User login
Cardiovascular disease: Innovations in devices and techniques
Supplement Editor:
Maan A. Fares, MD
Contents
Cardiovascular disease: Innovations in devices and techniques
Maan A. Fares
Transcatheter mitral valve replacement: A frontier in cardiac intervention
Amar Krishnaswamy, Stephanie Mick, Jose Navia, A. Marc Gillinov, E. Murrat Tuzcu, and Samir R. Kapadia
Bioresorbable stents: The future of Interventional cardiology?
Stephen G. Ellis and Haris Riaz
Leadless cardiac pacing: What primary care providers and non-EP cardiologists should know
Erich L. Kiehl and Daniel J. Cantillon
PCSK9 inhibition: A promise fulfilled?
Khendi White, Chaitra Mohan, and Michael Rocco
Fibromuscular dysplasia: Advances in understanding and management
Ellen K. Brinza and Heather L. Gornik
Supplement Editor:
Maan A. Fares, MD
Contents
Cardiovascular disease: Innovations in devices and techniques
Maan A. Fares
Transcatheter mitral valve replacement: A frontier in cardiac intervention
Amar Krishnaswamy, Stephanie Mick, Jose Navia, A. Marc Gillinov, E. Murrat Tuzcu, and Samir R. Kapadia
Bioresorbable stents: The future of Interventional cardiology?
Stephen G. Ellis and Haris Riaz
Leadless cardiac pacing: What primary care providers and non-EP cardiologists should know
Erich L. Kiehl and Daniel J. Cantillon
PCSK9 inhibition: A promise fulfilled?
Khendi White, Chaitra Mohan, and Michael Rocco
Fibromuscular dysplasia: Advances in understanding and management
Ellen K. Brinza and Heather L. Gornik
Supplement Editor:
Maan A. Fares, MD
Contents
Cardiovascular disease: Innovations in devices and techniques
Maan A. Fares
Transcatheter mitral valve replacement: A frontier in cardiac intervention
Amar Krishnaswamy, Stephanie Mick, Jose Navia, A. Marc Gillinov, E. Murrat Tuzcu, and Samir R. Kapadia
Bioresorbable stents: The future of Interventional cardiology?
Stephen G. Ellis and Haris Riaz
Leadless cardiac pacing: What primary care providers and non-EP cardiologists should know
Erich L. Kiehl and Daniel J. Cantillon
PCSK9 inhibition: A promise fulfilled?
Khendi White, Chaitra Mohan, and Michael Rocco
Fibromuscular dysplasia: Advances in understanding and management
Ellen K. Brinza and Heather L. Gornik
Why ustekinumab dosing differs in Crohn’s disease
ORLANDO – Preclinical studies and years of clinical experience using the monoclonal antibody ustekinumab (Stelara, Janssen Biotech) in psoriasis and psoriatic arthritis offer important clues to any gastroenterologist perplexed by the official Food and Drug Administration indication, dosing frequency, and intensity for Crohn’s disease. Phase II and phase III findings also reveal where the monoclonal antibody may offer particular advantages, compared with other agents.
“Ustekinumab landed in your lap in September. You’re probably all trying to figure out how to get the ID formulation paid for with insurance,” William J. Sanborn, MD, professor and chief of the division of gastroenterology at the University of California, San Diego, said at the Advances in Inflammatory Bowel Diseases meeting. “But this is now the reality that you have this in your Crohn’s practice.”
The FDA approved ustekinumab to treat adults with moderately to severely active Crohn’s disease who 1) failed or were intolerant to immune modulators or corticosteroids but did not fail tumor necrosis factor (TNF) blockers or 2) failed or were intolerant to one or more TNF blockers. Dr. Sanborn and colleagues observed a significant induction of clinical response in a subgroup of patients who previously failed a TNF blocker in an early efficacy study (Gastroenterology. 2008;135:1130-41). “This is where the idea of initially focusing on TNF failures came from,” he added at the meeting sponsored by the Crohn’s & Colitis Foundation of America.
Induction dosing in Crohn’s disease is intravenous versus subcutaneous in psoriasis and psoriatic arthritis, in part because of the same study. “It looked like relatively better bioavailability and relatively better effect with intravenous dosing,” Dr. Sanborn said. “In Crohn’s disease, it’s a completely different animal.”
Official induction dosing is approximately 6 mg/kg in three fixed doses according to patient weight in Crohn’s disease. The 6-mg/kg dose yielded the most consistent response, compared with 1-mg/kg or 3-mg/kg doses in a subsequent phase IIb study (N Engl J Med. 2012;367:1519-28).
The most consistent induction results at weeks 6 and 8 were observed with 6 mg/kg ustekinumab versus 1 mg/kg or 3 mg/kg.
Dr. Sanborn and coinvestigators also saw “numeric differences in drug versus placebo for remission at 6 and 8 weeks “but it was not that clear from the phase II trial what the remission efficacy was, so that needed more exploration to really understand.”
Another distinction for ustekinumab in Crohn’s disease is the approved maintenance dosing of 90 mg subcutaneously every 8 weeks versus a 12-week interval recommended for psoriasis. “Why so much more in Crohn’s disease, and is that necessary?” Dr. Sanborn asked.
Based on changes in C-reactive protein levels and a “rapid drop” in Crohn’s Disease Activity Index scores by 4 weeks, “clearly efficacy was there for induction,” he said. Ustekinumab has a “quick onset – analogous to the TNF blockers.”
“These were quite encouraging data, and paved the way to move on to phase III [studies],” Dr. Sanborn said. The preclinical studies up to this point focused on patients with Crohn’s disease who previously failed TNF blockers. However, “in clinical practice, we would be interested to know if it would work in anti-TNF naive or nonfailures as well.”
So two subsequent studies assessed safety and efficacy in a TNF blocker–failure population (UNITI-1 trial. Inflamm. Bowel Dis. 2016 Mar;22 Suppl 1:S1) and a non-TNF failure population of patients who did fail previous conventional therapy such as steroids or immunomodulators (UNITI-2 trial).
Clinical response and remission steadily rose following induction up to a significant difference versus placebo at 8 weeks in the non–TNF failure population. “Remember, in the phase IIa study, the remission rates were not as clear-cut, so this really nails down this as a good drug in both patient populations,” Dr. Sanborn said.
To evaluate long-term maintenance, investigators rerandomized all participants in the UNITI-1 and UNITI-2 studies. They saw a 15% gain in clinical remission out to week 44, compared with placebo. Dr. Sanborn noted that ustekinumab has a relatively long half-life, so the difference in patients switched to placebo may not have been as striking. “In practice it’s important to know the on-time and off-time of this agent, and I think the clinical trials make that clear.”
The trials also show that 12-week dosing works, Dr. Sanborn said. “You see about 20% gain for every 8-week dosing. You get extra 5% or 10% extra on all outcome measures at 8 weeks, compared to 12 weeks dosing, with no difference in safety signals.” He added, “So more intensive dosing of 90 mg every 8 weeks is what ended up getting approved in the United States.”
Safety profile
So what does all the preclinical evidence suggest about safety of ustekinumab? The UNITI trials combined included more than 1,000 patients, and there were no deaths, Dr. Sanborn said. “Usually with TNF blockers in 1,000 patients you would see a few deaths.”
Patient withdrawals from the preclinical studies were also relatively low, Dr. Sanborn reported. “With ustekinumab monotherapy, drug withdrawal is only 3% or 4%, so it seems to be different from TNF blockers in that sense [too].”
In addition, the rates of adverse events were similar between placebo (83.5%) and ustekinumab’s combined every 8 week and every 12 week dosing groups through 44 weeks (81.0%), Dr. Sanborn said. The rates of serious adverse events were likewise similar, 15.0% and 11.0%, respectively. Reported malignancy included two cases of basal cell skin cancers, one in the placebo group and one in the every-8-week dosing group, he added.
“So all those black box warnings you’re used to worrying about with TNF blockers – serious infections, about opportunistic infections, malignancy – there is no black box warning with this agent around that.”
Dr. Sanborn noted that the FDA labeling reports infections. “We know Crohn’s disease patients are [also] getting azathioprine, steroids, methotrexate, so you will see some infections, but there wasn’t a consistent opportunistic infection signal.”
One case of reversible posterior leukoencephalopathy syndrome is included on the labeling. Dr. Sanborn also put this in perspective: “With all the experience in psoriasis and psoriatic arthritis, and the clinical trials [in IBD], there is just one case. So the relationship is not very clear.”
“The safety signals with ustekinumab are really very good. It seems to be an extremely safe agent – we really don’t see much in terms of infections,” Brian Feagan, MD, an internist and gastroenterologist at the University of Western Ontario in London, said in a separate presentation at the conference. “We don’t have a lot of long-term experience with ustekinumab in Crohn’s disease, but we have a lot of experience in psoriasis, and it’s a safe drug.”
“Ustekinumab may be our first really valid monotherapy, with less immunogenicity,” Dr. Feagan said.
ORLANDO – Preclinical studies and years of clinical experience using the monoclonal antibody ustekinumab (Stelara, Janssen Biotech) in psoriasis and psoriatic arthritis offer important clues to any gastroenterologist perplexed by the official Food and Drug Administration indication, dosing frequency, and intensity for Crohn’s disease. Phase II and phase III findings also reveal where the monoclonal antibody may offer particular advantages, compared with other agents.
“Ustekinumab landed in your lap in September. You’re probably all trying to figure out how to get the ID formulation paid for with insurance,” William J. Sanborn, MD, professor and chief of the division of gastroenterology at the University of California, San Diego, said at the Advances in Inflammatory Bowel Diseases meeting. “But this is now the reality that you have this in your Crohn’s practice.”
The FDA approved ustekinumab to treat adults with moderately to severely active Crohn’s disease who 1) failed or were intolerant to immune modulators or corticosteroids but did not fail tumor necrosis factor (TNF) blockers or 2) failed or were intolerant to one or more TNF blockers. Dr. Sanborn and colleagues observed a significant induction of clinical response in a subgroup of patients who previously failed a TNF blocker in an early efficacy study (Gastroenterology. 2008;135:1130-41). “This is where the idea of initially focusing on TNF failures came from,” he added at the meeting sponsored by the Crohn’s & Colitis Foundation of America.
Induction dosing in Crohn’s disease is intravenous versus subcutaneous in psoriasis and psoriatic arthritis, in part because of the same study. “It looked like relatively better bioavailability and relatively better effect with intravenous dosing,” Dr. Sanborn said. “In Crohn’s disease, it’s a completely different animal.”
Official induction dosing is approximately 6 mg/kg in three fixed doses according to patient weight in Crohn’s disease. The 6-mg/kg dose yielded the most consistent response, compared with 1-mg/kg or 3-mg/kg doses in a subsequent phase IIb study (N Engl J Med. 2012;367:1519-28).
The most consistent induction results at weeks 6 and 8 were observed with 6 mg/kg ustekinumab versus 1 mg/kg or 3 mg/kg.
Dr. Sanborn and coinvestigators also saw “numeric differences in drug versus placebo for remission at 6 and 8 weeks “but it was not that clear from the phase II trial what the remission efficacy was, so that needed more exploration to really understand.”
Another distinction for ustekinumab in Crohn’s disease is the approved maintenance dosing of 90 mg subcutaneously every 8 weeks versus a 12-week interval recommended for psoriasis. “Why so much more in Crohn’s disease, and is that necessary?” Dr. Sanborn asked.
Based on changes in C-reactive protein levels and a “rapid drop” in Crohn’s Disease Activity Index scores by 4 weeks, “clearly efficacy was there for induction,” he said. Ustekinumab has a “quick onset – analogous to the TNF blockers.”
“These were quite encouraging data, and paved the way to move on to phase III [studies],” Dr. Sanborn said. The preclinical studies up to this point focused on patients with Crohn’s disease who previously failed TNF blockers. However, “in clinical practice, we would be interested to know if it would work in anti-TNF naive or nonfailures as well.”
So two subsequent studies assessed safety and efficacy in a TNF blocker–failure population (UNITI-1 trial. Inflamm. Bowel Dis. 2016 Mar;22 Suppl 1:S1) and a non-TNF failure population of patients who did fail previous conventional therapy such as steroids or immunomodulators (UNITI-2 trial).
Clinical response and remission steadily rose following induction up to a significant difference versus placebo at 8 weeks in the non–TNF failure population. “Remember, in the phase IIa study, the remission rates were not as clear-cut, so this really nails down this as a good drug in both patient populations,” Dr. Sanborn said.
To evaluate long-term maintenance, investigators rerandomized all participants in the UNITI-1 and UNITI-2 studies. They saw a 15% gain in clinical remission out to week 44, compared with placebo. Dr. Sanborn noted that ustekinumab has a relatively long half-life, so the difference in patients switched to placebo may not have been as striking. “In practice it’s important to know the on-time and off-time of this agent, and I think the clinical trials make that clear.”
The trials also show that 12-week dosing works, Dr. Sanborn said. “You see about 20% gain for every 8-week dosing. You get extra 5% or 10% extra on all outcome measures at 8 weeks, compared to 12 weeks dosing, with no difference in safety signals.” He added, “So more intensive dosing of 90 mg every 8 weeks is what ended up getting approved in the United States.”
Safety profile
So what does all the preclinical evidence suggest about safety of ustekinumab? The UNITI trials combined included more than 1,000 patients, and there were no deaths, Dr. Sanborn said. “Usually with TNF blockers in 1,000 patients you would see a few deaths.”
Patient withdrawals from the preclinical studies were also relatively low, Dr. Sanborn reported. “With ustekinumab monotherapy, drug withdrawal is only 3% or 4%, so it seems to be different from TNF blockers in that sense [too].”
In addition, the rates of adverse events were similar between placebo (83.5%) and ustekinumab’s combined every 8 week and every 12 week dosing groups through 44 weeks (81.0%), Dr. Sanborn said. The rates of serious adverse events were likewise similar, 15.0% and 11.0%, respectively. Reported malignancy included two cases of basal cell skin cancers, one in the placebo group and one in the every-8-week dosing group, he added.
“So all those black box warnings you’re used to worrying about with TNF blockers – serious infections, about opportunistic infections, malignancy – there is no black box warning with this agent around that.”
Dr. Sanborn noted that the FDA labeling reports infections. “We know Crohn’s disease patients are [also] getting azathioprine, steroids, methotrexate, so you will see some infections, but there wasn’t a consistent opportunistic infection signal.”
One case of reversible posterior leukoencephalopathy syndrome is included on the labeling. Dr. Sanborn also put this in perspective: “With all the experience in psoriasis and psoriatic arthritis, and the clinical trials [in IBD], there is just one case. So the relationship is not very clear.”
“The safety signals with ustekinumab are really very good. It seems to be an extremely safe agent – we really don’t see much in terms of infections,” Brian Feagan, MD, an internist and gastroenterologist at the University of Western Ontario in London, said in a separate presentation at the conference. “We don’t have a lot of long-term experience with ustekinumab in Crohn’s disease, but we have a lot of experience in psoriasis, and it’s a safe drug.”
“Ustekinumab may be our first really valid monotherapy, with less immunogenicity,” Dr. Feagan said.
ORLANDO – Preclinical studies and years of clinical experience using the monoclonal antibody ustekinumab (Stelara, Janssen Biotech) in psoriasis and psoriatic arthritis offer important clues to any gastroenterologist perplexed by the official Food and Drug Administration indication, dosing frequency, and intensity for Crohn’s disease. Phase II and phase III findings also reveal where the monoclonal antibody may offer particular advantages, compared with other agents.
“Ustekinumab landed in your lap in September. You’re probably all trying to figure out how to get the ID formulation paid for with insurance,” William J. Sanborn, MD, professor and chief of the division of gastroenterology at the University of California, San Diego, said at the Advances in Inflammatory Bowel Diseases meeting. “But this is now the reality that you have this in your Crohn’s practice.”
The FDA approved ustekinumab to treat adults with moderately to severely active Crohn’s disease who 1) failed or were intolerant to immune modulators or corticosteroids but did not fail tumor necrosis factor (TNF) blockers or 2) failed or were intolerant to one or more TNF blockers. Dr. Sanborn and colleagues observed a significant induction of clinical response in a subgroup of patients who previously failed a TNF blocker in an early efficacy study (Gastroenterology. 2008;135:1130-41). “This is where the idea of initially focusing on TNF failures came from,” he added at the meeting sponsored by the Crohn’s & Colitis Foundation of America.
Induction dosing in Crohn’s disease is intravenous versus subcutaneous in psoriasis and psoriatic arthritis, in part because of the same study. “It looked like relatively better bioavailability and relatively better effect with intravenous dosing,” Dr. Sanborn said. “In Crohn’s disease, it’s a completely different animal.”
Official induction dosing is approximately 6 mg/kg in three fixed doses according to patient weight in Crohn’s disease. The 6-mg/kg dose yielded the most consistent response, compared with 1-mg/kg or 3-mg/kg doses in a subsequent phase IIb study (N Engl J Med. 2012;367:1519-28).
The most consistent induction results at weeks 6 and 8 were observed with 6 mg/kg ustekinumab versus 1 mg/kg or 3 mg/kg.
Dr. Sanborn and coinvestigators also saw “numeric differences in drug versus placebo for remission at 6 and 8 weeks “but it was not that clear from the phase II trial what the remission efficacy was, so that needed more exploration to really understand.”
Another distinction for ustekinumab in Crohn’s disease is the approved maintenance dosing of 90 mg subcutaneously every 8 weeks versus a 12-week interval recommended for psoriasis. “Why so much more in Crohn’s disease, and is that necessary?” Dr. Sanborn asked.
Based on changes in C-reactive protein levels and a “rapid drop” in Crohn’s Disease Activity Index scores by 4 weeks, “clearly efficacy was there for induction,” he said. Ustekinumab has a “quick onset – analogous to the TNF blockers.”
“These were quite encouraging data, and paved the way to move on to phase III [studies],” Dr. Sanborn said. The preclinical studies up to this point focused on patients with Crohn’s disease who previously failed TNF blockers. However, “in clinical practice, we would be interested to know if it would work in anti-TNF naive or nonfailures as well.”
So two subsequent studies assessed safety and efficacy in a TNF blocker–failure population (UNITI-1 trial. Inflamm. Bowel Dis. 2016 Mar;22 Suppl 1:S1) and a non-TNF failure population of patients who did fail previous conventional therapy such as steroids or immunomodulators (UNITI-2 trial).
Clinical response and remission steadily rose following induction up to a significant difference versus placebo at 8 weeks in the non–TNF failure population. “Remember, in the phase IIa study, the remission rates were not as clear-cut, so this really nails down this as a good drug in both patient populations,” Dr. Sanborn said.
To evaluate long-term maintenance, investigators rerandomized all participants in the UNITI-1 and UNITI-2 studies. They saw a 15% gain in clinical remission out to week 44, compared with placebo. Dr. Sanborn noted that ustekinumab has a relatively long half-life, so the difference in patients switched to placebo may not have been as striking. “In practice it’s important to know the on-time and off-time of this agent, and I think the clinical trials make that clear.”
The trials also show that 12-week dosing works, Dr. Sanborn said. “You see about 20% gain for every 8-week dosing. You get extra 5% or 10% extra on all outcome measures at 8 weeks, compared to 12 weeks dosing, with no difference in safety signals.” He added, “So more intensive dosing of 90 mg every 8 weeks is what ended up getting approved in the United States.”
Safety profile
So what does all the preclinical evidence suggest about safety of ustekinumab? The UNITI trials combined included more than 1,000 patients, and there were no deaths, Dr. Sanborn said. “Usually with TNF blockers in 1,000 patients you would see a few deaths.”
Patient withdrawals from the preclinical studies were also relatively low, Dr. Sanborn reported. “With ustekinumab monotherapy, drug withdrawal is only 3% or 4%, so it seems to be different from TNF blockers in that sense [too].”
In addition, the rates of adverse events were similar between placebo (83.5%) and ustekinumab’s combined every 8 week and every 12 week dosing groups through 44 weeks (81.0%), Dr. Sanborn said. The rates of serious adverse events were likewise similar, 15.0% and 11.0%, respectively. Reported malignancy included two cases of basal cell skin cancers, one in the placebo group and one in the every-8-week dosing group, he added.
“So all those black box warnings you’re used to worrying about with TNF blockers – serious infections, about opportunistic infections, malignancy – there is no black box warning with this agent around that.”
Dr. Sanborn noted that the FDA labeling reports infections. “We know Crohn’s disease patients are [also] getting azathioprine, steroids, methotrexate, so you will see some infections, but there wasn’t a consistent opportunistic infection signal.”
One case of reversible posterior leukoencephalopathy syndrome is included on the labeling. Dr. Sanborn also put this in perspective: “With all the experience in psoriasis and psoriatic arthritis, and the clinical trials [in IBD], there is just one case. So the relationship is not very clear.”
“The safety signals with ustekinumab are really very good. It seems to be an extremely safe agent – we really don’t see much in terms of infections,” Brian Feagan, MD, an internist and gastroenterologist at the University of Western Ontario in London, said in a separate presentation at the conference. “We don’t have a lot of long-term experience with ustekinumab in Crohn’s disease, but we have a lot of experience in psoriasis, and it’s a safe drug.”
“Ustekinumab may be our first really valid monotherapy, with less immunogenicity,” Dr. Feagan said.
EXPERT ANALYSIS FROM AIBD 2016
Clinical Guidelines: Hospital-acquired and ventilator-associated pneumonia
Hospital-acquired pneumonia (HAP) is pneumonia that presents at least 48 hours after admission to the hospital. In contrast, ventilator-associated pneumonia (VAP), is pneumonia that clinically presents 48 hours after endotracheal intubation. Together, these are some of the most common hospital-acquired infections in the United States and pose a considerable burden on hospitals nationwide.
The Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) recently updated their management guidelines for HAP and VAP with a goal of striking a balance between providing appropriate early antibiotic coverage and avoiding unnecessary treatment that can lead to adverse effects such as Clostridium difficile infections and development of antibiotic resistance.1 This update eliminated the concept of Healthcare Associated Pneumonia (HCAP), often used for patients in skilled care facilities, because newer evidence has shown that patients who had met these criteria did not have a higher incidence of multidrug resistant pathogens; rather, they have microbial etiologies and sensitivities that are similar to adults with community acquired pneumonia (CAP).
Hospital-acquired pneumonia
Reasons to cover for MRSA in HAP:
Risk factors:
• IV antibiotic treatment within 90 days
• Treatment in a unit where the prevalence of MRSA is greater than 20% or unknown
• Prior detection of MRSA by culture or nonculture screening (weaker risk factor)
High risk of mortality: • Septic shock
• Need for ventilator support
MRSA should be covered with use of either vancomycin or linezolid in these cases.
In addition, patients with HAP should be covered for Pseudomonas aeruginosa and other gram-negative bacilli. For patients with risk factors for pseudomonas or other gram-negative infection or a high risk for mortality, then two antipseudomonal antibiotics from different classes are recommended, such as piperacillin-tazobactam/tobramycin or cefepime/amikacin.
Use two antipseudomonal antibiotics in HAP if the patient has these risk factors:
Pseudomonas risk factors:
• IV antibiotic treatment within 90 days
• Structural lung disease increasing the risk of gram-negative infection (bronchiectasis, cystic fibrosis)
• High-quality gram stain from respiratory specimen showing predominant and numerous gram-negative bacilli
High risk of mortality:
• Septic shock
• Need for ventilator support
Ventilator-associated pneumonia
General management of VAP is similar to HAP in that empiric treatment should be tailored to the local distribution and susceptibilities of pathogens based on each hospital’s antibiogram. All regimens should cover for S. aureus, P. aeruginosa, and other gram-negative bacilli based on the risk of mortality associated with the need for ventilator support. MSSA should be covered for VAP unless the patient has methicillin-resistant risk factors (see below).
MRSA should be covered for VAP if:
• Patient has had IV antibiotic use within past 90 days
• Hospital unit has greater than 10%-20% of S. aureus isolates are MRSA or MRSA prevalence unknown
Only one antipseudomonal agent should be used unless there are one of the following characteristics present, as described below.
Use two antipseudomonal agents in VAP if:
• Prior IV antibiotic use within 90 days
• Septic shock at time of VAP
• Acute respiratory distress syndrome preceding VAP
• 5 or more days of hospitalization prior to the occurrence of VAP
• Acute renal replacement therapy prior to VAP onset
• Greater than 10% of gram-negative isolates are resistant to an agent being considered for monotherapy
• Local antibiotic susceptibility rates unknown
In both HAP and VAP, antibiotics should be de-escalated to those with a narrower spectrum after initial empiric therapy, ideally within 72 hours and based on sputum or blood culture results. The guidelines support obtaining noninvasive sputum cultures in patients with VAP (endotracheal aspirates) and HAP (spontaneous expectoration, induced sputum, or nasotracheal suctioning in a patient who is unable to cooperate to produce a sputum sample). Patients who are improving clinically may be switched to appropriate oral therapy based on the susceptibility of an identified organism. Another key change is that of the standard duration of therapy. Previously, patients were treated for up to 2-3 weeks with antibiotics. The new IDSA/ATS guidelines recommend that patients should be treated with 7 days of antibiotics rather than a longer course.
The bottom line
Empiric therapy for HAP and VAP should be tailored to each hospital’s local pathogen distribution and antimicrobial susceptibilities, as detailed in an antibiogram. In HAP and VAP, empiric antibiotics should cover for S. aureus, but it only needs to target MRSA if risk factors are present, prevalence is greater than 20% or unknown, and – if HAP – a high risk of mortality. P. aeruginosa and other gram-negative bacilli should also be covered in empiric regimens. Dual antipseudomonal antibiotics is only recommended to be used in HAP if there are specific pseudomonal risk factors or a high risk of mortality. They should be used in VAP if there are multidrug-resistant risk factors present or there is a high/unknown prevalence of resistant organisms. All antibiotic regimens should be deescalated rather than maintained, and both HAP and VAP patients ought to be treated for 7 days.
References
1. Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016 Sep 1;63(5):557-82.
2. Beardsley JR, Williamson JC, Johnson JW, Ohl CA, Karchmer TB, Bowton DL. Using local microbiologic data to develop institution-specific guidelines for the treatment of hospital-acquired pneumonia. Chest. 2006 Sep;130(3):787-93.
Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Jefferson Medical College, Philadelphia. Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Jefferson Medical College, Philadelphia. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Hospital-acquired pneumonia (HAP) is pneumonia that presents at least 48 hours after admission to the hospital. In contrast, ventilator-associated pneumonia (VAP), is pneumonia that clinically presents 48 hours after endotracheal intubation. Together, these are some of the most common hospital-acquired infections in the United States and pose a considerable burden on hospitals nationwide.
The Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) recently updated their management guidelines for HAP and VAP with a goal of striking a balance between providing appropriate early antibiotic coverage and avoiding unnecessary treatment that can lead to adverse effects such as Clostridium difficile infections and development of antibiotic resistance.1 This update eliminated the concept of Healthcare Associated Pneumonia (HCAP), often used for patients in skilled care facilities, because newer evidence has shown that patients who had met these criteria did not have a higher incidence of multidrug resistant pathogens; rather, they have microbial etiologies and sensitivities that are similar to adults with community acquired pneumonia (CAP).
Hospital-acquired pneumonia
Reasons to cover for MRSA in HAP:
Risk factors:
• IV antibiotic treatment within 90 days
• Treatment in a unit where the prevalence of MRSA is greater than 20% or unknown
• Prior detection of MRSA by culture or nonculture screening (weaker risk factor)
High risk of mortality: • Septic shock
• Need for ventilator support
MRSA should be covered with use of either vancomycin or linezolid in these cases.
In addition, patients with HAP should be covered for Pseudomonas aeruginosa and other gram-negative bacilli. For patients with risk factors for pseudomonas or other gram-negative infection or a high risk for mortality, then two antipseudomonal antibiotics from different classes are recommended, such as piperacillin-tazobactam/tobramycin or cefepime/amikacin.
Use two antipseudomonal antibiotics in HAP if the patient has these risk factors:
Pseudomonas risk factors:
• IV antibiotic treatment within 90 days
• Structural lung disease increasing the risk of gram-negative infection (bronchiectasis, cystic fibrosis)
• High-quality gram stain from respiratory specimen showing predominant and numerous gram-negative bacilli
High risk of mortality:
• Septic shock
• Need for ventilator support
Ventilator-associated pneumonia
General management of VAP is similar to HAP in that empiric treatment should be tailored to the local distribution and susceptibilities of pathogens based on each hospital’s antibiogram. All regimens should cover for S. aureus, P. aeruginosa, and other gram-negative bacilli based on the risk of mortality associated with the need for ventilator support. MSSA should be covered for VAP unless the patient has methicillin-resistant risk factors (see below).
MRSA should be covered for VAP if:
• Patient has had IV antibiotic use within past 90 days
• Hospital unit has greater than 10%-20% of S. aureus isolates are MRSA or MRSA prevalence unknown
Only one antipseudomonal agent should be used unless there are one of the following characteristics present, as described below.
Use two antipseudomonal agents in VAP if:
• Prior IV antibiotic use within 90 days
• Septic shock at time of VAP
• Acute respiratory distress syndrome preceding VAP
• 5 or more days of hospitalization prior to the occurrence of VAP
• Acute renal replacement therapy prior to VAP onset
• Greater than 10% of gram-negative isolates are resistant to an agent being considered for monotherapy
• Local antibiotic susceptibility rates unknown
In both HAP and VAP, antibiotics should be de-escalated to those with a narrower spectrum after initial empiric therapy, ideally within 72 hours and based on sputum or blood culture results. The guidelines support obtaining noninvasive sputum cultures in patients with VAP (endotracheal aspirates) and HAP (spontaneous expectoration, induced sputum, or nasotracheal suctioning in a patient who is unable to cooperate to produce a sputum sample). Patients who are improving clinically may be switched to appropriate oral therapy based on the susceptibility of an identified organism. Another key change is that of the standard duration of therapy. Previously, patients were treated for up to 2-3 weeks with antibiotics. The new IDSA/ATS guidelines recommend that patients should be treated with 7 days of antibiotics rather than a longer course.
The bottom line
Empiric therapy for HAP and VAP should be tailored to each hospital’s local pathogen distribution and antimicrobial susceptibilities, as detailed in an antibiogram. In HAP and VAP, empiric antibiotics should cover for S. aureus, but it only needs to target MRSA if risk factors are present, prevalence is greater than 20% or unknown, and – if HAP – a high risk of mortality. P. aeruginosa and other gram-negative bacilli should also be covered in empiric regimens. Dual antipseudomonal antibiotics is only recommended to be used in HAP if there are specific pseudomonal risk factors or a high risk of mortality. They should be used in VAP if there are multidrug-resistant risk factors present or there is a high/unknown prevalence of resistant organisms. All antibiotic regimens should be deescalated rather than maintained, and both HAP and VAP patients ought to be treated for 7 days.
References
1. Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016 Sep 1;63(5):557-82.
2. Beardsley JR, Williamson JC, Johnson JW, Ohl CA, Karchmer TB, Bowton DL. Using local microbiologic data to develop institution-specific guidelines for the treatment of hospital-acquired pneumonia. Chest. 2006 Sep;130(3):787-93.
Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Jefferson Medical College, Philadelphia. Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Jefferson Medical College, Philadelphia. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Hospital-acquired pneumonia (HAP) is pneumonia that presents at least 48 hours after admission to the hospital. In contrast, ventilator-associated pneumonia (VAP), is pneumonia that clinically presents 48 hours after endotracheal intubation. Together, these are some of the most common hospital-acquired infections in the United States and pose a considerable burden on hospitals nationwide.
The Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) recently updated their management guidelines for HAP and VAP with a goal of striking a balance between providing appropriate early antibiotic coverage and avoiding unnecessary treatment that can lead to adverse effects such as Clostridium difficile infections and development of antibiotic resistance.1 This update eliminated the concept of Healthcare Associated Pneumonia (HCAP), often used for patients in skilled care facilities, because newer evidence has shown that patients who had met these criteria did not have a higher incidence of multidrug resistant pathogens; rather, they have microbial etiologies and sensitivities that are similar to adults with community acquired pneumonia (CAP).
Hospital-acquired pneumonia
Reasons to cover for MRSA in HAP:
Risk factors:
• IV antibiotic treatment within 90 days
• Treatment in a unit where the prevalence of MRSA is greater than 20% or unknown
• Prior detection of MRSA by culture or nonculture screening (weaker risk factor)
High risk of mortality: • Septic shock
• Need for ventilator support
MRSA should be covered with use of either vancomycin or linezolid in these cases.
In addition, patients with HAP should be covered for Pseudomonas aeruginosa and other gram-negative bacilli. For patients with risk factors for pseudomonas or other gram-negative infection or a high risk for mortality, then two antipseudomonal antibiotics from different classes are recommended, such as piperacillin-tazobactam/tobramycin or cefepime/amikacin.
Use two antipseudomonal antibiotics in HAP if the patient has these risk factors:
Pseudomonas risk factors:
• IV antibiotic treatment within 90 days
• Structural lung disease increasing the risk of gram-negative infection (bronchiectasis, cystic fibrosis)
• High-quality gram stain from respiratory specimen showing predominant and numerous gram-negative bacilli
High risk of mortality:
• Septic shock
• Need for ventilator support
Ventilator-associated pneumonia
General management of VAP is similar to HAP in that empiric treatment should be tailored to the local distribution and susceptibilities of pathogens based on each hospital’s antibiogram. All regimens should cover for S. aureus, P. aeruginosa, and other gram-negative bacilli based on the risk of mortality associated with the need for ventilator support. MSSA should be covered for VAP unless the patient has methicillin-resistant risk factors (see below).
MRSA should be covered for VAP if:
• Patient has had IV antibiotic use within past 90 days
• Hospital unit has greater than 10%-20% of S. aureus isolates are MRSA or MRSA prevalence unknown
Only one antipseudomonal agent should be used unless there are one of the following characteristics present, as described below.
Use two antipseudomonal agents in VAP if:
• Prior IV antibiotic use within 90 days
• Septic shock at time of VAP
• Acute respiratory distress syndrome preceding VAP
• 5 or more days of hospitalization prior to the occurrence of VAP
• Acute renal replacement therapy prior to VAP onset
• Greater than 10% of gram-negative isolates are resistant to an agent being considered for monotherapy
• Local antibiotic susceptibility rates unknown
In both HAP and VAP, antibiotics should be de-escalated to those with a narrower spectrum after initial empiric therapy, ideally within 72 hours and based on sputum or blood culture results. The guidelines support obtaining noninvasive sputum cultures in patients with VAP (endotracheal aspirates) and HAP (spontaneous expectoration, induced sputum, or nasotracheal suctioning in a patient who is unable to cooperate to produce a sputum sample). Patients who are improving clinically may be switched to appropriate oral therapy based on the susceptibility of an identified organism. Another key change is that of the standard duration of therapy. Previously, patients were treated for up to 2-3 weeks with antibiotics. The new IDSA/ATS guidelines recommend that patients should be treated with 7 days of antibiotics rather than a longer course.
The bottom line
Empiric therapy for HAP and VAP should be tailored to each hospital’s local pathogen distribution and antimicrobial susceptibilities, as detailed in an antibiogram. In HAP and VAP, empiric antibiotics should cover for S. aureus, but it only needs to target MRSA if risk factors are present, prevalence is greater than 20% or unknown, and – if HAP – a high risk of mortality. P. aeruginosa and other gram-negative bacilli should also be covered in empiric regimens. Dual antipseudomonal antibiotics is only recommended to be used in HAP if there are specific pseudomonal risk factors or a high risk of mortality. They should be used in VAP if there are multidrug-resistant risk factors present or there is a high/unknown prevalence of resistant organisms. All antibiotic regimens should be deescalated rather than maintained, and both HAP and VAP patients ought to be treated for 7 days.
References
1. Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016 Sep 1;63(5):557-82.
2. Beardsley JR, Williamson JC, Johnson JW, Ohl CA, Karchmer TB, Bowton DL. Using local microbiologic data to develop institution-specific guidelines for the treatment of hospital-acquired pneumonia. Chest. 2006 Sep;130(3):787-93.
Dr. Botti is a second-year resident in the family medicine residency program department of family and community medicine at Jefferson Medical College, Philadelphia. Dr. Mills is assistant residency program director and assistant professor in the department of family and community medicine and department of physiology at Jefferson Medical College, Philadelphia. Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia.
Neurosurgical Subspecialty Bedside Guide Improves Nursing Confidence
The VA Portland Healthcare System (VAPHCS) is a 277-bed facility that serves more than 85,000 inpatient and 880,000 outpatient visits each year from veterans in Oregon and southwestern Washington. The VAPHCS consists of a main tertiary care VAMC with an acute medical and surgical facility that includes 30 beds serving qualifying veterans. Supported surgical specialties include urology, general surgery, vascular surgery, otolaryngology, orthopedic surgery, ophthalmology, cardiothoracic surgery, transplant surgery, and neurological surgery. Neurosurgical patients account for about 12% to 13% of annual surgical patients. The VAPHCS also is partnered with Oregon Health & Science University in the training of health care professionals, such as physicians and nurses.
The expectation at the VAPHCS is that medical-surgical nurses care for 4 to 5 concurrent patients, often from different surgical services. Caring for patients with different medical and surgical needs, variable ambulatory, swallowing, and elimination functions, and different physician teams can become confusing; even within a single surgical service, postoperative care due to procedure complexity, specificity of care orders, and the real possibility of medical catastrophe can seem overwhelming. Therefore, subspecialty nursing training poses a challenge that requires technical in-service and didactic education and allocation of resources.
Despite systems level subspecialty nursing training, medical emergencies identified at the bedside can be mismanaged.1 Errors in care can be due to an incomplete knowledge of the patient’s procedure and misunderstanding of positioning and activity limitations.
To encourage medical-surgical nurses to become more engaged and confident in subspecialty patient care, the authors developed a bedside neurosurgical nursing guide to allow for independent procedure related education. The comprehensive guide summarized the clinical course for postoperative neurosurgical patients undergoing cranial and spinal surgeries. This guide included appropriate surgery-related images, procedure overviews, management decisions, potential postoperative complications, and wound care directions. The guide was distributed to medical-surgical nurses caring for neurosurgical patients. The authors hypothesized that the guide would enable nurses to better predict adverse outcomes and respond appropriately and would improve confidence in patient care.
Methods
For educational purposes, a bedside neurosurgical nursing guide (text and graphics) was created for the 16 surgical subspecialty nurses at the VAPHCS. The guide detailed the most common cranial and spinal neurosurgical procedures performed at VAPHCS and was written based on a typical postoperative course for each procedure by the chief neurosurgery resident at VAPHCS with collaboration from the attending neurosurgeons (Figure).
A quality improvement (QI) project was undertaken to assess nursing confidence with neurosurgical patients’ care pre- and postfamiliarity with the bedside neurosurgical nursing guide. A literature search revealed no validated survey assessing nursing confidence, so one was created using the Likert scale. Specifically, an anonymous 6-question survey was completed by all 16 surgical nurses prior to familiarization with the guide. Responses were recorded as scores of 1 to 5 for questions 1, 3, and 4, with a response of 1 indicative of no comfort or confidence and a response of 5 indicative of the highest level of comfort or confidence. Responses were recorded as either true or false for questions 2 and 6, and never, occasionally, frequently, or always for question 5.
The guide was made available to nurses for 6 months without encouragement to use it. After 6 months, a 3-week period of familiarization with and education about the availability of the guide was instituted at morning nursing reports; the total availability of the guide to nursing staff was 6 months 3 weeks. After this period the same 6-question survey was distributed, and data were collected.
Survey responses were categorized into 2 groups. Responses to questions 1, 3, and 4 were categorized as group 1, and responses to questions 4 and 5 were categorized as group 2. Responses (never and occasionally) to question 5, were categorized as group 1 and responses (frequently and always) as group 2 (Table). Responses to questions 2 and 6 were grouped 1 for true and 2 for false. Nurses participating in this study ranged in age from 22 to 57 years, education level ranged from registered nurse to a bachelor of science in nursing, and years of experience ranged from < 1 year to 27 years.
Statistics were calculated using chi-square analysis with Yates correction online calculator. For the chi-square analysis, the prefamiliarization data for groups 1 and 2 were used as the expected values, and the postfamiliarization data were used for the observed values. In this manner, differences were discerned between the before and after questionnaire responses. The VAPHCS institutional review board determined that the study was not human research and exempt from review.
Findings
Anonymous survey responses were collected from all 16 surgical subspecialty nurses both prior and after familiarization with the nursing guide.The response rate was 100% with only a few incomplete responses excluded from the analysis. Three questions in the prefamiliarization questionnaire had no appropriate response, and 1 question in the postfamiliarization survey had no appropriate response.
Improvement was statistically significant in responses for questions 1, 3, 5, and 6 (P = .026, .008, .004, and .033, respectively). No significant differences were found for questions 2 and 4 (P = .974 and .116, respectively). It is possible that there was no significant difference in question 2 because prefamiliarization responses were already favorable. Even if nurses did not feel comfortable taking care of neurosurgical patients (as assessed in question 1), they noted confidence improvement by working on the ward and through informal assimilation of knowledge and skill, which would have accumulated naturally over 1 year.
Prior to familiarization with the guide, 7 nurses did not feel confident in assessing the need to contact a physician (question 4). After familiarization with the nursing guide, favorable responses increased from 9 to 14 nurses. Results trended toward but did not reach statistical significance, likely due to the small sample size.
Ultimately, in the 16 surgical subspecialty nurses surveyed, familiarization with the nursing guide was shown to improve comfort in taking care of neurosurgical patients and increase confidence in patient care skills. At the end of the QI project (6 months, 3 weeks), all nurses knew where to locate the bedside neurosurgical nursing guide and were familiar with it and its use. The guide remains accessible to the medical-surgical nurses and continues to be used.
Discussion
Nursing confidence has an undervalued effect on patient care.2 Confidence, or a belief in one’s own ability, varies directly with competence. Systematic quantification of nursing competence has been extensively studied using self-report questionnaires and clinical simulations.2,3 Competency can be quantified and normalized using formal assessment; however, confidence is somewhat intangible. Nursing confidence is a situation-dependent subjective feeling of security and is derived from an internalized assessment of skills that are commensurate with patient needs. Nursing confidence is further influenced by an intuited value within the care team, adequate knowledge of the patient’s condition, and procedures and protocols.4
A similar but less specific definition deconstructs nursing confidence as “significance of a professional network of coworkers” and the “importance of confirmation of professional role and competence.”5 The professional network of coworkers is invaluable as it underlies the essence of patient-centered care. The adaptive leadership framework is integral to the modern delivery of patient care, and via this framework frontline clinical staff, including nurses, are empowered.6,7
The second portion of Haavardsholm and Nåden’s definition, “importance of confirmation of professional role and competence” describes the association of the most easily augmented correlate of confidence: competency.5 Nursing competency is supplemented continuously with in-service training and recertification processes; however, despite this, demands placed on nurses can be technologically advanced and extremely varied. Nursing competency is known to directly correlate with increasing education, as nurses holding a master’s degree have been shown to outperform those with a bachelor of nursing degree.3
Increased formal education as well as increased work experience (> 5 years) are correlated with increased critical thinking ability.4,5 The critical thinking ability of health care providers can be fortified by clinical simulation, which leads to statistically significant improvement in clinical competency.2,3
A literature review of Medline and the National Library of Medicine PubMed online databases for search terms (nurs*, confidence, bedside, guide) was performed but did not result in original research assessing nurse confidence related to bedside guides. In this population, nurses were anonymously compared against their own historical data obviating any effect of education or experience on survey measures.
Nursing Self-Confidence
Evidence suggests that nursing confidence is a complex manifestation of the security felt within the care team and the comfort of one’s own professional abilities.4 Patients’ trust in the team caring for them is based on the confidence exuded by the team.8 In this way, nursing confidence can affect the patient-care team profoundly. Value is maximized when a nurse’s self-confidence engenders patient confidence and trust. Due to the varied patient load and complexity of subspecialty nursing care, it is hypothesized that bedside manuals/guidelines can be used to educate the subspecialty nurses on specific patient-related issues.
Nursing practice competence and confidence is vital to providing care for patients with complex postsurgical health care needs. Patient safety and outcome are paramount. This can be intimidating for newly qualified surgical subspecialty nurses who have not yet had experience with or adequate exposure to patients with complex postsurgical needs. Surgical nursing continuing education places an emphasis on adaptation to ever-changing specialized surgical procedures and postoperative patient care. Nevertheless, it is difficult for surgical subspecialty nurses to learn and retain all the possible complexities of individual cases and to confidently, appropriately, and safely care for patients especially when adverse events arise.
Recognizing that leadership is personal and not dependent on hierarchy, surgical subspecialty nurses may be better suited to specific bedside training and counseling.6,9 A key factor influencing nursing confidence is communication and collaboration with physicians.9 The role of the physician at VA medical facilities is no longer to be a commanding figure with complete medical autonomy; rather, a unified team of specialized practitioners collaboratively facilitate and deliver patient care.
There is no specific research detailing the use of bedside nursing guides in caring for postoperative patients. However, at VAPHCS, nurses created supplemental material regarding postoperative acute care of vascular surgery patients, which was found to be subjectively helpful in elevating nursing confidence. To the authors’ knowledge, no such supplemental information/guide exists for other specialty surgical services.
The surgical nursing guide created here detailed visuals of many common neurosurgical procedures performed at VAPHCS and included a prioritized checklist, which the 16 surgical subspecialty nurses could reference postoperatively. The authors hypothesized that this would enhance the nurses’ ability to efficiently manage specific situations while bridging communication gaps between surgical teams and nurses. The survey results agree with previous reports that suggested that the application of an adaptive leadership framework would empower nurses to deliver excellent patient-centered care, care that can be augmented with subspecialty nursing guides.7,10
Based on these results the authors propose that subspecialty surgical services consider use of a practical nursing guide for all surgical subspecialty nurses to reference, improve familiarity with procedures, and provide guidance to manage adverse events. Since implementing this reader-friendly paradigm within neurosurgical care, a nurse driven expansion has now included other subspecialty services at the VAPHCS with success.
Limitations
Survey responses have inherent bias and sampling error rates. The sample size for this survey was small. Data were grouped for data analysis. Competency and patient outcomes were not measured.
Future Directions
Despite specific surgical specialty postoperative patient care training, an overall lack of confidence can persist. A physician-created neurosurgical nursing guide that detailed the most common neurosurgical procedures, expected postoperative care, and potential emergencies was shown to improve nursing confidence. Collaborative (physician and nursing leaders) QI projects, such as described here; development of specific surgical specialty initiatives designed to improve confidence and quality; and nurse-physician communication and teamwork could lead to improved patient satisfaction and outcome.
The costs associated with developing and using bedside nursing guides are relatively low, and efficiency can be considered high. Competency improvement could be measured by creating a specialty-specific case scenario question bank. Effects on patient satisfaction and outcome could be measured by a patient satisfaction survey. Improvements in beside catastrophe management could be prospectively tracked; for example, rates of mismanagement of mobility status, emergent transfers to the intensive care unit, or poor wound care could be compared pre- and postfamiliarization with a subspecialty guide.
Conclusion
Familiarization with the VAPHCS neurosurgical nursing guide had a positive impact on the confidence of medical-surgical nurses caring for neurosurgical patients. Medical-surgical nurses were more comfortable taking care of neurosurgical patients; they felt the guide helped improve skills and noted improved knowledge regarding involvement of physician oversight. Although objective parameters were not assessed, improvement in nursing confidence in general leads to improved overall nurse-physician communication and patient management. A further study might target objective parameters associated with guide usage, such as changes in the number of emergencies or calls to physicians regarding management.
Acknowledgments
The authors thank Andy Rekito, MS, for illustrative assistance.
1. Pusateri ME, Prior MM, Kiely SC. The role of the non-ICU staff nurse on a medical emergency team: perceptions and understanding. Am J Nurs. 2011;111(5):22-29, quiz 30-31.
2. Bambini D, Washburn J, Perkins R. Outcomes of clinical simulation for novice nursing students: communication, confidence, clinical judgment. Nurs Educ Perspect. 2009;30(2):79-82.
3. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21-22):3224-3232.
4. Perry P. Concept analysis: confidence/self-confidence. Nurs Forum. 2011;46(4):218-230.
5. Haavardsholm I, Nåden D. The concept of confidence—the nurse’s perception. Eur J Cancer Care (Engl). 2009;18(5):483-491.
6. Bailey DE Jr, Docherty SL, Adams JA, et al. Studying the clinical encounter with the Adaptive Leadership framework. J Healthc Leadersh. 2012;2012(4):83-91.
7. Hall C, McCutcheon H, Deuter K, Matricciani L. Evaluating and improving a model of nursing care delivery: a process of partnership. Collegian. 2012;19(4):203-210.
8. Williams AM, Irurita VF. Therapeutic and non-therapeutic interpersonal interactions: the patient’s perspective. J Clin Nurs. 2004;13(7):806-815.
9. Carryer J. Collaboration between doctors and nurses. J Prim Health Care. 2011;3(1):77-79.
10. Chadwick MM. Creating order out of chaos: a leadership approach. AORN J. 2010;91(1):154-170.
The VA Portland Healthcare System (VAPHCS) is a 277-bed facility that serves more than 85,000 inpatient and 880,000 outpatient visits each year from veterans in Oregon and southwestern Washington. The VAPHCS consists of a main tertiary care VAMC with an acute medical and surgical facility that includes 30 beds serving qualifying veterans. Supported surgical specialties include urology, general surgery, vascular surgery, otolaryngology, orthopedic surgery, ophthalmology, cardiothoracic surgery, transplant surgery, and neurological surgery. Neurosurgical patients account for about 12% to 13% of annual surgical patients. The VAPHCS also is partnered with Oregon Health & Science University in the training of health care professionals, such as physicians and nurses.
The expectation at the VAPHCS is that medical-surgical nurses care for 4 to 5 concurrent patients, often from different surgical services. Caring for patients with different medical and surgical needs, variable ambulatory, swallowing, and elimination functions, and different physician teams can become confusing; even within a single surgical service, postoperative care due to procedure complexity, specificity of care orders, and the real possibility of medical catastrophe can seem overwhelming. Therefore, subspecialty nursing training poses a challenge that requires technical in-service and didactic education and allocation of resources.
Despite systems level subspecialty nursing training, medical emergencies identified at the bedside can be mismanaged.1 Errors in care can be due to an incomplete knowledge of the patient’s procedure and misunderstanding of positioning and activity limitations.
To encourage medical-surgical nurses to become more engaged and confident in subspecialty patient care, the authors developed a bedside neurosurgical nursing guide to allow for independent procedure related education. The comprehensive guide summarized the clinical course for postoperative neurosurgical patients undergoing cranial and spinal surgeries. This guide included appropriate surgery-related images, procedure overviews, management decisions, potential postoperative complications, and wound care directions. The guide was distributed to medical-surgical nurses caring for neurosurgical patients. The authors hypothesized that the guide would enable nurses to better predict adverse outcomes and respond appropriately and would improve confidence in patient care.
Methods
For educational purposes, a bedside neurosurgical nursing guide (text and graphics) was created for the 16 surgical subspecialty nurses at the VAPHCS. The guide detailed the most common cranial and spinal neurosurgical procedures performed at VAPHCS and was written based on a typical postoperative course for each procedure by the chief neurosurgery resident at VAPHCS with collaboration from the attending neurosurgeons (Figure).
A quality improvement (QI) project was undertaken to assess nursing confidence with neurosurgical patients’ care pre- and postfamiliarity with the bedside neurosurgical nursing guide. A literature search revealed no validated survey assessing nursing confidence, so one was created using the Likert scale. Specifically, an anonymous 6-question survey was completed by all 16 surgical nurses prior to familiarization with the guide. Responses were recorded as scores of 1 to 5 for questions 1, 3, and 4, with a response of 1 indicative of no comfort or confidence and a response of 5 indicative of the highest level of comfort or confidence. Responses were recorded as either true or false for questions 2 and 6, and never, occasionally, frequently, or always for question 5.
The guide was made available to nurses for 6 months without encouragement to use it. After 6 months, a 3-week period of familiarization with and education about the availability of the guide was instituted at morning nursing reports; the total availability of the guide to nursing staff was 6 months 3 weeks. After this period the same 6-question survey was distributed, and data were collected.
Survey responses were categorized into 2 groups. Responses to questions 1, 3, and 4 were categorized as group 1, and responses to questions 4 and 5 were categorized as group 2. Responses (never and occasionally) to question 5, were categorized as group 1 and responses (frequently and always) as group 2 (Table). Responses to questions 2 and 6 were grouped 1 for true and 2 for false. Nurses participating in this study ranged in age from 22 to 57 years, education level ranged from registered nurse to a bachelor of science in nursing, and years of experience ranged from < 1 year to 27 years.
Statistics were calculated using chi-square analysis with Yates correction online calculator. For the chi-square analysis, the prefamiliarization data for groups 1 and 2 were used as the expected values, and the postfamiliarization data were used for the observed values. In this manner, differences were discerned between the before and after questionnaire responses. The VAPHCS institutional review board determined that the study was not human research and exempt from review.
Findings
Anonymous survey responses were collected from all 16 surgical subspecialty nurses both prior and after familiarization with the nursing guide.The response rate was 100% with only a few incomplete responses excluded from the analysis. Three questions in the prefamiliarization questionnaire had no appropriate response, and 1 question in the postfamiliarization survey had no appropriate response.
Improvement was statistically significant in responses for questions 1, 3, 5, and 6 (P = .026, .008, .004, and .033, respectively). No significant differences were found for questions 2 and 4 (P = .974 and .116, respectively). It is possible that there was no significant difference in question 2 because prefamiliarization responses were already favorable. Even if nurses did not feel comfortable taking care of neurosurgical patients (as assessed in question 1), they noted confidence improvement by working on the ward and through informal assimilation of knowledge and skill, which would have accumulated naturally over 1 year.
Prior to familiarization with the guide, 7 nurses did not feel confident in assessing the need to contact a physician (question 4). After familiarization with the nursing guide, favorable responses increased from 9 to 14 nurses. Results trended toward but did not reach statistical significance, likely due to the small sample size.
Ultimately, in the 16 surgical subspecialty nurses surveyed, familiarization with the nursing guide was shown to improve comfort in taking care of neurosurgical patients and increase confidence in patient care skills. At the end of the QI project (6 months, 3 weeks), all nurses knew where to locate the bedside neurosurgical nursing guide and were familiar with it and its use. The guide remains accessible to the medical-surgical nurses and continues to be used.
Discussion
Nursing confidence has an undervalued effect on patient care.2 Confidence, or a belief in one’s own ability, varies directly with competence. Systematic quantification of nursing competence has been extensively studied using self-report questionnaires and clinical simulations.2,3 Competency can be quantified and normalized using formal assessment; however, confidence is somewhat intangible. Nursing confidence is a situation-dependent subjective feeling of security and is derived from an internalized assessment of skills that are commensurate with patient needs. Nursing confidence is further influenced by an intuited value within the care team, adequate knowledge of the patient’s condition, and procedures and protocols.4
A similar but less specific definition deconstructs nursing confidence as “significance of a professional network of coworkers” and the “importance of confirmation of professional role and competence.”5 The professional network of coworkers is invaluable as it underlies the essence of patient-centered care. The adaptive leadership framework is integral to the modern delivery of patient care, and via this framework frontline clinical staff, including nurses, are empowered.6,7
The second portion of Haavardsholm and Nåden’s definition, “importance of confirmation of professional role and competence” describes the association of the most easily augmented correlate of confidence: competency.5 Nursing competency is supplemented continuously with in-service training and recertification processes; however, despite this, demands placed on nurses can be technologically advanced and extremely varied. Nursing competency is known to directly correlate with increasing education, as nurses holding a master’s degree have been shown to outperform those with a bachelor of nursing degree.3
Increased formal education as well as increased work experience (> 5 years) are correlated with increased critical thinking ability.4,5 The critical thinking ability of health care providers can be fortified by clinical simulation, which leads to statistically significant improvement in clinical competency.2,3
A literature review of Medline and the National Library of Medicine PubMed online databases for search terms (nurs*, confidence, bedside, guide) was performed but did not result in original research assessing nurse confidence related to bedside guides. In this population, nurses were anonymously compared against their own historical data obviating any effect of education or experience on survey measures.
Nursing Self-Confidence
Evidence suggests that nursing confidence is a complex manifestation of the security felt within the care team and the comfort of one’s own professional abilities.4 Patients’ trust in the team caring for them is based on the confidence exuded by the team.8 In this way, nursing confidence can affect the patient-care team profoundly. Value is maximized when a nurse’s self-confidence engenders patient confidence and trust. Due to the varied patient load and complexity of subspecialty nursing care, it is hypothesized that bedside manuals/guidelines can be used to educate the subspecialty nurses on specific patient-related issues.
Nursing practice competence and confidence is vital to providing care for patients with complex postsurgical health care needs. Patient safety and outcome are paramount. This can be intimidating for newly qualified surgical subspecialty nurses who have not yet had experience with or adequate exposure to patients with complex postsurgical needs. Surgical nursing continuing education places an emphasis on adaptation to ever-changing specialized surgical procedures and postoperative patient care. Nevertheless, it is difficult for surgical subspecialty nurses to learn and retain all the possible complexities of individual cases and to confidently, appropriately, and safely care for patients especially when adverse events arise.
Recognizing that leadership is personal and not dependent on hierarchy, surgical subspecialty nurses may be better suited to specific bedside training and counseling.6,9 A key factor influencing nursing confidence is communication and collaboration with physicians.9 The role of the physician at VA medical facilities is no longer to be a commanding figure with complete medical autonomy; rather, a unified team of specialized practitioners collaboratively facilitate and deliver patient care.
There is no specific research detailing the use of bedside nursing guides in caring for postoperative patients. However, at VAPHCS, nurses created supplemental material regarding postoperative acute care of vascular surgery patients, which was found to be subjectively helpful in elevating nursing confidence. To the authors’ knowledge, no such supplemental information/guide exists for other specialty surgical services.
The surgical nursing guide created here detailed visuals of many common neurosurgical procedures performed at VAPHCS and included a prioritized checklist, which the 16 surgical subspecialty nurses could reference postoperatively. The authors hypothesized that this would enhance the nurses’ ability to efficiently manage specific situations while bridging communication gaps between surgical teams and nurses. The survey results agree with previous reports that suggested that the application of an adaptive leadership framework would empower nurses to deliver excellent patient-centered care, care that can be augmented with subspecialty nursing guides.7,10
Based on these results the authors propose that subspecialty surgical services consider use of a practical nursing guide for all surgical subspecialty nurses to reference, improve familiarity with procedures, and provide guidance to manage adverse events. Since implementing this reader-friendly paradigm within neurosurgical care, a nurse driven expansion has now included other subspecialty services at the VAPHCS with success.
Limitations
Survey responses have inherent bias and sampling error rates. The sample size for this survey was small. Data were grouped for data analysis. Competency and patient outcomes were not measured.
Future Directions
Despite specific surgical specialty postoperative patient care training, an overall lack of confidence can persist. A physician-created neurosurgical nursing guide that detailed the most common neurosurgical procedures, expected postoperative care, and potential emergencies was shown to improve nursing confidence. Collaborative (physician and nursing leaders) QI projects, such as described here; development of specific surgical specialty initiatives designed to improve confidence and quality; and nurse-physician communication and teamwork could lead to improved patient satisfaction and outcome.
The costs associated with developing and using bedside nursing guides are relatively low, and efficiency can be considered high. Competency improvement could be measured by creating a specialty-specific case scenario question bank. Effects on patient satisfaction and outcome could be measured by a patient satisfaction survey. Improvements in beside catastrophe management could be prospectively tracked; for example, rates of mismanagement of mobility status, emergent transfers to the intensive care unit, or poor wound care could be compared pre- and postfamiliarization with a subspecialty guide.
Conclusion
Familiarization with the VAPHCS neurosurgical nursing guide had a positive impact on the confidence of medical-surgical nurses caring for neurosurgical patients. Medical-surgical nurses were more comfortable taking care of neurosurgical patients; they felt the guide helped improve skills and noted improved knowledge regarding involvement of physician oversight. Although objective parameters were not assessed, improvement in nursing confidence in general leads to improved overall nurse-physician communication and patient management. A further study might target objective parameters associated with guide usage, such as changes in the number of emergencies or calls to physicians regarding management.
Acknowledgments
The authors thank Andy Rekito, MS, for illustrative assistance.
The VA Portland Healthcare System (VAPHCS) is a 277-bed facility that serves more than 85,000 inpatient and 880,000 outpatient visits each year from veterans in Oregon and southwestern Washington. The VAPHCS consists of a main tertiary care VAMC with an acute medical and surgical facility that includes 30 beds serving qualifying veterans. Supported surgical specialties include urology, general surgery, vascular surgery, otolaryngology, orthopedic surgery, ophthalmology, cardiothoracic surgery, transplant surgery, and neurological surgery. Neurosurgical patients account for about 12% to 13% of annual surgical patients. The VAPHCS also is partnered with Oregon Health & Science University in the training of health care professionals, such as physicians and nurses.
The expectation at the VAPHCS is that medical-surgical nurses care for 4 to 5 concurrent patients, often from different surgical services. Caring for patients with different medical and surgical needs, variable ambulatory, swallowing, and elimination functions, and different physician teams can become confusing; even within a single surgical service, postoperative care due to procedure complexity, specificity of care orders, and the real possibility of medical catastrophe can seem overwhelming. Therefore, subspecialty nursing training poses a challenge that requires technical in-service and didactic education and allocation of resources.
Despite systems level subspecialty nursing training, medical emergencies identified at the bedside can be mismanaged.1 Errors in care can be due to an incomplete knowledge of the patient’s procedure and misunderstanding of positioning and activity limitations.
To encourage medical-surgical nurses to become more engaged and confident in subspecialty patient care, the authors developed a bedside neurosurgical nursing guide to allow for independent procedure related education. The comprehensive guide summarized the clinical course for postoperative neurosurgical patients undergoing cranial and spinal surgeries. This guide included appropriate surgery-related images, procedure overviews, management decisions, potential postoperative complications, and wound care directions. The guide was distributed to medical-surgical nurses caring for neurosurgical patients. The authors hypothesized that the guide would enable nurses to better predict adverse outcomes and respond appropriately and would improve confidence in patient care.
Methods
For educational purposes, a bedside neurosurgical nursing guide (text and graphics) was created for the 16 surgical subspecialty nurses at the VAPHCS. The guide detailed the most common cranial and spinal neurosurgical procedures performed at VAPHCS and was written based on a typical postoperative course for each procedure by the chief neurosurgery resident at VAPHCS with collaboration from the attending neurosurgeons (Figure).
A quality improvement (QI) project was undertaken to assess nursing confidence with neurosurgical patients’ care pre- and postfamiliarity with the bedside neurosurgical nursing guide. A literature search revealed no validated survey assessing nursing confidence, so one was created using the Likert scale. Specifically, an anonymous 6-question survey was completed by all 16 surgical nurses prior to familiarization with the guide. Responses were recorded as scores of 1 to 5 for questions 1, 3, and 4, with a response of 1 indicative of no comfort or confidence and a response of 5 indicative of the highest level of comfort or confidence. Responses were recorded as either true or false for questions 2 and 6, and never, occasionally, frequently, or always for question 5.
The guide was made available to nurses for 6 months without encouragement to use it. After 6 months, a 3-week period of familiarization with and education about the availability of the guide was instituted at morning nursing reports; the total availability of the guide to nursing staff was 6 months 3 weeks. After this period the same 6-question survey was distributed, and data were collected.
Survey responses were categorized into 2 groups. Responses to questions 1, 3, and 4 were categorized as group 1, and responses to questions 4 and 5 were categorized as group 2. Responses (never and occasionally) to question 5, were categorized as group 1 and responses (frequently and always) as group 2 (Table). Responses to questions 2 and 6 were grouped 1 for true and 2 for false. Nurses participating in this study ranged in age from 22 to 57 years, education level ranged from registered nurse to a bachelor of science in nursing, and years of experience ranged from < 1 year to 27 years.
Statistics were calculated using chi-square analysis with Yates correction online calculator. For the chi-square analysis, the prefamiliarization data for groups 1 and 2 were used as the expected values, and the postfamiliarization data were used for the observed values. In this manner, differences were discerned between the before and after questionnaire responses. The VAPHCS institutional review board determined that the study was not human research and exempt from review.
Findings
Anonymous survey responses were collected from all 16 surgical subspecialty nurses both prior and after familiarization with the nursing guide.The response rate was 100% with only a few incomplete responses excluded from the analysis. Three questions in the prefamiliarization questionnaire had no appropriate response, and 1 question in the postfamiliarization survey had no appropriate response.
Improvement was statistically significant in responses for questions 1, 3, 5, and 6 (P = .026, .008, .004, and .033, respectively). No significant differences were found for questions 2 and 4 (P = .974 and .116, respectively). It is possible that there was no significant difference in question 2 because prefamiliarization responses were already favorable. Even if nurses did not feel comfortable taking care of neurosurgical patients (as assessed in question 1), they noted confidence improvement by working on the ward and through informal assimilation of knowledge and skill, which would have accumulated naturally over 1 year.
Prior to familiarization with the guide, 7 nurses did not feel confident in assessing the need to contact a physician (question 4). After familiarization with the nursing guide, favorable responses increased from 9 to 14 nurses. Results trended toward but did not reach statistical significance, likely due to the small sample size.
Ultimately, in the 16 surgical subspecialty nurses surveyed, familiarization with the nursing guide was shown to improve comfort in taking care of neurosurgical patients and increase confidence in patient care skills. At the end of the QI project (6 months, 3 weeks), all nurses knew where to locate the bedside neurosurgical nursing guide and were familiar with it and its use. The guide remains accessible to the medical-surgical nurses and continues to be used.
Discussion
Nursing confidence has an undervalued effect on patient care.2 Confidence, or a belief in one’s own ability, varies directly with competence. Systematic quantification of nursing competence has been extensively studied using self-report questionnaires and clinical simulations.2,3 Competency can be quantified and normalized using formal assessment; however, confidence is somewhat intangible. Nursing confidence is a situation-dependent subjective feeling of security and is derived from an internalized assessment of skills that are commensurate with patient needs. Nursing confidence is further influenced by an intuited value within the care team, adequate knowledge of the patient’s condition, and procedures and protocols.4
A similar but less specific definition deconstructs nursing confidence as “significance of a professional network of coworkers” and the “importance of confirmation of professional role and competence.”5 The professional network of coworkers is invaluable as it underlies the essence of patient-centered care. The adaptive leadership framework is integral to the modern delivery of patient care, and via this framework frontline clinical staff, including nurses, are empowered.6,7
The second portion of Haavardsholm and Nåden’s definition, “importance of confirmation of professional role and competence” describes the association of the most easily augmented correlate of confidence: competency.5 Nursing competency is supplemented continuously with in-service training and recertification processes; however, despite this, demands placed on nurses can be technologically advanced and extremely varied. Nursing competency is known to directly correlate with increasing education, as nurses holding a master’s degree have been shown to outperform those with a bachelor of nursing degree.3
Increased formal education as well as increased work experience (> 5 years) are correlated with increased critical thinking ability.4,5 The critical thinking ability of health care providers can be fortified by clinical simulation, which leads to statistically significant improvement in clinical competency.2,3
A literature review of Medline and the National Library of Medicine PubMed online databases for search terms (nurs*, confidence, bedside, guide) was performed but did not result in original research assessing nurse confidence related to bedside guides. In this population, nurses were anonymously compared against their own historical data obviating any effect of education or experience on survey measures.
Nursing Self-Confidence
Evidence suggests that nursing confidence is a complex manifestation of the security felt within the care team and the comfort of one’s own professional abilities.4 Patients’ trust in the team caring for them is based on the confidence exuded by the team.8 In this way, nursing confidence can affect the patient-care team profoundly. Value is maximized when a nurse’s self-confidence engenders patient confidence and trust. Due to the varied patient load and complexity of subspecialty nursing care, it is hypothesized that bedside manuals/guidelines can be used to educate the subspecialty nurses on specific patient-related issues.
Nursing practice competence and confidence is vital to providing care for patients with complex postsurgical health care needs. Patient safety and outcome are paramount. This can be intimidating for newly qualified surgical subspecialty nurses who have not yet had experience with or adequate exposure to patients with complex postsurgical needs. Surgical nursing continuing education places an emphasis on adaptation to ever-changing specialized surgical procedures and postoperative patient care. Nevertheless, it is difficult for surgical subspecialty nurses to learn and retain all the possible complexities of individual cases and to confidently, appropriately, and safely care for patients especially when adverse events arise.
Recognizing that leadership is personal and not dependent on hierarchy, surgical subspecialty nurses may be better suited to specific bedside training and counseling.6,9 A key factor influencing nursing confidence is communication and collaboration with physicians.9 The role of the physician at VA medical facilities is no longer to be a commanding figure with complete medical autonomy; rather, a unified team of specialized practitioners collaboratively facilitate and deliver patient care.
There is no specific research detailing the use of bedside nursing guides in caring for postoperative patients. However, at VAPHCS, nurses created supplemental material regarding postoperative acute care of vascular surgery patients, which was found to be subjectively helpful in elevating nursing confidence. To the authors’ knowledge, no such supplemental information/guide exists for other specialty surgical services.
The surgical nursing guide created here detailed visuals of many common neurosurgical procedures performed at VAPHCS and included a prioritized checklist, which the 16 surgical subspecialty nurses could reference postoperatively. The authors hypothesized that this would enhance the nurses’ ability to efficiently manage specific situations while bridging communication gaps between surgical teams and nurses. The survey results agree with previous reports that suggested that the application of an adaptive leadership framework would empower nurses to deliver excellent patient-centered care, care that can be augmented with subspecialty nursing guides.7,10
Based on these results the authors propose that subspecialty surgical services consider use of a practical nursing guide for all surgical subspecialty nurses to reference, improve familiarity with procedures, and provide guidance to manage adverse events. Since implementing this reader-friendly paradigm within neurosurgical care, a nurse driven expansion has now included other subspecialty services at the VAPHCS with success.
Limitations
Survey responses have inherent bias and sampling error rates. The sample size for this survey was small. Data were grouped for data analysis. Competency and patient outcomes were not measured.
Future Directions
Despite specific surgical specialty postoperative patient care training, an overall lack of confidence can persist. A physician-created neurosurgical nursing guide that detailed the most common neurosurgical procedures, expected postoperative care, and potential emergencies was shown to improve nursing confidence. Collaborative (physician and nursing leaders) QI projects, such as described here; development of specific surgical specialty initiatives designed to improve confidence and quality; and nurse-physician communication and teamwork could lead to improved patient satisfaction and outcome.
The costs associated with developing and using bedside nursing guides are relatively low, and efficiency can be considered high. Competency improvement could be measured by creating a specialty-specific case scenario question bank. Effects on patient satisfaction and outcome could be measured by a patient satisfaction survey. Improvements in beside catastrophe management could be prospectively tracked; for example, rates of mismanagement of mobility status, emergent transfers to the intensive care unit, or poor wound care could be compared pre- and postfamiliarization with a subspecialty guide.
Conclusion
Familiarization with the VAPHCS neurosurgical nursing guide had a positive impact on the confidence of medical-surgical nurses caring for neurosurgical patients. Medical-surgical nurses were more comfortable taking care of neurosurgical patients; they felt the guide helped improve skills and noted improved knowledge regarding involvement of physician oversight. Although objective parameters were not assessed, improvement in nursing confidence in general leads to improved overall nurse-physician communication and patient management. A further study might target objective parameters associated with guide usage, such as changes in the number of emergencies or calls to physicians regarding management.
Acknowledgments
The authors thank Andy Rekito, MS, for illustrative assistance.
1. Pusateri ME, Prior MM, Kiely SC. The role of the non-ICU staff nurse on a medical emergency team: perceptions and understanding. Am J Nurs. 2011;111(5):22-29, quiz 30-31.
2. Bambini D, Washburn J, Perkins R. Outcomes of clinical simulation for novice nursing students: communication, confidence, clinical judgment. Nurs Educ Perspect. 2009;30(2):79-82.
3. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21-22):3224-3232.
4. Perry P. Concept analysis: confidence/self-confidence. Nurs Forum. 2011;46(4):218-230.
5. Haavardsholm I, Nåden D. The concept of confidence—the nurse’s perception. Eur J Cancer Care (Engl). 2009;18(5):483-491.
6. Bailey DE Jr, Docherty SL, Adams JA, et al. Studying the clinical encounter with the Adaptive Leadership framework. J Healthc Leadersh. 2012;2012(4):83-91.
7. Hall C, McCutcheon H, Deuter K, Matricciani L. Evaluating and improving a model of nursing care delivery: a process of partnership. Collegian. 2012;19(4):203-210.
8. Williams AM, Irurita VF. Therapeutic and non-therapeutic interpersonal interactions: the patient’s perspective. J Clin Nurs. 2004;13(7):806-815.
9. Carryer J. Collaboration between doctors and nurses. J Prim Health Care. 2011;3(1):77-79.
10. Chadwick MM. Creating order out of chaos: a leadership approach. AORN J. 2010;91(1):154-170.
1. Pusateri ME, Prior MM, Kiely SC. The role of the non-ICU staff nurse on a medical emergency team: perceptions and understanding. Am J Nurs. 2011;111(5):22-29, quiz 30-31.
2. Bambini D, Washburn J, Perkins R. Outcomes of clinical simulation for novice nursing students: communication, confidence, clinical judgment. Nurs Educ Perspect. 2009;30(2):79-82.
3. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20(21-22):3224-3232.
4. Perry P. Concept analysis: confidence/self-confidence. Nurs Forum. 2011;46(4):218-230.
5. Haavardsholm I, Nåden D. The concept of confidence—the nurse’s perception. Eur J Cancer Care (Engl). 2009;18(5):483-491.
6. Bailey DE Jr, Docherty SL, Adams JA, et al. Studying the clinical encounter with the Adaptive Leadership framework. J Healthc Leadersh. 2012;2012(4):83-91.
7. Hall C, McCutcheon H, Deuter K, Matricciani L. Evaluating and improving a model of nursing care delivery: a process of partnership. Collegian. 2012;19(4):203-210.
8. Williams AM, Irurita VF. Therapeutic and non-therapeutic interpersonal interactions: the patient’s perspective. J Clin Nurs. 2004;13(7):806-815.
9. Carryer J. Collaboration between doctors and nurses. J Prim Health Care. 2011;3(1):77-79.
10. Chadwick MM. Creating order out of chaos: a leadership approach. AORN J. 2010;91(1):154-170.
CAR met primary endpoint at interim analysis in DLBCL

2016 ASH Annual Meeting
SAN DIEGO—The chimeric antigen receptor (CAR) T-cell therapy KTE-C19 has met its primary endpoint at the pre-specified interim analysis of the phase 2 ZUMA-1 trial in diffuse large B-cell lymphoma (DLBCL), according to data presented at the 2016 ASH Annual Meeting.
DLBCL patients had an overall response rate (ORR) of 76% and a complete response (CR) rate of 47% (P<0.0001) after 3 months or more of follow-up. And most responses were evident by day 30, the researchers report.
ZUMA-1 is the first multicenter trial of an anti-CD19 CAR T-cell therapy in refractory, aggressive non-Hodgkin lymphoma (NHL).
A second NHL cohort of primary mediastinal B-cell lymphoma or transformed follicular lymphoma (PMBCL/TFL) patients were also treated. Together, the cohorts achieved an ORR of 79% and a CR rate of 52%.
Sattva Neelapu, MD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, presented the results as a late-breaking abstract (LBA-6*).
Detailed results of the PMBCL/TFL cohort were presented separately (abstract 998) at the meeting.
Earlier data from the phase 2 study have been reported in Hematology Times.
Phase 2 interim analysis
The study enrolled 111 patients, all of whom underwent leukapheresis. Seven of these patients were not treated, 5 due to serious adverse events (SAEs), 1 due to unavailable product, and 2 due to non-measurable disease.
“Importantly, there was no bridging therapy allowed on the study,” Dr Neelapu pointed out.
Patients then received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days. Two patients experienced SAEs after the conditioning regimen, making it a total of 10 patients who could not be treated.
Two days after the conditioning regimen was completed, investigators dosed 101 patients with KTE-C19 at a target dose of 2 × 106 anti-CD19 CAR T cells/kg.
“The majority of patients that were enrolled on the study were treated,” Dr Neelapu emphasized. “In fact, 91% of the 111 patients enrolled were treated and received the target dose of KTE-C19.”
Dr Neelapu noted that the success rate for manufacturing the CAR T cells was 99%, and the average turnaround time from apheresis to delivery to the clinical site was 17 days.
The study called for a pre-specified interim efficacy analysis when 50 patients in cohort 1—DLBCL patients—had at least 3 months of follow-up. This occurred on August 24, 2016, and the data was analyzed as of that date.
The primary endpoint was ORR of P<0.0001 using an exact binomial test comparing observed ORR to a historical control assumption of 20%. Key secondary endpoints included duration of response, overall survival, safety, and levels of CAR T cells and cytokines.
At the time of the pre-specified interim analysis, 93 patients had at least 1 month of follow-up. Fifty-one patients with DLBCL and 11 patients with PMBCL/TFL had at least 3 months of follow-up.
Patient characteristics
Dr Neelapu reported data on 73 DLBCL patients (cohort 1) and 20 PMBCL/TFL patients (cohort 2) evaluable with at least 1 month of follow-up at the time of the presentation.
The median age of all 93 patients was 59 (range, 25-76), and about half were 60 years or older.
Two-thirds of patients in cohort 1 and three-quarters in cohort 2 were male. Sixty-six percent of cohort 1 and 40% of cohort 2 had an ECOG performance status of 1.
Cohort 1 had a median of 3 prior therapies (range, 1-7), and 44% had an International Prognostic Index (IPI) risk score of 3-4. Cohort 2 had a median of 4 prior therapies (range, 2-12), and 45% had an IPI risk score of 3-4.
Fifty-six DLBCL patients (77%) were refractory to their second or later line of therapy, and 15 (21%) had relapsed after autologous stem cell transplant.
Sixteen PMBCL/TFL patients (80%) were refractory to their second or later line of therapy, and 4 (20%) relapsed after autologous stem cell transplant.
Results
Dr Neelapu indicated that patients responded rapidly to treatment, and most responses were evident at the first tumor assessment.
At 3 months’ follow-up or longer, the ORR was 76% and the CR rate 47% for the 51 DLBCL patients in cohort 1. This was a 6-fold higher CR rate compared with historical outcomes.
For the 11 PMBCL/TFL patients in cohort 2, the ORR was 91% and the CR rate was 73% at 3 months or longer.
Both cohorts combined yielded an ORR of 79% and a CR rate of 52%.
The treatment effect was consistent across key covariates—refractory patients, disease stage, IPI risk score, CD4/CD8 ratio, and steroid and tocilizumab use.
Dr Neelapu described the case of a 62-year-old male with refractory DLBCL who had 4 prior rituximab-based therapies. He had no response to his last 3 therapies combining rituximab with GDP (gemcitabine, cisplatin, and dexamethasone), ICE (ifosfamide, carboplatin, and etoposide), or lenalidomide.
After KTE-C19 therapy, the patient has an ongoing CR that has lasted more than 9 months.
Adverse events
Sixty-eight DLBCL patients (93%) experienced grade 3 or higher adverse events (AEs). These included 10 patients (14%) with cytokine release syndrome (CRS) and 18 (25%) with neurologic events.
Eighteen PMBCL/TFL patients (90%) experienced grade 3 or higher AEs, 2 (10%) with grade 3 or higher CRS and 9 (45%) with grade 3 or higher neurologic events.
CRS and neurological events were generally reversible, Dr Neelapu said. All CRS events resolved except 1 in the PMBCL/TFL cohort.
In both cohorts combined, 38% of patients received tocilizumab, 17% received corticosteroids, and 17% received both.
Three neurological events were ongoing at the data cut-off—grade 1 memory impairment, grade 1 tremor, and grade 2 tremor.
There were no cases of cerebral edema.
Three patients died from causes other than progressive disease—1 DLBCL patient and 2 in the PMBCL/TFL cohort.
Investigators considered the DLBCL patient death (due to hemophagocytic lymphohistiocytosis) and 1 death in the PMBCL/TFL arm (due to cardiac arrest) to be treatment-related.
Investigators did not consider the other death in the PMBCL/TFL arm (due to pulmonary embolism) to be treatment-related.
The most frequent grade 3 or higher treatment-emergent AEs in both arms combined included neutropenia (63%), anemia (42%), leukopenia (40%), febrile neutropenia (29%), thrombocytopenia (26%), encephalopathy (19%), hypophosphatemia (17%), and decreased lymphocyte count (17%).
Peak CAR T-cell expansion occurred between 7 and 14 days and was associated with ongoing CRs and grade 3 or greater neurological events, but not with CRS.
AEs were managed effectively across the 22 study sites, Dr Neelapu added, and most sites had no prior CAR T-cell therapy experience.
Dr Neelapu noted that the ZUMA-1 results are consistent with earlier KTE-C19 trials in aggressive NHL.
The primary analysis for this phase 2 study is expected to occur when all treated patients have 6 months of follow-up in the first quarter of 2017.
The study is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program. ![]()
*Information in the abstract differs from that presented at the meeting.

2016 ASH Annual Meeting
SAN DIEGO—The chimeric antigen receptor (CAR) T-cell therapy KTE-C19 has met its primary endpoint at the pre-specified interim analysis of the phase 2 ZUMA-1 trial in diffuse large B-cell lymphoma (DLBCL), according to data presented at the 2016 ASH Annual Meeting.
DLBCL patients had an overall response rate (ORR) of 76% and a complete response (CR) rate of 47% (P<0.0001) after 3 months or more of follow-up. And most responses were evident by day 30, the researchers report.
ZUMA-1 is the first multicenter trial of an anti-CD19 CAR T-cell therapy in refractory, aggressive non-Hodgkin lymphoma (NHL).
A second NHL cohort of primary mediastinal B-cell lymphoma or transformed follicular lymphoma (PMBCL/TFL) patients were also treated. Together, the cohorts achieved an ORR of 79% and a CR rate of 52%.
Sattva Neelapu, MD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, presented the results as a late-breaking abstract (LBA-6*).
Detailed results of the PMBCL/TFL cohort were presented separately (abstract 998) at the meeting.
Earlier data from the phase 2 study have been reported in Hematology Times.
Phase 2 interim analysis
The study enrolled 111 patients, all of whom underwent leukapheresis. Seven of these patients were not treated, 5 due to serious adverse events (SAEs), 1 due to unavailable product, and 2 due to non-measurable disease.
“Importantly, there was no bridging therapy allowed on the study,” Dr Neelapu pointed out.
Patients then received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days. Two patients experienced SAEs after the conditioning regimen, making it a total of 10 patients who could not be treated.
Two days after the conditioning regimen was completed, investigators dosed 101 patients with KTE-C19 at a target dose of 2 × 106 anti-CD19 CAR T cells/kg.
“The majority of patients that were enrolled on the study were treated,” Dr Neelapu emphasized. “In fact, 91% of the 111 patients enrolled were treated and received the target dose of KTE-C19.”
Dr Neelapu noted that the success rate for manufacturing the CAR T cells was 99%, and the average turnaround time from apheresis to delivery to the clinical site was 17 days.
The study called for a pre-specified interim efficacy analysis when 50 patients in cohort 1—DLBCL patients—had at least 3 months of follow-up. This occurred on August 24, 2016, and the data was analyzed as of that date.
The primary endpoint was ORR of P<0.0001 using an exact binomial test comparing observed ORR to a historical control assumption of 20%. Key secondary endpoints included duration of response, overall survival, safety, and levels of CAR T cells and cytokines.
At the time of the pre-specified interim analysis, 93 patients had at least 1 month of follow-up. Fifty-one patients with DLBCL and 11 patients with PMBCL/TFL had at least 3 months of follow-up.
Patient characteristics
Dr Neelapu reported data on 73 DLBCL patients (cohort 1) and 20 PMBCL/TFL patients (cohort 2) evaluable with at least 1 month of follow-up at the time of the presentation.
The median age of all 93 patients was 59 (range, 25-76), and about half were 60 years or older.
Two-thirds of patients in cohort 1 and three-quarters in cohort 2 were male. Sixty-six percent of cohort 1 and 40% of cohort 2 had an ECOG performance status of 1.
Cohort 1 had a median of 3 prior therapies (range, 1-7), and 44% had an International Prognostic Index (IPI) risk score of 3-4. Cohort 2 had a median of 4 prior therapies (range, 2-12), and 45% had an IPI risk score of 3-4.
Fifty-six DLBCL patients (77%) were refractory to their second or later line of therapy, and 15 (21%) had relapsed after autologous stem cell transplant.
Sixteen PMBCL/TFL patients (80%) were refractory to their second or later line of therapy, and 4 (20%) relapsed after autologous stem cell transplant.
Results
Dr Neelapu indicated that patients responded rapidly to treatment, and most responses were evident at the first tumor assessment.
At 3 months’ follow-up or longer, the ORR was 76% and the CR rate 47% for the 51 DLBCL patients in cohort 1. This was a 6-fold higher CR rate compared with historical outcomes.
For the 11 PMBCL/TFL patients in cohort 2, the ORR was 91% and the CR rate was 73% at 3 months or longer.
Both cohorts combined yielded an ORR of 79% and a CR rate of 52%.
The treatment effect was consistent across key covariates—refractory patients, disease stage, IPI risk score, CD4/CD8 ratio, and steroid and tocilizumab use.
Dr Neelapu described the case of a 62-year-old male with refractory DLBCL who had 4 prior rituximab-based therapies. He had no response to his last 3 therapies combining rituximab with GDP (gemcitabine, cisplatin, and dexamethasone), ICE (ifosfamide, carboplatin, and etoposide), or lenalidomide.
After KTE-C19 therapy, the patient has an ongoing CR that has lasted more than 9 months.
Adverse events
Sixty-eight DLBCL patients (93%) experienced grade 3 or higher adverse events (AEs). These included 10 patients (14%) with cytokine release syndrome (CRS) and 18 (25%) with neurologic events.
Eighteen PMBCL/TFL patients (90%) experienced grade 3 or higher AEs, 2 (10%) with grade 3 or higher CRS and 9 (45%) with grade 3 or higher neurologic events.
CRS and neurological events were generally reversible, Dr Neelapu said. All CRS events resolved except 1 in the PMBCL/TFL cohort.
In both cohorts combined, 38% of patients received tocilizumab, 17% received corticosteroids, and 17% received both.
Three neurological events were ongoing at the data cut-off—grade 1 memory impairment, grade 1 tremor, and grade 2 tremor.
There were no cases of cerebral edema.
Three patients died from causes other than progressive disease—1 DLBCL patient and 2 in the PMBCL/TFL cohort.
Investigators considered the DLBCL patient death (due to hemophagocytic lymphohistiocytosis) and 1 death in the PMBCL/TFL arm (due to cardiac arrest) to be treatment-related.
Investigators did not consider the other death in the PMBCL/TFL arm (due to pulmonary embolism) to be treatment-related.
The most frequent grade 3 or higher treatment-emergent AEs in both arms combined included neutropenia (63%), anemia (42%), leukopenia (40%), febrile neutropenia (29%), thrombocytopenia (26%), encephalopathy (19%), hypophosphatemia (17%), and decreased lymphocyte count (17%).
Peak CAR T-cell expansion occurred between 7 and 14 days and was associated with ongoing CRs and grade 3 or greater neurological events, but not with CRS.
AEs were managed effectively across the 22 study sites, Dr Neelapu added, and most sites had no prior CAR T-cell therapy experience.
Dr Neelapu noted that the ZUMA-1 results are consistent with earlier KTE-C19 trials in aggressive NHL.
The primary analysis for this phase 2 study is expected to occur when all treated patients have 6 months of follow-up in the first quarter of 2017.
The study is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program. ![]()
*Information in the abstract differs from that presented at the meeting.

2016 ASH Annual Meeting
SAN DIEGO—The chimeric antigen receptor (CAR) T-cell therapy KTE-C19 has met its primary endpoint at the pre-specified interim analysis of the phase 2 ZUMA-1 trial in diffuse large B-cell lymphoma (DLBCL), according to data presented at the 2016 ASH Annual Meeting.
DLBCL patients had an overall response rate (ORR) of 76% and a complete response (CR) rate of 47% (P<0.0001) after 3 months or more of follow-up. And most responses were evident by day 30, the researchers report.
ZUMA-1 is the first multicenter trial of an anti-CD19 CAR T-cell therapy in refractory, aggressive non-Hodgkin lymphoma (NHL).
A second NHL cohort of primary mediastinal B-cell lymphoma or transformed follicular lymphoma (PMBCL/TFL) patients were also treated. Together, the cohorts achieved an ORR of 79% and a CR rate of 52%.
Sattva Neelapu, MD, of The University of Texas MD Anderson Cancer Center in Houston, Texas, presented the results as a late-breaking abstract (LBA-6*).
Detailed results of the PMBCL/TFL cohort were presented separately (abstract 998) at the meeting.
Earlier data from the phase 2 study have been reported in Hematology Times.
Phase 2 interim analysis
The study enrolled 111 patients, all of whom underwent leukapheresis. Seven of these patients were not treated, 5 due to serious adverse events (SAEs), 1 due to unavailable product, and 2 due to non-measurable disease.
“Importantly, there was no bridging therapy allowed on the study,” Dr Neelapu pointed out.
Patients then received a conditioning regimen of cyclophosphamide (500 mg/m2) and fludarabine (30 mg/m2) for 3 days. Two patients experienced SAEs after the conditioning regimen, making it a total of 10 patients who could not be treated.
Two days after the conditioning regimen was completed, investigators dosed 101 patients with KTE-C19 at a target dose of 2 × 106 anti-CD19 CAR T cells/kg.
“The majority of patients that were enrolled on the study were treated,” Dr Neelapu emphasized. “In fact, 91% of the 111 patients enrolled were treated and received the target dose of KTE-C19.”
Dr Neelapu noted that the success rate for manufacturing the CAR T cells was 99%, and the average turnaround time from apheresis to delivery to the clinical site was 17 days.
The study called for a pre-specified interim efficacy analysis when 50 patients in cohort 1—DLBCL patients—had at least 3 months of follow-up. This occurred on August 24, 2016, and the data was analyzed as of that date.
The primary endpoint was ORR of P<0.0001 using an exact binomial test comparing observed ORR to a historical control assumption of 20%. Key secondary endpoints included duration of response, overall survival, safety, and levels of CAR T cells and cytokines.
At the time of the pre-specified interim analysis, 93 patients had at least 1 month of follow-up. Fifty-one patients with DLBCL and 11 patients with PMBCL/TFL had at least 3 months of follow-up.
Patient characteristics
Dr Neelapu reported data on 73 DLBCL patients (cohort 1) and 20 PMBCL/TFL patients (cohort 2) evaluable with at least 1 month of follow-up at the time of the presentation.
The median age of all 93 patients was 59 (range, 25-76), and about half were 60 years or older.
Two-thirds of patients in cohort 1 and three-quarters in cohort 2 were male. Sixty-six percent of cohort 1 and 40% of cohort 2 had an ECOG performance status of 1.
Cohort 1 had a median of 3 prior therapies (range, 1-7), and 44% had an International Prognostic Index (IPI) risk score of 3-4. Cohort 2 had a median of 4 prior therapies (range, 2-12), and 45% had an IPI risk score of 3-4.
Fifty-six DLBCL patients (77%) were refractory to their second or later line of therapy, and 15 (21%) had relapsed after autologous stem cell transplant.
Sixteen PMBCL/TFL patients (80%) were refractory to their second or later line of therapy, and 4 (20%) relapsed after autologous stem cell transplant.
Results
Dr Neelapu indicated that patients responded rapidly to treatment, and most responses were evident at the first tumor assessment.
At 3 months’ follow-up or longer, the ORR was 76% and the CR rate 47% for the 51 DLBCL patients in cohort 1. This was a 6-fold higher CR rate compared with historical outcomes.
For the 11 PMBCL/TFL patients in cohort 2, the ORR was 91% and the CR rate was 73% at 3 months or longer.
Both cohorts combined yielded an ORR of 79% and a CR rate of 52%.
The treatment effect was consistent across key covariates—refractory patients, disease stage, IPI risk score, CD4/CD8 ratio, and steroid and tocilizumab use.
Dr Neelapu described the case of a 62-year-old male with refractory DLBCL who had 4 prior rituximab-based therapies. He had no response to his last 3 therapies combining rituximab with GDP (gemcitabine, cisplatin, and dexamethasone), ICE (ifosfamide, carboplatin, and etoposide), or lenalidomide.
After KTE-C19 therapy, the patient has an ongoing CR that has lasted more than 9 months.
Adverse events
Sixty-eight DLBCL patients (93%) experienced grade 3 or higher adverse events (AEs). These included 10 patients (14%) with cytokine release syndrome (CRS) and 18 (25%) with neurologic events.
Eighteen PMBCL/TFL patients (90%) experienced grade 3 or higher AEs, 2 (10%) with grade 3 or higher CRS and 9 (45%) with grade 3 or higher neurologic events.
CRS and neurological events were generally reversible, Dr Neelapu said. All CRS events resolved except 1 in the PMBCL/TFL cohort.
In both cohorts combined, 38% of patients received tocilizumab, 17% received corticosteroids, and 17% received both.
Three neurological events were ongoing at the data cut-off—grade 1 memory impairment, grade 1 tremor, and grade 2 tremor.
There were no cases of cerebral edema.
Three patients died from causes other than progressive disease—1 DLBCL patient and 2 in the PMBCL/TFL cohort.
Investigators considered the DLBCL patient death (due to hemophagocytic lymphohistiocytosis) and 1 death in the PMBCL/TFL arm (due to cardiac arrest) to be treatment-related.
Investigators did not consider the other death in the PMBCL/TFL arm (due to pulmonary embolism) to be treatment-related.
The most frequent grade 3 or higher treatment-emergent AEs in both arms combined included neutropenia (63%), anemia (42%), leukopenia (40%), febrile neutropenia (29%), thrombocytopenia (26%), encephalopathy (19%), hypophosphatemia (17%), and decreased lymphocyte count (17%).
Peak CAR T-cell expansion occurred between 7 and 14 days and was associated with ongoing CRs and grade 3 or greater neurological events, but not with CRS.
AEs were managed effectively across the 22 study sites, Dr Neelapu added, and most sites had no prior CAR T-cell therapy experience.
Dr Neelapu noted that the ZUMA-1 results are consistent with earlier KTE-C19 trials in aggressive NHL.
The primary analysis for this phase 2 study is expected to occur when all treated patients have 6 months of follow-up in the first quarter of 2017.
The study is sponsored by Kite Pharma but is also funded, in part, by the Leukemia and Lymphoma Society Therapy Acceleration Program. ![]()
*Information in the abstract differs from that presented at the meeting.
Predicting the risk of CKD in sickle cell anemia

and normal red blood cells
Image by Graham Beards
Researchers say they have identified a genetic risk profile that can be used to predict which patients with sickle cell anemia (SCA) are likely to develop chronic kidney disease (CKD).
The team found evidence to suggest that a profile incorporating APOL1 G1/G2, α-thalassemia, and BCL11A can help physicians categorize SCA patients as having a high or low risk of CKD.
The researchers reported these findings in Haematologica.
Identifying SCA patients at the greatest risk of CKD can help physicians develop proactive, individualized strategies to reduce the high rate of early mortality due to CKD, said study author Santosh Saraf, MD, of the University of Illinois at Chicago.
“We looked at the genetic factors already known to be associated with kidney disease or the degree of red blood cell hemolysis and examined the relationship they had with the condition in sickle cell patients,” Dr Saraf said.
“Our hypothesis was that a genetic risk profile that integrated APOL1, α-thalassemia, and BCL11A would improve our ability to predict a patient’s risk for developing chronic kidney disease.”
To test this theory, Dr Saraf and his colleagues recruited 262 adult patients with SCA treated at a single center between 2010 and 2016. The team collected patient data, drew blood, analyzed genetic markers, and prospectively followed the patients to see if they developed CKD.
Stratification
The researchers used their genetic profile to stratify patients according to risk for CKD.
Patients were considered high-risk if they had APOL1 G1/G2 and wild-type BCL11A but did not have α-thalassemia.
Patients were considered low-risk if they were negative for APOL1 G1/G2 but had α-thalassemia (either α-/αα or α-/α-) and the BCL11A rs1427407 T allele (either G/T or T/T).
The researchers defined all other combinations as intermediate-risk.
The team found the genetic profile identified SCA patients at high and low risk for albuminuria or an estimated glomerular filtration rate less than 60 mL/min/1.73m2.
The researchers also said application of the genetic profile revealed progressively higher rates of CKD progression.
Mechanisms
Dr Saraf and his colleagues noted that homozygosity or compound heterozygosity for APOL1 G1/G2 is the strongest genetic association for CKD in African Americans, and APOL1 G1/G2 is associated with proteinuria and albuminuria in SCA patients.
The researchers pointed out that APOL1 G1/G2 variants associate with CKD in African
Americans by unknown mechanisms, but the team found an association with
hemolysis in SCA, as reflected by hemoglobinuria.
As for α-thalassemia, it’s associated with reduced hemolysis and protection from albuminuria. The researchers said α-thalassemia reduces hemolysis in SCA by decreasing the
intra-erythrocyte concentration of sickle hemoglobin (HbS) and reducing
HbS polymerization.
Finally, Dr Saraf and his colleagues noted that BCL11A rs1427407 leads to higher fetal hemoglobin (HbF) levels, reduced hemolysis, and amelioration of SCA-related complications. The team said the BCL11A rs1427407 T variant leads to decreased function of BCL11A at the HbF promoter and therefore increases HbF, leading to decreased HbS polymerization.
“The results of this study are encouraging,” Dr Saraf said. “By understanding more about the genetic risk factors of kidney disease in sickle cell patients, we are one step closer to improving the length and quality of life for the millions of people worldwide living with sickle cell disease.”
“Using combinations of genes to better predict complications in sickle cell anemia is a new approach,” added study author Victor Gordeuk, MD, of the University of Illinois at Chicago.
“The results of this study indicate that it is effective and probably can be improved on in the future to be an important part of our evaluation of patients.”
The researchers said the small sample size and observational nature of this study are limitations, and they hope to validate the results with larger studies. ![]()

and normal red blood cells
Image by Graham Beards
Researchers say they have identified a genetic risk profile that can be used to predict which patients with sickle cell anemia (SCA) are likely to develop chronic kidney disease (CKD).
The team found evidence to suggest that a profile incorporating APOL1 G1/G2, α-thalassemia, and BCL11A can help physicians categorize SCA patients as having a high or low risk of CKD.
The researchers reported these findings in Haematologica.
Identifying SCA patients at the greatest risk of CKD can help physicians develop proactive, individualized strategies to reduce the high rate of early mortality due to CKD, said study author Santosh Saraf, MD, of the University of Illinois at Chicago.
“We looked at the genetic factors already known to be associated with kidney disease or the degree of red blood cell hemolysis and examined the relationship they had with the condition in sickle cell patients,” Dr Saraf said.
“Our hypothesis was that a genetic risk profile that integrated APOL1, α-thalassemia, and BCL11A would improve our ability to predict a patient’s risk for developing chronic kidney disease.”
To test this theory, Dr Saraf and his colleagues recruited 262 adult patients with SCA treated at a single center between 2010 and 2016. The team collected patient data, drew blood, analyzed genetic markers, and prospectively followed the patients to see if they developed CKD.
Stratification
The researchers used their genetic profile to stratify patients according to risk for CKD.
Patients were considered high-risk if they had APOL1 G1/G2 and wild-type BCL11A but did not have α-thalassemia.
Patients were considered low-risk if they were negative for APOL1 G1/G2 but had α-thalassemia (either α-/αα or α-/α-) and the BCL11A rs1427407 T allele (either G/T or T/T).
The researchers defined all other combinations as intermediate-risk.
The team found the genetic profile identified SCA patients at high and low risk for albuminuria or an estimated glomerular filtration rate less than 60 mL/min/1.73m2.
The researchers also said application of the genetic profile revealed progressively higher rates of CKD progression.
Mechanisms
Dr Saraf and his colleagues noted that homozygosity or compound heterozygosity for APOL1 G1/G2 is the strongest genetic association for CKD in African Americans, and APOL1 G1/G2 is associated with proteinuria and albuminuria in SCA patients.
The researchers pointed out that APOL1 G1/G2 variants associate with CKD in African
Americans by unknown mechanisms, but the team found an association with
hemolysis in SCA, as reflected by hemoglobinuria.
As for α-thalassemia, it’s associated with reduced hemolysis and protection from albuminuria. The researchers said α-thalassemia reduces hemolysis in SCA by decreasing the
intra-erythrocyte concentration of sickle hemoglobin (HbS) and reducing
HbS polymerization.
Finally, Dr Saraf and his colleagues noted that BCL11A rs1427407 leads to higher fetal hemoglobin (HbF) levels, reduced hemolysis, and amelioration of SCA-related complications. The team said the BCL11A rs1427407 T variant leads to decreased function of BCL11A at the HbF promoter and therefore increases HbF, leading to decreased HbS polymerization.
“The results of this study are encouraging,” Dr Saraf said. “By understanding more about the genetic risk factors of kidney disease in sickle cell patients, we are one step closer to improving the length and quality of life for the millions of people worldwide living with sickle cell disease.”
“Using combinations of genes to better predict complications in sickle cell anemia is a new approach,” added study author Victor Gordeuk, MD, of the University of Illinois at Chicago.
“The results of this study indicate that it is effective and probably can be improved on in the future to be an important part of our evaluation of patients.”
The researchers said the small sample size and observational nature of this study are limitations, and they hope to validate the results with larger studies. ![]()

and normal red blood cells
Image by Graham Beards
Researchers say they have identified a genetic risk profile that can be used to predict which patients with sickle cell anemia (SCA) are likely to develop chronic kidney disease (CKD).
The team found evidence to suggest that a profile incorporating APOL1 G1/G2, α-thalassemia, and BCL11A can help physicians categorize SCA patients as having a high or low risk of CKD.
The researchers reported these findings in Haematologica.
Identifying SCA patients at the greatest risk of CKD can help physicians develop proactive, individualized strategies to reduce the high rate of early mortality due to CKD, said study author Santosh Saraf, MD, of the University of Illinois at Chicago.
“We looked at the genetic factors already known to be associated with kidney disease or the degree of red blood cell hemolysis and examined the relationship they had with the condition in sickle cell patients,” Dr Saraf said.
“Our hypothesis was that a genetic risk profile that integrated APOL1, α-thalassemia, and BCL11A would improve our ability to predict a patient’s risk for developing chronic kidney disease.”
To test this theory, Dr Saraf and his colleagues recruited 262 adult patients with SCA treated at a single center between 2010 and 2016. The team collected patient data, drew blood, analyzed genetic markers, and prospectively followed the patients to see if they developed CKD.
Stratification
The researchers used their genetic profile to stratify patients according to risk for CKD.
Patients were considered high-risk if they had APOL1 G1/G2 and wild-type BCL11A but did not have α-thalassemia.
Patients were considered low-risk if they were negative for APOL1 G1/G2 but had α-thalassemia (either α-/αα or α-/α-) and the BCL11A rs1427407 T allele (either G/T or T/T).
The researchers defined all other combinations as intermediate-risk.
The team found the genetic profile identified SCA patients at high and low risk for albuminuria or an estimated glomerular filtration rate less than 60 mL/min/1.73m2.
The researchers also said application of the genetic profile revealed progressively higher rates of CKD progression.
Mechanisms
Dr Saraf and his colleagues noted that homozygosity or compound heterozygosity for APOL1 G1/G2 is the strongest genetic association for CKD in African Americans, and APOL1 G1/G2 is associated with proteinuria and albuminuria in SCA patients.
The researchers pointed out that APOL1 G1/G2 variants associate with CKD in African
Americans by unknown mechanisms, but the team found an association with
hemolysis in SCA, as reflected by hemoglobinuria.
As for α-thalassemia, it’s associated with reduced hemolysis and protection from albuminuria. The researchers said α-thalassemia reduces hemolysis in SCA by decreasing the
intra-erythrocyte concentration of sickle hemoglobin (HbS) and reducing
HbS polymerization.
Finally, Dr Saraf and his colleagues noted that BCL11A rs1427407 leads to higher fetal hemoglobin (HbF) levels, reduced hemolysis, and amelioration of SCA-related complications. The team said the BCL11A rs1427407 T variant leads to decreased function of BCL11A at the HbF promoter and therefore increases HbF, leading to decreased HbS polymerization.
“The results of this study are encouraging,” Dr Saraf said. “By understanding more about the genetic risk factors of kidney disease in sickle cell patients, we are one step closer to improving the length and quality of life for the millions of people worldwide living with sickle cell disease.”
“Using combinations of genes to better predict complications in sickle cell anemia is a new approach,” added study author Victor Gordeuk, MD, of the University of Illinois at Chicago.
“The results of this study indicate that it is effective and probably can be improved on in the future to be an important part of our evaluation of patients.”
The researchers said the small sample size and observational nature of this study are limitations, and they hope to validate the results with larger studies. ![]()
Chemical could aid malaria control

Photo courtesy of the CDC
A chemical that disrupts hormone signaling in mosquitoes may reduce their ability to transmit malaria, according to a study published in PLOS Pathogens.
The findings suggest a potential new approach to combat spread of the disease.
“As insecticide resistance is spreading, new intervention methods to control mosquitoes are urgently needed,” said study author Flaminia Catteruccia, PhD, of the Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“Our study provides a new strategy based on the use of a non-toxic compound that prevents transmission of malaria parasites without killing the mosquito.”
Dr Catteruccia and her colleagues treated adult female Anopheles gambiae mosquitoes with a chemical known as dibenzoylhydrazine (DBH) to see how it would impact their biological processes.
DBH mimics the action of the steroid hormone 20-hydroxyecdysone, which plays a key role in the reproductive cycle of the female mosquito.
The researchers found various aspects of the mosquitoes’ life cycle to be disrupted after treatment with DBH.
DBH-treated mosquitoes produced and laid fewer eggs, didn’t mate successfully, and died more rapidly than non-treated mosquitoes. The effects were greater the higher the DBH dose.
And DBH-treated mosquitoes were less likely to be infected by malaria parasites.
To further explore the potential of hormone targeting as a malaria control tactic, the researchers fed their experimental results into a mathematical model of the mosquito life cycle.
The results suggest that applying DBH to bed nets or spraying it indoors could potentially reduce malaria transmission as effectively as insecticides.
The researchers noted that DBH compounds are not toxic to mammals, which would make them ideally suited for use in bed nets, where low toxicity is essential. ![]()

Photo courtesy of the CDC
A chemical that disrupts hormone signaling in mosquitoes may reduce their ability to transmit malaria, according to a study published in PLOS Pathogens.
The findings suggest a potential new approach to combat spread of the disease.
“As insecticide resistance is spreading, new intervention methods to control mosquitoes are urgently needed,” said study author Flaminia Catteruccia, PhD, of the Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“Our study provides a new strategy based on the use of a non-toxic compound that prevents transmission of malaria parasites without killing the mosquito.”
Dr Catteruccia and her colleagues treated adult female Anopheles gambiae mosquitoes with a chemical known as dibenzoylhydrazine (DBH) to see how it would impact their biological processes.
DBH mimics the action of the steroid hormone 20-hydroxyecdysone, which plays a key role in the reproductive cycle of the female mosquito.
The researchers found various aspects of the mosquitoes’ life cycle to be disrupted after treatment with DBH.
DBH-treated mosquitoes produced and laid fewer eggs, didn’t mate successfully, and died more rapidly than non-treated mosquitoes. The effects were greater the higher the DBH dose.
And DBH-treated mosquitoes were less likely to be infected by malaria parasites.
To further explore the potential of hormone targeting as a malaria control tactic, the researchers fed their experimental results into a mathematical model of the mosquito life cycle.
The results suggest that applying DBH to bed nets or spraying it indoors could potentially reduce malaria transmission as effectively as insecticides.
The researchers noted that DBH compounds are not toxic to mammals, which would make them ideally suited for use in bed nets, where low toxicity is essential. ![]()

Photo courtesy of the CDC
A chemical that disrupts hormone signaling in mosquitoes may reduce their ability to transmit malaria, according to a study published in PLOS Pathogens.
The findings suggest a potential new approach to combat spread of the disease.
“As insecticide resistance is spreading, new intervention methods to control mosquitoes are urgently needed,” said study author Flaminia Catteruccia, PhD, of the Harvard T. H. Chan School of Public Health in Boston, Massachusetts.
“Our study provides a new strategy based on the use of a non-toxic compound that prevents transmission of malaria parasites without killing the mosquito.”
Dr Catteruccia and her colleagues treated adult female Anopheles gambiae mosquitoes with a chemical known as dibenzoylhydrazine (DBH) to see how it would impact their biological processes.
DBH mimics the action of the steroid hormone 20-hydroxyecdysone, which plays a key role in the reproductive cycle of the female mosquito.
The researchers found various aspects of the mosquitoes’ life cycle to be disrupted after treatment with DBH.
DBH-treated mosquitoes produced and laid fewer eggs, didn’t mate successfully, and died more rapidly than non-treated mosquitoes. The effects were greater the higher the DBH dose.
And DBH-treated mosquitoes were less likely to be infected by malaria parasites.
To further explore the potential of hormone targeting as a malaria control tactic, the researchers fed their experimental results into a mathematical model of the mosquito life cycle.
The results suggest that applying DBH to bed nets or spraying it indoors could potentially reduce malaria transmission as effectively as insecticides.
The researchers noted that DBH compounds are not toxic to mammals, which would make them ideally suited for use in bed nets, where low toxicity is essential. ![]()
Congenital CMV linked to increased risk of ALL

Photo by Vera Kratochvil
Newborns with congenital cytomegalovirus (CMV) infection may have an increased risk of developing acute lymphoblastic leukemia (ALL), according to a study published in Blood.
The data also suggest the risk may be particularly high among Hispanic children.
Researchers said this is the first study to suggest that congenital CMV infection is a risk factor for childhood ALL and is more prominent in Hispanic children.
To conduct this study, the researchers first identified all known infections present in the bone marrow of 127 children diagnosed with ALL and 38 children diagnosed with acute myeloid leukemia (AML).
The team found CMV infection was prevalent in children with ALL but rare in those with AML.
Next, the researchers looked for CMV in newborn blood samples from 268 children who went on to develop ALL. The team compared the samples with samples from 270 healthy children.
“Our goal in tracking CMV back from the time of diagnosis to the womb was to establish that this infection occurred well before initiation of disease,” said lead study author Stephen Francis, PhD, of the University of Nevada and University of California, San Francisco.
He and his colleagues found that children who went on to develop ALL were nearly 4 times more likely than control subjects to be CMV-positive at birth. The odds ratio was 3.71 (P=0.0016).
The odds ratio was 5.9 in Hispanic children and 2.1 in non-Hispanic whites. The researchers said this finding is particularly interesting because of the high rate of ALL observed in Hispanics.
“If it’s true that in utero CMV is one of the initiating events in the development of childhood leukemia, then control of the virus has the potential to be a prevention target,” Dr Francis said. “That’s the real take-home message.”
While this research is in the early stages, the researchers hope these results will inspire more studies that will validate these findings and lead to the development of a CMV vaccine.
“This is the first step, but if we do end up finding a causal link to the most common childhood cancer, we hope that will light a fire in terms of stopping mother-to-child transmission of CMV,” Dr Francis said. ![]()

Photo by Vera Kratochvil
Newborns with congenital cytomegalovirus (CMV) infection may have an increased risk of developing acute lymphoblastic leukemia (ALL), according to a study published in Blood.
The data also suggest the risk may be particularly high among Hispanic children.
Researchers said this is the first study to suggest that congenital CMV infection is a risk factor for childhood ALL and is more prominent in Hispanic children.
To conduct this study, the researchers first identified all known infections present in the bone marrow of 127 children diagnosed with ALL and 38 children diagnosed with acute myeloid leukemia (AML).
The team found CMV infection was prevalent in children with ALL but rare in those with AML.
Next, the researchers looked for CMV in newborn blood samples from 268 children who went on to develop ALL. The team compared the samples with samples from 270 healthy children.
“Our goal in tracking CMV back from the time of diagnosis to the womb was to establish that this infection occurred well before initiation of disease,” said lead study author Stephen Francis, PhD, of the University of Nevada and University of California, San Francisco.
He and his colleagues found that children who went on to develop ALL were nearly 4 times more likely than control subjects to be CMV-positive at birth. The odds ratio was 3.71 (P=0.0016).
The odds ratio was 5.9 in Hispanic children and 2.1 in non-Hispanic whites. The researchers said this finding is particularly interesting because of the high rate of ALL observed in Hispanics.
“If it’s true that in utero CMV is one of the initiating events in the development of childhood leukemia, then control of the virus has the potential to be a prevention target,” Dr Francis said. “That’s the real take-home message.”
While this research is in the early stages, the researchers hope these results will inspire more studies that will validate these findings and lead to the development of a CMV vaccine.
“This is the first step, but if we do end up finding a causal link to the most common childhood cancer, we hope that will light a fire in terms of stopping mother-to-child transmission of CMV,” Dr Francis said. ![]()

Photo by Vera Kratochvil
Newborns with congenital cytomegalovirus (CMV) infection may have an increased risk of developing acute lymphoblastic leukemia (ALL), according to a study published in Blood.
The data also suggest the risk may be particularly high among Hispanic children.
Researchers said this is the first study to suggest that congenital CMV infection is a risk factor for childhood ALL and is more prominent in Hispanic children.
To conduct this study, the researchers first identified all known infections present in the bone marrow of 127 children diagnosed with ALL and 38 children diagnosed with acute myeloid leukemia (AML).
The team found CMV infection was prevalent in children with ALL but rare in those with AML.
Next, the researchers looked for CMV in newborn blood samples from 268 children who went on to develop ALL. The team compared the samples with samples from 270 healthy children.
“Our goal in tracking CMV back from the time of diagnosis to the womb was to establish that this infection occurred well before initiation of disease,” said lead study author Stephen Francis, PhD, of the University of Nevada and University of California, San Francisco.
He and his colleagues found that children who went on to develop ALL were nearly 4 times more likely than control subjects to be CMV-positive at birth. The odds ratio was 3.71 (P=0.0016).
The odds ratio was 5.9 in Hispanic children and 2.1 in non-Hispanic whites. The researchers said this finding is particularly interesting because of the high rate of ALL observed in Hispanics.
“If it’s true that in utero CMV is one of the initiating events in the development of childhood leukemia, then control of the virus has the potential to be a prevention target,” Dr Francis said. “That’s the real take-home message.”
While this research is in the early stages, the researchers hope these results will inspire more studies that will validate these findings and lead to the development of a CMV vaccine.
“This is the first step, but if we do end up finding a causal link to the most common childhood cancer, we hope that will light a fire in terms of stopping mother-to-child transmission of CMV,” Dr Francis said. ![]()
How to Categorize Pediatric Asthma
Does Chronic Complaining Mask Acute Problem?
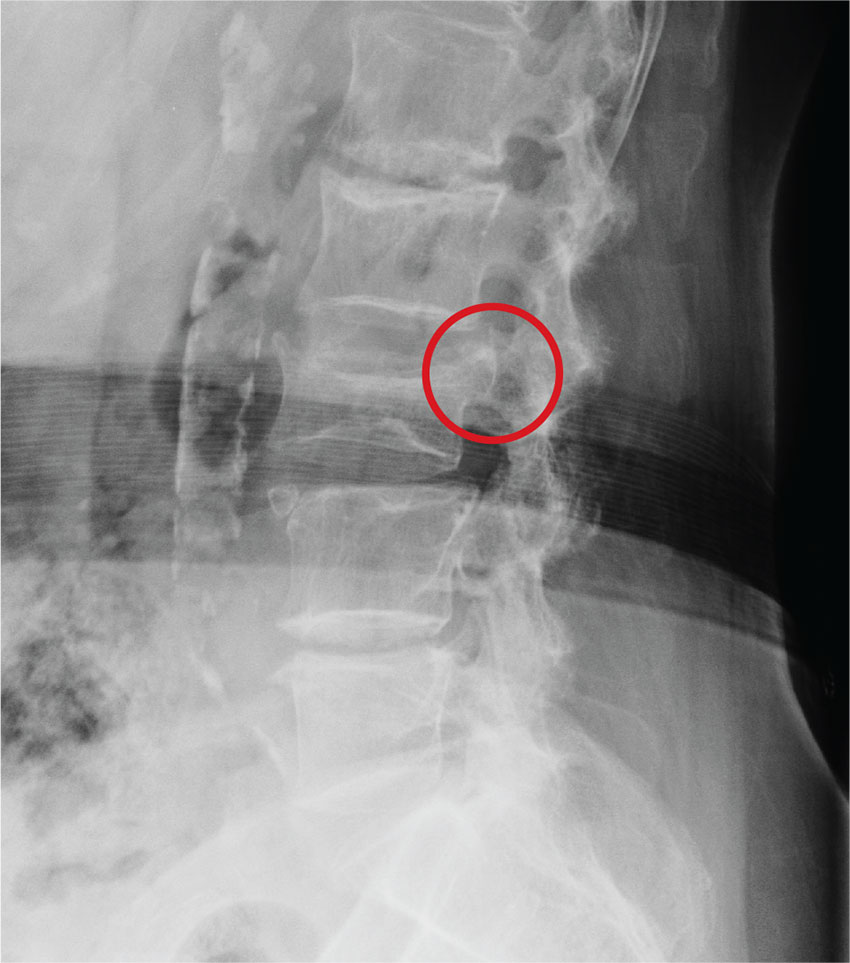
ANSWER
The radiograph demonstrates age-related degenerative changes. Of note is a moderate compression fracture of L3 with close to 50% loss of height. It is difficult to say for sure the fracture is acute; by plain film alone, it would be deemed age indeterminate.
Of concern, though, is the posterior portion of the superior endplate of L3, which appears to be posteriorly displaced into the spinal canal. This finding suggests possible retropulsion and, if this fracture was in fact acute, would suggest a possible unstable fracture. Further imaging is warranted.
The patient underwent noncontrast CT of the lumbar spine, which demonstrated that the fracture was acute. It also indicated that there was dorsal retropulsion causing close to 50% canal compromise. The patient was subsequently admitted for further workup and evaluation.
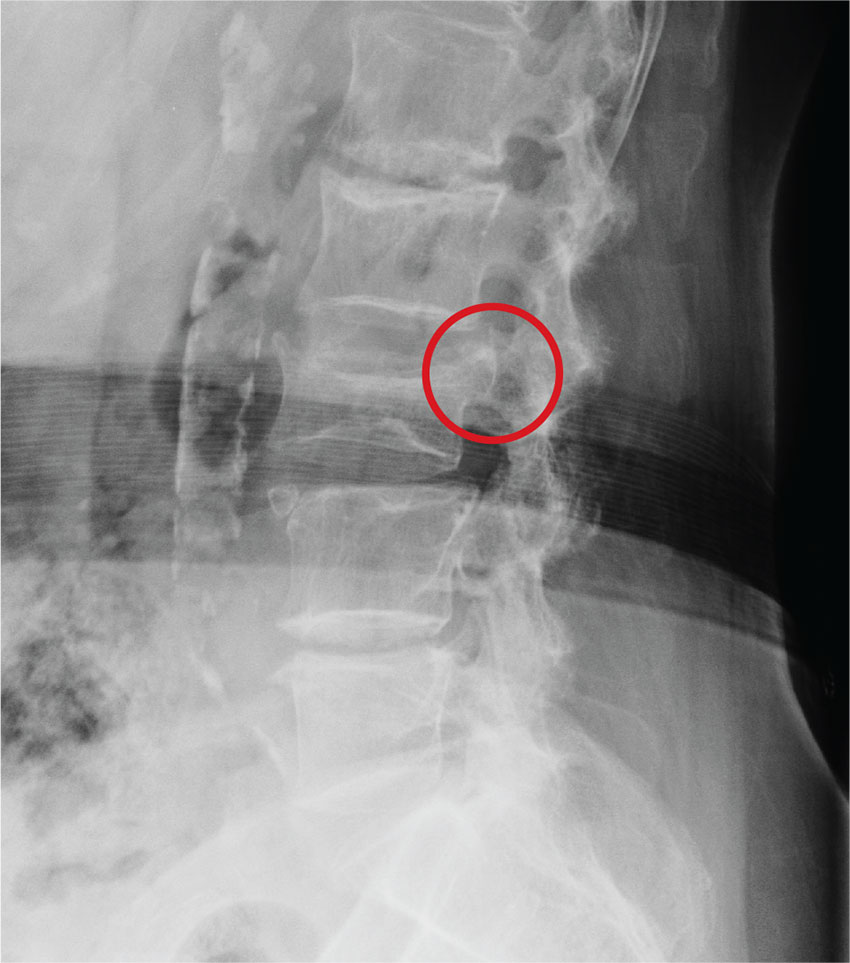
ANSWER
The radiograph demonstrates age-related degenerative changes. Of note is a moderate compression fracture of L3 with close to 50% loss of height. It is difficult to say for sure the fracture is acute; by plain film alone, it would be deemed age indeterminate.
Of concern, though, is the posterior portion of the superior endplate of L3, which appears to be posteriorly displaced into the spinal canal. This finding suggests possible retropulsion and, if this fracture was in fact acute, would suggest a possible unstable fracture. Further imaging is warranted.
The patient underwent noncontrast CT of the lumbar spine, which demonstrated that the fracture was acute. It also indicated that there was dorsal retropulsion causing close to 50% canal compromise. The patient was subsequently admitted for further workup and evaluation.
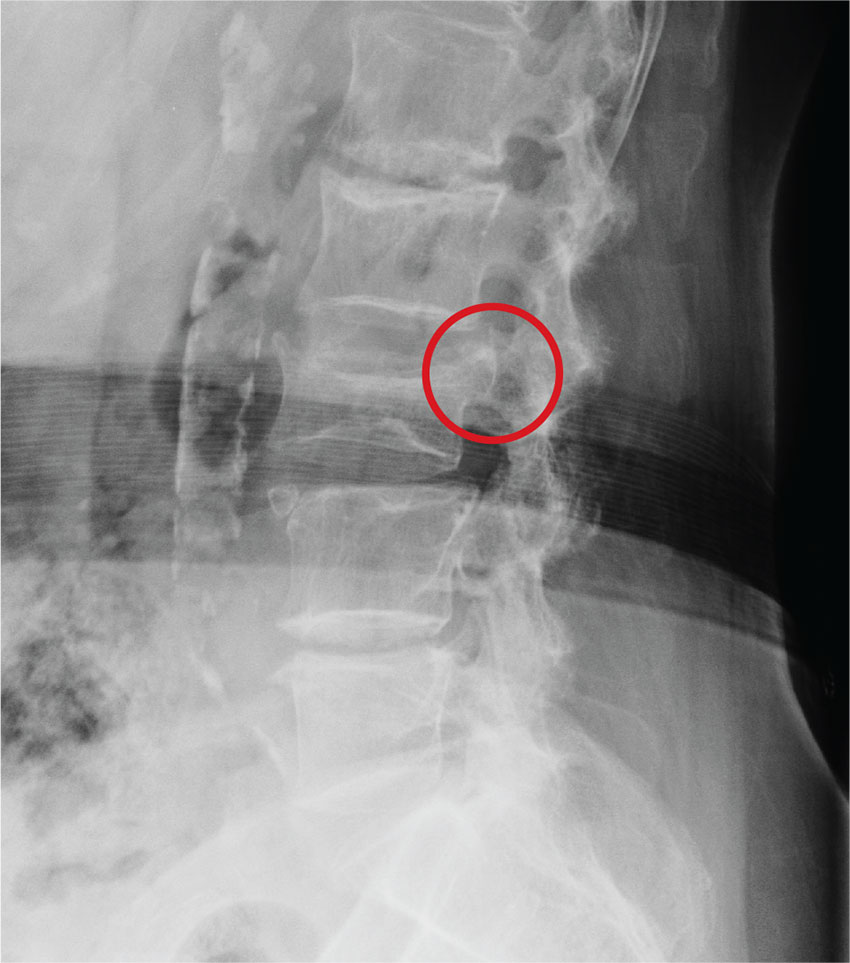
ANSWER
The radiograph demonstrates age-related degenerative changes. Of note is a moderate compression fracture of L3 with close to 50% loss of height. It is difficult to say for sure the fracture is acute; by plain film alone, it would be deemed age indeterminate.
Of concern, though, is the posterior portion of the superior endplate of L3, which appears to be posteriorly displaced into the spinal canal. This finding suggests possible retropulsion and, if this fracture was in fact acute, would suggest a possible unstable fracture. Further imaging is warranted.
The patient underwent noncontrast CT of the lumbar spine, which demonstrated that the fracture was acute. It also indicated that there was dorsal retropulsion causing close to 50% canal compromise. The patient was subsequently admitted for further workup and evaluation.
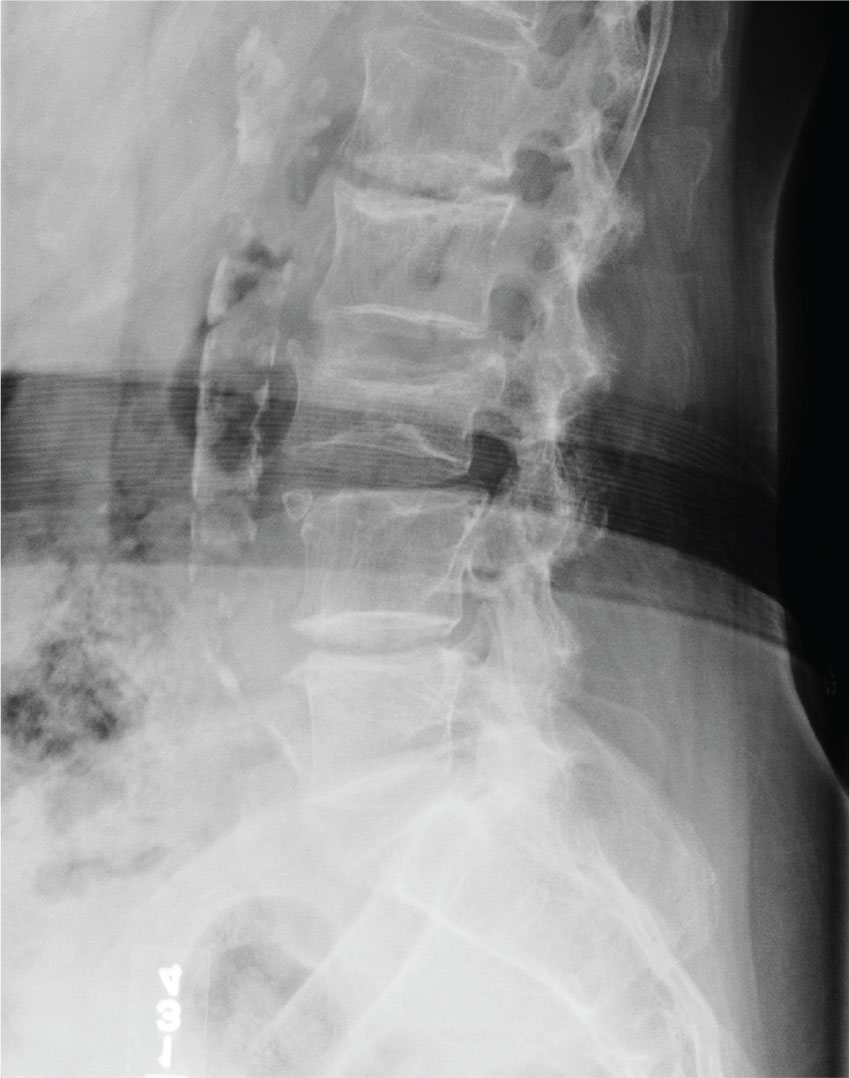
An 80-year-old woman who resides in a nursing home is sent to urgent care for evaluation of back pain. There have been no witnessed injuries or falls. The notes from the nursing home staff indicate that the patient, who has severe dementia, tends to chronically complain about one ailment or another. However, the patient’s family seems to feel she is complaining more than usual.
Her only other medical history is controlled hypertension. Her vital signs are stable. On physical exam, you note an elderly female who is pleasant but very confused. She is able to follow simple commands and appears to be able to move all her extremities well, with no obvious neurologic compromise. Inspection of her back does not demonstrate any obvious wounds, bruising, or step-offs. She does have generalized tenderness as you palpate her lumbar region.
The triage nurse already ordered lumbar spine radiographs, which have been completed. The lateral view is shown. What is your impression?