User login
2017 Update on pelvic floor dysfunction
The International Continence Society (ICS) defines overactive bladder (OAB) as a syndrome of "urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence (UUI), in the absence of urinary tract infection [UTI] or obvious pathology."1 The Agency for Healthcare Research and Quality (AHRQ) reported OAB prevalence to be 15% in US women, with 11% reporting UUI.2 OAB represents a significant health care burden that impacts nearly every aspect of life, including physical, emotional, and psychological domains.3,4 The economic impact is notable; the projected cost is estimated to reach $82.6 billion annually by 2020.5
The American Urological Association (AUA) and the Society for Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) have endorsed an algorithm for use in the evaluation of idiopathic OAB (FIGURE).6 If the patient's symptoms are certain, minimal evaluation is needed and it is reasonable to proceed with first-line therapy, which includes fluid management (decreasing caffeine intake and limiting evening fluid intake), bladder retraining drills such as timed voiding, and improving pelvic floor muscles with the use of biofeedback and functional electrical stimulation.6,7 Pelvic floor muscle training can be facilitated with a referral to a physical therapist trained in pelvic floor muscle education.
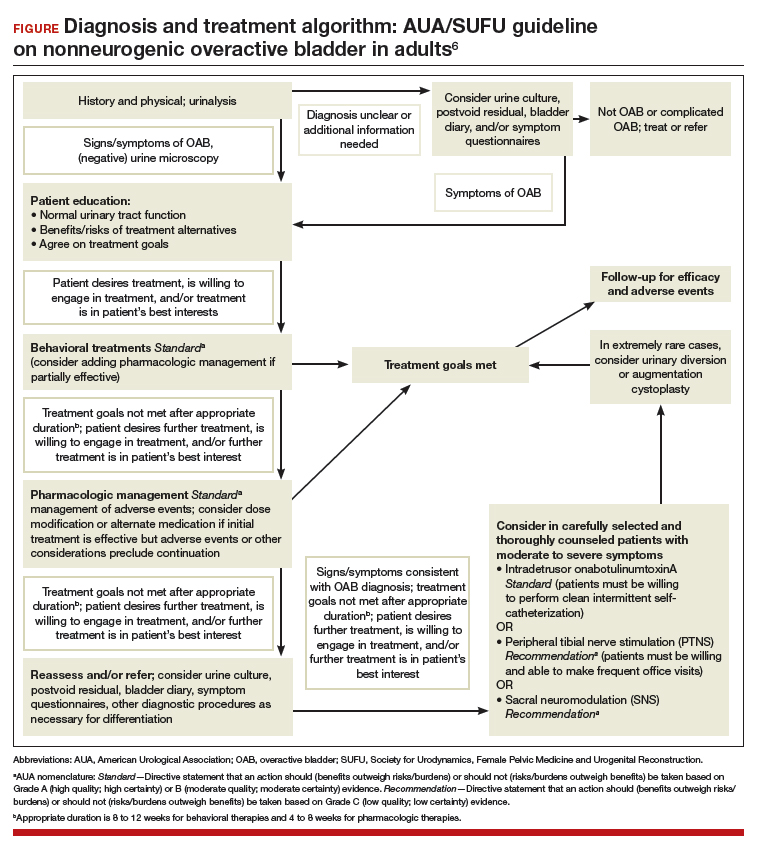
If treatment goals are not met with first-line strategies, second-line therapy may be initiated with anticholinergic or β3-adrenergic receptor agonist medications. If symptoms persist after 4 to 8 weeks of pharmacologic therapy, clinicians are encouraged to reassess or refer the patient to a specialist. Further evaluation may include a bladder diary in which the patient documents voided volumes, voiding frequency, and number of incontinent episodes; symptom-specific questionnaires; and/or urodynamic testing.
Related article:
The latest treatments for urinary and fecal incontinence: Which hold water?
Based on that evaluation, the patient may be a candidate for third-line therapy with either intradetrusor onabotulinumtoxinA, posterior tibial nerve stimulation (PTNS), or sacral neuromodulation.
There is a paucity of information comparing third-line therapies. In this Update, we focus on 4 randomized clinical trials that compare third-line treatment options for idiopathic OAB.
Read about how anticholinergic medication and onabotulinumtoxinA compare for treating UUI.
Anticholinergic therapy and onabotulinumtoxinA produce equivalent reductions in the frequency of daily UUI episodes
Visco AG, Brubaker L, Richter HE, et al; for the Pelvic Floor Disorders Network. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. N Engl J Med. 2012;367(19):1803-1813.
In a double-blind, double-placebo-controlled randomized trial, Visco and colleagues compared anticholinergic medication with onabotulinumtoxinA 100 U for the treatment of women with UUI.
Details of the study
Two hundred forty-one women with moderate to severe UUI received either 6 months of oral anticholinergic therapy (solifenacin 5 mg daily with the option of dose escalation to 10 mg daily or change to trospium XR 60 mg daily based on the Patient Global Symptom Control score) plus a single intradetrusor injection of saline, or a single intradetrusor injection of onabotulinumtoxinA 100 U plus a 6-month oral placebo regimen.
Inclusion criteria were 5 or more UUI episodes on a 3-day diary, insufficient resolution of symptoms after 2 medications, or being drug naive. Exclusions included a postvoid residual (PVR) urine volume greater than 150 mL or previous therapy with onabotulinumtoxinA.
Participants were scheduled for follow up every 2 to 6 months post randomization, at which time all study medications were discontinued. The primary outcome was reduction from baseline in the mean number of UUI episodes per day over the 6-month period, as recorded in the monthly 3-day bladder diaries. Secondary outcomes included the proportion of participants with complete resolution of UUI, the proportion of participants with 75% or more reduction in UUI episodes, Overactive Bladder Questionnaire Short Form (OABq-SF) scores, other symptom-specific questionnaire scores, and adverse events.
Related article:
Which treatments for pelvic floor disorders are backed by evidence?
Both treatments significantly reduced UUI episodes
At baseline, participants reported a mean (SD) of 5.0 (2.7) UUI episodes per day, and 41% of participants were drug naive. Both treatment groups experienced significant reductions compared with baseline in mean UUI episodes, and the reductions were similar between the 2 groups (reduction of 3.4 episodes per day in the anticholinergic group, reduction of 3.3 episodes in the onabotulinumtoxinA group; P = .81). Complete resolution of UUI was more common in the onabotulinumtoxinA group (27%) as compared with the anticholinergic group (13%) (P = .003). There were no differences in improvement in OABq-SF scores (37.05 in the anticholinergic group vs 37.13 in the onabotulinumtoxinA group; P = .98) or other quality-of-life measures.
Adverse events. The anticholinergic group experienced a higher rate of dry mouth compared with the onabotulinumtoxinA group (46% vs 31%; P = .02) but had lower rates of intermittent catheterization use at 2 months (0% vs 5%, P = .01) and UTIs (13% vs 33%, P<.001).
Strengths and limitations. This was a well-designed, multicenter, randomized double-blind, double placebo-controlled trial. The study design allowed for dose escalation and change to another medication for inadequate symptom control and included drug-naive participants, which increases the generalizability of the results. However, current guidelines recommend reserving onabotulinumtoxinA therapy for third-line therapy, thus deterring this treatment's use in the drug-naive population. Additionally, the lack of a pure placebo arm makes it difficult to interpret the extent to which a placebo effect contributed to observed improvements in clinical symptoms.
Through 6 months, both a single intradetrusor injection of onabotulinumtoxinA 100 U and anticholinergic therapy reduce UUI episodes and improve quality-of-life measures in women who have failed medications or are drug naive. Use of onabotulinumtoxinA, however, more likely will lead to complete resolution of UUI, although with an increased risk of transient urinary retention and UTI. Even given the study findings supporting the use of onabotulinumtoxinA over anticholinergic therapy for complete resolution of UUI, it is most appropriate to align with current practice, which includes a trial of pharmacotherapy before proceeding with third-line onabotulinumtoxinA.
Read: onabotulinumtoxinA vs PTNS for OAB.
OnabotulinumtoxinA has greater 9-month durability for OAB symptoms compared with12 weeks of PTNS
Sherif H, Khalil M, Omar R. Management of refractory idiopathic overactive bladder: intradetrusor injection of botulinum toxin type A versus posterior tibial nerve stimulation. Can J Urol. 2017;24(3):8838-8846.
In this randomized clinical trial, Sherif and colleagues compared the safety and efficacy of a single intradetrusor injection of onabotulinumtoxinA 100 U with that of PTNS for OAB.
Details of the study
Sixty adult men and women with OAB who did not respond to medical therapy were randomly assigned to treatment with either onabotulinumtoxinA 100 U or PTNS. Criteria for exclusion were current UTI, PVR urine volume of more than 150 mL, previous radiation therapy or chemotherapy, previous incontinence surgery or bladder malignancy, or presence of mixed urinary incontinence.
At baseline, participants completed a 3-day bladder diary, an OAB symptom score (OABSS) questionnaire, and urodynamic testing. The OABSS questionnaire included 7 questions (scoring range, 0-28), with higher scores indicating worse symptoms, and included subscales for urgency and quality-of-life measures. Total OABSS, urgency score, quality-of-life score, bladder diary records, and urodynamic testing parameters were assessed at 6, 12, 24, and 36 weeks, along with adverse events.
OnabotulinumtoxinA injections were performed under spinal anesthesia. If PVR urine volume was greater than 200 mL at any follow-up visit, participants were instructed to begin clean intermittent self-catheterization. PTNS was administered as weekly 30-minute sessions for 12 consecutive weeks.
Participants' baseline demographics and symptoms were similar. Average age was 45 years. Averages (SD) for duration of anticholinergic use was 13 (0.8) weeks, UUI episode score was 4.5 (1) on 3-day bladder diary, and OABSS was 22 (2.7). Nine-month data were available for 29 participants in the onabotulinumtoxinA group and for 8 in the PTNS group.
Related article:
Update on pelvic floor dysfunction: Focus on urinary incontinence
OnabotulinumtoxinA treatment benefits sustained for 9 months
Through 6 months, compared with baseline assessments, both treatment groups had significant improvements in clinical symptoms and OABSS total score, as well as urgency and quality-of-life subscales. At 3 months, urodynamic study parameters were similarly improved from baseline in both groups.
At 9 months, however, only the onabotulinumtoxinA group, compared with the PTNS group, maintained the significant improvement from baseline in 3-day bladder diary voiding episodes (average [SD], 10.7 [1.01] vs 11.6 [1.09]; P = .009), 3-day bladder diary nocturia episodes (average [SD], 3.8 [1.09] vs 4.4 [0.8]; P = .02), and average [SD] UUI episodes over 3 days (3.5 [1.2] vs 4.2 [1.04]; P = .02). Similarly, onabotulinumtoxinA-treated participants, compared with those treated with PTNS, maintained improvements at 9 months in average (SD): OABSS total score (19.2 [2.4] vs 20.4 [1.7]; P = .03), urgency scores (10.9 [1.3] vs 11.8 [1.4]; P = .009), urine volume at first desire (177.8 [9.2] vs 171.8 [7.7]), maximum cystometric capacity (304 [17.6] vs 290 [13.1]), and Qmax (mL/sec) (20.7 [1.6] vs 22.2 [1.2]).
Adverse events. Average PVR urine volumes were higher in the onabotulinumtoxinA group compared with the PTNS group (36.8 [2.7] vs 32.4 [3.03]; P = .0001) at all time points, and self-catheterization was required in 6.6% of onabotulinumtoxinA-treated participants. Urinary tract infection occurred in 6.6% of participants in the onabotulinumtoxinA group and in none of the PTNS group. In the PTNS group, few experienced pain and minor bleeding at the needle site.
Strengths and limitations. This randomized, open-label trial comparing treatment with onabotulinumtoxinA 100 U and PTNS included both men and women with idiopathic OAB symptoms. The participants were assessed at regular intervals with various measures, and follow-up adherence was good. The sample size was small, so the study may not have been powered to see differences prior to 9 months.
Although at 9 months only the onabotulinumtoxinA group maintained significant improvement over baseline levels, the improvement was diminished, and therefore the clinical meaningfulness is uncertain. Further, participants in the PTNS group did not undergo monthly maintenance therapy after 3 months, which is recommended for those with a 12-week therapeutic response; this may have affected 9-month outcomes in this group. Since the one-time onabotulinumtoxinA 100 U injection was performed under spinal anesthesia, cost comparisons should be considered, since future onabotulinumtoxinA injections would be necessary.
A one-time onabotulinumtoxinA 100 U injection and 12 weeks of PTNS therapy are reasonable short-term options for symptomatic OAB relief after unsuccessful therapy with medications. OnabotulinumtoxinA injection may provide more durable OAB symptom control at 9 months but with a risk of UTI and need for self-catheterization.
Read about using different doses of onabotulinumtoxinA for OAB.
OnabotulinumtoxinA 200-U injection provides longer OAB symptom improvement than 100-U injection
Abdelwahab O, Sherif H, Soliman T, Elbarky I, Eshazly A. Efficacy of botulinum toxin type A 100 units versus 200 units for treatment of refractory idiopathic overactive bladder. Int Braz J Urol. 2015;41(6):1132-1140.
Abdelwahab and colleagues conducted a single-center, randomized clinical trial to investigate the safety and efficacy of a single injection of intradetrusor onabotulinumtoxinA in 2 different doses (100 U and 200 U) for treatment of OAB.
Details of the study
Eighty adults (63 women, 17 men) who did not benefit from anticholinergic medication during the previous 3 months were randomly assigned to receive either a 100-U (n = 40) or a 200-U (n = 40) injection of onabotulinumtoxinA. Exclusion criteria were PVR urine volume greater than 150 mL and previous radiation therapy or chemotherapy.
Initial assessments -- completed at baseline and at 1, 3, 6, and 9 months -- included the health-related quality-of-life (HR-QOL) questionnaire (maximum score, 100; higher score indicates better quality of life), an abbreviated OABSS questionnaire (4 questions; score range, 0-15; higher score indicates more severe symptoms), and urodynamic evaluation. Outcomes included OABSS, HR-QOL score, and urodynamic parameters at the various time points.
Related article:
Is there a link between impaired mobility and urinary incontinence in elderly, community-dwelling women?
Higher dose, greater symptom improvement and higher adverse event rate
At baseline, participants (average age, 31 years) had an average (SD) OABSS of 1.7 (1.6). OnabotulinumtoxinA treatment with both a 100-U and a 200-U dose resulted in significant improvements (compared with baseline levels) in frequency, nocturia, UUI episodes, OABSS, and urodynamic parameters throughout the 9 months. At 9 months, however, the group treated with the 200-U dose had greater improvements, compared with the group who received a 100-U dose, in urinary frequency symptom scores (mean [SD], 0.32 [0.47] vs 1.1 [0.51]; P<.05), nocturia symptom scores (mean [SD], 0.13 [0.34] vs 0.36 [0.49]; P<.05), UUI symptom scores (mean [SD], 0.68 [0.16] vs 1.26 [1.1]; P<.05), and mean (SD) total OABSS (2.6 [2.31] vs 5.3 [2.11]; P<.05). Similarly, at 9 months the 200-U dose resulted in greater improvements in volume at first desire (mean [SD], 291.8 [42.8] vs 246.8 [53.8] mL; P<.05), volume at strong desire (mean [SD], 392.1 [37.3] vs 313.1 [67.4] mL; P<.05), detrusor pressure (mean [SD], 10.4 [4.0] vs 19.2 [7.8] cm H2O; P<.05), and maximum cystometric capacity (mean [SD], 430.5 [34.2] vs 350 [69.1] mL; P<.05) compared with the 100-U dose.
Adverse events. No participant had a PVR urine volume greater than 100 mL at any follow-up visit. Postoperative hematuria occurred in 23% of the group treated with onabotulinumtoxinA 200 U versus in 15% of those treated with a 100-U dose. Similarly, UTIs occurred in 17.5% of the 200-U dose group and in 7.5% of the 100-U dose group. Dysuria was reported in 37.5% and 15% of the 200-U and 100-U dose groups, respectively.
Strengths and limitations. This randomized, open-label trial comparing a single injection of 100 U versus 200 U of onabotulinumtoxinA included mostly women. OAB symptoms and urodynamic parameters improved after treatment with both dose levels, but a longer duration of improvement was seen with the 200-U dose. The cohort had a low baseline OAB severity, based on the OABSS questionnaire, and a young average age of participants, which limits the generalizability of the study results to a population with refractory OAB. The 0% rate of clean intermittent self-catheterization postinjection might be based on the study's criteria for requiring clean intermittent catheterization. In addition, the initial postinjection visit occurred at 1 month, possibly missing participants who had symptoms of retention soon after injection.
Two dose levels (100 U and 200 U) of a single injection of onabotulinumtoxinA are associated with comparable OAB symptom and urodyanamic improvements. The benefits of a longer duration of effect with the 200-U dose must be weighed against the possible higher risks of transient hematuria, dysuria, and UTI.
Read: onabotulinumtoxinA vs sacral neuromodulation therapy for UUI.
Treatment with onabotulinumtoxinA may control UUI symptoms better than sacral neuromodulation therapy
Amundsen CL, Richter HE, Menefee SA, et al; Pelvic Floor Disorders Network. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: a randomized clinical trial. JAMA. 2016;316(13):1366-1374.
In this multicenter open-label randomized trial, Amundsen and colleagues compared the efficacy and safety of onabotulinumtoxinA 200 U with that of sacral neuromodulation.
Details of the study
Three hundred sixty-four women with UUI had data available for primary analysis at 6 months. Women were considered eligible for the study if they had 6 or more UUI episodes on a 3-day bladder diary, persistent symptoms despite anticholinergic therapy, a PVR urine volume of less than 150 mL, and had never previously received either study treatment.
There were no differences in baseline characteristics of the participants. The average (SD) age of the study population was 63 (11.6) years, with an average (SD) daily number of UUI episodes of 5.3 (2.8). The average (SD) body mass index was 32 (8) kg/m2.
Participants were randomly assigned to undergo either sacral neuromodulation (n = 174) or intradetrusor injection of onabotulinumtoxinA 200 U (n = 190). The primary outcome was change from baseline in mean number of daily UUI episodes averaged over 6 months as recorded on a monthly 3-day bladder diary. Secondary outcomes included complete resolution of urgency incontinence, 75% or more reduction in UUI episodes, the Overactive Bladder Questionnaire Short Form (SF) score (range, 0-100; higher score indicates higher symptom severity), the Overactive Bladder Satisfaction of Treatment questionnaire (range, 0-100; higher score indicates better satisfaction), other quality-of-life measures, and adverse events.
Related article:
2015 Update on pelvic floor dysfunction: Bladder pain syndrome
Greater symptom bother improvement, treatment satisfaction with onabotulinumtoxinA 200 U
Participants treated with onabotulinumtoxinA had a greater mean reduction of 3.9 UUI episodes per day than the sacral neuromodulation group's reduction of 3.3 UUI episodes per day (mean difference, 0.63; 95% confidence interval [CI], 0.13-1.14; P = .01). In addition, complete UUI resolution was higher in the onabotulinumtoxinA group as compared with the sacral neuromodulation group (20% vs 4%; P<.001). The onabotulinumtoxinA group also had higher rates of 75% or more reduction of UUI episodes compared with the sacral neuromodulation group (46% vs 26%; P<.001). Over 6 months, both groups had improvements in all quality-of-life measures, but the onabotulinumtoxinA group had greater improvement in symptom bother compared with the sacral neuromodulation group (-46.7 vs -38.6; mean difference, 8.1; 95% CI, 3.0-13.3; P = .002). Furthermore, the onabotulinumtoxinA group had greater treatment satisfaction compared with the sacral neuromodulation group (mean difference, 7.8; 95% CI, 1.6-14.1; P = .01).
Adverse events. Six women (3%) underwent sacral neuromodulation device revision or removal. Approximately 8% of onabotulinumtoxinA-treated participants required intermittent self-catheterization at 1 month, 4% at 3 months, and 2% at 6 months. The risk of UTI was higher in the onabotulinumtoxinA group compared with the sacral neuromodulation group (35% vs 11%; risk difference, 23%; 95% CI, -33% to -13%; P<.001).
Strengths and limitations. This is a well-designed randomized clinical trial comparing clinical outcomes and adverse events after treatment with onabotulinumtoxinA 200-U versus sacral neuromodulation. The interventions were standardized across investigators at multiple sites, and the study design required close follow-up to assess efficacy and adverse events. The study used a 200-U dose based on reported durability of effect at that time and findings of equivalency between onabotulinumtoxinA 100 U and anticholinergic therapy. The US Food and Drug Administration's recommendation to use a 100-U dose in all patients with idiopathic OAB might dissuade clinicians from considering the higher dose of onabotulinumtoxinA. The study was limited by the lack of a placebo group.
Both onabotulinumtoxinA 200 U and sacral neuromodulation provide significant improvement in UUI episodes and quality of life over 6 months. However, while treatment with onabotulinumtoxinA has a likelihood of complete UUI resolution, greater improvements in symptom bother and treatment satisfaction, these benefits must be weighed against the risks of transient catheterization and UTI.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Haylen BT, de Ridder D, Freeman RM, et al; International Urogynecological Association; International Continence Society. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4-20.
- Hartmann KE, McPheeters ML, Biller DH, et al. Treatment of overactive bladder in women. Evid Rep Technol Assess (Full Rep). 2009;187:1-120.
- Reynolds,WS, Fowke J, Dmochowski, R. The burden of overactive bladder on US public health. Curr Bladder Dysfunct Rep. 2016;11(1):8-13.
- Willis-Gray MG, Dieter AA, Geller EJ. Evaluation and management of overactive bladder: strategies for optimizing care. Res Rep Urol. 2016;8:113-122.
- Ganz ML, Smalarz AM, Krupski TL, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75(3):526-532.
- Gormley EA, Lightner DJ, Faraday M, Vasavada SP; American Urological Association; Society of Urodyndamics, Female Pelvic Medicine. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol. 2015; 193(5):1572-1580.
- Gormley EA, Lightner DJ, Burgio KL, et al; American Urological Association; Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol. 2012;188(6 suppl):2455-2463.
The International Continence Society (ICS) defines overactive bladder (OAB) as a syndrome of "urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence (UUI), in the absence of urinary tract infection [UTI] or obvious pathology."1 The Agency for Healthcare Research and Quality (AHRQ) reported OAB prevalence to be 15% in US women, with 11% reporting UUI.2 OAB represents a significant health care burden that impacts nearly every aspect of life, including physical, emotional, and psychological domains.3,4 The economic impact is notable; the projected cost is estimated to reach $82.6 billion annually by 2020.5
The American Urological Association (AUA) and the Society for Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) have endorsed an algorithm for use in the evaluation of idiopathic OAB (FIGURE).6 If the patient's symptoms are certain, minimal evaluation is needed and it is reasonable to proceed with first-line therapy, which includes fluid management (decreasing caffeine intake and limiting evening fluid intake), bladder retraining drills such as timed voiding, and improving pelvic floor muscles with the use of biofeedback and functional electrical stimulation.6,7 Pelvic floor muscle training can be facilitated with a referral to a physical therapist trained in pelvic floor muscle education.
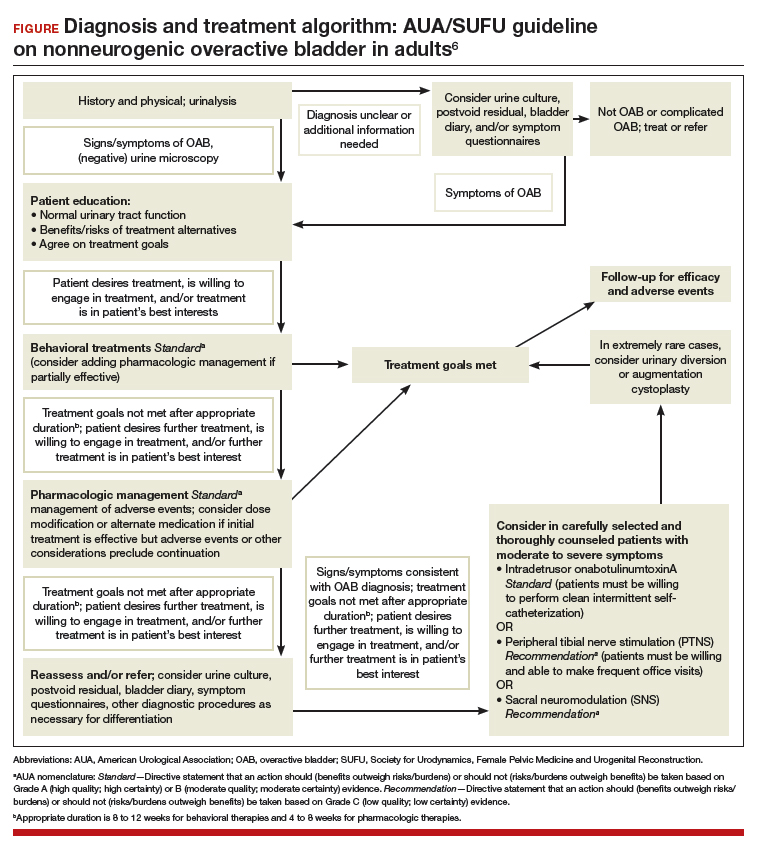
If treatment goals are not met with first-line strategies, second-line therapy may be initiated with anticholinergic or β3-adrenergic receptor agonist medications. If symptoms persist after 4 to 8 weeks of pharmacologic therapy, clinicians are encouraged to reassess or refer the patient to a specialist. Further evaluation may include a bladder diary in which the patient documents voided volumes, voiding frequency, and number of incontinent episodes; symptom-specific questionnaires; and/or urodynamic testing.
Related article:
The latest treatments for urinary and fecal incontinence: Which hold water?
Based on that evaluation, the patient may be a candidate for third-line therapy with either intradetrusor onabotulinumtoxinA, posterior tibial nerve stimulation (PTNS), or sacral neuromodulation.
There is a paucity of information comparing third-line therapies. In this Update, we focus on 4 randomized clinical trials that compare third-line treatment options for idiopathic OAB.
Read about how anticholinergic medication and onabotulinumtoxinA compare for treating UUI.
Anticholinergic therapy and onabotulinumtoxinA produce equivalent reductions in the frequency of daily UUI episodes
Visco AG, Brubaker L, Richter HE, et al; for the Pelvic Floor Disorders Network. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. N Engl J Med. 2012;367(19):1803-1813.
In a double-blind, double-placebo-controlled randomized trial, Visco and colleagues compared anticholinergic medication with onabotulinumtoxinA 100 U for the treatment of women with UUI.
Details of the study
Two hundred forty-one women with moderate to severe UUI received either 6 months of oral anticholinergic therapy (solifenacin 5 mg daily with the option of dose escalation to 10 mg daily or change to trospium XR 60 mg daily based on the Patient Global Symptom Control score) plus a single intradetrusor injection of saline, or a single intradetrusor injection of onabotulinumtoxinA 100 U plus a 6-month oral placebo regimen.
Inclusion criteria were 5 or more UUI episodes on a 3-day diary, insufficient resolution of symptoms after 2 medications, or being drug naive. Exclusions included a postvoid residual (PVR) urine volume greater than 150 mL or previous therapy with onabotulinumtoxinA.
Participants were scheduled for follow up every 2 to 6 months post randomization, at which time all study medications were discontinued. The primary outcome was reduction from baseline in the mean number of UUI episodes per day over the 6-month period, as recorded in the monthly 3-day bladder diaries. Secondary outcomes included the proportion of participants with complete resolution of UUI, the proportion of participants with 75% or more reduction in UUI episodes, Overactive Bladder Questionnaire Short Form (OABq-SF) scores, other symptom-specific questionnaire scores, and adverse events.
Related article:
Which treatments for pelvic floor disorders are backed by evidence?
Both treatments significantly reduced UUI episodes
At baseline, participants reported a mean (SD) of 5.0 (2.7) UUI episodes per day, and 41% of participants were drug naive. Both treatment groups experienced significant reductions compared with baseline in mean UUI episodes, and the reductions were similar between the 2 groups (reduction of 3.4 episodes per day in the anticholinergic group, reduction of 3.3 episodes in the onabotulinumtoxinA group; P = .81). Complete resolution of UUI was more common in the onabotulinumtoxinA group (27%) as compared with the anticholinergic group (13%) (P = .003). There were no differences in improvement in OABq-SF scores (37.05 in the anticholinergic group vs 37.13 in the onabotulinumtoxinA group; P = .98) or other quality-of-life measures.
Adverse events. The anticholinergic group experienced a higher rate of dry mouth compared with the onabotulinumtoxinA group (46% vs 31%; P = .02) but had lower rates of intermittent catheterization use at 2 months (0% vs 5%, P = .01) and UTIs (13% vs 33%, P<.001).
Strengths and limitations. This was a well-designed, multicenter, randomized double-blind, double placebo-controlled trial. The study design allowed for dose escalation and change to another medication for inadequate symptom control and included drug-naive participants, which increases the generalizability of the results. However, current guidelines recommend reserving onabotulinumtoxinA therapy for third-line therapy, thus deterring this treatment's use in the drug-naive population. Additionally, the lack of a pure placebo arm makes it difficult to interpret the extent to which a placebo effect contributed to observed improvements in clinical symptoms.
Through 6 months, both a single intradetrusor injection of onabotulinumtoxinA 100 U and anticholinergic therapy reduce UUI episodes and improve quality-of-life measures in women who have failed medications or are drug naive. Use of onabotulinumtoxinA, however, more likely will lead to complete resolution of UUI, although with an increased risk of transient urinary retention and UTI. Even given the study findings supporting the use of onabotulinumtoxinA over anticholinergic therapy for complete resolution of UUI, it is most appropriate to align with current practice, which includes a trial of pharmacotherapy before proceeding with third-line onabotulinumtoxinA.
Read: onabotulinumtoxinA vs PTNS for OAB.
OnabotulinumtoxinA has greater 9-month durability for OAB symptoms compared with12 weeks of PTNS
Sherif H, Khalil M, Omar R. Management of refractory idiopathic overactive bladder: intradetrusor injection of botulinum toxin type A versus posterior tibial nerve stimulation. Can J Urol. 2017;24(3):8838-8846.
In this randomized clinical trial, Sherif and colleagues compared the safety and efficacy of a single intradetrusor injection of onabotulinumtoxinA 100 U with that of PTNS for OAB.
Details of the study
Sixty adult men and women with OAB who did not respond to medical therapy were randomly assigned to treatment with either onabotulinumtoxinA 100 U or PTNS. Criteria for exclusion were current UTI, PVR urine volume of more than 150 mL, previous radiation therapy or chemotherapy, previous incontinence surgery or bladder malignancy, or presence of mixed urinary incontinence.
At baseline, participants completed a 3-day bladder diary, an OAB symptom score (OABSS) questionnaire, and urodynamic testing. The OABSS questionnaire included 7 questions (scoring range, 0-28), with higher scores indicating worse symptoms, and included subscales for urgency and quality-of-life measures. Total OABSS, urgency score, quality-of-life score, bladder diary records, and urodynamic testing parameters were assessed at 6, 12, 24, and 36 weeks, along with adverse events.
OnabotulinumtoxinA injections were performed under spinal anesthesia. If PVR urine volume was greater than 200 mL at any follow-up visit, participants were instructed to begin clean intermittent self-catheterization. PTNS was administered as weekly 30-minute sessions for 12 consecutive weeks.
Participants' baseline demographics and symptoms were similar. Average age was 45 years. Averages (SD) for duration of anticholinergic use was 13 (0.8) weeks, UUI episode score was 4.5 (1) on 3-day bladder diary, and OABSS was 22 (2.7). Nine-month data were available for 29 participants in the onabotulinumtoxinA group and for 8 in the PTNS group.
Related article:
Update on pelvic floor dysfunction: Focus on urinary incontinence
OnabotulinumtoxinA treatment benefits sustained for 9 months
Through 6 months, compared with baseline assessments, both treatment groups had significant improvements in clinical symptoms and OABSS total score, as well as urgency and quality-of-life subscales. At 3 months, urodynamic study parameters were similarly improved from baseline in both groups.
At 9 months, however, only the onabotulinumtoxinA group, compared with the PTNS group, maintained the significant improvement from baseline in 3-day bladder diary voiding episodes (average [SD], 10.7 [1.01] vs 11.6 [1.09]; P = .009), 3-day bladder diary nocturia episodes (average [SD], 3.8 [1.09] vs 4.4 [0.8]; P = .02), and average [SD] UUI episodes over 3 days (3.5 [1.2] vs 4.2 [1.04]; P = .02). Similarly, onabotulinumtoxinA-treated participants, compared with those treated with PTNS, maintained improvements at 9 months in average (SD): OABSS total score (19.2 [2.4] vs 20.4 [1.7]; P = .03), urgency scores (10.9 [1.3] vs 11.8 [1.4]; P = .009), urine volume at first desire (177.8 [9.2] vs 171.8 [7.7]), maximum cystometric capacity (304 [17.6] vs 290 [13.1]), and Qmax (mL/sec) (20.7 [1.6] vs 22.2 [1.2]).
Adverse events. Average PVR urine volumes were higher in the onabotulinumtoxinA group compared with the PTNS group (36.8 [2.7] vs 32.4 [3.03]; P = .0001) at all time points, and self-catheterization was required in 6.6% of onabotulinumtoxinA-treated participants. Urinary tract infection occurred in 6.6% of participants in the onabotulinumtoxinA group and in none of the PTNS group. In the PTNS group, few experienced pain and minor bleeding at the needle site.
Strengths and limitations. This randomized, open-label trial comparing treatment with onabotulinumtoxinA 100 U and PTNS included both men and women with idiopathic OAB symptoms. The participants were assessed at regular intervals with various measures, and follow-up adherence was good. The sample size was small, so the study may not have been powered to see differences prior to 9 months.
Although at 9 months only the onabotulinumtoxinA group maintained significant improvement over baseline levels, the improvement was diminished, and therefore the clinical meaningfulness is uncertain. Further, participants in the PTNS group did not undergo monthly maintenance therapy after 3 months, which is recommended for those with a 12-week therapeutic response; this may have affected 9-month outcomes in this group. Since the one-time onabotulinumtoxinA 100 U injection was performed under spinal anesthesia, cost comparisons should be considered, since future onabotulinumtoxinA injections would be necessary.
A one-time onabotulinumtoxinA 100 U injection and 12 weeks of PTNS therapy are reasonable short-term options for symptomatic OAB relief after unsuccessful therapy with medications. OnabotulinumtoxinA injection may provide more durable OAB symptom control at 9 months but with a risk of UTI and need for self-catheterization.
Read about using different doses of onabotulinumtoxinA for OAB.
OnabotulinumtoxinA 200-U injection provides longer OAB symptom improvement than 100-U injection
Abdelwahab O, Sherif H, Soliman T, Elbarky I, Eshazly A. Efficacy of botulinum toxin type A 100 units versus 200 units for treatment of refractory idiopathic overactive bladder. Int Braz J Urol. 2015;41(6):1132-1140.
Abdelwahab and colleagues conducted a single-center, randomized clinical trial to investigate the safety and efficacy of a single injection of intradetrusor onabotulinumtoxinA in 2 different doses (100 U and 200 U) for treatment of OAB.
Details of the study
Eighty adults (63 women, 17 men) who did not benefit from anticholinergic medication during the previous 3 months were randomly assigned to receive either a 100-U (n = 40) or a 200-U (n = 40) injection of onabotulinumtoxinA. Exclusion criteria were PVR urine volume greater than 150 mL and previous radiation therapy or chemotherapy.
Initial assessments -- completed at baseline and at 1, 3, 6, and 9 months -- included the health-related quality-of-life (HR-QOL) questionnaire (maximum score, 100; higher score indicates better quality of life), an abbreviated OABSS questionnaire (4 questions; score range, 0-15; higher score indicates more severe symptoms), and urodynamic evaluation. Outcomes included OABSS, HR-QOL score, and urodynamic parameters at the various time points.
Related article:
Is there a link between impaired mobility and urinary incontinence in elderly, community-dwelling women?
Higher dose, greater symptom improvement and higher adverse event rate
At baseline, participants (average age, 31 years) had an average (SD) OABSS of 1.7 (1.6). OnabotulinumtoxinA treatment with both a 100-U and a 200-U dose resulted in significant improvements (compared with baseline levels) in frequency, nocturia, UUI episodes, OABSS, and urodynamic parameters throughout the 9 months. At 9 months, however, the group treated with the 200-U dose had greater improvements, compared with the group who received a 100-U dose, in urinary frequency symptom scores (mean [SD], 0.32 [0.47] vs 1.1 [0.51]; P<.05), nocturia symptom scores (mean [SD], 0.13 [0.34] vs 0.36 [0.49]; P<.05), UUI symptom scores (mean [SD], 0.68 [0.16] vs 1.26 [1.1]; P<.05), and mean (SD) total OABSS (2.6 [2.31] vs 5.3 [2.11]; P<.05). Similarly, at 9 months the 200-U dose resulted in greater improvements in volume at first desire (mean [SD], 291.8 [42.8] vs 246.8 [53.8] mL; P<.05), volume at strong desire (mean [SD], 392.1 [37.3] vs 313.1 [67.4] mL; P<.05), detrusor pressure (mean [SD], 10.4 [4.0] vs 19.2 [7.8] cm H2O; P<.05), and maximum cystometric capacity (mean [SD], 430.5 [34.2] vs 350 [69.1] mL; P<.05) compared with the 100-U dose.
Adverse events. No participant had a PVR urine volume greater than 100 mL at any follow-up visit. Postoperative hematuria occurred in 23% of the group treated with onabotulinumtoxinA 200 U versus in 15% of those treated with a 100-U dose. Similarly, UTIs occurred in 17.5% of the 200-U dose group and in 7.5% of the 100-U dose group. Dysuria was reported in 37.5% and 15% of the 200-U and 100-U dose groups, respectively.
Strengths and limitations. This randomized, open-label trial comparing a single injection of 100 U versus 200 U of onabotulinumtoxinA included mostly women. OAB symptoms and urodynamic parameters improved after treatment with both dose levels, but a longer duration of improvement was seen with the 200-U dose. The cohort had a low baseline OAB severity, based on the OABSS questionnaire, and a young average age of participants, which limits the generalizability of the study results to a population with refractory OAB. The 0% rate of clean intermittent self-catheterization postinjection might be based on the study's criteria for requiring clean intermittent catheterization. In addition, the initial postinjection visit occurred at 1 month, possibly missing participants who had symptoms of retention soon after injection.
Two dose levels (100 U and 200 U) of a single injection of onabotulinumtoxinA are associated with comparable OAB symptom and urodyanamic improvements. The benefits of a longer duration of effect with the 200-U dose must be weighed against the possible higher risks of transient hematuria, dysuria, and UTI.
Read: onabotulinumtoxinA vs sacral neuromodulation therapy for UUI.
Treatment with onabotulinumtoxinA may control UUI symptoms better than sacral neuromodulation therapy
Amundsen CL, Richter HE, Menefee SA, et al; Pelvic Floor Disorders Network. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: a randomized clinical trial. JAMA. 2016;316(13):1366-1374.
In this multicenter open-label randomized trial, Amundsen and colleagues compared the efficacy and safety of onabotulinumtoxinA 200 U with that of sacral neuromodulation.
Details of the study
Three hundred sixty-four women with UUI had data available for primary analysis at 6 months. Women were considered eligible for the study if they had 6 or more UUI episodes on a 3-day bladder diary, persistent symptoms despite anticholinergic therapy, a PVR urine volume of less than 150 mL, and had never previously received either study treatment.
There were no differences in baseline characteristics of the participants. The average (SD) age of the study population was 63 (11.6) years, with an average (SD) daily number of UUI episodes of 5.3 (2.8). The average (SD) body mass index was 32 (8) kg/m2.
Participants were randomly assigned to undergo either sacral neuromodulation (n = 174) or intradetrusor injection of onabotulinumtoxinA 200 U (n = 190). The primary outcome was change from baseline in mean number of daily UUI episodes averaged over 6 months as recorded on a monthly 3-day bladder diary. Secondary outcomes included complete resolution of urgency incontinence, 75% or more reduction in UUI episodes, the Overactive Bladder Questionnaire Short Form (SF) score (range, 0-100; higher score indicates higher symptom severity), the Overactive Bladder Satisfaction of Treatment questionnaire (range, 0-100; higher score indicates better satisfaction), other quality-of-life measures, and adverse events.
Related article:
2015 Update on pelvic floor dysfunction: Bladder pain syndrome
Greater symptom bother improvement, treatment satisfaction with onabotulinumtoxinA 200 U
Participants treated with onabotulinumtoxinA had a greater mean reduction of 3.9 UUI episodes per day than the sacral neuromodulation group's reduction of 3.3 UUI episodes per day (mean difference, 0.63; 95% confidence interval [CI], 0.13-1.14; P = .01). In addition, complete UUI resolution was higher in the onabotulinumtoxinA group as compared with the sacral neuromodulation group (20% vs 4%; P<.001). The onabotulinumtoxinA group also had higher rates of 75% or more reduction of UUI episodes compared with the sacral neuromodulation group (46% vs 26%; P<.001). Over 6 months, both groups had improvements in all quality-of-life measures, but the onabotulinumtoxinA group had greater improvement in symptom bother compared with the sacral neuromodulation group (-46.7 vs -38.6; mean difference, 8.1; 95% CI, 3.0-13.3; P = .002). Furthermore, the onabotulinumtoxinA group had greater treatment satisfaction compared with the sacral neuromodulation group (mean difference, 7.8; 95% CI, 1.6-14.1; P = .01).
Adverse events. Six women (3%) underwent sacral neuromodulation device revision or removal. Approximately 8% of onabotulinumtoxinA-treated participants required intermittent self-catheterization at 1 month, 4% at 3 months, and 2% at 6 months. The risk of UTI was higher in the onabotulinumtoxinA group compared with the sacral neuromodulation group (35% vs 11%; risk difference, 23%; 95% CI, -33% to -13%; P<.001).
Strengths and limitations. This is a well-designed randomized clinical trial comparing clinical outcomes and adverse events after treatment with onabotulinumtoxinA 200-U versus sacral neuromodulation. The interventions were standardized across investigators at multiple sites, and the study design required close follow-up to assess efficacy and adverse events. The study used a 200-U dose based on reported durability of effect at that time and findings of equivalency between onabotulinumtoxinA 100 U and anticholinergic therapy. The US Food and Drug Administration's recommendation to use a 100-U dose in all patients with idiopathic OAB might dissuade clinicians from considering the higher dose of onabotulinumtoxinA. The study was limited by the lack of a placebo group.
Both onabotulinumtoxinA 200 U and sacral neuromodulation provide significant improvement in UUI episodes and quality of life over 6 months. However, while treatment with onabotulinumtoxinA has a likelihood of complete UUI resolution, greater improvements in symptom bother and treatment satisfaction, these benefits must be weighed against the risks of transient catheterization and UTI.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
The International Continence Society (ICS) defines overactive bladder (OAB) as a syndrome of "urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence (UUI), in the absence of urinary tract infection [UTI] or obvious pathology."1 The Agency for Healthcare Research and Quality (AHRQ) reported OAB prevalence to be 15% in US women, with 11% reporting UUI.2 OAB represents a significant health care burden that impacts nearly every aspect of life, including physical, emotional, and psychological domains.3,4 The economic impact is notable; the projected cost is estimated to reach $82.6 billion annually by 2020.5
The American Urological Association (AUA) and the Society for Urodynamics, Female Pelvic Medicine and Urogenital Reconstruction (SUFU) have endorsed an algorithm for use in the evaluation of idiopathic OAB (FIGURE).6 If the patient's symptoms are certain, minimal evaluation is needed and it is reasonable to proceed with first-line therapy, which includes fluid management (decreasing caffeine intake and limiting evening fluid intake), bladder retraining drills such as timed voiding, and improving pelvic floor muscles with the use of biofeedback and functional electrical stimulation.6,7 Pelvic floor muscle training can be facilitated with a referral to a physical therapist trained in pelvic floor muscle education.
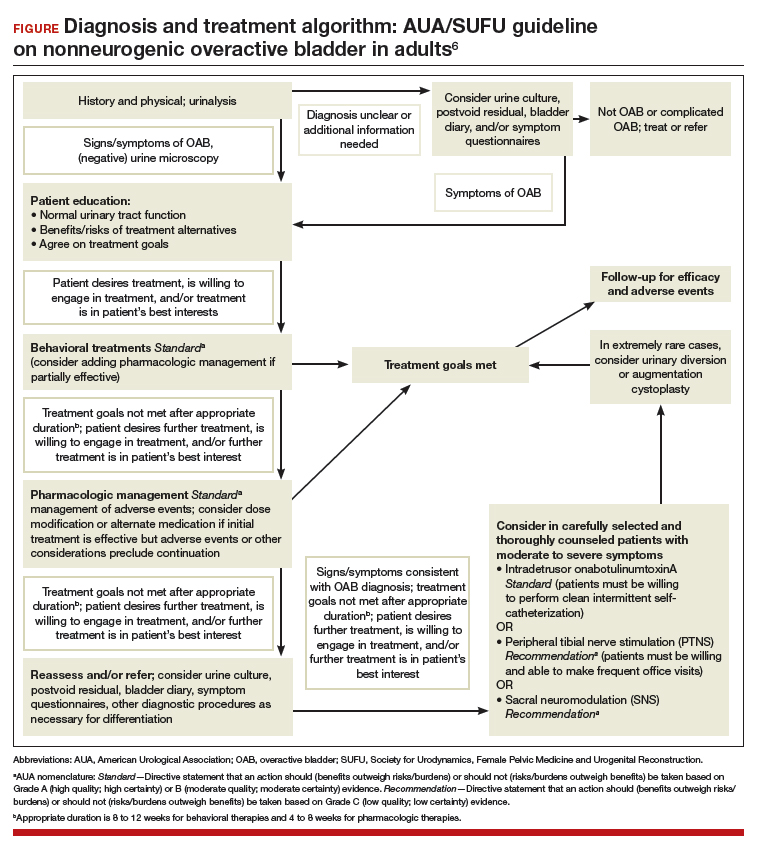
If treatment goals are not met with first-line strategies, second-line therapy may be initiated with anticholinergic or β3-adrenergic receptor agonist medications. If symptoms persist after 4 to 8 weeks of pharmacologic therapy, clinicians are encouraged to reassess or refer the patient to a specialist. Further evaluation may include a bladder diary in which the patient documents voided volumes, voiding frequency, and number of incontinent episodes; symptom-specific questionnaires; and/or urodynamic testing.
Related article:
The latest treatments for urinary and fecal incontinence: Which hold water?
Based on that evaluation, the patient may be a candidate for third-line therapy with either intradetrusor onabotulinumtoxinA, posterior tibial nerve stimulation (PTNS), or sacral neuromodulation.
There is a paucity of information comparing third-line therapies. In this Update, we focus on 4 randomized clinical trials that compare third-line treatment options for idiopathic OAB.
Read about how anticholinergic medication and onabotulinumtoxinA compare for treating UUI.
Anticholinergic therapy and onabotulinumtoxinA produce equivalent reductions in the frequency of daily UUI episodes
Visco AG, Brubaker L, Richter HE, et al; for the Pelvic Floor Disorders Network. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. N Engl J Med. 2012;367(19):1803-1813.
In a double-blind, double-placebo-controlled randomized trial, Visco and colleagues compared anticholinergic medication with onabotulinumtoxinA 100 U for the treatment of women with UUI.
Details of the study
Two hundred forty-one women with moderate to severe UUI received either 6 months of oral anticholinergic therapy (solifenacin 5 mg daily with the option of dose escalation to 10 mg daily or change to trospium XR 60 mg daily based on the Patient Global Symptom Control score) plus a single intradetrusor injection of saline, or a single intradetrusor injection of onabotulinumtoxinA 100 U plus a 6-month oral placebo regimen.
Inclusion criteria were 5 or more UUI episodes on a 3-day diary, insufficient resolution of symptoms after 2 medications, or being drug naive. Exclusions included a postvoid residual (PVR) urine volume greater than 150 mL or previous therapy with onabotulinumtoxinA.
Participants were scheduled for follow up every 2 to 6 months post randomization, at which time all study medications were discontinued. The primary outcome was reduction from baseline in the mean number of UUI episodes per day over the 6-month period, as recorded in the monthly 3-day bladder diaries. Secondary outcomes included the proportion of participants with complete resolution of UUI, the proportion of participants with 75% or more reduction in UUI episodes, Overactive Bladder Questionnaire Short Form (OABq-SF) scores, other symptom-specific questionnaire scores, and adverse events.
Related article:
Which treatments for pelvic floor disorders are backed by evidence?
Both treatments significantly reduced UUI episodes
At baseline, participants reported a mean (SD) of 5.0 (2.7) UUI episodes per day, and 41% of participants were drug naive. Both treatment groups experienced significant reductions compared with baseline in mean UUI episodes, and the reductions were similar between the 2 groups (reduction of 3.4 episodes per day in the anticholinergic group, reduction of 3.3 episodes in the onabotulinumtoxinA group; P = .81). Complete resolution of UUI was more common in the onabotulinumtoxinA group (27%) as compared with the anticholinergic group (13%) (P = .003). There were no differences in improvement in OABq-SF scores (37.05 in the anticholinergic group vs 37.13 in the onabotulinumtoxinA group; P = .98) or other quality-of-life measures.
Adverse events. The anticholinergic group experienced a higher rate of dry mouth compared with the onabotulinumtoxinA group (46% vs 31%; P = .02) but had lower rates of intermittent catheterization use at 2 months (0% vs 5%, P = .01) and UTIs (13% vs 33%, P<.001).
Strengths and limitations. This was a well-designed, multicenter, randomized double-blind, double placebo-controlled trial. The study design allowed for dose escalation and change to another medication for inadequate symptom control and included drug-naive participants, which increases the generalizability of the results. However, current guidelines recommend reserving onabotulinumtoxinA therapy for third-line therapy, thus deterring this treatment's use in the drug-naive population. Additionally, the lack of a pure placebo arm makes it difficult to interpret the extent to which a placebo effect contributed to observed improvements in clinical symptoms.
Through 6 months, both a single intradetrusor injection of onabotulinumtoxinA 100 U and anticholinergic therapy reduce UUI episodes and improve quality-of-life measures in women who have failed medications or are drug naive. Use of onabotulinumtoxinA, however, more likely will lead to complete resolution of UUI, although with an increased risk of transient urinary retention and UTI. Even given the study findings supporting the use of onabotulinumtoxinA over anticholinergic therapy for complete resolution of UUI, it is most appropriate to align with current practice, which includes a trial of pharmacotherapy before proceeding with third-line onabotulinumtoxinA.
Read: onabotulinumtoxinA vs PTNS for OAB.
OnabotulinumtoxinA has greater 9-month durability for OAB symptoms compared with12 weeks of PTNS
Sherif H, Khalil M, Omar R. Management of refractory idiopathic overactive bladder: intradetrusor injection of botulinum toxin type A versus posterior tibial nerve stimulation. Can J Urol. 2017;24(3):8838-8846.
In this randomized clinical trial, Sherif and colleagues compared the safety and efficacy of a single intradetrusor injection of onabotulinumtoxinA 100 U with that of PTNS for OAB.
Details of the study
Sixty adult men and women with OAB who did not respond to medical therapy were randomly assigned to treatment with either onabotulinumtoxinA 100 U or PTNS. Criteria for exclusion were current UTI, PVR urine volume of more than 150 mL, previous radiation therapy or chemotherapy, previous incontinence surgery or bladder malignancy, or presence of mixed urinary incontinence.
At baseline, participants completed a 3-day bladder diary, an OAB symptom score (OABSS) questionnaire, and urodynamic testing. The OABSS questionnaire included 7 questions (scoring range, 0-28), with higher scores indicating worse symptoms, and included subscales for urgency and quality-of-life measures. Total OABSS, urgency score, quality-of-life score, bladder diary records, and urodynamic testing parameters were assessed at 6, 12, 24, and 36 weeks, along with adverse events.
OnabotulinumtoxinA injections were performed under spinal anesthesia. If PVR urine volume was greater than 200 mL at any follow-up visit, participants were instructed to begin clean intermittent self-catheterization. PTNS was administered as weekly 30-minute sessions for 12 consecutive weeks.
Participants' baseline demographics and symptoms were similar. Average age was 45 years. Averages (SD) for duration of anticholinergic use was 13 (0.8) weeks, UUI episode score was 4.5 (1) on 3-day bladder diary, and OABSS was 22 (2.7). Nine-month data were available for 29 participants in the onabotulinumtoxinA group and for 8 in the PTNS group.
Related article:
Update on pelvic floor dysfunction: Focus on urinary incontinence
OnabotulinumtoxinA treatment benefits sustained for 9 months
Through 6 months, compared with baseline assessments, both treatment groups had significant improvements in clinical symptoms and OABSS total score, as well as urgency and quality-of-life subscales. At 3 months, urodynamic study parameters were similarly improved from baseline in both groups.
At 9 months, however, only the onabotulinumtoxinA group, compared with the PTNS group, maintained the significant improvement from baseline in 3-day bladder diary voiding episodes (average [SD], 10.7 [1.01] vs 11.6 [1.09]; P = .009), 3-day bladder diary nocturia episodes (average [SD], 3.8 [1.09] vs 4.4 [0.8]; P = .02), and average [SD] UUI episodes over 3 days (3.5 [1.2] vs 4.2 [1.04]; P = .02). Similarly, onabotulinumtoxinA-treated participants, compared with those treated with PTNS, maintained improvements at 9 months in average (SD): OABSS total score (19.2 [2.4] vs 20.4 [1.7]; P = .03), urgency scores (10.9 [1.3] vs 11.8 [1.4]; P = .009), urine volume at first desire (177.8 [9.2] vs 171.8 [7.7]), maximum cystometric capacity (304 [17.6] vs 290 [13.1]), and Qmax (mL/sec) (20.7 [1.6] vs 22.2 [1.2]).
Adverse events. Average PVR urine volumes were higher in the onabotulinumtoxinA group compared with the PTNS group (36.8 [2.7] vs 32.4 [3.03]; P = .0001) at all time points, and self-catheterization was required in 6.6% of onabotulinumtoxinA-treated participants. Urinary tract infection occurred in 6.6% of participants in the onabotulinumtoxinA group and in none of the PTNS group. In the PTNS group, few experienced pain and minor bleeding at the needle site.
Strengths and limitations. This randomized, open-label trial comparing treatment with onabotulinumtoxinA 100 U and PTNS included both men and women with idiopathic OAB symptoms. The participants were assessed at regular intervals with various measures, and follow-up adherence was good. The sample size was small, so the study may not have been powered to see differences prior to 9 months.
Although at 9 months only the onabotulinumtoxinA group maintained significant improvement over baseline levels, the improvement was diminished, and therefore the clinical meaningfulness is uncertain. Further, participants in the PTNS group did not undergo monthly maintenance therapy after 3 months, which is recommended for those with a 12-week therapeutic response; this may have affected 9-month outcomes in this group. Since the one-time onabotulinumtoxinA 100 U injection was performed under spinal anesthesia, cost comparisons should be considered, since future onabotulinumtoxinA injections would be necessary.
A one-time onabotulinumtoxinA 100 U injection and 12 weeks of PTNS therapy are reasonable short-term options for symptomatic OAB relief after unsuccessful therapy with medications. OnabotulinumtoxinA injection may provide more durable OAB symptom control at 9 months but with a risk of UTI and need for self-catheterization.
Read about using different doses of onabotulinumtoxinA for OAB.
OnabotulinumtoxinA 200-U injection provides longer OAB symptom improvement than 100-U injection
Abdelwahab O, Sherif H, Soliman T, Elbarky I, Eshazly A. Efficacy of botulinum toxin type A 100 units versus 200 units for treatment of refractory idiopathic overactive bladder. Int Braz J Urol. 2015;41(6):1132-1140.
Abdelwahab and colleagues conducted a single-center, randomized clinical trial to investigate the safety and efficacy of a single injection of intradetrusor onabotulinumtoxinA in 2 different doses (100 U and 200 U) for treatment of OAB.
Details of the study
Eighty adults (63 women, 17 men) who did not benefit from anticholinergic medication during the previous 3 months were randomly assigned to receive either a 100-U (n = 40) or a 200-U (n = 40) injection of onabotulinumtoxinA. Exclusion criteria were PVR urine volume greater than 150 mL and previous radiation therapy or chemotherapy.
Initial assessments -- completed at baseline and at 1, 3, 6, and 9 months -- included the health-related quality-of-life (HR-QOL) questionnaire (maximum score, 100; higher score indicates better quality of life), an abbreviated OABSS questionnaire (4 questions; score range, 0-15; higher score indicates more severe symptoms), and urodynamic evaluation. Outcomes included OABSS, HR-QOL score, and urodynamic parameters at the various time points.
Related article:
Is there a link between impaired mobility and urinary incontinence in elderly, community-dwelling women?
Higher dose, greater symptom improvement and higher adverse event rate
At baseline, participants (average age, 31 years) had an average (SD) OABSS of 1.7 (1.6). OnabotulinumtoxinA treatment with both a 100-U and a 200-U dose resulted in significant improvements (compared with baseline levels) in frequency, nocturia, UUI episodes, OABSS, and urodynamic parameters throughout the 9 months. At 9 months, however, the group treated with the 200-U dose had greater improvements, compared with the group who received a 100-U dose, in urinary frequency symptom scores (mean [SD], 0.32 [0.47] vs 1.1 [0.51]; P<.05), nocturia symptom scores (mean [SD], 0.13 [0.34] vs 0.36 [0.49]; P<.05), UUI symptom scores (mean [SD], 0.68 [0.16] vs 1.26 [1.1]; P<.05), and mean (SD) total OABSS (2.6 [2.31] vs 5.3 [2.11]; P<.05). Similarly, at 9 months the 200-U dose resulted in greater improvements in volume at first desire (mean [SD], 291.8 [42.8] vs 246.8 [53.8] mL; P<.05), volume at strong desire (mean [SD], 392.1 [37.3] vs 313.1 [67.4] mL; P<.05), detrusor pressure (mean [SD], 10.4 [4.0] vs 19.2 [7.8] cm H2O; P<.05), and maximum cystometric capacity (mean [SD], 430.5 [34.2] vs 350 [69.1] mL; P<.05) compared with the 100-U dose.
Adverse events. No participant had a PVR urine volume greater than 100 mL at any follow-up visit. Postoperative hematuria occurred in 23% of the group treated with onabotulinumtoxinA 200 U versus in 15% of those treated with a 100-U dose. Similarly, UTIs occurred in 17.5% of the 200-U dose group and in 7.5% of the 100-U dose group. Dysuria was reported in 37.5% and 15% of the 200-U and 100-U dose groups, respectively.
Strengths and limitations. This randomized, open-label trial comparing a single injection of 100 U versus 200 U of onabotulinumtoxinA included mostly women. OAB symptoms and urodynamic parameters improved after treatment with both dose levels, but a longer duration of improvement was seen with the 200-U dose. The cohort had a low baseline OAB severity, based on the OABSS questionnaire, and a young average age of participants, which limits the generalizability of the study results to a population with refractory OAB. The 0% rate of clean intermittent self-catheterization postinjection might be based on the study's criteria for requiring clean intermittent catheterization. In addition, the initial postinjection visit occurred at 1 month, possibly missing participants who had symptoms of retention soon after injection.
Two dose levels (100 U and 200 U) of a single injection of onabotulinumtoxinA are associated with comparable OAB symptom and urodyanamic improvements. The benefits of a longer duration of effect with the 200-U dose must be weighed against the possible higher risks of transient hematuria, dysuria, and UTI.
Read: onabotulinumtoxinA vs sacral neuromodulation therapy for UUI.
Treatment with onabotulinumtoxinA may control UUI symptoms better than sacral neuromodulation therapy
Amundsen CL, Richter HE, Menefee SA, et al; Pelvic Floor Disorders Network. OnabotulinumtoxinA vs sacral neuromodulation on refractory urgency urinary incontinence in women: a randomized clinical trial. JAMA. 2016;316(13):1366-1374.
In this multicenter open-label randomized trial, Amundsen and colleagues compared the efficacy and safety of onabotulinumtoxinA 200 U with that of sacral neuromodulation.
Details of the study
Three hundred sixty-four women with UUI had data available for primary analysis at 6 months. Women were considered eligible for the study if they had 6 or more UUI episodes on a 3-day bladder diary, persistent symptoms despite anticholinergic therapy, a PVR urine volume of less than 150 mL, and had never previously received either study treatment.
There were no differences in baseline characteristics of the participants. The average (SD) age of the study population was 63 (11.6) years, with an average (SD) daily number of UUI episodes of 5.3 (2.8). The average (SD) body mass index was 32 (8) kg/m2.
Participants were randomly assigned to undergo either sacral neuromodulation (n = 174) or intradetrusor injection of onabotulinumtoxinA 200 U (n = 190). The primary outcome was change from baseline in mean number of daily UUI episodes averaged over 6 months as recorded on a monthly 3-day bladder diary. Secondary outcomes included complete resolution of urgency incontinence, 75% or more reduction in UUI episodes, the Overactive Bladder Questionnaire Short Form (SF) score (range, 0-100; higher score indicates higher symptom severity), the Overactive Bladder Satisfaction of Treatment questionnaire (range, 0-100; higher score indicates better satisfaction), other quality-of-life measures, and adverse events.
Related article:
2015 Update on pelvic floor dysfunction: Bladder pain syndrome
Greater symptom bother improvement, treatment satisfaction with onabotulinumtoxinA 200 U
Participants treated with onabotulinumtoxinA had a greater mean reduction of 3.9 UUI episodes per day than the sacral neuromodulation group's reduction of 3.3 UUI episodes per day (mean difference, 0.63; 95% confidence interval [CI], 0.13-1.14; P = .01). In addition, complete UUI resolution was higher in the onabotulinumtoxinA group as compared with the sacral neuromodulation group (20% vs 4%; P<.001). The onabotulinumtoxinA group also had higher rates of 75% or more reduction of UUI episodes compared with the sacral neuromodulation group (46% vs 26%; P<.001). Over 6 months, both groups had improvements in all quality-of-life measures, but the onabotulinumtoxinA group had greater improvement in symptom bother compared with the sacral neuromodulation group (-46.7 vs -38.6; mean difference, 8.1; 95% CI, 3.0-13.3; P = .002). Furthermore, the onabotulinumtoxinA group had greater treatment satisfaction compared with the sacral neuromodulation group (mean difference, 7.8; 95% CI, 1.6-14.1; P = .01).
Adverse events. Six women (3%) underwent sacral neuromodulation device revision or removal. Approximately 8% of onabotulinumtoxinA-treated participants required intermittent self-catheterization at 1 month, 4% at 3 months, and 2% at 6 months. The risk of UTI was higher in the onabotulinumtoxinA group compared with the sacral neuromodulation group (35% vs 11%; risk difference, 23%; 95% CI, -33% to -13%; P<.001).
Strengths and limitations. This is a well-designed randomized clinical trial comparing clinical outcomes and adverse events after treatment with onabotulinumtoxinA 200-U versus sacral neuromodulation. The interventions were standardized across investigators at multiple sites, and the study design required close follow-up to assess efficacy and adverse events. The study used a 200-U dose based on reported durability of effect at that time and findings of equivalency between onabotulinumtoxinA 100 U and anticholinergic therapy. The US Food and Drug Administration's recommendation to use a 100-U dose in all patients with idiopathic OAB might dissuade clinicians from considering the higher dose of onabotulinumtoxinA. The study was limited by the lack of a placebo group.
Both onabotulinumtoxinA 200 U and sacral neuromodulation provide significant improvement in UUI episodes and quality of life over 6 months. However, while treatment with onabotulinumtoxinA has a likelihood of complete UUI resolution, greater improvements in symptom bother and treatment satisfaction, these benefits must be weighed against the risks of transient catheterization and UTI.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Haylen BT, de Ridder D, Freeman RM, et al; International Urogynecological Association; International Continence Society. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4-20.
- Hartmann KE, McPheeters ML, Biller DH, et al. Treatment of overactive bladder in women. Evid Rep Technol Assess (Full Rep). 2009;187:1-120.
- Reynolds,WS, Fowke J, Dmochowski, R. The burden of overactive bladder on US public health. Curr Bladder Dysfunct Rep. 2016;11(1):8-13.
- Willis-Gray MG, Dieter AA, Geller EJ. Evaluation and management of overactive bladder: strategies for optimizing care. Res Rep Urol. 2016;8:113-122.
- Ganz ML, Smalarz AM, Krupski TL, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75(3):526-532.
- Gormley EA, Lightner DJ, Faraday M, Vasavada SP; American Urological Association; Society of Urodyndamics, Female Pelvic Medicine. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol. 2015; 193(5):1572-1580.
- Gormley EA, Lightner DJ, Burgio KL, et al; American Urological Association; Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol. 2012;188(6 suppl):2455-2463.
- Haylen BT, de Ridder D, Freeman RM, et al; International Urogynecological Association; International Continence Society. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4-20.
- Hartmann KE, McPheeters ML, Biller DH, et al. Treatment of overactive bladder in women. Evid Rep Technol Assess (Full Rep). 2009;187:1-120.
- Reynolds,WS, Fowke J, Dmochowski, R. The burden of overactive bladder on US public health. Curr Bladder Dysfunct Rep. 2016;11(1):8-13.
- Willis-Gray MG, Dieter AA, Geller EJ. Evaluation and management of overactive bladder: strategies for optimizing care. Res Rep Urol. 2016;8:113-122.
- Ganz ML, Smalarz AM, Krupski TL, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75(3):526-532.
- Gormley EA, Lightner DJ, Faraday M, Vasavada SP; American Urological Association; Society of Urodyndamics, Female Pelvic Medicine. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment. J Urol. 2015; 193(5):1572-1580.
- Gormley EA, Lightner DJ, Burgio KL, et al; American Urological Association; Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol. 2012;188(6 suppl):2455-2463.
Bringing up the rear: Disorders of the rectum and colon
The final session of the course opened with Uri Ladabaum, MD, entertaining the question “Colon cancer screening and surveillance: who, when, and how?” Dr. Ladabaum pointed out that there is consensus that colorectal cancer screening for average-risk individuals should begin at age 50 with a choice of modalities and that surveillance depends on the findings on each colonoscopy. He reviewed the evidence for screening modalities and for surveillance and offered perspectives on the role of the gastroenterologist/colonoscopist in the quality of colonsocopy. Douglas K. Rex, MD, AGAF followed by asking “Does every big polyp need EMR?” Dr. Rex discussed the available approaches to the large colonic polyp, including endoscopic mucosal resection, endoscopic submucosal dissection, and surgery. He provided evidence for the advantages and expanded use of EMR, with the conclusion that almost every large benign polyp needs EMR.
Jennifer A. Christie, MD, then spoke on “Pelvic floor dysfunction and constipation.” Dr. Christie stressed the importance of a good history and the digital rectal exam in diagnosis of pelvic floor dysfunction. When over-the-counter or prescribed medications are not effective, the work-up should include anorectal manometry, balloon expulsion, and colonic transit testing. Attempts should be made to remove all potential offending agents, such as anticholinergics, narcotics, calcium channel blockers, and beta-blockers. Biofeedback is a safe and effective treatment for pelvic floor dysfunction. Lin Chang, MD, AGAF, continued with a talk on irritable bowel syndrome, which can be considered a combination of disorders, with clusters of symptoms and subgroups. There must be recurrent abdominal pain or discomfort at least 1 day/week for the prior 3 months, associated with 2 or more of the following: a relationship to defecation, change in stool frequency, or stool form/appearance. Risk includes genetic and environmental factors, stress/abuse, and acute gastroenteritis. After a structured evaluation, a graded treatment response is undertaken, ranging from diet/lifestyle counseling to pharmacotherapy to psychological therapies.
Neil Hyman, MD, concluded the session with a talk entitled “Disorders of the anorectum,” also stressing that the history is key to the diagnosis, with an emphasis on asking the right questions. Pain may be related to fissures, thrombosed hemorrhoids, abscesses, and proctalgia/levator spasm. New technologies, and pharmacological and surgical approaches were discussed.
This is a summary provided by the moderator of one of the AGA Postgraduate Courses held at DDW 2017. Dr. Cohen is the chief of the division of gastroenterology and hepatology in the Weill department of medicine, New York–Presbyterian Hospital Center, New York.
The final session of the course opened with Uri Ladabaum, MD, entertaining the question “Colon cancer screening and surveillance: who, when, and how?” Dr. Ladabaum pointed out that there is consensus that colorectal cancer screening for average-risk individuals should begin at age 50 with a choice of modalities and that surveillance depends on the findings on each colonoscopy. He reviewed the evidence for screening modalities and for surveillance and offered perspectives on the role of the gastroenterologist/colonoscopist in the quality of colonsocopy. Douglas K. Rex, MD, AGAF followed by asking “Does every big polyp need EMR?” Dr. Rex discussed the available approaches to the large colonic polyp, including endoscopic mucosal resection, endoscopic submucosal dissection, and surgery. He provided evidence for the advantages and expanded use of EMR, with the conclusion that almost every large benign polyp needs EMR.
Jennifer A. Christie, MD, then spoke on “Pelvic floor dysfunction and constipation.” Dr. Christie stressed the importance of a good history and the digital rectal exam in diagnosis of pelvic floor dysfunction. When over-the-counter or prescribed medications are not effective, the work-up should include anorectal manometry, balloon expulsion, and colonic transit testing. Attempts should be made to remove all potential offending agents, such as anticholinergics, narcotics, calcium channel blockers, and beta-blockers. Biofeedback is a safe and effective treatment for pelvic floor dysfunction. Lin Chang, MD, AGAF, continued with a talk on irritable bowel syndrome, which can be considered a combination of disorders, with clusters of symptoms and subgroups. There must be recurrent abdominal pain or discomfort at least 1 day/week for the prior 3 months, associated with 2 or more of the following: a relationship to defecation, change in stool frequency, or stool form/appearance. Risk includes genetic and environmental factors, stress/abuse, and acute gastroenteritis. After a structured evaluation, a graded treatment response is undertaken, ranging from diet/lifestyle counseling to pharmacotherapy to psychological therapies.
Neil Hyman, MD, concluded the session with a talk entitled “Disorders of the anorectum,” also stressing that the history is key to the diagnosis, with an emphasis on asking the right questions. Pain may be related to fissures, thrombosed hemorrhoids, abscesses, and proctalgia/levator spasm. New technologies, and pharmacological and surgical approaches were discussed.
This is a summary provided by the moderator of one of the AGA Postgraduate Courses held at DDW 2017. Dr. Cohen is the chief of the division of gastroenterology and hepatology in the Weill department of medicine, New York–Presbyterian Hospital Center, New York.
The final session of the course opened with Uri Ladabaum, MD, entertaining the question “Colon cancer screening and surveillance: who, when, and how?” Dr. Ladabaum pointed out that there is consensus that colorectal cancer screening for average-risk individuals should begin at age 50 with a choice of modalities and that surveillance depends on the findings on each colonoscopy. He reviewed the evidence for screening modalities and for surveillance and offered perspectives on the role of the gastroenterologist/colonoscopist in the quality of colonsocopy. Douglas K. Rex, MD, AGAF followed by asking “Does every big polyp need EMR?” Dr. Rex discussed the available approaches to the large colonic polyp, including endoscopic mucosal resection, endoscopic submucosal dissection, and surgery. He provided evidence for the advantages and expanded use of EMR, with the conclusion that almost every large benign polyp needs EMR.
Jennifer A. Christie, MD, then spoke on “Pelvic floor dysfunction and constipation.” Dr. Christie stressed the importance of a good history and the digital rectal exam in diagnosis of pelvic floor dysfunction. When over-the-counter or prescribed medications are not effective, the work-up should include anorectal manometry, balloon expulsion, and colonic transit testing. Attempts should be made to remove all potential offending agents, such as anticholinergics, narcotics, calcium channel blockers, and beta-blockers. Biofeedback is a safe and effective treatment for pelvic floor dysfunction. Lin Chang, MD, AGAF, continued with a talk on irritable bowel syndrome, which can be considered a combination of disorders, with clusters of symptoms and subgroups. There must be recurrent abdominal pain or discomfort at least 1 day/week for the prior 3 months, associated with 2 or more of the following: a relationship to defecation, change in stool frequency, or stool form/appearance. Risk includes genetic and environmental factors, stress/abuse, and acute gastroenteritis. After a structured evaluation, a graded treatment response is undertaken, ranging from diet/lifestyle counseling to pharmacotherapy to psychological therapies.
Neil Hyman, MD, concluded the session with a talk entitled “Disorders of the anorectum,” also stressing that the history is key to the diagnosis, with an emphasis on asking the right questions. Pain may be related to fissures, thrombosed hemorrhoids, abscesses, and proctalgia/levator spasm. New technologies, and pharmacological and surgical approaches were discussed.
This is a summary provided by the moderator of one of the AGA Postgraduate Courses held at DDW 2017. Dr. Cohen is the chief of the division of gastroenterology and hepatology in the Weill department of medicine, New York–Presbyterian Hospital Center, New York.
Hospital-acquired anemia
Clinical question: Is hospital acquired anemia associated with increased postdischarge adverse outcomes?
Background: Hospital acquired anemia (HAA) is defined as the development of anemia during the course of a hospitalization when starting with a normal hemoglobin on admission. The incidence of HAA is at least 25% when using the last hemoglobin prior to discharge as the index value. HAA is felt to be potentially preventable and usually iatrogenic due to phlebotomy.
Setting: Six northern Texas hospitals.
Synopsis: There were 11,309 index hospitalizations with a median hematocrit value on admission of 40.6 g/dL. The authors defined HAA as a normal hematocrit value within the first 24 hours of admission and a hematocrit value lower than the WHO sex-specific cut points at the time of discharge: mild HAA (hematocrit greater than 33% and less than 36% in women, greater than 33% and less than 40% in men), moderate HAA (greater than 27% and less than 33%), and severe HAA (less than 27%). Mild HAA occurred in 21.6% of patients, with 10.1% of patients developing moderate HAA, and 1.4% developing severe HAA (85% underwent major procedure, diagnosis of hemorrhage or coagulation/hemorrhagic disorder). Predictors of developing moderate/severe HAA included undergoing a major diagnostic or therapeutic procedure, female sex, elective admission, hospital LOS, BUN to creatinine ratio greater than 20:1, and serum creatinine on admission. Development of severe HAA was associated with a 41% increase in the odds of 30-day readmission and a 39% increase in the odds of the composite outcome (30-day mortality and 30-day readmission).
Bottom line: Severe HAA had significant increased odds of 30-day readmission and mortality, but might not be as preventable as initially thought given the frequency of major procedures and hemorrhage in those that developed severe HAA.
Citation: Makam AN, Nguyen OK, Clark C, Halm EA. Incidence, predictors, and outcomes of hospital-acquired anemia. J Hosp Med. 2017;12(5):317-22.
Dr. Newsom is a hospitalist at Ochsner Health System, New Orleans.
Clinical question: Is hospital acquired anemia associated with increased postdischarge adverse outcomes?
Background: Hospital acquired anemia (HAA) is defined as the development of anemia during the course of a hospitalization when starting with a normal hemoglobin on admission. The incidence of HAA is at least 25% when using the last hemoglobin prior to discharge as the index value. HAA is felt to be potentially preventable and usually iatrogenic due to phlebotomy.
Setting: Six northern Texas hospitals.
Synopsis: There were 11,309 index hospitalizations with a median hematocrit value on admission of 40.6 g/dL. The authors defined HAA as a normal hematocrit value within the first 24 hours of admission and a hematocrit value lower than the WHO sex-specific cut points at the time of discharge: mild HAA (hematocrit greater than 33% and less than 36% in women, greater than 33% and less than 40% in men), moderate HAA (greater than 27% and less than 33%), and severe HAA (less than 27%). Mild HAA occurred in 21.6% of patients, with 10.1% of patients developing moderate HAA, and 1.4% developing severe HAA (85% underwent major procedure, diagnosis of hemorrhage or coagulation/hemorrhagic disorder). Predictors of developing moderate/severe HAA included undergoing a major diagnostic or therapeutic procedure, female sex, elective admission, hospital LOS, BUN to creatinine ratio greater than 20:1, and serum creatinine on admission. Development of severe HAA was associated with a 41% increase in the odds of 30-day readmission and a 39% increase in the odds of the composite outcome (30-day mortality and 30-day readmission).
Bottom line: Severe HAA had significant increased odds of 30-day readmission and mortality, but might not be as preventable as initially thought given the frequency of major procedures and hemorrhage in those that developed severe HAA.
Citation: Makam AN, Nguyen OK, Clark C, Halm EA. Incidence, predictors, and outcomes of hospital-acquired anemia. J Hosp Med. 2017;12(5):317-22.
Dr. Newsom is a hospitalist at Ochsner Health System, New Orleans.
Clinical question: Is hospital acquired anemia associated with increased postdischarge adverse outcomes?
Background: Hospital acquired anemia (HAA) is defined as the development of anemia during the course of a hospitalization when starting with a normal hemoglobin on admission. The incidence of HAA is at least 25% when using the last hemoglobin prior to discharge as the index value. HAA is felt to be potentially preventable and usually iatrogenic due to phlebotomy.
Setting: Six northern Texas hospitals.
Synopsis: There were 11,309 index hospitalizations with a median hematocrit value on admission of 40.6 g/dL. The authors defined HAA as a normal hematocrit value within the first 24 hours of admission and a hematocrit value lower than the WHO sex-specific cut points at the time of discharge: mild HAA (hematocrit greater than 33% and less than 36% in women, greater than 33% and less than 40% in men), moderate HAA (greater than 27% and less than 33%), and severe HAA (less than 27%). Mild HAA occurred in 21.6% of patients, with 10.1% of patients developing moderate HAA, and 1.4% developing severe HAA (85% underwent major procedure, diagnosis of hemorrhage or coagulation/hemorrhagic disorder). Predictors of developing moderate/severe HAA included undergoing a major diagnostic or therapeutic procedure, female sex, elective admission, hospital LOS, BUN to creatinine ratio greater than 20:1, and serum creatinine on admission. Development of severe HAA was associated with a 41% increase in the odds of 30-day readmission and a 39% increase in the odds of the composite outcome (30-day mortality and 30-day readmission).
Bottom line: Severe HAA had significant increased odds of 30-day readmission and mortality, but might not be as preventable as initially thought given the frequency of major procedures and hemorrhage in those that developed severe HAA.
Citation: Makam AN, Nguyen OK, Clark C, Halm EA. Incidence, predictors, and outcomes of hospital-acquired anemia. J Hosp Med. 2017;12(5):317-22.
Dr. Newsom is a hospitalist at Ochsner Health System, New Orleans.
Biotin interference a concern in hormonal assays
Biotin supplementation showed signs of interference with biotinylated assays in a crossover trial.
The proposed benefits of biotin (vitamin B7), including stimulating hair growth and assisting in the treatment of various forms of diabetes, have made it a popular supplement. Supplementation generally leads to artificially high levels of biotin, which was shown to cause inaccurate results in biotinylated assays, according to Danni Li, PhD, of the advanced research and diagnostic laboratory at the University of Minnesota, Minneapolis, and her colleagues.
They analyzed the results of both biotinylated and nonbiotinylated assays of six patients – two women and four men – who ingested 10 mg/day of biotin supplement for 7 days. Two blood samples were obtained in the course of the study: one prior to starting biotin supplementation as a baseline and one a week ofter biotin supplementation had ended. The assays tested the presence of nine hormones and two nonhormones using multiple diagnostic systems to run the assays. In total, 37 immunoassays were conducted on each sample (JAMA. 2017;318[12]:1150-60. doi: 10.1001/jama.2017.13705).
Two immunoassay testing techniques were used in the diagnostic assays. The sandwich technique was used in testing TSH, parathyroid hormone (PTH), prolactin, N-terminal pro-brain natriuretic peptide (NT-proBNP), PSA, and ferritin and competitive technique was used in testing total T4, total T3, free T4, free T3, and 25-OHD. In assays utilizing competitive techniques, false highs were reported in three Roche cobas e602 machines and one Siemens Vista Dimension 1500 machine.
Assays utilizing the sandwich technique experienced false decreases in TSH, PTH, and NT-proBNP when compared with baseline measurements in Roche cobas e602 and OCD Vitros 5600 machines. A predominance of the falsely low results were present in the assays conducted by the OCD Vitros machine, with significant changes from baseline measurements. TSH experienced a 94% decrease of 1.67 mIU/L, PTH experienced a 61% decrease of 25.8 pg/mL, and NT-proBNP falsely decreased by more than 13.9 pg/mL. In Roche cobas e602 assays, TSH levels were falsely low and measurements decreased by 0.72 mIU/L (37%) when compared with baseline measurements.
Biotin did not interfere in all biotinylated assays and was only observed in 9 of the 23 (39%) of the assays conducted. Specifically, 4 of 15 (27%) sandwich immunoassays were falsely decreased while five of eight (63%) competitive binding assays were falsely increased.
“Among the 23 biotinylated assays studied, biotin interference was of greatest clinical significance in the OCD Vitros TSH assay, where falsely decreased TSH concentrations (to less than 0.15 mU/L) could have resulted in misdiagnosis of thyrotoxicosis in otherwise euthyroid individuals,” according to Dr. Li and her associates, “Likewise, falsely decreased OCD Vitros NT-proBNP, to lower than assay detection limits, could possibly result in failure to identify congestive heart failure.”
One investigator received funding and nonfinanical support from Siemens Healthcare Diagnostics, one reported receiving financial support from Abbott Laboratories, and another reported receiving personal fees from Roche and Abbott Laboratories. Dr. Li and the other researchers had no relevant financial disclosures.
Biotin supplementation showed signs of interference with biotinylated assays in a crossover trial.
The proposed benefits of biotin (vitamin B7), including stimulating hair growth and assisting in the treatment of various forms of diabetes, have made it a popular supplement. Supplementation generally leads to artificially high levels of biotin, which was shown to cause inaccurate results in biotinylated assays, according to Danni Li, PhD, of the advanced research and diagnostic laboratory at the University of Minnesota, Minneapolis, and her colleagues.
They analyzed the results of both biotinylated and nonbiotinylated assays of six patients – two women and four men – who ingested 10 mg/day of biotin supplement for 7 days. Two blood samples were obtained in the course of the study: one prior to starting biotin supplementation as a baseline and one a week ofter biotin supplementation had ended. The assays tested the presence of nine hormones and two nonhormones using multiple diagnostic systems to run the assays. In total, 37 immunoassays were conducted on each sample (JAMA. 2017;318[12]:1150-60. doi: 10.1001/jama.2017.13705).
Two immunoassay testing techniques were used in the diagnostic assays. The sandwich technique was used in testing TSH, parathyroid hormone (PTH), prolactin, N-terminal pro-brain natriuretic peptide (NT-proBNP), PSA, and ferritin and competitive technique was used in testing total T4, total T3, free T4, free T3, and 25-OHD. In assays utilizing competitive techniques, false highs were reported in three Roche cobas e602 machines and one Siemens Vista Dimension 1500 machine.
Assays utilizing the sandwich technique experienced false decreases in TSH, PTH, and NT-proBNP when compared with baseline measurements in Roche cobas e602 and OCD Vitros 5600 machines. A predominance of the falsely low results were present in the assays conducted by the OCD Vitros machine, with significant changes from baseline measurements. TSH experienced a 94% decrease of 1.67 mIU/L, PTH experienced a 61% decrease of 25.8 pg/mL, and NT-proBNP falsely decreased by more than 13.9 pg/mL. In Roche cobas e602 assays, TSH levels were falsely low and measurements decreased by 0.72 mIU/L (37%) when compared with baseline measurements.
Biotin did not interfere in all biotinylated assays and was only observed in 9 of the 23 (39%) of the assays conducted. Specifically, 4 of 15 (27%) sandwich immunoassays were falsely decreased while five of eight (63%) competitive binding assays were falsely increased.
“Among the 23 biotinylated assays studied, biotin interference was of greatest clinical significance in the OCD Vitros TSH assay, where falsely decreased TSH concentrations (to less than 0.15 mU/L) could have resulted in misdiagnosis of thyrotoxicosis in otherwise euthyroid individuals,” according to Dr. Li and her associates, “Likewise, falsely decreased OCD Vitros NT-proBNP, to lower than assay detection limits, could possibly result in failure to identify congestive heart failure.”
One investigator received funding and nonfinanical support from Siemens Healthcare Diagnostics, one reported receiving financial support from Abbott Laboratories, and another reported receiving personal fees from Roche and Abbott Laboratories. Dr. Li and the other researchers had no relevant financial disclosures.
Biotin supplementation showed signs of interference with biotinylated assays in a crossover trial.
The proposed benefits of biotin (vitamin B7), including stimulating hair growth and assisting in the treatment of various forms of diabetes, have made it a popular supplement. Supplementation generally leads to artificially high levels of biotin, which was shown to cause inaccurate results in biotinylated assays, according to Danni Li, PhD, of the advanced research and diagnostic laboratory at the University of Minnesota, Minneapolis, and her colleagues.
They analyzed the results of both biotinylated and nonbiotinylated assays of six patients – two women and four men – who ingested 10 mg/day of biotin supplement for 7 days. Two blood samples were obtained in the course of the study: one prior to starting biotin supplementation as a baseline and one a week ofter biotin supplementation had ended. The assays tested the presence of nine hormones and two nonhormones using multiple diagnostic systems to run the assays. In total, 37 immunoassays were conducted on each sample (JAMA. 2017;318[12]:1150-60. doi: 10.1001/jama.2017.13705).
Two immunoassay testing techniques were used in the diagnostic assays. The sandwich technique was used in testing TSH, parathyroid hormone (PTH), prolactin, N-terminal pro-brain natriuretic peptide (NT-proBNP), PSA, and ferritin and competitive technique was used in testing total T4, total T3, free T4, free T3, and 25-OHD. In assays utilizing competitive techniques, false highs were reported in three Roche cobas e602 machines and one Siemens Vista Dimension 1500 machine.
Assays utilizing the sandwich technique experienced false decreases in TSH, PTH, and NT-proBNP when compared with baseline measurements in Roche cobas e602 and OCD Vitros 5600 machines. A predominance of the falsely low results were present in the assays conducted by the OCD Vitros machine, with significant changes from baseline measurements. TSH experienced a 94% decrease of 1.67 mIU/L, PTH experienced a 61% decrease of 25.8 pg/mL, and NT-proBNP falsely decreased by more than 13.9 pg/mL. In Roche cobas e602 assays, TSH levels were falsely low and measurements decreased by 0.72 mIU/L (37%) when compared with baseline measurements.
Biotin did not interfere in all biotinylated assays and was only observed in 9 of the 23 (39%) of the assays conducted. Specifically, 4 of 15 (27%) sandwich immunoassays were falsely decreased while five of eight (63%) competitive binding assays were falsely increased.
“Among the 23 biotinylated assays studied, biotin interference was of greatest clinical significance in the OCD Vitros TSH assay, where falsely decreased TSH concentrations (to less than 0.15 mU/L) could have resulted in misdiagnosis of thyrotoxicosis in otherwise euthyroid individuals,” according to Dr. Li and her associates, “Likewise, falsely decreased OCD Vitros NT-proBNP, to lower than assay detection limits, could possibly result in failure to identify congestive heart failure.”
One investigator received funding and nonfinanical support from Siemens Healthcare Diagnostics, one reported receiving financial support from Abbott Laboratories, and another reported receiving personal fees from Roche and Abbott Laboratories. Dr. Li and the other researchers had no relevant financial disclosures.
FROM JAMA
Key clinical point:
Major finding: 9 of 23 biotinylated (39%) showed signs of interference from biotin ingestion.
Data source: Nonrandomized crossover trial of six participants at an academic medical center.
Disclosures: One investigator received funding and nonfinanical support from Siemens Healthcare Diagnostics, one reported receiving financial support from Abbott Laboratories, and another reported receiving personal fees from Roche and Abbott Laboratories. Dr. Li and the other researchers had no relevant financial disclosures.
It’s a beautiful day to discuss inflammatory bowel disease
Uma Mahadevan, MD, AGAF, and I moderated this session on IBD, and we were fortunate enough to secure four of the best IBD educators in the AGA.
David Rubin, MD, AGAF, opened with “Selecting the correct therapy for your outpatients with IBD: From mesalamine to biologics.” Treatment goals have evolved from symptom control to remission based on measures of inflammation (e.g., serum C-reactive protein, fecal calprotectin, or endoscopy). For ulcerative colitis (UC), high-risk markers include extensive disease, deep ulcers, younger age at diagnosis, elevated biomarkers, and early need for steroids or hospitalization. For Crohn’s disease (CD), these include younger age, extensive involvement, and fistulizing disease. The 5-aminosalicylate drugs remain a backbone in mild to moderate UC. Judicious use of corticosteroids is reasonable, but we need an exit strategy. The thiopurines are decent drugs, but studies have called into question their efficacy as monotherapy, and safety issues persist. Methotrexate is underutilized. The anti–tumor necrosis factor (TNF) biologics are excellent therapies but controversies persist as to whether these drugs require combination therapy or if they can be managed as “optimized monotherapy” with therapeutic drug monitoring (TDM). There are now two infliximab biosimilars available in the U.S.. Vedolizumab is an efficacious gut-selective anti-integrin (for both CD and UC). Ustekinumab, an anti-IL-12/23 antibody, is now available for moderate to severe CD, and has a favorable safety profile.
Fernando Velayos, MD, AGAF, discussed “Surveillance for dysplasia: What is the standard of care in 2017?” General principles for surveillance colonoscopy in IBD include having quiescent disease, since inflammation can reduce ability to detect lesions, and good colonic preparation. The three U.S. society guidelines recommend starting surveillance after 8 years of disease. Patients with concomitant primary schlerosing cholangitis should begin surveillance immediately. Frequency of surveillance ranges every 1-3 years depending on histology. A meta-analysis showed a higher incremental dysplasia yield with chromoendoscopy compared to standard white-light colonoscopy. If visible dysplasia can be endoscopically resected, then continued surveillance rather than colectomy is recommended.
Sunanda Kane, MD, AGAF, discussed “Managing special populations: the transitioning adolescent, the gravid, and the elderly.” The transition from pediatric to adult IBD care is a high-risk time because the patient may be lost to follow-up or not adhere to the medical regimen, resulting in increased risk of flare. Successful transition requires developmental maturity of the patient, a certain style of parental involvement, and care coordination of the medical team. For women with IBD considering pregnancy, active IBD at the time of conception significantly increases the risk of flare. Women with CD who have no history of perianal disease don’t have an increased risk of perianal disease with vaginal delivery. A meta-analysis of the risk of congenital malformations with thiopurines found no significant association. Infliximab levels were likely to rise in the mother during the second and third trimesters (versus no increase with adalimumab), so one could consider TDM to guide dosing. In the PIANO study, anti-TNF therapy in the third trimester was neither associated with adverse pregnancy outcomes nor with infections up to 1 year for children. Patients who develop IBD later in life are more likely to have colonic inflammation. Elderly UC patients are more likely to require surgery, and postop mortality is higher for both CD and UC.
This is a summary provided by the moderator of one of the AGA Postgraduate Courses held at DDW 2017. Dr. Loftus is a professor of medicine, division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn.
Uma Mahadevan, MD, AGAF, and I moderated this session on IBD, and we were fortunate enough to secure four of the best IBD educators in the AGA.
David Rubin, MD, AGAF, opened with “Selecting the correct therapy for your outpatients with IBD: From mesalamine to biologics.” Treatment goals have evolved from symptom control to remission based on measures of inflammation (e.g., serum C-reactive protein, fecal calprotectin, or endoscopy). For ulcerative colitis (UC), high-risk markers include extensive disease, deep ulcers, younger age at diagnosis, elevated biomarkers, and early need for steroids or hospitalization. For Crohn’s disease (CD), these include younger age, extensive involvement, and fistulizing disease. The 5-aminosalicylate drugs remain a backbone in mild to moderate UC. Judicious use of corticosteroids is reasonable, but we need an exit strategy. The thiopurines are decent drugs, but studies have called into question their efficacy as monotherapy, and safety issues persist. Methotrexate is underutilized. The anti–tumor necrosis factor (TNF) biologics are excellent therapies but controversies persist as to whether these drugs require combination therapy or if they can be managed as “optimized monotherapy” with therapeutic drug monitoring (TDM). There are now two infliximab biosimilars available in the U.S.. Vedolizumab is an efficacious gut-selective anti-integrin (for both CD and UC). Ustekinumab, an anti-IL-12/23 antibody, is now available for moderate to severe CD, and has a favorable safety profile.
Fernando Velayos, MD, AGAF, discussed “Surveillance for dysplasia: What is the standard of care in 2017?” General principles for surveillance colonoscopy in IBD include having quiescent disease, since inflammation can reduce ability to detect lesions, and good colonic preparation. The three U.S. society guidelines recommend starting surveillance after 8 years of disease. Patients with concomitant primary schlerosing cholangitis should begin surveillance immediately. Frequency of surveillance ranges every 1-3 years depending on histology. A meta-analysis showed a higher incremental dysplasia yield with chromoendoscopy compared to standard white-light colonoscopy. If visible dysplasia can be endoscopically resected, then continued surveillance rather than colectomy is recommended.
Sunanda Kane, MD, AGAF, discussed “Managing special populations: the transitioning adolescent, the gravid, and the elderly.” The transition from pediatric to adult IBD care is a high-risk time because the patient may be lost to follow-up or not adhere to the medical regimen, resulting in increased risk of flare. Successful transition requires developmental maturity of the patient, a certain style of parental involvement, and care coordination of the medical team. For women with IBD considering pregnancy, active IBD at the time of conception significantly increases the risk of flare. Women with CD who have no history of perianal disease don’t have an increased risk of perianal disease with vaginal delivery. A meta-analysis of the risk of congenital malformations with thiopurines found no significant association. Infliximab levels were likely to rise in the mother during the second and third trimesters (versus no increase with adalimumab), so one could consider TDM to guide dosing. In the PIANO study, anti-TNF therapy in the third trimester was neither associated with adverse pregnancy outcomes nor with infections up to 1 year for children. Patients who develop IBD later in life are more likely to have colonic inflammation. Elderly UC patients are more likely to require surgery, and postop mortality is higher for both CD and UC.
This is a summary provided by the moderator of one of the AGA Postgraduate Courses held at DDW 2017. Dr. Loftus is a professor of medicine, division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn.
Uma Mahadevan, MD, AGAF, and I moderated this session on IBD, and we were fortunate enough to secure four of the best IBD educators in the AGA.
David Rubin, MD, AGAF, opened with “Selecting the correct therapy for your outpatients with IBD: From mesalamine to biologics.” Treatment goals have evolved from symptom control to remission based on measures of inflammation (e.g., serum C-reactive protein, fecal calprotectin, or endoscopy). For ulcerative colitis (UC), high-risk markers include extensive disease, deep ulcers, younger age at diagnosis, elevated biomarkers, and early need for steroids or hospitalization. For Crohn’s disease (CD), these include younger age, extensive involvement, and fistulizing disease. The 5-aminosalicylate drugs remain a backbone in mild to moderate UC. Judicious use of corticosteroids is reasonable, but we need an exit strategy. The thiopurines are decent drugs, but studies have called into question their efficacy as monotherapy, and safety issues persist. Methotrexate is underutilized. The anti–tumor necrosis factor (TNF) biologics are excellent therapies but controversies persist as to whether these drugs require combination therapy or if they can be managed as “optimized monotherapy” with therapeutic drug monitoring (TDM). There are now two infliximab biosimilars available in the U.S.. Vedolizumab is an efficacious gut-selective anti-integrin (for both CD and UC). Ustekinumab, an anti-IL-12/23 antibody, is now available for moderate to severe CD, and has a favorable safety profile.
Fernando Velayos, MD, AGAF, discussed “Surveillance for dysplasia: What is the standard of care in 2017?” General principles for surveillance colonoscopy in IBD include having quiescent disease, since inflammation can reduce ability to detect lesions, and good colonic preparation. The three U.S. society guidelines recommend starting surveillance after 8 years of disease. Patients with concomitant primary schlerosing cholangitis should begin surveillance immediately. Frequency of surveillance ranges every 1-3 years depending on histology. A meta-analysis showed a higher incremental dysplasia yield with chromoendoscopy compared to standard white-light colonoscopy. If visible dysplasia can be endoscopically resected, then continued surveillance rather than colectomy is recommended.
Sunanda Kane, MD, AGAF, discussed “Managing special populations: the transitioning adolescent, the gravid, and the elderly.” The transition from pediatric to adult IBD care is a high-risk time because the patient may be lost to follow-up or not adhere to the medical regimen, resulting in increased risk of flare. Successful transition requires developmental maturity of the patient, a certain style of parental involvement, and care coordination of the medical team. For women with IBD considering pregnancy, active IBD at the time of conception significantly increases the risk of flare. Women with CD who have no history of perianal disease don’t have an increased risk of perianal disease with vaginal delivery. A meta-analysis of the risk of congenital malformations with thiopurines found no significant association. Infliximab levels were likely to rise in the mother during the second and third trimesters (versus no increase with adalimumab), so one could consider TDM to guide dosing. In the PIANO study, anti-TNF therapy in the third trimester was neither associated with adverse pregnancy outcomes nor with infections up to 1 year for children. Patients who develop IBD later in life are more likely to have colonic inflammation. Elderly UC patients are more likely to require surgery, and postop mortality is higher for both CD and UC.
This is a summary provided by the moderator of one of the AGA Postgraduate Courses held at DDW 2017. Dr. Loftus is a professor of medicine, division of gastroenterology and hepatology, Mayo Clinic, Rochester, Minn.
Cultivating competencies for value-based care
It is my privilege this month to assume responsibility for the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology. I am honored to join an impressive board of editors led by Dr Fasiha Kanwal, and anchored by global leaders in the field of gastroenterology and hepatology. This board of editors promises to continue the high level of excellence that has propelled the journal to its preeminent position among clinical journals. I am confident that the practice management section will uphold that tradition and continue to meet the expectation of our readers. I would like to mark this transition by acknowledging the history of the practice management section of Clinical Gastroenterology and Hepatology and outlining a vision for the future.
The section was introduced in 2010 under the leadership of Dr. Joel V. Brill. The section, titled “Practice Management: Opportunities and Challenges,” aimed to help practices navigate the disparate issues facing the field. Some of these issues included use of capnography in endoscopy, the importance of registries for quality reporting, and the burdens of meaningful use on physician practices. Dr Brill introduced this section in a video in May 2010 (https://www.youtube.com/watch?v=8FMsc2Wl5E8). Dr. Brill’s reference to these “interesting and challenging times” in gastroenterology resonates even more loudly today.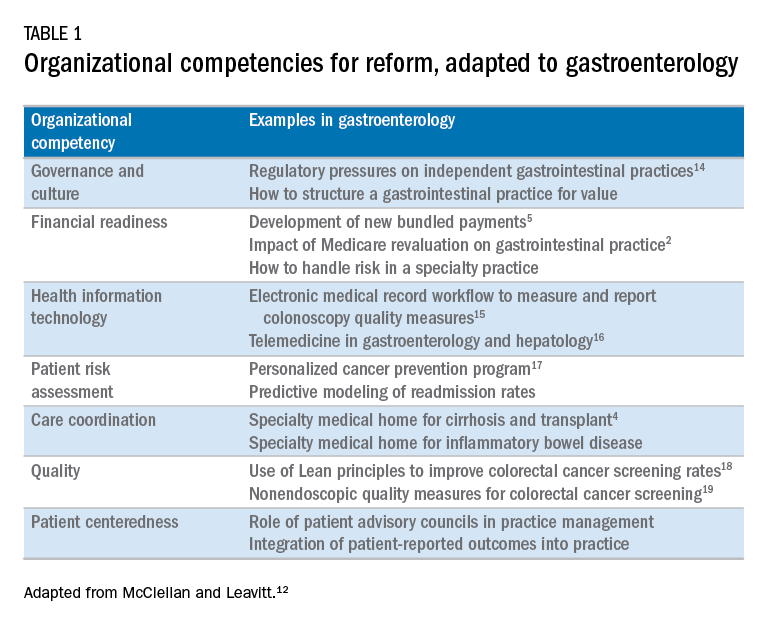
Over the next 5 years, the Road Ahead section will continue and strengthen its focus on the current and emerging issues facing gastroenterology and hepatology practices. I believe that high-value care will continue to be a high priority for patients and payers alike. Early results with payment reform around value have been mixed, in large part because of challenges in health systems and practices developing the competencies required for such reform.12 These competencies include governance and culture, financial readiness, health information technology, patient risk assessment, care coordination, quality, and patient centeredness. I will use this conceptual framework of organizational competencies, and their application in gastroenterology and hepatology, to help curate the Road Ahead section (Table 1). Key themes will include the following:
- • Governance and culture: The structure of health delivery systems, as conceptualized by Donabedian,13 is a key determinant of quality. Structural attributes include regulatory requirements on gastrointestinal practices, such as the rules governing use of anesthesia providers in ambulatory surgical settings; role of allied health professionals in clinical settings; and the impact of financial incentives in driving provider behavior.
- • Financial readiness: Value-based reimbursement, accountable care, medical homes, reference pricing, and physician tiering are some of the new terms in this era of value-based medicine. It is important for practices to assess patient costs longitudinally and manage financial risks. The Road Ahead section will continue to include papers that describe the impact of these reforms on gastroenterology and hepatology practices while providing guidance on implementation of these new models of care. Some examples include papers on the effect of payment policy on specialty practices, the development of a medical home in inflammatory bowel disease, and the physician experience with episode-based payments for colonoscopy.
- • Health information technology: All of the organizational competencies required for reform rely on a robust information technology platform that collects meaningful data and harnesses that data for analytic purposes. These platforms can be enterprise systems deployed by large health delivery systems or smaller, more nimble platforms, created by innovative start-up companies. The Road Ahead will include papers that share best practices in the use of these platforms to provide high-quality and cost-efficient care. In addition, the Road Ahead will continue to explore the use of health information technology to expand the reach of clinicians beyond brick and mortar clinics.
- • Patient risk assessment: Tailoring interventions to high-risk patients is necessary to deploy limited resources in a cost-effective manner. Risk assessment is also needed to more accurately and effectively personalize care for patients with chronic conditions. The Road Ahead will include papers that evaluate risk assessment tools and/or describe real-life implementation of these tools in different contexts.
- • Care coordination: The ability to provide team-based longitudinal care across the continuum of care will be integral to providing high value health care. The Road Ahead will serve as a means to disseminate best practices and innovative methods to care for increasingly complex patients, especially those with chronic diseases, such as cirrhosis and inflammatory bowel disease. For example, papers will explore the implementation of specialty medical homes, patient navigators, community-based care services, and involvement of patients in their own care.
- • Quality improvement: Providing high-value care by definition will require clinicians to accurately measure the quality of care provided to patients and use data to guide process improvement. The Road Ahead will continue to serve as an educational resource for clinicians with papers that discuss challenges and opportunities in quality measurement and improvement. Similarly, this section will present data on novel or impactful quality-improvement initiatives.
- • Patient centeredness: Patient experience measures and patient-reported outcomes are becoming increasingly important as meaningful indicators of quality. These measures are designed to ensure that patient perspectives are incorporated into the governance, design, and delivery of health care. The Road Ahead will serve as a dissemination mechanism for sharing best practices in developing, validating, implementing, and tracking patient-reported outcomes.
I consider Dr. Brill and Dr. Allen as mentors who have taught me tremendously about the business of medicine and the importance of physician leadership. I had the opportunity to coauthor several papers and book chapters with them. More recently, I have had the privilege to work closely with them in my role as the Chair of the American Gastroenterological Association Quality Measures Committee. It is an honor to now join their league as the editor for the Road Ahead section of Clinical Gastroenterology and Hepatology. These are indeed big shoes to fill. The section will retain the “Road Ahead” title in an acknowledgement of the continued importance of the issues outlined by Dr Allen. We will build on this theme to focus on not just the destination, but also the bumps in the road, the unexpected curves, the rest areas, beautiful vistas, and the indulgent road food. Hopefully no accidents along the way!
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Dorn, S.D., Vesy, C.J. Medicare’s revaluation of gastrointestinal endoscopic procedures: implications for academic and community-based practices. Clin Gastroenterol Hepatol. 2017;14:924-8.
3. Dorn, S.D. The road ahead 3.0: changing payments, changing practice. Clin Gastroenterol Hepatol. 2016;14:785-9.
4. Meier, S.K., Shah, N.D., Talwalkar, J.A. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14:492-6.
5. Mehta, S.J. Bundled payment for gastrointestinal hemorrhage. Clin Gastroenterol Hepatol. 2016;14:1681-4.
6. Weizman, A.V., Mosko, J., Bollegala, N., et al. Quality improvement primer series: launching a quality improvement initiative. Clin Gastroenterol Hepatol. 2017;14:1067-71.
7. Bernstein, M., Hou, J.K., Weizman, A.V., et al. Quality improvement primer series: how to sustain a quality improvement effort. Clin Gastroenterol Hepatol. 2017;14:1371-5.
8. Bollegala, N., Patel, K., Mosko, J.D., et al. Quality improvement primer series: the plan-do-study-act cycle and data display. Clin Gastroenterol Hepatol. 2016;14:1230-3.
9. Adams, M.A. Covert recording by patients of encounters with gastroenterology providers: path to empowerment or breach of trust?. Clin Gastroenterol Hepatol. 2017;15:13-6.
10. Oza, V.M., El-Dika, S., and Adams, M.A. Reaching safe harbor: legal implications of clinical practice guidelines. Clin Gastroenterol Hepatol. 2016;14:172-4.
11. Lin, M., Pappas, S.C., Sellin, J., et al. Curbside consultations: the good, the bad, and the ugly. Clin Gastroenterol Hepatol. 2016;14:2-4.
12. McClellan, M.B., Leavitt, M.O. Competencies and tools to shift payments from volume to value. JAMA. 2016; 316: 1655–1656
13. Donabedian, A. Evaluating the quality of medical care. Milbank Q. 1966;44:166-203.
14. Rosenberg, F.B., Kim, L.S., Ketover, S.R. Challenges facing independent integrated gastroenterology. Clin Gastroenterol Hepatol. 2017;15:335-8.
15. Leiman, D.A., Metz, D.C., Ginsberg, G.G., et al. A novel electronic medical record-based workflow to measure and report colonoscopy quality measures. Clin Gastroenterol Hepatol. 2016;14:333-7.
16. Cross, R.K., Kane, S. Integration of telemedicine into clinical gastroenterology and hepatology Practice. Clin Gastroenterol Hepatol. 2017;15:175-81.
17. Llor, X. Building a cancer genetics and prevention program. Clin Gastroenterol Hepatol. 2016;14:1516-20.
18. Patel, K.K., Cummings, S., Sellin, J., et al. Applying Lean design principles to a gastrointestinal endoscopy program for uninsured patients improves health care utilization. Clin Gastroenterol Hepatol. 2015;13:1556-9.
19. Saini, S.D., Adams, M.A., Brill, J.V., et al. Colorectal cancer screening quality measures: beyond colonoscopy. Clin Gastroenterol Hepatol. 2016;14:644-7.
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Durham VA Medical Center, Durham, N.C.; and Duke Clinical Research Institute, Durham, N.C. He reports a consulting relationship with Merck & Co. and he is also a cofounder and equity holder in Higgs Boson, LLC. He is funded by Veterans Affairs Health Services Research and Development Career Development Award (CDA 14-158 ).
It is my privilege this month to assume responsibility for the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology. I am honored to join an impressive board of editors led by Dr Fasiha Kanwal, and anchored by global leaders in the field of gastroenterology and hepatology. This board of editors promises to continue the high level of excellence that has propelled the journal to its preeminent position among clinical journals. I am confident that the practice management section will uphold that tradition and continue to meet the expectation of our readers. I would like to mark this transition by acknowledging the history of the practice management section of Clinical Gastroenterology and Hepatology and outlining a vision for the future.
The section was introduced in 2010 under the leadership of Dr. Joel V. Brill. The section, titled “Practice Management: Opportunities and Challenges,” aimed to help practices navigate the disparate issues facing the field. Some of these issues included use of capnography in endoscopy, the importance of registries for quality reporting, and the burdens of meaningful use on physician practices. Dr Brill introduced this section in a video in May 2010 (https://www.youtube.com/watch?v=8FMsc2Wl5E8). Dr. Brill’s reference to these “interesting and challenging times” in gastroenterology resonates even more loudly today.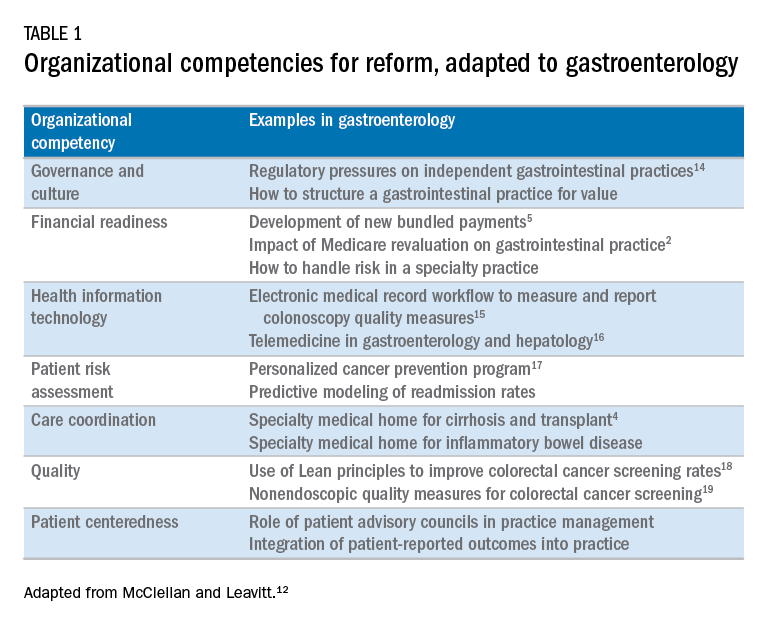
Over the next 5 years, the Road Ahead section will continue and strengthen its focus on the current and emerging issues facing gastroenterology and hepatology practices. I believe that high-value care will continue to be a high priority for patients and payers alike. Early results with payment reform around value have been mixed, in large part because of challenges in health systems and practices developing the competencies required for such reform.12 These competencies include governance and culture, financial readiness, health information technology, patient risk assessment, care coordination, quality, and patient centeredness. I will use this conceptual framework of organizational competencies, and their application in gastroenterology and hepatology, to help curate the Road Ahead section (Table 1). Key themes will include the following:
- • Governance and culture: The structure of health delivery systems, as conceptualized by Donabedian,13 is a key determinant of quality. Structural attributes include regulatory requirements on gastrointestinal practices, such as the rules governing use of anesthesia providers in ambulatory surgical settings; role of allied health professionals in clinical settings; and the impact of financial incentives in driving provider behavior.
- • Financial readiness: Value-based reimbursement, accountable care, medical homes, reference pricing, and physician tiering are some of the new terms in this era of value-based medicine. It is important for practices to assess patient costs longitudinally and manage financial risks. The Road Ahead section will continue to include papers that describe the impact of these reforms on gastroenterology and hepatology practices while providing guidance on implementation of these new models of care. Some examples include papers on the effect of payment policy on specialty practices, the development of a medical home in inflammatory bowel disease, and the physician experience with episode-based payments for colonoscopy.
- • Health information technology: All of the organizational competencies required for reform rely on a robust information technology platform that collects meaningful data and harnesses that data for analytic purposes. These platforms can be enterprise systems deployed by large health delivery systems or smaller, more nimble platforms, created by innovative start-up companies. The Road Ahead will include papers that share best practices in the use of these platforms to provide high-quality and cost-efficient care. In addition, the Road Ahead will continue to explore the use of health information technology to expand the reach of clinicians beyond brick and mortar clinics.
- • Patient risk assessment: Tailoring interventions to high-risk patients is necessary to deploy limited resources in a cost-effective manner. Risk assessment is also needed to more accurately and effectively personalize care for patients with chronic conditions. The Road Ahead will include papers that evaluate risk assessment tools and/or describe real-life implementation of these tools in different contexts.
- • Care coordination: The ability to provide team-based longitudinal care across the continuum of care will be integral to providing high value health care. The Road Ahead will serve as a means to disseminate best practices and innovative methods to care for increasingly complex patients, especially those with chronic diseases, such as cirrhosis and inflammatory bowel disease. For example, papers will explore the implementation of specialty medical homes, patient navigators, community-based care services, and involvement of patients in their own care.
- • Quality improvement: Providing high-value care by definition will require clinicians to accurately measure the quality of care provided to patients and use data to guide process improvement. The Road Ahead will continue to serve as an educational resource for clinicians with papers that discuss challenges and opportunities in quality measurement and improvement. Similarly, this section will present data on novel or impactful quality-improvement initiatives.
- • Patient centeredness: Patient experience measures and patient-reported outcomes are becoming increasingly important as meaningful indicators of quality. These measures are designed to ensure that patient perspectives are incorporated into the governance, design, and delivery of health care. The Road Ahead will serve as a dissemination mechanism for sharing best practices in developing, validating, implementing, and tracking patient-reported outcomes.
I consider Dr. Brill and Dr. Allen as mentors who have taught me tremendously about the business of medicine and the importance of physician leadership. I had the opportunity to coauthor several papers and book chapters with them. More recently, I have had the privilege to work closely with them in my role as the Chair of the American Gastroenterological Association Quality Measures Committee. It is an honor to now join their league as the editor for the Road Ahead section of Clinical Gastroenterology and Hepatology. These are indeed big shoes to fill. The section will retain the “Road Ahead” title in an acknowledgement of the continued importance of the issues outlined by Dr Allen. We will build on this theme to focus on not just the destination, but also the bumps in the road, the unexpected curves, the rest areas, beautiful vistas, and the indulgent road food. Hopefully no accidents along the way!
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Dorn, S.D., Vesy, C.J. Medicare’s revaluation of gastrointestinal endoscopic procedures: implications for academic and community-based practices. Clin Gastroenterol Hepatol. 2017;14:924-8.
3. Dorn, S.D. The road ahead 3.0: changing payments, changing practice. Clin Gastroenterol Hepatol. 2016;14:785-9.
4. Meier, S.K., Shah, N.D., Talwalkar, J.A. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14:492-6.
5. Mehta, S.J. Bundled payment for gastrointestinal hemorrhage. Clin Gastroenterol Hepatol. 2016;14:1681-4.
6. Weizman, A.V., Mosko, J., Bollegala, N., et al. Quality improvement primer series: launching a quality improvement initiative. Clin Gastroenterol Hepatol. 2017;14:1067-71.
7. Bernstein, M., Hou, J.K., Weizman, A.V., et al. Quality improvement primer series: how to sustain a quality improvement effort. Clin Gastroenterol Hepatol. 2017;14:1371-5.
8. Bollegala, N., Patel, K., Mosko, J.D., et al. Quality improvement primer series: the plan-do-study-act cycle and data display. Clin Gastroenterol Hepatol. 2016;14:1230-3.
9. Adams, M.A. Covert recording by patients of encounters with gastroenterology providers: path to empowerment or breach of trust?. Clin Gastroenterol Hepatol. 2017;15:13-6.
10. Oza, V.M., El-Dika, S., and Adams, M.A. Reaching safe harbor: legal implications of clinical practice guidelines. Clin Gastroenterol Hepatol. 2016;14:172-4.
11. Lin, M., Pappas, S.C., Sellin, J., et al. Curbside consultations: the good, the bad, and the ugly. Clin Gastroenterol Hepatol. 2016;14:2-4.
12. McClellan, M.B., Leavitt, M.O. Competencies and tools to shift payments from volume to value. JAMA. 2016; 316: 1655–1656
13. Donabedian, A. Evaluating the quality of medical care. Milbank Q. 1966;44:166-203.
14. Rosenberg, F.B., Kim, L.S., Ketover, S.R. Challenges facing independent integrated gastroenterology. Clin Gastroenterol Hepatol. 2017;15:335-8.
15. Leiman, D.A., Metz, D.C., Ginsberg, G.G., et al. A novel electronic medical record-based workflow to measure and report colonoscopy quality measures. Clin Gastroenterol Hepatol. 2016;14:333-7.
16. Cross, R.K., Kane, S. Integration of telemedicine into clinical gastroenterology and hepatology Practice. Clin Gastroenterol Hepatol. 2017;15:175-81.
17. Llor, X. Building a cancer genetics and prevention program. Clin Gastroenterol Hepatol. 2016;14:1516-20.
18. Patel, K.K., Cummings, S., Sellin, J., et al. Applying Lean design principles to a gastrointestinal endoscopy program for uninsured patients improves health care utilization. Clin Gastroenterol Hepatol. 2015;13:1556-9.
19. Saini, S.D., Adams, M.A., Brill, J.V., et al. Colorectal cancer screening quality measures: beyond colonoscopy. Clin Gastroenterol Hepatol. 2016;14:644-7.
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Durham VA Medical Center, Durham, N.C.; and Duke Clinical Research Institute, Durham, N.C. He reports a consulting relationship with Merck & Co. and he is also a cofounder and equity holder in Higgs Boson, LLC. He is funded by Veterans Affairs Health Services Research and Development Career Development Award (CDA 14-158 ).
It is my privilege this month to assume responsibility for the “Practice Management: The Road Ahead” section of Clinical Gastroenterology and Hepatology. I am honored to join an impressive board of editors led by Dr Fasiha Kanwal, and anchored by global leaders in the field of gastroenterology and hepatology. This board of editors promises to continue the high level of excellence that has propelled the journal to its preeminent position among clinical journals. I am confident that the practice management section will uphold that tradition and continue to meet the expectation of our readers. I would like to mark this transition by acknowledging the history of the practice management section of Clinical Gastroenterology and Hepatology and outlining a vision for the future.
The section was introduced in 2010 under the leadership of Dr. Joel V. Brill. The section, titled “Practice Management: Opportunities and Challenges,” aimed to help practices navigate the disparate issues facing the field. Some of these issues included use of capnography in endoscopy, the importance of registries for quality reporting, and the burdens of meaningful use on physician practices. Dr Brill introduced this section in a video in May 2010 (https://www.youtube.com/watch?v=8FMsc2Wl5E8). Dr. Brill’s reference to these “interesting and challenging times” in gastroenterology resonates even more loudly today.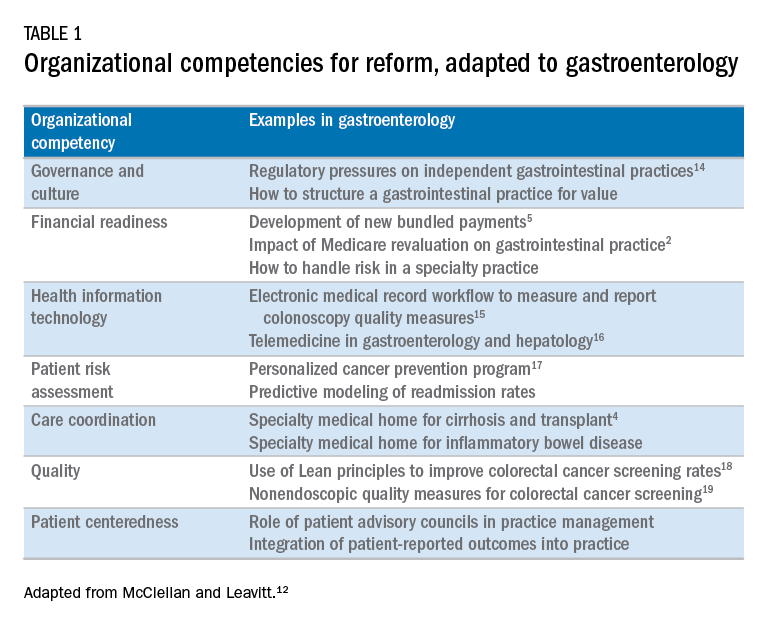
Over the next 5 years, the Road Ahead section will continue and strengthen its focus on the current and emerging issues facing gastroenterology and hepatology practices. I believe that high-value care will continue to be a high priority for patients and payers alike. Early results with payment reform around value have been mixed, in large part because of challenges in health systems and practices developing the competencies required for such reform.12 These competencies include governance and culture, financial readiness, health information technology, patient risk assessment, care coordination, quality, and patient centeredness. I will use this conceptual framework of organizational competencies, and their application in gastroenterology and hepatology, to help curate the Road Ahead section (Table 1). Key themes will include the following:
- • Governance and culture: The structure of health delivery systems, as conceptualized by Donabedian,13 is a key determinant of quality. Structural attributes include regulatory requirements on gastrointestinal practices, such as the rules governing use of anesthesia providers in ambulatory surgical settings; role of allied health professionals in clinical settings; and the impact of financial incentives in driving provider behavior.
- • Financial readiness: Value-based reimbursement, accountable care, medical homes, reference pricing, and physician tiering are some of the new terms in this era of value-based medicine. It is important for practices to assess patient costs longitudinally and manage financial risks. The Road Ahead section will continue to include papers that describe the impact of these reforms on gastroenterology and hepatology practices while providing guidance on implementation of these new models of care. Some examples include papers on the effect of payment policy on specialty practices, the development of a medical home in inflammatory bowel disease, and the physician experience with episode-based payments for colonoscopy.
- • Health information technology: All of the organizational competencies required for reform rely on a robust information technology platform that collects meaningful data and harnesses that data for analytic purposes. These platforms can be enterprise systems deployed by large health delivery systems or smaller, more nimble platforms, created by innovative start-up companies. The Road Ahead will include papers that share best practices in the use of these platforms to provide high-quality and cost-efficient care. In addition, the Road Ahead will continue to explore the use of health information technology to expand the reach of clinicians beyond brick and mortar clinics.
- • Patient risk assessment: Tailoring interventions to high-risk patients is necessary to deploy limited resources in a cost-effective manner. Risk assessment is also needed to more accurately and effectively personalize care for patients with chronic conditions. The Road Ahead will include papers that evaluate risk assessment tools and/or describe real-life implementation of these tools in different contexts.
- • Care coordination: The ability to provide team-based longitudinal care across the continuum of care will be integral to providing high value health care. The Road Ahead will serve as a means to disseminate best practices and innovative methods to care for increasingly complex patients, especially those with chronic diseases, such as cirrhosis and inflammatory bowel disease. For example, papers will explore the implementation of specialty medical homes, patient navigators, community-based care services, and involvement of patients in their own care.
- • Quality improvement: Providing high-value care by definition will require clinicians to accurately measure the quality of care provided to patients and use data to guide process improvement. The Road Ahead will continue to serve as an educational resource for clinicians with papers that discuss challenges and opportunities in quality measurement and improvement. Similarly, this section will present data on novel or impactful quality-improvement initiatives.
- • Patient centeredness: Patient experience measures and patient-reported outcomes are becoming increasingly important as meaningful indicators of quality. These measures are designed to ensure that patient perspectives are incorporated into the governance, design, and delivery of health care. The Road Ahead will serve as a dissemination mechanism for sharing best practices in developing, validating, implementing, and tracking patient-reported outcomes.
I consider Dr. Brill and Dr. Allen as mentors who have taught me tremendously about the business of medicine and the importance of physician leadership. I had the opportunity to coauthor several papers and book chapters with them. More recently, I have had the privilege to work closely with them in my role as the Chair of the American Gastroenterological Association Quality Measures Committee. It is an honor to now join their league as the editor for the Road Ahead section of Clinical Gastroenterology and Hepatology. These are indeed big shoes to fill. The section will retain the “Road Ahead” title in an acknowledgement of the continued importance of the issues outlined by Dr Allen. We will build on this theme to focus on not just the destination, but also the bumps in the road, the unexpected curves, the rest areas, beautiful vistas, and the indulgent road food. Hopefully no accidents along the way!
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Dorn, S.D., Vesy, C.J. Medicare’s revaluation of gastrointestinal endoscopic procedures: implications for academic and community-based practices. Clin Gastroenterol Hepatol. 2017;14:924-8.
3. Dorn, S.D. The road ahead 3.0: changing payments, changing practice. Clin Gastroenterol Hepatol. 2016;14:785-9.
4. Meier, S.K., Shah, N.D., Talwalkar, J.A. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14:492-6.
5. Mehta, S.J. Bundled payment for gastrointestinal hemorrhage. Clin Gastroenterol Hepatol. 2016;14:1681-4.
6. Weizman, A.V., Mosko, J., Bollegala, N., et al. Quality improvement primer series: launching a quality improvement initiative. Clin Gastroenterol Hepatol. 2017;14:1067-71.
7. Bernstein, M., Hou, J.K., Weizman, A.V., et al. Quality improvement primer series: how to sustain a quality improvement effort. Clin Gastroenterol Hepatol. 2017;14:1371-5.
8. Bollegala, N., Patel, K., Mosko, J.D., et al. Quality improvement primer series: the plan-do-study-act cycle and data display. Clin Gastroenterol Hepatol. 2016;14:1230-3.
9. Adams, M.A. Covert recording by patients of encounters with gastroenterology providers: path to empowerment or breach of trust?. Clin Gastroenterol Hepatol. 2017;15:13-6.
10. Oza, V.M., El-Dika, S., and Adams, M.A. Reaching safe harbor: legal implications of clinical practice guidelines. Clin Gastroenterol Hepatol. 2016;14:172-4.
11. Lin, M., Pappas, S.C., Sellin, J., et al. Curbside consultations: the good, the bad, and the ugly. Clin Gastroenterol Hepatol. 2016;14:2-4.
12. McClellan, M.B., Leavitt, M.O. Competencies and tools to shift payments from volume to value. JAMA. 2016; 316: 1655–1656
13. Donabedian, A. Evaluating the quality of medical care. Milbank Q. 1966;44:166-203.
14. Rosenberg, F.B., Kim, L.S., Ketover, S.R. Challenges facing independent integrated gastroenterology. Clin Gastroenterol Hepatol. 2017;15:335-8.
15. Leiman, D.A., Metz, D.C., Ginsberg, G.G., et al. A novel electronic medical record-based workflow to measure and report colonoscopy quality measures. Clin Gastroenterol Hepatol. 2016;14:333-7.
16. Cross, R.K., Kane, S. Integration of telemedicine into clinical gastroenterology and hepatology Practice. Clin Gastroenterol Hepatol. 2017;15:175-81.
17. Llor, X. Building a cancer genetics and prevention program. Clin Gastroenterol Hepatol. 2016;14:1516-20.
18. Patel, K.K., Cummings, S., Sellin, J., et al. Applying Lean design principles to a gastrointestinal endoscopy program for uninsured patients improves health care utilization. Clin Gastroenterol Hepatol. 2015;13:1556-9.
19. Saini, S.D., Adams, M.A., Brill, J.V., et al. Colorectal cancer screening quality measures: beyond colonoscopy. Clin Gastroenterol Hepatol. 2016;14:644-7.
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Durham VA Medical Center, Durham, N.C.; and Duke Clinical Research Institute, Durham, N.C. He reports a consulting relationship with Merck & Co. and he is also a cofounder and equity holder in Higgs Boson, LLC. He is funded by Veterans Affairs Health Services Research and Development Career Development Award (CDA 14-158 ).
Top translator apps can help you communicate with patients who have limited English proficiency
As the population of patients with limited English proficiency increases throughout English-speaking countries, health care providers often need translator services. Medical translator smartphone applications (apps) are useful tools that can provide ad hoc translator services.
According to the US Census Bureau in 2015, more than 60 million individuals — about 19% of Americans — reported speaking a language other than English at home, and more than 25 million said that they speak English “less than very well.”1,2 The top 5 non-English languages spoken at home were Spanish, French, Chinese, Tagalog, and Vietnamese, encompassing 72% of non-English speakers.
In the health care sector, translator services are essential for providing accurate and culturally competent care. Current options for translator services include face-to-face interpreters, phone-based translator services, and translator apps on mobile devices. In settings where face-to-face interpreters or phone-based translator services are not available, translator apps may provide reasonable alternatives. My colleagues, Dr. Amrin Khander and Dr. Sara Farag, and I identified and evaluated medical translator apps that are available from the Apple iTunes and Google Play stores to aid clinicians in using such apps during clinical encounters.3
Three types of translator apps
Preset medical phrase translator apps require the user to search for or find a question or statement in order to facilitate a conversation. With these types of apps, a health care provider can choose fully conjugated sentences, which then can be played or read back to the patient in the chosen translated language. Within this group of apps, Canopy Speak and Universal Doctor Speaker are highly accessible, since both apps are available from the Apple iTunes and Google Play stores and both are free.
Medical dictionary apps require the user to search for a medical term in one language to receive a translation in another language. These apps are less useful, but they can help providers find and define specific terms in a given language.
General language translator apps require the user to enter a term, statement, or question in one language and then provide a translation in another language. Google Translate and Vocre Translate are examples.
The top recommended translator apps are listed in the TABLE alphabetically and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, and important special features).4 I hope the apps described here will help you enhance communication with your patients who have limited English proficiency.
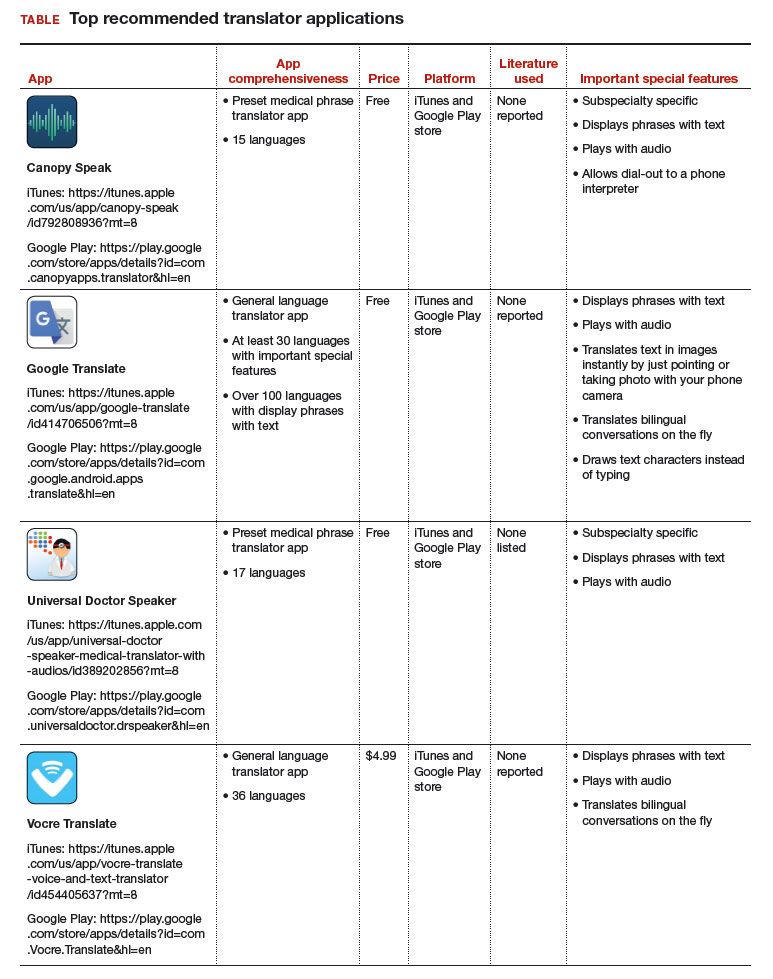
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- United States Census Bureau. Detailed language spoken at home and ability to speak English for the population 5 years and over: 2009–2013. http://www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Published October 2015. Accessed August 31, 2017.
- United States Census Bureau. US population world clock. http://www.census.gov/popclock/?intcmp=home_pop. Accessed August 31, 2017.
- Khander A, Farag S, Chen KT. Identification and rating of medical translator mobile applications using the APPLICATIONS scoring system [abstract 321]. Obstet Gynecol. 2017;129(5 suppl):101S. doi:10.1097/01.AOG.0000514971.96123.20
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125(6):1478–1483.
As the population of patients with limited English proficiency increases throughout English-speaking countries, health care providers often need translator services. Medical translator smartphone applications (apps) are useful tools that can provide ad hoc translator services.
According to the US Census Bureau in 2015, more than 60 million individuals — about 19% of Americans — reported speaking a language other than English at home, and more than 25 million said that they speak English “less than very well.”1,2 The top 5 non-English languages spoken at home were Spanish, French, Chinese, Tagalog, and Vietnamese, encompassing 72% of non-English speakers.
In the health care sector, translator services are essential for providing accurate and culturally competent care. Current options for translator services include face-to-face interpreters, phone-based translator services, and translator apps on mobile devices. In settings where face-to-face interpreters or phone-based translator services are not available, translator apps may provide reasonable alternatives. My colleagues, Dr. Amrin Khander and Dr. Sara Farag, and I identified and evaluated medical translator apps that are available from the Apple iTunes and Google Play stores to aid clinicians in using such apps during clinical encounters.3
Three types of translator apps
Preset medical phrase translator apps require the user to search for or find a question or statement in order to facilitate a conversation. With these types of apps, a health care provider can choose fully conjugated sentences, which then can be played or read back to the patient in the chosen translated language. Within this group of apps, Canopy Speak and Universal Doctor Speaker are highly accessible, since both apps are available from the Apple iTunes and Google Play stores and both are free.
Medical dictionary apps require the user to search for a medical term in one language to receive a translation in another language. These apps are less useful, but they can help providers find and define specific terms in a given language.
General language translator apps require the user to enter a term, statement, or question in one language and then provide a translation in another language. Google Translate and Vocre Translate are examples.
The top recommended translator apps are listed in the TABLE alphabetically and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, and important special features).4 I hope the apps described here will help you enhance communication with your patients who have limited English proficiency.
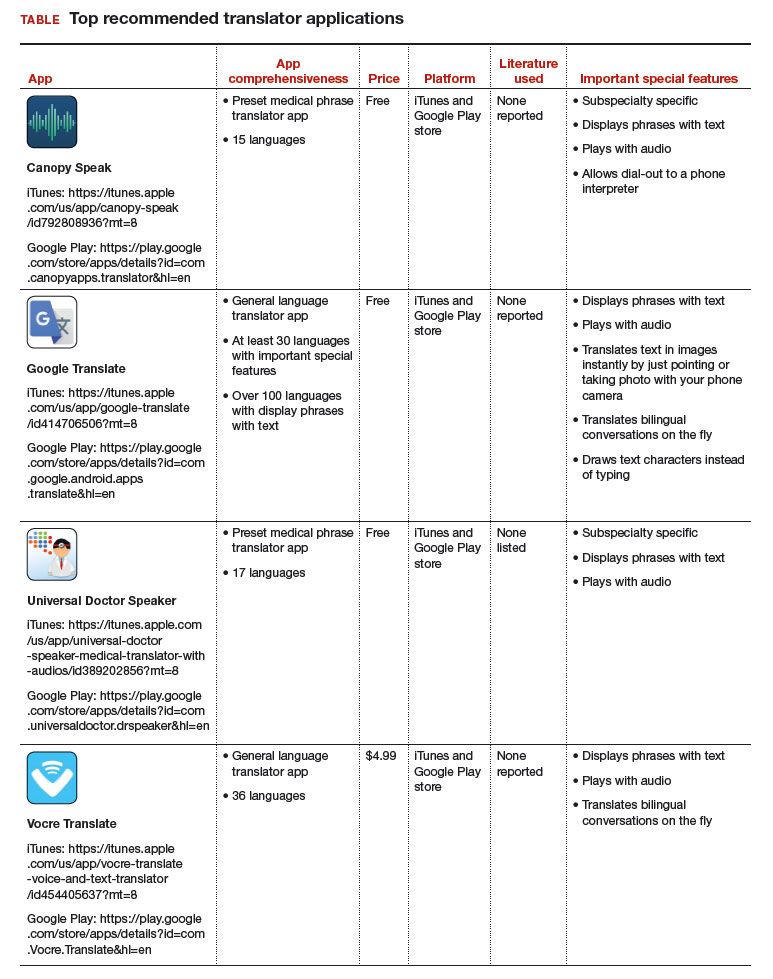
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
As the population of patients with limited English proficiency increases throughout English-speaking countries, health care providers often need translator services. Medical translator smartphone applications (apps) are useful tools that can provide ad hoc translator services.
According to the US Census Bureau in 2015, more than 60 million individuals — about 19% of Americans — reported speaking a language other than English at home, and more than 25 million said that they speak English “less than very well.”1,2 The top 5 non-English languages spoken at home were Spanish, French, Chinese, Tagalog, and Vietnamese, encompassing 72% of non-English speakers.
In the health care sector, translator services are essential for providing accurate and culturally competent care. Current options for translator services include face-to-face interpreters, phone-based translator services, and translator apps on mobile devices. In settings where face-to-face interpreters or phone-based translator services are not available, translator apps may provide reasonable alternatives. My colleagues, Dr. Amrin Khander and Dr. Sara Farag, and I identified and evaluated medical translator apps that are available from the Apple iTunes and Google Play stores to aid clinicians in using such apps during clinical encounters.3
Three types of translator apps
Preset medical phrase translator apps require the user to search for or find a question or statement in order to facilitate a conversation. With these types of apps, a health care provider can choose fully conjugated sentences, which then can be played or read back to the patient in the chosen translated language. Within this group of apps, Canopy Speak and Universal Doctor Speaker are highly accessible, since both apps are available from the Apple iTunes and Google Play stores and both are free.
Medical dictionary apps require the user to search for a medical term in one language to receive a translation in another language. These apps are less useful, but they can help providers find and define specific terms in a given language.
General language translator apps require the user to enter a term, statement, or question in one language and then provide a translation in another language. Google Translate and Vocre Translate are examples.
The top recommended translator apps are listed in the TABLE alphabetically and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, and important special features).4 I hope the apps described here will help you enhance communication with your patients who have limited English proficiency.
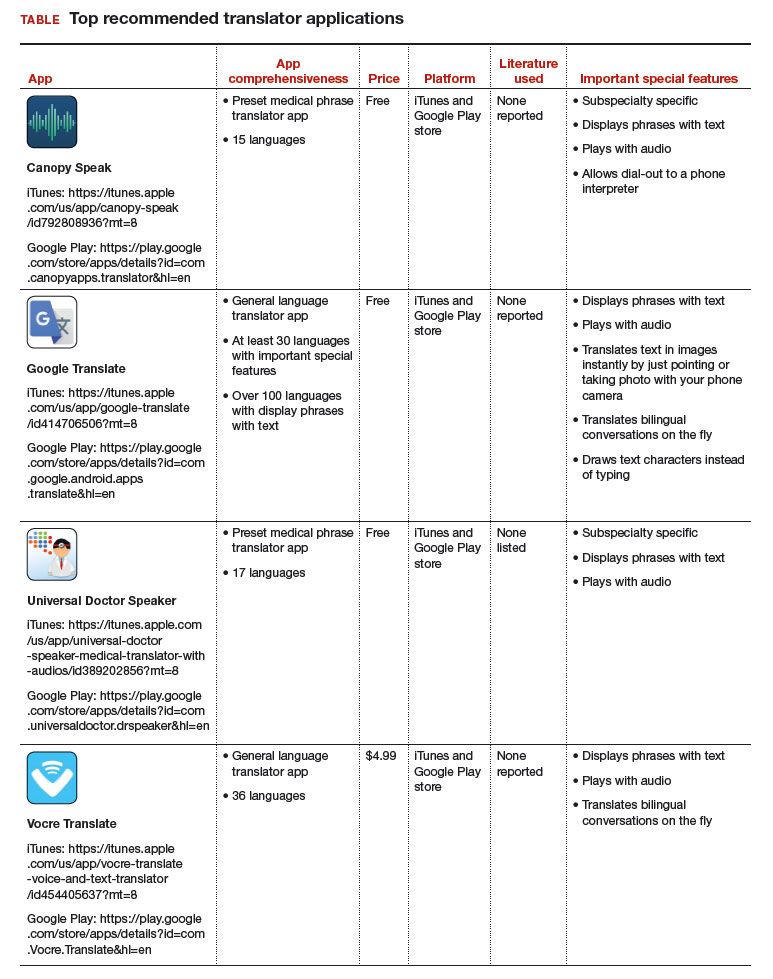
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- United States Census Bureau. Detailed language spoken at home and ability to speak English for the population 5 years and over: 2009–2013. http://www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Published October 2015. Accessed August 31, 2017.
- United States Census Bureau. US population world clock. http://www.census.gov/popclock/?intcmp=home_pop. Accessed August 31, 2017.
- Khander A, Farag S, Chen KT. Identification and rating of medical translator mobile applications using the APPLICATIONS scoring system [abstract 321]. Obstet Gynecol. 2017;129(5 suppl):101S. doi:10.1097/01.AOG.0000514971.96123.20
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125(6):1478–1483.
- United States Census Bureau. Detailed language spoken at home and ability to speak English for the population 5 years and over: 2009–2013. http://www.census.gov/data/tables/2013/demo/2009-2013-lang-tables.html. Published October 2015. Accessed August 31, 2017.
- United States Census Bureau. US population world clock. http://www.census.gov/popclock/?intcmp=home_pop. Accessed August 31, 2017.
- Khander A, Farag S, Chen KT. Identification and rating of medical translator mobile applications using the APPLICATIONS scoring system [abstract 321]. Obstet Gynecol. 2017;129(5 suppl):101S. doi:10.1097/01.AOG.0000514971.96123.20
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125(6):1478–1483.
No benefit seen for routine low-dose oxygen after stroke
Routine use of low-dose oxygen supplementation in the first days after stroke doesn’t improve overall survival or reduce disability, according to a large new study.
The poststroke death and disability odds ratio was 0.97 for those receiving one of two continuous low-dose oxygen protocols, compared with the control group (95% confidence interval, 0.89-1.05; P = .47).
Participants, who were not hypoxic at enrollment, were randomized 1:1:1 to receive continuous oxygen supplementation for the first 72 hours after stroke, to receive supplementation only at night, or to receive oxygen when indicated by usual care protocols. The average participant age was 72 years and 55% were men in all study arms, and all stroke severity levels were included in the study.
Patients in the two intervention arms received 2 L of oxygen by nasal cannula when their baseline oxygen saturation was greater than 93%, and 3 L when oxygen saturation at baseline was 93% or less. Participation in the study did not preclude more intensive respiratory support when clinically indicated.
Nocturnal supplementation was included as a study arm for two reasons: Poststroke hypoxia is more common at night, and night-only supplementation would avoid any interference with early rehabilitation caused by cumbersome oxygen apparatus and tubing.
Not only was no benefit seen for patients in the pooled intervention arm cohorts, but no benefit was seen for night-time versus continuous oxygen as well. The odds ratio for a better outcome was 1.03 when comparing those receiving continuous oxygen to those who only received nocturnal supplementation (95% CI, 0.93-1.13; P = .61).
First author Christine Roffe, MD, and her collaborators in the Stroke Oxygen Study Collaborative Group also performed subgroup analyses and did not see benefit of oxygen supplementation for older or younger patients, or for patients with chronic obstructive pulmonary disease, heart failure, or more severe strokes.
“Supplemental oxygen could improve outcomes by preventing hypoxia and secondary brain damage but could also have adverse effects,” according to Dr. Roffe, consultant at Keele (England) University and her collaborators.
A much smaller SOS pilot study, they said, had shown improved early neurologic recovery for patients who received supplemental oxygen after stroke, but the pilot also “suggested that oxygen might adversely affect outcome in patients with mild strokes, possibly through formation of toxic free radicals,” wrote the investigators.
These were effects not seen in the larger SO2S study, which was designed to have statistical power to detect even small differences and to do detailed subgroup analysis. For patients like those included in the study, “These findings do not support low-dose oxygen in this setting,” wrote Dr. Roffe and her collaborators.
Dr. Roffe reported receiving compensation from Air Liquide. The study was funded by the United Kingdom’s National Institute for Health Research.
[email protected]
On Twitter @karioakes
Routine use of low-dose oxygen supplementation in the first days after stroke doesn’t improve overall survival or reduce disability, according to a large new study.
The poststroke death and disability odds ratio was 0.97 for those receiving one of two continuous low-dose oxygen protocols, compared with the control group (95% confidence interval, 0.89-1.05; P = .47).
Participants, who were not hypoxic at enrollment, were randomized 1:1:1 to receive continuous oxygen supplementation for the first 72 hours after stroke, to receive supplementation only at night, or to receive oxygen when indicated by usual care protocols. The average participant age was 72 years and 55% were men in all study arms, and all stroke severity levels were included in the study.
Patients in the two intervention arms received 2 L of oxygen by nasal cannula when their baseline oxygen saturation was greater than 93%, and 3 L when oxygen saturation at baseline was 93% or less. Participation in the study did not preclude more intensive respiratory support when clinically indicated.
Nocturnal supplementation was included as a study arm for two reasons: Poststroke hypoxia is more common at night, and night-only supplementation would avoid any interference with early rehabilitation caused by cumbersome oxygen apparatus and tubing.
Not only was no benefit seen for patients in the pooled intervention arm cohorts, but no benefit was seen for night-time versus continuous oxygen as well. The odds ratio for a better outcome was 1.03 when comparing those receiving continuous oxygen to those who only received nocturnal supplementation (95% CI, 0.93-1.13; P = .61).
First author Christine Roffe, MD, and her collaborators in the Stroke Oxygen Study Collaborative Group also performed subgroup analyses and did not see benefit of oxygen supplementation for older or younger patients, or for patients with chronic obstructive pulmonary disease, heart failure, or more severe strokes.
“Supplemental oxygen could improve outcomes by preventing hypoxia and secondary brain damage but could also have adverse effects,” according to Dr. Roffe, consultant at Keele (England) University and her collaborators.
A much smaller SOS pilot study, they said, had shown improved early neurologic recovery for patients who received supplemental oxygen after stroke, but the pilot also “suggested that oxygen might adversely affect outcome in patients with mild strokes, possibly through formation of toxic free radicals,” wrote the investigators.
These were effects not seen in the larger SO2S study, which was designed to have statistical power to detect even small differences and to do detailed subgroup analysis. For patients like those included in the study, “These findings do not support low-dose oxygen in this setting,” wrote Dr. Roffe and her collaborators.
Dr. Roffe reported receiving compensation from Air Liquide. The study was funded by the United Kingdom’s National Institute for Health Research.
[email protected]
On Twitter @karioakes
Routine use of low-dose oxygen supplementation in the first days after stroke doesn’t improve overall survival or reduce disability, according to a large new study.
The poststroke death and disability odds ratio was 0.97 for those receiving one of two continuous low-dose oxygen protocols, compared with the control group (95% confidence interval, 0.89-1.05; P = .47).
Participants, who were not hypoxic at enrollment, were randomized 1:1:1 to receive continuous oxygen supplementation for the first 72 hours after stroke, to receive supplementation only at night, or to receive oxygen when indicated by usual care protocols. The average participant age was 72 years and 55% were men in all study arms, and all stroke severity levels were included in the study.
Patients in the two intervention arms received 2 L of oxygen by nasal cannula when their baseline oxygen saturation was greater than 93%, and 3 L when oxygen saturation at baseline was 93% or less. Participation in the study did not preclude more intensive respiratory support when clinically indicated.
Nocturnal supplementation was included as a study arm for two reasons: Poststroke hypoxia is more common at night, and night-only supplementation would avoid any interference with early rehabilitation caused by cumbersome oxygen apparatus and tubing.
Not only was no benefit seen for patients in the pooled intervention arm cohorts, but no benefit was seen for night-time versus continuous oxygen as well. The odds ratio for a better outcome was 1.03 when comparing those receiving continuous oxygen to those who only received nocturnal supplementation (95% CI, 0.93-1.13; P = .61).
First author Christine Roffe, MD, and her collaborators in the Stroke Oxygen Study Collaborative Group also performed subgroup analyses and did not see benefit of oxygen supplementation for older or younger patients, or for patients with chronic obstructive pulmonary disease, heart failure, or more severe strokes.
“Supplemental oxygen could improve outcomes by preventing hypoxia and secondary brain damage but could also have adverse effects,” according to Dr. Roffe, consultant at Keele (England) University and her collaborators.
A much smaller SOS pilot study, they said, had shown improved early neurologic recovery for patients who received supplemental oxygen after stroke, but the pilot also “suggested that oxygen might adversely affect outcome in patients with mild strokes, possibly through formation of toxic free radicals,” wrote the investigators.
These were effects not seen in the larger SO2S study, which was designed to have statistical power to detect even small differences and to do detailed subgroup analysis. For patients like those included in the study, “These findings do not support low-dose oxygen in this setting,” wrote Dr. Roffe and her collaborators.
Dr. Roffe reported receiving compensation from Air Liquide. The study was funded by the United Kingdom’s National Institute for Health Research.
[email protected]
On Twitter @karioakes
FROM JAMA
Key clinical point:
Major finding: The poststroke death and disability odds ratio was 0.97 for those receiving continuous low-dose oxygen, compared with controls.
Data source: Single-blind, multisite, randomized, controlled trial of 8,003 patients admitted with acute stroke.
Disclosures: Dr. Roffe reported receiving compensation from Air Liquide. The study was funded by the United Kingdom’s National Institute for Health Research.
Sen. Collins deals likely fatal blow to GOP’s health bill
Sen. Susan Collins (R-Maine) became the third GOP senator to confirm a no vote on the latest Republican attempt to repeal and replace the Affordable Care Act (ACA), a move that likely seals the bill’s fate.
The bill has the support of President Trump and many GOP leaders but has been roundly criticized by medical groups for insuring fewer Americans, failing to provide adequate protections for people with preexisting conditions, and barring Planned Parenthood from Medicaid participation.
“Sweeping reforms to our health care system and to Medicaid can’t be done well in a compressed time frame, especially when the actual bill is a moving target,” Sen. Collins said in a Sept. 25 statement announcing her opposition to a bill sponsored by Sen. Lindsey Graham (R-S.C.), Sen. Bill Cassidy (R-La.), Sen. Dean Heller (R-Nev.), and Sen. Ron Johnson (R-Wis.).
Since its introduction in mid September, the bill has undergone at least four published revisions, including providing additional funding to Maine and Alaska in an effort to flip Sen. Collins and Sen. Lisa Murkowski (R-Alaska) to the yes column. Both were no votes that helped kill a previous ACA repeal and replace effort.
“The fact is, Maine still loses money under whichever version of the Graham-Cassidy bill we consider because the bill uses what could be described as a ‘give with one hand, take with the other’ distribution model” to maintain the budget neutrality of the Medicaid block grants sent to states, Sen. Collins said. “Huge Medicaid cuts down the road more than offset any short-term influx of money.”
Sen. Collins’ opposition came on the heels of a damaging analysis from the Congressional Budget Office (CBO). The preliminary analysis looked at an earlier version of the bill and found that the number of people with comprehensive health insurance would be reduced by millions and the impact would be particularly large starting in 2020, when the bill would make changes to Medicaid funding and the nongroup insurance market.
Since Senate Republicans are using the budget reconciliation process to pass this legislation, they only need 50 votes to pass the legislation, with Vice President Mike Pence providing the tie-breaking vote. But with a slim 52-seat majority, there was little margin for error. Sen. John McCain (R-Ariz.) had already announced his opposition to the Graham-Cassidy bill on Sept. 22, primarily on process grounds.
“We should not be content to pass health care legislation on a party-line basis, as Democrats did when they rammed Obamacare through Congress in 2009. If we do, our success could be as short-lived as theirs, when the political winds shift, as they regularly do,” Sen. McCain said in a statement. “The issue is too important, and too many lives are at risk, for us to leave the American people guessing from one election to the next whether and how they will acquire health insurance. A bill of this impact requires a bipartisan approach.”
He praised the work of Senate Health, Education, Labor & Pensions Committee Chairman Lamar Alexander (R-Tenn.) and Ranking Member Patty Murray (D-Wash.), who have been working together on a small, focused package aimed at stabilizing the individual insurance market.
“Senators Alexander and Murray have been negotiating in good faith to fix some of the problems with Obamacare,” Sen. McCain said. “But I fear that the prospect of one last attempt at a strictly Republican bill has left the impression that their efforts cannot succeed. I hope they will resume their work should this last attempt at a partisan solution fail.”
Sen. Rand Paul (R-Ky.) also came out publicly against the Graham-Cassidy bill, though his opposition stems from it not going far enough in repealing elements of the ACA.
During a Sept. 25 Senate Finance Committee hearing on the Graham-Cassidy bill, Teresa Miller, acting secretary of the Pennsylvania Department of Human Services, testified that the real problem – the cost of health care – is getting pushed aside as everyone focuses on the coverage issue.
“This whole debate, for the last several years, has been about coverage and we haven’t been talking about the cost of health care,” Ms. Miller told the committee. “At the end of the day, insurance is a reflection of the cost of health care. So if we don’t have a debate in this county and discussion about how we get at the underlying cost of care, we have a major problem. That’s really the debate we should be having.”
Senate Majority Leader Mitch McConnell (R-Ky.) has not signaled whether he would still bring Graham-Cassidy to a vote, given that it appears not to have the votes needed for passage. If he chooses to move forward with the bill, the vote would need to happen before the end of the day on Sept. 30 to use the budget reconciliation process and gain passage with a simple majority.
Sen. Susan Collins (R-Maine) became the third GOP senator to confirm a no vote on the latest Republican attempt to repeal and replace the Affordable Care Act (ACA), a move that likely seals the bill’s fate.
The bill has the support of President Trump and many GOP leaders but has been roundly criticized by medical groups for insuring fewer Americans, failing to provide adequate protections for people with preexisting conditions, and barring Planned Parenthood from Medicaid participation.
“Sweeping reforms to our health care system and to Medicaid can’t be done well in a compressed time frame, especially when the actual bill is a moving target,” Sen. Collins said in a Sept. 25 statement announcing her opposition to a bill sponsored by Sen. Lindsey Graham (R-S.C.), Sen. Bill Cassidy (R-La.), Sen. Dean Heller (R-Nev.), and Sen. Ron Johnson (R-Wis.).
Since its introduction in mid September, the bill has undergone at least four published revisions, including providing additional funding to Maine and Alaska in an effort to flip Sen. Collins and Sen. Lisa Murkowski (R-Alaska) to the yes column. Both were no votes that helped kill a previous ACA repeal and replace effort.
“The fact is, Maine still loses money under whichever version of the Graham-Cassidy bill we consider because the bill uses what could be described as a ‘give with one hand, take with the other’ distribution model” to maintain the budget neutrality of the Medicaid block grants sent to states, Sen. Collins said. “Huge Medicaid cuts down the road more than offset any short-term influx of money.”
Sen. Collins’ opposition came on the heels of a damaging analysis from the Congressional Budget Office (CBO). The preliminary analysis looked at an earlier version of the bill and found that the number of people with comprehensive health insurance would be reduced by millions and the impact would be particularly large starting in 2020, when the bill would make changes to Medicaid funding and the nongroup insurance market.
Since Senate Republicans are using the budget reconciliation process to pass this legislation, they only need 50 votes to pass the legislation, with Vice President Mike Pence providing the tie-breaking vote. But with a slim 52-seat majority, there was little margin for error. Sen. John McCain (R-Ariz.) had already announced his opposition to the Graham-Cassidy bill on Sept. 22, primarily on process grounds.
“We should not be content to pass health care legislation on a party-line basis, as Democrats did when they rammed Obamacare through Congress in 2009. If we do, our success could be as short-lived as theirs, when the political winds shift, as they regularly do,” Sen. McCain said in a statement. “The issue is too important, and too many lives are at risk, for us to leave the American people guessing from one election to the next whether and how they will acquire health insurance. A bill of this impact requires a bipartisan approach.”
He praised the work of Senate Health, Education, Labor & Pensions Committee Chairman Lamar Alexander (R-Tenn.) and Ranking Member Patty Murray (D-Wash.), who have been working together on a small, focused package aimed at stabilizing the individual insurance market.
“Senators Alexander and Murray have been negotiating in good faith to fix some of the problems with Obamacare,” Sen. McCain said. “But I fear that the prospect of one last attempt at a strictly Republican bill has left the impression that their efforts cannot succeed. I hope they will resume their work should this last attempt at a partisan solution fail.”
Sen. Rand Paul (R-Ky.) also came out publicly against the Graham-Cassidy bill, though his opposition stems from it not going far enough in repealing elements of the ACA.
During a Sept. 25 Senate Finance Committee hearing on the Graham-Cassidy bill, Teresa Miller, acting secretary of the Pennsylvania Department of Human Services, testified that the real problem – the cost of health care – is getting pushed aside as everyone focuses on the coverage issue.
“This whole debate, for the last several years, has been about coverage and we haven’t been talking about the cost of health care,” Ms. Miller told the committee. “At the end of the day, insurance is a reflection of the cost of health care. So if we don’t have a debate in this county and discussion about how we get at the underlying cost of care, we have a major problem. That’s really the debate we should be having.”
Senate Majority Leader Mitch McConnell (R-Ky.) has not signaled whether he would still bring Graham-Cassidy to a vote, given that it appears not to have the votes needed for passage. If he chooses to move forward with the bill, the vote would need to happen before the end of the day on Sept. 30 to use the budget reconciliation process and gain passage with a simple majority.
Sen. Susan Collins (R-Maine) became the third GOP senator to confirm a no vote on the latest Republican attempt to repeal and replace the Affordable Care Act (ACA), a move that likely seals the bill’s fate.
The bill has the support of President Trump and many GOP leaders but has been roundly criticized by medical groups for insuring fewer Americans, failing to provide adequate protections for people with preexisting conditions, and barring Planned Parenthood from Medicaid participation.
“Sweeping reforms to our health care system and to Medicaid can’t be done well in a compressed time frame, especially when the actual bill is a moving target,” Sen. Collins said in a Sept. 25 statement announcing her opposition to a bill sponsored by Sen. Lindsey Graham (R-S.C.), Sen. Bill Cassidy (R-La.), Sen. Dean Heller (R-Nev.), and Sen. Ron Johnson (R-Wis.).
Since its introduction in mid September, the bill has undergone at least four published revisions, including providing additional funding to Maine and Alaska in an effort to flip Sen. Collins and Sen. Lisa Murkowski (R-Alaska) to the yes column. Both were no votes that helped kill a previous ACA repeal and replace effort.
“The fact is, Maine still loses money under whichever version of the Graham-Cassidy bill we consider because the bill uses what could be described as a ‘give with one hand, take with the other’ distribution model” to maintain the budget neutrality of the Medicaid block grants sent to states, Sen. Collins said. “Huge Medicaid cuts down the road more than offset any short-term influx of money.”
Sen. Collins’ opposition came on the heels of a damaging analysis from the Congressional Budget Office (CBO). The preliminary analysis looked at an earlier version of the bill and found that the number of people with comprehensive health insurance would be reduced by millions and the impact would be particularly large starting in 2020, when the bill would make changes to Medicaid funding and the nongroup insurance market.
Since Senate Republicans are using the budget reconciliation process to pass this legislation, they only need 50 votes to pass the legislation, with Vice President Mike Pence providing the tie-breaking vote. But with a slim 52-seat majority, there was little margin for error. Sen. John McCain (R-Ariz.) had already announced his opposition to the Graham-Cassidy bill on Sept. 22, primarily on process grounds.
“We should not be content to pass health care legislation on a party-line basis, as Democrats did when they rammed Obamacare through Congress in 2009. If we do, our success could be as short-lived as theirs, when the political winds shift, as they regularly do,” Sen. McCain said in a statement. “The issue is too important, and too many lives are at risk, for us to leave the American people guessing from one election to the next whether and how they will acquire health insurance. A bill of this impact requires a bipartisan approach.”
He praised the work of Senate Health, Education, Labor & Pensions Committee Chairman Lamar Alexander (R-Tenn.) and Ranking Member Patty Murray (D-Wash.), who have been working together on a small, focused package aimed at stabilizing the individual insurance market.
“Senators Alexander and Murray have been negotiating in good faith to fix some of the problems with Obamacare,” Sen. McCain said. “But I fear that the prospect of one last attempt at a strictly Republican bill has left the impression that their efforts cannot succeed. I hope they will resume their work should this last attempt at a partisan solution fail.”
Sen. Rand Paul (R-Ky.) also came out publicly against the Graham-Cassidy bill, though his opposition stems from it not going far enough in repealing elements of the ACA.
During a Sept. 25 Senate Finance Committee hearing on the Graham-Cassidy bill, Teresa Miller, acting secretary of the Pennsylvania Department of Human Services, testified that the real problem – the cost of health care – is getting pushed aside as everyone focuses on the coverage issue.
“This whole debate, for the last several years, has been about coverage and we haven’t been talking about the cost of health care,” Ms. Miller told the committee. “At the end of the day, insurance is a reflection of the cost of health care. So if we don’t have a debate in this county and discussion about how we get at the underlying cost of care, we have a major problem. That’s really the debate we should be having.”
Senate Majority Leader Mitch McConnell (R-Ky.) has not signaled whether he would still bring Graham-Cassidy to a vote, given that it appears not to have the votes needed for passage. If he chooses to move forward with the bill, the vote would need to happen before the end of the day on Sept. 30 to use the budget reconciliation process and gain passage with a simple majority.
Breast density and optimal screening for breast cancer
MY STORY: Prologue
My aunt received a breast cancer diagnosis at age 40, and she died at age 60, in 1970. Then, in 1975, my mother’s breast cancer was found at age 55, but only after she was examined for nipple retraction; on mammography, the cancer had been obscured by dense breast tissue. Mom had 2 metastatic nodes but participated in the earliest clinical trials of chemotherapy and lived free of breast cancer for another 41 years. Naturally I thought that, were I to develop this disease, I would want it found earlier. Ironically, it was, but only because I had spent my career trying to understand the optimal screening approaches for women with dense breasts—women like me.
Cancers are masked on mammography in dense breasts
For women, screening mammography is an important step in reducing the risk of dying from breast cancer. The greatest benefits are realized by those who start annual screening at age 40, or 45 at the latest.1 As it takes 9 to 10 years to see a benefit from breast cancer screening at the population level, it is not logical to continue this testing when life expectancy is less than 10 years, as is the case with women age 85 or older, even those in the healthiest quartile.2–4 However, despite recent advances, the development of 3D mammography (tomosynthesis) (FIGURE 1) in particular, cancers can still be masked by dense breast tissue. Both 2D and 3D mammograms are x-rays; both dense tissue and cancers absorb x-rays and appear white.
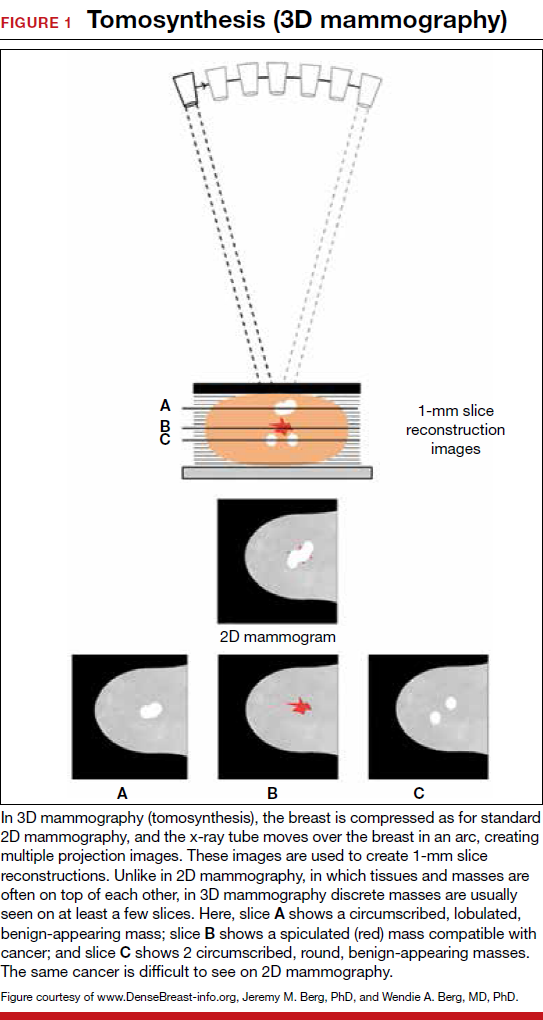
Breast density is determined on mammography and is categorized as fatty, scattered fibroglandular, heterogeneously dense, or extremely dense (FIGURE 2).5 Tissue in the heterogeneous and extreme categories is considered dense. More than half of women in their 40s have dense breasts; with some fatty involution occurring around menopause, the proportion drops to 25% for women in their 60s.6 About half of breast cancers have calcifications, which on mammography are usually easily visible even in dense breasts. The problem is with noncalcified invasive cancers that can be hidden by dense tissue (FIGURE 3).
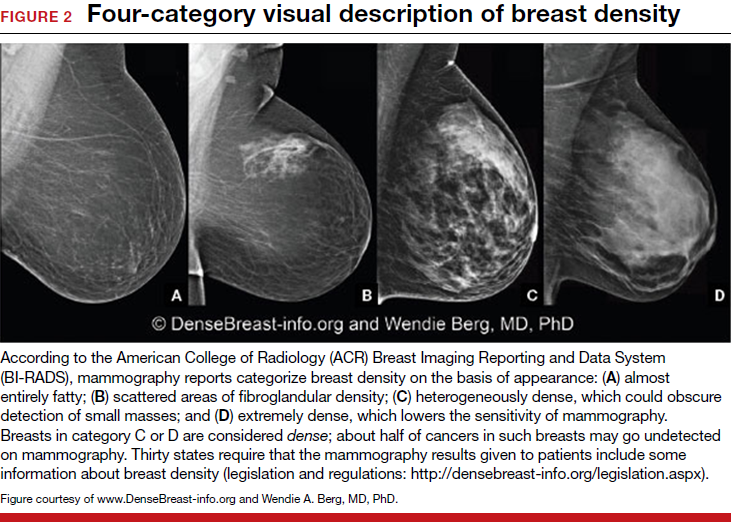
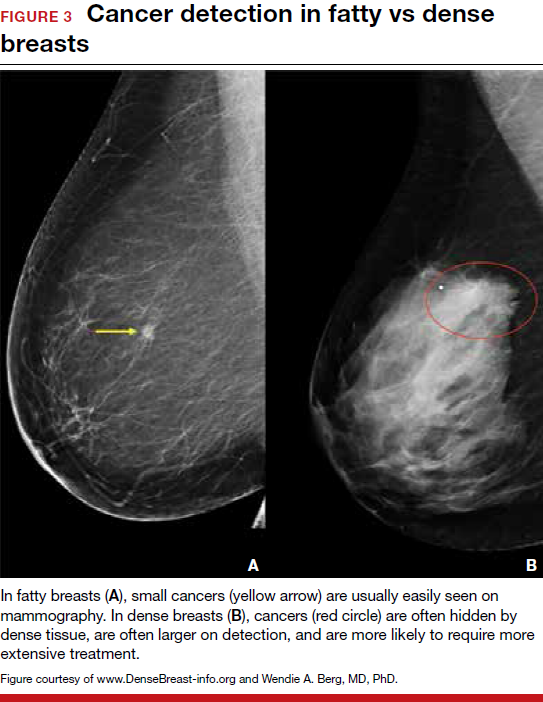
3D mammography improves cancer detection but is of minimal benefit in extremely dense breasts
Although 3D mammography improves cancer detection in most women, any benefit is minimal in women with extremely dense breasts, as there is no inherent soft-tissue contrast.7 Masked cancers are often only discovered because of a lump after a normal screening mammogram, as so-called “interval cancers.” Compared with screen-detected cancers, interval cancers tend to be more biologically aggressive, to have spread to lymph nodes, and to have worse prognoses. However, even some small screen-detected cancers are biologically aggressive and can spread to lymph nodes quickly, and no screening test or combination of screening tests can prevent this occurrence completely, regardless of breast density.
Related article:
Get smart about dense breasts
MRI provides early detection across all breast densities
In all tissue densities, contrast-enhanced magnetic resonance imaging (MRI) is far better than mammography in detecting breast cancer.8 Women at high risk for breast cancer caused by mutations in BRCA1, BRCA2, p53, and other genes have poor outcomes with screening mammography alone—up to 50% of cancers are interval cancers. Annual screening MRI reduces this percentage significantly, to 11% in women with pathogenic BRCA1 mutations and to 4% in women with BRCA2 mutations.9 Warner and colleagues found a decrease in late-stage cancers in high-risk women who underwent annual MRI screenings compared to high-risk women unable to have MRI.10
The use of MRI for screening is limited by availability, patient tolerance,11 and high cost. Research is being conducted to further validate approaches using shortened screening MRI times (so-called “abbreviated” or “fast” MRI) and, thereby, improve access, tolerance, and reduce associated costs; several investigators already have reported promising results, and a few centers offer this modality directly to patients willing to pay $300 to $350 out of pocket.12,13 Even in normal-risk women, MRI significantly increases detection of early breast cancer after a normal mammogram and ultrasound, and the cancer detection benefit of MRI is seen across all breast densities.14
Most health insurance plans cover screening MRI only for women who meet defined risk criteria, including women who have a known disease-causing mutation—or are suspected of having one, given a family history of breast cancer with higher than 20% to 25% lifetime risk by a model that predicts mutation carrier status—as well as women who had chest radiation therapy before age 30, typically for Hodgkin lymphoma, and at least 8 years earlier.15 In addition, MRI can be considered in women with atypical breast biopsy results or a personal history of lobular carcinoma in situ (LCIS).16
Screening MRI should start by age 25 in women with disease-causing mutations, or at the time of atypical or LCIS biopsy results, and should be performed annually unless the woman is pregnant or has a metallic implant, renal insufficiency, or another contraindication to MRI. MRI can be beneficial in women with a personal history of cancer, although annual mammography remains the standard of care.17–19
MRI and mammography can be performed at the same time or on an alternating 6-month basis, with mammography usually starting only after age 30 because of the small risk that radiation poses for younger women. There are a few other impediments to having breast MRI: The woman must lie on her stomach within a confined space (tunnel), the contrast that is injected may not be well tolerated, and insurance does not cover the test for women who do not meet the defined risk criteria.11
Read why mammography supplemented by US is best for women with dense breasts.
Ultrasonography supplements mammography
Mammography supplemented with ultrasonography (US) has been studied as a “Goldilocks” or best-fit solution for the screening of women with dense breasts, as detection of invasive cancers is improved with the 2 modalities over mammography alone, and US is less invasive, better tolerated, and lower in cost than the more sensitive MRI.
In women with dense breasts, US has been found to improve cancer detection over mammography alone, and early results suggest a larger cancer detection benefit from US than from 3D mammography, although research is ongoing.20 Adding US reduces the interval cancer rate in women with dense breasts to less than 10% of all cancers found—similar to results for women with fatty breasts.17,21,22
US can be performed by a trained technologist or a physician using a small transducer, which usually provides diagnostic images (so that most callbacks would be for a true finding), or a larger transducer and an automated system can be used to create more than a thousand images for radiologist review.23,24 Use of a hybrid system, a small transducer with an automated arm, has been validated as well.25 Screening US is not available universally, and with all these approaches optimal performance requires trained personnel. Supplemental screening US usually is covered by insurance but is nearly always subject to a deductible/copay.
Related article:
Educate patients about dense breasts and cancer risk
Reducing false-positives, callbacks, and additional testing
Mammography carries a risk of false-positives. On average, 11% to 12% of women are called back for additional testing after a screening mammogram, and in more than 95% of women brought back for extra testing, no cancer is found.26 Women with dense breasts are more likely than those with less dense breasts to be called back.27 US and MRI improve cancer detection and therefore yield additional positive, but also false-positive, findings. Notably, callbacks decrease after the first round of screening with any modality or combination of tests, as long as prior examinations are available for comparison.
One advantage of 3D over 2D mammography is a decrease in extra testing for areas of asymmetry, which are often recognizable on 3D mammography as representing normal superimposed tissue.28–30 Architectural distortion, which is better seen on 3D mammography and usually represents either cancer or a benign radial scar, can lead to false-positive biopsies, although the average biopsy rate is no higher for 3D than for 2D alone.31 Typically, the 3D and 2D examinations are performed together (slightly more than doubling the radiation dose), or synthetic 2D images can be created from the 3D slices (resulting in a total radiation dose almost the same as standard 2D alone).
Most additional cancers seen on 3D mammography or US are lower-grade invasive cancers with good prognoses. Some aggressive high-grade breast cancers go undetected even when mammography is supplemented with US, either because they are too small to be seen or because they resemble common benign masses and may not be recognized. MRI is particularly effective in depicting high-grade cancers, even small ones.
The TABLE summarizes the relative rates of cancer detection and additional testing by various breast screening tests or combinations of tests. Neither clinical breast examination by a physician or other health care professional nor routine breast self-examination reduces the number of deaths caused by breast cancer. Nevertheless, women should monitor any changes in their breasts and report these changes to their clinician. A new lump, skin or nipple retraction, or a spontaneous clear or bloody nipple discharge merits diagnostic breast imaging even if a recent screening mammogram was normal.

FIGURE 4 is an updated decision support tool that suggests strategies for optimizingcancer detection with widely available screening methods.
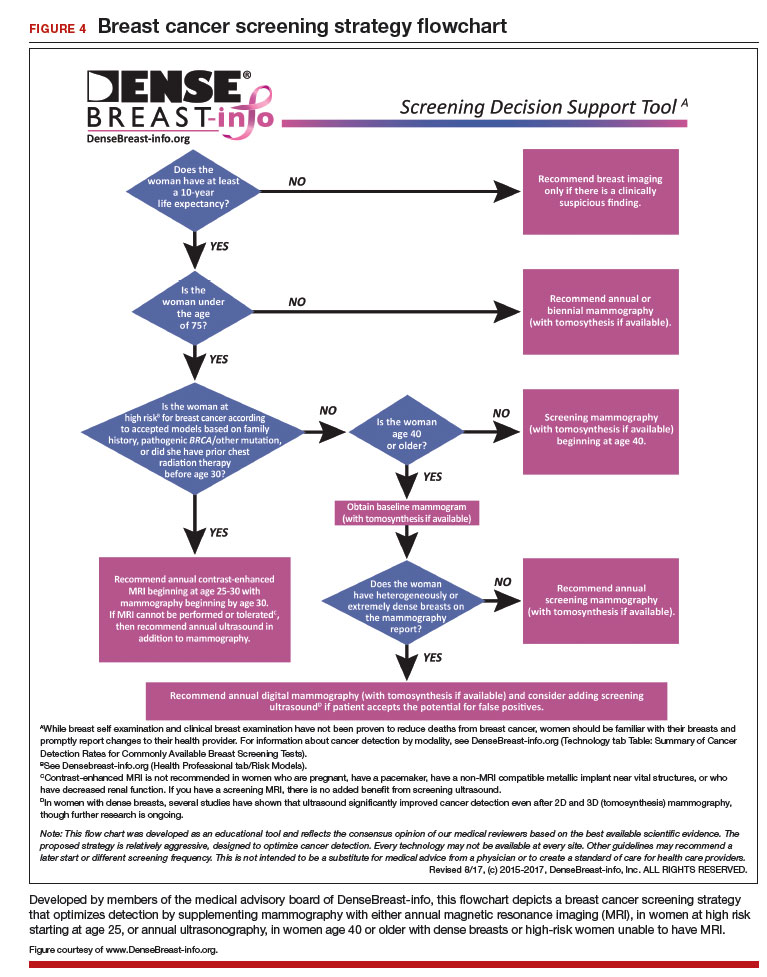
Read how to take advantage of today’s technology for breast density screening
MY STORY: Epilogue
My annual 3D mammograms were normal, even the year my cancer was present. In 2014, I entered my family history into the IBIS Breast Cancer Risk Evaluation Tool (Tyrer-Cuzick model of breast cancer risk) (http://www.ems-trials.org/riskevaluator/) and calculated my lifetime risk at 19.7%. That is when I decided to have a screening MRI. My invasive breast cancer was easily seen on MRI and then on US. The cancer was node-negative, easily confirmed with needle biopsy, and treated with lumpectomy and radiation. There was no need for chemotherapy.
My personal experience prompted me to join JoAnn Pushkin and Cindy Henke-Sarmento, RT(R)(M), BA, in developing a website, www.DenseBreast-info.org, to give women and their physicians easy access to information on making decisions about screening in dense breasts.
My colleagues and I are often asked what is the best way to order supplemental imaging for a patient who may have dense breasts. Even in cases in which a mammogram does not exist or is unavailable, the following prescription can be implemented easily at centers that offer US: “2D plus 3D mammogram if available; if dense, perform ultrasound as needed.”
Related article:
DenseBreast-info.org: What this resource can offer you, and your patients
Breast density screening: Take advantage of today’s technology
Breast screening and diagnostic imaging have improved significantly since the 1970s, when many of the randomized trials of mammography were conducted. Breast density is one of the most common and important risk factors for development of breast cancer and is now incorporated into the Breast Cancer Surveillance Consortium model (https://tools.bcsc-scc.org/BC5yearRisk/calculator.htm) and the Tyrer-Cuzick model (see also http://densebreast-info.org/explanation-of-dense-breast-risk-models.aspx).32 Although we continue to validate newer approaches, women should take advantage of the improved methods of early cancer detection, particularly if they have dense breasts or are at high risk for breast cancer.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al; American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. 2003;361(9367):1405–1410.
- Lee SJ, Boscardin WJ, Stijacic-Cenzer I, Conell-Price J, O’Brien S, Walter LC. Time lag to benefit after screening for breast and colorectal cancer: meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark. BMJ. 2013;346:e8441.
- Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. JAMA. 2001;285(21):2750–2756.
- Sickles EA, D’Orsi CJ, Bassett LW, et al. ACR BI-RADS mammography. In: D’Orsi CJ, Sickles EA, Mendelson EB, et al, eds. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th ed. Reston, VA: American College of Radiology; 2013.
- Sprague BL, Gangnon RE, Burt V, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014;106(10).
- Rafferty EA, Durand MA, Conant EF, et al. Breast cancer screening using tomosynthesis and digital mammography in dense and nondense breasts. JAMA. 2016;315(16):1784–1786.
- Berg WA. Tailored supplemental screening for breast cancer: what now and what next? AJR Am J Roentgenol. 2009;192(2):390–399.
- Heijnsdijk EA, Warner E, Gilbert FJ, et al. Differences in natural history between breast cancers in BRCA1 and BRCA2 mutation carriers and effects of MRI screening—MRISC, MARIBS, and Canadian studies combined. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1458–1468.
- Warner E, Hill K, Causer P, et al. Prospective study of breast cancer incidence in women with a BRCA1 or BRCA2 mutation under surveillance with and without magnetic resonance imaging. J Clin Oncol. 2011;29(13):1664–1669.
- Berg WA, Blume JD, Adams AM, et al. Reasons women at elevated risk of breast cancer refuse breast MR imaging screening: ACRIN 6666. Radiology. 2010;254(1):79–87.
- Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection—a novel approach to breast cancer screening with MRI. J Clin Oncol. 2014;32(22):2304–2310.
- Strahle DA, Pathak DR, Sierra A, Saha S, Strahle C, Devisetty K. Systematic development of an abbreviated protocol for screening breast magnetic resonance imaging. Breast Cancer Res Treat. 2017;162(2):283–295.
- Kuhl CK, Strobel K, Bieling H, Leutner C, Schild HH, Schrading S. Supplemental breast MR imaging screening of women with average risk of breast cancer. Radiology. 2017;283(2):361–370.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
- National Comprehensive Cancer Network. NCCN guidelines for detection, prevention, and risk reduction: breast cancer screening and diagnosis. https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf.
- Berg WA, Zhang Z, Lehrer D, et al; ACRIN 6666 Investigators. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394–1404.
- Brennan S, Liberman L, Dershaw DD, Morris E. Breast MRI screening of women with a personal history of breast cancer. AJR Am J Roentgenol. 2010;195(2):510–516.
- Lehman CD, Lee JM, DeMartini WB, et al. Screening MRI in women with a personal history of breast cancer. J Natl Cancer Inst. 2016;108(3).
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2016]. J Clin Oncol. JCO634147.
- Corsetti V, Houssami N, Ghirardi M, et al. Evidence of the effect of adjunct ultrasound screening in women with mammography-negative dense breasts: interval breast cancers at 1 year follow-up. Eur J Cancer. 2011;47(7):1021–1026.
- Ohuchi N, Suzuki A, Sobue T, et al; J-START Investigator Groups. Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan Strategic Anti-Cancer Randomized Trial (J-START): a randomised controlled trial. Lancet. 2016;387(10016):341–348.
- Berg WA, Mendelson EB. Technologist-performed handheld screening breast US imaging: how is it performed and what are the outcomes to date? Radiology. 2014;272(1):12–27.
- Brem RF, Tabár L, Duffy SW, et al. Assessing improvement in detection of breast cancer with three-dimensional automated breast US in women with dense breast tissue: the SomoInsight study. Radiology. 2015;274(3):663–673.
- Kelly KM, Dean J, Comulada WS, Lee SJ. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010;20(3):734–742.
- Lehman CD, Arao RF, Sprague BL, et al. National performance benchmarks for modern screening digital mammography: update from the Breast Cancer Surveillance Consortium. Radiology. 2017;283(1):49–58.
- Kerlikowske K, Zhu W, Hubbard RA, et al; Breast Cancer Surveillance Consortium. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern Med. 2013;173(9):807–816.
- Friedewald SM, Rafferty EA, Rose SL, et al. Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA. 2014;311(24):2499–2507.
- Skaane P, Bandos AI, Gullien R, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267(1):47–56.
- Ciatto S, Houssami N, Bernardi D, et al. Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): a prospective comparison study. Lancet Oncol. 2013;14(7):583–589.
- Bahl M, Lamb LR, Lehman CD. Pathologic outcomes of architectural distortion on digital 2D versus tomosynthesis mammography [published online ahead of print August 23, 2017]. AJR Am J Roentgenol. doi:10.2214/AJR.17.17979.
- Engmann NJ, Golmakani MK, Miglioretti DL, Sprague BL, Kerlikowske K; Breast Cancer Surveillance Consortium. Population-attributable risk proportion of clinical risk factors for breast cancer [published online ahead of print February 2, 2017]. JAMA Oncol. doi:10.1001/jamaoncol.2016.6326.
MY STORY: Prologue
My aunt received a breast cancer diagnosis at age 40, and she died at age 60, in 1970. Then, in 1975, my mother’s breast cancer was found at age 55, but only after she was examined for nipple retraction; on mammography, the cancer had been obscured by dense breast tissue. Mom had 2 metastatic nodes but participated in the earliest clinical trials of chemotherapy and lived free of breast cancer for another 41 years. Naturally I thought that, were I to develop this disease, I would want it found earlier. Ironically, it was, but only because I had spent my career trying to understand the optimal screening approaches for women with dense breasts—women like me.
Cancers are masked on mammography in dense breasts
For women, screening mammography is an important step in reducing the risk of dying from breast cancer. The greatest benefits are realized by those who start annual screening at age 40, or 45 at the latest.1 As it takes 9 to 10 years to see a benefit from breast cancer screening at the population level, it is not logical to continue this testing when life expectancy is less than 10 years, as is the case with women age 85 or older, even those in the healthiest quartile.2–4 However, despite recent advances, the development of 3D mammography (tomosynthesis) (FIGURE 1) in particular, cancers can still be masked by dense breast tissue. Both 2D and 3D mammograms are x-rays; both dense tissue and cancers absorb x-rays and appear white.
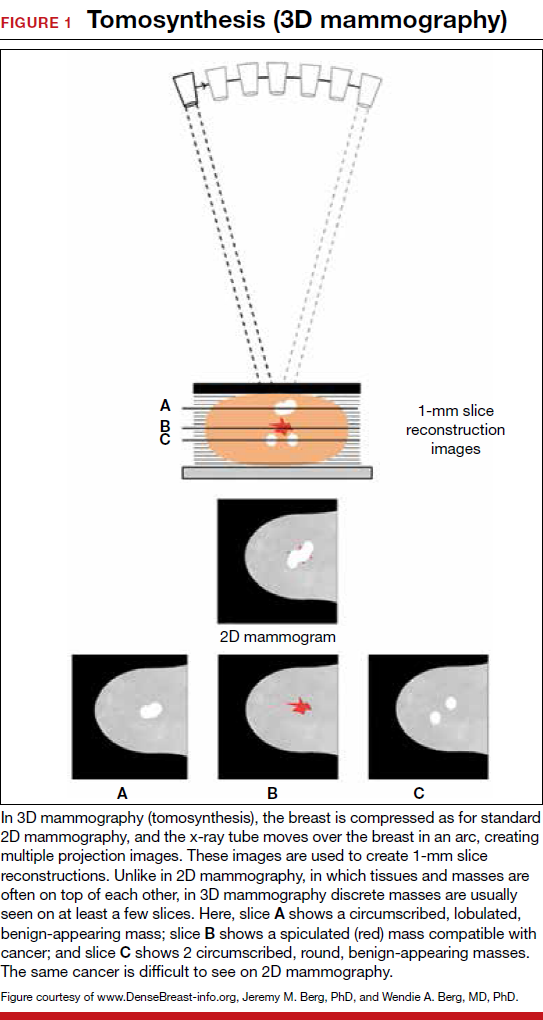
Breast density is determined on mammography and is categorized as fatty, scattered fibroglandular, heterogeneously dense, or extremely dense (FIGURE 2).5 Tissue in the heterogeneous and extreme categories is considered dense. More than half of women in their 40s have dense breasts; with some fatty involution occurring around menopause, the proportion drops to 25% for women in their 60s.6 About half of breast cancers have calcifications, which on mammography are usually easily visible even in dense breasts. The problem is with noncalcified invasive cancers that can be hidden by dense tissue (FIGURE 3).
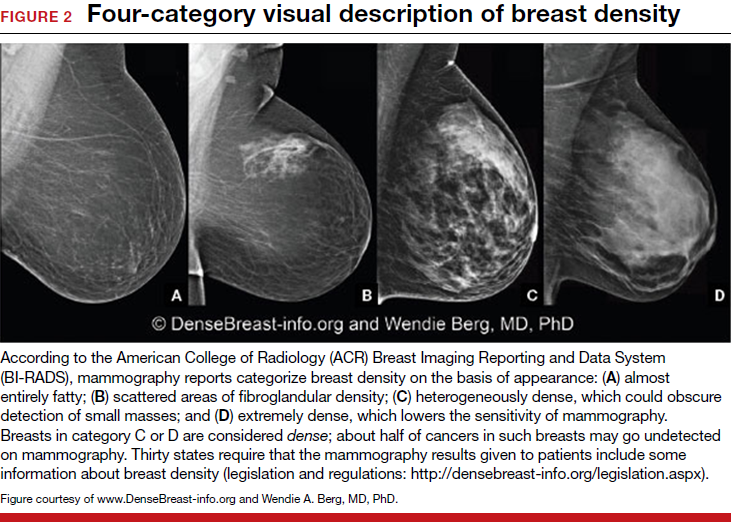
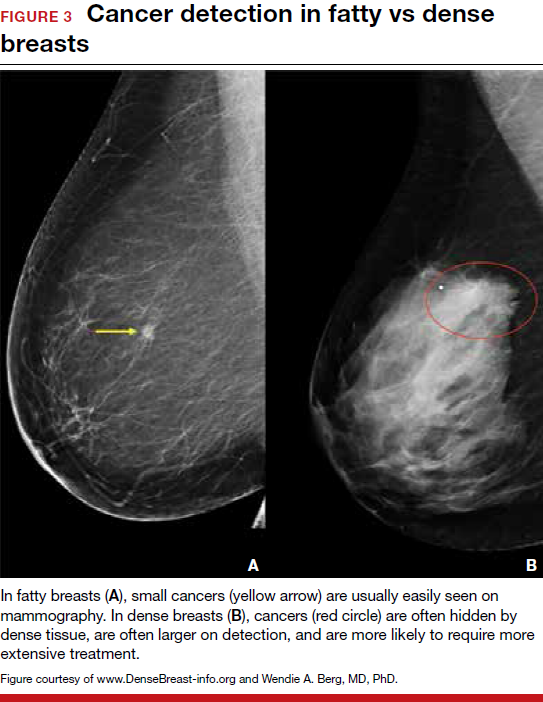
3D mammography improves cancer detection but is of minimal benefit in extremely dense breasts
Although 3D mammography improves cancer detection in most women, any benefit is minimal in women with extremely dense breasts, as there is no inherent soft-tissue contrast.7 Masked cancers are often only discovered because of a lump after a normal screening mammogram, as so-called “interval cancers.” Compared with screen-detected cancers, interval cancers tend to be more biologically aggressive, to have spread to lymph nodes, and to have worse prognoses. However, even some small screen-detected cancers are biologically aggressive and can spread to lymph nodes quickly, and no screening test or combination of screening tests can prevent this occurrence completely, regardless of breast density.
Related article:
Get smart about dense breasts
MRI provides early detection across all breast densities
In all tissue densities, contrast-enhanced magnetic resonance imaging (MRI) is far better than mammography in detecting breast cancer.8 Women at high risk for breast cancer caused by mutations in BRCA1, BRCA2, p53, and other genes have poor outcomes with screening mammography alone—up to 50% of cancers are interval cancers. Annual screening MRI reduces this percentage significantly, to 11% in women with pathogenic BRCA1 mutations and to 4% in women with BRCA2 mutations.9 Warner and colleagues found a decrease in late-stage cancers in high-risk women who underwent annual MRI screenings compared to high-risk women unable to have MRI.10
The use of MRI for screening is limited by availability, patient tolerance,11 and high cost. Research is being conducted to further validate approaches using shortened screening MRI times (so-called “abbreviated” or “fast” MRI) and, thereby, improve access, tolerance, and reduce associated costs; several investigators already have reported promising results, and a few centers offer this modality directly to patients willing to pay $300 to $350 out of pocket.12,13 Even in normal-risk women, MRI significantly increases detection of early breast cancer after a normal mammogram and ultrasound, and the cancer detection benefit of MRI is seen across all breast densities.14
Most health insurance plans cover screening MRI only for women who meet defined risk criteria, including women who have a known disease-causing mutation—or are suspected of having one, given a family history of breast cancer with higher than 20% to 25% lifetime risk by a model that predicts mutation carrier status—as well as women who had chest radiation therapy before age 30, typically for Hodgkin lymphoma, and at least 8 years earlier.15 In addition, MRI can be considered in women with atypical breast biopsy results or a personal history of lobular carcinoma in situ (LCIS).16
Screening MRI should start by age 25 in women with disease-causing mutations, or at the time of atypical or LCIS biopsy results, and should be performed annually unless the woman is pregnant or has a metallic implant, renal insufficiency, or another contraindication to MRI. MRI can be beneficial in women with a personal history of cancer, although annual mammography remains the standard of care.17–19
MRI and mammography can be performed at the same time or on an alternating 6-month basis, with mammography usually starting only after age 30 because of the small risk that radiation poses for younger women. There are a few other impediments to having breast MRI: The woman must lie on her stomach within a confined space (tunnel), the contrast that is injected may not be well tolerated, and insurance does not cover the test for women who do not meet the defined risk criteria.11
Read why mammography supplemented by US is best for women with dense breasts.
Ultrasonography supplements mammography
Mammography supplemented with ultrasonography (US) has been studied as a “Goldilocks” or best-fit solution for the screening of women with dense breasts, as detection of invasive cancers is improved with the 2 modalities over mammography alone, and US is less invasive, better tolerated, and lower in cost than the more sensitive MRI.
In women with dense breasts, US has been found to improve cancer detection over mammography alone, and early results suggest a larger cancer detection benefit from US than from 3D mammography, although research is ongoing.20 Adding US reduces the interval cancer rate in women with dense breasts to less than 10% of all cancers found—similar to results for women with fatty breasts.17,21,22
US can be performed by a trained technologist or a physician using a small transducer, which usually provides diagnostic images (so that most callbacks would be for a true finding), or a larger transducer and an automated system can be used to create more than a thousand images for radiologist review.23,24 Use of a hybrid system, a small transducer with an automated arm, has been validated as well.25 Screening US is not available universally, and with all these approaches optimal performance requires trained personnel. Supplemental screening US usually is covered by insurance but is nearly always subject to a deductible/copay.
Related article:
Educate patients about dense breasts and cancer risk
Reducing false-positives, callbacks, and additional testing
Mammography carries a risk of false-positives. On average, 11% to 12% of women are called back for additional testing after a screening mammogram, and in more than 95% of women brought back for extra testing, no cancer is found.26 Women with dense breasts are more likely than those with less dense breasts to be called back.27 US and MRI improve cancer detection and therefore yield additional positive, but also false-positive, findings. Notably, callbacks decrease after the first round of screening with any modality or combination of tests, as long as prior examinations are available for comparison.
One advantage of 3D over 2D mammography is a decrease in extra testing for areas of asymmetry, which are often recognizable on 3D mammography as representing normal superimposed tissue.28–30 Architectural distortion, which is better seen on 3D mammography and usually represents either cancer or a benign radial scar, can lead to false-positive biopsies, although the average biopsy rate is no higher for 3D than for 2D alone.31 Typically, the 3D and 2D examinations are performed together (slightly more than doubling the radiation dose), or synthetic 2D images can be created from the 3D slices (resulting in a total radiation dose almost the same as standard 2D alone).
Most additional cancers seen on 3D mammography or US are lower-grade invasive cancers with good prognoses. Some aggressive high-grade breast cancers go undetected even when mammography is supplemented with US, either because they are too small to be seen or because they resemble common benign masses and may not be recognized. MRI is particularly effective in depicting high-grade cancers, even small ones.
The TABLE summarizes the relative rates of cancer detection and additional testing by various breast screening tests or combinations of tests. Neither clinical breast examination by a physician or other health care professional nor routine breast self-examination reduces the number of deaths caused by breast cancer. Nevertheless, women should monitor any changes in their breasts and report these changes to their clinician. A new lump, skin or nipple retraction, or a spontaneous clear or bloody nipple discharge merits diagnostic breast imaging even if a recent screening mammogram was normal.

FIGURE 4 is an updated decision support tool that suggests strategies for optimizingcancer detection with widely available screening methods.
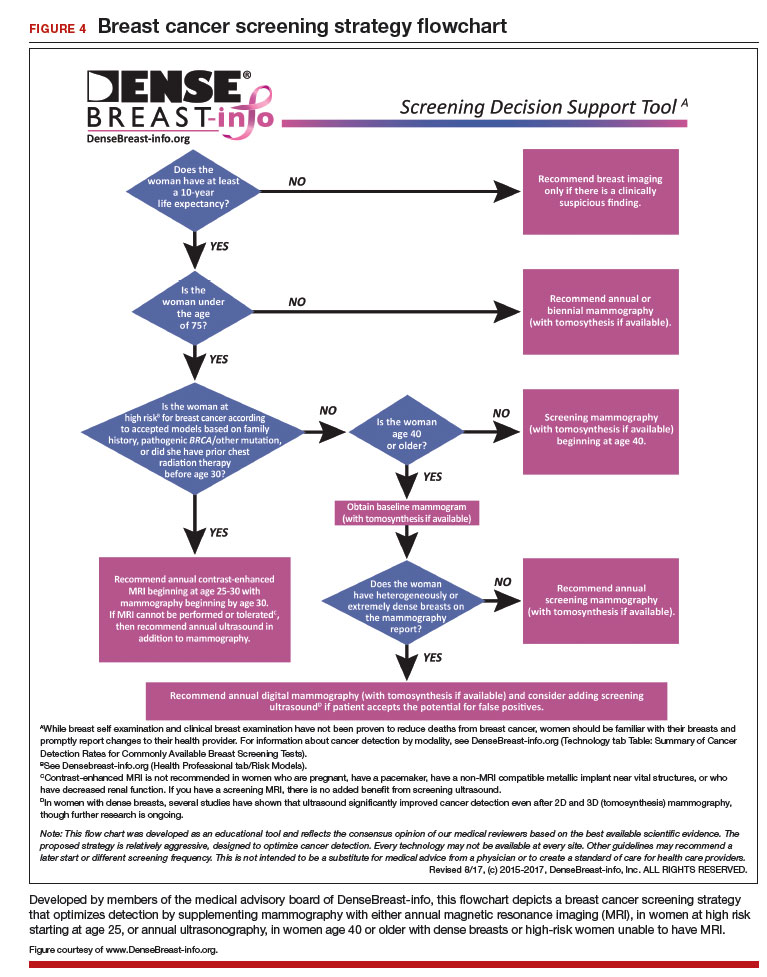
Read how to take advantage of today’s technology for breast density screening
MY STORY: Epilogue
My annual 3D mammograms were normal, even the year my cancer was present. In 2014, I entered my family history into the IBIS Breast Cancer Risk Evaluation Tool (Tyrer-Cuzick model of breast cancer risk) (http://www.ems-trials.org/riskevaluator/) and calculated my lifetime risk at 19.7%. That is when I decided to have a screening MRI. My invasive breast cancer was easily seen on MRI and then on US. The cancer was node-negative, easily confirmed with needle biopsy, and treated with lumpectomy and radiation. There was no need for chemotherapy.
My personal experience prompted me to join JoAnn Pushkin and Cindy Henke-Sarmento, RT(R)(M), BA, in developing a website, www.DenseBreast-info.org, to give women and their physicians easy access to information on making decisions about screening in dense breasts.
My colleagues and I are often asked what is the best way to order supplemental imaging for a patient who may have dense breasts. Even in cases in which a mammogram does not exist or is unavailable, the following prescription can be implemented easily at centers that offer US: “2D plus 3D mammogram if available; if dense, perform ultrasound as needed.”
Related article:
DenseBreast-info.org: What this resource can offer you, and your patients
Breast density screening: Take advantage of today’s technology
Breast screening and diagnostic imaging have improved significantly since the 1970s, when many of the randomized trials of mammography were conducted. Breast density is one of the most common and important risk factors for development of breast cancer and is now incorporated into the Breast Cancer Surveillance Consortium model (https://tools.bcsc-scc.org/BC5yearRisk/calculator.htm) and the Tyrer-Cuzick model (see also http://densebreast-info.org/explanation-of-dense-breast-risk-models.aspx).32 Although we continue to validate newer approaches, women should take advantage of the improved methods of early cancer detection, particularly if they have dense breasts or are at high risk for breast cancer.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
MY STORY: Prologue
My aunt received a breast cancer diagnosis at age 40, and she died at age 60, in 1970. Then, in 1975, my mother’s breast cancer was found at age 55, but only after she was examined for nipple retraction; on mammography, the cancer had been obscured by dense breast tissue. Mom had 2 metastatic nodes but participated in the earliest clinical trials of chemotherapy and lived free of breast cancer for another 41 years. Naturally I thought that, were I to develop this disease, I would want it found earlier. Ironically, it was, but only because I had spent my career trying to understand the optimal screening approaches for women with dense breasts—women like me.
Cancers are masked on mammography in dense breasts
For women, screening mammography is an important step in reducing the risk of dying from breast cancer. The greatest benefits are realized by those who start annual screening at age 40, or 45 at the latest.1 As it takes 9 to 10 years to see a benefit from breast cancer screening at the population level, it is not logical to continue this testing when life expectancy is less than 10 years, as is the case with women age 85 or older, even those in the healthiest quartile.2–4 However, despite recent advances, the development of 3D mammography (tomosynthesis) (FIGURE 1) in particular, cancers can still be masked by dense breast tissue. Both 2D and 3D mammograms are x-rays; both dense tissue and cancers absorb x-rays and appear white.
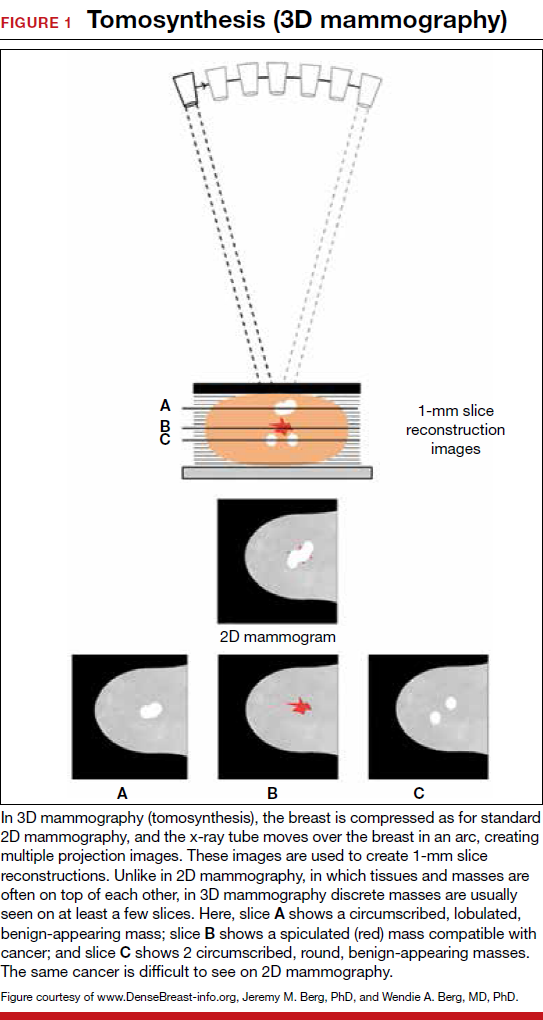
Breast density is determined on mammography and is categorized as fatty, scattered fibroglandular, heterogeneously dense, or extremely dense (FIGURE 2).5 Tissue in the heterogeneous and extreme categories is considered dense. More than half of women in their 40s have dense breasts; with some fatty involution occurring around menopause, the proportion drops to 25% for women in their 60s.6 About half of breast cancers have calcifications, which on mammography are usually easily visible even in dense breasts. The problem is with noncalcified invasive cancers that can be hidden by dense tissue (FIGURE 3).
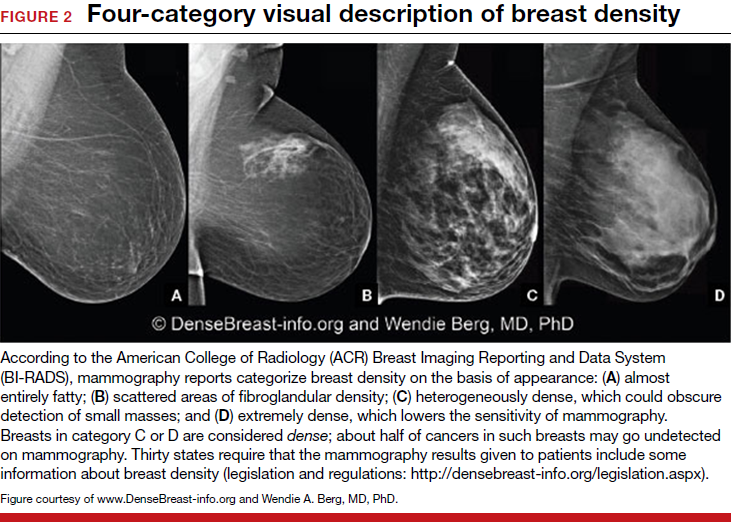
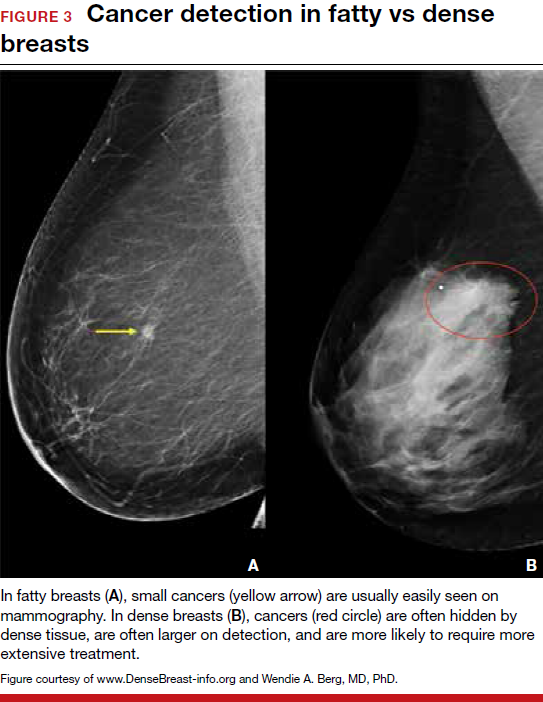
3D mammography improves cancer detection but is of minimal benefit in extremely dense breasts
Although 3D mammography improves cancer detection in most women, any benefit is minimal in women with extremely dense breasts, as there is no inherent soft-tissue contrast.7 Masked cancers are often only discovered because of a lump after a normal screening mammogram, as so-called “interval cancers.” Compared with screen-detected cancers, interval cancers tend to be more biologically aggressive, to have spread to lymph nodes, and to have worse prognoses. However, even some small screen-detected cancers are biologically aggressive and can spread to lymph nodes quickly, and no screening test or combination of screening tests can prevent this occurrence completely, regardless of breast density.
Related article:
Get smart about dense breasts
MRI provides early detection across all breast densities
In all tissue densities, contrast-enhanced magnetic resonance imaging (MRI) is far better than mammography in detecting breast cancer.8 Women at high risk for breast cancer caused by mutations in BRCA1, BRCA2, p53, and other genes have poor outcomes with screening mammography alone—up to 50% of cancers are interval cancers. Annual screening MRI reduces this percentage significantly, to 11% in women with pathogenic BRCA1 mutations and to 4% in women with BRCA2 mutations.9 Warner and colleagues found a decrease in late-stage cancers in high-risk women who underwent annual MRI screenings compared to high-risk women unable to have MRI.10
The use of MRI for screening is limited by availability, patient tolerance,11 and high cost. Research is being conducted to further validate approaches using shortened screening MRI times (so-called “abbreviated” or “fast” MRI) and, thereby, improve access, tolerance, and reduce associated costs; several investigators already have reported promising results, and a few centers offer this modality directly to patients willing to pay $300 to $350 out of pocket.12,13 Even in normal-risk women, MRI significantly increases detection of early breast cancer after a normal mammogram and ultrasound, and the cancer detection benefit of MRI is seen across all breast densities.14
Most health insurance plans cover screening MRI only for women who meet defined risk criteria, including women who have a known disease-causing mutation—or are suspected of having one, given a family history of breast cancer with higher than 20% to 25% lifetime risk by a model that predicts mutation carrier status—as well as women who had chest radiation therapy before age 30, typically for Hodgkin lymphoma, and at least 8 years earlier.15 In addition, MRI can be considered in women with atypical breast biopsy results or a personal history of lobular carcinoma in situ (LCIS).16
Screening MRI should start by age 25 in women with disease-causing mutations, or at the time of atypical or LCIS biopsy results, and should be performed annually unless the woman is pregnant or has a metallic implant, renal insufficiency, or another contraindication to MRI. MRI can be beneficial in women with a personal history of cancer, although annual mammography remains the standard of care.17–19
MRI and mammography can be performed at the same time or on an alternating 6-month basis, with mammography usually starting only after age 30 because of the small risk that radiation poses for younger women. There are a few other impediments to having breast MRI: The woman must lie on her stomach within a confined space (tunnel), the contrast that is injected may not be well tolerated, and insurance does not cover the test for women who do not meet the defined risk criteria.11
Read why mammography supplemented by US is best for women with dense breasts.
Ultrasonography supplements mammography
Mammography supplemented with ultrasonography (US) has been studied as a “Goldilocks” or best-fit solution for the screening of women with dense breasts, as detection of invasive cancers is improved with the 2 modalities over mammography alone, and US is less invasive, better tolerated, and lower in cost than the more sensitive MRI.
In women with dense breasts, US has been found to improve cancer detection over mammography alone, and early results suggest a larger cancer detection benefit from US than from 3D mammography, although research is ongoing.20 Adding US reduces the interval cancer rate in women with dense breasts to less than 10% of all cancers found—similar to results for women with fatty breasts.17,21,22
US can be performed by a trained technologist or a physician using a small transducer, which usually provides diagnostic images (so that most callbacks would be for a true finding), or a larger transducer and an automated system can be used to create more than a thousand images for radiologist review.23,24 Use of a hybrid system, a small transducer with an automated arm, has been validated as well.25 Screening US is not available universally, and with all these approaches optimal performance requires trained personnel. Supplemental screening US usually is covered by insurance but is nearly always subject to a deductible/copay.
Related article:
Educate patients about dense breasts and cancer risk
Reducing false-positives, callbacks, and additional testing
Mammography carries a risk of false-positives. On average, 11% to 12% of women are called back for additional testing after a screening mammogram, and in more than 95% of women brought back for extra testing, no cancer is found.26 Women with dense breasts are more likely than those with less dense breasts to be called back.27 US and MRI improve cancer detection and therefore yield additional positive, but also false-positive, findings. Notably, callbacks decrease after the first round of screening with any modality or combination of tests, as long as prior examinations are available for comparison.
One advantage of 3D over 2D mammography is a decrease in extra testing for areas of asymmetry, which are often recognizable on 3D mammography as representing normal superimposed tissue.28–30 Architectural distortion, which is better seen on 3D mammography and usually represents either cancer or a benign radial scar, can lead to false-positive biopsies, although the average biopsy rate is no higher for 3D than for 2D alone.31 Typically, the 3D and 2D examinations are performed together (slightly more than doubling the radiation dose), or synthetic 2D images can be created from the 3D slices (resulting in a total radiation dose almost the same as standard 2D alone).
Most additional cancers seen on 3D mammography or US are lower-grade invasive cancers with good prognoses. Some aggressive high-grade breast cancers go undetected even when mammography is supplemented with US, either because they are too small to be seen or because they resemble common benign masses and may not be recognized. MRI is particularly effective in depicting high-grade cancers, even small ones.
The TABLE summarizes the relative rates of cancer detection and additional testing by various breast screening tests or combinations of tests. Neither clinical breast examination by a physician or other health care professional nor routine breast self-examination reduces the number of deaths caused by breast cancer. Nevertheless, women should monitor any changes in their breasts and report these changes to their clinician. A new lump, skin or nipple retraction, or a spontaneous clear or bloody nipple discharge merits diagnostic breast imaging even if a recent screening mammogram was normal.

FIGURE 4 is an updated decision support tool that suggests strategies for optimizingcancer detection with widely available screening methods.
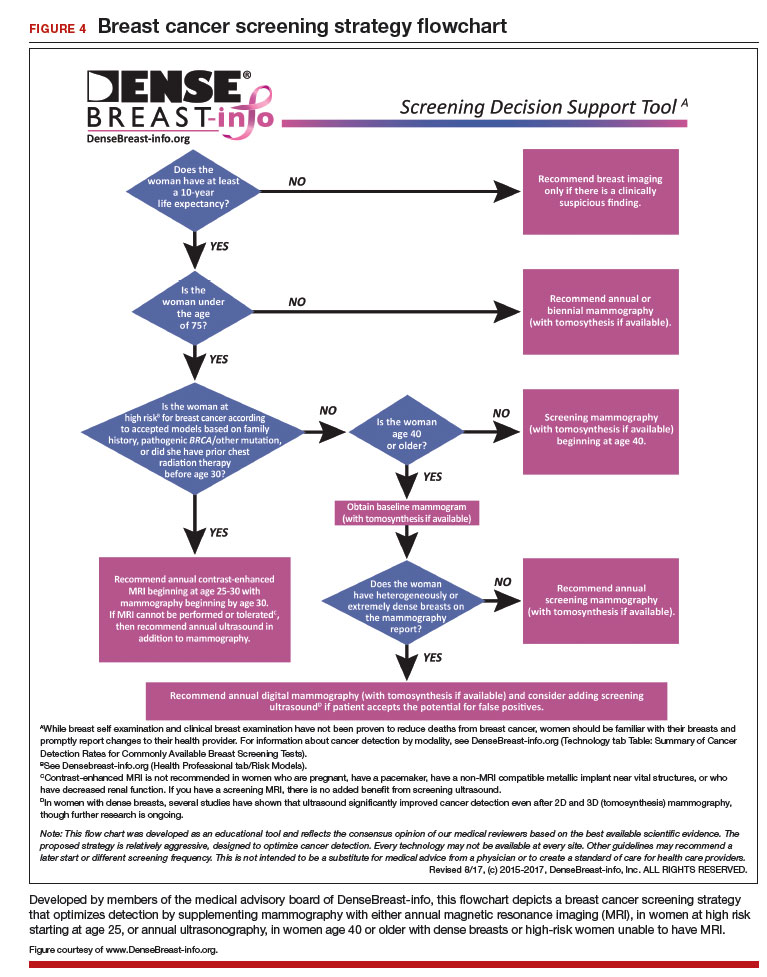
Read how to take advantage of today’s technology for breast density screening
MY STORY: Epilogue
My annual 3D mammograms were normal, even the year my cancer was present. In 2014, I entered my family history into the IBIS Breast Cancer Risk Evaluation Tool (Tyrer-Cuzick model of breast cancer risk) (http://www.ems-trials.org/riskevaluator/) and calculated my lifetime risk at 19.7%. That is when I decided to have a screening MRI. My invasive breast cancer was easily seen on MRI and then on US. The cancer was node-negative, easily confirmed with needle biopsy, and treated with lumpectomy and radiation. There was no need for chemotherapy.
My personal experience prompted me to join JoAnn Pushkin and Cindy Henke-Sarmento, RT(R)(M), BA, in developing a website, www.DenseBreast-info.org, to give women and their physicians easy access to information on making decisions about screening in dense breasts.
My colleagues and I are often asked what is the best way to order supplemental imaging for a patient who may have dense breasts. Even in cases in which a mammogram does not exist or is unavailable, the following prescription can be implemented easily at centers that offer US: “2D plus 3D mammogram if available; if dense, perform ultrasound as needed.”
Related article:
DenseBreast-info.org: What this resource can offer you, and your patients
Breast density screening: Take advantage of today’s technology
Breast screening and diagnostic imaging have improved significantly since the 1970s, when many of the randomized trials of mammography were conducted. Breast density is one of the most common and important risk factors for development of breast cancer and is now incorporated into the Breast Cancer Surveillance Consortium model (https://tools.bcsc-scc.org/BC5yearRisk/calculator.htm) and the Tyrer-Cuzick model (see also http://densebreast-info.org/explanation-of-dense-breast-risk-models.aspx).32 Although we continue to validate newer approaches, women should take advantage of the improved methods of early cancer detection, particularly if they have dense breasts or are at high risk for breast cancer.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
- Oeffinger KC, Fontham ET, Etzioni R, et al; American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. 2003;361(9367):1405–1410.
- Lee SJ, Boscardin WJ, Stijacic-Cenzer I, Conell-Price J, O’Brien S, Walter LC. Time lag to benefit after screening for breast and colorectal cancer: meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark. BMJ. 2013;346:e8441.
- Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. JAMA. 2001;285(21):2750–2756.
- Sickles EA, D’Orsi CJ, Bassett LW, et al. ACR BI-RADS mammography. In: D’Orsi CJ, Sickles EA, Mendelson EB, et al, eds. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th ed. Reston, VA: American College of Radiology; 2013.
- Sprague BL, Gangnon RE, Burt V, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014;106(10).
- Rafferty EA, Durand MA, Conant EF, et al. Breast cancer screening using tomosynthesis and digital mammography in dense and nondense breasts. JAMA. 2016;315(16):1784–1786.
- Berg WA. Tailored supplemental screening for breast cancer: what now and what next? AJR Am J Roentgenol. 2009;192(2):390–399.
- Heijnsdijk EA, Warner E, Gilbert FJ, et al. Differences in natural history between breast cancers in BRCA1 and BRCA2 mutation carriers and effects of MRI screening—MRISC, MARIBS, and Canadian studies combined. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1458–1468.
- Warner E, Hill K, Causer P, et al. Prospective study of breast cancer incidence in women with a BRCA1 or BRCA2 mutation under surveillance with and without magnetic resonance imaging. J Clin Oncol. 2011;29(13):1664–1669.
- Berg WA, Blume JD, Adams AM, et al. Reasons women at elevated risk of breast cancer refuse breast MR imaging screening: ACRIN 6666. Radiology. 2010;254(1):79–87.
- Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection—a novel approach to breast cancer screening with MRI. J Clin Oncol. 2014;32(22):2304–2310.
- Strahle DA, Pathak DR, Sierra A, Saha S, Strahle C, Devisetty K. Systematic development of an abbreviated protocol for screening breast magnetic resonance imaging. Breast Cancer Res Treat. 2017;162(2):283–295.
- Kuhl CK, Strobel K, Bieling H, Leutner C, Schild HH, Schrading S. Supplemental breast MR imaging screening of women with average risk of breast cancer. Radiology. 2017;283(2):361–370.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
- National Comprehensive Cancer Network. NCCN guidelines for detection, prevention, and risk reduction: breast cancer screening and diagnosis. https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf.
- Berg WA, Zhang Z, Lehrer D, et al; ACRIN 6666 Investigators. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394–1404.
- Brennan S, Liberman L, Dershaw DD, Morris E. Breast MRI screening of women with a personal history of breast cancer. AJR Am J Roentgenol. 2010;195(2):510–516.
- Lehman CD, Lee JM, DeMartini WB, et al. Screening MRI in women with a personal history of breast cancer. J Natl Cancer Inst. 2016;108(3).
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2016]. J Clin Oncol. JCO634147.
- Corsetti V, Houssami N, Ghirardi M, et al. Evidence of the effect of adjunct ultrasound screening in women with mammography-negative dense breasts: interval breast cancers at 1 year follow-up. Eur J Cancer. 2011;47(7):1021–1026.
- Ohuchi N, Suzuki A, Sobue T, et al; J-START Investigator Groups. Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan Strategic Anti-Cancer Randomized Trial (J-START): a randomised controlled trial. Lancet. 2016;387(10016):341–348.
- Berg WA, Mendelson EB. Technologist-performed handheld screening breast US imaging: how is it performed and what are the outcomes to date? Radiology. 2014;272(1):12–27.
- Brem RF, Tabár L, Duffy SW, et al. Assessing improvement in detection of breast cancer with three-dimensional automated breast US in women with dense breast tissue: the SomoInsight study. Radiology. 2015;274(3):663–673.
- Kelly KM, Dean J, Comulada WS, Lee SJ. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010;20(3):734–742.
- Lehman CD, Arao RF, Sprague BL, et al. National performance benchmarks for modern screening digital mammography: update from the Breast Cancer Surveillance Consortium. Radiology. 2017;283(1):49–58.
- Kerlikowske K, Zhu W, Hubbard RA, et al; Breast Cancer Surveillance Consortium. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern Med. 2013;173(9):807–816.
- Friedewald SM, Rafferty EA, Rose SL, et al. Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA. 2014;311(24):2499–2507.
- Skaane P, Bandos AI, Gullien R, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267(1):47–56.
- Ciatto S, Houssami N, Bernardi D, et al. Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): a prospective comparison study. Lancet Oncol. 2013;14(7):583–589.
- Bahl M, Lamb LR, Lehman CD. Pathologic outcomes of architectural distortion on digital 2D versus tomosynthesis mammography [published online ahead of print August 23, 2017]. AJR Am J Roentgenol. doi:10.2214/AJR.17.17979.
- Engmann NJ, Golmakani MK, Miglioretti DL, Sprague BL, Kerlikowske K; Breast Cancer Surveillance Consortium. Population-attributable risk proportion of clinical risk factors for breast cancer [published online ahead of print February 2, 2017]. JAMA Oncol. doi:10.1001/jamaoncol.2016.6326.
- Oeffinger KC, Fontham ET, Etzioni R, et al; American Cancer Society. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599–1614.
- Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW. Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet. 2003;361(9367):1405–1410.
- Lee SJ, Boscardin WJ, Stijacic-Cenzer I, Conell-Price J, O’Brien S, Walter LC. Time lag to benefit after screening for breast and colorectal cancer: meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark. BMJ. 2013;346:e8441.
- Walter LC, Covinsky KE. Cancer screening in elderly patients: a framework for individualized decision making. JAMA. 2001;285(21):2750–2756.
- Sickles EA, D’Orsi CJ, Bassett LW, et al. ACR BI-RADS mammography. In: D’Orsi CJ, Sickles EA, Mendelson EB, et al, eds. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. 5th ed. Reston, VA: American College of Radiology; 2013.
- Sprague BL, Gangnon RE, Burt V, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014;106(10).
- Rafferty EA, Durand MA, Conant EF, et al. Breast cancer screening using tomosynthesis and digital mammography in dense and nondense breasts. JAMA. 2016;315(16):1784–1786.
- Berg WA. Tailored supplemental screening for breast cancer: what now and what next? AJR Am J Roentgenol. 2009;192(2):390–399.
- Heijnsdijk EA, Warner E, Gilbert FJ, et al. Differences in natural history between breast cancers in BRCA1 and BRCA2 mutation carriers and effects of MRI screening—MRISC, MARIBS, and Canadian studies combined. Cancer Epidemiol Biomarkers Prev. 2012;21(9):1458–1468.
- Warner E, Hill K, Causer P, et al. Prospective study of breast cancer incidence in women with a BRCA1 or BRCA2 mutation under surveillance with and without magnetic resonance imaging. J Clin Oncol. 2011;29(13):1664–1669.
- Berg WA, Blume JD, Adams AM, et al. Reasons women at elevated risk of breast cancer refuse breast MR imaging screening: ACRIN 6666. Radiology. 2010;254(1):79–87.
- Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection—a novel approach to breast cancer screening with MRI. J Clin Oncol. 2014;32(22):2304–2310.
- Strahle DA, Pathak DR, Sierra A, Saha S, Strahle C, Devisetty K. Systematic development of an abbreviated protocol for screening breast magnetic resonance imaging. Breast Cancer Res Treat. 2017;162(2):283–295.
- Kuhl CK, Strobel K, Bieling H, Leutner C, Schild HH, Schrading S. Supplemental breast MR imaging screening of women with average risk of breast cancer. Radiology. 2017;283(2):361–370.
- Saslow D, Boetes C, Burke W, et al; American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
- National Comprehensive Cancer Network. NCCN guidelines for detection, prevention, and risk reduction: breast cancer screening and diagnosis. https://www.nccn.org/professionals/physician_gls/pdf/breast-screening.pdf.
- Berg WA, Zhang Z, Lehrer D, et al; ACRIN 6666 Investigators. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394–1404.
- Brennan S, Liberman L, Dershaw DD, Morris E. Breast MRI screening of women with a personal history of breast cancer. AJR Am J Roentgenol. 2010;195(2):510–516.
- Lehman CD, Lee JM, DeMartini WB, et al. Screening MRI in women with a personal history of breast cancer. J Natl Cancer Inst. 2016;108(3).
- Tagliafico AS, Calabrese M, Mariscotti G, et al. Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial [published online ahead of print March 9, 2016]. J Clin Oncol. JCO634147.
- Corsetti V, Houssami N, Ghirardi M, et al. Evidence of the effect of adjunct ultrasound screening in women with mammography-negative dense breasts: interval breast cancers at 1 year follow-up. Eur J Cancer. 2011;47(7):1021–1026.
- Ohuchi N, Suzuki A, Sobue T, et al; J-START Investigator Groups. Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan Strategic Anti-Cancer Randomized Trial (J-START): a randomised controlled trial. Lancet. 2016;387(10016):341–348.
- Berg WA, Mendelson EB. Technologist-performed handheld screening breast US imaging: how is it performed and what are the outcomes to date? Radiology. 2014;272(1):12–27.
- Brem RF, Tabár L, Duffy SW, et al. Assessing improvement in detection of breast cancer with three-dimensional automated breast US in women with dense breast tissue: the SomoInsight study. Radiology. 2015;274(3):663–673.
- Kelly KM, Dean J, Comulada WS, Lee SJ. Breast cancer detection using automated whole breast ultrasound and mammography in radiographically dense breasts. Eur Radiol. 2010;20(3):734–742.
- Lehman CD, Arao RF, Sprague BL, et al. National performance benchmarks for modern screening digital mammography: update from the Breast Cancer Surveillance Consortium. Radiology. 2017;283(1):49–58.
- Kerlikowske K, Zhu W, Hubbard RA, et al; Breast Cancer Surveillance Consortium. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern Med. 2013;173(9):807–816.
- Friedewald SM, Rafferty EA, Rose SL, et al. Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA. 2014;311(24):2499–2507.
- Skaane P, Bandos AI, Gullien R, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013;267(1):47–56.
- Ciatto S, Houssami N, Bernardi D, et al. Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): a prospective comparison study. Lancet Oncol. 2013;14(7):583–589.
- Bahl M, Lamb LR, Lehman CD. Pathologic outcomes of architectural distortion on digital 2D versus tomosynthesis mammography [published online ahead of print August 23, 2017]. AJR Am J Roentgenol. doi:10.2214/AJR.17.17979.
- Engmann NJ, Golmakani MK, Miglioretti DL, Sprague BL, Kerlikowske K; Breast Cancer Surveillance Consortium. Population-attributable risk proportion of clinical risk factors for breast cancer [published online ahead of print February 2, 2017]. JAMA Oncol. doi:10.1001/jamaoncol.2016.6326.