User login
Catch and Treat a Stealth Diagnosis: Obsessive-Compulsive Disorder
“Allie” is a 16-year-old African American female, presenting to her primary care provider for a routine well-child visit. She gets straight As in school, has a boyfriend, and works as a lifeguard. She is always on her phone using Snapchat, TikTok, and Instagram. Over the past year, it’s been taking her longer to turn off the phone and electronics at night. She needs to close the apps one by one and check the power sources a number of times. In the past few months, this ritual has become longer, includes more checks, and is interfering with sleep. She reports knowing this is abnormal and thinking she is “just kind of crazy” but she cannot stop. Her parents reassure her each evening. They now help her doublecheck that her devices are plugged in at least twice.
Unlike its depiction in the movies, many symptoms of obsessive-compulsive disorder (OCD) happen internally. Often patients are aware that these are “not normal” and cover up their experiences. It can be hard for treaters to learn about these challenges. Children spend years suffering from OCD and even regularly attend nonspecific therapy without being diagnosed. However,
OCD impacts 2.3% of the population in their lifetime but more than 28% of people report symptoms consistent with OCD traits.1 OCD symptoms have increased since the pandemic2 so it is showing up in primary care more frequently. Younger patients meet criteria when their symptoms on the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) are sufficiently present, and impact the ability to function. The youngest patients with OCD are more likely to be male1 and children are most likely to be identified between ages 8-12 and during the later teenage years,3 although symptoms can occur at any time in life.
Usually, symptom onset happens gradually and then waxes and wanes. Often OCD has been present over months to years but not identified until they reach a functional tipping point. Alternatively, symptoms caused by PANDAS/PANS occur out of the blue and should be treated according to infectious disease/autoimmune workup protocols. Other differential diagnosis for OCD include other anxiety disorders, mood disorders, eating disorders, psychotic disorders, and other compulsive behaviors. OCD, tics, and ADHD are a combination seen more frequently in younger patients.4 Comorbidities frequently occur, including anxiety disorders, mood disorders, impulse control disorders, and substance use disorders.1 PTSD frequently presents with comorbid OCD symptoms.1 Finding the underlying cause is key to effective treatment.
How do I identify OCD in primary care?
Administer the CY-BOCS if these symptoms cause inability to function. The cut off for moderate symptoms is a score of 16 or above. Like all mental health screening, clinical judgment should be used to interpret the score. Many therapists do not screen for OCD.
How do I treat OCD in primary care?
Exposure Therapy with Response Prevention (ERP) is the gold-standard therapy and medication management is most effective when paired with ERP. ERP helps patients list their obsessions and compulsions in order of how much anxiety they cause, then work on gradual exposure starting with those that cause the least amount of anxiety. Picking up on any sneaky internal or external “responses” is important. An example response could include externally checking the rearview mirror to make sure the patient didn’t run over a puppy after they hit a pothole, or internally reassuring themselves. This “response prevention” can be the trickiest part of the therapy and is key to efficacy.
How to access ERP?
The International OCD Foundation offers a list of therapists trained in ERP, and most states’ psychiatry access lines can help primary care providers find available targeted resources. Despite these resources, it can be frustrating to help a family try find any available therapist who takes insurance, let alone a specialist. A recent JAMA article review found that IInternet-based treatment with both therapist- and non-therapist–guided interventions resulted in symptom improvements.2 Interventions that include parents are most helpful for children.
Other therapy options include:
- MGH/McLean/ (iocd.org) hosts an online, low cost ($65 per family) OCD camp for those age 6-17 and caregivers found here.
- Many workbooks are available, Standing Up to OCD Workbook for Kids by Tyson Reuter, PhD, is one good option.
- A book for parents about how not to accidentally reinforce anxiety is Anxious Kids, Anxious Parents: 7 Ways to Stop the Worry Cycle by Lynn Lyons and Reid Wilson.
- Sometimes a therapist without expertise can work with families using workbooks and other supports to help with ERP.
Medication options
Medications alone do not cure OCD, but can help patients better participate in ERP therapy. When the most likely cause of OCD symptoms is OCD (ruling out family history of bipolar or other psychiatric illness), using SSRIs to treat symptoms is the gold standard for medications. There is FDA approval for sertraline (≥ age 6) and fluoxetine (≥ age 7) as first-line options. If tolerated, up-titrate to efficacy. Clomipramine and fluvoxamine also have FDA approval but have more side effects so are not first line. Citalopram has randomized clinical trial support.5
Allie’s primary care provider administered and scored the CY-BOCS, started her on an SSRI, and up-titrated to efficacy over 4 months. The family signed up for an online OCD camp and learned more about OCD at iocdf.org. They talked with her therapist and worked through an OCD workbook together as no specialist was available. Her parents decreased their reassurances. Because of her primary care provider’s intervention, Allie got the care she required and was better prepared to face future exacerbations.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. Ruscio AM et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010 Jan;15(1):53-63. doi: 10.1038/mp.2008.94.
2. Lattie EG, Stamatis CA. Focusing on accessibility of evidence-based treatments for obsessive-compulsive disorder. JAMA Netw Open. 2022;5(3):e221978. doi: 10.1001/jamanetworkopen.2022.1978.
3. International OCD Foundation pediatric OCD for professionals. https://kids.iocdf.org/professionals/md/pediatric-ocd/. Accessed December 27, 2023.
4. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 2013. https://doi.org/10.1176/appi.books.9780890425596. Accessed December 27, 2023.5. Hilt RJ, Nussbaum AM. DSM-5 pocket guide to child and adolescent mental health. Arlington, Virginia: American Psychiatric Association Publishing, 2015.
“Allie” is a 16-year-old African American female, presenting to her primary care provider for a routine well-child visit. She gets straight As in school, has a boyfriend, and works as a lifeguard. She is always on her phone using Snapchat, TikTok, and Instagram. Over the past year, it’s been taking her longer to turn off the phone and electronics at night. She needs to close the apps one by one and check the power sources a number of times. In the past few months, this ritual has become longer, includes more checks, and is interfering with sleep. She reports knowing this is abnormal and thinking she is “just kind of crazy” but she cannot stop. Her parents reassure her each evening. They now help her doublecheck that her devices are plugged in at least twice.
Unlike its depiction in the movies, many symptoms of obsessive-compulsive disorder (OCD) happen internally. Often patients are aware that these are “not normal” and cover up their experiences. It can be hard for treaters to learn about these challenges. Children spend years suffering from OCD and even regularly attend nonspecific therapy without being diagnosed. However,
OCD impacts 2.3% of the population in their lifetime but more than 28% of people report symptoms consistent with OCD traits.1 OCD symptoms have increased since the pandemic2 so it is showing up in primary care more frequently. Younger patients meet criteria when their symptoms on the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) are sufficiently present, and impact the ability to function. The youngest patients with OCD are more likely to be male1 and children are most likely to be identified between ages 8-12 and during the later teenage years,3 although symptoms can occur at any time in life.
Usually, symptom onset happens gradually and then waxes and wanes. Often OCD has been present over months to years but not identified until they reach a functional tipping point. Alternatively, symptoms caused by PANDAS/PANS occur out of the blue and should be treated according to infectious disease/autoimmune workup protocols. Other differential diagnosis for OCD include other anxiety disorders, mood disorders, eating disorders, psychotic disorders, and other compulsive behaviors. OCD, tics, and ADHD are a combination seen more frequently in younger patients.4 Comorbidities frequently occur, including anxiety disorders, mood disorders, impulse control disorders, and substance use disorders.1 PTSD frequently presents with comorbid OCD symptoms.1 Finding the underlying cause is key to effective treatment.
How do I identify OCD in primary care?
Administer the CY-BOCS if these symptoms cause inability to function. The cut off for moderate symptoms is a score of 16 or above. Like all mental health screening, clinical judgment should be used to interpret the score. Many therapists do not screen for OCD.
How do I treat OCD in primary care?
Exposure Therapy with Response Prevention (ERP) is the gold-standard therapy and medication management is most effective when paired with ERP. ERP helps patients list their obsessions and compulsions in order of how much anxiety they cause, then work on gradual exposure starting with those that cause the least amount of anxiety. Picking up on any sneaky internal or external “responses” is important. An example response could include externally checking the rearview mirror to make sure the patient didn’t run over a puppy after they hit a pothole, or internally reassuring themselves. This “response prevention” can be the trickiest part of the therapy and is key to efficacy.
How to access ERP?
The International OCD Foundation offers a list of therapists trained in ERP, and most states’ psychiatry access lines can help primary care providers find available targeted resources. Despite these resources, it can be frustrating to help a family try find any available therapist who takes insurance, let alone a specialist. A recent JAMA article review found that IInternet-based treatment with both therapist- and non-therapist–guided interventions resulted in symptom improvements.2 Interventions that include parents are most helpful for children.
Other therapy options include:
- MGH/McLean/ (iocd.org) hosts an online, low cost ($65 per family) OCD camp for those age 6-17 and caregivers found here.
- Many workbooks are available, Standing Up to OCD Workbook for Kids by Tyson Reuter, PhD, is one good option.
- A book for parents about how not to accidentally reinforce anxiety is Anxious Kids, Anxious Parents: 7 Ways to Stop the Worry Cycle by Lynn Lyons and Reid Wilson.
- Sometimes a therapist without expertise can work with families using workbooks and other supports to help with ERP.
Medication options
Medications alone do not cure OCD, but can help patients better participate in ERP therapy. When the most likely cause of OCD symptoms is OCD (ruling out family history of bipolar or other psychiatric illness), using SSRIs to treat symptoms is the gold standard for medications. There is FDA approval for sertraline (≥ age 6) and fluoxetine (≥ age 7) as first-line options. If tolerated, up-titrate to efficacy. Clomipramine and fluvoxamine also have FDA approval but have more side effects so are not first line. Citalopram has randomized clinical trial support.5
Allie’s primary care provider administered and scored the CY-BOCS, started her on an SSRI, and up-titrated to efficacy over 4 months. The family signed up for an online OCD camp and learned more about OCD at iocdf.org. They talked with her therapist and worked through an OCD workbook together as no specialist was available. Her parents decreased their reassurances. Because of her primary care provider’s intervention, Allie got the care she required and was better prepared to face future exacerbations.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. Ruscio AM et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010 Jan;15(1):53-63. doi: 10.1038/mp.2008.94.
2. Lattie EG, Stamatis CA. Focusing on accessibility of evidence-based treatments for obsessive-compulsive disorder. JAMA Netw Open. 2022;5(3):e221978. doi: 10.1001/jamanetworkopen.2022.1978.
3. International OCD Foundation pediatric OCD for professionals. https://kids.iocdf.org/professionals/md/pediatric-ocd/. Accessed December 27, 2023.
4. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 2013. https://doi.org/10.1176/appi.books.9780890425596. Accessed December 27, 2023.5. Hilt RJ, Nussbaum AM. DSM-5 pocket guide to child and adolescent mental health. Arlington, Virginia: American Psychiatric Association Publishing, 2015.
“Allie” is a 16-year-old African American female, presenting to her primary care provider for a routine well-child visit. She gets straight As in school, has a boyfriend, and works as a lifeguard. She is always on her phone using Snapchat, TikTok, and Instagram. Over the past year, it’s been taking her longer to turn off the phone and electronics at night. She needs to close the apps one by one and check the power sources a number of times. In the past few months, this ritual has become longer, includes more checks, and is interfering with sleep. She reports knowing this is abnormal and thinking she is “just kind of crazy” but she cannot stop. Her parents reassure her each evening. They now help her doublecheck that her devices are plugged in at least twice.
Unlike its depiction in the movies, many symptoms of obsessive-compulsive disorder (OCD) happen internally. Often patients are aware that these are “not normal” and cover up their experiences. It can be hard for treaters to learn about these challenges. Children spend years suffering from OCD and even regularly attend nonspecific therapy without being diagnosed. However,
OCD impacts 2.3% of the population in their lifetime but more than 28% of people report symptoms consistent with OCD traits.1 OCD symptoms have increased since the pandemic2 so it is showing up in primary care more frequently. Younger patients meet criteria when their symptoms on the Children’s Yale-Brown Obsessive Compulsive Scale (CY-BOCS) are sufficiently present, and impact the ability to function. The youngest patients with OCD are more likely to be male1 and children are most likely to be identified between ages 8-12 and during the later teenage years,3 although symptoms can occur at any time in life.
Usually, symptom onset happens gradually and then waxes and wanes. Often OCD has been present over months to years but not identified until they reach a functional tipping point. Alternatively, symptoms caused by PANDAS/PANS occur out of the blue and should be treated according to infectious disease/autoimmune workup protocols. Other differential diagnosis for OCD include other anxiety disorders, mood disorders, eating disorders, psychotic disorders, and other compulsive behaviors. OCD, tics, and ADHD are a combination seen more frequently in younger patients.4 Comorbidities frequently occur, including anxiety disorders, mood disorders, impulse control disorders, and substance use disorders.1 PTSD frequently presents with comorbid OCD symptoms.1 Finding the underlying cause is key to effective treatment.
How do I identify OCD in primary care?
Administer the CY-BOCS if these symptoms cause inability to function. The cut off for moderate symptoms is a score of 16 or above. Like all mental health screening, clinical judgment should be used to interpret the score. Many therapists do not screen for OCD.
How do I treat OCD in primary care?
Exposure Therapy with Response Prevention (ERP) is the gold-standard therapy and medication management is most effective when paired with ERP. ERP helps patients list their obsessions and compulsions in order of how much anxiety they cause, then work on gradual exposure starting with those that cause the least amount of anxiety. Picking up on any sneaky internal or external “responses” is important. An example response could include externally checking the rearview mirror to make sure the patient didn’t run over a puppy after they hit a pothole, or internally reassuring themselves. This “response prevention” can be the trickiest part of the therapy and is key to efficacy.
How to access ERP?
The International OCD Foundation offers a list of therapists trained in ERP, and most states’ psychiatry access lines can help primary care providers find available targeted resources. Despite these resources, it can be frustrating to help a family try find any available therapist who takes insurance, let alone a specialist. A recent JAMA article review found that IInternet-based treatment with both therapist- and non-therapist–guided interventions resulted in symptom improvements.2 Interventions that include parents are most helpful for children.
Other therapy options include:
- MGH/McLean/ (iocd.org) hosts an online, low cost ($65 per family) OCD camp for those age 6-17 and caregivers found here.
- Many workbooks are available, Standing Up to OCD Workbook for Kids by Tyson Reuter, PhD, is one good option.
- A book for parents about how not to accidentally reinforce anxiety is Anxious Kids, Anxious Parents: 7 Ways to Stop the Worry Cycle by Lynn Lyons and Reid Wilson.
- Sometimes a therapist without expertise can work with families using workbooks and other supports to help with ERP.
Medication options
Medications alone do not cure OCD, but can help patients better participate in ERP therapy. When the most likely cause of OCD symptoms is OCD (ruling out family history of bipolar or other psychiatric illness), using SSRIs to treat symptoms is the gold standard for medications. There is FDA approval for sertraline (≥ age 6) and fluoxetine (≥ age 7) as first-line options. If tolerated, up-titrate to efficacy. Clomipramine and fluvoxamine also have FDA approval but have more side effects so are not first line. Citalopram has randomized clinical trial support.5
Allie’s primary care provider administered and scored the CY-BOCS, started her on an SSRI, and up-titrated to efficacy over 4 months. The family signed up for an online OCD camp and learned more about OCD at iocdf.org. They talked with her therapist and worked through an OCD workbook together as no specialist was available. Her parents decreased their reassurances. Because of her primary care provider’s intervention, Allie got the care she required and was better prepared to face future exacerbations.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. Ruscio AM et al. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. 2010 Jan;15(1):53-63. doi: 10.1038/mp.2008.94.
2. Lattie EG, Stamatis CA. Focusing on accessibility of evidence-based treatments for obsessive-compulsive disorder. JAMA Netw Open. 2022;5(3):e221978. doi: 10.1001/jamanetworkopen.2022.1978.
3. International OCD Foundation pediatric OCD for professionals. https://kids.iocdf.org/professionals/md/pediatric-ocd/. Accessed December 27, 2023.
4. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 2013. https://doi.org/10.1176/appi.books.9780890425596. Accessed December 27, 2023.5. Hilt RJ, Nussbaum AM. DSM-5 pocket guide to child and adolescent mental health. Arlington, Virginia: American Psychiatric Association Publishing, 2015.
Nodal Radiation May Make BC Axillary Dissection Unnecessary
SAN ANTONIO — Axillary lymph node dissection may be unnecessary if breast cancer patients with one or two positive sentinel lymph nodes plan to have adjuvant nodal radiation, according to a major Scandinavian trial presented at the San Antonio Breast Cancer Symposium.
“It means that you don’t need to dissect the axilla if you” are going to “radiate the axilla.” “For the U.S., that’s the conclusion because there are still centers that do both, and that’s out,” lead investigator Jana de Boniface, MD, PhD, a breast cancer surgeon at the Karolinska Institutet, Stockholm, said in an interview.
Some even wondered if 5 years of endocrine therapy is necessary.
Dr. Boniface shared her thoughts after presenting the Scandinavian trial, SENOMAC, which she led.
SENOMAC randomized 1,204 patients with one or two positive sentinel lymph nodes to axillary dissection; 1,335 with the same finding were randomized to no dissection.
Subjects had clinically T1-3, N0 primary breast cancer. About 89% in both arms went on to adjuvant radiation, including nodal radiation, and almost all also went on to systemic therapy, which included endocrine therapy in over 90%. Only about 2% of subjects had neoadjuvant therapy.
At a median follow-up of nearly 4 years, recurrence-free survival was virtually identical in both groups, with 8% of patients in the dissection arm and 7.1% in the no-dissection group having recurrences. Estimated 5-year recurrence-free survival was just shy of 90% in both groups. Skipping dissection was strongly non-inferior to having one (P < .001).
SENOMAC “clearly shows that you don’t need to dissect the axilla if you have one to two positive sentinel lymph nodes” so long as patients have adjuvant nodal radiation. Recurrence-free survival “curves practically overlap, and we cannot see any difference between the two groups,” Dr. Boniface said.
Meanwhile, the dissection group fared worse on patient reported outcomes. Overall survival outcomes, the primary endpoint of the trial, are expected within 2 years.
The goal of the trial, the largest to date to look into the issue, was to fill gaps in the literature. Similar outcomes were reported around a decade ago in patients with low sentinel lymph node burdens, but the extensive exclusion criteria raised questions about general applicability.
In contrast, SENOMAC was widely inclusive. Over a third of patients had mastectomies, over a third had sentinel lymph node extracapsular extension, almost 6% had T3 disease, almost 20% had lobular carcinoma, 40% were 65 years or older, and tumors were as large as 15.5 cm.
The findings held regardless of those and other factors on subgroup analyses, including estrogen receptor and HER2 status and the number of additional positive nodes retrieved in the dissection group.
Andrea V. Barrio, MD, the study discussant and a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York, agreed with the message from SENOMAC.
“Based on this, ALND [axillary lymph node dissection] should not be considered standard in patients with clinical T1-3, N0 breast cancer with one to two positive sentinel nodes, with or without microscopic extracapsular extension, undergoing lumpectomy or mastectomy,” provided nodal adjuvant radiotherapy is indicated, she said.
Although adjuvant nodal radiation for patients with one to three positive sentinel nodes is standard of care in Denmark and Sweden, where most of the patients in SENOMAC were located, practices vary widely in the United States. If adjuvant radiation isn’t used, “then ALND [is still] indicated,” Dr. Barrio said, but in either case, “only one is needed.”
In keeping with the de-escalation theme at the 2023 symposium, both Dr. Boniface and Dr. Barrio noted that trials are now underway to find patients who can avoid any axillary treatment at all if they have just one or two positive sentinel lymph nodes.
Preoperative axillary ultrasound was mandatory in SENOMAC and patients with non-palpable suspicious axillary lymph nodes were enrolled.
Thirty-six were positive on fine needle aspiration and randomized into the study, but when asked, Dr. Boniface didn’t have the data immediately at hand on how they fared.
The work was funded by the Swedish Research Council, Nordic Cancer Union, and others. Dr. Boniface and Dr. Barrio didn’t have any disclosures.
SAN ANTONIO — Axillary lymph node dissection may be unnecessary if breast cancer patients with one or two positive sentinel lymph nodes plan to have adjuvant nodal radiation, according to a major Scandinavian trial presented at the San Antonio Breast Cancer Symposium.
“It means that you don’t need to dissect the axilla if you” are going to “radiate the axilla.” “For the U.S., that’s the conclusion because there are still centers that do both, and that’s out,” lead investigator Jana de Boniface, MD, PhD, a breast cancer surgeon at the Karolinska Institutet, Stockholm, said in an interview.
Some even wondered if 5 years of endocrine therapy is necessary.
Dr. Boniface shared her thoughts after presenting the Scandinavian trial, SENOMAC, which she led.
SENOMAC randomized 1,204 patients with one or two positive sentinel lymph nodes to axillary dissection; 1,335 with the same finding were randomized to no dissection.
Subjects had clinically T1-3, N0 primary breast cancer. About 89% in both arms went on to adjuvant radiation, including nodal radiation, and almost all also went on to systemic therapy, which included endocrine therapy in over 90%. Only about 2% of subjects had neoadjuvant therapy.
At a median follow-up of nearly 4 years, recurrence-free survival was virtually identical in both groups, with 8% of patients in the dissection arm and 7.1% in the no-dissection group having recurrences. Estimated 5-year recurrence-free survival was just shy of 90% in both groups. Skipping dissection was strongly non-inferior to having one (P < .001).
SENOMAC “clearly shows that you don’t need to dissect the axilla if you have one to two positive sentinel lymph nodes” so long as patients have adjuvant nodal radiation. Recurrence-free survival “curves practically overlap, and we cannot see any difference between the two groups,” Dr. Boniface said.
Meanwhile, the dissection group fared worse on patient reported outcomes. Overall survival outcomes, the primary endpoint of the trial, are expected within 2 years.
The goal of the trial, the largest to date to look into the issue, was to fill gaps in the literature. Similar outcomes were reported around a decade ago in patients with low sentinel lymph node burdens, but the extensive exclusion criteria raised questions about general applicability.
In contrast, SENOMAC was widely inclusive. Over a third of patients had mastectomies, over a third had sentinel lymph node extracapsular extension, almost 6% had T3 disease, almost 20% had lobular carcinoma, 40% were 65 years or older, and tumors were as large as 15.5 cm.
The findings held regardless of those and other factors on subgroup analyses, including estrogen receptor and HER2 status and the number of additional positive nodes retrieved in the dissection group.
Andrea V. Barrio, MD, the study discussant and a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York, agreed with the message from SENOMAC.
“Based on this, ALND [axillary lymph node dissection] should not be considered standard in patients with clinical T1-3, N0 breast cancer with one to two positive sentinel nodes, with or without microscopic extracapsular extension, undergoing lumpectomy or mastectomy,” provided nodal adjuvant radiotherapy is indicated, she said.
Although adjuvant nodal radiation for patients with one to three positive sentinel nodes is standard of care in Denmark and Sweden, where most of the patients in SENOMAC were located, practices vary widely in the United States. If adjuvant radiation isn’t used, “then ALND [is still] indicated,” Dr. Barrio said, but in either case, “only one is needed.”
In keeping with the de-escalation theme at the 2023 symposium, both Dr. Boniface and Dr. Barrio noted that trials are now underway to find patients who can avoid any axillary treatment at all if they have just one or two positive sentinel lymph nodes.
Preoperative axillary ultrasound was mandatory in SENOMAC and patients with non-palpable suspicious axillary lymph nodes were enrolled.
Thirty-six were positive on fine needle aspiration and randomized into the study, but when asked, Dr. Boniface didn’t have the data immediately at hand on how they fared.
The work was funded by the Swedish Research Council, Nordic Cancer Union, and others. Dr. Boniface and Dr. Barrio didn’t have any disclosures.
SAN ANTONIO — Axillary lymph node dissection may be unnecessary if breast cancer patients with one or two positive sentinel lymph nodes plan to have adjuvant nodal radiation, according to a major Scandinavian trial presented at the San Antonio Breast Cancer Symposium.
“It means that you don’t need to dissect the axilla if you” are going to “radiate the axilla.” “For the U.S., that’s the conclusion because there are still centers that do both, and that’s out,” lead investigator Jana de Boniface, MD, PhD, a breast cancer surgeon at the Karolinska Institutet, Stockholm, said in an interview.
Some even wondered if 5 years of endocrine therapy is necessary.
Dr. Boniface shared her thoughts after presenting the Scandinavian trial, SENOMAC, which she led.
SENOMAC randomized 1,204 patients with one or two positive sentinel lymph nodes to axillary dissection; 1,335 with the same finding were randomized to no dissection.
Subjects had clinically T1-3, N0 primary breast cancer. About 89% in both arms went on to adjuvant radiation, including nodal radiation, and almost all also went on to systemic therapy, which included endocrine therapy in over 90%. Only about 2% of subjects had neoadjuvant therapy.
At a median follow-up of nearly 4 years, recurrence-free survival was virtually identical in both groups, with 8% of patients in the dissection arm and 7.1% in the no-dissection group having recurrences. Estimated 5-year recurrence-free survival was just shy of 90% in both groups. Skipping dissection was strongly non-inferior to having one (P < .001).
SENOMAC “clearly shows that you don’t need to dissect the axilla if you have one to two positive sentinel lymph nodes” so long as patients have adjuvant nodal radiation. Recurrence-free survival “curves practically overlap, and we cannot see any difference between the two groups,” Dr. Boniface said.
Meanwhile, the dissection group fared worse on patient reported outcomes. Overall survival outcomes, the primary endpoint of the trial, are expected within 2 years.
The goal of the trial, the largest to date to look into the issue, was to fill gaps in the literature. Similar outcomes were reported around a decade ago in patients with low sentinel lymph node burdens, but the extensive exclusion criteria raised questions about general applicability.
In contrast, SENOMAC was widely inclusive. Over a third of patients had mastectomies, over a third had sentinel lymph node extracapsular extension, almost 6% had T3 disease, almost 20% had lobular carcinoma, 40% were 65 years or older, and tumors were as large as 15.5 cm.
The findings held regardless of those and other factors on subgroup analyses, including estrogen receptor and HER2 status and the number of additional positive nodes retrieved in the dissection group.
Andrea V. Barrio, MD, the study discussant and a breast cancer surgeon at Memorial Sloan Kettering Cancer Center, New York, agreed with the message from SENOMAC.
“Based on this, ALND [axillary lymph node dissection] should not be considered standard in patients with clinical T1-3, N0 breast cancer with one to two positive sentinel nodes, with or without microscopic extracapsular extension, undergoing lumpectomy or mastectomy,” provided nodal adjuvant radiotherapy is indicated, she said.
Although adjuvant nodal radiation for patients with one to three positive sentinel nodes is standard of care in Denmark and Sweden, where most of the patients in SENOMAC were located, practices vary widely in the United States. If adjuvant radiation isn’t used, “then ALND [is still] indicated,” Dr. Barrio said, but in either case, “only one is needed.”
In keeping with the de-escalation theme at the 2023 symposium, both Dr. Boniface and Dr. Barrio noted that trials are now underway to find patients who can avoid any axillary treatment at all if they have just one or two positive sentinel lymph nodes.
Preoperative axillary ultrasound was mandatory in SENOMAC and patients with non-palpable suspicious axillary lymph nodes were enrolled.
Thirty-six were positive on fine needle aspiration and randomized into the study, but when asked, Dr. Boniface didn’t have the data immediately at hand on how they fared.
The work was funded by the Swedish Research Council, Nordic Cancer Union, and others. Dr. Boniface and Dr. Barrio didn’t have any disclosures.
FROM SABCS 2023
Diagnosing Adrenal Insufficiency: The ‘Quick and Dirty’ Method
Matthew F. Watto, MD: Welcome back to The Curbsiders. I’m Dr. Matthew Watto, here with America’s primary care physician, Dr. Paul Nelson Williams. Paul, are you ready to talk about some adrenal insufficiency? We had a great conversation with Dr. Atil Kargi, and I’d like you to start us off.
Paul N. Williams, MD: How about thinking about it? It’s a good place to start.
That’s one of the ways this episode changed my approach a little bit. I never really thought about the fact that . It’s such a protean sort of nonspecific presentation. But if you have someone with chronic malaise and poor appetite and maybe unexplained weight loss, and your GI workup is not really leading you anywhere, it’s probably worth thinking about adrenal insufficiency. Even though primary adrenal insufficiency is pretty rare — we’re talking cases per millions — secondary adrenal insufficiency is actually fairly common. It’s probably worth thinking about and testing for more often than I have in the past. So for me, it’s having a lower threshold to start looking for it.
Dr. Watto: When it’s adrenal crisis, you probably think about it, but then it’s too late. Ideally, you would think about it before that happens. But the symptoms can be quite vague. The mineralocorticoid symptoms, like salt cravings, dizziness, near syncope, muscle cramps, might make me think of it because they sound more like something endocrine is going on. But if it’s just a little weight loss, a little fatigue, or a little nausea, that’s everybody.
Dr. Williams: Right. If a patient came to me saying, “I’m craving salt,” that might hasten the workup a little bit, but that’s not the typical presentation.
Dr. Watto: If you are going to check a cortisol level, you should really check it in the morning, between 7 AM and 9 AM. If you check it too early, it might not have peaked yet, so you might get a level that looks low. But if you had checked an hour or 2 later, it might have been above a threshold, and then you would know you could rule out the diagnosis. The cutoffs depend on your source: < 3-5 µg/dL that early in the morning is pretty much diagnostic of adrenal insufficiency. If it’s > 15 µg/dL, that’s a pretty robust cortisol and the patient probably doesn’t have adrenal insufficiency. But if the level is between 5 µg/dL and 15 µg/dL, you’re in a gray zone, and that’s where you might think about doing a stimulation (stim) test.
Dr. Kargi gave us a quick and dirty version of the stim test. Paul, have you had a chance to try this yet?
Dr. Williams: I have not. Have you? I’m sure you’ve been just waiting for the chance.
Dr. Watto: I would love to do this. I don›t know whether I›m set up to do it in the office right now. But this is an aspirational goal for my practice, and I›m sure some physicians are set up in their office already to do it. You can give either intramuscular or subcutaneous cosyntropin 250 µg. You don›t even have to get a baseline cortisol level right before the injection. Let›s say the patient›s previous cortisol level was between 5 µg/dL and 15 µg/dL, so you weren›t sure about the diagnosis. You bring them back to the office one day, give them a shot of cosyntropin, and then 30-60 minutes later, have a random cortisol drawn. If it›s > 19 µg/dL, you›ve ruled out adrenal insufficiency. If it›s anything else, send them to an endocrinologist to sort it out. You might be able to make the diagnosis yourself doing that.
Any treatment pearls to leave the audience with?
Dr. Williams: I hope endocrinologists don›t take issue with this. I say this with respect and admiration, but it feels kind of vibe-based to me. Without a lab value to guide treatment, you are dependent on the patient telling you how they feel much of the time. You have to let their symptoms guide you. It is probably worth noting that because hydrocortisone has a relatively short half-life, within hours, in fact, you typically have to do twice-daily dosing, sometimes even three times daily dosing to get patients to where they feel okay. It sounds like there›s a fair amount of trial and error and some adjustments that you have to make depending on what›s going on with the patient at any given time. You land somewhere between a dose of 15-30 mg per day, but there will be some variability, even within an individual patient, depending on what›s going on with them from a physiologic standpoint.
Dr. Watto: They are going to take one dose in the morning and then a second dose in the afternoon, but they don’t want them to take it too late in the evening because it could cause insomnia, and you want to try to mimic physiologic levels as much as you can. Two thirds of the daily dose is given early in the morning and then another third of the daily dose later in the day if you are prescribing two times daily dosing.
And Dr. Kargi had a low threshold for doubling the dose. If the patient has a cold, double the dose for 2 or 3 days. With a high fever, triple the dose for a few days. If they are going for surgery, they are probably going to be getting some intravenous hydrocortisone while they’re in the hospital.
We really turned over like every stone we could possibly think of on this podcast. There were so many great pearls that we don’t have time to go through them all here. But we talked about steroid tapers and a lot more. You can check it out here.
Dr. Watto has disclosed no relevant financial relationships.
Dr. Williams has disclosed the following relevant financial relationships:Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: The CurbsidersReceived income in an amount equal to or greater than $250 from: The Curbsiders.
A version of this article appeared on Medscape.com.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I’m Dr. Matthew Watto, here with America’s primary care physician, Dr. Paul Nelson Williams. Paul, are you ready to talk about some adrenal insufficiency? We had a great conversation with Dr. Atil Kargi, and I’d like you to start us off.
Paul N. Williams, MD: How about thinking about it? It’s a good place to start.
That’s one of the ways this episode changed my approach a little bit. I never really thought about the fact that . It’s such a protean sort of nonspecific presentation. But if you have someone with chronic malaise and poor appetite and maybe unexplained weight loss, and your GI workup is not really leading you anywhere, it’s probably worth thinking about adrenal insufficiency. Even though primary adrenal insufficiency is pretty rare — we’re talking cases per millions — secondary adrenal insufficiency is actually fairly common. It’s probably worth thinking about and testing for more often than I have in the past. So for me, it’s having a lower threshold to start looking for it.
Dr. Watto: When it’s adrenal crisis, you probably think about it, but then it’s too late. Ideally, you would think about it before that happens. But the symptoms can be quite vague. The mineralocorticoid symptoms, like salt cravings, dizziness, near syncope, muscle cramps, might make me think of it because they sound more like something endocrine is going on. But if it’s just a little weight loss, a little fatigue, or a little nausea, that’s everybody.
Dr. Williams: Right. If a patient came to me saying, “I’m craving salt,” that might hasten the workup a little bit, but that’s not the typical presentation.
Dr. Watto: If you are going to check a cortisol level, you should really check it in the morning, between 7 AM and 9 AM. If you check it too early, it might not have peaked yet, so you might get a level that looks low. But if you had checked an hour or 2 later, it might have been above a threshold, and then you would know you could rule out the diagnosis. The cutoffs depend on your source: < 3-5 µg/dL that early in the morning is pretty much diagnostic of adrenal insufficiency. If it’s > 15 µg/dL, that’s a pretty robust cortisol and the patient probably doesn’t have adrenal insufficiency. But if the level is between 5 µg/dL and 15 µg/dL, you’re in a gray zone, and that’s where you might think about doing a stimulation (stim) test.
Dr. Kargi gave us a quick and dirty version of the stim test. Paul, have you had a chance to try this yet?
Dr. Williams: I have not. Have you? I’m sure you’ve been just waiting for the chance.
Dr. Watto: I would love to do this. I don›t know whether I›m set up to do it in the office right now. But this is an aspirational goal for my practice, and I›m sure some physicians are set up in their office already to do it. You can give either intramuscular or subcutaneous cosyntropin 250 µg. You don›t even have to get a baseline cortisol level right before the injection. Let›s say the patient›s previous cortisol level was between 5 µg/dL and 15 µg/dL, so you weren›t sure about the diagnosis. You bring them back to the office one day, give them a shot of cosyntropin, and then 30-60 minutes later, have a random cortisol drawn. If it›s > 19 µg/dL, you›ve ruled out adrenal insufficiency. If it›s anything else, send them to an endocrinologist to sort it out. You might be able to make the diagnosis yourself doing that.
Any treatment pearls to leave the audience with?
Dr. Williams: I hope endocrinologists don›t take issue with this. I say this with respect and admiration, but it feels kind of vibe-based to me. Without a lab value to guide treatment, you are dependent on the patient telling you how they feel much of the time. You have to let their symptoms guide you. It is probably worth noting that because hydrocortisone has a relatively short half-life, within hours, in fact, you typically have to do twice-daily dosing, sometimes even three times daily dosing to get patients to where they feel okay. It sounds like there›s a fair amount of trial and error and some adjustments that you have to make depending on what›s going on with the patient at any given time. You land somewhere between a dose of 15-30 mg per day, but there will be some variability, even within an individual patient, depending on what›s going on with them from a physiologic standpoint.
Dr. Watto: They are going to take one dose in the morning and then a second dose in the afternoon, but they don’t want them to take it too late in the evening because it could cause insomnia, and you want to try to mimic physiologic levels as much as you can. Two thirds of the daily dose is given early in the morning and then another third of the daily dose later in the day if you are prescribing two times daily dosing.
And Dr. Kargi had a low threshold for doubling the dose. If the patient has a cold, double the dose for 2 or 3 days. With a high fever, triple the dose for a few days. If they are going for surgery, they are probably going to be getting some intravenous hydrocortisone while they’re in the hospital.
We really turned over like every stone we could possibly think of on this podcast. There were so many great pearls that we don’t have time to go through them all here. But we talked about steroid tapers and a lot more. You can check it out here.
Dr. Watto has disclosed no relevant financial relationships.
Dr. Williams has disclosed the following relevant financial relationships:Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: The CurbsidersReceived income in an amount equal to or greater than $250 from: The Curbsiders.
A version of this article appeared on Medscape.com.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I’m Dr. Matthew Watto, here with America’s primary care physician, Dr. Paul Nelson Williams. Paul, are you ready to talk about some adrenal insufficiency? We had a great conversation with Dr. Atil Kargi, and I’d like you to start us off.
Paul N. Williams, MD: How about thinking about it? It’s a good place to start.
That’s one of the ways this episode changed my approach a little bit. I never really thought about the fact that . It’s such a protean sort of nonspecific presentation. But if you have someone with chronic malaise and poor appetite and maybe unexplained weight loss, and your GI workup is not really leading you anywhere, it’s probably worth thinking about adrenal insufficiency. Even though primary adrenal insufficiency is pretty rare — we’re talking cases per millions — secondary adrenal insufficiency is actually fairly common. It’s probably worth thinking about and testing for more often than I have in the past. So for me, it’s having a lower threshold to start looking for it.
Dr. Watto: When it’s adrenal crisis, you probably think about it, but then it’s too late. Ideally, you would think about it before that happens. But the symptoms can be quite vague. The mineralocorticoid symptoms, like salt cravings, dizziness, near syncope, muscle cramps, might make me think of it because they sound more like something endocrine is going on. But if it’s just a little weight loss, a little fatigue, or a little nausea, that’s everybody.
Dr. Williams: Right. If a patient came to me saying, “I’m craving salt,” that might hasten the workup a little bit, but that’s not the typical presentation.
Dr. Watto: If you are going to check a cortisol level, you should really check it in the morning, between 7 AM and 9 AM. If you check it too early, it might not have peaked yet, so you might get a level that looks low. But if you had checked an hour or 2 later, it might have been above a threshold, and then you would know you could rule out the diagnosis. The cutoffs depend on your source: < 3-5 µg/dL that early in the morning is pretty much diagnostic of adrenal insufficiency. If it’s > 15 µg/dL, that’s a pretty robust cortisol and the patient probably doesn’t have adrenal insufficiency. But if the level is between 5 µg/dL and 15 µg/dL, you’re in a gray zone, and that’s where you might think about doing a stimulation (stim) test.
Dr. Kargi gave us a quick and dirty version of the stim test. Paul, have you had a chance to try this yet?
Dr. Williams: I have not. Have you? I’m sure you’ve been just waiting for the chance.
Dr. Watto: I would love to do this. I don›t know whether I›m set up to do it in the office right now. But this is an aspirational goal for my practice, and I›m sure some physicians are set up in their office already to do it. You can give either intramuscular or subcutaneous cosyntropin 250 µg. You don›t even have to get a baseline cortisol level right before the injection. Let›s say the patient›s previous cortisol level was between 5 µg/dL and 15 µg/dL, so you weren›t sure about the diagnosis. You bring them back to the office one day, give them a shot of cosyntropin, and then 30-60 minutes later, have a random cortisol drawn. If it›s > 19 µg/dL, you›ve ruled out adrenal insufficiency. If it›s anything else, send them to an endocrinologist to sort it out. You might be able to make the diagnosis yourself doing that.
Any treatment pearls to leave the audience with?
Dr. Williams: I hope endocrinologists don›t take issue with this. I say this with respect and admiration, but it feels kind of vibe-based to me. Without a lab value to guide treatment, you are dependent on the patient telling you how they feel much of the time. You have to let their symptoms guide you. It is probably worth noting that because hydrocortisone has a relatively short half-life, within hours, in fact, you typically have to do twice-daily dosing, sometimes even three times daily dosing to get patients to where they feel okay. It sounds like there›s a fair amount of trial and error and some adjustments that you have to make depending on what›s going on with the patient at any given time. You land somewhere between a dose of 15-30 mg per day, but there will be some variability, even within an individual patient, depending on what›s going on with them from a physiologic standpoint.
Dr. Watto: They are going to take one dose in the morning and then a second dose in the afternoon, but they don’t want them to take it too late in the evening because it could cause insomnia, and you want to try to mimic physiologic levels as much as you can. Two thirds of the daily dose is given early in the morning and then another third of the daily dose later in the day if you are prescribing two times daily dosing.
And Dr. Kargi had a low threshold for doubling the dose. If the patient has a cold, double the dose for 2 or 3 days. With a high fever, triple the dose for a few days. If they are going for surgery, they are probably going to be getting some intravenous hydrocortisone while they’re in the hospital.
We really turned over like every stone we could possibly think of on this podcast. There were so many great pearls that we don’t have time to go through them all here. But we talked about steroid tapers and a lot more. You can check it out here.
Dr. Watto has disclosed no relevant financial relationships.
Dr. Williams has disclosed the following relevant financial relationships:Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: The CurbsidersReceived income in an amount equal to or greater than $250 from: The Curbsiders.
A version of this article appeared on Medscape.com.
Artificial Sweeteners Alter the Duodenal Microbiome
TOPLINE:
and composition and levels of circulating inflammatory markers.
METHODOLOGY:
- Researchers analyzed samples from the REIMAGINE (Revealing the Entire Intestinal Microbiota and its Associations with the Genetic, Immunologic, and Neuroendocrine Ecosystem) study to assess the potential effects of NSS consumption on the duodenal luminal microbiome.
- They analyzed subjects consuming non-aspartame nonsugar sweeteners (NANS; n = 35) and aspartame only (ASP; n = 9), who were compared with 55 control participants matched for age, sex, and body mass index.
- A subset of 40 participants provided stool samples for additional analysis.
TAKEAWAY:
- Duodenal alpha diversity was lower in NANS consumers vs controls.
- Duodenal relative abundance (RA) of Escherichia, Klebsiella, and Salmonella was lower in both NANS and ASP vs controls, whereas stool RA of these phylum Proteobacteria was increased in both NANS and ASP.
- Compared with controls, NANS and ASP differed in how they altered predicted duodenal microbial metabolic pathways, with NANS impacting polysaccharides biosynthesis and D-galactose degradation and ASP significantly enriching biosynthesis of cylindrospermopsin, a potential cancer-causing agent known to adversely impact the liver and nervous system.
- Circulating levels of interleukin (IL)-1b, a pro-inflammatory cytokine that plays a key role in the immune response, were significantly decreased in NANS vs controls, whereas IL-6 and IL-10, two cytokines with protective properties, were decreased in the ASP group vs controls.
IN PRACTICE:
“Given the crucial role played by small intestinal microbes in digestion, nutrient absorption, immune regulation, and endocrine functions, coupled with the substantial prevalence of NSS consumption among US adults (estimated at 41.4%), our findings have potential implications for metabolic and gastrointestinal health in a considerable proportion of the American adult population.”
SOURCE:
The study, conducted by Ava Hosseini, MPH, and colleagues at Cedars-Sinai, Los Angeles, was published online on November 22, 2023, in iScience.
LIMITATIONS:
The study population may not be representative of healthy individuals as they underwent upper endoscopy for various reasons (eg, evaluation of intestinal complaints). After exclusions, the duodenal sample size for the aspartame group was small. Samples were collected at a single timepoint, limiting the ability to establish causal relationships.
DISCLOSURES:
This research was supported by Frank Lee, the Monica Lester Charitable Trust, and the Elias, Genevieve, and Georgianna Atol Charitable Trust through their support of the Medically Associated Science and Technology Program, Cedars-Sinai, Los Angeles. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
and composition and levels of circulating inflammatory markers.
METHODOLOGY:
- Researchers analyzed samples from the REIMAGINE (Revealing the Entire Intestinal Microbiota and its Associations with the Genetic, Immunologic, and Neuroendocrine Ecosystem) study to assess the potential effects of NSS consumption on the duodenal luminal microbiome.
- They analyzed subjects consuming non-aspartame nonsugar sweeteners (NANS; n = 35) and aspartame only (ASP; n = 9), who were compared with 55 control participants matched for age, sex, and body mass index.
- A subset of 40 participants provided stool samples for additional analysis.
TAKEAWAY:
- Duodenal alpha diversity was lower in NANS consumers vs controls.
- Duodenal relative abundance (RA) of Escherichia, Klebsiella, and Salmonella was lower in both NANS and ASP vs controls, whereas stool RA of these phylum Proteobacteria was increased in both NANS and ASP.
- Compared with controls, NANS and ASP differed in how they altered predicted duodenal microbial metabolic pathways, with NANS impacting polysaccharides biosynthesis and D-galactose degradation and ASP significantly enriching biosynthesis of cylindrospermopsin, a potential cancer-causing agent known to adversely impact the liver and nervous system.
- Circulating levels of interleukin (IL)-1b, a pro-inflammatory cytokine that plays a key role in the immune response, were significantly decreased in NANS vs controls, whereas IL-6 and IL-10, two cytokines with protective properties, were decreased in the ASP group vs controls.
IN PRACTICE:
“Given the crucial role played by small intestinal microbes in digestion, nutrient absorption, immune regulation, and endocrine functions, coupled with the substantial prevalence of NSS consumption among US adults (estimated at 41.4%), our findings have potential implications for metabolic and gastrointestinal health in a considerable proportion of the American adult population.”
SOURCE:
The study, conducted by Ava Hosseini, MPH, and colleagues at Cedars-Sinai, Los Angeles, was published online on November 22, 2023, in iScience.
LIMITATIONS:
The study population may not be representative of healthy individuals as they underwent upper endoscopy for various reasons (eg, evaluation of intestinal complaints). After exclusions, the duodenal sample size for the aspartame group was small. Samples were collected at a single timepoint, limiting the ability to establish causal relationships.
DISCLOSURES:
This research was supported by Frank Lee, the Monica Lester Charitable Trust, and the Elias, Genevieve, and Georgianna Atol Charitable Trust through their support of the Medically Associated Science and Technology Program, Cedars-Sinai, Los Angeles. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
and composition and levels of circulating inflammatory markers.
METHODOLOGY:
- Researchers analyzed samples from the REIMAGINE (Revealing the Entire Intestinal Microbiota and its Associations with the Genetic, Immunologic, and Neuroendocrine Ecosystem) study to assess the potential effects of NSS consumption on the duodenal luminal microbiome.
- They analyzed subjects consuming non-aspartame nonsugar sweeteners (NANS; n = 35) and aspartame only (ASP; n = 9), who were compared with 55 control participants matched for age, sex, and body mass index.
- A subset of 40 participants provided stool samples for additional analysis.
TAKEAWAY:
- Duodenal alpha diversity was lower in NANS consumers vs controls.
- Duodenal relative abundance (RA) of Escherichia, Klebsiella, and Salmonella was lower in both NANS and ASP vs controls, whereas stool RA of these phylum Proteobacteria was increased in both NANS and ASP.
- Compared with controls, NANS and ASP differed in how they altered predicted duodenal microbial metabolic pathways, with NANS impacting polysaccharides biosynthesis and D-galactose degradation and ASP significantly enriching biosynthesis of cylindrospermopsin, a potential cancer-causing agent known to adversely impact the liver and nervous system.
- Circulating levels of interleukin (IL)-1b, a pro-inflammatory cytokine that plays a key role in the immune response, were significantly decreased in NANS vs controls, whereas IL-6 and IL-10, two cytokines with protective properties, were decreased in the ASP group vs controls.
IN PRACTICE:
“Given the crucial role played by small intestinal microbes in digestion, nutrient absorption, immune regulation, and endocrine functions, coupled with the substantial prevalence of NSS consumption among US adults (estimated at 41.4%), our findings have potential implications for metabolic and gastrointestinal health in a considerable proportion of the American adult population.”
SOURCE:
The study, conducted by Ava Hosseini, MPH, and colleagues at Cedars-Sinai, Los Angeles, was published online on November 22, 2023, in iScience.
LIMITATIONS:
The study population may not be representative of healthy individuals as they underwent upper endoscopy for various reasons (eg, evaluation of intestinal complaints). After exclusions, the duodenal sample size for the aspartame group was small. Samples were collected at a single timepoint, limiting the ability to establish causal relationships.
DISCLOSURES:
This research was supported by Frank Lee, the Monica Lester Charitable Trust, and the Elias, Genevieve, and Georgianna Atol Charitable Trust through their support of the Medically Associated Science and Technology Program, Cedars-Sinai, Los Angeles. The authors declared no conflicts of interest.
A version of this article appeared on Medscape.com.
Ascending Thoracic Aortic Aneurysms: A ‘Silver Lining’?
Often known as a “silent killer,” ascending thoracic aortic aneurysms (ATAAs) may grow asymptomatically until they rupture, at which point, mortality is over 90%.
But and by extension, for those who have one, a significantly reduced risk for coronary artery disease and myocardial infarction (MI).
“We noticed in the operating room that many patients we worked on who had an ATAA had pristine arteries, like a teenager’s,” said John Elefteriades, MD, William W.L. Glenn Professor of Cardiothoracic Surgery and former chief of cardiothoracic surgery at Yale University and Yale New Haven Hospital, New Haven, Connecticut. “The same was true of the femoral artery, which we use to hook up to the heart-lung machine.”
Elefteriades and colleagues have been investigating the implications of this association for more than two decades. Many of their studies are highlighted in a recent review of the evidence supporting the protective relationship between ATAAs and the development of atherosclerosis and the possible mechanisms driving the relationship.
“We see four different layers of protection,” said Sandip Mukherjee, MD, medical director of the Aortic Institute at Yale New Haven Hospital and a senior editor of the journal AORTA. Mukherjee collaborated with Elefteriades on many of the studies.
The first layer of protection is lower intima-media thickness, specifically, 0.131 mm lower than in individuals without an ATAA. “It may not seem like very much, but one point can actually translate into a 13%-15% decline in the rate of myocardial infarction or stroke,” Dr. Mukherjee said.
The second layer is lower levels of low-density lipoprotein (LDL) cholesterol. Lower LDL cholesterol levels (75 mg/dL) were associated with increased odds of ATAAs (odds ratio [OR], 1.21), whereas elevated levels (150 mg/dL and 200 mg/dL) were associated with decreased odds of ATAAs (OR, 0.62 and 0.29, respectively).
Lower calcification scores for the coronary arteries are the third layer of protection (6.73 vs 9.36 in one study).
The fourth protective layer is a significantly reduced prevalence of coronary artery disease. A study of individuals with ATAA compared to controls found 61 of those with ATAA had coronary artery disease vs 140 of controls, and 11 vs 83 had experienced an MI. Of note, patients with ATAAs were protected despite having higher body mass indices than controls.
Other MI risk factors such as age increased the risk even among those with an ATAA but, again, much less so than among controls; a multivariable binary logistic regression of data in the team’s review showed that patients with ATAAs were 298, 250, and 232 times less likely to have an MI than if they had a family history of MI, dyslipidemia, or hypertension, respectively.
Why the Protection?
The ligamentum arteriosum separates the ascending from the descending (thoracoabdominal) aorta. ATAAs, located above the ligamentum, tend to be pro-aneurysmal but anti-atherosclerotic. In the descending aorta, below the ligamentum, atherosclerotic aneurysms develop.
The differences between the two sections of the aorta originate in the germ layer in the embryo, Dr. Elefteriades said. “The fundamental difference in tissue of origin translates into marked differences in the character of aneurysms in the different aortic segments.”
What specifically underlies the reduced cardiovascular risk? “We don’t really know, but we think that there may be two possible etiologies,” Dr. Mukherjee said. One hypothesis involves transforming growth factor–beta (TGF-beta), which is overexpressed in patients with ATAA and seems to increase their vulnerability to aneurysms while also conferring protection from coronary disease risk.
Some studies have shown differences in cellular responses to TGF-beta between the thoracic and abdominal aorta, including collagen production and contractility. Others have shown that some patients who have had an MI have polymorphisms that decrease their levels of TGF-beta.
Furthermore, TGF-beta plays a key role in the development of the intimal layer, which could underpin the lack of intimal thickening in patients with ATAA.
But overall, studies have been mixed and challenging to interpret, Dr. Elefteriades and Dr. Mukherjee agreed. TGF-beta has multiple remodeling roles in the body, and it is difficult at this point to isolate its exact role in aortic disease.
Another hypothesis involves matrix metalloproteinases (MMPs), which are dysregulated in patients with ATAA and may confer some protection, Mukherjee said. Several studies have shown higher plasma levels of certain MMPs in patients with ATAAs. MMPs also were found to be elevated in the thoracic aortic walls of patients with ATAA who had an aortic dissection, as well as in the aortic smooth muscle cells in the intima and media.
In addition, some studies have shown increased levels of MMP-2 in the aortas of patients with ATAAs compared with patients with coronary artery disease.
Adding to the mix of possibilities, “We recently found a gene that’s dysregulated in our aneurysm patients that is very intimately related to atherosclerosis,” Dr. Elefteriades said. “But the work is too preliminary to say anything more at this point.”
“It would be fabulous to prove what it is causing this protection,” Dr. Mukherjee added. “But the truth is we don’t know. These are hypotheses.”
“The most important message from our work is that most clinicians need to dissociate an ATAA from the concept of atherosclerosis,” Dr. Elefteriades said. “The ascending aorta is not an atherosclerotic phenomenon.”
How to Manage Patients With ATAA
What does the distinct character of ATAAs mean for patient management? “Finding a drug to treat ATAAs — to prevent growth, rupture, or dissection — has been like a search for the Holy Grail,” Dr. Elefteriades said. “Statins are not necessary, as this is a non-atherosclerotic process. Although sporadic studies have reported beneficial effects from beta-blockers or angiotensin II receptor blockers (ARBs), this has often been based on ‘soft’ evidence, requiring a combination of outcome measures to achieve significance.”
That said, he noted, “The mainstay, common sense treatment is to keep blood pressure controlled. This is usually achieved by a beta-blocker and an ARB, even if the benefit is not via a direct biologic effect on the aneurysmal degenerative process, but via simple hemodynamics — discouraging rupture by keeping pressure in the aorta low.”
Dr. Mukherjee suggested that these patients should be referred to a specialty aneurysm center where their genes will be evaluated, and then the aneurysm will be followed very closely.
“If the aneurysm is larger than 4.5 cm, we screen the patient every single year, and if they have chest pain, we treat them the same way as we treat other aneurysms,” he said. “As a rule of thumb, if the aneurysm reaches 5 cm, it should come out, although the size at which this should happen may differ between 4.5 cm and 5.5 cm, depending on the patient’s body size.”
As for lifestyle management, Dr. Elefteriades said, “Protection from atherosclerosis and MI won’t go away after the aneurysm is removed. We think it’s in the body’s chemistry. But even though it’s very hard for those patients to have a heart attack, we don’t recommend they eat roast beef every night — although I do think they’d be protected from such lifestyle aberrations.”
For now, he added, “Our team is on a hunt to find a drug to treat ascending disease directly and effectively. We have ongoing laboratory experiments with two drugs undergoing investigation at some level. We hope to embark soon on clinical trials.”
‘A Milestone’
James Hamilton Black III, MD, vice chair of the writing committee for the 2022 American College of Cardiology/American Heart Association Aortic Disease Guideline and chief of Division of Vascular Surgery and Endovascular Therapy at Johns Hopkins Medicine, Baltimore, commented on the review and the concept of ATAA’s atherosclerotic protection.
“The association of ascending aortic aneurysms with a lower risk for MI is an interesting one, but it’s probably influenced, at least in part, by the patient population.” That population is at least partially curated since people are coming to an academic center. In addition, Dr. Black noted, “the patients with ATAAs are younger, and so age may be a confounding factor in the analyses. We wouldn’t expect them to have the same burden of atherosclerosis” as older patients.
Nevertheless, he said, “the findings speak to an emerging body of literature suggesting that although the aorta is a single organ, there are certainly different areas, and these would respond quite differently to environmental or genetic or heritable stressors. This isn’t surprising, and there probably are a lot of factors involved.”
Overall, he said, the findings underscore “the precision medicine approaches we need to take with patients with aortic diseases.”
In a commentary on the team’s review article, published in 2022, John G.T. Augoustides, MD, professor of anesthesiology and critical care at the Perelman School of Medicine in Philadelphia, Pennsylvania, suggested that ATAA’s “silver lining” could advance the understanding of thoracic aortic aneurysm (TAA) management, be integrated with the expanding horizons in hereditary thoracic aortic disease, and might be explored in the context of bicuspid aortic valve disease.
Highlighting the “relative absence” of atherosclerosis in ascending aortic aneurysms and its importance is a “milestone in our understanding,” he concluded. “It is likely that future advances in TAAs will be significantly influenced by this observation.”
Dr. Elefteriades, Dr. Mukherjee, and Dr. Black have no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Often known as a “silent killer,” ascending thoracic aortic aneurysms (ATAAs) may grow asymptomatically until they rupture, at which point, mortality is over 90%.
But and by extension, for those who have one, a significantly reduced risk for coronary artery disease and myocardial infarction (MI).
“We noticed in the operating room that many patients we worked on who had an ATAA had pristine arteries, like a teenager’s,” said John Elefteriades, MD, William W.L. Glenn Professor of Cardiothoracic Surgery and former chief of cardiothoracic surgery at Yale University and Yale New Haven Hospital, New Haven, Connecticut. “The same was true of the femoral artery, which we use to hook up to the heart-lung machine.”
Elefteriades and colleagues have been investigating the implications of this association for more than two decades. Many of their studies are highlighted in a recent review of the evidence supporting the protective relationship between ATAAs and the development of atherosclerosis and the possible mechanisms driving the relationship.
“We see four different layers of protection,” said Sandip Mukherjee, MD, medical director of the Aortic Institute at Yale New Haven Hospital and a senior editor of the journal AORTA. Mukherjee collaborated with Elefteriades on many of the studies.
The first layer of protection is lower intima-media thickness, specifically, 0.131 mm lower than in individuals without an ATAA. “It may not seem like very much, but one point can actually translate into a 13%-15% decline in the rate of myocardial infarction or stroke,” Dr. Mukherjee said.
The second layer is lower levels of low-density lipoprotein (LDL) cholesterol. Lower LDL cholesterol levels (75 mg/dL) were associated with increased odds of ATAAs (odds ratio [OR], 1.21), whereas elevated levels (150 mg/dL and 200 mg/dL) were associated with decreased odds of ATAAs (OR, 0.62 and 0.29, respectively).
Lower calcification scores for the coronary arteries are the third layer of protection (6.73 vs 9.36 in one study).
The fourth protective layer is a significantly reduced prevalence of coronary artery disease. A study of individuals with ATAA compared to controls found 61 of those with ATAA had coronary artery disease vs 140 of controls, and 11 vs 83 had experienced an MI. Of note, patients with ATAAs were protected despite having higher body mass indices than controls.
Other MI risk factors such as age increased the risk even among those with an ATAA but, again, much less so than among controls; a multivariable binary logistic regression of data in the team’s review showed that patients with ATAAs were 298, 250, and 232 times less likely to have an MI than if they had a family history of MI, dyslipidemia, or hypertension, respectively.
Why the Protection?
The ligamentum arteriosum separates the ascending from the descending (thoracoabdominal) aorta. ATAAs, located above the ligamentum, tend to be pro-aneurysmal but anti-atherosclerotic. In the descending aorta, below the ligamentum, atherosclerotic aneurysms develop.
The differences between the two sections of the aorta originate in the germ layer in the embryo, Dr. Elefteriades said. “The fundamental difference in tissue of origin translates into marked differences in the character of aneurysms in the different aortic segments.”
What specifically underlies the reduced cardiovascular risk? “We don’t really know, but we think that there may be two possible etiologies,” Dr. Mukherjee said. One hypothesis involves transforming growth factor–beta (TGF-beta), which is overexpressed in patients with ATAA and seems to increase their vulnerability to aneurysms while also conferring protection from coronary disease risk.
Some studies have shown differences in cellular responses to TGF-beta between the thoracic and abdominal aorta, including collagen production and contractility. Others have shown that some patients who have had an MI have polymorphisms that decrease their levels of TGF-beta.
Furthermore, TGF-beta plays a key role in the development of the intimal layer, which could underpin the lack of intimal thickening in patients with ATAA.
But overall, studies have been mixed and challenging to interpret, Dr. Elefteriades and Dr. Mukherjee agreed. TGF-beta has multiple remodeling roles in the body, and it is difficult at this point to isolate its exact role in aortic disease.
Another hypothesis involves matrix metalloproteinases (MMPs), which are dysregulated in patients with ATAA and may confer some protection, Mukherjee said. Several studies have shown higher plasma levels of certain MMPs in patients with ATAAs. MMPs also were found to be elevated in the thoracic aortic walls of patients with ATAA who had an aortic dissection, as well as in the aortic smooth muscle cells in the intima and media.
In addition, some studies have shown increased levels of MMP-2 in the aortas of patients with ATAAs compared with patients with coronary artery disease.
Adding to the mix of possibilities, “We recently found a gene that’s dysregulated in our aneurysm patients that is very intimately related to atherosclerosis,” Dr. Elefteriades said. “But the work is too preliminary to say anything more at this point.”
“It would be fabulous to prove what it is causing this protection,” Dr. Mukherjee added. “But the truth is we don’t know. These are hypotheses.”
“The most important message from our work is that most clinicians need to dissociate an ATAA from the concept of atherosclerosis,” Dr. Elefteriades said. “The ascending aorta is not an atherosclerotic phenomenon.”
How to Manage Patients With ATAA
What does the distinct character of ATAAs mean for patient management? “Finding a drug to treat ATAAs — to prevent growth, rupture, or dissection — has been like a search for the Holy Grail,” Dr. Elefteriades said. “Statins are not necessary, as this is a non-atherosclerotic process. Although sporadic studies have reported beneficial effects from beta-blockers or angiotensin II receptor blockers (ARBs), this has often been based on ‘soft’ evidence, requiring a combination of outcome measures to achieve significance.”
That said, he noted, “The mainstay, common sense treatment is to keep blood pressure controlled. This is usually achieved by a beta-blocker and an ARB, even if the benefit is not via a direct biologic effect on the aneurysmal degenerative process, but via simple hemodynamics — discouraging rupture by keeping pressure in the aorta low.”
Dr. Mukherjee suggested that these patients should be referred to a specialty aneurysm center where their genes will be evaluated, and then the aneurysm will be followed very closely.
“If the aneurysm is larger than 4.5 cm, we screen the patient every single year, and if they have chest pain, we treat them the same way as we treat other aneurysms,” he said. “As a rule of thumb, if the aneurysm reaches 5 cm, it should come out, although the size at which this should happen may differ between 4.5 cm and 5.5 cm, depending on the patient’s body size.”
As for lifestyle management, Dr. Elefteriades said, “Protection from atherosclerosis and MI won’t go away after the aneurysm is removed. We think it’s in the body’s chemistry. But even though it’s very hard for those patients to have a heart attack, we don’t recommend they eat roast beef every night — although I do think they’d be protected from such lifestyle aberrations.”
For now, he added, “Our team is on a hunt to find a drug to treat ascending disease directly and effectively. We have ongoing laboratory experiments with two drugs undergoing investigation at some level. We hope to embark soon on clinical trials.”
‘A Milestone’
James Hamilton Black III, MD, vice chair of the writing committee for the 2022 American College of Cardiology/American Heart Association Aortic Disease Guideline and chief of Division of Vascular Surgery and Endovascular Therapy at Johns Hopkins Medicine, Baltimore, commented on the review and the concept of ATAA’s atherosclerotic protection.
“The association of ascending aortic aneurysms with a lower risk for MI is an interesting one, but it’s probably influenced, at least in part, by the patient population.” That population is at least partially curated since people are coming to an academic center. In addition, Dr. Black noted, “the patients with ATAAs are younger, and so age may be a confounding factor in the analyses. We wouldn’t expect them to have the same burden of atherosclerosis” as older patients.
Nevertheless, he said, “the findings speak to an emerging body of literature suggesting that although the aorta is a single organ, there are certainly different areas, and these would respond quite differently to environmental or genetic or heritable stressors. This isn’t surprising, and there probably are a lot of factors involved.”
Overall, he said, the findings underscore “the precision medicine approaches we need to take with patients with aortic diseases.”
In a commentary on the team’s review article, published in 2022, John G.T. Augoustides, MD, professor of anesthesiology and critical care at the Perelman School of Medicine in Philadelphia, Pennsylvania, suggested that ATAA’s “silver lining” could advance the understanding of thoracic aortic aneurysm (TAA) management, be integrated with the expanding horizons in hereditary thoracic aortic disease, and might be explored in the context of bicuspid aortic valve disease.
Highlighting the “relative absence” of atherosclerosis in ascending aortic aneurysms and its importance is a “milestone in our understanding,” he concluded. “It is likely that future advances in TAAs will be significantly influenced by this observation.”
Dr. Elefteriades, Dr. Mukherjee, and Dr. Black have no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
Often known as a “silent killer,” ascending thoracic aortic aneurysms (ATAAs) may grow asymptomatically until they rupture, at which point, mortality is over 90%.
But and by extension, for those who have one, a significantly reduced risk for coronary artery disease and myocardial infarction (MI).
“We noticed in the operating room that many patients we worked on who had an ATAA had pristine arteries, like a teenager’s,” said John Elefteriades, MD, William W.L. Glenn Professor of Cardiothoracic Surgery and former chief of cardiothoracic surgery at Yale University and Yale New Haven Hospital, New Haven, Connecticut. “The same was true of the femoral artery, which we use to hook up to the heart-lung machine.”
Elefteriades and colleagues have been investigating the implications of this association for more than two decades. Many of their studies are highlighted in a recent review of the evidence supporting the protective relationship between ATAAs and the development of atherosclerosis and the possible mechanisms driving the relationship.
“We see four different layers of protection,” said Sandip Mukherjee, MD, medical director of the Aortic Institute at Yale New Haven Hospital and a senior editor of the journal AORTA. Mukherjee collaborated with Elefteriades on many of the studies.
The first layer of protection is lower intima-media thickness, specifically, 0.131 mm lower than in individuals without an ATAA. “It may not seem like very much, but one point can actually translate into a 13%-15% decline in the rate of myocardial infarction or stroke,” Dr. Mukherjee said.
The second layer is lower levels of low-density lipoprotein (LDL) cholesterol. Lower LDL cholesterol levels (75 mg/dL) were associated with increased odds of ATAAs (odds ratio [OR], 1.21), whereas elevated levels (150 mg/dL and 200 mg/dL) were associated with decreased odds of ATAAs (OR, 0.62 and 0.29, respectively).
Lower calcification scores for the coronary arteries are the third layer of protection (6.73 vs 9.36 in one study).
The fourth protective layer is a significantly reduced prevalence of coronary artery disease. A study of individuals with ATAA compared to controls found 61 of those with ATAA had coronary artery disease vs 140 of controls, and 11 vs 83 had experienced an MI. Of note, patients with ATAAs were protected despite having higher body mass indices than controls.
Other MI risk factors such as age increased the risk even among those with an ATAA but, again, much less so than among controls; a multivariable binary logistic regression of data in the team’s review showed that patients with ATAAs were 298, 250, and 232 times less likely to have an MI than if they had a family history of MI, dyslipidemia, or hypertension, respectively.
Why the Protection?
The ligamentum arteriosum separates the ascending from the descending (thoracoabdominal) aorta. ATAAs, located above the ligamentum, tend to be pro-aneurysmal but anti-atherosclerotic. In the descending aorta, below the ligamentum, atherosclerotic aneurysms develop.
The differences between the two sections of the aorta originate in the germ layer in the embryo, Dr. Elefteriades said. “The fundamental difference in tissue of origin translates into marked differences in the character of aneurysms in the different aortic segments.”
What specifically underlies the reduced cardiovascular risk? “We don’t really know, but we think that there may be two possible etiologies,” Dr. Mukherjee said. One hypothesis involves transforming growth factor–beta (TGF-beta), which is overexpressed in patients with ATAA and seems to increase their vulnerability to aneurysms while also conferring protection from coronary disease risk.
Some studies have shown differences in cellular responses to TGF-beta between the thoracic and abdominal aorta, including collagen production and contractility. Others have shown that some patients who have had an MI have polymorphisms that decrease their levels of TGF-beta.
Furthermore, TGF-beta plays a key role in the development of the intimal layer, which could underpin the lack of intimal thickening in patients with ATAA.
But overall, studies have been mixed and challenging to interpret, Dr. Elefteriades and Dr. Mukherjee agreed. TGF-beta has multiple remodeling roles in the body, and it is difficult at this point to isolate its exact role in aortic disease.
Another hypothesis involves matrix metalloproteinases (MMPs), which are dysregulated in patients with ATAA and may confer some protection, Mukherjee said. Several studies have shown higher plasma levels of certain MMPs in patients with ATAAs. MMPs also were found to be elevated in the thoracic aortic walls of patients with ATAA who had an aortic dissection, as well as in the aortic smooth muscle cells in the intima and media.
In addition, some studies have shown increased levels of MMP-2 in the aortas of patients with ATAAs compared with patients with coronary artery disease.
Adding to the mix of possibilities, “We recently found a gene that’s dysregulated in our aneurysm patients that is very intimately related to atherosclerosis,” Dr. Elefteriades said. “But the work is too preliminary to say anything more at this point.”
“It would be fabulous to prove what it is causing this protection,” Dr. Mukherjee added. “But the truth is we don’t know. These are hypotheses.”
“The most important message from our work is that most clinicians need to dissociate an ATAA from the concept of atherosclerosis,” Dr. Elefteriades said. “The ascending aorta is not an atherosclerotic phenomenon.”
How to Manage Patients With ATAA
What does the distinct character of ATAAs mean for patient management? “Finding a drug to treat ATAAs — to prevent growth, rupture, or dissection — has been like a search for the Holy Grail,” Dr. Elefteriades said. “Statins are not necessary, as this is a non-atherosclerotic process. Although sporadic studies have reported beneficial effects from beta-blockers or angiotensin II receptor blockers (ARBs), this has often been based on ‘soft’ evidence, requiring a combination of outcome measures to achieve significance.”
That said, he noted, “The mainstay, common sense treatment is to keep blood pressure controlled. This is usually achieved by a beta-blocker and an ARB, even if the benefit is not via a direct biologic effect on the aneurysmal degenerative process, but via simple hemodynamics — discouraging rupture by keeping pressure in the aorta low.”
Dr. Mukherjee suggested that these patients should be referred to a specialty aneurysm center where their genes will be evaluated, and then the aneurysm will be followed very closely.
“If the aneurysm is larger than 4.5 cm, we screen the patient every single year, and if they have chest pain, we treat them the same way as we treat other aneurysms,” he said. “As a rule of thumb, if the aneurysm reaches 5 cm, it should come out, although the size at which this should happen may differ between 4.5 cm and 5.5 cm, depending on the patient’s body size.”
As for lifestyle management, Dr. Elefteriades said, “Protection from atherosclerosis and MI won’t go away after the aneurysm is removed. We think it’s in the body’s chemistry. But even though it’s very hard for those patients to have a heart attack, we don’t recommend they eat roast beef every night — although I do think they’d be protected from such lifestyle aberrations.”
For now, he added, “Our team is on a hunt to find a drug to treat ascending disease directly and effectively. We have ongoing laboratory experiments with two drugs undergoing investigation at some level. We hope to embark soon on clinical trials.”
‘A Milestone’
James Hamilton Black III, MD, vice chair of the writing committee for the 2022 American College of Cardiology/American Heart Association Aortic Disease Guideline and chief of Division of Vascular Surgery and Endovascular Therapy at Johns Hopkins Medicine, Baltimore, commented on the review and the concept of ATAA’s atherosclerotic protection.
“The association of ascending aortic aneurysms with a lower risk for MI is an interesting one, but it’s probably influenced, at least in part, by the patient population.” That population is at least partially curated since people are coming to an academic center. In addition, Dr. Black noted, “the patients with ATAAs are younger, and so age may be a confounding factor in the analyses. We wouldn’t expect them to have the same burden of atherosclerosis” as older patients.
Nevertheless, he said, “the findings speak to an emerging body of literature suggesting that although the aorta is a single organ, there are certainly different areas, and these would respond quite differently to environmental or genetic or heritable stressors. This isn’t surprising, and there probably are a lot of factors involved.”
Overall, he said, the findings underscore “the precision medicine approaches we need to take with patients with aortic diseases.”
In a commentary on the team’s review article, published in 2022, John G.T. Augoustides, MD, professor of anesthesiology and critical care at the Perelman School of Medicine in Philadelphia, Pennsylvania, suggested that ATAA’s “silver lining” could advance the understanding of thoracic aortic aneurysm (TAA) management, be integrated with the expanding horizons in hereditary thoracic aortic disease, and might be explored in the context of bicuspid aortic valve disease.
Highlighting the “relative absence” of atherosclerosis in ascending aortic aneurysms and its importance is a “milestone in our understanding,” he concluded. “It is likely that future advances in TAAs will be significantly influenced by this observation.”
Dr. Elefteriades, Dr. Mukherjee, and Dr. Black have no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
What Is the Best Way to Manage Axial Spondyloarthritis in Primary Care?
When axial spondyloarthritis (SpA) is suspected, a “prompt referral to a rheumatologist” is in order. But with the referral possibly taking several weeks, if not months in some parts of the world, how can primary care practitioners manage patients with this type of chronic back pain in the meantime? And what is the long-term role of the primary care practitioner in managing someone diagnosed with the condition? This news organization asked rheumatologist Marina Magrey, MD, and general internal medicine physician Debra Leizman, MD, for their expert advice.
Steps to Manage Suspected Axial SpA
“As [primary care practitioners] identify patients who they suspect may have axial spondyloarthritis, the first thing they should do is a prompt referral to a rheumatologist so that there is a timely diagnosis,” said Dr. Magrey, who heads up the division of rheumatology at University Hospitals Cleveland Medical Center and is professor of medicine at Case Western Reserve University School of Medicine in Cleveland, Ohio.
Importantly, the referral should “explicitly say that they’re suspecting axial spondyloarthritis” and not just chronic back pain, Dr. Magrey added, otherwise it may not “hit the radar” that patients need to be seen as soon as possible. Results of lab tests such as C-reactive protein, erythrocyte sedimentation rate, and human leukocyte antigen B27, along with basic pelvic imaging results, are useful to note on the referral. “If the patient comes with that information, it makes it much easier for the rheumatologist,” she said.
Additionally,
First-Line Treatment Options
“The goal is to improve the quality of life for our patients: To reduce pain, fatigue, inflammation,” Dr. Magrey noted. “So, starting a nonsteroidal anti-inflammatory drug [NSAID] with physical therapy is very useful” in primary care, she added. These remain the “cornerstone” of treatment for axial SpA even in secondary care.
Dr. Leizman agreed that her “go to” treatment for suspected axial SpA is physical therapy alongside one of the many NSAIDs available, such as naproxen or celecoxib. She may also use topical treatments such as lidocaine or diclofenac.
“I’m not going to start any biologics; I leave that for my rheumatologist,” said Dr. Leizman, who is a senior attending physician in the division of general internal medicine at University Hospitals Cleveland Medical Center and associate professor of medicine at Case Western Reserve University.
“If I think it’s a possibility that the patient will be going on to a biologic; however, I will try to check their TB status, immunizations, and vaccination titers, making sure that the patient is up to date and as healthy otherwise as possible so that they will be primed and ready, hopefully, to go on to the biologics,” she added.
Dr. Magrey cautioned that disease-modifying antirheumatic drugs, such as methotrexate and sulfasalazine, and systemic steroids such as oral prednisone “do not work in axial spondyloarthritis, so they are not recommended.”
Does the Choice of NSAID Matter?
The choice of NSAID is really down to the personal choice of the physician in agreement with the patient, and of course whether the medical insurance will cover it, Dr. Magrey observed. There appears to be little difference between the available NSAIDs, and it doesn’t appear to matter whether they are long-acting and taken once a day — which may be a convenient option for some patients — or short-acting and taken twice a day. The important point is that patients are taking these drugs continuously and not on demand and that they are being given at full dose.
“Start with one NSAID at the maximum strength, and then you try that for 2-4 weeks. If that doesn’t work, switch to another one,” Dr. Magrey advised.
American College of Rheumatology (ACR) guidelines for axial SpA recommend that a trial of at least two NSAIDs is undertaken before any biologic treatment is considered, but because the presentation of axial SpA is so heterogeneous, the decision to escalate treatment — usually to a tumor necrosis factor inhibitor first — is best left until after the referral and the diagnosis had been confirmed, she suggested.
What Type of Physical Therapy Works?
Physical therapy and nonpharmacologic ways to help people are integral to optimal patient management. But these still need to be prescribed and administered by a qualified physiotherapist, which means another, separate referral that can also take time, as it’s important to match the patient to the right physiotherapist, Dr. Leizman observed.
Patients need to be informed about the benefits of regular exercise, and suggesting low-impact exercises for the back can be helpful, Dr. Magrey noted.
“Supervised physical therapy is preferred over unsupervised back exercises,” Dr. Magrey said, summarizing current ACR recommendations, which also suggest that land-based activities are preferred over water-based exercises and group physical therapy rather than home-based exercises, according to the available evidence, although it is of low-to-moderate quality.
What type of physical therapy to recommend really boils down to what services are available, what facilities the patient has access to, and what they feel they are capable of doing or are willing to do.
Back pain can be frustrating for patients, said Dr. Leizman, because they hurt when they move, and there’s not a simple solution of “do this or that and you’ll get better.”
“If it’s possible for a patient to do aqua therapy, that has been a good option for many of my patients who are unable to get moving on land without pain,” she said, and “I’ve had some great success with some yoga therapists who work with my patients.”
Long-term Role of the Primary Care Practitioner
Once referred, patients with axial SpA will usually be seen by their rheumatologists at least twice a year to monitor their response to treatment. Primary care practitioners will also continue to see these people for other reasons and can help monitor for drug toxicity by performing blood and liver function tests, as well as looking for signs of associated conditions such as uveitis, psoriasis, and inflammatory bowel disease and referring patients on to other specialists as required.
Treating the inflammatory back pain may sometimes help treat the related conditions and vice versa, but not always, noted Dr. Leizman. Communication between professionals is thus very important to ensure that everyone is on the same page, and regular updates help enormously.
Dr. Leizman tries to see all her patients regularly, at least once a year, but it can be once or twice a year, depending on their age, how healthy they are, and what underlying conditions they may have that she is also managing along with the inflammatory back condition. It is a balancing act to prevent too many appointments, she said, but also helps patients manage the multiple recommendations.
At these appointments, she’ll not only check on patients’ progress and ensure that they have had all the tests that they should have, but she’ll also discuss general measures that may help with patients’ general health, such as weight control, their ability to manage disease processes with other daily activities of living, and other creative coping mechanisms.
“The weight discussion is never easy, but it is helpful to address the impact of weight if it may be contributing to their discomfort,” Dr. Leizman said. “I also think that there are diets patients can choose that are less inflammatory and that can be beneficial.”
Ultimately, “I want my patients to be on the least amount of medicine possible,” Dr. Leizman said. “If they need medications, I support my rheumatologists’ recommendations. I help my patients as they try whatever works to make them feel better, both the nonpharmaceutical options and the medications,” she said.
“Importantly, I am there for support as a resource and a partner,” Leizman added. “I’m the main quarterback for my patients.”
Key Takeaways
- Prompt referral to a rheumatologist remains key.
- The treatment goal is to improve patients’ quality of life by reducing symptoms such as pain and fatigue.
- Physical therapy and NSAIDs remain first-line treatment in primary care.
- NSAID treatment should be at the full recommended dose and given continuously, not as needed.
- The choice of NSAID does not matter; try switching the NSAID if no effects are seen.
- Physical therapy such as water-based activities and yoga may be beneficial, but exercise programs should be prescribed by a qualified therapist.
- Remember general health advice regarding diet and nutrition can be helpful.
A version of this article appeared on Medscape.com.
When axial spondyloarthritis (SpA) is suspected, a “prompt referral to a rheumatologist” is in order. But with the referral possibly taking several weeks, if not months in some parts of the world, how can primary care practitioners manage patients with this type of chronic back pain in the meantime? And what is the long-term role of the primary care practitioner in managing someone diagnosed with the condition? This news organization asked rheumatologist Marina Magrey, MD, and general internal medicine physician Debra Leizman, MD, for their expert advice.
Steps to Manage Suspected Axial SpA
“As [primary care practitioners] identify patients who they suspect may have axial spondyloarthritis, the first thing they should do is a prompt referral to a rheumatologist so that there is a timely diagnosis,” said Dr. Magrey, who heads up the division of rheumatology at University Hospitals Cleveland Medical Center and is professor of medicine at Case Western Reserve University School of Medicine in Cleveland, Ohio.
Importantly, the referral should “explicitly say that they’re suspecting axial spondyloarthritis” and not just chronic back pain, Dr. Magrey added, otherwise it may not “hit the radar” that patients need to be seen as soon as possible. Results of lab tests such as C-reactive protein, erythrocyte sedimentation rate, and human leukocyte antigen B27, along with basic pelvic imaging results, are useful to note on the referral. “If the patient comes with that information, it makes it much easier for the rheumatologist,” she said.
Additionally,
First-Line Treatment Options
“The goal is to improve the quality of life for our patients: To reduce pain, fatigue, inflammation,” Dr. Magrey noted. “So, starting a nonsteroidal anti-inflammatory drug [NSAID] with physical therapy is very useful” in primary care, she added. These remain the “cornerstone” of treatment for axial SpA even in secondary care.
Dr. Leizman agreed that her “go to” treatment for suspected axial SpA is physical therapy alongside one of the many NSAIDs available, such as naproxen or celecoxib. She may also use topical treatments such as lidocaine or diclofenac.
“I’m not going to start any biologics; I leave that for my rheumatologist,” said Dr. Leizman, who is a senior attending physician in the division of general internal medicine at University Hospitals Cleveland Medical Center and associate professor of medicine at Case Western Reserve University.
“If I think it’s a possibility that the patient will be going on to a biologic; however, I will try to check their TB status, immunizations, and vaccination titers, making sure that the patient is up to date and as healthy otherwise as possible so that they will be primed and ready, hopefully, to go on to the biologics,” she added.
Dr. Magrey cautioned that disease-modifying antirheumatic drugs, such as methotrexate and sulfasalazine, and systemic steroids such as oral prednisone “do not work in axial spondyloarthritis, so they are not recommended.”
Does the Choice of NSAID Matter?
The choice of NSAID is really down to the personal choice of the physician in agreement with the patient, and of course whether the medical insurance will cover it, Dr. Magrey observed. There appears to be little difference between the available NSAIDs, and it doesn’t appear to matter whether they are long-acting and taken once a day — which may be a convenient option for some patients — or short-acting and taken twice a day. The important point is that patients are taking these drugs continuously and not on demand and that they are being given at full dose.
“Start with one NSAID at the maximum strength, and then you try that for 2-4 weeks. If that doesn’t work, switch to another one,” Dr. Magrey advised.
American College of Rheumatology (ACR) guidelines for axial SpA recommend that a trial of at least two NSAIDs is undertaken before any biologic treatment is considered, but because the presentation of axial SpA is so heterogeneous, the decision to escalate treatment — usually to a tumor necrosis factor inhibitor first — is best left until after the referral and the diagnosis had been confirmed, she suggested.
What Type of Physical Therapy Works?
Physical therapy and nonpharmacologic ways to help people are integral to optimal patient management. But these still need to be prescribed and administered by a qualified physiotherapist, which means another, separate referral that can also take time, as it’s important to match the patient to the right physiotherapist, Dr. Leizman observed.
Patients need to be informed about the benefits of regular exercise, and suggesting low-impact exercises for the back can be helpful, Dr. Magrey noted.
“Supervised physical therapy is preferred over unsupervised back exercises,” Dr. Magrey said, summarizing current ACR recommendations, which also suggest that land-based activities are preferred over water-based exercises and group physical therapy rather than home-based exercises, according to the available evidence, although it is of low-to-moderate quality.
What type of physical therapy to recommend really boils down to what services are available, what facilities the patient has access to, and what they feel they are capable of doing or are willing to do.
Back pain can be frustrating for patients, said Dr. Leizman, because they hurt when they move, and there’s not a simple solution of “do this or that and you’ll get better.”
“If it’s possible for a patient to do aqua therapy, that has been a good option for many of my patients who are unable to get moving on land without pain,” she said, and “I’ve had some great success with some yoga therapists who work with my patients.”
Long-term Role of the Primary Care Practitioner
Once referred, patients with axial SpA will usually be seen by their rheumatologists at least twice a year to monitor their response to treatment. Primary care practitioners will also continue to see these people for other reasons and can help monitor for drug toxicity by performing blood and liver function tests, as well as looking for signs of associated conditions such as uveitis, psoriasis, and inflammatory bowel disease and referring patients on to other specialists as required.
Treating the inflammatory back pain may sometimes help treat the related conditions and vice versa, but not always, noted Dr. Leizman. Communication between professionals is thus very important to ensure that everyone is on the same page, and regular updates help enormously.
Dr. Leizman tries to see all her patients regularly, at least once a year, but it can be once or twice a year, depending on their age, how healthy they are, and what underlying conditions they may have that she is also managing along with the inflammatory back condition. It is a balancing act to prevent too many appointments, she said, but also helps patients manage the multiple recommendations.
At these appointments, she’ll not only check on patients’ progress and ensure that they have had all the tests that they should have, but she’ll also discuss general measures that may help with patients’ general health, such as weight control, their ability to manage disease processes with other daily activities of living, and other creative coping mechanisms.
“The weight discussion is never easy, but it is helpful to address the impact of weight if it may be contributing to their discomfort,” Dr. Leizman said. “I also think that there are diets patients can choose that are less inflammatory and that can be beneficial.”
Ultimately, “I want my patients to be on the least amount of medicine possible,” Dr. Leizman said. “If they need medications, I support my rheumatologists’ recommendations. I help my patients as they try whatever works to make them feel better, both the nonpharmaceutical options and the medications,” she said.
“Importantly, I am there for support as a resource and a partner,” Leizman added. “I’m the main quarterback for my patients.”
Key Takeaways
- Prompt referral to a rheumatologist remains key.
- The treatment goal is to improve patients’ quality of life by reducing symptoms such as pain and fatigue.
- Physical therapy and NSAIDs remain first-line treatment in primary care.
- NSAID treatment should be at the full recommended dose and given continuously, not as needed.
- The choice of NSAID does not matter; try switching the NSAID if no effects are seen.
- Physical therapy such as water-based activities and yoga may be beneficial, but exercise programs should be prescribed by a qualified therapist.
- Remember general health advice regarding diet and nutrition can be helpful.
A version of this article appeared on Medscape.com.
When axial spondyloarthritis (SpA) is suspected, a “prompt referral to a rheumatologist” is in order. But with the referral possibly taking several weeks, if not months in some parts of the world, how can primary care practitioners manage patients with this type of chronic back pain in the meantime? And what is the long-term role of the primary care practitioner in managing someone diagnosed with the condition? This news organization asked rheumatologist Marina Magrey, MD, and general internal medicine physician Debra Leizman, MD, for their expert advice.
Steps to Manage Suspected Axial SpA
“As [primary care practitioners] identify patients who they suspect may have axial spondyloarthritis, the first thing they should do is a prompt referral to a rheumatologist so that there is a timely diagnosis,” said Dr. Magrey, who heads up the division of rheumatology at University Hospitals Cleveland Medical Center and is professor of medicine at Case Western Reserve University School of Medicine in Cleveland, Ohio.
Importantly, the referral should “explicitly say that they’re suspecting axial spondyloarthritis” and not just chronic back pain, Dr. Magrey added, otherwise it may not “hit the radar” that patients need to be seen as soon as possible. Results of lab tests such as C-reactive protein, erythrocyte sedimentation rate, and human leukocyte antigen B27, along with basic pelvic imaging results, are useful to note on the referral. “If the patient comes with that information, it makes it much easier for the rheumatologist,” she said.
Additionally,
First-Line Treatment Options
“The goal is to improve the quality of life for our patients: To reduce pain, fatigue, inflammation,” Dr. Magrey noted. “So, starting a nonsteroidal anti-inflammatory drug [NSAID] with physical therapy is very useful” in primary care, she added. These remain the “cornerstone” of treatment for axial SpA even in secondary care.
Dr. Leizman agreed that her “go to” treatment for suspected axial SpA is physical therapy alongside one of the many NSAIDs available, such as naproxen or celecoxib. She may also use topical treatments such as lidocaine or diclofenac.
“I’m not going to start any biologics; I leave that for my rheumatologist,” said Dr. Leizman, who is a senior attending physician in the division of general internal medicine at University Hospitals Cleveland Medical Center and associate professor of medicine at Case Western Reserve University.
“If I think it’s a possibility that the patient will be going on to a biologic; however, I will try to check their TB status, immunizations, and vaccination titers, making sure that the patient is up to date and as healthy otherwise as possible so that they will be primed and ready, hopefully, to go on to the biologics,” she added.
Dr. Magrey cautioned that disease-modifying antirheumatic drugs, such as methotrexate and sulfasalazine, and systemic steroids such as oral prednisone “do not work in axial spondyloarthritis, so they are not recommended.”
Does the Choice of NSAID Matter?
The choice of NSAID is really down to the personal choice of the physician in agreement with the patient, and of course whether the medical insurance will cover it, Dr. Magrey observed. There appears to be little difference between the available NSAIDs, and it doesn’t appear to matter whether they are long-acting and taken once a day — which may be a convenient option for some patients — or short-acting and taken twice a day. The important point is that patients are taking these drugs continuously and not on demand and that they are being given at full dose.
“Start with one NSAID at the maximum strength, and then you try that for 2-4 weeks. If that doesn’t work, switch to another one,” Dr. Magrey advised.
American College of Rheumatology (ACR) guidelines for axial SpA recommend that a trial of at least two NSAIDs is undertaken before any biologic treatment is considered, but because the presentation of axial SpA is so heterogeneous, the decision to escalate treatment — usually to a tumor necrosis factor inhibitor first — is best left until after the referral and the diagnosis had been confirmed, she suggested.
What Type of Physical Therapy Works?
Physical therapy and nonpharmacologic ways to help people are integral to optimal patient management. But these still need to be prescribed and administered by a qualified physiotherapist, which means another, separate referral that can also take time, as it’s important to match the patient to the right physiotherapist, Dr. Leizman observed.
Patients need to be informed about the benefits of regular exercise, and suggesting low-impact exercises for the back can be helpful, Dr. Magrey noted.
“Supervised physical therapy is preferred over unsupervised back exercises,” Dr. Magrey said, summarizing current ACR recommendations, which also suggest that land-based activities are preferred over water-based exercises and group physical therapy rather than home-based exercises, according to the available evidence, although it is of low-to-moderate quality.
What type of physical therapy to recommend really boils down to what services are available, what facilities the patient has access to, and what they feel they are capable of doing or are willing to do.
Back pain can be frustrating for patients, said Dr. Leizman, because they hurt when they move, and there’s not a simple solution of “do this or that and you’ll get better.”
“If it’s possible for a patient to do aqua therapy, that has been a good option for many of my patients who are unable to get moving on land without pain,” she said, and “I’ve had some great success with some yoga therapists who work with my patients.”
Long-term Role of the Primary Care Practitioner
Once referred, patients with axial SpA will usually be seen by their rheumatologists at least twice a year to monitor their response to treatment. Primary care practitioners will also continue to see these people for other reasons and can help monitor for drug toxicity by performing blood and liver function tests, as well as looking for signs of associated conditions such as uveitis, psoriasis, and inflammatory bowel disease and referring patients on to other specialists as required.
Treating the inflammatory back pain may sometimes help treat the related conditions and vice versa, but not always, noted Dr. Leizman. Communication between professionals is thus very important to ensure that everyone is on the same page, and regular updates help enormously.
Dr. Leizman tries to see all her patients regularly, at least once a year, but it can be once or twice a year, depending on their age, how healthy they are, and what underlying conditions they may have that she is also managing along with the inflammatory back condition. It is a balancing act to prevent too many appointments, she said, but also helps patients manage the multiple recommendations.
At these appointments, she’ll not only check on patients’ progress and ensure that they have had all the tests that they should have, but she’ll also discuss general measures that may help with patients’ general health, such as weight control, their ability to manage disease processes with other daily activities of living, and other creative coping mechanisms.
“The weight discussion is never easy, but it is helpful to address the impact of weight if it may be contributing to their discomfort,” Dr. Leizman said. “I also think that there are diets patients can choose that are less inflammatory and that can be beneficial.”
Ultimately, “I want my patients to be on the least amount of medicine possible,” Dr. Leizman said. “If they need medications, I support my rheumatologists’ recommendations. I help my patients as they try whatever works to make them feel better, both the nonpharmaceutical options and the medications,” she said.
“Importantly, I am there for support as a resource and a partner,” Leizman added. “I’m the main quarterback for my patients.”
Key Takeaways
- Prompt referral to a rheumatologist remains key.
- The treatment goal is to improve patients’ quality of life by reducing symptoms such as pain and fatigue.
- Physical therapy and NSAIDs remain first-line treatment in primary care.
- NSAID treatment should be at the full recommended dose and given continuously, not as needed.
- The choice of NSAID does not matter; try switching the NSAID if no effects are seen.
- Physical therapy such as water-based activities and yoga may be beneficial, but exercise programs should be prescribed by a qualified therapist.
- Remember general health advice regarding diet and nutrition can be helpful.
A version of this article appeared on Medscape.com.
Migratory Nodules in a Traveler
The Diagnosis: Gnathostomiasis
The biopsy demonstrated a dense, eosinophilic, granulomatous infiltrate surrounding sections of a parasite with skeletal muscle bundles and intestines containing a brush border and luminal debris (Figure), which was consistent with a diagnosis of gnathostomiasis. Upon further questioning, he revealed that while in Peru he frequently consumed ceviche, which is a dish typically made from fresh raw fish cured in lemon or lime juice. He subsequently was treated with oral ivermectin 0.2 mg/kg once daily for 2 days with no evidence of recurrence 12 months later.
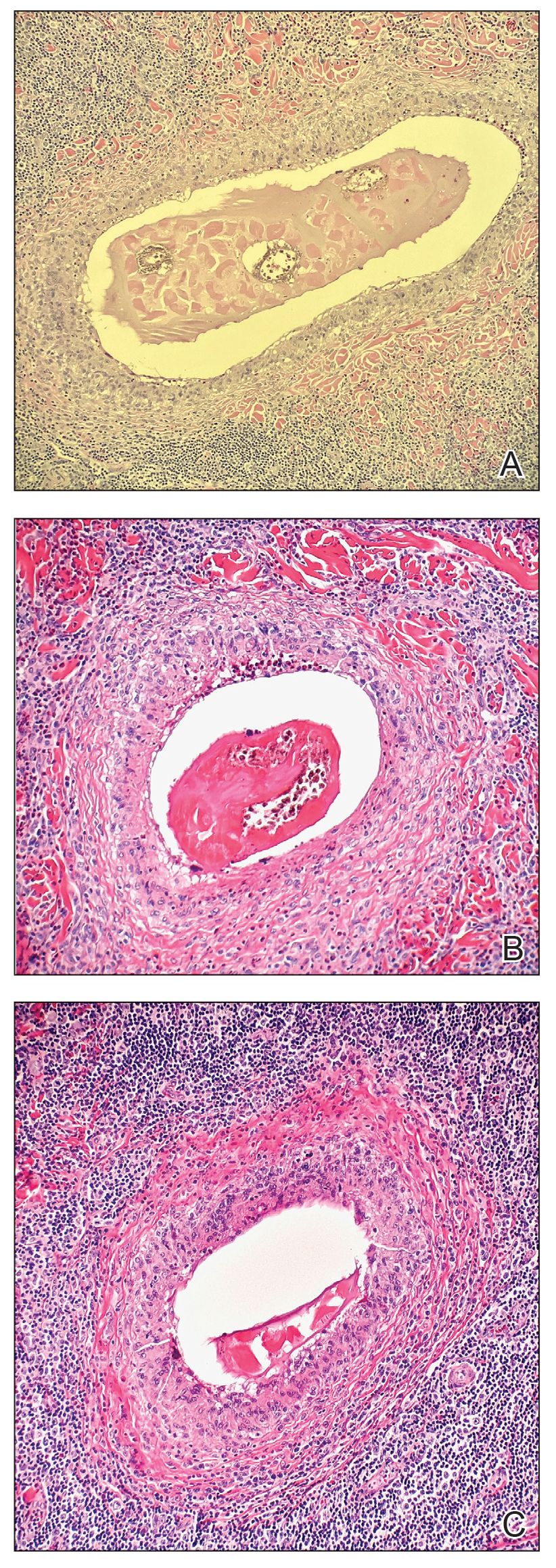
Cutaneous gnathostomiasis is the most common manifestation of infection caused by the third-stage larvae of the genus Gnathostoma. The nematode is endemic to tropical and subtropical regions of Japan and Southeast Asia, particularly Thailand. The disease has been increasingly observed in Central and South America. Humans can become infected through ingestion of undercooked meats, particularly freshwater fish but also poultry, snakes, or frogs. Few cases have been reported in North America and Europe presumably due to more stringent regulations governing the sourcing and storage of fish for consumption.1-3 Restaurants in endemic regions also may use cheaper local freshwater or brackish fish compared to restaurants in the West, which use more expensive saltwater fish that do not harbor Gnathostoma species.1 There is a false belief among restauranteurs and consumers that the larvae can be reliably killed by marinating meat in citrus juice or with concurrent consumption of alcohol or hot spices.2 Adequately cooking or freezing meat to 20 °C for 3 to 5 days are the only effective ways to ensure that the larvae are killed.1-3
The parasite requires its natural definitive hosts—fish-eating mammals such as pigs, cats, and dogs—to complete its life cycle and reproduce. Humans are accidental hosts in whom the parasite fails to reach sexual maturity.1-3 Consequently, symptoms commonly are due to the migration of only 1 larva, but occasionally infection with 2 or more has been observed.1,4
Human infection initially may result in malaise, fever, anorexia, abdominal pain, nausea, vomiting, and diarrhea as the parasite migrates through the stomach, intestines, and liver. After 2 to 4 weeks, larvae may reach the skin where they most commonly create ill-defined, erythematous, indurated, round or oval plaques or nodules described as nodular migratory panniculitis. These lesions tend to develop on the trunk or arms and correspond to the location of the migrating worm.1,3,5 The larvae have been observed to migrate at 1 cm/h.6 Symptoms often wax and wane, with individual nodules lasting approximately 1 to 2 weeks. Uniquely, larval migration can result in a trail of subcutaneous hemorrhage that is considered pathognomonic and helps to differentiate gnathostomiasis from other forms of parasitosis such as strongyloidiasis and sparganosis.1,3 Larvae are highly motile and invasive, and they are capable of producing a wide range of symptoms affecting virtually any part of the body.1,2 Depending on the anatomic location of the migrating worm, infection also may result in neurologic, gastrointestinal, pulmonary, or ocular symptoms.1-3,7 Eosinophilia is common but can subside in the chronic stage, as seen in our patient.1
The classic triad of intermittent migratory nodules, eosinophilia, and a history of travel to Southeast Asia or another endemic region should raise suspicion for gnathostomiasis.1-3,5,7 Unfortunately, confirmatory testing such as Gnathostoma serology is not readily available in the United States, and available serologic tests demonstrate frequent false positives and incomplete crossreactivity.1,2,8 Accordingly, the diagnosis most commonly is solidified by combining cardinal clinical features with histologic findings of a dense eosinophilic inflammatory infiltrate involving the dermis and hypodermis.2,5 In one study, the larva itself was only found in 12 of 66 (18%) skin biopsy specimens from patients with gnathostomiasis.5 If the larva is detected within the sections, it ranges from 2.5 to 12.5 mm in length and 0.4 to 1.2 mm in width and can exhibit cuticular spines, intestinal cells, and characteristic large lateral chords.1,5
The treatment of choice is surgical removal of the worm. Oral albendazole (400–800 mg/d for 21 days) also is considered a first-line treatment and results in clinical cure in approximately 90% of cases. Two doses of oral ivermectin (0.2 mg/kg) spaced 24 to 48 hours apart is an acceptable alternative with comparable efficacy.1-3 Care should be taken if involvement of the central nervous system is suspected, as antihelminthic treatment theoretically could be deleterious due to an inflammatory response to the dying larvae.1,2,9
In the differential diagnosis, loiasis can resemble gnathostomiasis, but the former is endemic to Africa.3 Cutaneous larva migrans most frequently is caused by hookworms from the genus Ancylostoma, which classically leads to superficial serpiginous linear plaques that migrate at a rate of several millimeters per day. However, the larvae are believed to lack the collagenase enzyme required to penetrate the epidermal basement membrane and thus are not capable of producing deep-seated nodules or visceral symptoms.3 Strongyloidiasis (larva currens) generally exhibits a more linear morphology, and infection would result in positive Strongyloides serology.7 Erythema nodosum is a septal panniculitis that can be triggered by infection, pregnancy, medications, connective tissue diseases, inflammatory conditions, and underlying malignancy.10
- Herman JS, Chiodini PL. Gnathostomiasis, another emerging imported disease. Clin Microbiol Rev. 2009;22:484-492.
- Liu GH, Sun MM, Elsheikha HM, et al. Human gnathostomiasis: a neglected food-borne zoonosis. Parasit Vectors. 2020;13:616.
- Tyring SK. Gnathostomiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. 2nd ed. Elsevier; 2017:77-78.
- Rusnak JM, Lucey DR. Clinical gnathostomiasis: case report and review of the English-language literature. Clin Infect Dis. 1993;16:33-50.
- Magaña M, Messina M, Bustamante F, et al. Gnathostomiasis: clinicopathologic study. Am J Dermatopathol. 2004;26:91-95.
- Chandenier J, Husson J, Canaple S, et al. Medullary gnathostomiasis in a white patient: use of immunodiagnosis and magnetic resonance imaging. Clin Infect Dis. 2001;32:E154-E157.
- Hamilton WL, Agranoff D. Imported gnathostomiasis manifesting as cutaneous larva migrans and Löffler’s syndrome. BMJ Case Rep. 2018;2018:bcr2017223132.
- Neumayr A, Ollague J, Bravo F, et al. Cross-reactivity pattern of Asian and American human gnathostomiasis in western blot assays using crude antigens prepared from Gnathostoma spinigerum and Gnathostoma binucleatum third-stage larvae. Am J Trop Med Hyg. 2016;95:413-416.
- Kraivichian K, Nuchprayoon S, Sitichalernchai P, et al. Treatment of cutaneous gnathostomiasis with ivermectin. Am J Trop Med Hyg. 2004;71:623-628.
- Pérez-Garza DM, Chavez-Alvarez S, Ocampo-Candiani J, et al. Erythema nodosum: a practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-378.
The Diagnosis: Gnathostomiasis
The biopsy demonstrated a dense, eosinophilic, granulomatous infiltrate surrounding sections of a parasite with skeletal muscle bundles and intestines containing a brush border and luminal debris (Figure), which was consistent with a diagnosis of gnathostomiasis. Upon further questioning, he revealed that while in Peru he frequently consumed ceviche, which is a dish typically made from fresh raw fish cured in lemon or lime juice. He subsequently was treated with oral ivermectin 0.2 mg/kg once daily for 2 days with no evidence of recurrence 12 months later.
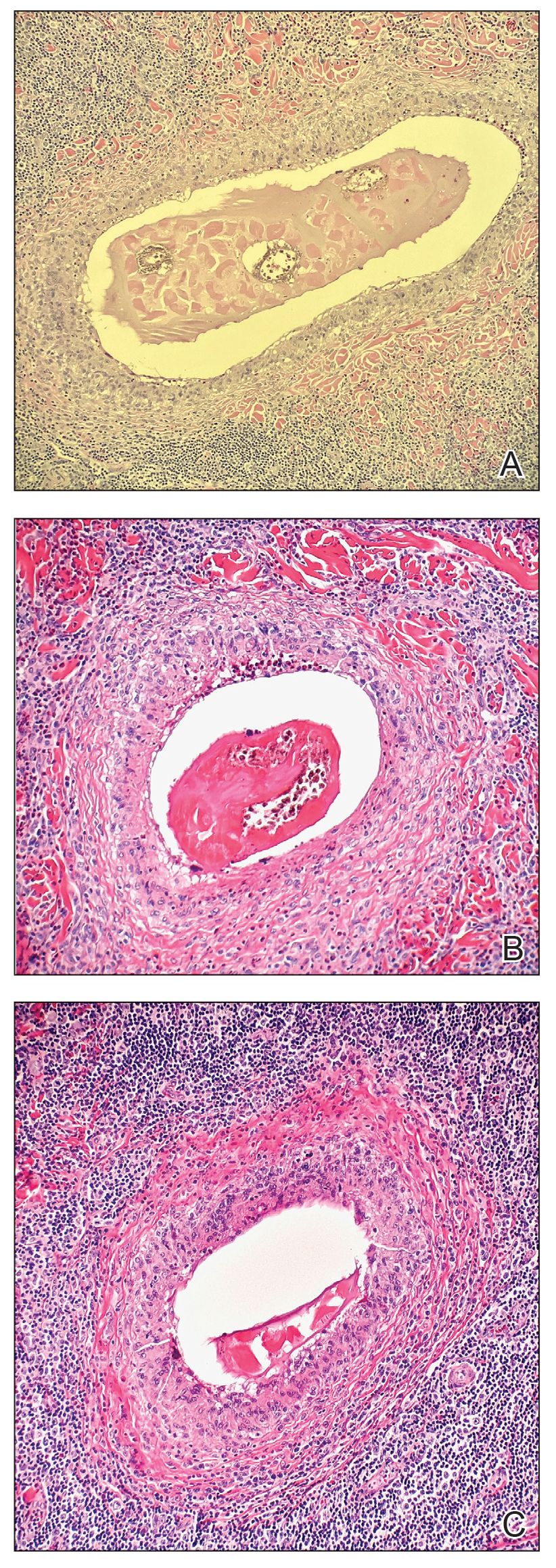
Cutaneous gnathostomiasis is the most common manifestation of infection caused by the third-stage larvae of the genus Gnathostoma. The nematode is endemic to tropical and subtropical regions of Japan and Southeast Asia, particularly Thailand. The disease has been increasingly observed in Central and South America. Humans can become infected through ingestion of undercooked meats, particularly freshwater fish but also poultry, snakes, or frogs. Few cases have been reported in North America and Europe presumably due to more stringent regulations governing the sourcing and storage of fish for consumption.1-3 Restaurants in endemic regions also may use cheaper local freshwater or brackish fish compared to restaurants in the West, which use more expensive saltwater fish that do not harbor Gnathostoma species.1 There is a false belief among restauranteurs and consumers that the larvae can be reliably killed by marinating meat in citrus juice or with concurrent consumption of alcohol or hot spices.2 Adequately cooking or freezing meat to 20 °C for 3 to 5 days are the only effective ways to ensure that the larvae are killed.1-3
The parasite requires its natural definitive hosts—fish-eating mammals such as pigs, cats, and dogs—to complete its life cycle and reproduce. Humans are accidental hosts in whom the parasite fails to reach sexual maturity.1-3 Consequently, symptoms commonly are due to the migration of only 1 larva, but occasionally infection with 2 or more has been observed.1,4
Human infection initially may result in malaise, fever, anorexia, abdominal pain, nausea, vomiting, and diarrhea as the parasite migrates through the stomach, intestines, and liver. After 2 to 4 weeks, larvae may reach the skin where they most commonly create ill-defined, erythematous, indurated, round or oval plaques or nodules described as nodular migratory panniculitis. These lesions tend to develop on the trunk or arms and correspond to the location of the migrating worm.1,3,5 The larvae have been observed to migrate at 1 cm/h.6 Symptoms often wax and wane, with individual nodules lasting approximately 1 to 2 weeks. Uniquely, larval migration can result in a trail of subcutaneous hemorrhage that is considered pathognomonic and helps to differentiate gnathostomiasis from other forms of parasitosis such as strongyloidiasis and sparganosis.1,3 Larvae are highly motile and invasive, and they are capable of producing a wide range of symptoms affecting virtually any part of the body.1,2 Depending on the anatomic location of the migrating worm, infection also may result in neurologic, gastrointestinal, pulmonary, or ocular symptoms.1-3,7 Eosinophilia is common but can subside in the chronic stage, as seen in our patient.1
The classic triad of intermittent migratory nodules, eosinophilia, and a history of travel to Southeast Asia or another endemic region should raise suspicion for gnathostomiasis.1-3,5,7 Unfortunately, confirmatory testing such as Gnathostoma serology is not readily available in the United States, and available serologic tests demonstrate frequent false positives and incomplete crossreactivity.1,2,8 Accordingly, the diagnosis most commonly is solidified by combining cardinal clinical features with histologic findings of a dense eosinophilic inflammatory infiltrate involving the dermis and hypodermis.2,5 In one study, the larva itself was only found in 12 of 66 (18%) skin biopsy specimens from patients with gnathostomiasis.5 If the larva is detected within the sections, it ranges from 2.5 to 12.5 mm in length and 0.4 to 1.2 mm in width and can exhibit cuticular spines, intestinal cells, and characteristic large lateral chords.1,5
The treatment of choice is surgical removal of the worm. Oral albendazole (400–800 mg/d for 21 days) also is considered a first-line treatment and results in clinical cure in approximately 90% of cases. Two doses of oral ivermectin (0.2 mg/kg) spaced 24 to 48 hours apart is an acceptable alternative with comparable efficacy.1-3 Care should be taken if involvement of the central nervous system is suspected, as antihelminthic treatment theoretically could be deleterious due to an inflammatory response to the dying larvae.1,2,9
In the differential diagnosis, loiasis can resemble gnathostomiasis, but the former is endemic to Africa.3 Cutaneous larva migrans most frequently is caused by hookworms from the genus Ancylostoma, which classically leads to superficial serpiginous linear plaques that migrate at a rate of several millimeters per day. However, the larvae are believed to lack the collagenase enzyme required to penetrate the epidermal basement membrane and thus are not capable of producing deep-seated nodules or visceral symptoms.3 Strongyloidiasis (larva currens) generally exhibits a more linear morphology, and infection would result in positive Strongyloides serology.7 Erythema nodosum is a septal panniculitis that can be triggered by infection, pregnancy, medications, connective tissue diseases, inflammatory conditions, and underlying malignancy.10
The Diagnosis: Gnathostomiasis
The biopsy demonstrated a dense, eosinophilic, granulomatous infiltrate surrounding sections of a parasite with skeletal muscle bundles and intestines containing a brush border and luminal debris (Figure), which was consistent with a diagnosis of gnathostomiasis. Upon further questioning, he revealed that while in Peru he frequently consumed ceviche, which is a dish typically made from fresh raw fish cured in lemon or lime juice. He subsequently was treated with oral ivermectin 0.2 mg/kg once daily for 2 days with no evidence of recurrence 12 months later.
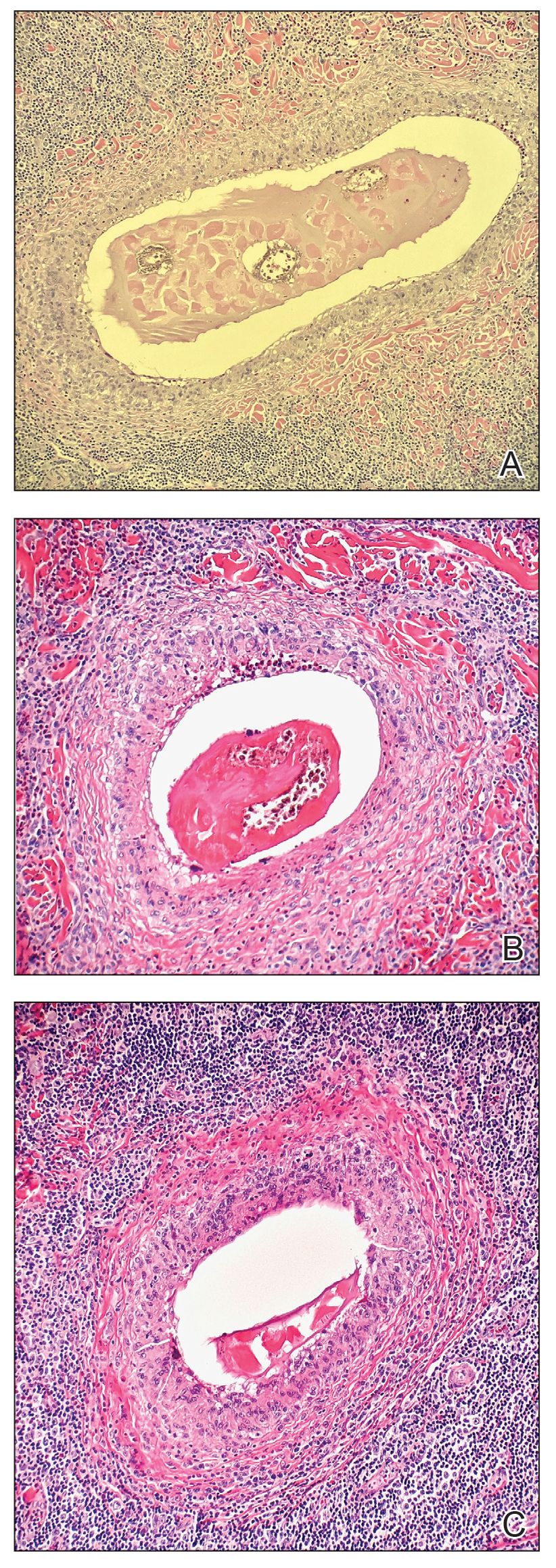
Cutaneous gnathostomiasis is the most common manifestation of infection caused by the third-stage larvae of the genus Gnathostoma. The nematode is endemic to tropical and subtropical regions of Japan and Southeast Asia, particularly Thailand. The disease has been increasingly observed in Central and South America. Humans can become infected through ingestion of undercooked meats, particularly freshwater fish but also poultry, snakes, or frogs. Few cases have been reported in North America and Europe presumably due to more stringent regulations governing the sourcing and storage of fish for consumption.1-3 Restaurants in endemic regions also may use cheaper local freshwater or brackish fish compared to restaurants in the West, which use more expensive saltwater fish that do not harbor Gnathostoma species.1 There is a false belief among restauranteurs and consumers that the larvae can be reliably killed by marinating meat in citrus juice or with concurrent consumption of alcohol or hot spices.2 Adequately cooking or freezing meat to 20 °C for 3 to 5 days are the only effective ways to ensure that the larvae are killed.1-3
The parasite requires its natural definitive hosts—fish-eating mammals such as pigs, cats, and dogs—to complete its life cycle and reproduce. Humans are accidental hosts in whom the parasite fails to reach sexual maturity.1-3 Consequently, symptoms commonly are due to the migration of only 1 larva, but occasionally infection with 2 or more has been observed.1,4
Human infection initially may result in malaise, fever, anorexia, abdominal pain, nausea, vomiting, and diarrhea as the parasite migrates through the stomach, intestines, and liver. After 2 to 4 weeks, larvae may reach the skin where they most commonly create ill-defined, erythematous, indurated, round or oval plaques or nodules described as nodular migratory panniculitis. These lesions tend to develop on the trunk or arms and correspond to the location of the migrating worm.1,3,5 The larvae have been observed to migrate at 1 cm/h.6 Symptoms often wax and wane, with individual nodules lasting approximately 1 to 2 weeks. Uniquely, larval migration can result in a trail of subcutaneous hemorrhage that is considered pathognomonic and helps to differentiate gnathostomiasis from other forms of parasitosis such as strongyloidiasis and sparganosis.1,3 Larvae are highly motile and invasive, and they are capable of producing a wide range of symptoms affecting virtually any part of the body.1,2 Depending on the anatomic location of the migrating worm, infection also may result in neurologic, gastrointestinal, pulmonary, or ocular symptoms.1-3,7 Eosinophilia is common but can subside in the chronic stage, as seen in our patient.1
The classic triad of intermittent migratory nodules, eosinophilia, and a history of travel to Southeast Asia or another endemic region should raise suspicion for gnathostomiasis.1-3,5,7 Unfortunately, confirmatory testing such as Gnathostoma serology is not readily available in the United States, and available serologic tests demonstrate frequent false positives and incomplete crossreactivity.1,2,8 Accordingly, the diagnosis most commonly is solidified by combining cardinal clinical features with histologic findings of a dense eosinophilic inflammatory infiltrate involving the dermis and hypodermis.2,5 In one study, the larva itself was only found in 12 of 66 (18%) skin biopsy specimens from patients with gnathostomiasis.5 If the larva is detected within the sections, it ranges from 2.5 to 12.5 mm in length and 0.4 to 1.2 mm in width and can exhibit cuticular spines, intestinal cells, and characteristic large lateral chords.1,5
The treatment of choice is surgical removal of the worm. Oral albendazole (400–800 mg/d for 21 days) also is considered a first-line treatment and results in clinical cure in approximately 90% of cases. Two doses of oral ivermectin (0.2 mg/kg) spaced 24 to 48 hours apart is an acceptable alternative with comparable efficacy.1-3 Care should be taken if involvement of the central nervous system is suspected, as antihelminthic treatment theoretically could be deleterious due to an inflammatory response to the dying larvae.1,2,9
In the differential diagnosis, loiasis can resemble gnathostomiasis, but the former is endemic to Africa.3 Cutaneous larva migrans most frequently is caused by hookworms from the genus Ancylostoma, which classically leads to superficial serpiginous linear plaques that migrate at a rate of several millimeters per day. However, the larvae are believed to lack the collagenase enzyme required to penetrate the epidermal basement membrane and thus are not capable of producing deep-seated nodules or visceral symptoms.3 Strongyloidiasis (larva currens) generally exhibits a more linear morphology, and infection would result in positive Strongyloides serology.7 Erythema nodosum is a septal panniculitis that can be triggered by infection, pregnancy, medications, connective tissue diseases, inflammatory conditions, and underlying malignancy.10
- Herman JS, Chiodini PL. Gnathostomiasis, another emerging imported disease. Clin Microbiol Rev. 2009;22:484-492.
- Liu GH, Sun MM, Elsheikha HM, et al. Human gnathostomiasis: a neglected food-borne zoonosis. Parasit Vectors. 2020;13:616.
- Tyring SK. Gnathostomiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. 2nd ed. Elsevier; 2017:77-78.
- Rusnak JM, Lucey DR. Clinical gnathostomiasis: case report and review of the English-language literature. Clin Infect Dis. 1993;16:33-50.
- Magaña M, Messina M, Bustamante F, et al. Gnathostomiasis: clinicopathologic study. Am J Dermatopathol. 2004;26:91-95.
- Chandenier J, Husson J, Canaple S, et al. Medullary gnathostomiasis in a white patient: use of immunodiagnosis and magnetic resonance imaging. Clin Infect Dis. 2001;32:E154-E157.
- Hamilton WL, Agranoff D. Imported gnathostomiasis manifesting as cutaneous larva migrans and Löffler’s syndrome. BMJ Case Rep. 2018;2018:bcr2017223132.
- Neumayr A, Ollague J, Bravo F, et al. Cross-reactivity pattern of Asian and American human gnathostomiasis in western blot assays using crude antigens prepared from Gnathostoma spinigerum and Gnathostoma binucleatum third-stage larvae. Am J Trop Med Hyg. 2016;95:413-416.
- Kraivichian K, Nuchprayoon S, Sitichalernchai P, et al. Treatment of cutaneous gnathostomiasis with ivermectin. Am J Trop Med Hyg. 2004;71:623-628.
- Pérez-Garza DM, Chavez-Alvarez S, Ocampo-Candiani J, et al. Erythema nodosum: a practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-378.
- Herman JS, Chiodini PL. Gnathostomiasis, another emerging imported disease. Clin Microbiol Rev. 2009;22:484-492.
- Liu GH, Sun MM, Elsheikha HM, et al. Human gnathostomiasis: a neglected food-borne zoonosis. Parasit Vectors. 2020;13:616.
- Tyring SK. Gnathostomiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. 2nd ed. Elsevier; 2017:77-78.
- Rusnak JM, Lucey DR. Clinical gnathostomiasis: case report and review of the English-language literature. Clin Infect Dis. 1993;16:33-50.
- Magaña M, Messina M, Bustamante F, et al. Gnathostomiasis: clinicopathologic study. Am J Dermatopathol. 2004;26:91-95.
- Chandenier J, Husson J, Canaple S, et al. Medullary gnathostomiasis in a white patient: use of immunodiagnosis and magnetic resonance imaging. Clin Infect Dis. 2001;32:E154-E157.
- Hamilton WL, Agranoff D. Imported gnathostomiasis manifesting as cutaneous larva migrans and Löffler’s syndrome. BMJ Case Rep. 2018;2018:bcr2017223132.
- Neumayr A, Ollague J, Bravo F, et al. Cross-reactivity pattern of Asian and American human gnathostomiasis in western blot assays using crude antigens prepared from Gnathostoma spinigerum and Gnathostoma binucleatum third-stage larvae. Am J Trop Med Hyg. 2016;95:413-416.
- Kraivichian K, Nuchprayoon S, Sitichalernchai P, et al. Treatment of cutaneous gnathostomiasis with ivermectin. Am J Trop Med Hyg. 2004;71:623-628.
- Pérez-Garza DM, Chavez-Alvarez S, Ocampo-Candiani J, et al. Erythema nodosum: a practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-378.
A 41-year-old man presented to a dermatology clinic in the United States with a migratory subcutaneous nodule overlying the left upper chest that initially developed 12 months prior and continued to migrate along the trunk and proximal aspect of the arms. The patient had spent the last 3 years residing in Peru. He never observed more than 1 nodule at a time and denied associated fever, headache, visual changes, chest pain, cough, abdominal pain, and diarrhea. Laboratory studies including a blood eosinophil count and serum Strongyloides immunoglobulins were within reference range. An excisional biopsy was performed.

Public Citizen seeks stronger warning for Botox, related products
.
The nonprofit watchdog group successfully petitioned the FDA in 2008 to require a warning for Botox and related products regarding the risk of distant spread of the toxin. In its latest petition to the agency, it says that the injectables need additional warnings about the possibility of iatrogenic botulism with initial and repeated doses and that individuals who contract the condition may need botulinum antitoxin to avert temporary muscle paralysis, hospitalization, and death.
The current warning does not contain any information about the potential need for antitoxin and downplays the need for giving antitoxin in the settings of excessive dosing, accidental injection, and oral ingestion, said Public Citizen.
“Our petition is based on clear postmarketing evidence that refutes industry propaganda claiming that Botox and related drugs are ‘always safe’ and that no ‘definitive’ cases of botulism have occurred with recommended doses,” Azza AbuDagga, PhD, health services researcher at Public Citizen’s Health Research Group, said in a statement.
Public Citizen said that using data from the FDA’s Adverse Event Reporting System (FAERS), it found 5414 reports of serious outcomes from botulinum toxin products from January 1989 through March 2021. Almost 22% involved cosmetic indications and about 78% involved therapeutic indications.
Of the 5414 reports, 121 (2%) specified botulism as an adverse reaction; 89 involved therapeutic uses of a botulinum toxin products, and 32 involved cosmetic uses. Many of those 121 reports involved doses within the recommended range for the indication, according to Public Citizen.
The group is also asking the FDA to remove what it calls misleading promotional statements in the labeling of Botox and Botox Cosmetic and from the medication guides for those products. The labels state that there have been “no definitive serious adverse event reports of distant spread of toxin effect” with either the cosmetic use or for use in treating chronic migraine, severe underarm sweating, blepharospasm, or strabismus. These statements do not appear in similar labeling in other countries, such as Canada and the United Kingdom, said Public Citizen.
“The FDA needs to implement our two requested actions quickly to warn the public in unambiguous terms about the risk of botulism associated with the use of Botox and related drugs,” Dr. AbuDagga said in the Public Citizen statement. “This will allow health care professionals and patients to make more informed decisions about the benefit-risk profile of these widely used drugs.”
The Public Citizen petition would apply to all seven approved botulinum toxin biological products: abobotulinumtoxinA (Dysport), daxibotulinumtoxinA-lanm (Daxxify), incobotulinumtoxinA (Xeomin), onabotulinumtoxinA (Botox, Botox Cosmetic), prabotulinumtoxinA-xvfs (Jeuveau) and rimabotulinumtoxinB (Myobloc).
An FDA spokesperson said the agency is reviewing the citizen petition, and that generally the agency does not comment on pending petitions. “When we respond to the petition, we will respond directly to the petitioner and post the response in the designated agency docket,” the spokesperson told this news organization. At press time, Botox manufacturer AbbVie had not responded to a request for a comment.
Botulinum toxin is the most-used product for nonsurgical cosmetic procedures, according to the International Society of Aesthetic Plastic Surgery (ISAPS). The ISAPS reported that there were more than 7 million botulinum toxin procedures performed by plastic surgeons worldwide in 2021.
The American Society of Plastic Surgery reported that its members performed 4.4 million Botox procedures in 2020, while the American Society of Dermatologic Surgery (ASDS) said its members performed 2.3 million wrinkle-relaxing procedures in 2019, a 60% increase since 2012.
.
The nonprofit watchdog group successfully petitioned the FDA in 2008 to require a warning for Botox and related products regarding the risk of distant spread of the toxin. In its latest petition to the agency, it says that the injectables need additional warnings about the possibility of iatrogenic botulism with initial and repeated doses and that individuals who contract the condition may need botulinum antitoxin to avert temporary muscle paralysis, hospitalization, and death.
The current warning does not contain any information about the potential need for antitoxin and downplays the need for giving antitoxin in the settings of excessive dosing, accidental injection, and oral ingestion, said Public Citizen.
“Our petition is based on clear postmarketing evidence that refutes industry propaganda claiming that Botox and related drugs are ‘always safe’ and that no ‘definitive’ cases of botulism have occurred with recommended doses,” Azza AbuDagga, PhD, health services researcher at Public Citizen’s Health Research Group, said in a statement.
Public Citizen said that using data from the FDA’s Adverse Event Reporting System (FAERS), it found 5414 reports of serious outcomes from botulinum toxin products from January 1989 through March 2021. Almost 22% involved cosmetic indications and about 78% involved therapeutic indications.
Of the 5414 reports, 121 (2%) specified botulism as an adverse reaction; 89 involved therapeutic uses of a botulinum toxin products, and 32 involved cosmetic uses. Many of those 121 reports involved doses within the recommended range for the indication, according to Public Citizen.
The group is also asking the FDA to remove what it calls misleading promotional statements in the labeling of Botox and Botox Cosmetic and from the medication guides for those products. The labels state that there have been “no definitive serious adverse event reports of distant spread of toxin effect” with either the cosmetic use or for use in treating chronic migraine, severe underarm sweating, blepharospasm, or strabismus. These statements do not appear in similar labeling in other countries, such as Canada and the United Kingdom, said Public Citizen.
“The FDA needs to implement our two requested actions quickly to warn the public in unambiguous terms about the risk of botulism associated with the use of Botox and related drugs,” Dr. AbuDagga said in the Public Citizen statement. “This will allow health care professionals and patients to make more informed decisions about the benefit-risk profile of these widely used drugs.”
The Public Citizen petition would apply to all seven approved botulinum toxin biological products: abobotulinumtoxinA (Dysport), daxibotulinumtoxinA-lanm (Daxxify), incobotulinumtoxinA (Xeomin), onabotulinumtoxinA (Botox, Botox Cosmetic), prabotulinumtoxinA-xvfs (Jeuveau) and rimabotulinumtoxinB (Myobloc).
An FDA spokesperson said the agency is reviewing the citizen petition, and that generally the agency does not comment on pending petitions. “When we respond to the petition, we will respond directly to the petitioner and post the response in the designated agency docket,” the spokesperson told this news organization. At press time, Botox manufacturer AbbVie had not responded to a request for a comment.
Botulinum toxin is the most-used product for nonsurgical cosmetic procedures, according to the International Society of Aesthetic Plastic Surgery (ISAPS). The ISAPS reported that there were more than 7 million botulinum toxin procedures performed by plastic surgeons worldwide in 2021.
The American Society of Plastic Surgery reported that its members performed 4.4 million Botox procedures in 2020, while the American Society of Dermatologic Surgery (ASDS) said its members performed 2.3 million wrinkle-relaxing procedures in 2019, a 60% increase since 2012.
.
The nonprofit watchdog group successfully petitioned the FDA in 2008 to require a warning for Botox and related products regarding the risk of distant spread of the toxin. In its latest petition to the agency, it says that the injectables need additional warnings about the possibility of iatrogenic botulism with initial and repeated doses and that individuals who contract the condition may need botulinum antitoxin to avert temporary muscle paralysis, hospitalization, and death.
The current warning does not contain any information about the potential need for antitoxin and downplays the need for giving antitoxin in the settings of excessive dosing, accidental injection, and oral ingestion, said Public Citizen.
“Our petition is based on clear postmarketing evidence that refutes industry propaganda claiming that Botox and related drugs are ‘always safe’ and that no ‘definitive’ cases of botulism have occurred with recommended doses,” Azza AbuDagga, PhD, health services researcher at Public Citizen’s Health Research Group, said in a statement.
Public Citizen said that using data from the FDA’s Adverse Event Reporting System (FAERS), it found 5414 reports of serious outcomes from botulinum toxin products from January 1989 through March 2021. Almost 22% involved cosmetic indications and about 78% involved therapeutic indications.
Of the 5414 reports, 121 (2%) specified botulism as an adverse reaction; 89 involved therapeutic uses of a botulinum toxin products, and 32 involved cosmetic uses. Many of those 121 reports involved doses within the recommended range for the indication, according to Public Citizen.
The group is also asking the FDA to remove what it calls misleading promotional statements in the labeling of Botox and Botox Cosmetic and from the medication guides for those products. The labels state that there have been “no definitive serious adverse event reports of distant spread of toxin effect” with either the cosmetic use or for use in treating chronic migraine, severe underarm sweating, blepharospasm, or strabismus. These statements do not appear in similar labeling in other countries, such as Canada and the United Kingdom, said Public Citizen.
“The FDA needs to implement our two requested actions quickly to warn the public in unambiguous terms about the risk of botulism associated with the use of Botox and related drugs,” Dr. AbuDagga said in the Public Citizen statement. “This will allow health care professionals and patients to make more informed decisions about the benefit-risk profile of these widely used drugs.”
The Public Citizen petition would apply to all seven approved botulinum toxin biological products: abobotulinumtoxinA (Dysport), daxibotulinumtoxinA-lanm (Daxxify), incobotulinumtoxinA (Xeomin), onabotulinumtoxinA (Botox, Botox Cosmetic), prabotulinumtoxinA-xvfs (Jeuveau) and rimabotulinumtoxinB (Myobloc).
An FDA spokesperson said the agency is reviewing the citizen petition, and that generally the agency does not comment on pending petitions. “When we respond to the petition, we will respond directly to the petitioner and post the response in the designated agency docket,” the spokesperson told this news organization. At press time, Botox manufacturer AbbVie had not responded to a request for a comment.
Botulinum toxin is the most-used product for nonsurgical cosmetic procedures, according to the International Society of Aesthetic Plastic Surgery (ISAPS). The ISAPS reported that there were more than 7 million botulinum toxin procedures performed by plastic surgeons worldwide in 2021.
The American Society of Plastic Surgery reported that its members performed 4.4 million Botox procedures in 2020, while the American Society of Dermatologic Surgery (ASDS) said its members performed 2.3 million wrinkle-relaxing procedures in 2019, a 60% increase since 2012.
Clinical Takeaways in Thrombocytopenia From ASH 2023
The clinical takeaways in immune thrombocytopenia (ITP) from the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition include the relative merits of advanced therapies, efficacy of novel therapies, and infection risk for patients with chronic ITP.
Dr Howard Liebman, of the Keck School of Medicine in Los Angeles, California, opens with a database analysis of patients with primary ITP who were first-time users of advanced therapies, such as rituximab and thrombopoietin (TPO) receptor agonists. The analysis found that despite their relative merits, all the drugs carried a significant risk for adverse events.
Next, he reports on a study examining whether newly diagnosed patients or patients with chronic ITP had better results from the use of avatrombopag, a TPO receptor agonist. Reassuringly, there were no differences in outcomes.
Dr Liebman then discusses the updated results of an ongoing study of rilzabrutinib, a Bruton kinase inhibitor. This analysis showed that the drug achieved rapid, stable, and durable platelet responses.
He next turns to a Danish registry study on infection in patients with chronic ITP, which revealed an ongoing, cumulative risk for infection over 10 years.
Finally, Dr Liebman reports on a study that showed women who develop ITP during pregnancy require more interventions than do women with chronic ITP who become pregnant, and many develop chronic disease after delivery.
--
Howard A. Liebman, MD, Professor of Medicine and Pathology, University of Southern California, Keck School of Medicine; Attending Physician, Department of Medicine, Hematology, Norris Comprehensive Cancer Center, Keck Medicine at University of Southern California, Los Angeles, California
Howard A. Liebman, MD, has disclosed the following relevant financial relationships:
Serve(d) as a consultant for: Novartis; Sanofi; Sobi
Received research grant from: Janssen Pharmaceuticals; Sanofi
The clinical takeaways in immune thrombocytopenia (ITP) from the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition include the relative merits of advanced therapies, efficacy of novel therapies, and infection risk for patients with chronic ITP.
Dr Howard Liebman, of the Keck School of Medicine in Los Angeles, California, opens with a database analysis of patients with primary ITP who were first-time users of advanced therapies, such as rituximab and thrombopoietin (TPO) receptor agonists. The analysis found that despite their relative merits, all the drugs carried a significant risk for adverse events.
Next, he reports on a study examining whether newly diagnosed patients or patients with chronic ITP had better results from the use of avatrombopag, a TPO receptor agonist. Reassuringly, there were no differences in outcomes.
Dr Liebman then discusses the updated results of an ongoing study of rilzabrutinib, a Bruton kinase inhibitor. This analysis showed that the drug achieved rapid, stable, and durable platelet responses.
He next turns to a Danish registry study on infection in patients with chronic ITP, which revealed an ongoing, cumulative risk for infection over 10 years.
Finally, Dr Liebman reports on a study that showed women who develop ITP during pregnancy require more interventions than do women with chronic ITP who become pregnant, and many develop chronic disease after delivery.
--
Howard A. Liebman, MD, Professor of Medicine and Pathology, University of Southern California, Keck School of Medicine; Attending Physician, Department of Medicine, Hematology, Norris Comprehensive Cancer Center, Keck Medicine at University of Southern California, Los Angeles, California
Howard A. Liebman, MD, has disclosed the following relevant financial relationships:
Serve(d) as a consultant for: Novartis; Sanofi; Sobi
Received research grant from: Janssen Pharmaceuticals; Sanofi
The clinical takeaways in immune thrombocytopenia (ITP) from the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition include the relative merits of advanced therapies, efficacy of novel therapies, and infection risk for patients with chronic ITP.
Dr Howard Liebman, of the Keck School of Medicine in Los Angeles, California, opens with a database analysis of patients with primary ITP who were first-time users of advanced therapies, such as rituximab and thrombopoietin (TPO) receptor agonists. The analysis found that despite their relative merits, all the drugs carried a significant risk for adverse events.
Next, he reports on a study examining whether newly diagnosed patients or patients with chronic ITP had better results from the use of avatrombopag, a TPO receptor agonist. Reassuringly, there were no differences in outcomes.
Dr Liebman then discusses the updated results of an ongoing study of rilzabrutinib, a Bruton kinase inhibitor. This analysis showed that the drug achieved rapid, stable, and durable platelet responses.
He next turns to a Danish registry study on infection in patients with chronic ITP, which revealed an ongoing, cumulative risk for infection over 10 years.
Finally, Dr Liebman reports on a study that showed women who develop ITP during pregnancy require more interventions than do women with chronic ITP who become pregnant, and many develop chronic disease after delivery.
--
Howard A. Liebman, MD, Professor of Medicine and Pathology, University of Southern California, Keck School of Medicine; Attending Physician, Department of Medicine, Hematology, Norris Comprehensive Cancer Center, Keck Medicine at University of Southern California, Los Angeles, California
Howard A. Liebman, MD, has disclosed the following relevant financial relationships:
Serve(d) as a consultant for: Novartis; Sanofi; Sobi
Received research grant from: Janssen Pharmaceuticals; Sanofi

Diffuse Large B-Cell Lymphoma Highlights From ASH 2023
Highlights in diffuse large B-cell lymphoma (DLBCL) from the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition that are particularly relevant to Veterans Health Administration (VHA) patients are reported by Dr Nicholas Burwick of Puget Sound VA Health Care System.
Dr Burwick begins with a large VHA study examining racial disparities in DLBCL outcomes among veterans. Importantly, overall survival was not significantly different across racial groups.
He next covers two studies in the DLBCL frontline setting. The first examines the efficacy of standard-dose R-CHOP; reduced-intensity R-CHOP; and an anthracycline alternative regimen among older patients. Standard-dose R-CHOP yielded superior results in patients aged 70- to 79-years but not for those older than 80 years, a group that merits further study.
The second frontline study focused on the chemotherapy-free regimen mosunetuzumab plus the antibody-drug conjugate polatuzumab vedotin (pola) in patients who are older and unfit for chemotherapy. The combination showed good preliminary efficacy.
Turning to relapsed/refractory patients, Dr Burwick discusses a real-world study examining response rates to tafasitamab in White vs Black/African American patients and non-Hispanic vs Hispanic patients. Differences between the two groups proved minimal.
Finally, he discusses a study of the bispecific antibody glofitamab and pola in heavily pretreated patients that showed promising results in this population.
--
Nicholas R. Burwick, MD, Associate Professor, Department of Medicine, Division of Hematology, University of Washington; Staff Physician, Department of Medicine, Division of Hematology, Puget Sound VA Health Care System, Seattle, Washington
Nicholas R. Burwick, MD, has disclosed no relevant financial relationships
Highlights in diffuse large B-cell lymphoma (DLBCL) from the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition that are particularly relevant to Veterans Health Administration (VHA) patients are reported by Dr Nicholas Burwick of Puget Sound VA Health Care System.
Dr Burwick begins with a large VHA study examining racial disparities in DLBCL outcomes among veterans. Importantly, overall survival was not significantly different across racial groups.
He next covers two studies in the DLBCL frontline setting. The first examines the efficacy of standard-dose R-CHOP; reduced-intensity R-CHOP; and an anthracycline alternative regimen among older patients. Standard-dose R-CHOP yielded superior results in patients aged 70- to 79-years but not for those older than 80 years, a group that merits further study.
The second frontline study focused on the chemotherapy-free regimen mosunetuzumab plus the antibody-drug conjugate polatuzumab vedotin (pola) in patients who are older and unfit for chemotherapy. The combination showed good preliminary efficacy.
Turning to relapsed/refractory patients, Dr Burwick discusses a real-world study examining response rates to tafasitamab in White vs Black/African American patients and non-Hispanic vs Hispanic patients. Differences between the two groups proved minimal.
Finally, he discusses a study of the bispecific antibody glofitamab and pola in heavily pretreated patients that showed promising results in this population.
--
Nicholas R. Burwick, MD, Associate Professor, Department of Medicine, Division of Hematology, University of Washington; Staff Physician, Department of Medicine, Division of Hematology, Puget Sound VA Health Care System, Seattle, Washington
Nicholas R. Burwick, MD, has disclosed no relevant financial relationships
Highlights in diffuse large B-cell lymphoma (DLBCL) from the 2023 American Society of Hematology (ASH) Annual Meeting and Exposition that are particularly relevant to Veterans Health Administration (VHA) patients are reported by Dr Nicholas Burwick of Puget Sound VA Health Care System.
Dr Burwick begins with a large VHA study examining racial disparities in DLBCL outcomes among veterans. Importantly, overall survival was not significantly different across racial groups.
He next covers two studies in the DLBCL frontline setting. The first examines the efficacy of standard-dose R-CHOP; reduced-intensity R-CHOP; and an anthracycline alternative regimen among older patients. Standard-dose R-CHOP yielded superior results in patients aged 70- to 79-years but not for those older than 80 years, a group that merits further study.
The second frontline study focused on the chemotherapy-free regimen mosunetuzumab plus the antibody-drug conjugate polatuzumab vedotin (pola) in patients who are older and unfit for chemotherapy. The combination showed good preliminary efficacy.
Turning to relapsed/refractory patients, Dr Burwick discusses a real-world study examining response rates to tafasitamab in White vs Black/African American patients and non-Hispanic vs Hispanic patients. Differences between the two groups proved minimal.
Finally, he discusses a study of the bispecific antibody glofitamab and pola in heavily pretreated patients that showed promising results in this population.
--
Nicholas R. Burwick, MD, Associate Professor, Department of Medicine, Division of Hematology, University of Washington; Staff Physician, Department of Medicine, Division of Hematology, Puget Sound VA Health Care System, Seattle, Washington
Nicholas R. Burwick, MD, has disclosed no relevant financial relationships



