User login
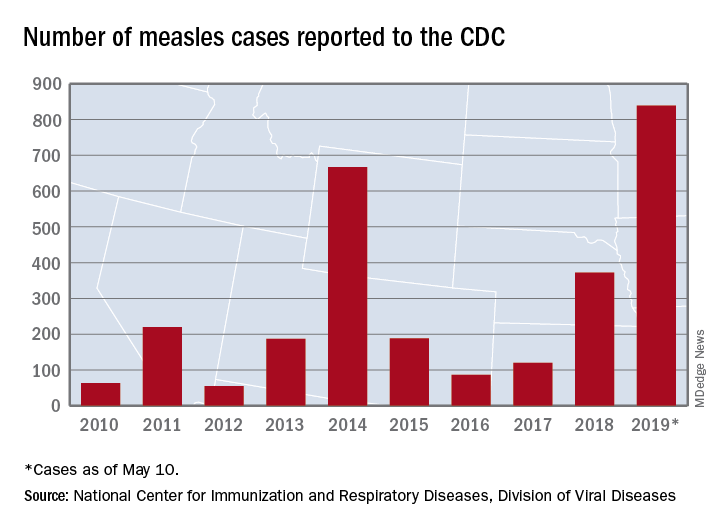
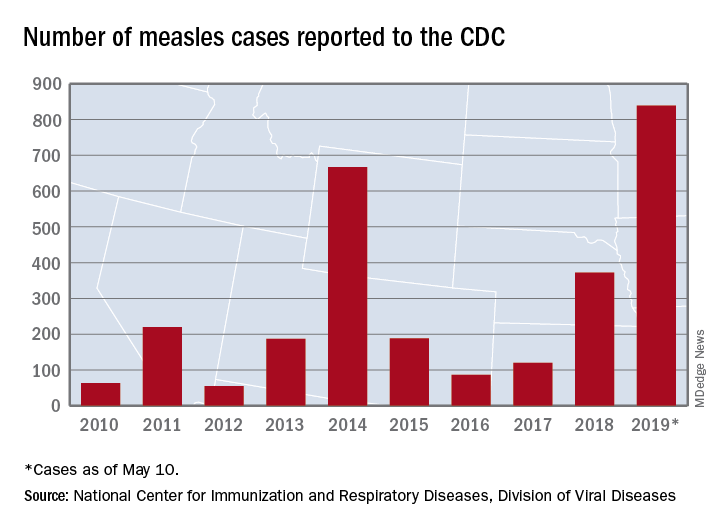
U.S. measles cases climb to over 800 for the year
according to the Centers for Disease Control and Prevention.
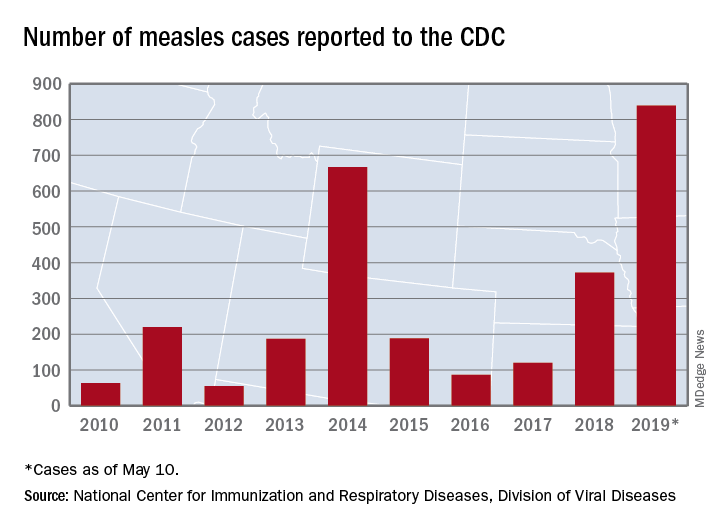
There are 10 states dealing with ongoing outbreaks now that Pennsylvania has been added to the list, the CDC reported May 13. The state has had five cases so far, all in Allegheny County. New York City continued to have the most active outbreak, adding 43 more cases in Brooklyn last week for a total of 410 in the city since the beginning of 2019, NYC Health said.
Several of this year’s outbreaks were predicted in an analysis published in the Lancet Infectious Diseases (2019 May 9. doi: 10.1016/S1473-3099(19)30231-2). Investigators identified the 25 counties most likely to experience a measles outbreak in 2019 – a list that includes Queens, N.Y. (adjacent to Brooklyn), Multnomah, Ore. (adjacent to Clark County, Wash., where 71 people were infected earlier this year), and San Mateo, Calif., where 4 cases have been reported.
“We recommend that public health officials and policymakers prioritize monitoring the counties we identify to be at high risk that have not yet reported cases, especially those that lie adjacent to counties with ongoing outbreaks and those that house large international airports,” senior author Lauren Gardner of Johns Hopkins University, Baltimore, said in a written statement.
The outbreak in Clark County was declared over in late April, but Gov. Jay Inslee signed a bill on May 10 that removes the personal/philosophical exemption for the MMR vaccine from the state’s school and child care immunization requirements. “We must step up our leadership to educate the public about the critical role vaccines have in keeping us healthy and safe, and continue working with communities to improve vaccination rates,” Washington State Secretary of Health John Wiesman said in a written statement.
In Oregon, a bill that would eliminate religious and philosophical exemptions to child vaccination requirements passed the state house of representatives by a 35-25 vote and is moving to the senate. Gov. Kate Brown has said that she plans to sign the bill, according to OregonLive.com.
according to the Centers for Disease Control and Prevention.
There are 10 states dealing with ongoing outbreaks now that Pennsylvania has been added to the list, the CDC reported May 13. The state has had five cases so far, all in Allegheny County. New York City continued to have the most active outbreak, adding 43 more cases in Brooklyn last week for a total of 410 in the city since the beginning of 2019, NYC Health said.
Several of this year’s outbreaks were predicted in an analysis published in the Lancet Infectious Diseases (2019 May 9. doi: 10.1016/S1473-3099(19)30231-2). Investigators identified the 25 counties most likely to experience a measles outbreak in 2019 – a list that includes Queens, N.Y. (adjacent to Brooklyn), Multnomah, Ore. (adjacent to Clark County, Wash., where 71 people were infected earlier this year), and San Mateo, Calif., where 4 cases have been reported.
“We recommend that public health officials and policymakers prioritize monitoring the counties we identify to be at high risk that have not yet reported cases, especially those that lie adjacent to counties with ongoing outbreaks and those that house large international airports,” senior author Lauren Gardner of Johns Hopkins University, Baltimore, said in a written statement.
The outbreak in Clark County was declared over in late April, but Gov. Jay Inslee signed a bill on May 10 that removes the personal/philosophical exemption for the MMR vaccine from the state’s school and child care immunization requirements. “We must step up our leadership to educate the public about the critical role vaccines have in keeping us healthy and safe, and continue working with communities to improve vaccination rates,” Washington State Secretary of Health John Wiesman said in a written statement.
In Oregon, a bill that would eliminate religious and philosophical exemptions to child vaccination requirements passed the state house of representatives by a 35-25 vote and is moving to the senate. Gov. Kate Brown has said that she plans to sign the bill, according to OregonLive.com.
according to the Centers for Disease Control and Prevention.
There are 10 states dealing with ongoing outbreaks now that Pennsylvania has been added to the list, the CDC reported May 13. The state has had five cases so far, all in Allegheny County. New York City continued to have the most active outbreak, adding 43 more cases in Brooklyn last week for a total of 410 in the city since the beginning of 2019, NYC Health said.
Several of this year’s outbreaks were predicted in an analysis published in the Lancet Infectious Diseases (2019 May 9. doi: 10.1016/S1473-3099(19)30231-2). Investigators identified the 25 counties most likely to experience a measles outbreak in 2019 – a list that includes Queens, N.Y. (adjacent to Brooklyn), Multnomah, Ore. (adjacent to Clark County, Wash., where 71 people were infected earlier this year), and San Mateo, Calif., where 4 cases have been reported.
“We recommend that public health officials and policymakers prioritize monitoring the counties we identify to be at high risk that have not yet reported cases, especially those that lie adjacent to counties with ongoing outbreaks and those that house large international airports,” senior author Lauren Gardner of Johns Hopkins University, Baltimore, said in a written statement.
The outbreak in Clark County was declared over in late April, but Gov. Jay Inslee signed a bill on May 10 that removes the personal/philosophical exemption for the MMR vaccine from the state’s school and child care immunization requirements. “We must step up our leadership to educate the public about the critical role vaccines have in keeping us healthy and safe, and continue working with communities to improve vaccination rates,” Washington State Secretary of Health John Wiesman said in a written statement.
In Oregon, a bill that would eliminate religious and philosophical exemptions to child vaccination requirements passed the state house of representatives by a 35-25 vote and is moving to the senate. Gov. Kate Brown has said that she plans to sign the bill, according to OregonLive.com.
Pilot program trains residents in telemedicine
WASHINGTON – while still providing the same quality of care during clinic visits, according to the results of a new pilot program.
While telephone visits have been shown to be an effective alternative to face-to-face visits for physicians, residents are not trained to perform telemedicine.
“We have no structured training program on how to teach these residents these skills. We assume that the same skills needed in the clinic are applicable through telephone medicine and we’re not sure about that yet,” Jenna L. Laughlin, DO, said at the annual meeting of the Society of General Internal Medicine.
The pilot study took place at Christiana Care Health System, Wilmington, Del., from October 2016 through December 2018. Nine residents were enrolled in the study, but only six participated.
The objective of the pilot was to demonstrate the feasibility of adding telephone visits into the internal medicine residency practice. This feasibility was measured by templating, scheduling, and supervision, noted Dr. Laughlin, an internist at Christiana Care Health System in Newark, Del. Templating was a term used to describe the designing of the program. For example, the researcher templated 1-hour telephone visit blocks, meaning they designed this structure to integrate into the resident’s training program.
Each resident had 1 hour within the weekly schedule to conduct telephone visits. First-year residents were allowed to do one telephone visit during that hour, second-year residents could do two telephone visits within the hour, and third-year residents could do three telephone visits in that hour.
“There were some challenges associated with scheduling and templating, such as initial schedule templates and a high utilization learning curve,” said Dr. Laughlin, lead author of the study and the program’s leader.
Some didn’t schedule enough telemedicine visits; those residents were assigned to acute clinic visits during the times that they should have been practicing telemedicine.
The program’s second objective was to evaluate the resident experience of scheduled telemedicine visits. This included provider-patient continuity and patient ownership.
The six residents who were surveyed about their experiences said these telephone visits increased their patient ownership and allowed them to build rapport with patients. They said the level of supervision they received was appropriate.
In terms of continuity of care, out the 273 telephone visits scheduled, 179 (65%) were with the patient’s primary care provider and 71 (26.0%) were within the primary care provider’s firm.
“As we build primary care practices in the future, there will be many alternative methods of working with our patients, compared to the traditional face-to-face encounters. I think these are increasingly going to be something that our medical residents need for their future,” Dr. Laughlin said.
The authors reported no conflicts of interest.
WASHINGTON – while still providing the same quality of care during clinic visits, according to the results of a new pilot program.
While telephone visits have been shown to be an effective alternative to face-to-face visits for physicians, residents are not trained to perform telemedicine.
“We have no structured training program on how to teach these residents these skills. We assume that the same skills needed in the clinic are applicable through telephone medicine and we’re not sure about that yet,” Jenna L. Laughlin, DO, said at the annual meeting of the Society of General Internal Medicine.
The pilot study took place at Christiana Care Health System, Wilmington, Del., from October 2016 through December 2018. Nine residents were enrolled in the study, but only six participated.
The objective of the pilot was to demonstrate the feasibility of adding telephone visits into the internal medicine residency practice. This feasibility was measured by templating, scheduling, and supervision, noted Dr. Laughlin, an internist at Christiana Care Health System in Newark, Del. Templating was a term used to describe the designing of the program. For example, the researcher templated 1-hour telephone visit blocks, meaning they designed this structure to integrate into the resident’s training program.
Each resident had 1 hour within the weekly schedule to conduct telephone visits. First-year residents were allowed to do one telephone visit during that hour, second-year residents could do two telephone visits within the hour, and third-year residents could do three telephone visits in that hour.
“There were some challenges associated with scheduling and templating, such as initial schedule templates and a high utilization learning curve,” said Dr. Laughlin, lead author of the study and the program’s leader.
Some didn’t schedule enough telemedicine visits; those residents were assigned to acute clinic visits during the times that they should have been practicing telemedicine.
The program’s second objective was to evaluate the resident experience of scheduled telemedicine visits. This included provider-patient continuity and patient ownership.
The six residents who were surveyed about their experiences said these telephone visits increased their patient ownership and allowed them to build rapport with patients. They said the level of supervision they received was appropriate.
In terms of continuity of care, out the 273 telephone visits scheduled, 179 (65%) were with the patient’s primary care provider and 71 (26.0%) were within the primary care provider’s firm.
“As we build primary care practices in the future, there will be many alternative methods of working with our patients, compared to the traditional face-to-face encounters. I think these are increasingly going to be something that our medical residents need for their future,” Dr. Laughlin said.
The authors reported no conflicts of interest.
WASHINGTON – while still providing the same quality of care during clinic visits, according to the results of a new pilot program.
While telephone visits have been shown to be an effective alternative to face-to-face visits for physicians, residents are not trained to perform telemedicine.
“We have no structured training program on how to teach these residents these skills. We assume that the same skills needed in the clinic are applicable through telephone medicine and we’re not sure about that yet,” Jenna L. Laughlin, DO, said at the annual meeting of the Society of General Internal Medicine.
The pilot study took place at Christiana Care Health System, Wilmington, Del., from October 2016 through December 2018. Nine residents were enrolled in the study, but only six participated.
The objective of the pilot was to demonstrate the feasibility of adding telephone visits into the internal medicine residency practice. This feasibility was measured by templating, scheduling, and supervision, noted Dr. Laughlin, an internist at Christiana Care Health System in Newark, Del. Templating was a term used to describe the designing of the program. For example, the researcher templated 1-hour telephone visit blocks, meaning they designed this structure to integrate into the resident’s training program.
Each resident had 1 hour within the weekly schedule to conduct telephone visits. First-year residents were allowed to do one telephone visit during that hour, second-year residents could do two telephone visits within the hour, and third-year residents could do three telephone visits in that hour.
“There were some challenges associated with scheduling and templating, such as initial schedule templates and a high utilization learning curve,” said Dr. Laughlin, lead author of the study and the program’s leader.
Some didn’t schedule enough telemedicine visits; those residents were assigned to acute clinic visits during the times that they should have been practicing telemedicine.
The program’s second objective was to evaluate the resident experience of scheduled telemedicine visits. This included provider-patient continuity and patient ownership.
The six residents who were surveyed about their experiences said these telephone visits increased their patient ownership and allowed them to build rapport with patients. They said the level of supervision they received was appropriate.
In terms of continuity of care, out the 273 telephone visits scheduled, 179 (65%) were with the patient’s primary care provider and 71 (26.0%) were within the primary care provider’s firm.
“As we build primary care practices in the future, there will be many alternative methods of working with our patients, compared to the traditional face-to-face encounters. I think these are increasingly going to be something that our medical residents need for their future,” Dr. Laughlin said.
The authors reported no conflicts of interest.
REPORTING FROM SGIM 2019
Pediatrician knowledge of tampon safety is low
BALTIMORE – and a remarkably high proportion of them lack adequate knowledge themselves about the topic, a new survey-based study found.
“Significant knowledge gaps [were] noted, for instance, [such as] the maximum time a tampon can safely remain in the body,” Miriam Singer of Cohen Children’s Medical Center of New York told attendees of the Pediatric Academic Societies annual meeting.
More than 80% of females aged 17-21 years have used tampons by themselves or with pads, Ms. Singer noted in her background information, yet many teens have low knowledge about their use and safety.
Past research has found that only 35% of high school junior and senior girls heard about tampon use from their mothers, yet many of these mothers showed low knowledge about proper tampon use as well. That same research found that less than 15% of girls aged 10-19 years reported getting information from a health professional about products for menstruation despite recommendations from the American Academy of Pediatrics to instruct girls on feminine hygiene product usage.
Other research has found minimal to no education about menstruation in schools “due to time constraints and stigma associated with menstruation,” Ms. Singer said.
She and her colleagues emailed 2,500 AAP members in November-December 2018 a 53-question online questionnaire about their self-rated and measured knowledge of proper tampon usage and safety and how frequently they discussed tampons with their female adolescent patients. The survey included questions asking pediatricians to self-rate their knowledge about tampon use and safety on a Likert scale of 1 (not at all knowledgeable) to 5 (extremely knowledgeable).
Two incentives provided for completing the survey were a Feminine Hygiene Fact Sheet offered in the first email and an ADHD Medication Guide offered in the third and final email.
Among the 518 pediatricians who responded (21% response rate), 462 met the inclusion criteria of being a primary care pediatrician currently practicing in the United States. Most were women (79%) and white (79%). Just over half of the pediatricians worked only in private practice (54%) and in a suburban area (52%). About a quarter (26%) were in an urban area and 20% in a rural area. Distribution of years in practice (from 1-5 years to over 25 years in 5-year increments) was fairly even across respondents.
Only 9% of respondents reported they very often or almost always talk to their female adolescent patients about how to insert a tampon. The most common tampon-related conversation pediatricians reported was how often to change tampons, which only 35% of respondents said they very often or almost always do.
Yet a similar proportion, 36%, rarely or almost never discuss how often to change tampons, and 62% said they rarely or almost never discuss how to insert a tampon or talk about using tampons while sleeping. Half of respondents (51%) almost never discuss using tampons while swimming (only 21% very often or almost always do), and 77% have not discussed how tampons might affect the hymen with their patients.
More pediatricians (36%) reported almost never discussing the risks of tampon use with female teens than those who sometimes (32%) or very often/almost always (31%) discussed risks.
Respondents also were generally much more willing to discuss tampons with older adolescents than younger ones. Only 18% of respondents said they were highly likely to discuss them with 12- and 13-year-olds, compared with almost twice as many (33%) who would discuss tampons with 16- and 17-year-olds (P less than .001).
Male pediatricians were significantly less likely to discuss any of these topics with their female adolescent patients than female pediatricians (P less than .001 for all questions except risks [P = .01] and hymen [P = .04]). They also rated their knowledge about tampons as significantly lower than self ratings by female pediatricians (P less than .001). Less than half of pediatricians (43%) rated their knowledge about tampons as high or very high, and one in five (20%) rated it as low.
Actual measured knowledge reflected the self-ratings, but still revealed substantial gaps in knowledge among male and female providers. Just over half of male pediatricians (52%) answered all questions about tampon use and safety correctly; however, female pediatricians were only slightly better, with 71% answering all questions correctly (P less than .001). Less than half of male and female pediatricians knew the maximum time a tampon could stay in before it should be removed to reduce risk of toxic shock syndrome (8 hours).
The only two questions that more than half of male pediatricians answered correctly were that girls can swim in the ocean while wearing a tampon and that it can, rarely but not typically, tear the hymen. Less than half knew girls could sleep while wearing a tampon and that a girl could start using a tampon with her first menstruation.
More than half of female pediatricians answered all these questions correctly, although only about two-thirds gave correct answers on how tampons can affect the hymen (the only question that more male pediatricians than female answered correctly), whether a girl can sleep in a tampon, and that patients should use the lowest effective absorbency tampon to minimize toxic shock syndrome risk.
Although the study is limited by a nonvalidated knowledge assessment instrument, self-reporting and potential selection bias means the study may not accurately represent U.S. primary care pediatricians nationwide; however, the findings still demonstrate notably low self-rated and measured knowledge about tampons.
“Given the AAP’s recommendation that pediatricians instruct girls on the use of feminine products, pediatricians must take steps to ensure they are educating patients about tampons,” Ms. Singer said. She also recommended the development of web-based resources targeting the improvement of pediatrician knowledge about tampon use and safety, and the need for the AAP to raise awareness about the importance of discussing tampons with female adolescent patients.
The study did not use external funding, and the authors reported no relevant financial disclosures.
BALTIMORE – and a remarkably high proportion of them lack adequate knowledge themselves about the topic, a new survey-based study found.
“Significant knowledge gaps [were] noted, for instance, [such as] the maximum time a tampon can safely remain in the body,” Miriam Singer of Cohen Children’s Medical Center of New York told attendees of the Pediatric Academic Societies annual meeting.
More than 80% of females aged 17-21 years have used tampons by themselves or with pads, Ms. Singer noted in her background information, yet many teens have low knowledge about their use and safety.
Past research has found that only 35% of high school junior and senior girls heard about tampon use from their mothers, yet many of these mothers showed low knowledge about proper tampon use as well. That same research found that less than 15% of girls aged 10-19 years reported getting information from a health professional about products for menstruation despite recommendations from the American Academy of Pediatrics to instruct girls on feminine hygiene product usage.
Other research has found minimal to no education about menstruation in schools “due to time constraints and stigma associated with menstruation,” Ms. Singer said.
She and her colleagues emailed 2,500 AAP members in November-December 2018 a 53-question online questionnaire about their self-rated and measured knowledge of proper tampon usage and safety and how frequently they discussed tampons with their female adolescent patients. The survey included questions asking pediatricians to self-rate their knowledge about tampon use and safety on a Likert scale of 1 (not at all knowledgeable) to 5 (extremely knowledgeable).
Two incentives provided for completing the survey were a Feminine Hygiene Fact Sheet offered in the first email and an ADHD Medication Guide offered in the third and final email.
Among the 518 pediatricians who responded (21% response rate), 462 met the inclusion criteria of being a primary care pediatrician currently practicing in the United States. Most were women (79%) and white (79%). Just over half of the pediatricians worked only in private practice (54%) and in a suburban area (52%). About a quarter (26%) were in an urban area and 20% in a rural area. Distribution of years in practice (from 1-5 years to over 25 years in 5-year increments) was fairly even across respondents.
Only 9% of respondents reported they very often or almost always talk to their female adolescent patients about how to insert a tampon. The most common tampon-related conversation pediatricians reported was how often to change tampons, which only 35% of respondents said they very often or almost always do.
Yet a similar proportion, 36%, rarely or almost never discuss how often to change tampons, and 62% said they rarely or almost never discuss how to insert a tampon or talk about using tampons while sleeping. Half of respondents (51%) almost never discuss using tampons while swimming (only 21% very often or almost always do), and 77% have not discussed how tampons might affect the hymen with their patients.
More pediatricians (36%) reported almost never discussing the risks of tampon use with female teens than those who sometimes (32%) or very often/almost always (31%) discussed risks.
Respondents also were generally much more willing to discuss tampons with older adolescents than younger ones. Only 18% of respondents said they were highly likely to discuss them with 12- and 13-year-olds, compared with almost twice as many (33%) who would discuss tampons with 16- and 17-year-olds (P less than .001).
Male pediatricians were significantly less likely to discuss any of these topics with their female adolescent patients than female pediatricians (P less than .001 for all questions except risks [P = .01] and hymen [P = .04]). They also rated their knowledge about tampons as significantly lower than self ratings by female pediatricians (P less than .001). Less than half of pediatricians (43%) rated their knowledge about tampons as high or very high, and one in five (20%) rated it as low.
Actual measured knowledge reflected the self-ratings, but still revealed substantial gaps in knowledge among male and female providers. Just over half of male pediatricians (52%) answered all questions about tampon use and safety correctly; however, female pediatricians were only slightly better, with 71% answering all questions correctly (P less than .001). Less than half of male and female pediatricians knew the maximum time a tampon could stay in before it should be removed to reduce risk of toxic shock syndrome (8 hours).
The only two questions that more than half of male pediatricians answered correctly were that girls can swim in the ocean while wearing a tampon and that it can, rarely but not typically, tear the hymen. Less than half knew girls could sleep while wearing a tampon and that a girl could start using a tampon with her first menstruation.
More than half of female pediatricians answered all these questions correctly, although only about two-thirds gave correct answers on how tampons can affect the hymen (the only question that more male pediatricians than female answered correctly), whether a girl can sleep in a tampon, and that patients should use the lowest effective absorbency tampon to minimize toxic shock syndrome risk.
Although the study is limited by a nonvalidated knowledge assessment instrument, self-reporting and potential selection bias means the study may not accurately represent U.S. primary care pediatricians nationwide; however, the findings still demonstrate notably low self-rated and measured knowledge about tampons.
“Given the AAP’s recommendation that pediatricians instruct girls on the use of feminine products, pediatricians must take steps to ensure they are educating patients about tampons,” Ms. Singer said. She also recommended the development of web-based resources targeting the improvement of pediatrician knowledge about tampon use and safety, and the need for the AAP to raise awareness about the importance of discussing tampons with female adolescent patients.
The study did not use external funding, and the authors reported no relevant financial disclosures.
BALTIMORE – and a remarkably high proportion of them lack adequate knowledge themselves about the topic, a new survey-based study found.
“Significant knowledge gaps [were] noted, for instance, [such as] the maximum time a tampon can safely remain in the body,” Miriam Singer of Cohen Children’s Medical Center of New York told attendees of the Pediatric Academic Societies annual meeting.
More than 80% of females aged 17-21 years have used tampons by themselves or with pads, Ms. Singer noted in her background information, yet many teens have low knowledge about their use and safety.
Past research has found that only 35% of high school junior and senior girls heard about tampon use from their mothers, yet many of these mothers showed low knowledge about proper tampon use as well. That same research found that less than 15% of girls aged 10-19 years reported getting information from a health professional about products for menstruation despite recommendations from the American Academy of Pediatrics to instruct girls on feminine hygiene product usage.
Other research has found minimal to no education about menstruation in schools “due to time constraints and stigma associated with menstruation,” Ms. Singer said.
She and her colleagues emailed 2,500 AAP members in November-December 2018 a 53-question online questionnaire about their self-rated and measured knowledge of proper tampon usage and safety and how frequently they discussed tampons with their female adolescent patients. The survey included questions asking pediatricians to self-rate their knowledge about tampon use and safety on a Likert scale of 1 (not at all knowledgeable) to 5 (extremely knowledgeable).
Two incentives provided for completing the survey were a Feminine Hygiene Fact Sheet offered in the first email and an ADHD Medication Guide offered in the third and final email.
Among the 518 pediatricians who responded (21% response rate), 462 met the inclusion criteria of being a primary care pediatrician currently practicing in the United States. Most were women (79%) and white (79%). Just over half of the pediatricians worked only in private practice (54%) and in a suburban area (52%). About a quarter (26%) were in an urban area and 20% in a rural area. Distribution of years in practice (from 1-5 years to over 25 years in 5-year increments) was fairly even across respondents.
Only 9% of respondents reported they very often or almost always talk to their female adolescent patients about how to insert a tampon. The most common tampon-related conversation pediatricians reported was how often to change tampons, which only 35% of respondents said they very often or almost always do.
Yet a similar proportion, 36%, rarely or almost never discuss how often to change tampons, and 62% said they rarely or almost never discuss how to insert a tampon or talk about using tampons while sleeping. Half of respondents (51%) almost never discuss using tampons while swimming (only 21% very often or almost always do), and 77% have not discussed how tampons might affect the hymen with their patients.
More pediatricians (36%) reported almost never discussing the risks of tampon use with female teens than those who sometimes (32%) or very often/almost always (31%) discussed risks.
Respondents also were generally much more willing to discuss tampons with older adolescents than younger ones. Only 18% of respondents said they were highly likely to discuss them with 12- and 13-year-olds, compared with almost twice as many (33%) who would discuss tampons with 16- and 17-year-olds (P less than .001).
Male pediatricians were significantly less likely to discuss any of these topics with their female adolescent patients than female pediatricians (P less than .001 for all questions except risks [P = .01] and hymen [P = .04]). They also rated their knowledge about tampons as significantly lower than self ratings by female pediatricians (P less than .001). Less than half of pediatricians (43%) rated their knowledge about tampons as high or very high, and one in five (20%) rated it as low.
Actual measured knowledge reflected the self-ratings, but still revealed substantial gaps in knowledge among male and female providers. Just over half of male pediatricians (52%) answered all questions about tampon use and safety correctly; however, female pediatricians were only slightly better, with 71% answering all questions correctly (P less than .001). Less than half of male and female pediatricians knew the maximum time a tampon could stay in before it should be removed to reduce risk of toxic shock syndrome (8 hours).
The only two questions that more than half of male pediatricians answered correctly were that girls can swim in the ocean while wearing a tampon and that it can, rarely but not typically, tear the hymen. Less than half knew girls could sleep while wearing a tampon and that a girl could start using a tampon with her first menstruation.
More than half of female pediatricians answered all these questions correctly, although only about two-thirds gave correct answers on how tampons can affect the hymen (the only question that more male pediatricians than female answered correctly), whether a girl can sleep in a tampon, and that patients should use the lowest effective absorbency tampon to minimize toxic shock syndrome risk.
Although the study is limited by a nonvalidated knowledge assessment instrument, self-reporting and potential selection bias means the study may not accurately represent U.S. primary care pediatricians nationwide; however, the findings still demonstrate notably low self-rated and measured knowledge about tampons.
“Given the AAP’s recommendation that pediatricians instruct girls on the use of feminine products, pediatricians must take steps to ensure they are educating patients about tampons,” Ms. Singer said. She also recommended the development of web-based resources targeting the improvement of pediatrician knowledge about tampon use and safety, and the need for the AAP to raise awareness about the importance of discussing tampons with female adolescent patients.
The study did not use external funding, and the authors reported no relevant financial disclosures.
REPORTING FROM PAS 2019
Key clinical point: U.S. pediatricians have low knowledge of and willingness to discuss proper tampon use and safety with adolescent patients.
Major finding: 35% of U.S. pediatricians reported they very often/almost always discuss how long to wear a tampon before removing it.
Study details: The findings are based on a survey of 462 U.S. pediatricians who responded to a 53-question online survey.
Disclosures: The study did not use external funding, and the authors reported no relevant financial disclosures.
AAA Screening to be held in DC
For the first time ever, the SVS Foundation is teaming up with the Society for Vascular Nursing and the Society for Vascular Ultrasound to provide free AAA and peripheral artery disease ultrasound screenings. The event will take place from 8am to 12pm, June 8 at the Medical Faculty Associates Department of Surgery in Washington, DC. Spread the word if you know someone in the DC area who might be interested in attending. Appointments may be scheduled by calling 888-871-3801. View the full details here.
For the first time ever, the SVS Foundation is teaming up with the Society for Vascular Nursing and the Society for Vascular Ultrasound to provide free AAA and peripheral artery disease ultrasound screenings. The event will take place from 8am to 12pm, June 8 at the Medical Faculty Associates Department of Surgery in Washington, DC. Spread the word if you know someone in the DC area who might be interested in attending. Appointments may be scheduled by calling 888-871-3801. View the full details here.
For the first time ever, the SVS Foundation is teaming up with the Society for Vascular Nursing and the Society for Vascular Ultrasound to provide free AAA and peripheral artery disease ultrasound screenings. The event will take place from 8am to 12pm, June 8 at the Medical Faculty Associates Department of Surgery in Washington, DC. Spread the word if you know someone in the DC area who might be interested in attending. Appointments may be scheduled by calling 888-871-3801. View the full details here.
Register for the UCLA-SVS Review Course
Register today for the Fourth Annual UCLA / SVS Symposium. This year’s program, “A Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery” will be held Aug. 24 to 26 at the Beverly Hilton, Beverly Hills, Calif. The course, a joint effort of the Division of Vascular and Endovascular Surgery at UCLA and the Society for Vascular Surgery, will offer an in-depth review of the specialty to those preparing to take the vascular board examinations. It will also provide basic didactic education for vascular residents and fellows in training. Read the full details and register here.
Register today for the Fourth Annual UCLA / SVS Symposium. This year’s program, “A Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery” will be held Aug. 24 to 26 at the Beverly Hilton, Beverly Hills, Calif. The course, a joint effort of the Division of Vascular and Endovascular Surgery at UCLA and the Society for Vascular Surgery, will offer an in-depth review of the specialty to those preparing to take the vascular board examinations. It will also provide basic didactic education for vascular residents and fellows in training. Read the full details and register here.
Register today for the Fourth Annual UCLA / SVS Symposium. This year’s program, “A Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery” will be held Aug. 24 to 26 at the Beverly Hilton, Beverly Hills, Calif. The course, a joint effort of the Division of Vascular and Endovascular Surgery at UCLA and the Society for Vascular Surgery, will offer an in-depth review of the specialty to those preparing to take the vascular board examinations. It will also provide basic didactic education for vascular residents and fellows in training. Read the full details and register here.
Attend PA Programming at VAM
PA programming is set to take place from 1:15 – 5:15pm Thursday, June 13. There will be a PA networking lunch before the section session from 12-1pm, and a PA networking meet-up afterwards at 5:30 in the exhibit hall. The entire Vascular Annual Meeting has been reviewed by the AAPA Review Panel and is compliant with AAPA CME Criteria. This activity is designated for 30 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation. Register for VAM today.
PA programming is set to take place from 1:15 – 5:15pm Thursday, June 13. There will be a PA networking lunch before the section session from 12-1pm, and a PA networking meet-up afterwards at 5:30 in the exhibit hall. The entire Vascular Annual Meeting has been reviewed by the AAPA Review Panel and is compliant with AAPA CME Criteria. This activity is designated for 30 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation. Register for VAM today.
PA programming is set to take place from 1:15 – 5:15pm Thursday, June 13. There will be a PA networking lunch before the section session from 12-1pm, and a PA networking meet-up afterwards at 5:30 in the exhibit hall. The entire Vascular Annual Meeting has been reviewed by the AAPA Review Panel and is compliant with AAPA CME Criteria. This activity is designated for 30 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation. Register for VAM today.
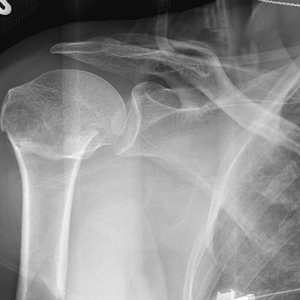
Give Her a Shoulder to Cry on
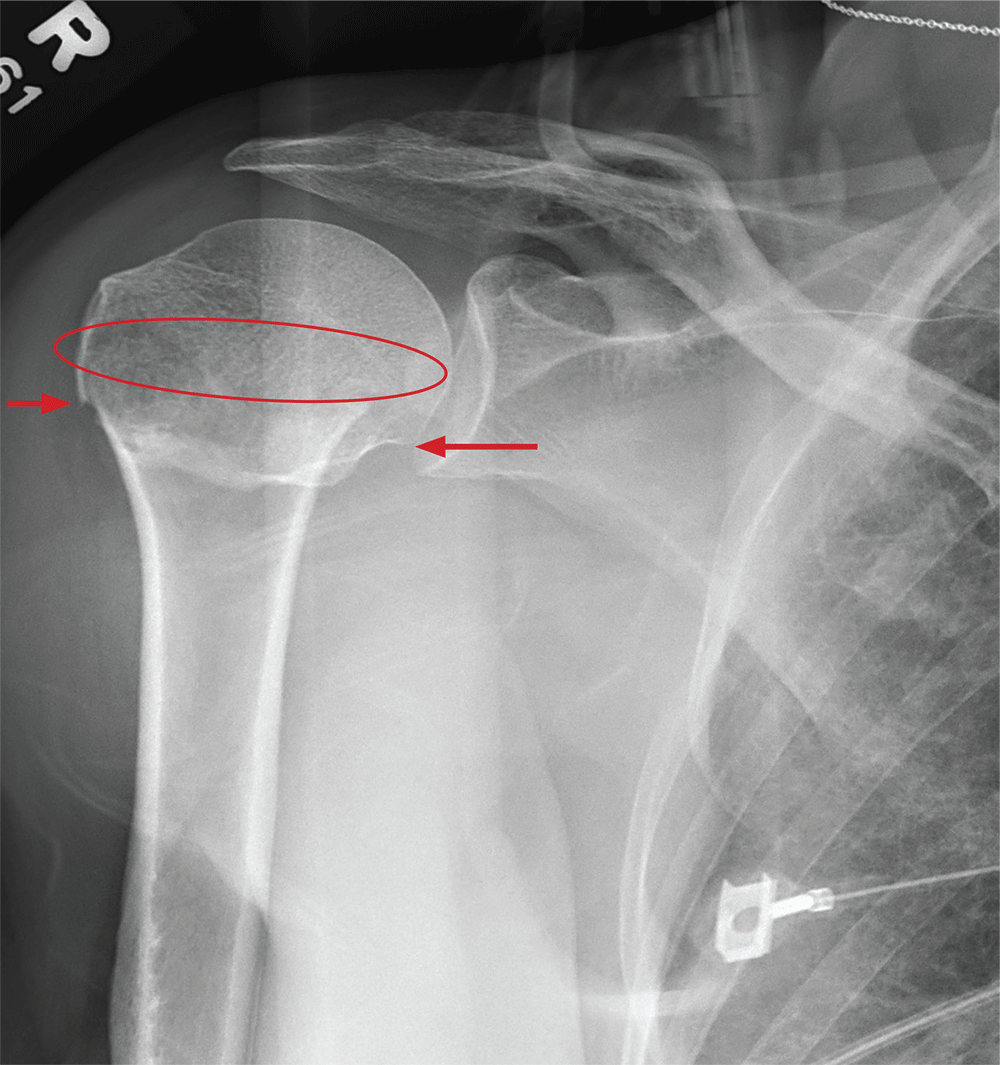
ANSWER
The radiograph demonstrates an acute horizontal fracture through the humeral neck. There is some slight lateral displacement of the fracture fragment.
The patient’s right arm was placed in a sling. Prompt orthopedic consultation was then obtained.
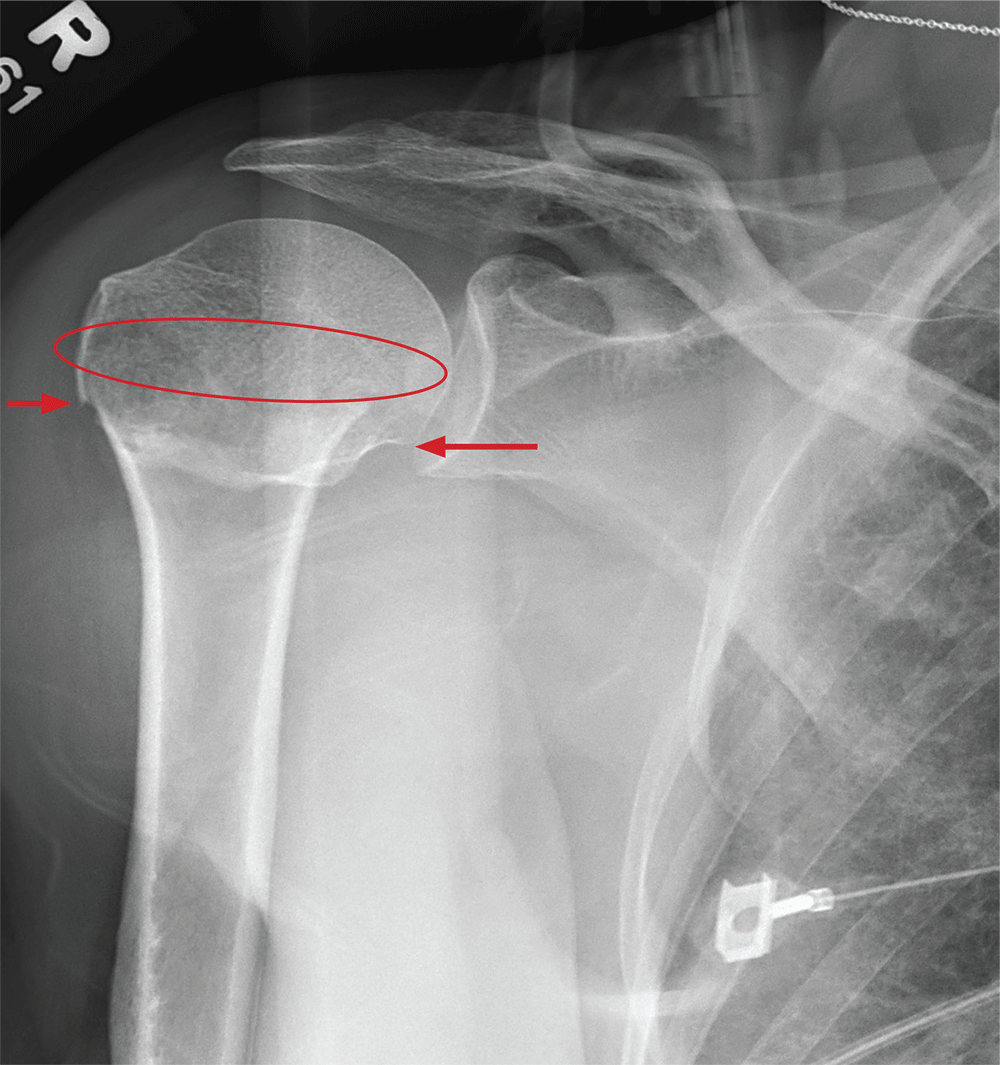
ANSWER
The radiograph demonstrates an acute horizontal fracture through the humeral neck. There is some slight lateral displacement of the fracture fragment.
The patient’s right arm was placed in a sling. Prompt orthopedic consultation was then obtained.
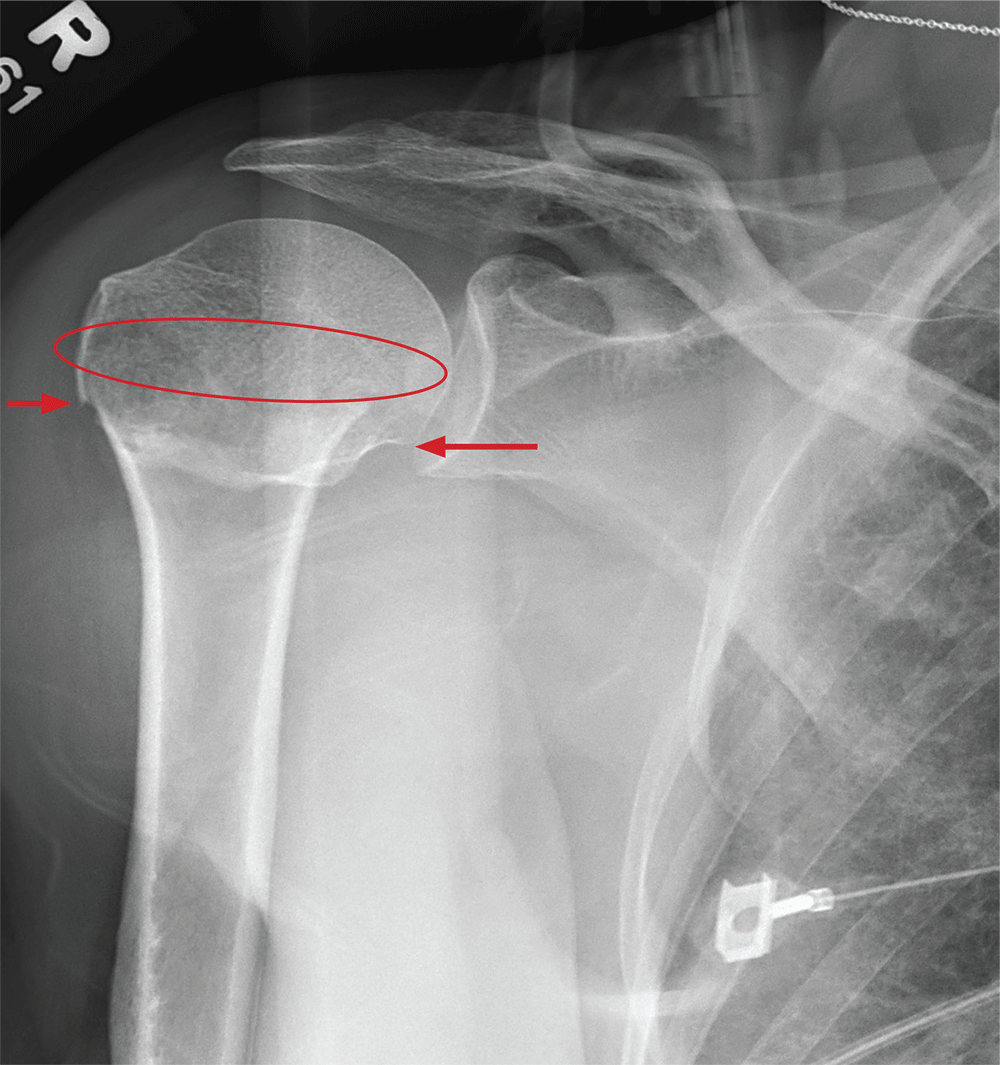
ANSWER
The radiograph demonstrates an acute horizontal fracture through the humeral neck. There is some slight lateral displacement of the fracture fragment.
The patient’s right arm was placed in a sling. Prompt orthopedic consultation was then obtained.
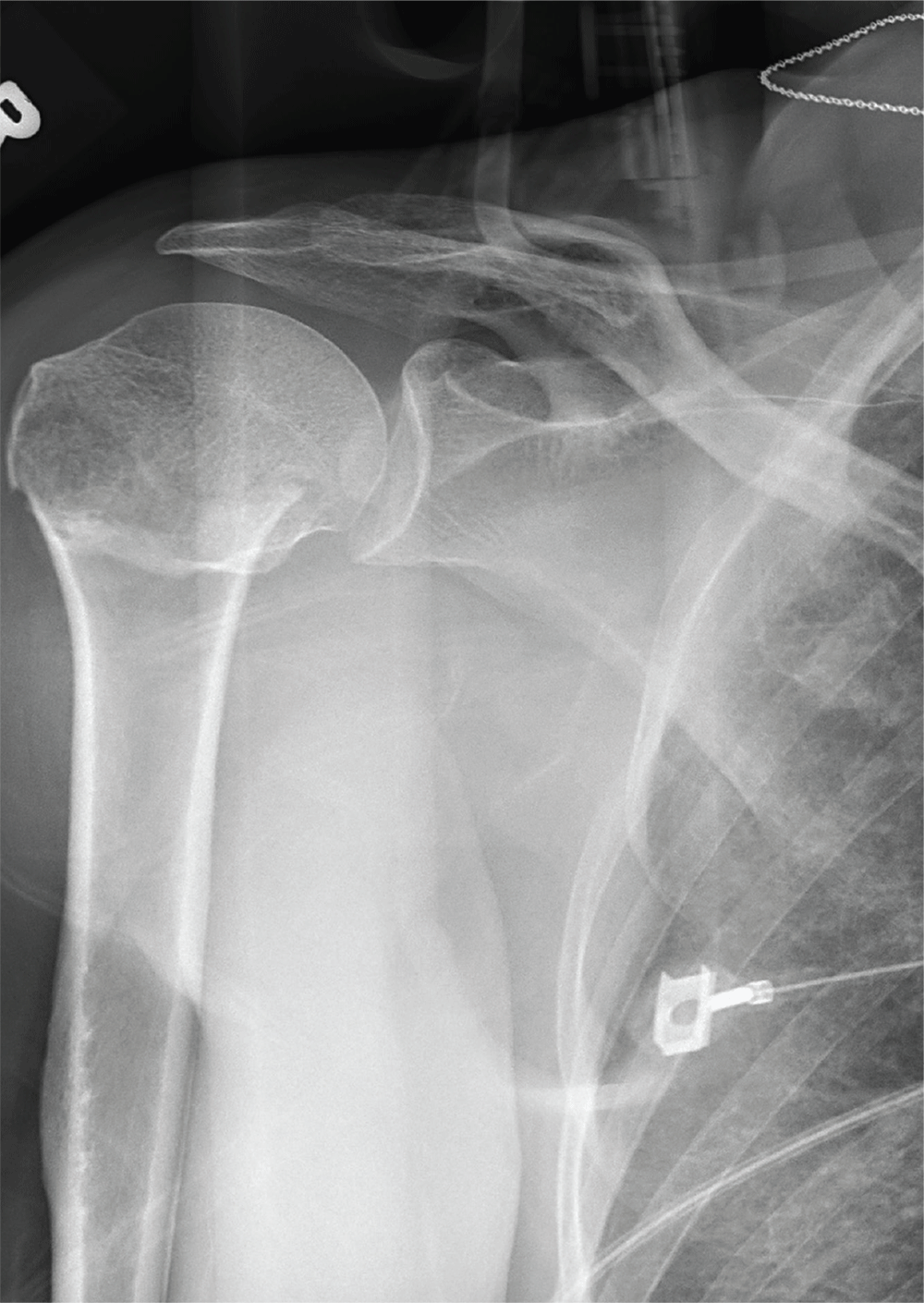
After a motor vehicle collision, a 70-year-old woman is brought to your emergency department by EMS personnel. She was a restrained driver in a vehicle crossing an intersection when she was broadsided by a tractor trailer traveling at high speed. Her airbags deployed, and she believes she briefly lost consciousness. Her biggest complaint is pain in her right shoulder.
Her medical history is significant for hypertension and hypothyroidism. On primary survey, you note an elderly woman who is in full cervical spine immobilization on a long backboard. Her Glasgow Coma Scale score is 15. She is in mild distress but has normal vital signs.
The patient has scattered abrasions and bruises on her body. Her right shoulder has mild to moderate tenderness to palpation and a decreased range of motion. Distally in that arm, she has good pulses and is neurovascularly intact.
You obtain a portable radiograph of the right shoulder (shown). What is your impression?
CardioMEMS cuts heart failure hospitalizations in post-approval study
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
[email protected]
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
[email protected]
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
[email protected]
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
REPORTING FROM ACC 2019
Ocrelizumab effective, safe in relapsing-remitting MS patients
PHILADELPHIA – Ocrelizumab is effective and safe in patients with relapsing-remitting multiple sclerosis who had inadequate responses to previous disease-modifying treatments, said an investigator reporting interim results of a recent nonrandomized study.
The findings of the 600+ patient CHORDS study suggest a positive risk-to-benefit ratio over nearly 1 year for this anti-CD20 monoclonal antibody, said Thomas P. Leist, MD, of Thomas Jefferson University, Philadelphia, at the annual meeting of the American Academy of Neurology (AAN).
“MRI activity has been significantly attenuated in these individuals, particularly, in the period from 24 to 48 weeks, and the overall safety that has been observed to date has been in line with what has been observed in clinical trials with this medication,” Dr. Leist said in a podium presentation.
While previous investigations demonstrated superiority to treatment with interferon in patients with relapsing multiple sclerosis, this phase IIIb study was needed to further clarify the effects of the treatment following suboptimal response to several disease modifying treatments, according to Dr. Leist and his co-investigators.
The intention-to-treat population of CHORDS consisted of 608 patients who received disease-modifying therapy for 6 or more months and discontinued it due to suboptimal response, which was defined as one or more clinically reported relapses, one or more T1 gadolinium-enhancing lesions, or two or more enlarging T2 lesions. They all received a 600 mg dose of ocrelizumab every 24 weeks for as many as 96 weeks.
With 48 weeks of follow-up, the majority of patients had no relapses, no enhancing T1 lesions, no new or enlarging T2 lesions, and no confirmed progression of disability. In all, 54.5% of the patients experienced none of those events, according to Dr. Leist.
The adjusted annualized relapse rate in this cohort was 0.065, he reported.
New MRI activity included 48 new T1 gadolinium-enhancing lesions in 1,174 MRI scans, for an adjusted rate of 0.023, he also reported, while there were 679 new or enlarging T2 lesions on 1,175 scans, for an adjusted rate of 0.581.
The safety in this population was comparable to the overall safety profile of ocrelizumab seen in other studies, according to Dr. Leist. A total of 25 patients, or 4.1%, experienced a serious adverse event, though none led to treatment withdrawal and only one led to a dose modification or interruption, the data show.
Dr. Leist reported disclosures related to Alkermes, Bayer, Biogen, EMD Serono, Genentech, Inc., Novartis, Sanofi Genzyme, Sun Pharma, and Teva Neuroscience.
SOURCE: Leist TP, et al. Presented at the 2019 American Academy of Neurology (AAN) Annual Meeting, May 4-10, 2019. Philadelphia. Presentation S56.007.
PHILADELPHIA – Ocrelizumab is effective and safe in patients with relapsing-remitting multiple sclerosis who had inadequate responses to previous disease-modifying treatments, said an investigator reporting interim results of a recent nonrandomized study.
The findings of the 600+ patient CHORDS study suggest a positive risk-to-benefit ratio over nearly 1 year for this anti-CD20 monoclonal antibody, said Thomas P. Leist, MD, of Thomas Jefferson University, Philadelphia, at the annual meeting of the American Academy of Neurology (AAN).
“MRI activity has been significantly attenuated in these individuals, particularly, in the period from 24 to 48 weeks, and the overall safety that has been observed to date has been in line with what has been observed in clinical trials with this medication,” Dr. Leist said in a podium presentation.
While previous investigations demonstrated superiority to treatment with interferon in patients with relapsing multiple sclerosis, this phase IIIb study was needed to further clarify the effects of the treatment following suboptimal response to several disease modifying treatments, according to Dr. Leist and his co-investigators.
The intention-to-treat population of CHORDS consisted of 608 patients who received disease-modifying therapy for 6 or more months and discontinued it due to suboptimal response, which was defined as one or more clinically reported relapses, one or more T1 gadolinium-enhancing lesions, or two or more enlarging T2 lesions. They all received a 600 mg dose of ocrelizumab every 24 weeks for as many as 96 weeks.
With 48 weeks of follow-up, the majority of patients had no relapses, no enhancing T1 lesions, no new or enlarging T2 lesions, and no confirmed progression of disability. In all, 54.5% of the patients experienced none of those events, according to Dr. Leist.
The adjusted annualized relapse rate in this cohort was 0.065, he reported.
New MRI activity included 48 new T1 gadolinium-enhancing lesions in 1,174 MRI scans, for an adjusted rate of 0.023, he also reported, while there were 679 new or enlarging T2 lesions on 1,175 scans, for an adjusted rate of 0.581.
The safety in this population was comparable to the overall safety profile of ocrelizumab seen in other studies, according to Dr. Leist. A total of 25 patients, or 4.1%, experienced a serious adverse event, though none led to treatment withdrawal and only one led to a dose modification or interruption, the data show.
Dr. Leist reported disclosures related to Alkermes, Bayer, Biogen, EMD Serono, Genentech, Inc., Novartis, Sanofi Genzyme, Sun Pharma, and Teva Neuroscience.
SOURCE: Leist TP, et al. Presented at the 2019 American Academy of Neurology (AAN) Annual Meeting, May 4-10, 2019. Philadelphia. Presentation S56.007.
PHILADELPHIA – Ocrelizumab is effective and safe in patients with relapsing-remitting multiple sclerosis who had inadequate responses to previous disease-modifying treatments, said an investigator reporting interim results of a recent nonrandomized study.
The findings of the 600+ patient CHORDS study suggest a positive risk-to-benefit ratio over nearly 1 year for this anti-CD20 monoclonal antibody, said Thomas P. Leist, MD, of Thomas Jefferson University, Philadelphia, at the annual meeting of the American Academy of Neurology (AAN).
“MRI activity has been significantly attenuated in these individuals, particularly, in the period from 24 to 48 weeks, and the overall safety that has been observed to date has been in line with what has been observed in clinical trials with this medication,” Dr. Leist said in a podium presentation.
While previous investigations demonstrated superiority to treatment with interferon in patients with relapsing multiple sclerosis, this phase IIIb study was needed to further clarify the effects of the treatment following suboptimal response to several disease modifying treatments, according to Dr. Leist and his co-investigators.
The intention-to-treat population of CHORDS consisted of 608 patients who received disease-modifying therapy for 6 or more months and discontinued it due to suboptimal response, which was defined as one or more clinically reported relapses, one or more T1 gadolinium-enhancing lesions, or two or more enlarging T2 lesions. They all received a 600 mg dose of ocrelizumab every 24 weeks for as many as 96 weeks.
With 48 weeks of follow-up, the majority of patients had no relapses, no enhancing T1 lesions, no new or enlarging T2 lesions, and no confirmed progression of disability. In all, 54.5% of the patients experienced none of those events, according to Dr. Leist.
The adjusted annualized relapse rate in this cohort was 0.065, he reported.
New MRI activity included 48 new T1 gadolinium-enhancing lesions in 1,174 MRI scans, for an adjusted rate of 0.023, he also reported, while there were 679 new or enlarging T2 lesions on 1,175 scans, for an adjusted rate of 0.581.
The safety in this population was comparable to the overall safety profile of ocrelizumab seen in other studies, according to Dr. Leist. A total of 25 patients, or 4.1%, experienced a serious adverse event, though none led to treatment withdrawal and only one led to a dose modification or interruption, the data show.
Dr. Leist reported disclosures related to Alkermes, Bayer, Biogen, EMD Serono, Genentech, Inc., Novartis, Sanofi Genzyme, Sun Pharma, and Teva Neuroscience.
SOURCE: Leist TP, et al. Presented at the 2019 American Academy of Neurology (AAN) Annual Meeting, May 4-10, 2019. Philadelphia. Presentation S56.007.
FROM AAN 2019
Gentamicin restores wound healing in hereditary epidermolysis bullosa
Rare progress seen in challenging disease
CHICAGO – Topical gentamicin counters the nonsense mutations that inhibit production of laminin 332 in infants with Herlitz junctional epidermolysis bullosa (H-JEB) to allow lesion healing, according to results of a small clinical study presented at the annual meeting of the Society for Investigative Dermatology.
“All of the children treated so far have responded,” reported Andrew Kwong, who will soon graduate from the Keck School of Medicine at the University of Southern California, Los Angeles.
H-JEB is an inherited blistering skin disease associated with nonsense mutations in the LAMA3, LAMB3, or LAMC2 genes that result in impaired production of functional laminin 332, an essential protein for epidermal-dermal adherence. At this time there are no effective therapies, and the disease is fatal.
The small clinical study was initiated after in vitro studies demonstrated that gentamicin restored functional laminin 332 in cultured keratinocytes from infants with H-JEB. The dose-dependent effect was credited to the ability of gentamicin to induce readthrough of premature stop codons that block production of laminin 332.
Data were presented on the first three infants with H-JEB treated with oral gentamicin. In each child, lesions were treated with topical 0.5% gentamicin twice daily for two weeks. Biopsies were taken prior to the initiation of treatment and at one and three months after treatment. The primary outcome was change in laminin 332, but clinical improvement was also monitored.
Although none of the infants had measurable laminin 332 prior to treatment, all lesions treated with topical gentamicin developed localized laminin 332 at the dermal-epidermal junction of the skin, Mr. Kwong reported. This expression, which was about 40% to 60% of that seen in normal skin, still persisted when evaluated three months after treatment.
The expression was associated with resolution of existing lesions and a reduced risk of developing new lesions, according to Mr. Kwong. In lesions that went untreated, there was no change.
Other molecular changes in the skin, such as increased expression and polarization of beta-4 integrin, were consistent with the ability of gentamicin to address the underlying pathophysiology of H-JEB. There were no adverse events observed.
By restoring functional laminin 332 in the skin, topical gentamicin appears to address the underlying cause of the bullae associated with H-JEB, but Mr. Kwong said that the next step is to determine whether intravenous gentamicin can address the systemic effects. If so, this treatment has the potential to improve survival. He reported that an infant with H-JEB was recently started on intravenous treatment, and initial results were encouraging.
Asked whether he would recommend topical gentamicin on the basis of these findings, Mr. Kwong cautioned that the case series remains very small, but he noted that the uniformity of the positive response is encouraging. He expects that off-label use of this novel and low-cost approach might be warranted in a population that has very limited therapeutic options.
SOURCE: Kwong A. SID 2019;S102, Abstract 594. Annual meeting of the Society for Investigative Dermatology.
Rare progress seen in challenging disease
Rare progress seen in challenging disease
CHICAGO – Topical gentamicin counters the nonsense mutations that inhibit production of laminin 332 in infants with Herlitz junctional epidermolysis bullosa (H-JEB) to allow lesion healing, according to results of a small clinical study presented at the annual meeting of the Society for Investigative Dermatology.
“All of the children treated so far have responded,” reported Andrew Kwong, who will soon graduate from the Keck School of Medicine at the University of Southern California, Los Angeles.
H-JEB is an inherited blistering skin disease associated with nonsense mutations in the LAMA3, LAMB3, or LAMC2 genes that result in impaired production of functional laminin 332, an essential protein for epidermal-dermal adherence. At this time there are no effective therapies, and the disease is fatal.
The small clinical study was initiated after in vitro studies demonstrated that gentamicin restored functional laminin 332 in cultured keratinocytes from infants with H-JEB. The dose-dependent effect was credited to the ability of gentamicin to induce readthrough of premature stop codons that block production of laminin 332.
Data were presented on the first three infants with H-JEB treated with oral gentamicin. In each child, lesions were treated with topical 0.5% gentamicin twice daily for two weeks. Biopsies were taken prior to the initiation of treatment and at one and three months after treatment. The primary outcome was change in laminin 332, but clinical improvement was also monitored.
Although none of the infants had measurable laminin 332 prior to treatment, all lesions treated with topical gentamicin developed localized laminin 332 at the dermal-epidermal junction of the skin, Mr. Kwong reported. This expression, which was about 40% to 60% of that seen in normal skin, still persisted when evaluated three months after treatment.
The expression was associated with resolution of existing lesions and a reduced risk of developing new lesions, according to Mr. Kwong. In lesions that went untreated, there was no change.
Other molecular changes in the skin, such as increased expression and polarization of beta-4 integrin, were consistent with the ability of gentamicin to address the underlying pathophysiology of H-JEB. There were no adverse events observed.
By restoring functional laminin 332 in the skin, topical gentamicin appears to address the underlying cause of the bullae associated with H-JEB, but Mr. Kwong said that the next step is to determine whether intravenous gentamicin can address the systemic effects. If so, this treatment has the potential to improve survival. He reported that an infant with H-JEB was recently started on intravenous treatment, and initial results were encouraging.
Asked whether he would recommend topical gentamicin on the basis of these findings, Mr. Kwong cautioned that the case series remains very small, but he noted that the uniformity of the positive response is encouraging. He expects that off-label use of this novel and low-cost approach might be warranted in a population that has very limited therapeutic options.
SOURCE: Kwong A. SID 2019;S102, Abstract 594. Annual meeting of the Society for Investigative Dermatology.
CHICAGO – Topical gentamicin counters the nonsense mutations that inhibit production of laminin 332 in infants with Herlitz junctional epidermolysis bullosa (H-JEB) to allow lesion healing, according to results of a small clinical study presented at the annual meeting of the Society for Investigative Dermatology.
“All of the children treated so far have responded,” reported Andrew Kwong, who will soon graduate from the Keck School of Medicine at the University of Southern California, Los Angeles.
H-JEB is an inherited blistering skin disease associated with nonsense mutations in the LAMA3, LAMB3, or LAMC2 genes that result in impaired production of functional laminin 332, an essential protein for epidermal-dermal adherence. At this time there are no effective therapies, and the disease is fatal.
The small clinical study was initiated after in vitro studies demonstrated that gentamicin restored functional laminin 332 in cultured keratinocytes from infants with H-JEB. The dose-dependent effect was credited to the ability of gentamicin to induce readthrough of premature stop codons that block production of laminin 332.
Data were presented on the first three infants with H-JEB treated with oral gentamicin. In each child, lesions were treated with topical 0.5% gentamicin twice daily for two weeks. Biopsies were taken prior to the initiation of treatment and at one and three months after treatment. The primary outcome was change in laminin 332, but clinical improvement was also monitored.
Although none of the infants had measurable laminin 332 prior to treatment, all lesions treated with topical gentamicin developed localized laminin 332 at the dermal-epidermal junction of the skin, Mr. Kwong reported. This expression, which was about 40% to 60% of that seen in normal skin, still persisted when evaluated three months after treatment.
The expression was associated with resolution of existing lesions and a reduced risk of developing new lesions, according to Mr. Kwong. In lesions that went untreated, there was no change.
Other molecular changes in the skin, such as increased expression and polarization of beta-4 integrin, were consistent with the ability of gentamicin to address the underlying pathophysiology of H-JEB. There were no adverse events observed.
By restoring functional laminin 332 in the skin, topical gentamicin appears to address the underlying cause of the bullae associated with H-JEB, but Mr. Kwong said that the next step is to determine whether intravenous gentamicin can address the systemic effects. If so, this treatment has the potential to improve survival. He reported that an infant with H-JEB was recently started on intravenous treatment, and initial results were encouraging.
Asked whether he would recommend topical gentamicin on the basis of these findings, Mr. Kwong cautioned that the case series remains very small, but he noted that the uniformity of the positive response is encouraging. He expects that off-label use of this novel and low-cost approach might be warranted in a population that has very limited therapeutic options.
SOURCE: Kwong A. SID 2019;S102, Abstract 594. Annual meeting of the Society for Investigative Dermatology.
REPORTING FROM SID 2019