User login
To fast or not to fast before elective cardiac catheterization
No restriction of oral food intake prior to nonemergent cardiac catheterization is as safe as the current traditional NPO [nothing by mouth] strategy, results from a large, single-center, randomized controlled trial showed.
According to lead investigator Abhishek Mishra, MD, NPO after midnight has been a standard practice before major surgery requiring general anesthesia since Mendelson Syndrome was first described in 1946. “The rational for keeping NPO after midnight has been to keep the stomach empty, to reduce gastric contents and acidity – which would reduce emesis – and eventually reduce the risk of aspiration,” Dr. Mishra, a cardiologist at the Heart and Vascular Institute at Vidant Health in Greenville, N.C., said at the at the Society for Cardiovascular Angiography & Interventions virtual annual scientific sessions. “The rationale of NPO in the setting of cardiac catheterization is to reduce the risk of aspiration, and more so, of a patient needing emergent cardiac surgery.” The clinical question was, do we really need to keep our patients NPO prior to elective cardiac catheterization? So far, no large randomized study has been done to answer this question.”
To find out, Dr. Mishra and colleagues carried out CHOW NOW (Can We Safely Have Our Patients Eat With Cardiac Catheterization – Nix or Allow), a single-center, prospective, randomized, single-blinded study that compared the safety of a nonfasting strategy with the current fasting protocol strategies in 599 patients who underwent nonemergent cardiac catheterization at The Guthrie Clinic/Robert Packer Hospital in Sayre, Pa.
Patients in the fasting group were instructed to be NPO after midnight, but could have clear liquids up to 2 hours prior to the procedure, while those in the nonfasting group had no restriction of oral intake, irrespective of time of cardiac catheterization. The primary outcome was a composite of aspiration pneumonia, preprocedural hypertension, preprocedural hypoglycemia or hyperglycemia, incidence of nausea/vomiting, and contrast-induced neuropathy. Secondary outcomes included total cost of the index hospitalization, patient satisfaction via a questionnaire containing seven questions, and in-hospital mortality.
Of the 599 patients, 306 were assigned to the standard fasting group and the remaining 293 to the nonfasting group. Their mean age was 67 years, 45% were on a proton pump inhibitor or H2 blockers, and 33% had diabetes. In addition, 40% had acute coronary syndrome, and 23% underwent percutaneous intervention.
The researchers observed no statistically significant difference in the primary or secondary outcomes between the study groups. In the nonfasting group, 11.3% of patients met the primary endpoint, compared with 9.8% of the patients in the standard fasting group (P = .65). In addition, the nonfasting strategy was found to be noninferior to the standard fasting strategy for the primary outcome at a noninferiority margin threshold of 0.059.
Dr. Mishra and colleagues observed no differences between the standard fasting and nonfasting groups with respect to in-hospital mortality (0.3% vs. 0.7%, respectively; P = .616), patient satisfaction score (a mean of 4.4 vs. a mean of 4.5; P = .257), and mean total cost of hospitalization ($8,446 vs. $6,960; P = .654).
“In this randomized, controlled trial, we found that there was no significant difference in the rate of overall adverse events with an approach of unrestricted oral intake prior to cardiac catheterization compared to strict fasting, and it was associated with better patient satisfaction and lower cost of care, especially for hospitalized patients,” concluded Dr. Mishra, who conducted the research during his fellowship at The Guthrie Clinic.
He acknowledged certain limitations of the trial, including the fact that results are applicable only to cardiac catheterization procedures, including coronary angiographies, percutaneous coronary interventions, and left heart catheterizations. “These results are not applicable to certain high-risk coronary procedures that required the use of a large-bore access or any valve procedures,” he said.
One of the session’s invited panelists, Cindy L. Grines, MD,, said that she and other interventional cardiologists have “gone around and around” on the issue of NPO prior to nonemergent cardiac catheterization. “I actually let my patients get fluids up until the time they’re put on the cath lab table,” said Dr. Grines, chief scientific officer of the Northside Cardiovascular Institute in Atlanta. “I haven’t been giving them solid food like this, though.”
Another panelist, Timothy D. Henry, MD, said that in his clinical experience, “patients don’t like being NPO, and I think we’ve all seen cases where patients are actually volume-depleted in the morning.” Dr. Henry, medical director of The Carl and Edyth Lindner Center for Research and Education at The Christ Hospital in Cincinnati, pointed out that most NPO policy “is not dictated by us as interventional cardiologists; it’s dictated by hospital policies or by anesthesiologists. Will [the results of this study] change what we do?”
The Donald Guthrie Research Foundation funded the study. Daniel P. Sporn, MD, FACC, was the study’s principal investigator. Dr. Mishra reported having no financial disclosures.
SOURCE: Mishra A et al., SCAI 2020, abstract 11758.
No restriction of oral food intake prior to nonemergent cardiac catheterization is as safe as the current traditional NPO [nothing by mouth] strategy, results from a large, single-center, randomized controlled trial showed.
According to lead investigator Abhishek Mishra, MD, NPO after midnight has been a standard practice before major surgery requiring general anesthesia since Mendelson Syndrome was first described in 1946. “The rational for keeping NPO after midnight has been to keep the stomach empty, to reduce gastric contents and acidity – which would reduce emesis – and eventually reduce the risk of aspiration,” Dr. Mishra, a cardiologist at the Heart and Vascular Institute at Vidant Health in Greenville, N.C., said at the at the Society for Cardiovascular Angiography & Interventions virtual annual scientific sessions. “The rationale of NPO in the setting of cardiac catheterization is to reduce the risk of aspiration, and more so, of a patient needing emergent cardiac surgery.” The clinical question was, do we really need to keep our patients NPO prior to elective cardiac catheterization? So far, no large randomized study has been done to answer this question.”
To find out, Dr. Mishra and colleagues carried out CHOW NOW (Can We Safely Have Our Patients Eat With Cardiac Catheterization – Nix or Allow), a single-center, prospective, randomized, single-blinded study that compared the safety of a nonfasting strategy with the current fasting protocol strategies in 599 patients who underwent nonemergent cardiac catheterization at The Guthrie Clinic/Robert Packer Hospital in Sayre, Pa.
Patients in the fasting group were instructed to be NPO after midnight, but could have clear liquids up to 2 hours prior to the procedure, while those in the nonfasting group had no restriction of oral intake, irrespective of time of cardiac catheterization. The primary outcome was a composite of aspiration pneumonia, preprocedural hypertension, preprocedural hypoglycemia or hyperglycemia, incidence of nausea/vomiting, and contrast-induced neuropathy. Secondary outcomes included total cost of the index hospitalization, patient satisfaction via a questionnaire containing seven questions, and in-hospital mortality.
Of the 599 patients, 306 were assigned to the standard fasting group and the remaining 293 to the nonfasting group. Their mean age was 67 years, 45% were on a proton pump inhibitor or H2 blockers, and 33% had diabetes. In addition, 40% had acute coronary syndrome, and 23% underwent percutaneous intervention.
The researchers observed no statistically significant difference in the primary or secondary outcomes between the study groups. In the nonfasting group, 11.3% of patients met the primary endpoint, compared with 9.8% of the patients in the standard fasting group (P = .65). In addition, the nonfasting strategy was found to be noninferior to the standard fasting strategy for the primary outcome at a noninferiority margin threshold of 0.059.
Dr. Mishra and colleagues observed no differences between the standard fasting and nonfasting groups with respect to in-hospital mortality (0.3% vs. 0.7%, respectively; P = .616), patient satisfaction score (a mean of 4.4 vs. a mean of 4.5; P = .257), and mean total cost of hospitalization ($8,446 vs. $6,960; P = .654).
“In this randomized, controlled trial, we found that there was no significant difference in the rate of overall adverse events with an approach of unrestricted oral intake prior to cardiac catheterization compared to strict fasting, and it was associated with better patient satisfaction and lower cost of care, especially for hospitalized patients,” concluded Dr. Mishra, who conducted the research during his fellowship at The Guthrie Clinic.
He acknowledged certain limitations of the trial, including the fact that results are applicable only to cardiac catheterization procedures, including coronary angiographies, percutaneous coronary interventions, and left heart catheterizations. “These results are not applicable to certain high-risk coronary procedures that required the use of a large-bore access or any valve procedures,” he said.
One of the session’s invited panelists, Cindy L. Grines, MD,, said that she and other interventional cardiologists have “gone around and around” on the issue of NPO prior to nonemergent cardiac catheterization. “I actually let my patients get fluids up until the time they’re put on the cath lab table,” said Dr. Grines, chief scientific officer of the Northside Cardiovascular Institute in Atlanta. “I haven’t been giving them solid food like this, though.”
Another panelist, Timothy D. Henry, MD, said that in his clinical experience, “patients don’t like being NPO, and I think we’ve all seen cases where patients are actually volume-depleted in the morning.” Dr. Henry, medical director of The Carl and Edyth Lindner Center for Research and Education at The Christ Hospital in Cincinnati, pointed out that most NPO policy “is not dictated by us as interventional cardiologists; it’s dictated by hospital policies or by anesthesiologists. Will [the results of this study] change what we do?”
The Donald Guthrie Research Foundation funded the study. Daniel P. Sporn, MD, FACC, was the study’s principal investigator. Dr. Mishra reported having no financial disclosures.
SOURCE: Mishra A et al., SCAI 2020, abstract 11758.
No restriction of oral food intake prior to nonemergent cardiac catheterization is as safe as the current traditional NPO [nothing by mouth] strategy, results from a large, single-center, randomized controlled trial showed.
According to lead investigator Abhishek Mishra, MD, NPO after midnight has been a standard practice before major surgery requiring general anesthesia since Mendelson Syndrome was first described in 1946. “The rational for keeping NPO after midnight has been to keep the stomach empty, to reduce gastric contents and acidity – which would reduce emesis – and eventually reduce the risk of aspiration,” Dr. Mishra, a cardiologist at the Heart and Vascular Institute at Vidant Health in Greenville, N.C., said at the at the Society for Cardiovascular Angiography & Interventions virtual annual scientific sessions. “The rationale of NPO in the setting of cardiac catheterization is to reduce the risk of aspiration, and more so, of a patient needing emergent cardiac surgery.” The clinical question was, do we really need to keep our patients NPO prior to elective cardiac catheterization? So far, no large randomized study has been done to answer this question.”
To find out, Dr. Mishra and colleagues carried out CHOW NOW (Can We Safely Have Our Patients Eat With Cardiac Catheterization – Nix or Allow), a single-center, prospective, randomized, single-blinded study that compared the safety of a nonfasting strategy with the current fasting protocol strategies in 599 patients who underwent nonemergent cardiac catheterization at The Guthrie Clinic/Robert Packer Hospital in Sayre, Pa.
Patients in the fasting group were instructed to be NPO after midnight, but could have clear liquids up to 2 hours prior to the procedure, while those in the nonfasting group had no restriction of oral intake, irrespective of time of cardiac catheterization. The primary outcome was a composite of aspiration pneumonia, preprocedural hypertension, preprocedural hypoglycemia or hyperglycemia, incidence of nausea/vomiting, and contrast-induced neuropathy. Secondary outcomes included total cost of the index hospitalization, patient satisfaction via a questionnaire containing seven questions, and in-hospital mortality.
Of the 599 patients, 306 were assigned to the standard fasting group and the remaining 293 to the nonfasting group. Their mean age was 67 years, 45% were on a proton pump inhibitor or H2 blockers, and 33% had diabetes. In addition, 40% had acute coronary syndrome, and 23% underwent percutaneous intervention.
The researchers observed no statistically significant difference in the primary or secondary outcomes between the study groups. In the nonfasting group, 11.3% of patients met the primary endpoint, compared with 9.8% of the patients in the standard fasting group (P = .65). In addition, the nonfasting strategy was found to be noninferior to the standard fasting strategy for the primary outcome at a noninferiority margin threshold of 0.059.
Dr. Mishra and colleagues observed no differences between the standard fasting and nonfasting groups with respect to in-hospital mortality (0.3% vs. 0.7%, respectively; P = .616), patient satisfaction score (a mean of 4.4 vs. a mean of 4.5; P = .257), and mean total cost of hospitalization ($8,446 vs. $6,960; P = .654).
“In this randomized, controlled trial, we found that there was no significant difference in the rate of overall adverse events with an approach of unrestricted oral intake prior to cardiac catheterization compared to strict fasting, and it was associated with better patient satisfaction and lower cost of care, especially for hospitalized patients,” concluded Dr. Mishra, who conducted the research during his fellowship at The Guthrie Clinic.
He acknowledged certain limitations of the trial, including the fact that results are applicable only to cardiac catheterization procedures, including coronary angiographies, percutaneous coronary interventions, and left heart catheterizations. “These results are not applicable to certain high-risk coronary procedures that required the use of a large-bore access or any valve procedures,” he said.
One of the session’s invited panelists, Cindy L. Grines, MD,, said that she and other interventional cardiologists have “gone around and around” on the issue of NPO prior to nonemergent cardiac catheterization. “I actually let my patients get fluids up until the time they’re put on the cath lab table,” said Dr. Grines, chief scientific officer of the Northside Cardiovascular Institute in Atlanta. “I haven’t been giving them solid food like this, though.”
Another panelist, Timothy D. Henry, MD, said that in his clinical experience, “patients don’t like being NPO, and I think we’ve all seen cases where patients are actually volume-depleted in the morning.” Dr. Henry, medical director of The Carl and Edyth Lindner Center for Research and Education at The Christ Hospital in Cincinnati, pointed out that most NPO policy “is not dictated by us as interventional cardiologists; it’s dictated by hospital policies or by anesthesiologists. Will [the results of this study] change what we do?”
The Donald Guthrie Research Foundation funded the study. Daniel P. Sporn, MD, FACC, was the study’s principal investigator. Dr. Mishra reported having no financial disclosures.
SOURCE: Mishra A et al., SCAI 2020, abstract 11758.
REPORTING FROM SCAI 2020
Remdesivir in Hospitalized Adults With Severe COVID-19: Lessons Learned From the First Randomized Trial
Study Overview
Objective. To assess the efficacy, safety, and clinical benefit of remdesivir in hospitalized adults with confirmed pneumonia due to severe SARS-CoV-2 infection.
Design. Randomized, investigator-initiated, placebo-controlled, double-blind, multicenter trial.
Setting and participants. The trial took place between February 6, 2020 and March 12, 2020, at 10 hospitals in Wuhan, China. Study participants included adult patients (aged ≥ 18 years) admitted to hospital who tested positive for SARS-CoV-2 by reverse transcription polymerase chain reaction assay and had the following clinical characteristics: radiographic evidence of pneumonia; hypoxia with oxygen saturation ≤ 94% on room air or a ratio of arterial oxygen partial pressure to fractional inspired oxygen ≤ 300 mm Hg; and symptom onset to enrollment ≤ 12 days. Some of the exclusion criteria for participation in the study were pregnancy or breast feeding, liver cirrhosis, abnormal liver enzymes ≥ 5 times the upper limit of normal, severe renal impairment or receipt of renal replacement therapy, plan for transfer to a non-study hospital, and enrollment in a trial for COVID-19 within the previous month.
Intervention. Participants were randomized in a 2:1 ratio to the remdesivir group or the placebo group and were administered either intravenous infusions of remdesivir (200 mg on day 1 followed by 100 mg daily on days 2-10) or the same volume of placebo for 10 days. Clinical and safety data assessed included laboratory testing, electrocardiogram, and medication adverse effects. Testing of oropharyngeal and nasopharyngeal swab samples, anal swab samples, sputum, and stool was performed for viral RNA detection and quantification on days 1, 3, 5, 7, 10, 14, 21, and 28.
Main outcome measures. The primary endpoint of this study was time to clinical improvement within 28 days after randomization. Clinical improvement was defined as a 2-point reduction in participants’ admission status on a 6-point ordinal scale (1 = discharged or clinical recovery, 6 = death) or live discharge from hospital, whichever came first. Secondary outcomes included all-cause mortality at day 28 and duration of hospital admission, oxygen support, and invasive mechanical ventilation. Virological measures and safety outcomes ascertained included treatment-emergent adverse events, serious adverse events, and premature discontinuation of remdesivir.
The sample size estimate for the original study design was a total of 453 patients (302 in the remdesivir group and 151 in the placebo group). This sample size would provide 80% power, assuming a hazard ratio (HR) of 1.4 comparing remdesivir to placebo, and corresponding to a change in time to clinical improvement of 6 days. The analysis of primary outcome was performed on an intention-to-treat basis. Time to clinical improvement within 28 days was assessed with Kaplan-Meier plots.
Main results. A total of 255 patients were screened, of whom 237 were enrolled and randomized to remdesivir (158) or placebo (79) group. Of the participants in the remdesivir group, 155 started study treatment and 150 completed treatment per protocol. For the participants in the placebo group, 78 started study treatment and 76 completed treatment per-protocol. Study enrollment was terminated after March 12, 2020, before attaining the prespecified sample size, because no additional patients met study eligibility criteria due to various public health measures implemented in Wuhan. The median age of participants was 65 years (IQR, 56-71), the majority were men (56% in remdesivir group vs 65% in placebo group), and the most common comorbidities included hypertension, diabetes, and coronary artery disease. Median time from symptom onset to study enrollment was 10 days (IQR, 9-12). The time to clinical improvement between treatments (21 days for remdesivir group vs 23 days for placebo group) was not significantly different (HR, 1.23; 95% confidence interval [CI], 0.87-1.75). In addition, in participants who received treatment within 10 days of symptom onset, those who were administered remdesivir had a nonsignificant (HR, 1.52; 95% CI, 0.95-2.43) but faster time (18 days) to clinical improvement, compared to those administered placebo (23 days). Moreover, treatment with remdesivir versus placebo did not lead to differences in secondary outcomes (eg, 28-day mortality and duration of hospital stay, oxygen support, and invasive mechanical ventilation), changes in viral load over time, or adverse events between the groups.
Conclusion. This study found that, compared with placebo, intravenous remdesivir did not significantly improve the time to clinical improvement, mortality, or time to clearance of SARS-CoV-2 in hospitalized adults with severe COVID-19. A numeric reduction in time to clinical improvement with early remdesivir treatment (ie, within 10 days of symptom onset) that approached statistical significance was observed in this underpowered study.
Commentary
Within a few short months since its emergence. SARS-CoV-2 infection has caused a global pandemic, posing a dire threat to public health due to its adverse effects on morbidity (eg, respiratory failure, thromboembolic diseases, multiorgan failure) and mortality. To date, no pharmacologic treatment has been shown to effectively improve clinical outcomes in patients with COVID-19. Multiple ongoing clinical trials are being conducted globally to determine potential therapeutic treatments for severe COVID-19. The first clinical trials of hydroxychloroquine and lopinavir-ritonavir, agents traditionally used for other indications, such as malaria and HIV, did not show a clear benefit in COVID-19.1,2 Remdesivir, a nucleoside analogue prodrug, is a broad-spectrum antiviral agent that was previously used for treatment of Ebola and has been shown to have inhibitory effects on pathogenic coronaviruses. The study reported by Wang and colleagues was the first randomized controlled trial (RCT) aimed at evaluating whether remdesivir improves outcomes in patients with severe COVID-19. Thus, the worsening COVID-19 pandemic, coupled with the absence of a curative treatment, underscore the urgency of this trial.
The study was grounded on observational data from several recent case reports and case series centering on the potential efficacy of remdesivir in treating COVID-19.3 The study itself was designed well (ie, randomized, placebo-controlled, double-blind, multicenter) and carefully implemented (ie, high protocol adherence to treatments, no loss to follow-up). The principal limitation of this study was its inability to reach the estimated statistical power of study. Due to successful epidemic control in Wuhan, which led to marked reductions in hospital admission of patients with COVID-19, and implementation of stringent termination criteria per the study protocol, only 237 participants were enrolled, instead of the 453, as specified by the sample estimate. This corresponded to a reduction of statistical power from 80% to 58%. Due to this limitation, the study was underpowered, rendering its findings inconclusive.
Despite this limitation, the study found that those treated with remdesivir within 10 days of symptom onset had a numerically faster time (although not statistically significant) to clinical improvement. This leads to an interesting question: whether remdesivir administration early in COVID-19 course could improve clinical outcomes, a question that warrants further investigation by an adequately powered trial. Also, data from this study provided evidence that intravenous remdesivir administration is likely safe in adults during the treatment period, although the long-term drug effects, as well as the safety profile in pediatric patients, remain unknown at this time.
While the study reported by Wang and colleagues was underpowered and is thus inconclusive, several other ongoing RCTs are evaluating the potential clinical benefit of remdesivir treatment in patients hospitalized with COVID-19. On the date of online publication of this report in The Lancet, the National Institutes of Health (NIH) published a news release summarizing preliminary findings from the Adaptive COVID-19 Treatment Trial (ACTT), which showed positive effects of remdesivir on clinical recovery from advanced COVID-19.4 The ACTT, the first RCT launched in the United States to evaluate experimental treatment for COVID-19, included 1063 hospitalized participants with advanced COVID-19 and lung involvement. Participants who were administered remdesivir had a 31% faster time to recovery compared to those in the placebo group (median time to recovery, 11 days vs 15 days, respectively; P < 0.001), and had near statistically significant improved survival (mortality rate, 8.0% vs 11.6%, respectively; P = 0.059). In response to these findings, the US Food and Drug Administration (FDA) issued an emergency use authorization for remdesivir on May 1, 2020, for the treatment of suspected or laboratory-confirmed COVID-19 in adults and children hospitalized with severe disease.5 While the findings noted from the NIH news release are very encouraging and provide the first evidence of a potentially beneficial antiviral treatment for severe COVID-19 in humans, the scientific community awaits the peer-reviewed publication of the ACTT to better assess the safety and effectiveness of remdesivir therapy and determine the trial’s implications in the management of COVID-19.
Applications for Clinical Practice
The discovery of an effective pharmacologic intervention for COVID-19 is of utmost urgency. While the present study was unable to answer the question of whether remdesivir is effective in improving clinical outcomes in patients with severe COVID-19, other ongoing or completed (ie, ACTT) studies will likely address this knowledge gap in the coming months. The FDA’s emergency use authorization for remdesivir provides a glimpse into this possibility.
–Katerina Oikonomou, MD, Brookdale Department of Geriatrics & Palliative Medicine, Icahn School of Medicine at Mount Sinai, New York, NY
–Fred Ko, MD
1. Tang W, Cao Z, Han M, et al. Hydroxychloroquine in patients with COVID-19: an open-label, randomized, controlled trial [published online April 14, 2020]. medRxiv.org. doi:10.1101/2020.04.10.20060558.
2. Cao B, Wang Y, Wen D, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe COVID-19. N Engl J Med. 2020;382:1787-1799.
3. Grein J, Ohmagari N, Shin D, et al. Compassionate use of remdesivir for patients with severe COVID-19 [published online April 10, 2020]. N Engl J Med. doi:10.1056/NEJMoa2007016.
4. NIH clinical trial shows remdesivir accelerates recovery from advanced COVID-19. www.niaid.nih.gov/news-events/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19. Accessed May 9, 2020
5. Coronavirus (COVID-19) update: FDA issues Emergency Use Authorization for potential COVID-19 treatment. www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment. Accessed May 9, 2020.
Study Overview
Objective. To assess the efficacy, safety, and clinical benefit of remdesivir in hospitalized adults with confirmed pneumonia due to severe SARS-CoV-2 infection.
Design. Randomized, investigator-initiated, placebo-controlled, double-blind, multicenter trial.
Setting and participants. The trial took place between February 6, 2020 and March 12, 2020, at 10 hospitals in Wuhan, China. Study participants included adult patients (aged ≥ 18 years) admitted to hospital who tested positive for SARS-CoV-2 by reverse transcription polymerase chain reaction assay and had the following clinical characteristics: radiographic evidence of pneumonia; hypoxia with oxygen saturation ≤ 94% on room air or a ratio of arterial oxygen partial pressure to fractional inspired oxygen ≤ 300 mm Hg; and symptom onset to enrollment ≤ 12 days. Some of the exclusion criteria for participation in the study were pregnancy or breast feeding, liver cirrhosis, abnormal liver enzymes ≥ 5 times the upper limit of normal, severe renal impairment or receipt of renal replacement therapy, plan for transfer to a non-study hospital, and enrollment in a trial for COVID-19 within the previous month.
Intervention. Participants were randomized in a 2:1 ratio to the remdesivir group or the placebo group and were administered either intravenous infusions of remdesivir (200 mg on day 1 followed by 100 mg daily on days 2-10) or the same volume of placebo for 10 days. Clinical and safety data assessed included laboratory testing, electrocardiogram, and medication adverse effects. Testing of oropharyngeal and nasopharyngeal swab samples, anal swab samples, sputum, and stool was performed for viral RNA detection and quantification on days 1, 3, 5, 7, 10, 14, 21, and 28.
Main outcome measures. The primary endpoint of this study was time to clinical improvement within 28 days after randomization. Clinical improvement was defined as a 2-point reduction in participants’ admission status on a 6-point ordinal scale (1 = discharged or clinical recovery, 6 = death) or live discharge from hospital, whichever came first. Secondary outcomes included all-cause mortality at day 28 and duration of hospital admission, oxygen support, and invasive mechanical ventilation. Virological measures and safety outcomes ascertained included treatment-emergent adverse events, serious adverse events, and premature discontinuation of remdesivir.
The sample size estimate for the original study design was a total of 453 patients (302 in the remdesivir group and 151 in the placebo group). This sample size would provide 80% power, assuming a hazard ratio (HR) of 1.4 comparing remdesivir to placebo, and corresponding to a change in time to clinical improvement of 6 days. The analysis of primary outcome was performed on an intention-to-treat basis. Time to clinical improvement within 28 days was assessed with Kaplan-Meier plots.
Main results. A total of 255 patients were screened, of whom 237 were enrolled and randomized to remdesivir (158) or placebo (79) group. Of the participants in the remdesivir group, 155 started study treatment and 150 completed treatment per protocol. For the participants in the placebo group, 78 started study treatment and 76 completed treatment per-protocol. Study enrollment was terminated after March 12, 2020, before attaining the prespecified sample size, because no additional patients met study eligibility criteria due to various public health measures implemented in Wuhan. The median age of participants was 65 years (IQR, 56-71), the majority were men (56% in remdesivir group vs 65% in placebo group), and the most common comorbidities included hypertension, diabetes, and coronary artery disease. Median time from symptom onset to study enrollment was 10 days (IQR, 9-12). The time to clinical improvement between treatments (21 days for remdesivir group vs 23 days for placebo group) was not significantly different (HR, 1.23; 95% confidence interval [CI], 0.87-1.75). In addition, in participants who received treatment within 10 days of symptom onset, those who were administered remdesivir had a nonsignificant (HR, 1.52; 95% CI, 0.95-2.43) but faster time (18 days) to clinical improvement, compared to those administered placebo (23 days). Moreover, treatment with remdesivir versus placebo did not lead to differences in secondary outcomes (eg, 28-day mortality and duration of hospital stay, oxygen support, and invasive mechanical ventilation), changes in viral load over time, or adverse events between the groups.
Conclusion. This study found that, compared with placebo, intravenous remdesivir did not significantly improve the time to clinical improvement, mortality, or time to clearance of SARS-CoV-2 in hospitalized adults with severe COVID-19. A numeric reduction in time to clinical improvement with early remdesivir treatment (ie, within 10 days of symptom onset) that approached statistical significance was observed in this underpowered study.
Commentary
Within a few short months since its emergence. SARS-CoV-2 infection has caused a global pandemic, posing a dire threat to public health due to its adverse effects on morbidity (eg, respiratory failure, thromboembolic diseases, multiorgan failure) and mortality. To date, no pharmacologic treatment has been shown to effectively improve clinical outcomes in patients with COVID-19. Multiple ongoing clinical trials are being conducted globally to determine potential therapeutic treatments for severe COVID-19. The first clinical trials of hydroxychloroquine and lopinavir-ritonavir, agents traditionally used for other indications, such as malaria and HIV, did not show a clear benefit in COVID-19.1,2 Remdesivir, a nucleoside analogue prodrug, is a broad-spectrum antiviral agent that was previously used for treatment of Ebola and has been shown to have inhibitory effects on pathogenic coronaviruses. The study reported by Wang and colleagues was the first randomized controlled trial (RCT) aimed at evaluating whether remdesivir improves outcomes in patients with severe COVID-19. Thus, the worsening COVID-19 pandemic, coupled with the absence of a curative treatment, underscore the urgency of this trial.
The study was grounded on observational data from several recent case reports and case series centering on the potential efficacy of remdesivir in treating COVID-19.3 The study itself was designed well (ie, randomized, placebo-controlled, double-blind, multicenter) and carefully implemented (ie, high protocol adherence to treatments, no loss to follow-up). The principal limitation of this study was its inability to reach the estimated statistical power of study. Due to successful epidemic control in Wuhan, which led to marked reductions in hospital admission of patients with COVID-19, and implementation of stringent termination criteria per the study protocol, only 237 participants were enrolled, instead of the 453, as specified by the sample estimate. This corresponded to a reduction of statistical power from 80% to 58%. Due to this limitation, the study was underpowered, rendering its findings inconclusive.
Despite this limitation, the study found that those treated with remdesivir within 10 days of symptom onset had a numerically faster time (although not statistically significant) to clinical improvement. This leads to an interesting question: whether remdesivir administration early in COVID-19 course could improve clinical outcomes, a question that warrants further investigation by an adequately powered trial. Also, data from this study provided evidence that intravenous remdesivir administration is likely safe in adults during the treatment period, although the long-term drug effects, as well as the safety profile in pediatric patients, remain unknown at this time.
While the study reported by Wang and colleagues was underpowered and is thus inconclusive, several other ongoing RCTs are evaluating the potential clinical benefit of remdesivir treatment in patients hospitalized with COVID-19. On the date of online publication of this report in The Lancet, the National Institutes of Health (NIH) published a news release summarizing preliminary findings from the Adaptive COVID-19 Treatment Trial (ACTT), which showed positive effects of remdesivir on clinical recovery from advanced COVID-19.4 The ACTT, the first RCT launched in the United States to evaluate experimental treatment for COVID-19, included 1063 hospitalized participants with advanced COVID-19 and lung involvement. Participants who were administered remdesivir had a 31% faster time to recovery compared to those in the placebo group (median time to recovery, 11 days vs 15 days, respectively; P < 0.001), and had near statistically significant improved survival (mortality rate, 8.0% vs 11.6%, respectively; P = 0.059). In response to these findings, the US Food and Drug Administration (FDA) issued an emergency use authorization for remdesivir on May 1, 2020, for the treatment of suspected or laboratory-confirmed COVID-19 in adults and children hospitalized with severe disease.5 While the findings noted from the NIH news release are very encouraging and provide the first evidence of a potentially beneficial antiviral treatment for severe COVID-19 in humans, the scientific community awaits the peer-reviewed publication of the ACTT to better assess the safety and effectiveness of remdesivir therapy and determine the trial’s implications in the management of COVID-19.
Applications for Clinical Practice
The discovery of an effective pharmacologic intervention for COVID-19 is of utmost urgency. While the present study was unable to answer the question of whether remdesivir is effective in improving clinical outcomes in patients with severe COVID-19, other ongoing or completed (ie, ACTT) studies will likely address this knowledge gap in the coming months. The FDA’s emergency use authorization for remdesivir provides a glimpse into this possibility.
–Katerina Oikonomou, MD, Brookdale Department of Geriatrics & Palliative Medicine, Icahn School of Medicine at Mount Sinai, New York, NY
–Fred Ko, MD
Study Overview
Objective. To assess the efficacy, safety, and clinical benefit of remdesivir in hospitalized adults with confirmed pneumonia due to severe SARS-CoV-2 infection.
Design. Randomized, investigator-initiated, placebo-controlled, double-blind, multicenter trial.
Setting and participants. The trial took place between February 6, 2020 and March 12, 2020, at 10 hospitals in Wuhan, China. Study participants included adult patients (aged ≥ 18 years) admitted to hospital who tested positive for SARS-CoV-2 by reverse transcription polymerase chain reaction assay and had the following clinical characteristics: radiographic evidence of pneumonia; hypoxia with oxygen saturation ≤ 94% on room air or a ratio of arterial oxygen partial pressure to fractional inspired oxygen ≤ 300 mm Hg; and symptom onset to enrollment ≤ 12 days. Some of the exclusion criteria for participation in the study were pregnancy or breast feeding, liver cirrhosis, abnormal liver enzymes ≥ 5 times the upper limit of normal, severe renal impairment or receipt of renal replacement therapy, plan for transfer to a non-study hospital, and enrollment in a trial for COVID-19 within the previous month.
Intervention. Participants were randomized in a 2:1 ratio to the remdesivir group or the placebo group and were administered either intravenous infusions of remdesivir (200 mg on day 1 followed by 100 mg daily on days 2-10) or the same volume of placebo for 10 days. Clinical and safety data assessed included laboratory testing, electrocardiogram, and medication adverse effects. Testing of oropharyngeal and nasopharyngeal swab samples, anal swab samples, sputum, and stool was performed for viral RNA detection and quantification on days 1, 3, 5, 7, 10, 14, 21, and 28.
Main outcome measures. The primary endpoint of this study was time to clinical improvement within 28 days after randomization. Clinical improvement was defined as a 2-point reduction in participants’ admission status on a 6-point ordinal scale (1 = discharged or clinical recovery, 6 = death) or live discharge from hospital, whichever came first. Secondary outcomes included all-cause mortality at day 28 and duration of hospital admission, oxygen support, and invasive mechanical ventilation. Virological measures and safety outcomes ascertained included treatment-emergent adverse events, serious adverse events, and premature discontinuation of remdesivir.
The sample size estimate for the original study design was a total of 453 patients (302 in the remdesivir group and 151 in the placebo group). This sample size would provide 80% power, assuming a hazard ratio (HR) of 1.4 comparing remdesivir to placebo, and corresponding to a change in time to clinical improvement of 6 days. The analysis of primary outcome was performed on an intention-to-treat basis. Time to clinical improvement within 28 days was assessed with Kaplan-Meier plots.
Main results. A total of 255 patients were screened, of whom 237 were enrolled and randomized to remdesivir (158) or placebo (79) group. Of the participants in the remdesivir group, 155 started study treatment and 150 completed treatment per protocol. For the participants in the placebo group, 78 started study treatment and 76 completed treatment per-protocol. Study enrollment was terminated after March 12, 2020, before attaining the prespecified sample size, because no additional patients met study eligibility criteria due to various public health measures implemented in Wuhan. The median age of participants was 65 years (IQR, 56-71), the majority were men (56% in remdesivir group vs 65% in placebo group), and the most common comorbidities included hypertension, diabetes, and coronary artery disease. Median time from symptom onset to study enrollment was 10 days (IQR, 9-12). The time to clinical improvement between treatments (21 days for remdesivir group vs 23 days for placebo group) was not significantly different (HR, 1.23; 95% confidence interval [CI], 0.87-1.75). In addition, in participants who received treatment within 10 days of symptom onset, those who were administered remdesivir had a nonsignificant (HR, 1.52; 95% CI, 0.95-2.43) but faster time (18 days) to clinical improvement, compared to those administered placebo (23 days). Moreover, treatment with remdesivir versus placebo did not lead to differences in secondary outcomes (eg, 28-day mortality and duration of hospital stay, oxygen support, and invasive mechanical ventilation), changes in viral load over time, or adverse events between the groups.
Conclusion. This study found that, compared with placebo, intravenous remdesivir did not significantly improve the time to clinical improvement, mortality, or time to clearance of SARS-CoV-2 in hospitalized adults with severe COVID-19. A numeric reduction in time to clinical improvement with early remdesivir treatment (ie, within 10 days of symptom onset) that approached statistical significance was observed in this underpowered study.
Commentary
Within a few short months since its emergence. SARS-CoV-2 infection has caused a global pandemic, posing a dire threat to public health due to its adverse effects on morbidity (eg, respiratory failure, thromboembolic diseases, multiorgan failure) and mortality. To date, no pharmacologic treatment has been shown to effectively improve clinical outcomes in patients with COVID-19. Multiple ongoing clinical trials are being conducted globally to determine potential therapeutic treatments for severe COVID-19. The first clinical trials of hydroxychloroquine and lopinavir-ritonavir, agents traditionally used for other indications, such as malaria and HIV, did not show a clear benefit in COVID-19.1,2 Remdesivir, a nucleoside analogue prodrug, is a broad-spectrum antiviral agent that was previously used for treatment of Ebola and has been shown to have inhibitory effects on pathogenic coronaviruses. The study reported by Wang and colleagues was the first randomized controlled trial (RCT) aimed at evaluating whether remdesivir improves outcomes in patients with severe COVID-19. Thus, the worsening COVID-19 pandemic, coupled with the absence of a curative treatment, underscore the urgency of this trial.
The study was grounded on observational data from several recent case reports and case series centering on the potential efficacy of remdesivir in treating COVID-19.3 The study itself was designed well (ie, randomized, placebo-controlled, double-blind, multicenter) and carefully implemented (ie, high protocol adherence to treatments, no loss to follow-up). The principal limitation of this study was its inability to reach the estimated statistical power of study. Due to successful epidemic control in Wuhan, which led to marked reductions in hospital admission of patients with COVID-19, and implementation of stringent termination criteria per the study protocol, only 237 participants were enrolled, instead of the 453, as specified by the sample estimate. This corresponded to a reduction of statistical power from 80% to 58%. Due to this limitation, the study was underpowered, rendering its findings inconclusive.
Despite this limitation, the study found that those treated with remdesivir within 10 days of symptom onset had a numerically faster time (although not statistically significant) to clinical improvement. This leads to an interesting question: whether remdesivir administration early in COVID-19 course could improve clinical outcomes, a question that warrants further investigation by an adequately powered trial. Also, data from this study provided evidence that intravenous remdesivir administration is likely safe in adults during the treatment period, although the long-term drug effects, as well as the safety profile in pediatric patients, remain unknown at this time.
While the study reported by Wang and colleagues was underpowered and is thus inconclusive, several other ongoing RCTs are evaluating the potential clinical benefit of remdesivir treatment in patients hospitalized with COVID-19. On the date of online publication of this report in The Lancet, the National Institutes of Health (NIH) published a news release summarizing preliminary findings from the Adaptive COVID-19 Treatment Trial (ACTT), which showed positive effects of remdesivir on clinical recovery from advanced COVID-19.4 The ACTT, the first RCT launched in the United States to evaluate experimental treatment for COVID-19, included 1063 hospitalized participants with advanced COVID-19 and lung involvement. Participants who were administered remdesivir had a 31% faster time to recovery compared to those in the placebo group (median time to recovery, 11 days vs 15 days, respectively; P < 0.001), and had near statistically significant improved survival (mortality rate, 8.0% vs 11.6%, respectively; P = 0.059). In response to these findings, the US Food and Drug Administration (FDA) issued an emergency use authorization for remdesivir on May 1, 2020, for the treatment of suspected or laboratory-confirmed COVID-19 in adults and children hospitalized with severe disease.5 While the findings noted from the NIH news release are very encouraging and provide the first evidence of a potentially beneficial antiviral treatment for severe COVID-19 in humans, the scientific community awaits the peer-reviewed publication of the ACTT to better assess the safety and effectiveness of remdesivir therapy and determine the trial’s implications in the management of COVID-19.
Applications for Clinical Practice
The discovery of an effective pharmacologic intervention for COVID-19 is of utmost urgency. While the present study was unable to answer the question of whether remdesivir is effective in improving clinical outcomes in patients with severe COVID-19, other ongoing or completed (ie, ACTT) studies will likely address this knowledge gap in the coming months. The FDA’s emergency use authorization for remdesivir provides a glimpse into this possibility.
–Katerina Oikonomou, MD, Brookdale Department of Geriatrics & Palliative Medicine, Icahn School of Medicine at Mount Sinai, New York, NY
–Fred Ko, MD
1. Tang W, Cao Z, Han M, et al. Hydroxychloroquine in patients with COVID-19: an open-label, randomized, controlled trial [published online April 14, 2020]. medRxiv.org. doi:10.1101/2020.04.10.20060558.
2. Cao B, Wang Y, Wen D, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe COVID-19. N Engl J Med. 2020;382:1787-1799.
3. Grein J, Ohmagari N, Shin D, et al. Compassionate use of remdesivir for patients with severe COVID-19 [published online April 10, 2020]. N Engl J Med. doi:10.1056/NEJMoa2007016.
4. NIH clinical trial shows remdesivir accelerates recovery from advanced COVID-19. www.niaid.nih.gov/news-events/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19. Accessed May 9, 2020
5. Coronavirus (COVID-19) update: FDA issues Emergency Use Authorization for potential COVID-19 treatment. www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment. Accessed May 9, 2020.
1. Tang W, Cao Z, Han M, et al. Hydroxychloroquine in patients with COVID-19: an open-label, randomized, controlled trial [published online April 14, 2020]. medRxiv.org. doi:10.1101/2020.04.10.20060558.
2. Cao B, Wang Y, Wen D, et al. A trial of lopinavir–ritonavir in adults hospitalized with severe COVID-19. N Engl J Med. 2020;382:1787-1799.
3. Grein J, Ohmagari N, Shin D, et al. Compassionate use of remdesivir for patients with severe COVID-19 [published online April 10, 2020]. N Engl J Med. doi:10.1056/NEJMoa2007016.
4. NIH clinical trial shows remdesivir accelerates recovery from advanced COVID-19. www.niaid.nih.gov/news-events/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19. Accessed May 9, 2020
5. Coronavirus (COVID-19) update: FDA issues Emergency Use Authorization for potential COVID-19 treatment. www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-issues-emergency-use-authorization-potential-covid-19-treatment. Accessed May 9, 2020.
Pedometer use improves postcesarean mobility for high-risk patients
based on data from a randomized trial of 215 patients.
“Patient immobility after surgery is associated with an increased risk of VTE [venous thromboembolism], whereas adequate mobility offers the benefits of enhanced bowel movement resumption and decreasing hospitalization length,” wrote Hadas Ganer Herman, MD, of Tel Aviv University, and colleagues.
In a study published in Obstetrics & Gynecology, the researchers randomized 108 women to a personalized feedback program using pedometers to promote mobility after cesarean delivery; 107 served as controls. Patient demographics and intrapartum experiences, including age, body mass index, and gestation week at delivery, were similar between the groups, as were postpartum complications and the use of analgesics.
Patients who used the pedometers took significantly more steps, compared with controls (5,918 vs. 4,161, P < .001). In addition, women in the pedometer group reported improved physical and mental postpartum recovery and higher levels of satisfaction with their delivery experience, the researchers noted.
The study findings were limited by several factors including potential selection bias among patients who completed the full follow-up, as well as the effect of preset visits from the research team during the study and lack of blinding of the participants. In addition, data on thromboembolic events after hospital discharge were available only through patient phone calls, the researchers noted.
“Our trial is notable for its novelty in exploring an intervention to improve postcesarean delivery mobility, using an objective means of digital step counters,” and for focusing on high-risk patients of clinical interest, Dr. Herman and associates wrote.
Larger studies are needed to explore interventions to improve mobility after cesarean deliveries, they emphasized. However, “because the integration between technology and medicine has continued to evolve and has successfully been proven for additional patient care issues in obstetrics, the current trial offers a basis for interpretation, with the possible use of low-cost interventions such as smart phone applications in maternity wards and simple digital feedback.”
“VTEs are still among the leading causes of maternal morbidity and mortality with peak incidence in the immediate postpartum period,” Martina L. Badell, MD, of Emory University, Atlanta, said in an interview. “As the age and body mass index of our pregnant patients continues to increase, focused attention to prevent VTEs in high-risk populations is very important.”
Dr. Badell said that pedometers are a feasible strategy “provided there is funding available to pay for and provide them.” Pedometers “don’t cause pain/discomfort and can be easily worn and reused. If the hospital isn’t able to provide them, however, then cost could be a barrier to high-risk women using pedometers in the immediate postpartum period.”
“The take-home message is that wearing a pedometer is a simple, low-risk strategy to encourage increased ambulation in a high-risk postpartum population with good patient satisfaction,” Dr. Badell said. The next step for research in this area “is to determine how many steps during the immediate postpartum period is optimal to reduce not only VTE risk, but potentially other postoperative markers such as pain and infection,” she added. Another research question is whether “focused feedback-based pedometers during the prolonged postpartum period result in improved weight loss.”
The researchers had no relevant financial disclosures. Dr. Badell said she had no relevant financial disclosures.
SOURCE: Herman HG et al. Obstet Gynecol. 2020 May 7. doi: 10.1097/AOG.0000000000003879.
based on data from a randomized trial of 215 patients.
“Patient immobility after surgery is associated with an increased risk of VTE [venous thromboembolism], whereas adequate mobility offers the benefits of enhanced bowel movement resumption and decreasing hospitalization length,” wrote Hadas Ganer Herman, MD, of Tel Aviv University, and colleagues.
In a study published in Obstetrics & Gynecology, the researchers randomized 108 women to a personalized feedback program using pedometers to promote mobility after cesarean delivery; 107 served as controls. Patient demographics and intrapartum experiences, including age, body mass index, and gestation week at delivery, were similar between the groups, as were postpartum complications and the use of analgesics.
Patients who used the pedometers took significantly more steps, compared with controls (5,918 vs. 4,161, P < .001). In addition, women in the pedometer group reported improved physical and mental postpartum recovery and higher levels of satisfaction with their delivery experience, the researchers noted.
The study findings were limited by several factors including potential selection bias among patients who completed the full follow-up, as well as the effect of preset visits from the research team during the study and lack of blinding of the participants. In addition, data on thromboembolic events after hospital discharge were available only through patient phone calls, the researchers noted.
“Our trial is notable for its novelty in exploring an intervention to improve postcesarean delivery mobility, using an objective means of digital step counters,” and for focusing on high-risk patients of clinical interest, Dr. Herman and associates wrote.
Larger studies are needed to explore interventions to improve mobility after cesarean deliveries, they emphasized. However, “because the integration between technology and medicine has continued to evolve and has successfully been proven for additional patient care issues in obstetrics, the current trial offers a basis for interpretation, with the possible use of low-cost interventions such as smart phone applications in maternity wards and simple digital feedback.”
“VTEs are still among the leading causes of maternal morbidity and mortality with peak incidence in the immediate postpartum period,” Martina L. Badell, MD, of Emory University, Atlanta, said in an interview. “As the age and body mass index of our pregnant patients continues to increase, focused attention to prevent VTEs in high-risk populations is very important.”
Dr. Badell said that pedometers are a feasible strategy “provided there is funding available to pay for and provide them.” Pedometers “don’t cause pain/discomfort and can be easily worn and reused. If the hospital isn’t able to provide them, however, then cost could be a barrier to high-risk women using pedometers in the immediate postpartum period.”
“The take-home message is that wearing a pedometer is a simple, low-risk strategy to encourage increased ambulation in a high-risk postpartum population with good patient satisfaction,” Dr. Badell said. The next step for research in this area “is to determine how many steps during the immediate postpartum period is optimal to reduce not only VTE risk, but potentially other postoperative markers such as pain and infection,” she added. Another research question is whether “focused feedback-based pedometers during the prolonged postpartum period result in improved weight loss.”
The researchers had no relevant financial disclosures. Dr. Badell said she had no relevant financial disclosures.
SOURCE: Herman HG et al. Obstet Gynecol. 2020 May 7. doi: 10.1097/AOG.0000000000003879.
based on data from a randomized trial of 215 patients.
“Patient immobility after surgery is associated with an increased risk of VTE [venous thromboembolism], whereas adequate mobility offers the benefits of enhanced bowel movement resumption and decreasing hospitalization length,” wrote Hadas Ganer Herman, MD, of Tel Aviv University, and colleagues.
In a study published in Obstetrics & Gynecology, the researchers randomized 108 women to a personalized feedback program using pedometers to promote mobility after cesarean delivery; 107 served as controls. Patient demographics and intrapartum experiences, including age, body mass index, and gestation week at delivery, were similar between the groups, as were postpartum complications and the use of analgesics.
Patients who used the pedometers took significantly more steps, compared with controls (5,918 vs. 4,161, P < .001). In addition, women in the pedometer group reported improved physical and mental postpartum recovery and higher levels of satisfaction with their delivery experience, the researchers noted.
The study findings were limited by several factors including potential selection bias among patients who completed the full follow-up, as well as the effect of preset visits from the research team during the study and lack of blinding of the participants. In addition, data on thromboembolic events after hospital discharge were available only through patient phone calls, the researchers noted.
“Our trial is notable for its novelty in exploring an intervention to improve postcesarean delivery mobility, using an objective means of digital step counters,” and for focusing on high-risk patients of clinical interest, Dr. Herman and associates wrote.
Larger studies are needed to explore interventions to improve mobility after cesarean deliveries, they emphasized. However, “because the integration between technology and medicine has continued to evolve and has successfully been proven for additional patient care issues in obstetrics, the current trial offers a basis for interpretation, with the possible use of low-cost interventions such as smart phone applications in maternity wards and simple digital feedback.”
“VTEs are still among the leading causes of maternal morbidity and mortality with peak incidence in the immediate postpartum period,” Martina L. Badell, MD, of Emory University, Atlanta, said in an interview. “As the age and body mass index of our pregnant patients continues to increase, focused attention to prevent VTEs in high-risk populations is very important.”
Dr. Badell said that pedometers are a feasible strategy “provided there is funding available to pay for and provide them.” Pedometers “don’t cause pain/discomfort and can be easily worn and reused. If the hospital isn’t able to provide them, however, then cost could be a barrier to high-risk women using pedometers in the immediate postpartum period.”
“The take-home message is that wearing a pedometer is a simple, low-risk strategy to encourage increased ambulation in a high-risk postpartum population with good patient satisfaction,” Dr. Badell said. The next step for research in this area “is to determine how many steps during the immediate postpartum period is optimal to reduce not only VTE risk, but potentially other postoperative markers such as pain and infection,” she added. Another research question is whether “focused feedback-based pedometers during the prolonged postpartum period result in improved weight loss.”
The researchers had no relevant financial disclosures. Dr. Badell said she had no relevant financial disclosures.
SOURCE: Herman HG et al. Obstet Gynecol. 2020 May 7. doi: 10.1097/AOG.0000000000003879.
FROM OBSTETRICS & GYNECOLOGY
BMD preserved with investigational drug for uterine fibroid bleeding
Combination therapy with relugolix, an investigational oral gonadotropin-releasing hormone antagonist, estradiol, and norethindrone acetate effectively preserved bone mineral density (BMD) in two replicate phase 3 studies enrolling women with heavy menstrual bleeding associated with uterine fibroids.
The BMD findings, released ahead of the study’s scheduled presentation at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists, build upon previously reported positive primary endpoint data from the LIBERTY 1 and LIBERTY 2 studies. ACOG canceled the meeting and released abstracts for press coverage.
The developer of the drug, Myovant Sciences, plans to submit a new drug application to the Food and Drug Administration for approval of the single-tablet combination therapy for women with uterine fibroids, according to Albert Liao, the company’s director of corporate communications.
The two multinational LIBERTY studies randomized women who had a monthly menstrual blood loss volume of at least 80 mL in two consecutive cycles (or 160 mL in one cycle) in a 1:1:1 ratio to one of three groups: relugolix combination therapy for 24 weeks (once-daily relugolix 40 mg plus estradiol 1.0 mg plus norethindrone acetate 0.5 mg); relugolix alone (40 mg once daily) for 12 weeks followed by relugolix combination therapy for 12 weeks; or placebo for 24 weeks.
In October 2019 at the American Society for Reproductive Medicine Scientific Congress, investigators reported that 73% of women receiving combination therapy in the LIBERTY 1 trial achieved a menstrual blood loss of less than 80 mL and a 50% or greater reduction from baseline over the last 35 days of treatment, compared with 19% in the placebo group. The mean percent reduction in menstrual blood loss from baseline at week 24 was 84% for combination therapy and 23% for placebo.
Earlier in 2019, Myovant Sciences announced that, in the LIBERTY 2 study, 71% of women receiving combination therapy met the primary endpoints, compared with 15% in the placebo group. The reduction in menstrual blood loss in this study’s combination therapy arm was also 84%, according to a company press release from June 2019.
Each of the two clinical trials enrolled upwards of 380 women.
The new abstract released for press coverage by ACOG and published in Obstetrics & Gynecology reports that women receiving relugolix combination therapy in the LIBERTY 1 and LIBERTY 2 studies had a mean change in lumbar spine BMD of –0.36% and –0.13%, respectively, from baseline to 24 weeks. Percent change in lumbar spine BMD in the delayed combination therapy groups (12 initial weeks of relugolix monotherapy) was –1.82% and –2.12%. In the placebo groups, the change was 0.05% and 0.32%.
Michael R. McClung, MD, who is the lead author of the abstract and was scheduled to present the findings at the ACOG meeting, said in an interview that the slight decreases in lumbar spine BMD with combination therapy were noted largely at week 12 and are “clinically insignificant in my opinion.” BMD by dual-energy x-ray absorptiometry was assessed at weeks 12 and 24.
“There was no further increase [after week 12] and [in some patients] there was even a return to baseline,” said Dr. McClung, of the Oregon Osteoporosis Center in Portland.
The safety and efficacy of longer-term treatment with relugolix combination therapy has been investigated thus far through an open-label extension study that brought the treatment period to 52 weeks. The 1-year data has been positive and will be presented or published soon, said Mr. Liao. In addition, a “second, 52-week randomized withdrawal study has been designed to provide 2-year safety and efficacy data … and to evaluate the need for maintenance therapy.”
It’s important, Dr. McClung said, “for clinicians to be confident that BMD loss is prevented or minimized with longer-term relugolix combination therapy since treatment for uterine fibroids is not a short-term proposition. Given the stability of BMD values between weeks 12 and 24 in the LIBERTY studies, I’d anticipate that we will see stable values with longer-term treatment.”
Dr. McClung disclosed that he has served as a consultant/advisory board member and speaker for Amgen and a consultant/advisory board member for Myovant. Several of his coauthors disclosed employment and ownerships interests in Myovant.
SOURCE: McClung MR et al. Obstet Gynecol. 2020 May. doi: 10.1097/01.AOG.0000662944.34860.b4.
Combination therapy with relugolix, an investigational oral gonadotropin-releasing hormone antagonist, estradiol, and norethindrone acetate effectively preserved bone mineral density (BMD) in two replicate phase 3 studies enrolling women with heavy menstrual bleeding associated with uterine fibroids.
The BMD findings, released ahead of the study’s scheduled presentation at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists, build upon previously reported positive primary endpoint data from the LIBERTY 1 and LIBERTY 2 studies. ACOG canceled the meeting and released abstracts for press coverage.
The developer of the drug, Myovant Sciences, plans to submit a new drug application to the Food and Drug Administration for approval of the single-tablet combination therapy for women with uterine fibroids, according to Albert Liao, the company’s director of corporate communications.
The two multinational LIBERTY studies randomized women who had a monthly menstrual blood loss volume of at least 80 mL in two consecutive cycles (or 160 mL in one cycle) in a 1:1:1 ratio to one of three groups: relugolix combination therapy for 24 weeks (once-daily relugolix 40 mg plus estradiol 1.0 mg plus norethindrone acetate 0.5 mg); relugolix alone (40 mg once daily) for 12 weeks followed by relugolix combination therapy for 12 weeks; or placebo for 24 weeks.
In October 2019 at the American Society for Reproductive Medicine Scientific Congress, investigators reported that 73% of women receiving combination therapy in the LIBERTY 1 trial achieved a menstrual blood loss of less than 80 mL and a 50% or greater reduction from baseline over the last 35 days of treatment, compared with 19% in the placebo group. The mean percent reduction in menstrual blood loss from baseline at week 24 was 84% for combination therapy and 23% for placebo.
Earlier in 2019, Myovant Sciences announced that, in the LIBERTY 2 study, 71% of women receiving combination therapy met the primary endpoints, compared with 15% in the placebo group. The reduction in menstrual blood loss in this study’s combination therapy arm was also 84%, according to a company press release from June 2019.
Each of the two clinical trials enrolled upwards of 380 women.
The new abstract released for press coverage by ACOG and published in Obstetrics & Gynecology reports that women receiving relugolix combination therapy in the LIBERTY 1 and LIBERTY 2 studies had a mean change in lumbar spine BMD of –0.36% and –0.13%, respectively, from baseline to 24 weeks. Percent change in lumbar spine BMD in the delayed combination therapy groups (12 initial weeks of relugolix monotherapy) was –1.82% and –2.12%. In the placebo groups, the change was 0.05% and 0.32%.
Michael R. McClung, MD, who is the lead author of the abstract and was scheduled to present the findings at the ACOG meeting, said in an interview that the slight decreases in lumbar spine BMD with combination therapy were noted largely at week 12 and are “clinically insignificant in my opinion.” BMD by dual-energy x-ray absorptiometry was assessed at weeks 12 and 24.
“There was no further increase [after week 12] and [in some patients] there was even a return to baseline,” said Dr. McClung, of the Oregon Osteoporosis Center in Portland.
The safety and efficacy of longer-term treatment with relugolix combination therapy has been investigated thus far through an open-label extension study that brought the treatment period to 52 weeks. The 1-year data has been positive and will be presented or published soon, said Mr. Liao. In addition, a “second, 52-week randomized withdrawal study has been designed to provide 2-year safety and efficacy data … and to evaluate the need for maintenance therapy.”
It’s important, Dr. McClung said, “for clinicians to be confident that BMD loss is prevented or minimized with longer-term relugolix combination therapy since treatment for uterine fibroids is not a short-term proposition. Given the stability of BMD values between weeks 12 and 24 in the LIBERTY studies, I’d anticipate that we will see stable values with longer-term treatment.”
Dr. McClung disclosed that he has served as a consultant/advisory board member and speaker for Amgen and a consultant/advisory board member for Myovant. Several of his coauthors disclosed employment and ownerships interests in Myovant.
SOURCE: McClung MR et al. Obstet Gynecol. 2020 May. doi: 10.1097/01.AOG.0000662944.34860.b4.
Combination therapy with relugolix, an investigational oral gonadotropin-releasing hormone antagonist, estradiol, and norethindrone acetate effectively preserved bone mineral density (BMD) in two replicate phase 3 studies enrolling women with heavy menstrual bleeding associated with uterine fibroids.
The BMD findings, released ahead of the study’s scheduled presentation at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists, build upon previously reported positive primary endpoint data from the LIBERTY 1 and LIBERTY 2 studies. ACOG canceled the meeting and released abstracts for press coverage.
The developer of the drug, Myovant Sciences, plans to submit a new drug application to the Food and Drug Administration for approval of the single-tablet combination therapy for women with uterine fibroids, according to Albert Liao, the company’s director of corporate communications.
The two multinational LIBERTY studies randomized women who had a monthly menstrual blood loss volume of at least 80 mL in two consecutive cycles (or 160 mL in one cycle) in a 1:1:1 ratio to one of three groups: relugolix combination therapy for 24 weeks (once-daily relugolix 40 mg plus estradiol 1.0 mg plus norethindrone acetate 0.5 mg); relugolix alone (40 mg once daily) for 12 weeks followed by relugolix combination therapy for 12 weeks; or placebo for 24 weeks.
In October 2019 at the American Society for Reproductive Medicine Scientific Congress, investigators reported that 73% of women receiving combination therapy in the LIBERTY 1 trial achieved a menstrual blood loss of less than 80 mL and a 50% or greater reduction from baseline over the last 35 days of treatment, compared with 19% in the placebo group. The mean percent reduction in menstrual blood loss from baseline at week 24 was 84% for combination therapy and 23% for placebo.
Earlier in 2019, Myovant Sciences announced that, in the LIBERTY 2 study, 71% of women receiving combination therapy met the primary endpoints, compared with 15% in the placebo group. The reduction in menstrual blood loss in this study’s combination therapy arm was also 84%, according to a company press release from June 2019.
Each of the two clinical trials enrolled upwards of 380 women.
The new abstract released for press coverage by ACOG and published in Obstetrics & Gynecology reports that women receiving relugolix combination therapy in the LIBERTY 1 and LIBERTY 2 studies had a mean change in lumbar spine BMD of –0.36% and –0.13%, respectively, from baseline to 24 weeks. Percent change in lumbar spine BMD in the delayed combination therapy groups (12 initial weeks of relugolix monotherapy) was –1.82% and –2.12%. In the placebo groups, the change was 0.05% and 0.32%.
Michael R. McClung, MD, who is the lead author of the abstract and was scheduled to present the findings at the ACOG meeting, said in an interview that the slight decreases in lumbar spine BMD with combination therapy were noted largely at week 12 and are “clinically insignificant in my opinion.” BMD by dual-energy x-ray absorptiometry was assessed at weeks 12 and 24.
“There was no further increase [after week 12] and [in some patients] there was even a return to baseline,” said Dr. McClung, of the Oregon Osteoporosis Center in Portland.
The safety and efficacy of longer-term treatment with relugolix combination therapy has been investigated thus far through an open-label extension study that brought the treatment period to 52 weeks. The 1-year data has been positive and will be presented or published soon, said Mr. Liao. In addition, a “second, 52-week randomized withdrawal study has been designed to provide 2-year safety and efficacy data … and to evaluate the need for maintenance therapy.”
It’s important, Dr. McClung said, “for clinicians to be confident that BMD loss is prevented or minimized with longer-term relugolix combination therapy since treatment for uterine fibroids is not a short-term proposition. Given the stability of BMD values between weeks 12 and 24 in the LIBERTY studies, I’d anticipate that we will see stable values with longer-term treatment.”
Dr. McClung disclosed that he has served as a consultant/advisory board member and speaker for Amgen and a consultant/advisory board member for Myovant. Several of his coauthors disclosed employment and ownerships interests in Myovant.
SOURCE: McClung MR et al. Obstet Gynecol. 2020 May. doi: 10.1097/01.AOG.0000662944.34860.b4.
FROM ACOG 2020
Chilblain-like lesions reported in children thought to have COVID-19
Two and elsewhere.
These symptoms should be considered a sign of infection with the virus, but the symptoms themselves typically don’t require treatment, according to the authors of the two new reports, from hospitals in Milan and Madrid, published in Pediatric Dermatology.
In the first study, Cristiana Colonna, MD, and colleagues at Hospital Maggiore Polyclinic in Milan described four cases of chilblain-like lesions in children ages 5-11 years with mild COVID-19 symptoms.
In the second, David Andina, MD, and colleagues in the ED and the departments of dermatology and pathology at the Child Jesus University Children’s Hospital in Madrid published a retrospective study of 22 cases in children and adolescents ages 6-17 years who reported to the hospital ED from April 6 to 17, the peak of the pandemic in Madrid.
In all four of the Milan cases, the skin lesions appeared several days after the onset of COVID-19 symptoms, although all four patients initially tested negative for COVID-19. However, Dr. Colonna and colleagues wrote that, “given the fact that the sensitivity and specificity of both nasopharyngeal swabs and antibody tests for COVID-19 (when available) are not 100% reliable, the question of the origin of these strange chilblain-like lesions is still elusive.” Until further studies are available, they emphasized that clinicians should be “alert to the presentation of chilblain-like findings” in children with mild symptoms “as a possible sign of COVID-19 infection.”
All the patients had lesions on their feet or toes, and a 5-year-old boy also had lesions on the right hand. One patient, an 11-year-old girl, had a biopsy that revealed dense lymphocytic perivascular cuffing and periadnexal infiltration.
“The finding of an elevated d-dimer in one of our patients, along with the clinical features suggestive of a vasoocclusive phenomenon, supports consideration of laboratory evaluation for coagulation defects in asymptomatic or mildly symptomatic children with acrovasculitis-like findings,” Dr. Colonna and colleagues wrote. None of the four cases in Milan required treatment, with three cases resolving within 5 days.
Like the Milan cases, all 22 patients in the Madrid series had foot or toe lesions and three had lesions on the fingers. This larger series also reported more detailed symptoms about the lesions: pruritus in nine patients (41%) and mild pain in seven (32%). A total of 10 patients had systemic symptoms of COVID-19, predominantly cough and rhinorrhea in 9 patients (41%), but 2 (9%) had abdominal pain and diarrhea. These symptoms, the authors said, appeared a median of 14 days (range, 1-28 days) before they developed chilblains.
A total of 19 patients were tested for COVID-19, but only 1 was positive.
This retrospective study also included contact information, with one patient having household contact with a single confirmed case of COVID-19; 12 patients recalled household contact who were considered probable cases of COVID-19, with respiratory symptoms.
Skin biopsies were obtained from the acral lesions in six patients, all showing similar results, although with varying degrees of intensity. All biopsies showed features of lymphocytic vasculopathy. Some cases showed mild dermal and perieccrine mucinosis, lymphocytic eccrine hidradenitis, vascular ectasia, red cell extravasation and focal thrombosis described as “mostly confined to scattered papillary dermal capillaries, but also in vessels of the reticular dermis.”
The only treatments Dr. Andina and colleagues reported were oral analgesics for pain and oral antihistamines for pruritus when needed. One patient was given topical corticosteroids and another a short course of oral steroids, both for erythema multiforme.
Dr. Andina and colleagues wrote that the skin lesions in these patients “were unequivocally categorized as chilblains, both clinically and histopathologically,” and, after 7-10 days, began to fade. None of the patients had complications, and had an “excellent outcome,” they noted.
Dr. Colonna and colleagues had no conflicts of interest to declare. Dr. Andina and colleagues provided no disclosure statement.
SOURCES: Colonna C et al. Ped Derm. 2020 May 6. doi: 10.1111/pde.14210; Andina D et al. Ped Derm. 2020 May 9. doi: 10.1111/pde.14215.
Two and elsewhere.
These symptoms should be considered a sign of infection with the virus, but the symptoms themselves typically don’t require treatment, according to the authors of the two new reports, from hospitals in Milan and Madrid, published in Pediatric Dermatology.
In the first study, Cristiana Colonna, MD, and colleagues at Hospital Maggiore Polyclinic in Milan described four cases of chilblain-like lesions in children ages 5-11 years with mild COVID-19 symptoms.
In the second, David Andina, MD, and colleagues in the ED and the departments of dermatology and pathology at the Child Jesus University Children’s Hospital in Madrid published a retrospective study of 22 cases in children and adolescents ages 6-17 years who reported to the hospital ED from April 6 to 17, the peak of the pandemic in Madrid.
In all four of the Milan cases, the skin lesions appeared several days after the onset of COVID-19 symptoms, although all four patients initially tested negative for COVID-19. However, Dr. Colonna and colleagues wrote that, “given the fact that the sensitivity and specificity of both nasopharyngeal swabs and antibody tests for COVID-19 (when available) are not 100% reliable, the question of the origin of these strange chilblain-like lesions is still elusive.” Until further studies are available, they emphasized that clinicians should be “alert to the presentation of chilblain-like findings” in children with mild symptoms “as a possible sign of COVID-19 infection.”
All the patients had lesions on their feet or toes, and a 5-year-old boy also had lesions on the right hand. One patient, an 11-year-old girl, had a biopsy that revealed dense lymphocytic perivascular cuffing and periadnexal infiltration.
“The finding of an elevated d-dimer in one of our patients, along with the clinical features suggestive of a vasoocclusive phenomenon, supports consideration of laboratory evaluation for coagulation defects in asymptomatic or mildly symptomatic children with acrovasculitis-like findings,” Dr. Colonna and colleagues wrote. None of the four cases in Milan required treatment, with three cases resolving within 5 days.
Like the Milan cases, all 22 patients in the Madrid series had foot or toe lesions and three had lesions on the fingers. This larger series also reported more detailed symptoms about the lesions: pruritus in nine patients (41%) and mild pain in seven (32%). A total of 10 patients had systemic symptoms of COVID-19, predominantly cough and rhinorrhea in 9 patients (41%), but 2 (9%) had abdominal pain and diarrhea. These symptoms, the authors said, appeared a median of 14 days (range, 1-28 days) before they developed chilblains.
A total of 19 patients were tested for COVID-19, but only 1 was positive.
This retrospective study also included contact information, with one patient having household contact with a single confirmed case of COVID-19; 12 patients recalled household contact who were considered probable cases of COVID-19, with respiratory symptoms.
Skin biopsies were obtained from the acral lesions in six patients, all showing similar results, although with varying degrees of intensity. All biopsies showed features of lymphocytic vasculopathy. Some cases showed mild dermal and perieccrine mucinosis, lymphocytic eccrine hidradenitis, vascular ectasia, red cell extravasation and focal thrombosis described as “mostly confined to scattered papillary dermal capillaries, but also in vessels of the reticular dermis.”
The only treatments Dr. Andina and colleagues reported were oral analgesics for pain and oral antihistamines for pruritus when needed. One patient was given topical corticosteroids and another a short course of oral steroids, both for erythema multiforme.
Dr. Andina and colleagues wrote that the skin lesions in these patients “were unequivocally categorized as chilblains, both clinically and histopathologically,” and, after 7-10 days, began to fade. None of the patients had complications, and had an “excellent outcome,” they noted.
Dr. Colonna and colleagues had no conflicts of interest to declare. Dr. Andina and colleagues provided no disclosure statement.
SOURCES: Colonna C et al. Ped Derm. 2020 May 6. doi: 10.1111/pde.14210; Andina D et al. Ped Derm. 2020 May 9. doi: 10.1111/pde.14215.
Two and elsewhere.
These symptoms should be considered a sign of infection with the virus, but the symptoms themselves typically don’t require treatment, according to the authors of the two new reports, from hospitals in Milan and Madrid, published in Pediatric Dermatology.
In the first study, Cristiana Colonna, MD, and colleagues at Hospital Maggiore Polyclinic in Milan described four cases of chilblain-like lesions in children ages 5-11 years with mild COVID-19 symptoms.
In the second, David Andina, MD, and colleagues in the ED and the departments of dermatology and pathology at the Child Jesus University Children’s Hospital in Madrid published a retrospective study of 22 cases in children and adolescents ages 6-17 years who reported to the hospital ED from April 6 to 17, the peak of the pandemic in Madrid.
In all four of the Milan cases, the skin lesions appeared several days after the onset of COVID-19 symptoms, although all four patients initially tested negative for COVID-19. However, Dr. Colonna and colleagues wrote that, “given the fact that the sensitivity and specificity of both nasopharyngeal swabs and antibody tests for COVID-19 (when available) are not 100% reliable, the question of the origin of these strange chilblain-like lesions is still elusive.” Until further studies are available, they emphasized that clinicians should be “alert to the presentation of chilblain-like findings” in children with mild symptoms “as a possible sign of COVID-19 infection.”
All the patients had lesions on their feet or toes, and a 5-year-old boy also had lesions on the right hand. One patient, an 11-year-old girl, had a biopsy that revealed dense lymphocytic perivascular cuffing and periadnexal infiltration.
“The finding of an elevated d-dimer in one of our patients, along with the clinical features suggestive of a vasoocclusive phenomenon, supports consideration of laboratory evaluation for coagulation defects in asymptomatic or mildly symptomatic children with acrovasculitis-like findings,” Dr. Colonna and colleagues wrote. None of the four cases in Milan required treatment, with three cases resolving within 5 days.
Like the Milan cases, all 22 patients in the Madrid series had foot or toe lesions and three had lesions on the fingers. This larger series also reported more detailed symptoms about the lesions: pruritus in nine patients (41%) and mild pain in seven (32%). A total of 10 patients had systemic symptoms of COVID-19, predominantly cough and rhinorrhea in 9 patients (41%), but 2 (9%) had abdominal pain and diarrhea. These symptoms, the authors said, appeared a median of 14 days (range, 1-28 days) before they developed chilblains.
A total of 19 patients were tested for COVID-19, but only 1 was positive.
This retrospective study also included contact information, with one patient having household contact with a single confirmed case of COVID-19; 12 patients recalled household contact who were considered probable cases of COVID-19, with respiratory symptoms.
Skin biopsies were obtained from the acral lesions in six patients, all showing similar results, although with varying degrees of intensity. All biopsies showed features of lymphocytic vasculopathy. Some cases showed mild dermal and perieccrine mucinosis, lymphocytic eccrine hidradenitis, vascular ectasia, red cell extravasation and focal thrombosis described as “mostly confined to scattered papillary dermal capillaries, but also in vessels of the reticular dermis.”
The only treatments Dr. Andina and colleagues reported were oral analgesics for pain and oral antihistamines for pruritus when needed. One patient was given topical corticosteroids and another a short course of oral steroids, both for erythema multiforme.
Dr. Andina and colleagues wrote that the skin lesions in these patients “were unequivocally categorized as chilblains, both clinically and histopathologically,” and, after 7-10 days, began to fade. None of the patients had complications, and had an “excellent outcome,” they noted.
Dr. Colonna and colleagues had no conflicts of interest to declare. Dr. Andina and colleagues provided no disclosure statement.
SOURCES: Colonna C et al. Ped Derm. 2020 May 6. doi: 10.1111/pde.14210; Andina D et al. Ped Derm. 2020 May 9. doi: 10.1111/pde.14215.
FROM PEDIATRIC DERMATOLOGY
Dermatologists saw small income drop before pandemic
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
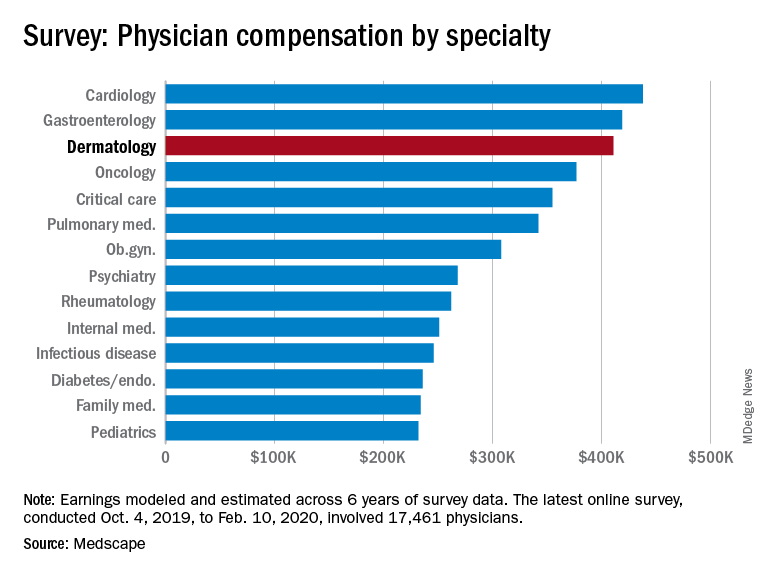
Back then, it turns out, earnings were down. Average compensation reported by dermatologists dropped from $419,000 in 2019 to $411,000 this year, a 1.9% decrease. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for this year of the pandemic are not better. “Specialists are currently having more troubles than [primary care physicians] because they’re dependent on elective cases, which can’t be directly addressed by telemedicine,” Joel Greenwald, MD, the CEO of Greenwald Wealth Management in St. Louis Park, Minn., told Medscape.
Despite the drop in earnings, 65% of dermatologists said that they were fairly compensated, which is more than the 61% who expressed that opinion in 2015 and more than 22 of the 29 specialties included in this year’s survey, Medscape noted.
Dermatologists (76%) were just below the average for all physicians (77%) when asked if they would choose medicine again, but they were near the top when asked if they would choose the same specialty (95%). Only orthopedics (97%) and oncology (96%) were higher, the survey data show.
The biggest problem area for dermatologists, by a small margin, is difficult patients. The most challenging part of their job, according to 24% of those responding, is “dealing with difficult patients,” with 23% choosing “having so many rules and regulations.” Among all physicians, rules/regulations was the leading choice with 27% of the vote, Medscape said.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
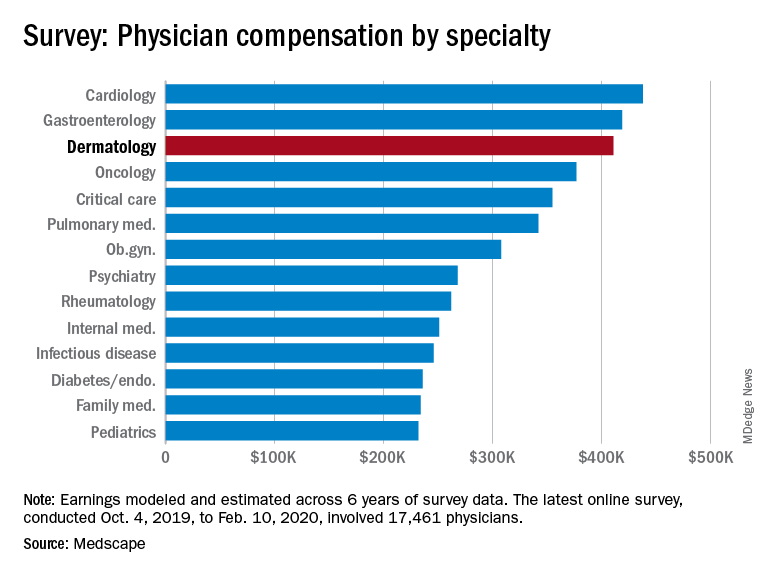
Back then, it turns out, earnings were down. Average compensation reported by dermatologists dropped from $419,000 in 2019 to $411,000 this year, a 1.9% decrease. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for this year of the pandemic are not better. “Specialists are currently having more troubles than [primary care physicians] because they’re dependent on elective cases, which can’t be directly addressed by telemedicine,” Joel Greenwald, MD, the CEO of Greenwald Wealth Management in St. Louis Park, Minn., told Medscape.
Despite the drop in earnings, 65% of dermatologists said that they were fairly compensated, which is more than the 61% who expressed that opinion in 2015 and more than 22 of the 29 specialties included in this year’s survey, Medscape noted.
Dermatologists (76%) were just below the average for all physicians (77%) when asked if they would choose medicine again, but they were near the top when asked if they would choose the same specialty (95%). Only orthopedics (97%) and oncology (96%) were higher, the survey data show.
The biggest problem area for dermatologists, by a small margin, is difficult patients. The most challenging part of their job, according to 24% of those responding, is “dealing with difficult patients,” with 23% choosing “having so many rules and regulations.” Among all physicians, rules/regulations was the leading choice with 27% of the vote, Medscape said.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
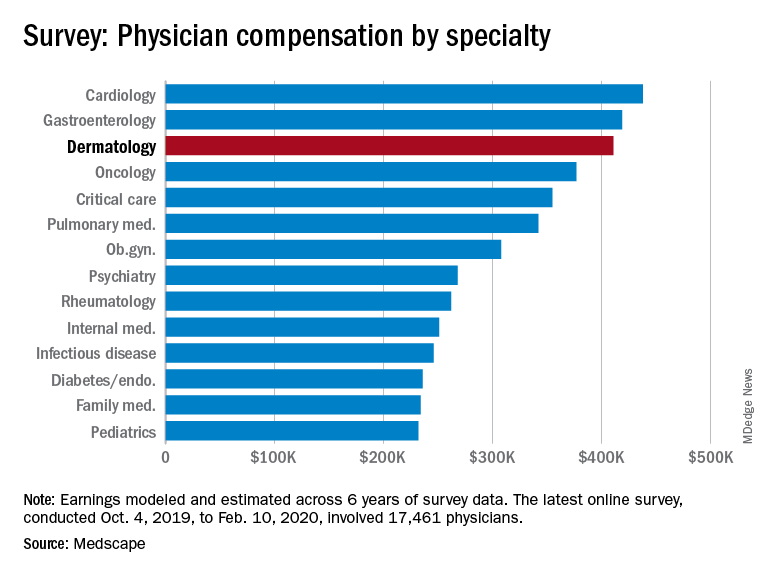
Back then, it turns out, earnings were down. Average compensation reported by dermatologists dropped from $419,000 in 2019 to $411,000 this year, a 1.9% decrease. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for this year of the pandemic are not better. “Specialists are currently having more troubles than [primary care physicians] because they’re dependent on elective cases, which can’t be directly addressed by telemedicine,” Joel Greenwald, MD, the CEO of Greenwald Wealth Management in St. Louis Park, Minn., told Medscape.
Despite the drop in earnings, 65% of dermatologists said that they were fairly compensated, which is more than the 61% who expressed that opinion in 2015 and more than 22 of the 29 specialties included in this year’s survey, Medscape noted.
Dermatologists (76%) were just below the average for all physicians (77%) when asked if they would choose medicine again, but they were near the top when asked if they would choose the same specialty (95%). Only orthopedics (97%) and oncology (96%) were higher, the survey data show.
The biggest problem area for dermatologists, by a small margin, is difficult patients. The most challenging part of their job, according to 24% of those responding, is “dealing with difficult patients,” with 23% choosing “having so many rules and regulations.” Among all physicians, rules/regulations was the leading choice with 27% of the vote, Medscape said.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
Ob.gyns. income is in the middle of the pack of specialties
Obstetrician/gynecologists reported making $308,000 between Oct. 4, 2019, and Feb. 10, 2020, which is slightly below middle among the specialties included in Medscape’s Physician Compensation Report 2020.
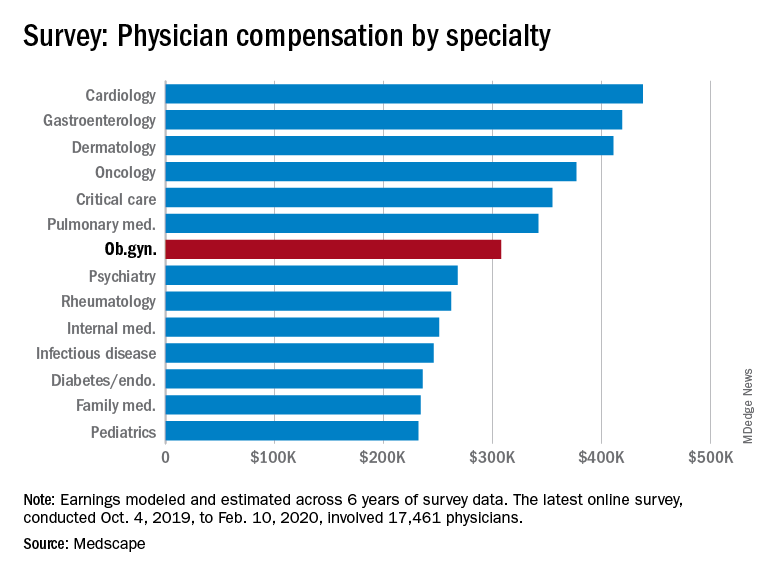
This occurs although male and female ob.gyns. reported working about the same hours per week (40.2 vs. 39).
The average incentive bonus for ob.gyns. was about $44,000, which is on the low side among specialties included in the report. Although 42% of ob.gyns. achieve 100% of this bonus and 17% achieve 76%-99% of their bonus, slightly less than a quarter (22%) achieve only 25% or less.
About 51% of ob.gyns. reported feeling fairly compensated, which put them in the bottom fifth of the 29 specialties asked that question.
Among ob.gyns., 38% reported that gratitude and relationships with patients is the most rewarding part of their job, while 20% said that helping others or being good at what they do is the most rewarding aspect of their job. About even proportions of ob.gyns. complained that the most challenging part of their job is dealing with EHRs (18%), working long hours (17%), or navigating rules and regulations (16%).
The data in the Medscape report were gathered before COVID-19 had really taken hold in the United States – before states began issuing stay-at-home orders and before practices began implementing their own precautions. Although in the best interest of patients and providers, switching to telemedicine, eliminating most elective procedures, and making other changes to improve safety will have significant financial consequences. It is unclear at this time how this ongoing pandemic will affect physician compensation and income.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
Obstetrician/gynecologists reported making $308,000 between Oct. 4, 2019, and Feb. 10, 2020, which is slightly below middle among the specialties included in Medscape’s Physician Compensation Report 2020.
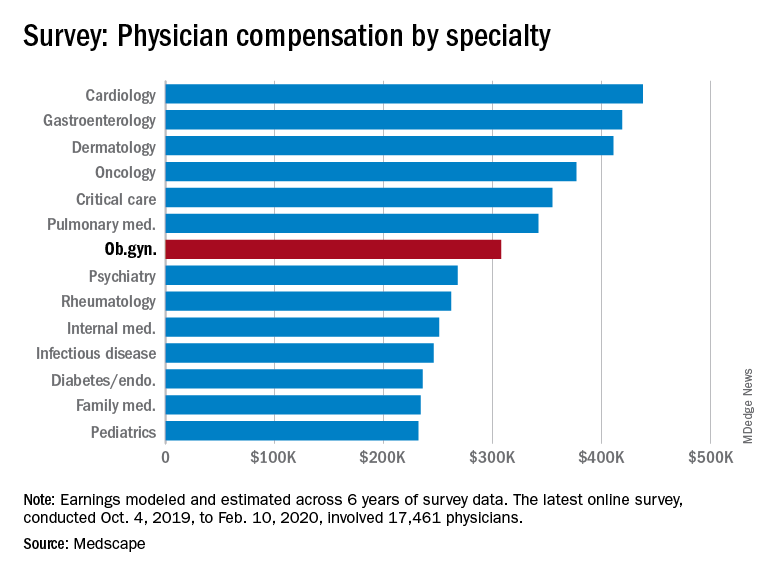
This occurs although male and female ob.gyns. reported working about the same hours per week (40.2 vs. 39).
The average incentive bonus for ob.gyns. was about $44,000, which is on the low side among specialties included in the report. Although 42% of ob.gyns. achieve 100% of this bonus and 17% achieve 76%-99% of their bonus, slightly less than a quarter (22%) achieve only 25% or less.
About 51% of ob.gyns. reported feeling fairly compensated, which put them in the bottom fifth of the 29 specialties asked that question.
Among ob.gyns., 38% reported that gratitude and relationships with patients is the most rewarding part of their job, while 20% said that helping others or being good at what they do is the most rewarding aspect of their job. About even proportions of ob.gyns. complained that the most challenging part of their job is dealing with EHRs (18%), working long hours (17%), or navigating rules and regulations (16%).
The data in the Medscape report were gathered before COVID-19 had really taken hold in the United States – before states began issuing stay-at-home orders and before practices began implementing their own precautions. Although in the best interest of patients and providers, switching to telemedicine, eliminating most elective procedures, and making other changes to improve safety will have significant financial consequences. It is unclear at this time how this ongoing pandemic will affect physician compensation and income.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
Obstetrician/gynecologists reported making $308,000 between Oct. 4, 2019, and Feb. 10, 2020, which is slightly below middle among the specialties included in Medscape’s Physician Compensation Report 2020.
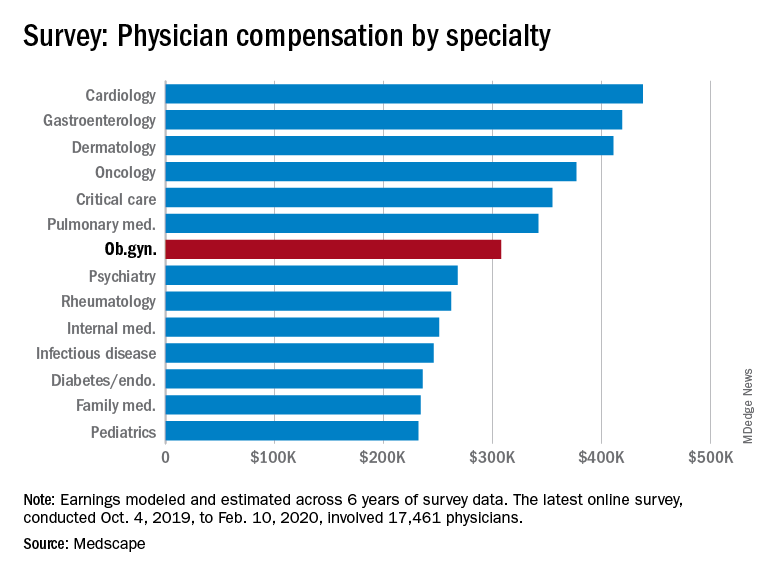
This occurs although male and female ob.gyns. reported working about the same hours per week (40.2 vs. 39).
The average incentive bonus for ob.gyns. was about $44,000, which is on the low side among specialties included in the report. Although 42% of ob.gyns. achieve 100% of this bonus and 17% achieve 76%-99% of their bonus, slightly less than a quarter (22%) achieve only 25% or less.
About 51% of ob.gyns. reported feeling fairly compensated, which put them in the bottom fifth of the 29 specialties asked that question.
Among ob.gyns., 38% reported that gratitude and relationships with patients is the most rewarding part of their job, while 20% said that helping others or being good at what they do is the most rewarding aspect of their job. About even proportions of ob.gyns. complained that the most challenging part of their job is dealing with EHRs (18%), working long hours (17%), or navigating rules and regulations (16%).
The data in the Medscape report were gathered before COVID-19 had really taken hold in the United States – before states began issuing stay-at-home orders and before practices began implementing their own precautions. Although in the best interest of patients and providers, switching to telemedicine, eliminating most elective procedures, and making other changes to improve safety will have significant financial consequences. It is unclear at this time how this ongoing pandemic will affect physician compensation and income.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
Pediatrics earnings were on the upswing before pandemic
As the COVID-19 spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and personal protective equipment was plentiful.
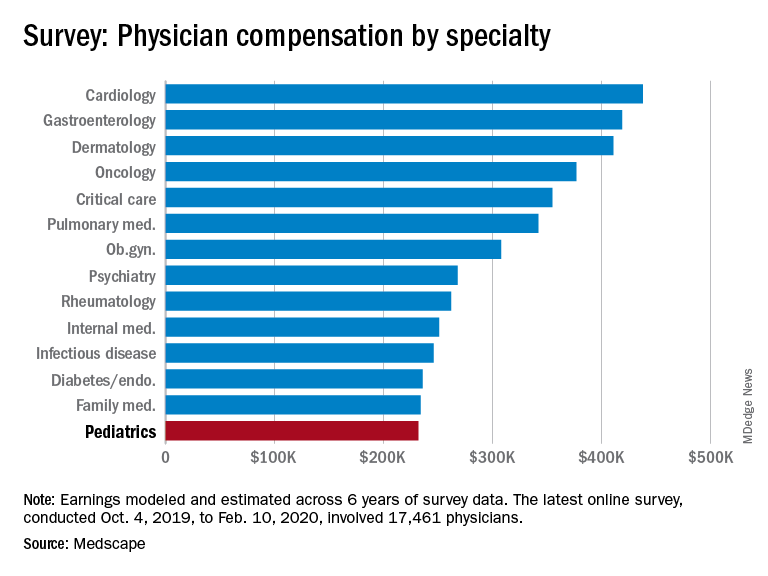
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pediatrics looked like just before the coronavirus arrived.
Back then, earnings were up. Average income for all primary care physicians was $243,000 in this year’s survey – 2.5% higher than the $237,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 53% of pediatricians said that they were fairly compensated, right between internists at 52% and family physicians at 54% and in the middle of the overall specialty pack, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%, the survey data show.
Primary care physicians and specialists were nearly equal in hours spent seeing patients each week – 37.6 for primary care and 38.0 for specialists – but family physicians and internists both averaged more hours than pediatricians doing paperwork and administration each week, at 15.9 and 18.5 versus 14.7, respectively, Medscape said.
Pediatricians (38%) were more likely than the average physician (27%) to say that “gratitude/relationships with patients” was the most rewarding part of their job, and less likely to say that “having so many rules and regulations” was the most challenging part (22% vs. 26%), according to the survey.
When asked if they would choose medicine again, 78% of pediatricians said yes, just above the 77% for all physicians. Pediatricians, however, were much more likely (83%) to say they would choose the same specialty, compared with family physicians (70%) and internists (66%), Medscape found.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID-19 spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and personal protective equipment was plentiful.
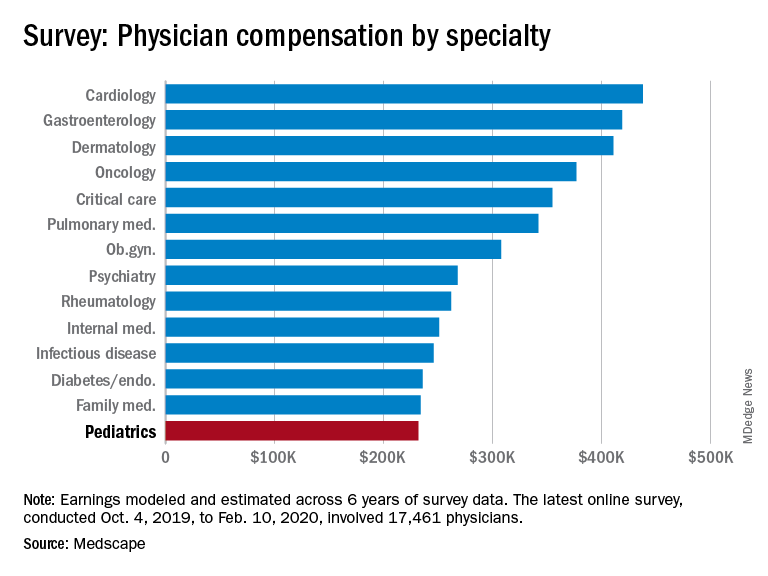
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pediatrics looked like just before the coronavirus arrived.
Back then, earnings were up. Average income for all primary care physicians was $243,000 in this year’s survey – 2.5% higher than the $237,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 53% of pediatricians said that they were fairly compensated, right between internists at 52% and family physicians at 54% and in the middle of the overall specialty pack, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%, the survey data show.
Primary care physicians and specialists were nearly equal in hours spent seeing patients each week – 37.6 for primary care and 38.0 for specialists – but family physicians and internists both averaged more hours than pediatricians doing paperwork and administration each week, at 15.9 and 18.5 versus 14.7, respectively, Medscape said.
Pediatricians (38%) were more likely than the average physician (27%) to say that “gratitude/relationships with patients” was the most rewarding part of their job, and less likely to say that “having so many rules and regulations” was the most challenging part (22% vs. 26%), according to the survey.
When asked if they would choose medicine again, 78% of pediatricians said yes, just above the 77% for all physicians. Pediatricians, however, were much more likely (83%) to say they would choose the same specialty, compared with family physicians (70%) and internists (66%), Medscape found.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID-19 spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and personal protective equipment was plentiful.
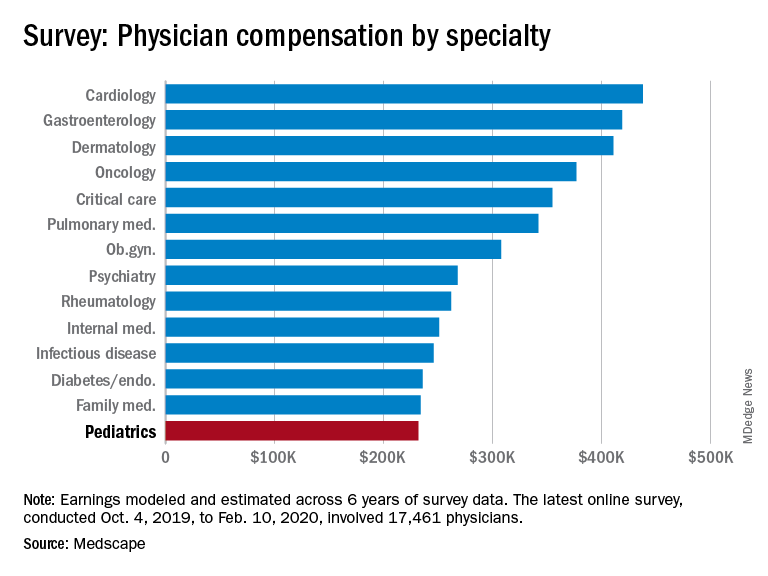
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pediatrics looked like just before the coronavirus arrived.
Back then, earnings were up. Average income for all primary care physicians was $243,000 in this year’s survey – 2.5% higher than the $237,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 53% of pediatricians said that they were fairly compensated, right between internists at 52% and family physicians at 54% and in the middle of the overall specialty pack, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%, the survey data show.
Primary care physicians and specialists were nearly equal in hours spent seeing patients each week – 37.6 for primary care and 38.0 for specialists – but family physicians and internists both averaged more hours than pediatricians doing paperwork and administration each week, at 15.9 and 18.5 versus 14.7, respectively, Medscape said.
Pediatricians (38%) were more likely than the average physician (27%) to say that “gratitude/relationships with patients” was the most rewarding part of their job, and less likely to say that “having so many rules and regulations” was the most challenging part (22% vs. 26%), according to the survey.
When asked if they would choose medicine again, 78% of pediatricians said yes, just above the 77% for all physicians. Pediatricians, however, were much more likely (83%) to say they would choose the same specialty, compared with family physicians (70%) and internists (66%), Medscape found.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
Before pandemic, rheumatologists saw small salary increase
COVID-19 has changed many things in the medical landscape as practices have closed, many physicians are transitioning to telemedicine, and EDs struggle to provide safe environments for their employees.
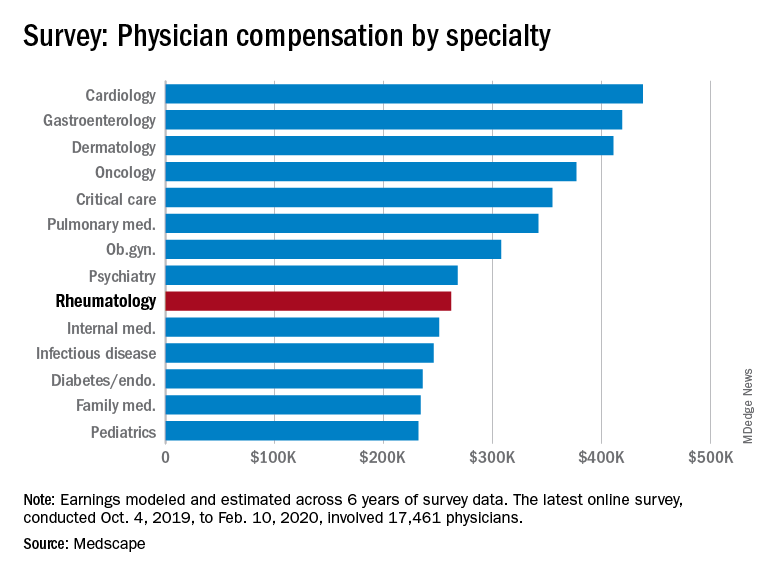
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, illustrates what rheumatology looked like just before the coronavirus arrived.
Rheumatologists saw a small increase in average salary in 2020, rising from $259,000 in 2019 to $262,000, an increase of 1.16%. In comparison, average income for all specialists was $346,000 in this year’s survey, up by 1.5% from the $341,000 earned in 2019, Medscape reported. Male rheumatologists earned significantly more than women at $288,000 versus $240,000.
Prospects for next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 55% of rheumatologists felt they were fairly compensated. This was about average among the 29 specialties included in the survey, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%.
Rheumatologists were more likely than the average physician to report that “having so many rules and regulations” was the most challenging part of their job, according to the survey. A similar number of rheumatologists said that “gratitude/relationships with patients” was the most rewarding part of the job at 27%.
When asked if they would choose medicine again, 79% of rheumatologists said yes, slightly more than the 77% for all physicians; 81% said that they’d choose rheumatology again.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
COVID-19 has changed many things in the medical landscape as practices have closed, many physicians are transitioning to telemedicine, and EDs struggle to provide safe environments for their employees.
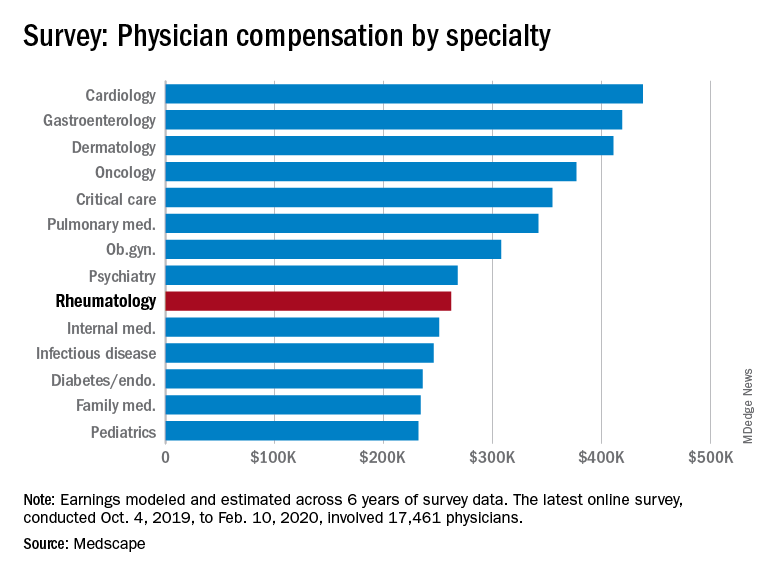
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, illustrates what rheumatology looked like just before the coronavirus arrived.
Rheumatologists saw a small increase in average salary in 2020, rising from $259,000 in 2019 to $262,000, an increase of 1.16%. In comparison, average income for all specialists was $346,000 in this year’s survey, up by 1.5% from the $341,000 earned in 2019, Medscape reported. Male rheumatologists earned significantly more than women at $288,000 versus $240,000.
Prospects for next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 55% of rheumatologists felt they were fairly compensated. This was about average among the 29 specialties included in the survey, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%.
Rheumatologists were more likely than the average physician to report that “having so many rules and regulations” was the most challenging part of their job, according to the survey. A similar number of rheumatologists said that “gratitude/relationships with patients” was the most rewarding part of the job at 27%.
When asked if they would choose medicine again, 79% of rheumatologists said yes, slightly more than the 77% for all physicians; 81% said that they’d choose rheumatology again.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
COVID-19 has changed many things in the medical landscape as practices have closed, many physicians are transitioning to telemedicine, and EDs struggle to provide safe environments for their employees.
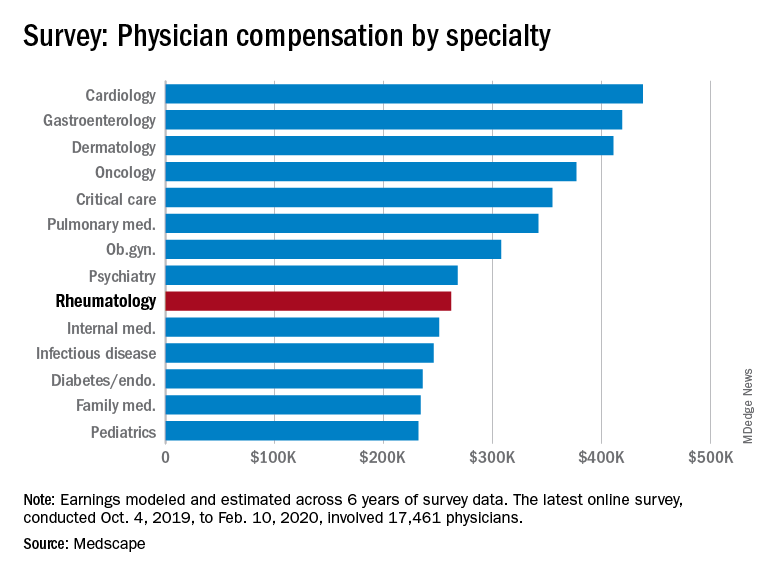
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, illustrates what rheumatology looked like just before the coronavirus arrived.
Rheumatologists saw a small increase in average salary in 2020, rising from $259,000 in 2019 to $262,000, an increase of 1.16%. In comparison, average income for all specialists was $346,000 in this year’s survey, up by 1.5% from the $341,000 earned in 2019, Medscape reported. Male rheumatologists earned significantly more than women at $288,000 versus $240,000.
Prospects for next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 55% of rheumatologists felt they were fairly compensated. This was about average among the 29 specialties included in the survey, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%.
Rheumatologists were more likely than the average physician to report that “having so many rules and regulations” was the most challenging part of their job, according to the survey. A similar number of rheumatologists said that “gratitude/relationships with patients” was the most rewarding part of the job at 27%.
When asked if they would choose medicine again, 79% of rheumatologists said yes, slightly more than the 77% for all physicians; 81% said that they’d choose rheumatology again.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
Pulmonology, critical care earnings on the upswing before pandemic
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
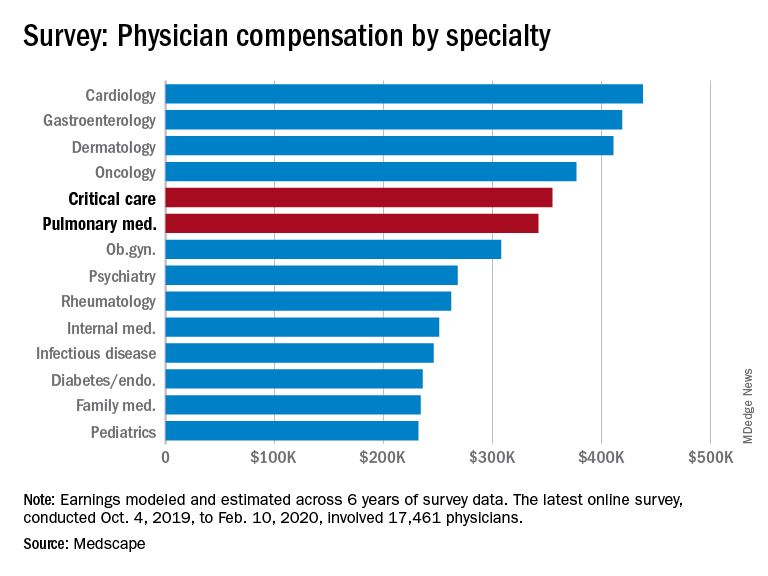
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
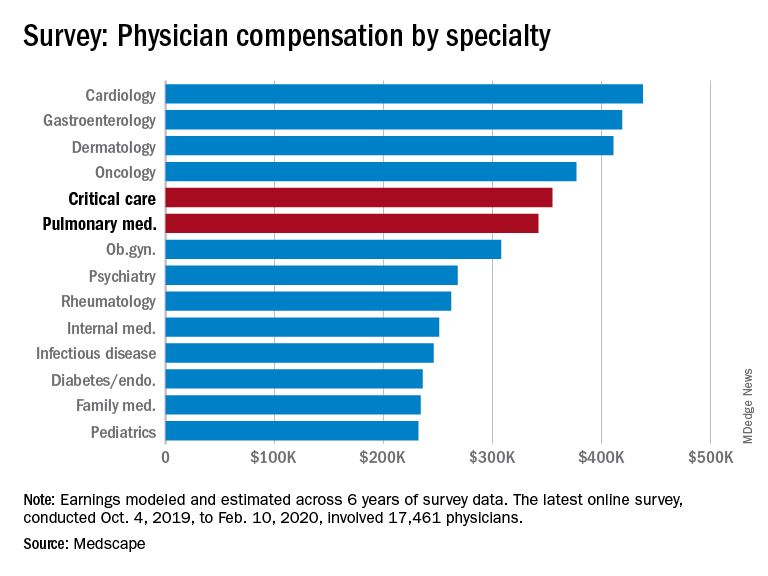
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
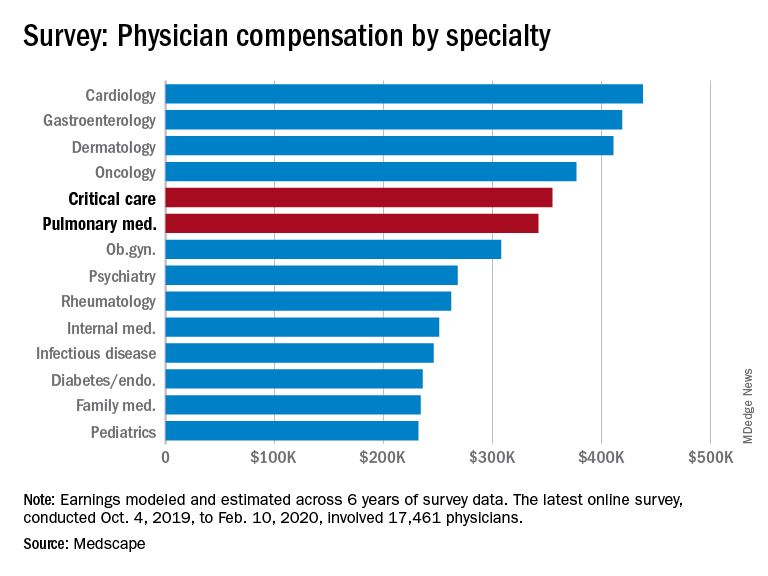
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.