User login
A Review of ACR Convergence Abstracts on Systemic Lupus Erythematosus
The American College of Rheumatology hosted its first-ever all-virtual annual meeting this year. Convergence 2020 highlighted several important treatment abstracts related to systemic lupus erythematosus.
Dr Michelle Petri, of Johns Hopkins University, reports on the use of hydroxychloroquine, which was not found to be associated with QTc length in a large cohort of patients with lupus and rheumatoid arthritis. This is notable because hydroxychloroquine was implicated in ventricular arrhythmias in patients with COVID-19 who were also given azithromycin.
Dr Petri also looks at the results of two trials focusing on the effects of belimumab and obinutuzumab on renal outcomes.
In the belimumab trial, the primary outcome was a 700-mg reduction in the urine protein to creatinine ratio, and it met that outcome with a 10.8% delta that was statistically significant. It also met the complete renal response outcome of less than 500 mg with a 10% delta, which is statistically significant.
In the other study, obinutuzumab showed a marked improvement over rituximab as a B-cell depleter.
The completion of the phase 2 trial means that there are now 2 years of data showing a 19% delta between obinutuzumab and standard-of-care treatment.
Finally, Dr Petri highlights two studies focusing on nonrenal lupus and the use of both BIIB059 and iberdomide.
--
Michelle Petri, MD, MPH, Professor, Department of Medicine, Division of Rheumatology, Johns Hopkins University School of Medicine; Director, Johns Hopkins Lupus Center, Johns Hopkins Hospital, Baltimore, Maryland.
Michelle Petri, MD, MPH, has disclosed the following relevant financial relationships:
Received research grant from: GlaxoSmithKline; Eli Lilly and Company; Thermo Fisher; Hexagen; AstraZeneca
Received income in an amount equal to or greater than $250 from: AbbVie; Amgen; AstraZeneca; Blackrock; Bristol-Myers Squibb; Hexagen; Glenmark; GlaxoSmithKline; IQVIA; Janssen; Eli Lilly and Company; Merck; EMD Serono; Novartis; Sanofi; Thermo Fisher; UCB
The American College of Rheumatology hosted its first-ever all-virtual annual meeting this year. Convergence 2020 highlighted several important treatment abstracts related to systemic lupus erythematosus.
Dr Michelle Petri, of Johns Hopkins University, reports on the use of hydroxychloroquine, which was not found to be associated with QTc length in a large cohort of patients with lupus and rheumatoid arthritis. This is notable because hydroxychloroquine was implicated in ventricular arrhythmias in patients with COVID-19 who were also given azithromycin.
Dr Petri also looks at the results of two trials focusing on the effects of belimumab and obinutuzumab on renal outcomes.
In the belimumab trial, the primary outcome was a 700-mg reduction in the urine protein to creatinine ratio, and it met that outcome with a 10.8% delta that was statistically significant. It also met the complete renal response outcome of less than 500 mg with a 10% delta, which is statistically significant.
In the other study, obinutuzumab showed a marked improvement over rituximab as a B-cell depleter.
The completion of the phase 2 trial means that there are now 2 years of data showing a 19% delta between obinutuzumab and standard-of-care treatment.
Finally, Dr Petri highlights two studies focusing on nonrenal lupus and the use of both BIIB059 and iberdomide.
--
Michelle Petri, MD, MPH, Professor, Department of Medicine, Division of Rheumatology, Johns Hopkins University School of Medicine; Director, Johns Hopkins Lupus Center, Johns Hopkins Hospital, Baltimore, Maryland.
Michelle Petri, MD, MPH, has disclosed the following relevant financial relationships:
Received research grant from: GlaxoSmithKline; Eli Lilly and Company; Thermo Fisher; Hexagen; AstraZeneca
Received income in an amount equal to or greater than $250 from: AbbVie; Amgen; AstraZeneca; Blackrock; Bristol-Myers Squibb; Hexagen; Glenmark; GlaxoSmithKline; IQVIA; Janssen; Eli Lilly and Company; Merck; EMD Serono; Novartis; Sanofi; Thermo Fisher; UCB
The American College of Rheumatology hosted its first-ever all-virtual annual meeting this year. Convergence 2020 highlighted several important treatment abstracts related to systemic lupus erythematosus.
Dr Michelle Petri, of Johns Hopkins University, reports on the use of hydroxychloroquine, which was not found to be associated with QTc length in a large cohort of patients with lupus and rheumatoid arthritis. This is notable because hydroxychloroquine was implicated in ventricular arrhythmias in patients with COVID-19 who were also given azithromycin.
Dr Petri also looks at the results of two trials focusing on the effects of belimumab and obinutuzumab on renal outcomes.
In the belimumab trial, the primary outcome was a 700-mg reduction in the urine protein to creatinine ratio, and it met that outcome with a 10.8% delta that was statistically significant. It also met the complete renal response outcome of less than 500 mg with a 10% delta, which is statistically significant.
In the other study, obinutuzumab showed a marked improvement over rituximab as a B-cell depleter.
The completion of the phase 2 trial means that there are now 2 years of data showing a 19% delta between obinutuzumab and standard-of-care treatment.
Finally, Dr Petri highlights two studies focusing on nonrenal lupus and the use of both BIIB059 and iberdomide.
--
Michelle Petri, MD, MPH, Professor, Department of Medicine, Division of Rheumatology, Johns Hopkins University School of Medicine; Director, Johns Hopkins Lupus Center, Johns Hopkins Hospital, Baltimore, Maryland.
Michelle Petri, MD, MPH, has disclosed the following relevant financial relationships:
Received research grant from: GlaxoSmithKline; Eli Lilly and Company; Thermo Fisher; Hexagen; AstraZeneca
Received income in an amount equal to or greater than $250 from: AbbVie; Amgen; AstraZeneca; Blackrock; Bristol-Myers Squibb; Hexagen; Glenmark; GlaxoSmithKline; IQVIA; Janssen; Eli Lilly and Company; Merck; EMD Serono; Novartis; Sanofi; Thermo Fisher; UCB

50.6 million tobacco users are not a homogeneous group
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
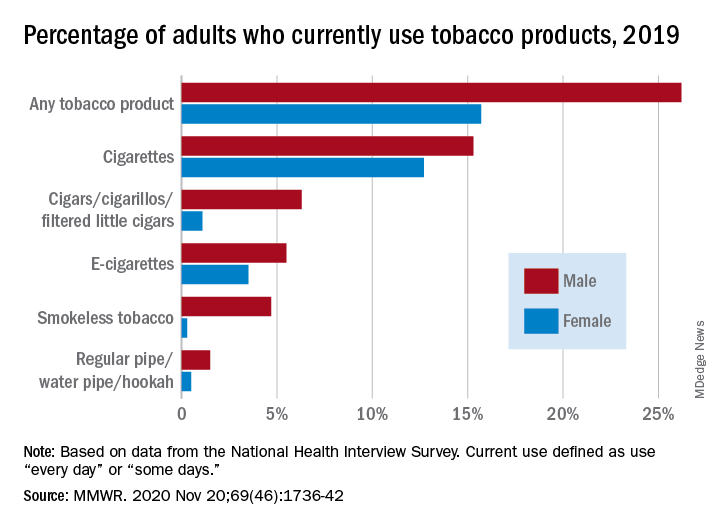
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
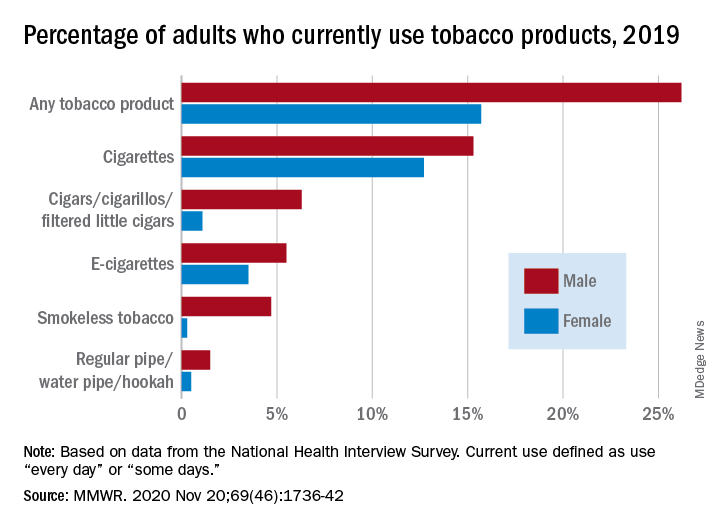
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
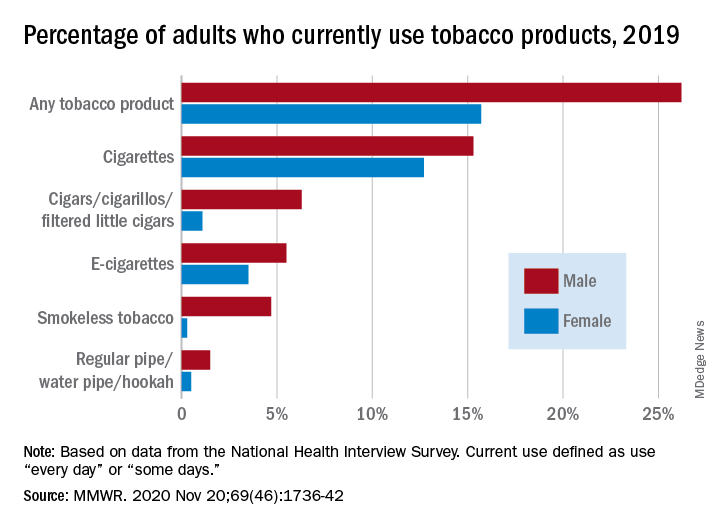
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
FROM MMWR
Metformin improves most outcomes for T2D during pregnancy
including reduced weight gain, reduced insulin doses, and fewer large-for-gestational-age babies, suggest the results of a randomized controlled trial.
However, the drug was associated with an increased risk of small-for-gestational-age babies, which poses the question as to risk versus benefit of metformin on the health of offspring.
“Better understanding of the short- and long-term implications of these effects on infants will be important to properly advise patients with type 2 diabetes contemplating use of metformin during pregnancy,” said lead author Denice S. Feig, MD, Mount Sinai Hospital, Toronto.
The research was presented at the Diabetes UK Professional Conference: Online Series on Nov. 17 and recently published in The Lancet Diabetes & Endocrinology.
Summing up, Dr. Feig said that, on balance, she would be inclined to give metformin to most pregnant women with type 2 diabetes, perhaps with the exception of those who may have risk factors for small-for-gestational-age babies; for example, women who’ve had intrauterine growth restriction, who are smokers, and have significant renal disease, or have a lower body mass index.
Increased prevalence of type 2 diabetes in pregnancy
Dr. Feig said that across the developed world there have been huge increases in the prevalence of type 2 diabetes in pregnancy in recent years.
Insulin is the standard treatment for the management of type 2 diabetes in pregnancy, but these women have marked insulin resistance that worsens in pregnancy, which means their insulin requirements increase, leading to weight gain, painful injections, high cost, and noncompliance.
So despite treatment with insulin, these women continue to face increased rates of adverse maternal and fetal outcomes.
And although metformin is increasingly being used in women with type 2 diabetes during pregnancy, there is a scarcity of data on the benefits and harms of metformin use on pregnancy outcomes in these women.
The MiTy trial was therefore undertaken to determine whether metformin could improve outcomes.
The team recruited 502 women from 29 sites in Canada and Australia who had type 2 diabetes prior to pregnancy or were diagnosed during pregnancy, before 20 weeks’ gestation. The women were randomized to metformin 1 g twice daily or placebo, in addition to their usual insulin regimen, at between 6 and 28 weeks’ gestation.
Type 2 diabetes was diagnosed prior to pregnancy in 83% of women in the metformin group and in 90% of those assigned to placebo. The mean hemoglobin A1c level at randomization was 47 mmol/mol (6.5%) in both groups.
The average maternal age at baseline was approximately 35 years and mean gestational age at randomization was 16 weeks. Mean prepregnancy BMI was approximately 34 kg/m2.
Of note, only 30% were of European ethnicity.
Less weight gain, lower A1c, less insulin needed with metformin
Dr. Feig reported that there was no significant difference between the treatment groups in terms of the proportion of women with the composite primary outcome of pregnancy loss, preterm birth, birth injury, respiratory distress, neonatal hypoglycemia, or admission to neonatal intensive care lasting more than 24 hours (P = 0.86).
However, women in the metformin group had significantly less overall weight gain during pregnancy than did those in the placebo group, at –1.8 kg (P < .0001).
They also had a significantly lower last A1c level in pregnancy, at 41 mmol/mol (5.9%) versus 43.2 mmol/mol (6.1%) in those given placebo (P = .015), and required fewer insulin doses, at 1.1 versus 1.5 units/kg/day (P < .0001), which translated to a reduction of almost 44 units/day.
Women given metformin were also less likely to require Cesarean section delivery, at 53.4% versus 62.7% in the placebo group (P = .03), although there was no difference between groups in terms of gestational hypertension or preeclampsia.
The most common adverse events were gastrointestinal complications, which occurred in 27.3% of women in the metformin group and 22.3% of those given placebo.
There were no significant differences between the metformin and placebo groups in rates of pregnancy loss (P = .81), preterm birth (P = .16), birth injury (P = .37), respiratory distress (P = .49), and congenital anomalies (P = .16).
Average birth weight lower with metformin
However, Dr. Feig showed that the average birth weight was lower for offspring of women given metformin than those assigned to placebo, at 3.2 kg (7.05 lb) versus 3.4 kg (7.4 lb) (P = .002).
Women given metformin were also less likely to have a baby with a birth weight of 4 kg (8.8 lb) or more, at 12.1% versus 19.2%, or a relative risk of 0.65 (P = .046), and a baby that was extremely large for gestational age, at 8.6% versus 14.8%, or a relative risk of 0.58 (P = .046).
But of concern, metformin was associated with an increased risk of small-for-gestational-age babies, at 12.9% versus 6.6% with placebo, or a relative risk of 1.96 (P = .03).
Dr. Feig suggested that this may be due to a direct effect of metformin “because as we know metformin inhibits the mTOR pathway,” which is a “primary nutrient sensor in the placenta” and could “attenuate nutrient flux and fetal growth.”
She said it is not clear whether the small-for-gestational-age babies were “healthy or unhealthy.”
To investigate further, the team has launched the MiTy Kids study, which will follow the offspring in the MiTy trial to determine whether metformin during pregnancy is associated with a reduction in adiposity and improvement in insulin resistance in the babies at 2 years of age.
Who should be given metformin?
During the discussion, Helen R. Murphy, MD, PhD, Norwich Medical School, University of East Anglia, England, asked whether Dr. Feig would recommend continuing metformin in pregnancy if it was started preconception for fertility issues rather than diabetes.
She replied: “If they don’t have diabetes and it’s simply for PCOS [polycystic ovary syndrome], then I have either stopped it as soon as they got pregnant or sometimes continued it through the first trimester, and then stopped.
“If the person has diabetes, however, I think given this work, for most people I would continue it,” she said.
The study was funded by the Canadian Institutes of Health Research, Lunenfeld-Tanenbaum Research Institute, and the University of Toronto. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
including reduced weight gain, reduced insulin doses, and fewer large-for-gestational-age babies, suggest the results of a randomized controlled trial.
However, the drug was associated with an increased risk of small-for-gestational-age babies, which poses the question as to risk versus benefit of metformin on the health of offspring.
“Better understanding of the short- and long-term implications of these effects on infants will be important to properly advise patients with type 2 diabetes contemplating use of metformin during pregnancy,” said lead author Denice S. Feig, MD, Mount Sinai Hospital, Toronto.
The research was presented at the Diabetes UK Professional Conference: Online Series on Nov. 17 and recently published in The Lancet Diabetes & Endocrinology.
Summing up, Dr. Feig said that, on balance, she would be inclined to give metformin to most pregnant women with type 2 diabetes, perhaps with the exception of those who may have risk factors for small-for-gestational-age babies; for example, women who’ve had intrauterine growth restriction, who are smokers, and have significant renal disease, or have a lower body mass index.
Increased prevalence of type 2 diabetes in pregnancy
Dr. Feig said that across the developed world there have been huge increases in the prevalence of type 2 diabetes in pregnancy in recent years.
Insulin is the standard treatment for the management of type 2 diabetes in pregnancy, but these women have marked insulin resistance that worsens in pregnancy, which means their insulin requirements increase, leading to weight gain, painful injections, high cost, and noncompliance.
So despite treatment with insulin, these women continue to face increased rates of adverse maternal and fetal outcomes.
And although metformin is increasingly being used in women with type 2 diabetes during pregnancy, there is a scarcity of data on the benefits and harms of metformin use on pregnancy outcomes in these women.
The MiTy trial was therefore undertaken to determine whether metformin could improve outcomes.
The team recruited 502 women from 29 sites in Canada and Australia who had type 2 diabetes prior to pregnancy or were diagnosed during pregnancy, before 20 weeks’ gestation. The women were randomized to metformin 1 g twice daily or placebo, in addition to their usual insulin regimen, at between 6 and 28 weeks’ gestation.
Type 2 diabetes was diagnosed prior to pregnancy in 83% of women in the metformin group and in 90% of those assigned to placebo. The mean hemoglobin A1c level at randomization was 47 mmol/mol (6.5%) in both groups.
The average maternal age at baseline was approximately 35 years and mean gestational age at randomization was 16 weeks. Mean prepregnancy BMI was approximately 34 kg/m2.
Of note, only 30% were of European ethnicity.
Less weight gain, lower A1c, less insulin needed with metformin
Dr. Feig reported that there was no significant difference between the treatment groups in terms of the proportion of women with the composite primary outcome of pregnancy loss, preterm birth, birth injury, respiratory distress, neonatal hypoglycemia, or admission to neonatal intensive care lasting more than 24 hours (P = 0.86).
However, women in the metformin group had significantly less overall weight gain during pregnancy than did those in the placebo group, at –1.8 kg (P < .0001).
They also had a significantly lower last A1c level in pregnancy, at 41 mmol/mol (5.9%) versus 43.2 mmol/mol (6.1%) in those given placebo (P = .015), and required fewer insulin doses, at 1.1 versus 1.5 units/kg/day (P < .0001), which translated to a reduction of almost 44 units/day.
Women given metformin were also less likely to require Cesarean section delivery, at 53.4% versus 62.7% in the placebo group (P = .03), although there was no difference between groups in terms of gestational hypertension or preeclampsia.
The most common adverse events were gastrointestinal complications, which occurred in 27.3% of women in the metformin group and 22.3% of those given placebo.
There were no significant differences between the metformin and placebo groups in rates of pregnancy loss (P = .81), preterm birth (P = .16), birth injury (P = .37), respiratory distress (P = .49), and congenital anomalies (P = .16).
Average birth weight lower with metformin
However, Dr. Feig showed that the average birth weight was lower for offspring of women given metformin than those assigned to placebo, at 3.2 kg (7.05 lb) versus 3.4 kg (7.4 lb) (P = .002).
Women given metformin were also less likely to have a baby with a birth weight of 4 kg (8.8 lb) or more, at 12.1% versus 19.2%, or a relative risk of 0.65 (P = .046), and a baby that was extremely large for gestational age, at 8.6% versus 14.8%, or a relative risk of 0.58 (P = .046).
But of concern, metformin was associated with an increased risk of small-for-gestational-age babies, at 12.9% versus 6.6% with placebo, or a relative risk of 1.96 (P = .03).
Dr. Feig suggested that this may be due to a direct effect of metformin “because as we know metformin inhibits the mTOR pathway,” which is a “primary nutrient sensor in the placenta” and could “attenuate nutrient flux and fetal growth.”
She said it is not clear whether the small-for-gestational-age babies were “healthy or unhealthy.”
To investigate further, the team has launched the MiTy Kids study, which will follow the offspring in the MiTy trial to determine whether metformin during pregnancy is associated with a reduction in adiposity and improvement in insulin resistance in the babies at 2 years of age.
Who should be given metformin?
During the discussion, Helen R. Murphy, MD, PhD, Norwich Medical School, University of East Anglia, England, asked whether Dr. Feig would recommend continuing metformin in pregnancy if it was started preconception for fertility issues rather than diabetes.
She replied: “If they don’t have diabetes and it’s simply for PCOS [polycystic ovary syndrome], then I have either stopped it as soon as they got pregnant or sometimes continued it through the first trimester, and then stopped.
“If the person has diabetes, however, I think given this work, for most people I would continue it,” she said.
The study was funded by the Canadian Institutes of Health Research, Lunenfeld-Tanenbaum Research Institute, and the University of Toronto. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
including reduced weight gain, reduced insulin doses, and fewer large-for-gestational-age babies, suggest the results of a randomized controlled trial.
However, the drug was associated with an increased risk of small-for-gestational-age babies, which poses the question as to risk versus benefit of metformin on the health of offspring.
“Better understanding of the short- and long-term implications of these effects on infants will be important to properly advise patients with type 2 diabetes contemplating use of metformin during pregnancy,” said lead author Denice S. Feig, MD, Mount Sinai Hospital, Toronto.
The research was presented at the Diabetes UK Professional Conference: Online Series on Nov. 17 and recently published in The Lancet Diabetes & Endocrinology.
Summing up, Dr. Feig said that, on balance, she would be inclined to give metformin to most pregnant women with type 2 diabetes, perhaps with the exception of those who may have risk factors for small-for-gestational-age babies; for example, women who’ve had intrauterine growth restriction, who are smokers, and have significant renal disease, or have a lower body mass index.
Increased prevalence of type 2 diabetes in pregnancy
Dr. Feig said that across the developed world there have been huge increases in the prevalence of type 2 diabetes in pregnancy in recent years.
Insulin is the standard treatment for the management of type 2 diabetes in pregnancy, but these women have marked insulin resistance that worsens in pregnancy, which means their insulin requirements increase, leading to weight gain, painful injections, high cost, and noncompliance.
So despite treatment with insulin, these women continue to face increased rates of adverse maternal and fetal outcomes.
And although metformin is increasingly being used in women with type 2 diabetes during pregnancy, there is a scarcity of data on the benefits and harms of metformin use on pregnancy outcomes in these women.
The MiTy trial was therefore undertaken to determine whether metformin could improve outcomes.
The team recruited 502 women from 29 sites in Canada and Australia who had type 2 diabetes prior to pregnancy or were diagnosed during pregnancy, before 20 weeks’ gestation. The women were randomized to metformin 1 g twice daily or placebo, in addition to their usual insulin regimen, at between 6 and 28 weeks’ gestation.
Type 2 diabetes was diagnosed prior to pregnancy in 83% of women in the metformin group and in 90% of those assigned to placebo. The mean hemoglobin A1c level at randomization was 47 mmol/mol (6.5%) in both groups.
The average maternal age at baseline was approximately 35 years and mean gestational age at randomization was 16 weeks. Mean prepregnancy BMI was approximately 34 kg/m2.
Of note, only 30% were of European ethnicity.
Less weight gain, lower A1c, less insulin needed with metformin
Dr. Feig reported that there was no significant difference between the treatment groups in terms of the proportion of women with the composite primary outcome of pregnancy loss, preterm birth, birth injury, respiratory distress, neonatal hypoglycemia, or admission to neonatal intensive care lasting more than 24 hours (P = 0.86).
However, women in the metformin group had significantly less overall weight gain during pregnancy than did those in the placebo group, at –1.8 kg (P < .0001).
They also had a significantly lower last A1c level in pregnancy, at 41 mmol/mol (5.9%) versus 43.2 mmol/mol (6.1%) in those given placebo (P = .015), and required fewer insulin doses, at 1.1 versus 1.5 units/kg/day (P < .0001), which translated to a reduction of almost 44 units/day.
Women given metformin were also less likely to require Cesarean section delivery, at 53.4% versus 62.7% in the placebo group (P = .03), although there was no difference between groups in terms of gestational hypertension or preeclampsia.
The most common adverse events were gastrointestinal complications, which occurred in 27.3% of women in the metformin group and 22.3% of those given placebo.
There were no significant differences between the metformin and placebo groups in rates of pregnancy loss (P = .81), preterm birth (P = .16), birth injury (P = .37), respiratory distress (P = .49), and congenital anomalies (P = .16).
Average birth weight lower with metformin
However, Dr. Feig showed that the average birth weight was lower for offspring of women given metformin than those assigned to placebo, at 3.2 kg (7.05 lb) versus 3.4 kg (7.4 lb) (P = .002).
Women given metformin were also less likely to have a baby with a birth weight of 4 kg (8.8 lb) or more, at 12.1% versus 19.2%, or a relative risk of 0.65 (P = .046), and a baby that was extremely large for gestational age, at 8.6% versus 14.8%, or a relative risk of 0.58 (P = .046).
But of concern, metformin was associated with an increased risk of small-for-gestational-age babies, at 12.9% versus 6.6% with placebo, or a relative risk of 1.96 (P = .03).
Dr. Feig suggested that this may be due to a direct effect of metformin “because as we know metformin inhibits the mTOR pathway,” which is a “primary nutrient sensor in the placenta” and could “attenuate nutrient flux and fetal growth.”
She said it is not clear whether the small-for-gestational-age babies were “healthy or unhealthy.”
To investigate further, the team has launched the MiTy Kids study, which will follow the offspring in the MiTy trial to determine whether metformin during pregnancy is associated with a reduction in adiposity and improvement in insulin resistance in the babies at 2 years of age.
Who should be given metformin?
During the discussion, Helen R. Murphy, MD, PhD, Norwich Medical School, University of East Anglia, England, asked whether Dr. Feig would recommend continuing metformin in pregnancy if it was started preconception for fertility issues rather than diabetes.
She replied: “If they don’t have diabetes and it’s simply for PCOS [polycystic ovary syndrome], then I have either stopped it as soon as they got pregnant or sometimes continued it through the first trimester, and then stopped.
“If the person has diabetes, however, I think given this work, for most people I would continue it,” she said.
The study was funded by the Canadian Institutes of Health Research, Lunenfeld-Tanenbaum Research Institute, and the University of Toronto. The authors have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Immunodeficiency strongly linked to mental illness, suicidal behavior
Patients with a primary humoral immunodeficiency (PID) are 91% more likely to have a psychiatric disorder and 84% more likely to exhibit suicidal behavior, compared against those without the condition, new research shows.
Results showed that this association, which was stronger in women, could not be fully explained by comorbid autoimmune diseases or by familial confounding.
These findings have important clinical implications, study investigator Josef Isung, MD, PhD, Centre for Psychiatry Research, Karolinska Institute, Stockholm, Sweden, told Medscape Medical News.
Clinicians managing patients with PID “should be aware of this increased association with psychiatric disorders and perhaps screen for them,” said Isung.
The study was published in the November issue of JAMA Psychiatry.
Registry study
Mounting evidence suggests immune disruption plays a role in psychiatric disorders through a range of mechanisms, including altered neurodevelopment. However, little is known about the neuropsychiatric consequences resulting from the underproduction of homeostatic antibodies.
They’re associated with an increased risk for recurrent infections and of developing autoimmune diseases.
The immunodeficiency can be severe, even life threatening, but can also be relatively mild. One of the less severe PID types is selective IgA deficiency, which is linked to increased infections within the mucosa-associated lymphoid tissue (MALT), an important immune barrier.
Experts have long suspected that infections within the MALT are associated with certain forms of psychopathology in children, particularly obsessive-compulsive disorder and chronic tic disorders.
While patients with this selective IgA subtype may be at some increased risk for infection and autoimmune disease, their overall health otherwise is good, said Isung.
The prevalence of PIDs ranges from about 1:250 to 1:20,000, depending on the type of humoral immunodeficiency, although most would fall into the relatively rare category, he added.
Using several linked national Swedish registries, researchers identified individuals with any PID diagnosis affecting immunoglobulin levels, their full siblings, and those with a lifetime diagnosis of selective IgA deficiency. In addition, they collected data on autoimmune diseases.
The study outcome was a lifetime record of a psychiatric disorder, a suicide attempt, or death by suicide.
Strong link to autism
Researchers identified 8378 patients (59% women) with PID affecting immunoglobulin levels (median age at first diagnosis, 47.8 years). They compared this group with almost 14.3 million subjects without PID.
In those with PID, 27.6% had an autoimmune disease vs 6.8% of those without PID, a statistically significant difference (P < .001).
About 20.5% of those with PID and 10.7% of unexposed subjects had at least one diagnosis of a psychiatric disorder.
In a model adjusted for year of birth, sex, and history of autoimmune disease, subjects with PID had a 91% higher likelihood of any psychiatric disorder (adjusted odds ratio [AOR] 1.91; 95% CI, 1.81 - 2.01; P < .001) vs their counterparts without PID.
The AORs for individual psychiatric disorders ranged from 1.34 (95% CI, 1.17 - 1.54; P < .001) for schizophrenia and other psychotic disorders to 2.99 (95% CI, 2.42 - 3.70; P < .001) for autism spectrum disorders (ASDs)
It’s unclear why the association with PID was strongest for autism, “but being a neurodevelopmental disorder, maybe autism is logically more associated with this type of disruption,” said Isung.
Research suggests that immunologic disruption may play a role in ASD, either through altered maternal immune function in utero or through immune disruption after birth, the researchers note.
Compared to those without PID, individuals with it had a significantly increased likelihood of any suicidal behavior (AOR, 1.84; 95% CI, 1.66 - 2.04, P < .001) as well as individual outcomes of death by suicide and suicide attempts.
The association with psychiatric disorders and suicidal behavior was markedly stronger for exposure to both PID and autoimmune disease than for exposure to either of these alone, which suggest an additive effect for these immune-related conditions.
Sex differences
“It was unclear to us why women seemed particularly vulnerable,” said Isung. He noted that PIDs are generally about as common in women as in men, but women tend to have higher rates of psychiatric disorders.
The analysis of the sibling cohort also revealed an elevated risk for psychiatric disorders, including ASD and suicidal behavior, but to a lesser degree.
“From this we could infer that at least part of the associations would be genetic, but part would be related to the disruption in itself,” said Isung.
An analysis examining selective IgA subtype also revealed a link with psychiatric disorders and suicidal behavior, suggesting this link is not exclusive to severe PID cases.
“Our conclusion here was that it seems like PID itself, or the immune disruption in itself, could explain the association rather than the burden of illness,” said Isung.
However, he acknowledged that the long-term stress and mental health fallout of having a chronic illness like PID may also explain some of the increased risk for psychiatric disorders.
This study, he said, provides more evidence that immune disruptions affect neurodevelopment and the brain. However, he added, the underlying mechanism still isn’t fully understood.
The results highlight the need to raise awareness of the association between immunodeficiency and mental illness, including suicidality among clinicians, patients, and advocates.
These findings may also have implications in patients with other immune deficiencies, said Isung, noting, “it would be interesting to further explore associations with other immunocompromised populations.”
No surprises
Commenting on the findings for Medscape Medical News, Igor Galynker, MD, professor of psychiatry at Icahn School of Medicine at Mount Sinai, New York City, said the study was “very well-done” and used “reliable and well-controlled” databases.
However, he added, the results “are neither particularly dramatic nor conclusive” as it makes sense that medical illnesses like PID would “increase risk of psychopathology,” said Galynker.
PID patients are much more likely to have contact with clinicians and to receive a psychiatric diagnosis, he said.
“People with a chronic illness are more stressed and generally have high incidences of depression, anxiety, and suicidal behavior. In addition to that, they may be more likely to be diagnosed with those conditions because they see a clinician more frequently.”
However, that reasoning doesn’t apply to autism, which manifests in early childhood and so is unlikely to be the result of stress, said Galynker, which is why he believes the finding that ASD is the psychiatric outcome most strongly associated with PID is “the most convincing.”
Galynker wasn’t surprised that the association between PID and psychiatric illnesses, and suicidal behaviors, was stronger among women.
“Women attempt suicide four times more often than men to begin with, so you would expect this to be more pronounced” in those with PID.
The study was supported by grants from the Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institute; Stockholm Care Services; the Soderstrom Konig Foundation; and the Fredrik & Ingrid Thurings Foundation. Isung and Galynker have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with a primary humoral immunodeficiency (PID) are 91% more likely to have a psychiatric disorder and 84% more likely to exhibit suicidal behavior, compared against those without the condition, new research shows.
Results showed that this association, which was stronger in women, could not be fully explained by comorbid autoimmune diseases or by familial confounding.
These findings have important clinical implications, study investigator Josef Isung, MD, PhD, Centre for Psychiatry Research, Karolinska Institute, Stockholm, Sweden, told Medscape Medical News.
Clinicians managing patients with PID “should be aware of this increased association with psychiatric disorders and perhaps screen for them,” said Isung.
The study was published in the November issue of JAMA Psychiatry.
Registry study
Mounting evidence suggests immune disruption plays a role in psychiatric disorders through a range of mechanisms, including altered neurodevelopment. However, little is known about the neuropsychiatric consequences resulting from the underproduction of homeostatic antibodies.
They’re associated with an increased risk for recurrent infections and of developing autoimmune diseases.
The immunodeficiency can be severe, even life threatening, but can also be relatively mild. One of the less severe PID types is selective IgA deficiency, which is linked to increased infections within the mucosa-associated lymphoid tissue (MALT), an important immune barrier.
Experts have long suspected that infections within the MALT are associated with certain forms of psychopathology in children, particularly obsessive-compulsive disorder and chronic tic disorders.
While patients with this selective IgA subtype may be at some increased risk for infection and autoimmune disease, their overall health otherwise is good, said Isung.
The prevalence of PIDs ranges from about 1:250 to 1:20,000, depending on the type of humoral immunodeficiency, although most would fall into the relatively rare category, he added.
Using several linked national Swedish registries, researchers identified individuals with any PID diagnosis affecting immunoglobulin levels, their full siblings, and those with a lifetime diagnosis of selective IgA deficiency. In addition, they collected data on autoimmune diseases.
The study outcome was a lifetime record of a psychiatric disorder, a suicide attempt, or death by suicide.
Strong link to autism
Researchers identified 8378 patients (59% women) with PID affecting immunoglobulin levels (median age at first diagnosis, 47.8 years). They compared this group with almost 14.3 million subjects without PID.
In those with PID, 27.6% had an autoimmune disease vs 6.8% of those without PID, a statistically significant difference (P < .001).
About 20.5% of those with PID and 10.7% of unexposed subjects had at least one diagnosis of a psychiatric disorder.
In a model adjusted for year of birth, sex, and history of autoimmune disease, subjects with PID had a 91% higher likelihood of any psychiatric disorder (adjusted odds ratio [AOR] 1.91; 95% CI, 1.81 - 2.01; P < .001) vs their counterparts without PID.
The AORs for individual psychiatric disorders ranged from 1.34 (95% CI, 1.17 - 1.54; P < .001) for schizophrenia and other psychotic disorders to 2.99 (95% CI, 2.42 - 3.70; P < .001) for autism spectrum disorders (ASDs)
It’s unclear why the association with PID was strongest for autism, “but being a neurodevelopmental disorder, maybe autism is logically more associated with this type of disruption,” said Isung.
Research suggests that immunologic disruption may play a role in ASD, either through altered maternal immune function in utero or through immune disruption after birth, the researchers note.
Compared to those without PID, individuals with it had a significantly increased likelihood of any suicidal behavior (AOR, 1.84; 95% CI, 1.66 - 2.04, P < .001) as well as individual outcomes of death by suicide and suicide attempts.
The association with psychiatric disorders and suicidal behavior was markedly stronger for exposure to both PID and autoimmune disease than for exposure to either of these alone, which suggest an additive effect for these immune-related conditions.
Sex differences
“It was unclear to us why women seemed particularly vulnerable,” said Isung. He noted that PIDs are generally about as common in women as in men, but women tend to have higher rates of psychiatric disorders.
The analysis of the sibling cohort also revealed an elevated risk for psychiatric disorders, including ASD and suicidal behavior, but to a lesser degree.
“From this we could infer that at least part of the associations would be genetic, but part would be related to the disruption in itself,” said Isung.
An analysis examining selective IgA subtype also revealed a link with psychiatric disorders and suicidal behavior, suggesting this link is not exclusive to severe PID cases.
“Our conclusion here was that it seems like PID itself, or the immune disruption in itself, could explain the association rather than the burden of illness,” said Isung.
However, he acknowledged that the long-term stress and mental health fallout of having a chronic illness like PID may also explain some of the increased risk for psychiatric disorders.
This study, he said, provides more evidence that immune disruptions affect neurodevelopment and the brain. However, he added, the underlying mechanism still isn’t fully understood.
The results highlight the need to raise awareness of the association between immunodeficiency and mental illness, including suicidality among clinicians, patients, and advocates.
These findings may also have implications in patients with other immune deficiencies, said Isung, noting, “it would be interesting to further explore associations with other immunocompromised populations.”
No surprises
Commenting on the findings for Medscape Medical News, Igor Galynker, MD, professor of psychiatry at Icahn School of Medicine at Mount Sinai, New York City, said the study was “very well-done” and used “reliable and well-controlled” databases.
However, he added, the results “are neither particularly dramatic nor conclusive” as it makes sense that medical illnesses like PID would “increase risk of psychopathology,” said Galynker.
PID patients are much more likely to have contact with clinicians and to receive a psychiatric diagnosis, he said.
“People with a chronic illness are more stressed and generally have high incidences of depression, anxiety, and suicidal behavior. In addition to that, they may be more likely to be diagnosed with those conditions because they see a clinician more frequently.”
However, that reasoning doesn’t apply to autism, which manifests in early childhood and so is unlikely to be the result of stress, said Galynker, which is why he believes the finding that ASD is the psychiatric outcome most strongly associated with PID is “the most convincing.”
Galynker wasn’t surprised that the association between PID and psychiatric illnesses, and suicidal behaviors, was stronger among women.
“Women attempt suicide four times more often than men to begin with, so you would expect this to be more pronounced” in those with PID.
The study was supported by grants from the Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institute; Stockholm Care Services; the Soderstrom Konig Foundation; and the Fredrik & Ingrid Thurings Foundation. Isung and Galynker have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Patients with a primary humoral immunodeficiency (PID) are 91% more likely to have a psychiatric disorder and 84% more likely to exhibit suicidal behavior, compared against those without the condition, new research shows.
Results showed that this association, which was stronger in women, could not be fully explained by comorbid autoimmune diseases or by familial confounding.
These findings have important clinical implications, study investigator Josef Isung, MD, PhD, Centre for Psychiatry Research, Karolinska Institute, Stockholm, Sweden, told Medscape Medical News.
Clinicians managing patients with PID “should be aware of this increased association with psychiatric disorders and perhaps screen for them,” said Isung.
The study was published in the November issue of JAMA Psychiatry.
Registry study
Mounting evidence suggests immune disruption plays a role in psychiatric disorders through a range of mechanisms, including altered neurodevelopment. However, little is known about the neuropsychiatric consequences resulting from the underproduction of homeostatic antibodies.
They’re associated with an increased risk for recurrent infections and of developing autoimmune diseases.
The immunodeficiency can be severe, even life threatening, but can also be relatively mild. One of the less severe PID types is selective IgA deficiency, which is linked to increased infections within the mucosa-associated lymphoid tissue (MALT), an important immune barrier.
Experts have long suspected that infections within the MALT are associated with certain forms of psychopathology in children, particularly obsessive-compulsive disorder and chronic tic disorders.
While patients with this selective IgA subtype may be at some increased risk for infection and autoimmune disease, their overall health otherwise is good, said Isung.
The prevalence of PIDs ranges from about 1:250 to 1:20,000, depending on the type of humoral immunodeficiency, although most would fall into the relatively rare category, he added.
Using several linked national Swedish registries, researchers identified individuals with any PID diagnosis affecting immunoglobulin levels, their full siblings, and those with a lifetime diagnosis of selective IgA deficiency. In addition, they collected data on autoimmune diseases.
The study outcome was a lifetime record of a psychiatric disorder, a suicide attempt, or death by suicide.
Strong link to autism
Researchers identified 8378 patients (59% women) with PID affecting immunoglobulin levels (median age at first diagnosis, 47.8 years). They compared this group with almost 14.3 million subjects without PID.
In those with PID, 27.6% had an autoimmune disease vs 6.8% of those without PID, a statistically significant difference (P < .001).
About 20.5% of those with PID and 10.7% of unexposed subjects had at least one diagnosis of a psychiatric disorder.
In a model adjusted for year of birth, sex, and history of autoimmune disease, subjects with PID had a 91% higher likelihood of any psychiatric disorder (adjusted odds ratio [AOR] 1.91; 95% CI, 1.81 - 2.01; P < .001) vs their counterparts without PID.
The AORs for individual psychiatric disorders ranged from 1.34 (95% CI, 1.17 - 1.54; P < .001) for schizophrenia and other psychotic disorders to 2.99 (95% CI, 2.42 - 3.70; P < .001) for autism spectrum disorders (ASDs)
It’s unclear why the association with PID was strongest for autism, “but being a neurodevelopmental disorder, maybe autism is logically more associated with this type of disruption,” said Isung.
Research suggests that immunologic disruption may play a role in ASD, either through altered maternal immune function in utero or through immune disruption after birth, the researchers note.
Compared to those without PID, individuals with it had a significantly increased likelihood of any suicidal behavior (AOR, 1.84; 95% CI, 1.66 - 2.04, P < .001) as well as individual outcomes of death by suicide and suicide attempts.
The association with psychiatric disorders and suicidal behavior was markedly stronger for exposure to both PID and autoimmune disease than for exposure to either of these alone, which suggest an additive effect for these immune-related conditions.
Sex differences
“It was unclear to us why women seemed particularly vulnerable,” said Isung. He noted that PIDs are generally about as common in women as in men, but women tend to have higher rates of psychiatric disorders.
The analysis of the sibling cohort also revealed an elevated risk for psychiatric disorders, including ASD and suicidal behavior, but to a lesser degree.
“From this we could infer that at least part of the associations would be genetic, but part would be related to the disruption in itself,” said Isung.
An analysis examining selective IgA subtype also revealed a link with psychiatric disorders and suicidal behavior, suggesting this link is not exclusive to severe PID cases.
“Our conclusion here was that it seems like PID itself, or the immune disruption in itself, could explain the association rather than the burden of illness,” said Isung.
However, he acknowledged that the long-term stress and mental health fallout of having a chronic illness like PID may also explain some of the increased risk for psychiatric disorders.
This study, he said, provides more evidence that immune disruptions affect neurodevelopment and the brain. However, he added, the underlying mechanism still isn’t fully understood.
The results highlight the need to raise awareness of the association between immunodeficiency and mental illness, including suicidality among clinicians, patients, and advocates.
These findings may also have implications in patients with other immune deficiencies, said Isung, noting, “it would be interesting to further explore associations with other immunocompromised populations.”
No surprises
Commenting on the findings for Medscape Medical News, Igor Galynker, MD, professor of psychiatry at Icahn School of Medicine at Mount Sinai, New York City, said the study was “very well-done” and used “reliable and well-controlled” databases.
However, he added, the results “are neither particularly dramatic nor conclusive” as it makes sense that medical illnesses like PID would “increase risk of psychopathology,” said Galynker.
PID patients are much more likely to have contact with clinicians and to receive a psychiatric diagnosis, he said.
“People with a chronic illness are more stressed and generally have high incidences of depression, anxiety, and suicidal behavior. In addition to that, they may be more likely to be diagnosed with those conditions because they see a clinician more frequently.”
However, that reasoning doesn’t apply to autism, which manifests in early childhood and so is unlikely to be the result of stress, said Galynker, which is why he believes the finding that ASD is the psychiatric outcome most strongly associated with PID is “the most convincing.”
Galynker wasn’t surprised that the association between PID and psychiatric illnesses, and suicidal behaviors, was stronger among women.
“Women attempt suicide four times more often than men to begin with, so you would expect this to be more pronounced” in those with PID.
The study was supported by grants from the Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institute; Stockholm Care Services; the Soderstrom Konig Foundation; and the Fredrik & Ingrid Thurings Foundation. Isung and Galynker have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Liquid oxygen recommended for mobile patients with lung disease
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
Neoadjuvant immunotherapy combo produces high response rate in melanoma
A neoadjuvant strategy combining two immunostimulatory agents with differing mechanisms of action is efficacious and safe in patients with high-risk, resectable melanoma, according to final results of the phase 2 Neo-C-Nivo trial.
The two agents are the PD-1 inhibitor nivolumab and CMP-001, an investigational Toll-like receptor 9 agonist that activates tumor-associated plasmacytoid dendritic cells.
CMP-001 and nivolumab produced a major pathologic response in 60% of patients, and these patients had a 1-year relapse-free survival rate of 89%. About 23% of patients had grade 3 treatment-related adverse events, and there were no grade 4-5 treatment-related events.
These data were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Stage III melanoma is a very, very high risk disease. Despite appropriate management, which involves surgical resection followed by adjuvant immunotherapy, a large number of patients still relapse,” noted study author Diwakar Davar, MD, of the University of Pittsburgh Hillman Cancer Center.
“Neoadjuvant immunotherapy in this setting enhances the systemic T-cell response to tumor antigens,” he explained. “As a result, there is greater detection and killing of micrometastatic disease. And, indeed, neoadjuvant immunotherapy with anti–[programmed death–1] monotherapy or with anti-PD1 and anti-CTLA4 combination therapy produces high response rates, although the combination therapy is associated with significant toxicity.”
Patients, treatment, and response
The Neo-C-Nivo trial enrolled 31 patients with resectable stage IIIB/C/D melanoma having clinically apparent lymph node disease.
The patients were treated with three cycles of nivolumab given every 2 weeks. They also received seven weekly injections of CMP-001 subcutaneously and then intratumorally. After surgical resection, the patients received more of the same immunotherapy.
At a median follow-up of 15 months, 60% of patients had a major pathologic response, 50% had a complete response, and 10% had a major response. Some 70% of patients (after additionally including partial responders) had any pathologic response.
“More than half of the patients that we treated had more than one injectable lesion,” Dr. Davar noted. “I want to emphasize that only one lesion was injected, so the results we got illustrate that the rest of the patients who had more than one injectable lesion had regression in their injected and uninjected lesions.”
Biomarker analyses showed that response was associated with evidence of immune activation, both in the tumor and in the blood. With immunotherapy, the density of CD8 tumor-infiltrating lymphocytes increased by a median of 10.3-fold in pathologic responders as compared with only 0.8-fold in nonresponders (P < .05). In addition, responders had evidence of activated CD8-positive T cells peripherally, as well as presence of plasmacytoid dendritic cells within the tumor microenvironment.
Survival and safety
Patients had better median relapse-free survival if they attained a major pathologic response (not reached in either group, P = .0106) or any pathologic response (not reached vs. 5 months, P = .0001).
The landmark 1-year relapse-free survival rate was 89% for major pathologic responders and 90% for all pathologic responders.
Overall, 22.6% of patients experienced grade 3 treatment-related adverse events, the majority of which did not require medical intervention and none of which delayed planned surgery. There were no grade 4-5 treatment-related adverse events.
Cytokine release syndrome was uncommon, seen in 16.1% of patients, possibly because the cohort received prophylaxis, Dr. Davar proposed.
Another treatment option?
“Intratumoral CMP-001 increases clinical efficacy of PD-1 blockade with minimal additional toxicity in patients with regionally advanced melanoma. Further study of this combination in high-risk resectable melanoma is planned,” Dr. Davar concluded.
“This combination achieved high response rates and certainly should be considered for a larger trial,” agreed session cochair Brian Gastman, MD, of the Cleveland (Ohio) Clinic.
However, long-term outcomes are pending, and it is not clear how efficacy of the studied combination will ultimately stack up against that of other treatment options, Dr. Gastman cautioned in an interview. “For example, it’s hard to tell if this will lead to better results versus, say, T-VEC [talimogene laherparepvec] with an anti-PD-1 agent,” he elaborated.
Nonetheless, “the implication of these findings is that there is another potential injectable option that can be combined with checkpoint inhibitors, and it may be useful for patients with refractory disease,” Dr. Gastman concluded.
The trial was funded by Checkmate Pharmaceuticals. Dr. Davar disclosed relationships with Checkmate Pharmaceuticals, Array Biopharma, Merck, Shionogi, Vedanta, Bristol-Myers Squibb, CellSight Technologies, GlaxoSmithKline/Tesaro, and Medpacto. Dr. Gastman disclosed no relevant conflicts of interest.
SOURCE: Davar D et al. SITC 2020, Abstract 303.
A neoadjuvant strategy combining two immunostimulatory agents with differing mechanisms of action is efficacious and safe in patients with high-risk, resectable melanoma, according to final results of the phase 2 Neo-C-Nivo trial.
The two agents are the PD-1 inhibitor nivolumab and CMP-001, an investigational Toll-like receptor 9 agonist that activates tumor-associated plasmacytoid dendritic cells.
CMP-001 and nivolumab produced a major pathologic response in 60% of patients, and these patients had a 1-year relapse-free survival rate of 89%. About 23% of patients had grade 3 treatment-related adverse events, and there were no grade 4-5 treatment-related events.
These data were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Stage III melanoma is a very, very high risk disease. Despite appropriate management, which involves surgical resection followed by adjuvant immunotherapy, a large number of patients still relapse,” noted study author Diwakar Davar, MD, of the University of Pittsburgh Hillman Cancer Center.
“Neoadjuvant immunotherapy in this setting enhances the systemic T-cell response to tumor antigens,” he explained. “As a result, there is greater detection and killing of micrometastatic disease. And, indeed, neoadjuvant immunotherapy with anti–[programmed death–1] monotherapy or with anti-PD1 and anti-CTLA4 combination therapy produces high response rates, although the combination therapy is associated with significant toxicity.”
Patients, treatment, and response
The Neo-C-Nivo trial enrolled 31 patients with resectable stage IIIB/C/D melanoma having clinically apparent lymph node disease.
The patients were treated with three cycles of nivolumab given every 2 weeks. They also received seven weekly injections of CMP-001 subcutaneously and then intratumorally. After surgical resection, the patients received more of the same immunotherapy.
At a median follow-up of 15 months, 60% of patients had a major pathologic response, 50% had a complete response, and 10% had a major response. Some 70% of patients (after additionally including partial responders) had any pathologic response.
“More than half of the patients that we treated had more than one injectable lesion,” Dr. Davar noted. “I want to emphasize that only one lesion was injected, so the results we got illustrate that the rest of the patients who had more than one injectable lesion had regression in their injected and uninjected lesions.”
Biomarker analyses showed that response was associated with evidence of immune activation, both in the tumor and in the blood. With immunotherapy, the density of CD8 tumor-infiltrating lymphocytes increased by a median of 10.3-fold in pathologic responders as compared with only 0.8-fold in nonresponders (P < .05). In addition, responders had evidence of activated CD8-positive T cells peripherally, as well as presence of plasmacytoid dendritic cells within the tumor microenvironment.
Survival and safety
Patients had better median relapse-free survival if they attained a major pathologic response (not reached in either group, P = .0106) or any pathologic response (not reached vs. 5 months, P = .0001).
The landmark 1-year relapse-free survival rate was 89% for major pathologic responders and 90% for all pathologic responders.
Overall, 22.6% of patients experienced grade 3 treatment-related adverse events, the majority of which did not require medical intervention and none of which delayed planned surgery. There were no grade 4-5 treatment-related adverse events.
Cytokine release syndrome was uncommon, seen in 16.1% of patients, possibly because the cohort received prophylaxis, Dr. Davar proposed.
Another treatment option?
“Intratumoral CMP-001 increases clinical efficacy of PD-1 blockade with minimal additional toxicity in patients with regionally advanced melanoma. Further study of this combination in high-risk resectable melanoma is planned,” Dr. Davar concluded.
“This combination achieved high response rates and certainly should be considered for a larger trial,” agreed session cochair Brian Gastman, MD, of the Cleveland (Ohio) Clinic.
However, long-term outcomes are pending, and it is not clear how efficacy of the studied combination will ultimately stack up against that of other treatment options, Dr. Gastman cautioned in an interview. “For example, it’s hard to tell if this will lead to better results versus, say, T-VEC [talimogene laherparepvec] with an anti-PD-1 agent,” he elaborated.
Nonetheless, “the implication of these findings is that there is another potential injectable option that can be combined with checkpoint inhibitors, and it may be useful for patients with refractory disease,” Dr. Gastman concluded.
The trial was funded by Checkmate Pharmaceuticals. Dr. Davar disclosed relationships with Checkmate Pharmaceuticals, Array Biopharma, Merck, Shionogi, Vedanta, Bristol-Myers Squibb, CellSight Technologies, GlaxoSmithKline/Tesaro, and Medpacto. Dr. Gastman disclosed no relevant conflicts of interest.
SOURCE: Davar D et al. SITC 2020, Abstract 303.
A neoadjuvant strategy combining two immunostimulatory agents with differing mechanisms of action is efficacious and safe in patients with high-risk, resectable melanoma, according to final results of the phase 2 Neo-C-Nivo trial.
The two agents are the PD-1 inhibitor nivolumab and CMP-001, an investigational Toll-like receptor 9 agonist that activates tumor-associated plasmacytoid dendritic cells.
CMP-001 and nivolumab produced a major pathologic response in 60% of patients, and these patients had a 1-year relapse-free survival rate of 89%. About 23% of patients had grade 3 treatment-related adverse events, and there were no grade 4-5 treatment-related events.
These data were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Stage III melanoma is a very, very high risk disease. Despite appropriate management, which involves surgical resection followed by adjuvant immunotherapy, a large number of patients still relapse,” noted study author Diwakar Davar, MD, of the University of Pittsburgh Hillman Cancer Center.
“Neoadjuvant immunotherapy in this setting enhances the systemic T-cell response to tumor antigens,” he explained. “As a result, there is greater detection and killing of micrometastatic disease. And, indeed, neoadjuvant immunotherapy with anti–[programmed death–1] monotherapy or with anti-PD1 and anti-CTLA4 combination therapy produces high response rates, although the combination therapy is associated with significant toxicity.”
Patients, treatment, and response
The Neo-C-Nivo trial enrolled 31 patients with resectable stage IIIB/C/D melanoma having clinically apparent lymph node disease.
The patients were treated with three cycles of nivolumab given every 2 weeks. They also received seven weekly injections of CMP-001 subcutaneously and then intratumorally. After surgical resection, the patients received more of the same immunotherapy.
At a median follow-up of 15 months, 60% of patients had a major pathologic response, 50% had a complete response, and 10% had a major response. Some 70% of patients (after additionally including partial responders) had any pathologic response.
“More than half of the patients that we treated had more than one injectable lesion,” Dr. Davar noted. “I want to emphasize that only one lesion was injected, so the results we got illustrate that the rest of the patients who had more than one injectable lesion had regression in their injected and uninjected lesions.”
Biomarker analyses showed that response was associated with evidence of immune activation, both in the tumor and in the blood. With immunotherapy, the density of CD8 tumor-infiltrating lymphocytes increased by a median of 10.3-fold in pathologic responders as compared with only 0.8-fold in nonresponders (P < .05). In addition, responders had evidence of activated CD8-positive T cells peripherally, as well as presence of plasmacytoid dendritic cells within the tumor microenvironment.
Survival and safety
Patients had better median relapse-free survival if they attained a major pathologic response (not reached in either group, P = .0106) or any pathologic response (not reached vs. 5 months, P = .0001).
The landmark 1-year relapse-free survival rate was 89% for major pathologic responders and 90% for all pathologic responders.
Overall, 22.6% of patients experienced grade 3 treatment-related adverse events, the majority of which did not require medical intervention and none of which delayed planned surgery. There were no grade 4-5 treatment-related adverse events.
Cytokine release syndrome was uncommon, seen in 16.1% of patients, possibly because the cohort received prophylaxis, Dr. Davar proposed.
Another treatment option?
“Intratumoral CMP-001 increases clinical efficacy of PD-1 blockade with minimal additional toxicity in patients with regionally advanced melanoma. Further study of this combination in high-risk resectable melanoma is planned,” Dr. Davar concluded.
“This combination achieved high response rates and certainly should be considered for a larger trial,” agreed session cochair Brian Gastman, MD, of the Cleveland (Ohio) Clinic.
However, long-term outcomes are pending, and it is not clear how efficacy of the studied combination will ultimately stack up against that of other treatment options, Dr. Gastman cautioned in an interview. “For example, it’s hard to tell if this will lead to better results versus, say, T-VEC [talimogene laherparepvec] with an anti-PD-1 agent,” he elaborated.
Nonetheless, “the implication of these findings is that there is another potential injectable option that can be combined with checkpoint inhibitors, and it may be useful for patients with refractory disease,” Dr. Gastman concluded.
The trial was funded by Checkmate Pharmaceuticals. Dr. Davar disclosed relationships with Checkmate Pharmaceuticals, Array Biopharma, Merck, Shionogi, Vedanta, Bristol-Myers Squibb, CellSight Technologies, GlaxoSmithKline/Tesaro, and Medpacto. Dr. Gastman disclosed no relevant conflicts of interest.
SOURCE: Davar D et al. SITC 2020, Abstract 303.
FROM SITC 2020
New findings on ‘exceptional responders’ to cancer therapies
An ongoing research project is studying why some patients have exceptional responses. The researchers have found particular molecular features in the tumors of about a quarter of these patients. In some cases, there are multiple rare genetic changes in the tumor genome. In other cases, the tumors are infiltrated with certain types of immune cells.
The findings were published online November 19 in Cancer Cell. They come from a genomic analysis of tumor biopsy specimens from 111 patients who were identified by the National Cancer Institute’s (NCI’s) Exceptional Responders Initiative, a national project launched in 2014.
An exceptional responder is defined as an individual who achieves a partial or complete response to a treatment that would be effective in fewer than 10% of similar patients. For exceptional response, the duration of response is at least three times longer than the usual median response time.
In this study of 111 such patients, about one quarter (24%, n = 26 patients) were found to have tumors in which there were molecular features that could potentially explain exceptional responses to treatment.
“We won’t be able to identify, in every patient, which particular drugs will be beneficial,” said Louis Staudt, MD, PhD, director of the NCI’s Center for Cancer Genomics, who co-led the study. “We are nowhere near that. But what it does say is that we have identified particular mutations, some of which we knew about in some types of cancer but can also occur less commonly in other cancer types.”
Staudt noted that these mutations can “illuminate” the path that the cancer will take — and potentially can be used to predict whether the cancer will be aggressive and will require treatment or could be managed with surveillance. This is why this research can be useful in the short term, he said.
“In the longer term, this is the kind of research that inspires future work,” he told Medscape Medical News. “That would encompass clinical trials involving drugs that target some of the pathways we found to be genetically inactivated in some of these responders.”
These results support the use of genetic testing in routine clinical care, he said.
Earlier this year, the NCI team published the results of a pilot study that affirmed the feasibility of this approach. Of the more than 100 cases that were analyzed, six were identified as involving potentially clinically actionable germline mutations.
‘Curiosity drove the research’
“We had these wonderful and gratifying experiences with our patients, so we were immediately curious how that happened, so it was pretty much that curiosity that drove a lot of this work,” said Staudt.
In the current study, Staudt and colleagues used multiple genomic methodologies to detect mutations, copy number changes, aberrant methylation, outlier gene expression, and the cellular makeup of the tumor microenvironment.
The hypothesized mechanisms for exceptional responses were broadly divided into the following four categories: DNA damage response (n = 15), intracellular signaling pathway (n = 9), prognostic genetics (n = 9), and immunologic engagement (n = 16). For many patients, two or more of these mechanisms were involved.
The authors note that the “predominance of plausible DNA damage response mechanisms parallels the frequent use of cytotoxic chemotherapy in routine cancer treatment reflected in this cohort.”
Twenty-six patients were identified as exceptional responders. Among these patients, a variety of cancer types was represented: brain (8); gastrointestinal tract (6); breast (4); cholangiocarcinoma (2); lung (2); pancreas, endometrium, ovarian, and bladder (1 each). Many of these patients (65%, n = 17) were treated with chemotherapy that included DNA-damaging agents. For more than half (54%, n = 14), targeted therapies were used, and some patients received both.
The authors highlight several patients as examples of exceptional responders:
- One patient with glioblastoma multiforme (GBM) was treated sequentially with surgery, localized carmustine, and radiotherapy. When the cancer recurred, temozolomide was administered. This induced a complete response that has lasted for more than a decade.
- A patient with metastatic colon adenocarcinoma has had an ongoing and nearly complete response that has lasted 45 months (last follow-up) after receiving temozolomide in combination with the investigational drug TRC102 (methoxyamine, under development by Tracon) in a phase 1 clinical trial. TRC102 is an inhibitor of the DNA base excision repair pathway, which is a pathway that causes resistance to alkylating and antimetabolite chemotherapeutics.
- A patient with metastatic, estrogen receptor–positive breast cancer received trastuzumab because of a high-level ERBB2 amplification, together with anastrozole. This resulted in an ongoing 2.4-year partial response.
- Although the patient was clinically HER2 positive, her tumor had exceedingly low expression of ERBB2 mRNA. Molecular profiling had classified the tumor as of the basal-like subtype rather than the HER2-enriched subtype. This meant that it was unlikely that trastuzumab contributed to the exceptional response, the authors note. Because the patient was estrogen-receptor positive, she received anastrozole, an inhibitor of aromatase (CYP19A), which converts testosterone into estradiol.
- A patient who had a gastrointestinal stromal tumor with a deletion of KIT exon 11 experienced relapse after an initial response to imatinib, which targets KIT and other tyrosine kinases, but then achieved a complete response with sunitinib. Gene expression profiling revealed high expression not only of KIT but also of genes encoding several tyrosine kinases that are targeted by sunitinib (KDR, FLT1, and FLT3). This may have accounted for the patient’s response.
Favorable genomic characteristics
The authors defined a “prognostic genetics” category of tumors, characterized by genetic lesions that are now known to be associated with a favorable prognosis but that were not addressed through routine care that these patients received when they were first diagnosed. Although the patients experienced relapse after first-line treatment, their exceptional survival after salvage therapy could be linked to favorable genomic characteristics.
For example, several of the patients with high-grade GBMs and astrocytomas had genetic lesions that are generally more common in low-grade glioma and that have been associated with an indolent clinical course following standard therapy.
The authors also assessed immune response. Examining immune cell infiltration in responder tumors in comparison with control cases, the team found that signatures of B cells and activated (CD56dim) natural killer cells were higher in exceptional-responder tumors.
In one patient with metastatic urothelial cancer who experienced disease progression after chemotherapy, radiotherapy, and surgery, treatment with nivolumab produced a complete response that lasted 7 months. Such an outcome occurs in only about 3% of bladder cancer patients. The tumor expressed high mRNA levels of PDCD1, which encodes the nivolumab target PD-1, and CD274, which encodes the PD-1 ligand PD-L1. There was also a high level of amplification of IFNG, which encodes interferon-gamma, a cytokine that has been linked to favorable response to immune checkpoint blockade.
Moving to precision medicine
“It is very valuable to be tested up front and again when the disease progresses, because there may have been some genetic changes, and this may change the treatment,” said co–lead author S. Percy Ivy, MD, of the NCI’s Division of Cancer Treatment and Diagnosis.
“The goal of this study was to understand what was unique about these patients and their genetic makeup that led them to be classified as exceptional responders, and hopefully we will be able to tease that out,” she added.
“As researchers, we have a lot to learn from these patients, and they have a lot to teach us,” she added. “In the future, they will help us as we move closer to the goal of delivering precision oncology to all of our patients. We’re not there yet, but every time we study more deeply and learn more, we are able to provide better care.”
To encourage participation in this effort by investigators around the world, the NCI team and their colleagues have made their molecular profiling results and clinical information publicly available in the NCI Genomic Data Commons.
The study was supported by the NCI’s Intramural Research Program, the National Institutes of Health, the Center for Cancer Research, and the NCI’s Center for Cancer Genomics. Staudt and Ivy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
An ongoing research project is studying why some patients have exceptional responses. The researchers have found particular molecular features in the tumors of about a quarter of these patients. In some cases, there are multiple rare genetic changes in the tumor genome. In other cases, the tumors are infiltrated with certain types of immune cells.
The findings were published online November 19 in Cancer Cell. They come from a genomic analysis of tumor biopsy specimens from 111 patients who were identified by the National Cancer Institute’s (NCI’s) Exceptional Responders Initiative, a national project launched in 2014.
An exceptional responder is defined as an individual who achieves a partial or complete response to a treatment that would be effective in fewer than 10% of similar patients. For exceptional response, the duration of response is at least three times longer than the usual median response time.
In this study of 111 such patients, about one quarter (24%, n = 26 patients) were found to have tumors in which there were molecular features that could potentially explain exceptional responses to treatment.
“We won’t be able to identify, in every patient, which particular drugs will be beneficial,” said Louis Staudt, MD, PhD, director of the NCI’s Center for Cancer Genomics, who co-led the study. “We are nowhere near that. But what it does say is that we have identified particular mutations, some of which we knew about in some types of cancer but can also occur less commonly in other cancer types.”
Staudt noted that these mutations can “illuminate” the path that the cancer will take — and potentially can be used to predict whether the cancer will be aggressive and will require treatment or could be managed with surveillance. This is why this research can be useful in the short term, he said.
“In the longer term, this is the kind of research that inspires future work,” he told Medscape Medical News. “That would encompass clinical trials involving drugs that target some of the pathways we found to be genetically inactivated in some of these responders.”
These results support the use of genetic testing in routine clinical care, he said.
Earlier this year, the NCI team published the results of a pilot study that affirmed the feasibility of this approach. Of the more than 100 cases that were analyzed, six were identified as involving potentially clinically actionable germline mutations.
‘Curiosity drove the research’
“We had these wonderful and gratifying experiences with our patients, so we were immediately curious how that happened, so it was pretty much that curiosity that drove a lot of this work,” said Staudt.
In the current study, Staudt and colleagues used multiple genomic methodologies to detect mutations, copy number changes, aberrant methylation, outlier gene expression, and the cellular makeup of the tumor microenvironment.
The hypothesized mechanisms for exceptional responses were broadly divided into the following four categories: DNA damage response (n = 15), intracellular signaling pathway (n = 9), prognostic genetics (n = 9), and immunologic engagement (n = 16). For many patients, two or more of these mechanisms were involved.
The authors note that the “predominance of plausible DNA damage response mechanisms parallels the frequent use of cytotoxic chemotherapy in routine cancer treatment reflected in this cohort.”
Twenty-six patients were identified as exceptional responders. Among these patients, a variety of cancer types was represented: brain (8); gastrointestinal tract (6); breast (4); cholangiocarcinoma (2); lung (2); pancreas, endometrium, ovarian, and bladder (1 each). Many of these patients (65%, n = 17) were treated with chemotherapy that included DNA-damaging agents. For more than half (54%, n = 14), targeted therapies were used, and some patients received both.
The authors highlight several patients as examples of exceptional responders:
- One patient with glioblastoma multiforme (GBM) was treated sequentially with surgery, localized carmustine, and radiotherapy. When the cancer recurred, temozolomide was administered. This induced a complete response that has lasted for more than a decade.
- A patient with metastatic colon adenocarcinoma has had an ongoing and nearly complete response that has lasted 45 months (last follow-up) after receiving temozolomide in combination with the investigational drug TRC102 (methoxyamine, under development by Tracon) in a phase 1 clinical trial. TRC102 is an inhibitor of the DNA base excision repair pathway, which is a pathway that causes resistance to alkylating and antimetabolite chemotherapeutics.
- A patient with metastatic, estrogen receptor–positive breast cancer received trastuzumab because of a high-level ERBB2 amplification, together with anastrozole. This resulted in an ongoing 2.4-year partial response.
- Although the patient was clinically HER2 positive, her tumor had exceedingly low expression of ERBB2 mRNA. Molecular profiling had classified the tumor as of the basal-like subtype rather than the HER2-enriched subtype. This meant that it was unlikely that trastuzumab contributed to the exceptional response, the authors note. Because the patient was estrogen-receptor positive, she received anastrozole, an inhibitor of aromatase (CYP19A), which converts testosterone into estradiol.
- A patient who had a gastrointestinal stromal tumor with a deletion of KIT exon 11 experienced relapse after an initial response to imatinib, which targets KIT and other tyrosine kinases, but then achieved a complete response with sunitinib. Gene expression profiling revealed high expression not only of KIT but also of genes encoding several tyrosine kinases that are targeted by sunitinib (KDR, FLT1, and FLT3). This may have accounted for the patient’s response.
Favorable genomic characteristics
The authors defined a “prognostic genetics” category of tumors, characterized by genetic lesions that are now known to be associated with a favorable prognosis but that were not addressed through routine care that these patients received when they were first diagnosed. Although the patients experienced relapse after first-line treatment, their exceptional survival after salvage therapy could be linked to favorable genomic characteristics.
For example, several of the patients with high-grade GBMs and astrocytomas had genetic lesions that are generally more common in low-grade glioma and that have been associated with an indolent clinical course following standard therapy.
The authors also assessed immune response. Examining immune cell infiltration in responder tumors in comparison with control cases, the team found that signatures of B cells and activated (CD56dim) natural killer cells were higher in exceptional-responder tumors.
In one patient with metastatic urothelial cancer who experienced disease progression after chemotherapy, radiotherapy, and surgery, treatment with nivolumab produced a complete response that lasted 7 months. Such an outcome occurs in only about 3% of bladder cancer patients. The tumor expressed high mRNA levels of PDCD1, which encodes the nivolumab target PD-1, and CD274, which encodes the PD-1 ligand PD-L1. There was also a high level of amplification of IFNG, which encodes interferon-gamma, a cytokine that has been linked to favorable response to immune checkpoint blockade.
Moving to precision medicine
“It is very valuable to be tested up front and again when the disease progresses, because there may have been some genetic changes, and this may change the treatment,” said co–lead author S. Percy Ivy, MD, of the NCI’s Division of Cancer Treatment and Diagnosis.
“The goal of this study was to understand what was unique about these patients and their genetic makeup that led them to be classified as exceptional responders, and hopefully we will be able to tease that out,” she added.
“As researchers, we have a lot to learn from these patients, and they have a lot to teach us,” she added. “In the future, they will help us as we move closer to the goal of delivering precision oncology to all of our patients. We’re not there yet, but every time we study more deeply and learn more, we are able to provide better care.”
To encourage participation in this effort by investigators around the world, the NCI team and their colleagues have made their molecular profiling results and clinical information publicly available in the NCI Genomic Data Commons.
The study was supported by the NCI’s Intramural Research Program, the National Institutes of Health, the Center for Cancer Research, and the NCI’s Center for Cancer Genomics. Staudt and Ivy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
An ongoing research project is studying why some patients have exceptional responses. The researchers have found particular molecular features in the tumors of about a quarter of these patients. In some cases, there are multiple rare genetic changes in the tumor genome. In other cases, the tumors are infiltrated with certain types of immune cells.
The findings were published online November 19 in Cancer Cell. They come from a genomic analysis of tumor biopsy specimens from 111 patients who were identified by the National Cancer Institute’s (NCI’s) Exceptional Responders Initiative, a national project launched in 2014.
An exceptional responder is defined as an individual who achieves a partial or complete response to a treatment that would be effective in fewer than 10% of similar patients. For exceptional response, the duration of response is at least three times longer than the usual median response time.
In this study of 111 such patients, about one quarter (24%, n = 26 patients) were found to have tumors in which there were molecular features that could potentially explain exceptional responses to treatment.
“We won’t be able to identify, in every patient, which particular drugs will be beneficial,” said Louis Staudt, MD, PhD, director of the NCI’s Center for Cancer Genomics, who co-led the study. “We are nowhere near that. But what it does say is that we have identified particular mutations, some of which we knew about in some types of cancer but can also occur less commonly in other cancer types.”
Staudt noted that these mutations can “illuminate” the path that the cancer will take — and potentially can be used to predict whether the cancer will be aggressive and will require treatment or could be managed with surveillance. This is why this research can be useful in the short term, he said.
“In the longer term, this is the kind of research that inspires future work,” he told Medscape Medical News. “That would encompass clinical trials involving drugs that target some of the pathways we found to be genetically inactivated in some of these responders.”
These results support the use of genetic testing in routine clinical care, he said.
Earlier this year, the NCI team published the results of a pilot study that affirmed the feasibility of this approach. Of the more than 100 cases that were analyzed, six were identified as involving potentially clinically actionable germline mutations.
‘Curiosity drove the research’
“We had these wonderful and gratifying experiences with our patients, so we were immediately curious how that happened, so it was pretty much that curiosity that drove a lot of this work,” said Staudt.
In the current study, Staudt and colleagues used multiple genomic methodologies to detect mutations, copy number changes, aberrant methylation, outlier gene expression, and the cellular makeup of the tumor microenvironment.
The hypothesized mechanisms for exceptional responses were broadly divided into the following four categories: DNA damage response (n = 15), intracellular signaling pathway (n = 9), prognostic genetics (n = 9), and immunologic engagement (n = 16). For many patients, two or more of these mechanisms were involved.
The authors note that the “predominance of plausible DNA damage response mechanisms parallels the frequent use of cytotoxic chemotherapy in routine cancer treatment reflected in this cohort.”
Twenty-six patients were identified as exceptional responders. Among these patients, a variety of cancer types was represented: brain (8); gastrointestinal tract (6); breast (4); cholangiocarcinoma (2); lung (2); pancreas, endometrium, ovarian, and bladder (1 each). Many of these patients (65%, n = 17) were treated with chemotherapy that included DNA-damaging agents. For more than half (54%, n = 14), targeted therapies were used, and some patients received both.
The authors highlight several patients as examples of exceptional responders:
- One patient with glioblastoma multiforme (GBM) was treated sequentially with surgery, localized carmustine, and radiotherapy. When the cancer recurred, temozolomide was administered. This induced a complete response that has lasted for more than a decade.
- A patient with metastatic colon adenocarcinoma has had an ongoing and nearly complete response that has lasted 45 months (last follow-up) after receiving temozolomide in combination with the investigational drug TRC102 (methoxyamine, under development by Tracon) in a phase 1 clinical trial. TRC102 is an inhibitor of the DNA base excision repair pathway, which is a pathway that causes resistance to alkylating and antimetabolite chemotherapeutics.
- A patient with metastatic, estrogen receptor–positive breast cancer received trastuzumab because of a high-level ERBB2 amplification, together with anastrozole. This resulted in an ongoing 2.4-year partial response.
- Although the patient was clinically HER2 positive, her tumor had exceedingly low expression of ERBB2 mRNA. Molecular profiling had classified the tumor as of the basal-like subtype rather than the HER2-enriched subtype. This meant that it was unlikely that trastuzumab contributed to the exceptional response, the authors note. Because the patient was estrogen-receptor positive, she received anastrozole, an inhibitor of aromatase (CYP19A), which converts testosterone into estradiol.
- A patient who had a gastrointestinal stromal tumor with a deletion of KIT exon 11 experienced relapse after an initial response to imatinib, which targets KIT and other tyrosine kinases, but then achieved a complete response with sunitinib. Gene expression profiling revealed high expression not only of KIT but also of genes encoding several tyrosine kinases that are targeted by sunitinib (KDR, FLT1, and FLT3). This may have accounted for the patient’s response.
Favorable genomic characteristics
The authors defined a “prognostic genetics” category of tumors, characterized by genetic lesions that are now known to be associated with a favorable prognosis but that were not addressed through routine care that these patients received when they were first diagnosed. Although the patients experienced relapse after first-line treatment, their exceptional survival after salvage therapy could be linked to favorable genomic characteristics.
For example, several of the patients with high-grade GBMs and astrocytomas had genetic lesions that are generally more common in low-grade glioma and that have been associated with an indolent clinical course following standard therapy.
The authors also assessed immune response. Examining immune cell infiltration in responder tumors in comparison with control cases, the team found that signatures of B cells and activated (CD56dim) natural killer cells were higher in exceptional-responder tumors.
In one patient with metastatic urothelial cancer who experienced disease progression after chemotherapy, radiotherapy, and surgery, treatment with nivolumab produced a complete response that lasted 7 months. Such an outcome occurs in only about 3% of bladder cancer patients. The tumor expressed high mRNA levels of PDCD1, which encodes the nivolumab target PD-1, and CD274, which encodes the PD-1 ligand PD-L1. There was also a high level of amplification of IFNG, which encodes interferon-gamma, a cytokine that has been linked to favorable response to immune checkpoint blockade.
Moving to precision medicine
“It is very valuable to be tested up front and again when the disease progresses, because there may have been some genetic changes, and this may change the treatment,” said co–lead author S. Percy Ivy, MD, of the NCI’s Division of Cancer Treatment and Diagnosis.
“The goal of this study was to understand what was unique about these patients and their genetic makeup that led them to be classified as exceptional responders, and hopefully we will be able to tease that out,” she added.
“As researchers, we have a lot to learn from these patients, and they have a lot to teach us,” she added. “In the future, they will help us as we move closer to the goal of delivering precision oncology to all of our patients. We’re not there yet, but every time we study more deeply and learn more, we are able to provide better care.”
To encourage participation in this effort by investigators around the world, the NCI team and their colleagues have made their molecular profiling results and clinical information publicly available in the NCI Genomic Data Commons.
The study was supported by the NCI’s Intramural Research Program, the National Institutes of Health, the Center for Cancer Research, and the NCI’s Center for Cancer Genomics. Staudt and Ivy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Hospitalist movers and shakers – November 2020
Erin Shaughnessy, MD, assumed the role of director of pediatric hospital medicine at the University of Alabama at Birmingham and Children’s of Alabama, also in Birmingham, on Sept. 1. Dr. Shaughnessy has done research in improving outcomes in hospitalized children, as well as improving communication between physicians and pediatric patients’ families during care transitions.
Prior to joining UAB and Children’s of Alabama, Dr. Shaughnessy was division chief of hospital medicine at Phoenix (Ariz.) Children’s Hospital while also serving as an associate professor at the University of Arizona, Phoenix.
Chandra Lingisetty, MD, MBA, MHCM, was recently named chief administrative officer for Baptist Health Physician Partners, Arkansas. BHPP is Baptist Health’s clinically integrated network (CIN) with more than 1,600 providers across the state.
Baptist Health Arkansas is the state’s largest not for profit health system with 12 hospitals, hundreds of provider clinics, a nursing school, and a graduate medical education residency program. Prior to his promotion, he worked in Baptist Health System as a hospitalist for 10 years, served on the board of managers at BHPP, and strategized COVID-19 care management protocols and medical staff preparedness as part of surge planning and capacity expansion. In his new role, he is focused on leading the clinically integrated network toward value-based care. He is also the cofounder and inaugural president of the Arkansas state chapter of the Society of Hospital Medicine.
Grace Farris, MD, recently accepted a position with the division of hospital medicine at the Dell Medical School in Austin where she will be an assistant professor of internal medicine, as well as a working hospitalist.
Dr. Farris worked as chief of hospital medicine at Mount Sinai West Hospital in Manhattan from January 2017 until accepting her new position with Dell. In addition, she publishes a monthly comics column in the Annals of Internal Medicine.
Her visual storytelling through comics has appeared in several media outlets, and she has penned literal columns as well, including one recently in the New York Times about living apart from her children while treating COVID-19 patients in the emergency room.
Dell Medical School has also named a new division chief of hospital medicine. Read Pierce, MD, made the move to Texas from the University of Colorado at Denver, Aurora. Dr. Pierce will also serve as associate chair of faculty development of internal medicine at Dell. He is eager to build on his experience and passion for developing people, creating outstanding culture, and changing complex systems in innovative, sustainable ways.
Dr. Pierce worked at University of Colorado for the past 8 years, serving as the associate director of the school’s Institute for Healthcare Quality, Safety and Efficiency (IHQSE), a program he co-founded. Prior to that, Dr. Pierce was chief resident at the University of San Francisco medical school and later founded the hospital medicine center at the San Francisco VA Medical Center.
Gurinder Kaur, MD, was recently named medical director of the Health Hospitalist Program at St. Joseph’s Health Rome (N.Y.) Memorial Hospital. Dr. Kaur’s focus will be on improving infrastructure to allow for the highest quality of care possible. She will oversee the facility’s crew of eight hospitalists, who rotate to be available 24 hours per day.
Dr. Kaur comes to Rome from St. Joseph’s Health in Syracuse, N.Y., where she was chief resident and a member of the hospitalist team.
Colin McMahon, MD, was recently appointed chief of hospital medicine at Eastern Niagara Hospital in Lockport, N.Y., where he will oversee the hospitalist program. He comes to ENH after serving as medical director of hospital operations at Buffalo (N.Y.) General Medical Center.
Dr. McMahon has worked in medicine for a quarter of a century. He also is the president and founder of Dimensions of Internal Medicine and Pediatric Care, PC (DMP). Associates from DMP Medicine make up the hospitalist team at ENH.
Sam Antonios, MD, has been promoted to chief clinical officer of Ascension Kansas, the parent group of Ascension Via Christi Hospital in Wichita, where Dr. Antonios has served as chief medical officer for the past 4 years. Dr. Antonios has emerged as a leader within Ascension Kansas during the COVID-19 pandemic.
Prior to his appointment at Via Christi, he worked at that facility as a hospitalist and as medical director of information systems. Dr. Antonios is a board-certified internist.
Bret J. Rudy, MD, was named a Top 25 Healthcare Innovator by Modern Healthcare magazine. Dr. Rudy is chief of hospital operations and senior vice president at NYU Langone Hospital-Brooklyn in New York, and the magazine cited his efforts in elevating the quality, safety, and accountability of the facility, which merged with NYU Langone Health in 2016.
Dr. Rudy has established a 24-hour hospitalist service, added full-time emergency faculty, and reduced hospital wait times, among other patient-experience benchmarks, since his appointment at Langone-Brooklyn.
Dr. Rudy is a board-certified pediatrician who has served on the National Institutes of Health’s HIV research networks, including a spot on the White House Advisory Committee on Adolescents for the Office of National AIDS Policy.
Nasim Afsar, MD, MBA, SFHM, a past president of SHM, was recently named chief operating officer at UCI Health in Orange, Calif. Dr. Afsar served previously as chief ambulatory officer and chief medical officer for accountable care organizations at UCI Health.
Anthony J. Macchiavelli, MD, FHM, was recognized by Continental Who’s Who as a “Top Distinguished Hospitalist” with AtlantiCare Regional Medical Center, in Atlantic City, N.J. He has been with AtlantiCare for the past ten years, and currently serves as medical director for the PACE program, as well as medical director for the Anticoagulation Clinic.
Dr. Macchiavelli has been involved in the development of 3 different hospital medicine programs throughout his career and was the founder of the Associates in Hospital Medicine program at Methodist Division of Thomas Jefferson University Hospitals. He serves as a mentor for SHM’s VTE-FAST Program, and has served on the Standards Review Panel for the Joint Commission developing the National Patient Safety Goal for anticoagulation therapy.
Erin Shaughnessy, MD, assumed the role of director of pediatric hospital medicine at the University of Alabama at Birmingham and Children’s of Alabama, also in Birmingham, on Sept. 1. Dr. Shaughnessy has done research in improving outcomes in hospitalized children, as well as improving communication between physicians and pediatric patients’ families during care transitions.
Prior to joining UAB and Children’s of Alabama, Dr. Shaughnessy was division chief of hospital medicine at Phoenix (Ariz.) Children’s Hospital while also serving as an associate professor at the University of Arizona, Phoenix.
Chandra Lingisetty, MD, MBA, MHCM, was recently named chief administrative officer for Baptist Health Physician Partners, Arkansas. BHPP is Baptist Health’s clinically integrated network (CIN) with more than 1,600 providers across the state.
Baptist Health Arkansas is the state’s largest not for profit health system with 12 hospitals, hundreds of provider clinics, a nursing school, and a graduate medical education residency program. Prior to his promotion, he worked in Baptist Health System as a hospitalist for 10 years, served on the board of managers at BHPP, and strategized COVID-19 care management protocols and medical staff preparedness as part of surge planning and capacity expansion. In his new role, he is focused on leading the clinically integrated network toward value-based care. He is also the cofounder and inaugural president of the Arkansas state chapter of the Society of Hospital Medicine.
Grace Farris, MD, recently accepted a position with the division of hospital medicine at the Dell Medical School in Austin where she will be an assistant professor of internal medicine, as well as a working hospitalist.
Dr. Farris worked as chief of hospital medicine at Mount Sinai West Hospital in Manhattan from January 2017 until accepting her new position with Dell. In addition, she publishes a monthly comics column in the Annals of Internal Medicine.
Her visual storytelling through comics has appeared in several media outlets, and she has penned literal columns as well, including one recently in the New York Times about living apart from her children while treating COVID-19 patients in the emergency room.
Dell Medical School has also named a new division chief of hospital medicine. Read Pierce, MD, made the move to Texas from the University of Colorado at Denver, Aurora. Dr. Pierce will also serve as associate chair of faculty development of internal medicine at Dell. He is eager to build on his experience and passion for developing people, creating outstanding culture, and changing complex systems in innovative, sustainable ways.
Dr. Pierce worked at University of Colorado for the past 8 years, serving as the associate director of the school’s Institute for Healthcare Quality, Safety and Efficiency (IHQSE), a program he co-founded. Prior to that, Dr. Pierce was chief resident at the University of San Francisco medical school and later founded the hospital medicine center at the San Francisco VA Medical Center.
Gurinder Kaur, MD, was recently named medical director of the Health Hospitalist Program at St. Joseph’s Health Rome (N.Y.) Memorial Hospital. Dr. Kaur’s focus will be on improving infrastructure to allow for the highest quality of care possible. She will oversee the facility’s crew of eight hospitalists, who rotate to be available 24 hours per day.
Dr. Kaur comes to Rome from St. Joseph’s Health in Syracuse, N.Y., where she was chief resident and a member of the hospitalist team.
Colin McMahon, MD, was recently appointed chief of hospital medicine at Eastern Niagara Hospital in Lockport, N.Y., where he will oversee the hospitalist program. He comes to ENH after serving as medical director of hospital operations at Buffalo (N.Y.) General Medical Center.
Dr. McMahon has worked in medicine for a quarter of a century. He also is the president and founder of Dimensions of Internal Medicine and Pediatric Care, PC (DMP). Associates from DMP Medicine make up the hospitalist team at ENH.
Sam Antonios, MD, has been promoted to chief clinical officer of Ascension Kansas, the parent group of Ascension Via Christi Hospital in Wichita, where Dr. Antonios has served as chief medical officer for the past 4 years. Dr. Antonios has emerged as a leader within Ascension Kansas during the COVID-19 pandemic.
Prior to his appointment at Via Christi, he worked at that facility as a hospitalist and as medical director of information systems. Dr. Antonios is a board-certified internist.
Bret J. Rudy, MD, was named a Top 25 Healthcare Innovator by Modern Healthcare magazine. Dr. Rudy is chief of hospital operations and senior vice president at NYU Langone Hospital-Brooklyn in New York, and the magazine cited his efforts in elevating the quality, safety, and accountability of the facility, which merged with NYU Langone Health in 2016.
Dr. Rudy has established a 24-hour hospitalist service, added full-time emergency faculty, and reduced hospital wait times, among other patient-experience benchmarks, since his appointment at Langone-Brooklyn.
Dr. Rudy is a board-certified pediatrician who has served on the National Institutes of Health’s HIV research networks, including a spot on the White House Advisory Committee on Adolescents for the Office of National AIDS Policy.
Nasim Afsar, MD, MBA, SFHM, a past president of SHM, was recently named chief operating officer at UCI Health in Orange, Calif. Dr. Afsar served previously as chief ambulatory officer and chief medical officer for accountable care organizations at UCI Health.
Anthony J. Macchiavelli, MD, FHM, was recognized by Continental Who’s Who as a “Top Distinguished Hospitalist” with AtlantiCare Regional Medical Center, in Atlantic City, N.J. He has been with AtlantiCare for the past ten years, and currently serves as medical director for the PACE program, as well as medical director for the Anticoagulation Clinic.
Dr. Macchiavelli has been involved in the development of 3 different hospital medicine programs throughout his career and was the founder of the Associates in Hospital Medicine program at Methodist Division of Thomas Jefferson University Hospitals. He serves as a mentor for SHM’s VTE-FAST Program, and has served on the Standards Review Panel for the Joint Commission developing the National Patient Safety Goal for anticoagulation therapy.
Erin Shaughnessy, MD, assumed the role of director of pediatric hospital medicine at the University of Alabama at Birmingham and Children’s of Alabama, also in Birmingham, on Sept. 1. Dr. Shaughnessy has done research in improving outcomes in hospitalized children, as well as improving communication between physicians and pediatric patients’ families during care transitions.
Prior to joining UAB and Children’s of Alabama, Dr. Shaughnessy was division chief of hospital medicine at Phoenix (Ariz.) Children’s Hospital while also serving as an associate professor at the University of Arizona, Phoenix.
Chandra Lingisetty, MD, MBA, MHCM, was recently named chief administrative officer for Baptist Health Physician Partners, Arkansas. BHPP is Baptist Health’s clinically integrated network (CIN) with more than 1,600 providers across the state.
Baptist Health Arkansas is the state’s largest not for profit health system with 12 hospitals, hundreds of provider clinics, a nursing school, and a graduate medical education residency program. Prior to his promotion, he worked in Baptist Health System as a hospitalist for 10 years, served on the board of managers at BHPP, and strategized COVID-19 care management protocols and medical staff preparedness as part of surge planning and capacity expansion. In his new role, he is focused on leading the clinically integrated network toward value-based care. He is also the cofounder and inaugural president of the Arkansas state chapter of the Society of Hospital Medicine.
Grace Farris, MD, recently accepted a position with the division of hospital medicine at the Dell Medical School in Austin where she will be an assistant professor of internal medicine, as well as a working hospitalist.
Dr. Farris worked as chief of hospital medicine at Mount Sinai West Hospital in Manhattan from January 2017 until accepting her new position with Dell. In addition, she publishes a monthly comics column in the Annals of Internal Medicine.
Her visual storytelling through comics has appeared in several media outlets, and she has penned literal columns as well, including one recently in the New York Times about living apart from her children while treating COVID-19 patients in the emergency room.
Dell Medical School has also named a new division chief of hospital medicine. Read Pierce, MD, made the move to Texas from the University of Colorado at Denver, Aurora. Dr. Pierce will also serve as associate chair of faculty development of internal medicine at Dell. He is eager to build on his experience and passion for developing people, creating outstanding culture, and changing complex systems in innovative, sustainable ways.
Dr. Pierce worked at University of Colorado for the past 8 years, serving as the associate director of the school’s Institute for Healthcare Quality, Safety and Efficiency (IHQSE), a program he co-founded. Prior to that, Dr. Pierce was chief resident at the University of San Francisco medical school and later founded the hospital medicine center at the San Francisco VA Medical Center.
Gurinder Kaur, MD, was recently named medical director of the Health Hospitalist Program at St. Joseph’s Health Rome (N.Y.) Memorial Hospital. Dr. Kaur’s focus will be on improving infrastructure to allow for the highest quality of care possible. She will oversee the facility’s crew of eight hospitalists, who rotate to be available 24 hours per day.
Dr. Kaur comes to Rome from St. Joseph’s Health in Syracuse, N.Y., where she was chief resident and a member of the hospitalist team.
Colin McMahon, MD, was recently appointed chief of hospital medicine at Eastern Niagara Hospital in Lockport, N.Y., where he will oversee the hospitalist program. He comes to ENH after serving as medical director of hospital operations at Buffalo (N.Y.) General Medical Center.
Dr. McMahon has worked in medicine for a quarter of a century. He also is the president and founder of Dimensions of Internal Medicine and Pediatric Care, PC (DMP). Associates from DMP Medicine make up the hospitalist team at ENH.
Sam Antonios, MD, has been promoted to chief clinical officer of Ascension Kansas, the parent group of Ascension Via Christi Hospital in Wichita, where Dr. Antonios has served as chief medical officer for the past 4 years. Dr. Antonios has emerged as a leader within Ascension Kansas during the COVID-19 pandemic.
Prior to his appointment at Via Christi, he worked at that facility as a hospitalist and as medical director of information systems. Dr. Antonios is a board-certified internist.
Bret J. Rudy, MD, was named a Top 25 Healthcare Innovator by Modern Healthcare magazine. Dr. Rudy is chief of hospital operations and senior vice president at NYU Langone Hospital-Brooklyn in New York, and the magazine cited his efforts in elevating the quality, safety, and accountability of the facility, which merged with NYU Langone Health in 2016.
Dr. Rudy has established a 24-hour hospitalist service, added full-time emergency faculty, and reduced hospital wait times, among other patient-experience benchmarks, since his appointment at Langone-Brooklyn.
Dr. Rudy is a board-certified pediatrician who has served on the National Institutes of Health’s HIV research networks, including a spot on the White House Advisory Committee on Adolescents for the Office of National AIDS Policy.
Nasim Afsar, MD, MBA, SFHM, a past president of SHM, was recently named chief operating officer at UCI Health in Orange, Calif. Dr. Afsar served previously as chief ambulatory officer and chief medical officer for accountable care organizations at UCI Health.
Anthony J. Macchiavelli, MD, FHM, was recognized by Continental Who’s Who as a “Top Distinguished Hospitalist” with AtlantiCare Regional Medical Center, in Atlantic City, N.J. He has been with AtlantiCare for the past ten years, and currently serves as medical director for the PACE program, as well as medical director for the Anticoagulation Clinic.
Dr. Macchiavelli has been involved in the development of 3 different hospital medicine programs throughout his career and was the founder of the Associates in Hospital Medicine program at Methodist Division of Thomas Jefferson University Hospitals. He serves as a mentor for SHM’s VTE-FAST Program, and has served on the Standards Review Panel for the Joint Commission developing the National Patient Safety Goal for anticoagulation therapy.
TNF inhibitor–induced psoriasis treatment algorithm maintains TNF inhibitor if possible
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Is a pelvic examination necessary 6 weeks after hysterectomy?
Doctors commonly perform pelvic examinations approximately 6 weeks following hysterectomy to assess the integrity of the vaginal cuff. But this practice may not be necessary if patients do not have symptoms, a study suggests.
“The 6-week posthysterectomy pelvic examination in asymptomatic women may not be necessary, as it neither detected cuff dehiscence nor negated future risk for dehiscence,” Ritchie Mae Delara, MD, said at the meeting sponsored by AAGL, held virtually this year.
Dr. Delara, of the Mayo Clinic in Phoenix, and colleagues conducted a retrospective cohort study of data from more than 2,000 patients to assess the utility of the 6-week posthysterectomy pelvic examination in detecting cuff dehiscence in asymptomatic women.
An unpredictable complication
Vaginal cuff dehiscence is a rare complication of hysterectomy that can occur days or decades after surgery, which makes “identifying an optimal time for cuff evaluation difficult,” Dr. Delara said. “Currently there is neither evidence demonstrating benefit of routine posthysterectomy examination in detecting vaginal cuff dehiscence, nor data demonstrating the best time to perform posthysterectomy examination.”
For their study, which was also published in the Journal of Minimally Invasive Gynecology, the researchers examined data from 2,051 women who underwent hysterectomy at a single institution during a 6-year period. Patients received at least one postoperative evaluation within 90 days of surgery. Examination of the vaginal cuff routinely was performed approximately 6 weeks after hysterectomy. Patients’ posthysterectomy symptoms and pelvic examination findings were recorded.
About 80% of patients were asymptomatic at the 6-week visit.
Asymptomatic patients were more likely to have normal pelvic examination findings, compared with patients with posthysterectomy symptoms (86.4% vs. 54.3%).
In all, 13 patients experienced complete cuff dehiscence. All of them had an intact vaginal cuff at their 6-week examination. Three had symptoms at that time, including vaginal bleeding in one patient and pelvic pain in two patients.
One patient experienced a complete cuff dehiscence that was provoked by intercourse prior to her examination. The patient subsequently developed two additional episodes of dehiscence provoked by intercourse.
Dehiscence may present differently after benign and oncologic hysterectomies, the study indicated.
Eight patients who experienced complete cuff dehiscence after benign hysterectomy had symptoms such as pelvic pain and vaginal bleeding at the time of presentation for dehiscence, which mainly occurred after intercourse.
Five patients who experienced dehiscence after oncologic hysterectomy were more likely to present without symptoms or provocation.
The median time to dehiscence after benign hysterectomy was about 19 weeks, whereas the median time to dehiscence after oncologic hysterectomy was about 81 weeks.
Surgeons should educate patients about symptoms of dehiscence and the potential for events such as coitus to provoke its occurrence, and patients should promptly seek evaluation if symptoms occur, Dr. Delara said.
Patients with risk factors such as malignancy may benefit from continued routine evaluation, she added.
Timely research
The findings may be especially relevant during the COVID-19 pandemic, when states have issued shelter-in-place orders and doctors have increased their use of telemedicine to reduce in-person visits, Dr. Delara noted.
In that sense, the study is “extremely timely” and may inform and support practice changes, commented Emad Mikhail, MD, in a discussion following the research presentation.
Whether the results generalize to other centers, including smaller centers that perform fewer surgeries, is unclear, said Dr. Mikhail, of the University of South Florida, Tampa.
“It takes vision and critical thinking to challenge these traditional practices,” he said. “I applaud Dr. Delara for challenging one of these.”
Dr. Delara and Dr. Mikhail had no relevant disclosures.
SOURCE: Delara RMM et al. J Minim Invasive Gynecol. 2020 Nov 1. doi: 10.1016/j.jmig.2020.08.306.
Doctors commonly perform pelvic examinations approximately 6 weeks following hysterectomy to assess the integrity of the vaginal cuff. But this practice may not be necessary if patients do not have symptoms, a study suggests.
“The 6-week posthysterectomy pelvic examination in asymptomatic women may not be necessary, as it neither detected cuff dehiscence nor negated future risk for dehiscence,” Ritchie Mae Delara, MD, said at the meeting sponsored by AAGL, held virtually this year.
Dr. Delara, of the Mayo Clinic in Phoenix, and colleagues conducted a retrospective cohort study of data from more than 2,000 patients to assess the utility of the 6-week posthysterectomy pelvic examination in detecting cuff dehiscence in asymptomatic women.
An unpredictable complication
Vaginal cuff dehiscence is a rare complication of hysterectomy that can occur days or decades after surgery, which makes “identifying an optimal time for cuff evaluation difficult,” Dr. Delara said. “Currently there is neither evidence demonstrating benefit of routine posthysterectomy examination in detecting vaginal cuff dehiscence, nor data demonstrating the best time to perform posthysterectomy examination.”
For their study, which was also published in the Journal of Minimally Invasive Gynecology, the researchers examined data from 2,051 women who underwent hysterectomy at a single institution during a 6-year period. Patients received at least one postoperative evaluation within 90 days of surgery. Examination of the vaginal cuff routinely was performed approximately 6 weeks after hysterectomy. Patients’ posthysterectomy symptoms and pelvic examination findings were recorded.
About 80% of patients were asymptomatic at the 6-week visit.
Asymptomatic patients were more likely to have normal pelvic examination findings, compared with patients with posthysterectomy symptoms (86.4% vs. 54.3%).
In all, 13 patients experienced complete cuff dehiscence. All of them had an intact vaginal cuff at their 6-week examination. Three had symptoms at that time, including vaginal bleeding in one patient and pelvic pain in two patients.
One patient experienced a complete cuff dehiscence that was provoked by intercourse prior to her examination. The patient subsequently developed two additional episodes of dehiscence provoked by intercourse.
Dehiscence may present differently after benign and oncologic hysterectomies, the study indicated.
Eight patients who experienced complete cuff dehiscence after benign hysterectomy had symptoms such as pelvic pain and vaginal bleeding at the time of presentation for dehiscence, which mainly occurred after intercourse.
Five patients who experienced dehiscence after oncologic hysterectomy were more likely to present without symptoms or provocation.
The median time to dehiscence after benign hysterectomy was about 19 weeks, whereas the median time to dehiscence after oncologic hysterectomy was about 81 weeks.
Surgeons should educate patients about symptoms of dehiscence and the potential for events such as coitus to provoke its occurrence, and patients should promptly seek evaluation if symptoms occur, Dr. Delara said.
Patients with risk factors such as malignancy may benefit from continued routine evaluation, she added.
Timely research
The findings may be especially relevant during the COVID-19 pandemic, when states have issued shelter-in-place orders and doctors have increased their use of telemedicine to reduce in-person visits, Dr. Delara noted.
In that sense, the study is “extremely timely” and may inform and support practice changes, commented Emad Mikhail, MD, in a discussion following the research presentation.
Whether the results generalize to other centers, including smaller centers that perform fewer surgeries, is unclear, said Dr. Mikhail, of the University of South Florida, Tampa.
“It takes vision and critical thinking to challenge these traditional practices,” he said. “I applaud Dr. Delara for challenging one of these.”
Dr. Delara and Dr. Mikhail had no relevant disclosures.
SOURCE: Delara RMM et al. J Minim Invasive Gynecol. 2020 Nov 1. doi: 10.1016/j.jmig.2020.08.306.
Doctors commonly perform pelvic examinations approximately 6 weeks following hysterectomy to assess the integrity of the vaginal cuff. But this practice may not be necessary if patients do not have symptoms, a study suggests.
“The 6-week posthysterectomy pelvic examination in asymptomatic women may not be necessary, as it neither detected cuff dehiscence nor negated future risk for dehiscence,” Ritchie Mae Delara, MD, said at the meeting sponsored by AAGL, held virtually this year.
Dr. Delara, of the Mayo Clinic in Phoenix, and colleagues conducted a retrospective cohort study of data from more than 2,000 patients to assess the utility of the 6-week posthysterectomy pelvic examination in detecting cuff dehiscence in asymptomatic women.
An unpredictable complication
Vaginal cuff dehiscence is a rare complication of hysterectomy that can occur days or decades after surgery, which makes “identifying an optimal time for cuff evaluation difficult,” Dr. Delara said. “Currently there is neither evidence demonstrating benefit of routine posthysterectomy examination in detecting vaginal cuff dehiscence, nor data demonstrating the best time to perform posthysterectomy examination.”
For their study, which was also published in the Journal of Minimally Invasive Gynecology, the researchers examined data from 2,051 women who underwent hysterectomy at a single institution during a 6-year period. Patients received at least one postoperative evaluation within 90 days of surgery. Examination of the vaginal cuff routinely was performed approximately 6 weeks after hysterectomy. Patients’ posthysterectomy symptoms and pelvic examination findings were recorded.
About 80% of patients were asymptomatic at the 6-week visit.
Asymptomatic patients were more likely to have normal pelvic examination findings, compared with patients with posthysterectomy symptoms (86.4% vs. 54.3%).
In all, 13 patients experienced complete cuff dehiscence. All of them had an intact vaginal cuff at their 6-week examination. Three had symptoms at that time, including vaginal bleeding in one patient and pelvic pain in two patients.
One patient experienced a complete cuff dehiscence that was provoked by intercourse prior to her examination. The patient subsequently developed two additional episodes of dehiscence provoked by intercourse.
Dehiscence may present differently after benign and oncologic hysterectomies, the study indicated.
Eight patients who experienced complete cuff dehiscence after benign hysterectomy had symptoms such as pelvic pain and vaginal bleeding at the time of presentation for dehiscence, which mainly occurred after intercourse.
Five patients who experienced dehiscence after oncologic hysterectomy were more likely to present without symptoms or provocation.
The median time to dehiscence after benign hysterectomy was about 19 weeks, whereas the median time to dehiscence after oncologic hysterectomy was about 81 weeks.
Surgeons should educate patients about symptoms of dehiscence and the potential for events such as coitus to provoke its occurrence, and patients should promptly seek evaluation if symptoms occur, Dr. Delara said.
Patients with risk factors such as malignancy may benefit from continued routine evaluation, she added.
Timely research
The findings may be especially relevant during the COVID-19 pandemic, when states have issued shelter-in-place orders and doctors have increased their use of telemedicine to reduce in-person visits, Dr. Delara noted.
In that sense, the study is “extremely timely” and may inform and support practice changes, commented Emad Mikhail, MD, in a discussion following the research presentation.
Whether the results generalize to other centers, including smaller centers that perform fewer surgeries, is unclear, said Dr. Mikhail, of the University of South Florida, Tampa.
“It takes vision and critical thinking to challenge these traditional practices,” he said. “I applaud Dr. Delara for challenging one of these.”
Dr. Delara and Dr. Mikhail had no relevant disclosures.
SOURCE: Delara RMM et al. J Minim Invasive Gynecol. 2020 Nov 1. doi: 10.1016/j.jmig.2020.08.306.
FROM AAGL GLOBAL CONGRESS






