User login
Widespread liver disease missed in patients with T2D
Among these calls is a pending statement from the Endocrine Society, the American Association of Clinical Endocrinologists, the American Gastroenterology Association, and other groups on what the growing appreciation of highly prevalent liver disease in patients with type 2 diabetes (T2D) means for assessing and managing patients. Publication of the statement is expected by spring 2021, said Christos S. Mantzoros, MD, DSc, PhD, chief of endocrinology for the Veterans Affairs Boston Healthcare System and a representative from the Endocrine Society to the statement-writing panel.
This upcoming “Call to Action” from these groups argues for a “need to collaborate across disciplines, and work together on establishing clinical guidelines, and creating new diagnostics and therapeutics,” said Dr. Mantzoros in an interview.
“Over time, it is becoming clearer that management of NAFLD [nonalcoholic fatty liver disease]/NASH [nonalcoholic steatohepatitis] requires a multidisciplinary panel of doctors ranging from primary care practitioners, to endocrinologists, and hepatologists. Given that the nature of the disease crosses scientific discipline boundaries, and that the number of patients is so large (it is estimated that about one in four U.S. adults have NAFLD), not all patients can be treated at the limited number of hepatology centers.
“However, not all stakeholders have fully realized this fact, and no effort had been undertaken so far by any professional society to develop a coordinated approach and clinical care pathway for NAFLD/NASH. The ‘Call to Action’ meeting can be considered as a starting point for such an important effort,” said Dr. Mantzoros, who is also a professor of medicine at Harvard Medical School and director of the human nutrition unit at Beth Israel Deaconess Medical Center, both in Boston.
Dramatic prevalence rates in patients with T2D
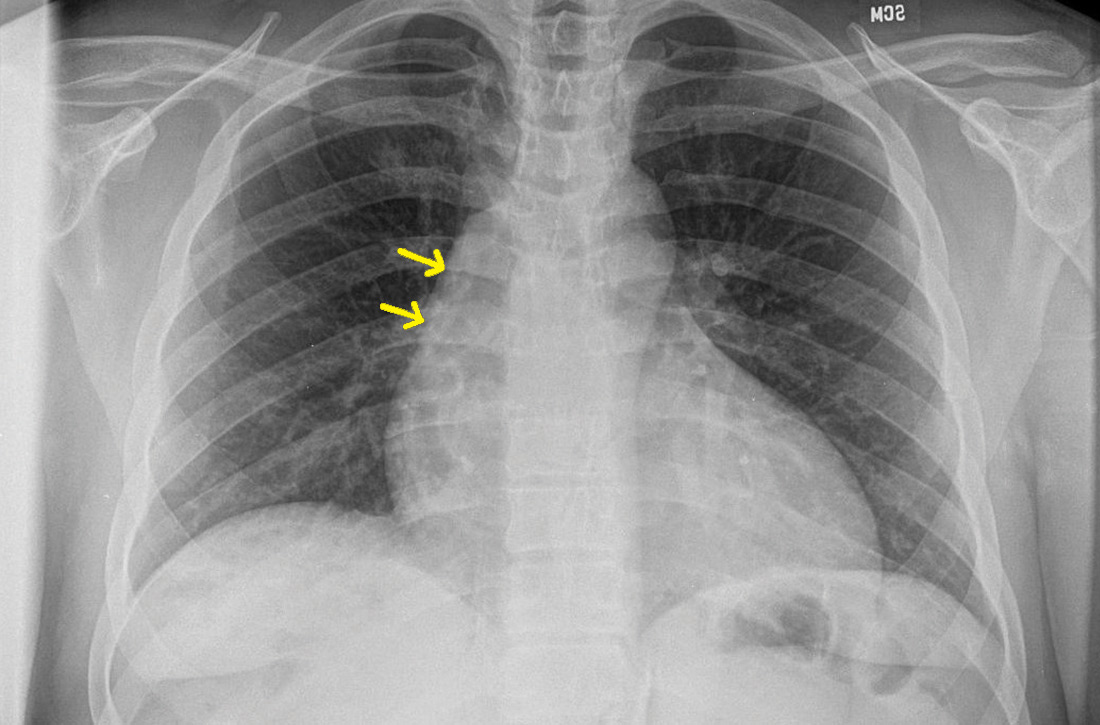
Results from two independent epidemiology reports, published in December 2020, documented steatosis (the fatty liver of NAFLD) in 70%-74% of unselected U.S. patients with T2D, advanced liver fibrosis accompanying this disease in 6%-15%, and previously unrecognized cirrhosis in 3%-8%.
One of these reports analyzed 825 patients with T2D included in the National Health and Nutritional Examination Survey of 2017-2018 run by the Centers for Disease Control and Prevention. All these patients, selected to be representative of the overall U.S. adult population with T2D, underwent transient elastography to identify steatosis and fibrosis, the first U.S. National Health Survey to run this type of population-based survey. The results showed an overall steatosis prevalence of 74% with grade 3 steatosis in 58%, advanced liver fibrosis in 15%, and cirrhosis in 8%, reported the team of Italian researchers who analyzed the data .
The second study focused on a single-center series of 561 patients with T2D who also underwent screening by transient elastography during 2018-2020 and had no history of NAFLD or other liver disease, or alcohol abuse. The imaging results showed a NAFLD prevalence of 70%, with 54% of the entire group diagnosed with severe steatosis, severe fibrosis in 6%, and cirrhosis in 3%. Among the 54% of patients with severe steatosis, 30% also had severe liver fibrosis. About 70% of the 561 patients assessed came from either the family medicine or general internal medicine clinics of the University of Florida, Gainesville, with the remaining 30% enrolled from the center’s endocrinology/diabetes outpatient clinic.
Neither report documented a NASH prevalence, which cannot receive definitive diagnosis by imaging alone. “This is the first study of its kind in the U.S. to establish the magnitude of [liver] disease burden in random patients with T2D seeking regular outpatient care,” wrote the University of Florida research team, led by Kenneth Cusi, MD, professor and chief of the university’s division of endocrinology, diabetes, and metabolism. Their finding that patients with T2D and previously unknown to have NAFLD had a 15% prevalence of moderate or advanced liver fibrosis “should trigger a call to action by all clinicians taking care of patients with T2D. Patient and physician awareness of the hepatic and extrahepatic complications of NASH, and reversing current diagnosis and treatment inertia will be the only way to avert the looming epidemic of cirrhosis in patients with diabetes.”
“Endocrinologists don’t ‘see’ NAFLD and NASH” in their patients with T2D “ because they don’t think about it,” Dr. Mantzoros declared.
“Why is NASH underdiagnosed and undertreated? Because many physicians aren’t aware of it,” agreed Dr. Cusi during a talk in December 2020 at the 18th World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease (WCIRDC). “You never find what you don’t look for.”
“Endocrinologists should do the tests for NASH [in patients with T2D], but we’re all guilty of not doing it enough,” Tracey McLaughlin, MD, an endocrinologist and professor of medicine at Stanford (Calif.) University, commented during the WCIRDC.
These prevalence numbers demand that clinicians suspect liver disease “in any patient with diabetes, especially patients with obesity who are older and have components of metabolic syndrome,” said Dr. Mantzoros. “We need to screen, refer the most advanced cases, and treat the early- and mid-stage cases.”
How to find NASH
Both the American Diabetes Association and the European Association for the Study of Diabetes call for routine screening of patients with T2D, starting with a check of liver enzymes, such as ALT, but no clear consensus exists for the specifics of screening beyond that. Dr. Mantzoros, Dr. Cusi, and other experts agree that the scheme for assessing liver disease in patients with T2D starts with regular monitoring of elevations in liver enzymes including ALT. Next is noninvasive ultrasound assessment of the extent of liver fibrosis inferred from the organ’s stiffness using transient elastography. Another frequently cited initial screening tool is the Fibrosis-4 (FIB-4) score, which incorporates a patient’s age, platelet count, and levels of ALT and a second liver enzyme, AST.
“There is more consensus about FIB-4 and then elastography, but some people use tests other than FIB-4. Unfortunately there is no perfect diagnostic test today. A top priority is to define the best diagnostic test,” said Dr. Mantzoros, who is leading an effort to try to refine screening using artificial intelligence.
“FIB-4 is simple, easy, and well validated,” commented Dr. Cusi during the WCIRDC last December. “FIB-4 and elastography should get you pretty close” to identifying patients with T2D and significant liver disease.
But in a recent editorial, Dr. Cusi agreed on the need for “more reliable tests for the diagnosis of NASH and advanced fibrosis in patients with T2D. Significant work is being done in the field to validate novel and more sophisticated fibrosis biomarkers. Future studies will help us enter a new era of precision medicine where biomarkers will identify and target therapy to those with more active disease at risk for cirrhosis,” he wrote.
“The ultimate goal is to diagnose fibrosis at an early stage to prevent people from developing cirrhosis,” Dr. Cusi said in a recent written statement. “We’re trying to identify these problems before they’re unfixable. Once someone has cirrhosis, there isn’t a whole lot you can do.”
Pioglitazone remains the best-documented treatment
Perhaps some of the inertia in diagnosing NAFLD, NASH, and liver fibrosis in patients with T2D is dissatisfaction with current treatment options, although several proven options exist, notably weight loss and diet, and thiazolidinedione (TZD) pioglitazone. But weight loss and diet pose issues for patient compliance and durability of the intervention, and many clinicians consider pioglitazone flawed by its potential adverse effects.
“When we don’t have an established treatment for something, we tend to not measure it or go after it. That’s been true of liver disease” in patients with T2D, said Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of the Metabolic Institute of America in Tarzana, Calif., during the WCIRDC.
Treatment with pioglitazone has resolved NASH in about a third of patients compared with placebo, prevented fibrosis progression, and cut cardiovascular disease events, noted Dr. Cusi during the WCIRDC.
“Pioglitazone is used in only 8% of patients with T2D, or less, but we need to use it more often because of its proven efficacy in patients with T2D and NASH” said Dr. Mantzoros. “The problem is that pioglitazone has side effects, including weight gain and fluid retention, that makes it less attractive unless one thinks about the diagnosis of NASH.”
Others highlight that the adverse effects of pioglitazone have been either misunderstood, or can be effectively minimized with careful dosing.
“The data with the TZDs are much stronger than the data from anything else. TZDs have gotten a bad name because they also work in the kidney and enhance fluid reabsorption. We use modest dosages of pioglitazone, 15 mg or 30 mg a day, to avoid excess fluid retention,” Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio, said during the WCIRDC. “The best drug for NASH is pioglitazone. No other drug beats it” based on current data, Dr. DeFronzo asserted.
Other strategies include the potential to pair pioglitazone with other interventions that can blunt a weight-gain effect. One intriguing combination would combine pioglitazone with a GLP-1 receptor agonist, a drug class that can produce significant weight loss. Results from a phase 2 study showed promise for semaglutide (Rybelsus) in treating patients with NASH.
Getting the name right
Another factor that may be keeping NAFLD and NASH from achieving a higher profile for patients with T2D are those names, which focus on what the diseases are not – nonalcoholic – rather than what they are.
A series of recent publications in both the endocrinology and hepatology literature have called for renaming these disorders either “metabolic (dysfunction)–associated fatty liver disease (MALFD)”, or “dysmetabolism-associated fatty liver disease (DALFD)”.
“The names NAFLD and NASH indicate absence of alcohol as a cause, but the disease is also characterized by the absence of other causes, such as autoimmune disorders or hepatitis. The names were coined when we did not know much about these diseases. We now know that it is dysmetabolism that causes these conditions, and so we need to adopt a new, more accurate name,” explained Dr. Mantzoros, who has published support for a name change.
While many agree, some have raised concerns as to whether a name change now is premature. A group of hepatologists recently published a rebuttal to an immediate name change , saying that, “although we are in agreement that metabolic fatty liver disease may more accurately and positively reflect the relevant risk factors better than the age-old term nonalcoholic fatty liver disease, the term still leaves a great deal of ambiguity. A name change will be appropriate when informed by a new understanding of the molecular basis of the disease entity, insights that fundamentally change risk stratification, or other important aspects of the disease. We may be on the cusp of this, but we are not there yet.”
Dr. Mantzoros agreed, but for somewhat different reasons.
“We need to be careful and deliberate, because there is a significant body of knowledge and a lot of data from clinical trials collected using the old definitions. We need to find an appropriate time frame for a [name] transition. We need to find a nice and robust way to productively bridge the old to the new,” he said. “We also need new diagnostic criteria, and new therapies. A new name and definition will facilitate progress.”
Dr. Mantzoros been a shareholder of and consultant to Coherus and Pangea, he has been a consultant to AstraZeneca, Eisai, Genfit, Intercept, Novo Nordisk, P.E.S., and Regeneron, and has received travel support from the Metabolic Institute of America and the California Walnut Commission. Dr. Cusi has been a consultant to and has received research funding from numerous drug companies. Dr. McLaughlin is a consultant to January AI. Dr. Handelsman has been a consultant to numerous drug companies. Dr. DeFronzo received research grants from AstraZeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk.
Among these calls is a pending statement from the Endocrine Society, the American Association of Clinical Endocrinologists, the American Gastroenterology Association, and other groups on what the growing appreciation of highly prevalent liver disease in patients with type 2 diabetes (T2D) means for assessing and managing patients. Publication of the statement is expected by spring 2021, said Christos S. Mantzoros, MD, DSc, PhD, chief of endocrinology for the Veterans Affairs Boston Healthcare System and a representative from the Endocrine Society to the statement-writing panel.
This upcoming “Call to Action” from these groups argues for a “need to collaborate across disciplines, and work together on establishing clinical guidelines, and creating new diagnostics and therapeutics,” said Dr. Mantzoros in an interview.
“Over time, it is becoming clearer that management of NAFLD [nonalcoholic fatty liver disease]/NASH [nonalcoholic steatohepatitis] requires a multidisciplinary panel of doctors ranging from primary care practitioners, to endocrinologists, and hepatologists. Given that the nature of the disease crosses scientific discipline boundaries, and that the number of patients is so large (it is estimated that about one in four U.S. adults have NAFLD), not all patients can be treated at the limited number of hepatology centers.
“However, not all stakeholders have fully realized this fact, and no effort had been undertaken so far by any professional society to develop a coordinated approach and clinical care pathway for NAFLD/NASH. The ‘Call to Action’ meeting can be considered as a starting point for such an important effort,” said Dr. Mantzoros, who is also a professor of medicine at Harvard Medical School and director of the human nutrition unit at Beth Israel Deaconess Medical Center, both in Boston.
Dramatic prevalence rates in patients with T2D
Results from two independent epidemiology reports, published in December 2020, documented steatosis (the fatty liver of NAFLD) in 70%-74% of unselected U.S. patients with T2D, advanced liver fibrosis accompanying this disease in 6%-15%, and previously unrecognized cirrhosis in 3%-8%.
One of these reports analyzed 825 patients with T2D included in the National Health and Nutritional Examination Survey of 2017-2018 run by the Centers for Disease Control and Prevention. All these patients, selected to be representative of the overall U.S. adult population with T2D, underwent transient elastography to identify steatosis and fibrosis, the first U.S. National Health Survey to run this type of population-based survey. The results showed an overall steatosis prevalence of 74% with grade 3 steatosis in 58%, advanced liver fibrosis in 15%, and cirrhosis in 8%, reported the team of Italian researchers who analyzed the data .
The second study focused on a single-center series of 561 patients with T2D who also underwent screening by transient elastography during 2018-2020 and had no history of NAFLD or other liver disease, or alcohol abuse. The imaging results showed a NAFLD prevalence of 70%, with 54% of the entire group diagnosed with severe steatosis, severe fibrosis in 6%, and cirrhosis in 3%. Among the 54% of patients with severe steatosis, 30% also had severe liver fibrosis. About 70% of the 561 patients assessed came from either the family medicine or general internal medicine clinics of the University of Florida, Gainesville, with the remaining 30% enrolled from the center’s endocrinology/diabetes outpatient clinic.
Neither report documented a NASH prevalence, which cannot receive definitive diagnosis by imaging alone. “This is the first study of its kind in the U.S. to establish the magnitude of [liver] disease burden in random patients with T2D seeking regular outpatient care,” wrote the University of Florida research team, led by Kenneth Cusi, MD, professor and chief of the university’s division of endocrinology, diabetes, and metabolism. Their finding that patients with T2D and previously unknown to have NAFLD had a 15% prevalence of moderate or advanced liver fibrosis “should trigger a call to action by all clinicians taking care of patients with T2D. Patient and physician awareness of the hepatic and extrahepatic complications of NASH, and reversing current diagnosis and treatment inertia will be the only way to avert the looming epidemic of cirrhosis in patients with diabetes.”
“Endocrinologists don’t ‘see’ NAFLD and NASH” in their patients with T2D “ because they don’t think about it,” Dr. Mantzoros declared.
“Why is NASH underdiagnosed and undertreated? Because many physicians aren’t aware of it,” agreed Dr. Cusi during a talk in December 2020 at the 18th World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease (WCIRDC). “You never find what you don’t look for.”
“Endocrinologists should do the tests for NASH [in patients with T2D], but we’re all guilty of not doing it enough,” Tracey McLaughlin, MD, an endocrinologist and professor of medicine at Stanford (Calif.) University, commented during the WCIRDC.
These prevalence numbers demand that clinicians suspect liver disease “in any patient with diabetes, especially patients with obesity who are older and have components of metabolic syndrome,” said Dr. Mantzoros. “We need to screen, refer the most advanced cases, and treat the early- and mid-stage cases.”
How to find NASH
Both the American Diabetes Association and the European Association for the Study of Diabetes call for routine screening of patients with T2D, starting with a check of liver enzymes, such as ALT, but no clear consensus exists for the specifics of screening beyond that. Dr. Mantzoros, Dr. Cusi, and other experts agree that the scheme for assessing liver disease in patients with T2D starts with regular monitoring of elevations in liver enzymes including ALT. Next is noninvasive ultrasound assessment of the extent of liver fibrosis inferred from the organ’s stiffness using transient elastography. Another frequently cited initial screening tool is the Fibrosis-4 (FIB-4) score, which incorporates a patient’s age, platelet count, and levels of ALT and a second liver enzyme, AST.
“There is more consensus about FIB-4 and then elastography, but some people use tests other than FIB-4. Unfortunately there is no perfect diagnostic test today. A top priority is to define the best diagnostic test,” said Dr. Mantzoros, who is leading an effort to try to refine screening using artificial intelligence.
“FIB-4 is simple, easy, and well validated,” commented Dr. Cusi during the WCIRDC last December. “FIB-4 and elastography should get you pretty close” to identifying patients with T2D and significant liver disease.
But in a recent editorial, Dr. Cusi agreed on the need for “more reliable tests for the diagnosis of NASH and advanced fibrosis in patients with T2D. Significant work is being done in the field to validate novel and more sophisticated fibrosis biomarkers. Future studies will help us enter a new era of precision medicine where biomarkers will identify and target therapy to those with more active disease at risk for cirrhosis,” he wrote.
“The ultimate goal is to diagnose fibrosis at an early stage to prevent people from developing cirrhosis,” Dr. Cusi said in a recent written statement. “We’re trying to identify these problems before they’re unfixable. Once someone has cirrhosis, there isn’t a whole lot you can do.”
Pioglitazone remains the best-documented treatment
Perhaps some of the inertia in diagnosing NAFLD, NASH, and liver fibrosis in patients with T2D is dissatisfaction with current treatment options, although several proven options exist, notably weight loss and diet, and thiazolidinedione (TZD) pioglitazone. But weight loss and diet pose issues for patient compliance and durability of the intervention, and many clinicians consider pioglitazone flawed by its potential adverse effects.
“When we don’t have an established treatment for something, we tend to not measure it or go after it. That’s been true of liver disease” in patients with T2D, said Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of the Metabolic Institute of America in Tarzana, Calif., during the WCIRDC.
Treatment with pioglitazone has resolved NASH in about a third of patients compared with placebo, prevented fibrosis progression, and cut cardiovascular disease events, noted Dr. Cusi during the WCIRDC.
“Pioglitazone is used in only 8% of patients with T2D, or less, but we need to use it more often because of its proven efficacy in patients with T2D and NASH” said Dr. Mantzoros. “The problem is that pioglitazone has side effects, including weight gain and fluid retention, that makes it less attractive unless one thinks about the diagnosis of NASH.”
Others highlight that the adverse effects of pioglitazone have been either misunderstood, or can be effectively minimized with careful dosing.
“The data with the TZDs are much stronger than the data from anything else. TZDs have gotten a bad name because they also work in the kidney and enhance fluid reabsorption. We use modest dosages of pioglitazone, 15 mg or 30 mg a day, to avoid excess fluid retention,” Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio, said during the WCIRDC. “The best drug for NASH is pioglitazone. No other drug beats it” based on current data, Dr. DeFronzo asserted.
Other strategies include the potential to pair pioglitazone with other interventions that can blunt a weight-gain effect. One intriguing combination would combine pioglitazone with a GLP-1 receptor agonist, a drug class that can produce significant weight loss. Results from a phase 2 study showed promise for semaglutide (Rybelsus) in treating patients with NASH.
Getting the name right
Another factor that may be keeping NAFLD and NASH from achieving a higher profile for patients with T2D are those names, which focus on what the diseases are not – nonalcoholic – rather than what they are.
A series of recent publications in both the endocrinology and hepatology literature have called for renaming these disorders either “metabolic (dysfunction)–associated fatty liver disease (MALFD)”, or “dysmetabolism-associated fatty liver disease (DALFD)”.
“The names NAFLD and NASH indicate absence of alcohol as a cause, but the disease is also characterized by the absence of other causes, such as autoimmune disorders or hepatitis. The names were coined when we did not know much about these diseases. We now know that it is dysmetabolism that causes these conditions, and so we need to adopt a new, more accurate name,” explained Dr. Mantzoros, who has published support for a name change.
While many agree, some have raised concerns as to whether a name change now is premature. A group of hepatologists recently published a rebuttal to an immediate name change , saying that, “although we are in agreement that metabolic fatty liver disease may more accurately and positively reflect the relevant risk factors better than the age-old term nonalcoholic fatty liver disease, the term still leaves a great deal of ambiguity. A name change will be appropriate when informed by a new understanding of the molecular basis of the disease entity, insights that fundamentally change risk stratification, or other important aspects of the disease. We may be on the cusp of this, but we are not there yet.”
Dr. Mantzoros agreed, but for somewhat different reasons.
“We need to be careful and deliberate, because there is a significant body of knowledge and a lot of data from clinical trials collected using the old definitions. We need to find an appropriate time frame for a [name] transition. We need to find a nice and robust way to productively bridge the old to the new,” he said. “We also need new diagnostic criteria, and new therapies. A new name and definition will facilitate progress.”
Dr. Mantzoros been a shareholder of and consultant to Coherus and Pangea, he has been a consultant to AstraZeneca, Eisai, Genfit, Intercept, Novo Nordisk, P.E.S., and Regeneron, and has received travel support from the Metabolic Institute of America and the California Walnut Commission. Dr. Cusi has been a consultant to and has received research funding from numerous drug companies. Dr. McLaughlin is a consultant to January AI. Dr. Handelsman has been a consultant to numerous drug companies. Dr. DeFronzo received research grants from AstraZeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk.
Among these calls is a pending statement from the Endocrine Society, the American Association of Clinical Endocrinologists, the American Gastroenterology Association, and other groups on what the growing appreciation of highly prevalent liver disease in patients with type 2 diabetes (T2D) means for assessing and managing patients. Publication of the statement is expected by spring 2021, said Christos S. Mantzoros, MD, DSc, PhD, chief of endocrinology for the Veterans Affairs Boston Healthcare System and a representative from the Endocrine Society to the statement-writing panel.
This upcoming “Call to Action” from these groups argues for a “need to collaborate across disciplines, and work together on establishing clinical guidelines, and creating new diagnostics and therapeutics,” said Dr. Mantzoros in an interview.
“Over time, it is becoming clearer that management of NAFLD [nonalcoholic fatty liver disease]/NASH [nonalcoholic steatohepatitis] requires a multidisciplinary panel of doctors ranging from primary care practitioners, to endocrinologists, and hepatologists. Given that the nature of the disease crosses scientific discipline boundaries, and that the number of patients is so large (it is estimated that about one in four U.S. adults have NAFLD), not all patients can be treated at the limited number of hepatology centers.
“However, not all stakeholders have fully realized this fact, and no effort had been undertaken so far by any professional society to develop a coordinated approach and clinical care pathway for NAFLD/NASH. The ‘Call to Action’ meeting can be considered as a starting point for such an important effort,” said Dr. Mantzoros, who is also a professor of medicine at Harvard Medical School and director of the human nutrition unit at Beth Israel Deaconess Medical Center, both in Boston.
Dramatic prevalence rates in patients with T2D
Results from two independent epidemiology reports, published in December 2020, documented steatosis (the fatty liver of NAFLD) in 70%-74% of unselected U.S. patients with T2D, advanced liver fibrosis accompanying this disease in 6%-15%, and previously unrecognized cirrhosis in 3%-8%.
One of these reports analyzed 825 patients with T2D included in the National Health and Nutritional Examination Survey of 2017-2018 run by the Centers for Disease Control and Prevention. All these patients, selected to be representative of the overall U.S. adult population with T2D, underwent transient elastography to identify steatosis and fibrosis, the first U.S. National Health Survey to run this type of population-based survey. The results showed an overall steatosis prevalence of 74% with grade 3 steatosis in 58%, advanced liver fibrosis in 15%, and cirrhosis in 8%, reported the team of Italian researchers who analyzed the data .
The second study focused on a single-center series of 561 patients with T2D who also underwent screening by transient elastography during 2018-2020 and had no history of NAFLD or other liver disease, or alcohol abuse. The imaging results showed a NAFLD prevalence of 70%, with 54% of the entire group diagnosed with severe steatosis, severe fibrosis in 6%, and cirrhosis in 3%. Among the 54% of patients with severe steatosis, 30% also had severe liver fibrosis. About 70% of the 561 patients assessed came from either the family medicine or general internal medicine clinics of the University of Florida, Gainesville, with the remaining 30% enrolled from the center’s endocrinology/diabetes outpatient clinic.
Neither report documented a NASH prevalence, which cannot receive definitive diagnosis by imaging alone. “This is the first study of its kind in the U.S. to establish the magnitude of [liver] disease burden in random patients with T2D seeking regular outpatient care,” wrote the University of Florida research team, led by Kenneth Cusi, MD, professor and chief of the university’s division of endocrinology, diabetes, and metabolism. Their finding that patients with T2D and previously unknown to have NAFLD had a 15% prevalence of moderate or advanced liver fibrosis “should trigger a call to action by all clinicians taking care of patients with T2D. Patient and physician awareness of the hepatic and extrahepatic complications of NASH, and reversing current diagnosis and treatment inertia will be the only way to avert the looming epidemic of cirrhosis in patients with diabetes.”
“Endocrinologists don’t ‘see’ NAFLD and NASH” in their patients with T2D “ because they don’t think about it,” Dr. Mantzoros declared.
“Why is NASH underdiagnosed and undertreated? Because many physicians aren’t aware of it,” agreed Dr. Cusi during a talk in December 2020 at the 18th World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease (WCIRDC). “You never find what you don’t look for.”
“Endocrinologists should do the tests for NASH [in patients with T2D], but we’re all guilty of not doing it enough,” Tracey McLaughlin, MD, an endocrinologist and professor of medicine at Stanford (Calif.) University, commented during the WCIRDC.
These prevalence numbers demand that clinicians suspect liver disease “in any patient with diabetes, especially patients with obesity who are older and have components of metabolic syndrome,” said Dr. Mantzoros. “We need to screen, refer the most advanced cases, and treat the early- and mid-stage cases.”
How to find NASH
Both the American Diabetes Association and the European Association for the Study of Diabetes call for routine screening of patients with T2D, starting with a check of liver enzymes, such as ALT, but no clear consensus exists for the specifics of screening beyond that. Dr. Mantzoros, Dr. Cusi, and other experts agree that the scheme for assessing liver disease in patients with T2D starts with regular monitoring of elevations in liver enzymes including ALT. Next is noninvasive ultrasound assessment of the extent of liver fibrosis inferred from the organ’s stiffness using transient elastography. Another frequently cited initial screening tool is the Fibrosis-4 (FIB-4) score, which incorporates a patient’s age, platelet count, and levels of ALT and a second liver enzyme, AST.
“There is more consensus about FIB-4 and then elastography, but some people use tests other than FIB-4. Unfortunately there is no perfect diagnostic test today. A top priority is to define the best diagnostic test,” said Dr. Mantzoros, who is leading an effort to try to refine screening using artificial intelligence.
“FIB-4 is simple, easy, and well validated,” commented Dr. Cusi during the WCIRDC last December. “FIB-4 and elastography should get you pretty close” to identifying patients with T2D and significant liver disease.
But in a recent editorial, Dr. Cusi agreed on the need for “more reliable tests for the diagnosis of NASH and advanced fibrosis in patients with T2D. Significant work is being done in the field to validate novel and more sophisticated fibrosis biomarkers. Future studies will help us enter a new era of precision medicine where biomarkers will identify and target therapy to those with more active disease at risk for cirrhosis,” he wrote.
“The ultimate goal is to diagnose fibrosis at an early stage to prevent people from developing cirrhosis,” Dr. Cusi said in a recent written statement. “We’re trying to identify these problems before they’re unfixable. Once someone has cirrhosis, there isn’t a whole lot you can do.”
Pioglitazone remains the best-documented treatment
Perhaps some of the inertia in diagnosing NAFLD, NASH, and liver fibrosis in patients with T2D is dissatisfaction with current treatment options, although several proven options exist, notably weight loss and diet, and thiazolidinedione (TZD) pioglitazone. But weight loss and diet pose issues for patient compliance and durability of the intervention, and many clinicians consider pioglitazone flawed by its potential adverse effects.
“When we don’t have an established treatment for something, we tend to not measure it or go after it. That’s been true of liver disease” in patients with T2D, said Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of the Metabolic Institute of America in Tarzana, Calif., during the WCIRDC.
Treatment with pioglitazone has resolved NASH in about a third of patients compared with placebo, prevented fibrosis progression, and cut cardiovascular disease events, noted Dr. Cusi during the WCIRDC.
“Pioglitazone is used in only 8% of patients with T2D, or less, but we need to use it more often because of its proven efficacy in patients with T2D and NASH” said Dr. Mantzoros. “The problem is that pioglitazone has side effects, including weight gain and fluid retention, that makes it less attractive unless one thinks about the diagnosis of NASH.”
Others highlight that the adverse effects of pioglitazone have been either misunderstood, or can be effectively minimized with careful dosing.
“The data with the TZDs are much stronger than the data from anything else. TZDs have gotten a bad name because they also work in the kidney and enhance fluid reabsorption. We use modest dosages of pioglitazone, 15 mg or 30 mg a day, to avoid excess fluid retention,” Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio, said during the WCIRDC. “The best drug for NASH is pioglitazone. No other drug beats it” based on current data, Dr. DeFronzo asserted.
Other strategies include the potential to pair pioglitazone with other interventions that can blunt a weight-gain effect. One intriguing combination would combine pioglitazone with a GLP-1 receptor agonist, a drug class that can produce significant weight loss. Results from a phase 2 study showed promise for semaglutide (Rybelsus) in treating patients with NASH.
Getting the name right
Another factor that may be keeping NAFLD and NASH from achieving a higher profile for patients with T2D are those names, which focus on what the diseases are not – nonalcoholic – rather than what they are.
A series of recent publications in both the endocrinology and hepatology literature have called for renaming these disorders either “metabolic (dysfunction)–associated fatty liver disease (MALFD)”, or “dysmetabolism-associated fatty liver disease (DALFD)”.
“The names NAFLD and NASH indicate absence of alcohol as a cause, but the disease is also characterized by the absence of other causes, such as autoimmune disorders or hepatitis. The names were coined when we did not know much about these diseases. We now know that it is dysmetabolism that causes these conditions, and so we need to adopt a new, more accurate name,” explained Dr. Mantzoros, who has published support for a name change.
While many agree, some have raised concerns as to whether a name change now is premature. A group of hepatologists recently published a rebuttal to an immediate name change , saying that, “although we are in agreement that metabolic fatty liver disease may more accurately and positively reflect the relevant risk factors better than the age-old term nonalcoholic fatty liver disease, the term still leaves a great deal of ambiguity. A name change will be appropriate when informed by a new understanding of the molecular basis of the disease entity, insights that fundamentally change risk stratification, or other important aspects of the disease. We may be on the cusp of this, but we are not there yet.”
Dr. Mantzoros agreed, but for somewhat different reasons.
“We need to be careful and deliberate, because there is a significant body of knowledge and a lot of data from clinical trials collected using the old definitions. We need to find an appropriate time frame for a [name] transition. We need to find a nice and robust way to productively bridge the old to the new,” he said. “We also need new diagnostic criteria, and new therapies. A new name and definition will facilitate progress.”
Dr. Mantzoros been a shareholder of and consultant to Coherus and Pangea, he has been a consultant to AstraZeneca, Eisai, Genfit, Intercept, Novo Nordisk, P.E.S., and Regeneron, and has received travel support from the Metabolic Institute of America and the California Walnut Commission. Dr. Cusi has been a consultant to and has received research funding from numerous drug companies. Dr. McLaughlin is a consultant to January AI. Dr. Handelsman has been a consultant to numerous drug companies. Dr. DeFronzo received research grants from AstraZeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk.
President Biden signs 10 new orders to help fight COVID-19
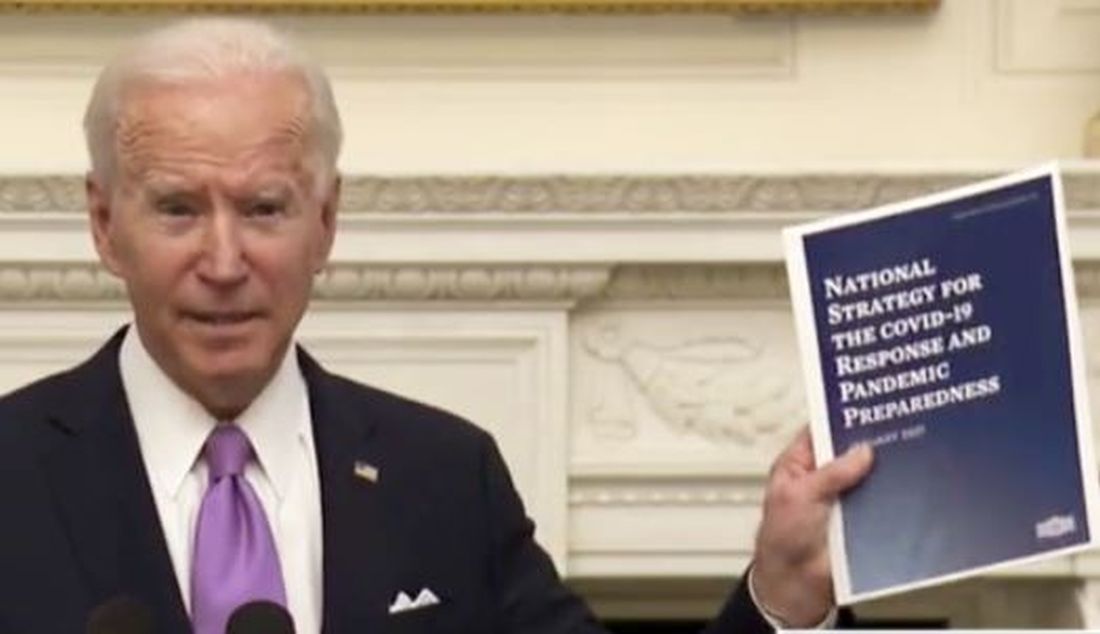
“For the past year, we couldn’t rely on the federal government to act with the urgency and focus and coordination we needed, and we have seen the tragic cost of that failure,” Mr. Biden said in remarks from the White House, unveiling his 198-page National Strategy for the COVID-19 Response and Pandemic Preparedness.
He said as many as 500,000 Americans will have died by February. “It’s going to take months for us to turn things around,” he said.
“Our national strategy is comprehensive – it’s based on science, not politics; it’s based on truth, not denial,” Mr. Biden said. He also promised to restore public trust, in part by having scientists and public health experts speak to the public. “That’s why you’ll be hearing a lot more from Dr. Fauci again, not from the president,” he said, adding that the experts will be “free from political interference.”
While the president’s executive orders can help accomplish some of the plan’s proposals, the majority will require new funding from Congress and will be included in the $1.9 trillion American Rescue package that Mr. Biden hopes legislators will approve.
Ten new orders
The 10 new pandemic-related orders Biden signed on Jan. 21 follow two he signed on his first day in office.
One establishes a COVID-19 Response Office responsible for coordinating the pandemic response across all federal departments and agencies and also reestablishes the White House Directorate on Global Health Security and Biodefense, which was disabled by the Trump administration.
The other order requires masks and physical distancing in all federal buildings, on all federal lands, and by federal employees and contractors.
Among the new orders will be directives that:
- Require individuals to also wear masks in airports and planes, and when using other modes of public transportation including trains, boats, and intercity buses, and also require international travelers to produce proof of a recent negative COVID-19 test prior to entry and to quarantine after entry.
- Federal agencies use all powers, including the Defense Production Act, to accelerate manufacturing and delivery of supplies such as N95 masks, gowns, gloves, swabs, reagents, pipette tips, rapid test kits, and nitrocellulose material for rapid antigen tests, and all equipment and material needed to accelerate manufacture, delivery, and administration of COVID-19 vaccine.
- Create a Pandemic Testing Board to expand supply and access, to promote more surge capacity, and to ensure equitable access to tests.
- Facilitate discovery, development, and trials of potential COVID-19 treatments, as well as expand access to programs that can meet the long-term health needs of those recovering from the disease.
- Facilitate more and better data sharing that will allow businesses, schools, hospitals, and individuals to make real-time decisions based on spread in their community.
- Direct the Education and Health & Human Services departments to provide schools and child-care operations guidance on how to reopen and operate safely.
- Direct the Occupational Safety and Health Administration (OSHA) to immediately release clear guidance for employers to help keep workers safe and to enforce health and safety requirements.
The plan also sets goals for vaccination – including 100 million shots in the administration’s first 100 days. President Biden had already previewed his goals for vaccination, including setting up mass vaccination sites and mobile vaccination sites. During his remarks, Mr. Biden said that he had already directed the Federal Emergency Management Agency (FEMA) to begin setting up the vaccination centers.
The administration is also going to look into improving reimbursement for giving vaccines. As a start, the HHS will ask the Centers for Medicare & Medicaid Services to consider if a higher rate “may more accurately compensate providers,” according to the Biden plan.
“But the brutal truth is it will take months before we can get the majority of Americans vaccinated,” said Mr. Biden.
As part of the goal of ensuring an equitable pandemic response, the president will sign an order that establishes a COVID-19 Health Equity Task Force. The task force is charged with providing recommendations for allocating resources and funding in communities with inequities in COVID-19 outcomes by race, ethnicity, geography, disability, and other considerations.
Finally, the administration has committed to being more transparent and sharing more information. The national plan calls for the federal government to conduct regular, expert-led, science-based public briefings and to release regular reports on the pandemic. The administration said it will launch massive science-based public information campaigns – in multiple languages – to educate Americans on masks, testing, and vaccines, and also work to counter misinformation and disinformation.
The American Academy of Family Physicians (AAFP) applauded Mr. Biden’s initiative. “If enacted, this bold legislative agenda will provide much-needed support to American families struggling during the pandemic – especially communities of color and those hardest hit by the virus,” Ada D. Stewart, MD, AAFP president, said in a statement.
Dr. Stewart also noted that family physicians “are uniquely positioned in their communities to educate patients, prioritize access, and coordinate administration of the COVID-19 vaccines,” and urged the administration to ensure that family physicians and staff be vaccinated as soon as possible, to help them “more safely provide care to their communities.”
A version of this article first appeared on Medscape.com.
“For the past year, we couldn’t rely on the federal government to act with the urgency and focus and coordination we needed, and we have seen the tragic cost of that failure,” Mr. Biden said in remarks from the White House, unveiling his 198-page National Strategy for the COVID-19 Response and Pandemic Preparedness.
He said as many as 500,000 Americans will have died by February. “It’s going to take months for us to turn things around,” he said.
“Our national strategy is comprehensive – it’s based on science, not politics; it’s based on truth, not denial,” Mr. Biden said. He also promised to restore public trust, in part by having scientists and public health experts speak to the public. “That’s why you’ll be hearing a lot more from Dr. Fauci again, not from the president,” he said, adding that the experts will be “free from political interference.”
While the president’s executive orders can help accomplish some of the plan’s proposals, the majority will require new funding from Congress and will be included in the $1.9 trillion American Rescue package that Mr. Biden hopes legislators will approve.
Ten new orders
The 10 new pandemic-related orders Biden signed on Jan. 21 follow two he signed on his first day in office.
One establishes a COVID-19 Response Office responsible for coordinating the pandemic response across all federal departments and agencies and also reestablishes the White House Directorate on Global Health Security and Biodefense, which was disabled by the Trump administration.
The other order requires masks and physical distancing in all federal buildings, on all federal lands, and by federal employees and contractors.
Among the new orders will be directives that:
- Require individuals to also wear masks in airports and planes, and when using other modes of public transportation including trains, boats, and intercity buses, and also require international travelers to produce proof of a recent negative COVID-19 test prior to entry and to quarantine after entry.
- Federal agencies use all powers, including the Defense Production Act, to accelerate manufacturing and delivery of supplies such as N95 masks, gowns, gloves, swabs, reagents, pipette tips, rapid test kits, and nitrocellulose material for rapid antigen tests, and all equipment and material needed to accelerate manufacture, delivery, and administration of COVID-19 vaccine.
- Create a Pandemic Testing Board to expand supply and access, to promote more surge capacity, and to ensure equitable access to tests.
- Facilitate discovery, development, and trials of potential COVID-19 treatments, as well as expand access to programs that can meet the long-term health needs of those recovering from the disease.
- Facilitate more and better data sharing that will allow businesses, schools, hospitals, and individuals to make real-time decisions based on spread in their community.
- Direct the Education and Health & Human Services departments to provide schools and child-care operations guidance on how to reopen and operate safely.
- Direct the Occupational Safety and Health Administration (OSHA) to immediately release clear guidance for employers to help keep workers safe and to enforce health and safety requirements.
The plan also sets goals for vaccination – including 100 million shots in the administration’s first 100 days. President Biden had already previewed his goals for vaccination, including setting up mass vaccination sites and mobile vaccination sites. During his remarks, Mr. Biden said that he had already directed the Federal Emergency Management Agency (FEMA) to begin setting up the vaccination centers.
The administration is also going to look into improving reimbursement for giving vaccines. As a start, the HHS will ask the Centers for Medicare & Medicaid Services to consider if a higher rate “may more accurately compensate providers,” according to the Biden plan.
“But the brutal truth is it will take months before we can get the majority of Americans vaccinated,” said Mr. Biden.
As part of the goal of ensuring an equitable pandemic response, the president will sign an order that establishes a COVID-19 Health Equity Task Force. The task force is charged with providing recommendations for allocating resources and funding in communities with inequities in COVID-19 outcomes by race, ethnicity, geography, disability, and other considerations.
Finally, the administration has committed to being more transparent and sharing more information. The national plan calls for the federal government to conduct regular, expert-led, science-based public briefings and to release regular reports on the pandemic. The administration said it will launch massive science-based public information campaigns – in multiple languages – to educate Americans on masks, testing, and vaccines, and also work to counter misinformation and disinformation.
The American Academy of Family Physicians (AAFP) applauded Mr. Biden’s initiative. “If enacted, this bold legislative agenda will provide much-needed support to American families struggling during the pandemic – especially communities of color and those hardest hit by the virus,” Ada D. Stewart, MD, AAFP president, said in a statement.
Dr. Stewart also noted that family physicians “are uniquely positioned in their communities to educate patients, prioritize access, and coordinate administration of the COVID-19 vaccines,” and urged the administration to ensure that family physicians and staff be vaccinated as soon as possible, to help them “more safely provide care to their communities.”
A version of this article first appeared on Medscape.com.
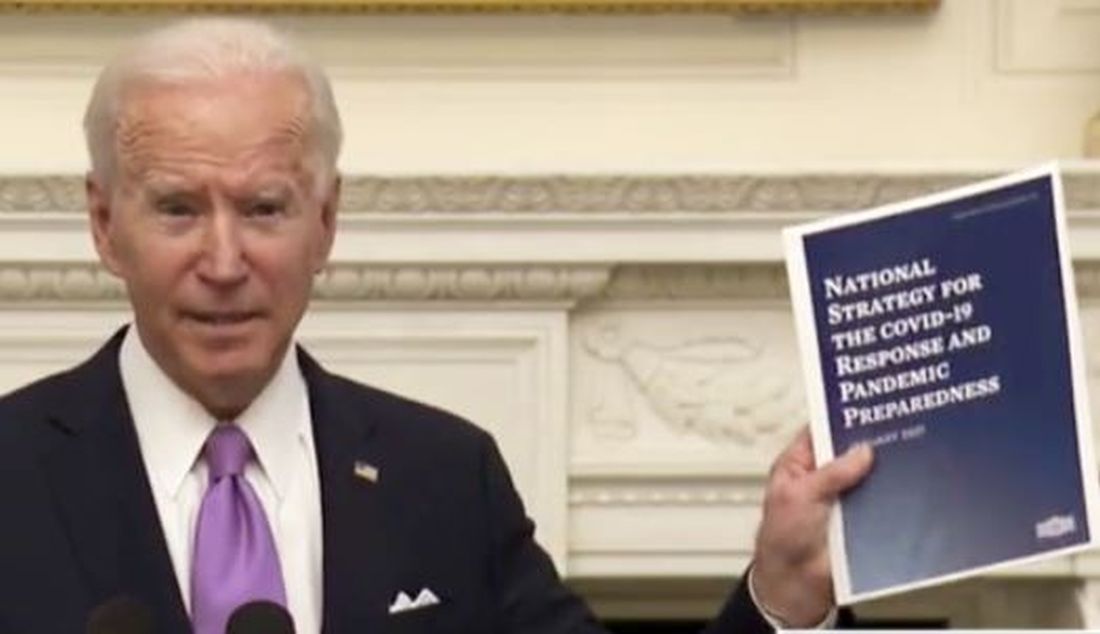
“For the past year, we couldn’t rely on the federal government to act with the urgency and focus and coordination we needed, and we have seen the tragic cost of that failure,” Mr. Biden said in remarks from the White House, unveiling his 198-page National Strategy for the COVID-19 Response and Pandemic Preparedness.
He said as many as 500,000 Americans will have died by February. “It’s going to take months for us to turn things around,” he said.
“Our national strategy is comprehensive – it’s based on science, not politics; it’s based on truth, not denial,” Mr. Biden said. He also promised to restore public trust, in part by having scientists and public health experts speak to the public. “That’s why you’ll be hearing a lot more from Dr. Fauci again, not from the president,” he said, adding that the experts will be “free from political interference.”
While the president’s executive orders can help accomplish some of the plan’s proposals, the majority will require new funding from Congress and will be included in the $1.9 trillion American Rescue package that Mr. Biden hopes legislators will approve.
Ten new orders
The 10 new pandemic-related orders Biden signed on Jan. 21 follow two he signed on his first day in office.
One establishes a COVID-19 Response Office responsible for coordinating the pandemic response across all federal departments and agencies and also reestablishes the White House Directorate on Global Health Security and Biodefense, which was disabled by the Trump administration.
The other order requires masks and physical distancing in all federal buildings, on all federal lands, and by federal employees and contractors.
Among the new orders will be directives that:
- Require individuals to also wear masks in airports and planes, and when using other modes of public transportation including trains, boats, and intercity buses, and also require international travelers to produce proof of a recent negative COVID-19 test prior to entry and to quarantine after entry.
- Federal agencies use all powers, including the Defense Production Act, to accelerate manufacturing and delivery of supplies such as N95 masks, gowns, gloves, swabs, reagents, pipette tips, rapid test kits, and nitrocellulose material for rapid antigen tests, and all equipment and material needed to accelerate manufacture, delivery, and administration of COVID-19 vaccine.
- Create a Pandemic Testing Board to expand supply and access, to promote more surge capacity, and to ensure equitable access to tests.
- Facilitate discovery, development, and trials of potential COVID-19 treatments, as well as expand access to programs that can meet the long-term health needs of those recovering from the disease.
- Facilitate more and better data sharing that will allow businesses, schools, hospitals, and individuals to make real-time decisions based on spread in their community.
- Direct the Education and Health & Human Services departments to provide schools and child-care operations guidance on how to reopen and operate safely.
- Direct the Occupational Safety and Health Administration (OSHA) to immediately release clear guidance for employers to help keep workers safe and to enforce health and safety requirements.
The plan also sets goals for vaccination – including 100 million shots in the administration’s first 100 days. President Biden had already previewed his goals for vaccination, including setting up mass vaccination sites and mobile vaccination sites. During his remarks, Mr. Biden said that he had already directed the Federal Emergency Management Agency (FEMA) to begin setting up the vaccination centers.
The administration is also going to look into improving reimbursement for giving vaccines. As a start, the HHS will ask the Centers for Medicare & Medicaid Services to consider if a higher rate “may more accurately compensate providers,” according to the Biden plan.
“But the brutal truth is it will take months before we can get the majority of Americans vaccinated,” said Mr. Biden.
As part of the goal of ensuring an equitable pandemic response, the president will sign an order that establishes a COVID-19 Health Equity Task Force. The task force is charged with providing recommendations for allocating resources and funding in communities with inequities in COVID-19 outcomes by race, ethnicity, geography, disability, and other considerations.
Finally, the administration has committed to being more transparent and sharing more information. The national plan calls for the federal government to conduct regular, expert-led, science-based public briefings and to release regular reports on the pandemic. The administration said it will launch massive science-based public information campaigns – in multiple languages – to educate Americans on masks, testing, and vaccines, and also work to counter misinformation and disinformation.
The American Academy of Family Physicians (AAFP) applauded Mr. Biden’s initiative. “If enacted, this bold legislative agenda will provide much-needed support to American families struggling during the pandemic – especially communities of color and those hardest hit by the virus,” Ada D. Stewart, MD, AAFP president, said in a statement.
Dr. Stewart also noted that family physicians “are uniquely positioned in their communities to educate patients, prioritize access, and coordinate administration of the COVID-19 vaccines,” and urged the administration to ensure that family physicians and staff be vaccinated as soon as possible, to help them “more safely provide care to their communities.”
A version of this article first appeared on Medscape.com.
Metformin treatment again linked to fewer deaths from COVID-19
People with type 2 diabetes who develop COVID-19 show a substantially reduced risk of dying if they are taking metformin, shows a study that adds to prior research indicating the drug might somehow play a role in reducing the severity of infection.
“Unlike several previous analyses, this was a study in a racially diverse population with a high proportion of Blacks/African Americans and [it] revealed that metformin treatment of diabetes prior to diagnosis with COVID-19 was associated with a dramatic threefold reduced mortality in subjects with type 2 diabetes, even after correcting for multiple covariates,” first author Anath Shalev, MD, of the Comprehensive Diabetes Center at the University of Alabama at Birmingham, said in an interview.
But Anne Peters, MD, a professor of clinical medicine at the University of Southern California, Los Angeles, said caution is needed when interpreting these findings.
“It’s hard to tease out the true effects because, for instance, those treated with insulin may be a sicker subset of patients with diabetes than those on metformin, or those with comorbidities such as renal insufficiency may not be treated with metformin” she said in an interview.
“In general, though, treatment obviously matters and people who are better treated tend to do better, so while I think this study raises the question of what role metformin plays in the risk of mortality and COVID-19, I don’t think it necessarily proves the association,” Dr. Peters asserted.
Diverse population
The new study, published this month in Frontiers of Endocrinology, included 25,326 individuals who were tested for COVID-19 at the University of Alabama at Birmingham Hospital between February and June 2020.
Overall, 2.4% tested positive for COVID-19 (n = 604), which the authors note is likely a low figure because screening included asymptomatic hospital staff and patients having elective procedures.
Black/African American patients had a significantly higher risk of COVID-19 positivity, compared with White patients (odds ratio, 2.6; P < .0001). Rates were also higher among those with hypertension (OR, 2.46), diabetes (OR, 2.11), and obesity (OR, 1.93), compared with those without each condition (all P < .0001).
The overall mortality rate in COVID-19-positive patients was 11%. Diabetes was associated with a dramatically increased risk of death (OR, 3.62; P < .0001), and remained an independent risk factor even after adjusting for age, race, sex, obesity, and hypertension.
Notably, the reduction in mortality among those with diabetes taking metformin prior to COVID-19 diagnosis was significant: 11% of those patients died, compared with 23% of those with diabetes not taking metformin (OR, 0.33; P = .021).
Similar findings reported across varied populations
The study adds to mounting research suggesting metformin could have a protective effect on COVID-19 mortality, including an early report from Wuhan, China, findings from the French CORONADO study, and a U.S. study linking treatment with decreased mortality among women with COVID-19.
Of note, the effects of metformin on mortality in the current study were observed in men and women alike, as well as in high-risk subgroups including African Americans.
“The fact that such similar results were obtained in different populations from around the world suggests that the observed reduction in mortality risk, associated with metformin use in subjects with type 2 diabetes and COVID-19, might be generalizable,” the authors wrote.
“Furthermore, these findings underline the importance of following general diabetes treatment and prevention guidelines and not delaying or discontinuing any metformin treatment,” they add.
Speculation of mechanisms includes anti-inflammatory effects
While the mechanisms behind metformin’s potential role in reducing mortality risk in COVID-19 are unknown, the authors note that the most obvious assumption – that improved glycemic control may be a key factor – is disputed by the study’s finding that blood glucose levels and hemoglobin A1c were not significantly different among COVID-19 survivors taking versus not taking metformin.
They point instead to metformin’s known anti-inflammatory and antithrombotic properties.
“We therefore hypothesize that, by exerting some of these effects, metformin might improve outcomes and we are now in the process of investigating this possibility further,” Dr. Shalev said.
Dr. Peters noted that anti-inflammatory properties, themselves, are not necessarily unique to metformin in the treatment of diabetes.
“Many other agents, such as sodium-glucose cotransporter 2 (SGLT2) inhibitors can reduce inflammation, so I don’t know if that would explain it, but it certainly could help,” she said. “[Reducing inflammation] is a hypothesis you see commonly with diabetes drugs, but I think there are also a lot of metabolic benefits from metformin.”
“It was fascinating that they had the A1c data and that survival with metformin didn’t appear to be as related to A1c levels as one might think,” she added.
Notably, a key advantage, should the effects and mechanisms be validated, is metformin’s high accessibility, Dr. Peters added.
“This doesn’t necessarily tell us what we can do to reduce the health care disparities surrounding COVID-19, but the fact that metformin is low cost and easily available is very important, so maybe it will help as we try to grapple with other risk factors.”
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with type 2 diabetes who develop COVID-19 show a substantially reduced risk of dying if they are taking metformin, shows a study that adds to prior research indicating the drug might somehow play a role in reducing the severity of infection.
“Unlike several previous analyses, this was a study in a racially diverse population with a high proportion of Blacks/African Americans and [it] revealed that metformin treatment of diabetes prior to diagnosis with COVID-19 was associated with a dramatic threefold reduced mortality in subjects with type 2 diabetes, even after correcting for multiple covariates,” first author Anath Shalev, MD, of the Comprehensive Diabetes Center at the University of Alabama at Birmingham, said in an interview.
But Anne Peters, MD, a professor of clinical medicine at the University of Southern California, Los Angeles, said caution is needed when interpreting these findings.
“It’s hard to tease out the true effects because, for instance, those treated with insulin may be a sicker subset of patients with diabetes than those on metformin, or those with comorbidities such as renal insufficiency may not be treated with metformin” she said in an interview.
“In general, though, treatment obviously matters and people who are better treated tend to do better, so while I think this study raises the question of what role metformin plays in the risk of mortality and COVID-19, I don’t think it necessarily proves the association,” Dr. Peters asserted.
Diverse population
The new study, published this month in Frontiers of Endocrinology, included 25,326 individuals who were tested for COVID-19 at the University of Alabama at Birmingham Hospital between February and June 2020.
Overall, 2.4% tested positive for COVID-19 (n = 604), which the authors note is likely a low figure because screening included asymptomatic hospital staff and patients having elective procedures.
Black/African American patients had a significantly higher risk of COVID-19 positivity, compared with White patients (odds ratio, 2.6; P < .0001). Rates were also higher among those with hypertension (OR, 2.46), diabetes (OR, 2.11), and obesity (OR, 1.93), compared with those without each condition (all P < .0001).
The overall mortality rate in COVID-19-positive patients was 11%. Diabetes was associated with a dramatically increased risk of death (OR, 3.62; P < .0001), and remained an independent risk factor even after adjusting for age, race, sex, obesity, and hypertension.
Notably, the reduction in mortality among those with diabetes taking metformin prior to COVID-19 diagnosis was significant: 11% of those patients died, compared with 23% of those with diabetes not taking metformin (OR, 0.33; P = .021).
Similar findings reported across varied populations
The study adds to mounting research suggesting metformin could have a protective effect on COVID-19 mortality, including an early report from Wuhan, China, findings from the French CORONADO study, and a U.S. study linking treatment with decreased mortality among women with COVID-19.
Of note, the effects of metformin on mortality in the current study were observed in men and women alike, as well as in high-risk subgroups including African Americans.
“The fact that such similar results were obtained in different populations from around the world suggests that the observed reduction in mortality risk, associated with metformin use in subjects with type 2 diabetes and COVID-19, might be generalizable,” the authors wrote.
“Furthermore, these findings underline the importance of following general diabetes treatment and prevention guidelines and not delaying or discontinuing any metformin treatment,” they add.
Speculation of mechanisms includes anti-inflammatory effects
While the mechanisms behind metformin’s potential role in reducing mortality risk in COVID-19 are unknown, the authors note that the most obvious assumption – that improved glycemic control may be a key factor – is disputed by the study’s finding that blood glucose levels and hemoglobin A1c were not significantly different among COVID-19 survivors taking versus not taking metformin.
They point instead to metformin’s known anti-inflammatory and antithrombotic properties.
“We therefore hypothesize that, by exerting some of these effects, metformin might improve outcomes and we are now in the process of investigating this possibility further,” Dr. Shalev said.
Dr. Peters noted that anti-inflammatory properties, themselves, are not necessarily unique to metformin in the treatment of diabetes.
“Many other agents, such as sodium-glucose cotransporter 2 (SGLT2) inhibitors can reduce inflammation, so I don’t know if that would explain it, but it certainly could help,” she said. “[Reducing inflammation] is a hypothesis you see commonly with diabetes drugs, but I think there are also a lot of metabolic benefits from metformin.”
“It was fascinating that they had the A1c data and that survival with metformin didn’t appear to be as related to A1c levels as one might think,” she added.
Notably, a key advantage, should the effects and mechanisms be validated, is metformin’s high accessibility, Dr. Peters added.
“This doesn’t necessarily tell us what we can do to reduce the health care disparities surrounding COVID-19, but the fact that metformin is low cost and easily available is very important, so maybe it will help as we try to grapple with other risk factors.”
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with type 2 diabetes who develop COVID-19 show a substantially reduced risk of dying if they are taking metformin, shows a study that adds to prior research indicating the drug might somehow play a role in reducing the severity of infection.
“Unlike several previous analyses, this was a study in a racially diverse population with a high proportion of Blacks/African Americans and [it] revealed that metformin treatment of diabetes prior to diagnosis with COVID-19 was associated with a dramatic threefold reduced mortality in subjects with type 2 diabetes, even after correcting for multiple covariates,” first author Anath Shalev, MD, of the Comprehensive Diabetes Center at the University of Alabama at Birmingham, said in an interview.
But Anne Peters, MD, a professor of clinical medicine at the University of Southern California, Los Angeles, said caution is needed when interpreting these findings.
“It’s hard to tease out the true effects because, for instance, those treated with insulin may be a sicker subset of patients with diabetes than those on metformin, or those with comorbidities such as renal insufficiency may not be treated with metformin” she said in an interview.
“In general, though, treatment obviously matters and people who are better treated tend to do better, so while I think this study raises the question of what role metformin plays in the risk of mortality and COVID-19, I don’t think it necessarily proves the association,” Dr. Peters asserted.
Diverse population
The new study, published this month in Frontiers of Endocrinology, included 25,326 individuals who were tested for COVID-19 at the University of Alabama at Birmingham Hospital between February and June 2020.
Overall, 2.4% tested positive for COVID-19 (n = 604), which the authors note is likely a low figure because screening included asymptomatic hospital staff and patients having elective procedures.
Black/African American patients had a significantly higher risk of COVID-19 positivity, compared with White patients (odds ratio, 2.6; P < .0001). Rates were also higher among those with hypertension (OR, 2.46), diabetes (OR, 2.11), and obesity (OR, 1.93), compared with those without each condition (all P < .0001).
The overall mortality rate in COVID-19-positive patients was 11%. Diabetes was associated with a dramatically increased risk of death (OR, 3.62; P < .0001), and remained an independent risk factor even after adjusting for age, race, sex, obesity, and hypertension.
Notably, the reduction in mortality among those with diabetes taking metformin prior to COVID-19 diagnosis was significant: 11% of those patients died, compared with 23% of those with diabetes not taking metformin (OR, 0.33; P = .021).
Similar findings reported across varied populations
The study adds to mounting research suggesting metformin could have a protective effect on COVID-19 mortality, including an early report from Wuhan, China, findings from the French CORONADO study, and a U.S. study linking treatment with decreased mortality among women with COVID-19.
Of note, the effects of metformin on mortality in the current study were observed in men and women alike, as well as in high-risk subgroups including African Americans.
“The fact that such similar results were obtained in different populations from around the world suggests that the observed reduction in mortality risk, associated with metformin use in subjects with type 2 diabetes and COVID-19, might be generalizable,” the authors wrote.
“Furthermore, these findings underline the importance of following general diabetes treatment and prevention guidelines and not delaying or discontinuing any metformin treatment,” they add.
Speculation of mechanisms includes anti-inflammatory effects
While the mechanisms behind metformin’s potential role in reducing mortality risk in COVID-19 are unknown, the authors note that the most obvious assumption – that improved glycemic control may be a key factor – is disputed by the study’s finding that blood glucose levels and hemoglobin A1c were not significantly different among COVID-19 survivors taking versus not taking metformin.
They point instead to metformin’s known anti-inflammatory and antithrombotic properties.
“We therefore hypothesize that, by exerting some of these effects, metformin might improve outcomes and we are now in the process of investigating this possibility further,” Dr. Shalev said.
Dr. Peters noted that anti-inflammatory properties, themselves, are not necessarily unique to metformin in the treatment of diabetes.
“Many other agents, such as sodium-glucose cotransporter 2 (SGLT2) inhibitors can reduce inflammation, so I don’t know if that would explain it, but it certainly could help,” she said. “[Reducing inflammation] is a hypothesis you see commonly with diabetes drugs, but I think there are also a lot of metabolic benefits from metformin.”
“It was fascinating that they had the A1c data and that survival with metformin didn’t appear to be as related to A1c levels as one might think,” she added.
Notably, a key advantage, should the effects and mechanisms be validated, is metformin’s high accessibility, Dr. Peters added.
“This doesn’t necessarily tell us what we can do to reduce the health care disparities surrounding COVID-19, but the fact that metformin is low cost and easily available is very important, so maybe it will help as we try to grapple with other risk factors.”
The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Seven ways President Biden could now change health care
President Joe Biden has come into office after an unexpected shift in Congress. On Jan. 5, Democrats scored an upset by winning two U.S. Senate seats in runoff elections in Georgia, giving them control of the Senate.
Now the Democrats have control of all three levers of power – the Senate, the House, and the presidency – for the first time since the early years of the Obama administration.
How will President Biden use this new concentration of power to shape health care policy?
Democrats’ small majorities in both houses of Congress suggest that moderation and bipartisanship will be necessary to get things done. Moreover, Mr. Biden himself is calling for bipartisanship. “On this January day,” he said in his inauguration speech, “my whole soul is in this: Bringing America together, uniting our people, uniting our nation.”
Key health care actions that Mr. Biden could pursue include the following.
1. Passing a new COVID-19 relief bill
Above all, Mr. Biden is focused on overcoming the COVID-19 pandemic, which has been registering record deaths recently, and getting newly released vaccines to Americans.
“Dealing with the coronavirus pandemic is one of the most important battles our administration will face, and I will be informed by science and by experts,” the president said.
“There is no question that the pandemic is the highest priority for the Biden administration,” said Larry Levitt, executive vice president for health policy at the Henry J. Kaiser Family Foundation. “COVID will dominate the early weeks and months of this administration. His success rests, in particular, on improving the rollout of vaccines.”
Five days before his inauguration, the president-elect unveiled the American Rescue Plan, a massive, $1.9 trillion legislative package intended to hasten rollout of COVID-19 vaccines, improve COVID-19 testing, and provide financial help to businesses and individuals, among many other things.
The bill would add $1,400 to the recently passed $600 government relief payments for each American, amounting to a $2,000 check. It would also enact many non-COVID-19 measures, such as a $15-an-hour minimum wage and measures to bolster the Affordable Care Act (ACA).
If Democrats cannot reach a deal with the Republicans, they might turn the proposal into a reconciliation bill, which could then be passed with a simple majority. However, drafting a reconciliation bill is a long, complicated process that would require removing provisions that don’t meet the requirements of reconciliation, said Hazen Marshall, a Washington lobbyist and former staffer for Sen. Mitch McConnell.
Most importantly, Mr. Marshall said, reconciliation bills bring out diehard partisanship. “They involve a sledgehammer mentality,” he says. “You’re telling the other side that their views aren’t going to matter.” The final version of the ACA, for example, was passed as a reconciliation bill, with not one Republican vote.
In the Trump years, “the last four reconciliation bills did not get any votes from the minority,” added Rodney Whitlock, PhD, a political consultant at McDermott+Consulting, who worked 21 years for Republicans in the House. “When the majority chooses to use reconciliation, it is an admission that it has no interest in working with the minority.”
Hammering out a compromise will be tough, but Robert Pearl MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University, said that if anyone can do it, it would be President Biden. Having served in the Senate for 36 years, “Biden knows Congress better than any president since Lyndon Johnson,” he said. “He can reach across the aisle and get legislation passed as much as anyone could these days.”
2. Restoring Obamacare
Mr. Biden has vowed to undo a gradual dismantling of the ACA that went on during the Trump administration through executive orders, rule-making, and new laws. “Reinvigorating the ACA was a central part of Biden’s platform as a candidate,” Mr. Levitt said.
Each Trump action against the ACA must be undone in the same way. Presidential orders must be met with presidential orders, regulations with regulations, and legislation with legislation.
The ACA is also being challenged in the Supreme Court. Republicans under Trump passed a law that reduced the penalty for not buying health insurance under the ACA to zero. Then a group of 20 states, led by Texas, filed a lawsuit asserting that this change makes the ACA unconstitutional.
The lawsuit was heard by the Supreme Court in November. From remarks made by the justices then, it appears that the court might well uphold the law when a verdict comes down in June.
But just in case, Mr. Biden wants Congress to enact a small penalty for not buying health insurance, which would remove the basis of the lawsuit.
Mr. Biden’s choice for secretary of Health and Human Services shows his level of commitment to protecting the ACA. His HHS nominee is California Attorney General Xavier Becerra, who led a group of 17 states defending the ACA in the current lawsuit.
In addition to undoing Trump’s changes, Mr. Biden plans to expand the ACA beyond the original legislation. The new COVID-19 bill contains provisions that would expand subsidies to buy insurance on the exchanges and would lower the maximum percentage of income that anyone has to pay for health insurance to 8.5%.
Dealing with Medicaid is also related to the ACA. In 2012, the Supreme Court struck down a mandate that states expand their Medicaid programs, with substantial funding from the federal government.
To date, 12 states still do not participate in the Medicaid expansion. To lure them into the expansion, the Democrat-controlled House last session passed a bill that would offer to pay the entire bill for the first 3 years of Medicaid expansion if they chose to enact an expansion.
3. Undoing other Trump actions in health care
In addition to changes in the ACA, Trump also enacted a number of other changes in health care that President Biden could undo. For example, Mr. Biden says he will reenter the World Health Organization (WHO) so that the United States could better coordinate a COVID-19 response with other nations. Trump exited the WHO with the stroke of a pen, and Mr. Biden can do the same in reverse.
Under Trump, the Centers for Medicare & Medicaid Services used waivers to weaken the ACA and allow states to alter their Medicaid programs. One waiver allows Georgia to leave the ACA exchanges and put brokers in charge of buying coverage. Other waivers allow states to transform federal Medicaid payments into block grants, which several states are planning to do.
The Trump CMS has allowed several states to use Medicaid waivers to add work requirements for Medicaid recipients. The courts have blocked the work rules so far, and the Biden CMS may decide to reverse these waivers or modify them.
“Undoing waivers is normally a fairly simple thing,” Mr. Levitt said. In January, however, the Trump CMS asked some waiver states to sign new contracts in which the CMS pledges not to end a waiver without 9 months’ notice. It’s unclear how many states signed such contracts and what obligation the Biden CMS has to enforce them.
The Trump CMS also stopped reimbursing insurers for waiving deductibles and copayments for low-income customers, as directed by the ACA. Without federal reimbursement, some insurers raised premiums by as much as 20% to cover the costs. It is unclear how the Biden CMS would tackle this change.
4. Negotiating lower drug prices
Allowing Medicare to negotiate drug prices, a major plank in Mr. Biden’s campaign, would seem like a slam dunk for the Democrats. This approach is backed by 89% of Americans, including 84% of Republicans, according to a Kaiser Family Foundation survey in December.
“With that level of support, it’s hard to go wrong politically on this issue,” Mr. Levitt said.
Many Republicans, however, do not favor negotiating drug prices, and the two parties continue to be far apart on how to control drug prices. Trump signed an action that allows Americans to buy cheaper drugs abroad, an approach that Mr. Biden also supports, but it is now tied up in the courts.
“A drug pricing bill has always been difficult to pass,” Dr. Whitlock said. “The issue is popular with the public, but change does not come easily. The drug lobby is one the strongest in Washington, and now it may be even stronger, since it was the drug companies that gave us the COVID vaccines.”
Dr. Whitlock said Republicans will want Democrats to compromise on drug pricing, but he doubts they will do so. The House passed a bill to negotiate drug prices last year, which never was voted on in the Senate. “It is difficult to imagine that the Democrats will be able to move rightward from that House bill,” Dr. Whitlock said. “Democrats are likely to stand pat on drug pricing.”
5. Introducing a public option
President Biden’s campaign proposal for a public option – health insurance offered by the federal government – and to lower the age for Medicare eligibility from 65 years to 60 years, resulted from a compromise between two factions of the Democratic party on how to expand coverage.
Although Mr. Biden and other moderates wanted to focus on fixing the ACA, Democrats led by Sen. Bernie Sanders of Vermont called for a single-payer system, dubbed “Medicare for all.” A public option was seen as the middle ground between the two camps.
“A public option would be a very controversial,” Dr. Whitlock said. Critics say it would pay at Medicare rates, which would reduce doctors’ reimbursements, and save very little money compared with a single-payer system.
Dr. Pearl sees similar problems with lowering the Medicare age. “This would be an expensive change that the federal government could not afford, particularly with all the spending on the pandemic,” he said. “And it would be tough on doctors and hospitals, because Medicare pays less than the private insurance payment they are now getting.”
“The public option is likely to get serious discussion within the Democratic caucus and get onto the Senate floor,” Mr. Levitt said. “The party won’t ignore it.” He notes that in the new Senate, Sen. Sanders chairs the budget committee, and from that position he is likely to push for expanding access to care.
Mr. Levitt says the Biden CMS might allow states to experiment with a statewide public option or even a single-payer model, but he concedes that states, with their budgets ravaged by COVID-19, do not currently have the money to launch such programs.
6. Reviving the CMS
Under President Obama, the CMS was the engine that implemented the ACA and shepherded wider use of value-based reimbursements, which reward providers for quality and outcomes rather than volume.
Under the Trump administration, CMS leadership continued to uphold value-based reimbursement, Dr. Pearl observed. “CMS leadership championed value-based payments, but they encountered a lot of pushback from doctors and hospitals and had to scale back their goals,” he said.
On the other hand, the Trump CMS took a 180-degree turn on the ACA and worked to take it apart. This took a toll on staff morale, according to Donald M. Berwick, MD, who ran the CMS under President Obama. “Many people in CMS did not feel supported during the Trump administration, and some of them left,” Dr. Berwick said.
The CMS needs experienced staff on board to write comprehensible rules and regulations that can overcome court challenges.
Having a fully functioning CMS also requires consistent leadership, which was a problem for Obama. When Mr. Obama nominated Dr. Berwick, 60 Senate votes were needed to confirm him, and Republicans would not vote for him. Mr. Obama eventually brought Dr. Berwick in as a recess appointment, but it meant he could serve for only 17 months.
Since then, Senate confirmation rules have changed so that only a simple majority is needed to confirm appointments. This is important for Biden’s nominees, Dr. Berwick said. “For a president, having your team in place means you are able to execute the policies you want,” he said. “You need to have consistent leadership.”
7. Potentially changing health care without Congress
Even with their newly won control of the Senate, the Democrats’ thin majorities in both houses of Congress may not be enough to pass much legislation if Republicans are solidly opposed.
Democrats in the House also have a narrow path this session in which to pass legislation. The Democratic leadership has an 11-vote majority, but it must contend with 15 moderate representatives in purple districts (where Democrats and Republicans have about equal support).
A bigger problem looms before the Democrats. In 2022, the party may well lose its majorities in both houses. Mr. Whitlock notes that the party of an incoming president normally loses seats in the first midterm election. “The last incoming president to keep both houses of Congress in his first midterm was Jimmy Carter,” he said.
If this happens, President Biden would have to govern without the support of Congress, which is what Barack Obama had to do through most of his presidency. As Mr. Obama’s vice president, Mr. Biden is well aware how that goes. Governing without Congress means relying on presidential orders and decrees.
In health care, Mr. Biden has a powerful policy-making tool, the Center for Medicare & Medicaid Innovation (CMMI). The CMMI was empowered by the ACA to initiate pilot programs for new payment models.
So far, the CMMI’s work has been mainly limited to accountable care organizations, bundled payments, and patient-centered medical homes, but it could also be used to enact new federal policies that would normally require Congressional action, Mr. Levitt said.
Conclusion
Expectations have been very high for what President Joe Biden can do in health care. He needs to unite a very divided political system to defeat a deadly pandemic, restore Obamacare, and sign landmark legislation, such as a drug-pricing bill.
But shepherding bills through Congress will be a challenge. “You need to have accountability, unity, and civility, which is a Herculean task,” Mr. Whitlock said. “You have to keep policies off the table that could blow up the bipartisanship.”
A version of this article first appeared on Medscape.com.
President Joe Biden has come into office after an unexpected shift in Congress. On Jan. 5, Democrats scored an upset by winning two U.S. Senate seats in runoff elections in Georgia, giving them control of the Senate.
Now the Democrats have control of all three levers of power – the Senate, the House, and the presidency – for the first time since the early years of the Obama administration.
How will President Biden use this new concentration of power to shape health care policy?
Democrats’ small majorities in both houses of Congress suggest that moderation and bipartisanship will be necessary to get things done. Moreover, Mr. Biden himself is calling for bipartisanship. “On this January day,” he said in his inauguration speech, “my whole soul is in this: Bringing America together, uniting our people, uniting our nation.”
Key health care actions that Mr. Biden could pursue include the following.
1. Passing a new COVID-19 relief bill
Above all, Mr. Biden is focused on overcoming the COVID-19 pandemic, which has been registering record deaths recently, and getting newly released vaccines to Americans.
“Dealing with the coronavirus pandemic is one of the most important battles our administration will face, and I will be informed by science and by experts,” the president said.
“There is no question that the pandemic is the highest priority for the Biden administration,” said Larry Levitt, executive vice president for health policy at the Henry J. Kaiser Family Foundation. “COVID will dominate the early weeks and months of this administration. His success rests, in particular, on improving the rollout of vaccines.”
Five days before his inauguration, the president-elect unveiled the American Rescue Plan, a massive, $1.9 trillion legislative package intended to hasten rollout of COVID-19 vaccines, improve COVID-19 testing, and provide financial help to businesses and individuals, among many other things.
The bill would add $1,400 to the recently passed $600 government relief payments for each American, amounting to a $2,000 check. It would also enact many non-COVID-19 measures, such as a $15-an-hour minimum wage and measures to bolster the Affordable Care Act (ACA).
If Democrats cannot reach a deal with the Republicans, they might turn the proposal into a reconciliation bill, which could then be passed with a simple majority. However, drafting a reconciliation bill is a long, complicated process that would require removing provisions that don’t meet the requirements of reconciliation, said Hazen Marshall, a Washington lobbyist and former staffer for Sen. Mitch McConnell.
Most importantly, Mr. Marshall said, reconciliation bills bring out diehard partisanship. “They involve a sledgehammer mentality,” he says. “You’re telling the other side that their views aren’t going to matter.” The final version of the ACA, for example, was passed as a reconciliation bill, with not one Republican vote.
In the Trump years, “the last four reconciliation bills did not get any votes from the minority,” added Rodney Whitlock, PhD, a political consultant at McDermott+Consulting, who worked 21 years for Republicans in the House. “When the majority chooses to use reconciliation, it is an admission that it has no interest in working with the minority.”
Hammering out a compromise will be tough, but Robert Pearl MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University, said that if anyone can do it, it would be President Biden. Having served in the Senate for 36 years, “Biden knows Congress better than any president since Lyndon Johnson,” he said. “He can reach across the aisle and get legislation passed as much as anyone could these days.”
2. Restoring Obamacare
Mr. Biden has vowed to undo a gradual dismantling of the ACA that went on during the Trump administration through executive orders, rule-making, and new laws. “Reinvigorating the ACA was a central part of Biden’s platform as a candidate,” Mr. Levitt said.
Each Trump action against the ACA must be undone in the same way. Presidential orders must be met with presidential orders, regulations with regulations, and legislation with legislation.
The ACA is also being challenged in the Supreme Court. Republicans under Trump passed a law that reduced the penalty for not buying health insurance under the ACA to zero. Then a group of 20 states, led by Texas, filed a lawsuit asserting that this change makes the ACA unconstitutional.
The lawsuit was heard by the Supreme Court in November. From remarks made by the justices then, it appears that the court might well uphold the law when a verdict comes down in June.
But just in case, Mr. Biden wants Congress to enact a small penalty for not buying health insurance, which would remove the basis of the lawsuit.
Mr. Biden’s choice for secretary of Health and Human Services shows his level of commitment to protecting the ACA. His HHS nominee is California Attorney General Xavier Becerra, who led a group of 17 states defending the ACA in the current lawsuit.
In addition to undoing Trump’s changes, Mr. Biden plans to expand the ACA beyond the original legislation. The new COVID-19 bill contains provisions that would expand subsidies to buy insurance on the exchanges and would lower the maximum percentage of income that anyone has to pay for health insurance to 8.5%.
Dealing with Medicaid is also related to the ACA. In 2012, the Supreme Court struck down a mandate that states expand their Medicaid programs, with substantial funding from the federal government.
To date, 12 states still do not participate in the Medicaid expansion. To lure them into the expansion, the Democrat-controlled House last session passed a bill that would offer to pay the entire bill for the first 3 years of Medicaid expansion if they chose to enact an expansion.
3. Undoing other Trump actions in health care
In addition to changes in the ACA, Trump also enacted a number of other changes in health care that President Biden could undo. For example, Mr. Biden says he will reenter the World Health Organization (WHO) so that the United States could better coordinate a COVID-19 response with other nations. Trump exited the WHO with the stroke of a pen, and Mr. Biden can do the same in reverse.
Under Trump, the Centers for Medicare & Medicaid Services used waivers to weaken the ACA and allow states to alter their Medicaid programs. One waiver allows Georgia to leave the ACA exchanges and put brokers in charge of buying coverage. Other waivers allow states to transform federal Medicaid payments into block grants, which several states are planning to do.
The Trump CMS has allowed several states to use Medicaid waivers to add work requirements for Medicaid recipients. The courts have blocked the work rules so far, and the Biden CMS may decide to reverse these waivers or modify them.
“Undoing waivers is normally a fairly simple thing,” Mr. Levitt said. In January, however, the Trump CMS asked some waiver states to sign new contracts in which the CMS pledges not to end a waiver without 9 months’ notice. It’s unclear how many states signed such contracts and what obligation the Biden CMS has to enforce them.
The Trump CMS also stopped reimbursing insurers for waiving deductibles and copayments for low-income customers, as directed by the ACA. Without federal reimbursement, some insurers raised premiums by as much as 20% to cover the costs. It is unclear how the Biden CMS would tackle this change.
4. Negotiating lower drug prices
Allowing Medicare to negotiate drug prices, a major plank in Mr. Biden’s campaign, would seem like a slam dunk for the Democrats. This approach is backed by 89% of Americans, including 84% of Republicans, according to a Kaiser Family Foundation survey in December.
“With that level of support, it’s hard to go wrong politically on this issue,” Mr. Levitt said.
Many Republicans, however, do not favor negotiating drug prices, and the two parties continue to be far apart on how to control drug prices. Trump signed an action that allows Americans to buy cheaper drugs abroad, an approach that Mr. Biden also supports, but it is now tied up in the courts.
“A drug pricing bill has always been difficult to pass,” Dr. Whitlock said. “The issue is popular with the public, but change does not come easily. The drug lobby is one the strongest in Washington, and now it may be even stronger, since it was the drug companies that gave us the COVID vaccines.”
Dr. Whitlock said Republicans will want Democrats to compromise on drug pricing, but he doubts they will do so. The House passed a bill to negotiate drug prices last year, which never was voted on in the Senate. “It is difficult to imagine that the Democrats will be able to move rightward from that House bill,” Dr. Whitlock said. “Democrats are likely to stand pat on drug pricing.”
5. Introducing a public option
President Biden’s campaign proposal for a public option – health insurance offered by the federal government – and to lower the age for Medicare eligibility from 65 years to 60 years, resulted from a compromise between two factions of the Democratic party on how to expand coverage.
Although Mr. Biden and other moderates wanted to focus on fixing the ACA, Democrats led by Sen. Bernie Sanders of Vermont called for a single-payer system, dubbed “Medicare for all.” A public option was seen as the middle ground between the two camps.
“A public option would be a very controversial,” Dr. Whitlock said. Critics say it would pay at Medicare rates, which would reduce doctors’ reimbursements, and save very little money compared with a single-payer system.
Dr. Pearl sees similar problems with lowering the Medicare age. “This would be an expensive change that the federal government could not afford, particularly with all the spending on the pandemic,” he said. “And it would be tough on doctors and hospitals, because Medicare pays less than the private insurance payment they are now getting.”
“The public option is likely to get serious discussion within the Democratic caucus and get onto the Senate floor,” Mr. Levitt said. “The party won’t ignore it.” He notes that in the new Senate, Sen. Sanders chairs the budget committee, and from that position he is likely to push for expanding access to care.
Mr. Levitt says the Biden CMS might allow states to experiment with a statewide public option or even a single-payer model, but he concedes that states, with their budgets ravaged by COVID-19, do not currently have the money to launch such programs.
6. Reviving the CMS
Under President Obama, the CMS was the engine that implemented the ACA and shepherded wider use of value-based reimbursements, which reward providers for quality and outcomes rather than volume.
Under the Trump administration, CMS leadership continued to uphold value-based reimbursement, Dr. Pearl observed. “CMS leadership championed value-based payments, but they encountered a lot of pushback from doctors and hospitals and had to scale back their goals,” he said.
On the other hand, the Trump CMS took a 180-degree turn on the ACA and worked to take it apart. This took a toll on staff morale, according to Donald M. Berwick, MD, who ran the CMS under President Obama. “Many people in CMS did not feel supported during the Trump administration, and some of them left,” Dr. Berwick said.
The CMS needs experienced staff on board to write comprehensible rules and regulations that can overcome court challenges.
Having a fully functioning CMS also requires consistent leadership, which was a problem for Obama. When Mr. Obama nominated Dr. Berwick, 60 Senate votes were needed to confirm him, and Republicans would not vote for him. Mr. Obama eventually brought Dr. Berwick in as a recess appointment, but it meant he could serve for only 17 months.
Since then, Senate confirmation rules have changed so that only a simple majority is needed to confirm appointments. This is important for Biden’s nominees, Dr. Berwick said. “For a president, having your team in place means you are able to execute the policies you want,” he said. “You need to have consistent leadership.”
7. Potentially changing health care without Congress
Even with their newly won control of the Senate, the Democrats’ thin majorities in both houses of Congress may not be enough to pass much legislation if Republicans are solidly opposed.
Democrats in the House also have a narrow path this session in which to pass legislation. The Democratic leadership has an 11-vote majority, but it must contend with 15 moderate representatives in purple districts (where Democrats and Republicans have about equal support).
A bigger problem looms before the Democrats. In 2022, the party may well lose its majorities in both houses. Mr. Whitlock notes that the party of an incoming president normally loses seats in the first midterm election. “The last incoming president to keep both houses of Congress in his first midterm was Jimmy Carter,” he said.
If this happens, President Biden would have to govern without the support of Congress, which is what Barack Obama had to do through most of his presidency. As Mr. Obama’s vice president, Mr. Biden is well aware how that goes. Governing without Congress means relying on presidential orders and decrees.
In health care, Mr. Biden has a powerful policy-making tool, the Center for Medicare & Medicaid Innovation (CMMI). The CMMI was empowered by the ACA to initiate pilot programs for new payment models.
So far, the CMMI’s work has been mainly limited to accountable care organizations, bundled payments, and patient-centered medical homes, but it could also be used to enact new federal policies that would normally require Congressional action, Mr. Levitt said.
Conclusion
Expectations have been very high for what President Joe Biden can do in health care. He needs to unite a very divided political system to defeat a deadly pandemic, restore Obamacare, and sign landmark legislation, such as a drug-pricing bill.
But shepherding bills through Congress will be a challenge. “You need to have accountability, unity, and civility, which is a Herculean task,” Mr. Whitlock said. “You have to keep policies off the table that could blow up the bipartisanship.”
A version of this article first appeared on Medscape.com.
President Joe Biden has come into office after an unexpected shift in Congress. On Jan. 5, Democrats scored an upset by winning two U.S. Senate seats in runoff elections in Georgia, giving them control of the Senate.
Now the Democrats have control of all three levers of power – the Senate, the House, and the presidency – for the first time since the early years of the Obama administration.
How will President Biden use this new concentration of power to shape health care policy?
Democrats’ small majorities in both houses of Congress suggest that moderation and bipartisanship will be necessary to get things done. Moreover, Mr. Biden himself is calling for bipartisanship. “On this January day,” he said in his inauguration speech, “my whole soul is in this: Bringing America together, uniting our people, uniting our nation.”
Key health care actions that Mr. Biden could pursue include the following.
1. Passing a new COVID-19 relief bill
Above all, Mr. Biden is focused on overcoming the COVID-19 pandemic, which has been registering record deaths recently, and getting newly released vaccines to Americans.
“Dealing with the coronavirus pandemic is one of the most important battles our administration will face, and I will be informed by science and by experts,” the president said.
“There is no question that the pandemic is the highest priority for the Biden administration,” said Larry Levitt, executive vice president for health policy at the Henry J. Kaiser Family Foundation. “COVID will dominate the early weeks and months of this administration. His success rests, in particular, on improving the rollout of vaccines.”
Five days before his inauguration, the president-elect unveiled the American Rescue Plan, a massive, $1.9 trillion legislative package intended to hasten rollout of COVID-19 vaccines, improve COVID-19 testing, and provide financial help to businesses and individuals, among many other things.
The bill would add $1,400 to the recently passed $600 government relief payments for each American, amounting to a $2,000 check. It would also enact many non-COVID-19 measures, such as a $15-an-hour minimum wage and measures to bolster the Affordable Care Act (ACA).
If Democrats cannot reach a deal with the Republicans, they might turn the proposal into a reconciliation bill, which could then be passed with a simple majority. However, drafting a reconciliation bill is a long, complicated process that would require removing provisions that don’t meet the requirements of reconciliation, said Hazen Marshall, a Washington lobbyist and former staffer for Sen. Mitch McConnell.
Most importantly, Mr. Marshall said, reconciliation bills bring out diehard partisanship. “They involve a sledgehammer mentality,” he says. “You’re telling the other side that their views aren’t going to matter.” The final version of the ACA, for example, was passed as a reconciliation bill, with not one Republican vote.
In the Trump years, “the last four reconciliation bills did not get any votes from the minority,” added Rodney Whitlock, PhD, a political consultant at McDermott+Consulting, who worked 21 years for Republicans in the House. “When the majority chooses to use reconciliation, it is an admission that it has no interest in working with the minority.”
Hammering out a compromise will be tough, but Robert Pearl MD, former CEO of the Permanente Medical Group and a professor at Stanford (Calif.) University, said that if anyone can do it, it would be President Biden. Having served in the Senate for 36 years, “Biden knows Congress better than any president since Lyndon Johnson,” he said. “He can reach across the aisle and get legislation passed as much as anyone could these days.”
2. Restoring Obamacare
Mr. Biden has vowed to undo a gradual dismantling of the ACA that went on during the Trump administration through executive orders, rule-making, and new laws. “Reinvigorating the ACA was a central part of Biden’s platform as a candidate,” Mr. Levitt said.
Each Trump action against the ACA must be undone in the same way. Presidential orders must be met with presidential orders, regulations with regulations, and legislation with legislation.
The ACA is also being challenged in the Supreme Court. Republicans under Trump passed a law that reduced the penalty for not buying health insurance under the ACA to zero. Then a group of 20 states, led by Texas, filed a lawsuit asserting that this change makes the ACA unconstitutional.
The lawsuit was heard by the Supreme Court in November. From remarks made by the justices then, it appears that the court might well uphold the law when a verdict comes down in June.
But just in case, Mr. Biden wants Congress to enact a small penalty for not buying health insurance, which would remove the basis of the lawsuit.
Mr. Biden’s choice for secretary of Health and Human Services shows his level of commitment to protecting the ACA. His HHS nominee is California Attorney General Xavier Becerra, who led a group of 17 states defending the ACA in the current lawsuit.
In addition to undoing Trump’s changes, Mr. Biden plans to expand the ACA beyond the original legislation. The new COVID-19 bill contains provisions that would expand subsidies to buy insurance on the exchanges and would lower the maximum percentage of income that anyone has to pay for health insurance to 8.5%.
Dealing with Medicaid is also related to the ACA. In 2012, the Supreme Court struck down a mandate that states expand their Medicaid programs, with substantial funding from the federal government.
To date, 12 states still do not participate in the Medicaid expansion. To lure them into the expansion, the Democrat-controlled House last session passed a bill that would offer to pay the entire bill for the first 3 years of Medicaid expansion if they chose to enact an expansion.
3. Undoing other Trump actions in health care
In addition to changes in the ACA, Trump also enacted a number of other changes in health care that President Biden could undo. For example, Mr. Biden says he will reenter the World Health Organization (WHO) so that the United States could better coordinate a COVID-19 response with other nations. Trump exited the WHO with the stroke of a pen, and Mr. Biden can do the same in reverse.
Under Trump, the Centers for Medicare & Medicaid Services used waivers to weaken the ACA and allow states to alter their Medicaid programs. One waiver allows Georgia to leave the ACA exchanges and put brokers in charge of buying coverage. Other waivers allow states to transform federal Medicaid payments into block grants, which several states are planning to do.
The Trump CMS has allowed several states to use Medicaid waivers to add work requirements for Medicaid recipients. The courts have blocked the work rules so far, and the Biden CMS may decide to reverse these waivers or modify them.
“Undoing waivers is normally a fairly simple thing,” Mr. Levitt said. In January, however, the Trump CMS asked some waiver states to sign new contracts in which the CMS pledges not to end a waiver without 9 months’ notice. It’s unclear how many states signed such contracts and what obligation the Biden CMS has to enforce them.
The Trump CMS also stopped reimbursing insurers for waiving deductibles and copayments for low-income customers, as directed by the ACA. Without federal reimbursement, some insurers raised premiums by as much as 20% to cover the costs. It is unclear how the Biden CMS would tackle this change.
4. Negotiating lower drug prices
Allowing Medicare to negotiate drug prices, a major plank in Mr. Biden’s campaign, would seem like a slam dunk for the Democrats. This approach is backed by 89% of Americans, including 84% of Republicans, according to a Kaiser Family Foundation survey in December.
“With that level of support, it’s hard to go wrong politically on this issue,” Mr. Levitt said.
Many Republicans, however, do not favor negotiating drug prices, and the two parties continue to be far apart on how to control drug prices. Trump signed an action that allows Americans to buy cheaper drugs abroad, an approach that Mr. Biden also supports, but it is now tied up in the courts.
“A drug pricing bill has always been difficult to pass,” Dr. Whitlock said. “The issue is popular with the public, but change does not come easily. The drug lobby is one the strongest in Washington, and now it may be even stronger, since it was the drug companies that gave us the COVID vaccines.”
Dr. Whitlock said Republicans will want Democrats to compromise on drug pricing, but he doubts they will do so. The House passed a bill to negotiate drug prices last year, which never was voted on in the Senate. “It is difficult to imagine that the Democrats will be able to move rightward from that House bill,” Dr. Whitlock said. “Democrats are likely to stand pat on drug pricing.”
5. Introducing a public option
President Biden’s campaign proposal for a public option – health insurance offered by the federal government – and to lower the age for Medicare eligibility from 65 years to 60 years, resulted from a compromise between two factions of the Democratic party on how to expand coverage.
Although Mr. Biden and other moderates wanted to focus on fixing the ACA, Democrats led by Sen. Bernie Sanders of Vermont called for a single-payer system, dubbed “Medicare for all.” A public option was seen as the middle ground between the two camps.
“A public option would be a very controversial,” Dr. Whitlock said. Critics say it would pay at Medicare rates, which would reduce doctors’ reimbursements, and save very little money compared with a single-payer system.
Dr. Pearl sees similar problems with lowering the Medicare age. “This would be an expensive change that the federal government could not afford, particularly with all the spending on the pandemic,” he said. “And it would be tough on doctors and hospitals, because Medicare pays less than the private insurance payment they are now getting.”
“The public option is likely to get serious discussion within the Democratic caucus and get onto the Senate floor,” Mr. Levitt said. “The party won’t ignore it.” He notes that in the new Senate, Sen. Sanders chairs the budget committee, and from that position he is likely to push for expanding access to care.
Mr. Levitt says the Biden CMS might allow states to experiment with a statewide public option or even a single-payer model, but he concedes that states, with their budgets ravaged by COVID-19, do not currently have the money to launch such programs.
6. Reviving the CMS
Under President Obama, the CMS was the engine that implemented the ACA and shepherded wider use of value-based reimbursements, which reward providers for quality and outcomes rather than volume.
Under the Trump administration, CMS leadership continued to uphold value-based reimbursement, Dr. Pearl observed. “CMS leadership championed value-based payments, but they encountered a lot of pushback from doctors and hospitals and had to scale back their goals,” he said.
On the other hand, the Trump CMS took a 180-degree turn on the ACA and worked to take it apart. This took a toll on staff morale, according to Donald M. Berwick, MD, who ran the CMS under President Obama. “Many people in CMS did not feel supported during the Trump administration, and some of them left,” Dr. Berwick said.
The CMS needs experienced staff on board to write comprehensible rules and regulations that can overcome court challenges.
Having a fully functioning CMS also requires consistent leadership, which was a problem for Obama. When Mr. Obama nominated Dr. Berwick, 60 Senate votes were needed to confirm him, and Republicans would not vote for him. Mr. Obama eventually brought Dr. Berwick in as a recess appointment, but it meant he could serve for only 17 months.
Since then, Senate confirmation rules have changed so that only a simple majority is needed to confirm appointments. This is important for Biden’s nominees, Dr. Berwick said. “For a president, having your team in place means you are able to execute the policies you want,” he said. “You need to have consistent leadership.”
7. Potentially changing health care without Congress
Even with their newly won control of the Senate, the Democrats’ thin majorities in both houses of Congress may not be enough to pass much legislation if Republicans are solidly opposed.
Democrats in the House also have a narrow path this session in which to pass legislation. The Democratic leadership has an 11-vote majority, but it must contend with 15 moderate representatives in purple districts (where Democrats and Republicans have about equal support).
A bigger problem looms before the Democrats. In 2022, the party may well lose its majorities in both houses. Mr. Whitlock notes that the party of an incoming president normally loses seats in the first midterm election. “The last incoming president to keep both houses of Congress in his first midterm was Jimmy Carter,” he said.
If this happens, President Biden would have to govern without the support of Congress, which is what Barack Obama had to do through most of his presidency. As Mr. Obama’s vice president, Mr. Biden is well aware how that goes. Governing without Congress means relying on presidential orders and decrees.
In health care, Mr. Biden has a powerful policy-making tool, the Center for Medicare & Medicaid Innovation (CMMI). The CMMI was empowered by the ACA to initiate pilot programs for new payment models.
So far, the CMMI’s work has been mainly limited to accountable care organizations, bundled payments, and patient-centered medical homes, but it could also be used to enact new federal policies that would normally require Congressional action, Mr. Levitt said.
Conclusion
Expectations have been very high for what President Joe Biden can do in health care. He needs to unite a very divided political system to defeat a deadly pandemic, restore Obamacare, and sign landmark legislation, such as a drug-pricing bill.
But shepherding bills through Congress will be a challenge. “You need to have accountability, unity, and civility, which is a Herculean task,” Mr. Whitlock said. “You have to keep policies off the table that could blow up the bipartisanship.”
A version of this article first appeared on Medscape.com.
Generalized pruritic blisters and bullous lesions
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
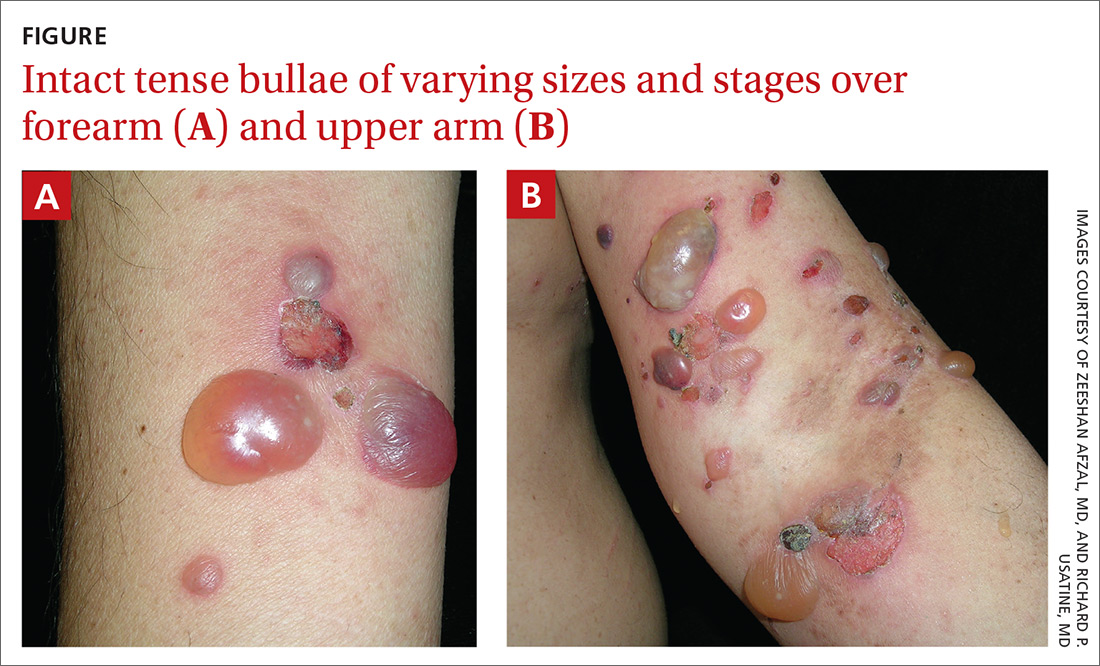
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
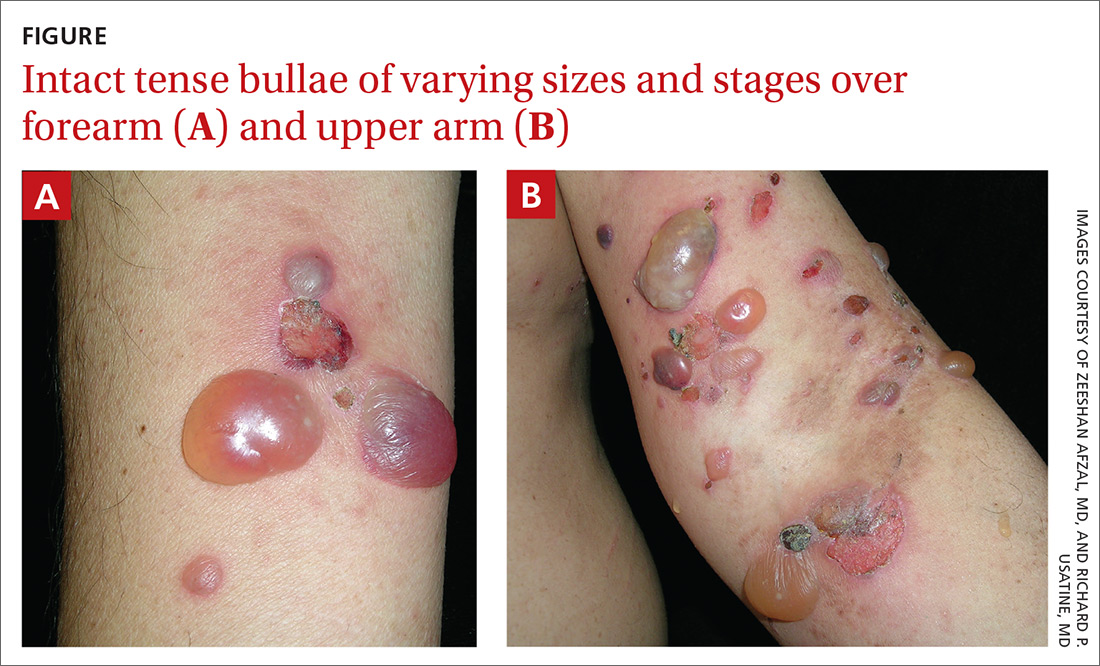
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
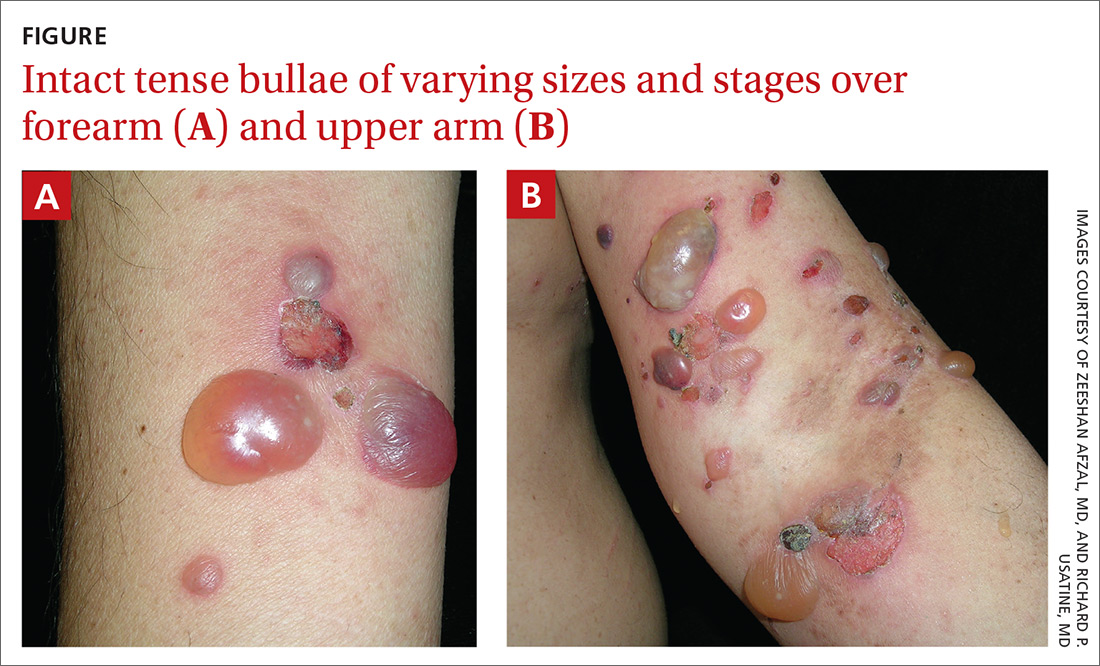
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
20-year-old man • sudden-onset chest pain • worsening pain with cough and exertion • Dx?
THE CASE
A 20-year-old man presented to our clinic with a 3-day history of nonradiating chest pain located at the center of his chest. Past medical history included idiopathic neonatal giant-cell hepatitis and subsequent liver transplant at 1 month of age; he had been followed by the transplant team without rejection or infection and was in otherwise good health prior to the chest pain.
On the day of symptom onset, he was walking inside his house and fell to his knees with a chest pain described as “a punch” to the center of the chest that lasted for a few seconds. He was able to continue his daily activities without limitation despite a constant, squeezing, centrally located chest pain. The pain worsened with cough and exertion.
A few hours later, he went to an urgent care center for evaluation. There, he reported, his chest radiograph and electrocardiogram (EKG) results were normal and he was given a diagnosis of musculoskeletal chest pain. Over the next 3 days, his chest pain persisted but did not worsen. He was taking 500 mg of naproxen every 8 hours with no improvement. No other acute or chronic medications were being taken. He had no significant family history. A review of systems was otherwise negative.
On physical exam, his vital statistics included a height of 6’4”; weight, 261 lb; body mass index, 31.8; temperature, 98.7 °F; blood pressure, 134/77 mm Hg; heart rate, 92 beats/min; respiratory rate, 18 breaths/min; and oxygen saturation, 96%. Throughout the exam, he demonstrated no acute distress, appeared well, and was talkative; however, he reported having a “constant, squeezing” chest pain that did not worsen with palpation of the chest. The rest of his physical exam was unremarkable.
Although he reported that his EKG and chest radiograph were normal 3 days prior, repeat chest radiograph and EKG were ordered due to his unexplained, active chest pain and the lack of immediate access to the prior results.
THE DIAGNOSIS
The chest radiograph (FIGURE 1A) showed a “mildly ectatic ascending thoracic aorta” that had increased since a chest radiograph from 6 years prior (FIGURE 1B) and “was concerning for an aneurysm.” Computed tomography (CT) angiography (FIGURE 2) then confirmed a 7-cm aneurysm of the ascending aorta, with findings suggestive of a retrograde ascending aortic dissection.
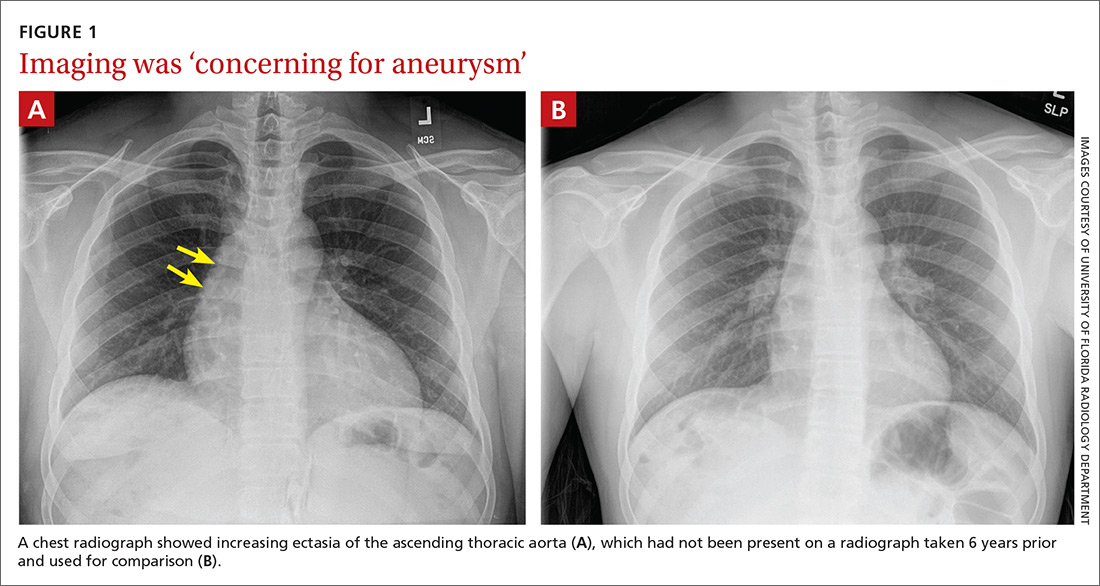
DISCUSSION
The average age of a patient with acute aortic dissection (AAD) is 63 years; only 7% occur in people younger than 40.1 AAD is often accompanied by a predisposing risk factor such as a connective tissue disease, bicuspid aortic valve, longstanding hypertension, trauma, or larger aortic dimensions.2,3 Younger patients are more likely to have predisposing risk factors of Marfan syndrome, prior aortic surgery, or a bicuspid aortic valve.3
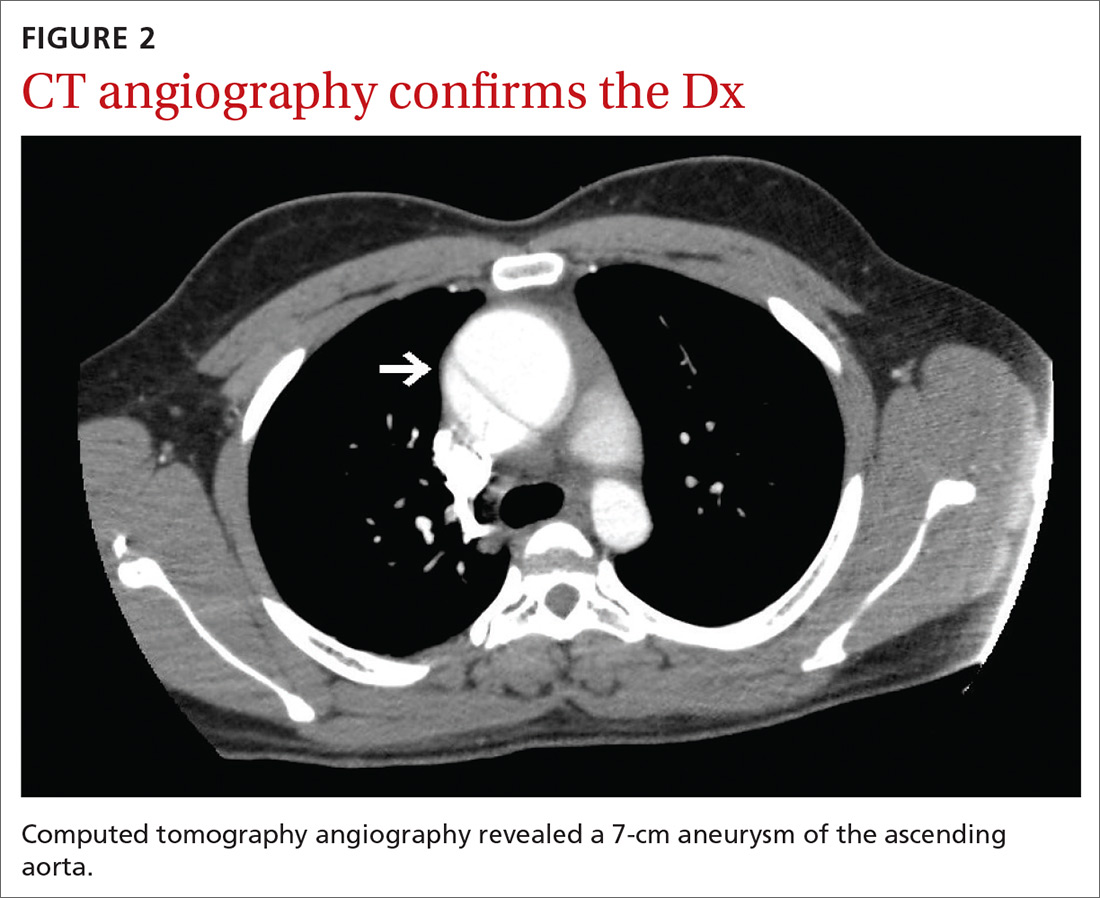
Continue to: A literature review did not reveal...
A literature review did not reveal any known correlation between the patient’s history of giant-cell hepatitis or antirejection therapy with thoracic aortic dissection. Furthermore, liver transplant is not known to be a specific risk factor for AAD in pediatric patients or outside the immediate postoperative period. Therefore, there were no known predisposing risk factors for AAD in our patient.
The most common clinical feature of AAD is chest pain, which occurs in 75% of patients.1 Other clinical symptoms include hypertension and diaphoresis.2,4 However, classic clinical findings are not always displayed, making the diagnosis difficult.2,4 The classical description of “tearing pain” is seen in only 51% of patients, and 5% to 15% of patients present without any pain.1
Commonly missed or misdiagnosed. The diagnosis of AAD has been missed during the initial exam in 38% of patients.4 As seen in our case, symptoms may be initially diagnosed as musculoskeletal chest pain. Based on symptoms, AAD can be incorrectly diagnosed as an acute myocardial infarction or vascular embolization.2,4
Every hour after symptom onset, the mortality rate of untreated AAD increases 1% to 2%,with no difference based on age.3,4 Different reports have shown mortality rates between 7% and 30%.4
Effective imaging is crucial to the diagnosis and treatment of AAD, given the occurrence of atypical presentation, missed diagnosis, and high mortality rate.4 A chest radiograph will show a widened mediastinum, but the preferred diagnostic tests are a CT or transthoracic echocardiogram.2,4 Once the diagnosis of AAD is confirmed, an aortic angiogram is the preferred test to determine the extent of the dissection prior to surgical treatment.2
Continue to: Classification dictates treatment
Classification dictates treatment. AAD is classified based on where the dissection of the aorta occurs. If the dissection involves the ascending aorta, it is classified as a type A AAD and should immediately be treated with emergent surgery in order to prevent complications including myocardial infarction, cardiac tamponade, and aortic rupture.2,4,5 If the dissection is limited to the descending aorta, it is classified as a type B AAD and can be medically managed by controlling pain and lowering blood pressure; if symptoms persist, surgical management may be required.2 After hospital discharge, AAD patients are followed closely with medical therapy, serial imaging, and reoperation if necessary.4
Our patient underwent emergent surgery for aortic root/ascending aortic replacement with a mechanical valve. He tolerated the procedure well. Surgical tissue pathology of the aortic segment showed a wall of elastic vessel with medial degeneration and dissection, and the tissue pathology of the aorta leaflets showed valvular tissue with myxoid degeneration.
THE TAKEAWAY
It is critical to keep AAD in the differential diagnosis of a patient presenting with acute onset of chest pain, as AAD often has an atypical presentation and can easily be misdiagnosed. Effective imaging is crucial to diagnosis, and immediate treatment is essential to patient survival.
CORRESPONDENCE
Rachel A. Reedy, PA, University of Florida, Department of General Pediatrics, 7046 SW Archer Road, Gainesville, FL 32608; [email protected]
1. Pineault J, Ouimet D, Pichette V, Vallée M. A case of aortic dissection in a young adult: a refresher of the literature of this “great masquerader.” Int J Gen Med. 2011;4:889-893.
2. Agabegi SS, Agabegi ElD, Ring AC. Diseases of the cardiovascular system. In: Jackson A, ed. Step-up to Medicine. 3rd ed. Lippincott Williams & Wilkins; 2012:54-55.
3. Januzzi JL, Isselbacher EM, Fattori R, et al. Characterizing the young patient with aortic dissection: results from the International Registry of Aortic Dissection (IRAD). J Am Coll Cardiol. 2004;43:665-669.
4. Tsai TT, Trimarchi S, Nienaber CA. Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg. 2009;37:149-159.
5. Trimarchi S, Eagle KA, Nienaber CA, et al. Role of age in acute type A aortic dissection outcome: Report from the International Registry of Acute Aortic Dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140:784-789.
THE CASE
A 20-year-old man presented to our clinic with a 3-day history of nonradiating chest pain located at the center of his chest. Past medical history included idiopathic neonatal giant-cell hepatitis and subsequent liver transplant at 1 month of age; he had been followed by the transplant team without rejection or infection and was in otherwise good health prior to the chest pain.
On the day of symptom onset, he was walking inside his house and fell to his knees with a chest pain described as “a punch” to the center of the chest that lasted for a few seconds. He was able to continue his daily activities without limitation despite a constant, squeezing, centrally located chest pain. The pain worsened with cough and exertion.
A few hours later, he went to an urgent care center for evaluation. There, he reported, his chest radiograph and electrocardiogram (EKG) results were normal and he was given a diagnosis of musculoskeletal chest pain. Over the next 3 days, his chest pain persisted but did not worsen. He was taking 500 mg of naproxen every 8 hours with no improvement. No other acute or chronic medications were being taken. He had no significant family history. A review of systems was otherwise negative.
On physical exam, his vital statistics included a height of 6’4”; weight, 261 lb; body mass index, 31.8; temperature, 98.7 °F; blood pressure, 134/77 mm Hg; heart rate, 92 beats/min; respiratory rate, 18 breaths/min; and oxygen saturation, 96%. Throughout the exam, he demonstrated no acute distress, appeared well, and was talkative; however, he reported having a “constant, squeezing” chest pain that did not worsen with palpation of the chest. The rest of his physical exam was unremarkable.
Although he reported that his EKG and chest radiograph were normal 3 days prior, repeat chest radiograph and EKG were ordered due to his unexplained, active chest pain and the lack of immediate access to the prior results.
THE DIAGNOSIS
The chest radiograph (FIGURE 1A) showed a “mildly ectatic ascending thoracic aorta” that had increased since a chest radiograph from 6 years prior (FIGURE 1B) and “was concerning for an aneurysm.” Computed tomography (CT) angiography (FIGURE 2) then confirmed a 7-cm aneurysm of the ascending aorta, with findings suggestive of a retrograde ascending aortic dissection.
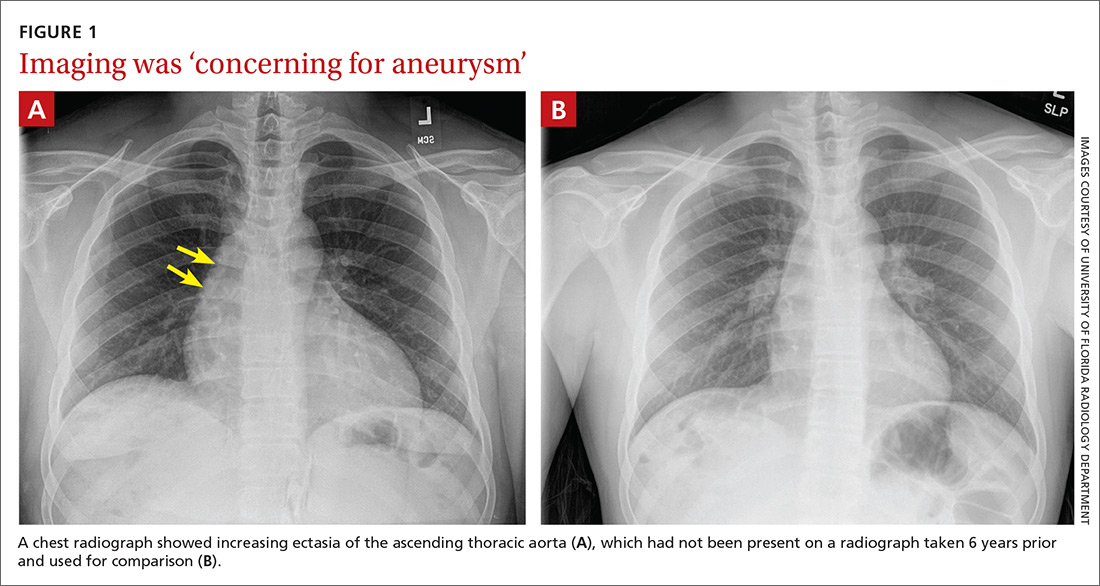
DISCUSSION
The average age of a patient with acute aortic dissection (AAD) is 63 years; only 7% occur in people younger than 40.1 AAD is often accompanied by a predisposing risk factor such as a connective tissue disease, bicuspid aortic valve, longstanding hypertension, trauma, or larger aortic dimensions.2,3 Younger patients are more likely to have predisposing risk factors of Marfan syndrome, prior aortic surgery, or a bicuspid aortic valve.3
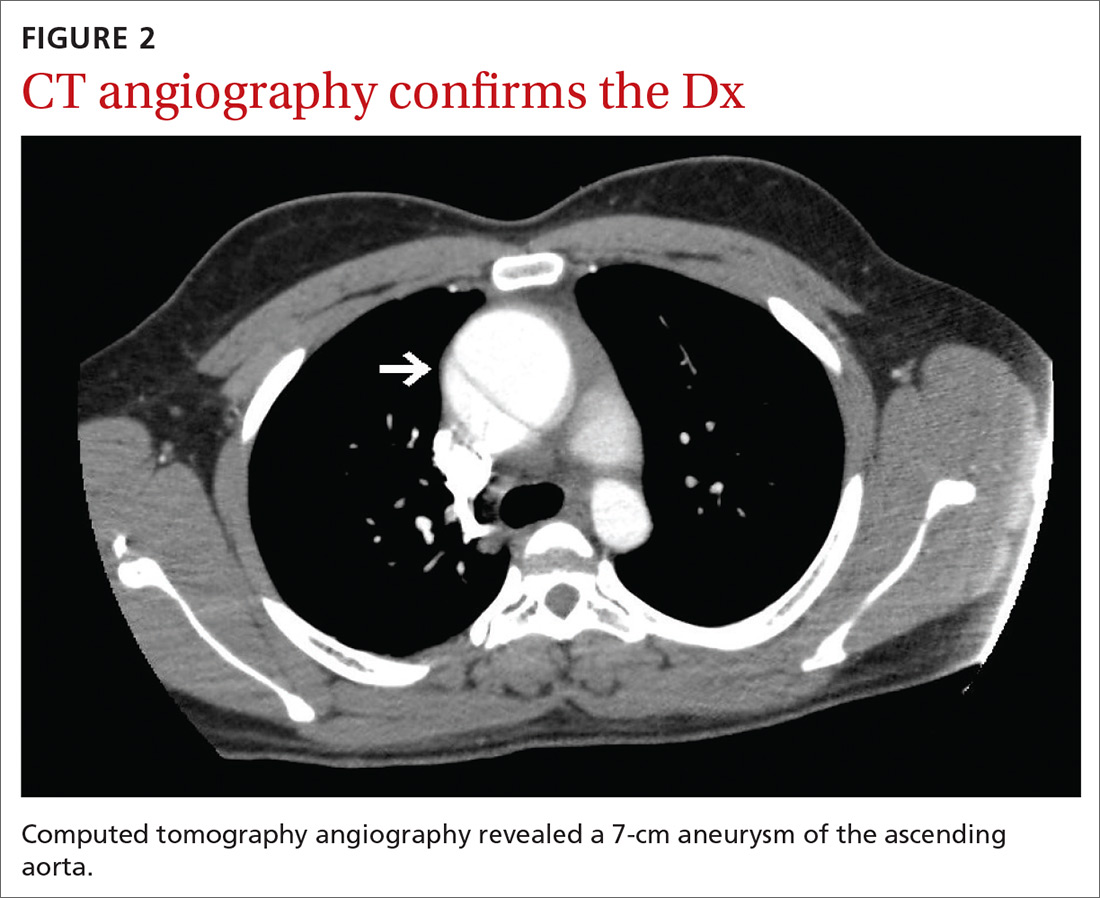
Continue to: A literature review did not reveal...
A literature review did not reveal any known correlation between the patient’s history of giant-cell hepatitis or antirejection therapy with thoracic aortic dissection. Furthermore, liver transplant is not known to be a specific risk factor for AAD in pediatric patients or outside the immediate postoperative period. Therefore, there were no known predisposing risk factors for AAD in our patient.
The most common clinical feature of AAD is chest pain, which occurs in 75% of patients.1 Other clinical symptoms include hypertension and diaphoresis.2,4 However, classic clinical findings are not always displayed, making the diagnosis difficult.2,4 The classical description of “tearing pain” is seen in only 51% of patients, and 5% to 15% of patients present without any pain.1
Commonly missed or misdiagnosed. The diagnosis of AAD has been missed during the initial exam in 38% of patients.4 As seen in our case, symptoms may be initially diagnosed as musculoskeletal chest pain. Based on symptoms, AAD can be incorrectly diagnosed as an acute myocardial infarction or vascular embolization.2,4
Every hour after symptom onset, the mortality rate of untreated AAD increases 1% to 2%,with no difference based on age.3,4 Different reports have shown mortality rates between 7% and 30%.4
Effective imaging is crucial to the diagnosis and treatment of AAD, given the occurrence of atypical presentation, missed diagnosis, and high mortality rate.4 A chest radiograph will show a widened mediastinum, but the preferred diagnostic tests are a CT or transthoracic echocardiogram.2,4 Once the diagnosis of AAD is confirmed, an aortic angiogram is the preferred test to determine the extent of the dissection prior to surgical treatment.2
Continue to: Classification dictates treatment
Classification dictates treatment. AAD is classified based on where the dissection of the aorta occurs. If the dissection involves the ascending aorta, it is classified as a type A AAD and should immediately be treated with emergent surgery in order to prevent complications including myocardial infarction, cardiac tamponade, and aortic rupture.2,4,5 If the dissection is limited to the descending aorta, it is classified as a type B AAD and can be medically managed by controlling pain and lowering blood pressure; if symptoms persist, surgical management may be required.2 After hospital discharge, AAD patients are followed closely with medical therapy, serial imaging, and reoperation if necessary.4
Our patient underwent emergent surgery for aortic root/ascending aortic replacement with a mechanical valve. He tolerated the procedure well. Surgical tissue pathology of the aortic segment showed a wall of elastic vessel with medial degeneration and dissection, and the tissue pathology of the aorta leaflets showed valvular tissue with myxoid degeneration.
THE TAKEAWAY
It is critical to keep AAD in the differential diagnosis of a patient presenting with acute onset of chest pain, as AAD often has an atypical presentation and can easily be misdiagnosed. Effective imaging is crucial to diagnosis, and immediate treatment is essential to patient survival.
CORRESPONDENCE
Rachel A. Reedy, PA, University of Florida, Department of General Pediatrics, 7046 SW Archer Road, Gainesville, FL 32608; [email protected]
THE CASE
A 20-year-old man presented to our clinic with a 3-day history of nonradiating chest pain located at the center of his chest. Past medical history included idiopathic neonatal giant-cell hepatitis and subsequent liver transplant at 1 month of age; he had been followed by the transplant team without rejection or infection and was in otherwise good health prior to the chest pain.
On the day of symptom onset, he was walking inside his house and fell to his knees with a chest pain described as “a punch” to the center of the chest that lasted for a few seconds. He was able to continue his daily activities without limitation despite a constant, squeezing, centrally located chest pain. The pain worsened with cough and exertion.
A few hours later, he went to an urgent care center for evaluation. There, he reported, his chest radiograph and electrocardiogram (EKG) results were normal and he was given a diagnosis of musculoskeletal chest pain. Over the next 3 days, his chest pain persisted but did not worsen. He was taking 500 mg of naproxen every 8 hours with no improvement. No other acute or chronic medications were being taken. He had no significant family history. A review of systems was otherwise negative.
On physical exam, his vital statistics included a height of 6’4”; weight, 261 lb; body mass index, 31.8; temperature, 98.7 °F; blood pressure, 134/77 mm Hg; heart rate, 92 beats/min; respiratory rate, 18 breaths/min; and oxygen saturation, 96%. Throughout the exam, he demonstrated no acute distress, appeared well, and was talkative; however, he reported having a “constant, squeezing” chest pain that did not worsen with palpation of the chest. The rest of his physical exam was unremarkable.
Although he reported that his EKG and chest radiograph were normal 3 days prior, repeat chest radiograph and EKG were ordered due to his unexplained, active chest pain and the lack of immediate access to the prior results.
THE DIAGNOSIS
The chest radiograph (FIGURE 1A) showed a “mildly ectatic ascending thoracic aorta” that had increased since a chest radiograph from 6 years prior (FIGURE 1B) and “was concerning for an aneurysm.” Computed tomography (CT) angiography (FIGURE 2) then confirmed a 7-cm aneurysm of the ascending aorta, with findings suggestive of a retrograde ascending aortic dissection.
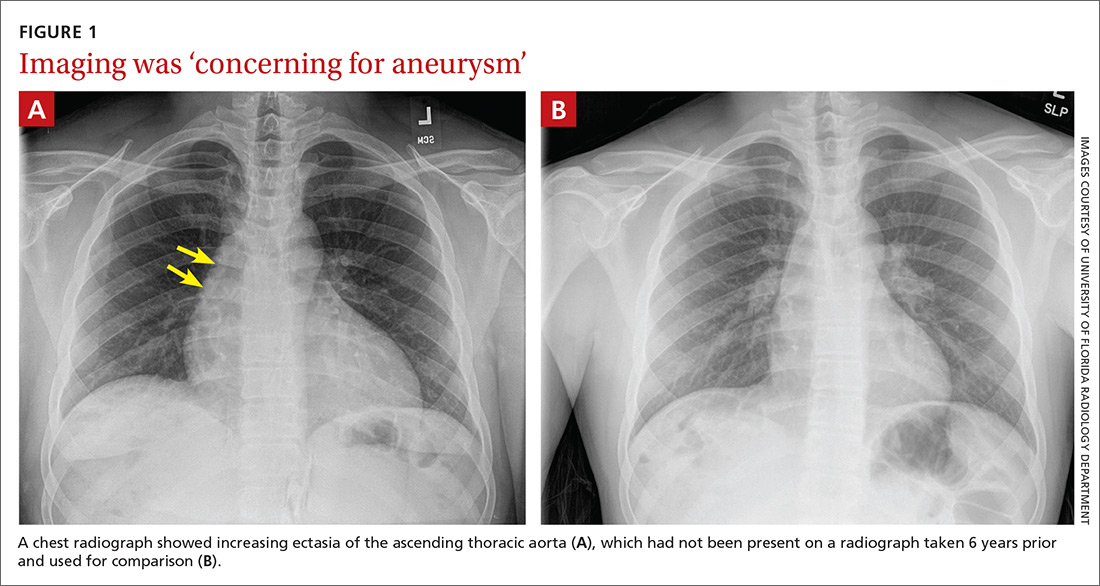
DISCUSSION
The average age of a patient with acute aortic dissection (AAD) is 63 years; only 7% occur in people younger than 40.1 AAD is often accompanied by a predisposing risk factor such as a connective tissue disease, bicuspid aortic valve, longstanding hypertension, trauma, or larger aortic dimensions.2,3 Younger patients are more likely to have predisposing risk factors of Marfan syndrome, prior aortic surgery, or a bicuspid aortic valve.3
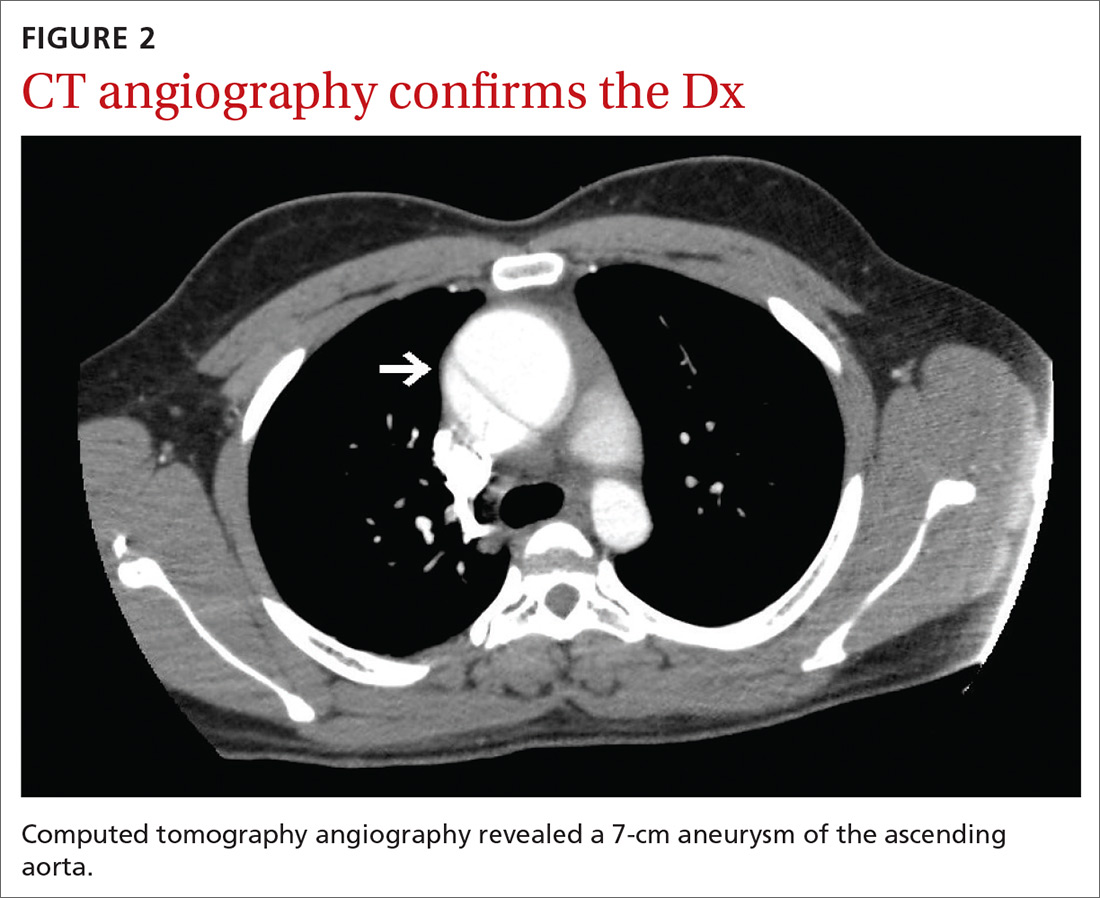
Continue to: A literature review did not reveal...
A literature review did not reveal any known correlation between the patient’s history of giant-cell hepatitis or antirejection therapy with thoracic aortic dissection. Furthermore, liver transplant is not known to be a specific risk factor for AAD in pediatric patients or outside the immediate postoperative period. Therefore, there were no known predisposing risk factors for AAD in our patient.
The most common clinical feature of AAD is chest pain, which occurs in 75% of patients.1 Other clinical symptoms include hypertension and diaphoresis.2,4 However, classic clinical findings are not always displayed, making the diagnosis difficult.2,4 The classical description of “tearing pain” is seen in only 51% of patients, and 5% to 15% of patients present without any pain.1
Commonly missed or misdiagnosed. The diagnosis of AAD has been missed during the initial exam in 38% of patients.4 As seen in our case, symptoms may be initially diagnosed as musculoskeletal chest pain. Based on symptoms, AAD can be incorrectly diagnosed as an acute myocardial infarction or vascular embolization.2,4
Every hour after symptom onset, the mortality rate of untreated AAD increases 1% to 2%,with no difference based on age.3,4 Different reports have shown mortality rates between 7% and 30%.4
Effective imaging is crucial to the diagnosis and treatment of AAD, given the occurrence of atypical presentation, missed diagnosis, and high mortality rate.4 A chest radiograph will show a widened mediastinum, but the preferred diagnostic tests are a CT or transthoracic echocardiogram.2,4 Once the diagnosis of AAD is confirmed, an aortic angiogram is the preferred test to determine the extent of the dissection prior to surgical treatment.2
Continue to: Classification dictates treatment
Classification dictates treatment. AAD is classified based on where the dissection of the aorta occurs. If the dissection involves the ascending aorta, it is classified as a type A AAD and should immediately be treated with emergent surgery in order to prevent complications including myocardial infarction, cardiac tamponade, and aortic rupture.2,4,5 If the dissection is limited to the descending aorta, it is classified as a type B AAD and can be medically managed by controlling pain and lowering blood pressure; if symptoms persist, surgical management may be required.2 After hospital discharge, AAD patients are followed closely with medical therapy, serial imaging, and reoperation if necessary.4
Our patient underwent emergent surgery for aortic root/ascending aortic replacement with a mechanical valve. He tolerated the procedure well. Surgical tissue pathology of the aortic segment showed a wall of elastic vessel with medial degeneration and dissection, and the tissue pathology of the aorta leaflets showed valvular tissue with myxoid degeneration.
THE TAKEAWAY
It is critical to keep AAD in the differential diagnosis of a patient presenting with acute onset of chest pain, as AAD often has an atypical presentation and can easily be misdiagnosed. Effective imaging is crucial to diagnosis, and immediate treatment is essential to patient survival.
CORRESPONDENCE
Rachel A. Reedy, PA, University of Florida, Department of General Pediatrics, 7046 SW Archer Road, Gainesville, FL 32608; [email protected]
1. Pineault J, Ouimet D, Pichette V, Vallée M. A case of aortic dissection in a young adult: a refresher of the literature of this “great masquerader.” Int J Gen Med. 2011;4:889-893.
2. Agabegi SS, Agabegi ElD, Ring AC. Diseases of the cardiovascular system. In: Jackson A, ed. Step-up to Medicine. 3rd ed. Lippincott Williams & Wilkins; 2012:54-55.
3. Januzzi JL, Isselbacher EM, Fattori R, et al. Characterizing the young patient with aortic dissection: results from the International Registry of Aortic Dissection (IRAD). J Am Coll Cardiol. 2004;43:665-669.
4. Tsai TT, Trimarchi S, Nienaber CA. Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg. 2009;37:149-159.
5. Trimarchi S, Eagle KA, Nienaber CA, et al. Role of age in acute type A aortic dissection outcome: Report from the International Registry of Acute Aortic Dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140:784-789.
1. Pineault J, Ouimet D, Pichette V, Vallée M. A case of aortic dissection in a young adult: a refresher of the literature of this “great masquerader.” Int J Gen Med. 2011;4:889-893.
2. Agabegi SS, Agabegi ElD, Ring AC. Diseases of the cardiovascular system. In: Jackson A, ed. Step-up to Medicine. 3rd ed. Lippincott Williams & Wilkins; 2012:54-55.
3. Januzzi JL, Isselbacher EM, Fattori R, et al. Characterizing the young patient with aortic dissection: results from the International Registry of Aortic Dissection (IRAD). J Am Coll Cardiol. 2004;43:665-669.
4. Tsai TT, Trimarchi S, Nienaber CA. Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg. 2009;37:149-159.
5. Trimarchi S, Eagle KA, Nienaber CA, et al. Role of age in acute type A aortic dissection outcome: Report from the International Registry of Acute Aortic Dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140:784-789.
Reproductive psychiatry in 2021: Old questions and new challenges
Across this period of the pandemic, we’ve spent considerable attention focusing on adaptations to clinical care for pregnant and postpartum women across the board. From the start, this has included a shift to telemedicine for the majority of our patients who come to see us with psychiatric disorders either before, during, or after pregnancy.
Specific issues for perinatal patients since the early days of COVID-19 have included the shifts in women’s plans with respect to delivery as well as the limitation on women’s ability to configure the types of support that they had originally planned on with family, friends, and others during delivery. Telemedicine again helped, at least in part, to fill that void by having online digital support by individuals or groups for both pregnant and postpartum women. These supports were always available, but quickly scaled up during the first 6-9 months of the pandemic and have likely seen their greatest increase in participation in the history of support groups for pregnant and postpartum women.
Similarly, at our own center, we have seen a dramatic increase across the last 10 months in requests for consultation by women with psychiatric disorders who have hopes and plans to conceive, to those who are pregnant or post partum and who are trying to sustain emotional well-being despite the added burden of the pandemic. As we heard similar stories regarding interactions with perinatal patients from reproductive psychiatrists across the country, my colleagues and I had to set up an additional resource, Virtual Rounds at the Center for Women’s Mental Health at Massachusetts General Hospital, Boston, which has been mentioned in previous columns, which has only grown during the last 6 months of the pandemic. We have colleagues across the country joining us from 2 p.m. to 3 p.m. on Wednesdays after our own faculty rounds, where we perform case reviews of our own patients, and invite our colleagues to share cases that are then reviewed with expert panelists together with our own faculty in a collaborative environment. Feedback from the community of clinicians has indicated that these virtual rounds have been invaluable to their efforts in taking care of women with perinatal psychiatric issues, particularly during the pandemic.
Of particular note during consultations on our service is the number of women coming to see us for questions about the reproductive safety of the medications on which they are maintained. Hundreds of women present to the center each year for the most up-to-date information regarding the reproductive safety of the most commonly used psychiatric medications in reproductive-age women, including antidepressants (SSRIs, serotonin norepinephrine reuptake inhibitor), mood stabilizers, lithium, lamotrigine, and atypical antipsychotics, as well as other medicines used to treat symptoms that have been a particular issue during the pandemic, such as insomnia and anxiety (benzodiazepines, nonbenzodiazepines, sedative hypnotics, and medicines such as gabapentin).
While consultation regarding risk of fetal exposure to psychotropics has been the cornerstone of our clinical work for 25 years, it has taken on a particularly critical dimension during the pandemic given the wish that women stay euthymic during the pandemic to limit the possibility of patients needing to present in a clinical space that would increase their risk for COVID-19, and to also minimize their risk for postpartum depression. (Psychiatric disorder during pregnancy remains the strongest predictor of emergence or worsening of underlying illness during the postpartum period.)
It is also noteworthy that, during a pandemic year, publications in reproductive psychiatry have been numerous, and we continue to make an effort at our own center to keep up with this and to share with our colleagues our impression of that literature using the weekly blog at womensmentalhealth.org. Last year brought the largest audience to the blog and visits to womensmentalhealth.org in the history of our center.
A case recently at our center presents a unique opportunity to review a confusing question in reproductive psychiatry over the last 15 years. A woman with a longstanding history of mixed anxiety and depression recently came to see us on a regimen of escitalopram and low-dose benzodiazepine. She was doing well, and she and her husband of 4 years were hopeful about starting to try to conceive despite the pandemic. We reviewed the reproductive safety data of the medicines on which she was maintained and made plans to follow-up as her plans galvanized. She notified me several months later that she had become pregnant but had experienced an early miscarriage. The patient was obviously upset and, as she reflected on her decision to maintain treatment with SSRI during her attempts to conceive and across a very early pregnancy, she queried about the extent to which her SSRI use might have contributed to her miscarriage.
The question about the possible association of antidepressant use during pregnancy and increased risk for miscarriage goes back at least 15 years when there were reports of an increased risk of miscarriage in women taking SSRIs during pregnancy. In that early work, there was an apparent increase in miscarriage in women taking SSRIs relative to a control group, but the rate did not exceed the prevalence of miscarriage in the general population. Since those early reports, we are lucky to have had multiple investigators look very closely at this issue, including one meta-analysis of 11 studies done approximately 8 years ago that failed to show an increased risk of miscarriage in the setting of first trimester exposure to SSRIs.
What has been most problematic methodologically, however, has been the failure to account for the potential role of depression in models that predict risk. A subsequent large epidemiologic study from Denmark evaluating over a million women has looked at this question further. The authors found a slightly increased risk of spontaneous abortion associated with the use of antidepressants (12.0% in women with antidepressant exposure vs. 11.1% in women with no exposure). However, looking only at women with a diagnosis of depression, the adjusted risk ratio for spontaneous abortion after any antidepressant exposure was 1.00 (95% confidence interval, 0.80-1.24). Thus, the researchers concluded that exposure to depression – but not exposure to antidepressant – is associated with a slightly higher risk of miscarriage.
Even more recently, a follow-up study examining this question supports the large epidemiologic study by Kjaersgaard and colleagues. For most readers, this effectively answers this very important question for women about rates of miscarriage associated with fetal exposure to SSRIs.
For the patient who presented at the center, reassuring her with this information felt particularly good, especially within the context of the pandemic. After several months of trying to conceive, she again became pregnant and delivered without difficulty. What was palpable in that clinical scenario, as it relates to the practice of reproductive psychiatry during the pandemic, is the even-greater emotional valence that questions about using psychiatric medications during pregnancy has taken on across these past months. While attention and thoughtful consideration about the relative risks of using psychiatric medications during pregnancy should be standard clinical practice, the level of anxiety associated with decisions to sustain or to discontinue treatment during pregnancy seems to have increased for some patients during the pandemic.
Even as the COVID-19 vaccine initiative across the United States is rolled out, 2021 will continue to be a complicated time for women and families. We still need to be vigilant. In addition to screening for perinatal depression during pregnancy and the postpartum period, we should be equally mindful of screening and treating perinatal anxiety, particularly during this challenging time. The challenge to keep pregnant and postpartum women well is perhaps even greater now, 10 months into the pandemic, than it was when we were in crisis mode in March 2020. As clinicians, we need to mobilize the spectrum of both pharmacologic and nonpharmacologic treatment options to sustain emotional well-being among women planning to conceive as well as those who are pregnant or postpartum as we navigate our way to safer times.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Across this period of the pandemic, we’ve spent considerable attention focusing on adaptations to clinical care for pregnant and postpartum women across the board. From the start, this has included a shift to telemedicine for the majority of our patients who come to see us with psychiatric disorders either before, during, or after pregnancy.
Specific issues for perinatal patients since the early days of COVID-19 have included the shifts in women’s plans with respect to delivery as well as the limitation on women’s ability to configure the types of support that they had originally planned on with family, friends, and others during delivery. Telemedicine again helped, at least in part, to fill that void by having online digital support by individuals or groups for both pregnant and postpartum women. These supports were always available, but quickly scaled up during the first 6-9 months of the pandemic and have likely seen their greatest increase in participation in the history of support groups for pregnant and postpartum women.
Similarly, at our own center, we have seen a dramatic increase across the last 10 months in requests for consultation by women with psychiatric disorders who have hopes and plans to conceive, to those who are pregnant or post partum and who are trying to sustain emotional well-being despite the added burden of the pandemic. As we heard similar stories regarding interactions with perinatal patients from reproductive psychiatrists across the country, my colleagues and I had to set up an additional resource, Virtual Rounds at the Center for Women’s Mental Health at Massachusetts General Hospital, Boston, which has been mentioned in previous columns, which has only grown during the last 6 months of the pandemic. We have colleagues across the country joining us from 2 p.m. to 3 p.m. on Wednesdays after our own faculty rounds, where we perform case reviews of our own patients, and invite our colleagues to share cases that are then reviewed with expert panelists together with our own faculty in a collaborative environment. Feedback from the community of clinicians has indicated that these virtual rounds have been invaluable to their efforts in taking care of women with perinatal psychiatric issues, particularly during the pandemic.
Of particular note during consultations on our service is the number of women coming to see us for questions about the reproductive safety of the medications on which they are maintained. Hundreds of women present to the center each year for the most up-to-date information regarding the reproductive safety of the most commonly used psychiatric medications in reproductive-age women, including antidepressants (SSRIs, serotonin norepinephrine reuptake inhibitor), mood stabilizers, lithium, lamotrigine, and atypical antipsychotics, as well as other medicines used to treat symptoms that have been a particular issue during the pandemic, such as insomnia and anxiety (benzodiazepines, nonbenzodiazepines, sedative hypnotics, and medicines such as gabapentin).
While consultation regarding risk of fetal exposure to psychotropics has been the cornerstone of our clinical work for 25 years, it has taken on a particularly critical dimension during the pandemic given the wish that women stay euthymic during the pandemic to limit the possibility of patients needing to present in a clinical space that would increase their risk for COVID-19, and to also minimize their risk for postpartum depression. (Psychiatric disorder during pregnancy remains the strongest predictor of emergence or worsening of underlying illness during the postpartum period.)
It is also noteworthy that, during a pandemic year, publications in reproductive psychiatry have been numerous, and we continue to make an effort at our own center to keep up with this and to share with our colleagues our impression of that literature using the weekly blog at womensmentalhealth.org. Last year brought the largest audience to the blog and visits to womensmentalhealth.org in the history of our center.
A case recently at our center presents a unique opportunity to review a confusing question in reproductive psychiatry over the last 15 years. A woman with a longstanding history of mixed anxiety and depression recently came to see us on a regimen of escitalopram and low-dose benzodiazepine. She was doing well, and she and her husband of 4 years were hopeful about starting to try to conceive despite the pandemic. We reviewed the reproductive safety data of the medicines on which she was maintained and made plans to follow-up as her plans galvanized. She notified me several months later that she had become pregnant but had experienced an early miscarriage. The patient was obviously upset and, as she reflected on her decision to maintain treatment with SSRI during her attempts to conceive and across a very early pregnancy, she queried about the extent to which her SSRI use might have contributed to her miscarriage.
The question about the possible association of antidepressant use during pregnancy and increased risk for miscarriage goes back at least 15 years when there were reports of an increased risk of miscarriage in women taking SSRIs during pregnancy. In that early work, there was an apparent increase in miscarriage in women taking SSRIs relative to a control group, but the rate did not exceed the prevalence of miscarriage in the general population. Since those early reports, we are lucky to have had multiple investigators look very closely at this issue, including one meta-analysis of 11 studies done approximately 8 years ago that failed to show an increased risk of miscarriage in the setting of first trimester exposure to SSRIs.
What has been most problematic methodologically, however, has been the failure to account for the potential role of depression in models that predict risk. A subsequent large epidemiologic study from Denmark evaluating over a million women has looked at this question further. The authors found a slightly increased risk of spontaneous abortion associated with the use of antidepressants (12.0% in women with antidepressant exposure vs. 11.1% in women with no exposure). However, looking only at women with a diagnosis of depression, the adjusted risk ratio for spontaneous abortion after any antidepressant exposure was 1.00 (95% confidence interval, 0.80-1.24). Thus, the researchers concluded that exposure to depression – but not exposure to antidepressant – is associated with a slightly higher risk of miscarriage.
Even more recently, a follow-up study examining this question supports the large epidemiologic study by Kjaersgaard and colleagues. For most readers, this effectively answers this very important question for women about rates of miscarriage associated with fetal exposure to SSRIs.
For the patient who presented at the center, reassuring her with this information felt particularly good, especially within the context of the pandemic. After several months of trying to conceive, she again became pregnant and delivered without difficulty. What was palpable in that clinical scenario, as it relates to the practice of reproductive psychiatry during the pandemic, is the even-greater emotional valence that questions about using psychiatric medications during pregnancy has taken on across these past months. While attention and thoughtful consideration about the relative risks of using psychiatric medications during pregnancy should be standard clinical practice, the level of anxiety associated with decisions to sustain or to discontinue treatment during pregnancy seems to have increased for some patients during the pandemic.
Even as the COVID-19 vaccine initiative across the United States is rolled out, 2021 will continue to be a complicated time for women and families. We still need to be vigilant. In addition to screening for perinatal depression during pregnancy and the postpartum period, we should be equally mindful of screening and treating perinatal anxiety, particularly during this challenging time. The challenge to keep pregnant and postpartum women well is perhaps even greater now, 10 months into the pandemic, than it was when we were in crisis mode in March 2020. As clinicians, we need to mobilize the spectrum of both pharmacologic and nonpharmacologic treatment options to sustain emotional well-being among women planning to conceive as well as those who are pregnant or postpartum as we navigate our way to safer times.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
Across this period of the pandemic, we’ve spent considerable attention focusing on adaptations to clinical care for pregnant and postpartum women across the board. From the start, this has included a shift to telemedicine for the majority of our patients who come to see us with psychiatric disorders either before, during, or after pregnancy.
Specific issues for perinatal patients since the early days of COVID-19 have included the shifts in women’s plans with respect to delivery as well as the limitation on women’s ability to configure the types of support that they had originally planned on with family, friends, and others during delivery. Telemedicine again helped, at least in part, to fill that void by having online digital support by individuals or groups for both pregnant and postpartum women. These supports were always available, but quickly scaled up during the first 6-9 months of the pandemic and have likely seen their greatest increase in participation in the history of support groups for pregnant and postpartum women.
Similarly, at our own center, we have seen a dramatic increase across the last 10 months in requests for consultation by women with psychiatric disorders who have hopes and plans to conceive, to those who are pregnant or post partum and who are trying to sustain emotional well-being despite the added burden of the pandemic. As we heard similar stories regarding interactions with perinatal patients from reproductive psychiatrists across the country, my colleagues and I had to set up an additional resource, Virtual Rounds at the Center for Women’s Mental Health at Massachusetts General Hospital, Boston, which has been mentioned in previous columns, which has only grown during the last 6 months of the pandemic. We have colleagues across the country joining us from 2 p.m. to 3 p.m. on Wednesdays after our own faculty rounds, where we perform case reviews of our own patients, and invite our colleagues to share cases that are then reviewed with expert panelists together with our own faculty in a collaborative environment. Feedback from the community of clinicians has indicated that these virtual rounds have been invaluable to their efforts in taking care of women with perinatal psychiatric issues, particularly during the pandemic.
Of particular note during consultations on our service is the number of women coming to see us for questions about the reproductive safety of the medications on which they are maintained. Hundreds of women present to the center each year for the most up-to-date information regarding the reproductive safety of the most commonly used psychiatric medications in reproductive-age women, including antidepressants (SSRIs, serotonin norepinephrine reuptake inhibitor), mood stabilizers, lithium, lamotrigine, and atypical antipsychotics, as well as other medicines used to treat symptoms that have been a particular issue during the pandemic, such as insomnia and anxiety (benzodiazepines, nonbenzodiazepines, sedative hypnotics, and medicines such as gabapentin).
While consultation regarding risk of fetal exposure to psychotropics has been the cornerstone of our clinical work for 25 years, it has taken on a particularly critical dimension during the pandemic given the wish that women stay euthymic during the pandemic to limit the possibility of patients needing to present in a clinical space that would increase their risk for COVID-19, and to also minimize their risk for postpartum depression. (Psychiatric disorder during pregnancy remains the strongest predictor of emergence or worsening of underlying illness during the postpartum period.)
It is also noteworthy that, during a pandemic year, publications in reproductive psychiatry have been numerous, and we continue to make an effort at our own center to keep up with this and to share with our colleagues our impression of that literature using the weekly blog at womensmentalhealth.org. Last year brought the largest audience to the blog and visits to womensmentalhealth.org in the history of our center.
A case recently at our center presents a unique opportunity to review a confusing question in reproductive psychiatry over the last 15 years. A woman with a longstanding history of mixed anxiety and depression recently came to see us on a regimen of escitalopram and low-dose benzodiazepine. She was doing well, and she and her husband of 4 years were hopeful about starting to try to conceive despite the pandemic. We reviewed the reproductive safety data of the medicines on which she was maintained and made plans to follow-up as her plans galvanized. She notified me several months later that she had become pregnant but had experienced an early miscarriage. The patient was obviously upset and, as she reflected on her decision to maintain treatment with SSRI during her attempts to conceive and across a very early pregnancy, she queried about the extent to which her SSRI use might have contributed to her miscarriage.
The question about the possible association of antidepressant use during pregnancy and increased risk for miscarriage goes back at least 15 years when there were reports of an increased risk of miscarriage in women taking SSRIs during pregnancy. In that early work, there was an apparent increase in miscarriage in women taking SSRIs relative to a control group, but the rate did not exceed the prevalence of miscarriage in the general population. Since those early reports, we are lucky to have had multiple investigators look very closely at this issue, including one meta-analysis of 11 studies done approximately 8 years ago that failed to show an increased risk of miscarriage in the setting of first trimester exposure to SSRIs.
What has been most problematic methodologically, however, has been the failure to account for the potential role of depression in models that predict risk. A subsequent large epidemiologic study from Denmark evaluating over a million women has looked at this question further. The authors found a slightly increased risk of spontaneous abortion associated with the use of antidepressants (12.0% in women with antidepressant exposure vs. 11.1% in women with no exposure). However, looking only at women with a diagnosis of depression, the adjusted risk ratio for spontaneous abortion after any antidepressant exposure was 1.00 (95% confidence interval, 0.80-1.24). Thus, the researchers concluded that exposure to depression – but not exposure to antidepressant – is associated with a slightly higher risk of miscarriage.
Even more recently, a follow-up study examining this question supports the large epidemiologic study by Kjaersgaard and colleagues. For most readers, this effectively answers this very important question for women about rates of miscarriage associated with fetal exposure to SSRIs.
For the patient who presented at the center, reassuring her with this information felt particularly good, especially within the context of the pandemic. After several months of trying to conceive, she again became pregnant and delivered without difficulty. What was palpable in that clinical scenario, as it relates to the practice of reproductive psychiatry during the pandemic, is the even-greater emotional valence that questions about using psychiatric medications during pregnancy has taken on across these past months. While attention and thoughtful consideration about the relative risks of using psychiatric medications during pregnancy should be standard clinical practice, the level of anxiety associated with decisions to sustain or to discontinue treatment during pregnancy seems to have increased for some patients during the pandemic.
Even as the COVID-19 vaccine initiative across the United States is rolled out, 2021 will continue to be a complicated time for women and families. We still need to be vigilant. In addition to screening for perinatal depression during pregnancy and the postpartum period, we should be equally mindful of screening and treating perinatal anxiety, particularly during this challenging time. The challenge to keep pregnant and postpartum women well is perhaps even greater now, 10 months into the pandemic, than it was when we were in crisis mode in March 2020. As clinicians, we need to mobilize the spectrum of both pharmacologic and nonpharmacologic treatment options to sustain emotional well-being among women planning to conceive as well as those who are pregnant or postpartum as we navigate our way to safer times.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
On receiving the COVID-19 vaccine
This moment, for which I am so grateful and fortunate, represents a link in a remarkable chain of events that spans decades and represents the acme of human achievement.
My gratitude starts with scientists who years before this pandemic, perfected the ability to extract DNA from viruses, sequence it, and transcribe it to RNA. From there my gratitude goes to scientists who years ago developed an ingenious animal model for mRNA vaccines. The next link of gratitude is for scientists who at the start of this year quickly identified a deadly novel coronavirus and to scientists who rapidly sequenced its villainous DNA.
Next, I give thanks to scientists who promptly identified the segment of that DNA that codes for the spike proteins that the virus uses to invade our cells. And then I am grateful to the scientists who made the mRNA that corresponds to that specific DNA sequence, and to the scientists who figured out how create a lipid womb to protect that precious mRNA payload during its perilous journey from factory floor to the depths of our deltoid musculature.
I am no less grateful to the brave people who volunteered for the Pfizer trial, taking the risk of being the first humans ever to participate in an mRNA trial with stakes so high, and to the investigators who ran that trial and the scientists at Pfizer, the Food and Drug Administration, and the Western Coalition who reviewed the data and approved the vaccine without bowing to political pressure.
My gratitude extends to the factory workers who manufactured the vaccine in mass quantities, and the workers who manufactured the equipment that those factories rely on, and the pilots of planes and drivers of trucks who transported the vaccine to my hospital in Seattle, and to the workers who made those planes and trucks that carried that precious cargo. And the workers who devised super-cold storage systems and the workers who built those systems, and the people who fed them and clothed them and housed them so that they could do this life-saving work.
And to the leaders at my hospital who devised our immunization plan, and the ethicists who figured out who should go first (thanks Nancy), and the workers who made the glass vials to hold the vaccine, the plastic syringes to deliver it precisely, and surgically sharp needles so that there would be no pain whatsoever when those beautiful little mRNA filled lipid particles got injected into my left deltoid muscle by a highly skilled and compassionate nurse.
From there, the miracle of nature takes hold causing my cells to transcribe that RNA into spike proteins which will trigger my magical B-cells and T-cells to recognize that nasty spike protein as foreign in case it ever shows its ugly head to my respiratory mucosa, where these cells and the antibodies and chemicals they produce would stomp that wretched virus down without me ever knowing it or missing a beat, and keep me safe not only to live and thrive another day but also hopefully prevent me from spreading the virus to those I love and others I don’t even know but pass within just feet of.
For these miracles of nature and the chain of human toil and genius involving innumerable individuals over many years, many whom will never be thanked or recognized, I am truly and forever grateful.
Dr. Aaronson is a hospitalist and chief medical informatics officer at Virginia Mason Medical Center in Seattle.
This moment, for which I am so grateful and fortunate, represents a link in a remarkable chain of events that spans decades and represents the acme of human achievement.
My gratitude starts with scientists who years before this pandemic, perfected the ability to extract DNA from viruses, sequence it, and transcribe it to RNA. From there my gratitude goes to scientists who years ago developed an ingenious animal model for mRNA vaccines. The next link of gratitude is for scientists who at the start of this year quickly identified a deadly novel coronavirus and to scientists who rapidly sequenced its villainous DNA.
Next, I give thanks to scientists who promptly identified the segment of that DNA that codes for the spike proteins that the virus uses to invade our cells. And then I am grateful to the scientists who made the mRNA that corresponds to that specific DNA sequence, and to the scientists who figured out how create a lipid womb to protect that precious mRNA payload during its perilous journey from factory floor to the depths of our deltoid musculature.
I am no less grateful to the brave people who volunteered for the Pfizer trial, taking the risk of being the first humans ever to participate in an mRNA trial with stakes so high, and to the investigators who ran that trial and the scientists at Pfizer, the Food and Drug Administration, and the Western Coalition who reviewed the data and approved the vaccine without bowing to political pressure.
My gratitude extends to the factory workers who manufactured the vaccine in mass quantities, and the workers who manufactured the equipment that those factories rely on, and the pilots of planes and drivers of trucks who transported the vaccine to my hospital in Seattle, and to the workers who made those planes and trucks that carried that precious cargo. And the workers who devised super-cold storage systems and the workers who built those systems, and the people who fed them and clothed them and housed them so that they could do this life-saving work.
And to the leaders at my hospital who devised our immunization plan, and the ethicists who figured out who should go first (thanks Nancy), and the workers who made the glass vials to hold the vaccine, the plastic syringes to deliver it precisely, and surgically sharp needles so that there would be no pain whatsoever when those beautiful little mRNA filled lipid particles got injected into my left deltoid muscle by a highly skilled and compassionate nurse.
From there, the miracle of nature takes hold causing my cells to transcribe that RNA into spike proteins which will trigger my magical B-cells and T-cells to recognize that nasty spike protein as foreign in case it ever shows its ugly head to my respiratory mucosa, where these cells and the antibodies and chemicals they produce would stomp that wretched virus down without me ever knowing it or missing a beat, and keep me safe not only to live and thrive another day but also hopefully prevent me from spreading the virus to those I love and others I don’t even know but pass within just feet of.
For these miracles of nature and the chain of human toil and genius involving innumerable individuals over many years, many whom will never be thanked or recognized, I am truly and forever grateful.
Dr. Aaronson is a hospitalist and chief medical informatics officer at Virginia Mason Medical Center in Seattle.
This moment, for which I am so grateful and fortunate, represents a link in a remarkable chain of events that spans decades and represents the acme of human achievement.
My gratitude starts with scientists who years before this pandemic, perfected the ability to extract DNA from viruses, sequence it, and transcribe it to RNA. From there my gratitude goes to scientists who years ago developed an ingenious animal model for mRNA vaccines. The next link of gratitude is for scientists who at the start of this year quickly identified a deadly novel coronavirus and to scientists who rapidly sequenced its villainous DNA.
Next, I give thanks to scientists who promptly identified the segment of that DNA that codes for the spike proteins that the virus uses to invade our cells. And then I am grateful to the scientists who made the mRNA that corresponds to that specific DNA sequence, and to the scientists who figured out how create a lipid womb to protect that precious mRNA payload during its perilous journey from factory floor to the depths of our deltoid musculature.
I am no less grateful to the brave people who volunteered for the Pfizer trial, taking the risk of being the first humans ever to participate in an mRNA trial with stakes so high, and to the investigators who ran that trial and the scientists at Pfizer, the Food and Drug Administration, and the Western Coalition who reviewed the data and approved the vaccine without bowing to political pressure.
My gratitude extends to the factory workers who manufactured the vaccine in mass quantities, and the workers who manufactured the equipment that those factories rely on, and the pilots of planes and drivers of trucks who transported the vaccine to my hospital in Seattle, and to the workers who made those planes and trucks that carried that precious cargo. And the workers who devised super-cold storage systems and the workers who built those systems, and the people who fed them and clothed them and housed them so that they could do this life-saving work.
And to the leaders at my hospital who devised our immunization plan, and the ethicists who figured out who should go first (thanks Nancy), and the workers who made the glass vials to hold the vaccine, the plastic syringes to deliver it precisely, and surgically sharp needles so that there would be no pain whatsoever when those beautiful little mRNA filled lipid particles got injected into my left deltoid muscle by a highly skilled and compassionate nurse.
From there, the miracle of nature takes hold causing my cells to transcribe that RNA into spike proteins which will trigger my magical B-cells and T-cells to recognize that nasty spike protein as foreign in case it ever shows its ugly head to my respiratory mucosa, where these cells and the antibodies and chemicals they produce would stomp that wretched virus down without me ever knowing it or missing a beat, and keep me safe not only to live and thrive another day but also hopefully prevent me from spreading the virus to those I love and others I don’t even know but pass within just feet of.
For these miracles of nature and the chain of human toil and genius involving innumerable individuals over many years, many whom will never be thanked or recognized, I am truly and forever grateful.
Dr. Aaronson is a hospitalist and chief medical informatics officer at Virginia Mason Medical Center in Seattle.
Can viscous fiber lower glycemic markers in type 2 diabetes?
ILLUSTRATIVE CASE
A 57-year-old man who was given a diagnosis of T2D a year ago presents for an office visit. His hemoglobin A1C level at diagnosis was 8.3%. He is otherwise healthy and has been adhering well to a plan of metformin 1000 mg twice daily, regular exercise, and a low-carbohydrate diet you recommended. His most recent hemoglobin A1C is 7.3%. He is pleased with his progress, so he is discouraged when you tell him that he is not yet at goal. He asks if there are other things that he can do to further lower his hemoglobin A1C. What can you recommend for him?
According to the National Diabetes Statistics Report, 2020 from the Centers for Disease Control and Prevention, approximately 34.1 million US adults ≥ 18 years of age (13% of the adult population) have diabetes, 50% of whom have a hemoglobin A1C > 7%. The report also states that approximately 88 million US adults—more than one-third of the population—have prediabetes.2
The American Diabetes Association (ADA) estimated that diabetes-related health care costs in the United States for 2017 totaled $237 billion, an increase of 26% from 2012. More than $30 billion of this expense comes directly from diabetes medications; the remainder of these costs are related to lost wages, clinic visits, hospitalizations, and treatment for diabetic complications and comorbidities. After controlling for age and gender, medical expenditures for people with diabetes are 2.3 times higher than for those without diabetes.3
The 2019
STUDY SUMMARY
Effect on A1C exceeded the FDA threshold for new drugs
This systematic review and meta-analysis searched MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials to identify randomized controlled trials that studied the effects of viscous fiber supplementation on glycemic control in patients with T2D. Eligible studies included those that: (1) had a duration ≥ 3 weeks; (2) allowed isolation of the viscous fiber effects; and (3) reported at least 1 of the following glycemic measures: hemoglobin A1C (n = 1148 patients), fasting glucose (n = 1394), fasting insulin (n = 228),
Data were pooled using the generic inverse variance method and expressed as mean difference (MD) with 95% confidence intervals (CIs). Heterogeneity was assessed and quantified (Cochran Q and I2 statistics, respectively). I2 ≥ 50% indicates substantial heterogeneity. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to evaluate the overall strength of evidence.
Twenty-eight eligible studies were compared. The median age of included patients was 60 years. The median dose of viscous fiber was 13.1 g/d (range, 2.55-21). Viscous fiber type varied between the studies and included psyllium, guar gum, β-glucan, and konjac, and was consumed in powder, tablet, capsule, and limited food-based forms (in 1 of the included studies). The median trial duration was 8 weeks, with 11 trials lasting ≥ 12 weeks.
Continue to: The study found...
The study found moderate-grade evidence that, when added to standard of care, viscous fiber supplementation reduced hemoglobin A1C (MD = –0.58%; 95% CI, –0.88 to –0.28; P = .0002; I2 = 91%), fasting glucose (MD = –14.8 mg/dL; 95% CI, –23.8 to –5.58; P = .001; I2 = 92%), and HOMA-IR (MD = –1.89; 95% CI, –3.45 to –0.33; P = .02; I2 = 94%) compared with control. The effect on hemoglobin A1C exceeds the ≥ 0.3% threshold established by the US Food and Drug Administration for new antihyperglycemic drug development. There was no significant effect on fasting insulin or fructosamine, although the sample size for fructosamine was small. No significant evidence of a dose-dependent response effect was found. The studies had substantial heterogeneity. No evaluation of potential or real harm was noted in the analysis.
WHAT’S NEW
Potential glycemic benefit without large dietary increase
The glucose-lowering effects of increased fiber intake have often been hypothesized, but this meta-analysis is the first to focus specifically on the effect of viscous fiber supplements in patients with T2D. Prior meta-analyses, including those cited in the 2019 ADA recommendations mentioned above, included primarily whole-food dietary sources of fiber in the treatment arms and generally had more modest effects on outcomes.4,6,7
By focusing on viscous fiber supplements, this study isolated the effect of these supplements vs fiber-rich dietary changes. It illustrates a greater potential benefit with supplements than whole-food dietary sources of fiber, and at a lower dose of fiber than was seen in prior studies without requiring substantial increases in caloric intake. Viscous fiber supplementation is a potential adjunct to the usual evidence-based standards of care for glycemic control in patients with T2D.
CAVEATS
Limited study durations may raise uncertainty about long-term benefits
This meta-analysis does have its limitations. The heterogeneity among the studies analyzed makes it difficult to establish a single recommendation regarding dose, type, and brand of fiber to be used. Only 11 of the 28 studies lasted longer than 12 weeks, with a median duration of 8 weeks, making any long-term effects on hemoglobin A1C unknown. No adverse effects or reactions were described to evaluate safety and tolerability of the viscous fiber supplementation. No patient-oriented outcomes were reported.
CHALLENGES TO IMPLEMENTATION
Patients may not be eager to supplement with viscous fiber
The biggest challenge to implementation is patient compliance. Some forms of supplemental fiber are less palatable than others and may cause unpleasant gastrointestinal adverse effects, which may be an impediment for some patients. Cost may also be an issue for some patients. Diabetes medications can be expensive; however, they are often covered, at least partially, by medical insurance. Over-the-counter supplements are unlikely to be covered for most patients.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Jovanovski E, Khayyat R, Zurbau A, et al. Should viscous fiber supplements be considered in diabetes control? Results from a systematic review and meta-analysis of randomized controlled tria ls. Diabetes Care. 2019;42:755-766. Published correction appears in Diabetes Care. 2019;42:1604.
2. CDC. National Diabetes Statistics Report, 2020. Estimates of Diabetes and Its Burden in the United States. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2020.
3. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41:917-928.
4. Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42:731-754.
5. American Diabetes Association. 5. Lifestyle management: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(suppl 1):S46-S60.
6. Post RE, Mainous AG III, King DE, et al. Dietary fiber for the treatment of type 2 diabetes mellitus: a meta-analysis. J Am Board Fam Med. 2012;25:16-23.
7. Jenkins DJA, Kendall CWC, Augustin LSA, et al. Effect of legumes as part of a low glycemic index diet on glycemic control and cardiovascular risk factors in type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2012;172:1653-1660.
ILLUSTRATIVE CASE
A 57-year-old man who was given a diagnosis of T2D a year ago presents for an office visit. His hemoglobin A1C level at diagnosis was 8.3%. He is otherwise healthy and has been adhering well to a plan of metformin 1000 mg twice daily, regular exercise, and a low-carbohydrate diet you recommended. His most recent hemoglobin A1C is 7.3%. He is pleased with his progress, so he is discouraged when you tell him that he is not yet at goal. He asks if there are other things that he can do to further lower his hemoglobin A1C. What can you recommend for him?
According to the National Diabetes Statistics Report, 2020 from the Centers for Disease Control and Prevention, approximately 34.1 million US adults ≥ 18 years of age (13% of the adult population) have diabetes, 50% of whom have a hemoglobin A1C > 7%. The report also states that approximately 88 million US adults—more than one-third of the population—have prediabetes.2
The American Diabetes Association (ADA) estimated that diabetes-related health care costs in the United States for 2017 totaled $237 billion, an increase of 26% from 2012. More than $30 billion of this expense comes directly from diabetes medications; the remainder of these costs are related to lost wages, clinic visits, hospitalizations, and treatment for diabetic complications and comorbidities. After controlling for age and gender, medical expenditures for people with diabetes are 2.3 times higher than for those without diabetes.3
The 2019
STUDY SUMMARY
Effect on A1C exceeded the FDA threshold for new drugs
This systematic review and meta-analysis searched MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials to identify randomized controlled trials that studied the effects of viscous fiber supplementation on glycemic control in patients with T2D. Eligible studies included those that: (1) had a duration ≥ 3 weeks; (2) allowed isolation of the viscous fiber effects; and (3) reported at least 1 of the following glycemic measures: hemoglobin A1C (n = 1148 patients), fasting glucose (n = 1394), fasting insulin (n = 228),
Data were pooled using the generic inverse variance method and expressed as mean difference (MD) with 95% confidence intervals (CIs). Heterogeneity was assessed and quantified (Cochran Q and I2 statistics, respectively). I2 ≥ 50% indicates substantial heterogeneity. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to evaluate the overall strength of evidence.
Twenty-eight eligible studies were compared. The median age of included patients was 60 years. The median dose of viscous fiber was 13.1 g/d (range, 2.55-21). Viscous fiber type varied between the studies and included psyllium, guar gum, β-glucan, and konjac, and was consumed in powder, tablet, capsule, and limited food-based forms (in 1 of the included studies). The median trial duration was 8 weeks, with 11 trials lasting ≥ 12 weeks.
Continue to: The study found...
The study found moderate-grade evidence that, when added to standard of care, viscous fiber supplementation reduced hemoglobin A1C (MD = –0.58%; 95% CI, –0.88 to –0.28; P = .0002; I2 = 91%), fasting glucose (MD = –14.8 mg/dL; 95% CI, –23.8 to –5.58; P = .001; I2 = 92%), and HOMA-IR (MD = –1.89; 95% CI, –3.45 to –0.33; P = .02; I2 = 94%) compared with control. The effect on hemoglobin A1C exceeds the ≥ 0.3% threshold established by the US Food and Drug Administration for new antihyperglycemic drug development. There was no significant effect on fasting insulin or fructosamine, although the sample size for fructosamine was small. No significant evidence of a dose-dependent response effect was found. The studies had substantial heterogeneity. No evaluation of potential or real harm was noted in the analysis.
WHAT’S NEW
Potential glycemic benefit without large dietary increase
The glucose-lowering effects of increased fiber intake have often been hypothesized, but this meta-analysis is the first to focus specifically on the effect of viscous fiber supplements in patients with T2D. Prior meta-analyses, including those cited in the 2019 ADA recommendations mentioned above, included primarily whole-food dietary sources of fiber in the treatment arms and generally had more modest effects on outcomes.4,6,7
By focusing on viscous fiber supplements, this study isolated the effect of these supplements vs fiber-rich dietary changes. It illustrates a greater potential benefit with supplements than whole-food dietary sources of fiber, and at a lower dose of fiber than was seen in prior studies without requiring substantial increases in caloric intake. Viscous fiber supplementation is a potential adjunct to the usual evidence-based standards of care for glycemic control in patients with T2D.
CAVEATS
Limited study durations may raise uncertainty about long-term benefits
This meta-analysis does have its limitations. The heterogeneity among the studies analyzed makes it difficult to establish a single recommendation regarding dose, type, and brand of fiber to be used. Only 11 of the 28 studies lasted longer than 12 weeks, with a median duration of 8 weeks, making any long-term effects on hemoglobin A1C unknown. No adverse effects or reactions were described to evaluate safety and tolerability of the viscous fiber supplementation. No patient-oriented outcomes were reported.
CHALLENGES TO IMPLEMENTATION
Patients may not be eager to supplement with viscous fiber
The biggest challenge to implementation is patient compliance. Some forms of supplemental fiber are less palatable than others and may cause unpleasant gastrointestinal adverse effects, which may be an impediment for some patients. Cost may also be an issue for some patients. Diabetes medications can be expensive; however, they are often covered, at least partially, by medical insurance. Over-the-counter supplements are unlikely to be covered for most patients.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 57-year-old man who was given a diagnosis of T2D a year ago presents for an office visit. His hemoglobin A1C level at diagnosis was 8.3%. He is otherwise healthy and has been adhering well to a plan of metformin 1000 mg twice daily, regular exercise, and a low-carbohydrate diet you recommended. His most recent hemoglobin A1C is 7.3%. He is pleased with his progress, so he is discouraged when you tell him that he is not yet at goal. He asks if there are other things that he can do to further lower his hemoglobin A1C. What can you recommend for him?
According to the National Diabetes Statistics Report, 2020 from the Centers for Disease Control and Prevention, approximately 34.1 million US adults ≥ 18 years of age (13% of the adult population) have diabetes, 50% of whom have a hemoglobin A1C > 7%. The report also states that approximately 88 million US adults—more than one-third of the population—have prediabetes.2
The American Diabetes Association (ADA) estimated that diabetes-related health care costs in the United States for 2017 totaled $237 billion, an increase of 26% from 2012. More than $30 billion of this expense comes directly from diabetes medications; the remainder of these costs are related to lost wages, clinic visits, hospitalizations, and treatment for diabetic complications and comorbidities. After controlling for age and gender, medical expenditures for people with diabetes are 2.3 times higher than for those without diabetes.3
The 2019
STUDY SUMMARY
Effect on A1C exceeded the FDA threshold for new drugs
This systematic review and meta-analysis searched MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials to identify randomized controlled trials that studied the effects of viscous fiber supplementation on glycemic control in patients with T2D. Eligible studies included those that: (1) had a duration ≥ 3 weeks; (2) allowed isolation of the viscous fiber effects; and (3) reported at least 1 of the following glycemic measures: hemoglobin A1C (n = 1148 patients), fasting glucose (n = 1394), fasting insulin (n = 228),
Data were pooled using the generic inverse variance method and expressed as mean difference (MD) with 95% confidence intervals (CIs). Heterogeneity was assessed and quantified (Cochran Q and I2 statistics, respectively). I2 ≥ 50% indicates substantial heterogeneity. The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to evaluate the overall strength of evidence.
Twenty-eight eligible studies were compared. The median age of included patients was 60 years. The median dose of viscous fiber was 13.1 g/d (range, 2.55-21). Viscous fiber type varied between the studies and included psyllium, guar gum, β-glucan, and konjac, and was consumed in powder, tablet, capsule, and limited food-based forms (in 1 of the included studies). The median trial duration was 8 weeks, with 11 trials lasting ≥ 12 weeks.
Continue to: The study found...
The study found moderate-grade evidence that, when added to standard of care, viscous fiber supplementation reduced hemoglobin A1C (MD = –0.58%; 95% CI, –0.88 to –0.28; P = .0002; I2 = 91%), fasting glucose (MD = –14.8 mg/dL; 95% CI, –23.8 to –5.58; P = .001; I2 = 92%), and HOMA-IR (MD = –1.89; 95% CI, –3.45 to –0.33; P = .02; I2 = 94%) compared with control. The effect on hemoglobin A1C exceeds the ≥ 0.3% threshold established by the US Food and Drug Administration for new antihyperglycemic drug development. There was no significant effect on fasting insulin or fructosamine, although the sample size for fructosamine was small. No significant evidence of a dose-dependent response effect was found. The studies had substantial heterogeneity. No evaluation of potential or real harm was noted in the analysis.
WHAT’S NEW
Potential glycemic benefit without large dietary increase
The glucose-lowering effects of increased fiber intake have often been hypothesized, but this meta-analysis is the first to focus specifically on the effect of viscous fiber supplements in patients with T2D. Prior meta-analyses, including those cited in the 2019 ADA recommendations mentioned above, included primarily whole-food dietary sources of fiber in the treatment arms and generally had more modest effects on outcomes.4,6,7
By focusing on viscous fiber supplements, this study isolated the effect of these supplements vs fiber-rich dietary changes. It illustrates a greater potential benefit with supplements than whole-food dietary sources of fiber, and at a lower dose of fiber than was seen in prior studies without requiring substantial increases in caloric intake. Viscous fiber supplementation is a potential adjunct to the usual evidence-based standards of care for glycemic control in patients with T2D.
CAVEATS
Limited study durations may raise uncertainty about long-term benefits
This meta-analysis does have its limitations. The heterogeneity among the studies analyzed makes it difficult to establish a single recommendation regarding dose, type, and brand of fiber to be used. Only 11 of the 28 studies lasted longer than 12 weeks, with a median duration of 8 weeks, making any long-term effects on hemoglobin A1C unknown. No adverse effects or reactions were described to evaluate safety and tolerability of the viscous fiber supplementation. No patient-oriented outcomes were reported.
CHALLENGES TO IMPLEMENTATION
Patients may not be eager to supplement with viscous fiber
The biggest challenge to implementation is patient compliance. Some forms of supplemental fiber are less palatable than others and may cause unpleasant gastrointestinal adverse effects, which may be an impediment for some patients. Cost may also be an issue for some patients. Diabetes medications can be expensive; however, they are often covered, at least partially, by medical insurance. Over-the-counter supplements are unlikely to be covered for most patients.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
1. Jovanovski E, Khayyat R, Zurbau A, et al. Should viscous fiber supplements be considered in diabetes control? Results from a systematic review and meta-analysis of randomized controlled tria ls. Diabetes Care. 2019;42:755-766. Published correction appears in Diabetes Care. 2019;42:1604.
2. CDC. National Diabetes Statistics Report, 2020. Estimates of Diabetes and Its Burden in the United States. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2020.
3. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41:917-928.
4. Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42:731-754.
5. American Diabetes Association. 5. Lifestyle management: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(suppl 1):S46-S60.
6. Post RE, Mainous AG III, King DE, et al. Dietary fiber for the treatment of type 2 diabetes mellitus: a meta-analysis. J Am Board Fam Med. 2012;25:16-23.
7. Jenkins DJA, Kendall CWC, Augustin LSA, et al. Effect of legumes as part of a low glycemic index diet on glycemic control and cardiovascular risk factors in type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2012;172:1653-1660.
1. Jovanovski E, Khayyat R, Zurbau A, et al. Should viscous fiber supplements be considered in diabetes control? Results from a systematic review and meta-analysis of randomized controlled tria ls. Diabetes Care. 2019;42:755-766. Published correction appears in Diabetes Care. 2019;42:1604.
2. CDC. National Diabetes Statistics Report, 2020. Estimates of Diabetes and Its Burden in the United States. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2020.
3. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41:917-928.
4. Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42:731-754.
5. American Diabetes Association. 5. Lifestyle management: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(suppl 1):S46-S60.
6. Post RE, Mainous AG III, King DE, et al. Dietary fiber for the treatment of type 2 diabetes mellitus: a meta-analysis. J Am Board Fam Med. 2012;25:16-23.
7. Jenkins DJA, Kendall CWC, Augustin LSA, et al. Effect of legumes as part of a low glycemic index diet on glycemic control and cardiovascular risk factors in type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2012;172:1653-1660.
PRACTICE CHANGER
Unless contraindicated, recommend viscous fiber supplementation to your patients with type 2 diabetes (T2D), in addition to the usual evidence-based standards of care, to improve markers of glycemic control.
STRENGTH OF RECOMMENDATION
C: Based on a meta-analysis and systematic review of 28 randomized controlled trials, without discussion of patient-oriented outcomes.1
Jovanovski E, Khayyat R, Zurbau A, et al. Should viscous fiber supplements be considered in diabetes control? Results from a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2019;42:755-766. Published correction appears in Diabetes Care. 2019;42:1604.
Recognizing and intervening in child sex trafficking
THE CASE
Emily T.* is a 15-year-old, cisgender, homeless runaway. While on the streets, she was lured to a hotel where a “pimp” informed her she was going to work for him. She repeatedly tried to leave, but he would strike her, so she eventually succumbed. She was forced to have sex with several men and rarely allowed to use condoms.
On 1 occasion, when she went to a hospital with her pimp to visit a patient, her aunt (a nurse on duty at that facility) saw Ms. T and called the police. The pimp was arrested. Ms. T was interviewed by the police and gave a statement but refused a forensic exam.
Because of her involvement with the pimp, she was incarcerated. In prison, she was seen by a physician. On evaluation, she reported difficulty sleeping, flashbacks, and feelings of shame and guilt.1
●
* The patient’s name has been changed to protect her identity.
Child and adolescent sex trafficking is defined as the sexual exploitation of minors through force, fraud, or coercion. Specifically, it includes the recruitment, harboring, transportation, or advertising of a minor, and includes the exchange of anything of value in return for sexual activity. Commercial sexual exploitation and sex trafficking against minors include crimes such as prostitution; survival sex (exchanging sex/sexual acts for money or something of value, such as shelter, food, or drugs); pornography; sex tourism, mail-order-bride trade, and early marriage; or sexual performances (peep shows or strip clubs).2
Providing optimal care for children and adolescents exploited by sex trafficking depends on knowing risk factors, having an awareness of recommended screening and assessment tools, and employing a trauma-informed approach to interviews, examination, and support.2
Continue to: Recognize clues to trafficking
Recognize clues to trafficking
The Centers for Disease Control and Prevention (CDC) offers a framework for trafficking prevention. Health care providers are encouraged to use the CDC Social-Ecological Model which describes targeted prevention strategies at the individual, relationship, community, and societal levels.3
Risk factors for entering trafficking. Younger age increases a child’s vulnerability to exploitation, due to a lack of maturity, limited cognitive development, and ease of deception. The mean age of trafficking survivors is 15 years.4 History of child abuse and other traumatic experiences can lead children to run away from home. It is estimated that, once on the streets, most teens will be recruited by a trafficker within 48 hours.5 Poor self-esteem, depression, substance abuse, history of truancy, and early sexual maturation also increase the risk of becoming involved in trafficking (TABLE 1).2,6-8
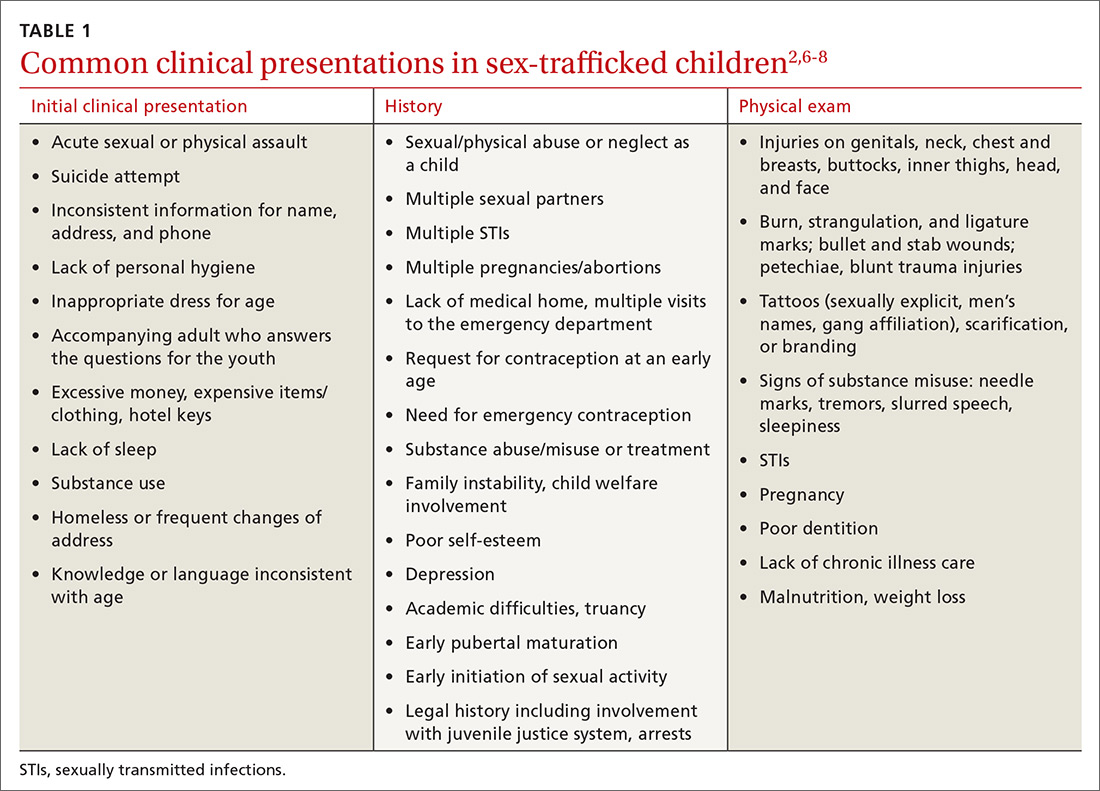
Clinical findings suggestive of trafficking. Many physicians grasp the critical role they play in confronting trafficking, but they lack specific training, experience, and assessment tools.3 Notably, in 1 retrospective study, 46% of victims had been seen by a provider within the previous 2 months.6 One of the major challenges to identifying survivors of trafficking is to recognize critical signs, of which there are many (TABLE 12,6-8). Often these include a history of sexual assault, multiple pregnancies, requests for contraception at an early age, or evidence of physical injury.
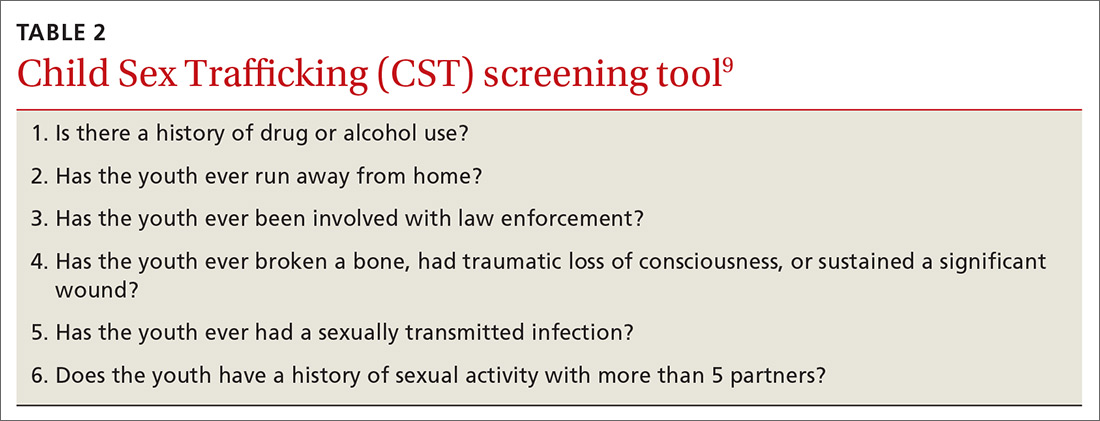
Screen to identify trafficking
Universal, validated screening tools to accurately identify trafficked youth is an area of growing research. Some tools have been validated, but only for specific populations such as homeless or incarcerated youth or in emergency department (ED) patients. Tools for sex trafficking identification that may be useful in primary care include the Child Sex Trafficking (CST) screen validated in ED settings (TABLE 2),9 the Commercial Sexual Exploitation-Identification Tool (CSE-IT) in multiple settings (TABLE 3),10,11 and the Quick Youth Indicators for Trafficking (QYIT) in homeless youth (TABLE 4).11 The QYIT is the first validated labor and sex trafficking screening tool in homeless young adults. Children who screen positive for sex trafficking should be further assessed using a comprehensive tool.

Barriers to effective recognition of trafficked individuals. Financial factors limit access to health care. Also, survivors have cited multiple barriers for health professionals that prevent identification of survivors’ trafficked status.12,13 Once in the medical setting, disclosure is impacted by time constraints, fear of judgment by clinicians, and the risk of re-traumatization. Survivors have also cited lack of privacy, control strategies by their traffickers, lack of provider empathy, and fear of police as barriers to disclosure.14
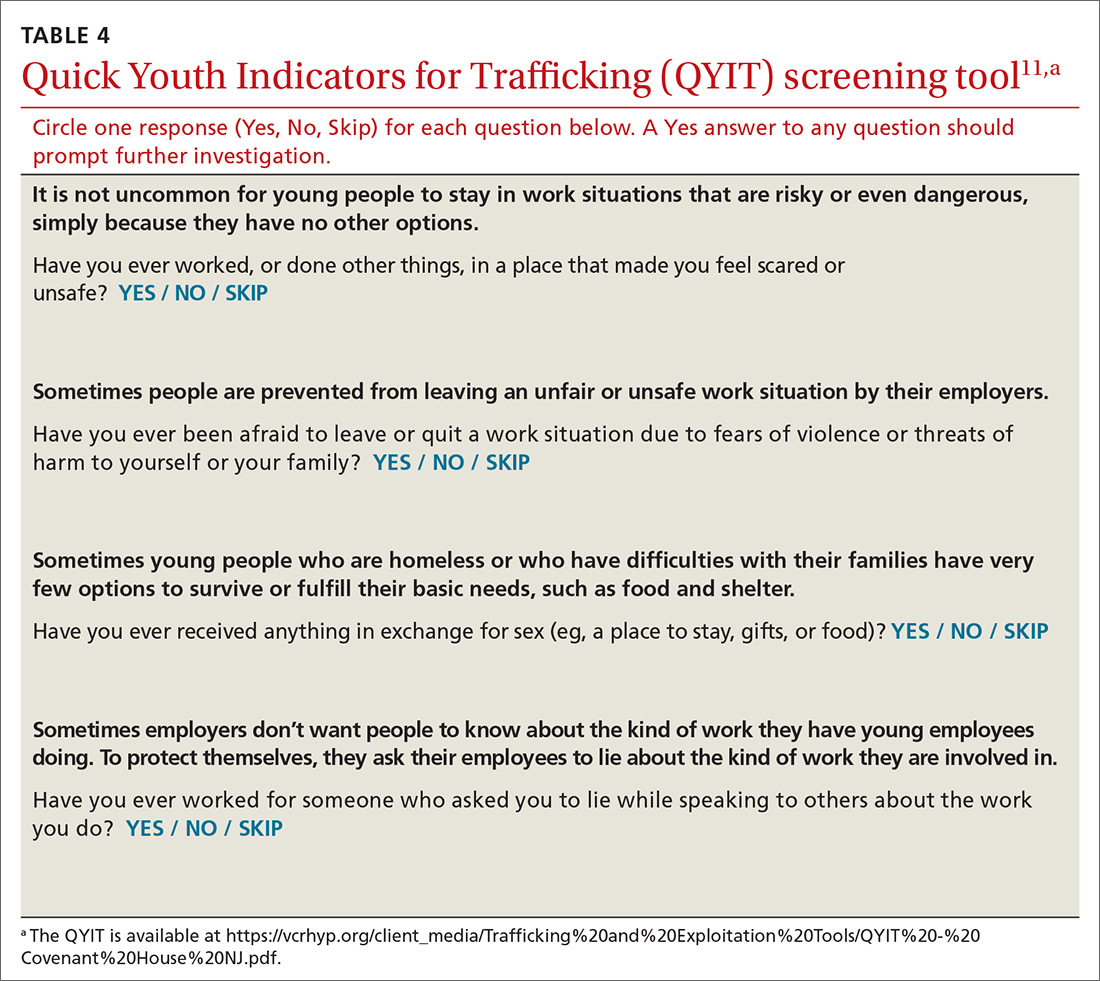
Continue to: The medical impact of trafficking
The medical impact of trafficking
Sexual exploitation is a traumatic experience that is known to cause harm across multiple domains including serious physical injuries related to violence, as well as reproductive and mental health consequences.15,16
Acute and chronic illnesses. In an initial evaluation, assess the survivor’s acute medical conditions (TABLE 5).15,16 Common acute issues include physical injuries due to assault, infections, and reproductive complications.17 Health concerns can also result from stressors such as deprivation of food and sleep, hazardous living conditions, and limited access to care.17
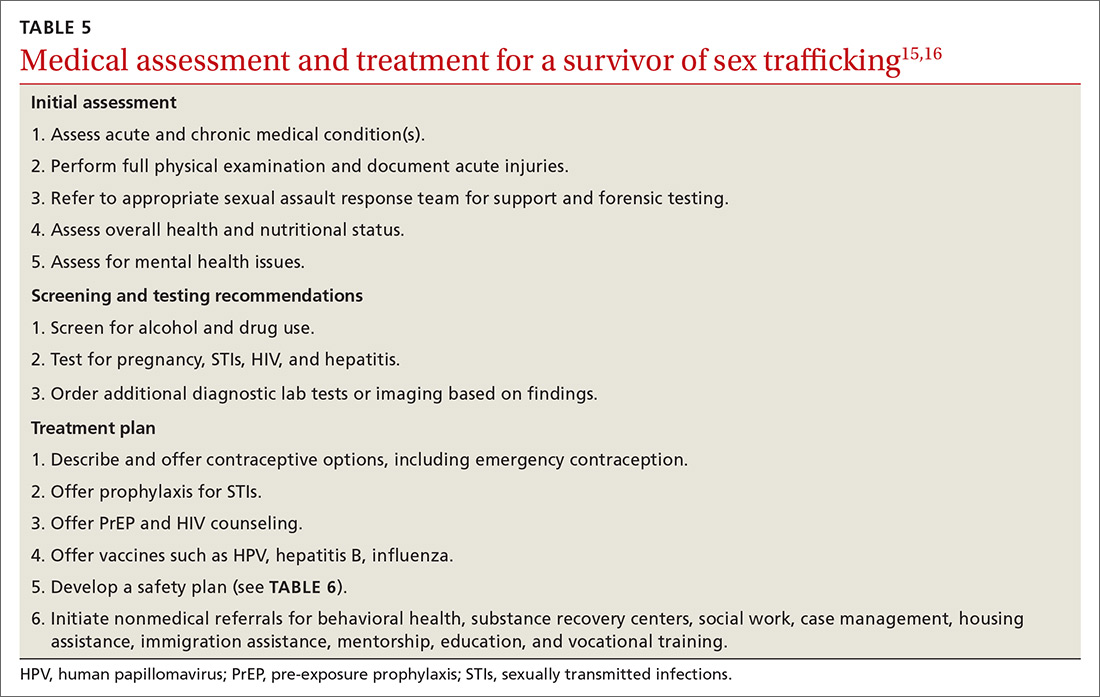
As part of caring for sex-trafficking survivors, assess for, and treat, chronic health issues such as pain, gastrointestinal complaints, poor dental care, malnutrition, and fatigue.16,18 Substance use, as well as chronic mental health concerns (eg, anxiety, depression, posttraumatic stress disorder [PTSD]) may also influence the clinical presentation.
Physical injuries. A cross-sectional study of female survivors of sex trafficking in the United States found that 89% sustained physical injury resulting from violence, including fractures, open wounds, head injury, dental problems, burns, and anogenital trauma.16,17 In many cases, acute injury may not be present in the clinical setting since care is often delayed, but a full examination can reveal signs of prior trauma.16
Reproductive health concerns. Significant, long-term impact on reproductive health can result due to forced penetration by multiple perpetrators, sodomy, and sex without protection or lubricants. Survivors are therefore at high risk for unplanned and unwanted pregnancies, sexually transmitted infections (STIs), pelvic pain, and infertility.16
Continue to: Psychological effects and trauma exposure
Psychological effects and trauma exposure. Survivors often have experienced abuse and neglect prior to commercial exploitation, and they may exhibit long-term sequelae. Survivors may present with major depression, anxiety, panic attacks, suicidality, addiction, PTSD, or aggression.16 Long-term sequelae for patients can include dysfunctional relationships due to an inability to trust, self-destructive behaviors, and significant shame.2,18
Care and treatment of trafficked youth
Initial presentation may occur in a variety of health care settings. Use a trauma-informed approach emphasizing physical and emotional safety and positive relationships, to reduce risk to the survivor, staff, and providers.19 Establishing trust and rapport may provide better short-term safety, as well as help build stronger long-term relationships that can lead to better health outcomes.
Clinical examination. Provide traumatized patients with a sense of safety, control, and autonomy in the health care setting. During the physical exam, be aware of the impact of re-traumatization as patients are asked to undress, endure sensitive examinations, and undergo invasive procedures. Explain the examination, ask for permission at each step, and use slow movements. Allow the patient to guide certain sensitive exams.15 Adopt an approach that recognizes the impact of trauma, avoids revictimization, and acknowledges the resilience of survivors.20
Treatment plan. After the initial exam, treat acute physical injuries and determine if any further testing is needed. Offer emergency contraception, STI prophylaxis, pre-exposure prophylaxis, and vaccines.15 After assessing patient readiness, offer local resources, identify safe methods for communication, identify individuals who could intervene in a crisis, and consider a safety plan (TABLE 6).
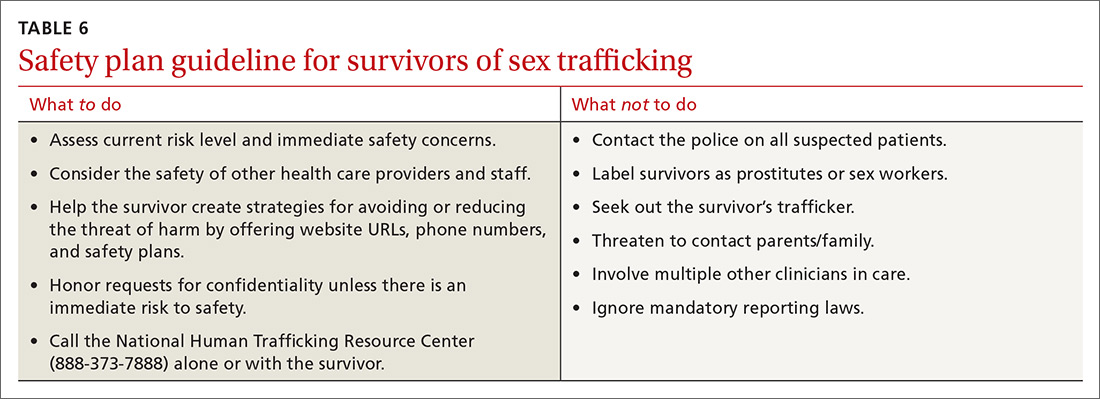
Coordination of care. Consider referrals to behavioral health services, substance recovery centers, food programs, housing resources, and a primary care clinic.15 ED clinicians may be asked to complete a sexual or physical assault forensic examination. After obtaining informed consent, one needs to19
- document skin signs such as scars, bites, strangulation marks, and tattoos. Note the size, shape, color, location, and other characteristics of each lesion.
- perform an oral, genital, and rectal examination and use a sexual assault evidence kit as indicated.
- use body diagrams and take photographs of all injuries/physical findings.
- order diagnostic testing as appropriate (eg, imaging to assess fractures).
Continue to: THE CASE
THE CASE
During Ms. T’s incarceration, she was tested for STIs and treated for gonorrhea, trichomonas, and bacterial vaginosis. She was educated about sexual health, was counseled on contraception, and accepted condoms. She was referred to a therapist and given information on additional community resources she could contact upon her release.
A year after her release, she was incarcerated again. She also had an unplanned pregnancy. With the support she received from community programs, social workers, and her primary care provider, she moved in with her family, where she is currently living. She denies any ongoing trafficking activity.
CORRESPONDENCE
Piali Basu, DO, MPH, UCSF Primary Care, 185 Berry Street, Lobby 1, Suite 1000, San Francisco, CA 94107; [email protected]
1. Samko Tracey (Department of Pediatrics, LA County + University of Southern California, Los Angeles, CA). Conversation with: Vidhi Doshi (Department of Internal Medicine, University of California San Francisco, San Francisco, CA). July 8, 2019.
2. Institute of Medicine; National Research Council. Confronting Commercial Sexual Exploitation and Sex Trafficking of Minors in the United States. Washington, DC: The National Academies Press; 2013.
3. Greenbaum VJ, Titchen K, Walker-Descartes I, et al. Multi-level prevention of human trafficking: the role of health care professionals. Prev Med. 2018;114:164-167.
4. Smith LA, Vardman SH, Snow MA. The national report on domestic minor sex trafficking: America’s prostituted children. 2009. Accessed January 11, 2021. http://sharedhope.org/wp-content/uploads/2012/09/SHI_National_Report_on_DMST_2009.pdf
5. Know the facts: commercial sexual exploitation of children. In: Connections. Summer 2011. Washington Coalition of Sexual Assault Programs. Accessed January 11, 2021. www.wcsap.org/sites/default/files/uploads/resources_publications/connections/Commercial_Sexual_Exploitation_of_Youth_2011.pdf
6. Varma S, Gillespie S, McCracken C, et al. Characteristics of child commercial sexual exploitation and sex trafficking victims presenting for medical care in the United States. Child Abuse Negl. 2015;44:98-105.
7. Walker K, California Child Welfare Council. Ending the commercial sexual exploitation of children: a call for multi-system collaboration in California. 2013. Accessed January 11, 2021. https://youthlaw.org/wp-content/uploads/2015/01/Ending-CSEC-A-Call-for-Multi-System_Collaboration-in-CA.pdf
8. Landers M, McGrath K, Johnson MH, et al. Baseline characteristics of dependent youth who have been commercially sexually exploited: findings from a specialized treatment program. J Child Sex Abus. 2017;26:692-709.
9. Greenbaum VJ, Dodd M, McCracken C. A short screening tool to identify victims of child sex trafficking in the health care setting. Pediatr Emerg Care. 2018;34:33-37.
10. Sy E, Quach T, Lee J, et al. Responding to commercially sexually exploited children (CSEC): a community health center‘s journey towards creating a primary care clinical CSEC screening tool in the United States. Inter J Soc Sci Stud. 2016;4:45-51.
11. Chisolm-Straker M, Sze J, Einbond J, et al. Screening for human trafficking among homeless young adults. Childr Youth Serv Rev. 2019;98:72-79.
12. Richie-Zavaleta AC, Villanueva A, Martinez-Donate A, et al. Sex trafficking victims at their junction with the healthcare setting—a mixed-methods inquiry. J Hum Traffick. 2020;6:1-29.
13. Chisolm-Straker M, Miller CL, Duke G, et al. A framework for the development of healthcare provider education programs on human trafficking part two: survivors. J Hum Traffick. 2019;5:410-424.
14. Heilemann T, Santhiveeran J. How do female adolescents cope and survive the hardships of prostitution? A content analysis of existing literature. J Ethn Cult Divers Soc Work. 2011;20:57-76.
15. Greenbaum J, Crawford-Jakubiak JE, Committee on Child Abuse and Neglect. Child sex trafficking and commercial sexual exploitation: health care needs of victims. Pediatrics. 2015;135:566-574.
16. Barnert E, Iqbal Z, Bruce J, et al. Commercial sexual exploitation and sex trafficking of children and adolescents: a narrative review. Acad Pediatr. 2017;17:825-829.
17. Dovydaitis T. Human trafficking: the role of the health care provider. J Midwifery Womens Health. 2010;55:462-467.
18. English A, Kivlahan C. Human rights and human trafficking of adolescents: legal and clinical perspectives. In: Titchen K, Miller E, Eds. Medical Perspectives on Human Trafficking in Adolescents. Springer Nature; 2020:21-41.
19. Price K, Nelson BD, Macias-Konstantopoulos WL. Understanding health care access disparities among human trafficking survivors: profiles of health care experiences, access, and engagement. J Interpers Violence. 2019; doi: 10.1177/0886260519889934.
20. Chambers R, Ravi A, Paulus S. Human trafficking: how family physicians can recognize and assist victims. Am Fam Physician. 2019;100:202-204.
THE CASE
Emily T.* is a 15-year-old, cisgender, homeless runaway. While on the streets, she was lured to a hotel where a “pimp” informed her she was going to work for him. She repeatedly tried to leave, but he would strike her, so she eventually succumbed. She was forced to have sex with several men and rarely allowed to use condoms.
On 1 occasion, when she went to a hospital with her pimp to visit a patient, her aunt (a nurse on duty at that facility) saw Ms. T and called the police. The pimp was arrested. Ms. T was interviewed by the police and gave a statement but refused a forensic exam.
Because of her involvement with the pimp, she was incarcerated. In prison, she was seen by a physician. On evaluation, she reported difficulty sleeping, flashbacks, and feelings of shame and guilt.1
●
* The patient’s name has been changed to protect her identity.
Child and adolescent sex trafficking is defined as the sexual exploitation of minors through force, fraud, or coercion. Specifically, it includes the recruitment, harboring, transportation, or advertising of a minor, and includes the exchange of anything of value in return for sexual activity. Commercial sexual exploitation and sex trafficking against minors include crimes such as prostitution; survival sex (exchanging sex/sexual acts for money or something of value, such as shelter, food, or drugs); pornography; sex tourism, mail-order-bride trade, and early marriage; or sexual performances (peep shows or strip clubs).2
Providing optimal care for children and adolescents exploited by sex trafficking depends on knowing risk factors, having an awareness of recommended screening and assessment tools, and employing a trauma-informed approach to interviews, examination, and support.2
Continue to: Recognize clues to trafficking
Recognize clues to trafficking
The Centers for Disease Control and Prevention (CDC) offers a framework for trafficking prevention. Health care providers are encouraged to use the CDC Social-Ecological Model which describes targeted prevention strategies at the individual, relationship, community, and societal levels.3
Risk factors for entering trafficking. Younger age increases a child’s vulnerability to exploitation, due to a lack of maturity, limited cognitive development, and ease of deception. The mean age of trafficking survivors is 15 years.4 History of child abuse and other traumatic experiences can lead children to run away from home. It is estimated that, once on the streets, most teens will be recruited by a trafficker within 48 hours.5 Poor self-esteem, depression, substance abuse, history of truancy, and early sexual maturation also increase the risk of becoming involved in trafficking (TABLE 1).2,6-8
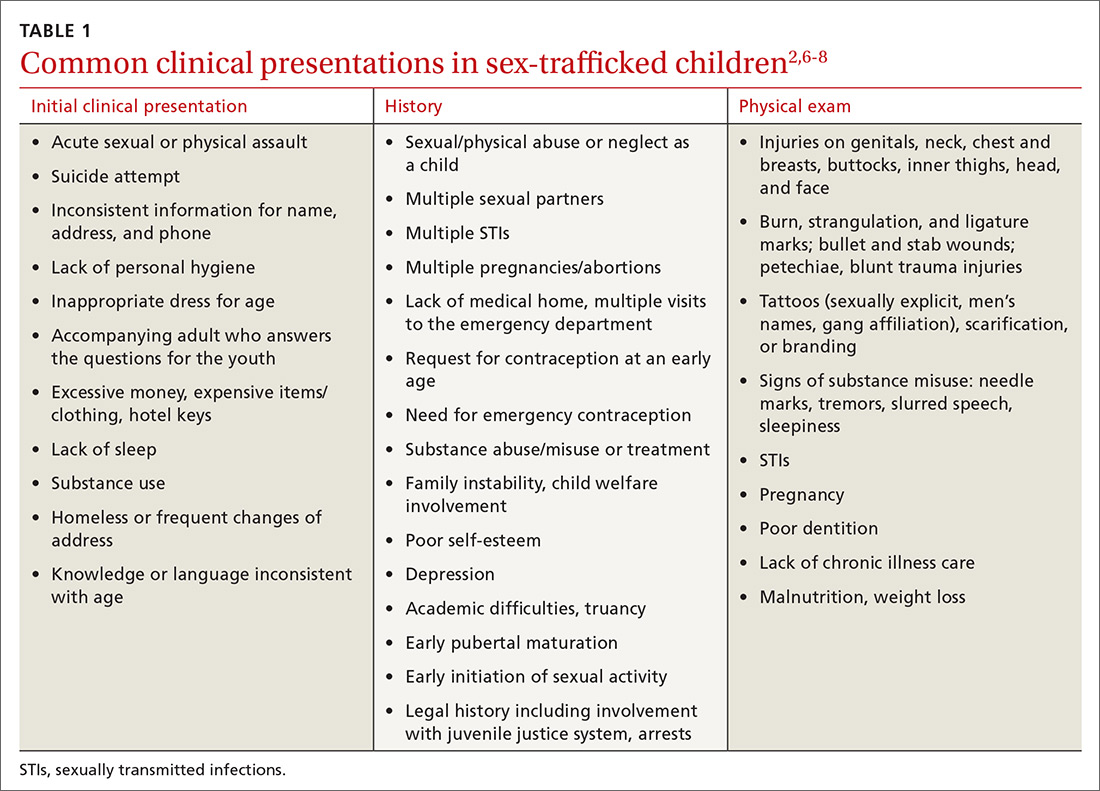
Clinical findings suggestive of trafficking. Many physicians grasp the critical role they play in confronting trafficking, but they lack specific training, experience, and assessment tools.3 Notably, in 1 retrospective study, 46% of victims had been seen by a provider within the previous 2 months.6 One of the major challenges to identifying survivors of trafficking is to recognize critical signs, of which there are many (TABLE 12,6-8). Often these include a history of sexual assault, multiple pregnancies, requests for contraception at an early age, or evidence of physical injury.
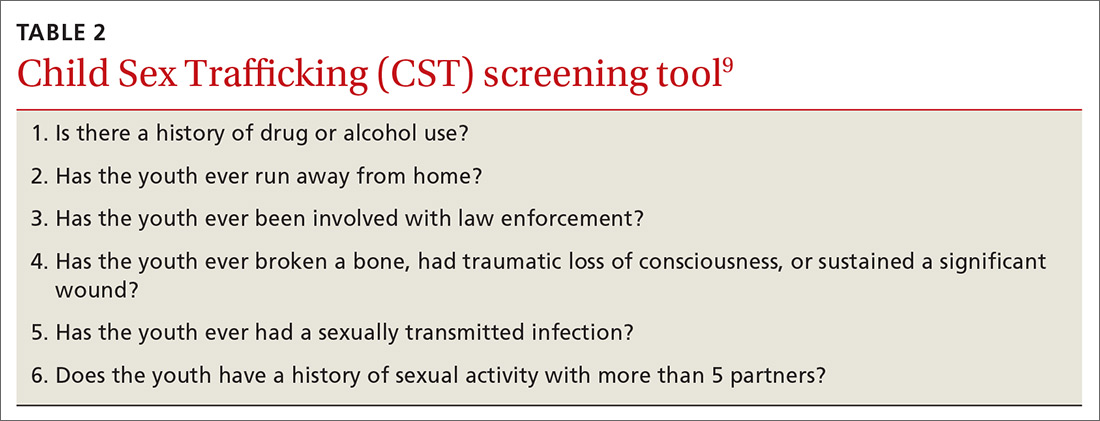
Screen to identify trafficking
Universal, validated screening tools to accurately identify trafficked youth is an area of growing research. Some tools have been validated, but only for specific populations such as homeless or incarcerated youth or in emergency department (ED) patients. Tools for sex trafficking identification that may be useful in primary care include the Child Sex Trafficking (CST) screen validated in ED settings (TABLE 2),9 the Commercial Sexual Exploitation-Identification Tool (CSE-IT) in multiple settings (TABLE 3),10,11 and the Quick Youth Indicators for Trafficking (QYIT) in homeless youth (TABLE 4).11 The QYIT is the first validated labor and sex trafficking screening tool in homeless young adults. Children who screen positive for sex trafficking should be further assessed using a comprehensive tool.

Barriers to effective recognition of trafficked individuals. Financial factors limit access to health care. Also, survivors have cited multiple barriers for health professionals that prevent identification of survivors’ trafficked status.12,13 Once in the medical setting, disclosure is impacted by time constraints, fear of judgment by clinicians, and the risk of re-traumatization. Survivors have also cited lack of privacy, control strategies by their traffickers, lack of provider empathy, and fear of police as barriers to disclosure.14
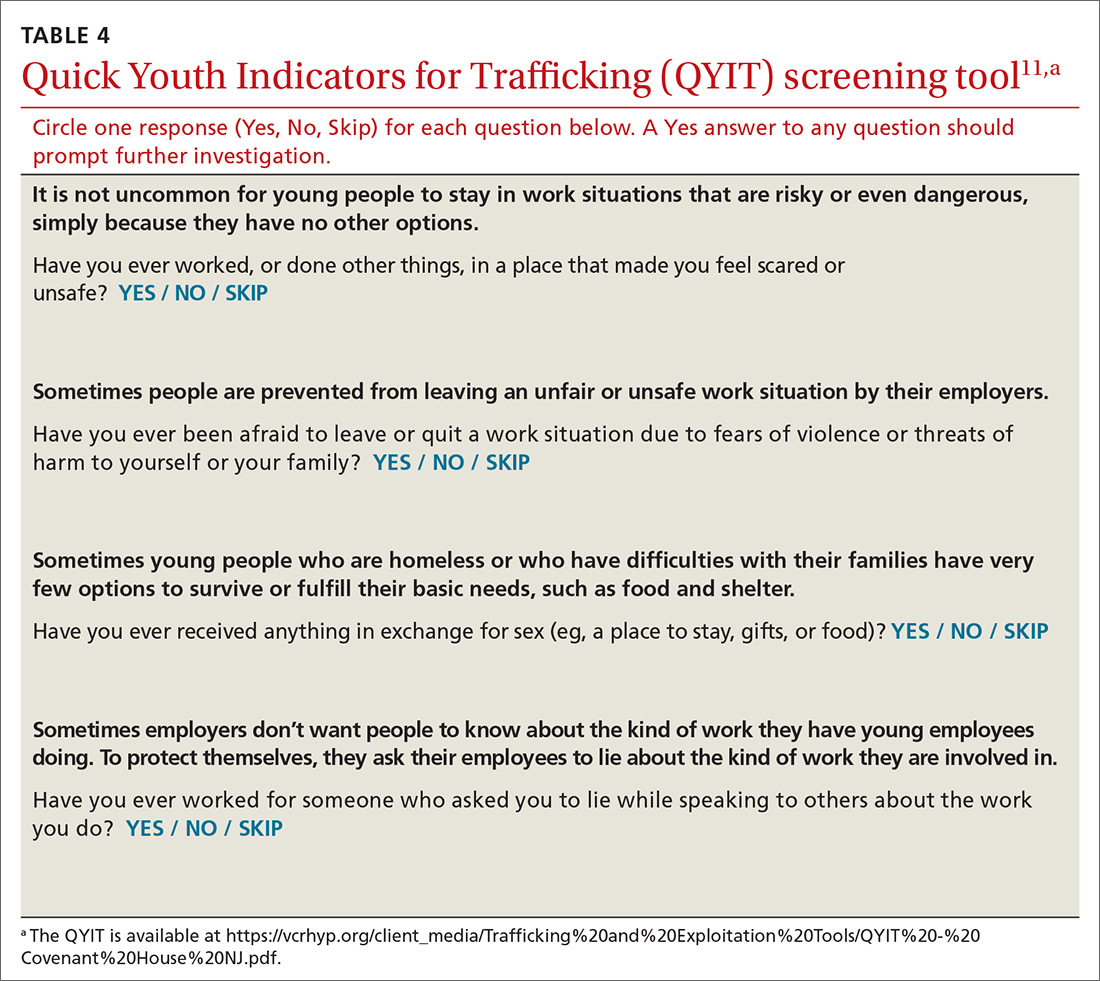
Continue to: The medical impact of trafficking
The medical impact of trafficking
Sexual exploitation is a traumatic experience that is known to cause harm across multiple domains including serious physical injuries related to violence, as well as reproductive and mental health consequences.15,16
Acute and chronic illnesses. In an initial evaluation, assess the survivor’s acute medical conditions (TABLE 5).15,16 Common acute issues include physical injuries due to assault, infections, and reproductive complications.17 Health concerns can also result from stressors such as deprivation of food and sleep, hazardous living conditions, and limited access to care.17
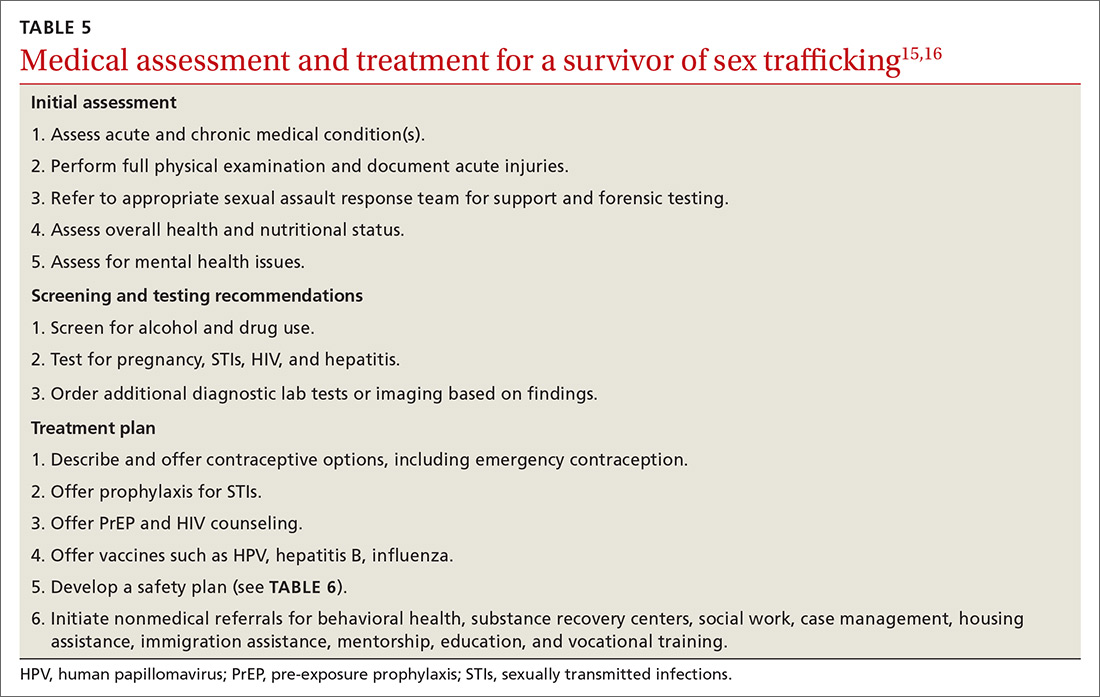
As part of caring for sex-trafficking survivors, assess for, and treat, chronic health issues such as pain, gastrointestinal complaints, poor dental care, malnutrition, and fatigue.16,18 Substance use, as well as chronic mental health concerns (eg, anxiety, depression, posttraumatic stress disorder [PTSD]) may also influence the clinical presentation.
Physical injuries. A cross-sectional study of female survivors of sex trafficking in the United States found that 89% sustained physical injury resulting from violence, including fractures, open wounds, head injury, dental problems, burns, and anogenital trauma.16,17 In many cases, acute injury may not be present in the clinical setting since care is often delayed, but a full examination can reveal signs of prior trauma.16
Reproductive health concerns. Significant, long-term impact on reproductive health can result due to forced penetration by multiple perpetrators, sodomy, and sex without protection or lubricants. Survivors are therefore at high risk for unplanned and unwanted pregnancies, sexually transmitted infections (STIs), pelvic pain, and infertility.16
Continue to: Psychological effects and trauma exposure
Psychological effects and trauma exposure. Survivors often have experienced abuse and neglect prior to commercial exploitation, and they may exhibit long-term sequelae. Survivors may present with major depression, anxiety, panic attacks, suicidality, addiction, PTSD, or aggression.16 Long-term sequelae for patients can include dysfunctional relationships due to an inability to trust, self-destructive behaviors, and significant shame.2,18
Care and treatment of trafficked youth
Initial presentation may occur in a variety of health care settings. Use a trauma-informed approach emphasizing physical and emotional safety and positive relationships, to reduce risk to the survivor, staff, and providers.19 Establishing trust and rapport may provide better short-term safety, as well as help build stronger long-term relationships that can lead to better health outcomes.
Clinical examination. Provide traumatized patients with a sense of safety, control, and autonomy in the health care setting. During the physical exam, be aware of the impact of re-traumatization as patients are asked to undress, endure sensitive examinations, and undergo invasive procedures. Explain the examination, ask for permission at each step, and use slow movements. Allow the patient to guide certain sensitive exams.15 Adopt an approach that recognizes the impact of trauma, avoids revictimization, and acknowledges the resilience of survivors.20
Treatment plan. After the initial exam, treat acute physical injuries and determine if any further testing is needed. Offer emergency contraception, STI prophylaxis, pre-exposure prophylaxis, and vaccines.15 After assessing patient readiness, offer local resources, identify safe methods for communication, identify individuals who could intervene in a crisis, and consider a safety plan (TABLE 6).
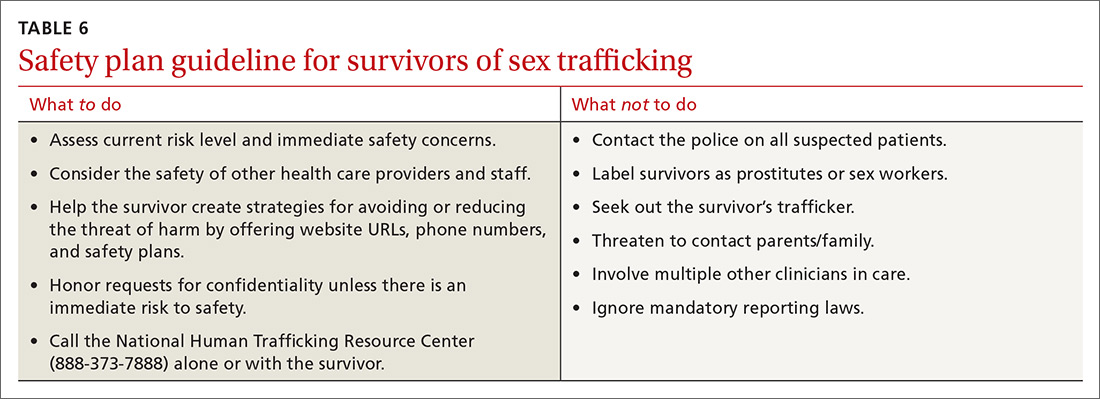
Coordination of care. Consider referrals to behavioral health services, substance recovery centers, food programs, housing resources, and a primary care clinic.15 ED clinicians may be asked to complete a sexual or physical assault forensic examination. After obtaining informed consent, one needs to19
- document skin signs such as scars, bites, strangulation marks, and tattoos. Note the size, shape, color, location, and other characteristics of each lesion.
- perform an oral, genital, and rectal examination and use a sexual assault evidence kit as indicated.
- use body diagrams and take photographs of all injuries/physical findings.
- order diagnostic testing as appropriate (eg, imaging to assess fractures).
Continue to: THE CASE
THE CASE
During Ms. T’s incarceration, she was tested for STIs and treated for gonorrhea, trichomonas, and bacterial vaginosis. She was educated about sexual health, was counseled on contraception, and accepted condoms. She was referred to a therapist and given information on additional community resources she could contact upon her release.
A year after her release, she was incarcerated again. She also had an unplanned pregnancy. With the support she received from community programs, social workers, and her primary care provider, she moved in with her family, where she is currently living. She denies any ongoing trafficking activity.
CORRESPONDENCE
Piali Basu, DO, MPH, UCSF Primary Care, 185 Berry Street, Lobby 1, Suite 1000, San Francisco, CA 94107; [email protected]
THE CASE
Emily T.* is a 15-year-old, cisgender, homeless runaway. While on the streets, she was lured to a hotel where a “pimp” informed her she was going to work for him. She repeatedly tried to leave, but he would strike her, so she eventually succumbed. She was forced to have sex with several men and rarely allowed to use condoms.
On 1 occasion, when she went to a hospital with her pimp to visit a patient, her aunt (a nurse on duty at that facility) saw Ms. T and called the police. The pimp was arrested. Ms. T was interviewed by the police and gave a statement but refused a forensic exam.
Because of her involvement with the pimp, she was incarcerated. In prison, she was seen by a physician. On evaluation, she reported difficulty sleeping, flashbacks, and feelings of shame and guilt.1
●
* The patient’s name has been changed to protect her identity.
Child and adolescent sex trafficking is defined as the sexual exploitation of minors through force, fraud, or coercion. Specifically, it includes the recruitment, harboring, transportation, or advertising of a minor, and includes the exchange of anything of value in return for sexual activity. Commercial sexual exploitation and sex trafficking against minors include crimes such as prostitution; survival sex (exchanging sex/sexual acts for money or something of value, such as shelter, food, or drugs); pornography; sex tourism, mail-order-bride trade, and early marriage; or sexual performances (peep shows or strip clubs).2
Providing optimal care for children and adolescents exploited by sex trafficking depends on knowing risk factors, having an awareness of recommended screening and assessment tools, and employing a trauma-informed approach to interviews, examination, and support.2
Continue to: Recognize clues to trafficking
Recognize clues to trafficking
The Centers for Disease Control and Prevention (CDC) offers a framework for trafficking prevention. Health care providers are encouraged to use the CDC Social-Ecological Model which describes targeted prevention strategies at the individual, relationship, community, and societal levels.3
Risk factors for entering trafficking. Younger age increases a child’s vulnerability to exploitation, due to a lack of maturity, limited cognitive development, and ease of deception. The mean age of trafficking survivors is 15 years.4 History of child abuse and other traumatic experiences can lead children to run away from home. It is estimated that, once on the streets, most teens will be recruited by a trafficker within 48 hours.5 Poor self-esteem, depression, substance abuse, history of truancy, and early sexual maturation also increase the risk of becoming involved in trafficking (TABLE 1).2,6-8
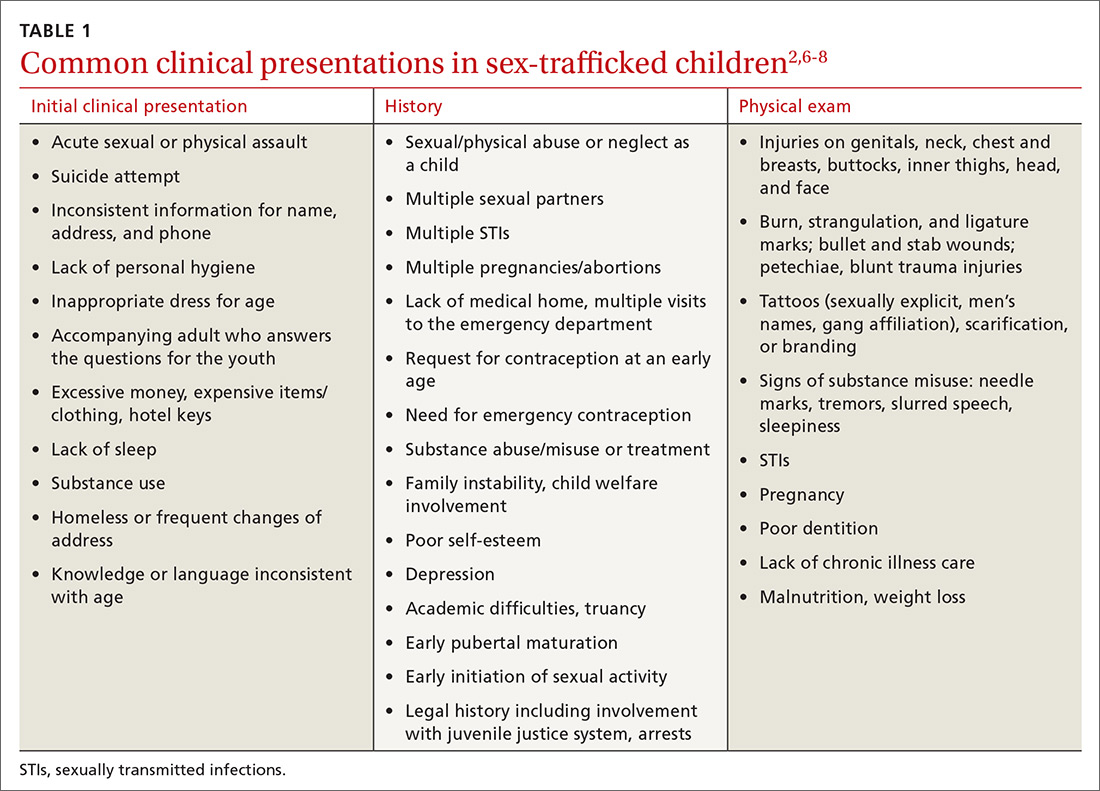
Clinical findings suggestive of trafficking. Many physicians grasp the critical role they play in confronting trafficking, but they lack specific training, experience, and assessment tools.3 Notably, in 1 retrospective study, 46% of victims had been seen by a provider within the previous 2 months.6 One of the major challenges to identifying survivors of trafficking is to recognize critical signs, of which there are many (TABLE 12,6-8). Often these include a history of sexual assault, multiple pregnancies, requests for contraception at an early age, or evidence of physical injury.
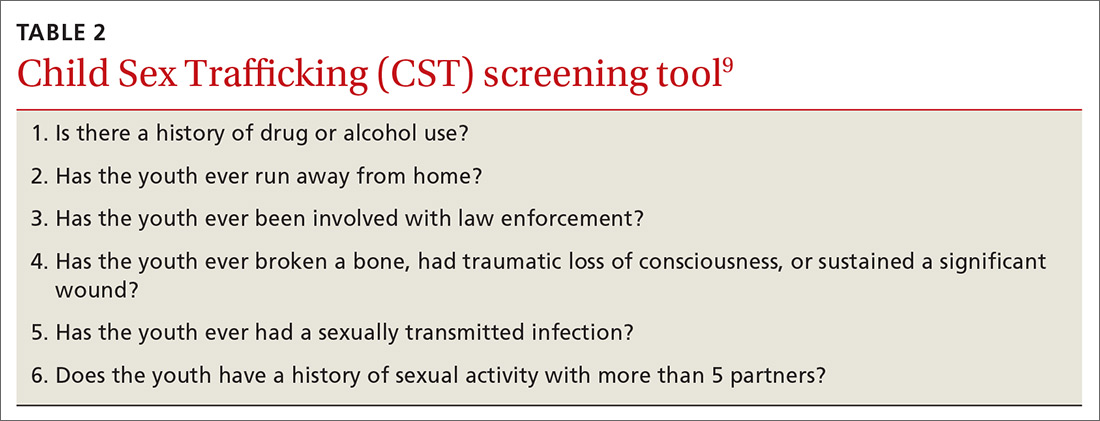
Screen to identify trafficking
Universal, validated screening tools to accurately identify trafficked youth is an area of growing research. Some tools have been validated, but only for specific populations such as homeless or incarcerated youth or in emergency department (ED) patients. Tools for sex trafficking identification that may be useful in primary care include the Child Sex Trafficking (CST) screen validated in ED settings (TABLE 2),9 the Commercial Sexual Exploitation-Identification Tool (CSE-IT) in multiple settings (TABLE 3),10,11 and the Quick Youth Indicators for Trafficking (QYIT) in homeless youth (TABLE 4).11 The QYIT is the first validated labor and sex trafficking screening tool in homeless young adults. Children who screen positive for sex trafficking should be further assessed using a comprehensive tool.

Barriers to effective recognition of trafficked individuals. Financial factors limit access to health care. Also, survivors have cited multiple barriers for health professionals that prevent identification of survivors’ trafficked status.12,13 Once in the medical setting, disclosure is impacted by time constraints, fear of judgment by clinicians, and the risk of re-traumatization. Survivors have also cited lack of privacy, control strategies by their traffickers, lack of provider empathy, and fear of police as barriers to disclosure.14
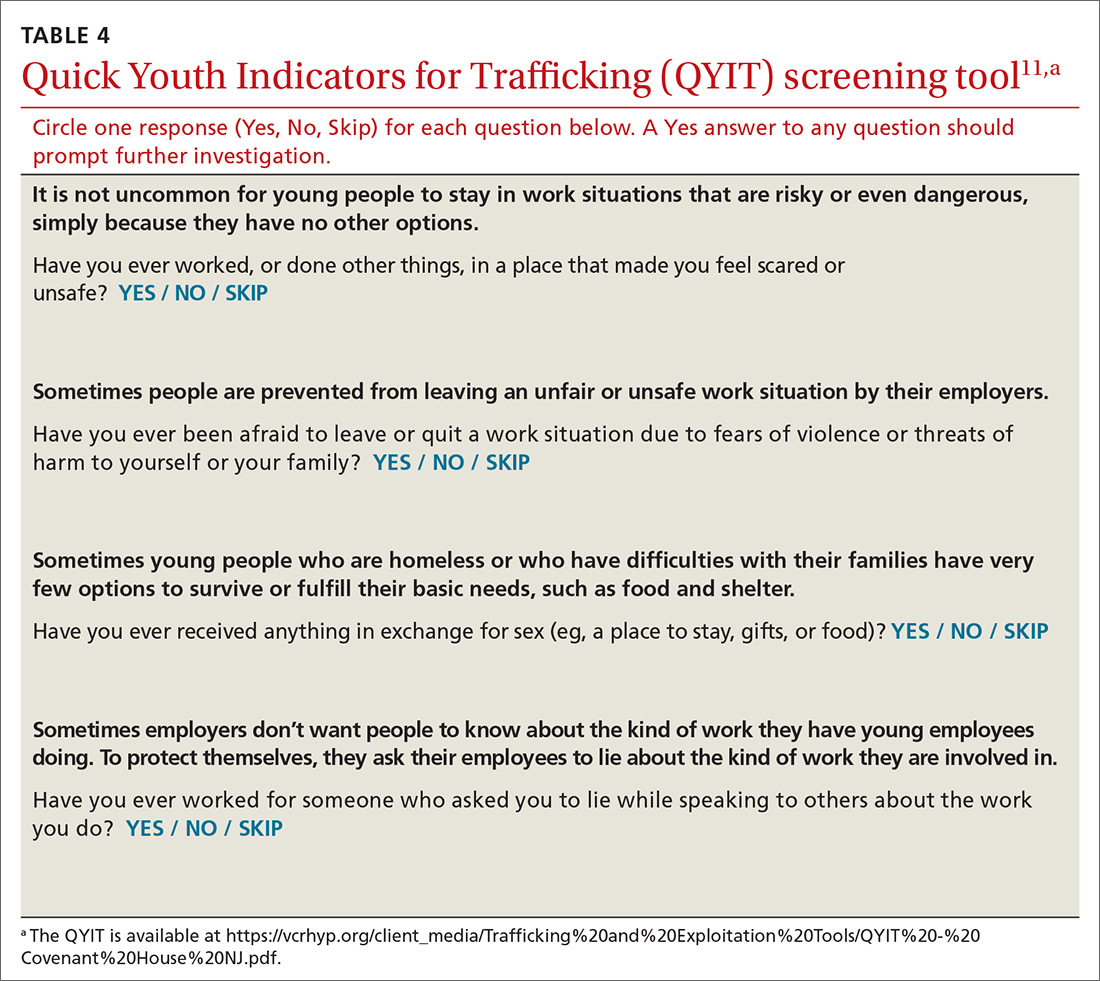
Continue to: The medical impact of trafficking
The medical impact of trafficking
Sexual exploitation is a traumatic experience that is known to cause harm across multiple domains including serious physical injuries related to violence, as well as reproductive and mental health consequences.15,16
Acute and chronic illnesses. In an initial evaluation, assess the survivor’s acute medical conditions (TABLE 5).15,16 Common acute issues include physical injuries due to assault, infections, and reproductive complications.17 Health concerns can also result from stressors such as deprivation of food and sleep, hazardous living conditions, and limited access to care.17
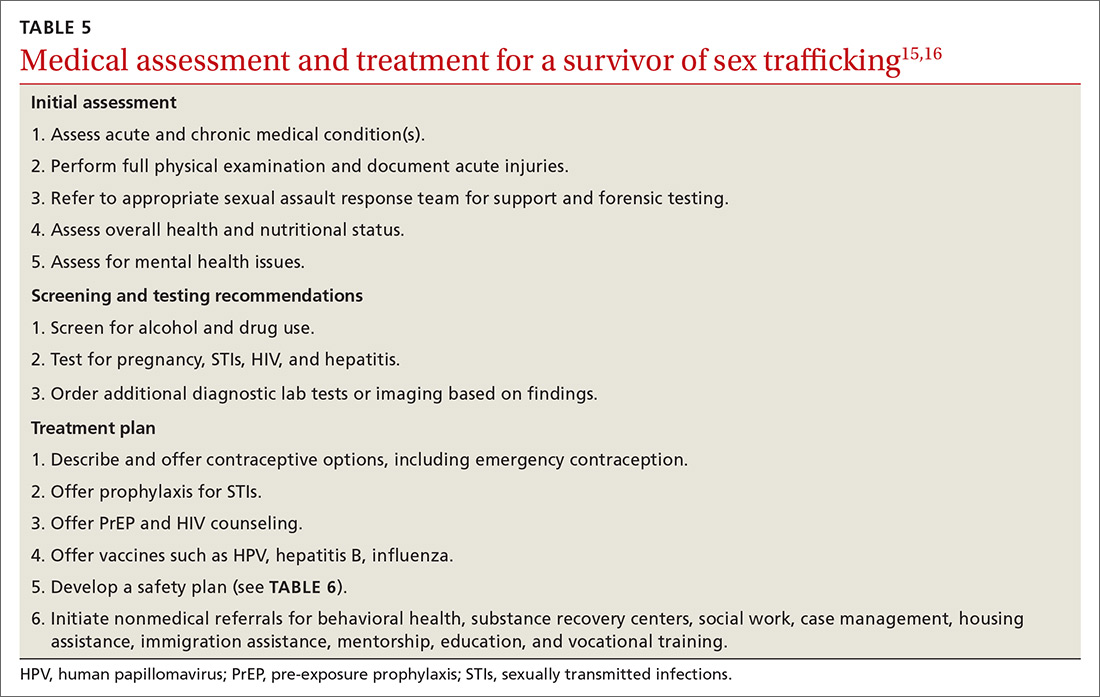
As part of caring for sex-trafficking survivors, assess for, and treat, chronic health issues such as pain, gastrointestinal complaints, poor dental care, malnutrition, and fatigue.16,18 Substance use, as well as chronic mental health concerns (eg, anxiety, depression, posttraumatic stress disorder [PTSD]) may also influence the clinical presentation.
Physical injuries. A cross-sectional study of female survivors of sex trafficking in the United States found that 89% sustained physical injury resulting from violence, including fractures, open wounds, head injury, dental problems, burns, and anogenital trauma.16,17 In many cases, acute injury may not be present in the clinical setting since care is often delayed, but a full examination can reveal signs of prior trauma.16
Reproductive health concerns. Significant, long-term impact on reproductive health can result due to forced penetration by multiple perpetrators, sodomy, and sex without protection or lubricants. Survivors are therefore at high risk for unplanned and unwanted pregnancies, sexually transmitted infections (STIs), pelvic pain, and infertility.16
Continue to: Psychological effects and trauma exposure
Psychological effects and trauma exposure. Survivors often have experienced abuse and neglect prior to commercial exploitation, and they may exhibit long-term sequelae. Survivors may present with major depression, anxiety, panic attacks, suicidality, addiction, PTSD, or aggression.16 Long-term sequelae for patients can include dysfunctional relationships due to an inability to trust, self-destructive behaviors, and significant shame.2,18
Care and treatment of trafficked youth
Initial presentation may occur in a variety of health care settings. Use a trauma-informed approach emphasizing physical and emotional safety and positive relationships, to reduce risk to the survivor, staff, and providers.19 Establishing trust and rapport may provide better short-term safety, as well as help build stronger long-term relationships that can lead to better health outcomes.
Clinical examination. Provide traumatized patients with a sense of safety, control, and autonomy in the health care setting. During the physical exam, be aware of the impact of re-traumatization as patients are asked to undress, endure sensitive examinations, and undergo invasive procedures. Explain the examination, ask for permission at each step, and use slow movements. Allow the patient to guide certain sensitive exams.15 Adopt an approach that recognizes the impact of trauma, avoids revictimization, and acknowledges the resilience of survivors.20
Treatment plan. After the initial exam, treat acute physical injuries and determine if any further testing is needed. Offer emergency contraception, STI prophylaxis, pre-exposure prophylaxis, and vaccines.15 After assessing patient readiness, offer local resources, identify safe methods for communication, identify individuals who could intervene in a crisis, and consider a safety plan (TABLE 6).
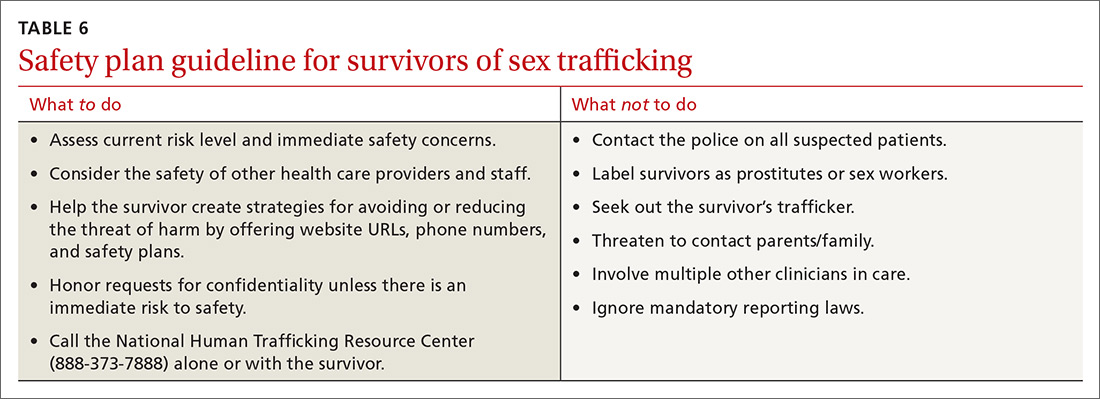
Coordination of care. Consider referrals to behavioral health services, substance recovery centers, food programs, housing resources, and a primary care clinic.15 ED clinicians may be asked to complete a sexual or physical assault forensic examination. After obtaining informed consent, one needs to19
- document skin signs such as scars, bites, strangulation marks, and tattoos. Note the size, shape, color, location, and other characteristics of each lesion.
- perform an oral, genital, and rectal examination and use a sexual assault evidence kit as indicated.
- use body diagrams and take photographs of all injuries/physical findings.
- order diagnostic testing as appropriate (eg, imaging to assess fractures).
Continue to: THE CASE
THE CASE
During Ms. T’s incarceration, she was tested for STIs and treated for gonorrhea, trichomonas, and bacterial vaginosis. She was educated about sexual health, was counseled on contraception, and accepted condoms. She was referred to a therapist and given information on additional community resources she could contact upon her release.
A year after her release, she was incarcerated again. She also had an unplanned pregnancy. With the support she received from community programs, social workers, and her primary care provider, she moved in with her family, where she is currently living. She denies any ongoing trafficking activity.
CORRESPONDENCE
Piali Basu, DO, MPH, UCSF Primary Care, 185 Berry Street, Lobby 1, Suite 1000, San Francisco, CA 94107; [email protected]
1. Samko Tracey (Department of Pediatrics, LA County + University of Southern California, Los Angeles, CA). Conversation with: Vidhi Doshi (Department of Internal Medicine, University of California San Francisco, San Francisco, CA). July 8, 2019.
2. Institute of Medicine; National Research Council. Confronting Commercial Sexual Exploitation and Sex Trafficking of Minors in the United States. Washington, DC: The National Academies Press; 2013.
3. Greenbaum VJ, Titchen K, Walker-Descartes I, et al. Multi-level prevention of human trafficking: the role of health care professionals. Prev Med. 2018;114:164-167.
4. Smith LA, Vardman SH, Snow MA. The national report on domestic minor sex trafficking: America’s prostituted children. 2009. Accessed January 11, 2021. http://sharedhope.org/wp-content/uploads/2012/09/SHI_National_Report_on_DMST_2009.pdf
5. Know the facts: commercial sexual exploitation of children. In: Connections. Summer 2011. Washington Coalition of Sexual Assault Programs. Accessed January 11, 2021. www.wcsap.org/sites/default/files/uploads/resources_publications/connections/Commercial_Sexual_Exploitation_of_Youth_2011.pdf
6. Varma S, Gillespie S, McCracken C, et al. Characteristics of child commercial sexual exploitation and sex trafficking victims presenting for medical care in the United States. Child Abuse Negl. 2015;44:98-105.
7. Walker K, California Child Welfare Council. Ending the commercial sexual exploitation of children: a call for multi-system collaboration in California. 2013. Accessed January 11, 2021. https://youthlaw.org/wp-content/uploads/2015/01/Ending-CSEC-A-Call-for-Multi-System_Collaboration-in-CA.pdf
8. Landers M, McGrath K, Johnson MH, et al. Baseline characteristics of dependent youth who have been commercially sexually exploited: findings from a specialized treatment program. J Child Sex Abus. 2017;26:692-709.
9. Greenbaum VJ, Dodd M, McCracken C. A short screening tool to identify victims of child sex trafficking in the health care setting. Pediatr Emerg Care. 2018;34:33-37.
10. Sy E, Quach T, Lee J, et al. Responding to commercially sexually exploited children (CSEC): a community health center‘s journey towards creating a primary care clinical CSEC screening tool in the United States. Inter J Soc Sci Stud. 2016;4:45-51.
11. Chisolm-Straker M, Sze J, Einbond J, et al. Screening for human trafficking among homeless young adults. Childr Youth Serv Rev. 2019;98:72-79.
12. Richie-Zavaleta AC, Villanueva A, Martinez-Donate A, et al. Sex trafficking victims at their junction with the healthcare setting—a mixed-methods inquiry. J Hum Traffick. 2020;6:1-29.
13. Chisolm-Straker M, Miller CL, Duke G, et al. A framework for the development of healthcare provider education programs on human trafficking part two: survivors. J Hum Traffick. 2019;5:410-424.
14. Heilemann T, Santhiveeran J. How do female adolescents cope and survive the hardships of prostitution? A content analysis of existing literature. J Ethn Cult Divers Soc Work. 2011;20:57-76.
15. Greenbaum J, Crawford-Jakubiak JE, Committee on Child Abuse and Neglect. Child sex trafficking and commercial sexual exploitation: health care needs of victims. Pediatrics. 2015;135:566-574.
16. Barnert E, Iqbal Z, Bruce J, et al. Commercial sexual exploitation and sex trafficking of children and adolescents: a narrative review. Acad Pediatr. 2017;17:825-829.
17. Dovydaitis T. Human trafficking: the role of the health care provider. J Midwifery Womens Health. 2010;55:462-467.
18. English A, Kivlahan C. Human rights and human trafficking of adolescents: legal and clinical perspectives. In: Titchen K, Miller E, Eds. Medical Perspectives on Human Trafficking in Adolescents. Springer Nature; 2020:21-41.
19. Price K, Nelson BD, Macias-Konstantopoulos WL. Understanding health care access disparities among human trafficking survivors: profiles of health care experiences, access, and engagement. J Interpers Violence. 2019; doi: 10.1177/0886260519889934.
20. Chambers R, Ravi A, Paulus S. Human trafficking: how family physicians can recognize and assist victims. Am Fam Physician. 2019;100:202-204.
1. Samko Tracey (Department of Pediatrics, LA County + University of Southern California, Los Angeles, CA). Conversation with: Vidhi Doshi (Department of Internal Medicine, University of California San Francisco, San Francisco, CA). July 8, 2019.
2. Institute of Medicine; National Research Council. Confronting Commercial Sexual Exploitation and Sex Trafficking of Minors in the United States. Washington, DC: The National Academies Press; 2013.
3. Greenbaum VJ, Titchen K, Walker-Descartes I, et al. Multi-level prevention of human trafficking: the role of health care professionals. Prev Med. 2018;114:164-167.
4. Smith LA, Vardman SH, Snow MA. The national report on domestic minor sex trafficking: America’s prostituted children. 2009. Accessed January 11, 2021. http://sharedhope.org/wp-content/uploads/2012/09/SHI_National_Report_on_DMST_2009.pdf
5. Know the facts: commercial sexual exploitation of children. In: Connections. Summer 2011. Washington Coalition of Sexual Assault Programs. Accessed January 11, 2021. www.wcsap.org/sites/default/files/uploads/resources_publications/connections/Commercial_Sexual_Exploitation_of_Youth_2011.pdf
6. Varma S, Gillespie S, McCracken C, et al. Characteristics of child commercial sexual exploitation and sex trafficking victims presenting for medical care in the United States. Child Abuse Negl. 2015;44:98-105.
7. Walker K, California Child Welfare Council. Ending the commercial sexual exploitation of children: a call for multi-system collaboration in California. 2013. Accessed January 11, 2021. https://youthlaw.org/wp-content/uploads/2015/01/Ending-CSEC-A-Call-for-Multi-System_Collaboration-in-CA.pdf
8. Landers M, McGrath K, Johnson MH, et al. Baseline characteristics of dependent youth who have been commercially sexually exploited: findings from a specialized treatment program. J Child Sex Abus. 2017;26:692-709.
9. Greenbaum VJ, Dodd M, McCracken C. A short screening tool to identify victims of child sex trafficking in the health care setting. Pediatr Emerg Care. 2018;34:33-37.
10. Sy E, Quach T, Lee J, et al. Responding to commercially sexually exploited children (CSEC): a community health center‘s journey towards creating a primary care clinical CSEC screening tool in the United States. Inter J Soc Sci Stud. 2016;4:45-51.
11. Chisolm-Straker M, Sze J, Einbond J, et al. Screening for human trafficking among homeless young adults. Childr Youth Serv Rev. 2019;98:72-79.
12. Richie-Zavaleta AC, Villanueva A, Martinez-Donate A, et al. Sex trafficking victims at their junction with the healthcare setting—a mixed-methods inquiry. J Hum Traffick. 2020;6:1-29.
13. Chisolm-Straker M, Miller CL, Duke G, et al. A framework for the development of healthcare provider education programs on human trafficking part two: survivors. J Hum Traffick. 2019;5:410-424.
14. Heilemann T, Santhiveeran J. How do female adolescents cope and survive the hardships of prostitution? A content analysis of existing literature. J Ethn Cult Divers Soc Work. 2011;20:57-76.
15. Greenbaum J, Crawford-Jakubiak JE, Committee on Child Abuse and Neglect. Child sex trafficking and commercial sexual exploitation: health care needs of victims. Pediatrics. 2015;135:566-574.
16. Barnert E, Iqbal Z, Bruce J, et al. Commercial sexual exploitation and sex trafficking of children and adolescents: a narrative review. Acad Pediatr. 2017;17:825-829.
17. Dovydaitis T. Human trafficking: the role of the health care provider. J Midwifery Womens Health. 2010;55:462-467.
18. English A, Kivlahan C. Human rights and human trafficking of adolescents: legal and clinical perspectives. In: Titchen K, Miller E, Eds. Medical Perspectives on Human Trafficking in Adolescents. Springer Nature; 2020:21-41.
19. Price K, Nelson BD, Macias-Konstantopoulos WL. Understanding health care access disparities among human trafficking survivors: profiles of health care experiences, access, and engagement. J Interpers Violence. 2019; doi: 10.1177/0886260519889934.
20. Chambers R, Ravi A, Paulus S. Human trafficking: how family physicians can recognize and assist victims. Am Fam Physician. 2019;100:202-204.