User login
Could tamoxifen dose be slashed down to 2.5 mg?
Tamoxifen has long been used in breast cancer, both in the adjuvant and preventive setting, but uptake and adherence are notoriously low, mainly because of adverse events.
Using a much lower dose to reduce the incidence of side effects would be a “way forward,” reasoned Swedish researchers. They report that a substantially lower dose of tamoxifen (2.5 mg) may be as effective as the standard dose (20 mg), but reduced by half the incidence of severe vasomotor symptoms, including hot flashes, cold sweats, and night sweats.
The research was published online March 18 in the Journal of Clinical Oncology.
The study involved 1,439 women (aged 40-74 years) who were participating in the Swedish mammography screening program and tested tamoxifen at various doses.
“We performed a dose determination study that we hope will initiate follow-up studies that in turn will influence both adjuvant treatment and prevention of breast cancer,” said lead author Per Hall, MD, PhD, head of the department of medical epidemiology and biostatistics at Karolinska Institutet in Stockholm.
The study measured the effects of the different doses (1, 2.5, 5, 10, and 20 mg) on mammographic breast density.
Dr. Hall emphasized that breast density was used as a proxy for therapy response. “We do not know how that translates to actual clinical effect,” he said in an interview. “This is step one.”
Previous studies have also used breast density changes as a proxy endpoint for tamoxifen therapy response, in both prophylactic and adjuvant settings, the authors note. There is some data to suggest that this does translate to a clinical effect. A recent study showed that tamoxifen at 5 mg/day taken for 3 years reduced the recurrence of breast intraepithelial neoplasia by 50% and contralateral breast cancer by 75%, with a symptom profile similar to placebo (J Clin Oncol. 2019;37:1629-1637).
Lower density, fewer symptoms
In the current study, Dr. Hall and colleagues found that the mammographic breast density (mean overall area) was decreased by 9.6% in the 20 mg tamoxifen group, and similar decreases were seen in the 2.5 and 10 mg dose groups, but not in the placebo and 1 mg dose groups.
These changes were driven primarily by changes observed among premenopausal women where the 20 mg mean decrease was 18.5% (P < .001 for interaction with menopausal status) with decreases of 13.4% in the 2.5 mg group, 19.6% in the 5 mg group, and 17% in the 10 mg group.
The results were quite different in postmenopausal participants, where those who received the 20 mg dose had a density mean decrease of 4%, which was not substantially different to the placebo, 1 mg, 2.5 mg, and 10 mg treatment arms.
The authors point out that the difference in density decrease between premenopausal and postmenopausal women was not dependent on differences in baseline density.
When reviewing adverse events with the various doses, the team found a large decrease in severe vasomotor symptoms with the lower doses of tamoxifen. These adverse events were reported by 34% of women taking 20 mg, 24.4% on 5 mg, 20.5% on 2.5 mg, 18.5% on 1 mg, and 13.7% of women taking placebo. There were no similar trends seen for gynecologic, sexual, or musculoskeletal symptoms.
Future studies should test whether 2.5 mg of tamoxifen reduces the risk of primary breast cancer, Dr. Hall commented.
“We are planning a trial now where women are offered risk assessment when attending mammography screening,” Dr. Hall said. “For those at very high risk, low-dose tamoxifen will be offered.”
The study received support from the Kamprad Foundation, Swedish Research Council, Marit and Hans Rausing’s Initiative Against Breast Cancer, Swedish Cancer Society, and Stockholm County Council.
Dr. Hall reports several relationships with industry, had a pending patent on compositions and methods for prevention of breast cancer with an option to license to Atossa Therapeutics, and has licensed an algorithm for risk prediction based on analyses of mammographic features to iCAD Travel. Several co-authors have also declared relationships with industry.
A version of this article first appeared on Medscape.com.
Tamoxifen has long been used in breast cancer, both in the adjuvant and preventive setting, but uptake and adherence are notoriously low, mainly because of adverse events.
Using a much lower dose to reduce the incidence of side effects would be a “way forward,” reasoned Swedish researchers. They report that a substantially lower dose of tamoxifen (2.5 mg) may be as effective as the standard dose (20 mg), but reduced by half the incidence of severe vasomotor symptoms, including hot flashes, cold sweats, and night sweats.
The research was published online March 18 in the Journal of Clinical Oncology.
The study involved 1,439 women (aged 40-74 years) who were participating in the Swedish mammography screening program and tested tamoxifen at various doses.
“We performed a dose determination study that we hope will initiate follow-up studies that in turn will influence both adjuvant treatment and prevention of breast cancer,” said lead author Per Hall, MD, PhD, head of the department of medical epidemiology and biostatistics at Karolinska Institutet in Stockholm.
The study measured the effects of the different doses (1, 2.5, 5, 10, and 20 mg) on mammographic breast density.
Dr. Hall emphasized that breast density was used as a proxy for therapy response. “We do not know how that translates to actual clinical effect,” he said in an interview. “This is step one.”
Previous studies have also used breast density changes as a proxy endpoint for tamoxifen therapy response, in both prophylactic and adjuvant settings, the authors note. There is some data to suggest that this does translate to a clinical effect. A recent study showed that tamoxifen at 5 mg/day taken for 3 years reduced the recurrence of breast intraepithelial neoplasia by 50% and contralateral breast cancer by 75%, with a symptom profile similar to placebo (J Clin Oncol. 2019;37:1629-1637).
Lower density, fewer symptoms
In the current study, Dr. Hall and colleagues found that the mammographic breast density (mean overall area) was decreased by 9.6% in the 20 mg tamoxifen group, and similar decreases were seen in the 2.5 and 10 mg dose groups, but not in the placebo and 1 mg dose groups.
These changes were driven primarily by changes observed among premenopausal women where the 20 mg mean decrease was 18.5% (P < .001 for interaction with menopausal status) with decreases of 13.4% in the 2.5 mg group, 19.6% in the 5 mg group, and 17% in the 10 mg group.
The results were quite different in postmenopausal participants, where those who received the 20 mg dose had a density mean decrease of 4%, which was not substantially different to the placebo, 1 mg, 2.5 mg, and 10 mg treatment arms.
The authors point out that the difference in density decrease between premenopausal and postmenopausal women was not dependent on differences in baseline density.
When reviewing adverse events with the various doses, the team found a large decrease in severe vasomotor symptoms with the lower doses of tamoxifen. These adverse events were reported by 34% of women taking 20 mg, 24.4% on 5 mg, 20.5% on 2.5 mg, 18.5% on 1 mg, and 13.7% of women taking placebo. There were no similar trends seen for gynecologic, sexual, or musculoskeletal symptoms.
Future studies should test whether 2.5 mg of tamoxifen reduces the risk of primary breast cancer, Dr. Hall commented.
“We are planning a trial now where women are offered risk assessment when attending mammography screening,” Dr. Hall said. “For those at very high risk, low-dose tamoxifen will be offered.”
The study received support from the Kamprad Foundation, Swedish Research Council, Marit and Hans Rausing’s Initiative Against Breast Cancer, Swedish Cancer Society, and Stockholm County Council.
Dr. Hall reports several relationships with industry, had a pending patent on compositions and methods for prevention of breast cancer with an option to license to Atossa Therapeutics, and has licensed an algorithm for risk prediction based on analyses of mammographic features to iCAD Travel. Several co-authors have also declared relationships with industry.
A version of this article first appeared on Medscape.com.
Tamoxifen has long been used in breast cancer, both in the adjuvant and preventive setting, but uptake and adherence are notoriously low, mainly because of adverse events.
Using a much lower dose to reduce the incidence of side effects would be a “way forward,” reasoned Swedish researchers. They report that a substantially lower dose of tamoxifen (2.5 mg) may be as effective as the standard dose (20 mg), but reduced by half the incidence of severe vasomotor symptoms, including hot flashes, cold sweats, and night sweats.
The research was published online March 18 in the Journal of Clinical Oncology.
The study involved 1,439 women (aged 40-74 years) who were participating in the Swedish mammography screening program and tested tamoxifen at various doses.
“We performed a dose determination study that we hope will initiate follow-up studies that in turn will influence both adjuvant treatment and prevention of breast cancer,” said lead author Per Hall, MD, PhD, head of the department of medical epidemiology and biostatistics at Karolinska Institutet in Stockholm.
The study measured the effects of the different doses (1, 2.5, 5, 10, and 20 mg) on mammographic breast density.
Dr. Hall emphasized that breast density was used as a proxy for therapy response. “We do not know how that translates to actual clinical effect,” he said in an interview. “This is step one.”
Previous studies have also used breast density changes as a proxy endpoint for tamoxifen therapy response, in both prophylactic and adjuvant settings, the authors note. There is some data to suggest that this does translate to a clinical effect. A recent study showed that tamoxifen at 5 mg/day taken for 3 years reduced the recurrence of breast intraepithelial neoplasia by 50% and contralateral breast cancer by 75%, with a symptom profile similar to placebo (J Clin Oncol. 2019;37:1629-1637).
Lower density, fewer symptoms
In the current study, Dr. Hall and colleagues found that the mammographic breast density (mean overall area) was decreased by 9.6% in the 20 mg tamoxifen group, and similar decreases were seen in the 2.5 and 10 mg dose groups, but not in the placebo and 1 mg dose groups.
These changes were driven primarily by changes observed among premenopausal women where the 20 mg mean decrease was 18.5% (P < .001 for interaction with menopausal status) with decreases of 13.4% in the 2.5 mg group, 19.6% in the 5 mg group, and 17% in the 10 mg group.
The results were quite different in postmenopausal participants, where those who received the 20 mg dose had a density mean decrease of 4%, which was not substantially different to the placebo, 1 mg, 2.5 mg, and 10 mg treatment arms.
The authors point out that the difference in density decrease between premenopausal and postmenopausal women was not dependent on differences in baseline density.
When reviewing adverse events with the various doses, the team found a large decrease in severe vasomotor symptoms with the lower doses of tamoxifen. These adverse events were reported by 34% of women taking 20 mg, 24.4% on 5 mg, 20.5% on 2.5 mg, 18.5% on 1 mg, and 13.7% of women taking placebo. There were no similar trends seen for gynecologic, sexual, or musculoskeletal symptoms.
Future studies should test whether 2.5 mg of tamoxifen reduces the risk of primary breast cancer, Dr. Hall commented.
“We are planning a trial now where women are offered risk assessment when attending mammography screening,” Dr. Hall said. “For those at very high risk, low-dose tamoxifen will be offered.”
The study received support from the Kamprad Foundation, Swedish Research Council, Marit and Hans Rausing’s Initiative Against Breast Cancer, Swedish Cancer Society, and Stockholm County Council.
Dr. Hall reports several relationships with industry, had a pending patent on compositions and methods for prevention of breast cancer with an option to license to Atossa Therapeutics, and has licensed an algorithm for risk prediction based on analyses of mammographic features to iCAD Travel. Several co-authors have also declared relationships with industry.
A version of this article first appeared on Medscape.com.
Paving the way for diversity in clinical trials
“I’m the first person in my circle of family and friends to participate in a clinical trial.”
Five years ago, Rhonda Long was diagnosed with cholangiocarcinoma, a rare bile duct cancer that’s seen in only about 8,000 Americans each year.
At the time, Mrs. Long, who is Black, said her doctor in Dayton, Ohio, told her she was not a candidate for surgery and suggested palliative care. After seeking a second opinion at Duke University Medical Center, Durham, N.C., where her sister worked, the 51-year-old wife and mother of two had surgery, radiation, and chemotherapy there in North Carolina. When the chemo stopped working after 3 months, her oncologist at Duke referred her to a colleague at Massachusetts General Hospital in Boston, where she was accepted into a clinical trial.
“In 2019, I traveled to Boston from Dayton, Ohio, every 3 weeks for labs and scans, to make sure that the drug wasn’t doing more harm than good, making sure that the drug as developed was maintaining, shrinking, or even eliminating the disease. Physically and financially, it takes a toll on you and loved ones.”
Her medical insurance did not cover the direct expenses from the clinical trial, and she was spending $1,000-$1,500 each trip. Sometimes they drove the 15 hours to Boston, and sometimes they flew on the cheapest flight they could find.
It’s not an unfamiliar story: people traveling, often long distances, to take part in clinical trials they hope will save their lives.
The Lazarex Cancer Foundation of Danville, Calif., helped Mrs. Long do just that.
Marya Shegog, PhD, health equity and diversity coordinator at Lazarex, said that a patient travels an average of 500 miles to participate in a trial.
The financial hurdles often prevent patients from taking part in clinical trials, Dr. Shegog said. “When you are sick, and you have a disease that may be terminal, you start thinking about setting your things in order.”
Many patients have to make a decision.
“Do I bankrupt my family on trying and hoping that this drug works and helps me live longer, or do I start setting things in order so that when I’m gone, they’re okay or at least better than if I wouldn’t have spent all the money traveling back and forth.”
Dr. Shegog, a 17-year cancer survivor, says when she was battling cervical cancer, a clinical trial was never offered or explored.
Lazarex has been helping cancer patients who have run out of options for 15 years. It identifies clinical trial opportunities and reimburses patients for all travel costs. Last year, Lazarex reimbursed more than 1,000 cancer patients. And it has supported more than 6,000 people since opening its doors.
“Lazarex exists to help remove the barriers of people not being able to participate in trials,” Dr. Shegog said. “It’s systemic that the medical system does not treat patients the same and oftentimes does not offer or make aware the opportunities for African Americans to participate.”
But now, thanks in part to COVID-19, new possibilities are taking shape. The pandemic has changed the landscape for trials, forcing many of them to go virtual, which allows patients to schedule telehealth visits and get some services like bloodwork and CT or MRI scans closer to home. Mrs. Long’s trial eventually went virtual.
“It was absolutely fantastic,” she said. “Having the trial locally, it saves us money, it saves wear and tear on my body. Being in the car, being in an airport or in a plane and in a hotel, all of that wears on you physically.”
The move to virtual studies may have lasting effects on research and treatment.
“The current pandemic has forced us to reexamine all of the traditional burdens we place on patients as it relates to receiving cancer treatment,” said Hala Borno, MD, an assistant professor of medicine at the University of California, San Francisco. “Whether they’re coming to our health care facility to see a clinician, for diagnostics such as blood draws and scans, or to receive therapy, this pandemic has challenged us to explore other possibilities that minimize the risk of exposure to SARS-CoV-2. What I find striking is that it has helped us operationalize use of telemedicine and the delivery of care closer to home.”
This is especially encouraging news for minority patients whose participation in trials has for years lagged well behind that of Whites.
But travel is not the only reason. Racial disparities in clinical trials have long been an issue that’s just another part of the implicit bias in health care.
Compared with White people, Black people are largely at higher risk for heart disease, cancer, stroke, diabetes, asthma, and even mental health problems.
And it’s not just African Americans. Asians, Hispanics, Native Americans, and Alaska Natives are all underrepresented in trials at a time when there is growing evidence that drugs may have different effects on different populations.
Dr. Borno is an oncologist who specializes in prostate cancer, a disease that she says shows a “significant disparity,” where Black men are two times more likely to die from advanced prostate cancer, compared with white men. Yet Black men make up just 3% of advanced therapeutic trials.
“A lack of diversity and inclusion in clinical trials is unacceptable,” she said. “If we continue to underrecruit racial/ethnic minorities and older adults to therapeutic clinical trials, we will not be powered to make valid conclusions regarding safety and efficacy in those patient populations. As a result, we can do harm.”
Dr. Borno said that telehealth and telemedicine are not cure-alls, and digital health solutions don’t work for all patients. Approaches, she says, must be tailored to the individual, or disparities could worsen.
In 2020, the Food and Drug Administration approved 53 new drugs. Overall, 32,000 patients took part in these trials. On average, 75% were White, 8% were Black, 6% were Asian, and 11% were Hispanic.
Here’s one stark example of the issue. In 2015, the FDA approved ixazomib (Ninlaro), a promising new drug for multiple myeloma, a blood cancer that affects Black people at disproportionately higher rates than White people. In the United States, one in five people diagnosed with multiple myeloma are Black people. They are more than twice as likely to get the disease as White people. Yet during the clinical trial of 722 participants, only 13 patients, or 1.8%, were Black.
The American Cancer Society estimates that more than 600,000 Americans will die from cancer this year. Historically, Black Americans have the highest death rate and the shortest survival of any racial or ethnic group, stemming largely, it concluded, from centuries of structural racism.
According to Jamie Freedman, MD, head of U.S. medical affairs at Genentech, a global pharmaceutical company, the lack of diversity is often tied to where studies are run.
“Companies tend to choose major academic medical centers where there is a high volume of clinical trial work. When you go to the same tried and true hospitals repeatedly, the pool of patients becomes very homogeneous and tends to be primarily white,” he said. “It’s critical to bring more trials into the community setting by including new sites that can reach underrepresented groups, and Genentech is making significant progress in that area.”
Dr. Freedman believes that, while access is a big hurdle, it doesn’t end there.
“Many patients have a lack of trust in the health care system,” he said. “There are also issues around underserved communities being able to afford quality care, so it’s important to keep time and financial burdens in mind when designing trials to help mitigate barriers such as travel, parking, time off work, and child care.”
Genentech started its diversity and inclusion effort several years ago. Dr. Freeman said that, until more trials become diverse, Black Americans will continue to pay the price. “I think they’re losing their lives in part due to lack of access to these trials. And that is why Genentech and all of us in the health care industry need to change how we design and enroll these studies. We have a long way to go, but I think the steps we’re taking are leading us in the right direction.”
Jennifer Jones-McMeans, PhD, director of global clinical affairs at Abbott Pharmaceuticals, is a clinical research scientist who has designed and led many clinical trials.
She said that Abbott is actively working on solutions.
“We have designed our trials to reduce the barriers to participation and expand access,” she said. “This can be as simple as providing transportation services or home visits for those who are housebound. We’re taking it a step further and providing home health services where someone comes to the home and provides follow-up visits there.”
They also provide interpretation services to address any language barriers.
“We are reaching out to a new set of talented investigators who work closely with underrepresented communities. They are very much wedded and supportive of the communities they treat. By working with doctors within these communities, it expands access to new therapies.”
Spokesperson Keanna Ghazvini said that Pfizer Pharmaceuticals is also committed to increasing minority participation in trials.
“We know that if historically underserved populations are left out of clinical trials, they risk not benefiting from medical breakthroughs down the line,” she said.
The National Institutes of Health’s National Library of Medicine maintains the clinicaltrials.gov database.
There, you can find information on nearly 372,000 publicly and privately supported clinical trials happening in all 50 states and 219 countries. Many are funded by the NIH, but not all of these studies have been evaluated by the U.S. government.
Andrea Denicoff, a nurse consultant at the National Cancer Institute and head of clinical trials operations for the NCI’s National Clinical Trials Network, has been involved in clinical research at the NIH for 35 years.
“It’s really important that our publicly funded trials represent the people of the country,” she said. “There are some cancers that we’re doing a good job in enrolling minorities, and other cancers we need to do a much better job in having a diverse representation in our trials.”
Ms. Denicoff believed opening trials in places where people live is key, but having a diverse clinical trials team is as important.
“We need to reinforce that cancer centers across the country have open doors, and anyone with cancer feels comfortable getting care at that center, and that also includes discussing the option to participate in clinical trials when one might be available. We know from research that when people are invited and asked about trial participation and educated about them, they’ll be much more interested in joining them.”
Ms. Denicoff said that, during the pandemic, the NCI quickly came up with guidance to allow trial sites to send patients their oral study drugs and set up virtual visits. She believes it may help increase future access.
‘Lola Fashoyin-Aje, MD, associate director for science and policy to address disparities in the Oncology Center of Excellence at the FDA, says the agency firmly believes clinical trials should represent the patients who will ultimately get the drug if it’s approved.
But the FDA’s power to require diversity in trials is limited.
“It is important to point out that there are legal constraints which limit’s FDA’s authority to require specific proportional representation in clinical trials by demographic factors,” Dr. Fashoyin-Aje said.
Still, some researchers feel the FDA should play a bigger role. The question is: Should diversity be mandated?
Rhonda Long is now back in Boston to start a new trial, with a new drug that targets her specific mutation. She will be there for 2 months. Once again, Lazarex will help cover some of the cost.
She wants people of color to understand that they are missing out on the promise of new cancer drugs and extended life.
“I feel like there’s not enough emphasis on clinical trials, I don’t believe there’s enough emphasis on second opinions, I don’t think there’s enough emphasis that medicine happens outside our borders, outside of our communities. Clinical trials that don’t have a broad range of participants, how do we know how effective they are if Black and brown people, Asian or Latin American people aren’t represented in the trial?”
And with more trials adopting virtual elements, she said it’s time for minorities to get on board.
Dr. Freedman believed the groundwork is being laid for that to happen. “I don’t think we’ll ever return back to the way we used to do things, where everything has to be done at the clinical trial site. I just don’t think we’re ever going back.”
A version of this article first appeared on WebMD.com.
“I’m the first person in my circle of family and friends to participate in a clinical trial.”
Five years ago, Rhonda Long was diagnosed with cholangiocarcinoma, a rare bile duct cancer that’s seen in only about 8,000 Americans each year.
At the time, Mrs. Long, who is Black, said her doctor in Dayton, Ohio, told her she was not a candidate for surgery and suggested palliative care. After seeking a second opinion at Duke University Medical Center, Durham, N.C., where her sister worked, the 51-year-old wife and mother of two had surgery, radiation, and chemotherapy there in North Carolina. When the chemo stopped working after 3 months, her oncologist at Duke referred her to a colleague at Massachusetts General Hospital in Boston, where she was accepted into a clinical trial.
“In 2019, I traveled to Boston from Dayton, Ohio, every 3 weeks for labs and scans, to make sure that the drug wasn’t doing more harm than good, making sure that the drug as developed was maintaining, shrinking, or even eliminating the disease. Physically and financially, it takes a toll on you and loved ones.”
Her medical insurance did not cover the direct expenses from the clinical trial, and she was spending $1,000-$1,500 each trip. Sometimes they drove the 15 hours to Boston, and sometimes they flew on the cheapest flight they could find.
It’s not an unfamiliar story: people traveling, often long distances, to take part in clinical trials they hope will save their lives.
The Lazarex Cancer Foundation of Danville, Calif., helped Mrs. Long do just that.
Marya Shegog, PhD, health equity and diversity coordinator at Lazarex, said that a patient travels an average of 500 miles to participate in a trial.
The financial hurdles often prevent patients from taking part in clinical trials, Dr. Shegog said. “When you are sick, and you have a disease that may be terminal, you start thinking about setting your things in order.”
Many patients have to make a decision.
“Do I bankrupt my family on trying and hoping that this drug works and helps me live longer, or do I start setting things in order so that when I’m gone, they’re okay or at least better than if I wouldn’t have spent all the money traveling back and forth.”
Dr. Shegog, a 17-year cancer survivor, says when she was battling cervical cancer, a clinical trial was never offered or explored.
Lazarex has been helping cancer patients who have run out of options for 15 years. It identifies clinical trial opportunities and reimburses patients for all travel costs. Last year, Lazarex reimbursed more than 1,000 cancer patients. And it has supported more than 6,000 people since opening its doors.
“Lazarex exists to help remove the barriers of people not being able to participate in trials,” Dr. Shegog said. “It’s systemic that the medical system does not treat patients the same and oftentimes does not offer or make aware the opportunities for African Americans to participate.”
But now, thanks in part to COVID-19, new possibilities are taking shape. The pandemic has changed the landscape for trials, forcing many of them to go virtual, which allows patients to schedule telehealth visits and get some services like bloodwork and CT or MRI scans closer to home. Mrs. Long’s trial eventually went virtual.
“It was absolutely fantastic,” she said. “Having the trial locally, it saves us money, it saves wear and tear on my body. Being in the car, being in an airport or in a plane and in a hotel, all of that wears on you physically.”
The move to virtual studies may have lasting effects on research and treatment.
“The current pandemic has forced us to reexamine all of the traditional burdens we place on patients as it relates to receiving cancer treatment,” said Hala Borno, MD, an assistant professor of medicine at the University of California, San Francisco. “Whether they’re coming to our health care facility to see a clinician, for diagnostics such as blood draws and scans, or to receive therapy, this pandemic has challenged us to explore other possibilities that minimize the risk of exposure to SARS-CoV-2. What I find striking is that it has helped us operationalize use of telemedicine and the delivery of care closer to home.”
This is especially encouraging news for minority patients whose participation in trials has for years lagged well behind that of Whites.
But travel is not the only reason. Racial disparities in clinical trials have long been an issue that’s just another part of the implicit bias in health care.
Compared with White people, Black people are largely at higher risk for heart disease, cancer, stroke, diabetes, asthma, and even mental health problems.
And it’s not just African Americans. Asians, Hispanics, Native Americans, and Alaska Natives are all underrepresented in trials at a time when there is growing evidence that drugs may have different effects on different populations.
Dr. Borno is an oncologist who specializes in prostate cancer, a disease that she says shows a “significant disparity,” where Black men are two times more likely to die from advanced prostate cancer, compared with white men. Yet Black men make up just 3% of advanced therapeutic trials.
“A lack of diversity and inclusion in clinical trials is unacceptable,” she said. “If we continue to underrecruit racial/ethnic minorities and older adults to therapeutic clinical trials, we will not be powered to make valid conclusions regarding safety and efficacy in those patient populations. As a result, we can do harm.”
Dr. Borno said that telehealth and telemedicine are not cure-alls, and digital health solutions don’t work for all patients. Approaches, she says, must be tailored to the individual, or disparities could worsen.
In 2020, the Food and Drug Administration approved 53 new drugs. Overall, 32,000 patients took part in these trials. On average, 75% were White, 8% were Black, 6% were Asian, and 11% were Hispanic.
Here’s one stark example of the issue. In 2015, the FDA approved ixazomib (Ninlaro), a promising new drug for multiple myeloma, a blood cancer that affects Black people at disproportionately higher rates than White people. In the United States, one in five people diagnosed with multiple myeloma are Black people. They are more than twice as likely to get the disease as White people. Yet during the clinical trial of 722 participants, only 13 patients, or 1.8%, were Black.
The American Cancer Society estimates that more than 600,000 Americans will die from cancer this year. Historically, Black Americans have the highest death rate and the shortest survival of any racial or ethnic group, stemming largely, it concluded, from centuries of structural racism.
According to Jamie Freedman, MD, head of U.S. medical affairs at Genentech, a global pharmaceutical company, the lack of diversity is often tied to where studies are run.
“Companies tend to choose major academic medical centers where there is a high volume of clinical trial work. When you go to the same tried and true hospitals repeatedly, the pool of patients becomes very homogeneous and tends to be primarily white,” he said. “It’s critical to bring more trials into the community setting by including new sites that can reach underrepresented groups, and Genentech is making significant progress in that area.”
Dr. Freedman believes that, while access is a big hurdle, it doesn’t end there.
“Many patients have a lack of trust in the health care system,” he said. “There are also issues around underserved communities being able to afford quality care, so it’s important to keep time and financial burdens in mind when designing trials to help mitigate barriers such as travel, parking, time off work, and child care.”
Genentech started its diversity and inclusion effort several years ago. Dr. Freeman said that, until more trials become diverse, Black Americans will continue to pay the price. “I think they’re losing their lives in part due to lack of access to these trials. And that is why Genentech and all of us in the health care industry need to change how we design and enroll these studies. We have a long way to go, but I think the steps we’re taking are leading us in the right direction.”
Jennifer Jones-McMeans, PhD, director of global clinical affairs at Abbott Pharmaceuticals, is a clinical research scientist who has designed and led many clinical trials.
She said that Abbott is actively working on solutions.
“We have designed our trials to reduce the barriers to participation and expand access,” she said. “This can be as simple as providing transportation services or home visits for those who are housebound. We’re taking it a step further and providing home health services where someone comes to the home and provides follow-up visits there.”
They also provide interpretation services to address any language barriers.
“We are reaching out to a new set of talented investigators who work closely with underrepresented communities. They are very much wedded and supportive of the communities they treat. By working with doctors within these communities, it expands access to new therapies.”
Spokesperson Keanna Ghazvini said that Pfizer Pharmaceuticals is also committed to increasing minority participation in trials.
“We know that if historically underserved populations are left out of clinical trials, they risk not benefiting from medical breakthroughs down the line,” she said.
The National Institutes of Health’s National Library of Medicine maintains the clinicaltrials.gov database.
There, you can find information on nearly 372,000 publicly and privately supported clinical trials happening in all 50 states and 219 countries. Many are funded by the NIH, but not all of these studies have been evaluated by the U.S. government.
Andrea Denicoff, a nurse consultant at the National Cancer Institute and head of clinical trials operations for the NCI’s National Clinical Trials Network, has been involved in clinical research at the NIH for 35 years.
“It’s really important that our publicly funded trials represent the people of the country,” she said. “There are some cancers that we’re doing a good job in enrolling minorities, and other cancers we need to do a much better job in having a diverse representation in our trials.”
Ms. Denicoff believed opening trials in places where people live is key, but having a diverse clinical trials team is as important.
“We need to reinforce that cancer centers across the country have open doors, and anyone with cancer feels comfortable getting care at that center, and that also includes discussing the option to participate in clinical trials when one might be available. We know from research that when people are invited and asked about trial participation and educated about them, they’ll be much more interested in joining them.”
Ms. Denicoff said that, during the pandemic, the NCI quickly came up with guidance to allow trial sites to send patients their oral study drugs and set up virtual visits. She believes it may help increase future access.
‘Lola Fashoyin-Aje, MD, associate director for science and policy to address disparities in the Oncology Center of Excellence at the FDA, says the agency firmly believes clinical trials should represent the patients who will ultimately get the drug if it’s approved.
But the FDA’s power to require diversity in trials is limited.
“It is important to point out that there are legal constraints which limit’s FDA’s authority to require specific proportional representation in clinical trials by demographic factors,” Dr. Fashoyin-Aje said.
Still, some researchers feel the FDA should play a bigger role. The question is: Should diversity be mandated?
Rhonda Long is now back in Boston to start a new trial, with a new drug that targets her specific mutation. She will be there for 2 months. Once again, Lazarex will help cover some of the cost.
She wants people of color to understand that they are missing out on the promise of new cancer drugs and extended life.
“I feel like there’s not enough emphasis on clinical trials, I don’t believe there’s enough emphasis on second opinions, I don’t think there’s enough emphasis that medicine happens outside our borders, outside of our communities. Clinical trials that don’t have a broad range of participants, how do we know how effective they are if Black and brown people, Asian or Latin American people aren’t represented in the trial?”
And with more trials adopting virtual elements, she said it’s time for minorities to get on board.
Dr. Freedman believed the groundwork is being laid for that to happen. “I don’t think we’ll ever return back to the way we used to do things, where everything has to be done at the clinical trial site. I just don’t think we’re ever going back.”
A version of this article first appeared on WebMD.com.
“I’m the first person in my circle of family and friends to participate in a clinical trial.”
Five years ago, Rhonda Long was diagnosed with cholangiocarcinoma, a rare bile duct cancer that’s seen in only about 8,000 Americans each year.
At the time, Mrs. Long, who is Black, said her doctor in Dayton, Ohio, told her she was not a candidate for surgery and suggested palliative care. After seeking a second opinion at Duke University Medical Center, Durham, N.C., where her sister worked, the 51-year-old wife and mother of two had surgery, radiation, and chemotherapy there in North Carolina. When the chemo stopped working after 3 months, her oncologist at Duke referred her to a colleague at Massachusetts General Hospital in Boston, where she was accepted into a clinical trial.
“In 2019, I traveled to Boston from Dayton, Ohio, every 3 weeks for labs and scans, to make sure that the drug wasn’t doing more harm than good, making sure that the drug as developed was maintaining, shrinking, or even eliminating the disease. Physically and financially, it takes a toll on you and loved ones.”
Her medical insurance did not cover the direct expenses from the clinical trial, and she was spending $1,000-$1,500 each trip. Sometimes they drove the 15 hours to Boston, and sometimes they flew on the cheapest flight they could find.
It’s not an unfamiliar story: people traveling, often long distances, to take part in clinical trials they hope will save their lives.
The Lazarex Cancer Foundation of Danville, Calif., helped Mrs. Long do just that.
Marya Shegog, PhD, health equity and diversity coordinator at Lazarex, said that a patient travels an average of 500 miles to participate in a trial.
The financial hurdles often prevent patients from taking part in clinical trials, Dr. Shegog said. “When you are sick, and you have a disease that may be terminal, you start thinking about setting your things in order.”
Many patients have to make a decision.
“Do I bankrupt my family on trying and hoping that this drug works and helps me live longer, or do I start setting things in order so that when I’m gone, they’re okay or at least better than if I wouldn’t have spent all the money traveling back and forth.”
Dr. Shegog, a 17-year cancer survivor, says when she was battling cervical cancer, a clinical trial was never offered or explored.
Lazarex has been helping cancer patients who have run out of options for 15 years. It identifies clinical trial opportunities and reimburses patients for all travel costs. Last year, Lazarex reimbursed more than 1,000 cancer patients. And it has supported more than 6,000 people since opening its doors.
“Lazarex exists to help remove the barriers of people not being able to participate in trials,” Dr. Shegog said. “It’s systemic that the medical system does not treat patients the same and oftentimes does not offer or make aware the opportunities for African Americans to participate.”
But now, thanks in part to COVID-19, new possibilities are taking shape. The pandemic has changed the landscape for trials, forcing many of them to go virtual, which allows patients to schedule telehealth visits and get some services like bloodwork and CT or MRI scans closer to home. Mrs. Long’s trial eventually went virtual.
“It was absolutely fantastic,” she said. “Having the trial locally, it saves us money, it saves wear and tear on my body. Being in the car, being in an airport or in a plane and in a hotel, all of that wears on you physically.”
The move to virtual studies may have lasting effects on research and treatment.
“The current pandemic has forced us to reexamine all of the traditional burdens we place on patients as it relates to receiving cancer treatment,” said Hala Borno, MD, an assistant professor of medicine at the University of California, San Francisco. “Whether they’re coming to our health care facility to see a clinician, for diagnostics such as blood draws and scans, or to receive therapy, this pandemic has challenged us to explore other possibilities that minimize the risk of exposure to SARS-CoV-2. What I find striking is that it has helped us operationalize use of telemedicine and the delivery of care closer to home.”
This is especially encouraging news for minority patients whose participation in trials has for years lagged well behind that of Whites.
But travel is not the only reason. Racial disparities in clinical trials have long been an issue that’s just another part of the implicit bias in health care.
Compared with White people, Black people are largely at higher risk for heart disease, cancer, stroke, diabetes, asthma, and even mental health problems.
And it’s not just African Americans. Asians, Hispanics, Native Americans, and Alaska Natives are all underrepresented in trials at a time when there is growing evidence that drugs may have different effects on different populations.
Dr. Borno is an oncologist who specializes in prostate cancer, a disease that she says shows a “significant disparity,” where Black men are two times more likely to die from advanced prostate cancer, compared with white men. Yet Black men make up just 3% of advanced therapeutic trials.
“A lack of diversity and inclusion in clinical trials is unacceptable,” she said. “If we continue to underrecruit racial/ethnic minorities and older adults to therapeutic clinical trials, we will not be powered to make valid conclusions regarding safety and efficacy in those patient populations. As a result, we can do harm.”
Dr. Borno said that telehealth and telemedicine are not cure-alls, and digital health solutions don’t work for all patients. Approaches, she says, must be tailored to the individual, or disparities could worsen.
In 2020, the Food and Drug Administration approved 53 new drugs. Overall, 32,000 patients took part in these trials. On average, 75% were White, 8% were Black, 6% were Asian, and 11% were Hispanic.
Here’s one stark example of the issue. In 2015, the FDA approved ixazomib (Ninlaro), a promising new drug for multiple myeloma, a blood cancer that affects Black people at disproportionately higher rates than White people. In the United States, one in five people diagnosed with multiple myeloma are Black people. They are more than twice as likely to get the disease as White people. Yet during the clinical trial of 722 participants, only 13 patients, or 1.8%, were Black.
The American Cancer Society estimates that more than 600,000 Americans will die from cancer this year. Historically, Black Americans have the highest death rate and the shortest survival of any racial or ethnic group, stemming largely, it concluded, from centuries of structural racism.
According to Jamie Freedman, MD, head of U.S. medical affairs at Genentech, a global pharmaceutical company, the lack of diversity is often tied to where studies are run.
“Companies tend to choose major academic medical centers where there is a high volume of clinical trial work. When you go to the same tried and true hospitals repeatedly, the pool of patients becomes very homogeneous and tends to be primarily white,” he said. “It’s critical to bring more trials into the community setting by including new sites that can reach underrepresented groups, and Genentech is making significant progress in that area.”
Dr. Freedman believes that, while access is a big hurdle, it doesn’t end there.
“Many patients have a lack of trust in the health care system,” he said. “There are also issues around underserved communities being able to afford quality care, so it’s important to keep time and financial burdens in mind when designing trials to help mitigate barriers such as travel, parking, time off work, and child care.”
Genentech started its diversity and inclusion effort several years ago. Dr. Freeman said that, until more trials become diverse, Black Americans will continue to pay the price. “I think they’re losing their lives in part due to lack of access to these trials. And that is why Genentech and all of us in the health care industry need to change how we design and enroll these studies. We have a long way to go, but I think the steps we’re taking are leading us in the right direction.”
Jennifer Jones-McMeans, PhD, director of global clinical affairs at Abbott Pharmaceuticals, is a clinical research scientist who has designed and led many clinical trials.
She said that Abbott is actively working on solutions.
“We have designed our trials to reduce the barriers to participation and expand access,” she said. “This can be as simple as providing transportation services or home visits for those who are housebound. We’re taking it a step further and providing home health services where someone comes to the home and provides follow-up visits there.”
They also provide interpretation services to address any language barriers.
“We are reaching out to a new set of talented investigators who work closely with underrepresented communities. They are very much wedded and supportive of the communities they treat. By working with doctors within these communities, it expands access to new therapies.”
Spokesperson Keanna Ghazvini said that Pfizer Pharmaceuticals is also committed to increasing minority participation in trials.
“We know that if historically underserved populations are left out of clinical trials, they risk not benefiting from medical breakthroughs down the line,” she said.
The National Institutes of Health’s National Library of Medicine maintains the clinicaltrials.gov database.
There, you can find information on nearly 372,000 publicly and privately supported clinical trials happening in all 50 states and 219 countries. Many are funded by the NIH, but not all of these studies have been evaluated by the U.S. government.
Andrea Denicoff, a nurse consultant at the National Cancer Institute and head of clinical trials operations for the NCI’s National Clinical Trials Network, has been involved in clinical research at the NIH for 35 years.
“It’s really important that our publicly funded trials represent the people of the country,” she said. “There are some cancers that we’re doing a good job in enrolling minorities, and other cancers we need to do a much better job in having a diverse representation in our trials.”
Ms. Denicoff believed opening trials in places where people live is key, but having a diverse clinical trials team is as important.
“We need to reinforce that cancer centers across the country have open doors, and anyone with cancer feels comfortable getting care at that center, and that also includes discussing the option to participate in clinical trials when one might be available. We know from research that when people are invited and asked about trial participation and educated about them, they’ll be much more interested in joining them.”
Ms. Denicoff said that, during the pandemic, the NCI quickly came up with guidance to allow trial sites to send patients their oral study drugs and set up virtual visits. She believes it may help increase future access.
‘Lola Fashoyin-Aje, MD, associate director for science and policy to address disparities in the Oncology Center of Excellence at the FDA, says the agency firmly believes clinical trials should represent the patients who will ultimately get the drug if it’s approved.
But the FDA’s power to require diversity in trials is limited.
“It is important to point out that there are legal constraints which limit’s FDA’s authority to require specific proportional representation in clinical trials by demographic factors,” Dr. Fashoyin-Aje said.
Still, some researchers feel the FDA should play a bigger role. The question is: Should diversity be mandated?
Rhonda Long is now back in Boston to start a new trial, with a new drug that targets her specific mutation. She will be there for 2 months. Once again, Lazarex will help cover some of the cost.
She wants people of color to understand that they are missing out on the promise of new cancer drugs and extended life.
“I feel like there’s not enough emphasis on clinical trials, I don’t believe there’s enough emphasis on second opinions, I don’t think there’s enough emphasis that medicine happens outside our borders, outside of our communities. Clinical trials that don’t have a broad range of participants, how do we know how effective they are if Black and brown people, Asian or Latin American people aren’t represented in the trial?”
And with more trials adopting virtual elements, she said it’s time for minorities to get on board.
Dr. Freedman believed the groundwork is being laid for that to happen. “I don’t think we’ll ever return back to the way we used to do things, where everything has to be done at the clinical trial site. I just don’t think we’re ever going back.”
A version of this article first appeared on WebMD.com.
Dapagliflozin may cut risk of HF hospitalization in patients with type 2 diabetes
Background: Dapagliflozin is a selective inhibitor of sodium-glucose transporter 2 (SGLT2) in the kidney; the drug blocks glucose reabsorption in the proximal tubule. It is taken once daily by mouth. An initial study sponsored by AstraZeneca was published January 2019 in the New England Journal of Medicine – “Dapagliflozin and cardiovascular outcomes in type 2 diabetes.” Until recently there was not an FDA-approved indication for the drug.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: 882 clinical sites in 33 countries.
Synopsis: The study randomized approximately 17,000 patients to receive either dapagliflozin or placebo in addition to any other diabetes treatments prescribed by their physician. This study demonstrated its primary safety outcome, which was that patients on dapagliflozin did not have any more major adverse cardiac events (MACE), compared with placebo. There were two primary efficacy outcomes. First, there was no change in MACE with dapagliflozin, compared with placebo. Second, and pertinent to this drug’s approval, was that dapagliflozin reduced risk of hospitalization for heart failure (HF) from 5.8% to 4.9%, compared to placebo; this includes both HF with both preserved and reduced ejection fractions.
Bottom line: Dapagliflozin now has an FDA-approved indication to reduce hospitalizations for HF in patients with type 2 diabetes. Based on this study, the number needed to treat with dapagliflozin is 111 patients to prevent one hospitalization for HF.
Citation: Farxiga approved in the US to reduce the risk of hospitalization for heart failure in patients with type-2 diabetes. AstraZeneca Press Release, 2019 Oct 21.
Dr. Como is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Dapagliflozin is a selective inhibitor of sodium-glucose transporter 2 (SGLT2) in the kidney; the drug blocks glucose reabsorption in the proximal tubule. It is taken once daily by mouth. An initial study sponsored by AstraZeneca was published January 2019 in the New England Journal of Medicine – “Dapagliflozin and cardiovascular outcomes in type 2 diabetes.” Until recently there was not an FDA-approved indication for the drug.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: 882 clinical sites in 33 countries.
Synopsis: The study randomized approximately 17,000 patients to receive either dapagliflozin or placebo in addition to any other diabetes treatments prescribed by their physician. This study demonstrated its primary safety outcome, which was that patients on dapagliflozin did not have any more major adverse cardiac events (MACE), compared with placebo. There were two primary efficacy outcomes. First, there was no change in MACE with dapagliflozin, compared with placebo. Second, and pertinent to this drug’s approval, was that dapagliflozin reduced risk of hospitalization for heart failure (HF) from 5.8% to 4.9%, compared to placebo; this includes both HF with both preserved and reduced ejection fractions.
Bottom line: Dapagliflozin now has an FDA-approved indication to reduce hospitalizations for HF in patients with type 2 diabetes. Based on this study, the number needed to treat with dapagliflozin is 111 patients to prevent one hospitalization for HF.
Citation: Farxiga approved in the US to reduce the risk of hospitalization for heart failure in patients with type-2 diabetes. AstraZeneca Press Release, 2019 Oct 21.
Dr. Como is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
Background: Dapagliflozin is a selective inhibitor of sodium-glucose transporter 2 (SGLT2) in the kidney; the drug blocks glucose reabsorption in the proximal tubule. It is taken once daily by mouth. An initial study sponsored by AstraZeneca was published January 2019 in the New England Journal of Medicine – “Dapagliflozin and cardiovascular outcomes in type 2 diabetes.” Until recently there was not an FDA-approved indication for the drug.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: 882 clinical sites in 33 countries.
Synopsis: The study randomized approximately 17,000 patients to receive either dapagliflozin or placebo in addition to any other diabetes treatments prescribed by their physician. This study demonstrated its primary safety outcome, which was that patients on dapagliflozin did not have any more major adverse cardiac events (MACE), compared with placebo. There were two primary efficacy outcomes. First, there was no change in MACE with dapagliflozin, compared with placebo. Second, and pertinent to this drug’s approval, was that dapagliflozin reduced risk of hospitalization for heart failure (HF) from 5.8% to 4.9%, compared to placebo; this includes both HF with both preserved and reduced ejection fractions.
Bottom line: Dapagliflozin now has an FDA-approved indication to reduce hospitalizations for HF in patients with type 2 diabetes. Based on this study, the number needed to treat with dapagliflozin is 111 patients to prevent one hospitalization for HF.
Citation: Farxiga approved in the US to reduce the risk of hospitalization for heart failure in patients with type-2 diabetes. AstraZeneca Press Release, 2019 Oct 21.
Dr. Como is a hospitalist and clinical instructor of medicine at the University of Utah, Salt Lake City.
FDA warning letters target OTC cannabidiol product claims for pain relief
The Food and Drug Administration has warned two manufacturers about illegal marketing of drugs containing cannabidiol (CBD) for over-the-counter use without an approved new drug application, for using substandard manufacturing processes, and for failure to comply with current good manufacturing practices. These warnings add to 51 previous warning letters issued by the FDA since 2015 to other manufacturers of products containing CBD who were violating the Federal Food, Drug, and Cosmetic Act.
In a news release, the agency explained that its two most recent letters, sent to Honest Globe Inc. on March 15 and BioLyte Laboratories LLC on March 18, were issued because CBD has “known pharmacologic effects on humans, with demonstrated risks, it cannot be legally marketed as an inactive ingredient in OTC drug products that are not reviewed and approved by the FDA.” They also describe the companies’ failures to comply with current good manufacturing practices.
“The FDA continues to alert the public to potential safety and efficacy concerns with unapproved CBD products sold online and in stores across the country,” FDA Principal Deputy Commissioner Amy P. Abernethy, MD, PhD, said in the release. “It’s important that consumers understand that the FDA has only approved one drug containing CBD as an ingredient [Epidiolex]. These other, unapproved, CBD products may have dangerous health impacts and side effects. We remain focused on exploring potential pathways for CBD products to be lawfully marketed while also educating the public about these outstanding questions of CBD’s safety. Meanwhile, we will continue to monitor and take action, as needed, against companies that unlawfully market their products – prioritizing those that pose a risk to public health.”
The specific products from Santa Ana, Calif.–based Honest Globe that the FDA called unapproved new drugs and misbranded under the Federal Food, Drug, and Cosmetic Act included Elixicure Original Pain Relief and Elixicure Lavender Pain Relief, both of which were described as containing CBD. Products from Grand Rapids, Mich.–based BioLyte Laboratories LLC that the FDA similarly cited for violations included Silver Gel, Silver Gel with Aloe, Silver Liquid Supplement, Therapeutic Pain Gel, Pain Relief Cream, and Magnesium Oil Spray.
The agency has asked the two companies to respond to its letters within 15 working days, “stating how they will address these violations or providing their reasoning and supporting information as to why they believe these products are not in violation of the law. Failure to adequately address the violations promptly may result in legal action, including product seizure and/or injunction.”
The Food and Drug Administration has warned two manufacturers about illegal marketing of drugs containing cannabidiol (CBD) for over-the-counter use without an approved new drug application, for using substandard manufacturing processes, and for failure to comply with current good manufacturing practices. These warnings add to 51 previous warning letters issued by the FDA since 2015 to other manufacturers of products containing CBD who were violating the Federal Food, Drug, and Cosmetic Act.
In a news release, the agency explained that its two most recent letters, sent to Honest Globe Inc. on March 15 and BioLyte Laboratories LLC on March 18, were issued because CBD has “known pharmacologic effects on humans, with demonstrated risks, it cannot be legally marketed as an inactive ingredient in OTC drug products that are not reviewed and approved by the FDA.” They also describe the companies’ failures to comply with current good manufacturing practices.
“The FDA continues to alert the public to potential safety and efficacy concerns with unapproved CBD products sold online and in stores across the country,” FDA Principal Deputy Commissioner Amy P. Abernethy, MD, PhD, said in the release. “It’s important that consumers understand that the FDA has only approved one drug containing CBD as an ingredient [Epidiolex]. These other, unapproved, CBD products may have dangerous health impacts and side effects. We remain focused on exploring potential pathways for CBD products to be lawfully marketed while also educating the public about these outstanding questions of CBD’s safety. Meanwhile, we will continue to monitor and take action, as needed, against companies that unlawfully market their products – prioritizing those that pose a risk to public health.”
The specific products from Santa Ana, Calif.–based Honest Globe that the FDA called unapproved new drugs and misbranded under the Federal Food, Drug, and Cosmetic Act included Elixicure Original Pain Relief and Elixicure Lavender Pain Relief, both of which were described as containing CBD. Products from Grand Rapids, Mich.–based BioLyte Laboratories LLC that the FDA similarly cited for violations included Silver Gel, Silver Gel with Aloe, Silver Liquid Supplement, Therapeutic Pain Gel, Pain Relief Cream, and Magnesium Oil Spray.
The agency has asked the two companies to respond to its letters within 15 working days, “stating how they will address these violations or providing their reasoning and supporting information as to why they believe these products are not in violation of the law. Failure to adequately address the violations promptly may result in legal action, including product seizure and/or injunction.”
The Food and Drug Administration has warned two manufacturers about illegal marketing of drugs containing cannabidiol (CBD) for over-the-counter use without an approved new drug application, for using substandard manufacturing processes, and for failure to comply with current good manufacturing practices. These warnings add to 51 previous warning letters issued by the FDA since 2015 to other manufacturers of products containing CBD who were violating the Federal Food, Drug, and Cosmetic Act.
In a news release, the agency explained that its two most recent letters, sent to Honest Globe Inc. on March 15 and BioLyte Laboratories LLC on March 18, were issued because CBD has “known pharmacologic effects on humans, with demonstrated risks, it cannot be legally marketed as an inactive ingredient in OTC drug products that are not reviewed and approved by the FDA.” They also describe the companies’ failures to comply with current good manufacturing practices.
“The FDA continues to alert the public to potential safety and efficacy concerns with unapproved CBD products sold online and in stores across the country,” FDA Principal Deputy Commissioner Amy P. Abernethy, MD, PhD, said in the release. “It’s important that consumers understand that the FDA has only approved one drug containing CBD as an ingredient [Epidiolex]. These other, unapproved, CBD products may have dangerous health impacts and side effects. We remain focused on exploring potential pathways for CBD products to be lawfully marketed while also educating the public about these outstanding questions of CBD’s safety. Meanwhile, we will continue to monitor and take action, as needed, against companies that unlawfully market their products – prioritizing those that pose a risk to public health.”
The specific products from Santa Ana, Calif.–based Honest Globe that the FDA called unapproved new drugs and misbranded under the Federal Food, Drug, and Cosmetic Act included Elixicure Original Pain Relief and Elixicure Lavender Pain Relief, both of which were described as containing CBD. Products from Grand Rapids, Mich.–based BioLyte Laboratories LLC that the FDA similarly cited for violations included Silver Gel, Silver Gel with Aloe, Silver Liquid Supplement, Therapeutic Pain Gel, Pain Relief Cream, and Magnesium Oil Spray.
The agency has asked the two companies to respond to its letters within 15 working days, “stating how they will address these violations or providing their reasoning and supporting information as to why they believe these products are not in violation of the law. Failure to adequately address the violations promptly may result in legal action, including product seizure and/or injunction.”
Low concordance between troponin assays for ACS
Clinicians should be aware that the discordance between high-sensitivity cardiac troponin (hs-cTn) assays is significant enough that management recommendations may change, for example, for a patient assessed for suspected acute coronary syndrome (ACS) in one hospital and transferred to another that uses a different assay, according to a team of international researchers.
When hs-cTn concentrations were measured using the three Food and Drug Administration–approved assays, only 37.4% (384 of 1,027 samples) of blood samples were classified into the same analytical benchmark category.
“We didn’t expect such low concordance, to be honest, but I have to stress that this first assessment used just one-time blood testing and serial testing is what is more commonly recommended now,” said Júlia Karády, MD, from Massachusetts General Hospital and Harvard Medical School, both in Boston.
To see if concordance improved with serial testing, the researchers looked at the 242 patients for whom serial samples were available and saw concordance of management recommendations across assays rise to 74.8%.
“We tested the 0/2-hour algorithm and found that the overall agreement almost doubled, so I think that a very important message from our study is that serial testing improves the agreement between the assays in terms of clinical management and patient stratification,” said Dr. Karády.
Dr. Karády and colleagues published their findings in the Journal of the American College of Cardiology.
The researchers tested three assays referred to clinically as high-sensitivity assays: Elecsys 2010 platform (Roche Diagnostics); ARCHITECT i2000SR (Abbott Diagnostics); and hsVista (Siemens Diagnostics). All three have received FDA approval, starting with Elecsys in 2017.
The proportion of patients with similar management recommendations differed between the assays for both “rule-out” (87.2%, 73.1%, and 78.5% for Roche, Abbott, and Siemens, respectively) and “observe” (9.5%, 24%, and 17.8%; both P < .001). For the purposes of “rule-in,” no difference was noted (3.3%, 2.9%, and 3.7%).
“It’s important to note that this was a highly selected population of patients with an intermediate likelihood for ACS, not an all-comer population. This group comprises about 20% of the [emergency department] population and actually is the group we struggle with the most, which is hardest to diagnose because it excludes the very low– and very high–risk patients,” said Dr. Karády.
The patients included in this study all had suspected ACS and were enrolled in the ROMICAT-I and II trials.
Among 1,027 samples from 624 patients (mean age, 52.8 years; 39.4% women), samples were classified as below the limit of detection (LOD) in 56.3%, 10.4%, and 41.2% (P < .001) by Roche, Abbott, and Siemens, respectively.
The proportion of sample with a troponin measurement between LOD to the 99th percentile also differed significantly between the assays at 36.5%, 83.5%, and 52.6%, respectively (P < .001).
Only the proportion classified greater than 99th percentile did not differ (7.2%, 6.0%, and 6.2%; P = .114).
When the researchers looked at sex-specific difference, no differences were seen in rule-in numbers for men, but significant differences were seen for women.
“One possible explanation for this could be differences in the representation of men and women in the various reference populations used to develop the 99th percentile values for these assays,” suggested Dr. Karády.
They estimate around 30%-40% of U.S. centers are currently using high-sensitivity troponin assays and this number is “rapidly rising.”
The diagnostic algorithms developed for use with high-sensitivity assays, such as the 0/2-h algorithm, acknowledge differences in performance characteristics and recommend that assay-specific cut points be used for clinical decision-making rather than relying on generally applicable thresholds.
Joseph S. Alpert, MD, University of Arizona, Tucson, and coauthors of an accompanying editorial said the take-home message here is caveat emptor.
“First, ‘let the buyer (i.e., the clinician) beware’ when patients are transferred from one hospital to another, where different hs-cTn assays may be used,” they wrote. This is particularly true in women and in those with troponin levels in the “observe (gray zone)” clinical management recommendation.
Dr. Karády has received grant support from the Fulbright Visiting Researcher Grant and the Rosztoczy Foundation. One of the coauthors of the editorial comment consults or has consulted for most of the major diagnostic companies, including the manufacturers of the three assays tested in this study. Dr. Alpert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clinicians should be aware that the discordance between high-sensitivity cardiac troponin (hs-cTn) assays is significant enough that management recommendations may change, for example, for a patient assessed for suspected acute coronary syndrome (ACS) in one hospital and transferred to another that uses a different assay, according to a team of international researchers.
When hs-cTn concentrations were measured using the three Food and Drug Administration–approved assays, only 37.4% (384 of 1,027 samples) of blood samples were classified into the same analytical benchmark category.
“We didn’t expect such low concordance, to be honest, but I have to stress that this first assessment used just one-time blood testing and serial testing is what is more commonly recommended now,” said Júlia Karády, MD, from Massachusetts General Hospital and Harvard Medical School, both in Boston.
To see if concordance improved with serial testing, the researchers looked at the 242 patients for whom serial samples were available and saw concordance of management recommendations across assays rise to 74.8%.
“We tested the 0/2-hour algorithm and found that the overall agreement almost doubled, so I think that a very important message from our study is that serial testing improves the agreement between the assays in terms of clinical management and patient stratification,” said Dr. Karády.
Dr. Karády and colleagues published their findings in the Journal of the American College of Cardiology.
The researchers tested three assays referred to clinically as high-sensitivity assays: Elecsys 2010 platform (Roche Diagnostics); ARCHITECT i2000SR (Abbott Diagnostics); and hsVista (Siemens Diagnostics). All three have received FDA approval, starting with Elecsys in 2017.
The proportion of patients with similar management recommendations differed between the assays for both “rule-out” (87.2%, 73.1%, and 78.5% for Roche, Abbott, and Siemens, respectively) and “observe” (9.5%, 24%, and 17.8%; both P < .001). For the purposes of “rule-in,” no difference was noted (3.3%, 2.9%, and 3.7%).
“It’s important to note that this was a highly selected population of patients with an intermediate likelihood for ACS, not an all-comer population. This group comprises about 20% of the [emergency department] population and actually is the group we struggle with the most, which is hardest to diagnose because it excludes the very low– and very high–risk patients,” said Dr. Karády.
The patients included in this study all had suspected ACS and were enrolled in the ROMICAT-I and II trials.
Among 1,027 samples from 624 patients (mean age, 52.8 years; 39.4% women), samples were classified as below the limit of detection (LOD) in 56.3%, 10.4%, and 41.2% (P < .001) by Roche, Abbott, and Siemens, respectively.
The proportion of sample with a troponin measurement between LOD to the 99th percentile also differed significantly between the assays at 36.5%, 83.5%, and 52.6%, respectively (P < .001).
Only the proportion classified greater than 99th percentile did not differ (7.2%, 6.0%, and 6.2%; P = .114).
When the researchers looked at sex-specific difference, no differences were seen in rule-in numbers for men, but significant differences were seen for women.
“One possible explanation for this could be differences in the representation of men and women in the various reference populations used to develop the 99th percentile values for these assays,” suggested Dr. Karády.
They estimate around 30%-40% of U.S. centers are currently using high-sensitivity troponin assays and this number is “rapidly rising.”
The diagnostic algorithms developed for use with high-sensitivity assays, such as the 0/2-h algorithm, acknowledge differences in performance characteristics and recommend that assay-specific cut points be used for clinical decision-making rather than relying on generally applicable thresholds.
Joseph S. Alpert, MD, University of Arizona, Tucson, and coauthors of an accompanying editorial said the take-home message here is caveat emptor.
“First, ‘let the buyer (i.e., the clinician) beware’ when patients are transferred from one hospital to another, where different hs-cTn assays may be used,” they wrote. This is particularly true in women and in those with troponin levels in the “observe (gray zone)” clinical management recommendation.
Dr. Karády has received grant support from the Fulbright Visiting Researcher Grant and the Rosztoczy Foundation. One of the coauthors of the editorial comment consults or has consulted for most of the major diagnostic companies, including the manufacturers of the three assays tested in this study. Dr. Alpert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clinicians should be aware that the discordance between high-sensitivity cardiac troponin (hs-cTn) assays is significant enough that management recommendations may change, for example, for a patient assessed for suspected acute coronary syndrome (ACS) in one hospital and transferred to another that uses a different assay, according to a team of international researchers.
When hs-cTn concentrations were measured using the three Food and Drug Administration–approved assays, only 37.4% (384 of 1,027 samples) of blood samples were classified into the same analytical benchmark category.
“We didn’t expect such low concordance, to be honest, but I have to stress that this first assessment used just one-time blood testing and serial testing is what is more commonly recommended now,” said Júlia Karády, MD, from Massachusetts General Hospital and Harvard Medical School, both in Boston.
To see if concordance improved with serial testing, the researchers looked at the 242 patients for whom serial samples were available and saw concordance of management recommendations across assays rise to 74.8%.
“We tested the 0/2-hour algorithm and found that the overall agreement almost doubled, so I think that a very important message from our study is that serial testing improves the agreement between the assays in terms of clinical management and patient stratification,” said Dr. Karády.
Dr. Karády and colleagues published their findings in the Journal of the American College of Cardiology.
The researchers tested three assays referred to clinically as high-sensitivity assays: Elecsys 2010 platform (Roche Diagnostics); ARCHITECT i2000SR (Abbott Diagnostics); and hsVista (Siemens Diagnostics). All three have received FDA approval, starting with Elecsys in 2017.
The proportion of patients with similar management recommendations differed between the assays for both “rule-out” (87.2%, 73.1%, and 78.5% for Roche, Abbott, and Siemens, respectively) and “observe” (9.5%, 24%, and 17.8%; both P < .001). For the purposes of “rule-in,” no difference was noted (3.3%, 2.9%, and 3.7%).
“It’s important to note that this was a highly selected population of patients with an intermediate likelihood for ACS, not an all-comer population. This group comprises about 20% of the [emergency department] population and actually is the group we struggle with the most, which is hardest to diagnose because it excludes the very low– and very high–risk patients,” said Dr. Karády.
The patients included in this study all had suspected ACS and were enrolled in the ROMICAT-I and II trials.
Among 1,027 samples from 624 patients (mean age, 52.8 years; 39.4% women), samples were classified as below the limit of detection (LOD) in 56.3%, 10.4%, and 41.2% (P < .001) by Roche, Abbott, and Siemens, respectively.
The proportion of sample with a troponin measurement between LOD to the 99th percentile also differed significantly between the assays at 36.5%, 83.5%, and 52.6%, respectively (P < .001).
Only the proportion classified greater than 99th percentile did not differ (7.2%, 6.0%, and 6.2%; P = .114).
When the researchers looked at sex-specific difference, no differences were seen in rule-in numbers for men, but significant differences were seen for women.
“One possible explanation for this could be differences in the representation of men and women in the various reference populations used to develop the 99th percentile values for these assays,” suggested Dr. Karády.
They estimate around 30%-40% of U.S. centers are currently using high-sensitivity troponin assays and this number is “rapidly rising.”
The diagnostic algorithms developed for use with high-sensitivity assays, such as the 0/2-h algorithm, acknowledge differences in performance characteristics and recommend that assay-specific cut points be used for clinical decision-making rather than relying on generally applicable thresholds.
Joseph S. Alpert, MD, University of Arizona, Tucson, and coauthors of an accompanying editorial said the take-home message here is caveat emptor.
“First, ‘let the buyer (i.e., the clinician) beware’ when patients are transferred from one hospital to another, where different hs-cTn assays may be used,” they wrote. This is particularly true in women and in those with troponin levels in the “observe (gray zone)” clinical management recommendation.
Dr. Karády has received grant support from the Fulbright Visiting Researcher Grant and the Rosztoczy Foundation. One of the coauthors of the editorial comment consults or has consulted for most of the major diagnostic companies, including the manufacturers of the three assays tested in this study. Dr. Alpert disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Artifactual hypoglycemia: When there’s a problem in the tube
If you are looking for zebras you might consider adrenal insufficiency, which could cause both hyperkalemia and hypoglycemia, but this would make no sense in someone asymptomatic.
This pattern is one I have seen commonly when I am on call, and I am contacted about abnormal labs. The lab reported no hemolysis seen, but this is the typical pattern seen with hemolytic specimens and/or specimens that have been held a long time before they are analyzed.
Lippi and colleagues reported on the clinically significant increase in potassium in samples that visually appeared not to be hemolyzed.1 Hemolyzed specimens can also drop glucose values, but not as profoundly as raising potassium values. When left unprocessed, glycolysis occurs in the white blood cells of a blood sample and may consume 5%-7% of the sample’s glucose content per hour.2
Khaled and colleagues looked at the drop in glucose levels in samples over time based on what anticoagulants were used.3 They found that, at 3 hours, glucose measurements were decreased by 28.4 mg/dL when sodium citrate is used, 58 mg/dL when EDTA was used, 15.4 mg/dL when fluoride oxalate was used, and 60.2 mg/dL when no anticoagulant is used.
Low blood sugars caused by elevated WBCs in blood samples has been well described.4 It has been described with moderate and very high WBC counts, as well as with the leukocytosis seen with polycythemia vera.5 The term “leukocyte larceny” has been used to describe high WBC counts that can not only utilize glucose, but also oxygen.
Saccheti and colleagues described a patient with a WBC greater than 500,000 who had repeatedly low oxygen levels on blood gases, that did not correlate with the normal oxygen saturations measured by pulse oximetry.6 This same issue has been seen in patients with extreme thrombocytosis.7Pearl: When labs don’t make sense clinically, always look at the possibility that there may be a problem in the tube and not in the person. Especially think of this when blood samples may have been held for a long time before they are run, such as with visiting nurse visits and blood draws at shelters and nursing homes.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Lippi G et al. Clin Chem Lab Med. 2006;44(3):311-6.
2. Mikesh LM and Bruns DE. Clin Chem. 2008 May;54(5):930-2.
3. Khaled S et al. Al-Mukhtar Journal of Sciences. 2018;33(2):100-6.
4. Goodenow TJ and Malarkey WB. JAMA. 1977;237(18):1961-2.
5. R Arem et al. Arch Intern Med. 1982 Nov;142(12):2199-201.
6. Sacchetti A et al. J Emerg Med. 1990;8:567–569.
7. A Mehta et al. Eur Respir J. 2008 Feb;31(2):469-72.
If you are looking for zebras you might consider adrenal insufficiency, which could cause both hyperkalemia and hypoglycemia, but this would make no sense in someone asymptomatic.
This pattern is one I have seen commonly when I am on call, and I am contacted about abnormal labs. The lab reported no hemolysis seen, but this is the typical pattern seen with hemolytic specimens and/or specimens that have been held a long time before they are analyzed.
Lippi and colleagues reported on the clinically significant increase in potassium in samples that visually appeared not to be hemolyzed.1 Hemolyzed specimens can also drop glucose values, but not as profoundly as raising potassium values. When left unprocessed, glycolysis occurs in the white blood cells of a blood sample and may consume 5%-7% of the sample’s glucose content per hour.2
Khaled and colleagues looked at the drop in glucose levels in samples over time based on what anticoagulants were used.3 They found that, at 3 hours, glucose measurements were decreased by 28.4 mg/dL when sodium citrate is used, 58 mg/dL when EDTA was used, 15.4 mg/dL when fluoride oxalate was used, and 60.2 mg/dL when no anticoagulant is used.
Low blood sugars caused by elevated WBCs in blood samples has been well described.4 It has been described with moderate and very high WBC counts, as well as with the leukocytosis seen with polycythemia vera.5 The term “leukocyte larceny” has been used to describe high WBC counts that can not only utilize glucose, but also oxygen.
Saccheti and colleagues described a patient with a WBC greater than 500,000 who had repeatedly low oxygen levels on blood gases, that did not correlate with the normal oxygen saturations measured by pulse oximetry.6 This same issue has been seen in patients with extreme thrombocytosis.7Pearl: When labs don’t make sense clinically, always look at the possibility that there may be a problem in the tube and not in the person. Especially think of this when blood samples may have been held for a long time before they are run, such as with visiting nurse visits and blood draws at shelters and nursing homes.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Lippi G et al. Clin Chem Lab Med. 2006;44(3):311-6.
2. Mikesh LM and Bruns DE. Clin Chem. 2008 May;54(5):930-2.
3. Khaled S et al. Al-Mukhtar Journal of Sciences. 2018;33(2):100-6.
4. Goodenow TJ and Malarkey WB. JAMA. 1977;237(18):1961-2.
5. R Arem et al. Arch Intern Med. 1982 Nov;142(12):2199-201.
6. Sacchetti A et al. J Emerg Med. 1990;8:567–569.
7. A Mehta et al. Eur Respir J. 2008 Feb;31(2):469-72.
If you are looking for zebras you might consider adrenal insufficiency, which could cause both hyperkalemia and hypoglycemia, but this would make no sense in someone asymptomatic.
This pattern is one I have seen commonly when I am on call, and I am contacted about abnormal labs. The lab reported no hemolysis seen, but this is the typical pattern seen with hemolytic specimens and/or specimens that have been held a long time before they are analyzed.
Lippi and colleagues reported on the clinically significant increase in potassium in samples that visually appeared not to be hemolyzed.1 Hemolyzed specimens can also drop glucose values, but not as profoundly as raising potassium values. When left unprocessed, glycolysis occurs in the white blood cells of a blood sample and may consume 5%-7% of the sample’s glucose content per hour.2
Khaled and colleagues looked at the drop in glucose levels in samples over time based on what anticoagulants were used.3 They found that, at 3 hours, glucose measurements were decreased by 28.4 mg/dL when sodium citrate is used, 58 mg/dL when EDTA was used, 15.4 mg/dL when fluoride oxalate was used, and 60.2 mg/dL when no anticoagulant is used.
Low blood sugars caused by elevated WBCs in blood samples has been well described.4 It has been described with moderate and very high WBC counts, as well as with the leukocytosis seen with polycythemia vera.5 The term “leukocyte larceny” has been used to describe high WBC counts that can not only utilize glucose, but also oxygen.
Saccheti and colleagues described a patient with a WBC greater than 500,000 who had repeatedly low oxygen levels on blood gases, that did not correlate with the normal oxygen saturations measured by pulse oximetry.6 This same issue has been seen in patients with extreme thrombocytosis.7Pearl: When labs don’t make sense clinically, always look at the possibility that there may be a problem in the tube and not in the person. Especially think of this when blood samples may have been held for a long time before they are run, such as with visiting nurse visits and blood draws at shelters and nursing homes.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Lippi G et al. Clin Chem Lab Med. 2006;44(3):311-6.
2. Mikesh LM and Bruns DE. Clin Chem. 2008 May;54(5):930-2.
3. Khaled S et al. Al-Mukhtar Journal of Sciences. 2018;33(2):100-6.
4. Goodenow TJ and Malarkey WB. JAMA. 1977;237(18):1961-2.
5. R Arem et al. Arch Intern Med. 1982 Nov;142(12):2199-201.
6. Sacchetti A et al. J Emerg Med. 1990;8:567–569.
7. A Mehta et al. Eur Respir J. 2008 Feb;31(2):469-72.
Gynecologic cancer patients at risk of insurance loss, ‘catastrophic’ costs
A retrospective study of respondents to the Medical Expenditure Panel Survey showed that more than one in five gynecologic cancer patients reported losing health insurance for at least 1 month every year, and more than one in four reported having catastrophic health expenses annually.
Benjamin Albright, MD, of Duke University Medical Center in Durham, N.C., presented these results at the Society of Gynecologic Oncology’s Virtual Annual Meeting on Women’s Cancer (Abstract 10303).
“We found gynecologic cancer patients to have high rates of insurance churn and catastrophic health expenditures, particularly among the poor,” Dr. Albright said. “Traditional static measurements clearly underestimate the impact of uninsurance, with over 20% of patients reporting some period of uninsurance annually.”
There was no evidence of improvement in any outcome after the implementation of the ACA, compared with the pre-ACA period, “though our assessment was limited in estimate precision by small sample size,” Dr. Albright acknowledged.
Dynamic, not static
Oncology researchers who study access to care and financial toxicities often consider insurance status as a static characteristic, but in the U.S. health care system, the reality is quite different, with insurance status fluctuating by employment or ability to pay, sometimes on a month-to-month basis, according to Dr. Albright.
Citing the Commonwealth Fund’s definition of catastrophic health expenditures as “spending over 10% of income on health care,” Dr. Albright noted that the prevalence of catastrophic out-of-pocket costs “is also relatively poorly described among cancer patients, particularly in accounting for family spending and income dynamics.
“The Affordable Care Act contained measures to address both of these concerns, including coverage protections and expansions, and spending regulations,” he said.
Dr. Albright and colleagues at Duke and Memorial Sloan Kettering Cancer Center in New York assessed insurance churn and catastrophic health expenditures among gynecologic cancer patients, attempting to determine whether the ACA had helped to limit insurance churn and keep costs manageable.
Representative sample
The investigators conducted a retrospective study of data from Medical Expenditure Panel Survey respondents from 2006 through 2017, a period that spanned the implementation of the ACA in 2010.
The sample included 684 women younger than 65 years reporting care in the given year related to a gynecologic cancer diagnosis. The civilian, noninstitutionalized sample was weighted to represent an estimated average annual population of 533,000 persons. The population was majority White (87%) and non-Hispanic (85.5%).
The investigators found that, compared with the overall U.S. population of people under 65, gynecologic cancer patients were more likely to have incomes of 250% or less of the federal poverty line (45.1% vs. 32.2%, P < .001).
The cancer patients were more likely than was the general population to have less than full-time employment, with 15.2% and 10.5%, respectively, reporting a job change or job loss; 55.3% and 44.1%, respectively, being employed only part of a given year; and 38.6% and 32.4%, respectively, being unemployed for a full year (P < .05 for each comparison).
Gynecologic cancer patients continued to experience insurance troubles and financial hardships after the ACA went into effect, with 8.8% reporting loss of insurance, 18.7% reporting a change in insurance, 21.7% being uninsured for at least 1 month, and 8.4% being uninsured for an entire year.
In addition, 12.8% of gynecologic cancer patients reported catastrophic health expenditures in out-of-pocket costs alone, and 28.0% spent more than 10% of their income on health care when the cost of premiums was factored in.
The numbers were even worse for non-White and Hispanic patients, with 25.9% reporting an insurance change (vs. 16.3% for non-Hispanic Whites) and 30.2% reporting a period of not being insured (vs. 18.7% for non-Hispanic Whites). There were no differences in catastrophic health expenditures by race/ethnicity, however.
Not surprisingly, patients from low-income families had significantly higher probability of having catastrophic expenditures, at 22.7% vs. 3.0% for higher-income families for out-of-pocket expenses alone (P < .001), and 35.3% vs. 20.8%, respectively, when the cost of premiums was included (P = .01).
On the other hand, patients with full-year Medicaid coverage were less likely to suffer from catastrophic costs than were privately-insured patients, at 15.3% vs. 31.3% in the overall sample (P = .02), and 11.5% vs. 62.1% of low-income vs. higher-income patients (P < .001).
There was a trend toward lower catastrophic health expenditures among low-income patients after full implementation of the ACA – 2014-2017 – compared with 2006-2009, but this difference was not statistically significant.
How to change it
In a panel discussion following the presentation, comoderator Eloise Chapman-Davis, MD, of Weill Cornell Medicine in New York, said to Dr. Albright, “As we look to improve equity within our subspecialty, I would like to ask you to comment on how you believe your abstract will inform our gyn-oncology culture and speak to what changes that you believe are needed to better advocate for our patients.”
“I think that our abstract really shows the prevalence of the problems of financial toxicity and of instability in the insurance market in the U.S.,” he replied. “I think it points out that we need to be more proactive about identifying patients and seeking out patients who may be having issues related to financial toxicity, to try to refer people to resources sooner and upfront.”
The investigators did not list a funding source for the study. Dr. Albright and Dr. Chapman-Davis reported having no conflicts of interest.
A retrospective study of respondents to the Medical Expenditure Panel Survey showed that more than one in five gynecologic cancer patients reported losing health insurance for at least 1 month every year, and more than one in four reported having catastrophic health expenses annually.
Benjamin Albright, MD, of Duke University Medical Center in Durham, N.C., presented these results at the Society of Gynecologic Oncology’s Virtual Annual Meeting on Women’s Cancer (Abstract 10303).
“We found gynecologic cancer patients to have high rates of insurance churn and catastrophic health expenditures, particularly among the poor,” Dr. Albright said. “Traditional static measurements clearly underestimate the impact of uninsurance, with over 20% of patients reporting some period of uninsurance annually.”
There was no evidence of improvement in any outcome after the implementation of the ACA, compared with the pre-ACA period, “though our assessment was limited in estimate precision by small sample size,” Dr. Albright acknowledged.
Dynamic, not static
Oncology researchers who study access to care and financial toxicities often consider insurance status as a static characteristic, but in the U.S. health care system, the reality is quite different, with insurance status fluctuating by employment or ability to pay, sometimes on a month-to-month basis, according to Dr. Albright.
Citing the Commonwealth Fund’s definition of catastrophic health expenditures as “spending over 10% of income on health care,” Dr. Albright noted that the prevalence of catastrophic out-of-pocket costs “is also relatively poorly described among cancer patients, particularly in accounting for family spending and income dynamics.
“The Affordable Care Act contained measures to address both of these concerns, including coverage protections and expansions, and spending regulations,” he said.
Dr. Albright and colleagues at Duke and Memorial Sloan Kettering Cancer Center in New York assessed insurance churn and catastrophic health expenditures among gynecologic cancer patients, attempting to determine whether the ACA had helped to limit insurance churn and keep costs manageable.
Representative sample
The investigators conducted a retrospective study of data from Medical Expenditure Panel Survey respondents from 2006 through 2017, a period that spanned the implementation of the ACA in 2010.
The sample included 684 women younger than 65 years reporting care in the given year related to a gynecologic cancer diagnosis. The civilian, noninstitutionalized sample was weighted to represent an estimated average annual population of 533,000 persons. The population was majority White (87%) and non-Hispanic (85.5%).
The investigators found that, compared with the overall U.S. population of people under 65, gynecologic cancer patients were more likely to have incomes of 250% or less of the federal poverty line (45.1% vs. 32.2%, P < .001).
The cancer patients were more likely than was the general population to have less than full-time employment, with 15.2% and 10.5%, respectively, reporting a job change or job loss; 55.3% and 44.1%, respectively, being employed only part of a given year; and 38.6% and 32.4%, respectively, being unemployed for a full year (P < .05 for each comparison).
Gynecologic cancer patients continued to experience insurance troubles and financial hardships after the ACA went into effect, with 8.8% reporting loss of insurance, 18.7% reporting a change in insurance, 21.7% being uninsured for at least 1 month, and 8.4% being uninsured for an entire year.
In addition, 12.8% of gynecologic cancer patients reported catastrophic health expenditures in out-of-pocket costs alone, and 28.0% spent more than 10% of their income on health care when the cost of premiums was factored in.
The numbers were even worse for non-White and Hispanic patients, with 25.9% reporting an insurance change (vs. 16.3% for non-Hispanic Whites) and 30.2% reporting a period of not being insured (vs. 18.7% for non-Hispanic Whites). There were no differences in catastrophic health expenditures by race/ethnicity, however.
Not surprisingly, patients from low-income families had significantly higher probability of having catastrophic expenditures, at 22.7% vs. 3.0% for higher-income families for out-of-pocket expenses alone (P < .001), and 35.3% vs. 20.8%, respectively, when the cost of premiums was included (P = .01).
On the other hand, patients with full-year Medicaid coverage were less likely to suffer from catastrophic costs than were privately-insured patients, at 15.3% vs. 31.3% in the overall sample (P = .02), and 11.5% vs. 62.1% of low-income vs. higher-income patients (P < .001).
There was a trend toward lower catastrophic health expenditures among low-income patients after full implementation of the ACA – 2014-2017 – compared with 2006-2009, but this difference was not statistically significant.
How to change it
In a panel discussion following the presentation, comoderator Eloise Chapman-Davis, MD, of Weill Cornell Medicine in New York, said to Dr. Albright, “As we look to improve equity within our subspecialty, I would like to ask you to comment on how you believe your abstract will inform our gyn-oncology culture and speak to what changes that you believe are needed to better advocate for our patients.”
“I think that our abstract really shows the prevalence of the problems of financial toxicity and of instability in the insurance market in the U.S.,” he replied. “I think it points out that we need to be more proactive about identifying patients and seeking out patients who may be having issues related to financial toxicity, to try to refer people to resources sooner and upfront.”
The investigators did not list a funding source for the study. Dr. Albright and Dr. Chapman-Davis reported having no conflicts of interest.
A retrospective study of respondents to the Medical Expenditure Panel Survey showed that more than one in five gynecologic cancer patients reported losing health insurance for at least 1 month every year, and more than one in four reported having catastrophic health expenses annually.
Benjamin Albright, MD, of Duke University Medical Center in Durham, N.C., presented these results at the Society of Gynecologic Oncology’s Virtual Annual Meeting on Women’s Cancer (Abstract 10303).
“We found gynecologic cancer patients to have high rates of insurance churn and catastrophic health expenditures, particularly among the poor,” Dr. Albright said. “Traditional static measurements clearly underestimate the impact of uninsurance, with over 20% of patients reporting some period of uninsurance annually.”
There was no evidence of improvement in any outcome after the implementation of the ACA, compared with the pre-ACA period, “though our assessment was limited in estimate precision by small sample size,” Dr. Albright acknowledged.
Dynamic, not static
Oncology researchers who study access to care and financial toxicities often consider insurance status as a static characteristic, but in the U.S. health care system, the reality is quite different, with insurance status fluctuating by employment or ability to pay, sometimes on a month-to-month basis, according to Dr. Albright.
Citing the Commonwealth Fund’s definition of catastrophic health expenditures as “spending over 10% of income on health care,” Dr. Albright noted that the prevalence of catastrophic out-of-pocket costs “is also relatively poorly described among cancer patients, particularly in accounting for family spending and income dynamics.
“The Affordable Care Act contained measures to address both of these concerns, including coverage protections and expansions, and spending regulations,” he said.
Dr. Albright and colleagues at Duke and Memorial Sloan Kettering Cancer Center in New York assessed insurance churn and catastrophic health expenditures among gynecologic cancer patients, attempting to determine whether the ACA had helped to limit insurance churn and keep costs manageable.
Representative sample
The investigators conducted a retrospective study of data from Medical Expenditure Panel Survey respondents from 2006 through 2017, a period that spanned the implementation of the ACA in 2010.
The sample included 684 women younger than 65 years reporting care in the given year related to a gynecologic cancer diagnosis. The civilian, noninstitutionalized sample was weighted to represent an estimated average annual population of 533,000 persons. The population was majority White (87%) and non-Hispanic (85.5%).
The investigators found that, compared with the overall U.S. population of people under 65, gynecologic cancer patients were more likely to have incomes of 250% or less of the federal poverty line (45.1% vs. 32.2%, P < .001).
The cancer patients were more likely than was the general population to have less than full-time employment, with 15.2% and 10.5%, respectively, reporting a job change or job loss; 55.3% and 44.1%, respectively, being employed only part of a given year; and 38.6% and 32.4%, respectively, being unemployed for a full year (P < .05 for each comparison).
Gynecologic cancer patients continued to experience insurance troubles and financial hardships after the ACA went into effect, with 8.8% reporting loss of insurance, 18.7% reporting a change in insurance, 21.7% being uninsured for at least 1 month, and 8.4% being uninsured for an entire year.
In addition, 12.8% of gynecologic cancer patients reported catastrophic health expenditures in out-of-pocket costs alone, and 28.0% spent more than 10% of their income on health care when the cost of premiums was factored in.
The numbers were even worse for non-White and Hispanic patients, with 25.9% reporting an insurance change (vs. 16.3% for non-Hispanic Whites) and 30.2% reporting a period of not being insured (vs. 18.7% for non-Hispanic Whites). There were no differences in catastrophic health expenditures by race/ethnicity, however.
Not surprisingly, patients from low-income families had significantly higher probability of having catastrophic expenditures, at 22.7% vs. 3.0% for higher-income families for out-of-pocket expenses alone (P < .001), and 35.3% vs. 20.8%, respectively, when the cost of premiums was included (P = .01).
On the other hand, patients with full-year Medicaid coverage were less likely to suffer from catastrophic costs than were privately-insured patients, at 15.3% vs. 31.3% in the overall sample (P = .02), and 11.5% vs. 62.1% of low-income vs. higher-income patients (P < .001).
There was a trend toward lower catastrophic health expenditures among low-income patients after full implementation of the ACA – 2014-2017 – compared with 2006-2009, but this difference was not statistically significant.
How to change it
In a panel discussion following the presentation, comoderator Eloise Chapman-Davis, MD, of Weill Cornell Medicine in New York, said to Dr. Albright, “As we look to improve equity within our subspecialty, I would like to ask you to comment on how you believe your abstract will inform our gyn-oncology culture and speak to what changes that you believe are needed to better advocate for our patients.”
“I think that our abstract really shows the prevalence of the problems of financial toxicity and of instability in the insurance market in the U.S.,” he replied. “I think it points out that we need to be more proactive about identifying patients and seeking out patients who may be having issues related to financial toxicity, to try to refer people to resources sooner and upfront.”
The investigators did not list a funding source for the study. Dr. Albright and Dr. Chapman-Davis reported having no conflicts of interest.
FROM SGO 2021
Recurrent miscarriage: What’s the evidence-based evaluation and management?
A pregnancy loss at any gestational age is devastating. Women and/or couples may, unfairly, self-blame as they desperately seek substantive answers. Their support systems, including health care providers, offer some, albeit fleeting, comfort. Conception is merely the start of an emotionally arduous first trimester that often results in a learned helplessness. This month, we focus on the comprehensive evaluation and the medical evidence–based approach to recurrent pregnancy loss (RPL).
RPL is defined by the American Society for Reproductive Medicine as two or more clinical pregnancy losses of less than 20 weeks’ gestation with a prevalence of approximately 5%. Embryo aneuploidy is the most common reason for a spontaneous miscarriage, occurring in 50%-70% of losses. The risk of spontaneous miscarriage during the reproductive years follows a J-shaped pattern. The lowest percentage is in women aged 25-29 years (9.8%), with a nadir at age 27 (9.5%), then an increasingly steep rise after age 35 to a peak at age 45 and over (53.6%). The loss rate is closer to 50% of all fertilizations since many spontaneous miscarriages occur at 2-4 weeks, before a pregnancy can be clinically diagnosed. The frequency of embryo aneuploidy significantly decreases and embryo euploidy increases with successive numbers of spontaneous miscarriages.
After three or more spontaneous miscarriages, nulliparous women appear to have a higher rate of subsequent pregnancy loss, compared with parous women (BMJ. 2000;320:1708). We recommend an evaluation following two losses given the lack of evidence for a difference in diagnostic yield following two versus three miscarriages and particularly because of the emotional effects of impact of RPL.
RPL causes, percentages of contribution, and evaluation
1. Genetic (2%-5%). Because of the risk of an embryo with an unbalanced chromosomal rearrangement inherited from a translocation present in either of the couple, a blood karyotype of the couple is essential despite a history of one or more successful live births. While in vitro fertilization (IVF) with preimplantation genetic testing for structural rearrangements (PGT-SR) can successfully diagnose affected embryos to avoid their intrauterine transfer, overall live birth rates are similar when comparing natural conception attempts with PGT-SR, although the latter may reduce miscarriages.
2. Anatomic (10%-15%). Hysteroscopy, hysterosalpingogram, or saline ultrasound can be used to image the uterine cavity to evaluate for polyps, fibroids, scarring, or a congenital septum – all of which can be surgically corrected. Chronic endometritis has been found in 27% of patients with recurrent miscarriage (and in 14% with recurrent implantation failure), therefore testing by biopsy is reasonable. An elevated level of homocysteine has been reported to impair DNA methylation and gene expression, causing defective chorionic villous vascularization in spontaneous miscarriage tissues. We recommend folic acid supplementation and the avoidance of testing for MTHFR (methylenetetrahydrofolate reductase). Of note, the recent TRUST study showed no significant benefit from metroplasty in comparison with expectant management in 12 months of observation resulting in a live birth rate of 31% versus 35%, respectively.
3. Acquired thrombophilias (20%). Medical evidence supports testing for the antiphospholipid antibody syndrome (APS), i.e., RPL with either the presence of lupus anticoagulant (LAC), anticardiolipin antibodies, or anti-beta2 glycoprotein for IgG and IgM. Persistent LAC or elevations of antibodies greater than 40 GPL or greater than the 99th percentile for more than 12 weeks justifies the use of low-molecular-weight heparin (LMWH). APS has been shown to cause RPL, thrombosis, and/or autoimmune thrombocytopenia. There is no definitive evidence to support testing for MTHFR or any other thrombophilias for first trimester RPL. APS has up to a 90% fetal loss rate without therapeutic intervention. Treatment includes low-dose aspirin (81 mg daily) and LMWH. These medications are thought to help prevent thrombosis in the placenta, helping to maintain pregnancies.
4. Hormonal (17%-20%). The most common hormonal disorders increasing the risk for miscarriage is thyroid dysfunction (both hyper- and hypothyroid), prolactin elevations, and lack of glucose control. While the concern for a luteal phase (LPD) prevails, there is no accepted definition or treatment. There is recent evidence that antibodies to thyroid peroxidase may increase miscarriage and that low-dose thyroid replacement may reduce this risk. One other important area is the polycystic ovarian syndrome (PCOS). This hormonal abnormality affects 6%-20% of all reproductive aged women and may increase miscarriage.
5. Unexplained (40%-50%). The most frustrating but most common reason for RPL. Nevertheless, close monitoring and supportive care throughout the first trimester has been demonstrated in medical studies to improve outcome.
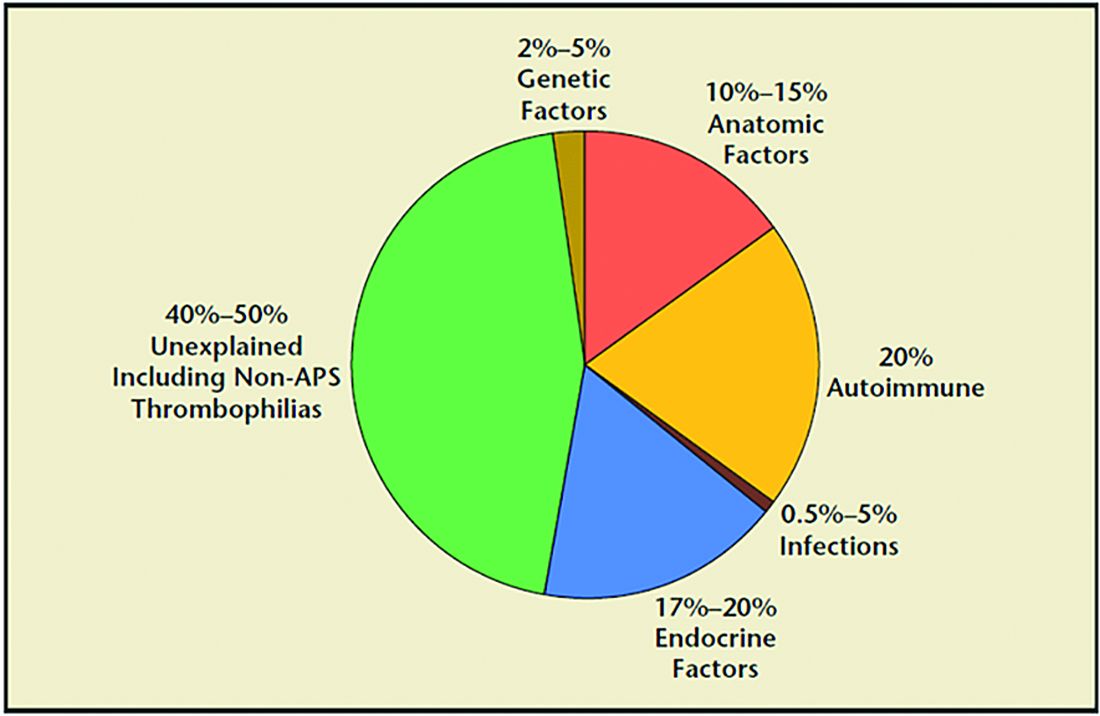
Seven surprising facts about recurrent miscarriage
1. Folic acid 4 mg daily may decrease embryo chromosomal abnormalities and miscarriage.
Folic acid in doses of at least 0.4 mg daily have long been advocated to reduce spina bifida and neural tube defects. It is optimal to begin folic acid for several months prior to conception attempts. There is evidence it may help treat RPL by reducing the chance for chromosomal errors.
2. A randomized trial did not demonstrate an improved live birth rate using progesterone in the first trimester. However, women enrolled may not have begun progesterone until 6 weeks of pregnancy, begging the question if earlier progesterone would have demonstrated improvement.
Dydrogesterone, a progestogen that is highly selective for the progesterone receptor, lacks estrogenic, androgenic, anabolic, and corticoid properties. Although not available in the United States, dydrogesterone appears to reduce the rate of idiopathic recurrent miscarriage (two or more losses). Also, progesterone support has been shown to reduce loss in threatened miscarriage – 17 OHPC 500 mg IM weekly in the first trimester.
3. No benefit of aspirin and/or heparin to treat unexplained RM.
The use of aspirin and/or heparin-like medication has convincingly been shown to not improve live birth rates in RPL.
4. Inherited thrombophilias are NOT associated with RM and should not be tested.
Screening for factor V (Leiden mutation), factor II (Prothrombin G20210A), and MTHFR have not been shown to cause RM and no treatment, such as aspirin and/or heparin-like medications, improves the live birth rate.
5. Close monitoring and empathetic care improves outcomes.
For unknown reasons, clinics providing close monitoring, emotional support, and education to patients with unexplained RM report higher live birth rates, compared with patients not receiving this level of care.
6. Behavior changes reduce miscarriage.
Elevations in body mass index (BMI) and cigarette smoking both increase the risk of miscarriage. As a result, a healthy BMI and eliminating tobacco use reduce the risk of pregnancy loss. Excessive caffeine use (more than two equivalent cups of caffeine in coffee per day) also may increase spontaneous miscarriage.
7. Fertility medications, intrauterine insemination, in vitro fertilization, or preimplantation genetic testing for aneuploidy (PGT-A) do not improve outcomes.
While patients and, often, health care providers, feel compelled to proceed with fertility treatment, ovulation induction medications, intrauterine insemination, in vitro fertilization, or PGT-A have not been shown to improve the chance for a live birth. PGT-A did not reduce the risk of miscarriage in women with recurrent pregnancy loss.
In summary, following two or more pregnancy losses, I recommend obtaining chromosomal testing of the couple, viewing the uterine cavity, blood testing for thyroid, prolactin, and glucose control, and acquired thrombophilias (as above). Fortunately, when the cause is unexplained, the woman has a 70%-80% chance of a spontaneous live birth over the next 10 years from diagnosis. By further understanding, knowing how to diagnose, and, finally, treating the cause of RPL we can hopefully prevent the heartbreak women and couples endure.
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
A pregnancy loss at any gestational age is devastating. Women and/or couples may, unfairly, self-blame as they desperately seek substantive answers. Their support systems, including health care providers, offer some, albeit fleeting, comfort. Conception is merely the start of an emotionally arduous first trimester that often results in a learned helplessness. This month, we focus on the comprehensive evaluation and the medical evidence–based approach to recurrent pregnancy loss (RPL).
RPL is defined by the American Society for Reproductive Medicine as two or more clinical pregnancy losses of less than 20 weeks’ gestation with a prevalence of approximately 5%. Embryo aneuploidy is the most common reason for a spontaneous miscarriage, occurring in 50%-70% of losses. The risk of spontaneous miscarriage during the reproductive years follows a J-shaped pattern. The lowest percentage is in women aged 25-29 years (9.8%), with a nadir at age 27 (9.5%), then an increasingly steep rise after age 35 to a peak at age 45 and over (53.6%). The loss rate is closer to 50% of all fertilizations since many spontaneous miscarriages occur at 2-4 weeks, before a pregnancy can be clinically diagnosed. The frequency of embryo aneuploidy significantly decreases and embryo euploidy increases with successive numbers of spontaneous miscarriages.
After three or more spontaneous miscarriages, nulliparous women appear to have a higher rate of subsequent pregnancy loss, compared with parous women (BMJ. 2000;320:1708). We recommend an evaluation following two losses given the lack of evidence for a difference in diagnostic yield following two versus three miscarriages and particularly because of the emotional effects of impact of RPL.
RPL causes, percentages of contribution, and evaluation
1. Genetic (2%-5%). Because of the risk of an embryo with an unbalanced chromosomal rearrangement inherited from a translocation present in either of the couple, a blood karyotype of the couple is essential despite a history of one or more successful live births. While in vitro fertilization (IVF) with preimplantation genetic testing for structural rearrangements (PGT-SR) can successfully diagnose affected embryos to avoid their intrauterine transfer, overall live birth rates are similar when comparing natural conception attempts with PGT-SR, although the latter may reduce miscarriages.
2. Anatomic (10%-15%). Hysteroscopy, hysterosalpingogram, or saline ultrasound can be used to image the uterine cavity to evaluate for polyps, fibroids, scarring, or a congenital septum – all of which can be surgically corrected. Chronic endometritis has been found in 27% of patients with recurrent miscarriage (and in 14% with recurrent implantation failure), therefore testing by biopsy is reasonable. An elevated level of homocysteine has been reported to impair DNA methylation and gene expression, causing defective chorionic villous vascularization in spontaneous miscarriage tissues. We recommend folic acid supplementation and the avoidance of testing for MTHFR (methylenetetrahydrofolate reductase). Of note, the recent TRUST study showed no significant benefit from metroplasty in comparison with expectant management in 12 months of observation resulting in a live birth rate of 31% versus 35%, respectively.
3. Acquired thrombophilias (20%). Medical evidence supports testing for the antiphospholipid antibody syndrome (APS), i.e., RPL with either the presence of lupus anticoagulant (LAC), anticardiolipin antibodies, or anti-beta2 glycoprotein for IgG and IgM. Persistent LAC or elevations of antibodies greater than 40 GPL or greater than the 99th percentile for more than 12 weeks justifies the use of low-molecular-weight heparin (LMWH). APS has been shown to cause RPL, thrombosis, and/or autoimmune thrombocytopenia. There is no definitive evidence to support testing for MTHFR or any other thrombophilias for first trimester RPL. APS has up to a 90% fetal loss rate without therapeutic intervention. Treatment includes low-dose aspirin (81 mg daily) and LMWH. These medications are thought to help prevent thrombosis in the placenta, helping to maintain pregnancies.
4. Hormonal (17%-20%). The most common hormonal disorders increasing the risk for miscarriage is thyroid dysfunction (both hyper- and hypothyroid), prolactin elevations, and lack of glucose control. While the concern for a luteal phase (LPD) prevails, there is no accepted definition or treatment. There is recent evidence that antibodies to thyroid peroxidase may increase miscarriage and that low-dose thyroid replacement may reduce this risk. One other important area is the polycystic ovarian syndrome (PCOS). This hormonal abnormality affects 6%-20% of all reproductive aged women and may increase miscarriage.
5. Unexplained (40%-50%). The most frustrating but most common reason for RPL. Nevertheless, close monitoring and supportive care throughout the first trimester has been demonstrated in medical studies to improve outcome.
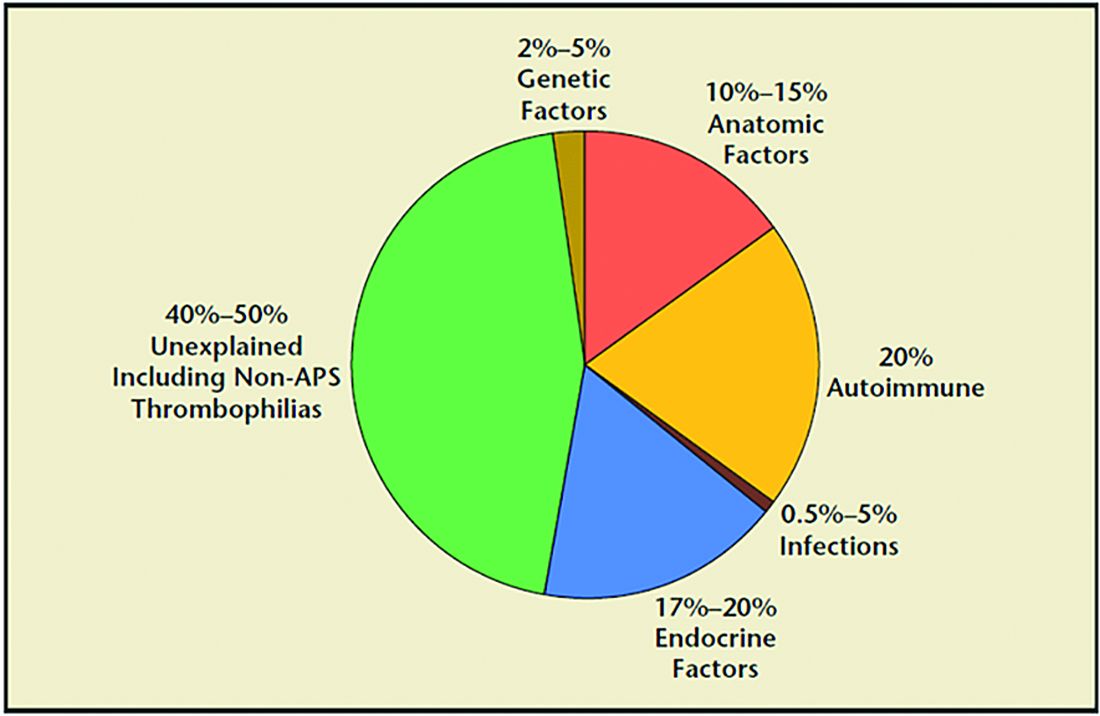
Seven surprising facts about recurrent miscarriage
1. Folic acid 4 mg daily may decrease embryo chromosomal abnormalities and miscarriage.
Folic acid in doses of at least 0.4 mg daily have long been advocated to reduce spina bifida and neural tube defects. It is optimal to begin folic acid for several months prior to conception attempts. There is evidence it may help treat RPL by reducing the chance for chromosomal errors.
2. A randomized trial did not demonstrate an improved live birth rate using progesterone in the first trimester. However, women enrolled may not have begun progesterone until 6 weeks of pregnancy, begging the question if earlier progesterone would have demonstrated improvement.
Dydrogesterone, a progestogen that is highly selective for the progesterone receptor, lacks estrogenic, androgenic, anabolic, and corticoid properties. Although not available in the United States, dydrogesterone appears to reduce the rate of idiopathic recurrent miscarriage (two or more losses). Also, progesterone support has been shown to reduce loss in threatened miscarriage – 17 OHPC 500 mg IM weekly in the first trimester.
3. No benefit of aspirin and/or heparin to treat unexplained RM.
The use of aspirin and/or heparin-like medication has convincingly been shown to not improve live birth rates in RPL.
4. Inherited thrombophilias are NOT associated with RM and should not be tested.
Screening for factor V (Leiden mutation), factor II (Prothrombin G20210A), and MTHFR have not been shown to cause RM and no treatment, such as aspirin and/or heparin-like medications, improves the live birth rate.
5. Close monitoring and empathetic care improves outcomes.
For unknown reasons, clinics providing close monitoring, emotional support, and education to patients with unexplained RM report higher live birth rates, compared with patients not receiving this level of care.
6. Behavior changes reduce miscarriage.
Elevations in body mass index (BMI) and cigarette smoking both increase the risk of miscarriage. As a result, a healthy BMI and eliminating tobacco use reduce the risk of pregnancy loss. Excessive caffeine use (more than two equivalent cups of caffeine in coffee per day) also may increase spontaneous miscarriage.
7. Fertility medications, intrauterine insemination, in vitro fertilization, or preimplantation genetic testing for aneuploidy (PGT-A) do not improve outcomes.
While patients and, often, health care providers, feel compelled to proceed with fertility treatment, ovulation induction medications, intrauterine insemination, in vitro fertilization, or PGT-A have not been shown to improve the chance for a live birth. PGT-A did not reduce the risk of miscarriage in women with recurrent pregnancy loss.
In summary, following two or more pregnancy losses, I recommend obtaining chromosomal testing of the couple, viewing the uterine cavity, blood testing for thyroid, prolactin, and glucose control, and acquired thrombophilias (as above). Fortunately, when the cause is unexplained, the woman has a 70%-80% chance of a spontaneous live birth over the next 10 years from diagnosis. By further understanding, knowing how to diagnose, and, finally, treating the cause of RPL we can hopefully prevent the heartbreak women and couples endure.
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
A pregnancy loss at any gestational age is devastating. Women and/or couples may, unfairly, self-blame as they desperately seek substantive answers. Their support systems, including health care providers, offer some, albeit fleeting, comfort. Conception is merely the start of an emotionally arduous first trimester that often results in a learned helplessness. This month, we focus on the comprehensive evaluation and the medical evidence–based approach to recurrent pregnancy loss (RPL).
RPL is defined by the American Society for Reproductive Medicine as two or more clinical pregnancy losses of less than 20 weeks’ gestation with a prevalence of approximately 5%. Embryo aneuploidy is the most common reason for a spontaneous miscarriage, occurring in 50%-70% of losses. The risk of spontaneous miscarriage during the reproductive years follows a J-shaped pattern. The lowest percentage is in women aged 25-29 years (9.8%), with a nadir at age 27 (9.5%), then an increasingly steep rise after age 35 to a peak at age 45 and over (53.6%). The loss rate is closer to 50% of all fertilizations since many spontaneous miscarriages occur at 2-4 weeks, before a pregnancy can be clinically diagnosed. The frequency of embryo aneuploidy significantly decreases and embryo euploidy increases with successive numbers of spontaneous miscarriages.
After three or more spontaneous miscarriages, nulliparous women appear to have a higher rate of subsequent pregnancy loss, compared with parous women (BMJ. 2000;320:1708). We recommend an evaluation following two losses given the lack of evidence for a difference in diagnostic yield following two versus three miscarriages and particularly because of the emotional effects of impact of RPL.
RPL causes, percentages of contribution, and evaluation
1. Genetic (2%-5%). Because of the risk of an embryo with an unbalanced chromosomal rearrangement inherited from a translocation present in either of the couple, a blood karyotype of the couple is essential despite a history of one or more successful live births. While in vitro fertilization (IVF) with preimplantation genetic testing for structural rearrangements (PGT-SR) can successfully diagnose affected embryos to avoid their intrauterine transfer, overall live birth rates are similar when comparing natural conception attempts with PGT-SR, although the latter may reduce miscarriages.
2. Anatomic (10%-15%). Hysteroscopy, hysterosalpingogram, or saline ultrasound can be used to image the uterine cavity to evaluate for polyps, fibroids, scarring, or a congenital septum – all of which can be surgically corrected. Chronic endometritis has been found in 27% of patients with recurrent miscarriage (and in 14% with recurrent implantation failure), therefore testing by biopsy is reasonable. An elevated level of homocysteine has been reported to impair DNA methylation and gene expression, causing defective chorionic villous vascularization in spontaneous miscarriage tissues. We recommend folic acid supplementation and the avoidance of testing for MTHFR (methylenetetrahydrofolate reductase). Of note, the recent TRUST study showed no significant benefit from metroplasty in comparison with expectant management in 12 months of observation resulting in a live birth rate of 31% versus 35%, respectively.
3. Acquired thrombophilias (20%). Medical evidence supports testing for the antiphospholipid antibody syndrome (APS), i.e., RPL with either the presence of lupus anticoagulant (LAC), anticardiolipin antibodies, or anti-beta2 glycoprotein for IgG and IgM. Persistent LAC or elevations of antibodies greater than 40 GPL or greater than the 99th percentile for more than 12 weeks justifies the use of low-molecular-weight heparin (LMWH). APS has been shown to cause RPL, thrombosis, and/or autoimmune thrombocytopenia. There is no definitive evidence to support testing for MTHFR or any other thrombophilias for first trimester RPL. APS has up to a 90% fetal loss rate without therapeutic intervention. Treatment includes low-dose aspirin (81 mg daily) and LMWH. These medications are thought to help prevent thrombosis in the placenta, helping to maintain pregnancies.
4. Hormonal (17%-20%). The most common hormonal disorders increasing the risk for miscarriage is thyroid dysfunction (both hyper- and hypothyroid), prolactin elevations, and lack of glucose control. While the concern for a luteal phase (LPD) prevails, there is no accepted definition or treatment. There is recent evidence that antibodies to thyroid peroxidase may increase miscarriage and that low-dose thyroid replacement may reduce this risk. One other important area is the polycystic ovarian syndrome (PCOS). This hormonal abnormality affects 6%-20% of all reproductive aged women and may increase miscarriage.
5. Unexplained (40%-50%). The most frustrating but most common reason for RPL. Nevertheless, close monitoring and supportive care throughout the first trimester has been demonstrated in medical studies to improve outcome.
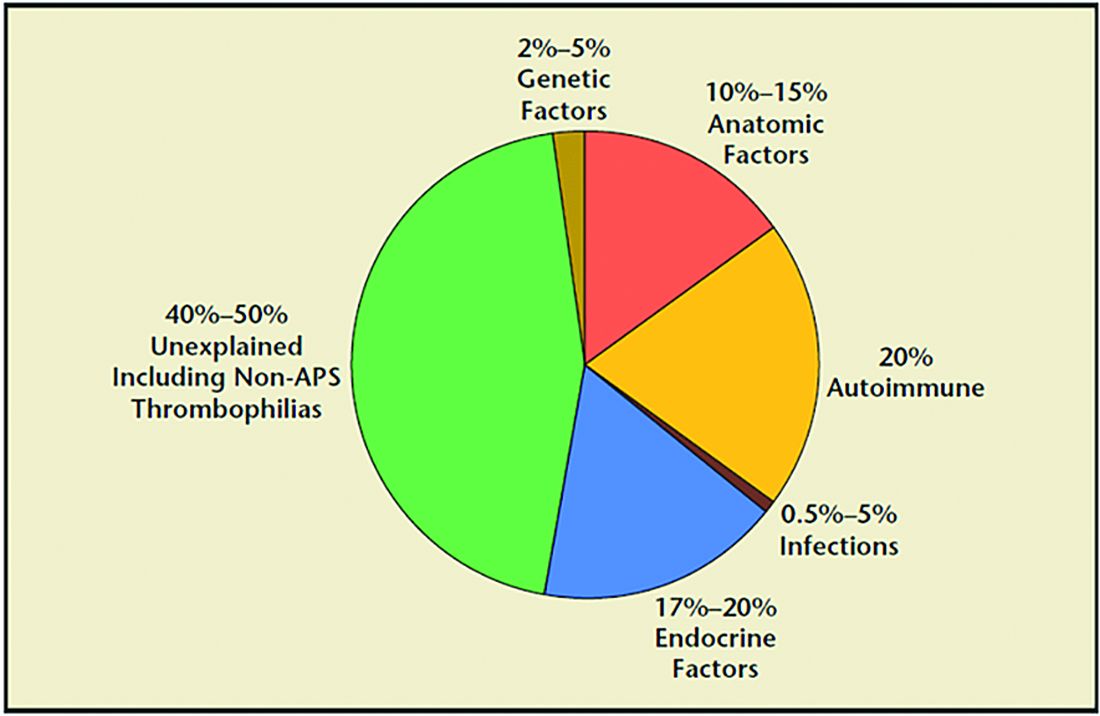
Seven surprising facts about recurrent miscarriage
1. Folic acid 4 mg daily may decrease embryo chromosomal abnormalities and miscarriage.
Folic acid in doses of at least 0.4 mg daily have long been advocated to reduce spina bifida and neural tube defects. It is optimal to begin folic acid for several months prior to conception attempts. There is evidence it may help treat RPL by reducing the chance for chromosomal errors.
2. A randomized trial did not demonstrate an improved live birth rate using progesterone in the first trimester. However, women enrolled may not have begun progesterone until 6 weeks of pregnancy, begging the question if earlier progesterone would have demonstrated improvement.
Dydrogesterone, a progestogen that is highly selective for the progesterone receptor, lacks estrogenic, androgenic, anabolic, and corticoid properties. Although not available in the United States, dydrogesterone appears to reduce the rate of idiopathic recurrent miscarriage (two or more losses). Also, progesterone support has been shown to reduce loss in threatened miscarriage – 17 OHPC 500 mg IM weekly in the first trimester.
3. No benefit of aspirin and/or heparin to treat unexplained RM.
The use of aspirin and/or heparin-like medication has convincingly been shown to not improve live birth rates in RPL.
4. Inherited thrombophilias are NOT associated with RM and should not be tested.
Screening for factor V (Leiden mutation), factor II (Prothrombin G20210A), and MTHFR have not been shown to cause RM and no treatment, such as aspirin and/or heparin-like medications, improves the live birth rate.
5. Close monitoring and empathetic care improves outcomes.
For unknown reasons, clinics providing close monitoring, emotional support, and education to patients with unexplained RM report higher live birth rates, compared with patients not receiving this level of care.
6. Behavior changes reduce miscarriage.
Elevations in body mass index (BMI) and cigarette smoking both increase the risk of miscarriage. As a result, a healthy BMI and eliminating tobacco use reduce the risk of pregnancy loss. Excessive caffeine use (more than two equivalent cups of caffeine in coffee per day) also may increase spontaneous miscarriage.
7. Fertility medications, intrauterine insemination, in vitro fertilization, or preimplantation genetic testing for aneuploidy (PGT-A) do not improve outcomes.
While patients and, often, health care providers, feel compelled to proceed with fertility treatment, ovulation induction medications, intrauterine insemination, in vitro fertilization, or PGT-A have not been shown to improve the chance for a live birth. PGT-A did not reduce the risk of miscarriage in women with recurrent pregnancy loss.
In summary, following two or more pregnancy losses, I recommend obtaining chromosomal testing of the couple, viewing the uterine cavity, blood testing for thyroid, prolactin, and glucose control, and acquired thrombophilias (as above). Fortunately, when the cause is unexplained, the woman has a 70%-80% chance of a spontaneous live birth over the next 10 years from diagnosis. By further understanding, knowing how to diagnose, and, finally, treating the cause of RPL we can hopefully prevent the heartbreak women and couples endure.
Dr. Trolice is director of Fertility CARE – The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Contact allergen of the year found in foam in shin guards, footwear
.
The announcement was made by Donald V. Belsito, MD, professor of dermatology, Columbia University, New York, during a presentation at the annual meeting of the American Contact Dermatitis Society, held virtually this year. In his opinion, he said, the most exciting selections occur when international cooperation results in the identification of a new allergen that could become problematic, and acetophenone azine falls into this category.
The chemical formula of acetophenone azine is C16H16N2.
Acetophenone azine was highlighted as a contact allergen in a recent report in Dermatitis. The authors, Nadia Raison-Peyron, MD, from the department of dermatology at the University of Montpelier (France), and Denis Sasseville, MD, from the division of dermatology at McGill University Health Center, Quebec, described publications and reports of about 12 cases of severe allergic contact dermatitis secondary to shin pads or footwear, mainly in children and teens in Europe (one case was in Canada).
A common feature of these cases was the presence of a foam used for cushioning, made of ethyl vinyl acetate (EVA) used in the relevant products.
In one case, a 13-year-old boy who wore shin pads for soccer developed contact dermatitis on both shins that spread, and was described as severe. Patch testing revealed the EVA foam in the shin pads as the only positive reaction. Similar cases have been reported after exposure to EVA-containing products, including shin pads, sneakers, flip-flops, ski boots, insoles, swimming goggles, and bicycle seats, according to the authors.
In some reports, cases related to footwear presented as dyshidrosiform, vesiculobullous eczema, with or without palmar lesions, or presented as plantar hyperkeratotic dermatitis, they wrote. In other cases, patients experienced scarring and postinflammatory hypopigmentation.
The compound is likely not added to EVA intentionally, they added, but instead is thought to result from reactions between additives during the manufacturing process. The presence of acetophenone azine is not well explained, but the current theory is that it results from a combination of “the degradation of the initiator dicumylperoxide and hydrazine from the foaming agent azodicarbonamide,” the authors said.
In the paper, Dr. Raison-Peyron and Dr. Sasseville recommended a patch testing concentration of 0.1% in acetone or petrolatum, as acetophenone azine is not currently available from path test suppliers, although it can be obtained from chemical product distributors.
“Given the recent discovery of this allergen, it is presumed that cases of allergic contact dermatitis would have been missed and labeled irritant contact dermatitis or dyshidrosis,” they noted. To avoid missing more cases, acetophenone azine should be added to the patch testing shoe series, as well as plastics and glues series, they emphasized.
Although no cases of allergic reactions to acetophenone azine have been reported in the United States to date, it is an emerging allergen that should be on the radar for U.S. dermatologists, Amber Atwater, MD, outgoing ACDS president, said in an interview. The lack of reported cases may be in part attributed to the fact that acetophenone azine is not yet available to purchase for testing in the United States, and the allergen could be present in shin guards and other products identified in reported cases, added Dr. Atwater, associate professor of dermatology, Duke University, Durham, N.C.
.
The announcement was made by Donald V. Belsito, MD, professor of dermatology, Columbia University, New York, during a presentation at the annual meeting of the American Contact Dermatitis Society, held virtually this year. In his opinion, he said, the most exciting selections occur when international cooperation results in the identification of a new allergen that could become problematic, and acetophenone azine falls into this category.
The chemical formula of acetophenone azine is C16H16N2.
Acetophenone azine was highlighted as a contact allergen in a recent report in Dermatitis. The authors, Nadia Raison-Peyron, MD, from the department of dermatology at the University of Montpelier (France), and Denis Sasseville, MD, from the division of dermatology at McGill University Health Center, Quebec, described publications and reports of about 12 cases of severe allergic contact dermatitis secondary to shin pads or footwear, mainly in children and teens in Europe (one case was in Canada).
A common feature of these cases was the presence of a foam used for cushioning, made of ethyl vinyl acetate (EVA) used in the relevant products.
In one case, a 13-year-old boy who wore shin pads for soccer developed contact dermatitis on both shins that spread, and was described as severe. Patch testing revealed the EVA foam in the shin pads as the only positive reaction. Similar cases have been reported after exposure to EVA-containing products, including shin pads, sneakers, flip-flops, ski boots, insoles, swimming goggles, and bicycle seats, according to the authors.
In some reports, cases related to footwear presented as dyshidrosiform, vesiculobullous eczema, with or without palmar lesions, or presented as plantar hyperkeratotic dermatitis, they wrote. In other cases, patients experienced scarring and postinflammatory hypopigmentation.
The compound is likely not added to EVA intentionally, they added, but instead is thought to result from reactions between additives during the manufacturing process. The presence of acetophenone azine is not well explained, but the current theory is that it results from a combination of “the degradation of the initiator dicumylperoxide and hydrazine from the foaming agent azodicarbonamide,” the authors said.
In the paper, Dr. Raison-Peyron and Dr. Sasseville recommended a patch testing concentration of 0.1% in acetone or petrolatum, as acetophenone azine is not currently available from path test suppliers, although it can be obtained from chemical product distributors.
“Given the recent discovery of this allergen, it is presumed that cases of allergic contact dermatitis would have been missed and labeled irritant contact dermatitis or dyshidrosis,” they noted. To avoid missing more cases, acetophenone azine should be added to the patch testing shoe series, as well as plastics and glues series, they emphasized.
Although no cases of allergic reactions to acetophenone azine have been reported in the United States to date, it is an emerging allergen that should be on the radar for U.S. dermatologists, Amber Atwater, MD, outgoing ACDS president, said in an interview. The lack of reported cases may be in part attributed to the fact that acetophenone azine is not yet available to purchase for testing in the United States, and the allergen could be present in shin guards and other products identified in reported cases, added Dr. Atwater, associate professor of dermatology, Duke University, Durham, N.C.
.
The announcement was made by Donald V. Belsito, MD, professor of dermatology, Columbia University, New York, during a presentation at the annual meeting of the American Contact Dermatitis Society, held virtually this year. In his opinion, he said, the most exciting selections occur when international cooperation results in the identification of a new allergen that could become problematic, and acetophenone azine falls into this category.
The chemical formula of acetophenone azine is C16H16N2.
Acetophenone azine was highlighted as a contact allergen in a recent report in Dermatitis. The authors, Nadia Raison-Peyron, MD, from the department of dermatology at the University of Montpelier (France), and Denis Sasseville, MD, from the division of dermatology at McGill University Health Center, Quebec, described publications and reports of about 12 cases of severe allergic contact dermatitis secondary to shin pads or footwear, mainly in children and teens in Europe (one case was in Canada).
A common feature of these cases was the presence of a foam used for cushioning, made of ethyl vinyl acetate (EVA) used in the relevant products.
In one case, a 13-year-old boy who wore shin pads for soccer developed contact dermatitis on both shins that spread, and was described as severe. Patch testing revealed the EVA foam in the shin pads as the only positive reaction. Similar cases have been reported after exposure to EVA-containing products, including shin pads, sneakers, flip-flops, ski boots, insoles, swimming goggles, and bicycle seats, according to the authors.
In some reports, cases related to footwear presented as dyshidrosiform, vesiculobullous eczema, with or without palmar lesions, or presented as plantar hyperkeratotic dermatitis, they wrote. In other cases, patients experienced scarring and postinflammatory hypopigmentation.
The compound is likely not added to EVA intentionally, they added, but instead is thought to result from reactions between additives during the manufacturing process. The presence of acetophenone azine is not well explained, but the current theory is that it results from a combination of “the degradation of the initiator dicumylperoxide and hydrazine from the foaming agent azodicarbonamide,” the authors said.
In the paper, Dr. Raison-Peyron and Dr. Sasseville recommended a patch testing concentration of 0.1% in acetone or petrolatum, as acetophenone azine is not currently available from path test suppliers, although it can be obtained from chemical product distributors.
“Given the recent discovery of this allergen, it is presumed that cases of allergic contact dermatitis would have been missed and labeled irritant contact dermatitis or dyshidrosis,” they noted. To avoid missing more cases, acetophenone azine should be added to the patch testing shoe series, as well as plastics and glues series, they emphasized.
Although no cases of allergic reactions to acetophenone azine have been reported in the United States to date, it is an emerging allergen that should be on the radar for U.S. dermatologists, Amber Atwater, MD, outgoing ACDS president, said in an interview. The lack of reported cases may be in part attributed to the fact that acetophenone azine is not yet available to purchase for testing in the United States, and the allergen could be present in shin guards and other products identified in reported cases, added Dr. Atwater, associate professor of dermatology, Duke University, Durham, N.C.
FROM ACDS 2021







