User login
Considerations for the surgical management of diaphragmatic endometriosis
Severe obesity persists, takes high cardiovascular toll
In a U.K. cohort of more than 260,000 mostly middle-aged adults in primary care with overweight or obesity, body mass index remained relatively stable over a decade.
However, compared to overweight individuals, those with severe (class 3) obesity were more socioeconomically disadvantaged and had triple the risk for incident heart failure or all-cause or cardiovascular disease (CVD)–related mortality in a study published online April 15 in BMC Public Health.
“This is the first study to evaluate the long-term impact of overweight and obese individuals’ BMI trajectory on cardiovascular endpoints, heart failure, and mortality outcomes,” wrote Barbara Iyen, PhD, University of Nottingham, England, and colleagues.
The findings emphasize “the high cardiovascular toll exacted by continuing failure to tackle obesity, particularly among more socioeconomically deprived populations,” they warned.
“We have found that despite widespread efforts to prevent and manage obesity, the majority of adults who are overweight or obese in the general population continue to remain so in the long term,” Dr. Iyen said in a statement from her university.
“More effective policies and weight-management interventions are needed urgently to address this increasing burden and associated adverse health outcomes,” she stressed.
Invited to comment, Sadiya S. Khan, MD, Northwestern University, Chicago, said in an interview: “This research adds to the growing body of evidence [that] earlier and more intensive interventions for weight loss are necessary to promote cardiovascular health and reduce morbidity and mortality.
“Adjunctive pharmacotherapy and bariatric surgery are both options that should be considered in addition to intensive lifestyle interventions in overweight and obesity groups,” she added.
“I would always advocate for earlier prevention efforts focused on weight loss, because years lived with obesity are associated with future CVD, so every year counts,” Dr. Khan said.
Does BMI remain elevated, predict worse heart health?
Although obesity is a well-recognized risk factor for CVD, long-term changes in BMI and the impact of BMI on the risk for heart failure, CVD, and mortality have not been quantified among adults with overweight and obesity, Dr. Iyen and colleagues explained.
The researchers examined data from the UK Clinical Practice Research Datalink and secondary care and mortality records to determine BMI trajectories among adults with overweight or obesity and to quantify the risk for heart failure, CVD (defined as coronary heart disease, stroke, transient ischemic attack, or peripheral vascular disease, CVD-related mortality, and all-cause mortality.
They identified 264,230 adults with overweight or obesity who were seen in 790 primary care practices in the United Kingdom from 1999 to 2018 and who did not initially have heart failure or CVD and for whom baseline BMI measurements and at least one other BMI measurement 2, 5, 8, and 10 years later was available.
The researchers divided the cohort into four groups on the basis of initial BMI: overweight (36% of patients; mean BMI, 28.7 kg/m2); class 1 obesity (40%; mean BMI, 33.7 kg/m2); class 2 obesity (19%; mean BMI, 39.9 kg/m2), and class 3 obesity (5%; mean BMI, 49.1 kg/m2).
The mean age of the individuals was 50 years, and 64% were White. Race/ethnicity data were unavailable for 31%. Asian Indian, Asian, and Black patients comprised 5% of the cohort.
“Strong significant gradient in heart failure risk”
Compared to the overweight (reference) group, the severe-obesity group comprised a higher percentage of women (74% vs. 70%), and the prevalence of comorbidities and socioeconomic deprivation was higher.
BMI remained relatively stable in each BMI group. The mean BMI increase was 1.06 kg/m2 during a median follow-up of 10.9 years.
There were 30,400 incident cases of CVD, 7,662 incident cases of heart failure, and 24,022 deaths, of which 2,827 (11.8%) were from CVD.
The risk for heart failure and CVD-related or all-cause mortality increased with increasing obesity severity.
Compared with overweight individuals, those with class 3 obesity were at significantly increased risk for heart failure (hazard ratio [HR], 3.26), all-cause mortality (HR, 2.72), and CVD-related mortality (HR, 3.31) after adjustment for age, sex, and comorbidities (hypertension, type 2 diabetes, atrial fibrillation, and chronic kidney disease).
The risk for stroke/TIA or coronary heart disease was similar among those with severe obesity and the other individuals. The risk for PVD was significantly lower (HR, 0.73).
The reduced risk for PVD in the most severely obese group is similar to findings in the Framingham heart study, the authors noted, and may be due to underdiagnosis or differences in the underlying mechanism.
Compelling evidence of poor health outcomes associated with obesity
Study limitations include the fact that the findings may not be generalizable to other race/ethnicity groups, the lack of information on diet and exercise, and the fact that BMI was used as a surrogate of adiposity. As such, it does not account for an age-related decrease in heavier-than-fat muscle mass and differences between sexes and ethnic groups.
The finding of stable obesity over time accords with two smaller studies that included Canadian and American adults.
The current study did not uncover an obesity paradox, unlike some studies that included patients with preexisting CVD or a history of acute coronary events. Those studies reported better clinical outcomes among patients with overweight or obesity.
The current study included individuals who did not initially have CVD. Those with more severe obesity were younger than individuals with overweight at the time of the occurrence of incident CVD (age 64 vs. 66) and at the age of death (age 67 vs. age 75), which “provides compelling evidence of poor health outcomes associated with obesity,” the authors emphasized.
“Further research is ... needed to explore whether interventions to change BMI trajectories would have an impact on future CVD outcomes,” they concluded.
Dr. Iyen’s clinical academic lectureship is fully funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and are not necessarily those of the National Health Service, the NIHR, or the Department of Health and Social Care. Dr. Khan has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a U.K. cohort of more than 260,000 mostly middle-aged adults in primary care with overweight or obesity, body mass index remained relatively stable over a decade.
However, compared to overweight individuals, those with severe (class 3) obesity were more socioeconomically disadvantaged and had triple the risk for incident heart failure or all-cause or cardiovascular disease (CVD)–related mortality in a study published online April 15 in BMC Public Health.
“This is the first study to evaluate the long-term impact of overweight and obese individuals’ BMI trajectory on cardiovascular endpoints, heart failure, and mortality outcomes,” wrote Barbara Iyen, PhD, University of Nottingham, England, and colleagues.
The findings emphasize “the high cardiovascular toll exacted by continuing failure to tackle obesity, particularly among more socioeconomically deprived populations,” they warned.
“We have found that despite widespread efforts to prevent and manage obesity, the majority of adults who are overweight or obese in the general population continue to remain so in the long term,” Dr. Iyen said in a statement from her university.
“More effective policies and weight-management interventions are needed urgently to address this increasing burden and associated adverse health outcomes,” she stressed.
Invited to comment, Sadiya S. Khan, MD, Northwestern University, Chicago, said in an interview: “This research adds to the growing body of evidence [that] earlier and more intensive interventions for weight loss are necessary to promote cardiovascular health and reduce morbidity and mortality.
“Adjunctive pharmacotherapy and bariatric surgery are both options that should be considered in addition to intensive lifestyle interventions in overweight and obesity groups,” she added.
“I would always advocate for earlier prevention efforts focused on weight loss, because years lived with obesity are associated with future CVD, so every year counts,” Dr. Khan said.
Does BMI remain elevated, predict worse heart health?
Although obesity is a well-recognized risk factor for CVD, long-term changes in BMI and the impact of BMI on the risk for heart failure, CVD, and mortality have not been quantified among adults with overweight and obesity, Dr. Iyen and colleagues explained.
The researchers examined data from the UK Clinical Practice Research Datalink and secondary care and mortality records to determine BMI trajectories among adults with overweight or obesity and to quantify the risk for heart failure, CVD (defined as coronary heart disease, stroke, transient ischemic attack, or peripheral vascular disease, CVD-related mortality, and all-cause mortality.
They identified 264,230 adults with overweight or obesity who were seen in 790 primary care practices in the United Kingdom from 1999 to 2018 and who did not initially have heart failure or CVD and for whom baseline BMI measurements and at least one other BMI measurement 2, 5, 8, and 10 years later was available.
The researchers divided the cohort into four groups on the basis of initial BMI: overweight (36% of patients; mean BMI, 28.7 kg/m2); class 1 obesity (40%; mean BMI, 33.7 kg/m2); class 2 obesity (19%; mean BMI, 39.9 kg/m2), and class 3 obesity (5%; mean BMI, 49.1 kg/m2).
The mean age of the individuals was 50 years, and 64% were White. Race/ethnicity data were unavailable for 31%. Asian Indian, Asian, and Black patients comprised 5% of the cohort.
“Strong significant gradient in heart failure risk”
Compared to the overweight (reference) group, the severe-obesity group comprised a higher percentage of women (74% vs. 70%), and the prevalence of comorbidities and socioeconomic deprivation was higher.
BMI remained relatively stable in each BMI group. The mean BMI increase was 1.06 kg/m2 during a median follow-up of 10.9 years.
There were 30,400 incident cases of CVD, 7,662 incident cases of heart failure, and 24,022 deaths, of which 2,827 (11.8%) were from CVD.
The risk for heart failure and CVD-related or all-cause mortality increased with increasing obesity severity.
Compared with overweight individuals, those with class 3 obesity were at significantly increased risk for heart failure (hazard ratio [HR], 3.26), all-cause mortality (HR, 2.72), and CVD-related mortality (HR, 3.31) after adjustment for age, sex, and comorbidities (hypertension, type 2 diabetes, atrial fibrillation, and chronic kidney disease).
The risk for stroke/TIA or coronary heart disease was similar among those with severe obesity and the other individuals. The risk for PVD was significantly lower (HR, 0.73).
The reduced risk for PVD in the most severely obese group is similar to findings in the Framingham heart study, the authors noted, and may be due to underdiagnosis or differences in the underlying mechanism.
Compelling evidence of poor health outcomes associated with obesity
Study limitations include the fact that the findings may not be generalizable to other race/ethnicity groups, the lack of information on diet and exercise, and the fact that BMI was used as a surrogate of adiposity. As such, it does not account for an age-related decrease in heavier-than-fat muscle mass and differences between sexes and ethnic groups.
The finding of stable obesity over time accords with two smaller studies that included Canadian and American adults.
The current study did not uncover an obesity paradox, unlike some studies that included patients with preexisting CVD or a history of acute coronary events. Those studies reported better clinical outcomes among patients with overweight or obesity.
The current study included individuals who did not initially have CVD. Those with more severe obesity were younger than individuals with overweight at the time of the occurrence of incident CVD (age 64 vs. 66) and at the age of death (age 67 vs. age 75), which “provides compelling evidence of poor health outcomes associated with obesity,” the authors emphasized.
“Further research is ... needed to explore whether interventions to change BMI trajectories would have an impact on future CVD outcomes,” they concluded.
Dr. Iyen’s clinical academic lectureship is fully funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and are not necessarily those of the National Health Service, the NIHR, or the Department of Health and Social Care. Dr. Khan has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a U.K. cohort of more than 260,000 mostly middle-aged adults in primary care with overweight or obesity, body mass index remained relatively stable over a decade.
However, compared to overweight individuals, those with severe (class 3) obesity were more socioeconomically disadvantaged and had triple the risk for incident heart failure or all-cause or cardiovascular disease (CVD)–related mortality in a study published online April 15 in BMC Public Health.
“This is the first study to evaluate the long-term impact of overweight and obese individuals’ BMI trajectory on cardiovascular endpoints, heart failure, and mortality outcomes,” wrote Barbara Iyen, PhD, University of Nottingham, England, and colleagues.
The findings emphasize “the high cardiovascular toll exacted by continuing failure to tackle obesity, particularly among more socioeconomically deprived populations,” they warned.
“We have found that despite widespread efforts to prevent and manage obesity, the majority of adults who are overweight or obese in the general population continue to remain so in the long term,” Dr. Iyen said in a statement from her university.
“More effective policies and weight-management interventions are needed urgently to address this increasing burden and associated adverse health outcomes,” she stressed.
Invited to comment, Sadiya S. Khan, MD, Northwestern University, Chicago, said in an interview: “This research adds to the growing body of evidence [that] earlier and more intensive interventions for weight loss are necessary to promote cardiovascular health and reduce morbidity and mortality.
“Adjunctive pharmacotherapy and bariatric surgery are both options that should be considered in addition to intensive lifestyle interventions in overweight and obesity groups,” she added.
“I would always advocate for earlier prevention efforts focused on weight loss, because years lived with obesity are associated with future CVD, so every year counts,” Dr. Khan said.
Does BMI remain elevated, predict worse heart health?
Although obesity is a well-recognized risk factor for CVD, long-term changes in BMI and the impact of BMI on the risk for heart failure, CVD, and mortality have not been quantified among adults with overweight and obesity, Dr. Iyen and colleagues explained.
The researchers examined data from the UK Clinical Practice Research Datalink and secondary care and mortality records to determine BMI trajectories among adults with overweight or obesity and to quantify the risk for heart failure, CVD (defined as coronary heart disease, stroke, transient ischemic attack, or peripheral vascular disease, CVD-related mortality, and all-cause mortality.
They identified 264,230 adults with overweight or obesity who were seen in 790 primary care practices in the United Kingdom from 1999 to 2018 and who did not initially have heart failure or CVD and for whom baseline BMI measurements and at least one other BMI measurement 2, 5, 8, and 10 years later was available.
The researchers divided the cohort into four groups on the basis of initial BMI: overweight (36% of patients; mean BMI, 28.7 kg/m2); class 1 obesity (40%; mean BMI, 33.7 kg/m2); class 2 obesity (19%; mean BMI, 39.9 kg/m2), and class 3 obesity (5%; mean BMI, 49.1 kg/m2).
The mean age of the individuals was 50 years, and 64% were White. Race/ethnicity data were unavailable for 31%. Asian Indian, Asian, and Black patients comprised 5% of the cohort.
“Strong significant gradient in heart failure risk”
Compared to the overweight (reference) group, the severe-obesity group comprised a higher percentage of women (74% vs. 70%), and the prevalence of comorbidities and socioeconomic deprivation was higher.
BMI remained relatively stable in each BMI group. The mean BMI increase was 1.06 kg/m2 during a median follow-up of 10.9 years.
There were 30,400 incident cases of CVD, 7,662 incident cases of heart failure, and 24,022 deaths, of which 2,827 (11.8%) were from CVD.
The risk for heart failure and CVD-related or all-cause mortality increased with increasing obesity severity.
Compared with overweight individuals, those with class 3 obesity were at significantly increased risk for heart failure (hazard ratio [HR], 3.26), all-cause mortality (HR, 2.72), and CVD-related mortality (HR, 3.31) after adjustment for age, sex, and comorbidities (hypertension, type 2 diabetes, atrial fibrillation, and chronic kidney disease).
The risk for stroke/TIA or coronary heart disease was similar among those with severe obesity and the other individuals. The risk for PVD was significantly lower (HR, 0.73).
The reduced risk for PVD in the most severely obese group is similar to findings in the Framingham heart study, the authors noted, and may be due to underdiagnosis or differences in the underlying mechanism.
Compelling evidence of poor health outcomes associated with obesity
Study limitations include the fact that the findings may not be generalizable to other race/ethnicity groups, the lack of information on diet and exercise, and the fact that BMI was used as a surrogate of adiposity. As such, it does not account for an age-related decrease in heavier-than-fat muscle mass and differences between sexes and ethnic groups.
The finding of stable obesity over time accords with two smaller studies that included Canadian and American adults.
The current study did not uncover an obesity paradox, unlike some studies that included patients with preexisting CVD or a history of acute coronary events. Those studies reported better clinical outcomes among patients with overweight or obesity.
The current study included individuals who did not initially have CVD. Those with more severe obesity were younger than individuals with overweight at the time of the occurrence of incident CVD (age 64 vs. 66) and at the age of death (age 67 vs. age 75), which “provides compelling evidence of poor health outcomes associated with obesity,” the authors emphasized.
“Further research is ... needed to explore whether interventions to change BMI trajectories would have an impact on future CVD outcomes,” they concluded.
Dr. Iyen’s clinical academic lectureship is fully funded by the National Institute for Health Research (NIHR). The views expressed are those of the authors and are not necessarily those of the National Health Service, the NIHR, or the Department of Health and Social Care. Dr. Khan has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Early palliative care consultation in the medical ICU
Background: Mortality rates in critically ill patients remain in excess of 20% in many institutions. In the last 2 decades, palliative care has become a core component of ICU care. Current literature recommends a palliative care consult in the ICU setting; however, implementing this recommendation in a meaningful way has been challenging. The purpose of this study is to evaluate whether consulting palliative care in ICU earlier improves patient outcomes.
Study design: Single-center cluster randomized crossover trial.
Setting: Two medical ICUs at Barnes Jewish Hospital, St. Louis.
Synopsis: 199 patients were enrolled using palliative care criteria to identify patients at high risk for morbidity and mortality. In the intervention arm patients received a palliative care consultation from an inter-professional team led by board-certified palliative care providers within 48 hours of ICU admission.
The primary outcome of this study was a change in code status to Do Not Resuscitate/Do Not Intubate (DNR/DNI), which was significantly higher in the intervention group (50.5% vs. 23.4%; P less than .0001). The intervention group also had more hospice discharges, fewer ventilated days, a lower rate of tracheostomy, and fewer hospital readmissions. However, mortality and ICU/hospital length of stay were not significantly different between the two arms. Limitations of this study include using a single academic center and the fact that establishing a DNR/DNI may not measure quality of life or patient/family satisfaction. Further studies are needed to focus on clinical outcomes as well as patient and family satisfaction.
Bottom line: Early goal-directed palliative care consults with experienced clinicians board certified in palliative care influences goals of care, code status, and discharge plans for the critically ill and can improve medical resource utilization.
Citation: Ma J et al. Early palliative care consultation in the medical ICU: A cluster randomized crossover trial. Crit Care Med. 2019 Dec;47: 1707-15.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Mortality rates in critically ill patients remain in excess of 20% in many institutions. In the last 2 decades, palliative care has become a core component of ICU care. Current literature recommends a palliative care consult in the ICU setting; however, implementing this recommendation in a meaningful way has been challenging. The purpose of this study is to evaluate whether consulting palliative care in ICU earlier improves patient outcomes.
Study design: Single-center cluster randomized crossover trial.
Setting: Two medical ICUs at Barnes Jewish Hospital, St. Louis.
Synopsis: 199 patients were enrolled using palliative care criteria to identify patients at high risk for morbidity and mortality. In the intervention arm patients received a palliative care consultation from an inter-professional team led by board-certified palliative care providers within 48 hours of ICU admission.
The primary outcome of this study was a change in code status to Do Not Resuscitate/Do Not Intubate (DNR/DNI), which was significantly higher in the intervention group (50.5% vs. 23.4%; P less than .0001). The intervention group also had more hospice discharges, fewer ventilated days, a lower rate of tracheostomy, and fewer hospital readmissions. However, mortality and ICU/hospital length of stay were not significantly different between the two arms. Limitations of this study include using a single academic center and the fact that establishing a DNR/DNI may not measure quality of life or patient/family satisfaction. Further studies are needed to focus on clinical outcomes as well as patient and family satisfaction.
Bottom line: Early goal-directed palliative care consults with experienced clinicians board certified in palliative care influences goals of care, code status, and discharge plans for the critically ill and can improve medical resource utilization.
Citation: Ma J et al. Early palliative care consultation in the medical ICU: A cluster randomized crossover trial. Crit Care Med. 2019 Dec;47: 1707-15.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Mortality rates in critically ill patients remain in excess of 20% in many institutions. In the last 2 decades, palliative care has become a core component of ICU care. Current literature recommends a palliative care consult in the ICU setting; however, implementing this recommendation in a meaningful way has been challenging. The purpose of this study is to evaluate whether consulting palliative care in ICU earlier improves patient outcomes.
Study design: Single-center cluster randomized crossover trial.
Setting: Two medical ICUs at Barnes Jewish Hospital, St. Louis.
Synopsis: 199 patients were enrolled using palliative care criteria to identify patients at high risk for morbidity and mortality. In the intervention arm patients received a palliative care consultation from an inter-professional team led by board-certified palliative care providers within 48 hours of ICU admission.
The primary outcome of this study was a change in code status to Do Not Resuscitate/Do Not Intubate (DNR/DNI), which was significantly higher in the intervention group (50.5% vs. 23.4%; P less than .0001). The intervention group also had more hospice discharges, fewer ventilated days, a lower rate of tracheostomy, and fewer hospital readmissions. However, mortality and ICU/hospital length of stay were not significantly different between the two arms. Limitations of this study include using a single academic center and the fact that establishing a DNR/DNI may not measure quality of life or patient/family satisfaction. Further studies are needed to focus on clinical outcomes as well as patient and family satisfaction.
Bottom line: Early goal-directed palliative care consults with experienced clinicians board certified in palliative care influences goals of care, code status, and discharge plans for the critically ill and can improve medical resource utilization.
Citation: Ma J et al. Early palliative care consultation in the medical ICU: A cluster randomized crossover trial. Crit Care Med. 2019 Dec;47: 1707-15.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Tislelizumab bests docetaxel in NSCLC
The results were presented at the American Association for Cancer Research Annual Meeting 2021: Week 1 (Abstract CT039).
Tislelizumab is an anti–PD-1 antibody engineered to minimize Fc-gamma receptor binding on macrophages, a mechanism of T-cell clearance and potential anti–PD-1 resistance, according to investigator Caicun Zhou, MD, PhD, of Shanghai (China) Pulmonary Hospital.
Tislelizumab is approved for the treatment of relapsed/refractory classical Hodgkin lymphoma, the second-line treatment of locally advanced or metastatic urothelial carcinoma, and first-line treatment of advanced squamous NSCLC in China.
In patients with locally advanced or metastatic NSCLC whose disease has progressed after initial platinum-based chemotherapy, anti–PD-1/PD-L1 therapies have been shown to improve OS by 2-4 months versus docetaxel, Dr. Zhou said. A phase 1/2 study of second-line tislelizumab demonstrated antitumor activity in multiple advanced solid tumors, including NSCLC.
The phase 3 RATIONALE 303 study (NCT3358875) was designed to investigate the efficacy and safety of tislelizumab, compared with docetaxel in patients with locally advanced or metastatic NSCLC whose disease had progressed during or after platinum-containing doublet chemotherapy.
Study details
RATIONALE 303 enrolled 805 patients who had received up to two prior lines of systemic therapy and had no known EGFR mutations or ALK fusions.
The patients’ median age was 61 years, about 77% were male, about 80% were Asian, and about 70% were current or former smokers. Roughly 46% of patients had squamous histology, and about 43% had PD-L1 expression of 25% or greater.
Patients were stratified according to histology (squamous vs. nonsquamous), lines of prior therapy (second vs. third), and PD-L1 status (<25% vs. ≥25%).
Patients were randomized 2:1 to receive IV tislelizumab at 200 mg every 3 weeks (n = 535) or IV docetaxel at 75 mg/m2 every 3 weeks (n = 270) until unacceptable toxicity or disease progression.
The dual primary endpoints were OS in the intention-to-treat (ITT) population and in patients with PD-L1 expression of 25% or higher.
Survival and safety
In the ITT population, the 1-year OS rate was 61.9% in the tislelizumab arm and 49.8% in the docetaxel arm. At 2 years, the OS rates were 39.4% and 25.0%, respectively.
The median OS was 17.2 months in the tislelizumab arm and 11.9 months in the docetaxel arm (hazard ratio, 0.64; 95% CI, 0.53-0.78; P < .0001).
In the PD-L1–high subgroup, the median OS was 19.1 months with tislelizumab and 11.9 months with docetaxel (HR, 0.52; 95% CI, 0.38-0.71; P < .0001). The 1-year OS rates in this group were 67.5% and 49.1%, respectively, and the 2-year OS rates were 44.7% and 24.5%, respectively.
The OS benefit with tislelizumab was observed across nearly all subgroups, Dr. Zhou noted.
In the ITT population, benefits were seen with tislelizumab over docetaxel for progression-free survival (4.1 months vs. 2.6 months, P < .0001), objective response rate (21.9% vs. 7.1%, P < .0001), and median duration of response (13.5 months vs. 6.2 months, P < .0001).
The rate of treatment-related adverse events (TRAEs) was 73.0% in the tislelizumab arm and 93.8% in the docetaxel arm. Rates of grade 3 or higher TRAEs were 14.4% and 66.3%, respectively. Rates of TRAEs leading to permanent discontinuation of treatment were 6.0% and 9.7%, respectively, and rates of TRAEs leading to death were 1.5% and 1.6%, respectively.
The most common treatment-emergent adverse events were anemia in the tislelizumab arm (28.5%) and alopecia in the docetaxel arm (47.3%). The most common grade 3 or higher treatment-emergent adverse event was neutropenia in the docetaxel arm (27.9% vs. 0.6% with tislelizumab).
‘Very important trial’
“RATIONALE 303 demonstrated that, as second- or third-line therapy in patients with advanced NSCLC, tislelizumab was tolerable and prolonged overall survival by 5-7 months. It also improved progression-free survival and objective response rate versus docetaxel, regardless of histology or PD-L1 expression,” Dr. Zhou concluded.
Session moderator Marina Chiara Garassino, MD, of the University of Chicago called RATIONALE 303 a “very important trial.”
Citing the range of immunotherapies available for NSCLC, Dr. Garassino said, “We have a very crowded space in the treatment of NSCLC. ... It is difficult to do a direct comparison [of immunotherapy trials] because we know that populations can be different and other factors can play a role. In the near future, we have to understand if they are all the same and interchangeable or if they are different.”
RATIONALE 303 was funded by BeiGene. Dr. Zhou disclosed relationships with Lily China, Sanofi, Roche, and several other companies, not including BeiGene. Dr. Garassino disclosed relationships with AstraZeneca, Novartis, Bristol-Myers Squibb, and several other companies, not including BeiGene.
The results were presented at the American Association for Cancer Research Annual Meeting 2021: Week 1 (Abstract CT039).
Tislelizumab is an anti–PD-1 antibody engineered to minimize Fc-gamma receptor binding on macrophages, a mechanism of T-cell clearance and potential anti–PD-1 resistance, according to investigator Caicun Zhou, MD, PhD, of Shanghai (China) Pulmonary Hospital.
Tislelizumab is approved for the treatment of relapsed/refractory classical Hodgkin lymphoma, the second-line treatment of locally advanced or metastatic urothelial carcinoma, and first-line treatment of advanced squamous NSCLC in China.
In patients with locally advanced or metastatic NSCLC whose disease has progressed after initial platinum-based chemotherapy, anti–PD-1/PD-L1 therapies have been shown to improve OS by 2-4 months versus docetaxel, Dr. Zhou said. A phase 1/2 study of second-line tislelizumab demonstrated antitumor activity in multiple advanced solid tumors, including NSCLC.
The phase 3 RATIONALE 303 study (NCT3358875) was designed to investigate the efficacy and safety of tislelizumab, compared with docetaxel in patients with locally advanced or metastatic NSCLC whose disease had progressed during or after platinum-containing doublet chemotherapy.
Study details
RATIONALE 303 enrolled 805 patients who had received up to two prior lines of systemic therapy and had no known EGFR mutations or ALK fusions.
The patients’ median age was 61 years, about 77% were male, about 80% were Asian, and about 70% were current or former smokers. Roughly 46% of patients had squamous histology, and about 43% had PD-L1 expression of 25% or greater.
Patients were stratified according to histology (squamous vs. nonsquamous), lines of prior therapy (second vs. third), and PD-L1 status (<25% vs. ≥25%).
Patients were randomized 2:1 to receive IV tislelizumab at 200 mg every 3 weeks (n = 535) or IV docetaxel at 75 mg/m2 every 3 weeks (n = 270) until unacceptable toxicity or disease progression.
The dual primary endpoints were OS in the intention-to-treat (ITT) population and in patients with PD-L1 expression of 25% or higher.
Survival and safety
In the ITT population, the 1-year OS rate was 61.9% in the tislelizumab arm and 49.8% in the docetaxel arm. At 2 years, the OS rates were 39.4% and 25.0%, respectively.
The median OS was 17.2 months in the tislelizumab arm and 11.9 months in the docetaxel arm (hazard ratio, 0.64; 95% CI, 0.53-0.78; P < .0001).
In the PD-L1–high subgroup, the median OS was 19.1 months with tislelizumab and 11.9 months with docetaxel (HR, 0.52; 95% CI, 0.38-0.71; P < .0001). The 1-year OS rates in this group were 67.5% and 49.1%, respectively, and the 2-year OS rates were 44.7% and 24.5%, respectively.
The OS benefit with tislelizumab was observed across nearly all subgroups, Dr. Zhou noted.
In the ITT population, benefits were seen with tislelizumab over docetaxel for progression-free survival (4.1 months vs. 2.6 months, P < .0001), objective response rate (21.9% vs. 7.1%, P < .0001), and median duration of response (13.5 months vs. 6.2 months, P < .0001).
The rate of treatment-related adverse events (TRAEs) was 73.0% in the tislelizumab arm and 93.8% in the docetaxel arm. Rates of grade 3 or higher TRAEs were 14.4% and 66.3%, respectively. Rates of TRAEs leading to permanent discontinuation of treatment were 6.0% and 9.7%, respectively, and rates of TRAEs leading to death were 1.5% and 1.6%, respectively.
The most common treatment-emergent adverse events were anemia in the tislelizumab arm (28.5%) and alopecia in the docetaxel arm (47.3%). The most common grade 3 or higher treatment-emergent adverse event was neutropenia in the docetaxel arm (27.9% vs. 0.6% with tislelizumab).
‘Very important trial’
“RATIONALE 303 demonstrated that, as second- or third-line therapy in patients with advanced NSCLC, tislelizumab was tolerable and prolonged overall survival by 5-7 months. It also improved progression-free survival and objective response rate versus docetaxel, regardless of histology or PD-L1 expression,” Dr. Zhou concluded.
Session moderator Marina Chiara Garassino, MD, of the University of Chicago called RATIONALE 303 a “very important trial.”
Citing the range of immunotherapies available for NSCLC, Dr. Garassino said, “We have a very crowded space in the treatment of NSCLC. ... It is difficult to do a direct comparison [of immunotherapy trials] because we know that populations can be different and other factors can play a role. In the near future, we have to understand if they are all the same and interchangeable or if they are different.”
RATIONALE 303 was funded by BeiGene. Dr. Zhou disclosed relationships with Lily China, Sanofi, Roche, and several other companies, not including BeiGene. Dr. Garassino disclosed relationships with AstraZeneca, Novartis, Bristol-Myers Squibb, and several other companies, not including BeiGene.
The results were presented at the American Association for Cancer Research Annual Meeting 2021: Week 1 (Abstract CT039).
Tislelizumab is an anti–PD-1 antibody engineered to minimize Fc-gamma receptor binding on macrophages, a mechanism of T-cell clearance and potential anti–PD-1 resistance, according to investigator Caicun Zhou, MD, PhD, of Shanghai (China) Pulmonary Hospital.
Tislelizumab is approved for the treatment of relapsed/refractory classical Hodgkin lymphoma, the second-line treatment of locally advanced or metastatic urothelial carcinoma, and first-line treatment of advanced squamous NSCLC in China.
In patients with locally advanced or metastatic NSCLC whose disease has progressed after initial platinum-based chemotherapy, anti–PD-1/PD-L1 therapies have been shown to improve OS by 2-4 months versus docetaxel, Dr. Zhou said. A phase 1/2 study of second-line tislelizumab demonstrated antitumor activity in multiple advanced solid tumors, including NSCLC.
The phase 3 RATIONALE 303 study (NCT3358875) was designed to investigate the efficacy and safety of tislelizumab, compared with docetaxel in patients with locally advanced or metastatic NSCLC whose disease had progressed during or after platinum-containing doublet chemotherapy.
Study details
RATIONALE 303 enrolled 805 patients who had received up to two prior lines of systemic therapy and had no known EGFR mutations or ALK fusions.
The patients’ median age was 61 years, about 77% were male, about 80% were Asian, and about 70% were current or former smokers. Roughly 46% of patients had squamous histology, and about 43% had PD-L1 expression of 25% or greater.
Patients were stratified according to histology (squamous vs. nonsquamous), lines of prior therapy (second vs. third), and PD-L1 status (<25% vs. ≥25%).
Patients were randomized 2:1 to receive IV tislelizumab at 200 mg every 3 weeks (n = 535) or IV docetaxel at 75 mg/m2 every 3 weeks (n = 270) until unacceptable toxicity or disease progression.
The dual primary endpoints were OS in the intention-to-treat (ITT) population and in patients with PD-L1 expression of 25% or higher.
Survival and safety
In the ITT population, the 1-year OS rate was 61.9% in the tislelizumab arm and 49.8% in the docetaxel arm. At 2 years, the OS rates were 39.4% and 25.0%, respectively.
The median OS was 17.2 months in the tislelizumab arm and 11.9 months in the docetaxel arm (hazard ratio, 0.64; 95% CI, 0.53-0.78; P < .0001).
In the PD-L1–high subgroup, the median OS was 19.1 months with tislelizumab and 11.9 months with docetaxel (HR, 0.52; 95% CI, 0.38-0.71; P < .0001). The 1-year OS rates in this group were 67.5% and 49.1%, respectively, and the 2-year OS rates were 44.7% and 24.5%, respectively.
The OS benefit with tislelizumab was observed across nearly all subgroups, Dr. Zhou noted.
In the ITT population, benefits were seen with tislelizumab over docetaxel for progression-free survival (4.1 months vs. 2.6 months, P < .0001), objective response rate (21.9% vs. 7.1%, P < .0001), and median duration of response (13.5 months vs. 6.2 months, P < .0001).
The rate of treatment-related adverse events (TRAEs) was 73.0% in the tislelizumab arm and 93.8% in the docetaxel arm. Rates of grade 3 or higher TRAEs were 14.4% and 66.3%, respectively. Rates of TRAEs leading to permanent discontinuation of treatment were 6.0% and 9.7%, respectively, and rates of TRAEs leading to death were 1.5% and 1.6%, respectively.
The most common treatment-emergent adverse events were anemia in the tislelizumab arm (28.5%) and alopecia in the docetaxel arm (47.3%). The most common grade 3 or higher treatment-emergent adverse event was neutropenia in the docetaxel arm (27.9% vs. 0.6% with tislelizumab).
‘Very important trial’
“RATIONALE 303 demonstrated that, as second- or third-line therapy in patients with advanced NSCLC, tislelizumab was tolerable and prolonged overall survival by 5-7 months. It also improved progression-free survival and objective response rate versus docetaxel, regardless of histology or PD-L1 expression,” Dr. Zhou concluded.
Session moderator Marina Chiara Garassino, MD, of the University of Chicago called RATIONALE 303 a “very important trial.”
Citing the range of immunotherapies available for NSCLC, Dr. Garassino said, “We have a very crowded space in the treatment of NSCLC. ... It is difficult to do a direct comparison [of immunotherapy trials] because we know that populations can be different and other factors can play a role. In the near future, we have to understand if they are all the same and interchangeable or if they are different.”
RATIONALE 303 was funded by BeiGene. Dr. Zhou disclosed relationships with Lily China, Sanofi, Roche, and several other companies, not including BeiGene. Dr. Garassino disclosed relationships with AstraZeneca, Novartis, Bristol-Myers Squibb, and several other companies, not including BeiGene.
FROM AACR 2021
Frontline brentuximab vedotin shows promise in high-risk pediatric Hodgkin lymphoma
A frontline treatment regimen including brentuximab vedotin (Bv) was well tolerated, was highly effective, and significantly reduced radiation exposure in pediatric patients with high-risk Hodgkin lymphoma, according to the results of an open-label, phase 2 trial.
Of 77 patients enrolled in the investigator-initiated, single-arm, multicenter trial, 27 (35%) achieved complete remission (CR) without radiation at the early response assessment (ERA) after two cycles of therapy, reported Monika L. Metzger, MD, of St. Jude Children’s Research Hospital, Memphis, Tenn. and colleagues. The report was published online in the Journal of Clinical Oncology.
The addition of Bv also resulted in superior event-free survival (97.4%) and overall survival (98.7%) at median follow-up of 3.4 years, compared with previously published pediatric trials, such as the HOD99 trial (EFS and OS of 80.8% and 96.5%, respectively), the authors noted.
Bv chemotherapy
Bv, a targeted anti-CD30 antibody-drug conjugate, received expanded Food and Drug Administration approval in March 2018 for frontline use in combination with chemotherapy in adults with stage III or IV classical Hodgkin lymphoma (HL). The current study is the first to include Bv as part of a chemotherapy regimen in the frontline setting for pediatric classical HL, the authors noted, adding that their primary aim was to reduce prescribed radiation thereby limiting late toxicities associated with radiation in this population.
Patients enrolled were children and adolescents aged 18 years and under with stage IIB, IIIB, or IV classical HL. Bv was used in place of vincristine in the standard OEPA/COPDac (vincristine, etoposide, prednisone, and doxorubicin/cyclophosphamide, vincristine, prednisone, and dacarbazine) frontline regimen for pediatric HL.
The Bv-based chemotherapy regimen was well tolerated and mostly limited to low-grade nausea, vomiting, and constipation, and the most common adverse events were hematologic events occurring mainly during the first two cycles of chemotherapy.
“Notably, we observed a very low incidence of neuropathy (4%) by both clinician and patient report, and no participants required Bv dose reduction or discontinuation,” they wrote, explaining that neuropathy is more common with vincristine.
Radiation exposure
Residual node radiotherapy (RNRT) was delivered at a prescribed dose of 25.5 Gy in 17 fractions of 1.5 Gy, 2-4 weeks after completion of chemotherapy only to nodal sites that did not achieve a CR at the early response assessment (ERA) after two cycles of therapy.
“Patients treated with RNRT had significantly lower integral radiation dose compared with patients treated on HOD99 with [involved-field radiation therapy] (78.1 J vs. 249.6 J),” the authors wrote. “Doses to specific organs were also compared ... [t]he mean heart dose was reduced to 5.29 Gy from 16.9 Gy, and the mean thyroid dose was reduced to 4.46 Gy from 25.9 Gy.”
Women also had significantly less breast radiation exposure (mean of 3.21 Gy vs. 6.85 Gy in HOD99).
One irradiated patient experienced disease progression at the end of therapy, but remained disease free more than 6 years following salvage therapy, and one unexpected death occurred, the authors said.
“We have already reduced the use of radiation for low-risk Hodgkin lymphoma patients. In this study we’ve shown that it is also possible to either omit or reduce the extent of radiation for high-risk patients, using highly focal methods such as proton beam radiation or intensity modulated radiation,” co–senior author Matthew Krasin, MD, of St. Jude’s department of radiation oncology, stated in a press release.
Next steps
Co–senior author Melissa Hudson, MD, the St. Jude cancer survivorship division director, added that “[b]eing able to offer Hodgkin lymphoma patients a targeted therapy in the frontline setting is an exciting development.
“The favorable safety and toxicity profile of Bv in combination with chemotherapy for high-risk pediatric patients supports its prospective evaluation in a randomized trial,” the authors concluded, noting that “[l]onger follow-up is required to establish if this approach reduces risk of late-occurring toxicities such as second malignant neoplasms in this cohort of minimally irradiated patients.”
The study was sponsored by Seattle Genetics. The research at St. Jude was funded in part by grants from the National Cancer Institute and ALSAC (American Lebanese Syrian Associated Charities), St. Jude’s fundraising and awareness organization. Dr. Metzger reported research funding from Seattle Genetics. Dr. Krasin reported a consulting or advisory role for Debiopharm Group. Dr. Hudson reported a consulting or advisory role for Oncology Research Information Exchange Network, Princess Máxima Center.
A frontline treatment regimen including brentuximab vedotin (Bv) was well tolerated, was highly effective, and significantly reduced radiation exposure in pediatric patients with high-risk Hodgkin lymphoma, according to the results of an open-label, phase 2 trial.
Of 77 patients enrolled in the investigator-initiated, single-arm, multicenter trial, 27 (35%) achieved complete remission (CR) without radiation at the early response assessment (ERA) after two cycles of therapy, reported Monika L. Metzger, MD, of St. Jude Children’s Research Hospital, Memphis, Tenn. and colleagues. The report was published online in the Journal of Clinical Oncology.
The addition of Bv also resulted in superior event-free survival (97.4%) and overall survival (98.7%) at median follow-up of 3.4 years, compared with previously published pediatric trials, such as the HOD99 trial (EFS and OS of 80.8% and 96.5%, respectively), the authors noted.
Bv chemotherapy
Bv, a targeted anti-CD30 antibody-drug conjugate, received expanded Food and Drug Administration approval in March 2018 for frontline use in combination with chemotherapy in adults with stage III or IV classical Hodgkin lymphoma (HL). The current study is the first to include Bv as part of a chemotherapy regimen in the frontline setting for pediatric classical HL, the authors noted, adding that their primary aim was to reduce prescribed radiation thereby limiting late toxicities associated with radiation in this population.
Patients enrolled were children and adolescents aged 18 years and under with stage IIB, IIIB, or IV classical HL. Bv was used in place of vincristine in the standard OEPA/COPDac (vincristine, etoposide, prednisone, and doxorubicin/cyclophosphamide, vincristine, prednisone, and dacarbazine) frontline regimen for pediatric HL.
The Bv-based chemotherapy regimen was well tolerated and mostly limited to low-grade nausea, vomiting, and constipation, and the most common adverse events were hematologic events occurring mainly during the first two cycles of chemotherapy.
“Notably, we observed a very low incidence of neuropathy (4%) by both clinician and patient report, and no participants required Bv dose reduction or discontinuation,” they wrote, explaining that neuropathy is more common with vincristine.
Radiation exposure
Residual node radiotherapy (RNRT) was delivered at a prescribed dose of 25.5 Gy in 17 fractions of 1.5 Gy, 2-4 weeks after completion of chemotherapy only to nodal sites that did not achieve a CR at the early response assessment (ERA) after two cycles of therapy.
“Patients treated with RNRT had significantly lower integral radiation dose compared with patients treated on HOD99 with [involved-field radiation therapy] (78.1 J vs. 249.6 J),” the authors wrote. “Doses to specific organs were also compared ... [t]he mean heart dose was reduced to 5.29 Gy from 16.9 Gy, and the mean thyroid dose was reduced to 4.46 Gy from 25.9 Gy.”
Women also had significantly less breast radiation exposure (mean of 3.21 Gy vs. 6.85 Gy in HOD99).
One irradiated patient experienced disease progression at the end of therapy, but remained disease free more than 6 years following salvage therapy, and one unexpected death occurred, the authors said.
“We have already reduced the use of radiation for low-risk Hodgkin lymphoma patients. In this study we’ve shown that it is also possible to either omit or reduce the extent of radiation for high-risk patients, using highly focal methods such as proton beam radiation or intensity modulated radiation,” co–senior author Matthew Krasin, MD, of St. Jude’s department of radiation oncology, stated in a press release.
Next steps
Co–senior author Melissa Hudson, MD, the St. Jude cancer survivorship division director, added that “[b]eing able to offer Hodgkin lymphoma patients a targeted therapy in the frontline setting is an exciting development.
“The favorable safety and toxicity profile of Bv in combination with chemotherapy for high-risk pediatric patients supports its prospective evaluation in a randomized trial,” the authors concluded, noting that “[l]onger follow-up is required to establish if this approach reduces risk of late-occurring toxicities such as second malignant neoplasms in this cohort of minimally irradiated patients.”
The study was sponsored by Seattle Genetics. The research at St. Jude was funded in part by grants from the National Cancer Institute and ALSAC (American Lebanese Syrian Associated Charities), St. Jude’s fundraising and awareness organization. Dr. Metzger reported research funding from Seattle Genetics. Dr. Krasin reported a consulting or advisory role for Debiopharm Group. Dr. Hudson reported a consulting or advisory role for Oncology Research Information Exchange Network, Princess Máxima Center.
A frontline treatment regimen including brentuximab vedotin (Bv) was well tolerated, was highly effective, and significantly reduced radiation exposure in pediatric patients with high-risk Hodgkin lymphoma, according to the results of an open-label, phase 2 trial.
Of 77 patients enrolled in the investigator-initiated, single-arm, multicenter trial, 27 (35%) achieved complete remission (CR) without radiation at the early response assessment (ERA) after two cycles of therapy, reported Monika L. Metzger, MD, of St. Jude Children’s Research Hospital, Memphis, Tenn. and colleagues. The report was published online in the Journal of Clinical Oncology.
The addition of Bv also resulted in superior event-free survival (97.4%) and overall survival (98.7%) at median follow-up of 3.4 years, compared with previously published pediatric trials, such as the HOD99 trial (EFS and OS of 80.8% and 96.5%, respectively), the authors noted.
Bv chemotherapy
Bv, a targeted anti-CD30 antibody-drug conjugate, received expanded Food and Drug Administration approval in March 2018 for frontline use in combination with chemotherapy in adults with stage III or IV classical Hodgkin lymphoma (HL). The current study is the first to include Bv as part of a chemotherapy regimen in the frontline setting for pediatric classical HL, the authors noted, adding that their primary aim was to reduce prescribed radiation thereby limiting late toxicities associated with radiation in this population.
Patients enrolled were children and adolescents aged 18 years and under with stage IIB, IIIB, or IV classical HL. Bv was used in place of vincristine in the standard OEPA/COPDac (vincristine, etoposide, prednisone, and doxorubicin/cyclophosphamide, vincristine, prednisone, and dacarbazine) frontline regimen for pediatric HL.
The Bv-based chemotherapy regimen was well tolerated and mostly limited to low-grade nausea, vomiting, and constipation, and the most common adverse events were hematologic events occurring mainly during the first two cycles of chemotherapy.
“Notably, we observed a very low incidence of neuropathy (4%) by both clinician and patient report, and no participants required Bv dose reduction or discontinuation,” they wrote, explaining that neuropathy is more common with vincristine.
Radiation exposure
Residual node radiotherapy (RNRT) was delivered at a prescribed dose of 25.5 Gy in 17 fractions of 1.5 Gy, 2-4 weeks after completion of chemotherapy only to nodal sites that did not achieve a CR at the early response assessment (ERA) after two cycles of therapy.
“Patients treated with RNRT had significantly lower integral radiation dose compared with patients treated on HOD99 with [involved-field radiation therapy] (78.1 J vs. 249.6 J),” the authors wrote. “Doses to specific organs were also compared ... [t]he mean heart dose was reduced to 5.29 Gy from 16.9 Gy, and the mean thyroid dose was reduced to 4.46 Gy from 25.9 Gy.”
Women also had significantly less breast radiation exposure (mean of 3.21 Gy vs. 6.85 Gy in HOD99).
One irradiated patient experienced disease progression at the end of therapy, but remained disease free more than 6 years following salvage therapy, and one unexpected death occurred, the authors said.
“We have already reduced the use of radiation for low-risk Hodgkin lymphoma patients. In this study we’ve shown that it is also possible to either omit or reduce the extent of radiation for high-risk patients, using highly focal methods such as proton beam radiation or intensity modulated radiation,” co–senior author Matthew Krasin, MD, of St. Jude’s department of radiation oncology, stated in a press release.
Next steps
Co–senior author Melissa Hudson, MD, the St. Jude cancer survivorship division director, added that “[b]eing able to offer Hodgkin lymphoma patients a targeted therapy in the frontline setting is an exciting development.
“The favorable safety and toxicity profile of Bv in combination with chemotherapy for high-risk pediatric patients supports its prospective evaluation in a randomized trial,” the authors concluded, noting that “[l]onger follow-up is required to establish if this approach reduces risk of late-occurring toxicities such as second malignant neoplasms in this cohort of minimally irradiated patients.”
The study was sponsored by Seattle Genetics. The research at St. Jude was funded in part by grants from the National Cancer Institute and ALSAC (American Lebanese Syrian Associated Charities), St. Jude’s fundraising and awareness organization. Dr. Metzger reported research funding from Seattle Genetics. Dr. Krasin reported a consulting or advisory role for Debiopharm Group. Dr. Hudson reported a consulting or advisory role for Oncology Research Information Exchange Network, Princess Máxima Center.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
GENUINE improvements: Ublituximab plus ibrutinib for CLL
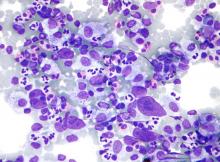
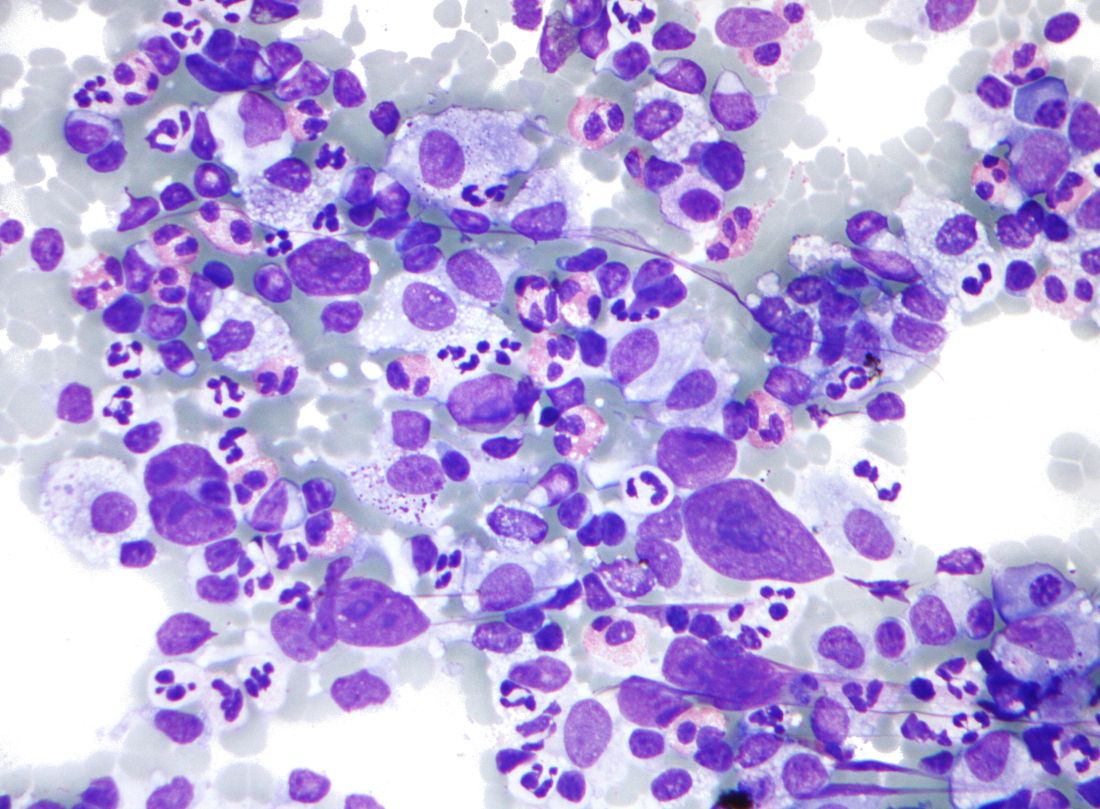
Chronic lymphocytic leukemia (CLL) is a clinically heterogeneous disease associated with several known genetic abnormalities, including 17p deletion (del[17p]), 11q deletion (del[11q]), and TP53 gene mutations, which are adverse prognostic markers among patients treated with chemoimmunotherapy.
The Bruton tyrosine kinase (BTK) inhibitor ibrutinib is approved for patients with untreated, relapsed, or refractory disease, including those with del(17p). Clinicians will soon have the chance to pair it with ublituximab, a next-generation, glycoengineered, type I, anti-CD20 monoclonal antibody that binds to a unique epitope on CD20, differentiating it from rituximab, ofatumumab, and obinutuzumab. Results from the phase 3 GENUINE trial, which were recently published in The Lancet Haematology, showed that ublituximab plus ibrutinib was superior to ibrutinib alone for patients with relapsed or refractory high-risk CLL.
This news organization spoke with Jennifer R. Brown, MD, PhD, director of the CLL Center and institute physician at the Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, both in Boston, about the GENUINE trial and its potential impact on treatment choices going forward.
What type of patients were treated in the GENUINE trial?
Dr. Brown: This is a trial among relapsed/refractory CLL patients with 17p or 11q deletion or TP53 mutation. Patients aged 18 years or older with CLL who warranted treatment, as defined by International Workshop on CLL criteria, were eligible if they had previously received at least two cycles of at least one standard treatment regimen, had an Eastern Cooperative Oncology Group performance status of 2 or lower, and had high-risk cytogenetics, defined as the presence of at least one of del(17p), del(11q), or TP53 mutation confirmed by a central laboratory with fluorescence in situ hybridization and/or next-generation sequencing.
What were the main outcomes of the trial?
Originally, the GENUINE trial had coprimary endpoints of progression-free survival (PFS) and overall response rate. Because of slow accrual, it was amended to have one primary endpoint of independent review committee (IRC)–assessed ORR.
IRC-assessed ORR was improved from 65% to 83% with the addition of ublituximab. PFS also improved significantly in the ublituximab group, with an even greater improvement when the analysis was limited to those with del(17p) or TP53 aberrancy, but this outcome was limited by the reduced sample size of the study as well as the relatively short PFS of the ibrutinib arm.
After a median follow-up of 41.6 months, the median IRC-assessed PFS in all treated patients was not reached in the ublituximab plus ibrutinib group after 15 PFS events but was 35.9 months in the ibrutinib group after 25 PFS events (hazard ratio, 0.46; 95% confidence interval, 0.24-0.87; P = .016).
Undetectable minimal residual disease was also seen in 42% of the combination arm, compared with 6% of the ibrutinib arm.
What types of adverse events were found in the trial?
The researchers found mostly mild and known side effects of ibrutinib. More atrial fibrillation and neutropenia were seen in the antibody group, but this was not marked.
Most adverse events were of grade 1 or 2. The most common grade 3 and 4 adverse events were neutropenia (11 [19%] patients in the ublituximab plus ibrutinib group and 7 [12%] in the ibrutinib group), anemia (5 [8%] and 5 [9%], respectively), and diarrhea (6 [10%] and 3 [5%], respectively).
What about serious adverse events?
Hospitalization from infection was seen, as expected. There were two cardiac arrests and an unexplained death, across both arms, which was concerning, given the known association of ibrutinib with ventricular arrhythmia and sudden death. There were also several hemorrhages, including one fatal one, which was again consistent with the known side effects of ibrutinib.
Are there treatments comparable with ublituximab plus ibrutinib that clinicians should perhaps first consider using?
In terms of other anti-CD20 antibodies, we have two randomized trials that have failed to show a benefit from adding rituximab to ibrutinib.
Obinutuzumab, like ublituximab, is also a next-generation glycoengineered antibody, and it is reasonably likely that it might lead to similar results. However, the only data we have on ibrutinib with obinutuzumab are from a single arm in a more heterogeneous, lower-risk patient population, and it is unlikely that a randomized comparison will ever be done.
On the basis of these trial results, how would you use the combination of ublituximab and ibrutinib for your patients?
I would consider the addition of ublituximab to a BTK inhibitor in high-risk patients (once ublituximab is approved). I already usually use a next-generation BTK inhibitor rather than ibrutinib.
Are there any other implications of the GENUINE trial?
I think this trial underscores the importance of studying genetic subgroups of patients separately. In this case, that was done in high-risk patients, but this observation likely also applies to low-risk patients.
Most trials to date have enrolled unselected patient populations, often without stratification, and their results therefore tend to obscure the outcomes in both the very high risk (as studied here) and in the low risk (patients with immunoglobulin heavy chain variable region gene mutations).
Dr. Brown has served as a consultant for AbbVie, Acerta/AstraZeneca, Beigene, Bristol-Myers Squibb/Juno/Celgene, Catapult, Genentech/Roche, Janssen, MEI Pharma, Morphosys, and Novartis, and has received research funding from Gilead, Loxo/Lilly, TG Therapeutics, Verastem/SecuraBio.
A version of this article first appeared on Medscape.com.
Chronic lymphocytic leukemia (CLL) is a clinically heterogeneous disease associated with several known genetic abnormalities, including 17p deletion (del[17p]), 11q deletion (del[11q]), and TP53 gene mutations, which are adverse prognostic markers among patients treated with chemoimmunotherapy.
The Bruton tyrosine kinase (BTK) inhibitor ibrutinib is approved for patients with untreated, relapsed, or refractory disease, including those with del(17p). Clinicians will soon have the chance to pair it with ublituximab, a next-generation, glycoengineered, type I, anti-CD20 monoclonal antibody that binds to a unique epitope on CD20, differentiating it from rituximab, ofatumumab, and obinutuzumab. Results from the phase 3 GENUINE trial, which were recently published in The Lancet Haematology, showed that ublituximab plus ibrutinib was superior to ibrutinib alone for patients with relapsed or refractory high-risk CLL.
This news organization spoke with Jennifer R. Brown, MD, PhD, director of the CLL Center and institute physician at the Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, both in Boston, about the GENUINE trial and its potential impact on treatment choices going forward.
What type of patients were treated in the GENUINE trial?
Dr. Brown: This is a trial among relapsed/refractory CLL patients with 17p or 11q deletion or TP53 mutation. Patients aged 18 years or older with CLL who warranted treatment, as defined by International Workshop on CLL criteria, were eligible if they had previously received at least two cycles of at least one standard treatment regimen, had an Eastern Cooperative Oncology Group performance status of 2 or lower, and had high-risk cytogenetics, defined as the presence of at least one of del(17p), del(11q), or TP53 mutation confirmed by a central laboratory with fluorescence in situ hybridization and/or next-generation sequencing.
What were the main outcomes of the trial?
Originally, the GENUINE trial had coprimary endpoints of progression-free survival (PFS) and overall response rate. Because of slow accrual, it was amended to have one primary endpoint of independent review committee (IRC)–assessed ORR.
IRC-assessed ORR was improved from 65% to 83% with the addition of ublituximab. PFS also improved significantly in the ublituximab group, with an even greater improvement when the analysis was limited to those with del(17p) or TP53 aberrancy, but this outcome was limited by the reduced sample size of the study as well as the relatively short PFS of the ibrutinib arm.
After a median follow-up of 41.6 months, the median IRC-assessed PFS in all treated patients was not reached in the ublituximab plus ibrutinib group after 15 PFS events but was 35.9 months in the ibrutinib group after 25 PFS events (hazard ratio, 0.46; 95% confidence interval, 0.24-0.87; P = .016).
Undetectable minimal residual disease was also seen in 42% of the combination arm, compared with 6% of the ibrutinib arm.
What types of adverse events were found in the trial?
The researchers found mostly mild and known side effects of ibrutinib. More atrial fibrillation and neutropenia were seen in the antibody group, but this was not marked.
Most adverse events were of grade 1 or 2. The most common grade 3 and 4 adverse events were neutropenia (11 [19%] patients in the ublituximab plus ibrutinib group and 7 [12%] in the ibrutinib group), anemia (5 [8%] and 5 [9%], respectively), and diarrhea (6 [10%] and 3 [5%], respectively).
What about serious adverse events?
Hospitalization from infection was seen, as expected. There were two cardiac arrests and an unexplained death, across both arms, which was concerning, given the known association of ibrutinib with ventricular arrhythmia and sudden death. There were also several hemorrhages, including one fatal one, which was again consistent with the known side effects of ibrutinib.
Are there treatments comparable with ublituximab plus ibrutinib that clinicians should perhaps first consider using?
In terms of other anti-CD20 antibodies, we have two randomized trials that have failed to show a benefit from adding rituximab to ibrutinib.
Obinutuzumab, like ublituximab, is also a next-generation glycoengineered antibody, and it is reasonably likely that it might lead to similar results. However, the only data we have on ibrutinib with obinutuzumab are from a single arm in a more heterogeneous, lower-risk patient population, and it is unlikely that a randomized comparison will ever be done.
On the basis of these trial results, how would you use the combination of ublituximab and ibrutinib for your patients?
I would consider the addition of ublituximab to a BTK inhibitor in high-risk patients (once ublituximab is approved). I already usually use a next-generation BTK inhibitor rather than ibrutinib.
Are there any other implications of the GENUINE trial?
I think this trial underscores the importance of studying genetic subgroups of patients separately. In this case, that was done in high-risk patients, but this observation likely also applies to low-risk patients.
Most trials to date have enrolled unselected patient populations, often without stratification, and their results therefore tend to obscure the outcomes in both the very high risk (as studied here) and in the low risk (patients with immunoglobulin heavy chain variable region gene mutations).
Dr. Brown has served as a consultant for AbbVie, Acerta/AstraZeneca, Beigene, Bristol-Myers Squibb/Juno/Celgene, Catapult, Genentech/Roche, Janssen, MEI Pharma, Morphosys, and Novartis, and has received research funding from Gilead, Loxo/Lilly, TG Therapeutics, Verastem/SecuraBio.
A version of this article first appeared on Medscape.com.
Chronic lymphocytic leukemia (CLL) is a clinically heterogeneous disease associated with several known genetic abnormalities, including 17p deletion (del[17p]), 11q deletion (del[11q]), and TP53 gene mutations, which are adverse prognostic markers among patients treated with chemoimmunotherapy.
The Bruton tyrosine kinase (BTK) inhibitor ibrutinib is approved for patients with untreated, relapsed, or refractory disease, including those with del(17p). Clinicians will soon have the chance to pair it with ublituximab, a next-generation, glycoengineered, type I, anti-CD20 monoclonal antibody that binds to a unique epitope on CD20, differentiating it from rituximab, ofatumumab, and obinutuzumab. Results from the phase 3 GENUINE trial, which were recently published in The Lancet Haematology, showed that ublituximab plus ibrutinib was superior to ibrutinib alone for patients with relapsed or refractory high-risk CLL.
This news organization spoke with Jennifer R. Brown, MD, PhD, director of the CLL Center and institute physician at the Dana-Farber Cancer Institute and professor of medicine at Harvard Medical School, both in Boston, about the GENUINE trial and its potential impact on treatment choices going forward.
What type of patients were treated in the GENUINE trial?
Dr. Brown: This is a trial among relapsed/refractory CLL patients with 17p or 11q deletion or TP53 mutation. Patients aged 18 years or older with CLL who warranted treatment, as defined by International Workshop on CLL criteria, were eligible if they had previously received at least two cycles of at least one standard treatment regimen, had an Eastern Cooperative Oncology Group performance status of 2 or lower, and had high-risk cytogenetics, defined as the presence of at least one of del(17p), del(11q), or TP53 mutation confirmed by a central laboratory with fluorescence in situ hybridization and/or next-generation sequencing.
What were the main outcomes of the trial?
Originally, the GENUINE trial had coprimary endpoints of progression-free survival (PFS) and overall response rate. Because of slow accrual, it was amended to have one primary endpoint of independent review committee (IRC)–assessed ORR.
IRC-assessed ORR was improved from 65% to 83% with the addition of ublituximab. PFS also improved significantly in the ublituximab group, with an even greater improvement when the analysis was limited to those with del(17p) or TP53 aberrancy, but this outcome was limited by the reduced sample size of the study as well as the relatively short PFS of the ibrutinib arm.
After a median follow-up of 41.6 months, the median IRC-assessed PFS in all treated patients was not reached in the ublituximab plus ibrutinib group after 15 PFS events but was 35.9 months in the ibrutinib group after 25 PFS events (hazard ratio, 0.46; 95% confidence interval, 0.24-0.87; P = .016).
Undetectable minimal residual disease was also seen in 42% of the combination arm, compared with 6% of the ibrutinib arm.
What types of adverse events were found in the trial?
The researchers found mostly mild and known side effects of ibrutinib. More atrial fibrillation and neutropenia were seen in the antibody group, but this was not marked.
Most adverse events were of grade 1 or 2. The most common grade 3 and 4 adverse events were neutropenia (11 [19%] patients in the ublituximab plus ibrutinib group and 7 [12%] in the ibrutinib group), anemia (5 [8%] and 5 [9%], respectively), and diarrhea (6 [10%] and 3 [5%], respectively).
What about serious adverse events?
Hospitalization from infection was seen, as expected. There were two cardiac arrests and an unexplained death, across both arms, which was concerning, given the known association of ibrutinib with ventricular arrhythmia and sudden death. There were also several hemorrhages, including one fatal one, which was again consistent with the known side effects of ibrutinib.
Are there treatments comparable with ublituximab plus ibrutinib that clinicians should perhaps first consider using?
In terms of other anti-CD20 antibodies, we have two randomized trials that have failed to show a benefit from adding rituximab to ibrutinib.
Obinutuzumab, like ublituximab, is also a next-generation glycoengineered antibody, and it is reasonably likely that it might lead to similar results. However, the only data we have on ibrutinib with obinutuzumab are from a single arm in a more heterogeneous, lower-risk patient population, and it is unlikely that a randomized comparison will ever be done.
On the basis of these trial results, how would you use the combination of ublituximab and ibrutinib for your patients?
I would consider the addition of ublituximab to a BTK inhibitor in high-risk patients (once ublituximab is approved). I already usually use a next-generation BTK inhibitor rather than ibrutinib.
Are there any other implications of the GENUINE trial?
I think this trial underscores the importance of studying genetic subgroups of patients separately. In this case, that was done in high-risk patients, but this observation likely also applies to low-risk patients.
Most trials to date have enrolled unselected patient populations, often without stratification, and their results therefore tend to obscure the outcomes in both the very high risk (as studied here) and in the low risk (patients with immunoglobulin heavy chain variable region gene mutations).
Dr. Brown has served as a consultant for AbbVie, Acerta/AstraZeneca, Beigene, Bristol-Myers Squibb/Juno/Celgene, Catapult, Genentech/Roche, Janssen, MEI Pharma, Morphosys, and Novartis, and has received research funding from Gilead, Loxo/Lilly, TG Therapeutics, Verastem/SecuraBio.
A version of this article first appeared on Medscape.com.
Antifungals during pregnancy and breastfeeding
There are three general classes of antifungal agents (number of agents): azole antifungals (9), echinocandins (3), and polyenes (5). The azole antifungals contain an azole ring and inhibit a wide range of fungi. Echinocandins target the fungal cell wall and the polyenes increase the fungal membrane permeability and lead to cell death.
Pregnancy
Azole antifungals inhibit the growth of fungi. Their trade names and molecular weights:
- Clotrimazole (Mycelex), an over-the-counter product, is available as a topical cream. Several studies have found no association between the drug and birth defects.
- Fluconazole (Diflucan) is a teratogen when doses of ≥400 mg/day are used during the first trimester. Smaller doses do not appear to cause embryo/fetal harm.
- Isavuconazonium (Cresemba) if used in pregnancy, exposure of the embryo/fetus would probably be low based on the >99% plasma protein binding, but the plasma half-life is 130 hours. Moreover, the drug is a potent animal teratogen and is best avoided in pregnancy.
- Itraconazole (Onmel, Sporanox, Tolsura), has a low risk, if any, of structural defects, according to what reported human experience suggests.
- Ketoconazole (Xolegel, Extina, Nizoral; 531) does not appear to adversely effect embryos and fetuses, but the human data are very limited. As with any drug, avoiding organogenesis is the best recommendation.
- Miconazole (Oravig) is usually used topically. Small amounts are absorbed from the vagina. The available evidence suggests that the drug does not increase the risk of congenital malformations.
- Posaconazole (Noxafil) does not have reported use in human pregnancy. The animal reproduction data suggest risk. Based on its molecular weight (about 701), the drug will most likely cross the placenta to the embryo/fetus. Thus, the best course is to avoid the drug during pregnancy, especially in the first trimester.
- Voriconazole (Vfend) has one human report of the drug use in pregnancy. The drug was started at about 19 weeks and continued until the woman gave birth at 35 weeks to a healthy male baby. At 6 months of age, the baby remained normal.
Echinocandin antifungals target the fungal cell wall by inhibiting its synthesis. Their trade names and molecular weights:
- Anidulafungin (Eraxis; 1,140) has no published human data. It is indicated for the treatment of candidemia and other forms of Candida infections. The animal data suggest low risk.
- Caspofungin (Cancidas; 1,213) has no published human data. It is indicated for presumed fungal infections in febrile, neutropenic patients. The animal data are suggestive of human risk, especially if exposure occurs in the first trimester. If possible, maternal treatment should be avoided in the first trimester.
- Micafungin (Mycamine; 1,292) has no published human data. It is indicated for the treatment of patients with esophageal candidiasis and for the prophylaxis of Candida infections in patients undergoing hematopoietic stem cell transplantation. The animal data in one species suggest high risk. If possible, maternal treatment should be avoided in the first trimester.
Polyene antifungals cause depolarization of the fungal cell membrane to increase the membrane permeability, which leads to cell death. Their trade names and molecular weights:
- Amphotericin b (Amphocin; Fungizone; 924) There are three other amphotericin agents: amphotericin b cholesteryl sulfate (Amphotec); amphotericin b lipid complex (Abelcet); amphotericin b liposomal (AmBisome). No reports linking amphotericin b with congenital defects have been found. The drug does cross the human placenta. Although there was a higher rate of spontaneous abortions in rabbits given amphotericin b, there was no fetal harm in rats and rabbits when given amphotericin b lipid complex.
- Nystatin (Bio-Statin; Mycostatin; Nilstat; 926). The drug does not appear to cause embryo-fetal harm. Based on published data, the drug can be used at any time in pregnancy.
Breastfeeding
Small amounts of all the above drugs are probably excreted into breast milk if they are used close to breastfeeding. Most can probably be used during breastfeeding, but there are no data for any of these agents. The safest decision is to not use these drugs when breastfeeding.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
There are three general classes of antifungal agents (number of agents): azole antifungals (9), echinocandins (3), and polyenes (5). The azole antifungals contain an azole ring and inhibit a wide range of fungi. Echinocandins target the fungal cell wall and the polyenes increase the fungal membrane permeability and lead to cell death.
Pregnancy
Azole antifungals inhibit the growth of fungi. Their trade names and molecular weights:
- Clotrimazole (Mycelex), an over-the-counter product, is available as a topical cream. Several studies have found no association between the drug and birth defects.
- Fluconazole (Diflucan) is a teratogen when doses of ≥400 mg/day are used during the first trimester. Smaller doses do not appear to cause embryo/fetal harm.
- Isavuconazonium (Cresemba) if used in pregnancy, exposure of the embryo/fetus would probably be low based on the >99% plasma protein binding, but the plasma half-life is 130 hours. Moreover, the drug is a potent animal teratogen and is best avoided in pregnancy.
- Itraconazole (Onmel, Sporanox, Tolsura), has a low risk, if any, of structural defects, according to what reported human experience suggests.
- Ketoconazole (Xolegel, Extina, Nizoral; 531) does not appear to adversely effect embryos and fetuses, but the human data are very limited. As with any drug, avoiding organogenesis is the best recommendation.
- Miconazole (Oravig) is usually used topically. Small amounts are absorbed from the vagina. The available evidence suggests that the drug does not increase the risk of congenital malformations.
- Posaconazole (Noxafil) does not have reported use in human pregnancy. The animal reproduction data suggest risk. Based on its molecular weight (about 701), the drug will most likely cross the placenta to the embryo/fetus. Thus, the best course is to avoid the drug during pregnancy, especially in the first trimester.
- Voriconazole (Vfend) has one human report of the drug use in pregnancy. The drug was started at about 19 weeks and continued until the woman gave birth at 35 weeks to a healthy male baby. At 6 months of age, the baby remained normal.
Echinocandin antifungals target the fungal cell wall by inhibiting its synthesis. Their trade names and molecular weights:
- Anidulafungin (Eraxis; 1,140) has no published human data. It is indicated for the treatment of candidemia and other forms of Candida infections. The animal data suggest low risk.
- Caspofungin (Cancidas; 1,213) has no published human data. It is indicated for presumed fungal infections in febrile, neutropenic patients. The animal data are suggestive of human risk, especially if exposure occurs in the first trimester. If possible, maternal treatment should be avoided in the first trimester.
- Micafungin (Mycamine; 1,292) has no published human data. It is indicated for the treatment of patients with esophageal candidiasis and for the prophylaxis of Candida infections in patients undergoing hematopoietic stem cell transplantation. The animal data in one species suggest high risk. If possible, maternal treatment should be avoided in the first trimester.
Polyene antifungals cause depolarization of the fungal cell membrane to increase the membrane permeability, which leads to cell death. Their trade names and molecular weights:
- Amphotericin b (Amphocin; Fungizone; 924) There are three other amphotericin agents: amphotericin b cholesteryl sulfate (Amphotec); amphotericin b lipid complex (Abelcet); amphotericin b liposomal (AmBisome). No reports linking amphotericin b with congenital defects have been found. The drug does cross the human placenta. Although there was a higher rate of spontaneous abortions in rabbits given amphotericin b, there was no fetal harm in rats and rabbits when given amphotericin b lipid complex.
- Nystatin (Bio-Statin; Mycostatin; Nilstat; 926). The drug does not appear to cause embryo-fetal harm. Based on published data, the drug can be used at any time in pregnancy.
Breastfeeding
Small amounts of all the above drugs are probably excreted into breast milk if they are used close to breastfeeding. Most can probably be used during breastfeeding, but there are no data for any of these agents. The safest decision is to not use these drugs when breastfeeding.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
There are three general classes of antifungal agents (number of agents): azole antifungals (9), echinocandins (3), and polyenes (5). The azole antifungals contain an azole ring and inhibit a wide range of fungi. Echinocandins target the fungal cell wall and the polyenes increase the fungal membrane permeability and lead to cell death.
Pregnancy
Azole antifungals inhibit the growth of fungi. Their trade names and molecular weights:
- Clotrimazole (Mycelex), an over-the-counter product, is available as a topical cream. Several studies have found no association between the drug and birth defects.
- Fluconazole (Diflucan) is a teratogen when doses of ≥400 mg/day are used during the first trimester. Smaller doses do not appear to cause embryo/fetal harm.
- Isavuconazonium (Cresemba) if used in pregnancy, exposure of the embryo/fetus would probably be low based on the >99% plasma protein binding, but the plasma half-life is 130 hours. Moreover, the drug is a potent animal teratogen and is best avoided in pregnancy.
- Itraconazole (Onmel, Sporanox, Tolsura), has a low risk, if any, of structural defects, according to what reported human experience suggests.
- Ketoconazole (Xolegel, Extina, Nizoral; 531) does not appear to adversely effect embryos and fetuses, but the human data are very limited. As with any drug, avoiding organogenesis is the best recommendation.
- Miconazole (Oravig) is usually used topically. Small amounts are absorbed from the vagina. The available evidence suggests that the drug does not increase the risk of congenital malformations.
- Posaconazole (Noxafil) does not have reported use in human pregnancy. The animal reproduction data suggest risk. Based on its molecular weight (about 701), the drug will most likely cross the placenta to the embryo/fetus. Thus, the best course is to avoid the drug during pregnancy, especially in the first trimester.
- Voriconazole (Vfend) has one human report of the drug use in pregnancy. The drug was started at about 19 weeks and continued until the woman gave birth at 35 weeks to a healthy male baby. At 6 months of age, the baby remained normal.
Echinocandin antifungals target the fungal cell wall by inhibiting its synthesis. Their trade names and molecular weights:
- Anidulafungin (Eraxis; 1,140) has no published human data. It is indicated for the treatment of candidemia and other forms of Candida infections. The animal data suggest low risk.
- Caspofungin (Cancidas; 1,213) has no published human data. It is indicated for presumed fungal infections in febrile, neutropenic patients. The animal data are suggestive of human risk, especially if exposure occurs in the first trimester. If possible, maternal treatment should be avoided in the first trimester.
- Micafungin (Mycamine; 1,292) has no published human data. It is indicated for the treatment of patients with esophageal candidiasis and for the prophylaxis of Candida infections in patients undergoing hematopoietic stem cell transplantation. The animal data in one species suggest high risk. If possible, maternal treatment should be avoided in the first trimester.
Polyene antifungals cause depolarization of the fungal cell membrane to increase the membrane permeability, which leads to cell death. Their trade names and molecular weights:
- Amphotericin b (Amphocin; Fungizone; 924) There are three other amphotericin agents: amphotericin b cholesteryl sulfate (Amphotec); amphotericin b lipid complex (Abelcet); amphotericin b liposomal (AmBisome). No reports linking amphotericin b with congenital defects have been found. The drug does cross the human placenta. Although there was a higher rate of spontaneous abortions in rabbits given amphotericin b, there was no fetal harm in rats and rabbits when given amphotericin b lipid complex.
- Nystatin (Bio-Statin; Mycostatin; Nilstat; 926). The drug does not appear to cause embryo-fetal harm. Based on published data, the drug can be used at any time in pregnancy.
Breastfeeding
Small amounts of all the above drugs are probably excreted into breast milk if they are used close to breastfeeding. Most can probably be used during breastfeeding, but there are no data for any of these agents. The safest decision is to not use these drugs when breastfeeding.
Mr. Briggs is clinical professor of pharmacy at the University of California, San Francisco, and adjunct professor of pharmacy at the University of Southern California, Los Angeles, as well as at Washington State University, Spokane. Mr. Briggs said he had no relevant financial disclosures. Email him at [email protected].
Study shows how COVID-19 disrupted RA meds
During the first 3 months of the COVID-19 pandemic last year, about one-third of people with rheumatoid arthritis in the United States made changes in their RA medications, and, before the American College of Rheumatology tweaked its guidelines midway through that period, they were about twice as likely to make medication changes on their own than before the pandemic, according to an analysis of data in FORWARD, the National Databank for Rheumatic Diseases.
The study, published in Arthritis Care & Research, also found that about 10% of RA patients on hydroxychloroquine lost access to the drug at a time it was drawing interest as a treatment for COVID-19. Another finding was that a high percentage of patients on non–tumor necrosis factor biologic disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase (JAK) inhibitors canceled or postponed appointments.
“Our results show that persons with RA who had medication changes in the first 3 months of the COVID-19 pandemic in the U.S. were more likely to have worse disease activity and higher exposure to prior DMARDs, but no statistical difference was found in terms of comorbidities,” first author Kaleb Michaud, PhD, and coauthors wrote. Dr. Michaud is with the National Databank for Rheumatic Diseases, Wichita, Kan., and the University of Nebraska Medical Center, Omaha.
The study evaluated responses from 734 adults who participated in FORWARD, an observational, multidisease registry. They answered online surveys about COVID-19 in May 2020 and had provided data on their medication use before the pandemic. A total of 30% (n = 221) reported medication changes in that period.
Details on medication changes
Medication changers were more likely to use glucocorticoids (GCs) (32.6% vs. 18.1%) and less likely to use nonhydroxychloroquine conventional DMARDs (49.3% vs. 62%) pre-COVID. Changers also reported higher rates of economic hardship during the pandemic (22.6% vs. 14.6%).
In the midst of the study period, the ACR issued a clinical guideline for treatment of rheumatic and musculoskeletal diseases (RMDs), emphasizing the need to maintain DMARD therapy, control disease activity, and reduce prednisone/GC use. The guideline advised continuing hydroxychloroquine and interleukin-6 inhibitor biologics in people with suspected or confirmed COVID-19.
Dr. Michaud and coauthors acknowledged the ongoing lack of knowledge about real-world treatment patterns for RA during the pandemic. They set out with this study to fill those knowledge gaps.
They noted that patients on bDMARDs (17.6%) and JAK inhibitors (17.1%) were more than twice as likely to discontinue medications than were those on conventional DMARDs (8.2%).
Switching to telehealth was the most common pandemic-related behavior change among patients in all DMARD groups, with rates ranging from 31% to 47.1%, followed by canceling or postponing appointments, with rates ranging from 27.9% to 36.4% depending on the DMARD group.
The study also found that RA patients widely adopted the behavior changes that the Centers for Disease Control and Prevention recommended during the pandemic, although the rates of restricting social contacts were significantly lower than the 90% reported in an early Italian study.
Dr. Michaud and coauthors also provided some explanation of why people on GCs and DMARDs were more likely than others to change medication patterns. “This may reflect efforts to reduce the perceived risk of infections due to GCs as well as the likely less-controlled disease activity associated with GC use,” they wrote. While the ACR’s early pandemic guidance followed the 2015 guidelines – that patients should continue on GCs at the “lowest possible dose” and not stop them “abruptly” – most U.S. rheumatologists reported cutting back on GC use during the pandemic.
The researchers acknowledged that evidence linking GC use with hospitalization for COVID-19, which emerged after they had surveyed study participants, was consistent their findings, but that the overall risk of COVID-19 in RA patients still isn’t known.
Pfizer funded the analysis, and a coauthor is an employee of Pfizer.
During the first 3 months of the COVID-19 pandemic last year, about one-third of people with rheumatoid arthritis in the United States made changes in their RA medications, and, before the American College of Rheumatology tweaked its guidelines midway through that period, they were about twice as likely to make medication changes on their own than before the pandemic, according to an analysis of data in FORWARD, the National Databank for Rheumatic Diseases.
The study, published in Arthritis Care & Research, also found that about 10% of RA patients on hydroxychloroquine lost access to the drug at a time it was drawing interest as a treatment for COVID-19. Another finding was that a high percentage of patients on non–tumor necrosis factor biologic disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase (JAK) inhibitors canceled or postponed appointments.
“Our results show that persons with RA who had medication changes in the first 3 months of the COVID-19 pandemic in the U.S. were more likely to have worse disease activity and higher exposure to prior DMARDs, but no statistical difference was found in terms of comorbidities,” first author Kaleb Michaud, PhD, and coauthors wrote. Dr. Michaud is with the National Databank for Rheumatic Diseases, Wichita, Kan., and the University of Nebraska Medical Center, Omaha.
The study evaluated responses from 734 adults who participated in FORWARD, an observational, multidisease registry. They answered online surveys about COVID-19 in May 2020 and had provided data on their medication use before the pandemic. A total of 30% (n = 221) reported medication changes in that period.
Details on medication changes
Medication changers were more likely to use glucocorticoids (GCs) (32.6% vs. 18.1%) and less likely to use nonhydroxychloroquine conventional DMARDs (49.3% vs. 62%) pre-COVID. Changers also reported higher rates of economic hardship during the pandemic (22.6% vs. 14.6%).
In the midst of the study period, the ACR issued a clinical guideline for treatment of rheumatic and musculoskeletal diseases (RMDs), emphasizing the need to maintain DMARD therapy, control disease activity, and reduce prednisone/GC use. The guideline advised continuing hydroxychloroquine and interleukin-6 inhibitor biologics in people with suspected or confirmed COVID-19.
Dr. Michaud and coauthors acknowledged the ongoing lack of knowledge about real-world treatment patterns for RA during the pandemic. They set out with this study to fill those knowledge gaps.
They noted that patients on bDMARDs (17.6%) and JAK inhibitors (17.1%) were more than twice as likely to discontinue medications than were those on conventional DMARDs (8.2%).
Switching to telehealth was the most common pandemic-related behavior change among patients in all DMARD groups, with rates ranging from 31% to 47.1%, followed by canceling or postponing appointments, with rates ranging from 27.9% to 36.4% depending on the DMARD group.
The study also found that RA patients widely adopted the behavior changes that the Centers for Disease Control and Prevention recommended during the pandemic, although the rates of restricting social contacts were significantly lower than the 90% reported in an early Italian study.
Dr. Michaud and coauthors also provided some explanation of why people on GCs and DMARDs were more likely than others to change medication patterns. “This may reflect efforts to reduce the perceived risk of infections due to GCs as well as the likely less-controlled disease activity associated with GC use,” they wrote. While the ACR’s early pandemic guidance followed the 2015 guidelines – that patients should continue on GCs at the “lowest possible dose” and not stop them “abruptly” – most U.S. rheumatologists reported cutting back on GC use during the pandemic.
The researchers acknowledged that evidence linking GC use with hospitalization for COVID-19, which emerged after they had surveyed study participants, was consistent their findings, but that the overall risk of COVID-19 in RA patients still isn’t known.
Pfizer funded the analysis, and a coauthor is an employee of Pfizer.
During the first 3 months of the COVID-19 pandemic last year, about one-third of people with rheumatoid arthritis in the United States made changes in their RA medications, and, before the American College of Rheumatology tweaked its guidelines midway through that period, they were about twice as likely to make medication changes on their own than before the pandemic, according to an analysis of data in FORWARD, the National Databank for Rheumatic Diseases.
The study, published in Arthritis Care & Research, also found that about 10% of RA patients on hydroxychloroquine lost access to the drug at a time it was drawing interest as a treatment for COVID-19. Another finding was that a high percentage of patients on non–tumor necrosis factor biologic disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase (JAK) inhibitors canceled or postponed appointments.
“Our results show that persons with RA who had medication changes in the first 3 months of the COVID-19 pandemic in the U.S. were more likely to have worse disease activity and higher exposure to prior DMARDs, but no statistical difference was found in terms of comorbidities,” first author Kaleb Michaud, PhD, and coauthors wrote. Dr. Michaud is with the National Databank for Rheumatic Diseases, Wichita, Kan., and the University of Nebraska Medical Center, Omaha.
The study evaluated responses from 734 adults who participated in FORWARD, an observational, multidisease registry. They answered online surveys about COVID-19 in May 2020 and had provided data on their medication use before the pandemic. A total of 30% (n = 221) reported medication changes in that period.
Details on medication changes
Medication changers were more likely to use glucocorticoids (GCs) (32.6% vs. 18.1%) and less likely to use nonhydroxychloroquine conventional DMARDs (49.3% vs. 62%) pre-COVID. Changers also reported higher rates of economic hardship during the pandemic (22.6% vs. 14.6%).
In the midst of the study period, the ACR issued a clinical guideline for treatment of rheumatic and musculoskeletal diseases (RMDs), emphasizing the need to maintain DMARD therapy, control disease activity, and reduce prednisone/GC use. The guideline advised continuing hydroxychloroquine and interleukin-6 inhibitor biologics in people with suspected or confirmed COVID-19.
Dr. Michaud and coauthors acknowledged the ongoing lack of knowledge about real-world treatment patterns for RA during the pandemic. They set out with this study to fill those knowledge gaps.
They noted that patients on bDMARDs (17.6%) and JAK inhibitors (17.1%) were more than twice as likely to discontinue medications than were those on conventional DMARDs (8.2%).
Switching to telehealth was the most common pandemic-related behavior change among patients in all DMARD groups, with rates ranging from 31% to 47.1%, followed by canceling or postponing appointments, with rates ranging from 27.9% to 36.4% depending on the DMARD group.
The study also found that RA patients widely adopted the behavior changes that the Centers for Disease Control and Prevention recommended during the pandemic, although the rates of restricting social contacts were significantly lower than the 90% reported in an early Italian study.
Dr. Michaud and coauthors also provided some explanation of why people on GCs and DMARDs were more likely than others to change medication patterns. “This may reflect efforts to reduce the perceived risk of infections due to GCs as well as the likely less-controlled disease activity associated with GC use,” they wrote. While the ACR’s early pandemic guidance followed the 2015 guidelines – that patients should continue on GCs at the “lowest possible dose” and not stop them “abruptly” – most U.S. rheumatologists reported cutting back on GC use during the pandemic.
The researchers acknowledged that evidence linking GC use with hospitalization for COVID-19, which emerged after they had surveyed study participants, was consistent their findings, but that the overall risk of COVID-19 in RA patients still isn’t known.
Pfizer funded the analysis, and a coauthor is an employee of Pfizer.
FROM ARTHRITIS CARE & RESEARCH
Most patients with chronic inflammatory diseases have sufficient response to COVID-19 vaccination
Glucocorticoids and B-cell–depleting therapies are trouble spots
Although most patients with chronic inflammatory diseases mounted immune responses after two doses of mRNA-based COVID-19 vaccines, glucocorticoids and B-cell–depleting therapies markedly reduced the response, according to a recently published preprint of a new study.
The study, published on MedRxiv and not yet peer reviewed, involved a prospective look at 133 patients with chronic inflammatory disease (CID) and 53 patients with healthy immune systems at Washington University, St. Louis, and the University of California, San Francisco. It is regarded as the largest and most detailed study yet in how vaccines perform in people with immune-mediated inflammatory disease. The patients were enrolled between December 2020 and March 2021, and the most common diseases were inflammatory bowel disease (32%), rheumatoid arthritis (29%), spondyloarthritis (15%), and systemic lupus erythematosus (11%).
A ‘modest’ reduction in antibody response
Senior author Alfred Kim, MD, PhD, of the department of medicine at Washington University, said the overall results so far are encouraging.
“Most patients with an autoimmune disease that are on immunosuppression can mount antibody responses,” he said. “We’re seeing the majority of our subjects respond.”
The immune-healthy controls and most of the patients with CID had a robust immune response against the spike protein, although the CID group had a mean reduction in antibody titers that was three times lower than the controls (P = .0092). The CID group similarly had a 2.7-fold reduction in preventing neutralization, or halting the virus’ ability to infect (P < .0001), researchers reported.
This reduction in response is “modest,” he said.
“Is the level of reduction going to be detrimental for protection? Time will tell,” he said, adding that researchers anticipate that it won’t have a critical effect on protection because responses tended to be within the range of the immunocompetent controls, who themselves had wildly varied antibody titers across a 20-fold range. “ ‘Optimal’ isn’t necessarily the same as ‘sufficient.’ ”
Type of medication has big impact on antibody titers
But there was a wide variety of effects on the immune response depending on the medication. Glucorticoids resulted in a response that was 10 times lower than the immune-healthy controls, as well as fewer circulating plasmablasts after vaccination. Researchers found that 98% of controls were seropositive for antibody, compared with 92% of those with CID who were not taking prednisone, and 65% of CID patients on prednisone (P = .0006 and .0115, respectively). Prevention of neutralization of the virus was similarly reduced in those groups, compared with the controls. Dr. Kim noted this was a small sample size, with about 15 patients. These effects were seen regardless of the dose.
“We would’ve anticipated this would have been dose dependent, so this was a little bit surprising,” Dr. Kim said.
B-cell–depleting therapies, such as rituximab (Rituxan) and ocrelizumab (Ocrevus), reduced antibody titers by 36 times, compared with controls (P < .0001), with a similar reduction in preventing infection (P = .0066), the researchers found. The reduction in antibody titers was the most pronounced among those who had received B-cell–depleting therapies within the previous 6 months. Dr. Kim noted this was a small sample size, with about 10 patients.
CID study subjects taking an antimetabolite, including methotrexate, had an average of a two- to threefold reduction in antibody titers and in neutralization (P = .0006). This reduction was greatest with methotrexate, researchers found (P = .0027).
JAK inhibitors also significantly reduced antibody titers (P = .0066), but the reduction in neutralization of the virus was not significant. In addition, researchers found a reduction in antibody titers, the prevention of viral infection, and circulating plasmablasts among those on tumor necrosis factor (TNF) inhibitors, compared with controls, but these were insignificant statistically except for virus neutralization.
Dr. Kim said he hopes the glucocorticoid data spur physicians to try harder to wean patients off the drugs, when possible, in keeping with recommendations already in place.
“The general culture in rheumatology has been very lax about the need to reduce glucocorticoids,” he said. “This reinvigorates that call.” Questions about possible drug holidays from glucocorticoids remain, regarding how long a holiday would be needed, he said. He noted that many patients on glucocorticoids nonetheless mounted responses.
Those on B-cell–depleting therapies present a “much more difficult” question, he said. Some patients possibly could wait a bit longer than their normal, every-6-month schedule, but it’s an individual decision, he said. Since a booster of influenza vaccine has been found to enhance the response even within the 6-month window among ocrelizumab patients, a booster of COVID-19 vaccine might also help, although this remains to be studied.
The study group has already increased its sample size and is looking at adverse reactions and long-term immune responses, Dr. Kim said.
Encouraging, rather than discouraging, results
Leonard Calabrese, DO, professor of medicine at the Cleveland Clinic in Ohio, said the findings shouldn’t discourage clinicians from encouraging vaccination.
“There’s still a preponderance of people who will develop a robust antibody vaccine response,” he said.
He cautioned that the findings look only at antibodies to the spike protein and at plasmablasts. The reduction in these titers is “of concern,” he said, but “we don’t really know with certainty what are the effects of these drugs, and these data are on the overall biologic protective effect of the vaccine. There’s much more to a vaccine response than anti–spike protein and plasmablasts,” including cell-mediated immune response.
For an individual patient, the findings “mean a lot,” he said.
“I think that people who are on significant prednisone and B-cell–depleting agents, I think you have to share with them that there’s a reasonable chance that you’re not going to be making a response similar to healthy people,” he said. “Thus, even with your vaccine, we’re not going to cut you loose to do things that are violating social distancing and group settings. … Should you be hugging your grandchildren if you’re a rituximab vaccine recipient? I think I would wait until we have a little bit more data.”
Kevin Winthrop, MD, MPH, professor of ophthalmology at Oregon Health & Science University, Portland, where he studies vaccinations in the immunocompromised, said that glucocorticoids tend to have little effect on vaccinations generally at low doses.
When effects are seen they can be difficult to interpret, he said.
“It’s hard to extricate that from the effect of the underlying disease,” he said. The drug can be a proxy for worse disease control.
Although it’s a small study, it’s reassuring that overall the responses were similar to healthy controls.
For B-cell–depleting therapies, his usual guidance is to not give vaccine until a patient is at least 3 months out from their last dose, and not to restart until at least 2 weeks after vaccination.
“It’s not surprising that some of these DMARDs [disease-modifying antirheumatic drugs] do negatively affect vaccine response, particularly B-cell–depletion therapy. We need to do some studies to find a way to overcome that, or optimize delivery of the vaccine.”
Dr. Kim reported participating in consulting, advisory board, or speaker’s bureau for Alexion, Aurinia, Annexon Biosciences, Exagen Diagnostics, and GlaxoSmithKline, and receiving funding under a sponsored research agreement unrelated to the data in the paper from GlaxoSmithKline. Dr. Winthrop reported receiving consulting fees from Pfizer, AbbVie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Bristol-Myers Squibb, Regeneron, Sanofi, AstraZeneca, Novartis, and research grants from Bristol-Myers Squibb and Pfizer. Dr. Calabrese reported no relevant disclosures.
Glucocorticoids and B-cell–depleting therapies are trouble spots
Glucocorticoids and B-cell–depleting therapies are trouble spots
Although most patients with chronic inflammatory diseases mounted immune responses after two doses of mRNA-based COVID-19 vaccines, glucocorticoids and B-cell–depleting therapies markedly reduced the response, according to a recently published preprint of a new study.
The study, published on MedRxiv and not yet peer reviewed, involved a prospective look at 133 patients with chronic inflammatory disease (CID) and 53 patients with healthy immune systems at Washington University, St. Louis, and the University of California, San Francisco. It is regarded as the largest and most detailed study yet in how vaccines perform in people with immune-mediated inflammatory disease. The patients were enrolled between December 2020 and March 2021, and the most common diseases were inflammatory bowel disease (32%), rheumatoid arthritis (29%), spondyloarthritis (15%), and systemic lupus erythematosus (11%).
A ‘modest’ reduction in antibody response
Senior author Alfred Kim, MD, PhD, of the department of medicine at Washington University, said the overall results so far are encouraging.
“Most patients with an autoimmune disease that are on immunosuppression can mount antibody responses,” he said. “We’re seeing the majority of our subjects respond.”
The immune-healthy controls and most of the patients with CID had a robust immune response against the spike protein, although the CID group had a mean reduction in antibody titers that was three times lower than the controls (P = .0092). The CID group similarly had a 2.7-fold reduction in preventing neutralization, or halting the virus’ ability to infect (P < .0001), researchers reported.
This reduction in response is “modest,” he said.
“Is the level of reduction going to be detrimental for protection? Time will tell,” he said, adding that researchers anticipate that it won’t have a critical effect on protection because responses tended to be within the range of the immunocompetent controls, who themselves had wildly varied antibody titers across a 20-fold range. “ ‘Optimal’ isn’t necessarily the same as ‘sufficient.’ ”
Type of medication has big impact on antibody titers
But there was a wide variety of effects on the immune response depending on the medication. Glucorticoids resulted in a response that was 10 times lower than the immune-healthy controls, as well as fewer circulating plasmablasts after vaccination. Researchers found that 98% of controls were seropositive for antibody, compared with 92% of those with CID who were not taking prednisone, and 65% of CID patients on prednisone (P = .0006 and .0115, respectively). Prevention of neutralization of the virus was similarly reduced in those groups, compared with the controls. Dr. Kim noted this was a small sample size, with about 15 patients. These effects were seen regardless of the dose.
“We would’ve anticipated this would have been dose dependent, so this was a little bit surprising,” Dr. Kim said.
B-cell–depleting therapies, such as rituximab (Rituxan) and ocrelizumab (Ocrevus), reduced antibody titers by 36 times, compared with controls (P < .0001), with a similar reduction in preventing infection (P = .0066), the researchers found. The reduction in antibody titers was the most pronounced among those who had received B-cell–depleting therapies within the previous 6 months. Dr. Kim noted this was a small sample size, with about 10 patients.
CID study subjects taking an antimetabolite, including methotrexate, had an average of a two- to threefold reduction in antibody titers and in neutralization (P = .0006). This reduction was greatest with methotrexate, researchers found (P = .0027).
JAK inhibitors also significantly reduced antibody titers (P = .0066), but the reduction in neutralization of the virus was not significant. In addition, researchers found a reduction in antibody titers, the prevention of viral infection, and circulating plasmablasts among those on tumor necrosis factor (TNF) inhibitors, compared with controls, but these were insignificant statistically except for virus neutralization.
Dr. Kim said he hopes the glucocorticoid data spur physicians to try harder to wean patients off the drugs, when possible, in keeping with recommendations already in place.
“The general culture in rheumatology has been very lax about the need to reduce glucocorticoids,” he said. “This reinvigorates that call.” Questions about possible drug holidays from glucocorticoids remain, regarding how long a holiday would be needed, he said. He noted that many patients on glucocorticoids nonetheless mounted responses.
Those on B-cell–depleting therapies present a “much more difficult” question, he said. Some patients possibly could wait a bit longer than their normal, every-6-month schedule, but it’s an individual decision, he said. Since a booster of influenza vaccine has been found to enhance the response even within the 6-month window among ocrelizumab patients, a booster of COVID-19 vaccine might also help, although this remains to be studied.
The study group has already increased its sample size and is looking at adverse reactions and long-term immune responses, Dr. Kim said.
Encouraging, rather than discouraging, results
Leonard Calabrese, DO, professor of medicine at the Cleveland Clinic in Ohio, said the findings shouldn’t discourage clinicians from encouraging vaccination.
“There’s still a preponderance of people who will develop a robust antibody vaccine response,” he said.
He cautioned that the findings look only at antibodies to the spike protein and at plasmablasts. The reduction in these titers is “of concern,” he said, but “we don’t really know with certainty what are the effects of these drugs, and these data are on the overall biologic protective effect of the vaccine. There’s much more to a vaccine response than anti–spike protein and plasmablasts,” including cell-mediated immune response.
For an individual patient, the findings “mean a lot,” he said.
“I think that people who are on significant prednisone and B-cell–depleting agents, I think you have to share with them that there’s a reasonable chance that you’re not going to be making a response similar to healthy people,” he said. “Thus, even with your vaccine, we’re not going to cut you loose to do things that are violating social distancing and group settings. … Should you be hugging your grandchildren if you’re a rituximab vaccine recipient? I think I would wait until we have a little bit more data.”
Kevin Winthrop, MD, MPH, professor of ophthalmology at Oregon Health & Science University, Portland, where he studies vaccinations in the immunocompromised, said that glucocorticoids tend to have little effect on vaccinations generally at low doses.
When effects are seen they can be difficult to interpret, he said.
“It’s hard to extricate that from the effect of the underlying disease,” he said. The drug can be a proxy for worse disease control.
Although it’s a small study, it’s reassuring that overall the responses were similar to healthy controls.
For B-cell–depleting therapies, his usual guidance is to not give vaccine until a patient is at least 3 months out from their last dose, and not to restart until at least 2 weeks after vaccination.
“It’s not surprising that some of these DMARDs [disease-modifying antirheumatic drugs] do negatively affect vaccine response, particularly B-cell–depletion therapy. We need to do some studies to find a way to overcome that, or optimize delivery of the vaccine.”
Dr. Kim reported participating in consulting, advisory board, or speaker’s bureau for Alexion, Aurinia, Annexon Biosciences, Exagen Diagnostics, and GlaxoSmithKline, and receiving funding under a sponsored research agreement unrelated to the data in the paper from GlaxoSmithKline. Dr. Winthrop reported receiving consulting fees from Pfizer, AbbVie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Bristol-Myers Squibb, Regeneron, Sanofi, AstraZeneca, Novartis, and research grants from Bristol-Myers Squibb and Pfizer. Dr. Calabrese reported no relevant disclosures.
Although most patients with chronic inflammatory diseases mounted immune responses after two doses of mRNA-based COVID-19 vaccines, glucocorticoids and B-cell–depleting therapies markedly reduced the response, according to a recently published preprint of a new study.
The study, published on MedRxiv and not yet peer reviewed, involved a prospective look at 133 patients with chronic inflammatory disease (CID) and 53 patients with healthy immune systems at Washington University, St. Louis, and the University of California, San Francisco. It is regarded as the largest and most detailed study yet in how vaccines perform in people with immune-mediated inflammatory disease. The patients were enrolled between December 2020 and March 2021, and the most common diseases were inflammatory bowel disease (32%), rheumatoid arthritis (29%), spondyloarthritis (15%), and systemic lupus erythematosus (11%).
A ‘modest’ reduction in antibody response
Senior author Alfred Kim, MD, PhD, of the department of medicine at Washington University, said the overall results so far are encouraging.
“Most patients with an autoimmune disease that are on immunosuppression can mount antibody responses,” he said. “We’re seeing the majority of our subjects respond.”
The immune-healthy controls and most of the patients with CID had a robust immune response against the spike protein, although the CID group had a mean reduction in antibody titers that was three times lower than the controls (P = .0092). The CID group similarly had a 2.7-fold reduction in preventing neutralization, or halting the virus’ ability to infect (P < .0001), researchers reported.
This reduction in response is “modest,” he said.
“Is the level of reduction going to be detrimental for protection? Time will tell,” he said, adding that researchers anticipate that it won’t have a critical effect on protection because responses tended to be within the range of the immunocompetent controls, who themselves had wildly varied antibody titers across a 20-fold range. “ ‘Optimal’ isn’t necessarily the same as ‘sufficient.’ ”
Type of medication has big impact on antibody titers
But there was a wide variety of effects on the immune response depending on the medication. Glucorticoids resulted in a response that was 10 times lower than the immune-healthy controls, as well as fewer circulating plasmablasts after vaccination. Researchers found that 98% of controls were seropositive for antibody, compared with 92% of those with CID who were not taking prednisone, and 65% of CID patients on prednisone (P = .0006 and .0115, respectively). Prevention of neutralization of the virus was similarly reduced in those groups, compared with the controls. Dr. Kim noted this was a small sample size, with about 15 patients. These effects were seen regardless of the dose.
“We would’ve anticipated this would have been dose dependent, so this was a little bit surprising,” Dr. Kim said.
B-cell–depleting therapies, such as rituximab (Rituxan) and ocrelizumab (Ocrevus), reduced antibody titers by 36 times, compared with controls (P < .0001), with a similar reduction in preventing infection (P = .0066), the researchers found. The reduction in antibody titers was the most pronounced among those who had received B-cell–depleting therapies within the previous 6 months. Dr. Kim noted this was a small sample size, with about 10 patients.
CID study subjects taking an antimetabolite, including methotrexate, had an average of a two- to threefold reduction in antibody titers and in neutralization (P = .0006). This reduction was greatest with methotrexate, researchers found (P = .0027).
JAK inhibitors also significantly reduced antibody titers (P = .0066), but the reduction in neutralization of the virus was not significant. In addition, researchers found a reduction in antibody titers, the prevention of viral infection, and circulating plasmablasts among those on tumor necrosis factor (TNF) inhibitors, compared with controls, but these were insignificant statistically except for virus neutralization.
Dr. Kim said he hopes the glucocorticoid data spur physicians to try harder to wean patients off the drugs, when possible, in keeping with recommendations already in place.
“The general culture in rheumatology has been very lax about the need to reduce glucocorticoids,” he said. “This reinvigorates that call.” Questions about possible drug holidays from glucocorticoids remain, regarding how long a holiday would be needed, he said. He noted that many patients on glucocorticoids nonetheless mounted responses.
Those on B-cell–depleting therapies present a “much more difficult” question, he said. Some patients possibly could wait a bit longer than their normal, every-6-month schedule, but it’s an individual decision, he said. Since a booster of influenza vaccine has been found to enhance the response even within the 6-month window among ocrelizumab patients, a booster of COVID-19 vaccine might also help, although this remains to be studied.
The study group has already increased its sample size and is looking at adverse reactions and long-term immune responses, Dr. Kim said.
Encouraging, rather than discouraging, results
Leonard Calabrese, DO, professor of medicine at the Cleveland Clinic in Ohio, said the findings shouldn’t discourage clinicians from encouraging vaccination.
“There’s still a preponderance of people who will develop a robust antibody vaccine response,” he said.
He cautioned that the findings look only at antibodies to the spike protein and at plasmablasts. The reduction in these titers is “of concern,” he said, but “we don’t really know with certainty what are the effects of these drugs, and these data are on the overall biologic protective effect of the vaccine. There’s much more to a vaccine response than anti–spike protein and plasmablasts,” including cell-mediated immune response.
For an individual patient, the findings “mean a lot,” he said.
“I think that people who are on significant prednisone and B-cell–depleting agents, I think you have to share with them that there’s a reasonable chance that you’re not going to be making a response similar to healthy people,” he said. “Thus, even with your vaccine, we’re not going to cut you loose to do things that are violating social distancing and group settings. … Should you be hugging your grandchildren if you’re a rituximab vaccine recipient? I think I would wait until we have a little bit more data.”
Kevin Winthrop, MD, MPH, professor of ophthalmology at Oregon Health & Science University, Portland, where he studies vaccinations in the immunocompromised, said that glucocorticoids tend to have little effect on vaccinations generally at low doses.
When effects are seen they can be difficult to interpret, he said.
“It’s hard to extricate that from the effect of the underlying disease,” he said. The drug can be a proxy for worse disease control.
Although it’s a small study, it’s reassuring that overall the responses were similar to healthy controls.
For B-cell–depleting therapies, his usual guidance is to not give vaccine until a patient is at least 3 months out from their last dose, and not to restart until at least 2 weeks after vaccination.
“It’s not surprising that some of these DMARDs [disease-modifying antirheumatic drugs] do negatively affect vaccine response, particularly B-cell–depletion therapy. We need to do some studies to find a way to overcome that, or optimize delivery of the vaccine.”
Dr. Kim reported participating in consulting, advisory board, or speaker’s bureau for Alexion, Aurinia, Annexon Biosciences, Exagen Diagnostics, and GlaxoSmithKline, and receiving funding under a sponsored research agreement unrelated to the data in the paper from GlaxoSmithKline. Dr. Winthrop reported receiving consulting fees from Pfizer, AbbVie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Bristol-Myers Squibb, Regeneron, Sanofi, AstraZeneca, Novartis, and research grants from Bristol-Myers Squibb and Pfizer. Dr. Calabrese reported no relevant disclosures.
FROM MEDRXIV
Oral contraceptive with new estrogen earns approval
The Food and Drug Administration has approved a new estrogen for the first time in more than 50 years.
The novel combined oral contraceptive, marketed as Nextstellis, contains 3 mg drospirenone (DRSP) and 14.2 mg of estetrol (E4) in tablet form. Estetrol is an estrogen that is naturally produced during pregnancy, but will now be produced from a plant source; it has not previously been used in oral contraceptives.
Approval of the unique estetrol/drospirenone combination was based on data from a pair of phase 3 clinical trials including 3,725 women. Overall, Nextstellis was safe and effective while meeting its primary endpoint of pregnancy prevention, according to a company press release. Participants also reported favorable results on secondary endpoints including cycle control, bleeding profile, safety, and tolerability.
Although many women take short-acting contraceptives containing estrogen and progestin, concerns persist about side effects, said Mitchell Creinin, MD, of the University of California, in the press release. In addition to providing effective contraception, the drug showed minimal impact on specific markers of concern, including triglycerides, cholesterol, and glucose, as well as weight and endocrine markers, Dr. Creinin said.
Nextstellis was developed by the Belgian biotech company Mithra Pharmaceuticals, and the drug is licensed for distribution in Australia and the United States by Mayne Pharma, with an expected launch at the end of June 2021.
The Food and Drug Administration has approved a new estrogen for the first time in more than 50 years.
The novel combined oral contraceptive, marketed as Nextstellis, contains 3 mg drospirenone (DRSP) and 14.2 mg of estetrol (E4) in tablet form. Estetrol is an estrogen that is naturally produced during pregnancy, but will now be produced from a plant source; it has not previously been used in oral contraceptives.
Approval of the unique estetrol/drospirenone combination was based on data from a pair of phase 3 clinical trials including 3,725 women. Overall, Nextstellis was safe and effective while meeting its primary endpoint of pregnancy prevention, according to a company press release. Participants also reported favorable results on secondary endpoints including cycle control, bleeding profile, safety, and tolerability.
Although many women take short-acting contraceptives containing estrogen and progestin, concerns persist about side effects, said Mitchell Creinin, MD, of the University of California, in the press release. In addition to providing effective contraception, the drug showed minimal impact on specific markers of concern, including triglycerides, cholesterol, and glucose, as well as weight and endocrine markers, Dr. Creinin said.
Nextstellis was developed by the Belgian biotech company Mithra Pharmaceuticals, and the drug is licensed for distribution in Australia and the United States by Mayne Pharma, with an expected launch at the end of June 2021.
The Food and Drug Administration has approved a new estrogen for the first time in more than 50 years.
The novel combined oral contraceptive, marketed as Nextstellis, contains 3 mg drospirenone (DRSP) and 14.2 mg of estetrol (E4) in tablet form. Estetrol is an estrogen that is naturally produced during pregnancy, but will now be produced from a plant source; it has not previously been used in oral contraceptives.
Approval of the unique estetrol/drospirenone combination was based on data from a pair of phase 3 clinical trials including 3,725 women. Overall, Nextstellis was safe and effective while meeting its primary endpoint of pregnancy prevention, according to a company press release. Participants also reported favorable results on secondary endpoints including cycle control, bleeding profile, safety, and tolerability.
Although many women take short-acting contraceptives containing estrogen and progestin, concerns persist about side effects, said Mitchell Creinin, MD, of the University of California, in the press release. In addition to providing effective contraception, the drug showed minimal impact on specific markers of concern, including triglycerides, cholesterol, and glucose, as well as weight and endocrine markers, Dr. Creinin said.
Nextstellis was developed by the Belgian biotech company Mithra Pharmaceuticals, and the drug is licensed for distribution in Australia and the United States by Mayne Pharma, with an expected launch at the end of June 2021.