User login
Fever following cesarean delivery: What are your steps for management?
CASE Woman who has undergone recent cesarean delivery
A 23-year-old woman had a primary cesarean delivery 72 hours ago due to an arrest of dilation at 6 cm. She was in labor for 22 hours, and her membranes were ruptured for 18 hours. She had 10 internal vaginal examinations, and the duration of internal fetal monitoring was 12 hours; 24 hours after delivery, she developed a fever of 39°C, in association with lower abdominal pain and tenderness. She was presumptively treated for endometritis with cefepime; 48 hours after the initiation of antibiotics, she remains febrile and symptomatic.
- What are the most likely causes of her persistent fever?
- What should be the next steps in her evaluation?
Cesarean delivery background
Cesarean delivery is now the most common major operation performed in US hospitals. Cesarean delivery rates hover between 25% and 30% in most medical centers in the United States.1 The most common postoperative complication of cesarean delivery is infection. Infection typically takes 1 of 3 forms: endometritis (organ space infection), wound infection (surgical site infection), and urinary tract infection (UTI).1 This article will review the initial differential diagnosis, evaluation, and management of the patient with a postoperative fever and also will describe the appropriate assessment and treatment of the patient who has a persistent postoperative fever despite therapy. The article will also highlight key interventions that help to prevent postoperative infections.
Initial evaluation of the febrile patient
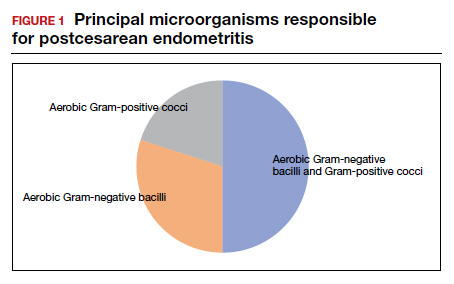
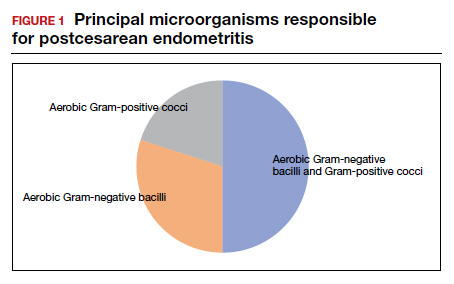
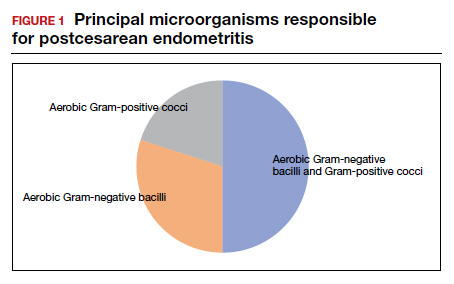
In the first 24 to 48 hours after cesarean delivery, the most common cause of fever is endometritis (organ space infection). This condition is a polymicrobial, mixed aerobic-anaerobic infection (FIGURE). The principal pathogens include anaerobic gram-positive cocci (
The major risk factors for postcesarean endometritis are extended duration of labor and ruptured membranes, multiple internal vaginal examinations, invasive fetal monitoring, and pre-existing colonization with group B Streptococcus and/or the organisms that cause bacterial vaginosis. Affected patients typically have a fever in the range of 38 to 39°C, tachycardia, mild tachypnea, lower abdominal pain and tenderness, and purulent lochia in some individuals.1
Differential for postoperative fever
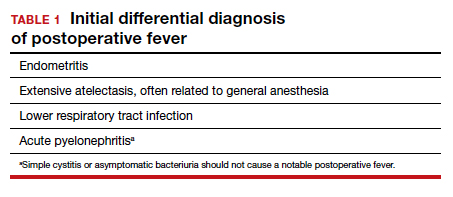
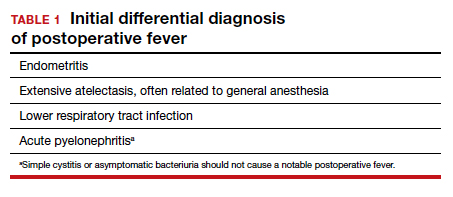
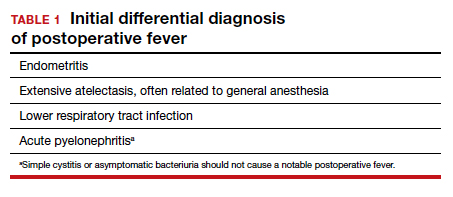
The initial differential diagnosis of postoperative fever is relatively limited (TABLE 1). In addition to endometritis, it includes extensive atelectasis, perhaps resulting from general anesthesia; lower respiratory tract infection, either viral influenza or bacterial pneumonia; and acute pyelonephritis. A simple infection of the bladder (cystitis or asymptomatic bacteriuria) should not cause a substantial temperature elevation and systemic symptoms.1
Differentiation between these entities usually is possible based on physical examination and a few laboratory tests. The peripheral white blood cell count usually is elevated, and a left shift may be evident. If a respiratory tract infection is suspected, chest radiography is indicated. A urine culture should be obtained if acute pyelonephritis strongly is considered. Lower genital tract cultures are rarely of value, and uncontaminated upper tract cultures are difficult to obtain. I do not believe that blood cultures should be performed as a matter of routine. They are expensive, and the results are often not available until after the patient has cleared her infection and left the hospital. However, I would obtain blood cultures in patients who meet one of these criteria1,2:
- They are immunocompromised (eg, HIV infection).
- They have a cardiac or vascular prosthesis and, thus, are at increased risk of complications related to bacteremia.
- They seem critically ill at the onset of evaluation.
- They fail to respond appropriately to initial therapy.
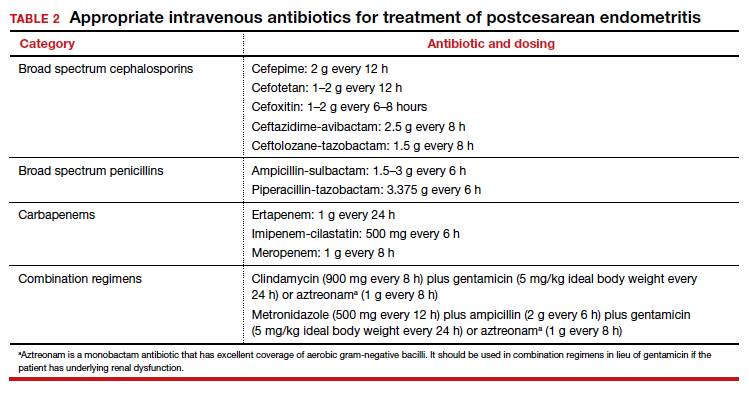
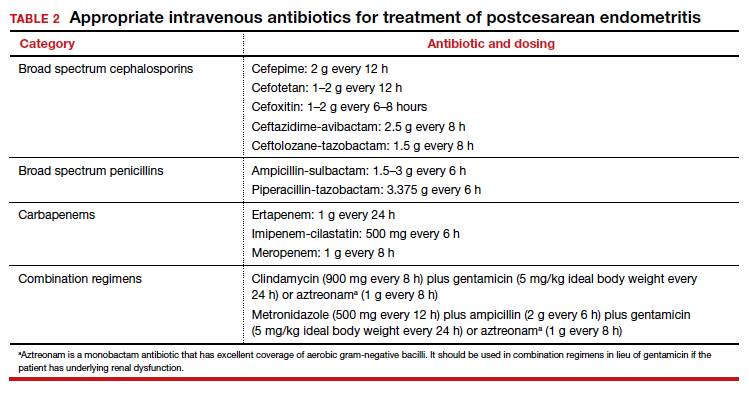
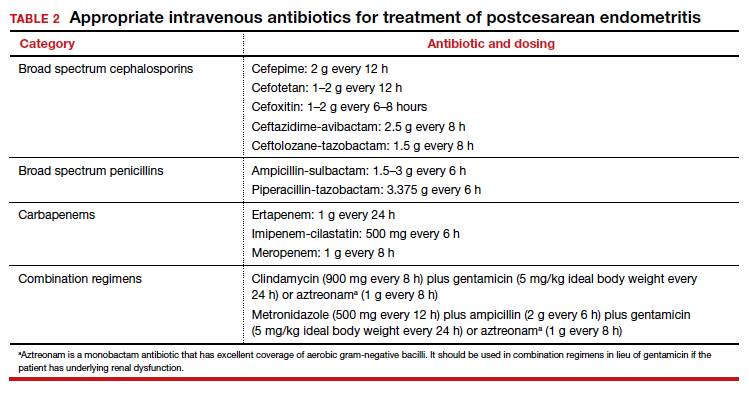
The cornerstone of therapy is broad spectrum antibiotics that target the multiple organisms responsible for endometritis.3 There are several single agents and several combination antibiotic regimens that provide excellent coverage against the usual pelvic pathogens (TABLE 2). I personally favor the generic combination regimen (clindamycin plus gentamicin) because it is relatively inexpensive and has been very well validated in multiple studies. In patients who have underlying renal dysfunction, aztreonam can be substituted for gentamicin.
Approximately 90% of patients will show clear evidence of clinical improvement (ie, decrease in temperature and resolution of abdominopelvic pain) within 48 hours of starting antibiotics. Patients should then continue therapy until they have been afebrile and asymptomatic for approximately 24 hours. At that point, antibiotics should be discontinued, and the patient can be discharged. With rare exceptions, there is no indication for administration of oral antibiotics on an outpatient basis.1,4
Continue to: Persistent postoperative fever...
Persistent postoperative fever
Resistant microorganism
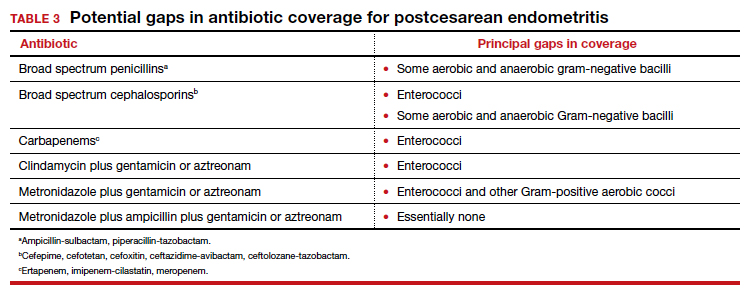
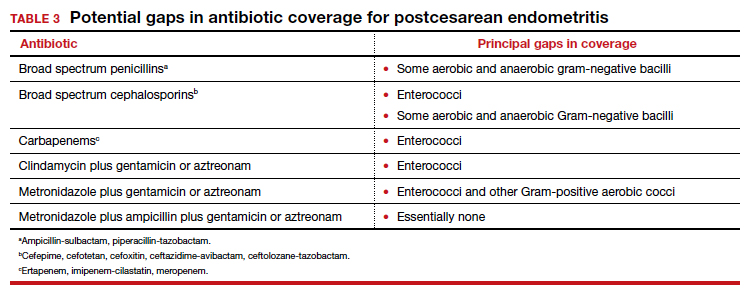
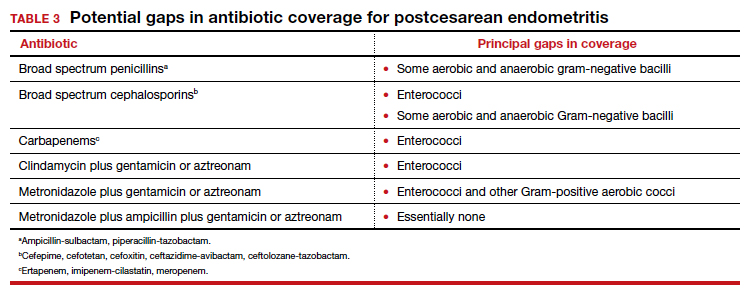
The most common cause of a persistent fever after initiating antibiotic therapy is a resistant microorganism. There are potential gaps in coverage for the antibiotic regimens commonly used to treat postcesarean endometritis (TABLE 3).1,4 Assuming there is no other obvious cause for treatment failure, I recommend that therapy be changed to the triple combination of metronidazole plus ampicillin plus gentamicin (or aztreonam). The first drug provides superb coverage against anaerobes; the second covers enterococci. Gentamicin or aztreonam cover virtually all aerobic Gram-negative bacilli likely to cause postcesarean infection. I prefer metronidazole rather than clindamycin in this regimen because, unlike clindamycin, it is less likely to trigger diarrhea when used in combination with ampicillin. The 3-drug regimen should be continued until the patient has been afebrile and asymptomatic for approximately 24 hours.1,3,4
Wound infection
The second most common reason for a poor response to initial antibiotic therapy is a wound (surgical site) infection. Wound infections are caused by many of the same pelvic pathogens responsible for endometritis combined with skin flora, notably Streptococcus and Staphylococcus species, including methicillin-resistant Staphylococcus aureus (MRSA).1,4
Wound infections typically take one of two forms. The first is an actual incisional abscess. The patient is febrile; the margins of the wound are warm, indurated, erythematous, and tender; and purulent material drains from the incision. In this situation, the wound should be opened widely to drain the purulent collection. The fascia should then be probed to be certain that dehiscence has not occurred. In addition, intravenous vancomycin (1 g every 12 h) should be included in the antibiotic regimen to ensure adequate coverage of hospital-acquired MRSA.1,4
The second common presentation of a wound infection is cellulitis. The patient is febrile, and there is a spreading area of erythema, warmth, and exquisite tenderness extending from the edges of the incision; however, no purulent drainage is apparent. In this second scenario, the wound should not be opened, but intravenous vancomycin should be added to the treatment regimen.1,3,4
A third and very rare form of wound infection is necrotizing fasciitis. In affected patients, the margins of the wound are darkened and necrotic rather than erythematous and indurated. Two other key physical findings are crepitance and loss of sensation along the margins of the wound. Necrotizing fasciitis is truly a life-threatening emergency and requires immediate and extensive debridement of the devitalized tissue, combined with broad spectrum therapy with antibiotics that provide excellent coverage against anaerobes, aerobic streptococci (particularly group A streptococci), and staphylococci. The requirement for debridement may be so extensive that a skin graft subsequently is necessary to close the defect.1,4
Continue to: Unusual causes of persistent postoperative fever...
Unusual causes of persistent postoperative fever
If a resistant microorganism and wound infection can be excluded, the clinician then must begin a diligent search for “zebras” (ie, uncommon but potentially serious causes of persistent fever).1,4 One possible cause is a pelvic abscess. These purulent collections typically form in the retrovesicle space as a result of infection of a hematoma that formed between the posterior bladder wall and the lower uterine segment, in the leaves of the broad ligament, or in the posterior cul-de-sac. The abscess may or may not be palpable. The patient’s peripheral white blood cell count usually is elevated, with a preponderance of neutrophils. The best imaging test for an abscess is a computed tomography (CT) scan. Abscesses require drainage, which usually can be accomplished by insertion of a percutaneous drain under ultrasonographic or CT guidance.
A second unusual cause of persistent fever is septic pelvic vein thrombophlebitis. The infected venous emboli usually are present in the ovarian veins, with the right side predominant. The patient’s peripheral white blood cell count usually is elevated, and the infected clots are best imaged by CT scan with contrast or magnetic resonance angiography. The appropriate treatment is continuation of broad-spectrum antibiotics and administration of therapeutic doses of parenteral anticoagulants such as enoxaparin or unfractionated heparin.
A third explanation for persistent fever is retained products of conception. This diagnosis is best made by ultrasonography. The placental fragments should be removed by sharp curettage.
A fourth consideration when evaluating the patient with persistent fever is an allergic drug reaction. In most instances, the increase in the patient’s temperature will correspond with administration of the offending antibiotic(s). Affected patients typically have an increased number of eosinophils in their peripheral white blood cell count. The appropriate management of drug fever is discontinuation of antibiotics.
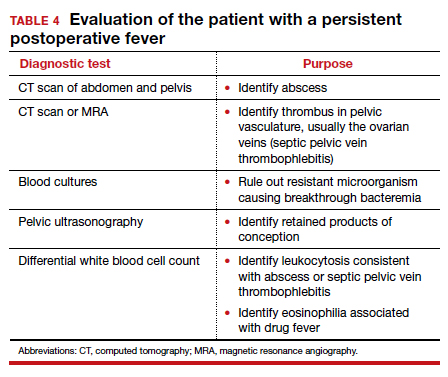
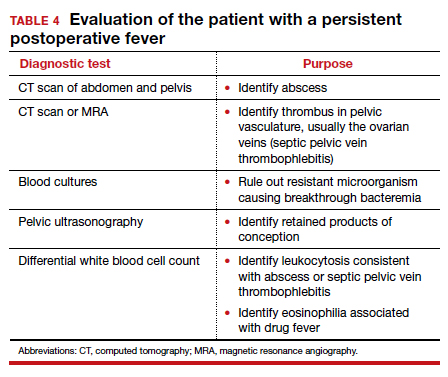
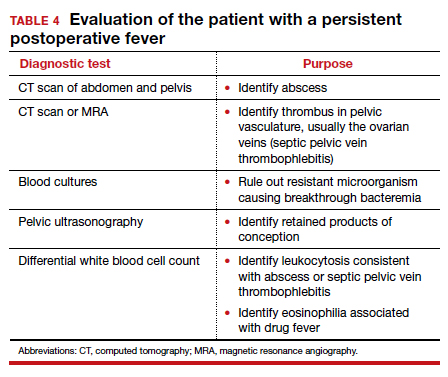
A final and distinctly unusual consideration is recrudescence of a connective tissue disorder such as systemic lupus erythematosus. The best test to confirm this diagnosis is the serum complement assay, which will demonstrate a decreased serum concentration of complement, reflecting consumption of this serum protein during the inflammatory process. The correct management for this condition is administration of a short course of systemic glucocorticoids. TABLE 4 summarizes a simple, systematic plan for evaluation of the patient with a persistent postoperative fever.
Preventive measures
We all remember the simple but profound statement by Benjamin Franklin, “An ounce of prevention is worth a pound of cure.” That folksy adage rings true with respect to postoperative infection because this complication extends hospital stay, increases hospital expense, and causes considerable discomfort and inconvenience for the patient. Therefore, we would do well to prevent as many instances of postoperative infection as possible.
Endometritis
On the basis of well-designed, prospective, randomized trials (Level 1 evidence), 3 interventions have proven effective in reducing the frequency of postcesarean endometritis. The first is irrigation of the vaginal canal preoperatively with an iodophor solution.5,6 The second is preoperative administration of systemic antibiotics.7-9 The combination of cefazolin (2 g IV within 30 minutes of incision) plus azithromycin (500 mg IV over 1 hour prior to incision) is superior to cefazolin alone.10,11 The third important preventive measure is removing the placenta by traction on the umbilical cord rather than by manual extraction.12,13
Wound infection
Several interventions are of proven effectiveness in reducing the frequency of postcesarean wound (surgical site) infection. The first is removal of hair at the incision site by clipping rather than by shaving (Level 2 evidence).14 The second is cleansing of the skin with chlorhexidine rather than iodophor (Level 1 evidence).15 The third is closing of the deep subcutaneous layer of the incision if it exceeds 2 cm in depth (Level 1 evidence).16,17 The fourth is closure of the skin with subcutaneous sutures rather than staples (Level 1 evidence).18 The monofilament suture poliglecaprone 25 is superior to the multifilament suture polyglactin 910 for this purpose (Level 1 evidence).19 Finally, in obese patients (body mass index >30 kg/m2), application of a negative pressure wound vacuum dressing may offer additional protection against infection (Level 1 evidence).20 Such dressings are too expensive, however, to be used routinely in all patients.
Urinary tract infection
The most important measures for preventing postoperative UTIs are identifying and clearing asymptomatic bacteriuria prior to delivery, inserting the urinary catheter prior to surgery using strict sterile technique, and removing the catheter as soon as possible after surgery, ideally within 12 hours.1,4
CASE Resolved
The 2 most likely causes for this patient’s poor response to initial therapy are resistant microorganism and wound infection. If a wound infection can be excluded by physical examination, the patient’s antibiotic regimen should be changed to metronidazole plus ampicillin plus gentamicin (or aztreonam). If an incisional abscess is identified, the incision should be opened and drained, and vancomycin should be added to the treatment regimen. If a wound cellulitis is evident, the incision should not be opened, but vancomycin should be added to the treatment regimen to enhance coverage against aerobic Streptococcus and Staphylococcus species. ●
- Duff WP. Maternal and perinatal infection in pregnancy: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2020:1124-1146.
- Locksmith GJ, Duff P. Assessment of the value of routine blood cultures in the evaluation and treatment of patients with chorioamnionitis. Infect Dis Obstet Gynecol. 1994;2:111-114.
- Duff P. Antibiotic selection in obstetric patients. Infect Dis Clin N Am. 1997;11:1-12.
- Duff P. Maternal and fetal infections. In: Creasy RK, Resnik R, Iams, JD, et al, eds. Creasy & Resnik’s Maternal Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
- Haas DM, Morgan S, Contreras K. Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections. Cochrane Database Syst Rev. 2014;12:CD007892.
- Caissutti C, Saccone G, Zullo F, et al. Vaginal cleansing before cesarean delivery. a systematic review and meta-analysis. Obstet Gynecol. 2017;130:527-538.
- Sullivan SA, Smith T, Change E, et al. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity; a randomized controlled trial. Am J Obstet Gynecol. 2007;196:455.e1-455.e5.
- Tita ATN, Hauth JC, Grimes A, et al. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111:51-56.
- Tita ATN, Owen J, Stamm AM, et al. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199: 303.e1-303.e3.
- Tita ATN, Szchowski JM, Boggess K, et al. Two antibiotics before cesarean delivery reduce infection rates further than one agent. N Engl J Med. 2016;375:1231-1241.
- Harper LM, Kilgore M, Szychowski JM, et al. Economic evaluation of adjunctive azithromycin prophylaxis for cesarean delivery. Obstet Gynecol. 2017;130:328-334.
- Lasley DS, Eblen A, Yancey MK, et al. The effect of placental removal method on the incidence of postcesarean infections. Am J Obstet Gynecol. 1997;176:1250-1254.
- Anorlu RI, Maholwana B, Hofmeyr GJ. Methods of delivering the placenta at cesarean section. Cochrane Database Syst Rev. 2008;3:CD004737.
- Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-209.
- Tuuli MG, Liu J, Stout MJ, et al. A randomized trial comparing skin antiseptic agents at cesarean delivery. N Engl J Med. 2016;374:657-665.
- Del Valle GO, Combs P, Qualls C, et al. Does closure of camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
- Chelmow D. Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103:974-980.
- Tuuli MG, Rampersod RM, Carbone JF, et al. Staples compared with subcuticular suture for skin closure after cesarean delivery. a systematic review and meta-analysis. Obstet Gynecol. 2011;117:682-690.
- Buresch AM, Arsdale AV, Ferzli M, et al. Comparison of subcuticular suture type for skin closure after cesarean delivery. a randomized controlled trial. Obstet Gynecol. 2017;130:521-526.
- Yu L, Kronen RJ, Simon LE, et al. Prophylactic negative-pressure wound therapy after cesarean is associated with reduced risk of surgical site infection: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:200-210.
CASE Woman who has undergone recent cesarean delivery
A 23-year-old woman had a primary cesarean delivery 72 hours ago due to an arrest of dilation at 6 cm. She was in labor for 22 hours, and her membranes were ruptured for 18 hours. She had 10 internal vaginal examinations, and the duration of internal fetal monitoring was 12 hours; 24 hours after delivery, she developed a fever of 39°C, in association with lower abdominal pain and tenderness. She was presumptively treated for endometritis with cefepime; 48 hours after the initiation of antibiotics, she remains febrile and symptomatic.
- What are the most likely causes of her persistent fever?
- What should be the next steps in her evaluation?
Cesarean delivery background
Cesarean delivery is now the most common major operation performed in US hospitals. Cesarean delivery rates hover between 25% and 30% in most medical centers in the United States.1 The most common postoperative complication of cesarean delivery is infection. Infection typically takes 1 of 3 forms: endometritis (organ space infection), wound infection (surgical site infection), and urinary tract infection (UTI).1 This article will review the initial differential diagnosis, evaluation, and management of the patient with a postoperative fever and also will describe the appropriate assessment and treatment of the patient who has a persistent postoperative fever despite therapy. The article will also highlight key interventions that help to prevent postoperative infections.
Initial evaluation of the febrile patient
In the first 24 to 48 hours after cesarean delivery, the most common cause of fever is endometritis (organ space infection). This condition is a polymicrobial, mixed aerobic-anaerobic infection (FIGURE). The principal pathogens include anaerobic gram-positive cocci (
The major risk factors for postcesarean endometritis are extended duration of labor and ruptured membranes, multiple internal vaginal examinations, invasive fetal monitoring, and pre-existing colonization with group B Streptococcus and/or the organisms that cause bacterial vaginosis. Affected patients typically have a fever in the range of 38 to 39°C, tachycardia, mild tachypnea, lower abdominal pain and tenderness, and purulent lochia in some individuals.1
Differential for postoperative fever
The initial differential diagnosis of postoperative fever is relatively limited (TABLE 1). In addition to endometritis, it includes extensive atelectasis, perhaps resulting from general anesthesia; lower respiratory tract infection, either viral influenza or bacterial pneumonia; and acute pyelonephritis. A simple infection of the bladder (cystitis or asymptomatic bacteriuria) should not cause a substantial temperature elevation and systemic symptoms.1
Differentiation between these entities usually is possible based on physical examination and a few laboratory tests. The peripheral white blood cell count usually is elevated, and a left shift may be evident. If a respiratory tract infection is suspected, chest radiography is indicated. A urine culture should be obtained if acute pyelonephritis strongly is considered. Lower genital tract cultures are rarely of value, and uncontaminated upper tract cultures are difficult to obtain. I do not believe that blood cultures should be performed as a matter of routine. They are expensive, and the results are often not available until after the patient has cleared her infection and left the hospital. However, I would obtain blood cultures in patients who meet one of these criteria1,2:
- They are immunocompromised (eg, HIV infection).
- They have a cardiac or vascular prosthesis and, thus, are at increased risk of complications related to bacteremia.
- They seem critically ill at the onset of evaluation.
- They fail to respond appropriately to initial therapy.
The cornerstone of therapy is broad spectrum antibiotics that target the multiple organisms responsible for endometritis.3 There are several single agents and several combination antibiotic regimens that provide excellent coverage against the usual pelvic pathogens (TABLE 2). I personally favor the generic combination regimen (clindamycin plus gentamicin) because it is relatively inexpensive and has been very well validated in multiple studies. In patients who have underlying renal dysfunction, aztreonam can be substituted for gentamicin.
Approximately 90% of patients will show clear evidence of clinical improvement (ie, decrease in temperature and resolution of abdominopelvic pain) within 48 hours of starting antibiotics. Patients should then continue therapy until they have been afebrile and asymptomatic for approximately 24 hours. At that point, antibiotics should be discontinued, and the patient can be discharged. With rare exceptions, there is no indication for administration of oral antibiotics on an outpatient basis.1,4
Continue to: Persistent postoperative fever...
Persistent postoperative fever
Resistant microorganism
The most common cause of a persistent fever after initiating antibiotic therapy is a resistant microorganism. There are potential gaps in coverage for the antibiotic regimens commonly used to treat postcesarean endometritis (TABLE 3).1,4 Assuming there is no other obvious cause for treatment failure, I recommend that therapy be changed to the triple combination of metronidazole plus ampicillin plus gentamicin (or aztreonam). The first drug provides superb coverage against anaerobes; the second covers enterococci. Gentamicin or aztreonam cover virtually all aerobic Gram-negative bacilli likely to cause postcesarean infection. I prefer metronidazole rather than clindamycin in this regimen because, unlike clindamycin, it is less likely to trigger diarrhea when used in combination with ampicillin. The 3-drug regimen should be continued until the patient has been afebrile and asymptomatic for approximately 24 hours.1,3,4
Wound infection
The second most common reason for a poor response to initial antibiotic therapy is a wound (surgical site) infection. Wound infections are caused by many of the same pelvic pathogens responsible for endometritis combined with skin flora, notably Streptococcus and Staphylococcus species, including methicillin-resistant Staphylococcus aureus (MRSA).1,4
Wound infections typically take one of two forms. The first is an actual incisional abscess. The patient is febrile; the margins of the wound are warm, indurated, erythematous, and tender; and purulent material drains from the incision. In this situation, the wound should be opened widely to drain the purulent collection. The fascia should then be probed to be certain that dehiscence has not occurred. In addition, intravenous vancomycin (1 g every 12 h) should be included in the antibiotic regimen to ensure adequate coverage of hospital-acquired MRSA.1,4
The second common presentation of a wound infection is cellulitis. The patient is febrile, and there is a spreading area of erythema, warmth, and exquisite tenderness extending from the edges of the incision; however, no purulent drainage is apparent. In this second scenario, the wound should not be opened, but intravenous vancomycin should be added to the treatment regimen.1,3,4
A third and very rare form of wound infection is necrotizing fasciitis. In affected patients, the margins of the wound are darkened and necrotic rather than erythematous and indurated. Two other key physical findings are crepitance and loss of sensation along the margins of the wound. Necrotizing fasciitis is truly a life-threatening emergency and requires immediate and extensive debridement of the devitalized tissue, combined with broad spectrum therapy with antibiotics that provide excellent coverage against anaerobes, aerobic streptococci (particularly group A streptococci), and staphylococci. The requirement for debridement may be so extensive that a skin graft subsequently is necessary to close the defect.1,4
Continue to: Unusual causes of persistent postoperative fever...
Unusual causes of persistent postoperative fever
If a resistant microorganism and wound infection can be excluded, the clinician then must begin a diligent search for “zebras” (ie, uncommon but potentially serious causes of persistent fever).1,4 One possible cause is a pelvic abscess. These purulent collections typically form in the retrovesicle space as a result of infection of a hematoma that formed between the posterior bladder wall and the lower uterine segment, in the leaves of the broad ligament, or in the posterior cul-de-sac. The abscess may or may not be palpable. The patient’s peripheral white blood cell count usually is elevated, with a preponderance of neutrophils. The best imaging test for an abscess is a computed tomography (CT) scan. Abscesses require drainage, which usually can be accomplished by insertion of a percutaneous drain under ultrasonographic or CT guidance.
A second unusual cause of persistent fever is septic pelvic vein thrombophlebitis. The infected venous emboli usually are present in the ovarian veins, with the right side predominant. The patient’s peripheral white blood cell count usually is elevated, and the infected clots are best imaged by CT scan with contrast or magnetic resonance angiography. The appropriate treatment is continuation of broad-spectrum antibiotics and administration of therapeutic doses of parenteral anticoagulants such as enoxaparin or unfractionated heparin.
A third explanation for persistent fever is retained products of conception. This diagnosis is best made by ultrasonography. The placental fragments should be removed by sharp curettage.
A fourth consideration when evaluating the patient with persistent fever is an allergic drug reaction. In most instances, the increase in the patient’s temperature will correspond with administration of the offending antibiotic(s). Affected patients typically have an increased number of eosinophils in their peripheral white blood cell count. The appropriate management of drug fever is discontinuation of antibiotics.
A final and distinctly unusual consideration is recrudescence of a connective tissue disorder such as systemic lupus erythematosus. The best test to confirm this diagnosis is the serum complement assay, which will demonstrate a decreased serum concentration of complement, reflecting consumption of this serum protein during the inflammatory process. The correct management for this condition is administration of a short course of systemic glucocorticoids. TABLE 4 summarizes a simple, systematic plan for evaluation of the patient with a persistent postoperative fever.
Preventive measures
We all remember the simple but profound statement by Benjamin Franklin, “An ounce of prevention is worth a pound of cure.” That folksy adage rings true with respect to postoperative infection because this complication extends hospital stay, increases hospital expense, and causes considerable discomfort and inconvenience for the patient. Therefore, we would do well to prevent as many instances of postoperative infection as possible.
Endometritis
On the basis of well-designed, prospective, randomized trials (Level 1 evidence), 3 interventions have proven effective in reducing the frequency of postcesarean endometritis. The first is irrigation of the vaginal canal preoperatively with an iodophor solution.5,6 The second is preoperative administration of systemic antibiotics.7-9 The combination of cefazolin (2 g IV within 30 minutes of incision) plus azithromycin (500 mg IV over 1 hour prior to incision) is superior to cefazolin alone.10,11 The third important preventive measure is removing the placenta by traction on the umbilical cord rather than by manual extraction.12,13
Wound infection
Several interventions are of proven effectiveness in reducing the frequency of postcesarean wound (surgical site) infection. The first is removal of hair at the incision site by clipping rather than by shaving (Level 2 evidence).14 The second is cleansing of the skin with chlorhexidine rather than iodophor (Level 1 evidence).15 The third is closing of the deep subcutaneous layer of the incision if it exceeds 2 cm in depth (Level 1 evidence).16,17 The fourth is closure of the skin with subcutaneous sutures rather than staples (Level 1 evidence).18 The monofilament suture poliglecaprone 25 is superior to the multifilament suture polyglactin 910 for this purpose (Level 1 evidence).19 Finally, in obese patients (body mass index >30 kg/m2), application of a negative pressure wound vacuum dressing may offer additional protection against infection (Level 1 evidence).20 Such dressings are too expensive, however, to be used routinely in all patients.
Urinary tract infection
The most important measures for preventing postoperative UTIs are identifying and clearing asymptomatic bacteriuria prior to delivery, inserting the urinary catheter prior to surgery using strict sterile technique, and removing the catheter as soon as possible after surgery, ideally within 12 hours.1,4
CASE Resolved
The 2 most likely causes for this patient’s poor response to initial therapy are resistant microorganism and wound infection. If a wound infection can be excluded by physical examination, the patient’s antibiotic regimen should be changed to metronidazole plus ampicillin plus gentamicin (or aztreonam). If an incisional abscess is identified, the incision should be opened and drained, and vancomycin should be added to the treatment regimen. If a wound cellulitis is evident, the incision should not be opened, but vancomycin should be added to the treatment regimen to enhance coverage against aerobic Streptococcus and Staphylococcus species. ●
CASE Woman who has undergone recent cesarean delivery
A 23-year-old woman had a primary cesarean delivery 72 hours ago due to an arrest of dilation at 6 cm. She was in labor for 22 hours, and her membranes were ruptured for 18 hours. She had 10 internal vaginal examinations, and the duration of internal fetal monitoring was 12 hours; 24 hours after delivery, she developed a fever of 39°C, in association with lower abdominal pain and tenderness. She was presumptively treated for endometritis with cefepime; 48 hours after the initiation of antibiotics, she remains febrile and symptomatic.
- What are the most likely causes of her persistent fever?
- What should be the next steps in her evaluation?
Cesarean delivery background
Cesarean delivery is now the most common major operation performed in US hospitals. Cesarean delivery rates hover between 25% and 30% in most medical centers in the United States.1 The most common postoperative complication of cesarean delivery is infection. Infection typically takes 1 of 3 forms: endometritis (organ space infection), wound infection (surgical site infection), and urinary tract infection (UTI).1 This article will review the initial differential diagnosis, evaluation, and management of the patient with a postoperative fever and also will describe the appropriate assessment and treatment of the patient who has a persistent postoperative fever despite therapy. The article will also highlight key interventions that help to prevent postoperative infections.
Initial evaluation of the febrile patient
In the first 24 to 48 hours after cesarean delivery, the most common cause of fever is endometritis (organ space infection). This condition is a polymicrobial, mixed aerobic-anaerobic infection (FIGURE). The principal pathogens include anaerobic gram-positive cocci (
The major risk factors for postcesarean endometritis are extended duration of labor and ruptured membranes, multiple internal vaginal examinations, invasive fetal monitoring, and pre-existing colonization with group B Streptococcus and/or the organisms that cause bacterial vaginosis. Affected patients typically have a fever in the range of 38 to 39°C, tachycardia, mild tachypnea, lower abdominal pain and tenderness, and purulent lochia in some individuals.1
Differential for postoperative fever
The initial differential diagnosis of postoperative fever is relatively limited (TABLE 1). In addition to endometritis, it includes extensive atelectasis, perhaps resulting from general anesthesia; lower respiratory tract infection, either viral influenza or bacterial pneumonia; and acute pyelonephritis. A simple infection of the bladder (cystitis or asymptomatic bacteriuria) should not cause a substantial temperature elevation and systemic symptoms.1
Differentiation between these entities usually is possible based on physical examination and a few laboratory tests. The peripheral white blood cell count usually is elevated, and a left shift may be evident. If a respiratory tract infection is suspected, chest radiography is indicated. A urine culture should be obtained if acute pyelonephritis strongly is considered. Lower genital tract cultures are rarely of value, and uncontaminated upper tract cultures are difficult to obtain. I do not believe that blood cultures should be performed as a matter of routine. They are expensive, and the results are often not available until after the patient has cleared her infection and left the hospital. However, I would obtain blood cultures in patients who meet one of these criteria1,2:
- They are immunocompromised (eg, HIV infection).
- They have a cardiac or vascular prosthesis and, thus, are at increased risk of complications related to bacteremia.
- They seem critically ill at the onset of evaluation.
- They fail to respond appropriately to initial therapy.
The cornerstone of therapy is broad spectrum antibiotics that target the multiple organisms responsible for endometritis.3 There are several single agents and several combination antibiotic regimens that provide excellent coverage against the usual pelvic pathogens (TABLE 2). I personally favor the generic combination regimen (clindamycin plus gentamicin) because it is relatively inexpensive and has been very well validated in multiple studies. In patients who have underlying renal dysfunction, aztreonam can be substituted for gentamicin.
Approximately 90% of patients will show clear evidence of clinical improvement (ie, decrease in temperature and resolution of abdominopelvic pain) within 48 hours of starting antibiotics. Patients should then continue therapy until they have been afebrile and asymptomatic for approximately 24 hours. At that point, antibiotics should be discontinued, and the patient can be discharged. With rare exceptions, there is no indication for administration of oral antibiotics on an outpatient basis.1,4
Continue to: Persistent postoperative fever...
Persistent postoperative fever
Resistant microorganism
The most common cause of a persistent fever after initiating antibiotic therapy is a resistant microorganism. There are potential gaps in coverage for the antibiotic regimens commonly used to treat postcesarean endometritis (TABLE 3).1,4 Assuming there is no other obvious cause for treatment failure, I recommend that therapy be changed to the triple combination of metronidazole plus ampicillin plus gentamicin (or aztreonam). The first drug provides superb coverage against anaerobes; the second covers enterococci. Gentamicin or aztreonam cover virtually all aerobic Gram-negative bacilli likely to cause postcesarean infection. I prefer metronidazole rather than clindamycin in this regimen because, unlike clindamycin, it is less likely to trigger diarrhea when used in combination with ampicillin. The 3-drug regimen should be continued until the patient has been afebrile and asymptomatic for approximately 24 hours.1,3,4
Wound infection
The second most common reason for a poor response to initial antibiotic therapy is a wound (surgical site) infection. Wound infections are caused by many of the same pelvic pathogens responsible for endometritis combined with skin flora, notably Streptococcus and Staphylococcus species, including methicillin-resistant Staphylococcus aureus (MRSA).1,4
Wound infections typically take one of two forms. The first is an actual incisional abscess. The patient is febrile; the margins of the wound are warm, indurated, erythematous, and tender; and purulent material drains from the incision. In this situation, the wound should be opened widely to drain the purulent collection. The fascia should then be probed to be certain that dehiscence has not occurred. In addition, intravenous vancomycin (1 g every 12 h) should be included in the antibiotic regimen to ensure adequate coverage of hospital-acquired MRSA.1,4
The second common presentation of a wound infection is cellulitis. The patient is febrile, and there is a spreading area of erythema, warmth, and exquisite tenderness extending from the edges of the incision; however, no purulent drainage is apparent. In this second scenario, the wound should not be opened, but intravenous vancomycin should be added to the treatment regimen.1,3,4
A third and very rare form of wound infection is necrotizing fasciitis. In affected patients, the margins of the wound are darkened and necrotic rather than erythematous and indurated. Two other key physical findings are crepitance and loss of sensation along the margins of the wound. Necrotizing fasciitis is truly a life-threatening emergency and requires immediate and extensive debridement of the devitalized tissue, combined with broad spectrum therapy with antibiotics that provide excellent coverage against anaerobes, aerobic streptococci (particularly group A streptococci), and staphylococci. The requirement for debridement may be so extensive that a skin graft subsequently is necessary to close the defect.1,4
Continue to: Unusual causes of persistent postoperative fever...
Unusual causes of persistent postoperative fever
If a resistant microorganism and wound infection can be excluded, the clinician then must begin a diligent search for “zebras” (ie, uncommon but potentially serious causes of persistent fever).1,4 One possible cause is a pelvic abscess. These purulent collections typically form in the retrovesicle space as a result of infection of a hematoma that formed between the posterior bladder wall and the lower uterine segment, in the leaves of the broad ligament, or in the posterior cul-de-sac. The abscess may or may not be palpable. The patient’s peripheral white blood cell count usually is elevated, with a preponderance of neutrophils. The best imaging test for an abscess is a computed tomography (CT) scan. Abscesses require drainage, which usually can be accomplished by insertion of a percutaneous drain under ultrasonographic or CT guidance.
A second unusual cause of persistent fever is septic pelvic vein thrombophlebitis. The infected venous emboli usually are present in the ovarian veins, with the right side predominant. The patient’s peripheral white blood cell count usually is elevated, and the infected clots are best imaged by CT scan with contrast or magnetic resonance angiography. The appropriate treatment is continuation of broad-spectrum antibiotics and administration of therapeutic doses of parenteral anticoagulants such as enoxaparin or unfractionated heparin.
A third explanation for persistent fever is retained products of conception. This diagnosis is best made by ultrasonography. The placental fragments should be removed by sharp curettage.
A fourth consideration when evaluating the patient with persistent fever is an allergic drug reaction. In most instances, the increase in the patient’s temperature will correspond with administration of the offending antibiotic(s). Affected patients typically have an increased number of eosinophils in their peripheral white blood cell count. The appropriate management of drug fever is discontinuation of antibiotics.
A final and distinctly unusual consideration is recrudescence of a connective tissue disorder such as systemic lupus erythematosus. The best test to confirm this diagnosis is the serum complement assay, which will demonstrate a decreased serum concentration of complement, reflecting consumption of this serum protein during the inflammatory process. The correct management for this condition is administration of a short course of systemic glucocorticoids. TABLE 4 summarizes a simple, systematic plan for evaluation of the patient with a persistent postoperative fever.
Preventive measures
We all remember the simple but profound statement by Benjamin Franklin, “An ounce of prevention is worth a pound of cure.” That folksy adage rings true with respect to postoperative infection because this complication extends hospital stay, increases hospital expense, and causes considerable discomfort and inconvenience for the patient. Therefore, we would do well to prevent as many instances of postoperative infection as possible.
Endometritis
On the basis of well-designed, prospective, randomized trials (Level 1 evidence), 3 interventions have proven effective in reducing the frequency of postcesarean endometritis. The first is irrigation of the vaginal canal preoperatively with an iodophor solution.5,6 The second is preoperative administration of systemic antibiotics.7-9 The combination of cefazolin (2 g IV within 30 minutes of incision) plus azithromycin (500 mg IV over 1 hour prior to incision) is superior to cefazolin alone.10,11 The third important preventive measure is removing the placenta by traction on the umbilical cord rather than by manual extraction.12,13
Wound infection
Several interventions are of proven effectiveness in reducing the frequency of postcesarean wound (surgical site) infection. The first is removal of hair at the incision site by clipping rather than by shaving (Level 2 evidence).14 The second is cleansing of the skin with chlorhexidine rather than iodophor (Level 1 evidence).15 The third is closing of the deep subcutaneous layer of the incision if it exceeds 2 cm in depth (Level 1 evidence).16,17 The fourth is closure of the skin with subcutaneous sutures rather than staples (Level 1 evidence).18 The monofilament suture poliglecaprone 25 is superior to the multifilament suture polyglactin 910 for this purpose (Level 1 evidence).19 Finally, in obese patients (body mass index >30 kg/m2), application of a negative pressure wound vacuum dressing may offer additional protection against infection (Level 1 evidence).20 Such dressings are too expensive, however, to be used routinely in all patients.
Urinary tract infection
The most important measures for preventing postoperative UTIs are identifying and clearing asymptomatic bacteriuria prior to delivery, inserting the urinary catheter prior to surgery using strict sterile technique, and removing the catheter as soon as possible after surgery, ideally within 12 hours.1,4
CASE Resolved
The 2 most likely causes for this patient’s poor response to initial therapy are resistant microorganism and wound infection. If a wound infection can be excluded by physical examination, the patient’s antibiotic regimen should be changed to metronidazole plus ampicillin plus gentamicin (or aztreonam). If an incisional abscess is identified, the incision should be opened and drained, and vancomycin should be added to the treatment regimen. If a wound cellulitis is evident, the incision should not be opened, but vancomycin should be added to the treatment regimen to enhance coverage against aerobic Streptococcus and Staphylococcus species. ●
- Duff WP. Maternal and perinatal infection in pregnancy: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2020:1124-1146.
- Locksmith GJ, Duff P. Assessment of the value of routine blood cultures in the evaluation and treatment of patients with chorioamnionitis. Infect Dis Obstet Gynecol. 1994;2:111-114.
- Duff P. Antibiotic selection in obstetric patients. Infect Dis Clin N Am. 1997;11:1-12.
- Duff P. Maternal and fetal infections. In: Creasy RK, Resnik R, Iams, JD, et al, eds. Creasy & Resnik’s Maternal Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
- Haas DM, Morgan S, Contreras K. Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections. Cochrane Database Syst Rev. 2014;12:CD007892.
- Caissutti C, Saccone G, Zullo F, et al. Vaginal cleansing before cesarean delivery. a systematic review and meta-analysis. Obstet Gynecol. 2017;130:527-538.
- Sullivan SA, Smith T, Change E, et al. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity; a randomized controlled trial. Am J Obstet Gynecol. 2007;196:455.e1-455.e5.
- Tita ATN, Hauth JC, Grimes A, et al. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111:51-56.
- Tita ATN, Owen J, Stamm AM, et al. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199: 303.e1-303.e3.
- Tita ATN, Szchowski JM, Boggess K, et al. Two antibiotics before cesarean delivery reduce infection rates further than one agent. N Engl J Med. 2016;375:1231-1241.
- Harper LM, Kilgore M, Szychowski JM, et al. Economic evaluation of adjunctive azithromycin prophylaxis for cesarean delivery. Obstet Gynecol. 2017;130:328-334.
- Lasley DS, Eblen A, Yancey MK, et al. The effect of placental removal method on the incidence of postcesarean infections. Am J Obstet Gynecol. 1997;176:1250-1254.
- Anorlu RI, Maholwana B, Hofmeyr GJ. Methods of delivering the placenta at cesarean section. Cochrane Database Syst Rev. 2008;3:CD004737.
- Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-209.
- Tuuli MG, Liu J, Stout MJ, et al. A randomized trial comparing skin antiseptic agents at cesarean delivery. N Engl J Med. 2016;374:657-665.
- Del Valle GO, Combs P, Qualls C, et al. Does closure of camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
- Chelmow D. Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103:974-980.
- Tuuli MG, Rampersod RM, Carbone JF, et al. Staples compared with subcuticular suture for skin closure after cesarean delivery. a systematic review and meta-analysis. Obstet Gynecol. 2011;117:682-690.
- Buresch AM, Arsdale AV, Ferzli M, et al. Comparison of subcuticular suture type for skin closure after cesarean delivery. a randomized controlled trial. Obstet Gynecol. 2017;130:521-526.
- Yu L, Kronen RJ, Simon LE, et al. Prophylactic negative-pressure wound therapy after cesarean is associated with reduced risk of surgical site infection: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:200-210.
- Duff WP. Maternal and perinatal infection in pregnancy: bacterial. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe’s Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2020:1124-1146.
- Locksmith GJ, Duff P. Assessment of the value of routine blood cultures in the evaluation and treatment of patients with chorioamnionitis. Infect Dis Obstet Gynecol. 1994;2:111-114.
- Duff P. Antibiotic selection in obstetric patients. Infect Dis Clin N Am. 1997;11:1-12.
- Duff P. Maternal and fetal infections. In: Creasy RK, Resnik R, Iams, JD, et al, eds. Creasy & Resnik’s Maternal Fetal Medicine: Principles and Practice. 8th ed. Elsevier; 2019:862-919.
- Haas DM, Morgan S, Contreras K. Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections. Cochrane Database Syst Rev. 2014;12:CD007892.
- Caissutti C, Saccone G, Zullo F, et al. Vaginal cleansing before cesarean delivery. a systematic review and meta-analysis. Obstet Gynecol. 2017;130:527-538.
- Sullivan SA, Smith T, Change E, et al. Administration of cefazolin prior to skin incision is superior to cefazolin at cord clamping in preventing postcesarean infectious morbidity; a randomized controlled trial. Am J Obstet Gynecol. 2007;196:455.e1-455.e5.
- Tita ATN, Hauth JC, Grimes A, et al. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstet Gynecol. 2008;111:51-56.
- Tita ATN, Owen J, Stamm AM, et al. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. Am J Obstet Gynecol. 2008;199: 303.e1-303.e3.
- Tita ATN, Szchowski JM, Boggess K, et al. Two antibiotics before cesarean delivery reduce infection rates further than one agent. N Engl J Med. 2016;375:1231-1241.
- Harper LM, Kilgore M, Szychowski JM, et al. Economic evaluation of adjunctive azithromycin prophylaxis for cesarean delivery. Obstet Gynecol. 2017;130:328-334.
- Lasley DS, Eblen A, Yancey MK, et al. The effect of placental removal method on the incidence of postcesarean infections. Am J Obstet Gynecol. 1997;176:1250-1254.
- Anorlu RI, Maholwana B, Hofmeyr GJ. Methods of delivering the placenta at cesarean section. Cochrane Database Syst Rev. 2008;3:CD004737.
- Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206-209.
- Tuuli MG, Liu J, Stout MJ, et al. A randomized trial comparing skin antiseptic agents at cesarean delivery. N Engl J Med. 2016;374:657-665.
- Del Valle GO, Combs P, Qualls C, et al. Does closure of camper fascia reduce the incidence of post-cesarean superficial wound disruption? Obstet Gynecol. 1992;80:1013-1016.
- Chelmow D. Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103:974-980.
- Tuuli MG, Rampersod RM, Carbone JF, et al. Staples compared with subcuticular suture for skin closure after cesarean delivery. a systematic review and meta-analysis. Obstet Gynecol. 2011;117:682-690.
- Buresch AM, Arsdale AV, Ferzli M, et al. Comparison of subcuticular suture type for skin closure after cesarean delivery. a randomized controlled trial. Obstet Gynecol. 2017;130:521-526.
- Yu L, Kronen RJ, Simon LE, et al. Prophylactic negative-pressure wound therapy after cesarean is associated with reduced risk of surgical site infection: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:200-210.
Does prophylactic manual rotation of OP and OT positions in early second stage of labor decrease operative vaginal and/or CDs?
Blanc J, Castel P, Mauviel F, et al. Prophylactic manual rotation of occiput posterior and transverse positions to decrease operative delivery: the PROPOP randomized clinical trial. Am J Obstet Gynecol. 2021;225:444.e1-444.e8. doi: 10.1016/j.ajog.2021.05.020.
EXPERT COMMENTARY
Occiput posterior or occiput transverse positions are reported at a rate of 20% in labor, with 5% persistent at the time of delivery. These lead to a higher risk of maternal complications, such as cesarean delivery (CD), prolonged second stage, severe perineal lacerations, postpartum hemorrhage, chorioamnionitis, and operative vaginal delivery.
Several options are available for rotation to occiput anterior (OA) to increase the likelihood of spontaneous delivery. These include instrument (which requires forceps or vacuum experience in rotation), maternal positioning changes, or manual rotation. Timing of manual rotation can be at full dilation (“prophylactic”) or at failure to progress (“therapeutic”), with the latter less likely to succeed.
Although the existing literature is somewhat limited, both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine recommend consideration of manual rotation to reduce the rate of operative delivery. A recent study by Blanc and colleagues sought to add to the evidence for the effectiveness of manual rotation in reducing operative delivery.
Details of the study
The multicenter, open-label, randomized clinical trial included 257 patients at 4 French hospitals (2 academic, 2 community). The 126 patients in the intervention group underwent a trial of prophylactic manual rotation, while the 131 in the standard group had no trial of prophylactic manual rotation. The study’s primary objective was to determine the effect of prophylactic manual rotation on operative delivery (vaginal or cesarean). The hypothesis was that manual rotation would decrease the risk of operative delivery.
The inclusion criteria were patients with a singleton pregnancy at more than 37 weeks, epidural anesthesia, and OP or OT presentation (confirmed by ultrasonography) in the early second stage of labor at diagnosis of full dilation. Manual rotation was attempted using the previously described Tarnier and Chantreiul technique, and all investigators were trained in this technique at the beginning of the study using a mannequin.
The primary outcome was vaginal or cesarean operative delivery. Secondary outcomes included length of the second stage of labor as well as maternal and neonatal complications.
Results. The intervention group had a significantly lower rate of operative delivery (29.4%) compared with the standard group (41.2%). Length of the second stage was also lower in the intervention group (146.7 minutes) compared with that of the standard group (164.4 minutes). The 5-minute Apgar score was reported as significantly higher in the intervention group as well (9.8 vs 9.6). There were no other differences between the groups in either maternal or neonatal complications.
Study strengths and limitations
The strengths of this study included randomization and no loss to follow-up. The 4 different study sites with different levels of care and acuity added to the generalizability of the results. Given the potential for inaccuracy of digital exam for fetal head positioning, the use of ultrasonography for confirmation of the OP or OT position is a study strength. Additional strengths are the prestudy training in the maneuver using simulation and the high level of success in the rotations (89.7%).
The study’s main limitation is that it was not double blinded; therefore, bias in management was a possibility. Additionally, the study looked only at short-term outcomes for the delivery itself and not at the potential long-term pelvic floor outcomes. The authors reported that the study was underpowered for operative vaginal delivery and cesarean delivery separately, as well as the secondary outcomes. Other limitations were the high frequency of operative vaginal delivery, low rate of consent for the study, and lack of patient satisfaction data. ●
In this study, a trial of prophylactic manual rotation of the occiput posterior or occiput transverse presentation decreased the rate of operative delivery and reduced the length of the second stage of labor without differences in maternal or neonatal complications. Obstetrical providers should consider this strategy to resolve the OP or OT presentation prior to performing an operative vaginal delivery or cesarean delivery. Simulation training in this maneuver may be a useful adjunct for both trainees and providers unfamiliar with the procedure.
JAIMEY M. PAULI, MD
Blanc J, Castel P, Mauviel F, et al. Prophylactic manual rotation of occiput posterior and transverse positions to decrease operative delivery: the PROPOP randomized clinical trial. Am J Obstet Gynecol. 2021;225:444.e1-444.e8. doi: 10.1016/j.ajog.2021.05.020.
EXPERT COMMENTARY
Occiput posterior or occiput transverse positions are reported at a rate of 20% in labor, with 5% persistent at the time of delivery. These lead to a higher risk of maternal complications, such as cesarean delivery (CD), prolonged second stage, severe perineal lacerations, postpartum hemorrhage, chorioamnionitis, and operative vaginal delivery.
Several options are available for rotation to occiput anterior (OA) to increase the likelihood of spontaneous delivery. These include instrument (which requires forceps or vacuum experience in rotation), maternal positioning changes, or manual rotation. Timing of manual rotation can be at full dilation (“prophylactic”) or at failure to progress (“therapeutic”), with the latter less likely to succeed.
Although the existing literature is somewhat limited, both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine recommend consideration of manual rotation to reduce the rate of operative delivery. A recent study by Blanc and colleagues sought to add to the evidence for the effectiveness of manual rotation in reducing operative delivery.
Details of the study
The multicenter, open-label, randomized clinical trial included 257 patients at 4 French hospitals (2 academic, 2 community). The 126 patients in the intervention group underwent a trial of prophylactic manual rotation, while the 131 in the standard group had no trial of prophylactic manual rotation. The study’s primary objective was to determine the effect of prophylactic manual rotation on operative delivery (vaginal or cesarean). The hypothesis was that manual rotation would decrease the risk of operative delivery.
The inclusion criteria were patients with a singleton pregnancy at more than 37 weeks, epidural anesthesia, and OP or OT presentation (confirmed by ultrasonography) in the early second stage of labor at diagnosis of full dilation. Manual rotation was attempted using the previously described Tarnier and Chantreiul technique, and all investigators were trained in this technique at the beginning of the study using a mannequin.
The primary outcome was vaginal or cesarean operative delivery. Secondary outcomes included length of the second stage of labor as well as maternal and neonatal complications.
Results. The intervention group had a significantly lower rate of operative delivery (29.4%) compared with the standard group (41.2%). Length of the second stage was also lower in the intervention group (146.7 minutes) compared with that of the standard group (164.4 minutes). The 5-minute Apgar score was reported as significantly higher in the intervention group as well (9.8 vs 9.6). There were no other differences between the groups in either maternal or neonatal complications.
Study strengths and limitations
The strengths of this study included randomization and no loss to follow-up. The 4 different study sites with different levels of care and acuity added to the generalizability of the results. Given the potential for inaccuracy of digital exam for fetal head positioning, the use of ultrasonography for confirmation of the OP or OT position is a study strength. Additional strengths are the prestudy training in the maneuver using simulation and the high level of success in the rotations (89.7%).
The study’s main limitation is that it was not double blinded; therefore, bias in management was a possibility. Additionally, the study looked only at short-term outcomes for the delivery itself and not at the potential long-term pelvic floor outcomes. The authors reported that the study was underpowered for operative vaginal delivery and cesarean delivery separately, as well as the secondary outcomes. Other limitations were the high frequency of operative vaginal delivery, low rate of consent for the study, and lack of patient satisfaction data. ●
In this study, a trial of prophylactic manual rotation of the occiput posterior or occiput transverse presentation decreased the rate of operative delivery and reduced the length of the second stage of labor without differences in maternal or neonatal complications. Obstetrical providers should consider this strategy to resolve the OP or OT presentation prior to performing an operative vaginal delivery or cesarean delivery. Simulation training in this maneuver may be a useful adjunct for both trainees and providers unfamiliar with the procedure.
JAIMEY M. PAULI, MD
Blanc J, Castel P, Mauviel F, et al. Prophylactic manual rotation of occiput posterior and transverse positions to decrease operative delivery: the PROPOP randomized clinical trial. Am J Obstet Gynecol. 2021;225:444.e1-444.e8. doi: 10.1016/j.ajog.2021.05.020.
EXPERT COMMENTARY
Occiput posterior or occiput transverse positions are reported at a rate of 20% in labor, with 5% persistent at the time of delivery. These lead to a higher risk of maternal complications, such as cesarean delivery (CD), prolonged second stage, severe perineal lacerations, postpartum hemorrhage, chorioamnionitis, and operative vaginal delivery.
Several options are available for rotation to occiput anterior (OA) to increase the likelihood of spontaneous delivery. These include instrument (which requires forceps or vacuum experience in rotation), maternal positioning changes, or manual rotation. Timing of manual rotation can be at full dilation (“prophylactic”) or at failure to progress (“therapeutic”), with the latter less likely to succeed.
Although the existing literature is somewhat limited, both the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine recommend consideration of manual rotation to reduce the rate of operative delivery. A recent study by Blanc and colleagues sought to add to the evidence for the effectiveness of manual rotation in reducing operative delivery.
Details of the study
The multicenter, open-label, randomized clinical trial included 257 patients at 4 French hospitals (2 academic, 2 community). The 126 patients in the intervention group underwent a trial of prophylactic manual rotation, while the 131 in the standard group had no trial of prophylactic manual rotation. The study’s primary objective was to determine the effect of prophylactic manual rotation on operative delivery (vaginal or cesarean). The hypothesis was that manual rotation would decrease the risk of operative delivery.
The inclusion criteria were patients with a singleton pregnancy at more than 37 weeks, epidural anesthesia, and OP or OT presentation (confirmed by ultrasonography) in the early second stage of labor at diagnosis of full dilation. Manual rotation was attempted using the previously described Tarnier and Chantreiul technique, and all investigators were trained in this technique at the beginning of the study using a mannequin.
The primary outcome was vaginal or cesarean operative delivery. Secondary outcomes included length of the second stage of labor as well as maternal and neonatal complications.
Results. The intervention group had a significantly lower rate of operative delivery (29.4%) compared with the standard group (41.2%). Length of the second stage was also lower in the intervention group (146.7 minutes) compared with that of the standard group (164.4 minutes). The 5-minute Apgar score was reported as significantly higher in the intervention group as well (9.8 vs 9.6). There were no other differences between the groups in either maternal or neonatal complications.
Study strengths and limitations
The strengths of this study included randomization and no loss to follow-up. The 4 different study sites with different levels of care and acuity added to the generalizability of the results. Given the potential for inaccuracy of digital exam for fetal head positioning, the use of ultrasonography for confirmation of the OP or OT position is a study strength. Additional strengths are the prestudy training in the maneuver using simulation and the high level of success in the rotations (89.7%).
The study’s main limitation is that it was not double blinded; therefore, bias in management was a possibility. Additionally, the study looked only at short-term outcomes for the delivery itself and not at the potential long-term pelvic floor outcomes. The authors reported that the study was underpowered for operative vaginal delivery and cesarean delivery separately, as well as the secondary outcomes. Other limitations were the high frequency of operative vaginal delivery, low rate of consent for the study, and lack of patient satisfaction data. ●
In this study, a trial of prophylactic manual rotation of the occiput posterior or occiput transverse presentation decreased the rate of operative delivery and reduced the length of the second stage of labor without differences in maternal or neonatal complications. Obstetrical providers should consider this strategy to resolve the OP or OT presentation prior to performing an operative vaginal delivery or cesarean delivery. Simulation training in this maneuver may be a useful adjunct for both trainees and providers unfamiliar with the procedure.
JAIMEY M. PAULI, MD
Reduce the use of perioperative opioids with a multimodal pain management strategy
Opioid-related deaths are a major cause of mortality in the United States. The Centers for Disease Control and Prevention (CDC) reported 72,151 and 93,331 drug overdose deaths in 2019 and 2020, respectively, and drug overdose deaths have continued to increase in 2021.1 The majority of drug overdose deaths are due to opioids. There are many factors contributing to this rise, including an incredibly high rate of opioid prescriptions in this country.2 The CDC reported that in 3.6% of US counties, there are more opioid prescriptions filled each year than number of residents in the county.3 The consumption of opioids per person in the US is approximately four times greater than countries with excellent health outcomes, including Sweden, Netherlands, Norway, and the United Kingdom.4 Some US physicians have opioid prescribing practices that are inconsistent with good medical practice in other countries, prescribing powerful opioids and an excessive number of pills per opioid prescription.2 We must continue to evolve our clinical practices to reduce opioid use while continually improving patient outcomes.
Cesarean birth is one of the most common major surgical procedures performed in the United States. The National Center for Health Statistics reported that in 2020 there were approximately 1,150,000 US cesarean births.5 Following cesarean birth, patients who were previously naïve to opioid medications were reported to have a 0.33% to 2.2% probability of transitioning to the persistent use of opioid prescriptions.6-8 Predictors of persistent opioid use after cesarean birth included a history of tobacco use, back pain, migraine headaches, and antidepressant or benzodiazepine use.6 The use of cesarean birth pain management protocols that prioritize multimodal analgesia and opioid sparing is warranted.
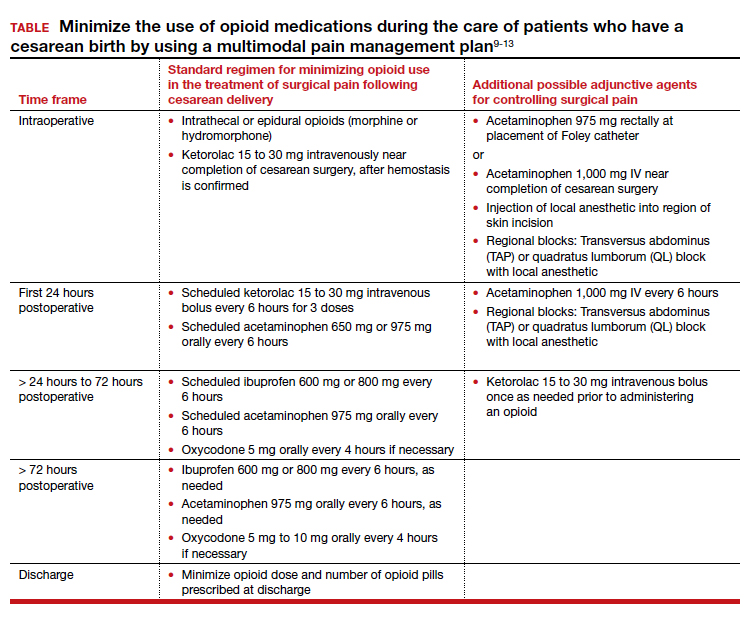
Multimodal pain management protocols for cesarean birth have been shown to reduce the use of opioid medications in the hospital and at discharge without a clinically significant increase in pain scores or a reduction in patient satisfaction (TABLE).9-13 For example, Holland and colleagues9 reported that the implementation of a multimodal pain management protocol reduced the percent of patients using oral opioids during hospitalization for cesarean birth from 68% to 45%, pre- and post-intervention, respectively. Mehraban and colleagues12 reported that the percent of patients using opioids during hospitalization for cesarean birth was reduced from 45% preintervention to 18% postintervention. In addition, these studies showed that multimodal pain management protocols for cesarean birth also reduced opioid prescribing at discharge. Holland and colleagues9 reported that the percent of patients provided an opioid prescription at discharge was reduced from 91% to 40%, pre- and post-intervention, respectively. Mehraban and colleagues12 reported that the percent of patients who took opioids after discharge was reduced from 24% preintervention to 9% postintervention. These studies were not randomized controlled clinical trials, but they do provide strong evidence that a focused intervention to reduce opioid medications in the management of pain after cesarean surgery can be successful without decreasing patient satisfaction or increasing reported pain scores. In these studies, it is likely that the influence, enthusiasm, and commitment of the study leaders to the change process contributed to the success of these opioid-sparing pain management programs.
Continue to: Key features of a multimodal analgesia intervention for cesarean surgery...
Key features of a multimodal analgesia intervention for cesarean surgery
Fundamental inclusions of multimodal analgesia for cesarean surgery include:
- exquisite attention to pain control during the surgical procedure by both the anesthesiologist and surgeon, with prioritization of spinal anesthesia that includes morphine and fentanyl
- regularly scheduled administration of intravenous ketorolac during the first 24 hours postcesarean
- regularly scheduled administration of both acetaminophen and ibuprofen, rather than “as needed” dosing
- using analgesics that work through different molecular pathways (ibuprofen and acetaminophen) (See Table.).
The significance of neuraxial and truncal nerve blockade for post-cesarean delivery pain control
Administration of a long-acting intrathecal opioid such as morphine lengthens time to first analgesic request after surgery and lowers 24-hour post‒cesarean delivery opioid requirement.14 If a patient requires general anesthesia and receives no spinal opioid, a transversus abdominis plane (TAP) block or quadratus lumborum (QL) block for postpartum pain control can lower associated postpartum opioid consumption. However, TAP or QL blocks confer no additional benefit to patients who receive spinal morphine,15 nor do they confer added benefit when combined with a multimodal pain management regimen postdelivery vs the multimodal regimen alone.16). TAP blocks administered to patients with severe breakthrough pain after spinal anesthesia help to lower opioid consumption.17 Further research is warranted on the use of TAP, QL, or other truncal blocks to spare opioid requirement after cesarean delivery in women with chronic pain, opioid use disorder, or those undergoing higher-complexity surgery such as cesarean hysterectomy for placenta accreta spectrum.
NSAIDs: Potential adverse effects
As we decrease the use of opioid medications and increase the use of nonsteroidal anti-inflammatory drugs (NSAIDs), we should reflect on the potential adverse effects of NSAID treatment in some patients. Specifically, the impact of ketorolac on hypertension, platelet function, and breastfeeding warrant consideration.
In the past, some studies reported that NSAID treatment is associated with a modest increase in blood pressure (BP), with a mean increase of 5 mm Hg.18 However, multiple recent studies report that in women with preeclampsia with and without severe features, postpartum administration of ibuprofen and ketorolac did not increase BP or delay resolution of hypertension.19-22 In a meta-analysis of randomized controlled studies comparing the effects of ibuprofen and acetaminophen on BP, neither medication was associated with an increase in BP.19 The American College of Obstetricians and Gynecologists supports the use of NSAIDs as one component of multimodal analgesia to help reduce the use of opioids.23
NSAIDs can inhibit platelet function and this effect is of clinical concern for people with platelet defects. However, a meta-analysis of clinical trials reported no difference in bleeding between surgical patients administered ketorolac or control participants.24 Alternative opioid-sparing adjuncts (TAP or QL blocks) may be considered for patients who cannot receive ketorolac based on a history of platelet deficiency. Furthermore, patients with ongoing coagulation defects after surgery from severe postpartum hemorrhage, hyperfibrinolysis, disseminated intravascular coagulation, or dilutional coagulopathy may have both limited platelet reserves and acute kidney injury. The need to postpone the initiation of NSAIDs in such patients should prompt alternate options such as TAP or QL blocks or dosing of an indwelling epidural when possible, in conjunction with acetaminophen. Patients who have a contraindication to ketorolac due to peptic ulcer disease or renal insufficiency may also benefit from TAP and QL blocks after cesarean delivery, although more studies are needed in these patients.
Both ketorolac and ibuprofen transfer to breast milk. The relative infant dose for ketorolac and ibuprofen is very low—0.2% and 0.9%, respectively.25,26 The World Health Organization advises that ibuprofen is compatible with breastfeeding.27 Of interest, in an enhanced recovery after cesarean clinical trial, scheduled ketorolac administration resulted in more mothers exclusively breastfeeding at discharge compared with “as needed” ketorolac treatment, 67% versus 48%, respectively; P = .046.28
Conclusion
Many factors influence a person’s experience of their surgery, including their pain symptoms. Factors that modulate a person’s perception of pain following surgery include their personality, social supports, and genetic factors. The technical skill of the anesthesiologist, surgeon, and nurses, and the confidence of the patient in the surgical care team are important factors influencing a person’s global experience of their surgery, including their experience of pain. Patients’ expectations regarding postoperative pain and psychological distress surrounding surgery may also influence their pain experience. Assuring patients that their pain will be addressed adequately, and helping them manage peripartum anxiety, also may favorably impact their pain experience.
Following a surgical procedure, a surgeon’s top goal is the full recovery of the patient to normal activity as soon as possible with as few complications as possible. Persistent opioid dependence is a serious long-term complication of surgery. Decades ago, most heroin users reported that heroin was the first opioid they used. However, the gateway drug to heroin use has evolved. In a recent study, 75% of heroin users reported that the first opioid they used was a prescription opioid.29 In managing surgical pain we want to minimize the use of opioids and reduce the risk of persistent opioid use following discharge. We believe that implementing a multimodal approach to the management of pain with additional targeted therapy for patients at risk for higher opioid requirement will reduce the perioperative and postdischarge use of opioid analgesics. ●
- Drug overdose deaths in the U.S. up 30% in 2020. Centers for Disease Control and Prevention web- site. July 14, 2020. https://www.cdc.gov/nchs /pressroom/nchs_press_releases/2021/20210714 .htm. Last reviewed July 14, 2021
- Jani M, Girard N, Bates DW, et al. Opioid prescribing among new users for non-cancer pain in the USA, Canada, UK, and Taiwan: a population-based cohort study. PLoS Med. 2021;18:e1003829.
- U.S. opioid dispensing rate maps. Centers for Disease Control and Prevention website. https://www. cdc.gov/drugoverdose/rxrate-maps/index.html. Last reviewed November 10, 2021.
- Richards GC, Aronson JK, Mahtani KR, et al. Global, regional, and national consumption of controlled opioids: a cross-sectional study of 214 countries and non-metropolitan areas. British J Pain. 2021. https://doi .org/10.1177/20494637211013052.
- Hamilton BE, Martin JA, Osterman MJK. Births: Provisional data for 2020. Vital Statistics Rapid Release; no 12. Hyattsville MD: National Center for Health Statistics. May 2021.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215:353.e1-e8. doi: 10.1016/j.ajog.2016.03.016.
- Osmundson SS, Wiese AD, Min JY, et al. Delivery type, opioid prescribing and the risk of persistent opioid use after delivery. Am J Obstet Gynecol. 2019;220:405-407. doi: 10.1016/j.ajog.2018.10.026.
- Peahl AF, Dalton VK, Montgomery JR, et al. Rates of new persistent opioid use after vaginal or cesarean birth among U.S. women. JAMA Netw Open. 2019;e197863. doi: 10.1001/jamanetworkopen.2019.7863.
- Holland E, Bateman BT, Cole N, et al. Evaluation of a quality improvement intervention that eliminated routine use of opioids after cesarean delivery. Obstet Gynecol. 2019;133:91-97. doi: 10.1097/AOG.0000000000003010.
- Smith AM, Young P, Blosser CC, et al. Multimodal stepwise approach to reducing in-hospital opioid use after cesarean delivery. Obstet Gynecol. 2019;133:700-706. doi: 10.1097/AOG.0000000000003156.
- Herbert KA, Yuraschevich M, Fuller M, et al. Impact of multimodeal analgesic protocol modification on opioid consumption after cesarean delivery: a retrospective cohort study. J Matern Fetal Neonatal Med. 2021;3:1-7. doi: 10.1080/14767058.2020.1863364.
- Mehraban SS, Suddle R, Mehraban S, et al. Opioid-free multimodal analgesia pathway to decrease opioid utilization after cesarean delivery. J Obstet Gynaecol Res. 2021;47:873-881. doi: 10.1111/jog.14582.
- Meyer MF, Broman AT, Gnadt SE, et al. A standardized post-cesarean analgesia regimen reduces postpartum opioid use. J Matern Fetal Neonatal Med. 2021;26:1-8. doi: 10.1080/14767058.2021.1970132.
- Seki H, Shiga T, Mihara T, et al. Effects of intrathecal opioids on cesarean section: a systematic review and Bayesian network meta-analysis of randomized controlled trials. J Anesth. 2021;35:911-927. doi: 10.1007/s00540-021-02980-2.
- Yang TR, He XM, Li XH, et al. Intrathecal morphine versus transversus abdominis plane block for cesarean delivery: a systematic review and meta-analysis. BMC Anesthesiol. 2021;21:174. doi: 10.1186/s12871-021-01392-9.
- Yu Y, Gao S, Yuen VMY, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane (TAP) block combined with oral multimodal analgesia in comparison with oral multimodal analgesia after cesarean delivery: a randomized controlled trial. BMC Anesthesiol. 2021;21:7. doi: 10.1186/s12871-020-01223-3.
- Mirza F, Carvalho B. Transversus abdominis plane blocks for rescue analgesia following cesarean delivery: a case series. Can J Anesth. 2013;60:299-303.
- Johnson AG, Nguyen TV, Day RO. Do nonsteroidal anti-inflammatory drugs affect blood pressure? A meta-analysis. Ann Int Med. 1994;121:289-300.
- Wang B, Yang X, Yu H, et al. The comparison of ibuprofen versus acetaminophen for blood pressure in preeclampsia: a meta-analysis of randomized controlled studies. J Matern Fetal Neonatal Med. 2020:1-6. doi: 10.1080/14767058.2020.1720641.
- Viteri OA, England JA, Alrais MA, et al. Association of nonsteroidal anti-inflammatory drugs and postpartum hypertension in women with preeclampsia with severe features. Obstet Gynecol. 2017;130:830. doi: 10.1097/AOG.0000000000002247.
- Blue NR, Murray-Krezan C, Drake-Lavelle S, et al. Effect of ibuprofen vs acetaminophen on postpartum hypertension in preeclampsia with severe features: a double-masked, randomized controlled trial. Am J Obstet Gynecol. 2018;218:616.e1. doi: 10.1016/j.ajog.2018.02.016.
- Penfield CA, McNulty JA, Oakes MC, et al. Ibuprofen and postpartum blood pressure in women with hypertensive disorders of pregnancy: a randomized controlled trial. Obstet Gynecol. 2019;134:1219. doi: 10.1097/AOG.0000000000003553.
- American College of Obstetricians and Gynecologists. Pharmacologic stepwise multimodal approach for postpartum pain management. Obstet Gynecol. 2021;138:507-517. doi: 10.1097/AOG.0000000000004517.
- Gobble RM, Hoang HLT, Kachniarz B, et al. Ketorolac does not increase perioperative bleeding: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2014;133:741. doi: 10.1097/01.prs.0000438459.60474.b5.
- Wischik A, Manth SM, Lloyd J, et al. The excretion of ketorolac tromethamine into breast milk after multiple oral dosing. Eur J Clin Pharmacol. 1989;36:521-524. doi: 10.1007/BF00558080.
- Rigourd V, de Villepin B, Amirouche A, et al. Ibuprofen concentrations in human mature milk-first data about pharmacokinetics study in breast milk with AOR-10127 “Antalait” study. The Drug Monit. 2014;36:590-596. doi: 10.1097/FTD.0000000000000058.
- World Health Organization. Breastfeeding and maternal medication, recommendations for drugs in the eleventh WHO model list of essential drugs. 2002. http://www.who.int/maternal _child_adolescent/documents/55732/en/.
- Teigen NC, Sahasrabudhe N, Doulaveris G. Enhanced recovery after surgery at cesarean delivery to reduce postoperative length of stay: a randomized controlled trial. Am J Obstet Gynecol. 2020;222:372.e1-e10. doi: 10.1016/j.ajog.2019.10.009.
- Cicero T, Ellis MS, Surratt HL, et al. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71:821-826. doi: 10.1001 /jamapsychiatry.2014.366.
Opioid-related deaths are a major cause of mortality in the United States. The Centers for Disease Control and Prevention (CDC) reported 72,151 and 93,331 drug overdose deaths in 2019 and 2020, respectively, and drug overdose deaths have continued to increase in 2021.1 The majority of drug overdose deaths are due to opioids. There are many factors contributing to this rise, including an incredibly high rate of opioid prescriptions in this country.2 The CDC reported that in 3.6% of US counties, there are more opioid prescriptions filled each year than number of residents in the county.3 The consumption of opioids per person in the US is approximately four times greater than countries with excellent health outcomes, including Sweden, Netherlands, Norway, and the United Kingdom.4 Some US physicians have opioid prescribing practices that are inconsistent with good medical practice in other countries, prescribing powerful opioids and an excessive number of pills per opioid prescription.2 We must continue to evolve our clinical practices to reduce opioid use while continually improving patient outcomes.
Cesarean birth is one of the most common major surgical procedures performed in the United States. The National Center for Health Statistics reported that in 2020 there were approximately 1,150,000 US cesarean births.5 Following cesarean birth, patients who were previously naïve to opioid medications were reported to have a 0.33% to 2.2% probability of transitioning to the persistent use of opioid prescriptions.6-8 Predictors of persistent opioid use after cesarean birth included a history of tobacco use, back pain, migraine headaches, and antidepressant or benzodiazepine use.6 The use of cesarean birth pain management protocols that prioritize multimodal analgesia and opioid sparing is warranted.
Multimodal pain management protocols for cesarean birth have been shown to reduce the use of opioid medications in the hospital and at discharge without a clinically significant increase in pain scores or a reduction in patient satisfaction (TABLE).9-13 For example, Holland and colleagues9 reported that the implementation of a multimodal pain management protocol reduced the percent of patients using oral opioids during hospitalization for cesarean birth from 68% to 45%, pre- and post-intervention, respectively. Mehraban and colleagues12 reported that the percent of patients using opioids during hospitalization for cesarean birth was reduced from 45% preintervention to 18% postintervention. In addition, these studies showed that multimodal pain management protocols for cesarean birth also reduced opioid prescribing at discharge. Holland and colleagues9 reported that the percent of patients provided an opioid prescription at discharge was reduced from 91% to 40%, pre- and post-intervention, respectively. Mehraban and colleagues12 reported that the percent of patients who took opioids after discharge was reduced from 24% preintervention to 9% postintervention. These studies were not randomized controlled clinical trials, but they do provide strong evidence that a focused intervention to reduce opioid medications in the management of pain after cesarean surgery can be successful without decreasing patient satisfaction or increasing reported pain scores. In these studies, it is likely that the influence, enthusiasm, and commitment of the study leaders to the change process contributed to the success of these opioid-sparing pain management programs.
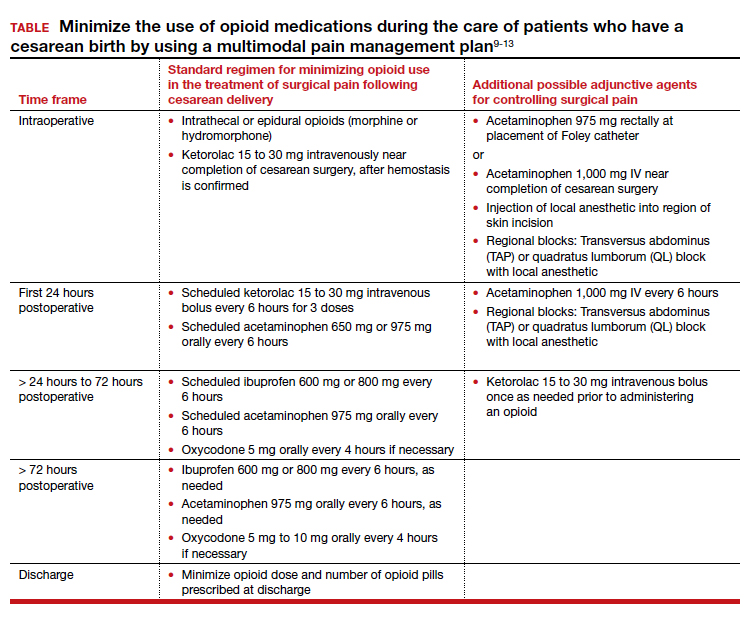
Continue to: Key features of a multimodal analgesia intervention for cesarean surgery...
Key features of a multimodal analgesia intervention for cesarean surgery
Fundamental inclusions of multimodal analgesia for cesarean surgery include:
- exquisite attention to pain control during the surgical procedure by both the anesthesiologist and surgeon, with prioritization of spinal anesthesia that includes morphine and fentanyl
- regularly scheduled administration of intravenous ketorolac during the first 24 hours postcesarean
- regularly scheduled administration of both acetaminophen and ibuprofen, rather than “as needed” dosing
- using analgesics that work through different molecular pathways (ibuprofen and acetaminophen) (See Table.).
The significance of neuraxial and truncal nerve blockade for post-cesarean delivery pain control
Administration of a long-acting intrathecal opioid such as morphine lengthens time to first analgesic request after surgery and lowers 24-hour post‒cesarean delivery opioid requirement.14 If a patient requires general anesthesia and receives no spinal opioid, a transversus abdominis plane (TAP) block or quadratus lumborum (QL) block for postpartum pain control can lower associated postpartum opioid consumption. However, TAP or QL blocks confer no additional benefit to patients who receive spinal morphine,15 nor do they confer added benefit when combined with a multimodal pain management regimen postdelivery vs the multimodal regimen alone.16). TAP blocks administered to patients with severe breakthrough pain after spinal anesthesia help to lower opioid consumption.17 Further research is warranted on the use of TAP, QL, or other truncal blocks to spare opioid requirement after cesarean delivery in women with chronic pain, opioid use disorder, or those undergoing higher-complexity surgery such as cesarean hysterectomy for placenta accreta spectrum.
NSAIDs: Potential adverse effects
As we decrease the use of opioid medications and increase the use of nonsteroidal anti-inflammatory drugs (NSAIDs), we should reflect on the potential adverse effects of NSAID treatment in some patients. Specifically, the impact of ketorolac on hypertension, platelet function, and breastfeeding warrant consideration.
In the past, some studies reported that NSAID treatment is associated with a modest increase in blood pressure (BP), with a mean increase of 5 mm Hg.18 However, multiple recent studies report that in women with preeclampsia with and without severe features, postpartum administration of ibuprofen and ketorolac did not increase BP or delay resolution of hypertension.19-22 In a meta-analysis of randomized controlled studies comparing the effects of ibuprofen and acetaminophen on BP, neither medication was associated with an increase in BP.19 The American College of Obstetricians and Gynecologists supports the use of NSAIDs as one component of multimodal analgesia to help reduce the use of opioids.23
NSAIDs can inhibit platelet function and this effect is of clinical concern for people with platelet defects. However, a meta-analysis of clinical trials reported no difference in bleeding between surgical patients administered ketorolac or control participants.24 Alternative opioid-sparing adjuncts (TAP or QL blocks) may be considered for patients who cannot receive ketorolac based on a history of platelet deficiency. Furthermore, patients with ongoing coagulation defects after surgery from severe postpartum hemorrhage, hyperfibrinolysis, disseminated intravascular coagulation, or dilutional coagulopathy may have both limited platelet reserves and acute kidney injury. The need to postpone the initiation of NSAIDs in such patients should prompt alternate options such as TAP or QL blocks or dosing of an indwelling epidural when possible, in conjunction with acetaminophen. Patients who have a contraindication to ketorolac due to peptic ulcer disease or renal insufficiency may also benefit from TAP and QL blocks after cesarean delivery, although more studies are needed in these patients.
Both ketorolac and ibuprofen transfer to breast milk. The relative infant dose for ketorolac and ibuprofen is very low—0.2% and 0.9%, respectively.25,26 The World Health Organization advises that ibuprofen is compatible with breastfeeding.27 Of interest, in an enhanced recovery after cesarean clinical trial, scheduled ketorolac administration resulted in more mothers exclusively breastfeeding at discharge compared with “as needed” ketorolac treatment, 67% versus 48%, respectively; P = .046.28
Conclusion
Many factors influence a person’s experience of their surgery, including their pain symptoms. Factors that modulate a person’s perception of pain following surgery include their personality, social supports, and genetic factors. The technical skill of the anesthesiologist, surgeon, and nurses, and the confidence of the patient in the surgical care team are important factors influencing a person’s global experience of their surgery, including their experience of pain. Patients’ expectations regarding postoperative pain and psychological distress surrounding surgery may also influence their pain experience. Assuring patients that their pain will be addressed adequately, and helping them manage peripartum anxiety, also may favorably impact their pain experience.
Following a surgical procedure, a surgeon’s top goal is the full recovery of the patient to normal activity as soon as possible with as few complications as possible. Persistent opioid dependence is a serious long-term complication of surgery. Decades ago, most heroin users reported that heroin was the first opioid they used. However, the gateway drug to heroin use has evolved. In a recent study, 75% of heroin users reported that the first opioid they used was a prescription opioid.29 In managing surgical pain we want to minimize the use of opioids and reduce the risk of persistent opioid use following discharge. We believe that implementing a multimodal approach to the management of pain with additional targeted therapy for patients at risk for higher opioid requirement will reduce the perioperative and postdischarge use of opioid analgesics. ●
Opioid-related deaths are a major cause of mortality in the United States. The Centers for Disease Control and Prevention (CDC) reported 72,151 and 93,331 drug overdose deaths in 2019 and 2020, respectively, and drug overdose deaths have continued to increase in 2021.1 The majority of drug overdose deaths are due to opioids. There are many factors contributing to this rise, including an incredibly high rate of opioid prescriptions in this country.2 The CDC reported that in 3.6% of US counties, there are more opioid prescriptions filled each year than number of residents in the county.3 The consumption of opioids per person in the US is approximately four times greater than countries with excellent health outcomes, including Sweden, Netherlands, Norway, and the United Kingdom.4 Some US physicians have opioid prescribing practices that are inconsistent with good medical practice in other countries, prescribing powerful opioids and an excessive number of pills per opioid prescription.2 We must continue to evolve our clinical practices to reduce opioid use while continually improving patient outcomes.
Cesarean birth is one of the most common major surgical procedures performed in the United States. The National Center for Health Statistics reported that in 2020 there were approximately 1,150,000 US cesarean births.5 Following cesarean birth, patients who were previously naïve to opioid medications were reported to have a 0.33% to 2.2% probability of transitioning to the persistent use of opioid prescriptions.6-8 Predictors of persistent opioid use after cesarean birth included a history of tobacco use, back pain, migraine headaches, and antidepressant or benzodiazepine use.6 The use of cesarean birth pain management protocols that prioritize multimodal analgesia and opioid sparing is warranted.
Multimodal pain management protocols for cesarean birth have been shown to reduce the use of opioid medications in the hospital and at discharge without a clinically significant increase in pain scores or a reduction in patient satisfaction (TABLE).9-13 For example, Holland and colleagues9 reported that the implementation of a multimodal pain management protocol reduced the percent of patients using oral opioids during hospitalization for cesarean birth from 68% to 45%, pre- and post-intervention, respectively. Mehraban and colleagues12 reported that the percent of patients using opioids during hospitalization for cesarean birth was reduced from 45% preintervention to 18% postintervention. In addition, these studies showed that multimodal pain management protocols for cesarean birth also reduced opioid prescribing at discharge. Holland and colleagues9 reported that the percent of patients provided an opioid prescription at discharge was reduced from 91% to 40%, pre- and post-intervention, respectively. Mehraban and colleagues12 reported that the percent of patients who took opioids after discharge was reduced from 24% preintervention to 9% postintervention. These studies were not randomized controlled clinical trials, but they do provide strong evidence that a focused intervention to reduce opioid medications in the management of pain after cesarean surgery can be successful without decreasing patient satisfaction or increasing reported pain scores. In these studies, it is likely that the influence, enthusiasm, and commitment of the study leaders to the change process contributed to the success of these opioid-sparing pain management programs.
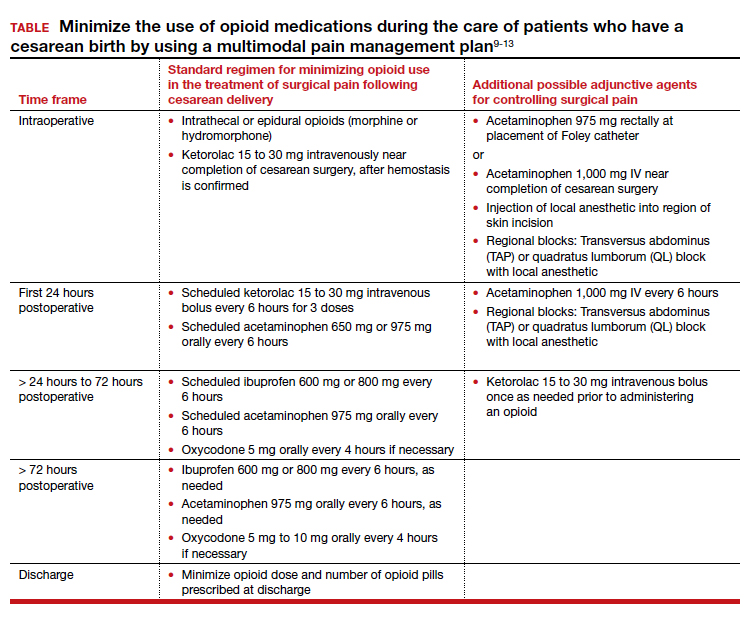
Continue to: Key features of a multimodal analgesia intervention for cesarean surgery...
Key features of a multimodal analgesia intervention for cesarean surgery
Fundamental inclusions of multimodal analgesia for cesarean surgery include:
- exquisite attention to pain control during the surgical procedure by both the anesthesiologist and surgeon, with prioritization of spinal anesthesia that includes morphine and fentanyl
- regularly scheduled administration of intravenous ketorolac during the first 24 hours postcesarean
- regularly scheduled administration of both acetaminophen and ibuprofen, rather than “as needed” dosing
- using analgesics that work through different molecular pathways (ibuprofen and acetaminophen) (See Table.).
The significance of neuraxial and truncal nerve blockade for post-cesarean delivery pain control
Administration of a long-acting intrathecal opioid such as morphine lengthens time to first analgesic request after surgery and lowers 24-hour post‒cesarean delivery opioid requirement.14 If a patient requires general anesthesia and receives no spinal opioid, a transversus abdominis plane (TAP) block or quadratus lumborum (QL) block for postpartum pain control can lower associated postpartum opioid consumption. However, TAP or QL blocks confer no additional benefit to patients who receive spinal morphine,15 nor do they confer added benefit when combined with a multimodal pain management regimen postdelivery vs the multimodal regimen alone.16). TAP blocks administered to patients with severe breakthrough pain after spinal anesthesia help to lower opioid consumption.17 Further research is warranted on the use of TAP, QL, or other truncal blocks to spare opioid requirement after cesarean delivery in women with chronic pain, opioid use disorder, or those undergoing higher-complexity surgery such as cesarean hysterectomy for placenta accreta spectrum.
NSAIDs: Potential adverse effects
As we decrease the use of opioid medications and increase the use of nonsteroidal anti-inflammatory drugs (NSAIDs), we should reflect on the potential adverse effects of NSAID treatment in some patients. Specifically, the impact of ketorolac on hypertension, platelet function, and breastfeeding warrant consideration.
In the past, some studies reported that NSAID treatment is associated with a modest increase in blood pressure (BP), with a mean increase of 5 mm Hg.18 However, multiple recent studies report that in women with preeclampsia with and without severe features, postpartum administration of ibuprofen and ketorolac did not increase BP or delay resolution of hypertension.19-22 In a meta-analysis of randomized controlled studies comparing the effects of ibuprofen and acetaminophen on BP, neither medication was associated with an increase in BP.19 The American College of Obstetricians and Gynecologists supports the use of NSAIDs as one component of multimodal analgesia to help reduce the use of opioids.23
NSAIDs can inhibit platelet function and this effect is of clinical concern for people with platelet defects. However, a meta-analysis of clinical trials reported no difference in bleeding between surgical patients administered ketorolac or control participants.24 Alternative opioid-sparing adjuncts (TAP or QL blocks) may be considered for patients who cannot receive ketorolac based on a history of platelet deficiency. Furthermore, patients with ongoing coagulation defects after surgery from severe postpartum hemorrhage, hyperfibrinolysis, disseminated intravascular coagulation, or dilutional coagulopathy may have both limited platelet reserves and acute kidney injury. The need to postpone the initiation of NSAIDs in such patients should prompt alternate options such as TAP or QL blocks or dosing of an indwelling epidural when possible, in conjunction with acetaminophen. Patients who have a contraindication to ketorolac due to peptic ulcer disease or renal insufficiency may also benefit from TAP and QL blocks after cesarean delivery, although more studies are needed in these patients.
Both ketorolac and ibuprofen transfer to breast milk. The relative infant dose for ketorolac and ibuprofen is very low—0.2% and 0.9%, respectively.25,26 The World Health Organization advises that ibuprofen is compatible with breastfeeding.27 Of interest, in an enhanced recovery after cesarean clinical trial, scheduled ketorolac administration resulted in more mothers exclusively breastfeeding at discharge compared with “as needed” ketorolac treatment, 67% versus 48%, respectively; P = .046.28
Conclusion
Many factors influence a person’s experience of their surgery, including their pain symptoms. Factors that modulate a person’s perception of pain following surgery include their personality, social supports, and genetic factors. The technical skill of the anesthesiologist, surgeon, and nurses, and the confidence of the patient in the surgical care team are important factors influencing a person’s global experience of their surgery, including their experience of pain. Patients’ expectations regarding postoperative pain and psychological distress surrounding surgery may also influence their pain experience. Assuring patients that their pain will be addressed adequately, and helping them manage peripartum anxiety, also may favorably impact their pain experience.
Following a surgical procedure, a surgeon’s top goal is the full recovery of the patient to normal activity as soon as possible with as few complications as possible. Persistent opioid dependence is a serious long-term complication of surgery. Decades ago, most heroin users reported that heroin was the first opioid they used. However, the gateway drug to heroin use has evolved. In a recent study, 75% of heroin users reported that the first opioid they used was a prescription opioid.29 In managing surgical pain we want to minimize the use of opioids and reduce the risk of persistent opioid use following discharge. We believe that implementing a multimodal approach to the management of pain with additional targeted therapy for patients at risk for higher opioid requirement will reduce the perioperative and postdischarge use of opioid analgesics. ●
- Drug overdose deaths in the U.S. up 30% in 2020. Centers for Disease Control and Prevention web- site. July 14, 2020. https://www.cdc.gov/nchs /pressroom/nchs_press_releases/2021/20210714 .htm. Last reviewed July 14, 2021
- Jani M, Girard N, Bates DW, et al. Opioid prescribing among new users for non-cancer pain in the USA, Canada, UK, and Taiwan: a population-based cohort study. PLoS Med. 2021;18:e1003829.
- U.S. opioid dispensing rate maps. Centers for Disease Control and Prevention website. https://www. cdc.gov/drugoverdose/rxrate-maps/index.html. Last reviewed November 10, 2021.
- Richards GC, Aronson JK, Mahtani KR, et al. Global, regional, and national consumption of controlled opioids: a cross-sectional study of 214 countries and non-metropolitan areas. British J Pain. 2021. https://doi .org/10.1177/20494637211013052.
- Hamilton BE, Martin JA, Osterman MJK. Births: Provisional data for 2020. Vital Statistics Rapid Release; no 12. Hyattsville MD: National Center for Health Statistics. May 2021.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215:353.e1-e8. doi: 10.1016/j.ajog.2016.03.016.
- Osmundson SS, Wiese AD, Min JY, et al. Delivery type, opioid prescribing and the risk of persistent opioid use after delivery. Am J Obstet Gynecol. 2019;220:405-407. doi: 10.1016/j.ajog.2018.10.026.
- Peahl AF, Dalton VK, Montgomery JR, et al. Rates of new persistent opioid use after vaginal or cesarean birth among U.S. women. JAMA Netw Open. 2019;e197863. doi: 10.1001/jamanetworkopen.2019.7863.
- Holland E, Bateman BT, Cole N, et al. Evaluation of a quality improvement intervention that eliminated routine use of opioids after cesarean delivery. Obstet Gynecol. 2019;133:91-97. doi: 10.1097/AOG.0000000000003010.
- Smith AM, Young P, Blosser CC, et al. Multimodal stepwise approach to reducing in-hospital opioid use after cesarean delivery. Obstet Gynecol. 2019;133:700-706. doi: 10.1097/AOG.0000000000003156.
- Herbert KA, Yuraschevich M, Fuller M, et al. Impact of multimodeal analgesic protocol modification on opioid consumption after cesarean delivery: a retrospective cohort study. J Matern Fetal Neonatal Med. 2021;3:1-7. doi: 10.1080/14767058.2020.1863364.
- Mehraban SS, Suddle R, Mehraban S, et al. Opioid-free multimodal analgesia pathway to decrease opioid utilization after cesarean delivery. J Obstet Gynaecol Res. 2021;47:873-881. doi: 10.1111/jog.14582.
- Meyer MF, Broman AT, Gnadt SE, et al. A standardized post-cesarean analgesia regimen reduces postpartum opioid use. J Matern Fetal Neonatal Med. 2021;26:1-8. doi: 10.1080/14767058.2021.1970132.
- Seki H, Shiga T, Mihara T, et al. Effects of intrathecal opioids on cesarean section: a systematic review and Bayesian network meta-analysis of randomized controlled trials. J Anesth. 2021;35:911-927. doi: 10.1007/s00540-021-02980-2.
- Yang TR, He XM, Li XH, et al. Intrathecal morphine versus transversus abdominis plane block for cesarean delivery: a systematic review and meta-analysis. BMC Anesthesiol. 2021;21:174. doi: 10.1186/s12871-021-01392-9.
- Yu Y, Gao S, Yuen VMY, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane (TAP) block combined with oral multimodal analgesia in comparison with oral multimodal analgesia after cesarean delivery: a randomized controlled trial. BMC Anesthesiol. 2021;21:7. doi: 10.1186/s12871-020-01223-3.
- Mirza F, Carvalho B. Transversus abdominis plane blocks for rescue analgesia following cesarean delivery: a case series. Can J Anesth. 2013;60:299-303.
- Johnson AG, Nguyen TV, Day RO. Do nonsteroidal anti-inflammatory drugs affect blood pressure? A meta-analysis. Ann Int Med. 1994;121:289-300.
- Wang B, Yang X, Yu H, et al. The comparison of ibuprofen versus acetaminophen for blood pressure in preeclampsia: a meta-analysis of randomized controlled studies. J Matern Fetal Neonatal Med. 2020:1-6. doi: 10.1080/14767058.2020.1720641.
- Viteri OA, England JA, Alrais MA, et al. Association of nonsteroidal anti-inflammatory drugs and postpartum hypertension in women with preeclampsia with severe features. Obstet Gynecol. 2017;130:830. doi: 10.1097/AOG.0000000000002247.
- Blue NR, Murray-Krezan C, Drake-Lavelle S, et al. Effect of ibuprofen vs acetaminophen on postpartum hypertension in preeclampsia with severe features: a double-masked, randomized controlled trial. Am J Obstet Gynecol. 2018;218:616.e1. doi: 10.1016/j.ajog.2018.02.016.
- Penfield CA, McNulty JA, Oakes MC, et al. Ibuprofen and postpartum blood pressure in women with hypertensive disorders of pregnancy: a randomized controlled trial. Obstet Gynecol. 2019;134:1219. doi: 10.1097/AOG.0000000000003553.
- American College of Obstetricians and Gynecologists. Pharmacologic stepwise multimodal approach for postpartum pain management. Obstet Gynecol. 2021;138:507-517. doi: 10.1097/AOG.0000000000004517.
- Gobble RM, Hoang HLT, Kachniarz B, et al. Ketorolac does not increase perioperative bleeding: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2014;133:741. doi: 10.1097/01.prs.0000438459.60474.b5.
- Wischik A, Manth SM, Lloyd J, et al. The excretion of ketorolac tromethamine into breast milk after multiple oral dosing. Eur J Clin Pharmacol. 1989;36:521-524. doi: 10.1007/BF00558080.
- Rigourd V, de Villepin B, Amirouche A, et al. Ibuprofen concentrations in human mature milk-first data about pharmacokinetics study in breast milk with AOR-10127 “Antalait” study. The Drug Monit. 2014;36:590-596. doi: 10.1097/FTD.0000000000000058.
- World Health Organization. Breastfeeding and maternal medication, recommendations for drugs in the eleventh WHO model list of essential drugs. 2002. http://www.who.int/maternal _child_adolescent/documents/55732/en/.
- Teigen NC, Sahasrabudhe N, Doulaveris G. Enhanced recovery after surgery at cesarean delivery to reduce postoperative length of stay: a randomized controlled trial. Am J Obstet Gynecol. 2020;222:372.e1-e10. doi: 10.1016/j.ajog.2019.10.009.
- Cicero T, Ellis MS, Surratt HL, et al. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71:821-826. doi: 10.1001 /jamapsychiatry.2014.366.
- Drug overdose deaths in the U.S. up 30% in 2020. Centers for Disease Control and Prevention web- site. July 14, 2020. https://www.cdc.gov/nchs /pressroom/nchs_press_releases/2021/20210714 .htm. Last reviewed July 14, 2021
- Jani M, Girard N, Bates DW, et al. Opioid prescribing among new users for non-cancer pain in the USA, Canada, UK, and Taiwan: a population-based cohort study. PLoS Med. 2021;18:e1003829.
- U.S. opioid dispensing rate maps. Centers for Disease Control and Prevention website. https://www. cdc.gov/drugoverdose/rxrate-maps/index.html. Last reviewed November 10, 2021.
- Richards GC, Aronson JK, Mahtani KR, et al. Global, regional, and national consumption of controlled opioids: a cross-sectional study of 214 countries and non-metropolitan areas. British J Pain. 2021. https://doi .org/10.1177/20494637211013052.
- Hamilton BE, Martin JA, Osterman MJK. Births: Provisional data for 2020. Vital Statistics Rapid Release; no 12. Hyattsville MD: National Center for Health Statistics. May 2021.
- Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naïve women. Am J Obstet Gynecol. 2016;215:353.e1-e8. doi: 10.1016/j.ajog.2016.03.016.
- Osmundson SS, Wiese AD, Min JY, et al. Delivery type, opioid prescribing and the risk of persistent opioid use after delivery. Am J Obstet Gynecol. 2019;220:405-407. doi: 10.1016/j.ajog.2018.10.026.
- Peahl AF, Dalton VK, Montgomery JR, et al. Rates of new persistent opioid use after vaginal or cesarean birth among U.S. women. JAMA Netw Open. 2019;e197863. doi: 10.1001/jamanetworkopen.2019.7863.
- Holland E, Bateman BT, Cole N, et al. Evaluation of a quality improvement intervention that eliminated routine use of opioids after cesarean delivery. Obstet Gynecol. 2019;133:91-97. doi: 10.1097/AOG.0000000000003010.
- Smith AM, Young P, Blosser CC, et al. Multimodal stepwise approach to reducing in-hospital opioid use after cesarean delivery. Obstet Gynecol. 2019;133:700-706. doi: 10.1097/AOG.0000000000003156.
- Herbert KA, Yuraschevich M, Fuller M, et al. Impact of multimodeal analgesic protocol modification on opioid consumption after cesarean delivery: a retrospective cohort study. J Matern Fetal Neonatal Med. 2021;3:1-7. doi: 10.1080/14767058.2020.1863364.
- Mehraban SS, Suddle R, Mehraban S, et al. Opioid-free multimodal analgesia pathway to decrease opioid utilization after cesarean delivery. J Obstet Gynaecol Res. 2021;47:873-881. doi: 10.1111/jog.14582.
- Meyer MF, Broman AT, Gnadt SE, et al. A standardized post-cesarean analgesia regimen reduces postpartum opioid use. J Matern Fetal Neonatal Med. 2021;26:1-8. doi: 10.1080/14767058.2021.1970132.
- Seki H, Shiga T, Mihara T, et al. Effects of intrathecal opioids on cesarean section: a systematic review and Bayesian network meta-analysis of randomized controlled trials. J Anesth. 2021;35:911-927. doi: 10.1007/s00540-021-02980-2.
- Yang TR, He XM, Li XH, et al. Intrathecal morphine versus transversus abdominis plane block for cesarean delivery: a systematic review and meta-analysis. BMC Anesthesiol. 2021;21:174. doi: 10.1186/s12871-021-01392-9.
- Yu Y, Gao S, Yuen VMY, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane (TAP) block combined with oral multimodal analgesia in comparison with oral multimodal analgesia after cesarean delivery: a randomized controlled trial. BMC Anesthesiol. 2021;21:7. doi: 10.1186/s12871-020-01223-3.
- Mirza F, Carvalho B. Transversus abdominis plane blocks for rescue analgesia following cesarean delivery: a case series. Can J Anesth. 2013;60:299-303.
- Johnson AG, Nguyen TV, Day RO. Do nonsteroidal anti-inflammatory drugs affect blood pressure? A meta-analysis. Ann Int Med. 1994;121:289-300.
- Wang B, Yang X, Yu H, et al. The comparison of ibuprofen versus acetaminophen for blood pressure in preeclampsia: a meta-analysis of randomized controlled studies. J Matern Fetal Neonatal Med. 2020:1-6. doi: 10.1080/14767058.2020.1720641.
- Viteri OA, England JA, Alrais MA, et al. Association of nonsteroidal anti-inflammatory drugs and postpartum hypertension in women with preeclampsia with severe features. Obstet Gynecol. 2017;130:830. doi: 10.1097/AOG.0000000000002247.
- Blue NR, Murray-Krezan C, Drake-Lavelle S, et al. Effect of ibuprofen vs acetaminophen on postpartum hypertension in preeclampsia with severe features: a double-masked, randomized controlled trial. Am J Obstet Gynecol. 2018;218:616.e1. doi: 10.1016/j.ajog.2018.02.016.
- Penfield CA, McNulty JA, Oakes MC, et al. Ibuprofen and postpartum blood pressure in women with hypertensive disorders of pregnancy: a randomized controlled trial. Obstet Gynecol. 2019;134:1219. doi: 10.1097/AOG.0000000000003553.
- American College of Obstetricians and Gynecologists. Pharmacologic stepwise multimodal approach for postpartum pain management. Obstet Gynecol. 2021;138:507-517. doi: 10.1097/AOG.0000000000004517.
- Gobble RM, Hoang HLT, Kachniarz B, et al. Ketorolac does not increase perioperative bleeding: a meta-analysis of randomized controlled trials. Plast Reconstr Surg. 2014;133:741. doi: 10.1097/01.prs.0000438459.60474.b5.
- Wischik A, Manth SM, Lloyd J, et al. The excretion of ketorolac tromethamine into breast milk after multiple oral dosing. Eur J Clin Pharmacol. 1989;36:521-524. doi: 10.1007/BF00558080.
- Rigourd V, de Villepin B, Amirouche A, et al. Ibuprofen concentrations in human mature milk-first data about pharmacokinetics study in breast milk with AOR-10127 “Antalait” study. The Drug Monit. 2014;36:590-596. doi: 10.1097/FTD.0000000000000058.
- World Health Organization. Breastfeeding and maternal medication, recommendations for drugs in the eleventh WHO model list of essential drugs. 2002. http://www.who.int/maternal _child_adolescent/documents/55732/en/.
- Teigen NC, Sahasrabudhe N, Doulaveris G. Enhanced recovery after surgery at cesarean delivery to reduce postoperative length of stay: a randomized controlled trial. Am J Obstet Gynecol. 2020;222:372.e1-e10. doi: 10.1016/j.ajog.2019.10.009.
- Cicero T, Ellis MS, Surratt HL, et al. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71:821-826. doi: 10.1001 /jamapsychiatry.2014.366.
Giant cell arteritis fast-track clinics pave way for greater ultrasound use in U.S.
Temporal artery biopsy has been the standard for diagnosing giant cell arteritis (GCA), but vascular ultrasound, a procedure that’s less invasive, less time-intensive, less expensive, and more convenient, has gained widespread use in Europe, and now clinics in the United States are adopting this approach and moving toward having rheumatologists take on the role of ultrasonographer.
However, directors at these clinics – known as GCA fast-track clinics – caution that the bar can be high for adopting vascular ultrasound (VUS) as a tool to diagnose GCA. Ultrasonographers need specialized training to perform the task and an adequate caseload to maintain their skills. Clinics also need to be outfitted with high-definition ultrasound machines.
“It definitely takes adequate training and learning of how to adjust the settings on the ultrasound machine to be able to visualize the findings appropriately,” said Minna Kohler, MD, director of the rheumatology and musculoskeletal ultrasound program at Massachusetts General Hospital in Boston, which has its own GCA fast-track clinic.
“And the clinical context is very important,” she said. “If you have a high suspicion for someone with temporal arteritis, or GCA, and the patient has been on steroids for weeks before you see them, the ultrasound findings may not show signs of the disease. In those cases in which the imaging is equivocal, we would still pursue a biopsy.”
The idea of the fast-track clinic is as the name implies: to quickly confirm the presence of GCA in a matter of hours, or days at the most, in an outpatient setting without the hassles of a biopsy. Temporal artery biopsy (TAB), by comparison, “is more costly because it requires operating room time, a surgical consultation, and surgery time, whereas ultrasound is a very inexpensive exam since it’s done in the clinic by the rheumatologist,” Dr. Kohler said.
European experience
Use of VUS to diagnose GCA is supplanting TAB in Europe and other countries. In Denmark alone – with a population of 6 million – three outpatient fast-track clinics are operating. The United States, with a population more than 50 times larger than Denmark’s, has six.
Stavros Chrysidis, MD, PhD, chief of rheumatology at the Hospital South West Jutland, one of the fast-track clinic sites in Denmark, led a recent multicenter study, known as EUREKA, of VUS in patients with suspected GCA. He and his colleagues reported in The Lancet Rheumatology that the sensitivity and specificity of VUS was superior to TAB in confirming a diagnosis of GCA. Dr. Chrysidis has instructed U.S. rheumatologists and ultrasonographers in performing and interpreting VUS for GCA.
The study emphasizes the importance of training for ultrasonographers, said Dr. Chrysidis, who regularly performs VUS at his institution. “The most important finding is that, when we apply VUS by systematically trained ultrasonographers using appropriate equipment in appropriate settings, it has excellent diagnostic accuracy on GCA,” he told this news organization.
He noted that The Lancet Rheumatology report is the first multicenter study of VUS for diagnosing GCA in which all the ultrasonographers participated in a standardized training program, which his group developed. “Ultrasound is very operator dependent,” he said. “That’s why the training is very important.”
The training occurred over a year and included two workshops consisting of 5 days of theoretical training on VUS; supervised hands-on evaluation of healthy individuals and patients with known GCA; and evaluation of ultrasound images. Over the course of the year, trainees performed at least 50 VUS evaluations, half of which were in patients with confirmed GCA. During the training period, an external rheumatologist with broad experience in VUS made the final diagnosis.
“The equipment and settings are very important because ultrasound can be very time consuming if you are not educated well and if your equipment is not adjusted well,” Dr. Chrysidis said. The equipment must be calibrated beforehand “so you don’t spend time on adjustments.”
For diagnosing temporal artery anomalies, the ultrasound equipment must have a resolution of 0.3-0.4 mm, he said. “When you have a transducer of 10 MHz, you cannot visualize changes smaller than 5 mm.”
The EUREKA study stated that VUS could replace TAB as a first-line diagnostic tool for GCA – provided the ultrasonographers are systematically trained and the equipment and settings are appropriate. In the Jutland clinic, VUS already has replaced TAB, Dr. Chrysidis said.
“In my department since 2017, when we started the fast-track clinic after the EUREKA study was terminated, we have performed three temporal artery biopsies in the last 4 years, and we screen 60-70 patients per year because we use ultrasound as the primary imaging,” he said. In cases when the results are inconclusive, they order a PET scan. “We don’t perform biopsies anymore,” he said.
U.S. fast-track clinic models
The fast-track clinic models in the United States vary. Results of a survey of the U.S. clinics were presented as an abstract at the 2021 American College of Rheumatology annual meeting. Some centers have a vasculitis specialist obtain and interpret the imaging. At others, a vasculitis specialist refers patients to a VUS-trained rheumatologist to perform and interpret the test. Another approach is to have vasculitis specialists refer patients to ultrasound technicians trained in VUS, with a vascular surgeon interpreting the images and either a VUS-trained rheumatologist or vascular medicine specialist verifying the images.
The take-home message of that survey is that “ultrasound evaluation should be considered in the hands of experts, realizing that not everyone has that skill set, but if it is available, it’s a way to expedite diagnosis and it can be helpful in managing the GCA patient in an appropriate way, quicker than trying to schedule cross-sectional imaging,” said Massachusetts General’s Dr. Kohler, who is a coauthor of the abstract. “Certainly, cross-sectional imaging also plays an important role, but when it comes to confirming whether to continue with treatment or not for a very serious condition, ultrasound is a quick way to get the answer.”
In addition to the fast-track clinic at Massachusetts General, the survey included fast-track clinics at the University of Washington, Seattle; Brigham and Women’s Hospital, Boston; Loma Linda (Calif.) University; University of California, Los Angeles; and at a private practice, Arthritis and Rheumatism Associates in the Washington area.
Advantages of VUS vs. TAB
At Massachusetts General, some of the rheumatologists are trained to perform VUS. The rheumatologists also perform the clinical evaluation of suspected cases of GCA. The advantage of VUS, Dr. Kohler said, is that the answer is “right there”; that is, the imaging yields a diagnosis almost instantaneously whereas a biopsy must be sent to a lab for analysis.
“Since a lot of patients with suspected vasculitis may already come to us on steroid therapy, and if there’s a low probability or low suspicion for vasculitis, [VUS] actually confirms that, and we’re able to taper prednisone or steroids quickly rather than keep them on a prolonged course.”
Alison Bays, MD, MPH, of the department of rheumatology at the University of Washington, said that the advantages of avoiding biopsy aren’t to be overlooked. “Temporal artery biopsies are invasive and carry surgical risks, especially as many of our patients are elderly,” she told this news organization.
“These patients occasionally refuse biopsy, but the acceptance of ultrasound is high,” Dr. Bays said. “Scheduling surgery can be more complicated, resulting in delays to biopsy and potentially higher rates of false negatives. Additionally, ultrasound has resulted in a higher rate of diagnosis with GCA as TAB misses large-vessel involvement.” The fast-track clinic at the university has evaluated 250 patients since it opened in 2017.
Dr. Bays and colleagues published the first United States study of a fast-track protocol using vascular sonographers. “Our group has demonstrated that fast-track clinics can rapidly and effectively evaluate patients, and we demonstrated a different method of evaluation using vascular sonographers rather than rheumatologists to do the vascular ultrasound,” she said. “It utilizes the familiarity vascular sonographers already have with imaging blood vessels.”
She added that the TABUL study in the United Kingdom in 2016 demonstrated that VUS yielded a savings of $686 (£484 as reported in the study), compared with TAB. “Further studies need to be done in the United States,” she said. “Beyond direct comparison of costs, reduction in steroid burden due to quick evaluation and diagnosis may carry additional benefits.”
At Brigham and Women’s Hospital, the division of rheumatology and the vascular section of the cardiology division collaborate on the GCA evaluation, said Sara Tedeschi, MD, MPH, codirector of the fast-track clinic there. Trained vascular technologists credentialed in the procedure and specifically trained in using VUS for evaluating arteritis perform the VUS. Cardiologists with a subspecialty in vascular medicine interpret the studies.
VUS patients have a rheumatology evaluation just before they have the ultrasound. “The rheumatology evaluation is then able to incorporate information from the VUS together with laboratory data, the patient’s history, and physical examination,” Dr. Tedeschi said.
“If the rheumatologist recommends a temporal artery biopsy as a next step, we arrange this with vascular surgery,” she said. “If the rheumatologist recommends other imaging such as MRA [magnetic resonance angiography] or PET-CT, we frequently review the images together with our colleagues in cardiovascular radiology and/or nuclear medicine.”
But in the United States, it will take some time for GCA fast-track clinics to become the standard, Dr. Tedeschi said. “Temporal artery biopsy may be faster to arrange in certain practice settings if VUS is not already being employed for giant cell arteritis evaluation,” she said.
Dr. Bays recognized this limitation, saying, “We are hoping that in the future, the American College of Rheumatology will consider vascular ultrasound as a first-line diagnostic test in diagnosis as rheumatologists and vascular sonographers gain familiarity over time.”
But that would mean that centers performing VUS for GCA would have to meet rigorous standards for the procedure. “With that, standardization of a protocol, high-quality equipment, and adequate training are necessary to ensure quality and reduce the chance of false-positive or false-negative results,” she said.
Dr. Chrysidis, Dr. Bays, and Dr. Tedeschi have disclosed no relevant financial relationships. Dr. Kohler is a board member of Ultrasound School of North American Rheumatologists.
A version of this article first appeared on Medscape.com.
Temporal artery biopsy has been the standard for diagnosing giant cell arteritis (GCA), but vascular ultrasound, a procedure that’s less invasive, less time-intensive, less expensive, and more convenient, has gained widespread use in Europe, and now clinics in the United States are adopting this approach and moving toward having rheumatologists take on the role of ultrasonographer.
However, directors at these clinics – known as GCA fast-track clinics – caution that the bar can be high for adopting vascular ultrasound (VUS) as a tool to diagnose GCA. Ultrasonographers need specialized training to perform the task and an adequate caseload to maintain their skills. Clinics also need to be outfitted with high-definition ultrasound machines.
“It definitely takes adequate training and learning of how to adjust the settings on the ultrasound machine to be able to visualize the findings appropriately,” said Minna Kohler, MD, director of the rheumatology and musculoskeletal ultrasound program at Massachusetts General Hospital in Boston, which has its own GCA fast-track clinic.
“And the clinical context is very important,” she said. “If you have a high suspicion for someone with temporal arteritis, or GCA, and the patient has been on steroids for weeks before you see them, the ultrasound findings may not show signs of the disease. In those cases in which the imaging is equivocal, we would still pursue a biopsy.”
The idea of the fast-track clinic is as the name implies: to quickly confirm the presence of GCA in a matter of hours, or days at the most, in an outpatient setting without the hassles of a biopsy. Temporal artery biopsy (TAB), by comparison, “is more costly because it requires operating room time, a surgical consultation, and surgery time, whereas ultrasound is a very inexpensive exam since it’s done in the clinic by the rheumatologist,” Dr. Kohler said.
European experience
Use of VUS to diagnose GCA is supplanting TAB in Europe and other countries. In Denmark alone – with a population of 6 million – three outpatient fast-track clinics are operating. The United States, with a population more than 50 times larger than Denmark’s, has six.
Stavros Chrysidis, MD, PhD, chief of rheumatology at the Hospital South West Jutland, one of the fast-track clinic sites in Denmark, led a recent multicenter study, known as EUREKA, of VUS in patients with suspected GCA. He and his colleagues reported in The Lancet Rheumatology that the sensitivity and specificity of VUS was superior to TAB in confirming a diagnosis of GCA. Dr. Chrysidis has instructed U.S. rheumatologists and ultrasonographers in performing and interpreting VUS for GCA.
The study emphasizes the importance of training for ultrasonographers, said Dr. Chrysidis, who regularly performs VUS at his institution. “The most important finding is that, when we apply VUS by systematically trained ultrasonographers using appropriate equipment in appropriate settings, it has excellent diagnostic accuracy on GCA,” he told this news organization.
He noted that The Lancet Rheumatology report is the first multicenter study of VUS for diagnosing GCA in which all the ultrasonographers participated in a standardized training program, which his group developed. “Ultrasound is very operator dependent,” he said. “That’s why the training is very important.”
The training occurred over a year and included two workshops consisting of 5 days of theoretical training on VUS; supervised hands-on evaluation of healthy individuals and patients with known GCA; and evaluation of ultrasound images. Over the course of the year, trainees performed at least 50 VUS evaluations, half of which were in patients with confirmed GCA. During the training period, an external rheumatologist with broad experience in VUS made the final diagnosis.
“The equipment and settings are very important because ultrasound can be very time consuming if you are not educated well and if your equipment is not adjusted well,” Dr. Chrysidis said. The equipment must be calibrated beforehand “so you don’t spend time on adjustments.”
For diagnosing temporal artery anomalies, the ultrasound equipment must have a resolution of 0.3-0.4 mm, he said. “When you have a transducer of 10 MHz, you cannot visualize changes smaller than 5 mm.”
The EUREKA study stated that VUS could replace TAB as a first-line diagnostic tool for GCA – provided the ultrasonographers are systematically trained and the equipment and settings are appropriate. In the Jutland clinic, VUS already has replaced TAB, Dr. Chrysidis said.
“In my department since 2017, when we started the fast-track clinic after the EUREKA study was terminated, we have performed three temporal artery biopsies in the last 4 years, and we screen 60-70 patients per year because we use ultrasound as the primary imaging,” he said. In cases when the results are inconclusive, they order a PET scan. “We don’t perform biopsies anymore,” he said.
U.S. fast-track clinic models
The fast-track clinic models in the United States vary. Results of a survey of the U.S. clinics were presented as an abstract at the 2021 American College of Rheumatology annual meeting. Some centers have a vasculitis specialist obtain and interpret the imaging. At others, a vasculitis specialist refers patients to a VUS-trained rheumatologist to perform and interpret the test. Another approach is to have vasculitis specialists refer patients to ultrasound technicians trained in VUS, with a vascular surgeon interpreting the images and either a VUS-trained rheumatologist or vascular medicine specialist verifying the images.
The take-home message of that survey is that “ultrasound evaluation should be considered in the hands of experts, realizing that not everyone has that skill set, but if it is available, it’s a way to expedite diagnosis and it can be helpful in managing the GCA patient in an appropriate way, quicker than trying to schedule cross-sectional imaging,” said Massachusetts General’s Dr. Kohler, who is a coauthor of the abstract. “Certainly, cross-sectional imaging also plays an important role, but when it comes to confirming whether to continue with treatment or not for a very serious condition, ultrasound is a quick way to get the answer.”
In addition to the fast-track clinic at Massachusetts General, the survey included fast-track clinics at the University of Washington, Seattle; Brigham and Women’s Hospital, Boston; Loma Linda (Calif.) University; University of California, Los Angeles; and at a private practice, Arthritis and Rheumatism Associates in the Washington area.
Advantages of VUS vs. TAB
At Massachusetts General, some of the rheumatologists are trained to perform VUS. The rheumatologists also perform the clinical evaluation of suspected cases of GCA. The advantage of VUS, Dr. Kohler said, is that the answer is “right there”; that is, the imaging yields a diagnosis almost instantaneously whereas a biopsy must be sent to a lab for analysis.
“Since a lot of patients with suspected vasculitis may already come to us on steroid therapy, and if there’s a low probability or low suspicion for vasculitis, [VUS] actually confirms that, and we’re able to taper prednisone or steroids quickly rather than keep them on a prolonged course.”
Alison Bays, MD, MPH, of the department of rheumatology at the University of Washington, said that the advantages of avoiding biopsy aren’t to be overlooked. “Temporal artery biopsies are invasive and carry surgical risks, especially as many of our patients are elderly,” she told this news organization.
“These patients occasionally refuse biopsy, but the acceptance of ultrasound is high,” Dr. Bays said. “Scheduling surgery can be more complicated, resulting in delays to biopsy and potentially higher rates of false negatives. Additionally, ultrasound has resulted in a higher rate of diagnosis with GCA as TAB misses large-vessel involvement.” The fast-track clinic at the university has evaluated 250 patients since it opened in 2017.
Dr. Bays and colleagues published the first United States study of a fast-track protocol using vascular sonographers. “Our group has demonstrated that fast-track clinics can rapidly and effectively evaluate patients, and we demonstrated a different method of evaluation using vascular sonographers rather than rheumatologists to do the vascular ultrasound,” she said. “It utilizes the familiarity vascular sonographers already have with imaging blood vessels.”
She added that the TABUL study in the United Kingdom in 2016 demonstrated that VUS yielded a savings of $686 (£484 as reported in the study), compared with TAB. “Further studies need to be done in the United States,” she said. “Beyond direct comparison of costs, reduction in steroid burden due to quick evaluation and diagnosis may carry additional benefits.”
At Brigham and Women’s Hospital, the division of rheumatology and the vascular section of the cardiology division collaborate on the GCA evaluation, said Sara Tedeschi, MD, MPH, codirector of the fast-track clinic there. Trained vascular technologists credentialed in the procedure and specifically trained in using VUS for evaluating arteritis perform the VUS. Cardiologists with a subspecialty in vascular medicine interpret the studies.
VUS patients have a rheumatology evaluation just before they have the ultrasound. “The rheumatology evaluation is then able to incorporate information from the VUS together with laboratory data, the patient’s history, and physical examination,” Dr. Tedeschi said.
“If the rheumatologist recommends a temporal artery biopsy as a next step, we arrange this with vascular surgery,” she said. “If the rheumatologist recommends other imaging such as MRA [magnetic resonance angiography] or PET-CT, we frequently review the images together with our colleagues in cardiovascular radiology and/or nuclear medicine.”
But in the United States, it will take some time for GCA fast-track clinics to become the standard, Dr. Tedeschi said. “Temporal artery biopsy may be faster to arrange in certain practice settings if VUS is not already being employed for giant cell arteritis evaluation,” she said.
Dr. Bays recognized this limitation, saying, “We are hoping that in the future, the American College of Rheumatology will consider vascular ultrasound as a first-line diagnostic test in diagnosis as rheumatologists and vascular sonographers gain familiarity over time.”
But that would mean that centers performing VUS for GCA would have to meet rigorous standards for the procedure. “With that, standardization of a protocol, high-quality equipment, and adequate training are necessary to ensure quality and reduce the chance of false-positive or false-negative results,” she said.
Dr. Chrysidis, Dr. Bays, and Dr. Tedeschi have disclosed no relevant financial relationships. Dr. Kohler is a board member of Ultrasound School of North American Rheumatologists.
A version of this article first appeared on Medscape.com.
Temporal artery biopsy has been the standard for diagnosing giant cell arteritis (GCA), but vascular ultrasound, a procedure that’s less invasive, less time-intensive, less expensive, and more convenient, has gained widespread use in Europe, and now clinics in the United States are adopting this approach and moving toward having rheumatologists take on the role of ultrasonographer.
However, directors at these clinics – known as GCA fast-track clinics – caution that the bar can be high for adopting vascular ultrasound (VUS) as a tool to diagnose GCA. Ultrasonographers need specialized training to perform the task and an adequate caseload to maintain their skills. Clinics also need to be outfitted with high-definition ultrasound machines.
“It definitely takes adequate training and learning of how to adjust the settings on the ultrasound machine to be able to visualize the findings appropriately,” said Minna Kohler, MD, director of the rheumatology and musculoskeletal ultrasound program at Massachusetts General Hospital in Boston, which has its own GCA fast-track clinic.
“And the clinical context is very important,” she said. “If you have a high suspicion for someone with temporal arteritis, or GCA, and the patient has been on steroids for weeks before you see them, the ultrasound findings may not show signs of the disease. In those cases in which the imaging is equivocal, we would still pursue a biopsy.”
The idea of the fast-track clinic is as the name implies: to quickly confirm the presence of GCA in a matter of hours, or days at the most, in an outpatient setting without the hassles of a biopsy. Temporal artery biopsy (TAB), by comparison, “is more costly because it requires operating room time, a surgical consultation, and surgery time, whereas ultrasound is a very inexpensive exam since it’s done in the clinic by the rheumatologist,” Dr. Kohler said.
European experience
Use of VUS to diagnose GCA is supplanting TAB in Europe and other countries. In Denmark alone – with a population of 6 million – three outpatient fast-track clinics are operating. The United States, with a population more than 50 times larger than Denmark’s, has six.
Stavros Chrysidis, MD, PhD, chief of rheumatology at the Hospital South West Jutland, one of the fast-track clinic sites in Denmark, led a recent multicenter study, known as EUREKA, of VUS in patients with suspected GCA. He and his colleagues reported in The Lancet Rheumatology that the sensitivity and specificity of VUS was superior to TAB in confirming a diagnosis of GCA. Dr. Chrysidis has instructed U.S. rheumatologists and ultrasonographers in performing and interpreting VUS for GCA.
The study emphasizes the importance of training for ultrasonographers, said Dr. Chrysidis, who regularly performs VUS at his institution. “The most important finding is that, when we apply VUS by systematically trained ultrasonographers using appropriate equipment in appropriate settings, it has excellent diagnostic accuracy on GCA,” he told this news organization.
He noted that The Lancet Rheumatology report is the first multicenter study of VUS for diagnosing GCA in which all the ultrasonographers participated in a standardized training program, which his group developed. “Ultrasound is very operator dependent,” he said. “That’s why the training is very important.”
The training occurred over a year and included two workshops consisting of 5 days of theoretical training on VUS; supervised hands-on evaluation of healthy individuals and patients with known GCA; and evaluation of ultrasound images. Over the course of the year, trainees performed at least 50 VUS evaluations, half of which were in patients with confirmed GCA. During the training period, an external rheumatologist with broad experience in VUS made the final diagnosis.
“The equipment and settings are very important because ultrasound can be very time consuming if you are not educated well and if your equipment is not adjusted well,” Dr. Chrysidis said. The equipment must be calibrated beforehand “so you don’t spend time on adjustments.”
For diagnosing temporal artery anomalies, the ultrasound equipment must have a resolution of 0.3-0.4 mm, he said. “When you have a transducer of 10 MHz, you cannot visualize changes smaller than 5 mm.”
The EUREKA study stated that VUS could replace TAB as a first-line diagnostic tool for GCA – provided the ultrasonographers are systematically trained and the equipment and settings are appropriate. In the Jutland clinic, VUS already has replaced TAB, Dr. Chrysidis said.
“In my department since 2017, when we started the fast-track clinic after the EUREKA study was terminated, we have performed three temporal artery biopsies in the last 4 years, and we screen 60-70 patients per year because we use ultrasound as the primary imaging,” he said. In cases when the results are inconclusive, they order a PET scan. “We don’t perform biopsies anymore,” he said.
U.S. fast-track clinic models
The fast-track clinic models in the United States vary. Results of a survey of the U.S. clinics were presented as an abstract at the 2021 American College of Rheumatology annual meeting. Some centers have a vasculitis specialist obtain and interpret the imaging. At others, a vasculitis specialist refers patients to a VUS-trained rheumatologist to perform and interpret the test. Another approach is to have vasculitis specialists refer patients to ultrasound technicians trained in VUS, with a vascular surgeon interpreting the images and either a VUS-trained rheumatologist or vascular medicine specialist verifying the images.
The take-home message of that survey is that “ultrasound evaluation should be considered in the hands of experts, realizing that not everyone has that skill set, but if it is available, it’s a way to expedite diagnosis and it can be helpful in managing the GCA patient in an appropriate way, quicker than trying to schedule cross-sectional imaging,” said Massachusetts General’s Dr. Kohler, who is a coauthor of the abstract. “Certainly, cross-sectional imaging also plays an important role, but when it comes to confirming whether to continue with treatment or not for a very serious condition, ultrasound is a quick way to get the answer.”
In addition to the fast-track clinic at Massachusetts General, the survey included fast-track clinics at the University of Washington, Seattle; Brigham and Women’s Hospital, Boston; Loma Linda (Calif.) University; University of California, Los Angeles; and at a private practice, Arthritis and Rheumatism Associates in the Washington area.
Advantages of VUS vs. TAB
At Massachusetts General, some of the rheumatologists are trained to perform VUS. The rheumatologists also perform the clinical evaluation of suspected cases of GCA. The advantage of VUS, Dr. Kohler said, is that the answer is “right there”; that is, the imaging yields a diagnosis almost instantaneously whereas a biopsy must be sent to a lab for analysis.
“Since a lot of patients with suspected vasculitis may already come to us on steroid therapy, and if there’s a low probability or low suspicion for vasculitis, [VUS] actually confirms that, and we’re able to taper prednisone or steroids quickly rather than keep them on a prolonged course.”
Alison Bays, MD, MPH, of the department of rheumatology at the University of Washington, said that the advantages of avoiding biopsy aren’t to be overlooked. “Temporal artery biopsies are invasive and carry surgical risks, especially as many of our patients are elderly,” she told this news organization.
“These patients occasionally refuse biopsy, but the acceptance of ultrasound is high,” Dr. Bays said. “Scheduling surgery can be more complicated, resulting in delays to biopsy and potentially higher rates of false negatives. Additionally, ultrasound has resulted in a higher rate of diagnosis with GCA as TAB misses large-vessel involvement.” The fast-track clinic at the university has evaluated 250 patients since it opened in 2017.
Dr. Bays and colleagues published the first United States study of a fast-track protocol using vascular sonographers. “Our group has demonstrated that fast-track clinics can rapidly and effectively evaluate patients, and we demonstrated a different method of evaluation using vascular sonographers rather than rheumatologists to do the vascular ultrasound,” she said. “It utilizes the familiarity vascular sonographers already have with imaging blood vessels.”
She added that the TABUL study in the United Kingdom in 2016 demonstrated that VUS yielded a savings of $686 (£484 as reported in the study), compared with TAB. “Further studies need to be done in the United States,” she said. “Beyond direct comparison of costs, reduction in steroid burden due to quick evaluation and diagnosis may carry additional benefits.”
At Brigham and Women’s Hospital, the division of rheumatology and the vascular section of the cardiology division collaborate on the GCA evaluation, said Sara Tedeschi, MD, MPH, codirector of the fast-track clinic there. Trained vascular technologists credentialed in the procedure and specifically trained in using VUS for evaluating arteritis perform the VUS. Cardiologists with a subspecialty in vascular medicine interpret the studies.
VUS patients have a rheumatology evaluation just before they have the ultrasound. “The rheumatology evaluation is then able to incorporate information from the VUS together with laboratory data, the patient’s history, and physical examination,” Dr. Tedeschi said.
“If the rheumatologist recommends a temporal artery biopsy as a next step, we arrange this with vascular surgery,” she said. “If the rheumatologist recommends other imaging such as MRA [magnetic resonance angiography] or PET-CT, we frequently review the images together with our colleagues in cardiovascular radiology and/or nuclear medicine.”
But in the United States, it will take some time for GCA fast-track clinics to become the standard, Dr. Tedeschi said. “Temporal artery biopsy may be faster to arrange in certain practice settings if VUS is not already being employed for giant cell arteritis evaluation,” she said.
Dr. Bays recognized this limitation, saying, “We are hoping that in the future, the American College of Rheumatology will consider vascular ultrasound as a first-line diagnostic test in diagnosis as rheumatologists and vascular sonographers gain familiarity over time.”
But that would mean that centers performing VUS for GCA would have to meet rigorous standards for the procedure. “With that, standardization of a protocol, high-quality equipment, and adequate training are necessary to ensure quality and reduce the chance of false-positive or false-negative results,” she said.
Dr. Chrysidis, Dr. Bays, and Dr. Tedeschi have disclosed no relevant financial relationships. Dr. Kohler is a board member of Ultrasound School of North American Rheumatologists.
A version of this article first appeared on Medscape.com.
Don’t give up on relentless youth depression
As pediatricians, we are acutely aware of the increase in depression in our teen patients. Lifetime prevalence is now approaching 20%, and we are doing our best to help.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC, 2018) has advice on screening and primary care provider (PCP) management, verifying our role in care. But GLAD-PC also advises “referral to a mental health specialist” in patient scenarios we see multiple times per week. Even when patients are willing and able to go, mental health specialists are in short supply or have months-long waiting lists. What should we do to help the more severely depressed adolescent when immediate referral is not possible? What should we expect of specialist care for what is called treatment-resistant or treatment-refractory depression (TRD)?
To know what to do for a youth with TRD, first you need to know what constitutes an adequate trial of treatment. After diagnosis of major depressive disorder (MDD) from a validated screening tool or an interview based on DSM-5 criteria and an appropriate assessment (as described in GLAD-PC), patients and parents need education on symptoms, course, prognosis including suicide risk, and treatment options. Known TRD risk factors, besides longer or greater depression severity, anhedonia, and poor global functioning, can benefit from being specifically addressed: trauma, bullying, comorbid anxiety or substance use, subsyndromal mania, insomnia, hypothyroidism, nutritional deficiencies from eating disorders, certain genetic variants, LGBTQ identification, family conflict, and parental depression. Screening and assessment for suicidal ideation/attempts is needed initially and in follow-up as MDD increases risk of suicide 30 times.
PCPs can manage mild depression with regular visits every 1-2 weeks for active support for 6-8 weeks. Advise all depressed youth on healthy eating, adequate sleep and exercise, pleasurable activities, and refraining from substance use. With a full response (50%+ reduction in symptom score from baseline), monthly monitoring for symptoms, suicidality, and stressors (phone/televisits suffice) should continue for 6-24 months as half recur. Monitoring with ratings by both youth and parent are recommended and may be required by insurers. Scores below cutoff suggest “remission,” although functioning must be considered. Youth report symptoms best but parents may better report improved functioning and affect that can precede symptom reduction.
If there is no initial response (< 25% decrease in symptom score) or a partial response (25%-49% decrease), PCPs should begin treatment as for moderate depression with either a selective serotonin reuptake inhibitor (SSRI) or psychotherapy. Use of both has the best evidence; cognitive behavior therapy (CBT) and interpersonal psychotherapy for adolescents are equally effective.
Side effects from SSRIs are almost universal with GI upset, headaches, and sexual dysfunction most common, but activation (increased agitation or irritability) may occur. Educate patients about these and encourage tolerating them as they tend to subside in weeks, allowing continuation of these most effective medicines. Activation rarely indicates true mania, which would require stopping and referral.
Moderate depression with only comorbid anxiety may be addressed by PCPs with problem-focused supportive counseling and SSRIs, but mental health consultation or referral also are appropriate. Fluoxetine starting at 5-10 mg/day has best evidence and Food and Drug Administration approval for MDD from age 8. Starting at a higher dose may increase risk of suicidal ideation. Alternatively, escitalopram is FDA approved for MDD at age 12 starting at 10 mg/day, although meta-analyses do not distinguish effectiveness within the SSRI class. Although benefit usually appears within 2 weeks, a trial of at least 4 weeks should be used to assess effect.
If after 4 weeks, the SSRI is tolerated but has little or no response, reassess the diagnosis, try a different SSRI, e.g. sertraline, and add CBT (combined SSRI+CBT has an advantage). To switch SSRIs, reduce the first every 1-2 weeks (by 10-20 mg for fluoxetine; 5-10 for escitalopram) to reduce side effects. If overlapping, the replacement SSRI may start midway in the wean at low dose with patients educated about serotonin syndrome. If instead there was a partial response to the initial SSRI, progressively increase the dose (by 10 mg for fluoxetine or 5 mg for escitalopram monthly) as indicated by symptom change up to the maximum (60-80 mg fluoxetine or 20 mg escitalopram), if needed, and maintain for another 4 weeks. Alternatively, or in addition, start psychotherapy or ask to change current therapy, as therapy focus makes a difference in effect. Initial CBT focus on anxiety acts fastest when anxiety is comorbid.
Once a regimen produces a response, maintain it for 16-20 weeks, the longer for more severe depression. Although three-fourths of mildly to moderately depressed youth are late responders, emerging near 6 weeks, a rapid initial response is associated with better outcome. The recommended 8 weeks on a final tolerated dose constituting an adequate trial before changing may be shortened to 6 weeks in severe unremitting cases. Youth not remitting by 12 weeks should be offered alternative treatment. Referral is recommended for moderately severe depression with comorbidity or severe depression but also for unresponsive moderate depression or by family or clinician preference.
Treatment-resistant depression is defined as “clinically impairing depression symptoms despite an adequate trial of an evidence-based psychotherapy and an antidepressant with grade A evidence (fluoxetine, escitalopram, or sertraline),” sequentially or together; treatment-refractory depression comprises the above with failure on at least two antidepressants, with at least one being grade A. Unfortunately, TRD occurs in 30%-40% of children and remission is only 30%. Low adherence based on pill counts (> 30% missed) or with therapy (fewer than nine visits) should be considered in treatment failures.
With manageable factors addressed, the next step for TRD is treatment augmentation. The best evidence-based augmentation for TRD is CBT; 55% of those receiving CBT responded within 12 weeks. TRD augmentations and interventions with evidence in adults have either no evidence of effect in children (SNRIs, lithium), no randomized controlled trials, or support only from small suggestive studies, e.g., antipsychotics, 16 g/day omega-3 fatty acid supplementation, folic acid supplementation, repetitive transcranial magnetic stimulation, electroconvulsive therapy, or ketamine. Prompt referral to a child psychiatrist is essential for youth classified as TRD as earlier more aggressive treatment may avoid the long-term morbidity of chronic depression.
Fortunately, a meta-analysis of studies showed that PCP medication management visits with monitoring could improve outcomes, even for TRD.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Reference
Dwyer J et al. Annual research review: Defining and treating pediatric treatment-resistant depression. J Child Psychol Psychiatry. 2020 March;61(3):312-32.
As pediatricians, we are acutely aware of the increase in depression in our teen patients. Lifetime prevalence is now approaching 20%, and we are doing our best to help.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC, 2018) has advice on screening and primary care provider (PCP) management, verifying our role in care. But GLAD-PC also advises “referral to a mental health specialist” in patient scenarios we see multiple times per week. Even when patients are willing and able to go, mental health specialists are in short supply or have months-long waiting lists. What should we do to help the more severely depressed adolescent when immediate referral is not possible? What should we expect of specialist care for what is called treatment-resistant or treatment-refractory depression (TRD)?
To know what to do for a youth with TRD, first you need to know what constitutes an adequate trial of treatment. After diagnosis of major depressive disorder (MDD) from a validated screening tool or an interview based on DSM-5 criteria and an appropriate assessment (as described in GLAD-PC), patients and parents need education on symptoms, course, prognosis including suicide risk, and treatment options. Known TRD risk factors, besides longer or greater depression severity, anhedonia, and poor global functioning, can benefit from being specifically addressed: trauma, bullying, comorbid anxiety or substance use, subsyndromal mania, insomnia, hypothyroidism, nutritional deficiencies from eating disorders, certain genetic variants, LGBTQ identification, family conflict, and parental depression. Screening and assessment for suicidal ideation/attempts is needed initially and in follow-up as MDD increases risk of suicide 30 times.
PCPs can manage mild depression with regular visits every 1-2 weeks for active support for 6-8 weeks. Advise all depressed youth on healthy eating, adequate sleep and exercise, pleasurable activities, and refraining from substance use. With a full response (50%+ reduction in symptom score from baseline), monthly monitoring for symptoms, suicidality, and stressors (phone/televisits suffice) should continue for 6-24 months as half recur. Monitoring with ratings by both youth and parent are recommended and may be required by insurers. Scores below cutoff suggest “remission,” although functioning must be considered. Youth report symptoms best but parents may better report improved functioning and affect that can precede symptom reduction.
If there is no initial response (< 25% decrease in symptom score) or a partial response (25%-49% decrease), PCPs should begin treatment as for moderate depression with either a selective serotonin reuptake inhibitor (SSRI) or psychotherapy. Use of both has the best evidence; cognitive behavior therapy (CBT) and interpersonal psychotherapy for adolescents are equally effective.
Side effects from SSRIs are almost universal with GI upset, headaches, and sexual dysfunction most common, but activation (increased agitation or irritability) may occur. Educate patients about these and encourage tolerating them as they tend to subside in weeks, allowing continuation of these most effective medicines. Activation rarely indicates true mania, which would require stopping and referral.
Moderate depression with only comorbid anxiety may be addressed by PCPs with problem-focused supportive counseling and SSRIs, but mental health consultation or referral also are appropriate. Fluoxetine starting at 5-10 mg/day has best evidence and Food and Drug Administration approval for MDD from age 8. Starting at a higher dose may increase risk of suicidal ideation. Alternatively, escitalopram is FDA approved for MDD at age 12 starting at 10 mg/day, although meta-analyses do not distinguish effectiveness within the SSRI class. Although benefit usually appears within 2 weeks, a trial of at least 4 weeks should be used to assess effect.
If after 4 weeks, the SSRI is tolerated but has little or no response, reassess the diagnosis, try a different SSRI, e.g. sertraline, and add CBT (combined SSRI+CBT has an advantage). To switch SSRIs, reduce the first every 1-2 weeks (by 10-20 mg for fluoxetine; 5-10 for escitalopram) to reduce side effects. If overlapping, the replacement SSRI may start midway in the wean at low dose with patients educated about serotonin syndrome. If instead there was a partial response to the initial SSRI, progressively increase the dose (by 10 mg for fluoxetine or 5 mg for escitalopram monthly) as indicated by symptom change up to the maximum (60-80 mg fluoxetine or 20 mg escitalopram), if needed, and maintain for another 4 weeks. Alternatively, or in addition, start psychotherapy or ask to change current therapy, as therapy focus makes a difference in effect. Initial CBT focus on anxiety acts fastest when anxiety is comorbid.
Once a regimen produces a response, maintain it for 16-20 weeks, the longer for more severe depression. Although three-fourths of mildly to moderately depressed youth are late responders, emerging near 6 weeks, a rapid initial response is associated with better outcome. The recommended 8 weeks on a final tolerated dose constituting an adequate trial before changing may be shortened to 6 weeks in severe unremitting cases. Youth not remitting by 12 weeks should be offered alternative treatment. Referral is recommended for moderately severe depression with comorbidity or severe depression but also for unresponsive moderate depression or by family or clinician preference.
Treatment-resistant depression is defined as “clinically impairing depression symptoms despite an adequate trial of an evidence-based psychotherapy and an antidepressant with grade A evidence (fluoxetine, escitalopram, or sertraline),” sequentially or together; treatment-refractory depression comprises the above with failure on at least two antidepressants, with at least one being grade A. Unfortunately, TRD occurs in 30%-40% of children and remission is only 30%. Low adherence based on pill counts (> 30% missed) or with therapy (fewer than nine visits) should be considered in treatment failures.
With manageable factors addressed, the next step for TRD is treatment augmentation. The best evidence-based augmentation for TRD is CBT; 55% of those receiving CBT responded within 12 weeks. TRD augmentations and interventions with evidence in adults have either no evidence of effect in children (SNRIs, lithium), no randomized controlled trials, or support only from small suggestive studies, e.g., antipsychotics, 16 g/day omega-3 fatty acid supplementation, folic acid supplementation, repetitive transcranial magnetic stimulation, electroconvulsive therapy, or ketamine. Prompt referral to a child psychiatrist is essential for youth classified as TRD as earlier more aggressive treatment may avoid the long-term morbidity of chronic depression.
Fortunately, a meta-analysis of studies showed that PCP medication management visits with monitoring could improve outcomes, even for TRD.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Reference
Dwyer J et al. Annual research review: Defining and treating pediatric treatment-resistant depression. J Child Psychol Psychiatry. 2020 March;61(3):312-32.
As pediatricians, we are acutely aware of the increase in depression in our teen patients. Lifetime prevalence is now approaching 20%, and we are doing our best to help.
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC, 2018) has advice on screening and primary care provider (PCP) management, verifying our role in care. But GLAD-PC also advises “referral to a mental health specialist” in patient scenarios we see multiple times per week. Even when patients are willing and able to go, mental health specialists are in short supply or have months-long waiting lists. What should we do to help the more severely depressed adolescent when immediate referral is not possible? What should we expect of specialist care for what is called treatment-resistant or treatment-refractory depression (TRD)?
To know what to do for a youth with TRD, first you need to know what constitutes an adequate trial of treatment. After diagnosis of major depressive disorder (MDD) from a validated screening tool or an interview based on DSM-5 criteria and an appropriate assessment (as described in GLAD-PC), patients and parents need education on symptoms, course, prognosis including suicide risk, and treatment options. Known TRD risk factors, besides longer or greater depression severity, anhedonia, and poor global functioning, can benefit from being specifically addressed: trauma, bullying, comorbid anxiety or substance use, subsyndromal mania, insomnia, hypothyroidism, nutritional deficiencies from eating disorders, certain genetic variants, LGBTQ identification, family conflict, and parental depression. Screening and assessment for suicidal ideation/attempts is needed initially and in follow-up as MDD increases risk of suicide 30 times.
PCPs can manage mild depression with regular visits every 1-2 weeks for active support for 6-8 weeks. Advise all depressed youth on healthy eating, adequate sleep and exercise, pleasurable activities, and refraining from substance use. With a full response (50%+ reduction in symptom score from baseline), monthly monitoring for symptoms, suicidality, and stressors (phone/televisits suffice) should continue for 6-24 months as half recur. Monitoring with ratings by both youth and parent are recommended and may be required by insurers. Scores below cutoff suggest “remission,” although functioning must be considered. Youth report symptoms best but parents may better report improved functioning and affect that can precede symptom reduction.
If there is no initial response (< 25% decrease in symptom score) or a partial response (25%-49% decrease), PCPs should begin treatment as for moderate depression with either a selective serotonin reuptake inhibitor (SSRI) or psychotherapy. Use of both has the best evidence; cognitive behavior therapy (CBT) and interpersonal psychotherapy for adolescents are equally effective.
Side effects from SSRIs are almost universal with GI upset, headaches, and sexual dysfunction most common, but activation (increased agitation or irritability) may occur. Educate patients about these and encourage tolerating them as they tend to subside in weeks, allowing continuation of these most effective medicines. Activation rarely indicates true mania, which would require stopping and referral.
Moderate depression with only comorbid anxiety may be addressed by PCPs with problem-focused supportive counseling and SSRIs, but mental health consultation or referral also are appropriate. Fluoxetine starting at 5-10 mg/day has best evidence and Food and Drug Administration approval for MDD from age 8. Starting at a higher dose may increase risk of suicidal ideation. Alternatively, escitalopram is FDA approved for MDD at age 12 starting at 10 mg/day, although meta-analyses do not distinguish effectiveness within the SSRI class. Although benefit usually appears within 2 weeks, a trial of at least 4 weeks should be used to assess effect.
If after 4 weeks, the SSRI is tolerated but has little or no response, reassess the diagnosis, try a different SSRI, e.g. sertraline, and add CBT (combined SSRI+CBT has an advantage). To switch SSRIs, reduce the first every 1-2 weeks (by 10-20 mg for fluoxetine; 5-10 for escitalopram) to reduce side effects. If overlapping, the replacement SSRI may start midway in the wean at low dose with patients educated about serotonin syndrome. If instead there was a partial response to the initial SSRI, progressively increase the dose (by 10 mg for fluoxetine or 5 mg for escitalopram monthly) as indicated by symptom change up to the maximum (60-80 mg fluoxetine or 20 mg escitalopram), if needed, and maintain for another 4 weeks. Alternatively, or in addition, start psychotherapy or ask to change current therapy, as therapy focus makes a difference in effect. Initial CBT focus on anxiety acts fastest when anxiety is comorbid.
Once a regimen produces a response, maintain it for 16-20 weeks, the longer for more severe depression. Although three-fourths of mildly to moderately depressed youth are late responders, emerging near 6 weeks, a rapid initial response is associated with better outcome. The recommended 8 weeks on a final tolerated dose constituting an adequate trial before changing may be shortened to 6 weeks in severe unremitting cases. Youth not remitting by 12 weeks should be offered alternative treatment. Referral is recommended for moderately severe depression with comorbidity or severe depression but also for unresponsive moderate depression or by family or clinician preference.
Treatment-resistant depression is defined as “clinically impairing depression symptoms despite an adequate trial of an evidence-based psychotherapy and an antidepressant with grade A evidence (fluoxetine, escitalopram, or sertraline),” sequentially or together; treatment-refractory depression comprises the above with failure on at least two antidepressants, with at least one being grade A. Unfortunately, TRD occurs in 30%-40% of children and remission is only 30%. Low adherence based on pill counts (> 30% missed) or with therapy (fewer than nine visits) should be considered in treatment failures.
With manageable factors addressed, the next step for TRD is treatment augmentation. The best evidence-based augmentation for TRD is CBT; 55% of those receiving CBT responded within 12 weeks. TRD augmentations and interventions with evidence in adults have either no evidence of effect in children (SNRIs, lithium), no randomized controlled trials, or support only from small suggestive studies, e.g., antipsychotics, 16 g/day omega-3 fatty acid supplementation, folic acid supplementation, repetitive transcranial magnetic stimulation, electroconvulsive therapy, or ketamine. Prompt referral to a child psychiatrist is essential for youth classified as TRD as earlier more aggressive treatment may avoid the long-term morbidity of chronic depression.
Fortunately, a meta-analysis of studies showed that PCP medication management visits with monitoring could improve outcomes, even for TRD.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Reference
Dwyer J et al. Annual research review: Defining and treating pediatric treatment-resistant depression. J Child Psychol Psychiatry. 2020 March;61(3):312-32.
‘Highest survival’ with combo immunotherapy in advanced melanoma
An researchers say.
Nearly half the patients treated with nivolumab (Opdivo) and ipilimumab (Yervoy) were alive at 6½ years. Within this group, 77% had not received further systemic treatment after coming off the study drugs.
After a minimum follow-up of 77 months, median overall survival was 72.1 months in patients on the combination, which was more than three times longer than the 19.9 months with ipilimumab alone (hazard ratio, 0.52; 95% confidence interval, 0.43-0.64) and twice as long as the 36.9 months with nivolumab alone (HR, 0.84; 95% CI, 0.67-1.04).
The results represent the longest median overall survival seen in a phase 3 trial of advanced melanoma and are evidence of “a substantial development in the melanoma treatment landscape versus the standard median survival of 8 months a decade ago,” researchers wrote in a study published online in the Journal of Clinical Oncology.
However, lead author Jedd D. Wolchok, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, noted that the study was not designed to compare nivolumab alone with the combination. “It wasn’t powered for that. [But] what we can say is that the highest survival was in the combination group,” Dr. Wolchok told this news organization.
Dr. Wolchok cautioned that the combination therapy is not currently standard of care. “PD-1 blockade – either nivolumab or the combination – are both excellent options for care,” he added. “I can’t tell you that one of them is the standard of care because that’s too complex of a decision.”
For example, he explained, “for a patient who only has lung metastases, a single-agent PD-1 blockade might be sufficient. But if it has spread to other organs, such as the liver or bones, which are more difficult to treat, that’s when we often reach for the combination.”
Other factors that weigh into the therapeutic decision are the patient’s performance status and their so-called clinical reserve for tolerating side effects. “The likelihood of having a high-grade side effect with the combination is more than twice that of the single agent,” Dr. Wolchok said.
Until 2011, only two therapies were approved for metastatic melanoma: Chemotherapy with dacarbazine and immunotherapy with high-dose interleukin-2, neither of which was very effective at prolonging life. But patient survival changed with the advent of targeted therapies and immunotherapy. Some patients are now living for years, and as the current study shows, many have surpassed the 5-year mark and are treatment free.
The updated CheckMate 067 analysis included patients with previously untreated, unresectable stage III/IV melanoma who were randomly assigned to receive nivolumab 1 mg/kg plus ipilimumab 3 mg/kg every 3 weeks (four doses) followed by nivolumab 3 mg/kg every 2 weeks (n = 314), nivolumab 3 mg/kg every 2 weeks (n = 316), or ipilimumab 3 mg/ kg every 3 weeks (four doses; n = 315).
The authors reported the 5-year overall survival rates from the trial, published in the New England Journal of Medicine in 2019 – 52% with the combination, 44% with nivolumab alone, and 26% with ipilimumab alone.
In the updated study, overall survival at 6½ years had dropped slightly to 49%, 42%, and 23%, respectively. Patients with BRAF-mutant tumors had overall survival rates of 57%, 43%, and 25% versus 46%, 42%, and 22% in those with BRAF wild-type tumors.
Overall, median investigator-assessed progression-free survival was 11.5 months with the combination, 6.9 months with nivolumab alone, and 2.9 months with ipilimumab.
The new analysis also evaluated melanoma-specific survival (MSS), which removes competing causes of deaths from the long-term follow-up. The MSS was not reached in the combination group, and was 58.7 months in the nivolumab group and 21.9 months for ipilimumab, with MSS rates at 6.5 years of 56%, 48%, and 27%, respectively.
No new safety signals were detected, but there was more immune-mediated toxicity in the combination group, the researchers reported.
“The patients will continue to be followed,” said Dr. Wolchok, “And data are still being collected.”
The trial was supported by Bristol-Myers Squibb, the National Cancer Institute, and the National Institute for Health Research Royal Marsden–Institute of Cancer Research Biomedical Research Centre. Dr. Wolchok and coauthors reported relationships with Bristol-Myers Squibb and other drugmakers.
A version of this article first appeared on Medscape.com.
An researchers say.
Nearly half the patients treated with nivolumab (Opdivo) and ipilimumab (Yervoy) were alive at 6½ years. Within this group, 77% had not received further systemic treatment after coming off the study drugs.
After a minimum follow-up of 77 months, median overall survival was 72.1 months in patients on the combination, which was more than three times longer than the 19.9 months with ipilimumab alone (hazard ratio, 0.52; 95% confidence interval, 0.43-0.64) and twice as long as the 36.9 months with nivolumab alone (HR, 0.84; 95% CI, 0.67-1.04).
The results represent the longest median overall survival seen in a phase 3 trial of advanced melanoma and are evidence of “a substantial development in the melanoma treatment landscape versus the standard median survival of 8 months a decade ago,” researchers wrote in a study published online in the Journal of Clinical Oncology.
However, lead author Jedd D. Wolchok, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, noted that the study was not designed to compare nivolumab alone with the combination. “It wasn’t powered for that. [But] what we can say is that the highest survival was in the combination group,” Dr. Wolchok told this news organization.
Dr. Wolchok cautioned that the combination therapy is not currently standard of care. “PD-1 blockade – either nivolumab or the combination – are both excellent options for care,” he added. “I can’t tell you that one of them is the standard of care because that’s too complex of a decision.”
For example, he explained, “for a patient who only has lung metastases, a single-agent PD-1 blockade might be sufficient. But if it has spread to other organs, such as the liver or bones, which are more difficult to treat, that’s when we often reach for the combination.”
Other factors that weigh into the therapeutic decision are the patient’s performance status and their so-called clinical reserve for tolerating side effects. “The likelihood of having a high-grade side effect with the combination is more than twice that of the single agent,” Dr. Wolchok said.
Until 2011, only two therapies were approved for metastatic melanoma: Chemotherapy with dacarbazine and immunotherapy with high-dose interleukin-2, neither of which was very effective at prolonging life. But patient survival changed with the advent of targeted therapies and immunotherapy. Some patients are now living for years, and as the current study shows, many have surpassed the 5-year mark and are treatment free.
The updated CheckMate 067 analysis included patients with previously untreated, unresectable stage III/IV melanoma who were randomly assigned to receive nivolumab 1 mg/kg plus ipilimumab 3 mg/kg every 3 weeks (four doses) followed by nivolumab 3 mg/kg every 2 weeks (n = 314), nivolumab 3 mg/kg every 2 weeks (n = 316), or ipilimumab 3 mg/ kg every 3 weeks (four doses; n = 315).
The authors reported the 5-year overall survival rates from the trial, published in the New England Journal of Medicine in 2019 – 52% with the combination, 44% with nivolumab alone, and 26% with ipilimumab alone.
In the updated study, overall survival at 6½ years had dropped slightly to 49%, 42%, and 23%, respectively. Patients with BRAF-mutant tumors had overall survival rates of 57%, 43%, and 25% versus 46%, 42%, and 22% in those with BRAF wild-type tumors.
Overall, median investigator-assessed progression-free survival was 11.5 months with the combination, 6.9 months with nivolumab alone, and 2.9 months with ipilimumab.
The new analysis also evaluated melanoma-specific survival (MSS), which removes competing causes of deaths from the long-term follow-up. The MSS was not reached in the combination group, and was 58.7 months in the nivolumab group and 21.9 months for ipilimumab, with MSS rates at 6.5 years of 56%, 48%, and 27%, respectively.
No new safety signals were detected, but there was more immune-mediated toxicity in the combination group, the researchers reported.
“The patients will continue to be followed,” said Dr. Wolchok, “And data are still being collected.”
The trial was supported by Bristol-Myers Squibb, the National Cancer Institute, and the National Institute for Health Research Royal Marsden–Institute of Cancer Research Biomedical Research Centre. Dr. Wolchok and coauthors reported relationships with Bristol-Myers Squibb and other drugmakers.
A version of this article first appeared on Medscape.com.
An researchers say.
Nearly half the patients treated with nivolumab (Opdivo) and ipilimumab (Yervoy) were alive at 6½ years. Within this group, 77% had not received further systemic treatment after coming off the study drugs.
After a minimum follow-up of 77 months, median overall survival was 72.1 months in patients on the combination, which was more than three times longer than the 19.9 months with ipilimumab alone (hazard ratio, 0.52; 95% confidence interval, 0.43-0.64) and twice as long as the 36.9 months with nivolumab alone (HR, 0.84; 95% CI, 0.67-1.04).
The results represent the longest median overall survival seen in a phase 3 trial of advanced melanoma and are evidence of “a substantial development in the melanoma treatment landscape versus the standard median survival of 8 months a decade ago,” researchers wrote in a study published online in the Journal of Clinical Oncology.
However, lead author Jedd D. Wolchok, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, noted that the study was not designed to compare nivolumab alone with the combination. “It wasn’t powered for that. [But] what we can say is that the highest survival was in the combination group,” Dr. Wolchok told this news organization.
Dr. Wolchok cautioned that the combination therapy is not currently standard of care. “PD-1 blockade – either nivolumab or the combination – are both excellent options for care,” he added. “I can’t tell you that one of them is the standard of care because that’s too complex of a decision.”
For example, he explained, “for a patient who only has lung metastases, a single-agent PD-1 blockade might be sufficient. But if it has spread to other organs, such as the liver or bones, which are more difficult to treat, that’s when we often reach for the combination.”
Other factors that weigh into the therapeutic decision are the patient’s performance status and their so-called clinical reserve for tolerating side effects. “The likelihood of having a high-grade side effect with the combination is more than twice that of the single agent,” Dr. Wolchok said.
Until 2011, only two therapies were approved for metastatic melanoma: Chemotherapy with dacarbazine and immunotherapy with high-dose interleukin-2, neither of which was very effective at prolonging life. But patient survival changed with the advent of targeted therapies and immunotherapy. Some patients are now living for years, and as the current study shows, many have surpassed the 5-year mark and are treatment free.
The updated CheckMate 067 analysis included patients with previously untreated, unresectable stage III/IV melanoma who were randomly assigned to receive nivolumab 1 mg/kg plus ipilimumab 3 mg/kg every 3 weeks (four doses) followed by nivolumab 3 mg/kg every 2 weeks (n = 314), nivolumab 3 mg/kg every 2 weeks (n = 316), or ipilimumab 3 mg/ kg every 3 weeks (four doses; n = 315).
The authors reported the 5-year overall survival rates from the trial, published in the New England Journal of Medicine in 2019 – 52% with the combination, 44% with nivolumab alone, and 26% with ipilimumab alone.
In the updated study, overall survival at 6½ years had dropped slightly to 49%, 42%, and 23%, respectively. Patients with BRAF-mutant tumors had overall survival rates of 57%, 43%, and 25% versus 46%, 42%, and 22% in those with BRAF wild-type tumors.
Overall, median investigator-assessed progression-free survival was 11.5 months with the combination, 6.9 months with nivolumab alone, and 2.9 months with ipilimumab.
The new analysis also evaluated melanoma-specific survival (MSS), which removes competing causes of deaths from the long-term follow-up. The MSS was not reached in the combination group, and was 58.7 months in the nivolumab group and 21.9 months for ipilimumab, with MSS rates at 6.5 years of 56%, 48%, and 27%, respectively.
No new safety signals were detected, but there was more immune-mediated toxicity in the combination group, the researchers reported.
“The patients will continue to be followed,” said Dr. Wolchok, “And data are still being collected.”
The trial was supported by Bristol-Myers Squibb, the National Cancer Institute, and the National Institute for Health Research Royal Marsden–Institute of Cancer Research Biomedical Research Centre. Dr. Wolchok and coauthors reported relationships with Bristol-Myers Squibb and other drugmakers.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
AMA president calls on Congress to stabilize Medicare payments to physicians
Physician practices around the country took an unprecedented financial hit with the arrival of the COVID-19 pandemic in March 2020. Recent research from the American Medical Association reveals an estimated pandemic-related shortfall in Medicare physician fee spending of $13.9 billion, or a 14% reduction, across all states and all major specialties in 2020.
While the report pointed to a “strong recovery” in May and June, that recovery stalled in the second half of 2020, and spending never returned to pre–COVID-19 levels.
“Physicians experienced a significant and sustained drop in Medicare revenue during the first 10 months of the pandemic,” said AMA President Gerald Harmon, MD, in a statement. “Medical practices that have not buckled under financial strain continue to be stretched clinically, emotionally, and fiscally as the pandemic persists. Yet physicians face an array of planned cuts that would reduce Medicare physician payments by nearly 10% for 2022.”
The reduction in the Medicare physician fee schedule payments means providers may face payment cuts of more than 9% starting Jan. 1, 2022, when the cuts take effect. That is, unless Congress makes changes.
Medicare physician fee schedule spending on telehealth stood at $4.1 billion, or 5% of the total Medicare spent in 2020. From March 16 to June 30, $1.8 billion of this amount was on telehealth, while $1.1 billion came in during third and fourth quarters of 2020, respectively, per the report.
According to AMA’s research:
- Medicare physician fee schedule spending for 2020, relative to expected 2020 spending, dipped 32% between March 16 and June 30; spending was down during the last 6 months of the year by between 9% and 10%.
- The care settings hit the worst were ambulatory surgical centers, outpatient hospitals, and physician offices; the next worst off were hospital emergency departments, inpatient hospitals, and skilled nursing facilities.
- The specialties that fared worst included physical therapists (-28%), opthamologists (-19%), podiatrists (-18%), and dermatologists (-18%).
- Cumulative spending was down the most in Minnesota (-22%), Maine (-19%), and New York (-19%); less affected states included Idaho (-9%), Oklahoma (-9%), and South Carolina (9%).
AMA: Budget neutrality hurting physicians’ financial stability
Dr. Harmon is calling for financial stability in Medicare spending. In particular, the AMA is “strongly urging Congress to avert the planned payment cuts,” he said in a statement.
The challenge: The Medicare physician fee schedule is currently “budget neutral,” meaning that the budget is fixed, Dr. Harmon, a family medicine specialist in South Carolina, told this news organization.
“If you rob from Peter to pay Paul, Paul is going to be less efficient or less rewarded. It continues to be that there’s always a ‘pay for’ in these things. So budget neutrality is probably one of the first things we need to address,” he said.
Lack of routine care expected to affect health outcomes
The result of reduced screening and treatment during the pandemic could be as many as 10,000 excess deaths due to cancers of the breast and colon during the next 10 years, wrote Norman Sharpless, MD, director of the National Cancer Institute, in Science in June. Combined, breast cancer and colon cancer account for one-sixth of all cancers in the U.S., he wrote.
In addition, blood pressure control has gotten worse since the start of the pandemic, said Michael Rakotz, MD, FAHA, FAAFP, vice president of improving health outcomes at the AMA, in an AMA blog post.
Dr. Harmon’s advice for physician practices on getting patients in for routine care:
- Educate the area’s largest employers to encourage their employees.
- Engage with hospital employees, since hospitals are often the largest employers in many communities.
- Partner with health insurers.
- Show up at athletic events, which is a particularly good fit for “small town America,” said Dr. Harmon.
The AMA’s research doesn’t consider reimbursement from other public and private payers. It also doesn’t account for funding sources such as Provider Relief Fund grants, Paycheck Protection Program loans, and the temporary suspension of the Medicare sequester, per the report.
A version of this article first appeared on Medscape.com.
Physician practices around the country took an unprecedented financial hit with the arrival of the COVID-19 pandemic in March 2020. Recent research from the American Medical Association reveals an estimated pandemic-related shortfall in Medicare physician fee spending of $13.9 billion, or a 14% reduction, across all states and all major specialties in 2020.
While the report pointed to a “strong recovery” in May and June, that recovery stalled in the second half of 2020, and spending never returned to pre–COVID-19 levels.
“Physicians experienced a significant and sustained drop in Medicare revenue during the first 10 months of the pandemic,” said AMA President Gerald Harmon, MD, in a statement. “Medical practices that have not buckled under financial strain continue to be stretched clinically, emotionally, and fiscally as the pandemic persists. Yet physicians face an array of planned cuts that would reduce Medicare physician payments by nearly 10% for 2022.”
The reduction in the Medicare physician fee schedule payments means providers may face payment cuts of more than 9% starting Jan. 1, 2022, when the cuts take effect. That is, unless Congress makes changes.
Medicare physician fee schedule spending on telehealth stood at $4.1 billion, or 5% of the total Medicare spent in 2020. From March 16 to June 30, $1.8 billion of this amount was on telehealth, while $1.1 billion came in during third and fourth quarters of 2020, respectively, per the report.
According to AMA’s research:
- Medicare physician fee schedule spending for 2020, relative to expected 2020 spending, dipped 32% between March 16 and June 30; spending was down during the last 6 months of the year by between 9% and 10%.
- The care settings hit the worst were ambulatory surgical centers, outpatient hospitals, and physician offices; the next worst off were hospital emergency departments, inpatient hospitals, and skilled nursing facilities.
- The specialties that fared worst included physical therapists (-28%), opthamologists (-19%), podiatrists (-18%), and dermatologists (-18%).
- Cumulative spending was down the most in Minnesota (-22%), Maine (-19%), and New York (-19%); less affected states included Idaho (-9%), Oklahoma (-9%), and South Carolina (9%).
AMA: Budget neutrality hurting physicians’ financial stability
Dr. Harmon is calling for financial stability in Medicare spending. In particular, the AMA is “strongly urging Congress to avert the planned payment cuts,” he said in a statement.
The challenge: The Medicare physician fee schedule is currently “budget neutral,” meaning that the budget is fixed, Dr. Harmon, a family medicine specialist in South Carolina, told this news organization.
“If you rob from Peter to pay Paul, Paul is going to be less efficient or less rewarded. It continues to be that there’s always a ‘pay for’ in these things. So budget neutrality is probably one of the first things we need to address,” he said.
Lack of routine care expected to affect health outcomes
The result of reduced screening and treatment during the pandemic could be as many as 10,000 excess deaths due to cancers of the breast and colon during the next 10 years, wrote Norman Sharpless, MD, director of the National Cancer Institute, in Science in June. Combined, breast cancer and colon cancer account for one-sixth of all cancers in the U.S., he wrote.
In addition, blood pressure control has gotten worse since the start of the pandemic, said Michael Rakotz, MD, FAHA, FAAFP, vice president of improving health outcomes at the AMA, in an AMA blog post.
Dr. Harmon’s advice for physician practices on getting patients in for routine care:
- Educate the area’s largest employers to encourage their employees.
- Engage with hospital employees, since hospitals are often the largest employers in many communities.
- Partner with health insurers.
- Show up at athletic events, which is a particularly good fit for “small town America,” said Dr. Harmon.
The AMA’s research doesn’t consider reimbursement from other public and private payers. It also doesn’t account for funding sources such as Provider Relief Fund grants, Paycheck Protection Program loans, and the temporary suspension of the Medicare sequester, per the report.
A version of this article first appeared on Medscape.com.
Physician practices around the country took an unprecedented financial hit with the arrival of the COVID-19 pandemic in March 2020. Recent research from the American Medical Association reveals an estimated pandemic-related shortfall in Medicare physician fee spending of $13.9 billion, or a 14% reduction, across all states and all major specialties in 2020.
While the report pointed to a “strong recovery” in May and June, that recovery stalled in the second half of 2020, and spending never returned to pre–COVID-19 levels.
“Physicians experienced a significant and sustained drop in Medicare revenue during the first 10 months of the pandemic,” said AMA President Gerald Harmon, MD, in a statement. “Medical practices that have not buckled under financial strain continue to be stretched clinically, emotionally, and fiscally as the pandemic persists. Yet physicians face an array of planned cuts that would reduce Medicare physician payments by nearly 10% for 2022.”
The reduction in the Medicare physician fee schedule payments means providers may face payment cuts of more than 9% starting Jan. 1, 2022, when the cuts take effect. That is, unless Congress makes changes.
Medicare physician fee schedule spending on telehealth stood at $4.1 billion, or 5% of the total Medicare spent in 2020. From March 16 to June 30, $1.8 billion of this amount was on telehealth, while $1.1 billion came in during third and fourth quarters of 2020, respectively, per the report.
According to AMA’s research:
- Medicare physician fee schedule spending for 2020, relative to expected 2020 spending, dipped 32% between March 16 and June 30; spending was down during the last 6 months of the year by between 9% and 10%.
- The care settings hit the worst were ambulatory surgical centers, outpatient hospitals, and physician offices; the next worst off were hospital emergency departments, inpatient hospitals, and skilled nursing facilities.
- The specialties that fared worst included physical therapists (-28%), opthamologists (-19%), podiatrists (-18%), and dermatologists (-18%).
- Cumulative spending was down the most in Minnesota (-22%), Maine (-19%), and New York (-19%); less affected states included Idaho (-9%), Oklahoma (-9%), and South Carolina (9%).
AMA: Budget neutrality hurting physicians’ financial stability
Dr. Harmon is calling for financial stability in Medicare spending. In particular, the AMA is “strongly urging Congress to avert the planned payment cuts,” he said in a statement.
The challenge: The Medicare physician fee schedule is currently “budget neutral,” meaning that the budget is fixed, Dr. Harmon, a family medicine specialist in South Carolina, told this news organization.
“If you rob from Peter to pay Paul, Paul is going to be less efficient or less rewarded. It continues to be that there’s always a ‘pay for’ in these things. So budget neutrality is probably one of the first things we need to address,” he said.
Lack of routine care expected to affect health outcomes
The result of reduced screening and treatment during the pandemic could be as many as 10,000 excess deaths due to cancers of the breast and colon during the next 10 years, wrote Norman Sharpless, MD, director of the National Cancer Institute, in Science in June. Combined, breast cancer and colon cancer account for one-sixth of all cancers in the U.S., he wrote.
In addition, blood pressure control has gotten worse since the start of the pandemic, said Michael Rakotz, MD, FAHA, FAAFP, vice president of improving health outcomes at the AMA, in an AMA blog post.
Dr. Harmon’s advice for physician practices on getting patients in for routine care:
- Educate the area’s largest employers to encourage their employees.
- Engage with hospital employees, since hospitals are often the largest employers in many communities.
- Partner with health insurers.
- Show up at athletic events, which is a particularly good fit for “small town America,” said Dr. Harmon.
The AMA’s research doesn’t consider reimbursement from other public and private payers. It also doesn’t account for funding sources such as Provider Relief Fund grants, Paycheck Protection Program loans, and the temporary suspension of the Medicare sequester, per the report.
A version of this article first appeared on Medscape.com.
Physicians may be overprescribing immunotherapy for unfit cancer patients
.
The study, by Ravi B. Parikh, MD, an assistant professor of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia, is an analysis of patient data from 280 U.S.-based community oncology practices. It included 34,131 patients who received first-line systemic therapy with immune checkpoint inhibitors (ICIs), or other treatment, between January 2014 and December 2019 for newly diagnosed metastatic or recurrent non–small cell lung cancer (NSCLC), urothelial cell cancer (UCC), renal cell cancer (RCC), or hepatocellular carcinoma (HCC). Researchers examined survival outcomes between patients who were eligible to participate in clinical trials with those who were deemed ineligible but may have still received ICIs.
For patients with poor performance status or organ dysfunction, participating in randomized clinical trials for immune checkpoint inhibitors is largely out of reach because of advanced disease, but it is not unusual for these patients to be accepted into clinical trials, a decision sometimes referred to as “desperation oncology,” the authors wrote.
In this study of 34,131 patients, 9,318 were considered ineligible to participate in ICI clinical trials because of advanced disease or organ dysfunction, yet up to 30% of these patients were treated with ICIs by their physician outside of a clinical trial. Dr. Parikh and colleagues found no overall survival differences between patients deemed ineligible for clinical trials, but were ultimately treated with ICI monotherapy, ICI combination therapy, or other treatments at 12 and 36 months. In fact, ICI monotherapy appeared to be harmful within 6 months of starting treatment.
“Clinicians who care for patients with poor performance status or organ dysfunction should be cautious about ICI use and carefully weigh expected survival gains against the potential for early mortality and adverse effects,” the authors wrote. They found the efficacy of ICI treatment alone, or in combination with other treatment, can be worse among trial-ineligible patients than patients who met the criteria for clinical trials.
No survival benefit was found for trial-ineligible patients who were treated with ICI monotherapy or combination therapy. Overall survival rates were similar at 12 and 36 months for both treatment groups. The overall median survival was less than 10 months, but 40% of trial ineligible patients treated with ICIs died within 6 months.
The use of ICIs for patients with poor performance status was found to be associated with lower hospice enrollment, more inpatient deaths, and more treatment during the last month of life. “It is critical to ensure that vulnerable, trial-ineligible patients are not exposed to non–evidence-based therapies that could cause harm and contradict patient goals,” the authors wrote.
The harms of treating unfit patients
The use of immune checkpoint inhibitor monotherapy in trial-ineligible patients is concerning, the authors said, because for patients with UCC and NSCLC, the standard of care is platinum-based chemotherapy. For patients with HCC and RCC, the standard of care is oral anti–vascular endothelial growth factor therapy. Immune checkpoint inhibitors may be prescribed in these cases to avoid side effects associated with other therapies, despite the lack of evidence showing that ICIs are effective in these cases.
“Individuals with poor performance status and/or organ dysfunction are vulnerable to receiving treatments that may not benefit them or cause disproportionately high side effects,” Dr. Parikh said in an interview. “Immunotherapy causes fewer side effects overall and is an attractive option, but there is no good phase 3 evidence that immunotherapy has benefits in this population.
“Physicians are preferentially using immunotherapy for unfit patients despite the fact that these individuals are usually excluded from clinical trials. Trial-ineligible patients – despite making up 30% of the cancer population – are different from patients studied in clinical trials. They are generally sicker, older and more prone to treatment adverse effects (including death), However, excluding these groups means that we don’t have good data on what treatments could benefit this vulnerable group. Thus, we are usually left to extrapolating results from healthier patients to unhealthy patients which risks giving them the wrong treatment,” he said.
A review that looked at immunotherapy in older adults suggested that, while those aged 65 or older represent most cancer patients, they are under-represented in clinical trials, including studies that led to approval of immunotherapy agents. A 2019 report suggested that, while 11 pivotal phase 3, randomized clinical trials have estimated the activity of ICIs in locally advanced and advanced NSCLC, each trial excluded patients with poor performance status.
Phase 3 trials needed for patients with poor performance
This retrospective study included 34,131 patients (median age, 70 years; 42% women) of which 27.3% had poor performance status and/or organ dysfunction and were classed as trial ineligible. The researchers assessed the use and overall survival outcomes following first-line ICI and non-ICI therapy that was initiated from January 2014 through December 2019.
Over the course of the study, the proportion of patients receiving ICI monotherapy increased from 0%-30.2% among trial-ineligible patients and from 0.1%-19.4% among eligible patients. However, among trial-ineligible patients, there were no overall survival differences between treatment with ICI monotherapy, ICI combination therapy and non-ICI therapy at 12 and 36 months.
Among trial-ineligible patients, ICI use was linked to a 14%-19% greater risk of death during the first 6 months after ICI initiation, but a 20% lower risk of death among those who survived 6 months after ICI initiation. Further, ICI combination therapy was associated with potential early harm among trial-ineligible patients.
“Phase 3 trials are sorely needed in patients with poor performance status or organ dysfunction so that we can adequately counsel patients who are unfit about expectations with novel cancer therapies,” Dr. Parikh said.
The cohort only included patients who received systemic therapy, which is a limitation of the study, so conclusions cannot be made about the efficacy of systemic therapy versus no systemic therapy in trial-ineligible patients.
Dr. Parikh reported nonfinancial support from Flatiron Health, grants from Humana, personal fees and equity from GNS Healthcare and Onc.AI, along with personal fees from the Cancer Study Group and Nanology outside the submitted work.
.
The study, by Ravi B. Parikh, MD, an assistant professor of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia, is an analysis of patient data from 280 U.S.-based community oncology practices. It included 34,131 patients who received first-line systemic therapy with immune checkpoint inhibitors (ICIs), or other treatment, between January 2014 and December 2019 for newly diagnosed metastatic or recurrent non–small cell lung cancer (NSCLC), urothelial cell cancer (UCC), renal cell cancer (RCC), or hepatocellular carcinoma (HCC). Researchers examined survival outcomes between patients who were eligible to participate in clinical trials with those who were deemed ineligible but may have still received ICIs.
For patients with poor performance status or organ dysfunction, participating in randomized clinical trials for immune checkpoint inhibitors is largely out of reach because of advanced disease, but it is not unusual for these patients to be accepted into clinical trials, a decision sometimes referred to as “desperation oncology,” the authors wrote.
In this study of 34,131 patients, 9,318 were considered ineligible to participate in ICI clinical trials because of advanced disease or organ dysfunction, yet up to 30% of these patients were treated with ICIs by their physician outside of a clinical trial. Dr. Parikh and colleagues found no overall survival differences between patients deemed ineligible for clinical trials, but were ultimately treated with ICI monotherapy, ICI combination therapy, or other treatments at 12 and 36 months. In fact, ICI monotherapy appeared to be harmful within 6 months of starting treatment.
“Clinicians who care for patients with poor performance status or organ dysfunction should be cautious about ICI use and carefully weigh expected survival gains against the potential for early mortality and adverse effects,” the authors wrote. They found the efficacy of ICI treatment alone, or in combination with other treatment, can be worse among trial-ineligible patients than patients who met the criteria for clinical trials.
No survival benefit was found for trial-ineligible patients who were treated with ICI monotherapy or combination therapy. Overall survival rates were similar at 12 and 36 months for both treatment groups. The overall median survival was less than 10 months, but 40% of trial ineligible patients treated with ICIs died within 6 months.
The use of ICIs for patients with poor performance status was found to be associated with lower hospice enrollment, more inpatient deaths, and more treatment during the last month of life. “It is critical to ensure that vulnerable, trial-ineligible patients are not exposed to non–evidence-based therapies that could cause harm and contradict patient goals,” the authors wrote.
The harms of treating unfit patients
The use of immune checkpoint inhibitor monotherapy in trial-ineligible patients is concerning, the authors said, because for patients with UCC and NSCLC, the standard of care is platinum-based chemotherapy. For patients with HCC and RCC, the standard of care is oral anti–vascular endothelial growth factor therapy. Immune checkpoint inhibitors may be prescribed in these cases to avoid side effects associated with other therapies, despite the lack of evidence showing that ICIs are effective in these cases.
“Individuals with poor performance status and/or organ dysfunction are vulnerable to receiving treatments that may not benefit them or cause disproportionately high side effects,” Dr. Parikh said in an interview. “Immunotherapy causes fewer side effects overall and is an attractive option, but there is no good phase 3 evidence that immunotherapy has benefits in this population.
“Physicians are preferentially using immunotherapy for unfit patients despite the fact that these individuals are usually excluded from clinical trials. Trial-ineligible patients – despite making up 30% of the cancer population – are different from patients studied in clinical trials. They are generally sicker, older and more prone to treatment adverse effects (including death), However, excluding these groups means that we don’t have good data on what treatments could benefit this vulnerable group. Thus, we are usually left to extrapolating results from healthier patients to unhealthy patients which risks giving them the wrong treatment,” he said.
A review that looked at immunotherapy in older adults suggested that, while those aged 65 or older represent most cancer patients, they are under-represented in clinical trials, including studies that led to approval of immunotherapy agents. A 2019 report suggested that, while 11 pivotal phase 3, randomized clinical trials have estimated the activity of ICIs in locally advanced and advanced NSCLC, each trial excluded patients with poor performance status.
Phase 3 trials needed for patients with poor performance
This retrospective study included 34,131 patients (median age, 70 years; 42% women) of which 27.3% had poor performance status and/or organ dysfunction and were classed as trial ineligible. The researchers assessed the use and overall survival outcomes following first-line ICI and non-ICI therapy that was initiated from January 2014 through December 2019.
Over the course of the study, the proportion of patients receiving ICI monotherapy increased from 0%-30.2% among trial-ineligible patients and from 0.1%-19.4% among eligible patients. However, among trial-ineligible patients, there were no overall survival differences between treatment with ICI monotherapy, ICI combination therapy and non-ICI therapy at 12 and 36 months.
Among trial-ineligible patients, ICI use was linked to a 14%-19% greater risk of death during the first 6 months after ICI initiation, but a 20% lower risk of death among those who survived 6 months after ICI initiation. Further, ICI combination therapy was associated with potential early harm among trial-ineligible patients.
“Phase 3 trials are sorely needed in patients with poor performance status or organ dysfunction so that we can adequately counsel patients who are unfit about expectations with novel cancer therapies,” Dr. Parikh said.
The cohort only included patients who received systemic therapy, which is a limitation of the study, so conclusions cannot be made about the efficacy of systemic therapy versus no systemic therapy in trial-ineligible patients.
Dr. Parikh reported nonfinancial support from Flatiron Health, grants from Humana, personal fees and equity from GNS Healthcare and Onc.AI, along with personal fees from the Cancer Study Group and Nanology outside the submitted work.
.
The study, by Ravi B. Parikh, MD, an assistant professor of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia, is an analysis of patient data from 280 U.S.-based community oncology practices. It included 34,131 patients who received first-line systemic therapy with immune checkpoint inhibitors (ICIs), or other treatment, between January 2014 and December 2019 for newly diagnosed metastatic or recurrent non–small cell lung cancer (NSCLC), urothelial cell cancer (UCC), renal cell cancer (RCC), or hepatocellular carcinoma (HCC). Researchers examined survival outcomes between patients who were eligible to participate in clinical trials with those who were deemed ineligible but may have still received ICIs.
For patients with poor performance status or organ dysfunction, participating in randomized clinical trials for immune checkpoint inhibitors is largely out of reach because of advanced disease, but it is not unusual for these patients to be accepted into clinical trials, a decision sometimes referred to as “desperation oncology,” the authors wrote.
In this study of 34,131 patients, 9,318 were considered ineligible to participate in ICI clinical trials because of advanced disease or organ dysfunction, yet up to 30% of these patients were treated with ICIs by their physician outside of a clinical trial. Dr. Parikh and colleagues found no overall survival differences between patients deemed ineligible for clinical trials, but were ultimately treated with ICI monotherapy, ICI combination therapy, or other treatments at 12 and 36 months. In fact, ICI monotherapy appeared to be harmful within 6 months of starting treatment.
“Clinicians who care for patients with poor performance status or organ dysfunction should be cautious about ICI use and carefully weigh expected survival gains against the potential for early mortality and adverse effects,” the authors wrote. They found the efficacy of ICI treatment alone, or in combination with other treatment, can be worse among trial-ineligible patients than patients who met the criteria for clinical trials.
No survival benefit was found for trial-ineligible patients who were treated with ICI monotherapy or combination therapy. Overall survival rates were similar at 12 and 36 months for both treatment groups. The overall median survival was less than 10 months, but 40% of trial ineligible patients treated with ICIs died within 6 months.
The use of ICIs for patients with poor performance status was found to be associated with lower hospice enrollment, more inpatient deaths, and more treatment during the last month of life. “It is critical to ensure that vulnerable, trial-ineligible patients are not exposed to non–evidence-based therapies that could cause harm and contradict patient goals,” the authors wrote.
The harms of treating unfit patients
The use of immune checkpoint inhibitor monotherapy in trial-ineligible patients is concerning, the authors said, because for patients with UCC and NSCLC, the standard of care is platinum-based chemotherapy. For patients with HCC and RCC, the standard of care is oral anti–vascular endothelial growth factor therapy. Immune checkpoint inhibitors may be prescribed in these cases to avoid side effects associated with other therapies, despite the lack of evidence showing that ICIs are effective in these cases.
“Individuals with poor performance status and/or organ dysfunction are vulnerable to receiving treatments that may not benefit them or cause disproportionately high side effects,” Dr. Parikh said in an interview. “Immunotherapy causes fewer side effects overall and is an attractive option, but there is no good phase 3 evidence that immunotherapy has benefits in this population.
“Physicians are preferentially using immunotherapy for unfit patients despite the fact that these individuals are usually excluded from clinical trials. Trial-ineligible patients – despite making up 30% of the cancer population – are different from patients studied in clinical trials. They are generally sicker, older and more prone to treatment adverse effects (including death), However, excluding these groups means that we don’t have good data on what treatments could benefit this vulnerable group. Thus, we are usually left to extrapolating results from healthier patients to unhealthy patients which risks giving them the wrong treatment,” he said.
A review that looked at immunotherapy in older adults suggested that, while those aged 65 or older represent most cancer patients, they are under-represented in clinical trials, including studies that led to approval of immunotherapy agents. A 2019 report suggested that, while 11 pivotal phase 3, randomized clinical trials have estimated the activity of ICIs in locally advanced and advanced NSCLC, each trial excluded patients with poor performance status.
Phase 3 trials needed for patients with poor performance
This retrospective study included 34,131 patients (median age, 70 years; 42% women) of which 27.3% had poor performance status and/or organ dysfunction and were classed as trial ineligible. The researchers assessed the use and overall survival outcomes following first-line ICI and non-ICI therapy that was initiated from January 2014 through December 2019.
Over the course of the study, the proportion of patients receiving ICI monotherapy increased from 0%-30.2% among trial-ineligible patients and from 0.1%-19.4% among eligible patients. However, among trial-ineligible patients, there were no overall survival differences between treatment with ICI monotherapy, ICI combination therapy and non-ICI therapy at 12 and 36 months.
Among trial-ineligible patients, ICI use was linked to a 14%-19% greater risk of death during the first 6 months after ICI initiation, but a 20% lower risk of death among those who survived 6 months after ICI initiation. Further, ICI combination therapy was associated with potential early harm among trial-ineligible patients.
“Phase 3 trials are sorely needed in patients with poor performance status or organ dysfunction so that we can adequately counsel patients who are unfit about expectations with novel cancer therapies,” Dr. Parikh said.
The cohort only included patients who received systemic therapy, which is a limitation of the study, so conclusions cannot be made about the efficacy of systemic therapy versus no systemic therapy in trial-ineligible patients.
Dr. Parikh reported nonfinancial support from Flatiron Health, grants from Humana, personal fees and equity from GNS Healthcare and Onc.AI, along with personal fees from the Cancer Study Group and Nanology outside the submitted work.
FROM JAMA ONCOLOGY
The importance of self-compassion for hospitalists
A mindful way relate to ourselves
Physicians, clinicians, providers, healers, and now heroes, are some of the names we have been given throughout history. These titles bring together a universal concept in medicine that all human beings deserve compassion, understanding, and care. However, as health care providers we forget to show ourselves the same compassion we bestow upon others.
Self-compassion is a new way of relating to ourselves. As clinicians, we are trained investigators, delving deeper into what our patient is thinking and feeling. “Tell me more about that. How does that make you feel? That must have been (very painful/scary/frustrating).” These are a few statements we learned in patient interviewing to actively engage with patients, build rapport, solidify trust, validate their concerns, and ultimately obtain the information needed to diagnose and heal.
We know the importance of looking beyond the surface, as more often than not a deeper inspection reveals more to the story. We have uncovered cracks in the foundation, erosion of the roof, worn out siding, and a glimpse into the complexities that make up each individual. We look at our patients, loved ones, and the world with night-vision lenses to uncover what is deeper.
Clinicians are good at directing compassion toward others, but not as good at giving it to themselves.1 Many health care providers may see self-compassion as soft, weak, selfish, or unnecessary. However, mindful self-compassion is a positive practice that opens a pathway for healing, personal growth, and protection against the negative consequences of self-judgment, isolation, anxiety, burnout, and depression.
What is self-compassion?
Kristin Neff, PhD, an associate professor in educational psychology at the University of Texas at Austin, was the first to academically define self-compassion. Self-compassion brings together three core elements – kindness, humanity, and mindfulness.2 Self-compassion involves acting the same way toward yourself when you are having a difficult time as you would toward another person. Instead of mercilessly judging and criticizing yourself for self-perceived inadequacies or shortcomings, self-compassion allows you to ask yourself: “How can I give myself comfort and care in this moment?”
Mindfulness acknowledges a painful experience without resistance or judgment, while being present in the moment with things as they are. Self-compassion provides the emotional safety needed to mindfully open to our pain, disappointments, and defeats. Mindfulness and self-compassion both allow us to live with more acceptance toward ourselves and our lives. Mindfulness asks: “What am I experiencing right now?” Self-compassion asks: “What do I need right now?” When you feel compassion for yourself or another, you recognize that suffering, failure, and imperfection are all part of the shared human experience.
The physiology of self-compassion
When we practice self-compassion, we feel safe and cared for because there is a physiological pathway that explains this response. Self-compassion helps down-regulate the stress response (fight-flight-freeze). When we are triggered by a threat to our self-concept, we are likely to do one, two, or all of three things: we fight ourselves (self-criticism – often our first reaction when things go wrong), we flee from others (isolation), or we freeze (rumination).
Feeling threatened puts stress on the mind and body, and chronic stress leads to anxiety and depression, which hinders emotional and physical well-being. With self-criticism, we are both the attacker and the attacked. When we practice self-compassion, we are deactivating the threat-defense system and activating the care system, releasing oxytocin and endorphins, which reduce stress and increase feelings of safety and security.3
Why is self-compassion important to provider well-being?
Research has shown that individuals who are more self-compassionate tend to have greater happiness, life satisfaction, and motivation; better relationships and physical health; and less anxiety and depression. They also have the resilience needed to cope with stressful life events. The more we practice being kind and compassionate with ourselves, the more we’ll increase the habit of self-compassion, and extend compassion to our patients and loved ones in daily life.4
Why is self-compassion important? When we experience a setback at work or in life, we can become defensive, accuse others, or blame ourselves, especially when we are already under immense stress. These responses are not helpful, productive, or effective to the situation or our personal well-being. Although in the moment it may feel good to be reactive, it is a short-lived feeling that we trade for the longer-lasting effects of learning, resilience, and personal growth. Self-compassion teaches us to connect with our inner imperfections, and what makes us human, as to err is human.
To cultivate a habit of self-compassion itself, it is important to understand that self-compassion is a practice of goodwill, not good feelings. Self-compassion is aimed at the alleviation of suffering, but it does not erase any pain and suffering that does exist. The truth is, we can’t always control external forces – the events of 2020-2021 are a perfect example of this. As a result, we cannot utilize self-compassion as a practice to make our pain disappear or suppress strong emotions.
Instead, self-compassion helps us cultivate the resilience needed to mindfully acknowledge and accept a painful moment or experience, while reminding us to embrace ourselves with kindness and care in response. This builds our internal foundation with support, love, and self-care, while providing the optimal conditions for growth, resilience, and transformation
Self-compassion and the backdraft phenomenon
When you start the practice of self-compassion, you may experience backdraft, a phenomenon in which pain initially increases.5 Backdraft is similar to the stages of grief or when the flames of a burning house become larger when a door is opened and oxygen surges in. Practicing self-compassion may cause a tidal wave of emotions to come to the forefront, but it is likely that if this happens, it needs to happen.
Imagine yourself in a room with two versions of yourself. To the left is your best self that you present to the world, standing tall, organized, well kept, and without any noticeable imperfections. To the right, is the deepest part of your being, laying on the floor, filled with raw emotions – sadness, fear, anger, and love. This version of yourself is vulnerable, open, honest, and imperfect. When looking at each version of yourself, which one is the real you? The right? The left? Maybe it’s both?
Imagine what would happen if you walked over to the version of yourself on the right, sat down, and provided it comfort, and embraced yourself with love and kindness. What would happen if you gave that version of yourself a hug? Seeing your true self, with all the layers peeled away, at the very core of your being, vulnerable, and possibly broken, is a powerful and gut-wrenching experience. It may hurt at first, but once we embrace our own pain and suffering, that is where mindfulness and self-compassion intersect to begin the path to healing. It takes more strength and courage to be the version of ourselves on the right than the version on the left.
What is not self compassion?
Self-compassion is not self-pity, weakness, self-esteem, or selfishness. When individuals feel self-pity, they become immersed in their own problems and feel that they are the only ones in the world who are suffering. Self-compassion makes us more willing to accept, experience, and acknowledge difficult feelings with kindness. This paradoxically helps us process and let go of these feelings without long-term negative consequences, and with a better ability to recognize the suffering of others.
Self-compassion allows us to be our own inner ally and strengthens our ability to cope successfully when life gets hard. Self-compassion will not make you weak and vulnerable. It is a reliable source of inner strength that enhances resilience when faced with difficulties. Research shows self-compassionate people are better able to cope with tough situations like divorce, trauma, and crisis.
Self-compassion and self-esteem are important to well-being; however, they are not the same. Self-esteem refers to a judgment or evaluation of our sense of self-worth, perceived value, or how much we like ourselves. While self-compassion relates to the changing landscape of who we are with kindness and acceptance – especially in times when we feel useless, inadequate, or hopeless – self-esteem allows for greater self-clarity, independent of external circumstances, and acknowledges that all human beings deserve compassion and understanding, not because they possess certain traits or have a certain perceive valued, but because we share the human experience and the human condition of imperfection. Finally, self-compassion is not selfish, as practicing it helps people sustain the act of caring for others and decrease caregiver burnout.6,7
Strategies to practice self-compassion
There are many ways to practice self-compassion. Here are a few experiences created by Dr. Neff, a leader in the field.8
Experience 1: How would you treat a friend?
How do you think things might change if you responded to yourself in the same way you typically respond to a close friend when he or she is suffering? Why not try treating yourself like a good friend and see what happens.
Take out a sheet of paper and write down your answer to the following questions:
- First, think about times when a close friend feels really bad about him or herself or is really struggling in some way. How would you respond to your friend in this situation (especially when you’re at your best)? Write down what you typically do and say and note the tone in which you typically talk to your friends.
- Second, think about times when you feel bad about yourself or are struggling. How do you typically respond to yourself in these situations? Write down what you typically do and say, and note the tone in which you typically talk to your friends.
- Did you notice a difference? If so, ask yourself why. What factors or fears come into play that lead you to treat yourself and others so differently?
- Please write down how you think things might change if you responded to yourself in the same way you typically respond to a close friend when you’re suffering.
Experience 2: Take a self-compassion break
This practice can be used any time of day or night, with others or alone. It will help you remember to evoke the three aspects of self-compassion when you need it most.
Think of a situation in your life that is difficult, that is causing you stress. Call the situation to mind, and if you feel comfortable, allow yourself to experience these feelings and emotions, without judgment and without altering them to what you think they should be.
- Say to yourself one of the following: “This is a difficult moment,” “This is a moment of suffering,” “This is stress,” “This hurts,” or “Ouch.” Doing this step is “mindfulness”: A willingness to observe negative thoughts and emotions with openness and clarity, so that they are held in mindful awareness, without judgment.
- Find your equilibrium of observation with thoughts and feelings. Try not to suppress or deny them and try not to get caught up and swept away by them.
- Remind yourself of the shared human experience. Recognize that suffering and personal difficulty is something that we all go through rather than being something that happens to “me” alone. Remind yourself that “other people feel this way,” “I’m not alone,” and “we all have struggles in life.”
- Be kind to yourself and ask: “What do I need to hear right now to express kindness to myself?” Is there a phrase that speaks to you in your particular situation? For example: “May I give myself the compassion that I need; may I learn to accept myself as I am; may I forgive myself; may I be strong; may I be patient.” There is no wrong answer.
Exercise 3: Explore self-compassion through writing
Everybody has something about themselves that they don’t like; something that causes them to feel shame, to feel insecure, or not “good enough.” This exercise will help you write a letter to yourself about this issue from a place of acceptance and compassion. It can feel uncomfortable at first, but it gets easier with practice.
- Write about an issue you have that makes you feel inadequate or bad about yourself (physical appearance, work, or relationship issue) What emotions do you experience when you think about this aspect of yourself? Try to only feel your emotions exactly as they are – no more, no less – and then write about them.
- Write a letter as if you were talking to a dearly beloved friend who was struggling with the same concerns as you and has the same strengths and weaknesses as you. How would you convey deep compassion, especially for the pain you feel when they judge themselves so harshly? What would you write to your friend to remind them that they are only human, that all people have both strengths and weaknesses? As you write, try to infuse your letter with a strong sense of acceptance, kindness, caring, and desire for their health and happiness.
- After writing the letter, put it aside for a little while. Then come back and read it again, really letting the words sink in. Feel the compassion as it pours into you, soothing and comforting you. Love, connection, and acceptance are a part of your human right. To claim them you need only look within yourself.
Experience 4: Taking care of the caregiver
We work in the very stressful time of the COVID pandemic. As medical providers, we are caregivers to our patients and our families. Yet, we do not give ourselves time to rest, recover, and recharge. Remember, to care for others, you cannot pour from an empty cup.
- Give yourself permission to meet your own needs, recognizing that this will not only enhance your quality of life, it will also enhance your ability to be there for those that rely on you. Our time is limited but self-care can occur both at work and outside of work.
- When you are “off the clock,” be off the clock! Turn off notifications, don’t check email, and be present in your personal lives. If you are constantly answering patient calls or nursing questions until 10 p.m., that means your health care system is in need of an upgrade, as you need the appropriate coverage to give you time to care for yourself, just as well as you care for your patients.
- While at work you can practice self-care. Take 2 minutes to practice relaxation breathing. Take 1 minute to show yourself or another person gratitude. Take 5 minutes before you start writing your notes for the day to listen to relaxing music or a mindful podcast. Take 3 minutes to share three good things that happened in the day with your family or colleagues. Take 5-10 minutes to do chair yoga. Take a self-compassion break.
- Implement a 5-minute wellness break into your group’s daily function with some of the previous mentioned examples. This will allow you to care for and nurture yourself, while also caring for and nurturing others in an environment that cultivates your wellness goals.
As a hospitalist, I can attest that I did not show myself self-compassion nearly as often as I showed compassion to others. I am my own worst critic and my training taught me to suffer in silence, and not seek out others who are experiencing the same thing for fear of being perceived as weak, inadequate, or flawed.
This false notion that we need to always be tough, strong, and without emotion in order to be taken seriously, to advance, or be held in high regard is rubbish and only perpetuated by accepting it. In order to change the culture of medicine, we have to change the way we think and behave. I have practiced self-compassion exercises and it has enhanced my perspective to see that many of us are going through varying degrees of the same thing. It has shown me the positive effects on my inner being and my life. If you are ready to try something new that will benefit your psychological and emotional well-being, and help you through pain, suffering, struggles, and crisis, you have nothing to lose. Be the change, and show yourself self-compassion.
In summary, self-compassion is an attitude of warmth, curiosity, connection, and care. Learning to become more self-compassionate is a process of moving from striving to change our experience and ourselves toward embracing who we are already.9 The practice of self-compassion is giving ourselves what we need in the moment. Even if we are not ready, or it is too painful to fully accept or embrace, we can still plant the seeds that will, with time and patience, grow and bloom.
When we are mindful of our struggles, when we respond to ourselves with compassion, kindness, and give ourselves support in times of difficulty, we learn to embrace ourselves and our lives, our inner and outer imperfections, and provide ourselves with the strength needed to thrive in the most precarious and difficult situations. With self-compassion, we give the world the best of us, instead of what is left of us.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the medical executive committee.
References
1. Sanchez-Reilly S et al. Caring for oneself to care for others: Physicians and their self-care. J Community Support Oncol. 2013;11(2):75-81. doi: 10.12788/j.suponc.0003.
2. Neff K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity. 2010;2(2):85-101. doi: 10.1080/15298860309032.
3. Neff K et al. The forest and the trees: Examining the association of self-compassion and its positive and negative components with psychological functioning. Self Identity. 2018;17(6):627-45. doi: 10.1080/15298868.2018.1436587.
4. Zessin U et al. The relationship between self-compassion and well-being: A meta-analysis. Appl Psychol Health Well-Being. 2015;7(3):340-64. doi: 10.1111/aphw.12051.
5. Warren R et al. Self-criticism and self-compassion: Risk and resilience. Current Psychiatry. 2016 Dec;15(12):18-21,24-28,32.
6. Neff K. The Five Myths of Self-Compassion. Greater Good Magazine. 2015 Sep 30. https://greatergood.berkeley.edu/article/item/the_five_myths_of_self_compassion.
7. Neff KD and Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013 Jan;69(1):28-44. doi: 10.1002/jclp.21923.
8. Neff K. Self-Compassion Guided Meditations and Exercises. https://self-compassion.org/category/exercises/#exercises.
9. Germer C and Neff KD. Mindful Self-Compassion (MSC), in “The handbook of mindfulness-based programs.” (London: Routledge, 2019, pp. 357-67).
A mindful way relate to ourselves
A mindful way relate to ourselves
Physicians, clinicians, providers, healers, and now heroes, are some of the names we have been given throughout history. These titles bring together a universal concept in medicine that all human beings deserve compassion, understanding, and care. However, as health care providers we forget to show ourselves the same compassion we bestow upon others.
Self-compassion is a new way of relating to ourselves. As clinicians, we are trained investigators, delving deeper into what our patient is thinking and feeling. “Tell me more about that. How does that make you feel? That must have been (very painful/scary/frustrating).” These are a few statements we learned in patient interviewing to actively engage with patients, build rapport, solidify trust, validate their concerns, and ultimately obtain the information needed to diagnose and heal.
We know the importance of looking beyond the surface, as more often than not a deeper inspection reveals more to the story. We have uncovered cracks in the foundation, erosion of the roof, worn out siding, and a glimpse into the complexities that make up each individual. We look at our patients, loved ones, and the world with night-vision lenses to uncover what is deeper.
Clinicians are good at directing compassion toward others, but not as good at giving it to themselves.1 Many health care providers may see self-compassion as soft, weak, selfish, or unnecessary. However, mindful self-compassion is a positive practice that opens a pathway for healing, personal growth, and protection against the negative consequences of self-judgment, isolation, anxiety, burnout, and depression.
What is self-compassion?
Kristin Neff, PhD, an associate professor in educational psychology at the University of Texas at Austin, was the first to academically define self-compassion. Self-compassion brings together three core elements – kindness, humanity, and mindfulness.2 Self-compassion involves acting the same way toward yourself when you are having a difficult time as you would toward another person. Instead of mercilessly judging and criticizing yourself for self-perceived inadequacies or shortcomings, self-compassion allows you to ask yourself: “How can I give myself comfort and care in this moment?”
Mindfulness acknowledges a painful experience without resistance or judgment, while being present in the moment with things as they are. Self-compassion provides the emotional safety needed to mindfully open to our pain, disappointments, and defeats. Mindfulness and self-compassion both allow us to live with more acceptance toward ourselves and our lives. Mindfulness asks: “What am I experiencing right now?” Self-compassion asks: “What do I need right now?” When you feel compassion for yourself or another, you recognize that suffering, failure, and imperfection are all part of the shared human experience.
The physiology of self-compassion
When we practice self-compassion, we feel safe and cared for because there is a physiological pathway that explains this response. Self-compassion helps down-regulate the stress response (fight-flight-freeze). When we are triggered by a threat to our self-concept, we are likely to do one, two, or all of three things: we fight ourselves (self-criticism – often our first reaction when things go wrong), we flee from others (isolation), or we freeze (rumination).
Feeling threatened puts stress on the mind and body, and chronic stress leads to anxiety and depression, which hinders emotional and physical well-being. With self-criticism, we are both the attacker and the attacked. When we practice self-compassion, we are deactivating the threat-defense system and activating the care system, releasing oxytocin and endorphins, which reduce stress and increase feelings of safety and security.3
Why is self-compassion important to provider well-being?
Research has shown that individuals who are more self-compassionate tend to have greater happiness, life satisfaction, and motivation; better relationships and physical health; and less anxiety and depression. They also have the resilience needed to cope with stressful life events. The more we practice being kind and compassionate with ourselves, the more we’ll increase the habit of self-compassion, and extend compassion to our patients and loved ones in daily life.4
Why is self-compassion important? When we experience a setback at work or in life, we can become defensive, accuse others, or blame ourselves, especially when we are already under immense stress. These responses are not helpful, productive, or effective to the situation or our personal well-being. Although in the moment it may feel good to be reactive, it is a short-lived feeling that we trade for the longer-lasting effects of learning, resilience, and personal growth. Self-compassion teaches us to connect with our inner imperfections, and what makes us human, as to err is human.
To cultivate a habit of self-compassion itself, it is important to understand that self-compassion is a practice of goodwill, not good feelings. Self-compassion is aimed at the alleviation of suffering, but it does not erase any pain and suffering that does exist. The truth is, we can’t always control external forces – the events of 2020-2021 are a perfect example of this. As a result, we cannot utilize self-compassion as a practice to make our pain disappear or suppress strong emotions.
Instead, self-compassion helps us cultivate the resilience needed to mindfully acknowledge and accept a painful moment or experience, while reminding us to embrace ourselves with kindness and care in response. This builds our internal foundation with support, love, and self-care, while providing the optimal conditions for growth, resilience, and transformation
Self-compassion and the backdraft phenomenon
When you start the practice of self-compassion, you may experience backdraft, a phenomenon in which pain initially increases.5 Backdraft is similar to the stages of grief or when the flames of a burning house become larger when a door is opened and oxygen surges in. Practicing self-compassion may cause a tidal wave of emotions to come to the forefront, but it is likely that if this happens, it needs to happen.
Imagine yourself in a room with two versions of yourself. To the left is your best self that you present to the world, standing tall, organized, well kept, and without any noticeable imperfections. To the right, is the deepest part of your being, laying on the floor, filled with raw emotions – sadness, fear, anger, and love. This version of yourself is vulnerable, open, honest, and imperfect. When looking at each version of yourself, which one is the real you? The right? The left? Maybe it’s both?
Imagine what would happen if you walked over to the version of yourself on the right, sat down, and provided it comfort, and embraced yourself with love and kindness. What would happen if you gave that version of yourself a hug? Seeing your true self, with all the layers peeled away, at the very core of your being, vulnerable, and possibly broken, is a powerful and gut-wrenching experience. It may hurt at first, but once we embrace our own pain and suffering, that is where mindfulness and self-compassion intersect to begin the path to healing. It takes more strength and courage to be the version of ourselves on the right than the version on the left.
What is not self compassion?
Self-compassion is not self-pity, weakness, self-esteem, or selfishness. When individuals feel self-pity, they become immersed in their own problems and feel that they are the only ones in the world who are suffering. Self-compassion makes us more willing to accept, experience, and acknowledge difficult feelings with kindness. This paradoxically helps us process and let go of these feelings without long-term negative consequences, and with a better ability to recognize the suffering of others.
Self-compassion allows us to be our own inner ally and strengthens our ability to cope successfully when life gets hard. Self-compassion will not make you weak and vulnerable. It is a reliable source of inner strength that enhances resilience when faced with difficulties. Research shows self-compassionate people are better able to cope with tough situations like divorce, trauma, and crisis.
Self-compassion and self-esteem are important to well-being; however, they are not the same. Self-esteem refers to a judgment or evaluation of our sense of self-worth, perceived value, or how much we like ourselves. While self-compassion relates to the changing landscape of who we are with kindness and acceptance – especially in times when we feel useless, inadequate, or hopeless – self-esteem allows for greater self-clarity, independent of external circumstances, and acknowledges that all human beings deserve compassion and understanding, not because they possess certain traits or have a certain perceive valued, but because we share the human experience and the human condition of imperfection. Finally, self-compassion is not selfish, as practicing it helps people sustain the act of caring for others and decrease caregiver burnout.6,7
Strategies to practice self-compassion
There are many ways to practice self-compassion. Here are a few experiences created by Dr. Neff, a leader in the field.8
Experience 1: How would you treat a friend?
How do you think things might change if you responded to yourself in the same way you typically respond to a close friend when he or she is suffering? Why not try treating yourself like a good friend and see what happens.
Take out a sheet of paper and write down your answer to the following questions:
- First, think about times when a close friend feels really bad about him or herself or is really struggling in some way. How would you respond to your friend in this situation (especially when you’re at your best)? Write down what you typically do and say and note the tone in which you typically talk to your friends.
- Second, think about times when you feel bad about yourself or are struggling. How do you typically respond to yourself in these situations? Write down what you typically do and say, and note the tone in which you typically talk to your friends.
- Did you notice a difference? If so, ask yourself why. What factors or fears come into play that lead you to treat yourself and others so differently?
- Please write down how you think things might change if you responded to yourself in the same way you typically respond to a close friend when you’re suffering.
Experience 2: Take a self-compassion break
This practice can be used any time of day or night, with others or alone. It will help you remember to evoke the three aspects of self-compassion when you need it most.
Think of a situation in your life that is difficult, that is causing you stress. Call the situation to mind, and if you feel comfortable, allow yourself to experience these feelings and emotions, without judgment and without altering them to what you think they should be.
- Say to yourself one of the following: “This is a difficult moment,” “This is a moment of suffering,” “This is stress,” “This hurts,” or “Ouch.” Doing this step is “mindfulness”: A willingness to observe negative thoughts and emotions with openness and clarity, so that they are held in mindful awareness, without judgment.
- Find your equilibrium of observation with thoughts and feelings. Try not to suppress or deny them and try not to get caught up and swept away by them.
- Remind yourself of the shared human experience. Recognize that suffering and personal difficulty is something that we all go through rather than being something that happens to “me” alone. Remind yourself that “other people feel this way,” “I’m not alone,” and “we all have struggles in life.”
- Be kind to yourself and ask: “What do I need to hear right now to express kindness to myself?” Is there a phrase that speaks to you in your particular situation? For example: “May I give myself the compassion that I need; may I learn to accept myself as I am; may I forgive myself; may I be strong; may I be patient.” There is no wrong answer.
Exercise 3: Explore self-compassion through writing
Everybody has something about themselves that they don’t like; something that causes them to feel shame, to feel insecure, or not “good enough.” This exercise will help you write a letter to yourself about this issue from a place of acceptance and compassion. It can feel uncomfortable at first, but it gets easier with practice.
- Write about an issue you have that makes you feel inadequate or bad about yourself (physical appearance, work, or relationship issue) What emotions do you experience when you think about this aspect of yourself? Try to only feel your emotions exactly as they are – no more, no less – and then write about them.
- Write a letter as if you were talking to a dearly beloved friend who was struggling with the same concerns as you and has the same strengths and weaknesses as you. How would you convey deep compassion, especially for the pain you feel when they judge themselves so harshly? What would you write to your friend to remind them that they are only human, that all people have both strengths and weaknesses? As you write, try to infuse your letter with a strong sense of acceptance, kindness, caring, and desire for their health and happiness.
- After writing the letter, put it aside for a little while. Then come back and read it again, really letting the words sink in. Feel the compassion as it pours into you, soothing and comforting you. Love, connection, and acceptance are a part of your human right. To claim them you need only look within yourself.
Experience 4: Taking care of the caregiver
We work in the very stressful time of the COVID pandemic. As medical providers, we are caregivers to our patients and our families. Yet, we do not give ourselves time to rest, recover, and recharge. Remember, to care for others, you cannot pour from an empty cup.
- Give yourself permission to meet your own needs, recognizing that this will not only enhance your quality of life, it will also enhance your ability to be there for those that rely on you. Our time is limited but self-care can occur both at work and outside of work.
- When you are “off the clock,” be off the clock! Turn off notifications, don’t check email, and be present in your personal lives. If you are constantly answering patient calls or nursing questions until 10 p.m., that means your health care system is in need of an upgrade, as you need the appropriate coverage to give you time to care for yourself, just as well as you care for your patients.
- While at work you can practice self-care. Take 2 minutes to practice relaxation breathing. Take 1 minute to show yourself or another person gratitude. Take 5 minutes before you start writing your notes for the day to listen to relaxing music or a mindful podcast. Take 3 minutes to share three good things that happened in the day with your family or colleagues. Take 5-10 minutes to do chair yoga. Take a self-compassion break.
- Implement a 5-minute wellness break into your group’s daily function with some of the previous mentioned examples. This will allow you to care for and nurture yourself, while also caring for and nurturing others in an environment that cultivates your wellness goals.
As a hospitalist, I can attest that I did not show myself self-compassion nearly as often as I showed compassion to others. I am my own worst critic and my training taught me to suffer in silence, and not seek out others who are experiencing the same thing for fear of being perceived as weak, inadequate, or flawed.
This false notion that we need to always be tough, strong, and without emotion in order to be taken seriously, to advance, or be held in high regard is rubbish and only perpetuated by accepting it. In order to change the culture of medicine, we have to change the way we think and behave. I have practiced self-compassion exercises and it has enhanced my perspective to see that many of us are going through varying degrees of the same thing. It has shown me the positive effects on my inner being and my life. If you are ready to try something new that will benefit your psychological and emotional well-being, and help you through pain, suffering, struggles, and crisis, you have nothing to lose. Be the change, and show yourself self-compassion.
In summary, self-compassion is an attitude of warmth, curiosity, connection, and care. Learning to become more self-compassionate is a process of moving from striving to change our experience and ourselves toward embracing who we are already.9 The practice of self-compassion is giving ourselves what we need in the moment. Even if we are not ready, or it is too painful to fully accept or embrace, we can still plant the seeds that will, with time and patience, grow and bloom.
When we are mindful of our struggles, when we respond to ourselves with compassion, kindness, and give ourselves support in times of difficulty, we learn to embrace ourselves and our lives, our inner and outer imperfections, and provide ourselves with the strength needed to thrive in the most precarious and difficult situations. With self-compassion, we give the world the best of us, instead of what is left of us.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the medical executive committee.
References
1. Sanchez-Reilly S et al. Caring for oneself to care for others: Physicians and their self-care. J Community Support Oncol. 2013;11(2):75-81. doi: 10.12788/j.suponc.0003.
2. Neff K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity. 2010;2(2):85-101. doi: 10.1080/15298860309032.
3. Neff K et al. The forest and the trees: Examining the association of self-compassion and its positive and negative components with psychological functioning. Self Identity. 2018;17(6):627-45. doi: 10.1080/15298868.2018.1436587.
4. Zessin U et al. The relationship between self-compassion and well-being: A meta-analysis. Appl Psychol Health Well-Being. 2015;7(3):340-64. doi: 10.1111/aphw.12051.
5. Warren R et al. Self-criticism and self-compassion: Risk and resilience. Current Psychiatry. 2016 Dec;15(12):18-21,24-28,32.
6. Neff K. The Five Myths of Self-Compassion. Greater Good Magazine. 2015 Sep 30. https://greatergood.berkeley.edu/article/item/the_five_myths_of_self_compassion.
7. Neff KD and Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013 Jan;69(1):28-44. doi: 10.1002/jclp.21923.
8. Neff K. Self-Compassion Guided Meditations and Exercises. https://self-compassion.org/category/exercises/#exercises.
9. Germer C and Neff KD. Mindful Self-Compassion (MSC), in “The handbook of mindfulness-based programs.” (London: Routledge, 2019, pp. 357-67).
Physicians, clinicians, providers, healers, and now heroes, are some of the names we have been given throughout history. These titles bring together a universal concept in medicine that all human beings deserve compassion, understanding, and care. However, as health care providers we forget to show ourselves the same compassion we bestow upon others.
Self-compassion is a new way of relating to ourselves. As clinicians, we are trained investigators, delving deeper into what our patient is thinking and feeling. “Tell me more about that. How does that make you feel? That must have been (very painful/scary/frustrating).” These are a few statements we learned in patient interviewing to actively engage with patients, build rapport, solidify trust, validate their concerns, and ultimately obtain the information needed to diagnose and heal.
We know the importance of looking beyond the surface, as more often than not a deeper inspection reveals more to the story. We have uncovered cracks in the foundation, erosion of the roof, worn out siding, and a glimpse into the complexities that make up each individual. We look at our patients, loved ones, and the world with night-vision lenses to uncover what is deeper.
Clinicians are good at directing compassion toward others, but not as good at giving it to themselves.1 Many health care providers may see self-compassion as soft, weak, selfish, or unnecessary. However, mindful self-compassion is a positive practice that opens a pathway for healing, personal growth, and protection against the negative consequences of self-judgment, isolation, anxiety, burnout, and depression.
What is self-compassion?
Kristin Neff, PhD, an associate professor in educational psychology at the University of Texas at Austin, was the first to academically define self-compassion. Self-compassion brings together three core elements – kindness, humanity, and mindfulness.2 Self-compassion involves acting the same way toward yourself when you are having a difficult time as you would toward another person. Instead of mercilessly judging and criticizing yourself for self-perceived inadequacies or shortcomings, self-compassion allows you to ask yourself: “How can I give myself comfort and care in this moment?”
Mindfulness acknowledges a painful experience without resistance or judgment, while being present in the moment with things as they are. Self-compassion provides the emotional safety needed to mindfully open to our pain, disappointments, and defeats. Mindfulness and self-compassion both allow us to live with more acceptance toward ourselves and our lives. Mindfulness asks: “What am I experiencing right now?” Self-compassion asks: “What do I need right now?” When you feel compassion for yourself or another, you recognize that suffering, failure, and imperfection are all part of the shared human experience.
The physiology of self-compassion
When we practice self-compassion, we feel safe and cared for because there is a physiological pathway that explains this response. Self-compassion helps down-regulate the stress response (fight-flight-freeze). When we are triggered by a threat to our self-concept, we are likely to do one, two, or all of three things: we fight ourselves (self-criticism – often our first reaction when things go wrong), we flee from others (isolation), or we freeze (rumination).
Feeling threatened puts stress on the mind and body, and chronic stress leads to anxiety and depression, which hinders emotional and physical well-being. With self-criticism, we are both the attacker and the attacked. When we practice self-compassion, we are deactivating the threat-defense system and activating the care system, releasing oxytocin and endorphins, which reduce stress and increase feelings of safety and security.3
Why is self-compassion important to provider well-being?
Research has shown that individuals who are more self-compassionate tend to have greater happiness, life satisfaction, and motivation; better relationships and physical health; and less anxiety and depression. They also have the resilience needed to cope with stressful life events. The more we practice being kind and compassionate with ourselves, the more we’ll increase the habit of self-compassion, and extend compassion to our patients and loved ones in daily life.4
Why is self-compassion important? When we experience a setback at work or in life, we can become defensive, accuse others, or blame ourselves, especially when we are already under immense stress. These responses are not helpful, productive, or effective to the situation or our personal well-being. Although in the moment it may feel good to be reactive, it is a short-lived feeling that we trade for the longer-lasting effects of learning, resilience, and personal growth. Self-compassion teaches us to connect with our inner imperfections, and what makes us human, as to err is human.
To cultivate a habit of self-compassion itself, it is important to understand that self-compassion is a practice of goodwill, not good feelings. Self-compassion is aimed at the alleviation of suffering, but it does not erase any pain and suffering that does exist. The truth is, we can’t always control external forces – the events of 2020-2021 are a perfect example of this. As a result, we cannot utilize self-compassion as a practice to make our pain disappear or suppress strong emotions.
Instead, self-compassion helps us cultivate the resilience needed to mindfully acknowledge and accept a painful moment or experience, while reminding us to embrace ourselves with kindness and care in response. This builds our internal foundation with support, love, and self-care, while providing the optimal conditions for growth, resilience, and transformation
Self-compassion and the backdraft phenomenon
When you start the practice of self-compassion, you may experience backdraft, a phenomenon in which pain initially increases.5 Backdraft is similar to the stages of grief or when the flames of a burning house become larger when a door is opened and oxygen surges in. Practicing self-compassion may cause a tidal wave of emotions to come to the forefront, but it is likely that if this happens, it needs to happen.
Imagine yourself in a room with two versions of yourself. To the left is your best self that you present to the world, standing tall, organized, well kept, and without any noticeable imperfections. To the right, is the deepest part of your being, laying on the floor, filled with raw emotions – sadness, fear, anger, and love. This version of yourself is vulnerable, open, honest, and imperfect. When looking at each version of yourself, which one is the real you? The right? The left? Maybe it’s both?
Imagine what would happen if you walked over to the version of yourself on the right, sat down, and provided it comfort, and embraced yourself with love and kindness. What would happen if you gave that version of yourself a hug? Seeing your true self, with all the layers peeled away, at the very core of your being, vulnerable, and possibly broken, is a powerful and gut-wrenching experience. It may hurt at first, but once we embrace our own pain and suffering, that is where mindfulness and self-compassion intersect to begin the path to healing. It takes more strength and courage to be the version of ourselves on the right than the version on the left.
What is not self compassion?
Self-compassion is not self-pity, weakness, self-esteem, or selfishness. When individuals feel self-pity, they become immersed in their own problems and feel that they are the only ones in the world who are suffering. Self-compassion makes us more willing to accept, experience, and acknowledge difficult feelings with kindness. This paradoxically helps us process and let go of these feelings without long-term negative consequences, and with a better ability to recognize the suffering of others.
Self-compassion allows us to be our own inner ally and strengthens our ability to cope successfully when life gets hard. Self-compassion will not make you weak and vulnerable. It is a reliable source of inner strength that enhances resilience when faced with difficulties. Research shows self-compassionate people are better able to cope with tough situations like divorce, trauma, and crisis.
Self-compassion and self-esteem are important to well-being; however, they are not the same. Self-esteem refers to a judgment or evaluation of our sense of self-worth, perceived value, or how much we like ourselves. While self-compassion relates to the changing landscape of who we are with kindness and acceptance – especially in times when we feel useless, inadequate, or hopeless – self-esteem allows for greater self-clarity, independent of external circumstances, and acknowledges that all human beings deserve compassion and understanding, not because they possess certain traits or have a certain perceive valued, but because we share the human experience and the human condition of imperfection. Finally, self-compassion is not selfish, as practicing it helps people sustain the act of caring for others and decrease caregiver burnout.6,7
Strategies to practice self-compassion
There are many ways to practice self-compassion. Here are a few experiences created by Dr. Neff, a leader in the field.8
Experience 1: How would you treat a friend?
How do you think things might change if you responded to yourself in the same way you typically respond to a close friend when he or she is suffering? Why not try treating yourself like a good friend and see what happens.
Take out a sheet of paper and write down your answer to the following questions:
- First, think about times when a close friend feels really bad about him or herself or is really struggling in some way. How would you respond to your friend in this situation (especially when you’re at your best)? Write down what you typically do and say and note the tone in which you typically talk to your friends.
- Second, think about times when you feel bad about yourself or are struggling. How do you typically respond to yourself in these situations? Write down what you typically do and say, and note the tone in which you typically talk to your friends.
- Did you notice a difference? If so, ask yourself why. What factors or fears come into play that lead you to treat yourself and others so differently?
- Please write down how you think things might change if you responded to yourself in the same way you typically respond to a close friend when you’re suffering.
Experience 2: Take a self-compassion break
This practice can be used any time of day or night, with others or alone. It will help you remember to evoke the three aspects of self-compassion when you need it most.
Think of a situation in your life that is difficult, that is causing you stress. Call the situation to mind, and if you feel comfortable, allow yourself to experience these feelings and emotions, without judgment and without altering them to what you think they should be.
- Say to yourself one of the following: “This is a difficult moment,” “This is a moment of suffering,” “This is stress,” “This hurts,” or “Ouch.” Doing this step is “mindfulness”: A willingness to observe negative thoughts and emotions with openness and clarity, so that they are held in mindful awareness, without judgment.
- Find your equilibrium of observation with thoughts and feelings. Try not to suppress or deny them and try not to get caught up and swept away by them.
- Remind yourself of the shared human experience. Recognize that suffering and personal difficulty is something that we all go through rather than being something that happens to “me” alone. Remind yourself that “other people feel this way,” “I’m not alone,” and “we all have struggles in life.”
- Be kind to yourself and ask: “What do I need to hear right now to express kindness to myself?” Is there a phrase that speaks to you in your particular situation? For example: “May I give myself the compassion that I need; may I learn to accept myself as I am; may I forgive myself; may I be strong; may I be patient.” There is no wrong answer.
Exercise 3: Explore self-compassion through writing
Everybody has something about themselves that they don’t like; something that causes them to feel shame, to feel insecure, or not “good enough.” This exercise will help you write a letter to yourself about this issue from a place of acceptance and compassion. It can feel uncomfortable at first, but it gets easier with practice.
- Write about an issue you have that makes you feel inadequate or bad about yourself (physical appearance, work, or relationship issue) What emotions do you experience when you think about this aspect of yourself? Try to only feel your emotions exactly as they are – no more, no less – and then write about them.
- Write a letter as if you were talking to a dearly beloved friend who was struggling with the same concerns as you and has the same strengths and weaknesses as you. How would you convey deep compassion, especially for the pain you feel when they judge themselves so harshly? What would you write to your friend to remind them that they are only human, that all people have both strengths and weaknesses? As you write, try to infuse your letter with a strong sense of acceptance, kindness, caring, and desire for their health and happiness.
- After writing the letter, put it aside for a little while. Then come back and read it again, really letting the words sink in. Feel the compassion as it pours into you, soothing and comforting you. Love, connection, and acceptance are a part of your human right. To claim them you need only look within yourself.
Experience 4: Taking care of the caregiver
We work in the very stressful time of the COVID pandemic. As medical providers, we are caregivers to our patients and our families. Yet, we do not give ourselves time to rest, recover, and recharge. Remember, to care for others, you cannot pour from an empty cup.
- Give yourself permission to meet your own needs, recognizing that this will not only enhance your quality of life, it will also enhance your ability to be there for those that rely on you. Our time is limited but self-care can occur both at work and outside of work.
- When you are “off the clock,” be off the clock! Turn off notifications, don’t check email, and be present in your personal lives. If you are constantly answering patient calls or nursing questions until 10 p.m., that means your health care system is in need of an upgrade, as you need the appropriate coverage to give you time to care for yourself, just as well as you care for your patients.
- While at work you can practice self-care. Take 2 minutes to practice relaxation breathing. Take 1 minute to show yourself or another person gratitude. Take 5 minutes before you start writing your notes for the day to listen to relaxing music or a mindful podcast. Take 3 minutes to share three good things that happened in the day with your family or colleagues. Take 5-10 minutes to do chair yoga. Take a self-compassion break.
- Implement a 5-minute wellness break into your group’s daily function with some of the previous mentioned examples. This will allow you to care for and nurture yourself, while also caring for and nurturing others in an environment that cultivates your wellness goals.
As a hospitalist, I can attest that I did not show myself self-compassion nearly as often as I showed compassion to others. I am my own worst critic and my training taught me to suffer in silence, and not seek out others who are experiencing the same thing for fear of being perceived as weak, inadequate, or flawed.
This false notion that we need to always be tough, strong, and without emotion in order to be taken seriously, to advance, or be held in high regard is rubbish and only perpetuated by accepting it. In order to change the culture of medicine, we have to change the way we think and behave. I have practiced self-compassion exercises and it has enhanced my perspective to see that many of us are going through varying degrees of the same thing. It has shown me the positive effects on my inner being and my life. If you are ready to try something new that will benefit your psychological and emotional well-being, and help you through pain, suffering, struggles, and crisis, you have nothing to lose. Be the change, and show yourself self-compassion.
In summary, self-compassion is an attitude of warmth, curiosity, connection, and care. Learning to become more self-compassionate is a process of moving from striving to change our experience and ourselves toward embracing who we are already.9 The practice of self-compassion is giving ourselves what we need in the moment. Even if we are not ready, or it is too painful to fully accept or embrace, we can still plant the seeds that will, with time and patience, grow and bloom.
When we are mindful of our struggles, when we respond to ourselves with compassion, kindness, and give ourselves support in times of difficulty, we learn to embrace ourselves and our lives, our inner and outer imperfections, and provide ourselves with the strength needed to thrive in the most precarious and difficult situations. With self-compassion, we give the world the best of us, instead of what is left of us.
Dr. Williams is vice president of the Hampton Roads chapter of the Society of Hospital Medicine. She is a hospitalist at Sentara Careplex Hospital in Hampton, Va., where she also serves as vice president of the medical executive committee.
References
1. Sanchez-Reilly S et al. Caring for oneself to care for others: Physicians and their self-care. J Community Support Oncol. 2013;11(2):75-81. doi: 10.12788/j.suponc.0003.
2. Neff K. Self-Compassion: An Alternative Conceptualization of a Healthy Attitude Toward Oneself. Self Identity. 2010;2(2):85-101. doi: 10.1080/15298860309032.
3. Neff K et al. The forest and the trees: Examining the association of self-compassion and its positive and negative components with psychological functioning. Self Identity. 2018;17(6):627-45. doi: 10.1080/15298868.2018.1436587.
4. Zessin U et al. The relationship between self-compassion and well-being: A meta-analysis. Appl Psychol Health Well-Being. 2015;7(3):340-64. doi: 10.1111/aphw.12051.
5. Warren R et al. Self-criticism and self-compassion: Risk and resilience. Current Psychiatry. 2016 Dec;15(12):18-21,24-28,32.
6. Neff K. The Five Myths of Self-Compassion. Greater Good Magazine. 2015 Sep 30. https://greatergood.berkeley.edu/article/item/the_five_myths_of_self_compassion.
7. Neff KD and Germer CK. A pilot study and randomized controlled trial of the mindful self-compassion program. J Clin Psychol. 2013 Jan;69(1):28-44. doi: 10.1002/jclp.21923.
8. Neff K. Self-Compassion Guided Meditations and Exercises. https://self-compassion.org/category/exercises/#exercises.
9. Germer C and Neff KD. Mindful Self-Compassion (MSC), in “The handbook of mindfulness-based programs.” (London: Routledge, 2019, pp. 357-67).
Children and COVID-19: 7 million cases and still counting
Total COVID-19 cases in children surpassed the 7-million mark as new cases rose slightly after the previous week’s decline, according to the American Academy of Pediatrics and the Children’s Hospital Association.

, the AAP and CHA said in their weekly COVID-19 report. New cases had dropped the previous week after 3 straight weeks of increases since late October.
The Centers for Disease Control and Prevention puts the total number of child COVID-19 cases at 6.2 million, but both estimates are based on all-age totals – 40 million for the CDC and 41 million for the AAP/CHA – that are well short of the CDC’s latest cumulative figure, which is now just over 49 million, so the actual figures are undoubtedly higher.
Meanwhile, the 1-month anniversary of 5- to 11-year-olds’ vaccine eligibility brought many completions: 923,000 received their second dose during the week ending Dec. 6, compared with 405,000 the previous week. About 16.9% (4.9 million) of children aged 5-11 have gotten at least one dose of the COVID-19 vaccine thus far, of whom almost 1.5 million children (5.1% of the age group) are now fully vaccinated, the CDC said on its COVID-19 Data Tracker.
The pace of vaccinations, however, is much lower for older children. Weekly numbers for all COVID-19 vaccinations, both first and second doses, dropped from 84,000 (Nov. 23-29) to 70,000 (Nov. 30 to Dec. 6), for those aged 12-17 years. In that group, 61.6% have received at least one dose and 51.8% are fully vaccinated, the CDC said.
The pace of vaccinations varies for younger children as well, when geography is considered. The AAP analyzed the CDC’s data and found that 42% of all 5- to 11-year-olds in Vermont had received at least one dose as of Dec. 1, followed by Massachusetts (33%), Maine (30%), and Rhode Island (28%). At the other end of the vaccination scale are Alabama, Louisiana, Mississippi, and West Virginia, all with 4%, the AAP reported.
As the United States puts 7 million children infected with COVID-19 in its rear view mirror, another milestone is looming ahead: The CDC’s current count of deaths in children is 974.
Total COVID-19 cases in children surpassed the 7-million mark as new cases rose slightly after the previous week’s decline, according to the American Academy of Pediatrics and the Children’s Hospital Association.

, the AAP and CHA said in their weekly COVID-19 report. New cases had dropped the previous week after 3 straight weeks of increases since late October.
The Centers for Disease Control and Prevention puts the total number of child COVID-19 cases at 6.2 million, but both estimates are based on all-age totals – 40 million for the CDC and 41 million for the AAP/CHA – that are well short of the CDC’s latest cumulative figure, which is now just over 49 million, so the actual figures are undoubtedly higher.
Meanwhile, the 1-month anniversary of 5- to 11-year-olds’ vaccine eligibility brought many completions: 923,000 received their second dose during the week ending Dec. 6, compared with 405,000 the previous week. About 16.9% (4.9 million) of children aged 5-11 have gotten at least one dose of the COVID-19 vaccine thus far, of whom almost 1.5 million children (5.1% of the age group) are now fully vaccinated, the CDC said on its COVID-19 Data Tracker.
The pace of vaccinations, however, is much lower for older children. Weekly numbers for all COVID-19 vaccinations, both first and second doses, dropped from 84,000 (Nov. 23-29) to 70,000 (Nov. 30 to Dec. 6), for those aged 12-17 years. In that group, 61.6% have received at least one dose and 51.8% are fully vaccinated, the CDC said.
The pace of vaccinations varies for younger children as well, when geography is considered. The AAP analyzed the CDC’s data and found that 42% of all 5- to 11-year-olds in Vermont had received at least one dose as of Dec. 1, followed by Massachusetts (33%), Maine (30%), and Rhode Island (28%). At the other end of the vaccination scale are Alabama, Louisiana, Mississippi, and West Virginia, all with 4%, the AAP reported.
As the United States puts 7 million children infected with COVID-19 in its rear view mirror, another milestone is looming ahead: The CDC’s current count of deaths in children is 974.
Total COVID-19 cases in children surpassed the 7-million mark as new cases rose slightly after the previous week’s decline, according to the American Academy of Pediatrics and the Children’s Hospital Association.

, the AAP and CHA said in their weekly COVID-19 report. New cases had dropped the previous week after 3 straight weeks of increases since late October.
The Centers for Disease Control and Prevention puts the total number of child COVID-19 cases at 6.2 million, but both estimates are based on all-age totals – 40 million for the CDC and 41 million for the AAP/CHA – that are well short of the CDC’s latest cumulative figure, which is now just over 49 million, so the actual figures are undoubtedly higher.
Meanwhile, the 1-month anniversary of 5- to 11-year-olds’ vaccine eligibility brought many completions: 923,000 received their second dose during the week ending Dec. 6, compared with 405,000 the previous week. About 16.9% (4.9 million) of children aged 5-11 have gotten at least one dose of the COVID-19 vaccine thus far, of whom almost 1.5 million children (5.1% of the age group) are now fully vaccinated, the CDC said on its COVID-19 Data Tracker.
The pace of vaccinations, however, is much lower for older children. Weekly numbers for all COVID-19 vaccinations, both first and second doses, dropped from 84,000 (Nov. 23-29) to 70,000 (Nov. 30 to Dec. 6), for those aged 12-17 years. In that group, 61.6% have received at least one dose and 51.8% are fully vaccinated, the CDC said.
The pace of vaccinations varies for younger children as well, when geography is considered. The AAP analyzed the CDC’s data and found that 42% of all 5- to 11-year-olds in Vermont had received at least one dose as of Dec. 1, followed by Massachusetts (33%), Maine (30%), and Rhode Island (28%). At the other end of the vaccination scale are Alabama, Louisiana, Mississippi, and West Virginia, all with 4%, the AAP reported.
As the United States puts 7 million children infected with COVID-19 in its rear view mirror, another milestone is looming ahead: The CDC’s current count of deaths in children is 974.












