User login
It’s the Television, Stupid
As more and more of us begin to feel (or believe we are feeling) the symptoms of aging, our language has begun to incorporate new words and phrases such as “aging in place” or “healthy aging.” In fact, some scientists have created a diagnostic criteria to define “healthy aging.” If you have reached your 70th birthday without mental health issues, memory issues, physical impairments, or chronic disease, according to some researchers at T.H. Chan School of Public Health and Brigham and Women’s Hospital, you should receive a gold star for healthy aging.
I am now nearly a decade past that milestone and can’t remember where I’ve put my gold star, or even if I had ever received one. But, I get up each morning looking forward to another day of activity and feeling “pretty good.”
Healthy aging is not something you start doing when you turn 65. Aging is something that goes on from the moment you are born. For the first couple decades we call it “maturing.” If you have lived well, the odds are you will age well. And, for that reason we should take note of some recent work by Boston-based researchers.
Looking at recent data from 45,000 participants in the well-known Nurses Health Study, the investigators found that for every 2-hour increase in daily sedentary behavior, the participants cut their chances of healthy aging by 12%. On the other hand, for every 2 hours of light physical activity, they increased their odds of healthy aging by 6 %.
There are two important messages sitting just below the surface of these two observations. First, we continue to overemphasize the importance of “exercise” in our attempt to help our patients achieve wellness. The word “exercise” carries with it whole carousel full of baggage including “fitness programs,” gym memberships, pulse rate monitors, pain, sweat, and spandex, to name just a few. Exercise can conjure up bad memories of suiting up for phys ed class, group showers, and being picked last when teams were being chosen.
It turns out the we should simply be promoting activity, and light activity at that — vacuuming the living room, walking around the block, rearranging the books on your bedroom book shelf, making a pot of soup, doing the laundry. Just getting up off one’s behind and doing something instead of being a passive spectator.
This somewhat counterintuitive notion of the benefit of light activity is beginning to get more attention. Earlier this year, I reported on a study by Andre O. Abaje MD, MPH, in which he showed that light physical activity in children was superior to more vigorous activity in lowering lipids.
The more important message embedded in this paper based on the Nurses Health Study is that the researchers used television watching time as their proxy for sedentary behavior. The investigators chose TV viewing because it is ubiquitous and includes prolonged sitting. Being semi-reclined on the couch or in a lounger requires very little muscle activity, which is in turn linked to disruption of glucose metabolism, increased inflammation, and altered blood flow to the brain, to name just a few of its collateral damages. I would add that TV viewing often prompts viewers to stay up well beyond their healthy bedtime. And, we know sleep deprivation is not compatible with health aging.
A traditional warning issued to new retirees was once “Don’t let the old rocking chair get ya.” In fact, I wonder how many folks watching television even have or use wood rocking chairs anymore, which, if rocked, might qualify as a light exercise if the viewer made the effort to rock. Instead I suspect most television viewing is done cocooned in soft recliners or curled up on a couch.
I will admit that this recent paper merely supports a suspicion I have harbored for decades. Like many of you, I have wondered how our society got to the point where obesity is frequent enough to be labeled a disease, attention deficit diagnoses are becoming increasingly prevalent, and our life expectancy is shrinking. There are dozens of factors, but if I had to pick one, I would paraphrase James Carville’s advice to Bill Clinton: “It’s the television, stupid.”
At least a couple of notches above “Are you wearing your seatbelt?” It can start with a nonjudgmental question such as “What are your favorite television shows?” And then deftly move toward compiling a tally of how many hours the patient watches each day.
How you manage the situation from there is up to you and can be based on the patient’s complaints and problem list. You might suggest he or she start by eliminating 2 hours of viewing a day. Then ask if he or she thinks that new schedule is achievable. If they ask for alternatives, be ready with a list of light activities that they might be surprised are healthier than their current behavior. Follow up with another visit or a call to see how they are doing. It’s that important, and your call will underscore your concern.
Sedentism is a serious health problem in this country and our emphasis on encouraging vigorous exercise isn’t working. Selling a television diet will be a tough sell, but it needs to be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As more and more of us begin to feel (or believe we are feeling) the symptoms of aging, our language has begun to incorporate new words and phrases such as “aging in place” or “healthy aging.” In fact, some scientists have created a diagnostic criteria to define “healthy aging.” If you have reached your 70th birthday without mental health issues, memory issues, physical impairments, or chronic disease, according to some researchers at T.H. Chan School of Public Health and Brigham and Women’s Hospital, you should receive a gold star for healthy aging.
I am now nearly a decade past that milestone and can’t remember where I’ve put my gold star, or even if I had ever received one. But, I get up each morning looking forward to another day of activity and feeling “pretty good.”
Healthy aging is not something you start doing when you turn 65. Aging is something that goes on from the moment you are born. For the first couple decades we call it “maturing.” If you have lived well, the odds are you will age well. And, for that reason we should take note of some recent work by Boston-based researchers.
Looking at recent data from 45,000 participants in the well-known Nurses Health Study, the investigators found that for every 2-hour increase in daily sedentary behavior, the participants cut their chances of healthy aging by 12%. On the other hand, for every 2 hours of light physical activity, they increased their odds of healthy aging by 6 %.
There are two important messages sitting just below the surface of these two observations. First, we continue to overemphasize the importance of “exercise” in our attempt to help our patients achieve wellness. The word “exercise” carries with it whole carousel full of baggage including “fitness programs,” gym memberships, pulse rate monitors, pain, sweat, and spandex, to name just a few. Exercise can conjure up bad memories of suiting up for phys ed class, group showers, and being picked last when teams were being chosen.
It turns out the we should simply be promoting activity, and light activity at that — vacuuming the living room, walking around the block, rearranging the books on your bedroom book shelf, making a pot of soup, doing the laundry. Just getting up off one’s behind and doing something instead of being a passive spectator.
This somewhat counterintuitive notion of the benefit of light activity is beginning to get more attention. Earlier this year, I reported on a study by Andre O. Abaje MD, MPH, in which he showed that light physical activity in children was superior to more vigorous activity in lowering lipids.
The more important message embedded in this paper based on the Nurses Health Study is that the researchers used television watching time as their proxy for sedentary behavior. The investigators chose TV viewing because it is ubiquitous and includes prolonged sitting. Being semi-reclined on the couch or in a lounger requires very little muscle activity, which is in turn linked to disruption of glucose metabolism, increased inflammation, and altered blood flow to the brain, to name just a few of its collateral damages. I would add that TV viewing often prompts viewers to stay up well beyond their healthy bedtime. And, we know sleep deprivation is not compatible with health aging.
A traditional warning issued to new retirees was once “Don’t let the old rocking chair get ya.” In fact, I wonder how many folks watching television even have or use wood rocking chairs anymore, which, if rocked, might qualify as a light exercise if the viewer made the effort to rock. Instead I suspect most television viewing is done cocooned in soft recliners or curled up on a couch.
I will admit that this recent paper merely supports a suspicion I have harbored for decades. Like many of you, I have wondered how our society got to the point where obesity is frequent enough to be labeled a disease, attention deficit diagnoses are becoming increasingly prevalent, and our life expectancy is shrinking. There are dozens of factors, but if I had to pick one, I would paraphrase James Carville’s advice to Bill Clinton: “It’s the television, stupid.”
At least a couple of notches above “Are you wearing your seatbelt?” It can start with a nonjudgmental question such as “What are your favorite television shows?” And then deftly move toward compiling a tally of how many hours the patient watches each day.
How you manage the situation from there is up to you and can be based on the patient’s complaints and problem list. You might suggest he or she start by eliminating 2 hours of viewing a day. Then ask if he or she thinks that new schedule is achievable. If they ask for alternatives, be ready with a list of light activities that they might be surprised are healthier than their current behavior. Follow up with another visit or a call to see how they are doing. It’s that important, and your call will underscore your concern.
Sedentism is a serious health problem in this country and our emphasis on encouraging vigorous exercise isn’t working. Selling a television diet will be a tough sell, but it needs to be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
As more and more of us begin to feel (or believe we are feeling) the symptoms of aging, our language has begun to incorporate new words and phrases such as “aging in place” or “healthy aging.” In fact, some scientists have created a diagnostic criteria to define “healthy aging.” If you have reached your 70th birthday without mental health issues, memory issues, physical impairments, or chronic disease, according to some researchers at T.H. Chan School of Public Health and Brigham and Women’s Hospital, you should receive a gold star for healthy aging.
I am now nearly a decade past that milestone and can’t remember where I’ve put my gold star, or even if I had ever received one. But, I get up each morning looking forward to another day of activity and feeling “pretty good.”
Healthy aging is not something you start doing when you turn 65. Aging is something that goes on from the moment you are born. For the first couple decades we call it “maturing.” If you have lived well, the odds are you will age well. And, for that reason we should take note of some recent work by Boston-based researchers.
Looking at recent data from 45,000 participants in the well-known Nurses Health Study, the investigators found that for every 2-hour increase in daily sedentary behavior, the participants cut their chances of healthy aging by 12%. On the other hand, for every 2 hours of light physical activity, they increased their odds of healthy aging by 6 %.
There are two important messages sitting just below the surface of these two observations. First, we continue to overemphasize the importance of “exercise” in our attempt to help our patients achieve wellness. The word “exercise” carries with it whole carousel full of baggage including “fitness programs,” gym memberships, pulse rate monitors, pain, sweat, and spandex, to name just a few. Exercise can conjure up bad memories of suiting up for phys ed class, group showers, and being picked last when teams were being chosen.
It turns out the we should simply be promoting activity, and light activity at that — vacuuming the living room, walking around the block, rearranging the books on your bedroom book shelf, making a pot of soup, doing the laundry. Just getting up off one’s behind and doing something instead of being a passive spectator.
This somewhat counterintuitive notion of the benefit of light activity is beginning to get more attention. Earlier this year, I reported on a study by Andre O. Abaje MD, MPH, in which he showed that light physical activity in children was superior to more vigorous activity in lowering lipids.
The more important message embedded in this paper based on the Nurses Health Study is that the researchers used television watching time as their proxy for sedentary behavior. The investigators chose TV viewing because it is ubiquitous and includes prolonged sitting. Being semi-reclined on the couch or in a lounger requires very little muscle activity, which is in turn linked to disruption of glucose metabolism, increased inflammation, and altered blood flow to the brain, to name just a few of its collateral damages. I would add that TV viewing often prompts viewers to stay up well beyond their healthy bedtime. And, we know sleep deprivation is not compatible with health aging.
A traditional warning issued to new retirees was once “Don’t let the old rocking chair get ya.” In fact, I wonder how many folks watching television even have or use wood rocking chairs anymore, which, if rocked, might qualify as a light exercise if the viewer made the effort to rock. Instead I suspect most television viewing is done cocooned in soft recliners or curled up on a couch.
I will admit that this recent paper merely supports a suspicion I have harbored for decades. Like many of you, I have wondered how our society got to the point where obesity is frequent enough to be labeled a disease, attention deficit diagnoses are becoming increasingly prevalent, and our life expectancy is shrinking. There are dozens of factors, but if I had to pick one, I would paraphrase James Carville’s advice to Bill Clinton: “It’s the television, stupid.”
At least a couple of notches above “Are you wearing your seatbelt?” It can start with a nonjudgmental question such as “What are your favorite television shows?” And then deftly move toward compiling a tally of how many hours the patient watches each day.
How you manage the situation from there is up to you and can be based on the patient’s complaints and problem list. You might suggest he or she start by eliminating 2 hours of viewing a day. Then ask if he or she thinks that new schedule is achievable. If they ask for alternatives, be ready with a list of light activities that they might be surprised are healthier than their current behavior. Follow up with another visit or a call to see how they are doing. It’s that important, and your call will underscore your concern.
Sedentism is a serious health problem in this country and our emphasis on encouraging vigorous exercise isn’t working. Selling a television diet will be a tough sell, but it needs to be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Giving Cash to Improve Health
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.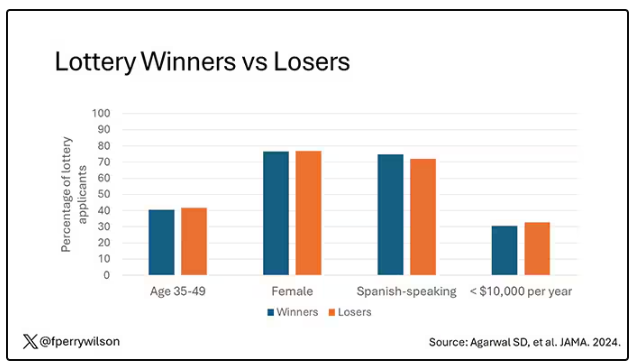
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.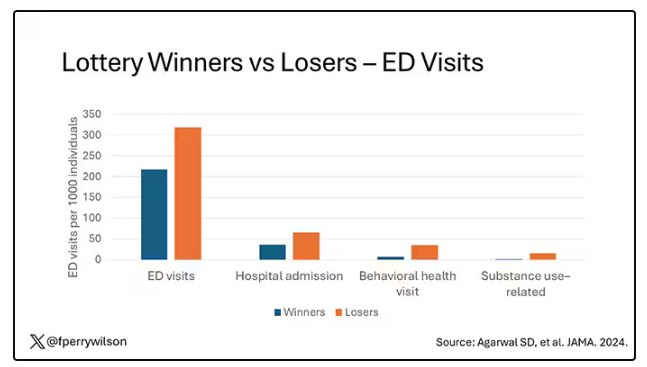
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.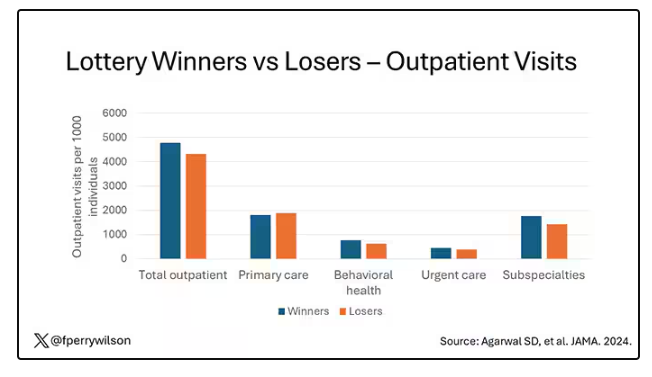
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.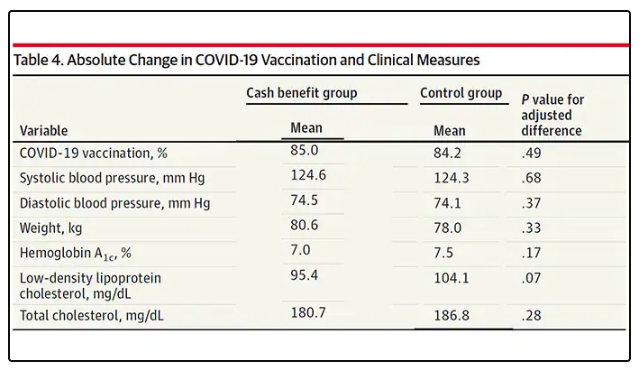
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions. 
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.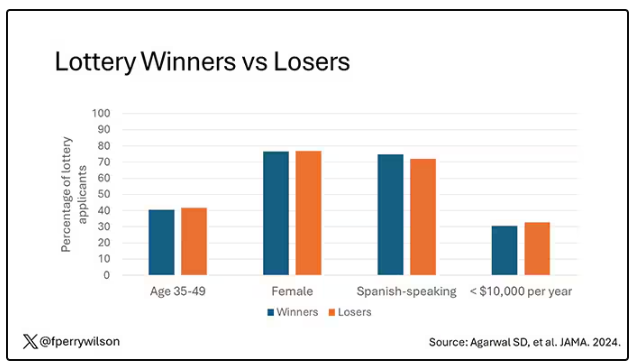
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.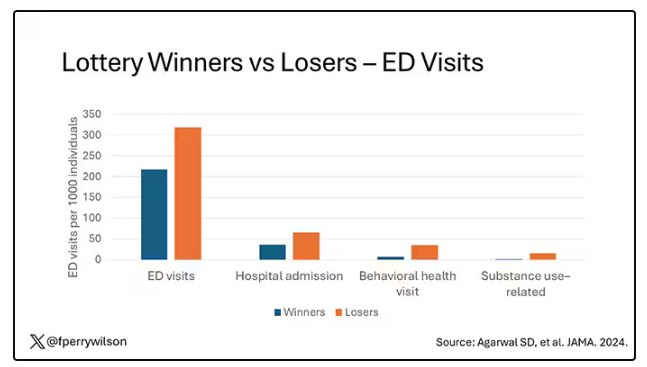
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.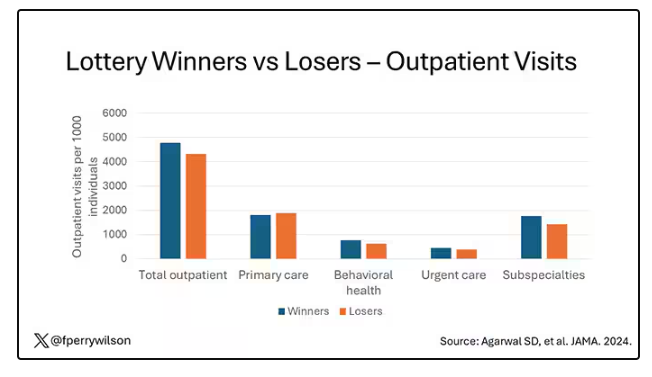
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.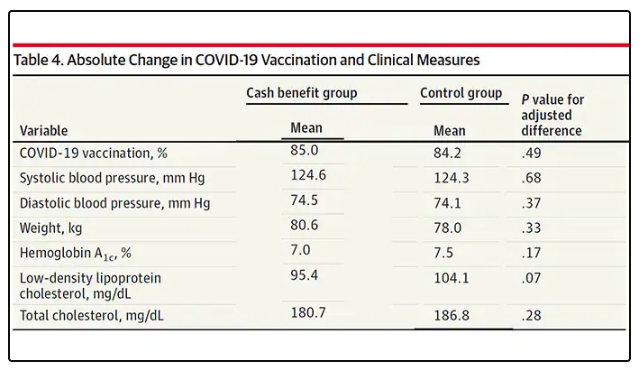
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions. 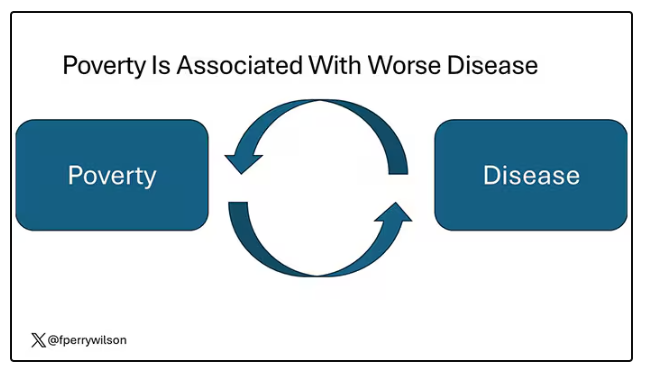
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It doesn’t really matter what disease you are looking at — cancer, heart disease, dementia, drug abuse, psychiatric disorders. In every case, poverty is associated with worse disease.
But the word “associated” is doing a lot of work there. Many of us feel that poverty itself is causally linked to worse disease outcomes through things like poor access to care and poor access to medicines.
And there is an argument that the arrow goes the other way; perhaps people with worse illness are more likely to be poor because, in this country at least, being sick is incredibly expensive.
Causality is what all medical research is fundamentally about. We want to know if A causes B, because if A causes B, then changing A changes B. If poverty causes bad health outcomes, then alleviating poverty should alleviate bad health outcomes.
But that’s a hard proposition to test. You can’t exactly randomize some people to get extra money and some not to, right? Actually, you can. And in Massachusetts, they did.
What happened in Chelsea, Massachusetts, wasn’t exactly a randomized trial of cash supplementation to avoid bad health outcomes. It was actually a government program instituted during the pandemic. Chelsea has a large immigrant population, many of whom are living in poverty. From April to August 2020, the city ran a food distribution program to aid those in need. But the decision was then made to convert the money spent on that program to cash distributions — free of obligations. Chelsea residents making less than 30% of the median income for the Boston metro area — around $30,000 per family — were invited to enter a lottery. Only one member of any given family could enter. If selected, an individual would receive $200 a month, or $300 for a family of two, or $400 for a family of three or more. These payments went on for about 9 months.
The key thing here is that not everyone won the lottery. The lottery picked winners randomly; 1746 individuals were selected to receive the benefits in the form of a reloadable gift card, and 1134 applied but did not receive any assistance.
This is a perfect natural experiment. As you can see here — and as expected, given that the lottery winners were chosen randomly — winners and losers were similar in terms of age, sex, race, language, income, and more.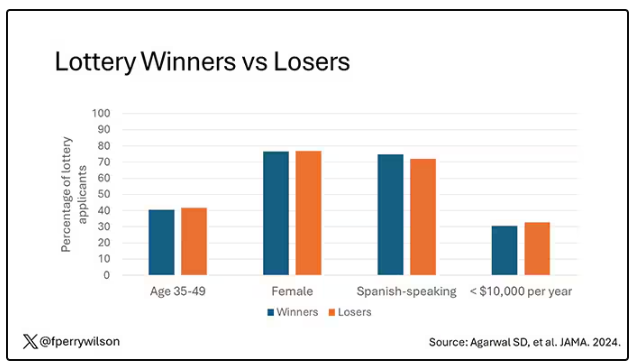
Researchers, led by Sumit Agarwal at the Brigham, leveraged that randomization to ask how these cash benefits would affect healthcare utilization. Their results appeared this week in JAMA.
I know what you’re thinking: Is $400 a month really enough to make a difference? Does $400 a month, less than $5000 a year, really fix poverty? We’ll get to that. But I will point out that the average family income of individuals in this study was about $1400 a month. An extra $400 might not change someone’s life, but it may really make a difference.
The primary outcome of this study was ED visits. There are a few ways this could go. Perhaps the money would lead to improved health and thus fewer ED visits. Or perhaps it would help people get transportation to primary care or other services that would offload the ED. Or maybe it would make things worse. Some folks have suggested that cash payments could increase the use of drugs and alcohol, and lead to more ED visits associated with the complications of using those substances.
Here are the actual data. Per 1000 individuals, there were 217 ED visits in the cash-benefit group, 318 in the no-benefit group. That was a statistically significant finding.
Breaking those ED visits down, you can see that fewer visits resulted in hospital admission, with fewer behavioral health–related visits and — a key finding — fewer visits for substance use disorder. This puts the lie to the idea that cash benefits increase drug use.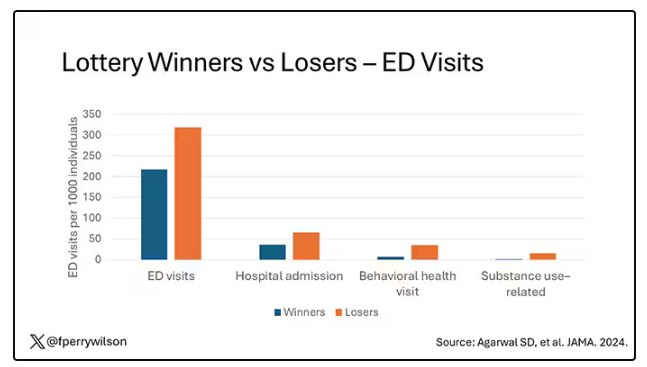
But the authors also looked at other causes of healthcare utilization. Outpatient visits were slightly higher in the cash-benefit group, driven largely by an increase in specialty care visits. The authors note that this is likely due to the fact that reaching a specialist often requires more travel, which can be costly. Indeed, this effect was most pronounced among the people living furthest from a specialty center.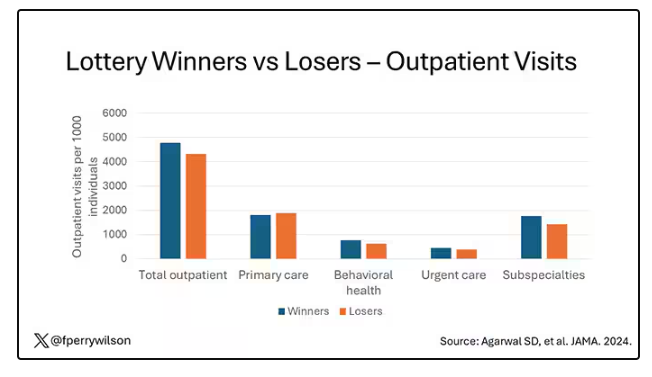
Outside of utilization, the researchers examined a variety of individual health markers — things like blood pressure — to see if the cash benefit had any effect. A bit of caution here because these data were available only among those who interacted with the healthcare system, which may bias the results a bit. Regardless, no major differences were seen in blood pressure, weight, hemoglobin A1c, cholesterol, or COVID vaccination.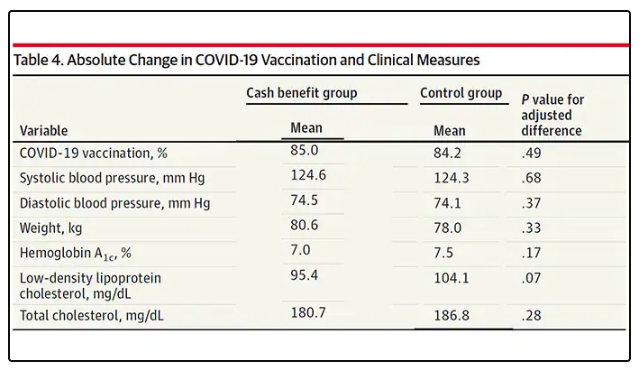
So, it seems that $400 a month doesn’t move the needle too much on risk factors for cardiovascular disease, but the effect on ED visits on their own is fairly impressive.
Is it worth it? The authors did their best to calculate the net effect of this program, accounting for the reduced ED visits and hospitalizations (that’s a big one), but also for the increased number of specialty visits. All told, the program saves about $450 per person in healthcare costs over 9 months. That’s about one seventh of the cost of the overall program.
But remember that they only looked at outcomes for the individual who got the gift cards; it’s likely that there were benefits to their family members as well. And, of course, programs like this can recoup costs indirectly though increases in economic activity, a phenomenon known as the multiplier effect.
I’m not here to tell you whether this program was a good idea; people tend to have quite strong feelings about this sort of thing. But I can tell you what it tells me about healthcare in America. It may not be surprising, but it confirms that access is far from fairly distributed.
I started this story asking about the arrow of causality between poverty and poor health. The truth is, you probably have causality in both directions. 
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Doctor on Death Row: Ahmad Reza Djalali Begins Hunger Strike
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Ahmad Reza Djalali, an Iranian-Swedish physician specializing in disaster medicine, has begun a hunger strike after being sentenced to death in 2017.
Last year, Iran set a grim record, leading the world in executions. The country carried out at least 853 executions, which accounted for three quarters of the officially recorded executions worldwide. The Iranian government uses the death penalty to intimidate political opponents, especially since the women’s uprising in 2022, and to exert pressure on Western states in diplomatic standoffs.
He emigrated to Sweden in 2009 and joined the Karolinska Institutet in Stockholm, Sweden. Over the years, he became one of Europe’s leading experts in disaster medicine. His work has been cited more than 700 times in medical literature, and he played a key role in establishing the emergency and disaster research center at the University of Piedmont.
In Italy, Denmark, and Sweden, Dr. Djalali helped hospitals and healthcare professionals in preparing for earthquakes, nuclear accidents, and terrorist attacks and designed several disaster medicine training programs.
‘Spreading Corruption’
Despite settling in Sweden with his family, Dr. Djalali never forgot his Iranian roots. His doctoral thesis was dedicated to the victims of the 2003 Bam earthquake in Iran, which killed 23,000 people. He expressed a desire to share his knowledge with his Iranian colleagues to help people. So when he was invited to participate in a 2016 conference at the University of Tehran, he accepted without hesitation.
Unfortunately, this decision had severe consequences. On April 25, 2016, as he was concluding his trip to Iran, the researcher was arrested by intelligence agents. After being held incommunicado for several days, he was officially accused of passing confidential information to Israeli intelligence services. According to his family, this accusation was baseless. They believed he was targeted for refusing to work for Iranian intelligence services in Europe.
On October 21, 2017, Dr. Djalali was sentenced to death for “spreading corruption on Earth,” a vague charge often used by Islamic courts against those who allegedly have challenged the regime. A few days later, a video of his “confessions” was broadcast on Iranian television. These confessions were coerced; Dr. Djalali later revealed that Iranian police had threatened to harm his mother in Iran and his family in Sweden.
Since then, Dr. Djalali and his loved ones have anxiously awaited the moment when the regime might carry out the sentence. Several times over the years, he has seemed on the verge of execution, only to receive a last-minute reprieve each time.
His imprisonment has taken a severe toll on his physical and mental health. He has reportedly lost 24 kg since his incarceration, and his family, who receive sporadic updates, suspect he has leukemia. Despite his deteriorating condition, the authorities have refused him access to a hematologist.
‘Forgotten’ in Exchange
The international medical community has rallied to secure Dr. Djalali’s release, but their efforts have so far been fruitless. The United Nations, the European Union, Amnesty International, several universities, and the World Medical Association have called for his release. In 2018, Sweden granted him citizenship in an attempt to increase pressure on Tehran, but Iranian law does not recognize dual citizenship.
On June 16, after nearly 7 years on death row, Dr. Djalali informed his family that he had begun a hunger strike. “It’s the only way to make my voice heard in the world,” he explained. “As a doctor, Ahmad Reza knows all too well that his fragile physical state makes a hunger strike potentially fatal, but he sees no other option. He suffers from cardiac arrhythmia, bradycardia, hypotension, chronic gastritis, anemia, and extreme weight loss following his two previous hunger strikes,” his wife told the press.
Aside from a potential (and unlikely) act of clemency by the Iranian authorities, Dr. Djalali’s best hope lies in a prisoner exchange. The Iranian government often imprisons foreign nationals to exchange them for Iranians detained in Western countries.
On June 15, Sweden agreed to release an Iranian dignitary serving a life sentence in exchange for the release of Swedish nationals detained in Iran. For a long time, Dr. Djalali’s family had hoped he would be included in this exchange.
However, to avoid jeopardizing the deal, the Swedish prime minister chose to accept the release of only two other Swedish nationals, leaving Dr. Djalali to his grim fate. “Mr Prime Minister, you have decided to abandon me at the enormous risk of being executed,” Dr. Djalali responded bitterly, knowing he could be hanged at any moment.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Disruptive Sleep Linked to Increased Susceptibility to COVID-19
Individuals with preexisting sleep disturbances including obstructive sleep apnea (OSA), insomnia, and abnormal sleep duration showed significantly increased vulnerability to COVID-19, as well as an increased risk for hospitalization, mortality, and long COVID, according to new data from more than 8 million individuals.
, wrote Jiawei Zhou, MD, of The First Hospital of China Medical University, Shenyang, China, and colleagues. Most previous research has focused on the impact of COVID-19 on sleep disturbances, not the impact of sleep disturbances on COVID-19, and most studies on the latter topic have focused only on OSA, the researchers wrote.
In a meta-analysis published in eClinicalMedicine, part of The Lancet Discovery Science, the researchers identified 48 observational studies published between October 27, 2023, and May 8, 2024, that involved COVID-19 and sleep disturbances including OSA, insomnia, abnormal sleep duration, and night shift work, among others. The study population included 8,664,026 adults.
The primary outcomes were COVID-19 susceptibility, hospitalization, mortality, and long COVID. Overall, the presence of preexisting sleep disturbances was associated with a significantly increased risk for each of these outcomes, with odds ratios (ORs) of 1.12, 1.25, 1.45, and 1.36, respectively.
In subgroup analyses, the association between preexisting sleep disturbances and greater susceptibility and hospitalization was higher in younger adults (younger than 60 years) than in older adults (aged 60 years and older), but the risk for death was lower in younger adults with sleep disturbances than in older adults with sleep disturbances (OR, 1.22 vs OR, 2.07, respectively). Men with sleep disturbances had a higher risk for COVID-19 mortality than women with sleep disturbances.
Preexisting sleep disturbances overall were significantly associated with long COVID and more so in a subgroup analysis of patients whose definition of long COVID was symptoms lasting 3 or more months vs those lasting 1 month (P = .029).
When the researchers broke down associations with COVID-19 outcomes and specific sleep disturbances, they found significant associations between OSA and all four primary outcomes. Abnormal sleep duration was associated with an increased risk for COVID-19 susceptibility, hospitalization, and long COVID. Night shift work was associated with an increased risk for COVID-19 susceptibility and hospitalization, and insomnia was associated with an increased risk for long COVID.
Although the exact mechanism behind the associations between preexisting sleep disturbances and COVID-19 outcomes is uncertain, persistent sleep deprivation could set the stage in various ways, including the promotion of elevated C-reactive protein and interleukin-6 levels, the researchers wrote.
“Overall, the compromised innate and adaptive immune functions combined with a persistent inflammatory state may explain the higher risk of susceptibility, severity, and longer recovery time observed in patients with sleep disturbances. Fortunately, early intervention for sleep disturbances could attenuate the adverse effects of COVID-19,” they noted in their discussion.
The findings were limited by several factors including the observational nature of the studies and the heterogeneity of outcomes, the researchers wrote. Looking ahead, randomized, controlled trials are needed to examine the effect of interventions for sleep disturbances in the prevention and course of COVID-19, they said.
However, the study is the first known to examine multiple types of sleep disturbances and their possible influences on the full clinical course of COVID-19 and support the need for early evaluation and intervention for individuals with sleep disturbances to reduce short-term and long-term effects of the disease, the researchers concluded.
Findings Reflect the Need to Address Sleep Issues Early
Although the results of the current study were not surprising, “it is always worth doing meta-analyses to see if there is a potential signal in the published data to suggest a need for a new study,” Arun Chatterjee, MD, professor of pulmonary, critical care, allergy, and immunologic diseases at Wake Forest University, Winston-Salem, North Carolina, said in an interview.
“Lack of sleep, whether acute active deprivation (zero sleep for one night) or subacute/chronic sleep debt, such as only 5 hours per night, has been demonstrated to affect lymphocyte proliferation, reduce immune globulin levels, increase inflammatory markers, shorten telomeres, and affect the immune system in various ways,” said Dr. Chatterjee, who was not involved in the meta-analysis.
The clinical takeaway from the current meta-analysis is that adequate sleep is important for various reasons, Dr. Chatterjee said. “Sleep disruption affects health across a spectrum of systems; adding an annual sleep wellness and screening event to healthcare visits is probably worth the investment,” he noted.
Much more is needed in the way of additional research, Dr. Chatterjee told this news organization. Notably, studies are needed to examine what sleep disruption does to immune status, as well as all other physiologic and mental health systems, he said.
The study was supported by the National Natural Science Foundation of China and the Key Laboratory of Respiratory Diseases of Liaoning Province. The researchers had no financial conflicts to disclose. Chatterjee had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Individuals with preexisting sleep disturbances including obstructive sleep apnea (OSA), insomnia, and abnormal sleep duration showed significantly increased vulnerability to COVID-19, as well as an increased risk for hospitalization, mortality, and long COVID, according to new data from more than 8 million individuals.
, wrote Jiawei Zhou, MD, of The First Hospital of China Medical University, Shenyang, China, and colleagues. Most previous research has focused on the impact of COVID-19 on sleep disturbances, not the impact of sleep disturbances on COVID-19, and most studies on the latter topic have focused only on OSA, the researchers wrote.
In a meta-analysis published in eClinicalMedicine, part of The Lancet Discovery Science, the researchers identified 48 observational studies published between October 27, 2023, and May 8, 2024, that involved COVID-19 and sleep disturbances including OSA, insomnia, abnormal sleep duration, and night shift work, among others. The study population included 8,664,026 adults.
The primary outcomes were COVID-19 susceptibility, hospitalization, mortality, and long COVID. Overall, the presence of preexisting sleep disturbances was associated with a significantly increased risk for each of these outcomes, with odds ratios (ORs) of 1.12, 1.25, 1.45, and 1.36, respectively.
In subgroup analyses, the association between preexisting sleep disturbances and greater susceptibility and hospitalization was higher in younger adults (younger than 60 years) than in older adults (aged 60 years and older), but the risk for death was lower in younger adults with sleep disturbances than in older adults with sleep disturbances (OR, 1.22 vs OR, 2.07, respectively). Men with sleep disturbances had a higher risk for COVID-19 mortality than women with sleep disturbances.
Preexisting sleep disturbances overall were significantly associated with long COVID and more so in a subgroup analysis of patients whose definition of long COVID was symptoms lasting 3 or more months vs those lasting 1 month (P = .029).
When the researchers broke down associations with COVID-19 outcomes and specific sleep disturbances, they found significant associations between OSA and all four primary outcomes. Abnormal sleep duration was associated with an increased risk for COVID-19 susceptibility, hospitalization, and long COVID. Night shift work was associated with an increased risk for COVID-19 susceptibility and hospitalization, and insomnia was associated with an increased risk for long COVID.
Although the exact mechanism behind the associations between preexisting sleep disturbances and COVID-19 outcomes is uncertain, persistent sleep deprivation could set the stage in various ways, including the promotion of elevated C-reactive protein and interleukin-6 levels, the researchers wrote.
“Overall, the compromised innate and adaptive immune functions combined with a persistent inflammatory state may explain the higher risk of susceptibility, severity, and longer recovery time observed in patients with sleep disturbances. Fortunately, early intervention for sleep disturbances could attenuate the adverse effects of COVID-19,” they noted in their discussion.
The findings were limited by several factors including the observational nature of the studies and the heterogeneity of outcomes, the researchers wrote. Looking ahead, randomized, controlled trials are needed to examine the effect of interventions for sleep disturbances in the prevention and course of COVID-19, they said.
However, the study is the first known to examine multiple types of sleep disturbances and their possible influences on the full clinical course of COVID-19 and support the need for early evaluation and intervention for individuals with sleep disturbances to reduce short-term and long-term effects of the disease, the researchers concluded.
Findings Reflect the Need to Address Sleep Issues Early
Although the results of the current study were not surprising, “it is always worth doing meta-analyses to see if there is a potential signal in the published data to suggest a need for a new study,” Arun Chatterjee, MD, professor of pulmonary, critical care, allergy, and immunologic diseases at Wake Forest University, Winston-Salem, North Carolina, said in an interview.
“Lack of sleep, whether acute active deprivation (zero sleep for one night) or subacute/chronic sleep debt, such as only 5 hours per night, has been demonstrated to affect lymphocyte proliferation, reduce immune globulin levels, increase inflammatory markers, shorten telomeres, and affect the immune system in various ways,” said Dr. Chatterjee, who was not involved in the meta-analysis.
The clinical takeaway from the current meta-analysis is that adequate sleep is important for various reasons, Dr. Chatterjee said. “Sleep disruption affects health across a spectrum of systems; adding an annual sleep wellness and screening event to healthcare visits is probably worth the investment,” he noted.
Much more is needed in the way of additional research, Dr. Chatterjee told this news organization. Notably, studies are needed to examine what sleep disruption does to immune status, as well as all other physiologic and mental health systems, he said.
The study was supported by the National Natural Science Foundation of China and the Key Laboratory of Respiratory Diseases of Liaoning Province. The researchers had no financial conflicts to disclose. Chatterjee had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Individuals with preexisting sleep disturbances including obstructive sleep apnea (OSA), insomnia, and abnormal sleep duration showed significantly increased vulnerability to COVID-19, as well as an increased risk for hospitalization, mortality, and long COVID, according to new data from more than 8 million individuals.
, wrote Jiawei Zhou, MD, of The First Hospital of China Medical University, Shenyang, China, and colleagues. Most previous research has focused on the impact of COVID-19 on sleep disturbances, not the impact of sleep disturbances on COVID-19, and most studies on the latter topic have focused only on OSA, the researchers wrote.
In a meta-analysis published in eClinicalMedicine, part of The Lancet Discovery Science, the researchers identified 48 observational studies published between October 27, 2023, and May 8, 2024, that involved COVID-19 and sleep disturbances including OSA, insomnia, abnormal sleep duration, and night shift work, among others. The study population included 8,664,026 adults.
The primary outcomes were COVID-19 susceptibility, hospitalization, mortality, and long COVID. Overall, the presence of preexisting sleep disturbances was associated with a significantly increased risk for each of these outcomes, with odds ratios (ORs) of 1.12, 1.25, 1.45, and 1.36, respectively.
In subgroup analyses, the association between preexisting sleep disturbances and greater susceptibility and hospitalization was higher in younger adults (younger than 60 years) than in older adults (aged 60 years and older), but the risk for death was lower in younger adults with sleep disturbances than in older adults with sleep disturbances (OR, 1.22 vs OR, 2.07, respectively). Men with sleep disturbances had a higher risk for COVID-19 mortality than women with sleep disturbances.
Preexisting sleep disturbances overall were significantly associated with long COVID and more so in a subgroup analysis of patients whose definition of long COVID was symptoms lasting 3 or more months vs those lasting 1 month (P = .029).
When the researchers broke down associations with COVID-19 outcomes and specific sleep disturbances, they found significant associations between OSA and all four primary outcomes. Abnormal sleep duration was associated with an increased risk for COVID-19 susceptibility, hospitalization, and long COVID. Night shift work was associated with an increased risk for COVID-19 susceptibility and hospitalization, and insomnia was associated with an increased risk for long COVID.
Although the exact mechanism behind the associations between preexisting sleep disturbances and COVID-19 outcomes is uncertain, persistent sleep deprivation could set the stage in various ways, including the promotion of elevated C-reactive protein and interleukin-6 levels, the researchers wrote.
“Overall, the compromised innate and adaptive immune functions combined with a persistent inflammatory state may explain the higher risk of susceptibility, severity, and longer recovery time observed in patients with sleep disturbances. Fortunately, early intervention for sleep disturbances could attenuate the adverse effects of COVID-19,” they noted in their discussion.
The findings were limited by several factors including the observational nature of the studies and the heterogeneity of outcomes, the researchers wrote. Looking ahead, randomized, controlled trials are needed to examine the effect of interventions for sleep disturbances in the prevention and course of COVID-19, they said.
However, the study is the first known to examine multiple types of sleep disturbances and their possible influences on the full clinical course of COVID-19 and support the need for early evaluation and intervention for individuals with sleep disturbances to reduce short-term and long-term effects of the disease, the researchers concluded.
Findings Reflect the Need to Address Sleep Issues Early
Although the results of the current study were not surprising, “it is always worth doing meta-analyses to see if there is a potential signal in the published data to suggest a need for a new study,” Arun Chatterjee, MD, professor of pulmonary, critical care, allergy, and immunologic diseases at Wake Forest University, Winston-Salem, North Carolina, said in an interview.
“Lack of sleep, whether acute active deprivation (zero sleep for one night) or subacute/chronic sleep debt, such as only 5 hours per night, has been demonstrated to affect lymphocyte proliferation, reduce immune globulin levels, increase inflammatory markers, shorten telomeres, and affect the immune system in various ways,” said Dr. Chatterjee, who was not involved in the meta-analysis.
The clinical takeaway from the current meta-analysis is that adequate sleep is important for various reasons, Dr. Chatterjee said. “Sleep disruption affects health across a spectrum of systems; adding an annual sleep wellness and screening event to healthcare visits is probably worth the investment,” he noted.
Much more is needed in the way of additional research, Dr. Chatterjee told this news organization. Notably, studies are needed to examine what sleep disruption does to immune status, as well as all other physiologic and mental health systems, he said.
The study was supported by the National Natural Science Foundation of China and the Key Laboratory of Respiratory Diseases of Liaoning Province. The researchers had no financial conflicts to disclose. Chatterjee had no financial conflicts to disclose.
A version of this article appeared on Medscape.com.
Managing Atopic Dermatitis in Older Adults: A Common, Unique Challenge
WASHINGTON, DC — Jonathan I. Silverberg, MD, PhD, MPH, said at the ElderDerm Conference on dermatology in the older patient hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC.
“I walked out of residency under the impression that if it didn’t start in the first year or two of life, it’s not AD,” said Dr. Silverberg, professor of dermatology and director of clinical research at George Washington University. “The numbers tell us a very different story.”
The prevalence of AD in the United States fluctuates between 6% and 8% through adulthood, including age categories up to 81-85 years, according to 2012 National Health Interview Survey data. And while persistence of childhood-onset AD is common, a systematic review and meta-analysis published in 2018 concluded that one in four adults with AD report adult-onset disease.
The investigators, including Dr. Silverberg, identified 25 observational studies — studies conducted across 16 countries and published during 1956-2017 — that included an analysis of age of onset beyond 10 years of age, and other inclusion criteria. Of the 25 studies, 17 reported age of onset after 16 years of age and had sufficient data for the meta-analysis. Using random-effects weighting, the investigators found a pooled proportion of adult-onset AD of 26.1% (95% CI, 16.5%-37.2%).
The research demonstrates that “the age of onset is distributed well throughout the lifespan,” Dr. Silverberg said, with the data “indicating there are many elderly-onset cases of true AD as well.” (Thirteen of the studies analyzed an age of onset from age ≥ 65, and several looked beyond age 80).
A 2021 study of a primary care database in the United Kingdom of 3.85 million children and adults found a “fascinating” bimodal distribution of incidence across the lifespan, with peaks in both infancy and older adulthood, he said. Incidence in adulthood was relatively stable from ages 18-49 years, after which, “into the 50s, 60s and beyond, you started to see a steady climb again.”
Also intriguing, Dr. Silverberg continued, are findings from a study of outpatient healthcare utilization for AD in which he and his coinvestigator analyzed data from the National Ambulatory Medical Care Survey (NAMCS). In the article, published in 2023 covering data from the 1993-2015 NAMCS, they reported that AD visits were more common among children aged 0-4 years (32.0%) and 5-9 years of age (10.6%), then decreased in adolescents aged 10-19 years (11.6%), remained fairly steady in patients aged 20-89 years (1.0%-4.7%), and increased in patients aged > 90 years (20.7%).
“The peak usage for dermatologists, primary care physicians, etc., is happening in the first few years of life, partially because that’s when the disease is more common and more severe but also partially because that’s when parents and caregivers are first learning [about] the disease and trying to understand how to gain control,” Dr. Silverberg said at the meeting, presenting data from an expanded, unpublished analysis of NAMCS data showing these same outpatient utilization patterns.
“It’s fascinating — there’s a much greater utilization in the elderly population. Why? The short answer is, we don’t know,” he said.
Risk Factors, Immune Differences
People with adult-onset AD were more likely to be women, smokers in adulthood, and have a lower childhood socioeconomic status than those whose AD started in childhood in a longitudinal study of two large birth cohorts from the United Kingdom , Dr. Silverberg pointed out.
Patients with childhood-onset AD, meanwhile, were more likely to have asthma, allergen-specific immunoglobulin E (IgE), and known genetic polymorphisms previously associated with AD. (Each cohort — the 1958 British Cohort Study and the 1970 British Cohort Study — had more than 17,000 participants who were followed from birth through middle age.)
Data is limited, but “mechanistically,” AD in much older adults appears to have a unique serum cytokine pattern, Dr. Silverberg said. He pointed to a cross-sectional study in China of 1312 children and adults with AD in which researchers analyzed clinical features, serum samples, and skin biopsy samples.
Adults aged > 60 years showed more lesions on the trunk and extensor sites of the extremities and lower levels of serum IgE and peripheral eosinophil counts than those in younger age groups. And “interestingly,” compared with healthy controls, older patients with AD had “higher levels of serum expression of a variety of cytokines, including IL [interleukin]-4 but also high TARC levels ... and a variety of cytokines related to the Th17, TH1 axes, etc.,” he said.
“So, we’re seeing a fascinating new profile that may be a little different than younger-onset cases,” he said, noting that TARC (thymus and activation-regulated chemokine) is regarded as a “decent biomarker” for AD.
In addition to higher levels of IL-4 and TARC, the study investigators reported significantly higher levels of IL-17A, IL-6, IL-22, IL-33, and thymic stromal lymphopoietin in older patients, compared with healthy controls.
Research also suggests that air pollution may play a role in the onset of AD in older age, Dr. Silverberg said, referencing a 2023 study that explored the association of air pollution and genetic risk with the onset of AD after age 50. The study analyzed 337,910 participants from the UK Biobank, with a median 12-year follow-up. Genetic risks were assessed as low, intermediate, and high, based on tertiles of polygenic risk scores. Exposure to various air pollutants was assessed using weighted quantile sum and also categorized into tertiles.
The incidence of older adult-onset AD was associated with medium and high air pollution compared with low air pollution, with hazard ratios (HRs) of 1.182 (P = .003) and 1.359 (P < .001), respectively. And “to a lesser extent,” Dr. Silverberg said, incidence was associated with medium and high genetic susceptibility, with HRs of 1.065 (P = .249) and 1.153 (P = .008).
The researchers calculated a greater population-attributable fraction of air pollution (15.5%) than genetic risk (6.4%). “This means that yes, genetics can contribute even to later-onset disease ... but environment may play an even more important role,” Dr. Silverberg said.
In the Clinic
In all patients, and especially in older adults, sleep disturbance associated with AD is a consideration for care. Data collected at the eczema clinic of Northwestern University, Chicago, Illinois, between 2014 and 2019 through previsit, self-administered questionnaires show that patients ≥ 65 years of age have more profound sleep disturbance (especially trouble staying asleep) than patients aged 18-64 years, despite having similar AD severity, said Dr. Silverberg, a coinvestigator of the study.
Older age was associated with having an increased number of nights of sleep disturbance (3-7 nights in the previous week) because of eczema (adjusted odds ratio [aOR], 2.14; 95% CI, 1.16-3.92). It was also associated with itching-attributed delays in falling asleep and nighttime awakenings in the prior 2 weeks (aOR, 1.88; 95% CI, 1.05-3.39).
“The aging population has dysregulated sleep patterns and altered circadian rhythms, so some of this is just natural predisposition,” Dr. Silverberg said. “But it’s amplified [with AD and itching], and it becomes a big clinical problem when we get into treatment because it’s our natural inclination to prescribe antihistamines for their sedative properties.”
Antihistamines can cause more profound sedation, more forgetfulness, and more anticholinergic side effects, he said, noting that “there’s some evidence that high-dose antihistamines may exacerbate dementia.”
Medication side effects and medication interactions, comorbidities, and decreased renal and hepatic clearance all can complicate treatment of AD in older adults. So can mobility, the extent of social/caregiving support, and other aspects of aging. For example, “I’m a big fan of ‘soak and smears’ ... but you have to ask, can you get out of a bathtub safely?” Dr. Silverberg said. “And you have to ask, can you reach the areas you need to [in order] to apply topicals?”
With oral Janus kinase inhibitors and other systemic medications, as with other drugs, “our older population is the most vulnerable from a safety perspective,” he said. A recently published post hoc analysis of four randomized trials of dupilumab in adults ≥ 60 years of age with moderate to severe AD demonstrated efficacy comparable with that in younger patients and “a really clean safety profile,” said Dr. Silverberg, the lead author. “We really need more of these types of post hocs to have some relative contextualization” for older adults.
Dr. Silverberg reported being a speaker for AbbVie, Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi-Genzyme; a consultant and/or advisory board member for Regeneron, Sanofi-Genzyme, and other companies; and an investigator for several companies.
A version of this article first appeared on Medscape.com.
WASHINGTON, DC — Jonathan I. Silverberg, MD, PhD, MPH, said at the ElderDerm Conference on dermatology in the older patient hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC.
“I walked out of residency under the impression that if it didn’t start in the first year or two of life, it’s not AD,” said Dr. Silverberg, professor of dermatology and director of clinical research at George Washington University. “The numbers tell us a very different story.”
The prevalence of AD in the United States fluctuates between 6% and 8% through adulthood, including age categories up to 81-85 years, according to 2012 National Health Interview Survey data. And while persistence of childhood-onset AD is common, a systematic review and meta-analysis published in 2018 concluded that one in four adults with AD report adult-onset disease.
The investigators, including Dr. Silverberg, identified 25 observational studies — studies conducted across 16 countries and published during 1956-2017 — that included an analysis of age of onset beyond 10 years of age, and other inclusion criteria. Of the 25 studies, 17 reported age of onset after 16 years of age and had sufficient data for the meta-analysis. Using random-effects weighting, the investigators found a pooled proportion of adult-onset AD of 26.1% (95% CI, 16.5%-37.2%).
The research demonstrates that “the age of onset is distributed well throughout the lifespan,” Dr. Silverberg said, with the data “indicating there are many elderly-onset cases of true AD as well.” (Thirteen of the studies analyzed an age of onset from age ≥ 65, and several looked beyond age 80).
A 2021 study of a primary care database in the United Kingdom of 3.85 million children and adults found a “fascinating” bimodal distribution of incidence across the lifespan, with peaks in both infancy and older adulthood, he said. Incidence in adulthood was relatively stable from ages 18-49 years, after which, “into the 50s, 60s and beyond, you started to see a steady climb again.”
Also intriguing, Dr. Silverberg continued, are findings from a study of outpatient healthcare utilization for AD in which he and his coinvestigator analyzed data from the National Ambulatory Medical Care Survey (NAMCS). In the article, published in 2023 covering data from the 1993-2015 NAMCS, they reported that AD visits were more common among children aged 0-4 years (32.0%) and 5-9 years of age (10.6%), then decreased in adolescents aged 10-19 years (11.6%), remained fairly steady in patients aged 20-89 years (1.0%-4.7%), and increased in patients aged > 90 years (20.7%).
“The peak usage for dermatologists, primary care physicians, etc., is happening in the first few years of life, partially because that’s when the disease is more common and more severe but also partially because that’s when parents and caregivers are first learning [about] the disease and trying to understand how to gain control,” Dr. Silverberg said at the meeting, presenting data from an expanded, unpublished analysis of NAMCS data showing these same outpatient utilization patterns.
“It’s fascinating — there’s a much greater utilization in the elderly population. Why? The short answer is, we don’t know,” he said.
Risk Factors, Immune Differences
People with adult-onset AD were more likely to be women, smokers in adulthood, and have a lower childhood socioeconomic status than those whose AD started in childhood in a longitudinal study of two large birth cohorts from the United Kingdom , Dr. Silverberg pointed out.
Patients with childhood-onset AD, meanwhile, were more likely to have asthma, allergen-specific immunoglobulin E (IgE), and known genetic polymorphisms previously associated with AD. (Each cohort — the 1958 British Cohort Study and the 1970 British Cohort Study — had more than 17,000 participants who were followed from birth through middle age.)
Data is limited, but “mechanistically,” AD in much older adults appears to have a unique serum cytokine pattern, Dr. Silverberg said. He pointed to a cross-sectional study in China of 1312 children and adults with AD in which researchers analyzed clinical features, serum samples, and skin biopsy samples.
Adults aged > 60 years showed more lesions on the trunk and extensor sites of the extremities and lower levels of serum IgE and peripheral eosinophil counts than those in younger age groups. And “interestingly,” compared with healthy controls, older patients with AD had “higher levels of serum expression of a variety of cytokines, including IL [interleukin]-4 but also high TARC levels ... and a variety of cytokines related to the Th17, TH1 axes, etc.,” he said.
“So, we’re seeing a fascinating new profile that may be a little different than younger-onset cases,” he said, noting that TARC (thymus and activation-regulated chemokine) is regarded as a “decent biomarker” for AD.
In addition to higher levels of IL-4 and TARC, the study investigators reported significantly higher levels of IL-17A, IL-6, IL-22, IL-33, and thymic stromal lymphopoietin in older patients, compared with healthy controls.
Research also suggests that air pollution may play a role in the onset of AD in older age, Dr. Silverberg said, referencing a 2023 study that explored the association of air pollution and genetic risk with the onset of AD after age 50. The study analyzed 337,910 participants from the UK Biobank, with a median 12-year follow-up. Genetic risks were assessed as low, intermediate, and high, based on tertiles of polygenic risk scores. Exposure to various air pollutants was assessed using weighted quantile sum and also categorized into tertiles.
The incidence of older adult-onset AD was associated with medium and high air pollution compared with low air pollution, with hazard ratios (HRs) of 1.182 (P = .003) and 1.359 (P < .001), respectively. And “to a lesser extent,” Dr. Silverberg said, incidence was associated with medium and high genetic susceptibility, with HRs of 1.065 (P = .249) and 1.153 (P = .008).
The researchers calculated a greater population-attributable fraction of air pollution (15.5%) than genetic risk (6.4%). “This means that yes, genetics can contribute even to later-onset disease ... but environment may play an even more important role,” Dr. Silverberg said.
In the Clinic
In all patients, and especially in older adults, sleep disturbance associated with AD is a consideration for care. Data collected at the eczema clinic of Northwestern University, Chicago, Illinois, between 2014 and 2019 through previsit, self-administered questionnaires show that patients ≥ 65 years of age have more profound sleep disturbance (especially trouble staying asleep) than patients aged 18-64 years, despite having similar AD severity, said Dr. Silverberg, a coinvestigator of the study.
Older age was associated with having an increased number of nights of sleep disturbance (3-7 nights in the previous week) because of eczema (adjusted odds ratio [aOR], 2.14; 95% CI, 1.16-3.92). It was also associated with itching-attributed delays in falling asleep and nighttime awakenings in the prior 2 weeks (aOR, 1.88; 95% CI, 1.05-3.39).
“The aging population has dysregulated sleep patterns and altered circadian rhythms, so some of this is just natural predisposition,” Dr. Silverberg said. “But it’s amplified [with AD and itching], and it becomes a big clinical problem when we get into treatment because it’s our natural inclination to prescribe antihistamines for their sedative properties.”
Antihistamines can cause more profound sedation, more forgetfulness, and more anticholinergic side effects, he said, noting that “there’s some evidence that high-dose antihistamines may exacerbate dementia.”
Medication side effects and medication interactions, comorbidities, and decreased renal and hepatic clearance all can complicate treatment of AD in older adults. So can mobility, the extent of social/caregiving support, and other aspects of aging. For example, “I’m a big fan of ‘soak and smears’ ... but you have to ask, can you get out of a bathtub safely?” Dr. Silverberg said. “And you have to ask, can you reach the areas you need to [in order] to apply topicals?”
With oral Janus kinase inhibitors and other systemic medications, as with other drugs, “our older population is the most vulnerable from a safety perspective,” he said. A recently published post hoc analysis of four randomized trials of dupilumab in adults ≥ 60 years of age with moderate to severe AD demonstrated efficacy comparable with that in younger patients and “a really clean safety profile,” said Dr. Silverberg, the lead author. “We really need more of these types of post hocs to have some relative contextualization” for older adults.
Dr. Silverberg reported being a speaker for AbbVie, Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi-Genzyme; a consultant and/or advisory board member for Regeneron, Sanofi-Genzyme, and other companies; and an investigator for several companies.
A version of this article first appeared on Medscape.com.
WASHINGTON, DC — Jonathan I. Silverberg, MD, PhD, MPH, said at the ElderDerm Conference on dermatology in the older patient hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC.
“I walked out of residency under the impression that if it didn’t start in the first year or two of life, it’s not AD,” said Dr. Silverberg, professor of dermatology and director of clinical research at George Washington University. “The numbers tell us a very different story.”
The prevalence of AD in the United States fluctuates between 6% and 8% through adulthood, including age categories up to 81-85 years, according to 2012 National Health Interview Survey data. And while persistence of childhood-onset AD is common, a systematic review and meta-analysis published in 2018 concluded that one in four adults with AD report adult-onset disease.
The investigators, including Dr. Silverberg, identified 25 observational studies — studies conducted across 16 countries and published during 1956-2017 — that included an analysis of age of onset beyond 10 years of age, and other inclusion criteria. Of the 25 studies, 17 reported age of onset after 16 years of age and had sufficient data for the meta-analysis. Using random-effects weighting, the investigators found a pooled proportion of adult-onset AD of 26.1% (95% CI, 16.5%-37.2%).
The research demonstrates that “the age of onset is distributed well throughout the lifespan,” Dr. Silverberg said, with the data “indicating there are many elderly-onset cases of true AD as well.” (Thirteen of the studies analyzed an age of onset from age ≥ 65, and several looked beyond age 80).
A 2021 study of a primary care database in the United Kingdom of 3.85 million children and adults found a “fascinating” bimodal distribution of incidence across the lifespan, with peaks in both infancy and older adulthood, he said. Incidence in adulthood was relatively stable from ages 18-49 years, after which, “into the 50s, 60s and beyond, you started to see a steady climb again.”
Also intriguing, Dr. Silverberg continued, are findings from a study of outpatient healthcare utilization for AD in which he and his coinvestigator analyzed data from the National Ambulatory Medical Care Survey (NAMCS). In the article, published in 2023 covering data from the 1993-2015 NAMCS, they reported that AD visits were more common among children aged 0-4 years (32.0%) and 5-9 years of age (10.6%), then decreased in adolescents aged 10-19 years (11.6%), remained fairly steady in patients aged 20-89 years (1.0%-4.7%), and increased in patients aged > 90 years (20.7%).
“The peak usage for dermatologists, primary care physicians, etc., is happening in the first few years of life, partially because that’s when the disease is more common and more severe but also partially because that’s when parents and caregivers are first learning [about] the disease and trying to understand how to gain control,” Dr. Silverberg said at the meeting, presenting data from an expanded, unpublished analysis of NAMCS data showing these same outpatient utilization patterns.
“It’s fascinating — there’s a much greater utilization in the elderly population. Why? The short answer is, we don’t know,” he said.
Risk Factors, Immune Differences
People with adult-onset AD were more likely to be women, smokers in adulthood, and have a lower childhood socioeconomic status than those whose AD started in childhood in a longitudinal study of two large birth cohorts from the United Kingdom , Dr. Silverberg pointed out.
Patients with childhood-onset AD, meanwhile, were more likely to have asthma, allergen-specific immunoglobulin E (IgE), and known genetic polymorphisms previously associated with AD. (Each cohort — the 1958 British Cohort Study and the 1970 British Cohort Study — had more than 17,000 participants who were followed from birth through middle age.)
Data is limited, but “mechanistically,” AD in much older adults appears to have a unique serum cytokine pattern, Dr. Silverberg said. He pointed to a cross-sectional study in China of 1312 children and adults with AD in which researchers analyzed clinical features, serum samples, and skin biopsy samples.
Adults aged > 60 years showed more lesions on the trunk and extensor sites of the extremities and lower levels of serum IgE and peripheral eosinophil counts than those in younger age groups. And “interestingly,” compared with healthy controls, older patients with AD had “higher levels of serum expression of a variety of cytokines, including IL [interleukin]-4 but also high TARC levels ... and a variety of cytokines related to the Th17, TH1 axes, etc.,” he said.
“So, we’re seeing a fascinating new profile that may be a little different than younger-onset cases,” he said, noting that TARC (thymus and activation-regulated chemokine) is regarded as a “decent biomarker” for AD.
In addition to higher levels of IL-4 and TARC, the study investigators reported significantly higher levels of IL-17A, IL-6, IL-22, IL-33, and thymic stromal lymphopoietin in older patients, compared with healthy controls.
Research also suggests that air pollution may play a role in the onset of AD in older age, Dr. Silverberg said, referencing a 2023 study that explored the association of air pollution and genetic risk with the onset of AD after age 50. The study analyzed 337,910 participants from the UK Biobank, with a median 12-year follow-up. Genetic risks were assessed as low, intermediate, and high, based on tertiles of polygenic risk scores. Exposure to various air pollutants was assessed using weighted quantile sum and also categorized into tertiles.
The incidence of older adult-onset AD was associated with medium and high air pollution compared with low air pollution, with hazard ratios (HRs) of 1.182 (P = .003) and 1.359 (P < .001), respectively. And “to a lesser extent,” Dr. Silverberg said, incidence was associated with medium and high genetic susceptibility, with HRs of 1.065 (P = .249) and 1.153 (P = .008).
The researchers calculated a greater population-attributable fraction of air pollution (15.5%) than genetic risk (6.4%). “This means that yes, genetics can contribute even to later-onset disease ... but environment may play an even more important role,” Dr. Silverberg said.
In the Clinic
In all patients, and especially in older adults, sleep disturbance associated with AD is a consideration for care. Data collected at the eczema clinic of Northwestern University, Chicago, Illinois, between 2014 and 2019 through previsit, self-administered questionnaires show that patients ≥ 65 years of age have more profound sleep disturbance (especially trouble staying asleep) than patients aged 18-64 years, despite having similar AD severity, said Dr. Silverberg, a coinvestigator of the study.
Older age was associated with having an increased number of nights of sleep disturbance (3-7 nights in the previous week) because of eczema (adjusted odds ratio [aOR], 2.14; 95% CI, 1.16-3.92). It was also associated with itching-attributed delays in falling asleep and nighttime awakenings in the prior 2 weeks (aOR, 1.88; 95% CI, 1.05-3.39).
“The aging population has dysregulated sleep patterns and altered circadian rhythms, so some of this is just natural predisposition,” Dr. Silverberg said. “But it’s amplified [with AD and itching], and it becomes a big clinical problem when we get into treatment because it’s our natural inclination to prescribe antihistamines for their sedative properties.”
Antihistamines can cause more profound sedation, more forgetfulness, and more anticholinergic side effects, he said, noting that “there’s some evidence that high-dose antihistamines may exacerbate dementia.”
Medication side effects and medication interactions, comorbidities, and decreased renal and hepatic clearance all can complicate treatment of AD in older adults. So can mobility, the extent of social/caregiving support, and other aspects of aging. For example, “I’m a big fan of ‘soak and smears’ ... but you have to ask, can you get out of a bathtub safely?” Dr. Silverberg said. “And you have to ask, can you reach the areas you need to [in order] to apply topicals?”
With oral Janus kinase inhibitors and other systemic medications, as with other drugs, “our older population is the most vulnerable from a safety perspective,” he said. A recently published post hoc analysis of four randomized trials of dupilumab in adults ≥ 60 years of age with moderate to severe AD demonstrated efficacy comparable with that in younger patients and “a really clean safety profile,” said Dr. Silverberg, the lead author. “We really need more of these types of post hocs to have some relative contextualization” for older adults.
Dr. Silverberg reported being a speaker for AbbVie, Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi-Genzyme; a consultant and/or advisory board member for Regeneron, Sanofi-Genzyme, and other companies; and an investigator for several companies.
A version of this article first appeared on Medscape.com.
FROM ELDERDERM 2024
Treatable Condition Misdiagnosed as Dementia in Almost 13% of Cases
, one of the main causes of the condition, new research suggests.
The study of more than 68,000 individuals in the general population diagnosed with dementia between 2009 and 2019 found that almost 13% had FIB-4 scores indicative of cirrhosis and potential hepatic encephalopathy.
The findings, recently published online in The American Journal of Medicine, corroborate and extend the researchers’ previous work, which showed that about 10% of US veterans with a dementia diagnosis may in fact have hepatic encephalopathy.
“We need to increase awareness that cirrhosis and related brain complications are common, silent, but treatable when found,” said corresponding author Jasmohan Bajaj, MD, of Virginia Commonwealth University and Richmond VA Medical Center, Richmond, Virginia. “Moreover, these are being increasingly diagnosed in older individuals.”
“Cirrhosis can also predispose patients to liver cancer and other complications, so diagnosing it in all patients is important, regardless of the hepatic encephalopathy-dementia connection,” he said.
FIB-4 Is Key
Dr. Bajaj and colleagues analyzed data from 72 healthcare centers on 68,807 nonveteran patients diagnosed with dementia at two or more physician visits between 2009 and 2019. Patients had no prior cirrhosis diagnosis, the mean age was 73 years, 44.7% were men, and 78% were White.
The team measured the prevalence of two high FIB-4 scores (> 2.67 and > 3.25), selected for their strong predictive value for advanced cirrhosis. Researchers also examined associations between high scores and multiple comorbidities and demographic factors.
Alanine aminotransferase (ALT), aspartate aminotransferase (AST), and platelet labs were collected up to 2 years after the index dementia diagnosis because they are used to calculate FIB-4.
The mean FIB-4 score was 1.78, mean ALT was 23.72 U/L, mean AST was 27.42 U/L, and mean platelets were 243.51 × 109/µL.
A total of 8683 participants (12.8%) had a FIB-4 score greater than 2.67 and 5185 (7.6%) had a score greater than 3.25.
In multivariable logistic regression models, FIB-4 greater than 3.25 was associated with viral hepatitis (odds ratio [OR], 2.23), congestive heart failure (OR,1.73), HIV (OR, 1.72), male gender (OR, 1.42), alcohol use disorder (OR, 1.39), and chronic kidney disease (OR, 1.38).
FIB-4 greater than 3.25 was inversely associated with White race (OR, 0.76) and diabetes (OR, 0.82).
The associations were similar when using a threshold score of greater than 2.67.
“With the aging population, including those with cirrhosis, the potential for overlap between hepatic encephalopathy and dementia has risen and should be considered in the differential diagnosis,” the authors wrote. “Undiagnosed cirrhosis and potential hepatic encephalopathy can be a treatable cause of or contributor towards cognitive impairment in patients diagnosed with dementia.”
Providers should use the FIB-4 index as a screening tool to detect cirrhosis in patients with dementia, they concluded.
The team’s next steps will include investigating barriers to the use of FIB-4 among practitioners, Dr. Bajaj said.
Incorporating use of the FIB-4 index into screening guidelines “with input from all stakeholders, including geriatricians, primary care providers, and neurologists … would greatly expand the diagnosis of cirrhosis and potentially hepatic encephalopathy in dementia patients,” Dr. Bajaj said.
The study had a few limitations, including the selected centers in the cohort database, lack of chart review to confirm diagnoses in individual cases, and the use of a modified FIB-4, with age capped at 65 years.
‘Easy to Miss’
Commenting on the research, Nancy Reau, MD, section chief of hepatology at Rush University Medical Center in Chicago, said that it is easy for physicians to miss asymptomatic liver disease that could progress and lead to cognitive decline.
“Most of my patients are already labeled with liver disease; however, it is not uncommon to receive a patient from another specialist who felt their presentation was more consistent with liver disease than the issue they were referred for,” she said.
Still, even in metabolic dysfunction–associated steatotic liver disease, which affects nearly one third of the population, the condition isn’t advanced enough in most patients to cause symptoms similar to those of dementia, said Dr. Reau, who was not associated with the study.
“It is more important for specialists in neurology to exclude liver disease and for hepatologists or gastroenterologists to be equipped with tools to exclude alternative explanations for neurocognitive presentations,” she said. “It is important to not label a patient as having HE and then miss alternative explanations.”
“Every presentation has a differential diagnosis. Using easy tools like FIB-4 can make sure you don’t miss liver disease as a contributing factor in a patient that presents with neurocognitive symptoms,” Dr. Reau said.
This work was partly supported by grants from Department of Veterans Affairs merit review program and the National Institutes of Health’s National Center for Advancing Translational Science. Dr. Bajaj and Dr. Reau reported no conflicts of interest.
A version of this article appeared on Medscape.com.
, one of the main causes of the condition, new research suggests.
The study of more than 68,000 individuals in the general population diagnosed with dementia between 2009 and 2019 found that almost 13% had FIB-4 scores indicative of cirrhosis and potential hepatic encephalopathy.
The findings, recently published online in The American Journal of Medicine, corroborate and extend the researchers’ previous work, which showed that about 10% of US veterans with a dementia diagnosis may in fact have hepatic encephalopathy.
“We need to increase awareness that cirrhosis and related brain complications are common, silent, but treatable when found,” said corresponding author Jasmohan Bajaj, MD, of Virginia Commonwealth University and Richmond VA Medical Center, Richmond, Virginia. “Moreover, these are being increasingly diagnosed in older individuals.”
“Cirrhosis can also predispose patients to liver cancer and other complications, so diagnosing it in all patients is important, regardless of the hepatic encephalopathy-dementia connection,” he said.
FIB-4 Is Key
Dr. Bajaj and colleagues analyzed data from 72 healthcare centers on 68,807 nonveteran patients diagnosed with dementia at two or more physician visits between 2009 and 2019. Patients had no prior cirrhosis diagnosis, the mean age was 73 years, 44.7% were men, and 78% were White.
The team measured the prevalence of two high FIB-4 scores (> 2.67 and > 3.25), selected for their strong predictive value for advanced cirrhosis. Researchers also examined associations between high scores and multiple comorbidities and demographic factors.
Alanine aminotransferase (ALT), aspartate aminotransferase (AST), and platelet labs were collected up to 2 years after the index dementia diagnosis because they are used to calculate FIB-4.
The mean FIB-4 score was 1.78, mean ALT was 23.72 U/L, mean AST was 27.42 U/L, and mean platelets were 243.51 × 109/µL.
A total of 8683 participants (12.8%) had a FIB-4 score greater than 2.67 and 5185 (7.6%) had a score greater than 3.25.
In multivariable logistic regression models, FIB-4 greater than 3.25 was associated with viral hepatitis (odds ratio [OR], 2.23), congestive heart failure (OR,1.73), HIV (OR, 1.72), male gender (OR, 1.42), alcohol use disorder (OR, 1.39), and chronic kidney disease (OR, 1.38).
FIB-4 greater than 3.25 was inversely associated with White race (OR, 0.76) and diabetes (OR, 0.82).
The associations were similar when using a threshold score of greater than 2.67.
“With the aging population, including those with cirrhosis, the potential for overlap between hepatic encephalopathy and dementia has risen and should be considered in the differential diagnosis,” the authors wrote. “Undiagnosed cirrhosis and potential hepatic encephalopathy can be a treatable cause of or contributor towards cognitive impairment in patients diagnosed with dementia.”
Providers should use the FIB-4 index as a screening tool to detect cirrhosis in patients with dementia, they concluded.
The team’s next steps will include investigating barriers to the use of FIB-4 among practitioners, Dr. Bajaj said.
Incorporating use of the FIB-4 index into screening guidelines “with input from all stakeholders, including geriatricians, primary care providers, and neurologists … would greatly expand the diagnosis of cirrhosis and potentially hepatic encephalopathy in dementia patients,” Dr. Bajaj said.
The study had a few limitations, including the selected centers in the cohort database, lack of chart review to confirm diagnoses in individual cases, and the use of a modified FIB-4, with age capped at 65 years.
‘Easy to Miss’
Commenting on the research, Nancy Reau, MD, section chief of hepatology at Rush University Medical Center in Chicago, said that it is easy for physicians to miss asymptomatic liver disease that could progress and lead to cognitive decline.
“Most of my patients are already labeled with liver disease; however, it is not uncommon to receive a patient from another specialist who felt their presentation was more consistent with liver disease than the issue they were referred for,” she said.
Still, even in metabolic dysfunction–associated steatotic liver disease, which affects nearly one third of the population, the condition isn’t advanced enough in most patients to cause symptoms similar to those of dementia, said Dr. Reau, who was not associated with the study.
“It is more important for specialists in neurology to exclude liver disease and for hepatologists or gastroenterologists to be equipped with tools to exclude alternative explanations for neurocognitive presentations,” she said. “It is important to not label a patient as having HE and then miss alternative explanations.”
“Every presentation has a differential diagnosis. Using easy tools like FIB-4 can make sure you don’t miss liver disease as a contributing factor in a patient that presents with neurocognitive symptoms,” Dr. Reau said.
This work was partly supported by grants from Department of Veterans Affairs merit review program and the National Institutes of Health’s National Center for Advancing Translational Science. Dr. Bajaj and Dr. Reau reported no conflicts of interest.
A version of this article appeared on Medscape.com.
, one of the main causes of the condition, new research suggests.
The study of more than 68,000 individuals in the general population diagnosed with dementia between 2009 and 2019 found that almost 13% had FIB-4 scores indicative of cirrhosis and potential hepatic encephalopathy.
The findings, recently published online in The American Journal of Medicine, corroborate and extend the researchers’ previous work, which showed that about 10% of US veterans with a dementia diagnosis may in fact have hepatic encephalopathy.
“We need to increase awareness that cirrhosis and related brain complications are common, silent, but treatable when found,” said corresponding author Jasmohan Bajaj, MD, of Virginia Commonwealth University and Richmond VA Medical Center, Richmond, Virginia. “Moreover, these are being increasingly diagnosed in older individuals.”
“Cirrhosis can also predispose patients to liver cancer and other complications, so diagnosing it in all patients is important, regardless of the hepatic encephalopathy-dementia connection,” he said.
FIB-4 Is Key
Dr. Bajaj and colleagues analyzed data from 72 healthcare centers on 68,807 nonveteran patients diagnosed with dementia at two or more physician visits between 2009 and 2019. Patients had no prior cirrhosis diagnosis, the mean age was 73 years, 44.7% were men, and 78% were White.
The team measured the prevalence of two high FIB-4 scores (> 2.67 and > 3.25), selected for their strong predictive value for advanced cirrhosis. Researchers also examined associations between high scores and multiple comorbidities and demographic factors.
Alanine aminotransferase (ALT), aspartate aminotransferase (AST), and platelet labs were collected up to 2 years after the index dementia diagnosis because they are used to calculate FIB-4.
The mean FIB-4 score was 1.78, mean ALT was 23.72 U/L, mean AST was 27.42 U/L, and mean platelets were 243.51 × 109/µL.
A total of 8683 participants (12.8%) had a FIB-4 score greater than 2.67 and 5185 (7.6%) had a score greater than 3.25.
In multivariable logistic regression models, FIB-4 greater than 3.25 was associated with viral hepatitis (odds ratio [OR], 2.23), congestive heart failure (OR,1.73), HIV (OR, 1.72), male gender (OR, 1.42), alcohol use disorder (OR, 1.39), and chronic kidney disease (OR, 1.38).
FIB-4 greater than 3.25 was inversely associated with White race (OR, 0.76) and diabetes (OR, 0.82).
The associations were similar when using a threshold score of greater than 2.67.
“With the aging population, including those with cirrhosis, the potential for overlap between hepatic encephalopathy and dementia has risen and should be considered in the differential diagnosis,” the authors wrote. “Undiagnosed cirrhosis and potential hepatic encephalopathy can be a treatable cause of or contributor towards cognitive impairment in patients diagnosed with dementia.”
Providers should use the FIB-4 index as a screening tool to detect cirrhosis in patients with dementia, they concluded.
The team’s next steps will include investigating barriers to the use of FIB-4 among practitioners, Dr. Bajaj said.
Incorporating use of the FIB-4 index into screening guidelines “with input from all stakeholders, including geriatricians, primary care providers, and neurologists … would greatly expand the diagnosis of cirrhosis and potentially hepatic encephalopathy in dementia patients,” Dr. Bajaj said.
The study had a few limitations, including the selected centers in the cohort database, lack of chart review to confirm diagnoses in individual cases, and the use of a modified FIB-4, with age capped at 65 years.
‘Easy to Miss’
Commenting on the research, Nancy Reau, MD, section chief of hepatology at Rush University Medical Center in Chicago, said that it is easy for physicians to miss asymptomatic liver disease that could progress and lead to cognitive decline.
“Most of my patients are already labeled with liver disease; however, it is not uncommon to receive a patient from another specialist who felt their presentation was more consistent with liver disease than the issue they were referred for,” she said.
Still, even in metabolic dysfunction–associated steatotic liver disease, which affects nearly one third of the population, the condition isn’t advanced enough in most patients to cause symptoms similar to those of dementia, said Dr. Reau, who was not associated with the study.
“It is more important for specialists in neurology to exclude liver disease and for hepatologists or gastroenterologists to be equipped with tools to exclude alternative explanations for neurocognitive presentations,” she said. “It is important to not label a patient as having HE and then miss alternative explanations.”
“Every presentation has a differential diagnosis. Using easy tools like FIB-4 can make sure you don’t miss liver disease as a contributing factor in a patient that presents with neurocognitive symptoms,” Dr. Reau said.
This work was partly supported by grants from Department of Veterans Affairs merit review program and the National Institutes of Health’s National Center for Advancing Translational Science. Dr. Bajaj and Dr. Reau reported no conflicts of interest.
A version of this article appeared on Medscape.com.
From the American Journal of Medicine
Debate: Should Dermatologists or Rheumatologists Manage Musculoskeletal Symptoms in Patients With Psoriasis?
SEATTLE — That was the subject of a debate between a dermatologist and a rheumatologist at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Fabian Proft, MD, the rheumatologist, spoke first and emphasized the potential that MSK symptoms are a sign of psoriatic arthritis (PsA) and therefore should be managed by a rheumatologist.
“Obviously, the rheumatologist perspective [is that] I should be in the driver’s seat when taking care of patient with psoriasis and MSK symptoms, but I will still need to have a copilot there: [The dermatologist] will have a slot,” said Dr. Proft, who is a rheumatologist at Charité — Universitätsmedizin Berlin.
“It’s so important that we make the correct and early diagnosis of [psoriatic arthritis and psoriasis] symptoms,” said Dr. Proft. He specifically called out cases where patients have symptoms that are difficult to determine, whether the cause is inflammatory, and when experience with imaging can be a key factor in the diagnosis.
It’s important not to overdiagnose or overtreat patients, he said, providing an example of a patient with psoriasis who had been training for a marathon. The MRI image suggested that his Achilles tendonitis pain was related to his athletic training, not PsA-associated inflammation. “So I think this is very important that you have the knowledge to read MRIs, and especially also carefully assessing them so as not to overdiagnose patients,” said Dr. Proft.
Dermatologist Rebuttal
In her rebuttal, Laura Savage, MD, PhD, emphasized the need for more of a coequal partnership between the two specialties because of the ability of dermatologists to intervene early in the treatment and prevention of PsA.
“Traditionally, I agree rheumatologists would solely be responsible for the assessment and the management of psoriatic arthritis, but I think that paradigm has shifted in part due to the increased recognition of the need for earlier intervention to limit disease progression and to reduce or even prevent functional limitation,” said Dr. Savage, who is a consultant dermatologist at Leeds Teaching Hospitals NHS Trust and a senior lecturer at the University of Leeds, Leeds, England.
Ideally, molecular biomarkers would be available to predict the development of PsA, but there aren’t any. Still, “we have a huge biomarker in the form of the skin, and it’s recognized that the majority of patients who will develop psoriatic arthritis will have antecedent psoriasis in about 70% of cases,” Dr. Savage said. “There’s a typical time delay of around 7-12 years between the onset of the skin [disease] and the patients developing psoriatic arthritis, and so many of them are going to be into the care of other healthcare practitioners, and particularly the care of dermatologists.”
Dermatologists may also be able to play a role in the prevention of PsA, according to Dr. Savage. In one retrospective study, treatment of skin lesions with biologics was associated with a reduced frequency of progression to PsA (11.1% vs 16.4%) over 10 years (P = .0006). Studies with tumor necrosis factor inhibitors and other interventions have shown similar results.
Such findings have led to the treat intercept strategy, which targets patients with psoriasis who have risk factors for transition to PsA — such as nail pitting, gluteal cleft disease, scalp disease, type 2 diabetes, obesity, and a first-degree relative with PsA — as well as symptoms of prodromal PSA, such as arthralgia and fatigue.
“I think dermatologists are aware of the need to not leave our patients languishing on these therapies and actually escalating them onto effective treatments that may also be able to treat early psoriatic arthritis. We could be more mindful about our choice of treatments for these patients, going on to thinking about their increased risk of PSA and trying to intercept,” Dr. Savage said. “What we don’t want is our patients to be developing these musculoskeletal symptoms of pain and stiffness and functional limitation and disability. We want to be treating the patients with musculoskeletal symptoms of that earlier prodromal phase when they’re developing arthralgia and fatigue.”
She conceded that more complicated patients are good candidates for care by the rheumatologist. “You can do your fancy imaging, and we’ll leave that to you, and the difficult-to-treat patients to [the rheumatologist], but actually we need to just get on and treat them,” she said. “One could argue as well that as a dermatologist, I’m likely to broaden my horizons in terms of choice of therapy and treat all of the domains of the patient. So I would argue that actually it should be the dermatologist who is in that driving seat, particularly when it comes to the management of early psoriatic arthritis, and actually what we should be doing is driving our patients and steering them to earlier intervention and better control for all domains of disease.”
Collaborative Care
During the follow-up discussion, both Dr. Proft and Dr. Savage agreed that dermatologists and rheumatologists should be working together in managing patients. “What we need to do is steer our patients toward collaborative care with our rheumatologists by trying to minimize delays to treatment, by working together in parallel clinics, combined clinics, and on virtual [multidisciplinary teams],” said Dr. Savage.
Dr. Proft agreed. “We should join forces and make decisions together.”
Dr. Savage and Dr. Proft did not provide any financial disclosures.
A version of this article appeared on Medscape.com.
SEATTLE — That was the subject of a debate between a dermatologist and a rheumatologist at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Fabian Proft, MD, the rheumatologist, spoke first and emphasized the potential that MSK symptoms are a sign of psoriatic arthritis (PsA) and therefore should be managed by a rheumatologist.
“Obviously, the rheumatologist perspective [is that] I should be in the driver’s seat when taking care of patient with psoriasis and MSK symptoms, but I will still need to have a copilot there: [The dermatologist] will have a slot,” said Dr. Proft, who is a rheumatologist at Charité — Universitätsmedizin Berlin.
“It’s so important that we make the correct and early diagnosis of [psoriatic arthritis and psoriasis] symptoms,” said Dr. Proft. He specifically called out cases where patients have symptoms that are difficult to determine, whether the cause is inflammatory, and when experience with imaging can be a key factor in the diagnosis.
It’s important not to overdiagnose or overtreat patients, he said, providing an example of a patient with psoriasis who had been training for a marathon. The MRI image suggested that his Achilles tendonitis pain was related to his athletic training, not PsA-associated inflammation. “So I think this is very important that you have the knowledge to read MRIs, and especially also carefully assessing them so as not to overdiagnose patients,” said Dr. Proft.
Dermatologist Rebuttal
In her rebuttal, Laura Savage, MD, PhD, emphasized the need for more of a coequal partnership between the two specialties because of the ability of dermatologists to intervene early in the treatment and prevention of PsA.
“Traditionally, I agree rheumatologists would solely be responsible for the assessment and the management of psoriatic arthritis, but I think that paradigm has shifted in part due to the increased recognition of the need for earlier intervention to limit disease progression and to reduce or even prevent functional limitation,” said Dr. Savage, who is a consultant dermatologist at Leeds Teaching Hospitals NHS Trust and a senior lecturer at the University of Leeds, Leeds, England.
Ideally, molecular biomarkers would be available to predict the development of PsA, but there aren’t any. Still, “we have a huge biomarker in the form of the skin, and it’s recognized that the majority of patients who will develop psoriatic arthritis will have antecedent psoriasis in about 70% of cases,” Dr. Savage said. “There’s a typical time delay of around 7-12 years between the onset of the skin [disease] and the patients developing psoriatic arthritis, and so many of them are going to be into the care of other healthcare practitioners, and particularly the care of dermatologists.”
Dermatologists may also be able to play a role in the prevention of PsA, according to Dr. Savage. In one retrospective study, treatment of skin lesions with biologics was associated with a reduced frequency of progression to PsA (11.1% vs 16.4%) over 10 years (P = .0006). Studies with tumor necrosis factor inhibitors and other interventions have shown similar results.
Such findings have led to the treat intercept strategy, which targets patients with psoriasis who have risk factors for transition to PsA — such as nail pitting, gluteal cleft disease, scalp disease, type 2 diabetes, obesity, and a first-degree relative with PsA — as well as symptoms of prodromal PSA, such as arthralgia and fatigue.
“I think dermatologists are aware of the need to not leave our patients languishing on these therapies and actually escalating them onto effective treatments that may also be able to treat early psoriatic arthritis. We could be more mindful about our choice of treatments for these patients, going on to thinking about their increased risk of PSA and trying to intercept,” Dr. Savage said. “What we don’t want is our patients to be developing these musculoskeletal symptoms of pain and stiffness and functional limitation and disability. We want to be treating the patients with musculoskeletal symptoms of that earlier prodromal phase when they’re developing arthralgia and fatigue.”
She conceded that more complicated patients are good candidates for care by the rheumatologist. “You can do your fancy imaging, and we’ll leave that to you, and the difficult-to-treat patients to [the rheumatologist], but actually we need to just get on and treat them,” she said. “One could argue as well that as a dermatologist, I’m likely to broaden my horizons in terms of choice of therapy and treat all of the domains of the patient. So I would argue that actually it should be the dermatologist who is in that driving seat, particularly when it comes to the management of early psoriatic arthritis, and actually what we should be doing is driving our patients and steering them to earlier intervention and better control for all domains of disease.”
Collaborative Care
During the follow-up discussion, both Dr. Proft and Dr. Savage agreed that dermatologists and rheumatologists should be working together in managing patients. “What we need to do is steer our patients toward collaborative care with our rheumatologists by trying to minimize delays to treatment, by working together in parallel clinics, combined clinics, and on virtual [multidisciplinary teams],” said Dr. Savage.
Dr. Proft agreed. “We should join forces and make decisions together.”
Dr. Savage and Dr. Proft did not provide any financial disclosures.
A version of this article appeared on Medscape.com.
SEATTLE — That was the subject of a debate between a dermatologist and a rheumatologist at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
Fabian Proft, MD, the rheumatologist, spoke first and emphasized the potential that MSK symptoms are a sign of psoriatic arthritis (PsA) and therefore should be managed by a rheumatologist.
“Obviously, the rheumatologist perspective [is that] I should be in the driver’s seat when taking care of patient with psoriasis and MSK symptoms, but I will still need to have a copilot there: [The dermatologist] will have a slot,” said Dr. Proft, who is a rheumatologist at Charité — Universitätsmedizin Berlin.
“It’s so important that we make the correct and early diagnosis of [psoriatic arthritis and psoriasis] symptoms,” said Dr. Proft. He specifically called out cases where patients have symptoms that are difficult to determine, whether the cause is inflammatory, and when experience with imaging can be a key factor in the diagnosis.
It’s important not to overdiagnose or overtreat patients, he said, providing an example of a patient with psoriasis who had been training for a marathon. The MRI image suggested that his Achilles tendonitis pain was related to his athletic training, not PsA-associated inflammation. “So I think this is very important that you have the knowledge to read MRIs, and especially also carefully assessing them so as not to overdiagnose patients,” said Dr. Proft.
Dermatologist Rebuttal
In her rebuttal, Laura Savage, MD, PhD, emphasized the need for more of a coequal partnership between the two specialties because of the ability of dermatologists to intervene early in the treatment and prevention of PsA.
“Traditionally, I agree rheumatologists would solely be responsible for the assessment and the management of psoriatic arthritis, but I think that paradigm has shifted in part due to the increased recognition of the need for earlier intervention to limit disease progression and to reduce or even prevent functional limitation,” said Dr. Savage, who is a consultant dermatologist at Leeds Teaching Hospitals NHS Trust and a senior lecturer at the University of Leeds, Leeds, England.
Ideally, molecular biomarkers would be available to predict the development of PsA, but there aren’t any. Still, “we have a huge biomarker in the form of the skin, and it’s recognized that the majority of patients who will develop psoriatic arthritis will have antecedent psoriasis in about 70% of cases,” Dr. Savage said. “There’s a typical time delay of around 7-12 years between the onset of the skin [disease] and the patients developing psoriatic arthritis, and so many of them are going to be into the care of other healthcare practitioners, and particularly the care of dermatologists.”
Dermatologists may also be able to play a role in the prevention of PsA, according to Dr. Savage. In one retrospective study, treatment of skin lesions with biologics was associated with a reduced frequency of progression to PsA (11.1% vs 16.4%) over 10 years (P = .0006). Studies with tumor necrosis factor inhibitors and other interventions have shown similar results.
Such findings have led to the treat intercept strategy, which targets patients with psoriasis who have risk factors for transition to PsA — such as nail pitting, gluteal cleft disease, scalp disease, type 2 diabetes, obesity, and a first-degree relative with PsA — as well as symptoms of prodromal PSA, such as arthralgia and fatigue.
“I think dermatologists are aware of the need to not leave our patients languishing on these therapies and actually escalating them onto effective treatments that may also be able to treat early psoriatic arthritis. We could be more mindful about our choice of treatments for these patients, going on to thinking about their increased risk of PSA and trying to intercept,” Dr. Savage said. “What we don’t want is our patients to be developing these musculoskeletal symptoms of pain and stiffness and functional limitation and disability. We want to be treating the patients with musculoskeletal symptoms of that earlier prodromal phase when they’re developing arthralgia and fatigue.”
She conceded that more complicated patients are good candidates for care by the rheumatologist. “You can do your fancy imaging, and we’ll leave that to you, and the difficult-to-treat patients to [the rheumatologist], but actually we need to just get on and treat them,” she said. “One could argue as well that as a dermatologist, I’m likely to broaden my horizons in terms of choice of therapy and treat all of the domains of the patient. So I would argue that actually it should be the dermatologist who is in that driving seat, particularly when it comes to the management of early psoriatic arthritis, and actually what we should be doing is driving our patients and steering them to earlier intervention and better control for all domains of disease.”
Collaborative Care
During the follow-up discussion, both Dr. Proft and Dr. Savage agreed that dermatologists and rheumatologists should be working together in managing patients. “What we need to do is steer our patients toward collaborative care with our rheumatologists by trying to minimize delays to treatment, by working together in parallel clinics, combined clinics, and on virtual [multidisciplinary teams],” said Dr. Savage.
Dr. Proft agreed. “We should join forces and make decisions together.”
Dr. Savage and Dr. Proft did not provide any financial disclosures.
A version of this article appeared on Medscape.com.
FROM GRAPPA 2024
Two New Studies on Benzoyl Peroxide Provide Reassuring Data on Safety
Two .
Earlier this year, controversy erupted after an independent lab Valisure petitioned the US Food and Drug Administration (FDA) to recall acne products with BP because it found extremely high levels of the carcinogen benzene. In the research, the lab directors contended that the products can form over 800 times the “conditionally restricted” FDA concentration limit of 2 parts per million (ppm) of benzene, with both prescription and over-the-counter (OTC) products affected. The issue, according to the lab’s report, is one of degradation, not contamination; BP can decompose into benzene. Exposures to benzene have been linked with a higher risk for leukemia and other blood cancers.
(“Conditionally restricted” means that the maximum of 2 ppm only applies to a drug product in which the use of benzene is unavoidable in order to produce a drug product with a significant therapeutic advance, according to FDA guidance.)
Critics of the report questioned the method used to test the products, calling for more “real-world” use data, and said the temperature used may not be what is expected with everyday use.
Now, both new studies are reassuring about the safety of the products, John Barbieri, MD, MBA, assistant professor of dermatology at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, said in a telephone interview. He was a coauthor of both studies. A leading dermatologist not involved in the new research reviewed the findings and agreed.
One study using data from the National Health and Nutrition Examination Survey compared blood levels of benzene between 14 people who had used BP products and 65 people without a history of BP product use, finding no difference between the groups .
The other, much larger study analyzed electronic health records of more than 27,000 patients with acne using BP products, comparing them with more than 27,000 controls who did not use the products. The patients were followed for 10 years after the use of BP products began, and no increased risk for cancer, either blood cancers or solid tumors, was found.
The studies were recently published in the Journal of the American Academy of Dermatology.
“Both studies are well done,” said Henry W. Lim, MD, former chair of the Department of Dermatology and senior vice president for academic affairs at Henry Ford Health, Detroit. Dr. Lim, a former president of the American Academy of Dermatology, reviewed the results of both studies.
“These studies indicate that [a] report of detection of benzene in [BP] products exposed to high temperature does not have any relevant clinical significance, both in terms of blood levels and in terms of internal cancer,” Dr. Lim said. “This is consistent with the clinical experience of practicing dermatologists; no internal side effects have been observed in patients using [BP products].”
Further Details
Under high temperatures, or over a long period, BP can decompose to benzene, a colorless, flammable liquid with a sweet odor. Benzene is formed from natural processes such as forest fires and volcanoes, according to the American Cancer Society, and is found in the air, cigarette smoke, some foods (at low levels), and contaminated drinking water. It’s one of the 20 widely used chemicals involved in making plastics, resins, detergents, and pesticides, among other products.
In the study evaluating blood levels, the researchers matched 14 people who used BP products currently with 65 controls who did not. Five (36%) of those using the products had detectable blood levels; 21 (32%) of those who did not use them did. There was no association between BP exposure and detectable blood benzene levels (odds ratio, 1.12; P = .80).
In the larger study, the researchers used the TriNetX US Collaborative Network database, comparing more than 27,000 patients treated with BP products for acne with more than 27,000 patients aged 12-40 years who had a diagnosis of nevus or seborrheic keratosis with no exposure to prescribed BP or any diagnosis of acne, hidradenitis suppurativa, or rosacea. The researchers looked at the database over the subsequent 10 years to determine the risk for either blood cancers or internal malignancies.
Compared with patients diagnosed with nevus or seborrheic keratosis, those with acne treated with BP had no significant difference in the risk for lymphoma (hazard ratio [HR], 1.00), leukemia (HR, 0.91), any lymphoma or leukemia (HR, 1.04), and internal malignancies (HR, 0.93).
The findings suggest no increased risk for malignancy, the researchers said, although they acknowledged study limitations, such as possible misclassification of BP exposure due to OTC availability and other issues.
Value of BP Treatments
BP is the “go-to” acne treatment, as Dr. Barbieri pointed out. “It’s probably the number one treatment for acne,” and there’s no substitute for it and it’s one of the most effective topical acne treatments, he noted.
Despite the reassuring findings, Dr. Barbieri repeated advice he gave soon after the Valisure report was released. Use common sense and don’t store BP-containing products in hot cars or other hot environments. In warmer climates, refrigeration could be considered, he said. Discard old products. Manufacturers should use cold-chain storage from the manufacturing site to retail or pharmacy sale sites, he added.
FDA and Citizen Petition Status
Asked about the status of the petition from Valisure, an FDA spokesperson said: “The FDA does not comment on the status of pending petitions.”
Dr. Barbieri and Dr. Lim had no relevant disclosures. There were no funding sources for either of the two studies.
A version of this article first appeared on Medscape.com.
Two .
Earlier this year, controversy erupted after an independent lab Valisure petitioned the US Food and Drug Administration (FDA) to recall acne products with BP because it found extremely high levels of the carcinogen benzene. In the research, the lab directors contended that the products can form over 800 times the “conditionally restricted” FDA concentration limit of 2 parts per million (ppm) of benzene, with both prescription and over-the-counter (OTC) products affected. The issue, according to the lab’s report, is one of degradation, not contamination; BP can decompose into benzene. Exposures to benzene have been linked with a higher risk for leukemia and other blood cancers.
(“Conditionally restricted” means that the maximum of 2 ppm only applies to a drug product in which the use of benzene is unavoidable in order to produce a drug product with a significant therapeutic advance, according to FDA guidance.)
Critics of the report questioned the method used to test the products, calling for more “real-world” use data, and said the temperature used may not be what is expected with everyday use.
Now, both new studies are reassuring about the safety of the products, John Barbieri, MD, MBA, assistant professor of dermatology at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, said in a telephone interview. He was a coauthor of both studies. A leading dermatologist not involved in the new research reviewed the findings and agreed.
One study using data from the National Health and Nutrition Examination Survey compared blood levels of benzene between 14 people who had used BP products and 65 people without a history of BP product use, finding no difference between the groups .
The other, much larger study analyzed electronic health records of more than 27,000 patients with acne using BP products, comparing them with more than 27,000 controls who did not use the products. The patients were followed for 10 years after the use of BP products began, and no increased risk for cancer, either blood cancers or solid tumors, was found.
The studies were recently published in the Journal of the American Academy of Dermatology.
“Both studies are well done,” said Henry W. Lim, MD, former chair of the Department of Dermatology and senior vice president for academic affairs at Henry Ford Health, Detroit. Dr. Lim, a former president of the American Academy of Dermatology, reviewed the results of both studies.
“These studies indicate that [a] report of detection of benzene in [BP] products exposed to high temperature does not have any relevant clinical significance, both in terms of blood levels and in terms of internal cancer,” Dr. Lim said. “This is consistent with the clinical experience of practicing dermatologists; no internal side effects have been observed in patients using [BP products].”
Further Details
Under high temperatures, or over a long period, BP can decompose to benzene, a colorless, flammable liquid with a sweet odor. Benzene is formed from natural processes such as forest fires and volcanoes, according to the American Cancer Society, and is found in the air, cigarette smoke, some foods (at low levels), and contaminated drinking water. It’s one of the 20 widely used chemicals involved in making plastics, resins, detergents, and pesticides, among other products.
In the study evaluating blood levels, the researchers matched 14 people who used BP products currently with 65 controls who did not. Five (36%) of those using the products had detectable blood levels; 21 (32%) of those who did not use them did. There was no association between BP exposure and detectable blood benzene levels (odds ratio, 1.12; P = .80).
In the larger study, the researchers used the TriNetX US Collaborative Network database, comparing more than 27,000 patients treated with BP products for acne with more than 27,000 patients aged 12-40 years who had a diagnosis of nevus or seborrheic keratosis with no exposure to prescribed BP or any diagnosis of acne, hidradenitis suppurativa, or rosacea. The researchers looked at the database over the subsequent 10 years to determine the risk for either blood cancers or internal malignancies.
Compared with patients diagnosed with nevus or seborrheic keratosis, those with acne treated with BP had no significant difference in the risk for lymphoma (hazard ratio [HR], 1.00), leukemia (HR, 0.91), any lymphoma or leukemia (HR, 1.04), and internal malignancies (HR, 0.93).
The findings suggest no increased risk for malignancy, the researchers said, although they acknowledged study limitations, such as possible misclassification of BP exposure due to OTC availability and other issues.
Value of BP Treatments
BP is the “go-to” acne treatment, as Dr. Barbieri pointed out. “It’s probably the number one treatment for acne,” and there’s no substitute for it and it’s one of the most effective topical acne treatments, he noted.
Despite the reassuring findings, Dr. Barbieri repeated advice he gave soon after the Valisure report was released. Use common sense and don’t store BP-containing products in hot cars or other hot environments. In warmer climates, refrigeration could be considered, he said. Discard old products. Manufacturers should use cold-chain storage from the manufacturing site to retail or pharmacy sale sites, he added.
FDA and Citizen Petition Status
Asked about the status of the petition from Valisure, an FDA spokesperson said: “The FDA does not comment on the status of pending petitions.”
Dr. Barbieri and Dr. Lim had no relevant disclosures. There were no funding sources for either of the two studies.
A version of this article first appeared on Medscape.com.
Two .
Earlier this year, controversy erupted after an independent lab Valisure petitioned the US Food and Drug Administration (FDA) to recall acne products with BP because it found extremely high levels of the carcinogen benzene. In the research, the lab directors contended that the products can form over 800 times the “conditionally restricted” FDA concentration limit of 2 parts per million (ppm) of benzene, with both prescription and over-the-counter (OTC) products affected. The issue, according to the lab’s report, is one of degradation, not contamination; BP can decompose into benzene. Exposures to benzene have been linked with a higher risk for leukemia and other blood cancers.
(“Conditionally restricted” means that the maximum of 2 ppm only applies to a drug product in which the use of benzene is unavoidable in order to produce a drug product with a significant therapeutic advance, according to FDA guidance.)
Critics of the report questioned the method used to test the products, calling for more “real-world” use data, and said the temperature used may not be what is expected with everyday use.
Now, both new studies are reassuring about the safety of the products, John Barbieri, MD, MBA, assistant professor of dermatology at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at Brigham and Women’s Hospital, Boston, said in a telephone interview. He was a coauthor of both studies. A leading dermatologist not involved in the new research reviewed the findings and agreed.
One study using data from the National Health and Nutrition Examination Survey compared blood levels of benzene between 14 people who had used BP products and 65 people without a history of BP product use, finding no difference between the groups .
The other, much larger study analyzed electronic health records of more than 27,000 patients with acne using BP products, comparing them with more than 27,000 controls who did not use the products. The patients were followed for 10 years after the use of BP products began, and no increased risk for cancer, either blood cancers or solid tumors, was found.
The studies were recently published in the Journal of the American Academy of Dermatology.
“Both studies are well done,” said Henry W. Lim, MD, former chair of the Department of Dermatology and senior vice president for academic affairs at Henry Ford Health, Detroit. Dr. Lim, a former president of the American Academy of Dermatology, reviewed the results of both studies.
“These studies indicate that [a] report of detection of benzene in [BP] products exposed to high temperature does not have any relevant clinical significance, both in terms of blood levels and in terms of internal cancer,” Dr. Lim said. “This is consistent with the clinical experience of practicing dermatologists; no internal side effects have been observed in patients using [BP products].”
Further Details
Under high temperatures, or over a long period, BP can decompose to benzene, a colorless, flammable liquid with a sweet odor. Benzene is formed from natural processes such as forest fires and volcanoes, according to the American Cancer Society, and is found in the air, cigarette smoke, some foods (at low levels), and contaminated drinking water. It’s one of the 20 widely used chemicals involved in making plastics, resins, detergents, and pesticides, among other products.
In the study evaluating blood levels, the researchers matched 14 people who used BP products currently with 65 controls who did not. Five (36%) of those using the products had detectable blood levels; 21 (32%) of those who did not use them did. There was no association between BP exposure and detectable blood benzene levels (odds ratio, 1.12; P = .80).
In the larger study, the researchers used the TriNetX US Collaborative Network database, comparing more than 27,000 patients treated with BP products for acne with more than 27,000 patients aged 12-40 years who had a diagnosis of nevus or seborrheic keratosis with no exposure to prescribed BP or any diagnosis of acne, hidradenitis suppurativa, or rosacea. The researchers looked at the database over the subsequent 10 years to determine the risk for either blood cancers or internal malignancies.
Compared with patients diagnosed with nevus or seborrheic keratosis, those with acne treated with BP had no significant difference in the risk for lymphoma (hazard ratio [HR], 1.00), leukemia (HR, 0.91), any lymphoma or leukemia (HR, 1.04), and internal malignancies (HR, 0.93).
The findings suggest no increased risk for malignancy, the researchers said, although they acknowledged study limitations, such as possible misclassification of BP exposure due to OTC availability and other issues.
Value of BP Treatments
BP is the “go-to” acne treatment, as Dr. Barbieri pointed out. “It’s probably the number one treatment for acne,” and there’s no substitute for it and it’s one of the most effective topical acne treatments, he noted.
Despite the reassuring findings, Dr. Barbieri repeated advice he gave soon after the Valisure report was released. Use common sense and don’t store BP-containing products in hot cars or other hot environments. In warmer climates, refrigeration could be considered, he said. Discard old products. Manufacturers should use cold-chain storage from the manufacturing site to retail or pharmacy sale sites, he added.
FDA and Citizen Petition Status
Asked about the status of the petition from Valisure, an FDA spokesperson said: “The FDA does not comment on the status of pending petitions.”
Dr. Barbieri and Dr. Lim had no relevant disclosures. There were no funding sources for either of the two studies.
A version of this article first appeared on Medscape.com.
Hemophilia: Novel Tx Also Cuts Bleeding in Kids
“In this study, once-weekly efanesoctocog alfa provided high sustained factor VIII activity and highly efficacious protection against bleeding episodes in children with severe hemophilia A, a population in which this goal has been difficult to achieve without burdensome treatment regimens,” report the authors in the study, published in The New England Journal of Medicine.
The results are from the phase 3, open-label XTEND-Kids study, in which first author Lynn Malec, MD, medical director of the Comprehensive Center for Bleeding Disorders and associate professor of medicine and pediatrics at The Medical College of Wisconsin, in Milwaukee, and colleagues enrolled 74 male pediatric patients with hemophilia A, including 38 under the age of 6 and 36 ages 6-12.
The participants received prophylaxis with once-weekly efanesoctocog alfa (50 IU per kg of body weight), for 52 weeks.
Prior to the treatment period, all patients had received factor VIII replacement therapy, with the exception of one who received the therapy on demand. Most (70%) received extended half-life products, such as doses twice a week or every 3 days, and the remaining 30% received standard half-life products, with dose regimens ranging from every 2 days to twice a week.
Over the course of the year-long study, none of the patients developed factor VIII inhibitors, neutralizing antibodies, a common complication in hemophilia A that prevents factor VIII replacement treatment from working to form clots.
In addition, no serious adverse events occurred that were determined to be related to efanesoctocog alfa.
“No inhibitors to factor VIII developed, most adverse events were not serious, and no adverse events led to discontinuation of efanesoctocog alfa,” the authors report.
In terms of efficacy, among 73 patients who were treated according to the protocol, the median annualized bleeding rate was 0.00 and the model-based mean rate was 0.61.
Overall, 47 patients (64%) experienced no treated bleeding episodes during the study, 65 (88%) had no spontaneous bleeding episodes, and 61 (82%) had no episodes of bleeding into joints.
Of 43 bleeding episodes, most (41; 95%) resolved with a single injection of efanesoctocog alfa.
Of note, “shortening the weekly administration interval was not deemed to be necessary in any patient during this study,” the authors add.
In comparison, other studies of children receiving other factor VIII products, including damoctocog alfa pegol, rurioctocog alfa pegol, and efmoroctocog alfa, show higher annualized bleeding rates of 2.9, 2.0, and 1.96, respectively, and studies showed the percentages of patients with no bleeding with those products were 23%, 38%, and 46%, respectively, compared with the 64% in the current study of efanesoctocog alfa.
“Although these clinical study results cannot be directly compared because of the differences in patient populations and study designs, the XTEND-Kids study showed favorable bleeding protection with efanesoctocog alfa prophylaxis as compared with these extended half-life factor VIII products,” the authors report.
Data on the once-weekly monoclonal antibody emicizumab, which has the important benefit of being administered subcutaneously instead of intravenously, is limited in children under age 12 with severe hemophilia A and without factor VIII inhibitors, the authors note.
However, the mean annualized bleeding rate with efanesoctocog alfa appears improved compared with that observed in a small Japanese study of 13 children who received emicizumab prophylaxis every 2 weeks or every 4 weeks, which showed annualized rates of treated bleeding episodes of 1.3 and 0.7 with the respective emicizumab regimens.
Results Compare With Findings in Adults
The results are similar to those reported among adults in the previous XTEND-1 phase 3 study, which was the basis for US Food and Drug Administration (FDA) approval of the drug in 2023 for routine prevention and on-demand treatment for the control of bleeding episodes, in addition to perioperative surgery for adults.
That approval was extended to children as well at the time, based on earlier interim results from the XTEND-Kids trial.
The annualized bleeding rate among adult patients treated with efanesoctocog alfa decreased from 2.96 to 0.69 over the 52 weeks, which was a significantly greater improvement compared with prestudy prophylaxis with conventional factor VIII prophylaxis (P < .001).
In children and adults alike, the decreased bleeding events were accompanied by improvements in physical health, pain, and joint health.
“Weekly prophylaxis with efanesoctocog alfa has the potential to provide long-term preservation of joint health,” the authors conclude.
Commenting in an editorial published concurrently with the study, Pratima Chowdary, MD, of the Katharine Dormandy Haemophilia and Thrombosis Centre, Royal Free Hospital, London, England, underscored the need for a longer duration of prophylaxis, particularly in children.
“In children, the factor VIII protein has a shorter half-life than in adults, and intravenous administration of coagulation factors is particularly challenging, owing to poor venous access,” she explains.
“In this context, a notable outcome in [the study] is the achievement of once-weekly prophylaxis in children with sustained factor VIII levels through the week, which augurs well for protection in the context of delayed or missed doses.”
Dr. Chowdary adds that limitations include that “the study participants had pre-existing tolerance of factor VIII, because only those with previous exposure to factor VIII and without inhibitors were eligible for enrollment.”
“As such, immunogenicity needs to be assessed in other patients, especially those with no previous treatment with factor VIII.”
Further commenting to this news organization, Dr. Chowdary emphasized “the key takeaway for patients with hemophilia is that the notion of a single, lifelong treatment is outdated.”
“Regular reviews and adjustments to prophylaxis are necessary to ensure optimal control of hemophilia, aiming for zero bleeds each year,” Dr. Chowdary noted.
Furthermore, “the treatment regimen to achieve this must also align with the life goals of both patients and their parents,” she said.
The study was supported by Sanofi and Sobi. The authors’ and Dr. Chowdary’s disclosures are published with the study and editorial, respectively.
“In this study, once-weekly efanesoctocog alfa provided high sustained factor VIII activity and highly efficacious protection against bleeding episodes in children with severe hemophilia A, a population in which this goal has been difficult to achieve without burdensome treatment regimens,” report the authors in the study, published in The New England Journal of Medicine.
The results are from the phase 3, open-label XTEND-Kids study, in which first author Lynn Malec, MD, medical director of the Comprehensive Center for Bleeding Disorders and associate professor of medicine and pediatrics at The Medical College of Wisconsin, in Milwaukee, and colleagues enrolled 74 male pediatric patients with hemophilia A, including 38 under the age of 6 and 36 ages 6-12.
The participants received prophylaxis with once-weekly efanesoctocog alfa (50 IU per kg of body weight), for 52 weeks.
Prior to the treatment period, all patients had received factor VIII replacement therapy, with the exception of one who received the therapy on demand. Most (70%) received extended half-life products, such as doses twice a week or every 3 days, and the remaining 30% received standard half-life products, with dose regimens ranging from every 2 days to twice a week.
Over the course of the year-long study, none of the patients developed factor VIII inhibitors, neutralizing antibodies, a common complication in hemophilia A that prevents factor VIII replacement treatment from working to form clots.
In addition, no serious adverse events occurred that were determined to be related to efanesoctocog alfa.
“No inhibitors to factor VIII developed, most adverse events were not serious, and no adverse events led to discontinuation of efanesoctocog alfa,” the authors report.
In terms of efficacy, among 73 patients who were treated according to the protocol, the median annualized bleeding rate was 0.00 and the model-based mean rate was 0.61.
Overall, 47 patients (64%) experienced no treated bleeding episodes during the study, 65 (88%) had no spontaneous bleeding episodes, and 61 (82%) had no episodes of bleeding into joints.
Of 43 bleeding episodes, most (41; 95%) resolved with a single injection of efanesoctocog alfa.
Of note, “shortening the weekly administration interval was not deemed to be necessary in any patient during this study,” the authors add.
In comparison, other studies of children receiving other factor VIII products, including damoctocog alfa pegol, rurioctocog alfa pegol, and efmoroctocog alfa, show higher annualized bleeding rates of 2.9, 2.0, and 1.96, respectively, and studies showed the percentages of patients with no bleeding with those products were 23%, 38%, and 46%, respectively, compared with the 64% in the current study of efanesoctocog alfa.
“Although these clinical study results cannot be directly compared because of the differences in patient populations and study designs, the XTEND-Kids study showed favorable bleeding protection with efanesoctocog alfa prophylaxis as compared with these extended half-life factor VIII products,” the authors report.
Data on the once-weekly monoclonal antibody emicizumab, which has the important benefit of being administered subcutaneously instead of intravenously, is limited in children under age 12 with severe hemophilia A and without factor VIII inhibitors, the authors note.
However, the mean annualized bleeding rate with efanesoctocog alfa appears improved compared with that observed in a small Japanese study of 13 children who received emicizumab prophylaxis every 2 weeks or every 4 weeks, which showed annualized rates of treated bleeding episodes of 1.3 and 0.7 with the respective emicizumab regimens.
Results Compare With Findings in Adults
The results are similar to those reported among adults in the previous XTEND-1 phase 3 study, which was the basis for US Food and Drug Administration (FDA) approval of the drug in 2023 for routine prevention and on-demand treatment for the control of bleeding episodes, in addition to perioperative surgery for adults.
That approval was extended to children as well at the time, based on earlier interim results from the XTEND-Kids trial.
The annualized bleeding rate among adult patients treated with efanesoctocog alfa decreased from 2.96 to 0.69 over the 52 weeks, which was a significantly greater improvement compared with prestudy prophylaxis with conventional factor VIII prophylaxis (P < .001).
In children and adults alike, the decreased bleeding events were accompanied by improvements in physical health, pain, and joint health.
“Weekly prophylaxis with efanesoctocog alfa has the potential to provide long-term preservation of joint health,” the authors conclude.
Commenting in an editorial published concurrently with the study, Pratima Chowdary, MD, of the Katharine Dormandy Haemophilia and Thrombosis Centre, Royal Free Hospital, London, England, underscored the need for a longer duration of prophylaxis, particularly in children.
“In children, the factor VIII protein has a shorter half-life than in adults, and intravenous administration of coagulation factors is particularly challenging, owing to poor venous access,” she explains.
“In this context, a notable outcome in [the study] is the achievement of once-weekly prophylaxis in children with sustained factor VIII levels through the week, which augurs well for protection in the context of delayed or missed doses.”
Dr. Chowdary adds that limitations include that “the study participants had pre-existing tolerance of factor VIII, because only those with previous exposure to factor VIII and without inhibitors were eligible for enrollment.”
“As such, immunogenicity needs to be assessed in other patients, especially those with no previous treatment with factor VIII.”
Further commenting to this news organization, Dr. Chowdary emphasized “the key takeaway for patients with hemophilia is that the notion of a single, lifelong treatment is outdated.”
“Regular reviews and adjustments to prophylaxis are necessary to ensure optimal control of hemophilia, aiming for zero bleeds each year,” Dr. Chowdary noted.
Furthermore, “the treatment regimen to achieve this must also align with the life goals of both patients and their parents,” she said.
The study was supported by Sanofi and Sobi. The authors’ and Dr. Chowdary’s disclosures are published with the study and editorial, respectively.
“In this study, once-weekly efanesoctocog alfa provided high sustained factor VIII activity and highly efficacious protection against bleeding episodes in children with severe hemophilia A, a population in which this goal has been difficult to achieve without burdensome treatment regimens,” report the authors in the study, published in The New England Journal of Medicine.
The results are from the phase 3, open-label XTEND-Kids study, in which first author Lynn Malec, MD, medical director of the Comprehensive Center for Bleeding Disorders and associate professor of medicine and pediatrics at The Medical College of Wisconsin, in Milwaukee, and colleagues enrolled 74 male pediatric patients with hemophilia A, including 38 under the age of 6 and 36 ages 6-12.
The participants received prophylaxis with once-weekly efanesoctocog alfa (50 IU per kg of body weight), for 52 weeks.
Prior to the treatment period, all patients had received factor VIII replacement therapy, with the exception of one who received the therapy on demand. Most (70%) received extended half-life products, such as doses twice a week or every 3 days, and the remaining 30% received standard half-life products, with dose regimens ranging from every 2 days to twice a week.
Over the course of the year-long study, none of the patients developed factor VIII inhibitors, neutralizing antibodies, a common complication in hemophilia A that prevents factor VIII replacement treatment from working to form clots.
In addition, no serious adverse events occurred that were determined to be related to efanesoctocog alfa.
“No inhibitors to factor VIII developed, most adverse events were not serious, and no adverse events led to discontinuation of efanesoctocog alfa,” the authors report.
In terms of efficacy, among 73 patients who were treated according to the protocol, the median annualized bleeding rate was 0.00 and the model-based mean rate was 0.61.
Overall, 47 patients (64%) experienced no treated bleeding episodes during the study, 65 (88%) had no spontaneous bleeding episodes, and 61 (82%) had no episodes of bleeding into joints.
Of 43 bleeding episodes, most (41; 95%) resolved with a single injection of efanesoctocog alfa.
Of note, “shortening the weekly administration interval was not deemed to be necessary in any patient during this study,” the authors add.
In comparison, other studies of children receiving other factor VIII products, including damoctocog alfa pegol, rurioctocog alfa pegol, and efmoroctocog alfa, show higher annualized bleeding rates of 2.9, 2.0, and 1.96, respectively, and studies showed the percentages of patients with no bleeding with those products were 23%, 38%, and 46%, respectively, compared with the 64% in the current study of efanesoctocog alfa.
“Although these clinical study results cannot be directly compared because of the differences in patient populations and study designs, the XTEND-Kids study showed favorable bleeding protection with efanesoctocog alfa prophylaxis as compared with these extended half-life factor VIII products,” the authors report.
Data on the once-weekly monoclonal antibody emicizumab, which has the important benefit of being administered subcutaneously instead of intravenously, is limited in children under age 12 with severe hemophilia A and without factor VIII inhibitors, the authors note.
However, the mean annualized bleeding rate with efanesoctocog alfa appears improved compared with that observed in a small Japanese study of 13 children who received emicizumab prophylaxis every 2 weeks or every 4 weeks, which showed annualized rates of treated bleeding episodes of 1.3 and 0.7 with the respective emicizumab regimens.
Results Compare With Findings in Adults
The results are similar to those reported among adults in the previous XTEND-1 phase 3 study, which was the basis for US Food and Drug Administration (FDA) approval of the drug in 2023 for routine prevention and on-demand treatment for the control of bleeding episodes, in addition to perioperative surgery for adults.
That approval was extended to children as well at the time, based on earlier interim results from the XTEND-Kids trial.
The annualized bleeding rate among adult patients treated with efanesoctocog alfa decreased from 2.96 to 0.69 over the 52 weeks, which was a significantly greater improvement compared with prestudy prophylaxis with conventional factor VIII prophylaxis (P < .001).
In children and adults alike, the decreased bleeding events were accompanied by improvements in physical health, pain, and joint health.
“Weekly prophylaxis with efanesoctocog alfa has the potential to provide long-term preservation of joint health,” the authors conclude.
Commenting in an editorial published concurrently with the study, Pratima Chowdary, MD, of the Katharine Dormandy Haemophilia and Thrombosis Centre, Royal Free Hospital, London, England, underscored the need for a longer duration of prophylaxis, particularly in children.
“In children, the factor VIII protein has a shorter half-life than in adults, and intravenous administration of coagulation factors is particularly challenging, owing to poor venous access,” she explains.
“In this context, a notable outcome in [the study] is the achievement of once-weekly prophylaxis in children with sustained factor VIII levels through the week, which augurs well for protection in the context of delayed or missed doses.”
Dr. Chowdary adds that limitations include that “the study participants had pre-existing tolerance of factor VIII, because only those with previous exposure to factor VIII and without inhibitors were eligible for enrollment.”
“As such, immunogenicity needs to be assessed in other patients, especially those with no previous treatment with factor VIII.”
Further commenting to this news organization, Dr. Chowdary emphasized “the key takeaway for patients with hemophilia is that the notion of a single, lifelong treatment is outdated.”
“Regular reviews and adjustments to prophylaxis are necessary to ensure optimal control of hemophilia, aiming for zero bleeds each year,” Dr. Chowdary noted.
Furthermore, “the treatment regimen to achieve this must also align with the life goals of both patients and their parents,” she said.
The study was supported by Sanofi and Sobi. The authors’ and Dr. Chowdary’s disclosures are published with the study and editorial, respectively.
Vitamin B1 May Reduce Constipation in Adults
TOPLINE:
Increased dietary intake of vitamin B1 is associated with a lower prevalence of constipation, particularly among men and individuals without hypertension or diabetes.
METHODOLOGY:
- Researchers conducted a cross-sectional study using National Health and Nutrition Examination Survey data from 2005-2010 involving 10,371 adults aged ≥ 20 years.
- Participants provided information on fecal characteristics and bowel movement frequency, which was documented for 30 days prior to data collection.
- Constipation was established by either frequency of bowel movements (fewer than three per week) or stool consistency (Bristol Stool Scale type 1 or 2).
- Data on vitamin B1 intake were collected through 24-hour total nutritional intake recall interviews. Patients were divided into three groups based on their level of B1 intake: 0.064-1.21 mg, 1.21-1.76 mg, and 1.76-12.61 mg.
TAKEAWAY:
- Overall, 10.8% of participants were identified as having constipation.
- Greater dietary vitamin B1 intake was associated with a 23% reduction in constipation risk (P = .034).
- Additionally, a subgroup analysis found that higher B1 intake was associated with a reduction in constipation risk of 20% in men, 16% in people without hypertension, and 14% in those without diabetes.
IN PRACTICE:
“This association suggests that enhanced intake of vitamin B1 through diet may facilitate softer stools and heightened intestinal motility, thereby potentially alleviating constipation symptoms. Consequently, healthcare professionals are advised to prioritize the promotion of a well-balanced diet as an initial therapeutic approach, preceding medical interventions,” the authors wrote.
SOURCE:
The study, led by Wenyi Du, the Affiliated Stomatological Hospital of Soochow University, Suzhou Stomatological Hospital, Suzhou, China, and Wuxi People’s Hospital Affiliated to Nanjing Medical University, Wuxi Medical Center, Wuxi, China, was published online in BMC Gastroenterology.
LIMITATIONS:
A causal relationship could not be established between vitamin B1 intake and constipation owing to the cross-sectional nature of the study. The study relied on patient interviews and patient self-reported data. Additionally, 24-hour dietary recalls may not have accurately reflected the long-term eating habits of the participants.
DISCLOSURES:
The study had no specific funding source. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Increased dietary intake of vitamin B1 is associated with a lower prevalence of constipation, particularly among men and individuals without hypertension or diabetes.
METHODOLOGY:
- Researchers conducted a cross-sectional study using National Health and Nutrition Examination Survey data from 2005-2010 involving 10,371 adults aged ≥ 20 years.
- Participants provided information on fecal characteristics and bowel movement frequency, which was documented for 30 days prior to data collection.
- Constipation was established by either frequency of bowel movements (fewer than three per week) or stool consistency (Bristol Stool Scale type 1 or 2).
- Data on vitamin B1 intake were collected through 24-hour total nutritional intake recall interviews. Patients were divided into three groups based on their level of B1 intake: 0.064-1.21 mg, 1.21-1.76 mg, and 1.76-12.61 mg.
TAKEAWAY:
- Overall, 10.8% of participants were identified as having constipation.
- Greater dietary vitamin B1 intake was associated with a 23% reduction in constipation risk (P = .034).
- Additionally, a subgroup analysis found that higher B1 intake was associated with a reduction in constipation risk of 20% in men, 16% in people without hypertension, and 14% in those without diabetes.
IN PRACTICE:
“This association suggests that enhanced intake of vitamin B1 through diet may facilitate softer stools and heightened intestinal motility, thereby potentially alleviating constipation symptoms. Consequently, healthcare professionals are advised to prioritize the promotion of a well-balanced diet as an initial therapeutic approach, preceding medical interventions,” the authors wrote.
SOURCE:
The study, led by Wenyi Du, the Affiliated Stomatological Hospital of Soochow University, Suzhou Stomatological Hospital, Suzhou, China, and Wuxi People’s Hospital Affiliated to Nanjing Medical University, Wuxi Medical Center, Wuxi, China, was published online in BMC Gastroenterology.
LIMITATIONS:
A causal relationship could not be established between vitamin B1 intake and constipation owing to the cross-sectional nature of the study. The study relied on patient interviews and patient self-reported data. Additionally, 24-hour dietary recalls may not have accurately reflected the long-term eating habits of the participants.
DISCLOSURES:
The study had no specific funding source. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Increased dietary intake of vitamin B1 is associated with a lower prevalence of constipation, particularly among men and individuals without hypertension or diabetes.
METHODOLOGY:
- Researchers conducted a cross-sectional study using National Health and Nutrition Examination Survey data from 2005-2010 involving 10,371 adults aged ≥ 20 years.
- Participants provided information on fecal characteristics and bowel movement frequency, which was documented for 30 days prior to data collection.
- Constipation was established by either frequency of bowel movements (fewer than three per week) or stool consistency (Bristol Stool Scale type 1 or 2).
- Data on vitamin B1 intake were collected through 24-hour total nutritional intake recall interviews. Patients were divided into three groups based on their level of B1 intake: 0.064-1.21 mg, 1.21-1.76 mg, and 1.76-12.61 mg.
TAKEAWAY:
- Overall, 10.8% of participants were identified as having constipation.
- Greater dietary vitamin B1 intake was associated with a 23% reduction in constipation risk (P = .034).
- Additionally, a subgroup analysis found that higher B1 intake was associated with a reduction in constipation risk of 20% in men, 16% in people without hypertension, and 14% in those without diabetes.
IN PRACTICE:
“This association suggests that enhanced intake of vitamin B1 through diet may facilitate softer stools and heightened intestinal motility, thereby potentially alleviating constipation symptoms. Consequently, healthcare professionals are advised to prioritize the promotion of a well-balanced diet as an initial therapeutic approach, preceding medical interventions,” the authors wrote.
SOURCE:
The study, led by Wenyi Du, the Affiliated Stomatological Hospital of Soochow University, Suzhou Stomatological Hospital, Suzhou, China, and Wuxi People’s Hospital Affiliated to Nanjing Medical University, Wuxi Medical Center, Wuxi, China, was published online in BMC Gastroenterology.
LIMITATIONS:
A causal relationship could not be established between vitamin B1 intake and constipation owing to the cross-sectional nature of the study. The study relied on patient interviews and patient self-reported data. Additionally, 24-hour dietary recalls may not have accurately reflected the long-term eating habits of the participants.
DISCLOSURES:
The study had no specific funding source. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.