User login
Indications and techniques for multifetal pregnancy reduction
Multifetal pregnancy reduction (MPR) was developed in the 1980s in the wake of significant increases in the incidence of triplets and other higher-order multiples emanating from assisted reproductive technologies (ART). It was offered to reduce fetal number and improve outcomes for remaining fetuses by reducing rates of preterm delivery, fetal growth restriction, and other adverse perinatal outcomes, as well as maternal complications such as preeclampsia and postpartum hemorrhage.
In recent years, improvements in ART – mainly changes in ovulation induction practices and limitations in the number of embryos implanted to two at most – have reversed the increase in higher-order multiples. However, with intrauterine insemination, higher-order multiples still occur, and even without any reproductive assistance, the reality is that multiple pregnancies – particularly twins – continue to exist. In 2018, twins comprised about 3% of births in the United States.1
Twin pregnancies have a significantly higher risk than singleton gestations of preterm birth, maternal complications, and neonatal morbidity and mortality. The pregnancies are complicated more often by preterm premature rupture of membranes, fetal growth restriction, and hypertensive disorders of pregnancy.
Monochorionic diamniotic twin pregnancies face additional, unique risks of twin-to-twin transfusion syndrome, twin reversed arterial perfusion sequence, and twin-anemia polycythemia sequence. These pregnancies account for about 20% of all twin gestations, and decades of experience with ART have shown us that monochorionic diamniotic gestations occur at a higher rate after in-vitro fertilization.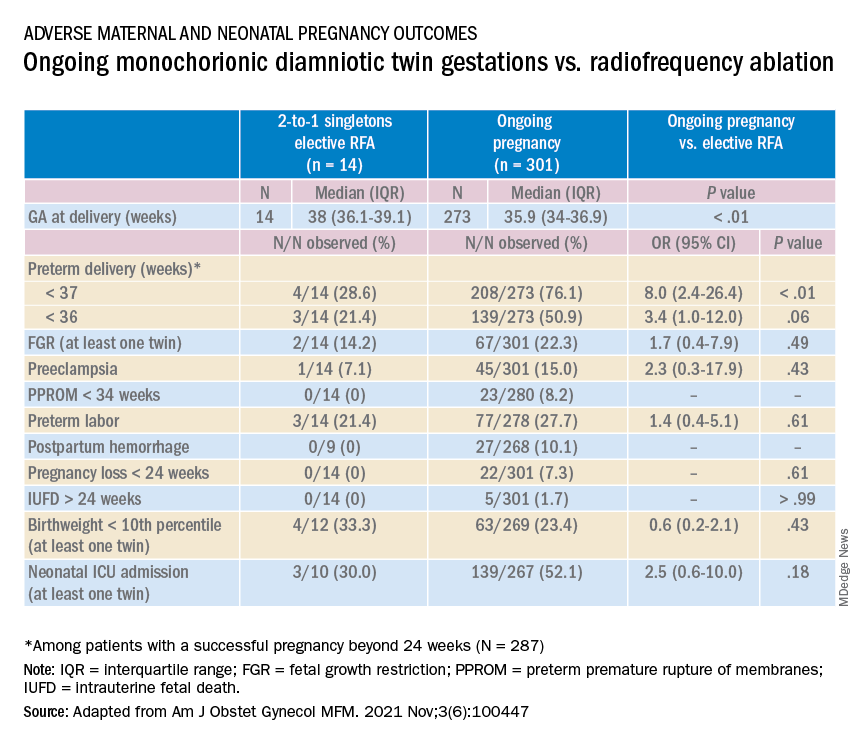
Although advances have improved the outcomes of multiple births, risks remain and elective MPR is still very relevant for twin gestations. Patients routinely receive counseling about the risks of twin gestations, but they often are not made aware of the option of elective fetal reduction.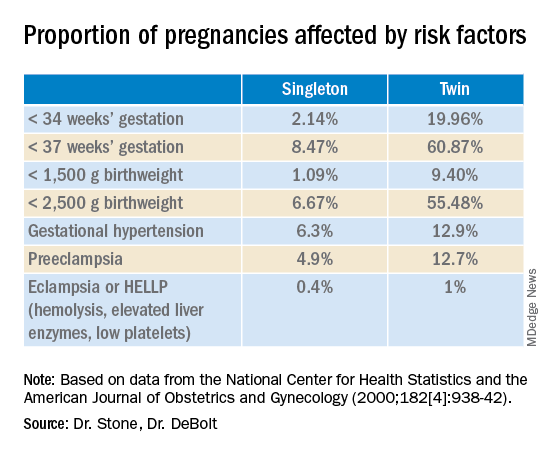
We have offered elective reduction (of nonanomalous fetuses) to a singleton for almost 30 years and have published several reports documenting that MPR in dichorionic diamniotic pregnancies reduces the risk of preterm delivery and other complications without increasing the risk of pregnancy loss.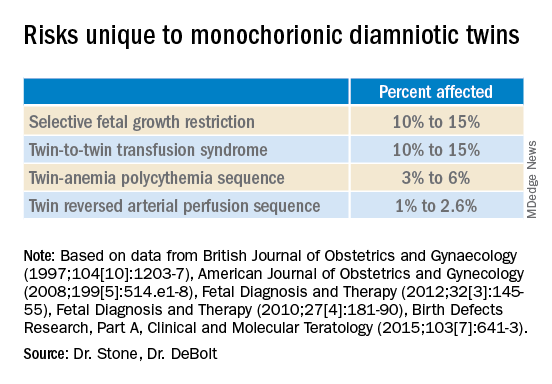
Most recently, we also published data comparing the outcomes of patients with monochorionic diamniotic gestations who underwent elective MPR by radiofrequency ablation (RFA) vs. those with ongoing monochorionic diamniotic gestations.2 While the numbers were small, the data show significantly lower rates of preterm birth without an increased risk of pregnancy loss.
Experience with dichorionic diamniotic twins, genetic testing
Our most recent review3 of outcomes in dichorionic diamniotic gestations covered 855 patients, 29% of whom underwent planned elective MPR at less than 15 weeks, and 71% of whom had ongoing twin gestations. Those with ongoing twin gestations had adjusted odds ratios of preterm delivery at less than 37 weeks and less than 34 weeks of 5.62 and 2.22, respectively (adjustments controlled for maternal characteristics such as maternal age, BMI, use of chorionic villus sampling [CVS], and history of preterm birth).
Ongoing twin pregnancies were also more likely to have preeclampsia (AOR, 3.33), preterm premature rupture of membranes (3.86), and low birthweight (under the 5th and 10th percentiles). There were no significant differences in the rate of unintended pregnancy loss (2.4% vs. 2.3%), and rates for total pregnancy loss at less than 24 weeks and less than 20 weeks were similar.
An important issue in the consideration of MPR is that prenatal diagnosis of chromosomal abnormalities is very safe in twins. Multiple gestations are at greater risk of chromosomal abnormalities, so performing MPR selectively – if a chromosomally abnormal fetus is present – is desirable for many parents.
A recent meta-analysis and systematic review of studies reporting fetal loss following amniocentesis or CVS in twin pregnancies found an exceedingly low risk of loss. Procedure-related fetal loss (the primary outcome) was lower than previously reported, and the rate of fetal loss before 24 weeks gestation or within 4 weeks after the procedure (secondary outcomes), did not differ from the background risk in twin pregnancies not undergoing invasive prenatal testing.4
Our data have shown no significant differences in pregnancy loss between patients who underwent CVS prior to MPR and those who did not. Looking specifically at reduction to a singleton gestation, patients who underwent CVS prior to MPR had a fourfold reduction in loss.5 Therefore, we counsel patients that CVS provides useful information – especially now with the common use of chromosomal microarray – at almost negligible risk.
MPR for monochorionic diamniotic twins
Most of the literature on MPR from twin to singleton gestations reports on intrathoracic potassium chloride injection used in dichorionic diamniotic twins.
MPR in monochorionic diamniotic twins is reserved in the United States for monochorionic pregnancies in which there are severe fetal anomalies, severe growth restriction, or other significant complications. It is performed in such cases around 20 weeks gestation. However, given the significant risks of monochorionic twin pregnancies, we also have been offering MPR electively and earlier in pregnancy. While many modalities of intrafetal cord occlusion exist, RFA at the cord insertion site into the fetal abdomen is our preferred technique.
In our retrospective review of 315 monochorionic diamniotic twin gestations, the 14 patients who had RFA electively had no pregnancy losses and a significantly lower rate of preterm birth at less than 37-weeks gestation, compared with 301 ongoing monochorionic diamniotic twin pregnancies (29% vs. 76%).5 Reduction with RFA, performed at a mean gestational age of 15 weeks, also eliminated the risks unique to monochorionic twins, such as twin-to-twin transfusion syndrome and twin-anemia polycythemia sequence. (Of the ongoing twin gestations, 12% required medically indicated RFA, fetoscopic laser ablation, and/or amnioreduction; 4% had unintended loss of one fetus; and 4% had unintended loss of both fetuses before 24 weeks’ gestation. Fewer than 70% of the ongoing twin gestations had none of the significant adverse outcomes unique to monochorionic twins.)
Interestingly, there were still a couple of cases of fetal growth restriction in patients who underwent elective MPR – a rate higher than that seen in singleton gestations – most likely because of the early timing of the procedure.
Our numbers of MPRs in this review were small, but the data offer at least preliminary evidence that planned elective RFA before 17 weeks gestation may be offered to patients who do not want to assume the risks of monochorionic diamniotic twin pregnancies.
Counseling in twin pregnancies
We perform thorough, early assessments of fetal anatomy in our twin pregnancies, and we undertake thorough medical and obstetrical histories to uncover birth complications or medical conditions that would increase risks of preeclampsia, preterm birth, fetal growth restriction, and other complications.
Because monochorionic gestations are at particularly high risk for heart defects, we also routinely perform fetal echocardiography in these pregnancies.
Genetic testing is offered to all twin pregnancies, and as mentioned above, we especially counsel those considering MPR that such testing provides useful information.
Patients are made aware of the option of MPR and receive nondirective counseling. It is the patient’s choice. We recognize that elective termination is a controversial procedure, but we believe that the option of MPR should be available to patients who want to improve outcomes for their pregnancy.
When anomalies are discovered and selective termination is chosen, we usually try to perform MPR as early as possible. After 16 weeks, we’ve found, the rate of pregnancy loss increases slightly.
Dr. Stone is the Ellen and Howard C. Katz Chairman’s Chair, and Dr. DeBolt is a clinical fellow in maternal-fetal medicine, in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai, New York.
References
1. Martin JA and Osterman MJK. National Center of Health Statistics. NCHS Data Brief, 2019;no 351.
2. Manasa GR et al. Am J Obstet Gynecol MFM 2021;3:100447.
3. Vieira LA et al. Am J. Obstet Gynecol. 2019;221:253.e1-8.
4. Di Mascio et al. Ultrasound Obstet Gynecol 2020 Nov;56(5):647-55.
5. Ferrara L et al. Am J Obstet Gynecol. 2008 Oct;199(4):408.e1-4.
Multifetal pregnancy reduction (MPR) was developed in the 1980s in the wake of significant increases in the incidence of triplets and other higher-order multiples emanating from assisted reproductive technologies (ART). It was offered to reduce fetal number and improve outcomes for remaining fetuses by reducing rates of preterm delivery, fetal growth restriction, and other adverse perinatal outcomes, as well as maternal complications such as preeclampsia and postpartum hemorrhage.
In recent years, improvements in ART – mainly changes in ovulation induction practices and limitations in the number of embryos implanted to two at most – have reversed the increase in higher-order multiples. However, with intrauterine insemination, higher-order multiples still occur, and even without any reproductive assistance, the reality is that multiple pregnancies – particularly twins – continue to exist. In 2018, twins comprised about 3% of births in the United States.1
Twin pregnancies have a significantly higher risk than singleton gestations of preterm birth, maternal complications, and neonatal morbidity and mortality. The pregnancies are complicated more often by preterm premature rupture of membranes, fetal growth restriction, and hypertensive disorders of pregnancy.
Monochorionic diamniotic twin pregnancies face additional, unique risks of twin-to-twin transfusion syndrome, twin reversed arterial perfusion sequence, and twin-anemia polycythemia sequence. These pregnancies account for about 20% of all twin gestations, and decades of experience with ART have shown us that monochorionic diamniotic gestations occur at a higher rate after in-vitro fertilization.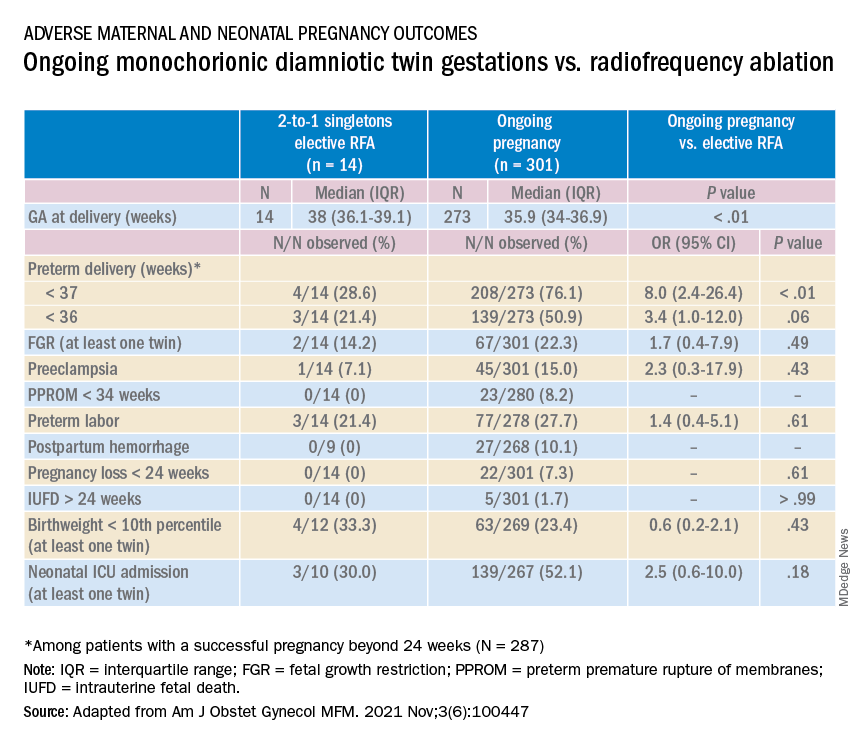
Although advances have improved the outcomes of multiple births, risks remain and elective MPR is still very relevant for twin gestations. Patients routinely receive counseling about the risks of twin gestations, but they often are not made aware of the option of elective fetal reduction.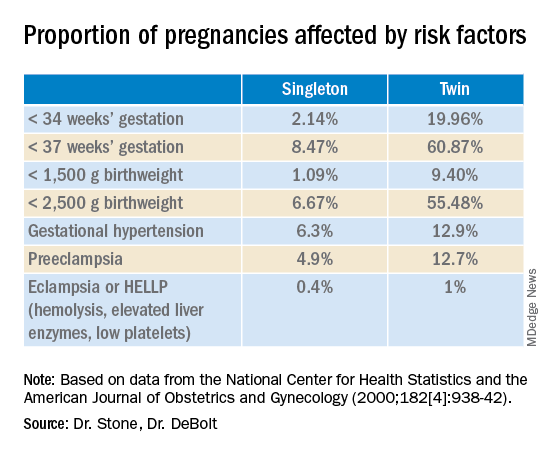
We have offered elective reduction (of nonanomalous fetuses) to a singleton for almost 30 years and have published several reports documenting that MPR in dichorionic diamniotic pregnancies reduces the risk of preterm delivery and other complications without increasing the risk of pregnancy loss.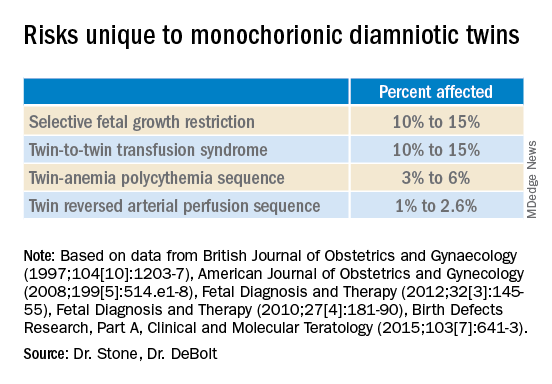
Most recently, we also published data comparing the outcomes of patients with monochorionic diamniotic gestations who underwent elective MPR by radiofrequency ablation (RFA) vs. those with ongoing monochorionic diamniotic gestations.2 While the numbers were small, the data show significantly lower rates of preterm birth without an increased risk of pregnancy loss.
Experience with dichorionic diamniotic twins, genetic testing
Our most recent review3 of outcomes in dichorionic diamniotic gestations covered 855 patients, 29% of whom underwent planned elective MPR at less than 15 weeks, and 71% of whom had ongoing twin gestations. Those with ongoing twin gestations had adjusted odds ratios of preterm delivery at less than 37 weeks and less than 34 weeks of 5.62 and 2.22, respectively (adjustments controlled for maternal characteristics such as maternal age, BMI, use of chorionic villus sampling [CVS], and history of preterm birth).
Ongoing twin pregnancies were also more likely to have preeclampsia (AOR, 3.33), preterm premature rupture of membranes (3.86), and low birthweight (under the 5th and 10th percentiles). There were no significant differences in the rate of unintended pregnancy loss (2.4% vs. 2.3%), and rates for total pregnancy loss at less than 24 weeks and less than 20 weeks were similar.
An important issue in the consideration of MPR is that prenatal diagnosis of chromosomal abnormalities is very safe in twins. Multiple gestations are at greater risk of chromosomal abnormalities, so performing MPR selectively – if a chromosomally abnormal fetus is present – is desirable for many parents.
A recent meta-analysis and systematic review of studies reporting fetal loss following amniocentesis or CVS in twin pregnancies found an exceedingly low risk of loss. Procedure-related fetal loss (the primary outcome) was lower than previously reported, and the rate of fetal loss before 24 weeks gestation or within 4 weeks after the procedure (secondary outcomes), did not differ from the background risk in twin pregnancies not undergoing invasive prenatal testing.4
Our data have shown no significant differences in pregnancy loss between patients who underwent CVS prior to MPR and those who did not. Looking specifically at reduction to a singleton gestation, patients who underwent CVS prior to MPR had a fourfold reduction in loss.5 Therefore, we counsel patients that CVS provides useful information – especially now with the common use of chromosomal microarray – at almost negligible risk.
MPR for monochorionic diamniotic twins
Most of the literature on MPR from twin to singleton gestations reports on intrathoracic potassium chloride injection used in dichorionic diamniotic twins.
MPR in monochorionic diamniotic twins is reserved in the United States for monochorionic pregnancies in which there are severe fetal anomalies, severe growth restriction, or other significant complications. It is performed in such cases around 20 weeks gestation. However, given the significant risks of monochorionic twin pregnancies, we also have been offering MPR electively and earlier in pregnancy. While many modalities of intrafetal cord occlusion exist, RFA at the cord insertion site into the fetal abdomen is our preferred technique.
In our retrospective review of 315 monochorionic diamniotic twin gestations, the 14 patients who had RFA electively had no pregnancy losses and a significantly lower rate of preterm birth at less than 37-weeks gestation, compared with 301 ongoing monochorionic diamniotic twin pregnancies (29% vs. 76%).5 Reduction with RFA, performed at a mean gestational age of 15 weeks, also eliminated the risks unique to monochorionic twins, such as twin-to-twin transfusion syndrome and twin-anemia polycythemia sequence. (Of the ongoing twin gestations, 12% required medically indicated RFA, fetoscopic laser ablation, and/or amnioreduction; 4% had unintended loss of one fetus; and 4% had unintended loss of both fetuses before 24 weeks’ gestation. Fewer than 70% of the ongoing twin gestations had none of the significant adverse outcomes unique to monochorionic twins.)
Interestingly, there were still a couple of cases of fetal growth restriction in patients who underwent elective MPR – a rate higher than that seen in singleton gestations – most likely because of the early timing of the procedure.
Our numbers of MPRs in this review were small, but the data offer at least preliminary evidence that planned elective RFA before 17 weeks gestation may be offered to patients who do not want to assume the risks of monochorionic diamniotic twin pregnancies.
Counseling in twin pregnancies
We perform thorough, early assessments of fetal anatomy in our twin pregnancies, and we undertake thorough medical and obstetrical histories to uncover birth complications or medical conditions that would increase risks of preeclampsia, preterm birth, fetal growth restriction, and other complications.
Because monochorionic gestations are at particularly high risk for heart defects, we also routinely perform fetal echocardiography in these pregnancies.
Genetic testing is offered to all twin pregnancies, and as mentioned above, we especially counsel those considering MPR that such testing provides useful information.
Patients are made aware of the option of MPR and receive nondirective counseling. It is the patient’s choice. We recognize that elective termination is a controversial procedure, but we believe that the option of MPR should be available to patients who want to improve outcomes for their pregnancy.
When anomalies are discovered and selective termination is chosen, we usually try to perform MPR as early as possible. After 16 weeks, we’ve found, the rate of pregnancy loss increases slightly.
Dr. Stone is the Ellen and Howard C. Katz Chairman’s Chair, and Dr. DeBolt is a clinical fellow in maternal-fetal medicine, in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai, New York.
References
1. Martin JA and Osterman MJK. National Center of Health Statistics. NCHS Data Brief, 2019;no 351.
2. Manasa GR et al. Am J Obstet Gynecol MFM 2021;3:100447.
3. Vieira LA et al. Am J. Obstet Gynecol. 2019;221:253.e1-8.
4. Di Mascio et al. Ultrasound Obstet Gynecol 2020 Nov;56(5):647-55.
5. Ferrara L et al. Am J Obstet Gynecol. 2008 Oct;199(4):408.e1-4.
Multifetal pregnancy reduction (MPR) was developed in the 1980s in the wake of significant increases in the incidence of triplets and other higher-order multiples emanating from assisted reproductive technologies (ART). It was offered to reduce fetal number and improve outcomes for remaining fetuses by reducing rates of preterm delivery, fetal growth restriction, and other adverse perinatal outcomes, as well as maternal complications such as preeclampsia and postpartum hemorrhage.
In recent years, improvements in ART – mainly changes in ovulation induction practices and limitations in the number of embryos implanted to two at most – have reversed the increase in higher-order multiples. However, with intrauterine insemination, higher-order multiples still occur, and even without any reproductive assistance, the reality is that multiple pregnancies – particularly twins – continue to exist. In 2018, twins comprised about 3% of births in the United States.1
Twin pregnancies have a significantly higher risk than singleton gestations of preterm birth, maternal complications, and neonatal morbidity and mortality. The pregnancies are complicated more often by preterm premature rupture of membranes, fetal growth restriction, and hypertensive disorders of pregnancy.
Monochorionic diamniotic twin pregnancies face additional, unique risks of twin-to-twin transfusion syndrome, twin reversed arterial perfusion sequence, and twin-anemia polycythemia sequence. These pregnancies account for about 20% of all twin gestations, and decades of experience with ART have shown us that monochorionic diamniotic gestations occur at a higher rate after in-vitro fertilization.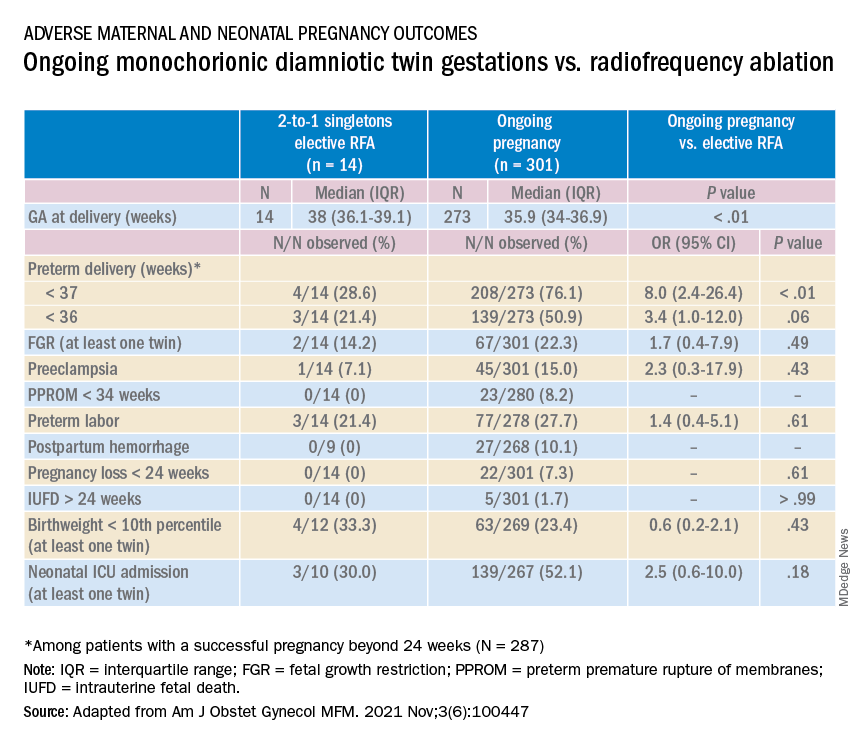
Although advances have improved the outcomes of multiple births, risks remain and elective MPR is still very relevant for twin gestations. Patients routinely receive counseling about the risks of twin gestations, but they often are not made aware of the option of elective fetal reduction.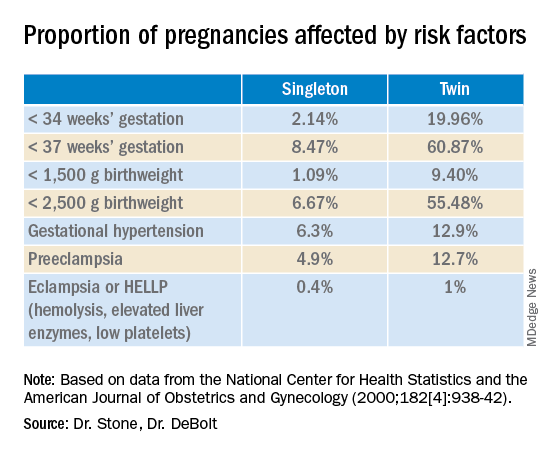
We have offered elective reduction (of nonanomalous fetuses) to a singleton for almost 30 years and have published several reports documenting that MPR in dichorionic diamniotic pregnancies reduces the risk of preterm delivery and other complications without increasing the risk of pregnancy loss.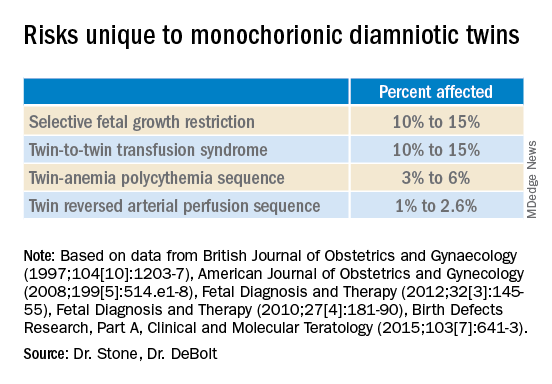
Most recently, we also published data comparing the outcomes of patients with monochorionic diamniotic gestations who underwent elective MPR by radiofrequency ablation (RFA) vs. those with ongoing monochorionic diamniotic gestations.2 While the numbers were small, the data show significantly lower rates of preterm birth without an increased risk of pregnancy loss.
Experience with dichorionic diamniotic twins, genetic testing
Our most recent review3 of outcomes in dichorionic diamniotic gestations covered 855 patients, 29% of whom underwent planned elective MPR at less than 15 weeks, and 71% of whom had ongoing twin gestations. Those with ongoing twin gestations had adjusted odds ratios of preterm delivery at less than 37 weeks and less than 34 weeks of 5.62 and 2.22, respectively (adjustments controlled for maternal characteristics such as maternal age, BMI, use of chorionic villus sampling [CVS], and history of preterm birth).
Ongoing twin pregnancies were also more likely to have preeclampsia (AOR, 3.33), preterm premature rupture of membranes (3.86), and low birthweight (under the 5th and 10th percentiles). There were no significant differences in the rate of unintended pregnancy loss (2.4% vs. 2.3%), and rates for total pregnancy loss at less than 24 weeks and less than 20 weeks were similar.
An important issue in the consideration of MPR is that prenatal diagnosis of chromosomal abnormalities is very safe in twins. Multiple gestations are at greater risk of chromosomal abnormalities, so performing MPR selectively – if a chromosomally abnormal fetus is present – is desirable for many parents.
A recent meta-analysis and systematic review of studies reporting fetal loss following amniocentesis or CVS in twin pregnancies found an exceedingly low risk of loss. Procedure-related fetal loss (the primary outcome) was lower than previously reported, and the rate of fetal loss before 24 weeks gestation or within 4 weeks after the procedure (secondary outcomes), did not differ from the background risk in twin pregnancies not undergoing invasive prenatal testing.4
Our data have shown no significant differences in pregnancy loss between patients who underwent CVS prior to MPR and those who did not. Looking specifically at reduction to a singleton gestation, patients who underwent CVS prior to MPR had a fourfold reduction in loss.5 Therefore, we counsel patients that CVS provides useful information – especially now with the common use of chromosomal microarray – at almost negligible risk.
MPR for monochorionic diamniotic twins
Most of the literature on MPR from twin to singleton gestations reports on intrathoracic potassium chloride injection used in dichorionic diamniotic twins.
MPR in monochorionic diamniotic twins is reserved in the United States for monochorionic pregnancies in which there are severe fetal anomalies, severe growth restriction, or other significant complications. It is performed in such cases around 20 weeks gestation. However, given the significant risks of monochorionic twin pregnancies, we also have been offering MPR electively and earlier in pregnancy. While many modalities of intrafetal cord occlusion exist, RFA at the cord insertion site into the fetal abdomen is our preferred technique.
In our retrospective review of 315 monochorionic diamniotic twin gestations, the 14 patients who had RFA electively had no pregnancy losses and a significantly lower rate of preterm birth at less than 37-weeks gestation, compared with 301 ongoing monochorionic diamniotic twin pregnancies (29% vs. 76%).5 Reduction with RFA, performed at a mean gestational age of 15 weeks, also eliminated the risks unique to monochorionic twins, such as twin-to-twin transfusion syndrome and twin-anemia polycythemia sequence. (Of the ongoing twin gestations, 12% required medically indicated RFA, fetoscopic laser ablation, and/or amnioreduction; 4% had unintended loss of one fetus; and 4% had unintended loss of both fetuses before 24 weeks’ gestation. Fewer than 70% of the ongoing twin gestations had none of the significant adverse outcomes unique to monochorionic twins.)
Interestingly, there were still a couple of cases of fetal growth restriction in patients who underwent elective MPR – a rate higher than that seen in singleton gestations – most likely because of the early timing of the procedure.
Our numbers of MPRs in this review were small, but the data offer at least preliminary evidence that planned elective RFA before 17 weeks gestation may be offered to patients who do not want to assume the risks of monochorionic diamniotic twin pregnancies.
Counseling in twin pregnancies
We perform thorough, early assessments of fetal anatomy in our twin pregnancies, and we undertake thorough medical and obstetrical histories to uncover birth complications or medical conditions that would increase risks of preeclampsia, preterm birth, fetal growth restriction, and other complications.
Because monochorionic gestations are at particularly high risk for heart defects, we also routinely perform fetal echocardiography in these pregnancies.
Genetic testing is offered to all twin pregnancies, and as mentioned above, we especially counsel those considering MPR that such testing provides useful information.
Patients are made aware of the option of MPR and receive nondirective counseling. It is the patient’s choice. We recognize that elective termination is a controversial procedure, but we believe that the option of MPR should be available to patients who want to improve outcomes for their pregnancy.
When anomalies are discovered and selective termination is chosen, we usually try to perform MPR as early as possible. After 16 weeks, we’ve found, the rate of pregnancy loss increases slightly.
Dr. Stone is the Ellen and Howard C. Katz Chairman’s Chair, and Dr. DeBolt is a clinical fellow in maternal-fetal medicine, in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai, New York.
References
1. Martin JA and Osterman MJK. National Center of Health Statistics. NCHS Data Brief, 2019;no 351.
2. Manasa GR et al. Am J Obstet Gynecol MFM 2021;3:100447.
3. Vieira LA et al. Am J. Obstet Gynecol. 2019;221:253.e1-8.
4. Di Mascio et al. Ultrasound Obstet Gynecol 2020 Nov;56(5):647-55.
5. Ferrara L et al. Am J Obstet Gynecol. 2008 Oct;199(4):408.e1-4.
Managing maternal mortality with multifetal pregnancy reduction
For over 2 years, the world has reeled from the COVID-19 pandemic. Life has changed dramatically, priorities have been re-examined, and the collective approach to health care has shifted tremendously. While concerns regarding coronavirus and its variants are warranted, another “pandemic” is ravaging the world and has yet to be fully addressed: pregnancy-related maternal mortality.
The rate of pregnancy-related deaths in the United States is unconscionable. Compared with other developed nations – such as Germany, the United Kingdom, and Canada – we lag far behind. Data published in 2020 showed that the rate of maternal deaths per 100,000 live births in the United States was 17.4, more than double that of France (8.7 deaths per 100,000 live births),1 the country with the next-highest rate. Americans like being first – first to invent the light bulb, first to perform a successful solid organ xenotransplantation, first to go to the moon – but holding “first place” in maternal mortality is not something we should wish to maintain.
Ob.gyns. have long raised the alarm regarding the exceedingly high rates of pregnancy-related deaths in the United States. While there have been many advances in antenatal care to reduce these severe adverse events – improvements in surveillance and data reporting, maternal-focused telemedicine services, multidisciplinary care team models, and numerous research initiatives by federal and nonprofit organizations2 – the recent wave of legislation restricting reproductive choice may also have the unintended consequence of further increasing the rate of pregnancy-related maternal morbidity and mortality.3
While we have an obligation to provide our maternal and fetal patients with the best possible care, under some circumstances, that care may require prioritizing the mother’s health above all else.
To discuss the judicious use of multifetal pregnancy reduction, we have invited Dr. Joanne Stone, The Ellen and Howard C. Katz Chairman’s Chair, and Dr. Chelsea DeBolt, clinical fellow in maternal-fetal medicine, both in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
References
1. Tikkanen R et al. The Commonwealth Fund. Nov 2020. doi: 10.26099/411v-9255
2. Ahn R et al. Ann Intern Med. 2020;173(11 Suppl):S3-10. doi: 10.7326/M19-3258.
3. Pabayo R et al. Int J Environ Res Public Health. 2020;17(11):3773. doi: 10.3390/ijerph17113773.
For over 2 years, the world has reeled from the COVID-19 pandemic. Life has changed dramatically, priorities have been re-examined, and the collective approach to health care has shifted tremendously. While concerns regarding coronavirus and its variants are warranted, another “pandemic” is ravaging the world and has yet to be fully addressed: pregnancy-related maternal mortality.
The rate of pregnancy-related deaths in the United States is unconscionable. Compared with other developed nations – such as Germany, the United Kingdom, and Canada – we lag far behind. Data published in 2020 showed that the rate of maternal deaths per 100,000 live births in the United States was 17.4, more than double that of France (8.7 deaths per 100,000 live births),1 the country with the next-highest rate. Americans like being first – first to invent the light bulb, first to perform a successful solid organ xenotransplantation, first to go to the moon – but holding “first place” in maternal mortality is not something we should wish to maintain.
Ob.gyns. have long raised the alarm regarding the exceedingly high rates of pregnancy-related deaths in the United States. While there have been many advances in antenatal care to reduce these severe adverse events – improvements in surveillance and data reporting, maternal-focused telemedicine services, multidisciplinary care team models, and numerous research initiatives by federal and nonprofit organizations2 – the recent wave of legislation restricting reproductive choice may also have the unintended consequence of further increasing the rate of pregnancy-related maternal morbidity and mortality.3
While we have an obligation to provide our maternal and fetal patients with the best possible care, under some circumstances, that care may require prioritizing the mother’s health above all else.
To discuss the judicious use of multifetal pregnancy reduction, we have invited Dr. Joanne Stone, The Ellen and Howard C. Katz Chairman’s Chair, and Dr. Chelsea DeBolt, clinical fellow in maternal-fetal medicine, both in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
References
1. Tikkanen R et al. The Commonwealth Fund. Nov 2020. doi: 10.26099/411v-9255
2. Ahn R et al. Ann Intern Med. 2020;173(11 Suppl):S3-10. doi: 10.7326/M19-3258.
3. Pabayo R et al. Int J Environ Res Public Health. 2020;17(11):3773. doi: 10.3390/ijerph17113773.
For over 2 years, the world has reeled from the COVID-19 pandemic. Life has changed dramatically, priorities have been re-examined, and the collective approach to health care has shifted tremendously. While concerns regarding coronavirus and its variants are warranted, another “pandemic” is ravaging the world and has yet to be fully addressed: pregnancy-related maternal mortality.
The rate of pregnancy-related deaths in the United States is unconscionable. Compared with other developed nations – such as Germany, the United Kingdom, and Canada – we lag far behind. Data published in 2020 showed that the rate of maternal deaths per 100,000 live births in the United States was 17.4, more than double that of France (8.7 deaths per 100,000 live births),1 the country with the next-highest rate. Americans like being first – first to invent the light bulb, first to perform a successful solid organ xenotransplantation, first to go to the moon – but holding “first place” in maternal mortality is not something we should wish to maintain.
Ob.gyns. have long raised the alarm regarding the exceedingly high rates of pregnancy-related deaths in the United States. While there have been many advances in antenatal care to reduce these severe adverse events – improvements in surveillance and data reporting, maternal-focused telemedicine services, multidisciplinary care team models, and numerous research initiatives by federal and nonprofit organizations2 – the recent wave of legislation restricting reproductive choice may also have the unintended consequence of further increasing the rate of pregnancy-related maternal morbidity and mortality.3
While we have an obligation to provide our maternal and fetal patients with the best possible care, under some circumstances, that care may require prioritizing the mother’s health above all else.
To discuss the judicious use of multifetal pregnancy reduction, we have invited Dr. Joanne Stone, The Ellen and Howard C. Katz Chairman’s Chair, and Dr. Chelsea DeBolt, clinical fellow in maternal-fetal medicine, both in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology, and Reproductive Science at the Icahn School of Medicine at Mount Sinai.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland, Baltimore, as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
References
1. Tikkanen R et al. The Commonwealth Fund. Nov 2020. doi: 10.26099/411v-9255
2. Ahn R et al. Ann Intern Med. 2020;173(11 Suppl):S3-10. doi: 10.7326/M19-3258.
3. Pabayo R et al. Int J Environ Res Public Health. 2020;17(11):3773. doi: 10.3390/ijerph17113773.
New combination med for severe mental illness tied to less weight gain
, new research suggests. However, at least one expert says the weight difference between the two drugs is of “questionable clinical benefit.”
Last year, the Food and Drug Administration approved the drug for the treatment of adults with schizophrenia or bipolar I disorder, as a maintenance monotherapy or as either monotherapy or an adjunct to lithium or valproate for acute manic or mixed episodes.
In the ENLIGHTEN-Early trial, researchers examined weight-gain profiles of more than 400 patients with early schizophrenia, schizophreniform disorder, or bipolar I disorder.
Results showed those given combination treatment gained just over half the amount of weight as those given monotherapy. They were also 36% less likely to gain at least 10% of their body weight during the 12-week treatment period.
They indicate that the weight-mitigating effects shown with olanzapine plus samidorphan are “consistent, regardless of the stage of illness,” Dr. Kahn added.
He presented the findings at the annual congress of the Schizophrenia International Research Society.
Potential benefit
“Early intervention with antipsychotic treatment is critical in shaping the course of treatment and the disease trajectory,” coinvestigator Christine Graham, PhD, with Alkermes, which manufactures the drug, told this news organization.
Olanzapine is a “highly effective antipsychotic, but it’s really avoided a lot in this population,” Dr. Graham said. Therefore, patients “could really stand to benefit” from a combination that delivers the same amount of antipsychotic effect, but “reduces the propensity” for clinically significant weight gain, she added.
Dr. Kahn noted in his meeting presentation that antipsychotics are the “cornerstone” of the treatment of serious mental illness, but that “many are associated with concerning weight gain and cardiometabolic effects.”
While olanzapine is an effective medication, it has “one of the highest weight gain” profiles of the available antipsychotics and patients early on in their illness are “especially vulnerable,” Dr. Kahn said.
Previous studies have shown the combination of olanzapine plus samidorphan is similarly effective as olanzapine, but is associated with less weight gain.
To determine its impact in recent-onset illness, the current researchers screened patients with schizophrenia, schizophreniform disorder, or bipolar I disorder. The patients were aged 16-39 years and had an initial onset of active phase symptoms less than 4 years previously. They had less than 24 weeks’ cumulative lifetime exposure to antipsychotics.
Participants were randomly assigned to receive olanzapine plus samidorphan or olanzapine alone for 12 weeks, and then followed up for safety assessment for a further 4 weeks.
A total of 426 patients were recruited and 76.5% completed the study. The mean age was 25.8 years, 66.2% were men, 66.4% were White, and 28.2% were Black.
The mean body mass index at baseline was 23.69 kg/m2. The most common diagnosis among the participants was schizophrenia (62.9%) followed by bipolar I disorder (21.6%).
Less weight gain
Results of the 12-week study showed a significant difference in percent change in body weight from baseline between the two treatment groups, with a gain of 4.91% for the olanzapine plus samidorphan group vs. 6.77% for the olanzapine-alone group (between-group difference, 1.87%; P = .012).
Dr. Kahn noted this equates to an average weight gain of 2.8 kg (6.2 pounds) with olanzapine plus samidorphan and a gain of about 5 kg (11pounds) with olanzapine.
“It’s not a huge difference, but it’s certainly a significant one,” he said. “I also think it’s clinically important and significant.”
The reduction in weight gain compared with olanzapine was even maintained in patients assigned to olanzapine plus samidorphan who dropped out and did not complete the study, Dr. Kahn reported. “No one really had a weight gain,” he said.
In contrast, patients in the olanzapine groups who dropped out of the study had weight gain larger than their counterparts who stayed in it.
Further analysis showed the proportion of patients who gained 10% or more of their body weight by week 12 was 21.9% for those receiving olanzapine plus samidorphan vs. 30.4% for those receiving just olanzapine (odds ratio, 0.64; P = .075).
As expected, the improvement in Clinical Global Impression–Severity scale scores was almost identical between the olanzapine + samidorphan and olanzapine-only groups.
For safety, Dr. Kahn said the adverse event rates were “very, very similar” between the two treatment arms, which was a pattern that was repeated for serious AEs. This led him to note that “nothing out of the ordinary” was observed.
Clinical impact 'questionable'
Commenting on the study, Laura LaChance, MD, a psychiatrist at St. Mary’s Hospital Centre, McGill University, Montreal, said the actual amount of weight loss shown in the study “is of questionable clinical significance.”
On the other hand, Dr. LaChance said she has achieved “better results with metformin, which has a great safety profile and is cheap and widely available.
“Cost is always a concern in patients with psychotic disorders,” she concluded.
The study was funded by Alkermes. Dr. Kahn reported having relationships with Alkermes, Angelini, Janssen, Sunovion, Otsuka, Merck, Minerva Neuroscience, Roche, and Teva. Dr. Graham is an employee of Alkermes.
A version of this article first appeared on Medscape.com.
, new research suggests. However, at least one expert says the weight difference between the two drugs is of “questionable clinical benefit.”
Last year, the Food and Drug Administration approved the drug for the treatment of adults with schizophrenia or bipolar I disorder, as a maintenance monotherapy or as either monotherapy or an adjunct to lithium or valproate for acute manic or mixed episodes.
In the ENLIGHTEN-Early trial, researchers examined weight-gain profiles of more than 400 patients with early schizophrenia, schizophreniform disorder, or bipolar I disorder.
Results showed those given combination treatment gained just over half the amount of weight as those given monotherapy. They were also 36% less likely to gain at least 10% of their body weight during the 12-week treatment period.
They indicate that the weight-mitigating effects shown with olanzapine plus samidorphan are “consistent, regardless of the stage of illness,” Dr. Kahn added.
He presented the findings at the annual congress of the Schizophrenia International Research Society.
Potential benefit
“Early intervention with antipsychotic treatment is critical in shaping the course of treatment and the disease trajectory,” coinvestigator Christine Graham, PhD, with Alkermes, which manufactures the drug, told this news organization.
Olanzapine is a “highly effective antipsychotic, but it’s really avoided a lot in this population,” Dr. Graham said. Therefore, patients “could really stand to benefit” from a combination that delivers the same amount of antipsychotic effect, but “reduces the propensity” for clinically significant weight gain, she added.
Dr. Kahn noted in his meeting presentation that antipsychotics are the “cornerstone” of the treatment of serious mental illness, but that “many are associated with concerning weight gain and cardiometabolic effects.”
While olanzapine is an effective medication, it has “one of the highest weight gain” profiles of the available antipsychotics and patients early on in their illness are “especially vulnerable,” Dr. Kahn said.
Previous studies have shown the combination of olanzapine plus samidorphan is similarly effective as olanzapine, but is associated with less weight gain.
To determine its impact in recent-onset illness, the current researchers screened patients with schizophrenia, schizophreniform disorder, or bipolar I disorder. The patients were aged 16-39 years and had an initial onset of active phase symptoms less than 4 years previously. They had less than 24 weeks’ cumulative lifetime exposure to antipsychotics.
Participants were randomly assigned to receive olanzapine plus samidorphan or olanzapine alone for 12 weeks, and then followed up for safety assessment for a further 4 weeks.
A total of 426 patients were recruited and 76.5% completed the study. The mean age was 25.8 years, 66.2% were men, 66.4% were White, and 28.2% were Black.
The mean body mass index at baseline was 23.69 kg/m2. The most common diagnosis among the participants was schizophrenia (62.9%) followed by bipolar I disorder (21.6%).
Less weight gain
Results of the 12-week study showed a significant difference in percent change in body weight from baseline between the two treatment groups, with a gain of 4.91% for the olanzapine plus samidorphan group vs. 6.77% for the olanzapine-alone group (between-group difference, 1.87%; P = .012).
Dr. Kahn noted this equates to an average weight gain of 2.8 kg (6.2 pounds) with olanzapine plus samidorphan and a gain of about 5 kg (11pounds) with olanzapine.
“It’s not a huge difference, but it’s certainly a significant one,” he said. “I also think it’s clinically important and significant.”
The reduction in weight gain compared with olanzapine was even maintained in patients assigned to olanzapine plus samidorphan who dropped out and did not complete the study, Dr. Kahn reported. “No one really had a weight gain,” he said.
In contrast, patients in the olanzapine groups who dropped out of the study had weight gain larger than their counterparts who stayed in it.
Further analysis showed the proportion of patients who gained 10% or more of their body weight by week 12 was 21.9% for those receiving olanzapine plus samidorphan vs. 30.4% for those receiving just olanzapine (odds ratio, 0.64; P = .075).
As expected, the improvement in Clinical Global Impression–Severity scale scores was almost identical between the olanzapine + samidorphan and olanzapine-only groups.
For safety, Dr. Kahn said the adverse event rates were “very, very similar” between the two treatment arms, which was a pattern that was repeated for serious AEs. This led him to note that “nothing out of the ordinary” was observed.
Clinical impact 'questionable'
Commenting on the study, Laura LaChance, MD, a psychiatrist at St. Mary’s Hospital Centre, McGill University, Montreal, said the actual amount of weight loss shown in the study “is of questionable clinical significance.”
On the other hand, Dr. LaChance said she has achieved “better results with metformin, which has a great safety profile and is cheap and widely available.
“Cost is always a concern in patients with psychotic disorders,” she concluded.
The study was funded by Alkermes. Dr. Kahn reported having relationships with Alkermes, Angelini, Janssen, Sunovion, Otsuka, Merck, Minerva Neuroscience, Roche, and Teva. Dr. Graham is an employee of Alkermes.
A version of this article first appeared on Medscape.com.
, new research suggests. However, at least one expert says the weight difference between the two drugs is of “questionable clinical benefit.”
Last year, the Food and Drug Administration approved the drug for the treatment of adults with schizophrenia or bipolar I disorder, as a maintenance monotherapy or as either monotherapy or an adjunct to lithium or valproate for acute manic or mixed episodes.
In the ENLIGHTEN-Early trial, researchers examined weight-gain profiles of more than 400 patients with early schizophrenia, schizophreniform disorder, or bipolar I disorder.
Results showed those given combination treatment gained just over half the amount of weight as those given monotherapy. They were also 36% less likely to gain at least 10% of their body weight during the 12-week treatment period.
They indicate that the weight-mitigating effects shown with olanzapine plus samidorphan are “consistent, regardless of the stage of illness,” Dr. Kahn added.
He presented the findings at the annual congress of the Schizophrenia International Research Society.
Potential benefit
“Early intervention with antipsychotic treatment is critical in shaping the course of treatment and the disease trajectory,” coinvestigator Christine Graham, PhD, with Alkermes, which manufactures the drug, told this news organization.
Olanzapine is a “highly effective antipsychotic, but it’s really avoided a lot in this population,” Dr. Graham said. Therefore, patients “could really stand to benefit” from a combination that delivers the same amount of antipsychotic effect, but “reduces the propensity” for clinically significant weight gain, she added.
Dr. Kahn noted in his meeting presentation that antipsychotics are the “cornerstone” of the treatment of serious mental illness, but that “many are associated with concerning weight gain and cardiometabolic effects.”
While olanzapine is an effective medication, it has “one of the highest weight gain” profiles of the available antipsychotics and patients early on in their illness are “especially vulnerable,” Dr. Kahn said.
Previous studies have shown the combination of olanzapine plus samidorphan is similarly effective as olanzapine, but is associated with less weight gain.
To determine its impact in recent-onset illness, the current researchers screened patients with schizophrenia, schizophreniform disorder, or bipolar I disorder. The patients were aged 16-39 years and had an initial onset of active phase symptoms less than 4 years previously. They had less than 24 weeks’ cumulative lifetime exposure to antipsychotics.
Participants were randomly assigned to receive olanzapine plus samidorphan or olanzapine alone for 12 weeks, and then followed up for safety assessment for a further 4 weeks.
A total of 426 patients were recruited and 76.5% completed the study. The mean age was 25.8 years, 66.2% were men, 66.4% were White, and 28.2% were Black.
The mean body mass index at baseline was 23.69 kg/m2. The most common diagnosis among the participants was schizophrenia (62.9%) followed by bipolar I disorder (21.6%).
Less weight gain
Results of the 12-week study showed a significant difference in percent change in body weight from baseline between the two treatment groups, with a gain of 4.91% for the olanzapine plus samidorphan group vs. 6.77% for the olanzapine-alone group (between-group difference, 1.87%; P = .012).
Dr. Kahn noted this equates to an average weight gain of 2.8 kg (6.2 pounds) with olanzapine plus samidorphan and a gain of about 5 kg (11pounds) with olanzapine.
“It’s not a huge difference, but it’s certainly a significant one,” he said. “I also think it’s clinically important and significant.”
The reduction in weight gain compared with olanzapine was even maintained in patients assigned to olanzapine plus samidorphan who dropped out and did not complete the study, Dr. Kahn reported. “No one really had a weight gain,” he said.
In contrast, patients in the olanzapine groups who dropped out of the study had weight gain larger than their counterparts who stayed in it.
Further analysis showed the proportion of patients who gained 10% or more of their body weight by week 12 was 21.9% for those receiving olanzapine plus samidorphan vs. 30.4% for those receiving just olanzapine (odds ratio, 0.64; P = .075).
As expected, the improvement in Clinical Global Impression–Severity scale scores was almost identical between the olanzapine + samidorphan and olanzapine-only groups.
For safety, Dr. Kahn said the adverse event rates were “very, very similar” between the two treatment arms, which was a pattern that was repeated for serious AEs. This led him to note that “nothing out of the ordinary” was observed.
Clinical impact 'questionable'
Commenting on the study, Laura LaChance, MD, a psychiatrist at St. Mary’s Hospital Centre, McGill University, Montreal, said the actual amount of weight loss shown in the study “is of questionable clinical significance.”
On the other hand, Dr. LaChance said she has achieved “better results with metformin, which has a great safety profile and is cheap and widely available.
“Cost is always a concern in patients with psychotic disorders,” she concluded.
The study was funded by Alkermes. Dr. Kahn reported having relationships with Alkermes, Angelini, Janssen, Sunovion, Otsuka, Merck, Minerva Neuroscience, Roche, and Teva. Dr. Graham is an employee of Alkermes.
A version of this article first appeared on Medscape.com.
FROM SIRS 2022
How effective are sterilization procedures? Study raises questions
Women opt for sterilization for a variety of reasons, but the goal is the same: to avoid getting pregnant.
But a head-to-head study of two forms of female sterilization has found surprisingly high rates of failure with the procedures.
The study compared the effectiveness of hysteroscopic sterilization, a nonincisional procedure, and minimally invasive laparoscopic sterilization. Although both methods prevented pregnancy in the vast majority of women, each was associated with more than a 6% failure rate 5 years after the procedure.
That figure is “much higher than expected,” said Aileen Gariepy, MD, MPH, the director of complex family planning at Weill Cornell Medicine, New York, who led the study.
The American College of Obstetricians and Gynecologists reported that the chance of pregnancy after sterilization is less than 1%, Dr. Gariepy said. “Women and pregnancy-capable people considering sterilization should be informed that, after the procedure, they have at least a 6% – not 1% – chance of pregnancy in the next 5 years.”
The study was published in Fertility and Sterility.
For laparoscopic sterilization, surgeons close or sever the fallopian tubes to prevent eggs from reaching the uterus and becoming fertilized.
Hysteroscopic sterilization involves the implantation of small, flexible metal coils into each fallopian tube, a process that produces inflammation and scarring that in turn prevents pregnancy. This method, called Essure and formerly marketed by Bayer, received approval by the Food and Drug Administration in 2002. But the agency received thousands of reports of adverse events with Essure, prompting regulators in 2016 to add a boxed warning to the product label about the risk for adverse events, including perforation, migration of the coils, allergic reactions, and pain.
Bayer pulled Essure from the market in 2019, citing decreased sales of the product. Some women did not have the device removed, however, and questions remain about its effectiveness, according to the researchers.
In the new study, Dr. Gariepy and colleagues examined Medicaid claims for 5906 hysteroscopic and 23,965 laparoscopic sterilizations performed in California between 2008 and 2014. They excluded sterilizations that were performed immediately after delivery, which involve a different approach.
The average age of the women in the study was 33 years.
The study found that, 5 years after the sterilization procedure, 6% of women in either group had become pregnant.
Despite the surprising new data, Chailee Moss, MD, an assistant professor of gynecology and obstetrics at Johns Hopkins University Medical Center, Baltimore, said she did not think the study would significantly affect the way she counsels her patients.
The main reason, she said, is that the study relied on an analysis of medical claims, which “is likely inferior to careful review of individual patient records or prospective collection of clinical data.” Home pregnancy tests may easily be excluded from such data and that patients can undergo ultrasound and termination procedures that would likely not be included in the data the researchers analyzed.
Dr. Moss added that the study was limited to California and that the researchers could not determine pregnancy rates for women who moved out of the state and thus received pregnancy care elsewhere. Nor did the authors account for the use of assistive reproductive technology, which can facilitate pregnancy after sterilization despite the success of the original procedure.
Dr. Gariepy, however, said the study may in fact have undercounted pregnancies and that the failure rates might be even higher than 6%, noting that California is “one of the largest, most populous and most diverse states” in terms of race, ethnicity, and other factors, making the new findings highly generalizable.
“I agree that study results should be confirmed by new nationwide study to determine risk of pregnancy after different sterilization methods,” she said. “Nevertheless, this retrospective cohort study delivers a strong signal that doctors and patients need to know about.”
Dr. Gariepy is on the board of directors of the Society of Family Planning. Dr. Moss has received research funding from Merck.
A version of this article first appeared on Medscape.com.
Women opt for sterilization for a variety of reasons, but the goal is the same: to avoid getting pregnant.
But a head-to-head study of two forms of female sterilization has found surprisingly high rates of failure with the procedures.
The study compared the effectiveness of hysteroscopic sterilization, a nonincisional procedure, and minimally invasive laparoscopic sterilization. Although both methods prevented pregnancy in the vast majority of women, each was associated with more than a 6% failure rate 5 years after the procedure.
That figure is “much higher than expected,” said Aileen Gariepy, MD, MPH, the director of complex family planning at Weill Cornell Medicine, New York, who led the study.
The American College of Obstetricians and Gynecologists reported that the chance of pregnancy after sterilization is less than 1%, Dr. Gariepy said. “Women and pregnancy-capable people considering sterilization should be informed that, after the procedure, they have at least a 6% – not 1% – chance of pregnancy in the next 5 years.”
The study was published in Fertility and Sterility.
For laparoscopic sterilization, surgeons close or sever the fallopian tubes to prevent eggs from reaching the uterus and becoming fertilized.
Hysteroscopic sterilization involves the implantation of small, flexible metal coils into each fallopian tube, a process that produces inflammation and scarring that in turn prevents pregnancy. This method, called Essure and formerly marketed by Bayer, received approval by the Food and Drug Administration in 2002. But the agency received thousands of reports of adverse events with Essure, prompting regulators in 2016 to add a boxed warning to the product label about the risk for adverse events, including perforation, migration of the coils, allergic reactions, and pain.
Bayer pulled Essure from the market in 2019, citing decreased sales of the product. Some women did not have the device removed, however, and questions remain about its effectiveness, according to the researchers.
In the new study, Dr. Gariepy and colleagues examined Medicaid claims for 5906 hysteroscopic and 23,965 laparoscopic sterilizations performed in California between 2008 and 2014. They excluded sterilizations that were performed immediately after delivery, which involve a different approach.
The average age of the women in the study was 33 years.
The study found that, 5 years after the sterilization procedure, 6% of women in either group had become pregnant.
Despite the surprising new data, Chailee Moss, MD, an assistant professor of gynecology and obstetrics at Johns Hopkins University Medical Center, Baltimore, said she did not think the study would significantly affect the way she counsels her patients.
The main reason, she said, is that the study relied on an analysis of medical claims, which “is likely inferior to careful review of individual patient records or prospective collection of clinical data.” Home pregnancy tests may easily be excluded from such data and that patients can undergo ultrasound and termination procedures that would likely not be included in the data the researchers analyzed.
Dr. Moss added that the study was limited to California and that the researchers could not determine pregnancy rates for women who moved out of the state and thus received pregnancy care elsewhere. Nor did the authors account for the use of assistive reproductive technology, which can facilitate pregnancy after sterilization despite the success of the original procedure.
Dr. Gariepy, however, said the study may in fact have undercounted pregnancies and that the failure rates might be even higher than 6%, noting that California is “one of the largest, most populous and most diverse states” in terms of race, ethnicity, and other factors, making the new findings highly generalizable.
“I agree that study results should be confirmed by new nationwide study to determine risk of pregnancy after different sterilization methods,” she said. “Nevertheless, this retrospective cohort study delivers a strong signal that doctors and patients need to know about.”
Dr. Gariepy is on the board of directors of the Society of Family Planning. Dr. Moss has received research funding from Merck.
A version of this article first appeared on Medscape.com.
Women opt for sterilization for a variety of reasons, but the goal is the same: to avoid getting pregnant.
But a head-to-head study of two forms of female sterilization has found surprisingly high rates of failure with the procedures.
The study compared the effectiveness of hysteroscopic sterilization, a nonincisional procedure, and minimally invasive laparoscopic sterilization. Although both methods prevented pregnancy in the vast majority of women, each was associated with more than a 6% failure rate 5 years after the procedure.
That figure is “much higher than expected,” said Aileen Gariepy, MD, MPH, the director of complex family planning at Weill Cornell Medicine, New York, who led the study.
The American College of Obstetricians and Gynecologists reported that the chance of pregnancy after sterilization is less than 1%, Dr. Gariepy said. “Women and pregnancy-capable people considering sterilization should be informed that, after the procedure, they have at least a 6% – not 1% – chance of pregnancy in the next 5 years.”
The study was published in Fertility and Sterility.
For laparoscopic sterilization, surgeons close or sever the fallopian tubes to prevent eggs from reaching the uterus and becoming fertilized.
Hysteroscopic sterilization involves the implantation of small, flexible metal coils into each fallopian tube, a process that produces inflammation and scarring that in turn prevents pregnancy. This method, called Essure and formerly marketed by Bayer, received approval by the Food and Drug Administration in 2002. But the agency received thousands of reports of adverse events with Essure, prompting regulators in 2016 to add a boxed warning to the product label about the risk for adverse events, including perforation, migration of the coils, allergic reactions, and pain.
Bayer pulled Essure from the market in 2019, citing decreased sales of the product. Some women did not have the device removed, however, and questions remain about its effectiveness, according to the researchers.
In the new study, Dr. Gariepy and colleagues examined Medicaid claims for 5906 hysteroscopic and 23,965 laparoscopic sterilizations performed in California between 2008 and 2014. They excluded sterilizations that were performed immediately after delivery, which involve a different approach.
The average age of the women in the study was 33 years.
The study found that, 5 years after the sterilization procedure, 6% of women in either group had become pregnant.
Despite the surprising new data, Chailee Moss, MD, an assistant professor of gynecology and obstetrics at Johns Hopkins University Medical Center, Baltimore, said she did not think the study would significantly affect the way she counsels her patients.
The main reason, she said, is that the study relied on an analysis of medical claims, which “is likely inferior to careful review of individual patient records or prospective collection of clinical data.” Home pregnancy tests may easily be excluded from such data and that patients can undergo ultrasound and termination procedures that would likely not be included in the data the researchers analyzed.
Dr. Moss added that the study was limited to California and that the researchers could not determine pregnancy rates for women who moved out of the state and thus received pregnancy care elsewhere. Nor did the authors account for the use of assistive reproductive technology, which can facilitate pregnancy after sterilization despite the success of the original procedure.
Dr. Gariepy, however, said the study may in fact have undercounted pregnancies and that the failure rates might be even higher than 6%, noting that California is “one of the largest, most populous and most diverse states” in terms of race, ethnicity, and other factors, making the new findings highly generalizable.
“I agree that study results should be confirmed by new nationwide study to determine risk of pregnancy after different sterilization methods,” she said. “Nevertheless, this retrospective cohort study delivers a strong signal that doctors and patients need to know about.”
Dr. Gariepy is on the board of directors of the Society of Family Planning. Dr. Moss has received research funding from Merck.
A version of this article first appeared on Medscape.com.
FROM FERTILITY AND STERILITY
Second-trimester blood test predicts preterm birth
A new blood test performed in the second trimester could help identify pregnancies at risk of early and very early spontaneous preterm birth (sPTB), based on a prospective cohort trial.
The cell-free RNA (cfRNA) profiling tool could guide patient and provider decision-making, while the underlying research illuminates biological pathways that may facilitate novel interventions, reported lead author Joan Camunas-Soler, PhD, of Mirvie, South San Francisco, and colleagues.
“Given the complex etiology of this heterogeneous syndrome, it would be advantageous to develop predictive tests that provide insight on the specific pathophysiology leading to preterm birth for each particular pregnancy,” Dr. Camunas-Soler and colleagues wrote in the American Journal of Obstetrics and Gynecology. “Such an approach could inform the development of preventive treatments and targeted therapeutics that are currently lacking/difficult to implement due to the heterogeneous etiology of sPTB.”
Currently, the best predictor of sPTB is previous sPTB, according to the investigators. Although a combination approach that incorporates cervical length and fetal fibronectin in cervicovaginal fluid is “of use,” they noted, “this is not standard of care in the U.S.A. nor recommended by the American College of Obstetricians and Gynecologists or the Society for Maternal-Fetal Medicine.” Existing molecular tests lack clinical data and may be inaccurate across diverse patient populations, they added.
The present study aimed to address these shortcomings by creating a second-trimester blood test for predicting sPTB. To identify relevant biomarkers, the investigators compared RNA profiles that were differentially expressed in three types of cases: term birth, early sPTB, and very early sPTB.
Among 242 women who contributed second-trimester blood samples for analysis, 194 went on to have a term birth. Of the remaining 48 women who gave birth spontaneously before 35 weeks’ gestation, 32 delivered between 25 and 35 weeks (early sPTB), while 16 delivered before 25 weeks’ gestation (very early sPTB). Slightly more than half of the patients were White, about one-third were Black, approximately 10% were Asian, and the remainder were of unknown race/ethnicity. Cases of preeclampsia were excluded.
The gene discovery and modeling process revealed 25 distinct genes that were significantly associated with early sPTB, offering a risk model with a sensitivity of 76% and a specificity of 72% (area under the curve, 0.80; 95% confidence interval, 0.72-0.87). Very early sPTB was associated with a set of 39 genes, giving a model with a sensitivity of 64% and a specificity of 80% (area under the curve = 0.76; 95% CI, 0.63-0.87).
Characterization of the two RNA profiles offered a glimpse into the underlying biological processes driving preterm birth. The genes predicting early sPTB are largely responsible for extracellular matrix degradation and remodeling, which could, “in terms of mechanism, reflect ongoing processes associated with cervical shortening, a feature often detected some weeks prior to sPTB,” the investigators wrote. In contrast, genes associated with very early sPTB are linked with insulinlike growth factor transport, which drives fetal growth and placentation. These findings could lead to development of pathway-specific interventions, Dr. Camunas-Soler and colleagues suggested.
According to coauthor Michal A. Elovitz, MD, the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health at the University of Pennsylvania, Philadelphia, and chief medical advisor at Mirvie, the proprietary RNA platform moves beyond “unreliable and at times biased clinical factors such as race, BMI, and maternal age” to offer a “precision-based approach to pregnancy health.”
Excluding traditional risk factors also “promises more equitable care than the use of broad sociodemographic factors that often result in bias,” she added, noting that this may help address the higher rate of pregnancy complications among Black patients.
When asked about the potential for false-positive results, considering reported specificity rates of 72%-80%, Dr. Elovitz suggested that such concerns among pregnant women are an “unfortunate misconception.”
“It is not reflective of what women want regarding knowledge about the health of their pregnancy,” she said in a written comment. “Rather than be left in the dark, women want to be prepared for what is to come in their pregnancy journey.”
In support of this statement, Dr. Elovitz cited a recent study involving women with preeclampsia and other hypertensive disorders in pregnancy. A questionnaire showed that women appreciated pregnancy risk models when making decisions, and reported that they would have greater peace of mind if such tests were available.
Laura Jelliffe-Pawlowski, PhD, of the University of California, San Francisco, California Preterm Birth Initiative, supported Dr. Elovitz’s viewpoint.
“If you talk to women who have delivered preterm most (but not all) say that they would have wanted to know their risk so they could have been better prepared,” she said in a written comment. “I think we need to shift the narrative to empowerment away from fear.”
Dr. Jelliffe-Pawlowski, who holds a patent for a separate test predicting preterm birth, said that the Mirvie RNA platform is “promising,” although she expressed concern that excluding patients with preeclampsia – representing approximately 4% of pregnancies in the United States – may have clouded accuracy results.
“What is unclear is how the test would perform more generally when a sample of all pregnancies was included,” she said. “Without that information, it is hard to compare their findings with other predictive models without such exclusions.”
Regardless of the model used, Dr. Jelliffe-Pawlowski said that more research is needed to determine best clinical responses when risk of sPTB is increased.
“Ultimately we want to connect action with results,” she said. “Okay, so [a woman] is at high risk for delivering preterm – now what? There is a lot of untapped potential once you start to focus more with women and birthing people you know have a high likelihood of preterm birth.”
The study was supported by Mirvie, Tommy’s Charity, and the National Institute for Health Research Biomedical Research Centre. The investigators disclosed financial relationships with Mirvie, including equity interest and/or intellectual property rights. Cohort contributors were remunerated for sample collection and/or shipping. Dr. Jelliffe-Pawlowski holds a patent for a different preterm birth prediction blood test.
*This story was updated on 4/26/2022.
A new blood test performed in the second trimester could help identify pregnancies at risk of early and very early spontaneous preterm birth (sPTB), based on a prospective cohort trial.
The cell-free RNA (cfRNA) profiling tool could guide patient and provider decision-making, while the underlying research illuminates biological pathways that may facilitate novel interventions, reported lead author Joan Camunas-Soler, PhD, of Mirvie, South San Francisco, and colleagues.
“Given the complex etiology of this heterogeneous syndrome, it would be advantageous to develop predictive tests that provide insight on the specific pathophysiology leading to preterm birth for each particular pregnancy,” Dr. Camunas-Soler and colleagues wrote in the American Journal of Obstetrics and Gynecology. “Such an approach could inform the development of preventive treatments and targeted therapeutics that are currently lacking/difficult to implement due to the heterogeneous etiology of sPTB.”
Currently, the best predictor of sPTB is previous sPTB, according to the investigators. Although a combination approach that incorporates cervical length and fetal fibronectin in cervicovaginal fluid is “of use,” they noted, “this is not standard of care in the U.S.A. nor recommended by the American College of Obstetricians and Gynecologists or the Society for Maternal-Fetal Medicine.” Existing molecular tests lack clinical data and may be inaccurate across diverse patient populations, they added.
The present study aimed to address these shortcomings by creating a second-trimester blood test for predicting sPTB. To identify relevant biomarkers, the investigators compared RNA profiles that were differentially expressed in three types of cases: term birth, early sPTB, and very early sPTB.
Among 242 women who contributed second-trimester blood samples for analysis, 194 went on to have a term birth. Of the remaining 48 women who gave birth spontaneously before 35 weeks’ gestation, 32 delivered between 25 and 35 weeks (early sPTB), while 16 delivered before 25 weeks’ gestation (very early sPTB). Slightly more than half of the patients were White, about one-third were Black, approximately 10% were Asian, and the remainder were of unknown race/ethnicity. Cases of preeclampsia were excluded.
The gene discovery and modeling process revealed 25 distinct genes that were significantly associated with early sPTB, offering a risk model with a sensitivity of 76% and a specificity of 72% (area under the curve, 0.80; 95% confidence interval, 0.72-0.87). Very early sPTB was associated with a set of 39 genes, giving a model with a sensitivity of 64% and a specificity of 80% (area under the curve = 0.76; 95% CI, 0.63-0.87).
Characterization of the two RNA profiles offered a glimpse into the underlying biological processes driving preterm birth. The genes predicting early sPTB are largely responsible for extracellular matrix degradation and remodeling, which could, “in terms of mechanism, reflect ongoing processes associated with cervical shortening, a feature often detected some weeks prior to sPTB,” the investigators wrote. In contrast, genes associated with very early sPTB are linked with insulinlike growth factor transport, which drives fetal growth and placentation. These findings could lead to development of pathway-specific interventions, Dr. Camunas-Soler and colleagues suggested.
According to coauthor Michal A. Elovitz, MD, the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health at the University of Pennsylvania, Philadelphia, and chief medical advisor at Mirvie, the proprietary RNA platform moves beyond “unreliable and at times biased clinical factors such as race, BMI, and maternal age” to offer a “precision-based approach to pregnancy health.”
Excluding traditional risk factors also “promises more equitable care than the use of broad sociodemographic factors that often result in bias,” she added, noting that this may help address the higher rate of pregnancy complications among Black patients.
When asked about the potential for false-positive results, considering reported specificity rates of 72%-80%, Dr. Elovitz suggested that such concerns among pregnant women are an “unfortunate misconception.”
“It is not reflective of what women want regarding knowledge about the health of their pregnancy,” she said in a written comment. “Rather than be left in the dark, women want to be prepared for what is to come in their pregnancy journey.”
In support of this statement, Dr. Elovitz cited a recent study involving women with preeclampsia and other hypertensive disorders in pregnancy. A questionnaire showed that women appreciated pregnancy risk models when making decisions, and reported that they would have greater peace of mind if such tests were available.
Laura Jelliffe-Pawlowski, PhD, of the University of California, San Francisco, California Preterm Birth Initiative, supported Dr. Elovitz’s viewpoint.
“If you talk to women who have delivered preterm most (but not all) say that they would have wanted to know their risk so they could have been better prepared,” she said in a written comment. “I think we need to shift the narrative to empowerment away from fear.”
Dr. Jelliffe-Pawlowski, who holds a patent for a separate test predicting preterm birth, said that the Mirvie RNA platform is “promising,” although she expressed concern that excluding patients with preeclampsia – representing approximately 4% of pregnancies in the United States – may have clouded accuracy results.
“What is unclear is how the test would perform more generally when a sample of all pregnancies was included,” she said. “Without that information, it is hard to compare their findings with other predictive models without such exclusions.”
Regardless of the model used, Dr. Jelliffe-Pawlowski said that more research is needed to determine best clinical responses when risk of sPTB is increased.
“Ultimately we want to connect action with results,” she said. “Okay, so [a woman] is at high risk for delivering preterm – now what? There is a lot of untapped potential once you start to focus more with women and birthing people you know have a high likelihood of preterm birth.”
The study was supported by Mirvie, Tommy’s Charity, and the National Institute for Health Research Biomedical Research Centre. The investigators disclosed financial relationships with Mirvie, including equity interest and/or intellectual property rights. Cohort contributors were remunerated for sample collection and/or shipping. Dr. Jelliffe-Pawlowski holds a patent for a different preterm birth prediction blood test.
*This story was updated on 4/26/2022.
A new blood test performed in the second trimester could help identify pregnancies at risk of early and very early spontaneous preterm birth (sPTB), based on a prospective cohort trial.
The cell-free RNA (cfRNA) profiling tool could guide patient and provider decision-making, while the underlying research illuminates biological pathways that may facilitate novel interventions, reported lead author Joan Camunas-Soler, PhD, of Mirvie, South San Francisco, and colleagues.
“Given the complex etiology of this heterogeneous syndrome, it would be advantageous to develop predictive tests that provide insight on the specific pathophysiology leading to preterm birth for each particular pregnancy,” Dr. Camunas-Soler and colleagues wrote in the American Journal of Obstetrics and Gynecology. “Such an approach could inform the development of preventive treatments and targeted therapeutics that are currently lacking/difficult to implement due to the heterogeneous etiology of sPTB.”
Currently, the best predictor of sPTB is previous sPTB, according to the investigators. Although a combination approach that incorporates cervical length and fetal fibronectin in cervicovaginal fluid is “of use,” they noted, “this is not standard of care in the U.S.A. nor recommended by the American College of Obstetricians and Gynecologists or the Society for Maternal-Fetal Medicine.” Existing molecular tests lack clinical data and may be inaccurate across diverse patient populations, they added.
The present study aimed to address these shortcomings by creating a second-trimester blood test for predicting sPTB. To identify relevant biomarkers, the investigators compared RNA profiles that were differentially expressed in three types of cases: term birth, early sPTB, and very early sPTB.
Among 242 women who contributed second-trimester blood samples for analysis, 194 went on to have a term birth. Of the remaining 48 women who gave birth spontaneously before 35 weeks’ gestation, 32 delivered between 25 and 35 weeks (early sPTB), while 16 delivered before 25 weeks’ gestation (very early sPTB). Slightly more than half of the patients were White, about one-third were Black, approximately 10% were Asian, and the remainder were of unknown race/ethnicity. Cases of preeclampsia were excluded.
The gene discovery and modeling process revealed 25 distinct genes that were significantly associated with early sPTB, offering a risk model with a sensitivity of 76% and a specificity of 72% (area under the curve, 0.80; 95% confidence interval, 0.72-0.87). Very early sPTB was associated with a set of 39 genes, giving a model with a sensitivity of 64% and a specificity of 80% (area under the curve = 0.76; 95% CI, 0.63-0.87).
Characterization of the two RNA profiles offered a glimpse into the underlying biological processes driving preterm birth. The genes predicting early sPTB are largely responsible for extracellular matrix degradation and remodeling, which could, “in terms of mechanism, reflect ongoing processes associated with cervical shortening, a feature often detected some weeks prior to sPTB,” the investigators wrote. In contrast, genes associated with very early sPTB are linked with insulinlike growth factor transport, which drives fetal growth and placentation. These findings could lead to development of pathway-specific interventions, Dr. Camunas-Soler and colleagues suggested.
According to coauthor Michal A. Elovitz, MD, the Hilarie L. Morgan and Mitchell L. Morgan President’s Distinguished Professor in Women’s Health at the University of Pennsylvania, Philadelphia, and chief medical advisor at Mirvie, the proprietary RNA platform moves beyond “unreliable and at times biased clinical factors such as race, BMI, and maternal age” to offer a “precision-based approach to pregnancy health.”
Excluding traditional risk factors also “promises more equitable care than the use of broad sociodemographic factors that often result in bias,” she added, noting that this may help address the higher rate of pregnancy complications among Black patients.
When asked about the potential for false-positive results, considering reported specificity rates of 72%-80%, Dr. Elovitz suggested that such concerns among pregnant women are an “unfortunate misconception.”
“It is not reflective of what women want regarding knowledge about the health of their pregnancy,” she said in a written comment. “Rather than be left in the dark, women want to be prepared for what is to come in their pregnancy journey.”
In support of this statement, Dr. Elovitz cited a recent study involving women with preeclampsia and other hypertensive disorders in pregnancy. A questionnaire showed that women appreciated pregnancy risk models when making decisions, and reported that they would have greater peace of mind if such tests were available.
Laura Jelliffe-Pawlowski, PhD, of the University of California, San Francisco, California Preterm Birth Initiative, supported Dr. Elovitz’s viewpoint.
“If you talk to women who have delivered preterm most (but not all) say that they would have wanted to know their risk so they could have been better prepared,” she said in a written comment. “I think we need to shift the narrative to empowerment away from fear.”
Dr. Jelliffe-Pawlowski, who holds a patent for a separate test predicting preterm birth, said that the Mirvie RNA platform is “promising,” although she expressed concern that excluding patients with preeclampsia – representing approximately 4% of pregnancies in the United States – may have clouded accuracy results.
“What is unclear is how the test would perform more generally when a sample of all pregnancies was included,” she said. “Without that information, it is hard to compare their findings with other predictive models without such exclusions.”
Regardless of the model used, Dr. Jelliffe-Pawlowski said that more research is needed to determine best clinical responses when risk of sPTB is increased.
“Ultimately we want to connect action with results,” she said. “Okay, so [a woman] is at high risk for delivering preterm – now what? There is a lot of untapped potential once you start to focus more with women and birthing people you know have a high likelihood of preterm birth.”
The study was supported by Mirvie, Tommy’s Charity, and the National Institute for Health Research Biomedical Research Centre. The investigators disclosed financial relationships with Mirvie, including equity interest and/or intellectual property rights. Cohort contributors were remunerated for sample collection and/or shipping. Dr. Jelliffe-Pawlowski holds a patent for a different preterm birth prediction blood test.
*This story was updated on 4/26/2022.
FROM AMERICAN JOURNAL OF OBSTETRICS AND GYNECOLOGY
Deep brain stimulation fails to halt depression in Parkinson’s disease
Treatment with deep brain stimulation improved motor function and quality of life, but depression scores increased after 1 year, based on data from 20 adults.
Subthalamic nucleus deep brain stimulation (STN-DBS) has emerged as an effective treatment for Parkinson’s disease symptoms, with evidence supporting improved motor symptoms and quality of life, wrote Francesca Mameli, PsyD, of Foundation IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, and colleagues.
However, the effect of STN-DBS on personality in Parkinson’s disease (PD) has not been well investigated they said.
In a study published in Neuromodulation, the researchers reviewed data from 12 women and 8 men with PD who underwent bilateral STN-DBS.
Depression was assessed via the Montgomery-Asberg Depressive Rating Scale (MADRS), personality characteristics were assessed via the Minnesota Multiphasic Personality Inventory–2 (MMPI-2), and motor disabilities were assessed via UPDRS-III-Motor. The motor disabilities score was obtained in medication on and medication off conditions; the off condition followed a 12-hour overnight withdrawal of dopaminergic medication. Quality of life was assessed via the Parkinson’s Disease Questionnaire–8 (PDQ-8).
After 12 months, scores on the MMPI-2 were significantly higher on the D subscale, increased from a baseline mean of 56.05 to a 12-month mean of 61.90 (P = .015).
Other MMPI-2 scales showing significant increases included the DEP scale, LSE scale, WRK scale, and TRT scale. No differences appeared between male and female patients.
No significant changes occurred from pre-DBS baseline to the 12-month follow-up in MADRS scale assessment, with mean scores of 8.18 and 9.22, respectively.
A 40% improvement in UPDRS measures of motor function occurred among patients in the “medication-off” condition, although there was no significant change following DBS in the medication-on condition, the researchers said. Among 18 patients with PDQ-8 assessments, quality of life scores were significantly higher at 12 months’ post DBS compared to baseline pre DBS (40.15 vs. 30.73, P = .011).
The researchers also examined the relationship between the total electrical energy delivered (TEED) and the occurrence of personality trait shift. In the TEED analysis, “only the energy on the right side was inversely correlated with the changes in depression,” they wrote.
“Because of the complexity of psychiatric phenomena, it would be advisable to take a cautious approach by including psychiatric evaluation by interview for a better selection of patients who score close to the pathological cutoffs in MADRS and MMPI-2,” the researchers wrote in their discussion.
The study findings were limited by several factors including the small sample size, lack of data on the prevalence and severity of apathy, the use of scales based on self-reports, and inability to control for all factors that might affect depressive traits, the researchers noted. In addition, more research is needed to explore the correlation between TEED and personality trait changes, they said.
However, the results support the value of DBS in PD, but emphasize the need to manage expectations, they emphasized. “Expectations should never be unrealistic, and the caring team should ensure not only that patients fully understand the risks and potential benefits of the DBS but also that it will not stop the neurodegenerative progression of the disease,” they said.
The study was supported in part by the Italian Ministry of Health. The researchers had no financial conflicts to disclose.
Treatment with deep brain stimulation improved motor function and quality of life, but depression scores increased after 1 year, based on data from 20 adults.
Subthalamic nucleus deep brain stimulation (STN-DBS) has emerged as an effective treatment for Parkinson’s disease symptoms, with evidence supporting improved motor symptoms and quality of life, wrote Francesca Mameli, PsyD, of Foundation IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, and colleagues.
However, the effect of STN-DBS on personality in Parkinson’s disease (PD) has not been well investigated they said.
In a study published in Neuromodulation, the researchers reviewed data from 12 women and 8 men with PD who underwent bilateral STN-DBS.
Depression was assessed via the Montgomery-Asberg Depressive Rating Scale (MADRS), personality characteristics were assessed via the Minnesota Multiphasic Personality Inventory–2 (MMPI-2), and motor disabilities were assessed via UPDRS-III-Motor. The motor disabilities score was obtained in medication on and medication off conditions; the off condition followed a 12-hour overnight withdrawal of dopaminergic medication. Quality of life was assessed via the Parkinson’s Disease Questionnaire–8 (PDQ-8).
After 12 months, scores on the MMPI-2 were significantly higher on the D subscale, increased from a baseline mean of 56.05 to a 12-month mean of 61.90 (P = .015).
Other MMPI-2 scales showing significant increases included the DEP scale, LSE scale, WRK scale, and TRT scale. No differences appeared between male and female patients.
No significant changes occurred from pre-DBS baseline to the 12-month follow-up in MADRS scale assessment, with mean scores of 8.18 and 9.22, respectively.
A 40% improvement in UPDRS measures of motor function occurred among patients in the “medication-off” condition, although there was no significant change following DBS in the medication-on condition, the researchers said. Among 18 patients with PDQ-8 assessments, quality of life scores were significantly higher at 12 months’ post DBS compared to baseline pre DBS (40.15 vs. 30.73, P = .011).
The researchers also examined the relationship between the total electrical energy delivered (TEED) and the occurrence of personality trait shift. In the TEED analysis, “only the energy on the right side was inversely correlated with the changes in depression,” they wrote.
“Because of the complexity of psychiatric phenomena, it would be advisable to take a cautious approach by including psychiatric evaluation by interview for a better selection of patients who score close to the pathological cutoffs in MADRS and MMPI-2,” the researchers wrote in their discussion.
The study findings were limited by several factors including the small sample size, lack of data on the prevalence and severity of apathy, the use of scales based on self-reports, and inability to control for all factors that might affect depressive traits, the researchers noted. In addition, more research is needed to explore the correlation between TEED and personality trait changes, they said.
However, the results support the value of DBS in PD, but emphasize the need to manage expectations, they emphasized. “Expectations should never be unrealistic, and the caring team should ensure not only that patients fully understand the risks and potential benefits of the DBS but also that it will not stop the neurodegenerative progression of the disease,” they said.
The study was supported in part by the Italian Ministry of Health. The researchers had no financial conflicts to disclose.
Treatment with deep brain stimulation improved motor function and quality of life, but depression scores increased after 1 year, based on data from 20 adults.
Subthalamic nucleus deep brain stimulation (STN-DBS) has emerged as an effective treatment for Parkinson’s disease symptoms, with evidence supporting improved motor symptoms and quality of life, wrote Francesca Mameli, PsyD, of Foundation IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, and colleagues.
However, the effect of STN-DBS on personality in Parkinson’s disease (PD) has not been well investigated they said.
In a study published in Neuromodulation, the researchers reviewed data from 12 women and 8 men with PD who underwent bilateral STN-DBS.
Depression was assessed via the Montgomery-Asberg Depressive Rating Scale (MADRS), personality characteristics were assessed via the Minnesota Multiphasic Personality Inventory–2 (MMPI-2), and motor disabilities were assessed via UPDRS-III-Motor. The motor disabilities score was obtained in medication on and medication off conditions; the off condition followed a 12-hour overnight withdrawal of dopaminergic medication. Quality of life was assessed via the Parkinson’s Disease Questionnaire–8 (PDQ-8).
After 12 months, scores on the MMPI-2 were significantly higher on the D subscale, increased from a baseline mean of 56.05 to a 12-month mean of 61.90 (P = .015).
Other MMPI-2 scales showing significant increases included the DEP scale, LSE scale, WRK scale, and TRT scale. No differences appeared between male and female patients.
No significant changes occurred from pre-DBS baseline to the 12-month follow-up in MADRS scale assessment, with mean scores of 8.18 and 9.22, respectively.
A 40% improvement in UPDRS measures of motor function occurred among patients in the “medication-off” condition, although there was no significant change following DBS in the medication-on condition, the researchers said. Among 18 patients with PDQ-8 assessments, quality of life scores were significantly higher at 12 months’ post DBS compared to baseline pre DBS (40.15 vs. 30.73, P = .011).
The researchers also examined the relationship between the total electrical energy delivered (TEED) and the occurrence of personality trait shift. In the TEED analysis, “only the energy on the right side was inversely correlated with the changes in depression,” they wrote.
“Because of the complexity of psychiatric phenomena, it would be advisable to take a cautious approach by including psychiatric evaluation by interview for a better selection of patients who score close to the pathological cutoffs in MADRS and MMPI-2,” the researchers wrote in their discussion.
The study findings were limited by several factors including the small sample size, lack of data on the prevalence and severity of apathy, the use of scales based on self-reports, and inability to control for all factors that might affect depressive traits, the researchers noted. In addition, more research is needed to explore the correlation between TEED and personality trait changes, they said.
However, the results support the value of DBS in PD, but emphasize the need to manage expectations, they emphasized. “Expectations should never be unrealistic, and the caring team should ensure not only that patients fully understand the risks and potential benefits of the DBS but also that it will not stop the neurodegenerative progression of the disease,” they said.
The study was supported in part by the Italian Ministry of Health. The researchers had no financial conflicts to disclose.
FROM NEUROMODULATION
Pandemic prompts spike in eating disorder hospitalization for adolescents
Hospital admission for children with eating disorders approximately tripled during the COVID-19 pandemic, based on data from 85 patients.
Eating disorders are common among adolescents and often require hospital admission for nutritional restoration, according to May Shum of Yale University, New Haven, Conn., and colleagues
During the COVID-19 pandemic, the volume of hospital admissions for adolescents with eating disorders has increased, the researchers wrote in a poster presented at the annual meeting of the Pediatric Academic Societies. This increase may be driven both by interruptions in medical care and increased psychological distress, but data on changes in patient characteristics and hospitalization course are lacking, they said.
The researchers reviewed charts from patients with eating disorders admitted to a single center between Jan. 1, 2017, and June 30, 2021. The majority of the patients were female (90.6%), and White (78.8%), had restrictive eating behaviors (97.2%), and had private insurance (80.0%).
Overall, the number of monthly admissions increased from 1.4 before the onset of the pandemic to 3.6 during the pandemic (P < .001).
Length of stay increased significantly from before to during pandemic cases (12.8 days vs. 17.3 days, P = .04) and age younger than 13 years was significantly associated with a longer length of stay (P < .001).
The number of patients for whom psychotropic medications were initiated or changed increased significantly (12.5% vs. 28.3%, P = .04); as did the proportion of patients discharged to partial hospitalization, residential, or inpatient psychiatric treatment rather than discharged home with outpatient therapy (56.2% vs. 75.0%, P = .04).
No significant differences were noted in demographics, comorbidities, admission parameters, EKG abnormalities, electrolyte repletion, or tube feeding.
The study findings were limited by the use of data from a single center. However, the results suggest an increase in severity of hospital admissions that have implications for use of hospital resources, the researchers said.
“In addition to an increase in hospital admissions for eating disorder management during the pandemic, longer inpatient stays of younger children with higher acuity at discharge is an added strain on hospital resources and warrants attention,” they concluded.
Considerations for younger patients
The current study is especially important at this time, Margaret Thew, DNP, FNP-BC, medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, said in an interview. “There have been reports of the rising numbers in eating disorders, but until research has been conducted, we cannot quantify the volumes,” said Ms. Thew, who was not involved in the study. “There have been many reports of the rise in mental health issues during the pandemic, so it seems accurate that the rate of eating disorders would rise,” she said. “Additionally, from a clinical perspective there seemed to be many younger-age patients with eating disorders presenting to the inpatient units who seemed sicker,” she noted.
Ms. Thew said she was not surprised by the study findings. “Working with adolescents with eating disorders we saw the increased numbers of both hospitalizations and outpatient referrals during the pandemic,” said Ms. Thew. “Length of stay was higher across the nation regarding admissions for concerns of eating disorders. These patients are sicker and fewer went home after medical stabilization,” she emphasized.
“Clinicians should be more aware of the rise in patients presenting with eating disorders at younger ages to their clinics and provide early interventions to prevent severe illness and medical instability,” said Ms. Thew. Clinicians also should be more proactive in managing younger children and adolescents who express mood disorders, disordered eating, or weight loss, given the significant rise in eating disorders and mental health concerns, she said.
Additional research is needed to continue following the rate of eating disorders into 2022, said Ms. Thew. More research is needed on early interventions and recognition of eating disorders for preteens and teens to prevent severe illness, as is research on how the younger patient with an eating disorder may present differently to the primary care doctor or emergency department, she said.
“We may need to study treatment of the younger population, as they may not do as well with admissions into behavioral health facilities,” Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Hospital admission for children with eating disorders approximately tripled during the COVID-19 pandemic, based on data from 85 patients.
Eating disorders are common among adolescents and often require hospital admission for nutritional restoration, according to May Shum of Yale University, New Haven, Conn., and colleagues
During the COVID-19 pandemic, the volume of hospital admissions for adolescents with eating disorders has increased, the researchers wrote in a poster presented at the annual meeting of the Pediatric Academic Societies. This increase may be driven both by interruptions in medical care and increased psychological distress, but data on changes in patient characteristics and hospitalization course are lacking, they said.
The researchers reviewed charts from patients with eating disorders admitted to a single center between Jan. 1, 2017, and June 30, 2021. The majority of the patients were female (90.6%), and White (78.8%), had restrictive eating behaviors (97.2%), and had private insurance (80.0%).
Overall, the number of monthly admissions increased from 1.4 before the onset of the pandemic to 3.6 during the pandemic (P < .001).
Length of stay increased significantly from before to during pandemic cases (12.8 days vs. 17.3 days, P = .04) and age younger than 13 years was significantly associated with a longer length of stay (P < .001).
The number of patients for whom psychotropic medications were initiated or changed increased significantly (12.5% vs. 28.3%, P = .04); as did the proportion of patients discharged to partial hospitalization, residential, or inpatient psychiatric treatment rather than discharged home with outpatient therapy (56.2% vs. 75.0%, P = .04).
No significant differences were noted in demographics, comorbidities, admission parameters, EKG abnormalities, electrolyte repletion, or tube feeding.
The study findings were limited by the use of data from a single center. However, the results suggest an increase in severity of hospital admissions that have implications for use of hospital resources, the researchers said.
“In addition to an increase in hospital admissions for eating disorder management during the pandemic, longer inpatient stays of younger children with higher acuity at discharge is an added strain on hospital resources and warrants attention,” they concluded.
Considerations for younger patients
The current study is especially important at this time, Margaret Thew, DNP, FNP-BC, medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, said in an interview. “There have been reports of the rising numbers in eating disorders, but until research has been conducted, we cannot quantify the volumes,” said Ms. Thew, who was not involved in the study. “There have been many reports of the rise in mental health issues during the pandemic, so it seems accurate that the rate of eating disorders would rise,” she said. “Additionally, from a clinical perspective there seemed to be many younger-age patients with eating disorders presenting to the inpatient units who seemed sicker,” she noted.
Ms. Thew said she was not surprised by the study findings. “Working with adolescents with eating disorders we saw the increased numbers of both hospitalizations and outpatient referrals during the pandemic,” said Ms. Thew. “Length of stay was higher across the nation regarding admissions for concerns of eating disorders. These patients are sicker and fewer went home after medical stabilization,” she emphasized.
“Clinicians should be more aware of the rise in patients presenting with eating disorders at younger ages to their clinics and provide early interventions to prevent severe illness and medical instability,” said Ms. Thew. Clinicians also should be more proactive in managing younger children and adolescents who express mood disorders, disordered eating, or weight loss, given the significant rise in eating disorders and mental health concerns, she said.
Additional research is needed to continue following the rate of eating disorders into 2022, said Ms. Thew. More research is needed on early interventions and recognition of eating disorders for preteens and teens to prevent severe illness, as is research on how the younger patient with an eating disorder may present differently to the primary care doctor or emergency department, she said.
“We may need to study treatment of the younger population, as they may not do as well with admissions into behavioral health facilities,” Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Hospital admission for children with eating disorders approximately tripled during the COVID-19 pandemic, based on data from 85 patients.
Eating disorders are common among adolescents and often require hospital admission for nutritional restoration, according to May Shum of Yale University, New Haven, Conn., and colleagues
During the COVID-19 pandemic, the volume of hospital admissions for adolescents with eating disorders has increased, the researchers wrote in a poster presented at the annual meeting of the Pediatric Academic Societies. This increase may be driven both by interruptions in medical care and increased psychological distress, but data on changes in patient characteristics and hospitalization course are lacking, they said.
The researchers reviewed charts from patients with eating disorders admitted to a single center between Jan. 1, 2017, and June 30, 2021. The majority of the patients were female (90.6%), and White (78.8%), had restrictive eating behaviors (97.2%), and had private insurance (80.0%).
Overall, the number of monthly admissions increased from 1.4 before the onset of the pandemic to 3.6 during the pandemic (P < .001).
Length of stay increased significantly from before to during pandemic cases (12.8 days vs. 17.3 days, P = .04) and age younger than 13 years was significantly associated with a longer length of stay (P < .001).
The number of patients for whom psychotropic medications were initiated or changed increased significantly (12.5% vs. 28.3%, P = .04); as did the proportion of patients discharged to partial hospitalization, residential, or inpatient psychiatric treatment rather than discharged home with outpatient therapy (56.2% vs. 75.0%, P = .04).
No significant differences were noted in demographics, comorbidities, admission parameters, EKG abnormalities, electrolyte repletion, or tube feeding.
The study findings were limited by the use of data from a single center. However, the results suggest an increase in severity of hospital admissions that have implications for use of hospital resources, the researchers said.
“In addition to an increase in hospital admissions for eating disorder management during the pandemic, longer inpatient stays of younger children with higher acuity at discharge is an added strain on hospital resources and warrants attention,” they concluded.
Considerations for younger patients
The current study is especially important at this time, Margaret Thew, DNP, FNP-BC, medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee, said in an interview. “There have been reports of the rising numbers in eating disorders, but until research has been conducted, we cannot quantify the volumes,” said Ms. Thew, who was not involved in the study. “There have been many reports of the rise in mental health issues during the pandemic, so it seems accurate that the rate of eating disorders would rise,” she said. “Additionally, from a clinical perspective there seemed to be many younger-age patients with eating disorders presenting to the inpatient units who seemed sicker,” she noted.
Ms. Thew said she was not surprised by the study findings. “Working with adolescents with eating disorders we saw the increased numbers of both hospitalizations and outpatient referrals during the pandemic,” said Ms. Thew. “Length of stay was higher across the nation regarding admissions for concerns of eating disorders. These patients are sicker and fewer went home after medical stabilization,” she emphasized.
“Clinicians should be more aware of the rise in patients presenting with eating disorders at younger ages to their clinics and provide early interventions to prevent severe illness and medical instability,” said Ms. Thew. Clinicians also should be more proactive in managing younger children and adolescents who express mood disorders, disordered eating, or weight loss, given the significant rise in eating disorders and mental health concerns, she said.
Additional research is needed to continue following the rate of eating disorders into 2022, said Ms. Thew. More research is needed on early interventions and recognition of eating disorders for preteens and teens to prevent severe illness, as is research on how the younger patient with an eating disorder may present differently to the primary care doctor or emergency department, she said.
“We may need to study treatment of the younger population, as they may not do as well with admissions into behavioral health facilities,” Ms. Thew added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Ms. Thew had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM PAS 2022
Water, water everywhere leads to leaner students
Elementary schools that provide easy access to drinking water and education about its benefits may help their students maintain a healthy weight, a new study found.
Researchers examined the health and drinking habits of 1,249 children in 26 low-income, ethnically diverse elementary schools in the San Francisco Bay Area. In half of the schools, water stations were placed throughout, along with signs explaining why water is healthier than sugary drinks. In addition, assemblies were held explaining the advantages of water over sugary drinks.
That simple message seemed to have had an outsized effect. Schools with water stations had significantly fewer overweight students than the other schools by the end of the 15-month study, according to Anisha Patel, MD, MSPH, MSHS, associate professor of pediatrics at Stanford (Calif.) University, who will be presenting the findings at the Pediatric Academic Societies (PAS) 2022 Meeting, Denver.
“Sugar-sweetened beverages are a huge contributor to obesity,” Dr. Patel told this news organization. “This provides a key strategy for schools to adopt, and the time is right for this type of work – in the pandemic period we’ve seen significant increases in obesity. Investments like this could help stem that.”
According to the U.S. Centers for Disease Control and Prevention, 14.4 million children aged 2-19 years in the United States – about 19% of all kids in that age range – were obese in 2017-2018. The agency said the rate of increase in body mass index among this group nearly doubled during the COVID-19 pandemic.
Children with obesity are at higher risk for chronic health problems, including diabetes, heart disease, depression, and high blood pressure.
Dr. Patel’s study, funded by the National Institutes of Health, was the culmination of a decade of interest in the area, she said.
Water stations and compostable or recyclable cups were placed in high-traffic areas of the schools, including playgrounds and cafeterias. The water was tested for lead, and if needed, researchers worked with school districts to remediate, Dr. Patel said in an interview.
The intervention included a kickoff assembly about the health benefits of water intake, and students who were seen drinking water with their lunches were given small prizes.
The researchers assessed body weight, height, and dietary intake of students throughout the study, including their consumption of water, sodas, fruit juices, and flavored and unflavored milk.
Promoting water didn’t lead to magical weight loss. At the start of the study, 49.5% of students in the intervention group were overweight – a figure that nudged up to 49.8% by the end of the study. In the control group, however, 47.7% of students began the study overweight – a number that climbed to 51.4% by the end of the trial (odds ratio, 0.3; P = .01), according to the researchers, who credited the increase to the lack of emphasis on opting for water over sweetened drinks.
“We were very excited the effect sizes were nearly double previous studies, which was great news,” Dr. Patel said.
Water intake began to decline at about the 15-month mark, signaling the need for more long-term, consistent education and incentive to foster lasting habits, Dr. Patel said.
The researchers noted that they were unable to collect data from eight of the target schools because of the pandemic. In addition, the study focused on schools with heavily Latino student populations, so the results might not be generalizable to other communities, they said.
Angie Cradock, a principal research scientist at the Harvard T. H. Chan School of Public Health, Boston, said the study “offers an important and practical strategy to promote student health.”
Ms. Cradock serves as deputy director of the Harvard Prevention Research Center on Nutrition and Physical Activity, which focuses on improving population nutrition, increasing physical activity, reducing obesity and chronic disease, and improving health equity.
Dr. Patel and her colleagues’ three-pronged approach of using education, promotion, and accessibility to increase student interest in drinking water could be employed at countless other schools, said Ms. Cradock, who was not involved in the study.
“Negative perceptions of tap water and drinking fountains are common,” she said. “Not all students have access to safe and appealing drinking water while at school, and this strategy seems like a recipe for success.”
Dr. Patel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Elementary schools that provide easy access to drinking water and education about its benefits may help their students maintain a healthy weight, a new study found.
Researchers examined the health and drinking habits of 1,249 children in 26 low-income, ethnically diverse elementary schools in the San Francisco Bay Area. In half of the schools, water stations were placed throughout, along with signs explaining why water is healthier than sugary drinks. In addition, assemblies were held explaining the advantages of water over sugary drinks.
That simple message seemed to have had an outsized effect. Schools with water stations had significantly fewer overweight students than the other schools by the end of the 15-month study, according to Anisha Patel, MD, MSPH, MSHS, associate professor of pediatrics at Stanford (Calif.) University, who will be presenting the findings at the Pediatric Academic Societies (PAS) 2022 Meeting, Denver.
“Sugar-sweetened beverages are a huge contributor to obesity,” Dr. Patel told this news organization. “This provides a key strategy for schools to adopt, and the time is right for this type of work – in the pandemic period we’ve seen significant increases in obesity. Investments like this could help stem that.”
According to the U.S. Centers for Disease Control and Prevention, 14.4 million children aged 2-19 years in the United States – about 19% of all kids in that age range – were obese in 2017-2018. The agency said the rate of increase in body mass index among this group nearly doubled during the COVID-19 pandemic.
Children with obesity are at higher risk for chronic health problems, including diabetes, heart disease, depression, and high blood pressure.
Dr. Patel’s study, funded by the National Institutes of Health, was the culmination of a decade of interest in the area, she said.
Water stations and compostable or recyclable cups were placed in high-traffic areas of the schools, including playgrounds and cafeterias. The water was tested for lead, and if needed, researchers worked with school districts to remediate, Dr. Patel said in an interview.
The intervention included a kickoff assembly about the health benefits of water intake, and students who were seen drinking water with their lunches were given small prizes.
The researchers assessed body weight, height, and dietary intake of students throughout the study, including their consumption of water, sodas, fruit juices, and flavored and unflavored milk.
Promoting water didn’t lead to magical weight loss. At the start of the study, 49.5% of students in the intervention group were overweight – a figure that nudged up to 49.8% by the end of the study. In the control group, however, 47.7% of students began the study overweight – a number that climbed to 51.4% by the end of the trial (odds ratio, 0.3; P = .01), according to the researchers, who credited the increase to the lack of emphasis on opting for water over sweetened drinks.
“We were very excited the effect sizes were nearly double previous studies, which was great news,” Dr. Patel said.
Water intake began to decline at about the 15-month mark, signaling the need for more long-term, consistent education and incentive to foster lasting habits, Dr. Patel said.
The researchers noted that they were unable to collect data from eight of the target schools because of the pandemic. In addition, the study focused on schools with heavily Latino student populations, so the results might not be generalizable to other communities, they said.
Angie Cradock, a principal research scientist at the Harvard T. H. Chan School of Public Health, Boston, said the study “offers an important and practical strategy to promote student health.”
Ms. Cradock serves as deputy director of the Harvard Prevention Research Center on Nutrition and Physical Activity, which focuses on improving population nutrition, increasing physical activity, reducing obesity and chronic disease, and improving health equity.
Dr. Patel and her colleagues’ three-pronged approach of using education, promotion, and accessibility to increase student interest in drinking water could be employed at countless other schools, said Ms. Cradock, who was not involved in the study.
“Negative perceptions of tap water and drinking fountains are common,” she said. “Not all students have access to safe and appealing drinking water while at school, and this strategy seems like a recipe for success.”
Dr. Patel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Elementary schools that provide easy access to drinking water and education about its benefits may help their students maintain a healthy weight, a new study found.
Researchers examined the health and drinking habits of 1,249 children in 26 low-income, ethnically diverse elementary schools in the San Francisco Bay Area. In half of the schools, water stations were placed throughout, along with signs explaining why water is healthier than sugary drinks. In addition, assemblies were held explaining the advantages of water over sugary drinks.
That simple message seemed to have had an outsized effect. Schools with water stations had significantly fewer overweight students than the other schools by the end of the 15-month study, according to Anisha Patel, MD, MSPH, MSHS, associate professor of pediatrics at Stanford (Calif.) University, who will be presenting the findings at the Pediatric Academic Societies (PAS) 2022 Meeting, Denver.
“Sugar-sweetened beverages are a huge contributor to obesity,” Dr. Patel told this news organization. “This provides a key strategy for schools to adopt, and the time is right for this type of work – in the pandemic period we’ve seen significant increases in obesity. Investments like this could help stem that.”
According to the U.S. Centers for Disease Control and Prevention, 14.4 million children aged 2-19 years in the United States – about 19% of all kids in that age range – were obese in 2017-2018. The agency said the rate of increase in body mass index among this group nearly doubled during the COVID-19 pandemic.
Children with obesity are at higher risk for chronic health problems, including diabetes, heart disease, depression, and high blood pressure.
Dr. Patel’s study, funded by the National Institutes of Health, was the culmination of a decade of interest in the area, she said.
Water stations and compostable or recyclable cups were placed in high-traffic areas of the schools, including playgrounds and cafeterias. The water was tested for lead, and if needed, researchers worked with school districts to remediate, Dr. Patel said in an interview.
The intervention included a kickoff assembly about the health benefits of water intake, and students who were seen drinking water with their lunches were given small prizes.
The researchers assessed body weight, height, and dietary intake of students throughout the study, including their consumption of water, sodas, fruit juices, and flavored and unflavored milk.
Promoting water didn’t lead to magical weight loss. At the start of the study, 49.5% of students in the intervention group were overweight – a figure that nudged up to 49.8% by the end of the study. In the control group, however, 47.7% of students began the study overweight – a number that climbed to 51.4% by the end of the trial (odds ratio, 0.3; P = .01), according to the researchers, who credited the increase to the lack of emphasis on opting for water over sweetened drinks.
“We were very excited the effect sizes were nearly double previous studies, which was great news,” Dr. Patel said.
Water intake began to decline at about the 15-month mark, signaling the need for more long-term, consistent education and incentive to foster lasting habits, Dr. Patel said.
The researchers noted that they were unable to collect data from eight of the target schools because of the pandemic. In addition, the study focused on schools with heavily Latino student populations, so the results might not be generalizable to other communities, they said.
Angie Cradock, a principal research scientist at the Harvard T. H. Chan School of Public Health, Boston, said the study “offers an important and practical strategy to promote student health.”
Ms. Cradock serves as deputy director of the Harvard Prevention Research Center on Nutrition and Physical Activity, which focuses on improving population nutrition, increasing physical activity, reducing obesity and chronic disease, and improving health equity.
Dr. Patel and her colleagues’ three-pronged approach of using education, promotion, and accessibility to increase student interest in drinking water could be employed at countless other schools, said Ms. Cradock, who was not involved in the study.
“Negative perceptions of tap water and drinking fountains are common,” she said. “Not all students have access to safe and appealing drinking water while at school, and this strategy seems like a recipe for success.”
Dr. Patel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Substance use disorders increase risk for death from COVID-19
MADRID, Spain – – compared with the general population. Such are the findings of a line of research led by Mexican psychiatrist Nora Volkow, MD, director of the U.S. National Institute on Drug Abuse (NIDA).
A pioneer in the use of brain imaging to investigate how substance use affects brain functions and one of Time magazine’s “Top 100 People Who Shape Our World,” she led the Inaugural Conference at the XXXI Congress of the Spanish Society of Clinical Pharmacology “Drugs and Actions During the Pandemic.” Dr. Volkow spoke about the effects that the current health crisis has had on drug use and the social challenges that arose from lockdowns. She also presented and discussed the results of studies being conducted at NIDA that “are aimed at reviewing what we’ve learned and what the consequences of COVID-19 have been with respect to substance abuse disorder.”
As Dr. Volkow pointed out, drugs affect much more than just the brain. “In particular, the heart, the lungs, the immune system – all of these are significantly harmed by substances like tobacco, alcohol, cocaine, and methamphetamine. This is why, since the beginning of the pandemic, we’ve been worried about seeing what consequences SARS-CoV-2 was going to have on users of these substances, especially in light of the great toll this disease takes on the respiratory system and the vascular system.”
Pulmonary ‘predisposition’ and race
Dr. Volkow and her team launched several studies to get a more thorough understanding of the link between substance abuse disorders and poor COVID-19 prognoses. One of them was based on analyses from electronic health records in the United States. The purpose was to determine COVID-19 risk and outcomes in patients based on the type of use disorder (for example, alcohol, opioid, cannabis, cocaine).
“The results showed that regardless of the drug type, all users of these substances had both a higher risk of being infected by COVID-19 and a higher death rate in comparison with the rest of the population,” said Dr. Volkow. “This surprised us, because there’s no evidence that drugs themselves make the virus more infectious. However, what the results did clearly indicate to us was that using these substances was associated with behavior that put these individuals at a greater risk for infection,” Dr. Volkow explained.
“In addition,” she continued, “using, for example, tobacco or cannabis causes inflammation in the lungs. It seems that, as a result, they end up being more vulnerable to infection by COVID. And this has consequences, above all, in terms of mortality.”
Another finding was that, among patients with substance use disorders, race had the largest effect on COVID risk. “From the very start, we saw that, compared with White individuals, Black individuals showed a much higher risk of not only getting COVID, but also dying from it,” said Dr. Volkow. “Therefore, on the one hand, our data show that drug users are more vulnerable to COVID-19 and, on the other hand, they reflect that within this group, Black individuals are even more vulnerable.”
In her presentation, Dr. Volkow drew particular attention to the impact that social surroundings have on these patients and the decisive role they played in terms of vulnerability. “It’s a very complex issue, what with the various factors at play: family, social environment. ... A person living in an at-risk situation can more easily get drugs or even prescription medication, which can also be abused.”
The psychiatrist stressed that when it comes to addictive disorders (and related questions such as prevention, treatment, and social reintegration), one of the most crucial factors has to do with the individual’s social support structures. “The studies also brought to light the role that social interaction has as an inhibitory factor with regard to drug use,” said Dr. Volkow. “And indeed, adequate adherence to treatment requires that the necessary support systems be maintained.”
In the context of the pandemic, this social aspect was also key, especially concerning the high death rate among substance use disorder patients with COVID-19. “There are very significant social determinants, such as the stigma associated with these groups – a stigma that makes these individuals more likely to hesitate to seek out treatment for diseases that may be starting to take hold, in this case COVID-19.”
On that note, Dr. Volkow emphasized the importance of treating drug addicts as though they had a chronic disease in need of treatment. “In fact, the prevalence of pathologies such as hypertension, diabetes, cancer, and dementia is much higher in these individuals than in the general population,” she said. “However, this isn’t widely known. The data reflect that not only the prevalence of these diseases, but also the severity of the symptoms, is higher, and this has a lot to do with these individuals’ reticence when it comes to reaching out for medical care. Added to that are the effects of their economic situation and other factors, such as stress (which can trigger a relapse), lack of ready access to medications, and limited access to community support or other sources of social connection.”
Opioids and COVID-19
As for drug use during the pandemic, Dr. Volkow provided context by mentioning that in the United States, the experts and authorities have spent two decades fighting the epidemic of opioid-related drug overdoses, which has caused many deaths. “And on top of this epidemic – one that we still haven’t been able to get control of – there’s the situation brought about by COVID-19. So, we had to see the consequences of a pandemic crossing paths with an epidemic.”
The United States’s epidemic of overdose deaths started with the use of opioid painkillers, medications which are overprescribed. Another issue that the United States faces is that many drugs are contaminated with fentanyl. This contamination has caused an increase in deaths.
“In the United States, fentanyl is everywhere,” said Dr. Volkow. “And what’s more concerning: almost a third of this fentanyl comes in pills that are sold as benzodiazepines. With this comes a high risk for overdose. In line with this, we saw overdose deaths among adolescents nearly double in 1 year, an increase which is likely related to these contaminated pills. It’s a risk that’s just below the surface. We’ve got to be vigilant, because this phenomenon is expected to eventually spread to Europe. After all, these pills are very cheap, hence the rapid increase in their use.”
To provide figures on drug use and overdose deaths since the beginning of the pandemic, Dr. Volkow referred to COVID-19 data provided by the National Center for Health Statistics (NCHS) at the U.S. Centers for Disease Control and Prevention. The data indicate that of the 70,630 drug overdose deaths that occurred in 2019, 49,860 involved opioids (whether prescribed or illicit). “And these numbers have continued to rise, so much so that the current situation can be classified as catastrophic – because this increase has been even greater during the pandemic due to the rise in the use of all drugs,” said Dr. Volkow.
Dr. Volkow referred to an NCHS study that looked at the period between September 2020 and September 2021, finding a 15.9% increase in the number of drug overdose deaths. A breakdown of these data shows that the highest percentage corresponds to deaths from “other psychostimulants,” primarily methamphetamines (35.7%). This category is followed by deaths involving synthetic opioids, mostly illicit fentanyl (25.8%), and deaths from cocaine (13.4%).
“These figures indicate that, for the first time in history, the United States had over 100,000 overdose deaths in 1 year,” said Dr. Volkow. “This is something that has never happened. We can only infer that the pandemic had a hand in making the overdose crisis even worse than it already was.”
As Dr. Volkow explained, policies related to handling overdoses and prescribing medications have been changed in the context of COVID-19. Addiction treatment consequently has been provided through a larger number of telehealth services, and measures such as greater access to treatment for comorbid conditions, expanded access to behavioral treatments, and the establishment of mental health hotlines have been undertaken.
Children’s cognitive development
Dr. Volkow also spoke about another of NIDA’s current subjects of research: The role that damage or compromise from drugs has on the neural circuits involved in reinforcement systems. “It’s important that we make people aware of the significance of what’s at play there, because the greatest damage that can be inflicted on the brain comes from using any type of drug during adolescence. In these cases, the likelihood of having an addictive disorder as an adult significantly increases.”
Within this framework, her team has also investigated the impact of the pandemic on the cognitive development of infants under 1 year of age. One of these studies was a pilot program in which pregnant women participated. “We found that children born during the pandemic had lower cognitive development: n = 112 versus n = 554 of those born before January 2019.”
“None of the mothers or children in the study had been infected with SARS-CoV-2,” Dr. Volkow explained. “But the results clearly reflect the negative effect of the circumstances brought about by the pandemic, especially the high level of stress, the isolation, and the lack of stimuli. Another study, currently in preprint, is based on imaging. It analyzed the impact on myelination in children not exposed to COVID-19 but born during the pandemic, compared with pre-pandemic infants. The data showed significantly reduced areas of myelin development (P < .05) in those born after 2019. And the researchers didn’t find significant differences in gestation duration or birth weight.”
The longitudinal characteristics of these studies will let us see whether a change in these individuals’ social circumstances over time also brings to light cognitive changes, even the recovery of lost or underdeveloped cognitive processes, Dr. Volkow concluded.
Dr. Volkow has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MADRID, Spain – – compared with the general population. Such are the findings of a line of research led by Mexican psychiatrist Nora Volkow, MD, director of the U.S. National Institute on Drug Abuse (NIDA).
A pioneer in the use of brain imaging to investigate how substance use affects brain functions and one of Time magazine’s “Top 100 People Who Shape Our World,” she led the Inaugural Conference at the XXXI Congress of the Spanish Society of Clinical Pharmacology “Drugs and Actions During the Pandemic.” Dr. Volkow spoke about the effects that the current health crisis has had on drug use and the social challenges that arose from lockdowns. She also presented and discussed the results of studies being conducted at NIDA that “are aimed at reviewing what we’ve learned and what the consequences of COVID-19 have been with respect to substance abuse disorder.”
As Dr. Volkow pointed out, drugs affect much more than just the brain. “In particular, the heart, the lungs, the immune system – all of these are significantly harmed by substances like tobacco, alcohol, cocaine, and methamphetamine. This is why, since the beginning of the pandemic, we’ve been worried about seeing what consequences SARS-CoV-2 was going to have on users of these substances, especially in light of the great toll this disease takes on the respiratory system and the vascular system.”
Pulmonary ‘predisposition’ and race
Dr. Volkow and her team launched several studies to get a more thorough understanding of the link between substance abuse disorders and poor COVID-19 prognoses. One of them was based on analyses from electronic health records in the United States. The purpose was to determine COVID-19 risk and outcomes in patients based on the type of use disorder (for example, alcohol, opioid, cannabis, cocaine).
“The results showed that regardless of the drug type, all users of these substances had both a higher risk of being infected by COVID-19 and a higher death rate in comparison with the rest of the population,” said Dr. Volkow. “This surprised us, because there’s no evidence that drugs themselves make the virus more infectious. However, what the results did clearly indicate to us was that using these substances was associated with behavior that put these individuals at a greater risk for infection,” Dr. Volkow explained.
“In addition,” she continued, “using, for example, tobacco or cannabis causes inflammation in the lungs. It seems that, as a result, they end up being more vulnerable to infection by COVID. And this has consequences, above all, in terms of mortality.”
Another finding was that, among patients with substance use disorders, race had the largest effect on COVID risk. “From the very start, we saw that, compared with White individuals, Black individuals showed a much higher risk of not only getting COVID, but also dying from it,” said Dr. Volkow. “Therefore, on the one hand, our data show that drug users are more vulnerable to COVID-19 and, on the other hand, they reflect that within this group, Black individuals are even more vulnerable.”
In her presentation, Dr. Volkow drew particular attention to the impact that social surroundings have on these patients and the decisive role they played in terms of vulnerability. “It’s a very complex issue, what with the various factors at play: family, social environment. ... A person living in an at-risk situation can more easily get drugs or even prescription medication, which can also be abused.”
The psychiatrist stressed that when it comes to addictive disorders (and related questions such as prevention, treatment, and social reintegration), one of the most crucial factors has to do with the individual’s social support structures. “The studies also brought to light the role that social interaction has as an inhibitory factor with regard to drug use,” said Dr. Volkow. “And indeed, adequate adherence to treatment requires that the necessary support systems be maintained.”
In the context of the pandemic, this social aspect was also key, especially concerning the high death rate among substance use disorder patients with COVID-19. “There are very significant social determinants, such as the stigma associated with these groups – a stigma that makes these individuals more likely to hesitate to seek out treatment for diseases that may be starting to take hold, in this case COVID-19.”
On that note, Dr. Volkow emphasized the importance of treating drug addicts as though they had a chronic disease in need of treatment. “In fact, the prevalence of pathologies such as hypertension, diabetes, cancer, and dementia is much higher in these individuals than in the general population,” she said. “However, this isn’t widely known. The data reflect that not only the prevalence of these diseases, but also the severity of the symptoms, is higher, and this has a lot to do with these individuals’ reticence when it comes to reaching out for medical care. Added to that are the effects of their economic situation and other factors, such as stress (which can trigger a relapse), lack of ready access to medications, and limited access to community support or other sources of social connection.”
Opioids and COVID-19
As for drug use during the pandemic, Dr. Volkow provided context by mentioning that in the United States, the experts and authorities have spent two decades fighting the epidemic of opioid-related drug overdoses, which has caused many deaths. “And on top of this epidemic – one that we still haven’t been able to get control of – there’s the situation brought about by COVID-19. So, we had to see the consequences of a pandemic crossing paths with an epidemic.”
The United States’s epidemic of overdose deaths started with the use of opioid painkillers, medications which are overprescribed. Another issue that the United States faces is that many drugs are contaminated with fentanyl. This contamination has caused an increase in deaths.
“In the United States, fentanyl is everywhere,” said Dr. Volkow. “And what’s more concerning: almost a third of this fentanyl comes in pills that are sold as benzodiazepines. With this comes a high risk for overdose. In line with this, we saw overdose deaths among adolescents nearly double in 1 year, an increase which is likely related to these contaminated pills. It’s a risk that’s just below the surface. We’ve got to be vigilant, because this phenomenon is expected to eventually spread to Europe. After all, these pills are very cheap, hence the rapid increase in their use.”
To provide figures on drug use and overdose deaths since the beginning of the pandemic, Dr. Volkow referred to COVID-19 data provided by the National Center for Health Statistics (NCHS) at the U.S. Centers for Disease Control and Prevention. The data indicate that of the 70,630 drug overdose deaths that occurred in 2019, 49,860 involved opioids (whether prescribed or illicit). “And these numbers have continued to rise, so much so that the current situation can be classified as catastrophic – because this increase has been even greater during the pandemic due to the rise in the use of all drugs,” said Dr. Volkow.
Dr. Volkow referred to an NCHS study that looked at the period between September 2020 and September 2021, finding a 15.9% increase in the number of drug overdose deaths. A breakdown of these data shows that the highest percentage corresponds to deaths from “other psychostimulants,” primarily methamphetamines (35.7%). This category is followed by deaths involving synthetic opioids, mostly illicit fentanyl (25.8%), and deaths from cocaine (13.4%).
“These figures indicate that, for the first time in history, the United States had over 100,000 overdose deaths in 1 year,” said Dr. Volkow. “This is something that has never happened. We can only infer that the pandemic had a hand in making the overdose crisis even worse than it already was.”
As Dr. Volkow explained, policies related to handling overdoses and prescribing medications have been changed in the context of COVID-19. Addiction treatment consequently has been provided through a larger number of telehealth services, and measures such as greater access to treatment for comorbid conditions, expanded access to behavioral treatments, and the establishment of mental health hotlines have been undertaken.
Children’s cognitive development
Dr. Volkow also spoke about another of NIDA’s current subjects of research: The role that damage or compromise from drugs has on the neural circuits involved in reinforcement systems. “It’s important that we make people aware of the significance of what’s at play there, because the greatest damage that can be inflicted on the brain comes from using any type of drug during adolescence. In these cases, the likelihood of having an addictive disorder as an adult significantly increases.”
Within this framework, her team has also investigated the impact of the pandemic on the cognitive development of infants under 1 year of age. One of these studies was a pilot program in which pregnant women participated. “We found that children born during the pandemic had lower cognitive development: n = 112 versus n = 554 of those born before January 2019.”
“None of the mothers or children in the study had been infected with SARS-CoV-2,” Dr. Volkow explained. “But the results clearly reflect the negative effect of the circumstances brought about by the pandemic, especially the high level of stress, the isolation, and the lack of stimuli. Another study, currently in preprint, is based on imaging. It analyzed the impact on myelination in children not exposed to COVID-19 but born during the pandemic, compared with pre-pandemic infants. The data showed significantly reduced areas of myelin development (P < .05) in those born after 2019. And the researchers didn’t find significant differences in gestation duration or birth weight.”
The longitudinal characteristics of these studies will let us see whether a change in these individuals’ social circumstances over time also brings to light cognitive changes, even the recovery of lost or underdeveloped cognitive processes, Dr. Volkow concluded.
Dr. Volkow has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MADRID, Spain – – compared with the general population. Such are the findings of a line of research led by Mexican psychiatrist Nora Volkow, MD, director of the U.S. National Institute on Drug Abuse (NIDA).
A pioneer in the use of brain imaging to investigate how substance use affects brain functions and one of Time magazine’s “Top 100 People Who Shape Our World,” she led the Inaugural Conference at the XXXI Congress of the Spanish Society of Clinical Pharmacology “Drugs and Actions During the Pandemic.” Dr. Volkow spoke about the effects that the current health crisis has had on drug use and the social challenges that arose from lockdowns. She also presented and discussed the results of studies being conducted at NIDA that “are aimed at reviewing what we’ve learned and what the consequences of COVID-19 have been with respect to substance abuse disorder.”
As Dr. Volkow pointed out, drugs affect much more than just the brain. “In particular, the heart, the lungs, the immune system – all of these are significantly harmed by substances like tobacco, alcohol, cocaine, and methamphetamine. This is why, since the beginning of the pandemic, we’ve been worried about seeing what consequences SARS-CoV-2 was going to have on users of these substances, especially in light of the great toll this disease takes on the respiratory system and the vascular system.”
Pulmonary ‘predisposition’ and race
Dr. Volkow and her team launched several studies to get a more thorough understanding of the link between substance abuse disorders and poor COVID-19 prognoses. One of them was based on analyses from electronic health records in the United States. The purpose was to determine COVID-19 risk and outcomes in patients based on the type of use disorder (for example, alcohol, opioid, cannabis, cocaine).
“The results showed that regardless of the drug type, all users of these substances had both a higher risk of being infected by COVID-19 and a higher death rate in comparison with the rest of the population,” said Dr. Volkow. “This surprised us, because there’s no evidence that drugs themselves make the virus more infectious. However, what the results did clearly indicate to us was that using these substances was associated with behavior that put these individuals at a greater risk for infection,” Dr. Volkow explained.
“In addition,” she continued, “using, for example, tobacco or cannabis causes inflammation in the lungs. It seems that, as a result, they end up being more vulnerable to infection by COVID. And this has consequences, above all, in terms of mortality.”
Another finding was that, among patients with substance use disorders, race had the largest effect on COVID risk. “From the very start, we saw that, compared with White individuals, Black individuals showed a much higher risk of not only getting COVID, but also dying from it,” said Dr. Volkow. “Therefore, on the one hand, our data show that drug users are more vulnerable to COVID-19 and, on the other hand, they reflect that within this group, Black individuals are even more vulnerable.”
In her presentation, Dr. Volkow drew particular attention to the impact that social surroundings have on these patients and the decisive role they played in terms of vulnerability. “It’s a very complex issue, what with the various factors at play: family, social environment. ... A person living in an at-risk situation can more easily get drugs or even prescription medication, which can also be abused.”
The psychiatrist stressed that when it comes to addictive disorders (and related questions such as prevention, treatment, and social reintegration), one of the most crucial factors has to do with the individual’s social support structures. “The studies also brought to light the role that social interaction has as an inhibitory factor with regard to drug use,” said Dr. Volkow. “And indeed, adequate adherence to treatment requires that the necessary support systems be maintained.”
In the context of the pandemic, this social aspect was also key, especially concerning the high death rate among substance use disorder patients with COVID-19. “There are very significant social determinants, such as the stigma associated with these groups – a stigma that makes these individuals more likely to hesitate to seek out treatment for diseases that may be starting to take hold, in this case COVID-19.”
On that note, Dr. Volkow emphasized the importance of treating drug addicts as though they had a chronic disease in need of treatment. “In fact, the prevalence of pathologies such as hypertension, diabetes, cancer, and dementia is much higher in these individuals than in the general population,” she said. “However, this isn’t widely known. The data reflect that not only the prevalence of these diseases, but also the severity of the symptoms, is higher, and this has a lot to do with these individuals’ reticence when it comes to reaching out for medical care. Added to that are the effects of their economic situation and other factors, such as stress (which can trigger a relapse), lack of ready access to medications, and limited access to community support or other sources of social connection.”
Opioids and COVID-19
As for drug use during the pandemic, Dr. Volkow provided context by mentioning that in the United States, the experts and authorities have spent two decades fighting the epidemic of opioid-related drug overdoses, which has caused many deaths. “And on top of this epidemic – one that we still haven’t been able to get control of – there’s the situation brought about by COVID-19. So, we had to see the consequences of a pandemic crossing paths with an epidemic.”
The United States’s epidemic of overdose deaths started with the use of opioid painkillers, medications which are overprescribed. Another issue that the United States faces is that many drugs are contaminated with fentanyl. This contamination has caused an increase in deaths.
“In the United States, fentanyl is everywhere,” said Dr. Volkow. “And what’s more concerning: almost a third of this fentanyl comes in pills that are sold as benzodiazepines. With this comes a high risk for overdose. In line with this, we saw overdose deaths among adolescents nearly double in 1 year, an increase which is likely related to these contaminated pills. It’s a risk that’s just below the surface. We’ve got to be vigilant, because this phenomenon is expected to eventually spread to Europe. After all, these pills are very cheap, hence the rapid increase in their use.”
To provide figures on drug use and overdose deaths since the beginning of the pandemic, Dr. Volkow referred to COVID-19 data provided by the National Center for Health Statistics (NCHS) at the U.S. Centers for Disease Control and Prevention. The data indicate that of the 70,630 drug overdose deaths that occurred in 2019, 49,860 involved opioids (whether prescribed or illicit). “And these numbers have continued to rise, so much so that the current situation can be classified as catastrophic – because this increase has been even greater during the pandemic due to the rise in the use of all drugs,” said Dr. Volkow.
Dr. Volkow referred to an NCHS study that looked at the period between September 2020 and September 2021, finding a 15.9% increase in the number of drug overdose deaths. A breakdown of these data shows that the highest percentage corresponds to deaths from “other psychostimulants,” primarily methamphetamines (35.7%). This category is followed by deaths involving synthetic opioids, mostly illicit fentanyl (25.8%), and deaths from cocaine (13.4%).
“These figures indicate that, for the first time in history, the United States had over 100,000 overdose deaths in 1 year,” said Dr. Volkow. “This is something that has never happened. We can only infer that the pandemic had a hand in making the overdose crisis even worse than it already was.”
As Dr. Volkow explained, policies related to handling overdoses and prescribing medications have been changed in the context of COVID-19. Addiction treatment consequently has been provided through a larger number of telehealth services, and measures such as greater access to treatment for comorbid conditions, expanded access to behavioral treatments, and the establishment of mental health hotlines have been undertaken.
Children’s cognitive development
Dr. Volkow also spoke about another of NIDA’s current subjects of research: The role that damage or compromise from drugs has on the neural circuits involved in reinforcement systems. “It’s important that we make people aware of the significance of what’s at play there, because the greatest damage that can be inflicted on the brain comes from using any type of drug during adolescence. In these cases, the likelihood of having an addictive disorder as an adult significantly increases.”
Within this framework, her team has also investigated the impact of the pandemic on the cognitive development of infants under 1 year of age. One of these studies was a pilot program in which pregnant women participated. “We found that children born during the pandemic had lower cognitive development: n = 112 versus n = 554 of those born before January 2019.”
“None of the mothers or children in the study had been infected with SARS-CoV-2,” Dr. Volkow explained. “But the results clearly reflect the negative effect of the circumstances brought about by the pandemic, especially the high level of stress, the isolation, and the lack of stimuli. Another study, currently in preprint, is based on imaging. It analyzed the impact on myelination in children not exposed to COVID-19 but born during the pandemic, compared with pre-pandemic infants. The data showed significantly reduced areas of myelin development (P < .05) in those born after 2019. And the researchers didn’t find significant differences in gestation duration or birth weight.”
The longitudinal characteristics of these studies will let us see whether a change in these individuals’ social circumstances over time also brings to light cognitive changes, even the recovery of lost or underdeveloped cognitive processes, Dr. Volkow concluded.
Dr. Volkow has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNUAL MEETING OF SPANISH SOCIETY OF CLINICAL PHARMACOLOGY
COVID-19 again the third-leading cause of U.S. deaths
the Centers for Disease Control and Prevention said April 22.
About 693,000 people died of heart disease in 2021, with 605,000 dying of cancer and 415,000 of COVID, the CDC said, citing provisional data that might be updated later.
Unintentional injuries were the fourth-leading cause of death, increasing to 219,000 in 2021 from 201,000 in 2020. Influenza and pneumonia dropped out of the top 10 leading causes of death and suicide moved into 10th place.
Overall, about 3,458,697 deaths were reported in the United States in 2021. The age-adjusted death rate was 841.6 deaths per 100,000 people, an increase of 0.7% from 2020. The 2021 death rate was the highest since 2003, the CDC said.
The overall number of COVID deaths in 2021 increased around 20% over 2020, when around 384,000 people died from the virus, the CDC said. COVID deaths in 2021 peaked for the weeks ending Jan. 16 and Sept. 11, following holiday periods.
The demographics of COVID mortality changed slightly, the CDC said in a second report.
Blacks accounted for 13.3% of COVID deaths in 2021 and Hispanics 16.5%, down several percentage points from 2020, the CDC said. Asians made up 3.1% of COVID deaths for 2021, a drop from 3.6% in 2020. White people accounted for 65.2% of COVID deaths in 2021, an increase from 59.6% in 2020.
Non-Hispanic American Indian/Alaskan Native and non-Hispanic Black or African American had the highest overall death rates for COVID, the CDC said.
Breaking the data down by age, the number of COVID deaths among people aged 75 years and older dropped to 178,000 in 2021 from around 207,000 in 2020. The numbers went up in other age groups. Among people aged 65-75, about 101,000 died of COVID in 2021, up from around 76,000 in 2020.
“The results of both studies highlight the need for greater effort to implement effective interventions,” the CDC said in a statement. “We must work to ensure equal treatment in all communities in proportion to their need for effective interventions that can prevent excess COVID-19 deaths.”
Since the pandemic began, about 991,000 people in the United States have died from COVID-related causes, the most among all nations in the world.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Prevention said April 22.
About 693,000 people died of heart disease in 2021, with 605,000 dying of cancer and 415,000 of COVID, the CDC said, citing provisional data that might be updated later.
Unintentional injuries were the fourth-leading cause of death, increasing to 219,000 in 2021 from 201,000 in 2020. Influenza and pneumonia dropped out of the top 10 leading causes of death and suicide moved into 10th place.
Overall, about 3,458,697 deaths were reported in the United States in 2021. The age-adjusted death rate was 841.6 deaths per 100,000 people, an increase of 0.7% from 2020. The 2021 death rate was the highest since 2003, the CDC said.
The overall number of COVID deaths in 2021 increased around 20% over 2020, when around 384,000 people died from the virus, the CDC said. COVID deaths in 2021 peaked for the weeks ending Jan. 16 and Sept. 11, following holiday periods.
The demographics of COVID mortality changed slightly, the CDC said in a second report.
Blacks accounted for 13.3% of COVID deaths in 2021 and Hispanics 16.5%, down several percentage points from 2020, the CDC said. Asians made up 3.1% of COVID deaths for 2021, a drop from 3.6% in 2020. White people accounted for 65.2% of COVID deaths in 2021, an increase from 59.6% in 2020.
Non-Hispanic American Indian/Alaskan Native and non-Hispanic Black or African American had the highest overall death rates for COVID, the CDC said.
Breaking the data down by age, the number of COVID deaths among people aged 75 years and older dropped to 178,000 in 2021 from around 207,000 in 2020. The numbers went up in other age groups. Among people aged 65-75, about 101,000 died of COVID in 2021, up from around 76,000 in 2020.
“The results of both studies highlight the need for greater effort to implement effective interventions,” the CDC said in a statement. “We must work to ensure equal treatment in all communities in proportion to their need for effective interventions that can prevent excess COVID-19 deaths.”
Since the pandemic began, about 991,000 people in the United States have died from COVID-related causes, the most among all nations in the world.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Prevention said April 22.
About 693,000 people died of heart disease in 2021, with 605,000 dying of cancer and 415,000 of COVID, the CDC said, citing provisional data that might be updated later.
Unintentional injuries were the fourth-leading cause of death, increasing to 219,000 in 2021 from 201,000 in 2020. Influenza and pneumonia dropped out of the top 10 leading causes of death and suicide moved into 10th place.
Overall, about 3,458,697 deaths were reported in the United States in 2021. The age-adjusted death rate was 841.6 deaths per 100,000 people, an increase of 0.7% from 2020. The 2021 death rate was the highest since 2003, the CDC said.
The overall number of COVID deaths in 2021 increased around 20% over 2020, when around 384,000 people died from the virus, the CDC said. COVID deaths in 2021 peaked for the weeks ending Jan. 16 and Sept. 11, following holiday periods.
The demographics of COVID mortality changed slightly, the CDC said in a second report.
Blacks accounted for 13.3% of COVID deaths in 2021 and Hispanics 16.5%, down several percentage points from 2020, the CDC said. Asians made up 3.1% of COVID deaths for 2021, a drop from 3.6% in 2020. White people accounted for 65.2% of COVID deaths in 2021, an increase from 59.6% in 2020.
Non-Hispanic American Indian/Alaskan Native and non-Hispanic Black or African American had the highest overall death rates for COVID, the CDC said.
Breaking the data down by age, the number of COVID deaths among people aged 75 years and older dropped to 178,000 in 2021 from around 207,000 in 2020. The numbers went up in other age groups. Among people aged 65-75, about 101,000 died of COVID in 2021, up from around 76,000 in 2020.
“The results of both studies highlight the need for greater effort to implement effective interventions,” the CDC said in a statement. “We must work to ensure equal treatment in all communities in proportion to their need for effective interventions that can prevent excess COVID-19 deaths.”
Since the pandemic began, about 991,000 people in the United States have died from COVID-related causes, the most among all nations in the world.
A version of this article first appeared on WebMD.com.
FROM THE MMWR








