User login
Early PT for lower back pain sends fewer patients to specialists
The study found that patients who were referred to physical therapists within 2 weeks of seeing their physicians for LBP were significantly less likely to make visits to a chiropractor, pain specialist, or orthopedist.
Patients also filed fewer claims for advanced imaging or epidural steroid injections and were half as likely to visit an emergency department (ED) within 30 days compared with those who did not start early physical therapy (PT), according to the study, published in BMC Health Services Research.
“Some lower back pain resolves itself, but often, that recovery is incomplete, leading to increased health care and opioid use,” said Richard L. Skolasky Jr., ScD, director of the Spine Outcomes Research Center at Johns Hopkins Medicine, Baltimore, and a coauthor of the study. “Our hope is this study helps more primary care physicians embrace nonpharmacologic, first-line treatments.”
LBP accounts for an estimated $1.8 billion annually in health care costs among the patients who do not receive surgery for the condition, according to a 2019 JAMA analysis of commercial insurance and Medicare claims. In addition, LBP accounts for approximately 2.7 million ED visits annually, a 2010 study published in Spine showed.
Dr. Skolasky and his colleagues assessed 980,000 outpatient claims over a period of almost 4 years that ended in 2014. The researchers used Truven MarketScan, a group of U.S.-based administrative commercial health care insurance claims databases. Patients who had a history of conditions that cause LBP, such as endometriosis and spinal fracture, were excluded from the analysis. Approximately 11% of patients in the total sample received early PT, defined as PT received within 2 weeks of their initial visit to a primary care clinician.
After adjustment for sex, age, and Charlson Morbidity Index, patients who received PT were about half as likely as were those who didn’t to see chiropractor or a pain specialist or have an ED visit within 30 days of their initial appointment. They were about one-third as likely to receive an epidural steroid injection, and they were 43% less likely to have claims for advanced imaging, according to the researchers (P < .001 for all).
In addition, the cost of claims was lower for patients who received early PT ($747 vs. $799), the researchers found.
The effects diminished somewhat over time but remained statistically significant.
At 1 year, patients who received early PT had slightly higher health care costs than did those who did not undergo PT ($2,588 vs. $2,510). Dr. Skolasky hypothesized that the increase was attributable to therapy visits and not having as many specialist visits. He said additional research could investigate whether early PT reduces the health care costs associated with LBP over a longer period.
“Physical therapy addresses a patient’s current pain and physical limitations and arms them with resources, exercises, and nonpharmacologic ways to deal with recurrences,” Dr. Skolasky said in an interview. “If we can follow patients even longer than a year, we may see a longer-term reduction in cost.”
Michael Knight, MD, associate chief quality and population health officer at George Washington University Medical Faculty Associates, Washington, said he refers patients to physical therapists if their pain has not resolved within 2 weeks of stretching at home and taking over-the-counter analgesics.
Dr. Knight recalled one patient who had strained her back doing yard work. When home exercises did not help, Dr. Knight referred her to a physical therapist, who created a customized treatment plan. Within 4 weeks, her condition had improved.
“She was then able to take what she learned and continue those exercises at home,” Dr. Knight said. “She got better, and we avoided MRI costs for her and the health care system.”
Dr. Skolasky and his fellow researchers found significant regional differences in the number of patients referred for early PT. The odds of PT utilization within 90 days after the onset of LBP were 1.6 times higher in the Northeast and 0.82 times lower in the South.
“There are health care deserts,” Dr. Skolasky said. “This study should spark a conversation about the inadequacy of distribution of physical resources to meet the needs of patients with LBP.”
Dr. Skolasky said telehealth could be one option for serving patients in these health care deserts – including those with LBP. He has conducted several studies that concluded that patients benefit from and are happy with telehealth PT.
Dr. Knight said Dr. Skolasky’s study will help patients better understand their options.
“Sometimes patients have an expectation – they want an MRI or pain medication when it’s not necessary,” he said. “This kind of evidence helps strengthen our recommendation for early intervention that really can help.”
The study was supported by a grant from the National Institutes of Health’s National Institute on Aging. Dr. Skolasky reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study found that patients who were referred to physical therapists within 2 weeks of seeing their physicians for LBP were significantly less likely to make visits to a chiropractor, pain specialist, or orthopedist.
Patients also filed fewer claims for advanced imaging or epidural steroid injections and were half as likely to visit an emergency department (ED) within 30 days compared with those who did not start early physical therapy (PT), according to the study, published in BMC Health Services Research.
“Some lower back pain resolves itself, but often, that recovery is incomplete, leading to increased health care and opioid use,” said Richard L. Skolasky Jr., ScD, director of the Spine Outcomes Research Center at Johns Hopkins Medicine, Baltimore, and a coauthor of the study. “Our hope is this study helps more primary care physicians embrace nonpharmacologic, first-line treatments.”
LBP accounts for an estimated $1.8 billion annually in health care costs among the patients who do not receive surgery for the condition, according to a 2019 JAMA analysis of commercial insurance and Medicare claims. In addition, LBP accounts for approximately 2.7 million ED visits annually, a 2010 study published in Spine showed.
Dr. Skolasky and his colleagues assessed 980,000 outpatient claims over a period of almost 4 years that ended in 2014. The researchers used Truven MarketScan, a group of U.S.-based administrative commercial health care insurance claims databases. Patients who had a history of conditions that cause LBP, such as endometriosis and spinal fracture, were excluded from the analysis. Approximately 11% of patients in the total sample received early PT, defined as PT received within 2 weeks of their initial visit to a primary care clinician.
After adjustment for sex, age, and Charlson Morbidity Index, patients who received PT were about half as likely as were those who didn’t to see chiropractor or a pain specialist or have an ED visit within 30 days of their initial appointment. They were about one-third as likely to receive an epidural steroid injection, and they were 43% less likely to have claims for advanced imaging, according to the researchers (P < .001 for all).
In addition, the cost of claims was lower for patients who received early PT ($747 vs. $799), the researchers found.
The effects diminished somewhat over time but remained statistically significant.
At 1 year, patients who received early PT had slightly higher health care costs than did those who did not undergo PT ($2,588 vs. $2,510). Dr. Skolasky hypothesized that the increase was attributable to therapy visits and not having as many specialist visits. He said additional research could investigate whether early PT reduces the health care costs associated with LBP over a longer period.
“Physical therapy addresses a patient’s current pain and physical limitations and arms them with resources, exercises, and nonpharmacologic ways to deal with recurrences,” Dr. Skolasky said in an interview. “If we can follow patients even longer than a year, we may see a longer-term reduction in cost.”
Michael Knight, MD, associate chief quality and population health officer at George Washington University Medical Faculty Associates, Washington, said he refers patients to physical therapists if their pain has not resolved within 2 weeks of stretching at home and taking over-the-counter analgesics.
Dr. Knight recalled one patient who had strained her back doing yard work. When home exercises did not help, Dr. Knight referred her to a physical therapist, who created a customized treatment plan. Within 4 weeks, her condition had improved.
“She was then able to take what she learned and continue those exercises at home,” Dr. Knight said. “She got better, and we avoided MRI costs for her and the health care system.”
Dr. Skolasky and his fellow researchers found significant regional differences in the number of patients referred for early PT. The odds of PT utilization within 90 days after the onset of LBP were 1.6 times higher in the Northeast and 0.82 times lower in the South.
“There are health care deserts,” Dr. Skolasky said. “This study should spark a conversation about the inadequacy of distribution of physical resources to meet the needs of patients with LBP.”
Dr. Skolasky said telehealth could be one option for serving patients in these health care deserts – including those with LBP. He has conducted several studies that concluded that patients benefit from and are happy with telehealth PT.
Dr. Knight said Dr. Skolasky’s study will help patients better understand their options.
“Sometimes patients have an expectation – they want an MRI or pain medication when it’s not necessary,” he said. “This kind of evidence helps strengthen our recommendation for early intervention that really can help.”
The study was supported by a grant from the National Institutes of Health’s National Institute on Aging. Dr. Skolasky reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study found that patients who were referred to physical therapists within 2 weeks of seeing their physicians for LBP were significantly less likely to make visits to a chiropractor, pain specialist, or orthopedist.
Patients also filed fewer claims for advanced imaging or epidural steroid injections and were half as likely to visit an emergency department (ED) within 30 days compared with those who did not start early physical therapy (PT), according to the study, published in BMC Health Services Research.
“Some lower back pain resolves itself, but often, that recovery is incomplete, leading to increased health care and opioid use,” said Richard L. Skolasky Jr., ScD, director of the Spine Outcomes Research Center at Johns Hopkins Medicine, Baltimore, and a coauthor of the study. “Our hope is this study helps more primary care physicians embrace nonpharmacologic, first-line treatments.”
LBP accounts for an estimated $1.8 billion annually in health care costs among the patients who do not receive surgery for the condition, according to a 2019 JAMA analysis of commercial insurance and Medicare claims. In addition, LBP accounts for approximately 2.7 million ED visits annually, a 2010 study published in Spine showed.
Dr. Skolasky and his colleagues assessed 980,000 outpatient claims over a period of almost 4 years that ended in 2014. The researchers used Truven MarketScan, a group of U.S.-based administrative commercial health care insurance claims databases. Patients who had a history of conditions that cause LBP, such as endometriosis and spinal fracture, were excluded from the analysis. Approximately 11% of patients in the total sample received early PT, defined as PT received within 2 weeks of their initial visit to a primary care clinician.
After adjustment for sex, age, and Charlson Morbidity Index, patients who received PT were about half as likely as were those who didn’t to see chiropractor or a pain specialist or have an ED visit within 30 days of their initial appointment. They were about one-third as likely to receive an epidural steroid injection, and they were 43% less likely to have claims for advanced imaging, according to the researchers (P < .001 for all).
In addition, the cost of claims was lower for patients who received early PT ($747 vs. $799), the researchers found.
The effects diminished somewhat over time but remained statistically significant.
At 1 year, patients who received early PT had slightly higher health care costs than did those who did not undergo PT ($2,588 vs. $2,510). Dr. Skolasky hypothesized that the increase was attributable to therapy visits and not having as many specialist visits. He said additional research could investigate whether early PT reduces the health care costs associated with LBP over a longer period.
“Physical therapy addresses a patient’s current pain and physical limitations and arms them with resources, exercises, and nonpharmacologic ways to deal with recurrences,” Dr. Skolasky said in an interview. “If we can follow patients even longer than a year, we may see a longer-term reduction in cost.”
Michael Knight, MD, associate chief quality and population health officer at George Washington University Medical Faculty Associates, Washington, said he refers patients to physical therapists if their pain has not resolved within 2 weeks of stretching at home and taking over-the-counter analgesics.
Dr. Knight recalled one patient who had strained her back doing yard work. When home exercises did not help, Dr. Knight referred her to a physical therapist, who created a customized treatment plan. Within 4 weeks, her condition had improved.
“She was then able to take what she learned and continue those exercises at home,” Dr. Knight said. “She got better, and we avoided MRI costs for her and the health care system.”
Dr. Skolasky and his fellow researchers found significant regional differences in the number of patients referred for early PT. The odds of PT utilization within 90 days after the onset of LBP were 1.6 times higher in the Northeast and 0.82 times lower in the South.
“There are health care deserts,” Dr. Skolasky said. “This study should spark a conversation about the inadequacy of distribution of physical resources to meet the needs of patients with LBP.”
Dr. Skolasky said telehealth could be one option for serving patients in these health care deserts – including those with LBP. He has conducted several studies that concluded that patients benefit from and are happy with telehealth PT.
Dr. Knight said Dr. Skolasky’s study will help patients better understand their options.
“Sometimes patients have an expectation – they want an MRI or pain medication when it’s not necessary,” he said. “This kind of evidence helps strengthen our recommendation for early intervention that really can help.”
The study was supported by a grant from the National Institutes of Health’s National Institute on Aging. Dr. Skolasky reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Commentary: Comparing Migraine Treatments, August 2022
Migraine is a unique neurologic condition, in that a person can't prove they have it and there are few objective tools neurologists have to guide their diagnostic process. The recognition of the role of the vasoactive peptide calcitonin gene-related peptide (CGRP) in the 1990s changed the way many researchers and clinicians conceptualized migraine. Subsequent studies have used CGRP as a human model for migraine, and most recently pituitary adenylate cyclase–activating polypeptide 38 (PACAP-38) has also been recognized for its important role in migraine propagation. All of the existing data have been in adults, and no studies until now have specifically investigated the presence of these peptides in children with migraine.
Pediatric migraine is unique in a number of ways. Children with migraine present less unilaterally, the duration of their attacks is typically shorter, and the associated symptoms can often be more prominent than the headache pain during an attack. There are unique pediatric migraine subtypes that are exceptionally rare in adults, such as periodic paralysis attacks and abdominal migraine. For this reason, it is not entirely clear whether the same biomarkers of disease in adults would also be present in the pediatric population.
In the study by Liu and colleagues, the investigators enrolled 76 pediatric patients with migraine (the diagnosis was confirmed by at least two neurologists). Patients were excluded if there was any analgesic medication use over the past 2 months; if there was concern for secondary headache; or any underlying mood disorders, congenital disease, or other major medical conditions. An additional 77 controls were matched for age and sex. Blood was collected from all participants after an 8-hour fast to avoid collecting after potentially ingesting a food trigger. Blood samples were obtained during an ictal period (within 8 hours of a migraine attack) as well as interictally (not taken if the participant had a migraine attack within the past 24 hours).
The plasma CGRP and PACAP-38 levels were significantly higher in pediatric patients with migraine than in those without a migraine history, in both the ictal state and the interictal state. Among patients with migraine, there was a nonsignificant trend toward a higher CGRP level in the ictal phase, and no difference in these phases with PACAP-38. There was no difference in the CGRP or PACAP-38 levels between participants with and those without aura. When different aura groups were compared (with the participants separated on the basis of a history of motor vs vision vs sensory aura), no difference was seen among the different aura groups. Binary logistic regression testing and analysis of variance also showed that CGRP and PACAP-38 are independent risk factors for pediatric migraine, and specific levels of each were associated with an 11 and a 13 times increased risk, respectively.
Biomarker testing is still not clinically performed for migraine either in adults or children. This is primarily due to cost and the fact that most commercially available laboratories do not currently offer these tests. The results above do shed additional light on migraine pathogenesis and indicate that the phenotypic differences seen in pediatric migraine are less likely related to differences in brain function in children.
Levetiracetam is a commonly used antiepileptic medication. Prior studies have investigated the use of this medication for migraine, both acutely and preventively. Other antiepileptic medications have been shown to be very effective for both of these indications. Topiramate and valproic acid are both commonly used for migraine: topiramate primarily preventively and valproic acid both for prevention and, commonly in its intravenous form, for acute treatment. Levetiracetam is currently not commonly used for migraine, although some institutions will use the intravenous formulation for severe refractory status migrainosus.
Evers and colleagues investigated the open label use of levetiracetam for migraine prevention at a dose of 1000 mg twice daily in a small population of 50 persons. The study participants were started at a dose of 500 mg twice daily for 4 weeks, then increased to 1000 mg twice daily for a total of 12 weeks. The primary endpoint was migraine attack frequency during the last 4 weeks of treatment.
A 50% reduction in headache frequency was seen in 46% of the enrolled participants. The most common reported side effects were sedation, nausea, and weight gain, as well as cognitive change (five patients dropped out of the study owing to intolerance of the treatment). A post hoc comparison between the patients with and without response to levetiracetam revealed that those who responded were those with a less refractory history — they had tried fewer medications and were using fewer acute medications as well.
The antiepileptic class of preventive migraine medications is notorious for issues with tolerance. Among the antiepileptic medications, levetiracetam is commonly used but also commonly stopped owing to mood and cognitive complaints. Although the researchers here do show early evidence for a moderate amount of efficacy for treating migraine, the fact that there are now more migraine-specific preventive medications that are better tolerated and overall more efficacious make choosing levetiracetam for prevention less necessary.
Now that there are multiple classes of migraine-specific acute medications, the outstanding question remains: What are the potential benefits and drawbacks for the use of triptans compared with the oral CGRP receptor antagonists (gepants)? Most obviously, triptan medications are contraindicated in patients with significant vascular risk factors; however, what is not known is whether some of the other adverse events associated with triptans are more or less prominent with gepant use. Lee and colleagues conducted a meta-analysis of 15 studies to review this data.
A previous meta-analysis demonstrated that oral CGRP receptor antagonists are more effective than placebo, but less effective than triptans against acute migraine. The most common intolerances for gepants are nausea, somnolence, and dry mouth, but the safety and tolerability of gepants have not been compared with that of triptans. These authors pooled the data on five gepant medications (BI44370TA, MK-3207, rimegepant, telcagepant, and ubrogepant). The primary outcome was incidence of treatment-related adverse events and the secondary outcome was the incidence of the specific intolerances of diarrhea, dizziness, dry mouth, fatigue, nausea, paresthesia, somnolence, upper abdominal pain, and vomiting.
Compared with placebo, the relative risk for any adverse event was found to be low, at 1.15, and the relative risk for treatment-related adverse events was only slightly higher, at 1.18. Gepants were found to be significantly more associated with an increased risk for fatigue, nausea, and somnolence vs placebo. Compared with triptans, the CGRP antagonists were associated with significantly less treatment-related adverse events as well as any adverse event. There was no significant difference in the incidence of diarrhea, nausea, and vomiting between the two groups.
This study helps elucidate some of the differences between the two classes of migraine-specific acute medications. As noted above, a prior meta-analysis did reveal some benefits with the triptan class, specifically better effectiveness. When choosing a better-tolerated medication for your patients, you may want to consider a gepant; when considering a stronger or more potent option, you might stick with a triptan.
Migraine is a unique neurologic condition, in that a person can't prove they have it and there are few objective tools neurologists have to guide their diagnostic process. The recognition of the role of the vasoactive peptide calcitonin gene-related peptide (CGRP) in the 1990s changed the way many researchers and clinicians conceptualized migraine. Subsequent studies have used CGRP as a human model for migraine, and most recently pituitary adenylate cyclase–activating polypeptide 38 (PACAP-38) has also been recognized for its important role in migraine propagation. All of the existing data have been in adults, and no studies until now have specifically investigated the presence of these peptides in children with migraine.
Pediatric migraine is unique in a number of ways. Children with migraine present less unilaterally, the duration of their attacks is typically shorter, and the associated symptoms can often be more prominent than the headache pain during an attack. There are unique pediatric migraine subtypes that are exceptionally rare in adults, such as periodic paralysis attacks and abdominal migraine. For this reason, it is not entirely clear whether the same biomarkers of disease in adults would also be present in the pediatric population.
In the study by Liu and colleagues, the investigators enrolled 76 pediatric patients with migraine (the diagnosis was confirmed by at least two neurologists). Patients were excluded if there was any analgesic medication use over the past 2 months; if there was concern for secondary headache; or any underlying mood disorders, congenital disease, or other major medical conditions. An additional 77 controls were matched for age and sex. Blood was collected from all participants after an 8-hour fast to avoid collecting after potentially ingesting a food trigger. Blood samples were obtained during an ictal period (within 8 hours of a migraine attack) as well as interictally (not taken if the participant had a migraine attack within the past 24 hours).
The plasma CGRP and PACAP-38 levels were significantly higher in pediatric patients with migraine than in those without a migraine history, in both the ictal state and the interictal state. Among patients with migraine, there was a nonsignificant trend toward a higher CGRP level in the ictal phase, and no difference in these phases with PACAP-38. There was no difference in the CGRP or PACAP-38 levels between participants with and those without aura. When different aura groups were compared (with the participants separated on the basis of a history of motor vs vision vs sensory aura), no difference was seen among the different aura groups. Binary logistic regression testing and analysis of variance also showed that CGRP and PACAP-38 are independent risk factors for pediatric migraine, and specific levels of each were associated with an 11 and a 13 times increased risk, respectively.
Biomarker testing is still not clinically performed for migraine either in adults or children. This is primarily due to cost and the fact that most commercially available laboratories do not currently offer these tests. The results above do shed additional light on migraine pathogenesis and indicate that the phenotypic differences seen in pediatric migraine are less likely related to differences in brain function in children.
Levetiracetam is a commonly used antiepileptic medication. Prior studies have investigated the use of this medication for migraine, both acutely and preventively. Other antiepileptic medications have been shown to be very effective for both of these indications. Topiramate and valproic acid are both commonly used for migraine: topiramate primarily preventively and valproic acid both for prevention and, commonly in its intravenous form, for acute treatment. Levetiracetam is currently not commonly used for migraine, although some institutions will use the intravenous formulation for severe refractory status migrainosus.
Evers and colleagues investigated the open label use of levetiracetam for migraine prevention at a dose of 1000 mg twice daily in a small population of 50 persons. The study participants were started at a dose of 500 mg twice daily for 4 weeks, then increased to 1000 mg twice daily for a total of 12 weeks. The primary endpoint was migraine attack frequency during the last 4 weeks of treatment.
A 50% reduction in headache frequency was seen in 46% of the enrolled participants. The most common reported side effects were sedation, nausea, and weight gain, as well as cognitive change (five patients dropped out of the study owing to intolerance of the treatment). A post hoc comparison between the patients with and without response to levetiracetam revealed that those who responded were those with a less refractory history — they had tried fewer medications and were using fewer acute medications as well.
The antiepileptic class of preventive migraine medications is notorious for issues with tolerance. Among the antiepileptic medications, levetiracetam is commonly used but also commonly stopped owing to mood and cognitive complaints. Although the researchers here do show early evidence for a moderate amount of efficacy for treating migraine, the fact that there are now more migraine-specific preventive medications that are better tolerated and overall more efficacious make choosing levetiracetam for prevention less necessary.
Now that there are multiple classes of migraine-specific acute medications, the outstanding question remains: What are the potential benefits and drawbacks for the use of triptans compared with the oral CGRP receptor antagonists (gepants)? Most obviously, triptan medications are contraindicated in patients with significant vascular risk factors; however, what is not known is whether some of the other adverse events associated with triptans are more or less prominent with gepant use. Lee and colleagues conducted a meta-analysis of 15 studies to review this data.
A previous meta-analysis demonstrated that oral CGRP receptor antagonists are more effective than placebo, but less effective than triptans against acute migraine. The most common intolerances for gepants are nausea, somnolence, and dry mouth, but the safety and tolerability of gepants have not been compared with that of triptans. These authors pooled the data on five gepant medications (BI44370TA, MK-3207, rimegepant, telcagepant, and ubrogepant). The primary outcome was incidence of treatment-related adverse events and the secondary outcome was the incidence of the specific intolerances of diarrhea, dizziness, dry mouth, fatigue, nausea, paresthesia, somnolence, upper abdominal pain, and vomiting.
Compared with placebo, the relative risk for any adverse event was found to be low, at 1.15, and the relative risk for treatment-related adverse events was only slightly higher, at 1.18. Gepants were found to be significantly more associated with an increased risk for fatigue, nausea, and somnolence vs placebo. Compared with triptans, the CGRP antagonists were associated with significantly less treatment-related adverse events as well as any adverse event. There was no significant difference in the incidence of diarrhea, nausea, and vomiting between the two groups.
This study helps elucidate some of the differences between the two classes of migraine-specific acute medications. As noted above, a prior meta-analysis did reveal some benefits with the triptan class, specifically better effectiveness. When choosing a better-tolerated medication for your patients, you may want to consider a gepant; when considering a stronger or more potent option, you might stick with a triptan.
Migraine is a unique neurologic condition, in that a person can't prove they have it and there are few objective tools neurologists have to guide their diagnostic process. The recognition of the role of the vasoactive peptide calcitonin gene-related peptide (CGRP) in the 1990s changed the way many researchers and clinicians conceptualized migraine. Subsequent studies have used CGRP as a human model for migraine, and most recently pituitary adenylate cyclase–activating polypeptide 38 (PACAP-38) has also been recognized for its important role in migraine propagation. All of the existing data have been in adults, and no studies until now have specifically investigated the presence of these peptides in children with migraine.
Pediatric migraine is unique in a number of ways. Children with migraine present less unilaterally, the duration of their attacks is typically shorter, and the associated symptoms can often be more prominent than the headache pain during an attack. There are unique pediatric migraine subtypes that are exceptionally rare in adults, such as periodic paralysis attacks and abdominal migraine. For this reason, it is not entirely clear whether the same biomarkers of disease in adults would also be present in the pediatric population.
In the study by Liu and colleagues, the investigators enrolled 76 pediatric patients with migraine (the diagnosis was confirmed by at least two neurologists). Patients were excluded if there was any analgesic medication use over the past 2 months; if there was concern for secondary headache; or any underlying mood disorders, congenital disease, or other major medical conditions. An additional 77 controls were matched for age and sex. Blood was collected from all participants after an 8-hour fast to avoid collecting after potentially ingesting a food trigger. Blood samples were obtained during an ictal period (within 8 hours of a migraine attack) as well as interictally (not taken if the participant had a migraine attack within the past 24 hours).
The plasma CGRP and PACAP-38 levels were significantly higher in pediatric patients with migraine than in those without a migraine history, in both the ictal state and the interictal state. Among patients with migraine, there was a nonsignificant trend toward a higher CGRP level in the ictal phase, and no difference in these phases with PACAP-38. There was no difference in the CGRP or PACAP-38 levels between participants with and those without aura. When different aura groups were compared (with the participants separated on the basis of a history of motor vs vision vs sensory aura), no difference was seen among the different aura groups. Binary logistic regression testing and analysis of variance also showed that CGRP and PACAP-38 are independent risk factors for pediatric migraine, and specific levels of each were associated with an 11 and a 13 times increased risk, respectively.
Biomarker testing is still not clinically performed for migraine either in adults or children. This is primarily due to cost and the fact that most commercially available laboratories do not currently offer these tests. The results above do shed additional light on migraine pathogenesis and indicate that the phenotypic differences seen in pediatric migraine are less likely related to differences in brain function in children.
Levetiracetam is a commonly used antiepileptic medication. Prior studies have investigated the use of this medication for migraine, both acutely and preventively. Other antiepileptic medications have been shown to be very effective for both of these indications. Topiramate and valproic acid are both commonly used for migraine: topiramate primarily preventively and valproic acid both for prevention and, commonly in its intravenous form, for acute treatment. Levetiracetam is currently not commonly used for migraine, although some institutions will use the intravenous formulation for severe refractory status migrainosus.
Evers and colleagues investigated the open label use of levetiracetam for migraine prevention at a dose of 1000 mg twice daily in a small population of 50 persons. The study participants were started at a dose of 500 mg twice daily for 4 weeks, then increased to 1000 mg twice daily for a total of 12 weeks. The primary endpoint was migraine attack frequency during the last 4 weeks of treatment.
A 50% reduction in headache frequency was seen in 46% of the enrolled participants. The most common reported side effects were sedation, nausea, and weight gain, as well as cognitive change (five patients dropped out of the study owing to intolerance of the treatment). A post hoc comparison between the patients with and without response to levetiracetam revealed that those who responded were those with a less refractory history — they had tried fewer medications and were using fewer acute medications as well.
The antiepileptic class of preventive migraine medications is notorious for issues with tolerance. Among the antiepileptic medications, levetiracetam is commonly used but also commonly stopped owing to mood and cognitive complaints. Although the researchers here do show early evidence for a moderate amount of efficacy for treating migraine, the fact that there are now more migraine-specific preventive medications that are better tolerated and overall more efficacious make choosing levetiracetam for prevention less necessary.
Now that there are multiple classes of migraine-specific acute medications, the outstanding question remains: What are the potential benefits and drawbacks for the use of triptans compared with the oral CGRP receptor antagonists (gepants)? Most obviously, triptan medications are contraindicated in patients with significant vascular risk factors; however, what is not known is whether some of the other adverse events associated with triptans are more or less prominent with gepant use. Lee and colleagues conducted a meta-analysis of 15 studies to review this data.
A previous meta-analysis demonstrated that oral CGRP receptor antagonists are more effective than placebo, but less effective than triptans against acute migraine. The most common intolerances for gepants are nausea, somnolence, and dry mouth, but the safety and tolerability of gepants have not been compared with that of triptans. These authors pooled the data on five gepant medications (BI44370TA, MK-3207, rimegepant, telcagepant, and ubrogepant). The primary outcome was incidence of treatment-related adverse events and the secondary outcome was the incidence of the specific intolerances of diarrhea, dizziness, dry mouth, fatigue, nausea, paresthesia, somnolence, upper abdominal pain, and vomiting.
Compared with placebo, the relative risk for any adverse event was found to be low, at 1.15, and the relative risk for treatment-related adverse events was only slightly higher, at 1.18. Gepants were found to be significantly more associated with an increased risk for fatigue, nausea, and somnolence vs placebo. Compared with triptans, the CGRP antagonists were associated with significantly less treatment-related adverse events as well as any adverse event. There was no significant difference in the incidence of diarrhea, nausea, and vomiting between the two groups.
This study helps elucidate some of the differences between the two classes of migraine-specific acute medications. As noted above, a prior meta-analysis did reveal some benefits with the triptan class, specifically better effectiveness. When choosing a better-tolerated medication for your patients, you may want to consider a gepant; when considering a stronger or more potent option, you might stick with a triptan.
Commentary: Concomitant Therapies May Affect NSCLC Survival, August 2022
A Danish population-based cohort study by Ehrenstein and colleagues involved 21,282 patients with non–small-cell lung cancer (NSCLC), 8758 of whom received a diagnosis at stage I-IIIA. Of those, 4071 (46%) were tested for epidermal growth factor receptor (EGFR) mutations at diagnosis. Median overall survival (OS) was 5.7 years among patients with EGFR mutation–positive status (n = 361) and 4.4 years among patients with EGFR mutation–negative status (n = 3710). EGFR mutation–positive status was associated with lower all-cause mortality in all subgroups. This is not surprising, because EGFR-mutated lung cancers are associated with never or light smoking history and the patients tend to be younger and have fewer medical comorbidities. Nevertheless, the lower risk for all-cause mortality was consistent across all subgroups (stage at diagnosis, age, sex, comorbidity, and surgery receipt), with hazard ratios (HR) ranging from 0.48 to 0.83. In addition, targeted therapies, such as osimertinib, improved OS and progression-free survival (PFS) in the metastatic setting as first-line treatment. Now that the ADAURA study has demonstrated a substantial disease-free survival benefit with osimertinib in the adjuvant setting in early-stage EGFR-mutated NSCLC (with final OS results still to come) it will be interesting to see whether this magnitude of difference in OS grows over time.
Wang and colleagues conducted a large meta-analysis of 10 retrospective studies and one prospective study including a total of 5892 patients with NSCLC who were receiving programmed cell death protein 1 (PD-1)/ programmed death-ligand 1 (PD-L1) inhibitors with the concomitant use of gastric acid suppressants (GAS). Use of PD-1/PD-L1 inhibitors with vs without GAS worsened PFS by 32% (HR 1.32; P < .001) and OS by 36% (HR 1.36; P < .001). The GAS in these studies were predominantly proton-pump inhibitors (PPI). There is still much to learn about medications that may influence outcomes to immune checkpoint blockade, such as steroids, antibiotics, GAS, and others. We are also learning that the microbiome probably plays an important role in contributing to activity of PD-1/PDL-1 antibodies and PPI may modify the microbiome. More research is needed, but it is reasonable to try and switch patients receiving PD-1/PDL-1 inhibitors from PPI to other GAS, if clinically appropriate.
Nazha and colleagues performed a SEER-Medicare database analysis evaluating 367,750 patients with lung cancer. A total of 11,061 patients had an initial prostate cancer diagnosis and subsequent lung cancer diagnosis, 3017 had an initial lung cancer diagnosis and subsequent prostate cancer diagnosis, and the remaining patients had an isolated lung cancer diagnosis. Patients who received androgen deprivation therapy (ADT) for a previously diagnosed prostate cancer showed improved survival after lung cancer diagnosis (adjusted HR for death 0.88; P = .02) and a shorter latency period to the diagnosis of lung cancer (40 vs 47 months; P < .001) compared with those who did not receive ADT. This finding applied mainly to White patients and may not apply to Black patients because there was an underrepresentation of Black patients in the study. The association of ADT for prostate cancer improving clinical outcomes in patients subsequently diagnosed with lung cancer is intriguing. There is known crosstalk between receptor kinase signaling and androgen receptor signaling that may biologically explain the findings in this study. This theoretically could apply more to certain molecular subtypes of lung cancer, such as EGFR-mutated lung cancer. However, further studies are needed to confirm this because confounding factors and immortal time bias (where patients receiving ADT may be more likely to have more frequent interactions in the healthcare system and thus receive an earlier lung cancer diagnosis) may in part explain the findings in this retrospective analysis. More research is needed to determine whether patients with prostate cancer receiving ADT had improved survival compared with those who did not receive ADT.
A Danish population-based cohort study by Ehrenstein and colleagues involved 21,282 patients with non–small-cell lung cancer (NSCLC), 8758 of whom received a diagnosis at stage I-IIIA. Of those, 4071 (46%) were tested for epidermal growth factor receptor (EGFR) mutations at diagnosis. Median overall survival (OS) was 5.7 years among patients with EGFR mutation–positive status (n = 361) and 4.4 years among patients with EGFR mutation–negative status (n = 3710). EGFR mutation–positive status was associated with lower all-cause mortality in all subgroups. This is not surprising, because EGFR-mutated lung cancers are associated with never or light smoking history and the patients tend to be younger and have fewer medical comorbidities. Nevertheless, the lower risk for all-cause mortality was consistent across all subgroups (stage at diagnosis, age, sex, comorbidity, and surgery receipt), with hazard ratios (HR) ranging from 0.48 to 0.83. In addition, targeted therapies, such as osimertinib, improved OS and progression-free survival (PFS) in the metastatic setting as first-line treatment. Now that the ADAURA study has demonstrated a substantial disease-free survival benefit with osimertinib in the adjuvant setting in early-stage EGFR-mutated NSCLC (with final OS results still to come) it will be interesting to see whether this magnitude of difference in OS grows over time.
Wang and colleagues conducted a large meta-analysis of 10 retrospective studies and one prospective study including a total of 5892 patients with NSCLC who were receiving programmed cell death protein 1 (PD-1)/ programmed death-ligand 1 (PD-L1) inhibitors with the concomitant use of gastric acid suppressants (GAS). Use of PD-1/PD-L1 inhibitors with vs without GAS worsened PFS by 32% (HR 1.32; P < .001) and OS by 36% (HR 1.36; P < .001). The GAS in these studies were predominantly proton-pump inhibitors (PPI). There is still much to learn about medications that may influence outcomes to immune checkpoint blockade, such as steroids, antibiotics, GAS, and others. We are also learning that the microbiome probably plays an important role in contributing to activity of PD-1/PDL-1 antibodies and PPI may modify the microbiome. More research is needed, but it is reasonable to try and switch patients receiving PD-1/PDL-1 inhibitors from PPI to other GAS, if clinically appropriate.
Nazha and colleagues performed a SEER-Medicare database analysis evaluating 367,750 patients with lung cancer. A total of 11,061 patients had an initial prostate cancer diagnosis and subsequent lung cancer diagnosis, 3017 had an initial lung cancer diagnosis and subsequent prostate cancer diagnosis, and the remaining patients had an isolated lung cancer diagnosis. Patients who received androgen deprivation therapy (ADT) for a previously diagnosed prostate cancer showed improved survival after lung cancer diagnosis (adjusted HR for death 0.88; P = .02) and a shorter latency period to the diagnosis of lung cancer (40 vs 47 months; P < .001) compared with those who did not receive ADT. This finding applied mainly to White patients and may not apply to Black patients because there was an underrepresentation of Black patients in the study. The association of ADT for prostate cancer improving clinical outcomes in patients subsequently diagnosed with lung cancer is intriguing. There is known crosstalk between receptor kinase signaling and androgen receptor signaling that may biologically explain the findings in this study. This theoretically could apply more to certain molecular subtypes of lung cancer, such as EGFR-mutated lung cancer. However, further studies are needed to confirm this because confounding factors and immortal time bias (where patients receiving ADT may be more likely to have more frequent interactions in the healthcare system and thus receive an earlier lung cancer diagnosis) may in part explain the findings in this retrospective analysis. More research is needed to determine whether patients with prostate cancer receiving ADT had improved survival compared with those who did not receive ADT.
A Danish population-based cohort study by Ehrenstein and colleagues involved 21,282 patients with non–small-cell lung cancer (NSCLC), 8758 of whom received a diagnosis at stage I-IIIA. Of those, 4071 (46%) were tested for epidermal growth factor receptor (EGFR) mutations at diagnosis. Median overall survival (OS) was 5.7 years among patients with EGFR mutation–positive status (n = 361) and 4.4 years among patients with EGFR mutation–negative status (n = 3710). EGFR mutation–positive status was associated with lower all-cause mortality in all subgroups. This is not surprising, because EGFR-mutated lung cancers are associated with never or light smoking history and the patients tend to be younger and have fewer medical comorbidities. Nevertheless, the lower risk for all-cause mortality was consistent across all subgroups (stage at diagnosis, age, sex, comorbidity, and surgery receipt), with hazard ratios (HR) ranging from 0.48 to 0.83. In addition, targeted therapies, such as osimertinib, improved OS and progression-free survival (PFS) in the metastatic setting as first-line treatment. Now that the ADAURA study has demonstrated a substantial disease-free survival benefit with osimertinib in the adjuvant setting in early-stage EGFR-mutated NSCLC (with final OS results still to come) it will be interesting to see whether this magnitude of difference in OS grows over time.
Wang and colleagues conducted a large meta-analysis of 10 retrospective studies and one prospective study including a total of 5892 patients with NSCLC who were receiving programmed cell death protein 1 (PD-1)/ programmed death-ligand 1 (PD-L1) inhibitors with the concomitant use of gastric acid suppressants (GAS). Use of PD-1/PD-L1 inhibitors with vs without GAS worsened PFS by 32% (HR 1.32; P < .001) and OS by 36% (HR 1.36; P < .001). The GAS in these studies were predominantly proton-pump inhibitors (PPI). There is still much to learn about medications that may influence outcomes to immune checkpoint blockade, such as steroids, antibiotics, GAS, and others. We are also learning that the microbiome probably plays an important role in contributing to activity of PD-1/PDL-1 antibodies and PPI may modify the microbiome. More research is needed, but it is reasonable to try and switch patients receiving PD-1/PDL-1 inhibitors from PPI to other GAS, if clinically appropriate.
Nazha and colleagues performed a SEER-Medicare database analysis evaluating 367,750 patients with lung cancer. A total of 11,061 patients had an initial prostate cancer diagnosis and subsequent lung cancer diagnosis, 3017 had an initial lung cancer diagnosis and subsequent prostate cancer diagnosis, and the remaining patients had an isolated lung cancer diagnosis. Patients who received androgen deprivation therapy (ADT) for a previously diagnosed prostate cancer showed improved survival after lung cancer diagnosis (adjusted HR for death 0.88; P = .02) and a shorter latency period to the diagnosis of lung cancer (40 vs 47 months; P < .001) compared with those who did not receive ADT. This finding applied mainly to White patients and may not apply to Black patients because there was an underrepresentation of Black patients in the study. The association of ADT for prostate cancer improving clinical outcomes in patients subsequently diagnosed with lung cancer is intriguing. There is known crosstalk between receptor kinase signaling and androgen receptor signaling that may biologically explain the findings in this study. This theoretically could apply more to certain molecular subtypes of lung cancer, such as EGFR-mutated lung cancer. However, further studies are needed to confirm this because confounding factors and immortal time bias (where patients receiving ADT may be more likely to have more frequent interactions in the healthcare system and thus receive an earlier lung cancer diagnosis) may in part explain the findings in this retrospective analysis. More research is needed to determine whether patients with prostate cancer receiving ADT had improved survival compared with those who did not receive ADT.
Federal Health Care Data Trends 2022: Military Sexual Trauma
- Hard truths and the duty to change: recommendations from the Independent Review Commission on Sexual Assault in the Military. Published July 1, 2022. Accessed May 20, 2022. https://media.defense.gov/2021/Jul/02/2002755437/-1/-1/0/IRC-FULL-REPORT-FINAL-1923-7-1-2.PDF
- Gross GM, Ronzitti S, Combellick JL, et al. Sex differences in military sexual trauma and severe self-directed violence. Am J Prev Med. 2020;58(5):675-682. http://doi.org/10.1016/j.amepre.2019.12.006
- Nitcher B, Holliday R, Monteith LL, et al. Military sexual trauma in the United States: results from a population-based study. J Affect Disord. 2022;306:19-27. http://doi.org/10.1016/j.jad.2022.03.016
- Lofgreen AM, Carroll KK, Dugan SA, Karnik NS. An overview of sexual trauma in the US Military. Focus (Am Psychiatr Publ). 2017;15(4):411-419. http://doi.org/10.1176/appi.focus.20170024
- Schuyler AC, Klemmer C, Mamey MR, et al. Experiences of sexual harassment, stalking, and sexual assault during military service among LGBT and non-LGBT service members. J Trauma Stress. 2020;33(3):257-266. http://doi.org/10.1002/jts.22506
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/DOD_Annual_Report_on_Sexual_Assault_in_the_Military_FY2020.pdf
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. Appendix B: statistical data on sexual assault. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/Appendix_B_Statistical_Data_On_Sexual_Assault_FY2020.pdf
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. Appendix C: metrics and non-metrics on sexual assault. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/Appendix_C_Metrics_and_NonMetrics_on_Sexual_Assault_FY2020.pdf
- Barth SK, Kimerling RE, Pavao J, et al. Military sexual trauma among recent veterans: correlates of sexual assault and sexual harassment. Am J Prev Med. 2016;50(1):77-86. http://doi.org/10.1016/j.amepre.2015.06.012
- Military sexual trauma. US Department of Veterans Affairs. Updated March 11, 2022. Accessed March 24, 2022. https://www.mentalhealth.va.gov/msthome/index.asp
- Hahn CK, Turchik J, Kimerling R. A latent class analysis of mental health beliefs related to military sexual trauma. J Trauma Stress. 2021;34(2):394-404. http://doi.org/10.1002/jts.22585
- Hard truths and the duty to change: recommendations from the Independent Review Commission on Sexual Assault in the Military. Published July 1, 2022. Accessed May 20, 2022. https://media.defense.gov/2021/Jul/02/2002755437/-1/-1/0/IRC-FULL-REPORT-FINAL-1923-7-1-2.PDF
- Gross GM, Ronzitti S, Combellick JL, et al. Sex differences in military sexual trauma and severe self-directed violence. Am J Prev Med. 2020;58(5):675-682. http://doi.org/10.1016/j.amepre.2019.12.006
- Nitcher B, Holliday R, Monteith LL, et al. Military sexual trauma in the United States: results from a population-based study. J Affect Disord. 2022;306:19-27. http://doi.org/10.1016/j.jad.2022.03.016
- Lofgreen AM, Carroll KK, Dugan SA, Karnik NS. An overview of sexual trauma in the US Military. Focus (Am Psychiatr Publ). 2017;15(4):411-419. http://doi.org/10.1176/appi.focus.20170024
- Schuyler AC, Klemmer C, Mamey MR, et al. Experiences of sexual harassment, stalking, and sexual assault during military service among LGBT and non-LGBT service members. J Trauma Stress. 2020;33(3):257-266. http://doi.org/10.1002/jts.22506
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/DOD_Annual_Report_on_Sexual_Assault_in_the_Military_FY2020.pdf
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. Appendix B: statistical data on sexual assault. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/Appendix_B_Statistical_Data_On_Sexual_Assault_FY2020.pdf
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. Appendix C: metrics and non-metrics on sexual assault. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/Appendix_C_Metrics_and_NonMetrics_on_Sexual_Assault_FY2020.pdf
- Barth SK, Kimerling RE, Pavao J, et al. Military sexual trauma among recent veterans: correlates of sexual assault and sexual harassment. Am J Prev Med. 2016;50(1):77-86. http://doi.org/10.1016/j.amepre.2015.06.012
- Military sexual trauma. US Department of Veterans Affairs. Updated March 11, 2022. Accessed March 24, 2022. https://www.mentalhealth.va.gov/msthome/index.asp
- Hahn CK, Turchik J, Kimerling R. A latent class analysis of mental health beliefs related to military sexual trauma. J Trauma Stress. 2021;34(2):394-404. http://doi.org/10.1002/jts.22585
- Hard truths and the duty to change: recommendations from the Independent Review Commission on Sexual Assault in the Military. Published July 1, 2022. Accessed May 20, 2022. https://media.defense.gov/2021/Jul/02/2002755437/-1/-1/0/IRC-FULL-REPORT-FINAL-1923-7-1-2.PDF
- Gross GM, Ronzitti S, Combellick JL, et al. Sex differences in military sexual trauma and severe self-directed violence. Am J Prev Med. 2020;58(5):675-682. http://doi.org/10.1016/j.amepre.2019.12.006
- Nitcher B, Holliday R, Monteith LL, et al. Military sexual trauma in the United States: results from a population-based study. J Affect Disord. 2022;306:19-27. http://doi.org/10.1016/j.jad.2022.03.016
- Lofgreen AM, Carroll KK, Dugan SA, Karnik NS. An overview of sexual trauma in the US Military. Focus (Am Psychiatr Publ). 2017;15(4):411-419. http://doi.org/10.1176/appi.focus.20170024
- Schuyler AC, Klemmer C, Mamey MR, et al. Experiences of sexual harassment, stalking, and sexual assault during military service among LGBT and non-LGBT service members. J Trauma Stress. 2020;33(3):257-266. http://doi.org/10.1002/jts.22506
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/DOD_Annual_Report_on_Sexual_Assault_in_the_Military_FY2020.pdf
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. Appendix B: statistical data on sexual assault. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/Appendix_B_Statistical_Data_On_Sexual_Assault_FY2020.pdf
- Department of Defense annual report on sexual assault in the military: fiscal year 2020. Appendix C: metrics and non-metrics on sexual assault. May 15, 2021. Accessed March 24, 2022. https://www.sapr.mil/sites/default/files/Appendix_C_Metrics_and_NonMetrics_on_Sexual_Assault_FY2020.pdf
- Barth SK, Kimerling RE, Pavao J, et al. Military sexual trauma among recent veterans: correlates of sexual assault and sexual harassment. Am J Prev Med. 2016;50(1):77-86. http://doi.org/10.1016/j.amepre.2015.06.012
- Military sexual trauma. US Department of Veterans Affairs. Updated March 11, 2022. Accessed March 24, 2022. https://www.mentalhealth.va.gov/msthome/index.asp
- Hahn CK, Turchik J, Kimerling R. A latent class analysis of mental health beliefs related to military sexual trauma. J Trauma Stress. 2021;34(2):394-404. http://doi.org/10.1002/jts.22585
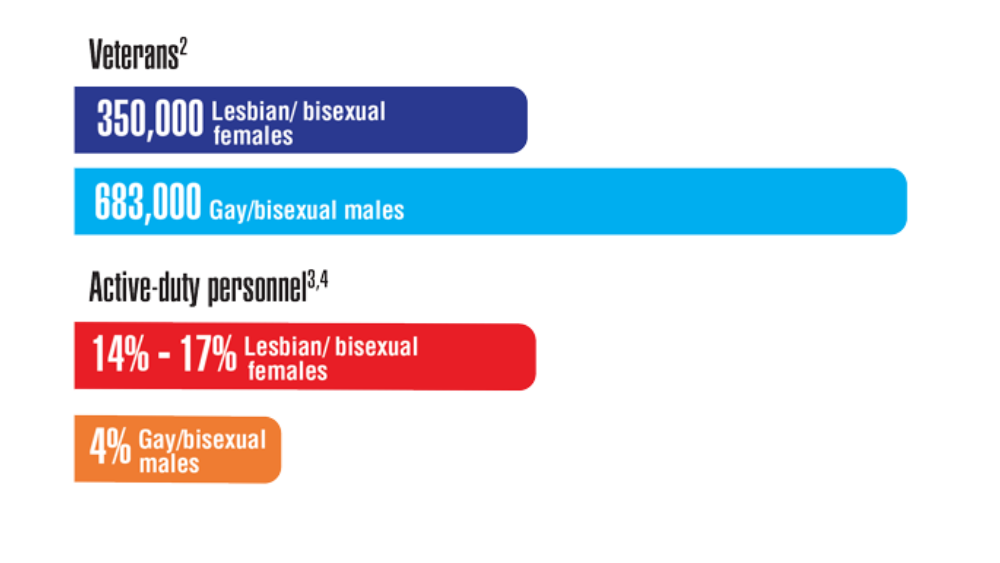
Federal Health Care Data Trends 2022: LGBTQ+ Veterans
- Ring T. VA eases the path to benefits for LGBTQ+ and HIV-positive vets. The Advocate. September 21, 2021. Accessed March 11, 2022. https://www.advocate.com/news/2021/9/21/va-eases-path-benefits-lgbtq-and-hiv-positive-vets
- Gay veterans top one million. Urban.org. Accessed March 11, 2022. https://www.urban.org/sites/default/files/publication/59711/900642-gay-veterans-top-one-million.pdf
- 2018 Workplace and Gender Relations Survey of Active Duty Members Overview Report. US Department of Defense. Published October 18, 2018. Accessed May 17, 2022. https://www.sapr.mil/sites/default/files/Annex_1_2018_WGRA_Overview_Report_0.pdf
- Meadows SO, Engel CC, Collins RL et al. 2018 Health related behaviors survey: sexual orientation and health among the active component. RAND Corporation. 2021. https://www.rand.org/pubs/research_briefs/RB10116z7.html
- Gates, GJ and Herman, JL. Transgender military service in the United States. Williams Institute, UCLA School of Law. Published May 1, 2014. Accessed May 17, 2022. https://escholarship.org/content/qt1t24j53h/qt1t24j53h.pdf?t=nsm5a0
- Downing J, Conron K, Herman JL, Blosnich JR. Transgender and cisgender US veterans have few health differences. Health Aff (Millwood). 2018;37(7):1160-1168. http://doi.org/10.1377/hlthaff.2018.0027
- Meadows SO, Engel CC, Collins RL, et al. 2015 Health related behaviors survey: sexual orientation, transgender identity, and health among U.S. active-duty service members. RAND Corporation. 2018. Accessed March 15, 2022. https://www.rand.org/pubs/research_briefs/RB9955z6.html
- Korshak L, Hilgeman MM, Lange-Altman T. Health disparities among LGBT veterans. Published July 2020. Accessed May 17, 2022. https://www.va.gov/HEALTHEQUITY/Health_Disparities_Among_LGBT_Veterans.asp
- Ring T. VA eases the path to benefits for LGBTQ+ and HIV-positive vets. The Advocate. September 21, 2021. Accessed March 11, 2022. https://www.advocate.com/news/2021/9/21/va-eases-path-benefits-lgbtq-and-hiv-positive-vets
- Gay veterans top one million. Urban.org. Accessed March 11, 2022. https://www.urban.org/sites/default/files/publication/59711/900642-gay-veterans-top-one-million.pdf
- 2018 Workplace and Gender Relations Survey of Active Duty Members Overview Report. US Department of Defense. Published October 18, 2018. Accessed May 17, 2022. https://www.sapr.mil/sites/default/files/Annex_1_2018_WGRA_Overview_Report_0.pdf
- Meadows SO, Engel CC, Collins RL et al. 2018 Health related behaviors survey: sexual orientation and health among the active component. RAND Corporation. 2021. https://www.rand.org/pubs/research_briefs/RB10116z7.html
- Gates, GJ and Herman, JL. Transgender military service in the United States. Williams Institute, UCLA School of Law. Published May 1, 2014. Accessed May 17, 2022. https://escholarship.org/content/qt1t24j53h/qt1t24j53h.pdf?t=nsm5a0
- Downing J, Conron K, Herman JL, Blosnich JR. Transgender and cisgender US veterans have few health differences. Health Aff (Millwood). 2018;37(7):1160-1168. http://doi.org/10.1377/hlthaff.2018.0027
- Meadows SO, Engel CC, Collins RL, et al. 2015 Health related behaviors survey: sexual orientation, transgender identity, and health among U.S. active-duty service members. RAND Corporation. 2018. Accessed March 15, 2022. https://www.rand.org/pubs/research_briefs/RB9955z6.html
- Korshak L, Hilgeman MM, Lange-Altman T. Health disparities among LGBT veterans. Published July 2020. Accessed May 17, 2022. https://www.va.gov/HEALTHEQUITY/Health_Disparities_Among_LGBT_Veterans.asp
- Ring T. VA eases the path to benefits for LGBTQ+ and HIV-positive vets. The Advocate. September 21, 2021. Accessed March 11, 2022. https://www.advocate.com/news/2021/9/21/va-eases-path-benefits-lgbtq-and-hiv-positive-vets
- Gay veterans top one million. Urban.org. Accessed March 11, 2022. https://www.urban.org/sites/default/files/publication/59711/900642-gay-veterans-top-one-million.pdf
- 2018 Workplace and Gender Relations Survey of Active Duty Members Overview Report. US Department of Defense. Published October 18, 2018. Accessed May 17, 2022. https://www.sapr.mil/sites/default/files/Annex_1_2018_WGRA_Overview_Report_0.pdf
- Meadows SO, Engel CC, Collins RL et al. 2018 Health related behaviors survey: sexual orientation and health among the active component. RAND Corporation. 2021. https://www.rand.org/pubs/research_briefs/RB10116z7.html
- Gates, GJ and Herman, JL. Transgender military service in the United States. Williams Institute, UCLA School of Law. Published May 1, 2014. Accessed May 17, 2022. https://escholarship.org/content/qt1t24j53h/qt1t24j53h.pdf?t=nsm5a0
- Downing J, Conron K, Herman JL, Blosnich JR. Transgender and cisgender US veterans have few health differences. Health Aff (Millwood). 2018;37(7):1160-1168. http://doi.org/10.1377/hlthaff.2018.0027
- Meadows SO, Engel CC, Collins RL, et al. 2015 Health related behaviors survey: sexual orientation, transgender identity, and health among U.S. active-duty service members. RAND Corporation. 2018. Accessed March 15, 2022. https://www.rand.org/pubs/research_briefs/RB9955z6.html
- Korshak L, Hilgeman MM, Lange-Altman T. Health disparities among LGBT veterans. Published July 2020. Accessed May 17, 2022. https://www.va.gov/HEALTHEQUITY/Health_Disparities_Among_LGBT_Veterans.asp
Federal Health Care Data Trends 2022: Mental Health and Related Disorders
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee to Evaluate the Department of Veterans Affairs Mental Health Services. Dimensions of quality in mental health care. In: Evaluation of the Department of Veterans Affairs Mental Health Services. National Academies Press; January 31, 2018; chap 7. Accessed April 25, 2022. https://www.ncbi.nlm.nih.gov/books/NBK499503
- Panza KE, Kline AC, Na PJ, Potenza MN, Norman SB, Pietrzak RH. Epidemiology of DSM-5 alcohol use disorder in U.S. military veterans: results from the National Health and Resilience in Veterans Study. Drug Alcohol Depend. 2022;231:109240. http://doi.org/10.1016/j.drugalcdep.2021.109240
- Warrener CD, Valentin EM, Gallin C, et al. The role of oxytocin signaling in depression and suicidality in returning war veterans. Psychoneuroendocrinology. 2021;126:105085. http://doi.org/10.1016/j.psyneuen.2020.105085
- Adams RE, Hu Y, Figley CR, et al. Risk and protective factors associated with mental health among female military veterans: results from the Veterans' Health Study. BMC Womens Health. 2021;21(1):55. http://doi.org/10.1186/s12905-021-01181-z
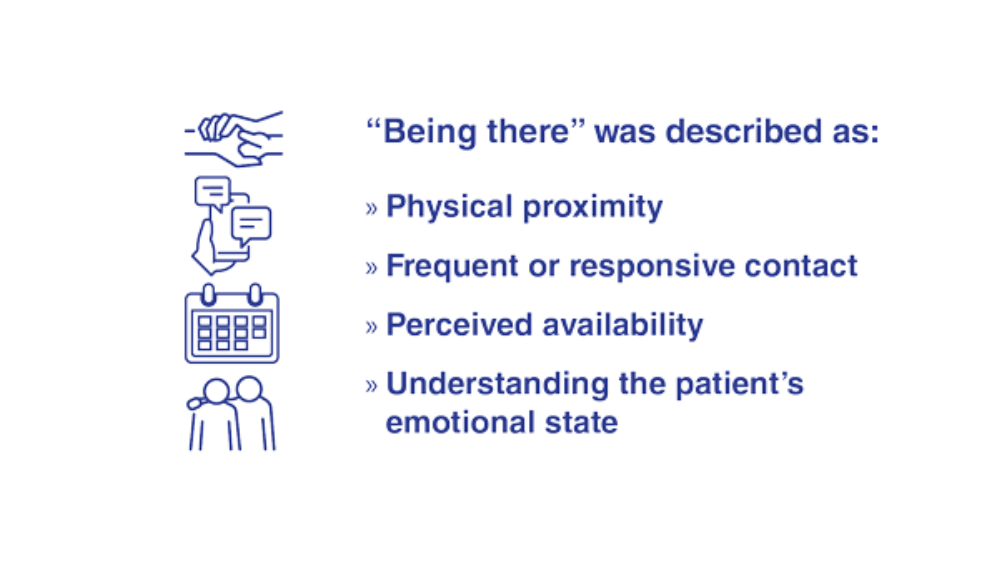
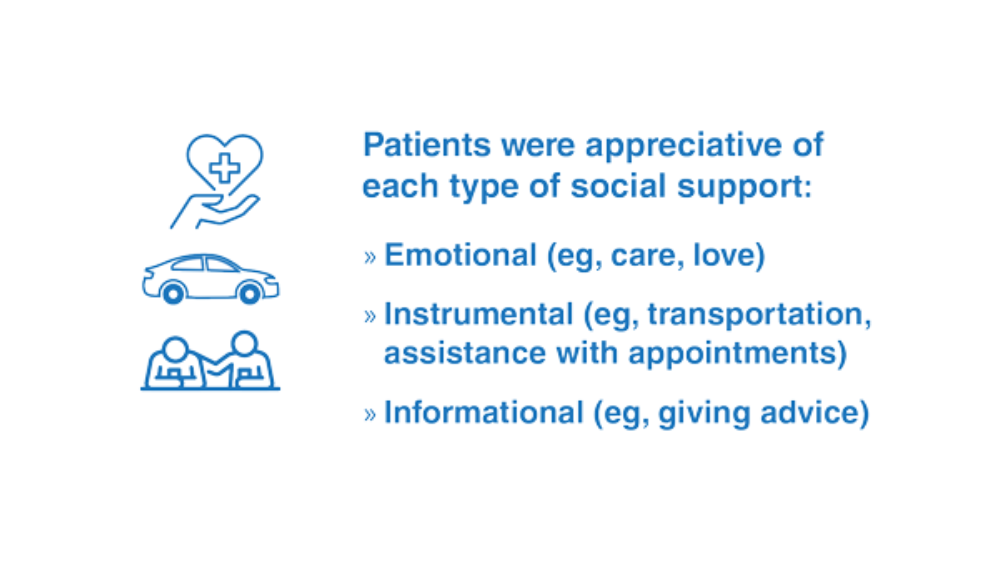
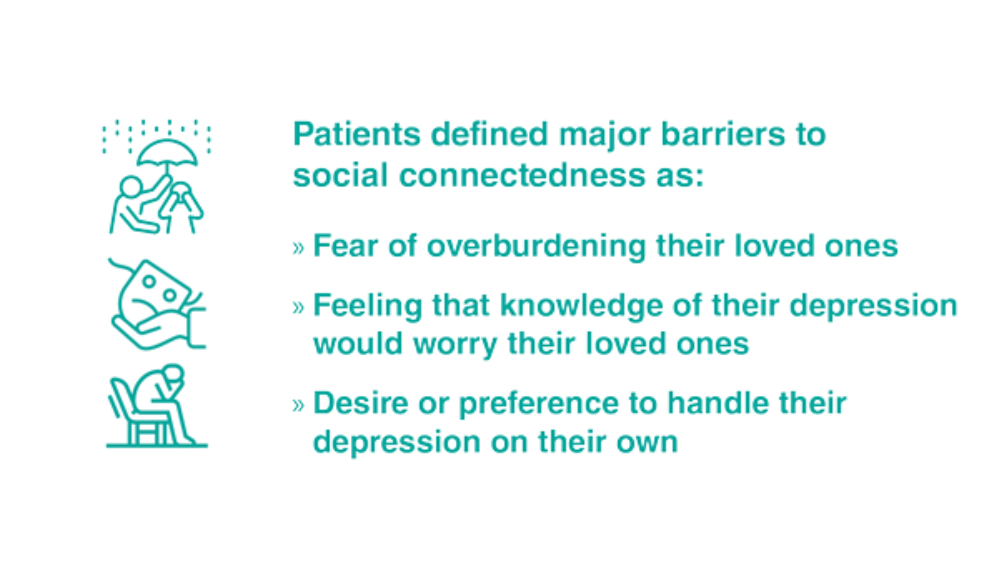
- Teo AR, Marsh HE, Ono SS, Nicolaidis C, Saha S, Dobscha SK. The importance of "being there": a qualitative study of what veterans with depression want in social support. J Gen Intern Med. 2020;35(7):1954-1962. http://doi.org/10.1007/s11606-020-05692-7
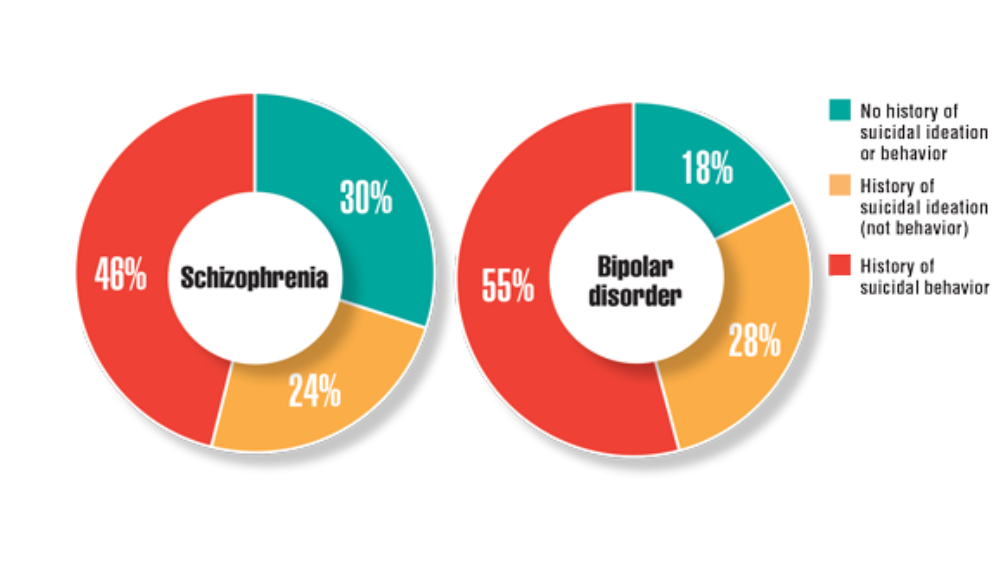
- Harvey PD, Bigdeli TB, Fanous AH, et al. Cooperative Studies Program (CSP) #572: a study of serious mental illness in veterans as a pathway to personalized medicine in schizophrenia and bipolar illness. Pers Med Psychiatry. 2021;27-28. http://doi.org/10.1016/j.pmip.2021.100078
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee to Evaluate the Department of Veterans Affairs Mental Health Services. Dimensions of quality in mental health care. In: Evaluation of the Department of Veterans Affairs Mental Health Services. National Academies Press; January 31, 2018; chap 7. Accessed April 25, 2022. https://www.ncbi.nlm.nih.gov/books/NBK499503
- Panza KE, Kline AC, Na PJ, Potenza MN, Norman SB, Pietrzak RH. Epidemiology of DSM-5 alcohol use disorder in U.S. military veterans: results from the National Health and Resilience in Veterans Study. Drug Alcohol Depend. 2022;231:109240. http://doi.org/10.1016/j.drugalcdep.2021.109240
- Warrener CD, Valentin EM, Gallin C, et al. The role of oxytocin signaling in depression and suicidality in returning war veterans. Psychoneuroendocrinology. 2021;126:105085. http://doi.org/10.1016/j.psyneuen.2020.105085
- Adams RE, Hu Y, Figley CR, et al. Risk and protective factors associated with mental health among female military veterans: results from the Veterans' Health Study. BMC Womens Health. 2021;21(1):55. http://doi.org/10.1186/s12905-021-01181-z
- Teo AR, Marsh HE, Ono SS, Nicolaidis C, Saha S, Dobscha SK. The importance of "being there": a qualitative study of what veterans with depression want in social support. J Gen Intern Med. 2020;35(7):1954-1962. http://doi.org/10.1007/s11606-020-05692-7
- Harvey PD, Bigdeli TB, Fanous AH, et al. Cooperative Studies Program (CSP) #572: a study of serious mental illness in veterans as a pathway to personalized medicine in schizophrenia and bipolar illness. Pers Med Psychiatry. 2021;27-28. http://doi.org/10.1016/j.pmip.2021.100078
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee to Evaluate the Department of Veterans Affairs Mental Health Services. Dimensions of quality in mental health care. In: Evaluation of the Department of Veterans Affairs Mental Health Services. National Academies Press; January 31, 2018; chap 7. Accessed April 25, 2022. https://www.ncbi.nlm.nih.gov/books/NBK499503
- Panza KE, Kline AC, Na PJ, Potenza MN, Norman SB, Pietrzak RH. Epidemiology of DSM-5 alcohol use disorder in U.S. military veterans: results from the National Health and Resilience in Veterans Study. Drug Alcohol Depend. 2022;231:109240. http://doi.org/10.1016/j.drugalcdep.2021.109240
- Warrener CD, Valentin EM, Gallin C, et al. The role of oxytocin signaling in depression and suicidality in returning war veterans. Psychoneuroendocrinology. 2021;126:105085. http://doi.org/10.1016/j.psyneuen.2020.105085
- Adams RE, Hu Y, Figley CR, et al. Risk and protective factors associated with mental health among female military veterans: results from the Veterans' Health Study. BMC Womens Health. 2021;21(1):55. http://doi.org/10.1186/s12905-021-01181-z
- Teo AR, Marsh HE, Ono SS, Nicolaidis C, Saha S, Dobscha SK. The importance of "being there": a qualitative study of what veterans with depression want in social support. J Gen Intern Med. 2020;35(7):1954-1962. http://doi.org/10.1007/s11606-020-05692-7
- Harvey PD, Bigdeli TB, Fanous AH, et al. Cooperative Studies Program (CSP) #572: a study of serious mental illness in veterans as a pathway to personalized medicine in schizophrenia and bipolar illness. Pers Med Psychiatry. 2021;27-28. http://doi.org/10.1016/j.pmip.2021.100078
Federal Health Care Data Trends 2022: Neurologic Disorders
- Williams KA. Headache management in a veteran population: First considerations. J Am Assoc Nurse Pract. 2020;32(11):758-763. https://doi.org/10.1097/JXX.0000000000000539
- Yin JH, Lin YK, Yang CP, et al. Prevalence and association of lifestyle and medical-, psychiatric-, and pain-related comorbidities in patients with migraine: a cross-sectional study. Headache. 2021;61(5):715-726. https://doi.org/10.1111/head.14106
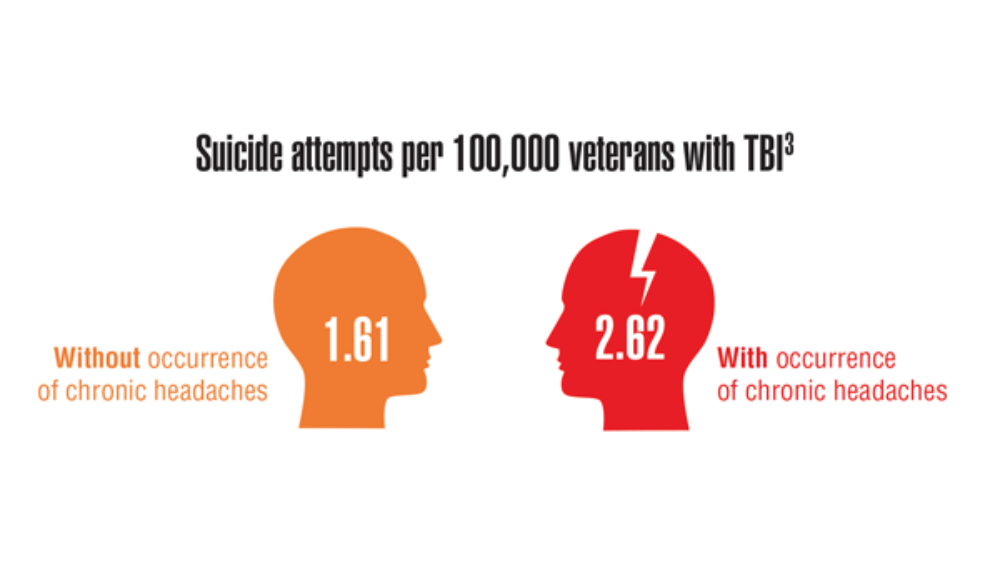
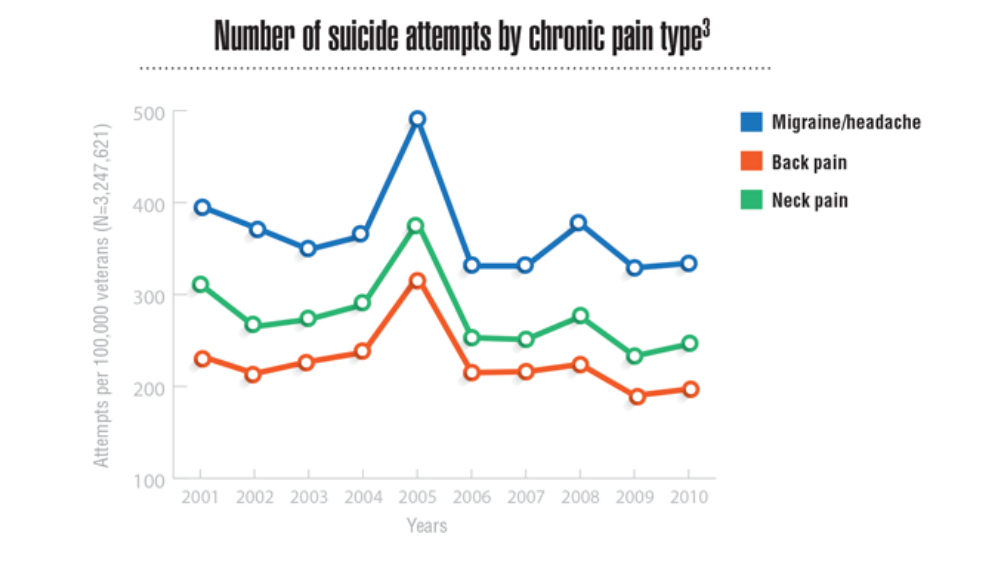
- Androulakis XM, Guo S, Zhang J, et al. Suicide attempts in US veterans with chronic headache disorders: a 10-year retrospective cohort study. J Pain Res. 2021;14:2629-2639. https://doi.org/10.2147/JPR.S322432
- Chen XY, Chen ZY, Dong Z, Liu MQ, Yu SY. Regional volume changes of the brain in migraine chronification. Neural Regen Res. 2020;15(9):1701-1708. https://doi.org/10.4103/1673-5374.276360
- Wallin MT, Whitham R, Maloni H, et al. The Multiple Sclerosis Surveillance Registry: a novel interactive database within the Veterans Health Administration. Fed Pract. 2020;37(suppl 1):S18-S23.
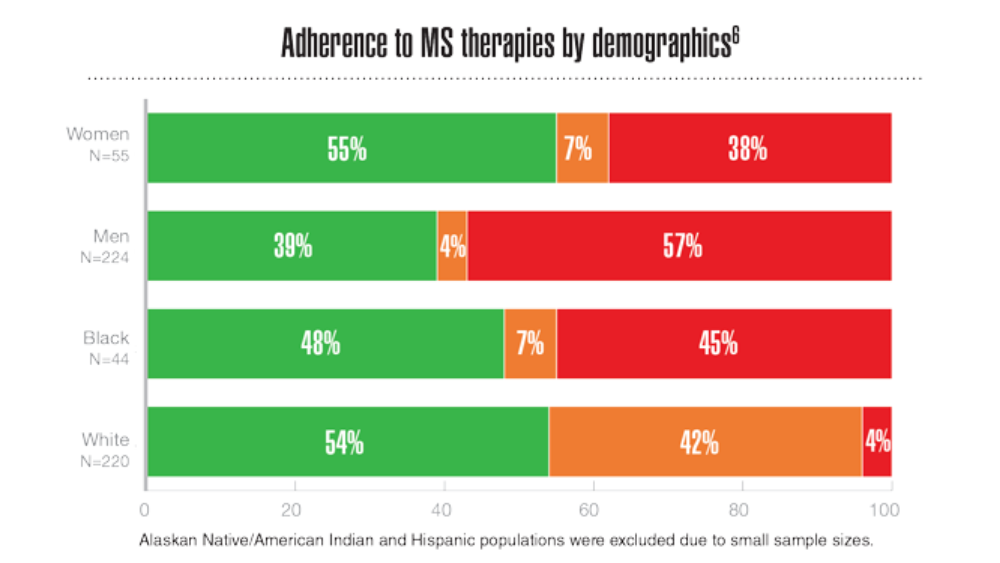
- Rabadi MH, Just K, Xu C. The impact of adherence to disease-modifying therapies on functional outcomes in veterans with multiple sclerosis. J Cent Nerv Syst Dis. 2021;13:11795735211028769. http://doi.org/10.1177/11795735211028769
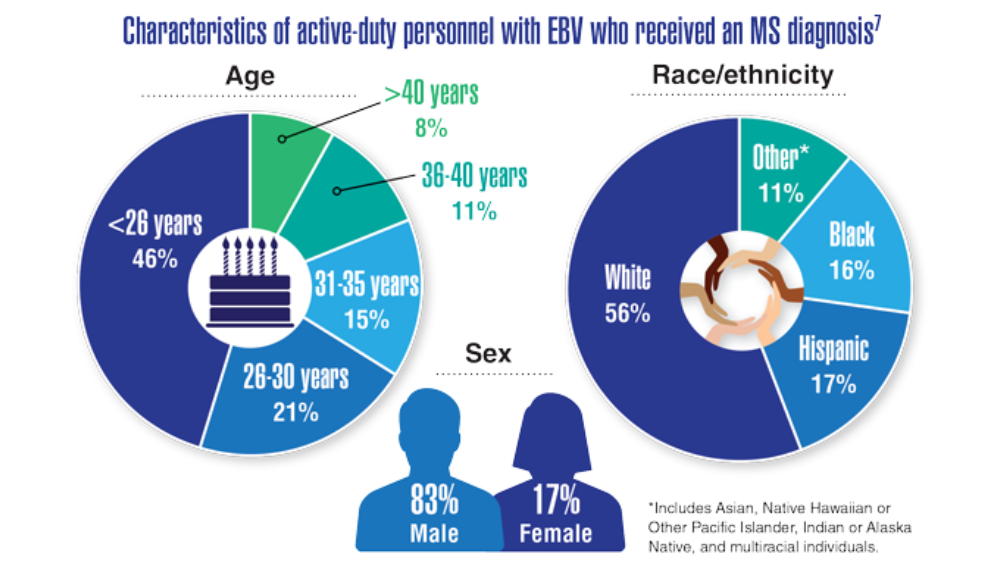
- Bjornevik K, Cortese M, Healy BC, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375(6578):296-301. http://doi.org/10.1126/science.abj8222
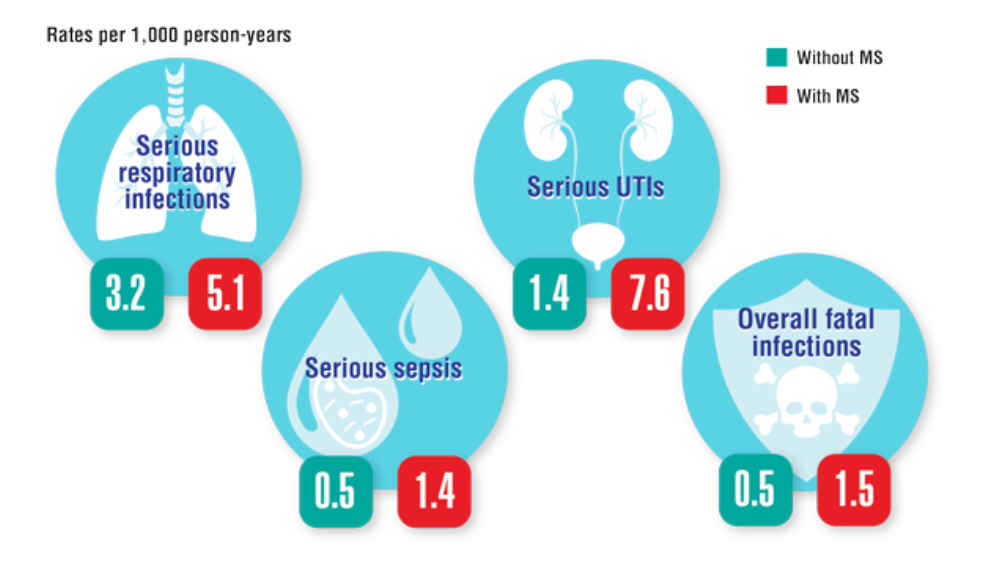
- Nelson RE, Xie Y, DuVall SL, et al. Multiple sclerosis and risk of infection-related hospitalization and death in US veterans. Int J MS Care. 2015;17(5):221-230. http://doi.org/10.7224/1537-2073.2014-035
- Williams KA. Headache management in a veteran population: First considerations. J Am Assoc Nurse Pract. 2020;32(11):758-763. https://doi.org/10.1097/JXX.0000000000000539
- Yin JH, Lin YK, Yang CP, et al. Prevalence and association of lifestyle and medical-, psychiatric-, and pain-related comorbidities in patients with migraine: a cross-sectional study. Headache. 2021;61(5):715-726. https://doi.org/10.1111/head.14106
- Androulakis XM, Guo S, Zhang J, et al. Suicide attempts in US veterans with chronic headache disorders: a 10-year retrospective cohort study. J Pain Res. 2021;14:2629-2639. https://doi.org/10.2147/JPR.S322432
- Chen XY, Chen ZY, Dong Z, Liu MQ, Yu SY. Regional volume changes of the brain in migraine chronification. Neural Regen Res. 2020;15(9):1701-1708. https://doi.org/10.4103/1673-5374.276360
- Wallin MT, Whitham R, Maloni H, et al. The Multiple Sclerosis Surveillance Registry: a novel interactive database within the Veterans Health Administration. Fed Pract. 2020;37(suppl 1):S18-S23.
- Rabadi MH, Just K, Xu C. The impact of adherence to disease-modifying therapies on functional outcomes in veterans with multiple sclerosis. J Cent Nerv Syst Dis. 2021;13:11795735211028769. http://doi.org/10.1177/11795735211028769
- Bjornevik K, Cortese M, Healy BC, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375(6578):296-301. http://doi.org/10.1126/science.abj8222
- Nelson RE, Xie Y, DuVall SL, et al. Multiple sclerosis and risk of infection-related hospitalization and death in US veterans. Int J MS Care. 2015;17(5):221-230. http://doi.org/10.7224/1537-2073.2014-035
- Williams KA. Headache management in a veteran population: First considerations. J Am Assoc Nurse Pract. 2020;32(11):758-763. https://doi.org/10.1097/JXX.0000000000000539
- Yin JH, Lin YK, Yang CP, et al. Prevalence and association of lifestyle and medical-, psychiatric-, and pain-related comorbidities in patients with migraine: a cross-sectional study. Headache. 2021;61(5):715-726. https://doi.org/10.1111/head.14106
- Androulakis XM, Guo S, Zhang J, et al. Suicide attempts in US veterans with chronic headache disorders: a 10-year retrospective cohort study. J Pain Res. 2021;14:2629-2639. https://doi.org/10.2147/JPR.S322432
- Chen XY, Chen ZY, Dong Z, Liu MQ, Yu SY. Regional volume changes of the brain in migraine chronification. Neural Regen Res. 2020;15(9):1701-1708. https://doi.org/10.4103/1673-5374.276360
- Wallin MT, Whitham R, Maloni H, et al. The Multiple Sclerosis Surveillance Registry: a novel interactive database within the Veterans Health Administration. Fed Pract. 2020;37(suppl 1):S18-S23.
- Rabadi MH, Just K, Xu C. The impact of adherence to disease-modifying therapies on functional outcomes in veterans with multiple sclerosis. J Cent Nerv Syst Dis. 2021;13:11795735211028769. http://doi.org/10.1177/11795735211028769
- Bjornevik K, Cortese M, Healy BC, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375(6578):296-301. http://doi.org/10.1126/science.abj8222
- Nelson RE, Xie Y, DuVall SL, et al. Multiple sclerosis and risk of infection-related hospitalization and death in US veterans. Int J MS Care. 2015;17(5):221-230. http://doi.org/10.7224/1537-2073.2014-035
Model may predict age-related mortality after TIPS implantation
Mortality after implantation of a transjugular intrahepatic portosystemic shunt (TIPS) is increased for patients aged 70 and older with cirrhosis, but creatinine and sodium levels can help with decision-making, according to a study published in Hepatology.
TIPS can improve survival in cirrhotic patients with refractory ascites or portal hypertensive bleeding, and age alone shouldn’t preclude older patients from receiving TIPS, wrote the researchers led by Francesco Vizzutti, MD, of the department of experimental and clinical medicine at the University of Florence in Italy.
“However, the indication for TIPS in older adult patients (70 years and over) is debated, and a specific prediction model developed in this particular setting is lacking,” they wrote.
Dr. Vizzutti and colleagues aimed to develop and validate a multivariable model to accurately predict mortality in older adults. They prospectively enrolled 411 patients at four Italian referral centers with de novo TIPS implantation for refractory ascites or secondary prophylaxis of variceal bleeding between October 2020 and March 2021.
All patients underwent TIPS placement using Viatorr-covered stent grafts. All patients had follow-up outpatient appointments every 6 months until the end of the study or when clinically indicated, such as recurrence of portal hypertension complications or TIPS dysfunction.
The research team created a competing risks model to predict liver-related mortality attributable to liver failure, portal hypertensive bleeding, hepatorenal syndrome, or hepatocellular carcinoma, with orthotopic liver transplant and death from extrahepatic causes considered as competing events. In older adults, the only competing event was death from extrahepatic causes because this age group could not receive orthotopic liver transplant.
Alcohol use disorder was the most common etiology at 37%, followed by viral infection at 30%. At the time of TIPS placement, alcohol use disorder was present as a main or concomitant etiology of liver disease in 181 patients, including 36 with active alcohol consumption.
Compared with younger patients, older adults had significantly higher prevalence of viral etiology (at 41%) and lower prevalence of alcohol use disorder (at 18%). In terms of liver function, older adults had significantly less advanced liver disease based on international normalized ratio levels, likely “reflecting a more careful selection by physicians when managing older adults,” the study authors wrote. However, older adults had significantly higher creatinine levels than younger patients, “underlining the importance of the assessment of kidney function when selecting patients for TIPS placement,” the authors wrote.
During a median follow-up time of about 20 months after TIPS placement, 99 of 411 (or 24%) of patients died of liver-related causes, 49 underwent a transplant, and 17 died of extrahepatic causes. Among the 99 older adults, 44 (or 44%) died of liver-related causes, and 7 patients died of extrahepatic causes.
In the overall cohort, the probabilities of liver-related death were 13% after 1 year, 17% after 2 years, and 24% after 3 years. The probabilities were higher in older adults, at 19% after 1 year, 30% after 2 years, and 41% after 3 years.
According to the model, age, alcoholic etiology, creatinine levels, and international normalized ratio levels were independently associated with a higher risk of liver-related death. In older adults, creatinine and sodium levels were the only independent risk factors for death.
Notably, older adult patients with favorable creatinine and sodium levels (1.2 mg/dL and 140 mEq/L, respectively) had survival probabilities of liver-related death at 1, 2, and 3 years from TIPS placement of 14%, 26%, and 34%, respectively, the authors wrote. In contrast, older adults with creatinine levels of 2.5 mg/dL and sodium levels of 130 mEq/L had worse outcomes, with risks of liver-related death of 71%, 92%, and 96%, respectively.
“These results suggest that older adult patients with preserved renal function and normal sodium levels could obtain a survival outcome after TIPS placement similar to younger patients,” they wrote. “Moreover, the occurrence of [hepatic encephalopathy] and/or recurrence of ascites or bleeding was not significantly different comparing the two groups of patients according to age.”
Future research should update the prediction model with larger sample sizes, the study authors wrote.
“The decision for or against TIPS should be made only after carefully weighing the risks and benefits, taking into consideration the available literature,” said Bubu Banini, MD, PhD, an assistant professor of digestive diseases and translational research director of the Metabolic Health and Weight Loss Program at Yale University, New Haven, Conn.
Dr. Banini, who wasn’t involved with the study, said the prediction model could be a useful tool to guide the decision-making process.
“As is usually the case with management of portal hypertension–related complications, a multidisciplinary discussion with evaluation of a multitude of factors, including quality of life, comorbidities, risks, and benefits, should guide decision-making,” she said.
Dr. Banini highlighted the finding that alcohol etiology for cirrhosis was associated with higher mortality compared with viral etiology.
“This is important in the context of unfortunately increasing trends in alcohol consumption in the pre- and peri-COVID era and the increased prevalence of alcohol-associated liver disease, especially in women,” she said.
The study was supported by grants from the University of Florence and the University of Modena and Reggio Emilia. The study authors have received lecture fees from Gore Medical, which creates stent grafts. Dr. Banini reported no relevant disclosures.
Mortality after implantation of a transjugular intrahepatic portosystemic shunt (TIPS) is increased for patients aged 70 and older with cirrhosis, but creatinine and sodium levels can help with decision-making, according to a study published in Hepatology.
TIPS can improve survival in cirrhotic patients with refractory ascites or portal hypertensive bleeding, and age alone shouldn’t preclude older patients from receiving TIPS, wrote the researchers led by Francesco Vizzutti, MD, of the department of experimental and clinical medicine at the University of Florence in Italy.
“However, the indication for TIPS in older adult patients (70 years and over) is debated, and a specific prediction model developed in this particular setting is lacking,” they wrote.
Dr. Vizzutti and colleagues aimed to develop and validate a multivariable model to accurately predict mortality in older adults. They prospectively enrolled 411 patients at four Italian referral centers with de novo TIPS implantation for refractory ascites or secondary prophylaxis of variceal bleeding between October 2020 and March 2021.
All patients underwent TIPS placement using Viatorr-covered stent grafts. All patients had follow-up outpatient appointments every 6 months until the end of the study or when clinically indicated, such as recurrence of portal hypertension complications or TIPS dysfunction.
The research team created a competing risks model to predict liver-related mortality attributable to liver failure, portal hypertensive bleeding, hepatorenal syndrome, or hepatocellular carcinoma, with orthotopic liver transplant and death from extrahepatic causes considered as competing events. In older adults, the only competing event was death from extrahepatic causes because this age group could not receive orthotopic liver transplant.
Alcohol use disorder was the most common etiology at 37%, followed by viral infection at 30%. At the time of TIPS placement, alcohol use disorder was present as a main or concomitant etiology of liver disease in 181 patients, including 36 with active alcohol consumption.
Compared with younger patients, older adults had significantly higher prevalence of viral etiology (at 41%) and lower prevalence of alcohol use disorder (at 18%). In terms of liver function, older adults had significantly less advanced liver disease based on international normalized ratio levels, likely “reflecting a more careful selection by physicians when managing older adults,” the study authors wrote. However, older adults had significantly higher creatinine levels than younger patients, “underlining the importance of the assessment of kidney function when selecting patients for TIPS placement,” the authors wrote.
During a median follow-up time of about 20 months after TIPS placement, 99 of 411 (or 24%) of patients died of liver-related causes, 49 underwent a transplant, and 17 died of extrahepatic causes. Among the 99 older adults, 44 (or 44%) died of liver-related causes, and 7 patients died of extrahepatic causes.
In the overall cohort, the probabilities of liver-related death were 13% after 1 year, 17% after 2 years, and 24% after 3 years. The probabilities were higher in older adults, at 19% after 1 year, 30% after 2 years, and 41% after 3 years.
According to the model, age, alcoholic etiology, creatinine levels, and international normalized ratio levels were independently associated with a higher risk of liver-related death. In older adults, creatinine and sodium levels were the only independent risk factors for death.
Notably, older adult patients with favorable creatinine and sodium levels (1.2 mg/dL and 140 mEq/L, respectively) had survival probabilities of liver-related death at 1, 2, and 3 years from TIPS placement of 14%, 26%, and 34%, respectively, the authors wrote. In contrast, older adults with creatinine levels of 2.5 mg/dL and sodium levels of 130 mEq/L had worse outcomes, with risks of liver-related death of 71%, 92%, and 96%, respectively.
“These results suggest that older adult patients with preserved renal function and normal sodium levels could obtain a survival outcome after TIPS placement similar to younger patients,” they wrote. “Moreover, the occurrence of [hepatic encephalopathy] and/or recurrence of ascites or bleeding was not significantly different comparing the two groups of patients according to age.”
Future research should update the prediction model with larger sample sizes, the study authors wrote.
“The decision for or against TIPS should be made only after carefully weighing the risks and benefits, taking into consideration the available literature,” said Bubu Banini, MD, PhD, an assistant professor of digestive diseases and translational research director of the Metabolic Health and Weight Loss Program at Yale University, New Haven, Conn.
Dr. Banini, who wasn’t involved with the study, said the prediction model could be a useful tool to guide the decision-making process.
“As is usually the case with management of portal hypertension–related complications, a multidisciplinary discussion with evaluation of a multitude of factors, including quality of life, comorbidities, risks, and benefits, should guide decision-making,” she said.
Dr. Banini highlighted the finding that alcohol etiology for cirrhosis was associated with higher mortality compared with viral etiology.
“This is important in the context of unfortunately increasing trends in alcohol consumption in the pre- and peri-COVID era and the increased prevalence of alcohol-associated liver disease, especially in women,” she said.
The study was supported by grants from the University of Florence and the University of Modena and Reggio Emilia. The study authors have received lecture fees from Gore Medical, which creates stent grafts. Dr. Banini reported no relevant disclosures.
Mortality after implantation of a transjugular intrahepatic portosystemic shunt (TIPS) is increased for patients aged 70 and older with cirrhosis, but creatinine and sodium levels can help with decision-making, according to a study published in Hepatology.
TIPS can improve survival in cirrhotic patients with refractory ascites or portal hypertensive bleeding, and age alone shouldn’t preclude older patients from receiving TIPS, wrote the researchers led by Francesco Vizzutti, MD, of the department of experimental and clinical medicine at the University of Florence in Italy.
“However, the indication for TIPS in older adult patients (70 years and over) is debated, and a specific prediction model developed in this particular setting is lacking,” they wrote.
Dr. Vizzutti and colleagues aimed to develop and validate a multivariable model to accurately predict mortality in older adults. They prospectively enrolled 411 patients at four Italian referral centers with de novo TIPS implantation for refractory ascites or secondary prophylaxis of variceal bleeding between October 2020 and March 2021.
All patients underwent TIPS placement using Viatorr-covered stent grafts. All patients had follow-up outpatient appointments every 6 months until the end of the study or when clinically indicated, such as recurrence of portal hypertension complications or TIPS dysfunction.
The research team created a competing risks model to predict liver-related mortality attributable to liver failure, portal hypertensive bleeding, hepatorenal syndrome, or hepatocellular carcinoma, with orthotopic liver transplant and death from extrahepatic causes considered as competing events. In older adults, the only competing event was death from extrahepatic causes because this age group could not receive orthotopic liver transplant.
Alcohol use disorder was the most common etiology at 37%, followed by viral infection at 30%. At the time of TIPS placement, alcohol use disorder was present as a main or concomitant etiology of liver disease in 181 patients, including 36 with active alcohol consumption.
Compared with younger patients, older adults had significantly higher prevalence of viral etiology (at 41%) and lower prevalence of alcohol use disorder (at 18%). In terms of liver function, older adults had significantly less advanced liver disease based on international normalized ratio levels, likely “reflecting a more careful selection by physicians when managing older adults,” the study authors wrote. However, older adults had significantly higher creatinine levels than younger patients, “underlining the importance of the assessment of kidney function when selecting patients for TIPS placement,” the authors wrote.
During a median follow-up time of about 20 months after TIPS placement, 99 of 411 (or 24%) of patients died of liver-related causes, 49 underwent a transplant, and 17 died of extrahepatic causes. Among the 99 older adults, 44 (or 44%) died of liver-related causes, and 7 patients died of extrahepatic causes.
In the overall cohort, the probabilities of liver-related death were 13% after 1 year, 17% after 2 years, and 24% after 3 years. The probabilities were higher in older adults, at 19% after 1 year, 30% after 2 years, and 41% after 3 years.
According to the model, age, alcoholic etiology, creatinine levels, and international normalized ratio levels were independently associated with a higher risk of liver-related death. In older adults, creatinine and sodium levels were the only independent risk factors for death.
Notably, older adult patients with favorable creatinine and sodium levels (1.2 mg/dL and 140 mEq/L, respectively) had survival probabilities of liver-related death at 1, 2, and 3 years from TIPS placement of 14%, 26%, and 34%, respectively, the authors wrote. In contrast, older adults with creatinine levels of 2.5 mg/dL and sodium levels of 130 mEq/L had worse outcomes, with risks of liver-related death of 71%, 92%, and 96%, respectively.
“These results suggest that older adult patients with preserved renal function and normal sodium levels could obtain a survival outcome after TIPS placement similar to younger patients,” they wrote. “Moreover, the occurrence of [hepatic encephalopathy] and/or recurrence of ascites or bleeding was not significantly different comparing the two groups of patients according to age.”
Future research should update the prediction model with larger sample sizes, the study authors wrote.
“The decision for or against TIPS should be made only after carefully weighing the risks and benefits, taking into consideration the available literature,” said Bubu Banini, MD, PhD, an assistant professor of digestive diseases and translational research director of the Metabolic Health and Weight Loss Program at Yale University, New Haven, Conn.
Dr. Banini, who wasn’t involved with the study, said the prediction model could be a useful tool to guide the decision-making process.
“As is usually the case with management of portal hypertension–related complications, a multidisciplinary discussion with evaluation of a multitude of factors, including quality of life, comorbidities, risks, and benefits, should guide decision-making,” she said.
Dr. Banini highlighted the finding that alcohol etiology for cirrhosis was associated with higher mortality compared with viral etiology.
“This is important in the context of unfortunately increasing trends in alcohol consumption in the pre- and peri-COVID era and the increased prevalence of alcohol-associated liver disease, especially in women,” she said.
The study was supported by grants from the University of Florence and the University of Modena and Reggio Emilia. The study authors have received lecture fees from Gore Medical, which creates stent grafts. Dr. Banini reported no relevant disclosures.
FROM HEPATOLOGY
Federal Health Care Data Trends 2022: Cardiovascular Diseases
- Howard JT, Stewart IJ, Kolaja CA, et al. Hypertension in military veterans is associated with combat exposure and combat injury. J Hypertens. 2020;38(7):1293-1301. http://doi.org/10.1097/HJH.0000000000002364
- Centers for Disease Control and Prevention (CDC). A closer look at African American men and high blood pressure control. Reviewed November 2, 2020. Accessed March 23, 2022. https://www.cdc.gov/bloodpressure/aa_sourcebook.htm
- CDC. National Health and Nutrition Examination Survey. What to expect and information collected. Reviewed November 16, 2021. Accessed March 23, 2022. https://www.cdc.gov/nchs/nhanes/participant/information-collected.htm
- Keaton JM, Hellwege JN, Giri A, et al. Associations of biogeographic ancestry with hypertension traits. J Hypertens. 2021;39(4):633-642. http://doi.org/10.1097/HJH.0000000000002701
- Groeneveld PW, Medvedeva EL, Walker L, Segal AG, Richardson DM, Epstein AJ. Outcomes of care for ischemic heart disease and chronic heart failure in the Veterans Health Administration. JAMA Cardiol. 2018;3(7):563-571. http://doi.org/10.1001/jamacardio.2018.1115
- Cho ME, Hansen JL, Sauer BC, Cheung AK, Agarwal A, Greene T. Heart failure hospitalization risk associated with iron status in veterans with CKD. Clin J Am Soc Nephrol. 2021;16(4):522-531. http://doi.org/10.2215/CJN.15360920
- Jackevicius CA, Lu L, Ghaznavi Z, Warner AL. Bleeding risk of direct oral anticoagulants in patients with heart failure and atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2021;14(2):e007230. http://doi.org/10.1161/CIRCOUTCOMES.120.007230
- Keithler AN, Wilson AS, Yuan A, Sosa JM, Bush KNV. Characteristics of United States military pilots with atrial fibrillation and deployment and retention rates. BMJ Mil Health. 2021;0:1-5. http://doi.org/10.1136/bmjmilitary-2020-001665
- Rouch L, Xia F, Bahorik A, Olgin J, Yaffe K. Atrial fibrillation is associated with greater risk of dementia in older veterans. J Geriatr Psychiatry. 2021;29(11):1092-1098. http://doi.org/10.1016/j.jagp.2021.02.038
- Shrauner W, Lord EM, Nguyen XMT, et al. Frailty and cardiovascular mortality in more than 3 million US veterans. Eur Heart J. 2022;43(8):818-826. http://doi.org/10.1093/eurheartj/ehab850
- Howard JT, Stewart IJ, Kolaja CA, et al. Hypertension in military veterans is associated with combat exposure and combat injury. J Hypertens. 2020;38(7):1293-1301. http://doi.org/10.1097/HJH.0000000000002364
- Centers for Disease Control and Prevention (CDC). A closer look at African American men and high blood pressure control. Reviewed November 2, 2020. Accessed March 23, 2022. https://www.cdc.gov/bloodpressure/aa_sourcebook.htm
- CDC. National Health and Nutrition Examination Survey. What to expect and information collected. Reviewed November 16, 2021. Accessed March 23, 2022. https://www.cdc.gov/nchs/nhanes/participant/information-collected.htm
- Keaton JM, Hellwege JN, Giri A, et al. Associations of biogeographic ancestry with hypertension traits. J Hypertens. 2021;39(4):633-642. http://doi.org/10.1097/HJH.0000000000002701
- Groeneveld PW, Medvedeva EL, Walker L, Segal AG, Richardson DM, Epstein AJ. Outcomes of care for ischemic heart disease and chronic heart failure in the Veterans Health Administration. JAMA Cardiol. 2018;3(7):563-571. http://doi.org/10.1001/jamacardio.2018.1115
- Cho ME, Hansen JL, Sauer BC, Cheung AK, Agarwal A, Greene T. Heart failure hospitalization risk associated with iron status in veterans with CKD. Clin J Am Soc Nephrol. 2021;16(4):522-531. http://doi.org/10.2215/CJN.15360920
- Jackevicius CA, Lu L, Ghaznavi Z, Warner AL. Bleeding risk of direct oral anticoagulants in patients with heart failure and atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2021;14(2):e007230. http://doi.org/10.1161/CIRCOUTCOMES.120.007230
- Keithler AN, Wilson AS, Yuan A, Sosa JM, Bush KNV. Characteristics of United States military pilots with atrial fibrillation and deployment and retention rates. BMJ Mil Health. 2021;0:1-5. http://doi.org/10.1136/bmjmilitary-2020-001665
- Rouch L, Xia F, Bahorik A, Olgin J, Yaffe K. Atrial fibrillation is associated with greater risk of dementia in older veterans. J Geriatr Psychiatry. 2021;29(11):1092-1098. http://doi.org/10.1016/j.jagp.2021.02.038
- Shrauner W, Lord EM, Nguyen XMT, et al. Frailty and cardiovascular mortality in more than 3 million US veterans. Eur Heart J. 2022;43(8):818-826. http://doi.org/10.1093/eurheartj/ehab850
- Howard JT, Stewart IJ, Kolaja CA, et al. Hypertension in military veterans is associated with combat exposure and combat injury. J Hypertens. 2020;38(7):1293-1301. http://doi.org/10.1097/HJH.0000000000002364
- Centers for Disease Control and Prevention (CDC). A closer look at African American men and high blood pressure control. Reviewed November 2, 2020. Accessed March 23, 2022. https://www.cdc.gov/bloodpressure/aa_sourcebook.htm
- CDC. National Health and Nutrition Examination Survey. What to expect and information collected. Reviewed November 16, 2021. Accessed March 23, 2022. https://www.cdc.gov/nchs/nhanes/participant/information-collected.htm
- Keaton JM, Hellwege JN, Giri A, et al. Associations of biogeographic ancestry with hypertension traits. J Hypertens. 2021;39(4):633-642. http://doi.org/10.1097/HJH.0000000000002701
- Groeneveld PW, Medvedeva EL, Walker L, Segal AG, Richardson DM, Epstein AJ. Outcomes of care for ischemic heart disease and chronic heart failure in the Veterans Health Administration. JAMA Cardiol. 2018;3(7):563-571. http://doi.org/10.1001/jamacardio.2018.1115
- Cho ME, Hansen JL, Sauer BC, Cheung AK, Agarwal A, Greene T. Heart failure hospitalization risk associated with iron status in veterans with CKD. Clin J Am Soc Nephrol. 2021;16(4):522-531. http://doi.org/10.2215/CJN.15360920
- Jackevicius CA, Lu L, Ghaznavi Z, Warner AL. Bleeding risk of direct oral anticoagulants in patients with heart failure and atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2021;14(2):e007230. http://doi.org/10.1161/CIRCOUTCOMES.120.007230
- Keithler AN, Wilson AS, Yuan A, Sosa JM, Bush KNV. Characteristics of United States military pilots with atrial fibrillation and deployment and retention rates. BMJ Mil Health. 2021;0:1-5. http://doi.org/10.1136/bmjmilitary-2020-001665
- Rouch L, Xia F, Bahorik A, Olgin J, Yaffe K. Atrial fibrillation is associated with greater risk of dementia in older veterans. J Geriatr Psychiatry. 2021;29(11):1092-1098. http://doi.org/10.1016/j.jagp.2021.02.038
- Shrauner W, Lord EM, Nguyen XMT, et al. Frailty and cardiovascular mortality in more than 3 million US veterans. Eur Heart J. 2022;43(8):818-826. http://doi.org/10.1093/eurheartj/ehab850
Vitamin D supplements during pregnancy may protect infants from atopic eczema
according to results of a clinical trial.
“Our data provide the first randomized controlled trial evidence of a protective effect of antenatal cholecalciferol supplementation on risk of infantile atopic eczema, with the effect only seen in infants that were breastfed for more than 1 month,” lead study author Sarah El-Heis, MRCP, DM, and colleagues wrote.
“The findings support a developmental influence on infantile atopic eczema and point to gestational cholecalciferol supplementation as a preventive strategy to reduce the burden of atopic eczema during infancy,” Dr. El-Heis, an academic clinical lecturer in dermatology at the Medical Research Council Lifecourse Epidemiology Center of the University of Southampton (England), said in a presentation at the annual meeting of the Society for Investigative Dermatology.
The study also was published in the British Journal of Dermatology.
Dr. El-Heis and colleagues analyzed data from one of the three U.K. study sites involved in the double-blind Maternal Vitamin D Osteoporosis Study (MAVIDOS), which enrolled participants between 2008 and 2014.
The women enrolled at the University of Southampton site were of age 18 or older, and had a singleton pregnancy. Serum 25-hydroxy vitamin D (25[OH]D) levels were 25-100 nmol/L, and calcium levels were less than 2.75 mmol/L.
Those who had metabolic bone disease, kidney stones, hyperparathyroidism, or hypercalciuria or who were taking more than 400 IU/day of vitamin D supplements or medication known to interfere with fetal growth or whose fetus had a major anomaly were excluded.
The study included 1,134 women. Half of the participants were randomly assigned to receive cholecalciferol 1,000 IU/day from around 14 weeks’ gestation until delivery, and half were assigned to receive placebo. Their babies were assessed for atopic eczema at 12, 24, and 48 months of age.
The maternal and infant characteristics were similar in both groups, but the treatment group tended to breastfeed longer.
Infants appear to be protected up to 1 year of age
Using logistic regression, the researchers analyzed links between maternal cholecalciferol 1,000 IU/day supplements or placebo and atopic eczema risk in their offspring.
After adjustments for breastfeeding duration, among the 636 infants assessed at 12 months, those whose mothers received cholecalciferol had lower odds ratios of atopic eczema than those whose mothers received placebo (OR, 0.55; 95% confidence interval, 0.32-0.97).
The risk of atopic eczema at 12 months was reduced only for children in the treatment group who were breastfed longer than 1 month (OR, 0.48; 95% CI, 0.24-0.94), further analysis showed. Those who were breastfed for less than 1 month showed no reduced risk.
The combined effect of vitamin D and breastfeeding for longer than 1 month weakened after 1 year and was not statistically significant among the 611 children assessed at 24 months and the 450 children assessed at 48 months. The ORs of atopic eczema in the treatment group and in the control group increased to 0.76 (95% CI, 0.47-1.23) and 0.75 (95% CI, 0.37-1.52), respectively.
At baseline, the mean maternal serum 25(OH)D levels in the treatment group (46.0 nmol/L) and in the control group (44.7 nmol/L) were similar. But by late pregnancy, maternal serum 25(OH)D levels in the treatment group were higher (67.4 nmol/L) than in the control group (42.4 nmol/L).
The authors note that strengths of the study include its design, the uniformity of criteria used to diagnose atopic eczema, and the similarity of both pregnant groups in their intake of vitamin D during the study.
Limitations included the lack of ultraviolet B light exposure data, the lack of non-White women in the study, the lack of measurement of cord blood and offspring 25(OH)D levels, and the exclusion of women with baseline 25(OH)D concentrations less than 25 nmol/L.
“This is an interesting study that brings up the possibility that maternal factors during pregnancy may impact atopic dermatitis,” Kalyani S. Marathe, MD, MPH, the director of the division of dermatology at Cincinnati Children’s Hospital Medical Center, told this news organization.
The results are mixed, though, she noted.
“While some impact on the risk of eczema is seen at 1 year of age, that protective effect is gone by 2 years and 4 years,” Dr. Marathe, who was not involved in the study, said in an email. “So if maternal supplementation does improve eczema, the effect is not long-lasting.
“The other complicating factor is that the babies who showed reduction in eczema were also the ones who were breastfed longer than 1 month,” she added. “We know that breastfeeding is associated with several factors, including socioeconomic status, so it is difficult to tease out the relationships here.
“Vitamin D has become a very hot topic lately and seems to have protective effects in many areas of health care,” Dr. Marathe said. “These results may motivate pregnant women to be compliant with their prenatal vitamins that contain the amount of vitamin D studied here.”
The study received grant support. Several authors disclosed financial relationships with pharmaceutical and nutritional products industries. Dr. El-Heis and Dr. Marathe reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to results of a clinical trial.
“Our data provide the first randomized controlled trial evidence of a protective effect of antenatal cholecalciferol supplementation on risk of infantile atopic eczema, with the effect only seen in infants that were breastfed for more than 1 month,” lead study author Sarah El-Heis, MRCP, DM, and colleagues wrote.
“The findings support a developmental influence on infantile atopic eczema and point to gestational cholecalciferol supplementation as a preventive strategy to reduce the burden of atopic eczema during infancy,” Dr. El-Heis, an academic clinical lecturer in dermatology at the Medical Research Council Lifecourse Epidemiology Center of the University of Southampton (England), said in a presentation at the annual meeting of the Society for Investigative Dermatology.
The study also was published in the British Journal of Dermatology.
Dr. El-Heis and colleagues analyzed data from one of the three U.K. study sites involved in the double-blind Maternal Vitamin D Osteoporosis Study (MAVIDOS), which enrolled participants between 2008 and 2014.
The women enrolled at the University of Southampton site were of age 18 or older, and had a singleton pregnancy. Serum 25-hydroxy vitamin D (25[OH]D) levels were 25-100 nmol/L, and calcium levels were less than 2.75 mmol/L.
Those who had metabolic bone disease, kidney stones, hyperparathyroidism, or hypercalciuria or who were taking more than 400 IU/day of vitamin D supplements or medication known to interfere with fetal growth or whose fetus had a major anomaly were excluded.
The study included 1,134 women. Half of the participants were randomly assigned to receive cholecalciferol 1,000 IU/day from around 14 weeks’ gestation until delivery, and half were assigned to receive placebo. Their babies were assessed for atopic eczema at 12, 24, and 48 months of age.
The maternal and infant characteristics were similar in both groups, but the treatment group tended to breastfeed longer.
Infants appear to be protected up to 1 year of age
Using logistic regression, the researchers analyzed links between maternal cholecalciferol 1,000 IU/day supplements or placebo and atopic eczema risk in their offspring.
After adjustments for breastfeeding duration, among the 636 infants assessed at 12 months, those whose mothers received cholecalciferol had lower odds ratios of atopic eczema than those whose mothers received placebo (OR, 0.55; 95% confidence interval, 0.32-0.97).
The risk of atopic eczema at 12 months was reduced only for children in the treatment group who were breastfed longer than 1 month (OR, 0.48; 95% CI, 0.24-0.94), further analysis showed. Those who were breastfed for less than 1 month showed no reduced risk.
The combined effect of vitamin D and breastfeeding for longer than 1 month weakened after 1 year and was not statistically significant among the 611 children assessed at 24 months and the 450 children assessed at 48 months. The ORs of atopic eczema in the treatment group and in the control group increased to 0.76 (95% CI, 0.47-1.23) and 0.75 (95% CI, 0.37-1.52), respectively.
At baseline, the mean maternal serum 25(OH)D levels in the treatment group (46.0 nmol/L) and in the control group (44.7 nmol/L) were similar. But by late pregnancy, maternal serum 25(OH)D levels in the treatment group were higher (67.4 nmol/L) than in the control group (42.4 nmol/L).
The authors note that strengths of the study include its design, the uniformity of criteria used to diagnose atopic eczema, and the similarity of both pregnant groups in their intake of vitamin D during the study.
Limitations included the lack of ultraviolet B light exposure data, the lack of non-White women in the study, the lack of measurement of cord blood and offspring 25(OH)D levels, and the exclusion of women with baseline 25(OH)D concentrations less than 25 nmol/L.
“This is an interesting study that brings up the possibility that maternal factors during pregnancy may impact atopic dermatitis,” Kalyani S. Marathe, MD, MPH, the director of the division of dermatology at Cincinnati Children’s Hospital Medical Center, told this news organization.
The results are mixed, though, she noted.
“While some impact on the risk of eczema is seen at 1 year of age, that protective effect is gone by 2 years and 4 years,” Dr. Marathe, who was not involved in the study, said in an email. “So if maternal supplementation does improve eczema, the effect is not long-lasting.
“The other complicating factor is that the babies who showed reduction in eczema were also the ones who were breastfed longer than 1 month,” she added. “We know that breastfeeding is associated with several factors, including socioeconomic status, so it is difficult to tease out the relationships here.
“Vitamin D has become a very hot topic lately and seems to have protective effects in many areas of health care,” Dr. Marathe said. “These results may motivate pregnant women to be compliant with their prenatal vitamins that contain the amount of vitamin D studied here.”
The study received grant support. Several authors disclosed financial relationships with pharmaceutical and nutritional products industries. Dr. El-Heis and Dr. Marathe reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to results of a clinical trial.
“Our data provide the first randomized controlled trial evidence of a protective effect of antenatal cholecalciferol supplementation on risk of infantile atopic eczema, with the effect only seen in infants that were breastfed for more than 1 month,” lead study author Sarah El-Heis, MRCP, DM, and colleagues wrote.
“The findings support a developmental influence on infantile atopic eczema and point to gestational cholecalciferol supplementation as a preventive strategy to reduce the burden of atopic eczema during infancy,” Dr. El-Heis, an academic clinical lecturer in dermatology at the Medical Research Council Lifecourse Epidemiology Center of the University of Southampton (England), said in a presentation at the annual meeting of the Society for Investigative Dermatology.
The study also was published in the British Journal of Dermatology.
Dr. El-Heis and colleagues analyzed data from one of the three U.K. study sites involved in the double-blind Maternal Vitamin D Osteoporosis Study (MAVIDOS), which enrolled participants between 2008 and 2014.
The women enrolled at the University of Southampton site were of age 18 or older, and had a singleton pregnancy. Serum 25-hydroxy vitamin D (25[OH]D) levels were 25-100 nmol/L, and calcium levels were less than 2.75 mmol/L.
Those who had metabolic bone disease, kidney stones, hyperparathyroidism, or hypercalciuria or who were taking more than 400 IU/day of vitamin D supplements or medication known to interfere with fetal growth or whose fetus had a major anomaly were excluded.
The study included 1,134 women. Half of the participants were randomly assigned to receive cholecalciferol 1,000 IU/day from around 14 weeks’ gestation until delivery, and half were assigned to receive placebo. Their babies were assessed for atopic eczema at 12, 24, and 48 months of age.
The maternal and infant characteristics were similar in both groups, but the treatment group tended to breastfeed longer.
Infants appear to be protected up to 1 year of age
Using logistic regression, the researchers analyzed links between maternal cholecalciferol 1,000 IU/day supplements or placebo and atopic eczema risk in their offspring.
After adjustments for breastfeeding duration, among the 636 infants assessed at 12 months, those whose mothers received cholecalciferol had lower odds ratios of atopic eczema than those whose mothers received placebo (OR, 0.55; 95% confidence interval, 0.32-0.97).
The risk of atopic eczema at 12 months was reduced only for children in the treatment group who were breastfed longer than 1 month (OR, 0.48; 95% CI, 0.24-0.94), further analysis showed. Those who were breastfed for less than 1 month showed no reduced risk.
The combined effect of vitamin D and breastfeeding for longer than 1 month weakened after 1 year and was not statistically significant among the 611 children assessed at 24 months and the 450 children assessed at 48 months. The ORs of atopic eczema in the treatment group and in the control group increased to 0.76 (95% CI, 0.47-1.23) and 0.75 (95% CI, 0.37-1.52), respectively.
At baseline, the mean maternal serum 25(OH)D levels in the treatment group (46.0 nmol/L) and in the control group (44.7 nmol/L) were similar. But by late pregnancy, maternal serum 25(OH)D levels in the treatment group were higher (67.4 nmol/L) than in the control group (42.4 nmol/L).
The authors note that strengths of the study include its design, the uniformity of criteria used to diagnose atopic eczema, and the similarity of both pregnant groups in their intake of vitamin D during the study.
Limitations included the lack of ultraviolet B light exposure data, the lack of non-White women in the study, the lack of measurement of cord blood and offspring 25(OH)D levels, and the exclusion of women with baseline 25(OH)D concentrations less than 25 nmol/L.
“This is an interesting study that brings up the possibility that maternal factors during pregnancy may impact atopic dermatitis,” Kalyani S. Marathe, MD, MPH, the director of the division of dermatology at Cincinnati Children’s Hospital Medical Center, told this news organization.
The results are mixed, though, she noted.
“While some impact on the risk of eczema is seen at 1 year of age, that protective effect is gone by 2 years and 4 years,” Dr. Marathe, who was not involved in the study, said in an email. “So if maternal supplementation does improve eczema, the effect is not long-lasting.
“The other complicating factor is that the babies who showed reduction in eczema were also the ones who were breastfed longer than 1 month,” she added. “We know that breastfeeding is associated with several factors, including socioeconomic status, so it is difficult to tease out the relationships here.
“Vitamin D has become a very hot topic lately and seems to have protective effects in many areas of health care,” Dr. Marathe said. “These results may motivate pregnant women to be compliant with their prenatal vitamins that contain the amount of vitamin D studied here.”
The study received grant support. Several authors disclosed financial relationships with pharmaceutical and nutritional products industries. Dr. El-Heis and Dr. Marathe reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SID 2022