User login
No Child Too Young for Eye Exam
STANFORD, CALIF. – Myths about pediatric eye abnormalities often mislead parents into thinking an eye evaluation is not necessary, according to Dr. Deborah M. Alcorn, chief of pediatric ophthalmology at Lucile Packard Children’s Hospital, Stanford.
At a pediatric update sponsored by Stanford University, she debunked the top 10 myths about eye problems in children:
1. My child is too young for an eye exam. Dr. Alcorn said she frequently gets called to the neonatal unit to evaluate babies who are only a few months old. Infant eye exams are very objective. The child’s age is irrelevant, except that it’s better to treat a problem earlier rather than later, she said.
2. Tearing must be due to a blocked tear duct. Yes, epiphora is most likely to be secondary to a nasolacrimal duct obstruction, but the differential diagnosis includes corneal abrasion and glaucoma.
Placing yellow fluorescein dye in the eye can easily identify nasolacrimal duct obstruction; within 2-3 minutes, the dye will come out the child’s nose. In infants, treatment with warm compresses and massage will open 95% of lacrimal obstructions by 1 year of age.
Persistent, excessive tearing, especially in the first few weeks of life, may be a sign of an associated dacryocystocele. These blue-domed cysts deserve aggressive treatment with systemic antibiotics, warm compresses, and massage, Dr. Alcorn said. Nasolacrimal duct probing may be needed. If the color of the dacryocystocele changes from blue to very red with erythema, hospitalize the child to treat infection, she said.
Tearing and discharge may be due to congenital nasolacrimal duct obstructions. If you see a child with silicone tubing poking out of the tear duct, don’t pull it out – it’s a stent to enlarge the lacrimal duct. "We like to leave it in for 6 months," she said.
Tearing from corneal abrasion is accompanied by pain, discomfort, and often photophobia. If you use a topical anesthetic to make the eye exam easier, do not dispense it to parents, Dr. Alcorn said. Repeated use will break down the child’s cornea. Treat a corneal abrasion with a topical antibiotic; children usually prefer drops to ointment, which blurs vision, she noted.
You may see tearing from congenital glaucoma, which produces big eyes on the baby that seem beautiful but are abnormal. Unlike adult glaucoma, congenital glaucoma deserves emergency surgery, she said.
3. All red eyes are contagious. Viral conjunctivitis is highly contagious, but the causes of red eye are diverse. Subconjunctival hemorrhage usually is benign and spontaneously resolves. Episcleritis usually resolves with eye drop therapy. Eyes may be red from pinguecula or pterygium – hyperkeratotic reactions to the sun that are slow growing and not malignant. "We’re starting to see more of these because kids are not wearing sunglasses," Dr. Alcorn said.
Treat pinguecula and pterygium with sunglasses, artificial tears, and vasoconstrictors, and consider surgical removal if the lesion is interfering with wearing contact lenses or the pterygium involves the visual axis.
Conjunctivitis can be bacterial, viral, or allergic. The two main clues to differentiate the three kinds of conjunctivitis are the discharge (which is purulent in bacterial conjunctivitis and watery in viral or allergic conjunctivitis) and itching (which is marked in allergic conjunctivitis but minimal with the other two forms).
Viral conjunctivitis is so contagious that Dr. Alcorn said she tries to not let these patients into her examination room, in order to avoid having to wash the room with bleach afterward. These patients usually have bilateral red eyes, preauricular lymphadenopathy, conjunctival inflammation, and watery discharge. Upper respiratory infection, sore throat, and fever are common.
This has been one of the worst years for seasonal allergies causing acute allergic conjunctivitis, in Dr. Alcorn’s experience. Bilateral red eyes, profuse pruritus, chemosis, and ropy mucous discharge are typical.
A variety of topical medications in eye drops can be used to treat allergic conjunctivitis. However, do not prescribe a topical steroid or combination antibiotic-steroid without close follow-up, because steroids can cause glaucoma or cataracts or potentiate infection, she said.
4. Children outgrow crossed eyes. "I don’t care how cute your kids are, they should have straight eyes," she said. Refer any patients with constant strabismus before 12 weeks of age or any strabismus at older ages.
An eye cover test is easy to do to diagnose strabismus. With the patient looking straight ahead, cover one eye, peek behind the cover, and you’ll see the eye turn in or drift outward.
Children with a wide nasal bridge, prominent epicanthal folds, or an abnormally small interpupillary distance may seem to have a crossed eye, but really don’t. Dr. Alcorn usually reevaluates children with pseudostrabismus in 6 months "to be sure we didn’t miss something," she said.
Glasses can fix accommodative esotropia (one eye moving toward the other), but must be worn all the time, except when bathing, swimming, or sleeping. Surgery is not indicated.
If the child is unable to abduct the eye (look outward from the nose), there may be an intracranial process or infection. The eye that can’t turn out will always be turned in if there’s a sixth nerve palsy. In contrast, Duane’s syndrome, a congenital miswiring that prevents an eye from looking outward, allows both eyes to look straight ahead.
The cover test also is very valuable in diagnosing exotropia (outward deviation of an eye), which is much less common than esotropia. These patients may need glasses or another intervention, and should be evaluated.
5. A bump on an eye will go away. Sties often go away with treatment, but chalazia (chronic sties) may need surgical removal. Treat both with warm compresses, topical antibiotic ointment, light massage, and daily oral flaxseed oil (generally 1 tablespoon per 100 pounds of body weight). Eventually, if needed, consider incision and curettage or possibly a steroid injection, she said.
Not all lumps and bumps are sties. Capillary hemangiomas occur in 1%-2% of newborns, usually appear by 6 months of age, and involute spontaneously. Congenital hemangiomas can be treated with topical timolol or oral propranolol, and should be monitored regularly; 50% will resolve by 5 years of age and 70% by 7 years. Orbital dermoids will not go away on their own and usually require surgical excision at age 4 or 5 years. Lymphangiomas typically present in the first decade of life and will grow. Rhabdomyosarcomas deserve emergency care – they can double in size in a day.
6. One eye is bigger, but it’s a family trait. A child with one eye bigger than the other deserves evaluation to determine if this is truly globe asymmetry or if there’s another diagnosis, such as microphthalmia, ptosis, congenital glaucoma, or proptosis from a mass pushing the eye out.
7. Glasses worsen a child’s prescription. No one is too young to wear glasses, which will not worsen vision over time, Dr. Alcorn said. Myopia is becoming a worldwide epidemic, especially in Asian populations, according to a recent report (Lancet 2012;379:1739-48).
Other data suggest that myopia is starting at earlier ages and occurring more frequently, she said. There is some literature to support letting children play outside more often to prevent myopia, so they won’t always be looking at things up close. Laser treatment is not approved in the United States for people younger than 21 years because the eyes are still growing.
Myopia is a "major global health concern" because it increases the risk for blindness, glaucoma, retinal detachment, and other problems. "We’re hoping for a cure," she said.
8. Abnormal light reflexes are just a bad picture. When a child has refractive asymmetry on a vision-screening photograph, be concerned. The child may simply need glasses, or could have leukokoria, a cataract, retinoblastoma, or another problem.
9. Different-colored eyes are cute. Maybe they are, but you wouldn’t want to miss an infection or Horner syndrome, which can affect eye color, Dr. Alcorn said.
10. Parents don’t know best. "Listen to parents," she said. "They know their children!"
Dr. Alcorn reported having no relevant financial disclosures.
STANFORD, CALIF. – Myths about pediatric eye abnormalities often mislead parents into thinking an eye evaluation is not necessary, according to Dr. Deborah M. Alcorn, chief of pediatric ophthalmology at Lucile Packard Children’s Hospital, Stanford.
At a pediatric update sponsored by Stanford University, she debunked the top 10 myths about eye problems in children:
1. My child is too young for an eye exam. Dr. Alcorn said she frequently gets called to the neonatal unit to evaluate babies who are only a few months old. Infant eye exams are very objective. The child’s age is irrelevant, except that it’s better to treat a problem earlier rather than later, she said.
2. Tearing must be due to a blocked tear duct. Yes, epiphora is most likely to be secondary to a nasolacrimal duct obstruction, but the differential diagnosis includes corneal abrasion and glaucoma.
Placing yellow fluorescein dye in the eye can easily identify nasolacrimal duct obstruction; within 2-3 minutes, the dye will come out the child’s nose. In infants, treatment with warm compresses and massage will open 95% of lacrimal obstructions by 1 year of age.
Persistent, excessive tearing, especially in the first few weeks of life, may be a sign of an associated dacryocystocele. These blue-domed cysts deserve aggressive treatment with systemic antibiotics, warm compresses, and massage, Dr. Alcorn said. Nasolacrimal duct probing may be needed. If the color of the dacryocystocele changes from blue to very red with erythema, hospitalize the child to treat infection, she said.
Tearing and discharge may be due to congenital nasolacrimal duct obstructions. If you see a child with silicone tubing poking out of the tear duct, don’t pull it out – it’s a stent to enlarge the lacrimal duct. "We like to leave it in for 6 months," she said.
Tearing from corneal abrasion is accompanied by pain, discomfort, and often photophobia. If you use a topical anesthetic to make the eye exam easier, do not dispense it to parents, Dr. Alcorn said. Repeated use will break down the child’s cornea. Treat a corneal abrasion with a topical antibiotic; children usually prefer drops to ointment, which blurs vision, she noted.
You may see tearing from congenital glaucoma, which produces big eyes on the baby that seem beautiful but are abnormal. Unlike adult glaucoma, congenital glaucoma deserves emergency surgery, she said.
3. All red eyes are contagious. Viral conjunctivitis is highly contagious, but the causes of red eye are diverse. Subconjunctival hemorrhage usually is benign and spontaneously resolves. Episcleritis usually resolves with eye drop therapy. Eyes may be red from pinguecula or pterygium – hyperkeratotic reactions to the sun that are slow growing and not malignant. "We’re starting to see more of these because kids are not wearing sunglasses," Dr. Alcorn said.
Treat pinguecula and pterygium with sunglasses, artificial tears, and vasoconstrictors, and consider surgical removal if the lesion is interfering with wearing contact lenses or the pterygium involves the visual axis.
Conjunctivitis can be bacterial, viral, or allergic. The two main clues to differentiate the three kinds of conjunctivitis are the discharge (which is purulent in bacterial conjunctivitis and watery in viral or allergic conjunctivitis) and itching (which is marked in allergic conjunctivitis but minimal with the other two forms).
Viral conjunctivitis is so contagious that Dr. Alcorn said she tries to not let these patients into her examination room, in order to avoid having to wash the room with bleach afterward. These patients usually have bilateral red eyes, preauricular lymphadenopathy, conjunctival inflammation, and watery discharge. Upper respiratory infection, sore throat, and fever are common.
This has been one of the worst years for seasonal allergies causing acute allergic conjunctivitis, in Dr. Alcorn’s experience. Bilateral red eyes, profuse pruritus, chemosis, and ropy mucous discharge are typical.
A variety of topical medications in eye drops can be used to treat allergic conjunctivitis. However, do not prescribe a topical steroid or combination antibiotic-steroid without close follow-up, because steroids can cause glaucoma or cataracts or potentiate infection, she said.
4. Children outgrow crossed eyes. "I don’t care how cute your kids are, they should have straight eyes," she said. Refer any patients with constant strabismus before 12 weeks of age or any strabismus at older ages.
An eye cover test is easy to do to diagnose strabismus. With the patient looking straight ahead, cover one eye, peek behind the cover, and you’ll see the eye turn in or drift outward.
Children with a wide nasal bridge, prominent epicanthal folds, or an abnormally small interpupillary distance may seem to have a crossed eye, but really don’t. Dr. Alcorn usually reevaluates children with pseudostrabismus in 6 months "to be sure we didn’t miss something," she said.
Glasses can fix accommodative esotropia (one eye moving toward the other), but must be worn all the time, except when bathing, swimming, or sleeping. Surgery is not indicated.
If the child is unable to abduct the eye (look outward from the nose), there may be an intracranial process or infection. The eye that can’t turn out will always be turned in if there’s a sixth nerve palsy. In contrast, Duane’s syndrome, a congenital miswiring that prevents an eye from looking outward, allows both eyes to look straight ahead.
The cover test also is very valuable in diagnosing exotropia (outward deviation of an eye), which is much less common than esotropia. These patients may need glasses or another intervention, and should be evaluated.
5. A bump on an eye will go away. Sties often go away with treatment, but chalazia (chronic sties) may need surgical removal. Treat both with warm compresses, topical antibiotic ointment, light massage, and daily oral flaxseed oil (generally 1 tablespoon per 100 pounds of body weight). Eventually, if needed, consider incision and curettage or possibly a steroid injection, she said.
Not all lumps and bumps are sties. Capillary hemangiomas occur in 1%-2% of newborns, usually appear by 6 months of age, and involute spontaneously. Congenital hemangiomas can be treated with topical timolol or oral propranolol, and should be monitored regularly; 50% will resolve by 5 years of age and 70% by 7 years. Orbital dermoids will not go away on their own and usually require surgical excision at age 4 or 5 years. Lymphangiomas typically present in the first decade of life and will grow. Rhabdomyosarcomas deserve emergency care – they can double in size in a day.
6. One eye is bigger, but it’s a family trait. A child with one eye bigger than the other deserves evaluation to determine if this is truly globe asymmetry or if there’s another diagnosis, such as microphthalmia, ptosis, congenital glaucoma, or proptosis from a mass pushing the eye out.
7. Glasses worsen a child’s prescription. No one is too young to wear glasses, which will not worsen vision over time, Dr. Alcorn said. Myopia is becoming a worldwide epidemic, especially in Asian populations, according to a recent report (Lancet 2012;379:1739-48).
Other data suggest that myopia is starting at earlier ages and occurring more frequently, she said. There is some literature to support letting children play outside more often to prevent myopia, so they won’t always be looking at things up close. Laser treatment is not approved in the United States for people younger than 21 years because the eyes are still growing.
Myopia is a "major global health concern" because it increases the risk for blindness, glaucoma, retinal detachment, and other problems. "We’re hoping for a cure," she said.
8. Abnormal light reflexes are just a bad picture. When a child has refractive asymmetry on a vision-screening photograph, be concerned. The child may simply need glasses, or could have leukokoria, a cataract, retinoblastoma, or another problem.
9. Different-colored eyes are cute. Maybe they are, but you wouldn’t want to miss an infection or Horner syndrome, which can affect eye color, Dr. Alcorn said.
10. Parents don’t know best. "Listen to parents," she said. "They know their children!"
Dr. Alcorn reported having no relevant financial disclosures.
STANFORD, CALIF. – Myths about pediatric eye abnormalities often mislead parents into thinking an eye evaluation is not necessary, according to Dr. Deborah M. Alcorn, chief of pediatric ophthalmology at Lucile Packard Children’s Hospital, Stanford.
At a pediatric update sponsored by Stanford University, she debunked the top 10 myths about eye problems in children:
1. My child is too young for an eye exam. Dr. Alcorn said she frequently gets called to the neonatal unit to evaluate babies who are only a few months old. Infant eye exams are very objective. The child’s age is irrelevant, except that it’s better to treat a problem earlier rather than later, she said.
2. Tearing must be due to a blocked tear duct. Yes, epiphora is most likely to be secondary to a nasolacrimal duct obstruction, but the differential diagnosis includes corneal abrasion and glaucoma.
Placing yellow fluorescein dye in the eye can easily identify nasolacrimal duct obstruction; within 2-3 minutes, the dye will come out the child’s nose. In infants, treatment with warm compresses and massage will open 95% of lacrimal obstructions by 1 year of age.
Persistent, excessive tearing, especially in the first few weeks of life, may be a sign of an associated dacryocystocele. These blue-domed cysts deserve aggressive treatment with systemic antibiotics, warm compresses, and massage, Dr. Alcorn said. Nasolacrimal duct probing may be needed. If the color of the dacryocystocele changes from blue to very red with erythema, hospitalize the child to treat infection, she said.
Tearing and discharge may be due to congenital nasolacrimal duct obstructions. If you see a child with silicone tubing poking out of the tear duct, don’t pull it out – it’s a stent to enlarge the lacrimal duct. "We like to leave it in for 6 months," she said.
Tearing from corneal abrasion is accompanied by pain, discomfort, and often photophobia. If you use a topical anesthetic to make the eye exam easier, do not dispense it to parents, Dr. Alcorn said. Repeated use will break down the child’s cornea. Treat a corneal abrasion with a topical antibiotic; children usually prefer drops to ointment, which blurs vision, she noted.
You may see tearing from congenital glaucoma, which produces big eyes on the baby that seem beautiful but are abnormal. Unlike adult glaucoma, congenital glaucoma deserves emergency surgery, she said.
3. All red eyes are contagious. Viral conjunctivitis is highly contagious, but the causes of red eye are diverse. Subconjunctival hemorrhage usually is benign and spontaneously resolves. Episcleritis usually resolves with eye drop therapy. Eyes may be red from pinguecula or pterygium – hyperkeratotic reactions to the sun that are slow growing and not malignant. "We’re starting to see more of these because kids are not wearing sunglasses," Dr. Alcorn said.
Treat pinguecula and pterygium with sunglasses, artificial tears, and vasoconstrictors, and consider surgical removal if the lesion is interfering with wearing contact lenses or the pterygium involves the visual axis.
Conjunctivitis can be bacterial, viral, or allergic. The two main clues to differentiate the three kinds of conjunctivitis are the discharge (which is purulent in bacterial conjunctivitis and watery in viral or allergic conjunctivitis) and itching (which is marked in allergic conjunctivitis but minimal with the other two forms).
Viral conjunctivitis is so contagious that Dr. Alcorn said she tries to not let these patients into her examination room, in order to avoid having to wash the room with bleach afterward. These patients usually have bilateral red eyes, preauricular lymphadenopathy, conjunctival inflammation, and watery discharge. Upper respiratory infection, sore throat, and fever are common.
This has been one of the worst years for seasonal allergies causing acute allergic conjunctivitis, in Dr. Alcorn’s experience. Bilateral red eyes, profuse pruritus, chemosis, and ropy mucous discharge are typical.
A variety of topical medications in eye drops can be used to treat allergic conjunctivitis. However, do not prescribe a topical steroid or combination antibiotic-steroid without close follow-up, because steroids can cause glaucoma or cataracts or potentiate infection, she said.
4. Children outgrow crossed eyes. "I don’t care how cute your kids are, they should have straight eyes," she said. Refer any patients with constant strabismus before 12 weeks of age or any strabismus at older ages.
An eye cover test is easy to do to diagnose strabismus. With the patient looking straight ahead, cover one eye, peek behind the cover, and you’ll see the eye turn in or drift outward.
Children with a wide nasal bridge, prominent epicanthal folds, or an abnormally small interpupillary distance may seem to have a crossed eye, but really don’t. Dr. Alcorn usually reevaluates children with pseudostrabismus in 6 months "to be sure we didn’t miss something," she said.
Glasses can fix accommodative esotropia (one eye moving toward the other), but must be worn all the time, except when bathing, swimming, or sleeping. Surgery is not indicated.
If the child is unable to abduct the eye (look outward from the nose), there may be an intracranial process or infection. The eye that can’t turn out will always be turned in if there’s a sixth nerve palsy. In contrast, Duane’s syndrome, a congenital miswiring that prevents an eye from looking outward, allows both eyes to look straight ahead.
The cover test also is very valuable in diagnosing exotropia (outward deviation of an eye), which is much less common than esotropia. These patients may need glasses or another intervention, and should be evaluated.
5. A bump on an eye will go away. Sties often go away with treatment, but chalazia (chronic sties) may need surgical removal. Treat both with warm compresses, topical antibiotic ointment, light massage, and daily oral flaxseed oil (generally 1 tablespoon per 100 pounds of body weight). Eventually, if needed, consider incision and curettage or possibly a steroid injection, she said.
Not all lumps and bumps are sties. Capillary hemangiomas occur in 1%-2% of newborns, usually appear by 6 months of age, and involute spontaneously. Congenital hemangiomas can be treated with topical timolol or oral propranolol, and should be monitored regularly; 50% will resolve by 5 years of age and 70% by 7 years. Orbital dermoids will not go away on their own and usually require surgical excision at age 4 or 5 years. Lymphangiomas typically present in the first decade of life and will grow. Rhabdomyosarcomas deserve emergency care – they can double in size in a day.
6. One eye is bigger, but it’s a family trait. A child with one eye bigger than the other deserves evaluation to determine if this is truly globe asymmetry or if there’s another diagnosis, such as microphthalmia, ptosis, congenital glaucoma, or proptosis from a mass pushing the eye out.
7. Glasses worsen a child’s prescription. No one is too young to wear glasses, which will not worsen vision over time, Dr. Alcorn said. Myopia is becoming a worldwide epidemic, especially in Asian populations, according to a recent report (Lancet 2012;379:1739-48).
Other data suggest that myopia is starting at earlier ages and occurring more frequently, she said. There is some literature to support letting children play outside more often to prevent myopia, so they won’t always be looking at things up close. Laser treatment is not approved in the United States for people younger than 21 years because the eyes are still growing.
Myopia is a "major global health concern" because it increases the risk for blindness, glaucoma, retinal detachment, and other problems. "We’re hoping for a cure," she said.
8. Abnormal light reflexes are just a bad picture. When a child has refractive asymmetry on a vision-screening photograph, be concerned. The child may simply need glasses, or could have leukokoria, a cataract, retinoblastoma, or another problem.
9. Different-colored eyes are cute. Maybe they are, but you wouldn’t want to miss an infection or Horner syndrome, which can affect eye color, Dr. Alcorn said.
10. Parents don’t know best. "Listen to parents," she said. "They know their children!"
Dr. Alcorn reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Therapy-Resistant Asthma May Be Neither
STANFORD, CALIF. – Therapy-resistant asthma usually isn’t.
Often it’s asthma that’s not really resistant to therapy, but a result of poor adherence to therapy, poor inhalation technique, or poor asthma control due to exposure to smoke or allergens.
And sometimes, it’s not even asthma. So, for a child with apparently severe asthma, first confirm the diagnosis and ensure that basic management strategies are in place and being followed, Dr. John D. Mark said at a pediatric update sponsored by Stanford University.
If you can improve the patient’s adherence to treatment, drug delivery, and exposure to environmental triggers, "you could fix nearly all ‘treatment-resistant asthma,’ " said Dr. Mark, a pediatric pulmonologist at Lucile Packard Children’s Hospital at Stanford.
He said he sees many patients referred for therapy-resistant asthma, but noted that there are not a lot of data on how to manage them.
Only 55 of 292 children with moderate to severe asthma, despite being prescribed at least 400 mcg/day of budesonide plus a long-acting beta-2 agonist, could be randomized after eligibility assessment in one treatment trial. Among the 237 who didn’t qualify, children either were nonadherent to treatment (38%) or were found to have mild or no asthma (25%) (J. Allergy Clin. Immunol. 2008;122:1138-44).
In a separate study of 780 patients aged 12-20 years with "severe asthma," the focus on basic asthma management during the run-in period of the trial improved symptoms so much that no clinically significant gains were achieved during the main part of the study by the use of exhaled nitric oxides as an indicator of control, even though this measure increased corticosteroid use (Lancet 2008;372:1065-72).
Another study found that 86% of 100 adults with chronic obstructive pulmonary disease or asthma were misusing their metered-dose inhaler (MDI) and 71% were misusing their Diskus dry powder inhaler (J. Gen. Intern. Med. 2011;26:635-42). A separate study of 127 children and adults found incorrect use of inhaler devices in 64% of MDI users and 26% of patients using the Rotahaler dry powder inhaler. Spacer devices seldom were used (J. Assoc. Physicians India 2005;53:681-4).
Dr. Mark said "therapy-resistant asthma" may fall into one of four categories:
• The wrong diagnosis. This is common, so do a diagnostic re-evaluation, he said.
• Asthma plus. Mild asthma exacerbated by one or more comorbidities is another common scenario. Some studies suggest that up to 15% of patients with severe or persistent asthma have dysfunctional breathing, such as vocal cord dysfunction. Rhinosinusitis, obesity, and food allergy can affect asthma control. Treating gastroesophageal reflux disorder usually does not improve asthma control much, Dr. Mark said.
• Difficult-to-treat asthma. This is a very common category in which poor treatment adherence or poor inhalation technique is the root of the problem. It often overlaps with the previous category.
• True resistance. Probably not common, this is severe therapy-resistant asthma that remains refractory to treatment even after dealing with reversible factors.
For diagnostic testing, start with lung function tests, he said. Spirometry is helpful, but the results may be normal even in cases of severe asthma. Longitudinal spirometry can be helpful, and bronchial responsiveness testing is helpful if the patient has persistent airflow limitation. Consider checking exhaled nitric oxide if that’s available and ordering complete lung function tests to evaluate lung volume and gas trapping. Look for markers of inflammation in induced sputum if the patient’s 1-second forced expiratory volume is more than 70% of predicted. An exercise challenge test also may be appropriate.
Perform an ear, nose, and throat or upper airway evaluation to look for vocal cord dysfunction. Assess tobacco smoke exposure by measuring cotinine in saliva or urine. If the patient has been prescribed theophylline, measure levels, Dr. Mark said.
Evaluate allergies by both skin prick testing and radioallergosorbent testing, looking for aeroallergens, fungi, and food allergens.
The role of bronchial challenge is not clear, and it can be dangerous if bronchial lability is present. There is no evidence to recommend routine high-resolution CT scans even in true severe, therapy-resistant pediatric asthma, he said.
For these tough cases, put on your Marcus Welby hat and make a home visit. "A home visit can be most rewarding," Dr. Mark said, because you can more accurately assess adherence to treatment, smoke exposure, allergens, and psychosocial factors such as acute and chronic stress, which are known to amplify the airway eosinophilic response to an allergen challenge.
A home visit helped solve the mystery of one 8-year-old boy with severe persistent asthma. Scans revealed no chronic sinusitis or bronchiectasis. But testing showed he was allergic to at least 32 substances, and a home inspection revealed mold throughout the house. Social services helped the family move to a new home, and Dr. Mark added itraconazole to the boy’s treatment regimen.
"You can figure it out," Dr. Mark said. "It took me around 3 years for this guy."
Dr. Mark reported having no relevant financial disclosures.
STANFORD, CALIF. – Therapy-resistant asthma usually isn’t.
Often it’s asthma that’s not really resistant to therapy, but a result of poor adherence to therapy, poor inhalation technique, or poor asthma control due to exposure to smoke or allergens.
And sometimes, it’s not even asthma. So, for a child with apparently severe asthma, first confirm the diagnosis and ensure that basic management strategies are in place and being followed, Dr. John D. Mark said at a pediatric update sponsored by Stanford University.
If you can improve the patient’s adherence to treatment, drug delivery, and exposure to environmental triggers, "you could fix nearly all ‘treatment-resistant asthma,’ " said Dr. Mark, a pediatric pulmonologist at Lucile Packard Children’s Hospital at Stanford.
He said he sees many patients referred for therapy-resistant asthma, but noted that there are not a lot of data on how to manage them.
Only 55 of 292 children with moderate to severe asthma, despite being prescribed at least 400 mcg/day of budesonide plus a long-acting beta-2 agonist, could be randomized after eligibility assessment in one treatment trial. Among the 237 who didn’t qualify, children either were nonadherent to treatment (38%) or were found to have mild or no asthma (25%) (J. Allergy Clin. Immunol. 2008;122:1138-44).
In a separate study of 780 patients aged 12-20 years with "severe asthma," the focus on basic asthma management during the run-in period of the trial improved symptoms so much that no clinically significant gains were achieved during the main part of the study by the use of exhaled nitric oxides as an indicator of control, even though this measure increased corticosteroid use (Lancet 2008;372:1065-72).
Another study found that 86% of 100 adults with chronic obstructive pulmonary disease or asthma were misusing their metered-dose inhaler (MDI) and 71% were misusing their Diskus dry powder inhaler (J. Gen. Intern. Med. 2011;26:635-42). A separate study of 127 children and adults found incorrect use of inhaler devices in 64% of MDI users and 26% of patients using the Rotahaler dry powder inhaler. Spacer devices seldom were used (J. Assoc. Physicians India 2005;53:681-4).
Dr. Mark said "therapy-resistant asthma" may fall into one of four categories:
• The wrong diagnosis. This is common, so do a diagnostic re-evaluation, he said.
• Asthma plus. Mild asthma exacerbated by one or more comorbidities is another common scenario. Some studies suggest that up to 15% of patients with severe or persistent asthma have dysfunctional breathing, such as vocal cord dysfunction. Rhinosinusitis, obesity, and food allergy can affect asthma control. Treating gastroesophageal reflux disorder usually does not improve asthma control much, Dr. Mark said.
• Difficult-to-treat asthma. This is a very common category in which poor treatment adherence or poor inhalation technique is the root of the problem. It often overlaps with the previous category.
• True resistance. Probably not common, this is severe therapy-resistant asthma that remains refractory to treatment even after dealing with reversible factors.
For diagnostic testing, start with lung function tests, he said. Spirometry is helpful, but the results may be normal even in cases of severe asthma. Longitudinal spirometry can be helpful, and bronchial responsiveness testing is helpful if the patient has persistent airflow limitation. Consider checking exhaled nitric oxide if that’s available and ordering complete lung function tests to evaluate lung volume and gas trapping. Look for markers of inflammation in induced sputum if the patient’s 1-second forced expiratory volume is more than 70% of predicted. An exercise challenge test also may be appropriate.
Perform an ear, nose, and throat or upper airway evaluation to look for vocal cord dysfunction. Assess tobacco smoke exposure by measuring cotinine in saliva or urine. If the patient has been prescribed theophylline, measure levels, Dr. Mark said.
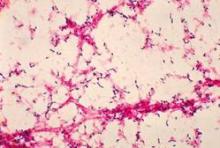
Evaluate allergies by both skin prick testing and radioallergosorbent testing, looking for aeroallergens, fungi, and food allergens.
The role of bronchial challenge is not clear, and it can be dangerous if bronchial lability is present. There is no evidence to recommend routine high-resolution CT scans even in true severe, therapy-resistant pediatric asthma, he said.
For these tough cases, put on your Marcus Welby hat and make a home visit. "A home visit can be most rewarding," Dr. Mark said, because you can more accurately assess adherence to treatment, smoke exposure, allergens, and psychosocial factors such as acute and chronic stress, which are known to amplify the airway eosinophilic response to an allergen challenge.
A home visit helped solve the mystery of one 8-year-old boy with severe persistent asthma. Scans revealed no chronic sinusitis or bronchiectasis. But testing showed he was allergic to at least 32 substances, and a home inspection revealed mold throughout the house. Social services helped the family move to a new home, and Dr. Mark added itraconazole to the boy’s treatment regimen.
"You can figure it out," Dr. Mark said. "It took me around 3 years for this guy."
Dr. Mark reported having no relevant financial disclosures.
STANFORD, CALIF. – Therapy-resistant asthma usually isn’t.
Often it’s asthma that’s not really resistant to therapy, but a result of poor adherence to therapy, poor inhalation technique, or poor asthma control due to exposure to smoke or allergens.
And sometimes, it’s not even asthma. So, for a child with apparently severe asthma, first confirm the diagnosis and ensure that basic management strategies are in place and being followed, Dr. John D. Mark said at a pediatric update sponsored by Stanford University.
If you can improve the patient’s adherence to treatment, drug delivery, and exposure to environmental triggers, "you could fix nearly all ‘treatment-resistant asthma,’ " said Dr. Mark, a pediatric pulmonologist at Lucile Packard Children’s Hospital at Stanford.
He said he sees many patients referred for therapy-resistant asthma, but noted that there are not a lot of data on how to manage them.
Only 55 of 292 children with moderate to severe asthma, despite being prescribed at least 400 mcg/day of budesonide plus a long-acting beta-2 agonist, could be randomized after eligibility assessment in one treatment trial. Among the 237 who didn’t qualify, children either were nonadherent to treatment (38%) or were found to have mild or no asthma (25%) (J. Allergy Clin. Immunol. 2008;122:1138-44).
In a separate study of 780 patients aged 12-20 years with "severe asthma," the focus on basic asthma management during the run-in period of the trial improved symptoms so much that no clinically significant gains were achieved during the main part of the study by the use of exhaled nitric oxides as an indicator of control, even though this measure increased corticosteroid use (Lancet 2008;372:1065-72).
Another study found that 86% of 100 adults with chronic obstructive pulmonary disease or asthma were misusing their metered-dose inhaler (MDI) and 71% were misusing their Diskus dry powder inhaler (J. Gen. Intern. Med. 2011;26:635-42). A separate study of 127 children and adults found incorrect use of inhaler devices in 64% of MDI users and 26% of patients using the Rotahaler dry powder inhaler. Spacer devices seldom were used (J. Assoc. Physicians India 2005;53:681-4).
Dr. Mark said "therapy-resistant asthma" may fall into one of four categories:
• The wrong diagnosis. This is common, so do a diagnostic re-evaluation, he said.
• Asthma plus. Mild asthma exacerbated by one or more comorbidities is another common scenario. Some studies suggest that up to 15% of patients with severe or persistent asthma have dysfunctional breathing, such as vocal cord dysfunction. Rhinosinusitis, obesity, and food allergy can affect asthma control. Treating gastroesophageal reflux disorder usually does not improve asthma control much, Dr. Mark said.
• Difficult-to-treat asthma. This is a very common category in which poor treatment adherence or poor inhalation technique is the root of the problem. It often overlaps with the previous category.
• True resistance. Probably not common, this is severe therapy-resistant asthma that remains refractory to treatment even after dealing with reversible factors.
For diagnostic testing, start with lung function tests, he said. Spirometry is helpful, but the results may be normal even in cases of severe asthma. Longitudinal spirometry can be helpful, and bronchial responsiveness testing is helpful if the patient has persistent airflow limitation. Consider checking exhaled nitric oxide if that’s available and ordering complete lung function tests to evaluate lung volume and gas trapping. Look for markers of inflammation in induced sputum if the patient’s 1-second forced expiratory volume is more than 70% of predicted. An exercise challenge test also may be appropriate.
Perform an ear, nose, and throat or upper airway evaluation to look for vocal cord dysfunction. Assess tobacco smoke exposure by measuring cotinine in saliva or urine. If the patient has been prescribed theophylline, measure levels, Dr. Mark said.
Evaluate allergies by both skin prick testing and radioallergosorbent testing, looking for aeroallergens, fungi, and food allergens.
The role of bronchial challenge is not clear, and it can be dangerous if bronchial lability is present. There is no evidence to recommend routine high-resolution CT scans even in true severe, therapy-resistant pediatric asthma, he said.
For these tough cases, put on your Marcus Welby hat and make a home visit. "A home visit can be most rewarding," Dr. Mark said, because you can more accurately assess adherence to treatment, smoke exposure, allergens, and psychosocial factors such as acute and chronic stress, which are known to amplify the airway eosinophilic response to an allergen challenge.
A home visit helped solve the mystery of one 8-year-old boy with severe persistent asthma. Scans revealed no chronic sinusitis or bronchiectasis. But testing showed he was allergic to at least 32 substances, and a home inspection revealed mold throughout the house. Social services helped the family move to a new home, and Dr. Mark added itraconazole to the boy’s treatment regimen.
"You can figure it out," Dr. Mark said. "It took me around 3 years for this guy."
Dr. Mark reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
X-Ray Illustrates Constipation Pain for Parents
STANFORD, CALIF. – An x-ray that shows that a child’s bowels are full of stool can help explain chronic abdominal pain to worried parents.
That’s a lot easier than convincing parents to accept the psychological causes behind functional abdominal pain, which is by far the No. 1 cause of chronic abdominal pain in children, Dr. Kenneth L. Cox said.
Constipation is – dare it be said – No. 2, he said at a pediatric update sponsored by Stanford University, and together these two problems account for about half of the cases of chronic abdominal pain that Dr. Cox sees in children.
Chronic abdominal pain is defined as intermittent or continuous pain that lasts for at least 1 month. Recurrent abdominal pain (defined as at least three episodes of pain occurring over 3 months or longer) affects 10%-25% of school-age children, and 80%-90% of it is functional abdominal pain, said Dr. Cox, chief of pediatric gastroenterology at Lucile Packard Children’s Hospital in Stanford, Calif.
In the evaluation of chronic abdominal pain in children, take a thorough history (especially psychosocial history), do a physical examination including a rectal exam, and ask the patient or parents to keep a pain log, he advised. Get a KUB (kidney, ureters, and bladder) x-ray, and consider ordering the following laboratory tests: CBC with differential; erythrocyte sedimentation rate; C-reactive protein; liver function tests; urinalysis; stool studies; and a spot urine amylase/creatinine ratio.
In the stool studies, order Hemoccult, fat, lactoferrin, Giardia enzyme immunoassay, Helicobacter pylori antigen, reducing substances, and pH, Dr. Cox added.
It’s important to rule out demonstrable disease to diagnose functional abdominal pain, which also requires continuous pain or at least one episode per week for 2 months or longer, he said.
The first step in treatment is reassuring the patient and family that functional pain is real and a common manifestation of stress, but that there is no organic disease. Treat with stress management; a high-fiber, high-fluid diet; drugs (which may include bulking agents, pain medications, anticholinergics, or antidepressants); and other therapies such as biofeedback, hypnosis, psychotherapy, imagery, yoga, or acupuncture.
The general screening studies will identify constipation as the cause of abdominal pain, which typically occurs in children who had difficulty around toilet training, Dr. Cox said.
Consider constipation to be chronic if the child has had at least two of the following problems for 12 weeks or more per year: fewer than three bowel movements per week and/or difficulty with more than a fourth of defecations (in the form of hard stool, straining, a feeling of incomplete evacuation, a sensation of anorectal obstruction, or the need for manual maneuvers to facilitate defecation).
These children have normal growth and normal anal tone with stool in the rectum. They’re usually at least 2 years old, and have encopresis.
Dr. Cox described a typical case of an 11-year-old boy complaining of 2 years of abdominal pain that was periumbilical, of short duration (usually lasting 1-3 hours), worse postprandially, and relieved by passing stool. The patient reported twice-weekly large, hard bowel movements, and he had smears of stool on his underwear (aka "skid marks"). His diet was low in fiber, with inadequate fluids.
With medical management, the constipation, encopresis, and pain will resolve. First, clean out retained or impacted stool using oral medications such as magnesium citrate, phosphor-soda, or polyethylene glycol. Enemas or suppositories also are options, but "I don’t like these," Dr. Cox said. "They’re a bit traumatic."
For maintenance therapy, prescribe a diet high in fluids and fiber. Add the child’s age plus 5 to calculate the number of grams per day of fiber that should be consumed, he said. Continue medications until the child has at least one bowel movement per day and no encopresis for 1 month. Teach the child to use the toilet after meals. Reward success with star charts or an age-appropriate reward, and avoid punishment, he said.
In patients who don’t respond, anal rectonometry may show abnormal defecation, such as an anal canal that does not relax during defecation. Biofeedback therapy incorporating video games can help train the child to relax the anal canal.
Besides constipation and functional abdominal pain, other common causes of chronic pediatric abdominal pain include gastroesophageal reflux, which often presents as pain in the abdomen (not chest), or abdominal wall injury from exercise. Drinking a lot of carbonated beverages can cause pain from aerophagia. Approximately half of chronic abdominal pain in adolescents involves lactose intolerance. Urinary tract infection, giardiasis, or H. pylori infection also are relatively common causes.
In rare cases, chronic abdominal pain in children is due to peptic ulcer disease, pancreatitis, inflammatory bowel disease, gallstones, renal stones, choledochal cysts, discitis, or abdominal migraine, although the last problem is "probably more common than is recognized," Dr. Cox said.
There’s approximately a 2% incidence of a syndrome of abdominal migraine and cyclic vomiting in school-age children, he estimated. The syndrome features recurrent, explosive bouts of vomiting and/or abdominal pain, punctuated by periods of normal health. In one study of 214 children with cyclic vomiting syndrome, 82% had associated migraines (J. Pediatr. 1999:134:567-72).
Dr. Cox reported having no relevant financial disclosures.
STANFORD, CALIF. – An x-ray that shows that a child’s bowels are full of stool can help explain chronic abdominal pain to worried parents.
That’s a lot easier than convincing parents to accept the psychological causes behind functional abdominal pain, which is by far the No. 1 cause of chronic abdominal pain in children, Dr. Kenneth L. Cox said.
Constipation is – dare it be said – No. 2, he said at a pediatric update sponsored by Stanford University, and together these two problems account for about half of the cases of chronic abdominal pain that Dr. Cox sees in children.
Chronic abdominal pain is defined as intermittent or continuous pain that lasts for at least 1 month. Recurrent abdominal pain (defined as at least three episodes of pain occurring over 3 months or longer) affects 10%-25% of school-age children, and 80%-90% of it is functional abdominal pain, said Dr. Cox, chief of pediatric gastroenterology at Lucile Packard Children’s Hospital in Stanford, Calif.
In the evaluation of chronic abdominal pain in children, take a thorough history (especially psychosocial history), do a physical examination including a rectal exam, and ask the patient or parents to keep a pain log, he advised. Get a KUB (kidney, ureters, and bladder) x-ray, and consider ordering the following laboratory tests: CBC with differential; erythrocyte sedimentation rate; C-reactive protein; liver function tests; urinalysis; stool studies; and a spot urine amylase/creatinine ratio.
In the stool studies, order Hemoccult, fat, lactoferrin, Giardia enzyme immunoassay, Helicobacter pylori antigen, reducing substances, and pH, Dr. Cox added.
It’s important to rule out demonstrable disease to diagnose functional abdominal pain, which also requires continuous pain or at least one episode per week for 2 months or longer, he said.
The first step in treatment is reassuring the patient and family that functional pain is real and a common manifestation of stress, but that there is no organic disease. Treat with stress management; a high-fiber, high-fluid diet; drugs (which may include bulking agents, pain medications, anticholinergics, or antidepressants); and other therapies such as biofeedback, hypnosis, psychotherapy, imagery, yoga, or acupuncture.
The general screening studies will identify constipation as the cause of abdominal pain, which typically occurs in children who had difficulty around toilet training, Dr. Cox said.
Consider constipation to be chronic if the child has had at least two of the following problems for 12 weeks or more per year: fewer than three bowel movements per week and/or difficulty with more than a fourth of defecations (in the form of hard stool, straining, a feeling of incomplete evacuation, a sensation of anorectal obstruction, or the need for manual maneuvers to facilitate defecation).
These children have normal growth and normal anal tone with stool in the rectum. They’re usually at least 2 years old, and have encopresis.
Dr. Cox described a typical case of an 11-year-old boy complaining of 2 years of abdominal pain that was periumbilical, of short duration (usually lasting 1-3 hours), worse postprandially, and relieved by passing stool. The patient reported twice-weekly large, hard bowel movements, and he had smears of stool on his underwear (aka "skid marks"). His diet was low in fiber, with inadequate fluids.
With medical management, the constipation, encopresis, and pain will resolve. First, clean out retained or impacted stool using oral medications such as magnesium citrate, phosphor-soda, or polyethylene glycol. Enemas or suppositories also are options, but "I don’t like these," Dr. Cox said. "They’re a bit traumatic."
For maintenance therapy, prescribe a diet high in fluids and fiber. Add the child’s age plus 5 to calculate the number of grams per day of fiber that should be consumed, he said. Continue medications until the child has at least one bowel movement per day and no encopresis for 1 month. Teach the child to use the toilet after meals. Reward success with star charts or an age-appropriate reward, and avoid punishment, he said.
In patients who don’t respond, anal rectonometry may show abnormal defecation, such as an anal canal that does not relax during defecation. Biofeedback therapy incorporating video games can help train the child to relax the anal canal.
Besides constipation and functional abdominal pain, other common causes of chronic pediatric abdominal pain include gastroesophageal reflux, which often presents as pain in the abdomen (not chest), or abdominal wall injury from exercise. Drinking a lot of carbonated beverages can cause pain from aerophagia. Approximately half of chronic abdominal pain in adolescents involves lactose intolerance. Urinary tract infection, giardiasis, or H. pylori infection also are relatively common causes.
In rare cases, chronic abdominal pain in children is due to peptic ulcer disease, pancreatitis, inflammatory bowel disease, gallstones, renal stones, choledochal cysts, discitis, or abdominal migraine, although the last problem is "probably more common than is recognized," Dr. Cox said.
There’s approximately a 2% incidence of a syndrome of abdominal migraine and cyclic vomiting in school-age children, he estimated. The syndrome features recurrent, explosive bouts of vomiting and/or abdominal pain, punctuated by periods of normal health. In one study of 214 children with cyclic vomiting syndrome, 82% had associated migraines (J. Pediatr. 1999:134:567-72).
Dr. Cox reported having no relevant financial disclosures.
STANFORD, CALIF. – An x-ray that shows that a child’s bowels are full of stool can help explain chronic abdominal pain to worried parents.
That’s a lot easier than convincing parents to accept the psychological causes behind functional abdominal pain, which is by far the No. 1 cause of chronic abdominal pain in children, Dr. Kenneth L. Cox said.
Constipation is – dare it be said – No. 2, he said at a pediatric update sponsored by Stanford University, and together these two problems account for about half of the cases of chronic abdominal pain that Dr. Cox sees in children.
Chronic abdominal pain is defined as intermittent or continuous pain that lasts for at least 1 month. Recurrent abdominal pain (defined as at least three episodes of pain occurring over 3 months or longer) affects 10%-25% of school-age children, and 80%-90% of it is functional abdominal pain, said Dr. Cox, chief of pediatric gastroenterology at Lucile Packard Children’s Hospital in Stanford, Calif.
In the evaluation of chronic abdominal pain in children, take a thorough history (especially psychosocial history), do a physical examination including a rectal exam, and ask the patient or parents to keep a pain log, he advised. Get a KUB (kidney, ureters, and bladder) x-ray, and consider ordering the following laboratory tests: CBC with differential; erythrocyte sedimentation rate; C-reactive protein; liver function tests; urinalysis; stool studies; and a spot urine amylase/creatinine ratio.
In the stool studies, order Hemoccult, fat, lactoferrin, Giardia enzyme immunoassay, Helicobacter pylori antigen, reducing substances, and pH, Dr. Cox added.
It’s important to rule out demonstrable disease to diagnose functional abdominal pain, which also requires continuous pain or at least one episode per week for 2 months or longer, he said.
The first step in treatment is reassuring the patient and family that functional pain is real and a common manifestation of stress, but that there is no organic disease. Treat with stress management; a high-fiber, high-fluid diet; drugs (which may include bulking agents, pain medications, anticholinergics, or antidepressants); and other therapies such as biofeedback, hypnosis, psychotherapy, imagery, yoga, or acupuncture.
The general screening studies will identify constipation as the cause of abdominal pain, which typically occurs in children who had difficulty around toilet training, Dr. Cox said.
Consider constipation to be chronic if the child has had at least two of the following problems for 12 weeks or more per year: fewer than three bowel movements per week and/or difficulty with more than a fourth of defecations (in the form of hard stool, straining, a feeling of incomplete evacuation, a sensation of anorectal obstruction, or the need for manual maneuvers to facilitate defecation).
These children have normal growth and normal anal tone with stool in the rectum. They’re usually at least 2 years old, and have encopresis.
Dr. Cox described a typical case of an 11-year-old boy complaining of 2 years of abdominal pain that was periumbilical, of short duration (usually lasting 1-3 hours), worse postprandially, and relieved by passing stool. The patient reported twice-weekly large, hard bowel movements, and he had smears of stool on his underwear (aka "skid marks"). His diet was low in fiber, with inadequate fluids.
With medical management, the constipation, encopresis, and pain will resolve. First, clean out retained or impacted stool using oral medications such as magnesium citrate, phosphor-soda, or polyethylene glycol. Enemas or suppositories also are options, but "I don’t like these," Dr. Cox said. "They’re a bit traumatic."
For maintenance therapy, prescribe a diet high in fluids and fiber. Add the child’s age plus 5 to calculate the number of grams per day of fiber that should be consumed, he said. Continue medications until the child has at least one bowel movement per day and no encopresis for 1 month. Teach the child to use the toilet after meals. Reward success with star charts or an age-appropriate reward, and avoid punishment, he said.
In patients who don’t respond, anal rectonometry may show abnormal defecation, such as an anal canal that does not relax during defecation. Biofeedback therapy incorporating video games can help train the child to relax the anal canal.
Besides constipation and functional abdominal pain, other common causes of chronic pediatric abdominal pain include gastroesophageal reflux, which often presents as pain in the abdomen (not chest), or abdominal wall injury from exercise. Drinking a lot of carbonated beverages can cause pain from aerophagia. Approximately half of chronic abdominal pain in adolescents involves lactose intolerance. Urinary tract infection, giardiasis, or H. pylori infection also are relatively common causes.
In rare cases, chronic abdominal pain in children is due to peptic ulcer disease, pancreatitis, inflammatory bowel disease, gallstones, renal stones, choledochal cysts, discitis, or abdominal migraine, although the last problem is "probably more common than is recognized," Dr. Cox said.
There’s approximately a 2% incidence of a syndrome of abdominal migraine and cyclic vomiting in school-age children, he estimated. The syndrome features recurrent, explosive bouts of vomiting and/or abdominal pain, punctuated by periods of normal health. In one study of 214 children with cyclic vomiting syndrome, 82% had associated migraines (J. Pediatr. 1999:134:567-72).
Dr. Cox reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Partner Violence, Reproductive Coercion Are Teen Problems
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
If your practice sees adolescent patients and you’re not identifying intimate partner violence or coercion on a regular basis, it’s time to ask, "Why not?"
It’s there, it’s more common than you may suspect, and it often produces lifelong health consequences. Not enough teenagers are reporting it – and not enough physicians are asking about it – for a slew of reasons.
Increased attention to these problems in recent years has generated some handy resources for physicians to improve prevention, detection, and responses to intimate partner violence and sexual or reproductive coercion.
More than half (53%) of 1,278 women aged 16-29 years who were seen at family planning clinics reported physical or sexual violence by intimate partners, 19% reported pregnancy coercion, and 15% reported birth control sabotage in one study (Contraception 2010;81:316-22).
Some 40% of 448 females aged 14-20 years who were seen at five urban adolescent clinics said they had experienced intimate partner violence in a separate study (Matern. Child Health J. 2010;14:910-7). A survey of 10th and 11th graders found that more than half of the girls and 13% of boys reported sexual coercion, defined as sexual behaviors involving verbal coercion, threats of force, or use of drugs or alcohol (Violence Vict. 1995;10:299-313).
In a survey of 1,430 seventh graders in three states that was conducted by the Robert Wood Johnson Foundation, 37% said they had witnessed physical dating violence against a peer, 37% reported experiencing psychological dating abuse, and – during the prior 6 month – 15% experienced physical dating abuse and 31% experienced electronic dating aggression.
In a survey of 305 school counselors, the majority (71%) had not received formal training on adolescent dating violence (ADV). Eighty-one percent said their school did not have a protocol to respond to incidents of ADV, and 83% said the school did not conduct periodic student surveys that included questions that mentioned ADV (Pediatrics 2012;130:202-10).
Adolescents overwhelmingly want health care providers to ask about intimate partner violence and coercion, other studies have shown. So, why aren’t they telling you about it, even if you ask?
You may not be asking in the right way, nor asking often enough, Dr. Harise Stein said at Stanford (Calif.) University’s annual pediatric update and preconference.
Teens aged 15-19 years have the highest rates of intimate partner violence and stalking of any age group, yet they report only an estimated 1 in 11 episodes of dating-related violence, said Dr. Stein, an ob.gyn at the university. She is a member of the Santa Clara County (Calif.) Domestic Violence Council.
One in six U.S. women experience rape – "which I think is a national disgrace," she said – and 32% of first rapes occur in female victims aged 12-17-years. In that age group, 36% of rapists are intimate partners, and 33% are acquaintances, according to a 2006 U.S. Department of Justice report.
Abuse during adolescence interferes with emotional development and has been associated with mental and physical illness both during the teen years and carried forward into adulthood, she said. It can exacerbate asthma, headaches, or other chronic illnesses. Consider abuse in the diagnostic differential when you see an adolescent who has developed school problems, increased isolation, personality changes, mental health issues, an eating disorder, substance abuse, cutting and other forms of self-harm, or suicidal ideology, Dr. Stein said.
Vague physical symptoms or symptoms that don’t make sense are red flags for possible abuse, as are chronic pain symptoms (especially headaches), or unexplained worsening of chronic illness. New sexually transmitted infections, an unplanned pregnancy, or a request for emergency contraception open a window to ask about abuse.
Suspicious injuries may result from abuse. Slap marks, scratches, bruises, welts, cuts, or muscle sprains are typical signs in adolescents, but most common are soft tissue injuries of the forearms (held up to defend against blows), face, head, and neck, Dr. Stein said.
The prevalence of being choked to unconsciousness is "very underappreciated by health care workers" because half the time choking leaves no immediate external signs on the neck, she said. The teenager may wake up on the floor and not remember what happened. Only 10 seconds of strangulation can induce unconsciousness, and every second after that causes brain damage. Laryngeal edema over the following 24-48 hours can create airway emergencies. Brain cell death from the choking may cause problems in memory, reasoning, and concentration for several weeks. At least 10% of adult abused women who obtain restraining orders are estimated to have been choked to unconsciousness. Data are lacking for teens.
Teens in abusive relationships are four to six times more likely to get pregnant than are other teens, and 25% of pregnant teens are in abusive relationships, compared with 4%-8% of pregnant adults, Dr. Stein said.
The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) recommend screening for dating abuse (Pediatrics 2009;124:393-402; Obstet. Gynecol. 2012;119:412-7) – perhaps starting as early at age 11, according to AAP’s Bright Futures – and educating preteens and teens about healthy relationships, she said.
Remember a key lesson from Adolescence 101: Teens are more likely to open up if you start with open-ended questions like "How’s school?" instead of pointed questions, or if you approach the topic obliquely by bringing up bullying as something a lot of people are talking about, and use that as a lead-in to talking about relationships. Focus on behaviors, not "abuse," Dr. Stein said.
Adolescents get most of their advice on health topics from peers, so use that to your advantage by giving your patients materials about healthy relationships and resources for abused teens, and telling them it’s "for a friend," if you suspect the patient or a friend is at risk.
To detect intimate partner violence and coercion, watch for it– but also make your office a place where teens will feel comfortable talking about it. Make informational materials available in nonconspicuous places. Explain confidentiality up front in teen visits.
Dr. Eve Espey learned some of these lessons in a vivid way. A patient and her boyfriend came to the emergency department, and an HCG test suggested that she had an ectopic pregnancy. She refused emergency treatment. Once the boyfriend left the room, she admitted that she’d just had an abortion, and didn’t want him to know because she feared he’d be violent. A nurse had screened her and asked specifically about domestic violence, but with the boyfriend in the room, she couldn’t discuss it.
"We made changes after that," said Dr. Espey, professor of ob.gyn. at the University of New Mexico, Albuquerque, and chair of ACOG’s Working Group on Long-Acting Reversible Contraception. "We talk to every woman by herself. We tell them it’s part of our protocol," she said at ACOG’s annual meeting.
A February 2012 opinion published by ACOG’s Committee on Health Care for Underserved Women calls on physicians to screen all women for intimate partner violence at periodic intervals, to offer ongoing support, and to review prevention and referral options with patients. Intimate partner violence is most common during the reproductive years, so it’s important to screen several times during obstetric care, including at the first prenatal visit, at least once per trimester, and at the postpartum checkup, the committee recommended. The opinion paper includes sample questions (Obstet. Gynecol. 2012;119:412-7).
Dr. Espey recommends that ob.gyns. screen patients for intimate partner violence and reproductive coercion at most contraceptive visits, again not by immediate blunt questions like, "Are you safe at home?" but in a more circuitous, conversational way.
"The goal is not disclosure. Just engaging in the conversation is a great first step," she said.
When a patient does reveal intimate partner violence but is not ready to make changes, help the patient avoid unintended pregnancy by separating out the issue of reproductive coercion (in which a partner sabotages birth control or coerces the person to have or terminate a pregnancy), Dr. Espey said.
Talk about contraceptive methods that are less detectable by partners, for example. Long-acting reversible contraceptive methods are less vulnerable to tampering, but hormonal methods that eliminate periods may not work for women whose cycles are being closely monitored by a partner. The string on an IUD can be cut before insertion so that a partner cannot pull it out. If the IUD already is inserted, you’ll need to remove it and cut the string and reinsert it, because cutting the string just at the cervix leaves it potentially detectable, she said. Pills for emergency contraception can be stored in a vitamin bottle to avoid detection.
Her practice keeps laminated copies handy of a color-coded chart from the Centers for Disease Control and Prevention that helps clinicians quickly identify which forms of contraception are medically appropriate for particular patients – and showing that long-active contraceptives usually are an option. The "Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use" is free.
She also lets patients who get an abortion know that they can say they’ve had a miscarriage, if they need to. "Women don’t realize that abortion cannot be detected. Tell them," she said.
These discussions plant the seeds for women to grow into readiness to leave abusive relationships, Dr. Espey said. Of course, keep in mind any legal requirements in your state to report abuse.
Adolescents often feel more comfortable being asked initially about abuse and coercion if it’s asked electronically, Virginia A. Duplessis said at ACOG’s annual meeting. In live conversations, "We’re moving from ‘Have you ever been punched, slapped, or kicked?’ to more nuanced conversation," said Ms. Duplessis, a program manager for Futures Without Violence, a nonprofit organization formerly known as the Family Violence Prevention Fund, headquartered in San Francisco.
Teens may not understand that violence and coercion are not acceptable ways to show love, she said.
Dr. Stein also pointed to a segment of the Tyra Banks television talk show that’s posted online, in which adolescents in the audience had trouble identifying types of abuse other than physical abuse.
Other times, the patient may have the knowledge, but feel unable to act on it. Ms. Duplessis described her frustration in a previous job as a community educator when teens who had condoms or birth control pills and knew how to use them kept reporting that they weren’t used. It’s not that they were dumb or apathetic, she finally learned; reproductive coercion often was the problem. The girls feared the consequences of negotiating condom use more than they feared pregnancy, or their partners threw away their pills.
That frustration with patients who do not follow a plan of care is one reason that clinicians don’t screen for intimate partner violence, she said. They also may not be comfortable starting conversations on this topic, or don’t ask because they don’t know what to do if a patient discloses intimate partner violence or coercion.
Futures Without Violence offers free materials to clinicians to simplify screening, such as folding wallet-size "safety cards" to give patients that list screening questions and resources.
Ms. Duplessis manages Project Connect, a national public health initiative to prevent violence against women through efforts focused on adolescent health, reproductive health, and home visiting programs. Funded by the U.S. Office on Women’s Health, Project Connect’s 10 geographically and ethnically diverse sites explore new ways to prevent, identify, and respond to domestic and sexual violence.
In a randomized, controlled pilot trial, a community-based intervention achieved some success (Contraception 2011;83:274-80). Clinicians asked 906 women at four family planning clinics questions about intimate partner violence and sexual and reproductive coercion, and reviewed the "safety cards" they gave to patients. The intervention took less than a minute of time in some cases, or longer if a positive screen led to more discussion.
Among women who had experienced recent partner violence, those in the intervention group were 71% less likely to report pregnancy coercion and 63% more likely to end an unhealthy or unsafe relationship, compared with a control group who got usual care.
Data suggest that reducing adolescent relationship abuse should reduce rates of substance abuse, teen pregnancy, depression, eating disorders, suicide, school dropouts, and adult intimate partner violence, Dr. Stein said.
For the past 4 years, she has reviewed the literature on the effects of abuse and has sent out monthly updates to interested parties. During that time, her monthly summary has grown from three to six pages. Attention to intimate partner violence and coercion is increasing, and every clinician plays a role, she said.
Dr. Stein, Dr. Espey and Ms. Duplessis recommended the following resources:
• ACOG and Futures Without Violence cobranded a guide for clinicians, "Addressing Intimate Partner Violence, Reproductive and Sexual Coercion." The 56-page pamphlet includes sample scripts for talking with patients, advice on managing someone who screens positive, quality assessment tools for clinical practices, and links to resources including a clinician training kit, "safety cards" for patients, and more.
• The "Healthcare Education, Assessment and Response Tool for Teen Relationships (HEART) Primer" is another free comprehensive toolkit to help clinicians recognize and decrease adolescent relationship abuse and sexual and reproductive coercion, offered by the California Adolescent Health Collaborative.
• The National Center for Youth Law created legal guides for Arizona, California, Maine, Michigan, and Ohio for "When Teens Disclose Dating Violence to Health Care Providers: A Guide to Confidentiality and Reporting Laws."
• Dr. Stein sends monthly e-mail updates about the literature on the effects of abuse. To get on her list, e-mail [email protected].
Dr. Stein, Dr. Espey, and Ms. Duplessis reported having no financial disclosures.
Include 'Legal Highs,' Designer Drugs in Screening
STANFORD, CALIF. – Dr. Leslie Gee walked into a local smoke shop near Stanford in May 2012 and bought a packet of synthetic cannabinoids 7 months after California banned similar versions.
That’s just one of many designer drugs that adolescents are using and abusing, with effects that may mimic illicit substances but also can cause unpredictable and sometimes serious adverse effects.
If you don’t ask about it, teenagers probably won’t tell.
Ask adolescent patients, "Are you using anything to get high?" Dr. Gee said at a pediatric update sponsored by Stanford (Calif.) University. Send acutely intoxicated teens to the emergency room or pediatric intensive care unit if needed, or provide supportive care and monitor them.
Call the American Association of Poison Control Centers help line at 800-222-1222 if you’re confused about what’s happening, and give the phone number to parents and families before they might need it, added Dr. Gee, a pediatrician at the university whose clinical focus is adolescent medicine.
A July 2012 federal law placed many synthetic cannabinoid ingredients into schedule I of the Controlled Substances Act, but manufacturers keep changing the ingredients, so they still can be bought legally.
Synthetic cannabinoids are available in shops and on the Internet, and adolescents are using them. In 2011, 11% of 12th graders reported using synthetic cannabinoids and 36% reported using marijuana, according to an annual survey of 50,000 teenagers by researchers at the University of Michigan.
The survey found that 7% of eighth graders and 3% of 12th graders abused inhalants in 2011. Prescription medications were abused by 15% percent of 12th graders. A total of 6% of 10th graders and 5% of 12th graders tried to get high from dextromethorphan, an ingredient in many over-the-counter cold medications that’s also sold as a powder online. About 6% of 12th graders tried chewing or smoking salvia, an herb in the mint family sold in smoke shops and on the Internet. There are no data yet on abuse of some of the newer designer drugs, such as so-called "bath salts," said Dr. Gee, who also is a postdoctoral research fellow in psychiatry and behavioral science.
Some of these substances can’t be detected by urine drug screens. But a laboratory screen for substance abuse generally is fairly useless in adolescents anyway, whether you’re concerned about legal or illegal drugs, Dr. Seth D. Ammerman said in a separate presentation at the meeting.
"Kids are a step ahead," said Dr. Ammerman, an adolescent medicine expert and medical director of the Teen Health Van at the university. "You can get a lot more out of a history than a drug screen."
Mnemonics such as HEADSSS, SBIRT, and CRAFT can help remind physicians about questions to ask when screening for substance abuse, but make sure any particular tool has been tested in teenagers before adopting it, he advised.
Most important, make substance abuse screening part of your routine, he urged. Screen for tobacco use at all adolescent encounters. Screen all adolescents for substance use at visits for preventive services. And screen for substance use in higher-risk patients, including teens brought in by parents because of behavioral issues or school problems, adolescents with acute medical problems such as GI disturbances or trauma, teens seen in emergency departments for any reason but especially for trauma, and residents of group homes, juvenile hall, foster homes, or shelters.
"We still have a ways to go to figure out the best way to screen adolescents for substance use. There’s much active research and some useful tools, but none include every question" that you may want to ask, Dr. Ammerman said.
A common way to start is the HEADSSS assessment, with questions about home; education or work; activities; drugs, alcohol and tobacco; sexuality; sadness; depression or suicidal ideation; and safety.
The SBIRT – Screening, Brief Intervention, and Referral for Treatment – doesn’t address tobacco use, but if you routinely screen for tobacco as a vital sign, you’ll have that covered, Dr. Ammerman said. Under SBIRT, ask if the patient has drunk alcohol, smoked marijuana, or used any other substance to get high including illicit drugs, over-the-counter preparations, prescription medications, inhalants, herbs, or plants.
If the patient says, "No" to all three questions, praise the patient and continue to encourage abstinence, he said. If there’s a "Yes" response, perform the CRAFFT screen for alcohol and drug use, Dr. Ammerman suggested. The acronym stands for Car, Relax, Alone, Forget, Friends/family, and Trouble. Have you driven or ridden in a Car in which anyone was high? Have you used substances to Relax or feel better about yourself? Have you used substances Alone? Ever done anything under the influence of substances that you Forgot? Have Friends or family commented on your use? Have you had any Trouble with parents, school, police, etc., related to substance use?
Adolescents who give at least two positive responses are increased risk of addiction and deserve further attention.
Many physicians received a screening tool in the mail last year from the National Institute on Alcohol Abuse and Alcoholism with specific questions for different age groups entitled "Alcohol Screening and Brief Intervention for Youth: A Practitioner’ Guide," but "I personally prefer the SBIRT," Dr. Ammerman said. "It’s validated and easy to use."
Dr. Gee described some of the common "legal highs" and designer drugs, and what to do besides taking a good history if you suspect adolescents are using them.
• Inhalants. The average U.S. household contains 30-50 products that can be used for inhalant abuse through sniffing, "bagging" (spraying or placing in a bag and then inhaling from the bag), or "huffing" (placing a rag soaked in chemicals on one’s face). Some contain hydrocarbons that depress the central nervous system. Others contain nitrite that cause vasodilation.
Inhalant abuse can cause asphyxia, suffocation, or "sudden sniffing death" from sensitization of the myocardium to catecholamines (especially Freon) and a catecholamine rush after exercise or masturbation, resulting in cardiovascular collapse, she said.
Clues to inhalant abuse include a "glue sniffer’s rash" on the face, cheeks, and nose. The family may notice empty containers around the house or a chemical smell on the teen’s breath, skin, or clothes.
Most inhalants won’t be detected by standard urine drug screens. Evaluate using pulse oximetry, an ECG, and cardiac monitoring for arrhythmias, complete blood count, complete metabolic panel, and urinalysis, she suggested. Depending on the substance being abused, consider checking methemoglobin and lead levels. Treat with supportive care.
• Prescription drugs. Prescribed narcotics, benzodiazepines, or medications for attention-deficit/hyperactivity disorder are found in many households. They may cause respiratory depression or organ failure. Evaluate with urine drug screening and manage with supportive care appropriate to the ingested substance.
• Dextromethorphan. It goes by at least 10 aliases: Robo; Skittles; Dex; and more. A typical dose for cold therapy is 15-30 mg four times a day. Higher doses produce side effects at different dose plateaus: mild inebriation or stimulation from 100-200 mg, and euphoria, mild hallucinations, slurred speech, and short-term memory loss after 200-400 mg. A dose of 300-600 mg can alter consciousness and impair vision and motor control. At 500-1,500 mg, the mind and body dissociate.
Abuse can produce life-threatening effects including serotonin syndrome, high fever, rhabdomyolysis, arrhythmias, loss of consciousness, and brain damage.
Treatment is supportive care. When you suspect dextromethorphan abuse, also screen and treat for coingestion of other substances, especially acetaminophen and selective serotonin reuptake inhibitors.
• Salvia. A perennial herb native to Mexico, salvia is not a controlled substance, but California prohibits its sale to minors. Effects kick in within 5-10 minutes of chewing or within 30 seconds of smoking 200-500 mcg, and include hallucinations, bright lights, vivid colors and shapes, body or object distortions, uncontrolled laughter, or a sense of body loss. Provide supportive care.
• Synthetic cannabinoids. Added to blends of herbs and sold legally in the United States as alternatives to marijuana from 2009 until the recent regulations, synthetic cannabinoids produce psychoactive and sedative effects similar to marijuana, although possibly less potent. They also may produce more adverse effects, including withdrawal symptoms, cardiac problems, or psychoses. "I’ve seen reports of acute MIs and arrhythmias" from these products, Dr. Gee said.
Standard urine drug screens won’t detect them, but newer screening tests are in development. Consider coingestion of other substances and contaminants and provide supportive care.
• Bath salts. These synthetic cathinones entered the United States from Europe around 2010. They contain methylenedioxypyrovalerone, methylone, 4-methylmethcathinone – all three of which became schedule I substances in 2011 – or an ever-new roster of similar drugs. "They’re just marketed as bath salts or plant food as a way to get around regulations," Dr. Gee said. "They’re not something you’d want to put in your bath or plants."
Snorting or consuming orally induce empathy, stimulation, alertness, and euphoria within 3-4 hours that last 6-8 hours – similar to the effects of cocaine, cathinone (khat), amphetamines, or 3,4-methylenedioxymethamphetamine (MDMA, or Ecstasy). But they also can cause intense, prolonged panic attacks, violent behavior, and psychosis. Some "dramatic, scary" news reports have linked bath salts with violent behavior, she said.
Standard drug screens won’t detect synthetic cathinones, but tests are being developed. Consider coingestion of other substances and contaminants if you suspect bath salts use, and provide supportive care for agitation and psychoses.
Some possible references to help with substance abuse screening follow:
• The U.S. Drug Enforcement Administration offers handouts, links, and information on legal issues surrounding drugs and chemicals of concern.
• The Partnership at drugfree.org produced a toolkit for parents about synthetic drugs.
• The U.S. Office of National Drug Control Policy soon will release a Synthetic Drug Prevention Toolkit, Dr. Gee said.
• A sort of wiki for drug use, the website Erowid.org posts accounts of personal experiences – what happened when someone tried a drug, how much they tried, etc. It’s a window for clinicians looking to understand more about drug use and abuse, she added.
• One physician in the audience recommended Millennium Laboratories of San Diego to test patient samples for any synthetic drug, with a 24-hour turnaround.
Dr. Gee and Dr. Ammerman reported having no relevant financial disclosures.
STANFORD, CALIF. – Dr. Leslie Gee walked into a local smoke shop near Stanford in May 2012 and bought a packet of synthetic cannabinoids 7 months after California banned similar versions.
That’s just one of many designer drugs that adolescents are using and abusing, with effects that may mimic illicit substances but also can cause unpredictable and sometimes serious adverse effects.
If you don’t ask about it, teenagers probably won’t tell.
Ask adolescent patients, "Are you using anything to get high?" Dr. Gee said at a pediatric update sponsored by Stanford (Calif.) University. Send acutely intoxicated teens to the emergency room or pediatric intensive care unit if needed, or provide supportive care and monitor them.
Call the American Association of Poison Control Centers help line at 800-222-1222 if you’re confused about what’s happening, and give the phone number to parents and families before they might need it, added Dr. Gee, a pediatrician at the university whose clinical focus is adolescent medicine.
A July 2012 federal law placed many synthetic cannabinoid ingredients into schedule I of the Controlled Substances Act, but manufacturers keep changing the ingredients, so they still can be bought legally.
Synthetic cannabinoids are available in shops and on the Internet, and adolescents are using them. In 2011, 11% of 12th graders reported using synthetic cannabinoids and 36% reported using marijuana, according to an annual survey of 50,000 teenagers by researchers at the University of Michigan.
The survey found that 7% of eighth graders and 3% of 12th graders abused inhalants in 2011. Prescription medications were abused by 15% percent of 12th graders. A total of 6% of 10th graders and 5% of 12th graders tried to get high from dextromethorphan, an ingredient in many over-the-counter cold medications that’s also sold as a powder online. About 6% of 12th graders tried chewing or smoking salvia, an herb in the mint family sold in smoke shops and on the Internet. There are no data yet on abuse of some of the newer designer drugs, such as so-called "bath salts," said Dr. Gee, who also is a postdoctoral research fellow in psychiatry and behavioral science.
Some of these substances can’t be detected by urine drug screens. But a laboratory screen for substance abuse generally is fairly useless in adolescents anyway, whether you’re concerned about legal or illegal drugs, Dr. Seth D. Ammerman said in a separate presentation at the meeting.
"Kids are a step ahead," said Dr. Ammerman, an adolescent medicine expert and medical director of the Teen Health Van at the university. "You can get a lot more out of a history than a drug screen."
Mnemonics such as HEADSSS, SBIRT, and CRAFT can help remind physicians about questions to ask when screening for substance abuse, but make sure any particular tool has been tested in teenagers before adopting it, he advised.
Most important, make substance abuse screening part of your routine, he urged. Screen for tobacco use at all adolescent encounters. Screen all adolescents for substance use at visits for preventive services. And screen for substance use in higher-risk patients, including teens brought in by parents because of behavioral issues or school problems, adolescents with acute medical problems such as GI disturbances or trauma, teens seen in emergency departments for any reason but especially for trauma, and residents of group homes, juvenile hall, foster homes, or shelters.
"We still have a ways to go to figure out the best way to screen adolescents for substance use. There’s much active research and some useful tools, but none include every question" that you may want to ask, Dr. Ammerman said.
A common way to start is the HEADSSS assessment, with questions about home; education or work; activities; drugs, alcohol and tobacco; sexuality; sadness; depression or suicidal ideation; and safety.
The SBIRT – Screening, Brief Intervention, and Referral for Treatment – doesn’t address tobacco use, but if you routinely screen for tobacco as a vital sign, you’ll have that covered, Dr. Ammerman said. Under SBIRT, ask if the patient has drunk alcohol, smoked marijuana, or used any other substance to get high including illicit drugs, over-the-counter preparations, prescription medications, inhalants, herbs, or plants.
If the patient says, "No" to all three questions, praise the patient and continue to encourage abstinence, he said. If there’s a "Yes" response, perform the CRAFFT screen for alcohol and drug use, Dr. Ammerman suggested. The acronym stands for Car, Relax, Alone, Forget, Friends/family, and Trouble. Have you driven or ridden in a Car in which anyone was high? Have you used substances to Relax or feel better about yourself? Have you used substances Alone? Ever done anything under the influence of substances that you Forgot? Have Friends or family commented on your use? Have you had any Trouble with parents, school, police, etc., related to substance use?
Adolescents who give at least two positive responses are increased risk of addiction and deserve further attention.
Many physicians received a screening tool in the mail last year from the National Institute on Alcohol Abuse and Alcoholism with specific questions for different age groups entitled "Alcohol Screening and Brief Intervention for Youth: A Practitioner’ Guide," but "I personally prefer the SBIRT," Dr. Ammerman said. "It’s validated and easy to use."
Dr. Gee described some of the common "legal highs" and designer drugs, and what to do besides taking a good history if you suspect adolescents are using them.
• Inhalants. The average U.S. household contains 30-50 products that can be used for inhalant abuse through sniffing, "bagging" (spraying or placing in a bag and then inhaling from the bag), or "huffing" (placing a rag soaked in chemicals on one’s face). Some contain hydrocarbons that depress the central nervous system. Others contain nitrite that cause vasodilation.
Inhalant abuse can cause asphyxia, suffocation, or "sudden sniffing death" from sensitization of the myocardium to catecholamines (especially Freon) and a catecholamine rush after exercise or masturbation, resulting in cardiovascular collapse, she said.
Clues to inhalant abuse include a "glue sniffer’s rash" on the face, cheeks, and nose. The family may notice empty containers around the house or a chemical smell on the teen’s breath, skin, or clothes.
Most inhalants won’t be detected by standard urine drug screens. Evaluate using pulse oximetry, an ECG, and cardiac monitoring for arrhythmias, complete blood count, complete metabolic panel, and urinalysis, she suggested. Depending on the substance being abused, consider checking methemoglobin and lead levels. Treat with supportive care.
• Prescription drugs. Prescribed narcotics, benzodiazepines, or medications for attention-deficit/hyperactivity disorder are found in many households. They may cause respiratory depression or organ failure. Evaluate with urine drug screening and manage with supportive care appropriate to the ingested substance.
• Dextromethorphan. It goes by at least 10 aliases: Robo; Skittles; Dex; and more. A typical dose for cold therapy is 15-30 mg four times a day. Higher doses produce side effects at different dose plateaus: mild inebriation or stimulation from 100-200 mg, and euphoria, mild hallucinations, slurred speech, and short-term memory loss after 200-400 mg. A dose of 300-600 mg can alter consciousness and impair vision and motor control. At 500-1,500 mg, the mind and body dissociate.
Abuse can produce life-threatening effects including serotonin syndrome, high fever, rhabdomyolysis, arrhythmias, loss of consciousness, and brain damage.
Treatment is supportive care. When you suspect dextromethorphan abuse, also screen and treat for coingestion of other substances, especially acetaminophen and selective serotonin reuptake inhibitors.
• Salvia. A perennial herb native to Mexico, salvia is not a controlled substance, but California prohibits its sale to minors. Effects kick in within 5-10 minutes of chewing or within 30 seconds of smoking 200-500 mcg, and include hallucinations, bright lights, vivid colors and shapes, body or object distortions, uncontrolled laughter, or a sense of body loss. Provide supportive care.
• Synthetic cannabinoids. Added to blends of herbs and sold legally in the United States as alternatives to marijuana from 2009 until the recent regulations, synthetic cannabinoids produce psychoactive and sedative effects similar to marijuana, although possibly less potent. They also may produce more adverse effects, including withdrawal symptoms, cardiac problems, or psychoses. "I’ve seen reports of acute MIs and arrhythmias" from these products, Dr. Gee said.
Standard urine drug screens won’t detect them, but newer screening tests are in development. Consider coingestion of other substances and contaminants and provide supportive care.
• Bath salts. These synthetic cathinones entered the United States from Europe around 2010. They contain methylenedioxypyrovalerone, methylone, 4-methylmethcathinone – all three of which became schedule I substances in 2011 – or an ever-new roster of similar drugs. "They’re just marketed as bath salts or plant food as a way to get around regulations," Dr. Gee said. "They’re not something you’d want to put in your bath or plants."
Snorting or consuming orally induce empathy, stimulation, alertness, and euphoria within 3-4 hours that last 6-8 hours – similar to the effects of cocaine, cathinone (khat), amphetamines, or 3,4-methylenedioxymethamphetamine (MDMA, or Ecstasy). But they also can cause intense, prolonged panic attacks, violent behavior, and psychosis. Some "dramatic, scary" news reports have linked bath salts with violent behavior, she said.
Standard drug screens won’t detect synthetic cathinones, but tests are being developed. Consider coingestion of other substances and contaminants if you suspect bath salts use, and provide supportive care for agitation and psychoses.
Some possible references to help with substance abuse screening follow:
• The U.S. Drug Enforcement Administration offers handouts, links, and information on legal issues surrounding drugs and chemicals of concern.
• The Partnership at drugfree.org produced a toolkit for parents about synthetic drugs.
• The U.S. Office of National Drug Control Policy soon will release a Synthetic Drug Prevention Toolkit, Dr. Gee said.
• A sort of wiki for drug use, the website Erowid.org posts accounts of personal experiences – what happened when someone tried a drug, how much they tried, etc. It’s a window for clinicians looking to understand more about drug use and abuse, she added.
• One physician in the audience recommended Millennium Laboratories of San Diego to test patient samples for any synthetic drug, with a 24-hour turnaround.
Dr. Gee and Dr. Ammerman reported having no relevant financial disclosures.
STANFORD, CALIF. – Dr. Leslie Gee walked into a local smoke shop near Stanford in May 2012 and bought a packet of synthetic cannabinoids 7 months after California banned similar versions.
That’s just one of many designer drugs that adolescents are using and abusing, with effects that may mimic illicit substances but also can cause unpredictable and sometimes serious adverse effects.
If you don’t ask about it, teenagers probably won’t tell.
Ask adolescent patients, "Are you using anything to get high?" Dr. Gee said at a pediatric update sponsored by Stanford (Calif.) University. Send acutely intoxicated teens to the emergency room or pediatric intensive care unit if needed, or provide supportive care and monitor them.
Call the American Association of Poison Control Centers help line at 800-222-1222 if you’re confused about what’s happening, and give the phone number to parents and families before they might need it, added Dr. Gee, a pediatrician at the university whose clinical focus is adolescent medicine.
A July 2012 federal law placed many synthetic cannabinoid ingredients into schedule I of the Controlled Substances Act, but manufacturers keep changing the ingredients, so they still can be bought legally.
Synthetic cannabinoids are available in shops and on the Internet, and adolescents are using them. In 2011, 11% of 12th graders reported using synthetic cannabinoids and 36% reported using marijuana, according to an annual survey of 50,000 teenagers by researchers at the University of Michigan.
The survey found that 7% of eighth graders and 3% of 12th graders abused inhalants in 2011. Prescription medications were abused by 15% percent of 12th graders. A total of 6% of 10th graders and 5% of 12th graders tried to get high from dextromethorphan, an ingredient in many over-the-counter cold medications that’s also sold as a powder online. About 6% of 12th graders tried chewing or smoking salvia, an herb in the mint family sold in smoke shops and on the Internet. There are no data yet on abuse of some of the newer designer drugs, such as so-called "bath salts," said Dr. Gee, who also is a postdoctoral research fellow in psychiatry and behavioral science.
Some of these substances can’t be detected by urine drug screens. But a laboratory screen for substance abuse generally is fairly useless in adolescents anyway, whether you’re concerned about legal or illegal drugs, Dr. Seth D. Ammerman said in a separate presentation at the meeting.
"Kids are a step ahead," said Dr. Ammerman, an adolescent medicine expert and medical director of the Teen Health Van at the university. "You can get a lot more out of a history than a drug screen."
Mnemonics such as HEADSSS, SBIRT, and CRAFT can help remind physicians about questions to ask when screening for substance abuse, but make sure any particular tool has been tested in teenagers before adopting it, he advised.
Most important, make substance abuse screening part of your routine, he urged. Screen for tobacco use at all adolescent encounters. Screen all adolescents for substance use at visits for preventive services. And screen for substance use in higher-risk patients, including teens brought in by parents because of behavioral issues or school problems, adolescents with acute medical problems such as GI disturbances or trauma, teens seen in emergency departments for any reason but especially for trauma, and residents of group homes, juvenile hall, foster homes, or shelters.
"We still have a ways to go to figure out the best way to screen adolescents for substance use. There’s much active research and some useful tools, but none include every question" that you may want to ask, Dr. Ammerman said.
A common way to start is the HEADSSS assessment, with questions about home; education or work; activities; drugs, alcohol and tobacco; sexuality; sadness; depression or suicidal ideation; and safety.
The SBIRT – Screening, Brief Intervention, and Referral for Treatment – doesn’t address tobacco use, but if you routinely screen for tobacco as a vital sign, you’ll have that covered, Dr. Ammerman said. Under SBIRT, ask if the patient has drunk alcohol, smoked marijuana, or used any other substance to get high including illicit drugs, over-the-counter preparations, prescription medications, inhalants, herbs, or plants.
If the patient says, "No" to all three questions, praise the patient and continue to encourage abstinence, he said. If there’s a "Yes" response, perform the CRAFFT screen for alcohol and drug use, Dr. Ammerman suggested. The acronym stands for Car, Relax, Alone, Forget, Friends/family, and Trouble. Have you driven or ridden in a Car in which anyone was high? Have you used substances to Relax or feel better about yourself? Have you used substances Alone? Ever done anything under the influence of substances that you Forgot? Have Friends or family commented on your use? Have you had any Trouble with parents, school, police, etc., related to substance use?
Adolescents who give at least two positive responses are increased risk of addiction and deserve further attention.
Many physicians received a screening tool in the mail last year from the National Institute on Alcohol Abuse and Alcoholism with specific questions for different age groups entitled "Alcohol Screening and Brief Intervention for Youth: A Practitioner’ Guide," but "I personally prefer the SBIRT," Dr. Ammerman said. "It’s validated and easy to use."
Dr. Gee described some of the common "legal highs" and designer drugs, and what to do besides taking a good history if you suspect adolescents are using them.
• Inhalants. The average U.S. household contains 30-50 products that can be used for inhalant abuse through sniffing, "bagging" (spraying or placing in a bag and then inhaling from the bag), or "huffing" (placing a rag soaked in chemicals on one’s face). Some contain hydrocarbons that depress the central nervous system. Others contain nitrite that cause vasodilation.
Inhalant abuse can cause asphyxia, suffocation, or "sudden sniffing death" from sensitization of the myocardium to catecholamines (especially Freon) and a catecholamine rush after exercise or masturbation, resulting in cardiovascular collapse, she said.
Clues to inhalant abuse include a "glue sniffer’s rash" on the face, cheeks, and nose. The family may notice empty containers around the house or a chemical smell on the teen’s breath, skin, or clothes.
Most inhalants won’t be detected by standard urine drug screens. Evaluate using pulse oximetry, an ECG, and cardiac monitoring for arrhythmias, complete blood count, complete metabolic panel, and urinalysis, she suggested. Depending on the substance being abused, consider checking methemoglobin and lead levels. Treat with supportive care.
• Prescription drugs. Prescribed narcotics, benzodiazepines, or medications for attention-deficit/hyperactivity disorder are found in many households. They may cause respiratory depression or organ failure. Evaluate with urine drug screening and manage with supportive care appropriate to the ingested substance.
• Dextromethorphan. It goes by at least 10 aliases: Robo; Skittles; Dex; and more. A typical dose for cold therapy is 15-30 mg four times a day. Higher doses produce side effects at different dose plateaus: mild inebriation or stimulation from 100-200 mg, and euphoria, mild hallucinations, slurred speech, and short-term memory loss after 200-400 mg. A dose of 300-600 mg can alter consciousness and impair vision and motor control. At 500-1,500 mg, the mind and body dissociate.
Abuse can produce life-threatening effects including serotonin syndrome, high fever, rhabdomyolysis, arrhythmias, loss of consciousness, and brain damage.
Treatment is supportive care. When you suspect dextromethorphan abuse, also screen and treat for coingestion of other substances, especially acetaminophen and selective serotonin reuptake inhibitors.
• Salvia. A perennial herb native to Mexico, salvia is not a controlled substance, but California prohibits its sale to minors. Effects kick in within 5-10 minutes of chewing or within 30 seconds of smoking 200-500 mcg, and include hallucinations, bright lights, vivid colors and shapes, body or object distortions, uncontrolled laughter, or a sense of body loss. Provide supportive care.
• Synthetic cannabinoids. Added to blends of herbs and sold legally in the United States as alternatives to marijuana from 2009 until the recent regulations, synthetic cannabinoids produce psychoactive and sedative effects similar to marijuana, although possibly less potent. They also may produce more adverse effects, including withdrawal symptoms, cardiac problems, or psychoses. "I’ve seen reports of acute MIs and arrhythmias" from these products, Dr. Gee said.
Standard urine drug screens won’t detect them, but newer screening tests are in development. Consider coingestion of other substances and contaminants and provide supportive care.
• Bath salts. These synthetic cathinones entered the United States from Europe around 2010. They contain methylenedioxypyrovalerone, methylone, 4-methylmethcathinone – all three of which became schedule I substances in 2011 – or an ever-new roster of similar drugs. "They’re just marketed as bath salts or plant food as a way to get around regulations," Dr. Gee said. "They’re not something you’d want to put in your bath or plants."
Snorting or consuming orally induce empathy, stimulation, alertness, and euphoria within 3-4 hours that last 6-8 hours – similar to the effects of cocaine, cathinone (khat), amphetamines, or 3,4-methylenedioxymethamphetamine (MDMA, or Ecstasy). But they also can cause intense, prolonged panic attacks, violent behavior, and psychosis. Some "dramatic, scary" news reports have linked bath salts with violent behavior, she said.
Standard drug screens won’t detect synthetic cathinones, but tests are being developed. Consider coingestion of other substances and contaminants if you suspect bath salts use, and provide supportive care for agitation and psychoses.
Some possible references to help with substance abuse screening follow:
• The U.S. Drug Enforcement Administration offers handouts, links, and information on legal issues surrounding drugs and chemicals of concern.
• The Partnership at drugfree.org produced a toolkit for parents about synthetic drugs.
• The U.S. Office of National Drug Control Policy soon will release a Synthetic Drug Prevention Toolkit, Dr. Gee said.
• A sort of wiki for drug use, the website Erowid.org posts accounts of personal experiences – what happened when someone tried a drug, how much they tried, etc. It’s a window for clinicians looking to understand more about drug use and abuse, she added.
• One physician in the audience recommended Millennium Laboratories of San Diego to test patient samples for any synthetic drug, with a 24-hour turnaround.
Dr. Gee and Dr. Ammerman reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC CONFERENCE
Fight Obesity with Specific, Countable Goals
STANFORD, CALIF. – Setting goals with families to reduce childhood obesity must be specific, explicit, and unambiguous to be effective.
Instead of encouraging them to walk or bike to school more often, try a goal of walking or biking to school 2 or more days per week. Don’t just say, "Watch less TV," but recommend that the child watch no television on school days, Dr. Thomas N. Robinson said at a pediatric update sponsored by Stanford University.
"Keep it simple," and only set one or two short-term goals at a time, said Dr. Robinson, the Irving Schulman M.D. Endowed Professor in Child Health at the university, and director of the Center for Healthy Weight at Lucile Packard Children’s Hospital at Stanford.
Talk with the child and parents to identify specific behaviors and routines that could be targets for change. "If you can’t count it, you can’t change it," he stressed.
If your aim is to modify eating behaviors, don’t focus on consumption of calories, fat, carbohydrates, fiber, or the energy density of foods, which are hard to track. It’s easier to focus on more specific categories like specific high-calorie foods, sweetened drinks, high-calorie food preparation methods (such as frying), eating out or eating fast food, or a specific eating pattern such as having multiple "dinners." A rule of thumb for a child’s "portion" is the size of a parent’s palm. Suggest that they use smaller plates or bowls for children, or never let the child eat something right out of the box.
To promote activity instead of inactivity, it’s relatively easy to count transportation to school, organized sports or classes, time spent playing outdoors, chores, physical education, and sedentary behaviors such as time with TV, video games, phones, or computers.
A more specific goal than exercising as a family might be to take a family hike every Sunday afternoon. Rather than, "Eat less junk food," perhaps aim to limit trips to McDonald’s to once a week, he said. "Drink less soda and juice" is not nearly as helpful and specific as "No soda or juice, only milk and water."
Parents can set goals for their own behaviors to help their children, such as not keeping sugar-sweetened beverages in the home, or keeping a bowl of fresh fruit in the kitchen and a bowl of cut vegetables in the refrigerator. Approximately 85% of school-aged children have televisions in their bedrooms (a practice that’s most likely in lower socioeconomic groups), so moving the TV out could be a parental goal, he said.
Parents may aim to offer no rides to school. "They can have a walking school bus where a parent walks home to home, picking up kids along the way to school. They can even have a wagon for backpacks," Dr. Robinson said. Or, starting new family routines or traditions could help, such as the Sunday afternoon hike.
Commonly, the parents of an obese child don’t perceive obesity to be a problem because everyone in the family is obese. Instead of focusing on weight loss, work with them to set short-term goals around nutrition and physical activity because those are about making their child healthy, he suggested. "Over time, you can talk about metabolic risk, etc., but start with short-term goals."
Think less of what motivates you, and more about what will motivate your patients. External rewards for a behavior – especially food or money – may work in the short term, but will backfire over time. Build intrinsic motivation by helping patients and families pick goals that are challenging but achievable, not too easy or too hard.
It’s extremely important that the child and parents know that they have choices and control. It’s the same concept employed in the strategy of getting a child to go to bed not by saying, "Time for bed," but by asking which they want to do first before going to bed: brushing teeth or putting on pajamas. Help children and parents identify the target behaviors that are motivating for them and individualized to them.
Contextualized fantasy (also called gamification) may build intrinsic motivation in children. For example, the parent might propose that they build a house out of vegetables and then eat it. Cooperation, competition, and social interaction – doing things in groups – also build intrinsic motivation.
"If you can’t count it, you can’t change it."
A behavior intervention doesn’t need to feel and smell like health education. Look for "stealth interventions" that are motivating in themselves and have the side effects of reducing inactivity or changing diets, Dr. Robinson suggested. Ethnic dance classes appeal to girls in his area, for example. Dr. Robinson and his associates created sports leagues specifically for overweight children, and the youngsters love it, he said.
Help parents consistently reward specific behavior changes, but avoid material rewards. Encourage them to be observant: If a child comes home from school and does homework without turning on the TV, give specific praise for that immediately or as soon as possible. Besides praise, other effective rewards might be an activity together, or an activity related to the goal. Extra privileges or extra time with a parent can be a motivating goal. Any "thing" used as a reward should be related to the goals, he said.
When the child is in the early stages of changing a behavior, reward success frequently, but make the rewards less frequent as the behavior becomes more established so that it is not contingent upon rewards. Parents might also consider making contracts with their children around the goals, even reciprocal contracts in which the parents reward the child and the child rewards the parents.
See patients regularly when trying to make these changes, Dr. Robinson said, and expect relapses. Problem-solve with patients and families to plan ahead for difficult scenarios, especially birthdays and holidays.
As behaviors begin to change, support that change with more intensity, greater frequency, or longer duration.
"Obesity is less about knowledge than about behavior and setting up behavioral systems," he said.
Dr. Robinson reported having no relevant financial disclosures.
STANFORD, CALIF. – Setting goals with families to reduce childhood obesity must be specific, explicit, and unambiguous to be effective.
Instead of encouraging them to walk or bike to school more often, try a goal of walking or biking to school 2 or more days per week. Don’t just say, "Watch less TV," but recommend that the child watch no television on school days, Dr. Thomas N. Robinson said at a pediatric update sponsored by Stanford University.
"Keep it simple," and only set one or two short-term goals at a time, said Dr. Robinson, the Irving Schulman M.D. Endowed Professor in Child Health at the university, and director of the Center for Healthy Weight at Lucile Packard Children’s Hospital at Stanford.
Talk with the child and parents to identify specific behaviors and routines that could be targets for change. "If you can’t count it, you can’t change it," he stressed.
If your aim is to modify eating behaviors, don’t focus on consumption of calories, fat, carbohydrates, fiber, or the energy density of foods, which are hard to track. It’s easier to focus on more specific categories like specific high-calorie foods, sweetened drinks, high-calorie food preparation methods (such as frying), eating out or eating fast food, or a specific eating pattern such as having multiple "dinners." A rule of thumb for a child’s "portion" is the size of a parent’s palm. Suggest that they use smaller plates or bowls for children, or never let the child eat something right out of the box.
To promote activity instead of inactivity, it’s relatively easy to count transportation to school, organized sports or classes, time spent playing outdoors, chores, physical education, and sedentary behaviors such as time with TV, video games, phones, or computers.
A more specific goal than exercising as a family might be to take a family hike every Sunday afternoon. Rather than, "Eat less junk food," perhaps aim to limit trips to McDonald’s to once a week, he said. "Drink less soda and juice" is not nearly as helpful and specific as "No soda or juice, only milk and water."
Parents can set goals for their own behaviors to help their children, such as not keeping sugar-sweetened beverages in the home, or keeping a bowl of fresh fruit in the kitchen and a bowl of cut vegetables in the refrigerator. Approximately 85% of school-aged children have televisions in their bedrooms (a practice that’s most likely in lower socioeconomic groups), so moving the TV out could be a parental goal, he said.
Parents may aim to offer no rides to school. "They can have a walking school bus where a parent walks home to home, picking up kids along the way to school. They can even have a wagon for backpacks," Dr. Robinson said. Or, starting new family routines or traditions could help, such as the Sunday afternoon hike.
Commonly, the parents of an obese child don’t perceive obesity to be a problem because everyone in the family is obese. Instead of focusing on weight loss, work with them to set short-term goals around nutrition and physical activity because those are about making their child healthy, he suggested. "Over time, you can talk about metabolic risk, etc., but start with short-term goals."
Think less of what motivates you, and more about what will motivate your patients. External rewards for a behavior – especially food or money – may work in the short term, but will backfire over time. Build intrinsic motivation by helping patients and families pick goals that are challenging but achievable, not too easy or too hard.
It’s extremely important that the child and parents know that they have choices and control. It’s the same concept employed in the strategy of getting a child to go to bed not by saying, "Time for bed," but by asking which they want to do first before going to bed: brushing teeth or putting on pajamas. Help children and parents identify the target behaviors that are motivating for them and individualized to them.
Contextualized fantasy (also called gamification) may build intrinsic motivation in children. For example, the parent might propose that they build a house out of vegetables and then eat it. Cooperation, competition, and social interaction – doing things in groups – also build intrinsic motivation.
"If you can’t count it, you can’t change it."
A behavior intervention doesn’t need to feel and smell like health education. Look for "stealth interventions" that are motivating in themselves and have the side effects of reducing inactivity or changing diets, Dr. Robinson suggested. Ethnic dance classes appeal to girls in his area, for example. Dr. Robinson and his associates created sports leagues specifically for overweight children, and the youngsters love it, he said.
Help parents consistently reward specific behavior changes, but avoid material rewards. Encourage them to be observant: If a child comes home from school and does homework without turning on the TV, give specific praise for that immediately or as soon as possible. Besides praise, other effective rewards might be an activity together, or an activity related to the goal. Extra privileges or extra time with a parent can be a motivating goal. Any "thing" used as a reward should be related to the goals, he said.
When the child is in the early stages of changing a behavior, reward success frequently, but make the rewards less frequent as the behavior becomes more established so that it is not contingent upon rewards. Parents might also consider making contracts with their children around the goals, even reciprocal contracts in which the parents reward the child and the child rewards the parents.
See patients regularly when trying to make these changes, Dr. Robinson said, and expect relapses. Problem-solve with patients and families to plan ahead for difficult scenarios, especially birthdays and holidays.
As behaviors begin to change, support that change with more intensity, greater frequency, or longer duration.
"Obesity is less about knowledge than about behavior and setting up behavioral systems," he said.
Dr. Robinson reported having no relevant financial disclosures.
STANFORD, CALIF. – Setting goals with families to reduce childhood obesity must be specific, explicit, and unambiguous to be effective.
Instead of encouraging them to walk or bike to school more often, try a goal of walking or biking to school 2 or more days per week. Don’t just say, "Watch less TV," but recommend that the child watch no television on school days, Dr. Thomas N. Robinson said at a pediatric update sponsored by Stanford University.
"Keep it simple," and only set one or two short-term goals at a time, said Dr. Robinson, the Irving Schulman M.D. Endowed Professor in Child Health at the university, and director of the Center for Healthy Weight at Lucile Packard Children’s Hospital at Stanford.
Talk with the child and parents to identify specific behaviors and routines that could be targets for change. "If you can’t count it, you can’t change it," he stressed.
If your aim is to modify eating behaviors, don’t focus on consumption of calories, fat, carbohydrates, fiber, or the energy density of foods, which are hard to track. It’s easier to focus on more specific categories like specific high-calorie foods, sweetened drinks, high-calorie food preparation methods (such as frying), eating out or eating fast food, or a specific eating pattern such as having multiple "dinners." A rule of thumb for a child’s "portion" is the size of a parent’s palm. Suggest that they use smaller plates or bowls for children, or never let the child eat something right out of the box.
To promote activity instead of inactivity, it’s relatively easy to count transportation to school, organized sports or classes, time spent playing outdoors, chores, physical education, and sedentary behaviors such as time with TV, video games, phones, or computers.
A more specific goal than exercising as a family might be to take a family hike every Sunday afternoon. Rather than, "Eat less junk food," perhaps aim to limit trips to McDonald’s to once a week, he said. "Drink less soda and juice" is not nearly as helpful and specific as "No soda or juice, only milk and water."
Parents can set goals for their own behaviors to help their children, such as not keeping sugar-sweetened beverages in the home, or keeping a bowl of fresh fruit in the kitchen and a bowl of cut vegetables in the refrigerator. Approximately 85% of school-aged children have televisions in their bedrooms (a practice that’s most likely in lower socioeconomic groups), so moving the TV out could be a parental goal, he said.
Parents may aim to offer no rides to school. "They can have a walking school bus where a parent walks home to home, picking up kids along the way to school. They can even have a wagon for backpacks," Dr. Robinson said. Or, starting new family routines or traditions could help, such as the Sunday afternoon hike.
Commonly, the parents of an obese child don’t perceive obesity to be a problem because everyone in the family is obese. Instead of focusing on weight loss, work with them to set short-term goals around nutrition and physical activity because those are about making their child healthy, he suggested. "Over time, you can talk about metabolic risk, etc., but start with short-term goals."
Think less of what motivates you, and more about what will motivate your patients. External rewards for a behavior – especially food or money – may work in the short term, but will backfire over time. Build intrinsic motivation by helping patients and families pick goals that are challenging but achievable, not too easy or too hard.
It’s extremely important that the child and parents know that they have choices and control. It’s the same concept employed in the strategy of getting a child to go to bed not by saying, "Time for bed," but by asking which they want to do first before going to bed: brushing teeth or putting on pajamas. Help children and parents identify the target behaviors that are motivating for them and individualized to them.
Contextualized fantasy (also called gamification) may build intrinsic motivation in children. For example, the parent might propose that they build a house out of vegetables and then eat it. Cooperation, competition, and social interaction – doing things in groups – also build intrinsic motivation.
"If you can’t count it, you can’t change it."
A behavior intervention doesn’t need to feel and smell like health education. Look for "stealth interventions" that are motivating in themselves and have the side effects of reducing inactivity or changing diets, Dr. Robinson suggested. Ethnic dance classes appeal to girls in his area, for example. Dr. Robinson and his associates created sports leagues specifically for overweight children, and the youngsters love it, he said.
Help parents consistently reward specific behavior changes, but avoid material rewards. Encourage them to be observant: If a child comes home from school and does homework without turning on the TV, give specific praise for that immediately or as soon as possible. Besides praise, other effective rewards might be an activity together, or an activity related to the goal. Extra privileges or extra time with a parent can be a motivating goal. Any "thing" used as a reward should be related to the goals, he said.
When the child is in the early stages of changing a behavior, reward success frequently, but make the rewards less frequent as the behavior becomes more established so that it is not contingent upon rewards. Parents might also consider making contracts with their children around the goals, even reciprocal contracts in which the parents reward the child and the child rewards the parents.
See patients regularly when trying to make these changes, Dr. Robinson said, and expect relapses. Problem-solve with patients and families to plan ahead for difficult scenarios, especially birthdays and holidays.
As behaviors begin to change, support that change with more intensity, greater frequency, or longer duration.
"Obesity is less about knowledge than about behavior and setting up behavioral systems," he said.
Dr. Robinson reported having no relevant financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Some Sports Injuries Greater for Girls
STANFORD, CALIF. – Help girls avoid the sports injuries that are more common for them than for boys by clearly explaining energy requirements, recommending prevention training programs, and educating about concussions.
Brains and knees face extra risk from sports injuries in girls than in boys, and only girls develop the Female Athlete Triad – disordered eating, amenorrhea and osteoporosis.
In gender-compatible sports such as soccer or basketball, girls have higher concussion rates than do boys and more postconcussion symptoms. Anterior cruciate ligament (ACL) injuries are two to eight times more common in females than in males. Approximately 1% of female high school athletes meet all three criteria of the Female Athlete Triad, 6% may meet two criteria, and approximately one in five may meet one of the criteria, Dr. Jennifer L. Carlson said at a pediatric update sponsored by Stanford University.
• Female athlete triad. The key to prevention is education. Dr. Carlson explains to patients that they should consume 2,200-2,400 kcal/day (depending on their age) if they are "active," meaning their daily activity is the equivalent of walking more than 3 miles/day at 3-4 mph. If they do more, they’re "very active" and need 2,500-4,000 kcal/day, depending on the sport and the number of hours spent training.
"Many have no idea that that’s what they need to be taking in," said Dr. Carlson of the university.
Girls also need to hear that losing one’s period is not a sign of fitness. And coaches may need to be asked to de-emphasize weight goals and abandon harmful weight-loss practices.
"I’ve had athletes in non–weight-class sports where the coach monitors weight" and even asks them to get a bone density scan, for no good reason, Dr. Carlson said.
One study of 170 female athletes in six Southern California high schools found that 1% met the three criteria for female athlete triad and 6% met two criteria. "But any one of the three criteria is pretty significant," Dr. Carlson said, and 18%-24% in the study had one of the individual criteria (Arch. Pediatr. Adolesc. Med. 2006;160:137-42).
The three criteria of disordered eating, amenorrhea, and osteoporosis that were identified in 1992 have evolved, and today would be described as low energy availability, menstrual disturbances, and low bone mineral density, she said. These can lead to fatigue, difficulty concentrating, emotional lability, impaired athletic performance, stress reactions, and fractures.
The triad is most likely in sports such as gymnastics in which the athlete is scored partly on aesthetics, endurance sports such as cross-country running that favor low body weight for better performance, sports like wrestling or crew that have different weight classes, or any sport in which clothing reveals body contours.
Physicians can find helpful resources about the syndrome from the Female Athlete Triad Coalition website, she said.
• ACL injuries. In females, ACL injuries most commonly come from noncontact maneuvers in sports involving sudden stopping and changing of direction, known as "cutting." The injuries range from small, mild tears to completely torn ligaments. Prevention focuses on awareness of risk factors and specific training programs.
Prevention training programs focus on minimizing risky positions (such as landing from a jump in an upright position instead of crouched), increasing balance and knee stiffness, and decreasing ACL strain. Training programs significantly reduced the risk for ACL injuries by 60% in a meta-analysis of six studies (Am. J. Sports Med. 2006;34:490-8).
The elite and collegiate-level sports programs incorporate prevention training programs. More and more experts advocate for them to be integrated into sports programs for prepubertal age groups, she said.
Greater friction on playing fields increases the risk of ACL injury. Generally, artificial turf is thought to be riskier, and wet surfaces may decrease risk of an ACL tear. Females may have higher risk because of neuromuscular or anatomic factors (such as wider hips) or less core stability, some think.
Biomechanical differences contribute to risk, compared with males. Hormones play a role, too. The peak time of female ACL injury is in the first phase of the menstrual cycle, and oral contraceptives seem to be protective, probably because of the action on neuromuscular junctions that hormones affect, Dr. Carlson said.
• Concussion. Higher rates of concussions in girls playing gender-comparable sports may be caused by reporting bias if boys are more reluctant than girls to report the injury, some speculate. In a recent study of 296 athletes, however, females had worse visual memory scores and more concussion symptoms than did males after a concussion, and neurocognitive impairments persisted as long as 10-21 days for high schoolers and 5-7 days for college athletes (Am. J. Sports Med. 2012;40:1303-12).
Possible reasons for these sex differences may include female sex hormones: rat studies show that estrogen has both protective and exacerbative effects, Dr. Carlson said. Cerebral blood flow and basal rate of glucose metabolism are higher in females than in males, and perhaps an increase in either of these after injury may cause concussion symptoms to persist or be more severe, she speculated.
There’s nothing gender specific about concussion-prevention efforts, except perhaps how they’re applied. Boys playing lacrosse are required to wear helmets, for example, but girls are not, she said. Concerns about universal use of headgear leading to more aggressive play and more collisions come from studies of boys, she added.
Regulations may play an increasing role in preventing concussions. A 2011 California law requires that players with suspected concussion must be pulled from school-based sports and not allowed to return without clearance from a health care profession, and they must get yearly head-trauma clearance.
Female participation in high school sports increased 900% in the past 40 years and increased 500% in collegiate sports. It’s not just the older girls who are at risk, though. Recent trends of increased participation in organized sports and greater specialization in sports at younger ages may contribute to overuse and sport-specific injuries at younger ages, Dr. Carlson said.
"My 3-year-old already gets flyers for soccer teams," she said.
Dr. Carlson reported having no financial disclosures.
STANFORD, CALIF. – Help girls avoid the sports injuries that are more common for them than for boys by clearly explaining energy requirements, recommending prevention training programs, and educating about concussions.
Brains and knees face extra risk from sports injuries in girls than in boys, and only girls develop the Female Athlete Triad – disordered eating, amenorrhea and osteoporosis.
In gender-compatible sports such as soccer or basketball, girls have higher concussion rates than do boys and more postconcussion symptoms. Anterior cruciate ligament (ACL) injuries are two to eight times more common in females than in males. Approximately 1% of female high school athletes meet all three criteria of the Female Athlete Triad, 6% may meet two criteria, and approximately one in five may meet one of the criteria, Dr. Jennifer L. Carlson said at a pediatric update sponsored by Stanford University.
• Female athlete triad. The key to prevention is education. Dr. Carlson explains to patients that they should consume 2,200-2,400 kcal/day (depending on their age) if they are "active," meaning their daily activity is the equivalent of walking more than 3 miles/day at 3-4 mph. If they do more, they’re "very active" and need 2,500-4,000 kcal/day, depending on the sport and the number of hours spent training.
"Many have no idea that that’s what they need to be taking in," said Dr. Carlson of the university.
Girls also need to hear that losing one’s period is not a sign of fitness. And coaches may need to be asked to de-emphasize weight goals and abandon harmful weight-loss practices.
"I’ve had athletes in non–weight-class sports where the coach monitors weight" and even asks them to get a bone density scan, for no good reason, Dr. Carlson said.
One study of 170 female athletes in six Southern California high schools found that 1% met the three criteria for female athlete triad and 6% met two criteria. "But any one of the three criteria is pretty significant," Dr. Carlson said, and 18%-24% in the study had one of the individual criteria (Arch. Pediatr. Adolesc. Med. 2006;160:137-42).
The three criteria of disordered eating, amenorrhea, and osteoporosis that were identified in 1992 have evolved, and today would be described as low energy availability, menstrual disturbances, and low bone mineral density, she said. These can lead to fatigue, difficulty concentrating, emotional lability, impaired athletic performance, stress reactions, and fractures.
The triad is most likely in sports such as gymnastics in which the athlete is scored partly on aesthetics, endurance sports such as cross-country running that favor low body weight for better performance, sports like wrestling or crew that have different weight classes, or any sport in which clothing reveals body contours.
Physicians can find helpful resources about the syndrome from the Female Athlete Triad Coalition website, she said.
• ACL injuries. In females, ACL injuries most commonly come from noncontact maneuvers in sports involving sudden stopping and changing of direction, known as "cutting." The injuries range from small, mild tears to completely torn ligaments. Prevention focuses on awareness of risk factors and specific training programs.
Prevention training programs focus on minimizing risky positions (such as landing from a jump in an upright position instead of crouched), increasing balance and knee stiffness, and decreasing ACL strain. Training programs significantly reduced the risk for ACL injuries by 60% in a meta-analysis of six studies (Am. J. Sports Med. 2006;34:490-8).
The elite and collegiate-level sports programs incorporate prevention training programs. More and more experts advocate for them to be integrated into sports programs for prepubertal age groups, she said.
Greater friction on playing fields increases the risk of ACL injury. Generally, artificial turf is thought to be riskier, and wet surfaces may decrease risk of an ACL tear. Females may have higher risk because of neuromuscular or anatomic factors (such as wider hips) or less core stability, some think.
Biomechanical differences contribute to risk, compared with males. Hormones play a role, too. The peak time of female ACL injury is in the first phase of the menstrual cycle, and oral contraceptives seem to be protective, probably because of the action on neuromuscular junctions that hormones affect, Dr. Carlson said.
• Concussion. Higher rates of concussions in girls playing gender-comparable sports may be caused by reporting bias if boys are more reluctant than girls to report the injury, some speculate. In a recent study of 296 athletes, however, females had worse visual memory scores and more concussion symptoms than did males after a concussion, and neurocognitive impairments persisted as long as 10-21 days for high schoolers and 5-7 days for college athletes (Am. J. Sports Med. 2012;40:1303-12).
Possible reasons for these sex differences may include female sex hormones: rat studies show that estrogen has both protective and exacerbative effects, Dr. Carlson said. Cerebral blood flow and basal rate of glucose metabolism are higher in females than in males, and perhaps an increase in either of these after injury may cause concussion symptoms to persist or be more severe, she speculated.
There’s nothing gender specific about concussion-prevention efforts, except perhaps how they’re applied. Boys playing lacrosse are required to wear helmets, for example, but girls are not, she said. Concerns about universal use of headgear leading to more aggressive play and more collisions come from studies of boys, she added.
Regulations may play an increasing role in preventing concussions. A 2011 California law requires that players with suspected concussion must be pulled from school-based sports and not allowed to return without clearance from a health care profession, and they must get yearly head-trauma clearance.
Female participation in high school sports increased 900% in the past 40 years and increased 500% in collegiate sports. It’s not just the older girls who are at risk, though. Recent trends of increased participation in organized sports and greater specialization in sports at younger ages may contribute to overuse and sport-specific injuries at younger ages, Dr. Carlson said.
"My 3-year-old already gets flyers for soccer teams," she said.
Dr. Carlson reported having no financial disclosures.
STANFORD, CALIF. – Help girls avoid the sports injuries that are more common for them than for boys by clearly explaining energy requirements, recommending prevention training programs, and educating about concussions.
Brains and knees face extra risk from sports injuries in girls than in boys, and only girls develop the Female Athlete Triad – disordered eating, amenorrhea and osteoporosis.
In gender-compatible sports such as soccer or basketball, girls have higher concussion rates than do boys and more postconcussion symptoms. Anterior cruciate ligament (ACL) injuries are two to eight times more common in females than in males. Approximately 1% of female high school athletes meet all three criteria of the Female Athlete Triad, 6% may meet two criteria, and approximately one in five may meet one of the criteria, Dr. Jennifer L. Carlson said at a pediatric update sponsored by Stanford University.
• Female athlete triad. The key to prevention is education. Dr. Carlson explains to patients that they should consume 2,200-2,400 kcal/day (depending on their age) if they are "active," meaning their daily activity is the equivalent of walking more than 3 miles/day at 3-4 mph. If they do more, they’re "very active" and need 2,500-4,000 kcal/day, depending on the sport and the number of hours spent training.
"Many have no idea that that’s what they need to be taking in," said Dr. Carlson of the university.
Girls also need to hear that losing one’s period is not a sign of fitness. And coaches may need to be asked to de-emphasize weight goals and abandon harmful weight-loss practices.
"I’ve had athletes in non–weight-class sports where the coach monitors weight" and even asks them to get a bone density scan, for no good reason, Dr. Carlson said.
One study of 170 female athletes in six Southern California high schools found that 1% met the three criteria for female athlete triad and 6% met two criteria. "But any one of the three criteria is pretty significant," Dr. Carlson said, and 18%-24% in the study had one of the individual criteria (Arch. Pediatr. Adolesc. Med. 2006;160:137-42).
The three criteria of disordered eating, amenorrhea, and osteoporosis that were identified in 1992 have evolved, and today would be described as low energy availability, menstrual disturbances, and low bone mineral density, she said. These can lead to fatigue, difficulty concentrating, emotional lability, impaired athletic performance, stress reactions, and fractures.
The triad is most likely in sports such as gymnastics in which the athlete is scored partly on aesthetics, endurance sports such as cross-country running that favor low body weight for better performance, sports like wrestling or crew that have different weight classes, or any sport in which clothing reveals body contours.
Physicians can find helpful resources about the syndrome from the Female Athlete Triad Coalition website, she said.
• ACL injuries. In females, ACL injuries most commonly come from noncontact maneuvers in sports involving sudden stopping and changing of direction, known as "cutting." The injuries range from small, mild tears to completely torn ligaments. Prevention focuses on awareness of risk factors and specific training programs.
Prevention training programs focus on minimizing risky positions (such as landing from a jump in an upright position instead of crouched), increasing balance and knee stiffness, and decreasing ACL strain. Training programs significantly reduced the risk for ACL injuries by 60% in a meta-analysis of six studies (Am. J. Sports Med. 2006;34:490-8).
The elite and collegiate-level sports programs incorporate prevention training programs. More and more experts advocate for them to be integrated into sports programs for prepubertal age groups, she said.
Greater friction on playing fields increases the risk of ACL injury. Generally, artificial turf is thought to be riskier, and wet surfaces may decrease risk of an ACL tear. Females may have higher risk because of neuromuscular or anatomic factors (such as wider hips) or less core stability, some think.
Biomechanical differences contribute to risk, compared with males. Hormones play a role, too. The peak time of female ACL injury is in the first phase of the menstrual cycle, and oral contraceptives seem to be protective, probably because of the action on neuromuscular junctions that hormones affect, Dr. Carlson said.
• Concussion. Higher rates of concussions in girls playing gender-comparable sports may be caused by reporting bias if boys are more reluctant than girls to report the injury, some speculate. In a recent study of 296 athletes, however, females had worse visual memory scores and more concussion symptoms than did males after a concussion, and neurocognitive impairments persisted as long as 10-21 days for high schoolers and 5-7 days for college athletes (Am. J. Sports Med. 2012;40:1303-12).
Possible reasons for these sex differences may include female sex hormones: rat studies show that estrogen has both protective and exacerbative effects, Dr. Carlson said. Cerebral blood flow and basal rate of glucose metabolism are higher in females than in males, and perhaps an increase in either of these after injury may cause concussion symptoms to persist or be more severe, she speculated.
There’s nothing gender specific about concussion-prevention efforts, except perhaps how they’re applied. Boys playing lacrosse are required to wear helmets, for example, but girls are not, she said. Concerns about universal use of headgear leading to more aggressive play and more collisions come from studies of boys, she added.
Regulations may play an increasing role in preventing concussions. A 2011 California law requires that players with suspected concussion must be pulled from school-based sports and not allowed to return without clearance from a health care profession, and they must get yearly head-trauma clearance.
Female participation in high school sports increased 900% in the past 40 years and increased 500% in collegiate sports. It’s not just the older girls who are at risk, though. Recent trends of increased participation in organized sports and greater specialization in sports at younger ages may contribute to overuse and sport-specific injuries at younger ages, Dr. Carlson said.
"My 3-year-old already gets flyers for soccer teams," she said.
Dr. Carlson reported having no financial disclosures.
EXPERT ANALYSIS FROM A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Infant Invasive Pneumococcal Disease Tanked in 2011
STANFORD, CALIF. – A huge drop in U.S. cases of invasive pneumococcal disease in infants younger than 2 years bodes well for possible similar trends in older age groups.
Preliminary data not yet published by the Centers for Disease Control and Prevention suggest that only 40 cases of invasive pneumococcal disease with serotypes covered by the previous vaccine were reported in infants under 2 years of age in 2011, Dr. Yvonne "Bonnie" Maldonado said at Stanford University’s pediatric update.
That’s a big, "exciting" drop from nearly 140-180 cases in infants under 2 years of age reported in each of 2006, 2007, 2008, and 2010, and it is most likely due to the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13) in 2010, said Dr. Maldonado, chief of pediatric infectious disease, and professor of pediatrics and of health research and policy at the university.
The previous PCV7 vaccine, introduced in 2000, lost some effectiveness over time as some covered serotypes mutated, and serotypes that were not included in the vaccine became more prominent.
With the introduction of the PCV13 vaccine, rates of invasive pneumococcal disease in this young age group "really dropped off dramatically," she said. "It bodes very well for our ability to significantly reduce the amount of pneumococcal disease in the population."
Data for cases of invasive pneumococcal disease in 2009 were not included in the analysis because pandemic influenza contributed to so many cases that year, she said.
The CDC now is analyzing data on invasive pneumococcal disease in age groups older than 2 months in 2011.
"I suspect that what’s going to happen, because it did happen with the PCV7 vaccine, is that you’re going to see this herd immunity affect older populations as well," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – A huge drop in U.S. cases of invasive pneumococcal disease in infants younger than 2 years bodes well for possible similar trends in older age groups.
Preliminary data not yet published by the Centers for Disease Control and Prevention suggest that only 40 cases of invasive pneumococcal disease with serotypes covered by the previous vaccine were reported in infants under 2 years of age in 2011, Dr. Yvonne "Bonnie" Maldonado said at Stanford University’s pediatric update.
That’s a big, "exciting" drop from nearly 140-180 cases in infants under 2 years of age reported in each of 2006, 2007, 2008, and 2010, and it is most likely due to the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13) in 2010, said Dr. Maldonado, chief of pediatric infectious disease, and professor of pediatrics and of health research and policy at the university.
The previous PCV7 vaccine, introduced in 2000, lost some effectiveness over time as some covered serotypes mutated, and serotypes that were not included in the vaccine became more prominent.
With the introduction of the PCV13 vaccine, rates of invasive pneumococcal disease in this young age group "really dropped off dramatically," she said. "It bodes very well for our ability to significantly reduce the amount of pneumococcal disease in the population."
Data for cases of invasive pneumococcal disease in 2009 were not included in the analysis because pandemic influenza contributed to so many cases that year, she said.
The CDC now is analyzing data on invasive pneumococcal disease in age groups older than 2 months in 2011.
"I suspect that what’s going to happen, because it did happen with the PCV7 vaccine, is that you’re going to see this herd immunity affect older populations as well," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – A huge drop in U.S. cases of invasive pneumococcal disease in infants younger than 2 years bodes well for possible similar trends in older age groups.
Preliminary data not yet published by the Centers for Disease Control and Prevention suggest that only 40 cases of invasive pneumococcal disease with serotypes covered by the previous vaccine were reported in infants under 2 years of age in 2011, Dr. Yvonne "Bonnie" Maldonado said at Stanford University’s pediatric update.
That’s a big, "exciting" drop from nearly 140-180 cases in infants under 2 years of age reported in each of 2006, 2007, 2008, and 2010, and it is most likely due to the introduction of the 13-valent pneumococcal conjugate vaccine (PCV13) in 2010, said Dr. Maldonado, chief of pediatric infectious disease, and professor of pediatrics and of health research and policy at the university.
The previous PCV7 vaccine, introduced in 2000, lost some effectiveness over time as some covered serotypes mutated, and serotypes that were not included in the vaccine became more prominent.
With the introduction of the PCV13 vaccine, rates of invasive pneumococcal disease in this young age group "really dropped off dramatically," she said. "It bodes very well for our ability to significantly reduce the amount of pneumococcal disease in the population."
Data for cases of invasive pneumococcal disease in 2009 were not included in the analysis because pandemic influenza contributed to so many cases that year, she said.
The CDC now is analyzing data on invasive pneumococcal disease in age groups older than 2 months in 2011.
"I suspect that what’s going to happen, because it did happen with the PCV7 vaccine, is that you’re going to see this herd immunity affect older populations as well," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
AT A PEDIATRIC UPDATE SPONSORED BY STANFORD UNIVERSITY
Younger Age for Measles Vaccine Debated
STANFORD, CALIF. – An expert panel is debating a possible change in federal immunization recommendations to lower the age of routine first measles vaccination to 6 months for infants who will be traveling to areas where measles is a problem.
The Centers for Disease Control and Prevention’s working group on measles, mumps and rubella (MMR) is talking to experts about a possible revamp of recommendations. "We probably aren’t going to change them very much, but one of the things we’ve been debating very strongly is whether or not we should recommend that if your child is under 12 months of age and going to an area where there’s measles, should the child get vaccinated?" Dr. Yvonne (Bonnie) Maldonado said at a pediatric update sponsored by Stanford University.
he debate is fueled by a recent CDC report showing the threat that imported measles creates for U.S. efforts to sustain elimination of endemic measles.
The 222 cases of measles reported in 2011 in the United States was the highest number since 1996, and it included 72 importations of measles from 20-22 countries – mainly from western Europe, the CDC reported recently (MMWR 2012;61:253-7). This compared with a median of 60 (37-140) cases and four (2-10) outbreaks reported annually during 2001-2010.
"That may not seem like a high number, but remember that measles is one of the most – if not the most – infectious viruses that we know of that affects humans," so a few cases could help the disease become endemic again, said Dr. Maldonado, one of the experts in the debate. She is chief of pediatric infectious diseases as well as professor of pediatrics and of health research and policy at Stanford.
With many Americans traveling to the Olympic Games in London, "the big concern for the Olympics is that people are going to go out there and be exposed, and come back and we’ll see more transmission in our children," she said.
Besides the clearly imported cases in 2011, most other cases were either linked to imported cases or involved a strain of measles virus that’s typically imported. The importations caused 17 outbreaks of measles in the United States – four times as many as usual – each with 3-21 more cases.
All in all, 88% of cases in 2011 were related to imported measles, and the other 12% of cases didn’t include enough information from the case history, the patient, or the viral strain to determine if they were related to importation.
Current recommendations call for first MMR vaccination routinely in infants aged 12-15 months, with a second dose at 4-6 years of age. Earlier this year, with the perspective of the 2011 data and with travel to the Olympics on the horizon, the CDC held media briefings and recommended that anyone older than 6 months who would be traveling internationally should receive the MMR vaccine, if needed. A second dose can be given as soon as 28 days after the first dose.
In fact, the Advisory Committee on Immunization Practices (MMWR 1998;47[RR-8]:20) and the American Academy of Pediatrics’ Red Book already allow for eligible children to be vaccinated against measles as young as 6 months of age, Dr. Maldonado said. "It’s buried in there," but the recommendations do allow it. The only caveat is that a vaccine dose given before 12 months of age doesn’t count toward the two recommended doses after 12 months of age. "They need to be revaccinated at 12 months and later on," she said.
Of the 70 U.S. patients hospitalized for measles in 2011, 14% were younger than 12 months of age, 38% were 1-4 years of age, and 21% were aged 5-19 years.
Most of the imported cases came from Europe because "there has been an ongoing endemic problem in Europe, primarily because of lack of vaccination due to issues around fears of autism" being caused by vaccines, she said. Many expert reports have discredited claims that the MMR vaccine causes autism. In 2011, 37,070 cases of measles were reported in Europe, with the highest proportion in France, accounting for 14% of cases. Seven people died of measles.
In the United States, 141 of the cases in 2011 occurred in people who were eligible for the vaccine, and so should have been preventable. These included measles in 9 infants aged 6-11 months who traveled abroad, and in 14 infants aged 12-15 months, 9 of whom traveled abroad.
"I think there’s not enough awareness about families bringing in their children for pretravel immunization updates. That’s something that’s really important," Dr. Maldonado said. "If you have children in your practice who are going to be traveling, it would be helpful if you would update the parents about what vaccinations they should be receiving."
The CDC declared that the United States had eliminated endemic measles (which is not quite the same thing as eradication) in 2000, and a recent review found that the elimination has been sustained but "is inherently a fragile state" that requires significant surveillance, investigation, and response to importation-related cases, Dr. Maldonado said.
The report will go to the World Health Organization, which is assessing the global status of measles, she added. "One of the things we found with polio, outside the United States, is that once countries feel that they have eliminated the disease, they kind of ease up on their vaccination practices. We really don’t think that’s advisable with measles because it’s so contagious," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – An expert panel is debating a possible change in federal immunization recommendations to lower the age of routine first measles vaccination to 6 months for infants who will be traveling to areas where measles is a problem.
The Centers for Disease Control and Prevention’s working group on measles, mumps and rubella (MMR) is talking to experts about a possible revamp of recommendations. "We probably aren’t going to change them very much, but one of the things we’ve been debating very strongly is whether or not we should recommend that if your child is under 12 months of age and going to an area where there’s measles, should the child get vaccinated?" Dr. Yvonne (Bonnie) Maldonado said at a pediatric update sponsored by Stanford University.
he debate is fueled by a recent CDC report showing the threat that imported measles creates for U.S. efforts to sustain elimination of endemic measles.
The 222 cases of measles reported in 2011 in the United States was the highest number since 1996, and it included 72 importations of measles from 20-22 countries – mainly from western Europe, the CDC reported recently (MMWR 2012;61:253-7). This compared with a median of 60 (37-140) cases and four (2-10) outbreaks reported annually during 2001-2010.
"That may not seem like a high number, but remember that measles is one of the most – if not the most – infectious viruses that we know of that affects humans," so a few cases could help the disease become endemic again, said Dr. Maldonado, one of the experts in the debate. She is chief of pediatric infectious diseases as well as professor of pediatrics and of health research and policy at Stanford.
With many Americans traveling to the Olympic Games in London, "the big concern for the Olympics is that people are going to go out there and be exposed, and come back and we’ll see more transmission in our children," she said.
Besides the clearly imported cases in 2011, most other cases were either linked to imported cases or involved a strain of measles virus that’s typically imported. The importations caused 17 outbreaks of measles in the United States – four times as many as usual – each with 3-21 more cases.
All in all, 88% of cases in 2011 were related to imported measles, and the other 12% of cases didn’t include enough information from the case history, the patient, or the viral strain to determine if they were related to importation.
Current recommendations call for first MMR vaccination routinely in infants aged 12-15 months, with a second dose at 4-6 years of age. Earlier this year, with the perspective of the 2011 data and with travel to the Olympics on the horizon, the CDC held media briefings and recommended that anyone older than 6 months who would be traveling internationally should receive the MMR vaccine, if needed. A second dose can be given as soon as 28 days after the first dose.
In fact, the Advisory Committee on Immunization Practices (MMWR 1998;47[RR-8]:20) and the American Academy of Pediatrics’ Red Book already allow for eligible children to be vaccinated against measles as young as 6 months of age, Dr. Maldonado said. "It’s buried in there," but the recommendations do allow it. The only caveat is that a vaccine dose given before 12 months of age doesn’t count toward the two recommended doses after 12 months of age. "They need to be revaccinated at 12 months and later on," she said.
Of the 70 U.S. patients hospitalized for measles in 2011, 14% were younger than 12 months of age, 38% were 1-4 years of age, and 21% were aged 5-19 years.
Most of the imported cases came from Europe because "there has been an ongoing endemic problem in Europe, primarily because of lack of vaccination due to issues around fears of autism" being caused by vaccines, she said. Many expert reports have discredited claims that the MMR vaccine causes autism. In 2011, 37,070 cases of measles were reported in Europe, with the highest proportion in France, accounting for 14% of cases. Seven people died of measles.
In the United States, 141 of the cases in 2011 occurred in people who were eligible for the vaccine, and so should have been preventable. These included measles in 9 infants aged 6-11 months who traveled abroad, and in 14 infants aged 12-15 months, 9 of whom traveled abroad.
"I think there’s not enough awareness about families bringing in their children for pretravel immunization updates. That’s something that’s really important," Dr. Maldonado said. "If you have children in your practice who are going to be traveling, it would be helpful if you would update the parents about what vaccinations they should be receiving."
The CDC declared that the United States had eliminated endemic measles (which is not quite the same thing as eradication) in 2000, and a recent review found that the elimination has been sustained but "is inherently a fragile state" that requires significant surveillance, investigation, and response to importation-related cases, Dr. Maldonado said.
The report will go to the World Health Organization, which is assessing the global status of measles, she added. "One of the things we found with polio, outside the United States, is that once countries feel that they have eliminated the disease, they kind of ease up on their vaccination practices. We really don’t think that’s advisable with measles because it’s so contagious," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
STANFORD, CALIF. – An expert panel is debating a possible change in federal immunization recommendations to lower the age of routine first measles vaccination to 6 months for infants who will be traveling to areas where measles is a problem.
The Centers for Disease Control and Prevention’s working group on measles, mumps and rubella (MMR) is talking to experts about a possible revamp of recommendations. "We probably aren’t going to change them very much, but one of the things we’ve been debating very strongly is whether or not we should recommend that if your child is under 12 months of age and going to an area where there’s measles, should the child get vaccinated?" Dr. Yvonne (Bonnie) Maldonado said at a pediatric update sponsored by Stanford University.
he debate is fueled by a recent CDC report showing the threat that imported measles creates for U.S. efforts to sustain elimination of endemic measles.
The 222 cases of measles reported in 2011 in the United States was the highest number since 1996, and it included 72 importations of measles from 20-22 countries – mainly from western Europe, the CDC reported recently (MMWR 2012;61:253-7). This compared with a median of 60 (37-140) cases and four (2-10) outbreaks reported annually during 2001-2010.
"That may not seem like a high number, but remember that measles is one of the most – if not the most – infectious viruses that we know of that affects humans," so a few cases could help the disease become endemic again, said Dr. Maldonado, one of the experts in the debate. She is chief of pediatric infectious diseases as well as professor of pediatrics and of health research and policy at Stanford.
With many Americans traveling to the Olympic Games in London, "the big concern for the Olympics is that people are going to go out there and be exposed, and come back and we’ll see more transmission in our children," she said.
Besides the clearly imported cases in 2011, most other cases were either linked to imported cases or involved a strain of measles virus that’s typically imported. The importations caused 17 outbreaks of measles in the United States – four times as many as usual – each with 3-21 more cases.
All in all, 88% of cases in 2011 were related to imported measles, and the other 12% of cases didn’t include enough information from the case history, the patient, or the viral strain to determine if they were related to importation.
Current recommendations call for first MMR vaccination routinely in infants aged 12-15 months, with a second dose at 4-6 years of age. Earlier this year, with the perspective of the 2011 data and with travel to the Olympics on the horizon, the CDC held media briefings and recommended that anyone older than 6 months who would be traveling internationally should receive the MMR vaccine, if needed. A second dose can be given as soon as 28 days after the first dose.
In fact, the Advisory Committee on Immunization Practices (MMWR 1998;47[RR-8]:20) and the American Academy of Pediatrics’ Red Book already allow for eligible children to be vaccinated against measles as young as 6 months of age, Dr. Maldonado said. "It’s buried in there," but the recommendations do allow it. The only caveat is that a vaccine dose given before 12 months of age doesn’t count toward the two recommended doses after 12 months of age. "They need to be revaccinated at 12 months and later on," she said.
Of the 70 U.S. patients hospitalized for measles in 2011, 14% were younger than 12 months of age, 38% were 1-4 years of age, and 21% were aged 5-19 years.
Most of the imported cases came from Europe because "there has been an ongoing endemic problem in Europe, primarily because of lack of vaccination due to issues around fears of autism" being caused by vaccines, she said. Many expert reports have discredited claims that the MMR vaccine causes autism. In 2011, 37,070 cases of measles were reported in Europe, with the highest proportion in France, accounting for 14% of cases. Seven people died of measles.
In the United States, 141 of the cases in 2011 occurred in people who were eligible for the vaccine, and so should have been preventable. These included measles in 9 infants aged 6-11 months who traveled abroad, and in 14 infants aged 12-15 months, 9 of whom traveled abroad.
"I think there’s not enough awareness about families bringing in their children for pretravel immunization updates. That’s something that’s really important," Dr. Maldonado said. "If you have children in your practice who are going to be traveling, it would be helpful if you would update the parents about what vaccinations they should be receiving."
The CDC declared that the United States had eliminated endemic measles (which is not quite the same thing as eradication) in 2000, and a recent review found that the elimination has been sustained but "is inherently a fragile state" that requires significant surveillance, investigation, and response to importation-related cases, Dr. Maldonado said.
The report will go to the World Health Organization, which is assessing the global status of measles, she added. "One of the things we found with polio, outside the United States, is that once countries feel that they have eliminated the disease, they kind of ease up on their vaccination practices. We really don’t think that’s advisable with measles because it’s so contagious," she said.
Dr. Maldonado has been a speaker for Merck and Novartis.
AT A PEDIATRIC UPDATE SPONOSORED BY STANFORD UNIVERSITY