User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
PT may lower risk of long-term opioid use after knee replacement
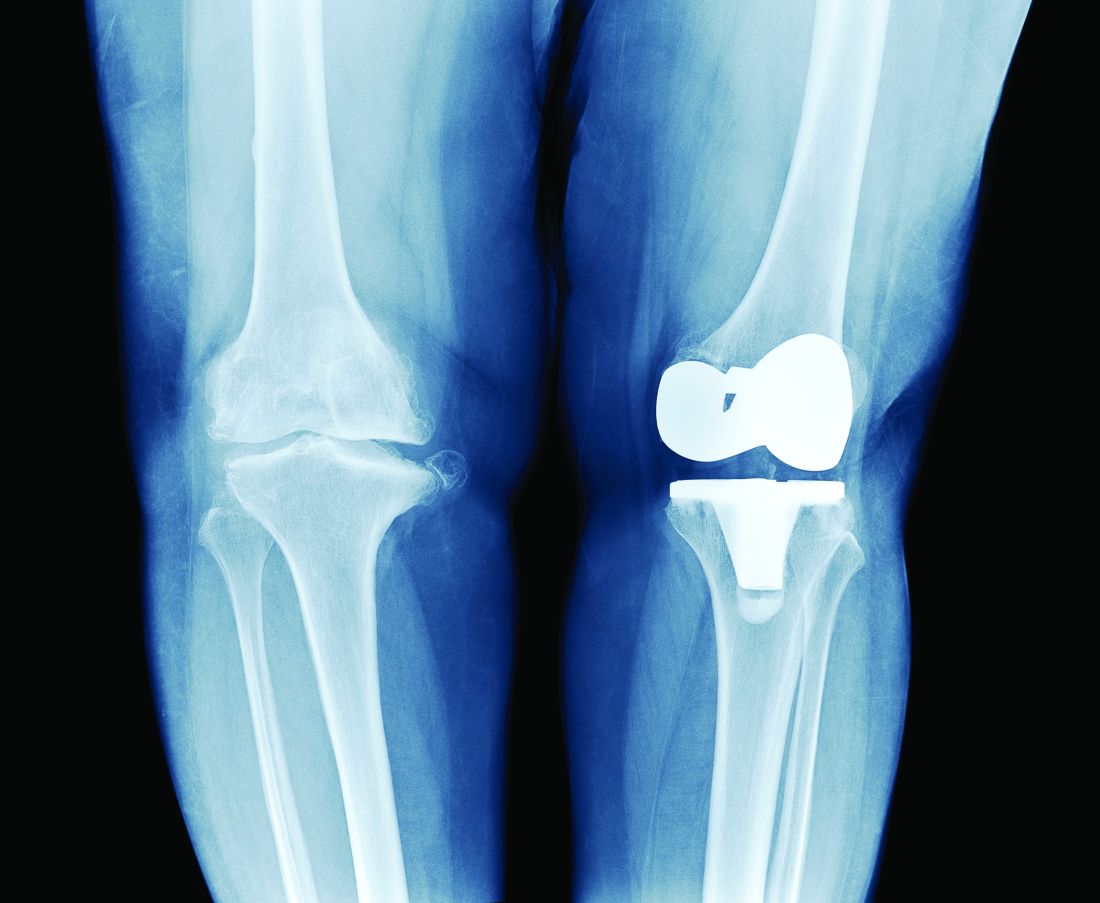
A new study has found that physical therapy may lead to a reduced risk of long-term opioid use in patients who have undergone total knee replacement (TKR).
“Greater number of PT intervention sessions and earlier initiation of outpatient PT care after TKR were associated with lower odds of long-term opioid use,” authors from Boston University wrote in their report on the study, which was published online Oct. 27 in JAMA Network Open.
“In previous large studies, we’ve seen that physical therapy can reduce pain in people with knee osteoarthritis, which is usually the primary indication for TKR,” study coauthor Deepak Kumar, PT, PhD, said in an interview. “But the association of physical therapy with opioid use in people with knee replacement has not yet been explored.
“The reason we focused on opioid use in these patients is because the number of knee replacement surgeries is going up exponentially,” Dr. Kumar said. “And, depending on which data you look at, from one-third to up to half of people who undergo knee replacement and have used opioids before end up becoming long-term users. Even in people who have not used them before, 5%-8% become long-term users after the surgery.
“Given how many surgeries are happening – and that number is expected to keep going up – the number of people who are becoming long-term opioid users is not trivial,” he said.
Study details
To assess the value of PT in reducing opioid use in this subset of patients, the authors reviewed records from the OptumLabs Data Warehouse insurance claims database to identify 67,322 eligible participants aged 40 or older who underwent TKR from Jan. 1, 2001, to Dec. 31, 2016. Of those patients, 38,408 were opioid naive and 28,914 had taken opioids before. The authors evaluated long-term opioid use – defined as 90 days or more of filled prescriptions – during a 12-month outcome assessment period that varied depending on differences in post-TKR PT start date and duration.
The researchers found a significantly lower likelihood of long-term opioid use associated with receipt of any PT before TKR among patients who had not taken opioids before (adjusted odds ratio [aOR], 0.75; 95% confidence interval, 0.60-0.95) and those who had taken opioids in the past (aOR, 0.75; 95% CI, 0.70-0.80).
Investigators found that 2.2% of participants in the opioid-naive group and 32.5% of those in the opioid-experienced group used opioids long-term after TKR. Approximately 76% of participants overall received outpatient PT within the 90 days after surgery, and the receipt of post-TKR PT at any point was associated with lower odds of long-term opioid use in the opioid-experienced group (aOR, 0.75; 95% CI, 0.70-0.79).
Among the opioid-experienced group, receiving between 6 and 12 PT sessions (aOR, 0.82; 95% CI, 0.75-0.90) or ≥ 13 sessions (aOR, 0.71; 95% CI, 0.65-0.77) were both associated with lower odds of long-term opioid use, compared with those who received 1-5 sessions. Beginning PT 31-60 days or 61-90 days after surgery was associated with greater odds of long-term opioid use across both cohorts, compared with those who initiated therapy within 30 days of TKR.
Physical therapy: Underexplored option for pain in knee replacement
One finding caught the researchers slightly off guard: There was no association between active physical therapy and reduced odds of long-term opioid use. “From prior studies, at least in people with knee osteoarthritis, we know that active interventions were more useful than passive interventions,” Dr. Kumar said.
That said, he added that there is still some professional uncertainty regarding “the right type or the right components of physical therapy for managing pain in this population.” Regardless, he believes their study emphasizes the benefits of PT as a pain alleviator in these patients, especially those who have previously used opioids.
“Pharmaceuticals have side effects. Injections are not super effective,” he said. “The idea behind focusing on physical therapy interventions is that it’s widely available, it does you no harm, and it could potentially be lower cost to both the payers and the providers.”
The authors acknowledged their study’s limitations, including not adjusting for opioid use within the 90 days after surgery as well as the different outcome assessment periods for pre-TKR and post-TKR PT exposures. In addition, they admitted that some of the patients who received PT could have been among those less likely to be treated with opioids, and vice versa. “A randomized clinical trial,” they wrote, “would be required to disentangle these issues.”
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Kumar reported receiving grants from the National Institutes of Health during the conduct of the study and grants from Pfizer for unrelated projects outside the submitted work. The full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
A new study has found that physical therapy may lead to a reduced risk of long-term opioid use in patients who have undergone total knee replacement (TKR).
“Greater number of PT intervention sessions and earlier initiation of outpatient PT care after TKR were associated with lower odds of long-term opioid use,” authors from Boston University wrote in their report on the study, which was published online Oct. 27 in JAMA Network Open.
“In previous large studies, we’ve seen that physical therapy can reduce pain in people with knee osteoarthritis, which is usually the primary indication for TKR,” study coauthor Deepak Kumar, PT, PhD, said in an interview. “But the association of physical therapy with opioid use in people with knee replacement has not yet been explored.
“The reason we focused on opioid use in these patients is because the number of knee replacement surgeries is going up exponentially,” Dr. Kumar said. “And, depending on which data you look at, from one-third to up to half of people who undergo knee replacement and have used opioids before end up becoming long-term users. Even in people who have not used them before, 5%-8% become long-term users after the surgery.
“Given how many surgeries are happening – and that number is expected to keep going up – the number of people who are becoming long-term opioid users is not trivial,” he said.
Study details
To assess the value of PT in reducing opioid use in this subset of patients, the authors reviewed records from the OptumLabs Data Warehouse insurance claims database to identify 67,322 eligible participants aged 40 or older who underwent TKR from Jan. 1, 2001, to Dec. 31, 2016. Of those patients, 38,408 were opioid naive and 28,914 had taken opioids before. The authors evaluated long-term opioid use – defined as 90 days or more of filled prescriptions – during a 12-month outcome assessment period that varied depending on differences in post-TKR PT start date and duration.
The researchers found a significantly lower likelihood of long-term opioid use associated with receipt of any PT before TKR among patients who had not taken opioids before (adjusted odds ratio [aOR], 0.75; 95% confidence interval, 0.60-0.95) and those who had taken opioids in the past (aOR, 0.75; 95% CI, 0.70-0.80).
Investigators found that 2.2% of participants in the opioid-naive group and 32.5% of those in the opioid-experienced group used opioids long-term after TKR. Approximately 76% of participants overall received outpatient PT within the 90 days after surgery, and the receipt of post-TKR PT at any point was associated with lower odds of long-term opioid use in the opioid-experienced group (aOR, 0.75; 95% CI, 0.70-0.79).
Among the opioid-experienced group, receiving between 6 and 12 PT sessions (aOR, 0.82; 95% CI, 0.75-0.90) or ≥ 13 sessions (aOR, 0.71; 95% CI, 0.65-0.77) were both associated with lower odds of long-term opioid use, compared with those who received 1-5 sessions. Beginning PT 31-60 days or 61-90 days after surgery was associated with greater odds of long-term opioid use across both cohorts, compared with those who initiated therapy within 30 days of TKR.
Physical therapy: Underexplored option for pain in knee replacement
One finding caught the researchers slightly off guard: There was no association between active physical therapy and reduced odds of long-term opioid use. “From prior studies, at least in people with knee osteoarthritis, we know that active interventions were more useful than passive interventions,” Dr. Kumar said.
That said, he added that there is still some professional uncertainty regarding “the right type or the right components of physical therapy for managing pain in this population.” Regardless, he believes their study emphasizes the benefits of PT as a pain alleviator in these patients, especially those who have previously used opioids.
“Pharmaceuticals have side effects. Injections are not super effective,” he said. “The idea behind focusing on physical therapy interventions is that it’s widely available, it does you no harm, and it could potentially be lower cost to both the payers and the providers.”
The authors acknowledged their study’s limitations, including not adjusting for opioid use within the 90 days after surgery as well as the different outcome assessment periods for pre-TKR and post-TKR PT exposures. In addition, they admitted that some of the patients who received PT could have been among those less likely to be treated with opioids, and vice versa. “A randomized clinical trial,” they wrote, “would be required to disentangle these issues.”
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Kumar reported receiving grants from the National Institutes of Health during the conduct of the study and grants from Pfizer for unrelated projects outside the submitted work. The full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
A new study has found that physical therapy may lead to a reduced risk of long-term opioid use in patients who have undergone total knee replacement (TKR).
“Greater number of PT intervention sessions and earlier initiation of outpatient PT care after TKR were associated with lower odds of long-term opioid use,” authors from Boston University wrote in their report on the study, which was published online Oct. 27 in JAMA Network Open.
“In previous large studies, we’ve seen that physical therapy can reduce pain in people with knee osteoarthritis, which is usually the primary indication for TKR,” study coauthor Deepak Kumar, PT, PhD, said in an interview. “But the association of physical therapy with opioid use in people with knee replacement has not yet been explored.
“The reason we focused on opioid use in these patients is because the number of knee replacement surgeries is going up exponentially,” Dr. Kumar said. “And, depending on which data you look at, from one-third to up to half of people who undergo knee replacement and have used opioids before end up becoming long-term users. Even in people who have not used them before, 5%-8% become long-term users after the surgery.
“Given how many surgeries are happening – and that number is expected to keep going up – the number of people who are becoming long-term opioid users is not trivial,” he said.
Study details
To assess the value of PT in reducing opioid use in this subset of patients, the authors reviewed records from the OptumLabs Data Warehouse insurance claims database to identify 67,322 eligible participants aged 40 or older who underwent TKR from Jan. 1, 2001, to Dec. 31, 2016. Of those patients, 38,408 were opioid naive and 28,914 had taken opioids before. The authors evaluated long-term opioid use – defined as 90 days or more of filled prescriptions – during a 12-month outcome assessment period that varied depending on differences in post-TKR PT start date and duration.
The researchers found a significantly lower likelihood of long-term opioid use associated with receipt of any PT before TKR among patients who had not taken opioids before (adjusted odds ratio [aOR], 0.75; 95% confidence interval, 0.60-0.95) and those who had taken opioids in the past (aOR, 0.75; 95% CI, 0.70-0.80).
Investigators found that 2.2% of participants in the opioid-naive group and 32.5% of those in the opioid-experienced group used opioids long-term after TKR. Approximately 76% of participants overall received outpatient PT within the 90 days after surgery, and the receipt of post-TKR PT at any point was associated with lower odds of long-term opioid use in the opioid-experienced group (aOR, 0.75; 95% CI, 0.70-0.79).
Among the opioid-experienced group, receiving between 6 and 12 PT sessions (aOR, 0.82; 95% CI, 0.75-0.90) or ≥ 13 sessions (aOR, 0.71; 95% CI, 0.65-0.77) were both associated with lower odds of long-term opioid use, compared with those who received 1-5 sessions. Beginning PT 31-60 days or 61-90 days after surgery was associated with greater odds of long-term opioid use across both cohorts, compared with those who initiated therapy within 30 days of TKR.
Physical therapy: Underexplored option for pain in knee replacement
One finding caught the researchers slightly off guard: There was no association between active physical therapy and reduced odds of long-term opioid use. “From prior studies, at least in people with knee osteoarthritis, we know that active interventions were more useful than passive interventions,” Dr. Kumar said.
That said, he added that there is still some professional uncertainty regarding “the right type or the right components of physical therapy for managing pain in this population.” Regardless, he believes their study emphasizes the benefits of PT as a pain alleviator in these patients, especially those who have previously used opioids.
“Pharmaceuticals have side effects. Injections are not super effective,” he said. “The idea behind focusing on physical therapy interventions is that it’s widely available, it does you no harm, and it could potentially be lower cost to both the payers and the providers.”
The authors acknowledged their study’s limitations, including not adjusting for opioid use within the 90 days after surgery as well as the different outcome assessment periods for pre-TKR and post-TKR PT exposures. In addition, they admitted that some of the patients who received PT could have been among those less likely to be treated with opioids, and vice versa. “A randomized clinical trial,” they wrote, “would be required to disentangle these issues.”
The study was supported by grants from the National Institutes of Health and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Kumar reported receiving grants from the National Institutes of Health during the conduct of the study and grants from Pfizer for unrelated projects outside the submitted work. The full list of author disclosures can be found with the original article.
A version of this article first appeared on Medscape.com.
Boxed warnings: Legal risks that many physicians never see coming
Almost all physicians write prescriptions, and each prescription requires a physician to assess the risks and benefits of the drug. If an adverse drug reaction occurs, physicians may be called on to defend their risk-benefit assessment in court.
The assessment of risk is complicated when there is a boxed warning that describes potentially serious and life-threatening adverse reactions associated with a drug. Some of our most commonly prescribed drugs have boxed warnings, and drugs that were initially approved by the Food and Drug Administration without boxed warnings may have them added years later.
One serious problem with boxed warnings is that there are no reliable mechanisms for making sure that physicians are aware of them. The warnings are typically not seen by physicians as printed product labels, just as physicians often don’t see the pills and capsules that they prescribe. Pharmacists who receive packaged drugs from manufacturers may be the only ones to see an actual printed boxed warning, but even those pharmacists have little reason to read each label and note changes when handling many bulk packages.
This problem is aggravated by misperceptions that many physicians have about boxed warnings and the increasingly intense scrutiny given to them by mass media and the courts. Lawyers can use boxed warnings to make a drug look dangerous, even when it’s not, and to make physicians look reckless when prescribing it. Therefore, it is important for physicians to understand what boxed warnings are, what they are not, the problems they cause, and how to minimize these problems.
What is a ‘boxed warning’?
The marketing and sale of drugs in the United States requires approval by the FDA. Approval requires manufacturers to prepare a document containing “Full Prescribing Information” for the drug and to include a printed copy in every package of the drug that is sold. This document is commonly called a “package insert,” but the FDA designates this document as the manufacturer’s product “label.”
In 1979, the FDA began requiring some labels to appear within thick, black rectangular borders; these have come to be known as boxed warnings. Boxed warnings are usually placed at the beginning of a label. They may be added to the label of a previously approved drug already on the market or included in the product label when first approved and marketed.
The requirement for a boxed warning most often arises when a signal appears during review of postmarketing surveillance data suggesting a possible and plausible association between a drug and an adverse reaction. Warnings may also be initiated in response to petitions from public interest groups, or upon the discovery of serious toxicity in animals. Regardless of their origin, the intent of a boxed warning is to highlight information that may have important therapeutic consequences and warrants heightened awareness among physicians.
What a boxed warning is not
A boxed warning is not “issued” by the FDA; it is merely required by the FDA. Specific wording or a template may be suggested by the FDA, but product labels and boxed warnings are written and issued by the manufacturer. This distinction may seem minor, but extensive litigation has occurred over whether manufacturers have met their duty to warn consumers about possible risks when using their products, and this duty cannot be shifted to the FDA.
A boxed warning may not be added to a product label at the option of a manufacturer. The FDA allows a boxed warning only if it requires the warning, to preserve its impact. It should be noted that some medical information sources (e.g., PDR.net) may include a “BOXED WARNING” in their drug monographs, but monographs not written by a manufacturer are not regulated by the FDA, and the text of their boxed warnings do not always correspond to the boxed warning that was approved by the FDA.
A boxed warning is not an indication that revocation of FDA approval is being considered or that it is likely to be revoked. FDA approval is subject to ongoing review and may be revoked at any time, without a prior boxed warning.
A boxed warning is not the highest level of warning. The FDA may require a manufacturer to send out a “Dear Health Care Provider” (DHCP) letter when an even higher or more urgent level of warning is deemed necessary. DHCP letters are usually accompanied by revisions of the product label, but most label revisions – and even most boxed warnings – are not accompanied by DHCP letters.
A boxed warning is not a statement about causation. Most warnings describe an “association” between a drug and an adverse effect, or “increased risk,” or instances of a particular adverse effect that “have been reported” in persons taking a drug. The words in a boxed warning are carefully chosen and require careful reading; in most cases they refrain from stating that a drug actually causes an adverse effect. The postmarketing surveillance data on which most warnings are based generally cannot provide the kind of evidence required to establish causation, and an association may be nothing more than an uncommon manifestation of the disorder for which the drug has been prescribed.
A boxed warning is not a statement about the probability of an adverse reaction occurring. The requirement for a boxed warning correlates better to the new recognition of a possible association than to the probability of an association. For example, penicillin has long been known to cause fatal anaphylaxis in 1/100,000 first-time administrations, but it does not have a boxed warning. The adverse consequences described in boxed warnings are often far less frequent – so much so that most physicians will never see them.
A boxed warning does not define the standard of care. The warning is a requirement imposed on the manufacturer, not on the practice of medicine. For legal purposes, the “standard of care” for the practice of medicine is defined state by state and is typically cast in terms such as “what most physicians would do in similar circumstances.” Physicians often prescribe drugs in spite of boxed warnings, just as they often prescribe drugs for “off label” indications, always balancing risk versus benefit.
A boxed warning does not constitute a contraindication to the use of a medication. Some warnings state that a drug is contraindicated in some situations, but product labels have another mandated section for listing contraindications, and most boxed warnings have no corresponding entry in that section.
A boxed warning does not necessarily constitute current information, nor is it always updated when new or contrary information becomes available. Revisions to boxed warnings, and to product labels in general, are made only after detailed review at the FDA, and the process of deciding whether an existing boxed warning continues to be appropriate may divert limited regulatory resources from more urgent priorities. Consequently, revisions to a boxed warning may lag behind the data that justify a revision by months or years. Revisions may never occur if softening or eliminating a boxed warning is deemed to be not worth the cost by a manufacturer.
Boxed warning problems for physicians
There is no reliable mechanism for manufacturers or the FDA to communicate boxed warnings directly to physicians, so it’s not clear how physicians are expected to stay informed about the issuance or revision of boxed warnings. They may first learn about new or revised warnings in the mass media, which is paying ever-increasing attention to press releases from the FDA. However, it can be difficult for the media to accurately convey the subtle and complex nature of a boxed warning in nontechnical terms.
Many physicians subscribe to various medical news alerts and attend continuing medical education (CME) programs, which often do an excellent job of highlighting new warnings, while hospitals, clinics, and pharmacies may broadcast news about boxed warnings in newsletters or other notices. But these notifications are ephemeral and may be missed by physicians who are overwhelmed by email, notices, newsletters, and CME programs.
The warnings that pop up in electronic medical records systems are often so numerous that physicians become trained to ignore them. Printed advertisements in professional journals must include mandated boxed warnings, but their visibility is waning as physicians increasingly read journals online.
Another conundrum is how to inform the public about boxed warnings.
Manufacturers are prohibited from direct-to-consumer advertising of drugs with boxed warnings, although the warnings are easily found on the Internet. Some patients expect and welcome detailed information from their physicians, so it’s a good policy to always and repeatedly review this information with them, especially if they are members of an identified risk group. However, that policy may be counterproductive if it dissuades anxious patients from needed therapy despite risk-benefit considerations that strongly favor it. Boxed warnings are well known to have “spillover effects” in which the aspersions cast by a boxed warning for a relatively small subgroup of patients causes use of a drug to decline among all patients.
Compounding this conundrum is that physicians rarely have sufficient information to gauge the magnitude of a risk, given that boxed warnings are often based on information from surveillance systems that cannot accurately quantify the risk or even establish a causal relationship. The text of a boxed warning generally does not provide the information needed for evidence-based clinical practice such as a quantitative estimate of effect, information about source and trustworthiness of the evidence, and guidance on implementation. For these and other reasons, FDA policies about various boxed warnings have been the target of significant criticism.
Medication guides are one mechanism to address the challenge of informing patients about the risks of drugs they are taking. FDA-approved medication guides are available for most drugs dispensed as outpatient prescriptions, they’re written in plain language for the consumer, and they include paraphrased versions of any boxed warning. Ideally, patients review these guides with their physicians or pharmacists, but the guides may be lengthy and raise questions that may not be answerable (e.g., about incidence rates). Patients may decline to review this information when a drug is prescribed or dispensed, and they may discard printed copies given to them without reading.
What can physicians do to minimize boxed warning problems?
Physicians should periodically review the product labels for drugs they commonly prescribe, including drugs they’ve prescribed for a long time. Prescription renewal requests can be used as a prompt to check for changes in a patient’s condition or other medications that might place a patient in the target population of a boxed warning. Physicians can subscribe to newsletters that announce and discuss significant product label changes, including alerts directly from the FDA. Physicians may also enlist their office staff to find and review boxed warnings for drugs being prescribed, noting which ones should require a conversation with any patient who has been or will be receiving this drug. They may want to make explicit mention in their encounter record that a boxed warning, medication guide, or overall risk-benefit assessment has been discussed.
Summary
The nature of boxed warnings, the means by which they are disseminated, and their role in clinical practice are all in great need of improvement. Until that occurs, boxed warnings offer some, but only very limited, help to patients and physicians who struggle to understand the risks of medications.
Dr. Axelsen is professor in the departments of pharmacology, biochemistry, and biophysics, and of medicine, infectious diseases section, University of Pennsylvania, Philadelphia. He disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Almost all physicians write prescriptions, and each prescription requires a physician to assess the risks and benefits of the drug. If an adverse drug reaction occurs, physicians may be called on to defend their risk-benefit assessment in court.
The assessment of risk is complicated when there is a boxed warning that describes potentially serious and life-threatening adverse reactions associated with a drug. Some of our most commonly prescribed drugs have boxed warnings, and drugs that were initially approved by the Food and Drug Administration without boxed warnings may have them added years later.
One serious problem with boxed warnings is that there are no reliable mechanisms for making sure that physicians are aware of them. The warnings are typically not seen by physicians as printed product labels, just as physicians often don’t see the pills and capsules that they prescribe. Pharmacists who receive packaged drugs from manufacturers may be the only ones to see an actual printed boxed warning, but even those pharmacists have little reason to read each label and note changes when handling many bulk packages.
This problem is aggravated by misperceptions that many physicians have about boxed warnings and the increasingly intense scrutiny given to them by mass media and the courts. Lawyers can use boxed warnings to make a drug look dangerous, even when it’s not, and to make physicians look reckless when prescribing it. Therefore, it is important for physicians to understand what boxed warnings are, what they are not, the problems they cause, and how to minimize these problems.
What is a ‘boxed warning’?
The marketing and sale of drugs in the United States requires approval by the FDA. Approval requires manufacturers to prepare a document containing “Full Prescribing Information” for the drug and to include a printed copy in every package of the drug that is sold. This document is commonly called a “package insert,” but the FDA designates this document as the manufacturer’s product “label.”
In 1979, the FDA began requiring some labels to appear within thick, black rectangular borders; these have come to be known as boxed warnings. Boxed warnings are usually placed at the beginning of a label. They may be added to the label of a previously approved drug already on the market or included in the product label when first approved and marketed.
The requirement for a boxed warning most often arises when a signal appears during review of postmarketing surveillance data suggesting a possible and plausible association between a drug and an adverse reaction. Warnings may also be initiated in response to petitions from public interest groups, or upon the discovery of serious toxicity in animals. Regardless of their origin, the intent of a boxed warning is to highlight information that may have important therapeutic consequences and warrants heightened awareness among physicians.
What a boxed warning is not
A boxed warning is not “issued” by the FDA; it is merely required by the FDA. Specific wording or a template may be suggested by the FDA, but product labels and boxed warnings are written and issued by the manufacturer. This distinction may seem minor, but extensive litigation has occurred over whether manufacturers have met their duty to warn consumers about possible risks when using their products, and this duty cannot be shifted to the FDA.
A boxed warning may not be added to a product label at the option of a manufacturer. The FDA allows a boxed warning only if it requires the warning, to preserve its impact. It should be noted that some medical information sources (e.g., PDR.net) may include a “BOXED WARNING” in their drug monographs, but monographs not written by a manufacturer are not regulated by the FDA, and the text of their boxed warnings do not always correspond to the boxed warning that was approved by the FDA.
A boxed warning is not an indication that revocation of FDA approval is being considered or that it is likely to be revoked. FDA approval is subject to ongoing review and may be revoked at any time, without a prior boxed warning.
A boxed warning is not the highest level of warning. The FDA may require a manufacturer to send out a “Dear Health Care Provider” (DHCP) letter when an even higher or more urgent level of warning is deemed necessary. DHCP letters are usually accompanied by revisions of the product label, but most label revisions – and even most boxed warnings – are not accompanied by DHCP letters.
A boxed warning is not a statement about causation. Most warnings describe an “association” between a drug and an adverse effect, or “increased risk,” or instances of a particular adverse effect that “have been reported” in persons taking a drug. The words in a boxed warning are carefully chosen and require careful reading; in most cases they refrain from stating that a drug actually causes an adverse effect. The postmarketing surveillance data on which most warnings are based generally cannot provide the kind of evidence required to establish causation, and an association may be nothing more than an uncommon manifestation of the disorder for which the drug has been prescribed.
A boxed warning is not a statement about the probability of an adverse reaction occurring. The requirement for a boxed warning correlates better to the new recognition of a possible association than to the probability of an association. For example, penicillin has long been known to cause fatal anaphylaxis in 1/100,000 first-time administrations, but it does not have a boxed warning. The adverse consequences described in boxed warnings are often far less frequent – so much so that most physicians will never see them.
A boxed warning does not define the standard of care. The warning is a requirement imposed on the manufacturer, not on the practice of medicine. For legal purposes, the “standard of care” for the practice of medicine is defined state by state and is typically cast in terms such as “what most physicians would do in similar circumstances.” Physicians often prescribe drugs in spite of boxed warnings, just as they often prescribe drugs for “off label” indications, always balancing risk versus benefit.
A boxed warning does not constitute a contraindication to the use of a medication. Some warnings state that a drug is contraindicated in some situations, but product labels have another mandated section for listing contraindications, and most boxed warnings have no corresponding entry in that section.
A boxed warning does not necessarily constitute current information, nor is it always updated when new or contrary information becomes available. Revisions to boxed warnings, and to product labels in general, are made only after detailed review at the FDA, and the process of deciding whether an existing boxed warning continues to be appropriate may divert limited regulatory resources from more urgent priorities. Consequently, revisions to a boxed warning may lag behind the data that justify a revision by months or years. Revisions may never occur if softening or eliminating a boxed warning is deemed to be not worth the cost by a manufacturer.
Boxed warning problems for physicians
There is no reliable mechanism for manufacturers or the FDA to communicate boxed warnings directly to physicians, so it’s not clear how physicians are expected to stay informed about the issuance or revision of boxed warnings. They may first learn about new or revised warnings in the mass media, which is paying ever-increasing attention to press releases from the FDA. However, it can be difficult for the media to accurately convey the subtle and complex nature of a boxed warning in nontechnical terms.
Many physicians subscribe to various medical news alerts and attend continuing medical education (CME) programs, which often do an excellent job of highlighting new warnings, while hospitals, clinics, and pharmacies may broadcast news about boxed warnings in newsletters or other notices. But these notifications are ephemeral and may be missed by physicians who are overwhelmed by email, notices, newsletters, and CME programs.
The warnings that pop up in electronic medical records systems are often so numerous that physicians become trained to ignore them. Printed advertisements in professional journals must include mandated boxed warnings, but their visibility is waning as physicians increasingly read journals online.
Another conundrum is how to inform the public about boxed warnings.
Manufacturers are prohibited from direct-to-consumer advertising of drugs with boxed warnings, although the warnings are easily found on the Internet. Some patients expect and welcome detailed information from their physicians, so it’s a good policy to always and repeatedly review this information with them, especially if they are members of an identified risk group. However, that policy may be counterproductive if it dissuades anxious patients from needed therapy despite risk-benefit considerations that strongly favor it. Boxed warnings are well known to have “spillover effects” in which the aspersions cast by a boxed warning for a relatively small subgroup of patients causes use of a drug to decline among all patients.
Compounding this conundrum is that physicians rarely have sufficient information to gauge the magnitude of a risk, given that boxed warnings are often based on information from surveillance systems that cannot accurately quantify the risk or even establish a causal relationship. The text of a boxed warning generally does not provide the information needed for evidence-based clinical practice such as a quantitative estimate of effect, information about source and trustworthiness of the evidence, and guidance on implementation. For these and other reasons, FDA policies about various boxed warnings have been the target of significant criticism.
Medication guides are one mechanism to address the challenge of informing patients about the risks of drugs they are taking. FDA-approved medication guides are available for most drugs dispensed as outpatient prescriptions, they’re written in plain language for the consumer, and they include paraphrased versions of any boxed warning. Ideally, patients review these guides with their physicians or pharmacists, but the guides may be lengthy and raise questions that may not be answerable (e.g., about incidence rates). Patients may decline to review this information when a drug is prescribed or dispensed, and they may discard printed copies given to them without reading.
What can physicians do to minimize boxed warning problems?
Physicians should periodically review the product labels for drugs they commonly prescribe, including drugs they’ve prescribed for a long time. Prescription renewal requests can be used as a prompt to check for changes in a patient’s condition or other medications that might place a patient in the target population of a boxed warning. Physicians can subscribe to newsletters that announce and discuss significant product label changes, including alerts directly from the FDA. Physicians may also enlist their office staff to find and review boxed warnings for drugs being prescribed, noting which ones should require a conversation with any patient who has been or will be receiving this drug. They may want to make explicit mention in their encounter record that a boxed warning, medication guide, or overall risk-benefit assessment has been discussed.
Summary
The nature of boxed warnings, the means by which they are disseminated, and their role in clinical practice are all in great need of improvement. Until that occurs, boxed warnings offer some, but only very limited, help to patients and physicians who struggle to understand the risks of medications.
Dr. Axelsen is professor in the departments of pharmacology, biochemistry, and biophysics, and of medicine, infectious diseases section, University of Pennsylvania, Philadelphia. He disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Almost all physicians write prescriptions, and each prescription requires a physician to assess the risks and benefits of the drug. If an adverse drug reaction occurs, physicians may be called on to defend their risk-benefit assessment in court.
The assessment of risk is complicated when there is a boxed warning that describes potentially serious and life-threatening adverse reactions associated with a drug. Some of our most commonly prescribed drugs have boxed warnings, and drugs that were initially approved by the Food and Drug Administration without boxed warnings may have them added years later.
One serious problem with boxed warnings is that there are no reliable mechanisms for making sure that physicians are aware of them. The warnings are typically not seen by physicians as printed product labels, just as physicians often don’t see the pills and capsules that they prescribe. Pharmacists who receive packaged drugs from manufacturers may be the only ones to see an actual printed boxed warning, but even those pharmacists have little reason to read each label and note changes when handling many bulk packages.
This problem is aggravated by misperceptions that many physicians have about boxed warnings and the increasingly intense scrutiny given to them by mass media and the courts. Lawyers can use boxed warnings to make a drug look dangerous, even when it’s not, and to make physicians look reckless when prescribing it. Therefore, it is important for physicians to understand what boxed warnings are, what they are not, the problems they cause, and how to minimize these problems.
What is a ‘boxed warning’?
The marketing and sale of drugs in the United States requires approval by the FDA. Approval requires manufacturers to prepare a document containing “Full Prescribing Information” for the drug and to include a printed copy in every package of the drug that is sold. This document is commonly called a “package insert,” but the FDA designates this document as the manufacturer’s product “label.”
In 1979, the FDA began requiring some labels to appear within thick, black rectangular borders; these have come to be known as boxed warnings. Boxed warnings are usually placed at the beginning of a label. They may be added to the label of a previously approved drug already on the market or included in the product label when first approved and marketed.
The requirement for a boxed warning most often arises when a signal appears during review of postmarketing surveillance data suggesting a possible and plausible association between a drug and an adverse reaction. Warnings may also be initiated in response to petitions from public interest groups, or upon the discovery of serious toxicity in animals. Regardless of their origin, the intent of a boxed warning is to highlight information that may have important therapeutic consequences and warrants heightened awareness among physicians.
What a boxed warning is not
A boxed warning is not “issued” by the FDA; it is merely required by the FDA. Specific wording or a template may be suggested by the FDA, but product labels and boxed warnings are written and issued by the manufacturer. This distinction may seem minor, but extensive litigation has occurred over whether manufacturers have met their duty to warn consumers about possible risks when using their products, and this duty cannot be shifted to the FDA.
A boxed warning may not be added to a product label at the option of a manufacturer. The FDA allows a boxed warning only if it requires the warning, to preserve its impact. It should be noted that some medical information sources (e.g., PDR.net) may include a “BOXED WARNING” in their drug monographs, but monographs not written by a manufacturer are not regulated by the FDA, and the text of their boxed warnings do not always correspond to the boxed warning that was approved by the FDA.
A boxed warning is not an indication that revocation of FDA approval is being considered or that it is likely to be revoked. FDA approval is subject to ongoing review and may be revoked at any time, without a prior boxed warning.
A boxed warning is not the highest level of warning. The FDA may require a manufacturer to send out a “Dear Health Care Provider” (DHCP) letter when an even higher or more urgent level of warning is deemed necessary. DHCP letters are usually accompanied by revisions of the product label, but most label revisions – and even most boxed warnings – are not accompanied by DHCP letters.
A boxed warning is not a statement about causation. Most warnings describe an “association” between a drug and an adverse effect, or “increased risk,” or instances of a particular adverse effect that “have been reported” in persons taking a drug. The words in a boxed warning are carefully chosen and require careful reading; in most cases they refrain from stating that a drug actually causes an adverse effect. The postmarketing surveillance data on which most warnings are based generally cannot provide the kind of evidence required to establish causation, and an association may be nothing more than an uncommon manifestation of the disorder for which the drug has been prescribed.
A boxed warning is not a statement about the probability of an adverse reaction occurring. The requirement for a boxed warning correlates better to the new recognition of a possible association than to the probability of an association. For example, penicillin has long been known to cause fatal anaphylaxis in 1/100,000 first-time administrations, but it does not have a boxed warning. The adverse consequences described in boxed warnings are often far less frequent – so much so that most physicians will never see them.
A boxed warning does not define the standard of care. The warning is a requirement imposed on the manufacturer, not on the practice of medicine. For legal purposes, the “standard of care” for the practice of medicine is defined state by state and is typically cast in terms such as “what most physicians would do in similar circumstances.” Physicians often prescribe drugs in spite of boxed warnings, just as they often prescribe drugs for “off label” indications, always balancing risk versus benefit.
A boxed warning does not constitute a contraindication to the use of a medication. Some warnings state that a drug is contraindicated in some situations, but product labels have another mandated section for listing contraindications, and most boxed warnings have no corresponding entry in that section.
A boxed warning does not necessarily constitute current information, nor is it always updated when new or contrary information becomes available. Revisions to boxed warnings, and to product labels in general, are made only after detailed review at the FDA, and the process of deciding whether an existing boxed warning continues to be appropriate may divert limited regulatory resources from more urgent priorities. Consequently, revisions to a boxed warning may lag behind the data that justify a revision by months or years. Revisions may never occur if softening or eliminating a boxed warning is deemed to be not worth the cost by a manufacturer.
Boxed warning problems for physicians
There is no reliable mechanism for manufacturers or the FDA to communicate boxed warnings directly to physicians, so it’s not clear how physicians are expected to stay informed about the issuance or revision of boxed warnings. They may first learn about new or revised warnings in the mass media, which is paying ever-increasing attention to press releases from the FDA. However, it can be difficult for the media to accurately convey the subtle and complex nature of a boxed warning in nontechnical terms.
Many physicians subscribe to various medical news alerts and attend continuing medical education (CME) programs, which often do an excellent job of highlighting new warnings, while hospitals, clinics, and pharmacies may broadcast news about boxed warnings in newsletters or other notices. But these notifications are ephemeral and may be missed by physicians who are overwhelmed by email, notices, newsletters, and CME programs.
The warnings that pop up in electronic medical records systems are often so numerous that physicians become trained to ignore them. Printed advertisements in professional journals must include mandated boxed warnings, but their visibility is waning as physicians increasingly read journals online.
Another conundrum is how to inform the public about boxed warnings.
Manufacturers are prohibited from direct-to-consumer advertising of drugs with boxed warnings, although the warnings are easily found on the Internet. Some patients expect and welcome detailed information from their physicians, so it’s a good policy to always and repeatedly review this information with them, especially if they are members of an identified risk group. However, that policy may be counterproductive if it dissuades anxious patients from needed therapy despite risk-benefit considerations that strongly favor it. Boxed warnings are well known to have “spillover effects” in which the aspersions cast by a boxed warning for a relatively small subgroup of patients causes use of a drug to decline among all patients.
Compounding this conundrum is that physicians rarely have sufficient information to gauge the magnitude of a risk, given that boxed warnings are often based on information from surveillance systems that cannot accurately quantify the risk or even establish a causal relationship. The text of a boxed warning generally does not provide the information needed for evidence-based clinical practice such as a quantitative estimate of effect, information about source and trustworthiness of the evidence, and guidance on implementation. For these and other reasons, FDA policies about various boxed warnings have been the target of significant criticism.
Medication guides are one mechanism to address the challenge of informing patients about the risks of drugs they are taking. FDA-approved medication guides are available for most drugs dispensed as outpatient prescriptions, they’re written in plain language for the consumer, and they include paraphrased versions of any boxed warning. Ideally, patients review these guides with their physicians or pharmacists, but the guides may be lengthy and raise questions that may not be answerable (e.g., about incidence rates). Patients may decline to review this information when a drug is prescribed or dispensed, and they may discard printed copies given to them without reading.
What can physicians do to minimize boxed warning problems?
Physicians should periodically review the product labels for drugs they commonly prescribe, including drugs they’ve prescribed for a long time. Prescription renewal requests can be used as a prompt to check for changes in a patient’s condition or other medications that might place a patient in the target population of a boxed warning. Physicians can subscribe to newsletters that announce and discuss significant product label changes, including alerts directly from the FDA. Physicians may also enlist their office staff to find and review boxed warnings for drugs being prescribed, noting which ones should require a conversation with any patient who has been or will be receiving this drug. They may want to make explicit mention in their encounter record that a boxed warning, medication guide, or overall risk-benefit assessment has been discussed.
Summary
The nature of boxed warnings, the means by which they are disseminated, and their role in clinical practice are all in great need of improvement. Until that occurs, boxed warnings offer some, but only very limited, help to patients and physicians who struggle to understand the risks of medications.
Dr. Axelsen is professor in the departments of pharmacology, biochemistry, and biophysics, and of medicine, infectious diseases section, University of Pennsylvania, Philadelphia. He disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
80% of Americans research recommendations post-visit
Confusion over health information and doctor advice is even higher among people who care for patients than among those who don’t provide care to their loved ones, the nationally representative survey from the AHIMA Foundation found.
The survey also shows that 80% of Americans – and an even higher portion of caregivers – are likely to research medical recommendations online after a doctor’s visit. But 1 in 4 people don’t know how to access their own medical records or find it difficult to do so.
The findings reflect the same low level of health literacy in the U.S. population that earlier surveys did. The results also indicate that little has changed since the Department of Health and Human Services released a National Action Plan to Improve Health Literacy in 2010.
That plan emphasized the need to develop and share accurate health information that helps people make decisions; to promote changes in the health care system that improve health information, communication, informed decision-making, and access to health services; and to increase the sharing and use of evidence-based health literacy practices.
According to the AHIMA Foundation report, 62% of Americans are not sure they understand their doctor’s advice and the health information discussed during a visit. Twenty-four percent say they don’t comprehend any of it, and 31% can’t remember what was said during the visit. Fifteen percent of those surveyed said they were more confused about their health than they were before the encounter with their doctor.
Caregivers have special issues
Forty-three percent of Americans are caregivers, the report notes, and 91% of those play an active role in managing someone else’s health. Millennials (65%) and Gen Xers (50%) are significantly more likely than Gen Zers (39%) and Boomers (20%) to be a caregiver.
Most caregivers have concerns about their loved ones’ ability to manage their own health. Most of them believe that doctors provide enough information, but 38% don’t believe a doctor can communicate effectively with the patient if the caregiver is not present.
Forty-three percent of caretakers don’t think their loved ones can understand medical information on their own. On the other hand, caregivers are more likely than people who don’t provide care to say the doctor confused them and to research the doctor’s advice after an appointment.
For many patients and caregivers, communications break down when they are with their health care provider. Twenty-two percent of Americans say they do not feel comfortable asking their doctor certain health questions. This inability to have a satisfactory dialogue with their doctor means that many patients leave their appointments without getting clear answers to their questions (24%) or without having an opportunity to ask any questions at all (17%).
This is not surprising, considering that a 2018 study found that doctors spend only 11 seconds, on average, listening to patients before interrupting them.
Depending on the internet
Overall, the AHIMA survey found, 42% of Americans research their doctor’s recommendations after an appointment. A higher percentage of caregivers than noncaregiver peers do so (47% vs. 38%). Eighty percent of respondents say they are “likely” to research their doctor’s advice online after a visit.
When they have a medical problem or a question about their condition, just as many Americans (59%) turn to the internet for an answer as contact their doctor directly, the survey found. Twenty-nine percent of the respondents consult friends, family, or colleagues; 23% look up medical records if they’re easily accessible; 19% ask pharmacists for advice; and 6% call an unspecified 800 number.
Americans feel secure in the health information they find on the internet. Among those who go online to look up information, 86% are confident that it is credible. And 42% report feeling relieved that they can find a lot of information about their health concerns. Respondents also say that the information they gather allows them to feel more confident in their doctor’s recommendations (35%) and that they feel better after having learned more on the internet than their doctor had told them (39%). Men are more likely than women to say that their confidence in their doctor’s recommendations increased after doing online research (40% vs. 30%).
Access to health records
Access to medical records would help people better understand their condition or diagnosis. But nearly half of Americans (48%) admit they don’t usually review their medical records until long after an appointment, and 52% say they rarely access their records at all.
One in four Americans say that they don’t know where to go to access their health information or that they didn’t find the process easy. More than half of those who have never had to find their records think the process would be difficult if they had to try.
Eighty-one percent of Americans use an online platform or portal to access their medical records or health information. Two-thirds of Americans who use an online portal trust that their medical information is kept safe and not shared with other people or organizations.
Four in five respondents agree that if they had access to all of their health information, including medical records, recommendations, conditions, and test results, they’d see an improvement in their health management. Fifty-nine percent of them believe they’d also be more confident about understanding their health, and 47% say they’d have greater trust in their doctor’s recommendations. Higher percentages of caregivers than noncaregivers say the same.
Younger people, those with a high school degree or less, and those who earn less than $50,000 are less likely than older, better educated, and more affluent people to understand their doctor’s health information and to ask questions of their providers.
People of color struggle with their relationships with doctors, are less satisfied than white people with the information they receive during visits, and are more likely than white peers to feel that if they had access to all their health information, they’d manage their health better and be more confident in their doctors’ recommendations, the survey found.
A version of this article first appeared on WebMD.com.
Confusion over health information and doctor advice is even higher among people who care for patients than among those who don’t provide care to their loved ones, the nationally representative survey from the AHIMA Foundation found.
The survey also shows that 80% of Americans – and an even higher portion of caregivers – are likely to research medical recommendations online after a doctor’s visit. But 1 in 4 people don’t know how to access their own medical records or find it difficult to do so.
The findings reflect the same low level of health literacy in the U.S. population that earlier surveys did. The results also indicate that little has changed since the Department of Health and Human Services released a National Action Plan to Improve Health Literacy in 2010.
That plan emphasized the need to develop and share accurate health information that helps people make decisions; to promote changes in the health care system that improve health information, communication, informed decision-making, and access to health services; and to increase the sharing and use of evidence-based health literacy practices.
According to the AHIMA Foundation report, 62% of Americans are not sure they understand their doctor’s advice and the health information discussed during a visit. Twenty-four percent say they don’t comprehend any of it, and 31% can’t remember what was said during the visit. Fifteen percent of those surveyed said they were more confused about their health than they were before the encounter with their doctor.
Caregivers have special issues
Forty-three percent of Americans are caregivers, the report notes, and 91% of those play an active role in managing someone else’s health. Millennials (65%) and Gen Xers (50%) are significantly more likely than Gen Zers (39%) and Boomers (20%) to be a caregiver.
Most caregivers have concerns about their loved ones’ ability to manage their own health. Most of them believe that doctors provide enough information, but 38% don’t believe a doctor can communicate effectively with the patient if the caregiver is not present.
Forty-three percent of caretakers don’t think their loved ones can understand medical information on their own. On the other hand, caregivers are more likely than people who don’t provide care to say the doctor confused them and to research the doctor’s advice after an appointment.
For many patients and caregivers, communications break down when they are with their health care provider. Twenty-two percent of Americans say they do not feel comfortable asking their doctor certain health questions. This inability to have a satisfactory dialogue with their doctor means that many patients leave their appointments without getting clear answers to their questions (24%) or without having an opportunity to ask any questions at all (17%).
This is not surprising, considering that a 2018 study found that doctors spend only 11 seconds, on average, listening to patients before interrupting them.
Depending on the internet
Overall, the AHIMA survey found, 42% of Americans research their doctor’s recommendations after an appointment. A higher percentage of caregivers than noncaregiver peers do so (47% vs. 38%). Eighty percent of respondents say they are “likely” to research their doctor’s advice online after a visit.
When they have a medical problem or a question about their condition, just as many Americans (59%) turn to the internet for an answer as contact their doctor directly, the survey found. Twenty-nine percent of the respondents consult friends, family, or colleagues; 23% look up medical records if they’re easily accessible; 19% ask pharmacists for advice; and 6% call an unspecified 800 number.
Americans feel secure in the health information they find on the internet. Among those who go online to look up information, 86% are confident that it is credible. And 42% report feeling relieved that they can find a lot of information about their health concerns. Respondents also say that the information they gather allows them to feel more confident in their doctor’s recommendations (35%) and that they feel better after having learned more on the internet than their doctor had told them (39%). Men are more likely than women to say that their confidence in their doctor’s recommendations increased after doing online research (40% vs. 30%).
Access to health records
Access to medical records would help people better understand their condition or diagnosis. But nearly half of Americans (48%) admit they don’t usually review their medical records until long after an appointment, and 52% say they rarely access their records at all.
One in four Americans say that they don’t know where to go to access their health information or that they didn’t find the process easy. More than half of those who have never had to find their records think the process would be difficult if they had to try.
Eighty-one percent of Americans use an online platform or portal to access their medical records or health information. Two-thirds of Americans who use an online portal trust that their medical information is kept safe and not shared with other people or organizations.
Four in five respondents agree that if they had access to all of their health information, including medical records, recommendations, conditions, and test results, they’d see an improvement in their health management. Fifty-nine percent of them believe they’d also be more confident about understanding their health, and 47% say they’d have greater trust in their doctor’s recommendations. Higher percentages of caregivers than noncaregivers say the same.
Younger people, those with a high school degree or less, and those who earn less than $50,000 are less likely than older, better educated, and more affluent people to understand their doctor’s health information and to ask questions of their providers.
People of color struggle with their relationships with doctors, are less satisfied than white people with the information they receive during visits, and are more likely than white peers to feel that if they had access to all their health information, they’d manage their health better and be more confident in their doctors’ recommendations, the survey found.
A version of this article first appeared on WebMD.com.
Confusion over health information and doctor advice is even higher among people who care for patients than among those who don’t provide care to their loved ones, the nationally representative survey from the AHIMA Foundation found.
The survey also shows that 80% of Americans – and an even higher portion of caregivers – are likely to research medical recommendations online after a doctor’s visit. But 1 in 4 people don’t know how to access their own medical records or find it difficult to do so.
The findings reflect the same low level of health literacy in the U.S. population that earlier surveys did. The results also indicate that little has changed since the Department of Health and Human Services released a National Action Plan to Improve Health Literacy in 2010.
That plan emphasized the need to develop and share accurate health information that helps people make decisions; to promote changes in the health care system that improve health information, communication, informed decision-making, and access to health services; and to increase the sharing and use of evidence-based health literacy practices.
According to the AHIMA Foundation report, 62% of Americans are not sure they understand their doctor’s advice and the health information discussed during a visit. Twenty-four percent say they don’t comprehend any of it, and 31% can’t remember what was said during the visit. Fifteen percent of those surveyed said they were more confused about their health than they were before the encounter with their doctor.
Caregivers have special issues
Forty-three percent of Americans are caregivers, the report notes, and 91% of those play an active role in managing someone else’s health. Millennials (65%) and Gen Xers (50%) are significantly more likely than Gen Zers (39%) and Boomers (20%) to be a caregiver.
Most caregivers have concerns about their loved ones’ ability to manage their own health. Most of them believe that doctors provide enough information, but 38% don’t believe a doctor can communicate effectively with the patient if the caregiver is not present.
Forty-three percent of caretakers don’t think their loved ones can understand medical information on their own. On the other hand, caregivers are more likely than people who don’t provide care to say the doctor confused them and to research the doctor’s advice after an appointment.
For many patients and caregivers, communications break down when they are with their health care provider. Twenty-two percent of Americans say they do not feel comfortable asking their doctor certain health questions. This inability to have a satisfactory dialogue with their doctor means that many patients leave their appointments without getting clear answers to their questions (24%) or without having an opportunity to ask any questions at all (17%).
This is not surprising, considering that a 2018 study found that doctors spend only 11 seconds, on average, listening to patients before interrupting them.
Depending on the internet
Overall, the AHIMA survey found, 42% of Americans research their doctor’s recommendations after an appointment. A higher percentage of caregivers than noncaregiver peers do so (47% vs. 38%). Eighty percent of respondents say they are “likely” to research their doctor’s advice online after a visit.
When they have a medical problem or a question about their condition, just as many Americans (59%) turn to the internet for an answer as contact their doctor directly, the survey found. Twenty-nine percent of the respondents consult friends, family, or colleagues; 23% look up medical records if they’re easily accessible; 19% ask pharmacists for advice; and 6% call an unspecified 800 number.
Americans feel secure in the health information they find on the internet. Among those who go online to look up information, 86% are confident that it is credible. And 42% report feeling relieved that they can find a lot of information about their health concerns. Respondents also say that the information they gather allows them to feel more confident in their doctor’s recommendations (35%) and that they feel better after having learned more on the internet than their doctor had told them (39%). Men are more likely than women to say that their confidence in their doctor’s recommendations increased after doing online research (40% vs. 30%).
Access to health records
Access to medical records would help people better understand their condition or diagnosis. But nearly half of Americans (48%) admit they don’t usually review their medical records until long after an appointment, and 52% say they rarely access their records at all.
One in four Americans say that they don’t know where to go to access their health information or that they didn’t find the process easy. More than half of those who have never had to find their records think the process would be difficult if they had to try.
Eighty-one percent of Americans use an online platform or portal to access their medical records or health information. Two-thirds of Americans who use an online portal trust that their medical information is kept safe and not shared with other people or organizations.
Four in five respondents agree that if they had access to all of their health information, including medical records, recommendations, conditions, and test results, they’d see an improvement in their health management. Fifty-nine percent of them believe they’d also be more confident about understanding their health, and 47% say they’d have greater trust in their doctor’s recommendations. Higher percentages of caregivers than noncaregivers say the same.
Younger people, those with a high school degree or less, and those who earn less than $50,000 are less likely than older, better educated, and more affluent people to understand their doctor’s health information and to ask questions of their providers.
People of color struggle with their relationships with doctors, are less satisfied than white people with the information they receive during visits, and are more likely than white peers to feel that if they had access to all their health information, they’d manage their health better and be more confident in their doctors’ recommendations, the survey found.
A version of this article first appeared on WebMD.com.
In and out surgeries become the norm during pandemic
Urologist Ronney Abaza, MD, a robotic surgery specialist in Dublin, Ohio, and colleagues, reviewed robotic surgeries at their hospital during COVID-19 restrictions on surgery in Ohio between March 17 and June 5, 2020, and compared them with robotic procedures before COVID-19 and after restrictions were lifted. They published their results in Urology.
Since 2016, the hospital has offered the option of same-day discharge (SDD) to all robotic urologic surgery patients, regardless of procedure or patient-specific factors.
Among patients who had surgery during COVID-19 restrictions, 98% (87/89 patients) opted for SDD versus 52% in the group having surgery before the restrictions (P < .00001). After the COVID-19 surgery restrictions were lifted, the higher rate of SDD remained at 98%.
“There were no differences in 30-day complications or readmissions between SDD and overnight patients,” the authors write.
The right patient, the right motivation for successful surgery
Brian Lane, MD, PhD, a urologic oncologist with Spectrum Health in Grand Rapids, Michigan, told this news organization that, for nephrectomies, uptake of same-day discharge will continue to be slow.
“You have to have the right patient, the right patient motivation, and the surgery has to go smoothly,” he said. “If you start sending everyone home the same day, you will certainly see readmissions,” he said.
Dr. Lane is part of the Michigan Urologic Surgery Improvement Collaborative and he said the group recently looked at same-day discharge outcomes after robotic prostatectomies with SDD as compared with 1-2 nights in the hospital.
The work has not yet been published but, “There was a slight signal that there were increased readmissions with same-day discharge vs. 0-1 day,” he said.
A paper on outcomes of same-day discharge in total knee arthroplasty in the Journal of Bone & Joint Surgery found a higher risk of perioperative complications “including component failure, surgical site infection, knee stiffness, and deep vein thrombosis.” Researchers compared outcomes between 4,391 patients who underwent outpatient TKA and 128,951 patients who underwent inpatient TKA.
But for other many surgeries, same-day discharge numbers are increasing without worsening outcomes.
A paper in the Journal of Robotic Surgery found that same-day discharge following robotic-assisted endometrial cancer staging is “safe and feasible.”
Stephen Bradley, MD, MPH, with the Minneapolis Heart Institute in Minneapolis, and colleagues write in the Journal of the American College of Cardiology: Cardiovascular Interventions that they found a large increase in the use of same-day discharge after elective percutaneous coronary intervention (PCI) was not associated with worse 30-day mortality rates or readmission.
In that study, 114,461 patients were discharged the same day they underwent PCI. The proportion of patients who had a same-day discharge increased from 4.5% in 2009 to 28.6% in the fourth quarter of 2017.
Risk-adjusted 30-day mortality did not change in that time, while risk-adjusted rehospitalization decreased over time and more quickly when patients had same-day discharge.
Deepak L. Bhatt, MD, MPH, and Jonathan G. Sung, MBCHB, both of Brigham and Women’s Hospital Heart & Vascular Center, Harvard Medical School, Boston, wrote in an accompanying article that, “Advances in the devices and techniques of PCI have improved the safety and efficacy of the procedure. In selected patients, same-day discharge has become possible, and overnight in-hospital observation can be avoided. By reducing unnecessary hospital stays, both patients and hospitals could benefit.”
Evan Garden, a medical student at Icahn School of Medicine at Mount Sinai in New York, presented findings at the American Urological Association 2021 annual meeting that show patients selected for same-day discharge after partial or radical nephrectomy did not have increased rates of postoperative complications or readmissions in the immediate postoperative period, compared with standard discharge of 1-3 days.
Case studies in nephrectomy
While several case studies have looked at the feasibility and safety of performing partial and radical nephrectomy with same-day discharge in select cases, “this topic has not been addressed on a national level,” Mr. Garden said.
Few patients who have partial or radical nephrectomies have same-day discharges. The researchers found that fewer than 1% of patients who have either procedure in the sample studied were discharged the same day.
Researchers used the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, a nationally representative deidentified database that prospectively tracks patient characteristics and 30-day perioperative outcomes for major inpatient and outpatient surgical procedures at more than 700 hospitals.
They extracted all minimally invasive partial and radical nephrectomies from 2012 to 2019 and refined the cohort to 28,140 patients who were theoretically eligible for same-day discharge: Of those, 237 (0.8%) had SSD, and 27,903 (99.2%) had a standard-length discharge (SLD).
The team found that there were no differences in 30-day complications or readmissions between same-day discharge (Clavien-Dindo [CD] I/II, 4.22%; CD III, 0%; CD IV, 1.27%; readmission, 4.64%); and SLD (CD I/II, 4.11%; CD III, 0.95%; CD IV, 0.79%; readmission, 3.90%; all P > .05).
Controlling for demographic and clinical variables, SDD was not associated with greater risk of 30-day complications or readmissions (CD I/II: odds ratio, 1.08; 95% confidence interval, 0.57-2.048; P = .813; CD IV: OR 1.699; 95% CI, 0.537-5.375; P = .367; readmission: OR, 1.254; 95% CI, 0.681-2.31; P = .467).
Mr. Garden and coauthors report no relevant financial relationships.
Dr. Lane reports no relevant financial relationships.
Urologist Ronney Abaza, MD, a robotic surgery specialist in Dublin, Ohio, and colleagues, reviewed robotic surgeries at their hospital during COVID-19 restrictions on surgery in Ohio between March 17 and June 5, 2020, and compared them with robotic procedures before COVID-19 and after restrictions were lifted. They published their results in Urology.
Since 2016, the hospital has offered the option of same-day discharge (SDD) to all robotic urologic surgery patients, regardless of procedure or patient-specific factors.
Among patients who had surgery during COVID-19 restrictions, 98% (87/89 patients) opted for SDD versus 52% in the group having surgery before the restrictions (P < .00001). After the COVID-19 surgery restrictions were lifted, the higher rate of SDD remained at 98%.
“There were no differences in 30-day complications or readmissions between SDD and overnight patients,” the authors write.
The right patient, the right motivation for successful surgery
Brian Lane, MD, PhD, a urologic oncologist with Spectrum Health in Grand Rapids, Michigan, told this news organization that, for nephrectomies, uptake of same-day discharge will continue to be slow.
“You have to have the right patient, the right patient motivation, and the surgery has to go smoothly,” he said. “If you start sending everyone home the same day, you will certainly see readmissions,” he said.
Dr. Lane is part of the Michigan Urologic Surgery Improvement Collaborative and he said the group recently looked at same-day discharge outcomes after robotic prostatectomies with SDD as compared with 1-2 nights in the hospital.
The work has not yet been published but, “There was a slight signal that there were increased readmissions with same-day discharge vs. 0-1 day,” he said.
A paper on outcomes of same-day discharge in total knee arthroplasty in the Journal of Bone & Joint Surgery found a higher risk of perioperative complications “including component failure, surgical site infection, knee stiffness, and deep vein thrombosis.” Researchers compared outcomes between 4,391 patients who underwent outpatient TKA and 128,951 patients who underwent inpatient TKA.
But for other many surgeries, same-day discharge numbers are increasing without worsening outcomes.
A paper in the Journal of Robotic Surgery found that same-day discharge following robotic-assisted endometrial cancer staging is “safe and feasible.”
Stephen Bradley, MD, MPH, with the Minneapolis Heart Institute in Minneapolis, and colleagues write in the Journal of the American College of Cardiology: Cardiovascular Interventions that they found a large increase in the use of same-day discharge after elective percutaneous coronary intervention (PCI) was not associated with worse 30-day mortality rates or readmission.
In that study, 114,461 patients were discharged the same day they underwent PCI. The proportion of patients who had a same-day discharge increased from 4.5% in 2009 to 28.6% in the fourth quarter of 2017.
Risk-adjusted 30-day mortality did not change in that time, while risk-adjusted rehospitalization decreased over time and more quickly when patients had same-day discharge.
Deepak L. Bhatt, MD, MPH, and Jonathan G. Sung, MBCHB, both of Brigham and Women’s Hospital Heart & Vascular Center, Harvard Medical School, Boston, wrote in an accompanying article that, “Advances in the devices and techniques of PCI have improved the safety and efficacy of the procedure. In selected patients, same-day discharge has become possible, and overnight in-hospital observation can be avoided. By reducing unnecessary hospital stays, both patients and hospitals could benefit.”
Evan Garden, a medical student at Icahn School of Medicine at Mount Sinai in New York, presented findings at the American Urological Association 2021 annual meeting that show patients selected for same-day discharge after partial or radical nephrectomy did not have increased rates of postoperative complications or readmissions in the immediate postoperative period, compared with standard discharge of 1-3 days.
Case studies in nephrectomy
While several case studies have looked at the feasibility and safety of performing partial and radical nephrectomy with same-day discharge in select cases, “this topic has not been addressed on a national level,” Mr. Garden said.
Few patients who have partial or radical nephrectomies have same-day discharges. The researchers found that fewer than 1% of patients who have either procedure in the sample studied were discharged the same day.
Researchers used the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, a nationally representative deidentified database that prospectively tracks patient characteristics and 30-day perioperative outcomes for major inpatient and outpatient surgical procedures at more than 700 hospitals.
They extracted all minimally invasive partial and radical nephrectomies from 2012 to 2019 and refined the cohort to 28,140 patients who were theoretically eligible for same-day discharge: Of those, 237 (0.8%) had SSD, and 27,903 (99.2%) had a standard-length discharge (SLD).
The team found that there were no differences in 30-day complications or readmissions between same-day discharge (Clavien-Dindo [CD] I/II, 4.22%; CD III, 0%; CD IV, 1.27%; readmission, 4.64%); and SLD (CD I/II, 4.11%; CD III, 0.95%; CD IV, 0.79%; readmission, 3.90%; all P > .05).
Controlling for demographic and clinical variables, SDD was not associated with greater risk of 30-day complications or readmissions (CD I/II: odds ratio, 1.08; 95% confidence interval, 0.57-2.048; P = .813; CD IV: OR 1.699; 95% CI, 0.537-5.375; P = .367; readmission: OR, 1.254; 95% CI, 0.681-2.31; P = .467).
Mr. Garden and coauthors report no relevant financial relationships.
Dr. Lane reports no relevant financial relationships.
Urologist Ronney Abaza, MD, a robotic surgery specialist in Dublin, Ohio, and colleagues, reviewed robotic surgeries at their hospital during COVID-19 restrictions on surgery in Ohio between March 17 and June 5, 2020, and compared them with robotic procedures before COVID-19 and after restrictions were lifted. They published their results in Urology.
Since 2016, the hospital has offered the option of same-day discharge (SDD) to all robotic urologic surgery patients, regardless of procedure or patient-specific factors.
Among patients who had surgery during COVID-19 restrictions, 98% (87/89 patients) opted for SDD versus 52% in the group having surgery before the restrictions (P < .00001). After the COVID-19 surgery restrictions were lifted, the higher rate of SDD remained at 98%.
“There were no differences in 30-day complications or readmissions between SDD and overnight patients,” the authors write.
The right patient, the right motivation for successful surgery
Brian Lane, MD, PhD, a urologic oncologist with Spectrum Health in Grand Rapids, Michigan, told this news organization that, for nephrectomies, uptake of same-day discharge will continue to be slow.
“You have to have the right patient, the right patient motivation, and the surgery has to go smoothly,” he said. “If you start sending everyone home the same day, you will certainly see readmissions,” he said.
Dr. Lane is part of the Michigan Urologic Surgery Improvement Collaborative and he said the group recently looked at same-day discharge outcomes after robotic prostatectomies with SDD as compared with 1-2 nights in the hospital.
The work has not yet been published but, “There was a slight signal that there were increased readmissions with same-day discharge vs. 0-1 day,” he said.
A paper on outcomes of same-day discharge in total knee arthroplasty in the Journal of Bone & Joint Surgery found a higher risk of perioperative complications “including component failure, surgical site infection, knee stiffness, and deep vein thrombosis.” Researchers compared outcomes between 4,391 patients who underwent outpatient TKA and 128,951 patients who underwent inpatient TKA.
But for other many surgeries, same-day discharge numbers are increasing without worsening outcomes.
A paper in the Journal of Robotic Surgery found that same-day discharge following robotic-assisted endometrial cancer staging is “safe and feasible.”
Stephen Bradley, MD, MPH, with the Minneapolis Heart Institute in Minneapolis, and colleagues write in the Journal of the American College of Cardiology: Cardiovascular Interventions that they found a large increase in the use of same-day discharge after elective percutaneous coronary intervention (PCI) was not associated with worse 30-day mortality rates or readmission.
In that study, 114,461 patients were discharged the same day they underwent PCI. The proportion of patients who had a same-day discharge increased from 4.5% in 2009 to 28.6% in the fourth quarter of 2017.
Risk-adjusted 30-day mortality did not change in that time, while risk-adjusted rehospitalization decreased over time and more quickly when patients had same-day discharge.
Deepak L. Bhatt, MD, MPH, and Jonathan G. Sung, MBCHB, both of Brigham and Women’s Hospital Heart & Vascular Center, Harvard Medical School, Boston, wrote in an accompanying article that, “Advances in the devices and techniques of PCI have improved the safety and efficacy of the procedure. In selected patients, same-day discharge has become possible, and overnight in-hospital observation can be avoided. By reducing unnecessary hospital stays, both patients and hospitals could benefit.”
Evan Garden, a medical student at Icahn School of Medicine at Mount Sinai in New York, presented findings at the American Urological Association 2021 annual meeting that show patients selected for same-day discharge after partial or radical nephrectomy did not have increased rates of postoperative complications or readmissions in the immediate postoperative period, compared with standard discharge of 1-3 days.
Case studies in nephrectomy
While several case studies have looked at the feasibility and safety of performing partial and radical nephrectomy with same-day discharge in select cases, “this topic has not been addressed on a national level,” Mr. Garden said.
Few patients who have partial or radical nephrectomies have same-day discharges. The researchers found that fewer than 1% of patients who have either procedure in the sample studied were discharged the same day.
Researchers used the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database, a nationally representative deidentified database that prospectively tracks patient characteristics and 30-day perioperative outcomes for major inpatient and outpatient surgical procedures at more than 700 hospitals.
They extracted all minimally invasive partial and radical nephrectomies from 2012 to 2019 and refined the cohort to 28,140 patients who were theoretically eligible for same-day discharge: Of those, 237 (0.8%) had SSD, and 27,903 (99.2%) had a standard-length discharge (SLD).
The team found that there were no differences in 30-day complications or readmissions between same-day discharge (Clavien-Dindo [CD] I/II, 4.22%; CD III, 0%; CD IV, 1.27%; readmission, 4.64%); and SLD (CD I/II, 4.11%; CD III, 0.95%; CD IV, 0.79%; readmission, 3.90%; all P > .05).
Controlling for demographic and clinical variables, SDD was not associated with greater risk of 30-day complications or readmissions (CD I/II: odds ratio, 1.08; 95% confidence interval, 0.57-2.048; P = .813; CD IV: OR 1.699; 95% CI, 0.537-5.375; P = .367; readmission: OR, 1.254; 95% CI, 0.681-2.31; P = .467).
Mr. Garden and coauthors report no relevant financial relationships.
Dr. Lane reports no relevant financial relationships.
Radiation underused as ‘bridge’ to transplant in liver cancer
CHICAGO –It is greatly underutilized compared to other liver-directed therapies, according to new findings.
“This highlights a real-world gap in the treatment armamentarium for hepatocellular carcinoma [HCC],” said Nima Nabavizadeh, MD, associate professor of radiation oncology and residency program director at the Oregon Health and Science University, Portland.
He was speaking at the annual meeting of the American Society for Radiation Oncology.
These new data suggest there is reluctance within transplant programs to utilize radiotherapy as a bridging therapy prior to liver transplant, said Hyun Kim, MD, chief, GI service, department of radiation oncology, Washington University and the Alvin J. Siteman Cancer Center, St. Louis.
“This is despite 10-year-old data from Princess Margaret and Toronto General Hospital showing that external-beam radiation is a safe and feasible bridging therapy,” he said. “More modern data from the same institutions indicate that patients bridged with stereotactic body radiotherapy ablative radiation doses delivered with high conformality have similar survival as patients bridged with radiofrequency ablation.”
Dr. Kim also noted that even after transplant, rates of intrahepatic recurrence can be as high as 10%. Approximately 60% of patients experience recurrence of any type within 3 years.
“Nonablative local therapies leave viable disease, which may permit metastatic progression while the patient awaits transplant,” he said in an interview. This new analysis highlights the need for well-designed clinical trials with modern endpoints to evaluate which bridging therapy is most beneficial for the patient, he added.
In this current “era of radiomics, deep learning, and liquid biopsies, we have unprecedented tools and responsibility to ensure that our practice continues to improve in a data-centric fashion and not remain paused in the paradigm of a previous era,” Dr. Kim said.
A leading cause of death worldwide
HCC is a leading cause of cancer death worldwide, and the incidence is rising within the United States. Transplant is often the best option for long-term survival for patients with localized HCC and advanced cirrhosis, Dr. Nabavizadeh told the meeting.
Because patients often have to wait months to over a year for a transplant, many patients receive liver-directed bridging therapy to prevent tumor growth or spread and to maintain their eligibility for transplant, he explained.
These bridging therapies include thermal ablation procedures, transarterial chemoembolization (TACE), and Y-90 radioembolization, as well as EBRT.
To investigate how these therapies were being used, Dr. Nabavizadeh and colleagues conducted a retrospective study in which they analyzed data from the United Network for Organ Sharing, a nonprofit organization that manages the only national liver transplant waiting list in the United States.
They identified patients on the transplant list who had applied for Model of End-Stage Liver Disease (MELD) exceptions so as to be prioritized on the waiting list.
A total of 18,447 HCC patients submitted MELD exception applications during the study period (October 2013 to June 2020). More than half of these patients (n = 11,171; 60.6%) received a transplant. After submitting the exception application, the median time for receiving a transplant was 7 months.
Of the total group, 15,759 patients (85.4%) received liver-directed therapy while waiting for the transplant, but only 658 patients (3.6% of the overall cohort) received EBRT, either alone or in combination with another therapy.
“The majority of patients received chemoembolization, and ERBT represents a very small percentage,” Dr. Nabavizadeh said.
During the study period, the use of transarterial chemoembolization decreased. It has largely been replaced by thermal ablation and Y-90 radioembolization. The analysis also showed that the use of EBRT had increased over the past several years, but its utilization still remained well below that of the other therapies.
TACE was the most utilized therapy. It was used for 39.6% of patients, followed by thermal ablation (12.8%) and radioembolization (8.7%). Almost a quarter of patients (22.2%) received a combination of non-EBRT therapies.
“We found that EBRT use significantly differed by region,” Dr. Nabavizadeh said. The highest usage (8.7%) was in Great Lakes states. In the Southeast, it was used for 1.7% patients.
No statistical differences were observed in clinicopathologic factors between the patients who received EBRT and those who did not.
Transplant is curative
Transplant is curative both for cancer and underlying cirrhosis, but patients may experience disease progression while waiting for transplant, noted Jessica Karen Wong, MD, assistant professor, department of radiation oncology, Fox Chase Cancer Center, Philadelphia, who was approached for comment.
“Radiation, specifically, stereotactic body radiation therapy, is a safe and effective bridging therapy but was only used in a small minority of eligible patients in this national database,” she said. “Although the use of radiation as bridging therapy is increasing over time, it continues to be underutilized. Increasing the use of radiation provides an opportunity to improve patient care for hepatocellular carcinoma patients awaiting a liver transplant.”
Dr. Nabavizadeh and Dr. Wong have disclosed no relevant financial relationships. Dr. Kim has received research funding and speaker honorarium from Varian and ViewRay.
A version of this article first appeared on Medscape.com.
CHICAGO –It is greatly underutilized compared to other liver-directed therapies, according to new findings.
“This highlights a real-world gap in the treatment armamentarium for hepatocellular carcinoma [HCC],” said Nima Nabavizadeh, MD, associate professor of radiation oncology and residency program director at the Oregon Health and Science University, Portland.
He was speaking at the annual meeting of the American Society for Radiation Oncology.
These new data suggest there is reluctance within transplant programs to utilize radiotherapy as a bridging therapy prior to liver transplant, said Hyun Kim, MD, chief, GI service, department of radiation oncology, Washington University and the Alvin J. Siteman Cancer Center, St. Louis.
“This is despite 10-year-old data from Princess Margaret and Toronto General Hospital showing that external-beam radiation is a safe and feasible bridging therapy,” he said. “More modern data from the same institutions indicate that patients bridged with stereotactic body radiotherapy ablative radiation doses delivered with high conformality have similar survival as patients bridged with radiofrequency ablation.”
Dr. Kim also noted that even after transplant, rates of intrahepatic recurrence can be as high as 10%. Approximately 60% of patients experience recurrence of any type within 3 years.
“Nonablative local therapies leave viable disease, which may permit metastatic progression while the patient awaits transplant,” he said in an interview. This new analysis highlights the need for well-designed clinical trials with modern endpoints to evaluate which bridging therapy is most beneficial for the patient, he added.
In this current “era of radiomics, deep learning, and liquid biopsies, we have unprecedented tools and responsibility to ensure that our practice continues to improve in a data-centric fashion and not remain paused in the paradigm of a previous era,” Dr. Kim said.
A leading cause of death worldwide
HCC is a leading cause of cancer death worldwide, and the incidence is rising within the United States. Transplant is often the best option for long-term survival for patients with localized HCC and advanced cirrhosis, Dr. Nabavizadeh told the meeting.
Because patients often have to wait months to over a year for a transplant, many patients receive liver-directed bridging therapy to prevent tumor growth or spread and to maintain their eligibility for transplant, he explained.
These bridging therapies include thermal ablation procedures, transarterial chemoembolization (TACE), and Y-90 radioembolization, as well as EBRT.
To investigate how these therapies were being used, Dr. Nabavizadeh and colleagues conducted a retrospective study in which they analyzed data from the United Network for Organ Sharing, a nonprofit organization that manages the only national liver transplant waiting list in the United States.
They identified patients on the transplant list who had applied for Model of End-Stage Liver Disease (MELD) exceptions so as to be prioritized on the waiting list.
A total of 18,447 HCC patients submitted MELD exception applications during the study period (October 2013 to June 2020). More than half of these patients (n = 11,171; 60.6%) received a transplant. After submitting the exception application, the median time for receiving a transplant was 7 months.
Of the total group, 15,759 patients (85.4%) received liver-directed therapy while waiting for the transplant, but only 658 patients (3.6% of the overall cohort) received EBRT, either alone or in combination with another therapy.
“The majority of patients received chemoembolization, and ERBT represents a very small percentage,” Dr. Nabavizadeh said.
During the study period, the use of transarterial chemoembolization decreased. It has largely been replaced by thermal ablation and Y-90 radioembolization. The analysis also showed that the use of EBRT had increased over the past several years, but its utilization still remained well below that of the other therapies.
TACE was the most utilized therapy. It was used for 39.6% of patients, followed by thermal ablation (12.8%) and radioembolization (8.7%). Almost a quarter of patients (22.2%) received a combination of non-EBRT therapies.
“We found that EBRT use significantly differed by region,” Dr. Nabavizadeh said. The highest usage (8.7%) was in Great Lakes states. In the Southeast, it was used for 1.7% patients.
No statistical differences were observed in clinicopathologic factors between the patients who received EBRT and those who did not.
Transplant is curative
Transplant is curative both for cancer and underlying cirrhosis, but patients may experience disease progression while waiting for transplant, noted Jessica Karen Wong, MD, assistant professor, department of radiation oncology, Fox Chase Cancer Center, Philadelphia, who was approached for comment.
“Radiation, specifically, stereotactic body radiation therapy, is a safe and effective bridging therapy but was only used in a small minority of eligible patients in this national database,” she said. “Although the use of radiation as bridging therapy is increasing over time, it continues to be underutilized. Increasing the use of radiation provides an opportunity to improve patient care for hepatocellular carcinoma patients awaiting a liver transplant.”
Dr. Nabavizadeh and Dr. Wong have disclosed no relevant financial relationships. Dr. Kim has received research funding and speaker honorarium from Varian and ViewRay.
A version of this article first appeared on Medscape.com.
CHICAGO –It is greatly underutilized compared to other liver-directed therapies, according to new findings.
“This highlights a real-world gap in the treatment armamentarium for hepatocellular carcinoma [HCC],” said Nima Nabavizadeh, MD, associate professor of radiation oncology and residency program director at the Oregon Health and Science University, Portland.
He was speaking at the annual meeting of the American Society for Radiation Oncology.
These new data suggest there is reluctance within transplant programs to utilize radiotherapy as a bridging therapy prior to liver transplant, said Hyun Kim, MD, chief, GI service, department of radiation oncology, Washington University and the Alvin J. Siteman Cancer Center, St. Louis.
“This is despite 10-year-old data from Princess Margaret and Toronto General Hospital showing that external-beam radiation is a safe and feasible bridging therapy,” he said. “More modern data from the same institutions indicate that patients bridged with stereotactic body radiotherapy ablative radiation doses delivered with high conformality have similar survival as patients bridged with radiofrequency ablation.”
Dr. Kim also noted that even after transplant, rates of intrahepatic recurrence can be as high as 10%. Approximately 60% of patients experience recurrence of any type within 3 years.
“Nonablative local therapies leave viable disease, which may permit metastatic progression while the patient awaits transplant,” he said in an interview. This new analysis highlights the need for well-designed clinical trials with modern endpoints to evaluate which bridging therapy is most beneficial for the patient, he added.
In this current “era of radiomics, deep learning, and liquid biopsies, we have unprecedented tools and responsibility to ensure that our practice continues to improve in a data-centric fashion and not remain paused in the paradigm of a previous era,” Dr. Kim said.
A leading cause of death worldwide
HCC is a leading cause of cancer death worldwide, and the incidence is rising within the United States. Transplant is often the best option for long-term survival for patients with localized HCC and advanced cirrhosis, Dr. Nabavizadeh told the meeting.
Because patients often have to wait months to over a year for a transplant, many patients receive liver-directed bridging therapy to prevent tumor growth or spread and to maintain their eligibility for transplant, he explained.
These bridging therapies include thermal ablation procedures, transarterial chemoembolization (TACE), and Y-90 radioembolization, as well as EBRT.
To investigate how these therapies were being used, Dr. Nabavizadeh and colleagues conducted a retrospective study in which they analyzed data from the United Network for Organ Sharing, a nonprofit organization that manages the only national liver transplant waiting list in the United States.
They identified patients on the transplant list who had applied for Model of End-Stage Liver Disease (MELD) exceptions so as to be prioritized on the waiting list.
A total of 18,447 HCC patients submitted MELD exception applications during the study period (October 2013 to June 2020). More than half of these patients (n = 11,171; 60.6%) received a transplant. After submitting the exception application, the median time for receiving a transplant was 7 months.
Of the total group, 15,759 patients (85.4%) received liver-directed therapy while waiting for the transplant, but only 658 patients (3.6% of the overall cohort) received EBRT, either alone or in combination with another therapy.
“The majority of patients received chemoembolization, and ERBT represents a very small percentage,” Dr. Nabavizadeh said.
During the study period, the use of transarterial chemoembolization decreased. It has largely been replaced by thermal ablation and Y-90 radioembolization. The analysis also showed that the use of EBRT had increased over the past several years, but its utilization still remained well below that of the other therapies.
TACE was the most utilized therapy. It was used for 39.6% of patients, followed by thermal ablation (12.8%) and radioembolization (8.7%). Almost a quarter of patients (22.2%) received a combination of non-EBRT therapies.
“We found that EBRT use significantly differed by region,” Dr. Nabavizadeh said. The highest usage (8.7%) was in Great Lakes states. In the Southeast, it was used for 1.7% patients.
No statistical differences were observed in clinicopathologic factors between the patients who received EBRT and those who did not.
Transplant is curative
Transplant is curative both for cancer and underlying cirrhosis, but patients may experience disease progression while waiting for transplant, noted Jessica Karen Wong, MD, assistant professor, department of radiation oncology, Fox Chase Cancer Center, Philadelphia, who was approached for comment.
“Radiation, specifically, stereotactic body radiation therapy, is a safe and effective bridging therapy but was only used in a small minority of eligible patients in this national database,” she said. “Although the use of radiation as bridging therapy is increasing over time, it continues to be underutilized. Increasing the use of radiation provides an opportunity to improve patient care for hepatocellular carcinoma patients awaiting a liver transplant.”
Dr. Nabavizadeh and Dr. Wong have disclosed no relevant financial relationships. Dr. Kim has received research funding and speaker honorarium from Varian and ViewRay.
A version of this article first appeared on Medscape.com.
FROM ASTRO 2021
Accused: Doc increases patient’s penis size with improper fillers; more
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
, as reported in NJ.com.
The physician, Muhammad A. Mirza, MD, is a board-certified internal medicine doctor and owner of Mirza Aesthetics, which has its main New Jersey office in Cedar Grove, a township in Essex County. The practice also leases space in New York, Pennsylvania, and Connecticut, where at press time Dr. Mirza was still licensed to practice medicine.
The acting New Jersey attorney general said that Dr. Mirza had deviated from the accepted standards of medical care in at least four key areas: he practiced in ways that put his patients in bodily danger; he lacked the formal training in and an adequate knowledge of aesthetic medicine; he practiced in office settings that inspectors found to be subpar; and he failed to safely store medical supplies or maintain proper medical records.
In one instance singled out by the attorney general’s office, Dr. Mirza used an injectable dermal filler to enhance a patient’s penis. As a result of that nonsurgical procedure, the patient needed to be rushed to a nearby hospital, where he underwent two emergency surgical interventions. Contacted by the emergency department doctor, Dr. Mirza allegedly failed to disclose the name of the filler he used, thereby complicating the patient’s recovery, according to the board complaint.
Dr. Mirza’s other alleged breaches of professional conduct include the following:
- Failure to wear a mask or surgical gloves during procedures
- Failure to keep electronic medical records of any kind
- Improper, off-label use of an injectable dermal filler in proximity to patients’ eyes
- Improper, off-label use of an injectable dermal filler for breast enhancement
- Use of a certain injectable dermal filler without first testing for skin allergies
In addition, site inspections of Dr. Mirza’s offices turned up substandard conditions. On April 23, 2021, in response to numerous patient complaints, the Enforcement Bureau of the Division of Consumer Affairs inspected Dr. Mirza’s Summit, N.J. office, one of several in the state.
Among other things, the inspection uncovered the following:
- The medical office was one large room. A curtain separated the reception area and the examination/treatment area, which consisted of only chairs and a fold-away table.
- “Duffle bags” were used to store injectable fillers. No medical storage refrigerators were observed.
- COVID-19 protocols were not followed. Inspectors could identify no barrier between receptionist and patients, no posted mask mandate, no social distancing policy, and no COVID-19 screening measures.
In addition to temporarily suspending Dr. Mirza’s license, the medical board has prohibited him from treating New Jersey patients in any of the out-of-state locations where he’s licensed to practice medicine.
Prosecutors have urged other patients who believe they’ve been injured by Mirza Aesthetics to file a complaint with the State Division of Consumer Affairs.
Dr. Mirza has agreed to the temporary suspension of his medical license, pending a hearing before an administrative law judge. In addition to facing civil penalties for each of the counts against him, he could be held responsible for paying investigative costs, attorney fees, trial costs, and other costs.
Doctor’s failure to diagnose results in mega award
In what is believed to be a record verdict in a wrongful death suit in Volusia County, Fla., a jury awarded $6.46 million to the family of a woman who died from an undiagnosed heart infection after being transferred from a local hospital, according to a report in The Daytona Beach News-Journal, among other news outlets.
In March 2016, Laura Staib went to what was then Florida Hospital DeLand — now AdventHealth DeLand — complaining of a variety of symptoms. There, she was examined by a doctor who was a member of a nearby cardiology group. His diagnosis: congestive heart failure, pneumonia, and sepsis. Transferred to a long-term care facility, Ms. Staib died 4 days later.
In their complaint against the cardiologist and his cardiology group, family members alleged that the doctor failed to identify Ms. Staib’s main problem: viral myocarditis.
“This was primarily a heart failure problem and a heart infection that was probably causing some problems in the lungs,” said the attorney representing the family. “A virus was attacking her heart, and they missed it,” he said. Claims against the hospital and other doctors were eventually resolved and dismissed.
The jury’s verdict will be appealed, said the attorney representing the cardiologist.
He argues that his client “did not cause that woman’s death. She died of an overwhelming lung infection...acute respiratory distress syndrome, caused by an overwhelming pneumonia that got worse after she was transferred to a facility where [my client] doesn’t practice.”
The bulk of the award will be in compensation for family members’ future pain and suffering and for other noneconomic damages.
Botched outpatient procedure leaves woman disfigured
In early September, a patient was allegedly administered the wrong drug during an outpatient procedure on her hand. She sued the Austin, Tex., hospital and surgical center where that procedure was performed, according to a story in Law/Street.
On January 9, 2020, Jessica Arguello went to HCA Healthcare’s South Austin Surgery Center to undergo a right-hand first metacarpophalangeal arthrodesis (fusion) and neuroma excision. In her suit against the hospital, Ms. Arguello claims that while her surgeon was preparing to close the incision after having irrigated the site, he called for a syringe containing an anesthetic. He was instead handed a syringe that contained formalin, the chemical used to preserve specimens for later review.
The mistake, Ms. Arguello claims, caused her to suffer massive chemical burns and necrosis of her flesh, which required four additional surgeries. In the end, she says, her right hand is disfigured and has limited mobility.
She adds that her injuries were preventable. Standard surgical procedure typically forbids chemicals such as formalin to be included among items on the prep tray. In addition to other compensation, she seeks damages for past and future medical expenses and past and future pain and suffering.
At press time, the defendants had not responded to Ms. Arguello’s complaint.
A version of this article first appeared on Medscape.com.
Lung cancer screening rates in U.S. nowhere near goal
according to a review and meta-analysis published in the Journal of Thoracic Oncology.
“Lung cancer screening is effective in reducing mortality, particularly when patients adhere to follow-up recommendations standardized by the Lung CT Screening Reporting & Data System (Lung-RADS),” Yannan Lin, MD, MPH, of the University of California, Los Angeles, and colleagues wrote. ”Patient adherence to Lung-RADS–recommended screening intervals is suboptimal across clinical lung cancer screening programs in the U.S., especially among patients with Lung-RADS category 1-2 results.”
Lung cancer screening can identify tumors at earlier, more treatable stages, but patients with lung cancer diagnoses based on new nodules at incidence screening have shown shortened survivals. The National Lung Screening Trial (NLST) has shown a 20% relative reduction in lung cancer mortality with low-dose chest CT screening relative to chest radiography. The Lung-RADS guidelines to standardize the reporting of lung cancer screening were developed based on findings from the NLST and other screening studies, partly to reduce false-positive rates. Lung-RADS scores are based upon nodule size, characteristics and location, with management guidelines specific to Lung-RADS categories, ranging from low-dose chest CT in 12 months for Lung-RADS 1-2 to chest CT, PET/CT, or tissue sampling for Lung-RADS 4B/X.
The rate of adherence to lung cancer screening based on Lung-RADS guidelines is unclear. This systematic review and meta-analysis looked at patient adherence to Lung-RADS recommended screening intervals in clinical practice.
The meta-analysis included 21 studies. The pooled adherence rate was 57% for defined adherence, which included an annual incidence screen performed within 15 months, among 6,689 patients and 65% for anytime adherence among 5,085 patients. The authors noted that overall rates of adherence to Lung-RADS recommended screening intervals in clinical practices is low as compared with the over 90% adherence seen in the NLST, adversely affecting the mortality benefits of lung cancer screening.
Higher adherence rates were found in patients with Lung-RADS 3 (risk for lung cancer, 1%-2%) and 4 (risk, >5%) than Lung-RADS 1 and 2 (risk, <1%; P < .05), which the authors said suggests that tailored interventions based on Lung-RADS categories may be beneficial.
“It is likely that patients and referrers are more concerned about nodules at a higher risk for lung cancer, prompting greater adherence to recommended screening intervals in Lung-RADS 3-4,” the authors wrote. “It is crucial that patients and referrers alike understand that screening is most effective when performed regularly, including for those with negative baseline screens, as de novo nodules, those detected after a negative screen, are more aggressive than those detected at baseline screen.”
These low adherence rates seen in the clinical practices could be explained by patient characteristics, insurance coverage and interventions to ensure adherence, among other factors.
Further, inconsistent reporting of adherence rates was observed. Standardized reporting of adherence rates to lung cancer screening is needed to identify interventions to improve adherence, the authors wrote.
The authors of this study noted no conflicts of interest.
according to a review and meta-analysis published in the Journal of Thoracic Oncology.
“Lung cancer screening is effective in reducing mortality, particularly when patients adhere to follow-up recommendations standardized by the Lung CT Screening Reporting & Data System (Lung-RADS),” Yannan Lin, MD, MPH, of the University of California, Los Angeles, and colleagues wrote. ”Patient adherence to Lung-RADS–recommended screening intervals is suboptimal across clinical lung cancer screening programs in the U.S., especially among patients with Lung-RADS category 1-2 results.”
Lung cancer screening can identify tumors at earlier, more treatable stages, but patients with lung cancer diagnoses based on new nodules at incidence screening have shown shortened survivals. The National Lung Screening Trial (NLST) has shown a 20% relative reduction in lung cancer mortality with low-dose chest CT screening relative to chest radiography. The Lung-RADS guidelines to standardize the reporting of lung cancer screening were developed based on findings from the NLST and other screening studies, partly to reduce false-positive rates. Lung-RADS scores are based upon nodule size, characteristics and location, with management guidelines specific to Lung-RADS categories, ranging from low-dose chest CT in 12 months for Lung-RADS 1-2 to chest CT, PET/CT, or tissue sampling for Lung-RADS 4B/X.
The rate of adherence to lung cancer screening based on Lung-RADS guidelines is unclear. This systematic review and meta-analysis looked at patient adherence to Lung-RADS recommended screening intervals in clinical practice.
The meta-analysis included 21 studies. The pooled adherence rate was 57% for defined adherence, which included an annual incidence screen performed within 15 months, among 6,689 patients and 65% for anytime adherence among 5,085 patients. The authors noted that overall rates of adherence to Lung-RADS recommended screening intervals in clinical practices is low as compared with the over 90% adherence seen in the NLST, adversely affecting the mortality benefits of lung cancer screening.
Higher adherence rates were found in patients with Lung-RADS 3 (risk for lung cancer, 1%-2%) and 4 (risk, >5%) than Lung-RADS 1 and 2 (risk, <1%; P < .05), which the authors said suggests that tailored interventions based on Lung-RADS categories may be beneficial.
“It is likely that patients and referrers are more concerned about nodules at a higher risk for lung cancer, prompting greater adherence to recommended screening intervals in Lung-RADS 3-4,” the authors wrote. “It is crucial that patients and referrers alike understand that screening is most effective when performed regularly, including for those with negative baseline screens, as de novo nodules, those detected after a negative screen, are more aggressive than those detected at baseline screen.”
These low adherence rates seen in the clinical practices could be explained by patient characteristics, insurance coverage and interventions to ensure adherence, among other factors.
Further, inconsistent reporting of adherence rates was observed. Standardized reporting of adherence rates to lung cancer screening is needed to identify interventions to improve adherence, the authors wrote.
The authors of this study noted no conflicts of interest.
according to a review and meta-analysis published in the Journal of Thoracic Oncology.
“Lung cancer screening is effective in reducing mortality, particularly when patients adhere to follow-up recommendations standardized by the Lung CT Screening Reporting & Data System (Lung-RADS),” Yannan Lin, MD, MPH, of the University of California, Los Angeles, and colleagues wrote. ”Patient adherence to Lung-RADS–recommended screening intervals is suboptimal across clinical lung cancer screening programs in the U.S., especially among patients with Lung-RADS category 1-2 results.”
Lung cancer screening can identify tumors at earlier, more treatable stages, but patients with lung cancer diagnoses based on new nodules at incidence screening have shown shortened survivals. The National Lung Screening Trial (NLST) has shown a 20% relative reduction in lung cancer mortality with low-dose chest CT screening relative to chest radiography. The Lung-RADS guidelines to standardize the reporting of lung cancer screening were developed based on findings from the NLST and other screening studies, partly to reduce false-positive rates. Lung-RADS scores are based upon nodule size, characteristics and location, with management guidelines specific to Lung-RADS categories, ranging from low-dose chest CT in 12 months for Lung-RADS 1-2 to chest CT, PET/CT, or tissue sampling for Lung-RADS 4B/X.
The rate of adherence to lung cancer screening based on Lung-RADS guidelines is unclear. This systematic review and meta-analysis looked at patient adherence to Lung-RADS recommended screening intervals in clinical practice.
The meta-analysis included 21 studies. The pooled adherence rate was 57% for defined adherence, which included an annual incidence screen performed within 15 months, among 6,689 patients and 65% for anytime adherence among 5,085 patients. The authors noted that overall rates of adherence to Lung-RADS recommended screening intervals in clinical practices is low as compared with the over 90% adherence seen in the NLST, adversely affecting the mortality benefits of lung cancer screening.
Higher adherence rates were found in patients with Lung-RADS 3 (risk for lung cancer, 1%-2%) and 4 (risk, >5%) than Lung-RADS 1 and 2 (risk, <1%; P < .05), which the authors said suggests that tailored interventions based on Lung-RADS categories may be beneficial.
“It is likely that patients and referrers are more concerned about nodules at a higher risk for lung cancer, prompting greater adherence to recommended screening intervals in Lung-RADS 3-4,” the authors wrote. “It is crucial that patients and referrers alike understand that screening is most effective when performed regularly, including for those with negative baseline screens, as de novo nodules, those detected after a negative screen, are more aggressive than those detected at baseline screen.”
These low adherence rates seen in the clinical practices could be explained by patient characteristics, insurance coverage and interventions to ensure adherence, among other factors.
Further, inconsistent reporting of adherence rates was observed. Standardized reporting of adherence rates to lung cancer screening is needed to identify interventions to improve adherence, the authors wrote.
The authors of this study noted no conflicts of interest.
FROM THE JOURNAL OF THORACIC ONCOLOGY
The devil in the (masking) details
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
The Devil’s own face covering?
It’s been over a year and a half since the COVID-19 emergency was declared in the United States, and we’ve been starting to wonder what our good friend SARS-CoV-2 has left to give. The collective cynic/optimist in us figures that the insanity can’t last forever, right?
Maybe not forever, but …
A group of parents is suing the Central Bucks (Pa.) School District over school mask mandates, suggesting that the district has no legal authority to enforce such measures. Most of their arguments, Philadelphia Magazine says, are pretty standard stuff: Masks are causing depression, anxiety, and discomfort in their children; masks are a violation of their constitutional rights; and “masks are being used as a control mechanism over the population.”
There are some unusual claims, though. One of the parents, Shannon Harris, said that “wearing masks interferes with their religious duty to spread the word of God and forces them to participate in a satanic ritual,” according to the Philadelphia Inquirer.
Philadelphia Magazine decided to check on that “satanic ritual” claim by asking an expert, in this case a spokesperson for the Church of Satan. The Reverend Raul Antony said that “simply ‘wearing a mask’ is not a Satanic ritual, and anyone that genuinely thinks otherwise is a blithering idiot,” adding that the group’s rituals were available on its website.
COVID, you never let us down.
You’re the (hurricane) wind beneath my wings
Marriage isn’t easy. From finances to everyday stressors like work and children, maintaining a solid relationship is tough. Then a natural disaster shows up on top of everything else, and marriages actually improve, researchers found.
In a study published by Psychological Science, researchers surveyed 231 newlywed couples about the satisfaction of their marriage before and after Hurricane Harvey in 2017. They found after the hurricane couples had a “significant boost” in the satisfaction of their relationship.
One would think something like this would create what researchers call a “stress spillover,” creating a decrease in relationship satisfaction. Destruction to your home or even displacement after a natural disaster seems pretty stressful. But, “a natural disaster can really put things in perspective. People realize how important their partner is to them when they are jolted out of the day-to-day stress of life,” said Hannah Williamson, PhD, the lead author of the study.
And although everyone saw an increase, the biggest jumps in relationship satisfaction belonged to the people who were most unhappy before the hurricane. Unfortunately, the researchers also found that the effects were only temporary and the dissatisfaction came back within a year.
Dr. Williamson thinks there may be something to these findings that can be beneficial from a therapy standpoint where “couples can shift their perspective in a similar way without having to go through a natural disaster.”
Let’s hope she’s right, because the alternative is to seek out a rampaging hurricane every time your relationship is on the rocks, and that just seems impractical after the second or third year.
Not-so-essential oils
Many people use essential oils as a way to unwind and relax. Stressed? Can’t sleep? There’s probably an essential oil for that. However, it seems like these days a lot of things we love and/or think are good for us have a side that’s not so.
According to the Centers for Disease Control and Prevention, a woman from Georgia died from a rare bacteria called Burkholderia pseudomallei. There have been three previous infections in Kansas, Minnesota, and Texas throughout 2021; two of the four infections were in children. Melioidosis, the disease caused by B. pseudomallei, is usually found in southeast Asia and isn’t obvious or easy to diagnose, especially in places like decidedly untropical Minnesota.
The Georgia case was the real break in this medical mystery, as the infection was traced back to a Walmart product called “Better Homes and Gardens Essential Oil Infused Aromatherapy Room Spray with Gemstones” (a very pithy name). The bacteria were in the lavender and chamomile scent. The CDC is investigating all other product scents, and Walmart has recalled all lots of the product.
If you’ve got that particular essential oil, it’s probably for the best that you stop using it. Don’t worry, we’re sure there’s plenty of other essential oil–infused aromatherapy room sprays with gemstones out there for your scent-based needs.
Welcome to the Ministry of Sleep-Deprived Walks
Walking is simple, right? You put one foot in front of the other, and soon you’re walking out the door. Little kids can do it. Even zombies can walk, and they don’t even have brains.
Research from MIT and the University of São Paulo has shown that walking is a little trickier than we might think. One researcher in particular noticed that student volunteers tended to perform worse toward the end of semesters, as project deadlines and multiple exams crashed over their heads and they were deprived of solid sleep schedules.
In a study published in Scientific Reports, our intrepid walking researchers had a collection of students monitor their sleep patterns for 2 weeks; on average, the students got 6 hours per night, though some were able to compensate on weekends. On the final day of a 14-day period, some students pulled all-nighters while the rest were allowed to sleep as usual. Then all students performed a walking test involving keeping time with a metronome.
To absolutely no one’s surprise, the students who performed all-nighters before being tested walked the worst, but between the other students, the ones who compensated for sleep deprivation on weekends did better than those who got 6 hours every night, despite getting a similar amount of sleep overall. This effect persisted even when the compensating students performed their walking tests late in the week, just before they got their weekend beauty sleep.
The moral of the story? Sleep is good, and you should get more of it. But if you can’t, sleep in on weekends. Science has given you permission. All those suburban dads looking to get their teenagers up at 8 in the morning must be sweating right now.
Which specialties get the biggest markups over Medicare rates?
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
Anesthesiologists charge private insurers more than 300% above Medicare rates, a markup that is higher than that of 16 other specialties, according to a study released by the Urban Institute.
The Washington-based nonprofit institute found that the lowest markups were in psychiatry, ophthalmology, ob.gyn., family medicine, gastroenterology, and internal medicine, at 110%-120% of Medicare rates. .
In the middle are cardiology and cardiovascular surgery (130%), urology (130%), general surgery, surgical and radiation oncology (all at 140%), and orthopedics (150%).
At the top end were radiology (180%), neurosurgery (220%), emergency and critical care (250%), and anesthesiology (330%).
The wide variation in payments could be cited in support of the idea of applying Medicare rates across all physician specialties, say the study authors. Although lowering practitioner payments might lead to savings, it “will also create more pushback from providers, especially if these rates are introduced in the employer market,” write researchers Stacey McMorrow, PhD, Robert A. Berenson, MD, and John Holahan, PhD.
It is not known whether lowering commercial payment rates might decrease patient access, they write.
The authors also note that specialties in which the potential for a fee reduction was greatest were also the specialties for which baseline compensation was highest – from $350,000 annually for emergency physicians to $800,000 a year for neurosurgeons. Annual compensation for ob.gyns., dermatologists, and opthalmologists is about $350,000 a year, which suggests that “these specialties are similarly well compensated by both Medicare and commercial insurers,” the authors write.
The investigators assessed the top 20 procedure codes by expenditure in each of 17 physician specialties. They estimated the commercial-to-Medicare payment ratio for each service and constructed weighted averages across services for each specialty at the national level and for 12 states for which data for all the specialties and services were available.
The researchers analyzed claims from the FAIR Health database between March 2019 and March 2020. That database represents 60 insurers covering 150 million people.
Pediatric and geriatric specialties, nonphysician practitioners, out-of-network clinicians, and ambulatory surgery center claims were excluded. Codes with modifiers, J codes, and clinical laboratory services were also not included.
The charges used in the study were not the actual contracted rates. The authors instead used “imputed allowed amounts” for each claim line. That method was used to protect the confidentiality of the negotiated rates.
With regard to all specialties, the lowest compensated services were procedures, evaluation and management, and tests, which received 140%-150% of the Medicare rate. Treatments and imaging were marked up 160%. Anesthesia was reimbursed at a rate 330% higher than the rate Medicare would pay.
The authors also assessed geographic variation for the 12 states for which they had data.
Similar to findings in other studies, the researchers found that the markup was lowest in Pennsylvania (120%) and highest in Wisconsin (260%). The U.S. average was 160%. California and Missouri were at 150%; Michigan was right at the average.
For physicians in Illinois, Louisiana, Colorado, Texas, and New York, markups were 170%-180% over the Medicare rate. Markups for clinicians in New Jersey (190%) and Arizona (200%) were closest to the Wisconsin rate.
The authors note some study limitations, including the fact that they excluded out-of-network practitioners, “and such payments may disproportionately affect certain specialties.”
A version of this article first appeared on Medscape.com.
PRP injections don’t top placebo for ankle osteoarthritis
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.
Platelet-rich plasma (PRP) injections did not significantly improve pain or function when compared with placebo injections in patients with ankle osteoarthritis (OA), a new study has found.
“Previous evidence for PRP injections in ankle osteoarthritis was limited to 4 small case series with methodological flaws,” wrote Liam D. A. Paget, MD, of the University of Amsterdam, and coauthors. The study was published online Oct. 26 in JAMA.
To assess the value of PRP injections as a treatment for ankle OA, the researchers launched a double-blind, randomized clinical trial of Dutch patients with notable ankle pain and tibiotalar joint space narrowing. From six sites in the Netherlands, 100 patients (45% women, mean age 56 years) were split into two groups: one that received two intra-articular injections of PRP 6 weeks apart (n = 48) and one that received two injections of saline placebo (n = 52).
At baseline, mean American Orthopaedic Foot and Ankle Society (AOFAS) scores were 63 in the PRP group and 64 in the placebo group (range 0-100, with higher scores indicating less pain and more function). At 26-week follow-up, the mean AOFAS score improved by 10 points in the PRP group (95% confidence interval, 6-14; P < .001) and by 11 points in the placebo group (95% CI, 7-15; P < .001). The adjusted between-group difference for AOFAS improvement over 26 weeks was –1 point (95% CI, –6 to 3; P = .56).
There was one serious adverse event in the placebo group – a transient ischemic attack 3 weeks after the first injection – but it was deemed unrelated.
Searching for answers regarding PRP and osteoarthritis
“From my standpoint, this study is a great step forward to where the field needs to be, which is honing in on longer-term studies that are standardizing PRP and teasing out its effects,” Prathap Jayaram, MD, director of regenerative sports medicine at the Baylor College of Medicine in Houston, said in an interview.
He highlighted the authors’ acknowledgment of previous studies in which PRP injections appeared effective in treating knee OA, including their statement that the “results reported here for ankle osteoarthritis were not consistent with these potentially beneficial effects in knee osteoarthritis.”
“They’re acknowledging that this does have some benefit in knees,” he said. “Could that translate toward the ankle?”
“PRP did lead to an improvement,” he added. “There just wasn’t a big enough difference to say one was superior to the other.”
Citing his team’s recent preclinical study that was published in Osteoarthritis and Cartilage, Dr. Jayaram emphasized the possibility that PRP could have much-needed disease-modifying effects in osteoarthritis. More work is needed to pin down the details.
“We need more mechanistic studies to be done so we can actually identify the therapeutic properties in PRP and leverage them to track reproducible outcomes,” he said, adding that “simply put, your blood and my blood might be different. There is going to be heterogeneity there. The analogy I give my patients is, when they take an antibiotic, we have a specific dose, a specific drug, and a specific duration. It’s very standardized. We’re just not there yet with PRP.”
The authors acknowledged their study’s limitations, including a likely inability to generalize their results to other platelet-rich blood products as well as a lack of composition analysis of the PRP they used. That said, they added that this particular PRP has been “analyzed previously” for another trial and noted that such analysis is not typically performed in a clinical setting.
The study was supported by a grant from the Dutch Arthritis Society. Its authors reported several potential conflicts of interest, including receiving their own grants from the Dutch Arthritis Society and other organizations, as well as accepting loaned Hettich centrifuges from a medical device company for the study.
A version of this article first appeared on Medscape.com.