User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Daily Recap: Transgender patients turn to DIY treatments; ACIP plans priority vaccine groups
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Ignored by doctors, transgender patients turn to DIY treatments
Without access to quality medical care, trans people around the world are seeking hormones from friends or through illegal online markets, even when the cost exceeds what it would through insurance. Although rare, others are resorting to self-surgery by cutting off their own penis and testicles or breasts.
Even with a doctor’s oversight, the health risks of transgender hormone therapy remain unclear, but without formal medical care, the do-it-yourself transition may be downright dangerous. To minimize these risks, some experts suggest health care reforms such as making it easier for primary care physicians to assess trans patients and prescribe hormones or creating specialized clinics where doctors prescribe hormones on demand.
Treating gender dysphoria should be just like treating a patient for any other condition. “It wouldn't be acceptable for someone to come into a primary care provider’s office with diabetes” and for the doctor to say “‘I can't actually treat you. Please leave,’” Zil Goldstein, associate medical director for transgender and gender non-binary health at the Callen-Lorde Community Health Center in New York City. Primary care providers need to see transgender care, she adds, “as a regular part of their practice.” Read more.
ACIP plans priority groups in advance of COVID-19 vaccine
Early plans for prioritizing vaccination when a COVID-19 vaccine becomes available include placing critical health care workers in the first tier, according to Sarah Mbaeyi, MD, MPH, of the CDC’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said. Read more.
‘Nietzsche was wrong’: Past stressors do not create psychological resilience.
The famous quote from the German philosopher Friedrich Nietzsche, “That which does not kill us makes us stronger,” may not be true after all – at least when it comes to mental health.
Results of a new study show that individuals who have a history of a stressful life events are more likely to develop PTSD and/or major depressive disorder (MDD) following a major natural disaster than their counterparts who do not have such a history.
The investigation of more than a thousand Chilean residents – all of whom experienced one of the most powerful earthquakes in the country’s history – showed that the odds of developing postdisaster PTSD or MDD increased according to the number of predisaster stressors participants had experienced.
“At the clinical level, these findings help the clinician know which patients are more likely to need more intensive services,” said Stephen L. Buka, PhD. “And the more trauma and hardship they’ve experienced, the more attention they need and the less likely they’re going to be able to cope and manage on their own.” Read more.
High-impact training can build bone in older women
Older adults, particularly postmenopausal women, are often advised to pursue low-impact, low-intensity exercise as a way to preserve joint health, but that approach might actually contribute to a decline in bone mineral density, researchers report.
Concerns about falls and fracture risk have led many clinicians to advise against higher-impact activities, like jumping, but that is exactly the type of activity that improves bone density and physical function, said Belinda Beck, PhD, professor at the Griffith University School of Allied Health Sciences in Southport, Australia. But new findings show that high-intensity resistance and impact training was a safe and effective way to improve bone mass.
“Once women hit 60, they’re somehow regarded as frail, but that becomes a self-fulfilling prophecy when we take this kinder, gentler approach to exercise,” said Vanessa Yingling, PhD. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
How racism contributes to the effects of SARS-CoV-2
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
ACIP plans priority groups in advance of COVID-19 vaccine
according to Sarah Mbaeyi, MD, MPH, of the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
“Preparing for vaccination during a pandemic has long been a priority of the CDC and the U.S. government,” said Dr. Mbaeyi. The work group is building on a tiered approach to vaccination that was updated in 2018 after the H1N1 flu pandemic, with occupational and high-risk populations placed in the highest-priority groups, Dr. Mbaeyi said.
There are important differences between COVID-19 and influenza, Dr. Mbaeyi said. “Vaccine prioritization is challenging due to incomplete information on COVID-19 epidemiology and vaccines, including characteristics, timing, and number of doses.”
However, guidance for vaccine prioritization developed after the H1N1 outbreak in 2018 can be adapted for COVID-19.
To help inform ACIP deliberations, the work group reviewed the epidemiology of COVID-19. A large proportion of the population remains susceptible, and prioritizations should be based on data to date and continually refined, she said.
The work group defined the objectives of the COVID-19 vaccine program as follows: “Ensure safety and effectiveness of COVID-19 vaccines; reduce transmission, morbidity, and mortality in the population; help minimize disruption to society and economy, including maintaining health care capacity; and ensure equity in vaccine allocation and distribution.”
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said.
However, vaccines will not be administered until safety and efficacy have been demonstrated, she emphasized. The timing and number of vaccine doses are unknown, and subprioritization may be needed, assuming the vaccine becomes available in incremental quantities over several months.
Next steps for the work group are refinement of priority groups based on ACIP feedback, and assignment of tiers to other groups such as children, pregnant women, and racial/ethnic groups at high risk, Dr. Mbaeyi said.
The goal of the work group is to have a prioritization framework for COVID-19 vaccination to present at the next ACIP meeting.
Committee member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., emphasized that “one of the things we need to know is how is the virus [is] transmitted and who is transmitting,” and that this information will be key to developing strategies for vaccination.
Sarah E. Oliver, MD, an epidemiologist at the National Center for Immunization and Respiratory Diseases, responded that household transmission studies are in progress that will help inform the prioritization process.
Dr. Mbaeyi and Dr. Oliver had no financial conflicts to disclose.
according to Sarah Mbaeyi, MD, MPH, of the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
“Preparing for vaccination during a pandemic has long been a priority of the CDC and the U.S. government,” said Dr. Mbaeyi. The work group is building on a tiered approach to vaccination that was updated in 2018 after the H1N1 flu pandemic, with occupational and high-risk populations placed in the highest-priority groups, Dr. Mbaeyi said.
There are important differences between COVID-19 and influenza, Dr. Mbaeyi said. “Vaccine prioritization is challenging due to incomplete information on COVID-19 epidemiology and vaccines, including characteristics, timing, and number of doses.”
However, guidance for vaccine prioritization developed after the H1N1 outbreak in 2018 can be adapted for COVID-19.
To help inform ACIP deliberations, the work group reviewed the epidemiology of COVID-19. A large proportion of the population remains susceptible, and prioritizations should be based on data to date and continually refined, she said.
The work group defined the objectives of the COVID-19 vaccine program as follows: “Ensure safety and effectiveness of COVID-19 vaccines; reduce transmission, morbidity, and mortality in the population; help minimize disruption to society and economy, including maintaining health care capacity; and ensure equity in vaccine allocation and distribution.”
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said.
However, vaccines will not be administered until safety and efficacy have been demonstrated, she emphasized. The timing and number of vaccine doses are unknown, and subprioritization may be needed, assuming the vaccine becomes available in incremental quantities over several months.
Next steps for the work group are refinement of priority groups based on ACIP feedback, and assignment of tiers to other groups such as children, pregnant women, and racial/ethnic groups at high risk, Dr. Mbaeyi said.
The goal of the work group is to have a prioritization framework for COVID-19 vaccination to present at the next ACIP meeting.
Committee member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., emphasized that “one of the things we need to know is how is the virus [is] transmitted and who is transmitting,” and that this information will be key to developing strategies for vaccination.
Sarah E. Oliver, MD, an epidemiologist at the National Center for Immunization and Respiratory Diseases, responded that household transmission studies are in progress that will help inform the prioritization process.
Dr. Mbaeyi and Dr. Oliver had no financial conflicts to disclose.
according to Sarah Mbaeyi, MD, MPH, of the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases.
A COVID-19 vaccine work group is developing strategies and identifying priority groups for vaccination to help inform discussions about the use of COVID-19 vaccines, Dr. Mbaeyi said at a virtual meeting of the CDC’s Advisory Committee on Immunization Practices.
“Preparing for vaccination during a pandemic has long been a priority of the CDC and the U.S. government,” said Dr. Mbaeyi. The work group is building on a tiered approach to vaccination that was updated in 2018 after the H1N1 flu pandemic, with occupational and high-risk populations placed in the highest-priority groups, Dr. Mbaeyi said.
There are important differences between COVID-19 and influenza, Dr. Mbaeyi said. “Vaccine prioritization is challenging due to incomplete information on COVID-19 epidemiology and vaccines, including characteristics, timing, and number of doses.”
However, guidance for vaccine prioritization developed after the H1N1 outbreak in 2018 can be adapted for COVID-19.
To help inform ACIP deliberations, the work group reviewed the epidemiology of COVID-19. A large proportion of the population remains susceptible, and prioritizations should be based on data to date and continually refined, she said.
The work group defined the objectives of the COVID-19 vaccine program as follows: “Ensure safety and effectiveness of COVID-19 vaccines; reduce transmission, morbidity, and mortality in the population; help minimize disruption to society and economy, including maintaining health care capacity; and ensure equity in vaccine allocation and distribution.”
Based on current information, the work group has proposed that vaccine priority be given to health care personnel, essential workers, adults aged 65 years and older, long-term care facility residents, and persons with high-risk medical conditions.
Among these groups “a subset of critical health care and other workers should receive initial doses,” Dr. Mbaeyi said.
However, vaccines will not be administered until safety and efficacy have been demonstrated, she emphasized. The timing and number of vaccine doses are unknown, and subprioritization may be needed, assuming the vaccine becomes available in incremental quantities over several months.
Next steps for the work group are refinement of priority groups based on ACIP feedback, and assignment of tiers to other groups such as children, pregnant women, and racial/ethnic groups at high risk, Dr. Mbaeyi said.
The goal of the work group is to have a prioritization framework for COVID-19 vaccination to present at the next ACIP meeting.
Committee member Helen Keipp Talbot, MD, of Vanderbilt University, Nashville, Tenn., emphasized that “one of the things we need to know is how is the virus [is] transmitted and who is transmitting,” and that this information will be key to developing strategies for vaccination.
Sarah E. Oliver, MD, an epidemiologist at the National Center for Immunization and Respiratory Diseases, responded that household transmission studies are in progress that will help inform the prioritization process.
Dr. Mbaeyi and Dr. Oliver had no financial conflicts to disclose.
Older adults boost muscle mass after bariatric surgery
Bariatric surgery may yield increases in muscle mass from baseline among older adults, findings from a small study suggest.
Although bariatric surgery can be used to treat obesity and related comorbidities in older adults, “here are concerns of excess loss of muscle mass after bariatric surgery, especially in elderly patients whose muscle tends to be less, compared to younger patients, at baseline,” wrote Moiz Dawood, MD, of Banner Gateway Medical Center, Gilbert, Ariz., and colleagues.
In a study presented in a poster at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education, the researchers reviewed data from 89 adults older than 65 years (74% women) who underwent either laparoscopic sleeve gastrectomy (87 patients) or Roux-en-Y gastric bypass (2 patients) between May 2015 and March 2017.
At baseline, the average total body weight was 251 pounds and the average muscle mass percent was 50%. At 12 months after surgery, the average weight of the patients decreased to 197 pounds and the percentage of muscle mass increased to 55% (P < .001 for both).
The study findings were limited by the small sample size and retrospective design. However, the results support the benefits of bariatric surgery for older adults, not only with reductions in total body weight loss, but also increasing the total percentage of muscle mass, the researchers said.
The study is important in light of the ongoing discussion regarding the age limit for bariatric surgery, Dr. Dawood said in an interview. “Currently there is no upper age cutoff for patients who undergo bariatric surgery, and understanding the relationship between muscle mass and bariatric surgery would help in determining if there was a negative relationship,” he said.
“The results definitely point toward evidence that suggests that elderly patients do not lose muscle mass to a significant degree,” Dr. Dawood noted. “Muscle mass definitions and calculations also include variables such as weight and fat content. With the additional loss in weight after surgery, it was expected that the muscle mass composition would be affected,” he explained. “However, the results clearly show that even up to 1 year after surgery, older patients who lose weight do not lose significant weight from their muscle mass,” he noted.
The take-home message for clinicians, said Dr. Dawood, is “to understand that metabolic and bariatric surgery, when performed cohesively in a unified program that focuses on lifestyle and dietary changes, is the best way to achieve sustained weight loss.” He added, “this study indicates that physiologic changes that occur after weight loss surgery are not detrimental in the elderly population.”
Next steps for research include further studies in the elderly population to examine the physiologic changes that occur after weight loss surgery, said Dr. Dawood. “Being able to characterize the metabolic changes will help in answering the question of whether there is an upper age cut-off for patients undergoing bariatric surgery.”
Global Academy for Medical Education and this news organization are owned by the same parent company. The researchers had no relevant financial conflicts to disclose.
Bariatric surgery may yield increases in muscle mass from baseline among older adults, findings from a small study suggest.
Although bariatric surgery can be used to treat obesity and related comorbidities in older adults, “here are concerns of excess loss of muscle mass after bariatric surgery, especially in elderly patients whose muscle tends to be less, compared to younger patients, at baseline,” wrote Moiz Dawood, MD, of Banner Gateway Medical Center, Gilbert, Ariz., and colleagues.
In a study presented in a poster at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education, the researchers reviewed data from 89 adults older than 65 years (74% women) who underwent either laparoscopic sleeve gastrectomy (87 patients) or Roux-en-Y gastric bypass (2 patients) between May 2015 and March 2017.
At baseline, the average total body weight was 251 pounds and the average muscle mass percent was 50%. At 12 months after surgery, the average weight of the patients decreased to 197 pounds and the percentage of muscle mass increased to 55% (P < .001 for both).
The study findings were limited by the small sample size and retrospective design. However, the results support the benefits of bariatric surgery for older adults, not only with reductions in total body weight loss, but also increasing the total percentage of muscle mass, the researchers said.
The study is important in light of the ongoing discussion regarding the age limit for bariatric surgery, Dr. Dawood said in an interview. “Currently there is no upper age cutoff for patients who undergo bariatric surgery, and understanding the relationship between muscle mass and bariatric surgery would help in determining if there was a negative relationship,” he said.
“The results definitely point toward evidence that suggests that elderly patients do not lose muscle mass to a significant degree,” Dr. Dawood noted. “Muscle mass definitions and calculations also include variables such as weight and fat content. With the additional loss in weight after surgery, it was expected that the muscle mass composition would be affected,” he explained. “However, the results clearly show that even up to 1 year after surgery, older patients who lose weight do not lose significant weight from their muscle mass,” he noted.
The take-home message for clinicians, said Dr. Dawood, is “to understand that metabolic and bariatric surgery, when performed cohesively in a unified program that focuses on lifestyle and dietary changes, is the best way to achieve sustained weight loss.” He added, “this study indicates that physiologic changes that occur after weight loss surgery are not detrimental in the elderly population.”
Next steps for research include further studies in the elderly population to examine the physiologic changes that occur after weight loss surgery, said Dr. Dawood. “Being able to characterize the metabolic changes will help in answering the question of whether there is an upper age cut-off for patients undergoing bariatric surgery.”
Global Academy for Medical Education and this news organization are owned by the same parent company. The researchers had no relevant financial conflicts to disclose.
Bariatric surgery may yield increases in muscle mass from baseline among older adults, findings from a small study suggest.
Although bariatric surgery can be used to treat obesity and related comorbidities in older adults, “here are concerns of excess loss of muscle mass after bariatric surgery, especially in elderly patients whose muscle tends to be less, compared to younger patients, at baseline,” wrote Moiz Dawood, MD, of Banner Gateway Medical Center, Gilbert, Ariz., and colleagues.
In a study presented in a poster at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education, the researchers reviewed data from 89 adults older than 65 years (74% women) who underwent either laparoscopic sleeve gastrectomy (87 patients) or Roux-en-Y gastric bypass (2 patients) between May 2015 and March 2017.
At baseline, the average total body weight was 251 pounds and the average muscle mass percent was 50%. At 12 months after surgery, the average weight of the patients decreased to 197 pounds and the percentage of muscle mass increased to 55% (P < .001 for both).
The study findings were limited by the small sample size and retrospective design. However, the results support the benefits of bariatric surgery for older adults, not only with reductions in total body weight loss, but also increasing the total percentage of muscle mass, the researchers said.
The study is important in light of the ongoing discussion regarding the age limit for bariatric surgery, Dr. Dawood said in an interview. “Currently there is no upper age cutoff for patients who undergo bariatric surgery, and understanding the relationship between muscle mass and bariatric surgery would help in determining if there was a negative relationship,” he said.
“The results definitely point toward evidence that suggests that elderly patients do not lose muscle mass to a significant degree,” Dr. Dawood noted. “Muscle mass definitions and calculations also include variables such as weight and fat content. With the additional loss in weight after surgery, it was expected that the muscle mass composition would be affected,” he explained. “However, the results clearly show that even up to 1 year after surgery, older patients who lose weight do not lose significant weight from their muscle mass,” he noted.
The take-home message for clinicians, said Dr. Dawood, is “to understand that metabolic and bariatric surgery, when performed cohesively in a unified program that focuses on lifestyle and dietary changes, is the best way to achieve sustained weight loss.” He added, “this study indicates that physiologic changes that occur after weight loss surgery are not detrimental in the elderly population.”
Next steps for research include further studies in the elderly population to examine the physiologic changes that occur after weight loss surgery, said Dr. Dawood. “Being able to characterize the metabolic changes will help in answering the question of whether there is an upper age cut-off for patients undergoing bariatric surgery.”
Global Academy for Medical Education and this news organization are owned by the same parent company. The researchers had no relevant financial conflicts to disclose.
FROM MISS
Daily Recap: Higher risk of severe COVID-19 seen in pregnancy, primary care practices at risk
Here are the stories our MDedge editors across specialties think you need to know about today:
Pregnant women at higher risk for severe COVID-19
Pregnant women may be at increased risk for severe COVID-19 illness, according to a report published online June 26 in Morbidity and Mortality Weekly Report.
Among reproductive-aged women (15-44 years) infected with SARS-CoV-2, pregnancy was associated with a greater likelihood of hospitalization, admission to the intensive care unit (ICU), and mechanical ventilation, but not death. Pregnant women were 5.4 times more likely to be hospitalized, 1.5 times more likely to be admitted to the ICU, and 1.7 times more likely to need mechanical ventilation, after adjustment for age, underlying conditions, and race/ethnicity.
CDC researchers said that preventing COVID-19 infection in pregnant women should be a priority and any potential barriers to compliance with preventive measures need to be removed.
“During pregnancy, women experience immunologic and physiologic changes that could increase their risk for more severe illness from respiratory infections,” they wrote. Read more.
Going out of business: Primary care practices at risk
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. In an interview with Kenny Lin, MD, MPH, a family physician, Dr. Frieden discussed the future of primary care.
Here is a sample of Dr. Frieden’s observations:
“When I’ve looked around the United States, I’ve been extremely concerned about both the risk that primary care practitioners are subjected to in their everyday practice and the economic risk that we could lose many of our primary care practices around the country. It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.” Read more.
Surge in out-of-hospital cardiac arrests
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests that placed a huge burden on first responders, according to a new analysis.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
Read more.
Fenfluramine approved for Dravet syndrome
The U.S. Food and Drug Administration has approved fenfluramine (Fintepla, Zogenix) oral solution, a Schedule IV controlled substance, for the treatment of seizures associated with Dravet syndrome in children age 2 years and older.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy.
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Pregnant women at higher risk for severe COVID-19
Pregnant women may be at increased risk for severe COVID-19 illness, according to a report published online June 26 in Morbidity and Mortality Weekly Report.
Among reproductive-aged women (15-44 years) infected with SARS-CoV-2, pregnancy was associated with a greater likelihood of hospitalization, admission to the intensive care unit (ICU), and mechanical ventilation, but not death. Pregnant women were 5.4 times more likely to be hospitalized, 1.5 times more likely to be admitted to the ICU, and 1.7 times more likely to need mechanical ventilation, after adjustment for age, underlying conditions, and race/ethnicity.
CDC researchers said that preventing COVID-19 infection in pregnant women should be a priority and any potential barriers to compliance with preventive measures need to be removed.
“During pregnancy, women experience immunologic and physiologic changes that could increase their risk for more severe illness from respiratory infections,” they wrote. Read more.
Going out of business: Primary care practices at risk
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. In an interview with Kenny Lin, MD, MPH, a family physician, Dr. Frieden discussed the future of primary care.
Here is a sample of Dr. Frieden’s observations:
“When I’ve looked around the United States, I’ve been extremely concerned about both the risk that primary care practitioners are subjected to in their everyday practice and the economic risk that we could lose many of our primary care practices around the country. It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.” Read more.
Surge in out-of-hospital cardiac arrests
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests that placed a huge burden on first responders, according to a new analysis.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
Read more.
Fenfluramine approved for Dravet syndrome
The U.S. Food and Drug Administration has approved fenfluramine (Fintepla, Zogenix) oral solution, a Schedule IV controlled substance, for the treatment of seizures associated with Dravet syndrome in children age 2 years and older.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy.
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Pregnant women at higher risk for severe COVID-19
Pregnant women may be at increased risk for severe COVID-19 illness, according to a report published online June 26 in Morbidity and Mortality Weekly Report.
Among reproductive-aged women (15-44 years) infected with SARS-CoV-2, pregnancy was associated with a greater likelihood of hospitalization, admission to the intensive care unit (ICU), and mechanical ventilation, but not death. Pregnant women were 5.4 times more likely to be hospitalized, 1.5 times more likely to be admitted to the ICU, and 1.7 times more likely to need mechanical ventilation, after adjustment for age, underlying conditions, and race/ethnicity.
CDC researchers said that preventing COVID-19 infection in pregnant women should be a priority and any potential barriers to compliance with preventive measures need to be removed.
“During pregnancy, women experience immunologic and physiologic changes that could increase their risk for more severe illness from respiratory infections,” they wrote. Read more.
Going out of business: Primary care practices at risk
In a recently published editorial, Tom Frieden, MD, MPH, former head of the Centers for Disease Control and Prevention, argued that primary care is in deep trouble, its long-standing financial problems exacerbated by the fallout from the COVID-19 pandemic. In an interview with Kenny Lin, MD, MPH, a family physician, Dr. Frieden discussed the future of primary care.
Here is a sample of Dr. Frieden’s observations:
“When I’ve looked around the United States, I’ve been extremely concerned about both the risk that primary care practitioners are subjected to in their everyday practice and the economic risk that we could lose many of our primary care practices around the country. It’s really striking to see that the number of visits has plummeted. Because of our payment structure, that means incomes have plummeted. We’re hearing about doctors’ offices getting boarded up and shuttering. As I write in the piece, it’s one thing for a theater or a restaurant or another important community entity to shut because of economic downturn, and these are real losses, but to lose their only primary care practice or one of the few in an area really is a matter of life and death for many communities.” Read more.
Surge in out-of-hospital cardiac arrests
The COVID-19 pandemic in New York City led to a surge in out-of-hospital cardiac arrests that placed a huge burden on first responders, according to a new analysis.
During the height of the pandemic in New York, there was a “dramatic increase in cardiopulmonary arrests, nearly all presented in non-shockable cardiac rhythms (> 90% fatality rate) and vulnerable patient populations were most affected,” David J. Prezant, MD, chief medical officer, Fire Department of New York (FDNY), said in an interview.
In a news release, Dr. Prezant noted that “relatively few, if any, patients were tested to confirm the presence of COVID-19,” making it impossible to distinguish between cardiac arrests as a result of COVID-19 and those that may have resulted from other health conditions.
“We also can’t rule out the possibility that some people may have died from delays in seeking or receiving treatment for non–COVID-19-related conditions. However, the dramatic increase in cardiac arrests compared to the same period in 2019 strongly indicates that the pandemic was directly or indirectly responsible for that surge in cardiac arrests and deaths,” said Dr. Prezant.
The study was published online June 19 in JAMA Cardiology.
Read more.
Fenfluramine approved for Dravet syndrome
The U.S. Food and Drug Administration has approved fenfluramine (Fintepla, Zogenix) oral solution, a Schedule IV controlled substance, for the treatment of seizures associated with Dravet syndrome in children age 2 years and older.
Dravet syndrome is a rare childhood-onset epilepsy characterized by frequent, drug-resistant convulsive seizures that may contribute to intellectual disability and impairments in motor control, behavior, and cognition, as well as an increased risk of sudden unexpected death in epilepsy.
Dravet syndrome takes a “tremendous toll on both patients and their families. Fintepla offers an additional effective treatment option for the treatment of seizures associated with Dravet syndrome,” Billy Dunn, MD, director, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, said in a news release. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Endoscopic full-thickness resection of colorectal lesions appears safe and effective
Endoscopic full-thickness resection (eFTR) of complex colorectal lesions appears safe and effective, based on prospective data from 20 Dutch hospitals.
Macroscopic complete en bloc resection was achieved in 83.9% of procedures with an adverse event rate of 9.3%, reported lead author Liselotte W. Zwager, a PhD candidate at the University of Amsterdam, and colleagues.
“With the advantage of enabling a transmural resection, eFTR offers an alternative to radical surgery in lesions considered incurable with current resection techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD),” the investigators wrote in Endoscopy.
But more data are needed for widespread adoption, they noted. “Several studies have reported encouraging results on the short-term safety and efficacy of eFTR for numerous indications. However, firm conclusions on clinical results will require analysis of large prospective series of patients in everyday clinical practice.”
The present study provided data from 362 patients who underwent 367 procedures at 5 academic and 15 nonacademic centers in the Netherlands.
Patients were eligible for eFTR if polyps were nonlifting or in difficult-to-reach locations, or if T1 colorectal cancer (CRC) was suspected. In addition, eFTR was performed for subepithelial tumors, and as secondary completion treatment after incomplete endoscopic resection of T1 CRC with a positive or nonassessable resection margin. Lesions greater than 30 mm were excluded because of device diameter constraints.
The primary outcome was macroscopic complete en bloc resection. Secondary outcomes included adverse events, full-thickness resection rate, and clinical success, the latter of which was defined by tumor-free resection margins (R0).
Out of 367 procedures, eFTR was most frequently conducted because of incomplete resection of T1 CRC (41%), followed by nonlifting or difficult-to-reach polyps (36%), suspected T1 CRC (19%), and least often, subepithelial tumors (4%).
Complete en bloc resection was achieved in 83.9% of procedures. Excluding 21 procedures in which eFTR was not performed because of inaccessibility of the lesion (n = 7) or immobility of tissue prohibiting retraction of the lesion into the cap (n = 14), R0 was achieved in 82.4% of cases. Among the same group, full-thickness resection rate was comparable, at 83.2%.
Adverse events occurred in 34 patients (9.3%), among whom 10 (2.7%) underwent emergency surgery for perforations or appendicitis.
“In conclusion,” the investigators wrote, “eFTR is an exciting, innovative resection technique that is clinically feasible and safe for complex colorectal lesions, with the potential to obviate the need for surgical resection. Further efficacy studies on eFTR as a primary and secondary treatment option for T1 CRC are needed, focusing on both the short- and long-term oncologic results.”
Peter V. Draganov, MD, of the University of Florida, Gainesville, called the R0 resection rate “respectable,” and suggested that the study “reconfirms on a larger scale that eFTR with the full-thickness resection device is successful in the majority of cases.”
“The full-thickness resection device expands our armamentarium to remove difficult polyps and early CRC,” he said.
Still, Dr. Draganov, who has previously advised careful patient selection for eFTR, noted certain drawbacks of the technique. “The presented data highlight some of the limitations of the full-thickness resection device, including the relatively small size of the lesion [median diameter, 23 mm] that can be resected, and challenges related to accessing and capturing the lesion due to the limited visibility and maneuverability of the device.”
Ultimately, Dr. Draganov supported the investigators’ call for more data. “Before eFTR becomes a primary modality for management of T1 CRC, we do need follow-up data on long-term cancer-related outcomes,” he said.
The study was supported by Ovesco Endoscopy. The investigators disclosed additional relationships with Cook, Ethicon, Olympus, and others.
SOURCE: Zwager LW et al. Endoscopy. 2020 Jun 4. doi: 10.1055/a-1176-1107.
Endoscopic full-thickness resection (eFTR) of complex colorectal lesions appears safe and effective, based on prospective data from 20 Dutch hospitals.
Macroscopic complete en bloc resection was achieved in 83.9% of procedures with an adverse event rate of 9.3%, reported lead author Liselotte W. Zwager, a PhD candidate at the University of Amsterdam, and colleagues.
“With the advantage of enabling a transmural resection, eFTR offers an alternative to radical surgery in lesions considered incurable with current resection techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD),” the investigators wrote in Endoscopy.
But more data are needed for widespread adoption, they noted. “Several studies have reported encouraging results on the short-term safety and efficacy of eFTR for numerous indications. However, firm conclusions on clinical results will require analysis of large prospective series of patients in everyday clinical practice.”
The present study provided data from 362 patients who underwent 367 procedures at 5 academic and 15 nonacademic centers in the Netherlands.
Patients were eligible for eFTR if polyps were nonlifting or in difficult-to-reach locations, or if T1 colorectal cancer (CRC) was suspected. In addition, eFTR was performed for subepithelial tumors, and as secondary completion treatment after incomplete endoscopic resection of T1 CRC with a positive or nonassessable resection margin. Lesions greater than 30 mm were excluded because of device diameter constraints.
The primary outcome was macroscopic complete en bloc resection. Secondary outcomes included adverse events, full-thickness resection rate, and clinical success, the latter of which was defined by tumor-free resection margins (R0).
Out of 367 procedures, eFTR was most frequently conducted because of incomplete resection of T1 CRC (41%), followed by nonlifting or difficult-to-reach polyps (36%), suspected T1 CRC (19%), and least often, subepithelial tumors (4%).
Complete en bloc resection was achieved in 83.9% of procedures. Excluding 21 procedures in which eFTR was not performed because of inaccessibility of the lesion (n = 7) or immobility of tissue prohibiting retraction of the lesion into the cap (n = 14), R0 was achieved in 82.4% of cases. Among the same group, full-thickness resection rate was comparable, at 83.2%.
Adverse events occurred in 34 patients (9.3%), among whom 10 (2.7%) underwent emergency surgery for perforations or appendicitis.
“In conclusion,” the investigators wrote, “eFTR is an exciting, innovative resection technique that is clinically feasible and safe for complex colorectal lesions, with the potential to obviate the need for surgical resection. Further efficacy studies on eFTR as a primary and secondary treatment option for T1 CRC are needed, focusing on both the short- and long-term oncologic results.”
Peter V. Draganov, MD, of the University of Florida, Gainesville, called the R0 resection rate “respectable,” and suggested that the study “reconfirms on a larger scale that eFTR with the full-thickness resection device is successful in the majority of cases.”
“The full-thickness resection device expands our armamentarium to remove difficult polyps and early CRC,” he said.
Still, Dr. Draganov, who has previously advised careful patient selection for eFTR, noted certain drawbacks of the technique. “The presented data highlight some of the limitations of the full-thickness resection device, including the relatively small size of the lesion [median diameter, 23 mm] that can be resected, and challenges related to accessing and capturing the lesion due to the limited visibility and maneuverability of the device.”
Ultimately, Dr. Draganov supported the investigators’ call for more data. “Before eFTR becomes a primary modality for management of T1 CRC, we do need follow-up data on long-term cancer-related outcomes,” he said.
The study was supported by Ovesco Endoscopy. The investigators disclosed additional relationships with Cook, Ethicon, Olympus, and others.
SOURCE: Zwager LW et al. Endoscopy. 2020 Jun 4. doi: 10.1055/a-1176-1107.
Endoscopic full-thickness resection (eFTR) of complex colorectal lesions appears safe and effective, based on prospective data from 20 Dutch hospitals.
Macroscopic complete en bloc resection was achieved in 83.9% of procedures with an adverse event rate of 9.3%, reported lead author Liselotte W. Zwager, a PhD candidate at the University of Amsterdam, and colleagues.
“With the advantage of enabling a transmural resection, eFTR offers an alternative to radical surgery in lesions considered incurable with current resection techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD),” the investigators wrote in Endoscopy.
But more data are needed for widespread adoption, they noted. “Several studies have reported encouraging results on the short-term safety and efficacy of eFTR for numerous indications. However, firm conclusions on clinical results will require analysis of large prospective series of patients in everyday clinical practice.”
The present study provided data from 362 patients who underwent 367 procedures at 5 academic and 15 nonacademic centers in the Netherlands.
Patients were eligible for eFTR if polyps were nonlifting or in difficult-to-reach locations, or if T1 colorectal cancer (CRC) was suspected. In addition, eFTR was performed for subepithelial tumors, and as secondary completion treatment after incomplete endoscopic resection of T1 CRC with a positive or nonassessable resection margin. Lesions greater than 30 mm were excluded because of device diameter constraints.
The primary outcome was macroscopic complete en bloc resection. Secondary outcomes included adverse events, full-thickness resection rate, and clinical success, the latter of which was defined by tumor-free resection margins (R0).
Out of 367 procedures, eFTR was most frequently conducted because of incomplete resection of T1 CRC (41%), followed by nonlifting or difficult-to-reach polyps (36%), suspected T1 CRC (19%), and least often, subepithelial tumors (4%).
Complete en bloc resection was achieved in 83.9% of procedures. Excluding 21 procedures in which eFTR was not performed because of inaccessibility of the lesion (n = 7) or immobility of tissue prohibiting retraction of the lesion into the cap (n = 14), R0 was achieved in 82.4% of cases. Among the same group, full-thickness resection rate was comparable, at 83.2%.
Adverse events occurred in 34 patients (9.3%), among whom 10 (2.7%) underwent emergency surgery for perforations or appendicitis.
“In conclusion,” the investigators wrote, “eFTR is an exciting, innovative resection technique that is clinically feasible and safe for complex colorectal lesions, with the potential to obviate the need for surgical resection. Further efficacy studies on eFTR as a primary and secondary treatment option for T1 CRC are needed, focusing on both the short- and long-term oncologic results.”
Peter V. Draganov, MD, of the University of Florida, Gainesville, called the R0 resection rate “respectable,” and suggested that the study “reconfirms on a larger scale that eFTR with the full-thickness resection device is successful in the majority of cases.”
“The full-thickness resection device expands our armamentarium to remove difficult polyps and early CRC,” he said.
Still, Dr. Draganov, who has previously advised careful patient selection for eFTR, noted certain drawbacks of the technique. “The presented data highlight some of the limitations of the full-thickness resection device, including the relatively small size of the lesion [median diameter, 23 mm] that can be resected, and challenges related to accessing and capturing the lesion due to the limited visibility and maneuverability of the device.”
Ultimately, Dr. Draganov supported the investigators’ call for more data. “Before eFTR becomes a primary modality for management of T1 CRC, we do need follow-up data on long-term cancer-related outcomes,” he said.
The study was supported by Ovesco Endoscopy. The investigators disclosed additional relationships with Cook, Ethicon, Olympus, and others.
SOURCE: Zwager LW et al. Endoscopy. 2020 Jun 4. doi: 10.1055/a-1176-1107.
FROM ENDOSCOPY
First reported U.S. case of COVID-19 linked to Guillain-Barré syndrome
further supporting a link between the virus and neurologic complications, including GBS.
Physicians in China reported the first case of COVID-19 that initially presented as acute GBS. The patient was a 61-year-old woman returning home from Wuhan during the pandemic.
Subsequently, physicians in Italy reported five cases of GBS in association with COVID-19.
The first U.S. case is described in the June issue of the Journal of Clinical Neuromuscular Disease.
Like cases from China and Italy, the U.S. patient’s symptoms of GBS reportedly occurred within days of being infected with SARS-CoV-2. “This onset is similar to a case report of acute Zika virus infection with concurrent GBS suggesting a parainfectious complication,” first author Sandeep Rana, MD, and colleagues noted.
The 54-year-old man was transferred to Allegheny General Hospital after developing ascending limb weakness and numbness that followed symptoms of a respiratory infection. Two weeks earlier, he initially developed rhinorrhea, odynophagia, fevers, chills, and night sweats. The man reported that his wife had tested positive for COVID-19 and that his symptoms started soon after her illness. The man also tested positive for COVID-19.
His deficits were characterized by quadriparesis and areflexia, burning dysesthesias, mild ophthalmoparesis, and dysautonomia. He did not have the loss of smell and taste documented in other COVID-19 patients. He briefly required mechanical ventilation and was successfully weaned after receiving a course of intravenous immunoglobulin.
Compared with other cases reported in the literature, the unique clinical features in the U.S. case are urinary retention secondary to dysautonomia and ocular symptoms of diplopia. These highlight the variability in the clinical presentation of GBS associated with COVID-19, the researchers noted.
They added that, with the Pittsburgh patient, electrophysiological findings were typical of demyelinating polyneuropathy seen in patients with GBS. The case series from Italy suggests that axonal variants could be as common in COVID-19–associated GBS.
“Although the number of documented cases internationally is notably small to date, it’s not completely surprising that a COVID-19 diagnosis may lead to a patient developing GBS. The increase of inflammation and inflammatory cells caused by the infection may trigger an irregular immune response that leads to the hallmark symptoms of this neurological disorder,” Dr. Rana said in a news release.
“Since GBS can significantly affect the respiratory system and other vital organs being pushed into overdrive during a COVID-19 immune response, it will be critically important to further investigate and understand this potential connection,” he added.
A version of this article originally appeared on Medscape.com.
further supporting a link between the virus and neurologic complications, including GBS.
Physicians in China reported the first case of COVID-19 that initially presented as acute GBS. The patient was a 61-year-old woman returning home from Wuhan during the pandemic.
Subsequently, physicians in Italy reported five cases of GBS in association with COVID-19.
The first U.S. case is described in the June issue of the Journal of Clinical Neuromuscular Disease.
Like cases from China and Italy, the U.S. patient’s symptoms of GBS reportedly occurred within days of being infected with SARS-CoV-2. “This onset is similar to a case report of acute Zika virus infection with concurrent GBS suggesting a parainfectious complication,” first author Sandeep Rana, MD, and colleagues noted.
The 54-year-old man was transferred to Allegheny General Hospital after developing ascending limb weakness and numbness that followed symptoms of a respiratory infection. Two weeks earlier, he initially developed rhinorrhea, odynophagia, fevers, chills, and night sweats. The man reported that his wife had tested positive for COVID-19 and that his symptoms started soon after her illness. The man also tested positive for COVID-19.
His deficits were characterized by quadriparesis and areflexia, burning dysesthesias, mild ophthalmoparesis, and dysautonomia. He did not have the loss of smell and taste documented in other COVID-19 patients. He briefly required mechanical ventilation and was successfully weaned after receiving a course of intravenous immunoglobulin.
Compared with other cases reported in the literature, the unique clinical features in the U.S. case are urinary retention secondary to dysautonomia and ocular symptoms of diplopia. These highlight the variability in the clinical presentation of GBS associated with COVID-19, the researchers noted.
They added that, with the Pittsburgh patient, electrophysiological findings were typical of demyelinating polyneuropathy seen in patients with GBS. The case series from Italy suggests that axonal variants could be as common in COVID-19–associated GBS.
“Although the number of documented cases internationally is notably small to date, it’s not completely surprising that a COVID-19 diagnosis may lead to a patient developing GBS. The increase of inflammation and inflammatory cells caused by the infection may trigger an irregular immune response that leads to the hallmark symptoms of this neurological disorder,” Dr. Rana said in a news release.
“Since GBS can significantly affect the respiratory system and other vital organs being pushed into overdrive during a COVID-19 immune response, it will be critically important to further investigate and understand this potential connection,” he added.
A version of this article originally appeared on Medscape.com.
further supporting a link between the virus and neurologic complications, including GBS.
Physicians in China reported the first case of COVID-19 that initially presented as acute GBS. The patient was a 61-year-old woman returning home from Wuhan during the pandemic.
Subsequently, physicians in Italy reported five cases of GBS in association with COVID-19.
The first U.S. case is described in the June issue of the Journal of Clinical Neuromuscular Disease.
Like cases from China and Italy, the U.S. patient’s symptoms of GBS reportedly occurred within days of being infected with SARS-CoV-2. “This onset is similar to a case report of acute Zika virus infection with concurrent GBS suggesting a parainfectious complication,” first author Sandeep Rana, MD, and colleagues noted.
The 54-year-old man was transferred to Allegheny General Hospital after developing ascending limb weakness and numbness that followed symptoms of a respiratory infection. Two weeks earlier, he initially developed rhinorrhea, odynophagia, fevers, chills, and night sweats. The man reported that his wife had tested positive for COVID-19 and that his symptoms started soon after her illness. The man also tested positive for COVID-19.
His deficits were characterized by quadriparesis and areflexia, burning dysesthesias, mild ophthalmoparesis, and dysautonomia. He did not have the loss of smell and taste documented in other COVID-19 patients. He briefly required mechanical ventilation and was successfully weaned after receiving a course of intravenous immunoglobulin.
Compared with other cases reported in the literature, the unique clinical features in the U.S. case are urinary retention secondary to dysautonomia and ocular symptoms of diplopia. These highlight the variability in the clinical presentation of GBS associated with COVID-19, the researchers noted.
They added that, with the Pittsburgh patient, electrophysiological findings were typical of demyelinating polyneuropathy seen in patients with GBS. The case series from Italy suggests that axonal variants could be as common in COVID-19–associated GBS.
“Although the number of documented cases internationally is notably small to date, it’s not completely surprising that a COVID-19 diagnosis may lead to a patient developing GBS. The increase of inflammation and inflammatory cells caused by the infection may trigger an irregular immune response that leads to the hallmark symptoms of this neurological disorder,” Dr. Rana said in a news release.
“Since GBS can significantly affect the respiratory system and other vital organs being pushed into overdrive during a COVID-19 immune response, it will be critically important to further investigate and understand this potential connection,” he added.
A version of this article originally appeared on Medscape.com.
What COVID-19 has taught us about senior care
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at [email protected]. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at [email protected].
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at [email protected]. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at [email protected].
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
Across the globe, there are marked differences in how countries responded to the COVID-19 outbreak, with varying degrees of success in limiting the spread of the virus. Some countries learned important lessons from previous outbreaks, including SARS and MERS, and put policies in place that contributed to lower infection and death rates from COVID-19 in these countries. Others struggled to respond appropriately to the outbreak.
The United States and most of the world was not affected significantly by SARS and MERS. Hence there is a need for different perspectives and observations on lessons that can be learned from this outbreak to help develop effective strategies and policies for the future. It also makes sense to focus intently on the demographic most affected by COVID-19 – the elderly.
Medical care, for the most part, is governed by protocols that clearly detail processes to be followed for the prevention and treatment of disease. Caring for older patients requires going above and beyond the protocols. That is one of the lessons learned from the COVID-19 pandemic – a wake-up call for a more proactive approach for at-risk patients, in this case everyone over the age of 60 years.
In this context, it is important for medical outreach to continue with the senior population long after the pandemic has run its course. Many seniors, particularly those susceptible to other illnesses or exhibiting ongoing issues, would benefit from a consistent and preplanned pattern of contacts by medical professionals and agencies that work with the aging population. These proactive follow-ups can facilitate prevention and treatment and, at the same time, reduce costs that would otherwise increase when health care is reactive.
Lessons in infectious disease containment
As COVID-19 spread globally, there were contrasting responses from individual countries in their efforts to contain the disease. Unfortunately, Italy suffered from its decision to lock down only specific regions of the country initially. The leadership in Italy may have ignored the advice of medical experts and been caught off guard by the intensity of the spread of COVID-19. In fact, they might not have taken strict actions right away because they did not want their responses to be viewed as an overreaction to the disease.
The government decided to shut down areas where the infection rates were high (“red zones”) rather than implement restrictions nationally. This may have inadvertently increased the spread as Italians vacated those “red zones” for other areas of the country not yet affected by COVID-19. Italy’s decentralized health care system also played a part in the effects of the disease, with some regions demonstrating more success in slowing the reach of the disease. According to an article in the Harvard Business Review, the neighboring regions of Lombardy and Veneto applied similar approaches to social distancing and retail closures. Veneto was more proactive, and its response to the outbreak was multipronged, including putting a “strong emphasis on home diagnosis and care” and “specific efforts to monitor and protect health care and other essential workers.” These measures most likely contributed to a slowdown of the spread of the disease in Veneto’s health care facilities, which lessened the load on medical providers.1
Conversely, Taiwan implemented proactive measures swiftly after learning about COVID-19. Taiwan was impacted adversely by the SARS outbreak in 2003 and, afterward, revised their medical policies and procedures to respond quickly to future infectious disease crises. In the beginning, little was known about COVID-19 or how it spread. However, Taiwan’s swift public health response to COVID-19 included early travel restrictions, patient screening, and quarantining of symptomatic patients. The government emphasized education and created real-time digital updates and alerts sent to their citizens, as well as partnering with media to broadcast crucial proactive health information and quickly disproving false information related to COVID-19. They coordinated with organizations throughout the country to increase supplies of personal protective equipment (PPE).2
Although countries and even cities within a country differ in terms of population demographics, health resources, government policies, and cultural practices, initial success stories have some similarities, including the following:
- Early travel restrictions from countries with positive cases, with some circumstances requiring compulsory quarantine periods and testing before entry.
- Extensive testing and proactive tracing of symptomatic cases early. Contacts of people testing positive were also tested, irrespective of being symptomatic or asymptomatic. If testing kits were unavailable, the contacts were self-quarantined.
- Emphasis on avoiding overburdening hospitals by having the public health infrastructure to divert people exhibiting symptoms, including using public health hotlines to send patients to dedicated testing sites and drive-through testing, rather than have patients presenting to emergency rooms and hospitals. This approach protected medical staff from exposure and allowed the focus to remain on treating severe symptomatic patients.
The vastly different response to the COVID-19 outbreak in these two countries illuminates the need for better preparation in the United States. At the onset of this outbreak, emergency room medical professionals, hospitalists, and outpatient primary care providers did not know how to screen for or treat this virus. Additionally, there was limited information on the most effective contact protocols for medical professionals, patients, and visitors. Finally, the lack of PPE and COVID-19 test kits hindered the U.S. response. Once the country is on the road to recovery from COVID-19, it is imperative to set the groundwork to prepare for future outbreaks and create mechanisms to quickly identify vulnerable populations when outbreaks occur.
Senior care in future infectious disease outbreaks
How can medical providers translate lessons learned from this outbreak into improving the quality of care for seniors? The National Institute on Aging (NIA) maintains a website with information about healthy aging. Seniors and their caregivers can use this website to learn more about chronic diseases, lifestyle modifications, disease prevention, and mental health.
In times of a pandemic, this website provides consistent and accurate information and education. One recommendation for reaching the elderly population during future outbreaks is for NIA to develop and implement strategies to increase the use of the website, including adding more audio and visual interfaces and developing a mobile app. Other recommendations for improving the quality of care for seniors include the following:
1. Identify which populations may be most affected when future outbreaks occur.
2. Consider nontraditional platforms, including social media, for communicating with the general population and for medical providers worldwide to learn from each other about new diseases, including the signs, symptoms, and treatment plans. Some medical professionals created specific WhatsApp groups to communicate, and the World Health Organization sent updated information about COVID-19 to anyone who texted them via WhatsApp.3
3. Create a checklist of signs and symptoms related to current infectious diseases and assess every vulnerable patient.
4. Share these guidelines with medical facilities that treat these populations, such as senior care, assisted living and rehabilitation facilities, hospitals, and outpatient treatment centers. Teach the staff at these medical facilities how to screen patients for signs and symptoms of the disease.
5. Implement social isolation strategies, travel and visitor restrictions, and testing and screening as soon as possible at these medical facilities.
6. Recognize that these strategies may affect the psychological and emotional well-being of seniors, increasing their risk for depression and anxiety and negatively affecting their immunity and mental health. Additionally, the use of PPE, either by the medical providers or the patient, may cause anxiety in seniors and those with mild cognitive impairment.
7. Encourage these medical facilities to improve coping strategies with older patients, such as incorporating communication technology that helps seniors stay connected with their families, and participating in physical and mental exercise, as well as religious activities.
8. Ask these medical facilities to create isolation or quarantine rooms for infected seniors.
9. Work with family members to proactively report to medical professionals any symptoms noticed in their senior relatives. Educate seniors to report symptoms earlier.
10. Offer incentives for medical professionals to conduct on-site testing in primary care offices or senior care facilities instead of sending patients to hospital emergency rooms for evaluation. This will only be effective if there are enough test kits available.
11. Urge insurance companies and Medicare to allow additional medical visits for screening vulnerable populations. Encourage the use of telemedicine in place of in-office visits (preferably billed at the same rate as an in-office visit) where appropriate, especially with nonambulatory patients or those with transportation issues. Many insurance companies, including Medicare, approved COVID-19–related coverage of telemedicine in place of office visits to limit the spread of the disease.
12. Provide community health care and integration and better coordination of local, state, and national health care.
13. Hold regular epidemic and pandemic preparedness exercises in every hospital, nursing home, and assisted living facility.
Proactive health care outreach
It is easier to identify the signs and symptoms of already identified infectious diseases as opposed to a novel one like COVID-19. The United States faced a steep learning curve with COVID-19. Hospitalists and other medical professionals were not able to learn about COVID-19 in a journal. At first, they did not know how to screen patients coming into the ER, how to protect staff, or what the treatment plan was for this new disease. As a result, the medical system experienced disorder and confusion. Investing in community health care and better coordination of local, state, and national health care resources is a priority.
The senior citizen population appears to be most vulnerable to this virus and may be just as vulnerable in future outbreaks. Yet the insights gained from this pandemic can lead to a more comprehensive outreach to senior patients and increased screenings for comorbidities and future contagious diseases. An emphasis on proactive health care and outreach for seniors, with a focus on identifying and treating comorbid conditions, improves the medical care system overall and may prevent or slow future community outbreaks.
Dr. Kasarla is a hospitalist with APOGEE Physicians at Wise Surgical at Parkway in Fort Worth, Tex. He did his internal medicine residency at Mercy Hospital & Medical Center, Chicago. Readers can contact him at [email protected]. Dr. Devireddy is a family physician at Positive Health Medical Center, Kingston, Jamaica. Contact him at [email protected].
References
1. Pisano GP et al. Lessons from Italy’s response to coronavirus. Harvard Business Review. 2020 Mar 27. https://hbr.org/2020/03/lessons-from-italys-response-to-coronavirus.
2. Tu C. Lessons from Taiwan’s experience with COVID-19. New Atlanticist. 2020 Apr 7. https://atlanticcouncil.org/blogs/new-atlanticist/lessons-from-taiwans-experience-with-covid-19/.
3. Newman LH. WhatsApp is at the center of coronavirus response. WIRED. 2020 Mar 20. https://www.wired.com/story/whatsapp-coronavirus-who-information-app/.
COVID-19: Medicare data show long hospital stays, disparities
according to a new analysis by the Centers for Medicare & Medicaid Services.
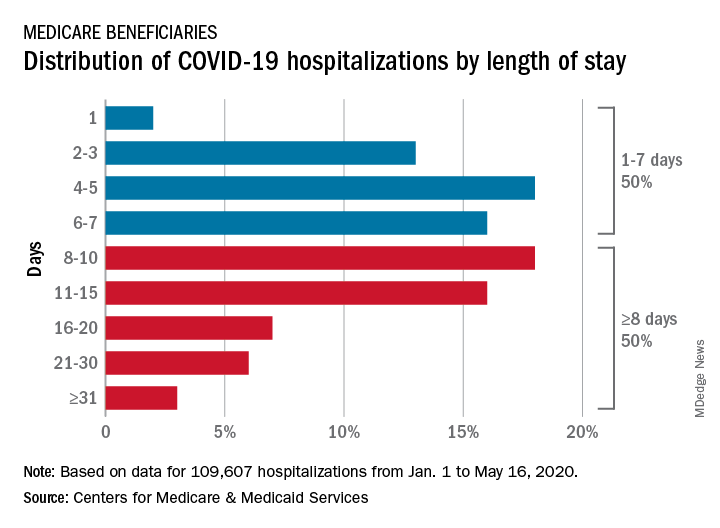
CMS encounter and claims data show almost 110,000 hospital stays for COVID-19 from Jan. 1 to May 16, 2020. Of the longer admissions, 18% were 8-10 days, 16% were 11-15 days, and another 16% were 16 days or longer, the CMS reported in a preliminary data snapshot released June 22.
The hospitalization rate for the Medicare population was 175 per 100,000 as of May 16, but the CMS data show a number of disparities involving race/ethnicity and other demographic characteristics were uncovered, such as the following:
- Black patients were hospitalized for COVID-19 at a much higher rate, at 465 per 100,000 beneficiaries, than were Hispanics (258), Asians (187), and whites (123).
- Residents of urban/suburban areas had a much higher hospitalization rate than did those living in rural areas: 205 versus 57 per 100,000.
- Beneficiaries enrolled in both Medicare and Medicaid had 473 hospitalizations per 100,000, but the rate for those with Medicare only was 112.
“The disparities in the data reflect longstanding challenges facing minority communities and low-income older adults, many of whom face structural challenges to their health that go far beyond what is traditionally considered ‘medical,’ ” CMS Administrator Seema Verma said in a separate statement.
according to a new analysis by the Centers for Medicare & Medicaid Services.
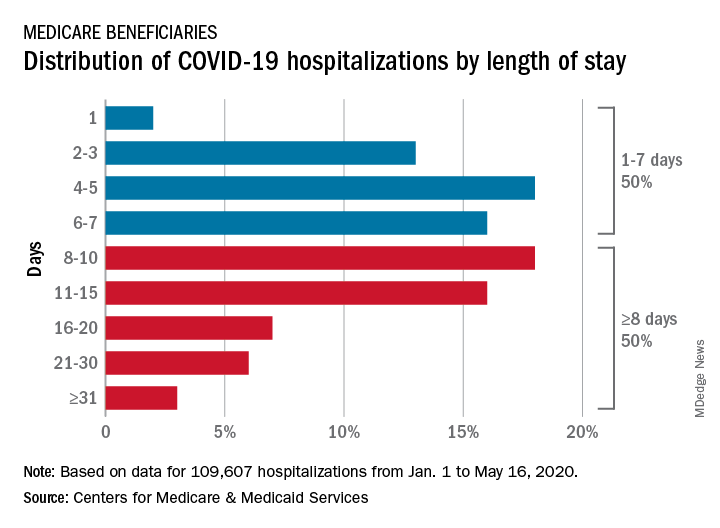
CMS encounter and claims data show almost 110,000 hospital stays for COVID-19 from Jan. 1 to May 16, 2020. Of the longer admissions, 18% were 8-10 days, 16% were 11-15 days, and another 16% were 16 days or longer, the CMS reported in a preliminary data snapshot released June 22.
The hospitalization rate for the Medicare population was 175 per 100,000 as of May 16, but the CMS data show a number of disparities involving race/ethnicity and other demographic characteristics were uncovered, such as the following:
- Black patients were hospitalized for COVID-19 at a much higher rate, at 465 per 100,000 beneficiaries, than were Hispanics (258), Asians (187), and whites (123).
- Residents of urban/suburban areas had a much higher hospitalization rate than did those living in rural areas: 205 versus 57 per 100,000.
- Beneficiaries enrolled in both Medicare and Medicaid had 473 hospitalizations per 100,000, but the rate for those with Medicare only was 112.
“The disparities in the data reflect longstanding challenges facing minority communities and low-income older adults, many of whom face structural challenges to their health that go far beyond what is traditionally considered ‘medical,’ ” CMS Administrator Seema Verma said in a separate statement.
according to a new analysis by the Centers for Medicare & Medicaid Services.
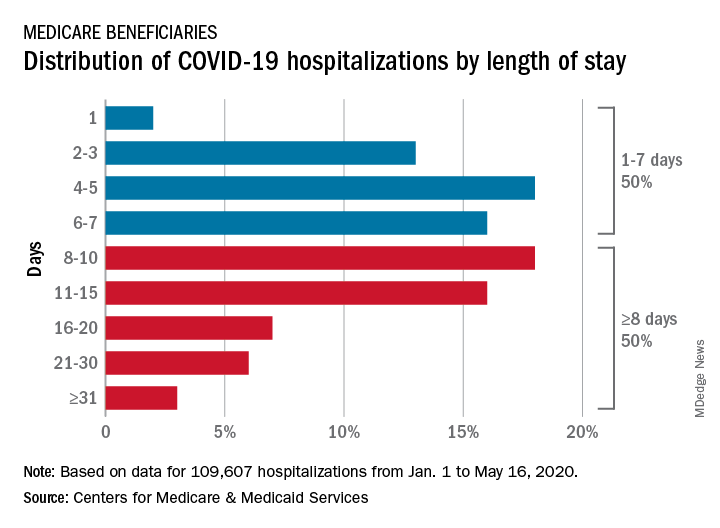
CMS encounter and claims data show almost 110,000 hospital stays for COVID-19 from Jan. 1 to May 16, 2020. Of the longer admissions, 18% were 8-10 days, 16% were 11-15 days, and another 16% were 16 days or longer, the CMS reported in a preliminary data snapshot released June 22.
The hospitalization rate for the Medicare population was 175 per 100,000 as of May 16, but the CMS data show a number of disparities involving race/ethnicity and other demographic characteristics were uncovered, such as the following:
- Black patients were hospitalized for COVID-19 at a much higher rate, at 465 per 100,000 beneficiaries, than were Hispanics (258), Asians (187), and whites (123).
- Residents of urban/suburban areas had a much higher hospitalization rate than did those living in rural areas: 205 versus 57 per 100,000.
- Beneficiaries enrolled in both Medicare and Medicaid had 473 hospitalizations per 100,000, but the rate for those with Medicare only was 112.
“The disparities in the data reflect longstanding challenges facing minority communities and low-income older adults, many of whom face structural challenges to their health that go far beyond what is traditionally considered ‘medical,’ ” CMS Administrator Seema Verma said in a separate statement.
Inside Mercy’s mission to care for non-COVID patients in Los Angeles
When the hospital ship USNS Mercy departed San Diego’s Naval Station North Island on March 23, 2020, to support the Department of Defense efforts in Los Angeles during the coronavirus outbreak, Commander Erin Blevins remembers the crew’s excitement was palpable.
“We normally do partnerships abroad and respond to tsunamis and earthquakes,” said Cdr. Blevins, MD, a pediatric hematologist-oncologist who served as director of medical services for the mission. “This was a slight change in situation, but still disaster relief in the form of a pandemic. We switched our mindset to putting together the best experts for an infectious disease pandemic versus an earthquake disaster relief.”
A new mission

The 1,000-bed Mercy ship – a converted San Clemente–class oil tanker that was delivered in 1986 – spent nearly 50 days pier side in Los Angeles as a referral hospital for non–COVID-19 patients, so that clinicians at Los Angeles area hospitals could care for an anticipated surge of COVID-19 patients. “We went into it with expectations of, ‘We’ll treat as many patients as you need us to take,” Cdr. Blevins recalled. “I don’t even think Los Angeles [health officials] knew exactly where they were going to peak and what the need was going to be.”
Between March 29 and May 15, about 1,071 medical personnel aboard the Mercy cared for 77 patients with an average age of 53 years who were referred from 11 Los Angeles area hospitals. The physicians, nurses, and other medical support personnel were drawn from military treatment facilities across the country. “We had additional people join us as we scoped the mission to be more medically heavy and surgically light,” said Captain John Rotruck, MD, an anesthesiologist who is commanding officer of Mercy’s medical treatment facility. “We did adjust to make sure that we had the right staffing mix to meet the parameters that we were assigned. That was the crux of the change: a change in flavors of staffing to ensure that we focused on ICU and ward medical care as opposed to very heavy surgical care in support of a combat operation.”
About 10% of the team consisted of reservists who volunteered for the mission. “There’s no way you could have walked around the ship and known who was active duty and who was reservist,” said Capt. Rotruck, who was formerly chief of staff at Walter Reed National Military Medical Center, Bethesda, Md. “They worked together so well, and I think that marriage of active duty who are used to working in a military medical treatment facility – in our case, a Navy medical treatment facility – together with our reservist physician colleagues who work in civilian facilities around the country, was beneficial. It was a synergistic relationship. I think both sides walked away learning quite a bit from each other.”
Start with screening
All crew members underwent a temperature check and completed a health screening questionnaire: once before departing their home of record and again before boarding Mercy. Based on those results, crew members and medical staff were screened for COVID-19 and tested as needed in order to minimize the risk of an outbreak aboard the ship.
Fewer than 1% of crew members developed COVID-19 or tested positive for the virus during the mission, according to Capt. Rotruck. Affected individuals were isolated and quarantined. “All staff have recovered and are doing well,” he said.
Mercy personnel worked with local health officials to ensure that all patients transferred to the ship tested negative for COVID-19. Physicians aboard the Mercy then worked directly with the patients’ civilian physician to ensure a safe and thorough turnover process before the patients were transferred.
From basic medical to trauma care

Care aboard the ship, which consists of open-bay medical wards, ranged from basic medical and surgical care to critical care and trauma. The most common procedures were cholecystectomies and orthopedic procedures, and the average length of stay was 4-5 days, according to Cdr. Blevins. Over the course of the mission, the medical professionals conducted 36 surgeries, 77 x-ray exams, 26 CT scans, and administered hundreds of ancillary studies ranging from routine labs to high-end x-rays and blood transfusion support.
“Within our ICU, we did have some end-of-life patients who ended up dying on our ship in comfort care,” Cdr. Blevins said. “Fortunately, we had a wonderful ICU team who had a great deal of experience with end-of-life care and were able to take care of these patients very comfortably and ensure good communication with family and loved ones during that time. In most instances we tried to make sure that people got to FaceTime or video chat with their loved one before they passed away.”

The Mercy, which includes 12 operating rooms, four x-ray units, and one CAT-scan unit, was not equipped to deliver pediatric or obstetrical care. Other unavailable services included psychiatry, oncology, cardiac and thoracic surgery, nuclear medicine, MRI, mammography, electrophysiology, cardiac catheterization, negative-pressure isolation, speech therapy, and occupational therapy.
Not your typical hospital experience
But for patients who did receive medical care aboard the Mercy – which made three 150-day deployments in recent years for the military-led humanitarian response known as Pacific Partnership in 2015, 2016, and 2018 – it was an experience that they are unlikely to forget.
“Every time a patient left the ship, our team on the ground surveyed them to see how their experience was and see what we could do to improve,” Cdr. Blevins said. “Across the board, they were all very appreciative of the medical care. We had a couple of veterans on board. They got [USNS Mercy] hats on their way out and seemed to very much enjoy a slightly different experience than they would get at a regular hospital.”
Capt. Rotruck added that the enthusiasm crew members had for supporting fellow Americans “really energized our team and really saturated that caring aspect of the people who interacted directly with patients,” he said. “It wasn’t just the physicians and nurses, but it was the staff delivering the food and coming to take blood samples and every other interaction that the patients had with our team. I think they really felt that enthusiasm for being there and supporting our neighbors in LA [Los Angeles].”
Crew life aboard the Mercy
Just as with any hospital on shore, personnel aboard the Mercy practiced preventive hygiene measures recommended by the Centers for Disease Control and Prevention to help prevent the spread of COVID-19, such as wearing cloth face masks, spacing out tables in the dining hall, closing indoor gyms, and devising creative ways to stay physically fit. Popular options included jogging around the perimeter of the ship and practicing yoga and calisthenics on the deck, “making sure you were physically distanced appropriately, and when you were done, putting your mask back on,” Cdr. Blevins said. Others supplemented their workouts with a pull-up bar on the deck. “In addition, we have a series of ramps that run on the starboard side of the ship that we can use for patient movement with litters on wheels or patient beds,” Capt. Rotruck said. “The uphill portion of those ramps represents a good workout opportunity as well.”
Downtime in an era of physical distancing also afforded crew members the opportunity to call or FaceTime with loved ones, watch streamed TV shows and movies, and work on their own professional development. Some continued with coursework for online degree programs offered by colleges and universities they were enrolled in, while some enlisted personnel used the time to complete the Navy Enlisted Warfare Qualification Programs Instruction, which issues the basic overarching requirements for the qualification and designation of all enlisted warfare programs.
“As you can imagine, people spend a lot of time learning how the ship works and how it integrates into larger naval forces and so forth,” Capt. Rotruck said. “Not just our ship but also other ships: their weapons systems and defense mechanisms and navigation systems. We had people spending a significant amount of time working on that. We had people complete their Enlisted Surface Warfare qualification while we were on the mission.”
End of the mission
Mercy returned to its home base in San Diego on May 15, but about 60 medical personnel stayed behind in Los Angeles to support Federal Emergency Management Agency (FEMA), state, and local health care professionals. Some worked at a site where clinicians provided care for COVID-19–positive patients who had been transferred from area skilled nursing facilities.
In addition, a team consisting of one nurse and five corpsmen “would go out to individual skilled nursing facilities and mainly conduct assessments and training, such as training in donning proper PPE [personal protective equipment] and determining what needs they had,” Capt. Rotruck said. “They met those needs if possible or [communicated with California officials] and let them know what the requirements were and what the needs were in that facility.” The assignment for those who stayed behind ended on May 31.
On the opposite coast, Mercy’s sister ship, USNS Comfort, arrived in New York Harbor from Norfolk, Va., on March 30 and spent 3½ weeks assisting area hospitals in the COVID-19 pandemic fight. A few days into the mission, Comfort’s internal spaces were reconfigured to create separate COVID-negative and COVID-positive sections. Medical teams aboard the ship cared for a total of 182 patients during the assignment.
Looking back on Mercy’s mission, Cdr. Blevins marveled at the sense of teamwork that unfolded. “We have quarterly training exercises with a core set of personnel, [and] we train getting ready for activation in 5 days,” she said. “All of that training kicks in and it comes to fruition in a mission like this. It was terrific to see a group of very disparate subject matter experts from all over the country come together with one purpose: which was to serve our own country during the pandemic.”
Capt. Rotruck pointed out that the experience enabled enlisted and nonenlisted physicians to maintain their skill sets during a time when military and civilian hospitals had stopped doing elective procedures and routine appointments. “The fact that those people were able to come on board the ship and continue to conduct their medical practice and maintain their skills and competencies in an environment that they weren’t quite used to is great,” he said. “Otherwise, some of those medical personnel would have been sitting idle, wherever they were from. This is the power of Navy medicine on behalf of our country.”
When the hospital ship USNS Mercy departed San Diego’s Naval Station North Island on March 23, 2020, to support the Department of Defense efforts in Los Angeles during the coronavirus outbreak, Commander Erin Blevins remembers the crew’s excitement was palpable.
“We normally do partnerships abroad and respond to tsunamis and earthquakes,” said Cdr. Blevins, MD, a pediatric hematologist-oncologist who served as director of medical services for the mission. “This was a slight change in situation, but still disaster relief in the form of a pandemic. We switched our mindset to putting together the best experts for an infectious disease pandemic versus an earthquake disaster relief.”
A new mission

The 1,000-bed Mercy ship – a converted San Clemente–class oil tanker that was delivered in 1986 – spent nearly 50 days pier side in Los Angeles as a referral hospital for non–COVID-19 patients, so that clinicians at Los Angeles area hospitals could care for an anticipated surge of COVID-19 patients. “We went into it with expectations of, ‘We’ll treat as many patients as you need us to take,” Cdr. Blevins recalled. “I don’t even think Los Angeles [health officials] knew exactly where they were going to peak and what the need was going to be.”
Between March 29 and May 15, about 1,071 medical personnel aboard the Mercy cared for 77 patients with an average age of 53 years who were referred from 11 Los Angeles area hospitals. The physicians, nurses, and other medical support personnel were drawn from military treatment facilities across the country. “We had additional people join us as we scoped the mission to be more medically heavy and surgically light,” said Captain John Rotruck, MD, an anesthesiologist who is commanding officer of Mercy’s medical treatment facility. “We did adjust to make sure that we had the right staffing mix to meet the parameters that we were assigned. That was the crux of the change: a change in flavors of staffing to ensure that we focused on ICU and ward medical care as opposed to very heavy surgical care in support of a combat operation.”
About 10% of the team consisted of reservists who volunteered for the mission. “There’s no way you could have walked around the ship and known who was active duty and who was reservist,” said Capt. Rotruck, who was formerly chief of staff at Walter Reed National Military Medical Center, Bethesda, Md. “They worked together so well, and I think that marriage of active duty who are used to working in a military medical treatment facility – in our case, a Navy medical treatment facility – together with our reservist physician colleagues who work in civilian facilities around the country, was beneficial. It was a synergistic relationship. I think both sides walked away learning quite a bit from each other.”
Start with screening
All crew members underwent a temperature check and completed a health screening questionnaire: once before departing their home of record and again before boarding Mercy. Based on those results, crew members and medical staff were screened for COVID-19 and tested as needed in order to minimize the risk of an outbreak aboard the ship.
Fewer than 1% of crew members developed COVID-19 or tested positive for the virus during the mission, according to Capt. Rotruck. Affected individuals were isolated and quarantined. “All staff have recovered and are doing well,” he said.
Mercy personnel worked with local health officials to ensure that all patients transferred to the ship tested negative for COVID-19. Physicians aboard the Mercy then worked directly with the patients’ civilian physician to ensure a safe and thorough turnover process before the patients were transferred.
From basic medical to trauma care

Care aboard the ship, which consists of open-bay medical wards, ranged from basic medical and surgical care to critical care and trauma. The most common procedures were cholecystectomies and orthopedic procedures, and the average length of stay was 4-5 days, according to Cdr. Blevins. Over the course of the mission, the medical professionals conducted 36 surgeries, 77 x-ray exams, 26 CT scans, and administered hundreds of ancillary studies ranging from routine labs to high-end x-rays and blood transfusion support.
“Within our ICU, we did have some end-of-life patients who ended up dying on our ship in comfort care,” Cdr. Blevins said. “Fortunately, we had a wonderful ICU team who had a great deal of experience with end-of-life care and were able to take care of these patients very comfortably and ensure good communication with family and loved ones during that time. In most instances we tried to make sure that people got to FaceTime or video chat with their loved one before they passed away.”

The Mercy, which includes 12 operating rooms, four x-ray units, and one CAT-scan unit, was not equipped to deliver pediatric or obstetrical care. Other unavailable services included psychiatry, oncology, cardiac and thoracic surgery, nuclear medicine, MRI, mammography, electrophysiology, cardiac catheterization, negative-pressure isolation, speech therapy, and occupational therapy.
Not your typical hospital experience
But for patients who did receive medical care aboard the Mercy – which made three 150-day deployments in recent years for the military-led humanitarian response known as Pacific Partnership in 2015, 2016, and 2018 – it was an experience that they are unlikely to forget.
“Every time a patient left the ship, our team on the ground surveyed them to see how their experience was and see what we could do to improve,” Cdr. Blevins said. “Across the board, they were all very appreciative of the medical care. We had a couple of veterans on board. They got [USNS Mercy] hats on their way out and seemed to very much enjoy a slightly different experience than they would get at a regular hospital.”
Capt. Rotruck added that the enthusiasm crew members had for supporting fellow Americans “really energized our team and really saturated that caring aspect of the people who interacted directly with patients,” he said. “It wasn’t just the physicians and nurses, but it was the staff delivering the food and coming to take blood samples and every other interaction that the patients had with our team. I think they really felt that enthusiasm for being there and supporting our neighbors in LA [Los Angeles].”
Crew life aboard the Mercy
Just as with any hospital on shore, personnel aboard the Mercy practiced preventive hygiene measures recommended by the Centers for Disease Control and Prevention to help prevent the spread of COVID-19, such as wearing cloth face masks, spacing out tables in the dining hall, closing indoor gyms, and devising creative ways to stay physically fit. Popular options included jogging around the perimeter of the ship and practicing yoga and calisthenics on the deck, “making sure you were physically distanced appropriately, and when you were done, putting your mask back on,” Cdr. Blevins said. Others supplemented their workouts with a pull-up bar on the deck. “In addition, we have a series of ramps that run on the starboard side of the ship that we can use for patient movement with litters on wheels or patient beds,” Capt. Rotruck said. “The uphill portion of those ramps represents a good workout opportunity as well.”
Downtime in an era of physical distancing also afforded crew members the opportunity to call or FaceTime with loved ones, watch streamed TV shows and movies, and work on their own professional development. Some continued with coursework for online degree programs offered by colleges and universities they were enrolled in, while some enlisted personnel used the time to complete the Navy Enlisted Warfare Qualification Programs Instruction, which issues the basic overarching requirements for the qualification and designation of all enlisted warfare programs.
“As you can imagine, people spend a lot of time learning how the ship works and how it integrates into larger naval forces and so forth,” Capt. Rotruck said. “Not just our ship but also other ships: their weapons systems and defense mechanisms and navigation systems. We had people spending a significant amount of time working on that. We had people complete their Enlisted Surface Warfare qualification while we were on the mission.”
End of the mission
Mercy returned to its home base in San Diego on May 15, but about 60 medical personnel stayed behind in Los Angeles to support Federal Emergency Management Agency (FEMA), state, and local health care professionals. Some worked at a site where clinicians provided care for COVID-19–positive patients who had been transferred from area skilled nursing facilities.
In addition, a team consisting of one nurse and five corpsmen “would go out to individual skilled nursing facilities and mainly conduct assessments and training, such as training in donning proper PPE [personal protective equipment] and determining what needs they had,” Capt. Rotruck said. “They met those needs if possible or [communicated with California officials] and let them know what the requirements were and what the needs were in that facility.” The assignment for those who stayed behind ended on May 31.
On the opposite coast, Mercy’s sister ship, USNS Comfort, arrived in New York Harbor from Norfolk, Va., on March 30 and spent 3½ weeks assisting area hospitals in the COVID-19 pandemic fight. A few days into the mission, Comfort’s internal spaces were reconfigured to create separate COVID-negative and COVID-positive sections. Medical teams aboard the ship cared for a total of 182 patients during the assignment.
Looking back on Mercy’s mission, Cdr. Blevins marveled at the sense of teamwork that unfolded. “We have quarterly training exercises with a core set of personnel, [and] we train getting ready for activation in 5 days,” she said. “All of that training kicks in and it comes to fruition in a mission like this. It was terrific to see a group of very disparate subject matter experts from all over the country come together with one purpose: which was to serve our own country during the pandemic.”
Capt. Rotruck pointed out that the experience enabled enlisted and nonenlisted physicians to maintain their skill sets during a time when military and civilian hospitals had stopped doing elective procedures and routine appointments. “The fact that those people were able to come on board the ship and continue to conduct their medical practice and maintain their skills and competencies in an environment that they weren’t quite used to is great,” he said. “Otherwise, some of those medical personnel would have been sitting idle, wherever they were from. This is the power of Navy medicine on behalf of our country.”
When the hospital ship USNS Mercy departed San Diego’s Naval Station North Island on March 23, 2020, to support the Department of Defense efforts in Los Angeles during the coronavirus outbreak, Commander Erin Blevins remembers the crew’s excitement was palpable.
“We normally do partnerships abroad and respond to tsunamis and earthquakes,” said Cdr. Blevins, MD, a pediatric hematologist-oncologist who served as director of medical services for the mission. “This was a slight change in situation, but still disaster relief in the form of a pandemic. We switched our mindset to putting together the best experts for an infectious disease pandemic versus an earthquake disaster relief.”
A new mission

The 1,000-bed Mercy ship – a converted San Clemente–class oil tanker that was delivered in 1986 – spent nearly 50 days pier side in Los Angeles as a referral hospital for non–COVID-19 patients, so that clinicians at Los Angeles area hospitals could care for an anticipated surge of COVID-19 patients. “We went into it with expectations of, ‘We’ll treat as many patients as you need us to take,” Cdr. Blevins recalled. “I don’t even think Los Angeles [health officials] knew exactly where they were going to peak and what the need was going to be.”
Between March 29 and May 15, about 1,071 medical personnel aboard the Mercy cared for 77 patients with an average age of 53 years who were referred from 11 Los Angeles area hospitals. The physicians, nurses, and other medical support personnel were drawn from military treatment facilities across the country. “We had additional people join us as we scoped the mission to be more medically heavy and surgically light,” said Captain John Rotruck, MD, an anesthesiologist who is commanding officer of Mercy’s medical treatment facility. “We did adjust to make sure that we had the right staffing mix to meet the parameters that we were assigned. That was the crux of the change: a change in flavors of staffing to ensure that we focused on ICU and ward medical care as opposed to very heavy surgical care in support of a combat operation.”
About 10% of the team consisted of reservists who volunteered for the mission. “There’s no way you could have walked around the ship and known who was active duty and who was reservist,” said Capt. Rotruck, who was formerly chief of staff at Walter Reed National Military Medical Center, Bethesda, Md. “They worked together so well, and I think that marriage of active duty who are used to working in a military medical treatment facility – in our case, a Navy medical treatment facility – together with our reservist physician colleagues who work in civilian facilities around the country, was beneficial. It was a synergistic relationship. I think both sides walked away learning quite a bit from each other.”
Start with screening
All crew members underwent a temperature check and completed a health screening questionnaire: once before departing their home of record and again before boarding Mercy. Based on those results, crew members and medical staff were screened for COVID-19 and tested as needed in order to minimize the risk of an outbreak aboard the ship.
Fewer than 1% of crew members developed COVID-19 or tested positive for the virus during the mission, according to Capt. Rotruck. Affected individuals were isolated and quarantined. “All staff have recovered and are doing well,” he said.
Mercy personnel worked with local health officials to ensure that all patients transferred to the ship tested negative for COVID-19. Physicians aboard the Mercy then worked directly with the patients’ civilian physician to ensure a safe and thorough turnover process before the patients were transferred.
From basic medical to trauma care

Care aboard the ship, which consists of open-bay medical wards, ranged from basic medical and surgical care to critical care and trauma. The most common procedures were cholecystectomies and orthopedic procedures, and the average length of stay was 4-5 days, according to Cdr. Blevins. Over the course of the mission, the medical professionals conducted 36 surgeries, 77 x-ray exams, 26 CT scans, and administered hundreds of ancillary studies ranging from routine labs to high-end x-rays and blood transfusion support.
“Within our ICU, we did have some end-of-life patients who ended up dying on our ship in comfort care,” Cdr. Blevins said. “Fortunately, we had a wonderful ICU team who had a great deal of experience with end-of-life care and were able to take care of these patients very comfortably and ensure good communication with family and loved ones during that time. In most instances we tried to make sure that people got to FaceTime or video chat with their loved one before they passed away.”

The Mercy, which includes 12 operating rooms, four x-ray units, and one CAT-scan unit, was not equipped to deliver pediatric or obstetrical care. Other unavailable services included psychiatry, oncology, cardiac and thoracic surgery, nuclear medicine, MRI, mammography, electrophysiology, cardiac catheterization, negative-pressure isolation, speech therapy, and occupational therapy.
Not your typical hospital experience
But for patients who did receive medical care aboard the Mercy – which made three 150-day deployments in recent years for the military-led humanitarian response known as Pacific Partnership in 2015, 2016, and 2018 – it was an experience that they are unlikely to forget.
“Every time a patient left the ship, our team on the ground surveyed them to see how their experience was and see what we could do to improve,” Cdr. Blevins said. “Across the board, they were all very appreciative of the medical care. We had a couple of veterans on board. They got [USNS Mercy] hats on their way out and seemed to very much enjoy a slightly different experience than they would get at a regular hospital.”
Capt. Rotruck added that the enthusiasm crew members had for supporting fellow Americans “really energized our team and really saturated that caring aspect of the people who interacted directly with patients,” he said. “It wasn’t just the physicians and nurses, but it was the staff delivering the food and coming to take blood samples and every other interaction that the patients had with our team. I think they really felt that enthusiasm for being there and supporting our neighbors in LA [Los Angeles].”
Crew life aboard the Mercy
Just as with any hospital on shore, personnel aboard the Mercy practiced preventive hygiene measures recommended by the Centers for Disease Control and Prevention to help prevent the spread of COVID-19, such as wearing cloth face masks, spacing out tables in the dining hall, closing indoor gyms, and devising creative ways to stay physically fit. Popular options included jogging around the perimeter of the ship and practicing yoga and calisthenics on the deck, “making sure you were physically distanced appropriately, and when you were done, putting your mask back on,” Cdr. Blevins said. Others supplemented their workouts with a pull-up bar on the deck. “In addition, we have a series of ramps that run on the starboard side of the ship that we can use for patient movement with litters on wheels or patient beds,” Capt. Rotruck said. “The uphill portion of those ramps represents a good workout opportunity as well.”
Downtime in an era of physical distancing also afforded crew members the opportunity to call or FaceTime with loved ones, watch streamed TV shows and movies, and work on their own professional development. Some continued with coursework for online degree programs offered by colleges and universities they were enrolled in, while some enlisted personnel used the time to complete the Navy Enlisted Warfare Qualification Programs Instruction, which issues the basic overarching requirements for the qualification and designation of all enlisted warfare programs.
“As you can imagine, people spend a lot of time learning how the ship works and how it integrates into larger naval forces and so forth,” Capt. Rotruck said. “Not just our ship but also other ships: their weapons systems and defense mechanisms and navigation systems. We had people spending a significant amount of time working on that. We had people complete their Enlisted Surface Warfare qualification while we were on the mission.”
End of the mission
Mercy returned to its home base in San Diego on May 15, but about 60 medical personnel stayed behind in Los Angeles to support Federal Emergency Management Agency (FEMA), state, and local health care professionals. Some worked at a site where clinicians provided care for COVID-19–positive patients who had been transferred from area skilled nursing facilities.
In addition, a team consisting of one nurse and five corpsmen “would go out to individual skilled nursing facilities and mainly conduct assessments and training, such as training in donning proper PPE [personal protective equipment] and determining what needs they had,” Capt. Rotruck said. “They met those needs if possible or [communicated with California officials] and let them know what the requirements were and what the needs were in that facility.” The assignment for those who stayed behind ended on May 31.
On the opposite coast, Mercy’s sister ship, USNS Comfort, arrived in New York Harbor from Norfolk, Va., on March 30 and spent 3½ weeks assisting area hospitals in the COVID-19 pandemic fight. A few days into the mission, Comfort’s internal spaces were reconfigured to create separate COVID-negative and COVID-positive sections. Medical teams aboard the ship cared for a total of 182 patients during the assignment.
Looking back on Mercy’s mission, Cdr. Blevins marveled at the sense of teamwork that unfolded. “We have quarterly training exercises with a core set of personnel, [and] we train getting ready for activation in 5 days,” she said. “All of that training kicks in and it comes to fruition in a mission like this. It was terrific to see a group of very disparate subject matter experts from all over the country come together with one purpose: which was to serve our own country during the pandemic.”
Capt. Rotruck pointed out that the experience enabled enlisted and nonenlisted physicians to maintain their skill sets during a time when military and civilian hospitals had stopped doing elective procedures and routine appointments. “The fact that those people were able to come on board the ship and continue to conduct their medical practice and maintain their skills and competencies in an environment that they weren’t quite used to is great,” he said. “Otherwise, some of those medical personnel would have been sitting idle, wherever they were from. This is the power of Navy medicine on behalf of our country.”