User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Noninjectable modes of insulin delivery coming of age
LOS ANGELES – Injections may be the most common way for patients with diabetes to take insulin, but other modes of delivery are coming of age.
George Grunberger, MD, chairman of the Grunberger Diabetes Institute in Bloomfield Township, Mich., said that at least seven different agents that are being studied for the oral delivery of biologics for diabetes.
He outlined several at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Oral insulin
ORMD-0801 from Oramed is an oral insulin capsule that prevents enzyme degradation and enhances intestinal absorption. Top-line, unpublished findings from a phase 2 study, which the company announced in November 2019, showed that ORMD-0801 significantly reduced hemoglobin A1c levels in patients with type 2 diabetes who were inadequately controlled on other standard-of-care drugs. ORMD-0801 dosed once daily reduced HbA1c by 0.60%, compared with 0.06% by placebo. “We’ll see when it’s going to wind up in the clinic,” Dr. Grunberger said. Oramed is also developing an oral glucagonlike peptide–1 analogue capsule, ORMD-0901, which has potential to be the first orally ingestible GLP-1 analogue.
Inhaled and absorbed insulin
Technosphere insulin (Affreza) is a novel inhalation powder for the treatment of diabetes that was developed by MannKind and approved by the Food and Drug Administration in 2014. Clinical studies have shown that Technosphere insulin delivers insulin with an ultrarapid pharmacokinetic profile that is different from all other insulin products, but similar to natural insulin release. “The idea was to develop a more patient-friendly device to deliver insulin directly into the lungs,” said Dr. Grunberger, who is also a clinical professor of internal medicine and molecular medicine and genetics at Wayne State University, Detroit. “When you inhale this into the lungs, there is one cell layer between the air sac and the circulation, so it works very quickly. The idea is to try to avoid injecting insulin to see if it helps. This is a prandial insulin – you inhale it before meals. The whole idea is that hopefully, you can reduce any fear of delayed postprandial hyperglycemia.”
In a randomized trial of 353 patients with inadequately controlled type 2 diabetes, those in the Technosphere insulin arm significantly reduced HbA1c by 0.8% from a baseline of 8.3%, compared with the placebo arm, which was reduced by 0.4% (P less than .0001; Diabetes Care. 2015;38[12]:2274-81). A greater number of patients treated with Technosphere insulin achieved an HbA1c of 7.0% or less, compared with placebo (38% vs. 19%; P = .0005). Dr. Grunberger noted that, in clinical trials lasting up to 2 years, patients treated with Technosphere insulin had a 40-mL greater decline from baseline in forced expiratory volume in 1 second (FEV1 ), compared with patients treated with comparator antidiabetes treatments. “But once you stop using the drug, FEV1 reverts to normal,” he said. “So, there does not appear to be lasting damage to your lungs and respiratory ability.”
In another development, Oral-Lyn from Generex Biotechnology, which delivers insulin through the oral mucosa, is being evaluated as a potential treatment option. In 2015, Generex partnered with the University of Toronto’s Center for Molecular Design and Preformulations to increase the bioavailability of insulin in the product and to reduce the number of sprays required to achieve effective prandial glucose control. In 2019, the company formed the NuGenerex Diabetes Research Center, which intended to accelerate the development of the reformulated Oral-Lyn-2, for type 2 diabetes, and Altsulin, for the treatment of type 1 diabetes. The programs are expected to initiate in the first quarter of 2020.
In the meantime, studies of intranasally delivered insulin continue to advance. “It works. It lowers glucose, but there is a whole slew of knowledge now about how it can also improve neurocognitive function,” Dr. Grunberger said.
Oral GLP-1 receptor agonists
Oral versions of glucagonlike peptide–1 (GLP-1) receptor agonists are also emerging as a treatment option. The FDA recently approved the first oral GLP-1 receptor agonist, semaglutide bound in the absorption enhancer sodium N‐(8‐[2‐hydroxybenzoyl] amino) caprylate (SNAC). According to data from manufacturer Novo Nordisk, SNAC facilitates local increase of pH, which leads to a higher solubility. SNAC interacts with cell membranes of gastric mucosa, facilitating absorption within 30 minutes, “so the drug can penetrate the mucosa without lasting damage,” Dr. Grunberger said. The SNAC effect is size dependent and fully reversible.
In PIONEER 3, researchers found that, in adults with type 2 diabetes uncontrolled with metformin with or without sulfonylurea, oral semaglutide at dosages of 7 and 14 mg/day resulted in significantly greater reductions in HbA1c over 26 weeks, compared with sitagliptin, but there was no significant benefit with the 3-mg/d dosage (JAMA. 2019;321[15]:1466-80). In PIONEER 4, researchers compared the efficacy and safety of oral semaglutide with subcutaneous liraglutide (Lancet. 2019;394[10192]:P39-50). “There was no difference in HbA1c effect between the two groups, but oral semaglutide beat out sitagliptin in terms of weight loss,” Dr. Grunberger said. “It’s going to be interesting to see what’s going to happen in the marketplace as the drug gets widely launched.”
Nasal glucagon
He closed out his presentation by discussing the July 2019 FDA approval of Eli Lilly’s nasal glucagon for severe hypoglycemia – the first such treatment that can be administered without an injection. The nasally administered dry powder, known as Baqsimi, is a welcome alternative to current glucagon kits, “which contain multiple components,” said Dr. Grunberger, who is also a past president of the American Association of Clinical Endocrinologists. An adult pivotal study showed that supraphysiologic levels of glucagon were achieved within 5 minutes with both nasal and intramuscular glucagon (Diabetes Care. 2016;39[2]:264-70). Headache and nasal symptoms occurred more frequently with nasal glucagon, but most were resolved within 1 day. In addition, nausea and vomiting occurred at similar frequencies with nasal and intramuscular glucacon, and most cases were resolved within 1 day.
Similar results were observed in a pediatric study of 48 patients with type 1 diabetes who were older than 4 years, (Diabetes Care. 2016;39[4]:555-62).
Dr. Grunberger disclosed that has research contracts with Medtronic and Eli Lilly, and that he serves on speakers bureaus of Eli Lilly, Janssen, Novo Nordisk, and Sanofi.
LOS ANGELES – Injections may be the most common way for patients with diabetes to take insulin, but other modes of delivery are coming of age.
George Grunberger, MD, chairman of the Grunberger Diabetes Institute in Bloomfield Township, Mich., said that at least seven different agents that are being studied for the oral delivery of biologics for diabetes.
He outlined several at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Oral insulin
ORMD-0801 from Oramed is an oral insulin capsule that prevents enzyme degradation and enhances intestinal absorption. Top-line, unpublished findings from a phase 2 study, which the company announced in November 2019, showed that ORMD-0801 significantly reduced hemoglobin A1c levels in patients with type 2 diabetes who were inadequately controlled on other standard-of-care drugs. ORMD-0801 dosed once daily reduced HbA1c by 0.60%, compared with 0.06% by placebo. “We’ll see when it’s going to wind up in the clinic,” Dr. Grunberger said. Oramed is also developing an oral glucagonlike peptide–1 analogue capsule, ORMD-0901, which has potential to be the first orally ingestible GLP-1 analogue.
Inhaled and absorbed insulin
Technosphere insulin (Affreza) is a novel inhalation powder for the treatment of diabetes that was developed by MannKind and approved by the Food and Drug Administration in 2014. Clinical studies have shown that Technosphere insulin delivers insulin with an ultrarapid pharmacokinetic profile that is different from all other insulin products, but similar to natural insulin release. “The idea was to develop a more patient-friendly device to deliver insulin directly into the lungs,” said Dr. Grunberger, who is also a clinical professor of internal medicine and molecular medicine and genetics at Wayne State University, Detroit. “When you inhale this into the lungs, there is one cell layer between the air sac and the circulation, so it works very quickly. The idea is to try to avoid injecting insulin to see if it helps. This is a prandial insulin – you inhale it before meals. The whole idea is that hopefully, you can reduce any fear of delayed postprandial hyperglycemia.”
In a randomized trial of 353 patients with inadequately controlled type 2 diabetes, those in the Technosphere insulin arm significantly reduced HbA1c by 0.8% from a baseline of 8.3%, compared with the placebo arm, which was reduced by 0.4% (P less than .0001; Diabetes Care. 2015;38[12]:2274-81). A greater number of patients treated with Technosphere insulin achieved an HbA1c of 7.0% or less, compared with placebo (38% vs. 19%; P = .0005). Dr. Grunberger noted that, in clinical trials lasting up to 2 years, patients treated with Technosphere insulin had a 40-mL greater decline from baseline in forced expiratory volume in 1 second (FEV1 ), compared with patients treated with comparator antidiabetes treatments. “But once you stop using the drug, FEV1 reverts to normal,” he said. “So, there does not appear to be lasting damage to your lungs and respiratory ability.”
In another development, Oral-Lyn from Generex Biotechnology, which delivers insulin through the oral mucosa, is being evaluated as a potential treatment option. In 2015, Generex partnered with the University of Toronto’s Center for Molecular Design and Preformulations to increase the bioavailability of insulin in the product and to reduce the number of sprays required to achieve effective prandial glucose control. In 2019, the company formed the NuGenerex Diabetes Research Center, which intended to accelerate the development of the reformulated Oral-Lyn-2, for type 2 diabetes, and Altsulin, for the treatment of type 1 diabetes. The programs are expected to initiate in the first quarter of 2020.
In the meantime, studies of intranasally delivered insulin continue to advance. “It works. It lowers glucose, but there is a whole slew of knowledge now about how it can also improve neurocognitive function,” Dr. Grunberger said.
Oral GLP-1 receptor agonists
Oral versions of glucagonlike peptide–1 (GLP-1) receptor agonists are also emerging as a treatment option. The FDA recently approved the first oral GLP-1 receptor agonist, semaglutide bound in the absorption enhancer sodium N‐(8‐[2‐hydroxybenzoyl] amino) caprylate (SNAC). According to data from manufacturer Novo Nordisk, SNAC facilitates local increase of pH, which leads to a higher solubility. SNAC interacts with cell membranes of gastric mucosa, facilitating absorption within 30 minutes, “so the drug can penetrate the mucosa without lasting damage,” Dr. Grunberger said. The SNAC effect is size dependent and fully reversible.
In PIONEER 3, researchers found that, in adults with type 2 diabetes uncontrolled with metformin with or without sulfonylurea, oral semaglutide at dosages of 7 and 14 mg/day resulted in significantly greater reductions in HbA1c over 26 weeks, compared with sitagliptin, but there was no significant benefit with the 3-mg/d dosage (JAMA. 2019;321[15]:1466-80). In PIONEER 4, researchers compared the efficacy and safety of oral semaglutide with subcutaneous liraglutide (Lancet. 2019;394[10192]:P39-50). “There was no difference in HbA1c effect between the two groups, but oral semaglutide beat out sitagliptin in terms of weight loss,” Dr. Grunberger said. “It’s going to be interesting to see what’s going to happen in the marketplace as the drug gets widely launched.”
Nasal glucagon
He closed out his presentation by discussing the July 2019 FDA approval of Eli Lilly’s nasal glucagon for severe hypoglycemia – the first such treatment that can be administered without an injection. The nasally administered dry powder, known as Baqsimi, is a welcome alternative to current glucagon kits, “which contain multiple components,” said Dr. Grunberger, who is also a past president of the American Association of Clinical Endocrinologists. An adult pivotal study showed that supraphysiologic levels of glucagon were achieved within 5 minutes with both nasal and intramuscular glucagon (Diabetes Care. 2016;39[2]:264-70). Headache and nasal symptoms occurred more frequently with nasal glucagon, but most were resolved within 1 day. In addition, nausea and vomiting occurred at similar frequencies with nasal and intramuscular glucacon, and most cases were resolved within 1 day.
Similar results were observed in a pediatric study of 48 patients with type 1 diabetes who were older than 4 years, (Diabetes Care. 2016;39[4]:555-62).
Dr. Grunberger disclosed that has research contracts with Medtronic and Eli Lilly, and that he serves on speakers bureaus of Eli Lilly, Janssen, Novo Nordisk, and Sanofi.
LOS ANGELES – Injections may be the most common way for patients with diabetes to take insulin, but other modes of delivery are coming of age.
George Grunberger, MD, chairman of the Grunberger Diabetes Institute in Bloomfield Township, Mich., said that at least seven different agents that are being studied for the oral delivery of biologics for diabetes.
He outlined several at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease.
Oral insulin
ORMD-0801 from Oramed is an oral insulin capsule that prevents enzyme degradation and enhances intestinal absorption. Top-line, unpublished findings from a phase 2 study, which the company announced in November 2019, showed that ORMD-0801 significantly reduced hemoglobin A1c levels in patients with type 2 diabetes who were inadequately controlled on other standard-of-care drugs. ORMD-0801 dosed once daily reduced HbA1c by 0.60%, compared with 0.06% by placebo. “We’ll see when it’s going to wind up in the clinic,” Dr. Grunberger said. Oramed is also developing an oral glucagonlike peptide–1 analogue capsule, ORMD-0901, which has potential to be the first orally ingestible GLP-1 analogue.
Inhaled and absorbed insulin
Technosphere insulin (Affreza) is a novel inhalation powder for the treatment of diabetes that was developed by MannKind and approved by the Food and Drug Administration in 2014. Clinical studies have shown that Technosphere insulin delivers insulin with an ultrarapid pharmacokinetic profile that is different from all other insulin products, but similar to natural insulin release. “The idea was to develop a more patient-friendly device to deliver insulin directly into the lungs,” said Dr. Grunberger, who is also a clinical professor of internal medicine and molecular medicine and genetics at Wayne State University, Detroit. “When you inhale this into the lungs, there is one cell layer between the air sac and the circulation, so it works very quickly. The idea is to try to avoid injecting insulin to see if it helps. This is a prandial insulin – you inhale it before meals. The whole idea is that hopefully, you can reduce any fear of delayed postprandial hyperglycemia.”
In a randomized trial of 353 patients with inadequately controlled type 2 diabetes, those in the Technosphere insulin arm significantly reduced HbA1c by 0.8% from a baseline of 8.3%, compared with the placebo arm, which was reduced by 0.4% (P less than .0001; Diabetes Care. 2015;38[12]:2274-81). A greater number of patients treated with Technosphere insulin achieved an HbA1c of 7.0% or less, compared with placebo (38% vs. 19%; P = .0005). Dr. Grunberger noted that, in clinical trials lasting up to 2 years, patients treated with Technosphere insulin had a 40-mL greater decline from baseline in forced expiratory volume in 1 second (FEV1 ), compared with patients treated with comparator antidiabetes treatments. “But once you stop using the drug, FEV1 reverts to normal,” he said. “So, there does not appear to be lasting damage to your lungs and respiratory ability.”
In another development, Oral-Lyn from Generex Biotechnology, which delivers insulin through the oral mucosa, is being evaluated as a potential treatment option. In 2015, Generex partnered with the University of Toronto’s Center for Molecular Design and Preformulations to increase the bioavailability of insulin in the product and to reduce the number of sprays required to achieve effective prandial glucose control. In 2019, the company formed the NuGenerex Diabetes Research Center, which intended to accelerate the development of the reformulated Oral-Lyn-2, for type 2 diabetes, and Altsulin, for the treatment of type 1 diabetes. The programs are expected to initiate in the first quarter of 2020.
In the meantime, studies of intranasally delivered insulin continue to advance. “It works. It lowers glucose, but there is a whole slew of knowledge now about how it can also improve neurocognitive function,” Dr. Grunberger said.
Oral GLP-1 receptor agonists
Oral versions of glucagonlike peptide–1 (GLP-1) receptor agonists are also emerging as a treatment option. The FDA recently approved the first oral GLP-1 receptor agonist, semaglutide bound in the absorption enhancer sodium N‐(8‐[2‐hydroxybenzoyl] amino) caprylate (SNAC). According to data from manufacturer Novo Nordisk, SNAC facilitates local increase of pH, which leads to a higher solubility. SNAC interacts with cell membranes of gastric mucosa, facilitating absorption within 30 minutes, “so the drug can penetrate the mucosa without lasting damage,” Dr. Grunberger said. The SNAC effect is size dependent and fully reversible.
In PIONEER 3, researchers found that, in adults with type 2 diabetes uncontrolled with metformin with or without sulfonylurea, oral semaglutide at dosages of 7 and 14 mg/day resulted in significantly greater reductions in HbA1c over 26 weeks, compared with sitagliptin, but there was no significant benefit with the 3-mg/d dosage (JAMA. 2019;321[15]:1466-80). In PIONEER 4, researchers compared the efficacy and safety of oral semaglutide with subcutaneous liraglutide (Lancet. 2019;394[10192]:P39-50). “There was no difference in HbA1c effect between the two groups, but oral semaglutide beat out sitagliptin in terms of weight loss,” Dr. Grunberger said. “It’s going to be interesting to see what’s going to happen in the marketplace as the drug gets widely launched.”
Nasal glucagon
He closed out his presentation by discussing the July 2019 FDA approval of Eli Lilly’s nasal glucagon for severe hypoglycemia – the first such treatment that can be administered without an injection. The nasally administered dry powder, known as Baqsimi, is a welcome alternative to current glucagon kits, “which contain multiple components,” said Dr. Grunberger, who is also a past president of the American Association of Clinical Endocrinologists. An adult pivotal study showed that supraphysiologic levels of glucagon were achieved within 5 minutes with both nasal and intramuscular glucagon (Diabetes Care. 2016;39[2]:264-70). Headache and nasal symptoms occurred more frequently with nasal glucagon, but most were resolved within 1 day. In addition, nausea and vomiting occurred at similar frequencies with nasal and intramuscular glucacon, and most cases were resolved within 1 day.
Similar results were observed in a pediatric study of 48 patients with type 1 diabetes who were older than 4 years, (Diabetes Care. 2016;39[4]:555-62).
Dr. Grunberger disclosed that has research contracts with Medtronic and Eli Lilly, and that he serves on speakers bureaus of Eli Lilly, Janssen, Novo Nordisk, and Sanofi.
EXPERT ANALYSIS FROM WCIRDC 2019
ECHELON-1 update: A+AVD bests ABVD in Hodgkin lymphoma
Brentuximab vedotin plus doxorubicin, vinblastine, and dacarbazine (A+AVD) provides “robust, sustained efficacy” in patients with Hodgkin lymphoma, according to investigators.
In the ECHELON-1 trial, investigators compared A+AVD to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for stage III or IV Hodgkin lymphoma. The 3-year progression-free survival (PFS) was superior in patients who received A+AVD, and this benefit was seen across most subgroups.
David J. Straus, MD, of Memorial Sloan Kettering Cancer Center in New York and his colleagues detailed these findings in Blood.
The phase 3 trial (NCT01712490) enrolled 1,334 patients with stage III or IV classical Hodgkin lymphoma. They were randomized to receive A+AVD (n = 664) or ABVD (n = 670). Baseline characteristics were similar between the treatment arms.
Positron emission tomography status after cycle 2 (PET2) was similar between the treatment arms as well. Most patients – 89% of the A+AVD arm and 86% of the ABVD arm – were PET2 negative. Treating physicians used PET2 status as a guide to potentially switch patients to an alternative regimen (radiotherapy or chemotherapy with or without transplant).
In a prior analysis, the study’s primary endpoint was modified PFS (time to progression, death, or noncomplete response after frontline therapy) per an independent review committee (N Engl J Med. 2018;378:331-44). The 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm (hazard ratio, 0.77; P = .04).
PFS update
In the current analysis, the main exploratory endpoint was PFS per investigator. The 3-year PFS rate was significantly higher in the A+AVD arm than in the ABVD arm – 83.1% and 76.0%, respectively (HR, 0.704; P = .005).
The investigators observed a “consistent improvement in PFS” in the A+AVD arm, regardless of disease stage, International Prognostic score, Eastern Cooperative Oncology Group status, sex, or age. There was a significant improvement in PFS with A+AVD in PET2-negative patients and a trend toward improvement in PET2-positive patients. In the PET2-negative patients, the 3-year PFS was 85.8% in the A+AVD arm and 79.5% in the ABVD arm (HR, 0.69; P = .009). In PET2-positive patients, the 3-year PFS was 67.7% and 51.5%, respectively (HR, 0.59; P = .077).
“These data highlight that A+AVD provides a durable efficacy benefit, compared with ABVD, for frontline stage III/IV cHL [classical Hodgkin lymphoma], which is consistent across key subgroups regardless of patient status at PET2,” Dr. Straus and his colleagues wrote.
Safety update
In both treatment arms, peripheral neuropathy continued to improve or resolve with longer follow-up. Among patients who developed peripheral neuropathy, 78% in the A+AVD arm and 83% in the ABVD arm had improvement or resolution of the condition at 3 years.
Most patients had complete resolution of peripheral neuropathy; 62% in the A+AVD arm and 73% in the ABVD arm. The median time to complete resolution was 28 weeks (range, 0-167 weeks) after stopping A+AVD and 14 weeks (range, 0-188 weeks) after stopping ABVD.
The incidence of secondary malignancies was similar between the treatment arms. There were 14 secondary malignancies in the A+AVD arm (6 solid tumors, 8 hematologic malignancies) and 20 in the ABVD arm (9 solid tumors, 11 hematologic malignancies).
“A+AVD provided a sustained PFS benefit with a predictable and manageable safety profile,” Dr. Straus and colleagues wrote. “These data further support the advantages of A+AVD versus ABVD as frontline treatment of patients with advanced stage III or IV cHL [classical Hodgkin lymphoma].”
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals (a subsidiary of Takeda) and Seattle Genetics. The investigators disclosed relationships with Millennium, Takeda, Seattle Genetics, and a range of other companies.
SOURCE: Straus DJ et al. Blood. 2020 Jan 16. pii: blood.2019003127. doi: 10.1182/blood.2019003127.
Brentuximab vedotin plus doxorubicin, vinblastine, and dacarbazine (A+AVD) provides “robust, sustained efficacy” in patients with Hodgkin lymphoma, according to investigators.
In the ECHELON-1 trial, investigators compared A+AVD to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for stage III or IV Hodgkin lymphoma. The 3-year progression-free survival (PFS) was superior in patients who received A+AVD, and this benefit was seen across most subgroups.
David J. Straus, MD, of Memorial Sloan Kettering Cancer Center in New York and his colleagues detailed these findings in Blood.
The phase 3 trial (NCT01712490) enrolled 1,334 patients with stage III or IV classical Hodgkin lymphoma. They were randomized to receive A+AVD (n = 664) or ABVD (n = 670). Baseline characteristics were similar between the treatment arms.
Positron emission tomography status after cycle 2 (PET2) was similar between the treatment arms as well. Most patients – 89% of the A+AVD arm and 86% of the ABVD arm – were PET2 negative. Treating physicians used PET2 status as a guide to potentially switch patients to an alternative regimen (radiotherapy or chemotherapy with or without transplant).
In a prior analysis, the study’s primary endpoint was modified PFS (time to progression, death, or noncomplete response after frontline therapy) per an independent review committee (N Engl J Med. 2018;378:331-44). The 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm (hazard ratio, 0.77; P = .04).
PFS update
In the current analysis, the main exploratory endpoint was PFS per investigator. The 3-year PFS rate was significantly higher in the A+AVD arm than in the ABVD arm – 83.1% and 76.0%, respectively (HR, 0.704; P = .005).
The investigators observed a “consistent improvement in PFS” in the A+AVD arm, regardless of disease stage, International Prognostic score, Eastern Cooperative Oncology Group status, sex, or age. There was a significant improvement in PFS with A+AVD in PET2-negative patients and a trend toward improvement in PET2-positive patients. In the PET2-negative patients, the 3-year PFS was 85.8% in the A+AVD arm and 79.5% in the ABVD arm (HR, 0.69; P = .009). In PET2-positive patients, the 3-year PFS was 67.7% and 51.5%, respectively (HR, 0.59; P = .077).
“These data highlight that A+AVD provides a durable efficacy benefit, compared with ABVD, for frontline stage III/IV cHL [classical Hodgkin lymphoma], which is consistent across key subgroups regardless of patient status at PET2,” Dr. Straus and his colleagues wrote.
Safety update
In both treatment arms, peripheral neuropathy continued to improve or resolve with longer follow-up. Among patients who developed peripheral neuropathy, 78% in the A+AVD arm and 83% in the ABVD arm had improvement or resolution of the condition at 3 years.
Most patients had complete resolution of peripheral neuropathy; 62% in the A+AVD arm and 73% in the ABVD arm. The median time to complete resolution was 28 weeks (range, 0-167 weeks) after stopping A+AVD and 14 weeks (range, 0-188 weeks) after stopping ABVD.
The incidence of secondary malignancies was similar between the treatment arms. There were 14 secondary malignancies in the A+AVD arm (6 solid tumors, 8 hematologic malignancies) and 20 in the ABVD arm (9 solid tumors, 11 hematologic malignancies).
“A+AVD provided a sustained PFS benefit with a predictable and manageable safety profile,” Dr. Straus and colleagues wrote. “These data further support the advantages of A+AVD versus ABVD as frontline treatment of patients with advanced stage III or IV cHL [classical Hodgkin lymphoma].”
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals (a subsidiary of Takeda) and Seattle Genetics. The investigators disclosed relationships with Millennium, Takeda, Seattle Genetics, and a range of other companies.
SOURCE: Straus DJ et al. Blood. 2020 Jan 16. pii: blood.2019003127. doi: 10.1182/blood.2019003127.
Brentuximab vedotin plus doxorubicin, vinblastine, and dacarbazine (A+AVD) provides “robust, sustained efficacy” in patients with Hodgkin lymphoma, according to investigators.
In the ECHELON-1 trial, investigators compared A+AVD to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for stage III or IV Hodgkin lymphoma. The 3-year progression-free survival (PFS) was superior in patients who received A+AVD, and this benefit was seen across most subgroups.
David J. Straus, MD, of Memorial Sloan Kettering Cancer Center in New York and his colleagues detailed these findings in Blood.
The phase 3 trial (NCT01712490) enrolled 1,334 patients with stage III or IV classical Hodgkin lymphoma. They were randomized to receive A+AVD (n = 664) or ABVD (n = 670). Baseline characteristics were similar between the treatment arms.
Positron emission tomography status after cycle 2 (PET2) was similar between the treatment arms as well. Most patients – 89% of the A+AVD arm and 86% of the ABVD arm – were PET2 negative. Treating physicians used PET2 status as a guide to potentially switch patients to an alternative regimen (radiotherapy or chemotherapy with or without transplant).
In a prior analysis, the study’s primary endpoint was modified PFS (time to progression, death, or noncomplete response after frontline therapy) per an independent review committee (N Engl J Med. 2018;378:331-44). The 2-year modified PFS rate was 82.1% in the A+AVD arm and 77.2% in the ABVD arm (hazard ratio, 0.77; P = .04).
PFS update
In the current analysis, the main exploratory endpoint was PFS per investigator. The 3-year PFS rate was significantly higher in the A+AVD arm than in the ABVD arm – 83.1% and 76.0%, respectively (HR, 0.704; P = .005).
The investigators observed a “consistent improvement in PFS” in the A+AVD arm, regardless of disease stage, International Prognostic score, Eastern Cooperative Oncology Group status, sex, or age. There was a significant improvement in PFS with A+AVD in PET2-negative patients and a trend toward improvement in PET2-positive patients. In the PET2-negative patients, the 3-year PFS was 85.8% in the A+AVD arm and 79.5% in the ABVD arm (HR, 0.69; P = .009). In PET2-positive patients, the 3-year PFS was 67.7% and 51.5%, respectively (HR, 0.59; P = .077).
“These data highlight that A+AVD provides a durable efficacy benefit, compared with ABVD, for frontline stage III/IV cHL [classical Hodgkin lymphoma], which is consistent across key subgroups regardless of patient status at PET2,” Dr. Straus and his colleagues wrote.
Safety update
In both treatment arms, peripheral neuropathy continued to improve or resolve with longer follow-up. Among patients who developed peripheral neuropathy, 78% in the A+AVD arm and 83% in the ABVD arm had improvement or resolution of the condition at 3 years.
Most patients had complete resolution of peripheral neuropathy; 62% in the A+AVD arm and 73% in the ABVD arm. The median time to complete resolution was 28 weeks (range, 0-167 weeks) after stopping A+AVD and 14 weeks (range, 0-188 weeks) after stopping ABVD.
The incidence of secondary malignancies was similar between the treatment arms. There were 14 secondary malignancies in the A+AVD arm (6 solid tumors, 8 hematologic malignancies) and 20 in the ABVD arm (9 solid tumors, 11 hematologic malignancies).
“A+AVD provided a sustained PFS benefit with a predictable and manageable safety profile,” Dr. Straus and colleagues wrote. “These data further support the advantages of A+AVD versus ABVD as frontline treatment of patients with advanced stage III or IV cHL [classical Hodgkin lymphoma].”
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals (a subsidiary of Takeda) and Seattle Genetics. The investigators disclosed relationships with Millennium, Takeda, Seattle Genetics, and a range of other companies.
SOURCE: Straus DJ et al. Blood. 2020 Jan 16. pii: blood.2019003127. doi: 10.1182/blood.2019003127.
FROM BLOOD
FDA okays Palforzia, first drug for peanut allergy in children
The Food and Drug Administration has approved the first drug to combat peanut allergy in children, (Palforzia, Aimmune Therapeutics), although those who take it must continue to avoid peanuts in their diets.
The peanut (Arachis hypogaea) allergen powder is also the first drug ever approved to treat a food allergy. It is not a cure, but it mitigates allergic reactions, including anaphylaxis, that may occur with accidental exposure to peanuts, the FDA said in a news release.
Treatment with the oral powder, which is mixed into semisolid food – such as applesauce or yogurt – can be started in children aged 4 through 17 years who have a confirmed peanut allergy and then continued as a maintenance medication. Some 1 million American children have peanut allergy, and only a fifth will outgrow the allergy, the agency said.
“Because there is no cure, allergic individuals must strictly avoid exposure to prevent severe and potentially life-threatening reactions,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in the statement.
An FDA advisory panel backed the medication in September 2019, but some committee members expressed concern about the large number of children in clinical trials who required epinephrine after receiving a dose of Palforzia.
The initial dose phase is given on a single day, while updosing consists of 11 increasing doses over several months. If the patient tolerates the first administration of an increased dose level, they may continue that dose daily at home. Daily maintenance begins after the completion of all updosing levels.
Palforzia will be available only through specially certified health care providers, health care settings, and pharmacies to patients enrolled in the REMS program, the agency said. Also, the initial dose escalation and first dose of each updosing level can be given only in a certified setting.
The agency said that patients or parents or caregivers must be counseled on the need for constant availability of injectable epinephrine, the need for continued dietary peanut avoidance, and on how to recognize the signs and symptoms of anaphylaxis.
‘Eagerly’ awaited
Palforzia’s effectiveness was based on a randomized, double-blind, placebo-controlled study involving about 500 peanut-allergic individuals that found that 67.2% of allergic patients tolerated an oral challenge with a single 600-mg dose of peanut protein with no more than mild allergic symptoms after 6 months of maintenance treatment, compared with 4% of placebo recipients, the FDA said.
In two double-blind, placebo-controlled studies looking at safety, the most commonly reported side effects among about 700 individuals involved in the research were abdominal pain, vomiting, nausea, tingling in the mouth, itching (including in the mouth and ears), cough, runny nose, throat irritation and tightness, hives, wheezing and shortness of breath, and anaphylaxis.
Palforzia should not be given to those with uncontrolled asthma and can’t be used for emergency treatment of allergic reactions, including anaphylaxis.
“The food allergy community has been eagerly awaiting an FDA-approved treatment that can help mitigate allergic reactions to peanut and, as allergists, we want nothing more than to have a treatment option to offer our patients that has demonstrated both the safety and efficacy to truly impact the lives of patients who live with peanut allergy,” said Christina Ciaccio, MD, chief of Allergy/Immunology and Pediatric Pulmonary Medicine at the University of Chicago Medical Center and Biological Sciences, in a company statement from Aimmune. “With today’s approval of Palforzia, we can – for the first time – offer children and teens with peanut allergy a proven medicine that employs an established therapeutic approach.”
This article first appeared on Medscape.com.
The Food and Drug Administration has approved the first drug to combat peanut allergy in children, (Palforzia, Aimmune Therapeutics), although those who take it must continue to avoid peanuts in their diets.
The peanut (Arachis hypogaea) allergen powder is also the first drug ever approved to treat a food allergy. It is not a cure, but it mitigates allergic reactions, including anaphylaxis, that may occur with accidental exposure to peanuts, the FDA said in a news release.
Treatment with the oral powder, which is mixed into semisolid food – such as applesauce or yogurt – can be started in children aged 4 through 17 years who have a confirmed peanut allergy and then continued as a maintenance medication. Some 1 million American children have peanut allergy, and only a fifth will outgrow the allergy, the agency said.
“Because there is no cure, allergic individuals must strictly avoid exposure to prevent severe and potentially life-threatening reactions,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in the statement.
An FDA advisory panel backed the medication in September 2019, but some committee members expressed concern about the large number of children in clinical trials who required epinephrine after receiving a dose of Palforzia.
The initial dose phase is given on a single day, while updosing consists of 11 increasing doses over several months. If the patient tolerates the first administration of an increased dose level, they may continue that dose daily at home. Daily maintenance begins after the completion of all updosing levels.
Palforzia will be available only through specially certified health care providers, health care settings, and pharmacies to patients enrolled in the REMS program, the agency said. Also, the initial dose escalation and first dose of each updosing level can be given only in a certified setting.
The agency said that patients or parents or caregivers must be counseled on the need for constant availability of injectable epinephrine, the need for continued dietary peanut avoidance, and on how to recognize the signs and symptoms of anaphylaxis.
‘Eagerly’ awaited
Palforzia’s effectiveness was based on a randomized, double-blind, placebo-controlled study involving about 500 peanut-allergic individuals that found that 67.2% of allergic patients tolerated an oral challenge with a single 600-mg dose of peanut protein with no more than mild allergic symptoms after 6 months of maintenance treatment, compared with 4% of placebo recipients, the FDA said.
In two double-blind, placebo-controlled studies looking at safety, the most commonly reported side effects among about 700 individuals involved in the research were abdominal pain, vomiting, nausea, tingling in the mouth, itching (including in the mouth and ears), cough, runny nose, throat irritation and tightness, hives, wheezing and shortness of breath, and anaphylaxis.
Palforzia should not be given to those with uncontrolled asthma and can’t be used for emergency treatment of allergic reactions, including anaphylaxis.
“The food allergy community has been eagerly awaiting an FDA-approved treatment that can help mitigate allergic reactions to peanut and, as allergists, we want nothing more than to have a treatment option to offer our patients that has demonstrated both the safety and efficacy to truly impact the lives of patients who live with peanut allergy,” said Christina Ciaccio, MD, chief of Allergy/Immunology and Pediatric Pulmonary Medicine at the University of Chicago Medical Center and Biological Sciences, in a company statement from Aimmune. “With today’s approval of Palforzia, we can – for the first time – offer children and teens with peanut allergy a proven medicine that employs an established therapeutic approach.”
This article first appeared on Medscape.com.
The Food and Drug Administration has approved the first drug to combat peanut allergy in children, (Palforzia, Aimmune Therapeutics), although those who take it must continue to avoid peanuts in their diets.
The peanut (Arachis hypogaea) allergen powder is also the first drug ever approved to treat a food allergy. It is not a cure, but it mitigates allergic reactions, including anaphylaxis, that may occur with accidental exposure to peanuts, the FDA said in a news release.
Treatment with the oral powder, which is mixed into semisolid food – such as applesauce or yogurt – can be started in children aged 4 through 17 years who have a confirmed peanut allergy and then continued as a maintenance medication. Some 1 million American children have peanut allergy, and only a fifth will outgrow the allergy, the agency said.
“Because there is no cure, allergic individuals must strictly avoid exposure to prevent severe and potentially life-threatening reactions,” said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in the statement.
An FDA advisory panel backed the medication in September 2019, but some committee members expressed concern about the large number of children in clinical trials who required epinephrine after receiving a dose of Palforzia.
The initial dose phase is given on a single day, while updosing consists of 11 increasing doses over several months. If the patient tolerates the first administration of an increased dose level, they may continue that dose daily at home. Daily maintenance begins after the completion of all updosing levels.
Palforzia will be available only through specially certified health care providers, health care settings, and pharmacies to patients enrolled in the REMS program, the agency said. Also, the initial dose escalation and first dose of each updosing level can be given only in a certified setting.
The agency said that patients or parents or caregivers must be counseled on the need for constant availability of injectable epinephrine, the need for continued dietary peanut avoidance, and on how to recognize the signs and symptoms of anaphylaxis.
‘Eagerly’ awaited
Palforzia’s effectiveness was based on a randomized, double-blind, placebo-controlled study involving about 500 peanut-allergic individuals that found that 67.2% of allergic patients tolerated an oral challenge with a single 600-mg dose of peanut protein with no more than mild allergic symptoms after 6 months of maintenance treatment, compared with 4% of placebo recipients, the FDA said.
In two double-blind, placebo-controlled studies looking at safety, the most commonly reported side effects among about 700 individuals involved in the research were abdominal pain, vomiting, nausea, tingling in the mouth, itching (including in the mouth and ears), cough, runny nose, throat irritation and tightness, hives, wheezing and shortness of breath, and anaphylaxis.
Palforzia should not be given to those with uncontrolled asthma and can’t be used for emergency treatment of allergic reactions, including anaphylaxis.
“The food allergy community has been eagerly awaiting an FDA-approved treatment that can help mitigate allergic reactions to peanut and, as allergists, we want nothing more than to have a treatment option to offer our patients that has demonstrated both the safety and efficacy to truly impact the lives of patients who live with peanut allergy,” said Christina Ciaccio, MD, chief of Allergy/Immunology and Pediatric Pulmonary Medicine at the University of Chicago Medical Center and Biological Sciences, in a company statement from Aimmune. “With today’s approval of Palforzia, we can – for the first time – offer children and teens with peanut allergy a proven medicine that employs an established therapeutic approach.”
This article first appeared on Medscape.com.
Dependent trait in chronic migraine may predict nonresponse to onabotulinumtoxin A
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
FROM HEADACHE
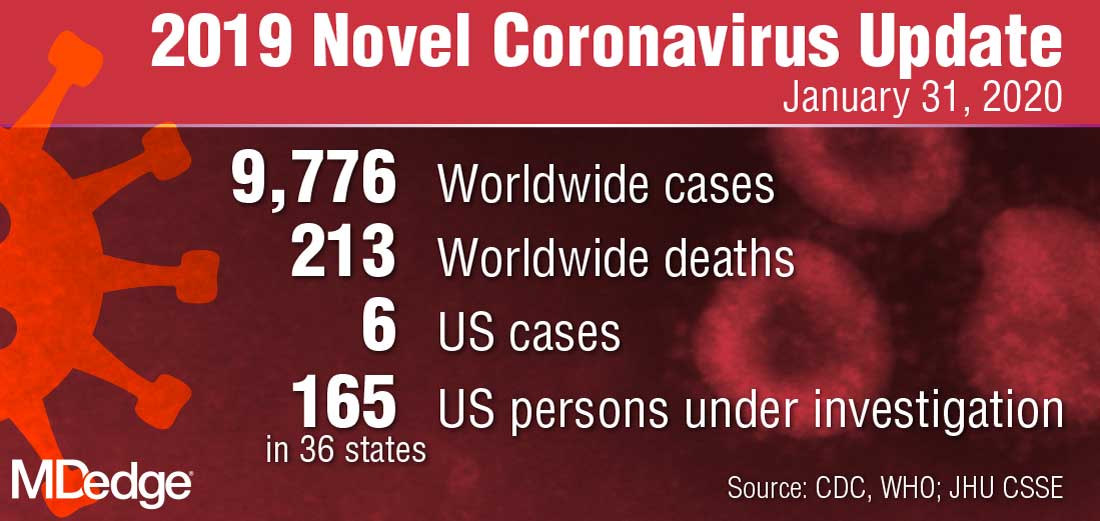
HHS declares coronavirus emergency, orders quarantine
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
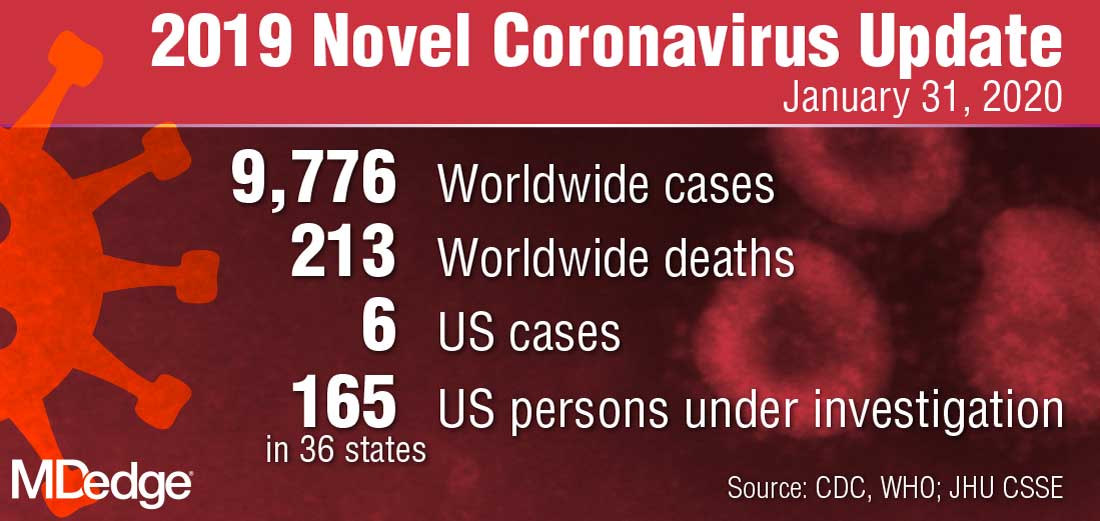
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
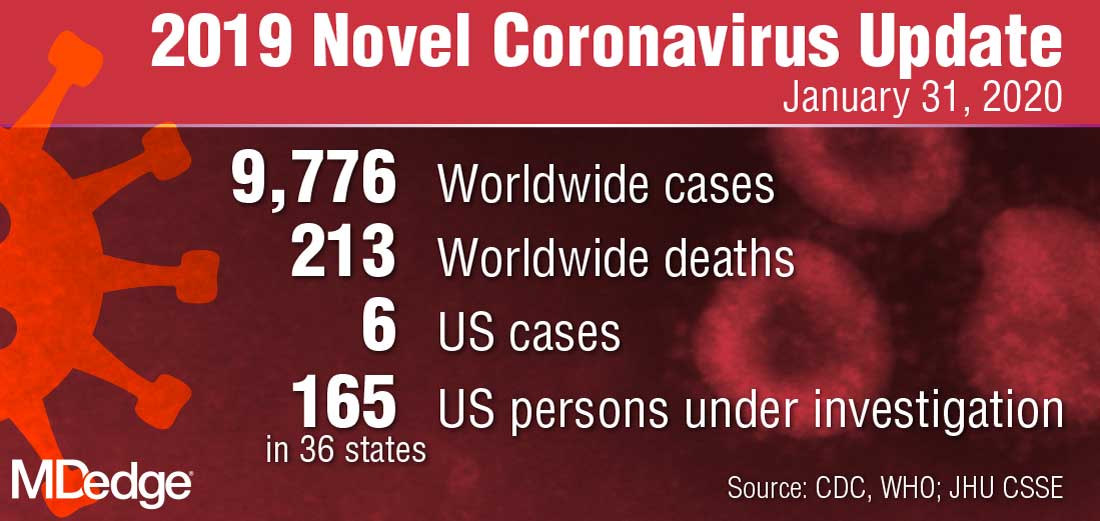
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
CDC: Opioid prescribing and use rates down since 2010
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
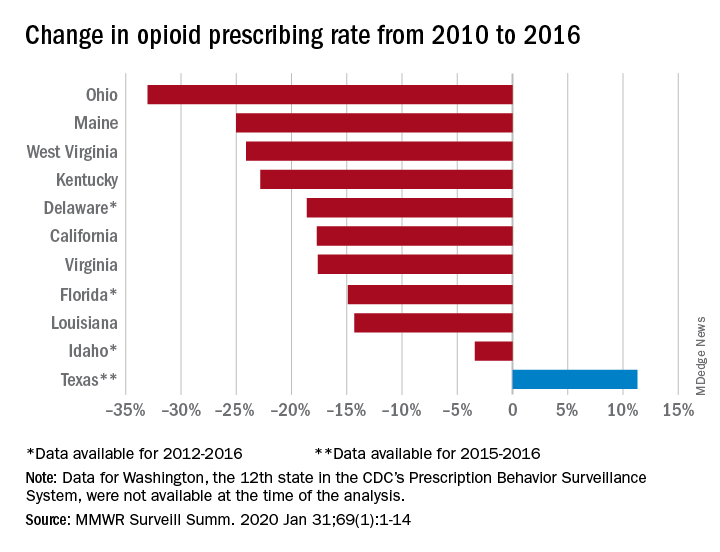
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
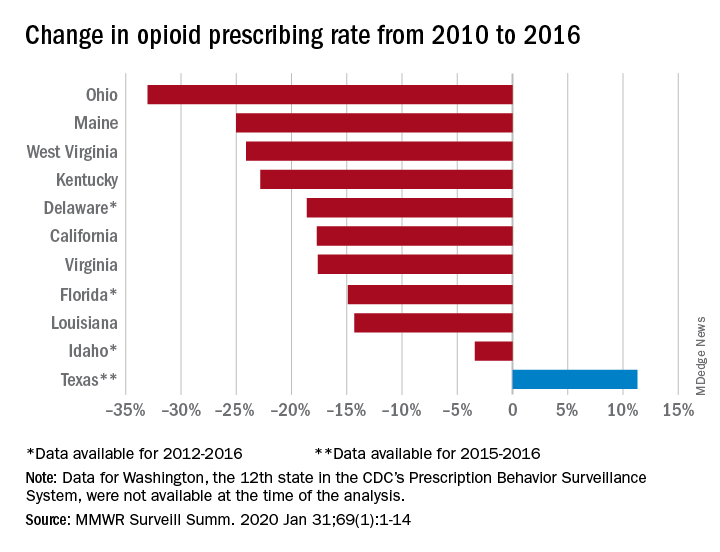
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
Trends in opioid prescribing and use from 2010 to 2016 offer some encouragement, but opioid-attributable deaths continued to increase over that period, according to the Centers for Disease Control and Prevention.
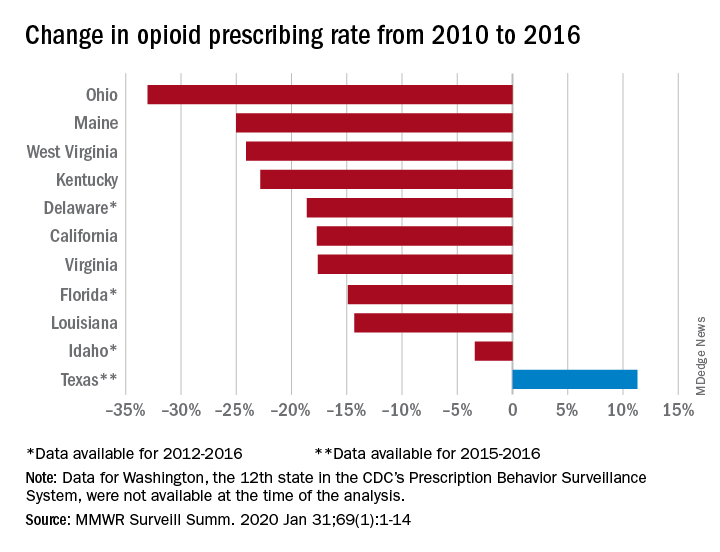
Prescribing rates dropped during that period, as did daily opioid dosage rates and the percentage of patients with high daily opioid dosages, Gail K. Strickler, PhD, of the Institute for Behavioral Health at Brandeis University in Waltham, Mass., and associates wrote in MMWR Surveillance Summaries.
Their analysis involved 11 of the 12 states (Washington was unable to provide data for the analysis) participating in the CDC’s Prescription Behavior Surveillance System, which uses data from the states’ prescription drug monitoring programs. The 11 states represented about 38% of the U.S. population in 2016.
The opioid prescribing rate fell in 10 of those 11 states, with declines varying from 3.4% in Idaho to 33.0% in Ohio. Prescribing went up in Texas by 11.3%, but the state only had data available for 2015 and 2016. Three other states – Delaware, Florida, and Idaho – were limited to data from 2012 to 2016, the investigators noted.
As for the other measures, all states showed declines for the mean daily opioid dosage. Texas had the smallest drop at 2.9% and Florida saw the largest, at 27.4%. All states also had reductions in the percentage of patients with high daily opioid dosage, with decreases varying from 5.7% in Idaho to 43.9% in Louisiana, Dr. Strickler and associates reported. A high daily dosage was defined as at least 90 morphine milligram equivalents for all class II-V opioid drugs.
“Despite these favorable trends ... opioid overdose deaths attributable to the most commonly prescribed opioids, the natural and semisynthetics (e.g., morphine and oxycodone), increased during 2010-2016,” they said.
It is possible that a change in mortality is lagging “behind changes in prescribing behaviors” or that “the trend in deaths related to these types of opioids has been driven by factors other than prescription opioid misuse rates, such as increasing mortality from heroin, which is frequently classified as morphine or found concomitantly with morphine postmortem, and a spike in deaths involving illicitly manufactured fentanyl combined with heroin and prescribed opioids since 2013,” the investigators suggested.
SOURCE: Strickler GK et al. MMWR Surveill Summ. 2020 Jan 31;69(1):1-14.
FROM MMWR SURVEILLANCE SUMMARIES
CDC: First person-to-person spread of novel coronavirus in U.S.
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
A Chicago woman in her 60s who tested positive for the 2019 Novel Coronavirus (2019-nCoV) after returning from Wuhan, China, earlier this month has infected her husband, becoming the first known instance of person-to-person transmission of the 2019-nCoV in the United States.
“Limited person-to-person spread of this new virus outside of China has already been seen in nine close contacts, where travelers were infected and transmitted the virus to someone else,” Robert R. Redfield, MD, director of the Centers for Disease Control and Prevention, said during a press briefing on Jan. 30, 2020. “However, the full picture of how easy and how sustainable this virus can spread is unclear. Today’s news underscores the important risk-dependent exposure. The vast majority of Americans have not had recent travel to China, where sustained human-to-human transmission is occurring. Individuals who are close personal contacts of cases, though, could have a risk.”
The affected man, also in his 60s, is the spouse of the first confirmed travel-associated case of 2019-nCoV to be reported in the state of Illinois, according to Ngozi O. Ezike, MD, director of the Illinois Department of Public Health. The man had no history of recent travel to China. “This person-to-person spread was between two very close contacts: a wife and husband,” said Dr. Ezike, who added that 21 individuals in the state are under investigation for 2019-nCoV. “The virus is not spreading widely across the community. At this time, we are not recommending that people in the general public take additional precautions such as canceling activities or avoiding going out. While there is concern with this second case, public health officials are actively monitoring close contacts, including health care workers, and we believe that people in Illinois are at low risk.”
Jennifer Layden, MD, state epidemiologist at the Illinois Department of Public Health, said that the infected Chicago woman returned from Wuhan, China on Jan. 13, 2020. She is hospitalized in stable condition “and continues to do well,” Dr. Layden said. “Public health officials have been actively and closely monitoring individuals who had contacts with her, including her husband, who had close contact for symptoms. He recently began reporting symptoms and was immediately admitted to the hospital and placed in an isolation room, where he is in stable condition. We are actively monitoring individuals such as health care workers, household contacts, and others who were in contact with either of the confirmed cases in the goal to contain and reduce the risk of additional transmission.”
Nancy Messonnier, MD, director, National Center for Immunization and Respiratory Diseases, expects that more cases of 2019-nCoV will transpire in the United States.
“More cases means the potential for more person-to-person spread,” Dr. Messonnier said. “We’re trying to strike a balance in our response right now. We want to be aggressive, but we want our actions to be evidence-based and appropriate for the current circumstance. For example, CDC does not currently recommend use of face masks for the general public. The virus is not spreading in the general community.”
ASCO issues guidelines on genetic testing in epithelial ovarian cancer
In new guidelines, the American Society of Clinical Oncology recommends offering germline genetic testing for BRCA1, BRCA2, and other ovarian cancer susceptibility genes to all women diagnosed with epithelial ovarian cancer, regardless of their clinical features or family history.
Testing should be offered at diagnosis or as soon as possible after that, Panagiotis A. Konstantinopoulos, MD, PhD, of the Dana-Farber Cancer Institute in Boston, and colleagues wrote in the Journal of Clinical Oncology.
For patients who do not carry a germline pathogenic or likely pathogenic BRCA1/2 variant, the guidelines recommend offering somatic tumor testing for BRCA1/2 pathogenic or likely pathogenic variants. This testing can be offered at the time of disease recurrence after up-front therapy.
The guidelines also recommend somatic tumor testing for mismatch repair deficiency in patients diagnosed with clear cell, endometrioid, or mucinous ovarian cancer. This testing may be offered to patients with other histologic types of epithelial ovarian cancer as well.
Genetic testing, as well as genetic risk evaluation and counseling, should be offered to first- or second-degree blood relatives of a patient with ovarian cancer and a known germline pathogenic cancer susceptibility gene variant, according to the guidelines.
According to the guidelines, genetic evaluations should be conducted in cooperation with other health care providers who are “familiar with the diagnosis and management of hereditary cancer syndromes to determine the most appropriate testing strategy and discuss implications of the findings.”
Patients with identified germline or somatic pathogenic or likely pathogenic BRCA1/2 variants should receive treatments approved for them by the Food and Drug Administration, according to the guidelines. The authors note that patients with these variants have responded well to FDA-approved poly (ADP-ribose) polymerase inhibitors, including niraparib (Zejula), olaparib (Lynparza), and rucaparib (Rubraca).
The guidelines also state that mismatch repair deficiency qualifies for FDA-approved treatment, so patients with recurrent epithelial ovarian cancer and mismatch repair deficiency should receive FDA-approved treatments under their labeled indications.
The guidelines note that clinical decisions should not be based on a variant of uncertain significance. When a patient has such a variant, “clinical features and family history should inform clinical decision making,” according to the guidelines.
Dr. Konstantinopoulos and colleagues formulated the guidelines after reviewing data from 19 studies, including 6 meta-analyses; 11 randomized, controlled trials; and 2 observational studies.
The authors reported relationships with a range of pharmaceutical companies, including those that market drugs for epithelial ovarian cancer.
SOURCE: Konstantinopoulos PA et al. J Clin Oncol. 2020 Jan 27. doi: 10.1200/JCO.19.02960.
In new guidelines, the American Society of Clinical Oncology recommends offering germline genetic testing for BRCA1, BRCA2, and other ovarian cancer susceptibility genes to all women diagnosed with epithelial ovarian cancer, regardless of their clinical features or family history.
Testing should be offered at diagnosis or as soon as possible after that, Panagiotis A. Konstantinopoulos, MD, PhD, of the Dana-Farber Cancer Institute in Boston, and colleagues wrote in the Journal of Clinical Oncology.
For patients who do not carry a germline pathogenic or likely pathogenic BRCA1/2 variant, the guidelines recommend offering somatic tumor testing for BRCA1/2 pathogenic or likely pathogenic variants. This testing can be offered at the time of disease recurrence after up-front therapy.
The guidelines also recommend somatic tumor testing for mismatch repair deficiency in patients diagnosed with clear cell, endometrioid, or mucinous ovarian cancer. This testing may be offered to patients with other histologic types of epithelial ovarian cancer as well.
Genetic testing, as well as genetic risk evaluation and counseling, should be offered to first- or second-degree blood relatives of a patient with ovarian cancer and a known germline pathogenic cancer susceptibility gene variant, according to the guidelines.
According to the guidelines, genetic evaluations should be conducted in cooperation with other health care providers who are “familiar with the diagnosis and management of hereditary cancer syndromes to determine the most appropriate testing strategy and discuss implications of the findings.”
Patients with identified germline or somatic pathogenic or likely pathogenic BRCA1/2 variants should receive treatments approved for them by the Food and Drug Administration, according to the guidelines. The authors note that patients with these variants have responded well to FDA-approved poly (ADP-ribose) polymerase inhibitors, including niraparib (Zejula), olaparib (Lynparza), and rucaparib (Rubraca).
The guidelines also state that mismatch repair deficiency qualifies for FDA-approved treatment, so patients with recurrent epithelial ovarian cancer and mismatch repair deficiency should receive FDA-approved treatments under their labeled indications.
The guidelines note that clinical decisions should not be based on a variant of uncertain significance. When a patient has such a variant, “clinical features and family history should inform clinical decision making,” according to the guidelines.
Dr. Konstantinopoulos and colleagues formulated the guidelines after reviewing data from 19 studies, including 6 meta-analyses; 11 randomized, controlled trials; and 2 observational studies.
The authors reported relationships with a range of pharmaceutical companies, including those that market drugs for epithelial ovarian cancer.
SOURCE: Konstantinopoulos PA et al. J Clin Oncol. 2020 Jan 27. doi: 10.1200/JCO.19.02960.
In new guidelines, the American Society of Clinical Oncology recommends offering germline genetic testing for BRCA1, BRCA2, and other ovarian cancer susceptibility genes to all women diagnosed with epithelial ovarian cancer, regardless of their clinical features or family history.
Testing should be offered at diagnosis or as soon as possible after that, Panagiotis A. Konstantinopoulos, MD, PhD, of the Dana-Farber Cancer Institute in Boston, and colleagues wrote in the Journal of Clinical Oncology.
For patients who do not carry a germline pathogenic or likely pathogenic BRCA1/2 variant, the guidelines recommend offering somatic tumor testing for BRCA1/2 pathogenic or likely pathogenic variants. This testing can be offered at the time of disease recurrence after up-front therapy.
The guidelines also recommend somatic tumor testing for mismatch repair deficiency in patients diagnosed with clear cell, endometrioid, or mucinous ovarian cancer. This testing may be offered to patients with other histologic types of epithelial ovarian cancer as well.
Genetic testing, as well as genetic risk evaluation and counseling, should be offered to first- or second-degree blood relatives of a patient with ovarian cancer and a known germline pathogenic cancer susceptibility gene variant, according to the guidelines.
According to the guidelines, genetic evaluations should be conducted in cooperation with other health care providers who are “familiar with the diagnosis and management of hereditary cancer syndromes to determine the most appropriate testing strategy and discuss implications of the findings.”
Patients with identified germline or somatic pathogenic or likely pathogenic BRCA1/2 variants should receive treatments approved for them by the Food and Drug Administration, according to the guidelines. The authors note that patients with these variants have responded well to FDA-approved poly (ADP-ribose) polymerase inhibitors, including niraparib (Zejula), olaparib (Lynparza), and rucaparib (Rubraca).
The guidelines also state that mismatch repair deficiency qualifies for FDA-approved treatment, so patients with recurrent epithelial ovarian cancer and mismatch repair deficiency should receive FDA-approved treatments under their labeled indications.
The guidelines note that clinical decisions should not be based on a variant of uncertain significance. When a patient has such a variant, “clinical features and family history should inform clinical decision making,” according to the guidelines.
Dr. Konstantinopoulos and colleagues formulated the guidelines after reviewing data from 19 studies, including 6 meta-analyses; 11 randomized, controlled trials; and 2 observational studies.
The authors reported relationships with a range of pharmaceutical companies, including those that market drugs for epithelial ovarian cancer.
SOURCE: Konstantinopoulos PA et al. J Clin Oncol. 2020 Jan 27. doi: 10.1200/JCO.19.02960.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Gestational diabetes: Treatment controversy rages on
WASHINGTON – Pharmacologic treatment of gestational diabetes remains controversial, with the American College of Obstetricians and Gynecologists and the American Diabetes Association firmly recommending insulin as the preferred first-line pharmacologic therapy, and the Society of Maternal-Fetal Medicine more accepting of metformin as a “reasonable and safe first-line” alternative to insulin and stating that there are no strong data supporting metformin over the sulfonylurea glyburide.
If there’s one main take-away, Mark B. Landon, MD, said at the biennial meeting of the Diabetes in Pregnancy Study Group of North America, it was that “the primary concern” about the use of oral agents for treating gestational diabetes mellitus (GDM) is that there is limited long-term follow-up of exposed offspring.
“The claim that long-term safety data are not available for any oral agent is probably the most valid warning [of any of the concerns voiced by professional organizations],” said Dr. Landon, Richard L. Meiling professor and chair of the department of obstetrics and gynecology at The Ohio State University Wexner Medical Center, Columbus.
Otherwise, he said, there are not enough data to firmly prioritize the drugs most commonly used for GDM, and “the superiority of insulin over oral agents simply remains questionable.”
ACOG’s 2017 level A recommendation for insulin as the first-line option when pharmacologic treatment is needed for treating GDM (Obstet Gynecol. 2017;130[1]:e17-37) was followed in 2018 by another updated practice bulletin on GDM (Obstet Gynecol. 2018;131[2]:e49-64) that considered several meta-analyses published in 2017 and reiterated a preference for insulin.
Those recent meta-analyses of pharmacologic treatment of GDM show that the available literature is generally of “poor trial quality,” and that studies are small and not designed to assess equivalence or noninferiority, Mark Turrentine, MD, chair of ACOG’s committee on practice bulletins, said in an interview. “Taking that into account and [considering] that oral antidiabetic medications are not approved by the Food and Drug Administration [for the treatment of GDM], that they cross the placenta, and that we currently lack long-term neonatal safety data ... we felt that insulin is the preferred treatment.”
In its 2017 and 2018 bulletins, ACOG said that metformin is a “reasonable alternative choice” for women who decline insulin therapy or who may be unable to safely administer it (a level B recommendation). The 2018 practice bulletin mentions one additional factor: affordability. “Insurance companies aren’t always covering [insulin],” said Dr. Turrentine, of the department of obstetrics and gynecology, Baylor College of Medicine, Houston. “It’s a challenge – no question.”
ACOG says glyburide should not be recommended as a first-line pharmacologic treatment, “because, in most studies, it does not yield outcomes equivalent to insulin or metformin,” Dr. Turrentine emphasized.
Glyburide’s role
Dr. Landon took issue with ACOG’s stance on the sulfonylurea. “Frankly, I think this [conclusion] is debatable,” he said. The trend in the United States – “at least after the 2017 ACOG document came out”– has been toward use of metformin over glyburide when an oral agent is [used], but “I think glyburide has been unfairly trashed. It probably still has a place.”
As Dr. Landon sees it, research published in 2015 put a damper on the use of glyburide, which “had become the number one agent” after an earlier, seminal trial, led by Oded Langer, MD, had shown equivalent glycemic control in about 400 women with GDM who were randomized to receive either insulin or glyburide (N Engl J Med. 2000;343;1134-8). The trial was not powered to evaluate other outcomes, but there were no significant differences in neonatal complications, Dr. Landon said.
One of the 2015 studies – a large, retrospective, population-based study of more than 9,000 women with GDM treated with glyburide or insulin – showed a higher risk of admission to the neonatal intensive care unit (relative risk, 1.41), hypoglycemia in the newborn (RR, 1.40), and large-for-gestational age (RR, 1.43) with glyburide, compared with insulin (JAMA Pediatr. 2015;169[5]:452-8).
A meta-analysis of glyburide, metformin, and insulin showed significant differences between glyburide and insulin in birth weight, macrosomia (RR, 2.62), and neonatal hypoglycemia (RR, 2.04; BMJ. 2015;350;h102). However, “this was basically a conglomeration of studies with about 50 [individuals] in each arm, and in which entry criteria for the diagnosis of GDM were rather heterogeneous,” said Dr. Landon. “There are real problems with this and other meta-analyses.”
The authors of a 2018 multicenter, noninferiority, randomized, controlled trial of about 900 women concluded that their study failed to show that the use of glyburide, compared with insulin, does not result in a greater frequency of perinatal complications. The authors also wrote, however, that the “increase in perinatal complications [with glyburide] may be no more than 10.5%, compared with insulin” (JAMA. 2018;319[17]:1773-80).
That increase, Dr. Landon said, was “not an absolute 10%, but 10% of the complication rate, which probably translates to about 2%.” The only component of a composite outcome (including macrosomia, hypoglycemia, and hyperbilirubinemia) that was significantly different, he noted, was hypoglycemia, which affected 12.2% of neonates in the glyburide group and 7.2% in the insulin group.
Glyburide’s role may well be substantiated in the future, Dr. Landon said during a discussion period at the meeting, through research underway at the University of Pittsburgh aimed at tailoring treatment to the underlying pathophysiology of a patient’s GDM.
The MATCh-GDM study (Metabolic Analysis for Treatment Choice in GDM) is randomizing women to receive usual, unmatched treatment or treatment matched to GDM mechanism – metformin for predominant insulin resistance, glyburide or insulin for predominant insulin secretion defects, and one of the three for combined mechanisms. The study’s principal investigator, Maisa Feghali, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of Pittsburgh, stressed in a presentation on the study that GDM is a heterogeneous condition and that research is needed to understand the impact of GDM subtypes on treatment response.
Metformin outcomes
Concerns about the impact of metformin on short-term perinatal outcomes focus on preterm birth, Dr. Landon said. The only study to date that has shown an increased rate of prematurity, however, is the “seminal” Metformin in Gestational Diabetes (MiG) trial led by Janet A. Rowan, MBChB, that randomized 751 women with GDM in Australia and New Zealand to treatment with metformin or insulin. The researchers found no significant differences between a composite of neonatal complications but did establish that severe hypoglycemia was less common in the metformin group and preterm birth was more common (N Engl J Med. 2008;358:2003-15).
A 2016 systematic review and meta-analysis of short- and long-term outcomes of metformin, compared with insulin, found that metformin did not increase preterm delivery (Diabet Med. 2017;34[1]:27-36). And while the 2015 BMJ meta-analysis found that metformin was associated with higher rates of preterm birth (RR, 1.50), the increased risk “was all driven by the Rowan study,” Dr. Landon said. The 2015 meta-analysis also found that metformin was associated with less maternal weight gain and fewer infants who were large for gestational age.
Metformin is also tainted by high rates of failure in GDM. In the 2008 Rowan study, 46% of patients on metformin failed to achieve glycemic control. “But this is a classic half-full, half-empty [phenomena],” Dr. Landon said. “Some people say this isn’t good, but on the other hand, 54% avoided insulin.”
Indeed, the Society of Maternal-Fetal Medicine (SMFM), in its 2018 statement on the pharmacologic treatment of GDM, said that oral hypoglycemic agents that are used as monotherapy work in “more than half” of GDM pregnancies. The need for adjunctive insulin to achieve glycemic control ranges between 26% and 46% for women using metformin, and 4% and 16% for women using glyburide, it says.
In the society’s view, recent meta-analyses and systemic reviews “support the efficacy and safety of oral agents,” and “although concerns have been raised for more frequent adverse neonatal outcomes with glyburide, including macrosomia and hypoglycemia, the evidence of benefit of one oral agent over the other remains limited.”
The society says that the difference between its statement and the ACOG recommendations is “based on the values placed by different experts and providers on the available evidence,” and it adds that more long-term data are needed.
But as Dr. Landon said, the SMFM is “a little more forgiving” in its interpretation of a limited body of literature. And clinicians, in the meantime, have to navigate the controversy. “The professional organizations don’t make it easy for [us],” he said. At this point, “insulin does not cross the placenta, and the oral agents do cross it. Informed consent is absolutely necessary when choosing oral agents for treating GDM.”
Offspring well-being
Of greater concern than neonatal outcomes are the potential long-term issues for offspring, Dr. Landon said. On the one hand, it is theorized that metformin may protect beta-cell function in offspring and thereby reduce the cross-generational effects of obesity and type 2 diabetes. On the other hand, it is theorized that the drug may cause a decrease in cell-cycle proliferation, which could have “unknown fetal programming effects,” and it may inhibit the mTOR signaling pathway, thus restricting the transport of glucose and amino acids across the placenta, he said. (Findings from in vitro research have suggested that glyburide treatment in GDM might be associated with enhanced transport across the placenta, he noted.)
Long-term follow-up studies of offspring are “clearly needed,” Dr. Landon said. At this point, in regard to long-term safety, he and other experts are concerned primarily about the potential for obesity and metabolic dysfunction in offspring who are exposed to metformin in utero. They are watching follow-up from Dr. Rowan’s MiG trial, as well as elsewhere in the literature, on metformin-exposed offspring from mothers with polycystic ovary syndrome.
A follow-up analysis of offspring from the MiG trial found that children of women with GDM who were exposed to metformin had larger measures of subcutaneous fat at age 2 years, compared with children of mothers treated with insulin alone, but that overall body fat was the same, Dr. Landon noted. The investigators postulated that these children may have less visceral fat and a more favorable pattern of fat distribution (Diab Care. 2011;34:2279-84).
A recently published follow-up analysis of two randomized, controlled trials of women with polycystic ovary syndrome is cause for more concern, he said. That analysis showed that offspring exposed to metformin in utero had a higher body mass index and an increased prevalence of obesity or overweight at age 4 years, compared with placebo groups (J Clin Endocrinol Metab. 2018;103[4]:1612-21).
That analysis of metformin-exposed offspring in the context of polycystic ovary syndrome was published after the SMFM statement, as was another follow-up analysis of MiG trial offspring – this one, at ages 7-9 years – that showed an increase in weight, size, and fat mass in one of two subsets analyzed, despite no difference in large-for-gestational age rates between the metformin- and insulin-exposed offspring (BMJ Open Diabetes Res Care. 2018;6[1]: e000456).
In 2018, a group of 17 prominent diabetes and maternal-fetal medicine researchers cited these findings in a response to the SMFM statement and cautioned against the widespread adoption of metformin use during pregnancy, writing that, based on “both pharmacologic and randomized trial evidence that metformin may create an atypical intrauterine environment ... we believe it is premature to embrace metformin as equivalent to insulin or as superior to glyburide, and that patients should be counseled on the limited long-term safety data and potential for adverse childhood metabolic effects” (Am J Obstet Gynecol. 2018;219[4]:367.e1-7).
WASHINGTON – Pharmacologic treatment of gestational diabetes remains controversial, with the American College of Obstetricians and Gynecologists and the American Diabetes Association firmly recommending insulin as the preferred first-line pharmacologic therapy, and the Society of Maternal-Fetal Medicine more accepting of metformin as a “reasonable and safe first-line” alternative to insulin and stating that there are no strong data supporting metformin over the sulfonylurea glyburide.
If there’s one main take-away, Mark B. Landon, MD, said at the biennial meeting of the Diabetes in Pregnancy Study Group of North America, it was that “the primary concern” about the use of oral agents for treating gestational diabetes mellitus (GDM) is that there is limited long-term follow-up of exposed offspring.
“The claim that long-term safety data are not available for any oral agent is probably the most valid warning [of any of the concerns voiced by professional organizations],” said Dr. Landon, Richard L. Meiling professor and chair of the department of obstetrics and gynecology at The Ohio State University Wexner Medical Center, Columbus.
Otherwise, he said, there are not enough data to firmly prioritize the drugs most commonly used for GDM, and “the superiority of insulin over oral agents simply remains questionable.”
ACOG’s 2017 level A recommendation for insulin as the first-line option when pharmacologic treatment is needed for treating GDM (Obstet Gynecol. 2017;130[1]:e17-37) was followed in 2018 by another updated practice bulletin on GDM (Obstet Gynecol. 2018;131[2]:e49-64) that considered several meta-analyses published in 2017 and reiterated a preference for insulin.
Those recent meta-analyses of pharmacologic treatment of GDM show that the available literature is generally of “poor trial quality,” and that studies are small and not designed to assess equivalence or noninferiority, Mark Turrentine, MD, chair of ACOG’s committee on practice bulletins, said in an interview. “Taking that into account and [considering] that oral antidiabetic medications are not approved by the Food and Drug Administration [for the treatment of GDM], that they cross the placenta, and that we currently lack long-term neonatal safety data ... we felt that insulin is the preferred treatment.”
In its 2017 and 2018 bulletins, ACOG said that metformin is a “reasonable alternative choice” for women who decline insulin therapy or who may be unable to safely administer it (a level B recommendation). The 2018 practice bulletin mentions one additional factor: affordability. “Insurance companies aren’t always covering [insulin],” said Dr. Turrentine, of the department of obstetrics and gynecology, Baylor College of Medicine, Houston. “It’s a challenge – no question.”
ACOG says glyburide should not be recommended as a first-line pharmacologic treatment, “because, in most studies, it does not yield outcomes equivalent to insulin or metformin,” Dr. Turrentine emphasized.
Glyburide’s role
Dr. Landon took issue with ACOG’s stance on the sulfonylurea. “Frankly, I think this [conclusion] is debatable,” he said. The trend in the United States – “at least after the 2017 ACOG document came out”– has been toward use of metformin over glyburide when an oral agent is [used], but “I think glyburide has been unfairly trashed. It probably still has a place.”
As Dr. Landon sees it, research published in 2015 put a damper on the use of glyburide, which “had become the number one agent” after an earlier, seminal trial, led by Oded Langer, MD, had shown equivalent glycemic control in about 400 women with GDM who were randomized to receive either insulin or glyburide (N Engl J Med. 2000;343;1134-8). The trial was not powered to evaluate other outcomes, but there were no significant differences in neonatal complications, Dr. Landon said.
One of the 2015 studies – a large, retrospective, population-based study of more than 9,000 women with GDM treated with glyburide or insulin – showed a higher risk of admission to the neonatal intensive care unit (relative risk, 1.41), hypoglycemia in the newborn (RR, 1.40), and large-for-gestational age (RR, 1.43) with glyburide, compared with insulin (JAMA Pediatr. 2015;169[5]:452-8).
A meta-analysis of glyburide, metformin, and insulin showed significant differences between glyburide and insulin in birth weight, macrosomia (RR, 2.62), and neonatal hypoglycemia (RR, 2.04; BMJ. 2015;350;h102). However, “this was basically a conglomeration of studies with about 50 [individuals] in each arm, and in which entry criteria for the diagnosis of GDM were rather heterogeneous,” said Dr. Landon. “There are real problems with this and other meta-analyses.”
The authors of a 2018 multicenter, noninferiority, randomized, controlled trial of about 900 women concluded that their study failed to show that the use of glyburide, compared with insulin, does not result in a greater frequency of perinatal complications. The authors also wrote, however, that the “increase in perinatal complications [with glyburide] may be no more than 10.5%, compared with insulin” (JAMA. 2018;319[17]:1773-80).
That increase, Dr. Landon said, was “not an absolute 10%, but 10% of the complication rate, which probably translates to about 2%.” The only component of a composite outcome (including macrosomia, hypoglycemia, and hyperbilirubinemia) that was significantly different, he noted, was hypoglycemia, which affected 12.2% of neonates in the glyburide group and 7.2% in the insulin group.
Glyburide’s role may well be substantiated in the future, Dr. Landon said during a discussion period at the meeting, through research underway at the University of Pittsburgh aimed at tailoring treatment to the underlying pathophysiology of a patient’s GDM.
The MATCh-GDM study (Metabolic Analysis for Treatment Choice in GDM) is randomizing women to receive usual, unmatched treatment or treatment matched to GDM mechanism – metformin for predominant insulin resistance, glyburide or insulin for predominant insulin secretion defects, and one of the three for combined mechanisms. The study’s principal investigator, Maisa Feghali, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of Pittsburgh, stressed in a presentation on the study that GDM is a heterogeneous condition and that research is needed to understand the impact of GDM subtypes on treatment response.
Metformin outcomes
Concerns about the impact of metformin on short-term perinatal outcomes focus on preterm birth, Dr. Landon said. The only study to date that has shown an increased rate of prematurity, however, is the “seminal” Metformin in Gestational Diabetes (MiG) trial led by Janet A. Rowan, MBChB, that randomized 751 women with GDM in Australia and New Zealand to treatment with metformin or insulin. The researchers found no significant differences between a composite of neonatal complications but did establish that severe hypoglycemia was less common in the metformin group and preterm birth was more common (N Engl J Med. 2008;358:2003-15).
A 2016 systematic review and meta-analysis of short- and long-term outcomes of metformin, compared with insulin, found that metformin did not increase preterm delivery (Diabet Med. 2017;34[1]:27-36). And while the 2015 BMJ meta-analysis found that metformin was associated with higher rates of preterm birth (RR, 1.50), the increased risk “was all driven by the Rowan study,” Dr. Landon said. The 2015 meta-analysis also found that metformin was associated with less maternal weight gain and fewer infants who were large for gestational age.
Metformin is also tainted by high rates of failure in GDM. In the 2008 Rowan study, 46% of patients on metformin failed to achieve glycemic control. “But this is a classic half-full, half-empty [phenomena],” Dr. Landon said. “Some people say this isn’t good, but on the other hand, 54% avoided insulin.”
Indeed, the Society of Maternal-Fetal Medicine (SMFM), in its 2018 statement on the pharmacologic treatment of GDM, said that oral hypoglycemic agents that are used as monotherapy work in “more than half” of GDM pregnancies. The need for adjunctive insulin to achieve glycemic control ranges between 26% and 46% for women using metformin, and 4% and 16% for women using glyburide, it says.
In the society’s view, recent meta-analyses and systemic reviews “support the efficacy and safety of oral agents,” and “although concerns have been raised for more frequent adverse neonatal outcomes with glyburide, including macrosomia and hypoglycemia, the evidence of benefit of one oral agent over the other remains limited.”
The society says that the difference between its statement and the ACOG recommendations is “based on the values placed by different experts and providers on the available evidence,” and it adds that more long-term data are needed.
But as Dr. Landon said, the SMFM is “a little more forgiving” in its interpretation of a limited body of literature. And clinicians, in the meantime, have to navigate the controversy. “The professional organizations don’t make it easy for [us],” he said. At this point, “insulin does not cross the placenta, and the oral agents do cross it. Informed consent is absolutely necessary when choosing oral agents for treating GDM.”
Offspring well-being
Of greater concern than neonatal outcomes are the potential long-term issues for offspring, Dr. Landon said. On the one hand, it is theorized that metformin may protect beta-cell function in offspring and thereby reduce the cross-generational effects of obesity and type 2 diabetes. On the other hand, it is theorized that the drug may cause a decrease in cell-cycle proliferation, which could have “unknown fetal programming effects,” and it may inhibit the mTOR signaling pathway, thus restricting the transport of glucose and amino acids across the placenta, he said. (Findings from in vitro research have suggested that glyburide treatment in GDM might be associated with enhanced transport across the placenta, he noted.)
Long-term follow-up studies of offspring are “clearly needed,” Dr. Landon said. At this point, in regard to long-term safety, he and other experts are concerned primarily about the potential for obesity and metabolic dysfunction in offspring who are exposed to metformin in utero. They are watching follow-up from Dr. Rowan’s MiG trial, as well as elsewhere in the literature, on metformin-exposed offspring from mothers with polycystic ovary syndrome.
A follow-up analysis of offspring from the MiG trial found that children of women with GDM who were exposed to metformin had larger measures of subcutaneous fat at age 2 years, compared with children of mothers treated with insulin alone, but that overall body fat was the same, Dr. Landon noted. The investigators postulated that these children may have less visceral fat and a more favorable pattern of fat distribution (Diab Care. 2011;34:2279-84).
A recently published follow-up analysis of two randomized, controlled trials of women with polycystic ovary syndrome is cause for more concern, he said. That analysis showed that offspring exposed to metformin in utero had a higher body mass index and an increased prevalence of obesity or overweight at age 4 years, compared with placebo groups (J Clin Endocrinol Metab. 2018;103[4]:1612-21).
That analysis of metformin-exposed offspring in the context of polycystic ovary syndrome was published after the SMFM statement, as was another follow-up analysis of MiG trial offspring – this one, at ages 7-9 years – that showed an increase in weight, size, and fat mass in one of two subsets analyzed, despite no difference in large-for-gestational age rates between the metformin- and insulin-exposed offspring (BMJ Open Diabetes Res Care. 2018;6[1]: e000456).
In 2018, a group of 17 prominent diabetes and maternal-fetal medicine researchers cited these findings in a response to the SMFM statement and cautioned against the widespread adoption of metformin use during pregnancy, writing that, based on “both pharmacologic and randomized trial evidence that metformin may create an atypical intrauterine environment ... we believe it is premature to embrace metformin as equivalent to insulin or as superior to glyburide, and that patients should be counseled on the limited long-term safety data and potential for adverse childhood metabolic effects” (Am J Obstet Gynecol. 2018;219[4]:367.e1-7).
WASHINGTON – Pharmacologic treatment of gestational diabetes remains controversial, with the American College of Obstetricians and Gynecologists and the American Diabetes Association firmly recommending insulin as the preferred first-line pharmacologic therapy, and the Society of Maternal-Fetal Medicine more accepting of metformin as a “reasonable and safe first-line” alternative to insulin and stating that there are no strong data supporting metformin over the sulfonylurea glyburide.
If there’s one main take-away, Mark B. Landon, MD, said at the biennial meeting of the Diabetes in Pregnancy Study Group of North America, it was that “the primary concern” about the use of oral agents for treating gestational diabetes mellitus (GDM) is that there is limited long-term follow-up of exposed offspring.
“The claim that long-term safety data are not available for any oral agent is probably the most valid warning [of any of the concerns voiced by professional organizations],” said Dr. Landon, Richard L. Meiling professor and chair of the department of obstetrics and gynecology at The Ohio State University Wexner Medical Center, Columbus.
Otherwise, he said, there are not enough data to firmly prioritize the drugs most commonly used for GDM, and “the superiority of insulin over oral agents simply remains questionable.”
ACOG’s 2017 level A recommendation for insulin as the first-line option when pharmacologic treatment is needed for treating GDM (Obstet Gynecol. 2017;130[1]:e17-37) was followed in 2018 by another updated practice bulletin on GDM (Obstet Gynecol. 2018;131[2]:e49-64) that considered several meta-analyses published in 2017 and reiterated a preference for insulin.
Those recent meta-analyses of pharmacologic treatment of GDM show that the available literature is generally of “poor trial quality,” and that studies are small and not designed to assess equivalence or noninferiority, Mark Turrentine, MD, chair of ACOG’s committee on practice bulletins, said in an interview. “Taking that into account and [considering] that oral antidiabetic medications are not approved by the Food and Drug Administration [for the treatment of GDM], that they cross the placenta, and that we currently lack long-term neonatal safety data ... we felt that insulin is the preferred treatment.”
In its 2017 and 2018 bulletins, ACOG said that metformin is a “reasonable alternative choice” for women who decline insulin therapy or who may be unable to safely administer it (a level B recommendation). The 2018 practice bulletin mentions one additional factor: affordability. “Insurance companies aren’t always covering [insulin],” said Dr. Turrentine, of the department of obstetrics and gynecology, Baylor College of Medicine, Houston. “It’s a challenge – no question.”
ACOG says glyburide should not be recommended as a first-line pharmacologic treatment, “because, in most studies, it does not yield outcomes equivalent to insulin or metformin,” Dr. Turrentine emphasized.
Glyburide’s role
Dr. Landon took issue with ACOG’s stance on the sulfonylurea. “Frankly, I think this [conclusion] is debatable,” he said. The trend in the United States – “at least after the 2017 ACOG document came out”– has been toward use of metformin over glyburide when an oral agent is [used], but “I think glyburide has been unfairly trashed. It probably still has a place.”
As Dr. Landon sees it, research published in 2015 put a damper on the use of glyburide, which “had become the number one agent” after an earlier, seminal trial, led by Oded Langer, MD, had shown equivalent glycemic control in about 400 women with GDM who were randomized to receive either insulin or glyburide (N Engl J Med. 2000;343;1134-8). The trial was not powered to evaluate other outcomes, but there were no significant differences in neonatal complications, Dr. Landon said.
One of the 2015 studies – a large, retrospective, population-based study of more than 9,000 women with GDM treated with glyburide or insulin – showed a higher risk of admission to the neonatal intensive care unit (relative risk, 1.41), hypoglycemia in the newborn (RR, 1.40), and large-for-gestational age (RR, 1.43) with glyburide, compared with insulin (JAMA Pediatr. 2015;169[5]:452-8).
A meta-analysis of glyburide, metformin, and insulin showed significant differences between glyburide and insulin in birth weight, macrosomia (RR, 2.62), and neonatal hypoglycemia (RR, 2.04; BMJ. 2015;350;h102). However, “this was basically a conglomeration of studies with about 50 [individuals] in each arm, and in which entry criteria for the diagnosis of GDM were rather heterogeneous,” said Dr. Landon. “There are real problems with this and other meta-analyses.”
The authors of a 2018 multicenter, noninferiority, randomized, controlled trial of about 900 women concluded that their study failed to show that the use of glyburide, compared with insulin, does not result in a greater frequency of perinatal complications. The authors also wrote, however, that the “increase in perinatal complications [with glyburide] may be no more than 10.5%, compared with insulin” (JAMA. 2018;319[17]:1773-80).
That increase, Dr. Landon said, was “not an absolute 10%, but 10% of the complication rate, which probably translates to about 2%.” The only component of a composite outcome (including macrosomia, hypoglycemia, and hyperbilirubinemia) that was significantly different, he noted, was hypoglycemia, which affected 12.2% of neonates in the glyburide group and 7.2% in the insulin group.
Glyburide’s role may well be substantiated in the future, Dr. Landon said during a discussion period at the meeting, through research underway at the University of Pittsburgh aimed at tailoring treatment to the underlying pathophysiology of a patient’s GDM.
The MATCh-GDM study (Metabolic Analysis for Treatment Choice in GDM) is randomizing women to receive usual, unmatched treatment or treatment matched to GDM mechanism – metformin for predominant insulin resistance, glyburide or insulin for predominant insulin secretion defects, and one of the three for combined mechanisms. The study’s principal investigator, Maisa Feghali, MD, of the department of obstetrics, gynecology, and reproductive sciences at the University of Pittsburgh, stressed in a presentation on the study that GDM is a heterogeneous condition and that research is needed to understand the impact of GDM subtypes on treatment response.
Metformin outcomes
Concerns about the impact of metformin on short-term perinatal outcomes focus on preterm birth, Dr. Landon said. The only study to date that has shown an increased rate of prematurity, however, is the “seminal” Metformin in Gestational Diabetes (MiG) trial led by Janet A. Rowan, MBChB, that randomized 751 women with GDM in Australia and New Zealand to treatment with metformin or insulin. The researchers found no significant differences between a composite of neonatal complications but did establish that severe hypoglycemia was less common in the metformin group and preterm birth was more common (N Engl J Med. 2008;358:2003-15).
A 2016 systematic review and meta-analysis of short- and long-term outcomes of metformin, compared with insulin, found that metformin did not increase preterm delivery (Diabet Med. 2017;34[1]:27-36). And while the 2015 BMJ meta-analysis found that metformin was associated with higher rates of preterm birth (RR, 1.50), the increased risk “was all driven by the Rowan study,” Dr. Landon said. The 2015 meta-analysis also found that metformin was associated with less maternal weight gain and fewer infants who were large for gestational age.
Metformin is also tainted by high rates of failure in GDM. In the 2008 Rowan study, 46% of patients on metformin failed to achieve glycemic control. “But this is a classic half-full, half-empty [phenomena],” Dr. Landon said. “Some people say this isn’t good, but on the other hand, 54% avoided insulin.”
Indeed, the Society of Maternal-Fetal Medicine (SMFM), in its 2018 statement on the pharmacologic treatment of GDM, said that oral hypoglycemic agents that are used as monotherapy work in “more than half” of GDM pregnancies. The need for adjunctive insulin to achieve glycemic control ranges between 26% and 46% for women using metformin, and 4% and 16% for women using glyburide, it says.
In the society’s view, recent meta-analyses and systemic reviews “support the efficacy and safety of oral agents,” and “although concerns have been raised for more frequent adverse neonatal outcomes with glyburide, including macrosomia and hypoglycemia, the evidence of benefit of one oral agent over the other remains limited.”
The society says that the difference between its statement and the ACOG recommendations is “based on the values placed by different experts and providers on the available evidence,” and it adds that more long-term data are needed.
But as Dr. Landon said, the SMFM is “a little more forgiving” in its interpretation of a limited body of literature. And clinicians, in the meantime, have to navigate the controversy. “The professional organizations don’t make it easy for [us],” he said. At this point, “insulin does not cross the placenta, and the oral agents do cross it. Informed consent is absolutely necessary when choosing oral agents for treating GDM.”
Offspring well-being
Of greater concern than neonatal outcomes are the potential long-term issues for offspring, Dr. Landon said. On the one hand, it is theorized that metformin may protect beta-cell function in offspring and thereby reduce the cross-generational effects of obesity and type 2 diabetes. On the other hand, it is theorized that the drug may cause a decrease in cell-cycle proliferation, which could have “unknown fetal programming effects,” and it may inhibit the mTOR signaling pathway, thus restricting the transport of glucose and amino acids across the placenta, he said. (Findings from in vitro research have suggested that glyburide treatment in GDM might be associated with enhanced transport across the placenta, he noted.)
Long-term follow-up studies of offspring are “clearly needed,” Dr. Landon said. At this point, in regard to long-term safety, he and other experts are concerned primarily about the potential for obesity and metabolic dysfunction in offspring who are exposed to metformin in utero. They are watching follow-up from Dr. Rowan’s MiG trial, as well as elsewhere in the literature, on metformin-exposed offspring from mothers with polycystic ovary syndrome.
A follow-up analysis of offspring from the MiG trial found that children of women with GDM who were exposed to metformin had larger measures of subcutaneous fat at age 2 years, compared with children of mothers treated with insulin alone, but that overall body fat was the same, Dr. Landon noted. The investigators postulated that these children may have less visceral fat and a more favorable pattern of fat distribution (Diab Care. 2011;34:2279-84).
A recently published follow-up analysis of two randomized, controlled trials of women with polycystic ovary syndrome is cause for more concern, he said. That analysis showed that offspring exposed to metformin in utero had a higher body mass index and an increased prevalence of obesity or overweight at age 4 years, compared with placebo groups (J Clin Endocrinol Metab. 2018;103[4]:1612-21).
That analysis of metformin-exposed offspring in the context of polycystic ovary syndrome was published after the SMFM statement, as was another follow-up analysis of MiG trial offspring – this one, at ages 7-9 years – that showed an increase in weight, size, and fat mass in one of two subsets analyzed, despite no difference in large-for-gestational age rates between the metformin- and insulin-exposed offspring (BMJ Open Diabetes Res Care. 2018;6[1]: e000456).
In 2018, a group of 17 prominent diabetes and maternal-fetal medicine researchers cited these findings in a response to the SMFM statement and cautioned against the widespread adoption of metformin use during pregnancy, writing that, based on “both pharmacologic and randomized trial evidence that metformin may create an atypical intrauterine environment ... we believe it is premature to embrace metformin as equivalent to insulin or as superior to glyburide, and that patients should be counseled on the limited long-term safety data and potential for adverse childhood metabolic effects” (Am J Obstet Gynecol. 2018;219[4]:367.e1-7).
EXPERT ANALYSIS FROM DPSG-NA 2019
Occult HCV infection is correlated to unfavorable genotypes in hemophilia patients
The presence of occult hepatitis C virus infection is determined by finding HCV RNA in the liver and peripheral blood mononuclear cells, with no HCV RNA in the serum. Researchers have shown that the presence of occult HCV infection (OCI) was correlated with unfavorable polymorphisms near interferon lambda-3/4 (IFNL3/4), which has been associated with spontaneous HCV clearance.
This study was conducted to assess the frequency of OCI in 450 hemophilia patients in Iran with negative HCV markers, and to evaluate the association of three IFNL3 single nucleotide polymorphisms (rs8099917, rs12979860, and rs12980275) and the IFNL4 ss469415590 SNP with OCI positivity.
The estimated OCI rate was 10.2%. Among the 46 OCI patients, 56.5%, 23.9%, and 19.6% were infected with HCV-1b, HCV-1a, and HCV-3a, respectively. The researchers found that, compared with patients without OCI, unfavorable IFNL3 rs12979860, IFNL3 rs8099917, IFNL3 rs12980275, and IFNL4 ss469415590 genotypes were more frequently found in OCI patients. Multivariate analysis showed that ALT, cholesterol, triglyceride, as well as the aforementioned unfavorable interferon SNP geneotypes were associated with OCI positivity.
“10.2% of anti-HCV seronegative Iranian patients with hemophilia had OCI in our study; therefore, risk of this infection should be taken into consideration. We also showed that patients with unfavorable IFNL3 SNPs and IFNL4 ss469415590 genotypes were exposed to a higher risk of OCI, compared to hemophilia patients with other genotypes,” the researchers concluded.
The authors reported that they had no disclosures.
SOURCE: Nafari AH et al. Infect Genet Evol. 2019 Dec 13. doi: 10.1016/j.meegid.2019.104144.
The presence of occult hepatitis C virus infection is determined by finding HCV RNA in the liver and peripheral blood mononuclear cells, with no HCV RNA in the serum. Researchers have shown that the presence of occult HCV infection (OCI) was correlated with unfavorable polymorphisms near interferon lambda-3/4 (IFNL3/4), which has been associated with spontaneous HCV clearance.
This study was conducted to assess the frequency of OCI in 450 hemophilia patients in Iran with negative HCV markers, and to evaluate the association of three IFNL3 single nucleotide polymorphisms (rs8099917, rs12979860, and rs12980275) and the IFNL4 ss469415590 SNP with OCI positivity.
The estimated OCI rate was 10.2%. Among the 46 OCI patients, 56.5%, 23.9%, and 19.6% were infected with HCV-1b, HCV-1a, and HCV-3a, respectively. The researchers found that, compared with patients without OCI, unfavorable IFNL3 rs12979860, IFNL3 rs8099917, IFNL3 rs12980275, and IFNL4 ss469415590 genotypes were more frequently found in OCI patients. Multivariate analysis showed that ALT, cholesterol, triglyceride, as well as the aforementioned unfavorable interferon SNP geneotypes were associated with OCI positivity.
“10.2% of anti-HCV seronegative Iranian patients with hemophilia had OCI in our study; therefore, risk of this infection should be taken into consideration. We also showed that patients with unfavorable IFNL3 SNPs and IFNL4 ss469415590 genotypes were exposed to a higher risk of OCI, compared to hemophilia patients with other genotypes,” the researchers concluded.
The authors reported that they had no disclosures.
SOURCE: Nafari AH et al. Infect Genet Evol. 2019 Dec 13. doi: 10.1016/j.meegid.2019.104144.
The presence of occult hepatitis C virus infection is determined by finding HCV RNA in the liver and peripheral blood mononuclear cells, with no HCV RNA in the serum. Researchers have shown that the presence of occult HCV infection (OCI) was correlated with unfavorable polymorphisms near interferon lambda-3/4 (IFNL3/4), which has been associated with spontaneous HCV clearance.
This study was conducted to assess the frequency of OCI in 450 hemophilia patients in Iran with negative HCV markers, and to evaluate the association of three IFNL3 single nucleotide polymorphisms (rs8099917, rs12979860, and rs12980275) and the IFNL4 ss469415590 SNP with OCI positivity.
The estimated OCI rate was 10.2%. Among the 46 OCI patients, 56.5%, 23.9%, and 19.6% were infected with HCV-1b, HCV-1a, and HCV-3a, respectively. The researchers found that, compared with patients without OCI, unfavorable IFNL3 rs12979860, IFNL3 rs8099917, IFNL3 rs12980275, and IFNL4 ss469415590 genotypes were more frequently found in OCI patients. Multivariate analysis showed that ALT, cholesterol, triglyceride, as well as the aforementioned unfavorable interferon SNP geneotypes were associated with OCI positivity.
“10.2% of anti-HCV seronegative Iranian patients with hemophilia had OCI in our study; therefore, risk of this infection should be taken into consideration. We also showed that patients with unfavorable IFNL3 SNPs and IFNL4 ss469415590 genotypes were exposed to a higher risk of OCI, compared to hemophilia patients with other genotypes,” the researchers concluded.
The authors reported that they had no disclosures.
SOURCE: Nafari AH et al. Infect Genet Evol. 2019 Dec 13. doi: 10.1016/j.meegid.2019.104144.
FROM INFECTION, GENETICS AND EVOLUTION