User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Real-world safety, efficacy found for fecal transplants
Fecal microbiota transplantation (FMT) appears safe and effective as a treatment for most Clostridioides difficile infections as it is currently being administered, researchers say.
“We actually didn’t see any infections that were definitely transmissible via fecal transplant,” Colleen Kelly, MD, an associate professor of medicine at Brown University, Providence, R.I., said in an interview.
The findings, published online Oct. 1 in the journal Gastroenterology, come from the American Gastroenterological Association (AGA) NIH-funded FMT National Registry and could allay concerns about a treatment that has yet to gain full approval by the Food and Drug Administration, despite successful clinical trials.
C. diff infections are common and increasing in the United States, often can’t be cured with conventional treatments such as antibiotics, and can be deadly.
Transplanting fecal matter from a donor to the patient appears to work by restoring beneficial microorganisms to the patient’s gut. The procedure is also under investigation for a wide range of other ailments, from irritable bowel syndrome to mood disorders.
But much remains unknown. Researchers have counted a thousand bacterial species along with viruses, bacteriophages, archaea, and fungi in the human gut that interact in complex ways, not all of them beneficial.
The FDA has not enforced regulations that would prohibit the procedure, but in March, it warned about infections with enteropathogenic Escherichia coli and Shiga toxin–producing E. coli following fecal transplants.
As a result of these reports, and the theoretical risk of spreading SARS-CoV-2, OpenBiome, the largest stool bank in the United States, has suspended shipments except for emergency orders, and asked clinicians to quarantine any of its products they already have on hand.
In the meantime, long-term effects of the treatment have not been well documented. And clinical trials have excluded patients who might benefit, such as those who have been immunocompromised or have inflammatory bowel disease.
National registry follows patients outside clinical trials
To better understand how patients fare outside these trials, AGA and other organizations developed a national registry, funded by a grant from the National Institute of Allergy and Infectious Diseases.
The current report summarizes results on 259 patients enrolled between Dec. 5, 2017, and Sept. 2, 2019 at 20 sites.
At baseline, 44% of these patients suffered moderate and 36% mild C. diff infections. The duration of the diagnosis ranged from less than 1 week to 9 years, with a median duration of 20 weeks. They ranged from 1 to 15 episodes with a mean of 3.5.
Almost all had received vancomycin, and 62% had at least two courses. About 40% had received metronidazole and 28% had received fidaxomicin.
Almost all participants received stool from an unknown donor, mostly from stool banks, with OpenBiome accounting for 67%. About 85% of the transplants were administered through colonoscopy and 6% by upper endoscopy.
Out of 222 patients who returned for a 1-month follow-up, 90% met the investigators’ definition of cure: resolution of diarrhea without need for further anti–C. diff therapy. About 98% received only one transplant. An intent to treat analysis produced a cure rate of 86%.
Results were good in patients with comorbidities, including 12% who had irritable bowel syndrome, 9% who had ulcerative colitis, and 7% who had Crohn’s disease, Dr. Kelly said. “I hope everybody sees the importance of it. In these patients that are more complicated, who may have underlying comorbidities, who may not have been in the clinical trials, it looks effective in that group, and also incredibly safe.”
She added that the risk of transmitting SARS-CoV-2 is minor. “I think it would be a very, very unlikely way for someone to get a respiratory pathogen.”
Of the 112 participants who were cured at 1 month and returned for follow-up after 6 months, 4 developed recurrent C. diff infection. Eleven patients who were not cured in the first month returned after 6 months. Of these, seven were reported cured at this later follow-up.
Three complications occurred as result of the procedure: one colonoscopic perforation and two episodes of gastrointestinal bleeding.
About 45% of participants reported at least one symptom, with diarrhea not related to C. difficile the most common, followed by abdominal pain, bloating, and constipation.
Eleven patients suffered infections, including two which the investigators thought might be related to the procedure: Bacteroides fragilis in one participant with severe diarrhea, and enteropathogenic E. coli in another with loose stools. Other infections included four urinary tract infections, three cases of pneumonia, one E. coli bacteremia and one tooth infection.
Within a month of the procedure, 27 patients were hospitalized, with 3 of these cases considered possibly related to the procedure.
Findings may not apply to all clinical settings
Vincent B. Young, MD, PhD, a professor of medicine and infectious diseases at the University of Michigan, Ann Arbor, pointed out that the findings might not apply to all clinical settings. The participating clinicians were almost all gastroenterologists working in academic centers.
“Most of them are not Joe Doctor at the doctor’s office,” said Dr. Young, who was not involved with the study. Clinicians in other specialties, such as infectious diseases, might be more inclined to administer fecal transplants through capsules rather than colonoscopies.
And he added that the study does not address effects of the transplant that might develop over years. “Some people talk about how changes in the microbiota lead to increased risk for long-term complications, things like cancer or heart disease. You’re not going to see those in 6 months.”
Also, the study didn’t yield any findings on indications other than C. diff. “In no way, shape, or form does it mean you can use it for autism, depression, heart disease, or [irritable bowel syndrome],” he said.
Still, he said, the study “confirms the fact that fecal cell transplantation is an effective treatment for recurrent C. diff infection when administered as they administered it.”
The National Institute of Allergy and Infectious Diseases funded the registry. Dr. Kelly reported a relationship with Finch Therapeutics. Dr. Young reports financial relationships with Vedanta Biosciences and Bio-K+.
This story was updated on Oct. 4, 2020.
A version of this article originally appeared on Medscape.com.
Fecal microbiota transplantation (FMT) appears safe and effective as a treatment for most Clostridioides difficile infections as it is currently being administered, researchers say.
“We actually didn’t see any infections that were definitely transmissible via fecal transplant,” Colleen Kelly, MD, an associate professor of medicine at Brown University, Providence, R.I., said in an interview.
The findings, published online Oct. 1 in the journal Gastroenterology, come from the American Gastroenterological Association (AGA) NIH-funded FMT National Registry and could allay concerns about a treatment that has yet to gain full approval by the Food and Drug Administration, despite successful clinical trials.
C. diff infections are common and increasing in the United States, often can’t be cured with conventional treatments such as antibiotics, and can be deadly.
Transplanting fecal matter from a donor to the patient appears to work by restoring beneficial microorganisms to the patient’s gut. The procedure is also under investigation for a wide range of other ailments, from irritable bowel syndrome to mood disorders.
But much remains unknown. Researchers have counted a thousand bacterial species along with viruses, bacteriophages, archaea, and fungi in the human gut that interact in complex ways, not all of them beneficial.
The FDA has not enforced regulations that would prohibit the procedure, but in March, it warned about infections with enteropathogenic Escherichia coli and Shiga toxin–producing E. coli following fecal transplants.
As a result of these reports, and the theoretical risk of spreading SARS-CoV-2, OpenBiome, the largest stool bank in the United States, has suspended shipments except for emergency orders, and asked clinicians to quarantine any of its products they already have on hand.
In the meantime, long-term effects of the treatment have not been well documented. And clinical trials have excluded patients who might benefit, such as those who have been immunocompromised or have inflammatory bowel disease.
National registry follows patients outside clinical trials
To better understand how patients fare outside these trials, AGA and other organizations developed a national registry, funded by a grant from the National Institute of Allergy and Infectious Diseases.
The current report summarizes results on 259 patients enrolled between Dec. 5, 2017, and Sept. 2, 2019 at 20 sites.
At baseline, 44% of these patients suffered moderate and 36% mild C. diff infections. The duration of the diagnosis ranged from less than 1 week to 9 years, with a median duration of 20 weeks. They ranged from 1 to 15 episodes with a mean of 3.5.
Almost all had received vancomycin, and 62% had at least two courses. About 40% had received metronidazole and 28% had received fidaxomicin.
Almost all participants received stool from an unknown donor, mostly from stool banks, with OpenBiome accounting for 67%. About 85% of the transplants were administered through colonoscopy and 6% by upper endoscopy.
Out of 222 patients who returned for a 1-month follow-up, 90% met the investigators’ definition of cure: resolution of diarrhea without need for further anti–C. diff therapy. About 98% received only one transplant. An intent to treat analysis produced a cure rate of 86%.
Results were good in patients with comorbidities, including 12% who had irritable bowel syndrome, 9% who had ulcerative colitis, and 7% who had Crohn’s disease, Dr. Kelly said. “I hope everybody sees the importance of it. In these patients that are more complicated, who may have underlying comorbidities, who may not have been in the clinical trials, it looks effective in that group, and also incredibly safe.”
She added that the risk of transmitting SARS-CoV-2 is minor. “I think it would be a very, very unlikely way for someone to get a respiratory pathogen.”
Of the 112 participants who were cured at 1 month and returned for follow-up after 6 months, 4 developed recurrent C. diff infection. Eleven patients who were not cured in the first month returned after 6 months. Of these, seven were reported cured at this later follow-up.
Three complications occurred as result of the procedure: one colonoscopic perforation and two episodes of gastrointestinal bleeding.
About 45% of participants reported at least one symptom, with diarrhea not related to C. difficile the most common, followed by abdominal pain, bloating, and constipation.
Eleven patients suffered infections, including two which the investigators thought might be related to the procedure: Bacteroides fragilis in one participant with severe diarrhea, and enteropathogenic E. coli in another with loose stools. Other infections included four urinary tract infections, three cases of pneumonia, one E. coli bacteremia and one tooth infection.
Within a month of the procedure, 27 patients were hospitalized, with 3 of these cases considered possibly related to the procedure.
Findings may not apply to all clinical settings
Vincent B. Young, MD, PhD, a professor of medicine and infectious diseases at the University of Michigan, Ann Arbor, pointed out that the findings might not apply to all clinical settings. The participating clinicians were almost all gastroenterologists working in academic centers.
“Most of them are not Joe Doctor at the doctor’s office,” said Dr. Young, who was not involved with the study. Clinicians in other specialties, such as infectious diseases, might be more inclined to administer fecal transplants through capsules rather than colonoscopies.
And he added that the study does not address effects of the transplant that might develop over years. “Some people talk about how changes in the microbiota lead to increased risk for long-term complications, things like cancer or heart disease. You’re not going to see those in 6 months.”
Also, the study didn’t yield any findings on indications other than C. diff. “In no way, shape, or form does it mean you can use it for autism, depression, heart disease, or [irritable bowel syndrome],” he said.
Still, he said, the study “confirms the fact that fecal cell transplantation is an effective treatment for recurrent C. diff infection when administered as they administered it.”
The National Institute of Allergy and Infectious Diseases funded the registry. Dr. Kelly reported a relationship with Finch Therapeutics. Dr. Young reports financial relationships with Vedanta Biosciences and Bio-K+.
This story was updated on Oct. 4, 2020.
A version of this article originally appeared on Medscape.com.
Fecal microbiota transplantation (FMT) appears safe and effective as a treatment for most Clostridioides difficile infections as it is currently being administered, researchers say.
“We actually didn’t see any infections that were definitely transmissible via fecal transplant,” Colleen Kelly, MD, an associate professor of medicine at Brown University, Providence, R.I., said in an interview.
The findings, published online Oct. 1 in the journal Gastroenterology, come from the American Gastroenterological Association (AGA) NIH-funded FMT National Registry and could allay concerns about a treatment that has yet to gain full approval by the Food and Drug Administration, despite successful clinical trials.
C. diff infections are common and increasing in the United States, often can’t be cured with conventional treatments such as antibiotics, and can be deadly.
Transplanting fecal matter from a donor to the patient appears to work by restoring beneficial microorganisms to the patient’s gut. The procedure is also under investigation for a wide range of other ailments, from irritable bowel syndrome to mood disorders.
But much remains unknown. Researchers have counted a thousand bacterial species along with viruses, bacteriophages, archaea, and fungi in the human gut that interact in complex ways, not all of them beneficial.
The FDA has not enforced regulations that would prohibit the procedure, but in March, it warned about infections with enteropathogenic Escherichia coli and Shiga toxin–producing E. coli following fecal transplants.
As a result of these reports, and the theoretical risk of spreading SARS-CoV-2, OpenBiome, the largest stool bank in the United States, has suspended shipments except for emergency orders, and asked clinicians to quarantine any of its products they already have on hand.
In the meantime, long-term effects of the treatment have not been well documented. And clinical trials have excluded patients who might benefit, such as those who have been immunocompromised or have inflammatory bowel disease.
National registry follows patients outside clinical trials
To better understand how patients fare outside these trials, AGA and other organizations developed a national registry, funded by a grant from the National Institute of Allergy and Infectious Diseases.
The current report summarizes results on 259 patients enrolled between Dec. 5, 2017, and Sept. 2, 2019 at 20 sites.
At baseline, 44% of these patients suffered moderate and 36% mild C. diff infections. The duration of the diagnosis ranged from less than 1 week to 9 years, with a median duration of 20 weeks. They ranged from 1 to 15 episodes with a mean of 3.5.
Almost all had received vancomycin, and 62% had at least two courses. About 40% had received metronidazole and 28% had received fidaxomicin.
Almost all participants received stool from an unknown donor, mostly from stool banks, with OpenBiome accounting for 67%. About 85% of the transplants were administered through colonoscopy and 6% by upper endoscopy.
Out of 222 patients who returned for a 1-month follow-up, 90% met the investigators’ definition of cure: resolution of diarrhea without need for further anti–C. diff therapy. About 98% received only one transplant. An intent to treat analysis produced a cure rate of 86%.
Results were good in patients with comorbidities, including 12% who had irritable bowel syndrome, 9% who had ulcerative colitis, and 7% who had Crohn’s disease, Dr. Kelly said. “I hope everybody sees the importance of it. In these patients that are more complicated, who may have underlying comorbidities, who may not have been in the clinical trials, it looks effective in that group, and also incredibly safe.”
She added that the risk of transmitting SARS-CoV-2 is minor. “I think it would be a very, very unlikely way for someone to get a respiratory pathogen.”
Of the 112 participants who were cured at 1 month and returned for follow-up after 6 months, 4 developed recurrent C. diff infection. Eleven patients who were not cured in the first month returned after 6 months. Of these, seven were reported cured at this later follow-up.
Three complications occurred as result of the procedure: one colonoscopic perforation and two episodes of gastrointestinal bleeding.
About 45% of participants reported at least one symptom, with diarrhea not related to C. difficile the most common, followed by abdominal pain, bloating, and constipation.
Eleven patients suffered infections, including two which the investigators thought might be related to the procedure: Bacteroides fragilis in one participant with severe diarrhea, and enteropathogenic E. coli in another with loose stools. Other infections included four urinary tract infections, three cases of pneumonia, one E. coli bacteremia and one tooth infection.
Within a month of the procedure, 27 patients were hospitalized, with 3 of these cases considered possibly related to the procedure.
Findings may not apply to all clinical settings
Vincent B. Young, MD, PhD, a professor of medicine and infectious diseases at the University of Michigan, Ann Arbor, pointed out that the findings might not apply to all clinical settings. The participating clinicians were almost all gastroenterologists working in academic centers.
“Most of them are not Joe Doctor at the doctor’s office,” said Dr. Young, who was not involved with the study. Clinicians in other specialties, such as infectious diseases, might be more inclined to administer fecal transplants through capsules rather than colonoscopies.
And he added that the study does not address effects of the transplant that might develop over years. “Some people talk about how changes in the microbiota lead to increased risk for long-term complications, things like cancer or heart disease. You’re not going to see those in 6 months.”
Also, the study didn’t yield any findings on indications other than C. diff. “In no way, shape, or form does it mean you can use it for autism, depression, heart disease, or [irritable bowel syndrome],” he said.
Still, he said, the study “confirms the fact that fecal cell transplantation is an effective treatment for recurrent C. diff infection when administered as they administered it.”
The National Institute of Allergy and Infectious Diseases funded the registry. Dr. Kelly reported a relationship with Finch Therapeutics. Dr. Young reports financial relationships with Vedanta Biosciences and Bio-K+.
This story was updated on Oct. 4, 2020.
A version of this article originally appeared on Medscape.com.
Mental illness tied to increased mortality in COVID-19
A psychiatric diagnosis for patients hospitalized with COVID-19 is linked to a significantly increased risk for death, new research shows.
Investigators found that patients who were hospitalized with COVID-19 and who had been diagnosed with a psychiatric disorder had a 50% increased risk for a COVID-related death in comparison with COVID-19 patients who had not received a psychiatric diagnosis.
“Pay attention and potentially address/treat a prior psychiatric diagnosis if a patient is hospitalized for COVID-19, as this risk factor can impact the patient’s outcome – death – while in the hospital,” lead investigator Luming Li, MD, assistant professor of psychiatry and associate medical director of quality improvement, Yale New Haven Psychiatric Hospital, New Haven, Conn., said in an interview.
The study was published Sept. 30 in JAMA Network Open.
Negative impact
“We were interested to learn more about the impact of psychiatric diagnoses on COVID-19 mortality, as prior large cohort studies included neurological and other medical conditions but did not assess for a priori psychiatric diagnoses,” said Dr. Li.
“We know from the literature that prior psychiatric diagnoses can have a negative impact on the outcomes of medical conditions, and therefore we tested our hypothesis on a cohort of patients who were hospitalized with COVID-19,” she added.
To investigate, the researchers analyzed data on 1,685 patients hospitalized with COVID-19 between Feb. 15 and April 25, 2020, and whose cases were followed to May 27, 2020. The patients (mean age, 65.2 years; 52.6% men) were drawn from the Yale New Haven Health System.
The median follow-up period was 8 days (interquartile range, 4-16 days) .
Of these patients, 28% had received a psychiatric diagnosis prior to hospitalization. (i.e., cancer, cerebrovascular disease, heart failure, diabetes, kidney disease, liver disease, MI, and/or HIV).
Psychiatric diagnoses were defined in accordance with ICD codes that included mental and behavioral health, Alzheimer’s disease, and self-injury.
Vulnerability to stress
In the unadjusted model, the risk for COVID-19–related hospital death was greater for those who had received any psychiatric diagnosis, compared with those had not (hazard ratio, 2.3; 95% CI, 1.8-2.9; P < .001).
In the adjusted model that controlled for demographic characteristics, other medical comorbidities, and hospital location, the mortality risk somewhat decreased but still remained significantly higher (HR, 1.5; 95% CI, 1.1-1.9; P = .003).
Dr. Li noted a number of factors that might account for the higher mortality rate among psychiatric patients who had COVID-19 in comparison with COVD-19 patients who did not have a psychiatric disorder. These included “potential inflammatory and stress responses that the body experiences related to prior psychiatric conditions,” she said.
Having been previously diagnosed with a psychiatric disorder may also “reflect existing neurochemical differences, compared to those who do not have a prior psychiatric diagnosis, [and] these differences may make the population with the prior psychiatric diagnosis more vulnerable to respond to an acute stressor such as COVID-19,” she said.
Quality care
Harold Pincus, MD, professor and vice chair of the department of psychiatry at Columbia University, New York, said it “adds to the fairly well-known and well-established phenomenon that people with mental illnesses have a high risk of all sorts of morbidity and mortality for non–mental health conditions.”
The researchers “adjusted for various expected [mortality] risks that would be independent of the presence of COVID-19,” so “there was something else going on associated with mortality,” said Dr. Pincus, who is also codirector of the Irving Institute for Clinical and Translation Research. He was not involved with the study.
Beyond the possibility of “some basic immunologic process affected by the presence of a mental disorder,” it is possible that the vulnerability is “related to access to quality care for the comorbid general condition that is not being effectively treated,” he said.
“The take-home message is that people with mental disorders are at higher risk for death, and we need to make sure that, irrespective of COVID-19, they get adequate preventive and chronic-disease care, which would be the most effective way to intervene and protect the impact of a serious disease like COVID-19,” he noted. This would include being appropriately vaccinated and receiving preventive healthcare to reduce smoking and encourage weight loss.
No source of funding for the study was provided. Dr. Li reported receiving grants from a Health and Aging Policy Fellowship during the conduct of the study. Dr. Pincus reported no relevant financial relationships.
A psychiatric diagnosis for patients hospitalized with COVID-19 is linked to a significantly increased risk for death, new research shows.
Investigators found that patients who were hospitalized with COVID-19 and who had been diagnosed with a psychiatric disorder had a 50% increased risk for a COVID-related death in comparison with COVID-19 patients who had not received a psychiatric diagnosis.
“Pay attention and potentially address/treat a prior psychiatric diagnosis if a patient is hospitalized for COVID-19, as this risk factor can impact the patient’s outcome – death – while in the hospital,” lead investigator Luming Li, MD, assistant professor of psychiatry and associate medical director of quality improvement, Yale New Haven Psychiatric Hospital, New Haven, Conn., said in an interview.
The study was published Sept. 30 in JAMA Network Open.
Negative impact
“We were interested to learn more about the impact of psychiatric diagnoses on COVID-19 mortality, as prior large cohort studies included neurological and other medical conditions but did not assess for a priori psychiatric diagnoses,” said Dr. Li.
“We know from the literature that prior psychiatric diagnoses can have a negative impact on the outcomes of medical conditions, and therefore we tested our hypothesis on a cohort of patients who were hospitalized with COVID-19,” she added.
To investigate, the researchers analyzed data on 1,685 patients hospitalized with COVID-19 between Feb. 15 and April 25, 2020, and whose cases were followed to May 27, 2020. The patients (mean age, 65.2 years; 52.6% men) were drawn from the Yale New Haven Health System.
The median follow-up period was 8 days (interquartile range, 4-16 days) .
Of these patients, 28% had received a psychiatric diagnosis prior to hospitalization. (i.e., cancer, cerebrovascular disease, heart failure, diabetes, kidney disease, liver disease, MI, and/or HIV).
Psychiatric diagnoses were defined in accordance with ICD codes that included mental and behavioral health, Alzheimer’s disease, and self-injury.
Vulnerability to stress
In the unadjusted model, the risk for COVID-19–related hospital death was greater for those who had received any psychiatric diagnosis, compared with those had not (hazard ratio, 2.3; 95% CI, 1.8-2.9; P < .001).
In the adjusted model that controlled for demographic characteristics, other medical comorbidities, and hospital location, the mortality risk somewhat decreased but still remained significantly higher (HR, 1.5; 95% CI, 1.1-1.9; P = .003).
Dr. Li noted a number of factors that might account for the higher mortality rate among psychiatric patients who had COVID-19 in comparison with COVD-19 patients who did not have a psychiatric disorder. These included “potential inflammatory and stress responses that the body experiences related to prior psychiatric conditions,” she said.
Having been previously diagnosed with a psychiatric disorder may also “reflect existing neurochemical differences, compared to those who do not have a prior psychiatric diagnosis, [and] these differences may make the population with the prior psychiatric diagnosis more vulnerable to respond to an acute stressor such as COVID-19,” she said.
Quality care
Harold Pincus, MD, professor and vice chair of the department of psychiatry at Columbia University, New York, said it “adds to the fairly well-known and well-established phenomenon that people with mental illnesses have a high risk of all sorts of morbidity and mortality for non–mental health conditions.”
The researchers “adjusted for various expected [mortality] risks that would be independent of the presence of COVID-19,” so “there was something else going on associated with mortality,” said Dr. Pincus, who is also codirector of the Irving Institute for Clinical and Translation Research. He was not involved with the study.
Beyond the possibility of “some basic immunologic process affected by the presence of a mental disorder,” it is possible that the vulnerability is “related to access to quality care for the comorbid general condition that is not being effectively treated,” he said.
“The take-home message is that people with mental disorders are at higher risk for death, and we need to make sure that, irrespective of COVID-19, they get adequate preventive and chronic-disease care, which would be the most effective way to intervene and protect the impact of a serious disease like COVID-19,” he noted. This would include being appropriately vaccinated and receiving preventive healthcare to reduce smoking and encourage weight loss.
No source of funding for the study was provided. Dr. Li reported receiving grants from a Health and Aging Policy Fellowship during the conduct of the study. Dr. Pincus reported no relevant financial relationships.
A psychiatric diagnosis for patients hospitalized with COVID-19 is linked to a significantly increased risk for death, new research shows.
Investigators found that patients who were hospitalized with COVID-19 and who had been diagnosed with a psychiatric disorder had a 50% increased risk for a COVID-related death in comparison with COVID-19 patients who had not received a psychiatric diagnosis.
“Pay attention and potentially address/treat a prior psychiatric diagnosis if a patient is hospitalized for COVID-19, as this risk factor can impact the patient’s outcome – death – while in the hospital,” lead investigator Luming Li, MD, assistant professor of psychiatry and associate medical director of quality improvement, Yale New Haven Psychiatric Hospital, New Haven, Conn., said in an interview.
The study was published Sept. 30 in JAMA Network Open.
Negative impact
“We were interested to learn more about the impact of psychiatric diagnoses on COVID-19 mortality, as prior large cohort studies included neurological and other medical conditions but did not assess for a priori psychiatric diagnoses,” said Dr. Li.
“We know from the literature that prior psychiatric diagnoses can have a negative impact on the outcomes of medical conditions, and therefore we tested our hypothesis on a cohort of patients who were hospitalized with COVID-19,” she added.
To investigate, the researchers analyzed data on 1,685 patients hospitalized with COVID-19 between Feb. 15 and April 25, 2020, and whose cases were followed to May 27, 2020. The patients (mean age, 65.2 years; 52.6% men) were drawn from the Yale New Haven Health System.
The median follow-up period was 8 days (interquartile range, 4-16 days) .
Of these patients, 28% had received a psychiatric diagnosis prior to hospitalization. (i.e., cancer, cerebrovascular disease, heart failure, diabetes, kidney disease, liver disease, MI, and/or HIV).
Psychiatric diagnoses were defined in accordance with ICD codes that included mental and behavioral health, Alzheimer’s disease, and self-injury.
Vulnerability to stress
In the unadjusted model, the risk for COVID-19–related hospital death was greater for those who had received any psychiatric diagnosis, compared with those had not (hazard ratio, 2.3; 95% CI, 1.8-2.9; P < .001).
In the adjusted model that controlled for demographic characteristics, other medical comorbidities, and hospital location, the mortality risk somewhat decreased but still remained significantly higher (HR, 1.5; 95% CI, 1.1-1.9; P = .003).
Dr. Li noted a number of factors that might account for the higher mortality rate among psychiatric patients who had COVID-19 in comparison with COVD-19 patients who did not have a psychiatric disorder. These included “potential inflammatory and stress responses that the body experiences related to prior psychiatric conditions,” she said.
Having been previously diagnosed with a psychiatric disorder may also “reflect existing neurochemical differences, compared to those who do not have a prior psychiatric diagnosis, [and] these differences may make the population with the prior psychiatric diagnosis more vulnerable to respond to an acute stressor such as COVID-19,” she said.
Quality care
Harold Pincus, MD, professor and vice chair of the department of psychiatry at Columbia University, New York, said it “adds to the fairly well-known and well-established phenomenon that people with mental illnesses have a high risk of all sorts of morbidity and mortality for non–mental health conditions.”
The researchers “adjusted for various expected [mortality] risks that would be independent of the presence of COVID-19,” so “there was something else going on associated with mortality,” said Dr. Pincus, who is also codirector of the Irving Institute for Clinical and Translation Research. He was not involved with the study.
Beyond the possibility of “some basic immunologic process affected by the presence of a mental disorder,” it is possible that the vulnerability is “related to access to quality care for the comorbid general condition that is not being effectively treated,” he said.
“The take-home message is that people with mental disorders are at higher risk for death, and we need to make sure that, irrespective of COVID-19, they get adequate preventive and chronic-disease care, which would be the most effective way to intervene and protect the impact of a serious disease like COVID-19,” he noted. This would include being appropriately vaccinated and receiving preventive healthcare to reduce smoking and encourage weight loss.
No source of funding for the study was provided. Dr. Li reported receiving grants from a Health and Aging Policy Fellowship during the conduct of the study. Dr. Pincus reported no relevant financial relationships.
‘Celebration’ will be ‘short-lived’ if COVID vaccine rushed: Experts
on Wednesday.
The career staff of the Food and Drug Administration can be counted on to appropriately weigh whether a vaccine should be cleared for use in preventing COVID-19, witnesses, including Paul A. Offit, MD, of Children’s Hospital of Philadelphia, told the House Energy and Commerce Committee’s oversight and investigations panel.
FDA staffers would object to attempts by the Trump administration to rush a vaccine to the public without proper vetting, as would veteran federal researchers, including National Institutes of Health Director Francis S. Collins, MD, PhD, and Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, Offit said.
“If COVID-19 vaccines are released before they’re ready to be released, you will hear from these people, and you will also hear from people like Dr. Francis Collins and Tony Fauci, both of whom are trusted by the American public, as well as many other academicians and researchers who wouldn’t stand for this,” he said.
“The public is already nervous about these vaccines,” said Offit, who serves on key FDA and Centers for Disease Control and Prevention committees overseeing vaccine policy. “If trusted health officials stand up and decry a premature release, the celebration by the administration will be short-lived.”
Overly optimistic estimates about a potential approval can only serve to erode the public’s trust in these crucial vaccines, said another witness, Ashish K. Jha, MD, MPH, the dean of Brown University’s School of Public Health, in Providence, Rhode Island.
“All political leaders need to stop talking about things like time lines,” Jha told the lawmakers.
President Donald Trump has several times suggested that a COVID vaccine might be approved ahead of the November 3 election, where he faces a significant challenge from his Democratic rival, former Vice President Joe Biden.
In a Tuesday night debate with Biden, Trump again raised the idea of a quick approval. “Now we’re weeks away from a vaccine,” Trump said during the debate.
Trump’s estimates, though, are not in line with those offered by most firms involved with making vaccines. The most optimistic projections have come from Pfizer Inc. The drugmaker’s chief executive, Albert Bourla, has spoken about his company possibly having data to present to the FDA as early as late October about the safety and effectiveness of a vaccine.
In a September 8 interview with the Today show, Bourla said there was a 60% chance his company would meet that goal. In response to a question, he made it clear his comments applied to a potential Pfizer application, not an approval or release of a vaccine by that time.
In response to concerns about political pressures, the FDA in June issued guidance outlining what its staff would require for approval of a COVID-19 vaccine.
Pushback on politics
Another witness at the Wednesday hearing, Mark McClellan, MD, PhD, a former FDA commissioner (2002 – 2004), pushed back on objections to a potential release of further guidance from the agency.
“Some recent statements from the White House have implied that FDA’s plan to release additional written guidance on its expectations for emergency use authorization of a vaccine is unnecessarily raising the bar on regulatory standards for authorization,” said McClellan in his testimony for the House panel. “That is not the case.”
Instead, further FDA guidance would be a welcome form of feedback for the firms trying to develop COVID-19 vaccines, according to McClellan, who also serves on the board of directors for Johnson & Johnson. Johnson & Johnson is among the firms that have advanced a COVID-19 vaccine candidate to phase 3 testing. In his role as a director, he serves on the board’s regulatory compliance committee.
Along with politics, recent stumbles at FDA with emergency use authorizations (EUAs) of treatments for COVID-19 have eroded the public’s confidence in the agency, Jha told the House panel. The FDA approved hydroxychloroquine, a medicine promoted by Trump for use in COVID, under an EUA in March and then revoked this clearance in June.
Jha said the FDA’s most serious misstep was its handling of convalescent plasma, which was approved through an EUA on August 23 “in a highly advertised and widely televised announcement including the president.
“The announcement solidified in the public conversation the impression that, increasingly with this administration, politics are taking over trusted, nonpartisan scientific institutions,” he said in his testimony.
Approving a COVID-19 vaccine on the limited evidence through an EUA would mark a serious departure from FDA policy, according to Jha.
“While we sometimes accept a certain level of potential harm in experimental treatments for those who are severely ill, vaccines are given to healthy people and therefore need to have a substantially higher measure of safety and effectiveness,” he explained.
Jha said the FDA has only once before used this EUA approach for a vaccine. That was for a vaccine against inhaled anthrax and was mostly distributed to high-risk soldiers and civilians in war zones.
COVID-19, in contrast, is an infection that has changed lives around the world. The virus has contributed to more than 1 million deaths, including more than 200,000 in the United States, according to the World Health Organization.
Scientists are hoping vaccines will help curb this infection, although much of the future success of vaccines depends on how widely they are used, witnesses told the House panel.
Debate on approaches for vaccine effectiveness
In his testimony, Jha also noted concerns about COVID-19 vaccine trials. He included a reference to a Sept. 22 opinion article titled, “These Coronavirus Trials Don›t Answer the One Question We Need to Know,” which was written by Peter Doshi, PhD, of the University of Maryland School of Pharmacy, in Baltimore, and Eric Topol, MD, a professor of molecular medicine at Scripps Research in La Jolla, Calif. Topol is also editor in chief of Medscape.
Topol and Doshi questioned why the firms Moderna, Pfizer, and AstraZeneca structured their competing trials such that “a vaccine could meet the companies’ benchmark for success if it lowered the risk of mild Covid-19, but was never shown to reduce moderate or severe forms of the disease, or the risk of hospitalization, admissions to the intensive care unit or death.”
“To say a vaccine works should mean that most people no longer run the risk of getting seriously sick,” Topol and Doshi wrote. “That’s not what these trials will determine.”
There was disagreement about this point at the hearing. U.S. Representative Morgan Griffith (R-Va.) read the section of the Doshi-Topol article quoted above and asked one witness, Offit, to weigh in.
“Do you agree with those concerns? And either way, tell me why,” Griffith asked.
“I don’t agree,” Offit responded.
“I think it’s actually much harder to prevent asymptomatic infection or mildly symptomatic infection,” he said. “If you can prevent that, you are much more likely to prevent moderate to severe disease. So I think they have it backwards.”
But other researchers also question the approaches used with the current crop of COVID-19 vaccines.
“With the current protocols, it is conceivable that a vaccine might be considered effective – and eventually approved – based primarily on its ability to prevent mild cases alone,” wrote William Haseltine, PhD, president of the nonprofit ACCESS Health International, in a September 22 opinion article in the Washington Post titled: “Beware of COVID-19 Vaccine Trials Designed to Succeed From the Start.”
In an interview with Medscape Medical News on Wednesday, Haseltine said he maintains these concerns about the tests. Earlier in his career, he was a leader in HIV research through his lab at Harvard University in Cambridge, Massachusetts, and he subsequently led a biotech company, Human Genome Sciences.
He fears consumers will not get what they might expect from the vaccines being tested.
“What people care about is if this is going to keep them out of the hospital and will it keep them alive. And that’s not even part of this protocol,” Haseltine said.
This article first appeared on Medscape.com.
on Wednesday.
The career staff of the Food and Drug Administration can be counted on to appropriately weigh whether a vaccine should be cleared for use in preventing COVID-19, witnesses, including Paul A. Offit, MD, of Children’s Hospital of Philadelphia, told the House Energy and Commerce Committee’s oversight and investigations panel.
FDA staffers would object to attempts by the Trump administration to rush a vaccine to the public without proper vetting, as would veteran federal researchers, including National Institutes of Health Director Francis S. Collins, MD, PhD, and Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, Offit said.
“If COVID-19 vaccines are released before they’re ready to be released, you will hear from these people, and you will also hear from people like Dr. Francis Collins and Tony Fauci, both of whom are trusted by the American public, as well as many other academicians and researchers who wouldn’t stand for this,” he said.
“The public is already nervous about these vaccines,” said Offit, who serves on key FDA and Centers for Disease Control and Prevention committees overseeing vaccine policy. “If trusted health officials stand up and decry a premature release, the celebration by the administration will be short-lived.”
Overly optimistic estimates about a potential approval can only serve to erode the public’s trust in these crucial vaccines, said another witness, Ashish K. Jha, MD, MPH, the dean of Brown University’s School of Public Health, in Providence, Rhode Island.
“All political leaders need to stop talking about things like time lines,” Jha told the lawmakers.
President Donald Trump has several times suggested that a COVID vaccine might be approved ahead of the November 3 election, where he faces a significant challenge from his Democratic rival, former Vice President Joe Biden.
In a Tuesday night debate with Biden, Trump again raised the idea of a quick approval. “Now we’re weeks away from a vaccine,” Trump said during the debate.
Trump’s estimates, though, are not in line with those offered by most firms involved with making vaccines. The most optimistic projections have come from Pfizer Inc. The drugmaker’s chief executive, Albert Bourla, has spoken about his company possibly having data to present to the FDA as early as late October about the safety and effectiveness of a vaccine.
In a September 8 interview with the Today show, Bourla said there was a 60% chance his company would meet that goal. In response to a question, he made it clear his comments applied to a potential Pfizer application, not an approval or release of a vaccine by that time.
In response to concerns about political pressures, the FDA in June issued guidance outlining what its staff would require for approval of a COVID-19 vaccine.
Pushback on politics
Another witness at the Wednesday hearing, Mark McClellan, MD, PhD, a former FDA commissioner (2002 – 2004), pushed back on objections to a potential release of further guidance from the agency.
“Some recent statements from the White House have implied that FDA’s plan to release additional written guidance on its expectations for emergency use authorization of a vaccine is unnecessarily raising the bar on regulatory standards for authorization,” said McClellan in his testimony for the House panel. “That is not the case.”
Instead, further FDA guidance would be a welcome form of feedback for the firms trying to develop COVID-19 vaccines, according to McClellan, who also serves on the board of directors for Johnson & Johnson. Johnson & Johnson is among the firms that have advanced a COVID-19 vaccine candidate to phase 3 testing. In his role as a director, he serves on the board’s regulatory compliance committee.
Along with politics, recent stumbles at FDA with emergency use authorizations (EUAs) of treatments for COVID-19 have eroded the public’s confidence in the agency, Jha told the House panel. The FDA approved hydroxychloroquine, a medicine promoted by Trump for use in COVID, under an EUA in March and then revoked this clearance in June.
Jha said the FDA’s most serious misstep was its handling of convalescent plasma, which was approved through an EUA on August 23 “in a highly advertised and widely televised announcement including the president.
“The announcement solidified in the public conversation the impression that, increasingly with this administration, politics are taking over trusted, nonpartisan scientific institutions,” he said in his testimony.
Approving a COVID-19 vaccine on the limited evidence through an EUA would mark a serious departure from FDA policy, according to Jha.
“While we sometimes accept a certain level of potential harm in experimental treatments for those who are severely ill, vaccines are given to healthy people and therefore need to have a substantially higher measure of safety and effectiveness,” he explained.
Jha said the FDA has only once before used this EUA approach for a vaccine. That was for a vaccine against inhaled anthrax and was mostly distributed to high-risk soldiers and civilians in war zones.
COVID-19, in contrast, is an infection that has changed lives around the world. The virus has contributed to more than 1 million deaths, including more than 200,000 in the United States, according to the World Health Organization.
Scientists are hoping vaccines will help curb this infection, although much of the future success of vaccines depends on how widely they are used, witnesses told the House panel.
Debate on approaches for vaccine effectiveness
In his testimony, Jha also noted concerns about COVID-19 vaccine trials. He included a reference to a Sept. 22 opinion article titled, “These Coronavirus Trials Don›t Answer the One Question We Need to Know,” which was written by Peter Doshi, PhD, of the University of Maryland School of Pharmacy, in Baltimore, and Eric Topol, MD, a professor of molecular medicine at Scripps Research in La Jolla, Calif. Topol is also editor in chief of Medscape.
Topol and Doshi questioned why the firms Moderna, Pfizer, and AstraZeneca structured their competing trials such that “a vaccine could meet the companies’ benchmark for success if it lowered the risk of mild Covid-19, but was never shown to reduce moderate or severe forms of the disease, or the risk of hospitalization, admissions to the intensive care unit or death.”
“To say a vaccine works should mean that most people no longer run the risk of getting seriously sick,” Topol and Doshi wrote. “That’s not what these trials will determine.”
There was disagreement about this point at the hearing. U.S. Representative Morgan Griffith (R-Va.) read the section of the Doshi-Topol article quoted above and asked one witness, Offit, to weigh in.
“Do you agree with those concerns? And either way, tell me why,” Griffith asked.
“I don’t agree,” Offit responded.
“I think it’s actually much harder to prevent asymptomatic infection or mildly symptomatic infection,” he said. “If you can prevent that, you are much more likely to prevent moderate to severe disease. So I think they have it backwards.”
But other researchers also question the approaches used with the current crop of COVID-19 vaccines.
“With the current protocols, it is conceivable that a vaccine might be considered effective – and eventually approved – based primarily on its ability to prevent mild cases alone,” wrote William Haseltine, PhD, president of the nonprofit ACCESS Health International, in a September 22 opinion article in the Washington Post titled: “Beware of COVID-19 Vaccine Trials Designed to Succeed From the Start.”
In an interview with Medscape Medical News on Wednesday, Haseltine said he maintains these concerns about the tests. Earlier in his career, he was a leader in HIV research through his lab at Harvard University in Cambridge, Massachusetts, and he subsequently led a biotech company, Human Genome Sciences.
He fears consumers will not get what they might expect from the vaccines being tested.
“What people care about is if this is going to keep them out of the hospital and will it keep them alive. And that’s not even part of this protocol,” Haseltine said.
This article first appeared on Medscape.com.
on Wednesday.
The career staff of the Food and Drug Administration can be counted on to appropriately weigh whether a vaccine should be cleared for use in preventing COVID-19, witnesses, including Paul A. Offit, MD, of Children’s Hospital of Philadelphia, told the House Energy and Commerce Committee’s oversight and investigations panel.
FDA staffers would object to attempts by the Trump administration to rush a vaccine to the public without proper vetting, as would veteran federal researchers, including National Institutes of Health Director Francis S. Collins, MD, PhD, and Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, Offit said.
“If COVID-19 vaccines are released before they’re ready to be released, you will hear from these people, and you will also hear from people like Dr. Francis Collins and Tony Fauci, both of whom are trusted by the American public, as well as many other academicians and researchers who wouldn’t stand for this,” he said.
“The public is already nervous about these vaccines,” said Offit, who serves on key FDA and Centers for Disease Control and Prevention committees overseeing vaccine policy. “If trusted health officials stand up and decry a premature release, the celebration by the administration will be short-lived.”
Overly optimistic estimates about a potential approval can only serve to erode the public’s trust in these crucial vaccines, said another witness, Ashish K. Jha, MD, MPH, the dean of Brown University’s School of Public Health, in Providence, Rhode Island.
“All political leaders need to stop talking about things like time lines,” Jha told the lawmakers.
President Donald Trump has several times suggested that a COVID vaccine might be approved ahead of the November 3 election, where he faces a significant challenge from his Democratic rival, former Vice President Joe Biden.
In a Tuesday night debate with Biden, Trump again raised the idea of a quick approval. “Now we’re weeks away from a vaccine,” Trump said during the debate.
Trump’s estimates, though, are not in line with those offered by most firms involved with making vaccines. The most optimistic projections have come from Pfizer Inc. The drugmaker’s chief executive, Albert Bourla, has spoken about his company possibly having data to present to the FDA as early as late October about the safety and effectiveness of a vaccine.
In a September 8 interview with the Today show, Bourla said there was a 60% chance his company would meet that goal. In response to a question, he made it clear his comments applied to a potential Pfizer application, not an approval or release of a vaccine by that time.
In response to concerns about political pressures, the FDA in June issued guidance outlining what its staff would require for approval of a COVID-19 vaccine.
Pushback on politics
Another witness at the Wednesday hearing, Mark McClellan, MD, PhD, a former FDA commissioner (2002 – 2004), pushed back on objections to a potential release of further guidance from the agency.
“Some recent statements from the White House have implied that FDA’s plan to release additional written guidance on its expectations for emergency use authorization of a vaccine is unnecessarily raising the bar on regulatory standards for authorization,” said McClellan in his testimony for the House panel. “That is not the case.”
Instead, further FDA guidance would be a welcome form of feedback for the firms trying to develop COVID-19 vaccines, according to McClellan, who also serves on the board of directors for Johnson & Johnson. Johnson & Johnson is among the firms that have advanced a COVID-19 vaccine candidate to phase 3 testing. In his role as a director, he serves on the board’s regulatory compliance committee.
Along with politics, recent stumbles at FDA with emergency use authorizations (EUAs) of treatments for COVID-19 have eroded the public’s confidence in the agency, Jha told the House panel. The FDA approved hydroxychloroquine, a medicine promoted by Trump for use in COVID, under an EUA in March and then revoked this clearance in June.
Jha said the FDA’s most serious misstep was its handling of convalescent plasma, which was approved through an EUA on August 23 “in a highly advertised and widely televised announcement including the president.
“The announcement solidified in the public conversation the impression that, increasingly with this administration, politics are taking over trusted, nonpartisan scientific institutions,” he said in his testimony.
Approving a COVID-19 vaccine on the limited evidence through an EUA would mark a serious departure from FDA policy, according to Jha.
“While we sometimes accept a certain level of potential harm in experimental treatments for those who are severely ill, vaccines are given to healthy people and therefore need to have a substantially higher measure of safety and effectiveness,” he explained.
Jha said the FDA has only once before used this EUA approach for a vaccine. That was for a vaccine against inhaled anthrax and was mostly distributed to high-risk soldiers and civilians in war zones.
COVID-19, in contrast, is an infection that has changed lives around the world. The virus has contributed to more than 1 million deaths, including more than 200,000 in the United States, according to the World Health Organization.
Scientists are hoping vaccines will help curb this infection, although much of the future success of vaccines depends on how widely they are used, witnesses told the House panel.
Debate on approaches for vaccine effectiveness
In his testimony, Jha also noted concerns about COVID-19 vaccine trials. He included a reference to a Sept. 22 opinion article titled, “These Coronavirus Trials Don›t Answer the One Question We Need to Know,” which was written by Peter Doshi, PhD, of the University of Maryland School of Pharmacy, in Baltimore, and Eric Topol, MD, a professor of molecular medicine at Scripps Research in La Jolla, Calif. Topol is also editor in chief of Medscape.
Topol and Doshi questioned why the firms Moderna, Pfizer, and AstraZeneca structured their competing trials such that “a vaccine could meet the companies’ benchmark for success if it lowered the risk of mild Covid-19, but was never shown to reduce moderate or severe forms of the disease, or the risk of hospitalization, admissions to the intensive care unit or death.”
“To say a vaccine works should mean that most people no longer run the risk of getting seriously sick,” Topol and Doshi wrote. “That’s not what these trials will determine.”
There was disagreement about this point at the hearing. U.S. Representative Morgan Griffith (R-Va.) read the section of the Doshi-Topol article quoted above and asked one witness, Offit, to weigh in.
“Do you agree with those concerns? And either way, tell me why,” Griffith asked.
“I don’t agree,” Offit responded.
“I think it’s actually much harder to prevent asymptomatic infection or mildly symptomatic infection,” he said. “If you can prevent that, you are much more likely to prevent moderate to severe disease. So I think they have it backwards.”
But other researchers also question the approaches used with the current crop of COVID-19 vaccines.
“With the current protocols, it is conceivable that a vaccine might be considered effective – and eventually approved – based primarily on its ability to prevent mild cases alone,” wrote William Haseltine, PhD, president of the nonprofit ACCESS Health International, in a September 22 opinion article in the Washington Post titled: “Beware of COVID-19 Vaccine Trials Designed to Succeed From the Start.”
In an interview with Medscape Medical News on Wednesday, Haseltine said he maintains these concerns about the tests. Earlier in his career, he was a leader in HIV research through his lab at Harvard University in Cambridge, Massachusetts, and he subsequently led a biotech company, Human Genome Sciences.
He fears consumers will not get what they might expect from the vaccines being tested.
“What people care about is if this is going to keep them out of the hospital and will it keep them alive. And that’s not even part of this protocol,” Haseltine said.
This article first appeared on Medscape.com.
Apatinib plus gefitinib: Better PFS but more toxicity
ACTIVE is the first phase 3 trial of an oral vascular epidermal growth factor receptor–2 (VEGFR2) tyrosine kinase inhibitor (TKI) added to an EGFR-TKI as first-line therapy in this population, according to Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
Dr. Zhang presented results from ACTIVE at the European Society for Medical Oncology Virtual Congress 2020.
“This dual oral regimen will provide more convenient treatment for patients who require long-term administration,” Dr. Zhang said. He added that apatinib plus gefitinib “is expected to become a new first-line treatment option for EGFR-mutant NSCLC.”
A discussant for the ACTIVE study was less optimistic, however, noting that the regimen proved tough to tolerate for some patients, and the PFS benefit may not translate to overall survival.
Study rationale and details
Sensitizing EGFR mutations occur in about 10% of White patients and up to 50% of Asian patients, Dr. Zhang noted. Unfortunately, most patients progress after first-line treatment with EGFR-TKIs because of acquired resistance.
Blocking VEGF receptor pathways has been shown to enhance EGFR-TKIs in EGFR-mutated NSCLC, and pilot study results have shown apatinib – an oral VEGFR2–TKI – to be safe and well-tolerated with promising efficacy in combination with gefitinib, Dr. Zhang added.
To expand upon those results, he and his colleagues tested apatinib with gefitinib in the phase 3, double-blind, placebo-controlled ACTIVE trial (CTONG1706).
The trial included 313 patients (median age, 58.5 years) with locally advanced, metastatic, or recurrent nonsquamous NSCLC. All were chemotherapy-naive and EGFR mutation-positive (exon 19 deletion or exon 21 L858R).
Patients were randomized 1:1 to first-line apatinib at 500 mg daily plus gefitinib at 250 mg daily (n = 157) or placebo plus gefitinib at 250 mg daily (n = 156) until progressive disease or unacceptable toxicity.
Efficacy and safety
The primary endpoint was PFS by independent review. The median follow-up was 15.8 months.
The median PFS was 13.7 months in the apatinib group and 10.2 months in the placebo group (hazard ratio, 0.71; P = .0189).
Objective response rates were similar for both groups – 77.1% with apatinib and 73.7% with placebo. However, depth of response ≥30% and depth of response ≥50% both favored the apatinib arm – 89.2% versus 79.5% for ≥ 30% (P = .0209) and 64.3% versus 52.6% for ≥50% (P = .0238).
In addition, the median duration of response was longer for the apatinib group – 12.9 months versus 9.3 months (HR, 0.64; P = .005).
Exploratory biomarker analyses showed the benefit of apatinib was more common in patients with TP53 exon 8 mutations.
The rate of grade 3 or higher treatment-emergent adverse events was 84.1% in the apatinib arm and 37.7% in the placebo arm. Diarrhea (73.2%) and hypertension (68.2%) were the most common treatment-emergent adverse events in the apatinib group.
Dose interruptions were more common in the apatinib group (59.5% vs. 22.7%) as were dose reductions (48.4% vs. 4.5%). However, treatment discontinuations attributable to treatment-emergent adverse events were few in both arms (5.1% in the apatinib arm and 3.2% in the placebo arm).
Cause for hesitation
“VEGFR-TKIs have not yet found a solid home in lung cancer,” said study discussant Lecia V. Sequist, MD, of Massachusetts General Hospital in Boston.
Listing 10 VEGFR-TKIs, Dr. Sequist noted: “None of them have changed practice.”
She added that, while an all-oral regimen is appealing, the benefit of adding apatinib to gefitinib was modest, and the regimen was “fairly difficult” to tolerate. “The PFS with apatinib plus gefitinib is well below what we see with other EGFR/VEGF first-line studies,” she said.
Dr. Sequist also observed that most studies have shown a PFS benefit but no overall survival benefit. “That, in combination with the toxicity, makes me a little hesitant about this regimen. The role of VEGF remains unclear in EGFR mutation–positive lung cancer in 2020,” she concluded.
The ACTIVE study was funded by Jiangsu HengRui Medicine, the Chinese Thoracic Oncology Group, and grants from Sun Yat-sen University and the National Key R&D Program of China. Dr. Zhang disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Pfizer, and Roche. Dr. Sequist disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Blueprint Medicines, and many other companies.
SOURCE: Zhang L et al. ESMO 2020, Abstract LBA50.
ACTIVE is the first phase 3 trial of an oral vascular epidermal growth factor receptor–2 (VEGFR2) tyrosine kinase inhibitor (TKI) added to an EGFR-TKI as first-line therapy in this population, according to Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
Dr. Zhang presented results from ACTIVE at the European Society for Medical Oncology Virtual Congress 2020.
“This dual oral regimen will provide more convenient treatment for patients who require long-term administration,” Dr. Zhang said. He added that apatinib plus gefitinib “is expected to become a new first-line treatment option for EGFR-mutant NSCLC.”
A discussant for the ACTIVE study was less optimistic, however, noting that the regimen proved tough to tolerate for some patients, and the PFS benefit may not translate to overall survival.
Study rationale and details
Sensitizing EGFR mutations occur in about 10% of White patients and up to 50% of Asian patients, Dr. Zhang noted. Unfortunately, most patients progress after first-line treatment with EGFR-TKIs because of acquired resistance.
Blocking VEGF receptor pathways has been shown to enhance EGFR-TKIs in EGFR-mutated NSCLC, and pilot study results have shown apatinib – an oral VEGFR2–TKI – to be safe and well-tolerated with promising efficacy in combination with gefitinib, Dr. Zhang added.
To expand upon those results, he and his colleagues tested apatinib with gefitinib in the phase 3, double-blind, placebo-controlled ACTIVE trial (CTONG1706).
The trial included 313 patients (median age, 58.5 years) with locally advanced, metastatic, or recurrent nonsquamous NSCLC. All were chemotherapy-naive and EGFR mutation-positive (exon 19 deletion or exon 21 L858R).
Patients were randomized 1:1 to first-line apatinib at 500 mg daily plus gefitinib at 250 mg daily (n = 157) or placebo plus gefitinib at 250 mg daily (n = 156) until progressive disease or unacceptable toxicity.
Efficacy and safety
The primary endpoint was PFS by independent review. The median follow-up was 15.8 months.
The median PFS was 13.7 months in the apatinib group and 10.2 months in the placebo group (hazard ratio, 0.71; P = .0189).
Objective response rates were similar for both groups – 77.1% with apatinib and 73.7% with placebo. However, depth of response ≥30% and depth of response ≥50% both favored the apatinib arm – 89.2% versus 79.5% for ≥ 30% (P = .0209) and 64.3% versus 52.6% for ≥50% (P = .0238).
In addition, the median duration of response was longer for the apatinib group – 12.9 months versus 9.3 months (HR, 0.64; P = .005).
Exploratory biomarker analyses showed the benefit of apatinib was more common in patients with TP53 exon 8 mutations.
The rate of grade 3 or higher treatment-emergent adverse events was 84.1% in the apatinib arm and 37.7% in the placebo arm. Diarrhea (73.2%) and hypertension (68.2%) were the most common treatment-emergent adverse events in the apatinib group.
Dose interruptions were more common in the apatinib group (59.5% vs. 22.7%) as were dose reductions (48.4% vs. 4.5%). However, treatment discontinuations attributable to treatment-emergent adverse events were few in both arms (5.1% in the apatinib arm and 3.2% in the placebo arm).
Cause for hesitation
“VEGFR-TKIs have not yet found a solid home in lung cancer,” said study discussant Lecia V. Sequist, MD, of Massachusetts General Hospital in Boston.
Listing 10 VEGFR-TKIs, Dr. Sequist noted: “None of them have changed practice.”
She added that, while an all-oral regimen is appealing, the benefit of adding apatinib to gefitinib was modest, and the regimen was “fairly difficult” to tolerate. “The PFS with apatinib plus gefitinib is well below what we see with other EGFR/VEGF first-line studies,” she said.
Dr. Sequist also observed that most studies have shown a PFS benefit but no overall survival benefit. “That, in combination with the toxicity, makes me a little hesitant about this regimen. The role of VEGF remains unclear in EGFR mutation–positive lung cancer in 2020,” she concluded.
The ACTIVE study was funded by Jiangsu HengRui Medicine, the Chinese Thoracic Oncology Group, and grants from Sun Yat-sen University and the National Key R&D Program of China. Dr. Zhang disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Pfizer, and Roche. Dr. Sequist disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Blueprint Medicines, and many other companies.
SOURCE: Zhang L et al. ESMO 2020, Abstract LBA50.
ACTIVE is the first phase 3 trial of an oral vascular epidermal growth factor receptor–2 (VEGFR2) tyrosine kinase inhibitor (TKI) added to an EGFR-TKI as first-line therapy in this population, according to Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
Dr. Zhang presented results from ACTIVE at the European Society for Medical Oncology Virtual Congress 2020.
“This dual oral regimen will provide more convenient treatment for patients who require long-term administration,” Dr. Zhang said. He added that apatinib plus gefitinib “is expected to become a new first-line treatment option for EGFR-mutant NSCLC.”
A discussant for the ACTIVE study was less optimistic, however, noting that the regimen proved tough to tolerate for some patients, and the PFS benefit may not translate to overall survival.
Study rationale and details
Sensitizing EGFR mutations occur in about 10% of White patients and up to 50% of Asian patients, Dr. Zhang noted. Unfortunately, most patients progress after first-line treatment with EGFR-TKIs because of acquired resistance.
Blocking VEGF receptor pathways has been shown to enhance EGFR-TKIs in EGFR-mutated NSCLC, and pilot study results have shown apatinib – an oral VEGFR2–TKI – to be safe and well-tolerated with promising efficacy in combination with gefitinib, Dr. Zhang added.
To expand upon those results, he and his colleagues tested apatinib with gefitinib in the phase 3, double-blind, placebo-controlled ACTIVE trial (CTONG1706).
The trial included 313 patients (median age, 58.5 years) with locally advanced, metastatic, or recurrent nonsquamous NSCLC. All were chemotherapy-naive and EGFR mutation-positive (exon 19 deletion or exon 21 L858R).
Patients were randomized 1:1 to first-line apatinib at 500 mg daily plus gefitinib at 250 mg daily (n = 157) or placebo plus gefitinib at 250 mg daily (n = 156) until progressive disease or unacceptable toxicity.
Efficacy and safety
The primary endpoint was PFS by independent review. The median follow-up was 15.8 months.
The median PFS was 13.7 months in the apatinib group and 10.2 months in the placebo group (hazard ratio, 0.71; P = .0189).
Objective response rates were similar for both groups – 77.1% with apatinib and 73.7% with placebo. However, depth of response ≥30% and depth of response ≥50% both favored the apatinib arm – 89.2% versus 79.5% for ≥ 30% (P = .0209) and 64.3% versus 52.6% for ≥50% (P = .0238).
In addition, the median duration of response was longer for the apatinib group – 12.9 months versus 9.3 months (HR, 0.64; P = .005).
Exploratory biomarker analyses showed the benefit of apatinib was more common in patients with TP53 exon 8 mutations.
The rate of grade 3 or higher treatment-emergent adverse events was 84.1% in the apatinib arm and 37.7% in the placebo arm. Diarrhea (73.2%) and hypertension (68.2%) were the most common treatment-emergent adverse events in the apatinib group.
Dose interruptions were more common in the apatinib group (59.5% vs. 22.7%) as were dose reductions (48.4% vs. 4.5%). However, treatment discontinuations attributable to treatment-emergent adverse events were few in both arms (5.1% in the apatinib arm and 3.2% in the placebo arm).
Cause for hesitation
“VEGFR-TKIs have not yet found a solid home in lung cancer,” said study discussant Lecia V. Sequist, MD, of Massachusetts General Hospital in Boston.
Listing 10 VEGFR-TKIs, Dr. Sequist noted: “None of them have changed practice.”
She added that, while an all-oral regimen is appealing, the benefit of adding apatinib to gefitinib was modest, and the regimen was “fairly difficult” to tolerate. “The PFS with apatinib plus gefitinib is well below what we see with other EGFR/VEGF first-line studies,” she said.
Dr. Sequist also observed that most studies have shown a PFS benefit but no overall survival benefit. “That, in combination with the toxicity, makes me a little hesitant about this regimen. The role of VEGF remains unclear in EGFR mutation–positive lung cancer in 2020,” she concluded.
The ACTIVE study was funded by Jiangsu HengRui Medicine, the Chinese Thoracic Oncology Group, and grants from Sun Yat-sen University and the National Key R&D Program of China. Dr. Zhang disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Pfizer, and Roche. Dr. Sequist disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Blueprint Medicines, and many other companies.
SOURCE: Zhang L et al. ESMO 2020, Abstract LBA50.
FROM ESMO 2020
Post-COVID clinics get jump-start from patients with lingering illness
Clarence Troutman survived a 2-month hospital stay with COVID-19, then went home in early June. But he’s far from over the disease, still suffering from limited endurance, shortness of breath and hands that can be stiff and swollen.
“Before COVID, I was a 59-year-old, relatively healthy man,” said the broadband technician from Denver. “If I had to say where I’m at now, I’d say about 50% of where I was, but when I first went home, I was at 20%.”
He credits much of his progress to the “motivation and education” gleaned from a new program for post-COVID patients at the University of Colorado at Denver, Aurora, one of a small but growing number of clinics aimed at treating and studying those who have had the unpredictable coronavirus.
As the election nears, much attention is focused on daily infection numbers or the climbing death toll, but another measure matters: Patients who survive but continue to wrestle with a range of physical or mental effects, including lung damage, heart or neurologic concerns, anxiety, and depression.
“We need to think about how we’re going to provide care for patients who may be recovering for years after the virus,” said Sarah Jolley, MD, a pulmonologist with UCHealth University of Colorado Hospital and director of UCHealth’s Post-Covid Clinic, where Mr. Troutman is seen.
That need has jump-started post-COVID clinics, which bring together a range of specialists into a one-stop shop.
One of the first and largest such clinics is at Mount Sinai in New York City, but programs have also launched at the University of California,San Francisco; Stanford (Calif.) University Medical Center; and the University of Pennsylvania, Philadelphia. The Cleveland Clinic plans to open one early next year. And it’s not just academic medical centers: St. John’s Well Child and Family Center, part of a network of community clinics in south central Los Angeles, said this month it aims to test thousands of its patients who were diagnosed with COVID-19 since March for long-term effects.
Mental health specialists are also involved, along with social workers and pharmacists. Many of the centers also do research studies, aiming to better understand why the virus hits certain patients so hard.
“Some of our patients, even those on a ventilator on death’s door, will come out remarkably unscathed,” said Lekshmi Santhosh, MD, an assistant professor of pulmonary critical care and a leader of the post-COVID program at UCSF, called the OPTIMAL clinic. “Others, even those who were never hospitalized, have disabling fatigue, ongoing chest pain, and shortness of breath, and there’s a whole spectrum in between.”
‘Staggering’ medical need
It’s too early to know how long the persistent medical effects and symptoms will linger, or to make accurate estimates on the percentage of patients affected.
Some early studies are sobering. An Austrian report released this month found that 76 of the first 86 patients studied had evidence of lung damage 6 weeks after hospital discharge, but that dropped to 48 patients at 12 weeks.
Some researchers and clinics say about 10% of U.S. COVID patients they see may have longer-running effects, said Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai, which has enrolled 400 patients so far.
If that estimate is correct – and Dr. Chen emphasized that more research is needed to make sure – it translates to patients entering the medical system in droves, often with multiple issues.
How health systems and insurers respond will be key, he said. More than 6.5 million U.S. residents have tested positive for the disease. If fewer than 10% – say 500,000 – already have long-lasting symptoms, “that number is staggering,” Dr. Chen said. “How much medical care will be needed for that?”
Though start-up costs could be a hurdle, the clinics themselves may eventually draw much-needed revenue to medical centers by attracting patients, many of whom have insurance to cover some or all of the cost of repeated visits.
Dr. Chen said the specialized centers can help lower health spending by providing more cost effective, coordinated care that avoids duplicative testing a patient might otherwise undergo.
“We’ve seen patients that when they come in, they’ve already had four MRI or CT scans and a stack of bloodwork,” he said.
The program consolidates those earlier results and determines if any additional testing is needed. Sometimes the answer to what’s causing patients’ long-lasting symptoms remains elusive. One problem for patients seeking help outside of dedicated clinics is that when there is no clear cause for their condition, they may be told the symptoms are imagined.
“I believe in the patients,” said Dr. Chen.
About half the clinic’s patients have received test results showing damage, said Dr. Chen, an endocrinologist and internal medicine physician. For those patients, the clinic can develop a treatment plan. But, frustratingly, the other half have inconclusive test results yet exhibit a range of symptoms.
“That makes it more difficult to treat,” said Dr. Chen.
Experts see parallels to a push in the past decade to establish special clinics to treat patients released from ICU wards, who may have problems related to long-term bed rest or the delirium many experience while hospitalized. Some of the current post-COVID clinics are modeled after the post-ICU clinics or are expanded versions of them.
The ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tenn., for instance, which opened in 2012, is accepting post-COVID patients.
There are about a dozen post-ICU clinics nationally, some of which are also now working with COVID patients, said James Jackson, director of long-term outcomes at the Vanderbilt center. In addition, he’s heard of at least another dozen post-COVID centers in development.
The centers generally do an initial assessment a few weeks after a patient is diagnosed or discharged from the hospital, often by video call. Check-in and repeat visits are scheduled every month or so after that.
“In an ideal world, with these post-COVID clinics, you can identify the patients and get them into rehab,” he said. “Even if the primary thing these clinics did was to say to patients: ‘This is real, it is not all in your head,’ that impact would be important.”
A question of feasibility
Financing is the largest obstacle, program proponents said. Many hospitals lost substantial revenue to canceled elective procedures during stay-at-home periods.
“So, it’s not a great time to be pitching a new activity that requires a start-up subsidy,” said Glenn Melnick, PhD, a professor of health economics at the University of Southern California.
At UCSF, a select group of faculty members staff the post-COVID clinics and some mental health professionals volunteer their time, said Dr. Santhosh.
Dr. Chen said he was able to recruit team members and support staff from the ranks of those whose elective patient caseload had dropped.
Dr. Jackson said unfortunately there’s not been enough research into the cost-and-clinical effectiveness of post-ICU centers.
“In the early days, there may have been questions about how much value does this add,” he noted. “Now, the question is not so much is it a good idea, but is it feasible?”
Right now, the post-COVID centers are foremost a research effort, said Len Nichols, an economist and nonresident fellow at the Urban Institute. “If these guys get good at treating long-term symptoms, that’s good for all of us. There’s not enough patients to make it a business model yet, but if they become the place to go when you get it, it could become a business model for some of the elite institutions.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Clarence Troutman survived a 2-month hospital stay with COVID-19, then went home in early June. But he’s far from over the disease, still suffering from limited endurance, shortness of breath and hands that can be stiff and swollen.
“Before COVID, I was a 59-year-old, relatively healthy man,” said the broadband technician from Denver. “If I had to say where I’m at now, I’d say about 50% of where I was, but when I first went home, I was at 20%.”
He credits much of his progress to the “motivation and education” gleaned from a new program for post-COVID patients at the University of Colorado at Denver, Aurora, one of a small but growing number of clinics aimed at treating and studying those who have had the unpredictable coronavirus.
As the election nears, much attention is focused on daily infection numbers or the climbing death toll, but another measure matters: Patients who survive but continue to wrestle with a range of physical or mental effects, including lung damage, heart or neurologic concerns, anxiety, and depression.
“We need to think about how we’re going to provide care for patients who may be recovering for years after the virus,” said Sarah Jolley, MD, a pulmonologist with UCHealth University of Colorado Hospital and director of UCHealth’s Post-Covid Clinic, where Mr. Troutman is seen.
That need has jump-started post-COVID clinics, which bring together a range of specialists into a one-stop shop.
One of the first and largest such clinics is at Mount Sinai in New York City, but programs have also launched at the University of California,San Francisco; Stanford (Calif.) University Medical Center; and the University of Pennsylvania, Philadelphia. The Cleveland Clinic plans to open one early next year. And it’s not just academic medical centers: St. John’s Well Child and Family Center, part of a network of community clinics in south central Los Angeles, said this month it aims to test thousands of its patients who were diagnosed with COVID-19 since March for long-term effects.
Mental health specialists are also involved, along with social workers and pharmacists. Many of the centers also do research studies, aiming to better understand why the virus hits certain patients so hard.
“Some of our patients, even those on a ventilator on death’s door, will come out remarkably unscathed,” said Lekshmi Santhosh, MD, an assistant professor of pulmonary critical care and a leader of the post-COVID program at UCSF, called the OPTIMAL clinic. “Others, even those who were never hospitalized, have disabling fatigue, ongoing chest pain, and shortness of breath, and there’s a whole spectrum in between.”
‘Staggering’ medical need
It’s too early to know how long the persistent medical effects and symptoms will linger, or to make accurate estimates on the percentage of patients affected.
Some early studies are sobering. An Austrian report released this month found that 76 of the first 86 patients studied had evidence of lung damage 6 weeks after hospital discharge, but that dropped to 48 patients at 12 weeks.
Some researchers and clinics say about 10% of U.S. COVID patients they see may have longer-running effects, said Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai, which has enrolled 400 patients so far.
If that estimate is correct – and Dr. Chen emphasized that more research is needed to make sure – it translates to patients entering the medical system in droves, often with multiple issues.
How health systems and insurers respond will be key, he said. More than 6.5 million U.S. residents have tested positive for the disease. If fewer than 10% – say 500,000 – already have long-lasting symptoms, “that number is staggering,” Dr. Chen said. “How much medical care will be needed for that?”
Though start-up costs could be a hurdle, the clinics themselves may eventually draw much-needed revenue to medical centers by attracting patients, many of whom have insurance to cover some or all of the cost of repeated visits.
Dr. Chen said the specialized centers can help lower health spending by providing more cost effective, coordinated care that avoids duplicative testing a patient might otherwise undergo.
“We’ve seen patients that when they come in, they’ve already had four MRI or CT scans and a stack of bloodwork,” he said.
The program consolidates those earlier results and determines if any additional testing is needed. Sometimes the answer to what’s causing patients’ long-lasting symptoms remains elusive. One problem for patients seeking help outside of dedicated clinics is that when there is no clear cause for their condition, they may be told the symptoms are imagined.
“I believe in the patients,” said Dr. Chen.
About half the clinic’s patients have received test results showing damage, said Dr. Chen, an endocrinologist and internal medicine physician. For those patients, the clinic can develop a treatment plan. But, frustratingly, the other half have inconclusive test results yet exhibit a range of symptoms.
“That makes it more difficult to treat,” said Dr. Chen.
Experts see parallels to a push in the past decade to establish special clinics to treat patients released from ICU wards, who may have problems related to long-term bed rest or the delirium many experience while hospitalized. Some of the current post-COVID clinics are modeled after the post-ICU clinics or are expanded versions of them.
The ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tenn., for instance, which opened in 2012, is accepting post-COVID patients.
There are about a dozen post-ICU clinics nationally, some of which are also now working with COVID patients, said James Jackson, director of long-term outcomes at the Vanderbilt center. In addition, he’s heard of at least another dozen post-COVID centers in development.
The centers generally do an initial assessment a few weeks after a patient is diagnosed or discharged from the hospital, often by video call. Check-in and repeat visits are scheduled every month or so after that.
“In an ideal world, with these post-COVID clinics, you can identify the patients and get them into rehab,” he said. “Even if the primary thing these clinics did was to say to patients: ‘This is real, it is not all in your head,’ that impact would be important.”
A question of feasibility
Financing is the largest obstacle, program proponents said. Many hospitals lost substantial revenue to canceled elective procedures during stay-at-home periods.
“So, it’s not a great time to be pitching a new activity that requires a start-up subsidy,” said Glenn Melnick, PhD, a professor of health economics at the University of Southern California.
At UCSF, a select group of faculty members staff the post-COVID clinics and some mental health professionals volunteer their time, said Dr. Santhosh.
Dr. Chen said he was able to recruit team members and support staff from the ranks of those whose elective patient caseload had dropped.
Dr. Jackson said unfortunately there’s not been enough research into the cost-and-clinical effectiveness of post-ICU centers.
“In the early days, there may have been questions about how much value does this add,” he noted. “Now, the question is not so much is it a good idea, but is it feasible?”
Right now, the post-COVID centers are foremost a research effort, said Len Nichols, an economist and nonresident fellow at the Urban Institute. “If these guys get good at treating long-term symptoms, that’s good for all of us. There’s not enough patients to make it a business model yet, but if they become the place to go when you get it, it could become a business model for some of the elite institutions.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Clarence Troutman survived a 2-month hospital stay with COVID-19, then went home in early June. But he’s far from over the disease, still suffering from limited endurance, shortness of breath and hands that can be stiff and swollen.
“Before COVID, I was a 59-year-old, relatively healthy man,” said the broadband technician from Denver. “If I had to say where I’m at now, I’d say about 50% of where I was, but when I first went home, I was at 20%.”
He credits much of his progress to the “motivation and education” gleaned from a new program for post-COVID patients at the University of Colorado at Denver, Aurora, one of a small but growing number of clinics aimed at treating and studying those who have had the unpredictable coronavirus.
As the election nears, much attention is focused on daily infection numbers or the climbing death toll, but another measure matters: Patients who survive but continue to wrestle with a range of physical or mental effects, including lung damage, heart or neurologic concerns, anxiety, and depression.
“We need to think about how we’re going to provide care for patients who may be recovering for years after the virus,” said Sarah Jolley, MD, a pulmonologist with UCHealth University of Colorado Hospital and director of UCHealth’s Post-Covid Clinic, where Mr. Troutman is seen.
That need has jump-started post-COVID clinics, which bring together a range of specialists into a one-stop shop.
One of the first and largest such clinics is at Mount Sinai in New York City, but programs have also launched at the University of California,San Francisco; Stanford (Calif.) University Medical Center; and the University of Pennsylvania, Philadelphia. The Cleveland Clinic plans to open one early next year. And it’s not just academic medical centers: St. John’s Well Child and Family Center, part of a network of community clinics in south central Los Angeles, said this month it aims to test thousands of its patients who were diagnosed with COVID-19 since March for long-term effects.
Mental health specialists are also involved, along with social workers and pharmacists. Many of the centers also do research studies, aiming to better understand why the virus hits certain patients so hard.
“Some of our patients, even those on a ventilator on death’s door, will come out remarkably unscathed,” said Lekshmi Santhosh, MD, an assistant professor of pulmonary critical care and a leader of the post-COVID program at UCSF, called the OPTIMAL clinic. “Others, even those who were never hospitalized, have disabling fatigue, ongoing chest pain, and shortness of breath, and there’s a whole spectrum in between.”
‘Staggering’ medical need
It’s too early to know how long the persistent medical effects and symptoms will linger, or to make accurate estimates on the percentage of patients affected.
Some early studies are sobering. An Austrian report released this month found that 76 of the first 86 patients studied had evidence of lung damage 6 weeks after hospital discharge, but that dropped to 48 patients at 12 weeks.
Some researchers and clinics say about 10% of U.S. COVID patients they see may have longer-running effects, said Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai, which has enrolled 400 patients so far.
If that estimate is correct – and Dr. Chen emphasized that more research is needed to make sure – it translates to patients entering the medical system in droves, often with multiple issues.
How health systems and insurers respond will be key, he said. More than 6.5 million U.S. residents have tested positive for the disease. If fewer than 10% – say 500,000 – already have long-lasting symptoms, “that number is staggering,” Dr. Chen said. “How much medical care will be needed for that?”
Though start-up costs could be a hurdle, the clinics themselves may eventually draw much-needed revenue to medical centers by attracting patients, many of whom have insurance to cover some or all of the cost of repeated visits.
Dr. Chen said the specialized centers can help lower health spending by providing more cost effective, coordinated care that avoids duplicative testing a patient might otherwise undergo.
“We’ve seen patients that when they come in, they’ve already had four MRI or CT scans and a stack of bloodwork,” he said.
The program consolidates those earlier results and determines if any additional testing is needed. Sometimes the answer to what’s causing patients’ long-lasting symptoms remains elusive. One problem for patients seeking help outside of dedicated clinics is that when there is no clear cause for their condition, they may be told the symptoms are imagined.
“I believe in the patients,” said Dr. Chen.
About half the clinic’s patients have received test results showing damage, said Dr. Chen, an endocrinologist and internal medicine physician. For those patients, the clinic can develop a treatment plan. But, frustratingly, the other half have inconclusive test results yet exhibit a range of symptoms.
“That makes it more difficult to treat,” said Dr. Chen.
Experts see parallels to a push in the past decade to establish special clinics to treat patients released from ICU wards, who may have problems related to long-term bed rest or the delirium many experience while hospitalized. Some of the current post-COVID clinics are modeled after the post-ICU clinics or are expanded versions of them.
The ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tenn., for instance, which opened in 2012, is accepting post-COVID patients.
There are about a dozen post-ICU clinics nationally, some of which are also now working with COVID patients, said James Jackson, director of long-term outcomes at the Vanderbilt center. In addition, he’s heard of at least another dozen post-COVID centers in development.
The centers generally do an initial assessment a few weeks after a patient is diagnosed or discharged from the hospital, often by video call. Check-in and repeat visits are scheduled every month or so after that.
“In an ideal world, with these post-COVID clinics, you can identify the patients and get them into rehab,” he said. “Even if the primary thing these clinics did was to say to patients: ‘This is real, it is not all in your head,’ that impact would be important.”
A question of feasibility
Financing is the largest obstacle, program proponents said. Many hospitals lost substantial revenue to canceled elective procedures during stay-at-home periods.
“So, it’s not a great time to be pitching a new activity that requires a start-up subsidy,” said Glenn Melnick, PhD, a professor of health economics at the University of Southern California.
At UCSF, a select group of faculty members staff the post-COVID clinics and some mental health professionals volunteer their time, said Dr. Santhosh.
Dr. Chen said he was able to recruit team members and support staff from the ranks of those whose elective patient caseload had dropped.
Dr. Jackson said unfortunately there’s not been enough research into the cost-and-clinical effectiveness of post-ICU centers.
“In the early days, there may have been questions about how much value does this add,” he noted. “Now, the question is not so much is it a good idea, but is it feasible?”
Right now, the post-COVID centers are foremost a research effort, said Len Nichols, an economist and nonresident fellow at the Urban Institute. “If these guys get good at treating long-term symptoms, that’s good for all of us. There’s not enough patients to make it a business model yet, but if they become the place to go when you get it, it could become a business model for some of the elite institutions.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Screening algorithm safely selects patients for OSA treatment before bariatric surgery
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
REPORTING FROM SLEEP 2020
Nerve damage linked to prone positioning in COVID-19
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
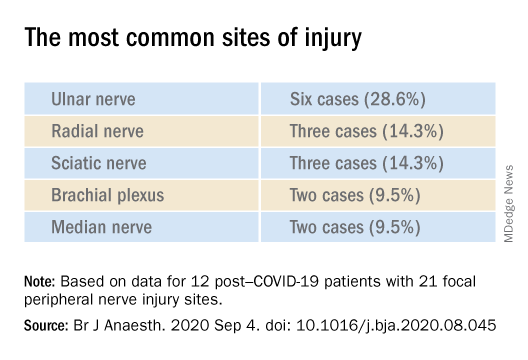
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
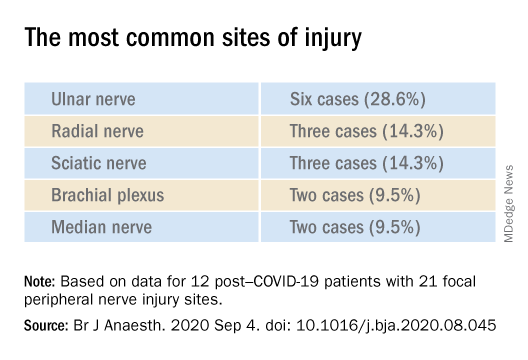
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
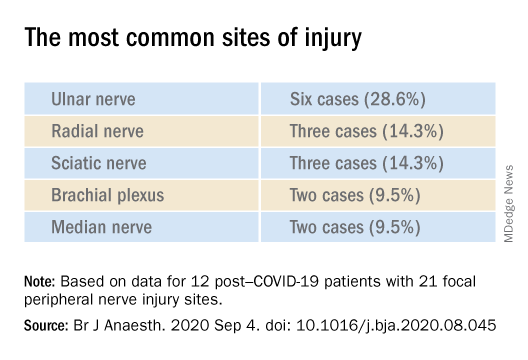
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF ANAESTHESIOLOGY
Trump signs Medicare loan relief bill delaying repayments
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
CRC risk: Raised by meat/alcohol, lowered by aspirin/NSAIDs
A new meta-analysis has largely confirmed what is already known about the lifestyle factors that increase and those that decrease the risk of developing colorectal cancer.
The use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) is associated with a decreased risk for colorectal cancer, the new article concludes. But it also adds a number of other factors that are associated with a decreased risk for the disease, including taking magnesium and folate supplements and eating dairy products, fiber, soy, and fruits and vegetables.
On the other hand, consumption of meat and alcohol was associated with an increased risk for colorectal cancer in almost all of the analyses included in this article.
The study was published online September 28 in Gut.
However, the authors pointed out that it is important to keep in mind that in most cases, the level of evidence is low or very low, primarily because of the heterogeneity of the various published studies, as well as the type of study.
“Furthermore, in most cases, we were unable to identify an optimal dose and duration of exposure/intake for any of the products, even in the case of low-dose aspirin and other compounds that have been extensively assessed,” they wrote.
The findings of this new meta-analysis echo previous findings on this issue.
A number of studies, for example, have found varying associations between the consumption of red meat and cancer. The American Institute for Cancer Research and the World Cancer Research Fund have published several reports during the past 10 years on the effect of diet, nutrition, and/or physical activity on risk for several cancer types. Their most recent study, published in 2017, concluded that eating red meat and processed meat may increase the risk for colorectal cancer, as may drinking two or more alcoholic beverages per day.
Another large meta-analysis published earlier this year found that regular use of aspirin reduced the risk for cancers of the digestive tract by 22%-38%, compared with nonuse.
Umbrella review
In the latest article in Gut, researchers led by Marc Bardou, MD, PhD, Centre Hospitalier Universitaire de Dijon (France), conducted an umbrella review of systematic reviews and meta-analyses of interventions that assessed chemopreventive products for colorectal cancer in an average-risk population.
A total of 80 meta-analyses of interventional and observational studies were included. The studies investigated a wide range of chemopreventive agents in an average-risk population and the risk for colorectal cancer. Agents included medications (aspirin, NSAIDs, statins), vitamins or supplements (magnesium; calcium; folic acid; vitamin A, B, C, E, and D; beta-carotene; and selenium), and dietary items (coffee, tea, fish, dairy products, fiber, fruits, vegetables, meat, and alcohol).
The studies included randomized controlled trials and observational studies. Most of the meta-analyses found a protective effect for aspirin, which lowered the risk by between 14% and 29% even at doses as low as 75 mg/day, with a dose-response effect of up to 325 mg/day. The certainty of evidence was moderate.
NSAID use was also associated with a protective effect, with a significant 26%-43% decrease in the incidence in colorectal cancer. The optimal duration for the observed protective effect remains unclear. Two meta-analyses suggested that NSAIDs may need to be taken for at least 5 years, although one article suggested a protective effect after the first year. The certainty of evidence was low.
Use of magnesium was found to be protective, with a relative risk (RR) of 0.78-0.87. High intake of folic acid was associated with a significant decrease in risk (RR, 0.85-0.88). The certainty of evidence was low and very low, respectively.
Consumption of dairy products was associated with 13%-19% lower risk for the disease. However, the authors note that, because of the small number of available meta-analyses, the multiplicity of outcomes, and the variety of dairy products, it was not possible to reach any firm conclusions about the amount needed or the duration necessary for a protective effect.
Another dietary item, fiber, was associated with a 22%-43% lower risk. Consumption of fruits and vegetables was associated with up to a 52% lower risk, with an added benefit for every additional 100 g/day increase in intake. Soy intake was also associated with a small but significant decrease in risk (8%-15%).
For many of the other items reviewed, evidence was either weak or no beneficial effect was seen.
Increased risk
Consumption of both meat and alcohol was found to increase the risk for colorectal cancer.
Most of the meta-analyses of observational studies have reported a significant increase in risk (RR, 1.12-1.21) with meat consumption (particularly red and processed) and the incidence of colorectal cancer. Studies of the dose effect reported a 10%-30% increased risk for each increment of 100 g/day of total or red meat.
Alcohol consumption was also associated with a significantly increased risk. The higher the intake, the greater the risk. The risk was evident even at the lowest consumption doses that were investigated (1-2 drinks per day).
Balanced for the individual patient
Commenting on the article, Thomas J. George Jr, MD, professor of medicine and director, GI Oncology Program, the University of Florida Health Cancer Center, Gainesville, feels that the take-home message for clinicians and patients alike is that these data help to reinforce behaviors that have already been recommended.
“We know that excessive alcohol and red meat consumption is not healthy, so seeing that there may be a negative effect on colorectal cancer is just more evidence that we should be avoiding that and recommend avoiding that,” said Dr. George. “So yes, I recommend minimizing those, and likewise, a diet that is inclusive of fruits, vegetables, fiber, soy – perhaps as an alternative to meat consumption – is healthier than a diet devoid of these, so again, more reassuring data to support doing what we should already be doing.”
However, he pointed out that there are risks associated with medications such as NSAIDs and aspirin, including bleeding, gastric ulcer formation, and kidney damage. “The risks are low but very real,” Dr. George said. “So I think those recommendations need to be considered on a very individual level, balancing any other risk factors that the patient may have for both colorectal cancer, as well as risks from the medications.”
The study had no outside funding. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new meta-analysis has largely confirmed what is already known about the lifestyle factors that increase and those that decrease the risk of developing colorectal cancer.
The use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) is associated with a decreased risk for colorectal cancer, the new article concludes. But it also adds a number of other factors that are associated with a decreased risk for the disease, including taking magnesium and folate supplements and eating dairy products, fiber, soy, and fruits and vegetables.
On the other hand, consumption of meat and alcohol was associated with an increased risk for colorectal cancer in almost all of the analyses included in this article.
The study was published online September 28 in Gut.
However, the authors pointed out that it is important to keep in mind that in most cases, the level of evidence is low or very low, primarily because of the heterogeneity of the various published studies, as well as the type of study.
“Furthermore, in most cases, we were unable to identify an optimal dose and duration of exposure/intake for any of the products, even in the case of low-dose aspirin and other compounds that have been extensively assessed,” they wrote.
The findings of this new meta-analysis echo previous findings on this issue.
A number of studies, for example, have found varying associations between the consumption of red meat and cancer. The American Institute for Cancer Research and the World Cancer Research Fund have published several reports during the past 10 years on the effect of diet, nutrition, and/or physical activity on risk for several cancer types. Their most recent study, published in 2017, concluded that eating red meat and processed meat may increase the risk for colorectal cancer, as may drinking two or more alcoholic beverages per day.
Another large meta-analysis published earlier this year found that regular use of aspirin reduced the risk for cancers of the digestive tract by 22%-38%, compared with nonuse.
Umbrella review
In the latest article in Gut, researchers led by Marc Bardou, MD, PhD, Centre Hospitalier Universitaire de Dijon (France), conducted an umbrella review of systematic reviews and meta-analyses of interventions that assessed chemopreventive products for colorectal cancer in an average-risk population.
A total of 80 meta-analyses of interventional and observational studies were included. The studies investigated a wide range of chemopreventive agents in an average-risk population and the risk for colorectal cancer. Agents included medications (aspirin, NSAIDs, statins), vitamins or supplements (magnesium; calcium; folic acid; vitamin A, B, C, E, and D; beta-carotene; and selenium), and dietary items (coffee, tea, fish, dairy products, fiber, fruits, vegetables, meat, and alcohol).
The studies included randomized controlled trials and observational studies. Most of the meta-analyses found a protective effect for aspirin, which lowered the risk by between 14% and 29% even at doses as low as 75 mg/day, with a dose-response effect of up to 325 mg/day. The certainty of evidence was moderate.
NSAID use was also associated with a protective effect, with a significant 26%-43% decrease in the incidence in colorectal cancer. The optimal duration for the observed protective effect remains unclear. Two meta-analyses suggested that NSAIDs may need to be taken for at least 5 years, although one article suggested a protective effect after the first year. The certainty of evidence was low.
Use of magnesium was found to be protective, with a relative risk (RR) of 0.78-0.87. High intake of folic acid was associated with a significant decrease in risk (RR, 0.85-0.88). The certainty of evidence was low and very low, respectively.
Consumption of dairy products was associated with 13%-19% lower risk for the disease. However, the authors note that, because of the small number of available meta-analyses, the multiplicity of outcomes, and the variety of dairy products, it was not possible to reach any firm conclusions about the amount needed or the duration necessary for a protective effect.
Another dietary item, fiber, was associated with a 22%-43% lower risk. Consumption of fruits and vegetables was associated with up to a 52% lower risk, with an added benefit for every additional 100 g/day increase in intake. Soy intake was also associated with a small but significant decrease in risk (8%-15%).
For many of the other items reviewed, evidence was either weak or no beneficial effect was seen.
Increased risk
Consumption of both meat and alcohol was found to increase the risk for colorectal cancer.
Most of the meta-analyses of observational studies have reported a significant increase in risk (RR, 1.12-1.21) with meat consumption (particularly red and processed) and the incidence of colorectal cancer. Studies of the dose effect reported a 10%-30% increased risk for each increment of 100 g/day of total or red meat.
Alcohol consumption was also associated with a significantly increased risk. The higher the intake, the greater the risk. The risk was evident even at the lowest consumption doses that were investigated (1-2 drinks per day).
Balanced for the individual patient
Commenting on the article, Thomas J. George Jr, MD, professor of medicine and director, GI Oncology Program, the University of Florida Health Cancer Center, Gainesville, feels that the take-home message for clinicians and patients alike is that these data help to reinforce behaviors that have already been recommended.
“We know that excessive alcohol and red meat consumption is not healthy, so seeing that there may be a negative effect on colorectal cancer is just more evidence that we should be avoiding that and recommend avoiding that,” said Dr. George. “So yes, I recommend minimizing those, and likewise, a diet that is inclusive of fruits, vegetables, fiber, soy – perhaps as an alternative to meat consumption – is healthier than a diet devoid of these, so again, more reassuring data to support doing what we should already be doing.”
However, he pointed out that there are risks associated with medications such as NSAIDs and aspirin, including bleeding, gastric ulcer formation, and kidney damage. “The risks are low but very real,” Dr. George said. “So I think those recommendations need to be considered on a very individual level, balancing any other risk factors that the patient may have for both colorectal cancer, as well as risks from the medications.”
The study had no outside funding. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new meta-analysis has largely confirmed what is already known about the lifestyle factors that increase and those that decrease the risk of developing colorectal cancer.
The use of aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) is associated with a decreased risk for colorectal cancer, the new article concludes. But it also adds a number of other factors that are associated with a decreased risk for the disease, including taking magnesium and folate supplements and eating dairy products, fiber, soy, and fruits and vegetables.
On the other hand, consumption of meat and alcohol was associated with an increased risk for colorectal cancer in almost all of the analyses included in this article.
The study was published online September 28 in Gut.
However, the authors pointed out that it is important to keep in mind that in most cases, the level of evidence is low or very low, primarily because of the heterogeneity of the various published studies, as well as the type of study.
“Furthermore, in most cases, we were unable to identify an optimal dose and duration of exposure/intake for any of the products, even in the case of low-dose aspirin and other compounds that have been extensively assessed,” they wrote.
The findings of this new meta-analysis echo previous findings on this issue.
A number of studies, for example, have found varying associations between the consumption of red meat and cancer. The American Institute for Cancer Research and the World Cancer Research Fund have published several reports during the past 10 years on the effect of diet, nutrition, and/or physical activity on risk for several cancer types. Their most recent study, published in 2017, concluded that eating red meat and processed meat may increase the risk for colorectal cancer, as may drinking two or more alcoholic beverages per day.
Another large meta-analysis published earlier this year found that regular use of aspirin reduced the risk for cancers of the digestive tract by 22%-38%, compared with nonuse.
Umbrella review
In the latest article in Gut, researchers led by Marc Bardou, MD, PhD, Centre Hospitalier Universitaire de Dijon (France), conducted an umbrella review of systematic reviews and meta-analyses of interventions that assessed chemopreventive products for colorectal cancer in an average-risk population.
A total of 80 meta-analyses of interventional and observational studies were included. The studies investigated a wide range of chemopreventive agents in an average-risk population and the risk for colorectal cancer. Agents included medications (aspirin, NSAIDs, statins), vitamins or supplements (magnesium; calcium; folic acid; vitamin A, B, C, E, and D; beta-carotene; and selenium), and dietary items (coffee, tea, fish, dairy products, fiber, fruits, vegetables, meat, and alcohol).
The studies included randomized controlled trials and observational studies. Most of the meta-analyses found a protective effect for aspirin, which lowered the risk by between 14% and 29% even at doses as low as 75 mg/day, with a dose-response effect of up to 325 mg/day. The certainty of evidence was moderate.
NSAID use was also associated with a protective effect, with a significant 26%-43% decrease in the incidence in colorectal cancer. The optimal duration for the observed protective effect remains unclear. Two meta-analyses suggested that NSAIDs may need to be taken for at least 5 years, although one article suggested a protective effect after the first year. The certainty of evidence was low.
Use of magnesium was found to be protective, with a relative risk (RR) of 0.78-0.87. High intake of folic acid was associated with a significant decrease in risk (RR, 0.85-0.88). The certainty of evidence was low and very low, respectively.
Consumption of dairy products was associated with 13%-19% lower risk for the disease. However, the authors note that, because of the small number of available meta-analyses, the multiplicity of outcomes, and the variety of dairy products, it was not possible to reach any firm conclusions about the amount needed or the duration necessary for a protective effect.
Another dietary item, fiber, was associated with a 22%-43% lower risk. Consumption of fruits and vegetables was associated with up to a 52% lower risk, with an added benefit for every additional 100 g/day increase in intake. Soy intake was also associated with a small but significant decrease in risk (8%-15%).
For many of the other items reviewed, evidence was either weak or no beneficial effect was seen.
Increased risk
Consumption of both meat and alcohol was found to increase the risk for colorectal cancer.
Most of the meta-analyses of observational studies have reported a significant increase in risk (RR, 1.12-1.21) with meat consumption (particularly red and processed) and the incidence of colorectal cancer. Studies of the dose effect reported a 10%-30% increased risk for each increment of 100 g/day of total or red meat.
Alcohol consumption was also associated with a significantly increased risk. The higher the intake, the greater the risk. The risk was evident even at the lowest consumption doses that were investigated (1-2 drinks per day).
Balanced for the individual patient
Commenting on the article, Thomas J. George Jr, MD, professor of medicine and director, GI Oncology Program, the University of Florida Health Cancer Center, Gainesville, feels that the take-home message for clinicians and patients alike is that these data help to reinforce behaviors that have already been recommended.
“We know that excessive alcohol and red meat consumption is not healthy, so seeing that there may be a negative effect on colorectal cancer is just more evidence that we should be avoiding that and recommend avoiding that,” said Dr. George. “So yes, I recommend minimizing those, and likewise, a diet that is inclusive of fruits, vegetables, fiber, soy – perhaps as an alternative to meat consumption – is healthier than a diet devoid of these, so again, more reassuring data to support doing what we should already be doing.”
However, he pointed out that there are risks associated with medications such as NSAIDs and aspirin, including bleeding, gastric ulcer formation, and kidney damage. “The risks are low but very real,” Dr. George said. “So I think those recommendations need to be considered on a very individual level, balancing any other risk factors that the patient may have for both colorectal cancer, as well as risks from the medications.”
The study had no outside funding. The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AHA scientific statement highlights cardiorenal benefit of new diabetes drugs
To protect the heart and kidneys, sodium-glucose transporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists should be considered for people with type 2 diabetes and chronic kidney disease (CKD), the American Heart Association advised in a new scientific statement.
Taken together, the results of relevant clinical trials indicate that SGLT2 inhibitors and GLP-1 receptor agonists safely and significantly reduce the risk for cardiovascular (CV) events, death, and the slow progression of CKD to end-stage kidney disease, including the risks for dialysis, transplantation, and death, the writing group says.
The scientific statement was published online Sept. 28 in Circulation.
“There has been rapid reporting of high-quality data in the cardio-renal-metabolic space with significant heart and kidney benefits, particularly with these two newer classes of antihyperglycemic agents,” Janani Rangaswami, MD, who chaired the writing group, said in an interview.
“More recent data show benefits in chronic kidney disease and heart failure even in patients without diabetes,” said Dr. Rangaswami, Einstein Medical Center and Sidney Kimmel Medical College, both in Philadelphia.
“These data are practice-changing in both cardiology and nephrology, and usher in a new era of disease-modifying therapies in heart and kidney disease,” Dr. Rangaswami added.
Recommendations at a glance
- Provide early and ongoing assessment of risks for CVD and CKD to patients who may benefit from SGLT2 inhibitors of GLP-1 receptor agonists.
- Tailor medication choices that meet the needs of individual patients. Realize that, given “consistent class-wide effects,” the choice of a specific SGLT2 inhibitor or GLP-1 receptor agonist may be dictated by affordability, coverage, and formulary considerations.
- Adjust all medications in tandem with these medicines and consider the burden of polypharmacy, which is common among people with type 2 diabetes. Adjust concomitant therapies and deprescribe where possible.
- Identify risks for hypoglycemia and educate patients on the signs so they can seek treatment quickly.
- Monitor and control high blood pressure.
- Counsel patients about the risks for and symptoms of euglycemic diabetic ketoacidosis when taking SGLT2 inhibitors, as well as classic DKA, which can be fatal.
- Regularly screen and counsel patients about foot care to prevent foot ulcers or blisters that can quickly become infected and lead to amputation.
The writing group identified two additional patient subgroups that may benefit from SGLT2 inhibitors and GLP-1 receptor agonists: those with heart failure with reduced ejection fraction with or without diabetes; and those with CKD who do not have diabetes. They say more data are anticipated to validate the use of SGLT2 inhibitors and GLP-1 receptor agonists in these “at-risk” patients.
Collaborative care model
The writing group proposed a collaborative care model, bridging cardiologists, nephrologists, endocrinologists, and primary care physicians, to help facilitate the “prompt and appropriate” integration of these new classes of medications in the management of patients with type 2 diabetes and CKD.
There is “an unmet need for a cardio-renal-metabolic care model that incorporates best practices in the real world to help align these therapies, especially with vulnerable high-risk patients with cardiorenal disease, and to overcome barriers toward uptake of these agents. Hopefully this statement provides some guidance to the cardiology and nephrology communities in that area,” Dr. Rangaswami said in an interview.
But old habits die hard, as research continues to show the slow adoption of these newer medications in the real world.
For example, a large observational study published last year showed a “striking” discordance between evidence-based, guideline-recommended use of SGLT2 inhibitors for the treatment of type 2 diabetes and their actual uptake in clinical practice.
Paradoxically, patients with CVD, heart failure, hypertension, CKD, and those at risk for hypoglycemia were less apt to receive an SGLT2 inhibitor than other patients.
“The relatively slow uptake of these agents is multifactorial,” Dr. Rangaswami said. “Cardiologists and nephrologists may suffer from some level of ‘therapeutic inertia’ when using new agents they are unfamiliar with and originally branded as ‘antidiabetic’ agents, with the perception of these agents being outside the scope of their practice.”
Two other factors are also at play. “The current health care system is based on ‘specialty silos,’ where specialists tend to stick to the traditional scope of their specialty and are reluctant to view these agents as part of their therapeutic armamentarium. Finally, insurance coverage barriers and affordability also limit the use on a widespread basis,” Dr. Rangaswami said.
A version of this article originally appeared on Medscape.com .
To protect the heart and kidneys, sodium-glucose transporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists should be considered for people with type 2 diabetes and chronic kidney disease (CKD), the American Heart Association advised in a new scientific statement.
Taken together, the results of relevant clinical trials indicate that SGLT2 inhibitors and GLP-1 receptor agonists safely and significantly reduce the risk for cardiovascular (CV) events, death, and the slow progression of CKD to end-stage kidney disease, including the risks for dialysis, transplantation, and death, the writing group says.
The scientific statement was published online Sept. 28 in Circulation.
“There has been rapid reporting of high-quality data in the cardio-renal-metabolic space with significant heart and kidney benefits, particularly with these two newer classes of antihyperglycemic agents,” Janani Rangaswami, MD, who chaired the writing group, said in an interview.
“More recent data show benefits in chronic kidney disease and heart failure even in patients without diabetes,” said Dr. Rangaswami, Einstein Medical Center and Sidney Kimmel Medical College, both in Philadelphia.
“These data are practice-changing in both cardiology and nephrology, and usher in a new era of disease-modifying therapies in heart and kidney disease,” Dr. Rangaswami added.
Recommendations at a glance
- Provide early and ongoing assessment of risks for CVD and CKD to patients who may benefit from SGLT2 inhibitors of GLP-1 receptor agonists.
- Tailor medication choices that meet the needs of individual patients. Realize that, given “consistent class-wide effects,” the choice of a specific SGLT2 inhibitor or GLP-1 receptor agonist may be dictated by affordability, coverage, and formulary considerations.
- Adjust all medications in tandem with these medicines and consider the burden of polypharmacy, which is common among people with type 2 diabetes. Adjust concomitant therapies and deprescribe where possible.
- Identify risks for hypoglycemia and educate patients on the signs so they can seek treatment quickly.
- Monitor and control high blood pressure.
- Counsel patients about the risks for and symptoms of euglycemic diabetic ketoacidosis when taking SGLT2 inhibitors, as well as classic DKA, which can be fatal.
- Regularly screen and counsel patients about foot care to prevent foot ulcers or blisters that can quickly become infected and lead to amputation.
The writing group identified two additional patient subgroups that may benefit from SGLT2 inhibitors and GLP-1 receptor agonists: those with heart failure with reduced ejection fraction with or without diabetes; and those with CKD who do not have diabetes. They say more data are anticipated to validate the use of SGLT2 inhibitors and GLP-1 receptor agonists in these “at-risk” patients.
Collaborative care model
The writing group proposed a collaborative care model, bridging cardiologists, nephrologists, endocrinologists, and primary care physicians, to help facilitate the “prompt and appropriate” integration of these new classes of medications in the management of patients with type 2 diabetes and CKD.
There is “an unmet need for a cardio-renal-metabolic care model that incorporates best practices in the real world to help align these therapies, especially with vulnerable high-risk patients with cardiorenal disease, and to overcome barriers toward uptake of these agents. Hopefully this statement provides some guidance to the cardiology and nephrology communities in that area,” Dr. Rangaswami said in an interview.
But old habits die hard, as research continues to show the slow adoption of these newer medications in the real world.
For example, a large observational study published last year showed a “striking” discordance between evidence-based, guideline-recommended use of SGLT2 inhibitors for the treatment of type 2 diabetes and their actual uptake in clinical practice.
Paradoxically, patients with CVD, heart failure, hypertension, CKD, and those at risk for hypoglycemia were less apt to receive an SGLT2 inhibitor than other patients.
“The relatively slow uptake of these agents is multifactorial,” Dr. Rangaswami said. “Cardiologists and nephrologists may suffer from some level of ‘therapeutic inertia’ when using new agents they are unfamiliar with and originally branded as ‘antidiabetic’ agents, with the perception of these agents being outside the scope of their practice.”
Two other factors are also at play. “The current health care system is based on ‘specialty silos,’ where specialists tend to stick to the traditional scope of their specialty and are reluctant to view these agents as part of their therapeutic armamentarium. Finally, insurance coverage barriers and affordability also limit the use on a widespread basis,” Dr. Rangaswami said.
A version of this article originally appeared on Medscape.com .
To protect the heart and kidneys, sodium-glucose transporter 2 (SGLT2) inhibitors and glucagonlike peptide–1 (GLP-1) receptor agonists should be considered for people with type 2 diabetes and chronic kidney disease (CKD), the American Heart Association advised in a new scientific statement.
Taken together, the results of relevant clinical trials indicate that SGLT2 inhibitors and GLP-1 receptor agonists safely and significantly reduce the risk for cardiovascular (CV) events, death, and the slow progression of CKD to end-stage kidney disease, including the risks for dialysis, transplantation, and death, the writing group says.
The scientific statement was published online Sept. 28 in Circulation.
“There has been rapid reporting of high-quality data in the cardio-renal-metabolic space with significant heart and kidney benefits, particularly with these two newer classes of antihyperglycemic agents,” Janani Rangaswami, MD, who chaired the writing group, said in an interview.
“More recent data show benefits in chronic kidney disease and heart failure even in patients without diabetes,” said Dr. Rangaswami, Einstein Medical Center and Sidney Kimmel Medical College, both in Philadelphia.
“These data are practice-changing in both cardiology and nephrology, and usher in a new era of disease-modifying therapies in heart and kidney disease,” Dr. Rangaswami added.
Recommendations at a glance
- Provide early and ongoing assessment of risks for CVD and CKD to patients who may benefit from SGLT2 inhibitors of GLP-1 receptor agonists.
- Tailor medication choices that meet the needs of individual patients. Realize that, given “consistent class-wide effects,” the choice of a specific SGLT2 inhibitor or GLP-1 receptor agonist may be dictated by affordability, coverage, and formulary considerations.
- Adjust all medications in tandem with these medicines and consider the burden of polypharmacy, which is common among people with type 2 diabetes. Adjust concomitant therapies and deprescribe where possible.
- Identify risks for hypoglycemia and educate patients on the signs so they can seek treatment quickly.
- Monitor and control high blood pressure.
- Counsel patients about the risks for and symptoms of euglycemic diabetic ketoacidosis when taking SGLT2 inhibitors, as well as classic DKA, which can be fatal.
- Regularly screen and counsel patients about foot care to prevent foot ulcers or blisters that can quickly become infected and lead to amputation.
The writing group identified two additional patient subgroups that may benefit from SGLT2 inhibitors and GLP-1 receptor agonists: those with heart failure with reduced ejection fraction with or without diabetes; and those with CKD who do not have diabetes. They say more data are anticipated to validate the use of SGLT2 inhibitors and GLP-1 receptor agonists in these “at-risk” patients.
Collaborative care model
The writing group proposed a collaborative care model, bridging cardiologists, nephrologists, endocrinologists, and primary care physicians, to help facilitate the “prompt and appropriate” integration of these new classes of medications in the management of patients with type 2 diabetes and CKD.
There is “an unmet need for a cardio-renal-metabolic care model that incorporates best practices in the real world to help align these therapies, especially with vulnerable high-risk patients with cardiorenal disease, and to overcome barriers toward uptake of these agents. Hopefully this statement provides some guidance to the cardiology and nephrology communities in that area,” Dr. Rangaswami said in an interview.
But old habits die hard, as research continues to show the slow adoption of these newer medications in the real world.
For example, a large observational study published last year showed a “striking” discordance between evidence-based, guideline-recommended use of SGLT2 inhibitors for the treatment of type 2 diabetes and their actual uptake in clinical practice.
Paradoxically, patients with CVD, heart failure, hypertension, CKD, and those at risk for hypoglycemia were less apt to receive an SGLT2 inhibitor than other patients.
“The relatively slow uptake of these agents is multifactorial,” Dr. Rangaswami said. “Cardiologists and nephrologists may suffer from some level of ‘therapeutic inertia’ when using new agents they are unfamiliar with and originally branded as ‘antidiabetic’ agents, with the perception of these agents being outside the scope of their practice.”
Two other factors are also at play. “The current health care system is based on ‘specialty silos,’ where specialists tend to stick to the traditional scope of their specialty and are reluctant to view these agents as part of their therapeutic armamentarium. Finally, insurance coverage barriers and affordability also limit the use on a widespread basis,” Dr. Rangaswami said.
A version of this article originally appeared on Medscape.com .