User login
-
HIV free 30 months after stem cell transplant, is the London patient cured?
A patient with HIV remission induced by stem cell transplantation continues to be disease free at the 30-month mark.
The individual, referred to as the London patient, received allogeneic hematopoietic stem cell transplantation (allo-HSCT) for stage IVB Hodgkin lymphoma. The transplant donor was homozygous for the CCR5 delta-32 mutation, which confers immunity to HIV because there’s no point of entry for the virus into immune cells.
After extensive sampling of various tissues, including gut, lymph node, blood, semen, and cerebrospinal fluid (CSF), Ravindra Kumar Gupta, MD, PhD, and colleagues found no detectable virus that was competent to replicate. However, they reported that the testing did detect some “fossilized” remnants of HIV DNA persisting in certain tissues.
The results were shared in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The London patient’s HIV status had been reported the previous year at CROI 2019, but only blood samples were used in that analysis.
In a commentary accompanying the simultaneously published study in the Lancet, Jennifer Zerbato, PhD, and Sharon Lewin, FRACP, PHD, FAAHMS, asked: “A key question now for the area of HIV cure is how soon can one know if someone has been cured of HIV?
“We will need more than a handful of patients cured of HIV to really understand the duration of follow-up needed and the likelihood of an unexpected late rebound in virus replication,” continued Dr. Zerbato, of the University of Melbourne, and Dr. Lewin, of the Royal Melbourne Hospital and Monash University, also in Melbourne.
In their ongoing analysis of data from the London patient, Dr. Gupta, a virologist at the University of Cambridge (England), and associates constructed a mathematical model that maps the probability for lifetime remission or cure of HIV against several factors, including the degree of chimerism achieved with the stem cell transplant.
In this model, when chimerism reaches 80% in total HIV target cells, the probability of remission for life is 98%; when donor chimerism reaches 90%, the probability of lifetime remission is greater than 99%. Peripheral T-cell chimerism in the London patient has held steady at 99%.
Dr. Gupta and associates obtained some testing opportunistically: A PET-CT scan revealed an axillary lymph node that was biopsied after it was found to have avid radiotracer uptake. Similarly, the CSF sample was obtained in the course of a work-up for some neurologic symptoms that the London patient was having.
In contrast to the first patient who achieved ongoing HIV remission from a pair of stem cell transplants received over 13 years ago – the Berlin patient – the London patient did not receive whole-body radiation, but rather underwent a reduced-intensity conditioning regimen. The London patient experienced a bout of gut graft-versus-host disease (GVHD) about 2 months after his transplant, but has been free of GVHD in the interval. He hasn’t taken cytotoxic agents or any GVHD prophylaxis since 6 months post transplant.
Though there’s no sign of HIV that’s competent to replicate, “the London patient has shown somewhat slow CD4 reconstitution,” said Dr. Gupta and coauthors in discussing the results.
The patient had a reactivation of Epstein-Barr virus (EBV) about 21 months after analytic treatment interruption (ATI) of antiretroviral therapy that was managed without any specific treatment, but he hasn’t experienced any opportunistic infections. However, his CD4 count didn’t rebound to pretransplant levels until 28 months after ATI. At that point, his CD4 count was 430 cells per mcL, or 23.5% of total T cells. The CD4:CD8 ratio was 0.86; normal range is 1.5-2.5.
The researchers used quantitative real-time polymerase chain reaction (rt-PCR) to look for packaging site and envelope (env) DNA fragments, and droplet digital PCR to quantify HIV-1 DNA.
The patient’s HIV-1 plasma load measured at 30 months post ATI on an ultrasensitive assay was below the lower limit of detection (less than 1 copy per mL). Semen viremia measured at 21 months was also below the lower limit of detection, as was CSF measured at 25 months.
Samples were taken from the patient’s rectum, cecum, sigmoid colon, and terminal ileum during a colonoscopy conducted 22 months post ATI; all tested negative for HIV DNA via droplet digital PCR.
The lymph node had large numbers of EBV-positive cells and was positive for HIV-1 env and long-terminal repeat by double-drop PCR, but no integrase DNA was detected. Additionally, no intact proviral DNA was found on assay.
Dr. Gupta and associates speculated that “EBV reactivation could have triggered EBV-specific CD4 and CD8 T-cell responses and proliferation, potentially including CD4 T cells containing HIV-1 DNA.” Supporting this hypothesis, EBV-specific CD8 T-cell responses in peripheral blood were “robust,” and the researchers also saw some CD4 response.
“Similar to the Berlin patient, highly sensitive tests showed very low levels of so-called fossilized HIV-1 DNA in some tissue samples from the London patient. Residual HIV-1 DNA and axillary lymph node tissue could represent a defective clone that expanded during hyperplasia within the lymph note sampled,” noted Dr. Gupta and coauthors.
Responses of CD4 and CD8 T cells to HIV have also remained below the limit of detection, though cytomegalovirus-specific responses persist in the London patient.
As with the Berlin patient, standard enzyme-linked immunosorbent assay (ELISA) testing has remained positive in the London patient. “Standard ELISA testing, therefore, cannot be used as a marker for cure, although more work needs to be done to assess the role of detuned low-avidity antibody assays in defining cure,” noted Dr. Gupta and associates.
The ongoing follow-up plan for the London patient is to obtain viral load testing twice yearly up to 5 years post ATI, and then obtain yearly tests for a total of 10 years. Ongoing testing will confirm the investigators’ belief that “these findings probably represent the second recorded HIV-1 cure after CCR5 delta-32/delta-32 allo-HSCT, with evidence of residual low-level HIV-1 DNA.”
Dr. Zerbato and Dr. Lewin advised cautious optimism and ongoing surveillance: “In view of the many cells sampled in this case, and the absence of any intact virus, is the London patient truly cured? The additional data provided in this follow-up case report is certainly exciting and encouraging but, in the end, only time will tell.”
Dr. Gupta reported being a consultant for ViiV Healthcare and Gilead Sciences; several coauthors also reported financial relationships with pharmaceutical companies. The work was funded by amfAR, the American Foundation for AIDS Research, and the Wellcome Trust. Dr. Lewin reported grants from the National Health and Medical Research Council of Australia, the National Institutes of Health, the American Foundation for AIDS Research, Gilead Sciences, Merck, ViiV Healthcare, Leidos, the Wellcome Trust, the Australian Centre for HIV and Hepatitis Virology Research, and the Melbourne HIV Cure Consortium. Dr. Zerbato reported grants from the Melbourne HIV Cure Consortium,
SOURCE: Gupta R et al. Lancet. 2020 Mar 10. doi: 10.1016/ S2352-3018(20)30069-2.
A patient with HIV remission induced by stem cell transplantation continues to be disease free at the 30-month mark.
The individual, referred to as the London patient, received allogeneic hematopoietic stem cell transplantation (allo-HSCT) for stage IVB Hodgkin lymphoma. The transplant donor was homozygous for the CCR5 delta-32 mutation, which confers immunity to HIV because there’s no point of entry for the virus into immune cells.
After extensive sampling of various tissues, including gut, lymph node, blood, semen, and cerebrospinal fluid (CSF), Ravindra Kumar Gupta, MD, PhD, and colleagues found no detectable virus that was competent to replicate. However, they reported that the testing did detect some “fossilized” remnants of HIV DNA persisting in certain tissues.
The results were shared in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The London patient’s HIV status had been reported the previous year at CROI 2019, but only blood samples were used in that analysis.
In a commentary accompanying the simultaneously published study in the Lancet, Jennifer Zerbato, PhD, and Sharon Lewin, FRACP, PHD, FAAHMS, asked: “A key question now for the area of HIV cure is how soon can one know if someone has been cured of HIV?
“We will need more than a handful of patients cured of HIV to really understand the duration of follow-up needed and the likelihood of an unexpected late rebound in virus replication,” continued Dr. Zerbato, of the University of Melbourne, and Dr. Lewin, of the Royal Melbourne Hospital and Monash University, also in Melbourne.
In their ongoing analysis of data from the London patient, Dr. Gupta, a virologist at the University of Cambridge (England), and associates constructed a mathematical model that maps the probability for lifetime remission or cure of HIV against several factors, including the degree of chimerism achieved with the stem cell transplant.
In this model, when chimerism reaches 80% in total HIV target cells, the probability of remission for life is 98%; when donor chimerism reaches 90%, the probability of lifetime remission is greater than 99%. Peripheral T-cell chimerism in the London patient has held steady at 99%.
Dr. Gupta and associates obtained some testing opportunistically: A PET-CT scan revealed an axillary lymph node that was biopsied after it was found to have avid radiotracer uptake. Similarly, the CSF sample was obtained in the course of a work-up for some neurologic symptoms that the London patient was having.
In contrast to the first patient who achieved ongoing HIV remission from a pair of stem cell transplants received over 13 years ago – the Berlin patient – the London patient did not receive whole-body radiation, but rather underwent a reduced-intensity conditioning regimen. The London patient experienced a bout of gut graft-versus-host disease (GVHD) about 2 months after his transplant, but has been free of GVHD in the interval. He hasn’t taken cytotoxic agents or any GVHD prophylaxis since 6 months post transplant.
Though there’s no sign of HIV that’s competent to replicate, “the London patient has shown somewhat slow CD4 reconstitution,” said Dr. Gupta and coauthors in discussing the results.
The patient had a reactivation of Epstein-Barr virus (EBV) about 21 months after analytic treatment interruption (ATI) of antiretroviral therapy that was managed without any specific treatment, but he hasn’t experienced any opportunistic infections. However, his CD4 count didn’t rebound to pretransplant levels until 28 months after ATI. At that point, his CD4 count was 430 cells per mcL, or 23.5% of total T cells. The CD4:CD8 ratio was 0.86; normal range is 1.5-2.5.
The researchers used quantitative real-time polymerase chain reaction (rt-PCR) to look for packaging site and envelope (env) DNA fragments, and droplet digital PCR to quantify HIV-1 DNA.
The patient’s HIV-1 plasma load measured at 30 months post ATI on an ultrasensitive assay was below the lower limit of detection (less than 1 copy per mL). Semen viremia measured at 21 months was also below the lower limit of detection, as was CSF measured at 25 months.
Samples were taken from the patient’s rectum, cecum, sigmoid colon, and terminal ileum during a colonoscopy conducted 22 months post ATI; all tested negative for HIV DNA via droplet digital PCR.
The lymph node had large numbers of EBV-positive cells and was positive for HIV-1 env and long-terminal repeat by double-drop PCR, but no integrase DNA was detected. Additionally, no intact proviral DNA was found on assay.
Dr. Gupta and associates speculated that “EBV reactivation could have triggered EBV-specific CD4 and CD8 T-cell responses and proliferation, potentially including CD4 T cells containing HIV-1 DNA.” Supporting this hypothesis, EBV-specific CD8 T-cell responses in peripheral blood were “robust,” and the researchers also saw some CD4 response.
“Similar to the Berlin patient, highly sensitive tests showed very low levels of so-called fossilized HIV-1 DNA in some tissue samples from the London patient. Residual HIV-1 DNA and axillary lymph node tissue could represent a defective clone that expanded during hyperplasia within the lymph note sampled,” noted Dr. Gupta and coauthors.
Responses of CD4 and CD8 T cells to HIV have also remained below the limit of detection, though cytomegalovirus-specific responses persist in the London patient.
As with the Berlin patient, standard enzyme-linked immunosorbent assay (ELISA) testing has remained positive in the London patient. “Standard ELISA testing, therefore, cannot be used as a marker for cure, although more work needs to be done to assess the role of detuned low-avidity antibody assays in defining cure,” noted Dr. Gupta and associates.
The ongoing follow-up plan for the London patient is to obtain viral load testing twice yearly up to 5 years post ATI, and then obtain yearly tests for a total of 10 years. Ongoing testing will confirm the investigators’ belief that “these findings probably represent the second recorded HIV-1 cure after CCR5 delta-32/delta-32 allo-HSCT, with evidence of residual low-level HIV-1 DNA.”
Dr. Zerbato and Dr. Lewin advised cautious optimism and ongoing surveillance: “In view of the many cells sampled in this case, and the absence of any intact virus, is the London patient truly cured? The additional data provided in this follow-up case report is certainly exciting and encouraging but, in the end, only time will tell.”
Dr. Gupta reported being a consultant for ViiV Healthcare and Gilead Sciences; several coauthors also reported financial relationships with pharmaceutical companies. The work was funded by amfAR, the American Foundation for AIDS Research, and the Wellcome Trust. Dr. Lewin reported grants from the National Health and Medical Research Council of Australia, the National Institutes of Health, the American Foundation for AIDS Research, Gilead Sciences, Merck, ViiV Healthcare, Leidos, the Wellcome Trust, the Australian Centre for HIV and Hepatitis Virology Research, and the Melbourne HIV Cure Consortium. Dr. Zerbato reported grants from the Melbourne HIV Cure Consortium,
SOURCE: Gupta R et al. Lancet. 2020 Mar 10. doi: 10.1016/ S2352-3018(20)30069-2.
A patient with HIV remission induced by stem cell transplantation continues to be disease free at the 30-month mark.
The individual, referred to as the London patient, received allogeneic hematopoietic stem cell transplantation (allo-HSCT) for stage IVB Hodgkin lymphoma. The transplant donor was homozygous for the CCR5 delta-32 mutation, which confers immunity to HIV because there’s no point of entry for the virus into immune cells.
After extensive sampling of various tissues, including gut, lymph node, blood, semen, and cerebrospinal fluid (CSF), Ravindra Kumar Gupta, MD, PhD, and colleagues found no detectable virus that was competent to replicate. However, they reported that the testing did detect some “fossilized” remnants of HIV DNA persisting in certain tissues.
The results were shared in a video presentation of the research during the Conference on Retroviruses & Opportunistic Infections, which was presented online this year. CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
The London patient’s HIV status had been reported the previous year at CROI 2019, but only blood samples were used in that analysis.
In a commentary accompanying the simultaneously published study in the Lancet, Jennifer Zerbato, PhD, and Sharon Lewin, FRACP, PHD, FAAHMS, asked: “A key question now for the area of HIV cure is how soon can one know if someone has been cured of HIV?
“We will need more than a handful of patients cured of HIV to really understand the duration of follow-up needed and the likelihood of an unexpected late rebound in virus replication,” continued Dr. Zerbato, of the University of Melbourne, and Dr. Lewin, of the Royal Melbourne Hospital and Monash University, also in Melbourne.
In their ongoing analysis of data from the London patient, Dr. Gupta, a virologist at the University of Cambridge (England), and associates constructed a mathematical model that maps the probability for lifetime remission or cure of HIV against several factors, including the degree of chimerism achieved with the stem cell transplant.
In this model, when chimerism reaches 80% in total HIV target cells, the probability of remission for life is 98%; when donor chimerism reaches 90%, the probability of lifetime remission is greater than 99%. Peripheral T-cell chimerism in the London patient has held steady at 99%.
Dr. Gupta and associates obtained some testing opportunistically: A PET-CT scan revealed an axillary lymph node that was biopsied after it was found to have avid radiotracer uptake. Similarly, the CSF sample was obtained in the course of a work-up for some neurologic symptoms that the London patient was having.
In contrast to the first patient who achieved ongoing HIV remission from a pair of stem cell transplants received over 13 years ago – the Berlin patient – the London patient did not receive whole-body radiation, but rather underwent a reduced-intensity conditioning regimen. The London patient experienced a bout of gut graft-versus-host disease (GVHD) about 2 months after his transplant, but has been free of GVHD in the interval. He hasn’t taken cytotoxic agents or any GVHD prophylaxis since 6 months post transplant.
Though there’s no sign of HIV that’s competent to replicate, “the London patient has shown somewhat slow CD4 reconstitution,” said Dr. Gupta and coauthors in discussing the results.
The patient had a reactivation of Epstein-Barr virus (EBV) about 21 months after analytic treatment interruption (ATI) of antiretroviral therapy that was managed without any specific treatment, but he hasn’t experienced any opportunistic infections. However, his CD4 count didn’t rebound to pretransplant levels until 28 months after ATI. At that point, his CD4 count was 430 cells per mcL, or 23.5% of total T cells. The CD4:CD8 ratio was 0.86; normal range is 1.5-2.5.
The researchers used quantitative real-time polymerase chain reaction (rt-PCR) to look for packaging site and envelope (env) DNA fragments, and droplet digital PCR to quantify HIV-1 DNA.
The patient’s HIV-1 plasma load measured at 30 months post ATI on an ultrasensitive assay was below the lower limit of detection (less than 1 copy per mL). Semen viremia measured at 21 months was also below the lower limit of detection, as was CSF measured at 25 months.
Samples were taken from the patient’s rectum, cecum, sigmoid colon, and terminal ileum during a colonoscopy conducted 22 months post ATI; all tested negative for HIV DNA via droplet digital PCR.
The lymph node had large numbers of EBV-positive cells and was positive for HIV-1 env and long-terminal repeat by double-drop PCR, but no integrase DNA was detected. Additionally, no intact proviral DNA was found on assay.
Dr. Gupta and associates speculated that “EBV reactivation could have triggered EBV-specific CD4 and CD8 T-cell responses and proliferation, potentially including CD4 T cells containing HIV-1 DNA.” Supporting this hypothesis, EBV-specific CD8 T-cell responses in peripheral blood were “robust,” and the researchers also saw some CD4 response.
“Similar to the Berlin patient, highly sensitive tests showed very low levels of so-called fossilized HIV-1 DNA in some tissue samples from the London patient. Residual HIV-1 DNA and axillary lymph node tissue could represent a defective clone that expanded during hyperplasia within the lymph note sampled,” noted Dr. Gupta and coauthors.
Responses of CD4 and CD8 T cells to HIV have also remained below the limit of detection, though cytomegalovirus-specific responses persist in the London patient.
As with the Berlin patient, standard enzyme-linked immunosorbent assay (ELISA) testing has remained positive in the London patient. “Standard ELISA testing, therefore, cannot be used as a marker for cure, although more work needs to be done to assess the role of detuned low-avidity antibody assays in defining cure,” noted Dr. Gupta and associates.
The ongoing follow-up plan for the London patient is to obtain viral load testing twice yearly up to 5 years post ATI, and then obtain yearly tests for a total of 10 years. Ongoing testing will confirm the investigators’ belief that “these findings probably represent the second recorded HIV-1 cure after CCR5 delta-32/delta-32 allo-HSCT, with evidence of residual low-level HIV-1 DNA.”
Dr. Zerbato and Dr. Lewin advised cautious optimism and ongoing surveillance: “In view of the many cells sampled in this case, and the absence of any intact virus, is the London patient truly cured? The additional data provided in this follow-up case report is certainly exciting and encouraging but, in the end, only time will tell.”
Dr. Gupta reported being a consultant for ViiV Healthcare and Gilead Sciences; several coauthors also reported financial relationships with pharmaceutical companies. The work was funded by amfAR, the American Foundation for AIDS Research, and the Wellcome Trust. Dr. Lewin reported grants from the National Health and Medical Research Council of Australia, the National Institutes of Health, the American Foundation for AIDS Research, Gilead Sciences, Merck, ViiV Healthcare, Leidos, the Wellcome Trust, the Australian Centre for HIV and Hepatitis Virology Research, and the Melbourne HIV Cure Consortium. Dr. Zerbato reported grants from the Melbourne HIV Cure Consortium,
SOURCE: Gupta R et al. Lancet. 2020 Mar 10. doi: 10.1016/ S2352-3018(20)30069-2.
FROM CROI 2020
Stored CD34 cells for multiple myeloma patients largely unused
ORLANDO – Collecting and storing extra stem cells on the off chance that a patient with multiple myeloma will need a salvage autologous stem cell transplant may not be worth the money or effort, investigators say.
Among patients with multiple myeloma who had adequate collection of mobilized and stored cells, only 3 of 146 eligible patients were given the stored cells in a second autologous stem cell transplant (ASCT), reported Nausheen Ahmed, MD, from the Case Western Reserve Cancer Center and University Hospitals Seidman Cancer Center, both in Cleveland.
“We found overall low utilization of salvage transplants and storage stem cells at our institution, which may not justify the strategy of early collection for all patients fit for transplant,” she said at the Transplantation and Cellular Therapy Meetings.
But Sergio Giralt, MD, a transplant specialist from Memorial Sloan Kettering Cancer Center, New York, who was not involved in the study, warned against changing practice “for the wrong reason, because it’s just a financial reason.”
Get them while they’re fresh
The rationale for collecting and storing extra cells is the risk that mobilization will fail in the future following prolonged maintenance with immunomodulatory agents such as lenalidomide (Revlimid), and the risk for genetic or epigenetic damage to cells from high-dose melphalan used in transplant-conditioning regimens, Dr. Ahmed noted at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“However, there are potential issues with early mobilization and storage, including cost, resources, apheresis scheduling, uncertainty of cell viability, and liability. There’s also risk of side effects with filgrastim and plerixafor use [for mobilization],” she said.
Dr. Ahmed and colleagues conducted a study to determine how stored stem cells for second ASCT were used, describe how second ASCTs are used in patients who meet the Mayo Consensus Stratification for Myeloma & Risk-Adapted Therapy (mSMART) criteria, and the costs of mobilizing and storing stem cells for a second ASCT.
They took a retrospective look at all adults aged 18 years and older with a diagnosis of multiple myeloma who received a first ASCT at their institution from 2009 to 2017. They excluded patients who had amyloidosis without myeloma or POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal plasma proliferative disorder, skin changes) syndrome.
Patients were considered eligible for a second ASCT based on mSMART recommendations if they had a relapse either 18 or more months without maintenance therapy or after at least 36 months on maintenance. The investigators defined an extra day of collection as an additional day of apheresis to obtain 2 million or more CD34 cells/kg for storage only.
They estimated costs from the institution’s charge master as the sum of cell processing, leukapheresis costs, additional plerixafor costs, and storage costs, and calculated the total duration of storage as months from the date of collection until the last follow-up.
The median age of the total study population of 179 patients was 61 years, with a majority of male and white patients. Of this group, 98% had an Eastern Cooperative Oncology Group performance score of 0-1. In all, 63.7% of the patients had standard-risk cytogenetics, 22.4% had high-risk disease, and the remainder had unknown cytogenetic risk.
At a median follow-up of 56.5 months, 95 patients (53.1%) had experienced a relapse after transplant with a median time to progression of 47.5 months. The majority of patients (166; 92.7%) had received a single transplant, 10 (5.6%) had received tandem transplants, and only 3 (1.6%) had a second transplant at relapse.
Looking at the use of second transplant in patients who met the criteria for salvage transplant based on mSMART (excluding patients who had undergone tandem transplant) and whose maintenance status was known, they identified 61 patients on maintenance therapy and 24 with no maintenance. A total of 31 patients (18 in the maintenance group and 13 in the no-maintenance group) met mSMART criteria for salvage ASCT.
Dr. Ahmed and colleagues next looked at the 146 patients who had at least 2 million stored cells/kg, and found that the stored cells were used for only three patients. Of the 146 patients, 66 had 1 extra collection day, 17 had 2 extra days, and 4 had 3 extra days, for an average additional cost per patient of $16,859.
‘Woefully underutilized’
Discussing the study, Dr. Giralt asked: “How valid are the SMART criteria of 36 months? And the answer is there is no data to support it, and if we actually go back to our oncology, any patient who has had more than 18 months without exposure to a drug can continue to have sensitivity to that drug, and that’s why if we used the ASBMT criteria of greater than 18 months you’d have a larger population” of patients eligible for salvage transplant.
He stated that, “we know these patients exist, we know they have cells in the freezer, but we’re not using those cells. Second transplant is woefully underutilized in myeloma patients,” and he added that stored cells could also be used to support those patients who develop cytopenias following chimeric antigen receptor (CAR) T-cell therapy.
Yago Nieto, MD, from the University of Texas MD Anderson Cancer Center, Houston, who comoderated the session where the data were presented, agreed with Dr. Giralt that stored stem cells are underutilized in the treatment of patients with multiple myeloma.
“I don’t think that the experience from Case Western, where the percentage of patients who are eligible for salvage transplant and actually got it was less than 10%, can be extrapolated to many other centers. I think that in most centers the actual percentage is higher than that,” he said in an interview.
“There are going to be therapies like CAR T that will compete with salvage transplants, but I think more patients should be considered for this salvage procedure,” he added.
No funding source for the story was disclosed. Dr. Ahmed reported no financial disclosures. Dr. Giralt reported consulting/advisory activities and receiving research funding from multiple companies. Dr. Nieto disclosed research funding from, and consultancy for, several companies.
SOURCE: Ahmed N et al. TCT 2020, Abstract 28.
ORLANDO – Collecting and storing extra stem cells on the off chance that a patient with multiple myeloma will need a salvage autologous stem cell transplant may not be worth the money or effort, investigators say.
Among patients with multiple myeloma who had adequate collection of mobilized and stored cells, only 3 of 146 eligible patients were given the stored cells in a second autologous stem cell transplant (ASCT), reported Nausheen Ahmed, MD, from the Case Western Reserve Cancer Center and University Hospitals Seidman Cancer Center, both in Cleveland.
“We found overall low utilization of salvage transplants and storage stem cells at our institution, which may not justify the strategy of early collection for all patients fit for transplant,” she said at the Transplantation and Cellular Therapy Meetings.
But Sergio Giralt, MD, a transplant specialist from Memorial Sloan Kettering Cancer Center, New York, who was not involved in the study, warned against changing practice “for the wrong reason, because it’s just a financial reason.”
Get them while they’re fresh
The rationale for collecting and storing extra cells is the risk that mobilization will fail in the future following prolonged maintenance with immunomodulatory agents such as lenalidomide (Revlimid), and the risk for genetic or epigenetic damage to cells from high-dose melphalan used in transplant-conditioning regimens, Dr. Ahmed noted at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“However, there are potential issues with early mobilization and storage, including cost, resources, apheresis scheduling, uncertainty of cell viability, and liability. There’s also risk of side effects with filgrastim and plerixafor use [for mobilization],” she said.
Dr. Ahmed and colleagues conducted a study to determine how stored stem cells for second ASCT were used, describe how second ASCTs are used in patients who meet the Mayo Consensus Stratification for Myeloma & Risk-Adapted Therapy (mSMART) criteria, and the costs of mobilizing and storing stem cells for a second ASCT.
They took a retrospective look at all adults aged 18 years and older with a diagnosis of multiple myeloma who received a first ASCT at their institution from 2009 to 2017. They excluded patients who had amyloidosis without myeloma or POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal plasma proliferative disorder, skin changes) syndrome.
Patients were considered eligible for a second ASCT based on mSMART recommendations if they had a relapse either 18 or more months without maintenance therapy or after at least 36 months on maintenance. The investigators defined an extra day of collection as an additional day of apheresis to obtain 2 million or more CD34 cells/kg for storage only.
They estimated costs from the institution’s charge master as the sum of cell processing, leukapheresis costs, additional plerixafor costs, and storage costs, and calculated the total duration of storage as months from the date of collection until the last follow-up.
The median age of the total study population of 179 patients was 61 years, with a majority of male and white patients. Of this group, 98% had an Eastern Cooperative Oncology Group performance score of 0-1. In all, 63.7% of the patients had standard-risk cytogenetics, 22.4% had high-risk disease, and the remainder had unknown cytogenetic risk.
At a median follow-up of 56.5 months, 95 patients (53.1%) had experienced a relapse after transplant with a median time to progression of 47.5 months. The majority of patients (166; 92.7%) had received a single transplant, 10 (5.6%) had received tandem transplants, and only 3 (1.6%) had a second transplant at relapse.
Looking at the use of second transplant in patients who met the criteria for salvage transplant based on mSMART (excluding patients who had undergone tandem transplant) and whose maintenance status was known, they identified 61 patients on maintenance therapy and 24 with no maintenance. A total of 31 patients (18 in the maintenance group and 13 in the no-maintenance group) met mSMART criteria for salvage ASCT.
Dr. Ahmed and colleagues next looked at the 146 patients who had at least 2 million stored cells/kg, and found that the stored cells were used for only three patients. Of the 146 patients, 66 had 1 extra collection day, 17 had 2 extra days, and 4 had 3 extra days, for an average additional cost per patient of $16,859.
‘Woefully underutilized’
Discussing the study, Dr. Giralt asked: “How valid are the SMART criteria of 36 months? And the answer is there is no data to support it, and if we actually go back to our oncology, any patient who has had more than 18 months without exposure to a drug can continue to have sensitivity to that drug, and that’s why if we used the ASBMT criteria of greater than 18 months you’d have a larger population” of patients eligible for salvage transplant.
He stated that, “we know these patients exist, we know they have cells in the freezer, but we’re not using those cells. Second transplant is woefully underutilized in myeloma patients,” and he added that stored cells could also be used to support those patients who develop cytopenias following chimeric antigen receptor (CAR) T-cell therapy.
Yago Nieto, MD, from the University of Texas MD Anderson Cancer Center, Houston, who comoderated the session where the data were presented, agreed with Dr. Giralt that stored stem cells are underutilized in the treatment of patients with multiple myeloma.
“I don’t think that the experience from Case Western, where the percentage of patients who are eligible for salvage transplant and actually got it was less than 10%, can be extrapolated to many other centers. I think that in most centers the actual percentage is higher than that,” he said in an interview.
“There are going to be therapies like CAR T that will compete with salvage transplants, but I think more patients should be considered for this salvage procedure,” he added.
No funding source for the story was disclosed. Dr. Ahmed reported no financial disclosures. Dr. Giralt reported consulting/advisory activities and receiving research funding from multiple companies. Dr. Nieto disclosed research funding from, and consultancy for, several companies.
SOURCE: Ahmed N et al. TCT 2020, Abstract 28.
ORLANDO – Collecting and storing extra stem cells on the off chance that a patient with multiple myeloma will need a salvage autologous stem cell transplant may not be worth the money or effort, investigators say.
Among patients with multiple myeloma who had adequate collection of mobilized and stored cells, only 3 of 146 eligible patients were given the stored cells in a second autologous stem cell transplant (ASCT), reported Nausheen Ahmed, MD, from the Case Western Reserve Cancer Center and University Hospitals Seidman Cancer Center, both in Cleveland.
“We found overall low utilization of salvage transplants and storage stem cells at our institution, which may not justify the strategy of early collection for all patients fit for transplant,” she said at the Transplantation and Cellular Therapy Meetings.
But Sergio Giralt, MD, a transplant specialist from Memorial Sloan Kettering Cancer Center, New York, who was not involved in the study, warned against changing practice “for the wrong reason, because it’s just a financial reason.”
Get them while they’re fresh
The rationale for collecting and storing extra cells is the risk that mobilization will fail in the future following prolonged maintenance with immunomodulatory agents such as lenalidomide (Revlimid), and the risk for genetic or epigenetic damage to cells from high-dose melphalan used in transplant-conditioning regimens, Dr. Ahmed noted at the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
“However, there are potential issues with early mobilization and storage, including cost, resources, apheresis scheduling, uncertainty of cell viability, and liability. There’s also risk of side effects with filgrastim and plerixafor use [for mobilization],” she said.
Dr. Ahmed and colleagues conducted a study to determine how stored stem cells for second ASCT were used, describe how second ASCTs are used in patients who meet the Mayo Consensus Stratification for Myeloma & Risk-Adapted Therapy (mSMART) criteria, and the costs of mobilizing and storing stem cells for a second ASCT.
They took a retrospective look at all adults aged 18 years and older with a diagnosis of multiple myeloma who received a first ASCT at their institution from 2009 to 2017. They excluded patients who had amyloidosis without myeloma or POEMS (polyneuropathy, organomegaly, endocrinopathy, monoclonal plasma proliferative disorder, skin changes) syndrome.
Patients were considered eligible for a second ASCT based on mSMART recommendations if they had a relapse either 18 or more months without maintenance therapy or after at least 36 months on maintenance. The investigators defined an extra day of collection as an additional day of apheresis to obtain 2 million or more CD34 cells/kg for storage only.
They estimated costs from the institution’s charge master as the sum of cell processing, leukapheresis costs, additional plerixafor costs, and storage costs, and calculated the total duration of storage as months from the date of collection until the last follow-up.
The median age of the total study population of 179 patients was 61 years, with a majority of male and white patients. Of this group, 98% had an Eastern Cooperative Oncology Group performance score of 0-1. In all, 63.7% of the patients had standard-risk cytogenetics, 22.4% had high-risk disease, and the remainder had unknown cytogenetic risk.
At a median follow-up of 56.5 months, 95 patients (53.1%) had experienced a relapse after transplant with a median time to progression of 47.5 months. The majority of patients (166; 92.7%) had received a single transplant, 10 (5.6%) had received tandem transplants, and only 3 (1.6%) had a second transplant at relapse.
Looking at the use of second transplant in patients who met the criteria for salvage transplant based on mSMART (excluding patients who had undergone tandem transplant) and whose maintenance status was known, they identified 61 patients on maintenance therapy and 24 with no maintenance. A total of 31 patients (18 in the maintenance group and 13 in the no-maintenance group) met mSMART criteria for salvage ASCT.
Dr. Ahmed and colleagues next looked at the 146 patients who had at least 2 million stored cells/kg, and found that the stored cells were used for only three patients. Of the 146 patients, 66 had 1 extra collection day, 17 had 2 extra days, and 4 had 3 extra days, for an average additional cost per patient of $16,859.
‘Woefully underutilized’
Discussing the study, Dr. Giralt asked: “How valid are the SMART criteria of 36 months? And the answer is there is no data to support it, and if we actually go back to our oncology, any patient who has had more than 18 months without exposure to a drug can continue to have sensitivity to that drug, and that’s why if we used the ASBMT criteria of greater than 18 months you’d have a larger population” of patients eligible for salvage transplant.
He stated that, “we know these patients exist, we know they have cells in the freezer, but we’re not using those cells. Second transplant is woefully underutilized in myeloma patients,” and he added that stored cells could also be used to support those patients who develop cytopenias following chimeric antigen receptor (CAR) T-cell therapy.
Yago Nieto, MD, from the University of Texas MD Anderson Cancer Center, Houston, who comoderated the session where the data were presented, agreed with Dr. Giralt that stored stem cells are underutilized in the treatment of patients with multiple myeloma.
“I don’t think that the experience from Case Western, where the percentage of patients who are eligible for salvage transplant and actually got it was less than 10%, can be extrapolated to many other centers. I think that in most centers the actual percentage is higher than that,” he said in an interview.
“There are going to be therapies like CAR T that will compete with salvage transplants, but I think more patients should be considered for this salvage procedure,” he added.
No funding source for the story was disclosed. Dr. Ahmed reported no financial disclosures. Dr. Giralt reported consulting/advisory activities and receiving research funding from multiple companies. Dr. Nieto disclosed research funding from, and consultancy for, several companies.
SOURCE: Ahmed N et al. TCT 2020, Abstract 28.
REPORTING FROM TCT 2020
Chimerism and the use of fludarabine associated with secondary graft failure in aplastic anemia
Inferior overall survival was observed in patients with aplastic anemia who had mixed or complete recipient-type chimerism or complete donor chimerism after hematopoietic stem cell transplantation (HSCT), according to the results of a registry database study in Japan.
Researchers examined four groups of patients with AA age greater than 15 years who underwent a first allogeneic bone marrow or peripheral blood stem cell transplantation and achieved engraftment.
Group 1 consisted of patients with mixed chimerism (MC) that did not require either granulocyte-colony stimulating factor (G-CSF) or transfusion support; group 2 consisted of MC (with no secondary graft failure (SGF) that required G-CSF and/or transfusion support ; group 3 consisted of patients with SGF with MC or complete recipient-type chimerism; and group 4 consisted of SGF with complete donor-type chimerism.
The overall median follow-up of survivors was 1,727 days. The overall survival (OS) was 90.4% at 1 year and 83.5% at 5 years in patients without MC or SGF (n = 340), which was not different from the OS in groups 1 and 2. However, inferior OS was observed in group 3 (1 year, 52.1%; 5 years, 52.1%) and group 4 (1 year, 82.4%; 5 years, 56.3%). In addition, multivariate analyses showed that the use of fludarabine (Flu) and the absence of irradiation in conditioning were associated with the development of SGF with MC or complete recipient-type chimerism. The use of Flu in conditioning also was associated with SGF with complete donor-type chimerism.
“The occurrence of SGF with both MC/recipient-type and donor-type chimerism after HSCT for AA was associated with inferior OS, and the conditioning regimens influenced the occurrence of SGF,” the researchers concluded.
The Japan Agency for Medical Research and Development funded the research. Two of the authors reported receiving honoraria or research funding from Sanofi KK and one from Shionogi.
SOURCE: Kako S et al. Biol Blood Marrow Transplant 2020. 26:445-50.
Inferior overall survival was observed in patients with aplastic anemia who had mixed or complete recipient-type chimerism or complete donor chimerism after hematopoietic stem cell transplantation (HSCT), according to the results of a registry database study in Japan.
Researchers examined four groups of patients with AA age greater than 15 years who underwent a first allogeneic bone marrow or peripheral blood stem cell transplantation and achieved engraftment.
Group 1 consisted of patients with mixed chimerism (MC) that did not require either granulocyte-colony stimulating factor (G-CSF) or transfusion support; group 2 consisted of MC (with no secondary graft failure (SGF) that required G-CSF and/or transfusion support ; group 3 consisted of patients with SGF with MC or complete recipient-type chimerism; and group 4 consisted of SGF with complete donor-type chimerism.
The overall median follow-up of survivors was 1,727 days. The overall survival (OS) was 90.4% at 1 year and 83.5% at 5 years in patients without MC or SGF (n = 340), which was not different from the OS in groups 1 and 2. However, inferior OS was observed in group 3 (1 year, 52.1%; 5 years, 52.1%) and group 4 (1 year, 82.4%; 5 years, 56.3%). In addition, multivariate analyses showed that the use of fludarabine (Flu) and the absence of irradiation in conditioning were associated with the development of SGF with MC or complete recipient-type chimerism. The use of Flu in conditioning also was associated with SGF with complete donor-type chimerism.
“The occurrence of SGF with both MC/recipient-type and donor-type chimerism after HSCT for AA was associated with inferior OS, and the conditioning regimens influenced the occurrence of SGF,” the researchers concluded.
The Japan Agency for Medical Research and Development funded the research. Two of the authors reported receiving honoraria or research funding from Sanofi KK and one from Shionogi.
SOURCE: Kako S et al. Biol Blood Marrow Transplant 2020. 26:445-50.
Inferior overall survival was observed in patients with aplastic anemia who had mixed or complete recipient-type chimerism or complete donor chimerism after hematopoietic stem cell transplantation (HSCT), according to the results of a registry database study in Japan.
Researchers examined four groups of patients with AA age greater than 15 years who underwent a first allogeneic bone marrow or peripheral blood stem cell transplantation and achieved engraftment.
Group 1 consisted of patients with mixed chimerism (MC) that did not require either granulocyte-colony stimulating factor (G-CSF) or transfusion support; group 2 consisted of MC (with no secondary graft failure (SGF) that required G-CSF and/or transfusion support ; group 3 consisted of patients with SGF with MC or complete recipient-type chimerism; and group 4 consisted of SGF with complete donor-type chimerism.
The overall median follow-up of survivors was 1,727 days. The overall survival (OS) was 90.4% at 1 year and 83.5% at 5 years in patients without MC or SGF (n = 340), which was not different from the OS in groups 1 and 2. However, inferior OS was observed in group 3 (1 year, 52.1%; 5 years, 52.1%) and group 4 (1 year, 82.4%; 5 years, 56.3%). In addition, multivariate analyses showed that the use of fludarabine (Flu) and the absence of irradiation in conditioning were associated with the development of SGF with MC or complete recipient-type chimerism. The use of Flu in conditioning also was associated with SGF with complete donor-type chimerism.
“The occurrence of SGF with both MC/recipient-type and donor-type chimerism after HSCT for AA was associated with inferior OS, and the conditioning regimens influenced the occurrence of SGF,” the researchers concluded.
The Japan Agency for Medical Research and Development funded the research. Two of the authors reported receiving honoraria or research funding from Sanofi KK and one from Shionogi.
SOURCE: Kako S et al. Biol Blood Marrow Transplant 2020. 26:445-50.
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
Survey: 2020 will see more attacks on ACA
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
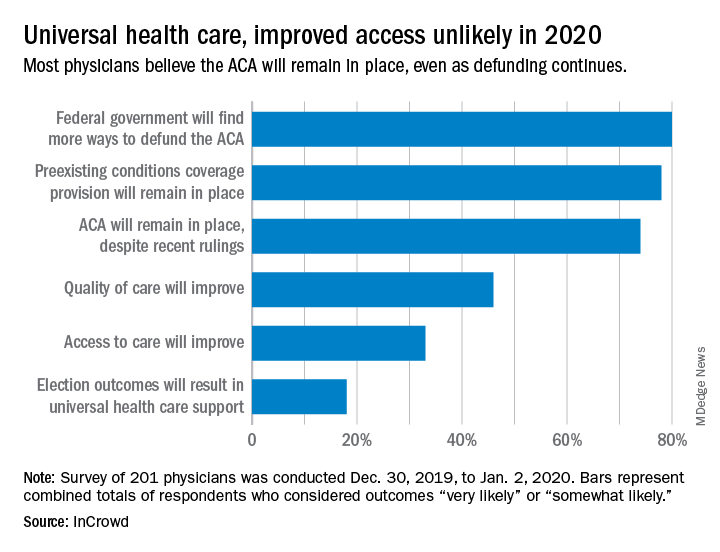
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
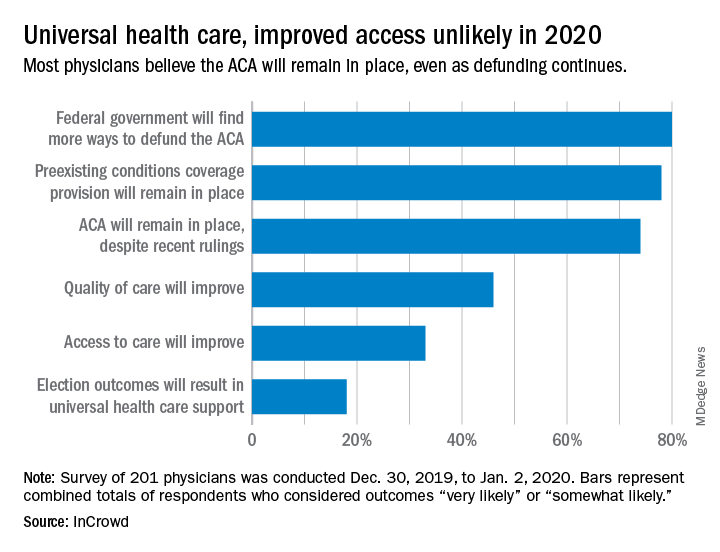
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
When physicians gaze into their crystal balls to predict what’s coming in 2020, they see continued efforts to defund the Affordable Care Act – meaning the ACA will still be around to be defunded – but they don’t see a lot of support for universal health care, according to health care market research company InCrowd.
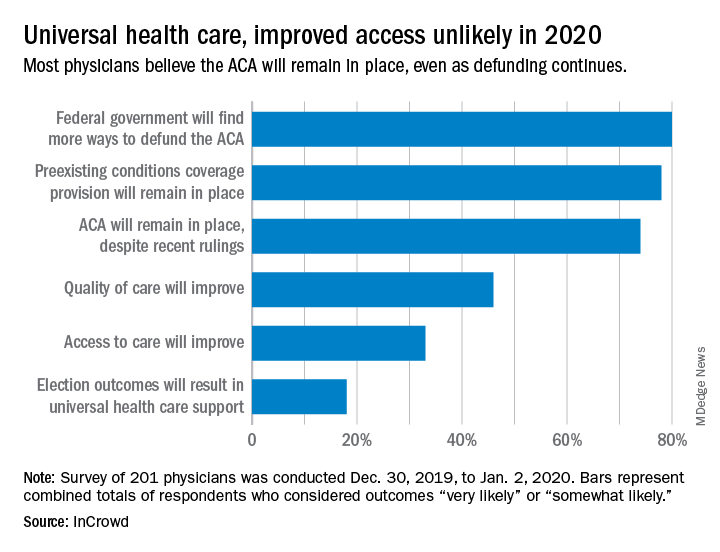
Expectations for universal health care came in at 18% of the 100 generalists and 101 specialists who responded to InCrowd’s fifth annual health care predictions survey, which left 82% who thought that “election outcomes will result in universal healthcare support” was somewhat or very unlikely in 2020.
One respondent, a specialist from California, commented that “the global data on universal healthcare for all shows that it results in overall improved population health. Unfortunately, we are so polarized in the US against universal healthcare driven by bias from health insurance companies and decision makers that are quick to ignore scientific data.”
This was the first time InCrowd asked physicians about universal health care, but ACA-related predictions have been included before, and all three scenarios presented were deemed to be increasingly likely, compared with 2019.
Respondents thought that federal government defunding was more likely to occur in 2020 (80%) than in 2019 (73%), but increased majorities also said that preexisting conditions coverage would continue (78% in 2020 vs. 70% in 2019) and that the ACA would remain in place (74% in 2020 vs. 60% in 2019), InCrowd reported after the survey, which was conducted from Dec. 30, 2019, to Jan. 2, 2020.
A respondent who thought the ACA will be eliminated said, “I have as many uninsured today as before the ACA. They are just different. Mainly younger patients who spend less in a year on healthcare than one month’s premium.” Another suggested that eliminateing it “will limit access to care and overload [emergency departments]. More people will die.”
Cost was addressed in a separate survey question that asked how physicians could help to reduce health care spending in 2020.
The leading answer, given by 37% of respondents, was for physicians to “inform themselves of costs and adapt cost-saving prescription practices.” Next came “limit use of expensive tests and scans” with 21%, followed by “prescribe generics when possible” at 20%, which was a substantial drop from the 38% it garnered in 2019, InCrowd noted.
“Participation in [shared savings] programs and risk-based incentive programs and pay-for-performance programs” would provide “better stewardship of resources,” a primary care physician from Michigan wrote.
When the survey turned to pharmaceutical industry predictions for 2020, cost was the major issue.
“What’s interesting about this year’s data is that we’re seeing less emphasis on the importance of bringing innovative, new therapies to market faster … versus expanding affordability, which was nearly a unanimous top priority for respondents,” Daniel S. Fitzgerald, InCrowd’s CEO and president, said in a separate statement.
AFib patients do best on a DOAC started 7-10 days post stroke
LOS ANGELES – When a patient with atrial fibrillation (AFib) has a cardioembolic stroke, the best blood thinner to start may be a direct-acting oral anticoagulant (DOAC), possibly beginning 7-10 days after the index stroke, according to an analysis of 90-day, observational outcomes data from nearly 1,300 patients.
The analysis also suggested that the use of “bridging” anticoagulant treatment by injection before a patient with atrial fibrillation (AFib) starts a daily oral anticoagulant regimen following a cardioembolic stroke is not a good idea. Patients who received bridging anticoagulation had a nearly threefold higher rate of symptomatic intracranial hemorrhage than did patients who did not, and their bridging treatment failed to protect them from recurrent ischemic events, Shadi Yaghi, MD, said at the International Stroke Conference, sponsored by the American Heart Association. The bridging regimens delivered either heparin or low-molecular-weight heparin.
Based on the findings, “it seems reasonable to avoid bridging unless absolutely necessary, to initiate a DOAC unless it’s contraindicated, and to start the DOAC on day 7-10 following the stroke in most patients,” said Dr. Yaghi, a vascular neurologist and director of stroke research at NYU Langone Health in New York.
“It’s been hard to develop a broad guideline on when to start oral anticoagulation” after a cardioembolic stroke in AFib patients. The best time “depends on a lot of variables and how the patient responded to acute treatment,” commented Alexis Simpkins, MD, a vascular and stroke neurologist at the University of Florida in Gainesville. “You want to start treatment before the patient has another stroke, but not so soon that the treatment causes symptomatic hemorrhagic transformation.”
Dr. Yaghi’s suggestion, based on his findings, to start treatment for most patients with a DOAC 7-10 days after their index stroke “shows consistency” with the prevailing guideline recommendation from the AHA/American Stroke Association to start oral anticoagulation in this patient population 4-14 days after the index stroke (Stroke. 2018 March;49[3]:e46-e99), she noted.
A recent article reviewed the uncertainty about the best time to start oral anticoagulation in AFib patients after a cardioembolic stroke and the subtle differences that distinguish various international medical groups that, like the ASA, have made recommendations (Lancet Neurol. 2019 Jan 1;18[1]:117-26). According to this review, a major limitation of these various recommendations has been the lack of actual evidence collected from AFib patients who began receiving a DOAC shortly after a cardioembolic stroke, although the article added that several studies in progress are collecting these data.
The study reported by Dr. Yaghi pooled data collected from 2,084 recent AFib patients with a cardioembolic stroke treated at any of eight comprehensive U.S. stroke centers. They excluded patients who died from causes unrelated to the primary endpoint, those who did not receive an anticoagulant or had incomplete data, and patients lost to follow-up, leaving 1,289 evaluable patients. During their 90-day follow-up, 10% of the patients had an ischemic event, a symptomatic intracranial hemorrhage, or an extracranial hemorrhage.
The study’s primary analysis showed no statistically significant difference in the incidence of recurrent ischemic events, symptomatic intracranial hemorrhage, or both based on when oral anticoagulant treatment began: 0-3 days, 4-14 days, or more than 14 days after the index stroke.
The investigators then subdivided patients into the subgroup that started treatment with a DOAC and the subgroup that started treatment with warfarin and also further subdivided the 4-14 day time window for starting treatment. Results of this analysis showed that patients who received a DOAC and began this treatment 7-10 days after their stroke had a 50% cut in their 90-day events compared with other patients, a difference that fell just short of statistical significance at P = .07. All the other combinations of oral anticoagulant and time of treatment initiation analyzed showed neutral effects that never came near statistical significance.
Secondary data analyses also showed that both patients with a history of a stroke prior to their index stroke and patients with ipsilateral atherosclerosis came close to having a statistically significant increased rate of a subsequent ischemic event during 90-day follow-up. Furthermore, women, patients with a history of hyperlipidemia, and patients who developed hemorrhagic transformation of their index stroke all had significantly increased rates of developing a symptomatic intracranial hemorrhage during 90-day follow-up. When the endpoint was limited to recurrent ischemic events only, patients who received a DOAC were 50% less likely to have an event than were patients treated with warfarin, a statistically significant difference.
Although starting a DOAC 7-10 days after the index stroke seems reasonable based on this analysis, the question needs a prospective, randomized study to create an appropriate evidence base, Dr. Yaghi said.
Dr. Yaghi disclosed a financial relationship with Medtronic. Dr. Simpkins had no disclosures.
SOURCE: Yaghi S et al. Stroke. 2020 Feb;51(suppl 1):A119.
LOS ANGELES – When a patient with atrial fibrillation (AFib) has a cardioembolic stroke, the best blood thinner to start may be a direct-acting oral anticoagulant (DOAC), possibly beginning 7-10 days after the index stroke, according to an analysis of 90-day, observational outcomes data from nearly 1,300 patients.
The analysis also suggested that the use of “bridging” anticoagulant treatment by injection before a patient with atrial fibrillation (AFib) starts a daily oral anticoagulant regimen following a cardioembolic stroke is not a good idea. Patients who received bridging anticoagulation had a nearly threefold higher rate of symptomatic intracranial hemorrhage than did patients who did not, and their bridging treatment failed to protect them from recurrent ischemic events, Shadi Yaghi, MD, said at the International Stroke Conference, sponsored by the American Heart Association. The bridging regimens delivered either heparin or low-molecular-weight heparin.
Based on the findings, “it seems reasonable to avoid bridging unless absolutely necessary, to initiate a DOAC unless it’s contraindicated, and to start the DOAC on day 7-10 following the stroke in most patients,” said Dr. Yaghi, a vascular neurologist and director of stroke research at NYU Langone Health in New York.
“It’s been hard to develop a broad guideline on when to start oral anticoagulation” after a cardioembolic stroke in AFib patients. The best time “depends on a lot of variables and how the patient responded to acute treatment,” commented Alexis Simpkins, MD, a vascular and stroke neurologist at the University of Florida in Gainesville. “You want to start treatment before the patient has another stroke, but not so soon that the treatment causes symptomatic hemorrhagic transformation.”
Dr. Yaghi’s suggestion, based on his findings, to start treatment for most patients with a DOAC 7-10 days after their index stroke “shows consistency” with the prevailing guideline recommendation from the AHA/American Stroke Association to start oral anticoagulation in this patient population 4-14 days after the index stroke (Stroke. 2018 March;49[3]:e46-e99), she noted.
A recent article reviewed the uncertainty about the best time to start oral anticoagulation in AFib patients after a cardioembolic stroke and the subtle differences that distinguish various international medical groups that, like the ASA, have made recommendations (Lancet Neurol. 2019 Jan 1;18[1]:117-26). According to this review, a major limitation of these various recommendations has been the lack of actual evidence collected from AFib patients who began receiving a DOAC shortly after a cardioembolic stroke, although the article added that several studies in progress are collecting these data.
The study reported by Dr. Yaghi pooled data collected from 2,084 recent AFib patients with a cardioembolic stroke treated at any of eight comprehensive U.S. stroke centers. They excluded patients who died from causes unrelated to the primary endpoint, those who did not receive an anticoagulant or had incomplete data, and patients lost to follow-up, leaving 1,289 evaluable patients. During their 90-day follow-up, 10% of the patients had an ischemic event, a symptomatic intracranial hemorrhage, or an extracranial hemorrhage.
The study’s primary analysis showed no statistically significant difference in the incidence of recurrent ischemic events, symptomatic intracranial hemorrhage, or both based on when oral anticoagulant treatment began: 0-3 days, 4-14 days, or more than 14 days after the index stroke.
The investigators then subdivided patients into the subgroup that started treatment with a DOAC and the subgroup that started treatment with warfarin and also further subdivided the 4-14 day time window for starting treatment. Results of this analysis showed that patients who received a DOAC and began this treatment 7-10 days after their stroke had a 50% cut in their 90-day events compared with other patients, a difference that fell just short of statistical significance at P = .07. All the other combinations of oral anticoagulant and time of treatment initiation analyzed showed neutral effects that never came near statistical significance.
Secondary data analyses also showed that both patients with a history of a stroke prior to their index stroke and patients with ipsilateral atherosclerosis came close to having a statistically significant increased rate of a subsequent ischemic event during 90-day follow-up. Furthermore, women, patients with a history of hyperlipidemia, and patients who developed hemorrhagic transformation of their index stroke all had significantly increased rates of developing a symptomatic intracranial hemorrhage during 90-day follow-up. When the endpoint was limited to recurrent ischemic events only, patients who received a DOAC were 50% less likely to have an event than were patients treated with warfarin, a statistically significant difference.
Although starting a DOAC 7-10 days after the index stroke seems reasonable based on this analysis, the question needs a prospective, randomized study to create an appropriate evidence base, Dr. Yaghi said.
Dr. Yaghi disclosed a financial relationship with Medtronic. Dr. Simpkins had no disclosures.
SOURCE: Yaghi S et al. Stroke. 2020 Feb;51(suppl 1):A119.
LOS ANGELES – When a patient with atrial fibrillation (AFib) has a cardioembolic stroke, the best blood thinner to start may be a direct-acting oral anticoagulant (DOAC), possibly beginning 7-10 days after the index stroke, according to an analysis of 90-day, observational outcomes data from nearly 1,300 patients.
The analysis also suggested that the use of “bridging” anticoagulant treatment by injection before a patient with atrial fibrillation (AFib) starts a daily oral anticoagulant regimen following a cardioembolic stroke is not a good idea. Patients who received bridging anticoagulation had a nearly threefold higher rate of symptomatic intracranial hemorrhage than did patients who did not, and their bridging treatment failed to protect them from recurrent ischemic events, Shadi Yaghi, MD, said at the International Stroke Conference, sponsored by the American Heart Association. The bridging regimens delivered either heparin or low-molecular-weight heparin.
Based on the findings, “it seems reasonable to avoid bridging unless absolutely necessary, to initiate a DOAC unless it’s contraindicated, and to start the DOAC on day 7-10 following the stroke in most patients,” said Dr. Yaghi, a vascular neurologist and director of stroke research at NYU Langone Health in New York.
“It’s been hard to develop a broad guideline on when to start oral anticoagulation” after a cardioembolic stroke in AFib patients. The best time “depends on a lot of variables and how the patient responded to acute treatment,” commented Alexis Simpkins, MD, a vascular and stroke neurologist at the University of Florida in Gainesville. “You want to start treatment before the patient has another stroke, but not so soon that the treatment causes symptomatic hemorrhagic transformation.”
Dr. Yaghi’s suggestion, based on his findings, to start treatment for most patients with a DOAC 7-10 days after their index stroke “shows consistency” with the prevailing guideline recommendation from the AHA/American Stroke Association to start oral anticoagulation in this patient population 4-14 days after the index stroke (Stroke. 2018 March;49[3]:e46-e99), she noted.
A recent article reviewed the uncertainty about the best time to start oral anticoagulation in AFib patients after a cardioembolic stroke and the subtle differences that distinguish various international medical groups that, like the ASA, have made recommendations (Lancet Neurol. 2019 Jan 1;18[1]:117-26). According to this review, a major limitation of these various recommendations has been the lack of actual evidence collected from AFib patients who began receiving a DOAC shortly after a cardioembolic stroke, although the article added that several studies in progress are collecting these data.
The study reported by Dr. Yaghi pooled data collected from 2,084 recent AFib patients with a cardioembolic stroke treated at any of eight comprehensive U.S. stroke centers. They excluded patients who died from causes unrelated to the primary endpoint, those who did not receive an anticoagulant or had incomplete data, and patients lost to follow-up, leaving 1,289 evaluable patients. During their 90-day follow-up, 10% of the patients had an ischemic event, a symptomatic intracranial hemorrhage, or an extracranial hemorrhage.
The study’s primary analysis showed no statistically significant difference in the incidence of recurrent ischemic events, symptomatic intracranial hemorrhage, or both based on when oral anticoagulant treatment began: 0-3 days, 4-14 days, or more than 14 days after the index stroke.
The investigators then subdivided patients into the subgroup that started treatment with a DOAC and the subgroup that started treatment with warfarin and also further subdivided the 4-14 day time window for starting treatment. Results of this analysis showed that patients who received a DOAC and began this treatment 7-10 days after their stroke had a 50% cut in their 90-day events compared with other patients, a difference that fell just short of statistical significance at P = .07. All the other combinations of oral anticoagulant and time of treatment initiation analyzed showed neutral effects that never came near statistical significance.
Secondary data analyses also showed that both patients with a history of a stroke prior to their index stroke and patients with ipsilateral atherosclerosis came close to having a statistically significant increased rate of a subsequent ischemic event during 90-day follow-up. Furthermore, women, patients with a history of hyperlipidemia, and patients who developed hemorrhagic transformation of their index stroke all had significantly increased rates of developing a symptomatic intracranial hemorrhage during 90-day follow-up. When the endpoint was limited to recurrent ischemic events only, patients who received a DOAC were 50% less likely to have an event than were patients treated with warfarin, a statistically significant difference.
Although starting a DOAC 7-10 days after the index stroke seems reasonable based on this analysis, the question needs a prospective, randomized study to create an appropriate evidence base, Dr. Yaghi said.
Dr. Yaghi disclosed a financial relationship with Medtronic. Dr. Simpkins had no disclosures.
SOURCE: Yaghi S et al. Stroke. 2020 Feb;51(suppl 1):A119.
REPORTING FROM ISC 2020
No reduction in oral mucositis with folinic acid post transplant
ORLANDO – Folinic acid does not prevent oral mucositis in patients who are receiving a calcineurin inhibitor and methotrexate for graft-vs.-host disease prophylaxis, results of a multicenter study from Israel suggest.
A randomized clinical trial to determine whether folinic acid rescue 24 hours after a methotrexate dose protects patients against severe oral mucositis was halted for futility after an interim analysis showed no advantage to adding folinic acid, reported Moshe Yeshrun, MD, of Rabin Medical Center at Tel Aviv University, Israel.
“Regarding the primary and secondary endpoints, we observed identical rates and duration of severe oral mucositis, as well as identical rates of oral mucositis of any grade in the folinic acid and placebo groups,” he said at the annual Transplantation and Cellular Therapy Meetings.
There were also no significant differences between the folinic acid and placebo control groups in time to neutrophil and platelet engraftment, rates of febrile neutropenia and bloodstream infections, veno-occlusive disease, need for opiates or total parenteral nutrition (TPN), or time from transplant to discharge, Dr. Yeshrun added at the meeting, held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Folinic acid therapy did not, however, appear to abrogate or interfere with the effects of methotrexate on prevention of either acute or chronic graft-vs-host disease (GVHD).
Severe adverse event
Oral mucositis can be a serious complication of therapy, associated with increased morbidity and mortality; significant pain; difficulty with eating or speaking; difficulty swallowing water, food, and medications; prolonged hospitalizations; and increased costs of care, Dr. Yeshrun noted.
The presence of oral mucositis sometimes leads clinicians to reduce or even skip methotrexate doses, thereby increasing risk for GVHD.
There are limited data from nonrandomized studies indicating that folinic acid (also called leucovorin) may reduce methotrexate-associated toxicities, and both the European Society for Blood and Marrow Transplantation and European LeukemiaNet working group recommend the use of folinic-acid rescue 24 hours following each methotrexate dose, Dr. Yeshrun said.
To see whether folinic acid rescue actually reduces the rate of methotrexate-induced toxicity and affects outcomes for patients who receive methotrexate post transplant for GVHD prophylaxis, Dr. Yeshrun and colleagues in three Israeli medical centers conducted a randomized, placebo-controlled trial.
The eligible study population included patients 18 and older with hematological malignancies in complete remission or minimal residual disease who underwent myeloablative conditioning and allogeneic transplant from HLA-matched or 1-antigen mismatched siblings or unrelated donors.
The patients were stratified by treatment center and intensity of the conditioning regimen, and then randomized on a 1:1 basis to receive folinic acid or placebo beginning 24 hours after each methotrexate dose, with the assigned medication given at a dose of 15 mg three times daily on the first day, and once daily on days 3 and 6.
Patients who received a transplant from an unrelated donor were also given anti-thymocyte globulin at a total dose of 15 mg/kg.
Supportive care included filgrastim (Neupogen) 5 mcg/kg from day 7 until neutrophil engraftment, infection prophylaxis, and ursodeoxycholic acid for prevention of veno-occlusive disease.
Trial stopped
Although the study was designed to enroll 116 patients to have a power of 80% to detect a 50% reduction in the rate of severe oral mucositis from an anticipated 50% in the placebo arm, a planned interim analysis conducted after approximately half of the target events occurred showed no difference in the rates of severe oral mucositis, and the trial was halted.
A total of 28 patients in the folinic acid group and 24 in the placebo group were available for the analysis.
The rate of grade 3 or 4 mucositis, the primary endpoint, was 46.6% in the folinic acid group, and 45.8% in the placebo group.
Respectively, the median duration of severe oral mucositis was 4 days in each group, days to neutrophil engraftment were a median of 12 and to platelet engraftment were a median of 13 days in each group, rates of febrile neutropenia were 57.1% and 58.3%, rates of bloodstream infections were 10.7% and 16.6%, rates of veno-occlusive disease were 7% and 12.5%, need for TPN occurred in 14.2% vs. 25%, need for opiates occurred in 78.5% vs. 66.6%, and median time to discharge was 18 and 19 days. As noted, none of the differences were statistically significant.
“These unequivocal interim results led to our decision to discontinue the study,” Dr. Yeshrun said.
Arnon Nagler, MD, MSc, from Sheba Medical Center Tel HaShomer at Tel Aviv University in Israel, who was not involved in the study, said in an interview “I think this is a very practical and important study, because we need evidence-based data such as this.”
Dr. Nagler, who comoderated the session where the data were presented, noted that the study was limited by the small number of patients and the lack of a subgroup analysis, but emphasized that the findings were important nonetheless.
His comoderator, Maria Gilleece, MD, director of the Yorkshire (England) Blood and Marrow Transplant Program, noted in an interview that folinic acid is frequently used in the United Kingdom for patients receiving high-dose methotrexate, ”and certainly, this study suggests that may be inappropriate.”
Rabin Medical Center sponsored the trial. Dr. Yeshrun, Dr. Nagler, and Dr. Gilleece reported no relevant conflicts of interest.
SOURCE: Yeshrun M. et al. TCT 2020. Abstract 61.
ORLANDO – Folinic acid does not prevent oral mucositis in patients who are receiving a calcineurin inhibitor and methotrexate for graft-vs.-host disease prophylaxis, results of a multicenter study from Israel suggest.
A randomized clinical trial to determine whether folinic acid rescue 24 hours after a methotrexate dose protects patients against severe oral mucositis was halted for futility after an interim analysis showed no advantage to adding folinic acid, reported Moshe Yeshrun, MD, of Rabin Medical Center at Tel Aviv University, Israel.
“Regarding the primary and secondary endpoints, we observed identical rates and duration of severe oral mucositis, as well as identical rates of oral mucositis of any grade in the folinic acid and placebo groups,” he said at the annual Transplantation and Cellular Therapy Meetings.
There were also no significant differences between the folinic acid and placebo control groups in time to neutrophil and platelet engraftment, rates of febrile neutropenia and bloodstream infections, veno-occlusive disease, need for opiates or total parenteral nutrition (TPN), or time from transplant to discharge, Dr. Yeshrun added at the meeting, held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Folinic acid therapy did not, however, appear to abrogate or interfere with the effects of methotrexate on prevention of either acute or chronic graft-vs-host disease (GVHD).
Severe adverse event
Oral mucositis can be a serious complication of therapy, associated with increased morbidity and mortality; significant pain; difficulty with eating or speaking; difficulty swallowing water, food, and medications; prolonged hospitalizations; and increased costs of care, Dr. Yeshrun noted.
The presence of oral mucositis sometimes leads clinicians to reduce or even skip methotrexate doses, thereby increasing risk for GVHD.
There are limited data from nonrandomized studies indicating that folinic acid (also called leucovorin) may reduce methotrexate-associated toxicities, and both the European Society for Blood and Marrow Transplantation and European LeukemiaNet working group recommend the use of folinic-acid rescue 24 hours following each methotrexate dose, Dr. Yeshrun said.
To see whether folinic acid rescue actually reduces the rate of methotrexate-induced toxicity and affects outcomes for patients who receive methotrexate post transplant for GVHD prophylaxis, Dr. Yeshrun and colleagues in three Israeli medical centers conducted a randomized, placebo-controlled trial.
The eligible study population included patients 18 and older with hematological malignancies in complete remission or minimal residual disease who underwent myeloablative conditioning and allogeneic transplant from HLA-matched or 1-antigen mismatched siblings or unrelated donors.
The patients were stratified by treatment center and intensity of the conditioning regimen, and then randomized on a 1:1 basis to receive folinic acid or placebo beginning 24 hours after each methotrexate dose, with the assigned medication given at a dose of 15 mg three times daily on the first day, and once daily on days 3 and 6.
Patients who received a transplant from an unrelated donor were also given anti-thymocyte globulin at a total dose of 15 mg/kg.
Supportive care included filgrastim (Neupogen) 5 mcg/kg from day 7 until neutrophil engraftment, infection prophylaxis, and ursodeoxycholic acid for prevention of veno-occlusive disease.
Trial stopped
Although the study was designed to enroll 116 patients to have a power of 80% to detect a 50% reduction in the rate of severe oral mucositis from an anticipated 50% in the placebo arm, a planned interim analysis conducted after approximately half of the target events occurred showed no difference in the rates of severe oral mucositis, and the trial was halted.
A total of 28 patients in the folinic acid group and 24 in the placebo group were available for the analysis.
The rate of grade 3 or 4 mucositis, the primary endpoint, was 46.6% in the folinic acid group, and 45.8% in the placebo group.
Respectively, the median duration of severe oral mucositis was 4 days in each group, days to neutrophil engraftment were a median of 12 and to platelet engraftment were a median of 13 days in each group, rates of febrile neutropenia were 57.1% and 58.3%, rates of bloodstream infections were 10.7% and 16.6%, rates of veno-occlusive disease were 7% and 12.5%, need for TPN occurred in 14.2% vs. 25%, need for opiates occurred in 78.5% vs. 66.6%, and median time to discharge was 18 and 19 days. As noted, none of the differences were statistically significant.
“These unequivocal interim results led to our decision to discontinue the study,” Dr. Yeshrun said.
Arnon Nagler, MD, MSc, from Sheba Medical Center Tel HaShomer at Tel Aviv University in Israel, who was not involved in the study, said in an interview “I think this is a very practical and important study, because we need evidence-based data such as this.”
Dr. Nagler, who comoderated the session where the data were presented, noted that the study was limited by the small number of patients and the lack of a subgroup analysis, but emphasized that the findings were important nonetheless.
His comoderator, Maria Gilleece, MD, director of the Yorkshire (England) Blood and Marrow Transplant Program, noted in an interview that folinic acid is frequently used in the United Kingdom for patients receiving high-dose methotrexate, ”and certainly, this study suggests that may be inappropriate.”
Rabin Medical Center sponsored the trial. Dr. Yeshrun, Dr. Nagler, and Dr. Gilleece reported no relevant conflicts of interest.
SOURCE: Yeshrun M. et al. TCT 2020. Abstract 61.
ORLANDO – Folinic acid does not prevent oral mucositis in patients who are receiving a calcineurin inhibitor and methotrexate for graft-vs.-host disease prophylaxis, results of a multicenter study from Israel suggest.
A randomized clinical trial to determine whether folinic acid rescue 24 hours after a methotrexate dose protects patients against severe oral mucositis was halted for futility after an interim analysis showed no advantage to adding folinic acid, reported Moshe Yeshrun, MD, of Rabin Medical Center at Tel Aviv University, Israel.
“Regarding the primary and secondary endpoints, we observed identical rates and duration of severe oral mucositis, as well as identical rates of oral mucositis of any grade in the folinic acid and placebo groups,” he said at the annual Transplantation and Cellular Therapy Meetings.
There were also no significant differences between the folinic acid and placebo control groups in time to neutrophil and platelet engraftment, rates of febrile neutropenia and bloodstream infections, veno-occlusive disease, need for opiates or total parenteral nutrition (TPN), or time from transplant to discharge, Dr. Yeshrun added at the meeting, held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Folinic acid therapy did not, however, appear to abrogate or interfere with the effects of methotrexate on prevention of either acute or chronic graft-vs-host disease (GVHD).
Severe adverse event
Oral mucositis can be a serious complication of therapy, associated with increased morbidity and mortality; significant pain; difficulty with eating or speaking; difficulty swallowing water, food, and medications; prolonged hospitalizations; and increased costs of care, Dr. Yeshrun noted.
The presence of oral mucositis sometimes leads clinicians to reduce or even skip methotrexate doses, thereby increasing risk for GVHD.
There are limited data from nonrandomized studies indicating that folinic acid (also called leucovorin) may reduce methotrexate-associated toxicities, and both the European Society for Blood and Marrow Transplantation and European LeukemiaNet working group recommend the use of folinic-acid rescue 24 hours following each methotrexate dose, Dr. Yeshrun said.
To see whether folinic acid rescue actually reduces the rate of methotrexate-induced toxicity and affects outcomes for patients who receive methotrexate post transplant for GVHD prophylaxis, Dr. Yeshrun and colleagues in three Israeli medical centers conducted a randomized, placebo-controlled trial.
The eligible study population included patients 18 and older with hematological malignancies in complete remission or minimal residual disease who underwent myeloablative conditioning and allogeneic transplant from HLA-matched or 1-antigen mismatched siblings or unrelated donors.
The patients were stratified by treatment center and intensity of the conditioning regimen, and then randomized on a 1:1 basis to receive folinic acid or placebo beginning 24 hours after each methotrexate dose, with the assigned medication given at a dose of 15 mg three times daily on the first day, and once daily on days 3 and 6.
Patients who received a transplant from an unrelated donor were also given anti-thymocyte globulin at a total dose of 15 mg/kg.
Supportive care included filgrastim (Neupogen) 5 mcg/kg from day 7 until neutrophil engraftment, infection prophylaxis, and ursodeoxycholic acid for prevention of veno-occlusive disease.
Trial stopped
Although the study was designed to enroll 116 patients to have a power of 80% to detect a 50% reduction in the rate of severe oral mucositis from an anticipated 50% in the placebo arm, a planned interim analysis conducted after approximately half of the target events occurred showed no difference in the rates of severe oral mucositis, and the trial was halted.
A total of 28 patients in the folinic acid group and 24 in the placebo group were available for the analysis.
The rate of grade 3 or 4 mucositis, the primary endpoint, was 46.6% in the folinic acid group, and 45.8% in the placebo group.
Respectively, the median duration of severe oral mucositis was 4 days in each group, days to neutrophil engraftment were a median of 12 and to platelet engraftment were a median of 13 days in each group, rates of febrile neutropenia were 57.1% and 58.3%, rates of bloodstream infections were 10.7% and 16.6%, rates of veno-occlusive disease were 7% and 12.5%, need for TPN occurred in 14.2% vs. 25%, need for opiates occurred in 78.5% vs. 66.6%, and median time to discharge was 18 and 19 days. As noted, none of the differences were statistically significant.
“These unequivocal interim results led to our decision to discontinue the study,” Dr. Yeshrun said.
Arnon Nagler, MD, MSc, from Sheba Medical Center Tel HaShomer at Tel Aviv University in Israel, who was not involved in the study, said in an interview “I think this is a very practical and important study, because we need evidence-based data such as this.”
Dr. Nagler, who comoderated the session where the data were presented, noted that the study was limited by the small number of patients and the lack of a subgroup analysis, but emphasized that the findings were important nonetheless.
His comoderator, Maria Gilleece, MD, director of the Yorkshire (England) Blood and Marrow Transplant Program, noted in an interview that folinic acid is frequently used in the United Kingdom for patients receiving high-dose methotrexate, ”and certainly, this study suggests that may be inappropriate.”
Rabin Medical Center sponsored the trial. Dr. Yeshrun, Dr. Nagler, and Dr. Gilleece reported no relevant conflicts of interest.
SOURCE: Yeshrun M. et al. TCT 2020. Abstract 61.
REPORTING FROM TCT 2020
What medical conferences are being canceled by coronavirus?
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
In a typical year, March marks the start of conference season, made all the more attractive by collegial gatherings and travel to warmer climes. But 2020 has already proven anything but typical as the number of novel coronavirus cases continues to increase around the globe. As a potential pandemic looms, these meetings – full of handshakes and crowded lecture halls – are also nirvana for opportunistic viruses. As are the airports, airplanes, and cabs required to get there.
So, as COVID-19 continues to spread, medical and scientific societies must make some difficult decisions. In Europe, at least a few societies have already suspended their upcoming meetings, while France has temporarily banned all gatherings over 5000 people.
In the United States, however, most medical conferences are moving forward as planned – at least for now. But one conference of 10,000 attendees, the American Physical Society annual meeting, which was scheduled for March 2-6 in Denver, was canceled the day before the meeting started. Although it’s not a medical conference, it speaks to the “rapidly escalating health concerns” that all conference organizers must grapple with.
APS Physics Meetings
@APSMeetings
Due to rapidly escalating health concerns relating to the spread of the coronavirus disease (COVID-19), the 2020 APS March Meeting in Denver, CO, has been canceled. Please do not travel to Denver to attend the March Meeting. More information will follow shortly. #apsmarch
734 9:59 PM - Feb 29, 2020
Just one smaller medical meeting, the Ataxia Conference, which was scheduled for March 6-7 in Denver, has been canceled.
Most societies hosting these meetings have put out statements to their attendees saying that they’re monitoring the situation and will adapt as necessary. The United States and Canadian Academy of Pathology, which is holding its annual meeting in Los Angeles this week, sent out an email beforehand asking international travelers to consider staying home. The Healthcare Information and Management Systems Society (HIMSS) Global Health Conference, which is slated to have about 50,000 attendees from around the world, has declared itself a “handshake-free” conference but otherwise intends to move ahead as planned.
All of these conferences will be pushing forward without at least one prominent group of attendees. New York University’s Langone Health has removed its employees from the decision-making process and instead is taking a proactive stance: The health system just declared a 60-day (minimum) ban preventing employees from attending any meetings or conferences and from all domestic and international work-related travel.
Here’s what some of the societies have said to attendees about their intent to proceed or modify their plans:
- Conference on Retroviruses and Opportunistic Infections (CROI), Boston, 3/8/20 - 3/11/20: Monitoring the situation and seeking input from local, state, and federal infectious-disease and public-health experts. Final decision expected by the evening of March 3.
- American Academy of Allergy, Asthma & Immunology (AAAAI), Philadelphia, 3/13/20 - 3/16/20: Monitoring developments but no plans to cancel or postpone at this time.
- American Academy of Orthopedic Surgeons (AAOS), Orlando, 3/24/20 - 3/28/20: Proceeding as planned.
- American Academy of Dermatology (AAD), Denver, 3/20/20 - 3/24/20: The AAD’s 2020 Annual Meeting is scheduled to take place as planned. The organization will increase the number of hand-sanitizing stations throughout the convention center, and it is adding a nursing station specifically designated for anyone with flu-like symptoms.
- American College of Cardiology (ACC), Chicago, 3/28/20 - 3/30/20: The organization is working with attendees, faculty, exhibitors, and other stakeholders in affected countries to ensure access to research and education from the meeting, but is otherwise proceeding as planned.
- Endocrine Society (ENDO), San Francisco, 3/28/20 - 3/31/20: ENDO 2020 will take place as scheduled, but this is an evolving situation worldwide. The society will continue to monitor and provide updates on its FAQ page.
- American College of Physicians Internal Medicine (ACP IM), Los Angeles, 4/23/20 - 4/25/20: ACP leadership is closely monitoring the COVID-19 situation and is actively working with the Centers for Disease Control and Prevention (CDC) to ensure authoritative communication of safety updates and recommendations as the situation evolves.
- American Association for Cancer Research (AACR), San Diego, 4/24/20 - 4/29/20: At this time, there is no plan to cancel or postpone any scheduled AACR meetings. The organization is tracking all travel restrictions as well as information and guidance from the CDC and World Health Organization.
- American Academy of Neurology (AAN), Toronto, 4/25/20 - 5/1/20: The group is continuing to closely monitor the situation in Toronto and will provide updates as the situation warrants.
This article originally appeared on Medscape.com.
FDA approves new drug for relapsed/refractory multiple myeloma
The U.S. Food and Drug Administration today approved isatuximab (Sarclisa, Sanofi) in combination with pomalidomide (Revlimid, Celgene) and dexamethasone for the treatment of adult patients with multiple myeloma who have received two or more prior therapies including lenalidomide and a proteasome inhibitor.
Isatuximab is an anti-CD38 monoclonal antibody administered by intravenous infusion that works by helping the immune system attack multiple myeloma cancer cells.
“While there is no cure for multiple myeloma, Sarclisa is now another CD38-directed treatment option added to the list of FDA-approved treatments of patients with multiple myeloma who have progressive disease after previous therapies,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research.
“In the clinical trial, there was a 40% reduction in the risk of disease progression or death with this therapy,” he added.
The new approval is based on results from ICARIA-MM, an open-label, randomized phase 3 clinical trial of isatuximab among 307 patients in this setting.
In the trial, at a median follow-up of 11.6 months, median progression-free survival was 11.5 months in the isatuximab-pomalidomide-dexamethasone group versus 6.5 months in the pomalidomide-dexamethasone group (hazard ratio, 0.60; P = .001), as reported last year. Overall response rates were 60.4% for the triplet-treated group versus 35.3% for the doublet-treated group.
The most common side effects for isatuximab included neutropenia, infusion-related reactions, pneumonia, upper respiratory tract infection, diarrhea, anemia, lymphopenia, and thrombocytopenia.
Deaths because of treatment-related adverse events were reported for one patient (less than 1%) in the isatuximab-pomalidomide-dexamethasone group (sepsis) and two patients (1%) in the pomalidomide-dexamethasone group (pneumonia and urinary tract infection).
The drug can also cause serious side effects, including IV infusion-related reactions. In the case of a grade 3 or higher reaction, the drug should be permanently discontinued and health care professionals should institute appropriate medical management.
The FDA notes there have been higher incidences of second primary malignancies observed in a controlled clinical trial of patients with multiple myeloma receiving the drug.
The FDA also highlighted that laboratory test interference may be caused by isatuximab and that blood banks should be informed that patients are receiving the drug. Isatuximab may interfere with, for example, antibody screening for patients who need a blood transfusion. Isatuximab may also interfere with the assays used to monitor M-protein, which may impact the determination of complete response.
This article originally appeared on Medscape.com.
The U.S. Food and Drug Administration today approved isatuximab (Sarclisa, Sanofi) in combination with pomalidomide (Revlimid, Celgene) and dexamethasone for the treatment of adult patients with multiple myeloma who have received two or more prior therapies including lenalidomide and a proteasome inhibitor.
Isatuximab is an anti-CD38 monoclonal antibody administered by intravenous infusion that works by helping the immune system attack multiple myeloma cancer cells.
“While there is no cure for multiple myeloma, Sarclisa is now another CD38-directed treatment option added to the list of FDA-approved treatments of patients with multiple myeloma who have progressive disease after previous therapies,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research.
“In the clinical trial, there was a 40% reduction in the risk of disease progression or death with this therapy,” he added.
The new approval is based on results from ICARIA-MM, an open-label, randomized phase 3 clinical trial of isatuximab among 307 patients in this setting.
In the trial, at a median follow-up of 11.6 months, median progression-free survival was 11.5 months in the isatuximab-pomalidomide-dexamethasone group versus 6.5 months in the pomalidomide-dexamethasone group (hazard ratio, 0.60; P = .001), as reported last year. Overall response rates were 60.4% for the triplet-treated group versus 35.3% for the doublet-treated group.
The most common side effects for isatuximab included neutropenia, infusion-related reactions, pneumonia, upper respiratory tract infection, diarrhea, anemia, lymphopenia, and thrombocytopenia.
Deaths because of treatment-related adverse events were reported for one patient (less than 1%) in the isatuximab-pomalidomide-dexamethasone group (sepsis) and two patients (1%) in the pomalidomide-dexamethasone group (pneumonia and urinary tract infection).
The drug can also cause serious side effects, including IV infusion-related reactions. In the case of a grade 3 or higher reaction, the drug should be permanently discontinued and health care professionals should institute appropriate medical management.
The FDA notes there have been higher incidences of second primary malignancies observed in a controlled clinical trial of patients with multiple myeloma receiving the drug.
The FDA also highlighted that laboratory test interference may be caused by isatuximab and that blood banks should be informed that patients are receiving the drug. Isatuximab may interfere with, for example, antibody screening for patients who need a blood transfusion. Isatuximab may also interfere with the assays used to monitor M-protein, which may impact the determination of complete response.
This article originally appeared on Medscape.com.
The U.S. Food and Drug Administration today approved isatuximab (Sarclisa, Sanofi) in combination with pomalidomide (Revlimid, Celgene) and dexamethasone for the treatment of adult patients with multiple myeloma who have received two or more prior therapies including lenalidomide and a proteasome inhibitor.
Isatuximab is an anti-CD38 monoclonal antibody administered by intravenous infusion that works by helping the immune system attack multiple myeloma cancer cells.
“While there is no cure for multiple myeloma, Sarclisa is now another CD38-directed treatment option added to the list of FDA-approved treatments of patients with multiple myeloma who have progressive disease after previous therapies,” said Richard Pazdur, MD, director of the FDA’s Oncology Center of Excellence and acting director of the Office of Oncologic Diseases in the FDA’s Center for Drug Evaluation and Research.
“In the clinical trial, there was a 40% reduction in the risk of disease progression or death with this therapy,” he added.
The new approval is based on results from ICARIA-MM, an open-label, randomized phase 3 clinical trial of isatuximab among 307 patients in this setting.
In the trial, at a median follow-up of 11.6 months, median progression-free survival was 11.5 months in the isatuximab-pomalidomide-dexamethasone group versus 6.5 months in the pomalidomide-dexamethasone group (hazard ratio, 0.60; P = .001), as reported last year. Overall response rates were 60.4% for the triplet-treated group versus 35.3% for the doublet-treated group.
The most common side effects for isatuximab included neutropenia, infusion-related reactions, pneumonia, upper respiratory tract infection, diarrhea, anemia, lymphopenia, and thrombocytopenia.
Deaths because of treatment-related adverse events were reported for one patient (less than 1%) in the isatuximab-pomalidomide-dexamethasone group (sepsis) and two patients (1%) in the pomalidomide-dexamethasone group (pneumonia and urinary tract infection).
The drug can also cause serious side effects, including IV infusion-related reactions. In the case of a grade 3 or higher reaction, the drug should be permanently discontinued and health care professionals should institute appropriate medical management.
The FDA notes there have been higher incidences of second primary malignancies observed in a controlled clinical trial of patients with multiple myeloma receiving the drug.
The FDA also highlighted that laboratory test interference may be caused by isatuximab and that blood banks should be informed that patients are receiving the drug. Isatuximab may interfere with, for example, antibody screening for patients who need a blood transfusion. Isatuximab may also interfere with the assays used to monitor M-protein, which may impact the determination of complete response.
This article originally appeared on Medscape.com.
The fate of the ACA now rests with the U.S. Supreme Court
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
The U.S. Supreme Court has agreed to hear Texas v. California, a closely watched case that could upend the Affordable Care Act.
The justices will hear oral arguments in the case in fall 2020, with a ruling likely in 2021.
The Texas case, consolidated with a similar challenge, stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Since the Trump administration declined to defend the ACA, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. On March 2, the U.S. Supreme Court granted two petitions by the defendants requesting that the high court review the appeals court decision.
The review follows a previous look at the ACA’s mandate by the Supreme Court in 2012. In National Federation of Independent Business v. Sebelius, justices upheld the ACA’s insurance mandate as constitutional, ruling the requirement was authorized by Congress’ power to levy taxes. The vote was 5-4, with Chief Justice John G. Roberts Jr. in agreement with the court’s four more liberal members.
Death from unintentional injury is higher in cancer patients
New research suggests the incidence of death from unintentional injury is higher among patients with cancer than among those in the general U.S. population.
The findings highlight the need for more initiatives to help recognize patients at risk of death from this category of injury, which is the third leading cause of death in the country, according to the study authors.
“The purpose of our study was to present a comprehensive analysis of death from unintentional injury among patients with cancer using a large population-based cohort,” wrote Kunyu Yang, MD, of Huazhong University of Science and Technology in China, and colleagues. Their report is in JAMA Network Open.
The retrospective study included 8,271,020 patients with cancer, 40,599 of whom died from unintentional injury. The researchers identified patients who received a new diagnosis of primary cancer between Jan. 1, 1973, and Dec. 31, 2015, from the Surveillance, Epidemiology, and End Results (SEER) database.
The mean age of study participants was 63.0 years, and most were diagnosed in the 2000-2009 period (41.6%) or the 2010-2015 period (27.6%).
The SEER data was compared with mortality data representative of the general U.S. population obtained from the National Center for Health Statistics. Standardized mortality ratios and rates of death from unintentional injury were measured in both groups.
The rates of death from unintentional injury were 81.90 per 100,000 person-years in cancer patients and 51.21 per 100,000 person-years in the general population. The standardized mortality ratio was 1.60 (95% confidence interval, 1.58-1.61).
Factors associated with higher rates of death from unintentional injury among cancer patients included male sex (relative risk, 1.69; P less than .001), age greater than 80 years at diagnosis (RR, 2.91; P less than .001), and being unmarried (RR, 1.23; P less than .001).
“Rates of death from unintentional injury were the highest in patients with cancers of the liver (200.37 per 100,000 person-years), brain (175.04 per 100,000 person-years), larynx (148.78 per 100,000 person-years), and esophagus (144.98 per 100,000 person-years),” the researchers reported.
They acknowledged that a key limitation of this study was the potential role of reporting bias in death certificate analyses. As a result, death due to unintentional injury and death from suicide and homicide could have been misclassified.
“Cancer-related suicides, like all suicides, are preventable and should be viewed as cancer-related mortality. It is a silent killer with a peak incidence weeks after diagnosis – an undeniably hectic time for most patients and clinicians getting to know their patients,” said Daniel C. McFarland, DO, of Memorial Sloan Kettering Cancer Center in New York. He was not involved in this study.
“Suicide screening with appropriate systems in place to address suicidal thoughts and behavior is crucial for cancer patients throughout the trajectory of their care,” he added.
As with death from unintentional injury, higher rates of suicide have been reported among cancer patients in comparison to the general population (Nat Commun. 2019;10[1]:207).
No funding sources were reported for this study. The authors and Dr. McFarland disclosed no conflicts of interest.
SOURCE: Yang K et al. JAMA Netw Open. 2020 Feb 21. doi: 10.1001/jamanetworkopen.2019.21647.
New research suggests the incidence of death from unintentional injury is higher among patients with cancer than among those in the general U.S. population.
The findings highlight the need for more initiatives to help recognize patients at risk of death from this category of injury, which is the third leading cause of death in the country, according to the study authors.
“The purpose of our study was to present a comprehensive analysis of death from unintentional injury among patients with cancer using a large population-based cohort,” wrote Kunyu Yang, MD, of Huazhong University of Science and Technology in China, and colleagues. Their report is in JAMA Network Open.
The retrospective study included 8,271,020 patients with cancer, 40,599 of whom died from unintentional injury. The researchers identified patients who received a new diagnosis of primary cancer between Jan. 1, 1973, and Dec. 31, 2015, from the Surveillance, Epidemiology, and End Results (SEER) database.
The mean age of study participants was 63.0 years, and most were diagnosed in the 2000-2009 period (41.6%) or the 2010-2015 period (27.6%).
The SEER data was compared with mortality data representative of the general U.S. population obtained from the National Center for Health Statistics. Standardized mortality ratios and rates of death from unintentional injury were measured in both groups.
The rates of death from unintentional injury were 81.90 per 100,000 person-years in cancer patients and 51.21 per 100,000 person-years in the general population. The standardized mortality ratio was 1.60 (95% confidence interval, 1.58-1.61).
Factors associated with higher rates of death from unintentional injury among cancer patients included male sex (relative risk, 1.69; P less than .001), age greater than 80 years at diagnosis (RR, 2.91; P less than .001), and being unmarried (RR, 1.23; P less than .001).
“Rates of death from unintentional injury were the highest in patients with cancers of the liver (200.37 per 100,000 person-years), brain (175.04 per 100,000 person-years), larynx (148.78 per 100,000 person-years), and esophagus (144.98 per 100,000 person-years),” the researchers reported.
They acknowledged that a key limitation of this study was the potential role of reporting bias in death certificate analyses. As a result, death due to unintentional injury and death from suicide and homicide could have been misclassified.
“Cancer-related suicides, like all suicides, are preventable and should be viewed as cancer-related mortality. It is a silent killer with a peak incidence weeks after diagnosis – an undeniably hectic time for most patients and clinicians getting to know their patients,” said Daniel C. McFarland, DO, of Memorial Sloan Kettering Cancer Center in New York. He was not involved in this study.
“Suicide screening with appropriate systems in place to address suicidal thoughts and behavior is crucial for cancer patients throughout the trajectory of their care,” he added.
As with death from unintentional injury, higher rates of suicide have been reported among cancer patients in comparison to the general population (Nat Commun. 2019;10[1]:207).
No funding sources were reported for this study. The authors and Dr. McFarland disclosed no conflicts of interest.
SOURCE: Yang K et al. JAMA Netw Open. 2020 Feb 21. doi: 10.1001/jamanetworkopen.2019.21647.
New research suggests the incidence of death from unintentional injury is higher among patients with cancer than among those in the general U.S. population.
The findings highlight the need for more initiatives to help recognize patients at risk of death from this category of injury, which is the third leading cause of death in the country, according to the study authors.
“The purpose of our study was to present a comprehensive analysis of death from unintentional injury among patients with cancer using a large population-based cohort,” wrote Kunyu Yang, MD, of Huazhong University of Science and Technology in China, and colleagues. Their report is in JAMA Network Open.
The retrospective study included 8,271,020 patients with cancer, 40,599 of whom died from unintentional injury. The researchers identified patients who received a new diagnosis of primary cancer between Jan. 1, 1973, and Dec. 31, 2015, from the Surveillance, Epidemiology, and End Results (SEER) database.
The mean age of study participants was 63.0 years, and most were diagnosed in the 2000-2009 period (41.6%) or the 2010-2015 period (27.6%).
The SEER data was compared with mortality data representative of the general U.S. population obtained from the National Center for Health Statistics. Standardized mortality ratios and rates of death from unintentional injury were measured in both groups.
The rates of death from unintentional injury were 81.90 per 100,000 person-years in cancer patients and 51.21 per 100,000 person-years in the general population. The standardized mortality ratio was 1.60 (95% confidence interval, 1.58-1.61).
Factors associated with higher rates of death from unintentional injury among cancer patients included male sex (relative risk, 1.69; P less than .001), age greater than 80 years at diagnosis (RR, 2.91; P less than .001), and being unmarried (RR, 1.23; P less than .001).
“Rates of death from unintentional injury were the highest in patients with cancers of the liver (200.37 per 100,000 person-years), brain (175.04 per 100,000 person-years), larynx (148.78 per 100,000 person-years), and esophagus (144.98 per 100,000 person-years),” the researchers reported.
They acknowledged that a key limitation of this study was the potential role of reporting bias in death certificate analyses. As a result, death due to unintentional injury and death from suicide and homicide could have been misclassified.
“Cancer-related suicides, like all suicides, are preventable and should be viewed as cancer-related mortality. It is a silent killer with a peak incidence weeks after diagnosis – an undeniably hectic time for most patients and clinicians getting to know their patients,” said Daniel C. McFarland, DO, of Memorial Sloan Kettering Cancer Center in New York. He was not involved in this study.
“Suicide screening with appropriate systems in place to address suicidal thoughts and behavior is crucial for cancer patients throughout the trajectory of their care,” he added.
As with death from unintentional injury, higher rates of suicide have been reported among cancer patients in comparison to the general population (Nat Commun. 2019;10[1]:207).
No funding sources were reported for this study. The authors and Dr. McFarland disclosed no conflicts of interest.
SOURCE: Yang K et al. JAMA Netw Open. 2020 Feb 21. doi: 10.1001/jamanetworkopen.2019.21647.
FROM JAMA NETWORK OPEN










