User login
-
See acute hepatitis? Consider COVID-19, N.Y. case suggests
A woman presented to the emergency department with high liver enzyme levels and dark urine. She developed fever on day 2 of care, and then tested positive for the new coronavirus, researchers at Northwell Health, in Hempstead, New York, report.
The authors say the case, published online in the American Journal of Gastroenterology, is the first documented instance of a patient with COVID-19 presenting with acute hepatitis as the primary symptom before developing respiratory symptoms.
Prior data show that the most common early indications of COVID-19 are respiratory symptoms with fever, shortness of breath, sore throat, and cough, and with imaging results consistent with pneumonia. However, liver enzyme abnormalities are not uncommon in the disease course.
“In patients who are now presenting with acute hepatitis, people need to think of COVID,” senior author David Bernstein, MD, chief of the Division of Hepatology at Northwell Health, told Medscape Medical News.
In addition to Bernstein, Praneet Wander, MD, also in Northwell’s hepatology division, and Marcia Epstein, MD, with Northwell’s Department of Infectious Disease, authored the case report.
Bernstein said Northwell currently has the largest number of COVID-19 cases in the nation and that many patients are presenting with abnormal liver test results and COVID-19 symptoms.
He said that anecdotally, colleagues elsewhere in the United States are also reporting the connection.
“It seems to be that the liver enzyme elevations are part and parcel of this disease,” he said.
Case Details
According to the case report, the 59-year-old woman, who lives alone, came to the emergency department with a chief complaint of dark urine. She was given a face mask and was isolated, per protocol.
“She denied cough, sore throat, shortness of breath, diarrhea, nausea, vomiting or abdominal pain,” the authors wrote. She denied having been in contact with someone who was sick.
She had well-controlled HIV, and recent outpatient liver test results were normal. Eighteen hours after she came to the ED, she was admitted, owing to concern regarding rising liver enzyme levels in conjunction with her being HIV positive.
On presentation, her temperature was 98.9° F. There were no skin indications, lungs were normal, and “there was no jaundice, right upper quadrant tenderness, hepatomegaly or splenomegaly.”
Liver enzyme levels were as follows: aspartate aminotransferase (AST), 1230 (IU/L); alanine aminotransferase (ALT), 697 IU/L (normal for both is < 50 IU/L); alkaline phosphatase, 141 IU/L (normal, < 125 IU/L).
The patient tested negative for hepatitis A, B, C, E, cytomegalovirus, and Epstein-Barr virus. A respiratory viral panel and autoimmune markers were normal.
Fever Appeared on Day 2
She was admitted, and 18 hours after she came to the ED, she developed a fever of 102.2° F. A chest x-ray showed interstitial opacities in both lungs.
Nasopharyngeal samples were taken, and polymerase chain reaction test results were positive for the novel coronavirus. The patient was placed on 3 L of oxygen.
On post admission day 4, a 5-day course of hydroxychloroquine (200 mg twice a day) was initiated.
The patient was discharged to home on hospital day 8. The serum bilirubin level was 0.6 mg/dL; AST, 114 IU/L; ALT, 227 IU/L; and alkaline phosphatase, 259 IU/L.
According to Bernstein, it’s hard to tell in what order COVID-19 symptoms occur because people are staying home with other complaints. They may only present to the emergency department after they develop more typical COVID-19 symptoms, such as shortness of breath.
In this case, the patient noticed a darkening of her urine, “but if she had come the next day, she would have had fever. I think we just happened to catch it early,” Bernstein said.
He added that he saw no connection between the underlying HIV and her liver abnormalities or COVID-19 diagnosis.
Bernstein notes that most COVID-19 patients are not admitted, and he said he worries that a COVID-19 test might not be on the radar of providers in the outpatient setting when a patient presents with elevated liver enzymes levels.
If elevated liver enzyme levels can predict disease course, the information could alter how and where the disease is treated, Bernstein said.
“This is a first report. We’re really right now in the beginning of learning,” he said.
This article first appeared on Medscape.com.
A woman presented to the emergency department with high liver enzyme levels and dark urine. She developed fever on day 2 of care, and then tested positive for the new coronavirus, researchers at Northwell Health, in Hempstead, New York, report.
The authors say the case, published online in the American Journal of Gastroenterology, is the first documented instance of a patient with COVID-19 presenting with acute hepatitis as the primary symptom before developing respiratory symptoms.
Prior data show that the most common early indications of COVID-19 are respiratory symptoms with fever, shortness of breath, sore throat, and cough, and with imaging results consistent with pneumonia. However, liver enzyme abnormalities are not uncommon in the disease course.
“In patients who are now presenting with acute hepatitis, people need to think of COVID,” senior author David Bernstein, MD, chief of the Division of Hepatology at Northwell Health, told Medscape Medical News.
In addition to Bernstein, Praneet Wander, MD, also in Northwell’s hepatology division, and Marcia Epstein, MD, with Northwell’s Department of Infectious Disease, authored the case report.
Bernstein said Northwell currently has the largest number of COVID-19 cases in the nation and that many patients are presenting with abnormal liver test results and COVID-19 symptoms.
He said that anecdotally, colleagues elsewhere in the United States are also reporting the connection.
“It seems to be that the liver enzyme elevations are part and parcel of this disease,” he said.
Case Details
According to the case report, the 59-year-old woman, who lives alone, came to the emergency department with a chief complaint of dark urine. She was given a face mask and was isolated, per protocol.
“She denied cough, sore throat, shortness of breath, diarrhea, nausea, vomiting or abdominal pain,” the authors wrote. She denied having been in contact with someone who was sick.
She had well-controlled HIV, and recent outpatient liver test results were normal. Eighteen hours after she came to the ED, she was admitted, owing to concern regarding rising liver enzyme levels in conjunction with her being HIV positive.
On presentation, her temperature was 98.9° F. There were no skin indications, lungs were normal, and “there was no jaundice, right upper quadrant tenderness, hepatomegaly or splenomegaly.”
Liver enzyme levels were as follows: aspartate aminotransferase (AST), 1230 (IU/L); alanine aminotransferase (ALT), 697 IU/L (normal for both is < 50 IU/L); alkaline phosphatase, 141 IU/L (normal, < 125 IU/L).
The patient tested negative for hepatitis A, B, C, E, cytomegalovirus, and Epstein-Barr virus. A respiratory viral panel and autoimmune markers were normal.
Fever Appeared on Day 2
She was admitted, and 18 hours after she came to the ED, she developed a fever of 102.2° F. A chest x-ray showed interstitial opacities in both lungs.
Nasopharyngeal samples were taken, and polymerase chain reaction test results were positive for the novel coronavirus. The patient was placed on 3 L of oxygen.
On post admission day 4, a 5-day course of hydroxychloroquine (200 mg twice a day) was initiated.
The patient was discharged to home on hospital day 8. The serum bilirubin level was 0.6 mg/dL; AST, 114 IU/L; ALT, 227 IU/L; and alkaline phosphatase, 259 IU/L.
According to Bernstein, it’s hard to tell in what order COVID-19 symptoms occur because people are staying home with other complaints. They may only present to the emergency department after they develop more typical COVID-19 symptoms, such as shortness of breath.
In this case, the patient noticed a darkening of her urine, “but if she had come the next day, she would have had fever. I think we just happened to catch it early,” Bernstein said.
He added that he saw no connection between the underlying HIV and her liver abnormalities or COVID-19 diagnosis.
Bernstein notes that most COVID-19 patients are not admitted, and he said he worries that a COVID-19 test might not be on the radar of providers in the outpatient setting when a patient presents with elevated liver enzymes levels.
If elevated liver enzyme levels can predict disease course, the information could alter how and where the disease is treated, Bernstein said.
“This is a first report. We’re really right now in the beginning of learning,” he said.
This article first appeared on Medscape.com.
A woman presented to the emergency department with high liver enzyme levels and dark urine. She developed fever on day 2 of care, and then tested positive for the new coronavirus, researchers at Northwell Health, in Hempstead, New York, report.
The authors say the case, published online in the American Journal of Gastroenterology, is the first documented instance of a patient with COVID-19 presenting with acute hepatitis as the primary symptom before developing respiratory symptoms.
Prior data show that the most common early indications of COVID-19 are respiratory symptoms with fever, shortness of breath, sore throat, and cough, and with imaging results consistent with pneumonia. However, liver enzyme abnormalities are not uncommon in the disease course.
“In patients who are now presenting with acute hepatitis, people need to think of COVID,” senior author David Bernstein, MD, chief of the Division of Hepatology at Northwell Health, told Medscape Medical News.
In addition to Bernstein, Praneet Wander, MD, also in Northwell’s hepatology division, and Marcia Epstein, MD, with Northwell’s Department of Infectious Disease, authored the case report.
Bernstein said Northwell currently has the largest number of COVID-19 cases in the nation and that many patients are presenting with abnormal liver test results and COVID-19 symptoms.
He said that anecdotally, colleagues elsewhere in the United States are also reporting the connection.
“It seems to be that the liver enzyme elevations are part and parcel of this disease,” he said.
Case Details
According to the case report, the 59-year-old woman, who lives alone, came to the emergency department with a chief complaint of dark urine. She was given a face mask and was isolated, per protocol.
“She denied cough, sore throat, shortness of breath, diarrhea, nausea, vomiting or abdominal pain,” the authors wrote. She denied having been in contact with someone who was sick.
She had well-controlled HIV, and recent outpatient liver test results were normal. Eighteen hours after she came to the ED, she was admitted, owing to concern regarding rising liver enzyme levels in conjunction with her being HIV positive.
On presentation, her temperature was 98.9° F. There were no skin indications, lungs were normal, and “there was no jaundice, right upper quadrant tenderness, hepatomegaly or splenomegaly.”
Liver enzyme levels were as follows: aspartate aminotransferase (AST), 1230 (IU/L); alanine aminotransferase (ALT), 697 IU/L (normal for both is < 50 IU/L); alkaline phosphatase, 141 IU/L (normal, < 125 IU/L).
The patient tested negative for hepatitis A, B, C, E, cytomegalovirus, and Epstein-Barr virus. A respiratory viral panel and autoimmune markers were normal.
Fever Appeared on Day 2
She was admitted, and 18 hours after she came to the ED, she developed a fever of 102.2° F. A chest x-ray showed interstitial opacities in both lungs.
Nasopharyngeal samples were taken, and polymerase chain reaction test results were positive for the novel coronavirus. The patient was placed on 3 L of oxygen.
On post admission day 4, a 5-day course of hydroxychloroquine (200 mg twice a day) was initiated.
The patient was discharged to home on hospital day 8. The serum bilirubin level was 0.6 mg/dL; AST, 114 IU/L; ALT, 227 IU/L; and alkaline phosphatase, 259 IU/L.
According to Bernstein, it’s hard to tell in what order COVID-19 symptoms occur because people are staying home with other complaints. They may only present to the emergency department after they develop more typical COVID-19 symptoms, such as shortness of breath.
In this case, the patient noticed a darkening of her urine, “but if she had come the next day, she would have had fever. I think we just happened to catch it early,” Bernstein said.
He added that he saw no connection between the underlying HIV and her liver abnormalities or COVID-19 diagnosis.
Bernstein notes that most COVID-19 patients are not admitted, and he said he worries that a COVID-19 test might not be on the radar of providers in the outpatient setting when a patient presents with elevated liver enzymes levels.
If elevated liver enzyme levels can predict disease course, the information could alter how and where the disease is treated, Bernstein said.
“This is a first report. We’re really right now in the beginning of learning,” he said.
This article first appeared on Medscape.com.
Abortion is essential health care
In my New Mexico reproductive health clinic one week in early April, I saw more than twice the number of patients usually scheduled, all seeking abortion care. Two-thirds of those patients were from Texas – some came from towns as close as 6 hours away, and at least two drove for more than 11 hours to receive care at our clinic. In addition to the many reasons women pursue abortion care, all of my patients had an overriding concern about the COVID-19 pandemic. Many worried for the safety of their parents and children; some worried about the safety of continuing a pregnancy during the pandemic; and many were worried for themselves because of the risk involved in their employment or their status as the sole breadwinner for their families. One patient chose an abortion for severe fetal anomalies diagnosed in the early second trimester; she had an appointment with a provider in Texas, which was canceled the day the Texas abortion ban was reinstated. New Mexico, more than 10 hours away, was the closest location to receive the care she needed; she traveled by car with her children.
I am fortunate to live in New Mexico. On March 24, New Mexico Secretary of Health Kathyleen “Kathy” Kunkel affirmed reproductive health care as an essential service. The American College of Obstetricians and Gynecologists, the U.S. professional organization for reproductive health care, agrees. In a joint statement with seven other professional organizations, they emphasize the importance of abortion access: “Abortion is an essential component of comprehensive health care. It is also a time-sensitive service. The consequences of being unable to obtain an abortion profoundly impact a person’s life, health, and well-being.”
Anti-abortion politicians are using the crisis as an opportunity to restrict health care access as they have done for my patients who have driven hundreds of miles for essential care they should receive in their home communities. My heart goes out to our patients and the burden they have been forced to take on at a time when our politicians should be protecting and ensuring their safety.
Dr. Espey is an obstetrician and gynecologist in New Mexico. She has no relevant financial disclosures. Dr. Espey is a member of the Ob.Gyn. News Editorial Advisory Board. Email her at [email protected].
In my New Mexico reproductive health clinic one week in early April, I saw more than twice the number of patients usually scheduled, all seeking abortion care. Two-thirds of those patients were from Texas – some came from towns as close as 6 hours away, and at least two drove for more than 11 hours to receive care at our clinic. In addition to the many reasons women pursue abortion care, all of my patients had an overriding concern about the COVID-19 pandemic. Many worried for the safety of their parents and children; some worried about the safety of continuing a pregnancy during the pandemic; and many were worried for themselves because of the risk involved in their employment or their status as the sole breadwinner for their families. One patient chose an abortion for severe fetal anomalies diagnosed in the early second trimester; she had an appointment with a provider in Texas, which was canceled the day the Texas abortion ban was reinstated. New Mexico, more than 10 hours away, was the closest location to receive the care she needed; she traveled by car with her children.
I am fortunate to live in New Mexico. On March 24, New Mexico Secretary of Health Kathyleen “Kathy” Kunkel affirmed reproductive health care as an essential service. The American College of Obstetricians and Gynecologists, the U.S. professional organization for reproductive health care, agrees. In a joint statement with seven other professional organizations, they emphasize the importance of abortion access: “Abortion is an essential component of comprehensive health care. It is also a time-sensitive service. The consequences of being unable to obtain an abortion profoundly impact a person’s life, health, and well-being.”
Anti-abortion politicians are using the crisis as an opportunity to restrict health care access as they have done for my patients who have driven hundreds of miles for essential care they should receive in their home communities. My heart goes out to our patients and the burden they have been forced to take on at a time when our politicians should be protecting and ensuring their safety.
Dr. Espey is an obstetrician and gynecologist in New Mexico. She has no relevant financial disclosures. Dr. Espey is a member of the Ob.Gyn. News Editorial Advisory Board. Email her at [email protected].
In my New Mexico reproductive health clinic one week in early April, I saw more than twice the number of patients usually scheduled, all seeking abortion care. Two-thirds of those patients were from Texas – some came from towns as close as 6 hours away, and at least two drove for more than 11 hours to receive care at our clinic. In addition to the many reasons women pursue abortion care, all of my patients had an overriding concern about the COVID-19 pandemic. Many worried for the safety of their parents and children; some worried about the safety of continuing a pregnancy during the pandemic; and many were worried for themselves because of the risk involved in their employment or their status as the sole breadwinner for their families. One patient chose an abortion for severe fetal anomalies diagnosed in the early second trimester; she had an appointment with a provider in Texas, which was canceled the day the Texas abortion ban was reinstated. New Mexico, more than 10 hours away, was the closest location to receive the care she needed; she traveled by car with her children.
I am fortunate to live in New Mexico. On March 24, New Mexico Secretary of Health Kathyleen “Kathy” Kunkel affirmed reproductive health care as an essential service. The American College of Obstetricians and Gynecologists, the U.S. professional organization for reproductive health care, agrees. In a joint statement with seven other professional organizations, they emphasize the importance of abortion access: “Abortion is an essential component of comprehensive health care. It is also a time-sensitive service. The consequences of being unable to obtain an abortion profoundly impact a person’s life, health, and well-being.”
Anti-abortion politicians are using the crisis as an opportunity to restrict health care access as they have done for my patients who have driven hundreds of miles for essential care they should receive in their home communities. My heart goes out to our patients and the burden they have been forced to take on at a time when our politicians should be protecting and ensuring their safety.
Dr. Espey is an obstetrician and gynecologist in New Mexico. She has no relevant financial disclosures. Dr. Espey is a member of the Ob.Gyn. News Editorial Advisory Board. Email her at [email protected].
Reproductive health care in the time of COVID-19
It is often said that a crisis brings out the best and worst in people, and I think we are definitely seeing that when it comes to the responses to reproductive health, family planning, and abortion care during this global pandemic.
Many national and international organizations have published strong statements of support for the importance of continuing reproductive health services. These organizations include the American College of Obstetricians and Gynecologists, American Board of Obstetrics & Gynecology, the American Society for Reproductive Medicine, the Society of Family Planning, the Society for Maternal-Fetal Medicine, Society of Family Planning, American Medical Association, the World Health Organization, and the Ethiopian Society of Obstetricians and Gynecologists. They state the obvious, which is that
We do not have complete knowledge of what the novel coronavirus 2019 does to a developing pregnancy, especially early in pregnancy. Many people who are struggling with all the uncertainty of this time – job, health, housing, food, school – may decide it is not the best moment to be adding to their family.
These concerns apply as well to the need to maintain and prioritize contraceptive services. Stay-at-home orders have put people in close quarters for long periods of time, and we are already getting reports of increased sexual intercourse, as well as increased sexual violence, both of which could result in a need for abortion if contraception is not accessible. Additionally, many women are expressing a concern for whether they will still have a job or have a job again when this first wave of the crisis passes, so they are wanting to access contraception now when they can afford to do so.
I was personally very proud of and grateful to Barbara A. Goff, MD, the chair of my department at the University of Washington, Seattle, for stating clearly in the first email she sent to faculty about canceling elective procedures and visits that family planning and abortion is not elective. My heart goes out to my colleagues and the patients who are in states that are using this opportunity to act poorly and use COVID-19 as another excuse to legislate against abortion and contraception. It demonstrates horrifying gender discrimination during a time when we should really be focusing on keeping everyone healthy.
I predict there will be an increase in the numbers of abortions after this crisis ebbs, and an increase in the numbers of term deliveries. The time to influence that is now.
Dr. Prager is professor of obstetrics and gynecology, chief of the family planning division, and director of the family planning fellowship at the University of Washington, Seattle. She also is professor of obstetrics and gynecology at St. Paul’s Hospital and Millennium Medical College in Addis Ababa, Ethiopia. Dr. Prager is a member of the Ob.Gyn. News editorial advisory board. She said she has no relevant financial disclosures. Email Dr. Prager at [email protected].
It is often said that a crisis brings out the best and worst in people, and I think we are definitely seeing that when it comes to the responses to reproductive health, family planning, and abortion care during this global pandemic.
Many national and international organizations have published strong statements of support for the importance of continuing reproductive health services. These organizations include the American College of Obstetricians and Gynecologists, American Board of Obstetrics & Gynecology, the American Society for Reproductive Medicine, the Society of Family Planning, the Society for Maternal-Fetal Medicine, Society of Family Planning, American Medical Association, the World Health Organization, and the Ethiopian Society of Obstetricians and Gynecologists. They state the obvious, which is that
We do not have complete knowledge of what the novel coronavirus 2019 does to a developing pregnancy, especially early in pregnancy. Many people who are struggling with all the uncertainty of this time – job, health, housing, food, school – may decide it is not the best moment to be adding to their family.
These concerns apply as well to the need to maintain and prioritize contraceptive services. Stay-at-home orders have put people in close quarters for long periods of time, and we are already getting reports of increased sexual intercourse, as well as increased sexual violence, both of which could result in a need for abortion if contraception is not accessible. Additionally, many women are expressing a concern for whether they will still have a job or have a job again when this first wave of the crisis passes, so they are wanting to access contraception now when they can afford to do so.
I was personally very proud of and grateful to Barbara A. Goff, MD, the chair of my department at the University of Washington, Seattle, for stating clearly in the first email she sent to faculty about canceling elective procedures and visits that family planning and abortion is not elective. My heart goes out to my colleagues and the patients who are in states that are using this opportunity to act poorly and use COVID-19 as another excuse to legislate against abortion and contraception. It demonstrates horrifying gender discrimination during a time when we should really be focusing on keeping everyone healthy.
I predict there will be an increase in the numbers of abortions after this crisis ebbs, and an increase in the numbers of term deliveries. The time to influence that is now.
Dr. Prager is professor of obstetrics and gynecology, chief of the family planning division, and director of the family planning fellowship at the University of Washington, Seattle. She also is professor of obstetrics and gynecology at St. Paul’s Hospital and Millennium Medical College in Addis Ababa, Ethiopia. Dr. Prager is a member of the Ob.Gyn. News editorial advisory board. She said she has no relevant financial disclosures. Email Dr. Prager at [email protected].
It is often said that a crisis brings out the best and worst in people, and I think we are definitely seeing that when it comes to the responses to reproductive health, family planning, and abortion care during this global pandemic.
Many national and international organizations have published strong statements of support for the importance of continuing reproductive health services. These organizations include the American College of Obstetricians and Gynecologists, American Board of Obstetrics & Gynecology, the American Society for Reproductive Medicine, the Society of Family Planning, the Society for Maternal-Fetal Medicine, Society of Family Planning, American Medical Association, the World Health Organization, and the Ethiopian Society of Obstetricians and Gynecologists. They state the obvious, which is that
We do not have complete knowledge of what the novel coronavirus 2019 does to a developing pregnancy, especially early in pregnancy. Many people who are struggling with all the uncertainty of this time – job, health, housing, food, school – may decide it is not the best moment to be adding to their family.
These concerns apply as well to the need to maintain and prioritize contraceptive services. Stay-at-home orders have put people in close quarters for long periods of time, and we are already getting reports of increased sexual intercourse, as well as increased sexual violence, both of which could result in a need for abortion if contraception is not accessible. Additionally, many women are expressing a concern for whether they will still have a job or have a job again when this first wave of the crisis passes, so they are wanting to access contraception now when they can afford to do so.
I was personally very proud of and grateful to Barbara A. Goff, MD, the chair of my department at the University of Washington, Seattle, for stating clearly in the first email she sent to faculty about canceling elective procedures and visits that family planning and abortion is not elective. My heart goes out to my colleagues and the patients who are in states that are using this opportunity to act poorly and use COVID-19 as another excuse to legislate against abortion and contraception. It demonstrates horrifying gender discrimination during a time when we should really be focusing on keeping everyone healthy.
I predict there will be an increase in the numbers of abortions after this crisis ebbs, and an increase in the numbers of term deliveries. The time to influence that is now.
Dr. Prager is professor of obstetrics and gynecology, chief of the family planning division, and director of the family planning fellowship at the University of Washington, Seattle. She also is professor of obstetrics and gynecology at St. Paul’s Hospital and Millennium Medical College in Addis Ababa, Ethiopia. Dr. Prager is a member of the Ob.Gyn. News editorial advisory board. She said she has no relevant financial disclosures. Email Dr. Prager at [email protected].
COVID-19: A guide to making telepsychiatry work
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
Changes prompted by social distancing could last beyond the pandemic
Changes prompted by social distancing could last beyond the pandemic
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
As the coronavirus pandemic persists, insurers and the federal government are making it easier for mental health professionals to deliver safe and effective psychiatric services to patients via Zoom, FaceTime, and other conferencing tools. Many psychiatrists, meanwhile, are embracing telepsychiatry for the first time – in some cases with urgency.
Jay H. Shore, MD, MPH, said in an interview that mental health providers at his medical center have gone entirely virtual in recent weeks.
“The genie is out of the bottle on this,” said Dr. Shore, director of telemedicine at the Helen and Arthur E. Johnson Depression Center and director of telemedicine programming for the department of psychiatry at the University of Colorado at Denver, Aurora. He thinks this is the beginning of a new era that will last beyond the pandemic. “There’s going to be a much wider and diffuse acceptance of telemedicine as we go forward,” he added.
Dr. Shore and several colleagues from across the country offered several tips about factors to consider while learning to use telepsychiatry as a treatment tool.
To start, Dr. Shore advised reviewing the American Psychiatric Association’s Telepsychiatry Practice Guidelines and its Telepsychiatry Toolkit, which include dozens of brief videos about topics such as room lighting and managing the content process.
Another resource is the joint APA–American Academy of Child and Adolescent Psychiatry Telepsychiatry Toolkit, said Shabana Khan, MD, an assistant professor and director of telemedicine for the department of child and adolescent psychiatry at New York University Langone Health.
One of the challenges is managing emergencies long distance. If a patient experiences a mental health emergency in a psychiatrist’s office, the clinician can call 911 or direct staff to seek help. “When they’re at their house,” said Dr. Shore, “it’s a little different.”
Staff members are not present at home offices, for example, and the patient might live in a different city and therefore have a different 911 system. “It’s important to know your protocol about how you plan to handle these emergencies before you start working with the patient,” Dr. Shore said.
Another tip is to ask staff to perform a test session to work out the technical kinks before the first patient appointment. “They can make the connection and make sure there’s a video signal with adequate quality,” Dr. Shore said. Failing to conduct a test run can lead to spending several minutes of a session trying to help patients figure out how to make video conferencing work properly.
“You can spend a lot of time acting as IT support,” he said.
It is important to ensure that virtual visits are not interrupted by technical glitches, Daniel Bristow, MD, said in an interview. If possible, hardwire your laptop or computer to an ethernet cable, said Dr. Bristow, president of the Oregon Psychiatric Physicians Association, the state’s branch of the APA. “This will lead to fewer fluctuations that you could see by using wifi,” said Dr. Bristow, who practices in Portland.
“Initially, I assumed that those with psychotic symptoms might struggle more. But I have been surprised at how well some patients have done,” said Andrew J. McLean, MD, MPH, clinical professor and chair of the department of psychiatry and behavioral science at the University of North Dakota, Grand Forks.
However, it might help to provide additional coaching to those patients, said Dr. Bristow. He offers a warning to these patients: “If you feel like you’re getting messages over the TV, my talking to you may make you feel worse.” However, “in every case, the patient was able to say, ‘I know you’re real.’ One patient even said: ‘I’ve heard these voices from my TV for years. But I know you’re a doctor, and you’re in an office trying to help me.’ ”
Dr. Shore thinks that video meetings have the potential to help psychiatrists and patients form better personal connections than in-person meetings. Patients with anxiety or PTSD, for example, “may feel safer since they’re in their own space, and they have a greater sense of control over the session than being in somebody’s office,” he said.
Dr. Khan agreed. “Some children, such as those with a significant trauma history or with significant anxiety, may feel more comfortable with this modality and may open up more during video sessions,” she said. In addition, “the distance that telepsychiatry provides may also enhance feelings of confidentiality and reduce potential stigma that may be associated with seeking mental health care.”
When it comes to using videoconferencing to treat children, take advantage of interactive features that are available, said Katherine Nguyen Williams, PhD. Zoom’s HIPAA-compliant health care software, for example, offers a “share screen” capability. “It allows for easy interactive activities,” said Dr. Nguyen Williams, director of strategic development and clinical innovation at Rady Children’s Hospital’s department of psychiatry at the University of California, San Diego. “Clinicians can play tic-tac-toe on the screen with the young patients, and they can work on cognitive-behavioral therapy worksheets together on the digital screen. Clinicians can even show a mindfulness video to the patient while actively coaching and giving feedback to the patient as they practice diaphragmatic breathing while viewing the video.
“There are so many more options for making virtual therapy as interactive as face-to-face therapy,” said Dr. Nguyen Williams, who also is an associate clinical professor at the university. “This is the key to getting and keeping the patient engaged in telepsychiatry.”
Despite the many positive aspects of using telepsychiatry as a treatment tool, some negative factors must be considered. “You lose some of the nuances, subtleties in terms of expression, movement, smell, etc.,” said Dr. McLean. “Also, there are rare instances where a part of a physical examination would be appropriate, which also is precluded.”
Videoconferencing software might allow the clinician to zoom in to take a closer look at a patient to look for subtle movements and tremors, Dr. McLean said. And, he added, he has asked nursing staff to check for particular signs and symptoms during visits and to describe them to him. “Still,” Dr. McLean said, “this does not take the place of being there.”
Dr. Shore suggested several other practical considerations. For example, while on a screen, keep the home environment as professional as the office would be, he said. Be clear with family members about the importance of not interrupting and make sure that privacy is maintained. The message should be: “I’m working from home, and I’m not available during these hours,” Dr. Shore said. “You need to be aware that, during this time, I need this for clinical work.”
Dr. Shore reported serving as chief medical officer of AccessCare Services, and receiving royalties from American Psychiatric Association Publishing and Springer. He also is coauthor with Peter Yellowlees, MD, of “Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals” (Arlington, Va.: American Psychiatric Association Publishing, 2018). Dr. Khan and Dr. McLean reported no relevant disclosures. Dr. Bristow reported relationships with MCG Health and Insight + Regroup Telehealth.
For more details about using telepsychiatry in the time of COVID-19, listen to the April 8 Psychcast Masterclass lecture by Dr. Shore.
Cardiology groups push back on hydroxychloroquine, azithromycin for COVID-19
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
The .
“Hydroxychloroquine and azithromycin have been touted for potential prophylaxis or treatment for COVID-19; both drugs are listed as definite causes of torsade de pointes” and increase in the risk of other arrhythmias and sudden death, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society said in a joint statement April 8 in Circulation.
The statement came amid ongoing promotion by the Trump administration of hydroxychloroquine, in particular, for COVID-19 despite lack of strong data.
In addition to underlying cardiovascular disease, “seriously ill patients often have comorbidities that can increase risk of serious arrhythmias,” including hypokalemia, hypomagnesemia, fever, and systemic inflammation, the groups said.
They recommended withholding the drugs in patients with baseline QT prolongation (e.g., QTc of at least 500 msec) or with known congenital long QT syndrome; monitoring cardiac rhythm and QT interval and withdrawing hydroxychloroquine and azithromycin if QTc exceeds 500 msec; correcting hypokalemia to levels greater than 4 mEq/L and hypomagnesemia to more than 2 mg/dL; and avoiding other QTc-prolonging agents when possible.
The groups noted that, “in patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible.” There is also a possible compounding arrhythmic effect when hydroxychloroquine and azithromycin are used together, but that has not been studied.
There’s a known risk of torsade de pointes with chloroquine and a possible risk with the antiviral HIV combination drug lopinavir-ritonavir, two other candidates for COVID-19 treatment. Hydroxychloroquine and chloroquine, both antimalarials, might help prevent or treat infection by interfering with angiotensin-converting enzyme 2 receptors, which the COVID-19 virus uses for cell entry, the groups said.
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” Robert A. Harrington, MD, AHA president and chair of the department of medicine at Stanford (Calif.) University, emphasized in a press release.
SOURCE: Roden DM et al. Circulation. 2020 Apr 8. doi:10.1161/CIRCULATIONAHA.120.047521.
COVID-19: Dramatic changes to telepsychiatry rules and regs
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
In the wake of the coronavirus pandemic,
Under the 1135 emergency waiver, Medicare has expanded telehealth services to include patients across the country – not just in rural areas or under other limited conditions, as was previously the case. In addition, there’s now a waiver to the Ryan Haight Act that allows the prescribing of controlled substances via telemedicine.
Peter Yellowlees, MD, from University of California, Davis, reported that outpatient service at his center was converted to an almost 100% telepsychiatry service from mid- to late March.
He and John Torous, MD, director of digital psychiatry at Beth Israel Deaconess Medical Center, Boston, led a free webinar late last month sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA).
During the hour-long event, they answered questions and offered tips on changes in licensure, patient safety, new prescribing rules, and equipment needed.
“Clinicians need to be aware of these changes so they can ensure they are reaching as many people as possible and taking advantage of the reduced barriers to offering safe and effective video visits,” Dr. Torous said in an interview.
‘This is huge’
The new 1135 waiver “basically says CMS will pay for any patient on Medicare who is seen by video by any provider who is correctly licensed in any state in this country,” Dr. Yellowlees told webinar attendees.
“You don’t need to be licensed in the state where the patient is if the patient is on Medicare. This opens up a huge number of patients we can now see on video,” he said. “And you can bill at normal Medicare rates for whatever you normally get for your in-person patients.”
Although this temporary rule only applies to Medicare and not to private insurers, or to patients on Medicaid, “these are really big changes. This is huge,” Dr. Torous said.
Previously, the “originating site” rule stated that, for the most part, clinicians had to be licensed in the state where the patient was located and not where the physician was stationed.
Asked about college students receiving mental health care who were in school in the psychiatrist’s area but are now back home in a state where the clinician doesn’t have a license, Dr. Yellowlees said that scenario could be a bit “tricky.”
“Most of those patients probably aren’t on Medicare. Legally, you [usually] can’t see them on video if they have private insurance or Medicaid. So, hopefully you can give them a 3-month supply of medication and then recommend they see a local provider,” he said.
Still, all states have their own rules, Dr. Yellowlees said. He and Dr. Torous noted that the Federation of State Medical Boards has a “very up-to-date” listing of policies at FSMB.org, all of which are organized by state. In addition, the American Psychiatric Association provides a telepsychiatry toolkit on its website.
Ryan Haight Act and prescribing
Physicians are now permitted to prescribe medication to patients assessed via telemedicine.
For those with substance use disorders, the U.S. Drug Enforcement Administration has announced a new waiver for the Ryan Haight Online Pharmacy Consumer Protection Act.
The waiver states that “practitioners in all areas of the United States may issue prescriptions for all schedule II-V controlled substances” – as long as it’s for a legitimate medical purpose; real-time, two-way interactive communication with patients has been used; and the clinician “is acting in accordance with applicable Federal and State laws.”
“It’s now possible to prescribe all the normal psychiatric drugs but also benzodiazepines, stimulants, and potentially narcotics over telepsychiatry,” even at a first visit via video, Dr. Yellowlees said.
However, he noted at this point the waiver is current for only 60 days. “This isn’t a permanent condition. It could be extended or even shortened at any given time.”
In addition, SAMHSA has relaxed some of its own regulations regarding telehealth and opioid treatment programs. An FAQ section on the organization’s website provides guidance for providing methadone and buprenorphine treatment.
“Some of the previous regulations will probably be put back in place later on, but the new changes are helpful now,” Dr. Yellowlees said.
Simple equipment needed
Regarding equipment, Dr. Yellowlees noted that the most important component is just a laptop, tablet, or smartphone – for the clinician and for the patient.
“You don’t need fancy new technology with a separate camera or microphone,” he said. However, it might be worth investing in a little better system down the line, he added.
Simple platforms that can be used to meet virtually with patients include FaceTime, Google Hangouts, and Skype.
Although some of these (such as FaceTime) are not HIPAA compliant, “that’s okay for now” under the new rules, Dr. Yellowlees said. While the health system/commercial version of Skype is compliant, the normal consumer-downloaded version is not, he noted.
“I would still strongly suggest using HIPAA-compliant video-conferencing programs in the long run,” he added.
Either way, it’s important for various safety practices to be put into place. For example, clinicians should be careful because the consumer version of Skype can show names of patients who were previously spoken with.
A business associate agreement (BAA) is something that HIPAA-compliant video systems will offer and which should be signed. It’s an agreement that “you’ll be, essentially, looking through a tunnel at the persona at the other end, and the company cannot get inside the tunnel and watch you while you’re having your interview,” said Dr. Yellowlees.
“There are multiple videoconferencing systems around that you can use,” he added. “The three major ones are from Zoom, Vidyo, and VSee, but there are probably 40 or 50 more.”
“There are a lot out there, and we’re certainly not endorsing any one of them,” Dr. Torous added.
When evaluating potential programs, Dr. Yellowlees suggested looking at Yelp-style reviews or telemedicine review sites, or talk with colleagues.
“Basically, you want systems that offer high-definition video quality and the ability to ‘lock’ and ‘unlock’ the rooms. And you want it to have an app so mobile devices can use it,” he said.
Phone vs. video
Some patients, especially older ones, may be resistant to the idea of video chats, preferring to talk via telephone instead.
“If you can use video, it’s better to do that if you can, especially when setting up the systems are relatively simple,” Dr. Yellowlees said, adding that it might just be an issue of patients needing help to get started.
However, “for some people, this is a barrier that we have to respect,” Dr. Torous said.
Either way, clinicians should check the American Medical Association’s website for information about coding for both video and phone visits.
Asked whether a clinician needs written consent from patients for conducting telepsychiatry visits, Dr. Yellowlees said it’s important to check state-by-state rules. For example, California allows a verbal consent.
In many cases, “simply jot down a note that consent was given and how” and write down the address where the patient is located at time of visit, such as for their home, he said.
If a patient wants to conduct a telehealth session while in their car, Dr. Yellowlees suggested getting the address of the parking lot. For safety, clinicians also are advised asking for the cell phone number of the patient as well as that of a loved one.
Vital signs
When it comes to checking vital signs, Dr. Yellowlees suggested asking patients to purchase an inexpensive blood pressure (BP) monitor, thermometer, etc, prior to an appointment.
“Ask them to do a BP test on video and show you the readings. For the AIMS [Abnormal Involuntary Movement Scale] test, or to check for tardive dyskinesia, instruct patients to come close to the camera to show movement.”
In addition, most psychiatric rating scales are available online, which patients can fill out before a telehealth visit. The Serious Mental Illness (SMI) Adviser mobile app also includes several of these scales, Dr. Torous noted.
Overall, “there have been dramatic changes in the rules and regulations governing [telepsychiatry] that, for the next 60 days, make it easier to offer telehealth to patients,” Dr. Torous said.
Therefore, all psychiatrists need to “get on board,” as soon as possible, Dr. Yellowlees added.
The webinar was funded in part by a grant from SAMHSA.
A version of this article originally appeared on Medscape.com.
Frailty indexes fail in sorting elderly MM patients
Despite the perceived benefits of their use in guiding treatment, frailty indexes were not reliable in differentiating elderly multiple myeloma (MM) patients, according to an analysis of a prospective cohort of 40 patients studied at a single institution.
The researchers examined three different models of frailty using data available in the Cancer and Aging Research Group tool to define frailty in their cohort: the international myeloma working group (IMWG) frailty model, the revised myeloma comorbidity index (R-MCI), and the Carolina Frailty Index (CFI).
The researchers found that, for their same population, applying the IMWG frailty index yielded 3 (7.5%) patients categorized as fit, 15 (37.5%) categorized as intermediate fit, and 22 (55%) categorized as frail. The R-MCI yielded 4 (10%) patients categorized as fit, 29 (72.5%) as intermediate, and 7 (17.5%) as frail. When using the CFI, 17 (42.5%) patients were categorized as fit, 8 (20%) were intermediate, and 15 (37.5%) were frail. Of particular note, among 28 patients categorized as frail by at least one of the three indexes, only 3 (11%) patients were categorized as frail by all three models.
The reasons for the differences were discussed by the authors, who pointed out that patients categorized as frail by the IMWG or R-MCI tended to be older than those categorized as frail by CFI, reflecting the fact that the IMWG and R-MCI both include age as a component of frailty, while the CFI does not. In addition, each index incorporates comorbidities into its assessment of frailty in a different way.
For example, falls and depression are incorporated as components of the CFI, reflected in the higher proportion of patients reporting a prior fall and more symptoms of depression in the group categorized as frail by the CFI model than in the IMWG or R-MCI. In the CFI as well, each of the individual instrumental activities of daily living is a component of the model, rather than the summary score, as in the IMWG and R-MCI.
“Our findings highlight the differences in currently available approaches to applying the concept of frailty to older adults with cancer. This problem is not unique to oncology, as there is a continued lack of consensus on defining the concept of frailty in the general geriatric population,” the researchers stated. “Further studies are needed to establish the role of frailty indexes in predicting toxicity of therapy and other outcomes of importance in older adults with multiple myeloma,” they concluded.
The study was funded by the National Cancer Institute and other U.S. government agencies. The authors reported having no conflicts.
SOURCE: Isaacs A et al. J Geriat Onc. 2020;11(2):311-15.
Despite the perceived benefits of their use in guiding treatment, frailty indexes were not reliable in differentiating elderly multiple myeloma (MM) patients, according to an analysis of a prospective cohort of 40 patients studied at a single institution.
The researchers examined three different models of frailty using data available in the Cancer and Aging Research Group tool to define frailty in their cohort: the international myeloma working group (IMWG) frailty model, the revised myeloma comorbidity index (R-MCI), and the Carolina Frailty Index (CFI).
The researchers found that, for their same population, applying the IMWG frailty index yielded 3 (7.5%) patients categorized as fit, 15 (37.5%) categorized as intermediate fit, and 22 (55%) categorized as frail. The R-MCI yielded 4 (10%) patients categorized as fit, 29 (72.5%) as intermediate, and 7 (17.5%) as frail. When using the CFI, 17 (42.5%) patients were categorized as fit, 8 (20%) were intermediate, and 15 (37.5%) were frail. Of particular note, among 28 patients categorized as frail by at least one of the three indexes, only 3 (11%) patients were categorized as frail by all three models.
The reasons for the differences were discussed by the authors, who pointed out that patients categorized as frail by the IMWG or R-MCI tended to be older than those categorized as frail by CFI, reflecting the fact that the IMWG and R-MCI both include age as a component of frailty, while the CFI does not. In addition, each index incorporates comorbidities into its assessment of frailty in a different way.
For example, falls and depression are incorporated as components of the CFI, reflected in the higher proportion of patients reporting a prior fall and more symptoms of depression in the group categorized as frail by the CFI model than in the IMWG or R-MCI. In the CFI as well, each of the individual instrumental activities of daily living is a component of the model, rather than the summary score, as in the IMWG and R-MCI.
“Our findings highlight the differences in currently available approaches to applying the concept of frailty to older adults with cancer. This problem is not unique to oncology, as there is a continued lack of consensus on defining the concept of frailty in the general geriatric population,” the researchers stated. “Further studies are needed to establish the role of frailty indexes in predicting toxicity of therapy and other outcomes of importance in older adults with multiple myeloma,” they concluded.
The study was funded by the National Cancer Institute and other U.S. government agencies. The authors reported having no conflicts.
SOURCE: Isaacs A et al. J Geriat Onc. 2020;11(2):311-15.
Despite the perceived benefits of their use in guiding treatment, frailty indexes were not reliable in differentiating elderly multiple myeloma (MM) patients, according to an analysis of a prospective cohort of 40 patients studied at a single institution.
The researchers examined three different models of frailty using data available in the Cancer and Aging Research Group tool to define frailty in their cohort: the international myeloma working group (IMWG) frailty model, the revised myeloma comorbidity index (R-MCI), and the Carolina Frailty Index (CFI).
The researchers found that, for their same population, applying the IMWG frailty index yielded 3 (7.5%) patients categorized as fit, 15 (37.5%) categorized as intermediate fit, and 22 (55%) categorized as frail. The R-MCI yielded 4 (10%) patients categorized as fit, 29 (72.5%) as intermediate, and 7 (17.5%) as frail. When using the CFI, 17 (42.5%) patients were categorized as fit, 8 (20%) were intermediate, and 15 (37.5%) were frail. Of particular note, among 28 patients categorized as frail by at least one of the three indexes, only 3 (11%) patients were categorized as frail by all three models.
The reasons for the differences were discussed by the authors, who pointed out that patients categorized as frail by the IMWG or R-MCI tended to be older than those categorized as frail by CFI, reflecting the fact that the IMWG and R-MCI both include age as a component of frailty, while the CFI does not. In addition, each index incorporates comorbidities into its assessment of frailty in a different way.
For example, falls and depression are incorporated as components of the CFI, reflected in the higher proportion of patients reporting a prior fall and more symptoms of depression in the group categorized as frail by the CFI model than in the IMWG or R-MCI. In the CFI as well, each of the individual instrumental activities of daily living is a component of the model, rather than the summary score, as in the IMWG and R-MCI.
“Our findings highlight the differences in currently available approaches to applying the concept of frailty to older adults with cancer. This problem is not unique to oncology, as there is a continued lack of consensus on defining the concept of frailty in the general geriatric population,” the researchers stated. “Further studies are needed to establish the role of frailty indexes in predicting toxicity of therapy and other outcomes of importance in older adults with multiple myeloma,” they concluded.
The study was funded by the National Cancer Institute and other U.S. government agencies. The authors reported having no conflicts.
SOURCE: Isaacs A et al. J Geriat Onc. 2020;11(2):311-15.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
Key clinical point:
Major finding: Although 28 multiple myeloma patients were deemed frail by at least one model, only 3 patients were deemed frail by all three models.
Study details: A total of 40 adults aged 65 years and over with MM were assessed by three frailty indexes.
Disclosures: The study was funded by the National Cancer Institute and other U.S. government agencies. The authors reported having no conflicts.
Source: Isaacs A et al. J Geriat Onc. 2020;11(2):311-5.
Comorbidities the rule in New York’s COVID-19 deaths
In New York state, just over 86% of reported COVID-19 deaths involved at least one comorbidity, according to the state’s department of health.
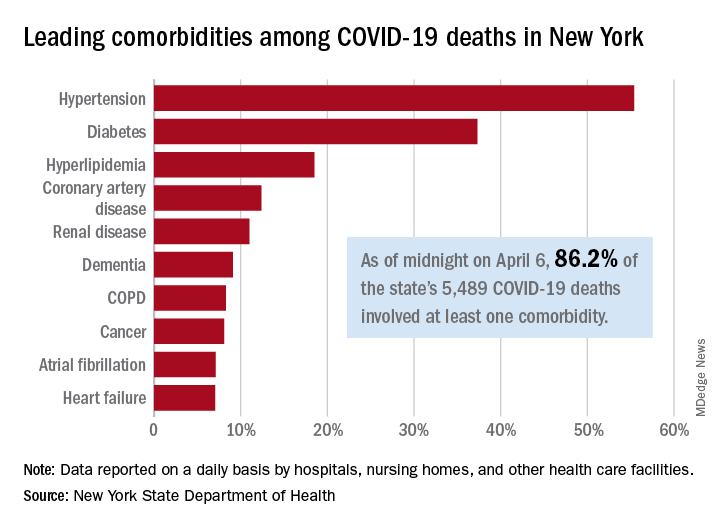
As of midnight on April 6, there had been 5,489 fatalities caused by COVID-19 in the state, of which 86.2% (4,732) had at least one underlying condition, the New York State Department of Health reported April 7 on its COVID-19 tracker.
The leading comorbidity, seen in 55.4% of all deaths, was hypertension. In comparison, a recent estimate from the U.S. Department of Health & Human Services put the prevalence of high blood pressure at about 45% in the overall adult population.
In New York, the rest of the 10 most common comorbidities in COVID-19 fatalities were diabetes (37.3%), hyperlipidemia (18.5%), coronary artery disease (12.4%), renal disease (11.0%), dementia (9.1%), chronic obstructive pulmonary disease (8.3%), cancer (8.1%), atrial fibrillation (7.1%), and heart failure (7.1%), the NYSDOH said.
Other data on the tracker site show that 63% of all deaths involved a patient who was aged 70 years or older and that 61% of COVID-19 patients who have died in New York were male and 38.8% were female (sex unknown for 0.2%). Among all individuals who have tested positive, 54.8% were male and 44.6% were female (sex unknown for 0.6%).
As of the end of day on April 6, a total of 340,058 persons had been tested in the state and 40.8% (138,863) were positive for the SARS-CoV-2 virus. By county, the highest positive rates are in New York City: Queens at 57.4%, Brooklyn at 52.4%, and the Bronx at 52.3%, according to the NYSDOH.
In New York state, just over 86% of reported COVID-19 deaths involved at least one comorbidity, according to the state’s department of health.
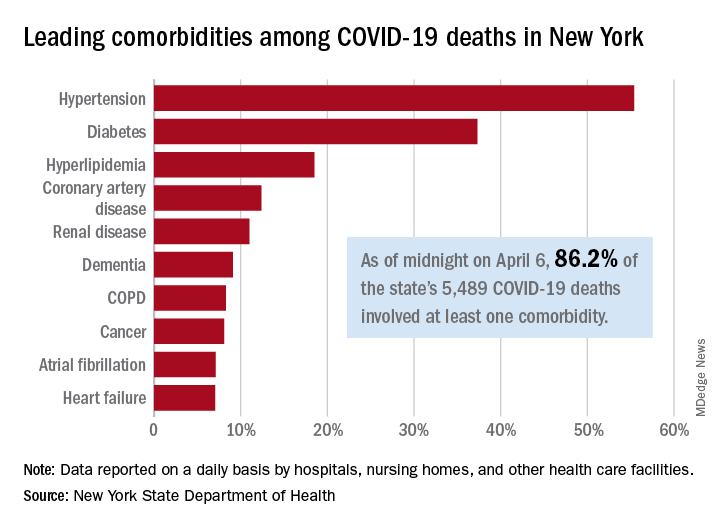
As of midnight on April 6, there had been 5,489 fatalities caused by COVID-19 in the state, of which 86.2% (4,732) had at least one underlying condition, the New York State Department of Health reported April 7 on its COVID-19 tracker.
The leading comorbidity, seen in 55.4% of all deaths, was hypertension. In comparison, a recent estimate from the U.S. Department of Health & Human Services put the prevalence of high blood pressure at about 45% in the overall adult population.
In New York, the rest of the 10 most common comorbidities in COVID-19 fatalities were diabetes (37.3%), hyperlipidemia (18.5%), coronary artery disease (12.4%), renal disease (11.0%), dementia (9.1%), chronic obstructive pulmonary disease (8.3%), cancer (8.1%), atrial fibrillation (7.1%), and heart failure (7.1%), the NYSDOH said.
Other data on the tracker site show that 63% of all deaths involved a patient who was aged 70 years or older and that 61% of COVID-19 patients who have died in New York were male and 38.8% were female (sex unknown for 0.2%). Among all individuals who have tested positive, 54.8% were male and 44.6% were female (sex unknown for 0.6%).
As of the end of day on April 6, a total of 340,058 persons had been tested in the state and 40.8% (138,863) were positive for the SARS-CoV-2 virus. By county, the highest positive rates are in New York City: Queens at 57.4%, Brooklyn at 52.4%, and the Bronx at 52.3%, according to the NYSDOH.
In New York state, just over 86% of reported COVID-19 deaths involved at least one comorbidity, according to the state’s department of health.
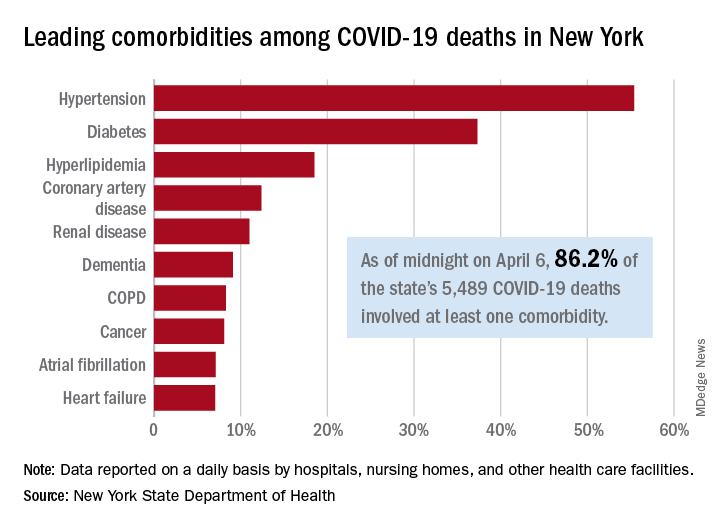
As of midnight on April 6, there had been 5,489 fatalities caused by COVID-19 in the state, of which 86.2% (4,732) had at least one underlying condition, the New York State Department of Health reported April 7 on its COVID-19 tracker.
The leading comorbidity, seen in 55.4% of all deaths, was hypertension. In comparison, a recent estimate from the U.S. Department of Health & Human Services put the prevalence of high blood pressure at about 45% in the overall adult population.
In New York, the rest of the 10 most common comorbidities in COVID-19 fatalities were diabetes (37.3%), hyperlipidemia (18.5%), coronary artery disease (12.4%), renal disease (11.0%), dementia (9.1%), chronic obstructive pulmonary disease (8.3%), cancer (8.1%), atrial fibrillation (7.1%), and heart failure (7.1%), the NYSDOH said.
Other data on the tracker site show that 63% of all deaths involved a patient who was aged 70 years or older and that 61% of COVID-19 patients who have died in New York were male and 38.8% were female (sex unknown for 0.2%). Among all individuals who have tested positive, 54.8% were male and 44.6% were female (sex unknown for 0.6%).
As of the end of day on April 6, a total of 340,058 persons had been tested in the state and 40.8% (138,863) were positive for the SARS-CoV-2 virus. By county, the highest positive rates are in New York City: Queens at 57.4%, Brooklyn at 52.4%, and the Bronx at 52.3%, according to the NYSDOH.
National Watchman registry reports impressive procedural safety
Early results from the massive National Cardiovascular Data Registry Left Atrial Appendage Occlusion Registry indicate that the rollout of the Watchman device into routine clinical practice is going smoothly, with a higher implant success rate and a substantially lower in-hospital complication rate than that seen in the pivotal randomized clinical trials, James V. Freeman, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
These real-world results are particularly impressive because the 38,158 registry participants were on average significantly older and sicker than were patients in the clinical trials. They were at higher risk of both stroke and bleeding, yet they fared better in terms of procedural safety, observed Dr. Freeman, an electrophysiologist and director of the Yale University Atrial Fibrillation Center in New Haven, Conn.
“You always worry that once you get outside of the clinical trials setting and you roll out to a large number of centers, including some that are relatively low volume, that you’re going to start to see higher rates of complications. And overall, broadly speaking, the rates of adverse events were quite reassuring,” he said.
The registry, maintained by the ACC, serves as the postmarketing surveillance tool mandated by the Food and Drug Administration and Centers for Medicare & Medicaid Services. The 38,158 participants make this registry the world’s largest patient experience with the Watchman device by many orders of magnitude. Dr. Freeman’s report included patients enrolled during 2016-2018 who were treated at 495 hospitals by 1,318 physician interventionalists. CMS reimbursement requires participation in the registry, which captures more than 95% of all Watchman procedures done in the United States. Although Dr. Freeman presented only the acute in-hospital outcomes, active follow-up for adverse events and medical therapy will be conducted at 45 days, 6 months, and 1 and 2 years.
Participants in the Left Atrial Appendage Occlusion (LAAO) Registry averaged 76.1 years of age, which is 2-4 years older than patients in the pivotal PROTECT-AF and PREVAIL trials or the 1,025-patient EWOLUTION registry. The LAAO Registry participants had a mean CHA2DS2-VASc score of 4.6, compared with 3.4 in PROTECT-AF and 3.8 in PREVAIL. Their mean HAS BLED score was 3.0. Thirty percent had a prior ischemic stroke or transient ischemic attack, 12% had a prior intracranial hemorrhage, and 69% had a history of clinically relevant bleeding. Thirty percent had heart failure, 92% were hypertensive, and 30% had diabetes.
“The take home here is that these patients were at moderate to high risk of stroke and they also carried a high risk of bleeding and therefore had some relative contraindication to anticoagulation,” according to the cardiologist. “The patient population overall is really in accordance with the CMS guidance. We’re not seeing a lot of patients who are getting this device for a lifestyle indication. Most of these patients are really stuck between a rock and a hard place.”
Most hospitals offering the Watchman did 10-40 cases per year. The median annual physician volume was 12 cases. However, there was substantial variation in both hospital and physician volumes.
The device was deployed in 93% of procedures attempted; roughly half of cancellations were cause by LAAO thrombus detected on the day of the procedure. The acute procedural success rate when the device was deployed was 98.3%, compared with 90.9% in PROTECT-AF and 95.1% in PREVAIL. The rate of device margin residual leak of 5 mm or more among registry participants with an acutely successful procedure was 0.2%.
The rate of any major in-hospital complication in the LAAO Registry was 2.16%, the most common of which was pericardial effusion requiring intervention, which occurred in 1.39% of cases. The major bleeding rate was 1.25%. The stroke/transient ischemic attack rate was 0.17%. Systemic arterial embolism was a rare event, occurring in less than 0.01% of patients, as was acute MI, with an incidence of 0.04%. Device embolization occurred in 0.07% of patients.
By comparison, the 7-day rate of pericardial effusion requiring intervention was 4.0% in PROTECT-AF and 1.9% in PREVAIL, with procedure-related stroke rates of 1.1% and 0.7%, respectively, and device embolization rates of 0.4% and 0.7%. The major bleeding rate in PROTECT-AF was 3.5%, nearly triple that in the real-world registry.
Discussant Mark A. Estes, MD, characterized the acute outcomes in the LAAO Registry as “an improvement – a considerable improvement – over some of the early data in PREVAIL and PROTECT-AF.” He credited this to the “very robust validation procedure” the Watchman closure device has undergone, which included the clinical trials, regulatory requirements for training and patient selection, and mandatory reporting of outcomes in the registry.
He noted that a lot is happening now with the Watchman device. There are a couple of dozen prospective clinical trials, including one on the Watchman versus direct oral anticoagulant (DOAC) therapy and another on left atrial ablation plus left atrial appendage closure versus a DOAC. A new-generation Watchman device, the Watchman FLX, is approved in Europe and undergoing an ongoing FDA-mandated approval trial in the United States.
“It has a lot of technical advantages,” according to Dr. Estes, an electrophysiologist and professor of medicine at the University of Pittsburgh.
Current guidelines give LAAO a class IIb rating, meaning it “could be considered” in patients with atrial fibrillation at increased risk of stroke who have a contraindication to long-term anticoagulation. Dr. Estes asked: Does the LAAO Registry data warrant a rating upgrade to a stronger recommendation?
Dr. Freeman replied that the new data should allay the guideline writers’ and government regulators’ concerns regarding acute procedural safety. But that’s only part of the picture. He and his coinvestigators are busy gathering data on intermediate-term outcomes, analyzing the impact of various strategies for periprocedural and long-term management of antiplatelet and anticoagulant medications with an eye toward identifying best practices, and investigating the relationship between procedural volume and outcomes, information, which could have an impact on the next iteration of the guidelines.
Simultaneous with his presentation at ACC 2020, the study was published online (J Am Coll Cardiol. 2020 Mar 13;75[13]1503-18).
In an accompanying editorial, Dhanunjaya Lakkireddy, MD, commented that an important contribution of the LAAO Registry is its inclusion of an enormous number of patients with contraindications to oral anticoagulation, a population excluded from the PROTECT-AF and PREVAIL randomized trials.
The short-term results of the registry suggest a relaxation of the current strict requirement for surgical backup during Watchman procedures is in order, added Dr. Lakkireddy, professor of medicine at the University of Missouri, Columbia, and medical director of the Kansas City Heart Rhythm Institute (J Am Coll Cardiol. 2020 Mar 13;75[13]:1519-22).
Dr. Freeman reported serving as a consultant to Boston Scientific, which markets the Watchman, as well as to Medtronic, Janssen, and Biosense Webster.
SOURCE: Freeman JF. ACC 2020, Abstract 409-10.
Early results from the massive National Cardiovascular Data Registry Left Atrial Appendage Occlusion Registry indicate that the rollout of the Watchman device into routine clinical practice is going smoothly, with a higher implant success rate and a substantially lower in-hospital complication rate than that seen in the pivotal randomized clinical trials, James V. Freeman, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
These real-world results are particularly impressive because the 38,158 registry participants were on average significantly older and sicker than were patients in the clinical trials. They were at higher risk of both stroke and bleeding, yet they fared better in terms of procedural safety, observed Dr. Freeman, an electrophysiologist and director of the Yale University Atrial Fibrillation Center in New Haven, Conn.
“You always worry that once you get outside of the clinical trials setting and you roll out to a large number of centers, including some that are relatively low volume, that you’re going to start to see higher rates of complications. And overall, broadly speaking, the rates of adverse events were quite reassuring,” he said.
The registry, maintained by the ACC, serves as the postmarketing surveillance tool mandated by the Food and Drug Administration and Centers for Medicare & Medicaid Services. The 38,158 participants make this registry the world’s largest patient experience with the Watchman device by many orders of magnitude. Dr. Freeman’s report included patients enrolled during 2016-2018 who were treated at 495 hospitals by 1,318 physician interventionalists. CMS reimbursement requires participation in the registry, which captures more than 95% of all Watchman procedures done in the United States. Although Dr. Freeman presented only the acute in-hospital outcomes, active follow-up for adverse events and medical therapy will be conducted at 45 days, 6 months, and 1 and 2 years.
Participants in the Left Atrial Appendage Occlusion (LAAO) Registry averaged 76.1 years of age, which is 2-4 years older than patients in the pivotal PROTECT-AF and PREVAIL trials or the 1,025-patient EWOLUTION registry. The LAAO Registry participants had a mean CHA2DS2-VASc score of 4.6, compared with 3.4 in PROTECT-AF and 3.8 in PREVAIL. Their mean HAS BLED score was 3.0. Thirty percent had a prior ischemic stroke or transient ischemic attack, 12% had a prior intracranial hemorrhage, and 69% had a history of clinically relevant bleeding. Thirty percent had heart failure, 92% were hypertensive, and 30% had diabetes.
“The take home here is that these patients were at moderate to high risk of stroke and they also carried a high risk of bleeding and therefore had some relative contraindication to anticoagulation,” according to the cardiologist. “The patient population overall is really in accordance with the CMS guidance. We’re not seeing a lot of patients who are getting this device for a lifestyle indication. Most of these patients are really stuck between a rock and a hard place.”
Most hospitals offering the Watchman did 10-40 cases per year. The median annual physician volume was 12 cases. However, there was substantial variation in both hospital and physician volumes.
The device was deployed in 93% of procedures attempted; roughly half of cancellations were cause by LAAO thrombus detected on the day of the procedure. The acute procedural success rate when the device was deployed was 98.3%, compared with 90.9% in PROTECT-AF and 95.1% in PREVAIL. The rate of device margin residual leak of 5 mm or more among registry participants with an acutely successful procedure was 0.2%.
The rate of any major in-hospital complication in the LAAO Registry was 2.16%, the most common of which was pericardial effusion requiring intervention, which occurred in 1.39% of cases. The major bleeding rate was 1.25%. The stroke/transient ischemic attack rate was 0.17%. Systemic arterial embolism was a rare event, occurring in less than 0.01% of patients, as was acute MI, with an incidence of 0.04%. Device embolization occurred in 0.07% of patients.
By comparison, the 7-day rate of pericardial effusion requiring intervention was 4.0% in PROTECT-AF and 1.9% in PREVAIL, with procedure-related stroke rates of 1.1% and 0.7%, respectively, and device embolization rates of 0.4% and 0.7%. The major bleeding rate in PROTECT-AF was 3.5%, nearly triple that in the real-world registry.
Discussant Mark A. Estes, MD, characterized the acute outcomes in the LAAO Registry as “an improvement – a considerable improvement – over some of the early data in PREVAIL and PROTECT-AF.” He credited this to the “very robust validation procedure” the Watchman closure device has undergone, which included the clinical trials, regulatory requirements for training and patient selection, and mandatory reporting of outcomes in the registry.
He noted that a lot is happening now with the Watchman device. There are a couple of dozen prospective clinical trials, including one on the Watchman versus direct oral anticoagulant (DOAC) therapy and another on left atrial ablation plus left atrial appendage closure versus a DOAC. A new-generation Watchman device, the Watchman FLX, is approved in Europe and undergoing an ongoing FDA-mandated approval trial in the United States.
“It has a lot of technical advantages,” according to Dr. Estes, an electrophysiologist and professor of medicine at the University of Pittsburgh.
Current guidelines give LAAO a class IIb rating, meaning it “could be considered” in patients with atrial fibrillation at increased risk of stroke who have a contraindication to long-term anticoagulation. Dr. Estes asked: Does the LAAO Registry data warrant a rating upgrade to a stronger recommendation?
Dr. Freeman replied that the new data should allay the guideline writers’ and government regulators’ concerns regarding acute procedural safety. But that’s only part of the picture. He and his coinvestigators are busy gathering data on intermediate-term outcomes, analyzing the impact of various strategies for periprocedural and long-term management of antiplatelet and anticoagulant medications with an eye toward identifying best practices, and investigating the relationship between procedural volume and outcomes, information, which could have an impact on the next iteration of the guidelines.
Simultaneous with his presentation at ACC 2020, the study was published online (J Am Coll Cardiol. 2020 Mar 13;75[13]1503-18).
In an accompanying editorial, Dhanunjaya Lakkireddy, MD, commented that an important contribution of the LAAO Registry is its inclusion of an enormous number of patients with contraindications to oral anticoagulation, a population excluded from the PROTECT-AF and PREVAIL randomized trials.
The short-term results of the registry suggest a relaxation of the current strict requirement for surgical backup during Watchman procedures is in order, added Dr. Lakkireddy, professor of medicine at the University of Missouri, Columbia, and medical director of the Kansas City Heart Rhythm Institute (J Am Coll Cardiol. 2020 Mar 13;75[13]:1519-22).
Dr. Freeman reported serving as a consultant to Boston Scientific, which markets the Watchman, as well as to Medtronic, Janssen, and Biosense Webster.
SOURCE: Freeman JF. ACC 2020, Abstract 409-10.
Early results from the massive National Cardiovascular Data Registry Left Atrial Appendage Occlusion Registry indicate that the rollout of the Watchman device into routine clinical practice is going smoothly, with a higher implant success rate and a substantially lower in-hospital complication rate than that seen in the pivotal randomized clinical trials, James V. Freeman, MD, reported at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The meeting was conducted online after its cancellation because of the COVID-19 pandemic.
These real-world results are particularly impressive because the 38,158 registry participants were on average significantly older and sicker than were patients in the clinical trials. They were at higher risk of both stroke and bleeding, yet they fared better in terms of procedural safety, observed Dr. Freeman, an electrophysiologist and director of the Yale University Atrial Fibrillation Center in New Haven, Conn.
“You always worry that once you get outside of the clinical trials setting and you roll out to a large number of centers, including some that are relatively low volume, that you’re going to start to see higher rates of complications. And overall, broadly speaking, the rates of adverse events were quite reassuring,” he said.
The registry, maintained by the ACC, serves as the postmarketing surveillance tool mandated by the Food and Drug Administration and Centers for Medicare & Medicaid Services. The 38,158 participants make this registry the world’s largest patient experience with the Watchman device by many orders of magnitude. Dr. Freeman’s report included patients enrolled during 2016-2018 who were treated at 495 hospitals by 1,318 physician interventionalists. CMS reimbursement requires participation in the registry, which captures more than 95% of all Watchman procedures done in the United States. Although Dr. Freeman presented only the acute in-hospital outcomes, active follow-up for adverse events and medical therapy will be conducted at 45 days, 6 months, and 1 and 2 years.
Participants in the Left Atrial Appendage Occlusion (LAAO) Registry averaged 76.1 years of age, which is 2-4 years older than patients in the pivotal PROTECT-AF and PREVAIL trials or the 1,025-patient EWOLUTION registry. The LAAO Registry participants had a mean CHA2DS2-VASc score of 4.6, compared with 3.4 in PROTECT-AF and 3.8 in PREVAIL. Their mean HAS BLED score was 3.0. Thirty percent had a prior ischemic stroke or transient ischemic attack, 12% had a prior intracranial hemorrhage, and 69% had a history of clinically relevant bleeding. Thirty percent had heart failure, 92% were hypertensive, and 30% had diabetes.
“The take home here is that these patients were at moderate to high risk of stroke and they also carried a high risk of bleeding and therefore had some relative contraindication to anticoagulation,” according to the cardiologist. “The patient population overall is really in accordance with the CMS guidance. We’re not seeing a lot of patients who are getting this device for a lifestyle indication. Most of these patients are really stuck between a rock and a hard place.”
Most hospitals offering the Watchman did 10-40 cases per year. The median annual physician volume was 12 cases. However, there was substantial variation in both hospital and physician volumes.
The device was deployed in 93% of procedures attempted; roughly half of cancellations were cause by LAAO thrombus detected on the day of the procedure. The acute procedural success rate when the device was deployed was 98.3%, compared with 90.9% in PROTECT-AF and 95.1% in PREVAIL. The rate of device margin residual leak of 5 mm or more among registry participants with an acutely successful procedure was 0.2%.
The rate of any major in-hospital complication in the LAAO Registry was 2.16%, the most common of which was pericardial effusion requiring intervention, which occurred in 1.39% of cases. The major bleeding rate was 1.25%. The stroke/transient ischemic attack rate was 0.17%. Systemic arterial embolism was a rare event, occurring in less than 0.01% of patients, as was acute MI, with an incidence of 0.04%. Device embolization occurred in 0.07% of patients.
By comparison, the 7-day rate of pericardial effusion requiring intervention was 4.0% in PROTECT-AF and 1.9% in PREVAIL, with procedure-related stroke rates of 1.1% and 0.7%, respectively, and device embolization rates of 0.4% and 0.7%. The major bleeding rate in PROTECT-AF was 3.5%, nearly triple that in the real-world registry.
Discussant Mark A. Estes, MD, characterized the acute outcomes in the LAAO Registry as “an improvement – a considerable improvement – over some of the early data in PREVAIL and PROTECT-AF.” He credited this to the “very robust validation procedure” the Watchman closure device has undergone, which included the clinical trials, regulatory requirements for training and patient selection, and mandatory reporting of outcomes in the registry.
He noted that a lot is happening now with the Watchman device. There are a couple of dozen prospective clinical trials, including one on the Watchman versus direct oral anticoagulant (DOAC) therapy and another on left atrial ablation plus left atrial appendage closure versus a DOAC. A new-generation Watchman device, the Watchman FLX, is approved in Europe and undergoing an ongoing FDA-mandated approval trial in the United States.
“It has a lot of technical advantages,” according to Dr. Estes, an electrophysiologist and professor of medicine at the University of Pittsburgh.
Current guidelines give LAAO a class IIb rating, meaning it “could be considered” in patients with atrial fibrillation at increased risk of stroke who have a contraindication to long-term anticoagulation. Dr. Estes asked: Does the LAAO Registry data warrant a rating upgrade to a stronger recommendation?
Dr. Freeman replied that the new data should allay the guideline writers’ and government regulators’ concerns regarding acute procedural safety. But that’s only part of the picture. He and his coinvestigators are busy gathering data on intermediate-term outcomes, analyzing the impact of various strategies for periprocedural and long-term management of antiplatelet and anticoagulant medications with an eye toward identifying best practices, and investigating the relationship between procedural volume and outcomes, information, which could have an impact on the next iteration of the guidelines.
Simultaneous with his presentation at ACC 2020, the study was published online (J Am Coll Cardiol. 2020 Mar 13;75[13]1503-18).
In an accompanying editorial, Dhanunjaya Lakkireddy, MD, commented that an important contribution of the LAAO Registry is its inclusion of an enormous number of patients with contraindications to oral anticoagulation, a population excluded from the PROTECT-AF and PREVAIL randomized trials.
The short-term results of the registry suggest a relaxation of the current strict requirement for surgical backup during Watchman procedures is in order, added Dr. Lakkireddy, professor of medicine at the University of Missouri, Columbia, and medical director of the Kansas City Heart Rhythm Institute (J Am Coll Cardiol. 2020 Mar 13;75[13]:1519-22).
Dr. Freeman reported serving as a consultant to Boston Scientific, which markets the Watchman, as well as to Medtronic, Janssen, and Biosense Webster.
SOURCE: Freeman JF. ACC 2020, Abstract 409-10.
FROM ACC 2020
SARS-CoV-2 escapes cotton, surgical masks of infected
June 9, 2020 — Editor’s note: The study on which this news story is based has been retracted by the journal. The retraction notice can be found here.
according to Seongman Bae, MD, of the University of Ulsan College of Medicine in Seoul, South Korea, and associates.
The report was published in Annals of Internal Medicine.
Because the COVID-19 pandemic has caused a shortage of N95 and surgical masks, cotton masks have gained interest as a substitute, as surgical masks have been shown to effectively filter influenza virus, the researchers wrote. However, the size of and concentrations of SARS-CoV-2 in aerosols generated during coughing are unknown.
To compare the effectiveness of cotton and surgical masks, a group of patients infected with SARS-CoV-2 coughed into petri dishes while wearing no mask, a surgical mask, and a cotton mask. The mask surfaces were swabbed afterward to assess viral positivity on the mask itself.
The median nasopharyngeal and saliva viral load was 5.66 log copies/mL and 4.00 log copies/mL, respectively. The median viral loads after coughing was 2.56 log copies/mL without a mask, 2.42 log copies/mL with a surgical mask, and 1.85 log copies/mL with a cotton mask. All outer surfaces of the mask were positive for SARS-CoV-2, while most inner surfaces were negative.
The investigators acknowledged that the test did not include N95 masks and does not reflect the actual infection transmission, and that they didn’t know whether cotton or surgical masks shorten the travel distance of droplets while coughing.
“Further study is needed to recommend whether face masks decrease transmission of virus from asymptomatic individuals or those with suspected COVID-19 who are not coughing,” they added.
The study was funded by a grant from the government-wide R&D Fund Project for Infectious Disease Research. The investigators reported that they had no conflicts of interest.
SOURCE: Bae S et al. Ann Intern Med. 2020 Apr 6. doi: 10.7326/M20-1342.
Correction, 4/9/20: The headline of an earlier version of this article misstated a finding of this study. Whether cotton and surgical masks can block transmission was not investigated.
June 9, 2020 — Editor’s note: The study on which this news story is based has been retracted by the journal. The retraction notice can be found here.
according to Seongman Bae, MD, of the University of Ulsan College of Medicine in Seoul, South Korea, and associates.
The report was published in Annals of Internal Medicine.
Because the COVID-19 pandemic has caused a shortage of N95 and surgical masks, cotton masks have gained interest as a substitute, as surgical masks have been shown to effectively filter influenza virus, the researchers wrote. However, the size of and concentrations of SARS-CoV-2 in aerosols generated during coughing are unknown.
To compare the effectiveness of cotton and surgical masks, a group of patients infected with SARS-CoV-2 coughed into petri dishes while wearing no mask, a surgical mask, and a cotton mask. The mask surfaces were swabbed afterward to assess viral positivity on the mask itself.
The median nasopharyngeal and saliva viral load was 5.66 log copies/mL and 4.00 log copies/mL, respectively. The median viral loads after coughing was 2.56 log copies/mL without a mask, 2.42 log copies/mL with a surgical mask, and 1.85 log copies/mL with a cotton mask. All outer surfaces of the mask were positive for SARS-CoV-2, while most inner surfaces were negative.
The investigators acknowledged that the test did not include N95 masks and does not reflect the actual infection transmission, and that they didn’t know whether cotton or surgical masks shorten the travel distance of droplets while coughing.
“Further study is needed to recommend whether face masks decrease transmission of virus from asymptomatic individuals or those with suspected COVID-19 who are not coughing,” they added.
The study was funded by a grant from the government-wide R&D Fund Project for Infectious Disease Research. The investigators reported that they had no conflicts of interest.
SOURCE: Bae S et al. Ann Intern Med. 2020 Apr 6. doi: 10.7326/M20-1342.
Correction, 4/9/20: The headline of an earlier version of this article misstated a finding of this study. Whether cotton and surgical masks can block transmission was not investigated.
June 9, 2020 — Editor’s note: The study on which this news story is based has been retracted by the journal. The retraction notice can be found here.
according to Seongman Bae, MD, of the University of Ulsan College of Medicine in Seoul, South Korea, and associates.
The report was published in Annals of Internal Medicine.
Because the COVID-19 pandemic has caused a shortage of N95 and surgical masks, cotton masks have gained interest as a substitute, as surgical masks have been shown to effectively filter influenza virus, the researchers wrote. However, the size of and concentrations of SARS-CoV-2 in aerosols generated during coughing are unknown.
To compare the effectiveness of cotton and surgical masks, a group of patients infected with SARS-CoV-2 coughed into petri dishes while wearing no mask, a surgical mask, and a cotton mask. The mask surfaces were swabbed afterward to assess viral positivity on the mask itself.
The median nasopharyngeal and saliva viral load was 5.66 log copies/mL and 4.00 log copies/mL, respectively. The median viral loads after coughing was 2.56 log copies/mL without a mask, 2.42 log copies/mL with a surgical mask, and 1.85 log copies/mL with a cotton mask. All outer surfaces of the mask were positive for SARS-CoV-2, while most inner surfaces were negative.
The investigators acknowledged that the test did not include N95 masks and does not reflect the actual infection transmission, and that they didn’t know whether cotton or surgical masks shorten the travel distance of droplets while coughing.
“Further study is needed to recommend whether face masks decrease transmission of virus from asymptomatic individuals or those with suspected COVID-19 who are not coughing,” they added.
The study was funded by a grant from the government-wide R&D Fund Project for Infectious Disease Research. The investigators reported that they had no conflicts of interest.
SOURCE: Bae S et al. Ann Intern Med. 2020 Apr 6. doi: 10.7326/M20-1342.
Correction, 4/9/20: The headline of an earlier version of this article misstated a finding of this study. Whether cotton and surgical masks can block transmission was not investigated.
FROM ANNALS OF INTERNAL MEDICINE















