User login
-
LAA Closure noninferior to DOACs to prevent AF-related events
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point:
Major finding: A composite primary outcome including stroke and death was not significantly different in high-risk patients randomized to left atrial appendage occlusion or direct oral anticoagulants at roughly 20 months’ follow-up (11% vs. 13%, respectively).
Study details: The data come from the PRAGUE-17 study, a randomized trial of 402 adults at increased risk for atrial fibrillation.
Disclosures: The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot.
Sources: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Hashtag medicine: #ShareTheMicNowMed highlights Black female physicians on social media
Prominent female physicians are handing over their social media platforms today to black female physicians as part of a campaign called #ShareTheMicNowMed.
The social media event, which will play out on both Twitter and Instagram, is an offshoot of #ShareTheMicNow, held earlier this month. For that event, more than 90 women, including A-list celebrities like Ellen DeGeneres, Julia Roberts, and Senator Elizabeth Warren, swapped accounts with women of color, such as “I’m Still Here” author Austin Channing Brown, Olympic fencer Ibtihaj Muhammad, and #MeToo founder Tarana Burke.
The physician event will feature 10 teams of two, with one physician handing over her account to her black female counterpart for the day. The takeover will allow the black physician to share her thoughts about the successes and challenges she faces as a woman of color in medicine.
“It was such an honor to be contacted by Arghavan Salles, MD, PhD, to participate in an event that has a goal of connecting like-minded women from various backgrounds to share a diverse perspective with a different audience,” Minnesota family medicine physician Jay-Sheree Allen, MD, told Medscape Medical News. “This event is not only incredibly important but timely.”
Only about 5% of all active physicians in 2018 identified as Black or African American, according to a report by the Association of American Medical Colleges. And of those, just over a third are female, the report found.
“I think that as we hear those small numbers we often celebrate the success of those people without looking back and understanding where all of the barriers are that are limiting talented black women from entering medicine at every stage,” another campaign participant, Chicago pediatrician Rebekah Fenton, MD, told Medscape Medical News.
Allen says that, amid continuing worldwide protests over racial injustice, prompted by the death of George Floyd while in Minneapolis police custody last month, the online event is very timely and an important way to advocate for black lives and engage in a productive conversation.
“I believe that with the #ShareTheMicNowMed movement we will start to show people how they can become allies. I always say that a candle loses nothing by lighting another candle, and sharing that stage is one of the many ways you can support the Black Lives Matters movement by amplifying black voices,” she said.
Allen went on to add that women in medicine have many of the same experiences as any other doctor but do face some unique challenges. This is especially true for female physicians of color, she noted.
To join the conversation follow the hashtag #ShareTheMicNowMed all day on Monday, June 22, 2020.
This article originally appeared on Medscape.com.
Prominent female physicians are handing over their social media platforms today to black female physicians as part of a campaign called #ShareTheMicNowMed.
The social media event, which will play out on both Twitter and Instagram, is an offshoot of #ShareTheMicNow, held earlier this month. For that event, more than 90 women, including A-list celebrities like Ellen DeGeneres, Julia Roberts, and Senator Elizabeth Warren, swapped accounts with women of color, such as “I’m Still Here” author Austin Channing Brown, Olympic fencer Ibtihaj Muhammad, and #MeToo founder Tarana Burke.
The physician event will feature 10 teams of two, with one physician handing over her account to her black female counterpart for the day. The takeover will allow the black physician to share her thoughts about the successes and challenges she faces as a woman of color in medicine.
“It was such an honor to be contacted by Arghavan Salles, MD, PhD, to participate in an event that has a goal of connecting like-minded women from various backgrounds to share a diverse perspective with a different audience,” Minnesota family medicine physician Jay-Sheree Allen, MD, told Medscape Medical News. “This event is not only incredibly important but timely.”
Only about 5% of all active physicians in 2018 identified as Black or African American, according to a report by the Association of American Medical Colleges. And of those, just over a third are female, the report found.
“I think that as we hear those small numbers we often celebrate the success of those people without looking back and understanding where all of the barriers are that are limiting talented black women from entering medicine at every stage,” another campaign participant, Chicago pediatrician Rebekah Fenton, MD, told Medscape Medical News.
Allen says that, amid continuing worldwide protests over racial injustice, prompted by the death of George Floyd while in Minneapolis police custody last month, the online event is very timely and an important way to advocate for black lives and engage in a productive conversation.
“I believe that with the #ShareTheMicNowMed movement we will start to show people how they can become allies. I always say that a candle loses nothing by lighting another candle, and sharing that stage is one of the many ways you can support the Black Lives Matters movement by amplifying black voices,” she said.
Allen went on to add that women in medicine have many of the same experiences as any other doctor but do face some unique challenges. This is especially true for female physicians of color, she noted.
To join the conversation follow the hashtag #ShareTheMicNowMed all day on Monday, June 22, 2020.
This article originally appeared on Medscape.com.
Prominent female physicians are handing over their social media platforms today to black female physicians as part of a campaign called #ShareTheMicNowMed.
The social media event, which will play out on both Twitter and Instagram, is an offshoot of #ShareTheMicNow, held earlier this month. For that event, more than 90 women, including A-list celebrities like Ellen DeGeneres, Julia Roberts, and Senator Elizabeth Warren, swapped accounts with women of color, such as “I’m Still Here” author Austin Channing Brown, Olympic fencer Ibtihaj Muhammad, and #MeToo founder Tarana Burke.
The physician event will feature 10 teams of two, with one physician handing over her account to her black female counterpart for the day. The takeover will allow the black physician to share her thoughts about the successes and challenges she faces as a woman of color in medicine.
“It was such an honor to be contacted by Arghavan Salles, MD, PhD, to participate in an event that has a goal of connecting like-minded women from various backgrounds to share a diverse perspective with a different audience,” Minnesota family medicine physician Jay-Sheree Allen, MD, told Medscape Medical News. “This event is not only incredibly important but timely.”
Only about 5% of all active physicians in 2018 identified as Black or African American, according to a report by the Association of American Medical Colleges. And of those, just over a third are female, the report found.
“I think that as we hear those small numbers we often celebrate the success of those people without looking back and understanding where all of the barriers are that are limiting talented black women from entering medicine at every stage,” another campaign participant, Chicago pediatrician Rebekah Fenton, MD, told Medscape Medical News.
Allen says that, amid continuing worldwide protests over racial injustice, prompted by the death of George Floyd while in Minneapolis police custody last month, the online event is very timely and an important way to advocate for black lives and engage in a productive conversation.
“I believe that with the #ShareTheMicNowMed movement we will start to show people how they can become allies. I always say that a candle loses nothing by lighting another candle, and sharing that stage is one of the many ways you can support the Black Lives Matters movement by amplifying black voices,” she said.
Allen went on to add that women in medicine have many of the same experiences as any other doctor but do face some unique challenges. This is especially true for female physicians of color, she noted.
To join the conversation follow the hashtag #ShareTheMicNowMed all day on Monday, June 22, 2020.
This article originally appeared on Medscape.com.
After the ICU: A ‘fraternity of people who are struggling’
By the time she was discharged from a suburban New Jersey hospital on April 10, Kathleen Ronan thought the worst was behind her. For a week before her husband rushed her to the emergency department (ED), incoherent and struggling to breathe, the novel coronavirus had ravaged her body. She tried to treat her fevers with acetaminophen and ice packs. Despite taking enough Tylenol to risk liver damage and packing herself on ice like the catch of the day, Ronan’s fever continued to rise. By the time her temperature reached 104.5° F, Ronan knew the time had come for more drastic measures.
A team of masked and gowned nurses greeted her at a triage tent outside the ED, and from there, everything becomes hazy for Ronan. She was immediately rushed to the hospital’s special COVID-19 intensive care unit (ICU), where she spent 5 days. But she has few distinct memories from this time. What she does remember is the exhaustion, the pain, the loneliness, and the fear. Her family couldn’t visit, and though Ronan works as a home health nurse, her brain was so addled with fever that she couldn’t make sense of what was happening. After a week in the hospital, 5 days of which were spent in the ICU, 51-year-old Ronan was discharged.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, who had supplemented long days on her feet caring for others as a nurse with regular trips to the gym, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article.
“It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, . Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
Nor is PICS simply a set of side effects that will go away on their own. It includes ongoing cognitive difficulties and physical weakness, both of which can lead to employment problems. Beyond that, depression and anxiety can exacerbate – and be exacerbated by – these challenges. Psychologist Jim Jackson, PsyD, assistant director of the ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tennessee, recently spoke with a former ICU patient who has struggled since her discharge 30 years ago.
“Her life essentially stopped with her critical care stay. She hasn’t been able to move forward,” he said. “She’s part of a whole fraternity of people who are struggling.”
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her.
Surviving the ICU
Although the new coronavirus has pushed the world’s critical care system to its limits, it was an outbreak in 1952 that inspired the creation of intensive care units. That summer, a wave of paralytic polio swept over Copenhagen, Denmark, and anesthesiologist Bjørn Ibsen, MD, PhD, used mechanical ventilation — physically operated by medical and dental students – to help 316 children breathe for weeks at a time while their small bodies worked to fight off the virus. The effort halved the mortality rate from polio that affected breathing, from 80% to 40%.
In these wards, dedicated to the very sickest, each patient was assigned his or her own nurse. Over the next decade, hospitals in the United Kingdom and the United States established their own ICUs to treat patients with a variety of conditions. Although it helped improve survival, mortality rates in critical care units remained stubbornly high, owing to the patients’ severe underlying illnesses.
“We thought we were doing a good job if the patient survived, but we had no idea what happened after discharge,” said Carla Sevin, MD, medical director of Vanderbilt’s ICU Recovery Center. Nor did their efforts to find out always bring answers. “We struggled to get people to come in for support — they were debilitated, physically burdened, and weak.”
Through further advances in life support, by the early 2000s, the average mortality rates in American ICUs had dropped to 8% to 19%. As the number of critical care survivors began to climb, clinical researchers noticed that the lives of these patients and their families were profoundly altered by their severe illness.
As Dale Needham, MD, PhD, began his pulmonology and critical care residency in Toronto, Canada, in 2005, a group of physicians there began a 5-year longitudinal study to assess long-term outcomes of patients who developed acute respiratory distress syndrome (ARDS). Although ARDS is an acute condition, the investigators found that patients felt effects for years. Younger patients recovered better than older ones, but none of the patients› physical functioning was equivalent to that of age-matched control persons. Even 5 years later, former ICU patients only reached 76% of expected physical functioning, according to results published in the New England Journal of Medicine. The study was a wake-up call.
At a meeting in Chicago in 2010, Needham, now an intensivist at Johns Hopkins Hospital in Baltimore, Maryland, gathered an interdisciplinary group of colleagues, including patients and caregivers, to clarify the phenomena they were seeing. What emerged from that meeting, published in 2012 in Critical Care Medicine, were the diagnostic criteria for PICS: According to the new definition, PICS is characterized by new or worsening physical and neuropsychiatric deficits that range from forgetfulness and loss of motivation to physical weakness and insomnia.
The issue, Needham says, is that although the trouble starts in the ICU, it only becomes clear once patients leave. “ICU doctors aren’t the ones dealing with this,” Needham said. “We need to build stronger bridges between critical care and other professions.” That’s where PICS comes in, a definition that exists explicitly to alert healthcare providers about the constellation of challenges many of these individuals face as they try to reenter “normal” life.
Defining the problem
As an ICU nurse at the Mayo Clinic in Rochester, Minnesota, Annie Johnson, ACNP-BC, knew lots about helping hospitalized patients, but she says she didn’t know anything about what to do after discharge – at least not until her own mother became a patient.
On the first day of retirement in October 2014, Johnson’s mother flatlined. Quick-thinking paramedics resuscitated her, and after several days in critical care, she was discharged. Since then, her heart has remained healthy. Johnson’s sister, who spent time worrying over her mother at the hospital, also had lingering effects. Both have since struggled, plagued by nightmares, flashbacks, and insomnia.
Johnson initially believed her mom’s and sister’s neuropsychiatric, post-ICU struggles were unique to her family. It was only a year later, at a seminar she was attending, that she first heard the words “post–intensive care syndrome.” Suddenly, Johnson had a name for her family’s experiences, and she began to create support groups and resources to help other families like hers.
“I thought of all the patients I had treated over the years who had been on ventilators for days and days and days. And if this happened to my mom after 48 hours, what must they be going through?” she asked.
Once physicians formally defined PICS, the Society for Critical Care Medicine helped create programs to educate ICU staff, patients, and families about potential post-discharge challenges. Researchers also began to investigate factors affecting post-ICU functioning. Follow-up studies of patients with delirium (ranging from general confusion about time and place to extreme agitation and violence) showed they had striking cognitive deficits. Problems with short-term memory, flexible thinking, and motivation plagued patients for years after their critical illness, similar to the physical deficiencies seen after ARDS. Delirium was one of the strongest risk factors for neuropsychiatric problems.
“Delirium is basically a stress test for the brain,” said Babar Khan, MD, a critical care specialist at Indiana University’s Regenstrief Institute, in Bloomington. But whether delirium accentuates preexisting cognitive difficulties or creates them afresh isn’t yet clear.
Sophia Wang, MD, a geriatric psychiatrist at Indiana University who works with many critical care patients, says patients who had experienced delirium in the ICU showed significant defects in memory and executive functioning long after their hospital stay. She points to a 2015 study that followed 47 ICU patients for a year post discharge. Among those who experienced delirium, brain volumes, as measured by MRI, were smaller at 3 months, something associated with cognitive problems at 1 year. Many struggled at work, and unemployment was common. Depression and posttraumatic stress compounded these difficulties. Among those with acute respiratory distress, ICU patients who are young, female, and unemployed are most likely to suffer from posttraumatic stress disorder after they are discharge.
Critical care medicine may have given these patients a second chance at life, Wang says, but the life they return to often looks nothing like the one they had before their illness.
Prolonged mechanical ventilation and the heavy sedation that often accompanies it are predictors of PICS severity. Some of these links could be explained by the gravity of the illness that landed someone in critical care, but others are more likely to be iatrogenic, says Gerald Weinhouse, MD, a pulmonology and critical care physician and co-director of the Critical Illness Recovery Program at the Brigham and Women’s Hospital in Boston. The involvement of loved ones at the patient’s bedside, however, improved the entire family’s outcome.
When Weinhouse saw those data, he and his colleagues founded a peer support program for ICU survivors. In a study published in 2019 in Critical Care Medicine, they identified six different models for peer support for those with PICS and their families, including both online and in-person approaches. An ongoing challenge for physicians, Weinhouse says, is getting patients to engage with these programs, given that their calendars are crowded with medical appointments and that they suffer from increased physical and mental disability.
Studies such as these led critical care physicians to form the ICU Liberation Collaborative to rethink critical care medicine. At Vanderbilt, Sevin and Jackson headed up one of the world’s first post-ICU clinics, which uses an interdisciplinary team to help patients maximize their functioning. They redesigned their critical care unit in a way that allows families to spend the night and that encourages patient mobility. Both Needham and Weinhouse continue tracking patient outcomes.
Even before the novel coronavirus struck, the United States — and the world — had begun to realize that graduating from the ICU was only the start of what was often an extensive recovery.
The long road back
When COVID-19 patients began flooding intensive care wards around the world, physicians scrambled to meet their complex and desperate acute medical needs. Over the past few months, physicians have focused on keeping these patients alive. “We’ve never seen anything like it ― not even during polio — with the sheer number of patients, all with respiratory distress,” Needham said.
But he and his colleagues know this is only the beginning.
“We’re aware that survivorship issues are coming. There’s going to be a wave of sick people who survived the coronavirus but are going to need more help,” Weinhouse said.
Intensivists have been drawing on PICS research in their fight to help COVID-19 patients. Work from the past few years has shown that although sedation is required during intubation itself, not everyone needs it while on a ventilator. Titrating down sedating medication helps reduce delirium, Wang says. Such medication has been shown to contribute to later cognitive problems. Needham’s studies showing that prolonged bedrest by ICU patients causes muscular atrophy has led him to encourage patients to move as much as possible. With the help of physical therapists, many patients on ventilators can be awake, alert, and moving around the ward.
One of the biggest challenges critical-care coronavirus patients face is prolonged isolation. The constant presence of a familiar face helps orient confused and delirious patients and provides emotional support during a frightening time. But because the immediate need for infection control outweighs these benefits, few hospitals allow visitors, especially for COVID-19 patients.
To address this, some units have been using video technology to allow loved ones to call in. At Johns Hopkins, physicians have also been relying on the expertise of occupational therapists (OTs). Needham says that one OT found that rubbing the hand and back of an agitated, delirious patient helped soothe and calm him better than many medications.
Ronan, who spent 5 days in intensive care, echoes that problem. She says she found the relative lack of human contact to be one of the most challenging parts of being in a bed on a COVID-19 ward. Separated from her husband and daughter, suffering from high fever and severe illness, she lost all track of time.
Her return home was difficult, too. Although her job as a home health nurse had prepared her on some level for the challenges she would face after discharge, Ronan says the hospital provided little practical help.
“Everything is so much harder at home, even little things like going to the bathroom,” she said. “I feel like I’m trying to bail out a sinking ship with a teacup.”
Khan and other physicians, aware of the challenges Ronan and others face once home, aim to create post-ICU clinics specifically for COVID-19 patients. They want to build what Khan calls a “one-stop shop” for all the support patients need to recover. Some of that can be provided via telehealth, which may also help ease the physical burden.
Because there’s so much physicians don’t know about the coronavirus, Johnson says, such clinics are not only a chance to help the sickest COVID-19 patients, they will also help researchers learn more about the virus and improve critical care for other illnesses.
Today, nearly 2 months after discharge, Ronan is back on the job but struggles with a persistent cough — likely due to the lung damage she sustained while ill. She has constant fatigue, as well as ongoing upset stomach from all the medications she took to reduce fever and body aches. When she dons a mask for work, the tangible reminder of her hospital stay sends her into a panic attack. Physically, she’s weaker than before.
Researchers are still trying to understand everything that Ronan and other COVID-19 patients need to move on with their lives after being in the ICU. Mysteries abound, but the ground laid by Sevin, Needham, Weinhouse, and others has provided a solid foundation on which to build.
This article first appeared on Medscape.com.
By the time she was discharged from a suburban New Jersey hospital on April 10, Kathleen Ronan thought the worst was behind her. For a week before her husband rushed her to the emergency department (ED), incoherent and struggling to breathe, the novel coronavirus had ravaged her body. She tried to treat her fevers with acetaminophen and ice packs. Despite taking enough Tylenol to risk liver damage and packing herself on ice like the catch of the day, Ronan’s fever continued to rise. By the time her temperature reached 104.5° F, Ronan knew the time had come for more drastic measures.
A team of masked and gowned nurses greeted her at a triage tent outside the ED, and from there, everything becomes hazy for Ronan. She was immediately rushed to the hospital’s special COVID-19 intensive care unit (ICU), where she spent 5 days. But she has few distinct memories from this time. What she does remember is the exhaustion, the pain, the loneliness, and the fear. Her family couldn’t visit, and though Ronan works as a home health nurse, her brain was so addled with fever that she couldn’t make sense of what was happening. After a week in the hospital, 5 days of which were spent in the ICU, 51-year-old Ronan was discharged.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, who had supplemented long days on her feet caring for others as a nurse with regular trips to the gym, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article.
“It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, . Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
Nor is PICS simply a set of side effects that will go away on their own. It includes ongoing cognitive difficulties and physical weakness, both of which can lead to employment problems. Beyond that, depression and anxiety can exacerbate – and be exacerbated by – these challenges. Psychologist Jim Jackson, PsyD, assistant director of the ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tennessee, recently spoke with a former ICU patient who has struggled since her discharge 30 years ago.
“Her life essentially stopped with her critical care stay. She hasn’t been able to move forward,” he said. “She’s part of a whole fraternity of people who are struggling.”
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her.
Surviving the ICU
Although the new coronavirus has pushed the world’s critical care system to its limits, it was an outbreak in 1952 that inspired the creation of intensive care units. That summer, a wave of paralytic polio swept over Copenhagen, Denmark, and anesthesiologist Bjørn Ibsen, MD, PhD, used mechanical ventilation — physically operated by medical and dental students – to help 316 children breathe for weeks at a time while their small bodies worked to fight off the virus. The effort halved the mortality rate from polio that affected breathing, from 80% to 40%.
In these wards, dedicated to the very sickest, each patient was assigned his or her own nurse. Over the next decade, hospitals in the United Kingdom and the United States established their own ICUs to treat patients with a variety of conditions. Although it helped improve survival, mortality rates in critical care units remained stubbornly high, owing to the patients’ severe underlying illnesses.
“We thought we were doing a good job if the patient survived, but we had no idea what happened after discharge,” said Carla Sevin, MD, medical director of Vanderbilt’s ICU Recovery Center. Nor did their efforts to find out always bring answers. “We struggled to get people to come in for support — they were debilitated, physically burdened, and weak.”
Through further advances in life support, by the early 2000s, the average mortality rates in American ICUs had dropped to 8% to 19%. As the number of critical care survivors began to climb, clinical researchers noticed that the lives of these patients and their families were profoundly altered by their severe illness.
As Dale Needham, MD, PhD, began his pulmonology and critical care residency in Toronto, Canada, in 2005, a group of physicians there began a 5-year longitudinal study to assess long-term outcomes of patients who developed acute respiratory distress syndrome (ARDS). Although ARDS is an acute condition, the investigators found that patients felt effects for years. Younger patients recovered better than older ones, but none of the patients› physical functioning was equivalent to that of age-matched control persons. Even 5 years later, former ICU patients only reached 76% of expected physical functioning, according to results published in the New England Journal of Medicine. The study was a wake-up call.
At a meeting in Chicago in 2010, Needham, now an intensivist at Johns Hopkins Hospital in Baltimore, Maryland, gathered an interdisciplinary group of colleagues, including patients and caregivers, to clarify the phenomena they were seeing. What emerged from that meeting, published in 2012 in Critical Care Medicine, were the diagnostic criteria for PICS: According to the new definition, PICS is characterized by new or worsening physical and neuropsychiatric deficits that range from forgetfulness and loss of motivation to physical weakness and insomnia.
The issue, Needham says, is that although the trouble starts in the ICU, it only becomes clear once patients leave. “ICU doctors aren’t the ones dealing with this,” Needham said. “We need to build stronger bridges between critical care and other professions.” That’s where PICS comes in, a definition that exists explicitly to alert healthcare providers about the constellation of challenges many of these individuals face as they try to reenter “normal” life.
Defining the problem
As an ICU nurse at the Mayo Clinic in Rochester, Minnesota, Annie Johnson, ACNP-BC, knew lots about helping hospitalized patients, but she says she didn’t know anything about what to do after discharge – at least not until her own mother became a patient.
On the first day of retirement in October 2014, Johnson’s mother flatlined. Quick-thinking paramedics resuscitated her, and after several days in critical care, she was discharged. Since then, her heart has remained healthy. Johnson’s sister, who spent time worrying over her mother at the hospital, also had lingering effects. Both have since struggled, plagued by nightmares, flashbacks, and insomnia.
Johnson initially believed her mom’s and sister’s neuropsychiatric, post-ICU struggles were unique to her family. It was only a year later, at a seminar she was attending, that she first heard the words “post–intensive care syndrome.” Suddenly, Johnson had a name for her family’s experiences, and she began to create support groups and resources to help other families like hers.
“I thought of all the patients I had treated over the years who had been on ventilators for days and days and days. And if this happened to my mom after 48 hours, what must they be going through?” she asked.
Once physicians formally defined PICS, the Society for Critical Care Medicine helped create programs to educate ICU staff, patients, and families about potential post-discharge challenges. Researchers also began to investigate factors affecting post-ICU functioning. Follow-up studies of patients with delirium (ranging from general confusion about time and place to extreme agitation and violence) showed they had striking cognitive deficits. Problems with short-term memory, flexible thinking, and motivation plagued patients for years after their critical illness, similar to the physical deficiencies seen after ARDS. Delirium was one of the strongest risk factors for neuropsychiatric problems.
“Delirium is basically a stress test for the brain,” said Babar Khan, MD, a critical care specialist at Indiana University’s Regenstrief Institute, in Bloomington. But whether delirium accentuates preexisting cognitive difficulties or creates them afresh isn’t yet clear.
Sophia Wang, MD, a geriatric psychiatrist at Indiana University who works with many critical care patients, says patients who had experienced delirium in the ICU showed significant defects in memory and executive functioning long after their hospital stay. She points to a 2015 study that followed 47 ICU patients for a year post discharge. Among those who experienced delirium, brain volumes, as measured by MRI, were smaller at 3 months, something associated with cognitive problems at 1 year. Many struggled at work, and unemployment was common. Depression and posttraumatic stress compounded these difficulties. Among those with acute respiratory distress, ICU patients who are young, female, and unemployed are most likely to suffer from posttraumatic stress disorder after they are discharge.
Critical care medicine may have given these patients a second chance at life, Wang says, but the life they return to often looks nothing like the one they had before their illness.
Prolonged mechanical ventilation and the heavy sedation that often accompanies it are predictors of PICS severity. Some of these links could be explained by the gravity of the illness that landed someone in critical care, but others are more likely to be iatrogenic, says Gerald Weinhouse, MD, a pulmonology and critical care physician and co-director of the Critical Illness Recovery Program at the Brigham and Women’s Hospital in Boston. The involvement of loved ones at the patient’s bedside, however, improved the entire family’s outcome.
When Weinhouse saw those data, he and his colleagues founded a peer support program for ICU survivors. In a study published in 2019 in Critical Care Medicine, they identified six different models for peer support for those with PICS and their families, including both online and in-person approaches. An ongoing challenge for physicians, Weinhouse says, is getting patients to engage with these programs, given that their calendars are crowded with medical appointments and that they suffer from increased physical and mental disability.
Studies such as these led critical care physicians to form the ICU Liberation Collaborative to rethink critical care medicine. At Vanderbilt, Sevin and Jackson headed up one of the world’s first post-ICU clinics, which uses an interdisciplinary team to help patients maximize their functioning. They redesigned their critical care unit in a way that allows families to spend the night and that encourages patient mobility. Both Needham and Weinhouse continue tracking patient outcomes.
Even before the novel coronavirus struck, the United States — and the world — had begun to realize that graduating from the ICU was only the start of what was often an extensive recovery.
The long road back
When COVID-19 patients began flooding intensive care wards around the world, physicians scrambled to meet their complex and desperate acute medical needs. Over the past few months, physicians have focused on keeping these patients alive. “We’ve never seen anything like it ― not even during polio — with the sheer number of patients, all with respiratory distress,” Needham said.
But he and his colleagues know this is only the beginning.
“We’re aware that survivorship issues are coming. There’s going to be a wave of sick people who survived the coronavirus but are going to need more help,” Weinhouse said.
Intensivists have been drawing on PICS research in their fight to help COVID-19 patients. Work from the past few years has shown that although sedation is required during intubation itself, not everyone needs it while on a ventilator. Titrating down sedating medication helps reduce delirium, Wang says. Such medication has been shown to contribute to later cognitive problems. Needham’s studies showing that prolonged bedrest by ICU patients causes muscular atrophy has led him to encourage patients to move as much as possible. With the help of physical therapists, many patients on ventilators can be awake, alert, and moving around the ward.
One of the biggest challenges critical-care coronavirus patients face is prolonged isolation. The constant presence of a familiar face helps orient confused and delirious patients and provides emotional support during a frightening time. But because the immediate need for infection control outweighs these benefits, few hospitals allow visitors, especially for COVID-19 patients.
To address this, some units have been using video technology to allow loved ones to call in. At Johns Hopkins, physicians have also been relying on the expertise of occupational therapists (OTs). Needham says that one OT found that rubbing the hand and back of an agitated, delirious patient helped soothe and calm him better than many medications.
Ronan, who spent 5 days in intensive care, echoes that problem. She says she found the relative lack of human contact to be one of the most challenging parts of being in a bed on a COVID-19 ward. Separated from her husband and daughter, suffering from high fever and severe illness, she lost all track of time.
Her return home was difficult, too. Although her job as a home health nurse had prepared her on some level for the challenges she would face after discharge, Ronan says the hospital provided little practical help.
“Everything is so much harder at home, even little things like going to the bathroom,” she said. “I feel like I’m trying to bail out a sinking ship with a teacup.”
Khan and other physicians, aware of the challenges Ronan and others face once home, aim to create post-ICU clinics specifically for COVID-19 patients. They want to build what Khan calls a “one-stop shop” for all the support patients need to recover. Some of that can be provided via telehealth, which may also help ease the physical burden.
Because there’s so much physicians don’t know about the coronavirus, Johnson says, such clinics are not only a chance to help the sickest COVID-19 patients, they will also help researchers learn more about the virus and improve critical care for other illnesses.
Today, nearly 2 months after discharge, Ronan is back on the job but struggles with a persistent cough — likely due to the lung damage she sustained while ill. She has constant fatigue, as well as ongoing upset stomach from all the medications she took to reduce fever and body aches. When she dons a mask for work, the tangible reminder of her hospital stay sends her into a panic attack. Physically, she’s weaker than before.
Researchers are still trying to understand everything that Ronan and other COVID-19 patients need to move on with their lives after being in the ICU. Mysteries abound, but the ground laid by Sevin, Needham, Weinhouse, and others has provided a solid foundation on which to build.
This article first appeared on Medscape.com.
By the time she was discharged from a suburban New Jersey hospital on April 10, Kathleen Ronan thought the worst was behind her. For a week before her husband rushed her to the emergency department (ED), incoherent and struggling to breathe, the novel coronavirus had ravaged her body. She tried to treat her fevers with acetaminophen and ice packs. Despite taking enough Tylenol to risk liver damage and packing herself on ice like the catch of the day, Ronan’s fever continued to rise. By the time her temperature reached 104.5° F, Ronan knew the time had come for more drastic measures.
A team of masked and gowned nurses greeted her at a triage tent outside the ED, and from there, everything becomes hazy for Ronan. She was immediately rushed to the hospital’s special COVID-19 intensive care unit (ICU), where she spent 5 days. But she has few distinct memories from this time. What she does remember is the exhaustion, the pain, the loneliness, and the fear. Her family couldn’t visit, and though Ronan works as a home health nurse, her brain was so addled with fever that she couldn’t make sense of what was happening. After a week in the hospital, 5 days of which were spent in the ICU, 51-year-old Ronan was discharged.
Her years of working as a home health nurse told her that the return home wouldn’t be easy, but nothing prepared her for just how much she would struggle. The once-active Ronan, who had supplemented long days on her feet caring for others as a nurse with regular trips to the gym, now needed a walker to traverse the few steps from her bed to the toilet, an effort that left her gasping for air. Her brain couldn’t even focus on an audiobook, let alone a short magazine article.
“It just completely knocked the stuffing out of me,” Ronan said.
Ronan’s lingering symptoms aren’t unique to COVID-19 patients. In as many as 80% of patients leaving the ICU, . Although underlying illness plays a role in these symptoms, the amount of time spent in critical care is a major factor.
Nor is PICS simply a set of side effects that will go away on their own. It includes ongoing cognitive difficulties and physical weakness, both of which can lead to employment problems. Beyond that, depression and anxiety can exacerbate – and be exacerbated by – these challenges. Psychologist Jim Jackson, PsyD, assistant director of the ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tennessee, recently spoke with a former ICU patient who has struggled since her discharge 30 years ago.
“Her life essentially stopped with her critical care stay. She hasn’t been able to move forward,” he said. “She’s part of a whole fraternity of people who are struggling.”
The good news is that over the past decade, researchers have made important strides in understanding what makes PICS symptoms worse and how critical care physicians can tweak ICU protocols to reduce PICS severity. Practitioners will need to draw on this knowledge to help Ronan and the thousands of COVID-19 ICU patients like her.
Surviving the ICU
Although the new coronavirus has pushed the world’s critical care system to its limits, it was an outbreak in 1952 that inspired the creation of intensive care units. That summer, a wave of paralytic polio swept over Copenhagen, Denmark, and anesthesiologist Bjørn Ibsen, MD, PhD, used mechanical ventilation — physically operated by medical and dental students – to help 316 children breathe for weeks at a time while their small bodies worked to fight off the virus. The effort halved the mortality rate from polio that affected breathing, from 80% to 40%.
In these wards, dedicated to the very sickest, each patient was assigned his or her own nurse. Over the next decade, hospitals in the United Kingdom and the United States established their own ICUs to treat patients with a variety of conditions. Although it helped improve survival, mortality rates in critical care units remained stubbornly high, owing to the patients’ severe underlying illnesses.
“We thought we were doing a good job if the patient survived, but we had no idea what happened after discharge,” said Carla Sevin, MD, medical director of Vanderbilt’s ICU Recovery Center. Nor did their efforts to find out always bring answers. “We struggled to get people to come in for support — they were debilitated, physically burdened, and weak.”
Through further advances in life support, by the early 2000s, the average mortality rates in American ICUs had dropped to 8% to 19%. As the number of critical care survivors began to climb, clinical researchers noticed that the lives of these patients and their families were profoundly altered by their severe illness.
As Dale Needham, MD, PhD, began his pulmonology and critical care residency in Toronto, Canada, in 2005, a group of physicians there began a 5-year longitudinal study to assess long-term outcomes of patients who developed acute respiratory distress syndrome (ARDS). Although ARDS is an acute condition, the investigators found that patients felt effects for years. Younger patients recovered better than older ones, but none of the patients› physical functioning was equivalent to that of age-matched control persons. Even 5 years later, former ICU patients only reached 76% of expected physical functioning, according to results published in the New England Journal of Medicine. The study was a wake-up call.
At a meeting in Chicago in 2010, Needham, now an intensivist at Johns Hopkins Hospital in Baltimore, Maryland, gathered an interdisciplinary group of colleagues, including patients and caregivers, to clarify the phenomena they were seeing. What emerged from that meeting, published in 2012 in Critical Care Medicine, were the diagnostic criteria for PICS: According to the new definition, PICS is characterized by new or worsening physical and neuropsychiatric deficits that range from forgetfulness and loss of motivation to physical weakness and insomnia.
The issue, Needham says, is that although the trouble starts in the ICU, it only becomes clear once patients leave. “ICU doctors aren’t the ones dealing with this,” Needham said. “We need to build stronger bridges between critical care and other professions.” That’s where PICS comes in, a definition that exists explicitly to alert healthcare providers about the constellation of challenges many of these individuals face as they try to reenter “normal” life.
Defining the problem
As an ICU nurse at the Mayo Clinic in Rochester, Minnesota, Annie Johnson, ACNP-BC, knew lots about helping hospitalized patients, but she says she didn’t know anything about what to do after discharge – at least not until her own mother became a patient.
On the first day of retirement in October 2014, Johnson’s mother flatlined. Quick-thinking paramedics resuscitated her, and after several days in critical care, she was discharged. Since then, her heart has remained healthy. Johnson’s sister, who spent time worrying over her mother at the hospital, also had lingering effects. Both have since struggled, plagued by nightmares, flashbacks, and insomnia.
Johnson initially believed her mom’s and sister’s neuropsychiatric, post-ICU struggles were unique to her family. It was only a year later, at a seminar she was attending, that she first heard the words “post–intensive care syndrome.” Suddenly, Johnson had a name for her family’s experiences, and she began to create support groups and resources to help other families like hers.
“I thought of all the patients I had treated over the years who had been on ventilators for days and days and days. And if this happened to my mom after 48 hours, what must they be going through?” she asked.
Once physicians formally defined PICS, the Society for Critical Care Medicine helped create programs to educate ICU staff, patients, and families about potential post-discharge challenges. Researchers also began to investigate factors affecting post-ICU functioning. Follow-up studies of patients with delirium (ranging from general confusion about time and place to extreme agitation and violence) showed they had striking cognitive deficits. Problems with short-term memory, flexible thinking, and motivation plagued patients for years after their critical illness, similar to the physical deficiencies seen after ARDS. Delirium was one of the strongest risk factors for neuropsychiatric problems.
“Delirium is basically a stress test for the brain,” said Babar Khan, MD, a critical care specialist at Indiana University’s Regenstrief Institute, in Bloomington. But whether delirium accentuates preexisting cognitive difficulties or creates them afresh isn’t yet clear.
Sophia Wang, MD, a geriatric psychiatrist at Indiana University who works with many critical care patients, says patients who had experienced delirium in the ICU showed significant defects in memory and executive functioning long after their hospital stay. She points to a 2015 study that followed 47 ICU patients for a year post discharge. Among those who experienced delirium, brain volumes, as measured by MRI, were smaller at 3 months, something associated with cognitive problems at 1 year. Many struggled at work, and unemployment was common. Depression and posttraumatic stress compounded these difficulties. Among those with acute respiratory distress, ICU patients who are young, female, and unemployed are most likely to suffer from posttraumatic stress disorder after they are discharge.
Critical care medicine may have given these patients a second chance at life, Wang says, but the life they return to often looks nothing like the one they had before their illness.
Prolonged mechanical ventilation and the heavy sedation that often accompanies it are predictors of PICS severity. Some of these links could be explained by the gravity of the illness that landed someone in critical care, but others are more likely to be iatrogenic, says Gerald Weinhouse, MD, a pulmonology and critical care physician and co-director of the Critical Illness Recovery Program at the Brigham and Women’s Hospital in Boston. The involvement of loved ones at the patient’s bedside, however, improved the entire family’s outcome.
When Weinhouse saw those data, he and his colleagues founded a peer support program for ICU survivors. In a study published in 2019 in Critical Care Medicine, they identified six different models for peer support for those with PICS and their families, including both online and in-person approaches. An ongoing challenge for physicians, Weinhouse says, is getting patients to engage with these programs, given that their calendars are crowded with medical appointments and that they suffer from increased physical and mental disability.
Studies such as these led critical care physicians to form the ICU Liberation Collaborative to rethink critical care medicine. At Vanderbilt, Sevin and Jackson headed up one of the world’s first post-ICU clinics, which uses an interdisciplinary team to help patients maximize their functioning. They redesigned their critical care unit in a way that allows families to spend the night and that encourages patient mobility. Both Needham and Weinhouse continue tracking patient outcomes.
Even before the novel coronavirus struck, the United States — and the world — had begun to realize that graduating from the ICU was only the start of what was often an extensive recovery.
The long road back
When COVID-19 patients began flooding intensive care wards around the world, physicians scrambled to meet their complex and desperate acute medical needs. Over the past few months, physicians have focused on keeping these patients alive. “We’ve never seen anything like it ― not even during polio — with the sheer number of patients, all with respiratory distress,” Needham said.
But he and his colleagues know this is only the beginning.
“We’re aware that survivorship issues are coming. There’s going to be a wave of sick people who survived the coronavirus but are going to need more help,” Weinhouse said.
Intensivists have been drawing on PICS research in their fight to help COVID-19 patients. Work from the past few years has shown that although sedation is required during intubation itself, not everyone needs it while on a ventilator. Titrating down sedating medication helps reduce delirium, Wang says. Such medication has been shown to contribute to later cognitive problems. Needham’s studies showing that prolonged bedrest by ICU patients causes muscular atrophy has led him to encourage patients to move as much as possible. With the help of physical therapists, many patients on ventilators can be awake, alert, and moving around the ward.
One of the biggest challenges critical-care coronavirus patients face is prolonged isolation. The constant presence of a familiar face helps orient confused and delirious patients and provides emotional support during a frightening time. But because the immediate need for infection control outweighs these benefits, few hospitals allow visitors, especially for COVID-19 patients.
To address this, some units have been using video technology to allow loved ones to call in. At Johns Hopkins, physicians have also been relying on the expertise of occupational therapists (OTs). Needham says that one OT found that rubbing the hand and back of an agitated, delirious patient helped soothe and calm him better than many medications.
Ronan, who spent 5 days in intensive care, echoes that problem. She says she found the relative lack of human contact to be one of the most challenging parts of being in a bed on a COVID-19 ward. Separated from her husband and daughter, suffering from high fever and severe illness, she lost all track of time.
Her return home was difficult, too. Although her job as a home health nurse had prepared her on some level for the challenges she would face after discharge, Ronan says the hospital provided little practical help.
“Everything is so much harder at home, even little things like going to the bathroom,” she said. “I feel like I’m trying to bail out a sinking ship with a teacup.”
Khan and other physicians, aware of the challenges Ronan and others face once home, aim to create post-ICU clinics specifically for COVID-19 patients. They want to build what Khan calls a “one-stop shop” for all the support patients need to recover. Some of that can be provided via telehealth, which may also help ease the physical burden.
Because there’s so much physicians don’t know about the coronavirus, Johnson says, such clinics are not only a chance to help the sickest COVID-19 patients, they will also help researchers learn more about the virus and improve critical care for other illnesses.
Today, nearly 2 months after discharge, Ronan is back on the job but struggles with a persistent cough — likely due to the lung damage she sustained while ill. She has constant fatigue, as well as ongoing upset stomach from all the medications she took to reduce fever and body aches. When she dons a mask for work, the tangible reminder of her hospital stay sends her into a panic attack. Physically, she’s weaker than before.
Researchers are still trying to understand everything that Ronan and other COVID-19 patients need to move on with their lives after being in the ICU. Mysteries abound, but the ground laid by Sevin, Needham, Weinhouse, and others has provided a solid foundation on which to build.
This article first appeared on Medscape.com.
FDA gives thumbs up to tazemetostat for follicular lymphoma
The US Food and Drug Administration (FDA) has granted accelerated approval of the EZH2 inhibitor tazemetostat (Tazverik, Epizyme, Inc) for the treatment of relapsed or refractory follicular lymphoma in adult patients with tumors harboring an EZH2 mutation.
Eligible patients must have already received at least two prior systemic therapies and have tumors that are positive for an EZH2 mutation, as detected by an FDA-approved test. The FDA has also approved the cobas EZH2 Mutation Test (Roche Molecular Systems, Inc) as a companion diagnostic test for tazemetostat.
The new indication is also for adult patients with relapsed/refractory follicular lymphoma who have no other satisfactory alternative treatment options.
“In our view, there remains no clear standard of care in the relapsed and/or refractory [follicular lymphoma] population, as not all patients benefit from today’s available therapies,” said Shefali Agarwal, MD, chief medical officer of Epizyme, in a company press release. “Based on this label, physicians will have the ability to use their clinical discretion to prescribe tazemetostat for their relapsed or refractory patients regardless of EZH2 mutational status and without regard to a specific line of treatment where other options are not satisfactory.”
This accelerated approval is based on overall response rate and duration of response. Continued approval for these indications may be contingent upon verification and description of clinical benefit in confirmatory trials, the FDA notes.
Tazemetostat acts as an inhibitor of EZH2 methyltransferase. Earlier this year, the drug was approved for the treatment of metastatic or locally advanced epithelioid sarcoma in cases in which complete resection is not possible. It is the first drug with this mechanism of action and is the first to be indicated for epithelioid sarcoma.
Promising Efficacy in Phase 2 Trial
The new approval for use in follicular lymphoma was based on results from an open-label, single-arm, multicenter phase 2 clinical trial involving patients who had experienced disease progression after being treated with at least two prior systemic regimens. The cohort was divided into two treatment groups: One group consisted of 45 patients with EZH2-activating mutations, the other included 54 patients with wild-type EZH2.
All patients received tazemetostat at 800 mg administered orally twice a day. The primary efficacy outcome measures were overall response rate and duration of response, in accordance with International Working Group Non-Hodgkin Lymphoma criteria.
The median duration of follow-up was 22 months for patients with EZH2-activating mutations and 36 months for those with wild-type tumors.
Among the 45 patients with an EZH2-activating mutation, the median number of lines of prior systemic therapy was 2.0 (range, 1 – 11). In 49% of patients, disease was refractory to rituximab, and in 49%, it was refractory to the patient’s last therapy.
The overall response rate was 69%; 12% of patients achieved a complete response, and 57% achieved a partial response. The median duration of response was 10.9 months and ongoing.
In the cohort of 54 patients with wild-type EZH2, the median number previous therapies was 3.0 (range, 1 – 8); in 59% of patients, disease was refractory to rituximab, and in 41%, it was refractory to the patient’s last therapy.
The overall response rate to tazemetostat treatment was 34%; 4% of patients achieved a complete response, and 30% achieved a partial response. The median duration of response was 13 months.
Serious adverse reactions occurred in 30% of patients. The most common were fatigue, upper respiratory tract infection, musculoskeletal pain, nausea, and abdominal pain. Eight patients (8%) discontinued treatment during the trial because of adverse events. There were no reported deaths. No black box warnings have been published, and there are no contraindications.
“The durable responses observed with this drug are notable in the context of the safety profile and route of oral, at-home administration, and will offer an important new option for physicians as we care for patients with relapsed/refractory follicular lymphoma,” said John Leonard, MD, in a company press release. He is associate dean for clinical research and Richard T. Silver Distinguished Professor of Hematology and Medical Oncology, Meyer Cancer Center, Weill Cornell Medicine and New York–Presbyterian Hospital, New York, and an investigator in the ongoing phase 1b/3 confirmatory trial for tazemetostat.
“Follicular lymphoma remains an incurable disease, and even with the availability of new drugs in recent years, there have remained important unmet needs in the treatment of follicular lymphoma,” he commented.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has granted accelerated approval of the EZH2 inhibitor tazemetostat (Tazverik, Epizyme, Inc) for the treatment of relapsed or refractory follicular lymphoma in adult patients with tumors harboring an EZH2 mutation.
Eligible patients must have already received at least two prior systemic therapies and have tumors that are positive for an EZH2 mutation, as detected by an FDA-approved test. The FDA has also approved the cobas EZH2 Mutation Test (Roche Molecular Systems, Inc) as a companion diagnostic test for tazemetostat.
The new indication is also for adult patients with relapsed/refractory follicular lymphoma who have no other satisfactory alternative treatment options.
“In our view, there remains no clear standard of care in the relapsed and/or refractory [follicular lymphoma] population, as not all patients benefit from today’s available therapies,” said Shefali Agarwal, MD, chief medical officer of Epizyme, in a company press release. “Based on this label, physicians will have the ability to use their clinical discretion to prescribe tazemetostat for their relapsed or refractory patients regardless of EZH2 mutational status and without regard to a specific line of treatment where other options are not satisfactory.”
This accelerated approval is based on overall response rate and duration of response. Continued approval for these indications may be contingent upon verification and description of clinical benefit in confirmatory trials, the FDA notes.
Tazemetostat acts as an inhibitor of EZH2 methyltransferase. Earlier this year, the drug was approved for the treatment of metastatic or locally advanced epithelioid sarcoma in cases in which complete resection is not possible. It is the first drug with this mechanism of action and is the first to be indicated for epithelioid sarcoma.
Promising Efficacy in Phase 2 Trial
The new approval for use in follicular lymphoma was based on results from an open-label, single-arm, multicenter phase 2 clinical trial involving patients who had experienced disease progression after being treated with at least two prior systemic regimens. The cohort was divided into two treatment groups: One group consisted of 45 patients with EZH2-activating mutations, the other included 54 patients with wild-type EZH2.
All patients received tazemetostat at 800 mg administered orally twice a day. The primary efficacy outcome measures were overall response rate and duration of response, in accordance with International Working Group Non-Hodgkin Lymphoma criteria.
The median duration of follow-up was 22 months for patients with EZH2-activating mutations and 36 months for those with wild-type tumors.
Among the 45 patients with an EZH2-activating mutation, the median number of lines of prior systemic therapy was 2.0 (range, 1 – 11). In 49% of patients, disease was refractory to rituximab, and in 49%, it was refractory to the patient’s last therapy.
The overall response rate was 69%; 12% of patients achieved a complete response, and 57% achieved a partial response. The median duration of response was 10.9 months and ongoing.
In the cohort of 54 patients with wild-type EZH2, the median number previous therapies was 3.0 (range, 1 – 8); in 59% of patients, disease was refractory to rituximab, and in 41%, it was refractory to the patient’s last therapy.
The overall response rate to tazemetostat treatment was 34%; 4% of patients achieved a complete response, and 30% achieved a partial response. The median duration of response was 13 months.
Serious adverse reactions occurred in 30% of patients. The most common were fatigue, upper respiratory tract infection, musculoskeletal pain, nausea, and abdominal pain. Eight patients (8%) discontinued treatment during the trial because of adverse events. There were no reported deaths. No black box warnings have been published, and there are no contraindications.
“The durable responses observed with this drug are notable in the context of the safety profile and route of oral, at-home administration, and will offer an important new option for physicians as we care for patients with relapsed/refractory follicular lymphoma,” said John Leonard, MD, in a company press release. He is associate dean for clinical research and Richard T. Silver Distinguished Professor of Hematology and Medical Oncology, Meyer Cancer Center, Weill Cornell Medicine and New York–Presbyterian Hospital, New York, and an investigator in the ongoing phase 1b/3 confirmatory trial for tazemetostat.
“Follicular lymphoma remains an incurable disease, and even with the availability of new drugs in recent years, there have remained important unmet needs in the treatment of follicular lymphoma,” he commented.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has granted accelerated approval of the EZH2 inhibitor tazemetostat (Tazverik, Epizyme, Inc) for the treatment of relapsed or refractory follicular lymphoma in adult patients with tumors harboring an EZH2 mutation.
Eligible patients must have already received at least two prior systemic therapies and have tumors that are positive for an EZH2 mutation, as detected by an FDA-approved test. The FDA has also approved the cobas EZH2 Mutation Test (Roche Molecular Systems, Inc) as a companion diagnostic test for tazemetostat.
The new indication is also for adult patients with relapsed/refractory follicular lymphoma who have no other satisfactory alternative treatment options.
“In our view, there remains no clear standard of care in the relapsed and/or refractory [follicular lymphoma] population, as not all patients benefit from today’s available therapies,” said Shefali Agarwal, MD, chief medical officer of Epizyme, in a company press release. “Based on this label, physicians will have the ability to use their clinical discretion to prescribe tazemetostat for their relapsed or refractory patients regardless of EZH2 mutational status and without regard to a specific line of treatment where other options are not satisfactory.”
This accelerated approval is based on overall response rate and duration of response. Continued approval for these indications may be contingent upon verification and description of clinical benefit in confirmatory trials, the FDA notes.
Tazemetostat acts as an inhibitor of EZH2 methyltransferase. Earlier this year, the drug was approved for the treatment of metastatic or locally advanced epithelioid sarcoma in cases in which complete resection is not possible. It is the first drug with this mechanism of action and is the first to be indicated for epithelioid sarcoma.
Promising Efficacy in Phase 2 Trial
The new approval for use in follicular lymphoma was based on results from an open-label, single-arm, multicenter phase 2 clinical trial involving patients who had experienced disease progression after being treated with at least two prior systemic regimens. The cohort was divided into two treatment groups: One group consisted of 45 patients with EZH2-activating mutations, the other included 54 patients with wild-type EZH2.
All patients received tazemetostat at 800 mg administered orally twice a day. The primary efficacy outcome measures were overall response rate and duration of response, in accordance with International Working Group Non-Hodgkin Lymphoma criteria.
The median duration of follow-up was 22 months for patients with EZH2-activating mutations and 36 months for those with wild-type tumors.
Among the 45 patients with an EZH2-activating mutation, the median number of lines of prior systemic therapy was 2.0 (range, 1 – 11). In 49% of patients, disease was refractory to rituximab, and in 49%, it was refractory to the patient’s last therapy.
The overall response rate was 69%; 12% of patients achieved a complete response, and 57% achieved a partial response. The median duration of response was 10.9 months and ongoing.
In the cohort of 54 patients with wild-type EZH2, the median number previous therapies was 3.0 (range, 1 – 8); in 59% of patients, disease was refractory to rituximab, and in 41%, it was refractory to the patient’s last therapy.
The overall response rate to tazemetostat treatment was 34%; 4% of patients achieved a complete response, and 30% achieved a partial response. The median duration of response was 13 months.
Serious adverse reactions occurred in 30% of patients. The most common were fatigue, upper respiratory tract infection, musculoskeletal pain, nausea, and abdominal pain. Eight patients (8%) discontinued treatment during the trial because of adverse events. There were no reported deaths. No black box warnings have been published, and there are no contraindications.
“The durable responses observed with this drug are notable in the context of the safety profile and route of oral, at-home administration, and will offer an important new option for physicians as we care for patients with relapsed/refractory follicular lymphoma,” said John Leonard, MD, in a company press release. He is associate dean for clinical research and Richard T. Silver Distinguished Professor of Hematology and Medical Oncology, Meyer Cancer Center, Weill Cornell Medicine and New York–Presbyterian Hospital, New York, and an investigator in the ongoing phase 1b/3 confirmatory trial for tazemetostat.
“Follicular lymphoma remains an incurable disease, and even with the availability of new drugs in recent years, there have remained important unmet needs in the treatment of follicular lymphoma,” he commented.
This article first appeared on Medscape.com.
The evolution of “COVIDists”
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).
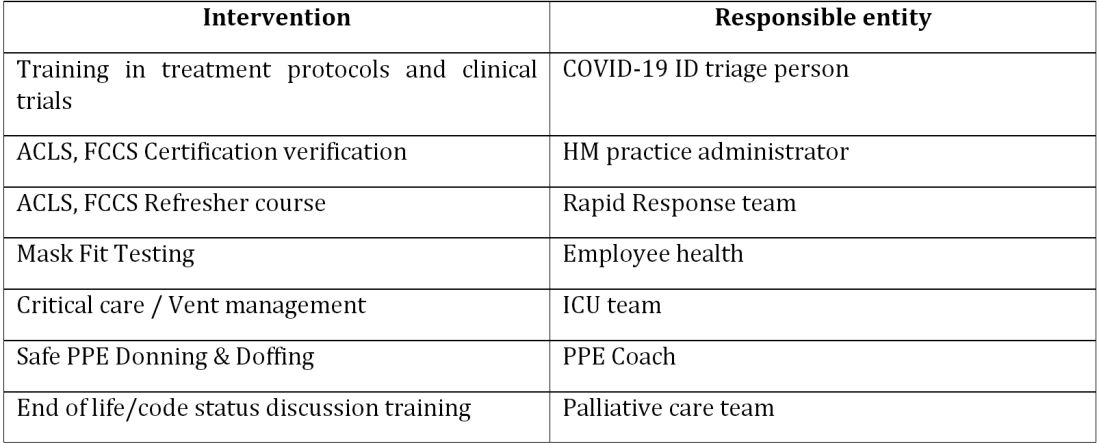
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).
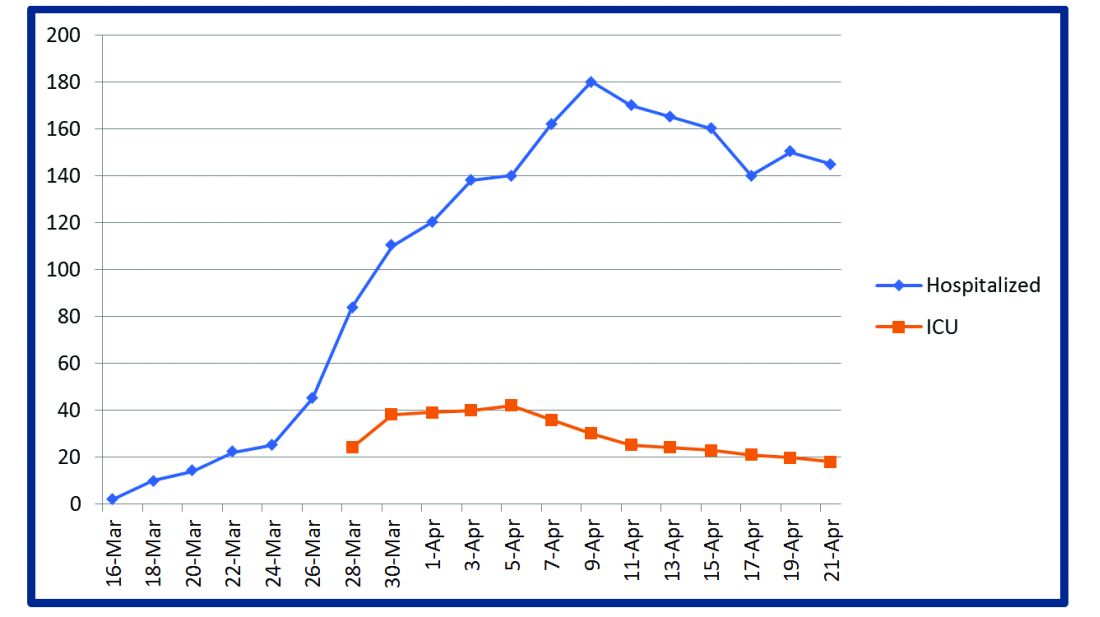
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
Adapting to the demands placed on hospital resources by COVID-19
Adapting to the demands placed on hospital resources by COVID-19
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).
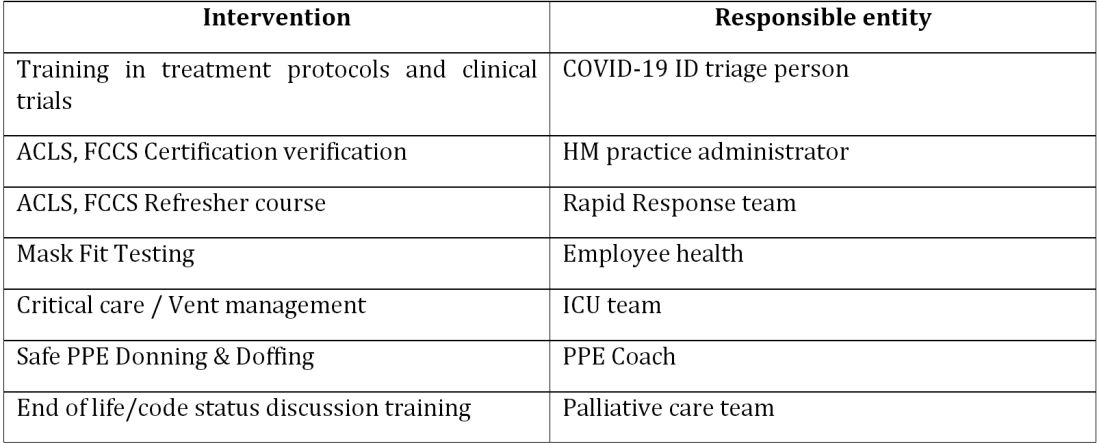
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).
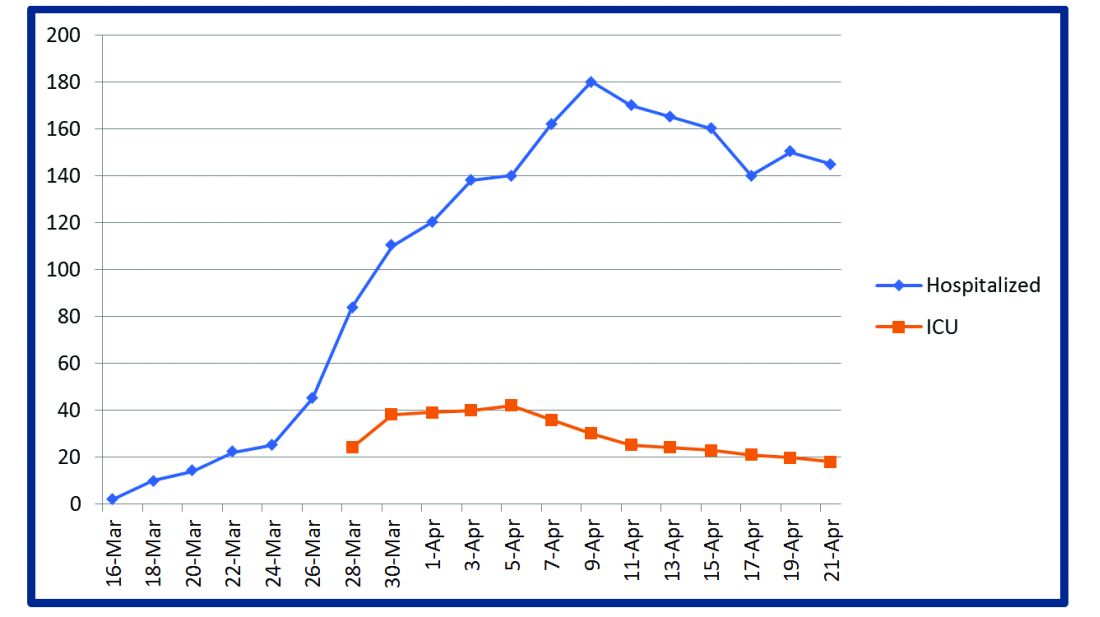
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
The challenges posed by COVID-19 have crippled health care systems around the globe. By February 2020, the first outbreak in the United States had been set off in Washington State. We quickly became the world’s epicenter of the epidemic, with over 1.8 million patients and over 110,000 deaths.1 The rapidity of spread and the severity of the disease created a tremendous strain on resources. It blindsided policymakers and hospital administrators, which left little time to react to the challenges placed on hospital operations all over the country.
The necessity of a new care model
Although health systems in the United States are adept in managing complications of common seasonal viral respiratory illnesses, COVID-19 presented an entirely different challenge with its significantly higher mortality rate. A respiratory disease turning into a multiorgan disease that causes debilitating cardiac, renal, neurological, hematological, and psychosocial complications2 was not something we had experience managing effectively. Additional challenges included a massive surge of COVID-19 patients, a limited supply of personal protective equipment (PPE), an inadequate number of intensivists for managing the anticipated ventilated patients, and most importantly, the potential of losing some of our workforce if they became infected.
Based on the experiences in China and Italy, and various predictive models, the division of hospital medicine at Baystate Health quickly realized the necessity of a new model of care for COVID-19 patients. We came up with an elaborate plan to manage the disease burden and the strain on resources effectively. The measures we put in place could be broadly divided into three categories following the timeline of the disease: the preparatory phase, the execution phase, and the maintenance phase.
The preparatory phase: From “Hospitalists” to “COVIDists”
As in most hospitals around the country, hospitalists are the backbone of inpatient clinical operations at our health system. A focused group of 10 hospitalists who volunteered to take care of COVID-19 patients with a particular interest in the pandemic and experience in critical care were selected, and the term “COVIDists” was coined to refer to them.
COVIDists were trained in various treatment protocols and ongoing clinical trials. They were given refresher training in Advanced Cardiac Life Support (ACLS) and Fundamental Critical Care Support (FCCS) courses and were taught in critical care/ventilator management by the intensivists through rapid indoctrination in the ICU. All of them had their N-95 mask fitting updated and were trained in the safe donning and doffing of all kinds of PPE by PPE coaches. The palliative care team trained them in conducting end-of-life/code status discussions with a focus on being unable to speak with family members at the bedside. COVIDists were also assigned as Code Blue leaders for any “COVID code blue” in the hospital.
In addition to the rapid training course, COVID-related updates were disseminated daily using three different modalities: brief huddles at the start of the day with the COVIDists; a COVID-19 newsletter summarizing daily updates, new treatments, strategies, and policies; and a WhatsApp group for instantly broadcasting information to the COVIDists (Table 1).
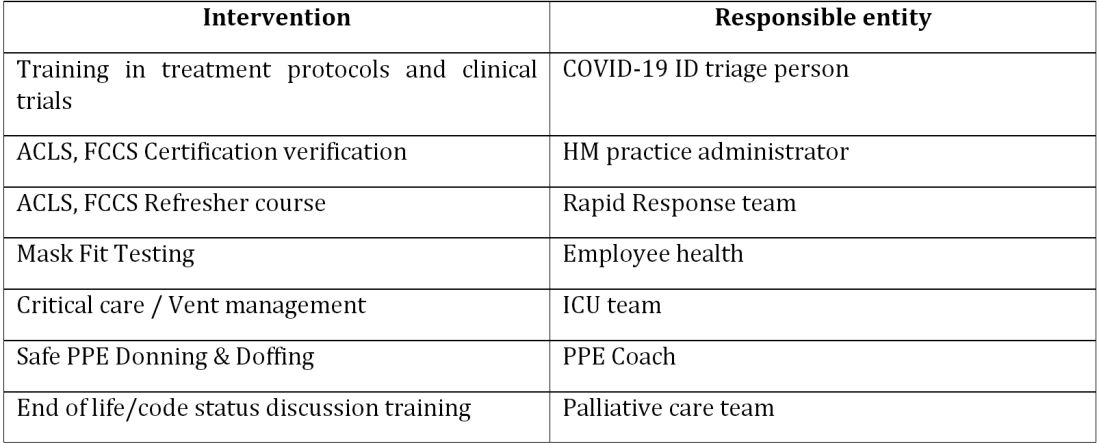
The execution phase
All the hospitalized COVID-19 patients were grouped together to COVID units, and the COVIDists were deployed to those units geographically. COVIDists were given lighter than usual patient loads to deal with the extra time needed for donning and doffing of PPE and for coordination with specialists. COVIDists were almost the only clinicians physically visiting the patients in most cases, and they became the “eyes and ears” of specialists since the specialists were advised to minimize exposure and pursue telemedicine consults. The COVIDists were also undertaking the most challenging part of the care – talking to families about end-of-life issues and the futility of aggressive care in certain patients with preexisting conditions.
Some COVIDists were deployed to the ICU to work alongside the intensivists and became an invaluable resource in ICU management when the ICU census skyrocketed during the initial phase of the outbreak. This helped in tiding the health system over during the initial crisis. Within a short time, we shifted away from an early intubation strategy, and most of the ICU patients were managed in the intermediate care units on high flow oxygen along with the awake-proning protocol. The COVIDists exclusively managed these units. They led multidisciplinary rounds two times a day with the ICU, rapid response team (RRT), the palliative care team, and the nursing team. This step drastically decreased the number of intubations, RRT activations, reduced ICU census,3 and helped with hospital capacity and patient flow (Tables 2 and 3).
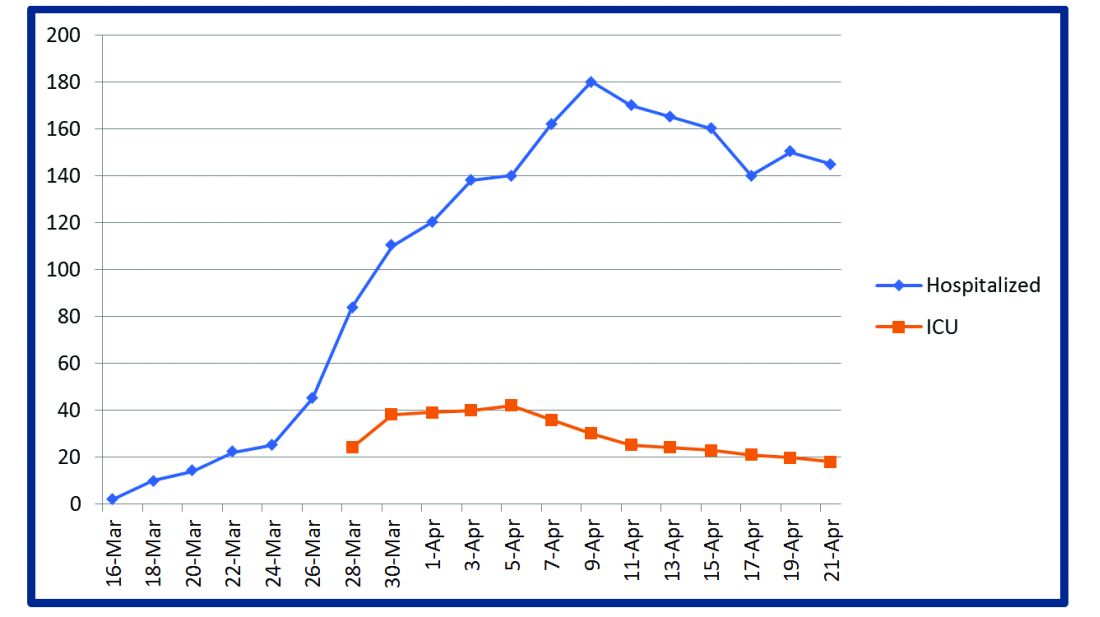
This strategy also helped build solidarity and camaraderie between all these groups, making the COVIDists feel that they were never alone and that the whole hospital supported them. We are currently evaluating clinical outcomes and attempting to identify effects on mortality, length of stay, days on the ventilator, and days in ICU.

The maintenance phase
It is already 2 months since the first devising COVIDists. There is no difference in sick callouts between COVIDists and non-COVIDists. One COVIDist and one non-COVIDist contracted the disease, but none of them required hospitalization. Although we initially thought that COVIDists would be needed for only a short period of time, the evolution of the disease is showing signs that it might be prolonged over the next several months. Hence, we are planning to continue COVIDist service for at least the next 6 months and reevaluate the need.
Hospital medicine leadership checked on COVIDists daily in regard to their physical health and, more importantly, their mental well-being. They were offered the chance to be taken off the schedule if they felt burned out, but no one wanted to come off their scheduled service before finishing their shifts. BlueCross MA recognized one of the COVIDists, Raghuveer Rakasi, MD, as a “hero on the front line.”4 In Dr. Rakasi’s words, “We took a nosedive into something without knowing its depth, and aware that we could have fatalities among ourselves. We took up new roles, faced new challenges, learned new things every day, evolving every step of the way. We had to change the way we practice medicine, finding new ways to treat patients, and protecting the workforce by limiting patient exposure, prioritizing investigations.” He added that “we have to adapt to a new normal; we should be prepared for this to come in waves. Putting aside our political views, we should stand united 6 feet apart, with a mask covering our brave faces, frequently washing our helping hands to overcome these uncertain times.”
Conclusion
The creation of a focused group of hospitalists called COVIDists and providing them with structured and rapid training (in various aspects of clinical care of COVID-19 patients, critical care/ventilator management, efficient and safe use of PPE) and daily information dissemination allowed our health system to prepare for the large volume of COVID-19 patients. It also helped in preserving the larger hospital workforce for a possible future surge.
The rapid development and implementation of the COVIDist strategy succeeded because of the intrinsic motivation of the providers to improve the outcomes of this high-risk patient population and the close collaboration of the stakeholders. Our institution remains successful in managing the pandemic in Western Massachusetts, with reserve capacity remaining even during the peak of the epidemic. A large part of this was because of creating and training a pool of COVIDists.
Dr. Medarametla is medical director, clinical operations, in the division of hospital medicine at Baystate Health, and assistant professor at University of Massachusetts, Worcester. Readers can contact him at [email protected]. Dr. Prabhakaran is unit medical director, geriatrics unit, in the division of hospital medicine at Baystate Health and assistant professor at University of Massachusetts. Dr. Bryson is associate program director of the Internal Medicine Residency at Baystate Health and assistant professor at University of Massachusetts. Dr. Umar is medical director, clinical operations, in the division of hospital medicine at Baystate Health. Dr. Natanasabapathy is division chief of hospital medicine at Baystate Health and assistant professor at University of Massachusetts.
References
1. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Updated Jun 10, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Westafer LM et al. A transdisciplinary COVID-19 early respiratory intervention protocol: An implementation story. J Hosp Med. 2020 May 21;15(6):372-374.
4. Miller J. “Heroes on the front line: Dr. Raghuveer Rakasi.” Coverage. May 18, 2020. https://coverage.bluecrossma.com/article/heroes-front-line-dr-raghuveer-rakasi
First-in-kind anti-CD47 antibody shows promise for MDS and AML treatment
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
Magrolimab plus azacitidine (AZA) improved outcomes in acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) patients according to the results of a phase 1b study (NCT03248479) presented at the virtual ASCO meeting. The combo especially was promising for the underserved patient population that have the TP53 (p53) mutation.
Magrolimab is a first-in-kind IgG anti-CD47 monoclonal antibody that promotes the elimination of tumor cells through macrophage phagocytosis. CD47 is a “do not eat me” signal on cancer cells that allows the cells to evade macrophages. Its increased expression is predictive of a worse outcome in AML patients, according to David A. Sallman, MD, of the Moffitt Cancer Center, Tampa, Fla., and colleagues.
Dr. Sallman presented the results of a study examining whether magrolimab would provide a synergistic benefit when combined with AZA (which induces other prophagocytic “eat me” signals such as calreticulin on cancer cells). The primary objectives of the study were to examine the safety of magrolimab alone or with AZA, and to assess the efficacy of the magrolimab/AZA combo in 29 untreated AML patients and 39 untreated MDS patients. The majority of both the MDS and AML patients were poor cytogenetic risk at 64% and 72%, respectively. Mutant p53 was present in 13% of the MDS patients and 45% of the AML patients.
No deaths occurred in the first 60 days of the study among either the MDS or AML patients and discontinuation of treatment because of drug-related adverse events was seen in only one of the patients (1.5%) treated with magrolimab/AZA. There was no significant neutropenia or thrombocytopenia caused by the therapy seen, and the majority of the patients improved their neutrophil and platelet counts while on therapy.
Anemia from CD47 blockade was mitigated by the use of a priming dose of magrolimab coupled to a maintenance-dose regimen, resulting in a mild hemoglobin drop on the first dose, which returned to baseline with a majority of patients experiencing significant hemoglobin improvement and a decrease in transfusion frequency over time, according to Dr. Sallman and his colleagues.
The results showed that magrolimab/AZA induced a 91% overall response rate (ORR), with a 42% complete remission (CR) that increased to 56% at 6 months, in the MDS patients. AML patients experienced a 64% ORR (56% CR/CRi [CR with incomplete hematological remission]). These results compare favorably with the CR rate of 6%-17% rate seen for AZA monotherapy, according to Dr. Sallman.
Red blood cell transfusion independence was achieved in 58% of the MDS patients and 64% of the AML patients, and a complete cytogenetic response was seen in 35% and 50% of the MDS and AML patients, respectively.
The combined treatment was especially effective in the patients with p53 mutations, with an overall response rate of 75% for both MDS and AML, and a complete response of 42% and 50%, respectively. During the reported time of the study, the median survival was not reached, which compares favorably with current therapies, according to Dr. Sallman.
“Specifically looking at a very-high-risk p53-mutant subset, complete remissions have been observed in the majority of patients. And again, these have been durable. Based on all of these data, expansion cohorts both in MDS and p53 and AML continue to accrue with registrational studies in progress for MDS and planned for p53-mutant AML,” Dr. Sallman concluded.
The trial was sponsored by Gilead Sciences, and funding was obtained from the California Institute for Regenerative Medicine. Dr. Sallman disclosed that he received research funding from Celgene and has acted in a consulting or advisory role for Agios, argenx, and Celyad. He was also on the speaker’s bureau for a variety of pharmaceutical/biotech companies.
SOURCE: Sallman DA et al. ASCO 2020, Abstract 7507.
FROM ASCO 2020
Examining bias
I have an automatic preference for white people over black people. This isn’t my opinion; rather, it is my implicit bias test result. I didn’t believe it at first. Trying hard to not be biased, I took the test again and received the same outcome. My reaction – disbelief – is typical for those like me: White people who believe they are good human beings.
We’ve all watched in horror the acts of violence against blacks in the news. I was shocked and disgusted. It was easy to believe, however, that I am in no way complicit in the injustice and racism I was watching. I think I’m fair and without prejudice. I have never intentionally discriminated against someone. Wanting to help, I listened to my black colleagues, staff, and patients. What I learned made me uncomfortable.
Through all this news, I’d said little to my colleagues and friends. I cannot identify with how a black person has felt recently. What if I said the wrong thing or caused offense? The safe option is to say nothing. I learned that this is a common reaction and the least helpful. The advice from one black colleague was simple: “Just ask us.” Instead of ignoring the issue, she advised me to say: “I wonder what this experience has been like for you. Would you like to share?” And, if you mean it, to add, “I stand with you.” The latter should be followed by “What can I do to help?” Or, more powerfully, “What have I done that makes me complicit?”
Some of these conversations will be uncomfortable. If you want to help, then sit with that. Feeling uncomfortable might mean you are beginning to understand.
I also heard about the excellent book “White Fragility,” by Robin DiAngelo, PhD. In it, she argues that it is difficult for white people to talk about racism because of a tendency to react with defensiveness, guilt, and sometimes anger.
Many of the chapters in the book were easy to read because they didn’t apply to me: I don’t get angry in equity, inclusion, and diversity meetings. I don’t resent affirmative action programs. But then Dr. DiAngelo got me: I believed because I’m a good person and I have no intention of being racist, I’m absolved. Her argument was enlightening. Like all white people in the United States, I have benefited from white privilege. Yes, I’ve worked hard, but I also grew up in a white family with a college-educated father. That alone afforded me academic and financial advantages, which pushed me ahead. I’ve benefited from the status quo.
I have also failed to speak up when white friends carried on about how unnecessary affirmative action programs have become. I’ve sat with sealed lips when I’ve heard comments like “As a white male, it’s a lot harder to get into prestigious schools now.” Having no intention to harm doesn’t matter; plenty of harm is done unintentionally.
I also believed that because I have good intentions, I have no racial bias. I was wrong. The test I took online is an excellent tool to combat this blind spot. It was created by Harvard researchers and is available to everyone: Take a Test. It asks you to categorize faces as good or bad and records your tiny reaction times. Based on these and other questions, it provides feedback on your personal biases.
I was surprised that I have an implicit preference for white people over black people. That’s the point. Most of us are unaware of our biases and falsely believe we are free of them. I encourage you to take the test and learn about yourself. If the result makes you uncomfortable, then sit with it. Try not to be defensive, as I was, and accept that, even if you are a good person, you can become a better one.
Based on what I’ve learned and heard in the last few weeks, I’ve committed to a few things: To acknowledge the harm done to my black and brown colleagues and my complicity even by acts of omission. To not avoid uncomfortable feelings or uncomfortable conversations. As a leader, to use my organizational status to advocate. To stand by my partners of color not only in dramatic one-time marches but also against the everyday perpetrators of microaggressions. To create a safe space and invite my colleagues, staff, friends, and patients to share.
Standing up against racism is all our responsibility. As Dr. Martin Luther King Jr. reminds us: “In the end, we will remember not the words of our enemies, but the silence of our friends.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no disclosures related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I have an automatic preference for white people over black people. This isn’t my opinion; rather, it is my implicit bias test result. I didn’t believe it at first. Trying hard to not be biased, I took the test again and received the same outcome. My reaction – disbelief – is typical for those like me: White people who believe they are good human beings.
We’ve all watched in horror the acts of violence against blacks in the news. I was shocked and disgusted. It was easy to believe, however, that I am in no way complicit in the injustice and racism I was watching. I think I’m fair and without prejudice. I have never intentionally discriminated against someone. Wanting to help, I listened to my black colleagues, staff, and patients. What I learned made me uncomfortable.
Through all this news, I’d said little to my colleagues and friends. I cannot identify with how a black person has felt recently. What if I said the wrong thing or caused offense? The safe option is to say nothing. I learned that this is a common reaction and the least helpful. The advice from one black colleague was simple: “Just ask us.” Instead of ignoring the issue, she advised me to say: “I wonder what this experience has been like for you. Would you like to share?” And, if you mean it, to add, “I stand with you.” The latter should be followed by “What can I do to help?” Or, more powerfully, “What have I done that makes me complicit?”
Some of these conversations will be uncomfortable. If you want to help, then sit with that. Feeling uncomfortable might mean you are beginning to understand.
I also heard about the excellent book “White Fragility,” by Robin DiAngelo, PhD. In it, she argues that it is difficult for white people to talk about racism because of a tendency to react with defensiveness, guilt, and sometimes anger.
Many of the chapters in the book were easy to read because they didn’t apply to me: I don’t get angry in equity, inclusion, and diversity meetings. I don’t resent affirmative action programs. But then Dr. DiAngelo got me: I believed because I’m a good person and I have no intention of being racist, I’m absolved. Her argument was enlightening. Like all white people in the United States, I have benefited from white privilege. Yes, I’ve worked hard, but I also grew up in a white family with a college-educated father. That alone afforded me academic and financial advantages, which pushed me ahead. I’ve benefited from the status quo.
I have also failed to speak up when white friends carried on about how unnecessary affirmative action programs have become. I’ve sat with sealed lips when I’ve heard comments like “As a white male, it’s a lot harder to get into prestigious schools now.” Having no intention to harm doesn’t matter; plenty of harm is done unintentionally.
I also believed that because I have good intentions, I have no racial bias. I was wrong. The test I took online is an excellent tool to combat this blind spot. It was created by Harvard researchers and is available to everyone: Take a Test. It asks you to categorize faces as good or bad and records your tiny reaction times. Based on these and other questions, it provides feedback on your personal biases.
I was surprised that I have an implicit preference for white people over black people. That’s the point. Most of us are unaware of our biases and falsely believe we are free of them. I encourage you to take the test and learn about yourself. If the result makes you uncomfortable, then sit with it. Try not to be defensive, as I was, and accept that, even if you are a good person, you can become a better one.
Based on what I’ve learned and heard in the last few weeks, I’ve committed to a few things: To acknowledge the harm done to my black and brown colleagues and my complicity even by acts of omission. To not avoid uncomfortable feelings or uncomfortable conversations. As a leader, to use my organizational status to advocate. To stand by my partners of color not only in dramatic one-time marches but also against the everyday perpetrators of microaggressions. To create a safe space and invite my colleagues, staff, friends, and patients to share.
Standing up against racism is all our responsibility. As Dr. Martin Luther King Jr. reminds us: “In the end, we will remember not the words of our enemies, but the silence of our friends.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no disclosures related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
I have an automatic preference for white people over black people. This isn’t my opinion; rather, it is my implicit bias test result. I didn’t believe it at first. Trying hard to not be biased, I took the test again and received the same outcome. My reaction – disbelief – is typical for those like me: White people who believe they are good human beings.
We’ve all watched in horror the acts of violence against blacks in the news. I was shocked and disgusted. It was easy to believe, however, that I am in no way complicit in the injustice and racism I was watching. I think I’m fair and without prejudice. I have never intentionally discriminated against someone. Wanting to help, I listened to my black colleagues, staff, and patients. What I learned made me uncomfortable.
Through all this news, I’d said little to my colleagues and friends. I cannot identify with how a black person has felt recently. What if I said the wrong thing or caused offense? The safe option is to say nothing. I learned that this is a common reaction and the least helpful. The advice from one black colleague was simple: “Just ask us.” Instead of ignoring the issue, she advised me to say: “I wonder what this experience has been like for you. Would you like to share?” And, if you mean it, to add, “I stand with you.” The latter should be followed by “What can I do to help?” Or, more powerfully, “What have I done that makes me complicit?”
Some of these conversations will be uncomfortable. If you want to help, then sit with that. Feeling uncomfortable might mean you are beginning to understand.
I also heard about the excellent book “White Fragility,” by Robin DiAngelo, PhD. In it, she argues that it is difficult for white people to talk about racism because of a tendency to react with defensiveness, guilt, and sometimes anger.
Many of the chapters in the book were easy to read because they didn’t apply to me: I don’t get angry in equity, inclusion, and diversity meetings. I don’t resent affirmative action programs. But then Dr. DiAngelo got me: I believed because I’m a good person and I have no intention of being racist, I’m absolved. Her argument was enlightening. Like all white people in the United States, I have benefited from white privilege. Yes, I’ve worked hard, but I also grew up in a white family with a college-educated father. That alone afforded me academic and financial advantages, which pushed me ahead. I’ve benefited from the status quo.
I have also failed to speak up when white friends carried on about how unnecessary affirmative action programs have become. I’ve sat with sealed lips when I’ve heard comments like “As a white male, it’s a lot harder to get into prestigious schools now.” Having no intention to harm doesn’t matter; plenty of harm is done unintentionally.
I also believed that because I have good intentions, I have no racial bias. I was wrong. The test I took online is an excellent tool to combat this blind spot. It was created by Harvard researchers and is available to everyone: Take a Test. It asks you to categorize faces as good or bad and records your tiny reaction times. Based on these and other questions, it provides feedback on your personal biases.
I was surprised that I have an implicit preference for white people over black people. That’s the point. Most of us are unaware of our biases and falsely believe we are free of them. I encourage you to take the test and learn about yourself. If the result makes you uncomfortable, then sit with it. Try not to be defensive, as I was, and accept that, even if you are a good person, you can become a better one.
Based on what I’ve learned and heard in the last few weeks, I’ve committed to a few things: To acknowledge the harm done to my black and brown colleagues and my complicity even by acts of omission. To not avoid uncomfortable feelings or uncomfortable conversations. As a leader, to use my organizational status to advocate. To stand by my partners of color not only in dramatic one-time marches but also against the everyday perpetrators of microaggressions. To create a safe space and invite my colleagues, staff, friends, and patients to share.
Standing up against racism is all our responsibility. As Dr. Martin Luther King Jr. reminds us: “In the end, we will remember not the words of our enemies, but the silence of our friends.”
Dr. Benabio is director of healthcare transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He has no disclosures related to this column. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Lung ultrasound works well in children with COVID-19
researchers wrote in Pediatrics.
They also noted the benefits that modality provides over other imaging techniques.
Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy, performed an observational study of eight children aged 0-17 years who were admitted to the hospital for COVID-19 between March 8 and 26, 2020. In seven of eight patients, the findings were concordant between imaging modalities; in the remaining patient, lung ultrasound (LUS) found an interstitial B-lines pattern that was not seen on radiography. In seven patients with pathologic ultrasound findings at baseline, the improvement or resolution of the subpleural consolidations or interstitial patterns was consistent with concomitant radiologic findings.
The authors cited the benefits of using point-of-care ultrasound instead of other modalities, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” they wrote. “Secondly, when performed at the bedside, LUS allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].”
One limitation of the study is the small sample size; however, the researchers felt the high concordance still suggests LUS is a reasonable method for COVID-19 patients.
There was no external funding for this study and the investigators had no relevant financial disclosures.
SOURCE: Denina M et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2020-1157.
researchers wrote in Pediatrics.
They also noted the benefits that modality provides over other imaging techniques.
Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy, performed an observational study of eight children aged 0-17 years who were admitted to the hospital for COVID-19 between March 8 and 26, 2020. In seven of eight patients, the findings were concordant between imaging modalities; in the remaining patient, lung ultrasound (LUS) found an interstitial B-lines pattern that was not seen on radiography. In seven patients with pathologic ultrasound findings at baseline, the improvement or resolution of the subpleural consolidations or interstitial patterns was consistent with concomitant radiologic findings.
The authors cited the benefits of using point-of-care ultrasound instead of other modalities, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” they wrote. “Secondly, when performed at the bedside, LUS allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].”
One limitation of the study is the small sample size; however, the researchers felt the high concordance still suggests LUS is a reasonable method for COVID-19 patients.
There was no external funding for this study and the investigators had no relevant financial disclosures.
SOURCE: Denina M et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2020-1157.
researchers wrote in Pediatrics.
They also noted the benefits that modality provides over other imaging techniques.
Marco Denina, MD, and colleagues from the pediatric infectious diseases unit at Regina Margherita Children’s Hospital in Turin, Italy, performed an observational study of eight children aged 0-17 years who were admitted to the hospital for COVID-19 between March 8 and 26, 2020. In seven of eight patients, the findings were concordant between imaging modalities; in the remaining patient, lung ultrasound (LUS) found an interstitial B-lines pattern that was not seen on radiography. In seven patients with pathologic ultrasound findings at baseline, the improvement or resolution of the subpleural consolidations or interstitial patterns was consistent with concomitant radiologic findings.
The authors cited the benefits of using point-of-care ultrasound instead of other modalities, such as CT. “First, it may reduce the number of radiologic examinations, lowering the radiation exposure of the patients,” they wrote. “Secondly, when performed at the bedside, LUS allows for the reduction of the patient’s movement within the hospital; thus, it lowers the number of health care workers and medical devices exposed to [SARS-CoV-2].”
One limitation of the study is the small sample size; however, the researchers felt the high concordance still suggests LUS is a reasonable method for COVID-19 patients.
There was no external funding for this study and the investigators had no relevant financial disclosures.
SOURCE: Denina M et al. Pediatrics. 2020 Jun. doi: 10.1542/peds.2020-1157.
FROM PEDIATRICS
‘I can’t breathe’: Health inequity and state-sanctioned violence
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
One might immediately think of the deaths of Eric Garner, George Floyd, or even the fictional character Radio Raheem from Spike Lee’s critically acclaimed film, “Do the Right Thing,” when they hear the words “I can’t breathe.” These words are a cry for help. The deaths of these unarmed black men is devastating and has led to a state of rage, palpable pain, and protest across the world.
However, in this moment, I am talking about the health inequity exposed by the COVID-19 pandemic. Whether it be acute respiratory distress syndrome (ARDS) secondary to severe COVID-19, or the subsequent hypercoagulable state of COVID-19 that leads to venous thromboembolism, many black people in this country are left breathless. Many black patients who had no employee-based health insurance also had no primary care physician to order a SARS-CoV2 PCR lab test for them. Many of these patients have preexisting conditions, such as asthma from living in redlined communities affected by environmental racism. Many grew up in food deserts, where no fresh-produce store was interested enough to set up shop in their neighborhoods. They have been eating fast food since early childhood, as a fast-food burger is still cheaper than a salad. The result is obesity, an epidemic that can lead to diabetes mellitus, hypertension that can lead to coronary artery disease, stroke, and end-stage renal disease.
Earlier in my career, I once had a colleague gleefully tell me that all black people drank Kool-Aid while in discussion of the effects of high-sugar diets in our patients; this colleague was sure I would agree. Not all black people drink Kool-Aid. Secondary to my fear of the backlash that can come from the discomfort of “white fragility” that Robin DiAngelo describes in her New York Times bestseller by the same name, ”White Fragility: Why It’s So Hard for White People to Talk About Racism,” I refrained from expressing my own hurt, and I did not offer explicit correction. I, instead, took a serious pause. That pause, which lasted only minutes, seemed to last 400 years. It was a brief reflection of the 400 years of systemic racism seeping into everyday life. This included the circumstances that would lead to the health inequities that result in the health disparities from which many black patients suffer. It is that same systemic racism that could create two America’s in which my colleague might not have to know the historic context in which that question could be hurtful. I retorted with modified shock and a chuckle so that I could muster up enough strength to repeat what was said and leave it open for reflection. The goal was for my colleague to realize the obvious implicit bias that lingered, despite intention. The chuckle was also to cover my pain.
Whether we know it or not, we all carry some form of implicit bias, regardless of race, class, gender, ethnicity, sexual preference, or socioeconomic status. In this case, it is the same implicit bias that causes physicians to ignore some black patients when they have said that they are in pain. A groundbreaking April 2016 article in Proceedings of the National Academy of Sciences, “Racial Bias in Pain Assessment and Treatment Recommendations, and False Beliefs about Biological Differences Between Blacks and Whites” (doi: 10.1073/pnas.1516047113), revealed that racial disparities in pain assessment and treatment recommendations can be directly connected to the racial bias of the provider. It could be possible that this phenomenon has affected black patients who have walked into clinics and emergency departments and said, “I’m short of breath. I think that I might have coronavirus and need to be tested.” It may be that same implicit bias that has cut the air supply to a patient encounter. Instead of inquiring further, the patient might be met with minimum questions while their provider obtains their history and physical. Assumptions and blame on behavior and lack of personal responsibility secretly replace questions that could have been asked. Differentials between exacerbations and other etiologies are not explored. Could that patient have been sent home without a SARS-CoV2 polymerase chain reaction test? Well, what if the tests were in short supply? Sometimes they may have been sent home without a chest x-ray. In most cases, there are no funds to send them home with a pulse oximeter.
The act of assuming a person’s story that we consider to be one dimensional is always dangerous – and even more so during this pandemic. That person we can relate to – secondary to a cool pop culture moment, a TikTok song, or a negative stereotype – is not one dimensional. That assumption and that stereotype can make room for implicit bias. That same implicit bias is the knee on a neck of any marginalized patient. Implicit bias is the choke hold that slowly removes the light and life from a person who has a story, who has a family, and who has been an essential worker who can’t work from home. That person is telling us that they can’t breathe, but sometimes the only things seen are comorbidities through a misinformed or biased lens that suggest an assumed lack of personal responsibility. In a May 2020 New England Journal of Medicine perspective, “Racial health disparities and Covid-19” (doi: 10.1056/NEJMp2012910), Merlin Chowkwanyun, PhD, MPH, and Adolph L. Reed Jr., PhD, caution us against creating race-based explanations for presumed behavioral patterns.
Systemic racism has created the myth that the playing field has been leveled since the end of enslavement. It hasn’t. That black man, woman, or nonbinary person is telling you “I can’t breathe. I’m tired. I’m short of breath ... I have a cough ... I’m feeling weak these days, Doc.” However, implicit bias is still that knee that won’t let up. It has not let up. Communities with lower-income black and Hispanic patients have already seen local hospitals and frontline workers fight to save their lives while losing their own to COVID-19. We all witnessed the battle for scarce resources and PPE [personal protective equipment]. In contrast, some wealthy neighborhoods have occupants who most likely have access to a primary care physician and more testing centers.
As we reexamine ourselves and look at these cases of police brutality against unarmed black men, women, and children with the appropriate shame and outrage, let us reflect upon the privileges that we enjoy. Let us find our voice as we speak up for black lives. Let us look deeply into the history of medicine as it relates to black patients by reading “Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present” by Harriet A. Washington. Let us examine that painful legacy, which, while having moments of good intention, still carries the stain of indifference, racism, neglect, and even experimentation without informed consent.
Why should we do these things? Because some of our black patients have also yelled or whispered, “I can’t breathe,” and we were not always listening either.
Dr. Ajala is a hospitalist and associate site director for education at Grady Memorial Hospital in Atlanta. She is a member of the executive council for SHM’s Care for Vulnerable Populations special interest group.
VIALE-A confirms survival benefit for venetoclax-azacitidine in hard-to-treat AML
Adding venetoclax to azacitidine significantly extended survival of patients with previously untreated acute myeloid leukemia (AML) who were ineligible for standard induction therapy, results of the phase 3 VIALE-A trial showed.
Median overall survival for patients treated with venetoclax (Venclexta) and azacitidine was 14.7 months, compared with 9.6 months for patients who received azacitidine with a placebo, reported Courtney DiNardo, MD, from the University of Texas MD Anderson Cancer Center, Houston.
“The combination of [azacitidine] and [venetoclax] was associated with statistically significant and clinically meaningful improvements in overall survival, response rates, duration of remission, and transfusion independence, representing a true paradigm shift in the treatment of our older patients with AML,” she said in a late-breaking abstract presentation at the virtual annual congress of the European Hematology Association.
Patients with newly diagnosed AML who are aged 75 years and older or have significant comorbidities are often not able to withstand the rigors of standard induction therapy for AML and have instead been treated with low-dose hypomethylating agents or cytarabine, but these therapies typically are associated with inferior outcomes, Dr. DiNardo said.
Venetoclax has shown good single-agent activity against relapsed/refractory AML. Early efficacy results of a phase 1b study, reported at the 2017 EHA Congress, showed that, among 100 patients age 65 years and older with previously untreated AML, the combination of venetoclax with either decitabine or azacitidine was associated with a 69% overall response rate, and that older patients were able to tolerate the regimen.
No surprise
The results of the VIALE-A study merely confirm what hematologists/oncologists have known for several years, said Joshua F. Zeidner, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill.
“Most leukemia clinicians have been using this regimen as a standard of care prior to these results,” he said in an interview. Dr. Zeidner was not involved in the study.
In November 2018, the Food and Drug Administration granted accelerated approval to venetoclax in combination with either azacitidine or decitabine or low-dose cytarabine in adults with newly diagnosed AML who because of age or comorbidities were ineligible for standard intensive induction regimens. Dr. Zeidner noted, however, that there are still questions about the combination in this population that need further exploration.
Despite being labeled as a “low-intensity” therapy, “I think low intensity is sort of a misnomer here,” he said. “It’s very challenging to give this regimen in the community because of all of the cytopenias, a high degree of transfusion dependence that these patients have, at least in the first few cycles, and all the rigorous laboratory monitoring and drug interactions that are common with venetoclax really lead to a lot of challenges in the community.”
Also still unanswered are questions about how to dose patients with early responses who have potential dose-limiting toxicities such as neutropenia and thrombocytopenia, he said.
It’s also unclear whether patients will require hospitalization during the ramp-up phase of venetoclax, as was done in some clinical trials, because of risk of tumor lysis syndrome. In the VIALE-A study, however, there were only three minor biochemical cases of tumor lysis syndrome in the experimental arm, and none of these cases required dose modification or treatment discontinuation.
“This begets the question whether patients need to be hospitalized at for the initiation of this treatment,” Dr. Zeidner said. Additional studies will also be needed to see whether certain subgroups of patients would be likely to derive particular benefit from venetoclax plus azacitidine, such as patients with IDH1 or IDH2 somatic mutations.
Randomized confirmatory trial
The VIALE-A study was a randomized, placebo-controlled trial designed to put the early promise of the combination to the test.
Investigators enrolled 433 adults with newly diagnosed AML who were ineligible for induction therapy either because they were 75 or older or were younger than 75 but had one or more of the following comorbidities: heart failure requiring treatment or a left ventricular ejection fraction of 50% or less, chronic stable angina, diffusion lung capacity for carbon monoxide of 65% or less or forced expiratory volume in 1 second of 65% or less, or Eastern Cooperative Oncology Group performance status score of 2-3.
After stratification by age, cytogenetic risk, and geographic region, the patients were randomized in a 2:1 fashion to receive azacitidine 75 mg/m2 either subcutaneously or intravenously on days 1-7 of each 28-day cycle, plus either oral venetoclax 400 mg daily following a 3-day ramp up in the first cycle (286 patients) or placebo (145 patients).
The median age in each arm was 76 years. Approximately 75% of patients in each arm had de novo AML.
Approximately half of all patients in each arm has bone marrow blast counts of 50% or greater. Two-thirds of patients had intermediate cytogenetic risk and one-third had poor risk disease. Somatic mutation rates, including mutations in IDH1/2, FLT3, NPM1 and TP53, were roughly comparable between the arms.
As noted before, median overall survival, the primary endpoint, was significantly longer with venetoclax, at 14.7 versus 9.6 months, translating into a hazard ratio for death with venetoclax of 0.66 (P < .001).
Although the numbers were relatively small, an analysis of overall survival by subgroups showed either a significant advantage or trend favoring venetoclax in all subgroups, notably among patients with difficult-to-treat disease, including patients 75 years and older and those with secondary AML, Dr. DiNardo said.
The combined complete response and CR with incomplete recovery (CRi) response rate was 66.4% with venetoclax, compared with 28.3% with azacitidine alone. The median time to a CR/CRi was shorter with the combination at 1.3 versus 2.8 months for azacitidine plus placebo, and the median duration of a CR/CRi response was longer, at 17.5 versus 13.4 months, respectively.
Response rates were also notably higher with venetoclax in all cytogenetic risk, AML subtype, molecular mutation, age, ECOG score, and bone marrow blast subgroups.
Additionally, significantly more patients treated with venetoclax/azacitidine were transfusion independent for a minimum of 8 weeks for platelets or combined red cells and platelets, Dr. DiNardo noted.
Median event-free survival – time from randomization to relapse, death, or treatment failure – was 9.8 months in the venetoclax arm versus 7 months in the placebo arm (HR, 0.63; P < .001).
All patients experienced at least one treatment-emergent adverse event. Grade 3 or greater hematologic adverse events were seen 82% of patients in the venetoclax arm and 68% in the placebo arm. The respective rates of grade 3 or greater neutropenia were 42% versus 29%, and febrile neutropenia were 42% versus 19%. Thrombocytopenia, anemia, and leukopenia rates were also higher among patients who received venetoclax.
Grade 1-2 gastrointestinal events were the most frequent nonhematologic adverse events. There was no increase in early deaths seen with the study combination.
The study was supported by AbbVie and Genentech. Dr. DiNardo disclosed research funding from and advisory board activities for those companies and from others. Dr. Zeidner disclosed serving on an independent review committee for AbbVie and advisory board activity for Genentech and others.
SOURCE: DiNardo C et al. EHA25, Abstract LB2601.
Adding venetoclax to azacitidine significantly extended survival of patients with previously untreated acute myeloid leukemia (AML) who were ineligible for standard induction therapy, results of the phase 3 VIALE-A trial showed.
Median overall survival for patients treated with venetoclax (Venclexta) and azacitidine was 14.7 months, compared with 9.6 months for patients who received azacitidine with a placebo, reported Courtney DiNardo, MD, from the University of Texas MD Anderson Cancer Center, Houston.
“The combination of [azacitidine] and [venetoclax] was associated with statistically significant and clinically meaningful improvements in overall survival, response rates, duration of remission, and transfusion independence, representing a true paradigm shift in the treatment of our older patients with AML,” she said in a late-breaking abstract presentation at the virtual annual congress of the European Hematology Association.
Patients with newly diagnosed AML who are aged 75 years and older or have significant comorbidities are often not able to withstand the rigors of standard induction therapy for AML and have instead been treated with low-dose hypomethylating agents or cytarabine, but these therapies typically are associated with inferior outcomes, Dr. DiNardo said.
Venetoclax has shown good single-agent activity against relapsed/refractory AML. Early efficacy results of a phase 1b study, reported at the 2017 EHA Congress, showed that, among 100 patients age 65 years and older with previously untreated AML, the combination of venetoclax with either decitabine or azacitidine was associated with a 69% overall response rate, and that older patients were able to tolerate the regimen.
No surprise
The results of the VIALE-A study merely confirm what hematologists/oncologists have known for several years, said Joshua F. Zeidner, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill.
“Most leukemia clinicians have been using this regimen as a standard of care prior to these results,” he said in an interview. Dr. Zeidner was not involved in the study.
In November 2018, the Food and Drug Administration granted accelerated approval to venetoclax in combination with either azacitidine or decitabine or low-dose cytarabine in adults with newly diagnosed AML who because of age or comorbidities were ineligible for standard intensive induction regimens. Dr. Zeidner noted, however, that there are still questions about the combination in this population that need further exploration.
Despite being labeled as a “low-intensity” therapy, “I think low intensity is sort of a misnomer here,” he said. “It’s very challenging to give this regimen in the community because of all of the cytopenias, a high degree of transfusion dependence that these patients have, at least in the first few cycles, and all the rigorous laboratory monitoring and drug interactions that are common with venetoclax really lead to a lot of challenges in the community.”
Also still unanswered are questions about how to dose patients with early responses who have potential dose-limiting toxicities such as neutropenia and thrombocytopenia, he said.
It’s also unclear whether patients will require hospitalization during the ramp-up phase of venetoclax, as was done in some clinical trials, because of risk of tumor lysis syndrome. In the VIALE-A study, however, there were only three minor biochemical cases of tumor lysis syndrome in the experimental arm, and none of these cases required dose modification or treatment discontinuation.
“This begets the question whether patients need to be hospitalized at for the initiation of this treatment,” Dr. Zeidner said. Additional studies will also be needed to see whether certain subgroups of patients would be likely to derive particular benefit from venetoclax plus azacitidine, such as patients with IDH1 or IDH2 somatic mutations.
Randomized confirmatory trial
The VIALE-A study was a randomized, placebo-controlled trial designed to put the early promise of the combination to the test.
Investigators enrolled 433 adults with newly diagnosed AML who were ineligible for induction therapy either because they were 75 or older or were younger than 75 but had one or more of the following comorbidities: heart failure requiring treatment or a left ventricular ejection fraction of 50% or less, chronic stable angina, diffusion lung capacity for carbon monoxide of 65% or less or forced expiratory volume in 1 second of 65% or less, or Eastern Cooperative Oncology Group performance status score of 2-3.
After stratification by age, cytogenetic risk, and geographic region, the patients were randomized in a 2:1 fashion to receive azacitidine 75 mg/m2 either subcutaneously or intravenously on days 1-7 of each 28-day cycle, plus either oral venetoclax 400 mg daily following a 3-day ramp up in the first cycle (286 patients) or placebo (145 patients).
The median age in each arm was 76 years. Approximately 75% of patients in each arm had de novo AML.
Approximately half of all patients in each arm has bone marrow blast counts of 50% or greater. Two-thirds of patients had intermediate cytogenetic risk and one-third had poor risk disease. Somatic mutation rates, including mutations in IDH1/2, FLT3, NPM1 and TP53, were roughly comparable between the arms.
As noted before, median overall survival, the primary endpoint, was significantly longer with venetoclax, at 14.7 versus 9.6 months, translating into a hazard ratio for death with venetoclax of 0.66 (P < .001).
Although the numbers were relatively small, an analysis of overall survival by subgroups showed either a significant advantage or trend favoring venetoclax in all subgroups, notably among patients with difficult-to-treat disease, including patients 75 years and older and those with secondary AML, Dr. DiNardo said.
The combined complete response and CR with incomplete recovery (CRi) response rate was 66.4% with venetoclax, compared with 28.3% with azacitidine alone. The median time to a CR/CRi was shorter with the combination at 1.3 versus 2.8 months for azacitidine plus placebo, and the median duration of a CR/CRi response was longer, at 17.5 versus 13.4 months, respectively.
Response rates were also notably higher with venetoclax in all cytogenetic risk, AML subtype, molecular mutation, age, ECOG score, and bone marrow blast subgroups.
Additionally, significantly more patients treated with venetoclax/azacitidine were transfusion independent for a minimum of 8 weeks for platelets or combined red cells and platelets, Dr. DiNardo noted.
Median event-free survival – time from randomization to relapse, death, or treatment failure – was 9.8 months in the venetoclax arm versus 7 months in the placebo arm (HR, 0.63; P < .001).
All patients experienced at least one treatment-emergent adverse event. Grade 3 or greater hematologic adverse events were seen 82% of patients in the venetoclax arm and 68% in the placebo arm. The respective rates of grade 3 or greater neutropenia were 42% versus 29%, and febrile neutropenia were 42% versus 19%. Thrombocytopenia, anemia, and leukopenia rates were also higher among patients who received venetoclax.
Grade 1-2 gastrointestinal events were the most frequent nonhematologic adverse events. There was no increase in early deaths seen with the study combination.
The study was supported by AbbVie and Genentech. Dr. DiNardo disclosed research funding from and advisory board activities for those companies and from others. Dr. Zeidner disclosed serving on an independent review committee for AbbVie and advisory board activity for Genentech and others.
SOURCE: DiNardo C et al. EHA25, Abstract LB2601.
Adding venetoclax to azacitidine significantly extended survival of patients with previously untreated acute myeloid leukemia (AML) who were ineligible for standard induction therapy, results of the phase 3 VIALE-A trial showed.
Median overall survival for patients treated with venetoclax (Venclexta) and azacitidine was 14.7 months, compared with 9.6 months for patients who received azacitidine with a placebo, reported Courtney DiNardo, MD, from the University of Texas MD Anderson Cancer Center, Houston.
“The combination of [azacitidine] and [venetoclax] was associated with statistically significant and clinically meaningful improvements in overall survival, response rates, duration of remission, and transfusion independence, representing a true paradigm shift in the treatment of our older patients with AML,” she said in a late-breaking abstract presentation at the virtual annual congress of the European Hematology Association.
Patients with newly diagnosed AML who are aged 75 years and older or have significant comorbidities are often not able to withstand the rigors of standard induction therapy for AML and have instead been treated with low-dose hypomethylating agents or cytarabine, but these therapies typically are associated with inferior outcomes, Dr. DiNardo said.
Venetoclax has shown good single-agent activity against relapsed/refractory AML. Early efficacy results of a phase 1b study, reported at the 2017 EHA Congress, showed that, among 100 patients age 65 years and older with previously untreated AML, the combination of venetoclax with either decitabine or azacitidine was associated with a 69% overall response rate, and that older patients were able to tolerate the regimen.
No surprise
The results of the VIALE-A study merely confirm what hematologists/oncologists have known for several years, said Joshua F. Zeidner, MD, from the University of North Carolina Lineberger Comprehensive Cancer Center in Chapel Hill.
“Most leukemia clinicians have been using this regimen as a standard of care prior to these results,” he said in an interview. Dr. Zeidner was not involved in the study.
In November 2018, the Food and Drug Administration granted accelerated approval to venetoclax in combination with either azacitidine or decitabine or low-dose cytarabine in adults with newly diagnosed AML who because of age or comorbidities were ineligible for standard intensive induction regimens. Dr. Zeidner noted, however, that there are still questions about the combination in this population that need further exploration.
Despite being labeled as a “low-intensity” therapy, “I think low intensity is sort of a misnomer here,” he said. “It’s very challenging to give this regimen in the community because of all of the cytopenias, a high degree of transfusion dependence that these patients have, at least in the first few cycles, and all the rigorous laboratory monitoring and drug interactions that are common with venetoclax really lead to a lot of challenges in the community.”
Also still unanswered are questions about how to dose patients with early responses who have potential dose-limiting toxicities such as neutropenia and thrombocytopenia, he said.
It’s also unclear whether patients will require hospitalization during the ramp-up phase of venetoclax, as was done in some clinical trials, because of risk of tumor lysis syndrome. In the VIALE-A study, however, there were only three minor biochemical cases of tumor lysis syndrome in the experimental arm, and none of these cases required dose modification or treatment discontinuation.
“This begets the question whether patients need to be hospitalized at for the initiation of this treatment,” Dr. Zeidner said. Additional studies will also be needed to see whether certain subgroups of patients would be likely to derive particular benefit from venetoclax plus azacitidine, such as patients with IDH1 or IDH2 somatic mutations.
Randomized confirmatory trial
The VIALE-A study was a randomized, placebo-controlled trial designed to put the early promise of the combination to the test.
Investigators enrolled 433 adults with newly diagnosed AML who were ineligible for induction therapy either because they were 75 or older or were younger than 75 but had one or more of the following comorbidities: heart failure requiring treatment or a left ventricular ejection fraction of 50% or less, chronic stable angina, diffusion lung capacity for carbon monoxide of 65% or less or forced expiratory volume in 1 second of 65% or less, or Eastern Cooperative Oncology Group performance status score of 2-3.
After stratification by age, cytogenetic risk, and geographic region, the patients were randomized in a 2:1 fashion to receive azacitidine 75 mg/m2 either subcutaneously or intravenously on days 1-7 of each 28-day cycle, plus either oral venetoclax 400 mg daily following a 3-day ramp up in the first cycle (286 patients) or placebo (145 patients).
The median age in each arm was 76 years. Approximately 75% of patients in each arm had de novo AML.
Approximately half of all patients in each arm has bone marrow blast counts of 50% or greater. Two-thirds of patients had intermediate cytogenetic risk and one-third had poor risk disease. Somatic mutation rates, including mutations in IDH1/2, FLT3, NPM1 and TP53, were roughly comparable between the arms.
As noted before, median overall survival, the primary endpoint, was significantly longer with venetoclax, at 14.7 versus 9.6 months, translating into a hazard ratio for death with venetoclax of 0.66 (P < .001).
Although the numbers were relatively small, an analysis of overall survival by subgroups showed either a significant advantage or trend favoring venetoclax in all subgroups, notably among patients with difficult-to-treat disease, including patients 75 years and older and those with secondary AML, Dr. DiNardo said.
The combined complete response and CR with incomplete recovery (CRi) response rate was 66.4% with venetoclax, compared with 28.3% with azacitidine alone. The median time to a CR/CRi was shorter with the combination at 1.3 versus 2.8 months for azacitidine plus placebo, and the median duration of a CR/CRi response was longer, at 17.5 versus 13.4 months, respectively.
Response rates were also notably higher with venetoclax in all cytogenetic risk, AML subtype, molecular mutation, age, ECOG score, and bone marrow blast subgroups.
Additionally, significantly more patients treated with venetoclax/azacitidine were transfusion independent for a minimum of 8 weeks for platelets or combined red cells and platelets, Dr. DiNardo noted.
Median event-free survival – time from randomization to relapse, death, or treatment failure – was 9.8 months in the venetoclax arm versus 7 months in the placebo arm (HR, 0.63; P < .001).
All patients experienced at least one treatment-emergent adverse event. Grade 3 or greater hematologic adverse events were seen 82% of patients in the venetoclax arm and 68% in the placebo arm. The respective rates of grade 3 or greater neutropenia were 42% versus 29%, and febrile neutropenia were 42% versus 19%. Thrombocytopenia, anemia, and leukopenia rates were also higher among patients who received venetoclax.
Grade 1-2 gastrointestinal events were the most frequent nonhematologic adverse events. There was no increase in early deaths seen with the study combination.
The study was supported by AbbVie and Genentech. Dr. DiNardo disclosed research funding from and advisory board activities for those companies and from others. Dr. Zeidner disclosed serving on an independent review committee for AbbVie and advisory board activity for Genentech and others.
SOURCE: DiNardo C et al. EHA25, Abstract LB2601.
FROM EHA CONGRESS