User login
-
Worry over family, friends the main driver of COVID-19 stress
Individuals are more worried about family members becoming ill with COVID-19 or about unknowingly transmitting the disease to family members than they are about contracting it themselves, results of a new survey show.
Investigators surveyed over 3,000 adults, using an online questionnaire. Of the respondents, about 20% were health care workers, and most were living in locations with active stay-at-home orders at the time of the survey.
Close to half of participants were worried about family members contracting the virus, one third were worried about unknowingly infecting others, and 20% were worried about contracting the virus themselves.
“We were a little surprised to see that people were more concerned about others than about themselves, specifically worrying about whether a family member would contract COVID-19 and whether they might unintentionally infect others,” lead author Ran Barzilay, MD, PhD, child and adolescent psychiatrist at the Children’s Hospital of Philadelphia (CHOP), told Medscape Medical News.
The study was published online August 20 in Translational Psychiatry.
Interactive platform
“The pandemic has provided a unique opportunity to study resilience in healthcare professionals and others,” said Barzilay, assistant professor at the Lifespan Brain Institute, a collaboration between CHOP and the University of Pennsylvania, under the directorship of Raquel Gur, MD, PhD.
“After the pandemic broke out in March, we launched a website in early April where we surveyed people for levels of resilience, mental health, and well-being during the outbreak,” he added.
Survey participants then shared it with their contacts.
“To date, over 7000 people have completed it – mostly from the US but also from Israel,” Barzilay said.
The survey was anonymous, but participants could choose to have follow-up contact. The survey included an interactive 21-item resilience questionnaire and an assessment of COVID-19-related items related to worries concerning the following: contracting, dying from, or currently having the illness; having a family member contract the illness; unknowingly infecting others; and experiencing significant financial burden.
A total of 1350 participants took a second survey on anxiety and depression that utilized the Generalized Anxiety Disorder–7 and the Patient Health Questionnaire–2.
“What makes the survey unique is that it’s not just a means of collecting data but also an interactive platform that gives participants immediate personalized feedback, based on their responses to the resilience and well-being surveys, with practical tips and recommendations for stress management and ways of boosting resilience,” Barzilay said.
Tend and befriend
Ten days into the survey, data were available on 3,042 participants (64% women, 54% with advanced education, 20.5% health care providers), who ranged in age from 18 to 70 years (mean [SD], 38.9 [11.9] years).
After accounting for covariates, the researchers found that participants reported more distress about family members contracting COVID-19 and about unknowingly infecting others than about getting COVID-19 themselves (48.5% and 36% vs. 19.9%, respectively; P < .0005).
Increased COVID-19-related worries were associated with 22% higher anxiety and 16.1% higher depression scores; women had higher scores than men on both.
Each 1-SD increase in the composite score of COVID-19 worries was associated with over twice the increased probability of generalized anxiety and depression (odds ratio, 2.23; 95% confidence interval, 1.88-2.65; and OR, 1.67; 95% CI, 1.41-1.98, respectively; for both, P < .001).
On the other hand, for every 1-SD increase in the resilience score, there was a 64.9% decrease in the possibility of screening positive for generalized anxiety disorder and a 69.3% decrease in the possibility of screening positive for depression (for both, P < .0001).
Compared to participants from Israel, US participants were “more stressed” about contracting, dying from, and currently having COVID-19 themselves. Overall, Israeli participants scored higher than US participants on the resilience scale.
Rates of anxiety and depression did not differ significantly between healthcare providers and others. Health care providers worried more about contracting COVID-19 themselves and worried less about finances after COVID-19.
The authors propose that survey participants were more worried about others than about themselves because of “prosocial behavior under stress” and “tend-and-befriend,” whereby, “in response to threat, humans tend to protect their close ones (tending) and seek out their social group for mutual defense (befriending).”
This type of altruistic behavior has been “described in acute situations throughout history” and has been “linked to mechanisms of resilience for overcoming adversity,” the authors indicate.
Demographic biases
Commenting on the findings for Medscape Medical News, Golnaz Tabibnia, PhD, a neuroscientist at the University of California, Irvine, who was not involved in the research, suggested that although higher resilience scores were associated with lower COVID-related worries, it is possible, “as the authors suggest, that having more resilience resources makes you less worried, but the causality could go the other direction as well, and less worry/rumination may lead to more resilience.”
Also commenting on the study for Medscape Medical News, Christiaan Vinkers, MD, PhD, a psychiatrist at the Amsterdam University Medical Center, Amsterdam, the Netherlands, said it was noteworthy that healthcare providers reported similar levels of mood and anxiety symptoms, compared to others.
“This is encouraging, as it suggests adequate resilience levels in professionals who work in the front lines of the COVID-19 pandemic,” he said.
Resilience occurs not only at the individual level but also at the community level, which may help explain the striking differences in COVID-19-related worries and anxiety between participants from the United States and Israel, Vinkers added.
E. Alison Holman, PhD, professor, Sue and Bill Gross School of Nursing, University of California, Irvine, noted that respondents were predominantly white, female, and had relatively high incomes, “suggesting strong demographic biases in those who chose to participate.”
Holman, who was not involved with the study, told Medscape Medical News that the “findings do not address the real impact of COVID-19 on the hardest-hit communities in America – poor, Black, and Latinx communities, where a large proportion of essential workers live.”
Barzilay acknowledged that, “unfortunately, because of the way the study was circulated, it did not reach minorities, which is one of the things we want to improve.”
The study is ongoing and has been translated into Spanish, French, and Hebrew. The team plans to collect data on diverse populations.
The study was supported by grants from the National Institute of Mental Health, the Lifespan Brain Institute of Children’s Hospital of Philadelphia, Penn Medicine, the University of Pennsylvania, and in part by the Zuckerman STEM Leadership Program. Barzilay serves on the scientific board and reports stock ownership in Taliaz Health. The other authors, Golnaz, Vinkers, and Holman have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Individuals are more worried about family members becoming ill with COVID-19 or about unknowingly transmitting the disease to family members than they are about contracting it themselves, results of a new survey show.
Investigators surveyed over 3,000 adults, using an online questionnaire. Of the respondents, about 20% were health care workers, and most were living in locations with active stay-at-home orders at the time of the survey.
Close to half of participants were worried about family members contracting the virus, one third were worried about unknowingly infecting others, and 20% were worried about contracting the virus themselves.
“We were a little surprised to see that people were more concerned about others than about themselves, specifically worrying about whether a family member would contract COVID-19 and whether they might unintentionally infect others,” lead author Ran Barzilay, MD, PhD, child and adolescent psychiatrist at the Children’s Hospital of Philadelphia (CHOP), told Medscape Medical News.
The study was published online August 20 in Translational Psychiatry.
Interactive platform
“The pandemic has provided a unique opportunity to study resilience in healthcare professionals and others,” said Barzilay, assistant professor at the Lifespan Brain Institute, a collaboration between CHOP and the University of Pennsylvania, under the directorship of Raquel Gur, MD, PhD.
“After the pandemic broke out in March, we launched a website in early April where we surveyed people for levels of resilience, mental health, and well-being during the outbreak,” he added.
Survey participants then shared it with their contacts.
“To date, over 7000 people have completed it – mostly from the US but also from Israel,” Barzilay said.
The survey was anonymous, but participants could choose to have follow-up contact. The survey included an interactive 21-item resilience questionnaire and an assessment of COVID-19-related items related to worries concerning the following: contracting, dying from, or currently having the illness; having a family member contract the illness; unknowingly infecting others; and experiencing significant financial burden.
A total of 1350 participants took a second survey on anxiety and depression that utilized the Generalized Anxiety Disorder–7 and the Patient Health Questionnaire–2.
“What makes the survey unique is that it’s not just a means of collecting data but also an interactive platform that gives participants immediate personalized feedback, based on their responses to the resilience and well-being surveys, with practical tips and recommendations for stress management and ways of boosting resilience,” Barzilay said.
Tend and befriend
Ten days into the survey, data were available on 3,042 participants (64% women, 54% with advanced education, 20.5% health care providers), who ranged in age from 18 to 70 years (mean [SD], 38.9 [11.9] years).
After accounting for covariates, the researchers found that participants reported more distress about family members contracting COVID-19 and about unknowingly infecting others than about getting COVID-19 themselves (48.5% and 36% vs. 19.9%, respectively; P < .0005).
Increased COVID-19-related worries were associated with 22% higher anxiety and 16.1% higher depression scores; women had higher scores than men on both.
Each 1-SD increase in the composite score of COVID-19 worries was associated with over twice the increased probability of generalized anxiety and depression (odds ratio, 2.23; 95% confidence interval, 1.88-2.65; and OR, 1.67; 95% CI, 1.41-1.98, respectively; for both, P < .001).
On the other hand, for every 1-SD increase in the resilience score, there was a 64.9% decrease in the possibility of screening positive for generalized anxiety disorder and a 69.3% decrease in the possibility of screening positive for depression (for both, P < .0001).
Compared to participants from Israel, US participants were “more stressed” about contracting, dying from, and currently having COVID-19 themselves. Overall, Israeli participants scored higher than US participants on the resilience scale.
Rates of anxiety and depression did not differ significantly between healthcare providers and others. Health care providers worried more about contracting COVID-19 themselves and worried less about finances after COVID-19.
The authors propose that survey participants were more worried about others than about themselves because of “prosocial behavior under stress” and “tend-and-befriend,” whereby, “in response to threat, humans tend to protect their close ones (tending) and seek out their social group for mutual defense (befriending).”
This type of altruistic behavior has been “described in acute situations throughout history” and has been “linked to mechanisms of resilience for overcoming adversity,” the authors indicate.
Demographic biases
Commenting on the findings for Medscape Medical News, Golnaz Tabibnia, PhD, a neuroscientist at the University of California, Irvine, who was not involved in the research, suggested that although higher resilience scores were associated with lower COVID-related worries, it is possible, “as the authors suggest, that having more resilience resources makes you less worried, but the causality could go the other direction as well, and less worry/rumination may lead to more resilience.”
Also commenting on the study for Medscape Medical News, Christiaan Vinkers, MD, PhD, a psychiatrist at the Amsterdam University Medical Center, Amsterdam, the Netherlands, said it was noteworthy that healthcare providers reported similar levels of mood and anxiety symptoms, compared to others.
“This is encouraging, as it suggests adequate resilience levels in professionals who work in the front lines of the COVID-19 pandemic,” he said.
Resilience occurs not only at the individual level but also at the community level, which may help explain the striking differences in COVID-19-related worries and anxiety between participants from the United States and Israel, Vinkers added.
E. Alison Holman, PhD, professor, Sue and Bill Gross School of Nursing, University of California, Irvine, noted that respondents were predominantly white, female, and had relatively high incomes, “suggesting strong demographic biases in those who chose to participate.”
Holman, who was not involved with the study, told Medscape Medical News that the “findings do not address the real impact of COVID-19 on the hardest-hit communities in America – poor, Black, and Latinx communities, where a large proportion of essential workers live.”
Barzilay acknowledged that, “unfortunately, because of the way the study was circulated, it did not reach minorities, which is one of the things we want to improve.”
The study is ongoing and has been translated into Spanish, French, and Hebrew. The team plans to collect data on diverse populations.
The study was supported by grants from the National Institute of Mental Health, the Lifespan Brain Institute of Children’s Hospital of Philadelphia, Penn Medicine, the University of Pennsylvania, and in part by the Zuckerman STEM Leadership Program. Barzilay serves on the scientific board and reports stock ownership in Taliaz Health. The other authors, Golnaz, Vinkers, and Holman have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Individuals are more worried about family members becoming ill with COVID-19 or about unknowingly transmitting the disease to family members than they are about contracting it themselves, results of a new survey show.
Investigators surveyed over 3,000 adults, using an online questionnaire. Of the respondents, about 20% were health care workers, and most were living in locations with active stay-at-home orders at the time of the survey.
Close to half of participants were worried about family members contracting the virus, one third were worried about unknowingly infecting others, and 20% were worried about contracting the virus themselves.
“We were a little surprised to see that people were more concerned about others than about themselves, specifically worrying about whether a family member would contract COVID-19 and whether they might unintentionally infect others,” lead author Ran Barzilay, MD, PhD, child and adolescent psychiatrist at the Children’s Hospital of Philadelphia (CHOP), told Medscape Medical News.
The study was published online August 20 in Translational Psychiatry.
Interactive platform
“The pandemic has provided a unique opportunity to study resilience in healthcare professionals and others,” said Barzilay, assistant professor at the Lifespan Brain Institute, a collaboration between CHOP and the University of Pennsylvania, under the directorship of Raquel Gur, MD, PhD.
“After the pandemic broke out in March, we launched a website in early April where we surveyed people for levels of resilience, mental health, and well-being during the outbreak,” he added.
Survey participants then shared it with their contacts.
“To date, over 7000 people have completed it – mostly from the US but also from Israel,” Barzilay said.
The survey was anonymous, but participants could choose to have follow-up contact. The survey included an interactive 21-item resilience questionnaire and an assessment of COVID-19-related items related to worries concerning the following: contracting, dying from, or currently having the illness; having a family member contract the illness; unknowingly infecting others; and experiencing significant financial burden.
A total of 1350 participants took a second survey on anxiety and depression that utilized the Generalized Anxiety Disorder–7 and the Patient Health Questionnaire–2.
“What makes the survey unique is that it’s not just a means of collecting data but also an interactive platform that gives participants immediate personalized feedback, based on their responses to the resilience and well-being surveys, with practical tips and recommendations for stress management and ways of boosting resilience,” Barzilay said.
Tend and befriend
Ten days into the survey, data were available on 3,042 participants (64% women, 54% with advanced education, 20.5% health care providers), who ranged in age from 18 to 70 years (mean [SD], 38.9 [11.9] years).
After accounting for covariates, the researchers found that participants reported more distress about family members contracting COVID-19 and about unknowingly infecting others than about getting COVID-19 themselves (48.5% and 36% vs. 19.9%, respectively; P < .0005).
Increased COVID-19-related worries were associated with 22% higher anxiety and 16.1% higher depression scores; women had higher scores than men on both.
Each 1-SD increase in the composite score of COVID-19 worries was associated with over twice the increased probability of generalized anxiety and depression (odds ratio, 2.23; 95% confidence interval, 1.88-2.65; and OR, 1.67; 95% CI, 1.41-1.98, respectively; for both, P < .001).
On the other hand, for every 1-SD increase in the resilience score, there was a 64.9% decrease in the possibility of screening positive for generalized anxiety disorder and a 69.3% decrease in the possibility of screening positive for depression (for both, P < .0001).
Compared to participants from Israel, US participants were “more stressed” about contracting, dying from, and currently having COVID-19 themselves. Overall, Israeli participants scored higher than US participants on the resilience scale.
Rates of anxiety and depression did not differ significantly between healthcare providers and others. Health care providers worried more about contracting COVID-19 themselves and worried less about finances after COVID-19.
The authors propose that survey participants were more worried about others than about themselves because of “prosocial behavior under stress” and “tend-and-befriend,” whereby, “in response to threat, humans tend to protect their close ones (tending) and seek out their social group for mutual defense (befriending).”
This type of altruistic behavior has been “described in acute situations throughout history” and has been “linked to mechanisms of resilience for overcoming adversity,” the authors indicate.
Demographic biases
Commenting on the findings for Medscape Medical News, Golnaz Tabibnia, PhD, a neuroscientist at the University of California, Irvine, who was not involved in the research, suggested that although higher resilience scores were associated with lower COVID-related worries, it is possible, “as the authors suggest, that having more resilience resources makes you less worried, but the causality could go the other direction as well, and less worry/rumination may lead to more resilience.”
Also commenting on the study for Medscape Medical News, Christiaan Vinkers, MD, PhD, a psychiatrist at the Amsterdam University Medical Center, Amsterdam, the Netherlands, said it was noteworthy that healthcare providers reported similar levels of mood and anxiety symptoms, compared to others.
“This is encouraging, as it suggests adequate resilience levels in professionals who work in the front lines of the COVID-19 pandemic,” he said.
Resilience occurs not only at the individual level but also at the community level, which may help explain the striking differences in COVID-19-related worries and anxiety between participants from the United States and Israel, Vinkers added.
E. Alison Holman, PhD, professor, Sue and Bill Gross School of Nursing, University of California, Irvine, noted that respondents were predominantly white, female, and had relatively high incomes, “suggesting strong demographic biases in those who chose to participate.”
Holman, who was not involved with the study, told Medscape Medical News that the “findings do not address the real impact of COVID-19 on the hardest-hit communities in America – poor, Black, and Latinx communities, where a large proportion of essential workers live.”
Barzilay acknowledged that, “unfortunately, because of the way the study was circulated, it did not reach minorities, which is one of the things we want to improve.”
The study is ongoing and has been translated into Spanish, French, and Hebrew. The team plans to collect data on diverse populations.
The study was supported by grants from the National Institute of Mental Health, the Lifespan Brain Institute of Children’s Hospital of Philadelphia, Penn Medicine, the University of Pennsylvania, and in part by the Zuckerman STEM Leadership Program. Barzilay serves on the scientific board and reports stock ownership in Taliaz Health. The other authors, Golnaz, Vinkers, and Holman have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
New billing code for added COVID practice expense
The American Medical Association on Sept. 8 announced that a new code, 99072, is intended to cover additional supplies, materials, and clinical staff time over and above those usually included in an office visit when performed during a declared public health emergency, as defined by law, attributable to respiratory-transmitted infectious disease, the AMA said in a release.
Fifty national medical specialty societies and other organizations worked with the AMA’s Specialty Society RVS Update Committee over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency. It has submitted recommendations to the Centers for Medicare & Medicaid Services seeking to persuade the federal agencies to recognize the new 99072 payment code.
The intention is to recognize the extra expenses involved in steps now routinely taken to reduce the risk for COVID transmission from office visits, Current Procedural Terminology Editorial Panel Chair Mark S. Synovec, MD, said in an interview. Some practices have adapted by having staff screen patients before they enter offices and making arrangements to keep patients at a safe distance from others during their visits, he said.
“Everyone’s life has significantly changed because of COVID and the health care system has dramatically changed,” Dr. Synovec said. “It was pretty clear that the status quo was not going to work.”
Physician practices will welcome this change, said Veronica Bradley, CPC, a senior industry adviser to the Medical Group Management Association. An office visit that in the past may have involved only basic infection control measures, such as donning a pair of gloves, now may involve clinicians taking the time to put on more extensive protective gear, she said.
“Now they are taking a heck of a lot more precautions, and there’s more time and more supplies being consumed,” Ms. Bradley said in an interview.
Code looks ahead to future use
The AMA explained how this new code differs from CPT code 99070, which is typically reported for supplies and materials that may be used or provided to patients during an office visit.
The new 99072 code applies only during declared public health emergencies and applies only to additional items required to support “a safe in-person provision” of evaluation, treatment, and procedures, the AMA said.
“These items contrast with those typically reported with code 99070, which focuses on additional supplies provided over and above those usually included with a specific service, such as drugs, intravenous catheters, or trays,” the AMA said.
The CPT panel sought to structure the new code for covering COVID practice expenses so that it could not be abused, and also looked ahead to the future, Dr. Synovec said.
“It’s a code that you would put on during a public health emergency as defined by law that would be related to a respiratory-transmitted infectious disease. Obviously we meant it for SARS-CoV-2,” he said. “Hopefully we can go another 100 years before we have another pandemic, but we also wanted to prepare something where if we have another airborne respiratory virus that requires additional practice expenses as seen this time, it would be available for use.”
The AMA also announced a second addition, CPT code 86413, that anticipates greater use of quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) provided by laboratory tests reported by other CPT codes.
More information is available on the AMA website.
A version of this article originally appeared on Medscape.com.
The American Medical Association on Sept. 8 announced that a new code, 99072, is intended to cover additional supplies, materials, and clinical staff time over and above those usually included in an office visit when performed during a declared public health emergency, as defined by law, attributable to respiratory-transmitted infectious disease, the AMA said in a release.
Fifty national medical specialty societies and other organizations worked with the AMA’s Specialty Society RVS Update Committee over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency. It has submitted recommendations to the Centers for Medicare & Medicaid Services seeking to persuade the federal agencies to recognize the new 99072 payment code.
The intention is to recognize the extra expenses involved in steps now routinely taken to reduce the risk for COVID transmission from office visits, Current Procedural Terminology Editorial Panel Chair Mark S. Synovec, MD, said in an interview. Some practices have adapted by having staff screen patients before they enter offices and making arrangements to keep patients at a safe distance from others during their visits, he said.
“Everyone’s life has significantly changed because of COVID and the health care system has dramatically changed,” Dr. Synovec said. “It was pretty clear that the status quo was not going to work.”
Physician practices will welcome this change, said Veronica Bradley, CPC, a senior industry adviser to the Medical Group Management Association. An office visit that in the past may have involved only basic infection control measures, such as donning a pair of gloves, now may involve clinicians taking the time to put on more extensive protective gear, she said.
“Now they are taking a heck of a lot more precautions, and there’s more time and more supplies being consumed,” Ms. Bradley said in an interview.
Code looks ahead to future use
The AMA explained how this new code differs from CPT code 99070, which is typically reported for supplies and materials that may be used or provided to patients during an office visit.
The new 99072 code applies only during declared public health emergencies and applies only to additional items required to support “a safe in-person provision” of evaluation, treatment, and procedures, the AMA said.
“These items contrast with those typically reported with code 99070, which focuses on additional supplies provided over and above those usually included with a specific service, such as drugs, intravenous catheters, or trays,” the AMA said.
The CPT panel sought to structure the new code for covering COVID practice expenses so that it could not be abused, and also looked ahead to the future, Dr. Synovec said.
“It’s a code that you would put on during a public health emergency as defined by law that would be related to a respiratory-transmitted infectious disease. Obviously we meant it for SARS-CoV-2,” he said. “Hopefully we can go another 100 years before we have another pandemic, but we also wanted to prepare something where if we have another airborne respiratory virus that requires additional practice expenses as seen this time, it would be available for use.”
The AMA also announced a second addition, CPT code 86413, that anticipates greater use of quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) provided by laboratory tests reported by other CPT codes.
More information is available on the AMA website.
A version of this article originally appeared on Medscape.com.
The American Medical Association on Sept. 8 announced that a new code, 99072, is intended to cover additional supplies, materials, and clinical staff time over and above those usually included in an office visit when performed during a declared public health emergency, as defined by law, attributable to respiratory-transmitted infectious disease, the AMA said in a release.
Fifty national medical specialty societies and other organizations worked with the AMA’s Specialty Society RVS Update Committee over the summer to collect data on the costs of maintaining safe medical offices during the public health emergency. It has submitted recommendations to the Centers for Medicare & Medicaid Services seeking to persuade the federal agencies to recognize the new 99072 payment code.
The intention is to recognize the extra expenses involved in steps now routinely taken to reduce the risk for COVID transmission from office visits, Current Procedural Terminology Editorial Panel Chair Mark S. Synovec, MD, said in an interview. Some practices have adapted by having staff screen patients before they enter offices and making arrangements to keep patients at a safe distance from others during their visits, he said.
“Everyone’s life has significantly changed because of COVID and the health care system has dramatically changed,” Dr. Synovec said. “It was pretty clear that the status quo was not going to work.”
Physician practices will welcome this change, said Veronica Bradley, CPC, a senior industry adviser to the Medical Group Management Association. An office visit that in the past may have involved only basic infection control measures, such as donning a pair of gloves, now may involve clinicians taking the time to put on more extensive protective gear, she said.
“Now they are taking a heck of a lot more precautions, and there’s more time and more supplies being consumed,” Ms. Bradley said in an interview.
Code looks ahead to future use
The AMA explained how this new code differs from CPT code 99070, which is typically reported for supplies and materials that may be used or provided to patients during an office visit.
The new 99072 code applies only during declared public health emergencies and applies only to additional items required to support “a safe in-person provision” of evaluation, treatment, and procedures, the AMA said.
“These items contrast with those typically reported with code 99070, which focuses on additional supplies provided over and above those usually included with a specific service, such as drugs, intravenous catheters, or trays,” the AMA said.
The CPT panel sought to structure the new code for covering COVID practice expenses so that it could not be abused, and also looked ahead to the future, Dr. Synovec said.
“It’s a code that you would put on during a public health emergency as defined by law that would be related to a respiratory-transmitted infectious disease. Obviously we meant it for SARS-CoV-2,” he said. “Hopefully we can go another 100 years before we have another pandemic, but we also wanted to prepare something where if we have another airborne respiratory virus that requires additional practice expenses as seen this time, it would be available for use.”
The AMA also announced a second addition, CPT code 86413, that anticipates greater use of quantitative measurements of SARS-CoV-2 antibodies, as opposed to a qualitative assessment (positive/negative) provided by laboratory tests reported by other CPT codes.
More information is available on the AMA website.
A version of this article originally appeared on Medscape.com.
Distinguishing COVID-19 from flu in kids remains challenging
For children with COVID-19, rates of hospitalization, ICU admission, and ventilator use were similar to those of children with influenza, but rates differed in other respects, according to results of a study published online Sept. 11 in JAMA Network Open.
As winter approaches, distinguishing patients with COVID-19 from those with influenza will become a problem. To assist with that, Xiaoyan Song, PhD, director of the office of infection control and epidemiology at Children’s National Hospital in Washington, D.C., and colleagues investigated commonalities and differences between the clinical symptoms of COVID-19 and influenza in children.
“Distinguishing COVID-19 from flu and other respiratory viral infections remains a challenge to clinicians. Although our study showed that patients with COVID-19 were more likely than patients with flu to report fever, gastrointestinal, and other clinical symptoms at the time of diagnosis, the two groups do have many overlapping clinical symptoms,” Dr. Song said. “Until future data show us otherwise, clinicians need to prepare for managing coinfections of COVID-19 with flu and/or other respiratory viral infections in the upcoming flu season.”
The retrospective cohort study included 315 children diagnosed with laboratory-confirmed COVID-19 between March 25 and May 15, 2020, and 1,402 children diagnosed with laboratory-confirmed seasonal influenza A or influenza B between Oct. 1, 2019, and June 6, 2020, at Children’s National Hospital. The investigation excluded asymptomatic patients who tested positive for COVID-19.
Patients with COVID-19 and patients with influenza were similar with respect to rates of hospitalization (17% vs. 21%; odds ratio, 0.8; 95% confidence interval, 0.6-1.1; P = .15), admission to the ICU (6% vs. 7%; OR, 0.8; 95% CI, 0.5-1.3; P = .42), and use of mechanical ventilation (3% vs. 2%; OR, 1.5; 95% CI, 0.9-2.6; P =.17).
The difference in the duration of ventilation for the two groups was not statistically significant. None of the patients who had COVID-19 or influenza B died, but two patients with influenza A did.
No patients had coinfections, which the researchers attribute to the mid-March shutdown of many schools, which they believe limited the spread of seasonal influenza.
Patients who were hospitalized with COVID-19 were older (median age, 9.7 years; range, 0.06-23.2 years) than those hospitalized with either type of influenza (median age, 4.2 years; range, 0.04-23.1). Patients older than 15 years made up 37% of patients with COVID-19 but only 6% of those with influenza.
Among patients hospitalized with COVID-19, 65% had at least one underlying medical condition, compared with 42% of those hospitalized for either type of influenza (OR, 2.6; 95% CI, 1.4-4.7; P = .002).
The most common underlying condition was neurologic problems from global developmental delay or seizures, identified in 11 patients (20%) hospitalized with COVID-19 and in 24 patients (8%) hospitalized with influenza (OR, 2.8; 95% CI, 1.3-6.2; P = .002). There was no significant difference between the two groups with respect to a history of asthma, cardiac disease, hematologic disease, and cancer.
For both groups, fever and cough were the most frequently reported symptoms at the time of diagnosis. However, more patients hospitalized with COVID-19 reported fever (76% vs. 55%; OR, 2.6; 95% CI, 1.4-5.1; P = 01), diarrhea or vomiting (26% vs. 12%; OR, 2.5; 95% CI, 1.2-5.0; P = .01), headache (11% vs. 3%; OR, 3.9; 95% CI, 1.3-11.5; P = .01), myalgia (22% vs. 7%; OR, 3.9; 95% CI, 1.8-8.5; P = .001), or chest pain (11% vs. 3%; OR, 3.9; 95% CI, 1.3-11.5; P = .01).
The researchers found no statistically significant differences between the two groups in rates of cough, congestion, sore throat, or shortness of breath.
Comparison of the symptom spectrum between COVID-19 and flu differed with respect to influenza type. More patients with COVID-19 reported fever, cough, diarrhea and vomiting, and myalgia than patients hospitalized with influenza A. But rates of fever, cough, diarrhea or vomiting, headache, or chest pain didn’t differ significantly in patients with COVID-19 and those with influenza B.
Larry K. Kociolek, MD, medical director of infection prevention and control at Ann and Robert H. Lurie Children’s Hospital of Chicago, noted the lower age of patients with flu. “Differentiating the two infections, which is difficult if not impossible based on symptoms alone, may have prognostic implications, depending on the age of the child. Because this study was performed outside peak influenza season, when coinfections would be less likely to occur, we must be vigilant about the potential clinical implications of influenza and SARS-CoV-2 coinfection this fall and winter.”
Clinicians will still have to use a combination of symptoms, examinations, and testing to distinguish the two diseases, said Aimee Sznewajs, MD, medical director of the pediatric hospital medicine department at Children’s Minnesota, Minneapolis. “We will continue to test for influenza and COVID-19 prior to hospitalizations and make decisions about whether to hospitalize based on other clinical factors, such as dehydration, oxygen requirement, and vital sign changes.”
Dr. Sznewajs stressed the importance of maintaining public health strategies, including “ensuring all children get the flu vaccine, encouraging mask wearing and hand hygiene, adequate testing to determine which virus is present, and other mitigation measures if the prevalence of COVID-19 is increasing in the community.”
Dr. Song reiterated those points, noting that clinicians need to make the most of the options they have. “Clinicians already have many great tools on hand. It is extremely important to get the flu vaccine now, especially for kids with underlying medical conditions. Diagnostic tests are available for both COVID-19 and flu. Antiviral treatment for flu is available. Judicious use of these tools will protect the health of providers, kids, and well-being at large.”
The authors noted several limitations for the study, including its retrospective design, that the data came from a single center, and that different platforms were used to detect the viruses.
A version of this article originally appeared on Medscape.com.
For children with COVID-19, rates of hospitalization, ICU admission, and ventilator use were similar to those of children with influenza, but rates differed in other respects, according to results of a study published online Sept. 11 in JAMA Network Open.
As winter approaches, distinguishing patients with COVID-19 from those with influenza will become a problem. To assist with that, Xiaoyan Song, PhD, director of the office of infection control and epidemiology at Children’s National Hospital in Washington, D.C., and colleagues investigated commonalities and differences between the clinical symptoms of COVID-19 and influenza in children.
“Distinguishing COVID-19 from flu and other respiratory viral infections remains a challenge to clinicians. Although our study showed that patients with COVID-19 were more likely than patients with flu to report fever, gastrointestinal, and other clinical symptoms at the time of diagnosis, the two groups do have many overlapping clinical symptoms,” Dr. Song said. “Until future data show us otherwise, clinicians need to prepare for managing coinfections of COVID-19 with flu and/or other respiratory viral infections in the upcoming flu season.”
The retrospective cohort study included 315 children diagnosed with laboratory-confirmed COVID-19 between March 25 and May 15, 2020, and 1,402 children diagnosed with laboratory-confirmed seasonal influenza A or influenza B between Oct. 1, 2019, and June 6, 2020, at Children’s National Hospital. The investigation excluded asymptomatic patients who tested positive for COVID-19.
Patients with COVID-19 and patients with influenza were similar with respect to rates of hospitalization (17% vs. 21%; odds ratio, 0.8; 95% confidence interval, 0.6-1.1; P = .15), admission to the ICU (6% vs. 7%; OR, 0.8; 95% CI, 0.5-1.3; P = .42), and use of mechanical ventilation (3% vs. 2%; OR, 1.5; 95% CI, 0.9-2.6; P =.17).
The difference in the duration of ventilation for the two groups was not statistically significant. None of the patients who had COVID-19 or influenza B died, but two patients with influenza A did.
No patients had coinfections, which the researchers attribute to the mid-March shutdown of many schools, which they believe limited the spread of seasonal influenza.
Patients who were hospitalized with COVID-19 were older (median age, 9.7 years; range, 0.06-23.2 years) than those hospitalized with either type of influenza (median age, 4.2 years; range, 0.04-23.1). Patients older than 15 years made up 37% of patients with COVID-19 but only 6% of those with influenza.
Among patients hospitalized with COVID-19, 65% had at least one underlying medical condition, compared with 42% of those hospitalized for either type of influenza (OR, 2.6; 95% CI, 1.4-4.7; P = .002).
The most common underlying condition was neurologic problems from global developmental delay or seizures, identified in 11 patients (20%) hospitalized with COVID-19 and in 24 patients (8%) hospitalized with influenza (OR, 2.8; 95% CI, 1.3-6.2; P = .002). There was no significant difference between the two groups with respect to a history of asthma, cardiac disease, hematologic disease, and cancer.
For both groups, fever and cough were the most frequently reported symptoms at the time of diagnosis. However, more patients hospitalized with COVID-19 reported fever (76% vs. 55%; OR, 2.6; 95% CI, 1.4-5.1; P = 01), diarrhea or vomiting (26% vs. 12%; OR, 2.5; 95% CI, 1.2-5.0; P = .01), headache (11% vs. 3%; OR, 3.9; 95% CI, 1.3-11.5; P = .01), myalgia (22% vs. 7%; OR, 3.9; 95% CI, 1.8-8.5; P = .001), or chest pain (11% vs. 3%; OR, 3.9; 95% CI, 1.3-11.5; P = .01).
The researchers found no statistically significant differences between the two groups in rates of cough, congestion, sore throat, or shortness of breath.
Comparison of the symptom spectrum between COVID-19 and flu differed with respect to influenza type. More patients with COVID-19 reported fever, cough, diarrhea and vomiting, and myalgia than patients hospitalized with influenza A. But rates of fever, cough, diarrhea or vomiting, headache, or chest pain didn’t differ significantly in patients with COVID-19 and those with influenza B.
Larry K. Kociolek, MD, medical director of infection prevention and control at Ann and Robert H. Lurie Children’s Hospital of Chicago, noted the lower age of patients with flu. “Differentiating the two infections, which is difficult if not impossible based on symptoms alone, may have prognostic implications, depending on the age of the child. Because this study was performed outside peak influenza season, when coinfections would be less likely to occur, we must be vigilant about the potential clinical implications of influenza and SARS-CoV-2 coinfection this fall and winter.”
Clinicians will still have to use a combination of symptoms, examinations, and testing to distinguish the two diseases, said Aimee Sznewajs, MD, medical director of the pediatric hospital medicine department at Children’s Minnesota, Minneapolis. “We will continue to test for influenza and COVID-19 prior to hospitalizations and make decisions about whether to hospitalize based on other clinical factors, such as dehydration, oxygen requirement, and vital sign changes.”
Dr. Sznewajs stressed the importance of maintaining public health strategies, including “ensuring all children get the flu vaccine, encouraging mask wearing and hand hygiene, adequate testing to determine which virus is present, and other mitigation measures if the prevalence of COVID-19 is increasing in the community.”
Dr. Song reiterated those points, noting that clinicians need to make the most of the options they have. “Clinicians already have many great tools on hand. It is extremely important to get the flu vaccine now, especially for kids with underlying medical conditions. Diagnostic tests are available for both COVID-19 and flu. Antiviral treatment for flu is available. Judicious use of these tools will protect the health of providers, kids, and well-being at large.”
The authors noted several limitations for the study, including its retrospective design, that the data came from a single center, and that different platforms were used to detect the viruses.
A version of this article originally appeared on Medscape.com.
For children with COVID-19, rates of hospitalization, ICU admission, and ventilator use were similar to those of children with influenza, but rates differed in other respects, according to results of a study published online Sept. 11 in JAMA Network Open.
As winter approaches, distinguishing patients with COVID-19 from those with influenza will become a problem. To assist with that, Xiaoyan Song, PhD, director of the office of infection control and epidemiology at Children’s National Hospital in Washington, D.C., and colleagues investigated commonalities and differences between the clinical symptoms of COVID-19 and influenza in children.
“Distinguishing COVID-19 from flu and other respiratory viral infections remains a challenge to clinicians. Although our study showed that patients with COVID-19 were more likely than patients with flu to report fever, gastrointestinal, and other clinical symptoms at the time of diagnosis, the two groups do have many overlapping clinical symptoms,” Dr. Song said. “Until future data show us otherwise, clinicians need to prepare for managing coinfections of COVID-19 with flu and/or other respiratory viral infections in the upcoming flu season.”
The retrospective cohort study included 315 children diagnosed with laboratory-confirmed COVID-19 between March 25 and May 15, 2020, and 1,402 children diagnosed with laboratory-confirmed seasonal influenza A or influenza B between Oct. 1, 2019, and June 6, 2020, at Children’s National Hospital. The investigation excluded asymptomatic patients who tested positive for COVID-19.
Patients with COVID-19 and patients with influenza were similar with respect to rates of hospitalization (17% vs. 21%; odds ratio, 0.8; 95% confidence interval, 0.6-1.1; P = .15), admission to the ICU (6% vs. 7%; OR, 0.8; 95% CI, 0.5-1.3; P = .42), and use of mechanical ventilation (3% vs. 2%; OR, 1.5; 95% CI, 0.9-2.6; P =.17).
The difference in the duration of ventilation for the two groups was not statistically significant. None of the patients who had COVID-19 or influenza B died, but two patients with influenza A did.
No patients had coinfections, which the researchers attribute to the mid-March shutdown of many schools, which they believe limited the spread of seasonal influenza.
Patients who were hospitalized with COVID-19 were older (median age, 9.7 years; range, 0.06-23.2 years) than those hospitalized with either type of influenza (median age, 4.2 years; range, 0.04-23.1). Patients older than 15 years made up 37% of patients with COVID-19 but only 6% of those with influenza.
Among patients hospitalized with COVID-19, 65% had at least one underlying medical condition, compared with 42% of those hospitalized for either type of influenza (OR, 2.6; 95% CI, 1.4-4.7; P = .002).
The most common underlying condition was neurologic problems from global developmental delay or seizures, identified in 11 patients (20%) hospitalized with COVID-19 and in 24 patients (8%) hospitalized with influenza (OR, 2.8; 95% CI, 1.3-6.2; P = .002). There was no significant difference between the two groups with respect to a history of asthma, cardiac disease, hematologic disease, and cancer.
For both groups, fever and cough were the most frequently reported symptoms at the time of diagnosis. However, more patients hospitalized with COVID-19 reported fever (76% vs. 55%; OR, 2.6; 95% CI, 1.4-5.1; P = 01), diarrhea or vomiting (26% vs. 12%; OR, 2.5; 95% CI, 1.2-5.0; P = .01), headache (11% vs. 3%; OR, 3.9; 95% CI, 1.3-11.5; P = .01), myalgia (22% vs. 7%; OR, 3.9; 95% CI, 1.8-8.5; P = .001), or chest pain (11% vs. 3%; OR, 3.9; 95% CI, 1.3-11.5; P = .01).
The researchers found no statistically significant differences between the two groups in rates of cough, congestion, sore throat, or shortness of breath.
Comparison of the symptom spectrum between COVID-19 and flu differed with respect to influenza type. More patients with COVID-19 reported fever, cough, diarrhea and vomiting, and myalgia than patients hospitalized with influenza A. But rates of fever, cough, diarrhea or vomiting, headache, or chest pain didn’t differ significantly in patients with COVID-19 and those with influenza B.
Larry K. Kociolek, MD, medical director of infection prevention and control at Ann and Robert H. Lurie Children’s Hospital of Chicago, noted the lower age of patients with flu. “Differentiating the two infections, which is difficult if not impossible based on symptoms alone, may have prognostic implications, depending on the age of the child. Because this study was performed outside peak influenza season, when coinfections would be less likely to occur, we must be vigilant about the potential clinical implications of influenza and SARS-CoV-2 coinfection this fall and winter.”
Clinicians will still have to use a combination of symptoms, examinations, and testing to distinguish the two diseases, said Aimee Sznewajs, MD, medical director of the pediatric hospital medicine department at Children’s Minnesota, Minneapolis. “We will continue to test for influenza and COVID-19 prior to hospitalizations and make decisions about whether to hospitalize based on other clinical factors, such as dehydration, oxygen requirement, and vital sign changes.”
Dr. Sznewajs stressed the importance of maintaining public health strategies, including “ensuring all children get the flu vaccine, encouraging mask wearing and hand hygiene, adequate testing to determine which virus is present, and other mitigation measures if the prevalence of COVID-19 is increasing in the community.”
Dr. Song reiterated those points, noting that clinicians need to make the most of the options they have. “Clinicians already have many great tools on hand. It is extremely important to get the flu vaccine now, especially for kids with underlying medical conditions. Diagnostic tests are available for both COVID-19 and flu. Antiviral treatment for flu is available. Judicious use of these tools will protect the health of providers, kids, and well-being at large.”
The authors noted several limitations for the study, including its retrospective design, that the data came from a single center, and that different platforms were used to detect the viruses.
A version of this article originally appeared on Medscape.com.
AI can pinpoint COVID-19 from chest x-rays
Conventional chest x-rays combined with artificial intelligence (AI) can identify lung damage from COVID-19 and differentiate coronavirus patients from other patients, improving triage efforts, new research suggests.
The AI tool – developed by Jason Fleischer, PhD, and graduate student Mohammad Tariqul Islam, both from Princeton (N.J.) University – can distinguish COVID-19 patients from those with pneumonia or normal lung tissue with an accuracy of more than 95%.
“We were able to separate the COVID-19 patients with very high fidelity,” Dr. Fleischer said in an interview. “If you give me an x-ray now, I can say with very high confidence whether a patient has COVID-19.”
The diagnostic tool pinpoints patterns on x-ray images that are too subtle for even trained experts to notice. The precision of CT scanning is similar to that of the AI tool, but CT costs much more and has other disadvantages, said Dr. Fleischer, who presented his findings at the virtual European Respiratory Society International Congress 2020.
“CT is more expensive and uses higher doses of radiation,” he said. “Another big thing is that not everyone has tomography facilities – including a lot of rural places and developing countries – so you need something that’s on the spot.”
With machine learning, Dr. Fleischer analyzed 2,300 x-ray images: 1,018 “normal” images from patients who had neither pneumonia nor COVID-19, 1,011 from patients with pneumonia, and 271 from patients with COVID-19.
The AI tool uses a neural network to refine the number and type of lung features being tracked. A UMAP (Uniform Manifold Approximation and Projection) clustering algorithm then looks for similarities and differences in those images, he explained.
“We, as users, knew which type each x-ray was – normal, pneumonia positive, or COVID-19 positive – but the network did not,” he added.
Clinicians have observed two basic types of lung problems in COVID-19 patients: pneumonia that fills lung air sacs with fluid and dangerously low blood-oxygen levels despite nearly normal breathing patterns. Because treatment can vary according to type, it would be beneficial to quickly distinguish between them, Dr. Fleischer said.
The AI tool showed that there is a distinct difference in chest x-rays from pneumonia-positive patients and healthy people, he said. It also demonstrated two distinct clusters of COVID-19–positive chest x-rays: those that looked like pneumonia and those with a more normal presentation.
The fact that “the AI system recognizes something unique in chest x-rays from COVID-19–positive patients” indicates that the computer is able to identify visual markers for coronavirus, he explained. “We currently do not know what these markers are.”
Dr. Fleischer said his goal is not to replace physician decision-making, but to supplement it.
“I’m uncomfortable with having computers make the final decision,” he said. “They often have a narrow focus, whereas doctors have the big picture in mind.”
This AI tool is “very interesting,” especially in the context of expanding AI applications in various specialties, said Thierry Fumeaux, MD, from Nyon (Switzerland) Hospital. Some physicians currently disagree on whether a chest x-ray or CT scan is the better tool to help diagnose COVID-19.
“It seems better than the human eye and brain” to pinpoint COVID-19 lung damage, “so it’s very attractive as a technology,” Dr. Fumeaux said in an interview.
And AI can be used to supplement the efforts of busy and fatigued clinicians who might be stretched thin by large caseloads. “I cannot read 200 chest x-rays in a day, but a computer can do that in 2 minutes,” he said.
But Dr. Fumeaux offered a caveat: “Pattern recognition is promising, but at the moment I’m not aware of papers showing that, by using AI, you’re changing anything in the outcome of a patient.”
Ideally, Dr. Fleischer said he hopes that AI will soon be able to accurately indicate which treatments are most effective for individual COVID-19 patients. And the technology might eventually be used to help with treatment decisions for patients with asthma or chronic obstructive pulmonary disease, he noted.
But he needs more data before results indicate whether a COVID-19 patient would benefit from ventilator support, for example, and the tool can be used more widely. To contribute data or collaborate with Dr. Fleischer’s efforts, contact him.
“Machine learning is all about data, so you can find these correlations,” he said. “It would be nice to be able to use it to reassure a worried patient that their prognosis is good; to say that most of the people with symptoms like yours will be just fine.”
Dr. Fleischer and Dr. Fumeaux have declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Conventional chest x-rays combined with artificial intelligence (AI) can identify lung damage from COVID-19 and differentiate coronavirus patients from other patients, improving triage efforts, new research suggests.
The AI tool – developed by Jason Fleischer, PhD, and graduate student Mohammad Tariqul Islam, both from Princeton (N.J.) University – can distinguish COVID-19 patients from those with pneumonia or normal lung tissue with an accuracy of more than 95%.
“We were able to separate the COVID-19 patients with very high fidelity,” Dr. Fleischer said in an interview. “If you give me an x-ray now, I can say with very high confidence whether a patient has COVID-19.”
The diagnostic tool pinpoints patterns on x-ray images that are too subtle for even trained experts to notice. The precision of CT scanning is similar to that of the AI tool, but CT costs much more and has other disadvantages, said Dr. Fleischer, who presented his findings at the virtual European Respiratory Society International Congress 2020.
“CT is more expensive and uses higher doses of radiation,” he said. “Another big thing is that not everyone has tomography facilities – including a lot of rural places and developing countries – so you need something that’s on the spot.”
With machine learning, Dr. Fleischer analyzed 2,300 x-ray images: 1,018 “normal” images from patients who had neither pneumonia nor COVID-19, 1,011 from patients with pneumonia, and 271 from patients with COVID-19.
The AI tool uses a neural network to refine the number and type of lung features being tracked. A UMAP (Uniform Manifold Approximation and Projection) clustering algorithm then looks for similarities and differences in those images, he explained.
“We, as users, knew which type each x-ray was – normal, pneumonia positive, or COVID-19 positive – but the network did not,” he added.
Clinicians have observed two basic types of lung problems in COVID-19 patients: pneumonia that fills lung air sacs with fluid and dangerously low blood-oxygen levels despite nearly normal breathing patterns. Because treatment can vary according to type, it would be beneficial to quickly distinguish between them, Dr. Fleischer said.
The AI tool showed that there is a distinct difference in chest x-rays from pneumonia-positive patients and healthy people, he said. It also demonstrated two distinct clusters of COVID-19–positive chest x-rays: those that looked like pneumonia and those with a more normal presentation.
The fact that “the AI system recognizes something unique in chest x-rays from COVID-19–positive patients” indicates that the computer is able to identify visual markers for coronavirus, he explained. “We currently do not know what these markers are.”
Dr. Fleischer said his goal is not to replace physician decision-making, but to supplement it.
“I’m uncomfortable with having computers make the final decision,” he said. “They often have a narrow focus, whereas doctors have the big picture in mind.”
This AI tool is “very interesting,” especially in the context of expanding AI applications in various specialties, said Thierry Fumeaux, MD, from Nyon (Switzerland) Hospital. Some physicians currently disagree on whether a chest x-ray or CT scan is the better tool to help diagnose COVID-19.
“It seems better than the human eye and brain” to pinpoint COVID-19 lung damage, “so it’s very attractive as a technology,” Dr. Fumeaux said in an interview.
And AI can be used to supplement the efforts of busy and fatigued clinicians who might be stretched thin by large caseloads. “I cannot read 200 chest x-rays in a day, but a computer can do that in 2 minutes,” he said.
But Dr. Fumeaux offered a caveat: “Pattern recognition is promising, but at the moment I’m not aware of papers showing that, by using AI, you’re changing anything in the outcome of a patient.”
Ideally, Dr. Fleischer said he hopes that AI will soon be able to accurately indicate which treatments are most effective for individual COVID-19 patients. And the technology might eventually be used to help with treatment decisions for patients with asthma or chronic obstructive pulmonary disease, he noted.
But he needs more data before results indicate whether a COVID-19 patient would benefit from ventilator support, for example, and the tool can be used more widely. To contribute data or collaborate with Dr. Fleischer’s efforts, contact him.
“Machine learning is all about data, so you can find these correlations,” he said. “It would be nice to be able to use it to reassure a worried patient that their prognosis is good; to say that most of the people with symptoms like yours will be just fine.”
Dr. Fleischer and Dr. Fumeaux have declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Conventional chest x-rays combined with artificial intelligence (AI) can identify lung damage from COVID-19 and differentiate coronavirus patients from other patients, improving triage efforts, new research suggests.
The AI tool – developed by Jason Fleischer, PhD, and graduate student Mohammad Tariqul Islam, both from Princeton (N.J.) University – can distinguish COVID-19 patients from those with pneumonia or normal lung tissue with an accuracy of more than 95%.
“We were able to separate the COVID-19 patients with very high fidelity,” Dr. Fleischer said in an interview. “If you give me an x-ray now, I can say with very high confidence whether a patient has COVID-19.”
The diagnostic tool pinpoints patterns on x-ray images that are too subtle for even trained experts to notice. The precision of CT scanning is similar to that of the AI tool, but CT costs much more and has other disadvantages, said Dr. Fleischer, who presented his findings at the virtual European Respiratory Society International Congress 2020.
“CT is more expensive and uses higher doses of radiation,” he said. “Another big thing is that not everyone has tomography facilities – including a lot of rural places and developing countries – so you need something that’s on the spot.”
With machine learning, Dr. Fleischer analyzed 2,300 x-ray images: 1,018 “normal” images from patients who had neither pneumonia nor COVID-19, 1,011 from patients with pneumonia, and 271 from patients with COVID-19.
The AI tool uses a neural network to refine the number and type of lung features being tracked. A UMAP (Uniform Manifold Approximation and Projection) clustering algorithm then looks for similarities and differences in those images, he explained.
“We, as users, knew which type each x-ray was – normal, pneumonia positive, or COVID-19 positive – but the network did not,” he added.
Clinicians have observed two basic types of lung problems in COVID-19 patients: pneumonia that fills lung air sacs with fluid and dangerously low blood-oxygen levels despite nearly normal breathing patterns. Because treatment can vary according to type, it would be beneficial to quickly distinguish between them, Dr. Fleischer said.
The AI tool showed that there is a distinct difference in chest x-rays from pneumonia-positive patients and healthy people, he said. It also demonstrated two distinct clusters of COVID-19–positive chest x-rays: those that looked like pneumonia and those with a more normal presentation.
The fact that “the AI system recognizes something unique in chest x-rays from COVID-19–positive patients” indicates that the computer is able to identify visual markers for coronavirus, he explained. “We currently do not know what these markers are.”
Dr. Fleischer said his goal is not to replace physician decision-making, but to supplement it.
“I’m uncomfortable with having computers make the final decision,” he said. “They often have a narrow focus, whereas doctors have the big picture in mind.”
This AI tool is “very interesting,” especially in the context of expanding AI applications in various specialties, said Thierry Fumeaux, MD, from Nyon (Switzerland) Hospital. Some physicians currently disagree on whether a chest x-ray or CT scan is the better tool to help diagnose COVID-19.
“It seems better than the human eye and brain” to pinpoint COVID-19 lung damage, “so it’s very attractive as a technology,” Dr. Fumeaux said in an interview.
And AI can be used to supplement the efforts of busy and fatigued clinicians who might be stretched thin by large caseloads. “I cannot read 200 chest x-rays in a day, but a computer can do that in 2 minutes,” he said.
But Dr. Fumeaux offered a caveat: “Pattern recognition is promising, but at the moment I’m not aware of papers showing that, by using AI, you’re changing anything in the outcome of a patient.”
Ideally, Dr. Fleischer said he hopes that AI will soon be able to accurately indicate which treatments are most effective for individual COVID-19 patients. And the technology might eventually be used to help with treatment decisions for patients with asthma or chronic obstructive pulmonary disease, he noted.
But he needs more data before results indicate whether a COVID-19 patient would benefit from ventilator support, for example, and the tool can be used more widely. To contribute data or collaborate with Dr. Fleischer’s efforts, contact him.
“Machine learning is all about data, so you can find these correlations,” he said. “It would be nice to be able to use it to reassure a worried patient that their prognosis is good; to say that most of the people with symptoms like yours will be just fine.”
Dr. Fleischer and Dr. Fumeaux have declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Social distancing impacts other infectious diseases
Diagnoses of 12 common pediatric infectious diseases in a large pediatric primary care network declined significantly in the weeks after COVID-19 social distancing (SD) was enacted in Massachusetts, compared with the same time period in 2019, an analysis of EHR data has shown.
While declines in infectious disease transmission with SD are not surprising, “these data demonstrate the extent to which transmission of common pediatric infections can be altered when close contact with other children is eliminated,” Jonathan Hatoun, MD, MPH of the Pediatric Physicians’ Organization at Children’s in Brookline, Mass., and coauthors wrote in Pediatrics . “Notably, three of the studied diseases, namely, influenza, croup, and bronchiolitis, essentially disappeared with [social distancing].”
The researchers analyzed the weekly incidence of each diagnosis for similar calendar periods in 2019 and 2020. A pre-SD period was defined as week 1-9, starting on Jan. 1, and a post-SD period was defined as week 13-18. (The several-week gap represented an implementation period as social distancing was enacted in the state earlier in 2020, from a declared statewide state of emergency through school closures and stay-at-home advisories.)
To isolate the effect of widespread SD, they performed a “difference-in-differences regression analysis, with diagnosis count as a function of calendar year, time period (pre-SD versus post-SD) and the interaction between the two.” The Massachusetts pediatric network provides care for approximately 375,000 children in 100 locations around the state.
In their research brief, Dr. Hatoun and coauthors presented weekly rates expressed as diagnoses per 100,000 patients per day. The rate of bronchiolitis, for instance, was 18 and 8 in the pre- and post-SD–equivalent weeks of 2019, respectively, and 20 and 0.6 in the pre- and post-SD weeks of 2020. Their analysis showed the rate in the 2020 post-SD period to be 10 diagnoses per 100,000 patients per day lower than they would have expected based on the 2019 trend.
Rates of pneumonia, acute otitis media, and streptococcal pharyngitis were similarly 14, 85, and 31 diagnoses per 100,000 patients per day lower, respectively. The prevalence of each of the other conditions analyzed – the common cold, croup, gastroenteritis, nonstreptococcal pharyngitis, sinusitis, skin and soft tissue infections, and urinary tract infection (UTI) – also was significantly lower in the 2020 post-SD period than would be expected based on 2019 data (P < .001 for all diagnoses).
Putting things in perspective
“This study puts numbers to the sense that we have all had in pediatrics – that social distancing appears to have had a dramatic impact on the transmission of common childhood infectious diseases, especially other respiratory viral pathogens,” Audrey R. John, MD, PhD, chief of the division of pediatric infectious disease at Children’s Hospital of Philadelphia, said in an interview.
The authors acknowledged the possible role of families not seeking care, but said that a smaller decrease in diagnoses of UTI – generally not a contagious disease – “suggests that changes in care-seeking behavior had a relatively modest effect on the other observed declines.” (The rate of UTI for the pre- and post-SD periods was 3.3 and 3.7 per 100,000 patients per day in 2019, and 3.4 and 2.4 in 2020, for a difference in differences of –1.5).
In an accompanying editorial, David W. Kimberlin, MD and Erica C. Bjornstad, MD, PhD, MPH, of the University of Alabama at Birmingham, called the report “provocative” and wrote that similar observations of infections dropping during periods of isolation – namely, dramatic declines in influenza and other respiratory viruses in Seattle after a record snowstorm in 2019 – combined with findings from other modeling studies “suggest that the decline [reported in Boston] is indeed real” (Pediatrics 2020. doi: 10.1542/peds.2020-019232).
However, “we also now know that immunization rates for American children have plummeted since the onset of the SARS-CoV-2 pandemic [because of a] ... dramatic decrease in the use of health care during the first months of the pandemic,” they wrote. “Viewed through this lens,” the declines reported in Boston may reflect inflections going “undiagnosed and untreated.”
Ultimately, Dr. Kimberlin and Dr. Bjornstad said, “the verdict remains out.”
Dr. John said that she and others are “concerned about children not seeking care in a timely manner, and [concerned] that reductions in reported infections might be due to a lack of recognition rather than a lack of transmission.”
In Philadelphia, however, declines in admissions for asthma exacerbations, “which are often caused by respiratory viral infections, suggests that this may not be the case,” said Dr. John, who was asked to comment on the study.
In addition, she said, the Massachusetts data showing that UTI diagnoses “are nearly as common this year as in 2019” are “reassuring.”
Are there lessons for the future?
Coauthor Louis Vernacchio, MD, MSc, chief medical officer of the Pediatric Physicians’ Organization at Children’s network, said in an interview that beyond the pandemic, it’s likely that “more careful attention to proven infection control practices in daycares and schools could reduce the burden of common infectious diseases in children.”
Dr. John similarly sees a long-term value of quantifying the impact of social distancing. “We’ve always known [for instance] that bronchiolitis is the result of viral infection.” Findings like the Massachusetts data “will help us advise families who might be trying to protect their premature infants (at risk for severe bronchiolitis) through social distancing.”
The analysis covered both in-person and telemedicine encounters occurring on weekdays.
The authors of the research brief indicated they have no relevant financial disclosures and there was no external funding. The authors of the commentary also reported they have no relevant financial disclosures, and Dr. John said she had no relevant financial disclosures.
SOURCE: Hatoun J et al. Pediatrics. 2020. doi: 10.1542/peds.2020-006460.
Diagnoses of 12 common pediatric infectious diseases in a large pediatric primary care network declined significantly in the weeks after COVID-19 social distancing (SD) was enacted in Massachusetts, compared with the same time period in 2019, an analysis of EHR data has shown.
While declines in infectious disease transmission with SD are not surprising, “these data demonstrate the extent to which transmission of common pediatric infections can be altered when close contact with other children is eliminated,” Jonathan Hatoun, MD, MPH of the Pediatric Physicians’ Organization at Children’s in Brookline, Mass., and coauthors wrote in Pediatrics . “Notably, three of the studied diseases, namely, influenza, croup, and bronchiolitis, essentially disappeared with [social distancing].”
The researchers analyzed the weekly incidence of each diagnosis for similar calendar periods in 2019 and 2020. A pre-SD period was defined as week 1-9, starting on Jan. 1, and a post-SD period was defined as week 13-18. (The several-week gap represented an implementation period as social distancing was enacted in the state earlier in 2020, from a declared statewide state of emergency through school closures and stay-at-home advisories.)
To isolate the effect of widespread SD, they performed a “difference-in-differences regression analysis, with diagnosis count as a function of calendar year, time period (pre-SD versus post-SD) and the interaction between the two.” The Massachusetts pediatric network provides care for approximately 375,000 children in 100 locations around the state.
In their research brief, Dr. Hatoun and coauthors presented weekly rates expressed as diagnoses per 100,000 patients per day. The rate of bronchiolitis, for instance, was 18 and 8 in the pre- and post-SD–equivalent weeks of 2019, respectively, and 20 and 0.6 in the pre- and post-SD weeks of 2020. Their analysis showed the rate in the 2020 post-SD period to be 10 diagnoses per 100,000 patients per day lower than they would have expected based on the 2019 trend.
Rates of pneumonia, acute otitis media, and streptococcal pharyngitis were similarly 14, 85, and 31 diagnoses per 100,000 patients per day lower, respectively. The prevalence of each of the other conditions analyzed – the common cold, croup, gastroenteritis, nonstreptococcal pharyngitis, sinusitis, skin and soft tissue infections, and urinary tract infection (UTI) – also was significantly lower in the 2020 post-SD period than would be expected based on 2019 data (P < .001 for all diagnoses).
Putting things in perspective
“This study puts numbers to the sense that we have all had in pediatrics – that social distancing appears to have had a dramatic impact on the transmission of common childhood infectious diseases, especially other respiratory viral pathogens,” Audrey R. John, MD, PhD, chief of the division of pediatric infectious disease at Children’s Hospital of Philadelphia, said in an interview.
The authors acknowledged the possible role of families not seeking care, but said that a smaller decrease in diagnoses of UTI – generally not a contagious disease – “suggests that changes in care-seeking behavior had a relatively modest effect on the other observed declines.” (The rate of UTI for the pre- and post-SD periods was 3.3 and 3.7 per 100,000 patients per day in 2019, and 3.4 and 2.4 in 2020, for a difference in differences of –1.5).
In an accompanying editorial, David W. Kimberlin, MD and Erica C. Bjornstad, MD, PhD, MPH, of the University of Alabama at Birmingham, called the report “provocative” and wrote that similar observations of infections dropping during periods of isolation – namely, dramatic declines in influenza and other respiratory viruses in Seattle after a record snowstorm in 2019 – combined with findings from other modeling studies “suggest that the decline [reported in Boston] is indeed real” (Pediatrics 2020. doi: 10.1542/peds.2020-019232).
However, “we also now know that immunization rates for American children have plummeted since the onset of the SARS-CoV-2 pandemic [because of a] ... dramatic decrease in the use of health care during the first months of the pandemic,” they wrote. “Viewed through this lens,” the declines reported in Boston may reflect inflections going “undiagnosed and untreated.”
Ultimately, Dr. Kimberlin and Dr. Bjornstad said, “the verdict remains out.”
Dr. John said that she and others are “concerned about children not seeking care in a timely manner, and [concerned] that reductions in reported infections might be due to a lack of recognition rather than a lack of transmission.”
In Philadelphia, however, declines in admissions for asthma exacerbations, “which are often caused by respiratory viral infections, suggests that this may not be the case,” said Dr. John, who was asked to comment on the study.
In addition, she said, the Massachusetts data showing that UTI diagnoses “are nearly as common this year as in 2019” are “reassuring.”
Are there lessons for the future?
Coauthor Louis Vernacchio, MD, MSc, chief medical officer of the Pediatric Physicians’ Organization at Children’s network, said in an interview that beyond the pandemic, it’s likely that “more careful attention to proven infection control practices in daycares and schools could reduce the burden of common infectious diseases in children.”
Dr. John similarly sees a long-term value of quantifying the impact of social distancing. “We’ve always known [for instance] that bronchiolitis is the result of viral infection.” Findings like the Massachusetts data “will help us advise families who might be trying to protect their premature infants (at risk for severe bronchiolitis) through social distancing.”
The analysis covered both in-person and telemedicine encounters occurring on weekdays.
The authors of the research brief indicated they have no relevant financial disclosures and there was no external funding. The authors of the commentary also reported they have no relevant financial disclosures, and Dr. John said she had no relevant financial disclosures.
SOURCE: Hatoun J et al. Pediatrics. 2020. doi: 10.1542/peds.2020-006460.
Diagnoses of 12 common pediatric infectious diseases in a large pediatric primary care network declined significantly in the weeks after COVID-19 social distancing (SD) was enacted in Massachusetts, compared with the same time period in 2019, an analysis of EHR data has shown.
While declines in infectious disease transmission with SD are not surprising, “these data demonstrate the extent to which transmission of common pediatric infections can be altered when close contact with other children is eliminated,” Jonathan Hatoun, MD, MPH of the Pediatric Physicians’ Organization at Children’s in Brookline, Mass., and coauthors wrote in Pediatrics . “Notably, three of the studied diseases, namely, influenza, croup, and bronchiolitis, essentially disappeared with [social distancing].”
The researchers analyzed the weekly incidence of each diagnosis for similar calendar periods in 2019 and 2020. A pre-SD period was defined as week 1-9, starting on Jan. 1, and a post-SD period was defined as week 13-18. (The several-week gap represented an implementation period as social distancing was enacted in the state earlier in 2020, from a declared statewide state of emergency through school closures and stay-at-home advisories.)
To isolate the effect of widespread SD, they performed a “difference-in-differences regression analysis, with diagnosis count as a function of calendar year, time period (pre-SD versus post-SD) and the interaction between the two.” The Massachusetts pediatric network provides care for approximately 375,000 children in 100 locations around the state.
In their research brief, Dr. Hatoun and coauthors presented weekly rates expressed as diagnoses per 100,000 patients per day. The rate of bronchiolitis, for instance, was 18 and 8 in the pre- and post-SD–equivalent weeks of 2019, respectively, and 20 and 0.6 in the pre- and post-SD weeks of 2020. Their analysis showed the rate in the 2020 post-SD period to be 10 diagnoses per 100,000 patients per day lower than they would have expected based on the 2019 trend.
Rates of pneumonia, acute otitis media, and streptococcal pharyngitis were similarly 14, 85, and 31 diagnoses per 100,000 patients per day lower, respectively. The prevalence of each of the other conditions analyzed – the common cold, croup, gastroenteritis, nonstreptococcal pharyngitis, sinusitis, skin and soft tissue infections, and urinary tract infection (UTI) – also was significantly lower in the 2020 post-SD period than would be expected based on 2019 data (P < .001 for all diagnoses).
Putting things in perspective
“This study puts numbers to the sense that we have all had in pediatrics – that social distancing appears to have had a dramatic impact on the transmission of common childhood infectious diseases, especially other respiratory viral pathogens,” Audrey R. John, MD, PhD, chief of the division of pediatric infectious disease at Children’s Hospital of Philadelphia, said in an interview.
The authors acknowledged the possible role of families not seeking care, but said that a smaller decrease in diagnoses of UTI – generally not a contagious disease – “suggests that changes in care-seeking behavior had a relatively modest effect on the other observed declines.” (The rate of UTI for the pre- and post-SD periods was 3.3 and 3.7 per 100,000 patients per day in 2019, and 3.4 and 2.4 in 2020, for a difference in differences of –1.5).
In an accompanying editorial, David W. Kimberlin, MD and Erica C. Bjornstad, MD, PhD, MPH, of the University of Alabama at Birmingham, called the report “provocative” and wrote that similar observations of infections dropping during periods of isolation – namely, dramatic declines in influenza and other respiratory viruses in Seattle after a record snowstorm in 2019 – combined with findings from other modeling studies “suggest that the decline [reported in Boston] is indeed real” (Pediatrics 2020. doi: 10.1542/peds.2020-019232).
However, “we also now know that immunization rates for American children have plummeted since the onset of the SARS-CoV-2 pandemic [because of a] ... dramatic decrease in the use of health care during the first months of the pandemic,” they wrote. “Viewed through this lens,” the declines reported in Boston may reflect inflections going “undiagnosed and untreated.”
Ultimately, Dr. Kimberlin and Dr. Bjornstad said, “the verdict remains out.”
Dr. John said that she and others are “concerned about children not seeking care in a timely manner, and [concerned] that reductions in reported infections might be due to a lack of recognition rather than a lack of transmission.”
In Philadelphia, however, declines in admissions for asthma exacerbations, “which are often caused by respiratory viral infections, suggests that this may not be the case,” said Dr. John, who was asked to comment on the study.
In addition, she said, the Massachusetts data showing that UTI diagnoses “are nearly as common this year as in 2019” are “reassuring.”
Are there lessons for the future?
Coauthor Louis Vernacchio, MD, MSc, chief medical officer of the Pediatric Physicians’ Organization at Children’s network, said in an interview that beyond the pandemic, it’s likely that “more careful attention to proven infection control practices in daycares and schools could reduce the burden of common infectious diseases in children.”
Dr. John similarly sees a long-term value of quantifying the impact of social distancing. “We’ve always known [for instance] that bronchiolitis is the result of viral infection.” Findings like the Massachusetts data “will help us advise families who might be trying to protect their premature infants (at risk for severe bronchiolitis) through social distancing.”
The analysis covered both in-person and telemedicine encounters occurring on weekdays.
The authors of the research brief indicated they have no relevant financial disclosures and there was no external funding. The authors of the commentary also reported they have no relevant financial disclosures, and Dr. John said she had no relevant financial disclosures.
SOURCE: Hatoun J et al. Pediatrics. 2020. doi: 10.1542/peds.2020-006460.
FROM PEDIATRICS
Low VWF levels or blood group O not linked to intracerebral hemorrhage risk
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
In contrast to findings of previous research, low levels of von Willebrand Factor (VWF) and blood group O were not associated with a first-ever intracerebral hemorrhage (ICH), according to a study published in Thrombosis Research.
The researchers compared 176 cases of ICH with 349 age- and sex-matched controls. The mean patient age was 57 years, and 50% were women. The median time from baseline blood sampling to the first ICH was 5.6 years, according to the study reported by Kristina Johansson of Umeå (Sweden) University and her colleagues.
Complicated picture
The level of VWF differed significantly among blood groups: In individuals with blood group O, the mean VWF level was 1.29 kIU/L; for blood group A, it was 1.52 kIU/L; for blood group AB, 1.59 kIU/L; and in blood group B, 1.76 kIU/L. However, there was no difference in VWF concentration between cases and controls.
The researchers found no association between blood group O and the risk of ICH, a finding previously seen in other studies. They did, however, find that, in the limited number of patients with blood group B there was an association with a lower risk of ICH, compared with blood group A (odds ratio, 0.47; 95% confidence interval, 0.23-0.95).
“To our knowledge this is the largest prospective study investigating the association between VWF, ABO blood group and ICH. We found no association between VWF or blood group O and risk of future ICH,” the researchers concluded.
The study was funded by public institutions in Sweden. The authors declared that they had no conflicts.
SOURCE: Johansson K et al. Thromb Res. 2020 Jul 5;195:77-80.
FROM THROMBOSIS RESEARCH
COVID-19: New guidance to stem mental health crisis in frontline HCPs
A new review offers fresh guidance to help stem the mental health toll of the COVID-19 pandemic on frontline clinicians.
Investigators gathered practice guidelines and resources from a wide range of health care organizations and professional societies to develop a conceptual framework of mental health support for health care professionals (HCPs) caring for COVID-19 patients.
“Support needs to be deployed in multiple dimensions – including individual, organizational, and societal levels – and include training in resilience, stress reduction, emotional awareness, and self-care strategies,” lead author Rachel Schwartz, PhD, health services researcher, Stanford (Calif.) University, said in an interview.
The review was published Aug. 21 in the Annals of Internal Medicine.
An opportune moment
Coauthor Rebecca Margolis, DO, director of well-being in the division of medical education and faculty development, Children’s Hospital of Los Angeles, said that this is “an opportune moment to look at how we treat frontline providers in this country.”
Studies of previous pandemics have shown heightened distress in HCPs, even years after the pandemic, and the unique challenges posed by the COVID-19 pandemic surpass those of previous pandemics, Dr. Margolis said in an interview.
Dr. Schwartz, Dr. Margolis, and coauthors Uma Anand, PhD, LP, and Jina Sinskey, MD, met through the Collaborative for Healing and Renewal in Medicine network, a group of medical educators, leaders in academic medicine, experts in burnout research and interventions, and trainees working together to promote well-being among trainees and practicing physicians.
“We were brought together on a conference call in March, when things were particularly bad in New York, and started looking to see what resources we could get to frontline providers who were suffering. It was great to lean on each other and stand on the shoulders of colleagues in New York, who were the ones we learned from on these calls,” said Dr. Margolis.
The authors recommended addressing clinicians’ basic practical needs, including ensuring essentials like meals and transportation, establishing a “well-being area” within hospitals for staff to rest, and providing well-stocked living quarters so clinicians can safely quarantine from family, as well as personal protective equipment and child care.
Clinicians are often asked to “assume new professional roles to meet evolving needs” during a pandemic, which can increase stress. The authors recommended targeted training, assessment of clinician skills before redeployment to a new clinical role, and clear communication practices around redeployment.
Recognition from hospital and government leaders improves morale and supports clinicians’ ability to continue delivering care. Leadership should “leverage communication strategies to provide clinicians with up-to-date information and reassurance,” they wrote.
‘Uniquely isolated’
Dr. Margolis noted that
“My colleagues feel a sense of moral injury, putting their lives on the line at work, performing the most perilous job, and their kids can’t hang out with other kids, which just puts salt on the wound,” she said.
Additional sources of moral injury are deciding which patients should receive life support in the event of inadequate resources and bearing witness to, or enforcing, policies that lead to patients dying alone.
Leaders should encourage clinicians to “seek informal support from colleagues, managers, or chaplains” and to “provide rapid access to professional help,” the authors noted.
Furthermore, they contended that leaders should “proactively and routinely monitor the psychological well-being of their teams,” since guilt and shame often prevent clinicians from disclosing feelings of moral injury.
“Being provided with routine mental health support should be normalized and it should be part of the job – not only during COVID-19 but in general,” Dr. Schwartz said.
‘Battle buddies’
Dr. Margolis recommended the “battle buddy” model for mutual peer support.
Dr. Anand, a mental health clinician at Mayo Medical School, Rochester, Minn., elaborated.
“We connect residents with each other, and they form pairs to support each other and watch for warning signs such as withdrawal from colleagues, being frequently tearful, not showing up at work or showing up late, missing assignments, making mistakes at work, increased use of alcohol, or verbalizing serious concerns,” Dr. Anand said.
If the buddy shows any of these warning signs, he or she can be directed to appropriate resources to get help.
Since the pandemic has interfered with the ability to connect with colleagues and family members, attention should be paid to addressing the social support needs of clinicians.
Dr. Anand suggested that clinicians maintain contact with counselors, friends, and family, even if they cannot be together in person and must connect “virtually.”
Resilience and strength training are “key” components of reducing clinician distress, but trainings as well as processing groups and support workshops should be offered during protected time, Dr. Margolis advised, since it can be burdensome for clinicians to wake up early or stay late to attend these sessions.
Leaders and administrators should “model self-care and well-being,” she noted. For example, sending emails to clinicians late at night or on weekends creates an expectation of a rapid reply, which leads to additional pressure for the clinician.
“This is of the most powerful unspoken curricula we can develop,” Dr. Margolis emphasized.
Self-care critical
Marcus S. Shaker, MD, MSc, associate professor of pediatrics, medicine, and community and family medicine, Children’s Hospital at Dartmouth-Hitchcock in Lebanon, N.H., and Geisel School of Medicine at Dartmouth, Hanover, N.H., said the study was “a much appreciated, timely reminder of the importance of clinician wellness.”
Moreover, “without self-care, our ability to help our patients withers. This article provides a useful conceptual framework for individuals and organizations to provide the right care at the right time in these unprecedented times,” said Dr. Shaker, who was not involved with the study.
The authors agreed, stating that clinicians “require proactive psychological protection specifically because they are a population known for putting others’ needs before their own.”
They recommended several resources for HCPs, including the Physician Support Line; Headspace, a mindfulness Web-based app for reducing stress and anxiety; the National Suicide Prevention Lifeline; and the Crisis Text Line.
The authors and Dr. Shaker disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new review offers fresh guidance to help stem the mental health toll of the COVID-19 pandemic on frontline clinicians.
Investigators gathered practice guidelines and resources from a wide range of health care organizations and professional societies to develop a conceptual framework of mental health support for health care professionals (HCPs) caring for COVID-19 patients.
“Support needs to be deployed in multiple dimensions – including individual, organizational, and societal levels – and include training in resilience, stress reduction, emotional awareness, and self-care strategies,” lead author Rachel Schwartz, PhD, health services researcher, Stanford (Calif.) University, said in an interview.
The review was published Aug. 21 in the Annals of Internal Medicine.
An opportune moment
Coauthor Rebecca Margolis, DO, director of well-being in the division of medical education and faculty development, Children’s Hospital of Los Angeles, said that this is “an opportune moment to look at how we treat frontline providers in this country.”
Studies of previous pandemics have shown heightened distress in HCPs, even years after the pandemic, and the unique challenges posed by the COVID-19 pandemic surpass those of previous pandemics, Dr. Margolis said in an interview.
Dr. Schwartz, Dr. Margolis, and coauthors Uma Anand, PhD, LP, and Jina Sinskey, MD, met through the Collaborative for Healing and Renewal in Medicine network, a group of medical educators, leaders in academic medicine, experts in burnout research and interventions, and trainees working together to promote well-being among trainees and practicing physicians.
“We were brought together on a conference call in March, when things were particularly bad in New York, and started looking to see what resources we could get to frontline providers who were suffering. It was great to lean on each other and stand on the shoulders of colleagues in New York, who were the ones we learned from on these calls,” said Dr. Margolis.
The authors recommended addressing clinicians’ basic practical needs, including ensuring essentials like meals and transportation, establishing a “well-being area” within hospitals for staff to rest, and providing well-stocked living quarters so clinicians can safely quarantine from family, as well as personal protective equipment and child care.
Clinicians are often asked to “assume new professional roles to meet evolving needs” during a pandemic, which can increase stress. The authors recommended targeted training, assessment of clinician skills before redeployment to a new clinical role, and clear communication practices around redeployment.
Recognition from hospital and government leaders improves morale and supports clinicians’ ability to continue delivering care. Leadership should “leverage communication strategies to provide clinicians with up-to-date information and reassurance,” they wrote.
‘Uniquely isolated’
Dr. Margolis noted that
“My colleagues feel a sense of moral injury, putting their lives on the line at work, performing the most perilous job, and their kids can’t hang out with other kids, which just puts salt on the wound,” she said.
Additional sources of moral injury are deciding which patients should receive life support in the event of inadequate resources and bearing witness to, or enforcing, policies that lead to patients dying alone.
Leaders should encourage clinicians to “seek informal support from colleagues, managers, or chaplains” and to “provide rapid access to professional help,” the authors noted.
Furthermore, they contended that leaders should “proactively and routinely monitor the psychological well-being of their teams,” since guilt and shame often prevent clinicians from disclosing feelings of moral injury.
“Being provided with routine mental health support should be normalized and it should be part of the job – not only during COVID-19 but in general,” Dr. Schwartz said.
‘Battle buddies’
Dr. Margolis recommended the “battle buddy” model for mutual peer support.
Dr. Anand, a mental health clinician at Mayo Medical School, Rochester, Minn., elaborated.
“We connect residents with each other, and they form pairs to support each other and watch for warning signs such as withdrawal from colleagues, being frequently tearful, not showing up at work or showing up late, missing assignments, making mistakes at work, increased use of alcohol, or verbalizing serious concerns,” Dr. Anand said.
If the buddy shows any of these warning signs, he or she can be directed to appropriate resources to get help.
Since the pandemic has interfered with the ability to connect with colleagues and family members, attention should be paid to addressing the social support needs of clinicians.
Dr. Anand suggested that clinicians maintain contact with counselors, friends, and family, even if they cannot be together in person and must connect “virtually.”
Resilience and strength training are “key” components of reducing clinician distress, but trainings as well as processing groups and support workshops should be offered during protected time, Dr. Margolis advised, since it can be burdensome for clinicians to wake up early or stay late to attend these sessions.
Leaders and administrators should “model self-care and well-being,” she noted. For example, sending emails to clinicians late at night or on weekends creates an expectation of a rapid reply, which leads to additional pressure for the clinician.
“This is of the most powerful unspoken curricula we can develop,” Dr. Margolis emphasized.
Self-care critical
Marcus S. Shaker, MD, MSc, associate professor of pediatrics, medicine, and community and family medicine, Children’s Hospital at Dartmouth-Hitchcock in Lebanon, N.H., and Geisel School of Medicine at Dartmouth, Hanover, N.H., said the study was “a much appreciated, timely reminder of the importance of clinician wellness.”
Moreover, “without self-care, our ability to help our patients withers. This article provides a useful conceptual framework for individuals and organizations to provide the right care at the right time in these unprecedented times,” said Dr. Shaker, who was not involved with the study.
The authors agreed, stating that clinicians “require proactive psychological protection specifically because they are a population known for putting others’ needs before their own.”
They recommended several resources for HCPs, including the Physician Support Line; Headspace, a mindfulness Web-based app for reducing stress and anxiety; the National Suicide Prevention Lifeline; and the Crisis Text Line.
The authors and Dr. Shaker disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new review offers fresh guidance to help stem the mental health toll of the COVID-19 pandemic on frontline clinicians.
Investigators gathered practice guidelines and resources from a wide range of health care organizations and professional societies to develop a conceptual framework of mental health support for health care professionals (HCPs) caring for COVID-19 patients.
“Support needs to be deployed in multiple dimensions – including individual, organizational, and societal levels – and include training in resilience, stress reduction, emotional awareness, and self-care strategies,” lead author Rachel Schwartz, PhD, health services researcher, Stanford (Calif.) University, said in an interview.
The review was published Aug. 21 in the Annals of Internal Medicine.
An opportune moment
Coauthor Rebecca Margolis, DO, director of well-being in the division of medical education and faculty development, Children’s Hospital of Los Angeles, said that this is “an opportune moment to look at how we treat frontline providers in this country.”
Studies of previous pandemics have shown heightened distress in HCPs, even years after the pandemic, and the unique challenges posed by the COVID-19 pandemic surpass those of previous pandemics, Dr. Margolis said in an interview.
Dr. Schwartz, Dr. Margolis, and coauthors Uma Anand, PhD, LP, and Jina Sinskey, MD, met through the Collaborative for Healing and Renewal in Medicine network, a group of medical educators, leaders in academic medicine, experts in burnout research and interventions, and trainees working together to promote well-being among trainees and practicing physicians.
“We were brought together on a conference call in March, when things were particularly bad in New York, and started looking to see what resources we could get to frontline providers who were suffering. It was great to lean on each other and stand on the shoulders of colleagues in New York, who were the ones we learned from on these calls,” said Dr. Margolis.
The authors recommended addressing clinicians’ basic practical needs, including ensuring essentials like meals and transportation, establishing a “well-being area” within hospitals for staff to rest, and providing well-stocked living quarters so clinicians can safely quarantine from family, as well as personal protective equipment and child care.
Clinicians are often asked to “assume new professional roles to meet evolving needs” during a pandemic, which can increase stress. The authors recommended targeted training, assessment of clinician skills before redeployment to a new clinical role, and clear communication practices around redeployment.
Recognition from hospital and government leaders improves morale and supports clinicians’ ability to continue delivering care. Leadership should “leverage communication strategies to provide clinicians with up-to-date information and reassurance,” they wrote.
‘Uniquely isolated’
Dr. Margolis noted that
“My colleagues feel a sense of moral injury, putting their lives on the line at work, performing the most perilous job, and their kids can’t hang out with other kids, which just puts salt on the wound,” she said.
Additional sources of moral injury are deciding which patients should receive life support in the event of inadequate resources and bearing witness to, or enforcing, policies that lead to patients dying alone.
Leaders should encourage clinicians to “seek informal support from colleagues, managers, or chaplains” and to “provide rapid access to professional help,” the authors noted.
Furthermore, they contended that leaders should “proactively and routinely monitor the psychological well-being of their teams,” since guilt and shame often prevent clinicians from disclosing feelings of moral injury.
“Being provided with routine mental health support should be normalized and it should be part of the job – not only during COVID-19 but in general,” Dr. Schwartz said.
‘Battle buddies’
Dr. Margolis recommended the “battle buddy” model for mutual peer support.
Dr. Anand, a mental health clinician at Mayo Medical School, Rochester, Minn., elaborated.
“We connect residents with each other, and they form pairs to support each other and watch for warning signs such as withdrawal from colleagues, being frequently tearful, not showing up at work or showing up late, missing assignments, making mistakes at work, increased use of alcohol, or verbalizing serious concerns,” Dr. Anand said.
If the buddy shows any of these warning signs, he or she can be directed to appropriate resources to get help.
Since the pandemic has interfered with the ability to connect with colleagues and family members, attention should be paid to addressing the social support needs of clinicians.
Dr. Anand suggested that clinicians maintain contact with counselors, friends, and family, even if they cannot be together in person and must connect “virtually.”
Resilience and strength training are “key” components of reducing clinician distress, but trainings as well as processing groups and support workshops should be offered during protected time, Dr. Margolis advised, since it can be burdensome for clinicians to wake up early or stay late to attend these sessions.
Leaders and administrators should “model self-care and well-being,” she noted. For example, sending emails to clinicians late at night or on weekends creates an expectation of a rapid reply, which leads to additional pressure for the clinician.
“This is of the most powerful unspoken curricula we can develop,” Dr. Margolis emphasized.
Self-care critical
Marcus S. Shaker, MD, MSc, associate professor of pediatrics, medicine, and community and family medicine, Children’s Hospital at Dartmouth-Hitchcock in Lebanon, N.H., and Geisel School of Medicine at Dartmouth, Hanover, N.H., said the study was “a much appreciated, timely reminder of the importance of clinician wellness.”
Moreover, “without self-care, our ability to help our patients withers. This article provides a useful conceptual framework for individuals and organizations to provide the right care at the right time in these unprecedented times,” said Dr. Shaker, who was not involved with the study.
The authors agreed, stating that clinicians “require proactive psychological protection specifically because they are a population known for putting others’ needs before their own.”
They recommended several resources for HCPs, including the Physician Support Line; Headspace, a mindfulness Web-based app for reducing stress and anxiety; the National Suicide Prevention Lifeline; and the Crisis Text Line.
The authors and Dr. Shaker disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Statins linked to improved survival in multiple myeloma
Statin use was associated with an overall reduction of the risk of death in multiple myeloma (MM) patients, according to a report published in Clinical Lymphoma, Myeloma & Leukemia.
Statins maintained their benefit in patients with multiple myeloma treated with modern-day chemotherapy regimens based on novel agents, but the benefit is less pronounced, reported Amber Afzal, MD, Washington University, St Louis, and colleagues.
Dr. Afzal and colleagues assessed results from 5,922 patients who were diagnosed with multiple myeloma within the study period between 2007 and 2013. The association of statins with mortality in patients with MM was determined using multivariate Cox proportional hazards regression analysis, and a subanalysis was also performed to investigate the effect of statins on mortality in those patients treated with novel agents.
Mortality reduction seen
The study found that the use of statins was associated with a 21% reduction in risk of death (adjusted hazard ratio,] 0.79; 95% confidence interval, 0.74-0.84) among all patients with MM. Among the patents treated with novel agents (n = 3,603), statins reduced mortality by 10% (aHR, 0.90; 95% CI, 0.83-0.98).
“Our current study is the first one to support the survival benefit of statins in patients with myeloma treated with modern-day regimens based on novel agents, although it appears the benefit may not be as pronounced. Therefore, as myeloma regimens become more effective, the benefits of statins may diminish,” the researchers concluded.
The authors reported that they had no relevant disclosures.
SOURCE: Afzal A et al. Clin Lymphoma Myeloma Leuk. 2020 Jul 16. doi: 10.1016/j.clml.2020.07.003.
Statin use was associated with an overall reduction of the risk of death in multiple myeloma (MM) patients, according to a report published in Clinical Lymphoma, Myeloma & Leukemia.
Statins maintained their benefit in patients with multiple myeloma treated with modern-day chemotherapy regimens based on novel agents, but the benefit is less pronounced, reported Amber Afzal, MD, Washington University, St Louis, and colleagues.
Dr. Afzal and colleagues assessed results from 5,922 patients who were diagnosed with multiple myeloma within the study period between 2007 and 2013. The association of statins with mortality in patients with MM was determined using multivariate Cox proportional hazards regression analysis, and a subanalysis was also performed to investigate the effect of statins on mortality in those patients treated with novel agents.
Mortality reduction seen
The study found that the use of statins was associated with a 21% reduction in risk of death (adjusted hazard ratio,] 0.79; 95% confidence interval, 0.74-0.84) among all patients with MM. Among the patents treated with novel agents (n = 3,603), statins reduced mortality by 10% (aHR, 0.90; 95% CI, 0.83-0.98).
“Our current study is the first one to support the survival benefit of statins in patients with myeloma treated with modern-day regimens based on novel agents, although it appears the benefit may not be as pronounced. Therefore, as myeloma regimens become more effective, the benefits of statins may diminish,” the researchers concluded.
The authors reported that they had no relevant disclosures.
SOURCE: Afzal A et al. Clin Lymphoma Myeloma Leuk. 2020 Jul 16. doi: 10.1016/j.clml.2020.07.003.
Statin use was associated with an overall reduction of the risk of death in multiple myeloma (MM) patients, according to a report published in Clinical Lymphoma, Myeloma & Leukemia.
Statins maintained their benefit in patients with multiple myeloma treated with modern-day chemotherapy regimens based on novel agents, but the benefit is less pronounced, reported Amber Afzal, MD, Washington University, St Louis, and colleagues.
Dr. Afzal and colleagues assessed results from 5,922 patients who were diagnosed with multiple myeloma within the study period between 2007 and 2013. The association of statins with mortality in patients with MM was determined using multivariate Cox proportional hazards regression analysis, and a subanalysis was also performed to investigate the effect of statins on mortality in those patients treated with novel agents.
Mortality reduction seen
The study found that the use of statins was associated with a 21% reduction in risk of death (adjusted hazard ratio,] 0.79; 95% confidence interval, 0.74-0.84) among all patients with MM. Among the patents treated with novel agents (n = 3,603), statins reduced mortality by 10% (aHR, 0.90; 95% CI, 0.83-0.98).
“Our current study is the first one to support the survival benefit of statins in patients with myeloma treated with modern-day regimens based on novel agents, although it appears the benefit may not be as pronounced. Therefore, as myeloma regimens become more effective, the benefits of statins may diminish,” the researchers concluded.
The authors reported that they had no relevant disclosures.
SOURCE: Afzal A et al. Clin Lymphoma Myeloma Leuk. 2020 Jul 16. doi: 10.1016/j.clml.2020.07.003.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Dangers behind antimaskers and antivaxxers: How to combat both
Niket Sonpal, MD, thought he’d heard most of the myths about wearing masks during the pandemic, but the recent claim from a patient was a new one for the New York City gastroenterologist.
The patient refused to wear a mask because she heard inhaling bad breath through a mask could be toxic. The woman said the rumor was circulating on Facebook. Sonpal calmly explained that breathing your own breath is not going to cause health problems, he said.
“There’s a lot of controversy on masks,” he said. “Unfortunately, it’s really just a lack of education and buy-in. Social media is the primary source of all this misinformation. These kinds of over-the-top hyperbole has basically led to a disbelief that masks are effective. The disbelief is hard to break up.”
As mask requirements have tightened amid the ongoing pandemic, debates about face coverings have emerged front and center, with a growing number of people opposing mask usage. So-called antimaskers dispute the benefits of wearing masks and many contend that face coverings decrease oxygen flow and can lead to illness. Sentiment against masks have led to protests nationwide, ignited public conflicts in some areas, and even generated lawsuits over mask mandates.
The issue presents an ongoing challenge for physicians as they strive to educate patients about the significance of masking against the flood of antimask messages on social media and beyond. Opposition to masks is particularly frustrating for health professionals who have witnessed patients, family, or friends become ill or die from the virus. Refusing to mask and failing to social distance have been linked to the rapid spread of the coronavirus and subsequent deaths.
“I have had colleagues pass away, and it’s extremely disheartening and frustrating to see science so easily disregarded,” Sonpal said. “Masks save lives and protect people and not wearing them is simply a lack of respect, not just for your fellow colleagues, but for a member of your species.”
Michael Rebresh, who helped create the antimask group Million Unmasked Patriots, says his group’s objections to masks are rational and reasonable. The group, which has more than 8,000 members, formed in response to guidance by Illinois state officials that children would only be allowed to return to school wearing a mask.
“Our objections are to the fact that masks on children in school have a greater propensity to make children sick from breathing in bacteria that forms on the inner layer of a mask worn for hours on end,” Rebresh said. “We have an objection to the increase of CO2 intake and a decrease in oxygen flow for kids who need all the oxygen they can get during a learning environment. We recognized the masking of ourselves and kids for what it is: A political move to separate the two parties in our November election and define and create division between the two.”
Million Unmasked Patriots is one of dozens of antimask groups on social media platforms such as Facebook, Instagram, and TikTok. In July, Facebook suspended one such group, Unmasking America, which boasts 9,600 members, for posting repeated claims that face masks obstruct oxygen flow and have negative mental health effects.
Experts say the antiscience rhetoric is far from new. The antimask movement in many ways, shares similarities with that of the anti-vaccine movement, says Todd Wolynn, MD, a Pittsburgh pediatrician and cofounder of Shots Heard Round the World, an organization that defends vaccine advocates against coordinated online attacks by antivaxxers.
“A lot of it is conspiracy-laden,” said Wolynn of the disinformation. “That Dr. [Anthony] Fauci somehow helped construct the pandemic and that it’s not real. That Bill Gates is funding the vaccine so he can inject people with microchips. All sorts of really out-there, ungrounded conspiracy theories. If you had Venn diagram of antimask and antivaxx, I would say there’s clearly overlap.”
Parallels between antimaskers, antivaxxers
Opponents to masks fall on a spectrum, explains Vineet Arora, MD, a hospitalist and associate chief medical officer–clinical learning environment at University of Chicago Medicine. People who believe conspiracy theories and push misinformation are on one end, she said. There are also those who generally don’t believe the seriousness of the pandemic, feel their risk is minimal, or doubt the benefits of masks.
The two trains of thought resemble the distinction among parents who are antivaccine and those who are simply “vaccine hesitant,” says Arora, who co-authored a recent article about masking and misinformation that addresses antivaccine attitudes.
“While the antimask sentiment gets a lot of attention, I think it’s important to highlight there’s a lot of vocal anti-mask sentiment since most people are supportive of masks,” she said. “There might be people sitting on the fence who are just unsure about wearing a mask. That’s understandable because the science and the communication has evolved. There was a lot of early mixed messages about masking. Anytime you have confusion about the science or the science is evolving, it’s easy to have misinformation and then have that take off as myth.”
Just as antivaxxers work to swing the opinion of the vaccine hesitant, antimaskers are vying with public health advocates for the support of the mask hesitant, she said. Creating doubt in public health authorities is one way they are gaining followers. Anti-maskers often question and scrutinize past messaging about masks by public health officials, claiming that because guidance on masks has changed over time, the science behind masks and current guidance can’t be trusted, Wolynn said. Similarly, antivaxxers frequently question past actions by public health officials, such as the Tuskegee Experiment (which began in 1932), to try to poke holes in the credibility of public health officials and their advice.
Both the antimask and antivaccine movements also tend to base their resistance on a personal liberties argument, adds Jacqueline Winfield Fincher, MD, president for the American College of Physicians and an internist based in Thomson, Georgia. Antimaskers contend they should be free to decide whether to wear face coverings and that rules requiring masks infringe upon their civil liberties. Similarly, antivaxxers argue they should be free to decide whether to vaccinate their children and contend vaccine mandates violate their personal liberties.
Taking a deeper look, fear and control are two likely drivers of antimasking and antivaccine attitudes, Fincher said. Those refusing to wear masks may feel they have no control over the pandemic or its impacts, but they can control how they respond to mask-wearing requirements, she said.
Antivaccine parents often want more control over their children’s healthcare and falsely believe that vaccines are injecting something harmful into their children or may lead to harmful reactions.
“It’s a control issue and a defense mechanism,” she said. “Some people may feel helpless to deal with the pandemic or believe since it is not affecting them or their family, that it is not real. ‘If I just deny it and I don’t acknowledge facts, I don’t have to worry about it or do anything about it, and therefore I will have more control over my day-to-day life.’”
Groups fueling each other
In some cases, antimask and antivaxx groups are joining forces or adopting dual causes.
In California for instance, longtime opponents to vaccines are now objecting to mask policies as similar infringement to their bodily autonomy. Demonstrations in Texas, Idaho, and Michigan against mask mandates and other COVID-19 requirements have drawn support from anti-vaccine activists and incorporated antivaccine propaganda.
In Illinois, Million Unmasked Patriots, formally the Million Unmasked March, has received widespread attention for protesting both masks for returning schoolchildren and a future COVID-19 vaccine requirement.
A July protest planned by the antimask group triggered a letter by Arora and 500 other healthcare professionals to Illinois lawmakers decrying the group’s views and urging the state to move forward with universal masking in schools.
“What’s happening is those who are distrustful of government and public health and science are joining together,” said Arora, who coauthored a piece about the problem on KevinMD.com. “It’s important to address both movements together because they can quickly feed off each other and build in momentum. At the heart of both is really this deep skepticism of science.”
Rebresh of Million Unmasked Patriots said most of his members are not opposed to all vaccines, but rather they are opposed to “untested vaccines.” The primary concern is the inability to research long-term effects of a COVID-19 vaccine before its approval, he said.
Rebresh disagrees with the antimask movement being compared with the antivaccine movement. The two groups are “motivated by different things and a different set of circumstances drive their opinions,” he said. However, Rebresh believes that potential harm resulting from “mass vaccinations” is a valid concern. For this reason, he and his wife chose for their children to receive their vaccinations individually over a series of weeks, rather than the “kiddie cocktail of vaccines,” at a single visit, he said.
Vaccine scientist Peter Hotez, MD, PhD, said the antivaccine movement appears to have grown stronger from the pandemic fueled by fresh conspiracies and new alliances. Antivaccine sentiment has been gaining steam over the last several years and collecting more allies from the far-right, said Hotez, dean for the National School of Tropical Medicine and codirector for the Texas Children’s Hospital Center for Vaccine Development.
“Now what you’re seeing is yet another expansion this year, with antivaccine groups, under the banner of ‘health freedom,’ campaigning against social distancing and wearing masks and contact tracing,” he said. “What was an antivaccine movement has now become a full-blown antiscience movement and an anti-public health movement. It’s causing a lot of damage and I believe costing a lot of American lives.”
Neil F. Johnson, PhD, who has studied the antivaccine movement and its social media proliferation during the pandemic, said online comments by antivaxxers frequently condemn mask usage and showcase memes making fun of masks.
“In those same narratives about opposing vaccines for COVID, we see a lot of discussion against masks,” said Johnson, a physics professor at George Washington University in Washington, D.C. “If you don’t believe in the official picture of COVID, you don’t believe the policies or the advice that’s given about COVID.”
An analysis by Johnson that examined 1,300 Facebook pages found that, while antivaxxers have fewer followers than provaccine pages, antivaccine pages are more numerous, faster growing, and are more often connected to unrelated, undecided pages. Conversely, pages that advocate the benefits of vaccinations and explain the science behind immunizations are largely disconnected from such undecided communities, according to the study, published May 13 in Nature.
The study suggests the antivaccine movement is making influential strides during the pandemic and connecting with people who are undecided, while public health advocates are not building the same bridges, Johnson said.
“I think it’s hugely dangerous, because I don’t know any other moment in science or in public health when there was so much uncertainty in something affecting everybody,” he said. “Every policy that will be coming, everything depends on people buying into the official message. Once you have the seeds of doubt, that’s a very difficult thing to overcome. It’s an unprecedented challenge.”
How physicians and clinicians can help
A more aggressive approach is necessary when it comes to taking down antiscience content on social media, says Hotez. Too often, misinformation and antiscience rhetoric is allowed to linger on popular sites such as Facebook and Amazon.
Wolynn agrees. On personal or business platforms, it’s crucial to ban, hide, and delete such comments as quickly as possible, he said. On public sites, purposeful disinformation should be immediately reported to the platform.
At the same time, Wolynn said it’s essential to support those who make sound, science-based comments in social media forums.
“If you see someone who is pushing accurate, evidence-based information, and they come under attack, they should be supported and defended and empowered,” Wolynn said. “Shots Heard Round the World is doing all of those things, including galvanizing and recruiting more people to help get their voices out there.”
Expanded visibility by physicians and scientists would greatly help counter the spread of antiscience sentiment, adds Hotez.
“Too often, antiscience movements are able to flourish because scientists and physicians are invisible,” he said. “They’re too focused on either clinical practices or in the case of physician scientists, on grants and papers and not enough attention to public engagement. We’re going to have to change that around. We need to hear more from scientists directly.”
To that end, Wolynn said health care professionals, including medical students and residents, need to have formal training in communications, media, and social media as part of their education – and more support from employers to engage through social media.
“That’s where the fight is,” Wolynn said. “You can be the best diagnostician, the best clinician. You can make the right diagnosis and prescribe the right medication, but if families don’t hear what you’re saying, you’re not going to be effective. If you can’t be on the platform where they’re being influenced, we’re losing the battle.”
Speaking to your mask-hesitant patients
Concentrating on those who are uncertain about masks is particularly key for physicians and public health advocates as the pandemic continues, says Arora.
“It’s important for us to focus on the mask-hesitant who often don’t get the attention they need,” she said.
She suggests bringing up the subject of masks with patients during visits, asking about mask usage, discussing rumors they’ve heard, and emphasizing why masks are important. Be a role model by wearing a mask in your community and on social media, she added.
Some patients have real concerns about not being able to breathe through masks or anxiety disorders that can be aggravated even by the thought of wearing a mask, noted Susan R. Bailey, MD, president for the American Medical Association. Bailey, an immunologist, recently counseled a patient with a deviated nasal septum in addition to a panic disorder who was worried about wearing a mask, she said. Bailey listened to the patient’s concerns, discussed his health conditions, and proposed an alternative face covering that might make him more comfortable.
“Every patient is different,” Bailey said. “It’s important for us to remember that each person who is reluctant to wear a mask has their own reasons. It’s important for us to express some empathy – to agree with them, yes, masks are hot and inconvenient – and help understand their questions, which you may be able to answer to their satisfaction. There are patients that have legitimate questions and a physician caring about how they feel, can make all the difference.”
Physicians can also get involved with the AMA’s #MaskUp campaign, an effort to normalize mask wearing and debunk myths associated with masks. The campaign includes social media materials, slogans doctors can tweet, and profile pictures they can use on social media. The campaign’s toolkit includes images, videos, and information that physicians can share with patients and the public.
Enforcing strong mask policies at your practice and ensuring all staff are modeling appropriate mask behavior is also important, adds Fincher of the ACP. The college recently issued a policy supporting mask usage in community settings.
If a patient conveys an antimask belief, Fincher suggests not directly challenging the person’s views, but listening to them and offering objective data, discussing the science behind masks, and directing them to credible sources.
“Doctors are used to this. We recommend a lot of things to patients that they don’t want to do,” Fincher said. “If a patient feels attacked, they act defensively. But if you base your explanation in more objective terms with data, numbers, and personalize the risks and benefits of a vaccine, a healthy change in behavior, or a medication, then patients are more likely to hear your concerns and do the right thing. Having a long-term relationship with a trusted physician makes all of these issues much easier to discuss and to implement the best plan for the individual patient.”
This article first appeared on Medscape.com.
Niket Sonpal, MD, thought he’d heard most of the myths about wearing masks during the pandemic, but the recent claim from a patient was a new one for the New York City gastroenterologist.
The patient refused to wear a mask because she heard inhaling bad breath through a mask could be toxic. The woman said the rumor was circulating on Facebook. Sonpal calmly explained that breathing your own breath is not going to cause health problems, he said.
“There’s a lot of controversy on masks,” he said. “Unfortunately, it’s really just a lack of education and buy-in. Social media is the primary source of all this misinformation. These kinds of over-the-top hyperbole has basically led to a disbelief that masks are effective. The disbelief is hard to break up.”
As mask requirements have tightened amid the ongoing pandemic, debates about face coverings have emerged front and center, with a growing number of people opposing mask usage. So-called antimaskers dispute the benefits of wearing masks and many contend that face coverings decrease oxygen flow and can lead to illness. Sentiment against masks have led to protests nationwide, ignited public conflicts in some areas, and even generated lawsuits over mask mandates.
The issue presents an ongoing challenge for physicians as they strive to educate patients about the significance of masking against the flood of antimask messages on social media and beyond. Opposition to masks is particularly frustrating for health professionals who have witnessed patients, family, or friends become ill or die from the virus. Refusing to mask and failing to social distance have been linked to the rapid spread of the coronavirus and subsequent deaths.
“I have had colleagues pass away, and it’s extremely disheartening and frustrating to see science so easily disregarded,” Sonpal said. “Masks save lives and protect people and not wearing them is simply a lack of respect, not just for your fellow colleagues, but for a member of your species.”
Michael Rebresh, who helped create the antimask group Million Unmasked Patriots, says his group’s objections to masks are rational and reasonable. The group, which has more than 8,000 members, formed in response to guidance by Illinois state officials that children would only be allowed to return to school wearing a mask.
“Our objections are to the fact that masks on children in school have a greater propensity to make children sick from breathing in bacteria that forms on the inner layer of a mask worn for hours on end,” Rebresh said. “We have an objection to the increase of CO2 intake and a decrease in oxygen flow for kids who need all the oxygen they can get during a learning environment. We recognized the masking of ourselves and kids for what it is: A political move to separate the two parties in our November election and define and create division between the two.”
Million Unmasked Patriots is one of dozens of antimask groups on social media platforms such as Facebook, Instagram, and TikTok. In July, Facebook suspended one such group, Unmasking America, which boasts 9,600 members, for posting repeated claims that face masks obstruct oxygen flow and have negative mental health effects.
Experts say the antiscience rhetoric is far from new. The antimask movement in many ways, shares similarities with that of the anti-vaccine movement, says Todd Wolynn, MD, a Pittsburgh pediatrician and cofounder of Shots Heard Round the World, an organization that defends vaccine advocates against coordinated online attacks by antivaxxers.
“A lot of it is conspiracy-laden,” said Wolynn of the disinformation. “That Dr. [Anthony] Fauci somehow helped construct the pandemic and that it’s not real. That Bill Gates is funding the vaccine so he can inject people with microchips. All sorts of really out-there, ungrounded conspiracy theories. If you had Venn diagram of antimask and antivaxx, I would say there’s clearly overlap.”
Parallels between antimaskers, antivaxxers
Opponents to masks fall on a spectrum, explains Vineet Arora, MD, a hospitalist and associate chief medical officer–clinical learning environment at University of Chicago Medicine. People who believe conspiracy theories and push misinformation are on one end, she said. There are also those who generally don’t believe the seriousness of the pandemic, feel their risk is minimal, or doubt the benefits of masks.
The two trains of thought resemble the distinction among parents who are antivaccine and those who are simply “vaccine hesitant,” says Arora, who co-authored a recent article about masking and misinformation that addresses antivaccine attitudes.
“While the antimask sentiment gets a lot of attention, I think it’s important to highlight there’s a lot of vocal anti-mask sentiment since most people are supportive of masks,” she said. “There might be people sitting on the fence who are just unsure about wearing a mask. That’s understandable because the science and the communication has evolved. There was a lot of early mixed messages about masking. Anytime you have confusion about the science or the science is evolving, it’s easy to have misinformation and then have that take off as myth.”
Just as antivaxxers work to swing the opinion of the vaccine hesitant, antimaskers are vying with public health advocates for the support of the mask hesitant, she said. Creating doubt in public health authorities is one way they are gaining followers. Anti-maskers often question and scrutinize past messaging about masks by public health officials, claiming that because guidance on masks has changed over time, the science behind masks and current guidance can’t be trusted, Wolynn said. Similarly, antivaxxers frequently question past actions by public health officials, such as the Tuskegee Experiment (which began in 1932), to try to poke holes in the credibility of public health officials and their advice.
Both the antimask and antivaccine movements also tend to base their resistance on a personal liberties argument, adds Jacqueline Winfield Fincher, MD, president for the American College of Physicians and an internist based in Thomson, Georgia. Antimaskers contend they should be free to decide whether to wear face coverings and that rules requiring masks infringe upon their civil liberties. Similarly, antivaxxers argue they should be free to decide whether to vaccinate their children and contend vaccine mandates violate their personal liberties.
Taking a deeper look, fear and control are two likely drivers of antimasking and antivaccine attitudes, Fincher said. Those refusing to wear masks may feel they have no control over the pandemic or its impacts, but they can control how they respond to mask-wearing requirements, she said.
Antivaccine parents often want more control over their children’s healthcare and falsely believe that vaccines are injecting something harmful into their children or may lead to harmful reactions.
“It’s a control issue and a defense mechanism,” she said. “Some people may feel helpless to deal with the pandemic or believe since it is not affecting them or their family, that it is not real. ‘If I just deny it and I don’t acknowledge facts, I don’t have to worry about it or do anything about it, and therefore I will have more control over my day-to-day life.’”
Groups fueling each other
In some cases, antimask and antivaxx groups are joining forces or adopting dual causes.
In California for instance, longtime opponents to vaccines are now objecting to mask policies as similar infringement to their bodily autonomy. Demonstrations in Texas, Idaho, and Michigan against mask mandates and other COVID-19 requirements have drawn support from anti-vaccine activists and incorporated antivaccine propaganda.
In Illinois, Million Unmasked Patriots, formally the Million Unmasked March, has received widespread attention for protesting both masks for returning schoolchildren and a future COVID-19 vaccine requirement.
A July protest planned by the antimask group triggered a letter by Arora and 500 other healthcare professionals to Illinois lawmakers decrying the group’s views and urging the state to move forward with universal masking in schools.
“What’s happening is those who are distrustful of government and public health and science are joining together,” said Arora, who coauthored a piece about the problem on KevinMD.com. “It’s important to address both movements together because they can quickly feed off each other and build in momentum. At the heart of both is really this deep skepticism of science.”
Rebresh of Million Unmasked Patriots said most of his members are not opposed to all vaccines, but rather they are opposed to “untested vaccines.” The primary concern is the inability to research long-term effects of a COVID-19 vaccine before its approval, he said.
Rebresh disagrees with the antimask movement being compared with the antivaccine movement. The two groups are “motivated by different things and a different set of circumstances drive their opinions,” he said. However, Rebresh believes that potential harm resulting from “mass vaccinations” is a valid concern. For this reason, he and his wife chose for their children to receive their vaccinations individually over a series of weeks, rather than the “kiddie cocktail of vaccines,” at a single visit, he said.
Vaccine scientist Peter Hotez, MD, PhD, said the antivaccine movement appears to have grown stronger from the pandemic fueled by fresh conspiracies and new alliances. Antivaccine sentiment has been gaining steam over the last several years and collecting more allies from the far-right, said Hotez, dean for the National School of Tropical Medicine and codirector for the Texas Children’s Hospital Center for Vaccine Development.
“Now what you’re seeing is yet another expansion this year, with antivaccine groups, under the banner of ‘health freedom,’ campaigning against social distancing and wearing masks and contact tracing,” he said. “What was an antivaccine movement has now become a full-blown antiscience movement and an anti-public health movement. It’s causing a lot of damage and I believe costing a lot of American lives.”
Neil F. Johnson, PhD, who has studied the antivaccine movement and its social media proliferation during the pandemic, said online comments by antivaxxers frequently condemn mask usage and showcase memes making fun of masks.
“In those same narratives about opposing vaccines for COVID, we see a lot of discussion against masks,” said Johnson, a physics professor at George Washington University in Washington, D.C. “If you don’t believe in the official picture of COVID, you don’t believe the policies or the advice that’s given about COVID.”
An analysis by Johnson that examined 1,300 Facebook pages found that, while antivaxxers have fewer followers than provaccine pages, antivaccine pages are more numerous, faster growing, and are more often connected to unrelated, undecided pages. Conversely, pages that advocate the benefits of vaccinations and explain the science behind immunizations are largely disconnected from such undecided communities, according to the study, published May 13 in Nature.
The study suggests the antivaccine movement is making influential strides during the pandemic and connecting with people who are undecided, while public health advocates are not building the same bridges, Johnson said.
“I think it’s hugely dangerous, because I don’t know any other moment in science or in public health when there was so much uncertainty in something affecting everybody,” he said. “Every policy that will be coming, everything depends on people buying into the official message. Once you have the seeds of doubt, that’s a very difficult thing to overcome. It’s an unprecedented challenge.”
How physicians and clinicians can help
A more aggressive approach is necessary when it comes to taking down antiscience content on social media, says Hotez. Too often, misinformation and antiscience rhetoric is allowed to linger on popular sites such as Facebook and Amazon.
Wolynn agrees. On personal or business platforms, it’s crucial to ban, hide, and delete such comments as quickly as possible, he said. On public sites, purposeful disinformation should be immediately reported to the platform.
At the same time, Wolynn said it’s essential to support those who make sound, science-based comments in social media forums.
“If you see someone who is pushing accurate, evidence-based information, and they come under attack, they should be supported and defended and empowered,” Wolynn said. “Shots Heard Round the World is doing all of those things, including galvanizing and recruiting more people to help get their voices out there.”
Expanded visibility by physicians and scientists would greatly help counter the spread of antiscience sentiment, adds Hotez.
“Too often, antiscience movements are able to flourish because scientists and physicians are invisible,” he said. “They’re too focused on either clinical practices or in the case of physician scientists, on grants and papers and not enough attention to public engagement. We’re going to have to change that around. We need to hear more from scientists directly.”
To that end, Wolynn said health care professionals, including medical students and residents, need to have formal training in communications, media, and social media as part of their education – and more support from employers to engage through social media.
“That’s where the fight is,” Wolynn said. “You can be the best diagnostician, the best clinician. You can make the right diagnosis and prescribe the right medication, but if families don’t hear what you’re saying, you’re not going to be effective. If you can’t be on the platform where they’re being influenced, we’re losing the battle.”
Speaking to your mask-hesitant patients
Concentrating on those who are uncertain about masks is particularly key for physicians and public health advocates as the pandemic continues, says Arora.
“It’s important for us to focus on the mask-hesitant who often don’t get the attention they need,” she said.
She suggests bringing up the subject of masks with patients during visits, asking about mask usage, discussing rumors they’ve heard, and emphasizing why masks are important. Be a role model by wearing a mask in your community and on social media, she added.
Some patients have real concerns about not being able to breathe through masks or anxiety disorders that can be aggravated even by the thought of wearing a mask, noted Susan R. Bailey, MD, president for the American Medical Association. Bailey, an immunologist, recently counseled a patient with a deviated nasal septum in addition to a panic disorder who was worried about wearing a mask, she said. Bailey listened to the patient’s concerns, discussed his health conditions, and proposed an alternative face covering that might make him more comfortable.
“Every patient is different,” Bailey said. “It’s important for us to remember that each person who is reluctant to wear a mask has their own reasons. It’s important for us to express some empathy – to agree with them, yes, masks are hot and inconvenient – and help understand their questions, which you may be able to answer to their satisfaction. There are patients that have legitimate questions and a physician caring about how they feel, can make all the difference.”
Physicians can also get involved with the AMA’s #MaskUp campaign, an effort to normalize mask wearing and debunk myths associated with masks. The campaign includes social media materials, slogans doctors can tweet, and profile pictures they can use on social media. The campaign’s toolkit includes images, videos, and information that physicians can share with patients and the public.
Enforcing strong mask policies at your practice and ensuring all staff are modeling appropriate mask behavior is also important, adds Fincher of the ACP. The college recently issued a policy supporting mask usage in community settings.
If a patient conveys an antimask belief, Fincher suggests not directly challenging the person’s views, but listening to them and offering objective data, discussing the science behind masks, and directing them to credible sources.
“Doctors are used to this. We recommend a lot of things to patients that they don’t want to do,” Fincher said. “If a patient feels attacked, they act defensively. But if you base your explanation in more objective terms with data, numbers, and personalize the risks and benefits of a vaccine, a healthy change in behavior, or a medication, then patients are more likely to hear your concerns and do the right thing. Having a long-term relationship with a trusted physician makes all of these issues much easier to discuss and to implement the best plan for the individual patient.”
This article first appeared on Medscape.com.
Niket Sonpal, MD, thought he’d heard most of the myths about wearing masks during the pandemic, but the recent claim from a patient was a new one for the New York City gastroenterologist.
The patient refused to wear a mask because she heard inhaling bad breath through a mask could be toxic. The woman said the rumor was circulating on Facebook. Sonpal calmly explained that breathing your own breath is not going to cause health problems, he said.
“There’s a lot of controversy on masks,” he said. “Unfortunately, it’s really just a lack of education and buy-in. Social media is the primary source of all this misinformation. These kinds of over-the-top hyperbole has basically led to a disbelief that masks are effective. The disbelief is hard to break up.”
As mask requirements have tightened amid the ongoing pandemic, debates about face coverings have emerged front and center, with a growing number of people opposing mask usage. So-called antimaskers dispute the benefits of wearing masks and many contend that face coverings decrease oxygen flow and can lead to illness. Sentiment against masks have led to protests nationwide, ignited public conflicts in some areas, and even generated lawsuits over mask mandates.
The issue presents an ongoing challenge for physicians as they strive to educate patients about the significance of masking against the flood of antimask messages on social media and beyond. Opposition to masks is particularly frustrating for health professionals who have witnessed patients, family, or friends become ill or die from the virus. Refusing to mask and failing to social distance have been linked to the rapid spread of the coronavirus and subsequent deaths.
“I have had colleagues pass away, and it’s extremely disheartening and frustrating to see science so easily disregarded,” Sonpal said. “Masks save lives and protect people and not wearing them is simply a lack of respect, not just for your fellow colleagues, but for a member of your species.”
Michael Rebresh, who helped create the antimask group Million Unmasked Patriots, says his group’s objections to masks are rational and reasonable. The group, which has more than 8,000 members, formed in response to guidance by Illinois state officials that children would only be allowed to return to school wearing a mask.
“Our objections are to the fact that masks on children in school have a greater propensity to make children sick from breathing in bacteria that forms on the inner layer of a mask worn for hours on end,” Rebresh said. “We have an objection to the increase of CO2 intake and a decrease in oxygen flow for kids who need all the oxygen they can get during a learning environment. We recognized the masking of ourselves and kids for what it is: A political move to separate the two parties in our November election and define and create division between the two.”
Million Unmasked Patriots is one of dozens of antimask groups on social media platforms such as Facebook, Instagram, and TikTok. In July, Facebook suspended one such group, Unmasking America, which boasts 9,600 members, for posting repeated claims that face masks obstruct oxygen flow and have negative mental health effects.
Experts say the antiscience rhetoric is far from new. The antimask movement in many ways, shares similarities with that of the anti-vaccine movement, says Todd Wolynn, MD, a Pittsburgh pediatrician and cofounder of Shots Heard Round the World, an organization that defends vaccine advocates against coordinated online attacks by antivaxxers.
“A lot of it is conspiracy-laden,” said Wolynn of the disinformation. “That Dr. [Anthony] Fauci somehow helped construct the pandemic and that it’s not real. That Bill Gates is funding the vaccine so he can inject people with microchips. All sorts of really out-there, ungrounded conspiracy theories. If you had Venn diagram of antimask and antivaxx, I would say there’s clearly overlap.”
Parallels between antimaskers, antivaxxers
Opponents to masks fall on a spectrum, explains Vineet Arora, MD, a hospitalist and associate chief medical officer–clinical learning environment at University of Chicago Medicine. People who believe conspiracy theories and push misinformation are on one end, she said. There are also those who generally don’t believe the seriousness of the pandemic, feel their risk is minimal, or doubt the benefits of masks.
The two trains of thought resemble the distinction among parents who are antivaccine and those who are simply “vaccine hesitant,” says Arora, who co-authored a recent article about masking and misinformation that addresses antivaccine attitudes.
“While the antimask sentiment gets a lot of attention, I think it’s important to highlight there’s a lot of vocal anti-mask sentiment since most people are supportive of masks,” she said. “There might be people sitting on the fence who are just unsure about wearing a mask. That’s understandable because the science and the communication has evolved. There was a lot of early mixed messages about masking. Anytime you have confusion about the science or the science is evolving, it’s easy to have misinformation and then have that take off as myth.”
Just as antivaxxers work to swing the opinion of the vaccine hesitant, antimaskers are vying with public health advocates for the support of the mask hesitant, she said. Creating doubt in public health authorities is one way they are gaining followers. Anti-maskers often question and scrutinize past messaging about masks by public health officials, claiming that because guidance on masks has changed over time, the science behind masks and current guidance can’t be trusted, Wolynn said. Similarly, antivaxxers frequently question past actions by public health officials, such as the Tuskegee Experiment (which began in 1932), to try to poke holes in the credibility of public health officials and their advice.
Both the antimask and antivaccine movements also tend to base their resistance on a personal liberties argument, adds Jacqueline Winfield Fincher, MD, president for the American College of Physicians and an internist based in Thomson, Georgia. Antimaskers contend they should be free to decide whether to wear face coverings and that rules requiring masks infringe upon their civil liberties. Similarly, antivaxxers argue they should be free to decide whether to vaccinate their children and contend vaccine mandates violate their personal liberties.
Taking a deeper look, fear and control are two likely drivers of antimasking and antivaccine attitudes, Fincher said. Those refusing to wear masks may feel they have no control over the pandemic or its impacts, but they can control how they respond to mask-wearing requirements, she said.
Antivaccine parents often want more control over their children’s healthcare and falsely believe that vaccines are injecting something harmful into their children or may lead to harmful reactions.
“It’s a control issue and a defense mechanism,” she said. “Some people may feel helpless to deal with the pandemic or believe since it is not affecting them or their family, that it is not real. ‘If I just deny it and I don’t acknowledge facts, I don’t have to worry about it or do anything about it, and therefore I will have more control over my day-to-day life.’”
Groups fueling each other
In some cases, antimask and antivaxx groups are joining forces or adopting dual causes.
In California for instance, longtime opponents to vaccines are now objecting to mask policies as similar infringement to their bodily autonomy. Demonstrations in Texas, Idaho, and Michigan against mask mandates and other COVID-19 requirements have drawn support from anti-vaccine activists and incorporated antivaccine propaganda.
In Illinois, Million Unmasked Patriots, formally the Million Unmasked March, has received widespread attention for protesting both masks for returning schoolchildren and a future COVID-19 vaccine requirement.
A July protest planned by the antimask group triggered a letter by Arora and 500 other healthcare professionals to Illinois lawmakers decrying the group’s views and urging the state to move forward with universal masking in schools.
“What’s happening is those who are distrustful of government and public health and science are joining together,” said Arora, who coauthored a piece about the problem on KevinMD.com. “It’s important to address both movements together because they can quickly feed off each other and build in momentum. At the heart of both is really this deep skepticism of science.”
Rebresh of Million Unmasked Patriots said most of his members are not opposed to all vaccines, but rather they are opposed to “untested vaccines.” The primary concern is the inability to research long-term effects of a COVID-19 vaccine before its approval, he said.
Rebresh disagrees with the antimask movement being compared with the antivaccine movement. The two groups are “motivated by different things and a different set of circumstances drive their opinions,” he said. However, Rebresh believes that potential harm resulting from “mass vaccinations” is a valid concern. For this reason, he and his wife chose for their children to receive their vaccinations individually over a series of weeks, rather than the “kiddie cocktail of vaccines,” at a single visit, he said.
Vaccine scientist Peter Hotez, MD, PhD, said the antivaccine movement appears to have grown stronger from the pandemic fueled by fresh conspiracies and new alliances. Antivaccine sentiment has been gaining steam over the last several years and collecting more allies from the far-right, said Hotez, dean for the National School of Tropical Medicine and codirector for the Texas Children’s Hospital Center for Vaccine Development.
“Now what you’re seeing is yet another expansion this year, with antivaccine groups, under the banner of ‘health freedom,’ campaigning against social distancing and wearing masks and contact tracing,” he said. “What was an antivaccine movement has now become a full-blown antiscience movement and an anti-public health movement. It’s causing a lot of damage and I believe costing a lot of American lives.”
Neil F. Johnson, PhD, who has studied the antivaccine movement and its social media proliferation during the pandemic, said online comments by antivaxxers frequently condemn mask usage and showcase memes making fun of masks.
“In those same narratives about opposing vaccines for COVID, we see a lot of discussion against masks,” said Johnson, a physics professor at George Washington University in Washington, D.C. “If you don’t believe in the official picture of COVID, you don’t believe the policies or the advice that’s given about COVID.”
An analysis by Johnson that examined 1,300 Facebook pages found that, while antivaxxers have fewer followers than provaccine pages, antivaccine pages are more numerous, faster growing, and are more often connected to unrelated, undecided pages. Conversely, pages that advocate the benefits of vaccinations and explain the science behind immunizations are largely disconnected from such undecided communities, according to the study, published May 13 in Nature.
The study suggests the antivaccine movement is making influential strides during the pandemic and connecting with people who are undecided, while public health advocates are not building the same bridges, Johnson said.
“I think it’s hugely dangerous, because I don’t know any other moment in science or in public health when there was so much uncertainty in something affecting everybody,” he said. “Every policy that will be coming, everything depends on people buying into the official message. Once you have the seeds of doubt, that’s a very difficult thing to overcome. It’s an unprecedented challenge.”
How physicians and clinicians can help
A more aggressive approach is necessary when it comes to taking down antiscience content on social media, says Hotez. Too often, misinformation and antiscience rhetoric is allowed to linger on popular sites such as Facebook and Amazon.
Wolynn agrees. On personal or business platforms, it’s crucial to ban, hide, and delete such comments as quickly as possible, he said. On public sites, purposeful disinformation should be immediately reported to the platform.
At the same time, Wolynn said it’s essential to support those who make sound, science-based comments in social media forums.
“If you see someone who is pushing accurate, evidence-based information, and they come under attack, they should be supported and defended and empowered,” Wolynn said. “Shots Heard Round the World is doing all of those things, including galvanizing and recruiting more people to help get their voices out there.”
Expanded visibility by physicians and scientists would greatly help counter the spread of antiscience sentiment, adds Hotez.
“Too often, antiscience movements are able to flourish because scientists and physicians are invisible,” he said. “They’re too focused on either clinical practices or in the case of physician scientists, on grants and papers and not enough attention to public engagement. We’re going to have to change that around. We need to hear more from scientists directly.”
To that end, Wolynn said health care professionals, including medical students and residents, need to have formal training in communications, media, and social media as part of their education – and more support from employers to engage through social media.
“That’s where the fight is,” Wolynn said. “You can be the best diagnostician, the best clinician. You can make the right diagnosis and prescribe the right medication, but if families don’t hear what you’re saying, you’re not going to be effective. If you can’t be on the platform where they’re being influenced, we’re losing the battle.”
Speaking to your mask-hesitant patients
Concentrating on those who are uncertain about masks is particularly key for physicians and public health advocates as the pandemic continues, says Arora.
“It’s important for us to focus on the mask-hesitant who often don’t get the attention they need,” she said.
She suggests bringing up the subject of masks with patients during visits, asking about mask usage, discussing rumors they’ve heard, and emphasizing why masks are important. Be a role model by wearing a mask in your community and on social media, she added.
Some patients have real concerns about not being able to breathe through masks or anxiety disorders that can be aggravated even by the thought of wearing a mask, noted Susan R. Bailey, MD, president for the American Medical Association. Bailey, an immunologist, recently counseled a patient with a deviated nasal septum in addition to a panic disorder who was worried about wearing a mask, she said. Bailey listened to the patient’s concerns, discussed his health conditions, and proposed an alternative face covering that might make him more comfortable.
“Every patient is different,” Bailey said. “It’s important for us to remember that each person who is reluctant to wear a mask has their own reasons. It’s important for us to express some empathy – to agree with them, yes, masks are hot and inconvenient – and help understand their questions, which you may be able to answer to their satisfaction. There are patients that have legitimate questions and a physician caring about how they feel, can make all the difference.”
Physicians can also get involved with the AMA’s #MaskUp campaign, an effort to normalize mask wearing and debunk myths associated with masks. The campaign includes social media materials, slogans doctors can tweet, and profile pictures they can use on social media. The campaign’s toolkit includes images, videos, and information that physicians can share with patients and the public.
Enforcing strong mask policies at your practice and ensuring all staff are modeling appropriate mask behavior is also important, adds Fincher of the ACP. The college recently issued a policy supporting mask usage in community settings.
If a patient conveys an antimask belief, Fincher suggests not directly challenging the person’s views, but listening to them and offering objective data, discussing the science behind masks, and directing them to credible sources.
“Doctors are used to this. We recommend a lot of things to patients that they don’t want to do,” Fincher said. “If a patient feels attacked, they act defensively. But if you base your explanation in more objective terms with data, numbers, and personalize the risks and benefits of a vaccine, a healthy change in behavior, or a medication, then patients are more likely to hear your concerns and do the right thing. Having a long-term relationship with a trusted physician makes all of these issues much easier to discuss and to implement the best plan for the individual patient.”
This article first appeared on Medscape.com.
U.S. tops 500,000 COVID-19 cases in children
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
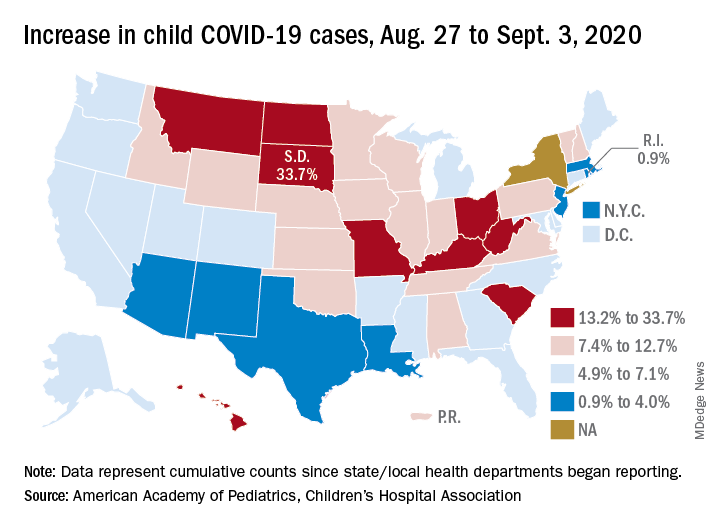
States have reported 513,415 cases of COVID-19 in children since the beginning of the pandemic, with almost 37,000 coming in the last week, the AAP and the CHA said Sept. 8 in the weekly report. That figure includes New York City – the rest of New York State is not reporting ages for COVID-19 patients – as well as Puerto Rico, the District of Columbia, and Guam.
“These numbers are a chilling reminder of why we need to take this virus seriously,” AAP President Sara Goza, MD, said in a written statement.
Children now represent 9.8% of the almost 5.3 million cases that have been reported in Americans of all ages. The proportion of child cases has continued to increase as the pandemic has progressed – it was 8.0% as of mid-July and 5.2% in early June, the data show.
“Throughout the summer, surges in the virus have occurred in Southern, Western, and Midwestern states,” the AAP statement said.
The latest AAP/CHA report shows that, from Aug. 27 to Sept. 3, the total number of child cases jumped by 33.7% in South Dakota, more than any other state. North Dakota was next at 22.7%, followed by Hawaii (18.1%), Missouri (16.8%), and Kentucky (16.4%).
“This rapid rise in positive cases occurred over the summer, and as the weather cools, we know people will spend more time indoors,” said Sean O’Leary, MD, MPH, vice chair of the AAP Committee on Infectious Diseases. “The goal is to get children back into schools for in-person learning, but in many communities, this is not possible as the virus spreads unchecked.”
The smallest increase over the last week, just 0.9%, came in Rhode Island, with Massachusetts just a bit higher at 1.0%. Also at the low end of the increase scale are Arizona (3.3%) and Louisiana (4.0%), two states that have very high rates of cumulative cases: 1,380 per 100,000 children for Arizona and 1,234 per 100,000 for Louisiana, the report said.
To give those figures some context, Tennessee has the highest cumulative count of any state at 1,553 cases per 100,000 children and Vermont has the lowest at 151, based on the data gathered by the AAP and CHA.
“While much remains unknown about COVID-19, we do know that the spread among children reflects what is happening in the broader communities. A disproportionate number of cases are reported in Black and Hispanic children and in places where there is high poverty. We must work harder to address societal inequities that contribute to these disparities,” Dr. Goza said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
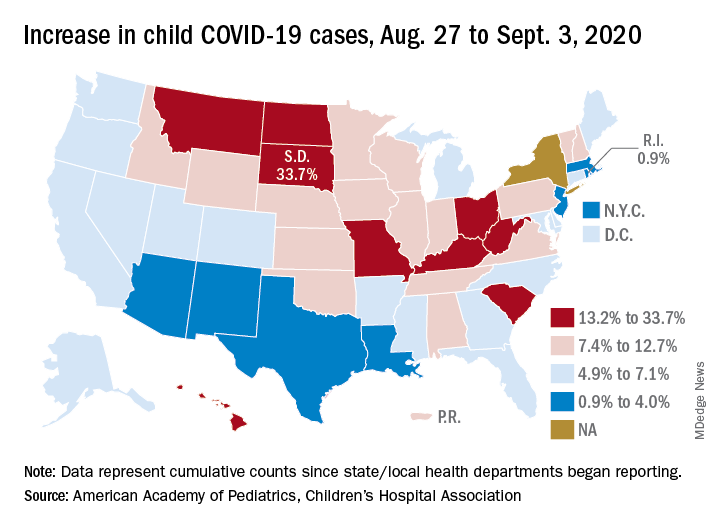
States have reported 513,415 cases of COVID-19 in children since the beginning of the pandemic, with almost 37,000 coming in the last week, the AAP and the CHA said Sept. 8 in the weekly report. That figure includes New York City – the rest of New York State is not reporting ages for COVID-19 patients – as well as Puerto Rico, the District of Columbia, and Guam.
“These numbers are a chilling reminder of why we need to take this virus seriously,” AAP President Sara Goza, MD, said in a written statement.
Children now represent 9.8% of the almost 5.3 million cases that have been reported in Americans of all ages. The proportion of child cases has continued to increase as the pandemic has progressed – it was 8.0% as of mid-July and 5.2% in early June, the data show.
“Throughout the summer, surges in the virus have occurred in Southern, Western, and Midwestern states,” the AAP statement said.
The latest AAP/CHA report shows that, from Aug. 27 to Sept. 3, the total number of child cases jumped by 33.7% in South Dakota, more than any other state. North Dakota was next at 22.7%, followed by Hawaii (18.1%), Missouri (16.8%), and Kentucky (16.4%).
“This rapid rise in positive cases occurred over the summer, and as the weather cools, we know people will spend more time indoors,” said Sean O’Leary, MD, MPH, vice chair of the AAP Committee on Infectious Diseases. “The goal is to get children back into schools for in-person learning, but in many communities, this is not possible as the virus spreads unchecked.”
The smallest increase over the last week, just 0.9%, came in Rhode Island, with Massachusetts just a bit higher at 1.0%. Also at the low end of the increase scale are Arizona (3.3%) and Louisiana (4.0%), two states that have very high rates of cumulative cases: 1,380 per 100,000 children for Arizona and 1,234 per 100,000 for Louisiana, the report said.
To give those figures some context, Tennessee has the highest cumulative count of any state at 1,553 cases per 100,000 children and Vermont has the lowest at 151, based on the data gathered by the AAP and CHA.
“While much remains unknown about COVID-19, we do know that the spread among children reflects what is happening in the broader communities. A disproportionate number of cases are reported in Black and Hispanic children and in places where there is high poverty. We must work harder to address societal inequities that contribute to these disparities,” Dr. Goza said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
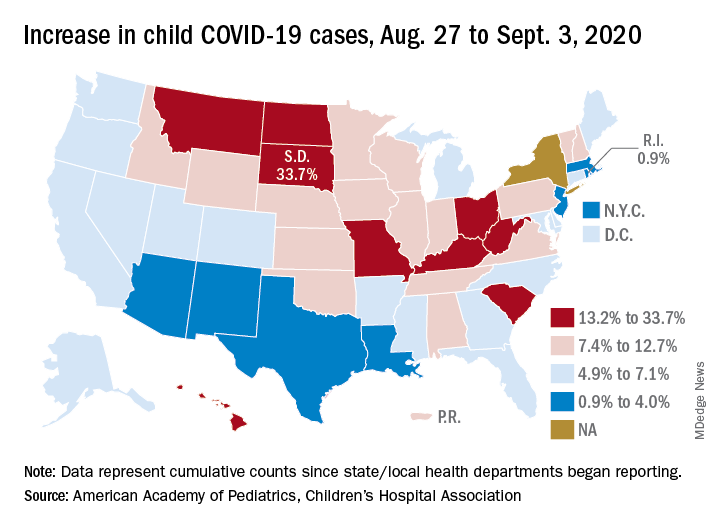
States have reported 513,415 cases of COVID-19 in children since the beginning of the pandemic, with almost 37,000 coming in the last week, the AAP and the CHA said Sept. 8 in the weekly report. That figure includes New York City – the rest of New York State is not reporting ages for COVID-19 patients – as well as Puerto Rico, the District of Columbia, and Guam.
“These numbers are a chilling reminder of why we need to take this virus seriously,” AAP President Sara Goza, MD, said in a written statement.
Children now represent 9.8% of the almost 5.3 million cases that have been reported in Americans of all ages. The proportion of child cases has continued to increase as the pandemic has progressed – it was 8.0% as of mid-July and 5.2% in early June, the data show.
“Throughout the summer, surges in the virus have occurred in Southern, Western, and Midwestern states,” the AAP statement said.
The latest AAP/CHA report shows that, from Aug. 27 to Sept. 3, the total number of child cases jumped by 33.7% in South Dakota, more than any other state. North Dakota was next at 22.7%, followed by Hawaii (18.1%), Missouri (16.8%), and Kentucky (16.4%).
“This rapid rise in positive cases occurred over the summer, and as the weather cools, we know people will spend more time indoors,” said Sean O’Leary, MD, MPH, vice chair of the AAP Committee on Infectious Diseases. “The goal is to get children back into schools for in-person learning, but in many communities, this is not possible as the virus spreads unchecked.”
The smallest increase over the last week, just 0.9%, came in Rhode Island, with Massachusetts just a bit higher at 1.0%. Also at the low end of the increase scale are Arizona (3.3%) and Louisiana (4.0%), two states that have very high rates of cumulative cases: 1,380 per 100,000 children for Arizona and 1,234 per 100,000 for Louisiana, the report said.
To give those figures some context, Tennessee has the highest cumulative count of any state at 1,553 cases per 100,000 children and Vermont has the lowest at 151, based on the data gathered by the AAP and CHA.
“While much remains unknown about COVID-19, we do know that the spread among children reflects what is happening in the broader communities. A disproportionate number of cases are reported in Black and Hispanic children and in places where there is high poverty. We must work harder to address societal inequities that contribute to these disparities,” Dr. Goza said.














