User login
AVAHO
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]


Genomic prostate score does not improve risk assessment
A genomic prostate score (GPS) has little value in predicting adverse outcomes in men who have undergone a period of active surveillance before having a radical prostatectomy, according to a study published in the Journal of Clinical of Oncology.
The hazard ratio for adverse pathology using the 17-gene Oncotype DX Genomic Prostate Score did not reach statistical significance in a multivariate model (HR, 1.17; P = .066). This model took into account factors such as the prostate-specific antigen density (PSAD) and the Gleason grade group at diagnosis.
“In our study, the independent association of GPS with adverse pathology after initial active surveillance was not statistically significant,” Daniel W. Lin, MD, of the Fred Hutchinson Cancer Research Center in Seattle, and colleagues wrote.
There was also no association between the GPS and having upgraded biopsy findings during active surveillance.
Active surveillance is the “preferred management strategy” for men with low-risk prostate cancer, observed Dr. Lin and colleagues, but its use is often tempered by the worry that there may be underlying pathology that is not detected using routine clinical measures such as prostate-specific antigen testing. In their study, the investigators looked to see if using the GPS could help risk-stratify men undergoing active surveillance.
They noted that the biopsy-based genomic test had been shown to predict adverse surgical pathology and recurrence in men with low- and intermediate-risk prostate cancer who had undergone immediate radical prostatectomy. The team therefore wanted to clarify the test’s role in men who had been initially managed with a period of active surveillance.
To calculate the GPS, the investigators retrospectively analyzed diagnostic biopsy samples that had been prospectively collected from 432 men in the Canary Prostate Active Surveillance Study. The primary endpoint was adverse pathology in men who underwent radical prostatectomy after initial surveillance. Adverse pathology was defined as a Gleason grade of 3 or greater, a staging of pT3a or higher (with or without N1), or both.
After a median follow-up of 4.6 years, 167 (39%) men experienced upgrading of their prostate cancer at a surveillance biopsy, with 51 (12%) being upgraded to a Gleason grade group of 3 or higher. A total of 101 (23%) men had radical prostatectomy at a median of 2.1 years after their diagnostic biopsy, and just over half (n = 52; 51%) had adverse pathology at this time point.
GPS was associated with adverse pathology when the diagnostic Gleason grade group was taken into account (HR, 1.18; P = .030) but not when the investigators adjusted for both PSAD and diagnostic Gleason grade group. By contrast, PSAD (HR, 1.75; P = .025) was significantly associated with adverse pathology.
“Adding GPS to a model containing PSAD and diagnostic [Gleason grade group] did not significantly improve stratification of risk for [adverse pathology] over the clinical variables alone,” Dr. Lin and colleagues concluded.
This work was supported by the Canary Foundation, the Department of Defense, the National Institutes of Health, and Genomic Health. The authors disclosed relationships with Genomic Health and other companies.
SOURCE: Lin DW et al. J Clin Oncol. 2020 Mar 4. doi: 10.1200/JCO.19.02267.
A genomic prostate score (GPS) has little value in predicting adverse outcomes in men who have undergone a period of active surveillance before having a radical prostatectomy, according to a study published in the Journal of Clinical of Oncology.
The hazard ratio for adverse pathology using the 17-gene Oncotype DX Genomic Prostate Score did not reach statistical significance in a multivariate model (HR, 1.17; P = .066). This model took into account factors such as the prostate-specific antigen density (PSAD) and the Gleason grade group at diagnosis.
“In our study, the independent association of GPS with adverse pathology after initial active surveillance was not statistically significant,” Daniel W. Lin, MD, of the Fred Hutchinson Cancer Research Center in Seattle, and colleagues wrote.
There was also no association between the GPS and having upgraded biopsy findings during active surveillance.
Active surveillance is the “preferred management strategy” for men with low-risk prostate cancer, observed Dr. Lin and colleagues, but its use is often tempered by the worry that there may be underlying pathology that is not detected using routine clinical measures such as prostate-specific antigen testing. In their study, the investigators looked to see if using the GPS could help risk-stratify men undergoing active surveillance.
They noted that the biopsy-based genomic test had been shown to predict adverse surgical pathology and recurrence in men with low- and intermediate-risk prostate cancer who had undergone immediate radical prostatectomy. The team therefore wanted to clarify the test’s role in men who had been initially managed with a period of active surveillance.
To calculate the GPS, the investigators retrospectively analyzed diagnostic biopsy samples that had been prospectively collected from 432 men in the Canary Prostate Active Surveillance Study. The primary endpoint was adverse pathology in men who underwent radical prostatectomy after initial surveillance. Adverse pathology was defined as a Gleason grade of 3 or greater, a staging of pT3a or higher (with or without N1), or both.
After a median follow-up of 4.6 years, 167 (39%) men experienced upgrading of their prostate cancer at a surveillance biopsy, with 51 (12%) being upgraded to a Gleason grade group of 3 or higher. A total of 101 (23%) men had radical prostatectomy at a median of 2.1 years after their diagnostic biopsy, and just over half (n = 52; 51%) had adverse pathology at this time point.
GPS was associated with adverse pathology when the diagnostic Gleason grade group was taken into account (HR, 1.18; P = .030) but not when the investigators adjusted for both PSAD and diagnostic Gleason grade group. By contrast, PSAD (HR, 1.75; P = .025) was significantly associated with adverse pathology.
“Adding GPS to a model containing PSAD and diagnostic [Gleason grade group] did not significantly improve stratification of risk for [adverse pathology] over the clinical variables alone,” Dr. Lin and colleagues concluded.
This work was supported by the Canary Foundation, the Department of Defense, the National Institutes of Health, and Genomic Health. The authors disclosed relationships with Genomic Health and other companies.
SOURCE: Lin DW et al. J Clin Oncol. 2020 Mar 4. doi: 10.1200/JCO.19.02267.
A genomic prostate score (GPS) has little value in predicting adverse outcomes in men who have undergone a period of active surveillance before having a radical prostatectomy, according to a study published in the Journal of Clinical of Oncology.
The hazard ratio for adverse pathology using the 17-gene Oncotype DX Genomic Prostate Score did not reach statistical significance in a multivariate model (HR, 1.17; P = .066). This model took into account factors such as the prostate-specific antigen density (PSAD) and the Gleason grade group at diagnosis.
“In our study, the independent association of GPS with adverse pathology after initial active surveillance was not statistically significant,” Daniel W. Lin, MD, of the Fred Hutchinson Cancer Research Center in Seattle, and colleagues wrote.
There was also no association between the GPS and having upgraded biopsy findings during active surveillance.
Active surveillance is the “preferred management strategy” for men with low-risk prostate cancer, observed Dr. Lin and colleagues, but its use is often tempered by the worry that there may be underlying pathology that is not detected using routine clinical measures such as prostate-specific antigen testing. In their study, the investigators looked to see if using the GPS could help risk-stratify men undergoing active surveillance.
They noted that the biopsy-based genomic test had been shown to predict adverse surgical pathology and recurrence in men with low- and intermediate-risk prostate cancer who had undergone immediate radical prostatectomy. The team therefore wanted to clarify the test’s role in men who had been initially managed with a period of active surveillance.
To calculate the GPS, the investigators retrospectively analyzed diagnostic biopsy samples that had been prospectively collected from 432 men in the Canary Prostate Active Surveillance Study. The primary endpoint was adverse pathology in men who underwent radical prostatectomy after initial surveillance. Adverse pathology was defined as a Gleason grade of 3 or greater, a staging of pT3a or higher (with or without N1), or both.
After a median follow-up of 4.6 years, 167 (39%) men experienced upgrading of their prostate cancer at a surveillance biopsy, with 51 (12%) being upgraded to a Gleason grade group of 3 or higher. A total of 101 (23%) men had radical prostatectomy at a median of 2.1 years after their diagnostic biopsy, and just over half (n = 52; 51%) had adverse pathology at this time point.
GPS was associated with adverse pathology when the diagnostic Gleason grade group was taken into account (HR, 1.18; P = .030) but not when the investigators adjusted for both PSAD and diagnostic Gleason grade group. By contrast, PSAD (HR, 1.75; P = .025) was significantly associated with adverse pathology.
“Adding GPS to a model containing PSAD and diagnostic [Gleason grade group] did not significantly improve stratification of risk for [adverse pathology] over the clinical variables alone,” Dr. Lin and colleagues concluded.
This work was supported by the Canary Foundation, the Department of Defense, the National Institutes of Health, and Genomic Health. The authors disclosed relationships with Genomic Health and other companies.
SOURCE: Lin DW et al. J Clin Oncol. 2020 Mar 4. doi: 10.1200/JCO.19.02267.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
How long is it safe to delay gynecologic cancer surgery?
As I write this column, there are more than 25,000 current cases of COVID-19 in the United States with an expected exponential rise in these numbers. Hospitals are issuing directives to cancel or postpone “elective” surgery to preserve the finite essential personal protective equipment (PPE), encourage social distancing, prevent exposure of at-risk patients within the hospital, and ensure bed and ventilator capacity for the impending surge in COVID-19 patients.
Many health systems have defined which surgeries they consider permissible, typically by using time parameters such as would not cause patient harm if not performed within 4 weeks, or 7 days, or 24 hours. This leaves surgeons in the unfamiliar position of rationing health care, a role with which, over the coming months, we may have to become increasingly comfortable. This is an enormous responsibility, the shift of resources between one population in need and another, and decisions should be based on data, not bias or hunch. We know that untreated cancer is life threatening, but there is a difference between untreated and delayed. What is a safe time to wait for gynecologic cancer surgery after diagnosis without negatively affecting survival from that cancer?
As I looked through my own upcoming surgical schedule, I sought guidance from the American College of Surgeons’ website, updated on March 17, 2020. In this site they tabulate an “Elective Surgery Acuity Scale” in which “most cancers” fit into tier 3a, which corresponds to high acuity surgery – “do not postpone.” This definition is fairly generalized and blunt; it does not account for the differences in cancers and occasional voluntary needs to postpone a patient’s cancer surgery for health optimization. There are limited data that measure the impact of surgical wait times on survival from gynecologic cancer. Most of this research is observational, and therefore, is influenced by confounders causing delay in surgery (e.g., comorbid conditions or socioeconomic factors that limit access to care). However, the current enforced delays are involuntary; driven by the system, not the patient; and access is universally restricted.
Endometrial cancer
Most data regarding outcomes and gynecologic cancer delay come from endometrial cancer. In 2016, Shalowitz et al. evaluated 182,000 endometrial cancer cases documented within the National Cancer Database (NCDB), which captures approximately 70% of cancer surgeries in the United States.1 They separated these patients into groups of low-grade (grade 1 and 2 endometrioid) and high-grade (grade 3 endometrioid and nonendometrioid) cancers, and evaluated the groups for their overall survival, stratified by the time period between diagnosis and surgery. Interestingly, those whose surgery was performed under 2 weeks from diagnosis had worse perioperative mortality and long-term survival. This seems to be a function of lack of medical optimization; low-volume, nonspecialized centers having less wait time; and the presentation of more advanced and symptomatic disease demanding a more urgent surgery. After those initial 2 weeks of worse outcomes, there was a period of stable outcomes and safety in waiting that extended up to 8 weeks for patients with low-grade cancers and up to 18 weeks for patients with high-grade cancers.
It may be counterintuitive to think that surgical delay affects patients with high-grade endometrial cancers less. These are more aggressive cancers, and there is patient and provider concern for metastatic spread with time elapsed. But an expedited surgery does not appear to be necessary for this group. The Shalowitz study demonstrated no risk for upstaging with surgical delay, meaning that advanced stage was not more likely to be identified in patients whose surgery was delayed, compared with those performed earlier. This observation suggests that the survival from high-grade endometrial cancers is largely determined by factors that cannot be controlled by the surgeon such as the stage at diagnosis, occult spread, and decreased responsiveness of the tumor to adjuvant therapy. In other words, fast-tracking these patients to surgery has limited influence on the outcomes for high-grade endometrial cancers.
For low-grade cancers, adverse outcomes were seen with a surgical delay of more than 8 weeks. But this may not have been caused by progression of disease (low-grade cancers also were not upstaged with delays), but rather may reflect that, in normal times, elective delays of more than 8 weeks are a function of necessary complex medical optimization of comorbidities (such as obesity-related disease). The survival that is measured by NCDB is not disease specific, and patients with comorbidities will be more likely to have impaired overall survival.
A systematic review of all papers that looked at endometrial cancer outcomes associated with surgical delay determined that it is reasonable to delay surgery for up to 8 weeks.2
Ovarian cancer
The data for ovarian cancer surgery is more limited. Most literature discusses the impact of delay in the time between surgery and the receipt of adjuvant chemotherapy, but there are limited data exploring how a delay in primary debulking negatively affects patients. This is perhaps because advanced ovarian cancer surgery rarely is delayed because of symptoms and apparent advanced stage at diagnosis. When a patient’s surgery does need to be voluntarily delayed, for example for medical optimization, there is the option of neoadjuvant chemotherapy (NACT) in which surgery is performed after three or more cycles of chemotherapy. NACT has been shown in multiple studies to have noninferior cancer outcomes, compared with primary debulking surgery.3,4
Perhaps in this current environment in which access to operating rooms and supplies is rationed, we should consider offering more, or all, patients NACT? Hospital stays after primary cytoreductive surgeries are typically 3-7 days in length, and these patients are at a higher risk, compared with other gynecologic cancer surgeries, of ICU admission and blood transfusions, both limited resources in this current environment. The disadvantage of this approach is that, while chemotherapy can keep patients out of the hospital so that they can practice social distancing, this particular therapy adds to the immunocompromised population. However, even patients who undergo primary surgical cytoreductive surgery will need to rapidly transition to immunosuppressive cytotoxic therapy; therefore it is unlikely that this can be avoided entirely during this time.
Lower genital tract cancers
Surgery for patients with lower genital tract cancers – such as cervical and vulvar cancer – also can probably be safely delayed for a 4-week period, and possibly longer. A Canadian retrospective study looked collectively at cervical, vaginal, and vulvar cancers evaluating for disease progression associated with delay to surgery, using 28 days as a benchmark for delayed surgery.5 They found no significant increased progression associated with surgical delay greater than 28 days. This study evaluated progression of cancer and did not measure cancer survival, although it is unlikely we would see impaired survival without a significant increase in disease progression.
We also can look to outcomes from delayed radical hysterectomy for stage I cervical cancer in pregnancy to provided us with some data. A retrospective cohort study observed no difference in survival when 28 women with early-stage cervical cancer who were diagnosed in pregnancy (average wait time 20 weeks from diagnosis to treatment) were compared with the outcomes of 52 matched nonpregnant control patients (average wait time 8 weeks). Their survival was 89% versus 94% respectively (P = .08).6
Summary
Synthesizing this data, it appears that, in an environment of competing needs and resources, it is reasonable and safe to delay surgery for patients with gynecologic cancers for 4-6 weeks and potentially longer. This includes patients with high-grade endometrial cancers. Clearly, these decisions should be individualized to patients and different health systems. For example, a patient who presents with a cancer-associated life-threatening bowel obstruction or hemorrhage may need an immediate intervention, and communities minimally affected by the coronavirus pandemic may have more allowances for surgery. With respect to patient anxiety, most patients with cancer are keen to have surgery promptly, and breaking the news to them that their surgery may be delayed because of institutional and public health needs will be difficult. However, the data support that this is likely safe.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. Am J Obstet Gynecol 2017;216(3):268 e1-68 e18.
2. Eur J Obstet Gynecol Reprod Biol 2020;246:1-6. doi: 10.1016/j.ejogrb.2020.01.004.
3. N Engl J Med 2010;363(10):943-53.
4. Lancet 2015;386(9990):249-57.
5. J Obstet Gynaecol Can 2015;37(4):338-44.
6. Am J Obstet Gynecol 2017;216(3):276 e1-76 e6. doi: 10.1016/j.ajog.2016.10.034.
As I write this column, there are more than 25,000 current cases of COVID-19 in the United States with an expected exponential rise in these numbers. Hospitals are issuing directives to cancel or postpone “elective” surgery to preserve the finite essential personal protective equipment (PPE), encourage social distancing, prevent exposure of at-risk patients within the hospital, and ensure bed and ventilator capacity for the impending surge in COVID-19 patients.
Many health systems have defined which surgeries they consider permissible, typically by using time parameters such as would not cause patient harm if not performed within 4 weeks, or 7 days, or 24 hours. This leaves surgeons in the unfamiliar position of rationing health care, a role with which, over the coming months, we may have to become increasingly comfortable. This is an enormous responsibility, the shift of resources between one population in need and another, and decisions should be based on data, not bias or hunch. We know that untreated cancer is life threatening, but there is a difference between untreated and delayed. What is a safe time to wait for gynecologic cancer surgery after diagnosis without negatively affecting survival from that cancer?
As I looked through my own upcoming surgical schedule, I sought guidance from the American College of Surgeons’ website, updated on March 17, 2020. In this site they tabulate an “Elective Surgery Acuity Scale” in which “most cancers” fit into tier 3a, which corresponds to high acuity surgery – “do not postpone.” This definition is fairly generalized and blunt; it does not account for the differences in cancers and occasional voluntary needs to postpone a patient’s cancer surgery for health optimization. There are limited data that measure the impact of surgical wait times on survival from gynecologic cancer. Most of this research is observational, and therefore, is influenced by confounders causing delay in surgery (e.g., comorbid conditions or socioeconomic factors that limit access to care). However, the current enforced delays are involuntary; driven by the system, not the patient; and access is universally restricted.
Endometrial cancer
Most data regarding outcomes and gynecologic cancer delay come from endometrial cancer. In 2016, Shalowitz et al. evaluated 182,000 endometrial cancer cases documented within the National Cancer Database (NCDB), which captures approximately 70% of cancer surgeries in the United States.1 They separated these patients into groups of low-grade (grade 1 and 2 endometrioid) and high-grade (grade 3 endometrioid and nonendometrioid) cancers, and evaluated the groups for their overall survival, stratified by the time period between diagnosis and surgery. Interestingly, those whose surgery was performed under 2 weeks from diagnosis had worse perioperative mortality and long-term survival. This seems to be a function of lack of medical optimization; low-volume, nonspecialized centers having less wait time; and the presentation of more advanced and symptomatic disease demanding a more urgent surgery. After those initial 2 weeks of worse outcomes, there was a period of stable outcomes and safety in waiting that extended up to 8 weeks for patients with low-grade cancers and up to 18 weeks for patients with high-grade cancers.
It may be counterintuitive to think that surgical delay affects patients with high-grade endometrial cancers less. These are more aggressive cancers, and there is patient and provider concern for metastatic spread with time elapsed. But an expedited surgery does not appear to be necessary for this group. The Shalowitz study demonstrated no risk for upstaging with surgical delay, meaning that advanced stage was not more likely to be identified in patients whose surgery was delayed, compared with those performed earlier. This observation suggests that the survival from high-grade endometrial cancers is largely determined by factors that cannot be controlled by the surgeon such as the stage at diagnosis, occult spread, and decreased responsiveness of the tumor to adjuvant therapy. In other words, fast-tracking these patients to surgery has limited influence on the outcomes for high-grade endometrial cancers.
For low-grade cancers, adverse outcomes were seen with a surgical delay of more than 8 weeks. But this may not have been caused by progression of disease (low-grade cancers also were not upstaged with delays), but rather may reflect that, in normal times, elective delays of more than 8 weeks are a function of necessary complex medical optimization of comorbidities (such as obesity-related disease). The survival that is measured by NCDB is not disease specific, and patients with comorbidities will be more likely to have impaired overall survival.
A systematic review of all papers that looked at endometrial cancer outcomes associated with surgical delay determined that it is reasonable to delay surgery for up to 8 weeks.2
Ovarian cancer
The data for ovarian cancer surgery is more limited. Most literature discusses the impact of delay in the time between surgery and the receipt of adjuvant chemotherapy, but there are limited data exploring how a delay in primary debulking negatively affects patients. This is perhaps because advanced ovarian cancer surgery rarely is delayed because of symptoms and apparent advanced stage at diagnosis. When a patient’s surgery does need to be voluntarily delayed, for example for medical optimization, there is the option of neoadjuvant chemotherapy (NACT) in which surgery is performed after three or more cycles of chemotherapy. NACT has been shown in multiple studies to have noninferior cancer outcomes, compared with primary debulking surgery.3,4
Perhaps in this current environment in which access to operating rooms and supplies is rationed, we should consider offering more, or all, patients NACT? Hospital stays after primary cytoreductive surgeries are typically 3-7 days in length, and these patients are at a higher risk, compared with other gynecologic cancer surgeries, of ICU admission and blood transfusions, both limited resources in this current environment. The disadvantage of this approach is that, while chemotherapy can keep patients out of the hospital so that they can practice social distancing, this particular therapy adds to the immunocompromised population. However, even patients who undergo primary surgical cytoreductive surgery will need to rapidly transition to immunosuppressive cytotoxic therapy; therefore it is unlikely that this can be avoided entirely during this time.
Lower genital tract cancers
Surgery for patients with lower genital tract cancers – such as cervical and vulvar cancer – also can probably be safely delayed for a 4-week period, and possibly longer. A Canadian retrospective study looked collectively at cervical, vaginal, and vulvar cancers evaluating for disease progression associated with delay to surgery, using 28 days as a benchmark for delayed surgery.5 They found no significant increased progression associated with surgical delay greater than 28 days. This study evaluated progression of cancer and did not measure cancer survival, although it is unlikely we would see impaired survival without a significant increase in disease progression.
We also can look to outcomes from delayed radical hysterectomy for stage I cervical cancer in pregnancy to provided us with some data. A retrospective cohort study observed no difference in survival when 28 women with early-stage cervical cancer who were diagnosed in pregnancy (average wait time 20 weeks from diagnosis to treatment) were compared with the outcomes of 52 matched nonpregnant control patients (average wait time 8 weeks). Their survival was 89% versus 94% respectively (P = .08).6
Summary
Synthesizing this data, it appears that, in an environment of competing needs and resources, it is reasonable and safe to delay surgery for patients with gynecologic cancers for 4-6 weeks and potentially longer. This includes patients with high-grade endometrial cancers. Clearly, these decisions should be individualized to patients and different health systems. For example, a patient who presents with a cancer-associated life-threatening bowel obstruction or hemorrhage may need an immediate intervention, and communities minimally affected by the coronavirus pandemic may have more allowances for surgery. With respect to patient anxiety, most patients with cancer are keen to have surgery promptly, and breaking the news to them that their surgery may be delayed because of institutional and public health needs will be difficult. However, the data support that this is likely safe.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. Am J Obstet Gynecol 2017;216(3):268 e1-68 e18.
2. Eur J Obstet Gynecol Reprod Biol 2020;246:1-6. doi: 10.1016/j.ejogrb.2020.01.004.
3. N Engl J Med 2010;363(10):943-53.
4. Lancet 2015;386(9990):249-57.
5. J Obstet Gynaecol Can 2015;37(4):338-44.
6. Am J Obstet Gynecol 2017;216(3):276 e1-76 e6. doi: 10.1016/j.ajog.2016.10.034.
As I write this column, there are more than 25,000 current cases of COVID-19 in the United States with an expected exponential rise in these numbers. Hospitals are issuing directives to cancel or postpone “elective” surgery to preserve the finite essential personal protective equipment (PPE), encourage social distancing, prevent exposure of at-risk patients within the hospital, and ensure bed and ventilator capacity for the impending surge in COVID-19 patients.
Many health systems have defined which surgeries they consider permissible, typically by using time parameters such as would not cause patient harm if not performed within 4 weeks, or 7 days, or 24 hours. This leaves surgeons in the unfamiliar position of rationing health care, a role with which, over the coming months, we may have to become increasingly comfortable. This is an enormous responsibility, the shift of resources between one population in need and another, and decisions should be based on data, not bias or hunch. We know that untreated cancer is life threatening, but there is a difference between untreated and delayed. What is a safe time to wait for gynecologic cancer surgery after diagnosis without negatively affecting survival from that cancer?
As I looked through my own upcoming surgical schedule, I sought guidance from the American College of Surgeons’ website, updated on March 17, 2020. In this site they tabulate an “Elective Surgery Acuity Scale” in which “most cancers” fit into tier 3a, which corresponds to high acuity surgery – “do not postpone.” This definition is fairly generalized and blunt; it does not account for the differences in cancers and occasional voluntary needs to postpone a patient’s cancer surgery for health optimization. There are limited data that measure the impact of surgical wait times on survival from gynecologic cancer. Most of this research is observational, and therefore, is influenced by confounders causing delay in surgery (e.g., comorbid conditions or socioeconomic factors that limit access to care). However, the current enforced delays are involuntary; driven by the system, not the patient; and access is universally restricted.
Endometrial cancer
Most data regarding outcomes and gynecologic cancer delay come from endometrial cancer. In 2016, Shalowitz et al. evaluated 182,000 endometrial cancer cases documented within the National Cancer Database (NCDB), which captures approximately 70% of cancer surgeries in the United States.1 They separated these patients into groups of low-grade (grade 1 and 2 endometrioid) and high-grade (grade 3 endometrioid and nonendometrioid) cancers, and evaluated the groups for their overall survival, stratified by the time period between diagnosis and surgery. Interestingly, those whose surgery was performed under 2 weeks from diagnosis had worse perioperative mortality and long-term survival. This seems to be a function of lack of medical optimization; low-volume, nonspecialized centers having less wait time; and the presentation of more advanced and symptomatic disease demanding a more urgent surgery. After those initial 2 weeks of worse outcomes, there was a period of stable outcomes and safety in waiting that extended up to 8 weeks for patients with low-grade cancers and up to 18 weeks for patients with high-grade cancers.
It may be counterintuitive to think that surgical delay affects patients with high-grade endometrial cancers less. These are more aggressive cancers, and there is patient and provider concern for metastatic spread with time elapsed. But an expedited surgery does not appear to be necessary for this group. The Shalowitz study demonstrated no risk for upstaging with surgical delay, meaning that advanced stage was not more likely to be identified in patients whose surgery was delayed, compared with those performed earlier. This observation suggests that the survival from high-grade endometrial cancers is largely determined by factors that cannot be controlled by the surgeon such as the stage at diagnosis, occult spread, and decreased responsiveness of the tumor to adjuvant therapy. In other words, fast-tracking these patients to surgery has limited influence on the outcomes for high-grade endometrial cancers.
For low-grade cancers, adverse outcomes were seen with a surgical delay of more than 8 weeks. But this may not have been caused by progression of disease (low-grade cancers also were not upstaged with delays), but rather may reflect that, in normal times, elective delays of more than 8 weeks are a function of necessary complex medical optimization of comorbidities (such as obesity-related disease). The survival that is measured by NCDB is not disease specific, and patients with comorbidities will be more likely to have impaired overall survival.
A systematic review of all papers that looked at endometrial cancer outcomes associated with surgical delay determined that it is reasonable to delay surgery for up to 8 weeks.2
Ovarian cancer
The data for ovarian cancer surgery is more limited. Most literature discusses the impact of delay in the time between surgery and the receipt of adjuvant chemotherapy, but there are limited data exploring how a delay in primary debulking negatively affects patients. This is perhaps because advanced ovarian cancer surgery rarely is delayed because of symptoms and apparent advanced stage at diagnosis. When a patient’s surgery does need to be voluntarily delayed, for example for medical optimization, there is the option of neoadjuvant chemotherapy (NACT) in which surgery is performed after three or more cycles of chemotherapy. NACT has been shown in multiple studies to have noninferior cancer outcomes, compared with primary debulking surgery.3,4
Perhaps in this current environment in which access to operating rooms and supplies is rationed, we should consider offering more, or all, patients NACT? Hospital stays after primary cytoreductive surgeries are typically 3-7 days in length, and these patients are at a higher risk, compared with other gynecologic cancer surgeries, of ICU admission and blood transfusions, both limited resources in this current environment. The disadvantage of this approach is that, while chemotherapy can keep patients out of the hospital so that they can practice social distancing, this particular therapy adds to the immunocompromised population. However, even patients who undergo primary surgical cytoreductive surgery will need to rapidly transition to immunosuppressive cytotoxic therapy; therefore it is unlikely that this can be avoided entirely during this time.
Lower genital tract cancers
Surgery for patients with lower genital tract cancers – such as cervical and vulvar cancer – also can probably be safely delayed for a 4-week period, and possibly longer. A Canadian retrospective study looked collectively at cervical, vaginal, and vulvar cancers evaluating for disease progression associated with delay to surgery, using 28 days as a benchmark for delayed surgery.5 They found no significant increased progression associated with surgical delay greater than 28 days. This study evaluated progression of cancer and did not measure cancer survival, although it is unlikely we would see impaired survival without a significant increase in disease progression.
We also can look to outcomes from delayed radical hysterectomy for stage I cervical cancer in pregnancy to provided us with some data. A retrospective cohort study observed no difference in survival when 28 women with early-stage cervical cancer who were diagnosed in pregnancy (average wait time 20 weeks from diagnosis to treatment) were compared with the outcomes of 52 matched nonpregnant control patients (average wait time 8 weeks). Their survival was 89% versus 94% respectively (P = .08).6
Summary
Synthesizing this data, it appears that, in an environment of competing needs and resources, it is reasonable and safe to delay surgery for patients with gynecologic cancers for 4-6 weeks and potentially longer. This includes patients with high-grade endometrial cancers. Clearly, these decisions should be individualized to patients and different health systems. For example, a patient who presents with a cancer-associated life-threatening bowel obstruction or hemorrhage may need an immediate intervention, and communities minimally affected by the coronavirus pandemic may have more allowances for surgery. With respect to patient anxiety, most patients with cancer are keen to have surgery promptly, and breaking the news to them that their surgery may be delayed because of institutional and public health needs will be difficult. However, the data support that this is likely safe.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She had no relevant financial disclosures. Email Dr. Rossi at [email protected].
References
1. Am J Obstet Gynecol 2017;216(3):268 e1-68 e18.
2. Eur J Obstet Gynecol Reprod Biol 2020;246:1-6. doi: 10.1016/j.ejogrb.2020.01.004.
3. N Engl J Med 2010;363(10):943-53.
4. Lancet 2015;386(9990):249-57.
5. J Obstet Gynaecol Can 2015;37(4):338-44.
6. Am J Obstet Gynecol 2017;216(3):276 e1-76 e6. doi: 10.1016/j.ajog.2016.10.034.
Cancer care and COVID-19 in Seattle, the first U.S. epicenter
Two months after the first patient with COVID-19 was identified in China, the first case was reported in the United States in the Seattle, Washington, metropolitan area.
Seattle rapidly became the first US epicenter for COVID-19, and local experts are now offering their expertise and advice on how to provide optimal cancer care during the pandemic in a special feature published online March 20 in the Journal of the National Comprehensive Cancer Network.
“We began implementing measures in early March, including infection control and screening of visitors, staff, and patients at the door,” said lead author Masumi Ueda, MD, who holds positions at the Seattle Cancer Care Alliance, the University of Washington, and the Fred Hutchinson Research Center.
“A lot of changes have been implemented, and it changes on a daily basis. We are responding to the growing rate of COVID-19 infection in the community,” she told Medscape Medical News.
Ueda notes that as a result of the quick implementation of new procedures, so far, very few cancer patients at their facilities have been infected by the virus. “It has not hit our cancer population hard, which is a good thing,” she said.
Create “Incident Command Structure”
In sharing their experience, the authors emphasize the importance of keeping channels of communication open between all stakeholders ― administrators and staff, patients, caregivers, and the general public. They also recommend that each facility create an “incident command structure” that can provide early coordination of institution-wide efforts and that can rapidly respond to changing information.
Ueda noted that their command structure was set up very early on, “so we could get communication set up and start building an infrastructure for response.”
Several areas of care that required new strategies were addressed, both to protect patients and to work around staff shortages caused by possible exposure and/or school closings, as well as projected shortages of supplies and hospital resources.
First and foremost was to identify patients and visitors who had respiratory symptoms and to provide them with masks. Although this is always routine practice during the respiratory virus season, screening has now been initiated at entry points throughout the system.
“We were lucky in Seattle and Washington state in that the University of Washington virology lab developed PCR [polymerase chain reaction] testing early on for COVID-19, which subsequently got FDA approval,” said Ueda. “So we were able to have local testing and didn’t have to rely on the state lab. Testing has also been rapidly scaled up.”
Initiating a comprehensive policy for testing staff, tracking results and exposures for persons under investigation, and defining when it is possible to return to work are essential elements for maintaining a stable workforce. In addition, reinforcing a strict “stay at home when ill” policy and providing access to testing for symptomatic staff have been key to limiting exposures.
“What is unique to our region is that we had testing early on, and we are turning it around in 24 hours,” she pointed out. “This is important for staff to be able to return to work.” Currently, staff, patients, and visitors are being tested only if they show the cardinal symptoms associated with COVID-19: fever, shortness of breath, and cough, although muscle aches have recently been added to their testing protocol.
“I think if we had unlimited capacity, we might consider testing people who are asymptomatic,” Ueda noted, “although if you don’t have symptoms, you may not have the viral load needed for an accurate test.”
Educational materials explaining infection control were also needed for patients and families, along with signs and a website to provide COVID-19 education. These were quickly developed.
In addition, a telephone triage line was established for patients with mild symptoms in order to minimize exposures in clinics and to lessen the number of patients presenting at emergency departments.
Outpatient Care
Because theirs is a referral center, many cancer patients come from out of town, and so there is concern about exposing nonlocal patients to COVID-19 as the virus spreads in the Seattle area. In addition, staffing shortages due to factors such as illness, exposure, and school closures are anticipated.
To address these problems, an initial priority was to establish a “multilayer” coverage system for the clinics in the event that practitioners had to be quarantined on short notice, the authors explain.
One decision was to reschedule all wellness visits for current patients or to use telemedicine. Capacity for that option expanded quickly, which was greatly helped by the recent decision by the Centers for Medicare & Medicaid Services to lift Medicare restrictions on the use of certain telemedicine services.
Another approach is to defer all consultations for second opinions for patients who were already undergoing treatment and to increase clinic hours of operations and capabilities for acute evaluations. This helps reserve emergency departments and hospital resources for patients who require higher-level care, the authors comment.
Treatment Decisions
Treatment decisions were more challenging to make, the authors note. One decision was that, despite the risk for COVID-19 for patients with solid tumors, adjuvant therapy with curative intent should proceed, they note. Similarly, patients with metastatic disease might lose the window of opportunity for treatment if it is delayed.
Treatment for aggressive hematologic malignancies is usually urgent, and stem cell transplant and cellular immunotherapies that provide curative treatments cannot be delayed in many cases.
Enrollment in clinical trials will most likely be limited to those trials that are most likely to benefit the patient.
Ueda noted that, because their patients come from all over the country, they are now conducting consultations for stem cell transplant by telephone so that nonlocal patients do not have to travel to Seattle. “If there is some way we can delay the treatment, we have taken that approach,” Ueda told Medscape Medical News. “If we can divert a patient to an area that is not as heavily affected, that’s another option we are taking.”
Although cancer surgery is not considered elective, surgical intervention needs to be prioritized, the authors comment. In the Seattle system, there is currently a 2-week ban on elective surgery in the healthcare system, owing to limited availability of personal protective equipment (PPE), staffing, and beds.
The oncology teams are currently reviewing treatment regimens to determine which treatments might lessen immunosuppression and which treatment options can be moved from the inpatient to the outpatient setting or can be delayed.
Inpatient Care
For hospitalized patients, several issues are being addressed. The priority is to prepare for an upcoming shortage of beds and resources because of the surge of patients with COVID-19 that is predicted. For both clinic and hospitalized patients, shortages of blood products have necessitated stricter adherence to thresholds for transfusion, and consideration is being given to lowering those thresholds.
Another important problem is the need to conserve PPE, which includes masks, gowns, gloves, and other products. The Seattle teams have implemented solutions such as favoring handwashing with soap and water over the use of hand gel for standard-precaution rooms, limiting the number of personnel entering patient rooms (so as to use less PPE), and reducing nursing procedures that require PPE, such as measuring urine output, unless they are necessary.
In addition, a no-visitor policy has been adopted in inpatient units to conserve PPE, with the exception of end-of-life situations.
The Future
The future trajectory of the COVID-19 pandemic is uncertain, Ueda commented. She emphasized that “we must continue to prepare for its widespread impact. The unknown is what we are looking at. We are expecting it to evolve, and the number of infections cannot go down.”
Ueda and coauthors end their article on a positive note. “To many of us, this has become the health care challenge of our generation, one that modern cancer therapy has never had to face. We will prevail, and when the pandemic ends, we will all be proud of what we did for our patients and each other in this critical moment for humanity.”
Two months after the first patient with COVID-19 was identified in China, the first case was reported in the United States in the Seattle, Washington, metropolitan area.
Seattle rapidly became the first US epicenter for COVID-19, and local experts are now offering their expertise and advice on how to provide optimal cancer care during the pandemic in a special feature published online March 20 in the Journal of the National Comprehensive Cancer Network.
“We began implementing measures in early March, including infection control and screening of visitors, staff, and patients at the door,” said lead author Masumi Ueda, MD, who holds positions at the Seattle Cancer Care Alliance, the University of Washington, and the Fred Hutchinson Research Center.
“A lot of changes have been implemented, and it changes on a daily basis. We are responding to the growing rate of COVID-19 infection in the community,” she told Medscape Medical News.
Ueda notes that as a result of the quick implementation of new procedures, so far, very few cancer patients at their facilities have been infected by the virus. “It has not hit our cancer population hard, which is a good thing,” she said.
Create “Incident Command Structure”
In sharing their experience, the authors emphasize the importance of keeping channels of communication open between all stakeholders ― administrators and staff, patients, caregivers, and the general public. They also recommend that each facility create an “incident command structure” that can provide early coordination of institution-wide efforts and that can rapidly respond to changing information.
Ueda noted that their command structure was set up very early on, “so we could get communication set up and start building an infrastructure for response.”
Several areas of care that required new strategies were addressed, both to protect patients and to work around staff shortages caused by possible exposure and/or school closings, as well as projected shortages of supplies and hospital resources.
First and foremost was to identify patients and visitors who had respiratory symptoms and to provide them with masks. Although this is always routine practice during the respiratory virus season, screening has now been initiated at entry points throughout the system.
“We were lucky in Seattle and Washington state in that the University of Washington virology lab developed PCR [polymerase chain reaction] testing early on for COVID-19, which subsequently got FDA approval,” said Ueda. “So we were able to have local testing and didn’t have to rely on the state lab. Testing has also been rapidly scaled up.”
Initiating a comprehensive policy for testing staff, tracking results and exposures for persons under investigation, and defining when it is possible to return to work are essential elements for maintaining a stable workforce. In addition, reinforcing a strict “stay at home when ill” policy and providing access to testing for symptomatic staff have been key to limiting exposures.
“What is unique to our region is that we had testing early on, and we are turning it around in 24 hours,” she pointed out. “This is important for staff to be able to return to work.” Currently, staff, patients, and visitors are being tested only if they show the cardinal symptoms associated with COVID-19: fever, shortness of breath, and cough, although muscle aches have recently been added to their testing protocol.
“I think if we had unlimited capacity, we might consider testing people who are asymptomatic,” Ueda noted, “although if you don’t have symptoms, you may not have the viral load needed for an accurate test.”
Educational materials explaining infection control were also needed for patients and families, along with signs and a website to provide COVID-19 education. These were quickly developed.
In addition, a telephone triage line was established for patients with mild symptoms in order to minimize exposures in clinics and to lessen the number of patients presenting at emergency departments.
Outpatient Care
Because theirs is a referral center, many cancer patients come from out of town, and so there is concern about exposing nonlocal patients to COVID-19 as the virus spreads in the Seattle area. In addition, staffing shortages due to factors such as illness, exposure, and school closures are anticipated.
To address these problems, an initial priority was to establish a “multilayer” coverage system for the clinics in the event that practitioners had to be quarantined on short notice, the authors explain.
One decision was to reschedule all wellness visits for current patients or to use telemedicine. Capacity for that option expanded quickly, which was greatly helped by the recent decision by the Centers for Medicare & Medicaid Services to lift Medicare restrictions on the use of certain telemedicine services.
Another approach is to defer all consultations for second opinions for patients who were already undergoing treatment and to increase clinic hours of operations and capabilities for acute evaluations. This helps reserve emergency departments and hospital resources for patients who require higher-level care, the authors comment.
Treatment Decisions
Treatment decisions were more challenging to make, the authors note. One decision was that, despite the risk for COVID-19 for patients with solid tumors, adjuvant therapy with curative intent should proceed, they note. Similarly, patients with metastatic disease might lose the window of opportunity for treatment if it is delayed.
Treatment for aggressive hematologic malignancies is usually urgent, and stem cell transplant and cellular immunotherapies that provide curative treatments cannot be delayed in many cases.
Enrollment in clinical trials will most likely be limited to those trials that are most likely to benefit the patient.
Ueda noted that, because their patients come from all over the country, they are now conducting consultations for stem cell transplant by telephone so that nonlocal patients do not have to travel to Seattle. “If there is some way we can delay the treatment, we have taken that approach,” Ueda told Medscape Medical News. “If we can divert a patient to an area that is not as heavily affected, that’s another option we are taking.”
Although cancer surgery is not considered elective, surgical intervention needs to be prioritized, the authors comment. In the Seattle system, there is currently a 2-week ban on elective surgery in the healthcare system, owing to limited availability of personal protective equipment (PPE), staffing, and beds.
The oncology teams are currently reviewing treatment regimens to determine which treatments might lessen immunosuppression and which treatment options can be moved from the inpatient to the outpatient setting or can be delayed.
Inpatient Care
For hospitalized patients, several issues are being addressed. The priority is to prepare for an upcoming shortage of beds and resources because of the surge of patients with COVID-19 that is predicted. For both clinic and hospitalized patients, shortages of blood products have necessitated stricter adherence to thresholds for transfusion, and consideration is being given to lowering those thresholds.
Another important problem is the need to conserve PPE, which includes masks, gowns, gloves, and other products. The Seattle teams have implemented solutions such as favoring handwashing with soap and water over the use of hand gel for standard-precaution rooms, limiting the number of personnel entering patient rooms (so as to use less PPE), and reducing nursing procedures that require PPE, such as measuring urine output, unless they are necessary.
In addition, a no-visitor policy has been adopted in inpatient units to conserve PPE, with the exception of end-of-life situations.
The Future
The future trajectory of the COVID-19 pandemic is uncertain, Ueda commented. She emphasized that “we must continue to prepare for its widespread impact. The unknown is what we are looking at. We are expecting it to evolve, and the number of infections cannot go down.”
Ueda and coauthors end their article on a positive note. “To many of us, this has become the health care challenge of our generation, one that modern cancer therapy has never had to face. We will prevail, and when the pandemic ends, we will all be proud of what we did for our patients and each other in this critical moment for humanity.”
Two months after the first patient with COVID-19 was identified in China, the first case was reported in the United States in the Seattle, Washington, metropolitan area.
Seattle rapidly became the first US epicenter for COVID-19, and local experts are now offering their expertise and advice on how to provide optimal cancer care during the pandemic in a special feature published online March 20 in the Journal of the National Comprehensive Cancer Network.
“We began implementing measures in early March, including infection control and screening of visitors, staff, and patients at the door,” said lead author Masumi Ueda, MD, who holds positions at the Seattle Cancer Care Alliance, the University of Washington, and the Fred Hutchinson Research Center.
“A lot of changes have been implemented, and it changes on a daily basis. We are responding to the growing rate of COVID-19 infection in the community,” she told Medscape Medical News.
Ueda notes that as a result of the quick implementation of new procedures, so far, very few cancer patients at their facilities have been infected by the virus. “It has not hit our cancer population hard, which is a good thing,” she said.
Create “Incident Command Structure”
In sharing their experience, the authors emphasize the importance of keeping channels of communication open between all stakeholders ― administrators and staff, patients, caregivers, and the general public. They also recommend that each facility create an “incident command structure” that can provide early coordination of institution-wide efforts and that can rapidly respond to changing information.
Ueda noted that their command structure was set up very early on, “so we could get communication set up and start building an infrastructure for response.”
Several areas of care that required new strategies were addressed, both to protect patients and to work around staff shortages caused by possible exposure and/or school closings, as well as projected shortages of supplies and hospital resources.
First and foremost was to identify patients and visitors who had respiratory symptoms and to provide them with masks. Although this is always routine practice during the respiratory virus season, screening has now been initiated at entry points throughout the system.
“We were lucky in Seattle and Washington state in that the University of Washington virology lab developed PCR [polymerase chain reaction] testing early on for COVID-19, which subsequently got FDA approval,” said Ueda. “So we were able to have local testing and didn’t have to rely on the state lab. Testing has also been rapidly scaled up.”
Initiating a comprehensive policy for testing staff, tracking results and exposures for persons under investigation, and defining when it is possible to return to work are essential elements for maintaining a stable workforce. In addition, reinforcing a strict “stay at home when ill” policy and providing access to testing for symptomatic staff have been key to limiting exposures.
“What is unique to our region is that we had testing early on, and we are turning it around in 24 hours,” she pointed out. “This is important for staff to be able to return to work.” Currently, staff, patients, and visitors are being tested only if they show the cardinal symptoms associated with COVID-19: fever, shortness of breath, and cough, although muscle aches have recently been added to their testing protocol.
“I think if we had unlimited capacity, we might consider testing people who are asymptomatic,” Ueda noted, “although if you don’t have symptoms, you may not have the viral load needed for an accurate test.”
Educational materials explaining infection control were also needed for patients and families, along with signs and a website to provide COVID-19 education. These were quickly developed.
In addition, a telephone triage line was established for patients with mild symptoms in order to minimize exposures in clinics and to lessen the number of patients presenting at emergency departments.
Outpatient Care
Because theirs is a referral center, many cancer patients come from out of town, and so there is concern about exposing nonlocal patients to COVID-19 as the virus spreads in the Seattle area. In addition, staffing shortages due to factors such as illness, exposure, and school closures are anticipated.
To address these problems, an initial priority was to establish a “multilayer” coverage system for the clinics in the event that practitioners had to be quarantined on short notice, the authors explain.
One decision was to reschedule all wellness visits for current patients or to use telemedicine. Capacity for that option expanded quickly, which was greatly helped by the recent decision by the Centers for Medicare & Medicaid Services to lift Medicare restrictions on the use of certain telemedicine services.
Another approach is to defer all consultations for second opinions for patients who were already undergoing treatment and to increase clinic hours of operations and capabilities for acute evaluations. This helps reserve emergency departments and hospital resources for patients who require higher-level care, the authors comment.
Treatment Decisions
Treatment decisions were more challenging to make, the authors note. One decision was that, despite the risk for COVID-19 for patients with solid tumors, adjuvant therapy with curative intent should proceed, they note. Similarly, patients with metastatic disease might lose the window of opportunity for treatment if it is delayed.
Treatment for aggressive hematologic malignancies is usually urgent, and stem cell transplant and cellular immunotherapies that provide curative treatments cannot be delayed in many cases.
Enrollment in clinical trials will most likely be limited to those trials that are most likely to benefit the patient.
Ueda noted that, because their patients come from all over the country, they are now conducting consultations for stem cell transplant by telephone so that nonlocal patients do not have to travel to Seattle. “If there is some way we can delay the treatment, we have taken that approach,” Ueda told Medscape Medical News. “If we can divert a patient to an area that is not as heavily affected, that’s another option we are taking.”
Although cancer surgery is not considered elective, surgical intervention needs to be prioritized, the authors comment. In the Seattle system, there is currently a 2-week ban on elective surgery in the healthcare system, owing to limited availability of personal protective equipment (PPE), staffing, and beds.
The oncology teams are currently reviewing treatment regimens to determine which treatments might lessen immunosuppression and which treatment options can be moved from the inpatient to the outpatient setting or can be delayed.
Inpatient Care
For hospitalized patients, several issues are being addressed. The priority is to prepare for an upcoming shortage of beds and resources because of the surge of patients with COVID-19 that is predicted. For both clinic and hospitalized patients, shortages of blood products have necessitated stricter adherence to thresholds for transfusion, and consideration is being given to lowering those thresholds.
Another important problem is the need to conserve PPE, which includes masks, gowns, gloves, and other products. The Seattle teams have implemented solutions such as favoring handwashing with soap and water over the use of hand gel for standard-precaution rooms, limiting the number of personnel entering patient rooms (so as to use less PPE), and reducing nursing procedures that require PPE, such as measuring urine output, unless they are necessary.
In addition, a no-visitor policy has been adopted in inpatient units to conserve PPE, with the exception of end-of-life situations.
The Future
The future trajectory of the COVID-19 pandemic is uncertain, Ueda commented. She emphasized that “we must continue to prepare for its widespread impact. The unknown is what we are looking at. We are expecting it to evolve, and the number of infections cannot go down.”
Ueda and coauthors end their article on a positive note. “To many of us, this has become the health care challenge of our generation, one that modern cancer therapy has never had to face. We will prevail, and when the pandemic ends, we will all be proud of what we did for our patients and each other in this critical moment for humanity.”
How is oncology adapting to COVID-19?
As the coronavirus pandemic escalates in the United States, Medscape Oncology reached out to a group of our contributors and asked them to provide their perspective on how their oncology departments and centers are preparing. Here are their responses to a number of issues facing oncologists in the US and around the world.
Have you shifted nonurgent follow-up visits to telemedicine, either via video or phone?
Kathy Miller, MD, Associate Director of Indiana University Simon Cancer Center: We are reviewing our clinic schedules and identifying “routine” follow-up patients who can be rescheduled. When patients are contacted to reschedule, they are asked if they have any urgent, immediate concerns that need to be addressed before the new appointment. If yes, they are offered a virtual visit.
Don Dizon, MD, Director of Women’s Cancers, Lifespan Cancer Institute; Director of Medical Oncology, Rhode Island Hospital: We have started to do this in preparation for a surge of people with COVID-19. Patients who are in long-term follow-up (no evidence of disease at 3 years or longer, being seen annually) or those in routine surveillance after curative treatment (that is, seen every 3 months) as well as those being seen for supportive care–type visits, like sexual health or survivorship, are all being contacted and visits are being moved to telehealth.
Jeffrey S. Weber, MD, PhD, Deputy Director of the Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center: Yes. Any follow-up, nontreatment visits are done by phone or video if the patient agrees. (They all have).
Have you delayed or canceled cancer surgeries?
Ravi B. Parikh, MD, MPP, Medical oncologist at the University of Pennsylvania and the Philadelphia VA Medical Center: The University of Pennsylvania has taken this seriously. We’ve canceled all elective surgeries, have ramped up our telemedicine (video and phone) capabilities significantly, are limiting our appointments mostly to on-treatment visits, and have been asked to reconsider regular scans and reviews.
Dizon: We have not done this. There are apparently differences in interpretation in what institutions might mean as “elective surgeries.” At our institution, surgery for invasive malignancies is not elective. However, this may (or will) change if resources become an issue.
Lidia Schapira, MD, Associate Professor of Medicine and Director of Cancer Survivorship at the Stanford Comprehensive Cancer Institute: Delaying elective surgery is something that hospitals here have already implemented, and I imagine that this trend will spread. But it may be difficult to decide in situations that are not exactly “life-saving” but where an earlier intervention could preserve function or improve quality of life.
Mark A. Lewis, MD, Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah: Cancer surgeries have not been deemed elective or delayed.
Have you delayed or altered the delivery of potentially immune-comprising treatments?
David Kerr, MD, Professor of Cancer Medicine at the University of Oxford in England: We are considering delaying initiation of our adjuvant colorectal cancer treatments, as we have data from our own QUASAR trials suggesting that patients who commence chemotherapy between 2 and 6 weeks do equally as well as those who begin 6-12 weeks after surgery.
Parikh: I personally haven’t delayed giving chemotherapy to avoid immune compromise, but I believe some others may have. It’s a delicate balance between wanting to ensure cancer control and making sure we are flattening the curve. As an example, though, I delayed three on-treatment visits for my clinic last Monday, and I converted 70% of my visits to telemedicine. However, I’m a genitourinary cancer specialist and the treatments I give are very different from others.
Lewis: The most difficult calculus is around adjuvant therapy. For metastatic patients, I am trying to use the least immunosuppressive regimen possible that will still control their disease. As you can imagine, it’s an assessment of competing risks.
Schapira: Patients who need essential anticancer therapy should still get it, but attempts to deintensify therapy should continue—for example, holding or postponing treatment without harm (based on evidence, not opinion). This may be possible for patients considering hormonal therapies for breast or prostate cancer.
Patients who need radiation should discuss the timing with their radiation oncologist. In some cases, it may be possible to delay treatment without affecting outcomes, but these decisions should be made carefully. Alternatively, shorter courses of radiation may be appropriate.
Have you advised your own patients differently given the high risk to cancer patients?
Kerr: We have factored potential infection with the virus into discussions where the benefits of chemotherapy are very marginal. This could tip the balance toward the patient deciding not to pursue chemotherapy.
Dizon: The data from China are not entirely crystal-clear. While they noted that people with active cancer and those who had a history of cancer are at increased risk for more severe infections and worse outcomes, the Chinese cohort was small, and compared with people without cancer, it tended to be much older and to be smokers (former or current). Having said this, we are counseling everyone about the importance of social distancing, washing hands, and not touching your face.
Lewis: If I have a complete blood count with a differential that includes lymphocytes, I can advise my lymphopenic patients (who are particularly vulnerable to viral infection) to take special precautions regarding social distancing in their own families.
Have any of your hospitalized patients been affected by policy changes to prepare beds/departments for the expected increase in COVID-19–positive patients?
Weber: Not yet.
Dizon: No, not at the moment.
Have you been asked to assist with other services or COVID-19 task forces?
Dizon: I am keenly involved in the preparations and modifications to procedures, including staffing decisions in outpatient, movement to telehealth, and work-from-home policies.
Lewis: I am engaged in system-wide COVID-19 efforts around oncology.
Kerr: Perhaps oddest of all, I am learning with some of our junior doctors to care for ventilated patients. I still consider myself enough of a general physician that I would hope to be able to contribute to the truly sick, but I accept that I do need an appropriate refresher course.
Bishal Gyawali, MD, PhD, medical oncologist at Queen’s University Cancer Research Institute: Queen’s Hospital medical students are now volunteering to help with daycare, groceries, and other tasks for staff who are working in the hospital.
Are you experiencing any shortages in personal protective equipment (PPE) at your center?
Miller: Some supplies are running short, though none are frankly out at this point. However, rationing and controls are in place to stretch the supplies as far as possible, including reusing some PPE.
Dizon: We are rationing face masks and N95 respirators, eye shields, and even surgical scrubs. We are talking about postponing elective surgery to save PPE but are not yet to that point. We’re asking that face masks be reused for at least 2 days, maybe longer. PPEs are one per day. Scrubs are kept secure.
Lewis: We are being very careful not to overuse PPE but currently have an adequate inventory. We have had to move gloves and masks to areas where they are not accessible to the general public, as otherwise they were being stolen (this started weeks ago).
Kerr: Our National Health System has an adequate supply of PPE equipment centrally, but there seems to be a problem with distribution, as some hospitals are reporting shortages.
Weber: Masks are in short supply, so they are being used for several days if not wet. We are short of plastic gowns and are using paper chemo gowns. Similar story at many places.
This article first appeared on Medscape.com.
As the coronavirus pandemic escalates in the United States, Medscape Oncology reached out to a group of our contributors and asked them to provide their perspective on how their oncology departments and centers are preparing. Here are their responses to a number of issues facing oncologists in the US and around the world.
Have you shifted nonurgent follow-up visits to telemedicine, either via video or phone?
Kathy Miller, MD, Associate Director of Indiana University Simon Cancer Center: We are reviewing our clinic schedules and identifying “routine” follow-up patients who can be rescheduled. When patients are contacted to reschedule, they are asked if they have any urgent, immediate concerns that need to be addressed before the new appointment. If yes, they are offered a virtual visit.
Don Dizon, MD, Director of Women’s Cancers, Lifespan Cancer Institute; Director of Medical Oncology, Rhode Island Hospital: We have started to do this in preparation for a surge of people with COVID-19. Patients who are in long-term follow-up (no evidence of disease at 3 years or longer, being seen annually) or those in routine surveillance after curative treatment (that is, seen every 3 months) as well as those being seen for supportive care–type visits, like sexual health or survivorship, are all being contacted and visits are being moved to telehealth.
Jeffrey S. Weber, MD, PhD, Deputy Director of the Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center: Yes. Any follow-up, nontreatment visits are done by phone or video if the patient agrees. (They all have).
Have you delayed or canceled cancer surgeries?
Ravi B. Parikh, MD, MPP, Medical oncologist at the University of Pennsylvania and the Philadelphia VA Medical Center: The University of Pennsylvania has taken this seriously. We’ve canceled all elective surgeries, have ramped up our telemedicine (video and phone) capabilities significantly, are limiting our appointments mostly to on-treatment visits, and have been asked to reconsider regular scans and reviews.
Dizon: We have not done this. There are apparently differences in interpretation in what institutions might mean as “elective surgeries.” At our institution, surgery for invasive malignancies is not elective. However, this may (or will) change if resources become an issue.
Lidia Schapira, MD, Associate Professor of Medicine and Director of Cancer Survivorship at the Stanford Comprehensive Cancer Institute: Delaying elective surgery is something that hospitals here have already implemented, and I imagine that this trend will spread. But it may be difficult to decide in situations that are not exactly “life-saving” but where an earlier intervention could preserve function or improve quality of life.
Mark A. Lewis, MD, Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah: Cancer surgeries have not been deemed elective or delayed.
Have you delayed or altered the delivery of potentially immune-comprising treatments?
David Kerr, MD, Professor of Cancer Medicine at the University of Oxford in England: We are considering delaying initiation of our adjuvant colorectal cancer treatments, as we have data from our own QUASAR trials suggesting that patients who commence chemotherapy between 2 and 6 weeks do equally as well as those who begin 6-12 weeks after surgery.
Parikh: I personally haven’t delayed giving chemotherapy to avoid immune compromise, but I believe some others may have. It’s a delicate balance between wanting to ensure cancer control and making sure we are flattening the curve. As an example, though, I delayed three on-treatment visits for my clinic last Monday, and I converted 70% of my visits to telemedicine. However, I’m a genitourinary cancer specialist and the treatments I give are very different from others.
Lewis: The most difficult calculus is around adjuvant therapy. For metastatic patients, I am trying to use the least immunosuppressive regimen possible that will still control their disease. As you can imagine, it’s an assessment of competing risks.
Schapira: Patients who need essential anticancer therapy should still get it, but attempts to deintensify therapy should continue—for example, holding or postponing treatment without harm (based on evidence, not opinion). This may be possible for patients considering hormonal therapies for breast or prostate cancer.
Patients who need radiation should discuss the timing with their radiation oncologist. In some cases, it may be possible to delay treatment without affecting outcomes, but these decisions should be made carefully. Alternatively, shorter courses of radiation may be appropriate.
Have you advised your own patients differently given the high risk to cancer patients?
Kerr: We have factored potential infection with the virus into discussions where the benefits of chemotherapy are very marginal. This could tip the balance toward the patient deciding not to pursue chemotherapy.
Dizon: The data from China are not entirely crystal-clear. While they noted that people with active cancer and those who had a history of cancer are at increased risk for more severe infections and worse outcomes, the Chinese cohort was small, and compared with people without cancer, it tended to be much older and to be smokers (former or current). Having said this, we are counseling everyone about the importance of social distancing, washing hands, and not touching your face.
Lewis: If I have a complete blood count with a differential that includes lymphocytes, I can advise my lymphopenic patients (who are particularly vulnerable to viral infection) to take special precautions regarding social distancing in their own families.
Have any of your hospitalized patients been affected by policy changes to prepare beds/departments for the expected increase in COVID-19–positive patients?
Weber: Not yet.
Dizon: No, not at the moment.
Have you been asked to assist with other services or COVID-19 task forces?
Dizon: I am keenly involved in the preparations and modifications to procedures, including staffing decisions in outpatient, movement to telehealth, and work-from-home policies.
Lewis: I am engaged in system-wide COVID-19 efforts around oncology.
Kerr: Perhaps oddest of all, I am learning with some of our junior doctors to care for ventilated patients. I still consider myself enough of a general physician that I would hope to be able to contribute to the truly sick, but I accept that I do need an appropriate refresher course.
Bishal Gyawali, MD, PhD, medical oncologist at Queen’s University Cancer Research Institute: Queen’s Hospital medical students are now volunteering to help with daycare, groceries, and other tasks for staff who are working in the hospital.
Are you experiencing any shortages in personal protective equipment (PPE) at your center?
Miller: Some supplies are running short, though none are frankly out at this point. However, rationing and controls are in place to stretch the supplies as far as possible, including reusing some PPE.
Dizon: We are rationing face masks and N95 respirators, eye shields, and even surgical scrubs. We are talking about postponing elective surgery to save PPE but are not yet to that point. We’re asking that face masks be reused for at least 2 days, maybe longer. PPEs are one per day. Scrubs are kept secure.
Lewis: We are being very careful not to overuse PPE but currently have an adequate inventory. We have had to move gloves and masks to areas where they are not accessible to the general public, as otherwise they were being stolen (this started weeks ago).
Kerr: Our National Health System has an adequate supply of PPE equipment centrally, but there seems to be a problem with distribution, as some hospitals are reporting shortages.
Weber: Masks are in short supply, so they are being used for several days if not wet. We are short of plastic gowns and are using paper chemo gowns. Similar story at many places.
This article first appeared on Medscape.com.
As the coronavirus pandemic escalates in the United States, Medscape Oncology reached out to a group of our contributors and asked them to provide their perspective on how their oncology departments and centers are preparing. Here are their responses to a number of issues facing oncologists in the US and around the world.
Have you shifted nonurgent follow-up visits to telemedicine, either via video or phone?
Kathy Miller, MD, Associate Director of Indiana University Simon Cancer Center: We are reviewing our clinic schedules and identifying “routine” follow-up patients who can be rescheduled. When patients are contacted to reschedule, they are asked if they have any urgent, immediate concerns that need to be addressed before the new appointment. If yes, they are offered a virtual visit.
Don Dizon, MD, Director of Women’s Cancers, Lifespan Cancer Institute; Director of Medical Oncology, Rhode Island Hospital: We have started to do this in preparation for a surge of people with COVID-19. Patients who are in long-term follow-up (no evidence of disease at 3 years or longer, being seen annually) or those in routine surveillance after curative treatment (that is, seen every 3 months) as well as those being seen for supportive care–type visits, like sexual health or survivorship, are all being contacted and visits are being moved to telehealth.
Jeffrey S. Weber, MD, PhD, Deputy Director of the Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center: Yes. Any follow-up, nontreatment visits are done by phone or video if the patient agrees. (They all have).
Have you delayed or canceled cancer surgeries?
Ravi B. Parikh, MD, MPP, Medical oncologist at the University of Pennsylvania and the Philadelphia VA Medical Center: The University of Pennsylvania has taken this seriously. We’ve canceled all elective surgeries, have ramped up our telemedicine (video and phone) capabilities significantly, are limiting our appointments mostly to on-treatment visits, and have been asked to reconsider regular scans and reviews.
Dizon: We have not done this. There are apparently differences in interpretation in what institutions might mean as “elective surgeries.” At our institution, surgery for invasive malignancies is not elective. However, this may (or will) change if resources become an issue.
Lidia Schapira, MD, Associate Professor of Medicine and Director of Cancer Survivorship at the Stanford Comprehensive Cancer Institute: Delaying elective surgery is something that hospitals here have already implemented, and I imagine that this trend will spread. But it may be difficult to decide in situations that are not exactly “life-saving” but where an earlier intervention could preserve function or improve quality of life.
Mark A. Lewis, MD, Director of Gastrointestinal Oncology at Intermountain Healthcare in Utah: Cancer surgeries have not been deemed elective or delayed.
Have you delayed or altered the delivery of potentially immune-comprising treatments?
David Kerr, MD, Professor of Cancer Medicine at the University of Oxford in England: We are considering delaying initiation of our adjuvant colorectal cancer treatments, as we have data from our own QUASAR trials suggesting that patients who commence chemotherapy between 2 and 6 weeks do equally as well as those who begin 6-12 weeks after surgery.
Parikh: I personally haven’t delayed giving chemotherapy to avoid immune compromise, but I believe some others may have. It’s a delicate balance between wanting to ensure cancer control and making sure we are flattening the curve. As an example, though, I delayed three on-treatment visits for my clinic last Monday, and I converted 70% of my visits to telemedicine. However, I’m a genitourinary cancer specialist and the treatments I give are very different from others.
Lewis: The most difficult calculus is around adjuvant therapy. For metastatic patients, I am trying to use the least immunosuppressive regimen possible that will still control their disease. As you can imagine, it’s an assessment of competing risks.
Schapira: Patients who need essential anticancer therapy should still get it, but attempts to deintensify therapy should continue—for example, holding or postponing treatment without harm (based on evidence, not opinion). This may be possible for patients considering hormonal therapies for breast or prostate cancer.
Patients who need radiation should discuss the timing with their radiation oncologist. In some cases, it may be possible to delay treatment without affecting outcomes, but these decisions should be made carefully. Alternatively, shorter courses of radiation may be appropriate.
Have you advised your own patients differently given the high risk to cancer patients?
Kerr: We have factored potential infection with the virus into discussions where the benefits of chemotherapy are very marginal. This could tip the balance toward the patient deciding not to pursue chemotherapy.
Dizon: The data from China are not entirely crystal-clear. While they noted that people with active cancer and those who had a history of cancer are at increased risk for more severe infections and worse outcomes, the Chinese cohort was small, and compared with people without cancer, it tended to be much older and to be smokers (former or current). Having said this, we are counseling everyone about the importance of social distancing, washing hands, and not touching your face.
Lewis: If I have a complete blood count with a differential that includes lymphocytes, I can advise my lymphopenic patients (who are particularly vulnerable to viral infection) to take special precautions regarding social distancing in their own families.
Have any of your hospitalized patients been affected by policy changes to prepare beds/departments for the expected increase in COVID-19–positive patients?
Weber: Not yet.
Dizon: No, not at the moment.
Have you been asked to assist with other services or COVID-19 task forces?
Dizon: I am keenly involved in the preparations and modifications to procedures, including staffing decisions in outpatient, movement to telehealth, and work-from-home policies.
Lewis: I am engaged in system-wide COVID-19 efforts around oncology.
Kerr: Perhaps oddest of all, I am learning with some of our junior doctors to care for ventilated patients. I still consider myself enough of a general physician that I would hope to be able to contribute to the truly sick, but I accept that I do need an appropriate refresher course.
Bishal Gyawali, MD, PhD, medical oncologist at Queen’s University Cancer Research Institute: Queen’s Hospital medical students are now volunteering to help with daycare, groceries, and other tasks for staff who are working in the hospital.
Are you experiencing any shortages in personal protective equipment (PPE) at your center?
Miller: Some supplies are running short, though none are frankly out at this point. However, rationing and controls are in place to stretch the supplies as far as possible, including reusing some PPE.
Dizon: We are rationing face masks and N95 respirators, eye shields, and even surgical scrubs. We are talking about postponing elective surgery to save PPE but are not yet to that point. We’re asking that face masks be reused for at least 2 days, maybe longer. PPEs are one per day. Scrubs are kept secure.
Lewis: We are being very careful not to overuse PPE but currently have an adequate inventory. We have had to move gloves and masks to areas where they are not accessible to the general public, as otherwise they were being stolen (this started weeks ago).
Kerr: Our National Health System has an adequate supply of PPE equipment centrally, but there seems to be a problem with distribution, as some hospitals are reporting shortages.
Weber: Masks are in short supply, so they are being used for several days if not wet. We are short of plastic gowns and are using paper chemo gowns. Similar story at many places.
This article first appeared on Medscape.com.
Disruptions in cancer care in the era of COVID-19
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Even in the midst of the COVID-19 pandemic, cancer care must go on, but changes may need to be made in the way some care is delivered.
“We’re headed for a time when there will be significant disruptions in the care of patients with cancer,” said Len Lichtenfeld, MD, deputy chief medical officer of the American Cancer Society (ACS), in a statement. “For some it may be as straightforward as a delay in having elective surgery. For others it may be delaying preventive care or adjuvant chemotherapy that’s meant to keep cancer from returning or rescheduling appointments.”
Lichtenfeld emphasized that cancer care teams are going to do the best they can to deliver care to those most in need. However, even in those circumstances, it won’t be life as usual. “It will require patience on everyone’s part as we go through this pandemic,” he said.
“The way we treat cancer over the next few months will change enormously,” writes a British oncologist in an article published in the Guardian.
“As oncologists, we will have to find a tenuous balance between undertreating people with cancer, resulting in more deaths from the disease in the medium to long term, and increasing deaths from COVID-19 in a vulnerable patient population. Alongside our patients we will have to make difficult decisions regarding treatments, with only low-quality evidence to guide us,” writes Lucy Gossage, MD, consultant oncologist at Nottingham University Hospital, UK.
The evidence to date (from reports from China in Lancet Oncology) suggests that people with cancer have a significantly higher risk of severe illness resulting in intensive care admissions or death when infected with COVID-19, particularly if they recently had chemotherapy or surgery.
“Many of the oncology treatments we currently use, especially those given after surgery to reduce risk of cancer recurrence, have relatively small benefits,” she writes.
“In the current climate, the balance of offering these treatments may shift; a small reduction in risk of cancer recurrence over the next 5 years may be outweighed by the potential for a short-term increase in risk of death from COVID-19. In the long term, more people’s cancer will return if we aren’t able to offer these treatments,” she adds.
Postpone Routine Screening
One thing that can go on the back burner for now is routine cancer screening, which can be postponed for now in order to conserve health system resources and reduce contact with healthcare facilities, says the ACS.
“Patients seeking routine cancer screenings should delay those until further notice,” said Lichtenfeld. “While timely screening is important, the need to prevent the spread of coronavirus and to reduce the strain on the medical system is more important right now.”
But as soon as restrictions to slow the spread of COVID-19 are lifted and routine visits to health facilities are safe, regular screening tests should be rescheduled.
Guidance From ASCO
The American Society of Clinical Oncology (ASCO) has issued new guidance on caring for patients with cancer during the COVID-19 outbreak.
First and foremost, ASCO encourages providers, facilities, and anyone caring for patients with cancer to follow the existing guidelines from the Center for Disease Control and Prevention when possible.
ASCO highlights the CDC’s general recommendation for healthcare facilities that suggests “elective surgeries” at inpatient facilities be rescheduled if possible, which has also been recommended by the American College of Surgeons.
However, in many cases, cancer surgery is not elective but essential, it points out. So this is largely an individual determination that clinicians and patients will need to make, taking into account the potential harms of delaying needed cancer-related surgery.
Systemic treatments, including chemotherapy and immunotherapy, leave cancer patients vulnerable to infection, but ASCO says there is no direct evidence to support changes in regimens during the pandemic. Therefore, routinely stopping anticancer or immunosuppressive therapy is not recommended, as the balance of potential harms that may result from delaying or interrupting treatment versus the potential benefits of possibly preventing or delaying COVID-19 infection remains very unclear.
Clinical decisions must be individualized, ASCO emphasized, and suggested the following practice points be considered:
- For patients already in deep remission who are receiving maintenance therapy, stopping treatment may be an option.
- Some patients may be able to switch from IV to oral therapies, which would decrease the frequency of clinic visits.
- Decisions on modifying or withholding chemotherapy need to consider both the indication and goals of care, as well as where the patient is in the treatment regimen and tolerance to the therapy. As an example, the risk–benefit assessment for proceeding with chemotherapy in patients with untreated extensive small-cell lung cancer is quite different than proceeding with maintenance pemetrexed for metastatic non–small cell lung cancer.
- If local coronavirus transmission is an issue at a particular cancer center, reasonable options may include taking a 2-week treatment break or arranging treatment at a different facility.
- Evaluate if home infusion is medically and logistically feasible.
- In some settings, delaying or modifying adjuvant treatment presents a higher risk of compromised disease control and long-term survival than in others, but in cases where the absolute benefit of adjuvant chemotherapy may be quite small and other options are available, the risk of COVID-19 may be considered an additional factor when evaluating care.
Delay Stem Cell Transplants
For patients who are candidates for allogeneic stem cell transplantation, a delay may be reasonable if the patient is currently well controlled with conventional treatment, ASCO comments. It also directs clinicians to follow the recommendations provided by the American Society of Transplantation and Cellular Therapy and from the European Society for Blood and Marrow Transplantation regarding this issue.
Finally, there is also the question of prophylactic antiviral therapy: Should it be considered for cancer patients undergoing active therapy?
The answer to that question is currently unknown, says ASCO, but “this is an active area of research and evidence may be available at any time.”
This article first appeared on Medscape.com.
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Even in the midst of the COVID-19 pandemic, cancer care must go on, but changes may need to be made in the way some care is delivered.
“We’re headed for a time when there will be significant disruptions in the care of patients with cancer,” said Len Lichtenfeld, MD, deputy chief medical officer of the American Cancer Society (ACS), in a statement. “For some it may be as straightforward as a delay in having elective surgery. For others it may be delaying preventive care or adjuvant chemotherapy that’s meant to keep cancer from returning or rescheduling appointments.”
Lichtenfeld emphasized that cancer care teams are going to do the best they can to deliver care to those most in need. However, even in those circumstances, it won’t be life as usual. “It will require patience on everyone’s part as we go through this pandemic,” he said.
“The way we treat cancer over the next few months will change enormously,” writes a British oncologist in an article published in the Guardian.
“As oncologists, we will have to find a tenuous balance between undertreating people with cancer, resulting in more deaths from the disease in the medium to long term, and increasing deaths from COVID-19 in a vulnerable patient population. Alongside our patients we will have to make difficult decisions regarding treatments, with only low-quality evidence to guide us,” writes Lucy Gossage, MD, consultant oncologist at Nottingham University Hospital, UK.
The evidence to date (from reports from China in Lancet Oncology) suggests that people with cancer have a significantly higher risk of severe illness resulting in intensive care admissions or death when infected with COVID-19, particularly if they recently had chemotherapy or surgery.
“Many of the oncology treatments we currently use, especially those given after surgery to reduce risk of cancer recurrence, have relatively small benefits,” she writes.
“In the current climate, the balance of offering these treatments may shift; a small reduction in risk of cancer recurrence over the next 5 years may be outweighed by the potential for a short-term increase in risk of death from COVID-19. In the long term, more people’s cancer will return if we aren’t able to offer these treatments,” she adds.
Postpone Routine Screening
One thing that can go on the back burner for now is routine cancer screening, which can be postponed for now in order to conserve health system resources and reduce contact with healthcare facilities, says the ACS.
“Patients seeking routine cancer screenings should delay those until further notice,” said Lichtenfeld. “While timely screening is important, the need to prevent the spread of coronavirus and to reduce the strain on the medical system is more important right now.”
But as soon as restrictions to slow the spread of COVID-19 are lifted and routine visits to health facilities are safe, regular screening tests should be rescheduled.
Guidance From ASCO
The American Society of Clinical Oncology (ASCO) has issued new guidance on caring for patients with cancer during the COVID-19 outbreak.
First and foremost, ASCO encourages providers, facilities, and anyone caring for patients with cancer to follow the existing guidelines from the Center for Disease Control and Prevention when possible.
ASCO highlights the CDC’s general recommendation for healthcare facilities that suggests “elective surgeries” at inpatient facilities be rescheduled if possible, which has also been recommended by the American College of Surgeons.
However, in many cases, cancer surgery is not elective but essential, it points out. So this is largely an individual determination that clinicians and patients will need to make, taking into account the potential harms of delaying needed cancer-related surgery.
Systemic treatments, including chemotherapy and immunotherapy, leave cancer patients vulnerable to infection, but ASCO says there is no direct evidence to support changes in regimens during the pandemic. Therefore, routinely stopping anticancer or immunosuppressive therapy is not recommended, as the balance of potential harms that may result from delaying or interrupting treatment versus the potential benefits of possibly preventing or delaying COVID-19 infection remains very unclear.
Clinical decisions must be individualized, ASCO emphasized, and suggested the following practice points be considered:
- For patients already in deep remission who are receiving maintenance therapy, stopping treatment may be an option.
- Some patients may be able to switch from IV to oral therapies, which would decrease the frequency of clinic visits.
- Decisions on modifying or withholding chemotherapy need to consider both the indication and goals of care, as well as where the patient is in the treatment regimen and tolerance to the therapy. As an example, the risk–benefit assessment for proceeding with chemotherapy in patients with untreated extensive small-cell lung cancer is quite different than proceeding with maintenance pemetrexed for metastatic non–small cell lung cancer.
- If local coronavirus transmission is an issue at a particular cancer center, reasonable options may include taking a 2-week treatment break or arranging treatment at a different facility.
- Evaluate if home infusion is medically and logistically feasible.
- In some settings, delaying or modifying adjuvant treatment presents a higher risk of compromised disease control and long-term survival than in others, but in cases where the absolute benefit of adjuvant chemotherapy may be quite small and other options are available, the risk of COVID-19 may be considered an additional factor when evaluating care.
Delay Stem Cell Transplants
For patients who are candidates for allogeneic stem cell transplantation, a delay may be reasonable if the patient is currently well controlled with conventional treatment, ASCO comments. It also directs clinicians to follow the recommendations provided by the American Society of Transplantation and Cellular Therapy and from the European Society for Blood and Marrow Transplantation regarding this issue.
Finally, there is also the question of prophylactic antiviral therapy: Should it be considered for cancer patients undergoing active therapy?
The answer to that question is currently unknown, says ASCO, but “this is an active area of research and evidence may be available at any time.”
This article first appeared on Medscape.com.
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Even in the midst of the COVID-19 pandemic, cancer care must go on, but changes may need to be made in the way some care is delivered.
“We’re headed for a time when there will be significant disruptions in the care of patients with cancer,” said Len Lichtenfeld, MD, deputy chief medical officer of the American Cancer Society (ACS), in a statement. “For some it may be as straightforward as a delay in having elective surgery. For others it may be delaying preventive care or adjuvant chemotherapy that’s meant to keep cancer from returning or rescheduling appointments.”
Lichtenfeld emphasized that cancer care teams are going to do the best they can to deliver care to those most in need. However, even in those circumstances, it won’t be life as usual. “It will require patience on everyone’s part as we go through this pandemic,” he said.
“The way we treat cancer over the next few months will change enormously,” writes a British oncologist in an article published in the Guardian.
“As oncologists, we will have to find a tenuous balance between undertreating people with cancer, resulting in more deaths from the disease in the medium to long term, and increasing deaths from COVID-19 in a vulnerable patient population. Alongside our patients we will have to make difficult decisions regarding treatments, with only low-quality evidence to guide us,” writes Lucy Gossage, MD, consultant oncologist at Nottingham University Hospital, UK.
The evidence to date (from reports from China in Lancet Oncology) suggests that people with cancer have a significantly higher risk of severe illness resulting in intensive care admissions or death when infected with COVID-19, particularly if they recently had chemotherapy or surgery.
“Many of the oncology treatments we currently use, especially those given after surgery to reduce risk of cancer recurrence, have relatively small benefits,” she writes.
“In the current climate, the balance of offering these treatments may shift; a small reduction in risk of cancer recurrence over the next 5 years may be outweighed by the potential for a short-term increase in risk of death from COVID-19. In the long term, more people’s cancer will return if we aren’t able to offer these treatments,” she adds.
Postpone Routine Screening
One thing that can go on the back burner for now is routine cancer screening, which can be postponed for now in order to conserve health system resources and reduce contact with healthcare facilities, says the ACS.
“Patients seeking routine cancer screenings should delay those until further notice,” said Lichtenfeld. “While timely screening is important, the need to prevent the spread of coronavirus and to reduce the strain on the medical system is more important right now.”
But as soon as restrictions to slow the spread of COVID-19 are lifted and routine visits to health facilities are safe, regular screening tests should be rescheduled.
Guidance From ASCO
The American Society of Clinical Oncology (ASCO) has issued new guidance on caring for patients with cancer during the COVID-19 outbreak.
First and foremost, ASCO encourages providers, facilities, and anyone caring for patients with cancer to follow the existing guidelines from the Center for Disease Control and Prevention when possible.
ASCO highlights the CDC’s general recommendation for healthcare facilities that suggests “elective surgeries” at inpatient facilities be rescheduled if possible, which has also been recommended by the American College of Surgeons.
However, in many cases, cancer surgery is not elective but essential, it points out. So this is largely an individual determination that clinicians and patients will need to make, taking into account the potential harms of delaying needed cancer-related surgery.
Systemic treatments, including chemotherapy and immunotherapy, leave cancer patients vulnerable to infection, but ASCO says there is no direct evidence to support changes in regimens during the pandemic. Therefore, routinely stopping anticancer or immunosuppressive therapy is not recommended, as the balance of potential harms that may result from delaying or interrupting treatment versus the potential benefits of possibly preventing or delaying COVID-19 infection remains very unclear.
Clinical decisions must be individualized, ASCO emphasized, and suggested the following practice points be considered:
- For patients already in deep remission who are receiving maintenance therapy, stopping treatment may be an option.
- Some patients may be able to switch from IV to oral therapies, which would decrease the frequency of clinic visits.
- Decisions on modifying or withholding chemotherapy need to consider both the indication and goals of care, as well as where the patient is in the treatment regimen and tolerance to the therapy. As an example, the risk–benefit assessment for proceeding with chemotherapy in patients with untreated extensive small-cell lung cancer is quite different than proceeding with maintenance pemetrexed for metastatic non–small cell lung cancer.
- If local coronavirus transmission is an issue at a particular cancer center, reasonable options may include taking a 2-week treatment break or arranging treatment at a different facility.
- Evaluate if home infusion is medically and logistically feasible.
- In some settings, delaying or modifying adjuvant treatment presents a higher risk of compromised disease control and long-term survival than in others, but in cases where the absolute benefit of adjuvant chemotherapy may be quite small and other options are available, the risk of COVID-19 may be considered an additional factor when evaluating care.
Delay Stem Cell Transplants
For patients who are candidates for allogeneic stem cell transplantation, a delay may be reasonable if the patient is currently well controlled with conventional treatment, ASCO comments. It also directs clinicians to follow the recommendations provided by the American Society of Transplantation and Cellular Therapy and from the European Society for Blood and Marrow Transplantation regarding this issue.
Finally, there is also the question of prophylactic antiviral therapy: Should it be considered for cancer patients undergoing active therapy?
The answer to that question is currently unknown, says ASCO, but “this is an active area of research and evidence may be available at any time.”
This article first appeared on Medscape.com.
New melanoma treatments linked to mortality decline
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
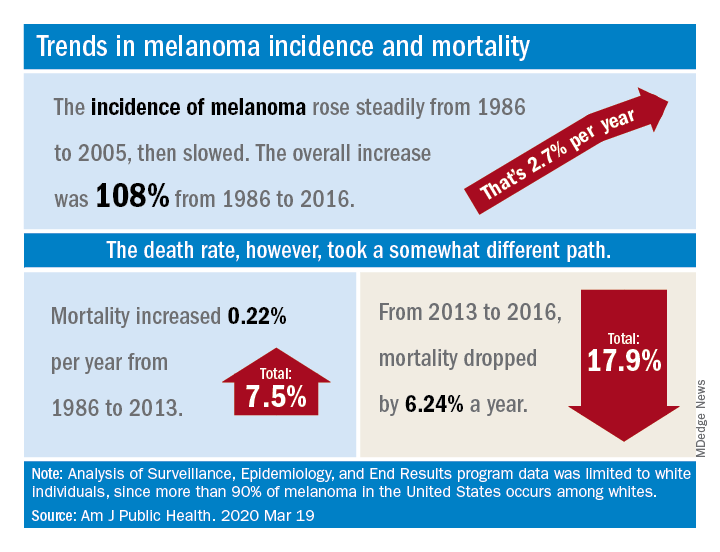
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
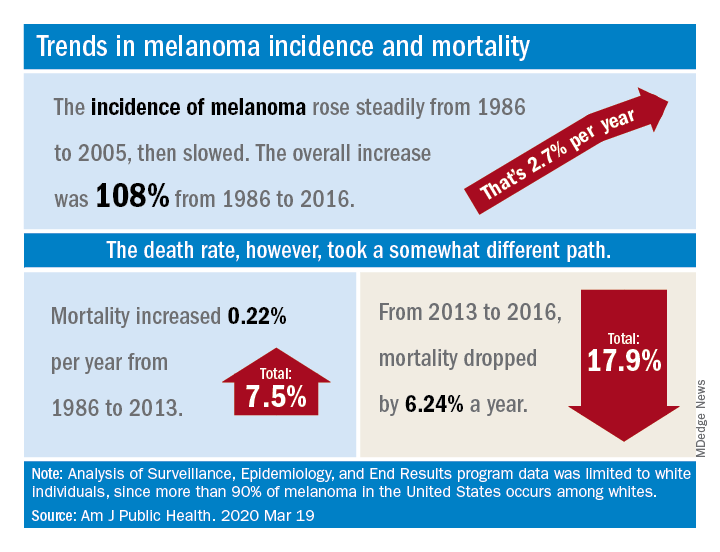
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
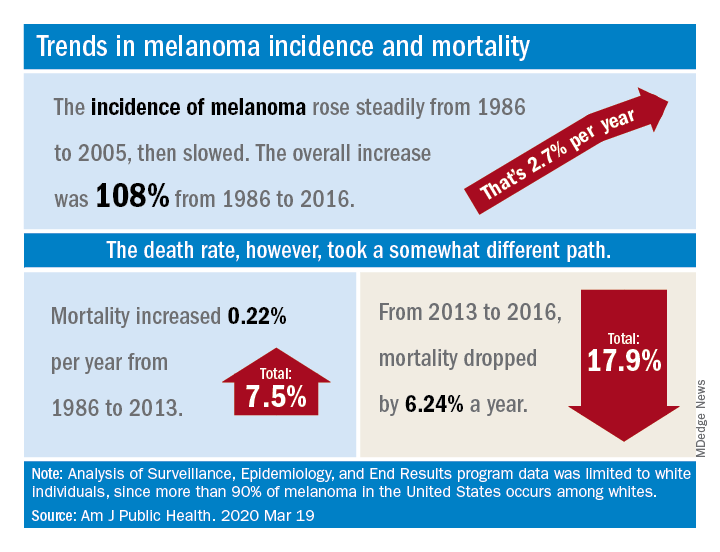
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.
FROM THE AMERICAN JOURNAL OF PUBLIC HEALTH
Doublet may be beneficial in wild-type, advanced NSCLC
Combination apatinib and vinorelbine “may have potential” for treating patients with wild-type, advanced non–small cell lung cancer (NSCLC) who failed at least two prior lines of chemotherapy, according to researchers.
In a phase 2 trial, apatinib plus vinorelbine produced an overall response rate of 36.7% and a disease control rate of 76.7%. Nearly half of patients required dose reductions, and 17% discontinued treatment due to adverse events.
Xiangyu Zhang, MD, of Hunan Cancer Hospital in Changsha, China, and colleagues conducted this trial (NCT03652857) and detailed the results in JAMA Network Open.
The researchers noted that there is no standard treatment strategy for patients who have advanced NSCLC without actionable mutations and have failed two or more lines of chemotherapy. So the team tested apatinib plus vinorelbine in 30 such patients.
The patients’ median age was 63 years (range, 34-78 years), 60% were men, and 90% had stage IV disease. They had received a median of 2 (range, 2-5) prior lines of chemotherapy.
In this study, patients received apatinib at 500 mg once daily and vinorelbine at 60 mg/m2 once weekly. The dose of apatinib could be interrupted or reduced to manage adverse events. Patients could receive 250 mg or 500 mg on alternate days or 250 mg once daily. Patients were treated until they progressed, withdrew, or had unacceptable adverse events.
Results
Patients were treated for a median of 4 months (range, 1-22 months), and the median follow-up was 11 months (range, 4.5-14.1 months). Most patients (n = 25) continued treatment until they progressed, 17 were able to remain on the 500-mg dose of apatinib, 13 received the 250-mg dose of apatinib, and 5 patients discontinued treatment due to adverse events.
The overall response rate was 36.7%, and the disease control rate, defined as the proportion of patients with complete response, partial response, and stable disease, was 76.7%. There were no complete responses, 11 partial responses, 12 patients with stable disease, and 7 patients who progressed. Rates of response, disease control, and progression were similar whether patients received the 500-mg dose of apatinib or the 250-mg dose.
The median progression-free survival was 4.5 months, and the median overall survival was 10 months.
Hand-foot syndrome was the most common adverse event, with grade 1-2 hand-foot syndrome occurring in 13 patients (43%), grade 3 occurring in 5 patients (17%), and grade 4 occurring in 1 patient (3%).
The adverse events that led to treatment discontinuation were grade 3 weakness (n = 1), pleural effusion (n = 1), fungal infection (n = 1), and grade 3 hand-foot syndrome (n = 2). There were no fatal adverse events.
“” the researchers concluded. “Further evaluation of this combination in phase 3 trials is warranted.”
The current study was funded by grants from the National Natural Science Foundation of China and the Hunan Natural Science Foundation. The researchers disclosed no conflicts of interest.
SOURCE: Zhang X et al. JAMA Netw Open. 2020;3(3):e201226. doi: 10.1001/jamanetworkopen.2020.12.
Combination apatinib and vinorelbine “may have potential” for treating patients with wild-type, advanced non–small cell lung cancer (NSCLC) who failed at least two prior lines of chemotherapy, according to researchers.
In a phase 2 trial, apatinib plus vinorelbine produced an overall response rate of 36.7% and a disease control rate of 76.7%. Nearly half of patients required dose reductions, and 17% discontinued treatment due to adverse events.
Xiangyu Zhang, MD, of Hunan Cancer Hospital in Changsha, China, and colleagues conducted this trial (NCT03652857) and detailed the results in JAMA Network Open.
The researchers noted that there is no standard treatment strategy for patients who have advanced NSCLC without actionable mutations and have failed two or more lines of chemotherapy. So the team tested apatinib plus vinorelbine in 30 such patients.
The patients’ median age was 63 years (range, 34-78 years), 60% were men, and 90% had stage IV disease. They had received a median of 2 (range, 2-5) prior lines of chemotherapy.
In this study, patients received apatinib at 500 mg once daily and vinorelbine at 60 mg/m2 once weekly. The dose of apatinib could be interrupted or reduced to manage adverse events. Patients could receive 250 mg or 500 mg on alternate days or 250 mg once daily. Patients were treated until they progressed, withdrew, or had unacceptable adverse events.
Results
Patients were treated for a median of 4 months (range, 1-22 months), and the median follow-up was 11 months (range, 4.5-14.1 months). Most patients (n = 25) continued treatment until they progressed, 17 were able to remain on the 500-mg dose of apatinib, 13 received the 250-mg dose of apatinib, and 5 patients discontinued treatment due to adverse events.
The overall response rate was 36.7%, and the disease control rate, defined as the proportion of patients with complete response, partial response, and stable disease, was 76.7%. There were no complete responses, 11 partial responses, 12 patients with stable disease, and 7 patients who progressed. Rates of response, disease control, and progression were similar whether patients received the 500-mg dose of apatinib or the 250-mg dose.
The median progression-free survival was 4.5 months, and the median overall survival was 10 months.
Hand-foot syndrome was the most common adverse event, with grade 1-2 hand-foot syndrome occurring in 13 patients (43%), grade 3 occurring in 5 patients (17%), and grade 4 occurring in 1 patient (3%).
The adverse events that led to treatment discontinuation were grade 3 weakness (n = 1), pleural effusion (n = 1), fungal infection (n = 1), and grade 3 hand-foot syndrome (n = 2). There were no fatal adverse events.
“” the researchers concluded. “Further evaluation of this combination in phase 3 trials is warranted.”
The current study was funded by grants from the National Natural Science Foundation of China and the Hunan Natural Science Foundation. The researchers disclosed no conflicts of interest.
SOURCE: Zhang X et al. JAMA Netw Open. 2020;3(3):e201226. doi: 10.1001/jamanetworkopen.2020.12.
Combination apatinib and vinorelbine “may have potential” for treating patients with wild-type, advanced non–small cell lung cancer (NSCLC) who failed at least two prior lines of chemotherapy, according to researchers.
In a phase 2 trial, apatinib plus vinorelbine produced an overall response rate of 36.7% and a disease control rate of 76.7%. Nearly half of patients required dose reductions, and 17% discontinued treatment due to adverse events.
Xiangyu Zhang, MD, of Hunan Cancer Hospital in Changsha, China, and colleagues conducted this trial (NCT03652857) and detailed the results in JAMA Network Open.
The researchers noted that there is no standard treatment strategy for patients who have advanced NSCLC without actionable mutations and have failed two or more lines of chemotherapy. So the team tested apatinib plus vinorelbine in 30 such patients.
The patients’ median age was 63 years (range, 34-78 years), 60% were men, and 90% had stage IV disease. They had received a median of 2 (range, 2-5) prior lines of chemotherapy.
In this study, patients received apatinib at 500 mg once daily and vinorelbine at 60 mg/m2 once weekly. The dose of apatinib could be interrupted or reduced to manage adverse events. Patients could receive 250 mg or 500 mg on alternate days or 250 mg once daily. Patients were treated until they progressed, withdrew, or had unacceptable adverse events.
Results
Patients were treated for a median of 4 months (range, 1-22 months), and the median follow-up was 11 months (range, 4.5-14.1 months). Most patients (n = 25) continued treatment until they progressed, 17 were able to remain on the 500-mg dose of apatinib, 13 received the 250-mg dose of apatinib, and 5 patients discontinued treatment due to adverse events.
The overall response rate was 36.7%, and the disease control rate, defined as the proportion of patients with complete response, partial response, and stable disease, was 76.7%. There were no complete responses, 11 partial responses, 12 patients with stable disease, and 7 patients who progressed. Rates of response, disease control, and progression were similar whether patients received the 500-mg dose of apatinib or the 250-mg dose.
The median progression-free survival was 4.5 months, and the median overall survival was 10 months.
Hand-foot syndrome was the most common adverse event, with grade 1-2 hand-foot syndrome occurring in 13 patients (43%), grade 3 occurring in 5 patients (17%), and grade 4 occurring in 1 patient (3%).
The adverse events that led to treatment discontinuation were grade 3 weakness (n = 1), pleural effusion (n = 1), fungal infection (n = 1), and grade 3 hand-foot syndrome (n = 2). There were no fatal adverse events.
“” the researchers concluded. “Further evaluation of this combination in phase 3 trials is warranted.”
The current study was funded by grants from the National Natural Science Foundation of China and the Hunan Natural Science Foundation. The researchers disclosed no conflicts of interest.
SOURCE: Zhang X et al. JAMA Netw Open. 2020;3(3):e201226. doi: 10.1001/jamanetworkopen.2020.12.
FROM JAMA NETWORK OPEN
‘Like a coin flip’: Assay denies some cancer patients new drug
In December, at a major breast cancer conference, some attendees couldn’t find a seat and were told to leave an overcrowded session on immunotherapy for metastatic triple-negative breast cancer (TNBC). They refused, and pushed in to hear what was being said.
The crowd might have been surprised to learn that the main draw of the event, a successful new drug, was not all it might have been for women with the disease, being handicapped by a test that determines who is eligible for it.
“That room was overpacked ― there were five people deep against the wall. ... It was amazing,” said Janice Cowden of Bradenton, Florida. She attended the meeting, the San Antonio Breast Cancer Symposium, as a patient advocate.
Cowden lives with metastatic TNBC, which is known for poor prognoses, aggressiveness, and a lack of targeted treatment options. “Stage IV is a state of desperation. We just want something to work,” she said.
That’s why the conference room was packed – the session was focused on something that had been found to work – the immunotherapy atezolizumab (Tecentriq, Genentech/Roche).
Atezolizumab had recently been conditionally approved for first-line use in advanced TNBC, having been shown to significantly slow disease progression and, in some patients, to possibly improve survival. A pair of medical oncologists reviewed the clinical trial data during the session.
One important point from the trial data was that the benefit was greater in patients whose tumors had the biomarker PD-L1, and so the Food and Drug Administration approval of the drug specified that it should be used only in those patients.
The drug approval was accompanied by approval of a companion diagnostic test used to identify this PD-L1-positive subgroup of patients, the Ventana SP142 Assay (Roche Diagnostics).
At the meeting, pathologist David Rimm, MD, of Yale University, New Haven, Connecticut, discussed the biomarker PD-L1 and the test. Rimm had a subtle but unsettling message about the crucial test: that the SP142 diagnostic assay, when used by increasing numbers of pathologists, resulted in increasing rates of PD-L1 scores that were not concordant.
A related meeting poster, presented the next day with Rimm as senior author, was more explicit and concluded that “more than half of the pathologists in real-world situations may mis- assign” patient scores with SP142 (and another Roche assay) because of wide variability in readouts.
“They’ve made a test that is inadequate – it just doesn’t work. It’s like flipping a coin,” he told Medscape Medical News about Roche’s SP142 assay in everyday practice.
The general problem is not a new one – for some years there have been problems with the use of PD-L1 as a biomarker for immunotherapy and with assays for that biomarker, with many groups questioning both accuracy and reproducibility. But the problems with SP142 are “the most egregious,” said Rimm, who has served as a paid consultant to Roche Diagnostics in the past.
In clinical practice, Rimm’s overall message is that because of the difficulty of reading SP142 assay results, some TNBC patients who were PD-L1-positive would not get the drug, and some who were not positive would get the drug.
Patient advocate Cowden was not worried about overtreatment. She was concerned about patients who “might die without receiving a potentially life-extending treatment.”
In an essay in the Pathologist, Rimm echoed that sentiment about undertreatment (as well as overtreatment) with atezolizumab for breast cancer: “In all cases, the patients are the potential victims, but this appears to be completely under the radar of the hype surrounding this new drug.”
Roche Disputes Problems With Assay
Roche, manufacturer of both atezolizumab and the companion diagnostic test, disputes that there is a problem.
The FDA and multiple health authorities worldwide have approved atezolizumab and the companion diagnostic SP142 assay for use in TNBC, points out Eslie Dennis, MD, vice president of medical affairs at Roche Tissue Diagnostics.
“The role of a companion diagnostic assay is to discriminate between responders and non-responders for a specific therapeutic product in a specific indication, with a cut-off based on clinical outcomes,” she wrote in an email to Medscape Medical News.
Data from the pivotal IMpassion130 trial show that the assay was effective at that task. Among the 369 patients in the 902-patient trial whose tumors were ≥1% positive for PD-L1, those treated with atezolizumab (and nab-paclitaxel; n = 185) had a median progression-free survival (PFS) of 7.4 months, vs. 4.8 months among those treated with placebo (and nab-paclitaxel; n = 184) (P < .0001).
“Exploratory analysis showed no [PFS] benefit in PD-L1-negative patients as tested by the SP142 assay [in IMpassion130],” Dennis and three other physicians write in a reply to Rimm in a letter published in July 2019 in the Pathologist.
The same held true for overall survival in exploratory analysis – there was no benefit with atezolizumab among the PD-L1-negative patients, they write.
Notably, overall survival benefit for patients who were PD-L1 positive was about 10 months (at the first interim analysis; at the second analysis, the benefit dropped to 7 months and was not statistically significant).
But Rimm points out that the pivotal trial used only one pathologist in a central lab to determine PD-L1 status, who was undoubtedly an expert with the SP142 assay.
Further, Rimm observes that additional data submitted to the FDA to show that SP142 test results are reproducible outside of the pivotal trial setting were performed with only three pathologists and thus unsurprisingly yielded high rates of agreement – all above 90%.
The data from both of these circumstances are problematic, Rimm said, because in the real world, hundreds of pathologists will score the SP142 assay – all in the context of a busy day reading a variety of other tests for other diseases.
It’s one thing to get an FDA approval for an assay, and it’s another thing to be a reliable, well-functioning assay in the real world, he summarized.
Last year, Roberto Salgado, MD, PhD, a pathologist at the Université Libre de Bruxelles, Belgium, commented that “a positive phase III trial should not be taken as a guarantee that the assay used in the trial can be implemented in daily practice” in an opinion piece in the Pathologist.
SP142 Identifies the “Fewest Possible Patients”
The SP142 assay has been shown in multiple studies to have lower sensitivity for PD-L1 than other competing PD-L1 assays, said Rimm, citing examples such as a 2017 study and a 2018 study.
Angela DeMichele, MD, a medical oncologist at the University of Pennsylvania in Philadelphia, agreed and explained what that meant in practical terms for women whose tumors are tested with SP142. “It means that the test is going to identify the fewest possible PD-L1-positive patients [relative to the other available assays],” she said. “It [the SP142 assay] is far from a perfect test for this situation,” added DeMichele, an expert on biomarkers in breast cancer clinical trials.
She said that biomarker tests, like many products of science, tend to become dated with the passage of time, as more is learned about the target and new assays are developed. “Unfortunately, you can’t change assays midstream,” said DeMichele. She has received a grant from Roche and Stand Up to Cancer to study atezolizumab and another drug in a clinical trial among patients with metastatic TNBC who have minimal residual disease.
DeMichele also said that “David Rimm is one of the most knowledgeable people in the world about this issue.”
But DeMichelle also points out the practical: “We’re stuck as clinicians” because regulatory bodies and insurance companies only pay for atezolizumab when the SP142 assay indicates PD-L1 positivity. That’s not the case in Europe, where health authorities do not specify which PD-L1 assay is to be used with atezolizumab for breast cancer, pointed out Belgium’s Salgado last year.
Another Level of Complexity
At the immunotherapy session in San Antonio, Rimm discussed the results of a study of 68 TNBC archived cases in which specimens were stained with the SP142 assay at Yale and were distributed via electronic images to 19 pathologists at 14 institutions across the United States for PD-L1 scoring.
The study, coauthored by academics from Iowa, Texas A&M, UC San Diego, Mayo Clinic, Memorial Sloan Kettering, and others, used a novel method to determine the minimum number of evaluators needed to estimate “concordance” or agreement about a test result among large numbers of readers. The consensus/agreement was as high as 80% when eight or fewer pathologists’ scores were compared, but was as low as 40% when results from more than eight pathologists were included, said Rimm.
These are some of the data that led him to declare that using the assay is no better than flipping a coin.
Yes, PD-L1 testing is a challenge, and it has “introduced another level of complexity” for pathologists in reading assays, write experts Emina Torlakovic, MD, University of Saskatchewan, Canada, and Allen Gown, MD, PhenoPath Laboratories, Seattle, in response to Rimm last year.
But there is “poor” consensus among pathologists, they point out, “for many scoring systems that are still clinically applied (such as Gleason grading).” Consensus “improves with education and training,” the pair add. To that end, Roche has initiated a global training program for pathologists using the SP142 assay for TNBC. At San Antonio, Roche’s Dennis reported that among 432 pathologists from 58 countries, there was overall agreement of 98.2% in scoring assays.
Rimm commented that such high agreement would not be a surprise if testing took place soon after any such training program.
In an email to Medscape Medical News, Torlakovic encouraged pathologists who wish to practice their skill in interpreting assays, including SP142, to visit CBQAReadout.ca, a testing site. The site, which was founded by Torlakovic and may be one of a kind, offers CME credits and is sponsored by independent pathology organizations, such as CAP-ACP and the Saskatchewan Health Authority, as well as pharmaceutical companies, including Roche.
No Clue
Patient advocate Cowden believes the controversy about PD-L1 testing for atezolizumab is largely unknown among breast cancer patients. She learned about SP142 assay ambiguities in San Antonio, when the Florida Breast Cancer Foundation funded her trip to the meeting and the Alamo Breast Cancer Foundation asked her to write a report on Rimm’s presentation.
Cowden is a member of a Facebook group for stage IV TNBC, which has about 1500 members. She estimates that 75%-80% would be willing to try atezolizumab “no matter what,” meaning they don’t care about PD-L1 positivity being associated with efficacy.
The Facebook group members “know there is a test and if you are positive, there is an immunotherapy for their breast cancer,” said Cowden.
None know that women may be excluded from treatment because of shortcomings with the SP142 test. “They have no clue,” she said.
Rimm and DeMichele have financial ties to Roche and other companies. Dennis is an employee of Roche. Torlakovic has ties to multiple companies, including Roche, for whom she has acted as a paid consultant, grant recipient, and paid lecturer. Gown did not respond to a request for financial disclosures. Cowden reports no relevant financial relationships.
This article first appeared on Medscape.com.
In December, at a major breast cancer conference, some attendees couldn’t find a seat and were told to leave an overcrowded session on immunotherapy for metastatic triple-negative breast cancer (TNBC). They refused, and pushed in to hear what was being said.
The crowd might have been surprised to learn that the main draw of the event, a successful new drug, was not all it might have been for women with the disease, being handicapped by a test that determines who is eligible for it.
“That room was overpacked ― there were five people deep against the wall. ... It was amazing,” said Janice Cowden of Bradenton, Florida. She attended the meeting, the San Antonio Breast Cancer Symposium, as a patient advocate.
Cowden lives with metastatic TNBC, which is known for poor prognoses, aggressiveness, and a lack of targeted treatment options. “Stage IV is a state of desperation. We just want something to work,” she said.
That’s why the conference room was packed – the session was focused on something that had been found to work – the immunotherapy atezolizumab (Tecentriq, Genentech/Roche).
Atezolizumab had recently been conditionally approved for first-line use in advanced TNBC, having been shown to significantly slow disease progression and, in some patients, to possibly improve survival. A pair of medical oncologists reviewed the clinical trial data during the session.
One important point from the trial data was that the benefit was greater in patients whose tumors had the biomarker PD-L1, and so the Food and Drug Administration approval of the drug specified that it should be used only in those patients.
The drug approval was accompanied by approval of a companion diagnostic test used to identify this PD-L1-positive subgroup of patients, the Ventana SP142 Assay (Roche Diagnostics).
At the meeting, pathologist David Rimm, MD, of Yale University, New Haven, Connecticut, discussed the biomarker PD-L1 and the test. Rimm had a subtle but unsettling message about the crucial test: that the SP142 diagnostic assay, when used by increasing numbers of pathologists, resulted in increasing rates of PD-L1 scores that were not concordant.
A related meeting poster, presented the next day with Rimm as senior author, was more explicit and concluded that “more than half of the pathologists in real-world situations may mis- assign” patient scores with SP142 (and another Roche assay) because of wide variability in readouts.
“They’ve made a test that is inadequate – it just doesn’t work. It’s like flipping a coin,” he told Medscape Medical News about Roche’s SP142 assay in everyday practice.
The general problem is not a new one – for some years there have been problems with the use of PD-L1 as a biomarker for immunotherapy and with assays for that biomarker, with many groups questioning both accuracy and reproducibility. But the problems with SP142 are “the most egregious,” said Rimm, who has served as a paid consultant to Roche Diagnostics in the past.
In clinical practice, Rimm’s overall message is that because of the difficulty of reading SP142 assay results, some TNBC patients who were PD-L1-positive would not get the drug, and some who were not positive would get the drug.
Patient advocate Cowden was not worried about overtreatment. She was concerned about patients who “might die without receiving a potentially life-extending treatment.”
In an essay in the Pathologist, Rimm echoed that sentiment about undertreatment (as well as overtreatment) with atezolizumab for breast cancer: “In all cases, the patients are the potential victims, but this appears to be completely under the radar of the hype surrounding this new drug.”
Roche Disputes Problems With Assay
Roche, manufacturer of both atezolizumab and the companion diagnostic test, disputes that there is a problem.
The FDA and multiple health authorities worldwide have approved atezolizumab and the companion diagnostic SP142 assay for use in TNBC, points out Eslie Dennis, MD, vice president of medical affairs at Roche Tissue Diagnostics.
“The role of a companion diagnostic assay is to discriminate between responders and non-responders for a specific therapeutic product in a specific indication, with a cut-off based on clinical outcomes,” she wrote in an email to Medscape Medical News.
Data from the pivotal IMpassion130 trial show that the assay was effective at that task. Among the 369 patients in the 902-patient trial whose tumors were ≥1% positive for PD-L1, those treated with atezolizumab (and nab-paclitaxel; n = 185) had a median progression-free survival (PFS) of 7.4 months, vs. 4.8 months among those treated with placebo (and nab-paclitaxel; n = 184) (P < .0001).
“Exploratory analysis showed no [PFS] benefit in PD-L1-negative patients as tested by the SP142 assay [in IMpassion130],” Dennis and three other physicians write in a reply to Rimm in a letter published in July 2019 in the Pathologist.
The same held true for overall survival in exploratory analysis – there was no benefit with atezolizumab among the PD-L1-negative patients, they write.
Notably, overall survival benefit for patients who were PD-L1 positive was about 10 months (at the first interim analysis; at the second analysis, the benefit dropped to 7 months and was not statistically significant).
But Rimm points out that the pivotal trial used only one pathologist in a central lab to determine PD-L1 status, who was undoubtedly an expert with the SP142 assay.
Further, Rimm observes that additional data submitted to the FDA to show that SP142 test results are reproducible outside of the pivotal trial setting were performed with only three pathologists and thus unsurprisingly yielded high rates of agreement – all above 90%.
The data from both of these circumstances are problematic, Rimm said, because in the real world, hundreds of pathologists will score the SP142 assay – all in the context of a busy day reading a variety of other tests for other diseases.
It’s one thing to get an FDA approval for an assay, and it’s another thing to be a reliable, well-functioning assay in the real world, he summarized.
Last year, Roberto Salgado, MD, PhD, a pathologist at the Université Libre de Bruxelles, Belgium, commented that “a positive phase III trial should not be taken as a guarantee that the assay used in the trial can be implemented in daily practice” in an opinion piece in the Pathologist.
SP142 Identifies the “Fewest Possible Patients”
The SP142 assay has been shown in multiple studies to have lower sensitivity for PD-L1 than other competing PD-L1 assays, said Rimm, citing examples such as a 2017 study and a 2018 study.
Angela DeMichele, MD, a medical oncologist at the University of Pennsylvania in Philadelphia, agreed and explained what that meant in practical terms for women whose tumors are tested with SP142. “It means that the test is going to identify the fewest possible PD-L1-positive patients [relative to the other available assays],” she said. “It [the SP142 assay] is far from a perfect test for this situation,” added DeMichele, an expert on biomarkers in breast cancer clinical trials.
She said that biomarker tests, like many products of science, tend to become dated with the passage of time, as more is learned about the target and new assays are developed. “Unfortunately, you can’t change assays midstream,” said DeMichele. She has received a grant from Roche and Stand Up to Cancer to study atezolizumab and another drug in a clinical trial among patients with metastatic TNBC who have minimal residual disease.
DeMichele also said that “David Rimm is one of the most knowledgeable people in the world about this issue.”
But DeMichelle also points out the practical: “We’re stuck as clinicians” because regulatory bodies and insurance companies only pay for atezolizumab when the SP142 assay indicates PD-L1 positivity. That’s not the case in Europe, where health authorities do not specify which PD-L1 assay is to be used with atezolizumab for breast cancer, pointed out Belgium’s Salgado last year.
Another Level of Complexity
At the immunotherapy session in San Antonio, Rimm discussed the results of a study of 68 TNBC archived cases in which specimens were stained with the SP142 assay at Yale and were distributed via electronic images to 19 pathologists at 14 institutions across the United States for PD-L1 scoring.
The study, coauthored by academics from Iowa, Texas A&M, UC San Diego, Mayo Clinic, Memorial Sloan Kettering, and others, used a novel method to determine the minimum number of evaluators needed to estimate “concordance” or agreement about a test result among large numbers of readers. The consensus/agreement was as high as 80% when eight or fewer pathologists’ scores were compared, but was as low as 40% when results from more than eight pathologists were included, said Rimm.
These are some of the data that led him to declare that using the assay is no better than flipping a coin.
Yes, PD-L1 testing is a challenge, and it has “introduced another level of complexity” for pathologists in reading assays, write experts Emina Torlakovic, MD, University of Saskatchewan, Canada, and Allen Gown, MD, PhenoPath Laboratories, Seattle, in response to Rimm last year.
But there is “poor” consensus among pathologists, they point out, “for many scoring systems that are still clinically applied (such as Gleason grading).” Consensus “improves with education and training,” the pair add. To that end, Roche has initiated a global training program for pathologists using the SP142 assay for TNBC. At San Antonio, Roche’s Dennis reported that among 432 pathologists from 58 countries, there was overall agreement of 98.2% in scoring assays.
Rimm commented that such high agreement would not be a surprise if testing took place soon after any such training program.
In an email to Medscape Medical News, Torlakovic encouraged pathologists who wish to practice their skill in interpreting assays, including SP142, to visit CBQAReadout.ca, a testing site. The site, which was founded by Torlakovic and may be one of a kind, offers CME credits and is sponsored by independent pathology organizations, such as CAP-ACP and the Saskatchewan Health Authority, as well as pharmaceutical companies, including Roche.
No Clue
Patient advocate Cowden believes the controversy about PD-L1 testing for atezolizumab is largely unknown among breast cancer patients. She learned about SP142 assay ambiguities in San Antonio, when the Florida Breast Cancer Foundation funded her trip to the meeting and the Alamo Breast Cancer Foundation asked her to write a report on Rimm’s presentation.
Cowden is a member of a Facebook group for stage IV TNBC, which has about 1500 members. She estimates that 75%-80% would be willing to try atezolizumab “no matter what,” meaning they don’t care about PD-L1 positivity being associated with efficacy.
The Facebook group members “know there is a test and if you are positive, there is an immunotherapy for their breast cancer,” said Cowden.
None know that women may be excluded from treatment because of shortcomings with the SP142 test. “They have no clue,” she said.
Rimm and DeMichele have financial ties to Roche and other companies. Dennis is an employee of Roche. Torlakovic has ties to multiple companies, including Roche, for whom she has acted as a paid consultant, grant recipient, and paid lecturer. Gown did not respond to a request for financial disclosures. Cowden reports no relevant financial relationships.
This article first appeared on Medscape.com.
In December, at a major breast cancer conference, some attendees couldn’t find a seat and were told to leave an overcrowded session on immunotherapy for metastatic triple-negative breast cancer (TNBC). They refused, and pushed in to hear what was being said.
The crowd might have been surprised to learn that the main draw of the event, a successful new drug, was not all it might have been for women with the disease, being handicapped by a test that determines who is eligible for it.
“That room was overpacked ― there were five people deep against the wall. ... It was amazing,” said Janice Cowden of Bradenton, Florida. She attended the meeting, the San Antonio Breast Cancer Symposium, as a patient advocate.
Cowden lives with metastatic TNBC, which is known for poor prognoses, aggressiveness, and a lack of targeted treatment options. “Stage IV is a state of desperation. We just want something to work,” she said.
That’s why the conference room was packed – the session was focused on something that had been found to work – the immunotherapy atezolizumab (Tecentriq, Genentech/Roche).
Atezolizumab had recently been conditionally approved for first-line use in advanced TNBC, having been shown to significantly slow disease progression and, in some patients, to possibly improve survival. A pair of medical oncologists reviewed the clinical trial data during the session.
One important point from the trial data was that the benefit was greater in patients whose tumors had the biomarker PD-L1, and so the Food and Drug Administration approval of the drug specified that it should be used only in those patients.
The drug approval was accompanied by approval of a companion diagnostic test used to identify this PD-L1-positive subgroup of patients, the Ventana SP142 Assay (Roche Diagnostics).
At the meeting, pathologist David Rimm, MD, of Yale University, New Haven, Connecticut, discussed the biomarker PD-L1 and the test. Rimm had a subtle but unsettling message about the crucial test: that the SP142 diagnostic assay, when used by increasing numbers of pathologists, resulted in increasing rates of PD-L1 scores that were not concordant.
A related meeting poster, presented the next day with Rimm as senior author, was more explicit and concluded that “more than half of the pathologists in real-world situations may mis- assign” patient scores with SP142 (and another Roche assay) because of wide variability in readouts.
“They’ve made a test that is inadequate – it just doesn’t work. It’s like flipping a coin,” he told Medscape Medical News about Roche’s SP142 assay in everyday practice.
The general problem is not a new one – for some years there have been problems with the use of PD-L1 as a biomarker for immunotherapy and with assays for that biomarker, with many groups questioning both accuracy and reproducibility. But the problems with SP142 are “the most egregious,” said Rimm, who has served as a paid consultant to Roche Diagnostics in the past.
In clinical practice, Rimm’s overall message is that because of the difficulty of reading SP142 assay results, some TNBC patients who were PD-L1-positive would not get the drug, and some who were not positive would get the drug.
Patient advocate Cowden was not worried about overtreatment. She was concerned about patients who “might die without receiving a potentially life-extending treatment.”
In an essay in the Pathologist, Rimm echoed that sentiment about undertreatment (as well as overtreatment) with atezolizumab for breast cancer: “In all cases, the patients are the potential victims, but this appears to be completely under the radar of the hype surrounding this new drug.”
Roche Disputes Problems With Assay
Roche, manufacturer of both atezolizumab and the companion diagnostic test, disputes that there is a problem.
The FDA and multiple health authorities worldwide have approved atezolizumab and the companion diagnostic SP142 assay for use in TNBC, points out Eslie Dennis, MD, vice president of medical affairs at Roche Tissue Diagnostics.
“The role of a companion diagnostic assay is to discriminate between responders and non-responders for a specific therapeutic product in a specific indication, with a cut-off based on clinical outcomes,” she wrote in an email to Medscape Medical News.
Data from the pivotal IMpassion130 trial show that the assay was effective at that task. Among the 369 patients in the 902-patient trial whose tumors were ≥1% positive for PD-L1, those treated with atezolizumab (and nab-paclitaxel; n = 185) had a median progression-free survival (PFS) of 7.4 months, vs. 4.8 months among those treated with placebo (and nab-paclitaxel; n = 184) (P < .0001).
“Exploratory analysis showed no [PFS] benefit in PD-L1-negative patients as tested by the SP142 assay [in IMpassion130],” Dennis and three other physicians write in a reply to Rimm in a letter published in July 2019 in the Pathologist.
The same held true for overall survival in exploratory analysis – there was no benefit with atezolizumab among the PD-L1-negative patients, they write.
Notably, overall survival benefit for patients who were PD-L1 positive was about 10 months (at the first interim analysis; at the second analysis, the benefit dropped to 7 months and was not statistically significant).
But Rimm points out that the pivotal trial used only one pathologist in a central lab to determine PD-L1 status, who was undoubtedly an expert with the SP142 assay.
Further, Rimm observes that additional data submitted to the FDA to show that SP142 test results are reproducible outside of the pivotal trial setting were performed with only three pathologists and thus unsurprisingly yielded high rates of agreement – all above 90%.
The data from both of these circumstances are problematic, Rimm said, because in the real world, hundreds of pathologists will score the SP142 assay – all in the context of a busy day reading a variety of other tests for other diseases.
It’s one thing to get an FDA approval for an assay, and it’s another thing to be a reliable, well-functioning assay in the real world, he summarized.
Last year, Roberto Salgado, MD, PhD, a pathologist at the Université Libre de Bruxelles, Belgium, commented that “a positive phase III trial should not be taken as a guarantee that the assay used in the trial can be implemented in daily practice” in an opinion piece in the Pathologist.
SP142 Identifies the “Fewest Possible Patients”
The SP142 assay has been shown in multiple studies to have lower sensitivity for PD-L1 than other competing PD-L1 assays, said Rimm, citing examples such as a 2017 study and a 2018 study.
Angela DeMichele, MD, a medical oncologist at the University of Pennsylvania in Philadelphia, agreed and explained what that meant in practical terms for women whose tumors are tested with SP142. “It means that the test is going to identify the fewest possible PD-L1-positive patients [relative to the other available assays],” she said. “It [the SP142 assay] is far from a perfect test for this situation,” added DeMichele, an expert on biomarkers in breast cancer clinical trials.
She said that biomarker tests, like many products of science, tend to become dated with the passage of time, as more is learned about the target and new assays are developed. “Unfortunately, you can’t change assays midstream,” said DeMichele. She has received a grant from Roche and Stand Up to Cancer to study atezolizumab and another drug in a clinical trial among patients with metastatic TNBC who have minimal residual disease.
DeMichele also said that “David Rimm is one of the most knowledgeable people in the world about this issue.”
But DeMichelle also points out the practical: “We’re stuck as clinicians” because regulatory bodies and insurance companies only pay for atezolizumab when the SP142 assay indicates PD-L1 positivity. That’s not the case in Europe, where health authorities do not specify which PD-L1 assay is to be used with atezolizumab for breast cancer, pointed out Belgium’s Salgado last year.
Another Level of Complexity
At the immunotherapy session in San Antonio, Rimm discussed the results of a study of 68 TNBC archived cases in which specimens were stained with the SP142 assay at Yale and were distributed via electronic images to 19 pathologists at 14 institutions across the United States for PD-L1 scoring.
The study, coauthored by academics from Iowa, Texas A&M, UC San Diego, Mayo Clinic, Memorial Sloan Kettering, and others, used a novel method to determine the minimum number of evaluators needed to estimate “concordance” or agreement about a test result among large numbers of readers. The consensus/agreement was as high as 80% when eight or fewer pathologists’ scores were compared, but was as low as 40% when results from more than eight pathologists were included, said Rimm.
These are some of the data that led him to declare that using the assay is no better than flipping a coin.
Yes, PD-L1 testing is a challenge, and it has “introduced another level of complexity” for pathologists in reading assays, write experts Emina Torlakovic, MD, University of Saskatchewan, Canada, and Allen Gown, MD, PhenoPath Laboratories, Seattle, in response to Rimm last year.
But there is “poor” consensus among pathologists, they point out, “for many scoring systems that are still clinically applied (such as Gleason grading).” Consensus “improves with education and training,” the pair add. To that end, Roche has initiated a global training program for pathologists using the SP142 assay for TNBC. At San Antonio, Roche’s Dennis reported that among 432 pathologists from 58 countries, there was overall agreement of 98.2% in scoring assays.
Rimm commented that such high agreement would not be a surprise if testing took place soon after any such training program.
In an email to Medscape Medical News, Torlakovic encouraged pathologists who wish to practice their skill in interpreting assays, including SP142, to visit CBQAReadout.ca, a testing site. The site, which was founded by Torlakovic and may be one of a kind, offers CME credits and is sponsored by independent pathology organizations, such as CAP-ACP and the Saskatchewan Health Authority, as well as pharmaceutical companies, including Roche.
No Clue
Patient advocate Cowden believes the controversy about PD-L1 testing for atezolizumab is largely unknown among breast cancer patients. She learned about SP142 assay ambiguities in San Antonio, when the Florida Breast Cancer Foundation funded her trip to the meeting and the Alamo Breast Cancer Foundation asked her to write a report on Rimm’s presentation.
Cowden is a member of a Facebook group for stage IV TNBC, which has about 1500 members. She estimates that 75%-80% would be willing to try atezolizumab “no matter what,” meaning they don’t care about PD-L1 positivity being associated with efficacy.
The Facebook group members “know there is a test and if you are positive, there is an immunotherapy for their breast cancer,” said Cowden.
None know that women may be excluded from treatment because of shortcomings with the SP142 test. “They have no clue,” she said.
Rimm and DeMichele have financial ties to Roche and other companies. Dennis is an employee of Roche. Torlakovic has ties to multiple companies, including Roche, for whom she has acted as a paid consultant, grant recipient, and paid lecturer. Gown did not respond to a request for financial disclosures. Cowden reports no relevant financial relationships.
This article first appeared on Medscape.com.
ASCO guidelines take global view of late-stage colorectal cancer
Ideally, all cases of colorectal cancer would be detected at an early and curable stage, but, as new guidelines for late-stage colorectal cancer suggest, the world is far from perfect.
“Different regions of the world, both among and within countries, differ with respect to access to early detection,” the guideline authors wrote in JCO Global Oncology. “Many regions do not have mass or even opportunistic screening, and even within regions with mass screening, subpopulations may not have access to screening.”
The guidelines were developed by the American Society of Clinical Oncology’s Resource-Stratified Guidelines Advisory Group. Based on and adapted from existing guidelines developed by four international agencies, the ASCO guidelines take into account economic and social realities and offer recommendations for diagnosis, staging, and treatment by resource level: basic, limited, enhanced, or maximal.
“We made these guidelines to apply to countries or regions that have basic resources,” lead author E. Gabriela Chiorean, MD, of the University of Washington, Seattle, and the Seattle Cancer Care Alliance, said in an interview.
“We decided what should be the most basic resources – diagnostics, imaging, and treatment – that should be available to patients, and we make recommendations for the use of limited resources and supplies,” she added.
The guidelines pose and answer seven questions about optimal initial symptom management, diagnosis, and staging; optimal first and later lines of therapy; liver-directed therapy options for patients with late-stage colorectal cancer and liver metastases; and optimal on-treatment surveillance and follow-up strategies for patients treated for metastatic colorectal cancer.
For each question, the document offers guidance based on the availability of resources. As defined by the authors, the recommendations are stratified according to the following categories:
- Basic resources – “Core resources or fundamental services that are absolutely necessary for any cancer health care system to function.”
- Limited resources – “Second-tier resources or services that are intended to produce major improvements in outcome, such as increased survival and cost effectiveness, and are attainable with limited financial means and modest infrastructure.”
- Enhanced resources – “Third-tier resources or services that are optional but important; enhanced-level resources should produce further improvements in outcome and increase the number and quality of options and patient choice.”
- Maximal resources – “High-level/state-of-the art resources or services that may be used/available in some high-resource regions and/or may be recommended by high-resource setting guidelines that do not adapt to resource constraints but that nonetheless should be considered a lower priority than those resources or services listed in the other categories on the basis of extreme cost and/or impracticality for broad use in a resource-limited environment.”
The guidelines address common elements of symptom management for patients with acute disease, such as diagnosis involving the primary tumor, endoscopy when possible, and staging to include digital rectal exam and/or imaging when possible. The guidelines also include information tailored to resource level about chemotherapy and surgical resection.
“If, for example, a patient presents with bleeding and you suspect it to be of colorectal origin, we make recommendations that if the patient has symptoms of obstruction and bleeding and is resectable, they should undergo surgery, which should be available in countries of all resource levels,” Dr. Chiorean said.
The guidelines also recommend following the ASCO palliative care guidelines (J Clin Oncol. 2017 Jan;35[1]:96-112) for those patients who present with clinically unstable disease because of bowel obstruction, uncontrolled bleeding, or uncontrolled pain. Patients with clinically stable disease and ongoing bleeding from the primary tumor site are recommended to undergo transfusion and primary-site resection if only basic resources are available or transfusion plus multidisciplinary specialized evaluation when higher-level resources are available.
The ASCO guidelines are adapted from guidelines developed by Cancer Council Australia; the European Society for Medical Oncology; the National Institute for Health and Care Excellence, including separate recommendation for therapy combinations (https://www.nice.org.uk/guidance/ta212, https://www.nice.org.uk/guidance/ta439); and the National Comprehensive Cancer Network. Some of these guidelines have been updated since the creation of the ASCO guidelines.
ASCO funds the guideline development process. Dr. Chiorean and other authors disclosed relationships with multiple companies.
SOURCE: Chiorean EG et al. JCO Glob Oncol. 2020 Mar;6:414-38.
Ideally, all cases of colorectal cancer would be detected at an early and curable stage, but, as new guidelines for late-stage colorectal cancer suggest, the world is far from perfect.
“Different regions of the world, both among and within countries, differ with respect to access to early detection,” the guideline authors wrote in JCO Global Oncology. “Many regions do not have mass or even opportunistic screening, and even within regions with mass screening, subpopulations may not have access to screening.”
The guidelines were developed by the American Society of Clinical Oncology’s Resource-Stratified Guidelines Advisory Group. Based on and adapted from existing guidelines developed by four international agencies, the ASCO guidelines take into account economic and social realities and offer recommendations for diagnosis, staging, and treatment by resource level: basic, limited, enhanced, or maximal.
“We made these guidelines to apply to countries or regions that have basic resources,” lead author E. Gabriela Chiorean, MD, of the University of Washington, Seattle, and the Seattle Cancer Care Alliance, said in an interview.
“We decided what should be the most basic resources – diagnostics, imaging, and treatment – that should be available to patients, and we make recommendations for the use of limited resources and supplies,” she added.
The guidelines pose and answer seven questions about optimal initial symptom management, diagnosis, and staging; optimal first and later lines of therapy; liver-directed therapy options for patients with late-stage colorectal cancer and liver metastases; and optimal on-treatment surveillance and follow-up strategies for patients treated for metastatic colorectal cancer.
For each question, the document offers guidance based on the availability of resources. As defined by the authors, the recommendations are stratified according to the following categories:
- Basic resources – “Core resources or fundamental services that are absolutely necessary for any cancer health care system to function.”
- Limited resources – “Second-tier resources or services that are intended to produce major improvements in outcome, such as increased survival and cost effectiveness, and are attainable with limited financial means and modest infrastructure.”
- Enhanced resources – “Third-tier resources or services that are optional but important; enhanced-level resources should produce further improvements in outcome and increase the number and quality of options and patient choice.”
- Maximal resources – “High-level/state-of-the art resources or services that may be used/available in some high-resource regions and/or may be recommended by high-resource setting guidelines that do not adapt to resource constraints but that nonetheless should be considered a lower priority than those resources or services listed in the other categories on the basis of extreme cost and/or impracticality for broad use in a resource-limited environment.”
The guidelines address common elements of symptom management for patients with acute disease, such as diagnosis involving the primary tumor, endoscopy when possible, and staging to include digital rectal exam and/or imaging when possible. The guidelines also include information tailored to resource level about chemotherapy and surgical resection.
“If, for example, a patient presents with bleeding and you suspect it to be of colorectal origin, we make recommendations that if the patient has symptoms of obstruction and bleeding and is resectable, they should undergo surgery, which should be available in countries of all resource levels,” Dr. Chiorean said.
The guidelines also recommend following the ASCO palliative care guidelines (J Clin Oncol. 2017 Jan;35[1]:96-112) for those patients who present with clinically unstable disease because of bowel obstruction, uncontrolled bleeding, or uncontrolled pain. Patients with clinically stable disease and ongoing bleeding from the primary tumor site are recommended to undergo transfusion and primary-site resection if only basic resources are available or transfusion plus multidisciplinary specialized evaluation when higher-level resources are available.
The ASCO guidelines are adapted from guidelines developed by Cancer Council Australia; the European Society for Medical Oncology; the National Institute for Health and Care Excellence, including separate recommendation for therapy combinations (https://www.nice.org.uk/guidance/ta212, https://www.nice.org.uk/guidance/ta439); and the National Comprehensive Cancer Network. Some of these guidelines have been updated since the creation of the ASCO guidelines.
ASCO funds the guideline development process. Dr. Chiorean and other authors disclosed relationships with multiple companies.
SOURCE: Chiorean EG et al. JCO Glob Oncol. 2020 Mar;6:414-38.
Ideally, all cases of colorectal cancer would be detected at an early and curable stage, but, as new guidelines for late-stage colorectal cancer suggest, the world is far from perfect.
“Different regions of the world, both among and within countries, differ with respect to access to early detection,” the guideline authors wrote in JCO Global Oncology. “Many regions do not have mass or even opportunistic screening, and even within regions with mass screening, subpopulations may not have access to screening.”
The guidelines were developed by the American Society of Clinical Oncology’s Resource-Stratified Guidelines Advisory Group. Based on and adapted from existing guidelines developed by four international agencies, the ASCO guidelines take into account economic and social realities and offer recommendations for diagnosis, staging, and treatment by resource level: basic, limited, enhanced, or maximal.
“We made these guidelines to apply to countries or regions that have basic resources,” lead author E. Gabriela Chiorean, MD, of the University of Washington, Seattle, and the Seattle Cancer Care Alliance, said in an interview.
“We decided what should be the most basic resources – diagnostics, imaging, and treatment – that should be available to patients, and we make recommendations for the use of limited resources and supplies,” she added.
The guidelines pose and answer seven questions about optimal initial symptom management, diagnosis, and staging; optimal first and later lines of therapy; liver-directed therapy options for patients with late-stage colorectal cancer and liver metastases; and optimal on-treatment surveillance and follow-up strategies for patients treated for metastatic colorectal cancer.
For each question, the document offers guidance based on the availability of resources. As defined by the authors, the recommendations are stratified according to the following categories:
- Basic resources – “Core resources or fundamental services that are absolutely necessary for any cancer health care system to function.”
- Limited resources – “Second-tier resources or services that are intended to produce major improvements in outcome, such as increased survival and cost effectiveness, and are attainable with limited financial means and modest infrastructure.”
- Enhanced resources – “Third-tier resources or services that are optional but important; enhanced-level resources should produce further improvements in outcome and increase the number and quality of options and patient choice.”
- Maximal resources – “High-level/state-of-the art resources or services that may be used/available in some high-resource regions and/or may be recommended by high-resource setting guidelines that do not adapt to resource constraints but that nonetheless should be considered a lower priority than those resources or services listed in the other categories on the basis of extreme cost and/or impracticality for broad use in a resource-limited environment.”
The guidelines address common elements of symptom management for patients with acute disease, such as diagnosis involving the primary tumor, endoscopy when possible, and staging to include digital rectal exam and/or imaging when possible. The guidelines also include information tailored to resource level about chemotherapy and surgical resection.
“If, for example, a patient presents with bleeding and you suspect it to be of colorectal origin, we make recommendations that if the patient has symptoms of obstruction and bleeding and is resectable, they should undergo surgery, which should be available in countries of all resource levels,” Dr. Chiorean said.
The guidelines also recommend following the ASCO palliative care guidelines (J Clin Oncol. 2017 Jan;35[1]:96-112) for those patients who present with clinically unstable disease because of bowel obstruction, uncontrolled bleeding, or uncontrolled pain. Patients with clinically stable disease and ongoing bleeding from the primary tumor site are recommended to undergo transfusion and primary-site resection if only basic resources are available or transfusion plus multidisciplinary specialized evaluation when higher-level resources are available.
The ASCO guidelines are adapted from guidelines developed by Cancer Council Australia; the European Society for Medical Oncology; the National Institute for Health and Care Excellence, including separate recommendation for therapy combinations (https://www.nice.org.uk/guidance/ta212, https://www.nice.org.uk/guidance/ta439); and the National Comprehensive Cancer Network. Some of these guidelines have been updated since the creation of the ASCO guidelines.
ASCO funds the guideline development process. Dr. Chiorean and other authors disclosed relationships with multiple companies.
SOURCE: Chiorean EG et al. JCO Glob Oncol. 2020 Mar;6:414-38.
FROM JCO GLOBAL ONCOLOGY
COVID-19: Older patients with cancer especially vulnerable
For oncologists and other clinicians caring for patients with cancer, the COVID-19 pandemic represents a dynamic clinical challenge that is changing daily and that can feel overwhelming at times, say experts.
“Oncology clinicians are well versed in caring for immunosuppressed patients with cancer, of all ages,” Merry-Jennifer Markham, MD, interim chief of the Division of Hematology and Oncology at the University of Florida Health, Gainesville, told Medscape Medical News.
However, she emphasized that, during this COVID-19 outbreak, “we must be especially diligent about screening for symptoms and exposure, and we must recognize that our older patients with cancer may be especially vulnerable.”
Patients with cancer who are in active treatment are immunosuppressed and are more susceptible to infection and to complications from infection, Markham pointed out. “While we don’t yet have much data on how COVID-19 impacts patients with cancer, I have to suspect that patients undergoing active cancer treatment may be especially vulnerable to the more severe illness associated with COVID-19,” she said.
Indeed, a recent report from China that was published in the Lancet Oncology supports this. The authors suggest that patients with cancer are at higher risk for COVID-19 and have a worse prognosis if they become infected than do those without cancer.
Commonsense rules
Commonsense rules apply for all patients with cancer, regardless of age, said Markham. Measures include thorough handwashing, staying home when sick, and avoiding sick contacts.
Markham, who acts as an expert spokesperson for the American Society of Clinical Oncology, provides information on what patients with cancer need to know about COVID-19 at Cancer.net, the society’s website for patients with cancer.
“Unfortunately, this outbreak of COVID-19 is happening rapidly and in real time,” Markham noted. “The entire medical community is learning as we go, rather than having the luxury of years of evidence-based literature to guide us.”
Another expert agrees. “Unfortunately, there are not a lot of data on how COVID-19 affects cancer patients,” Cardinale Smith, MD, PhD, director of Quality for Cancer Services in the Mount Sinai Health System, New York City, said in an interview.
“We need to minimize the risk for patients and minimize our own exposure by treating this situation like we would a really bad flu season,” Smith told Medscape Medical News. “Some patients have had a bad outcome, but the vast majority do not. The best we can do is stay calm and focused.”
At Mount Sinai, for patients with cancer, routine, nonurgent appointments are being rescheduled for May, Smith said. Those in active treatment are screened by telephone 24 to 48 hours before arrival, after which they undergo a full risk assessment in an isolation room. Those with a respiratory infection are given a mask.
“Patients are very anxious and worried about COVID-19,” said Smith, who has young children and an elderly parent at home. “We don’t have all the answers, and this can heighten anxiety.”
To help allay fears, social workers are asking patients with cancer who express anxiety to discuss their concerns and provide information. A one-page handout on both flu and COVID-10 is available in the waiting room.
The Web portal MyChart gives patients access to updated information on COVID-19 precautions and provides links to the hospital website and to the US Centers for Disease Control and Prevention. Patients who are not feeling well can speak to someone or get answers if they have additional questions.
When counseling patients, Smith advises them to use “an abundance of caution” and to be creative in efforts to minimize risk. “My suggestion is to use FaceTime and Skype to connect and communicate with your community,” she said.
Some churches are conducting services via teleconferencing to minimize risk, and seniors’ centers that offer yoga and other classes are also beginning to provide services virtually, she pointed out.
Data from China
A report published February 14 in the Lancet Oncology appears to be the first analysis in the literature to focus on COVID-19 in patients with cancer.
“Patients with cancer are more susceptible to infection than individuals without cancer because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments, such as chemotherapy or surgery,” write the authors, led by Wenhua Liang, MD, of Guangzhou Medical University. However, in correspondence published in the Lancet Oncology, other experts in China question some of Liang’s and colleagues’ findings.
The report by Liang and colleagues concerns a prospective cohort of 1590 patients with COVID-19.
There were 2007 laboratory-confirmed cases of COVID-19 among patients admitted to 575 hospitals throughout China as of January 31. Of those cases, 417 were excluded from the analysis because of insufficient information regarding disease history.
The team reports that of 18 patients with cancer and COVID-19, 39% were at significantly higher risk for “severe events.” By comparison, of 1572 patients with COVID-19 who did not have cancer, 8% were at significantly higher risk (P = .0003). These events included rapid clinical deterioration that required admission to intensive care; invasive ventilation; or death.
Patients with cancer experienced a much more rapid deterioration in clinical status than did those without cancer. The median time to severe events was 13 days, vs 43 days (hazard ratio [HR] adjusted for age, 3.56; P < .0001).
The analysis also shows that patients who underwent chemotherapy or surgery in the past month had a 75% risk of experiencing clinically severe events, compared with a 43% risk for those who had not received recent treatment.
After adjusting for other risk factors, including age and smoking history, older age was the only risk factor for severe events (odds ratio [OR], 1.43; 95% confidence interval [CI], 0.97 – 2.12; P = .072), the study authors say.
Patients with lung cancer did not have a higher probability of severe events compared with patients with other cancer types (20% vs 62%, respectively; P = .294).
Liang and colleagues conclude that these findings provide “a timely reminder to physicians that more intensive attention should be paid to patients with cancer, in case of rapid deterioration.”
The team also proposes three strategies for managing patients with cancer who are at risk for COVID-19 or any other severe infectious disease. They recommend that intentional postponement of adjuvant chemotherapy or elective surgery be considered for patients with stable cancer who live in areas where disease is endemic. Stronger “personal protection provisions” could also be made for patients with cancer or for cancer survivors. Lastly, for patients with cancer who have COVID-19, especially those who are older or who have comorbidities, more intensive surveillance or treatment should be considered.
However, in comments in the Lancet Oncology, other authors in China say these findings should be interpreted with caution.
One group suggests that the increased susceptibility to COVID-19 in patients with cancer could be the result of higher rates of smoking compared with patients who did not have cancer. “Overall, current evidence remains insufficient to explain a conclusive association between cancer and COVID-19,” say Huahao Shen, PhD, of Zhejiang University School of Medicine, Hangzhou, Zhejiang, and colleagues.
Another group suggests that the significantly higher median age of patients with cancer compared with noncancer patients (63 years vs 49 years) may have contributed to poor prognosis.
These authors, led by Li Zhang, MD, PhD, and Hanping Wang, MD, of Peking Union Medical College and the Chinese Academy of Medical Sciences, Beijing, emphasize that patients with cancer need online medical counseling and that critical cases need to be identified and treated.
“In endemic areas outside Wuhan, decisions on whether or not to postpone cancer treatment need to made on a patient-by-patient basis and according to the risk to the patient and the prevailing situation because delays could lead to tumor progression and ultimately poorer outcomes,” they write.
The study was funded by the China National Science Foundation and the Key Project of Guangzhou Scientific Research Project. Liang and coauthors, Shen and coauthors, Zhang, Wang, and Smith have disclosed no relevant financial relationships. Markham has relationships with Aduro Biotech, Lilly, Tesaro, Novartis, and VBL Therapeutics.
This article first appeared on Medscape.com.
For oncologists and other clinicians caring for patients with cancer, the COVID-19 pandemic represents a dynamic clinical challenge that is changing daily and that can feel overwhelming at times, say experts.
“Oncology clinicians are well versed in caring for immunosuppressed patients with cancer, of all ages,” Merry-Jennifer Markham, MD, interim chief of the Division of Hematology and Oncology at the University of Florida Health, Gainesville, told Medscape Medical News.
However, she emphasized that, during this COVID-19 outbreak, “we must be especially diligent about screening for symptoms and exposure, and we must recognize that our older patients with cancer may be especially vulnerable.”
Patients with cancer who are in active treatment are immunosuppressed and are more susceptible to infection and to complications from infection, Markham pointed out. “While we don’t yet have much data on how COVID-19 impacts patients with cancer, I have to suspect that patients undergoing active cancer treatment may be especially vulnerable to the more severe illness associated with COVID-19,” she said.
Indeed, a recent report from China that was published in the Lancet Oncology supports this. The authors suggest that patients with cancer are at higher risk for COVID-19 and have a worse prognosis if they become infected than do those without cancer.
Commonsense rules
Commonsense rules apply for all patients with cancer, regardless of age, said Markham. Measures include thorough handwashing, staying home when sick, and avoiding sick contacts.
Markham, who acts as an expert spokesperson for the American Society of Clinical Oncology, provides information on what patients with cancer need to know about COVID-19 at Cancer.net, the society’s website for patients with cancer.
“Unfortunately, this outbreak of COVID-19 is happening rapidly and in real time,” Markham noted. “The entire medical community is learning as we go, rather than having the luxury of years of evidence-based literature to guide us.”
Another expert agrees. “Unfortunately, there are not a lot of data on how COVID-19 affects cancer patients,” Cardinale Smith, MD, PhD, director of Quality for Cancer Services in the Mount Sinai Health System, New York City, said in an interview.
“We need to minimize the risk for patients and minimize our own exposure by treating this situation like we would a really bad flu season,” Smith told Medscape Medical News. “Some patients have had a bad outcome, but the vast majority do not. The best we can do is stay calm and focused.”
At Mount Sinai, for patients with cancer, routine, nonurgent appointments are being rescheduled for May, Smith said. Those in active treatment are screened by telephone 24 to 48 hours before arrival, after which they undergo a full risk assessment in an isolation room. Those with a respiratory infection are given a mask.
“Patients are very anxious and worried about COVID-19,” said Smith, who has young children and an elderly parent at home. “We don’t have all the answers, and this can heighten anxiety.”
To help allay fears, social workers are asking patients with cancer who express anxiety to discuss their concerns and provide information. A one-page handout on both flu and COVID-10 is available in the waiting room.
The Web portal MyChart gives patients access to updated information on COVID-19 precautions and provides links to the hospital website and to the US Centers for Disease Control and Prevention. Patients who are not feeling well can speak to someone or get answers if they have additional questions.
When counseling patients, Smith advises them to use “an abundance of caution” and to be creative in efforts to minimize risk. “My suggestion is to use FaceTime and Skype to connect and communicate with your community,” she said.
Some churches are conducting services via teleconferencing to minimize risk, and seniors’ centers that offer yoga and other classes are also beginning to provide services virtually, she pointed out.
Data from China
A report published February 14 in the Lancet Oncology appears to be the first analysis in the literature to focus on COVID-19 in patients with cancer.
“Patients with cancer are more susceptible to infection than individuals without cancer because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments, such as chemotherapy or surgery,” write the authors, led by Wenhua Liang, MD, of Guangzhou Medical University. However, in correspondence published in the Lancet Oncology, other experts in China question some of Liang’s and colleagues’ findings.
The report by Liang and colleagues concerns a prospective cohort of 1590 patients with COVID-19.
There were 2007 laboratory-confirmed cases of COVID-19 among patients admitted to 575 hospitals throughout China as of January 31. Of those cases, 417 were excluded from the analysis because of insufficient information regarding disease history.
The team reports that of 18 patients with cancer and COVID-19, 39% were at significantly higher risk for “severe events.” By comparison, of 1572 patients with COVID-19 who did not have cancer, 8% were at significantly higher risk (P = .0003). These events included rapid clinical deterioration that required admission to intensive care; invasive ventilation; or death.
Patients with cancer experienced a much more rapid deterioration in clinical status than did those without cancer. The median time to severe events was 13 days, vs 43 days (hazard ratio [HR] adjusted for age, 3.56; P < .0001).
The analysis also shows that patients who underwent chemotherapy or surgery in the past month had a 75% risk of experiencing clinically severe events, compared with a 43% risk for those who had not received recent treatment.
After adjusting for other risk factors, including age and smoking history, older age was the only risk factor for severe events (odds ratio [OR], 1.43; 95% confidence interval [CI], 0.97 – 2.12; P = .072), the study authors say.
Patients with lung cancer did not have a higher probability of severe events compared with patients with other cancer types (20% vs 62%, respectively; P = .294).
Liang and colleagues conclude that these findings provide “a timely reminder to physicians that more intensive attention should be paid to patients with cancer, in case of rapid deterioration.”
The team also proposes three strategies for managing patients with cancer who are at risk for COVID-19 or any other severe infectious disease. They recommend that intentional postponement of adjuvant chemotherapy or elective surgery be considered for patients with stable cancer who live in areas where disease is endemic. Stronger “personal protection provisions” could also be made for patients with cancer or for cancer survivors. Lastly, for patients with cancer who have COVID-19, especially those who are older or who have comorbidities, more intensive surveillance or treatment should be considered.
However, in comments in the Lancet Oncology, other authors in China say these findings should be interpreted with caution.
One group suggests that the increased susceptibility to COVID-19 in patients with cancer could be the result of higher rates of smoking compared with patients who did not have cancer. “Overall, current evidence remains insufficient to explain a conclusive association between cancer and COVID-19,” say Huahao Shen, PhD, of Zhejiang University School of Medicine, Hangzhou, Zhejiang, and colleagues.
Another group suggests that the significantly higher median age of patients with cancer compared with noncancer patients (63 years vs 49 years) may have contributed to poor prognosis.
These authors, led by Li Zhang, MD, PhD, and Hanping Wang, MD, of Peking Union Medical College and the Chinese Academy of Medical Sciences, Beijing, emphasize that patients with cancer need online medical counseling and that critical cases need to be identified and treated.
“In endemic areas outside Wuhan, decisions on whether or not to postpone cancer treatment need to made on a patient-by-patient basis and according to the risk to the patient and the prevailing situation because delays could lead to tumor progression and ultimately poorer outcomes,” they write.
The study was funded by the China National Science Foundation and the Key Project of Guangzhou Scientific Research Project. Liang and coauthors, Shen and coauthors, Zhang, Wang, and Smith have disclosed no relevant financial relationships. Markham has relationships with Aduro Biotech, Lilly, Tesaro, Novartis, and VBL Therapeutics.
This article first appeared on Medscape.com.
For oncologists and other clinicians caring for patients with cancer, the COVID-19 pandemic represents a dynamic clinical challenge that is changing daily and that can feel overwhelming at times, say experts.
“Oncology clinicians are well versed in caring for immunosuppressed patients with cancer, of all ages,” Merry-Jennifer Markham, MD, interim chief of the Division of Hematology and Oncology at the University of Florida Health, Gainesville, told Medscape Medical News.
However, she emphasized that, during this COVID-19 outbreak, “we must be especially diligent about screening for symptoms and exposure, and we must recognize that our older patients with cancer may be especially vulnerable.”
Patients with cancer who are in active treatment are immunosuppressed and are more susceptible to infection and to complications from infection, Markham pointed out. “While we don’t yet have much data on how COVID-19 impacts patients with cancer, I have to suspect that patients undergoing active cancer treatment may be especially vulnerable to the more severe illness associated with COVID-19,” she said.
Indeed, a recent report from China that was published in the Lancet Oncology supports this. The authors suggest that patients with cancer are at higher risk for COVID-19 and have a worse prognosis if they become infected than do those without cancer.
Commonsense rules
Commonsense rules apply for all patients with cancer, regardless of age, said Markham. Measures include thorough handwashing, staying home when sick, and avoiding sick contacts.
Markham, who acts as an expert spokesperson for the American Society of Clinical Oncology, provides information on what patients with cancer need to know about COVID-19 at Cancer.net, the society’s website for patients with cancer.
“Unfortunately, this outbreak of COVID-19 is happening rapidly and in real time,” Markham noted. “The entire medical community is learning as we go, rather than having the luxury of years of evidence-based literature to guide us.”
Another expert agrees. “Unfortunately, there are not a lot of data on how COVID-19 affects cancer patients,” Cardinale Smith, MD, PhD, director of Quality for Cancer Services in the Mount Sinai Health System, New York City, said in an interview.
“We need to minimize the risk for patients and minimize our own exposure by treating this situation like we would a really bad flu season,” Smith told Medscape Medical News. “Some patients have had a bad outcome, but the vast majority do not. The best we can do is stay calm and focused.”
At Mount Sinai, for patients with cancer, routine, nonurgent appointments are being rescheduled for May, Smith said. Those in active treatment are screened by telephone 24 to 48 hours before arrival, after which they undergo a full risk assessment in an isolation room. Those with a respiratory infection are given a mask.
“Patients are very anxious and worried about COVID-19,” said Smith, who has young children and an elderly parent at home. “We don’t have all the answers, and this can heighten anxiety.”
To help allay fears, social workers are asking patients with cancer who express anxiety to discuss their concerns and provide information. A one-page handout on both flu and COVID-10 is available in the waiting room.
The Web portal MyChart gives patients access to updated information on COVID-19 precautions and provides links to the hospital website and to the US Centers for Disease Control and Prevention. Patients who are not feeling well can speak to someone or get answers if they have additional questions.
When counseling patients, Smith advises them to use “an abundance of caution” and to be creative in efforts to minimize risk. “My suggestion is to use FaceTime and Skype to connect and communicate with your community,” she said.
Some churches are conducting services via teleconferencing to minimize risk, and seniors’ centers that offer yoga and other classes are also beginning to provide services virtually, she pointed out.
Data from China
A report published February 14 in the Lancet Oncology appears to be the first analysis in the literature to focus on COVID-19 in patients with cancer.
“Patients with cancer are more susceptible to infection than individuals without cancer because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments, such as chemotherapy or surgery,” write the authors, led by Wenhua Liang, MD, of Guangzhou Medical University. However, in correspondence published in the Lancet Oncology, other experts in China question some of Liang’s and colleagues’ findings.
The report by Liang and colleagues concerns a prospective cohort of 1590 patients with COVID-19.
There were 2007 laboratory-confirmed cases of COVID-19 among patients admitted to 575 hospitals throughout China as of January 31. Of those cases, 417 were excluded from the analysis because of insufficient information regarding disease history.
The team reports that of 18 patients with cancer and COVID-19, 39% were at significantly higher risk for “severe events.” By comparison, of 1572 patients with COVID-19 who did not have cancer, 8% were at significantly higher risk (P = .0003). These events included rapid clinical deterioration that required admission to intensive care; invasive ventilation; or death.
Patients with cancer experienced a much more rapid deterioration in clinical status than did those without cancer. The median time to severe events was 13 days, vs 43 days (hazard ratio [HR] adjusted for age, 3.56; P < .0001).
The analysis also shows that patients who underwent chemotherapy or surgery in the past month had a 75% risk of experiencing clinically severe events, compared with a 43% risk for those who had not received recent treatment.
After adjusting for other risk factors, including age and smoking history, older age was the only risk factor for severe events (odds ratio [OR], 1.43; 95% confidence interval [CI], 0.97 – 2.12; P = .072), the study authors say.
Patients with lung cancer did not have a higher probability of severe events compared with patients with other cancer types (20% vs 62%, respectively; P = .294).
Liang and colleagues conclude that these findings provide “a timely reminder to physicians that more intensive attention should be paid to patients with cancer, in case of rapid deterioration.”
The team also proposes three strategies for managing patients with cancer who are at risk for COVID-19 or any other severe infectious disease. They recommend that intentional postponement of adjuvant chemotherapy or elective surgery be considered for patients with stable cancer who live in areas where disease is endemic. Stronger “personal protection provisions” could also be made for patients with cancer or for cancer survivors. Lastly, for patients with cancer who have COVID-19, especially those who are older or who have comorbidities, more intensive surveillance or treatment should be considered.
However, in comments in the Lancet Oncology, other authors in China say these findings should be interpreted with caution.
One group suggests that the increased susceptibility to COVID-19 in patients with cancer could be the result of higher rates of smoking compared with patients who did not have cancer. “Overall, current evidence remains insufficient to explain a conclusive association between cancer and COVID-19,” say Huahao Shen, PhD, of Zhejiang University School of Medicine, Hangzhou, Zhejiang, and colleagues.
Another group suggests that the significantly higher median age of patients with cancer compared with noncancer patients (63 years vs 49 years) may have contributed to poor prognosis.
These authors, led by Li Zhang, MD, PhD, and Hanping Wang, MD, of Peking Union Medical College and the Chinese Academy of Medical Sciences, Beijing, emphasize that patients with cancer need online medical counseling and that critical cases need to be identified and treated.
“In endemic areas outside Wuhan, decisions on whether or not to postpone cancer treatment need to made on a patient-by-patient basis and according to the risk to the patient and the prevailing situation because delays could lead to tumor progression and ultimately poorer outcomes,” they write.
The study was funded by the China National Science Foundation and the Key Project of Guangzhou Scientific Research Project. Liang and coauthors, Shen and coauthors, Zhang, Wang, and Smith have disclosed no relevant financial relationships. Markham has relationships with Aduro Biotech, Lilly, Tesaro, Novartis, and VBL Therapeutics.
This article first appeared on Medscape.com.




