User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
New reports help nail down myocarditis risk with COVID-19 vaccine
Recent literature features new descriptions of myocarditis linked to the two available mRNA vaccines against SARS-CoV-2. They tell a story largely consistent with experience to date, and support what might be its most useful public health message: The associated myocarditis is usually mild and self-limiting, and is far less likely to occur than myocarditis or death in unvaccinated people with COVID-19.
In line with previous research, the new analyses suggest the myocarditis – with onset usually a few days to a week after injection – has an overall incidence that ranges from less than 1 to perhaps 3 per 100,000 people who received at least one of the full mRNA-vaccine regimen’s two injections. Also, as in earlier studies, the incidence climbed higher – sometimes sharply – in certain groups by age and sex, particularly in young men and older male teens.
The new studies “are confirmatory, in terms of the risk being low,” but underscore that clinicians still must be wary of myocarditis as a potential complication of the mRNA vaccines, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
Dr. Bozkurt, a leading heart failure specialist and researcher, did not contribute to any of the new reports but does study the myocarditis of COVID-19 and was lead author on a recent review of the potential vaccine complication’s features and possible mechanisms.
In the new myocarditis reports, she observed, more than 90% of the cases were mild and “resolved on their own without a major adverse outcome.” Dr. Bozkurt emphasized the need for perspective regarding the risk. For example, the myocarditis associated with SARS-CoV-2 infection is not only more likely than the vaccine-related myocarditis, but it’s also usually far more severe.
Dr. Bozkurt pointed to a recent study in which the mRNA vaccines, compared with no vaccination, appeared to escalate the myocarditis risk by a factor of 3, whereas the risk for myocarditis in SARS-CoV-2 infection was increased 18 times.
In contrast, she observed, the new myocarditis cases reported this week feature a few that are novel or are at least very rare, including the case of a patient who developed cardiogenic shock and another with fulminant myocarditis who died.
The Centers for Disease Control and Prevention in May publicly described the apparent link between myocarditis and the two available mRNA vaccines against SARS-CoV-2: BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). The next month, the Food and Drug Administration added a warning about the risk to the labeling.
Less than 1 case per 100,000
Fifteen confirmed cases of myocarditis were identified among about 2.4 million members of Kaiser Permanente Southern California aged 18 or older who received at least one injection of the Pfizer or Moderna mRNA vaccines between December 2020 and July 2021, in a report published in JAMA Internal Medicine. The study counted cases up to 10 days after the first or second injection, of which there were 2 and 13, respectively.
All eight patients who received the Pfizer BNT162b2 vaccine and the eight given the Moderna mRNA-1273 vaccine were male with a median age of 25 years (interquartile range, 20-32 years).
“The main takeaway messages from our study are that the incidence of myocarditis after COVID-19 mRNA vaccinations is very low, that this condition is primarily observed in young men within a few days after the second dose, and that most patients recover quickly,” senior author Mingsum Lee, MD, PhD, Kaiser Permanente Los Angeles Medical Center, told this news organization.
“The incidence of vaccine-related myocarditis was significantly lower than rates of COVID-19 hospitalization during the same period and population area,” she added.
The group saw a per-million incidence of 0.8 and 5.8 myocarditis cases in the 10 days after first and second injections, respectively. That made for an incidence of 0.58 per 100,000, or 1 case per 172,414 fully vaccinated adults.
The group also considered a cohort of 1,577,741 unvaccinated people with a median age of 39 years (interquartile range, 28-53 years) during the same period. Of the 75 cases of myocarditis, 52% were in men, they reported.
Comparing the vaccinated and unvaccinated cohorts, they saw a 10-day vaccine-associated myocarditis incidence rate ratio of 0.38 (95% confidence interval, 0.05-1.40; P = .15) after the first dose, and 2.7 (95% CI, 1.4-4.8; P = .004) after the second dose.
In a comparison of the vaccinated group with itself using data from a 10-day period in the previous year, the corresponding myocarditis IRRs were 1.0 (P > .99) and 3.3 (P = .03), respectively.
Dr. Lee said none of the 15 patients required admission to an intensive care unit. “All patients with myocarditis responded well to treatment and felt better quickly,” she noted.
Myocarditis after an mRNA vaccine injection is rare and, Dr. Lee said emphatically, and “the benefits of the COVID-19 vaccine greatly outweigh the risks.”
Sex- and age-stratified rates
In a separate analysis of 5,442,696 people given a first dose of the Pfizer BNT162b2 vaccine and 5,125,635 given a second dose, there were 142 cases of myocarditis with onset 21 days after dose 1 and 30 days after dose 2. Of those cases, 136 were documented as “definite or probable” in an Israeli Ministry of Health database that covered up to the end of May 2021.
There were also 40 cases among vaccinated people seen after the 30-day window, which were considered not related to the vaccination, and 101 cases among unvaccinated people; of the latter, 29 had confirmed diagnoses of COVID-19.
Of the 136 people with definite or probable cases, the myocarditis was “generally mild” in 129 and usually resolved on its own, notes the report on the study, published in the New England Journal of Medicine, with lead author Dror Mevorach, MD, Hadassah-Hebrew University Medical Center, Jerusalem.
The estimated myocarditis incidence after a second such vaccine dose across the entire Israeli population, based on the current study, was about one per 26,000 males and one per 218,000 females, the group writes. Those figures compare with one case per 10,857 among “the general unvaccinated population.”
Again, the risk was concentrated among younger men and male adolescents. In an analysis limited to vaccinated people aged 16-19 years, myocarditis in the 21 days after a second mRNA injection was seen in about one of 6,637 males and one of 99,853 females, the group reported.
The standardized incidence ratio of 5.34 (95% CI, 4.48-6.40) after a second injection, across all groups, “was driven mostly by the diagnosis of myocarditis in younger male recipients.” Among that male subgroup, the ratios by age group were 13.60 (95% CI, 9.30-19.20) for 16-19 years, 8.53 (95% CI, 5.57-12.50) for 20-24 years, and 6.96 (95% CI, 4.25-10.75) for 25-29 years.
Among people who received a second injection, compared with unvaccinated people, the 30-day rate ratio was 2.35 (95% CI, 1.10-5.02). Again, the effect was concentrated in males aged 16-19 years. Among them, the myocarditis rate ratios in the 30 days after a second mRNA vaccine injection were 8.96 (95% CI, 4.50-17.83) for the 16-19 years group, 6.13 (95% CI, 3.16-11.88) for the 20-24 group, and 3.58 (95% CI, 1.82-7.01) for 25-29 years.
Most of the patients with myocarditis showed “significant clinical improvement,” with a mean hospitalization time of only 3-4 days, the report notes. Treatment consisted of nonsteroidal anti-inflammatory drugs “with or without colchicine for presumed pericardial inflammation.”
However, seven patients (4.9%) developed important complications, including left-ventricular dysfunction, ventricular arrhythmias, and heart failure. Among them was a 22-year-old patient who died of fulminant myocarditis within 24 hours of diagnosis, the group wrote.
From an Israeli health care organization
Published by the same journal as the study by Dr. Menvorach and associates, an analysis of a separate database showed largely consistent findings among patients in the largest of Israel’s four health care organizations charged by the government to administer health services.
The report, with authors led by Guy Witberg, MD, Rabin Medical Center, Petah Tikva, Israel, focused on members of the health care organization aged 16 years or older who had received at least one Pfizer mRNA vaccine dose by the end of May 2021.
The cohorts from the two separate reports surely overlap substantially, as the Ministry of Health analysis from Dr. Mevorach and colleagues derived from a nationwide database, and – as Dr. Witberg and associates wrote – the health care organization providing their data covers 52% of the Israeli population.
Of 2,558,421 vaccinated people in the analysis, of whom 94% received two doses, 54 developed confirmed myocarditis in the 42 days after the first dose. Their median age was 27 years (interquartile range, 21-35 years) and all but three (94%) were male. Of those 54 cases, 41 were considered mild and 12 intermediate in severity, and one was fulminant with the patient in cardiogenic shock, the group writes. In addition, nonsustained ventricular tachycardia and atrial fibrillation developed in 5% and 3% of cases, respectively.
The estimated myocarditis incidence in the 42 days after administration of at least one mRNA vaccine dose was 2.13 per 100,000 vaccinated people. In that group, Dr. Witberg and colleagues note, the corresponding incidences per 100,000 were 4.12 and 0.23 for males and females, respectively.
Also in the current report, incidences per 100,000 vaccinated people aged 16-29 years, by sex, included 5.49 (95% CI, 3.59-7.39) overall, and 10.69 (95% CI, 6.93-14.46) for males (the highest rate in the report).
There was only one case in a female aged 16-29 years, and two cases in females 30 years or older.
Of note, some authors of the current study are also authors on the high-profile report from Noam Barda, MD, and colleagues published in the New England Journal of Medicine, that used the same database to arrive at an mRNA-vaccine-related incidence of myocarditis of 2.7 per 100,000. Eligibility criteria and follow-up time were different in that report, as were case ascertainment criteria.
The myocarditis risk associated with the two mRNA vaccines is small compared with “the morbidity and mortality of COVID-19 infection, in which up to 28% of hospitalized patients showed signs of myocardial injury,” wrote Vinay Guduguntla, MD, University of California, San Francisco, and Mitchell H. Katz, MD, NYC Health + Hospitals, New York, in an editorial accompanying the report from Dr. Lee and associates.
“Randomized clinical trials show that COVID-19 mRNA vaccines represent a safe and effective method of preventing infection,” they stated. “The identification of rare myocarditis does not change clinical decision-making.”
Dr. Bozkurt, who is immediate past president of the Heart Failure Society of America, has disclosed consulting for Bayer and scPharmaceuticals and serving on a clinical events committee for a trial supported by Abbott Pharmaceuticals and on a data and safety monitoring board for a trial supported by Liva Nova Pharmaceuticals. Dr. Lee and the report’s other authors had no disclosures. Dr. Mevorach discloses consulting for Enlivex Therapeutics; disclosures for the other authors are available at NEJM.org. Dr. Witberg said he has no interests to disclose; disclosures for the other authors are available at NEJM.org. Dr. Guduguntla is an editorial fellow and Dr. Katz a deputy editor at JAMA Internal Medicine; neither had disclosures.
A version of this article first appeared on Medscape.com.
Recent literature features new descriptions of myocarditis linked to the two available mRNA vaccines against SARS-CoV-2. They tell a story largely consistent with experience to date, and support what might be its most useful public health message: The associated myocarditis is usually mild and self-limiting, and is far less likely to occur than myocarditis or death in unvaccinated people with COVID-19.
In line with previous research, the new analyses suggest the myocarditis – with onset usually a few days to a week after injection – has an overall incidence that ranges from less than 1 to perhaps 3 per 100,000 people who received at least one of the full mRNA-vaccine regimen’s two injections. Also, as in earlier studies, the incidence climbed higher – sometimes sharply – in certain groups by age and sex, particularly in young men and older male teens.
The new studies “are confirmatory, in terms of the risk being low,” but underscore that clinicians still must be wary of myocarditis as a potential complication of the mRNA vaccines, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
Dr. Bozkurt, a leading heart failure specialist and researcher, did not contribute to any of the new reports but does study the myocarditis of COVID-19 and was lead author on a recent review of the potential vaccine complication’s features and possible mechanisms.
In the new myocarditis reports, she observed, more than 90% of the cases were mild and “resolved on their own without a major adverse outcome.” Dr. Bozkurt emphasized the need for perspective regarding the risk. For example, the myocarditis associated with SARS-CoV-2 infection is not only more likely than the vaccine-related myocarditis, but it’s also usually far more severe.
Dr. Bozkurt pointed to a recent study in which the mRNA vaccines, compared with no vaccination, appeared to escalate the myocarditis risk by a factor of 3, whereas the risk for myocarditis in SARS-CoV-2 infection was increased 18 times.
In contrast, she observed, the new myocarditis cases reported this week feature a few that are novel or are at least very rare, including the case of a patient who developed cardiogenic shock and another with fulminant myocarditis who died.
The Centers for Disease Control and Prevention in May publicly described the apparent link between myocarditis and the two available mRNA vaccines against SARS-CoV-2: BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). The next month, the Food and Drug Administration added a warning about the risk to the labeling.
Less than 1 case per 100,000
Fifteen confirmed cases of myocarditis were identified among about 2.4 million members of Kaiser Permanente Southern California aged 18 or older who received at least one injection of the Pfizer or Moderna mRNA vaccines between December 2020 and July 2021, in a report published in JAMA Internal Medicine. The study counted cases up to 10 days after the first or second injection, of which there were 2 and 13, respectively.
All eight patients who received the Pfizer BNT162b2 vaccine and the eight given the Moderna mRNA-1273 vaccine were male with a median age of 25 years (interquartile range, 20-32 years).
“The main takeaway messages from our study are that the incidence of myocarditis after COVID-19 mRNA vaccinations is very low, that this condition is primarily observed in young men within a few days after the second dose, and that most patients recover quickly,” senior author Mingsum Lee, MD, PhD, Kaiser Permanente Los Angeles Medical Center, told this news organization.
“The incidence of vaccine-related myocarditis was significantly lower than rates of COVID-19 hospitalization during the same period and population area,” she added.
The group saw a per-million incidence of 0.8 and 5.8 myocarditis cases in the 10 days after first and second injections, respectively. That made for an incidence of 0.58 per 100,000, or 1 case per 172,414 fully vaccinated adults.
The group also considered a cohort of 1,577,741 unvaccinated people with a median age of 39 years (interquartile range, 28-53 years) during the same period. Of the 75 cases of myocarditis, 52% were in men, they reported.
Comparing the vaccinated and unvaccinated cohorts, they saw a 10-day vaccine-associated myocarditis incidence rate ratio of 0.38 (95% confidence interval, 0.05-1.40; P = .15) after the first dose, and 2.7 (95% CI, 1.4-4.8; P = .004) after the second dose.
In a comparison of the vaccinated group with itself using data from a 10-day period in the previous year, the corresponding myocarditis IRRs were 1.0 (P > .99) and 3.3 (P = .03), respectively.
Dr. Lee said none of the 15 patients required admission to an intensive care unit. “All patients with myocarditis responded well to treatment and felt better quickly,” she noted.
Myocarditis after an mRNA vaccine injection is rare and, Dr. Lee said emphatically, and “the benefits of the COVID-19 vaccine greatly outweigh the risks.”
Sex- and age-stratified rates
In a separate analysis of 5,442,696 people given a first dose of the Pfizer BNT162b2 vaccine and 5,125,635 given a second dose, there were 142 cases of myocarditis with onset 21 days after dose 1 and 30 days after dose 2. Of those cases, 136 were documented as “definite or probable” in an Israeli Ministry of Health database that covered up to the end of May 2021.
There were also 40 cases among vaccinated people seen after the 30-day window, which were considered not related to the vaccination, and 101 cases among unvaccinated people; of the latter, 29 had confirmed diagnoses of COVID-19.
Of the 136 people with definite or probable cases, the myocarditis was “generally mild” in 129 and usually resolved on its own, notes the report on the study, published in the New England Journal of Medicine, with lead author Dror Mevorach, MD, Hadassah-Hebrew University Medical Center, Jerusalem.
The estimated myocarditis incidence after a second such vaccine dose across the entire Israeli population, based on the current study, was about one per 26,000 males and one per 218,000 females, the group writes. Those figures compare with one case per 10,857 among “the general unvaccinated population.”
Again, the risk was concentrated among younger men and male adolescents. In an analysis limited to vaccinated people aged 16-19 years, myocarditis in the 21 days after a second mRNA injection was seen in about one of 6,637 males and one of 99,853 females, the group reported.
The standardized incidence ratio of 5.34 (95% CI, 4.48-6.40) after a second injection, across all groups, “was driven mostly by the diagnosis of myocarditis in younger male recipients.” Among that male subgroup, the ratios by age group were 13.60 (95% CI, 9.30-19.20) for 16-19 years, 8.53 (95% CI, 5.57-12.50) for 20-24 years, and 6.96 (95% CI, 4.25-10.75) for 25-29 years.
Among people who received a second injection, compared with unvaccinated people, the 30-day rate ratio was 2.35 (95% CI, 1.10-5.02). Again, the effect was concentrated in males aged 16-19 years. Among them, the myocarditis rate ratios in the 30 days after a second mRNA vaccine injection were 8.96 (95% CI, 4.50-17.83) for the 16-19 years group, 6.13 (95% CI, 3.16-11.88) for the 20-24 group, and 3.58 (95% CI, 1.82-7.01) for 25-29 years.
Most of the patients with myocarditis showed “significant clinical improvement,” with a mean hospitalization time of only 3-4 days, the report notes. Treatment consisted of nonsteroidal anti-inflammatory drugs “with or without colchicine for presumed pericardial inflammation.”
However, seven patients (4.9%) developed important complications, including left-ventricular dysfunction, ventricular arrhythmias, and heart failure. Among them was a 22-year-old patient who died of fulminant myocarditis within 24 hours of diagnosis, the group wrote.
From an Israeli health care organization
Published by the same journal as the study by Dr. Menvorach and associates, an analysis of a separate database showed largely consistent findings among patients in the largest of Israel’s four health care organizations charged by the government to administer health services.
The report, with authors led by Guy Witberg, MD, Rabin Medical Center, Petah Tikva, Israel, focused on members of the health care organization aged 16 years or older who had received at least one Pfizer mRNA vaccine dose by the end of May 2021.
The cohorts from the two separate reports surely overlap substantially, as the Ministry of Health analysis from Dr. Mevorach and colleagues derived from a nationwide database, and – as Dr. Witberg and associates wrote – the health care organization providing their data covers 52% of the Israeli population.
Of 2,558,421 vaccinated people in the analysis, of whom 94% received two doses, 54 developed confirmed myocarditis in the 42 days after the first dose. Their median age was 27 years (interquartile range, 21-35 years) and all but three (94%) were male. Of those 54 cases, 41 were considered mild and 12 intermediate in severity, and one was fulminant with the patient in cardiogenic shock, the group writes. In addition, nonsustained ventricular tachycardia and atrial fibrillation developed in 5% and 3% of cases, respectively.
The estimated myocarditis incidence in the 42 days after administration of at least one mRNA vaccine dose was 2.13 per 100,000 vaccinated people. In that group, Dr. Witberg and colleagues note, the corresponding incidences per 100,000 were 4.12 and 0.23 for males and females, respectively.
Also in the current report, incidences per 100,000 vaccinated people aged 16-29 years, by sex, included 5.49 (95% CI, 3.59-7.39) overall, and 10.69 (95% CI, 6.93-14.46) for males (the highest rate in the report).
There was only one case in a female aged 16-29 years, and two cases in females 30 years or older.
Of note, some authors of the current study are also authors on the high-profile report from Noam Barda, MD, and colleagues published in the New England Journal of Medicine, that used the same database to arrive at an mRNA-vaccine-related incidence of myocarditis of 2.7 per 100,000. Eligibility criteria and follow-up time were different in that report, as were case ascertainment criteria.
The myocarditis risk associated with the two mRNA vaccines is small compared with “the morbidity and mortality of COVID-19 infection, in which up to 28% of hospitalized patients showed signs of myocardial injury,” wrote Vinay Guduguntla, MD, University of California, San Francisco, and Mitchell H. Katz, MD, NYC Health + Hospitals, New York, in an editorial accompanying the report from Dr. Lee and associates.
“Randomized clinical trials show that COVID-19 mRNA vaccines represent a safe and effective method of preventing infection,” they stated. “The identification of rare myocarditis does not change clinical decision-making.”
Dr. Bozkurt, who is immediate past president of the Heart Failure Society of America, has disclosed consulting for Bayer and scPharmaceuticals and serving on a clinical events committee for a trial supported by Abbott Pharmaceuticals and on a data and safety monitoring board for a trial supported by Liva Nova Pharmaceuticals. Dr. Lee and the report’s other authors had no disclosures. Dr. Mevorach discloses consulting for Enlivex Therapeutics; disclosures for the other authors are available at NEJM.org. Dr. Witberg said he has no interests to disclose; disclosures for the other authors are available at NEJM.org. Dr. Guduguntla is an editorial fellow and Dr. Katz a deputy editor at JAMA Internal Medicine; neither had disclosures.
A version of this article first appeared on Medscape.com.
Recent literature features new descriptions of myocarditis linked to the two available mRNA vaccines against SARS-CoV-2. They tell a story largely consistent with experience to date, and support what might be its most useful public health message: The associated myocarditis is usually mild and self-limiting, and is far less likely to occur than myocarditis or death in unvaccinated people with COVID-19.
In line with previous research, the new analyses suggest the myocarditis – with onset usually a few days to a week after injection – has an overall incidence that ranges from less than 1 to perhaps 3 per 100,000 people who received at least one of the full mRNA-vaccine regimen’s two injections. Also, as in earlier studies, the incidence climbed higher – sometimes sharply – in certain groups by age and sex, particularly in young men and older male teens.
The new studies “are confirmatory, in terms of the risk being low,” but underscore that clinicians still must be wary of myocarditis as a potential complication of the mRNA vaccines, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
Dr. Bozkurt, a leading heart failure specialist and researcher, did not contribute to any of the new reports but does study the myocarditis of COVID-19 and was lead author on a recent review of the potential vaccine complication’s features and possible mechanisms.
In the new myocarditis reports, she observed, more than 90% of the cases were mild and “resolved on their own without a major adverse outcome.” Dr. Bozkurt emphasized the need for perspective regarding the risk. For example, the myocarditis associated with SARS-CoV-2 infection is not only more likely than the vaccine-related myocarditis, but it’s also usually far more severe.
Dr. Bozkurt pointed to a recent study in which the mRNA vaccines, compared with no vaccination, appeared to escalate the myocarditis risk by a factor of 3, whereas the risk for myocarditis in SARS-CoV-2 infection was increased 18 times.
In contrast, she observed, the new myocarditis cases reported this week feature a few that are novel or are at least very rare, including the case of a patient who developed cardiogenic shock and another with fulminant myocarditis who died.
The Centers for Disease Control and Prevention in May publicly described the apparent link between myocarditis and the two available mRNA vaccines against SARS-CoV-2: BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). The next month, the Food and Drug Administration added a warning about the risk to the labeling.
Less than 1 case per 100,000
Fifteen confirmed cases of myocarditis were identified among about 2.4 million members of Kaiser Permanente Southern California aged 18 or older who received at least one injection of the Pfizer or Moderna mRNA vaccines between December 2020 and July 2021, in a report published in JAMA Internal Medicine. The study counted cases up to 10 days after the first or second injection, of which there were 2 and 13, respectively.
All eight patients who received the Pfizer BNT162b2 vaccine and the eight given the Moderna mRNA-1273 vaccine were male with a median age of 25 years (interquartile range, 20-32 years).
“The main takeaway messages from our study are that the incidence of myocarditis after COVID-19 mRNA vaccinations is very low, that this condition is primarily observed in young men within a few days after the second dose, and that most patients recover quickly,” senior author Mingsum Lee, MD, PhD, Kaiser Permanente Los Angeles Medical Center, told this news organization.
“The incidence of vaccine-related myocarditis was significantly lower than rates of COVID-19 hospitalization during the same period and population area,” she added.
The group saw a per-million incidence of 0.8 and 5.8 myocarditis cases in the 10 days after first and second injections, respectively. That made for an incidence of 0.58 per 100,000, or 1 case per 172,414 fully vaccinated adults.
The group also considered a cohort of 1,577,741 unvaccinated people with a median age of 39 years (interquartile range, 28-53 years) during the same period. Of the 75 cases of myocarditis, 52% were in men, they reported.
Comparing the vaccinated and unvaccinated cohorts, they saw a 10-day vaccine-associated myocarditis incidence rate ratio of 0.38 (95% confidence interval, 0.05-1.40; P = .15) after the first dose, and 2.7 (95% CI, 1.4-4.8; P = .004) after the second dose.
In a comparison of the vaccinated group with itself using data from a 10-day period in the previous year, the corresponding myocarditis IRRs were 1.0 (P > .99) and 3.3 (P = .03), respectively.
Dr. Lee said none of the 15 patients required admission to an intensive care unit. “All patients with myocarditis responded well to treatment and felt better quickly,” she noted.
Myocarditis after an mRNA vaccine injection is rare and, Dr. Lee said emphatically, and “the benefits of the COVID-19 vaccine greatly outweigh the risks.”
Sex- and age-stratified rates
In a separate analysis of 5,442,696 people given a first dose of the Pfizer BNT162b2 vaccine and 5,125,635 given a second dose, there were 142 cases of myocarditis with onset 21 days after dose 1 and 30 days after dose 2. Of those cases, 136 were documented as “definite or probable” in an Israeli Ministry of Health database that covered up to the end of May 2021.
There were also 40 cases among vaccinated people seen after the 30-day window, which were considered not related to the vaccination, and 101 cases among unvaccinated people; of the latter, 29 had confirmed diagnoses of COVID-19.
Of the 136 people with definite or probable cases, the myocarditis was “generally mild” in 129 and usually resolved on its own, notes the report on the study, published in the New England Journal of Medicine, with lead author Dror Mevorach, MD, Hadassah-Hebrew University Medical Center, Jerusalem.
The estimated myocarditis incidence after a second such vaccine dose across the entire Israeli population, based on the current study, was about one per 26,000 males and one per 218,000 females, the group writes. Those figures compare with one case per 10,857 among “the general unvaccinated population.”
Again, the risk was concentrated among younger men and male adolescents. In an analysis limited to vaccinated people aged 16-19 years, myocarditis in the 21 days after a second mRNA injection was seen in about one of 6,637 males and one of 99,853 females, the group reported.
The standardized incidence ratio of 5.34 (95% CI, 4.48-6.40) after a second injection, across all groups, “was driven mostly by the diagnosis of myocarditis in younger male recipients.” Among that male subgroup, the ratios by age group were 13.60 (95% CI, 9.30-19.20) for 16-19 years, 8.53 (95% CI, 5.57-12.50) for 20-24 years, and 6.96 (95% CI, 4.25-10.75) for 25-29 years.
Among people who received a second injection, compared with unvaccinated people, the 30-day rate ratio was 2.35 (95% CI, 1.10-5.02). Again, the effect was concentrated in males aged 16-19 years. Among them, the myocarditis rate ratios in the 30 days after a second mRNA vaccine injection were 8.96 (95% CI, 4.50-17.83) for the 16-19 years group, 6.13 (95% CI, 3.16-11.88) for the 20-24 group, and 3.58 (95% CI, 1.82-7.01) for 25-29 years.
Most of the patients with myocarditis showed “significant clinical improvement,” with a mean hospitalization time of only 3-4 days, the report notes. Treatment consisted of nonsteroidal anti-inflammatory drugs “with or without colchicine for presumed pericardial inflammation.”
However, seven patients (4.9%) developed important complications, including left-ventricular dysfunction, ventricular arrhythmias, and heart failure. Among them was a 22-year-old patient who died of fulminant myocarditis within 24 hours of diagnosis, the group wrote.
From an Israeli health care organization
Published by the same journal as the study by Dr. Menvorach and associates, an analysis of a separate database showed largely consistent findings among patients in the largest of Israel’s four health care organizations charged by the government to administer health services.
The report, with authors led by Guy Witberg, MD, Rabin Medical Center, Petah Tikva, Israel, focused on members of the health care organization aged 16 years or older who had received at least one Pfizer mRNA vaccine dose by the end of May 2021.
The cohorts from the two separate reports surely overlap substantially, as the Ministry of Health analysis from Dr. Mevorach and colleagues derived from a nationwide database, and – as Dr. Witberg and associates wrote – the health care organization providing their data covers 52% of the Israeli population.
Of 2,558,421 vaccinated people in the analysis, of whom 94% received two doses, 54 developed confirmed myocarditis in the 42 days after the first dose. Their median age was 27 years (interquartile range, 21-35 years) and all but three (94%) were male. Of those 54 cases, 41 were considered mild and 12 intermediate in severity, and one was fulminant with the patient in cardiogenic shock, the group writes. In addition, nonsustained ventricular tachycardia and atrial fibrillation developed in 5% and 3% of cases, respectively.
The estimated myocarditis incidence in the 42 days after administration of at least one mRNA vaccine dose was 2.13 per 100,000 vaccinated people. In that group, Dr. Witberg and colleagues note, the corresponding incidences per 100,000 were 4.12 and 0.23 for males and females, respectively.
Also in the current report, incidences per 100,000 vaccinated people aged 16-29 years, by sex, included 5.49 (95% CI, 3.59-7.39) overall, and 10.69 (95% CI, 6.93-14.46) for males (the highest rate in the report).
There was only one case in a female aged 16-29 years, and two cases in females 30 years or older.
Of note, some authors of the current study are also authors on the high-profile report from Noam Barda, MD, and colleagues published in the New England Journal of Medicine, that used the same database to arrive at an mRNA-vaccine-related incidence of myocarditis of 2.7 per 100,000. Eligibility criteria and follow-up time were different in that report, as were case ascertainment criteria.
The myocarditis risk associated with the two mRNA vaccines is small compared with “the morbidity and mortality of COVID-19 infection, in which up to 28% of hospitalized patients showed signs of myocardial injury,” wrote Vinay Guduguntla, MD, University of California, San Francisco, and Mitchell H. Katz, MD, NYC Health + Hospitals, New York, in an editorial accompanying the report from Dr. Lee and associates.
“Randomized clinical trials show that COVID-19 mRNA vaccines represent a safe and effective method of preventing infection,” they stated. “The identification of rare myocarditis does not change clinical decision-making.”
Dr. Bozkurt, who is immediate past president of the Heart Failure Society of America, has disclosed consulting for Bayer and scPharmaceuticals and serving on a clinical events committee for a trial supported by Abbott Pharmaceuticals and on a data and safety monitoring board for a trial supported by Liva Nova Pharmaceuticals. Dr. Lee and the report’s other authors had no disclosures. Dr. Mevorach discloses consulting for Enlivex Therapeutics; disclosures for the other authors are available at NEJM.org. Dr. Witberg said he has no interests to disclose; disclosures for the other authors are available at NEJM.org. Dr. Guduguntla is an editorial fellow and Dr. Katz a deputy editor at JAMA Internal Medicine; neither had disclosures.
A version of this article first appeared on Medscape.com.
Merck seeks FDA authorization for antiviral COVID-19 pill
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
, an experimental antiviral COVID-19 treatment.
If the FDA grants authorization, the drug would be the first oral antiviral treatment for COVID-19. The capsule, made by Merck and Ridgeback Biotherapeutics, is intended to treat mild to moderate COVID-19 in adults who are at risk of having severe COVID-19 or hospitalization.
“The extraordinary impact of this pandemic demands that we move with unprecedented urgency, and that is what our teams have done by submitting this application for molnupiravir to the FDA within 10 days of receiving the data,” Robert Davis, CEO and president of Merck, said in a statement. On Oct. 1, Merck and Ridgeback released interim data from its phase III clinical trial, which showed that molnupiravir reduced the risk of hospitalization or death by about 50%. About 7% of patients who received the drug were hospitalized within 30 days in the study, as compared with 14% of patients who took a placebo, the company said.
No deaths were reported in the group that received the drug, as compared with eight deaths in the group that received the placebo. None of the trial participants had been vaccinated.
“Medicines and vaccines are both essential to our collective efforts,” Mr. Davis said. “We look forward to working with the FDA on its review of our application, and to working with other regulatory agencies as we do everything we can to bring molnupiravir to patients around the world as quickly as possible.”
Merck has been producing molnupiravir in anticipation of the clinical trial results and FDA authorization. The company expects to produce 10 million courses of treatment by the end of the year, with more expected for 2022.
In June, Merck signed an agreement with the United States to supply 1.7 million courses of molnupiravir once the FDA authorizes the drug. The company has agreed to advance purchase agreements with other countries as well.
Earlier in the year, Merck also announced voluntary licensing agreements with several generics manufacturers in India to provide molnupiravir to more than 100 low- and middle-income countries after approval from local regulatory agencies.
Data from the company’s late-stage clinical trial has not yet been peer-reviewed or published.
Last week, Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said the clinical trial results were “very encouraging” but noted that the FDA should closely scrutinize the drug, CNN reported.
“It is very important that this now must go through the usual process of careful examination of the data by the Food and Drug Administration, both for effectiveness but also for safety, because whenever you introduce a new compound, safety is very important,” Dr. Fauci said, adding that vaccines remain “our best tools against COVID-19.”
A version of this article firsts appeared on WebMD.com.
High-dose omega-3s tied to higher AFib risk
Taking high-doses of marine omega-3 fatty acids, more than 1 gram daily, may raise the risk for atrial fibrillation (AFib), according to a meta-analysis of relevant research.
However, the risk of developing AFib appears to be “relatively small” for those taking 1 gram or less of fish oil per day, Christine M. Albert, MD, chair of the department of cardiology at the Smidt Heart Institute at Cedars-Sinai, Los Angeles, told this news organization.
The study was published online Oct. 6 in the journal Circulation.
It’s estimated that 7.8% of U.S. adults – almost 19 million in all – take fish oil supplements, often unbeknownst to their health care providers, the researchers noted. Yet, the literature on the effects of omega-3 fatty acid supplementation on cardiovascular outcomes are mixed.
“Some, but not all” large-scale randomized controlled trials investigating the effects of marine omega-3 fatty acid supplements on cardiovascular outcomes have reported increased risks for AFib. The potential reasons for differing findings may be dose related, the authors note in their paper.
The goal of this meta-analysis was to “bring clarity, answers, and actionable information” to doctors and patients, said Dr. Albert. The results suggest, however, that there may not be a “straightforward answer” to whether fish oil is good or bad for AFib. Instead, the answer may depend on the dose, she added.
Pooled data
After screening 4,049 articles and abstracts, the researchers included in their analysis seven large-scale randomized controlled trials reporting cardiovascular outcomes of marine omega-3 fatty acids.
The trials reported results for AFib, either as prespecified outcome, adverse event, or a reason for hospitalization. Each had a minimum of 500 patients and a median follow-up of at least 1 year.
Trials examining the effects of omega-3 fatty acids on recurrent AFib in patients with established AFib or postoperative AFib were excluded.
The seven trials enrolled a total of 81,210 patients (mean age, 65 years; 39% women); 72.6% of participants were enrolled in clinical trials testing ≤1 gram of marine omega-3 fatty acids per day and 27.4% were enrolled in clinical trials testing >1 gram of the supplement per day. The weighted average follow-up was 4.9 years.
Overall, use of omega-3 fatty acids was associated with a 25% increased risk for AFib (hazard ratio, 1.25; 95% confidence interval, 1.07-1.46; P = .013).
In analyses stratified by dose, the risk for AFib was “significantly more pronounced” in trials testing high doses of marine omega-3 fatty acid supplements (>1 gram per day: HR, 1.49; 95% CI, 1.04-2.15; P = .042) compared with those testing lower doses (≤1 gram per day: HR, 1.12; 95% CI, 1.03-1.22; P = .024; P for interaction < .001).
In meta-regression, the HR for AFib increased per 1 gram increase in daily omega-3 fatty acid dose (HR. 1.11; 95% CI, 1.06-1.15; P = .001).
Risk-benefit balance
“This meta-analysis adds new evidence regarding the risk of AFib in patients taking marine omega-3 fatty acid supplements,” wrote Dr. Albert and colleagues.
“Since the benefit of omega-3 fatty acids also appears to be dose dependent, the associated risk of AFib should be balanced against the benefit on atherosclerotic cardiovascular outcomes,” they suggested.
They cautioned that the meta-analysis pooled aggregate-level trial data, not individual patient data. Therefore, subgroup analyses by age or other patient level characteristics were not possible.
The risk of developing AFib increases with advancing age and is more common in men than in women. Additional risk factors include elevated blood pressure, coronary artery disease, heart failure, heart valve defects, obesity, and diabetes.
The authors said the potential risk of developing AFib with high doses of omega-3 fatty acid supplements should be discussed with patients and they should know the signs and symptoms of the condition.
The study had no specific funding. Dr. Albert has received grants from St. Jude Medical, Abbott, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
Taking high-doses of marine omega-3 fatty acids, more than 1 gram daily, may raise the risk for atrial fibrillation (AFib), according to a meta-analysis of relevant research.
However, the risk of developing AFib appears to be “relatively small” for those taking 1 gram or less of fish oil per day, Christine M. Albert, MD, chair of the department of cardiology at the Smidt Heart Institute at Cedars-Sinai, Los Angeles, told this news organization.
The study was published online Oct. 6 in the journal Circulation.
It’s estimated that 7.8% of U.S. adults – almost 19 million in all – take fish oil supplements, often unbeknownst to their health care providers, the researchers noted. Yet, the literature on the effects of omega-3 fatty acid supplementation on cardiovascular outcomes are mixed.
“Some, but not all” large-scale randomized controlled trials investigating the effects of marine omega-3 fatty acid supplements on cardiovascular outcomes have reported increased risks for AFib. The potential reasons for differing findings may be dose related, the authors note in their paper.
The goal of this meta-analysis was to “bring clarity, answers, and actionable information” to doctors and patients, said Dr. Albert. The results suggest, however, that there may not be a “straightforward answer” to whether fish oil is good or bad for AFib. Instead, the answer may depend on the dose, she added.
Pooled data
After screening 4,049 articles and abstracts, the researchers included in their analysis seven large-scale randomized controlled trials reporting cardiovascular outcomes of marine omega-3 fatty acids.
The trials reported results for AFib, either as prespecified outcome, adverse event, or a reason for hospitalization. Each had a minimum of 500 patients and a median follow-up of at least 1 year.
Trials examining the effects of omega-3 fatty acids on recurrent AFib in patients with established AFib or postoperative AFib were excluded.
The seven trials enrolled a total of 81,210 patients (mean age, 65 years; 39% women); 72.6% of participants were enrolled in clinical trials testing ≤1 gram of marine omega-3 fatty acids per day and 27.4% were enrolled in clinical trials testing >1 gram of the supplement per day. The weighted average follow-up was 4.9 years.
Overall, use of omega-3 fatty acids was associated with a 25% increased risk for AFib (hazard ratio, 1.25; 95% confidence interval, 1.07-1.46; P = .013).
In analyses stratified by dose, the risk for AFib was “significantly more pronounced” in trials testing high doses of marine omega-3 fatty acid supplements (>1 gram per day: HR, 1.49; 95% CI, 1.04-2.15; P = .042) compared with those testing lower doses (≤1 gram per day: HR, 1.12; 95% CI, 1.03-1.22; P = .024; P for interaction < .001).
In meta-regression, the HR for AFib increased per 1 gram increase in daily omega-3 fatty acid dose (HR. 1.11; 95% CI, 1.06-1.15; P = .001).
Risk-benefit balance
“This meta-analysis adds new evidence regarding the risk of AFib in patients taking marine omega-3 fatty acid supplements,” wrote Dr. Albert and colleagues.
“Since the benefit of omega-3 fatty acids also appears to be dose dependent, the associated risk of AFib should be balanced against the benefit on atherosclerotic cardiovascular outcomes,” they suggested.
They cautioned that the meta-analysis pooled aggregate-level trial data, not individual patient data. Therefore, subgroup analyses by age or other patient level characteristics were not possible.
The risk of developing AFib increases with advancing age and is more common in men than in women. Additional risk factors include elevated blood pressure, coronary artery disease, heart failure, heart valve defects, obesity, and diabetes.
The authors said the potential risk of developing AFib with high doses of omega-3 fatty acid supplements should be discussed with patients and they should know the signs and symptoms of the condition.
The study had no specific funding. Dr. Albert has received grants from St. Jude Medical, Abbott, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
Taking high-doses of marine omega-3 fatty acids, more than 1 gram daily, may raise the risk for atrial fibrillation (AFib), according to a meta-analysis of relevant research.
However, the risk of developing AFib appears to be “relatively small” for those taking 1 gram or less of fish oil per day, Christine M. Albert, MD, chair of the department of cardiology at the Smidt Heart Institute at Cedars-Sinai, Los Angeles, told this news organization.
The study was published online Oct. 6 in the journal Circulation.
It’s estimated that 7.8% of U.S. adults – almost 19 million in all – take fish oil supplements, often unbeknownst to their health care providers, the researchers noted. Yet, the literature on the effects of omega-3 fatty acid supplementation on cardiovascular outcomes are mixed.
“Some, but not all” large-scale randomized controlled trials investigating the effects of marine omega-3 fatty acid supplements on cardiovascular outcomes have reported increased risks for AFib. The potential reasons for differing findings may be dose related, the authors note in their paper.
The goal of this meta-analysis was to “bring clarity, answers, and actionable information” to doctors and patients, said Dr. Albert. The results suggest, however, that there may not be a “straightforward answer” to whether fish oil is good or bad for AFib. Instead, the answer may depend on the dose, she added.
Pooled data
After screening 4,049 articles and abstracts, the researchers included in their analysis seven large-scale randomized controlled trials reporting cardiovascular outcomes of marine omega-3 fatty acids.
The trials reported results for AFib, either as prespecified outcome, adverse event, or a reason for hospitalization. Each had a minimum of 500 patients and a median follow-up of at least 1 year.
Trials examining the effects of omega-3 fatty acids on recurrent AFib in patients with established AFib or postoperative AFib were excluded.
The seven trials enrolled a total of 81,210 patients (mean age, 65 years; 39% women); 72.6% of participants were enrolled in clinical trials testing ≤1 gram of marine omega-3 fatty acids per day and 27.4% were enrolled in clinical trials testing >1 gram of the supplement per day. The weighted average follow-up was 4.9 years.
Overall, use of omega-3 fatty acids was associated with a 25% increased risk for AFib (hazard ratio, 1.25; 95% confidence interval, 1.07-1.46; P = .013).
In analyses stratified by dose, the risk for AFib was “significantly more pronounced” in trials testing high doses of marine omega-3 fatty acid supplements (>1 gram per day: HR, 1.49; 95% CI, 1.04-2.15; P = .042) compared with those testing lower doses (≤1 gram per day: HR, 1.12; 95% CI, 1.03-1.22; P = .024; P for interaction < .001).
In meta-regression, the HR for AFib increased per 1 gram increase in daily omega-3 fatty acid dose (HR. 1.11; 95% CI, 1.06-1.15; P = .001).
Risk-benefit balance
“This meta-analysis adds new evidence regarding the risk of AFib in patients taking marine omega-3 fatty acid supplements,” wrote Dr. Albert and colleagues.
“Since the benefit of omega-3 fatty acids also appears to be dose dependent, the associated risk of AFib should be balanced against the benefit on atherosclerotic cardiovascular outcomes,” they suggested.
They cautioned that the meta-analysis pooled aggregate-level trial data, not individual patient data. Therefore, subgroup analyses by age or other patient level characteristics were not possible.
The risk of developing AFib increases with advancing age and is more common in men than in women. Additional risk factors include elevated blood pressure, coronary artery disease, heart failure, heart valve defects, obesity, and diabetes.
The authors said the potential risk of developing AFib with high doses of omega-3 fatty acid supplements should be discussed with patients and they should know the signs and symptoms of the condition.
The study had no specific funding. Dr. Albert has received grants from St. Jude Medical, Abbott, and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
Adding statins to steroids in thyroid eye disease improves outcomes
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
Treatment of Graves’ orbitopathy with statins in combination with glucocorticoids shows benefits among people with – and even without – high cholesterol, results from a new randomized clinical trial show.
“Our results [indicate] that adding atorvastatin to intravenous glucocorticoids seems to potentiate the effects of glucocorticoids,” senior author Michelle Marino, MD, associate professor of endocrinology in the department of clinical and experimental medicine at the University of Pisa, Italy, told this news organization.
“At least in hypercholesterolemic patients with moderate to severe and active Graves’ orbitopathy, atorvastatin should be considered in addition to intravenous glucocorticoids,” Dr. Marino said.
The study was presented by first author Giulia Lanzolla, MD, also of the University of Pisa and University Hospital of Pisa, at the virtual annual meeting of the American Thyroid Association.
Hypercholesterolemia, well known to promote systemic inflammation, has been previously linked to Graves’ orbitopathy, and the use of statins has also been shown to possibly provide a protective effect in the risk of developing the thyroid eye disease.
Furthermore, patients with Graves’ orbitopathy and high cholesterol levels, compared with those with normal cholesterol, have been shown to have poorer responses to treatment with glucocorticoids, which have long been the first line of treatment.
Asked for comment on the findings, Marius Stan, MD, a consultant in the division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn., said he didn’t think the outcome measure used – a composite of a variety of measures of thyroid eye disease – was best to truly understand the benefits.
Statins for Graves’ orbitopathy (STAGO) study details
For a better understanding of the effects with and without the addition of statins in a randomized trial, Dr. Lanzolla and colleagues enrolled 88 patients with high cholesterol and moderate to severe active Graves’ orbitopathy in the phase 2 STAGO trial.
Patients were randomized to two groups of 44 patients each to receive treatment either with intravenous (IV) methylprednisolone at 500 mg per week for 6 weeks, followed by 250 mg per week for another 6 weeks, in combination with atorvastatin 20 mg daily for 12 weeks, or methylprednisolone alone for 12 weeks.
The primary endpoint was a composite of Graves orbitopathy outcomes and included measures of exophthalmos, clinical activity score, eyelid aperture, diplopia, and visual acuity, as assessed in the modified intention-to-treat population.
The trial met the primary composite endpoint, with 51.2% of those treated with statins achieving the outcome (21 of 41) versus 28.2% (11 of 39) of those treated with glucocorticoids alone (odds ratio, 2.76; P = .03).
The study also achieved secondary outcomes, with 43.9% in the statin group having a response to treatment at 12 weeks versus 23% in the glucocorticoid group (OR 2.60; P = .05). The statin group also had a greater improvement in quality of life measures (P = .03).
The glucocorticoid-only group meanwhile had a significantly greater rate of Graves orbitopathy relapse at 24 weeks, with six relapses versus none in the statin group (15.3% vs. 0.0%; OR 0.06; P = .01).
There were no significant differences in low-density lipoprotein (LDL) cholesterol between those who did and did not respond to treatment in the statin group.
The most likely explanation for those findings is that “atorvastatin acts through its pleiotropic action, resulting in an anti-inflammatory effect,” Dr. Marino said.
“In addition, the effect may be related to the capability of statins to inhibit fibroblast proliferation,” Dr. Marino added.
“Total cholesterol had a behavior similar to LDL cholesterol, [while] HDL cholesterol did not change across the study.”
There were no major adverse events related to atorvastatin, with one patient in each group requiring treatment discontinuation.
In the rapidly evolving landscape of treatments for Graves’ orbitopathy, including the recent Food and Drug Administration approval for teprotumumab in thyroid eye disease, the potential role of statins remains to be seen, Dr. Marino noted.
“Graves’ orbitopathy is a rather complex disease, and in its mild to moderate forms it is very rare for a patient to require only a single treatment,” Dr. Marino explained. “Rehabilitative surgery is needed quite often once the disease is inactive.”
The authors noted that a composite overall Graves’ orbitopathy outcome was used as the primary endpoint because the alternative of a change in single eye features may not reflect a true modification of Graves’ orbitopathy and could be affected by a number of unrelated factors.
“By contrast, the composite evaluation offers a more realistic picture,” the authors wrote in the article, which was published in The Lancet Diabetes and Endocrinology.
Composite outcome not best way of assessing effects of statins
Dr. Stan extrapolated on his criticism of the trial.
“The study has interesting results but fails to show that any particular eye feature is benefited by the combination therapy, showing only the composite outcome to be improved,” he told this news organization.
“Unfortunately, that is hard to extrapolate to patient care, where one or another of Graves’ orbitopathy features are present and are the intended target of therapy,” he said.
Dr. Stan added that IV glucocorticoids are meanwhile also changing the landscape of treatment of thyroid eye disease.
“This ... current plan is to recommend a more individualized approach, depending on what is the main problem for that thyroid eye disease case,” he explained.
Dr. Marino noted that the authors are planning a double-blind, placebo-controlled phase 3 clinical trial of the statin/glucocorticoid combination to include patients regardless of their cholesterol levels.
The study received funding from Associazione Allievi Endocrinologia Pisana. The authors have reported no relevant financial relationships. Dr. Stan is on the advisory board for Horizon Pharma/Immunovant and provides general consulting for VasaraGen/Septerna and ValenzaBio/Medicxi.
A version of this article first appeared on Medscape.com.
FROM ATA 2021
HEPA filters may clean SARS-CoV-2 from the air: Study
, researchers report in the preprint server medRxiv.
The journal Nature reported Oct. 6 that the research, which has not been peer-reviewed, suggests the filters may help reduce the risk of hospital-acquired SARS-CoV-2.
Researchers, led by intensivist Andrew Conway-Morris, MBChB, PhD, with the division of anaesthesia in the school of clinical medicine at University of Cambridge, United Kingdom, write that earlier experiments assessed air filters’ ability to remove inactive particles in carefully controlled environments, but it was unknown how they would work in a real-world setting.
Co-author Vilas Navapurkar, MBChB, an ICU physician at Addenbrooke’s Hospital in Cambridge, United Kingdom, said that hospitals have used portable air filters when their isolation facilities are full, but evidence was needed as to whether such filters are effective or whether they provide a false sense of security.
The researchers installed the filters in two fully occupied COVID-19 wards — a general ward and an ICU. They chose HEPA filters because they can catch extremely small particles.
The team collected air samples from the wards during a week when the air filters were on and 2 weeks when they were turned off, then compared results.
According to the study, “airborne SARS-CoV-2 was detected in the ward on all five days before activation of air/UV filtration, but on none of the five days when the air/UV filter was operational; SARS-CoV-2 was again detected on four out of five days when the filter was off.”
Airborne SARS-CoV-2 was not frequently detected in the ICU, even when the filters were off.
Cheap and easy
According to the Nature article, the authors suggest several potential explanations for this, “including slower viral replication at later stages of the disease.” Therefore, the authors say, filtering the virus from the air might be more important in general wards than in ICUs.
The filters significantly reduced the other microbial bioaerosols in both the ward (48 pathogens detected before filtration, 2 after, P = .05) and the ICU (45 pathogens detected before filtration, 5 after P = .05).
National Institute for Occupational Safety and Health (NIOSH) cyclonic aerosol samplers and PCR tests were used to detect airborne SARS-CoV-2 and other microbial bioaerosol.
David Fisman, MD, an epidemiologist at the University of Toronto, who was not involved in the research, said in the Nature article, “This study suggests that HEPA air cleaners, which remain little-used in Canadian hospitals, are a cheap and easy way to reduce risk from airborne pathogens.”This work was supported by a Wellcome senior research fellowship to co-author Stephen Baker. Conway Morris is supported by a Clinician Scientist Fellowship from the Medical Research Council. Dr. Navapurkar is the founder, director, and shareholder of Cambridge Infection Diagnostics Ltd. Dr. Conway-Morris and several co-authors are members of the Scientific Advisory Board of Cambridge Infection Diagnostics Ltd. Co-author Theodore Gouliouris has received a research grant from Shionogi and co-author R. Andres Floto has received research grants and/or consultancy payments from GSK, AstraZeneca, Chiesi, Shionogi, Insmed, and Thirty Technology.
A version of this article first appeared on Medscape.com.
, researchers report in the preprint server medRxiv.
The journal Nature reported Oct. 6 that the research, which has not been peer-reviewed, suggests the filters may help reduce the risk of hospital-acquired SARS-CoV-2.
Researchers, led by intensivist Andrew Conway-Morris, MBChB, PhD, with the division of anaesthesia in the school of clinical medicine at University of Cambridge, United Kingdom, write that earlier experiments assessed air filters’ ability to remove inactive particles in carefully controlled environments, but it was unknown how they would work in a real-world setting.
Co-author Vilas Navapurkar, MBChB, an ICU physician at Addenbrooke’s Hospital in Cambridge, United Kingdom, said that hospitals have used portable air filters when their isolation facilities are full, but evidence was needed as to whether such filters are effective or whether they provide a false sense of security.
The researchers installed the filters in two fully occupied COVID-19 wards — a general ward and an ICU. They chose HEPA filters because they can catch extremely small particles.
The team collected air samples from the wards during a week when the air filters were on and 2 weeks when they were turned off, then compared results.
According to the study, “airborne SARS-CoV-2 was detected in the ward on all five days before activation of air/UV filtration, but on none of the five days when the air/UV filter was operational; SARS-CoV-2 was again detected on four out of five days when the filter was off.”
Airborne SARS-CoV-2 was not frequently detected in the ICU, even when the filters were off.
Cheap and easy
According to the Nature article, the authors suggest several potential explanations for this, “including slower viral replication at later stages of the disease.” Therefore, the authors say, filtering the virus from the air might be more important in general wards than in ICUs.
The filters significantly reduced the other microbial bioaerosols in both the ward (48 pathogens detected before filtration, 2 after, P = .05) and the ICU (45 pathogens detected before filtration, 5 after P = .05).
National Institute for Occupational Safety and Health (NIOSH) cyclonic aerosol samplers and PCR tests were used to detect airborne SARS-CoV-2 and other microbial bioaerosol.
David Fisman, MD, an epidemiologist at the University of Toronto, who was not involved in the research, said in the Nature article, “This study suggests that HEPA air cleaners, which remain little-used in Canadian hospitals, are a cheap and easy way to reduce risk from airborne pathogens.”This work was supported by a Wellcome senior research fellowship to co-author Stephen Baker. Conway Morris is supported by a Clinician Scientist Fellowship from the Medical Research Council. Dr. Navapurkar is the founder, director, and shareholder of Cambridge Infection Diagnostics Ltd. Dr. Conway-Morris and several co-authors are members of the Scientific Advisory Board of Cambridge Infection Diagnostics Ltd. Co-author Theodore Gouliouris has received a research grant from Shionogi and co-author R. Andres Floto has received research grants and/or consultancy payments from GSK, AstraZeneca, Chiesi, Shionogi, Insmed, and Thirty Technology.
A version of this article first appeared on Medscape.com.
, researchers report in the preprint server medRxiv.
The journal Nature reported Oct. 6 that the research, which has not been peer-reviewed, suggests the filters may help reduce the risk of hospital-acquired SARS-CoV-2.
Researchers, led by intensivist Andrew Conway-Morris, MBChB, PhD, with the division of anaesthesia in the school of clinical medicine at University of Cambridge, United Kingdom, write that earlier experiments assessed air filters’ ability to remove inactive particles in carefully controlled environments, but it was unknown how they would work in a real-world setting.
Co-author Vilas Navapurkar, MBChB, an ICU physician at Addenbrooke’s Hospital in Cambridge, United Kingdom, said that hospitals have used portable air filters when their isolation facilities are full, but evidence was needed as to whether such filters are effective or whether they provide a false sense of security.
The researchers installed the filters in two fully occupied COVID-19 wards — a general ward and an ICU. They chose HEPA filters because they can catch extremely small particles.
The team collected air samples from the wards during a week when the air filters were on and 2 weeks when they were turned off, then compared results.
According to the study, “airborne SARS-CoV-2 was detected in the ward on all five days before activation of air/UV filtration, but on none of the five days when the air/UV filter was operational; SARS-CoV-2 was again detected on four out of five days when the filter was off.”
Airborne SARS-CoV-2 was not frequently detected in the ICU, even when the filters were off.
Cheap and easy
According to the Nature article, the authors suggest several potential explanations for this, “including slower viral replication at later stages of the disease.” Therefore, the authors say, filtering the virus from the air might be more important in general wards than in ICUs.
The filters significantly reduced the other microbial bioaerosols in both the ward (48 pathogens detected before filtration, 2 after, P = .05) and the ICU (45 pathogens detected before filtration, 5 after P = .05).
National Institute for Occupational Safety and Health (NIOSH) cyclonic aerosol samplers and PCR tests were used to detect airborne SARS-CoV-2 and other microbial bioaerosol.
David Fisman, MD, an epidemiologist at the University of Toronto, who was not involved in the research, said in the Nature article, “This study suggests that HEPA air cleaners, which remain little-used in Canadian hospitals, are a cheap and easy way to reduce risk from airborne pathogens.”This work was supported by a Wellcome senior research fellowship to co-author Stephen Baker. Conway Morris is supported by a Clinician Scientist Fellowship from the Medical Research Council. Dr. Navapurkar is the founder, director, and shareholder of Cambridge Infection Diagnostics Ltd. Dr. Conway-Morris and several co-authors are members of the Scientific Advisory Board of Cambridge Infection Diagnostics Ltd. Co-author Theodore Gouliouris has received a research grant from Shionogi and co-author R. Andres Floto has received research grants and/or consultancy payments from GSK, AstraZeneca, Chiesi, Shionogi, Insmed, and Thirty Technology.
A version of this article first appeared on Medscape.com.
Abaloparatide significantly reduced fractures, increased BMD in women at high fracture risk
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).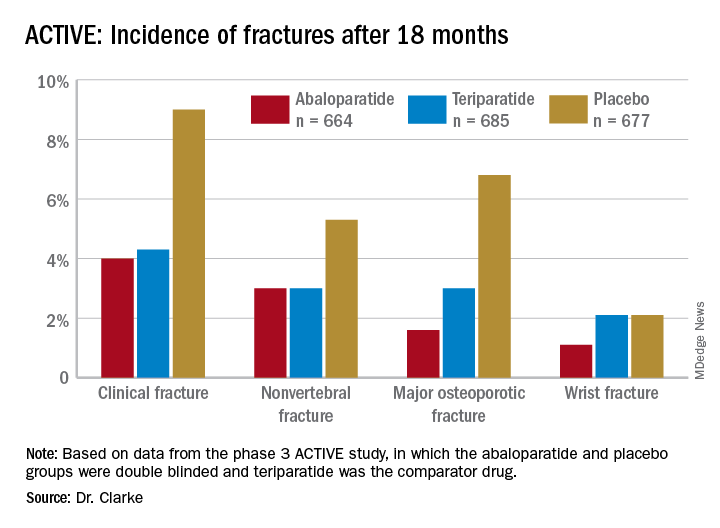
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).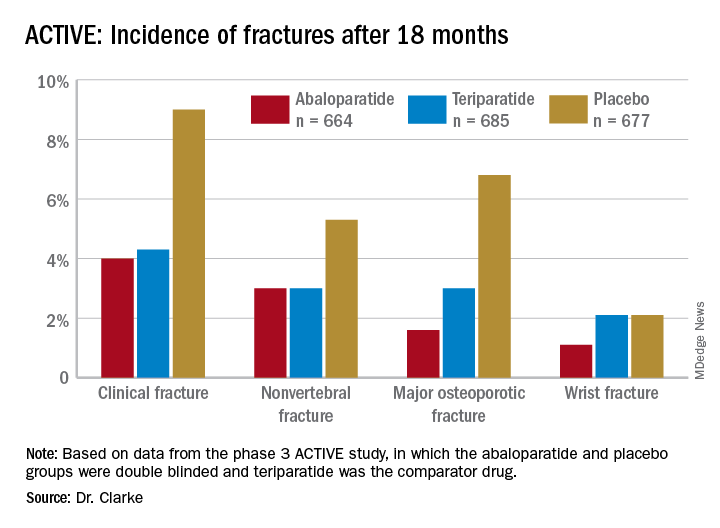
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
Postmenopausal women at high or very high risk of fracture gained significantly more bone mineral density and were significantly less likely to experience a fracture when taking abaloparatide for 18 months, according to new research presented at the hybrid annual meeting of the North American Menopause Society.
“The findings showed that abaloparatide was better than teriparatide in a number of parameters important in osteoporosis treatment, and similar in others, in high-risk and very-high-risk postmenopausal women with osteoporosis,” Bart Clarke, MD, a professor of medicine at Mayo Clinic in Rochester, Minn., said in an interview. “Abaloparatide is safe and effective for use in high-risk or very-high-risk postmenopausal women,” as defined by the new American Association of Clinical Endocrinology/American College of Endocrinology osteoporosis guidelines.
Ricardo R. Correa, MD, of the department of endocrinology and director of diversity for graduate medical education at the University of Arizona, Phoenix, said that the study demonstrates that abaloparatide and teriparatide have a very similar effect with abaloparatide providing a slightly better absolute risk reduction in fracture. Dr. Correa was not involved in the research.
“What will drive my decision in what to prescribe will be the cost and insurance coverage,” Dr. Correa said. “At the Veterans Administration hospital, the option that we have is abaloparatide, so this is the option that we use.”
Among women at least 65 years old who have already had one fracture, 1 in 10 will experience another fracture within the next year, and 30% will have another fracture within the next 5 years, the authors noted in their background material. Since phase 3 ACTIVE study data in 2016 showed that abaloparatide reduces fracture risk while increasing bone mineral density, compared with placebo, the researchers reanalyzed that data to assess the drug’s efficacy in patients at high or very high risk for fracture.
The study involved 2,463 postmenopausal women with osteoporosis who received one of three interventions: 80 mcg abaloparatide daily, placebo, or 20 mcg subcutaneous teriparatide daily. Only the abaloparatide and placebo groups were double blinded.
“Teriparatide was used as the comparator drug because teriparatide was previously approved as the first anabolic drug for osteoporosis,” Dr. Clarke said in an interview. “The hope was to show that abaloparatide was a better anabolic drug.”
Women were considered at high or very high risk of fracture if they met at least one of the following four criteria from the 2020 American Association of Clinical Endocrinology guidelines:
- Fracture within the past 12 months or prevalent vertebral fracture.
- Very low T-score (less than –3.0) at baseline at any site.
- Multiple fractures at baseline since age 45.
- Very high fracture risk based on the Fracture Risk Assessment Tool (FRAX) (at least 30% for major osteoporotic fracture or at least 4.5% for hip fracture).
Among the 2,026 patients who met at least one of these criteria, 664 received abaloparatide, 685 received teriparatide, and 677 received placebo. Both the abaloparatide and teriparatide significantly reduced new vertebral fracture risk, compared with placebo. In the abaloparatide group, 0.72% of women had a new vertebral fracture, compared with 0.99% in the teriparatide group and 4.77% in the placebo group (P < .0001).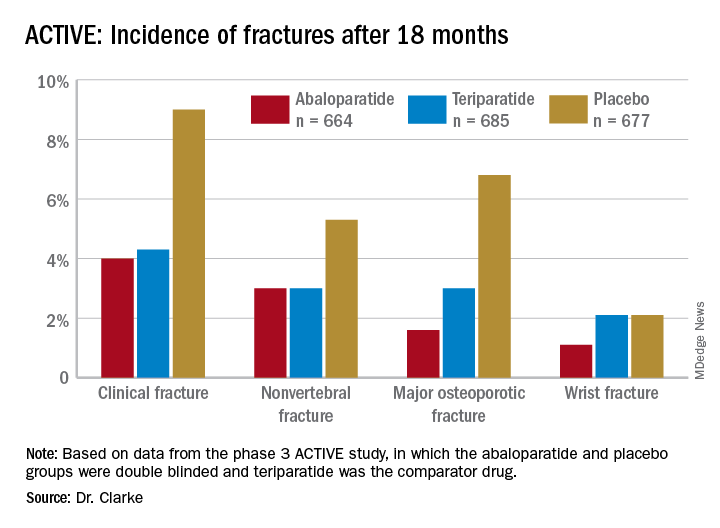
Abaloparatide and teriparatide also led to significant increases in lumbar spine, total hip, and femoral neck bone mineral density, compared with placebo (P < .0001).
The study was limited by its duration of 18 months and the Food and Drug Administration’s restriction on using abaloparatide for more than 2 years because of the theoretical risk of increasing osteosarcoma, although that risk has never been demonstrated in humans, Dr. Correa said. ”We need more data with abaloparitide in more than 2 years,” he added.
In determining which medication clinicians should first prescribe to manage osteoporosis, Dr. Correa said practitioners should consider the type of osteoporosis women have, their preferences, and their labs on kidney function.
With mild to moderate osteoporosis, bisphosphonates will be the first option while denosumab will be preferred for moderate to severe osteoporosis. Teriparatide and abaloparitide are the first-line options for severe osteoporosis, he said.
“If the glomerular filtration rate is low, we cannot use bisphosphonate and we will have to limit our use to denosumab,” he said. Route and frequency of delivery plays a role in patient preferences.
“If the patient prefers an infusion once a year or a pill, then bisphosphonate,” he said, but “if the patient is fine with an injection every 6 months, then denosumab.” Patients who need and can do an injection every day can take abaloparitide or teriparatide.
Failure of previous treatments also guide clinical decisions, he added. ”If the patient has been on one medication and has a fracture or the bone mineral density decreases, then we need to switch to another medication, usually teriparatide or abaloparitide, to build new bone.”
Contraindications for abaloparatide include a high serum calcium before therapy or prior allergic reactions to components in abaloparatide, Dr. Clarke said. No new safety signals showed up in the data analysis.
The research was funded by Radius Health. Dr. Clarke is an advisory board member of Amgen, and another author consults and speaks for Amgen and is a Radius Health Advisory Board member. Two other authors are Radius Health employees who own stock in the company. Dr Correa has no disclosures.
FROM NAMS 2021
Telehealth for heart failure during pandemic shown effective, safe
The rapid transition to and reliance on telehealth to manage patients with heart failure during the COVID-19 pandemic does not appear to impact clinical outcomes, according to real-world data.
HF outpatients managed with telehealth visits did not show a significantly higher adjusted risk for subsequent ED visits, hospital admissions, intensive care use, or death at 30 and 90 days, the investigators reported in JACC: Heart Failure.
“Telehealth is safe and effective in probably some of our highest-risk patients who traditionally have needed hands-on, in-person assessment and evaluation – those patients who have heart failure – so we shouldn’t be afraid to use it all the time, not when needed as a minimum,” senior author Brett W. Sperry, MD, said in an interview.
Heart failure is a perfect case example to examine telehealth because the chronic condition not only requires continual assessment and medication adjustments, but HF patients are also particularly vulnerable to complications related to COVID-19 infection, he noted. A small, single-center report on telehealth early in Italy’s outbreak showed fewer HF hospitalizations and similar mortality, compared with in-person visits in 2019 but, overall, few data exist.
The current analysis took a wider sweep, comparing HF patients seen from March 15 to June 15, 2020 with those seen during the same time period in 2018 and 2019 at 16 cardiology clinics in Saint Luke’s Health System, which serves the Kansas City metro area and surrounding suburbs in Missouri and Kansas.
Among 8,263 unique patients and 15,421 visits identified, telehealth was not used in 2018 or 2019 but accounted for 88.5% of visits during the study period in 2020, 70% of which were by telephone and 30% of which were by video.
“We had zero telehealth before March 2020 and basically built an entire telehealth apparatus in a week or 2,” explained Dr. Sperry. “Initially it was a lot of telephone visits while we were getting the video stuff figured out, which is reflected in the paper, and then went to mostly video visits.”
Despite the pandemic, however, more outpatients were seen in 2020 than in 2018 and 2019 (4,063 vs. 3675 and 3,619 patients, respectively). This likely reflects the shift of personnel and resources from hospital duties to outpatient virtual visits, which were strongly recommended by the Heart Failure Society of America and other professional societies to manage patients during the pandemic, he said.
Unadjusted analyses demonstrated fewer ED visits and hospital admissions and more ICU admissions and all-cause mortality in 2020 than in previous years.
A propensity-matched analysis involving 4541 pairs of patients, however, showed admissions to the ED or hospital were lower after the telehealth visits than after in-person visits at 30 days (6.8% vs 10.4%; P < .001) and 90 days (17.9% vs. 23.3%; P < .001).
Among hospitalized patients, there was no difference between telehealth and in-patient visits in ICU admissions at 30 or 90 days. Mortality was also similar at 30 days (0.8% vs. 0.7%; P = .465) and 90 days (2.9% vs. 2.4%; P = .133).
Dr. Sperry said the pendulum has swung since 2020 and that the team is back to seeing most people in person, with about 15% of his clinic visits that day done via video. Standardized quality of life assessments prior to outpatient visits can help triage patients to telehealth in-patient visits, but in-person visits will still be needed for cases with greater acuity, older patients, and those with limited or no access to quality telephone videos or the internet.
“It isn’t for everyone,” Dr. Sperry said. “You’re going to need some kind of hybrid model with both in-person and video visits available and be able to offer both for patients and be able to titrate that as the pandemic changes in the future.”
Ankit Bhatia, MD, an advanced HF cardiologist at Christ Hospital in Cincinnati, who was not part of the study, said in an interview the use of telehealth in 85% of patients may be higher than the norm at most centers but that the study provides much-needed data.
“I’m really appreciative of a study like this because we were all in such a rush last year to get patients seen that very few people thought how could we design a study to really ensure we’re treating our patients within an equipoise with prior practices,” he said.
“The fact that they were able to do that [85%] and demonstrate in a propensity-matched analysis that outcomes were similar really just shows that telehealth is a strategy that we can use well in patients with heart failure to extend our ability to take care of them,” said Dr. Bhatia, a member of the American College of Cardiology Health Care Innovation Council.
Even beyond the pandemic, he said, the trend in health care is for patients to want health care delivered closer to home and for health care systems to become more patient centric. “This accelerated that but what I think this study showed me was that it’s okay to have this be part of my care model and I’m not sacrificing on my patient care if I choose to intersperse telehealth with inpatient visits.”
Besides the inherent limitations of retrospective studies, the authors noted that diagnoses in the study were based on ICD-10 codes and that subsequent ED visits or hospitalizations outside the single system may have been underreported. A further limitation is that they could not identify the cause of death or reasons for hospital encounters.
“Further data are needed to confirm the relative safety of a telehealth strategy in the HF population over a more sustained period of time, although we hypothesize that greater risks would be observed early after telehealth visits, where patients’ acuity might be misjudged,” they wrote.
Dr. Sperry is a consultant to Pfizer and Alnylam. Coauthor John A. Spertus is the principal investigator of grants from National Institutes of Health, Abbott Vascular, and the American College of Cardiology Foundation; is a consultant to Janssen, Novartis, Amgen, Myokardia, AstraZeneca, Bayer, and Merck; serves on the scientific advisory board of United Healthcare and the board of directors for Blue Cross Blue Shield of Kansas City; owns the copyright to the Kansas City Cardiomyopathy Questionnaire, Seattle Angina Questionnaire, and Peripheral Artery Questionnaire; and has an equity interest in Health Outcomes Sciences. All other authors and Dr. Bhatia reported no relevant conflicts.
A version of this article first appeared on Medscape.com.
The rapid transition to and reliance on telehealth to manage patients with heart failure during the COVID-19 pandemic does not appear to impact clinical outcomes, according to real-world data.
HF outpatients managed with telehealth visits did not show a significantly higher adjusted risk for subsequent ED visits, hospital admissions, intensive care use, or death at 30 and 90 days, the investigators reported in JACC: Heart Failure.
“Telehealth is safe and effective in probably some of our highest-risk patients who traditionally have needed hands-on, in-person assessment and evaluation – those patients who have heart failure – so we shouldn’t be afraid to use it all the time, not when needed as a minimum,” senior author Brett W. Sperry, MD, said in an interview.
Heart failure is a perfect case example to examine telehealth because the chronic condition not only requires continual assessment and medication adjustments, but HF patients are also particularly vulnerable to complications related to COVID-19 infection, he noted. A small, single-center report on telehealth early in Italy’s outbreak showed fewer HF hospitalizations and similar mortality, compared with in-person visits in 2019 but, overall, few data exist.
The current analysis took a wider sweep, comparing HF patients seen from March 15 to June 15, 2020 with those seen during the same time period in 2018 and 2019 at 16 cardiology clinics in Saint Luke’s Health System, which serves the Kansas City metro area and surrounding suburbs in Missouri and Kansas.
Among 8,263 unique patients and 15,421 visits identified, telehealth was not used in 2018 or 2019 but accounted for 88.5% of visits during the study period in 2020, 70% of which were by telephone and 30% of which were by video.
“We had zero telehealth before March 2020 and basically built an entire telehealth apparatus in a week or 2,” explained Dr. Sperry. “Initially it was a lot of telephone visits while we were getting the video stuff figured out, which is reflected in the paper, and then went to mostly video visits.”
Despite the pandemic, however, more outpatients were seen in 2020 than in 2018 and 2019 (4,063 vs. 3675 and 3,619 patients, respectively). This likely reflects the shift of personnel and resources from hospital duties to outpatient virtual visits, which were strongly recommended by the Heart Failure Society of America and other professional societies to manage patients during the pandemic, he said.
Unadjusted analyses demonstrated fewer ED visits and hospital admissions and more ICU admissions and all-cause mortality in 2020 than in previous years.
A propensity-matched analysis involving 4541 pairs of patients, however, showed admissions to the ED or hospital were lower after the telehealth visits than after in-person visits at 30 days (6.8% vs 10.4%; P < .001) and 90 days (17.9% vs. 23.3%; P < .001).
Among hospitalized patients, there was no difference between telehealth and in-patient visits in ICU admissions at 30 or 90 days. Mortality was also similar at 30 days (0.8% vs. 0.7%; P = .465) and 90 days (2.9% vs. 2.4%; P = .133).
Dr. Sperry said the pendulum has swung since 2020 and that the team is back to seeing most people in person, with about 15% of his clinic visits that day done via video. Standardized quality of life assessments prior to outpatient visits can help triage patients to telehealth in-patient visits, but in-person visits will still be needed for cases with greater acuity, older patients, and those with limited or no access to quality telephone videos or the internet.
“It isn’t for everyone,” Dr. Sperry said. “You’re going to need some kind of hybrid model with both in-person and video visits available and be able to offer both for patients and be able to titrate that as the pandemic changes in the future.”
Ankit Bhatia, MD, an advanced HF cardiologist at Christ Hospital in Cincinnati, who was not part of the study, said in an interview the use of telehealth in 85% of patients may be higher than the norm at most centers but that the study provides much-needed data.
“I’m really appreciative of a study like this because we were all in such a rush last year to get patients seen that very few people thought how could we design a study to really ensure we’re treating our patients within an equipoise with prior practices,” he said.
“The fact that they were able to do that [85%] and demonstrate in a propensity-matched analysis that outcomes were similar really just shows that telehealth is a strategy that we can use well in patients with heart failure to extend our ability to take care of them,” said Dr. Bhatia, a member of the American College of Cardiology Health Care Innovation Council.
Even beyond the pandemic, he said, the trend in health care is for patients to want health care delivered closer to home and for health care systems to become more patient centric. “This accelerated that but what I think this study showed me was that it’s okay to have this be part of my care model and I’m not sacrificing on my patient care if I choose to intersperse telehealth with inpatient visits.”
Besides the inherent limitations of retrospective studies, the authors noted that diagnoses in the study were based on ICD-10 codes and that subsequent ED visits or hospitalizations outside the single system may have been underreported. A further limitation is that they could not identify the cause of death or reasons for hospital encounters.
“Further data are needed to confirm the relative safety of a telehealth strategy in the HF population over a more sustained period of time, although we hypothesize that greater risks would be observed early after telehealth visits, where patients’ acuity might be misjudged,” they wrote.
Dr. Sperry is a consultant to Pfizer and Alnylam. Coauthor John A. Spertus is the principal investigator of grants from National Institutes of Health, Abbott Vascular, and the American College of Cardiology Foundation; is a consultant to Janssen, Novartis, Amgen, Myokardia, AstraZeneca, Bayer, and Merck; serves on the scientific advisory board of United Healthcare and the board of directors for Blue Cross Blue Shield of Kansas City; owns the copyright to the Kansas City Cardiomyopathy Questionnaire, Seattle Angina Questionnaire, and Peripheral Artery Questionnaire; and has an equity interest in Health Outcomes Sciences. All other authors and Dr. Bhatia reported no relevant conflicts.
A version of this article first appeared on Medscape.com.
The rapid transition to and reliance on telehealth to manage patients with heart failure during the COVID-19 pandemic does not appear to impact clinical outcomes, according to real-world data.
HF outpatients managed with telehealth visits did not show a significantly higher adjusted risk for subsequent ED visits, hospital admissions, intensive care use, or death at 30 and 90 days, the investigators reported in JACC: Heart Failure.
“Telehealth is safe and effective in probably some of our highest-risk patients who traditionally have needed hands-on, in-person assessment and evaluation – those patients who have heart failure – so we shouldn’t be afraid to use it all the time, not when needed as a minimum,” senior author Brett W. Sperry, MD, said in an interview.
Heart failure is a perfect case example to examine telehealth because the chronic condition not only requires continual assessment and medication adjustments, but HF patients are also particularly vulnerable to complications related to COVID-19 infection, he noted. A small, single-center report on telehealth early in Italy’s outbreak showed fewer HF hospitalizations and similar mortality, compared with in-person visits in 2019 but, overall, few data exist.
The current analysis took a wider sweep, comparing HF patients seen from March 15 to June 15, 2020 with those seen during the same time period in 2018 and 2019 at 16 cardiology clinics in Saint Luke’s Health System, which serves the Kansas City metro area and surrounding suburbs in Missouri and Kansas.
Among 8,263 unique patients and 15,421 visits identified, telehealth was not used in 2018 or 2019 but accounted for 88.5% of visits during the study period in 2020, 70% of which were by telephone and 30% of which were by video.
“We had zero telehealth before March 2020 and basically built an entire telehealth apparatus in a week or 2,” explained Dr. Sperry. “Initially it was a lot of telephone visits while we were getting the video stuff figured out, which is reflected in the paper, and then went to mostly video visits.”
Despite the pandemic, however, more outpatients were seen in 2020 than in 2018 and 2019 (4,063 vs. 3675 and 3,619 patients, respectively). This likely reflects the shift of personnel and resources from hospital duties to outpatient virtual visits, which were strongly recommended by the Heart Failure Society of America and other professional societies to manage patients during the pandemic, he said.
Unadjusted analyses demonstrated fewer ED visits and hospital admissions and more ICU admissions and all-cause mortality in 2020 than in previous years.
A propensity-matched analysis involving 4541 pairs of patients, however, showed admissions to the ED or hospital were lower after the telehealth visits than after in-person visits at 30 days (6.8% vs 10.4%; P < .001) and 90 days (17.9% vs. 23.3%; P < .001).
Among hospitalized patients, there was no difference between telehealth and in-patient visits in ICU admissions at 30 or 90 days. Mortality was also similar at 30 days (0.8% vs. 0.7%; P = .465) and 90 days (2.9% vs. 2.4%; P = .133).
Dr. Sperry said the pendulum has swung since 2020 and that the team is back to seeing most people in person, with about 15% of his clinic visits that day done via video. Standardized quality of life assessments prior to outpatient visits can help triage patients to telehealth in-patient visits, but in-person visits will still be needed for cases with greater acuity, older patients, and those with limited or no access to quality telephone videos or the internet.
“It isn’t for everyone,” Dr. Sperry said. “You’re going to need some kind of hybrid model with both in-person and video visits available and be able to offer both for patients and be able to titrate that as the pandemic changes in the future.”
Ankit Bhatia, MD, an advanced HF cardiologist at Christ Hospital in Cincinnati, who was not part of the study, said in an interview the use of telehealth in 85% of patients may be higher than the norm at most centers but that the study provides much-needed data.
“I’m really appreciative of a study like this because we were all in such a rush last year to get patients seen that very few people thought how could we design a study to really ensure we’re treating our patients within an equipoise with prior practices,” he said.
“The fact that they were able to do that [85%] and demonstrate in a propensity-matched analysis that outcomes were similar really just shows that telehealth is a strategy that we can use well in patients with heart failure to extend our ability to take care of them,” said Dr. Bhatia, a member of the American College of Cardiology Health Care Innovation Council.
Even beyond the pandemic, he said, the trend in health care is for patients to want health care delivered closer to home and for health care systems to become more patient centric. “This accelerated that but what I think this study showed me was that it’s okay to have this be part of my care model and I’m not sacrificing on my patient care if I choose to intersperse telehealth with inpatient visits.”
Besides the inherent limitations of retrospective studies, the authors noted that diagnoses in the study were based on ICD-10 codes and that subsequent ED visits or hospitalizations outside the single system may have been underreported. A further limitation is that they could not identify the cause of death or reasons for hospital encounters.
“Further data are needed to confirm the relative safety of a telehealth strategy in the HF population over a more sustained period of time, although we hypothesize that greater risks would be observed early after telehealth visits, where patients’ acuity might be misjudged,” they wrote.
Dr. Sperry is a consultant to Pfizer and Alnylam. Coauthor John A. Spertus is the principal investigator of grants from National Institutes of Health, Abbott Vascular, and the American College of Cardiology Foundation; is a consultant to Janssen, Novartis, Amgen, Myokardia, AstraZeneca, Bayer, and Merck; serves on the scientific advisory board of United Healthcare and the board of directors for Blue Cross Blue Shield of Kansas City; owns the copyright to the Kansas City Cardiomyopathy Questionnaire, Seattle Angina Questionnaire, and Peripheral Artery Questionnaire; and has an equity interest in Health Outcomes Sciences. All other authors and Dr. Bhatia reported no relevant conflicts.
A version of this article first appeared on Medscape.com.
Psychiatrists shift stance on gender dysphoria, recommend therapy
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
A new position statement from the Royal Australian and New Zealand College of Psychiatrists (RANZCP) stresses the importance of a mental health evaluation for people with gender dysphoria – in particular for children and adolescents – before any firm decisions are made on whether to prescribe hormonal treatments to transition, or perform surgeries, often referred to as “gender-affirming care.”
“There is a paucity of quality evidence on the outcomes of those presenting with gender dysphoria. In particular, there is a need for better evidence in relation to outcomes for children and young people,” the guidance states.
Because gender dysphoria “is associated with significant distress ... each case should be assessed by a mental health professional, which will frequently be a psychiatrist, with the person at the center of care. It is important the psychological state and context in which gender dysphoria has arisen is explored to assess the most appropriate treatment,” it adds.
The move by the psychiatry body represents a big shift in the landscape regarding recommendations for the treatment of gender dysphoria in Australia and New Zealand.
Asked to explain the new RANZCP position, Philip Morris, MBBS, FRANZCP, said: “The College acknowledged the complexity of the issues and the legitimacy of different approaches.”
Exploration of a patient’s reasons for identifying as transgender is essential, he said in an interview, especially when it comes to young people.
“There may be other reasons for doing it, and we need to look for those, identify them and treat them. This needs to be done before initiating hormones and changing the whole physical nature of the child,” he said.
“A cautious psychotherapy-first approach makes sense. If we can do that with adolescents, then we will take a big step in the right direction,” stressed Dr. Morris, who is president of the National Association of Practising Psychiatrists in Australia.
Keira Bell case and Scandinavian stance lead to more open discussion
The rapid rise in gender dysphoria among adolescents in the Western world, referred to as “rapid-onset” or “late-onset” gender dysphoria, has seen a huge increase in the number of natal girls presenting and created frenzied debate that has intensified worldwide in the last 12 months about how to best treat youth with gender dysphoria.
Concerns have arisen that some transgender identification is due to social contagion, and there is a growing number of “detransitioners” – people who identified as transgender, transitioned to the opposite gender, but then regretted their decision, changed their minds, and “detransitioned” back to their birth sex. If they have had hormone therapy, and in some cases surgery, they are left with irreversible changes to their bodies.
As a result, Scandinavian countries, most notably Finland, once eager advocates of the gender-affirmative approach, have pulled back and issued new treatment guidelines in 2020 stating that psychotherapy, rather than gender reassignment, should be the first line of treatment for gender-dysphoric youth.
This, along with a landmark High Court decision in the U.K. regarding the use of puberty-blocking drugs for children with gender dysphoria, brought by detransitioner Keira Bell, which was recently overturned by the Appeal Court, but which Ms. Bell now says she will take to the Supreme Court, has led to a considerable shift in the conversation around treating transgender adolescents with hormonal therapy, says Dr. Morris.
“This [has moved from] ... a topic that could previously not be talked about freely to one that we can discuss more openly now. This is a big improvement. Previously, everyone thought it was all settled, but it’s not, certainly not from a medical angle,” he states.
At odds with prior Australian recommendations
The RANZCP had previously endorsed the standard guidelines of the Royal Children’s Hospital (RCH) Melbourne, followed by most gender-identity services in Australia and similar guidance from New Zealand, which both recommend gender-affirming care.
“Increasing evidence demonstrates that with supportive, gender-affirming care during childhood and adolescence, harms can be ameliorated and mental health and well-being outcomes can be significantly improved,” state the RCH guidelines.
But in 2019, RANZCP removed its endorsement of the RCH guidelines and started a consultation, which resulted in the new position statement.
However, Ken Pang, MD, of the Murdoch Children’s Research Institute in Melbourne and an author of the RCH guidelines, says the key recommendations of the new RANZCP position statement are consistent with their own guidelines.
The former note “the need for a skilled mental health clinician in providing comprehensive exploration of a child or adolescent’s biopsychosocial context,” Dr. Pang says.
However, it’s difficult not to see the contrast in stance when the new RANZCP statement maintains: “Research on gender dysphoria is still emerging. There are polarized views and mixed evidence regarding treatment options for people presenting with gender identity concerns, especially children and young people.”
Dr. Pang says the RCH guidelines do, however, recognize the need for further research in the field.
“I look forward to being able to incorporate such research, including from our own Trans20 study, into future revisions of our guidelines,” he told this news organization.
Watch your backs with affirmative therapy: Will there be a compromise?
Dr. Morris says there will obviously be cases where “the child might transition with a medical intervention, but that wouldn’t be the first step.”
And yet, he adds, “There are those who push the pro-trans view that everyone should be allowed to transition, and the doctors are only technicians that provide hormones with no questions asked.”
But from a doctor’s perspective, clinicians will still be held responsible in medical and legal terms for the treatments given, he stressed.
“I don’t think they will ever not be accountable for that. They will always need to determine in their own mind whether their actions have positive value that outweigh any disadvantages,” Dr. Morris continues.
The RANZCP statement does, in fact, stress just this.
All health care professionals need to “be aware of ethical and medicolegal dilemmas” pertaining to affirmative therapy, it indicates. “Psychiatrists should practice within the relevant laws and accepted professional standards in relation to assessing capacity and obtaining consent...”
Dr. Morris hopes there will ultimately be many more checks and balances in place and that courts and clinicians will need to step back and not assume every child who seeks to transition is doing it as a result of pure gender dysphoria.
He predicts that things will end in a compromise.
“In my view, this compromise will treat children with respect and approach them like any other patient that presents with a condition that requires proper assessment and treatment.”
“In the end, some cases will be transitioned, but there will be fewer than [are] transitioned at the moment,” he predicts.
Dr. Morris has reported no relevant financial relationships. Dr. Pang is a member of the Australian Professional Association for Trans Health and its research committee.
A version of this article first appeared on Medscape.com.
Lie down for orthostatic hypotension assessment
New research shows that supine orthostatic hypotension is more common and better predicts falls and orthostatic symptoms than seated OH, supporting a supine OH protocol in clinical practice, the researchers say.
“Older adults at risk for falls undergoing assessment for OH should lie supine rather than sitting prior to standing to get the most informative OH assessment,” study author Stephen Juraschek, MD, PhD, Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, said in an interview.
“The findings call for a change in current practice,” Dr. Juraschek said.
He presented the study Sept. 29 at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The seated position for detecting OH is “commonly used for convenience. Since many clinics already perform a seated blood pressure, it saves time for people to stand shortly afterward,” he explained.
“It has also been thought that the two are interchangeable [i.e., the change in blood pressure from seated to standing was just a lower magnitude than the change from supine to standing]. However, we showed that the physiology is on average quite different, questioning prior perspectives on the interchangeability of the two protocols,” he added.
The researchers studied 522 adults (mean age, 76 years; 42% women) at high risk for falls and with vitamin D levels in the insufficient/deficient range participating in the Study to Understand Fall Reduction and Vitamin D (STURDY).
The study showed that vitamin D supplementation was not associated with OH or the main study outcome of falls.
The study used two different OH assessment protocols – seated to standing and supine to standing – and Dr. Juraschek’s team used the data to gauge the impact of supine and seated positions on OH prevalence and its relation with fall risk and orthostatic symptoms.
OH was defined as a drop in systolic BP of at least 20 mm Hg or diastolic BP of at least 10 mm Hg.
At baseline, mean BP was 129/68 mm Hg. Mean BP increased 3.4/2.6 mm Hg after sitting, but decreased 3.7/0.7 mm Hg after lying supine.
Of the 953 OH assessments (supine and seated), OH was detected in 14.8% of the supine measurements but in only 2.2% of the seated measures.
Supine OH better predicted falls (hazard ratio, 1.60; 95% CI, 0.98-2.61; P = .06) than seated OH (HR, 0.70; 95% CI, 0.30-1.60; P = .39).
Although both were nonsignificant, “potentially due to power,” the association with falls was stronger for supine OH than for seated OH, Dr. Juraschek said.
In addition, seated OH was not associated with orthostatic symptoms, whereas supine OH was significantly associated with a greater risk of fainting, blacking out, seeing spots, room spinning, and headache in the previous month (P = .048-.002).
Useful study confirms anecdotal evidence
This is a “useful study” from a “reputable” group, “and the results reveal what I would have expected,” Robert Carey, MD, University of Virginia, Charlottesville, who wasn’t involved in the study, said in an interview.
The findings, Dr. Carey said, show that measuring supine, compared with standing, “actually correlates much better with the untoward effects of orthostatic hypotension which are falls and symptoms such as dizziness and spots before your eyes.”
“Seated BP is mostly used for convenience and a little bit shorter protocol. Most clinical trials do seated orthostatic hypotension measurements. I’ve always taught my medical students and others to use the supine to standing because I’ve just anecdotally felt that this was a much better way of detecting true orthostatic hypotension and that’s how we do it at the University of Virginia Hospital,” Dr. Carey said.
The study had no funding. Dr. Juraschek and Dr. Carey have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New research shows that supine orthostatic hypotension is more common and better predicts falls and orthostatic symptoms than seated OH, supporting a supine OH protocol in clinical practice, the researchers say.
“Older adults at risk for falls undergoing assessment for OH should lie supine rather than sitting prior to standing to get the most informative OH assessment,” study author Stephen Juraschek, MD, PhD, Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, said in an interview.
“The findings call for a change in current practice,” Dr. Juraschek said.
He presented the study Sept. 29 at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The seated position for detecting OH is “commonly used for convenience. Since many clinics already perform a seated blood pressure, it saves time for people to stand shortly afterward,” he explained.
“It has also been thought that the two are interchangeable [i.e., the change in blood pressure from seated to standing was just a lower magnitude than the change from supine to standing]. However, we showed that the physiology is on average quite different, questioning prior perspectives on the interchangeability of the two protocols,” he added.
The researchers studied 522 adults (mean age, 76 years; 42% women) at high risk for falls and with vitamin D levels in the insufficient/deficient range participating in the Study to Understand Fall Reduction and Vitamin D (STURDY).
The study showed that vitamin D supplementation was not associated with OH or the main study outcome of falls.
The study used two different OH assessment protocols – seated to standing and supine to standing – and Dr. Juraschek’s team used the data to gauge the impact of supine and seated positions on OH prevalence and its relation with fall risk and orthostatic symptoms.
OH was defined as a drop in systolic BP of at least 20 mm Hg or diastolic BP of at least 10 mm Hg.
At baseline, mean BP was 129/68 mm Hg. Mean BP increased 3.4/2.6 mm Hg after sitting, but decreased 3.7/0.7 mm Hg after lying supine.
Of the 953 OH assessments (supine and seated), OH was detected in 14.8% of the supine measurements but in only 2.2% of the seated measures.
Supine OH better predicted falls (hazard ratio, 1.60; 95% CI, 0.98-2.61; P = .06) than seated OH (HR, 0.70; 95% CI, 0.30-1.60; P = .39).
Although both were nonsignificant, “potentially due to power,” the association with falls was stronger for supine OH than for seated OH, Dr. Juraschek said.
In addition, seated OH was not associated with orthostatic symptoms, whereas supine OH was significantly associated with a greater risk of fainting, blacking out, seeing spots, room spinning, and headache in the previous month (P = .048-.002).
Useful study confirms anecdotal evidence
This is a “useful study” from a “reputable” group, “and the results reveal what I would have expected,” Robert Carey, MD, University of Virginia, Charlottesville, who wasn’t involved in the study, said in an interview.
The findings, Dr. Carey said, show that measuring supine, compared with standing, “actually correlates much better with the untoward effects of orthostatic hypotension which are falls and symptoms such as dizziness and spots before your eyes.”
“Seated BP is mostly used for convenience and a little bit shorter protocol. Most clinical trials do seated orthostatic hypotension measurements. I’ve always taught my medical students and others to use the supine to standing because I’ve just anecdotally felt that this was a much better way of detecting true orthostatic hypotension and that’s how we do it at the University of Virginia Hospital,” Dr. Carey said.
The study had no funding. Dr. Juraschek and Dr. Carey have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New research shows that supine orthostatic hypotension is more common and better predicts falls and orthostatic symptoms than seated OH, supporting a supine OH protocol in clinical practice, the researchers say.
“Older adults at risk for falls undergoing assessment for OH should lie supine rather than sitting prior to standing to get the most informative OH assessment,” study author Stephen Juraschek, MD, PhD, Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, said in an interview.
“The findings call for a change in current practice,” Dr. Juraschek said.
He presented the study Sept. 29 at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The seated position for detecting OH is “commonly used for convenience. Since many clinics already perform a seated blood pressure, it saves time for people to stand shortly afterward,” he explained.
“It has also been thought that the two are interchangeable [i.e., the change in blood pressure from seated to standing was just a lower magnitude than the change from supine to standing]. However, we showed that the physiology is on average quite different, questioning prior perspectives on the interchangeability of the two protocols,” he added.
The researchers studied 522 adults (mean age, 76 years; 42% women) at high risk for falls and with vitamin D levels in the insufficient/deficient range participating in the Study to Understand Fall Reduction and Vitamin D (STURDY).
The study showed that vitamin D supplementation was not associated with OH or the main study outcome of falls.
The study used two different OH assessment protocols – seated to standing and supine to standing – and Dr. Juraschek’s team used the data to gauge the impact of supine and seated positions on OH prevalence and its relation with fall risk and orthostatic symptoms.
OH was defined as a drop in systolic BP of at least 20 mm Hg or diastolic BP of at least 10 mm Hg.
At baseline, mean BP was 129/68 mm Hg. Mean BP increased 3.4/2.6 mm Hg after sitting, but decreased 3.7/0.7 mm Hg after lying supine.
Of the 953 OH assessments (supine and seated), OH was detected in 14.8% of the supine measurements but in only 2.2% of the seated measures.
Supine OH better predicted falls (hazard ratio, 1.60; 95% CI, 0.98-2.61; P = .06) than seated OH (HR, 0.70; 95% CI, 0.30-1.60; P = .39).
Although both were nonsignificant, “potentially due to power,” the association with falls was stronger for supine OH than for seated OH, Dr. Juraschek said.
In addition, seated OH was not associated with orthostatic symptoms, whereas supine OH was significantly associated with a greater risk of fainting, blacking out, seeing spots, room spinning, and headache in the previous month (P = .048-.002).
Useful study confirms anecdotal evidence
This is a “useful study” from a “reputable” group, “and the results reveal what I would have expected,” Robert Carey, MD, University of Virginia, Charlottesville, who wasn’t involved in the study, said in an interview.
The findings, Dr. Carey said, show that measuring supine, compared with standing, “actually correlates much better with the untoward effects of orthostatic hypotension which are falls and symptoms such as dizziness and spots before your eyes.”
“Seated BP is mostly used for convenience and a little bit shorter protocol. Most clinical trials do seated orthostatic hypotension measurements. I’ve always taught my medical students and others to use the supine to standing because I’ve just anecdotally felt that this was a much better way of detecting true orthostatic hypotension and that’s how we do it at the University of Virginia Hospital,” Dr. Carey said.
The study had no funding. Dr. Juraschek and Dr. Carey have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New nonhormonal therapies for hot flashes on the horizon
Hot flashes affect three out of four women and can last 7-10 years, but the current standard of care treatment isn’t necessarily appropriate for all women who experience vasomotor symptoms, according to Stephanie Faubion, MD, MBA, director of the Mayo Clinic Women’s Health Clinic in Jacksonville, Fla.
For the majority of women under age 60 who are within 10 years of menopause, hormone therapy currently remains the most effective management option for hot flashes where the benefits outweigh the risks, Dr. Faubion told attendees Sept. 25 during a plenary at the annual meeting of the North American Menopause Society. “But really, individualizing treatment is the goal, and there are some women who are going to need some other options.”
Contraindications for hormone therapy include having a history of breast cancer, coronary heart disease, active liver disease, unexplained vaginal bleeding, high-risk endometrial cancer, transient ischemic attack, and a previous venous thromboembolic event or stroke.
“Fortunately, we have things in development,” Dr. Faubion said. She reviewed a wide range of therapies that are not currently Food and Drug Administration approved for vasomotor symptoms but are either available off label or are in clinical trials.
One of these is oxybutynin, an antimuscarinic, anticholinergic agent currently used to treat overactive bladder and overactive sweating. In a 2016 trial, 73% of women taking 15 mg extended-release oxybutynin once daily rated their symptoms as “much better,” compared with 26% who received placebo. The women experienced reduced frequency and severity of hot flashes and better sleep.
Subsequent research found a 60% reduction in hot flash frequency with 2.5 mg twice a day and a 77% reduction with 5 mg twice a day, compared with a 27% reduction with placebo. The only reported side effect that occurred more often with oxybutynin was dry mouth, but there were no significant differences in reasons for discontinuation between the treatment and placebo groups.
There are, however, some potential long-term cognitive effects from oxybutynin, Dr. Faubion said. Some research has shown an increased risk of dementia from oxybutynin and from an overall higher cumulative use of anticholinergics.
“There’s some concern about that for long-term use,” she said, but it’s effective, it’s “probably not harmful [when] used short term in women with significant, bothersome hot flashes who are unwilling or unable to use hormone therapy, and the adverse effects are tolerable for most women.” Women with bladder symptoms would be especially ideal candidates since the drug already treats those.
Dr. Faubion then discussed a new estrogen called estetrol (E4), a naturally occurring estrogen with selection action in tissues that is produced by the fetal liver and crosses the placenta. It has a long half-life of 28-32 hours, and its potential mechanism may give it a different safety profile than estradiol (E2). “There may be a lower risk of drug-drug interactions; lower breast stimulation, pain or carcinogenic impact; lower impact on triglycerides; and a neutral impact on markers of coagulation,” she said.
Though estetrol was recently approved as an oral contraceptive under the name Estelle, it’s also under investigation as a postmenopausal regimen. Preliminary findings suggest it reduces vasomotor symptom severity by 44%, compared with 30% with placebo, at 15 mg, the apparent minimum effective dose. The safety profile showed no endometrial hyperplasia and no unexpected adverse events. In those taking 15 mg of estetrol, mean endometrial thickness increased from 2 to 6 mm but returned to baseline after progestin therapy.
“The 15-mg dose also positively influenced markers of bone turnover, increased HDL [cholesterol], improved glucose tolerance,” and had no effects on coagulation parameters or triglycerides, Dr. Faubion added.
Another group of potential agents being studied for hot flashes are NK3 antagonists, which aim to exploit the recent discovery that kisspeptin, neurokinin B, and dynorphin (KNDy) neurons may play an important role in the etiology of vasomotor symptoms. Development of one of these, MLE 4901, was halted despite a 45% reduction in hot flashes because 3 of 28 women developed transiently elevated liver function tests, about four to six times the upper limit of normal.
Two others, fezolinetant and NT-814, are in phase 2 trials and have shown a significant reduction in symptoms, compared with placebo. The most commonly reported adverse effect in the phase 2a trial was gastrointestinal effects, but none of the participants stopped the drug because of these, and no elevated liver tests occurred. In the larger phase 2b trial, the most commonly reported treatment-emergent adverse events included nausea, diarrhea, fatigue, urinary tract infection, sinusitis, upper respiratory infection, headache, and cough. Five women discontinued the drug because of elevated liver enzymes.
“Overall, NK3 inhibitors appear to be generally well tolerated,” Dr. Faubion said. “There does seem to be mild transaminase elevation,” though it’s not yet known if this is an effect from this class of drugs as a whole. She noted that follicle-stimulating hormone does not significantly increase, which is important because elevated FSH is associated with poor bone health, nor does estradiol significantly increase, which is clinically relevant for women at high risk of breast cancer.
“We don’t know the effects on the heart, the brain, the bone, mood, weight, or sexual health, so there’s a lot that is still not known,” Dr. Faubion said. “We still don’t know about long-term safety and efficacy with these chemical compounds,” but clinical trials of them are ongoing.
They “would be a welcome alternative to hormone therapy for those who can’t or prefer not to use a hormonal option,” Dr. Faubion said. “However, we may need broad education of clinicians to caution against widespread abandonment of hormone therapy, particularly in women with premature or early menopause.”
Donna Klassen, LCSW, the cofounder of Let’s Talk Menopause, asked whether any of these new therapies were being tested in women with breast cancer and whether anything was known about taking oxybutynin at the same time as letrozole.
“I suspect that most women with chronic diseases would have been excluded from these initial studies, but I can’t speak to that,” Dr. Faubion said, and she wasn’t aware of any data related to taking oxybutynin and letrozole concurrently.
James Simon, MD, medical director and founder of IntimMedicine and one of those who led the research on oxybutynin, responded that his trials excluded breast cancer survivors and anyone taking aromatase inhibitors.
“It will be unlikely that, in the very near future, that data will be available because all the clinical developments on these NK3s or KNDy neuron-modulating drugs exclude cancer patients,” Dr. Simon said.
However, another attendee, Lisa Larkin, MD, of Cincinnati, introduced herself as a breast cancer survivor who takes tamoxifen and said she feels “completely comfortable” prescribing oxybutynin to breast cancer survivors.
“In terms of side effects and effectiveness in patients on tamoxifen and aromatase inhibitors, I’ve had incredibly good luck with it, and I think it’s underutilized,” Dr. Larkin said. “The clinical pearl I would tell you is you can start really low, and the dry mouth really seems to improve with time.” She added that patients should be informed that it takes 2 weeks before it begins working, but the side effects eventually go away. “It becomes very tolerable, so I just encourage all of you to consider it as another great option.”
Dr. Faubion had no disclosures. Disclosure information was unavailable for Dr. Simon, Dr. Larkin, and Ms. Klassen.
Hot flashes affect three out of four women and can last 7-10 years, but the current standard of care treatment isn’t necessarily appropriate for all women who experience vasomotor symptoms, according to Stephanie Faubion, MD, MBA, director of the Mayo Clinic Women’s Health Clinic in Jacksonville, Fla.
For the majority of women under age 60 who are within 10 years of menopause, hormone therapy currently remains the most effective management option for hot flashes where the benefits outweigh the risks, Dr. Faubion told attendees Sept. 25 during a plenary at the annual meeting of the North American Menopause Society. “But really, individualizing treatment is the goal, and there are some women who are going to need some other options.”
Contraindications for hormone therapy include having a history of breast cancer, coronary heart disease, active liver disease, unexplained vaginal bleeding, high-risk endometrial cancer, transient ischemic attack, and a previous venous thromboembolic event or stroke.
“Fortunately, we have things in development,” Dr. Faubion said. She reviewed a wide range of therapies that are not currently Food and Drug Administration approved for vasomotor symptoms but are either available off label or are in clinical trials.
One of these is oxybutynin, an antimuscarinic, anticholinergic agent currently used to treat overactive bladder and overactive sweating. In a 2016 trial, 73% of women taking 15 mg extended-release oxybutynin once daily rated their symptoms as “much better,” compared with 26% who received placebo. The women experienced reduced frequency and severity of hot flashes and better sleep.
Subsequent research found a 60% reduction in hot flash frequency with 2.5 mg twice a day and a 77% reduction with 5 mg twice a day, compared with a 27% reduction with placebo. The only reported side effect that occurred more often with oxybutynin was dry mouth, but there were no significant differences in reasons for discontinuation between the treatment and placebo groups.
There are, however, some potential long-term cognitive effects from oxybutynin, Dr. Faubion said. Some research has shown an increased risk of dementia from oxybutynin and from an overall higher cumulative use of anticholinergics.
“There’s some concern about that for long-term use,” she said, but it’s effective, it’s “probably not harmful [when] used short term in women with significant, bothersome hot flashes who are unwilling or unable to use hormone therapy, and the adverse effects are tolerable for most women.” Women with bladder symptoms would be especially ideal candidates since the drug already treats those.
Dr. Faubion then discussed a new estrogen called estetrol (E4), a naturally occurring estrogen with selection action in tissues that is produced by the fetal liver and crosses the placenta. It has a long half-life of 28-32 hours, and its potential mechanism may give it a different safety profile than estradiol (E2). “There may be a lower risk of drug-drug interactions; lower breast stimulation, pain or carcinogenic impact; lower impact on triglycerides; and a neutral impact on markers of coagulation,” she said.
Though estetrol was recently approved as an oral contraceptive under the name Estelle, it’s also under investigation as a postmenopausal regimen. Preliminary findings suggest it reduces vasomotor symptom severity by 44%, compared with 30% with placebo, at 15 mg, the apparent minimum effective dose. The safety profile showed no endometrial hyperplasia and no unexpected adverse events. In those taking 15 mg of estetrol, mean endometrial thickness increased from 2 to 6 mm but returned to baseline after progestin therapy.
“The 15-mg dose also positively influenced markers of bone turnover, increased HDL [cholesterol], improved glucose tolerance,” and had no effects on coagulation parameters or triglycerides, Dr. Faubion added.
Another group of potential agents being studied for hot flashes are NK3 antagonists, which aim to exploit the recent discovery that kisspeptin, neurokinin B, and dynorphin (KNDy) neurons may play an important role in the etiology of vasomotor symptoms. Development of one of these, MLE 4901, was halted despite a 45% reduction in hot flashes because 3 of 28 women developed transiently elevated liver function tests, about four to six times the upper limit of normal.
Two others, fezolinetant and NT-814, are in phase 2 trials and have shown a significant reduction in symptoms, compared with placebo. The most commonly reported adverse effect in the phase 2a trial was gastrointestinal effects, but none of the participants stopped the drug because of these, and no elevated liver tests occurred. In the larger phase 2b trial, the most commonly reported treatment-emergent adverse events included nausea, diarrhea, fatigue, urinary tract infection, sinusitis, upper respiratory infection, headache, and cough. Five women discontinued the drug because of elevated liver enzymes.
“Overall, NK3 inhibitors appear to be generally well tolerated,” Dr. Faubion said. “There does seem to be mild transaminase elevation,” though it’s not yet known if this is an effect from this class of drugs as a whole. She noted that follicle-stimulating hormone does not significantly increase, which is important because elevated FSH is associated with poor bone health, nor does estradiol significantly increase, which is clinically relevant for women at high risk of breast cancer.
“We don’t know the effects on the heart, the brain, the bone, mood, weight, or sexual health, so there’s a lot that is still not known,” Dr. Faubion said. “We still don’t know about long-term safety and efficacy with these chemical compounds,” but clinical trials of them are ongoing.
They “would be a welcome alternative to hormone therapy for those who can’t or prefer not to use a hormonal option,” Dr. Faubion said. “However, we may need broad education of clinicians to caution against widespread abandonment of hormone therapy, particularly in women with premature or early menopause.”
Donna Klassen, LCSW, the cofounder of Let’s Talk Menopause, asked whether any of these new therapies were being tested in women with breast cancer and whether anything was known about taking oxybutynin at the same time as letrozole.
“I suspect that most women with chronic diseases would have been excluded from these initial studies, but I can’t speak to that,” Dr. Faubion said, and she wasn’t aware of any data related to taking oxybutynin and letrozole concurrently.
James Simon, MD, medical director and founder of IntimMedicine and one of those who led the research on oxybutynin, responded that his trials excluded breast cancer survivors and anyone taking aromatase inhibitors.
“It will be unlikely that, in the very near future, that data will be available because all the clinical developments on these NK3s or KNDy neuron-modulating drugs exclude cancer patients,” Dr. Simon said.
However, another attendee, Lisa Larkin, MD, of Cincinnati, introduced herself as a breast cancer survivor who takes tamoxifen and said she feels “completely comfortable” prescribing oxybutynin to breast cancer survivors.
“In terms of side effects and effectiveness in patients on tamoxifen and aromatase inhibitors, I’ve had incredibly good luck with it, and I think it’s underutilized,” Dr. Larkin said. “The clinical pearl I would tell you is you can start really low, and the dry mouth really seems to improve with time.” She added that patients should be informed that it takes 2 weeks before it begins working, but the side effects eventually go away. “It becomes very tolerable, so I just encourage all of you to consider it as another great option.”
Dr. Faubion had no disclosures. Disclosure information was unavailable for Dr. Simon, Dr. Larkin, and Ms. Klassen.
Hot flashes affect three out of four women and can last 7-10 years, but the current standard of care treatment isn’t necessarily appropriate for all women who experience vasomotor symptoms, according to Stephanie Faubion, MD, MBA, director of the Mayo Clinic Women’s Health Clinic in Jacksonville, Fla.
For the majority of women under age 60 who are within 10 years of menopause, hormone therapy currently remains the most effective management option for hot flashes where the benefits outweigh the risks, Dr. Faubion told attendees Sept. 25 during a plenary at the annual meeting of the North American Menopause Society. “But really, individualizing treatment is the goal, and there are some women who are going to need some other options.”
Contraindications for hormone therapy include having a history of breast cancer, coronary heart disease, active liver disease, unexplained vaginal bleeding, high-risk endometrial cancer, transient ischemic attack, and a previous venous thromboembolic event or stroke.
“Fortunately, we have things in development,” Dr. Faubion said. She reviewed a wide range of therapies that are not currently Food and Drug Administration approved for vasomotor symptoms but are either available off label or are in clinical trials.
One of these is oxybutynin, an antimuscarinic, anticholinergic agent currently used to treat overactive bladder and overactive sweating. In a 2016 trial, 73% of women taking 15 mg extended-release oxybutynin once daily rated their symptoms as “much better,” compared with 26% who received placebo. The women experienced reduced frequency and severity of hot flashes and better sleep.
Subsequent research found a 60% reduction in hot flash frequency with 2.5 mg twice a day and a 77% reduction with 5 mg twice a day, compared with a 27% reduction with placebo. The only reported side effect that occurred more often with oxybutynin was dry mouth, but there were no significant differences in reasons for discontinuation between the treatment and placebo groups.
There are, however, some potential long-term cognitive effects from oxybutynin, Dr. Faubion said. Some research has shown an increased risk of dementia from oxybutynin and from an overall higher cumulative use of anticholinergics.
“There’s some concern about that for long-term use,” she said, but it’s effective, it’s “probably not harmful [when] used short term in women with significant, bothersome hot flashes who are unwilling or unable to use hormone therapy, and the adverse effects are tolerable for most women.” Women with bladder symptoms would be especially ideal candidates since the drug already treats those.
Dr. Faubion then discussed a new estrogen called estetrol (E4), a naturally occurring estrogen with selection action in tissues that is produced by the fetal liver and crosses the placenta. It has a long half-life of 28-32 hours, and its potential mechanism may give it a different safety profile than estradiol (E2). “There may be a lower risk of drug-drug interactions; lower breast stimulation, pain or carcinogenic impact; lower impact on triglycerides; and a neutral impact on markers of coagulation,” she said.
Though estetrol was recently approved as an oral contraceptive under the name Estelle, it’s also under investigation as a postmenopausal regimen. Preliminary findings suggest it reduces vasomotor symptom severity by 44%, compared with 30% with placebo, at 15 mg, the apparent minimum effective dose. The safety profile showed no endometrial hyperplasia and no unexpected adverse events. In those taking 15 mg of estetrol, mean endometrial thickness increased from 2 to 6 mm but returned to baseline after progestin therapy.
“The 15-mg dose also positively influenced markers of bone turnover, increased HDL [cholesterol], improved glucose tolerance,” and had no effects on coagulation parameters or triglycerides, Dr. Faubion added.
Another group of potential agents being studied for hot flashes are NK3 antagonists, which aim to exploit the recent discovery that kisspeptin, neurokinin B, and dynorphin (KNDy) neurons may play an important role in the etiology of vasomotor symptoms. Development of one of these, MLE 4901, was halted despite a 45% reduction in hot flashes because 3 of 28 women developed transiently elevated liver function tests, about four to six times the upper limit of normal.
Two others, fezolinetant and NT-814, are in phase 2 trials and have shown a significant reduction in symptoms, compared with placebo. The most commonly reported adverse effect in the phase 2a trial was gastrointestinal effects, but none of the participants stopped the drug because of these, and no elevated liver tests occurred. In the larger phase 2b trial, the most commonly reported treatment-emergent adverse events included nausea, diarrhea, fatigue, urinary tract infection, sinusitis, upper respiratory infection, headache, and cough. Five women discontinued the drug because of elevated liver enzymes.
“Overall, NK3 inhibitors appear to be generally well tolerated,” Dr. Faubion said. “There does seem to be mild transaminase elevation,” though it’s not yet known if this is an effect from this class of drugs as a whole. She noted that follicle-stimulating hormone does not significantly increase, which is important because elevated FSH is associated with poor bone health, nor does estradiol significantly increase, which is clinically relevant for women at high risk of breast cancer.
“We don’t know the effects on the heart, the brain, the bone, mood, weight, or sexual health, so there’s a lot that is still not known,” Dr. Faubion said. “We still don’t know about long-term safety and efficacy with these chemical compounds,” but clinical trials of them are ongoing.
They “would be a welcome alternative to hormone therapy for those who can’t or prefer not to use a hormonal option,” Dr. Faubion said. “However, we may need broad education of clinicians to caution against widespread abandonment of hormone therapy, particularly in women with premature or early menopause.”
Donna Klassen, LCSW, the cofounder of Let’s Talk Menopause, asked whether any of these new therapies were being tested in women with breast cancer and whether anything was known about taking oxybutynin at the same time as letrozole.
“I suspect that most women with chronic diseases would have been excluded from these initial studies, but I can’t speak to that,” Dr. Faubion said, and she wasn’t aware of any data related to taking oxybutynin and letrozole concurrently.
James Simon, MD, medical director and founder of IntimMedicine and one of those who led the research on oxybutynin, responded that his trials excluded breast cancer survivors and anyone taking aromatase inhibitors.
“It will be unlikely that, in the very near future, that data will be available because all the clinical developments on these NK3s or KNDy neuron-modulating drugs exclude cancer patients,” Dr. Simon said.
However, another attendee, Lisa Larkin, MD, of Cincinnati, introduced herself as a breast cancer survivor who takes tamoxifen and said she feels “completely comfortable” prescribing oxybutynin to breast cancer survivors.
“In terms of side effects and effectiveness in patients on tamoxifen and aromatase inhibitors, I’ve had incredibly good luck with it, and I think it’s underutilized,” Dr. Larkin said. “The clinical pearl I would tell you is you can start really low, and the dry mouth really seems to improve with time.” She added that patients should be informed that it takes 2 weeks before it begins working, but the side effects eventually go away. “It becomes very tolerable, so I just encourage all of you to consider it as another great option.”
Dr. Faubion had no disclosures. Disclosure information was unavailable for Dr. Simon, Dr. Larkin, and Ms. Klassen.
FROM NAMS 2021