User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Spam filter failure: Selling physician emails equals big $$
Despite the best efforts of my institution’s spam filter, I’ve realized that I spend at least 4 minutes every day of the week removing junk email from my in basket: EMR vendors, predatory journals trying to lure me into paying their outrageous publication fees, people who want to help me with my billing software (evidently that .edu extension hasn’t clicked for them yet), headhunters trying to fill specialty positions in other states, market researchers offering a gift card for 40 minutes filling out a survey.
If you do the math, 4 minutes daily is 1,460 minutes per year. That’s an entire day of my life lost each year to this useless nonsense, which I never agreed to receive in the first place. Now multiply that by the 22 million health care workers in the United States, or even just by the 985,000 licensed physicians in this country. Then factor in the $638 per hour in gross revenue generated by the average primary care physician, as a conservative, well-documented value.
By my reckoning, these bozos owe the United States alone over $15 billion in lost GDP each year.
So why don’t we shut it down!? The CAN-SPAM Act of 2003 attempted to at least mitigate the problem. It applies only to commercial entities (I know, I’d love to report some political groups, too). To avoid violating the law and risking fines of up to $16,000 per individual email, senders must:
- Not use misleading header info (including domain name and email address)
- Not use deceptive subject lines
- Clearly label the email as an ad
- Give an actual physical address of the sender
- Tell recipients how to opt out of future emails
- Honor opt-out requests within 10 business days
- Monitor the activities of any subcontractor sending email on their behalf
I can say with certainty that much of the trash in my inbox violates at least one of these. But that doesn’t matter if there is not an efficient way to report the violators and ensure that they’ll be tracked down. Hard enough if they live here, impossible if the email is routed from overseas, as much of it clearly is.
If you receive email in violation of the act, experts recommend that you write down the email address and the business name of the sender, fill out a complaint form on the Federal Trade Commission website, or send an email to [email protected], then send an email to your Internet service provider’s abuse desk. If you’re not working within a big institution like mine that has hot and cold running IT personnel that operate their own abuse prevention office, the address you’ll need is likely abuse@domain_name or postmaster@domain_name. Just hitting the spam button at the top of your browser/email software may do the trick. There’s more good advice at the FTC’s consumer spam page.
The answer came, ironically, to my email inbox in the form of one of those emails that did indeed violate the law.
I rolled my eyes and started into my reporting subroutine but then stopped cold. Just 1 second. If this person is selling lists of email addresses of conference attendees, somebody within the conference structure must be providing them. How is that legal? I have never agreed, in registering for a medical conference, to allow them to share my email address with anyone. To think that they are making money from that is extremely galling.
Vermont, at least, has enacted a law requiring companies that traffic in such email lists to register with the state. Although it has been in effect for 2 years, the jury is out regarding its efficacy. Our European counterparts are protected by the General Data Protection Regulation, which specifies that commercial email can be sent only to individuals who have explicitly opted into such mailings, and that purchased email lists are not compliant with the requirement.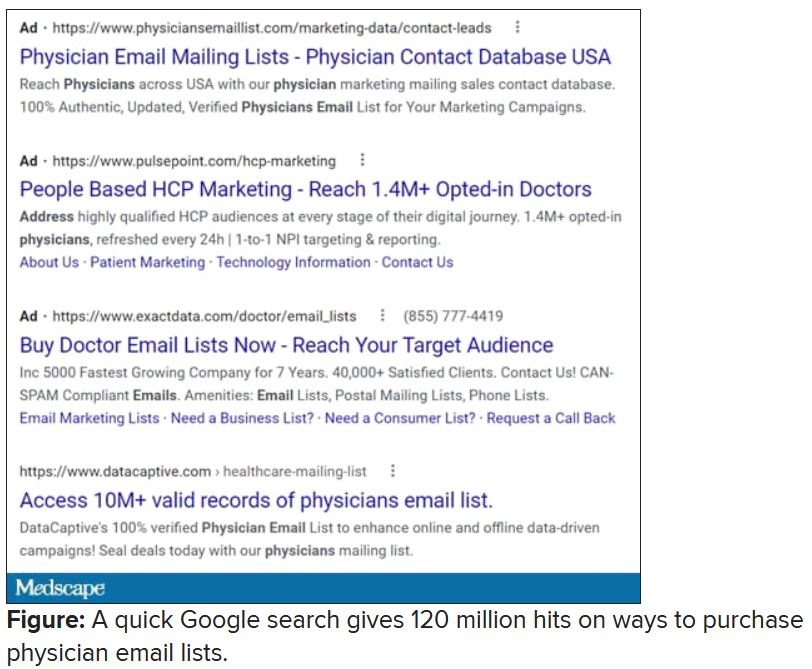
Anybody have the inside scoop on this? Can we demand that our professional societies safeguard their attendee databases so this won’t happen? If they won’t, why am I paying big money to attend their conferences, only for them to make even more money at my expense?
Dr. Hitchcock is assistant professor, department of radiation oncology, at the University of Florida, Gainesville. She reported receiving research grant money from Merck. A version of this article first appeared on Medscape.com.
Despite the best efforts of my institution’s spam filter, I’ve realized that I spend at least 4 minutes every day of the week removing junk email from my in basket: EMR vendors, predatory journals trying to lure me into paying their outrageous publication fees, people who want to help me with my billing software (evidently that .edu extension hasn’t clicked for them yet), headhunters trying to fill specialty positions in other states, market researchers offering a gift card for 40 minutes filling out a survey.
If you do the math, 4 minutes daily is 1,460 minutes per year. That’s an entire day of my life lost each year to this useless nonsense, which I never agreed to receive in the first place. Now multiply that by the 22 million health care workers in the United States, or even just by the 985,000 licensed physicians in this country. Then factor in the $638 per hour in gross revenue generated by the average primary care physician, as a conservative, well-documented value.
By my reckoning, these bozos owe the United States alone over $15 billion in lost GDP each year.
So why don’t we shut it down!? The CAN-SPAM Act of 2003 attempted to at least mitigate the problem. It applies only to commercial entities (I know, I’d love to report some political groups, too). To avoid violating the law and risking fines of up to $16,000 per individual email, senders must:
- Not use misleading header info (including domain name and email address)
- Not use deceptive subject lines
- Clearly label the email as an ad
- Give an actual physical address of the sender
- Tell recipients how to opt out of future emails
- Honor opt-out requests within 10 business days
- Monitor the activities of any subcontractor sending email on their behalf
I can say with certainty that much of the trash in my inbox violates at least one of these. But that doesn’t matter if there is not an efficient way to report the violators and ensure that they’ll be tracked down. Hard enough if they live here, impossible if the email is routed from overseas, as much of it clearly is.
If you receive email in violation of the act, experts recommend that you write down the email address and the business name of the sender, fill out a complaint form on the Federal Trade Commission website, or send an email to [email protected], then send an email to your Internet service provider’s abuse desk. If you’re not working within a big institution like mine that has hot and cold running IT personnel that operate their own abuse prevention office, the address you’ll need is likely abuse@domain_name or postmaster@domain_name. Just hitting the spam button at the top of your browser/email software may do the trick. There’s more good advice at the FTC’s consumer spam page.
The answer came, ironically, to my email inbox in the form of one of those emails that did indeed violate the law.
I rolled my eyes and started into my reporting subroutine but then stopped cold. Just 1 second. If this person is selling lists of email addresses of conference attendees, somebody within the conference structure must be providing them. How is that legal? I have never agreed, in registering for a medical conference, to allow them to share my email address with anyone. To think that they are making money from that is extremely galling.
Vermont, at least, has enacted a law requiring companies that traffic in such email lists to register with the state. Although it has been in effect for 2 years, the jury is out regarding its efficacy. Our European counterparts are protected by the General Data Protection Regulation, which specifies that commercial email can be sent only to individuals who have explicitly opted into such mailings, and that purchased email lists are not compliant with the requirement.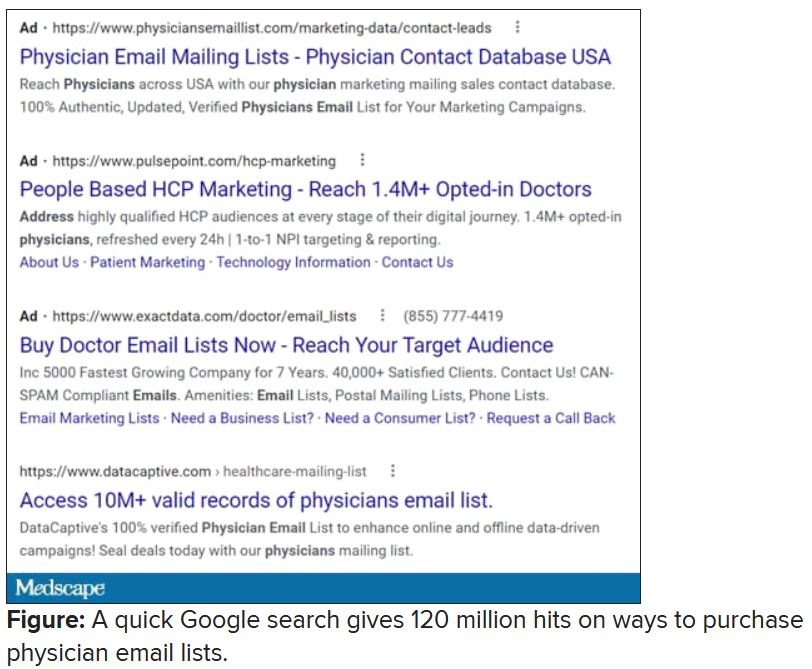
Anybody have the inside scoop on this? Can we demand that our professional societies safeguard their attendee databases so this won’t happen? If they won’t, why am I paying big money to attend their conferences, only for them to make even more money at my expense?
Dr. Hitchcock is assistant professor, department of radiation oncology, at the University of Florida, Gainesville. She reported receiving research grant money from Merck. A version of this article first appeared on Medscape.com.
Despite the best efforts of my institution’s spam filter, I’ve realized that I spend at least 4 minutes every day of the week removing junk email from my in basket: EMR vendors, predatory journals trying to lure me into paying their outrageous publication fees, people who want to help me with my billing software (evidently that .edu extension hasn’t clicked for them yet), headhunters trying to fill specialty positions in other states, market researchers offering a gift card for 40 minutes filling out a survey.
If you do the math, 4 minutes daily is 1,460 minutes per year. That’s an entire day of my life lost each year to this useless nonsense, which I never agreed to receive in the first place. Now multiply that by the 22 million health care workers in the United States, or even just by the 985,000 licensed physicians in this country. Then factor in the $638 per hour in gross revenue generated by the average primary care physician, as a conservative, well-documented value.
By my reckoning, these bozos owe the United States alone over $15 billion in lost GDP each year.
So why don’t we shut it down!? The CAN-SPAM Act of 2003 attempted to at least mitigate the problem. It applies only to commercial entities (I know, I’d love to report some political groups, too). To avoid violating the law and risking fines of up to $16,000 per individual email, senders must:
- Not use misleading header info (including domain name and email address)
- Not use deceptive subject lines
- Clearly label the email as an ad
- Give an actual physical address of the sender
- Tell recipients how to opt out of future emails
- Honor opt-out requests within 10 business days
- Monitor the activities of any subcontractor sending email on their behalf
I can say with certainty that much of the trash in my inbox violates at least one of these. But that doesn’t matter if there is not an efficient way to report the violators and ensure that they’ll be tracked down. Hard enough if they live here, impossible if the email is routed from overseas, as much of it clearly is.
If you receive email in violation of the act, experts recommend that you write down the email address and the business name of the sender, fill out a complaint form on the Federal Trade Commission website, or send an email to [email protected], then send an email to your Internet service provider’s abuse desk. If you’re not working within a big institution like mine that has hot and cold running IT personnel that operate their own abuse prevention office, the address you’ll need is likely abuse@domain_name or postmaster@domain_name. Just hitting the spam button at the top of your browser/email software may do the trick. There’s more good advice at the FTC’s consumer spam page.
The answer came, ironically, to my email inbox in the form of one of those emails that did indeed violate the law.
I rolled my eyes and started into my reporting subroutine but then stopped cold. Just 1 second. If this person is selling lists of email addresses of conference attendees, somebody within the conference structure must be providing them. How is that legal? I have never agreed, in registering for a medical conference, to allow them to share my email address with anyone. To think that they are making money from that is extremely galling.
Vermont, at least, has enacted a law requiring companies that traffic in such email lists to register with the state. Although it has been in effect for 2 years, the jury is out regarding its efficacy. Our European counterparts are protected by the General Data Protection Regulation, which specifies that commercial email can be sent only to individuals who have explicitly opted into such mailings, and that purchased email lists are not compliant with the requirement.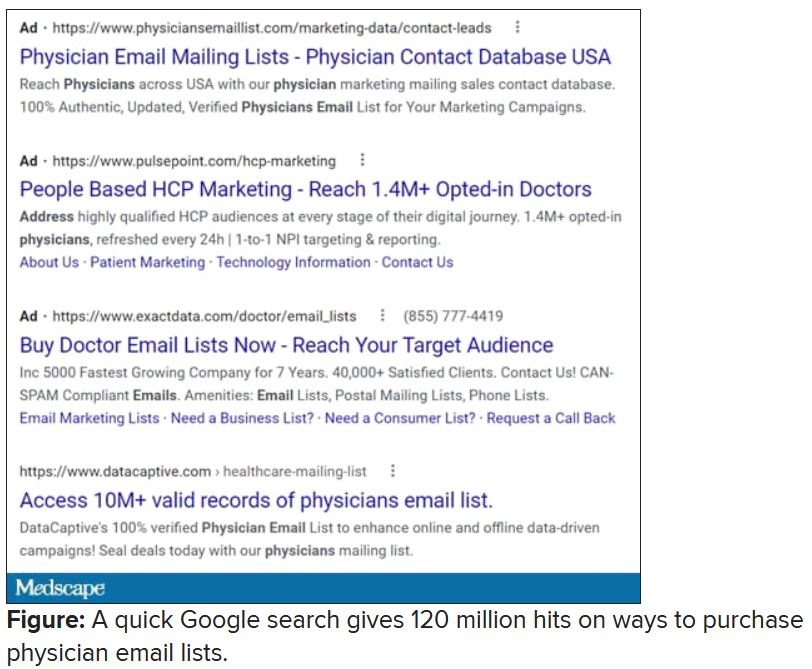
Anybody have the inside scoop on this? Can we demand that our professional societies safeguard their attendee databases so this won’t happen? If they won’t, why am I paying big money to attend their conferences, only for them to make even more money at my expense?
Dr. Hitchcock is assistant professor, department of radiation oncology, at the University of Florida, Gainesville. She reported receiving research grant money from Merck. A version of this article first appeared on Medscape.com.
Closing your practice
“I might have to close my office,” a colleague wrote me recently. “I can’t find reliable medical assistants; no one good applies. Sad, but oh, well.”
A paucity of good employees is just one of many reasons given by physicians who have decided to close up shop. (See my recent column, “Finding Employees During a Pandemic”).
to address in order to ensure a smooth exit.
First, this cannot (and should not) be a hasty process. You will need at least a year to do it correctly, because there is a lot to do.
Once you have settled on a closing date, inform your attorney. If the firm you are using does not have experience in medical practice sales or closures, ask them to recommend one that does. You will need expert legal guidance during many of the steps that follow.
Next, review all of your contracts and leases. Most of them cannot be terminated at the drop of a hat. Facility and equipment leases may require a year’s notice, or even longer. Contracts with managed care, maintenance, cleaning, and hazardous waste disposal companies, and others such as answering services and website managers, should be reviewed to determine what sort of advance notice you will need to give.
Another step to take well in advance is to contact your malpractice insurance carrier. Most carriers have specific guidelines for when to notify your patients – and that notification will vary from carrier to carrier, state to state, and situation to situation. If you have a claims-made policy, you also need to inquire about the necessity of purchasing “tail” coverage, which will protect you in the event of a lawsuit after your practice has closed. Many carriers include tail coverage at no charge if you are retiring completely, but if you expect to do part-time, locum tenens, or volunteer medical work, you will need to pay for it.
Once you have the basics nailed down, notify your employees. You will want them to hear the news from you, not through the grapevine, and certainly not from your patients. You may be worried that some will quit, but keeping them in the dark will not prevent that, as they will find out soon enough. Besides, if you help them by assisting in finding them new employment, they will most likely help you by staying to the end.
At this point, you should also begin thinking about disposition of your patients’ records. You can’t just shred them, much as you might be tempted. Your attorney and malpractice carrier will guide you in how long they must be retained; 7-10 years is typical in many states, but it could be longer in yours. Unless you are selling part or all of your practice to another physician, you will have to designate someone else to be the legal custodian of the records and obtain a written custodial agreement from that person or organization.
Once that is arranged, you can notify your patients. Send them a letter or e-mail (or both) informing them of the date that you intend to close the practice. Let them know where their records will be kept, who to contact for a copy, and that their written consent will be required to obtain it. Some states also require that a notice be placed in the local newspaper or online, including the date of closure and how to request records.
This is also the time to inform all your third-party payers, including Medicare and Medicaid if applicable, any hospitals where you have privileges, and referring physicians. Notify any business concerns not notified already, such as utilities and other ancillary services. Your state medical board and the Drug Enforcement Agency will need to know as well. Contact a liquidator or used equipment dealer to arrange for disposal of any office equipment that has resale value. It is also a good time to decide how you will handle patient collections that trickle in after closing, and where mail should be forwarded.
As the closing date approaches, determine how to properly dispose of any medications you have on-hand. Your state may have requirements for disposal of controlled substances, and possibly for noncontrolled pharmaceuticals as well. Check your state’s controlled substances reporting system and other applicable regulators. Once the office is closed, don’t forget to shred any blank prescription pads and dissolve your corporation, if you have one.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
“I might have to close my office,” a colleague wrote me recently. “I can’t find reliable medical assistants; no one good applies. Sad, but oh, well.”
A paucity of good employees is just one of many reasons given by physicians who have decided to close up shop. (See my recent column, “Finding Employees During a Pandemic”).
to address in order to ensure a smooth exit.
First, this cannot (and should not) be a hasty process. You will need at least a year to do it correctly, because there is a lot to do.
Once you have settled on a closing date, inform your attorney. If the firm you are using does not have experience in medical practice sales or closures, ask them to recommend one that does. You will need expert legal guidance during many of the steps that follow.
Next, review all of your contracts and leases. Most of them cannot be terminated at the drop of a hat. Facility and equipment leases may require a year’s notice, or even longer. Contracts with managed care, maintenance, cleaning, and hazardous waste disposal companies, and others such as answering services and website managers, should be reviewed to determine what sort of advance notice you will need to give.
Another step to take well in advance is to contact your malpractice insurance carrier. Most carriers have specific guidelines for when to notify your patients – and that notification will vary from carrier to carrier, state to state, and situation to situation. If you have a claims-made policy, you also need to inquire about the necessity of purchasing “tail” coverage, which will protect you in the event of a lawsuit after your practice has closed. Many carriers include tail coverage at no charge if you are retiring completely, but if you expect to do part-time, locum tenens, or volunteer medical work, you will need to pay for it.
Once you have the basics nailed down, notify your employees. You will want them to hear the news from you, not through the grapevine, and certainly not from your patients. You may be worried that some will quit, but keeping them in the dark will not prevent that, as they will find out soon enough. Besides, if you help them by assisting in finding them new employment, they will most likely help you by staying to the end.
At this point, you should also begin thinking about disposition of your patients’ records. You can’t just shred them, much as you might be tempted. Your attorney and malpractice carrier will guide you in how long they must be retained; 7-10 years is typical in many states, but it could be longer in yours. Unless you are selling part or all of your practice to another physician, you will have to designate someone else to be the legal custodian of the records and obtain a written custodial agreement from that person or organization.
Once that is arranged, you can notify your patients. Send them a letter or e-mail (or both) informing them of the date that you intend to close the practice. Let them know where their records will be kept, who to contact for a copy, and that their written consent will be required to obtain it. Some states also require that a notice be placed in the local newspaper or online, including the date of closure and how to request records.
This is also the time to inform all your third-party payers, including Medicare and Medicaid if applicable, any hospitals where you have privileges, and referring physicians. Notify any business concerns not notified already, such as utilities and other ancillary services. Your state medical board and the Drug Enforcement Agency will need to know as well. Contact a liquidator or used equipment dealer to arrange for disposal of any office equipment that has resale value. It is also a good time to decide how you will handle patient collections that trickle in after closing, and where mail should be forwarded.
As the closing date approaches, determine how to properly dispose of any medications you have on-hand. Your state may have requirements for disposal of controlled substances, and possibly for noncontrolled pharmaceuticals as well. Check your state’s controlled substances reporting system and other applicable regulators. Once the office is closed, don’t forget to shred any blank prescription pads and dissolve your corporation, if you have one.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
“I might have to close my office,” a colleague wrote me recently. “I can’t find reliable medical assistants; no one good applies. Sad, but oh, well.”
A paucity of good employees is just one of many reasons given by physicians who have decided to close up shop. (See my recent column, “Finding Employees During a Pandemic”).
to address in order to ensure a smooth exit.
First, this cannot (and should not) be a hasty process. You will need at least a year to do it correctly, because there is a lot to do.
Once you have settled on a closing date, inform your attorney. If the firm you are using does not have experience in medical practice sales or closures, ask them to recommend one that does. You will need expert legal guidance during many of the steps that follow.
Next, review all of your contracts and leases. Most of them cannot be terminated at the drop of a hat. Facility and equipment leases may require a year’s notice, or even longer. Contracts with managed care, maintenance, cleaning, and hazardous waste disposal companies, and others such as answering services and website managers, should be reviewed to determine what sort of advance notice you will need to give.
Another step to take well in advance is to contact your malpractice insurance carrier. Most carriers have specific guidelines for when to notify your patients – and that notification will vary from carrier to carrier, state to state, and situation to situation. If you have a claims-made policy, you also need to inquire about the necessity of purchasing “tail” coverage, which will protect you in the event of a lawsuit after your practice has closed. Many carriers include tail coverage at no charge if you are retiring completely, but if you expect to do part-time, locum tenens, or volunteer medical work, you will need to pay for it.
Once you have the basics nailed down, notify your employees. You will want them to hear the news from you, not through the grapevine, and certainly not from your patients. You may be worried that some will quit, but keeping them in the dark will not prevent that, as they will find out soon enough. Besides, if you help them by assisting in finding them new employment, they will most likely help you by staying to the end.
At this point, you should also begin thinking about disposition of your patients’ records. You can’t just shred them, much as you might be tempted. Your attorney and malpractice carrier will guide you in how long they must be retained; 7-10 years is typical in many states, but it could be longer in yours. Unless you are selling part or all of your practice to another physician, you will have to designate someone else to be the legal custodian of the records and obtain a written custodial agreement from that person or organization.
Once that is arranged, you can notify your patients. Send them a letter or e-mail (or both) informing them of the date that you intend to close the practice. Let them know where their records will be kept, who to contact for a copy, and that their written consent will be required to obtain it. Some states also require that a notice be placed in the local newspaper or online, including the date of closure and how to request records.
This is also the time to inform all your third-party payers, including Medicare and Medicaid if applicable, any hospitals where you have privileges, and referring physicians. Notify any business concerns not notified already, such as utilities and other ancillary services. Your state medical board and the Drug Enforcement Agency will need to know as well. Contact a liquidator or used equipment dealer to arrange for disposal of any office equipment that has resale value. It is also a good time to decide how you will handle patient collections that trickle in after closing, and where mail should be forwarded.
As the closing date approaches, determine how to properly dispose of any medications you have on-hand. Your state may have requirements for disposal of controlled substances, and possibly for noncontrolled pharmaceuticals as well. Check your state’s controlled substances reporting system and other applicable regulators. Once the office is closed, don’t forget to shred any blank prescription pads and dissolve your corporation, if you have one.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
A very strange place to find a tooth
A nose for the tooth
Have you ever had a stuffy nose that just wouldn’t go away? Those irritating head colds have nothing on the stuffy nose a man in New York recently had to go through. A stuffy nose to top all stuffy noses. One stuffy nose to rule them all, as it were.
This man went to a Mount Sinai clinic with difficulty breathing through his right nostril, a problem that had been going on for years. Let us repeat that: A stuffy nose that lasted for years. The exam revealed a white mass jutting through the back of the septum and a CT scan confirmed the diagnosis. Perhaps you’ve already guessed, since the headline does give things away. Yes, this man had a tooth growing into his nose.
The problem was a half-inch-long ectopic tooth. Ectopic teeth are rare, occurring in less than 1% of people, but an ectopic tooth growing backward into the nasal cavity? Well, that’s so uncommon that this man got a case report in the New England Journal of Medicine.
This story does have a happy ending. Not all ectopic teeth need to be treated, but this one really did have to go. The offending tooth was surgically removed and, at a 3-month follow-up, the stuffy nose issue was completely resolved. So our friend gets the best of both worlds: His issue gets cured and he gets a case report in a major medical publication. If that’s not living the dream, we don’t know what is, and that’s the tooth.
Lettuce recommend you a sleep aid
Lettuce is great for many things. The star in a salad? Of course. The fresh element in a BLT? Yep. A sleep aid? According to a TikTok hack with almost 5 million views, the pinch hitter in a sandwich is switching leagues to be used like a tea for faster sleep. But, does it really work? Researchers say yes and no, according to a recent report at Tyla.com.
Studies conducted in 2013 and 2017 pointed toward a compound called lactucin, which is found in the plant’s n-butanol fraction. In the 2013 study, mice that received n-butanol fraction fell asleep faster and stayed asleep longer. In 2017, researchers found that lettuce made mice sleep longer and helped protect against cell inflammation and damage.
OK, so it works on mice. But what about humans? In the TikTok video, user Shapla Hoque pours hot water on a few lettuce leaves in a mug with a peppermint tea bag (for flavor). After 10 minutes, when the leaves are soaked and soggy, she removes them and drinks the lettuce tea. By the end of the video she’s visibly drowsy and ready to crash. Does this hold water?
Here’s the no. Dr. Charlotte Norton of the Slimming Clinic told Tyla.com that yeah, there are some properties in lettuce that will help you fall asleep, such as lactucarium, which is prominent in romaine. But you would need a massive amount of lettuce to get any effect. The TikTok video, she said, is an example of the placebo effect.
Brains get a rise out of Viagra
A lot of medications are used off label. Antidepressants for COVID have taken the cake recently, but here’s a new one: Viagra for Alzheimer’s disease.
Although there’s no definite link yet between the two, neuron models derived from induced pluripotent stem cells from patients with Alzheimer’s suggest that sildenafil increases neurite growth and decreases phospho-tau expression, Jiansong Fang, PhD, of the Cleveland Clinic, and associates said in Nature Aging.
Their research is an attempt to find untapped sources of new treatments among existing drugs. They began the search with 1,600 approved drugs and focused on those that target the buildup of beta amyloid and tau proteins in the brain, according to the Daily Beast.
Since sildenafil is obviously for men, more research will need to be done on how this drug affects women. Don’t start stocking up just yet.
Omicron is not a social-distancing robot
COVID, safe to say, has not been your typical, run-of-the-mill pandemic. People have protested social distancing. People have protested lockdowns. People have protested mask mandates. People have protested vaccine mandates. People have protested people protesting vaccine mandates.
Someone used a fake arm to get a COVID vaccine card. People have tried to reverse their COVID vaccinations. People had COVID contamination parties.
The common denominator? People. Humans. Maybe what we need is a nonhuman intervention. To fight COVID, we need a hero. A robotic hero.
And where can we find such a hero? The University of Maryland, of course, where computer scientists and engineers are working on an autonomous mobile robot to enforce indoor social-distancing rules.
Their robot can detect lapses in social distancing using cameras, both thermal and visual, along with a LiDAR (Light Detection and Ranging) sensor. It then sorts the offenders into various groups depending on whether they are standing still or moving and predicts their future movement using a state-of-the-art hybrid collision avoidance method known as Frozone, Adarsh Jagan Sathyamoorthy and associates explained in PLOS One.
“Once it reaches the breach, the robot encourages people to move apart via text that appears on a mounted display,” ScienceDaily said.
Maybe you were expecting a Terminator-type robot coming to enforce social distancing requirements rather than a simple text message. Let’s just hope that all COVID guidelines are followed, including social distancing, so the pandemic will finally end and won’t “be back.”
A nose for the tooth
Have you ever had a stuffy nose that just wouldn’t go away? Those irritating head colds have nothing on the stuffy nose a man in New York recently had to go through. A stuffy nose to top all stuffy noses. One stuffy nose to rule them all, as it were.
This man went to a Mount Sinai clinic with difficulty breathing through his right nostril, a problem that had been going on for years. Let us repeat that: A stuffy nose that lasted for years. The exam revealed a white mass jutting through the back of the septum and a CT scan confirmed the diagnosis. Perhaps you’ve already guessed, since the headline does give things away. Yes, this man had a tooth growing into his nose.
The problem was a half-inch-long ectopic tooth. Ectopic teeth are rare, occurring in less than 1% of people, but an ectopic tooth growing backward into the nasal cavity? Well, that’s so uncommon that this man got a case report in the New England Journal of Medicine.
This story does have a happy ending. Not all ectopic teeth need to be treated, but this one really did have to go. The offending tooth was surgically removed and, at a 3-month follow-up, the stuffy nose issue was completely resolved. So our friend gets the best of both worlds: His issue gets cured and he gets a case report in a major medical publication. If that’s not living the dream, we don’t know what is, and that’s the tooth.
Lettuce recommend you a sleep aid
Lettuce is great for many things. The star in a salad? Of course. The fresh element in a BLT? Yep. A sleep aid? According to a TikTok hack with almost 5 million views, the pinch hitter in a sandwich is switching leagues to be used like a tea for faster sleep. But, does it really work? Researchers say yes and no, according to a recent report at Tyla.com.
Studies conducted in 2013 and 2017 pointed toward a compound called lactucin, which is found in the plant’s n-butanol fraction. In the 2013 study, mice that received n-butanol fraction fell asleep faster and stayed asleep longer. In 2017, researchers found that lettuce made mice sleep longer and helped protect against cell inflammation and damage.
OK, so it works on mice. But what about humans? In the TikTok video, user Shapla Hoque pours hot water on a few lettuce leaves in a mug with a peppermint tea bag (for flavor). After 10 minutes, when the leaves are soaked and soggy, she removes them and drinks the lettuce tea. By the end of the video she’s visibly drowsy and ready to crash. Does this hold water?
Here’s the no. Dr. Charlotte Norton of the Slimming Clinic told Tyla.com that yeah, there are some properties in lettuce that will help you fall asleep, such as lactucarium, which is prominent in romaine. But you would need a massive amount of lettuce to get any effect. The TikTok video, she said, is an example of the placebo effect.
Brains get a rise out of Viagra
A lot of medications are used off label. Antidepressants for COVID have taken the cake recently, but here’s a new one: Viagra for Alzheimer’s disease.
Although there’s no definite link yet between the two, neuron models derived from induced pluripotent stem cells from patients with Alzheimer’s suggest that sildenafil increases neurite growth and decreases phospho-tau expression, Jiansong Fang, PhD, of the Cleveland Clinic, and associates said in Nature Aging.
Their research is an attempt to find untapped sources of new treatments among existing drugs. They began the search with 1,600 approved drugs and focused on those that target the buildup of beta amyloid and tau proteins in the brain, according to the Daily Beast.
Since sildenafil is obviously for men, more research will need to be done on how this drug affects women. Don’t start stocking up just yet.
Omicron is not a social-distancing robot
COVID, safe to say, has not been your typical, run-of-the-mill pandemic. People have protested social distancing. People have protested lockdowns. People have protested mask mandates. People have protested vaccine mandates. People have protested people protesting vaccine mandates.
Someone used a fake arm to get a COVID vaccine card. People have tried to reverse their COVID vaccinations. People had COVID contamination parties.
The common denominator? People. Humans. Maybe what we need is a nonhuman intervention. To fight COVID, we need a hero. A robotic hero.
And where can we find such a hero? The University of Maryland, of course, where computer scientists and engineers are working on an autonomous mobile robot to enforce indoor social-distancing rules.
Their robot can detect lapses in social distancing using cameras, both thermal and visual, along with a LiDAR (Light Detection and Ranging) sensor. It then sorts the offenders into various groups depending on whether they are standing still or moving and predicts their future movement using a state-of-the-art hybrid collision avoidance method known as Frozone, Adarsh Jagan Sathyamoorthy and associates explained in PLOS One.
“Once it reaches the breach, the robot encourages people to move apart via text that appears on a mounted display,” ScienceDaily said.
Maybe you were expecting a Terminator-type robot coming to enforce social distancing requirements rather than a simple text message. Let’s just hope that all COVID guidelines are followed, including social distancing, so the pandemic will finally end and won’t “be back.”
A nose for the tooth
Have you ever had a stuffy nose that just wouldn’t go away? Those irritating head colds have nothing on the stuffy nose a man in New York recently had to go through. A stuffy nose to top all stuffy noses. One stuffy nose to rule them all, as it were.
This man went to a Mount Sinai clinic with difficulty breathing through his right nostril, a problem that had been going on for years. Let us repeat that: A stuffy nose that lasted for years. The exam revealed a white mass jutting through the back of the septum and a CT scan confirmed the diagnosis. Perhaps you’ve already guessed, since the headline does give things away. Yes, this man had a tooth growing into his nose.
The problem was a half-inch-long ectopic tooth. Ectopic teeth are rare, occurring in less than 1% of people, but an ectopic tooth growing backward into the nasal cavity? Well, that’s so uncommon that this man got a case report in the New England Journal of Medicine.
This story does have a happy ending. Not all ectopic teeth need to be treated, but this one really did have to go. The offending tooth was surgically removed and, at a 3-month follow-up, the stuffy nose issue was completely resolved. So our friend gets the best of both worlds: His issue gets cured and he gets a case report in a major medical publication. If that’s not living the dream, we don’t know what is, and that’s the tooth.
Lettuce recommend you a sleep aid
Lettuce is great for many things. The star in a salad? Of course. The fresh element in a BLT? Yep. A sleep aid? According to a TikTok hack with almost 5 million views, the pinch hitter in a sandwich is switching leagues to be used like a tea for faster sleep. But, does it really work? Researchers say yes and no, according to a recent report at Tyla.com.
Studies conducted in 2013 and 2017 pointed toward a compound called lactucin, which is found in the plant’s n-butanol fraction. In the 2013 study, mice that received n-butanol fraction fell asleep faster and stayed asleep longer. In 2017, researchers found that lettuce made mice sleep longer and helped protect against cell inflammation and damage.
OK, so it works on mice. But what about humans? In the TikTok video, user Shapla Hoque pours hot water on a few lettuce leaves in a mug with a peppermint tea bag (for flavor). After 10 minutes, when the leaves are soaked and soggy, she removes them and drinks the lettuce tea. By the end of the video she’s visibly drowsy and ready to crash. Does this hold water?
Here’s the no. Dr. Charlotte Norton of the Slimming Clinic told Tyla.com that yeah, there are some properties in lettuce that will help you fall asleep, such as lactucarium, which is prominent in romaine. But you would need a massive amount of lettuce to get any effect. The TikTok video, she said, is an example of the placebo effect.
Brains get a rise out of Viagra
A lot of medications are used off label. Antidepressants for COVID have taken the cake recently, but here’s a new one: Viagra for Alzheimer’s disease.
Although there’s no definite link yet between the two, neuron models derived from induced pluripotent stem cells from patients with Alzheimer’s suggest that sildenafil increases neurite growth and decreases phospho-tau expression, Jiansong Fang, PhD, of the Cleveland Clinic, and associates said in Nature Aging.
Their research is an attempt to find untapped sources of new treatments among existing drugs. They began the search with 1,600 approved drugs and focused on those that target the buildup of beta amyloid and tau proteins in the brain, according to the Daily Beast.
Since sildenafil is obviously for men, more research will need to be done on how this drug affects women. Don’t start stocking up just yet.
Omicron is not a social-distancing robot
COVID, safe to say, has not been your typical, run-of-the-mill pandemic. People have protested social distancing. People have protested lockdowns. People have protested mask mandates. People have protested vaccine mandates. People have protested people protesting vaccine mandates.
Someone used a fake arm to get a COVID vaccine card. People have tried to reverse their COVID vaccinations. People had COVID contamination parties.
The common denominator? People. Humans. Maybe what we need is a nonhuman intervention. To fight COVID, we need a hero. A robotic hero.
And where can we find such a hero? The University of Maryland, of course, where computer scientists and engineers are working on an autonomous mobile robot to enforce indoor social-distancing rules.
Their robot can detect lapses in social distancing using cameras, both thermal and visual, along with a LiDAR (Light Detection and Ranging) sensor. It then sorts the offenders into various groups depending on whether they are standing still or moving and predicts their future movement using a state-of-the-art hybrid collision avoidance method known as Frozone, Adarsh Jagan Sathyamoorthy and associates explained in PLOS One.
“Once it reaches the breach, the robot encourages people to move apart via text that appears on a mounted display,” ScienceDaily said.
Maybe you were expecting a Terminator-type robot coming to enforce social distancing requirements rather than a simple text message. Let’s just hope that all COVID guidelines are followed, including social distancing, so the pandemic will finally end and won’t “be back.”
Vaccine protection drops against Omicron, making boosters crucial
A raft of new
The new studies, from teams of researchers in Germany, South Africa, Sweden, and the drug company Pfizer, showed 25 to 40-fold drops in the ability of antibodies created by two doses of the Pfizer-BioNTech vaccine to neutralize the virus.
But there seemed to be a bright spot in the studies too. The virus didn’t completely escape the immunity from the vaccines, and giving a third, booster dose appeared to restore antibodies to a level that’s been associated with protection against variants in the past.
“One of the silver linings of this pandemic so far is that mRNA vaccines manufactured based on the ancestral SARS-CoV-2 continue to work in the laboratory and, importantly, in real life against variant strains,” said Hana El Sahly, MD, professor of molecular virology and microbiology at Baylor College of Medicine in Houston. “The strains so far vary by their degree of being neutralized by the antibodies from these vaccines, but they are being neutralized nonetheless.”
Dr. El Sahly points out that the Beta variant was associated with a 10-fold drop in antibodies, but two doses of the vaccines still protected against it.
President Biden hailed the study results as good news.
“That Pfizer lab report came back saying that the expectation is that the existing vaccines protect against Omicron. But if you get the booster, you’re really in good shape. And so that’s very encouraging,” he said in a press briefing Dec. 8.
More research needed
Other scientists, however, stressed that these studies are from lab tests, and don’t necessarily reflect what will happen with Omicron in the real world. They cautioned about a worldwide push for boosters with so many countries still struggling to give first doses of vaccines.
Soumya Swaminathan, MD, chief scientist for the World Health Organization, stressed in a press briefing Dec. 8 that the results from the four studies varied widely, showing dips in neutralizing activity with Omicron that ranged from 5-fold to 40-fold.
The types of lab tests that were run were different, too, and involved small numbers of blood samples from patients.
She stressed that immunity depends not just on neutralizing antibodies, which act as a first line of defense when a virus invades, but also on B cells and T cells, and so far, tests show that these crucial components — which are important for preventing severe disease and death — had been less impacted than antibodies.
“So, I think it’s premature to conclude that this reduction in neutralizing activity would result in a significant reduction in vaccine effectiveness,” she said.
Whether or not these first-generation vaccines will be enough to stop Omicron, though, remains to be seen. A study of the Pfizer, Moderna, and AstraZeneca vaccines, led by German physician Sandra Ciesek, MD, who directs the Institute of Medical Virology at the University of Frankfurt, shows a booster didn’t appear to hold up well over time.
Dr. Ciesek and her team exposed Omicron viruses to the antibodies of volunteers who had been boosted with the Pfizer vaccine 3 months prior.
She also compared the results to what happened to those same 3-month antibody levels against Delta variant viruses. She found only a 25% neutralization of Omicron compared with a 95% neutralization of Delta. That represented about a 37-fold reduction in the ability of the antibodies to neutralize Omicron vs Delta.
“The data confirm that developing a vaccine adapted for Omicron makes sense,” she tweeted as part of a long thread she posted on her results.
Retool the vaccines?
Both Pfizer and Moderna are retooling their vaccines to better match them to the changes in the Omicron variant. In a press release, Pfizer said it could start deliveries of that updated vaccine by March, pending U.S. Food and Drug Administration authorization.
“What the booster really does in neutralizing Omicron right now, they don’t know, they have no idea,” said Peter Palese, PhD, chair of the department of microbiology at the Mount Sinai School of Medicine in New York City.
Dr. Palese said he was definitely concerned about a possible Omicron wave.
“There are four major sites on the spike protein targeted by antibodies from the vaccines, and all four sites have mutations,” he said. “All these important antigenic sites are changed.
“If Omicron becomes the new Delta, and the old vaccines really aren’t good enough, then we have to make new Omicron vaccines. Then we have to revaccinate everybody twice,” he said, and the costs could be staggering. “I am worried.”
Tedros Adhanom Ghebreyesus, PhD, director general of the WHO, urged countries to move quickly.
“Don’t wait. Act now,” he said, even before all the science is in hand. “All of us, every government, every individual should use all the tools we have right now,” to drive down transmission, increase testing and surveillance, and share scientific findings.
“We can prevent Omicron [from] becoming a global crisis right now,” he said.
A version of this article first appeared on Medscape.com.
A raft of new
The new studies, from teams of researchers in Germany, South Africa, Sweden, and the drug company Pfizer, showed 25 to 40-fold drops in the ability of antibodies created by two doses of the Pfizer-BioNTech vaccine to neutralize the virus.
But there seemed to be a bright spot in the studies too. The virus didn’t completely escape the immunity from the vaccines, and giving a third, booster dose appeared to restore antibodies to a level that’s been associated with protection against variants in the past.
“One of the silver linings of this pandemic so far is that mRNA vaccines manufactured based on the ancestral SARS-CoV-2 continue to work in the laboratory and, importantly, in real life against variant strains,” said Hana El Sahly, MD, professor of molecular virology and microbiology at Baylor College of Medicine in Houston. “The strains so far vary by their degree of being neutralized by the antibodies from these vaccines, but they are being neutralized nonetheless.”
Dr. El Sahly points out that the Beta variant was associated with a 10-fold drop in antibodies, but two doses of the vaccines still protected against it.
President Biden hailed the study results as good news.
“That Pfizer lab report came back saying that the expectation is that the existing vaccines protect against Omicron. But if you get the booster, you’re really in good shape. And so that’s very encouraging,” he said in a press briefing Dec. 8.
More research needed
Other scientists, however, stressed that these studies are from lab tests, and don’t necessarily reflect what will happen with Omicron in the real world. They cautioned about a worldwide push for boosters with so many countries still struggling to give first doses of vaccines.
Soumya Swaminathan, MD, chief scientist for the World Health Organization, stressed in a press briefing Dec. 8 that the results from the four studies varied widely, showing dips in neutralizing activity with Omicron that ranged from 5-fold to 40-fold.
The types of lab tests that were run were different, too, and involved small numbers of blood samples from patients.
She stressed that immunity depends not just on neutralizing antibodies, which act as a first line of defense when a virus invades, but also on B cells and T cells, and so far, tests show that these crucial components — which are important for preventing severe disease and death — had been less impacted than antibodies.
“So, I think it’s premature to conclude that this reduction in neutralizing activity would result in a significant reduction in vaccine effectiveness,” she said.
Whether or not these first-generation vaccines will be enough to stop Omicron, though, remains to be seen. A study of the Pfizer, Moderna, and AstraZeneca vaccines, led by German physician Sandra Ciesek, MD, who directs the Institute of Medical Virology at the University of Frankfurt, shows a booster didn’t appear to hold up well over time.
Dr. Ciesek and her team exposed Omicron viruses to the antibodies of volunteers who had been boosted with the Pfizer vaccine 3 months prior.
She also compared the results to what happened to those same 3-month antibody levels against Delta variant viruses. She found only a 25% neutralization of Omicron compared with a 95% neutralization of Delta. That represented about a 37-fold reduction in the ability of the antibodies to neutralize Omicron vs Delta.
“The data confirm that developing a vaccine adapted for Omicron makes sense,” she tweeted as part of a long thread she posted on her results.
Retool the vaccines?
Both Pfizer and Moderna are retooling their vaccines to better match them to the changes in the Omicron variant. In a press release, Pfizer said it could start deliveries of that updated vaccine by March, pending U.S. Food and Drug Administration authorization.
“What the booster really does in neutralizing Omicron right now, they don’t know, they have no idea,” said Peter Palese, PhD, chair of the department of microbiology at the Mount Sinai School of Medicine in New York City.
Dr. Palese said he was definitely concerned about a possible Omicron wave.
“There are four major sites on the spike protein targeted by antibodies from the vaccines, and all four sites have mutations,” he said. “All these important antigenic sites are changed.
“If Omicron becomes the new Delta, and the old vaccines really aren’t good enough, then we have to make new Omicron vaccines. Then we have to revaccinate everybody twice,” he said, and the costs could be staggering. “I am worried.”
Tedros Adhanom Ghebreyesus, PhD, director general of the WHO, urged countries to move quickly.
“Don’t wait. Act now,” he said, even before all the science is in hand. “All of us, every government, every individual should use all the tools we have right now,” to drive down transmission, increase testing and surveillance, and share scientific findings.
“We can prevent Omicron [from] becoming a global crisis right now,” he said.
A version of this article first appeared on Medscape.com.
A raft of new
The new studies, from teams of researchers in Germany, South Africa, Sweden, and the drug company Pfizer, showed 25 to 40-fold drops in the ability of antibodies created by two doses of the Pfizer-BioNTech vaccine to neutralize the virus.
But there seemed to be a bright spot in the studies too. The virus didn’t completely escape the immunity from the vaccines, and giving a third, booster dose appeared to restore antibodies to a level that’s been associated with protection against variants in the past.
“One of the silver linings of this pandemic so far is that mRNA vaccines manufactured based on the ancestral SARS-CoV-2 continue to work in the laboratory and, importantly, in real life against variant strains,” said Hana El Sahly, MD, professor of molecular virology and microbiology at Baylor College of Medicine in Houston. “The strains so far vary by their degree of being neutralized by the antibodies from these vaccines, but they are being neutralized nonetheless.”
Dr. El Sahly points out that the Beta variant was associated with a 10-fold drop in antibodies, but two doses of the vaccines still protected against it.
President Biden hailed the study results as good news.
“That Pfizer lab report came back saying that the expectation is that the existing vaccines protect against Omicron. But if you get the booster, you’re really in good shape. And so that’s very encouraging,” he said in a press briefing Dec. 8.
More research needed
Other scientists, however, stressed that these studies are from lab tests, and don’t necessarily reflect what will happen with Omicron in the real world. They cautioned about a worldwide push for boosters with so many countries still struggling to give first doses of vaccines.
Soumya Swaminathan, MD, chief scientist for the World Health Organization, stressed in a press briefing Dec. 8 that the results from the four studies varied widely, showing dips in neutralizing activity with Omicron that ranged from 5-fold to 40-fold.
The types of lab tests that were run were different, too, and involved small numbers of blood samples from patients.
She stressed that immunity depends not just on neutralizing antibodies, which act as a first line of defense when a virus invades, but also on B cells and T cells, and so far, tests show that these crucial components — which are important for preventing severe disease and death — had been less impacted than antibodies.
“So, I think it’s premature to conclude that this reduction in neutralizing activity would result in a significant reduction in vaccine effectiveness,” she said.
Whether or not these first-generation vaccines will be enough to stop Omicron, though, remains to be seen. A study of the Pfizer, Moderna, and AstraZeneca vaccines, led by German physician Sandra Ciesek, MD, who directs the Institute of Medical Virology at the University of Frankfurt, shows a booster didn’t appear to hold up well over time.
Dr. Ciesek and her team exposed Omicron viruses to the antibodies of volunteers who had been boosted with the Pfizer vaccine 3 months prior.
She also compared the results to what happened to those same 3-month antibody levels against Delta variant viruses. She found only a 25% neutralization of Omicron compared with a 95% neutralization of Delta. That represented about a 37-fold reduction in the ability of the antibodies to neutralize Omicron vs Delta.
“The data confirm that developing a vaccine adapted for Omicron makes sense,” she tweeted as part of a long thread she posted on her results.
Retool the vaccines?
Both Pfizer and Moderna are retooling their vaccines to better match them to the changes in the Omicron variant. In a press release, Pfizer said it could start deliveries of that updated vaccine by March, pending U.S. Food and Drug Administration authorization.
“What the booster really does in neutralizing Omicron right now, they don’t know, they have no idea,” said Peter Palese, PhD, chair of the department of microbiology at the Mount Sinai School of Medicine in New York City.
Dr. Palese said he was definitely concerned about a possible Omicron wave.
“There are four major sites on the spike protein targeted by antibodies from the vaccines, and all four sites have mutations,” he said. “All these important antigenic sites are changed.
“If Omicron becomes the new Delta, and the old vaccines really aren’t good enough, then we have to make new Omicron vaccines. Then we have to revaccinate everybody twice,” he said, and the costs could be staggering. “I am worried.”
Tedros Adhanom Ghebreyesus, PhD, director general of the WHO, urged countries to move quickly.
“Don’t wait. Act now,” he said, even before all the science is in hand. “All of us, every government, every individual should use all the tools we have right now,” to drive down transmission, increase testing and surveillance, and share scientific findings.
“We can prevent Omicron [from] becoming a global crisis right now,” he said.
A version of this article first appeared on Medscape.com.
AHA challenges diet doctor’s study alleging COVID vax risks
An abstract and poster presentation questioning the safety of mRNA-based COVID-19 vaccines, embraced by some and lambasted by others, has drawn an “expression of concern” from the American Heart Association, along with a bid for correction.
The abstract in question concludes that COVID vaccines “dramatically increase” levels of certain inflammatory biomarkers, and therefore, the 5-year risk of acute coronary syndromes (ACS), based on pre- and post-vaccination results of an obscure blood panel called the PULS Cardiac Test (GD Biosciences). The findings were presented at the AHA’s 2021 Scientific Sessionsas, an uncontrolled observational study of 566 patients in a preventive cardiology practice.
Some on social media have seized on the abstract as evidence of serious potential harm from the two available mRNA-based SARS-CoV-2 vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). But others contend that the study’s described design and findings are specious and its conclusions overstated.
They also point to the notoriety of its one listed author, Steven R. Gundry, MD, who promotes his diet books and supplements as well as fringe, highly criticized theories about diet and disease on several websites, including drgundry.com. Dr. Gundry has not responded to requests for an interview.
Dr. Gundry’s abstract from the AHA Scientific Sessions 2021, available on the meeting’s program planner, was marked with an “expression of concern” by the AHA that is to stand “until a suitable correction is published, to indicate that the abstract in its current version may not be reliable.”
The expression of concern statement, also published online Nov. 24 in Circulation, says “potential errors in the abstract” were brought to the attention of the meeting planners. “Specifically, there are several typographical errors, there is no data in the abstract regarding myocardial T-cell infiltration, there are no statistical analyses for significance provided, and the author is not clear that only anecdotal data was used.”
The biomarker elevations on which the abstract’s conclusions are based included hepatocyte growth factor, “which serves as a marker for chemotaxis of T-cells into epithelium and cardiac tissue,” it states.
“The expression of concern about the abstract will remain in place until a correction is accepted and published” in Circulation, AHA spokesperson Suzanne Grant told this news organization by email.
“The specific data needed will be up to the abstract author to determine and supply,” she said, noting that Dr. Gundry “has been in communication with the journal throughout this process.”
Submitting researchers “must always attest to the validity of the abstract,” Ms. Grant said. “Abstracts are then curated by independent review panels, blinded to the identities of the abstract authors, and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting.”
Regarding the AHA’s system for vetting abstracts vying for acceptance to the scientific sessions, she said it is not primarily intended to “evaluate scientific validity” and that the organization is “currently reviewing its existing abstract submission processes.”
A recent Reuters report reviews the controversy and provides links to criticisms of the study on social media.
A version of this article first appeared on Medscape.com.
An abstract and poster presentation questioning the safety of mRNA-based COVID-19 vaccines, embraced by some and lambasted by others, has drawn an “expression of concern” from the American Heart Association, along with a bid for correction.
The abstract in question concludes that COVID vaccines “dramatically increase” levels of certain inflammatory biomarkers, and therefore, the 5-year risk of acute coronary syndromes (ACS), based on pre- and post-vaccination results of an obscure blood panel called the PULS Cardiac Test (GD Biosciences). The findings were presented at the AHA’s 2021 Scientific Sessionsas, an uncontrolled observational study of 566 patients in a preventive cardiology practice.
Some on social media have seized on the abstract as evidence of serious potential harm from the two available mRNA-based SARS-CoV-2 vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). But others contend that the study’s described design and findings are specious and its conclusions overstated.
They also point to the notoriety of its one listed author, Steven R. Gundry, MD, who promotes his diet books and supplements as well as fringe, highly criticized theories about diet and disease on several websites, including drgundry.com. Dr. Gundry has not responded to requests for an interview.
Dr. Gundry’s abstract from the AHA Scientific Sessions 2021, available on the meeting’s program planner, was marked with an “expression of concern” by the AHA that is to stand “until a suitable correction is published, to indicate that the abstract in its current version may not be reliable.”
The expression of concern statement, also published online Nov. 24 in Circulation, says “potential errors in the abstract” were brought to the attention of the meeting planners. “Specifically, there are several typographical errors, there is no data in the abstract regarding myocardial T-cell infiltration, there are no statistical analyses for significance provided, and the author is not clear that only anecdotal data was used.”
The biomarker elevations on which the abstract’s conclusions are based included hepatocyte growth factor, “which serves as a marker for chemotaxis of T-cells into epithelium and cardiac tissue,” it states.
“The expression of concern about the abstract will remain in place until a correction is accepted and published” in Circulation, AHA spokesperson Suzanne Grant told this news organization by email.
“The specific data needed will be up to the abstract author to determine and supply,” she said, noting that Dr. Gundry “has been in communication with the journal throughout this process.”
Submitting researchers “must always attest to the validity of the abstract,” Ms. Grant said. “Abstracts are then curated by independent review panels, blinded to the identities of the abstract authors, and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting.”
Regarding the AHA’s system for vetting abstracts vying for acceptance to the scientific sessions, she said it is not primarily intended to “evaluate scientific validity” and that the organization is “currently reviewing its existing abstract submission processes.”
A recent Reuters report reviews the controversy and provides links to criticisms of the study on social media.
A version of this article first appeared on Medscape.com.
An abstract and poster presentation questioning the safety of mRNA-based COVID-19 vaccines, embraced by some and lambasted by others, has drawn an “expression of concern” from the American Heart Association, along with a bid for correction.
The abstract in question concludes that COVID vaccines “dramatically increase” levels of certain inflammatory biomarkers, and therefore, the 5-year risk of acute coronary syndromes (ACS), based on pre- and post-vaccination results of an obscure blood panel called the PULS Cardiac Test (GD Biosciences). The findings were presented at the AHA’s 2021 Scientific Sessionsas, an uncontrolled observational study of 566 patients in a preventive cardiology practice.
Some on social media have seized on the abstract as evidence of serious potential harm from the two available mRNA-based SARS-CoV-2 vaccines, BNT162b2 (Pfizer-BioNTech) and mRNA-1273 (Moderna). But others contend that the study’s described design and findings are specious and its conclusions overstated.
They also point to the notoriety of its one listed author, Steven R. Gundry, MD, who promotes his diet books and supplements as well as fringe, highly criticized theories about diet and disease on several websites, including drgundry.com. Dr. Gundry has not responded to requests for an interview.
Dr. Gundry’s abstract from the AHA Scientific Sessions 2021, available on the meeting’s program planner, was marked with an “expression of concern” by the AHA that is to stand “until a suitable correction is published, to indicate that the abstract in its current version may not be reliable.”
The expression of concern statement, also published online Nov. 24 in Circulation, says “potential errors in the abstract” were brought to the attention of the meeting planners. “Specifically, there are several typographical errors, there is no data in the abstract regarding myocardial T-cell infiltration, there are no statistical analyses for significance provided, and the author is not clear that only anecdotal data was used.”
The biomarker elevations on which the abstract’s conclusions are based included hepatocyte growth factor, “which serves as a marker for chemotaxis of T-cells into epithelium and cardiac tissue,” it states.
“The expression of concern about the abstract will remain in place until a correction is accepted and published” in Circulation, AHA spokesperson Suzanne Grant told this news organization by email.
“The specific data needed will be up to the abstract author to determine and supply,” she said, noting that Dr. Gundry “has been in communication with the journal throughout this process.”
Submitting researchers “must always attest to the validity of the abstract,” Ms. Grant said. “Abstracts are then curated by independent review panels, blinded to the identities of the abstract authors, and are considered based on the potential to add to the diversity of scientific issues and views discussed at the meeting.”
Regarding the AHA’s system for vetting abstracts vying for acceptance to the scientific sessions, she said it is not primarily intended to “evaluate scientific validity” and that the organization is “currently reviewing its existing abstract submission processes.”
A recent Reuters report reviews the controversy and provides links to criticisms of the study on social media.
A version of this article first appeared on Medscape.com.
Higher resting heart rate tied to increased dementia risk
independent of the presence of cardiovascular disease (CVD) risk factors, new research shows.
“RHR is easy to measure and might be used to identify older people potentially at high risk of dementia and cognitive decline for early interventions,” Yume Imahori, MD, PhD, with the Aging Research Center, Karolinska Institutet, Stockholm, said in an interview.
“Health care professionals should be aware of potential cognitive consequences associated with elevated RHR in older people and may advise older people with high RHR to have a follow-up assessment of cognitive function,” Dr. Imahori said.
The study was published online Dec. 3, 2021, in Alzheimer’s & Dementia.
Heart-brain connection
The findings are based on 2,147 adults (62% women) aged 60 years and older (mean age, 70.6 years) from the population-based Swedish National Aging and Care in Kungsholmen (SNAC-K) study. All were free of dementia at baseline and were followed regularly from 2001-2004 to 2013-2016.
The average RHR at baseline was 65.7 bpm. Individuals in higher RHR groups were older, less educated, and were more likely to be smokers and sedentary and to have hypertension. There were no differences among RHR groups in the prevalence of CVD at baseline.
During a median follow-up of 11.4 years, 289 participants were diagnosed with dementia.
In the fully adjusted model, participants with RHR of 80 bpm or higher had a 55% increased risk of developing dementia, compared with peers with lower RHR of 60 to 69 bpm (hazard ratio, 1.55; 95% CI, 1.06-2.27).
“This association was not due to underlying cardiovascular diseases such as atrial fibrillation and heart failure, which is important because elevated RHR is often related to heart disease,” Dr. Imahori said in an interview.
Regarding cognitive function, Mini-Mental State Examination scores declined over time during the follow-up period in all RHR groups, but participants with RHR 70-79 and 80+ bpm had a greater decline, compared with those with lower RHR of 60-69 bpm.
Dr. Imahori said these findings are in line with data from the U.S. Atherosclerosis Risk in Communities study linking elevated RHR of 80+ bpm in midlife to dementia and cognitive decline in late life.
Public health implications
Reached for comment, Claire Sexton, DPhil, Alzheimer’s Association director of scientific programs and outreach, said this study adds to the “growing body of research showing the health of the heart and brain are closely connected. However, this study only shows a correlation between resting heart rate and cognition, not causation. More research is needed.
“Evidence shows that other risk factors for cardiovascular disease and stroke – obesity, high blood pressure, and diabetes – negatively impact your cognitive health,” Dr. Sexton said in an interview.
“The Alzheimer’s Association believes the conversation about heart health management is something everyone should be having with their doctor,” she said.
“There are things you can do today to lower your risk for cardiovascular disease, including regular exercise and maintaining a healthy diet. Improving your heart health is an important step to maintaining your brain health as you age,” Dr. Sexton added.
SNAC-K is supported by the Swedish Ministry of Health and Social Affairs and the participating county councils and municipalities and in part by additional grants from the Swedish Research Council and the Swedish Research Council for Health, Working Life and Welfare. Dr. Imahori and Dr. Sexton disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
independent of the presence of cardiovascular disease (CVD) risk factors, new research shows.
“RHR is easy to measure and might be used to identify older people potentially at high risk of dementia and cognitive decline for early interventions,” Yume Imahori, MD, PhD, with the Aging Research Center, Karolinska Institutet, Stockholm, said in an interview.
“Health care professionals should be aware of potential cognitive consequences associated with elevated RHR in older people and may advise older people with high RHR to have a follow-up assessment of cognitive function,” Dr. Imahori said.
The study was published online Dec. 3, 2021, in Alzheimer’s & Dementia.
Heart-brain connection
The findings are based on 2,147 adults (62% women) aged 60 years and older (mean age, 70.6 years) from the population-based Swedish National Aging and Care in Kungsholmen (SNAC-K) study. All were free of dementia at baseline and were followed regularly from 2001-2004 to 2013-2016.
The average RHR at baseline was 65.7 bpm. Individuals in higher RHR groups were older, less educated, and were more likely to be smokers and sedentary and to have hypertension. There were no differences among RHR groups in the prevalence of CVD at baseline.
During a median follow-up of 11.4 years, 289 participants were diagnosed with dementia.
In the fully adjusted model, participants with RHR of 80 bpm or higher had a 55% increased risk of developing dementia, compared with peers with lower RHR of 60 to 69 bpm (hazard ratio, 1.55; 95% CI, 1.06-2.27).
“This association was not due to underlying cardiovascular diseases such as atrial fibrillation and heart failure, which is important because elevated RHR is often related to heart disease,” Dr. Imahori said in an interview.
Regarding cognitive function, Mini-Mental State Examination scores declined over time during the follow-up period in all RHR groups, but participants with RHR 70-79 and 80+ bpm had a greater decline, compared with those with lower RHR of 60-69 bpm.
Dr. Imahori said these findings are in line with data from the U.S. Atherosclerosis Risk in Communities study linking elevated RHR of 80+ bpm in midlife to dementia and cognitive decline in late life.
Public health implications
Reached for comment, Claire Sexton, DPhil, Alzheimer’s Association director of scientific programs and outreach, said this study adds to the “growing body of research showing the health of the heart and brain are closely connected. However, this study only shows a correlation between resting heart rate and cognition, not causation. More research is needed.
“Evidence shows that other risk factors for cardiovascular disease and stroke – obesity, high blood pressure, and diabetes – negatively impact your cognitive health,” Dr. Sexton said in an interview.
“The Alzheimer’s Association believes the conversation about heart health management is something everyone should be having with their doctor,” she said.
“There are things you can do today to lower your risk for cardiovascular disease, including regular exercise and maintaining a healthy diet. Improving your heart health is an important step to maintaining your brain health as you age,” Dr. Sexton added.
SNAC-K is supported by the Swedish Ministry of Health and Social Affairs and the participating county councils and municipalities and in part by additional grants from the Swedish Research Council and the Swedish Research Council for Health, Working Life and Welfare. Dr. Imahori and Dr. Sexton disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
independent of the presence of cardiovascular disease (CVD) risk factors, new research shows.
“RHR is easy to measure and might be used to identify older people potentially at high risk of dementia and cognitive decline for early interventions,” Yume Imahori, MD, PhD, with the Aging Research Center, Karolinska Institutet, Stockholm, said in an interview.
“Health care professionals should be aware of potential cognitive consequences associated with elevated RHR in older people and may advise older people with high RHR to have a follow-up assessment of cognitive function,” Dr. Imahori said.
The study was published online Dec. 3, 2021, in Alzheimer’s & Dementia.
Heart-brain connection
The findings are based on 2,147 adults (62% women) aged 60 years and older (mean age, 70.6 years) from the population-based Swedish National Aging and Care in Kungsholmen (SNAC-K) study. All were free of dementia at baseline and were followed regularly from 2001-2004 to 2013-2016.
The average RHR at baseline was 65.7 bpm. Individuals in higher RHR groups were older, less educated, and were more likely to be smokers and sedentary and to have hypertension. There were no differences among RHR groups in the prevalence of CVD at baseline.
During a median follow-up of 11.4 years, 289 participants were diagnosed with dementia.
In the fully adjusted model, participants with RHR of 80 bpm or higher had a 55% increased risk of developing dementia, compared with peers with lower RHR of 60 to 69 bpm (hazard ratio, 1.55; 95% CI, 1.06-2.27).
“This association was not due to underlying cardiovascular diseases such as atrial fibrillation and heart failure, which is important because elevated RHR is often related to heart disease,” Dr. Imahori said in an interview.
Regarding cognitive function, Mini-Mental State Examination scores declined over time during the follow-up period in all RHR groups, but participants with RHR 70-79 and 80+ bpm had a greater decline, compared with those with lower RHR of 60-69 bpm.
Dr. Imahori said these findings are in line with data from the U.S. Atherosclerosis Risk in Communities study linking elevated RHR of 80+ bpm in midlife to dementia and cognitive decline in late life.
Public health implications
Reached for comment, Claire Sexton, DPhil, Alzheimer’s Association director of scientific programs and outreach, said this study adds to the “growing body of research showing the health of the heart and brain are closely connected. However, this study only shows a correlation between resting heart rate and cognition, not causation. More research is needed.
“Evidence shows that other risk factors for cardiovascular disease and stroke – obesity, high blood pressure, and diabetes – negatively impact your cognitive health,” Dr. Sexton said in an interview.
“The Alzheimer’s Association believes the conversation about heart health management is something everyone should be having with their doctor,” she said.
“There are things you can do today to lower your risk for cardiovascular disease, including regular exercise and maintaining a healthy diet. Improving your heart health is an important step to maintaining your brain health as you age,” Dr. Sexton added.
SNAC-K is supported by the Swedish Ministry of Health and Social Affairs and the participating county councils and municipalities and in part by additional grants from the Swedish Research Council and the Swedish Research Council for Health, Working Life and Welfare. Dr. Imahori and Dr. Sexton disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ALZHEIMER’S & DEMENTIA
Cancer-related thyroidectomy linked to increased diabetes risk
People with thyroid cancer treated with thyroidectomy have as much as a 40% increased risk of developing type 2 diabetes, regardless of their age, with the elevated risk observed with low as well as high doses of postoperative levothyroxine, new research shows.
“This is the first population-based study to demonstrate an elevated risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer, compared with that in matched controls,” wrote the authors of the research, published recently in the Journal of Clinical Endocrinology & Metabolism.
“Notably, there was a U-shaped relationship between postoperative levothyroxine dosage, a surrogate marker of TSH suppression, and the risk of type 2 diabetes,” said Hye Jin Yoo, MD, of the division of endocrinology and metabolism, Korea University College of Medicine, Seoul, and colleagues.
While other studies have linked thyroidectomy for thyroid cancer with an elevated risk for other metabolic conditions, including coronary heart disease and ischemic stroke, the relatively high diabetes risk is unexpected, said Tyler Drake, MD, an endocrinologist with the Minneapolis VA Health Care System.
“A 40% increased risk of diabetes is a big surprise,” he said in an interview.
“Diabetes is very common, with about one in 10 U.S. adults having type 2 diabetes, but a 40% increased risk in thyroid cancer patients is higher than I see in my clinical practice. [However], it is important to note that the [highest] risk was predominantly among the groups on the lowest and highest doses of levothyroxine,” said Dr. Drake, assistant professor of medicine at the University of Minnesota, Minneapolis.
U-shaped relationship between levothyroxine dose and diabetes risk
The findings are from a study of 36,377 patients with thyroid cancer in the National Health Insurance Service (NHIS) database in Korea who had undergone a thyroidectomy between 2004 and 2013.
The patients were matched 1:1 with controls who had nonthyroid cancers. Their mean age was 46.6 years, about 30% were male, and their mean body mass index was 23.8 kg/m2.
Over a mean follow-up of 6.6 years, the patients with thyroid cancer had a significantly higher risk of developing type 2 diabetes, at a rate of 47.5% (10,812) compared with 36.9% (9414; HR, 1.43; P < .001) in the control group, after adjustment for factors such as age, sex, BMI, smoking, drinking, systolic blood pressure, and fasting glucose.
The risk of type 2 diabetes among those with thyroid cancer was higher among the 83.2% of patients who underwent a total thyroidectomy compared with the 16.8% who had a unilateral lobectomy (HR, 1.06; P < .001).
In addition, those with thyroid cancer who received the lowest as well as highest dosages of levothyroxine had significantly higher risks of type 2 diabetes compared with controls (HR, 1.50 and 1.39, respectively; both P < .001).
A closer look at quartiles of levothyroxine dosing showed the first (lowest) quartile (defined as a mean levothyroxine dosage of < 101 mcg/day) was associated with an increased risk of type 2 diabetes compared with the second quartile group (101-127 mcg/day; HR, 1.45), as was the fourth quartile (≥ 150 mcg/day; HR, 1.37), while a decreased risk of type 2 diabetes was observed in the third quartile group (128-149 mcg/day versus the second quartile group; HR, 0.91).
“This result suggests a U-shaped relationship between the mean levothyroxine dosage and risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer,” the authors said.
However, “consistent with previous studies, the present study showed that the highest risk of type 2 diabetes was observed in patients with thyroid cancer who were treated with the lowest mean dosage of levothyroxine,” they noted.
“This result suggests that inadequate supplementation of thyroid hormones may worsen glucose metabolism and should therefore be avoided.”
Potential mechanisms
Abnormal thyroid function, including hypo- and hyperthyroidism, following thyroidectomy and subsequent treatment with levothyroxine, is known to have potentially detrimental effects on glucose regulation among patients with thyroid cancer.
The potential mechanisms linking hypothyroidism with diabetes specifically include the possibility that insulin becomes unable to promote the utilization of glucose by muscles and adipose tissue. However, thyroid hormone replacement has been associated with a normalization of insulin sensitivity, the authors noted.
Meanwhile, glucose intolerance is common among patients with hyperthyroidism, largely due to an increase in hepatic glucose production, and likewise, the normalization of thyroid levels among those treated with methimazole has been linked to normalization of glucose and lipid metabolism alterations.
Dr. Drake noted that an important study limitation is that patients were analyzed based on their levothyroxine dose and not their TSH values, which the authors explain was due to the unavailability of the TSH values.
“By looking at levothyroxine doses, and not TSH values, it is possible some patients were being improperly treated with either too much or too little levothyroxine,” Dr. Drake noted.
Control group should have had hypothyroidism
The findings nevertheless shed light on the risk of diabetes following thyroidectomy for thyroid cancer, Anupam Kotwal, MD, commented on the study.
“This study is significant because it addresses an important topic exploring the link between thyroid dysfunction and metabolic disease, in this case ... hypothyroidism, due to surgery for thyroid cancer and type 2 diabetes,” Dr. Kotwal, assistant professor of medicine in the division of diabetes, endocrinology & metabolism at the University of Nebraska Medical Center, Omaha, said in an interview.
In terms of other limitations, Dr. Kotwal noted that the controls did not have hypothyroidism; therefore, “from this study, it is impossible to confirm whether hypothyroidism from any cause would be associated with higher incidence of diabetes or if it is specific to thyroid surgery for thyroid cancer.
“It would have been useful to have a control group of autoimmune primary hypothyroidism to evaluate the rate of diabetes during a similar follow-up duration,” Dr. Kotwal said.
“Hence, cohort studies with more granular data such as degree of TSH suppression and having a control group of hypothyroid patients due to autoimmune thyroid disease are needed to better understand this risk.”
Dr. Kotwal and Dr. Drake have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with thyroid cancer treated with thyroidectomy have as much as a 40% increased risk of developing type 2 diabetes, regardless of their age, with the elevated risk observed with low as well as high doses of postoperative levothyroxine, new research shows.
“This is the first population-based study to demonstrate an elevated risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer, compared with that in matched controls,” wrote the authors of the research, published recently in the Journal of Clinical Endocrinology & Metabolism.
“Notably, there was a U-shaped relationship between postoperative levothyroxine dosage, a surrogate marker of TSH suppression, and the risk of type 2 diabetes,” said Hye Jin Yoo, MD, of the division of endocrinology and metabolism, Korea University College of Medicine, Seoul, and colleagues.
While other studies have linked thyroidectomy for thyroid cancer with an elevated risk for other metabolic conditions, including coronary heart disease and ischemic stroke, the relatively high diabetes risk is unexpected, said Tyler Drake, MD, an endocrinologist with the Minneapolis VA Health Care System.
“A 40% increased risk of diabetes is a big surprise,” he said in an interview.
“Diabetes is very common, with about one in 10 U.S. adults having type 2 diabetes, but a 40% increased risk in thyroid cancer patients is higher than I see in my clinical practice. [However], it is important to note that the [highest] risk was predominantly among the groups on the lowest and highest doses of levothyroxine,” said Dr. Drake, assistant professor of medicine at the University of Minnesota, Minneapolis.
U-shaped relationship between levothyroxine dose and diabetes risk
The findings are from a study of 36,377 patients with thyroid cancer in the National Health Insurance Service (NHIS) database in Korea who had undergone a thyroidectomy between 2004 and 2013.
The patients were matched 1:1 with controls who had nonthyroid cancers. Their mean age was 46.6 years, about 30% were male, and their mean body mass index was 23.8 kg/m2.
Over a mean follow-up of 6.6 years, the patients with thyroid cancer had a significantly higher risk of developing type 2 diabetes, at a rate of 47.5% (10,812) compared with 36.9% (9414; HR, 1.43; P < .001) in the control group, after adjustment for factors such as age, sex, BMI, smoking, drinking, systolic blood pressure, and fasting glucose.
The risk of type 2 diabetes among those with thyroid cancer was higher among the 83.2% of patients who underwent a total thyroidectomy compared with the 16.8% who had a unilateral lobectomy (HR, 1.06; P < .001).
In addition, those with thyroid cancer who received the lowest as well as highest dosages of levothyroxine had significantly higher risks of type 2 diabetes compared with controls (HR, 1.50 and 1.39, respectively; both P < .001).
A closer look at quartiles of levothyroxine dosing showed the first (lowest) quartile (defined as a mean levothyroxine dosage of < 101 mcg/day) was associated with an increased risk of type 2 diabetes compared with the second quartile group (101-127 mcg/day; HR, 1.45), as was the fourth quartile (≥ 150 mcg/day; HR, 1.37), while a decreased risk of type 2 diabetes was observed in the third quartile group (128-149 mcg/day versus the second quartile group; HR, 0.91).
“This result suggests a U-shaped relationship between the mean levothyroxine dosage and risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer,” the authors said.
However, “consistent with previous studies, the present study showed that the highest risk of type 2 diabetes was observed in patients with thyroid cancer who were treated with the lowest mean dosage of levothyroxine,” they noted.
“This result suggests that inadequate supplementation of thyroid hormones may worsen glucose metabolism and should therefore be avoided.”
Potential mechanisms
Abnormal thyroid function, including hypo- and hyperthyroidism, following thyroidectomy and subsequent treatment with levothyroxine, is known to have potentially detrimental effects on glucose regulation among patients with thyroid cancer.
The potential mechanisms linking hypothyroidism with diabetes specifically include the possibility that insulin becomes unable to promote the utilization of glucose by muscles and adipose tissue. However, thyroid hormone replacement has been associated with a normalization of insulin sensitivity, the authors noted.
Meanwhile, glucose intolerance is common among patients with hyperthyroidism, largely due to an increase in hepatic glucose production, and likewise, the normalization of thyroid levels among those treated with methimazole has been linked to normalization of glucose and lipid metabolism alterations.
Dr. Drake noted that an important study limitation is that patients were analyzed based on their levothyroxine dose and not their TSH values, which the authors explain was due to the unavailability of the TSH values.
“By looking at levothyroxine doses, and not TSH values, it is possible some patients were being improperly treated with either too much or too little levothyroxine,” Dr. Drake noted.
Control group should have had hypothyroidism
The findings nevertheless shed light on the risk of diabetes following thyroidectomy for thyroid cancer, Anupam Kotwal, MD, commented on the study.
“This study is significant because it addresses an important topic exploring the link between thyroid dysfunction and metabolic disease, in this case ... hypothyroidism, due to surgery for thyroid cancer and type 2 diabetes,” Dr. Kotwal, assistant professor of medicine in the division of diabetes, endocrinology & metabolism at the University of Nebraska Medical Center, Omaha, said in an interview.
In terms of other limitations, Dr. Kotwal noted that the controls did not have hypothyroidism; therefore, “from this study, it is impossible to confirm whether hypothyroidism from any cause would be associated with higher incidence of diabetes or if it is specific to thyroid surgery for thyroid cancer.
“It would have been useful to have a control group of autoimmune primary hypothyroidism to evaluate the rate of diabetes during a similar follow-up duration,” Dr. Kotwal said.
“Hence, cohort studies with more granular data such as degree of TSH suppression and having a control group of hypothyroid patients due to autoimmune thyroid disease are needed to better understand this risk.”
Dr. Kotwal and Dr. Drake have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
People with thyroid cancer treated with thyroidectomy have as much as a 40% increased risk of developing type 2 diabetes, regardless of their age, with the elevated risk observed with low as well as high doses of postoperative levothyroxine, new research shows.
“This is the first population-based study to demonstrate an elevated risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer, compared with that in matched controls,” wrote the authors of the research, published recently in the Journal of Clinical Endocrinology & Metabolism.
“Notably, there was a U-shaped relationship between postoperative levothyroxine dosage, a surrogate marker of TSH suppression, and the risk of type 2 diabetes,” said Hye Jin Yoo, MD, of the division of endocrinology and metabolism, Korea University College of Medicine, Seoul, and colleagues.
While other studies have linked thyroidectomy for thyroid cancer with an elevated risk for other metabolic conditions, including coronary heart disease and ischemic stroke, the relatively high diabetes risk is unexpected, said Tyler Drake, MD, an endocrinologist with the Minneapolis VA Health Care System.
“A 40% increased risk of diabetes is a big surprise,” he said in an interview.
“Diabetes is very common, with about one in 10 U.S. adults having type 2 diabetes, but a 40% increased risk in thyroid cancer patients is higher than I see in my clinical practice. [However], it is important to note that the [highest] risk was predominantly among the groups on the lowest and highest doses of levothyroxine,” said Dr. Drake, assistant professor of medicine at the University of Minnesota, Minneapolis.
U-shaped relationship between levothyroxine dose and diabetes risk
The findings are from a study of 36,377 patients with thyroid cancer in the National Health Insurance Service (NHIS) database in Korea who had undergone a thyroidectomy between 2004 and 2013.
The patients were matched 1:1 with controls who had nonthyroid cancers. Their mean age was 46.6 years, about 30% were male, and their mean body mass index was 23.8 kg/m2.
Over a mean follow-up of 6.6 years, the patients with thyroid cancer had a significantly higher risk of developing type 2 diabetes, at a rate of 47.5% (10,812) compared with 36.9% (9414; HR, 1.43; P < .001) in the control group, after adjustment for factors such as age, sex, BMI, smoking, drinking, systolic blood pressure, and fasting glucose.
The risk of type 2 diabetes among those with thyroid cancer was higher among the 83.2% of patients who underwent a total thyroidectomy compared with the 16.8% who had a unilateral lobectomy (HR, 1.06; P < .001).
In addition, those with thyroid cancer who received the lowest as well as highest dosages of levothyroxine had significantly higher risks of type 2 diabetes compared with controls (HR, 1.50 and 1.39, respectively; both P < .001).
A closer look at quartiles of levothyroxine dosing showed the first (lowest) quartile (defined as a mean levothyroxine dosage of < 101 mcg/day) was associated with an increased risk of type 2 diabetes compared with the second quartile group (101-127 mcg/day; HR, 1.45), as was the fourth quartile (≥ 150 mcg/day; HR, 1.37), while a decreased risk of type 2 diabetes was observed in the third quartile group (128-149 mcg/day versus the second quartile group; HR, 0.91).
“This result suggests a U-shaped relationship between the mean levothyroxine dosage and risk of type 2 diabetes in postthyroidectomy patients with thyroid cancer,” the authors said.
However, “consistent with previous studies, the present study showed that the highest risk of type 2 diabetes was observed in patients with thyroid cancer who were treated with the lowest mean dosage of levothyroxine,” they noted.
“This result suggests that inadequate supplementation of thyroid hormones may worsen glucose metabolism and should therefore be avoided.”
Potential mechanisms
Abnormal thyroid function, including hypo- and hyperthyroidism, following thyroidectomy and subsequent treatment with levothyroxine, is known to have potentially detrimental effects on glucose regulation among patients with thyroid cancer.
The potential mechanisms linking hypothyroidism with diabetes specifically include the possibility that insulin becomes unable to promote the utilization of glucose by muscles and adipose tissue. However, thyroid hormone replacement has been associated with a normalization of insulin sensitivity, the authors noted.
Meanwhile, glucose intolerance is common among patients with hyperthyroidism, largely due to an increase in hepatic glucose production, and likewise, the normalization of thyroid levels among those treated with methimazole has been linked to normalization of glucose and lipid metabolism alterations.
Dr. Drake noted that an important study limitation is that patients were analyzed based on their levothyroxine dose and not their TSH values, which the authors explain was due to the unavailability of the TSH values.
“By looking at levothyroxine doses, and not TSH values, it is possible some patients were being improperly treated with either too much or too little levothyroxine,” Dr. Drake noted.
Control group should have had hypothyroidism
The findings nevertheless shed light on the risk of diabetes following thyroidectomy for thyroid cancer, Anupam Kotwal, MD, commented on the study.
“This study is significant because it addresses an important topic exploring the link between thyroid dysfunction and metabolic disease, in this case ... hypothyroidism, due to surgery for thyroid cancer and type 2 diabetes,” Dr. Kotwal, assistant professor of medicine in the division of diabetes, endocrinology & metabolism at the University of Nebraska Medical Center, Omaha, said in an interview.
In terms of other limitations, Dr. Kotwal noted that the controls did not have hypothyroidism; therefore, “from this study, it is impossible to confirm whether hypothyroidism from any cause would be associated with higher incidence of diabetes or if it is specific to thyroid surgery for thyroid cancer.
“It would have been useful to have a control group of autoimmune primary hypothyroidism to evaluate the rate of diabetes during a similar follow-up duration,” Dr. Kotwal said.
“Hence, cohort studies with more granular data such as degree of TSH suppression and having a control group of hypothyroid patients due to autoimmune thyroid disease are needed to better understand this risk.”
Dr. Kotwal and Dr. Drake have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Blood pressure control worsened during COVID pandemic
Blood pressure control declined in both men and women with the onset of the COVID-19 pandemic in the United States in 2020, especially among women and older adults, according to a new analysis.
“We know that even small rises in blood pressure increase one’s risk of stroke and other adverse cardiovascular disease events,” lead author Luke J. Laffin, MD, codirector, Center for Blood Pressure Disorders, Cleveland Clinic, Ohio, said in a news release.
The researchers say increases in systolic BP among U.S. adults during the COVID-19 pandemic “could signal a forthcoming increase in incident cardiovascular disease mortality.”
Their study was published online Dec. 6 in Circulation.
Dr. Laffin and colleagues analyzed BP data from 464,585 U.S. adults (mean age, 46, 54% women) who had their BP measured as part of employee health screening annually from 2018 through 2020.
They found that BP levels went up between April and Dec. of 2020 – around the same time stay-at-home orders and other restrictions were put in place.
During this pandemic period, average monthly increases in BP ranged from 1.10 to 2.50 mm Hg higher for systolic BP and 0.14 to 0.53 mm Hg higher for diastolic BP, compared with the prepandemic period of April to Dec. 2019.
Increases in systolic and diastolic BP were seen among men and women and across age groups. Larger increases were evident in women for both systolic and diastolic BP: in older individuals for systolic BP and in younger individuals for diastolic BP (all P < .0001).
Dr. Laffin and colleagues also assessed changes in BP category based on current American Heart Association blood pressure guidelines (normal, elevated, stage 1, or stage 2 hypertension).
During the pandemic, more adults (26.8%) were recategorized to a higher BP category, whereas only 22% moved to a lower BP category, compared with before the pandemic.
“At the start of the pandemic, most people were not taking good care of themselves. Increases in blood pressure were likely related to changes in eating habits, increased alcohol consumption, less physical activity, decreased medication adherence, more emotional stress, and poor sleep,” Dr. Laffin said.
However, the increases in BP during the pandemic could not be explained by weight gain, the researchers note, because the observed changes in weight during the pandemic were similar to the prepandemic period among 86% of adults completing weight data.
The study authors are following up on these results to determine if this trend continued in 2021.
“Unfortunately, this research confirms what is being seen across the country – the COVID-19 pandemic has had and will continue to have long-reaching health impacts across the country and particularly related to uncontrolled hypertension,” Eduardo Sanchez, MD, MPH, the AHA’s chief medical officer for prevention, said in the news release.
“These results validate why the American Heart Association’s National Hypertension Control Initiative (NHCI) is critically important,” he said.
“With a particular emphasis on historically under-resourced communities in the United States, the comprehensive program supports health care teams at community health centers through regular blood pressure management training; technical assistance and resources that include the proper blood pressure measurement technique; self-measured blood pressure monitoring and management; medication adherence; and healthy lifestyle services,” Dr. Sanchez noted.
The study had no specific funding. Dr. Laffin is a paid consultant for Medtronic and medical advisor for LucidAct Health.
A version of this article first appeared on Medscape.com.
Blood pressure control declined in both men and women with the onset of the COVID-19 pandemic in the United States in 2020, especially among women and older adults, according to a new analysis.
“We know that even small rises in blood pressure increase one’s risk of stroke and other adverse cardiovascular disease events,” lead author Luke J. Laffin, MD, codirector, Center for Blood Pressure Disorders, Cleveland Clinic, Ohio, said in a news release.
The researchers say increases in systolic BP among U.S. adults during the COVID-19 pandemic “could signal a forthcoming increase in incident cardiovascular disease mortality.”
Their study was published online Dec. 6 in Circulation.
Dr. Laffin and colleagues analyzed BP data from 464,585 U.S. adults (mean age, 46, 54% women) who had their BP measured as part of employee health screening annually from 2018 through 2020.
They found that BP levels went up between April and Dec. of 2020 – around the same time stay-at-home orders and other restrictions were put in place.
During this pandemic period, average monthly increases in BP ranged from 1.10 to 2.50 mm Hg higher for systolic BP and 0.14 to 0.53 mm Hg higher for diastolic BP, compared with the prepandemic period of April to Dec. 2019.
Increases in systolic and diastolic BP were seen among men and women and across age groups. Larger increases were evident in women for both systolic and diastolic BP: in older individuals for systolic BP and in younger individuals for diastolic BP (all P < .0001).
Dr. Laffin and colleagues also assessed changes in BP category based on current American Heart Association blood pressure guidelines (normal, elevated, stage 1, or stage 2 hypertension).
During the pandemic, more adults (26.8%) were recategorized to a higher BP category, whereas only 22% moved to a lower BP category, compared with before the pandemic.
“At the start of the pandemic, most people were not taking good care of themselves. Increases in blood pressure were likely related to changes in eating habits, increased alcohol consumption, less physical activity, decreased medication adherence, more emotional stress, and poor sleep,” Dr. Laffin said.
However, the increases in BP during the pandemic could not be explained by weight gain, the researchers note, because the observed changes in weight during the pandemic were similar to the prepandemic period among 86% of adults completing weight data.
The study authors are following up on these results to determine if this trend continued in 2021.
“Unfortunately, this research confirms what is being seen across the country – the COVID-19 pandemic has had and will continue to have long-reaching health impacts across the country and particularly related to uncontrolled hypertension,” Eduardo Sanchez, MD, MPH, the AHA’s chief medical officer for prevention, said in the news release.
“These results validate why the American Heart Association’s National Hypertension Control Initiative (NHCI) is critically important,” he said.
“With a particular emphasis on historically under-resourced communities in the United States, the comprehensive program supports health care teams at community health centers through regular blood pressure management training; technical assistance and resources that include the proper blood pressure measurement technique; self-measured blood pressure monitoring and management; medication adherence; and healthy lifestyle services,” Dr. Sanchez noted.
The study had no specific funding. Dr. Laffin is a paid consultant for Medtronic and medical advisor for LucidAct Health.
A version of this article first appeared on Medscape.com.
Blood pressure control declined in both men and women with the onset of the COVID-19 pandemic in the United States in 2020, especially among women and older adults, according to a new analysis.
“We know that even small rises in blood pressure increase one’s risk of stroke and other adverse cardiovascular disease events,” lead author Luke J. Laffin, MD, codirector, Center for Blood Pressure Disorders, Cleveland Clinic, Ohio, said in a news release.
The researchers say increases in systolic BP among U.S. adults during the COVID-19 pandemic “could signal a forthcoming increase in incident cardiovascular disease mortality.”
Their study was published online Dec. 6 in Circulation.
Dr. Laffin and colleagues analyzed BP data from 464,585 U.S. adults (mean age, 46, 54% women) who had their BP measured as part of employee health screening annually from 2018 through 2020.
They found that BP levels went up between April and Dec. of 2020 – around the same time stay-at-home orders and other restrictions were put in place.
During this pandemic period, average monthly increases in BP ranged from 1.10 to 2.50 mm Hg higher for systolic BP and 0.14 to 0.53 mm Hg higher for diastolic BP, compared with the prepandemic period of April to Dec. 2019.
Increases in systolic and diastolic BP were seen among men and women and across age groups. Larger increases were evident in women for both systolic and diastolic BP: in older individuals for systolic BP and in younger individuals for diastolic BP (all P < .0001).
Dr. Laffin and colleagues also assessed changes in BP category based on current American Heart Association blood pressure guidelines (normal, elevated, stage 1, or stage 2 hypertension).
During the pandemic, more adults (26.8%) were recategorized to a higher BP category, whereas only 22% moved to a lower BP category, compared with before the pandemic.
“At the start of the pandemic, most people were not taking good care of themselves. Increases in blood pressure were likely related to changes in eating habits, increased alcohol consumption, less physical activity, decreased medication adherence, more emotional stress, and poor sleep,” Dr. Laffin said.
However, the increases in BP during the pandemic could not be explained by weight gain, the researchers note, because the observed changes in weight during the pandemic were similar to the prepandemic period among 86% of adults completing weight data.
The study authors are following up on these results to determine if this trend continued in 2021.
“Unfortunately, this research confirms what is being seen across the country – the COVID-19 pandemic has had and will continue to have long-reaching health impacts across the country and particularly related to uncontrolled hypertension,” Eduardo Sanchez, MD, MPH, the AHA’s chief medical officer for prevention, said in the news release.
“These results validate why the American Heart Association’s National Hypertension Control Initiative (NHCI) is critically important,” he said.
“With a particular emphasis on historically under-resourced communities in the United States, the comprehensive program supports health care teams at community health centers through regular blood pressure management training; technical assistance and resources that include the proper blood pressure measurement technique; self-measured blood pressure monitoring and management; medication adherence; and healthy lifestyle services,” Dr. Sanchez noted.
The study had no specific funding. Dr. Laffin is a paid consultant for Medtronic and medical advisor for LucidAct Health.
A version of this article first appeared on Medscape.com.
Is mindfulness key to helping physicians with mental health?
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
Are physician-owned large groups better than flying solo?
Large, physician-owned group practices are gaining ground as a popular form of practice, even as the number of physicians in solo and small practices declines, and employment maintains its appeal.
As physicians shift from owning private practices to employment in hospital systems, this countertrend is also taking place. Large group practices are growing in number, even as solo and small practices are in decline.
Do large, physician-owned groups bring benefits that beat employment? And how do large groups compare with smaller practices and new opportunities, such as private equity? You’ll find some answers here.
Working in large group practices
Large group practices with 50 or more physicians are enjoying a renaissance, even though physicians are still streaming into hospital systems. The share of physicians in large practices increased from 14.7% in 2018 to 17.2% in 2020, the largest 2-year change for this group, according to the American Medical Association.
“Physicians expect that large groups will treat them better than hospitals do,” says Robert Pearl, MD, former CEO of Permanente Medical Group, the nation’s largest physicians’ group.
Compared with hospitals, “doctors would prefer working in a group practice, if all other things are equal,” says Dr. Pearl, who is now a professor at Stanford (Calif.) University Medical School.
Large group practices can include both multispecialty groups and single-specialty groups. Groups in specialties like urology, orthopedics, and oncology have been growing in recent years, according to Gregory Mertz, managing director of Physician Strategies Group in Virginia Beach, Va.
A group practice could also be an independent physicians association – a federation of small practices that share functions like negotiations with insurers and management. Physicians can also form larger groups for single purposes like running an accountable care organization.
Some large group practices can have a mix of partners and employees. In these groups, “some doctors either don’t want a partnership or aren’t offered one,” says Nathan Miller, CEO of the Medicus Firm, a physician recruitment company in Dallas. The AMA reports that about 10% of physicians are employees of large practices.
“Large groups like the Permanente Medical Group are not partnerships,” Dr. Pearl says. “They tend to be a corporation with a board of directors, and all the physicians are employees, but it’s a physician-led organization.”
Doctors in these groups can enjoy a great deal of control. While Permanente Medical Group is exclusively affiliated with Kaiser, which runs hospitals and an HMO, the group is an independent corporation run by its doctors, who are both shareholders and employees, Dr. Pearl says.
The Cleveland Clinic and Mayo Clinic are not medical groups in the strict sense of the word. They describe themselves as academic medical centers, but Dr. Pearl says, “Doctors have a tremendous amount of control there, particularly those in the most remunerative specialties.”
Pros of large groups
Group practices are able to focus more on the physician participants’ needs and priorities, says Mr. Mertz. “In a hospital-based organization, physicians’ needs have to compete with the needs of the hospital. … In a large group, it can be easier to get policies changed and order equipment.”
However, for many physicians, their primary reason for joining a large group is having negotiating leverage with health insurance plans, and this leverage seems even more important today. It typically results in higher reimbursements, which could translate into higher pay. The higher practice income, however, could be negated by higher administrative overhead, which is endemic in large organizations.
Mr. Mertz says large groups also have the resources to recruit new doctors. Small practices, in contrast, often decide not to grow. The practice would at first need to guarantee the salary of a new partner, which could require existing partners to take a pay cut, which they often don’t want to do. “They’ll decide to ride the practice into the ground,” which means closing it down when they retire, he says.
Cons of large groups
One individual doctor may have relatively little input in decision-making in a large group, and strong leadership may be lacking. One study examining the pros and cons of large group practices found that lack of physician cooperation, investment, and leadership were the most frequently cited barriers in large groups.
Physicians in large groups can also divide into competing factions. Mr. Mertz says rifts are more likely to take place in multispecialty groups, where higher-reimbursed proceduralists resent having to financially support lower-reimbursed primary care physicians. But it’s rare that such rifts actually break up the practice, he says.
Private practice vs. employment
Even as more physicians enter large groups, physicians continue to flee private practice in general. In 2020, the AMA found that the number of physicians in private practices had dropped nearly 5 percentage points since 2018, the largest 2-year drop recorded by the AMA.
The hardest hit are small groups of 10 physicians or fewer, once the backbone of U.S. medicine. A 2020 survey found that 53.7% of physicians still work in small practices of 10 or fewer physicians, compared with 61.4% in 2012.
Private practices tend to be partnerships, but younger physicians, for their part, often don’t want to become a partner. In a 2016 survey, only 22% of medical residents surveyed said they anticipate owning a stake in a practice someday.
What’s good about private practice?
The obvious advantage of private practice is having control. Physician-owners can choose staff, oversee finances, and decide on the direction the practice should take. They don’t have to worry about being fired, because the partnership agreement virtually guarantees each doctor’s place in the group.
The atmosphere in a small practice is often more relaxed. “Private practices tend to offer a family-like environment,” Mr. Miller says. Owners of small practices tend to have lower burnout than large practices, a 2018 study found.
Unlike hospital-employed doctors, private practitioners get to keep their ancillary income. “Physicians own the equipment and receive income generated from ancillary services, not just professional fees,” says Mr. Miller.
What’s negative about private practice?
Since small groups have little negotiating power with private payers, they can’t get favorable reimbursement rates. And while partners are protected from being fired, the practice could still go bankrupt.
Running a private practice means putting on an entrepreneurial hat. To develop a strong practice, you need to learn about marketing, finance, IT, contract negotiations, and facility management. “Most young doctors have no interest in this work,” Mr. Mertz says.
Value-based contracting has added another disadvantage for small practices. “It can be harder for small, independent groups to compete,” says Mike Belkin, JD, a divisional vice president at Merritt Hawkins, a physician recruitment company based in Dallas. “They don’t have the data and integration of services that are necessary for this.”
Employment in hospital systems
More than one-third of all physicians worked for hospitals in 2018, and hospitals’ share has been growing since then. In 2020, for the first time, the AMA found that more than half of all physicians were employed, and employment is mainly a hospital phenomenon.
The trend shows no signs of stopping. In 2019 and 2020, hospitals and other corporate entities acquired 20,900 physician practices, representing 29,800 doctors. “This trend will continue,” Dr. Pearl says. “The bigger will get bigger. It’s all about market control. Everyone wants to be wider, more vertical, and more powerful.”
Pros of hospital employment
“The advantages of hospital employment are mostly financial,” Mr. Mertz says. Unlike a private practice, “there’s no financial risk to hospital employment because you don’t own it. You won’t be on the tab for any losses.”
“Hospitals usually offer a highly competitive salary with less emphasis on production than in a private practice,” he says. New physicians are typically paid a guaranteed salary in the first 1-3 years of employment.
“You don’t have any management responsibilities, as you would in a practice,” Mr. Mertz says. “The hospital has a professional management team to handle the business side. Most young doctors have no interest in this work.”
“Employed physicians have a built-in referral network at a hospital,” Mr. Miller says. This is especially an advantage for new physicians, who don’t yet have a referral network of their own.”
Cons of hospital employment
Physicians employed by a hospital lack control. “You don’t decide the hours you work, the schedules you follow, and the physical facility you work in, and, for the most part, you don’t pick your staff,” Mr. Mertz says.
Like any big organization, hospitals are bureaucratic. “If you want to purchase a new piece of equipment, your request goes up the chain of command,” Mr. Mertz says. “Your purchase has to fit into the budget.” (This can be the case with large groups, too.)
Many employed doctors chafe under this lack of control. In an earlier survey by Medscape, 45% of employed respondents didn’t like having limited influence in decision-making, and 32% said they had less control over their work or schedule.
It’s no wonder that a large percentage of physicians would rather work in practices than hospitals. According to a 2021 Medicus Firm survey, 23% of physicians are interested in working in hospitals, while 40% would rather work either in multispecialty or single-specialty groups, Mr. Miller reports.
Doctors have differing views of hospital employment
New physicians are apt to dismiss any negatives about hospitals. “Lack of autonomy often matters less to younger physicians, who were trained in team-based models,” Mr. Belkin says.
Many young doctors actually like working in a large organization. “Young doctors out of residency are used to having everything at their fingertips – labs and testing is in-house,” Mr. Mertz says.
On the other hand, doctors who were previously self-employed – a group that makes up almost one-third of all hospital-employed doctors – can often be dissatisfied with employment. In a 2014 Medscape survey, 26% of previously self-employed doctors said job satisfaction had not improved with employment.
Mr. Mertz says these doctors remember what it was like to be in charge of a practice. “If you once owned a practice, you can always compare what’s going on now with that experience, and that can make you frustrated.”
Hospitals have higher turnover
It’s much easier to leave an organization when you don’t have an ownership stake. The annual physician turnover rate at hospitals is 28%, compared with 7% at medical groups, according to a 2019 report.
Mr. Belkin says changing jobs has become a way of life for many doctors. “Staying at a job for only a few years is no longer a red flag,” he says. “Physicians are exploring different options. They might try group practice and switch to hospitals or vice versa.”
Physicians are now part of a high-turnover culture: Once in a new job, many are already thinking about the next one. A 2018 survey found that 46% of doctors planned to leave their position within 3 years.
Private equity ownership of practice
Selling majority control of your practice to a private equity firm is a relatively new phenomenon and accounts for a small share of physicians – just 4% in 2020. This trend was originally limited to certain specialties, such as anesthesiology, emergency medicine, and dermatology, but now many others are courted.
The deals work like this: Physicians sell majority control of their practice to investors in return for shares in the private equity practice, and they become employees of that practice. The private equity firm then adds more physicians to the practice and invests in infrastructure with the intention of selling the practice at a large profit, which is then shared with the original physicians.
Pros of private equity
The original owners of the practice stand to make a substantial profit if they are willing to wait several years for the practice to be built up and sold. “If they are patient, they could earn a bonanza,” Mr. Belkin says.
Private equity investment helps the practice expand. “It’s an alternative to going to the bank and borrowing money,” Mr. Mertz says.
Cons of private equity
Physicians lose control of their practice. A client of Mr. Mertz’s briefly considered a private equity offer and turned it down. “The private equity firm would have veto power over what the doctors wanted to do,” he says.
Mr. Belkin says the selling physicians typically lose income after the sale. “Money they earned from ancillary services now goes to the practice,” Mr. Belkin says. The selling doctors could potentially take up to a 30% cut in their compensation, according to Coker Capital Advisors.
A version of this article first appeared on Medscape.com.
Large, physician-owned group practices are gaining ground as a popular form of practice, even as the number of physicians in solo and small practices declines, and employment maintains its appeal.
As physicians shift from owning private practices to employment in hospital systems, this countertrend is also taking place. Large group practices are growing in number, even as solo and small practices are in decline.
Do large, physician-owned groups bring benefits that beat employment? And how do large groups compare with smaller practices and new opportunities, such as private equity? You’ll find some answers here.
Working in large group practices
Large group practices with 50 or more physicians are enjoying a renaissance, even though physicians are still streaming into hospital systems. The share of physicians in large practices increased from 14.7% in 2018 to 17.2% in 2020, the largest 2-year change for this group, according to the American Medical Association.
“Physicians expect that large groups will treat them better than hospitals do,” says Robert Pearl, MD, former CEO of Permanente Medical Group, the nation’s largest physicians’ group.
Compared with hospitals, “doctors would prefer working in a group practice, if all other things are equal,” says Dr. Pearl, who is now a professor at Stanford (Calif.) University Medical School.
Large group practices can include both multispecialty groups and single-specialty groups. Groups in specialties like urology, orthopedics, and oncology have been growing in recent years, according to Gregory Mertz, managing director of Physician Strategies Group in Virginia Beach, Va.
A group practice could also be an independent physicians association – a federation of small practices that share functions like negotiations with insurers and management. Physicians can also form larger groups for single purposes like running an accountable care organization.
Some large group practices can have a mix of partners and employees. In these groups, “some doctors either don’t want a partnership or aren’t offered one,” says Nathan Miller, CEO of the Medicus Firm, a physician recruitment company in Dallas. The AMA reports that about 10% of physicians are employees of large practices.
“Large groups like the Permanente Medical Group are not partnerships,” Dr. Pearl says. “They tend to be a corporation with a board of directors, and all the physicians are employees, but it’s a physician-led organization.”
Doctors in these groups can enjoy a great deal of control. While Permanente Medical Group is exclusively affiliated with Kaiser, which runs hospitals and an HMO, the group is an independent corporation run by its doctors, who are both shareholders and employees, Dr. Pearl says.
The Cleveland Clinic and Mayo Clinic are not medical groups in the strict sense of the word. They describe themselves as academic medical centers, but Dr. Pearl says, “Doctors have a tremendous amount of control there, particularly those in the most remunerative specialties.”
Pros of large groups
Group practices are able to focus more on the physician participants’ needs and priorities, says Mr. Mertz. “In a hospital-based organization, physicians’ needs have to compete with the needs of the hospital. … In a large group, it can be easier to get policies changed and order equipment.”
However, for many physicians, their primary reason for joining a large group is having negotiating leverage with health insurance plans, and this leverage seems even more important today. It typically results in higher reimbursements, which could translate into higher pay. The higher practice income, however, could be negated by higher administrative overhead, which is endemic in large organizations.
Mr. Mertz says large groups also have the resources to recruit new doctors. Small practices, in contrast, often decide not to grow. The practice would at first need to guarantee the salary of a new partner, which could require existing partners to take a pay cut, which they often don’t want to do. “They’ll decide to ride the practice into the ground,” which means closing it down when they retire, he says.
Cons of large groups
One individual doctor may have relatively little input in decision-making in a large group, and strong leadership may be lacking. One study examining the pros and cons of large group practices found that lack of physician cooperation, investment, and leadership were the most frequently cited barriers in large groups.
Physicians in large groups can also divide into competing factions. Mr. Mertz says rifts are more likely to take place in multispecialty groups, where higher-reimbursed proceduralists resent having to financially support lower-reimbursed primary care physicians. But it’s rare that such rifts actually break up the practice, he says.
Private practice vs. employment
Even as more physicians enter large groups, physicians continue to flee private practice in general. In 2020, the AMA found that the number of physicians in private practices had dropped nearly 5 percentage points since 2018, the largest 2-year drop recorded by the AMA.
The hardest hit are small groups of 10 physicians or fewer, once the backbone of U.S. medicine. A 2020 survey found that 53.7% of physicians still work in small practices of 10 or fewer physicians, compared with 61.4% in 2012.
Private practices tend to be partnerships, but younger physicians, for their part, often don’t want to become a partner. In a 2016 survey, only 22% of medical residents surveyed said they anticipate owning a stake in a practice someday.
What’s good about private practice?
The obvious advantage of private practice is having control. Physician-owners can choose staff, oversee finances, and decide on the direction the practice should take. They don’t have to worry about being fired, because the partnership agreement virtually guarantees each doctor’s place in the group.
The atmosphere in a small practice is often more relaxed. “Private practices tend to offer a family-like environment,” Mr. Miller says. Owners of small practices tend to have lower burnout than large practices, a 2018 study found.
Unlike hospital-employed doctors, private practitioners get to keep their ancillary income. “Physicians own the equipment and receive income generated from ancillary services, not just professional fees,” says Mr. Miller.
What’s negative about private practice?
Since small groups have little negotiating power with private payers, they can’t get favorable reimbursement rates. And while partners are protected from being fired, the practice could still go bankrupt.
Running a private practice means putting on an entrepreneurial hat. To develop a strong practice, you need to learn about marketing, finance, IT, contract negotiations, and facility management. “Most young doctors have no interest in this work,” Mr. Mertz says.
Value-based contracting has added another disadvantage for small practices. “It can be harder for small, independent groups to compete,” says Mike Belkin, JD, a divisional vice president at Merritt Hawkins, a physician recruitment company based in Dallas. “They don’t have the data and integration of services that are necessary for this.”
Employment in hospital systems
More than one-third of all physicians worked for hospitals in 2018, and hospitals’ share has been growing since then. In 2020, for the first time, the AMA found that more than half of all physicians were employed, and employment is mainly a hospital phenomenon.
The trend shows no signs of stopping. In 2019 and 2020, hospitals and other corporate entities acquired 20,900 physician practices, representing 29,800 doctors. “This trend will continue,” Dr. Pearl says. “The bigger will get bigger. It’s all about market control. Everyone wants to be wider, more vertical, and more powerful.”
Pros of hospital employment
“The advantages of hospital employment are mostly financial,” Mr. Mertz says. Unlike a private practice, “there’s no financial risk to hospital employment because you don’t own it. You won’t be on the tab for any losses.”
“Hospitals usually offer a highly competitive salary with less emphasis on production than in a private practice,” he says. New physicians are typically paid a guaranteed salary in the first 1-3 years of employment.
“You don’t have any management responsibilities, as you would in a practice,” Mr. Mertz says. “The hospital has a professional management team to handle the business side. Most young doctors have no interest in this work.”
“Employed physicians have a built-in referral network at a hospital,” Mr. Miller says. This is especially an advantage for new physicians, who don’t yet have a referral network of their own.”
Cons of hospital employment
Physicians employed by a hospital lack control. “You don’t decide the hours you work, the schedules you follow, and the physical facility you work in, and, for the most part, you don’t pick your staff,” Mr. Mertz says.
Like any big organization, hospitals are bureaucratic. “If you want to purchase a new piece of equipment, your request goes up the chain of command,” Mr. Mertz says. “Your purchase has to fit into the budget.” (This can be the case with large groups, too.)
Many employed doctors chafe under this lack of control. In an earlier survey by Medscape, 45% of employed respondents didn’t like having limited influence in decision-making, and 32% said they had less control over their work or schedule.
It’s no wonder that a large percentage of physicians would rather work in practices than hospitals. According to a 2021 Medicus Firm survey, 23% of physicians are interested in working in hospitals, while 40% would rather work either in multispecialty or single-specialty groups, Mr. Miller reports.
Doctors have differing views of hospital employment
New physicians are apt to dismiss any negatives about hospitals. “Lack of autonomy often matters less to younger physicians, who were trained in team-based models,” Mr. Belkin says.
Many young doctors actually like working in a large organization. “Young doctors out of residency are used to having everything at their fingertips – labs and testing is in-house,” Mr. Mertz says.
On the other hand, doctors who were previously self-employed – a group that makes up almost one-third of all hospital-employed doctors – can often be dissatisfied with employment. In a 2014 Medscape survey, 26% of previously self-employed doctors said job satisfaction had not improved with employment.
Mr. Mertz says these doctors remember what it was like to be in charge of a practice. “If you once owned a practice, you can always compare what’s going on now with that experience, and that can make you frustrated.”
Hospitals have higher turnover
It’s much easier to leave an organization when you don’t have an ownership stake. The annual physician turnover rate at hospitals is 28%, compared with 7% at medical groups, according to a 2019 report.
Mr. Belkin says changing jobs has become a way of life for many doctors. “Staying at a job for only a few years is no longer a red flag,” he says. “Physicians are exploring different options. They might try group practice and switch to hospitals or vice versa.”
Physicians are now part of a high-turnover culture: Once in a new job, many are already thinking about the next one. A 2018 survey found that 46% of doctors planned to leave their position within 3 years.
Private equity ownership of practice
Selling majority control of your practice to a private equity firm is a relatively new phenomenon and accounts for a small share of physicians – just 4% in 2020. This trend was originally limited to certain specialties, such as anesthesiology, emergency medicine, and dermatology, but now many others are courted.
The deals work like this: Physicians sell majority control of their practice to investors in return for shares in the private equity practice, and they become employees of that practice. The private equity firm then adds more physicians to the practice and invests in infrastructure with the intention of selling the practice at a large profit, which is then shared with the original physicians.
Pros of private equity
The original owners of the practice stand to make a substantial profit if they are willing to wait several years for the practice to be built up and sold. “If they are patient, they could earn a bonanza,” Mr. Belkin says.
Private equity investment helps the practice expand. “It’s an alternative to going to the bank and borrowing money,” Mr. Mertz says.
Cons of private equity
Physicians lose control of their practice. A client of Mr. Mertz’s briefly considered a private equity offer and turned it down. “The private equity firm would have veto power over what the doctors wanted to do,” he says.
Mr. Belkin says the selling physicians typically lose income after the sale. “Money they earned from ancillary services now goes to the practice,” Mr. Belkin says. The selling doctors could potentially take up to a 30% cut in their compensation, according to Coker Capital Advisors.
A version of this article first appeared on Medscape.com.
Large, physician-owned group practices are gaining ground as a popular form of practice, even as the number of physicians in solo and small practices declines, and employment maintains its appeal.
As physicians shift from owning private practices to employment in hospital systems, this countertrend is also taking place. Large group practices are growing in number, even as solo and small practices are in decline.
Do large, physician-owned groups bring benefits that beat employment? And how do large groups compare with smaller practices and new opportunities, such as private equity? You’ll find some answers here.
Working in large group practices
Large group practices with 50 or more physicians are enjoying a renaissance, even though physicians are still streaming into hospital systems. The share of physicians in large practices increased from 14.7% in 2018 to 17.2% in 2020, the largest 2-year change for this group, according to the American Medical Association.
“Physicians expect that large groups will treat them better than hospitals do,” says Robert Pearl, MD, former CEO of Permanente Medical Group, the nation’s largest physicians’ group.
Compared with hospitals, “doctors would prefer working in a group practice, if all other things are equal,” says Dr. Pearl, who is now a professor at Stanford (Calif.) University Medical School.
Large group practices can include both multispecialty groups and single-specialty groups. Groups in specialties like urology, orthopedics, and oncology have been growing in recent years, according to Gregory Mertz, managing director of Physician Strategies Group in Virginia Beach, Va.
A group practice could also be an independent physicians association – a federation of small practices that share functions like negotiations with insurers and management. Physicians can also form larger groups for single purposes like running an accountable care organization.
Some large group practices can have a mix of partners and employees. In these groups, “some doctors either don’t want a partnership or aren’t offered one,” says Nathan Miller, CEO of the Medicus Firm, a physician recruitment company in Dallas. The AMA reports that about 10% of physicians are employees of large practices.
“Large groups like the Permanente Medical Group are not partnerships,” Dr. Pearl says. “They tend to be a corporation with a board of directors, and all the physicians are employees, but it’s a physician-led organization.”
Doctors in these groups can enjoy a great deal of control. While Permanente Medical Group is exclusively affiliated with Kaiser, which runs hospitals and an HMO, the group is an independent corporation run by its doctors, who are both shareholders and employees, Dr. Pearl says.
The Cleveland Clinic and Mayo Clinic are not medical groups in the strict sense of the word. They describe themselves as academic medical centers, but Dr. Pearl says, “Doctors have a tremendous amount of control there, particularly those in the most remunerative specialties.”
Pros of large groups
Group practices are able to focus more on the physician participants’ needs and priorities, says Mr. Mertz. “In a hospital-based organization, physicians’ needs have to compete with the needs of the hospital. … In a large group, it can be easier to get policies changed and order equipment.”
However, for many physicians, their primary reason for joining a large group is having negotiating leverage with health insurance plans, and this leverage seems even more important today. It typically results in higher reimbursements, which could translate into higher pay. The higher practice income, however, could be negated by higher administrative overhead, which is endemic in large organizations.
Mr. Mertz says large groups also have the resources to recruit new doctors. Small practices, in contrast, often decide not to grow. The practice would at first need to guarantee the salary of a new partner, which could require existing partners to take a pay cut, which they often don’t want to do. “They’ll decide to ride the practice into the ground,” which means closing it down when they retire, he says.
Cons of large groups
One individual doctor may have relatively little input in decision-making in a large group, and strong leadership may be lacking. One study examining the pros and cons of large group practices found that lack of physician cooperation, investment, and leadership were the most frequently cited barriers in large groups.
Physicians in large groups can also divide into competing factions. Mr. Mertz says rifts are more likely to take place in multispecialty groups, where higher-reimbursed proceduralists resent having to financially support lower-reimbursed primary care physicians. But it’s rare that such rifts actually break up the practice, he says.
Private practice vs. employment
Even as more physicians enter large groups, physicians continue to flee private practice in general. In 2020, the AMA found that the number of physicians in private practices had dropped nearly 5 percentage points since 2018, the largest 2-year drop recorded by the AMA.
The hardest hit are small groups of 10 physicians or fewer, once the backbone of U.S. medicine. A 2020 survey found that 53.7% of physicians still work in small practices of 10 or fewer physicians, compared with 61.4% in 2012.
Private practices tend to be partnerships, but younger physicians, for their part, often don’t want to become a partner. In a 2016 survey, only 22% of medical residents surveyed said they anticipate owning a stake in a practice someday.
What’s good about private practice?
The obvious advantage of private practice is having control. Physician-owners can choose staff, oversee finances, and decide on the direction the practice should take. They don’t have to worry about being fired, because the partnership agreement virtually guarantees each doctor’s place in the group.
The atmosphere in a small practice is often more relaxed. “Private practices tend to offer a family-like environment,” Mr. Miller says. Owners of small practices tend to have lower burnout than large practices, a 2018 study found.
Unlike hospital-employed doctors, private practitioners get to keep their ancillary income. “Physicians own the equipment and receive income generated from ancillary services, not just professional fees,” says Mr. Miller.
What’s negative about private practice?
Since small groups have little negotiating power with private payers, they can’t get favorable reimbursement rates. And while partners are protected from being fired, the practice could still go bankrupt.
Running a private practice means putting on an entrepreneurial hat. To develop a strong practice, you need to learn about marketing, finance, IT, contract negotiations, and facility management. “Most young doctors have no interest in this work,” Mr. Mertz says.
Value-based contracting has added another disadvantage for small practices. “It can be harder for small, independent groups to compete,” says Mike Belkin, JD, a divisional vice president at Merritt Hawkins, a physician recruitment company based in Dallas. “They don’t have the data and integration of services that are necessary for this.”
Employment in hospital systems
More than one-third of all physicians worked for hospitals in 2018, and hospitals’ share has been growing since then. In 2020, for the first time, the AMA found that more than half of all physicians were employed, and employment is mainly a hospital phenomenon.
The trend shows no signs of stopping. In 2019 and 2020, hospitals and other corporate entities acquired 20,900 physician practices, representing 29,800 doctors. “This trend will continue,” Dr. Pearl says. “The bigger will get bigger. It’s all about market control. Everyone wants to be wider, more vertical, and more powerful.”
Pros of hospital employment
“The advantages of hospital employment are mostly financial,” Mr. Mertz says. Unlike a private practice, “there’s no financial risk to hospital employment because you don’t own it. You won’t be on the tab for any losses.”
“Hospitals usually offer a highly competitive salary with less emphasis on production than in a private practice,” he says. New physicians are typically paid a guaranteed salary in the first 1-3 years of employment.
“You don’t have any management responsibilities, as you would in a practice,” Mr. Mertz says. “The hospital has a professional management team to handle the business side. Most young doctors have no interest in this work.”
“Employed physicians have a built-in referral network at a hospital,” Mr. Miller says. This is especially an advantage for new physicians, who don’t yet have a referral network of their own.”
Cons of hospital employment
Physicians employed by a hospital lack control. “You don’t decide the hours you work, the schedules you follow, and the physical facility you work in, and, for the most part, you don’t pick your staff,” Mr. Mertz says.
Like any big organization, hospitals are bureaucratic. “If you want to purchase a new piece of equipment, your request goes up the chain of command,” Mr. Mertz says. “Your purchase has to fit into the budget.” (This can be the case with large groups, too.)
Many employed doctors chafe under this lack of control. In an earlier survey by Medscape, 45% of employed respondents didn’t like having limited influence in decision-making, and 32% said they had less control over their work or schedule.
It’s no wonder that a large percentage of physicians would rather work in practices than hospitals. According to a 2021 Medicus Firm survey, 23% of physicians are interested in working in hospitals, while 40% would rather work either in multispecialty or single-specialty groups, Mr. Miller reports.
Doctors have differing views of hospital employment
New physicians are apt to dismiss any negatives about hospitals. “Lack of autonomy often matters less to younger physicians, who were trained in team-based models,” Mr. Belkin says.
Many young doctors actually like working in a large organization. “Young doctors out of residency are used to having everything at their fingertips – labs and testing is in-house,” Mr. Mertz says.
On the other hand, doctors who were previously self-employed – a group that makes up almost one-third of all hospital-employed doctors – can often be dissatisfied with employment. In a 2014 Medscape survey, 26% of previously self-employed doctors said job satisfaction had not improved with employment.
Mr. Mertz says these doctors remember what it was like to be in charge of a practice. “If you once owned a practice, you can always compare what’s going on now with that experience, and that can make you frustrated.”
Hospitals have higher turnover
It’s much easier to leave an organization when you don’t have an ownership stake. The annual physician turnover rate at hospitals is 28%, compared with 7% at medical groups, according to a 2019 report.
Mr. Belkin says changing jobs has become a way of life for many doctors. “Staying at a job for only a few years is no longer a red flag,” he says. “Physicians are exploring different options. They might try group practice and switch to hospitals or vice versa.”
Physicians are now part of a high-turnover culture: Once in a new job, many are already thinking about the next one. A 2018 survey found that 46% of doctors planned to leave their position within 3 years.
Private equity ownership of practice
Selling majority control of your practice to a private equity firm is a relatively new phenomenon and accounts for a small share of physicians – just 4% in 2020. This trend was originally limited to certain specialties, such as anesthesiology, emergency medicine, and dermatology, but now many others are courted.
The deals work like this: Physicians sell majority control of their practice to investors in return for shares in the private equity practice, and they become employees of that practice. The private equity firm then adds more physicians to the practice and invests in infrastructure with the intention of selling the practice at a large profit, which is then shared with the original physicians.
Pros of private equity
The original owners of the practice stand to make a substantial profit if they are willing to wait several years for the practice to be built up and sold. “If they are patient, they could earn a bonanza,” Mr. Belkin says.
Private equity investment helps the practice expand. “It’s an alternative to going to the bank and borrowing money,” Mr. Mertz says.
Cons of private equity
Physicians lose control of their practice. A client of Mr. Mertz’s briefly considered a private equity offer and turned it down. “The private equity firm would have veto power over what the doctors wanted to do,” he says.
Mr. Belkin says the selling physicians typically lose income after the sale. “Money they earned from ancillary services now goes to the practice,” Mr. Belkin says. The selling doctors could potentially take up to a 30% cut in their compensation, according to Coker Capital Advisors.
A version of this article first appeared on Medscape.com.















