User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Changing terminology in LGBTQ+ spaces: How to keep up with the lingo
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
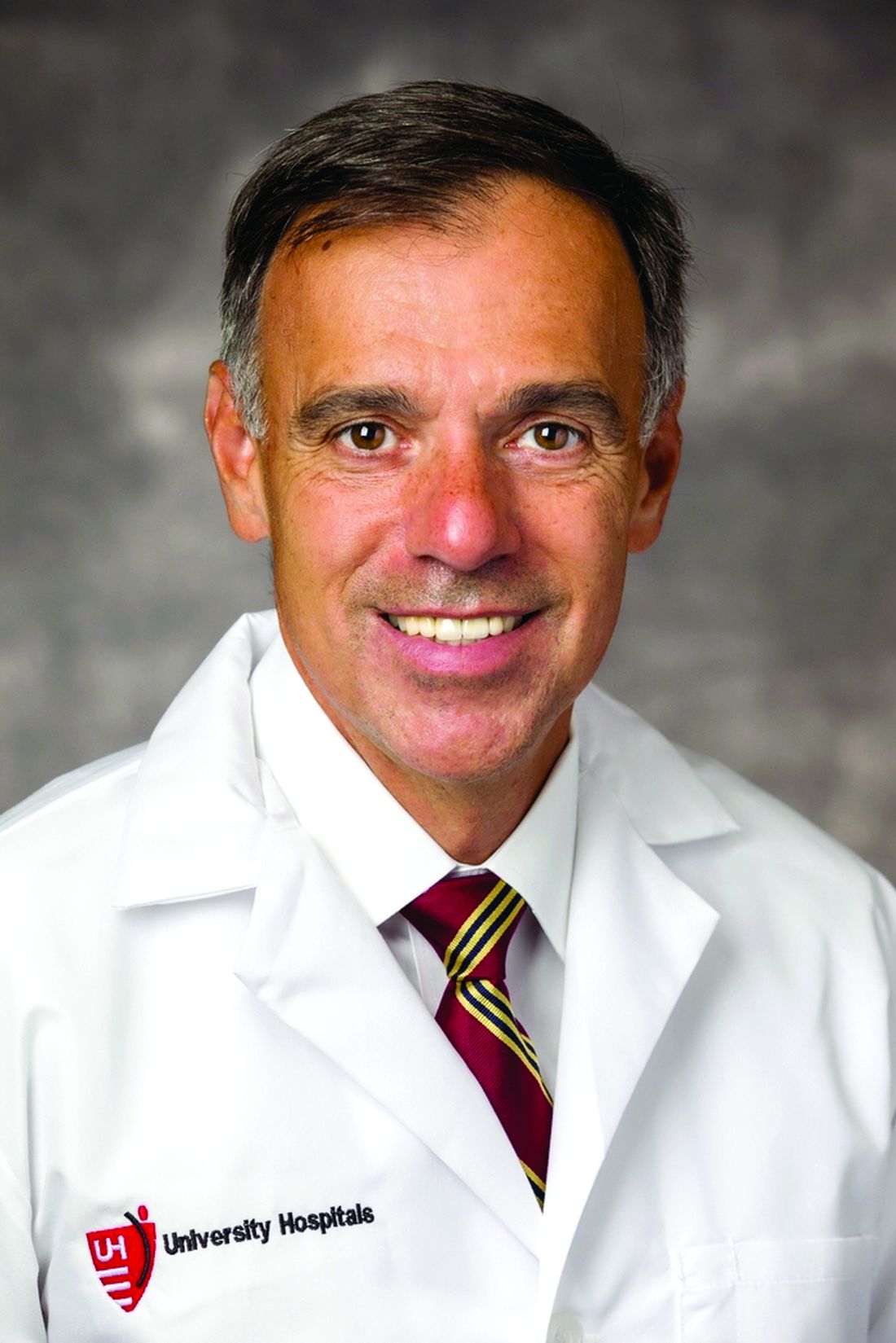
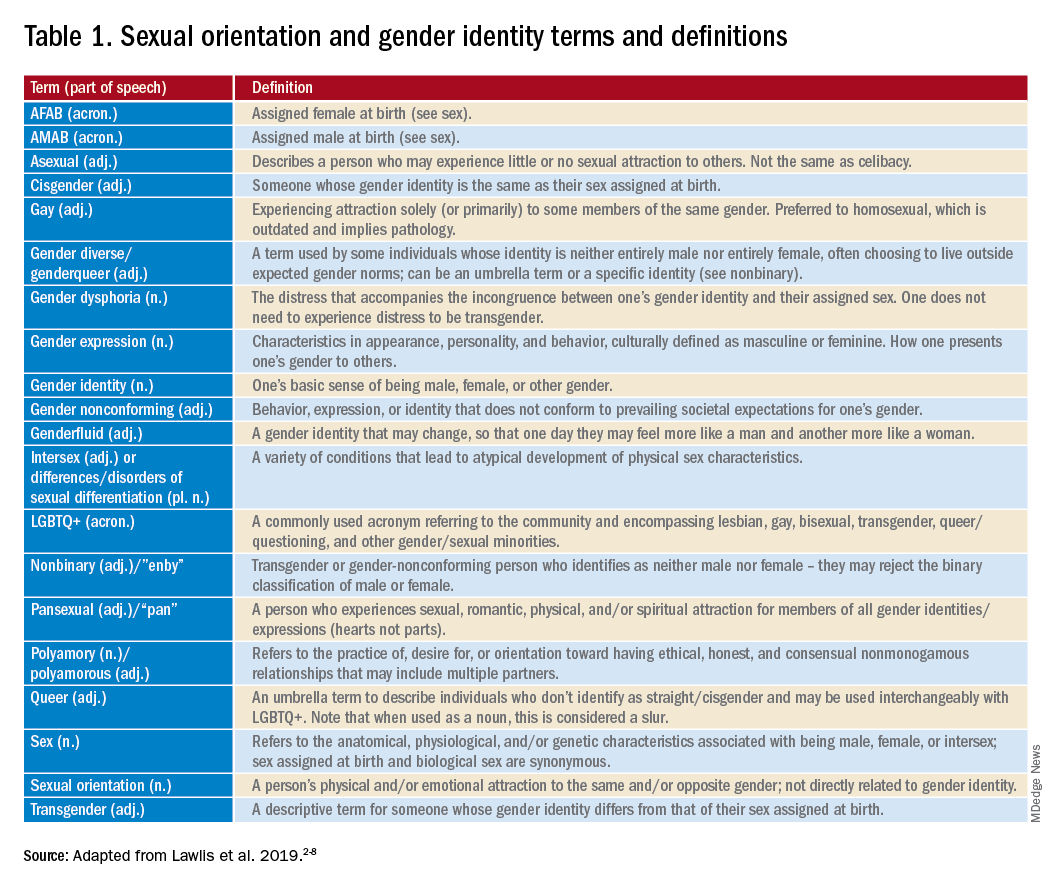
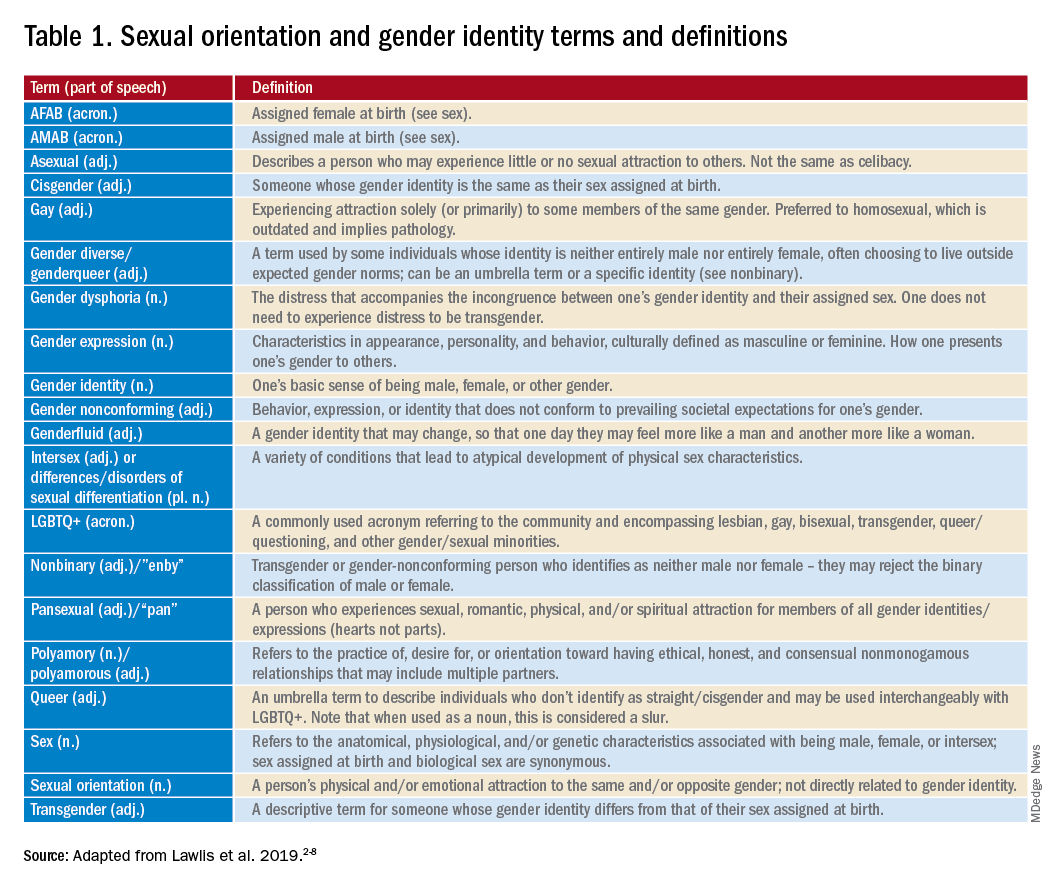
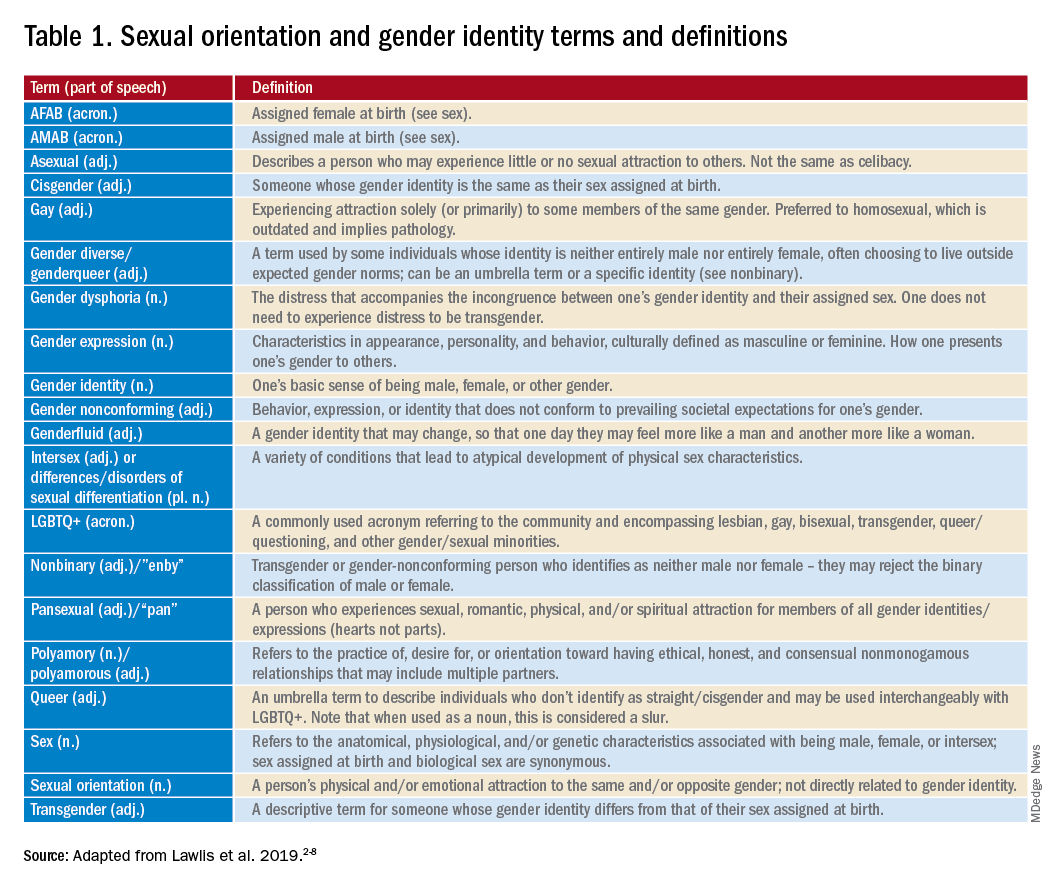
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
For those of us who see adolescent patients on a regular basis, it seems that they use new vocabulary almost every day. While you may not need to know what “lit” means, you probably do need to understand terms used to describe your patients’ identities. At times it feels like we, as providers, have to be on TikTok to keep up with our patients, and while this may be an amusing way to educate ourselves, a judicious Google search can be much more helpful. The interesting part about LGBTQ+ terminology is that it stems from the community and thus is frequently updated to reflect our evolving understanding of gender, sexuality, and identity. That being said, it can make it difficult for those who are not plugged in to the community to keep up to date. While we have learned in medicine to use accurate terminology and appropriate three-letter acronyms (or “TLAs” as one of my residents referenced them when I was a medical student) to describe medical conditions, the LGBTQ+ community has its own set of terms and acronyms. These new words may seem daunting, but they are often based in Latin roots or prefixes such as a-, demi-, poly-, and pan-, which may be familiar to those of us who use plenty of other Latin-based terms in medicine and our everyday lives. By paying attention to how people define and use terminology, we can better recognize their true identities and become better providers.
The first, and perhaps most important, piece of advice is to maintain cultural humility. Know when to admit you don’t recognize a term and politely ask the definition. For example, the first time I heard the term “demiboy” I said “I’m not familiar with that word. Can you explain what it means to you?” Phrasing the question as such is also helpful in that it gives the individuals a chance to really define their identity. In addition, some words may be used differently by various individuals and by asking what the word means to them, you can have a better understanding of how they are using the terminology. In this particular instance, the patient felt more masculine, but not 100%, partway between agender (meaning having no gender identity) and being “all male.” By embracing cultural humility, we place the patients in the role of expert on their own identity and orientation. According to Maria Ruud, DNP, of the University of Minnesota, Minneapolis, cultural humility is the “ongoing self-reflection and education …[seeking] to gain an awareness of their own assumptions and biases that may contribute to health disparities.”1
Another reason it is important to keep up on the language is that some adolescents, particularly younger adolescents, may not be using the terminology correctly. It can be very helpful to know the difference between polyamorous and pansexual when a 12-year-old describes themselves as polyamorous (having consenting, nonmonogamous relationships) but provides the definition for pansexual (being attracted to all gender identities). Yes, this has happened to me, and yes, my resident was appropriately confused. Correcting someone else’s vocabulary can be tricky and even inappropriate or condescending; therefore, tread cautiously. It may be appropriate, however, to correct colleagues’ or even patients’ family members’ language if they are using terms that may be hurtful to your patients. I do not allow slurs in my clinic, and when parents are using incorrect pronouns on purpose, I will often let them know that it is my job to respect their child’s identity where it is in the moment and that they have asked me to use specific pronouns, so I will continue to refer to their child with those pronouns. Reflecting the language of the patient can be a powerful statement providing them with the autonomy that they deserve as burgeoning adults navigating the complicated journey of identity.
As providers who often have to defend ourselves against “Dr. Google,” we may be leery of just searching randomly for the definition of a new word and hoping a site is credible. One site that I have used repeatedly is www.itspronouncedmetrosexual.com by Sam Killermann,2 a gender and sexuality educator.
Mr. Killermann has also produced an E-book that is regularly updated to reflect changing terminology, which can be obtained for a small donation. As Mr. Killermann explains, “New language can be intimidating, and the language of gender and sexuality is often that.”3 In reality, the definitions aren’t scary and often the words can describe something you already know exists but didn’t recognize had a specific term. Not everyone can know every term and its definition; in fact, many members of the LGBTQ+ community don’t know or even understand every term. Below is a shortened list with some of the more common terms you may encounter; however, individuals may use them differently so it is never out of place to clarify your understanding of the term’s definition.
With these resources, along with cultural humility and reflection of others’ language, we can all start to have more meaningful conversations with our patients around their identity and relationships with others.
Dr. Lawlis is an assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
References
1. Ruud M. Nursing for women’s health. 2018;22(3):255-63.
2. Killermann S. It’s Pronounced Metrosexual. 2020.
3. Killermann S. Defining LGBTQ+: A guide to gender and sexuality terminology. 2019, Feb 25.
4. The Joint Commission. Advancing effective communication, cultural competence, and patient- and family-centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: A field guide. Oak Brook, Ill. 2011.
5. LGBT health disparities. American Psychiatric Association Public Interest Government Relations Office. 2013 May.
6. Lawlis S et al. Health services for LGBTQ+ patients. Psychiatr Ann. 2019;49(10):426-35.
7. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
8. Center of Excellence for Transgender Health, department of family and community medicine, UCSF. Guidelines for the primary and gender-affirming care of transgender and gender nonbinary people. 2016 Jun 17.
Mayo Clinic fires 700 employees for refusing COVID vaccine
The medical center, which is Minnesota’s largest employer, has major campuses in Arizona, Florida, and Minnesota and operates hospitals in Iowa and Wisconsin.
Employees had until Jan. 3 to get vaccinated or receive approval for an exemption. On Jan. 4, the hospital fired those who didn’t meet the requirement, according to Action News Jax, a CBS affiliate in Florida.
The 700 employees make up about 1% of Mayo Clinic’s 73,000-person workforce. So far, none of the employees at the campus in Jacksonville, Fla., have been affected, the news outlet reported.
“Florida staff who are not in compliance with our vaccination program remain employed pending the outcome of litigation related to the Centers for Medicare & Medicaid Services requirements,” a Mayo Clinic spokesperson told Action News Jax.
The federal government and Florida remain at odds over vaccine mandates, and several lawsuits are winding through the court system. Florida Gov. Ron DeSantis signed legislation in November that bans private Florida employers from requiring all employees to get vaccinated and calls for various exemption options, according to The Florida Times-Union. The state law clashes with a federal rule that requires vaccinations for all health care workers at hospitals that receive Medicare and Medicaid funding.
The Mayo Clinic mandate required employees to receive at least one COVID-19 vaccine dose and not be “overdue” for a second dose, according to the statement. Only medical and religious exemptions were allowed, and most medical and religious exemptions were approved.
“While Mayo Clinic is saddened to lose valuable employees, we need to take all steps necessary to keep our patients, workforce, visitors, and communities safe,” Mayo Clinic wrote in its statement. “If individuals released from employment choose to get vaccinated at a later date, the opportunity exists for them to apply and return to Mayo Clinic for future job openings.”
With the latest surge in COVID-19 cases from the Omicron variant, the Mayo Clinic also encouraged unvaccinated people to get a shot and those who are eligible for a booster to get one “as soon as possible.”
“Based on science and data, it’s clear that vaccination keeps people out of the hospital and saves lives,” according to the statement. “That’s true for everyone in our communities – and it’s especially true for the many patients with serious or complex diseases who seek care at Mayo Clinic each day.”
A version of this article first appeared on WebMD.com.
The medical center, which is Minnesota’s largest employer, has major campuses in Arizona, Florida, and Minnesota and operates hospitals in Iowa and Wisconsin.
Employees had until Jan. 3 to get vaccinated or receive approval for an exemption. On Jan. 4, the hospital fired those who didn’t meet the requirement, according to Action News Jax, a CBS affiliate in Florida.
The 700 employees make up about 1% of Mayo Clinic’s 73,000-person workforce. So far, none of the employees at the campus in Jacksonville, Fla., have been affected, the news outlet reported.
“Florida staff who are not in compliance with our vaccination program remain employed pending the outcome of litigation related to the Centers for Medicare & Medicaid Services requirements,” a Mayo Clinic spokesperson told Action News Jax.
The federal government and Florida remain at odds over vaccine mandates, and several lawsuits are winding through the court system. Florida Gov. Ron DeSantis signed legislation in November that bans private Florida employers from requiring all employees to get vaccinated and calls for various exemption options, according to The Florida Times-Union. The state law clashes with a federal rule that requires vaccinations for all health care workers at hospitals that receive Medicare and Medicaid funding.
The Mayo Clinic mandate required employees to receive at least one COVID-19 vaccine dose and not be “overdue” for a second dose, according to the statement. Only medical and religious exemptions were allowed, and most medical and religious exemptions were approved.
“While Mayo Clinic is saddened to lose valuable employees, we need to take all steps necessary to keep our patients, workforce, visitors, and communities safe,” Mayo Clinic wrote in its statement. “If individuals released from employment choose to get vaccinated at a later date, the opportunity exists for them to apply and return to Mayo Clinic for future job openings.”
With the latest surge in COVID-19 cases from the Omicron variant, the Mayo Clinic also encouraged unvaccinated people to get a shot and those who are eligible for a booster to get one “as soon as possible.”
“Based on science and data, it’s clear that vaccination keeps people out of the hospital and saves lives,” according to the statement. “That’s true for everyone in our communities – and it’s especially true for the many patients with serious or complex diseases who seek care at Mayo Clinic each day.”
A version of this article first appeared on WebMD.com.
The medical center, which is Minnesota’s largest employer, has major campuses in Arizona, Florida, and Minnesota and operates hospitals in Iowa and Wisconsin.
Employees had until Jan. 3 to get vaccinated or receive approval for an exemption. On Jan. 4, the hospital fired those who didn’t meet the requirement, according to Action News Jax, a CBS affiliate in Florida.
The 700 employees make up about 1% of Mayo Clinic’s 73,000-person workforce. So far, none of the employees at the campus in Jacksonville, Fla., have been affected, the news outlet reported.
“Florida staff who are not in compliance with our vaccination program remain employed pending the outcome of litigation related to the Centers for Medicare & Medicaid Services requirements,” a Mayo Clinic spokesperson told Action News Jax.
The federal government and Florida remain at odds over vaccine mandates, and several lawsuits are winding through the court system. Florida Gov. Ron DeSantis signed legislation in November that bans private Florida employers from requiring all employees to get vaccinated and calls for various exemption options, according to The Florida Times-Union. The state law clashes with a federal rule that requires vaccinations for all health care workers at hospitals that receive Medicare and Medicaid funding.
The Mayo Clinic mandate required employees to receive at least one COVID-19 vaccine dose and not be “overdue” for a second dose, according to the statement. Only medical and religious exemptions were allowed, and most medical and religious exemptions were approved.
“While Mayo Clinic is saddened to lose valuable employees, we need to take all steps necessary to keep our patients, workforce, visitors, and communities safe,” Mayo Clinic wrote in its statement. “If individuals released from employment choose to get vaccinated at a later date, the opportunity exists for them to apply and return to Mayo Clinic for future job openings.”
With the latest surge in COVID-19 cases from the Omicron variant, the Mayo Clinic also encouraged unvaccinated people to get a shot and those who are eligible for a booster to get one “as soon as possible.”
“Based on science and data, it’s clear that vaccination keeps people out of the hospital and saves lives,” according to the statement. “That’s true for everyone in our communities – and it’s especially true for the many patients with serious or complex diseases who seek care at Mayo Clinic each day.”
A version of this article first appeared on WebMD.com.
Surgical groups push back against new revascularization guidelines
The new 2021 coronary revascularization guidelines are spurring controversy, as surgical associations raise concerns about the interpretation of the evidence behind key recommendations and the makeup of the writing committee.
The guideline was published in December by the American College of Cardiology, American Heart Association, and Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI), and replaces the 2011 coronary artery bypass surgery (CABG) and the 2011 and 2015 percutaneous coronary intervention (PCI) guidelines.
The American Association for Thoracic Surgery (AATS) and Society of Thoracic Surgeons (STS) were part of the development of the document but have withdrawn their support, citing three areas of concern in a recent editorial in Annals of Thoracic Surgery.
“I do have to emphasize this is not just the AATS and STS – the European societies, Latin American societies, Asian societies, and even cardiologists are all coming out against these guidelines,” Joseph F. Sabik III, MD, University Hospitals Cleveland Medical Center, lead author of the editorial, said in an interview. “So, I think that tells us that something didn’t go right here.”
The main objection is the downgrading of CABG surgery from a class 1 to weak 2b recommendation to improve survival in patients with three-vessel coronary artery disease (CAD) and normal left ventricular function.
The ISCHEMIA trial was used to support this two-level downgrade and a class 1 to 2a downgrade for CABG in three-vessel CAD with mild to moderate left ventricular dysfunction. But the trial wasn’t powered for survival, only 20% of patients underwent CABG as the initial invasive strategy, and patients were followed for less than 5 years, the editorialists observed.
At the same time, there’s plenty of observational and randomized studies such as SYNTAX, EXCEL, and FAME 3 showing a clear survival benefit of CABG over PCI, Dr. Sabik said. “The criticism is that these are old studies and aren’t applicable today, but we don’t understand downgrading without any evidence suggesting it [CABG] isn’t effective anymore.”
CABG and PCI treated as equal
AATS and STS also object to the new guidelines treating PCI and CABG as equivalent revascularization strategies in decreasing ischemic events. Both were given a 2b recommendation for survival with triple-vessel disease, but randomized trials have demonstrated not only lower mortality with surgery but fewer reinterventions and myocardial infarctions.
“None of that gets acknowledged in the guidelines; they are treated equally,” Dr. Sabik said. “So if you’re going to say that CABG isn’t any better than medical therapy, in our mind, you have to say that PCI is worse than medical therapy. And we don’t believe that, I want you to know. We just think that the logic doesn’t make any sense. The committee used what it wanted to but didn’t use many things that committees have used in the past to give CABG a level 1 recommendation.”
The downgrade is also at odds with the 2018 European Society of Cardiology (ESC)/ European Association for Cardio-Thoracic Surgery (EACTS) guidelines, which give CABG a class 1 recommendation in three-vessel CAD as well as one- or two-vessel CAD with proximal left atrial descending artery stenosis.
In a Dec. 14 letter to the ACC/AHA Joint Committee, the Latin American Association of Cardiac and Endovascular Surgery (LACES) also called out the guideline committee for the 2b class of recommendation (COR) for PCI and CABG, saying it contradicts the text, which “clearly considers” the need to give a weaker endorsement for PCI than for CABG in patients with multivessel CAD.
“Considering that this section has the most significant impact due to the prevalence of stable ischemic heart disease in patients with multivessel CAD, such a contradiction may affect the lives and survival of millions of patients worldwide and have a major socioeconomic impact,” the letter states.
“Therefore, LACES respectfully but vehemently believes the Task Force should seriously reconsider the wording and recommendations in this specific large group of patients.”
Class I for radial conduit
AATS and STS also express concern about the new class 1 recommendation for the radial artery as a conduit in CABG. They note this is higher than bilateral internal mammary artery grafting and based on a meta-analysis of six relatively small studies with very strict inclusion criteria favorable for radial artery usage and patency.
“There’s a lot of studies that showed if you use the radial artery incorrectly, you have worse outcomes, and that’s what scares us a bit,” Dr. Sabik said. “If they’re giving it a class 1 recommendation, does that mean that becomes standard of care and could that cause patient harm? We think that level 1 is too high and that a [class] 2a with qualifications would be appropriate.”
Unequal footing
In a Dec. 23 letter, EACTS said it is “extremely concerned” about downgrading the COR for CABG without new randomized controlled trials to support the decision or to reject previously held evidence.
“The downgrading of CABG, and placing PCI at the same COR, does not meet our interpretation of the evidence, and may lead to avoidable loss of life,” EACTS officials said. “These guidelines also have implications on patient care: A COR IIb entails that CABG may not be reimbursable in some countries.”
EACTS called on AHA, ACC, and SCAI to review the evidence and called out the makeup of the guideline writing committee. “It is astonishing that no surgical association was involved, coauthored, or endorsed these guidelines.”
The AATS and STS each had a single representative on the guidelines’ writing committee but note that the six remaining surgeons were chosen by the ACC and AHA. Surgeons were also in the minority and only a majority was needed to approve the guidelines, highlighting the need to revisit the guideline development process to ensure equal representation by multidisciplinary experts across specialties.
“I hope the cardiology and surgical societies can come together and figure out how we do this better in the future, and we take a look again at these guidelines and come up with what we think is appropriate, especially since this is not just AATS and STS,” Dr. Sabik said.
In an emailed statement, the ACC/AHA said the AATS and STS representatives “actively participated throughout the writing process the past 3 years” and that the AATS and STS were involved in the “extensive peer review process” for the document with a reviewer from each organization. Nevertheless, AATS and STS both elected not to endorse the guidelines when at the organizational approval stage.
“Consequently, the AATS representative chose to stay with the committee and be recognized as having been appointed on behalf of the ACC and the AHA,” according to the statement. “The STS representative chose to withdraw from the committee and is not listed as a writing committee member on the final guideline. The final guideline reflects the latest evidence-based recommendations for coronary artery revascularization, as agreed by the ACC, AHA, SCAI, and the full writing committee.”
Despite pleas from the surgical groups to reconsider the evidence, “there is no further review process for the revascularization guideline,” the ACC/AHA spokesperson noted.
Jennifer S. Lawton, MD, chief of cardiac surgery at Johns Hopkins University, Baltimore, and guideline writing committee chair, did not respond to numerous requests for comment.
A version of this article first appeared on Medscape.com.
The new 2021 coronary revascularization guidelines are spurring controversy, as surgical associations raise concerns about the interpretation of the evidence behind key recommendations and the makeup of the writing committee.
The guideline was published in December by the American College of Cardiology, American Heart Association, and Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI), and replaces the 2011 coronary artery bypass surgery (CABG) and the 2011 and 2015 percutaneous coronary intervention (PCI) guidelines.
The American Association for Thoracic Surgery (AATS) and Society of Thoracic Surgeons (STS) were part of the development of the document but have withdrawn their support, citing three areas of concern in a recent editorial in Annals of Thoracic Surgery.
“I do have to emphasize this is not just the AATS and STS – the European societies, Latin American societies, Asian societies, and even cardiologists are all coming out against these guidelines,” Joseph F. Sabik III, MD, University Hospitals Cleveland Medical Center, lead author of the editorial, said in an interview. “So, I think that tells us that something didn’t go right here.”
The main objection is the downgrading of CABG surgery from a class 1 to weak 2b recommendation to improve survival in patients with three-vessel coronary artery disease (CAD) and normal left ventricular function.
The ISCHEMIA trial was used to support this two-level downgrade and a class 1 to 2a downgrade for CABG in three-vessel CAD with mild to moderate left ventricular dysfunction. But the trial wasn’t powered for survival, only 20% of patients underwent CABG as the initial invasive strategy, and patients were followed for less than 5 years, the editorialists observed.
At the same time, there’s plenty of observational and randomized studies such as SYNTAX, EXCEL, and FAME 3 showing a clear survival benefit of CABG over PCI, Dr. Sabik said. “The criticism is that these are old studies and aren’t applicable today, but we don’t understand downgrading without any evidence suggesting it [CABG] isn’t effective anymore.”
CABG and PCI treated as equal
AATS and STS also object to the new guidelines treating PCI and CABG as equivalent revascularization strategies in decreasing ischemic events. Both were given a 2b recommendation for survival with triple-vessel disease, but randomized trials have demonstrated not only lower mortality with surgery but fewer reinterventions and myocardial infarctions.
“None of that gets acknowledged in the guidelines; they are treated equally,” Dr. Sabik said. “So if you’re going to say that CABG isn’t any better than medical therapy, in our mind, you have to say that PCI is worse than medical therapy. And we don’t believe that, I want you to know. We just think that the logic doesn’t make any sense. The committee used what it wanted to but didn’t use many things that committees have used in the past to give CABG a level 1 recommendation.”
The downgrade is also at odds with the 2018 European Society of Cardiology (ESC)/ European Association for Cardio-Thoracic Surgery (EACTS) guidelines, which give CABG a class 1 recommendation in three-vessel CAD as well as one- or two-vessel CAD with proximal left atrial descending artery stenosis.
In a Dec. 14 letter to the ACC/AHA Joint Committee, the Latin American Association of Cardiac and Endovascular Surgery (LACES) also called out the guideline committee for the 2b class of recommendation (COR) for PCI and CABG, saying it contradicts the text, which “clearly considers” the need to give a weaker endorsement for PCI than for CABG in patients with multivessel CAD.
“Considering that this section has the most significant impact due to the prevalence of stable ischemic heart disease in patients with multivessel CAD, such a contradiction may affect the lives and survival of millions of patients worldwide and have a major socioeconomic impact,” the letter states.
“Therefore, LACES respectfully but vehemently believes the Task Force should seriously reconsider the wording and recommendations in this specific large group of patients.”
Class I for radial conduit
AATS and STS also express concern about the new class 1 recommendation for the radial artery as a conduit in CABG. They note this is higher than bilateral internal mammary artery grafting and based on a meta-analysis of six relatively small studies with very strict inclusion criteria favorable for radial artery usage and patency.
“There’s a lot of studies that showed if you use the radial artery incorrectly, you have worse outcomes, and that’s what scares us a bit,” Dr. Sabik said. “If they’re giving it a class 1 recommendation, does that mean that becomes standard of care and could that cause patient harm? We think that level 1 is too high and that a [class] 2a with qualifications would be appropriate.”
Unequal footing
In a Dec. 23 letter, EACTS said it is “extremely concerned” about downgrading the COR for CABG without new randomized controlled trials to support the decision or to reject previously held evidence.
“The downgrading of CABG, and placing PCI at the same COR, does not meet our interpretation of the evidence, and may lead to avoidable loss of life,” EACTS officials said. “These guidelines also have implications on patient care: A COR IIb entails that CABG may not be reimbursable in some countries.”
EACTS called on AHA, ACC, and SCAI to review the evidence and called out the makeup of the guideline writing committee. “It is astonishing that no surgical association was involved, coauthored, or endorsed these guidelines.”
The AATS and STS each had a single representative on the guidelines’ writing committee but note that the six remaining surgeons were chosen by the ACC and AHA. Surgeons were also in the minority and only a majority was needed to approve the guidelines, highlighting the need to revisit the guideline development process to ensure equal representation by multidisciplinary experts across specialties.
“I hope the cardiology and surgical societies can come together and figure out how we do this better in the future, and we take a look again at these guidelines and come up with what we think is appropriate, especially since this is not just AATS and STS,” Dr. Sabik said.
In an emailed statement, the ACC/AHA said the AATS and STS representatives “actively participated throughout the writing process the past 3 years” and that the AATS and STS were involved in the “extensive peer review process” for the document with a reviewer from each organization. Nevertheless, AATS and STS both elected not to endorse the guidelines when at the organizational approval stage.
“Consequently, the AATS representative chose to stay with the committee and be recognized as having been appointed on behalf of the ACC and the AHA,” according to the statement. “The STS representative chose to withdraw from the committee and is not listed as a writing committee member on the final guideline. The final guideline reflects the latest evidence-based recommendations for coronary artery revascularization, as agreed by the ACC, AHA, SCAI, and the full writing committee.”
Despite pleas from the surgical groups to reconsider the evidence, “there is no further review process for the revascularization guideline,” the ACC/AHA spokesperson noted.
Jennifer S. Lawton, MD, chief of cardiac surgery at Johns Hopkins University, Baltimore, and guideline writing committee chair, did not respond to numerous requests for comment.
A version of this article first appeared on Medscape.com.
The new 2021 coronary revascularization guidelines are spurring controversy, as surgical associations raise concerns about the interpretation of the evidence behind key recommendations and the makeup of the writing committee.
The guideline was published in December by the American College of Cardiology, American Heart Association, and Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI), and replaces the 2011 coronary artery bypass surgery (CABG) and the 2011 and 2015 percutaneous coronary intervention (PCI) guidelines.
The American Association for Thoracic Surgery (AATS) and Society of Thoracic Surgeons (STS) were part of the development of the document but have withdrawn their support, citing three areas of concern in a recent editorial in Annals of Thoracic Surgery.
“I do have to emphasize this is not just the AATS and STS – the European societies, Latin American societies, Asian societies, and even cardiologists are all coming out against these guidelines,” Joseph F. Sabik III, MD, University Hospitals Cleveland Medical Center, lead author of the editorial, said in an interview. “So, I think that tells us that something didn’t go right here.”
The main objection is the downgrading of CABG surgery from a class 1 to weak 2b recommendation to improve survival in patients with three-vessel coronary artery disease (CAD) and normal left ventricular function.
The ISCHEMIA trial was used to support this two-level downgrade and a class 1 to 2a downgrade for CABG in three-vessel CAD with mild to moderate left ventricular dysfunction. But the trial wasn’t powered for survival, only 20% of patients underwent CABG as the initial invasive strategy, and patients were followed for less than 5 years, the editorialists observed.
At the same time, there’s plenty of observational and randomized studies such as SYNTAX, EXCEL, and FAME 3 showing a clear survival benefit of CABG over PCI, Dr. Sabik said. “The criticism is that these are old studies and aren’t applicable today, but we don’t understand downgrading without any evidence suggesting it [CABG] isn’t effective anymore.”
CABG and PCI treated as equal
AATS and STS also object to the new guidelines treating PCI and CABG as equivalent revascularization strategies in decreasing ischemic events. Both were given a 2b recommendation for survival with triple-vessel disease, but randomized trials have demonstrated not only lower mortality with surgery but fewer reinterventions and myocardial infarctions.
“None of that gets acknowledged in the guidelines; they are treated equally,” Dr. Sabik said. “So if you’re going to say that CABG isn’t any better than medical therapy, in our mind, you have to say that PCI is worse than medical therapy. And we don’t believe that, I want you to know. We just think that the logic doesn’t make any sense. The committee used what it wanted to but didn’t use many things that committees have used in the past to give CABG a level 1 recommendation.”
The downgrade is also at odds with the 2018 European Society of Cardiology (ESC)/ European Association for Cardio-Thoracic Surgery (EACTS) guidelines, which give CABG a class 1 recommendation in three-vessel CAD as well as one- or two-vessel CAD with proximal left atrial descending artery stenosis.
In a Dec. 14 letter to the ACC/AHA Joint Committee, the Latin American Association of Cardiac and Endovascular Surgery (LACES) also called out the guideline committee for the 2b class of recommendation (COR) for PCI and CABG, saying it contradicts the text, which “clearly considers” the need to give a weaker endorsement for PCI than for CABG in patients with multivessel CAD.
“Considering that this section has the most significant impact due to the prevalence of stable ischemic heart disease in patients with multivessel CAD, such a contradiction may affect the lives and survival of millions of patients worldwide and have a major socioeconomic impact,” the letter states.
“Therefore, LACES respectfully but vehemently believes the Task Force should seriously reconsider the wording and recommendations in this specific large group of patients.”
Class I for radial conduit
AATS and STS also express concern about the new class 1 recommendation for the radial artery as a conduit in CABG. They note this is higher than bilateral internal mammary artery grafting and based on a meta-analysis of six relatively small studies with very strict inclusion criteria favorable for radial artery usage and patency.
“There’s a lot of studies that showed if you use the radial artery incorrectly, you have worse outcomes, and that’s what scares us a bit,” Dr. Sabik said. “If they’re giving it a class 1 recommendation, does that mean that becomes standard of care and could that cause patient harm? We think that level 1 is too high and that a [class] 2a with qualifications would be appropriate.”
Unequal footing
In a Dec. 23 letter, EACTS said it is “extremely concerned” about downgrading the COR for CABG without new randomized controlled trials to support the decision or to reject previously held evidence.
“The downgrading of CABG, and placing PCI at the same COR, does not meet our interpretation of the evidence, and may lead to avoidable loss of life,” EACTS officials said. “These guidelines also have implications on patient care: A COR IIb entails that CABG may not be reimbursable in some countries.”
EACTS called on AHA, ACC, and SCAI to review the evidence and called out the makeup of the guideline writing committee. “It is astonishing that no surgical association was involved, coauthored, or endorsed these guidelines.”
The AATS and STS each had a single representative on the guidelines’ writing committee but note that the six remaining surgeons were chosen by the ACC and AHA. Surgeons were also in the minority and only a majority was needed to approve the guidelines, highlighting the need to revisit the guideline development process to ensure equal representation by multidisciplinary experts across specialties.
“I hope the cardiology and surgical societies can come together and figure out how we do this better in the future, and we take a look again at these guidelines and come up with what we think is appropriate, especially since this is not just AATS and STS,” Dr. Sabik said.
In an emailed statement, the ACC/AHA said the AATS and STS representatives “actively participated throughout the writing process the past 3 years” and that the AATS and STS were involved in the “extensive peer review process” for the document with a reviewer from each organization. Nevertheless, AATS and STS both elected not to endorse the guidelines when at the organizational approval stage.
“Consequently, the AATS representative chose to stay with the committee and be recognized as having been appointed on behalf of the ACC and the AHA,” according to the statement. “The STS representative chose to withdraw from the committee and is not listed as a writing committee member on the final guideline. The final guideline reflects the latest evidence-based recommendations for coronary artery revascularization, as agreed by the ACC, AHA, SCAI, and the full writing committee.”
Despite pleas from the surgical groups to reconsider the evidence, “there is no further review process for the revascularization guideline,” the ACC/AHA spokesperson noted.
Jennifer S. Lawton, MD, chief of cardiac surgery at Johns Hopkins University, Baltimore, and guideline writing committee chair, did not respond to numerous requests for comment.
A version of this article first appeared on Medscape.com.
SGLT2 inhibitors improve cardiovascular outcomes across groups
Sodium-glucose cotransporter 2 (SGLT2) inhibitors show “remarkable consistency of class benefit” for improving cardiovascular outcomes in high-risk people across age, sex, and race/ethnicity categories.
The findings, from a meta-analysis of 10 major randomized clinical trials, were published online Jan. 5, 2021, in JAMA Network Open by Mukul Bhattarai, MD, a cardiology fellow at Southern Illinois University, Springfield, and colleagues.
“Our meta-analysis evaluated a wide spectrum of efficacy outcomes, further characterizing the primary outcome in different subgroups from several well-designed large clinical trials. It supports that SGLT2 inhibitors have emerged as an effective class of drugs for improving cardiovascular morbidity and mortality, including the prevention of [hospitalization for heart failure] and reducing all-cause mortality in selected patients,” Dr. Bhattarai and colleagues wrote.
The cardiovascular outcomes of SGLT2 inhibitor therapy, they noted, “can be compared across all trials, and it demonstrates remarkable consistency of class benefit, despite the variations in populations enrolled.”
However, they also noted that SGLT inhibitors did not reduce the risk of acute MIn overall, and that most of the trials were short term, with a mean follow-up of just 2.3 years.
Ten trials, consistent cardiovascular benefits
Dr. Bhattarai and colleagues searched the literature through Jan. 10, 2021, as well as meeting presentations and other sources. They identified 10 placebo-controlled, randomized clinical trials in which participants had atherosclerotic cardiovascular disease or ASCVD risk factors, diabetes, or heart failure. Among a total of 71,553 high-risk patients, 39,053 received an SGLT2 inhibitor and 32,500 received a placebo.
The primary outcome of cardiovascular death or hospitalization for heart failure occurred in 8.10% randomized to SGLT2 inhibitors, compared with 11.56% in the placebo group, a significant difference with odds ratio 0.67 (P < .001). Both individual outcomes were lower in the SGLT2-inhibitor group, with a number needed to treat of 5.7 (P < .001).
Patients receiving SGLT2 inhibitors also had significantly lower rates of major adverse cardiovascular events, defined as death due to cardiovascular causes, nonfatal MI, or nonfatal stroke. Those events occurred in 9.82% versus 10.22%(OR, 0.90; P = .03).
Hospitalizations and ED visits with heart failure were also reduced with SGLT2 inhibitors (4.37% vs. 6.81%; OR, 0.67; P < .001), as was cardiovascular death (4.65% vs. 5.14%; OR, 0.87; P = .009). The reduction in heart failure is likely caused by a combination of a natriuretic effect and reduced interstitial fluid, along with inhibition of cardiac fibrosis, the authors said.
On the other hand, no reductions were seen in acute MI, evaluated in five of the studies. That event occurred in 4.66% taking SGLT2 inhibitors, compared with 4.70% of the placebo group, a nonsignificant difference with an OR of 0.95 (P = 0.22). This is likely because of the fact that SGLT2 inhibitors don’t have known antianginal properties or vasodilatory effects, they don’t reduce myocardial oxygen consumption, and they don’t prevent cardiac muscle remodeling, they noted.
All-cause mortality was significantly lower with SGLT2 inhibitors, though, at 7.09% versus 7.86% (odds ratio, 0.87; P = .004).
Benefits seen across age, sex, and race/ethnicity subgroups
While no differences in benefit were found between men and women when compared with placebo groups, the rates of cardiovascular death or heart failure hospitalizations were slightly higher in men than in women (9.01% [OR, 0.75; P < .001] vs. 5.34% [OR, 0.78; P = .002]).
By age, SGLT2 inhibitors benefited people both those younger than 65 years and those aged 65 years and older, although the primary outcome was slightly lower in the younger group (6.94% [OR, 0.79; P < 0.001] vs. 10.47% [OR, 0.78; P < .001]).
And by race, similar benefits from SGLT2 inhibitors were seen among individuals who were White, compared with those who were Asian, Black, or of other race/ethnicity, with event rates of 8.77% (OR, 0.82; P < .001) and 8.75% (OR, 0.66; P = .06), respectively.
“Owing to the short-term trial durations, future long-term prospective studies and postmarketing surveillance studies are warranted to discover the rate of cardiovascular outcomes,” Dr. Bhattarai and colleagues concluded.
The authors have no disclosures.
A version of this article first appeared on Medscape.com.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors show “remarkable consistency of class benefit” for improving cardiovascular outcomes in high-risk people across age, sex, and race/ethnicity categories.
The findings, from a meta-analysis of 10 major randomized clinical trials, were published online Jan. 5, 2021, in JAMA Network Open by Mukul Bhattarai, MD, a cardiology fellow at Southern Illinois University, Springfield, and colleagues.
“Our meta-analysis evaluated a wide spectrum of efficacy outcomes, further characterizing the primary outcome in different subgroups from several well-designed large clinical trials. It supports that SGLT2 inhibitors have emerged as an effective class of drugs for improving cardiovascular morbidity and mortality, including the prevention of [hospitalization for heart failure] and reducing all-cause mortality in selected patients,” Dr. Bhattarai and colleagues wrote.
The cardiovascular outcomes of SGLT2 inhibitor therapy, they noted, “can be compared across all trials, and it demonstrates remarkable consistency of class benefit, despite the variations in populations enrolled.”
However, they also noted that SGLT inhibitors did not reduce the risk of acute MIn overall, and that most of the trials were short term, with a mean follow-up of just 2.3 years.
Ten trials, consistent cardiovascular benefits
Dr. Bhattarai and colleagues searched the literature through Jan. 10, 2021, as well as meeting presentations and other sources. They identified 10 placebo-controlled, randomized clinical trials in which participants had atherosclerotic cardiovascular disease or ASCVD risk factors, diabetes, or heart failure. Among a total of 71,553 high-risk patients, 39,053 received an SGLT2 inhibitor and 32,500 received a placebo.
The primary outcome of cardiovascular death or hospitalization for heart failure occurred in 8.10% randomized to SGLT2 inhibitors, compared with 11.56% in the placebo group, a significant difference with odds ratio 0.67 (P < .001). Both individual outcomes were lower in the SGLT2-inhibitor group, with a number needed to treat of 5.7 (P < .001).
Patients receiving SGLT2 inhibitors also had significantly lower rates of major adverse cardiovascular events, defined as death due to cardiovascular causes, nonfatal MI, or nonfatal stroke. Those events occurred in 9.82% versus 10.22%(OR, 0.90; P = .03).
Hospitalizations and ED visits with heart failure were also reduced with SGLT2 inhibitors (4.37% vs. 6.81%; OR, 0.67; P < .001), as was cardiovascular death (4.65% vs. 5.14%; OR, 0.87; P = .009). The reduction in heart failure is likely caused by a combination of a natriuretic effect and reduced interstitial fluid, along with inhibition of cardiac fibrosis, the authors said.
On the other hand, no reductions were seen in acute MI, evaluated in five of the studies. That event occurred in 4.66% taking SGLT2 inhibitors, compared with 4.70% of the placebo group, a nonsignificant difference with an OR of 0.95 (P = 0.22). This is likely because of the fact that SGLT2 inhibitors don’t have known antianginal properties or vasodilatory effects, they don’t reduce myocardial oxygen consumption, and they don’t prevent cardiac muscle remodeling, they noted.
All-cause mortality was significantly lower with SGLT2 inhibitors, though, at 7.09% versus 7.86% (odds ratio, 0.87; P = .004).
Benefits seen across age, sex, and race/ethnicity subgroups
While no differences in benefit were found between men and women when compared with placebo groups, the rates of cardiovascular death or heart failure hospitalizations were slightly higher in men than in women (9.01% [OR, 0.75; P < .001] vs. 5.34% [OR, 0.78; P = .002]).
By age, SGLT2 inhibitors benefited people both those younger than 65 years and those aged 65 years and older, although the primary outcome was slightly lower in the younger group (6.94% [OR, 0.79; P < 0.001] vs. 10.47% [OR, 0.78; P < .001]).
And by race, similar benefits from SGLT2 inhibitors were seen among individuals who were White, compared with those who were Asian, Black, or of other race/ethnicity, with event rates of 8.77% (OR, 0.82; P < .001) and 8.75% (OR, 0.66; P = .06), respectively.
“Owing to the short-term trial durations, future long-term prospective studies and postmarketing surveillance studies are warranted to discover the rate of cardiovascular outcomes,” Dr. Bhattarai and colleagues concluded.
The authors have no disclosures.
A version of this article first appeared on Medscape.com.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors show “remarkable consistency of class benefit” for improving cardiovascular outcomes in high-risk people across age, sex, and race/ethnicity categories.
The findings, from a meta-analysis of 10 major randomized clinical trials, were published online Jan. 5, 2021, in JAMA Network Open by Mukul Bhattarai, MD, a cardiology fellow at Southern Illinois University, Springfield, and colleagues.
“Our meta-analysis evaluated a wide spectrum of efficacy outcomes, further characterizing the primary outcome in different subgroups from several well-designed large clinical trials. It supports that SGLT2 inhibitors have emerged as an effective class of drugs for improving cardiovascular morbidity and mortality, including the prevention of [hospitalization for heart failure] and reducing all-cause mortality in selected patients,” Dr. Bhattarai and colleagues wrote.
The cardiovascular outcomes of SGLT2 inhibitor therapy, they noted, “can be compared across all trials, and it demonstrates remarkable consistency of class benefit, despite the variations in populations enrolled.”
However, they also noted that SGLT inhibitors did not reduce the risk of acute MIn overall, and that most of the trials were short term, with a mean follow-up of just 2.3 years.
Ten trials, consistent cardiovascular benefits
Dr. Bhattarai and colleagues searched the literature through Jan. 10, 2021, as well as meeting presentations and other sources. They identified 10 placebo-controlled, randomized clinical trials in which participants had atherosclerotic cardiovascular disease or ASCVD risk factors, diabetes, or heart failure. Among a total of 71,553 high-risk patients, 39,053 received an SGLT2 inhibitor and 32,500 received a placebo.
The primary outcome of cardiovascular death or hospitalization for heart failure occurred in 8.10% randomized to SGLT2 inhibitors, compared with 11.56% in the placebo group, a significant difference with odds ratio 0.67 (P < .001). Both individual outcomes were lower in the SGLT2-inhibitor group, with a number needed to treat of 5.7 (P < .001).
Patients receiving SGLT2 inhibitors also had significantly lower rates of major adverse cardiovascular events, defined as death due to cardiovascular causes, nonfatal MI, or nonfatal stroke. Those events occurred in 9.82% versus 10.22%(OR, 0.90; P = .03).
Hospitalizations and ED visits with heart failure were also reduced with SGLT2 inhibitors (4.37% vs. 6.81%; OR, 0.67; P < .001), as was cardiovascular death (4.65% vs. 5.14%; OR, 0.87; P = .009). The reduction in heart failure is likely caused by a combination of a natriuretic effect and reduced interstitial fluid, along with inhibition of cardiac fibrosis, the authors said.
On the other hand, no reductions were seen in acute MI, evaluated in five of the studies. That event occurred in 4.66% taking SGLT2 inhibitors, compared with 4.70% of the placebo group, a nonsignificant difference with an OR of 0.95 (P = 0.22). This is likely because of the fact that SGLT2 inhibitors don’t have known antianginal properties or vasodilatory effects, they don’t reduce myocardial oxygen consumption, and they don’t prevent cardiac muscle remodeling, they noted.
All-cause mortality was significantly lower with SGLT2 inhibitors, though, at 7.09% versus 7.86% (odds ratio, 0.87; P = .004).
Benefits seen across age, sex, and race/ethnicity subgroups
While no differences in benefit were found between men and women when compared with placebo groups, the rates of cardiovascular death or heart failure hospitalizations were slightly higher in men than in women (9.01% [OR, 0.75; P < .001] vs. 5.34% [OR, 0.78; P = .002]).
By age, SGLT2 inhibitors benefited people both those younger than 65 years and those aged 65 years and older, although the primary outcome was slightly lower in the younger group (6.94% [OR, 0.79; P < 0.001] vs. 10.47% [OR, 0.78; P < .001]).
And by race, similar benefits from SGLT2 inhibitors were seen among individuals who were White, compared with those who were Asian, Black, or of other race/ethnicity, with event rates of 8.77% (OR, 0.82; P < .001) and 8.75% (OR, 0.66; P = .06), respectively.
“Owing to the short-term trial durations, future long-term prospective studies and postmarketing surveillance studies are warranted to discover the rate of cardiovascular outcomes,” Dr. Bhattarai and colleagues concluded.
The authors have no disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Medicare expands coverage of continuous glucose monitoring devices for diabetes
Proposed in November 2020, the final CMS rule applies primarily to CGMs that integrate with Medtronic insulin pumps. Those CGMs have not been approved by the Food and Drug Administration to replace the need for fingerstick blood glucose measurements in determining insulin or other glucose-lowering medication dosing.
Other CGM systems, Dexcom G6 and Abbott Libre, have “therapeutic” indications and were already covered under Medicare, as was the combined insulin pump–CGM Tandem Diabetes Care Control-IQ technology system.
The expanded coverage means that people using the Medtronic 770G or 630G hybrid closed-loop insulin delivery systems will receive coverage for all the systems’ components, and that people aging into Medicare won’t lose any coverage for those devices.
Medtronic will continue to offer its CGM Access Discount to all Medicare customers until the ruling takes effect. The proposed rule was finalized on Dec. 21, 2021, and will be effective starting 60 days after official publication.
A version of this article first appeared on Medscape.com.
Proposed in November 2020, the final CMS rule applies primarily to CGMs that integrate with Medtronic insulin pumps. Those CGMs have not been approved by the Food and Drug Administration to replace the need for fingerstick blood glucose measurements in determining insulin or other glucose-lowering medication dosing.
Other CGM systems, Dexcom G6 and Abbott Libre, have “therapeutic” indications and were already covered under Medicare, as was the combined insulin pump–CGM Tandem Diabetes Care Control-IQ technology system.
The expanded coverage means that people using the Medtronic 770G or 630G hybrid closed-loop insulin delivery systems will receive coverage for all the systems’ components, and that people aging into Medicare won’t lose any coverage for those devices.
Medtronic will continue to offer its CGM Access Discount to all Medicare customers until the ruling takes effect. The proposed rule was finalized on Dec. 21, 2021, and will be effective starting 60 days after official publication.
A version of this article first appeared on Medscape.com.
Proposed in November 2020, the final CMS rule applies primarily to CGMs that integrate with Medtronic insulin pumps. Those CGMs have not been approved by the Food and Drug Administration to replace the need for fingerstick blood glucose measurements in determining insulin or other glucose-lowering medication dosing.
Other CGM systems, Dexcom G6 and Abbott Libre, have “therapeutic” indications and were already covered under Medicare, as was the combined insulin pump–CGM Tandem Diabetes Care Control-IQ technology system.
The expanded coverage means that people using the Medtronic 770G or 630G hybrid closed-loop insulin delivery systems will receive coverage for all the systems’ components, and that people aging into Medicare won’t lose any coverage for those devices.
Medtronic will continue to offer its CGM Access Discount to all Medicare customers until the ruling takes effect. The proposed rule was finalized on Dec. 21, 2021, and will be effective starting 60 days after official publication.
A version of this article first appeared on Medscape.com.
New blood test could identify pregnant women who are at risk of preeclampsia
Pregnant women who are at risk of preeclampsia can now be identified early before symptoms develop, finds new research from Kings College London and Guy’s and St Thomas’ NHS Foundation Trust, published in Nature.
The study, supported by the National Institute for Health Research and in partnership with the Mirvie RNA platform, analyzed the genetic material from over 2,500 blood samples of pregnant women from eight independent cohorts with multiple demographics, including socioeconomic background, geographic location, ethnicity, and nationality, collected 14.5 weeks before delivery.
“Because the study drew upon samples for a diverse group of women, including participants recruited across King’s Health Partners, the molecular signature is very reliable and has potential to outperform currently available tests,” said Rachel Tribe, PhD, department of women and children’s health, King’s College London.
Researchers used plasma cell-free RNA (cfRNA) transcripts to examine the standard molecular mechanism between the fetus, maternal, and placental tissues in order to determine fetal development and healthy pregnancy progression. Deviation from the standard cfRNA expression was also observed to establish the molecular pathway for those at risk of preeclampsia before clinical presentation.
A cfRNA signal from a single blood sample showed a 32.3% positive-predictive value and 75% sensitivity, which exceeds current positive-predictive values from recent clinical state-of-the-art models.
In addition, 73% of participants with a positive-predictive value were identified “as destined to have a medically indicated preterm birth over 3 months in advance of the preeclampsia symptoms,” said the authors.
With up to 1 in 12 pregnancies affected by preeclampsia, and the diagnosis most often only being made in the third trimester, these results provide a promising outlook for pregnant women “so that they can be more closely monitored and treated by the clinicians involved,” commented Dr. Tribe.
“We are now focused on ongoing clinical research to further validate these results and improve the understanding of other pregnancy complications,” she said. “As a scientist, it was also extremely interesting to see that the molecular signature tells us something about mechanisms associated with health in pregnancy and complications including preeclampsia; such knowledge will aid development of treatment strategies in the future.”
A version of this article first appeared on Medscape.com.
Pregnant women who are at risk of preeclampsia can now be identified early before symptoms develop, finds new research from Kings College London and Guy’s and St Thomas’ NHS Foundation Trust, published in Nature.
The study, supported by the National Institute for Health Research and in partnership with the Mirvie RNA platform, analyzed the genetic material from over 2,500 blood samples of pregnant women from eight independent cohorts with multiple demographics, including socioeconomic background, geographic location, ethnicity, and nationality, collected 14.5 weeks before delivery.
“Because the study drew upon samples for a diverse group of women, including participants recruited across King’s Health Partners, the molecular signature is very reliable and has potential to outperform currently available tests,” said Rachel Tribe, PhD, department of women and children’s health, King’s College London.
Researchers used plasma cell-free RNA (cfRNA) transcripts to examine the standard molecular mechanism between the fetus, maternal, and placental tissues in order to determine fetal development and healthy pregnancy progression. Deviation from the standard cfRNA expression was also observed to establish the molecular pathway for those at risk of preeclampsia before clinical presentation.
A cfRNA signal from a single blood sample showed a 32.3% positive-predictive value and 75% sensitivity, which exceeds current positive-predictive values from recent clinical state-of-the-art models.
In addition, 73% of participants with a positive-predictive value were identified “as destined to have a medically indicated preterm birth over 3 months in advance of the preeclampsia symptoms,” said the authors.
With up to 1 in 12 pregnancies affected by preeclampsia, and the diagnosis most often only being made in the third trimester, these results provide a promising outlook for pregnant women “so that they can be more closely monitored and treated by the clinicians involved,” commented Dr. Tribe.
“We are now focused on ongoing clinical research to further validate these results and improve the understanding of other pregnancy complications,” she said. “As a scientist, it was also extremely interesting to see that the molecular signature tells us something about mechanisms associated with health in pregnancy and complications including preeclampsia; such knowledge will aid development of treatment strategies in the future.”
A version of this article first appeared on Medscape.com.
Pregnant women who are at risk of preeclampsia can now be identified early before symptoms develop, finds new research from Kings College London and Guy’s and St Thomas’ NHS Foundation Trust, published in Nature.
The study, supported by the National Institute for Health Research and in partnership with the Mirvie RNA platform, analyzed the genetic material from over 2,500 blood samples of pregnant women from eight independent cohorts with multiple demographics, including socioeconomic background, geographic location, ethnicity, and nationality, collected 14.5 weeks before delivery.
“Because the study drew upon samples for a diverse group of women, including participants recruited across King’s Health Partners, the molecular signature is very reliable and has potential to outperform currently available tests,” said Rachel Tribe, PhD, department of women and children’s health, King’s College London.
Researchers used plasma cell-free RNA (cfRNA) transcripts to examine the standard molecular mechanism between the fetus, maternal, and placental tissues in order to determine fetal development and healthy pregnancy progression. Deviation from the standard cfRNA expression was also observed to establish the molecular pathway for those at risk of preeclampsia before clinical presentation.
A cfRNA signal from a single blood sample showed a 32.3% positive-predictive value and 75% sensitivity, which exceeds current positive-predictive values from recent clinical state-of-the-art models.
In addition, 73% of participants with a positive-predictive value were identified “as destined to have a medically indicated preterm birth over 3 months in advance of the preeclampsia symptoms,” said the authors.
With up to 1 in 12 pregnancies affected by preeclampsia, and the diagnosis most often only being made in the third trimester, these results provide a promising outlook for pregnant women “so that they can be more closely monitored and treated by the clinicians involved,” commented Dr. Tribe.
“We are now focused on ongoing clinical research to further validate these results and improve the understanding of other pregnancy complications,” she said. “As a scientist, it was also extremely interesting to see that the molecular signature tells us something about mechanisms associated with health in pregnancy and complications including preeclampsia; such knowledge will aid development of treatment strategies in the future.”
A version of this article first appeared on Medscape.com.
FROM NATURE
Statin therapy seems safe in pregnancy
Statins may be safe when used during pregnancy, with no increase in risk for fetal anomalies, although there may be a higher risk for low birth weight and preterm labor, results of a large study from Taiwan suggest.
The Food and Drug Administration relaxed its warning on statins in July 2021, removing the drug’s blanket contraindication in all pregnant women.
Removal of the broadly worded contraindication should “enable health care professionals and patients to make individual decisions about benefit and risk, especially for those at very high risk of heart attack or stroke,” the FDA said in their announcement.
“Our findings suggested that statins may be used during pregnancy with no increase in the rate of congenital anomalies,” wrote Jui-Chun Chang, MD, from Taichung Veterans General Hospital, Taiwan, and colleagues in the new study, published online Dec. 30, 2021, in JAMA Network Open.
“For pregnant women at low risk, statins should be used carefully after assessing the risks of low birth weight and preterm birth,” they said. “For women with dyslipidemia or high-risk cardiovascular disease, as well as those who use statins before conception, statins may be continuously used with no increased risks of neonatal adverse effects.”
The study included more than 1.4 million pregnant women aged 18 years and older who gave birth to their first child between 2004 and 2014.
A total of 469 women (mean age, 32.6 years; mean gestational age, 38.4 weeks) who used statins during pregnancy were compared with 4,690 matched controls who had no statin exposure during pregnancy.
After controlling for maternal comorbidities and age, women who used statins during pregnancy were more apt to have low-birth-weight babies weighing less than 2,500 g (risk ratio, 1.51; 95% confidence interval, 1.05-2.16) and to deliver preterm (RR, 1.99; 95% CI, 1.46-2.71).
The statin-exposed babies were also more likely to have a lower 1-minute Apgar score (RR, 1.83; 95% CI, 1.04-3.20). Importantly, however, there was no increase in risk for fetal anomalies in the statin-exposed infants, the researchers said.
In addition, for women who used statins for more than 3 months prior to pregnancy, maintaining statin use during pregnancy did not increase the risk for adverse neonatal outcomes, including congenital anomalies, low birth weight, preterm birth, very low birth weight, low Apgar scores, and fetal distress.
The researchers called for further studies to confirm their observations.
Funding for the study was provided by Taichung Veterans General Hospital. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Statins may be safe when used during pregnancy, with no increase in risk for fetal anomalies, although there may be a higher risk for low birth weight and preterm labor, results of a large study from Taiwan suggest.
The Food and Drug Administration relaxed its warning on statins in July 2021, removing the drug’s blanket contraindication in all pregnant women.
Removal of the broadly worded contraindication should “enable health care professionals and patients to make individual decisions about benefit and risk, especially for those at very high risk of heart attack or stroke,” the FDA said in their announcement.
“Our findings suggested that statins may be used during pregnancy with no increase in the rate of congenital anomalies,” wrote Jui-Chun Chang, MD, from Taichung Veterans General Hospital, Taiwan, and colleagues in the new study, published online Dec. 30, 2021, in JAMA Network Open.
“For pregnant women at low risk, statins should be used carefully after assessing the risks of low birth weight and preterm birth,” they said. “For women with dyslipidemia or high-risk cardiovascular disease, as well as those who use statins before conception, statins may be continuously used with no increased risks of neonatal adverse effects.”
The study included more than 1.4 million pregnant women aged 18 years and older who gave birth to their first child between 2004 and 2014.
A total of 469 women (mean age, 32.6 years; mean gestational age, 38.4 weeks) who used statins during pregnancy were compared with 4,690 matched controls who had no statin exposure during pregnancy.
After controlling for maternal comorbidities and age, women who used statins during pregnancy were more apt to have low-birth-weight babies weighing less than 2,500 g (risk ratio, 1.51; 95% confidence interval, 1.05-2.16) and to deliver preterm (RR, 1.99; 95% CI, 1.46-2.71).
The statin-exposed babies were also more likely to have a lower 1-minute Apgar score (RR, 1.83; 95% CI, 1.04-3.20). Importantly, however, there was no increase in risk for fetal anomalies in the statin-exposed infants, the researchers said.
In addition, for women who used statins for more than 3 months prior to pregnancy, maintaining statin use during pregnancy did not increase the risk for adverse neonatal outcomes, including congenital anomalies, low birth weight, preterm birth, very low birth weight, low Apgar scores, and fetal distress.
The researchers called for further studies to confirm their observations.
Funding for the study was provided by Taichung Veterans General Hospital. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Statins may be safe when used during pregnancy, with no increase in risk for fetal anomalies, although there may be a higher risk for low birth weight and preterm labor, results of a large study from Taiwan suggest.
The Food and Drug Administration relaxed its warning on statins in July 2021, removing the drug’s blanket contraindication in all pregnant women.
Removal of the broadly worded contraindication should “enable health care professionals and patients to make individual decisions about benefit and risk, especially for those at very high risk of heart attack or stroke,” the FDA said in their announcement.
“Our findings suggested that statins may be used during pregnancy with no increase in the rate of congenital anomalies,” wrote Jui-Chun Chang, MD, from Taichung Veterans General Hospital, Taiwan, and colleagues in the new study, published online Dec. 30, 2021, in JAMA Network Open.
“For pregnant women at low risk, statins should be used carefully after assessing the risks of low birth weight and preterm birth,” they said. “For women with dyslipidemia or high-risk cardiovascular disease, as well as those who use statins before conception, statins may be continuously used with no increased risks of neonatal adverse effects.”
The study included more than 1.4 million pregnant women aged 18 years and older who gave birth to their first child between 2004 and 2014.
A total of 469 women (mean age, 32.6 years; mean gestational age, 38.4 weeks) who used statins during pregnancy were compared with 4,690 matched controls who had no statin exposure during pregnancy.
After controlling for maternal comorbidities and age, women who used statins during pregnancy were more apt to have low-birth-weight babies weighing less than 2,500 g (risk ratio, 1.51; 95% confidence interval, 1.05-2.16) and to deliver preterm (RR, 1.99; 95% CI, 1.46-2.71).
The statin-exposed babies were also more likely to have a lower 1-minute Apgar score (RR, 1.83; 95% CI, 1.04-3.20). Importantly, however, there was no increase in risk for fetal anomalies in the statin-exposed infants, the researchers said.
In addition, for women who used statins for more than 3 months prior to pregnancy, maintaining statin use during pregnancy did not increase the risk for adverse neonatal outcomes, including congenital anomalies, low birth weight, preterm birth, very low birth weight, low Apgar scores, and fetal distress.
The researchers called for further studies to confirm their observations.
Funding for the study was provided by Taichung Veterans General Hospital. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
First ‘flurona’ cases reported in the U.S.
The first known case was detected in Israel, but until the first week of January no cases had been reported in the United States.
In Los Angeles, a teenaged boy tested positive for both illnesses at a COVID testing site in Brentwood, the Los Angeles Times reported. The child’s mother tested positive for COVID the next day.
“This is the first one that we’re aware of,” Steve Farzam, chief operating officer of 911 COVID Testing, told the LA Times. “In and of itself, it’s not overly concerning; however, it is concerning and can be problematic for someone who has pre-existing medical conditions, anyone who is immunocompromised.”
The teen and his family of five had just returned from vacation in Cabo San Lucas, Mexico. All said they tested negative before the trip, but they tested again when they got home because one of the children had a runny nose, Mr. Farzam said.
The boy, who had not been vaccinated for COVID or the flu, doesn’t have serious symptoms and is recovering at home.
In Houston, a 17-year-old boy, his siblings, and his father felt sick a few days before Christmas and went in for testing, TV station KTRK reported. The teen tested positive for both the flu and COVID.
“I ended up getting tested the day before Christmas for strep throat, flu and COVID,” the teenager, Alec Zierlein, told KTRK. “I didn’t think I had any of the three. It felt like a mild cold.”
Health officials reported Jan. 5 that a flurona case was detected in Hays, Kan., TV station WIBW reported. The patient was being treated in the ICU. No other details were provided. In Israel, flurona was first found in an unvaccinated pregnant woman at Rabin Medical Center in Petach Tikva, according to the Times of Israel. She tested positive for both viruses when she arrived at the medical center, and doctors double-checked to confirm her diagnosis. The woman had mild symptoms and was released in good condition, the news outlet reported.
Public health officials in Israel said they are concerned that an increase in both viruses at the same time could lead to many hospitalizations.
A version of this article first appeared on WebMD.com.
The first known case was detected in Israel, but until the first week of January no cases had been reported in the United States.
In Los Angeles, a teenaged boy tested positive for both illnesses at a COVID testing site in Brentwood, the Los Angeles Times reported. The child’s mother tested positive for COVID the next day.
“This is the first one that we’re aware of,” Steve Farzam, chief operating officer of 911 COVID Testing, told the LA Times. “In and of itself, it’s not overly concerning; however, it is concerning and can be problematic for someone who has pre-existing medical conditions, anyone who is immunocompromised.”
The teen and his family of five had just returned from vacation in Cabo San Lucas, Mexico. All said they tested negative before the trip, but they tested again when they got home because one of the children had a runny nose, Mr. Farzam said.
The boy, who had not been vaccinated for COVID or the flu, doesn’t have serious symptoms and is recovering at home.
In Houston, a 17-year-old boy, his siblings, and his father felt sick a few days before Christmas and went in for testing, TV station KTRK reported. The teen tested positive for both the flu and COVID.
“I ended up getting tested the day before Christmas for strep throat, flu and COVID,” the teenager, Alec Zierlein, told KTRK. “I didn’t think I had any of the three. It felt like a mild cold.”
Health officials reported Jan. 5 that a flurona case was detected in Hays, Kan., TV station WIBW reported. The patient was being treated in the ICU. No other details were provided. In Israel, flurona was first found in an unvaccinated pregnant woman at Rabin Medical Center in Petach Tikva, according to the Times of Israel. She tested positive for both viruses when she arrived at the medical center, and doctors double-checked to confirm her diagnosis. The woman had mild symptoms and was released in good condition, the news outlet reported.
Public health officials in Israel said they are concerned that an increase in both viruses at the same time could lead to many hospitalizations.
A version of this article first appeared on WebMD.com.
The first known case was detected in Israel, but until the first week of January no cases had been reported in the United States.
In Los Angeles, a teenaged boy tested positive for both illnesses at a COVID testing site in Brentwood, the Los Angeles Times reported. The child’s mother tested positive for COVID the next day.
“This is the first one that we’re aware of,” Steve Farzam, chief operating officer of 911 COVID Testing, told the LA Times. “In and of itself, it’s not overly concerning; however, it is concerning and can be problematic for someone who has pre-existing medical conditions, anyone who is immunocompromised.”
The teen and his family of five had just returned from vacation in Cabo San Lucas, Mexico. All said they tested negative before the trip, but they tested again when they got home because one of the children had a runny nose, Mr. Farzam said.
The boy, who had not been vaccinated for COVID or the flu, doesn’t have serious symptoms and is recovering at home.
In Houston, a 17-year-old boy, his siblings, and his father felt sick a few days before Christmas and went in for testing, TV station KTRK reported. The teen tested positive for both the flu and COVID.
“I ended up getting tested the day before Christmas for strep throat, flu and COVID,” the teenager, Alec Zierlein, told KTRK. “I didn’t think I had any of the three. It felt like a mild cold.”
Health officials reported Jan. 5 that a flurona case was detected in Hays, Kan., TV station WIBW reported. The patient was being treated in the ICU. No other details were provided. In Israel, flurona was first found in an unvaccinated pregnant woman at Rabin Medical Center in Petach Tikva, according to the Times of Israel. She tested positive for both viruses when she arrived at the medical center, and doctors double-checked to confirm her diagnosis. The woman had mild symptoms and was released in good condition, the news outlet reported.
Public health officials in Israel said they are concerned that an increase in both viruses at the same time could lead to many hospitalizations.
A version of this article first appeared on WebMD.com.
Docs refused to pay the cyber attack ransom – and suffered
Ransomware attacks are driving some small practices out of business.
Michigan-based Brookside ENT and Hearing Center, a two-physician practice, closed its doors in 2019 after a ransomware attack. The criminals locked their computer system and files and then demanded a $6,500 ransom to restore access. The practice took the advice of law enforcement and refused to pay. The attackers wiped the computer systems clean – destroying all patient records, appointment schedules, and financial information. Rather than rebuild the entire practice, the two doctors took early retirement.
Wood Ranch Medical, in Simi, Calif., a small primary care practice, decided to shut its doors in 2019 after a ransomware attack damaged its servers and backup files, which affected more than 5,000 patient records. The criminals demanded a ransom to restore the technology and records, but the owners refused to pay. They couldn’t rebuild the system without the backup files, so they shuttered their business.
Several large practices have also been attacked by ransomware, including Imperial Health in Louisiana in 2019, that may have compromised more than 110,000 records. The practice didn’t pay the ransom and had access to its backup files and the resources to rebuild its computer systems and stay in business.
Medical practices of all sizes have experienced ransomware attacks.
All it takes is one employee clicking on a link or embedded file in an email to launch malware. A vicious code locks the electronic health record (EHR) system, and your practice grinds to a halt.
Cyber criminals demand a ransom in bitcoin to unlock the files. They may even threaten to post private patient data publicly or sell it on the dark web to get you to pay up.
But, is paying a ransom necessary or wise? What other steps should you take? Here’s what cyber security experts say criminals look for in targets, how they infiltrate and attack, and how you should respond and prevent future attacks.
How does it happen?
Email is a popular way for criminals to hack into a system. Criminals often research company websites and impersonate a company executive and send a legitimate-looking “phishing” email to employees hoping that someone will click on it and launch a malware attack.
Recently, cyber criminals found an easier way to infiltrate that doesn’t require identifying targets to gain access, said Drex DeFord, executive health care strategist at CrowdStrike, a cybersecurity technology company in Sunnyvale, Calif.
“Instead of hacking into the system, cyber criminals are just logging in. Most likely, they have acquired a user’s credentials (username/password) from another source – possibly purchasing it from the dark web, the part of the Internet that criminals use, through an ‘access broker,’ an organization that specializes in collecting and selling these kinds of credentials,” said Mr. DeFord.
After a ransomware attack last August on Eskenazi Health in Indianapolis, forensic investigators discovered that the criminals had logged into the IT system in May and had disabled security protections that could have detected their presence before they launched their cyber attack, according to a statement.
Responding to a ransomware attack
When employees or the IT department suspect a ransomware attack is underway, cyber experts recommend isolating the “infected” part of the network, shutting down the computer system to prevent further damage, and securing backups.
Soon afterward, cyber criminals typically communicate their ransom demands electronically with instructions for payment. One practice described seeing a “skull and bones image” on its laptops with a link to instructions to pay the ransom demand in bitcoin.
Although you never want to pay criminals, it’s ultimately a business decision that every organization that’s affected by ransomware has to make, said Kathy Hughes, chief information security officer at Northwell Health in New York. “They need to weigh the cost and impact from paying a ransom against what they are able to recover, how long will it take, and how much will it cost,” she said.
While it may be tempting to pay a small ransom, such as $5,000, cyber experts warn that it doesn’t guarantee full access to the original data. About one-third (34%) of health care organizations whose data were encrypted paid the ransom to get their data back, according to a June 2021 HHS Report on Ransomware Trends. However, only 69% of the encrypted data was restored, the report states.
Criminals may also demand another payment, called “double extortion,” by threatening to post any extracted private patient or employee data on the dark web, said Ms. Hughes.
Practices sometimes choose not to pay the ransom when they know they can restore the backup files and rebuild the system for less than the ransom amount. However, it can take weeks to rebuild a fully operational IT system; meanwhile, the organization is losing thousands of dollars in patient revenue.
Criminals may retaliate against a practice that doesn’t pay the ransom by wiping the hard drives clean or posting the extracted medical, financial, and demographic data of patients on the dark web. Patients whose information has been extracted have filed class-action lawsuits against medical practices and organizations such as Scripps Health, in San Diego, claiming that they should have done more to keep their private information safe.
Experts also advise reporting the attack to local law enforcement officials, who may have cyber security experts on staff who will come on site and investigate the nature of the attack. They may also request help from the FBI’s professional cyber security team.
Having a cyber insurance policy may help offset some of the costs of an attack. However, make sure you have a good cyber security program, advised Mr. DeFord.
He suggests that small practices partner with large health systems that can donate their cyber security technology and related services legally under the updated Stark safe harbor rules. Otherwise, they may not meet the insurer’s requirements, or they may have to pay significantly higher rates.
Who is an easy target?
Cyber criminals look for easy targets, said Ms. Hughes. “A lot of threat actors are not targeting a specific practice – they’re simply throwing out a net and looking for vulnerable systems on the Internet.”
Small medical practices are particularly vulnerable to ransomware attacks because they lack the resources to pay for dedicated IT or cyber security staff, said Ms. Hughes, who oversees security for more than 800 outpatient practices. They’re not replacing outdated or unsupported equipment, applying regular “patches” that fix, update, or improve operating systems, application software, and Internet browsers, or using password controls.
As large practices or health systems acquire medical practices with different EHR systems, security can be more challenging. “Our goal at Northwell is always to get them onto our standard platform, where we use best practices for technology and security controls,” Ms. Hughes said. “In the world of security, having fewer EHR systems is better so there are fewer things to watch, fewer systems to patch, and fewer servers to monitor. From our point of view, it makes sense to have a standardized and streamlined system.”
Still, some practices may feel strongly about using their EHR system, she said. When that happens, “We at least bring them up to our security standards by having them implement password controls and regular patches. We communicate and collaborate with them constantly to get them to a more secure posture.”
Cyber security lapses may have increased during the pandemic when practices had to pivot rapidly to allow administrative staff to work remotely and clinical staff to use telehealth with patients.
“In the rush to get people out of the building during the pandemic, health care organizations bent many of their own rules on remote access. As they moved quickly to new telehealth solutions, they skipped steps like auditing new vendors and cyber-testing new equipment and software. Many organizations are still cleaning up the security ‘exceptions’ they made earlier in the pandemic,” said Mr. DeFord.
Hackers are sophisticated criminals
“The version of a hacker a lot of us grew up with – someone in a basement hacking into your environment and possibly deploying ransomware – isn’t accurate,” said Mr. DeFord. What experts know now is that these cyber criminals operate more like companies that have hired, trained, and developed people to be stealth-like – getting inside your network without being detected.
“They are more sophisticated than the health care organizations they often target,” added Mr. DeFord. “Their developers write the encryption software; they use chatbots to make paying the ransom easy and refer to the people they ransom as clients, because it’s a lucrative business,” he said.
These groups also have specialized roles – one may come in and map your network’s vulnerabilities and sell that information to another group that is good at extracting data and that sells that information to another group that is good at setting off ransomware and negotiation, said Mr. DeFord. “By the time a ransomware attack occurs, we often find that the bad guys have owned the network for at least 6 months.”
Patient records are attractive targets because the information can be sold on the dark web, the part of the Internet that’s unavailable to search engines and requires an anonymous browser called Tor to gain access, said Ms. Hughes.
Criminals steal patient identifiers such as Social Security numbers and birth dates, payment or insurance information, as well as medical histories and prescription data. Other people buy the information for fraudulent purposes, such as filing false tax returns, obtaining medical services, and opening credit cards, said Ms. Hughes.
Lately, criminal gangs appear to be targeting the IT or EHR systems that practices rely on for clinical care and making them unavailable. By locking EHR files or databases and holding them for ransom, criminals hope practices will be more likely to pay, said Ms. Hughes.
They also don’t want to get caught, and this tactic “gets them in and out faster” than extracting and posting patient data, although criminals may use that as a threat to extort a ransom payment, she said.
Fines for lax privacy/security
Breaches of patient records have consequences that include being investigated by federal or state authorities for potential HIPAA privacy and security violations and fines. Recently, the HHS announced a $1.5 million settlement – the largest to date – with Athens Orthopedic Clinic, PA, in Georgia, for not complying with the HIPAA rules.
When breaches of 500 or more patient records occur, medical groups are required to notify the HHS Office of Civil Rights (OCR) within 60 days, as well as all the affected patients and the media. Some organizations offer free credit monitoring and identity theft protection services to their patients.
Information about the breaches, including company names and the number of affected individuals, is posted publicly on what cyber experts often call “OCR’s wall of shame.”
Strengthen your defenses
The FBI and the HHS warned health care professionals and organizations in 2020 about the threat of increasing cyber attacks and urged them to take precautions to protect their networks.
Here are five actions you can take:
- Back-up your files to the cloud or off-site services and test that the restoration works.
- Implement user training with simulated phishing attacks so the staff will recognize suspicious emails and avoid actions that could launch malware attacks.
- Ensure strong password controls and that systems are regularly patched.
- Require multifactor authentication for remote access to IT networks.
- Set anti-virus/anti-malware programs to conduct regular scans of IT network assets using up-to-date signatures.
A version of this article first appeared on Medscape.com.
Ransomware attacks are driving some small practices out of business.
Michigan-based Brookside ENT and Hearing Center, a two-physician practice, closed its doors in 2019 after a ransomware attack. The criminals locked their computer system and files and then demanded a $6,500 ransom to restore access. The practice took the advice of law enforcement and refused to pay. The attackers wiped the computer systems clean – destroying all patient records, appointment schedules, and financial information. Rather than rebuild the entire practice, the two doctors took early retirement.
Wood Ranch Medical, in Simi, Calif., a small primary care practice, decided to shut its doors in 2019 after a ransomware attack damaged its servers and backup files, which affected more than 5,000 patient records. The criminals demanded a ransom to restore the technology and records, but the owners refused to pay. They couldn’t rebuild the system without the backup files, so they shuttered their business.
Several large practices have also been attacked by ransomware, including Imperial Health in Louisiana in 2019, that may have compromised more than 110,000 records. The practice didn’t pay the ransom and had access to its backup files and the resources to rebuild its computer systems and stay in business.
Medical practices of all sizes have experienced ransomware attacks.
All it takes is one employee clicking on a link or embedded file in an email to launch malware. A vicious code locks the electronic health record (EHR) system, and your practice grinds to a halt.
Cyber criminals demand a ransom in bitcoin to unlock the files. They may even threaten to post private patient data publicly or sell it on the dark web to get you to pay up.
But, is paying a ransom necessary or wise? What other steps should you take? Here’s what cyber security experts say criminals look for in targets, how they infiltrate and attack, and how you should respond and prevent future attacks.
How does it happen?
Email is a popular way for criminals to hack into a system. Criminals often research company websites and impersonate a company executive and send a legitimate-looking “phishing” email to employees hoping that someone will click on it and launch a malware attack.
Recently, cyber criminals found an easier way to infiltrate that doesn’t require identifying targets to gain access, said Drex DeFord, executive health care strategist at CrowdStrike, a cybersecurity technology company in Sunnyvale, Calif.
“Instead of hacking into the system, cyber criminals are just logging in. Most likely, they have acquired a user’s credentials (username/password) from another source – possibly purchasing it from the dark web, the part of the Internet that criminals use, through an ‘access broker,’ an organization that specializes in collecting and selling these kinds of credentials,” said Mr. DeFord.
After a ransomware attack last August on Eskenazi Health in Indianapolis, forensic investigators discovered that the criminals had logged into the IT system in May and had disabled security protections that could have detected their presence before they launched their cyber attack, according to a statement.
Responding to a ransomware attack
When employees or the IT department suspect a ransomware attack is underway, cyber experts recommend isolating the “infected” part of the network, shutting down the computer system to prevent further damage, and securing backups.
Soon afterward, cyber criminals typically communicate their ransom demands electronically with instructions for payment. One practice described seeing a “skull and bones image” on its laptops with a link to instructions to pay the ransom demand in bitcoin.
Although you never want to pay criminals, it’s ultimately a business decision that every organization that’s affected by ransomware has to make, said Kathy Hughes, chief information security officer at Northwell Health in New York. “They need to weigh the cost and impact from paying a ransom against what they are able to recover, how long will it take, and how much will it cost,” she said.
While it may be tempting to pay a small ransom, such as $5,000, cyber experts warn that it doesn’t guarantee full access to the original data. About one-third (34%) of health care organizations whose data were encrypted paid the ransom to get their data back, according to a June 2021 HHS Report on Ransomware Trends. However, only 69% of the encrypted data was restored, the report states.
Criminals may also demand another payment, called “double extortion,” by threatening to post any extracted private patient or employee data on the dark web, said Ms. Hughes.
Practices sometimes choose not to pay the ransom when they know they can restore the backup files and rebuild the system for less than the ransom amount. However, it can take weeks to rebuild a fully operational IT system; meanwhile, the organization is losing thousands of dollars in patient revenue.
Criminals may retaliate against a practice that doesn’t pay the ransom by wiping the hard drives clean or posting the extracted medical, financial, and demographic data of patients on the dark web. Patients whose information has been extracted have filed class-action lawsuits against medical practices and organizations such as Scripps Health, in San Diego, claiming that they should have done more to keep their private information safe.
Experts also advise reporting the attack to local law enforcement officials, who may have cyber security experts on staff who will come on site and investigate the nature of the attack. They may also request help from the FBI’s professional cyber security team.
Having a cyber insurance policy may help offset some of the costs of an attack. However, make sure you have a good cyber security program, advised Mr. DeFord.
He suggests that small practices partner with large health systems that can donate their cyber security technology and related services legally under the updated Stark safe harbor rules. Otherwise, they may not meet the insurer’s requirements, or they may have to pay significantly higher rates.
Who is an easy target?
Cyber criminals look for easy targets, said Ms. Hughes. “A lot of threat actors are not targeting a specific practice – they’re simply throwing out a net and looking for vulnerable systems on the Internet.”
Small medical practices are particularly vulnerable to ransomware attacks because they lack the resources to pay for dedicated IT or cyber security staff, said Ms. Hughes, who oversees security for more than 800 outpatient practices. They’re not replacing outdated or unsupported equipment, applying regular “patches” that fix, update, or improve operating systems, application software, and Internet browsers, or using password controls.
As large practices or health systems acquire medical practices with different EHR systems, security can be more challenging. “Our goal at Northwell is always to get them onto our standard platform, where we use best practices for technology and security controls,” Ms. Hughes said. “In the world of security, having fewer EHR systems is better so there are fewer things to watch, fewer systems to patch, and fewer servers to monitor. From our point of view, it makes sense to have a standardized and streamlined system.”
Still, some practices may feel strongly about using their EHR system, she said. When that happens, “We at least bring them up to our security standards by having them implement password controls and regular patches. We communicate and collaborate with them constantly to get them to a more secure posture.”
Cyber security lapses may have increased during the pandemic when practices had to pivot rapidly to allow administrative staff to work remotely and clinical staff to use telehealth with patients.
“In the rush to get people out of the building during the pandemic, health care organizations bent many of their own rules on remote access. As they moved quickly to new telehealth solutions, they skipped steps like auditing new vendors and cyber-testing new equipment and software. Many organizations are still cleaning up the security ‘exceptions’ they made earlier in the pandemic,” said Mr. DeFord.
Hackers are sophisticated criminals
“The version of a hacker a lot of us grew up with – someone in a basement hacking into your environment and possibly deploying ransomware – isn’t accurate,” said Mr. DeFord. What experts know now is that these cyber criminals operate more like companies that have hired, trained, and developed people to be stealth-like – getting inside your network without being detected.
“They are more sophisticated than the health care organizations they often target,” added Mr. DeFord. “Their developers write the encryption software; they use chatbots to make paying the ransom easy and refer to the people they ransom as clients, because it’s a lucrative business,” he said.
These groups also have specialized roles – one may come in and map your network’s vulnerabilities and sell that information to another group that is good at extracting data and that sells that information to another group that is good at setting off ransomware and negotiation, said Mr. DeFord. “By the time a ransomware attack occurs, we often find that the bad guys have owned the network for at least 6 months.”
Patient records are attractive targets because the information can be sold on the dark web, the part of the Internet that’s unavailable to search engines and requires an anonymous browser called Tor to gain access, said Ms. Hughes.
Criminals steal patient identifiers such as Social Security numbers and birth dates, payment or insurance information, as well as medical histories and prescription data. Other people buy the information for fraudulent purposes, such as filing false tax returns, obtaining medical services, and opening credit cards, said Ms. Hughes.
Lately, criminal gangs appear to be targeting the IT or EHR systems that practices rely on for clinical care and making them unavailable. By locking EHR files or databases and holding them for ransom, criminals hope practices will be more likely to pay, said Ms. Hughes.
They also don’t want to get caught, and this tactic “gets them in and out faster” than extracting and posting patient data, although criminals may use that as a threat to extort a ransom payment, she said.
Fines for lax privacy/security
Breaches of patient records have consequences that include being investigated by federal or state authorities for potential HIPAA privacy and security violations and fines. Recently, the HHS announced a $1.5 million settlement – the largest to date – with Athens Orthopedic Clinic, PA, in Georgia, for not complying with the HIPAA rules.
When breaches of 500 or more patient records occur, medical groups are required to notify the HHS Office of Civil Rights (OCR) within 60 days, as well as all the affected patients and the media. Some organizations offer free credit monitoring and identity theft protection services to their patients.
Information about the breaches, including company names and the number of affected individuals, is posted publicly on what cyber experts often call “OCR’s wall of shame.”
Strengthen your defenses
The FBI and the HHS warned health care professionals and organizations in 2020 about the threat of increasing cyber attacks and urged them to take precautions to protect their networks.
Here are five actions you can take:
- Back-up your files to the cloud or off-site services and test that the restoration works.
- Implement user training with simulated phishing attacks so the staff will recognize suspicious emails and avoid actions that could launch malware attacks.
- Ensure strong password controls and that systems are regularly patched.
- Require multifactor authentication for remote access to IT networks.
- Set anti-virus/anti-malware programs to conduct regular scans of IT network assets using up-to-date signatures.
A version of this article first appeared on Medscape.com.
Ransomware attacks are driving some small practices out of business.
Michigan-based Brookside ENT and Hearing Center, a two-physician practice, closed its doors in 2019 after a ransomware attack. The criminals locked their computer system and files and then demanded a $6,500 ransom to restore access. The practice took the advice of law enforcement and refused to pay. The attackers wiped the computer systems clean – destroying all patient records, appointment schedules, and financial information. Rather than rebuild the entire practice, the two doctors took early retirement.
Wood Ranch Medical, in Simi, Calif., a small primary care practice, decided to shut its doors in 2019 after a ransomware attack damaged its servers and backup files, which affected more than 5,000 patient records. The criminals demanded a ransom to restore the technology and records, but the owners refused to pay. They couldn’t rebuild the system without the backup files, so they shuttered their business.
Several large practices have also been attacked by ransomware, including Imperial Health in Louisiana in 2019, that may have compromised more than 110,000 records. The practice didn’t pay the ransom and had access to its backup files and the resources to rebuild its computer systems and stay in business.
Medical practices of all sizes have experienced ransomware attacks.
All it takes is one employee clicking on a link or embedded file in an email to launch malware. A vicious code locks the electronic health record (EHR) system, and your practice grinds to a halt.
Cyber criminals demand a ransom in bitcoin to unlock the files. They may even threaten to post private patient data publicly or sell it on the dark web to get you to pay up.
But, is paying a ransom necessary or wise? What other steps should you take? Here’s what cyber security experts say criminals look for in targets, how they infiltrate and attack, and how you should respond and prevent future attacks.
How does it happen?
Email is a popular way for criminals to hack into a system. Criminals often research company websites and impersonate a company executive and send a legitimate-looking “phishing” email to employees hoping that someone will click on it and launch a malware attack.
Recently, cyber criminals found an easier way to infiltrate that doesn’t require identifying targets to gain access, said Drex DeFord, executive health care strategist at CrowdStrike, a cybersecurity technology company in Sunnyvale, Calif.
“Instead of hacking into the system, cyber criminals are just logging in. Most likely, they have acquired a user’s credentials (username/password) from another source – possibly purchasing it from the dark web, the part of the Internet that criminals use, through an ‘access broker,’ an organization that specializes in collecting and selling these kinds of credentials,” said Mr. DeFord.
After a ransomware attack last August on Eskenazi Health in Indianapolis, forensic investigators discovered that the criminals had logged into the IT system in May and had disabled security protections that could have detected their presence before they launched their cyber attack, according to a statement.
Responding to a ransomware attack
When employees or the IT department suspect a ransomware attack is underway, cyber experts recommend isolating the “infected” part of the network, shutting down the computer system to prevent further damage, and securing backups.
Soon afterward, cyber criminals typically communicate their ransom demands electronically with instructions for payment. One practice described seeing a “skull and bones image” on its laptops with a link to instructions to pay the ransom demand in bitcoin.
Although you never want to pay criminals, it’s ultimately a business decision that every organization that’s affected by ransomware has to make, said Kathy Hughes, chief information security officer at Northwell Health in New York. “They need to weigh the cost and impact from paying a ransom against what they are able to recover, how long will it take, and how much will it cost,” she said.
While it may be tempting to pay a small ransom, such as $5,000, cyber experts warn that it doesn’t guarantee full access to the original data. About one-third (34%) of health care organizations whose data were encrypted paid the ransom to get their data back, according to a June 2021 HHS Report on Ransomware Trends. However, only 69% of the encrypted data was restored, the report states.
Criminals may also demand another payment, called “double extortion,” by threatening to post any extracted private patient or employee data on the dark web, said Ms. Hughes.
Practices sometimes choose not to pay the ransom when they know they can restore the backup files and rebuild the system for less than the ransom amount. However, it can take weeks to rebuild a fully operational IT system; meanwhile, the organization is losing thousands of dollars in patient revenue.
Criminals may retaliate against a practice that doesn’t pay the ransom by wiping the hard drives clean or posting the extracted medical, financial, and demographic data of patients on the dark web. Patients whose information has been extracted have filed class-action lawsuits against medical practices and organizations such as Scripps Health, in San Diego, claiming that they should have done more to keep their private information safe.
Experts also advise reporting the attack to local law enforcement officials, who may have cyber security experts on staff who will come on site and investigate the nature of the attack. They may also request help from the FBI’s professional cyber security team.
Having a cyber insurance policy may help offset some of the costs of an attack. However, make sure you have a good cyber security program, advised Mr. DeFord.
He suggests that small practices partner with large health systems that can donate their cyber security technology and related services legally under the updated Stark safe harbor rules. Otherwise, they may not meet the insurer’s requirements, or they may have to pay significantly higher rates.
Who is an easy target?
Cyber criminals look for easy targets, said Ms. Hughes. “A lot of threat actors are not targeting a specific practice – they’re simply throwing out a net and looking for vulnerable systems on the Internet.”
Small medical practices are particularly vulnerable to ransomware attacks because they lack the resources to pay for dedicated IT or cyber security staff, said Ms. Hughes, who oversees security for more than 800 outpatient practices. They’re not replacing outdated or unsupported equipment, applying regular “patches” that fix, update, or improve operating systems, application software, and Internet browsers, or using password controls.
As large practices or health systems acquire medical practices with different EHR systems, security can be more challenging. “Our goal at Northwell is always to get them onto our standard platform, where we use best practices for technology and security controls,” Ms. Hughes said. “In the world of security, having fewer EHR systems is better so there are fewer things to watch, fewer systems to patch, and fewer servers to monitor. From our point of view, it makes sense to have a standardized and streamlined system.”
Still, some practices may feel strongly about using their EHR system, she said. When that happens, “We at least bring them up to our security standards by having them implement password controls and regular patches. We communicate and collaborate with them constantly to get them to a more secure posture.”
Cyber security lapses may have increased during the pandemic when practices had to pivot rapidly to allow administrative staff to work remotely and clinical staff to use telehealth with patients.
“In the rush to get people out of the building during the pandemic, health care organizations bent many of their own rules on remote access. As they moved quickly to new telehealth solutions, they skipped steps like auditing new vendors and cyber-testing new equipment and software. Many organizations are still cleaning up the security ‘exceptions’ they made earlier in the pandemic,” said Mr. DeFord.
Hackers are sophisticated criminals
“The version of a hacker a lot of us grew up with – someone in a basement hacking into your environment and possibly deploying ransomware – isn’t accurate,” said Mr. DeFord. What experts know now is that these cyber criminals operate more like companies that have hired, trained, and developed people to be stealth-like – getting inside your network without being detected.
“They are more sophisticated than the health care organizations they often target,” added Mr. DeFord. “Their developers write the encryption software; they use chatbots to make paying the ransom easy and refer to the people they ransom as clients, because it’s a lucrative business,” he said.
These groups also have specialized roles – one may come in and map your network’s vulnerabilities and sell that information to another group that is good at extracting data and that sells that information to another group that is good at setting off ransomware and negotiation, said Mr. DeFord. “By the time a ransomware attack occurs, we often find that the bad guys have owned the network for at least 6 months.”
Patient records are attractive targets because the information can be sold on the dark web, the part of the Internet that’s unavailable to search engines and requires an anonymous browser called Tor to gain access, said Ms. Hughes.
Criminals steal patient identifiers such as Social Security numbers and birth dates, payment or insurance information, as well as medical histories and prescription data. Other people buy the information for fraudulent purposes, such as filing false tax returns, obtaining medical services, and opening credit cards, said Ms. Hughes.
Lately, criminal gangs appear to be targeting the IT or EHR systems that practices rely on for clinical care and making them unavailable. By locking EHR files or databases and holding them for ransom, criminals hope practices will be more likely to pay, said Ms. Hughes.
They also don’t want to get caught, and this tactic “gets them in and out faster” than extracting and posting patient data, although criminals may use that as a threat to extort a ransom payment, she said.
Fines for lax privacy/security
Breaches of patient records have consequences that include being investigated by federal or state authorities for potential HIPAA privacy and security violations and fines. Recently, the HHS announced a $1.5 million settlement – the largest to date – with Athens Orthopedic Clinic, PA, in Georgia, for not complying with the HIPAA rules.
When breaches of 500 or more patient records occur, medical groups are required to notify the HHS Office of Civil Rights (OCR) within 60 days, as well as all the affected patients and the media. Some organizations offer free credit monitoring and identity theft protection services to their patients.
Information about the breaches, including company names and the number of affected individuals, is posted publicly on what cyber experts often call “OCR’s wall of shame.”
Strengthen your defenses
The FBI and the HHS warned health care professionals and organizations in 2020 about the threat of increasing cyber attacks and urged them to take precautions to protect their networks.
Here are five actions you can take:
- Back-up your files to the cloud or off-site services and test that the restoration works.
- Implement user training with simulated phishing attacks so the staff will recognize suspicious emails and avoid actions that could launch malware attacks.
- Ensure strong password controls and that systems are regularly patched.
- Require multifactor authentication for remote access to IT networks.
- Set anti-virus/anti-malware programs to conduct regular scans of IT network assets using up-to-date signatures.
A version of this article first appeared on Medscape.com.
Could the Omicron surge hasten the transition from pandemic to endemic?
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.
The record-setting surge in COVID-19 cases nationwide – including more than one million new infections reported on Jan. 3 – raises questions about whether the higher Omicron variant transmissibility will accelerate a transition from pandemic to endemic disease.
Furthermore,
Infectious disease experts weigh in on these possibilities.
An endemic eventuality?
Whether the current surge will mean the predicted switch to endemic COVID-19 will come sooner “is very hard to predict,” Michael Lin, MD, MPH, told this news organization.
“It’s an open question,” he said, “if another highly transmissible variant will emerge.”
On a positive note, “at this point many more people have received their vaccinations or been infected. And over time, repeated infections have led to milder symptoms,” added Dr. Lin, hospital epidemiologist at Rush Medical College, Chicago.
“It could end up being a seasonal variant,” he said.
COVID-19 going endemic is “a real possibility, but unfortunately ... it doesn’t seem necessarily that we’re going to have the same predictable pattern we have with the flu,” said Eleftherios Mylonakis, MD, PhD, chief of infectious diseases for Lifespan and its affiliates at Rhode Island Hospital and Miriam Hospital in Providence.
“We have a number of other viruses that don’t follow the same annual pattern,” he said.
Unknowns include how long individuals’ immune responses, including T-cell defenses, will last going forward.
A transition from pandemic to endemic is “not a light switch, and there are no metrics associated with what endemic means for COVID-19,” said Syra Madad, DHSc., MSc, MCP, an infectious disease epidemiologist at Harvard’s Belfer Center for Science and International Affairs, Boston.
“Instead, we should continue to focus on decreasing transmission rates and preventing our hospitals from getting overwhelmed,” she said.
A hastening to herd immunity?
“The short answer is yes,” Dr. Lin said when asked if the increased transmissibility and increased cases linked to the Omicron surge could get the U.S. closer to herd immunity.
“The twist in this whole story,” he said, “is the virus mutated enough to escape first-line immune defenses, specifically antibodies. That is why we are seeing breakthrough infections, even in highly vaccinated populations.”
Dr. Mylonakis was more skeptical regarding herd immunity.
“The concept of herd immunity with a rapidly evolving virus is very difficult” to address, he said.
One reason is the number of unknown factors, Dr. Mylonakis said. He predicted a clearer picture will emerge after the Omicrons surge subsides. Also, with so many people infected by the Omicron variant, immune protection should peak.
“People will have boosted immunity. Not everybody, unfortunately, because there are people who cannot really mount [a full immune response] because of age, because of immunosuppression, etc.,” said Dr. Mylonakis, who is also professor of infectious diseases at Brown University.
“But the majority of the population will be exposed and will mount some degree of immunity.”
Dr. Madad agreed. “The omicron variant will add much more immunity into our population by both the preferred pathway – which is through vaccination – as well as through those that are unvaccinated and get infected with omicron,” she said.
“The pathway to gain immunity from vaccination is the safest option, and already over 1 million doses of the COVID-19 vaccine are going into arms per day – this includes first, second, and additional doses like boosters,” added Dr. Madad, who is also senior director of the System-wide Special Pathogens Program at New York City Health and Hospitals.
A shorter, more intense surge?
The United Kingdom’s experience with COVID-19 has often served as a bellwether of what is likely to happen in the U.S. If that is the case with the Omicron surge, the peak should last about 4 weeks, Dr. Mylonakis said.
In other words, the accelerated spread of Omicron could mean this surge passes more quickly than Delta.
Furthermore, some evidence suggests neutralizing antibodies produced by Omicron infection remain effective against the Delta variant – thereby reducing the risk of Delta reinfections over time.
The ability to neutralize the Delta variant increased more than fourfold after a median 14 days, according to data from a preprint study posted Dec. 27 on MedRxiv.
At the same time, neutralization of the Omicron variant increased 14-fold as participants mounted an antibody response. The study was conducted in vaccinated and unvaccinated people infected by Omicron in South Africa shortly after symptoms started. It has yet to be peer reviewed.
Eric Topol, MD, editor-in-chief of Medscape, described the results as “especially good news” in a tweet.
The current surge could also mean enhanced protection in the future.
“As we look at getting to the other side of this Omicron wave, we will end up with more immunity,” Dr. Madad said. “And with more immunity means we’ll be better guarded against the next emerging variant.”
A version of this article first appeared on Medscape.com.