User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Growth in early life may predict early puberty
Faster gains in weight, length or height, or body mass index in the first 5 years of life were associated with an earlier onset of puberty in boys and girls, based on data from a cohort study of more than 7,000 children.
In recent decades, clinicians and parents have raised concerns about an earlier onset of puberty in children in the United States and other countries, Izzudin M. Aris, PhD, of Harvard Medical School, Boston, and colleagues wrote.
“Children with earlier pubertal onset not only may be at increased risk for long-term chronic diseases, but also may experience adverse consequences during adolescence, including psychosocial difficulties and dysmetabolism,” they said. However, the effect of growth in the first 5 years of life on pubertal onset has not been well studied.
In a study published in JAMA Network Open, the researchers identified 7,495 children from 36 cohorts participating in the Environmental Influences on Child Health Outcomes program from Jan. 1, 1986, to Dec. 31, 2015.
The study population included 3,772 girls and 3,723 boys; 60% reported as White, 23% as Black, 15% as Hispanic, 12% as one of the following: American Indian or Alaska Native, Native Hawaiian or Pacific Islander, multiple races, or other race. Most (84.1%) were born during or after the year 2000.
The primary outcome was the pubertal growth spurt, also known as age at peak height velocity (APHV). The researchers measured growth at 3 age periods in the first 5 years (early infancy, late infancy, and early childhood) and estimated rates of weight, length or height, and body mass index (BMI) gain. Secondary outcomes included self-reported pubic hair staging and scores on the Pubertal Development Scale.
Overall, weight and length or height gain velocities declined in the first 5 years of life, and boys had faster gains in early infancy, compared with girls.
APHV was negatively correlated with puberty scores and Tanner staging for pubic hair development in both boys and girls, while puberty score was positively correlated with Tanner staging for pubic hair in both sexes.
After controlling for maternal and child confounders including maternal age at delivery, maternal education level, and year of birth, faster gains in weight, length or height, or BMI at each of the three measurement periods in early life was associated with earlier APHV in boys. No effect was noted for race, maternal education level, or birth year.
In girls, faster gains in weight, length, or height, only at the latest measurement period (early childhood) were associated with younger APHV. No associations with APHV occurred for velocities of BMI gain at any age period in girls, the researchers noted. However, age at menarche was positively correlated with early APHV and negatively correlated with puberty score and Tanner staging for pubic hair.
The findings support previous studies of associations between child growth and pubertal onset, the researchers wrote. The mechanisms of action are many, and have not been explained, the researchers wrote in their discussion of the findings.
“We speculate that insulinlike growth factor 1 may be a factor in the associations observed in the present study, either directly or indirectly through sex steroid synthesis and secretion. Alternatively, in girls, androgens and adipokines may be factors in the observed associations for pubic hair staging and menarche, respectively,” they said. Genetics and other factors including social factors, environmental exposures, diet, and physical activity also affect growth in early life.
The study findings were limited by several factors including the use of child-reported measures of pubic hair staging and parent reports of pubertal scores, with the potential for error and misclassification, the researchers noted. Other limitations include a lack of data on maternal age at menarche and the use of weight-for-length rather than BMI for children younger than 2 years.
However, the results were strengthened by the large sample size, long-term follow-up, and especially the use of a nationally representative contemporary cohort that addresses gaps in the current literature from later time periods. The results support the associations of sex-specific early pubertal onset in children with faster growth early in life. “In the long term, results of the present study may inform future research that aims to develop and/or test preventive interventions to optimize nutrition, environmental exposures, physical activity, and other behaviors related to growth during these age periods,” they concluded.
Time and timing limit practical application of results
The current study addresses two issues that are ongoing concerns for clinicians, specifically, the rise in obesity in childhood and its potential link to an earlier age of entry into puberty, M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview.
“Authors in prior studies have suggested that earlier puberty, and indeed earlier menarche, in females may be associated with the potential of long-term health issues,” Dr. Jay noted. “It has also been suggested that both early maturing females and males may be impacted psychosocially. Others have suggested that the pathways through puberty are key and environmental factors as well as nutrition can have an impact on adolescence as well as health consequences later in life.”
The current study is important because it focused on children born in the present era of the obesity epidemic, while earlier studies were conducted on a group in the 1960s-1980s. “This study suggests that there are sex-specific associations of faster growth and earlier entry into puberty,” Dr. Jay said.
“While it is exciting to consider closer monitoring of pubertal progression in pediatric settings, often patients and families do not present in a timely manner for assessment,” she said. “Also, the authors suggest that preventive support may be offered to children who are traversing puberty at earlier ages. However, given the current stress on practices with COVID as well as stress on providers offering clinical services, identifying supportive interventions may be a stretch at best for practitioners already burdened by clinical and administrative demands.
“Ongoing studies are needed to address the knowledge gaps that exist in the arena of pubertal onset and growth during childhood across life periods,” said Dr. Jay. “In the long term, the present study may help direct research that could focus on preventive interventions to optimize nutrition, physical activity, environmental exposures, and other factors that intersect growth during infancy through early childhood, which may hasten early pubertal development’s later sequelae in adulthood.”
The study was supported by various grants to the researchers from the Environmental Influences on Child Health Outcomes program, Office of the Director, National Institutes of Health, as well as the Colorado Clinical and Translational Sciences Institute, University of Colorado at Denver. Lead author Dr. Aris had no financial conflicts to disclose. Dr. Jay had no conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Faster gains in weight, length or height, or body mass index in the first 5 years of life were associated with an earlier onset of puberty in boys and girls, based on data from a cohort study of more than 7,000 children.
In recent decades, clinicians and parents have raised concerns about an earlier onset of puberty in children in the United States and other countries, Izzudin M. Aris, PhD, of Harvard Medical School, Boston, and colleagues wrote.
“Children with earlier pubertal onset not only may be at increased risk for long-term chronic diseases, but also may experience adverse consequences during adolescence, including psychosocial difficulties and dysmetabolism,” they said. However, the effect of growth in the first 5 years of life on pubertal onset has not been well studied.
In a study published in JAMA Network Open, the researchers identified 7,495 children from 36 cohorts participating in the Environmental Influences on Child Health Outcomes program from Jan. 1, 1986, to Dec. 31, 2015.
The study population included 3,772 girls and 3,723 boys; 60% reported as White, 23% as Black, 15% as Hispanic, 12% as one of the following: American Indian or Alaska Native, Native Hawaiian or Pacific Islander, multiple races, or other race. Most (84.1%) were born during or after the year 2000.
The primary outcome was the pubertal growth spurt, also known as age at peak height velocity (APHV). The researchers measured growth at 3 age periods in the first 5 years (early infancy, late infancy, and early childhood) and estimated rates of weight, length or height, and body mass index (BMI) gain. Secondary outcomes included self-reported pubic hair staging and scores on the Pubertal Development Scale.
Overall, weight and length or height gain velocities declined in the first 5 years of life, and boys had faster gains in early infancy, compared with girls.
APHV was negatively correlated with puberty scores and Tanner staging for pubic hair development in both boys and girls, while puberty score was positively correlated with Tanner staging for pubic hair in both sexes.
After controlling for maternal and child confounders including maternal age at delivery, maternal education level, and year of birth, faster gains in weight, length or height, or BMI at each of the three measurement periods in early life was associated with earlier APHV in boys. No effect was noted for race, maternal education level, or birth year.
In girls, faster gains in weight, length, or height, only at the latest measurement period (early childhood) were associated with younger APHV. No associations with APHV occurred for velocities of BMI gain at any age period in girls, the researchers noted. However, age at menarche was positively correlated with early APHV and negatively correlated with puberty score and Tanner staging for pubic hair.
The findings support previous studies of associations between child growth and pubertal onset, the researchers wrote. The mechanisms of action are many, and have not been explained, the researchers wrote in their discussion of the findings.
“We speculate that insulinlike growth factor 1 may be a factor in the associations observed in the present study, either directly or indirectly through sex steroid synthesis and secretion. Alternatively, in girls, androgens and adipokines may be factors in the observed associations for pubic hair staging and menarche, respectively,” they said. Genetics and other factors including social factors, environmental exposures, diet, and physical activity also affect growth in early life.
The study findings were limited by several factors including the use of child-reported measures of pubic hair staging and parent reports of pubertal scores, with the potential for error and misclassification, the researchers noted. Other limitations include a lack of data on maternal age at menarche and the use of weight-for-length rather than BMI for children younger than 2 years.
However, the results were strengthened by the large sample size, long-term follow-up, and especially the use of a nationally representative contemporary cohort that addresses gaps in the current literature from later time periods. The results support the associations of sex-specific early pubertal onset in children with faster growth early in life. “In the long term, results of the present study may inform future research that aims to develop and/or test preventive interventions to optimize nutrition, environmental exposures, physical activity, and other behaviors related to growth during these age periods,” they concluded.
Time and timing limit practical application of results
The current study addresses two issues that are ongoing concerns for clinicians, specifically, the rise in obesity in childhood and its potential link to an earlier age of entry into puberty, M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview.
“Authors in prior studies have suggested that earlier puberty, and indeed earlier menarche, in females may be associated with the potential of long-term health issues,” Dr. Jay noted. “It has also been suggested that both early maturing females and males may be impacted psychosocially. Others have suggested that the pathways through puberty are key and environmental factors as well as nutrition can have an impact on adolescence as well as health consequences later in life.”
The current study is important because it focused on children born in the present era of the obesity epidemic, while earlier studies were conducted on a group in the 1960s-1980s. “This study suggests that there are sex-specific associations of faster growth and earlier entry into puberty,” Dr. Jay said.
“While it is exciting to consider closer monitoring of pubertal progression in pediatric settings, often patients and families do not present in a timely manner for assessment,” she said. “Also, the authors suggest that preventive support may be offered to children who are traversing puberty at earlier ages. However, given the current stress on practices with COVID as well as stress on providers offering clinical services, identifying supportive interventions may be a stretch at best for practitioners already burdened by clinical and administrative demands.
“Ongoing studies are needed to address the knowledge gaps that exist in the arena of pubertal onset and growth during childhood across life periods,” said Dr. Jay. “In the long term, the present study may help direct research that could focus on preventive interventions to optimize nutrition, physical activity, environmental exposures, and other factors that intersect growth during infancy through early childhood, which may hasten early pubertal development’s later sequelae in adulthood.”
The study was supported by various grants to the researchers from the Environmental Influences on Child Health Outcomes program, Office of the Director, National Institutes of Health, as well as the Colorado Clinical and Translational Sciences Institute, University of Colorado at Denver. Lead author Dr. Aris had no financial conflicts to disclose. Dr. Jay had no conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Faster gains in weight, length or height, or body mass index in the first 5 years of life were associated with an earlier onset of puberty in boys and girls, based on data from a cohort study of more than 7,000 children.
In recent decades, clinicians and parents have raised concerns about an earlier onset of puberty in children in the United States and other countries, Izzudin M. Aris, PhD, of Harvard Medical School, Boston, and colleagues wrote.
“Children with earlier pubertal onset not only may be at increased risk for long-term chronic diseases, but also may experience adverse consequences during adolescence, including psychosocial difficulties and dysmetabolism,” they said. However, the effect of growth in the first 5 years of life on pubertal onset has not been well studied.
In a study published in JAMA Network Open, the researchers identified 7,495 children from 36 cohorts participating in the Environmental Influences on Child Health Outcomes program from Jan. 1, 1986, to Dec. 31, 2015.
The study population included 3,772 girls and 3,723 boys; 60% reported as White, 23% as Black, 15% as Hispanic, 12% as one of the following: American Indian or Alaska Native, Native Hawaiian or Pacific Islander, multiple races, or other race. Most (84.1%) were born during or after the year 2000.
The primary outcome was the pubertal growth spurt, also known as age at peak height velocity (APHV). The researchers measured growth at 3 age periods in the first 5 years (early infancy, late infancy, and early childhood) and estimated rates of weight, length or height, and body mass index (BMI) gain. Secondary outcomes included self-reported pubic hair staging and scores on the Pubertal Development Scale.
Overall, weight and length or height gain velocities declined in the first 5 years of life, and boys had faster gains in early infancy, compared with girls.
APHV was negatively correlated with puberty scores and Tanner staging for pubic hair development in both boys and girls, while puberty score was positively correlated with Tanner staging for pubic hair in both sexes.
After controlling for maternal and child confounders including maternal age at delivery, maternal education level, and year of birth, faster gains in weight, length or height, or BMI at each of the three measurement periods in early life was associated with earlier APHV in boys. No effect was noted for race, maternal education level, or birth year.
In girls, faster gains in weight, length, or height, only at the latest measurement period (early childhood) were associated with younger APHV. No associations with APHV occurred for velocities of BMI gain at any age period in girls, the researchers noted. However, age at menarche was positively correlated with early APHV and negatively correlated with puberty score and Tanner staging for pubic hair.
The findings support previous studies of associations between child growth and pubertal onset, the researchers wrote. The mechanisms of action are many, and have not been explained, the researchers wrote in their discussion of the findings.
“We speculate that insulinlike growth factor 1 may be a factor in the associations observed in the present study, either directly or indirectly through sex steroid synthesis and secretion. Alternatively, in girls, androgens and adipokines may be factors in the observed associations for pubic hair staging and menarche, respectively,” they said. Genetics and other factors including social factors, environmental exposures, diet, and physical activity also affect growth in early life.
The study findings were limited by several factors including the use of child-reported measures of pubic hair staging and parent reports of pubertal scores, with the potential for error and misclassification, the researchers noted. Other limitations include a lack of data on maternal age at menarche and the use of weight-for-length rather than BMI for children younger than 2 years.
However, the results were strengthened by the large sample size, long-term follow-up, and especially the use of a nationally representative contemporary cohort that addresses gaps in the current literature from later time periods. The results support the associations of sex-specific early pubertal onset in children with faster growth early in life. “In the long term, results of the present study may inform future research that aims to develop and/or test preventive interventions to optimize nutrition, environmental exposures, physical activity, and other behaviors related to growth during these age periods,” they concluded.
Time and timing limit practical application of results
The current study addresses two issues that are ongoing concerns for clinicians, specifically, the rise in obesity in childhood and its potential link to an earlier age of entry into puberty, M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview.
“Authors in prior studies have suggested that earlier puberty, and indeed earlier menarche, in females may be associated with the potential of long-term health issues,” Dr. Jay noted. “It has also been suggested that both early maturing females and males may be impacted psychosocially. Others have suggested that the pathways through puberty are key and environmental factors as well as nutrition can have an impact on adolescence as well as health consequences later in life.”
The current study is important because it focused on children born in the present era of the obesity epidemic, while earlier studies were conducted on a group in the 1960s-1980s. “This study suggests that there are sex-specific associations of faster growth and earlier entry into puberty,” Dr. Jay said.
“While it is exciting to consider closer monitoring of pubertal progression in pediatric settings, often patients and families do not present in a timely manner for assessment,” she said. “Also, the authors suggest that preventive support may be offered to children who are traversing puberty at earlier ages. However, given the current stress on practices with COVID as well as stress on providers offering clinical services, identifying supportive interventions may be a stretch at best for practitioners already burdened by clinical and administrative demands.
“Ongoing studies are needed to address the knowledge gaps that exist in the arena of pubertal onset and growth during childhood across life periods,” said Dr. Jay. “In the long term, the present study may help direct research that could focus on preventive interventions to optimize nutrition, physical activity, environmental exposures, and other factors that intersect growth during infancy through early childhood, which may hasten early pubertal development’s later sequelae in adulthood.”
The study was supported by various grants to the researchers from the Environmental Influences on Child Health Outcomes program, Office of the Director, National Institutes of Health, as well as the Colorado Clinical and Translational Sciences Institute, University of Colorado at Denver. Lead author Dr. Aris had no financial conflicts to disclose. Dr. Jay had no conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM JAMA NETWORK OPEN
Heavy cannabis use tied to less diabetes in women
Women who used marijuana (cannabis) at least four times in the previous month (heavy users) were less likely to have type 2 diabetes than women who were light users or nonusers, in a nationally representative U.S. observational study.
In contrast, there were no differences in the prevalence of type 2 diabetes in men who were light or heavy cannabis users versus nonusers.
These findings are based on data from the 2013-2018 National Health and Nutrition Examination Survey (NHANES), whereby participants self-reported their cannabis use.
The study by Ayobami S. Ogunsola, MD, MPH, a graduate student at Texas A&M University, College Station, and colleagues was recently published in Cannabis and Cannabinoid Research.
What do the findings mean?
Although overall findings linking cannabis use and diabetes have been inconsistent, the gender differences in the current study are consistent with animal studies and some clinical studies, senior author Ibraheem M. Karaye, MD, MPH, said in an interview.
However, these gender differences need to be confirmed, and “we strongly recommend that more biological or biochemical studies be conducted that could actually tell us the mechanisms,” said Dr. Karaye, an assistant professor in the department of population health, Hofstra University, Hempstead, N.Y.
“It’s indisputable that medical marijuana has some medical benefits,” he added. “Women [who use cannabis] have been shown to lose more weight than men, for example.”
“If women [cannabis users] are less likely to develop diabetes or more likely to express improvement of symptoms of diabetes,” he noted, “this means that hyperglycemic medications that are being prescribed should be watched scrupulously. Otherwise, there is a risk that [women] may overrespond.”
That is, Dr. Karaye continued, women “may be at risk of developing hypoglycemia because the cannabis is acting synergistically with the regular drug that is being used to treat the diabetes.”
U.S. clinicians, especially in states with legalized medical marijuana, need to be aware of the potential synergy.
“One would have to consider the patient as a whole,” he stressed. “For example, a woman that uses medical marijuana may actually respond differently to hyperglycemic medication.”
Conflicting reports explained by sex differences?
Evidence on whether cannabis use is linked with type 2 diabetes is limited and conflicting, the researchers wrote. They hypothesized that these conflicting findings might be explained by sex differences.
To “help inform current diabetes prevention and mitigation efforts,” they investigated sex differences in cannabis use and prevalence of type 2 diabetes in 15,602 men and women in the 2013-2014, 2015-2016, and 2017-2018 NHANES surveys.
Participants were classified as having type 2 diabetes if they had a physician’s diagnosis; a 2-hour plasma glucose of at least 200 mg/dL (in a glucose tolerance test); fasting blood glucose of at least 126 mg/dL; or A1c of at least 6.5%.
About half of respondents were women (52%) and close to half (44%) were age 18-39.
More than a third (38%) had a body mass index (BMI) of at least 30 kg/m2, indicating obesity.
Roughly 1 in 10 had a diagnosis of type 2 diabetes (13.5%) or A1c of at least 6.5% (9.8%).
Close to a fifth smoked cigarettes (16%). Similarly, 14.5% used cannabis at least four times a week, 3.3% used it less often, and the rest did not use it. Half of participants were not physically active (49%).
Just over half had at least a college education (55%).
Heavy cannabis users were more likely to be younger than age 40 (57% of men, 57% of women), college graduates (54% of men, 63% of women), cigarette smokers (79% of men, 83% of women), and physically inactive (39% of men, 49% of women).
Among women, heavy cannabis users were 49% less likely to have type 2 diabetes than nonusers, after adjusting for age, sex, race/ethnicity, educational level, physical activity, tobacco use, alcohol use, marital status, difficulty walking, employment status, income, and BMI (adjusted odds ratio, 0.51; 95% confidence interval, 0.31-0.84).
There were no significant differences between light cannabis users versus nonusers and diabetes prevalence in women, or between light or heavy cannabis users versus nonusers and diabetes prevalence in men.
Limitations, yet biologically plausible
The researchers acknowledged several study limitations.
They do not know how long participants had used marijuana. The men and women may have underreported their cannabis use, especially in states where medical marijuana was not legal, and the NHANES data did not specify whether the cannabis was recreational or medicinal.
The study may have been underpowered to detect a smaller difference in men who used versus did not use marijuana.
And importantly, this was an observational study (a snapshot at one point in time), so it cannot say whether the heavy cannabis use in women caused a decreased likelihood of diabetes.
Nevertheless, the inverse association between cannabis use and presence of type 2 diabetes is biologically plausible, Dr. Ogunsola and colleagues wrote.
The two major cannabis compounds, cannabidiol and delta-9-tetrahydrocannabinol, stimulate CBD1 and CBD2 receptors in the central and peripheral nervous systems, respectively. And “activation of the CBD1 receptor increases insulin secretion, glucagon, and somatostatin, and activates metabolic processes in fat and skeletal muscles – mechanisms that improve glucose disposal,” they explained.
The researchers speculated that the sex differences they found for this association may be caused by differences in sex hormones, or the endocannabinoid system, or fat deposits.
Therefore, “additional studies are needed to investigate the sex-based heterogeneity reported in this study and to elucidate potential mechanisms for the observation,” they concluded.
The study did not receive any funding and the researchers have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Women who used marijuana (cannabis) at least four times in the previous month (heavy users) were less likely to have type 2 diabetes than women who were light users or nonusers, in a nationally representative U.S. observational study.
In contrast, there were no differences in the prevalence of type 2 diabetes in men who were light or heavy cannabis users versus nonusers.
These findings are based on data from the 2013-2018 National Health and Nutrition Examination Survey (NHANES), whereby participants self-reported their cannabis use.
The study by Ayobami S. Ogunsola, MD, MPH, a graduate student at Texas A&M University, College Station, and colleagues was recently published in Cannabis and Cannabinoid Research.
What do the findings mean?
Although overall findings linking cannabis use and diabetes have been inconsistent, the gender differences in the current study are consistent with animal studies and some clinical studies, senior author Ibraheem M. Karaye, MD, MPH, said in an interview.
However, these gender differences need to be confirmed, and “we strongly recommend that more biological or biochemical studies be conducted that could actually tell us the mechanisms,” said Dr. Karaye, an assistant professor in the department of population health, Hofstra University, Hempstead, N.Y.
“It’s indisputable that medical marijuana has some medical benefits,” he added. “Women [who use cannabis] have been shown to lose more weight than men, for example.”
“If women [cannabis users] are less likely to develop diabetes or more likely to express improvement of symptoms of diabetes,” he noted, “this means that hyperglycemic medications that are being prescribed should be watched scrupulously. Otherwise, there is a risk that [women] may overrespond.”
That is, Dr. Karaye continued, women “may be at risk of developing hypoglycemia because the cannabis is acting synergistically with the regular drug that is being used to treat the diabetes.”
U.S. clinicians, especially in states with legalized medical marijuana, need to be aware of the potential synergy.
“One would have to consider the patient as a whole,” he stressed. “For example, a woman that uses medical marijuana may actually respond differently to hyperglycemic medication.”
Conflicting reports explained by sex differences?
Evidence on whether cannabis use is linked with type 2 diabetes is limited and conflicting, the researchers wrote. They hypothesized that these conflicting findings might be explained by sex differences.
To “help inform current diabetes prevention and mitigation efforts,” they investigated sex differences in cannabis use and prevalence of type 2 diabetes in 15,602 men and women in the 2013-2014, 2015-2016, and 2017-2018 NHANES surveys.
Participants were classified as having type 2 diabetes if they had a physician’s diagnosis; a 2-hour plasma glucose of at least 200 mg/dL (in a glucose tolerance test); fasting blood glucose of at least 126 mg/dL; or A1c of at least 6.5%.
About half of respondents were women (52%) and close to half (44%) were age 18-39.
More than a third (38%) had a body mass index (BMI) of at least 30 kg/m2, indicating obesity.
Roughly 1 in 10 had a diagnosis of type 2 diabetes (13.5%) or A1c of at least 6.5% (9.8%).
Close to a fifth smoked cigarettes (16%). Similarly, 14.5% used cannabis at least four times a week, 3.3% used it less often, and the rest did not use it. Half of participants were not physically active (49%).
Just over half had at least a college education (55%).
Heavy cannabis users were more likely to be younger than age 40 (57% of men, 57% of women), college graduates (54% of men, 63% of women), cigarette smokers (79% of men, 83% of women), and physically inactive (39% of men, 49% of women).
Among women, heavy cannabis users were 49% less likely to have type 2 diabetes than nonusers, after adjusting for age, sex, race/ethnicity, educational level, physical activity, tobacco use, alcohol use, marital status, difficulty walking, employment status, income, and BMI (adjusted odds ratio, 0.51; 95% confidence interval, 0.31-0.84).
There were no significant differences between light cannabis users versus nonusers and diabetes prevalence in women, or between light or heavy cannabis users versus nonusers and diabetes prevalence in men.
Limitations, yet biologically plausible
The researchers acknowledged several study limitations.
They do not know how long participants had used marijuana. The men and women may have underreported their cannabis use, especially in states where medical marijuana was not legal, and the NHANES data did not specify whether the cannabis was recreational or medicinal.
The study may have been underpowered to detect a smaller difference in men who used versus did not use marijuana.
And importantly, this was an observational study (a snapshot at one point in time), so it cannot say whether the heavy cannabis use in women caused a decreased likelihood of diabetes.
Nevertheless, the inverse association between cannabis use and presence of type 2 diabetes is biologically plausible, Dr. Ogunsola and colleagues wrote.
The two major cannabis compounds, cannabidiol and delta-9-tetrahydrocannabinol, stimulate CBD1 and CBD2 receptors in the central and peripheral nervous systems, respectively. And “activation of the CBD1 receptor increases insulin secretion, glucagon, and somatostatin, and activates metabolic processes in fat and skeletal muscles – mechanisms that improve glucose disposal,” they explained.
The researchers speculated that the sex differences they found for this association may be caused by differences in sex hormones, or the endocannabinoid system, or fat deposits.
Therefore, “additional studies are needed to investigate the sex-based heterogeneity reported in this study and to elucidate potential mechanisms for the observation,” they concluded.
The study did not receive any funding and the researchers have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Women who used marijuana (cannabis) at least four times in the previous month (heavy users) were less likely to have type 2 diabetes than women who were light users or nonusers, in a nationally representative U.S. observational study.
In contrast, there were no differences in the prevalence of type 2 diabetes in men who were light or heavy cannabis users versus nonusers.
These findings are based on data from the 2013-2018 National Health and Nutrition Examination Survey (NHANES), whereby participants self-reported their cannabis use.
The study by Ayobami S. Ogunsola, MD, MPH, a graduate student at Texas A&M University, College Station, and colleagues was recently published in Cannabis and Cannabinoid Research.
What do the findings mean?
Although overall findings linking cannabis use and diabetes have been inconsistent, the gender differences in the current study are consistent with animal studies and some clinical studies, senior author Ibraheem M. Karaye, MD, MPH, said in an interview.
However, these gender differences need to be confirmed, and “we strongly recommend that more biological or biochemical studies be conducted that could actually tell us the mechanisms,” said Dr. Karaye, an assistant professor in the department of population health, Hofstra University, Hempstead, N.Y.
“It’s indisputable that medical marijuana has some medical benefits,” he added. “Women [who use cannabis] have been shown to lose more weight than men, for example.”
“If women [cannabis users] are less likely to develop diabetes or more likely to express improvement of symptoms of diabetes,” he noted, “this means that hyperglycemic medications that are being prescribed should be watched scrupulously. Otherwise, there is a risk that [women] may overrespond.”
That is, Dr. Karaye continued, women “may be at risk of developing hypoglycemia because the cannabis is acting synergistically with the regular drug that is being used to treat the diabetes.”
U.S. clinicians, especially in states with legalized medical marijuana, need to be aware of the potential synergy.
“One would have to consider the patient as a whole,” he stressed. “For example, a woman that uses medical marijuana may actually respond differently to hyperglycemic medication.”
Conflicting reports explained by sex differences?
Evidence on whether cannabis use is linked with type 2 diabetes is limited and conflicting, the researchers wrote. They hypothesized that these conflicting findings might be explained by sex differences.
To “help inform current diabetes prevention and mitigation efforts,” they investigated sex differences in cannabis use and prevalence of type 2 diabetes in 15,602 men and women in the 2013-2014, 2015-2016, and 2017-2018 NHANES surveys.
Participants were classified as having type 2 diabetes if they had a physician’s diagnosis; a 2-hour plasma glucose of at least 200 mg/dL (in a glucose tolerance test); fasting blood glucose of at least 126 mg/dL; or A1c of at least 6.5%.
About half of respondents were women (52%) and close to half (44%) were age 18-39.
More than a third (38%) had a body mass index (BMI) of at least 30 kg/m2, indicating obesity.
Roughly 1 in 10 had a diagnosis of type 2 diabetes (13.5%) or A1c of at least 6.5% (9.8%).
Close to a fifth smoked cigarettes (16%). Similarly, 14.5% used cannabis at least four times a week, 3.3% used it less often, and the rest did not use it. Half of participants were not physically active (49%).
Just over half had at least a college education (55%).
Heavy cannabis users were more likely to be younger than age 40 (57% of men, 57% of women), college graduates (54% of men, 63% of women), cigarette smokers (79% of men, 83% of women), and physically inactive (39% of men, 49% of women).
Among women, heavy cannabis users were 49% less likely to have type 2 diabetes than nonusers, after adjusting for age, sex, race/ethnicity, educational level, physical activity, tobacco use, alcohol use, marital status, difficulty walking, employment status, income, and BMI (adjusted odds ratio, 0.51; 95% confidence interval, 0.31-0.84).
There were no significant differences between light cannabis users versus nonusers and diabetes prevalence in women, or between light or heavy cannabis users versus nonusers and diabetes prevalence in men.
Limitations, yet biologically plausible
The researchers acknowledged several study limitations.
They do not know how long participants had used marijuana. The men and women may have underreported their cannabis use, especially in states where medical marijuana was not legal, and the NHANES data did not specify whether the cannabis was recreational or medicinal.
The study may have been underpowered to detect a smaller difference in men who used versus did not use marijuana.
And importantly, this was an observational study (a snapshot at one point in time), so it cannot say whether the heavy cannabis use in women caused a decreased likelihood of diabetes.
Nevertheless, the inverse association between cannabis use and presence of type 2 diabetes is biologically plausible, Dr. Ogunsola and colleagues wrote.
The two major cannabis compounds, cannabidiol and delta-9-tetrahydrocannabinol, stimulate CBD1 and CBD2 receptors in the central and peripheral nervous systems, respectively. And “activation of the CBD1 receptor increases insulin secretion, glucagon, and somatostatin, and activates metabolic processes in fat and skeletal muscles – mechanisms that improve glucose disposal,” they explained.
The researchers speculated that the sex differences they found for this association may be caused by differences in sex hormones, or the endocannabinoid system, or fat deposits.
Therefore, “additional studies are needed to investigate the sex-based heterogeneity reported in this study and to elucidate potential mechanisms for the observation,” they concluded.
The study did not receive any funding and the researchers have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FROM CANNABIS AND CANNABINOID RESEARCH
Limited benefits of early gestational diabetes screening
Screening pregnant women with obesity for gestational diabetes before 20 weeks of pregnancy did not lead to any improved maternal or neonatal outcomes compared with doing routine screening between 24 and 28 weeks, according to research presented Feb. 4 at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“There is increasing evidence that early screening does not reduce the risk of adverse perinatal outcomes,” Jennifer Thompson, MD, associate professor of ob.gyn. at Vanderbilt University, Nashville, Tenn., said in an interview. “The increasing number of studies that have demonstrated no benefit in reducing adverse perinatal outcomes leads to consideration to revise recommendations for early screening.”
However, she did note that early screening may be helpful in identifying patients with undiagnosed preexisting diabetes.
Michael Richley, MD, a maternal-fetal medicine fellow at the University of California, Los Angeles, said catching those previously undiagnosed cases is one of the goals of earlier screening with the expectation that earlier management will lead to better outcomes.
“If a patient then obtains the diagnosis of type 2 diabetes, introducing nutritional counseling and possible medical management early can lead to better outcomes,” said Dr. Richley, who attended the presentation but was not involved in the research. ”While catching undiagnosed type 2 diabetes is not common, it is becoming increasingly common lately.”
Obesity is a known risk factor for impaired glucose metabolism and for gestational diabetes, explained presenter Christopher A. Enakpene, MD, an ob.gyn. from Midland, Tex., who completed the study while completing his maternal-fetal medicine fellowship at the University of Illinois in Chicago. Dr. Enakpene reminded attendees that the American College of Obstetricians and Gynecologists (ACOG) currently recommends early screening for gestational diabetes in patients with certain risk factors, including obesity, a history of first-degree relatives with diabetes, or a history of gestational diabetes, impaired glucose tolerance, poor pregnancy outcomes, fetal demise, congenital abnormalities, or birth of an infant large for gestational age.
The researchers screened 7,126 patients for enrollment in the study from March 2017 through February 2019 and identified 600 who met the criteria: An adult with a singleton pregnancy and body mass index (BMI) of at least 30 kg/m2. Patients were excluded if they had preexisting diabetes, elevated blood glucose or impaired glucose tolerance, a history of gestational diabetes, any chromosomal anomalies or abnormalities in the pregnancy, or were past 20 weeks of pregnancy.
The prospective randomized controlled trial was open label and included 296 patients who were randomly assigned to early screening with a 1-hour glucose challenge test (GCT) and hemoglobin A1c before 20 weeks, followed by a 3-hour oral glucose tolerance test if the GCT result was between 140 and 200 mg/dL with an HbA1c of less than 6.5%. The other 304 patients were screened with a 1-hour GCT between 24 and 28 weeks but also had an HbA1c test before 20 weeks.
The primary outcome was macrosomia, defined as a birth weight at least 4,000 g, with various maternal and neonatal secondary outcomes. The only significant difference between the groups at baseline was a higher proportion of Hispanic participants in the early screening group (22.4%) compared to the routine screening group (13.7%).
The groups had no significant differences in birth weight or macrosomia, which occurred in 2.8% of the early screening group and 3.4% of the routine screening group (P = .7). There were no significant differences in gestational age at delivery, preeclampsia, polyhydramnios, shoulder dystocia, cesarean delivery, or NICU admission. However, the rate of gestational diabetes was significantly higher in the early screening group (22.5%) than in the routine screening group (15.7%; P < .05). In addition, more participants with gestational diabetes in the early screening group used insulin (34.4%) compared with those in the routine screening group (15.6%; P < .05).
Dr. Enakpene noted several reasons that the perinatal outcomes may have been similar between the groups, such as the increased rate of gestational diabetes requiring treatment in the early screening group or a higher proportion of participants using insulin in the early screening group.
“Hence, the similarity in adverse perinatal outcomes between the groups despite a higher proportion of gestational diabetes in the early group might be due to more utilization of insulin,” Dr. Enakpene said.
Dr. Richley was not surprised by the findings and hypothesized that the reason for not seeing a difference in outcomes might relate to using a 20-week cutoff for testing when type 2 diabetes would be evident at any stage of pregnancy.
“It would be interesting to have a study look at diabetes testing exclusively in the first trimester for high-risk patients that looks at neonatal outcomes and see if that would show a difference between the two groups,” Dr. Richley said.
Dr. Thompson was similarly interested in whether 20 weeks was an early enough time for early screening.
”I would also like to know the differences in management between the two groups and if the knowledge of early diagnosis impacted their management, such as timing of medication start, amount of medication required, and how that differed from the standard group,” Dr. Thompson said. ”Since patients with a hemoglobin A1c > 6.5% or glucose tolerance test > 200 [mg/dL] were excluded, I’m interested in the number of patients that were excluded since they likely have undiagnosed preexisting diabetes, which are the patients that may benefit most from early screening.”
Dr. Richley pointed out that the potential clinical implications of the study are limited right now.
“While their secondary outcomes of neonatal hypoglycemia, method of delivery, and other common obstetrical measures were not different, we cannot draw conclusions from this as the study was not powered to evaluate these findings,” Dr. Richley said. “I do still see a role in early screening for patients with risk factors but favor doing so at the first prenatal visit, whenever that is, as opposed to as late as mid-second trimester, though this is often when a patient’s first interaction with a health care system will be within their pregnancy.”
Dr. Enakpene, Dr. Thompson, and Dr. Richley reported no disclosures. External funding for the study was not noted.
Screening pregnant women with obesity for gestational diabetes before 20 weeks of pregnancy did not lead to any improved maternal or neonatal outcomes compared with doing routine screening between 24 and 28 weeks, according to research presented Feb. 4 at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“There is increasing evidence that early screening does not reduce the risk of adverse perinatal outcomes,” Jennifer Thompson, MD, associate professor of ob.gyn. at Vanderbilt University, Nashville, Tenn., said in an interview. “The increasing number of studies that have demonstrated no benefit in reducing adverse perinatal outcomes leads to consideration to revise recommendations for early screening.”
However, she did note that early screening may be helpful in identifying patients with undiagnosed preexisting diabetes.
Michael Richley, MD, a maternal-fetal medicine fellow at the University of California, Los Angeles, said catching those previously undiagnosed cases is one of the goals of earlier screening with the expectation that earlier management will lead to better outcomes.
“If a patient then obtains the diagnosis of type 2 diabetes, introducing nutritional counseling and possible medical management early can lead to better outcomes,” said Dr. Richley, who attended the presentation but was not involved in the research. ”While catching undiagnosed type 2 diabetes is not common, it is becoming increasingly common lately.”
Obesity is a known risk factor for impaired glucose metabolism and for gestational diabetes, explained presenter Christopher A. Enakpene, MD, an ob.gyn. from Midland, Tex., who completed the study while completing his maternal-fetal medicine fellowship at the University of Illinois in Chicago. Dr. Enakpene reminded attendees that the American College of Obstetricians and Gynecologists (ACOG) currently recommends early screening for gestational diabetes in patients with certain risk factors, including obesity, a history of first-degree relatives with diabetes, or a history of gestational diabetes, impaired glucose tolerance, poor pregnancy outcomes, fetal demise, congenital abnormalities, or birth of an infant large for gestational age.
The researchers screened 7,126 patients for enrollment in the study from March 2017 through February 2019 and identified 600 who met the criteria: An adult with a singleton pregnancy and body mass index (BMI) of at least 30 kg/m2. Patients were excluded if they had preexisting diabetes, elevated blood glucose or impaired glucose tolerance, a history of gestational diabetes, any chromosomal anomalies or abnormalities in the pregnancy, or were past 20 weeks of pregnancy.
The prospective randomized controlled trial was open label and included 296 patients who were randomly assigned to early screening with a 1-hour glucose challenge test (GCT) and hemoglobin A1c before 20 weeks, followed by a 3-hour oral glucose tolerance test if the GCT result was between 140 and 200 mg/dL with an HbA1c of less than 6.5%. The other 304 patients were screened with a 1-hour GCT between 24 and 28 weeks but also had an HbA1c test before 20 weeks.
The primary outcome was macrosomia, defined as a birth weight at least 4,000 g, with various maternal and neonatal secondary outcomes. The only significant difference between the groups at baseline was a higher proportion of Hispanic participants in the early screening group (22.4%) compared to the routine screening group (13.7%).
The groups had no significant differences in birth weight or macrosomia, which occurred in 2.8% of the early screening group and 3.4% of the routine screening group (P = .7). There were no significant differences in gestational age at delivery, preeclampsia, polyhydramnios, shoulder dystocia, cesarean delivery, or NICU admission. However, the rate of gestational diabetes was significantly higher in the early screening group (22.5%) than in the routine screening group (15.7%; P < .05). In addition, more participants with gestational diabetes in the early screening group used insulin (34.4%) compared with those in the routine screening group (15.6%; P < .05).
Dr. Enakpene noted several reasons that the perinatal outcomes may have been similar between the groups, such as the increased rate of gestational diabetes requiring treatment in the early screening group or a higher proportion of participants using insulin in the early screening group.
“Hence, the similarity in adverse perinatal outcomes between the groups despite a higher proportion of gestational diabetes in the early group might be due to more utilization of insulin,” Dr. Enakpene said.
Dr. Richley was not surprised by the findings and hypothesized that the reason for not seeing a difference in outcomes might relate to using a 20-week cutoff for testing when type 2 diabetes would be evident at any stage of pregnancy.
“It would be interesting to have a study look at diabetes testing exclusively in the first trimester for high-risk patients that looks at neonatal outcomes and see if that would show a difference between the two groups,” Dr. Richley said.
Dr. Thompson was similarly interested in whether 20 weeks was an early enough time for early screening.
”I would also like to know the differences in management between the two groups and if the knowledge of early diagnosis impacted their management, such as timing of medication start, amount of medication required, and how that differed from the standard group,” Dr. Thompson said. ”Since patients with a hemoglobin A1c > 6.5% or glucose tolerance test > 200 [mg/dL] were excluded, I’m interested in the number of patients that were excluded since they likely have undiagnosed preexisting diabetes, which are the patients that may benefit most from early screening.”
Dr. Richley pointed out that the potential clinical implications of the study are limited right now.
“While their secondary outcomes of neonatal hypoglycemia, method of delivery, and other common obstetrical measures were not different, we cannot draw conclusions from this as the study was not powered to evaluate these findings,” Dr. Richley said. “I do still see a role in early screening for patients with risk factors but favor doing so at the first prenatal visit, whenever that is, as opposed to as late as mid-second trimester, though this is often when a patient’s first interaction with a health care system will be within their pregnancy.”
Dr. Enakpene, Dr. Thompson, and Dr. Richley reported no disclosures. External funding for the study was not noted.
Screening pregnant women with obesity for gestational diabetes before 20 weeks of pregnancy did not lead to any improved maternal or neonatal outcomes compared with doing routine screening between 24 and 28 weeks, according to research presented Feb. 4 at the Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
“There is increasing evidence that early screening does not reduce the risk of adverse perinatal outcomes,” Jennifer Thompson, MD, associate professor of ob.gyn. at Vanderbilt University, Nashville, Tenn., said in an interview. “The increasing number of studies that have demonstrated no benefit in reducing adverse perinatal outcomes leads to consideration to revise recommendations for early screening.”
However, she did note that early screening may be helpful in identifying patients with undiagnosed preexisting diabetes.
Michael Richley, MD, a maternal-fetal medicine fellow at the University of California, Los Angeles, said catching those previously undiagnosed cases is one of the goals of earlier screening with the expectation that earlier management will lead to better outcomes.
“If a patient then obtains the diagnosis of type 2 diabetes, introducing nutritional counseling and possible medical management early can lead to better outcomes,” said Dr. Richley, who attended the presentation but was not involved in the research. ”While catching undiagnosed type 2 diabetes is not common, it is becoming increasingly common lately.”
Obesity is a known risk factor for impaired glucose metabolism and for gestational diabetes, explained presenter Christopher A. Enakpene, MD, an ob.gyn. from Midland, Tex., who completed the study while completing his maternal-fetal medicine fellowship at the University of Illinois in Chicago. Dr. Enakpene reminded attendees that the American College of Obstetricians and Gynecologists (ACOG) currently recommends early screening for gestational diabetes in patients with certain risk factors, including obesity, a history of first-degree relatives with diabetes, or a history of gestational diabetes, impaired glucose tolerance, poor pregnancy outcomes, fetal demise, congenital abnormalities, or birth of an infant large for gestational age.
The researchers screened 7,126 patients for enrollment in the study from March 2017 through February 2019 and identified 600 who met the criteria: An adult with a singleton pregnancy and body mass index (BMI) of at least 30 kg/m2. Patients were excluded if they had preexisting diabetes, elevated blood glucose or impaired glucose tolerance, a history of gestational diabetes, any chromosomal anomalies or abnormalities in the pregnancy, or were past 20 weeks of pregnancy.
The prospective randomized controlled trial was open label and included 296 patients who were randomly assigned to early screening with a 1-hour glucose challenge test (GCT) and hemoglobin A1c before 20 weeks, followed by a 3-hour oral glucose tolerance test if the GCT result was between 140 and 200 mg/dL with an HbA1c of less than 6.5%. The other 304 patients were screened with a 1-hour GCT between 24 and 28 weeks but also had an HbA1c test before 20 weeks.
The primary outcome was macrosomia, defined as a birth weight at least 4,000 g, with various maternal and neonatal secondary outcomes. The only significant difference between the groups at baseline was a higher proportion of Hispanic participants in the early screening group (22.4%) compared to the routine screening group (13.7%).
The groups had no significant differences in birth weight or macrosomia, which occurred in 2.8% of the early screening group and 3.4% of the routine screening group (P = .7). There were no significant differences in gestational age at delivery, preeclampsia, polyhydramnios, shoulder dystocia, cesarean delivery, or NICU admission. However, the rate of gestational diabetes was significantly higher in the early screening group (22.5%) than in the routine screening group (15.7%; P < .05). In addition, more participants with gestational diabetes in the early screening group used insulin (34.4%) compared with those in the routine screening group (15.6%; P < .05).
Dr. Enakpene noted several reasons that the perinatal outcomes may have been similar between the groups, such as the increased rate of gestational diabetes requiring treatment in the early screening group or a higher proportion of participants using insulin in the early screening group.
“Hence, the similarity in adverse perinatal outcomes between the groups despite a higher proportion of gestational diabetes in the early group might be due to more utilization of insulin,” Dr. Enakpene said.
Dr. Richley was not surprised by the findings and hypothesized that the reason for not seeing a difference in outcomes might relate to using a 20-week cutoff for testing when type 2 diabetes would be evident at any stage of pregnancy.
“It would be interesting to have a study look at diabetes testing exclusively in the first trimester for high-risk patients that looks at neonatal outcomes and see if that would show a difference between the two groups,” Dr. Richley said.
Dr. Thompson was similarly interested in whether 20 weeks was an early enough time for early screening.
”I would also like to know the differences in management between the two groups and if the knowledge of early diagnosis impacted their management, such as timing of medication start, amount of medication required, and how that differed from the standard group,” Dr. Thompson said. ”Since patients with a hemoglobin A1c > 6.5% or glucose tolerance test > 200 [mg/dL] were excluded, I’m interested in the number of patients that were excluded since they likely have undiagnosed preexisting diabetes, which are the patients that may benefit most from early screening.”
Dr. Richley pointed out that the potential clinical implications of the study are limited right now.
“While their secondary outcomes of neonatal hypoglycemia, method of delivery, and other common obstetrical measures were not different, we cannot draw conclusions from this as the study was not powered to evaluate these findings,” Dr. Richley said. “I do still see a role in early screening for patients with risk factors but favor doing so at the first prenatal visit, whenever that is, as opposed to as late as mid-second trimester, though this is often when a patient’s first interaction with a health care system will be within their pregnancy.”
Dr. Enakpene, Dr. Thompson, and Dr. Richley reported no disclosures. External funding for the study was not noted.
FROM THE PREGNANCY MEETING
If you’ve got 3 seconds, then you’ve got time to work out
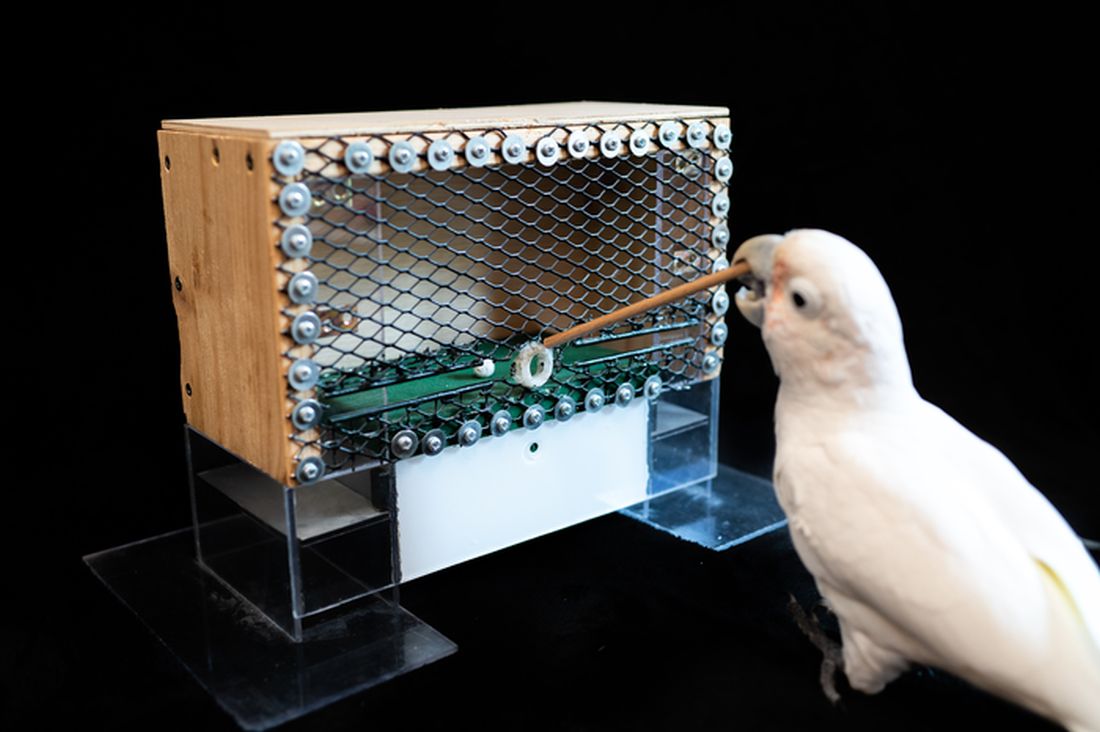
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Goffin’s cockatoo? More like golfin’ cockatoo
Can birds play golf? Of course not; it’s ridiculous. Humans can barely play golf, and we invented the sport. Anyway, moving on to “Brian retraction injury after elective aneurysm clipping.”
Hang on, we’re now hearing that a group of researchers, as part of a large international project comparing children’s innovation and problem-solving skills with those of cockatoos, have in fact taught a group of Goffin’s cockatoos how to play golf. Huh. What an oddly specific project. All right, fine, I guess we’ll go with the golf-playing birds.
Golf may seem very simple at its core. It is, essentially, whacking a ball with a stick. But the Scots who invented the game were undertaking a complex project involving combined usage of multiple tools, and until now, only primates were thought to be capable of utilizing compound tools to play games such as golf.
For this latest research, published in Scientific Reports, our intrepid birds were given a rudimentary form of golf to play (featuring a stick, a ball, and a closed box to get the ball through). Putting the ball through the hole gave the bird a reward. Not every cockatoo was able to hole out, but three did, with each inventing a unique way to manipulate the stick to hit the ball.
As entertaining as it would be to simply teach some birds how to play golf, we do loop back around to medical relevance. While children are perfectly capable of using tools, young children in particular are actually quite bad at using tools to solve novel solutions. Present a 5-year-old with a stick, a ball, and a hole, and that child might not figure out what the cockatoos did. The research really does give insight into the psychology behind the development of complex tools and technology by our ancient ancestors, according to the researchers.
We’re not entirely convinced this isn’t an elaborate ploy to get a bird out onto the PGA Tour. The LOTME staff can see the future headline already: “Painted bunting wins Valspar Championship in epic playoff.”
Work out now, sweat never
Okay, show of hands: Who’s familiar with “Name that tune?” The TV game show got a reboot last year, but some of us are old enough to remember the 1970s version hosted by national treasure Tom Kennedy.
The contestants try to identify a song as quickly as possible, claiming that they “can name that tune in five notes.” Or four notes, or three. Well, welcome to “Name that exercise study.”
Senior author Masatoshi Nakamura, PhD, and associates gathered together 39 students from Niigata (Japan) University of Health and Welfare and had them perform one isometric, concentric, or eccentric bicep curl with a dumbbell for 3 seconds a day at maximum effort for 5 days a week, over 4 weeks. And yes, we did say 3 seconds.
“Lifting the weight sees the bicep in concentric contraction, lowering the weight sees it in eccentric contraction, while holding the weight parallel to the ground is isometric,” they explained in a statement on Eurekalert.
The three exercise groups were compared with a group that did no exercise, and after 4 weeks of rigorous but brief science, the group doing eccentric contractions had the best results, as their overall muscle strength increased by 11.5%. After a total of just 60 seconds of exercise in 4 weeks. That’s 60 seconds. In 4 weeks.
Big news, but maybe we can do better. “Tom, we can do that exercise in 2 seconds.”
And one! And two! Whoa, feel the burn.
Tingling over anxiety
Apparently there are two kinds of people in this world. Those who love ASMR and those who just don’t get it.
ASMR, for those who don’t know, is the autonomous sensory meridian response. An online community has surfaced, with video creators making tapping sounds, whispering, or brushing mannequin hair to elicit “a pleasant tingling sensation originating from the scalp and neck which can spread to the rest of the body” from viewers, Charlotte M. Eid and associates said in PLOS One.
The people who are into these types of videos are more likely to have higher levels of neuroticism than those who aren’t, which gives ASMR the potential to be a nontraditional form of treatment for anxiety and/or neuroticism, they suggested.
The research involved a group of 64 volunteers who watched an ASMR video meant to trigger the tingles and then completed questionnaires to evaluate their levels of neuroticism, trait anxiety, and state anxiety, said Ms. Eid and associates of Northumbria University in Newcastle-upon-Tyne, England.
The people who had a history of producing tingles from ASMR videos in the past had higher levels of anxiety, compared with those who didn’t. Those who responded to triggers also received some benefit from the video in the study, reporting lower levels of neuroticism and anxiety after watching, the investigators found.
Although people who didn’t have a history of tingles didn’t feel any reduction in anxiety after the video, that didn’t stop the people who weren’t familiar with the genre from catching tingles.
So if you find yourself a little high strung or anxious, or if you can’t sleep, consider watching a person pretending to give you a makeover or using fingernails to tap on books for some relaxation. Don’t knock it until you try it!
Living in the past? Not so far-fetched
It’s usually an insult when people tell us to stop living in the past, but the joke’s on them because we really do live in the past. By 15 seconds, to be exact, according to researchers from the University of California, Berkeley.
But wait, did you just read that last sentence 15 seconds ago, even though it feels like real time? Did we just type these words now, or 15 seconds ago?
Think of your brain as a web page you’re constantly refreshing. We are constantly seeing new pictures, images, and colors, and your brain is responsible for keeping everything in chronological order. This new research suggests that our brains show us images from 15 seconds prior. Is your mind blown yet?
“One could say our brain is procrastinating. It’s too much work to constantly update images, so it sticks to the past because the past is a good predictor of the present. We recycle information from the past because it’s faster, more efficient and less work,” senior author David Whitney explained in a statement from the university.
It seems like the 15-second rule helps us not lose our minds by keeping a steady flow of information, but it could be a bit dangerous if someone, such as a surgeon, needs to see things with extreme precision.
And now we are definitely feeling a bit anxious about our upcoming heart/spleen/gallbladder replacement. … Where’s that link to the ASMR video?
Promising leads to crack long COVID discovered
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
It’s a story of promise at a time of urgent need.
They proposed many theories on what might be driving long COVID. A role for a virus “cryptic reservoir” that could reactivate at any time, “viral remnants” that trigger chronic inflammation, and action by “autoimmune antibodies” that cause ongoing symptoms are possibilities.
In fact, it’s likely that research will show long COVID is a condition with more than one cause, the experts said during a recent webinar.
People might experience post-infection problems, including organ damage that takes time to heal after initial COVID-19 illness. Or they may be living with post-immune factors, including ongoing immune system responses triggered by autoantibodies.
Determining the cause or causes of long COVID is essential for treatment. For example, if one person’s symptoms persist because of an overactive immune system, “we need to provide immunosuppressant therapies,” Akiko Iwasaki, PhD, said. “But we don’t want to give that to someone who has a persistent virus reservoir,” meaning remnants of the virus remain in their bodies.
Interestingly, a study preprint, which has not been peer reviewed, found dogs were accurate more than half the time in sniffing out long COVID, said Dr. Iwasaki, professor of immunobiology and developmental biology at Yale University, New Haven, Conn.
The dogs were tasked with identifying 45 people with long COVID versus 188 people without it. The findings suggest the presence of a unique chemical in the sweat of people with long COVID that could someday lead to a diagnostic test.
Viral persistence possible
If one of the main theories holds, it could be that the coronavirus somehow remains in the body in some form for some people after COVID-19.
Mady Hornig, MD, agreed this is a possibility that needs to be investigated further.
“A weakened immune response to an infection may mean that you have cryptic reservoirs of virus that are continuing to cause symptoms,” she said during the briefing. Dr. Hornig is a doctor-scientist specializing in epidemiology at Columbia University, New York.
“That may explain why some patients with long COVID feel better after vaccination,” because the vaccine creates a strong antibody response to fight COVID-19, Dr. Iwasaki said.
Researchers are unearthing additional potential factors contributing to long COVID.
Viral persistence could also reactivate other dormant viruses in the body, such as Epstein-Barr virus (EBV), said Lawrence Purpura, MD, MPH, an infectious disease specialist at New York Presbyterian/Columbia University. Reactivation of Epstein-Barr is one of four identifying signs of long COVID revealed in a Jan. 25 study published in the journal Cell.
Immune overactivation also possible?
For other people with long COVID, it’s not the virus sticking around but the body’s reaction that’s the issue.
Investigators suggest autoimmunity plays a role, and they point to the presence of autoantibodies, for example.
When these autoantibodies persist, they can cause tissue and organ damage over time.
Other investigators are proposing “immune exhaustion” in long COVID because of similarities to chronic fatigue syndrome, Dr. Hornig said.
“It should be ‘all hands on deck’ for research into long COVID,” she said. “The number of disabled individuals who will likely qualify for a diagnosis of [chronic fatigue syndrome] is growing by the second.”
Forging ahead on future research
It’s clear there is more work to do. There are investigators working on banking tissue samples from people with long COVID to learn more, for example.
Also, finding a biomarker unique to long COVID could vastly improve the precision of diagnosing long COVID, especially if the dog sniffing option does not pan out.
Of the thousands of biomarker possibilities, Dr. Hornig said, “maybe that’s one or two that ultimately make a real impact on patient care. So it’s going to be critical to find those quickly, translate them, and make them available.”
In the meantime, some answers might come from a large study sponsored by the National Institutes of Health. The NIH is funding the “Researching COVID to Enhance Recovery” project using $470 million from the American Rescue Plan. Investigators at NYU Langone Health are leading the effort and plan to share the wealth by funding more than 100 researchers at more than 30 institutions to create a “metacohort” to study long COVID. More information is available at recovercovid.org.
“Fortunately, through the global research effort, we are now really starting to expand our understanding of how long COVID manifests, how common it is, and what the underlying mechanisms may be,” Dr. Purpura said.
A version of this article first appeared on WebMD.com.
Endocrine Society and others to FDA: Restrict BPA
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
The chemical is used to make plastics in items such as food containers, pitchers, and inner linings of metal products. Small amounts of BPA can leak into food and beverages.
The petition points to a December 2021 report by the European Food Safety Authority titled: “Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs,” which summarizes evidence gathered since 2013.
It concludes that “there is a health concern from BPA exposure for all age groups.” Specific concerns include harm to the immune system and male and female reproductive systems.
Average American exposed to 5,000 times the safe level of BPA
The EFSA established a new “tolerable daily intake” of BPA of 0.04 ng/kg of body weight per day. By contrast, in 2014 the FDA estimated that the mean BPA intake for the U.S. population older than 2 years was 200 ng/kg bw/day and that the 90th percentile for BPA intake was 500 ng/kg of body weight per day.
“Using FDA’s own exposure estimates, the average American is exposed to more than 5000 times the safe level of 0.04 ng BPA/kg [body weight per day] set by the EFSA expert panel. Without a doubt, these values constitute a high health risk and support the conclusion that uses of BPA are not safe ... Given the magnitude of the overexposure, we request an expedited review by FDA,” the petition reads.
In addition to the Endocrine Society, which has long warned about the dangers of endocrine-disrupting chemicals, other signatories to the petition include the Environmental Defense Fund, Breast Cancer Prevention Partners, Clean Water Action/Clean Water Fund, Consumer Reports, Environmental Working Group, Healthy Babies Bright Futures, and the former director of the National Institute of Environmental Health Sciences and National Toxicology Program.
In a statement, Endocrine Society BPA expert Heather Patisaul, PhD, of North Carolina University, Raleigh, said the report’s findings “are extremely concerning and prove the point that even very low levels of BPA exposure can be harmful and lead to issues with reproductive health, breast cancer risk, behavior, and metabolism.”
“The FDA needs to acknowledge the science behind endocrine-disrupting chemicals and act accordingly to protect public health,” she urged.
The FDA is expected to decide within the next few days whether to open a docket to accept comments.
A final decision could take 6 months or longer, an Endocrine Society spokesperson told this news organization.
A version of this article first appeared on Medscape.com.
Eating dinner late ups diabetes risk; melatonin involved
which increase the risk of type 2 diabetes.
And people who are carriers of the G allele of the MTNR1B gene have greater impairment in glucose tolerance after eating a late dinner.
“In natural late eaters [in Spain], we simulated early and late dinner timing by administering a glucose drink and compared effects on blood sugar control over 2 hours,” said senior author Richa Saxena, PhD, a principal investigator at the Center for Genomic Medicine at Massachusetts General Hospital, Boston.
The study also compared outcomes in carriers and noncarriers of the G allele variant of the melatonin receptor gene, Dr. Saxena pointed out in a press release from the hospital.
“We found that late eating disturbed blood sugar control in the whole group,” added lead author Marta Garaulet, PhD.
“This impaired glucose control was predominantly seen in genetic risk variant carriers, representing about half of the cohort,” said Dr. Garaulet, professor of physiology and nutrition, University of Murcia (Spain).
The study results “may be important in the effort toward prevention of type 2 diabetes,” according to co–senior author Frank A.J.L. Scheer, PhD.
“Our findings are applicable to about a third of the population in the industrialized world who consume food close to bedtime, as well as other populations who eat at night, including shift workers, or those experiencing jet lag or night-eating disorders, as well as those who routinely use melatonin supplements close to food intake,” said Dr. Scheer, director of the medical chronobiology program at Brigham and Women’s Hospital, Boston.
The results suggest people should not eat within 2 hours of bedtime, said the researchers.
“Notably, our study does not include patients with diabetes, so additional studies are needed to examine the impact of food timing and its link with melatonin and receptor variation in patients with diabetes,” Dr. Scheer said.
The findings, from the MTNR1B SNP*Food Timing Interaction on Glucose Control (ONTIME-MT) randomized crossover study, were recently published in Diabetes Care.
Melatonin plays a key role in glucose metabolism
Melatonin, a hormone primarily released at night that helps control the sleep-wake cycle, typically rises around 2 hours before bedtime, the researchers explained.
The discovery of MTNR1B as a type 2 diabetes–associated gene “suggests that, beyond sleep and circadian regulation, melatonin plays a key role in glucose metabolism,” they noted. However, whether melatonin improves or impairs glucose control is controversial, and the effect of MTNR1B genotypes on glucose control is not clear.
“We decided to test if late eating that usually occurs with elevated melatonin levels results in disturbed blood sugar control,” Dr. Saxena explained.
To investigate this, researchers enrolled 845 adults in Spain who were 18-70 years old and did not have diabetes. Participants were a mean age of 38 years and 71% were women. They had a mean body mass index of 25.7 kg/m2 and 18% had obesity.
On average, they typically ate dinner at 21:38 (9:38 p.m.) and went to bed at 24:32 (12:32 a.m.).
DNA analysis from participants’ blood samples determined that 50% had the CC genotype of the MTNR1B gene, 40% had the CG genotype, and 10% had the GG genotype.
Each participant underwent two oral glucose tolerance tests. They fasted for 8 hours and then had a 2-hour 75-g oral glucose tolerance test either 1 hour before bedtime (simulating a late dinner) or 4 hours before bedtime (simulating an early dinner). Then they repeated the test at the opposite dinner time on another night.
The average serum melatonin values were 3.5-fold higher after the late dinner than after the early dinner, resulting in 6.7% lower insulin area under the curve and 8.3% higher glucose AUC.
Genotype differences in glucose tolerance were attributed to reductions in beta-cell function.
“Our results confirm that late eating acutely impairs glucose tolerance through a defect in insulin secretion,” the researchers reiterated.
ONTIME-MT was funded by the National Institutes of Health; the Spanish Government of Investigation, Development, and Innovation; and the Seneca Foundation. The researchers reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
which increase the risk of type 2 diabetes.
And people who are carriers of the G allele of the MTNR1B gene have greater impairment in glucose tolerance after eating a late dinner.
“In natural late eaters [in Spain], we simulated early and late dinner timing by administering a glucose drink and compared effects on blood sugar control over 2 hours,” said senior author Richa Saxena, PhD, a principal investigator at the Center for Genomic Medicine at Massachusetts General Hospital, Boston.
The study also compared outcomes in carriers and noncarriers of the G allele variant of the melatonin receptor gene, Dr. Saxena pointed out in a press release from the hospital.
“We found that late eating disturbed blood sugar control in the whole group,” added lead author Marta Garaulet, PhD.
“This impaired glucose control was predominantly seen in genetic risk variant carriers, representing about half of the cohort,” said Dr. Garaulet, professor of physiology and nutrition, University of Murcia (Spain).
The study results “may be important in the effort toward prevention of type 2 diabetes,” according to co–senior author Frank A.J.L. Scheer, PhD.
“Our findings are applicable to about a third of the population in the industrialized world who consume food close to bedtime, as well as other populations who eat at night, including shift workers, or those experiencing jet lag or night-eating disorders, as well as those who routinely use melatonin supplements close to food intake,” said Dr. Scheer, director of the medical chronobiology program at Brigham and Women’s Hospital, Boston.
The results suggest people should not eat within 2 hours of bedtime, said the researchers.
“Notably, our study does not include patients with diabetes, so additional studies are needed to examine the impact of food timing and its link with melatonin and receptor variation in patients with diabetes,” Dr. Scheer said.
The findings, from the MTNR1B SNP*Food Timing Interaction on Glucose Control (ONTIME-MT) randomized crossover study, were recently published in Diabetes Care.
Melatonin plays a key role in glucose metabolism
Melatonin, a hormone primarily released at night that helps control the sleep-wake cycle, typically rises around 2 hours before bedtime, the researchers explained.
The discovery of MTNR1B as a type 2 diabetes–associated gene “suggests that, beyond sleep and circadian regulation, melatonin plays a key role in glucose metabolism,” they noted. However, whether melatonin improves or impairs glucose control is controversial, and the effect of MTNR1B genotypes on glucose control is not clear.
“We decided to test if late eating that usually occurs with elevated melatonin levels results in disturbed blood sugar control,” Dr. Saxena explained.
To investigate this, researchers enrolled 845 adults in Spain who were 18-70 years old and did not have diabetes. Participants were a mean age of 38 years and 71% were women. They had a mean body mass index of 25.7 kg/m2 and 18% had obesity.
On average, they typically ate dinner at 21:38 (9:38 p.m.) and went to bed at 24:32 (12:32 a.m.).
DNA analysis from participants’ blood samples determined that 50% had the CC genotype of the MTNR1B gene, 40% had the CG genotype, and 10% had the GG genotype.
Each participant underwent two oral glucose tolerance tests. They fasted for 8 hours and then had a 2-hour 75-g oral glucose tolerance test either 1 hour before bedtime (simulating a late dinner) or 4 hours before bedtime (simulating an early dinner). Then they repeated the test at the opposite dinner time on another night.
The average serum melatonin values were 3.5-fold higher after the late dinner than after the early dinner, resulting in 6.7% lower insulin area under the curve and 8.3% higher glucose AUC.
Genotype differences in glucose tolerance were attributed to reductions in beta-cell function.
“Our results confirm that late eating acutely impairs glucose tolerance through a defect in insulin secretion,” the researchers reiterated.
ONTIME-MT was funded by the National Institutes of Health; the Spanish Government of Investigation, Development, and Innovation; and the Seneca Foundation. The researchers reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
which increase the risk of type 2 diabetes.
And people who are carriers of the G allele of the MTNR1B gene have greater impairment in glucose tolerance after eating a late dinner.
“In natural late eaters [in Spain], we simulated early and late dinner timing by administering a glucose drink and compared effects on blood sugar control over 2 hours,” said senior author Richa Saxena, PhD, a principal investigator at the Center for Genomic Medicine at Massachusetts General Hospital, Boston.
The study also compared outcomes in carriers and noncarriers of the G allele variant of the melatonin receptor gene, Dr. Saxena pointed out in a press release from the hospital.
“We found that late eating disturbed blood sugar control in the whole group,” added lead author Marta Garaulet, PhD.
“This impaired glucose control was predominantly seen in genetic risk variant carriers, representing about half of the cohort,” said Dr. Garaulet, professor of physiology and nutrition, University of Murcia (Spain).
The study results “may be important in the effort toward prevention of type 2 diabetes,” according to co–senior author Frank A.J.L. Scheer, PhD.
“Our findings are applicable to about a third of the population in the industrialized world who consume food close to bedtime, as well as other populations who eat at night, including shift workers, or those experiencing jet lag or night-eating disorders, as well as those who routinely use melatonin supplements close to food intake,” said Dr. Scheer, director of the medical chronobiology program at Brigham and Women’s Hospital, Boston.
The results suggest people should not eat within 2 hours of bedtime, said the researchers.
“Notably, our study does not include patients with diabetes, so additional studies are needed to examine the impact of food timing and its link with melatonin and receptor variation in patients with diabetes,” Dr. Scheer said.
The findings, from the MTNR1B SNP*Food Timing Interaction on Glucose Control (ONTIME-MT) randomized crossover study, were recently published in Diabetes Care.
Melatonin plays a key role in glucose metabolism
Melatonin, a hormone primarily released at night that helps control the sleep-wake cycle, typically rises around 2 hours before bedtime, the researchers explained.
The discovery of MTNR1B as a type 2 diabetes–associated gene “suggests that, beyond sleep and circadian regulation, melatonin plays a key role in glucose metabolism,” they noted. However, whether melatonin improves or impairs glucose control is controversial, and the effect of MTNR1B genotypes on glucose control is not clear.
“We decided to test if late eating that usually occurs with elevated melatonin levels results in disturbed blood sugar control,” Dr. Saxena explained.
To investigate this, researchers enrolled 845 adults in Spain who were 18-70 years old and did not have diabetes. Participants were a mean age of 38 years and 71% were women. They had a mean body mass index of 25.7 kg/m2 and 18% had obesity.
On average, they typically ate dinner at 21:38 (9:38 p.m.) and went to bed at 24:32 (12:32 a.m.).
DNA analysis from participants’ blood samples determined that 50% had the CC genotype of the MTNR1B gene, 40% had the CG genotype, and 10% had the GG genotype.
Each participant underwent two oral glucose tolerance tests. They fasted for 8 hours and then had a 2-hour 75-g oral glucose tolerance test either 1 hour before bedtime (simulating a late dinner) or 4 hours before bedtime (simulating an early dinner). Then they repeated the test at the opposite dinner time on another night.
The average serum melatonin values were 3.5-fold higher after the late dinner than after the early dinner, resulting in 6.7% lower insulin area under the curve and 8.3% higher glucose AUC.
Genotype differences in glucose tolerance were attributed to reductions in beta-cell function.
“Our results confirm that late eating acutely impairs glucose tolerance through a defect in insulin secretion,” the researchers reiterated.
ONTIME-MT was funded by the National Institutes of Health; the Spanish Government of Investigation, Development, and Innovation; and the Seneca Foundation. The researchers reported no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE
Updated endometriosis guidelines emphasize less laparoscopy, more hormone therapy
Updated guidelines for the management and treatment of endometriosis reflect changes in clinical practice to guide clinician and patient decision-making, according to a statement from the European Society of Human Reproduction and Embryology, which issued the guidelines in February 2022.
Although the exact prevalence of endometriosis remains unclear, estimates suggest that approximately 190 million women and adolescent girls are affected by endometriosis during their reproductive years, and women continue to suffer beyond menopause, according to the authors. Endometriosis has a significant impact on society through both direct and indirect health care costs comparable to those of type 2 diabetes, rheumatoid arthritis, and Crohn’s disease, they noted.
The guidelines are the first update on the topic of endometriosis since 2014, and include more than 100 recommendations, according to the European Society of Human Reproduction and Embryology (ESHRE). The target audience, according to the authors, is secondary and tertiary health care providers who treat women with endometriosis. The recommendations were based on research papers published up to Dec. 1, 2020.
Although most of the recent studies confirm previous ESHRE recommendations, several topics reflect significant changes in clinical practice.
Notably, laparoscopy is no longer recommended as the diagnostic gold standard, and should be used only in patients with negative imaging for whom empirical treatment was unsuccessful.
For pain management, studies support the use of GnRH antagonists as a second-line treatment, while laparoscopic uterosacral nerve ablation and presacral neurectomy are no longer included in the recommendations.
The guidelines include new information on pregnancy and fertility preservation for women with endometriosis. The Endometriosis Fertility Index (EFI) was added to support joint decision-making for women seeking pregnancy after surgery. However, the extended use of GnRH antagonist prior to assisted reproductive technology treatments to improve live birth rate is not recommended.
Endometriosis in adolescent patients is included in the guidelines for the first time, and strong recommendations include taking a careful history and using ultrasound if appropriate, but the use of serum biomarkers is not recommended for diagnosis. Strong recommendations for treatment strategies for adolescents include hormonal contraceptives or progestins as a first-line therapy.
Recommendations for managing endometriosis in menopause are more extensive than in previous guidelines and the strongest update is against the use of estrogen-only treatment in these patients. However, the guidelines continue to recommend treating women with a history of endometriosis after surgical menopause with combined estrogen-progestogen therapy “at least up to the age of natural menopause.”
Expanded recommendations related to endometriosis and cancer begin with a strong recommendation for clinicians to advise women that endometriosis is not associated with a significantly higher risk of cancer overall. “Although endometriosis is associated with a higher risk of ovarian, breast, and thyroid cancers in particular, the increase in absolute risk compared with women in the general population is low,” the authors wrote. Other strong recommendations include reassuring women with endometriosis of the low risk of malignancy associated with hormonal contraceptive use, and performing cancer screening according to the existing population-based guidelines without additional screening. Epidemiologic data show that complete excision of visible endometriosis may reduce the risk of ovarian cancer, but the potential benefits must be weighed against the risks of surgery, including morbidity, pain, and ovarian reserve, the authors said.
The guidelines include recommendations related to asymptomatic endometriosis, extrapelvic endometriosis, and primary prevention of endometriosis, but without major changes to the 2014 guidelines.
Guidelines expand strategies, but research gaps remain
In 2021, an international working group of the American Association of Gynecologic Laparoscopists, the European Society for Gynecologic Endoscopy, ESHRE, and the World Endometriosis Society defined endometriosis as “a disease characterized by the presence of endometrium-like epithelium and/or stroma outside the endometrium and myometrium, usually with an associated inflammatory process,” Mark P. Trolice, MD, director of The IVF Center, Orlando, Fla., and professor of obstetrics and gynecology at the University of Central Florida, said in an interview.
Although the current guidelines represent the second update since 2005, many unanswered questions remain, Dr. Trolice said. “There is a large diagnostic void between the onset of symptoms and the time to a reliable diagnosis averaging between 8 and 12 years,” he emphasized.
Dr. Trolice noted the change of the addition of an oral GnRH antagonist, “now FDA approved for the treatment of pain associated with endometriosis,” he said. However, “Extended GnRH agonist prior to ART is not recommended due to the lack of any clear benefit,” he noted.
Dr. Trolice noted the inclusion of the Endometriosis Fertility Index (EFI), published in 2010, “as a useful scoring system to predict postoperative non-IVF pregnancy rates (both by natural means and IUI [intrauterine insemination]) based on patient characteristics, revised ASRM staging, and ‘least function score of the adnexa.’ ” He agreed with the need for expanded information on the topics of endometriosis and adolescence and endometriosis and cancer.
The most important changes for clinical practice include reducing unnecessary laparoscopy and procedures without benefit, such as laparoscopic uterosacral nerve ablation and presacral neurectomy, and GnRH suppression using an oral antagonist, said Dr. Trolice. Other especially practical guidance includes the recommendation to discontinue advising patients that pregnancy will reduce symptoms of endometriosis, and to avoid prescribing estrogen-only treatment in menopause given the risk of malignant transformation of endometriosis, he said.
Another clinically useful recommendation, though not a significant update, is the need to identify extrapelvic endometriosis symptoms, such as cyclical shoulder pain, cyclical spontaneous pneumothorax, cyclical cough, or nodules that enlarge during menses, Dr. Trolice added.
Barriers to implementing the updated guidelines include lack of education of clinicians, including primary care providers, and the lack of definitive evidence for many areas, he noted.
As for additional research, more data are needed to explore the genetic, mutational, and epigenetic profile of endometriosis, and to identify biomarkers to noninvasively detect and provide a prognosis for endometriosis, and optimal methods for prevention and management, said Dr. Trolice. Other research gaps include “definitive medical and surgical treatment of endometriosis for improvement of fertility, quality of life, and reduction of pain,” he noted. From a fertility standpoint, more studies are needed on “the use of ovarian tissue or oocytes cryopreservation in adolescents and adults who undergo ovarian surgery for endometriomas, and the role of the EFI as a presurgical triage tool and to predict IUI outcomes,” said Dr. Trolice.
Overall, society recommendations such as these from ESHRE “serve as guides for physicians by providing evidence-based medicine and dispelling prior unproven practices so patients may receive the most effective care of endometriosis, throughout a woman’s life,” Dr. Trolice emphasized.
The current guideline will be considered for revision in 2025, and the full version is available on the ESHRE website.
Members of the ESHRE guideline development group received no payment for participating in the development process, although they were reimbursed for travel expenses related to guideline meetings.
Dr. Trolice had no financial conflicts to disclose and serves on the editorial advisory board of Ob.Gyn News.
Updated guidelines for the management and treatment of endometriosis reflect changes in clinical practice to guide clinician and patient decision-making, according to a statement from the European Society of Human Reproduction and Embryology, which issued the guidelines in February 2022.
Although the exact prevalence of endometriosis remains unclear, estimates suggest that approximately 190 million women and adolescent girls are affected by endometriosis during their reproductive years, and women continue to suffer beyond menopause, according to the authors. Endometriosis has a significant impact on society through both direct and indirect health care costs comparable to those of type 2 diabetes, rheumatoid arthritis, and Crohn’s disease, they noted.
The guidelines are the first update on the topic of endometriosis since 2014, and include more than 100 recommendations, according to the European Society of Human Reproduction and Embryology (ESHRE). The target audience, according to the authors, is secondary and tertiary health care providers who treat women with endometriosis. The recommendations were based on research papers published up to Dec. 1, 2020.
Although most of the recent studies confirm previous ESHRE recommendations, several topics reflect significant changes in clinical practice.
Notably, laparoscopy is no longer recommended as the diagnostic gold standard, and should be used only in patients with negative imaging for whom empirical treatment was unsuccessful.
For pain management, studies support the use of GnRH antagonists as a second-line treatment, while laparoscopic uterosacral nerve ablation and presacral neurectomy are no longer included in the recommendations.
The guidelines include new information on pregnancy and fertility preservation for women with endometriosis. The Endometriosis Fertility Index (EFI) was added to support joint decision-making for women seeking pregnancy after surgery. However, the extended use of GnRH antagonist prior to assisted reproductive technology treatments to improve live birth rate is not recommended.
Endometriosis in adolescent patients is included in the guidelines for the first time, and strong recommendations include taking a careful history and using ultrasound if appropriate, but the use of serum biomarkers is not recommended for diagnosis. Strong recommendations for treatment strategies for adolescents include hormonal contraceptives or progestins as a first-line therapy.
Recommendations for managing endometriosis in menopause are more extensive than in previous guidelines and the strongest update is against the use of estrogen-only treatment in these patients. However, the guidelines continue to recommend treating women with a history of endometriosis after surgical menopause with combined estrogen-progestogen therapy “at least up to the age of natural menopause.”
Expanded recommendations related to endometriosis and cancer begin with a strong recommendation for clinicians to advise women that endometriosis is not associated with a significantly higher risk of cancer overall. “Although endometriosis is associated with a higher risk of ovarian, breast, and thyroid cancers in particular, the increase in absolute risk compared with women in the general population is low,” the authors wrote. Other strong recommendations include reassuring women with endometriosis of the low risk of malignancy associated with hormonal contraceptive use, and performing cancer screening according to the existing population-based guidelines without additional screening. Epidemiologic data show that complete excision of visible endometriosis may reduce the risk of ovarian cancer, but the potential benefits must be weighed against the risks of surgery, including morbidity, pain, and ovarian reserve, the authors said.
The guidelines include recommendations related to asymptomatic endometriosis, extrapelvic endometriosis, and primary prevention of endometriosis, but without major changes to the 2014 guidelines.
Guidelines expand strategies, but research gaps remain
In 2021, an international working group of the American Association of Gynecologic Laparoscopists, the European Society for Gynecologic Endoscopy, ESHRE, and the World Endometriosis Society defined endometriosis as “a disease characterized by the presence of endometrium-like epithelium and/or stroma outside the endometrium and myometrium, usually with an associated inflammatory process,” Mark P. Trolice, MD, director of The IVF Center, Orlando, Fla., and professor of obstetrics and gynecology at the University of Central Florida, said in an interview.
Although the current guidelines represent the second update since 2005, many unanswered questions remain, Dr. Trolice said. “There is a large diagnostic void between the onset of symptoms and the time to a reliable diagnosis averaging between 8 and 12 years,” he emphasized.
Dr. Trolice noted the change of the addition of an oral GnRH antagonist, “now FDA approved for the treatment of pain associated with endometriosis,” he said. However, “Extended GnRH agonist prior to ART is not recommended due to the lack of any clear benefit,” he noted.
Dr. Trolice noted the inclusion of the Endometriosis Fertility Index (EFI), published in 2010, “as a useful scoring system to predict postoperative non-IVF pregnancy rates (both by natural means and IUI [intrauterine insemination]) based on patient characteristics, revised ASRM staging, and ‘least function score of the adnexa.’ ” He agreed with the need for expanded information on the topics of endometriosis and adolescence and endometriosis and cancer.
The most important changes for clinical practice include reducing unnecessary laparoscopy and procedures without benefit, such as laparoscopic uterosacral nerve ablation and presacral neurectomy, and GnRH suppression using an oral antagonist, said Dr. Trolice. Other especially practical guidance includes the recommendation to discontinue advising patients that pregnancy will reduce symptoms of endometriosis, and to avoid prescribing estrogen-only treatment in menopause given the risk of malignant transformation of endometriosis, he said.
Another clinically useful recommendation, though not a significant update, is the need to identify extrapelvic endometriosis symptoms, such as cyclical shoulder pain, cyclical spontaneous pneumothorax, cyclical cough, or nodules that enlarge during menses, Dr. Trolice added.
Barriers to implementing the updated guidelines include lack of education of clinicians, including primary care providers, and the lack of definitive evidence for many areas, he noted.
As for additional research, more data are needed to explore the genetic, mutational, and epigenetic profile of endometriosis, and to identify biomarkers to noninvasively detect and provide a prognosis for endometriosis, and optimal methods for prevention and management, said Dr. Trolice. Other research gaps include “definitive medical and surgical treatment of endometriosis for improvement of fertility, quality of life, and reduction of pain,” he noted. From a fertility standpoint, more studies are needed on “the use of ovarian tissue or oocytes cryopreservation in adolescents and adults who undergo ovarian surgery for endometriomas, and the role of the EFI as a presurgical triage tool and to predict IUI outcomes,” said Dr. Trolice.
Overall, society recommendations such as these from ESHRE “serve as guides for physicians by providing evidence-based medicine and dispelling prior unproven practices so patients may receive the most effective care of endometriosis, throughout a woman’s life,” Dr. Trolice emphasized.
The current guideline will be considered for revision in 2025, and the full version is available on the ESHRE website.
Members of the ESHRE guideline development group received no payment for participating in the development process, although they were reimbursed for travel expenses related to guideline meetings.
Dr. Trolice had no financial conflicts to disclose and serves on the editorial advisory board of Ob.Gyn News.
Updated guidelines for the management and treatment of endometriosis reflect changes in clinical practice to guide clinician and patient decision-making, according to a statement from the European Society of Human Reproduction and Embryology, which issued the guidelines in February 2022.
Although the exact prevalence of endometriosis remains unclear, estimates suggest that approximately 190 million women and adolescent girls are affected by endometriosis during their reproductive years, and women continue to suffer beyond menopause, according to the authors. Endometriosis has a significant impact on society through both direct and indirect health care costs comparable to those of type 2 diabetes, rheumatoid arthritis, and Crohn’s disease, they noted.
The guidelines are the first update on the topic of endometriosis since 2014, and include more than 100 recommendations, according to the European Society of Human Reproduction and Embryology (ESHRE). The target audience, according to the authors, is secondary and tertiary health care providers who treat women with endometriosis. The recommendations were based on research papers published up to Dec. 1, 2020.
Although most of the recent studies confirm previous ESHRE recommendations, several topics reflect significant changes in clinical practice.
Notably, laparoscopy is no longer recommended as the diagnostic gold standard, and should be used only in patients with negative imaging for whom empirical treatment was unsuccessful.
For pain management, studies support the use of GnRH antagonists as a second-line treatment, while laparoscopic uterosacral nerve ablation and presacral neurectomy are no longer included in the recommendations.
The guidelines include new information on pregnancy and fertility preservation for women with endometriosis. The Endometriosis Fertility Index (EFI) was added to support joint decision-making for women seeking pregnancy after surgery. However, the extended use of GnRH antagonist prior to assisted reproductive technology treatments to improve live birth rate is not recommended.
Endometriosis in adolescent patients is included in the guidelines for the first time, and strong recommendations include taking a careful history and using ultrasound if appropriate, but the use of serum biomarkers is not recommended for diagnosis. Strong recommendations for treatment strategies for adolescents include hormonal contraceptives or progestins as a first-line therapy.
Recommendations for managing endometriosis in menopause are more extensive than in previous guidelines and the strongest update is against the use of estrogen-only treatment in these patients. However, the guidelines continue to recommend treating women with a history of endometriosis after surgical menopause with combined estrogen-progestogen therapy “at least up to the age of natural menopause.”
Expanded recommendations related to endometriosis and cancer begin with a strong recommendation for clinicians to advise women that endometriosis is not associated with a significantly higher risk of cancer overall. “Although endometriosis is associated with a higher risk of ovarian, breast, and thyroid cancers in particular, the increase in absolute risk compared with women in the general population is low,” the authors wrote. Other strong recommendations include reassuring women with endometriosis of the low risk of malignancy associated with hormonal contraceptive use, and performing cancer screening according to the existing population-based guidelines without additional screening. Epidemiologic data show that complete excision of visible endometriosis may reduce the risk of ovarian cancer, but the potential benefits must be weighed against the risks of surgery, including morbidity, pain, and ovarian reserve, the authors said.
The guidelines include recommendations related to asymptomatic endometriosis, extrapelvic endometriosis, and primary prevention of endometriosis, but without major changes to the 2014 guidelines.
Guidelines expand strategies, but research gaps remain
In 2021, an international working group of the American Association of Gynecologic Laparoscopists, the European Society for Gynecologic Endoscopy, ESHRE, and the World Endometriosis Society defined endometriosis as “a disease characterized by the presence of endometrium-like epithelium and/or stroma outside the endometrium and myometrium, usually with an associated inflammatory process,” Mark P. Trolice, MD, director of The IVF Center, Orlando, Fla., and professor of obstetrics and gynecology at the University of Central Florida, said in an interview.
Although the current guidelines represent the second update since 2005, many unanswered questions remain, Dr. Trolice said. “There is a large diagnostic void between the onset of symptoms and the time to a reliable diagnosis averaging between 8 and 12 years,” he emphasized.
Dr. Trolice noted the change of the addition of an oral GnRH antagonist, “now FDA approved for the treatment of pain associated with endometriosis,” he said. However, “Extended GnRH agonist prior to ART is not recommended due to the lack of any clear benefit,” he noted.
Dr. Trolice noted the inclusion of the Endometriosis Fertility Index (EFI), published in 2010, “as a useful scoring system to predict postoperative non-IVF pregnancy rates (both by natural means and IUI [intrauterine insemination]) based on patient characteristics, revised ASRM staging, and ‘least function score of the adnexa.’ ” He agreed with the need for expanded information on the topics of endometriosis and adolescence and endometriosis and cancer.
The most important changes for clinical practice include reducing unnecessary laparoscopy and procedures without benefit, such as laparoscopic uterosacral nerve ablation and presacral neurectomy, and GnRH suppression using an oral antagonist, said Dr. Trolice. Other especially practical guidance includes the recommendation to discontinue advising patients that pregnancy will reduce symptoms of endometriosis, and to avoid prescribing estrogen-only treatment in menopause given the risk of malignant transformation of endometriosis, he said.
Another clinically useful recommendation, though not a significant update, is the need to identify extrapelvic endometriosis symptoms, such as cyclical shoulder pain, cyclical spontaneous pneumothorax, cyclical cough, or nodules that enlarge during menses, Dr. Trolice added.
Barriers to implementing the updated guidelines include lack of education of clinicians, including primary care providers, and the lack of definitive evidence for many areas, he noted.
As for additional research, more data are needed to explore the genetic, mutational, and epigenetic profile of endometriosis, and to identify biomarkers to noninvasively detect and provide a prognosis for endometriosis, and optimal methods for prevention and management, said Dr. Trolice. Other research gaps include “definitive medical and surgical treatment of endometriosis for improvement of fertility, quality of life, and reduction of pain,” he noted. From a fertility standpoint, more studies are needed on “the use of ovarian tissue or oocytes cryopreservation in adolescents and adults who undergo ovarian surgery for endometriomas, and the role of the EFI as a presurgical triage tool and to predict IUI outcomes,” said Dr. Trolice.
Overall, society recommendations such as these from ESHRE “serve as guides for physicians by providing evidence-based medicine and dispelling prior unproven practices so patients may receive the most effective care of endometriosis, throughout a woman’s life,” Dr. Trolice emphasized.
The current guideline will be considered for revision in 2025, and the full version is available on the ESHRE website.
Members of the ESHRE guideline development group received no payment for participating in the development process, although they were reimbursed for travel expenses related to guideline meetings.
Dr. Trolice had no financial conflicts to disclose and serves on the editorial advisory board of Ob.Gyn News.
LGBTQ parents fare worse giving birth
Members of the LGBTQ community who give birth appear to have a greater risk of hypertensive disorders of pregnancy and postpartum hemorrhage, according to new research presented at the annual meeting sponsored by the Society for Maternal-Fetal Medicine.
“Our study found that birthing patients in likely sexual and gender minority partnerships experienced disparities in clinical outcomes,” Stephanie Leonard, PhD, an epidemiology and biostatistics instructor at the Stanford (Calif.) University division of maternal-fetal medicine and obstetrics, told attendees at the meeting. The disparities are likely because of various social determinants and possibly higher use of assisted reproductive technology (ART). The findings establish “how these are significant disparities that have been largely overlooked and set the groundwork for doing further research on maybe ways that we can improve the inclusivity of obstetric care.”
Jenny Mei, MD, a maternal-fetal medicine fellow at the University of California, Los Angeles, who attended the presentation but was not involved in the research, said the findings were “overall unfortunate but not surprising given the existing studies looking at LGBTQ patients and their poorer health outcomes, largely due to lack of access to health care and discrimination in the health care setting.”
Dr. Leonard described the societal, interpersonal, and individual factors that can contribute to health disparities among gender and sexual minority patients.
“At the societal level, there are expectations of what it means to be pregnant, to give birth, and to be a parent. At the community level, there’s the clinical care environment, and at the interpersonal level, there’s an obstetrician’s relationship with the patient,” Dr. Leonard said. “At the individual level, most notably is minority stress, the biological effects of the chronic experience of discrimination.”
It has historically been difficult to collect data on this patient population, but a change in the design of the California birth certificate made it possible to gather more data than previously possible. The updated California birth certificate, issued in 2016, allows the parent not giving birth to check off whether they are the child’s mother, father, parent, or “not specified” instead of defaulting to “father.” In addition, the parent giving birth can select mother, father, parent or not specified instead of being “mother” by default.
The researchers classified sexual and gender minority (SGM) partnerships as those in which the parent giving birth was identified as the father and those where both parents were identified as mothers. Non-SGM minority partnerships were those in which the birthing parent was identified as the mother and the nonbirthing parent was identified as the father.
The population-based cohort study included data from all live birth hospitalizations from 2016-2019 in California, whose annual births represent one in eight babies born each year in the United States. The population of SGM patients different significantly from the non-SGM population in nearly every demographic and clinical factor except rates of pre-existing diabetes. For example, 42% of the SGM birthing patients were age 35 or older, compared with 23% of the non-SGM patients.
SGM patients were more likely to be born in the United States, were more likely to be White, and were less likely to be Asian or Hispanic. SGM patients had higher education levels and were more likely to have private insurance. They were also more likely to be nulliparous and have chronic hypertension. Average body mass index for SGM patients was 33 kg/m2, compared with 30 for non-SGM patients. SGM patients were also much more likely to have multifetal gestation: 7.1% of SGM patients versus 1.5% of non-SGM patients.
In terms of clinical outcomes, 14% of SGM patients had hypertensive disorders of pregnancy, compared with 8% of non-SGM patients. Before adjustment for potential confounders, SGM patients were also twice as likely to have postpartum hemorrhage (8% vs. 4% in non-SGM patients) and postterm birth at 42-44 weeks (0.6% vs 0.3% in non-SGM patients).
“Having increased postterm birth is a matter of declining induction of labor, as it is recommended to have an induction by 41 weeks of gestation in general,” Dr. Mei said in an interview. “It is also possible this patient cohort faces more barriers in access to care and possible discrimination as sexual/gender minority patients.”
Rates of severe preeclampsia, induction of labor, cesarean delivery, preterm birth, low birth weight, and a low Apgar score were also higher among SGM patients, but these associations were no longer significant after adjustment for age, education, payment method, parity, prepregnancy weight, comorbidities, and multifetal gestation. The difference in hypertensive disorders of pregnancy, postpartum hemorrhage, and postterm birth remained statistically significant after adjustment.
Past research has shown that only about a third of cisgender female same-sex marriages used ART, so the disparities cannot be completely explained by ART use, Dr. Leonard said.
“I think the main drivers are structural disparities,” Dr. Leonard said. “Every obstetric clinic is focused in a way that’s about mother-father, and many people who don’t feel like they fit into that paradigm feel excluded and disengage with health care.”
Elliott Main, MD, a clinical professor of obstetrics and gynecology at Stanford University and coauthor of the study noted that discrimination and stigma likely play a substantial role in the disparities.
“Sexual and/or gender minority people face this discrimination at structural and interpersonal levels on a regular basis, which can lead to chronic stress and its harmful physical effects as well as lower-quality health care,” Dr. Main said in an interview.
Another coauthor, Juno Obedin-Maliver, MD, an assistant professor of obstetrics and gynecology at Stanford, emphasized how much room for improvement exists in care for SGM obstetric patients.
“We hope that this study brings needed attention to the disparities in perinatal health experienced by sexual and/or gender minority people,” Dr. Obedin-Maliver said. “There is much we can do to better understand the family building goals of sexual and/or gender minority people and help those to be achieved with healthy outcomes for parents and their children.”
One limitation of the study is that it’s possible to misclassify individuals using the birth certificate data, and not everyone may be comfortable selecting the box that accurately represents their identity, particularly if they aren’t “out” or fear discrimination or stigma, so the population may underrepresent the actual numbers of sexual and gender minority individuals giving birth. Dr. Mei added that it would be helpful to see data on neonatal ICU admissions and use of ART.
It’s difficult to say how generalizable the findings are, Dr. Mei said. “It is possible the findings would be more exaggerated in the rest of the country outside of California, if we assume there is potentially lower health access and more stigma.” The fact that California offers different gender options for the birthing and nonbirthing parent is, by itself, an indication of a potentially more accepting social environment than might be found in other states.
”The take-home message is that this patient population is higher risk, likely partially due to baseline increased risk factors, such as older maternal age and likely use of ART, and partially due to possible lack of health access and stigma,” Dr. Mei said. “Health care providers should be notably cognizant of these increased risks, particularly in the psychosocial context and make efforts to reduce those burdens as much as possible.”
The research was funded by the Stanford Maternal and Child Health Research Institute. Dr. Obedin-Maliver has consulted for Sage Therapeutics, Ibis Reproductive Health, and Hims. Dr. Mei and the other authors had no disclosures.
Members of the LGBTQ community who give birth appear to have a greater risk of hypertensive disorders of pregnancy and postpartum hemorrhage, according to new research presented at the annual meeting sponsored by the Society for Maternal-Fetal Medicine.
“Our study found that birthing patients in likely sexual and gender minority partnerships experienced disparities in clinical outcomes,” Stephanie Leonard, PhD, an epidemiology and biostatistics instructor at the Stanford (Calif.) University division of maternal-fetal medicine and obstetrics, told attendees at the meeting. The disparities are likely because of various social determinants and possibly higher use of assisted reproductive technology (ART). The findings establish “how these are significant disparities that have been largely overlooked and set the groundwork for doing further research on maybe ways that we can improve the inclusivity of obstetric care.”
Jenny Mei, MD, a maternal-fetal medicine fellow at the University of California, Los Angeles, who attended the presentation but was not involved in the research, said the findings were “overall unfortunate but not surprising given the existing studies looking at LGBTQ patients and their poorer health outcomes, largely due to lack of access to health care and discrimination in the health care setting.”
Dr. Leonard described the societal, interpersonal, and individual factors that can contribute to health disparities among gender and sexual minority patients.
“At the societal level, there are expectations of what it means to be pregnant, to give birth, and to be a parent. At the community level, there’s the clinical care environment, and at the interpersonal level, there’s an obstetrician’s relationship with the patient,” Dr. Leonard said. “At the individual level, most notably is minority stress, the biological effects of the chronic experience of discrimination.”
It has historically been difficult to collect data on this patient population, but a change in the design of the California birth certificate made it possible to gather more data than previously possible. The updated California birth certificate, issued in 2016, allows the parent not giving birth to check off whether they are the child’s mother, father, parent, or “not specified” instead of defaulting to “father.” In addition, the parent giving birth can select mother, father, parent or not specified instead of being “mother” by default.
The researchers classified sexual and gender minority (SGM) partnerships as those in which the parent giving birth was identified as the father and those where both parents were identified as mothers. Non-SGM minority partnerships were those in which the birthing parent was identified as the mother and the nonbirthing parent was identified as the father.
The population-based cohort study included data from all live birth hospitalizations from 2016-2019 in California, whose annual births represent one in eight babies born each year in the United States. The population of SGM patients different significantly from the non-SGM population in nearly every demographic and clinical factor except rates of pre-existing diabetes. For example, 42% of the SGM birthing patients were age 35 or older, compared with 23% of the non-SGM patients.
SGM patients were more likely to be born in the United States, were more likely to be White, and were less likely to be Asian or Hispanic. SGM patients had higher education levels and were more likely to have private insurance. They were also more likely to be nulliparous and have chronic hypertension. Average body mass index for SGM patients was 33 kg/m2, compared with 30 for non-SGM patients. SGM patients were also much more likely to have multifetal gestation: 7.1% of SGM patients versus 1.5% of non-SGM patients.
In terms of clinical outcomes, 14% of SGM patients had hypertensive disorders of pregnancy, compared with 8% of non-SGM patients. Before adjustment for potential confounders, SGM patients were also twice as likely to have postpartum hemorrhage (8% vs. 4% in non-SGM patients) and postterm birth at 42-44 weeks (0.6% vs 0.3% in non-SGM patients).
“Having increased postterm birth is a matter of declining induction of labor, as it is recommended to have an induction by 41 weeks of gestation in general,” Dr. Mei said in an interview. “It is also possible this patient cohort faces more barriers in access to care and possible discrimination as sexual/gender minority patients.”
Rates of severe preeclampsia, induction of labor, cesarean delivery, preterm birth, low birth weight, and a low Apgar score were also higher among SGM patients, but these associations were no longer significant after adjustment for age, education, payment method, parity, prepregnancy weight, comorbidities, and multifetal gestation. The difference in hypertensive disorders of pregnancy, postpartum hemorrhage, and postterm birth remained statistically significant after adjustment.
Past research has shown that only about a third of cisgender female same-sex marriages used ART, so the disparities cannot be completely explained by ART use, Dr. Leonard said.
“I think the main drivers are structural disparities,” Dr. Leonard said. “Every obstetric clinic is focused in a way that’s about mother-father, and many people who don’t feel like they fit into that paradigm feel excluded and disengage with health care.”
Elliott Main, MD, a clinical professor of obstetrics and gynecology at Stanford University and coauthor of the study noted that discrimination and stigma likely play a substantial role in the disparities.
“Sexual and/or gender minority people face this discrimination at structural and interpersonal levels on a regular basis, which can lead to chronic stress and its harmful physical effects as well as lower-quality health care,” Dr. Main said in an interview.
Another coauthor, Juno Obedin-Maliver, MD, an assistant professor of obstetrics and gynecology at Stanford, emphasized how much room for improvement exists in care for SGM obstetric patients.
“We hope that this study brings needed attention to the disparities in perinatal health experienced by sexual and/or gender minority people,” Dr. Obedin-Maliver said. “There is much we can do to better understand the family building goals of sexual and/or gender minority people and help those to be achieved with healthy outcomes for parents and their children.”
One limitation of the study is that it’s possible to misclassify individuals using the birth certificate data, and not everyone may be comfortable selecting the box that accurately represents their identity, particularly if they aren’t “out” or fear discrimination or stigma, so the population may underrepresent the actual numbers of sexual and gender minority individuals giving birth. Dr. Mei added that it would be helpful to see data on neonatal ICU admissions and use of ART.
It’s difficult to say how generalizable the findings are, Dr. Mei said. “It is possible the findings would be more exaggerated in the rest of the country outside of California, if we assume there is potentially lower health access and more stigma.” The fact that California offers different gender options for the birthing and nonbirthing parent is, by itself, an indication of a potentially more accepting social environment than might be found in other states.
”The take-home message is that this patient population is higher risk, likely partially due to baseline increased risk factors, such as older maternal age and likely use of ART, and partially due to possible lack of health access and stigma,” Dr. Mei said. “Health care providers should be notably cognizant of these increased risks, particularly in the psychosocial context and make efforts to reduce those burdens as much as possible.”
The research was funded by the Stanford Maternal and Child Health Research Institute. Dr. Obedin-Maliver has consulted for Sage Therapeutics, Ibis Reproductive Health, and Hims. Dr. Mei and the other authors had no disclosures.
Members of the LGBTQ community who give birth appear to have a greater risk of hypertensive disorders of pregnancy and postpartum hemorrhage, according to new research presented at the annual meeting sponsored by the Society for Maternal-Fetal Medicine.
“Our study found that birthing patients in likely sexual and gender minority partnerships experienced disparities in clinical outcomes,” Stephanie Leonard, PhD, an epidemiology and biostatistics instructor at the Stanford (Calif.) University division of maternal-fetal medicine and obstetrics, told attendees at the meeting. The disparities are likely because of various social determinants and possibly higher use of assisted reproductive technology (ART). The findings establish “how these are significant disparities that have been largely overlooked and set the groundwork for doing further research on maybe ways that we can improve the inclusivity of obstetric care.”
Jenny Mei, MD, a maternal-fetal medicine fellow at the University of California, Los Angeles, who attended the presentation but was not involved in the research, said the findings were “overall unfortunate but not surprising given the existing studies looking at LGBTQ patients and their poorer health outcomes, largely due to lack of access to health care and discrimination in the health care setting.”
Dr. Leonard described the societal, interpersonal, and individual factors that can contribute to health disparities among gender and sexual minority patients.
“At the societal level, there are expectations of what it means to be pregnant, to give birth, and to be a parent. At the community level, there’s the clinical care environment, and at the interpersonal level, there’s an obstetrician’s relationship with the patient,” Dr. Leonard said. “At the individual level, most notably is minority stress, the biological effects of the chronic experience of discrimination.”
It has historically been difficult to collect data on this patient population, but a change in the design of the California birth certificate made it possible to gather more data than previously possible. The updated California birth certificate, issued in 2016, allows the parent not giving birth to check off whether they are the child’s mother, father, parent, or “not specified” instead of defaulting to “father.” In addition, the parent giving birth can select mother, father, parent or not specified instead of being “mother” by default.
The researchers classified sexual and gender minority (SGM) partnerships as those in which the parent giving birth was identified as the father and those where both parents were identified as mothers. Non-SGM minority partnerships were those in which the birthing parent was identified as the mother and the nonbirthing parent was identified as the father.
The population-based cohort study included data from all live birth hospitalizations from 2016-2019 in California, whose annual births represent one in eight babies born each year in the United States. The population of SGM patients different significantly from the non-SGM population in nearly every demographic and clinical factor except rates of pre-existing diabetes. For example, 42% of the SGM birthing patients were age 35 or older, compared with 23% of the non-SGM patients.
SGM patients were more likely to be born in the United States, were more likely to be White, and were less likely to be Asian or Hispanic. SGM patients had higher education levels and were more likely to have private insurance. They were also more likely to be nulliparous and have chronic hypertension. Average body mass index for SGM patients was 33 kg/m2, compared with 30 for non-SGM patients. SGM patients were also much more likely to have multifetal gestation: 7.1% of SGM patients versus 1.5% of non-SGM patients.
In terms of clinical outcomes, 14% of SGM patients had hypertensive disorders of pregnancy, compared with 8% of non-SGM patients. Before adjustment for potential confounders, SGM patients were also twice as likely to have postpartum hemorrhage (8% vs. 4% in non-SGM patients) and postterm birth at 42-44 weeks (0.6% vs 0.3% in non-SGM patients).
“Having increased postterm birth is a matter of declining induction of labor, as it is recommended to have an induction by 41 weeks of gestation in general,” Dr. Mei said in an interview. “It is also possible this patient cohort faces more barriers in access to care and possible discrimination as sexual/gender minority patients.”
Rates of severe preeclampsia, induction of labor, cesarean delivery, preterm birth, low birth weight, and a low Apgar score were also higher among SGM patients, but these associations were no longer significant after adjustment for age, education, payment method, parity, prepregnancy weight, comorbidities, and multifetal gestation. The difference in hypertensive disorders of pregnancy, postpartum hemorrhage, and postterm birth remained statistically significant after adjustment.
Past research has shown that only about a third of cisgender female same-sex marriages used ART, so the disparities cannot be completely explained by ART use, Dr. Leonard said.
“I think the main drivers are structural disparities,” Dr. Leonard said. “Every obstetric clinic is focused in a way that’s about mother-father, and many people who don’t feel like they fit into that paradigm feel excluded and disengage with health care.”
Elliott Main, MD, a clinical professor of obstetrics and gynecology at Stanford University and coauthor of the study noted that discrimination and stigma likely play a substantial role in the disparities.
“Sexual and/or gender minority people face this discrimination at structural and interpersonal levels on a regular basis, which can lead to chronic stress and its harmful physical effects as well as lower-quality health care,” Dr. Main said in an interview.
Another coauthor, Juno Obedin-Maliver, MD, an assistant professor of obstetrics and gynecology at Stanford, emphasized how much room for improvement exists in care for SGM obstetric patients.
“We hope that this study brings needed attention to the disparities in perinatal health experienced by sexual and/or gender minority people,” Dr. Obedin-Maliver said. “There is much we can do to better understand the family building goals of sexual and/or gender minority people and help those to be achieved with healthy outcomes for parents and their children.”
One limitation of the study is that it’s possible to misclassify individuals using the birth certificate data, and not everyone may be comfortable selecting the box that accurately represents their identity, particularly if they aren’t “out” or fear discrimination or stigma, so the population may underrepresent the actual numbers of sexual and gender minority individuals giving birth. Dr. Mei added that it would be helpful to see data on neonatal ICU admissions and use of ART.
It’s difficult to say how generalizable the findings are, Dr. Mei said. “It is possible the findings would be more exaggerated in the rest of the country outside of California, if we assume there is potentially lower health access and more stigma.” The fact that California offers different gender options for the birthing and nonbirthing parent is, by itself, an indication of a potentially more accepting social environment than might be found in other states.
”The take-home message is that this patient population is higher risk, likely partially due to baseline increased risk factors, such as older maternal age and likely use of ART, and partially due to possible lack of health access and stigma,” Dr. Mei said. “Health care providers should be notably cognizant of these increased risks, particularly in the psychosocial context and make efforts to reduce those burdens as much as possible.”
The research was funded by the Stanford Maternal and Child Health Research Institute. Dr. Obedin-Maliver has consulted for Sage Therapeutics, Ibis Reproductive Health, and Hims. Dr. Mei and the other authors had no disclosures.
FROM THE PREGNANCY MEETING
Picture warnings on sugary drinks could help fight childhood obesity
Sugary beverages – juice, soda, decadent lattes, sports drinks, and more – are the leading source of both calories and added sugar in the American diet, according to the Harvard T. H. Chan School of Public Health. But new research published in PLoS Medicine has found that
The new study, from researchers at the University of North Carolina at Chapel Hill, found that parents were 17% less likely to buy sugary drinks for their children when the beverages had the graphical – and graphic – warnings on the products.
The researchers turned a laboratory setting into a “minimart,” and parents were told to choose one drink and snack for their children, along with one household item (to disguise the purpose of the study).
Some parents were presented with sweetened drinks with images on the products reflecting type 2 diabetes and heart damage. Others were shown sugary drinks with a barcode label and no picture warning.
Forty-five percent of parents chose sugary drinks for their children when the products had no picture warning, but only 28% of parents chose sugary beverages with the cautionary images.
“When people make choices about what food to buy, they are juggling dozens of factors, like taste, cost, and advertising, and are looking at many products at once,” said Lindsey Smith Taillie, PhD, a nutrition researcher and the senior author of the paper.
“Showing that warnings can cut through the noise of everything else that’s happening in a food store is powerful evidence that they would help reduce sugary drink purchases in the real world.”
Children are particularly prone to overindulging on sugar, largely due to companies’ frequent marketing displays of pleasurable-looking and seemingly “thirst-quenching” sweet beverages.
Drink packaging also can be misleading.
Fruits and vegetables displayed on the front of many beverages often lead parents to buy what they believe are “healthy” options, when these drinks could be packed with sugar, according to a study published online Jan. 22 in the journal Appetite.
Parents are often “doing the best with what information they have,” so more education about nutrition, through picture warning labels, for example, would make a difference, said Caroline Fausel, a paleo food blogger, podcaster, and author of “Prep, Cook, Freeze: A Paleo Meal Planning Cookbook.”
Healthier choices on the rise
The American Beverage Association, an industry trade group, shared the current steps that major companies are taking to help lower Americans’ sugar intake.
Pepsi, Coca-Cola, and Keurig Dr Pepper joined forces in 2014 to create the Balance Calories Initiative, which aims to reduce beverage calories in the national diet.
Coca-Cola now offers 250 beverages with zero to low calories, and Keurig Dr Pepper has 158 products with 40 calories or less. Pepsi sells 7.5-ounce mini-cans, along with various other sizes, to encourage portion control.
“Beverage companies are fully transparent about the calories and sugar in our products, and we are offering more choices with less sugar than ever before,” William Dermody, vice president of media and public affairs for the American Beverage Association, said in a statement. “We agree that too much sugar is not good for anyone, and clear information about beverages is most helpful to consumers.”
Other big companies also are taking strides to lower sugar content in their products.
Kraft Heinz, which owns the popular line of Capri Sun drinks, has publicly shared its efforts to ramp up the nutritional value of its products.
The company has a goal to slash 60 million pounds of total sugar in Kraft Heinz products globally by 2025.
“As more people become aware of the harm that excessive sugar can cause in the body, my hope is that they continue to choose healthier alternatives,” Ms. Fausel said.
Creating new patterns
For children who consume sweetened juices and sodas regularly, the transition to healthier options might be challenging at first.
“Change can involve tantrums and unhappiness, and right now parents are at their max living pandemic parenting life,” said Jennifer Anderson, a registered dietitian and CEO of Kids Eat in Color, LLC, a resource for improving child nutrition and health through innovative education, meal plans, and tools. “Kids can get used to having sugary drinks, and they don’t want to give them up.”
One way to help make the switch is by having only water and milk as options while children are up and about, a technique that works particularly well for younger children, she said.
“This sort of ‘quiet restriction’ helps kids learn to love the healthier option without feeling deprived,” Ms. Anderson said. “They will eventually learn about juice, soda, chocolate milk, sports drinks, and more, but you can let them learn about those foods at a slower pace when you rarely or don’t serve them at home.”
The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sugary beverages – juice, soda, decadent lattes, sports drinks, and more – are the leading source of both calories and added sugar in the American diet, according to the Harvard T. H. Chan School of Public Health. But new research published in PLoS Medicine has found that
The new study, from researchers at the University of North Carolina at Chapel Hill, found that parents were 17% less likely to buy sugary drinks for their children when the beverages had the graphical – and graphic – warnings on the products.
The researchers turned a laboratory setting into a “minimart,” and parents were told to choose one drink and snack for their children, along with one household item (to disguise the purpose of the study).
Some parents were presented with sweetened drinks with images on the products reflecting type 2 diabetes and heart damage. Others were shown sugary drinks with a barcode label and no picture warning.
Forty-five percent of parents chose sugary drinks for their children when the products had no picture warning, but only 28% of parents chose sugary beverages with the cautionary images.
“When people make choices about what food to buy, they are juggling dozens of factors, like taste, cost, and advertising, and are looking at many products at once,” said Lindsey Smith Taillie, PhD, a nutrition researcher and the senior author of the paper.
“Showing that warnings can cut through the noise of everything else that’s happening in a food store is powerful evidence that they would help reduce sugary drink purchases in the real world.”
Children are particularly prone to overindulging on sugar, largely due to companies’ frequent marketing displays of pleasurable-looking and seemingly “thirst-quenching” sweet beverages.
Drink packaging also can be misleading.
Fruits and vegetables displayed on the front of many beverages often lead parents to buy what they believe are “healthy” options, when these drinks could be packed with sugar, according to a study published online Jan. 22 in the journal Appetite.
Parents are often “doing the best with what information they have,” so more education about nutrition, through picture warning labels, for example, would make a difference, said Caroline Fausel, a paleo food blogger, podcaster, and author of “Prep, Cook, Freeze: A Paleo Meal Planning Cookbook.”
Healthier choices on the rise
The American Beverage Association, an industry trade group, shared the current steps that major companies are taking to help lower Americans’ sugar intake.
Pepsi, Coca-Cola, and Keurig Dr Pepper joined forces in 2014 to create the Balance Calories Initiative, which aims to reduce beverage calories in the national diet.
Coca-Cola now offers 250 beverages with zero to low calories, and Keurig Dr Pepper has 158 products with 40 calories or less. Pepsi sells 7.5-ounce mini-cans, along with various other sizes, to encourage portion control.
“Beverage companies are fully transparent about the calories and sugar in our products, and we are offering more choices with less sugar than ever before,” William Dermody, vice president of media and public affairs for the American Beverage Association, said in a statement. “We agree that too much sugar is not good for anyone, and clear information about beverages is most helpful to consumers.”
Other big companies also are taking strides to lower sugar content in their products.
Kraft Heinz, which owns the popular line of Capri Sun drinks, has publicly shared its efforts to ramp up the nutritional value of its products.
The company has a goal to slash 60 million pounds of total sugar in Kraft Heinz products globally by 2025.
“As more people become aware of the harm that excessive sugar can cause in the body, my hope is that they continue to choose healthier alternatives,” Ms. Fausel said.
Creating new patterns
For children who consume sweetened juices and sodas regularly, the transition to healthier options might be challenging at first.
“Change can involve tantrums and unhappiness, and right now parents are at their max living pandemic parenting life,” said Jennifer Anderson, a registered dietitian and CEO of Kids Eat in Color, LLC, a resource for improving child nutrition and health through innovative education, meal plans, and tools. “Kids can get used to having sugary drinks, and they don’t want to give them up.”
One way to help make the switch is by having only water and milk as options while children are up and about, a technique that works particularly well for younger children, she said.
“This sort of ‘quiet restriction’ helps kids learn to love the healthier option without feeling deprived,” Ms. Anderson said. “They will eventually learn about juice, soda, chocolate milk, sports drinks, and more, but you can let them learn about those foods at a slower pace when you rarely or don’t serve them at home.”
The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sugary beverages – juice, soda, decadent lattes, sports drinks, and more – are the leading source of both calories and added sugar in the American diet, according to the Harvard T. H. Chan School of Public Health. But new research published in PLoS Medicine has found that
The new study, from researchers at the University of North Carolina at Chapel Hill, found that parents were 17% less likely to buy sugary drinks for their children when the beverages had the graphical – and graphic – warnings on the products.
The researchers turned a laboratory setting into a “minimart,” and parents were told to choose one drink and snack for their children, along with one household item (to disguise the purpose of the study).
Some parents were presented with sweetened drinks with images on the products reflecting type 2 diabetes and heart damage. Others were shown sugary drinks with a barcode label and no picture warning.
Forty-five percent of parents chose sugary drinks for their children when the products had no picture warning, but only 28% of parents chose sugary beverages with the cautionary images.
“When people make choices about what food to buy, they are juggling dozens of factors, like taste, cost, and advertising, and are looking at many products at once,” said Lindsey Smith Taillie, PhD, a nutrition researcher and the senior author of the paper.
“Showing that warnings can cut through the noise of everything else that’s happening in a food store is powerful evidence that they would help reduce sugary drink purchases in the real world.”
Children are particularly prone to overindulging on sugar, largely due to companies’ frequent marketing displays of pleasurable-looking and seemingly “thirst-quenching” sweet beverages.
Drink packaging also can be misleading.
Fruits and vegetables displayed on the front of many beverages often lead parents to buy what they believe are “healthy” options, when these drinks could be packed with sugar, according to a study published online Jan. 22 in the journal Appetite.
Parents are often “doing the best with what information they have,” so more education about nutrition, through picture warning labels, for example, would make a difference, said Caroline Fausel, a paleo food blogger, podcaster, and author of “Prep, Cook, Freeze: A Paleo Meal Planning Cookbook.”
Healthier choices on the rise
The American Beverage Association, an industry trade group, shared the current steps that major companies are taking to help lower Americans’ sugar intake.
Pepsi, Coca-Cola, and Keurig Dr Pepper joined forces in 2014 to create the Balance Calories Initiative, which aims to reduce beverage calories in the national diet.
Coca-Cola now offers 250 beverages with zero to low calories, and Keurig Dr Pepper has 158 products with 40 calories or less. Pepsi sells 7.5-ounce mini-cans, along with various other sizes, to encourage portion control.
“Beverage companies are fully transparent about the calories and sugar in our products, and we are offering more choices with less sugar than ever before,” William Dermody, vice president of media and public affairs for the American Beverage Association, said in a statement. “We agree that too much sugar is not good for anyone, and clear information about beverages is most helpful to consumers.”
Other big companies also are taking strides to lower sugar content in their products.
Kraft Heinz, which owns the popular line of Capri Sun drinks, has publicly shared its efforts to ramp up the nutritional value of its products.
The company has a goal to slash 60 million pounds of total sugar in Kraft Heinz products globally by 2025.
“As more people become aware of the harm that excessive sugar can cause in the body, my hope is that they continue to choose healthier alternatives,” Ms. Fausel said.
Creating new patterns
For children who consume sweetened juices and sodas regularly, the transition to healthier options might be challenging at first.
“Change can involve tantrums and unhappiness, and right now parents are at their max living pandemic parenting life,” said Jennifer Anderson, a registered dietitian and CEO of Kids Eat in Color, LLC, a resource for improving child nutrition and health through innovative education, meal plans, and tools. “Kids can get used to having sugary drinks, and they don’t want to give them up.”
One way to help make the switch is by having only water and milk as options while children are up and about, a technique that works particularly well for younger children, she said.
“This sort of ‘quiet restriction’ helps kids learn to love the healthier option without feeling deprived,” Ms. Anderson said. “They will eventually learn about juice, soda, chocolate milk, sports drinks, and more, but you can let them learn about those foods at a slower pace when you rarely or don’t serve them at home.”
The researchers reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PLOS MEDICINE