User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
2020 presidential election tied to spike in cardiac events
The analysis of nearly 6.4 million adults showed that the rate of hospitalization for acute cardiovascular disease (CVD) was 17% higher in the 5 days after the election than in a 5-day period 2 weeks earlier.
The rate of acute myocardial infarction (AMI) was 42% higher, with no significant difference for heart failure or stroke hospital admissions.
“These findings suggest that awareness of the heightened risk of CVD and strategies to mitigate risk during notable political events are needed,” write Matthew T. Mefford, PhD, of Kaiser Permanente Southern California, Pasadena, and colleagues.
The study was published in the April issue of JAMA Network Open.
Stress and the heart
In the American Psychological Association Stress in America 2020 survey conducted roughly 3 months before the 2020 presidential election, 77% of adults cited the future of the country as a substantial source of stress, enhanced by the ongoing COVID-19 pandemic, the authors note. More than two-thirds said the election was a substantial source of stress.
Dr. Mefford and colleagues compared CVD hospitalizations at Kaiser Permanente Southern and Northern California hospitals in the 5-day risk window of Nov. 4-8, 2020, with the control window of Oct. 21-25, 2020.
There were 666 CVD hospitalizations (760.47 per 100,000 person-years [PY]) in the risk window, compared with 569 (647.97 per 100,000 PY) in the control window (rate ratio, 1.17; 95% confidence interval, 1.05-1.31).
There were also significantly more hospitalizations for AMI immediately after the election than before (179 vs. 126 AMI hospitalizations; 204.4 vs. 143.5 per 100,000 PY; RR, 1.42; 95% CI, 1.13-1.79).
There was no significant difference between the risk and control periods for hospitalizations because of stroke or heart failure.
The study also suggests higher rates of acute CVD after the election in older adults, men, and White individuals. Political affiliation was not examined in the study.
“Importantly, results were consistent before and after excluding patients with confirmed COVID-19 infection,” the study team notes.
Yet, the potential influence of COVID-19 stressors on increasing CVD risk cannot be ruled out, they say.
However, COVID-19 stressors occurred over a much longer period and are less likely to explain the transient risks observed in the defined risk and control windows that are in close proximity to the 2020 election, the investigators point out.
There is growing evidence that psychological health contributes to CVD.
Previous studies shown a higher risk for acute CVD around population-wide psychosocial or environmental stressors, but less was known about acute CVD risk in relation to political events.
The researchers note future studies evaluating stress-relieving interventions may be important for understanding the intersection of political events, associated stress, and acute CVD risk.
Partial funding for the study was provided by a grant from the W.K. Kellogg Foundation. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The analysis of nearly 6.4 million adults showed that the rate of hospitalization for acute cardiovascular disease (CVD) was 17% higher in the 5 days after the election than in a 5-day period 2 weeks earlier.
The rate of acute myocardial infarction (AMI) was 42% higher, with no significant difference for heart failure or stroke hospital admissions.
“These findings suggest that awareness of the heightened risk of CVD and strategies to mitigate risk during notable political events are needed,” write Matthew T. Mefford, PhD, of Kaiser Permanente Southern California, Pasadena, and colleagues.
The study was published in the April issue of JAMA Network Open.
Stress and the heart
In the American Psychological Association Stress in America 2020 survey conducted roughly 3 months before the 2020 presidential election, 77% of adults cited the future of the country as a substantial source of stress, enhanced by the ongoing COVID-19 pandemic, the authors note. More than two-thirds said the election was a substantial source of stress.
Dr. Mefford and colleagues compared CVD hospitalizations at Kaiser Permanente Southern and Northern California hospitals in the 5-day risk window of Nov. 4-8, 2020, with the control window of Oct. 21-25, 2020.
There were 666 CVD hospitalizations (760.47 per 100,000 person-years [PY]) in the risk window, compared with 569 (647.97 per 100,000 PY) in the control window (rate ratio, 1.17; 95% confidence interval, 1.05-1.31).
There were also significantly more hospitalizations for AMI immediately after the election than before (179 vs. 126 AMI hospitalizations; 204.4 vs. 143.5 per 100,000 PY; RR, 1.42; 95% CI, 1.13-1.79).
There was no significant difference between the risk and control periods for hospitalizations because of stroke or heart failure.
The study also suggests higher rates of acute CVD after the election in older adults, men, and White individuals. Political affiliation was not examined in the study.
“Importantly, results were consistent before and after excluding patients with confirmed COVID-19 infection,” the study team notes.
Yet, the potential influence of COVID-19 stressors on increasing CVD risk cannot be ruled out, they say.
However, COVID-19 stressors occurred over a much longer period and are less likely to explain the transient risks observed in the defined risk and control windows that are in close proximity to the 2020 election, the investigators point out.
There is growing evidence that psychological health contributes to CVD.
Previous studies shown a higher risk for acute CVD around population-wide psychosocial or environmental stressors, but less was known about acute CVD risk in relation to political events.
The researchers note future studies evaluating stress-relieving interventions may be important for understanding the intersection of political events, associated stress, and acute CVD risk.
Partial funding for the study was provided by a grant from the W.K. Kellogg Foundation. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
The analysis of nearly 6.4 million adults showed that the rate of hospitalization for acute cardiovascular disease (CVD) was 17% higher in the 5 days after the election than in a 5-day period 2 weeks earlier.
The rate of acute myocardial infarction (AMI) was 42% higher, with no significant difference for heart failure or stroke hospital admissions.
“These findings suggest that awareness of the heightened risk of CVD and strategies to mitigate risk during notable political events are needed,” write Matthew T. Mefford, PhD, of Kaiser Permanente Southern California, Pasadena, and colleagues.
The study was published in the April issue of JAMA Network Open.
Stress and the heart
In the American Psychological Association Stress in America 2020 survey conducted roughly 3 months before the 2020 presidential election, 77% of adults cited the future of the country as a substantial source of stress, enhanced by the ongoing COVID-19 pandemic, the authors note. More than two-thirds said the election was a substantial source of stress.
Dr. Mefford and colleagues compared CVD hospitalizations at Kaiser Permanente Southern and Northern California hospitals in the 5-day risk window of Nov. 4-8, 2020, with the control window of Oct. 21-25, 2020.
There were 666 CVD hospitalizations (760.47 per 100,000 person-years [PY]) in the risk window, compared with 569 (647.97 per 100,000 PY) in the control window (rate ratio, 1.17; 95% confidence interval, 1.05-1.31).
There were also significantly more hospitalizations for AMI immediately after the election than before (179 vs. 126 AMI hospitalizations; 204.4 vs. 143.5 per 100,000 PY; RR, 1.42; 95% CI, 1.13-1.79).
There was no significant difference between the risk and control periods for hospitalizations because of stroke or heart failure.
The study also suggests higher rates of acute CVD after the election in older adults, men, and White individuals. Political affiliation was not examined in the study.
“Importantly, results were consistent before and after excluding patients with confirmed COVID-19 infection,” the study team notes.
Yet, the potential influence of COVID-19 stressors on increasing CVD risk cannot be ruled out, they say.
However, COVID-19 stressors occurred over a much longer period and are less likely to explain the transient risks observed in the defined risk and control windows that are in close proximity to the 2020 election, the investigators point out.
There is growing evidence that psychological health contributes to CVD.
Previous studies shown a higher risk for acute CVD around population-wide psychosocial or environmental stressors, but less was known about acute CVD risk in relation to political events.
The researchers note future studies evaluating stress-relieving interventions may be important for understanding the intersection of political events, associated stress, and acute CVD risk.
Partial funding for the study was provided by a grant from the W.K. Kellogg Foundation. The authors have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Endoscopic obesity treatments offer alternatives to surgery
SAN FRANCISCO – Endoscopic treatments for obesity are under-utilized but represent an opportunity for gastroenterologists to help address the metabolic epidemic that affects up to 40% of people in the United States, according to a presentation reviewing these techniques.
Lifestyle modification is the first intervention, but results in just a 5% average weight loss, according to Allison Schulman, MD, MPH, who discussed these options at the 2022 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. Although surgical interventions induce more weight loss and greater improvement of metabolic outcomes, they come with significant risks and many patients are reluctant to pursue them, she added. In fact, fewer than 1% of obese individuals who qualify for bariatric surgery ultimately undergo it.
Dr. Schulman emphasized another option: Endoscopic bariatric therapies fill this void in between those two extremes, as they are clearly less invasive” said Dr. Schulman, who is an assistant professor of gastroenterology and hepatology at the University of Michigan, Ann Arbor. “They may appeal to those who do not qualify or do not want bariatric surgery. They also could bridge a critical gap in the treatment of obesity, as they reach patients earlier, at BMIs [body mass indexes] where they may not be surgical candidates. Furthermore, these therapies are oftentimes repeatable and commonly can be used in combination [with other weight loss approaches].”
Endoscopic therapies for obesity include devices that occupy space in the stomach, such as intragastric balloons, gastric remodeling procedures like endoscopic sleeve gastroplasty (ESG), and aspiration therapy.
Potential candidates for noninvasive approaches include patients with a BMI over 30 kg/m2 who have not lost sufficient weight through nonsurgical methods or those who do not want to undergo surgery or require a bridge therapy to surgery.
Fluid-filled balloons can be placed and filled to an appropriate volume. One network meta-analysis found that fluid-filled balloons were more likely to lead to weight loss, but also more likely to be removed due to intolerance. She also noted that the Elipse balloon (Allurion Technologies) is designed to be swallowed and thus avoid procedures entirely; it is currently under review by Food and Drug Administration.
Although balloons are linked to 7%-10% weight loss in some studies and reviews, Dr. Schulman said, “we know … that the majority of these lead to much more weight loss in clinical practice, oftentimes closer to 13%-%15.”
One review found that balloons also lead to improvement in obesity-related comorbidities, compared with conventional nonsurgical approaches, and this benefit extends past 1 year. A study of 21 patients with nonalcoholic steatohepatitis (NASH) treated with intragastric balloons found that 90% had an improvement in nonalcoholic fatty liver disease activity score, with a median drop of 3 points, and 80% had a drop of at least 2 points. Of these patients, 50% also had an improvement in fibrosis determined by magnetic resonance elastography.
Balloon therapy should be highly individualized, according to Dr. Schulman.
Dr. Schulman also described ESG, which uses sutures to remodel the stomach and reduce volume by up to 70%. She outlined studies and reviews, such as those from Sharaiha and colleagues and Hedjoudje and colleagues, showing that ESG leads to significant and sustained weight loss. The procedure was also quite safe, with one large, single-center study showing that both fever and significant blood loss each occurred in less than 1% of patients (Gastrointest Endosc. 2019 Jun;89[6]:1132-8), while the systematic review and meta-analysis from Hedjoudje and colleagues found an adverse event frequency of 2.2%.
In a matched control study, laparoscopic sleeve gastrectomy led to more weight loss, but ESG had fewer adverse events (5.2% versus 16.9%; P < .01) and had a greater effect on gastroesophageal reflux disease.
ESG can be effective when repeated, while surgical revisions are associated with much higher morbidity, according to Dr. Schulman.
During her presentation, Dr. Schulman mentioned the AspireAssist device developed by Aspire Bariatrics, which is similar to a percutaneous endoscopic gastrostomy (PEG) tube. It leads to the removal of about 30% of calories consumed during a meal, with patients instructed to aspirate 20-30 minutes after a meal, two to three times a day. It gained Food and Drug Administration approval on the strength of the PATHWAY study, which showed significant weight loss.
“But perhaps more impressive is the overall patient satisfaction and willingness to recommend this device to others,” said Dr. Schulman.
Another approach she described is the transpyloric shuttle (TPS), which leads to faster filling times and delayed gastric emptying, though it must be removed endoscopically at 12 months.
Dr. Schulman also discussed endoscopic bariatric and metabolic therapy. This approach is currently a primary therapy for obesity, and is in development for the treatment of diabetes and non-alcoholic fatty liver disease. The approach is predicated on the idea that obesity is a disorder of energy homeostasis, and that enteric neurons in the small bowel are key players, possibly through reduced production of as yet unknown signaling molecules, leading to insulin resistance. It’s also known that diets high in fat and sugar alter the duodenum, which causes changes in nutrient signaling to the brain.
“It’s thought that this leads to duodenal endocrine hyperactivity and ultimately metabolic disease,” said Dr. Schulman.
Finally, she described small-bowel therapies like endobarrier sleeves, duodenal mucosal resurfacing, and an incisionless anastomosis system designed to improve glycemic control by altering the gut through noninvasive means.
Dr. Schulman has consulted for Apollo Endosurgery, Boston Scientific, Olympus, and MicroTech, and has received research support from GI Dynamics.
SAN FRANCISCO – Endoscopic treatments for obesity are under-utilized but represent an opportunity for gastroenterologists to help address the metabolic epidemic that affects up to 40% of people in the United States, according to a presentation reviewing these techniques.
Lifestyle modification is the first intervention, but results in just a 5% average weight loss, according to Allison Schulman, MD, MPH, who discussed these options at the 2022 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. Although surgical interventions induce more weight loss and greater improvement of metabolic outcomes, they come with significant risks and many patients are reluctant to pursue them, she added. In fact, fewer than 1% of obese individuals who qualify for bariatric surgery ultimately undergo it.
Dr. Schulman emphasized another option: Endoscopic bariatric therapies fill this void in between those two extremes, as they are clearly less invasive” said Dr. Schulman, who is an assistant professor of gastroenterology and hepatology at the University of Michigan, Ann Arbor. “They may appeal to those who do not qualify or do not want bariatric surgery. They also could bridge a critical gap in the treatment of obesity, as they reach patients earlier, at BMIs [body mass indexes] where they may not be surgical candidates. Furthermore, these therapies are oftentimes repeatable and commonly can be used in combination [with other weight loss approaches].”
Endoscopic therapies for obesity include devices that occupy space in the stomach, such as intragastric balloons, gastric remodeling procedures like endoscopic sleeve gastroplasty (ESG), and aspiration therapy.
Potential candidates for noninvasive approaches include patients with a BMI over 30 kg/m2 who have not lost sufficient weight through nonsurgical methods or those who do not want to undergo surgery or require a bridge therapy to surgery.
Fluid-filled balloons can be placed and filled to an appropriate volume. One network meta-analysis found that fluid-filled balloons were more likely to lead to weight loss, but also more likely to be removed due to intolerance. She also noted that the Elipse balloon (Allurion Technologies) is designed to be swallowed and thus avoid procedures entirely; it is currently under review by Food and Drug Administration.
Although balloons are linked to 7%-10% weight loss in some studies and reviews, Dr. Schulman said, “we know … that the majority of these lead to much more weight loss in clinical practice, oftentimes closer to 13%-%15.”
One review found that balloons also lead to improvement in obesity-related comorbidities, compared with conventional nonsurgical approaches, and this benefit extends past 1 year. A study of 21 patients with nonalcoholic steatohepatitis (NASH) treated with intragastric balloons found that 90% had an improvement in nonalcoholic fatty liver disease activity score, with a median drop of 3 points, and 80% had a drop of at least 2 points. Of these patients, 50% also had an improvement in fibrosis determined by magnetic resonance elastography.
Balloon therapy should be highly individualized, according to Dr. Schulman.
Dr. Schulman also described ESG, which uses sutures to remodel the stomach and reduce volume by up to 70%. She outlined studies and reviews, such as those from Sharaiha and colleagues and Hedjoudje and colleagues, showing that ESG leads to significant and sustained weight loss. The procedure was also quite safe, with one large, single-center study showing that both fever and significant blood loss each occurred in less than 1% of patients (Gastrointest Endosc. 2019 Jun;89[6]:1132-8), while the systematic review and meta-analysis from Hedjoudje and colleagues found an adverse event frequency of 2.2%.
In a matched control study, laparoscopic sleeve gastrectomy led to more weight loss, but ESG had fewer adverse events (5.2% versus 16.9%; P < .01) and had a greater effect on gastroesophageal reflux disease.
ESG can be effective when repeated, while surgical revisions are associated with much higher morbidity, according to Dr. Schulman.
During her presentation, Dr. Schulman mentioned the AspireAssist device developed by Aspire Bariatrics, which is similar to a percutaneous endoscopic gastrostomy (PEG) tube. It leads to the removal of about 30% of calories consumed during a meal, with patients instructed to aspirate 20-30 minutes after a meal, two to three times a day. It gained Food and Drug Administration approval on the strength of the PATHWAY study, which showed significant weight loss.
“But perhaps more impressive is the overall patient satisfaction and willingness to recommend this device to others,” said Dr. Schulman.
Another approach she described is the transpyloric shuttle (TPS), which leads to faster filling times and delayed gastric emptying, though it must be removed endoscopically at 12 months.
Dr. Schulman also discussed endoscopic bariatric and metabolic therapy. This approach is currently a primary therapy for obesity, and is in development for the treatment of diabetes and non-alcoholic fatty liver disease. The approach is predicated on the idea that obesity is a disorder of energy homeostasis, and that enteric neurons in the small bowel are key players, possibly through reduced production of as yet unknown signaling molecules, leading to insulin resistance. It’s also known that diets high in fat and sugar alter the duodenum, which causes changes in nutrient signaling to the brain.
“It’s thought that this leads to duodenal endocrine hyperactivity and ultimately metabolic disease,” said Dr. Schulman.
Finally, she described small-bowel therapies like endobarrier sleeves, duodenal mucosal resurfacing, and an incisionless anastomosis system designed to improve glycemic control by altering the gut through noninvasive means.
Dr. Schulman has consulted for Apollo Endosurgery, Boston Scientific, Olympus, and MicroTech, and has received research support from GI Dynamics.
SAN FRANCISCO – Endoscopic treatments for obesity are under-utilized but represent an opportunity for gastroenterologists to help address the metabolic epidemic that affects up to 40% of people in the United States, according to a presentation reviewing these techniques.
Lifestyle modification is the first intervention, but results in just a 5% average weight loss, according to Allison Schulman, MD, MPH, who discussed these options at the 2022 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. Although surgical interventions induce more weight loss and greater improvement of metabolic outcomes, they come with significant risks and many patients are reluctant to pursue them, she added. In fact, fewer than 1% of obese individuals who qualify for bariatric surgery ultimately undergo it.
Dr. Schulman emphasized another option: Endoscopic bariatric therapies fill this void in between those two extremes, as they are clearly less invasive” said Dr. Schulman, who is an assistant professor of gastroenterology and hepatology at the University of Michigan, Ann Arbor. “They may appeal to those who do not qualify or do not want bariatric surgery. They also could bridge a critical gap in the treatment of obesity, as they reach patients earlier, at BMIs [body mass indexes] where they may not be surgical candidates. Furthermore, these therapies are oftentimes repeatable and commonly can be used in combination [with other weight loss approaches].”
Endoscopic therapies for obesity include devices that occupy space in the stomach, such as intragastric balloons, gastric remodeling procedures like endoscopic sleeve gastroplasty (ESG), and aspiration therapy.
Potential candidates for noninvasive approaches include patients with a BMI over 30 kg/m2 who have not lost sufficient weight through nonsurgical methods or those who do not want to undergo surgery or require a bridge therapy to surgery.
Fluid-filled balloons can be placed and filled to an appropriate volume. One network meta-analysis found that fluid-filled balloons were more likely to lead to weight loss, but also more likely to be removed due to intolerance. She also noted that the Elipse balloon (Allurion Technologies) is designed to be swallowed and thus avoid procedures entirely; it is currently under review by Food and Drug Administration.
Although balloons are linked to 7%-10% weight loss in some studies and reviews, Dr. Schulman said, “we know … that the majority of these lead to much more weight loss in clinical practice, oftentimes closer to 13%-%15.”
One review found that balloons also lead to improvement in obesity-related comorbidities, compared with conventional nonsurgical approaches, and this benefit extends past 1 year. A study of 21 patients with nonalcoholic steatohepatitis (NASH) treated with intragastric balloons found that 90% had an improvement in nonalcoholic fatty liver disease activity score, with a median drop of 3 points, and 80% had a drop of at least 2 points. Of these patients, 50% also had an improvement in fibrosis determined by magnetic resonance elastography.
Balloon therapy should be highly individualized, according to Dr. Schulman.
Dr. Schulman also described ESG, which uses sutures to remodel the stomach and reduce volume by up to 70%. She outlined studies and reviews, such as those from Sharaiha and colleagues and Hedjoudje and colleagues, showing that ESG leads to significant and sustained weight loss. The procedure was also quite safe, with one large, single-center study showing that both fever and significant blood loss each occurred in less than 1% of patients (Gastrointest Endosc. 2019 Jun;89[6]:1132-8), while the systematic review and meta-analysis from Hedjoudje and colleagues found an adverse event frequency of 2.2%.
In a matched control study, laparoscopic sleeve gastrectomy led to more weight loss, but ESG had fewer adverse events (5.2% versus 16.9%; P < .01) and had a greater effect on gastroesophageal reflux disease.
ESG can be effective when repeated, while surgical revisions are associated with much higher morbidity, according to Dr. Schulman.
During her presentation, Dr. Schulman mentioned the AspireAssist device developed by Aspire Bariatrics, which is similar to a percutaneous endoscopic gastrostomy (PEG) tube. It leads to the removal of about 30% of calories consumed during a meal, with patients instructed to aspirate 20-30 minutes after a meal, two to three times a day. It gained Food and Drug Administration approval on the strength of the PATHWAY study, which showed significant weight loss.
“But perhaps more impressive is the overall patient satisfaction and willingness to recommend this device to others,” said Dr. Schulman.
Another approach she described is the transpyloric shuttle (TPS), which leads to faster filling times and delayed gastric emptying, though it must be removed endoscopically at 12 months.
Dr. Schulman also discussed endoscopic bariatric and metabolic therapy. This approach is currently a primary therapy for obesity, and is in development for the treatment of diabetes and non-alcoholic fatty liver disease. The approach is predicated on the idea that obesity is a disorder of energy homeostasis, and that enteric neurons in the small bowel are key players, possibly through reduced production of as yet unknown signaling molecules, leading to insulin resistance. It’s also known that diets high in fat and sugar alter the duodenum, which causes changes in nutrient signaling to the brain.
“It’s thought that this leads to duodenal endocrine hyperactivity and ultimately metabolic disease,” said Dr. Schulman.
Finally, she described small-bowel therapies like endobarrier sleeves, duodenal mucosal resurfacing, and an incisionless anastomosis system designed to improve glycemic control by altering the gut through noninvasive means.
Dr. Schulman has consulted for Apollo Endosurgery, Boston Scientific, Olympus, and MicroTech, and has received research support from GI Dynamics.
AT 2022 AGA TECH SUMMIT
Water, water everywhere leads to leaner students
Elementary schools that provide easy access to drinking water and education about its benefits may help their students maintain a healthy weight, a new study found.
Researchers examined the health and drinking habits of 1,249 children in 26 low-income, ethnically diverse elementary schools in the San Francisco Bay Area. In half of the schools, water stations were placed throughout, along with signs explaining why water is healthier than sugary drinks. In addition, assemblies were held explaining the advantages of water over sugary drinks.
That simple message seemed to have had an outsized effect. Schools with water stations had significantly fewer overweight students than the other schools by the end of the 15-month study, according to Anisha Patel, MD, MSPH, MSHS, associate professor of pediatrics at Stanford (Calif.) University, who will be presenting the findings at the Pediatric Academic Societies (PAS) 2022 Meeting, Denver.
“Sugar-sweetened beverages are a huge contributor to obesity,” Dr. Patel told this news organization. “This provides a key strategy for schools to adopt, and the time is right for this type of work – in the pandemic period we’ve seen significant increases in obesity. Investments like this could help stem that.”
According to the U.S. Centers for Disease Control and Prevention, 14.4 million children aged 2-19 years in the United States – about 19% of all kids in that age range – were obese in 2017-2018. The agency said the rate of increase in body mass index among this group nearly doubled during the COVID-19 pandemic.
Children with obesity are at higher risk for chronic health problems, including diabetes, heart disease, depression, and high blood pressure.
Dr. Patel’s study, funded by the National Institutes of Health, was the culmination of a decade of interest in the area, she said.
Water stations and compostable or recyclable cups were placed in high-traffic areas of the schools, including playgrounds and cafeterias. The water was tested for lead, and if needed, researchers worked with school districts to remediate, Dr. Patel said in an interview.
The intervention included a kickoff assembly about the health benefits of water intake, and students who were seen drinking water with their lunches were given small prizes.
The researchers assessed body weight, height, and dietary intake of students throughout the study, including their consumption of water, sodas, fruit juices, and flavored and unflavored milk.
Promoting water didn’t lead to magical weight loss. At the start of the study, 49.5% of students in the intervention group were overweight – a figure that nudged up to 49.8% by the end of the study. In the control group, however, 47.7% of students began the study overweight – a number that climbed to 51.4% by the end of the trial (odds ratio, 0.3; P = .01), according to the researchers, who credited the increase to the lack of emphasis on opting for water over sweetened drinks.
“We were very excited the effect sizes were nearly double previous studies, which was great news,” Dr. Patel said.
Water intake began to decline at about the 15-month mark, signaling the need for more long-term, consistent education and incentive to foster lasting habits, Dr. Patel said.
The researchers noted that they were unable to collect data from eight of the target schools because of the pandemic. In addition, the study focused on schools with heavily Latino student populations, so the results might not be generalizable to other communities, they said.
Angie Cradock, a principal research scientist at the Harvard T. H. Chan School of Public Health, Boston, said the study “offers an important and practical strategy to promote student health.”
Ms. Cradock serves as deputy director of the Harvard Prevention Research Center on Nutrition and Physical Activity, which focuses on improving population nutrition, increasing physical activity, reducing obesity and chronic disease, and improving health equity.
Dr. Patel and her colleagues’ three-pronged approach of using education, promotion, and accessibility to increase student interest in drinking water could be employed at countless other schools, said Ms. Cradock, who was not involved in the study.
“Negative perceptions of tap water and drinking fountains are common,” she said. “Not all students have access to safe and appealing drinking water while at school, and this strategy seems like a recipe for success.”
Dr. Patel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Elementary schools that provide easy access to drinking water and education about its benefits may help their students maintain a healthy weight, a new study found.
Researchers examined the health and drinking habits of 1,249 children in 26 low-income, ethnically diverse elementary schools in the San Francisco Bay Area. In half of the schools, water stations were placed throughout, along with signs explaining why water is healthier than sugary drinks. In addition, assemblies were held explaining the advantages of water over sugary drinks.
That simple message seemed to have had an outsized effect. Schools with water stations had significantly fewer overweight students than the other schools by the end of the 15-month study, according to Anisha Patel, MD, MSPH, MSHS, associate professor of pediatrics at Stanford (Calif.) University, who will be presenting the findings at the Pediatric Academic Societies (PAS) 2022 Meeting, Denver.
“Sugar-sweetened beverages are a huge contributor to obesity,” Dr. Patel told this news organization. “This provides a key strategy for schools to adopt, and the time is right for this type of work – in the pandemic period we’ve seen significant increases in obesity. Investments like this could help stem that.”
According to the U.S. Centers for Disease Control and Prevention, 14.4 million children aged 2-19 years in the United States – about 19% of all kids in that age range – were obese in 2017-2018. The agency said the rate of increase in body mass index among this group nearly doubled during the COVID-19 pandemic.
Children with obesity are at higher risk for chronic health problems, including diabetes, heart disease, depression, and high blood pressure.
Dr. Patel’s study, funded by the National Institutes of Health, was the culmination of a decade of interest in the area, she said.
Water stations and compostable or recyclable cups were placed in high-traffic areas of the schools, including playgrounds and cafeterias. The water was tested for lead, and if needed, researchers worked with school districts to remediate, Dr. Patel said in an interview.
The intervention included a kickoff assembly about the health benefits of water intake, and students who were seen drinking water with their lunches were given small prizes.
The researchers assessed body weight, height, and dietary intake of students throughout the study, including their consumption of water, sodas, fruit juices, and flavored and unflavored milk.
Promoting water didn’t lead to magical weight loss. At the start of the study, 49.5% of students in the intervention group were overweight – a figure that nudged up to 49.8% by the end of the study. In the control group, however, 47.7% of students began the study overweight – a number that climbed to 51.4% by the end of the trial (odds ratio, 0.3; P = .01), according to the researchers, who credited the increase to the lack of emphasis on opting for water over sweetened drinks.
“We were very excited the effect sizes were nearly double previous studies, which was great news,” Dr. Patel said.
Water intake began to decline at about the 15-month mark, signaling the need for more long-term, consistent education and incentive to foster lasting habits, Dr. Patel said.
The researchers noted that they were unable to collect data from eight of the target schools because of the pandemic. In addition, the study focused on schools with heavily Latino student populations, so the results might not be generalizable to other communities, they said.
Angie Cradock, a principal research scientist at the Harvard T. H. Chan School of Public Health, Boston, said the study “offers an important and practical strategy to promote student health.”
Ms. Cradock serves as deputy director of the Harvard Prevention Research Center on Nutrition and Physical Activity, which focuses on improving population nutrition, increasing physical activity, reducing obesity and chronic disease, and improving health equity.
Dr. Patel and her colleagues’ three-pronged approach of using education, promotion, and accessibility to increase student interest in drinking water could be employed at countless other schools, said Ms. Cradock, who was not involved in the study.
“Negative perceptions of tap water and drinking fountains are common,” she said. “Not all students have access to safe and appealing drinking water while at school, and this strategy seems like a recipe for success.”
Dr. Patel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Elementary schools that provide easy access to drinking water and education about its benefits may help their students maintain a healthy weight, a new study found.
Researchers examined the health and drinking habits of 1,249 children in 26 low-income, ethnically diverse elementary schools in the San Francisco Bay Area. In half of the schools, water stations were placed throughout, along with signs explaining why water is healthier than sugary drinks. In addition, assemblies were held explaining the advantages of water over sugary drinks.
That simple message seemed to have had an outsized effect. Schools with water stations had significantly fewer overweight students than the other schools by the end of the 15-month study, according to Anisha Patel, MD, MSPH, MSHS, associate professor of pediatrics at Stanford (Calif.) University, who will be presenting the findings at the Pediatric Academic Societies (PAS) 2022 Meeting, Denver.
“Sugar-sweetened beverages are a huge contributor to obesity,” Dr. Patel told this news organization. “This provides a key strategy for schools to adopt, and the time is right for this type of work – in the pandemic period we’ve seen significant increases in obesity. Investments like this could help stem that.”
According to the U.S. Centers for Disease Control and Prevention, 14.4 million children aged 2-19 years in the United States – about 19% of all kids in that age range – were obese in 2017-2018. The agency said the rate of increase in body mass index among this group nearly doubled during the COVID-19 pandemic.
Children with obesity are at higher risk for chronic health problems, including diabetes, heart disease, depression, and high blood pressure.
Dr. Patel’s study, funded by the National Institutes of Health, was the culmination of a decade of interest in the area, she said.
Water stations and compostable or recyclable cups were placed in high-traffic areas of the schools, including playgrounds and cafeterias. The water was tested for lead, and if needed, researchers worked with school districts to remediate, Dr. Patel said in an interview.
The intervention included a kickoff assembly about the health benefits of water intake, and students who were seen drinking water with their lunches were given small prizes.
The researchers assessed body weight, height, and dietary intake of students throughout the study, including their consumption of water, sodas, fruit juices, and flavored and unflavored milk.
Promoting water didn’t lead to magical weight loss. At the start of the study, 49.5% of students in the intervention group were overweight – a figure that nudged up to 49.8% by the end of the study. In the control group, however, 47.7% of students began the study overweight – a number that climbed to 51.4% by the end of the trial (odds ratio, 0.3; P = .01), according to the researchers, who credited the increase to the lack of emphasis on opting for water over sweetened drinks.
“We were very excited the effect sizes were nearly double previous studies, which was great news,” Dr. Patel said.
Water intake began to decline at about the 15-month mark, signaling the need for more long-term, consistent education and incentive to foster lasting habits, Dr. Patel said.
The researchers noted that they were unable to collect data from eight of the target schools because of the pandemic. In addition, the study focused on schools with heavily Latino student populations, so the results might not be generalizable to other communities, they said.
Angie Cradock, a principal research scientist at the Harvard T. H. Chan School of Public Health, Boston, said the study “offers an important and practical strategy to promote student health.”
Ms. Cradock serves as deputy director of the Harvard Prevention Research Center on Nutrition and Physical Activity, which focuses on improving population nutrition, increasing physical activity, reducing obesity and chronic disease, and improving health equity.
Dr. Patel and her colleagues’ three-pronged approach of using education, promotion, and accessibility to increase student interest in drinking water could be employed at countless other schools, said Ms. Cradock, who was not involved in the study.
“Negative perceptions of tap water and drinking fountains are common,” she said. “Not all students have access to safe and appealing drinking water while at school, and this strategy seems like a recipe for success.”
Dr. Patel reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 again the third-leading cause of U.S. deaths
the Centers for Disease Control and Prevention said April 22.
About 693,000 people died of heart disease in 2021, with 605,000 dying of cancer and 415,000 of COVID, the CDC said, citing provisional data that might be updated later.
Unintentional injuries were the fourth-leading cause of death, increasing to 219,000 in 2021 from 201,000 in 2020. Influenza and pneumonia dropped out of the top 10 leading causes of death and suicide moved into 10th place.
Overall, about 3,458,697 deaths were reported in the United States in 2021. The age-adjusted death rate was 841.6 deaths per 100,000 people, an increase of 0.7% from 2020. The 2021 death rate was the highest since 2003, the CDC said.
The overall number of COVID deaths in 2021 increased around 20% over 2020, when around 384,000 people died from the virus, the CDC said. COVID deaths in 2021 peaked for the weeks ending Jan. 16 and Sept. 11, following holiday periods.
The demographics of COVID mortality changed slightly, the CDC said in a second report.
Blacks accounted for 13.3% of COVID deaths in 2021 and Hispanics 16.5%, down several percentage points from 2020, the CDC said. Asians made up 3.1% of COVID deaths for 2021, a drop from 3.6% in 2020. White people accounted for 65.2% of COVID deaths in 2021, an increase from 59.6% in 2020.
Non-Hispanic American Indian/Alaskan Native and non-Hispanic Black or African American had the highest overall death rates for COVID, the CDC said.
Breaking the data down by age, the number of COVID deaths among people aged 75 years and older dropped to 178,000 in 2021 from around 207,000 in 2020. The numbers went up in other age groups. Among people aged 65-75, about 101,000 died of COVID in 2021, up from around 76,000 in 2020.
“The results of both studies highlight the need for greater effort to implement effective interventions,” the CDC said in a statement. “We must work to ensure equal treatment in all communities in proportion to their need for effective interventions that can prevent excess COVID-19 deaths.”
Since the pandemic began, about 991,000 people in the United States have died from COVID-related causes, the most among all nations in the world.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Prevention said April 22.
About 693,000 people died of heart disease in 2021, with 605,000 dying of cancer and 415,000 of COVID, the CDC said, citing provisional data that might be updated later.
Unintentional injuries were the fourth-leading cause of death, increasing to 219,000 in 2021 from 201,000 in 2020. Influenza and pneumonia dropped out of the top 10 leading causes of death and suicide moved into 10th place.
Overall, about 3,458,697 deaths were reported in the United States in 2021. The age-adjusted death rate was 841.6 deaths per 100,000 people, an increase of 0.7% from 2020. The 2021 death rate was the highest since 2003, the CDC said.
The overall number of COVID deaths in 2021 increased around 20% over 2020, when around 384,000 people died from the virus, the CDC said. COVID deaths in 2021 peaked for the weeks ending Jan. 16 and Sept. 11, following holiday periods.
The demographics of COVID mortality changed slightly, the CDC said in a second report.
Blacks accounted for 13.3% of COVID deaths in 2021 and Hispanics 16.5%, down several percentage points from 2020, the CDC said. Asians made up 3.1% of COVID deaths for 2021, a drop from 3.6% in 2020. White people accounted for 65.2% of COVID deaths in 2021, an increase from 59.6% in 2020.
Non-Hispanic American Indian/Alaskan Native and non-Hispanic Black or African American had the highest overall death rates for COVID, the CDC said.
Breaking the data down by age, the number of COVID deaths among people aged 75 years and older dropped to 178,000 in 2021 from around 207,000 in 2020. The numbers went up in other age groups. Among people aged 65-75, about 101,000 died of COVID in 2021, up from around 76,000 in 2020.
“The results of both studies highlight the need for greater effort to implement effective interventions,” the CDC said in a statement. “We must work to ensure equal treatment in all communities in proportion to their need for effective interventions that can prevent excess COVID-19 deaths.”
Since the pandemic began, about 991,000 people in the United States have died from COVID-related causes, the most among all nations in the world.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Prevention said April 22.
About 693,000 people died of heart disease in 2021, with 605,000 dying of cancer and 415,000 of COVID, the CDC said, citing provisional data that might be updated later.
Unintentional injuries were the fourth-leading cause of death, increasing to 219,000 in 2021 from 201,000 in 2020. Influenza and pneumonia dropped out of the top 10 leading causes of death and suicide moved into 10th place.
Overall, about 3,458,697 deaths were reported in the United States in 2021. The age-adjusted death rate was 841.6 deaths per 100,000 people, an increase of 0.7% from 2020. The 2021 death rate was the highest since 2003, the CDC said.
The overall number of COVID deaths in 2021 increased around 20% over 2020, when around 384,000 people died from the virus, the CDC said. COVID deaths in 2021 peaked for the weeks ending Jan. 16 and Sept. 11, following holiday periods.
The demographics of COVID mortality changed slightly, the CDC said in a second report.
Blacks accounted for 13.3% of COVID deaths in 2021 and Hispanics 16.5%, down several percentage points from 2020, the CDC said. Asians made up 3.1% of COVID deaths for 2021, a drop from 3.6% in 2020. White people accounted for 65.2% of COVID deaths in 2021, an increase from 59.6% in 2020.
Non-Hispanic American Indian/Alaskan Native and non-Hispanic Black or African American had the highest overall death rates for COVID, the CDC said.
Breaking the data down by age, the number of COVID deaths among people aged 75 years and older dropped to 178,000 in 2021 from around 207,000 in 2020. The numbers went up in other age groups. Among people aged 65-75, about 101,000 died of COVID in 2021, up from around 76,000 in 2020.
“The results of both studies highlight the need for greater effort to implement effective interventions,” the CDC said in a statement. “We must work to ensure equal treatment in all communities in proportion to their need for effective interventions that can prevent excess COVID-19 deaths.”
Since the pandemic began, about 991,000 people in the United States have died from COVID-related causes, the most among all nations in the world.
A version of this article first appeared on WebMD.com.
FROM THE MMWR
Three in four U.S. doctors are employed by hospitals, corporate entities: Report
Marcus Welby, MD, was a fictitious hometown doctor featured in a TV drama with the same name that was shown on ABC from 1969 to 1976. Played by actor Robert Young, Dr. Welby treated his patients through their bouts with breast cancer, impotence, and Alzheimer’s disease.
, according to a recent report sponsored by the Physicians Advocacy Institute and prepared by consulting firm Avalere Health.
“COVID-19 drove physicians to leave private practice for employment at an even more rapid pace than we’ve seen in recent years, and these trends continued to accelerate in 2021,” Kelly Kenney, chief executive officer of Physicians Advocacy Institute, said in an announcement. “This study underscores the fact that physicians across the nation are facing severe burnout and strain. The pressures of the pandemic forced many independent physicians to make difficult decisions to sell their practices, health insurers, or other corporate entities.”
Corporate entities are defined in the report as health insurers, private equity firms, and umbrella corporate entities that own multiple physician practices.
“The pandemic has been just brutal ... for nurses and physicians who are caring for patients,” Ms. Kenney told this news organization. “Between the financial stress that the pandemic certainly had on practices, because they certainly had little revenue for a while, and then also we know that the stress that physicians have felt mentally, you can’t overstate that.”
More than half of physician practices owned by hospitals, corporate entities
The Physicians Advocacy Institute has tracked changes in physician employment consistently since 2012, said Ms. Kenney. In 2012, 25% of physicians were employed; that has jumped to nearly 74%, which means the past decade has brought a world of change to the nation’s physicians.
“These are essentially small-business people ... and they were primarily trained to care for patients,” said Ms. Kenney, referring to physicians in independent practice. Still, she understands why physicians would seek employment in the face of “the crushing kind of pressure of having to deal with 20 different payers, pay overhead, and keep the lights on [at the practice].”
According to the report, 108,700 physicians left independent practice to enter employment with hospitals or other corporate entities in the 3-year period that ended in 2021. Seventy-six percent of that shift to employed status among physicians has occurred since the start of the COVID-19 pandemic in March 2020.
From a regional perspective, the report found continued growth among employed physicians across all U.S. regions in the last half of 2020. Hospital- or corporate-owned physician practices increased between 28% and 44%, while the percentage of hospital- or corporate-employed physicians increased between 13% and 24%.
Eighty percent of physicians in the Midwest are employed by hospitals or corporations, which leads the rest of the country, per the report. That’s followed by the Northeast, the West, and the South. Overall, the number of physicians working for such entities increased in all regions.
The report revealed that physician employment by corporations such as health insurers and venture capital firms grew from 92,400 in January 2019 to 142,900 in January 2022.
Hospitals and corporate entities acquired 36,200 physician practices (representing 38% growth) between 2019 and 2021, and the majority of these moves occurred since the pandemic’s start, according to the report.
Value-based care, venture capital firms driving change
Ms. Kenney pointed to value-based care as driving much of this activity by hospitals. “We all embrace [value-based payment], because we need to get a handle on cost, and we want better quality [but] those trends tend to favor integrated systems and systems that can handle a lot of risk and populations of patients.”
Still, the moves by private equity firms and health insurers in this space is relatively new, said Ms. Kenney, who added that her organization started tracking this trend 3 years ago. She pointed to a “marked acceleration” in the trend toward employing physicians and the sale of practices in the 18 months following the pandemic’s start; nonhospital corporate entities drove that steep increase, she said.
Ms. Kenney calls for further study and “guardrails” to respond to “that force in the health care system,” referring to the acquisition of practices by entities such as private equity firms. “Are these big [health care] systems going to continue to see patients in underserved areas, rural areas, and Medicaid patients if it doesn’t make sense financially to do so?
“That’s what we’re teeing up with this research,” added Ms. Kenney. “We are providing information that starts some conversations around what we might want to think about in terms of policies to ensure that we don’t impact patients’ access to care.”
The Physicians Advocacy Institute represents more than 170,000 physicians and medical students. Avalere Health used the IQVIA OneKey database for the report. The researchers studied the 3-year period from Jan. 1, 2019, to Jan. 1, 2022.
A version of this article first appeared on Medscape.com.
Marcus Welby, MD, was a fictitious hometown doctor featured in a TV drama with the same name that was shown on ABC from 1969 to 1976. Played by actor Robert Young, Dr. Welby treated his patients through their bouts with breast cancer, impotence, and Alzheimer’s disease.
, according to a recent report sponsored by the Physicians Advocacy Institute and prepared by consulting firm Avalere Health.
“COVID-19 drove physicians to leave private practice for employment at an even more rapid pace than we’ve seen in recent years, and these trends continued to accelerate in 2021,” Kelly Kenney, chief executive officer of Physicians Advocacy Institute, said in an announcement. “This study underscores the fact that physicians across the nation are facing severe burnout and strain. The pressures of the pandemic forced many independent physicians to make difficult decisions to sell their practices, health insurers, or other corporate entities.”
Corporate entities are defined in the report as health insurers, private equity firms, and umbrella corporate entities that own multiple physician practices.
“The pandemic has been just brutal ... for nurses and physicians who are caring for patients,” Ms. Kenney told this news organization. “Between the financial stress that the pandemic certainly had on practices, because they certainly had little revenue for a while, and then also we know that the stress that physicians have felt mentally, you can’t overstate that.”
More than half of physician practices owned by hospitals, corporate entities
The Physicians Advocacy Institute has tracked changes in physician employment consistently since 2012, said Ms. Kenney. In 2012, 25% of physicians were employed; that has jumped to nearly 74%, which means the past decade has brought a world of change to the nation’s physicians.
“These are essentially small-business people ... and they were primarily trained to care for patients,” said Ms. Kenney, referring to physicians in independent practice. Still, she understands why physicians would seek employment in the face of “the crushing kind of pressure of having to deal with 20 different payers, pay overhead, and keep the lights on [at the practice].”
According to the report, 108,700 physicians left independent practice to enter employment with hospitals or other corporate entities in the 3-year period that ended in 2021. Seventy-six percent of that shift to employed status among physicians has occurred since the start of the COVID-19 pandemic in March 2020.
From a regional perspective, the report found continued growth among employed physicians across all U.S. regions in the last half of 2020. Hospital- or corporate-owned physician practices increased between 28% and 44%, while the percentage of hospital- or corporate-employed physicians increased between 13% and 24%.
Eighty percent of physicians in the Midwest are employed by hospitals or corporations, which leads the rest of the country, per the report. That’s followed by the Northeast, the West, and the South. Overall, the number of physicians working for such entities increased in all regions.
The report revealed that physician employment by corporations such as health insurers and venture capital firms grew from 92,400 in January 2019 to 142,900 in January 2022.
Hospitals and corporate entities acquired 36,200 physician practices (representing 38% growth) between 2019 and 2021, and the majority of these moves occurred since the pandemic’s start, according to the report.
Value-based care, venture capital firms driving change
Ms. Kenney pointed to value-based care as driving much of this activity by hospitals. “We all embrace [value-based payment], because we need to get a handle on cost, and we want better quality [but] those trends tend to favor integrated systems and systems that can handle a lot of risk and populations of patients.”
Still, the moves by private equity firms and health insurers in this space is relatively new, said Ms. Kenney, who added that her organization started tracking this trend 3 years ago. She pointed to a “marked acceleration” in the trend toward employing physicians and the sale of practices in the 18 months following the pandemic’s start; nonhospital corporate entities drove that steep increase, she said.
Ms. Kenney calls for further study and “guardrails” to respond to “that force in the health care system,” referring to the acquisition of practices by entities such as private equity firms. “Are these big [health care] systems going to continue to see patients in underserved areas, rural areas, and Medicaid patients if it doesn’t make sense financially to do so?
“That’s what we’re teeing up with this research,” added Ms. Kenney. “We are providing information that starts some conversations around what we might want to think about in terms of policies to ensure that we don’t impact patients’ access to care.”
The Physicians Advocacy Institute represents more than 170,000 physicians and medical students. Avalere Health used the IQVIA OneKey database for the report. The researchers studied the 3-year period from Jan. 1, 2019, to Jan. 1, 2022.
A version of this article first appeared on Medscape.com.
Marcus Welby, MD, was a fictitious hometown doctor featured in a TV drama with the same name that was shown on ABC from 1969 to 1976. Played by actor Robert Young, Dr. Welby treated his patients through their bouts with breast cancer, impotence, and Alzheimer’s disease.
, according to a recent report sponsored by the Physicians Advocacy Institute and prepared by consulting firm Avalere Health.
“COVID-19 drove physicians to leave private practice for employment at an even more rapid pace than we’ve seen in recent years, and these trends continued to accelerate in 2021,” Kelly Kenney, chief executive officer of Physicians Advocacy Institute, said in an announcement. “This study underscores the fact that physicians across the nation are facing severe burnout and strain. The pressures of the pandemic forced many independent physicians to make difficult decisions to sell their practices, health insurers, or other corporate entities.”
Corporate entities are defined in the report as health insurers, private equity firms, and umbrella corporate entities that own multiple physician practices.
“The pandemic has been just brutal ... for nurses and physicians who are caring for patients,” Ms. Kenney told this news organization. “Between the financial stress that the pandemic certainly had on practices, because they certainly had little revenue for a while, and then also we know that the stress that physicians have felt mentally, you can’t overstate that.”
More than half of physician practices owned by hospitals, corporate entities
The Physicians Advocacy Institute has tracked changes in physician employment consistently since 2012, said Ms. Kenney. In 2012, 25% of physicians were employed; that has jumped to nearly 74%, which means the past decade has brought a world of change to the nation’s physicians.
“These are essentially small-business people ... and they were primarily trained to care for patients,” said Ms. Kenney, referring to physicians in independent practice. Still, she understands why physicians would seek employment in the face of “the crushing kind of pressure of having to deal with 20 different payers, pay overhead, and keep the lights on [at the practice].”
According to the report, 108,700 physicians left independent practice to enter employment with hospitals or other corporate entities in the 3-year period that ended in 2021. Seventy-six percent of that shift to employed status among physicians has occurred since the start of the COVID-19 pandemic in March 2020.
From a regional perspective, the report found continued growth among employed physicians across all U.S. regions in the last half of 2020. Hospital- or corporate-owned physician practices increased between 28% and 44%, while the percentage of hospital- or corporate-employed physicians increased between 13% and 24%.
Eighty percent of physicians in the Midwest are employed by hospitals or corporations, which leads the rest of the country, per the report. That’s followed by the Northeast, the West, and the South. Overall, the number of physicians working for such entities increased in all regions.
The report revealed that physician employment by corporations such as health insurers and venture capital firms grew from 92,400 in January 2019 to 142,900 in January 2022.
Hospitals and corporate entities acquired 36,200 physician practices (representing 38% growth) between 2019 and 2021, and the majority of these moves occurred since the pandemic’s start, according to the report.
Value-based care, venture capital firms driving change
Ms. Kenney pointed to value-based care as driving much of this activity by hospitals. “We all embrace [value-based payment], because we need to get a handle on cost, and we want better quality [but] those trends tend to favor integrated systems and systems that can handle a lot of risk and populations of patients.”
Still, the moves by private equity firms and health insurers in this space is relatively new, said Ms. Kenney, who added that her organization started tracking this trend 3 years ago. She pointed to a “marked acceleration” in the trend toward employing physicians and the sale of practices in the 18 months following the pandemic’s start; nonhospital corporate entities drove that steep increase, she said.
Ms. Kenney calls for further study and “guardrails” to respond to “that force in the health care system,” referring to the acquisition of practices by entities such as private equity firms. “Are these big [health care] systems going to continue to see patients in underserved areas, rural areas, and Medicaid patients if it doesn’t make sense financially to do so?
“That’s what we’re teeing up with this research,” added Ms. Kenney. “We are providing information that starts some conversations around what we might want to think about in terms of policies to ensure that we don’t impact patients’ access to care.”
The Physicians Advocacy Institute represents more than 170,000 physicians and medical students. Avalere Health used the IQVIA OneKey database for the report. The researchers studied the 3-year period from Jan. 1, 2019, to Jan. 1, 2022.
A version of this article first appeared on Medscape.com.
Icosapent ethyl’s CV mortality benefit magnified in patients with prior MI
In the placebo-controlled REDUCE-IT trial, icosapent ethyl (IPE) was linked to a significant reduction in major adverse cardiovascular events (MACE) when administered on top of LDL cholesterol control, but a new substudy suggests a greater relative advantage in those with a prior myocardial infarction.
In the study as a whole, IPE (Vascepa, Amarin) was tied to a 20% reduction in CV death (hazard ratio, 0.80; P = .03), but it climbed to a 30% reduction (HR, 0.70; P = .01) in the subgroup with a prior MI, reported a multinational team of investigators led by Prakriti Gaba, MD, a cardiologist at Brigham and Women’s Hospital, Boston.
On the basis of these data, “the imperative to treat patients who have a history of prior MI is even stronger,” said Deepak L. Bhatt, MD, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital.
The principal investigator of REDUCE-IT and a coauthor of this subanalysis, Dr. Bhatt said in an interview, “The significant reduction in cardiovascular mortality, as well as sudden cardiac death and cardiac arrest, really should make physicians strongly consider this therapy in eligible patients.”
The main results of the REDUCE-IT trial were published more than 3 years ago. It enrolled patients with established CV disease or diabetes with additional risk factors who were on a statin and had elevated triglyceride (TG) levels.
A 25% reduction in MACE reported
In those randomized to IPE, there was about a 25% reduction in the primary composite MACE outcome of cardiovascular death, nonfatal MI, nonfatal stroke, revascularization, and unstable angina relative to placebo. About the same relative reduction was achieved in the key secondary endpoint of CV death, nonfatal MI, and nonfatal stroke.
Some guidelines have been changed on the basis of these data. The National Lipid Association, for example, conferred a class 1 recommendation for adding IPE to other appropriate lipid-reducing therapies in any individual 45 years of age or older with atherosclerotic cardiovascular disease.
This new substudy (J Am Coll Cardiol. 2022 Apr 25; doi: 10.1016/j.jacc.2022.02.035), is likely to be influential for those guidelines not yet revised. In the substudy of the prior MI patients, the relative benefit of IPE for the primary and secondary MACE endpoints were of similar magnitude to the overall study population, but events occurred more frequently in the prior-MI subgroup, greatly increasing the statistical power of the advantage.
More MACE in prior MI patients
For example, the primary outcome was observed in 22% of the placebo patients in the overall REDUCE-IT analysis but in 26.1% of those with prior MI, so even though the relative risk reduction remained at about 25%, the statistical strength was a hundred-fold greater (P = .00001 vs. P < .001).
For the key secondary composite MACE endpoint, the relative reduction for those with a prior MI was modestly greater than the study as a whole (HR 0.71 vs. HR. 075) but the statistical strength was again magnified in those with a prior MI (P = .00006 vs. P < .001). In those with a prior MI , the advantage of receiving IPE was similar whether or not there had been a prior revascularization.
The 20% lower rate of all-cause mortality among prior MI patients receiving IPE rather than placebo fell just short of statistical significance (HR, 0.80; P = .054). Ischemic events on IPE were reduced by 35% (P = .0000001) and recurrent MI was reduced by 34% (P = .00009).
In the substudy as well as in the REDUCE-IT trial overall, IPE was well tolerated. A slightly higher rate of atrial fibrillation was reported in both.
The REDUCE-IT substudy evaluated 3,693 patients with a history of MI, representing 45% of the 8,179 patients randomized.
IPE, an ethyl ester of the omega-3 polyunsaturated fatty acid, initially attracted attention for its ability to reduce elevated TG. It was hoped this would address reduce residual risk in patients on maximally reduced LDL cholesterol. However, it is suspected that IPE exerts benefits additive to or independent of TG lowering, according to the authors of the REDUCE-IT substudy. These include attenuation of the inflammatory response, release of nitric oxide, and effects that support stabilization of atherosclerotic plaque.
The investigators reported that the pattern of response supports this theory. In the newly reported substudy, the primary event curves that included nonthrombotic events separated at about 1 year, but even curves for CV death and sudden cardiac death were more delayed.
This delay might be explained “by the slow but steady reduction in plaque volume, mitigation of inflammation, improvements in endothelial function, and membrane stabilization,” according to the authors, who cited studies suggesting each of these effects might not be wholly dependent on TG reductions alone.
Prior TG-lowering studies disappointing
In fact, several studies evaluating other strategies for TG reductions have been disappointing, according to an accompanying editorial (J Am Coll Cardiol. 2022 Apr 25; doi: 10.1016/j.jacc.2022.03.001). For example, the STRENGTH trial did not show clinical benefits despite a slightly greater reduction in TGs than that shown in REDUCE-IT (19% reduction vs. 18.3%).
Overall, the REDUCE-IT trial and the prior-MI REDUCE-IT substudy show that there is targetable residual risk in high risk patients on statin therapy. One of the authors of the editorial that accompanied the prior-MI substudy of REDUCE-IT, William E. Boden, MD, professor of medicine, Boston University, emphasized this point. On the basis of REDUCE-IT, he said he believes that IPE should be considered to have broad indications as an adjunctive treatment to other lipid-lowering strategies.
“My practice centers on optimizing secondary prevention in high-risk patients who have elevated TG levels despite well-controlled LDL levels on statins, ezetimibe, or even PCSK-9 [proprotein convertase subtilisin/kexin type 9] inhibitors,” Dr. Boden said in an interview. Patients with diabetes are notorious for presenting with this profile of dyslipidemia, but he added that “even nondiabetics with prior MI, acute coronary syndrome, or revascularization will benefit from the addition of IPE to high-potency statins.”
Although the American Heart Association and the American College of Cardiology have not yet updated their guidelines to include IPE, Dr. Boden pointed out that the European Society of Cardiology, the Canadian Cardiovascular Society, and the American Diabetes Society have.
Dr. Bhatt added that there is a clear message from REDUCE-IT that IPE addresses residual risk.
Targeting the subgroup of high-risk patients with elevated TGs “is easy” because they are so readily identifiable, according to Dr. Bhatt, but he said it should be used for any patient that meet the entry criteria used for REDUCE-IT.
“The overall results of REDUCE-IT were robustly positive, so I wouldn’t just use it in patients with prior MI,” Dr. Bhatt said.
Dr. Bhatt reports financial relationships with more than 20 pharmaceutical companies, including Amarin, which provided funding for this trial. Dr. Boden reports no potential conflicts of interest.
In the placebo-controlled REDUCE-IT trial, icosapent ethyl (IPE) was linked to a significant reduction in major adverse cardiovascular events (MACE) when administered on top of LDL cholesterol control, but a new substudy suggests a greater relative advantage in those with a prior myocardial infarction.
In the study as a whole, IPE (Vascepa, Amarin) was tied to a 20% reduction in CV death (hazard ratio, 0.80; P = .03), but it climbed to a 30% reduction (HR, 0.70; P = .01) in the subgroup with a prior MI, reported a multinational team of investigators led by Prakriti Gaba, MD, a cardiologist at Brigham and Women’s Hospital, Boston.
On the basis of these data, “the imperative to treat patients who have a history of prior MI is even stronger,” said Deepak L. Bhatt, MD, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital.
The principal investigator of REDUCE-IT and a coauthor of this subanalysis, Dr. Bhatt said in an interview, “The significant reduction in cardiovascular mortality, as well as sudden cardiac death and cardiac arrest, really should make physicians strongly consider this therapy in eligible patients.”
The main results of the REDUCE-IT trial were published more than 3 years ago. It enrolled patients with established CV disease or diabetes with additional risk factors who were on a statin and had elevated triglyceride (TG) levels.
A 25% reduction in MACE reported
In those randomized to IPE, there was about a 25% reduction in the primary composite MACE outcome of cardiovascular death, nonfatal MI, nonfatal stroke, revascularization, and unstable angina relative to placebo. About the same relative reduction was achieved in the key secondary endpoint of CV death, nonfatal MI, and nonfatal stroke.
Some guidelines have been changed on the basis of these data. The National Lipid Association, for example, conferred a class 1 recommendation for adding IPE to other appropriate lipid-reducing therapies in any individual 45 years of age or older with atherosclerotic cardiovascular disease.
This new substudy (J Am Coll Cardiol. 2022 Apr 25; doi: 10.1016/j.jacc.2022.02.035), is likely to be influential for those guidelines not yet revised. In the substudy of the prior MI patients, the relative benefit of IPE for the primary and secondary MACE endpoints were of similar magnitude to the overall study population, but events occurred more frequently in the prior-MI subgroup, greatly increasing the statistical power of the advantage.
More MACE in prior MI patients
For example, the primary outcome was observed in 22% of the placebo patients in the overall REDUCE-IT analysis but in 26.1% of those with prior MI, so even though the relative risk reduction remained at about 25%, the statistical strength was a hundred-fold greater (P = .00001 vs. P < .001).
For the key secondary composite MACE endpoint, the relative reduction for those with a prior MI was modestly greater than the study as a whole (HR 0.71 vs. HR. 075) but the statistical strength was again magnified in those with a prior MI (P = .00006 vs. P < .001). In those with a prior MI , the advantage of receiving IPE was similar whether or not there had been a prior revascularization.
The 20% lower rate of all-cause mortality among prior MI patients receiving IPE rather than placebo fell just short of statistical significance (HR, 0.80; P = .054). Ischemic events on IPE were reduced by 35% (P = .0000001) and recurrent MI was reduced by 34% (P = .00009).
In the substudy as well as in the REDUCE-IT trial overall, IPE was well tolerated. A slightly higher rate of atrial fibrillation was reported in both.
The REDUCE-IT substudy evaluated 3,693 patients with a history of MI, representing 45% of the 8,179 patients randomized.
IPE, an ethyl ester of the omega-3 polyunsaturated fatty acid, initially attracted attention for its ability to reduce elevated TG. It was hoped this would address reduce residual risk in patients on maximally reduced LDL cholesterol. However, it is suspected that IPE exerts benefits additive to or independent of TG lowering, according to the authors of the REDUCE-IT substudy. These include attenuation of the inflammatory response, release of nitric oxide, and effects that support stabilization of atherosclerotic plaque.
The investigators reported that the pattern of response supports this theory. In the newly reported substudy, the primary event curves that included nonthrombotic events separated at about 1 year, but even curves for CV death and sudden cardiac death were more delayed.
This delay might be explained “by the slow but steady reduction in plaque volume, mitigation of inflammation, improvements in endothelial function, and membrane stabilization,” according to the authors, who cited studies suggesting each of these effects might not be wholly dependent on TG reductions alone.
Prior TG-lowering studies disappointing
In fact, several studies evaluating other strategies for TG reductions have been disappointing, according to an accompanying editorial (J Am Coll Cardiol. 2022 Apr 25; doi: 10.1016/j.jacc.2022.03.001). For example, the STRENGTH trial did not show clinical benefits despite a slightly greater reduction in TGs than that shown in REDUCE-IT (19% reduction vs. 18.3%).
Overall, the REDUCE-IT trial and the prior-MI REDUCE-IT substudy show that there is targetable residual risk in high risk patients on statin therapy. One of the authors of the editorial that accompanied the prior-MI substudy of REDUCE-IT, William E. Boden, MD, professor of medicine, Boston University, emphasized this point. On the basis of REDUCE-IT, he said he believes that IPE should be considered to have broad indications as an adjunctive treatment to other lipid-lowering strategies.
“My practice centers on optimizing secondary prevention in high-risk patients who have elevated TG levels despite well-controlled LDL levels on statins, ezetimibe, or even PCSK-9 [proprotein convertase subtilisin/kexin type 9] inhibitors,” Dr. Boden said in an interview. Patients with diabetes are notorious for presenting with this profile of dyslipidemia, but he added that “even nondiabetics with prior MI, acute coronary syndrome, or revascularization will benefit from the addition of IPE to high-potency statins.”
Although the American Heart Association and the American College of Cardiology have not yet updated their guidelines to include IPE, Dr. Boden pointed out that the European Society of Cardiology, the Canadian Cardiovascular Society, and the American Diabetes Society have.
Dr. Bhatt added that there is a clear message from REDUCE-IT that IPE addresses residual risk.
Targeting the subgroup of high-risk patients with elevated TGs “is easy” because they are so readily identifiable, according to Dr. Bhatt, but he said it should be used for any patient that meet the entry criteria used for REDUCE-IT.
“The overall results of REDUCE-IT were robustly positive, so I wouldn’t just use it in patients with prior MI,” Dr. Bhatt said.
Dr. Bhatt reports financial relationships with more than 20 pharmaceutical companies, including Amarin, which provided funding for this trial. Dr. Boden reports no potential conflicts of interest.
In the placebo-controlled REDUCE-IT trial, icosapent ethyl (IPE) was linked to a significant reduction in major adverse cardiovascular events (MACE) when administered on top of LDL cholesterol control, but a new substudy suggests a greater relative advantage in those with a prior myocardial infarction.
In the study as a whole, IPE (Vascepa, Amarin) was tied to a 20% reduction in CV death (hazard ratio, 0.80; P = .03), but it climbed to a 30% reduction (HR, 0.70; P = .01) in the subgroup with a prior MI, reported a multinational team of investigators led by Prakriti Gaba, MD, a cardiologist at Brigham and Women’s Hospital, Boston.
On the basis of these data, “the imperative to treat patients who have a history of prior MI is even stronger,” said Deepak L. Bhatt, MD, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital.
The principal investigator of REDUCE-IT and a coauthor of this subanalysis, Dr. Bhatt said in an interview, “The significant reduction in cardiovascular mortality, as well as sudden cardiac death and cardiac arrest, really should make physicians strongly consider this therapy in eligible patients.”
The main results of the REDUCE-IT trial were published more than 3 years ago. It enrolled patients with established CV disease or diabetes with additional risk factors who were on a statin and had elevated triglyceride (TG) levels.
A 25% reduction in MACE reported
In those randomized to IPE, there was about a 25% reduction in the primary composite MACE outcome of cardiovascular death, nonfatal MI, nonfatal stroke, revascularization, and unstable angina relative to placebo. About the same relative reduction was achieved in the key secondary endpoint of CV death, nonfatal MI, and nonfatal stroke.
Some guidelines have been changed on the basis of these data. The National Lipid Association, for example, conferred a class 1 recommendation for adding IPE to other appropriate lipid-reducing therapies in any individual 45 years of age or older with atherosclerotic cardiovascular disease.
This new substudy (J Am Coll Cardiol. 2022 Apr 25; doi: 10.1016/j.jacc.2022.02.035), is likely to be influential for those guidelines not yet revised. In the substudy of the prior MI patients, the relative benefit of IPE for the primary and secondary MACE endpoints were of similar magnitude to the overall study population, but events occurred more frequently in the prior-MI subgroup, greatly increasing the statistical power of the advantage.
More MACE in prior MI patients
For example, the primary outcome was observed in 22% of the placebo patients in the overall REDUCE-IT analysis but in 26.1% of those with prior MI, so even though the relative risk reduction remained at about 25%, the statistical strength was a hundred-fold greater (P = .00001 vs. P < .001).
For the key secondary composite MACE endpoint, the relative reduction for those with a prior MI was modestly greater than the study as a whole (HR 0.71 vs. HR. 075) but the statistical strength was again magnified in those with a prior MI (P = .00006 vs. P < .001). In those with a prior MI , the advantage of receiving IPE was similar whether or not there had been a prior revascularization.
The 20% lower rate of all-cause mortality among prior MI patients receiving IPE rather than placebo fell just short of statistical significance (HR, 0.80; P = .054). Ischemic events on IPE were reduced by 35% (P = .0000001) and recurrent MI was reduced by 34% (P = .00009).
In the substudy as well as in the REDUCE-IT trial overall, IPE was well tolerated. A slightly higher rate of atrial fibrillation was reported in both.
The REDUCE-IT substudy evaluated 3,693 patients with a history of MI, representing 45% of the 8,179 patients randomized.
IPE, an ethyl ester of the omega-3 polyunsaturated fatty acid, initially attracted attention for its ability to reduce elevated TG. It was hoped this would address reduce residual risk in patients on maximally reduced LDL cholesterol. However, it is suspected that IPE exerts benefits additive to or independent of TG lowering, according to the authors of the REDUCE-IT substudy. These include attenuation of the inflammatory response, release of nitric oxide, and effects that support stabilization of atherosclerotic plaque.
The investigators reported that the pattern of response supports this theory. In the newly reported substudy, the primary event curves that included nonthrombotic events separated at about 1 year, but even curves for CV death and sudden cardiac death were more delayed.
This delay might be explained “by the slow but steady reduction in plaque volume, mitigation of inflammation, improvements in endothelial function, and membrane stabilization,” according to the authors, who cited studies suggesting each of these effects might not be wholly dependent on TG reductions alone.
Prior TG-lowering studies disappointing
In fact, several studies evaluating other strategies for TG reductions have been disappointing, according to an accompanying editorial (J Am Coll Cardiol. 2022 Apr 25; doi: 10.1016/j.jacc.2022.03.001). For example, the STRENGTH trial did not show clinical benefits despite a slightly greater reduction in TGs than that shown in REDUCE-IT (19% reduction vs. 18.3%).
Overall, the REDUCE-IT trial and the prior-MI REDUCE-IT substudy show that there is targetable residual risk in high risk patients on statin therapy. One of the authors of the editorial that accompanied the prior-MI substudy of REDUCE-IT, William E. Boden, MD, professor of medicine, Boston University, emphasized this point. On the basis of REDUCE-IT, he said he believes that IPE should be considered to have broad indications as an adjunctive treatment to other lipid-lowering strategies.
“My practice centers on optimizing secondary prevention in high-risk patients who have elevated TG levels despite well-controlled LDL levels on statins, ezetimibe, or even PCSK-9 [proprotein convertase subtilisin/kexin type 9] inhibitors,” Dr. Boden said in an interview. Patients with diabetes are notorious for presenting with this profile of dyslipidemia, but he added that “even nondiabetics with prior MI, acute coronary syndrome, or revascularization will benefit from the addition of IPE to high-potency statins.”
Although the American Heart Association and the American College of Cardiology have not yet updated their guidelines to include IPE, Dr. Boden pointed out that the European Society of Cardiology, the Canadian Cardiovascular Society, and the American Diabetes Society have.
Dr. Bhatt added that there is a clear message from REDUCE-IT that IPE addresses residual risk.
Targeting the subgroup of high-risk patients with elevated TGs “is easy” because they are so readily identifiable, according to Dr. Bhatt, but he said it should be used for any patient that meet the entry criteria used for REDUCE-IT.
“The overall results of REDUCE-IT were robustly positive, so I wouldn’t just use it in patients with prior MI,” Dr. Bhatt said.
Dr. Bhatt reports financial relationships with more than 20 pharmaceutical companies, including Amarin, which provided funding for this trial. Dr. Boden reports no potential conflicts of interest.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Mediterranean diet linked to lower risk for preeclampsia
Pregnant women who had a higher adherence to a Mediterranean-style diet had a lower risk of preeclampsia, according to the results of a new study.
“As an observational study, it obviously has limitations that need to be considered, but these results build on other evidence that Mediterranean diet reduces cardiovascular risk and extends those findings to pregnancy as preeclampsia is a cardiovascular outcome,” senior author Noel T. Mueller, PhD, associate professor at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in an interview.
The study was published online April 20 in the Journal of the American Heart Association.
The authors noted that preeclampsia, characterized by a range of symptoms including hypertension, proteinuria, and end-organ dysfunction, is a disorder that occurs in up to 5%-10% of all pregnant women worldwide, and is more common in Black women. It is a major cause of maternal and fetal morbidity and raises the risk for long-term cardiovascular disease (CVD), including chronic hypertension, coronary artery disease, ischemic stroke, and heart failure.
Children born to mothers with preeclampsia are at an elevated risk of having higher blood pressure and other abnormal cardiometabolic parameters.
The authors noted that multiple studies have demonstrated the benefit of the Mediterranean diet – characterized primarily by high intake of vegetables, fruits, and unsaturated fats – in reducing cardiovascular risk in the nonpregnant population. The current study was conducted to investigate whether benefits could also be seen in pregnant women in the form of a reduced risk of preeclampsia.
For the study, which used data from the Boston Birth Cohort, maternal sociodemographic and dietary data were obtained from 8,507 women via interview and food frequency questionnaire within 24-72 hours of giving birth. A Mediterranean-style diet score was calculated from the food frequency questionnaire. Additional clinical information, including physician diagnoses of preexisting conditions and preeclampsia, were extracted from medical records.
Of the women in the sample, 848 developed preeclampsia, of whom 47% were Black, and 28% were Hispanic.
After multivariable adjustment, the greatest adherence to a Mediterranean-style diet was associated with lower odds of developing preeclampsia (adjusted odds ratio comparing tertile 3 to tertile 1, 0.78; 95% confidence interval [CI], 0.64-0.96).
A subgroup analysis of Black women demonstrated a similar benefit with an adjusted odds ratio comparing tertile 3 to tertile 1 of 0.74 (95% CI, 0.76-0.96).
“In this racially and ethnically diverse cohort, women who had greater adherence to a Mediterranean-style diet during pregnancy had a greater than 20% lower odds of developing preeclampsia, after [adjustment] for potential confounders. In addition, the evidence for the protective effect of a Mediterranean-style diet against the odds of developing preeclampsia remained present in a subgroup analysis of Black women,” the researchers concluded.
Asked whether this would be enough evidence to recommend a Mediterranean diet to pregnant women, Dr. Mueller said that the organizations that issue dietary guidelines would probably require replication of these results and also possibly a randomized trial in a diverse population group before advocating such a diet.
“That is something we would like to do but this will take time and money,” he added.
Lead study author Anum Minhas, MD, Johns Hopkins University, Baltimore, said that in the meantime she would be recommending a Mediterranean diet to her pregnant patients.
“The Mediterranean diet is a very healthy way of eating. I can’t see any downside of following such a diet in pregnancy, especially for high-risk women – those with obesity, hypertension or gestational diabetes, and there are likely other potential benefits such as reduced weight gain and reduced gestational diabetes,” she said.
Dr. Mueller said he appreciated this pragmatic approach. “Sometimes there can be hesitation on making recommendations from observational studies, but the alternative to recommending this diet is either no recommendations on diet or recommending an alternative diet,” he said. “The Mediterranean diet or the DASH diet, which is quite similar, have shown by far the most evidence of cardioprotection of any diets. They have been shown to reduce blood pressure and lipids and improve cardiovascular risk, and I think we can now assume that that likely extends to pregnancy. I feel comfortable for this diet to be recommended to pregnant women.”
But he added: “Having said that, there is still a need for a randomized trial in pregnancy. We think it works but until we have a randomized trial we won’t know for sure, and we won’t know how much of a benefit we can get.”
Commenting on the study, JoAnn Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital, Boston, pointed out that this type of observational study is important for hypothesis generation but cannot prove cause and effect relationships.
“The evidence is promising enough,” said Dr. Manson, who was not involved with this study. But she added that to move forward, a randomized trial in women at elevated risk of preeclampsia would be needed, beginning in early pregnancy, if not earlier.
“In the meantime,” she noted, “several large-scale cohorts could be leveraged to look at diet assessed before or during pregnancy to see if this dietary pattern is prospectively related to lower risk of preeclampsia.
“With additional supportive data, and in view of the diet’s safety and general cardiovascular benefits, it could become a major tool for preventing adverse pregnancy outcomes.”
The Boston Birth Cohort study was supported in part by grants from the March of Dimes, the National Institutes of Health, and the Health Resources and Services Administration of the U.S. Department of Health and Human Services. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women who had a higher adherence to a Mediterranean-style diet had a lower risk of preeclampsia, according to the results of a new study.
“As an observational study, it obviously has limitations that need to be considered, but these results build on other evidence that Mediterranean diet reduces cardiovascular risk and extends those findings to pregnancy as preeclampsia is a cardiovascular outcome,” senior author Noel T. Mueller, PhD, associate professor at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in an interview.
The study was published online April 20 in the Journal of the American Heart Association.
The authors noted that preeclampsia, characterized by a range of symptoms including hypertension, proteinuria, and end-organ dysfunction, is a disorder that occurs in up to 5%-10% of all pregnant women worldwide, and is more common in Black women. It is a major cause of maternal and fetal morbidity and raises the risk for long-term cardiovascular disease (CVD), including chronic hypertension, coronary artery disease, ischemic stroke, and heart failure.
Children born to mothers with preeclampsia are at an elevated risk of having higher blood pressure and other abnormal cardiometabolic parameters.
The authors noted that multiple studies have demonstrated the benefit of the Mediterranean diet – characterized primarily by high intake of vegetables, fruits, and unsaturated fats – in reducing cardiovascular risk in the nonpregnant population. The current study was conducted to investigate whether benefits could also be seen in pregnant women in the form of a reduced risk of preeclampsia.
For the study, which used data from the Boston Birth Cohort, maternal sociodemographic and dietary data were obtained from 8,507 women via interview and food frequency questionnaire within 24-72 hours of giving birth. A Mediterranean-style diet score was calculated from the food frequency questionnaire. Additional clinical information, including physician diagnoses of preexisting conditions and preeclampsia, were extracted from medical records.
Of the women in the sample, 848 developed preeclampsia, of whom 47% were Black, and 28% were Hispanic.
After multivariable adjustment, the greatest adherence to a Mediterranean-style diet was associated with lower odds of developing preeclampsia (adjusted odds ratio comparing tertile 3 to tertile 1, 0.78; 95% confidence interval [CI], 0.64-0.96).
A subgroup analysis of Black women demonstrated a similar benefit with an adjusted odds ratio comparing tertile 3 to tertile 1 of 0.74 (95% CI, 0.76-0.96).
“In this racially and ethnically diverse cohort, women who had greater adherence to a Mediterranean-style diet during pregnancy had a greater than 20% lower odds of developing preeclampsia, after [adjustment] for potential confounders. In addition, the evidence for the protective effect of a Mediterranean-style diet against the odds of developing preeclampsia remained present in a subgroup analysis of Black women,” the researchers concluded.
Asked whether this would be enough evidence to recommend a Mediterranean diet to pregnant women, Dr. Mueller said that the organizations that issue dietary guidelines would probably require replication of these results and also possibly a randomized trial in a diverse population group before advocating such a diet.
“That is something we would like to do but this will take time and money,” he added.
Lead study author Anum Minhas, MD, Johns Hopkins University, Baltimore, said that in the meantime she would be recommending a Mediterranean diet to her pregnant patients.
“The Mediterranean diet is a very healthy way of eating. I can’t see any downside of following such a diet in pregnancy, especially for high-risk women – those with obesity, hypertension or gestational diabetes, and there are likely other potential benefits such as reduced weight gain and reduced gestational diabetes,” she said.
Dr. Mueller said he appreciated this pragmatic approach. “Sometimes there can be hesitation on making recommendations from observational studies, but the alternative to recommending this diet is either no recommendations on diet or recommending an alternative diet,” he said. “The Mediterranean diet or the DASH diet, which is quite similar, have shown by far the most evidence of cardioprotection of any diets. They have been shown to reduce blood pressure and lipids and improve cardiovascular risk, and I think we can now assume that that likely extends to pregnancy. I feel comfortable for this diet to be recommended to pregnant women.”
But he added: “Having said that, there is still a need for a randomized trial in pregnancy. We think it works but until we have a randomized trial we won’t know for sure, and we won’t know how much of a benefit we can get.”
Commenting on the study, JoAnn Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital, Boston, pointed out that this type of observational study is important for hypothesis generation but cannot prove cause and effect relationships.
“The evidence is promising enough,” said Dr. Manson, who was not involved with this study. But she added that to move forward, a randomized trial in women at elevated risk of preeclampsia would be needed, beginning in early pregnancy, if not earlier.
“In the meantime,” she noted, “several large-scale cohorts could be leveraged to look at diet assessed before or during pregnancy to see if this dietary pattern is prospectively related to lower risk of preeclampsia.
“With additional supportive data, and in view of the diet’s safety and general cardiovascular benefits, it could become a major tool for preventing adverse pregnancy outcomes.”
The Boston Birth Cohort study was supported in part by grants from the March of Dimes, the National Institutes of Health, and the Health Resources and Services Administration of the U.S. Department of Health and Human Services. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women who had a higher adherence to a Mediterranean-style diet had a lower risk of preeclampsia, according to the results of a new study.
“As an observational study, it obviously has limitations that need to be considered, but these results build on other evidence that Mediterranean diet reduces cardiovascular risk and extends those findings to pregnancy as preeclampsia is a cardiovascular outcome,” senior author Noel T. Mueller, PhD, associate professor at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in an interview.
The study was published online April 20 in the Journal of the American Heart Association.
The authors noted that preeclampsia, characterized by a range of symptoms including hypertension, proteinuria, and end-organ dysfunction, is a disorder that occurs in up to 5%-10% of all pregnant women worldwide, and is more common in Black women. It is a major cause of maternal and fetal morbidity and raises the risk for long-term cardiovascular disease (CVD), including chronic hypertension, coronary artery disease, ischemic stroke, and heart failure.
Children born to mothers with preeclampsia are at an elevated risk of having higher blood pressure and other abnormal cardiometabolic parameters.
The authors noted that multiple studies have demonstrated the benefit of the Mediterranean diet – characterized primarily by high intake of vegetables, fruits, and unsaturated fats – in reducing cardiovascular risk in the nonpregnant population. The current study was conducted to investigate whether benefits could also be seen in pregnant women in the form of a reduced risk of preeclampsia.
For the study, which used data from the Boston Birth Cohort, maternal sociodemographic and dietary data were obtained from 8,507 women via interview and food frequency questionnaire within 24-72 hours of giving birth. A Mediterranean-style diet score was calculated from the food frequency questionnaire. Additional clinical information, including physician diagnoses of preexisting conditions and preeclampsia, were extracted from medical records.
Of the women in the sample, 848 developed preeclampsia, of whom 47% were Black, and 28% were Hispanic.
After multivariable adjustment, the greatest adherence to a Mediterranean-style diet was associated with lower odds of developing preeclampsia (adjusted odds ratio comparing tertile 3 to tertile 1, 0.78; 95% confidence interval [CI], 0.64-0.96).
A subgroup analysis of Black women demonstrated a similar benefit with an adjusted odds ratio comparing tertile 3 to tertile 1 of 0.74 (95% CI, 0.76-0.96).
“In this racially and ethnically diverse cohort, women who had greater adherence to a Mediterranean-style diet during pregnancy had a greater than 20% lower odds of developing preeclampsia, after [adjustment] for potential confounders. In addition, the evidence for the protective effect of a Mediterranean-style diet against the odds of developing preeclampsia remained present in a subgroup analysis of Black women,” the researchers concluded.
Asked whether this would be enough evidence to recommend a Mediterranean diet to pregnant women, Dr. Mueller said that the organizations that issue dietary guidelines would probably require replication of these results and also possibly a randomized trial in a diverse population group before advocating such a diet.
“That is something we would like to do but this will take time and money,” he added.
Lead study author Anum Minhas, MD, Johns Hopkins University, Baltimore, said that in the meantime she would be recommending a Mediterranean diet to her pregnant patients.
“The Mediterranean diet is a very healthy way of eating. I can’t see any downside of following such a diet in pregnancy, especially for high-risk women – those with obesity, hypertension or gestational diabetes, and there are likely other potential benefits such as reduced weight gain and reduced gestational diabetes,” she said.
Dr. Mueller said he appreciated this pragmatic approach. “Sometimes there can be hesitation on making recommendations from observational studies, but the alternative to recommending this diet is either no recommendations on diet or recommending an alternative diet,” he said. “The Mediterranean diet or the DASH diet, which is quite similar, have shown by far the most evidence of cardioprotection of any diets. They have been shown to reduce blood pressure and lipids and improve cardiovascular risk, and I think we can now assume that that likely extends to pregnancy. I feel comfortable for this diet to be recommended to pregnant women.”
But he added: “Having said that, there is still a need for a randomized trial in pregnancy. We think it works but until we have a randomized trial we won’t know for sure, and we won’t know how much of a benefit we can get.”
Commenting on the study, JoAnn Manson, MD, chief of the division of preventive medicine at Brigham and Women’s Hospital, Boston, pointed out that this type of observational study is important for hypothesis generation but cannot prove cause and effect relationships.
“The evidence is promising enough,” said Dr. Manson, who was not involved with this study. But she added that to move forward, a randomized trial in women at elevated risk of preeclampsia would be needed, beginning in early pregnancy, if not earlier.
“In the meantime,” she noted, “several large-scale cohorts could be leveraged to look at diet assessed before or during pregnancy to see if this dietary pattern is prospectively related to lower risk of preeclampsia.
“With additional supportive data, and in view of the diet’s safety and general cardiovascular benefits, it could become a major tool for preventing adverse pregnancy outcomes.”
The Boston Birth Cohort study was supported in part by grants from the March of Dimes, the National Institutes of Health, and the Health Resources and Services Administration of the U.S. Department of Health and Human Services. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Myocarditis higher with Moderna COVID vax in young men
One of the largest studies to date on myocarditis after COVID-19 vaccination confirms an increased risk with both the Pfizer and Moderna vaccines in young men and shows that the risk is higher with the Moderna than with the Pfizer vaccine.
The study also suggests for the first time that in young men 16 to 24 years of age, the risk for myocarditis after vaccination with either the Pfizer or Moderna vaccine is higher than the risk for myocarditis after COVID-19 infection.
The population-based study involved data on 23.1 million residents across four Scandinavian countries – Denmark, Finland, Norway, and Sweden – 74% of whom had received two vaccine doses and 7% of whom had received one dose.
By linking data from high-quality nationwide health registers on COVID-19 vaccination, infection rates, and myocarditis diagnoses, the researchers were able to evaluate the risk for myocarditis by vaccine product, vaccination dose number, sex, and age.
The study was published online in JAMA Cardiology.
The results confirm that the risk for myocarditis after COVID-19 mRNA vaccines is highest in young men 16 to 24 years of age after the second dose.
For men in this age group who received two doses of the same vaccine, data were compatible, with between four and seven excess myocarditis events in 28 days per 100,000 individuals after the second dose of the Pfizer vaccine, and between nine and 28 per 100,000 individuals after the second dose of the Moderna vaccine.
“This is one of the largest studies on this topic to date. The first population studies were in Israel, with 5 million individuals, and looked at just the Pfizer vaccine. We have data on 23 million people from Scandinavia that include both the Pfizer and Moderna vaccines,” senior author Rickard Ljung, MD, Swedish Medical Products Agency, told this news organization.
“We show a clearly higher risk of myocarditis after the Moderna vaccine than after the Pfizer vaccine. This has been suggested before, but our data confirm definitively that the Moderna vaccine has a higher risk of myocarditis than the Pfizer vaccine,” he added.
“In the group at highest risk of myocarditis after COVID vaccination – young men aged 16 to 24 – the Pfizer vaccine shows a five times higher risk of myocarditis versus the unvaccinated cohort, while the Moderna vaccine shows a 15 times higher risk,” Dr. Ljung noted.
After seeing these data, the Swedish regulatory authority is no longer recommending use of the Moderna vaccine for people younger than 30 years, Dr. Ljung said. Similar recommendations have been made in Norway and Finland.
The researchers report that their finding of a higher risk for myocarditis after the Moderna vaccine than after the Pfizer vaccine in young men is in line with data from the Canada, France, the United Kingdom, and the United States. But they point out that, compared with previous studies, the current study had the advantage of data analyzed according to a common protocol from four different countries and that showed similar directions of associations, despite considerable differences in previous COVID-19 infection levels and lockdown policies.
Risk higher with vaccination than infection?
For what is believed to be the first time, the Scandinavian data also suggest a higher risk for myocarditis after COVID-19 vaccination with both the Pfizer and Moderna vaccines than after COVID-19 infection in young men 16 to 24 years.
Although previous studies have shown that males in this age group have the highest risk for myocarditis after vaccination, it has always been suggested that the risk after vaccination is lower than the risk after infection. The Scandinavian data suggest otherwise for this age group.
Dr. Ljung explained that the myocarditis risk after COVID infection is very hard to study.
“It is highly dependent on the testing strategy,” he said. “For example, in the first half of 2020, the only people being tested were those admitted to hospital, so studies would have included the sickest patients and would therefore likely have found a higher rate of myocarditis. But this current Scandinavian dataset only included individuals with a positive COVID test after August 2020, reflecting a broader range of people.”
The researchers found an excess rate of myocarditis of 3.26 per 100,000 individuals within 28 days of a positive COVID-19 test among all males, and 1.37 per 100,000 individuals among males 16 to 24 years of age.
“We show that the risk of myocarditis after COVID infection is lower in younger people and higher in older people, but the opposite is true after COVID vaccination, where the risk of myocarditis is higher in younger people and lower in older people,” Dr. Ljung said.
The study was not able to look at severity of myocarditis but did record length of hospital stay, which was similar in patients who developed myocarditis after vaccination and those in the unvaccinated cohort (4 to 5 days). Deaths were rare, with no deaths in people younger than 40 years.
“I think we can say that in people aged over 40, the risk of myocarditis is greater with infection than with vaccination, but in those under 40, it is not so clear. And our data suggest that for young men aged 16 to 24 years, the risk of myocarditis after COVID vaccination with either the Pfizer or Moderna vaccine is higher than after COVID infection,” Dr. Ljung commented.
Although the Swedish regulatory agency has already stopped recommending use of Moderna vaccine in those younger than 30 years on the basis of these data, Dr. Ljung was reluctant to make any recommendations regarding the use of the Pfizer vaccine in young males, saying it was up to individual public-health agencies to makes these decisions.
But he pointed out that the current study only looked at myocarditis, and COVID infection can result in many other complications that can lead to hospitalization and death, which needs to be taken into account when assessing the risk and benefit of vaccination.
Dr. Ljung noted that the current data only applied to the first two doses of the vaccines; data after booster injections have not been included, although the researchers are looking at that now.
What to advise patients?
In an accompanying Editor’s Note, Ann Marie Navar, MD, University of Texas Southwestern Medical Center, Dallas, who is editor of JAMA Cardiology, and Robert Bonow, MD, Northwestern University Feinberg School of Medicine, Chicago, who is deputy editor of JAMA Cardiology, try to explain how these data can inform the way health care professionals communicate with their patients about vaccination.
They point out the “good news,” that older adults who are at highest risk for COVID-19 complications appear to be at extremely low risk for vaccine-associated myocarditis.
They note that for both men and women older than 40 years, the excess number of cases of myocarditis after vaccination was fewer than two in 100,000 vaccinees across all vaccines studied, and the death toll from COVID-19 in the United States as of March was more than 200 per 100,000 population.
“Given the high rates of morbidity and mortality from COVID-19 infection in older adults and the efficacy of the vaccine in preventing severe infection and death, the benefits of immunization in those older than 40 years clearly outweigh the risks,” the editors say.
But given these data in young men, they suggest that health care professionals consider recommending the Pfizer vaccine over the Moderna vaccine for certain populations, including young men and other individuals for whom concerns about myocarditis present a barrier to immunization.
The editors also point out that although the risk for myocarditis after COVID-19 immunization is real, this low risk must be considered in the context of the overall benefit of the vaccine.
“At the individual level, immunization prevents not only COVID-19-related myocarditis but also severe disease, hospitalization, long-term complications after COVID-19 infection, and death. At the population level, immunization helps to decrease community spread, decrease the chances of new variants emerging, protect people who are immunocompromised, and ensure our health care system can continue to provide for our communities,” they conclude.
Dr. Ljung reports grants from Sanofi Aventis paid to his institution outside the submitted work and personal fees from Pfizer outside the submitted work. Dr. Navar reports personal fees from Pfizer and AstraZeneca, outside the scope of this work.
A version of this article first appeared on Medscape.com.
One of the largest studies to date on myocarditis after COVID-19 vaccination confirms an increased risk with both the Pfizer and Moderna vaccines in young men and shows that the risk is higher with the Moderna than with the Pfizer vaccine.
The study also suggests for the first time that in young men 16 to 24 years of age, the risk for myocarditis after vaccination with either the Pfizer or Moderna vaccine is higher than the risk for myocarditis after COVID-19 infection.
The population-based study involved data on 23.1 million residents across four Scandinavian countries – Denmark, Finland, Norway, and Sweden – 74% of whom had received two vaccine doses and 7% of whom had received one dose.
By linking data from high-quality nationwide health registers on COVID-19 vaccination, infection rates, and myocarditis diagnoses, the researchers were able to evaluate the risk for myocarditis by vaccine product, vaccination dose number, sex, and age.
The study was published online in JAMA Cardiology.
The results confirm that the risk for myocarditis after COVID-19 mRNA vaccines is highest in young men 16 to 24 years of age after the second dose.
For men in this age group who received two doses of the same vaccine, data were compatible, with between four and seven excess myocarditis events in 28 days per 100,000 individuals after the second dose of the Pfizer vaccine, and between nine and 28 per 100,000 individuals after the second dose of the Moderna vaccine.
“This is one of the largest studies on this topic to date. The first population studies were in Israel, with 5 million individuals, and looked at just the Pfizer vaccine. We have data on 23 million people from Scandinavia that include both the Pfizer and Moderna vaccines,” senior author Rickard Ljung, MD, Swedish Medical Products Agency, told this news organization.
“We show a clearly higher risk of myocarditis after the Moderna vaccine than after the Pfizer vaccine. This has been suggested before, but our data confirm definitively that the Moderna vaccine has a higher risk of myocarditis than the Pfizer vaccine,” he added.
“In the group at highest risk of myocarditis after COVID vaccination – young men aged 16 to 24 – the Pfizer vaccine shows a five times higher risk of myocarditis versus the unvaccinated cohort, while the Moderna vaccine shows a 15 times higher risk,” Dr. Ljung noted.
After seeing these data, the Swedish regulatory authority is no longer recommending use of the Moderna vaccine for people younger than 30 years, Dr. Ljung said. Similar recommendations have been made in Norway and Finland.
The researchers report that their finding of a higher risk for myocarditis after the Moderna vaccine than after the Pfizer vaccine in young men is in line with data from the Canada, France, the United Kingdom, and the United States. But they point out that, compared with previous studies, the current study had the advantage of data analyzed according to a common protocol from four different countries and that showed similar directions of associations, despite considerable differences in previous COVID-19 infection levels and lockdown policies.
Risk higher with vaccination than infection?
For what is believed to be the first time, the Scandinavian data also suggest a higher risk for myocarditis after COVID-19 vaccination with both the Pfizer and Moderna vaccines than after COVID-19 infection in young men 16 to 24 years.
Although previous studies have shown that males in this age group have the highest risk for myocarditis after vaccination, it has always been suggested that the risk after vaccination is lower than the risk after infection. The Scandinavian data suggest otherwise for this age group.
Dr. Ljung explained that the myocarditis risk after COVID infection is very hard to study.
“It is highly dependent on the testing strategy,” he said. “For example, in the first half of 2020, the only people being tested were those admitted to hospital, so studies would have included the sickest patients and would therefore likely have found a higher rate of myocarditis. But this current Scandinavian dataset only included individuals with a positive COVID test after August 2020, reflecting a broader range of people.”
The researchers found an excess rate of myocarditis of 3.26 per 100,000 individuals within 28 days of a positive COVID-19 test among all males, and 1.37 per 100,000 individuals among males 16 to 24 years of age.
“We show that the risk of myocarditis after COVID infection is lower in younger people and higher in older people, but the opposite is true after COVID vaccination, where the risk of myocarditis is higher in younger people and lower in older people,” Dr. Ljung said.
The study was not able to look at severity of myocarditis but did record length of hospital stay, which was similar in patients who developed myocarditis after vaccination and those in the unvaccinated cohort (4 to 5 days). Deaths were rare, with no deaths in people younger than 40 years.
“I think we can say that in people aged over 40, the risk of myocarditis is greater with infection than with vaccination, but in those under 40, it is not so clear. And our data suggest that for young men aged 16 to 24 years, the risk of myocarditis after COVID vaccination with either the Pfizer or Moderna vaccine is higher than after COVID infection,” Dr. Ljung commented.
Although the Swedish regulatory agency has already stopped recommending use of Moderna vaccine in those younger than 30 years on the basis of these data, Dr. Ljung was reluctant to make any recommendations regarding the use of the Pfizer vaccine in young males, saying it was up to individual public-health agencies to makes these decisions.
But he pointed out that the current study only looked at myocarditis, and COVID infection can result in many other complications that can lead to hospitalization and death, which needs to be taken into account when assessing the risk and benefit of vaccination.
Dr. Ljung noted that the current data only applied to the first two doses of the vaccines; data after booster injections have not been included, although the researchers are looking at that now.
What to advise patients?
In an accompanying Editor’s Note, Ann Marie Navar, MD, University of Texas Southwestern Medical Center, Dallas, who is editor of JAMA Cardiology, and Robert Bonow, MD, Northwestern University Feinberg School of Medicine, Chicago, who is deputy editor of JAMA Cardiology, try to explain how these data can inform the way health care professionals communicate with their patients about vaccination.
They point out the “good news,” that older adults who are at highest risk for COVID-19 complications appear to be at extremely low risk for vaccine-associated myocarditis.
They note that for both men and women older than 40 years, the excess number of cases of myocarditis after vaccination was fewer than two in 100,000 vaccinees across all vaccines studied, and the death toll from COVID-19 in the United States as of March was more than 200 per 100,000 population.
“Given the high rates of morbidity and mortality from COVID-19 infection in older adults and the efficacy of the vaccine in preventing severe infection and death, the benefits of immunization in those older than 40 years clearly outweigh the risks,” the editors say.
But given these data in young men, they suggest that health care professionals consider recommending the Pfizer vaccine over the Moderna vaccine for certain populations, including young men and other individuals for whom concerns about myocarditis present a barrier to immunization.
The editors also point out that although the risk for myocarditis after COVID-19 immunization is real, this low risk must be considered in the context of the overall benefit of the vaccine.
“At the individual level, immunization prevents not only COVID-19-related myocarditis but also severe disease, hospitalization, long-term complications after COVID-19 infection, and death. At the population level, immunization helps to decrease community spread, decrease the chances of new variants emerging, protect people who are immunocompromised, and ensure our health care system can continue to provide for our communities,” they conclude.
Dr. Ljung reports grants from Sanofi Aventis paid to his institution outside the submitted work and personal fees from Pfizer outside the submitted work. Dr. Navar reports personal fees from Pfizer and AstraZeneca, outside the scope of this work.
A version of this article first appeared on Medscape.com.
One of the largest studies to date on myocarditis after COVID-19 vaccination confirms an increased risk with both the Pfizer and Moderna vaccines in young men and shows that the risk is higher with the Moderna than with the Pfizer vaccine.
The study also suggests for the first time that in young men 16 to 24 years of age, the risk for myocarditis after vaccination with either the Pfizer or Moderna vaccine is higher than the risk for myocarditis after COVID-19 infection.
The population-based study involved data on 23.1 million residents across four Scandinavian countries – Denmark, Finland, Norway, and Sweden – 74% of whom had received two vaccine doses and 7% of whom had received one dose.
By linking data from high-quality nationwide health registers on COVID-19 vaccination, infection rates, and myocarditis diagnoses, the researchers were able to evaluate the risk for myocarditis by vaccine product, vaccination dose number, sex, and age.
The study was published online in JAMA Cardiology.
The results confirm that the risk for myocarditis after COVID-19 mRNA vaccines is highest in young men 16 to 24 years of age after the second dose.
For men in this age group who received two doses of the same vaccine, data were compatible, with between four and seven excess myocarditis events in 28 days per 100,000 individuals after the second dose of the Pfizer vaccine, and between nine and 28 per 100,000 individuals after the second dose of the Moderna vaccine.
“This is one of the largest studies on this topic to date. The first population studies were in Israel, with 5 million individuals, and looked at just the Pfizer vaccine. We have data on 23 million people from Scandinavia that include both the Pfizer and Moderna vaccines,” senior author Rickard Ljung, MD, Swedish Medical Products Agency, told this news organization.
“We show a clearly higher risk of myocarditis after the Moderna vaccine than after the Pfizer vaccine. This has been suggested before, but our data confirm definitively that the Moderna vaccine has a higher risk of myocarditis than the Pfizer vaccine,” he added.
“In the group at highest risk of myocarditis after COVID vaccination – young men aged 16 to 24 – the Pfizer vaccine shows a five times higher risk of myocarditis versus the unvaccinated cohort, while the Moderna vaccine shows a 15 times higher risk,” Dr. Ljung noted.
After seeing these data, the Swedish regulatory authority is no longer recommending use of the Moderna vaccine for people younger than 30 years, Dr. Ljung said. Similar recommendations have been made in Norway and Finland.
The researchers report that their finding of a higher risk for myocarditis after the Moderna vaccine than after the Pfizer vaccine in young men is in line with data from the Canada, France, the United Kingdom, and the United States. But they point out that, compared with previous studies, the current study had the advantage of data analyzed according to a common protocol from four different countries and that showed similar directions of associations, despite considerable differences in previous COVID-19 infection levels and lockdown policies.
Risk higher with vaccination than infection?
For what is believed to be the first time, the Scandinavian data also suggest a higher risk for myocarditis after COVID-19 vaccination with both the Pfizer and Moderna vaccines than after COVID-19 infection in young men 16 to 24 years.
Although previous studies have shown that males in this age group have the highest risk for myocarditis after vaccination, it has always been suggested that the risk after vaccination is lower than the risk after infection. The Scandinavian data suggest otherwise for this age group.
Dr. Ljung explained that the myocarditis risk after COVID infection is very hard to study.
“It is highly dependent on the testing strategy,” he said. “For example, in the first half of 2020, the only people being tested were those admitted to hospital, so studies would have included the sickest patients and would therefore likely have found a higher rate of myocarditis. But this current Scandinavian dataset only included individuals with a positive COVID test after August 2020, reflecting a broader range of people.”
The researchers found an excess rate of myocarditis of 3.26 per 100,000 individuals within 28 days of a positive COVID-19 test among all males, and 1.37 per 100,000 individuals among males 16 to 24 years of age.
“We show that the risk of myocarditis after COVID infection is lower in younger people and higher in older people, but the opposite is true after COVID vaccination, where the risk of myocarditis is higher in younger people and lower in older people,” Dr. Ljung said.
The study was not able to look at severity of myocarditis but did record length of hospital stay, which was similar in patients who developed myocarditis after vaccination and those in the unvaccinated cohort (4 to 5 days). Deaths were rare, with no deaths in people younger than 40 years.
“I think we can say that in people aged over 40, the risk of myocarditis is greater with infection than with vaccination, but in those under 40, it is not so clear. And our data suggest that for young men aged 16 to 24 years, the risk of myocarditis after COVID vaccination with either the Pfizer or Moderna vaccine is higher than after COVID infection,” Dr. Ljung commented.
Although the Swedish regulatory agency has already stopped recommending use of Moderna vaccine in those younger than 30 years on the basis of these data, Dr. Ljung was reluctant to make any recommendations regarding the use of the Pfizer vaccine in young males, saying it was up to individual public-health agencies to makes these decisions.
But he pointed out that the current study only looked at myocarditis, and COVID infection can result in many other complications that can lead to hospitalization and death, which needs to be taken into account when assessing the risk and benefit of vaccination.
Dr. Ljung noted that the current data only applied to the first two doses of the vaccines; data after booster injections have not been included, although the researchers are looking at that now.
What to advise patients?
In an accompanying Editor’s Note, Ann Marie Navar, MD, University of Texas Southwestern Medical Center, Dallas, who is editor of JAMA Cardiology, and Robert Bonow, MD, Northwestern University Feinberg School of Medicine, Chicago, who is deputy editor of JAMA Cardiology, try to explain how these data can inform the way health care professionals communicate with their patients about vaccination.
They point out the “good news,” that older adults who are at highest risk for COVID-19 complications appear to be at extremely low risk for vaccine-associated myocarditis.
They note that for both men and women older than 40 years, the excess number of cases of myocarditis after vaccination was fewer than two in 100,000 vaccinees across all vaccines studied, and the death toll from COVID-19 in the United States as of March was more than 200 per 100,000 population.
“Given the high rates of morbidity and mortality from COVID-19 infection in older adults and the efficacy of the vaccine in preventing severe infection and death, the benefits of immunization in those older than 40 years clearly outweigh the risks,” the editors say.
But given these data in young men, they suggest that health care professionals consider recommending the Pfizer vaccine over the Moderna vaccine for certain populations, including young men and other individuals for whom concerns about myocarditis present a barrier to immunization.
The editors also point out that although the risk for myocarditis after COVID-19 immunization is real, this low risk must be considered in the context of the overall benefit of the vaccine.
“At the individual level, immunization prevents not only COVID-19-related myocarditis but also severe disease, hospitalization, long-term complications after COVID-19 infection, and death. At the population level, immunization helps to decrease community spread, decrease the chances of new variants emerging, protect people who are immunocompromised, and ensure our health care system can continue to provide for our communities,” they conclude.
Dr. Ljung reports grants from Sanofi Aventis paid to his institution outside the submitted work and personal fees from Pfizer outside the submitted work. Dr. Navar reports personal fees from Pfizer and AstraZeneca, outside the scope of this work.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY
Depression strikes more than half of obese adolescents
More than 50% of obese adolescents met criteria for depression, which also was associated with several components of metabolic syndrome, based on data from 160 individuals.
Previous research shows that the metabolic consequences of obesity are worsened with the coexistence of depression in adults, but a similar relationship in obese adolescents has not been explored, according to Nisha Gupta, a medical student at the University of Texas Health Science Center, Houston, and colleagues.
“This relationship is explained by an overactive stress response and adoption of unhealthy lifestyle habits,” both of which increased during the COVID-19 pandemic, the researchers noted in their abstract.
In a study presented at the Pediatric Academic Societies annual meeting, the researchers reviewed data from 160 obese adolescents seen at a pediatric weight management clinic between July 1, 2018, and Dec. 3, 2021. The data included anthropometric, clinical, and laboratory information. Depression was assessed using the Patient Health Questionnaire–9 (PHQ-9). The goal of the study was to compare the prevalence of metabolic syndrome components in obese youth with and without diagnosed depression.
Overall, 46% of the patients had PHQ-9 scores less than 5, which was defined as no clinically significant depression. A total of 26% had current or prior diagnoses of depression, and 25% met the criteria for moderate to severe depression, with PHQ-9 scores of 10 or higher. Notably, 18% of individuals with no prior history of depression met criteria for moderate to severe depression, the researchers wrote.
Teens who reported daytime fatigue or trouble sleeping, and those who reported eating out seven or more times a week had higher scores than those without these reports.
In laboratory analyses, higher PHQ-9 scores were significantly associated with increasing weight, body mass index, body fat percentage, diastolic blood pressure, and fasting blood insulin (P < .02 for all).
The study findings were limited by the relatively small sample size, the researchers noted. However, the results suggest that depression is common, but often underdiagnosed in obese adolescents, and depression screening should be part of obesity management.
Study highlights need to screen
The current study is important because of the overall increase in obesity in the United States, which extends to children and teens, Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, said in an interview.
“With skyrocketing rates of obesity among children and teens over the last decades, we are seeing more ‘adult’ diseases seep into the younger ages, including type 2 diabetes, high blood pressure and now, depression,” he said.
“The results are a wake-up call for the need for better system-wide prevention and management of obesity in adolescents and the importance of screening and managing depression in obese teenagers,” he emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More than 50% of obese adolescents met criteria for depression, which also was associated with several components of metabolic syndrome, based on data from 160 individuals.
Previous research shows that the metabolic consequences of obesity are worsened with the coexistence of depression in adults, but a similar relationship in obese adolescents has not been explored, according to Nisha Gupta, a medical student at the University of Texas Health Science Center, Houston, and colleagues.
“This relationship is explained by an overactive stress response and adoption of unhealthy lifestyle habits,” both of which increased during the COVID-19 pandemic, the researchers noted in their abstract.
In a study presented at the Pediatric Academic Societies annual meeting, the researchers reviewed data from 160 obese adolescents seen at a pediatric weight management clinic between July 1, 2018, and Dec. 3, 2021. The data included anthropometric, clinical, and laboratory information. Depression was assessed using the Patient Health Questionnaire–9 (PHQ-9). The goal of the study was to compare the prevalence of metabolic syndrome components in obese youth with and without diagnosed depression.
Overall, 46% of the patients had PHQ-9 scores less than 5, which was defined as no clinically significant depression. A total of 26% had current or prior diagnoses of depression, and 25% met the criteria for moderate to severe depression, with PHQ-9 scores of 10 or higher. Notably, 18% of individuals with no prior history of depression met criteria for moderate to severe depression, the researchers wrote.
Teens who reported daytime fatigue or trouble sleeping, and those who reported eating out seven or more times a week had higher scores than those without these reports.
In laboratory analyses, higher PHQ-9 scores were significantly associated with increasing weight, body mass index, body fat percentage, diastolic blood pressure, and fasting blood insulin (P < .02 for all).
The study findings were limited by the relatively small sample size, the researchers noted. However, the results suggest that depression is common, but often underdiagnosed in obese adolescents, and depression screening should be part of obesity management.
Study highlights need to screen
The current study is important because of the overall increase in obesity in the United States, which extends to children and teens, Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, said in an interview.
“With skyrocketing rates of obesity among children and teens over the last decades, we are seeing more ‘adult’ diseases seep into the younger ages, including type 2 diabetes, high blood pressure and now, depression,” he said.
“The results are a wake-up call for the need for better system-wide prevention and management of obesity in adolescents and the importance of screening and managing depression in obese teenagers,” he emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
More than 50% of obese adolescents met criteria for depression, which also was associated with several components of metabolic syndrome, based on data from 160 individuals.
Previous research shows that the metabolic consequences of obesity are worsened with the coexistence of depression in adults, but a similar relationship in obese adolescents has not been explored, according to Nisha Gupta, a medical student at the University of Texas Health Science Center, Houston, and colleagues.
“This relationship is explained by an overactive stress response and adoption of unhealthy lifestyle habits,” both of which increased during the COVID-19 pandemic, the researchers noted in their abstract.
In a study presented at the Pediatric Academic Societies annual meeting, the researchers reviewed data from 160 obese adolescents seen at a pediatric weight management clinic between July 1, 2018, and Dec. 3, 2021. The data included anthropometric, clinical, and laboratory information. Depression was assessed using the Patient Health Questionnaire–9 (PHQ-9). The goal of the study was to compare the prevalence of metabolic syndrome components in obese youth with and without diagnosed depression.
Overall, 46% of the patients had PHQ-9 scores less than 5, which was defined as no clinically significant depression. A total of 26% had current or prior diagnoses of depression, and 25% met the criteria for moderate to severe depression, with PHQ-9 scores of 10 or higher. Notably, 18% of individuals with no prior history of depression met criteria for moderate to severe depression, the researchers wrote.
Teens who reported daytime fatigue or trouble sleeping, and those who reported eating out seven or more times a week had higher scores than those without these reports.
In laboratory analyses, higher PHQ-9 scores were significantly associated with increasing weight, body mass index, body fat percentage, diastolic blood pressure, and fasting blood insulin (P < .02 for all).
The study findings were limited by the relatively small sample size, the researchers noted. However, the results suggest that depression is common, but often underdiagnosed in obese adolescents, and depression screening should be part of obesity management.
Study highlights need to screen
The current study is important because of the overall increase in obesity in the United States, which extends to children and teens, Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, said in an interview.
“With skyrocketing rates of obesity among children and teens over the last decades, we are seeing more ‘adult’ diseases seep into the younger ages, including type 2 diabetes, high blood pressure and now, depression,” he said.
“The results are a wake-up call for the need for better system-wide prevention and management of obesity in adolescents and the importance of screening and managing depression in obese teenagers,” he emphasized.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM PAS 2022
Trans women in female sports: A sports scientist’s take
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
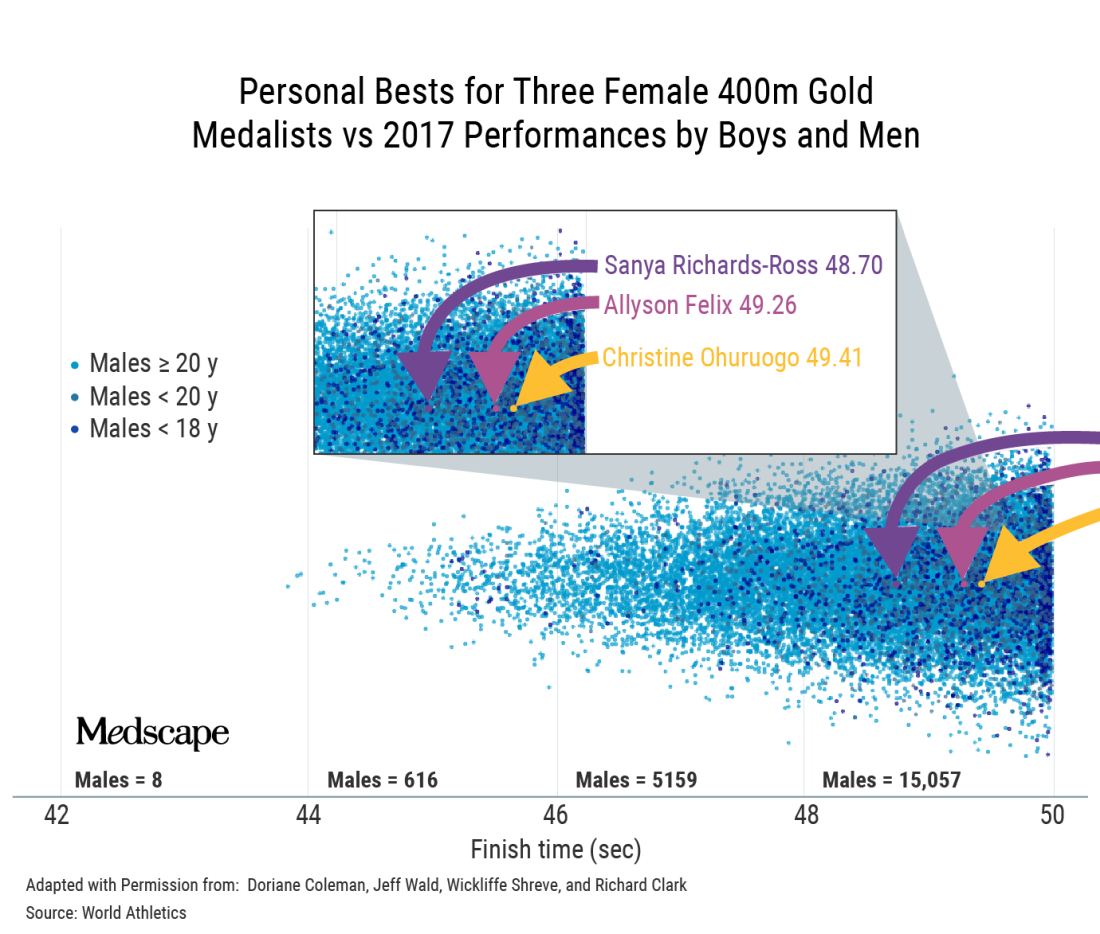
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
An interview with Ross Tucker, PhD
An interview with Ross Tucker, PhD
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
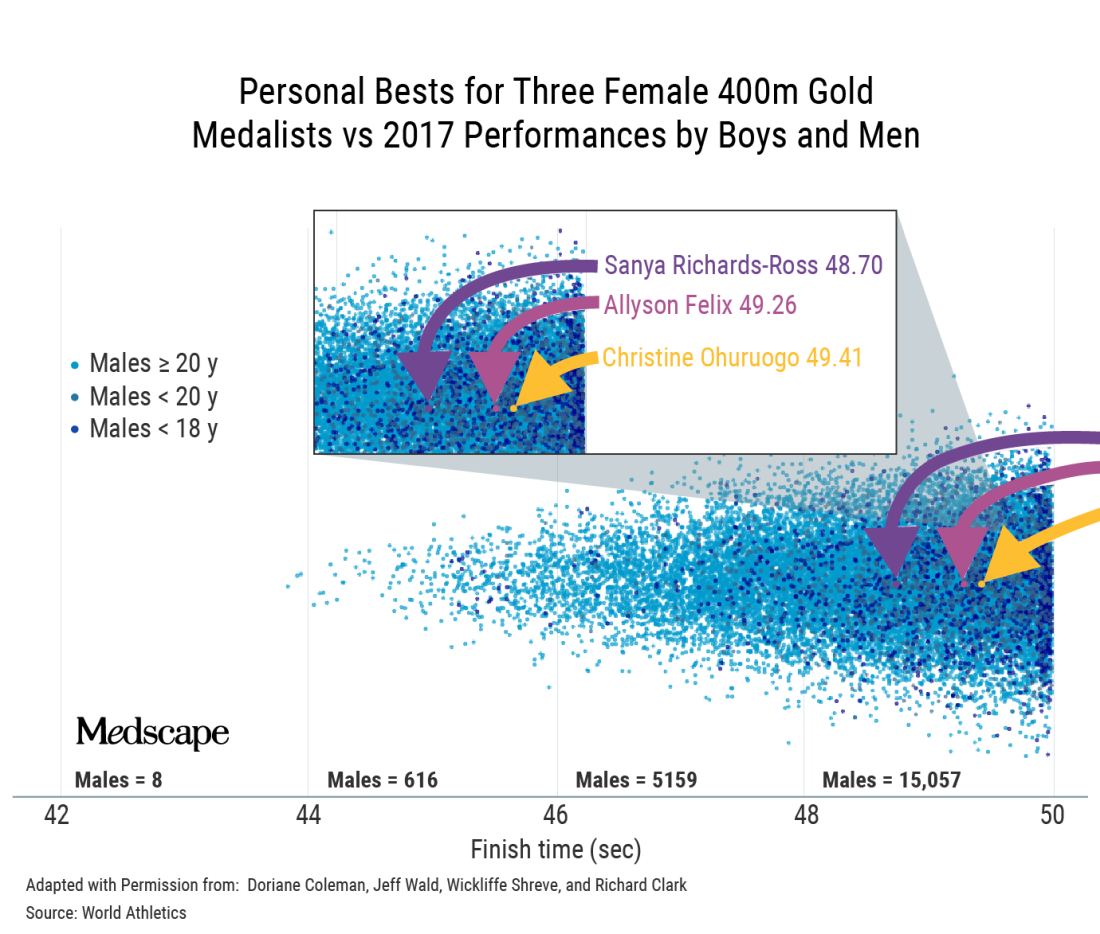
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.
When Lia Thomas won the women’s 500-yard freestyle at the 2022 NCAA Division 1 swimming championships, the issue of trans women’s participation in female sports ignited national headlines.
which prohibit trans women’s participation.
This interview has been edited for length and clarity.
Let’s start with the proinclusion argument that there are always advantages in sports.
That’s true. The whole point of sports is to recognize people who have advantages and reward them for it. By the time this argument comes out, people have already accepted that males have advantages, right?
Some do, some don’t.
If someone uses this argument to say that we should allow trans women, basically biological males, to compete in women’s sports, they’ve implicitly accepted that there are advantages. Otherwise, what advantage are you talking about?
They would say it’s like the advantage Michael Phelps has because of his wingspan.
To answer that, you have to start by asking why women’s sports exist.
Women’s sports exist because we recognize that male physiology has biological differences that create performance advantages. Women’s sports exist to ensure that male advantages are excluded. If you allow male advantage in, you’re allowing something to cross into a category that specifically tries to exclude it. That makes the advantage possessed by trans women conceptually and substantively different from an advantage that’s possessed by Michael Phelps because his advantage doesn’t cross a category boundary line.
If someone wants to allow natural advantages to be celebrated in sports, they’re arguing against the existence of any categories, because every single category in sports is trying to filter out certain advantages.
Weight categories in boxing exist to get rid of the advantage of being stronger, taller, with greater reach. Paralympic categories filter out the natural advantage that someone has if, for example, they are only mildly affected by cerebral palsy, compared with more severely affected.
If someone wants to allow natural advantages, they’re making an argument for all advantages to be eliminated from regulation, and we would end up with sports dominated by males between the ages of 20 and 28.
There are some people suggesting open categories by height and weight.
The problem is that for any height, males will be stronger, faster, more powerful than females. For any mass, and we know this because weightlifting has categories by mass, males lift about 30% heavier than females. They’ll be about 10%-15% faster at the same height and weight.
There’d be one or two sports where you might have some women, like gymnastics. Otherwise you would have to create categories that are so small – say, under 100 pounds. But in every other category, most sports would be completely dominated by males.
It’s not a viable solution for me unless we as a society are satisfied with filtering out women.
Another argument is that if trans women have an advantage, then they would be dominating.
That one misunderstands how you assess advantage. For a trans woman to win, she still has to be good enough at the base level without the advantage, in order to parlay that advantage into winning the women’s events.
If I was in the Tour de France and you gave me a bicycle with a 100-watt motor, I wouldn’t win the Tour de France. I’d do better than I would have done without it, but I wouldn’t win. Does my failure to win prove that motors don’t give an advantage? Of course not. My failure says more about my base level of performance than it does about the motor.
In terms of trans athletes, the retention of biological attributes creates the retention of performance advantages, which means that the person’s ranking relative to their peers’ will go up when they compare themselves to women rather than men. Someone who’s ranked 500 might improve to the 250s, but you still won’t see them on a podium.
It’s the change in performance that matters, not the final outcome.
Wasn’t Lia Thomas ranked in the 500s in the men’s division?
There’s some dispute as to whether it was 460 or 550 in the 200- and 65th in the 500-yard freestyle. But the concept is the same and we can use that case because we know the percentage performance change.
As Will Thomas, the performance was 4:18 in the 500-yard freestyle. As Lia Thomas, it’s 4:33. Ms. Thomas has slowed by 5.8% as a result of testosterone suppression. That’s fairly typical; most studies so far suggest performance impairments in that range.
The thing is that the male-female gap in swimming times is 10%-12% on average. That means that Ms. Thomas has retained about half the male advantage.
In strength events, for instance, weightlifting, where the gap is 30% or more, if you lost 10%, you’d still retain a 20% advantage and you’d jump more ranking places.
The retention of about half the male advantage is enough for No. 1 in the NCAA, but it’s not enough to move Ms. Thomas to No. 1 in the world.
The record set by Katie Ledecky in the 500 freestyle is 4:24. Thomas swam 4:18 as a man so could only afford to lose about 1% to be the record holder in women’s swimming.
When Ms. Thomas was beaten by cisgender women in other events, your point is that’s just because her baseline (pretransition) time wasn’t good enough.
Exactly. Are your performances in men’s sports close enough to the best woman such that you can turn that retained advantage into dominance, winning in women’s sports?
If the answer to that is yes, then you get Thomas in the 500. If the answer to that is not quite, then you get Thomas in the other distances.
On your podcast, you expressed frustration at having to keep debunking these arguments. Why do you think they persist?
There are a few things in play. There are nuances around the idea of advantage that people from outside sports don’t always appreciate.
But then the second thing comes into play and that’s the fact that this is an emotive issue. If you come to this debate wanting trans inclusion, then you reject the idea that it’s unfair. You will dismiss everything I’ve just said.
There’s a third thing. When people invoke the Phelps wingspan argument, they haven’t thought through the implications. If you could sit them down and say: “Okay. If you want to get rid of regulating natural advantages, then we would get rid of male and female categories,” what do you think would happen then?
They may still support inclusion because that’s their world view, but at least they’re honest now and understand the implications. But most people don’t go through that process.
I get that men are faster but I was shocked at how many are faster than elite women – for example, Allyson Felix.
There’s an amazing visual representation of that.
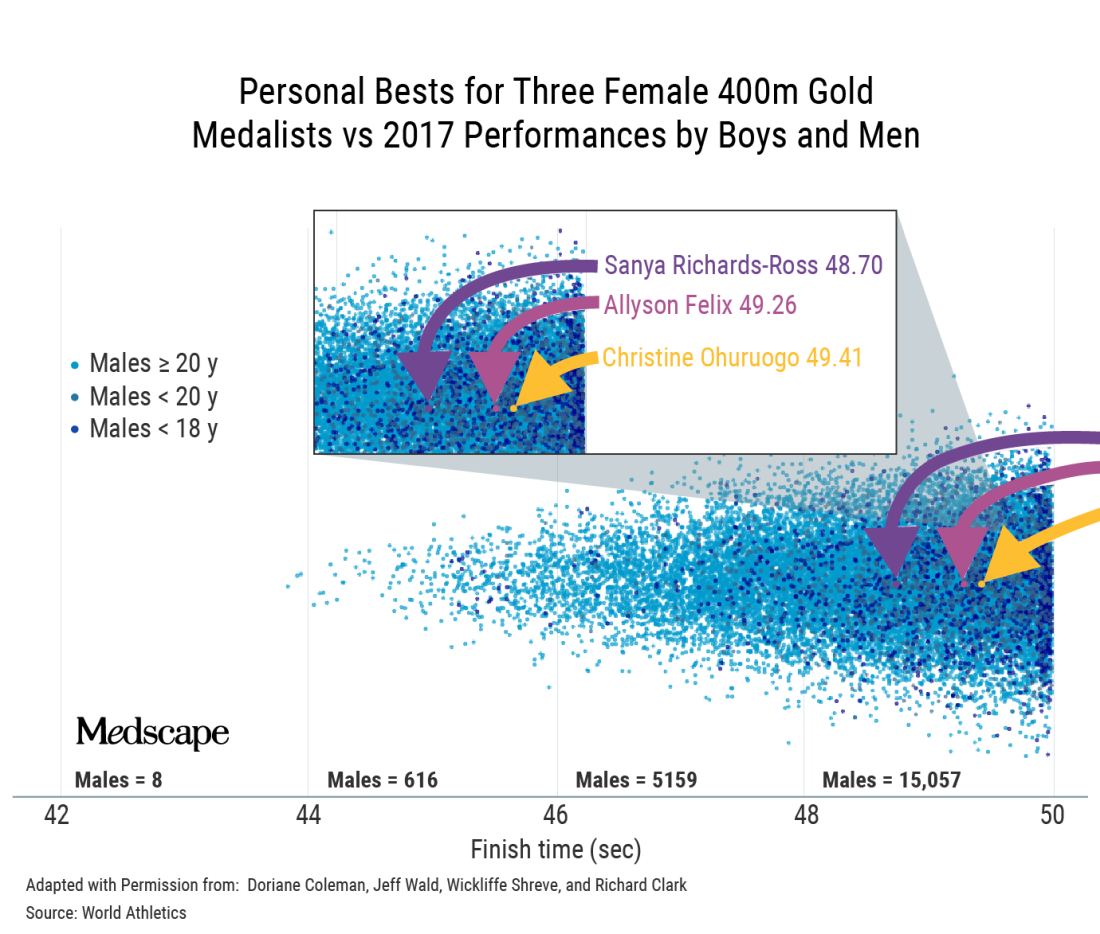
That’s a classic example where, if you’re immersed in sports, it becomes intuitive. If you’re not, you do a double-take and think, is that right? Position determines perspective.
Do you think some of it is because we’re constantly told that girls and women can do anything?
It’s a paradox that is difficult for people to get their minds around because in most walks of life, we can say that women can do anything. Of course, it’s arguably more difficult for women to become CEOs of Fortune 500 companies. This is a work in progress.
But sports are different. In sports, it’s not possible to directly compare male and female, and then tell girls they can be the best at whatever in the whole human race. That’s the uniqueness of sports and the reason categories exist in the first place. The biology does matter.
Speaking of biology, you’ve said that the focus on testosterone levels is a bit of a red herring.
Yes. The authorities were looking for a solution.
They grabbed onto the idea that lowering testosterone was the solution and perpetuated that as the mechanism by which we would ensure fairness. The problem is that my concentration of testosterone today is only a tiny part of the story.
I’ve been exposed to testosterone my whole life. My twin sister has not. There are many differences between us, but in terms of sports, the main biological difference is not that my testosterone is higher today; it’s that my testosterone has been higher my whole life. It’s the work done by that hormone over many years that makes a difference.
The key issue is, has this body, this physiology, been exposed to and benefited in the sports context, from male hormones – yes or no?
If your answer is yes, then that body belongs in male sports. With gender identity, we want to accommodate as far as possible, but we can’t take away that difference. That’s where we create this collision of rights between trans women and women.
Ultimately, your point is that we can’t have both fairness and inclusion.
When we sat down to do the World Rugby trans guidance, we had an epiphany: It doesn’t matter which way we go; we’re going to face hostility.
Once you accept that there are two parties that are affected and one of them will always be unhappy, then you start to see that fairness and inclusion can’t be balanced.
What about Joanna Harper’s proposal to make rules case by case and sport by sport?
First, it could be tricky legally because you’re effectively discriminating against some people within a subset of a subset. You’re going to end up saying to some trans women: “You can play because you don’t pose a safety or fairness issue.” But to another: “You can’t because you’re too strong.”
Then the problem is, how do you do that screening? It’s not like you can measure half a dozen variables and then have an algorithm spit out a performance level that tells you that this trans woman can compete here safely and fairly. It’s a theoretical solution that is practically impossible.
At a conference in Boston recently, Joanna said that when there are no medals, prize money, scholarships, or record times, we should allow inclusion. But just because a woman isn’t winning medals or going to the Olympics doesn’t mean there’s not considerable value for her if she were to make her school team, for instance.
There are only 11 places on the soccer field, eight lanes in a swimming pool. The moment you allow someone in, you potentially exclude someone else. And that happens everywhere, not only at the elite level.
Would you ever make a distinction between elite and subelite?
One of the beauties of sports is that it’s a meritocracy; it functions on a pathway system. I don’t think the level matters if you can track that this person’s presence denied a place on the team or a place at the competition to someone else.
With Lia Thomas, it’s not only denying the silver medalist gold or fourth place a bronze; it’s also the fact that there are only so many places at that meet. For some, that was their ambition and they weren’t able to realize it.
Now, a lot of sports are played outside that pathway. Say your local tennis club has a social league. There is little there to stand in the way of inclusion. Although I’m mindful that there may be a women’s league where it does matter to them.
We can try to accommodate trans women when the stakes are not high, provided that two requirements are met: One is that there’s no disruption to the selection/meritocracy pathway; and the second key point is that women must be okay with that inclusion, particularly if there are safety considerations, but even if it’s just a fairness consideration.
That’s where it gets tricky, because there are bigoted people in the world. Unfortunately, sometimes it’s difficult to tell whether people are using scientific arguments to prop up bigotry or whether they are genuine.
Joanna Harper has said that if you support inclusion, you have to be okay with trans women winning.
Winning the summer tennis league is not winning in the same sense as winning at the NCAA.
But the moment winning means selection and performance pathways, then I think we have to draw a line. The moment participation disrupts the natural order in sports, then it’s a problem.
In World Rugby, we proposed open competitions lower in contact to deal with the safety concerns. That was rejected by the trans community because they felt it was othering – that we were trying to squeeze them off to the side.
If you offered me one of two choices: no participation, or inclusion and they have to be able to win, I’d go for the former.
How did you get involved in this topic?
I got involved because I testified in the Caster Semenya case at the Court of Arbitration for Sport.
That is not a transgender issue; it’s a difference of sex development issue. What it has in common is the question of what to do with male-bodied biological advantage in sports.
When World Rugby joined the Olympic Games, we followed the IOC transgender policy. In 2019, it became apparent from the latest research that male advantage isn’t removed by testosterone suppression. We decided to delete the previous policy and make a new one.
The latest IOC policy is kind of no policy; it leaves it up to the governing bodies for each sport.
The one element of progress in what the IOC released, and it really is the only one, is that they’ve recognized that sports have to manage three imperatives: fairness, inclusion, and safety.
The 2015 IOC document says something like “sports should strive to be as inclusive as possible, but the overriding objective remains to guarantee a fair competition.” Basically, fair competition was nonnegotiable and must be guaranteed.
Of course, that policy allowed for testosterone suppression, and you’d have a difficult time convincing a physiologist that lowering testosterone guarantees fair competition.
Where there is merit in the current policy is that it’s clear that sports like rugby, boxing, taekwondo, and judo have a different equation with respect to safety, fairness, and inclusion than sports like equestrian, shooting, and archery. I think that’s wise to acknowledge.
However, the IOC policy doesn’t do anything to lead. In fact, what they said was extraordinary: There should be no presumption of advantage. If there’s no presumption of advantage for male-bodied athletes, then why do they persist with two categories? If there’s no presumption of advantage for trans women, are they saying that gender identity removes the advantage? We know that’s not true. We know that at the very least, you should presume that there is some advantage. How you manage it is up to you, but you can’t say that it’s not there.
This is a hostile debate. Have you ever thought: Maybe I’ll just shut up and stick to other sports topics?
Big time. The Lia Thomas case brought out a lot of vitriol. From about 2017, the situation we had with Ms. Thomas was predictable. The problem is that 95% of the world didn’t know this was happening and were taken by surprise.
The number of people who have opinions has exploded. A lot wade in without much thought. I’ve seen people question Lia Thomas’s motives. Presumably, Lia Thomas is trans, identifies as a woman, and therefore thinks she belongs in women’s sports. But I’ve seen people saying she only wants to swim in women’s sports because she knows she’ll win. And that’s not the worst of it. I’ve seen people saying Lia Thomas is only identifying as a woman so she can get into women’s changing rooms.
I don’t see how that helps the conversation. It just polarizes to the point that neither side is listening to the other. Before it was the trans community that wasn’t interested in talking about the idea of advantage, fairness, and safety. Their position is that trans women are women; how do you even have a discussion when they’ve got that dogma as their foundation?
Now, unfortunately, on the other side, we’re seeing unnecessary offensive tactics. For example, I’ve referred to Lia Thomas as “she.” I’ll have people shouting at me for using “she.” You’ve got to pick your battles, and that’s not the one you want to be fighting, in my opinion.
A version of this article first appeared on Medscape.com.





