User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
ADA updates on finerenone, SGLT2 inhibitors, and race-based eGFR
As it gears up for the first in-person scientific sessions for 3 years, the American Diabetes Association has issued an addendum to its most recent annual clinical practice recommendations published in December 2021, the 2022 Standards of Medical Care in Diabetes, based on recent trial evidence and consensus.
The update informs clinicians about:
- The effect of the nonsteroidal mineralocorticoid antagonist (Kerendia) on cardiovascular outcomes in patients with type 2 diabetes and chronic kidney disease.
- The effect of a sodium-glucose cotransporter 2 (SGLT2) inhibitor on heart failure and renal outcomes in patients with type 2 diabetes.
The National Kidney Foundation and the American Society of Nephrology Task Force recommendation to remove race in the formula for calculating estimated glomerular filtration rate (eGFR).
“This is the fifth year that we are able to update the Standards of Care after it has been published through our Living Standards of Care updates, making it possible to give diabetes care providers the most important information and the latest evidence relevant to their practice,” Robert A. Gabbay, MD, PhD, ADA chief scientific and medical officer, said in a press release from the organization.
The addendum, entitled, “Living Standards of Care,” updates Section 10, “Cardiovascular Disease and Risk Management,” and Section 11, “Chronic Kidney Disease and Risk Management” of the 2022 Standards of Medical Care in Diabetes.
The amendments were approved by the ADA Professional Practice Committee, which is responsible for developing the Standards of Care. The American College of Cardiology reviewed and endorsed the section on CVD and risk management.
The Living Standards Update was published online in Diabetes Care.
CVD and risk management
In the Addendum to Section 10, “Cardiovascular Disease and Risk Management,” the committee writes:
- “For patients with type 2 diabetes and chronic kidney disease treated with maximum tolerated doses of ACE inhibitors or angiotensin receptor blockers, addition of finerenone should be considered to improve cardiovascular outcomes and reduce the risk of chronic kidney disease progression. A”
- “Patients with type 2 diabetes and chronic kidney disease should be considered for treatment with finerenone to reduce cardiovascular outcomes and the risk of chronic kidney disease progression.”
- “In patients with type 2 diabetes and established heart failure with either preserved or reduced ejection fraction, an SGLT2 inhibitor [with proven benefit in this patient population] is recommended to reduce risk of worsening heart failure, hospitalizations for heart failure, and cardiovascular death. ”
In the section “Statin Treatment,” the addendum no longer states that “a prospective trial of a newer fibrate ... is ongoing,” because that trial investigating pemafibrate (Kowa), a novel selective peroxisome proliferator-activated receptor alpha modulator (or fibrate), has been discontinued.
Chronic kidney disease and risk management
In the Addendum to Section 11, “Chronic Kidney Disease and Risk Management,” the committee writes:
- “Traditionally, eGFR is calculated from serum creatinine using a validated formula. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is preferred. ... Historically, a correction factor for muscle mass was included in a modified equation for African Americans; however, due to various issues with inequities, it was decided to the equation such that it applies to all. Hence, a committee was convened, resulting in the recommendation for immediate implementation of the CKD-EPI creatinine equation refit without the race variable in all laboratories in the U.S.” (This is based on an National Kidney Foundation and American Society of Nephrology Task Force recommendation.)
- “Additionally, increased use of cystatin C, especially to confirm estimated GFR in adults who are at risk for or have chronic kidney disease, because combining filtration markers (creatinine and cystatin C) is more accurate and would support better clinical decisions than either marker alone.”
Evidence from clinical trials
The update is based on findings from the following clinical trials:
- Efficacy and Safety of Finerenone in Subjects With Type 2 Diabetes Mellitus and Diabetic Kidney Disease (FIDELIO-DKD)
- Efficacy and Safety of Finerenone in Subjects With Type 2 Diabetes Mellitus and the Clinical Diagnosis of Diabetic Kidney Disease (FIGARO-DKD)
- FIDELITY, a prespecified pooled analysis of FIDELIO-DKD and FIGARO-DKD
- Empagliflozin Outcome Trial in Patients With Chronic Heart Failure With Preserved Ejection Fraction (EMPEROR-Preserved)
- Effects of Dapagliflozin on Biomarkers, Symptoms and Functional Status in Patients with PRESERVED Ejection Fraction Heart Failure (PRESERVED-HF)
- Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Patients with Diabetes (PROMINENT).
A version of this article first appeared on Medscape.com.
As it gears up for the first in-person scientific sessions for 3 years, the American Diabetes Association has issued an addendum to its most recent annual clinical practice recommendations published in December 2021, the 2022 Standards of Medical Care in Diabetes, based on recent trial evidence and consensus.
The update informs clinicians about:
- The effect of the nonsteroidal mineralocorticoid antagonist (Kerendia) on cardiovascular outcomes in patients with type 2 diabetes and chronic kidney disease.
- The effect of a sodium-glucose cotransporter 2 (SGLT2) inhibitor on heart failure and renal outcomes in patients with type 2 diabetes.
The National Kidney Foundation and the American Society of Nephrology Task Force recommendation to remove race in the formula for calculating estimated glomerular filtration rate (eGFR).
“This is the fifth year that we are able to update the Standards of Care after it has been published through our Living Standards of Care updates, making it possible to give diabetes care providers the most important information and the latest evidence relevant to their practice,” Robert A. Gabbay, MD, PhD, ADA chief scientific and medical officer, said in a press release from the organization.
The addendum, entitled, “Living Standards of Care,” updates Section 10, “Cardiovascular Disease and Risk Management,” and Section 11, “Chronic Kidney Disease and Risk Management” of the 2022 Standards of Medical Care in Diabetes.
The amendments were approved by the ADA Professional Practice Committee, which is responsible for developing the Standards of Care. The American College of Cardiology reviewed and endorsed the section on CVD and risk management.
The Living Standards Update was published online in Diabetes Care.
CVD and risk management
In the Addendum to Section 10, “Cardiovascular Disease and Risk Management,” the committee writes:
- “For patients with type 2 diabetes and chronic kidney disease treated with maximum tolerated doses of ACE inhibitors or angiotensin receptor blockers, addition of finerenone should be considered to improve cardiovascular outcomes and reduce the risk of chronic kidney disease progression. A”
- “Patients with type 2 diabetes and chronic kidney disease should be considered for treatment with finerenone to reduce cardiovascular outcomes and the risk of chronic kidney disease progression.”
- “In patients with type 2 diabetes and established heart failure with either preserved or reduced ejection fraction, an SGLT2 inhibitor [with proven benefit in this patient population] is recommended to reduce risk of worsening heart failure, hospitalizations for heart failure, and cardiovascular death. ”
In the section “Statin Treatment,” the addendum no longer states that “a prospective trial of a newer fibrate ... is ongoing,” because that trial investigating pemafibrate (Kowa), a novel selective peroxisome proliferator-activated receptor alpha modulator (or fibrate), has been discontinued.
Chronic kidney disease and risk management
In the Addendum to Section 11, “Chronic Kidney Disease and Risk Management,” the committee writes:
- “Traditionally, eGFR is calculated from serum creatinine using a validated formula. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is preferred. ... Historically, a correction factor for muscle mass was included in a modified equation for African Americans; however, due to various issues with inequities, it was decided to the equation such that it applies to all. Hence, a committee was convened, resulting in the recommendation for immediate implementation of the CKD-EPI creatinine equation refit without the race variable in all laboratories in the U.S.” (This is based on an National Kidney Foundation and American Society of Nephrology Task Force recommendation.)
- “Additionally, increased use of cystatin C, especially to confirm estimated GFR in adults who are at risk for or have chronic kidney disease, because combining filtration markers (creatinine and cystatin C) is more accurate and would support better clinical decisions than either marker alone.”
Evidence from clinical trials
The update is based on findings from the following clinical trials:
- Efficacy and Safety of Finerenone in Subjects With Type 2 Diabetes Mellitus and Diabetic Kidney Disease (FIDELIO-DKD)
- Efficacy and Safety of Finerenone in Subjects With Type 2 Diabetes Mellitus and the Clinical Diagnosis of Diabetic Kidney Disease (FIGARO-DKD)
- FIDELITY, a prespecified pooled analysis of FIDELIO-DKD and FIGARO-DKD
- Empagliflozin Outcome Trial in Patients With Chronic Heart Failure With Preserved Ejection Fraction (EMPEROR-Preserved)
- Effects of Dapagliflozin on Biomarkers, Symptoms and Functional Status in Patients with PRESERVED Ejection Fraction Heart Failure (PRESERVED-HF)
- Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Patients with Diabetes (PROMINENT).
A version of this article first appeared on Medscape.com.
As it gears up for the first in-person scientific sessions for 3 years, the American Diabetes Association has issued an addendum to its most recent annual clinical practice recommendations published in December 2021, the 2022 Standards of Medical Care in Diabetes, based on recent trial evidence and consensus.
The update informs clinicians about:
- The effect of the nonsteroidal mineralocorticoid antagonist (Kerendia) on cardiovascular outcomes in patients with type 2 diabetes and chronic kidney disease.
- The effect of a sodium-glucose cotransporter 2 (SGLT2) inhibitor on heart failure and renal outcomes in patients with type 2 diabetes.
The National Kidney Foundation and the American Society of Nephrology Task Force recommendation to remove race in the formula for calculating estimated glomerular filtration rate (eGFR).
“This is the fifth year that we are able to update the Standards of Care after it has been published through our Living Standards of Care updates, making it possible to give diabetes care providers the most important information and the latest evidence relevant to their practice,” Robert A. Gabbay, MD, PhD, ADA chief scientific and medical officer, said in a press release from the organization.
The addendum, entitled, “Living Standards of Care,” updates Section 10, “Cardiovascular Disease and Risk Management,” and Section 11, “Chronic Kidney Disease and Risk Management” of the 2022 Standards of Medical Care in Diabetes.
The amendments were approved by the ADA Professional Practice Committee, which is responsible for developing the Standards of Care. The American College of Cardiology reviewed and endorsed the section on CVD and risk management.
The Living Standards Update was published online in Diabetes Care.
CVD and risk management
In the Addendum to Section 10, “Cardiovascular Disease and Risk Management,” the committee writes:
- “For patients with type 2 diabetes and chronic kidney disease treated with maximum tolerated doses of ACE inhibitors or angiotensin receptor blockers, addition of finerenone should be considered to improve cardiovascular outcomes and reduce the risk of chronic kidney disease progression. A”
- “Patients with type 2 diabetes and chronic kidney disease should be considered for treatment with finerenone to reduce cardiovascular outcomes and the risk of chronic kidney disease progression.”
- “In patients with type 2 diabetes and established heart failure with either preserved or reduced ejection fraction, an SGLT2 inhibitor [with proven benefit in this patient population] is recommended to reduce risk of worsening heart failure, hospitalizations for heart failure, and cardiovascular death. ”
In the section “Statin Treatment,” the addendum no longer states that “a prospective trial of a newer fibrate ... is ongoing,” because that trial investigating pemafibrate (Kowa), a novel selective peroxisome proliferator-activated receptor alpha modulator (or fibrate), has been discontinued.
Chronic kidney disease and risk management
In the Addendum to Section 11, “Chronic Kidney Disease and Risk Management,” the committee writes:
- “Traditionally, eGFR is calculated from serum creatinine using a validated formula. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is preferred. ... Historically, a correction factor for muscle mass was included in a modified equation for African Americans; however, due to various issues with inequities, it was decided to the equation such that it applies to all. Hence, a committee was convened, resulting in the recommendation for immediate implementation of the CKD-EPI creatinine equation refit without the race variable in all laboratories in the U.S.” (This is based on an National Kidney Foundation and American Society of Nephrology Task Force recommendation.)
- “Additionally, increased use of cystatin C, especially to confirm estimated GFR in adults who are at risk for or have chronic kidney disease, because combining filtration markers (creatinine and cystatin C) is more accurate and would support better clinical decisions than either marker alone.”
Evidence from clinical trials
The update is based on findings from the following clinical trials:
- Efficacy and Safety of Finerenone in Subjects With Type 2 Diabetes Mellitus and Diabetic Kidney Disease (FIDELIO-DKD)
- Efficacy and Safety of Finerenone in Subjects With Type 2 Diabetes Mellitus and the Clinical Diagnosis of Diabetic Kidney Disease (FIGARO-DKD)
- FIDELITY, a prespecified pooled analysis of FIDELIO-DKD and FIGARO-DKD
- Empagliflozin Outcome Trial in Patients With Chronic Heart Failure With Preserved Ejection Fraction (EMPEROR-Preserved)
- Effects of Dapagliflozin on Biomarkers, Symptoms and Functional Status in Patients with PRESERVED Ejection Fraction Heart Failure (PRESERVED-HF)
- Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Patients with Diabetes (PROMINENT).
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE
Parkinson’s disease could be hiding behind those nightmares
Living the dream, diagnosing the nightmare
Does a bad dream mean you should be consulting your doctor about an impending neurologic disease? Maybe.
New research published in eClinicalMedicine suggests that, for some people, bad dreams and nightmares have been associated with developing Parkinson’s disease later in life. Dr. Abidemi I. Otaiku of the University of Birmingham (England) analyzed data from a cohort study involving 3,818 older men, of whom 2.3% were diagnosed with Parkinson’s during the 12 years of follow-up.
Dr. Otaiku found those with frequent nightmares – at least once per week – were twice as likely to develop Parkinson’s than were those without, with most of the diagnoses coming in the first 5 years.
Although more research needs to be done, “identifying the significance of bad dreams and nightmares could indicate that individuals who experience changes to their dreams in older age – without any obvious trigger – should seek medical advice,” he said in a Eurekalert statement.
Dr. Otaiku pointed out that studying dreams can tell us a lot about how our brains work and are structured. By using electroencephalography, Dr. Otaiku plans to look into the biological reasons for why we dream the way we do.
So could it be that those killer clowns are actually giving you a heads up on your health?
Maybe next time try a paper route
There’s just no winning with teenagers sometimes. You tell them to go outside, they’ll sit in the dark playing video games all night. You tell them to get better grades, they’ll skip school. You tell them to get a hobby, they’ll scam the German government for millions of euros.
The COVID-19 pandemic has been tricky for governments to manage. Massive amounts of infrastructure needed to be set up, and that means corners got cut. Germany was no exception in this regard; the government entrusted the Kassenärztlichen Vereinigung, a doctor’s association, with overseeing COVID testing and payment at private test centers. To make things a bit easier, all they required private test centers to provide to receive reimbursement was an invoice.
This is where our 17-year-old from Freiburg comes in. In a spark of entrepreneurial genius, he decided to falsify documents and create an entirely fictional COVID test center. The KV approved it, and between March and July of 2021, he sent in thousands of fake invoices. Over that 4-month period, he submitted 500,000 invoices and received 5.7 million euros as compensation. That’s a few thousand tests per day, which was absolutely absurd, but he avoided scrutiny for months.
In the end, it wasn’t even the KV that noticed the fraud, but the bank. A bank employee noticed millions flowing into the account of a teenager and suspected money laundering, alerting the government. Fortunately for our young friend, since he was under 18 when he hatched his scheme, he was tried as a minor, avoiding jail time. His ill-gotten gains were confiscated, he has to pay a relatively minimal fine, and he will be on probation for 1 year. And presumably, he’ll be on the receiving end of the grounding of a lifetime.
You look like I need more sleep
Like most people, not getting our beauty sleep can make us look tired and feel less attractive, but a new study from Sweden shows that the sleep deprived also are more likely to find others less attractive. That’s probably not a good finding for singles who often go out trying to meet someone after a long day of work.
For the study, 45 young men and women were required to spend one night with no sleep and then another night with the possibility of 8 hours of sleep. The following mornings, eye-tracking technology was used as they looked at images of happy, angry, fearful, and neutral faces. The subjects then rated the faces for attractiveness, trustworthiness, and healthiness.
“The finding that sleep-deprived subjects in our experiment rated angry faces as less trustworthy and healthy-looking and neutral and fearful faces as less attractive indicates that sleep loss is associated with more negative social impressions of others,” senior author Christian Benedict of Uppsala University said in a statement.
When we are sleep deprived, the researchers added, we might not stop to really look at someone else, which has a negative impact on how we perceive people because we are not focusing on what their facial expressions are really telling us.
We already knew that not sleeping well has many negative effects on us, but now – thank you very much, science – we have something else to think about. Better hope your crush at work gets enough sleep so you’ll be accurately noticed.
The expanding-hole illusion of science
Time for a LOTME-style reality check: I think, therefore I am.
So far, so good. Next step: I think, therefore I am. I think.
Works for us. Now for the biggie: I think I am seeing the black hole in the middle of this image expanding.
Does that work for you? Do you perceive the black hole as expanding? If you do, then you fit in with the 86% of subjects in a recent study who perceived the same thing.
Lead author Bruno Laeng of the University of Oslo explained the effect in a statement from Frontiers Science News. “The circular smear or shadow gradient of the central black hole evokes a marked impression of optic flow, as if the observer were heading forward into a hole or tunnel. ... The pupil reacts to how we perceive light – even if this ‘light’ is imaginary like in the illusion – and not just to the amount of light energy that actually enters the eye.”
The illusion is so good at deceiving the brain “that it even prompts a dilation reflex of the pupils to let in more light, just as would happen if we were really moving into a dark area,” the investigators said.
Of the 50 men and women who had their eye movements measured while looking at the illusion, only 14% didn’t perceive the illusion when the hole was black. When the hole was a color, that figure went up to 20%. There also was a strong dilation reflex with black holes, but colored holes caused the subjects’ pupils to constrict, they noted.
Dr. Laeng and his associates can’t explain why some people don’t see the movement, but they did offer this: “Pupils’ dilation or contraction reflex is not a closed-loop mechanism, like a photocell opening a door, impervious to any other information than the actual amount of light stimulating the photoreceptor. Rather, the eye adjusts to perceived and even imagined light, not simply to physical energy.”
And now, back to our reality check: We think we perceive the light of a cheeseburger, therefore it’s time for lunch.
Living the dream, diagnosing the nightmare
Does a bad dream mean you should be consulting your doctor about an impending neurologic disease? Maybe.
New research published in eClinicalMedicine suggests that, for some people, bad dreams and nightmares have been associated with developing Parkinson’s disease later in life. Dr. Abidemi I. Otaiku of the University of Birmingham (England) analyzed data from a cohort study involving 3,818 older men, of whom 2.3% were diagnosed with Parkinson’s during the 12 years of follow-up.
Dr. Otaiku found those with frequent nightmares – at least once per week – were twice as likely to develop Parkinson’s than were those without, with most of the diagnoses coming in the first 5 years.
Although more research needs to be done, “identifying the significance of bad dreams and nightmares could indicate that individuals who experience changes to their dreams in older age – without any obvious trigger – should seek medical advice,” he said in a Eurekalert statement.
Dr. Otaiku pointed out that studying dreams can tell us a lot about how our brains work and are structured. By using electroencephalography, Dr. Otaiku plans to look into the biological reasons for why we dream the way we do.
So could it be that those killer clowns are actually giving you a heads up on your health?
Maybe next time try a paper route
There’s just no winning with teenagers sometimes. You tell them to go outside, they’ll sit in the dark playing video games all night. You tell them to get better grades, they’ll skip school. You tell them to get a hobby, they’ll scam the German government for millions of euros.
The COVID-19 pandemic has been tricky for governments to manage. Massive amounts of infrastructure needed to be set up, and that means corners got cut. Germany was no exception in this regard; the government entrusted the Kassenärztlichen Vereinigung, a doctor’s association, with overseeing COVID testing and payment at private test centers. To make things a bit easier, all they required private test centers to provide to receive reimbursement was an invoice.
This is where our 17-year-old from Freiburg comes in. In a spark of entrepreneurial genius, he decided to falsify documents and create an entirely fictional COVID test center. The KV approved it, and between March and July of 2021, he sent in thousands of fake invoices. Over that 4-month period, he submitted 500,000 invoices and received 5.7 million euros as compensation. That’s a few thousand tests per day, which was absolutely absurd, but he avoided scrutiny for months.
In the end, it wasn’t even the KV that noticed the fraud, but the bank. A bank employee noticed millions flowing into the account of a teenager and suspected money laundering, alerting the government. Fortunately for our young friend, since he was under 18 when he hatched his scheme, he was tried as a minor, avoiding jail time. His ill-gotten gains were confiscated, he has to pay a relatively minimal fine, and he will be on probation for 1 year. And presumably, he’ll be on the receiving end of the grounding of a lifetime.
You look like I need more sleep
Like most people, not getting our beauty sleep can make us look tired and feel less attractive, but a new study from Sweden shows that the sleep deprived also are more likely to find others less attractive. That’s probably not a good finding for singles who often go out trying to meet someone after a long day of work.
For the study, 45 young men and women were required to spend one night with no sleep and then another night with the possibility of 8 hours of sleep. The following mornings, eye-tracking technology was used as they looked at images of happy, angry, fearful, and neutral faces. The subjects then rated the faces for attractiveness, trustworthiness, and healthiness.
“The finding that sleep-deprived subjects in our experiment rated angry faces as less trustworthy and healthy-looking and neutral and fearful faces as less attractive indicates that sleep loss is associated with more negative social impressions of others,” senior author Christian Benedict of Uppsala University said in a statement.
When we are sleep deprived, the researchers added, we might not stop to really look at someone else, which has a negative impact on how we perceive people because we are not focusing on what their facial expressions are really telling us.
We already knew that not sleeping well has many negative effects on us, but now – thank you very much, science – we have something else to think about. Better hope your crush at work gets enough sleep so you’ll be accurately noticed.
The expanding-hole illusion of science
Time for a LOTME-style reality check: I think, therefore I am.
So far, so good. Next step: I think, therefore I am. I think.
Works for us. Now for the biggie: I think I am seeing the black hole in the middle of this image expanding.
Does that work for you? Do you perceive the black hole as expanding? If you do, then you fit in with the 86% of subjects in a recent study who perceived the same thing.
Lead author Bruno Laeng of the University of Oslo explained the effect in a statement from Frontiers Science News. “The circular smear or shadow gradient of the central black hole evokes a marked impression of optic flow, as if the observer were heading forward into a hole or tunnel. ... The pupil reacts to how we perceive light – even if this ‘light’ is imaginary like in the illusion – and not just to the amount of light energy that actually enters the eye.”
The illusion is so good at deceiving the brain “that it even prompts a dilation reflex of the pupils to let in more light, just as would happen if we were really moving into a dark area,” the investigators said.
Of the 50 men and women who had their eye movements measured while looking at the illusion, only 14% didn’t perceive the illusion when the hole was black. When the hole was a color, that figure went up to 20%. There also was a strong dilation reflex with black holes, but colored holes caused the subjects’ pupils to constrict, they noted.
Dr. Laeng and his associates can’t explain why some people don’t see the movement, but they did offer this: “Pupils’ dilation or contraction reflex is not a closed-loop mechanism, like a photocell opening a door, impervious to any other information than the actual amount of light stimulating the photoreceptor. Rather, the eye adjusts to perceived and even imagined light, not simply to physical energy.”
And now, back to our reality check: We think we perceive the light of a cheeseburger, therefore it’s time for lunch.
Living the dream, diagnosing the nightmare
Does a bad dream mean you should be consulting your doctor about an impending neurologic disease? Maybe.
New research published in eClinicalMedicine suggests that, for some people, bad dreams and nightmares have been associated with developing Parkinson’s disease later in life. Dr. Abidemi I. Otaiku of the University of Birmingham (England) analyzed data from a cohort study involving 3,818 older men, of whom 2.3% were diagnosed with Parkinson’s during the 12 years of follow-up.
Dr. Otaiku found those with frequent nightmares – at least once per week – were twice as likely to develop Parkinson’s than were those without, with most of the diagnoses coming in the first 5 years.
Although more research needs to be done, “identifying the significance of bad dreams and nightmares could indicate that individuals who experience changes to their dreams in older age – without any obvious trigger – should seek medical advice,” he said in a Eurekalert statement.
Dr. Otaiku pointed out that studying dreams can tell us a lot about how our brains work and are structured. By using electroencephalography, Dr. Otaiku plans to look into the biological reasons for why we dream the way we do.
So could it be that those killer clowns are actually giving you a heads up on your health?
Maybe next time try a paper route
There’s just no winning with teenagers sometimes. You tell them to go outside, they’ll sit in the dark playing video games all night. You tell them to get better grades, they’ll skip school. You tell them to get a hobby, they’ll scam the German government for millions of euros.
The COVID-19 pandemic has been tricky for governments to manage. Massive amounts of infrastructure needed to be set up, and that means corners got cut. Germany was no exception in this regard; the government entrusted the Kassenärztlichen Vereinigung, a doctor’s association, with overseeing COVID testing and payment at private test centers. To make things a bit easier, all they required private test centers to provide to receive reimbursement was an invoice.
This is where our 17-year-old from Freiburg comes in. In a spark of entrepreneurial genius, he decided to falsify documents and create an entirely fictional COVID test center. The KV approved it, and between March and July of 2021, he sent in thousands of fake invoices. Over that 4-month period, he submitted 500,000 invoices and received 5.7 million euros as compensation. That’s a few thousand tests per day, which was absolutely absurd, but he avoided scrutiny for months.
In the end, it wasn’t even the KV that noticed the fraud, but the bank. A bank employee noticed millions flowing into the account of a teenager and suspected money laundering, alerting the government. Fortunately for our young friend, since he was under 18 when he hatched his scheme, he was tried as a minor, avoiding jail time. His ill-gotten gains were confiscated, he has to pay a relatively minimal fine, and he will be on probation for 1 year. And presumably, he’ll be on the receiving end of the grounding of a lifetime.
You look like I need more sleep
Like most people, not getting our beauty sleep can make us look tired and feel less attractive, but a new study from Sweden shows that the sleep deprived also are more likely to find others less attractive. That’s probably not a good finding for singles who often go out trying to meet someone after a long day of work.
For the study, 45 young men and women were required to spend one night with no sleep and then another night with the possibility of 8 hours of sleep. The following mornings, eye-tracking technology was used as they looked at images of happy, angry, fearful, and neutral faces. The subjects then rated the faces for attractiveness, trustworthiness, and healthiness.
“The finding that sleep-deprived subjects in our experiment rated angry faces as less trustworthy and healthy-looking and neutral and fearful faces as less attractive indicates that sleep loss is associated with more negative social impressions of others,” senior author Christian Benedict of Uppsala University said in a statement.
When we are sleep deprived, the researchers added, we might not stop to really look at someone else, which has a negative impact on how we perceive people because we are not focusing on what their facial expressions are really telling us.
We already knew that not sleeping well has many negative effects on us, but now – thank you very much, science – we have something else to think about. Better hope your crush at work gets enough sleep so you’ll be accurately noticed.
The expanding-hole illusion of science
Time for a LOTME-style reality check: I think, therefore I am.
So far, so good. Next step: I think, therefore I am. I think.
Works for us. Now for the biggie: I think I am seeing the black hole in the middle of this image expanding.
Does that work for you? Do you perceive the black hole as expanding? If you do, then you fit in with the 86% of subjects in a recent study who perceived the same thing.
Lead author Bruno Laeng of the University of Oslo explained the effect in a statement from Frontiers Science News. “The circular smear or shadow gradient of the central black hole evokes a marked impression of optic flow, as if the observer were heading forward into a hole or tunnel. ... The pupil reacts to how we perceive light – even if this ‘light’ is imaginary like in the illusion – and not just to the amount of light energy that actually enters the eye.”
The illusion is so good at deceiving the brain “that it even prompts a dilation reflex of the pupils to let in more light, just as would happen if we were really moving into a dark area,” the investigators said.
Of the 50 men and women who had their eye movements measured while looking at the illusion, only 14% didn’t perceive the illusion when the hole was black. When the hole was a color, that figure went up to 20%. There also was a strong dilation reflex with black holes, but colored holes caused the subjects’ pupils to constrict, they noted.
Dr. Laeng and his associates can’t explain why some people don’t see the movement, but they did offer this: “Pupils’ dilation or contraction reflex is not a closed-loop mechanism, like a photocell opening a door, impervious to any other information than the actual amount of light stimulating the photoreceptor. Rather, the eye adjusts to perceived and even imagined light, not simply to physical energy.”
And now, back to our reality check: We think we perceive the light of a cheeseburger, therefore it’s time for lunch.
PCOS comes with high morbidity, medication use into late 40s
Women with polycystic ovary syndrome (PCOS) have an increased risk for several diseases and symptoms, many independent of body mass index (BMI), new research indicates.
Some diseases are linked for the first time to PCOS in this study, the authors wrote.
Researchers, led by Linda Kujanpää, MD, of the research unit for pediatrics, dermatology, clinical genetics, obstetrics, and gynecology at University of Oulu (Finland), found the morbidity risk is evident through the late reproductive years.
The paper was published online in Acta Obstetricia et Gynecologica Scandinavica.
This population-based follow-up study investigated comorbidities and medication and health care services use among women with PCOS in Finland at age 46 years via answers to a questionnaire.
The whole PCOS population (n = 280) consisted of women who reported both hirsutism and oligo/amenorrhea at age 31 (4.1%) and/or polycystic ovary morphology/PCOS at age 46 (3.1%), of which 246 replied to the 46-year questionnaire. They were compared with a control group of 1,573 women without PCOS.
Overall morbidity risk was 35% higher than for women without PCOS (risk ratio, 1.35; 95% confidence interval, 1.16-1.57). Medication use was 27% higher (RR, 1.27; 95% CI, 1.08-1.50), and the risk remained after adjusting for BMI.
Diagnoses with increased prevalence in women with PCOS were osteoarthritis, migraine, hypertension, tendinitis, and endometriosis. PCOS was also associated with autoimmune diseases and recurrent upper respiratory tract infections.
“BMI seems not to be solely responsible for the increased morbidity,” the researchers found. The average morbidity score of women with PCOS with a BMI of 25 kg/m2 or higher was similar to that of women with PCOS and lower BMI.
Mindy Christianson, MD, medical director at Johns Hopkins Fertility Center and associate professor of gynecology and obstetrics at Johns Hopkins University, both in Baltimore, said in an interview that the links to diseases independent of BMI are interesting because there’s so much focus on counseling women with PCOS to lose weight.
While that message is still important, it’s important to realize that some related diseases and conditions – such as autoimmune diseases and migraine – are not driven by BMI.
“It really drives home the point that polycystic ovary syndrome is really a chronic medical condition and puts patients at risk for a number of health conditions,” she said. “Having a good primary care physician is important to help them with their overall health.”
Women with PCOS said their health was poor or very poor almost three times more often than did women in the control group.
Surprisingly few studies have looked at overall comorbidity in women with PCOS, the authors wrote.
“This should be of high priority given the high cost to society resulting from PCOS-related morbidity,” they added. As an example, they pointed out that PCOS-related type 2 diabetes alone costs an estimated $1.77 billion in the United States and £237 million ($310 million) each year in the United Kingdom.
Additionally, the focus in previous research has typically been on women in their early or mid-reproductive years, and morbidity burden data in late reproductive years are scarce.
The study population was pulled from the longitudinal Northern Finland Birth Cohort 1966 and included all pregnancies with estimated date of delivery during 1966 in two provinces of Finland (5,889 women).
Dr. Christianson said she hopes this study will spur more research on PCOS, which has been severely underfunded, especially in the United States.
Part of the reason for that is there is a limited number of subspecialists in the country who work with patients with PCOS and do research in the area. PCOS often gets lost in the research priorities of infertility, diabetes, and thyroid disease.
The message in this study that PCOS is not just a fertility issue or an obesity issue but an overall health issue with a substantial cost to the health system may help raise awareness, Dr. Christianson said.
This study was supported by grants from The Finnish Medical Foundation, The Academy of Finland, The Sigrid Juselius Foundation, The Finnish Cultural Foundation, The Jalmari and Rauha Ahokas Foundation, The Päivikki and Sakari Sohlberg Foundation, Genesis Research Trust, The Medical Research Council, University of Oulu, Oulu University Hospital, Ministry of Health and Social Affairs, National Institute for Health and Welfare, Regional Institute of Occupational Health, and the European Regional Development Fund. The Study authors and Dr. Christianson reported no relevant financial relationships.
Women with polycystic ovary syndrome (PCOS) have an increased risk for several diseases and symptoms, many independent of body mass index (BMI), new research indicates.
Some diseases are linked for the first time to PCOS in this study, the authors wrote.
Researchers, led by Linda Kujanpää, MD, of the research unit for pediatrics, dermatology, clinical genetics, obstetrics, and gynecology at University of Oulu (Finland), found the morbidity risk is evident through the late reproductive years.
The paper was published online in Acta Obstetricia et Gynecologica Scandinavica.
This population-based follow-up study investigated comorbidities and medication and health care services use among women with PCOS in Finland at age 46 years via answers to a questionnaire.
The whole PCOS population (n = 280) consisted of women who reported both hirsutism and oligo/amenorrhea at age 31 (4.1%) and/or polycystic ovary morphology/PCOS at age 46 (3.1%), of which 246 replied to the 46-year questionnaire. They were compared with a control group of 1,573 women without PCOS.
Overall morbidity risk was 35% higher than for women without PCOS (risk ratio, 1.35; 95% confidence interval, 1.16-1.57). Medication use was 27% higher (RR, 1.27; 95% CI, 1.08-1.50), and the risk remained after adjusting for BMI.
Diagnoses with increased prevalence in women with PCOS were osteoarthritis, migraine, hypertension, tendinitis, and endometriosis. PCOS was also associated with autoimmune diseases and recurrent upper respiratory tract infections.
“BMI seems not to be solely responsible for the increased morbidity,” the researchers found. The average morbidity score of women with PCOS with a BMI of 25 kg/m2 or higher was similar to that of women with PCOS and lower BMI.
Mindy Christianson, MD, medical director at Johns Hopkins Fertility Center and associate professor of gynecology and obstetrics at Johns Hopkins University, both in Baltimore, said in an interview that the links to diseases independent of BMI are interesting because there’s so much focus on counseling women with PCOS to lose weight.
While that message is still important, it’s important to realize that some related diseases and conditions – such as autoimmune diseases and migraine – are not driven by BMI.
“It really drives home the point that polycystic ovary syndrome is really a chronic medical condition and puts patients at risk for a number of health conditions,” she said. “Having a good primary care physician is important to help them with their overall health.”
Women with PCOS said their health was poor or very poor almost three times more often than did women in the control group.
Surprisingly few studies have looked at overall comorbidity in women with PCOS, the authors wrote.
“This should be of high priority given the high cost to society resulting from PCOS-related morbidity,” they added. As an example, they pointed out that PCOS-related type 2 diabetes alone costs an estimated $1.77 billion in the United States and £237 million ($310 million) each year in the United Kingdom.
Additionally, the focus in previous research has typically been on women in their early or mid-reproductive years, and morbidity burden data in late reproductive years are scarce.
The study population was pulled from the longitudinal Northern Finland Birth Cohort 1966 and included all pregnancies with estimated date of delivery during 1966 in two provinces of Finland (5,889 women).
Dr. Christianson said she hopes this study will spur more research on PCOS, which has been severely underfunded, especially in the United States.
Part of the reason for that is there is a limited number of subspecialists in the country who work with patients with PCOS and do research in the area. PCOS often gets lost in the research priorities of infertility, diabetes, and thyroid disease.
The message in this study that PCOS is not just a fertility issue or an obesity issue but an overall health issue with a substantial cost to the health system may help raise awareness, Dr. Christianson said.
This study was supported by grants from The Finnish Medical Foundation, The Academy of Finland, The Sigrid Juselius Foundation, The Finnish Cultural Foundation, The Jalmari and Rauha Ahokas Foundation, The Päivikki and Sakari Sohlberg Foundation, Genesis Research Trust, The Medical Research Council, University of Oulu, Oulu University Hospital, Ministry of Health and Social Affairs, National Institute for Health and Welfare, Regional Institute of Occupational Health, and the European Regional Development Fund. The Study authors and Dr. Christianson reported no relevant financial relationships.
Women with polycystic ovary syndrome (PCOS) have an increased risk for several diseases and symptoms, many independent of body mass index (BMI), new research indicates.
Some diseases are linked for the first time to PCOS in this study, the authors wrote.
Researchers, led by Linda Kujanpää, MD, of the research unit for pediatrics, dermatology, clinical genetics, obstetrics, and gynecology at University of Oulu (Finland), found the morbidity risk is evident through the late reproductive years.
The paper was published online in Acta Obstetricia et Gynecologica Scandinavica.
This population-based follow-up study investigated comorbidities and medication and health care services use among women with PCOS in Finland at age 46 years via answers to a questionnaire.
The whole PCOS population (n = 280) consisted of women who reported both hirsutism and oligo/amenorrhea at age 31 (4.1%) and/or polycystic ovary morphology/PCOS at age 46 (3.1%), of which 246 replied to the 46-year questionnaire. They were compared with a control group of 1,573 women without PCOS.
Overall morbidity risk was 35% higher than for women without PCOS (risk ratio, 1.35; 95% confidence interval, 1.16-1.57). Medication use was 27% higher (RR, 1.27; 95% CI, 1.08-1.50), and the risk remained after adjusting for BMI.
Diagnoses with increased prevalence in women with PCOS were osteoarthritis, migraine, hypertension, tendinitis, and endometriosis. PCOS was also associated with autoimmune diseases and recurrent upper respiratory tract infections.
“BMI seems not to be solely responsible for the increased morbidity,” the researchers found. The average morbidity score of women with PCOS with a BMI of 25 kg/m2 or higher was similar to that of women with PCOS and lower BMI.
Mindy Christianson, MD, medical director at Johns Hopkins Fertility Center and associate professor of gynecology and obstetrics at Johns Hopkins University, both in Baltimore, said in an interview that the links to diseases independent of BMI are interesting because there’s so much focus on counseling women with PCOS to lose weight.
While that message is still important, it’s important to realize that some related diseases and conditions – such as autoimmune diseases and migraine – are not driven by BMI.
“It really drives home the point that polycystic ovary syndrome is really a chronic medical condition and puts patients at risk for a number of health conditions,” she said. “Having a good primary care physician is important to help them with their overall health.”
Women with PCOS said their health was poor or very poor almost three times more often than did women in the control group.
Surprisingly few studies have looked at overall comorbidity in women with PCOS, the authors wrote.
“This should be of high priority given the high cost to society resulting from PCOS-related morbidity,” they added. As an example, they pointed out that PCOS-related type 2 diabetes alone costs an estimated $1.77 billion in the United States and £237 million ($310 million) each year in the United Kingdom.
Additionally, the focus in previous research has typically been on women in their early or mid-reproductive years, and morbidity burden data in late reproductive years are scarce.
The study population was pulled from the longitudinal Northern Finland Birth Cohort 1966 and included all pregnancies with estimated date of delivery during 1966 in two provinces of Finland (5,889 women).
Dr. Christianson said she hopes this study will spur more research on PCOS, which has been severely underfunded, especially in the United States.
Part of the reason for that is there is a limited number of subspecialists in the country who work with patients with PCOS and do research in the area. PCOS often gets lost in the research priorities of infertility, diabetes, and thyroid disease.
The message in this study that PCOS is not just a fertility issue or an obesity issue but an overall health issue with a substantial cost to the health system may help raise awareness, Dr. Christianson said.
This study was supported by grants from The Finnish Medical Foundation, The Academy of Finland, The Sigrid Juselius Foundation, The Finnish Cultural Foundation, The Jalmari and Rauha Ahokas Foundation, The Päivikki and Sakari Sohlberg Foundation, Genesis Research Trust, The Medical Research Council, University of Oulu, Oulu University Hospital, Ministry of Health and Social Affairs, National Institute for Health and Welfare, Regional Institute of Occupational Health, and the European Regional Development Fund. The Study authors and Dr. Christianson reported no relevant financial relationships.
FROM ACTA OBSTETRICIA ET GYNECOLOGICA SCANDINAVICA
CTO PCI success rates rising, with blip during COVID-19, registry shows
Technical and procedural success rates for chronic total occlusion percutaneous coronary intervention (CTO PCI) have increased steadily over the past 6 years, with rates of in-hospital major adverse cardiac events (MACE) declining to the 2%-or-lower range in that time.
“CTO PCI technical and procedural success rates are high and continue to increase over time,” Spyridon Kostantinis, MD said in presenting updated results from the international PROGRESS-CTO registry at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
“The overall success rate increased from 81.6% in 2018 to 88.1% in 2021,” he added. The overall incidence of in-hospital MACE in that time was “an acceptable” 2.1% without significant changes over that period.
The analysis examined clinical, angiographic and procedural outcomes of 10,249 CTO PCIs performed on 10,019 patients from 63 centers in nine countries during 2016-2021. PROGRESS-CTO stands for Prospective Global Registry for the Study of Chronic Total Occlusion Intervention.
The target CTOs were highly complex, he said, with an average J-CTO (multicenter CTO registry in Japan) score of 2.4 ± 1.3 and PROGRESS-CTO score of 1.3 ± 1. The most common CTO target vessel was the right coronary artery (53%), followed by the left anterior descending artery (26%) and the circumflex artery (19%).
The registry also tracked how characteristics of the CTO PCI procedures themselves changed over time. “The septal and the epicardial collaterals were the most common collaterals used for retrograde crossing, with a decreasing trend for epicardial collaterals over time,” said Dr. Kostantinis, a research fellow at the Minneapolis Heart Institute.
Septal collateral use varied between 64% and 69% of cases from 2016 to 2021, but the share of epicardial collaterals declined from 35% to 22% in that time.
“Over time, the range of antegrade wiring as the final successfully crossing strategy increased from 46% in 2016 to 61% in 2021, with a decrease in antegrade dissection and re-entry (ADR) and no change in the retrograde approach,” Dr. Kostantinis said. The percentage of procedures using ADR as the final crossing strategy declined from 18% in 2016 to 12% in 2021, with the rate of retrograde crossings peaking at 21% in 2016 but leveling off to 18% or 19% in the subsequent years.
“An increasing use in the efficiency of antegrade wiring may reflect an improvement in guidewire retrograde crossing as well as the increasing operator expertise,” Dr. Kostantinis said.
The study also found that contrast volume, air kerma radiation dose, fluoroscopy time, and procedure time declined steadily over time. “The potential explanations for these are using new x-ray systems as well as the use of intravascular imaging,” Dr. Kostantinis said.
In 2020, the rates of technical and procedural success, as well as the number of overall procedures, declined from 2019, while MACE rates ticked upward that year, probably because of the COVID-19 pandemic, Dr. Kostantinis said.
“It is true that we noticed a rise in MACE rate from 1.6% in 2019 to 2.7% in 2020, but in 2021 that decreased again to 1.7%,” he said in an interview. “Another potential explanation is the higher angiographic complexity of CTOs treated during that year (2020) that resulted in more adverse events.”
Previous results from the PROGRESS-CTO registry reported the difference in MACE between 2019 and 2020 was significant (P = .01). “So, yes, the difference between those 2 years is significant,” Dr. Kostantinis said. However, he noted, the overall trend was not significant, with a P value of .194.
The risk profile of CTO PCI has improved “slowly” over time, said Kirk N. Garratt, MD, but “it’s not yet were it needs to be.”
He added, “Undoubtedly we’ve learned that, without any question, one method for minimizing the risk is to concentrate these cases in the hands of those that do many of them.” As the number of procedures fell – an “embedded” pandemic impact –“I worry that it’s inevitable that complication rates will tick up a bit,” said Dr. Garratt, director of the Center for Heart and Vascular Health at Christiana Care in Newark, Del.
By the same token, he added, this situation with regard to CTOs “parallels what’s happening elsewhere in interventional medicine and medicine broadly; numbers are increasing and we’re busy again. In most domains we’re not as busy as we had been prepandemic, and time will allow us to catch up.”
PROGRESS-CTO has received funding from the Joseph F. and Mary M. Fleischhacker Foundation and the Abbott Northwestern Hospital Foundation Innovation Grant.
Dr. Kostantinis has no disclosures. Dr. Garratt is an advisory board member for Abbott.
Technical and procedural success rates for chronic total occlusion percutaneous coronary intervention (CTO PCI) have increased steadily over the past 6 years, with rates of in-hospital major adverse cardiac events (MACE) declining to the 2%-or-lower range in that time.
“CTO PCI technical and procedural success rates are high and continue to increase over time,” Spyridon Kostantinis, MD said in presenting updated results from the international PROGRESS-CTO registry at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
“The overall success rate increased from 81.6% in 2018 to 88.1% in 2021,” he added. The overall incidence of in-hospital MACE in that time was “an acceptable” 2.1% without significant changes over that period.
The analysis examined clinical, angiographic and procedural outcomes of 10,249 CTO PCIs performed on 10,019 patients from 63 centers in nine countries during 2016-2021. PROGRESS-CTO stands for Prospective Global Registry for the Study of Chronic Total Occlusion Intervention.
The target CTOs were highly complex, he said, with an average J-CTO (multicenter CTO registry in Japan) score of 2.4 ± 1.3 and PROGRESS-CTO score of 1.3 ± 1. The most common CTO target vessel was the right coronary artery (53%), followed by the left anterior descending artery (26%) and the circumflex artery (19%).
The registry also tracked how characteristics of the CTO PCI procedures themselves changed over time. “The septal and the epicardial collaterals were the most common collaterals used for retrograde crossing, with a decreasing trend for epicardial collaterals over time,” said Dr. Kostantinis, a research fellow at the Minneapolis Heart Institute.
Septal collateral use varied between 64% and 69% of cases from 2016 to 2021, but the share of epicardial collaterals declined from 35% to 22% in that time.
“Over time, the range of antegrade wiring as the final successfully crossing strategy increased from 46% in 2016 to 61% in 2021, with a decrease in antegrade dissection and re-entry (ADR) and no change in the retrograde approach,” Dr. Kostantinis said. The percentage of procedures using ADR as the final crossing strategy declined from 18% in 2016 to 12% in 2021, with the rate of retrograde crossings peaking at 21% in 2016 but leveling off to 18% or 19% in the subsequent years.
“An increasing use in the efficiency of antegrade wiring may reflect an improvement in guidewire retrograde crossing as well as the increasing operator expertise,” Dr. Kostantinis said.
The study also found that contrast volume, air kerma radiation dose, fluoroscopy time, and procedure time declined steadily over time. “The potential explanations for these are using new x-ray systems as well as the use of intravascular imaging,” Dr. Kostantinis said.
In 2020, the rates of technical and procedural success, as well as the number of overall procedures, declined from 2019, while MACE rates ticked upward that year, probably because of the COVID-19 pandemic, Dr. Kostantinis said.
“It is true that we noticed a rise in MACE rate from 1.6% in 2019 to 2.7% in 2020, but in 2021 that decreased again to 1.7%,” he said in an interview. “Another potential explanation is the higher angiographic complexity of CTOs treated during that year (2020) that resulted in more adverse events.”
Previous results from the PROGRESS-CTO registry reported the difference in MACE between 2019 and 2020 was significant (P = .01). “So, yes, the difference between those 2 years is significant,” Dr. Kostantinis said. However, he noted, the overall trend was not significant, with a P value of .194.
The risk profile of CTO PCI has improved “slowly” over time, said Kirk N. Garratt, MD, but “it’s not yet were it needs to be.”
He added, “Undoubtedly we’ve learned that, without any question, one method for minimizing the risk is to concentrate these cases in the hands of those that do many of them.” As the number of procedures fell – an “embedded” pandemic impact –“I worry that it’s inevitable that complication rates will tick up a bit,” said Dr. Garratt, director of the Center for Heart and Vascular Health at Christiana Care in Newark, Del.
By the same token, he added, this situation with regard to CTOs “parallels what’s happening elsewhere in interventional medicine and medicine broadly; numbers are increasing and we’re busy again. In most domains we’re not as busy as we had been prepandemic, and time will allow us to catch up.”
PROGRESS-CTO has received funding from the Joseph F. and Mary M. Fleischhacker Foundation and the Abbott Northwestern Hospital Foundation Innovation Grant.
Dr. Kostantinis has no disclosures. Dr. Garratt is an advisory board member for Abbott.
Technical and procedural success rates for chronic total occlusion percutaneous coronary intervention (CTO PCI) have increased steadily over the past 6 years, with rates of in-hospital major adverse cardiac events (MACE) declining to the 2%-or-lower range in that time.
“CTO PCI technical and procedural success rates are high and continue to increase over time,” Spyridon Kostantinis, MD said in presenting updated results from the international PROGRESS-CTO registry at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
“The overall success rate increased from 81.6% in 2018 to 88.1% in 2021,” he added. The overall incidence of in-hospital MACE in that time was “an acceptable” 2.1% without significant changes over that period.
The analysis examined clinical, angiographic and procedural outcomes of 10,249 CTO PCIs performed on 10,019 patients from 63 centers in nine countries during 2016-2021. PROGRESS-CTO stands for Prospective Global Registry for the Study of Chronic Total Occlusion Intervention.
The target CTOs were highly complex, he said, with an average J-CTO (multicenter CTO registry in Japan) score of 2.4 ± 1.3 and PROGRESS-CTO score of 1.3 ± 1. The most common CTO target vessel was the right coronary artery (53%), followed by the left anterior descending artery (26%) and the circumflex artery (19%).
The registry also tracked how characteristics of the CTO PCI procedures themselves changed over time. “The septal and the epicardial collaterals were the most common collaterals used for retrograde crossing, with a decreasing trend for epicardial collaterals over time,” said Dr. Kostantinis, a research fellow at the Minneapolis Heart Institute.
Septal collateral use varied between 64% and 69% of cases from 2016 to 2021, but the share of epicardial collaterals declined from 35% to 22% in that time.
“Over time, the range of antegrade wiring as the final successfully crossing strategy increased from 46% in 2016 to 61% in 2021, with a decrease in antegrade dissection and re-entry (ADR) and no change in the retrograde approach,” Dr. Kostantinis said. The percentage of procedures using ADR as the final crossing strategy declined from 18% in 2016 to 12% in 2021, with the rate of retrograde crossings peaking at 21% in 2016 but leveling off to 18% or 19% in the subsequent years.
“An increasing use in the efficiency of antegrade wiring may reflect an improvement in guidewire retrograde crossing as well as the increasing operator expertise,” Dr. Kostantinis said.
The study also found that contrast volume, air kerma radiation dose, fluoroscopy time, and procedure time declined steadily over time. “The potential explanations for these are using new x-ray systems as well as the use of intravascular imaging,” Dr. Kostantinis said.
In 2020, the rates of technical and procedural success, as well as the number of overall procedures, declined from 2019, while MACE rates ticked upward that year, probably because of the COVID-19 pandemic, Dr. Kostantinis said.
“It is true that we noticed a rise in MACE rate from 1.6% in 2019 to 2.7% in 2020, but in 2021 that decreased again to 1.7%,” he said in an interview. “Another potential explanation is the higher angiographic complexity of CTOs treated during that year (2020) that resulted in more adverse events.”
Previous results from the PROGRESS-CTO registry reported the difference in MACE between 2019 and 2020 was significant (P = .01). “So, yes, the difference between those 2 years is significant,” Dr. Kostantinis said. However, he noted, the overall trend was not significant, with a P value of .194.
The risk profile of CTO PCI has improved “slowly” over time, said Kirk N. Garratt, MD, but “it’s not yet were it needs to be.”
He added, “Undoubtedly we’ve learned that, without any question, one method for minimizing the risk is to concentrate these cases in the hands of those that do many of them.” As the number of procedures fell – an “embedded” pandemic impact –“I worry that it’s inevitable that complication rates will tick up a bit,” said Dr. Garratt, director of the Center for Heart and Vascular Health at Christiana Care in Newark, Del.
By the same token, he added, this situation with regard to CTOs “parallels what’s happening elsewhere in interventional medicine and medicine broadly; numbers are increasing and we’re busy again. In most domains we’re not as busy as we had been prepandemic, and time will allow us to catch up.”
PROGRESS-CTO has received funding from the Joseph F. and Mary M. Fleischhacker Foundation and the Abbott Northwestern Hospital Foundation Innovation Grant.
Dr. Kostantinis has no disclosures. Dr. Garratt is an advisory board member for Abbott.
FROM SCAI 2022
Stem cell transplants could be ‘transformational’ in type 1 diabetes
NEW ORLEANS – Two patients with type 1 diabetes have now experienced improved blood glucose control with Vertex Pharmaceutical’s investigational allogeneic stem cell–derived islets (VX-880), with the first person now completely insulin independent at 9 months post transplant.
Prior to the procedure, both patients had hypoglycemic unawareness and had experienced multiple episodes of severe hypoglycemia, conditions considered severe enough to justify the risk of immune suppression (which is required for such stem cell–derived islet transplants as they are “foreign” to the recipient).
The first patient, a 64-year-old man with type 1 diabetes for more than 40 years, now has a hemoglobin A1c in the normal range without taking any insulin more than 9 months after the procedure. The second, a 35-year-old woman with type 1 diabetes for 10.7 years, experienced a 30% reduction in insulin use and significant increased time spent in target glucose range, by 5 months post transplant. Both patients were given just half the targeted VX-880 dose.
Data for those two patients – the first in Vertex’s phase 1/2 multicenter, single-arm, open-label clinical trial of VX-880 – were reported at the annual scientific sessions of the American Diabetes Association, by James F. Markmann, MD, PhD.
He has been transplanting pancreatic islet cells from deceased donors into humans via infusion into the hepatic portal vein for over 20 years.
Transplantation of pancreatic islet cells obtained from cadavers have been shown to eliminate severe hypoglycemia and improve glycemic control in patients with type 1 diabetes, but they’re limited in quantity and are of variable quality. Islets that are manufactured via differentiation from human pluripotent stem cells represent an alternative, explained Dr. Markmann, chief of the division of transplant surgery at Massachusetts General Hospital, Boston.
“This is a new area. ... We hope this will be the same or potentially better. With stem cell–derived islets the quality, consistency, and reliability might produce a better result than with cadaveric islets,” he commented during a press briefing here.
A third patient has recently received the full targeted VX-880 dose but was not part of the current report. The planned enrollment is 17 patients. The trial is currently on clinical hold per the Food and Drug Administration concerning the criteria around dose escalation, but Vertex is working with the FDA to sort that out. Meanwhile, enrollment remains open in Canada, Dr. Markmann said.
In answer to a question about how patient 1 is doing now, Dr. Markmann replied, “He’s doing great. He’s probably the most appreciative patient I’ve ever met. His life was being destroyed by diabetes. He couldn’t work. He crashed his motorcycle from [low blood sugar]. He really was tremendously appreciative that he could participate.”
When Dr. Markmann explained the potential uncertainties and risks to the patient prior to the procedure, the patient replied: “I want to participate. If I die from this and I help somebody else I’d be happy, but I can’t go on living the way I’m living.”
“These people really suffer and this, I think, brings hope to them,” Dr. Markmann said.
‘Beautiful data’ seen in two patients, with ‘transformational’ potential
Asked to comment, Marlon Pragnell, PhD, vice president for Research & Science at the ADA, told this news organization: “It’s beautiful data. People who have type 1 diabetes lack [pancreatic] beta cells ... it was impossible to get sufficient beta cells from cadaveric transplants. It’s just nowhere near enough. If this is safe and effective, if they continue to show safety and efficacy like patient 1, this will be transformational.”
Dr. Markmann presented data for the most recent study visit for each of the two patients, 270 days for patient 1 and 150 days for patient 2. Prior to the transplants, patient 1 had experienced five severe hypoglycemic events and patient 2 had experienced three.
Both had undetectable C-peptide levels at baseline. In response to a mixed-meal tolerance test, patient 1 showed a “robust” C-peptide response by day 90, which increased by day 180. Those levels had dropped but were still detectable by day 270, “possibly due to improved insulin sensitivity,” Dr. Markmann said.
Similarly, Patient 2 also had increased C-peptide that increased to detectable range by day 90 with improved glucose disposal.
Hemoglobin A1c dropped in patient 1 from 8.6% at baseline to 6.9% at day 180, to a “remarkable” 5.2% at day 270. For patient 2, the drop was from 7.5% to a nadir of 6.4% by day 57, then reversing back to 7.1% at day 150.
Both patients also had significant reductions in insulin dose. For patient 1, the dose reduction was more than 90% – from 34 units at baseline to 2.6 units by day 90. By day 210 he was able to stop insulin and by day 270 he met formal criteria for insulin independence.
Patient 2 also had a significant reduction in insulin dose, from 25.9 units to 18.7 by day 57 and remained stable thereafter, at 18.2 units by day 150.
Asked why Patient 2’s results weren’t quite as impressive as patient 1’s, Dr. Markmann replied “I think what’s important is that both patients did great. And since this was a half-dose, we might have expected that the outcome was going to be more like patient 2 rather than patient 1. So, I think we’re just going to have to [study this in] more patients to understand where it falls.”
Although patient 1 experienced a cluster of six severe hypoglycemic events early in the posttransplant period, he had no further events after day 35. Patient 2 had no severe hypoglycemic events.
Other safety events were generally consistent with that seen with the immunosuppressive regimen in the perioperative period. Patient 1 had a “mild and self-limited” rise in liver function test and also experienced two severe adverse events: A rash from the immune suppression that resolved spontaneously, and dehydration requiring hospitalization on day 186. Patient 2’s adverse events were all mild to moderate, most commonly headache and hypomagnesemia and not related to VX-880.
Immunosuppression: Work is ongoing
The immunosuppression regimen used comprises a depletion of lymphocytes at induction, followed by a maintenance regimen of two standard agents used in kidney transplant patients and found to be well tolerated, Dr. Markmann said.
Still, the risk of immunosuppression generally outweighs the potential benefit for most people with type 1 diabetes who are managing reasonably well with insulin treatment.
“This is part one of a two-part problem. One is to have a reliable, consistent, effective cell therapy. The second is to develop an approach that doesn’t require immunosuppression. ... But if we had a way of transplanting the cells without the need for immunosuppression, then it could be really widely available. That’s an opportunity for the future since these cells can be made in unlimited quantities,” Dr. Markmann commented during the press briefing.
Asked for his thoughts about the immunosuppression aspect, Dr. Pragnell told this news organization: “Immune suppression is a concern, but I feel that this is just the start of so much research in this area. They’re going to take this step by step. This is just the start. My understanding is they have additional strategies around immune suppression, and in the future they might not even need immunosuppression. But even at this stage right now, it’s amazing.”
He added: “The ‘artificial pancreas’ is a huge step forward, but it’s just a bridge to a cure, whereas if they’re able to show safety and efficacy, this is potentially a cure. ... I’m very excited about it.”
Dr. Markmann serves on advisory boards for iTolerance, eGenesis, and QihanBio. He is a consultant to Vertex Pharmaceuticals. Dr. Pragnell is an ADA employee and has no further disclosures.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Two patients with type 1 diabetes have now experienced improved blood glucose control with Vertex Pharmaceutical’s investigational allogeneic stem cell–derived islets (VX-880), with the first person now completely insulin independent at 9 months post transplant.
Prior to the procedure, both patients had hypoglycemic unawareness and had experienced multiple episodes of severe hypoglycemia, conditions considered severe enough to justify the risk of immune suppression (which is required for such stem cell–derived islet transplants as they are “foreign” to the recipient).
The first patient, a 64-year-old man with type 1 diabetes for more than 40 years, now has a hemoglobin A1c in the normal range without taking any insulin more than 9 months after the procedure. The second, a 35-year-old woman with type 1 diabetes for 10.7 years, experienced a 30% reduction in insulin use and significant increased time spent in target glucose range, by 5 months post transplant. Both patients were given just half the targeted VX-880 dose.
Data for those two patients – the first in Vertex’s phase 1/2 multicenter, single-arm, open-label clinical trial of VX-880 – were reported at the annual scientific sessions of the American Diabetes Association, by James F. Markmann, MD, PhD.
He has been transplanting pancreatic islet cells from deceased donors into humans via infusion into the hepatic portal vein for over 20 years.
Transplantation of pancreatic islet cells obtained from cadavers have been shown to eliminate severe hypoglycemia and improve glycemic control in patients with type 1 diabetes, but they’re limited in quantity and are of variable quality. Islets that are manufactured via differentiation from human pluripotent stem cells represent an alternative, explained Dr. Markmann, chief of the division of transplant surgery at Massachusetts General Hospital, Boston.
“This is a new area. ... We hope this will be the same or potentially better. With stem cell–derived islets the quality, consistency, and reliability might produce a better result than with cadaveric islets,” he commented during a press briefing here.
A third patient has recently received the full targeted VX-880 dose but was not part of the current report. The planned enrollment is 17 patients. The trial is currently on clinical hold per the Food and Drug Administration concerning the criteria around dose escalation, but Vertex is working with the FDA to sort that out. Meanwhile, enrollment remains open in Canada, Dr. Markmann said.
In answer to a question about how patient 1 is doing now, Dr. Markmann replied, “He’s doing great. He’s probably the most appreciative patient I’ve ever met. His life was being destroyed by diabetes. He couldn’t work. He crashed his motorcycle from [low blood sugar]. He really was tremendously appreciative that he could participate.”
When Dr. Markmann explained the potential uncertainties and risks to the patient prior to the procedure, the patient replied: “I want to participate. If I die from this and I help somebody else I’d be happy, but I can’t go on living the way I’m living.”
“These people really suffer and this, I think, brings hope to them,” Dr. Markmann said.
‘Beautiful data’ seen in two patients, with ‘transformational’ potential
Asked to comment, Marlon Pragnell, PhD, vice president for Research & Science at the ADA, told this news organization: “It’s beautiful data. People who have type 1 diabetes lack [pancreatic] beta cells ... it was impossible to get sufficient beta cells from cadaveric transplants. It’s just nowhere near enough. If this is safe and effective, if they continue to show safety and efficacy like patient 1, this will be transformational.”
Dr. Markmann presented data for the most recent study visit for each of the two patients, 270 days for patient 1 and 150 days for patient 2. Prior to the transplants, patient 1 had experienced five severe hypoglycemic events and patient 2 had experienced three.
Both had undetectable C-peptide levels at baseline. In response to a mixed-meal tolerance test, patient 1 showed a “robust” C-peptide response by day 90, which increased by day 180. Those levels had dropped but were still detectable by day 270, “possibly due to improved insulin sensitivity,” Dr. Markmann said.
Similarly, Patient 2 also had increased C-peptide that increased to detectable range by day 90 with improved glucose disposal.
Hemoglobin A1c dropped in patient 1 from 8.6% at baseline to 6.9% at day 180, to a “remarkable” 5.2% at day 270. For patient 2, the drop was from 7.5% to a nadir of 6.4% by day 57, then reversing back to 7.1% at day 150.
Both patients also had significant reductions in insulin dose. For patient 1, the dose reduction was more than 90% – from 34 units at baseline to 2.6 units by day 90. By day 210 he was able to stop insulin and by day 270 he met formal criteria for insulin independence.
Patient 2 also had a significant reduction in insulin dose, from 25.9 units to 18.7 by day 57 and remained stable thereafter, at 18.2 units by day 150.
Asked why Patient 2’s results weren’t quite as impressive as patient 1’s, Dr. Markmann replied “I think what’s important is that both patients did great. And since this was a half-dose, we might have expected that the outcome was going to be more like patient 2 rather than patient 1. So, I think we’re just going to have to [study this in] more patients to understand where it falls.”
Although patient 1 experienced a cluster of six severe hypoglycemic events early in the posttransplant period, he had no further events after day 35. Patient 2 had no severe hypoglycemic events.
Other safety events were generally consistent with that seen with the immunosuppressive regimen in the perioperative period. Patient 1 had a “mild and self-limited” rise in liver function test and also experienced two severe adverse events: A rash from the immune suppression that resolved spontaneously, and dehydration requiring hospitalization on day 186. Patient 2’s adverse events were all mild to moderate, most commonly headache and hypomagnesemia and not related to VX-880.
Immunosuppression: Work is ongoing
The immunosuppression regimen used comprises a depletion of lymphocytes at induction, followed by a maintenance regimen of two standard agents used in kidney transplant patients and found to be well tolerated, Dr. Markmann said.
Still, the risk of immunosuppression generally outweighs the potential benefit for most people with type 1 diabetes who are managing reasonably well with insulin treatment.
“This is part one of a two-part problem. One is to have a reliable, consistent, effective cell therapy. The second is to develop an approach that doesn’t require immunosuppression. ... But if we had a way of transplanting the cells without the need for immunosuppression, then it could be really widely available. That’s an opportunity for the future since these cells can be made in unlimited quantities,” Dr. Markmann commented during the press briefing.
Asked for his thoughts about the immunosuppression aspect, Dr. Pragnell told this news organization: “Immune suppression is a concern, but I feel that this is just the start of so much research in this area. They’re going to take this step by step. This is just the start. My understanding is they have additional strategies around immune suppression, and in the future they might not even need immunosuppression. But even at this stage right now, it’s amazing.”
He added: “The ‘artificial pancreas’ is a huge step forward, but it’s just a bridge to a cure, whereas if they’re able to show safety and efficacy, this is potentially a cure. ... I’m very excited about it.”
Dr. Markmann serves on advisory boards for iTolerance, eGenesis, and QihanBio. He is a consultant to Vertex Pharmaceuticals. Dr. Pragnell is an ADA employee and has no further disclosures.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Two patients with type 1 diabetes have now experienced improved blood glucose control with Vertex Pharmaceutical’s investigational allogeneic stem cell–derived islets (VX-880), with the first person now completely insulin independent at 9 months post transplant.
Prior to the procedure, both patients had hypoglycemic unawareness and had experienced multiple episodes of severe hypoglycemia, conditions considered severe enough to justify the risk of immune suppression (which is required for such stem cell–derived islet transplants as they are “foreign” to the recipient).
The first patient, a 64-year-old man with type 1 diabetes for more than 40 years, now has a hemoglobin A1c in the normal range without taking any insulin more than 9 months after the procedure. The second, a 35-year-old woman with type 1 diabetes for 10.7 years, experienced a 30% reduction in insulin use and significant increased time spent in target glucose range, by 5 months post transplant. Both patients were given just half the targeted VX-880 dose.
Data for those two patients – the first in Vertex’s phase 1/2 multicenter, single-arm, open-label clinical trial of VX-880 – were reported at the annual scientific sessions of the American Diabetes Association, by James F. Markmann, MD, PhD.
He has been transplanting pancreatic islet cells from deceased donors into humans via infusion into the hepatic portal vein for over 20 years.
Transplantation of pancreatic islet cells obtained from cadavers have been shown to eliminate severe hypoglycemia and improve glycemic control in patients with type 1 diabetes, but they’re limited in quantity and are of variable quality. Islets that are manufactured via differentiation from human pluripotent stem cells represent an alternative, explained Dr. Markmann, chief of the division of transplant surgery at Massachusetts General Hospital, Boston.
“This is a new area. ... We hope this will be the same or potentially better. With stem cell–derived islets the quality, consistency, and reliability might produce a better result than with cadaveric islets,” he commented during a press briefing here.
A third patient has recently received the full targeted VX-880 dose but was not part of the current report. The planned enrollment is 17 patients. The trial is currently on clinical hold per the Food and Drug Administration concerning the criteria around dose escalation, but Vertex is working with the FDA to sort that out. Meanwhile, enrollment remains open in Canada, Dr. Markmann said.
In answer to a question about how patient 1 is doing now, Dr. Markmann replied, “He’s doing great. He’s probably the most appreciative patient I’ve ever met. His life was being destroyed by diabetes. He couldn’t work. He crashed his motorcycle from [low blood sugar]. He really was tremendously appreciative that he could participate.”
When Dr. Markmann explained the potential uncertainties and risks to the patient prior to the procedure, the patient replied: “I want to participate. If I die from this and I help somebody else I’d be happy, but I can’t go on living the way I’m living.”
“These people really suffer and this, I think, brings hope to them,” Dr. Markmann said.
‘Beautiful data’ seen in two patients, with ‘transformational’ potential
Asked to comment, Marlon Pragnell, PhD, vice president for Research & Science at the ADA, told this news organization: “It’s beautiful data. People who have type 1 diabetes lack [pancreatic] beta cells ... it was impossible to get sufficient beta cells from cadaveric transplants. It’s just nowhere near enough. If this is safe and effective, if they continue to show safety and efficacy like patient 1, this will be transformational.”
Dr. Markmann presented data for the most recent study visit for each of the two patients, 270 days for patient 1 and 150 days for patient 2. Prior to the transplants, patient 1 had experienced five severe hypoglycemic events and patient 2 had experienced three.
Both had undetectable C-peptide levels at baseline. In response to a mixed-meal tolerance test, patient 1 showed a “robust” C-peptide response by day 90, which increased by day 180. Those levels had dropped but were still detectable by day 270, “possibly due to improved insulin sensitivity,” Dr. Markmann said.
Similarly, Patient 2 also had increased C-peptide that increased to detectable range by day 90 with improved glucose disposal.
Hemoglobin A1c dropped in patient 1 from 8.6% at baseline to 6.9% at day 180, to a “remarkable” 5.2% at day 270. For patient 2, the drop was from 7.5% to a nadir of 6.4% by day 57, then reversing back to 7.1% at day 150.
Both patients also had significant reductions in insulin dose. For patient 1, the dose reduction was more than 90% – from 34 units at baseline to 2.6 units by day 90. By day 210 he was able to stop insulin and by day 270 he met formal criteria for insulin independence.
Patient 2 also had a significant reduction in insulin dose, from 25.9 units to 18.7 by day 57 and remained stable thereafter, at 18.2 units by day 150.
Asked why Patient 2’s results weren’t quite as impressive as patient 1’s, Dr. Markmann replied “I think what’s important is that both patients did great. And since this was a half-dose, we might have expected that the outcome was going to be more like patient 2 rather than patient 1. So, I think we’re just going to have to [study this in] more patients to understand where it falls.”
Although patient 1 experienced a cluster of six severe hypoglycemic events early in the posttransplant period, he had no further events after day 35. Patient 2 had no severe hypoglycemic events.
Other safety events were generally consistent with that seen with the immunosuppressive regimen in the perioperative period. Patient 1 had a “mild and self-limited” rise in liver function test and also experienced two severe adverse events: A rash from the immune suppression that resolved spontaneously, and dehydration requiring hospitalization on day 186. Patient 2’s adverse events were all mild to moderate, most commonly headache and hypomagnesemia and not related to VX-880.
Immunosuppression: Work is ongoing
The immunosuppression regimen used comprises a depletion of lymphocytes at induction, followed by a maintenance regimen of two standard agents used in kidney transplant patients and found to be well tolerated, Dr. Markmann said.
Still, the risk of immunosuppression generally outweighs the potential benefit for most people with type 1 diabetes who are managing reasonably well with insulin treatment.
“This is part one of a two-part problem. One is to have a reliable, consistent, effective cell therapy. The second is to develop an approach that doesn’t require immunosuppression. ... But if we had a way of transplanting the cells without the need for immunosuppression, then it could be really widely available. That’s an opportunity for the future since these cells can be made in unlimited quantities,” Dr. Markmann commented during the press briefing.
Asked for his thoughts about the immunosuppression aspect, Dr. Pragnell told this news organization: “Immune suppression is a concern, but I feel that this is just the start of so much research in this area. They’re going to take this step by step. This is just the start. My understanding is they have additional strategies around immune suppression, and in the future they might not even need immunosuppression. But even at this stage right now, it’s amazing.”
He added: “The ‘artificial pancreas’ is a huge step forward, but it’s just a bridge to a cure, whereas if they’re able to show safety and efficacy, this is potentially a cure. ... I’m very excited about it.”
Dr. Markmann serves on advisory boards for iTolerance, eGenesis, and QihanBio. He is a consultant to Vertex Pharmaceuticals. Dr. Pragnell is an ADA employee and has no further disclosures.
A version of this article first appeared on Medscape.com.
AT ADA 2022
Substance use the main cause of physician license actions
Despite a sharp uptick in 2011, substance use–specific license actions taken against physicians dropped in frequency between 2004 and 2020.
More than three fourths (76.3%) of license actions taken against physicians were related to substance use, according to a recent study published in JAMA. Psychological impairment was the reason associated with more than 1 in 10 (11.5%) actions taken against physicians’ licenses, while physical impairment was the reason behind approximately 12% of such actions, per the study.
Researchers analyzed 5032 actions taken against the licenses of U.S. physicians. The actions were reported to the National Practitioner Data Bank and were related to substance use, psychological impairment, and physical impairment. The National Practitioner Data Bank is a web-based repository of reports with information on medical malpractice payments and certain adverse actions related to healthcare practitioners, providers, and suppliers. It is provided by the Department of Health & Human Services.
“While there has been increased attention [on] the mental health of physicians, we wanted to understand the extent to which changes in attitudes and practices were reflected in actions taken by hospitals or licensing boards, which are reported in the National Practitioner Data Bank,” Lisa Rotenstein, MD, a primary care physician at Boston’s Brigham and Women’s Hospital and lead author of the study, told this news organization.
Dr. Rotenstein, who is an assistant professor at Harvard Medical School, Boston, studies issues of mental health among physicians and trainees. Dr. Rotenstein was the lead author of a 2016 study that found that more than a quarter (27.2%) of medical students have depressive symptoms. She was also lead author of a 2018 study published in JAMA on the prevalence of burnout among attending physicians.
Actions against physicians trending downward
2011 marked the peak in actions taken against physicians’ licenses for substance use, per the study, but actions related to substance use have otherwise maintained a steady decline over the past 17 years. Researchers found that physicians with license actions as a result of substance use or psychological impairment were more likely to receive indefinite penalties, while also having emergency action taken against their license to practice.
In addition, physicians who had actions taken against their licenses because of substance use or psychological impairment were more likely to accrue a greater number of actions over the course of their careers, according to the study.
About 47% of physicians reported experiencing burnout per Medscape’s Physician Burnout and Depression Report 2022: Stress, Anxiety, and Anger report. Burnout among emergency physicians spiked from 43% in 2020 to 60% in 2021, according to the report.
More than one quarter (26%) of physicians reported drinking alcohol to cope with burnout in 2020, according to Medscape’s 2021 Physician Burnout and Suicide Report. Per the 2021 report, 48% of physicians chose exercise to deal with burnout, while 35% indulged in eating junk food.
Peter Grinspoon, MD, a Boston-based primary care physician, wrote in The Los Angeles Times in 2016 that the rate of substance abuse among physicians starts at 10% and can go as high as 15%; by comparison, rates of substance use among the general population are 8%-10%. “What appears to account for the difference is physician distress, and in the case of drug abuse, plentiful access,” he added.
Dr. Grinspoon wrote a 2016 book called “Free Refills: A Doctor Confronts His Addiction,” which chronicles his experience in recovery and relapse as a physician who was dependent on opioid painkillers.
The findings from the recent study in JAMA “suggest we have made some progress in addressing issues related to substance use in ways that don’t result in license actions or even in meeting physicians’ need for support related to substance use,” said Dr. Rotenstein.
Still, she insists that there’s “substantial opportunity to improve mental health and support offerings for physicians and to reduce stigma related to seeking and receiving mental health support, ideally averting the need for license actions.”
According to Dr. Rotenstein, the cases listed in the National Practitioner Data Bank represent the most severe cases; these reports have risen to a high level of attention or concern and are the result of adverse action reports submitted by healthcare institutions and state licensing boards.
“There are many, many more physicians whose cases are not represented here but who struggle with depression, anxiety, substance use, and more,” said Dr. Rotenstein.
A version of this article first appeared on Medscape.com.
Despite a sharp uptick in 2011, substance use–specific license actions taken against physicians dropped in frequency between 2004 and 2020.
More than three fourths (76.3%) of license actions taken against physicians were related to substance use, according to a recent study published in JAMA. Psychological impairment was the reason associated with more than 1 in 10 (11.5%) actions taken against physicians’ licenses, while physical impairment was the reason behind approximately 12% of such actions, per the study.
Researchers analyzed 5032 actions taken against the licenses of U.S. physicians. The actions were reported to the National Practitioner Data Bank and were related to substance use, psychological impairment, and physical impairment. The National Practitioner Data Bank is a web-based repository of reports with information on medical malpractice payments and certain adverse actions related to healthcare practitioners, providers, and suppliers. It is provided by the Department of Health & Human Services.
“While there has been increased attention [on] the mental health of physicians, we wanted to understand the extent to which changes in attitudes and practices were reflected in actions taken by hospitals or licensing boards, which are reported in the National Practitioner Data Bank,” Lisa Rotenstein, MD, a primary care physician at Boston’s Brigham and Women’s Hospital and lead author of the study, told this news organization.
Dr. Rotenstein, who is an assistant professor at Harvard Medical School, Boston, studies issues of mental health among physicians and trainees. Dr. Rotenstein was the lead author of a 2016 study that found that more than a quarter (27.2%) of medical students have depressive symptoms. She was also lead author of a 2018 study published in JAMA on the prevalence of burnout among attending physicians.
Actions against physicians trending downward
2011 marked the peak in actions taken against physicians’ licenses for substance use, per the study, but actions related to substance use have otherwise maintained a steady decline over the past 17 years. Researchers found that physicians with license actions as a result of substance use or psychological impairment were more likely to receive indefinite penalties, while also having emergency action taken against their license to practice.
In addition, physicians who had actions taken against their licenses because of substance use or psychological impairment were more likely to accrue a greater number of actions over the course of their careers, according to the study.
About 47% of physicians reported experiencing burnout per Medscape’s Physician Burnout and Depression Report 2022: Stress, Anxiety, and Anger report. Burnout among emergency physicians spiked from 43% in 2020 to 60% in 2021, according to the report.
More than one quarter (26%) of physicians reported drinking alcohol to cope with burnout in 2020, according to Medscape’s 2021 Physician Burnout and Suicide Report. Per the 2021 report, 48% of physicians chose exercise to deal with burnout, while 35% indulged in eating junk food.
Peter Grinspoon, MD, a Boston-based primary care physician, wrote in The Los Angeles Times in 2016 that the rate of substance abuse among physicians starts at 10% and can go as high as 15%; by comparison, rates of substance use among the general population are 8%-10%. “What appears to account for the difference is physician distress, and in the case of drug abuse, plentiful access,” he added.
Dr. Grinspoon wrote a 2016 book called “Free Refills: A Doctor Confronts His Addiction,” which chronicles his experience in recovery and relapse as a physician who was dependent on opioid painkillers.
The findings from the recent study in JAMA “suggest we have made some progress in addressing issues related to substance use in ways that don’t result in license actions or even in meeting physicians’ need for support related to substance use,” said Dr. Rotenstein.
Still, she insists that there’s “substantial opportunity to improve mental health and support offerings for physicians and to reduce stigma related to seeking and receiving mental health support, ideally averting the need for license actions.”
According to Dr. Rotenstein, the cases listed in the National Practitioner Data Bank represent the most severe cases; these reports have risen to a high level of attention or concern and are the result of adverse action reports submitted by healthcare institutions and state licensing boards.
“There are many, many more physicians whose cases are not represented here but who struggle with depression, anxiety, substance use, and more,” said Dr. Rotenstein.
A version of this article first appeared on Medscape.com.
Despite a sharp uptick in 2011, substance use–specific license actions taken against physicians dropped in frequency between 2004 and 2020.
More than three fourths (76.3%) of license actions taken against physicians were related to substance use, according to a recent study published in JAMA. Psychological impairment was the reason associated with more than 1 in 10 (11.5%) actions taken against physicians’ licenses, while physical impairment was the reason behind approximately 12% of such actions, per the study.
Researchers analyzed 5032 actions taken against the licenses of U.S. physicians. The actions were reported to the National Practitioner Data Bank and were related to substance use, psychological impairment, and physical impairment. The National Practitioner Data Bank is a web-based repository of reports with information on medical malpractice payments and certain adverse actions related to healthcare practitioners, providers, and suppliers. It is provided by the Department of Health & Human Services.
“While there has been increased attention [on] the mental health of physicians, we wanted to understand the extent to which changes in attitudes and practices were reflected in actions taken by hospitals or licensing boards, which are reported in the National Practitioner Data Bank,” Lisa Rotenstein, MD, a primary care physician at Boston’s Brigham and Women’s Hospital and lead author of the study, told this news organization.
Dr. Rotenstein, who is an assistant professor at Harvard Medical School, Boston, studies issues of mental health among physicians and trainees. Dr. Rotenstein was the lead author of a 2016 study that found that more than a quarter (27.2%) of medical students have depressive symptoms. She was also lead author of a 2018 study published in JAMA on the prevalence of burnout among attending physicians.
Actions against physicians trending downward
2011 marked the peak in actions taken against physicians’ licenses for substance use, per the study, but actions related to substance use have otherwise maintained a steady decline over the past 17 years. Researchers found that physicians with license actions as a result of substance use or psychological impairment were more likely to receive indefinite penalties, while also having emergency action taken against their license to practice.
In addition, physicians who had actions taken against their licenses because of substance use or psychological impairment were more likely to accrue a greater number of actions over the course of their careers, according to the study.
About 47% of physicians reported experiencing burnout per Medscape’s Physician Burnout and Depression Report 2022: Stress, Anxiety, and Anger report. Burnout among emergency physicians spiked from 43% in 2020 to 60% in 2021, according to the report.
More than one quarter (26%) of physicians reported drinking alcohol to cope with burnout in 2020, according to Medscape’s 2021 Physician Burnout and Suicide Report. Per the 2021 report, 48% of physicians chose exercise to deal with burnout, while 35% indulged in eating junk food.
Peter Grinspoon, MD, a Boston-based primary care physician, wrote in The Los Angeles Times in 2016 that the rate of substance abuse among physicians starts at 10% and can go as high as 15%; by comparison, rates of substance use among the general population are 8%-10%. “What appears to account for the difference is physician distress, and in the case of drug abuse, plentiful access,” he added.
Dr. Grinspoon wrote a 2016 book called “Free Refills: A Doctor Confronts His Addiction,” which chronicles his experience in recovery and relapse as a physician who was dependent on opioid painkillers.
The findings from the recent study in JAMA “suggest we have made some progress in addressing issues related to substance use in ways that don’t result in license actions or even in meeting physicians’ need for support related to substance use,” said Dr. Rotenstein.
Still, she insists that there’s “substantial opportunity to improve mental health and support offerings for physicians and to reduce stigma related to seeking and receiving mental health support, ideally averting the need for license actions.”
According to Dr. Rotenstein, the cases listed in the National Practitioner Data Bank represent the most severe cases; these reports have risen to a high level of attention or concern and are the result of adverse action reports submitted by healthcare institutions and state licensing boards.
“There are many, many more physicians whose cases are not represented here but who struggle with depression, anxiety, substance use, and more,” said Dr. Rotenstein.
A version of this article first appeared on Medscape.com.
FROM JAMA
FDA panel strongly backs protein-based Novavax COVID-19 vaccine
than the cutting-edge technology used in mRNA-based shots.
The Vaccines and Related Biological Products Advisory Committee of the Food and Drug Administration voted almost unanimously June 7 in favor of Novavax’s two-dose COVID-19 vaccine for those 18 or older – despite some concerns over rare events of myocarditis and pericarditis.
The tally was 21 “yes” votes, without any “no” votes, but one abstention from a panelist who then offered a largely positive take on this vaccine.
Panelist Bruce Gellin, MD, explained at the end of the meeting that he would have cast a conditional vote in favor of the Novavax vaccine, called NVX-CoV2373, had that been an option. Dr. Gellin, chief of global public health strategy for the Rockefeller Foundation and a vaccine expert, said he didn’t want his abstention to be considered as signaling opposition to the Novavax shot.
Instead, he said, he expects FDA officials will gather more data and evidence about the Novavax vaccine, especially in relation to certain manufacturing issues, before making its decision on the company’s application.
Earlier in the day, a top FDA vaccine reviewer, Doran Fink, MD, PhD, noted that there were important manufacturing differences between the Novavax vaccine supply used in different projects, complicating efforts to assess the company’s application for emergency use authorization (EUA).
But Dr. Fink noted that the FDA staff already had made a convincing case in its briefing document, with enough evidence for an initial conditional clearance to be found in available data.
The FDA is not bound to follow the suggestions of its advisory committees but it often does.
Using the ‘bully pulpit’
At the beginning of the meeting, Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said he was seizing the “bully pulpit” in addressing the need to persuade more people in the United States to take shots against COVID-19.
About 67% of people in the United States aged 18 and older are fully vaccinated, but only about 50% of those in this group have had a first booster, according to the Centers for Disease Control and Prevention.
The two-dose mRNA vaccines from Pfizer and Moderna have been the subject of intense misinformation campaigns on social media, despite efforts by the FDA and other public health officials to convey the message about their strong benefit-risk profile. The FDA in May limited the authorized use of Johnson & Johnson’s single-dose COVID-19 shot, which is based on a different technology, because of concerns about rare and potentially life-threatening blood clots.
Novavax has been described as a more traditional vaccine – a protein subunit shot similar to one people have long received for protection against influenza, pertussis (whooping cough), diphtheria, and tetanus.
“Having a protein-based alternative may be more comfortable for some in terms of their acceptance of vaccines,” Dr. Marks said. “We do have a problem with vaccine uptake that is very serious in the United States. And anything we can do to get people more comfortable to be able to accept these potentially life-saving medical products is something that we feel we are compelled to do.”
Dr. Marks offered these remarks in answer to an FDA panelist’s question about the need to consider an EUA for yet another vaccine.
EUAs are special clearances the FDA can grant in connection with public health emergencies such as the pandemic. The FDA used EUAs for the initial December 2020 clearances of the Pfizer-BioNTech and Moderna vaccines. It has since granted normal approvals for both of these mRNA-based vaccines, based on larger bodies of evidence gathered and submitted by their developers.
During the meeting, the FDA panelists in general appeared comfortable with the idea of granting another EUA for a vaccine. There was agreement that the shot appeared to work in key tests, although these were done before the rise of the Omicron variant.
In a key test, known as study 301, the Novavax vaccine was judged to be 90.4% effective. In the study, 17 of the 17,272 people who got the Novavax vaccine developed COVID-19, compared with 79 of the 8,385 in the placebo group.
Panelists expressed disappointment with the lack of information about how the shot would work now.
“We’re looking at the efficacy against strains that don’t exist any longer,” said panelist Eric J. Rubin, MD, PhD, a Harvard professor and editor of the New England Journal of Medicine.
Still, Dr. Rubin added that he agreed with the argument the FDA’s Dr. Marks had made earlier for an EUA for the Novavax vaccine.
“If there really is a population of patients who are willing to take this and not willing to take the existing vaccines, I think it’s pretty compelling,” Dr. Rubin said.
Other FDA panelists were skeptical of this argument. Jay Portnoy, MD, who was listed on the FDA roster as the panel’s consumer representative, said he has close friends who are vaccine skeptics.
“Their hesitancy is more ideological than technological,” said Dr. Portnoy of Children’s Mercy Hospital, Kansas City, Mo. “So I really doubt that this vaccine is going to crack that nut, but perhaps some individuals would get this when they wouldn’t get the other ones.”
Myocarditis, pericarditis
The Novavax vaccine is already authorized in other countries, including Canada. Novavax in February announced that it had begun shipping its first doses of the vaccine to European Union member states. The vaccine can be moved through existing vaccine supply and cold chain channels instead of requiring complex new delivery procedures.
That could prove an advantage in time, said FDA panelist Michael Nelson, MD, PhD, of the University of Virginia, Charlottesville.
“Who knows even with supply chain challenges down the road, it will be nice to have options going forward,” Dr. Nelson said.
As with other COVID-19 vaccines, clinicians and researchers are still working to understand the potential risk for inflammation of heart muscle and nearby tissue with vaccination. Most patients with myocarditis or pericarditis who sought medical care for these conditions responded well to medicine and rest and felt better quickly, the CDC says on its website. They usually return to their normal daily activities after their symptoms improve.
At the June 7 meeting, Dr. Nelson said there may be cases of myocarditis that go undetected.
“Our signals are those who get admitted to the emergency room and the hospital,” he said. “I’m quite convinced that there are others who are experiencing cardiac events of lesser severity that are worthy of being studied, both from mechanistic and outcomes standpoints. So we have a lot of work to do.”
In looking at results for an initial pool of 40,000 people who received the Novavax vaccine, there were five reported cases of myocarditis or pericarditis developing within 20 days of people getting the shot, the FDA staff said in its presentation on safety.
In a briefing document released ahead of the advisory committee meeting, the FDA staff flagged this number of cases in a relatively small database as a concern, noting it “could be higher than reported during postauthorization use of mRNA COVID-19 vaccines (for which no cases were identified in preauthorization evaluation).”
Novavax officials took a somewhat unusual step of responding in public. The Gaithersburg, Md.–based company on June 3 issued a statement saying researchers had come to “expect to see natural background events of myocarditis in any sufficiently large database, and that young males are at higher risk.”
The data from the company’s placebo-controlled studies show that, overall, in its clinical development program, the rate of myocarditis was balanced between the vaccine and placebo arms (0.007% and 0.005%), Novavax said.
At the June 7 meeting, FDA panelists including Dr. Nelson, and Paul A. Offit, MD, of Children’s Hospital of Philadelphia, urged continued study to try to determine whether and how the vaccines could trigger myocarditis. Investments made now in pursuing these questions related to COVID-19 shots may pay off later, Dr. Offit said.
“We can use that knowledge to make safer vaccines for a disease that is going to be with us for decades, if not longer,” he said.
A version of this article first appeared on Medscape.com.
than the cutting-edge technology used in mRNA-based shots.
The Vaccines and Related Biological Products Advisory Committee of the Food and Drug Administration voted almost unanimously June 7 in favor of Novavax’s two-dose COVID-19 vaccine for those 18 or older – despite some concerns over rare events of myocarditis and pericarditis.
The tally was 21 “yes” votes, without any “no” votes, but one abstention from a panelist who then offered a largely positive take on this vaccine.
Panelist Bruce Gellin, MD, explained at the end of the meeting that he would have cast a conditional vote in favor of the Novavax vaccine, called NVX-CoV2373, had that been an option. Dr. Gellin, chief of global public health strategy for the Rockefeller Foundation and a vaccine expert, said he didn’t want his abstention to be considered as signaling opposition to the Novavax shot.
Instead, he said, he expects FDA officials will gather more data and evidence about the Novavax vaccine, especially in relation to certain manufacturing issues, before making its decision on the company’s application.
Earlier in the day, a top FDA vaccine reviewer, Doran Fink, MD, PhD, noted that there were important manufacturing differences between the Novavax vaccine supply used in different projects, complicating efforts to assess the company’s application for emergency use authorization (EUA).
But Dr. Fink noted that the FDA staff already had made a convincing case in its briefing document, with enough evidence for an initial conditional clearance to be found in available data.
The FDA is not bound to follow the suggestions of its advisory committees but it often does.
Using the ‘bully pulpit’
At the beginning of the meeting, Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said he was seizing the “bully pulpit” in addressing the need to persuade more people in the United States to take shots against COVID-19.
About 67% of people in the United States aged 18 and older are fully vaccinated, but only about 50% of those in this group have had a first booster, according to the Centers for Disease Control and Prevention.
The two-dose mRNA vaccines from Pfizer and Moderna have been the subject of intense misinformation campaigns on social media, despite efforts by the FDA and other public health officials to convey the message about their strong benefit-risk profile. The FDA in May limited the authorized use of Johnson & Johnson’s single-dose COVID-19 shot, which is based on a different technology, because of concerns about rare and potentially life-threatening blood clots.
Novavax has been described as a more traditional vaccine – a protein subunit shot similar to one people have long received for protection against influenza, pertussis (whooping cough), diphtheria, and tetanus.
“Having a protein-based alternative may be more comfortable for some in terms of their acceptance of vaccines,” Dr. Marks said. “We do have a problem with vaccine uptake that is very serious in the United States. And anything we can do to get people more comfortable to be able to accept these potentially life-saving medical products is something that we feel we are compelled to do.”
Dr. Marks offered these remarks in answer to an FDA panelist’s question about the need to consider an EUA for yet another vaccine.
EUAs are special clearances the FDA can grant in connection with public health emergencies such as the pandemic. The FDA used EUAs for the initial December 2020 clearances of the Pfizer-BioNTech and Moderna vaccines. It has since granted normal approvals for both of these mRNA-based vaccines, based on larger bodies of evidence gathered and submitted by their developers.
During the meeting, the FDA panelists in general appeared comfortable with the idea of granting another EUA for a vaccine. There was agreement that the shot appeared to work in key tests, although these were done before the rise of the Omicron variant.
In a key test, known as study 301, the Novavax vaccine was judged to be 90.4% effective. In the study, 17 of the 17,272 people who got the Novavax vaccine developed COVID-19, compared with 79 of the 8,385 in the placebo group.
Panelists expressed disappointment with the lack of information about how the shot would work now.
“We’re looking at the efficacy against strains that don’t exist any longer,” said panelist Eric J. Rubin, MD, PhD, a Harvard professor and editor of the New England Journal of Medicine.
Still, Dr. Rubin added that he agreed with the argument the FDA’s Dr. Marks had made earlier for an EUA for the Novavax vaccine.
“If there really is a population of patients who are willing to take this and not willing to take the existing vaccines, I think it’s pretty compelling,” Dr. Rubin said.
Other FDA panelists were skeptical of this argument. Jay Portnoy, MD, who was listed on the FDA roster as the panel’s consumer representative, said he has close friends who are vaccine skeptics.
“Their hesitancy is more ideological than technological,” said Dr. Portnoy of Children’s Mercy Hospital, Kansas City, Mo. “So I really doubt that this vaccine is going to crack that nut, but perhaps some individuals would get this when they wouldn’t get the other ones.”
Myocarditis, pericarditis
The Novavax vaccine is already authorized in other countries, including Canada. Novavax in February announced that it had begun shipping its first doses of the vaccine to European Union member states. The vaccine can be moved through existing vaccine supply and cold chain channels instead of requiring complex new delivery procedures.
That could prove an advantage in time, said FDA panelist Michael Nelson, MD, PhD, of the University of Virginia, Charlottesville.
“Who knows even with supply chain challenges down the road, it will be nice to have options going forward,” Dr. Nelson said.
As with other COVID-19 vaccines, clinicians and researchers are still working to understand the potential risk for inflammation of heart muscle and nearby tissue with vaccination. Most patients with myocarditis or pericarditis who sought medical care for these conditions responded well to medicine and rest and felt better quickly, the CDC says on its website. They usually return to their normal daily activities after their symptoms improve.
At the June 7 meeting, Dr. Nelson said there may be cases of myocarditis that go undetected.
“Our signals are those who get admitted to the emergency room and the hospital,” he said. “I’m quite convinced that there are others who are experiencing cardiac events of lesser severity that are worthy of being studied, both from mechanistic and outcomes standpoints. So we have a lot of work to do.”
In looking at results for an initial pool of 40,000 people who received the Novavax vaccine, there were five reported cases of myocarditis or pericarditis developing within 20 days of people getting the shot, the FDA staff said in its presentation on safety.
In a briefing document released ahead of the advisory committee meeting, the FDA staff flagged this number of cases in a relatively small database as a concern, noting it “could be higher than reported during postauthorization use of mRNA COVID-19 vaccines (for which no cases were identified in preauthorization evaluation).”
Novavax officials took a somewhat unusual step of responding in public. The Gaithersburg, Md.–based company on June 3 issued a statement saying researchers had come to “expect to see natural background events of myocarditis in any sufficiently large database, and that young males are at higher risk.”
The data from the company’s placebo-controlled studies show that, overall, in its clinical development program, the rate of myocarditis was balanced between the vaccine and placebo arms (0.007% and 0.005%), Novavax said.
At the June 7 meeting, FDA panelists including Dr. Nelson, and Paul A. Offit, MD, of Children’s Hospital of Philadelphia, urged continued study to try to determine whether and how the vaccines could trigger myocarditis. Investments made now in pursuing these questions related to COVID-19 shots may pay off later, Dr. Offit said.
“We can use that knowledge to make safer vaccines for a disease that is going to be with us for decades, if not longer,” he said.
A version of this article first appeared on Medscape.com.
than the cutting-edge technology used in mRNA-based shots.
The Vaccines and Related Biological Products Advisory Committee of the Food and Drug Administration voted almost unanimously June 7 in favor of Novavax’s two-dose COVID-19 vaccine for those 18 or older – despite some concerns over rare events of myocarditis and pericarditis.
The tally was 21 “yes” votes, without any “no” votes, but one abstention from a panelist who then offered a largely positive take on this vaccine.
Panelist Bruce Gellin, MD, explained at the end of the meeting that he would have cast a conditional vote in favor of the Novavax vaccine, called NVX-CoV2373, had that been an option. Dr. Gellin, chief of global public health strategy for the Rockefeller Foundation and a vaccine expert, said he didn’t want his abstention to be considered as signaling opposition to the Novavax shot.
Instead, he said, he expects FDA officials will gather more data and evidence about the Novavax vaccine, especially in relation to certain manufacturing issues, before making its decision on the company’s application.
Earlier in the day, a top FDA vaccine reviewer, Doran Fink, MD, PhD, noted that there were important manufacturing differences between the Novavax vaccine supply used in different projects, complicating efforts to assess the company’s application for emergency use authorization (EUA).
But Dr. Fink noted that the FDA staff already had made a convincing case in its briefing document, with enough evidence for an initial conditional clearance to be found in available data.
The FDA is not bound to follow the suggestions of its advisory committees but it often does.
Using the ‘bully pulpit’
At the beginning of the meeting, Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, said he was seizing the “bully pulpit” in addressing the need to persuade more people in the United States to take shots against COVID-19.
About 67% of people in the United States aged 18 and older are fully vaccinated, but only about 50% of those in this group have had a first booster, according to the Centers for Disease Control and Prevention.
The two-dose mRNA vaccines from Pfizer and Moderna have been the subject of intense misinformation campaigns on social media, despite efforts by the FDA and other public health officials to convey the message about their strong benefit-risk profile. The FDA in May limited the authorized use of Johnson & Johnson’s single-dose COVID-19 shot, which is based on a different technology, because of concerns about rare and potentially life-threatening blood clots.
Novavax has been described as a more traditional vaccine – a protein subunit shot similar to one people have long received for protection against influenza, pertussis (whooping cough), diphtheria, and tetanus.
“Having a protein-based alternative may be more comfortable for some in terms of their acceptance of vaccines,” Dr. Marks said. “We do have a problem with vaccine uptake that is very serious in the United States. And anything we can do to get people more comfortable to be able to accept these potentially life-saving medical products is something that we feel we are compelled to do.”
Dr. Marks offered these remarks in answer to an FDA panelist’s question about the need to consider an EUA for yet another vaccine.
EUAs are special clearances the FDA can grant in connection with public health emergencies such as the pandemic. The FDA used EUAs for the initial December 2020 clearances of the Pfizer-BioNTech and Moderna vaccines. It has since granted normal approvals for both of these mRNA-based vaccines, based on larger bodies of evidence gathered and submitted by their developers.
During the meeting, the FDA panelists in general appeared comfortable with the idea of granting another EUA for a vaccine. There was agreement that the shot appeared to work in key tests, although these were done before the rise of the Omicron variant.
In a key test, known as study 301, the Novavax vaccine was judged to be 90.4% effective. In the study, 17 of the 17,272 people who got the Novavax vaccine developed COVID-19, compared with 79 of the 8,385 in the placebo group.
Panelists expressed disappointment with the lack of information about how the shot would work now.
“We’re looking at the efficacy against strains that don’t exist any longer,” said panelist Eric J. Rubin, MD, PhD, a Harvard professor and editor of the New England Journal of Medicine.
Still, Dr. Rubin added that he agreed with the argument the FDA’s Dr. Marks had made earlier for an EUA for the Novavax vaccine.
“If there really is a population of patients who are willing to take this and not willing to take the existing vaccines, I think it’s pretty compelling,” Dr. Rubin said.
Other FDA panelists were skeptical of this argument. Jay Portnoy, MD, who was listed on the FDA roster as the panel’s consumer representative, said he has close friends who are vaccine skeptics.
“Their hesitancy is more ideological than technological,” said Dr. Portnoy of Children’s Mercy Hospital, Kansas City, Mo. “So I really doubt that this vaccine is going to crack that nut, but perhaps some individuals would get this when they wouldn’t get the other ones.”
Myocarditis, pericarditis
The Novavax vaccine is already authorized in other countries, including Canada. Novavax in February announced that it had begun shipping its first doses of the vaccine to European Union member states. The vaccine can be moved through existing vaccine supply and cold chain channels instead of requiring complex new delivery procedures.
That could prove an advantage in time, said FDA panelist Michael Nelson, MD, PhD, of the University of Virginia, Charlottesville.
“Who knows even with supply chain challenges down the road, it will be nice to have options going forward,” Dr. Nelson said.
As with other COVID-19 vaccines, clinicians and researchers are still working to understand the potential risk for inflammation of heart muscle and nearby tissue with vaccination. Most patients with myocarditis or pericarditis who sought medical care for these conditions responded well to medicine and rest and felt better quickly, the CDC says on its website. They usually return to their normal daily activities after their symptoms improve.
At the June 7 meeting, Dr. Nelson said there may be cases of myocarditis that go undetected.
“Our signals are those who get admitted to the emergency room and the hospital,” he said. “I’m quite convinced that there are others who are experiencing cardiac events of lesser severity that are worthy of being studied, both from mechanistic and outcomes standpoints. So we have a lot of work to do.”
In looking at results for an initial pool of 40,000 people who received the Novavax vaccine, there were five reported cases of myocarditis or pericarditis developing within 20 days of people getting the shot, the FDA staff said in its presentation on safety.
In a briefing document released ahead of the advisory committee meeting, the FDA staff flagged this number of cases in a relatively small database as a concern, noting it “could be higher than reported during postauthorization use of mRNA COVID-19 vaccines (for which no cases were identified in preauthorization evaluation).”
Novavax officials took a somewhat unusual step of responding in public. The Gaithersburg, Md.–based company on June 3 issued a statement saying researchers had come to “expect to see natural background events of myocarditis in any sufficiently large database, and that young males are at higher risk.”
The data from the company’s placebo-controlled studies show that, overall, in its clinical development program, the rate of myocarditis was balanced between the vaccine and placebo arms (0.007% and 0.005%), Novavax said.
At the June 7 meeting, FDA panelists including Dr. Nelson, and Paul A. Offit, MD, of Children’s Hospital of Philadelphia, urged continued study to try to determine whether and how the vaccines could trigger myocarditis. Investments made now in pursuing these questions related to COVID-19 shots may pay off later, Dr. Offit said.
“We can use that knowledge to make safer vaccines for a disease that is going to be with us for decades, if not longer,” he said.
A version of this article first appeared on Medscape.com.
Antipsychotic tied to dose-related weight gain, higher cholesterol
new research suggests.
Investigators analyzed 1-year data for more than 400 patients who were taking risperidone and/or its metabolite paliperidone (Invega). Results showed increments of 1 mg of risperidone-equivalent doses were associated with an increase of 0.25% of weight within a year of follow-up.
“Although our findings report a positive and statistically significant dose-dependence of weight gain and cholesterol, both total and LDL [cholesterol], the size of the predicted changes of metabolic effects is clinically nonrelevant,” lead author Marianna Piras, PharmD, Centre for Psychiatric Neuroscience, Lausanne (Switzerland) University Hospital, said in an interview.
“Therefore, dose lowering would not have a beneficial effect on attenuating weight gain or cholesterol increases and could lead to psychiatric decompensation,” said Ms. Piras, who is also a PhD candidate in the unit of pharmacogenetics and clinical psychopharmacology at the University of Lausanne.
However, she added that because dose increments could increase risk for significant weight gain in the first month of treatment – the dose can be increased typically in a range of 1-10 grams – and strong dose increments could contribute to metabolic worsening over time, “risperidone minimum effective doses should be preferred.”
The findings were published online in the Journal of Clinical Psychiatry.
‘Serious public health issue’
Compared with the general population, patients with mental illness present with a greater prevalence of metabolic disorders. In addition, several psychotropic medications, including antipsychotics, can induce metabolic alterations such as weight gain, the investigators noted.
Antipsychotic-induced metabolic adverse effects “constitute a serious public health issue” because they are risk factors for cardiovascular diseases such as obesity and/or dyslipidemia, “which have been associated with a 10-year reduced life expectancy in the psychiatric population,” Ms. Piras said.
“The dose-dependence of metabolic adverse effects is a debated subject that needs to be assessed for each psychotropic drug known to induce weight gain,” she added.
Several previous studies have examined whether there is a dose-related effect of antipsychotics on metabolic parameters, “with some results suggesting that [weight gain] seems to develop even when low off-label doses are prescribed,” Ms. Piras noted.
She and her colleagues had already studied dose-related metabolic effects of quetiapine (Seroquel) and olanzapine (Zyprexa).
Risperidone is an antipsychotic with a “medium to high metabolic risk profile,” the researchers note, and few studies have examined the impact of risperidone on metabolic parameters other than weight gain.
For the current analysis, they analyzed data from a longitudinal study that included 438 patients (mean age, 40.7 years; 50.7% men) who started treatment with risperidone and/or paliperidone between 2007 and 2018.
The participants had diagnoses of schizophrenia, schizoaffective disorder, bipolar disorder, depression, “other,” or “unknown.”
Clinical follow-up periods were up to a year, but were no shorter than 3 weeks. The investigators also assessed the data at different time intervals at 1, 3, 6, and 12 months “to appreciate the evolution of the metabolic parameters.”
In addition, they collected demographic and clinical information, such as comorbidities, and measured patients’ weight, height, waist circumference, blood pressure, plasma glucose, and lipids at baseline and at 1, 3, and 12 months and then annually. Weight, waist circumference, and BP were also assessed at 2 and 6 months.
Doses of paliperidone were converted into risperidone-equivalent doses.
Significant weight gain over time
The mean duration of follow-up for the participants, of whom 374 were being treated with risperidone and 64 with paliperidone, was 153 days. Close to half (48.2%) were taking other psychotropic medications known to be associated with some degree of metabolic risk.
Patients were divided into two cohorts based on their daily dose intake (DDI): less than 3 mg/day (n = 201) and at least 3 mg/day (n = 237).
In the overall cohort, a “significant effect of time on weight change was found for each time point,” the investigators reported.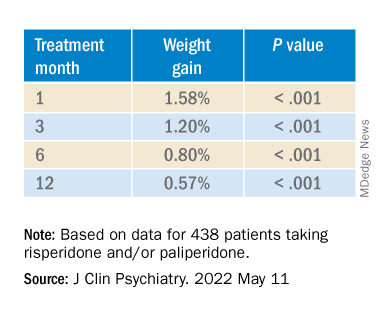
When the researchers looked at the changes according to DDI, they found that each 1-mg dose increase was associated with incremental weight gain at each time point.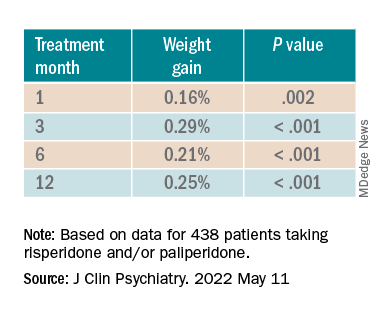
Patients who had 5% or greater weight gain in the first month continued to gain weight more than patients who did not reach that threshold, leading the researchers to call that early threshold a “strong predictor of important weight gain in the long term.” There was a weight gain of 6.68% at 3 months, of 7.36% at 6 months, and of 7.7% at 12 months.
After the patients were stratified by age, there were differences in the effect of DDI on various age groups at different time points.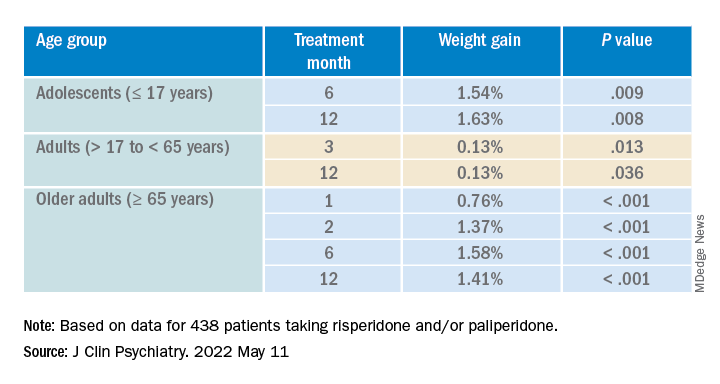
Dose was shown to have a significant effect on weight gain for women at all four time points (P ≥ .001), but for men only at 3 months (P = .003).
For each additional 1-mg dose, there was a 0.05 mmol/L (1.93 mg/dL) increase in total cholesterol (P = .018) after 1 year and a 0.04 mmol/L (1.54 mg/dL) increase in LDL cholesterol (P = .011).
There were no significant effects of time or DDI on triglycerides, HDL cholesterol, glucose levels, and systolic BP, and there was a negative effect of DDI on diastolic BP (P = .001).
The findings “provide evidence for a small dose effect of risperidone” on weight gain and total and LDL cholesterol levels, the investigators note.
Ms. Piras added that because each antipsychotic differs in its metabolic risk profile, “further analyses on other antipsychotics are ongoing in our laboratory, so far confirming our findings.”
Small increases, big changes
Commenting on the study, Erika Nurmi, MD, PhD, associate professor in the department of psychiatry and biobehavioral sciences at the Semel Institute for Neuroscience, University of California, Los Angeles, said the study is “unique in the field.”
It “leverages real-world data from a large patient registry to ask a long-unanswered question: Are weight and metabolic adverse effects proportional to dose? Big data approaches like these are very powerful, given the large number of participants that can be included,” said Dr. Nurmi, who was not involved with the research.
However, she cautioned, the “biggest drawback [is that] these data are by nature much more complex and prone to confounding effects.”
In this case, a “critical confounder” for the study was that the majority of individuals taking higher risperidone doses were also taking other drugs known to cause weight gain, whereas the majority of those on lower risperidone doses were not. “This difference may explain the dose relationship observed,” she said.
Because real-world, big data are “valuable but also messy, conclusions drawn from them must be interpreted with caution,” Dr. Nurmi said.
She added that it is generally wise to use the lowest effective dose possible.
“Clinicians should appreciate that even small doses of antipsychotics can cause big changes in weight. Risks and benefits of medications must be carefully considered in clinical practice,” Dr. Nurmi said.
The research was funded in part by the Swiss National Research Foundation. Piras reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Nurmi reported no relevant financial relationships, but she is an unpaid member of the Tourette Association of America’s medical advisory board and of the Myriad Genetics scientific advisory board.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators analyzed 1-year data for more than 400 patients who were taking risperidone and/or its metabolite paliperidone (Invega). Results showed increments of 1 mg of risperidone-equivalent doses were associated with an increase of 0.25% of weight within a year of follow-up.
“Although our findings report a positive and statistically significant dose-dependence of weight gain and cholesterol, both total and LDL [cholesterol], the size of the predicted changes of metabolic effects is clinically nonrelevant,” lead author Marianna Piras, PharmD, Centre for Psychiatric Neuroscience, Lausanne (Switzerland) University Hospital, said in an interview.
“Therefore, dose lowering would not have a beneficial effect on attenuating weight gain or cholesterol increases and could lead to psychiatric decompensation,” said Ms. Piras, who is also a PhD candidate in the unit of pharmacogenetics and clinical psychopharmacology at the University of Lausanne.
However, she added that because dose increments could increase risk for significant weight gain in the first month of treatment – the dose can be increased typically in a range of 1-10 grams – and strong dose increments could contribute to metabolic worsening over time, “risperidone minimum effective doses should be preferred.”
The findings were published online in the Journal of Clinical Psychiatry.
‘Serious public health issue’
Compared with the general population, patients with mental illness present with a greater prevalence of metabolic disorders. In addition, several psychotropic medications, including antipsychotics, can induce metabolic alterations such as weight gain, the investigators noted.
Antipsychotic-induced metabolic adverse effects “constitute a serious public health issue” because they are risk factors for cardiovascular diseases such as obesity and/or dyslipidemia, “which have been associated with a 10-year reduced life expectancy in the psychiatric population,” Ms. Piras said.
“The dose-dependence of metabolic adverse effects is a debated subject that needs to be assessed for each psychotropic drug known to induce weight gain,” she added.
Several previous studies have examined whether there is a dose-related effect of antipsychotics on metabolic parameters, “with some results suggesting that [weight gain] seems to develop even when low off-label doses are prescribed,” Ms. Piras noted.
She and her colleagues had already studied dose-related metabolic effects of quetiapine (Seroquel) and olanzapine (Zyprexa).
Risperidone is an antipsychotic with a “medium to high metabolic risk profile,” the researchers note, and few studies have examined the impact of risperidone on metabolic parameters other than weight gain.
For the current analysis, they analyzed data from a longitudinal study that included 438 patients (mean age, 40.7 years; 50.7% men) who started treatment with risperidone and/or paliperidone between 2007 and 2018.
The participants had diagnoses of schizophrenia, schizoaffective disorder, bipolar disorder, depression, “other,” or “unknown.”
Clinical follow-up periods were up to a year, but were no shorter than 3 weeks. The investigators also assessed the data at different time intervals at 1, 3, 6, and 12 months “to appreciate the evolution of the metabolic parameters.”
In addition, they collected demographic and clinical information, such as comorbidities, and measured patients’ weight, height, waist circumference, blood pressure, plasma glucose, and lipids at baseline and at 1, 3, and 12 months and then annually. Weight, waist circumference, and BP were also assessed at 2 and 6 months.
Doses of paliperidone were converted into risperidone-equivalent doses.
Significant weight gain over time
The mean duration of follow-up for the participants, of whom 374 were being treated with risperidone and 64 with paliperidone, was 153 days. Close to half (48.2%) were taking other psychotropic medications known to be associated with some degree of metabolic risk.
Patients were divided into two cohorts based on their daily dose intake (DDI): less than 3 mg/day (n = 201) and at least 3 mg/day (n = 237).
In the overall cohort, a “significant effect of time on weight change was found for each time point,” the investigators reported.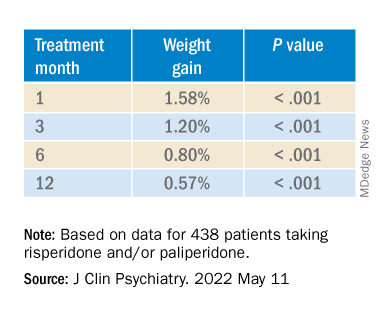
When the researchers looked at the changes according to DDI, they found that each 1-mg dose increase was associated with incremental weight gain at each time point.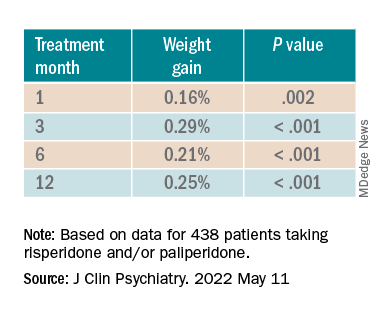
Patients who had 5% or greater weight gain in the first month continued to gain weight more than patients who did not reach that threshold, leading the researchers to call that early threshold a “strong predictor of important weight gain in the long term.” There was a weight gain of 6.68% at 3 months, of 7.36% at 6 months, and of 7.7% at 12 months.
After the patients were stratified by age, there were differences in the effect of DDI on various age groups at different time points.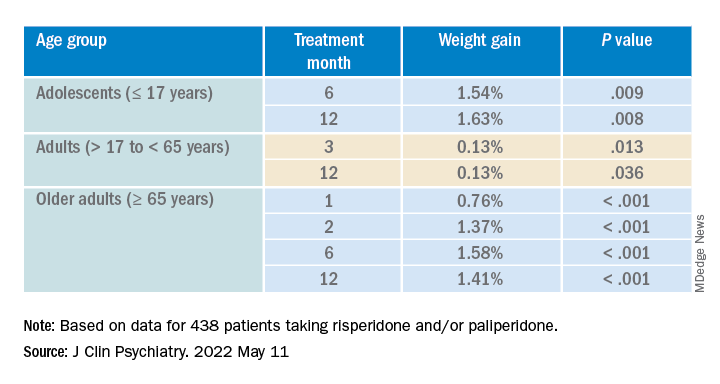
Dose was shown to have a significant effect on weight gain for women at all four time points (P ≥ .001), but for men only at 3 months (P = .003).
For each additional 1-mg dose, there was a 0.05 mmol/L (1.93 mg/dL) increase in total cholesterol (P = .018) after 1 year and a 0.04 mmol/L (1.54 mg/dL) increase in LDL cholesterol (P = .011).
There were no significant effects of time or DDI on triglycerides, HDL cholesterol, glucose levels, and systolic BP, and there was a negative effect of DDI on diastolic BP (P = .001).
The findings “provide evidence for a small dose effect of risperidone” on weight gain and total and LDL cholesterol levels, the investigators note.
Ms. Piras added that because each antipsychotic differs in its metabolic risk profile, “further analyses on other antipsychotics are ongoing in our laboratory, so far confirming our findings.”
Small increases, big changes
Commenting on the study, Erika Nurmi, MD, PhD, associate professor in the department of psychiatry and biobehavioral sciences at the Semel Institute for Neuroscience, University of California, Los Angeles, said the study is “unique in the field.”
It “leverages real-world data from a large patient registry to ask a long-unanswered question: Are weight and metabolic adverse effects proportional to dose? Big data approaches like these are very powerful, given the large number of participants that can be included,” said Dr. Nurmi, who was not involved with the research.
However, she cautioned, the “biggest drawback [is that] these data are by nature much more complex and prone to confounding effects.”
In this case, a “critical confounder” for the study was that the majority of individuals taking higher risperidone doses were also taking other drugs known to cause weight gain, whereas the majority of those on lower risperidone doses were not. “This difference may explain the dose relationship observed,” she said.
Because real-world, big data are “valuable but also messy, conclusions drawn from them must be interpreted with caution,” Dr. Nurmi said.
She added that it is generally wise to use the lowest effective dose possible.
“Clinicians should appreciate that even small doses of antipsychotics can cause big changes in weight. Risks and benefits of medications must be carefully considered in clinical practice,” Dr. Nurmi said.
The research was funded in part by the Swiss National Research Foundation. Piras reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Nurmi reported no relevant financial relationships, but she is an unpaid member of the Tourette Association of America’s medical advisory board and of the Myriad Genetics scientific advisory board.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators analyzed 1-year data for more than 400 patients who were taking risperidone and/or its metabolite paliperidone (Invega). Results showed increments of 1 mg of risperidone-equivalent doses were associated with an increase of 0.25% of weight within a year of follow-up.
“Although our findings report a positive and statistically significant dose-dependence of weight gain and cholesterol, both total and LDL [cholesterol], the size of the predicted changes of metabolic effects is clinically nonrelevant,” lead author Marianna Piras, PharmD, Centre for Psychiatric Neuroscience, Lausanne (Switzerland) University Hospital, said in an interview.
“Therefore, dose lowering would not have a beneficial effect on attenuating weight gain or cholesterol increases and could lead to psychiatric decompensation,” said Ms. Piras, who is also a PhD candidate in the unit of pharmacogenetics and clinical psychopharmacology at the University of Lausanne.
However, she added that because dose increments could increase risk for significant weight gain in the first month of treatment – the dose can be increased typically in a range of 1-10 grams – and strong dose increments could contribute to metabolic worsening over time, “risperidone minimum effective doses should be preferred.”
The findings were published online in the Journal of Clinical Psychiatry.
‘Serious public health issue’
Compared with the general population, patients with mental illness present with a greater prevalence of metabolic disorders. In addition, several psychotropic medications, including antipsychotics, can induce metabolic alterations such as weight gain, the investigators noted.
Antipsychotic-induced metabolic adverse effects “constitute a serious public health issue” because they are risk factors for cardiovascular diseases such as obesity and/or dyslipidemia, “which have been associated with a 10-year reduced life expectancy in the psychiatric population,” Ms. Piras said.
“The dose-dependence of metabolic adverse effects is a debated subject that needs to be assessed for each psychotropic drug known to induce weight gain,” she added.
Several previous studies have examined whether there is a dose-related effect of antipsychotics on metabolic parameters, “with some results suggesting that [weight gain] seems to develop even when low off-label doses are prescribed,” Ms. Piras noted.
She and her colleagues had already studied dose-related metabolic effects of quetiapine (Seroquel) and olanzapine (Zyprexa).
Risperidone is an antipsychotic with a “medium to high metabolic risk profile,” the researchers note, and few studies have examined the impact of risperidone on metabolic parameters other than weight gain.
For the current analysis, they analyzed data from a longitudinal study that included 438 patients (mean age, 40.7 years; 50.7% men) who started treatment with risperidone and/or paliperidone between 2007 and 2018.
The participants had diagnoses of schizophrenia, schizoaffective disorder, bipolar disorder, depression, “other,” or “unknown.”
Clinical follow-up periods were up to a year, but were no shorter than 3 weeks. The investigators also assessed the data at different time intervals at 1, 3, 6, and 12 months “to appreciate the evolution of the metabolic parameters.”
In addition, they collected demographic and clinical information, such as comorbidities, and measured patients’ weight, height, waist circumference, blood pressure, plasma glucose, and lipids at baseline and at 1, 3, and 12 months and then annually. Weight, waist circumference, and BP were also assessed at 2 and 6 months.
Doses of paliperidone were converted into risperidone-equivalent doses.
Significant weight gain over time
The mean duration of follow-up for the participants, of whom 374 were being treated with risperidone and 64 with paliperidone, was 153 days. Close to half (48.2%) were taking other psychotropic medications known to be associated with some degree of metabolic risk.
Patients were divided into two cohorts based on their daily dose intake (DDI): less than 3 mg/day (n = 201) and at least 3 mg/day (n = 237).
In the overall cohort, a “significant effect of time on weight change was found for each time point,” the investigators reported.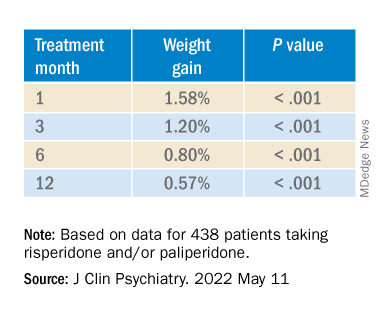
When the researchers looked at the changes according to DDI, they found that each 1-mg dose increase was associated with incremental weight gain at each time point.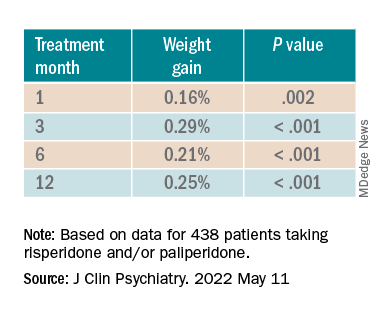
Patients who had 5% or greater weight gain in the first month continued to gain weight more than patients who did not reach that threshold, leading the researchers to call that early threshold a “strong predictor of important weight gain in the long term.” There was a weight gain of 6.68% at 3 months, of 7.36% at 6 months, and of 7.7% at 12 months.
After the patients were stratified by age, there were differences in the effect of DDI on various age groups at different time points.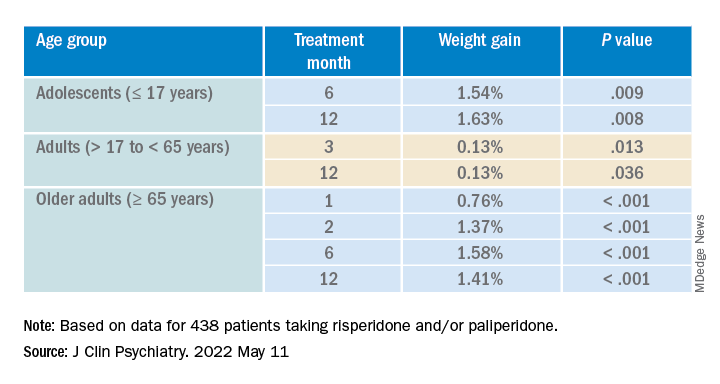
Dose was shown to have a significant effect on weight gain for women at all four time points (P ≥ .001), but for men only at 3 months (P = .003).
For each additional 1-mg dose, there was a 0.05 mmol/L (1.93 mg/dL) increase in total cholesterol (P = .018) after 1 year and a 0.04 mmol/L (1.54 mg/dL) increase in LDL cholesterol (P = .011).
There were no significant effects of time or DDI on triglycerides, HDL cholesterol, glucose levels, and systolic BP, and there was a negative effect of DDI on diastolic BP (P = .001).
The findings “provide evidence for a small dose effect of risperidone” on weight gain and total and LDL cholesterol levels, the investigators note.
Ms. Piras added that because each antipsychotic differs in its metabolic risk profile, “further analyses on other antipsychotics are ongoing in our laboratory, so far confirming our findings.”
Small increases, big changes
Commenting on the study, Erika Nurmi, MD, PhD, associate professor in the department of psychiatry and biobehavioral sciences at the Semel Institute for Neuroscience, University of California, Los Angeles, said the study is “unique in the field.”
It “leverages real-world data from a large patient registry to ask a long-unanswered question: Are weight and metabolic adverse effects proportional to dose? Big data approaches like these are very powerful, given the large number of participants that can be included,” said Dr. Nurmi, who was not involved with the research.
However, she cautioned, the “biggest drawback [is that] these data are by nature much more complex and prone to confounding effects.”
In this case, a “critical confounder” for the study was that the majority of individuals taking higher risperidone doses were also taking other drugs known to cause weight gain, whereas the majority of those on lower risperidone doses were not. “This difference may explain the dose relationship observed,” she said.
Because real-world, big data are “valuable but also messy, conclusions drawn from them must be interpreted with caution,” Dr. Nurmi said.
She added that it is generally wise to use the lowest effective dose possible.
“Clinicians should appreciate that even small doses of antipsychotics can cause big changes in weight. Risks and benefits of medications must be carefully considered in clinical practice,” Dr. Nurmi said.
The research was funded in part by the Swiss National Research Foundation. Piras reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Nurmi reported no relevant financial relationships, but she is an unpaid member of the Tourette Association of America’s medical advisory board and of the Myriad Genetics scientific advisory board.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
‘Remission is possible’ for patients with type 2 diabetes
A novel approach that involves sensors, artificial intelligence, and real-time individualized lifestyle guidance from an app and live coaches led to a high rate of remission of type 2 diabetes in a new study.
Specifically, among 199 patients with type 2 diabetes in India who received the app-delivered lifestyle guidance developed by Twin Health, Mountain View, Calif., mean hemoglobin A1c dropped from 9.0% to 5.7% at 6 months.
This is “huge,” Paramesh Shamanna, MD, told a press briefing at the annual scientific sessions of the American Diabetes Association. The research was presented as three posters by the group at the meeting.
Patients were a mean age of 43 and had diabetes for a mean of 3.7 years and up to 8 years.
An “unprecedented” 84% of patients had remission of diabetes at 6 months, Dr. Shamanna, medical director at Twin Health, noted.
Diabetes remission was defined according to the 2021 joint consensus statement from the ADA and other organizations as an A1c less than 6.5% without the use of diabetes medications for at least 3 months.
Importantly, patients’ time in range (percentage of time spent in target blood glucose range) increased from 53% to 81%, Dr. Shamanna pointed out. On average, patients’ waist circumference decreased by 10 cm (3.9 inches) and their weight dropped from 79 kg (approximately 174 lb) to 68 kg (150 lb).
These results are driven by “the continuous individualized and precise guidance regarding nutrition, activity, and sleep,” Dr. Shamanna said in an interview.
Remission is not reversal or cure ...
“Remission” from type 2 diabetes is not “reversal” or a “cure,” Robert A. Gabbay, MD, PhD, chief scientific and medical officer of the ADA, stressed to the press. Just like cancer, diabetes can return after remission
Therefore, it is important to follow the lifestyle guidance. Patients may still be at risk for diabetes complications after diabetes remission, so it’s also important to continue to be screened for eye disease, nerve damage, and lipid levels.
However, “remission can be made to last,” Dr. Shamanna said, by continuing to follow the lifestyle advice and getting back on track after a relapse.
“We’re in a different time right now,” Lisa Shah, MD, chief medical officer, Twin Health, noted. “This is very different from management of blood glucose to a certain number.”
This study shows that “remission [from type 2 diabetes] is possible. How you achieve it can be precise for you.”
The program is designed to consider the health and happiness of the patient, added Shashank R. Joshi, MD, chief scientist, Twin Health. “We want remission to be complication free. These findings give patients hope.”
“It’s exciting now that we can really start thinking about remission as an option for people with [type 2] diabetes, and that just provides such incredible hope for all of those living with [type 2] diabetes,” Dr. Gabbay said in an interview.
How the intervention works
The Twin Precision Treatment (TPT) intervention integrates multiple data – glucose values from a continuous glucose monitor (CGM); heart rate, activity, and sleep time from a fitness tracker; blood pressure values from a blood pressure cuff; food intake from the patient’s food log; and weight and body fat data from a smart scale – and provides the patient with precise, individualized nutrition and health guidance.
The four most critical sensors are the CGM, the fitness tracker, the smart scale, and the blood pressure cuff, Dr. Shah explained. The system gathers thousands of signals combined with patient self-reported data including mood or anxiety.
The CGM is used to build the initial nutrition guidance during the first 30 days. Once a patient is in remission, he or she can just keep the fitness tracker and smart scale.
The coaches who are part of this program include dietitians who are trained to provide compassionate patient education and help patients avoid diabetes relapse, and they are overseen by a licensed provider.
The program does not restrict calories. “It is not a diet,” Dr. Shah stressed.
The algorithm makes mini adjustments to the food a person is already eating to improve nutrition, Dr. Joshi explained. “This is personalized medicine at its best.” Patients eat food that they like and are guided to make small changes to get glucose under control and avoid glucose spikes.
The program is designed to safely deescalate diabetes medications as A1c decreases, Dr. Shamanna added.
U.S. clinical trial, health insurance coverage
The 1-year results of the current trial are expected in August, and the trial will continue for 2-=5 years, Dr. Shamanna said.
The company has started a clinical trial in the United States, with 5-year results expected in 2027.
“Currently, in the United States, we are partnering with self-insured employers and select health plans that offer [Twin Precision Treatment ] as an available benefit for their members,” Dr. Shah said. It “is suitable for most members living with type 2 diabetes, with rare exclusion situations.”
The study was funded by Twin Health. Dr. Shamanna, Dr. Shah, and Dr. Joshi are employees of Twin Health.
A version of this article first appeared on Medscape.com.
A novel approach that involves sensors, artificial intelligence, and real-time individualized lifestyle guidance from an app and live coaches led to a high rate of remission of type 2 diabetes in a new study.
Specifically, among 199 patients with type 2 diabetes in India who received the app-delivered lifestyle guidance developed by Twin Health, Mountain View, Calif., mean hemoglobin A1c dropped from 9.0% to 5.7% at 6 months.
This is “huge,” Paramesh Shamanna, MD, told a press briefing at the annual scientific sessions of the American Diabetes Association. The research was presented as three posters by the group at the meeting.
Patients were a mean age of 43 and had diabetes for a mean of 3.7 years and up to 8 years.
An “unprecedented” 84% of patients had remission of diabetes at 6 months, Dr. Shamanna, medical director at Twin Health, noted.
Diabetes remission was defined according to the 2021 joint consensus statement from the ADA and other organizations as an A1c less than 6.5% without the use of diabetes medications for at least 3 months.
Importantly, patients’ time in range (percentage of time spent in target blood glucose range) increased from 53% to 81%, Dr. Shamanna pointed out. On average, patients’ waist circumference decreased by 10 cm (3.9 inches) and their weight dropped from 79 kg (approximately 174 lb) to 68 kg (150 lb).
These results are driven by “the continuous individualized and precise guidance regarding nutrition, activity, and sleep,” Dr. Shamanna said in an interview.
Remission is not reversal or cure ...
“Remission” from type 2 diabetes is not “reversal” or a “cure,” Robert A. Gabbay, MD, PhD, chief scientific and medical officer of the ADA, stressed to the press. Just like cancer, diabetes can return after remission
Therefore, it is important to follow the lifestyle guidance. Patients may still be at risk for diabetes complications after diabetes remission, so it’s also important to continue to be screened for eye disease, nerve damage, and lipid levels.
However, “remission can be made to last,” Dr. Shamanna said, by continuing to follow the lifestyle advice and getting back on track after a relapse.
“We’re in a different time right now,” Lisa Shah, MD, chief medical officer, Twin Health, noted. “This is very different from management of blood glucose to a certain number.”
This study shows that “remission [from type 2 diabetes] is possible. How you achieve it can be precise for you.”
The program is designed to consider the health and happiness of the patient, added Shashank R. Joshi, MD, chief scientist, Twin Health. “We want remission to be complication free. These findings give patients hope.”
“It’s exciting now that we can really start thinking about remission as an option for people with [type 2] diabetes, and that just provides such incredible hope for all of those living with [type 2] diabetes,” Dr. Gabbay said in an interview.
How the intervention works
The Twin Precision Treatment (TPT) intervention integrates multiple data – glucose values from a continuous glucose monitor (CGM); heart rate, activity, and sleep time from a fitness tracker; blood pressure values from a blood pressure cuff; food intake from the patient’s food log; and weight and body fat data from a smart scale – and provides the patient with precise, individualized nutrition and health guidance.
The four most critical sensors are the CGM, the fitness tracker, the smart scale, and the blood pressure cuff, Dr. Shah explained. The system gathers thousands of signals combined with patient self-reported data including mood or anxiety.
The CGM is used to build the initial nutrition guidance during the first 30 days. Once a patient is in remission, he or she can just keep the fitness tracker and smart scale.
The coaches who are part of this program include dietitians who are trained to provide compassionate patient education and help patients avoid diabetes relapse, and they are overseen by a licensed provider.
The program does not restrict calories. “It is not a diet,” Dr. Shah stressed.
The algorithm makes mini adjustments to the food a person is already eating to improve nutrition, Dr. Joshi explained. “This is personalized medicine at its best.” Patients eat food that they like and are guided to make small changes to get glucose under control and avoid glucose spikes.
The program is designed to safely deescalate diabetes medications as A1c decreases, Dr. Shamanna added.
U.S. clinical trial, health insurance coverage
The 1-year results of the current trial are expected in August, and the trial will continue for 2-=5 years, Dr. Shamanna said.
The company has started a clinical trial in the United States, with 5-year results expected in 2027.
“Currently, in the United States, we are partnering with self-insured employers and select health plans that offer [Twin Precision Treatment ] as an available benefit for their members,” Dr. Shah said. It “is suitable for most members living with type 2 diabetes, with rare exclusion situations.”
The study was funded by Twin Health. Dr. Shamanna, Dr. Shah, and Dr. Joshi are employees of Twin Health.
A version of this article first appeared on Medscape.com.
A novel approach that involves sensors, artificial intelligence, and real-time individualized lifestyle guidance from an app and live coaches led to a high rate of remission of type 2 diabetes in a new study.
Specifically, among 199 patients with type 2 diabetes in India who received the app-delivered lifestyle guidance developed by Twin Health, Mountain View, Calif., mean hemoglobin A1c dropped from 9.0% to 5.7% at 6 months.
This is “huge,” Paramesh Shamanna, MD, told a press briefing at the annual scientific sessions of the American Diabetes Association. The research was presented as three posters by the group at the meeting.
Patients were a mean age of 43 and had diabetes for a mean of 3.7 years and up to 8 years.
An “unprecedented” 84% of patients had remission of diabetes at 6 months, Dr. Shamanna, medical director at Twin Health, noted.
Diabetes remission was defined according to the 2021 joint consensus statement from the ADA and other organizations as an A1c less than 6.5% without the use of diabetes medications for at least 3 months.
Importantly, patients’ time in range (percentage of time spent in target blood glucose range) increased from 53% to 81%, Dr. Shamanna pointed out. On average, patients’ waist circumference decreased by 10 cm (3.9 inches) and their weight dropped from 79 kg (approximately 174 lb) to 68 kg (150 lb).
These results are driven by “the continuous individualized and precise guidance regarding nutrition, activity, and sleep,” Dr. Shamanna said in an interview.
Remission is not reversal or cure ...
“Remission” from type 2 diabetes is not “reversal” or a “cure,” Robert A. Gabbay, MD, PhD, chief scientific and medical officer of the ADA, stressed to the press. Just like cancer, diabetes can return after remission
Therefore, it is important to follow the lifestyle guidance. Patients may still be at risk for diabetes complications after diabetes remission, so it’s also important to continue to be screened for eye disease, nerve damage, and lipid levels.
However, “remission can be made to last,” Dr. Shamanna said, by continuing to follow the lifestyle advice and getting back on track after a relapse.
“We’re in a different time right now,” Lisa Shah, MD, chief medical officer, Twin Health, noted. “This is very different from management of blood glucose to a certain number.”
This study shows that “remission [from type 2 diabetes] is possible. How you achieve it can be precise for you.”
The program is designed to consider the health and happiness of the patient, added Shashank R. Joshi, MD, chief scientist, Twin Health. “We want remission to be complication free. These findings give patients hope.”
“It’s exciting now that we can really start thinking about remission as an option for people with [type 2] diabetes, and that just provides such incredible hope for all of those living with [type 2] diabetes,” Dr. Gabbay said in an interview.
How the intervention works
The Twin Precision Treatment (TPT) intervention integrates multiple data – glucose values from a continuous glucose monitor (CGM); heart rate, activity, and sleep time from a fitness tracker; blood pressure values from a blood pressure cuff; food intake from the patient’s food log; and weight and body fat data from a smart scale – and provides the patient with precise, individualized nutrition and health guidance.
The four most critical sensors are the CGM, the fitness tracker, the smart scale, and the blood pressure cuff, Dr. Shah explained. The system gathers thousands of signals combined with patient self-reported data including mood or anxiety.
The CGM is used to build the initial nutrition guidance during the first 30 days. Once a patient is in remission, he or she can just keep the fitness tracker and smart scale.
The coaches who are part of this program include dietitians who are trained to provide compassionate patient education and help patients avoid diabetes relapse, and they are overseen by a licensed provider.
The program does not restrict calories. “It is not a diet,” Dr. Shah stressed.
The algorithm makes mini adjustments to the food a person is already eating to improve nutrition, Dr. Joshi explained. “This is personalized medicine at its best.” Patients eat food that they like and are guided to make small changes to get glucose under control and avoid glucose spikes.
The program is designed to safely deescalate diabetes medications as A1c decreases, Dr. Shamanna added.
U.S. clinical trial, health insurance coverage
The 1-year results of the current trial are expected in August, and the trial will continue for 2-=5 years, Dr. Shamanna said.
The company has started a clinical trial in the United States, with 5-year results expected in 2027.
“Currently, in the United States, we are partnering with self-insured employers and select health plans that offer [Twin Precision Treatment ] as an available benefit for their members,” Dr. Shah said. It “is suitable for most members living with type 2 diabetes, with rare exclusion situations.”
The study was funded by Twin Health. Dr. Shamanna, Dr. Shah, and Dr. Joshi are employees of Twin Health.
A version of this article first appeared on Medscape.com.
FROM ADA 2022
Antidiabetes drug costs keep patients away
NEW ORLEANS – , according to findings from two separate studies.
One study looked at the insurance records of more than 70,000 U.S. patients with type 2 diabetes and established cardiovascular disease who were already on metformin. The findings showed that, after adjustment for confounders, the quartile of patients with the highest out-of-pocket cost for an agent from the sodium-glucose cotransporter 2 (SGLT2)–inhibitor class filled a prescription for one of these drugs a significant 21% less often than did patients from the quartile with the lowest personal expense, after adjustment for a variety of potential confounding factors, reported Jing Luo, MD, at the annual scientific sessions of the American Diabetes Association.
A similar analysis run by Dr. Luo and his associates looking at glucagonlike peptide-1 (GLP-1) receptor agonists showed that the quartile of patients who had to pay the most for one of those drugs had an adjusted 12% lower rate of filling a prescription, compared with those with the lowest out-of-pocket expense, a difference that fell just short of significance.
“If we consistently see that high drug costs affect use of highly effective medications in patients with type 2 diabetes and risk factors, it’s quite problematic because it’s not just a matter of money, but it also makes a difference in the patient’s quality of care,” Dr. Luo said in an interview.
Prevention drug lists can help
Consistency turned up in a second report at the same ADA session that retrospectively reviewed data collected during 2004-2017 by a single large U.S. health insurer to identify 3,315 matched pairs of children and adults with diabetes who all had high-deductible health plans for their medical insurance, along with an associated health savings account.
One set of patients in each matched pair began to receive, at some point during follow-up, coverage with a prevention drug list (PDL; also called a formulary) that provided them with a variety of specified agents at no charge. They included oral antidiabetes agents, insulin, antihypertensives, and lipid-lowering drugs. The other half of the matched pairs of patients received no PDL coverage and had copays for their antidiabetes medications.
The findings showed that the rates of out-of-pocket costs for antidiabetes drugs, antidiabetic medications used, and acute diabetes complications all tracked extremely closely between the matched pairs before half of them started to receive their PDL coverage. However, after PDL coverage kicked in, out of pocket costs dropped by 32% for the people with PDL coverage, compared with those who did not receive this coverage. Oral antidiabetes medication use rose modestly, but acute diabetes complications “declined substantially,” with a 14% relative reduction overall in those with PDL coverage, compared with those without, reported J. Franklin Wharam, MBBCh, a professor and health policy researcher at Duke University in Durham, N.C. In the roughly half of the study cohort who fell into a low-income category based on where they lived, the rate of excess acute diabetes complications was 23% higher for those without a PDL, compared with those who had that coverage.
PDL coverage linked with “large reductions in acute, preventable diabetes complications,” concluded Dr. Wharam. “Policy makers and employers should incentivize PDL uptake among low-income patients with diabetes.”
Newer, more effective drugs cost a lot
“The more comorbidities that patients have, the greater is the strength of the evidence for using newer antidiabetes drugs that are more expensive,” but that would mean spending much more on this part of patient care, noted Dr. Luo, an internal medicine physician and researcher at the University of Pittsburgh. “It will cost a lot of money, and I’m not sure what the solution is. It’s a huge conundrum.”
About 30 million Americans have type 2 diabetes. If every one of them went on an SGLT2 inhibitor, or went on an SGLT2 inhibitor plus a GLP-1 receptor agonist, “it would bankrupt the U.S. health care system, so we can’t do that,” commented Sylvio E. Inzucchi, MD, in an interview. “The only thing holding this back is cost. We target these drugs to the patients most apt to benefit from them. If they were generic they would be used much more widely,” noted Dr. Inzucchi, professor and clinical chief of endocrinology at Yale University in New Haven, Conn.
The study run by Dr. Luo and his associates retrospectively reviewed data from 72,743 U.S. adults included in the Optum Clinformatics database during December 2017–December 2019. All included patients had type 2 diabetes, received metformin monotherapy, and had established atherosclerotic cardiovascular disease. They averaged 72 years of age, 56% were men, and 88% were on a Medicare Advantage plan, while the remainder had commercial insurance. Their average hemoglobin A1c level was 6.8%.
People in the quartile with the lowest copays spent an average of about $20/month for either an SGLT2 inhibitor or a GLP-1 receptor agonist. Those in the quartile with the highest copays spent roughly $100/month for agents from each of these two classes. The analysis followed patients for a median of 914 days.
In addition to finding disparate rates of drug use between these two quartiles, the analysis also showed that higher copays linked with longer times to initially fill prescriptions for these drugs. But while those with higher copays took longer to start both classes than did those with the smallest copays, even those with the lowest out-of-pocket costs averaged about a year to initiate treatment.
Dr. Luo attributed this delay to other factors besides costs to patients, such as clinicians prescribing other classes of second-line oral antidiabetes agents, clinical inertia, and lack of awareness by clinicians of the special benefits of SGLT2 inhibitors and GLP-1 receptor antagonists for patients with type 2 diabetes and cardiovascular disease.
“A lot of clinical and social factors drive medication use,” not just out-of-pocket cost, he explained.
Dr. Luo is a consultant to Alosa Health. Dr. Wharam had no disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk.
NEW ORLEANS – , according to findings from two separate studies.
One study looked at the insurance records of more than 70,000 U.S. patients with type 2 diabetes and established cardiovascular disease who were already on metformin. The findings showed that, after adjustment for confounders, the quartile of patients with the highest out-of-pocket cost for an agent from the sodium-glucose cotransporter 2 (SGLT2)–inhibitor class filled a prescription for one of these drugs a significant 21% less often than did patients from the quartile with the lowest personal expense, after adjustment for a variety of potential confounding factors, reported Jing Luo, MD, at the annual scientific sessions of the American Diabetes Association.
A similar analysis run by Dr. Luo and his associates looking at glucagonlike peptide-1 (GLP-1) receptor agonists showed that the quartile of patients who had to pay the most for one of those drugs had an adjusted 12% lower rate of filling a prescription, compared with those with the lowest out-of-pocket expense, a difference that fell just short of significance.
“If we consistently see that high drug costs affect use of highly effective medications in patients with type 2 diabetes and risk factors, it’s quite problematic because it’s not just a matter of money, but it also makes a difference in the patient’s quality of care,” Dr. Luo said in an interview.
Prevention drug lists can help
Consistency turned up in a second report at the same ADA session that retrospectively reviewed data collected during 2004-2017 by a single large U.S. health insurer to identify 3,315 matched pairs of children and adults with diabetes who all had high-deductible health plans for their medical insurance, along with an associated health savings account.
One set of patients in each matched pair began to receive, at some point during follow-up, coverage with a prevention drug list (PDL; also called a formulary) that provided them with a variety of specified agents at no charge. They included oral antidiabetes agents, insulin, antihypertensives, and lipid-lowering drugs. The other half of the matched pairs of patients received no PDL coverage and had copays for their antidiabetes medications.
The findings showed that the rates of out-of-pocket costs for antidiabetes drugs, antidiabetic medications used, and acute diabetes complications all tracked extremely closely between the matched pairs before half of them started to receive their PDL coverage. However, after PDL coverage kicked in, out of pocket costs dropped by 32% for the people with PDL coverage, compared with those who did not receive this coverage. Oral antidiabetes medication use rose modestly, but acute diabetes complications “declined substantially,” with a 14% relative reduction overall in those with PDL coverage, compared with those without, reported J. Franklin Wharam, MBBCh, a professor and health policy researcher at Duke University in Durham, N.C. In the roughly half of the study cohort who fell into a low-income category based on where they lived, the rate of excess acute diabetes complications was 23% higher for those without a PDL, compared with those who had that coverage.
PDL coverage linked with “large reductions in acute, preventable diabetes complications,” concluded Dr. Wharam. “Policy makers and employers should incentivize PDL uptake among low-income patients with diabetes.”
Newer, more effective drugs cost a lot
“The more comorbidities that patients have, the greater is the strength of the evidence for using newer antidiabetes drugs that are more expensive,” but that would mean spending much more on this part of patient care, noted Dr. Luo, an internal medicine physician and researcher at the University of Pittsburgh. “It will cost a lot of money, and I’m not sure what the solution is. It’s a huge conundrum.”
About 30 million Americans have type 2 diabetes. If every one of them went on an SGLT2 inhibitor, or went on an SGLT2 inhibitor plus a GLP-1 receptor agonist, “it would bankrupt the U.S. health care system, so we can’t do that,” commented Sylvio E. Inzucchi, MD, in an interview. “The only thing holding this back is cost. We target these drugs to the patients most apt to benefit from them. If they were generic they would be used much more widely,” noted Dr. Inzucchi, professor and clinical chief of endocrinology at Yale University in New Haven, Conn.
The study run by Dr. Luo and his associates retrospectively reviewed data from 72,743 U.S. adults included in the Optum Clinformatics database during December 2017–December 2019. All included patients had type 2 diabetes, received metformin monotherapy, and had established atherosclerotic cardiovascular disease. They averaged 72 years of age, 56% were men, and 88% were on a Medicare Advantage plan, while the remainder had commercial insurance. Their average hemoglobin A1c level was 6.8%.
People in the quartile with the lowest copays spent an average of about $20/month for either an SGLT2 inhibitor or a GLP-1 receptor agonist. Those in the quartile with the highest copays spent roughly $100/month for agents from each of these two classes. The analysis followed patients for a median of 914 days.
In addition to finding disparate rates of drug use between these two quartiles, the analysis also showed that higher copays linked with longer times to initially fill prescriptions for these drugs. But while those with higher copays took longer to start both classes than did those with the smallest copays, even those with the lowest out-of-pocket costs averaged about a year to initiate treatment.
Dr. Luo attributed this delay to other factors besides costs to patients, such as clinicians prescribing other classes of second-line oral antidiabetes agents, clinical inertia, and lack of awareness by clinicians of the special benefits of SGLT2 inhibitors and GLP-1 receptor antagonists for patients with type 2 diabetes and cardiovascular disease.
“A lot of clinical and social factors drive medication use,” not just out-of-pocket cost, he explained.
Dr. Luo is a consultant to Alosa Health. Dr. Wharam had no disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk.
NEW ORLEANS – , according to findings from two separate studies.
One study looked at the insurance records of more than 70,000 U.S. patients with type 2 diabetes and established cardiovascular disease who were already on metformin. The findings showed that, after adjustment for confounders, the quartile of patients with the highest out-of-pocket cost for an agent from the sodium-glucose cotransporter 2 (SGLT2)–inhibitor class filled a prescription for one of these drugs a significant 21% less often than did patients from the quartile with the lowest personal expense, after adjustment for a variety of potential confounding factors, reported Jing Luo, MD, at the annual scientific sessions of the American Diabetes Association.
A similar analysis run by Dr. Luo and his associates looking at glucagonlike peptide-1 (GLP-1) receptor agonists showed that the quartile of patients who had to pay the most for one of those drugs had an adjusted 12% lower rate of filling a prescription, compared with those with the lowest out-of-pocket expense, a difference that fell just short of significance.
“If we consistently see that high drug costs affect use of highly effective medications in patients with type 2 diabetes and risk factors, it’s quite problematic because it’s not just a matter of money, but it also makes a difference in the patient’s quality of care,” Dr. Luo said in an interview.
Prevention drug lists can help
Consistency turned up in a second report at the same ADA session that retrospectively reviewed data collected during 2004-2017 by a single large U.S. health insurer to identify 3,315 matched pairs of children and adults with diabetes who all had high-deductible health plans for their medical insurance, along with an associated health savings account.
One set of patients in each matched pair began to receive, at some point during follow-up, coverage with a prevention drug list (PDL; also called a formulary) that provided them with a variety of specified agents at no charge. They included oral antidiabetes agents, insulin, antihypertensives, and lipid-lowering drugs. The other half of the matched pairs of patients received no PDL coverage and had copays for their antidiabetes medications.
The findings showed that the rates of out-of-pocket costs for antidiabetes drugs, antidiabetic medications used, and acute diabetes complications all tracked extremely closely between the matched pairs before half of them started to receive their PDL coverage. However, after PDL coverage kicked in, out of pocket costs dropped by 32% for the people with PDL coverage, compared with those who did not receive this coverage. Oral antidiabetes medication use rose modestly, but acute diabetes complications “declined substantially,” with a 14% relative reduction overall in those with PDL coverage, compared with those without, reported J. Franklin Wharam, MBBCh, a professor and health policy researcher at Duke University in Durham, N.C. In the roughly half of the study cohort who fell into a low-income category based on where they lived, the rate of excess acute diabetes complications was 23% higher for those without a PDL, compared with those who had that coverage.
PDL coverage linked with “large reductions in acute, preventable diabetes complications,” concluded Dr. Wharam. “Policy makers and employers should incentivize PDL uptake among low-income patients with diabetes.”
Newer, more effective drugs cost a lot
“The more comorbidities that patients have, the greater is the strength of the evidence for using newer antidiabetes drugs that are more expensive,” but that would mean spending much more on this part of patient care, noted Dr. Luo, an internal medicine physician and researcher at the University of Pittsburgh. “It will cost a lot of money, and I’m not sure what the solution is. It’s a huge conundrum.”
About 30 million Americans have type 2 diabetes. If every one of them went on an SGLT2 inhibitor, or went on an SGLT2 inhibitor plus a GLP-1 receptor agonist, “it would bankrupt the U.S. health care system, so we can’t do that,” commented Sylvio E. Inzucchi, MD, in an interview. “The only thing holding this back is cost. We target these drugs to the patients most apt to benefit from them. If they were generic they would be used much more widely,” noted Dr. Inzucchi, professor and clinical chief of endocrinology at Yale University in New Haven, Conn.
The study run by Dr. Luo and his associates retrospectively reviewed data from 72,743 U.S. adults included in the Optum Clinformatics database during December 2017–December 2019. All included patients had type 2 diabetes, received metformin monotherapy, and had established atherosclerotic cardiovascular disease. They averaged 72 years of age, 56% were men, and 88% were on a Medicare Advantage plan, while the remainder had commercial insurance. Their average hemoglobin A1c level was 6.8%.
People in the quartile with the lowest copays spent an average of about $20/month for either an SGLT2 inhibitor or a GLP-1 receptor agonist. Those in the quartile with the highest copays spent roughly $100/month for agents from each of these two classes. The analysis followed patients for a median of 914 days.
In addition to finding disparate rates of drug use between these two quartiles, the analysis also showed that higher copays linked with longer times to initially fill prescriptions for these drugs. But while those with higher copays took longer to start both classes than did those with the smallest copays, even those with the lowest out-of-pocket costs averaged about a year to initiate treatment.
Dr. Luo attributed this delay to other factors besides costs to patients, such as clinicians prescribing other classes of second-line oral antidiabetes agents, clinical inertia, and lack of awareness by clinicians of the special benefits of SGLT2 inhibitors and GLP-1 receptor antagonists for patients with type 2 diabetes and cardiovascular disease.
“A lot of clinical and social factors drive medication use,” not just out-of-pocket cost, he explained.
Dr. Luo is a consultant to Alosa Health. Dr. Wharam had no disclosures. Dr. Inzucchi is an adviser to Abbott Diagnostics, Esperion Therapeutics, and vTv Therapeutics, a consultant to Merck and Pfizer, and has other relationships with AstraZeneca, Boehringer Ingelheim, Lexicon, and Novo Nordisk.
AT ADA 2022


















