User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Biden boosts LGBTQIA+ protections, bans conversion therapy
President Joe Biden issued an executive order on June 15 banning conversion therapy and offering other LBGTQIA+ protections as part of White House efforts to advance equality during Pride Month.
“My order will use the full force of the federal government to end inhumane practices of conversion therapy,” President Biden said in a speech before signing the order. “This is the first time the federal government is making a coordinated effort against this dangerous and discredited practice.”
Conversion therapy is any emotional or physical therapy used to “cure” or “repair” a person’s attraction to the same sex, or their gender identity and expression. Providers claim these therapies can make someone heterosexual or “straight.” But there’s no evidence to support this.
Medical and mental health experts have rejected conversion therapy practices as dangerous and discriminatory for decades.
The executive order also addresses:
- The LGBTQIA+ youth mental health crisis, in part by expanding suicide prevention resources for that at-risk population.
- Discrimination within the foster care system against LGBTQIA+ children and parents.
- Discrimination, poverty and isolation challenges faced by LGBTQIA+ seniors.
- Efforts to strengthen federal data collection in this population to counter homelessness, housing insecurity and barriers to health care access.
Enforcement of executive order will rely on legal experts, including the Justice Department.
President Biden’s order comes at a time when multiple states are promoting or passing anti-LGBTQIA+ laws.
“I don’t have to tell you about the ultra-MAGA agenda attacking our freedoms. There are more than 300 discriminatory bills introduced in states across this country,” President Biden said. “In Texas, they are knocking on front doors to investigate parents who are raising transgender children, and in Florida they are going after Mickey Mouse for God’s sake.”
First Lady Jill Biden, PhD, said the order will not solve all problems. “Prejudice and discrimination still lurk. We will not let the progress we fought for slip away. Pride is a celebration of the courage it takes to stand up for what’s right.”
The American Psychiatric Association applauded President Biden’s action. This executive order will “protect the mental health of LGBTQ+ people, particularly children. APA has long condemned the practice of so-called ‘conversion therapy’ and we welcome the federal government’s efforts to raise public awareness about its harms, alongside other practices that will help to end it.”
The goal of the order is to “improve the health, wellbeing, and safety of countless families across the country,” senior White House administration officials said in a June 15 media call. “And they will send a powerful signal from the president of the United States to LGBTQIA+ kids across the country – who may be feeling scared and hopeless – that their president has their back.”
Biden also called on Congress to pass the Equality Act “to enshrine the long overdue civil rights to protect all Americans.”
The event was held in the East Room of the White House at a Pride event attended by Vice President Kamala Harris and her husband, the first lady, Transportation Secretary Pete Buttigieg, and hundreds of LGBTQIA+ leaders.
Guidance on starting transgender treatment
In other LGBTQIA+-related news, an international group focusing on transgender health lowered the minimum ages they recommend for starting hormone therapy or surgery for transgender youth.
The World Professional Association for Transgender Health said that hormones could be started at 14, 2 years earlier than the group’s previous advice. The association also said some surgeries can be performed at age 15 or 17, a year or so earlier than their previous recommendations.
The group acknowledged potential risks but said it is unethical and harmful to withhold early treatment, according to a report from The Associated Press.
Transgender treatment for teens has been a controversial issue, with experts disagreeing about whether teenagers can fully understand the ramifications of such life-altering decisions.
During the White House background media call, senior administration officials pointed to existing policy regarding transgender care. “We’ve already put out guidance through HHS about civil rights protections and making clear that the denial of medical care based on someone’s gender identity is discriminatory and have invited the members of the public to file complaints with the Office of Civil Rights.”
A version of this article first appeared on WebMD.com.
President Joe Biden issued an executive order on June 15 banning conversion therapy and offering other LBGTQIA+ protections as part of White House efforts to advance equality during Pride Month.
“My order will use the full force of the federal government to end inhumane practices of conversion therapy,” President Biden said in a speech before signing the order. “This is the first time the federal government is making a coordinated effort against this dangerous and discredited practice.”
Conversion therapy is any emotional or physical therapy used to “cure” or “repair” a person’s attraction to the same sex, or their gender identity and expression. Providers claim these therapies can make someone heterosexual or “straight.” But there’s no evidence to support this.
Medical and mental health experts have rejected conversion therapy practices as dangerous and discriminatory for decades.
The executive order also addresses:
- The LGBTQIA+ youth mental health crisis, in part by expanding suicide prevention resources for that at-risk population.
- Discrimination within the foster care system against LGBTQIA+ children and parents.
- Discrimination, poverty and isolation challenges faced by LGBTQIA+ seniors.
- Efforts to strengthen federal data collection in this population to counter homelessness, housing insecurity and barriers to health care access.
Enforcement of executive order will rely on legal experts, including the Justice Department.
President Biden’s order comes at a time when multiple states are promoting or passing anti-LGBTQIA+ laws.
“I don’t have to tell you about the ultra-MAGA agenda attacking our freedoms. There are more than 300 discriminatory bills introduced in states across this country,” President Biden said. “In Texas, they are knocking on front doors to investigate parents who are raising transgender children, and in Florida they are going after Mickey Mouse for God’s sake.”
First Lady Jill Biden, PhD, said the order will not solve all problems. “Prejudice and discrimination still lurk. We will not let the progress we fought for slip away. Pride is a celebration of the courage it takes to stand up for what’s right.”
The American Psychiatric Association applauded President Biden’s action. This executive order will “protect the mental health of LGBTQ+ people, particularly children. APA has long condemned the practice of so-called ‘conversion therapy’ and we welcome the federal government’s efforts to raise public awareness about its harms, alongside other practices that will help to end it.”
The goal of the order is to “improve the health, wellbeing, and safety of countless families across the country,” senior White House administration officials said in a June 15 media call. “And they will send a powerful signal from the president of the United States to LGBTQIA+ kids across the country – who may be feeling scared and hopeless – that their president has their back.”
Biden also called on Congress to pass the Equality Act “to enshrine the long overdue civil rights to protect all Americans.”
The event was held in the East Room of the White House at a Pride event attended by Vice President Kamala Harris and her husband, the first lady, Transportation Secretary Pete Buttigieg, and hundreds of LGBTQIA+ leaders.
Guidance on starting transgender treatment
In other LGBTQIA+-related news, an international group focusing on transgender health lowered the minimum ages they recommend for starting hormone therapy or surgery for transgender youth.
The World Professional Association for Transgender Health said that hormones could be started at 14, 2 years earlier than the group’s previous advice. The association also said some surgeries can be performed at age 15 or 17, a year or so earlier than their previous recommendations.
The group acknowledged potential risks but said it is unethical and harmful to withhold early treatment, according to a report from The Associated Press.
Transgender treatment for teens has been a controversial issue, with experts disagreeing about whether teenagers can fully understand the ramifications of such life-altering decisions.
During the White House background media call, senior administration officials pointed to existing policy regarding transgender care. “We’ve already put out guidance through HHS about civil rights protections and making clear that the denial of medical care based on someone’s gender identity is discriminatory and have invited the members of the public to file complaints with the Office of Civil Rights.”
A version of this article first appeared on WebMD.com.
President Joe Biden issued an executive order on June 15 banning conversion therapy and offering other LBGTQIA+ protections as part of White House efforts to advance equality during Pride Month.
“My order will use the full force of the federal government to end inhumane practices of conversion therapy,” President Biden said in a speech before signing the order. “This is the first time the federal government is making a coordinated effort against this dangerous and discredited practice.”
Conversion therapy is any emotional or physical therapy used to “cure” or “repair” a person’s attraction to the same sex, or their gender identity and expression. Providers claim these therapies can make someone heterosexual or “straight.” But there’s no evidence to support this.
Medical and mental health experts have rejected conversion therapy practices as dangerous and discriminatory for decades.
The executive order also addresses:
- The LGBTQIA+ youth mental health crisis, in part by expanding suicide prevention resources for that at-risk population.
- Discrimination within the foster care system against LGBTQIA+ children and parents.
- Discrimination, poverty and isolation challenges faced by LGBTQIA+ seniors.
- Efforts to strengthen federal data collection in this population to counter homelessness, housing insecurity and barriers to health care access.
Enforcement of executive order will rely on legal experts, including the Justice Department.
President Biden’s order comes at a time when multiple states are promoting or passing anti-LGBTQIA+ laws.
“I don’t have to tell you about the ultra-MAGA agenda attacking our freedoms. There are more than 300 discriminatory bills introduced in states across this country,” President Biden said. “In Texas, they are knocking on front doors to investigate parents who are raising transgender children, and in Florida they are going after Mickey Mouse for God’s sake.”
First Lady Jill Biden, PhD, said the order will not solve all problems. “Prejudice and discrimination still lurk. We will not let the progress we fought for slip away. Pride is a celebration of the courage it takes to stand up for what’s right.”
The American Psychiatric Association applauded President Biden’s action. This executive order will “protect the mental health of LGBTQ+ people, particularly children. APA has long condemned the practice of so-called ‘conversion therapy’ and we welcome the federal government’s efforts to raise public awareness about its harms, alongside other practices that will help to end it.”
The goal of the order is to “improve the health, wellbeing, and safety of countless families across the country,” senior White House administration officials said in a June 15 media call. “And they will send a powerful signal from the president of the United States to LGBTQIA+ kids across the country – who may be feeling scared and hopeless – that their president has their back.”
Biden also called on Congress to pass the Equality Act “to enshrine the long overdue civil rights to protect all Americans.”
The event was held in the East Room of the White House at a Pride event attended by Vice President Kamala Harris and her husband, the first lady, Transportation Secretary Pete Buttigieg, and hundreds of LGBTQIA+ leaders.
Guidance on starting transgender treatment
In other LGBTQIA+-related news, an international group focusing on transgender health lowered the minimum ages they recommend for starting hormone therapy or surgery for transgender youth.
The World Professional Association for Transgender Health said that hormones could be started at 14, 2 years earlier than the group’s previous advice. The association also said some surgeries can be performed at age 15 or 17, a year or so earlier than their previous recommendations.
The group acknowledged potential risks but said it is unethical and harmful to withhold early treatment, according to a report from The Associated Press.
Transgender treatment for teens has been a controversial issue, with experts disagreeing about whether teenagers can fully understand the ramifications of such life-altering decisions.
During the White House background media call, senior administration officials pointed to existing policy regarding transgender care. “We’ve already put out guidance through HHS about civil rights protections and making clear that the denial of medical care based on someone’s gender identity is discriminatory and have invited the members of the public to file complaints with the Office of Civil Rights.”
A version of this article first appeared on WebMD.com.
Hypothyroidism: No more waiting to eat or drink with liquid thyroxine?
ATLANTA -- Liquid formulations of levothyroxine offer the possibility of allowing patients with hypothyroidism to take their medication with meals or coffee and skip the currently recommended 30- to 60-minute waiting period before doing either, new data suggest.
Because food, coffee, and certain medications can interfere with intestinal absorption of levothyroxine (also known as LT4), current guidelines recommend that the drug be taken in a fasting state, typically 30-60 minutes before breakfast. However, compliance may be difficult for some patients.
Now, a potential solution may come from new evidence that liquid levothyroxine formulations that bypass the gastric dissolution phase of absorption may mitigate the interference with food and coffee.
Findings from two bioavailability studies showing no difference in comparisons of Thyquidity (levothyroxine sodium oral solution, Vertice Pharma) with or without waiting periods before consuming coffee or a high-fat meal were presented at the annual meeting of the Endocrine Society (ENDO 2022), by Vertice Pharma Medical Director Kris Washington, PharmD.
And just last month, similar data were published in Thyroid for another levothyroxine oral solution, Tirosint-SOL (IBSA). No difference in pharmacokinetic properties were found with this product with a shorter versus a longer waiting period before consuming a high-fat meal.
Liquid thyroxine may be less affected by food/drink but is expensive
Both products have been approved by the U.S. Food and Drug Administration, but current labeling for both still calls for a 30- to 60-minute waiting period between taking the medication and eating or drinking. Thyquidity is an oral solution of 100 µg/mL levothyroxine sodium that has been shown to be bioequivalent to one of the most popular branded levothyroxine tablets, Synthroid (AbbVie), under fasting conditions. Tirosint-SOL is also an oral solution that comes in 15 different dosage ampules.
“It is important to note that while these findings are exciting and encouraging, we do want you to continue to follow the current FDA-approved label for Thyquidity, recommending that it be taken on an empty stomach 30-60 minutes prior to breakfast and that patients continue to follow all other label instructions,” Dr. Washington said during a press briefing at ENDO 2022.
When asked whether the new data would be submitted to the FDA for a possible amendment to this message, she replied: “We’re still discussing that. We’re exploring all options. ... This is fairly new data. ... It makes sense and certainly solves a lot of the challenges for people who can’t swallow or don’t choose to swallow, or the challenges of splitting or crushing with tablets.”
Asked to comment, Benjamin J. Gigliotti, MD, a clinical thyroidologist at the University of Rochester, New York, told this news organization: “Liquid levothyroxine has the potential to be a clinically useful formulation,” noting that these recent data corroborate prior findings from Europe and elsewhere that liquid levothyroxine is absorbed more rapidly and thus may be less impacted by food or beverages.
However, Dr. Gigliotti also pointed out, “I don’t think malabsorption is a major contributor to suboptimal treatment because if [patients] malabsorb the hormone, we typically just increase their dose a little bit or ask them to take it separately, and that works just fine for most people.”
And the higher cost of the liquid products is a major issue, he noted.
A quick search on GoodRx shows that the lowest price of Tirosint-SOL is $115.52 for a 1 month supply and Thyquidity is $181.04/month. “In the few patients where I tried to obtain Tirosint-SOL, it was not covered by insurance, even with a prior authorization,” Dr. Gigliotti commented.
In contrast, generic levothyroxine tablets are about $4/month, while a common brand name of levothyroxine tablets are $47.81/month.
“Until these liquid formulations are more widely covered by insurance for a reasonable copay, or come down in price compared to generic levothyroxine tablets, most of my patients have voiced that they’d rather deal with the inconveniences of a tablet compared to higher medication cost, especially with rising economic insecurity imposed by the COVID-19 pandemic and recent world events,” Dr. Gigliotti said.
Bioequivalence with shorter versus longer waits before coffee/breakfast
The Thyquidity coffee study was a single-center open-label, randomized, crossover study of 40 healthy adults randomized after a 10-hour overnight fast to 600 µg Thyquidity with water under fasting conditions or to the same dose given 5 minutes prior to drinking an 8-ounce cup of American coffee without milk or sweeteners. After a 40-day washout period, the same participants received the other treatment.
Mean serum thyroxine (T4) concentrations over 48 hours were nearly identical, demonstrating comparable bioavailability. Pharmacokinetics parameters, including area under the curve (AUC) and Cmax, were also comparable for both groups. The geometric least square mean ratios for baseline-adjusted LT4 were 96.0% for Cmax and 94% for AUC. And the corresponding 90% confidence intervals fell within the 80%-125% FDA acceptance range for absence of a food effect on bioavailability, said Dr. Washington when presenting the findings.
There was one adverse event, a decrease in blood glucose level, which was deemed to be mild and unrelated to study treatment. No deaths, serious adverse events, or discontinuations due to adverse events were reported. There were no significant changes in vital signs or on ECG.
In the second Thyquidity study of 38 healthy adults, after a 10-hour fast, the same doses were given 10 or 30 minutes prior to the consumption of a 950-calorie standardized high-fat breakfast.
Again, over 48 hours, mean serum T4 levels were comparable between the two groups. The geometric least squares mean ratios for both AUC and Cmax for baseline-adjusted LT4 were 88.7% and 85.1%, respectively. Again, the corresponding 90% confidence intervals fell within the FDA’s noninterference definition, again demonstrating lack of a food effect on bioavailability, Dr. Washington noted.
Four adverse events were reported in three participants, with three deemed to be possibly related to the medication. All were isolated lab abnormalities without clinical symptoms and deemed to be mild. Three were normal on repeat testing.
There were no deaths or serious adverse events or study discontinuations for adverse events and no significant findings for vital signs or on ECG.
Similar findings for Tirosint-SOL but longer-term studies needed
The recently published Tirosint-SOL study included 36 healthy volunteers randomized to single 600-µg doses of the LT4 oral solution after a 10-hour fast, either 15 or 30 minutes before eating a standardized high-fat, high-calorie meal. Mean serum total thyroxine concentration profiles were similar for both the 15- and 30-minute waits, with similar AUCs.
Geometric mean ratios for AUCs at 48 and 72 hours were 90% and 92%, respectively, and the 90% confidence intervals fell within the 80%-125% FDA boundaries, suggesting similar exposures whether taken 15 or 30 minutes before a meal.
Senior author Francesco S. Celi, MD, chair of the division of endocrinology, diabetes, and metabolism at Virginia Commonwealth University, Richmond, told this news organization: “There is an interest in providing more opportunities for patients and improving adherence to the medication. ... Whatever makes life a bit easier for patients and results in a more predictable response to treatment means down the road there will be fewer visits to the doctor to make adjustments.”
However, he said that in addition to the cost and reimbursement issue, all of these studies have been short term and not conducted in real-life settings.
“Another question is: What happens if the patient goes on low-dose LT4? The studies were conducted on much higher pharmacologic doses. But at least from a safety standpoint, there’s no specific concern.”
Dr. Washington is an employee of Vertice Pharma. Dr. Celi has received unrestricted research grants and worked as a consultant for IBSA. Dr. Gigliotti has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA -- Liquid formulations of levothyroxine offer the possibility of allowing patients with hypothyroidism to take their medication with meals or coffee and skip the currently recommended 30- to 60-minute waiting period before doing either, new data suggest.
Because food, coffee, and certain medications can interfere with intestinal absorption of levothyroxine (also known as LT4), current guidelines recommend that the drug be taken in a fasting state, typically 30-60 minutes before breakfast. However, compliance may be difficult for some patients.
Now, a potential solution may come from new evidence that liquid levothyroxine formulations that bypass the gastric dissolution phase of absorption may mitigate the interference with food and coffee.
Findings from two bioavailability studies showing no difference in comparisons of Thyquidity (levothyroxine sodium oral solution, Vertice Pharma) with or without waiting periods before consuming coffee or a high-fat meal were presented at the annual meeting of the Endocrine Society (ENDO 2022), by Vertice Pharma Medical Director Kris Washington, PharmD.
And just last month, similar data were published in Thyroid for another levothyroxine oral solution, Tirosint-SOL (IBSA). No difference in pharmacokinetic properties were found with this product with a shorter versus a longer waiting period before consuming a high-fat meal.
Liquid thyroxine may be less affected by food/drink but is expensive
Both products have been approved by the U.S. Food and Drug Administration, but current labeling for both still calls for a 30- to 60-minute waiting period between taking the medication and eating or drinking. Thyquidity is an oral solution of 100 µg/mL levothyroxine sodium that has been shown to be bioequivalent to one of the most popular branded levothyroxine tablets, Synthroid (AbbVie), under fasting conditions. Tirosint-SOL is also an oral solution that comes in 15 different dosage ampules.
“It is important to note that while these findings are exciting and encouraging, we do want you to continue to follow the current FDA-approved label for Thyquidity, recommending that it be taken on an empty stomach 30-60 minutes prior to breakfast and that patients continue to follow all other label instructions,” Dr. Washington said during a press briefing at ENDO 2022.
When asked whether the new data would be submitted to the FDA for a possible amendment to this message, she replied: “We’re still discussing that. We’re exploring all options. ... This is fairly new data. ... It makes sense and certainly solves a lot of the challenges for people who can’t swallow or don’t choose to swallow, or the challenges of splitting or crushing with tablets.”
Asked to comment, Benjamin J. Gigliotti, MD, a clinical thyroidologist at the University of Rochester, New York, told this news organization: “Liquid levothyroxine has the potential to be a clinically useful formulation,” noting that these recent data corroborate prior findings from Europe and elsewhere that liquid levothyroxine is absorbed more rapidly and thus may be less impacted by food or beverages.
However, Dr. Gigliotti also pointed out, “I don’t think malabsorption is a major contributor to suboptimal treatment because if [patients] malabsorb the hormone, we typically just increase their dose a little bit or ask them to take it separately, and that works just fine for most people.”
And the higher cost of the liquid products is a major issue, he noted.
A quick search on GoodRx shows that the lowest price of Tirosint-SOL is $115.52 for a 1 month supply and Thyquidity is $181.04/month. “In the few patients where I tried to obtain Tirosint-SOL, it was not covered by insurance, even with a prior authorization,” Dr. Gigliotti commented.
In contrast, generic levothyroxine tablets are about $4/month, while a common brand name of levothyroxine tablets are $47.81/month.
“Until these liquid formulations are more widely covered by insurance for a reasonable copay, or come down in price compared to generic levothyroxine tablets, most of my patients have voiced that they’d rather deal with the inconveniences of a tablet compared to higher medication cost, especially with rising economic insecurity imposed by the COVID-19 pandemic and recent world events,” Dr. Gigliotti said.
Bioequivalence with shorter versus longer waits before coffee/breakfast
The Thyquidity coffee study was a single-center open-label, randomized, crossover study of 40 healthy adults randomized after a 10-hour overnight fast to 600 µg Thyquidity with water under fasting conditions or to the same dose given 5 minutes prior to drinking an 8-ounce cup of American coffee without milk or sweeteners. After a 40-day washout period, the same participants received the other treatment.
Mean serum thyroxine (T4) concentrations over 48 hours were nearly identical, demonstrating comparable bioavailability. Pharmacokinetics parameters, including area under the curve (AUC) and Cmax, were also comparable for both groups. The geometric least square mean ratios for baseline-adjusted LT4 were 96.0% for Cmax and 94% for AUC. And the corresponding 90% confidence intervals fell within the 80%-125% FDA acceptance range for absence of a food effect on bioavailability, said Dr. Washington when presenting the findings.
There was one adverse event, a decrease in blood glucose level, which was deemed to be mild and unrelated to study treatment. No deaths, serious adverse events, or discontinuations due to adverse events were reported. There were no significant changes in vital signs or on ECG.
In the second Thyquidity study of 38 healthy adults, after a 10-hour fast, the same doses were given 10 or 30 minutes prior to the consumption of a 950-calorie standardized high-fat breakfast.
Again, over 48 hours, mean serum T4 levels were comparable between the two groups. The geometric least squares mean ratios for both AUC and Cmax for baseline-adjusted LT4 were 88.7% and 85.1%, respectively. Again, the corresponding 90% confidence intervals fell within the FDA’s noninterference definition, again demonstrating lack of a food effect on bioavailability, Dr. Washington noted.
Four adverse events were reported in three participants, with three deemed to be possibly related to the medication. All were isolated lab abnormalities without clinical symptoms and deemed to be mild. Three were normal on repeat testing.
There were no deaths or serious adverse events or study discontinuations for adverse events and no significant findings for vital signs or on ECG.
Similar findings for Tirosint-SOL but longer-term studies needed
The recently published Tirosint-SOL study included 36 healthy volunteers randomized to single 600-µg doses of the LT4 oral solution after a 10-hour fast, either 15 or 30 minutes before eating a standardized high-fat, high-calorie meal. Mean serum total thyroxine concentration profiles were similar for both the 15- and 30-minute waits, with similar AUCs.
Geometric mean ratios for AUCs at 48 and 72 hours were 90% and 92%, respectively, and the 90% confidence intervals fell within the 80%-125% FDA boundaries, suggesting similar exposures whether taken 15 or 30 minutes before a meal.
Senior author Francesco S. Celi, MD, chair of the division of endocrinology, diabetes, and metabolism at Virginia Commonwealth University, Richmond, told this news organization: “There is an interest in providing more opportunities for patients and improving adherence to the medication. ... Whatever makes life a bit easier for patients and results in a more predictable response to treatment means down the road there will be fewer visits to the doctor to make adjustments.”
However, he said that in addition to the cost and reimbursement issue, all of these studies have been short term and not conducted in real-life settings.
“Another question is: What happens if the patient goes on low-dose LT4? The studies were conducted on much higher pharmacologic doses. But at least from a safety standpoint, there’s no specific concern.”
Dr. Washington is an employee of Vertice Pharma. Dr. Celi has received unrestricted research grants and worked as a consultant for IBSA. Dr. Gigliotti has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ATLANTA -- Liquid formulations of levothyroxine offer the possibility of allowing patients with hypothyroidism to take their medication with meals or coffee and skip the currently recommended 30- to 60-minute waiting period before doing either, new data suggest.
Because food, coffee, and certain medications can interfere with intestinal absorption of levothyroxine (also known as LT4), current guidelines recommend that the drug be taken in a fasting state, typically 30-60 minutes before breakfast. However, compliance may be difficult for some patients.
Now, a potential solution may come from new evidence that liquid levothyroxine formulations that bypass the gastric dissolution phase of absorption may mitigate the interference with food and coffee.
Findings from two bioavailability studies showing no difference in comparisons of Thyquidity (levothyroxine sodium oral solution, Vertice Pharma) with or without waiting periods before consuming coffee or a high-fat meal were presented at the annual meeting of the Endocrine Society (ENDO 2022), by Vertice Pharma Medical Director Kris Washington, PharmD.
And just last month, similar data were published in Thyroid for another levothyroxine oral solution, Tirosint-SOL (IBSA). No difference in pharmacokinetic properties were found with this product with a shorter versus a longer waiting period before consuming a high-fat meal.
Liquid thyroxine may be less affected by food/drink but is expensive
Both products have been approved by the U.S. Food and Drug Administration, but current labeling for both still calls for a 30- to 60-minute waiting period between taking the medication and eating or drinking. Thyquidity is an oral solution of 100 µg/mL levothyroxine sodium that has been shown to be bioequivalent to one of the most popular branded levothyroxine tablets, Synthroid (AbbVie), under fasting conditions. Tirosint-SOL is also an oral solution that comes in 15 different dosage ampules.
“It is important to note that while these findings are exciting and encouraging, we do want you to continue to follow the current FDA-approved label for Thyquidity, recommending that it be taken on an empty stomach 30-60 minutes prior to breakfast and that patients continue to follow all other label instructions,” Dr. Washington said during a press briefing at ENDO 2022.
When asked whether the new data would be submitted to the FDA for a possible amendment to this message, she replied: “We’re still discussing that. We’re exploring all options. ... This is fairly new data. ... It makes sense and certainly solves a lot of the challenges for people who can’t swallow or don’t choose to swallow, or the challenges of splitting or crushing with tablets.”
Asked to comment, Benjamin J. Gigliotti, MD, a clinical thyroidologist at the University of Rochester, New York, told this news organization: “Liquid levothyroxine has the potential to be a clinically useful formulation,” noting that these recent data corroborate prior findings from Europe and elsewhere that liquid levothyroxine is absorbed more rapidly and thus may be less impacted by food or beverages.
However, Dr. Gigliotti also pointed out, “I don’t think malabsorption is a major contributor to suboptimal treatment because if [patients] malabsorb the hormone, we typically just increase their dose a little bit or ask them to take it separately, and that works just fine for most people.”
And the higher cost of the liquid products is a major issue, he noted.
A quick search on GoodRx shows that the lowest price of Tirosint-SOL is $115.52 for a 1 month supply and Thyquidity is $181.04/month. “In the few patients where I tried to obtain Tirosint-SOL, it was not covered by insurance, even with a prior authorization,” Dr. Gigliotti commented.
In contrast, generic levothyroxine tablets are about $4/month, while a common brand name of levothyroxine tablets are $47.81/month.
“Until these liquid formulations are more widely covered by insurance for a reasonable copay, or come down in price compared to generic levothyroxine tablets, most of my patients have voiced that they’d rather deal with the inconveniences of a tablet compared to higher medication cost, especially with rising economic insecurity imposed by the COVID-19 pandemic and recent world events,” Dr. Gigliotti said.
Bioequivalence with shorter versus longer waits before coffee/breakfast
The Thyquidity coffee study was a single-center open-label, randomized, crossover study of 40 healthy adults randomized after a 10-hour overnight fast to 600 µg Thyquidity with water under fasting conditions or to the same dose given 5 minutes prior to drinking an 8-ounce cup of American coffee without milk or sweeteners. After a 40-day washout period, the same participants received the other treatment.
Mean serum thyroxine (T4) concentrations over 48 hours were nearly identical, demonstrating comparable bioavailability. Pharmacokinetics parameters, including area under the curve (AUC) and Cmax, were also comparable for both groups. The geometric least square mean ratios for baseline-adjusted LT4 were 96.0% for Cmax and 94% for AUC. And the corresponding 90% confidence intervals fell within the 80%-125% FDA acceptance range for absence of a food effect on bioavailability, said Dr. Washington when presenting the findings.
There was one adverse event, a decrease in blood glucose level, which was deemed to be mild and unrelated to study treatment. No deaths, serious adverse events, or discontinuations due to adverse events were reported. There were no significant changes in vital signs or on ECG.
In the second Thyquidity study of 38 healthy adults, after a 10-hour fast, the same doses were given 10 or 30 minutes prior to the consumption of a 950-calorie standardized high-fat breakfast.
Again, over 48 hours, mean serum T4 levels were comparable between the two groups. The geometric least squares mean ratios for both AUC and Cmax for baseline-adjusted LT4 were 88.7% and 85.1%, respectively. Again, the corresponding 90% confidence intervals fell within the FDA’s noninterference definition, again demonstrating lack of a food effect on bioavailability, Dr. Washington noted.
Four adverse events were reported in three participants, with three deemed to be possibly related to the medication. All were isolated lab abnormalities without clinical symptoms and deemed to be mild. Three were normal on repeat testing.
There were no deaths or serious adverse events or study discontinuations for adverse events and no significant findings for vital signs or on ECG.
Similar findings for Tirosint-SOL but longer-term studies needed
The recently published Tirosint-SOL study included 36 healthy volunteers randomized to single 600-µg doses of the LT4 oral solution after a 10-hour fast, either 15 or 30 minutes before eating a standardized high-fat, high-calorie meal. Mean serum total thyroxine concentration profiles were similar for both the 15- and 30-minute waits, with similar AUCs.
Geometric mean ratios for AUCs at 48 and 72 hours were 90% and 92%, respectively, and the 90% confidence intervals fell within the 80%-125% FDA boundaries, suggesting similar exposures whether taken 15 or 30 minutes before a meal.
Senior author Francesco S. Celi, MD, chair of the division of endocrinology, diabetes, and metabolism at Virginia Commonwealth University, Richmond, told this news organization: “There is an interest in providing more opportunities for patients and improving adherence to the medication. ... Whatever makes life a bit easier for patients and results in a more predictable response to treatment means down the road there will be fewer visits to the doctor to make adjustments.”
However, he said that in addition to the cost and reimbursement issue, all of these studies have been short term and not conducted in real-life settings.
“Another question is: What happens if the patient goes on low-dose LT4? The studies were conducted on much higher pharmacologic doses. But at least from a safety standpoint, there’s no specific concern.”
Dr. Washington is an employee of Vertice Pharma. Dr. Celi has received unrestricted research grants and worked as a consultant for IBSA. Dr. Gigliotti has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ENDO 2022
New National Lipid Association statement on statin intolerance
The U.S. National Lipid Association has issued a new scientific statement on the management of patients with statin intolerance, which recommends different strategies to help patients stay on statin medications, and also suggests alternatives that can be used in patients who really cannot tolerate statin drugs.
The statement was published online in the Journal of Clinical Lipidology.
It notes that, although statins are generally well tolerated, statin intolerance is reported in 5%-30% of patients and contributes to reduced statin adherence and persistence, as well as higher risk for adverse cardiovascular outcomes.
The statement acknowledges the importance of identifying modifiable risk factors for statin intolerance and recognizes the possibility of a “nocebo” effect, basically the patient expectation of harm resulting in perceived side effects.
To identify a tolerable statin regimen, it recommends that clinicians consider using several different strategies (different statin, dose, and/or dosing frequency), and to classify a patient as having statin intolerance, a minimum of two statins should have been attempted, including at least one at the lowest-approved daily dosage.
The statement says that nonstatin therapy may be required for patients who cannot reach therapeutic objectives with lifestyle and maximal tolerated statin therapy, and in these cases, therapies with outcomes data from randomized trials showing reduced cardiovascular events are favored.
In high and very high-risk patients who are statin intolerant, clinicians should consider initiating nonstatin therapy while additional attempts are made to identify a tolerable statin in order to limit the time of exposure to elevated levels of atherogenic lipoproteins, it suggests.
“There is strong evidence that statins reduce risk of cardiovascular events particularly in patients with atherosclerotic cardiovascular disease, but recent research shows that only about half of patients with ASCVD are on a statin,” Kevin C. Maki, PhD, coauthor of the statement and current president of the National Lipid Association, said in an interview.
“There is an urgent problem with underutilization of statins and undertreatment of ASCVD. And we know that perceived side effects associated with statins are a common reason for discontinuation of these drugs and the consequent failure to manage ASCVD adequately,” he said.
Dr. Maki noted that the NLA’s first message is that, when experiencing symptoms taking statins, a large majority of patients can still tolerate a statin. “They can try a different agent or a different dose. But for those who still can’t tolerate a statin, we then recommend nonstatin therapies and we favor those therapies with evidence from randomized trials.”
He pointed out that many patients who believe they are experiencing side effects from taking statins still experience the same effects on a placebo, a condition known as the nocebo effect.
“Several studies have shown that the nocebo effect is very common and accounts for more than half of perceived statin side effects. It is therefore estimated that many of the complaints of statin intolerance are probably not directly related to the pharmacodynamic actions of the drugs,” Dr. Maki said.
One recent study on the nocebo effect, the SAMSON study, suggested that 90% of symptoms attributed to statins were elicited by placebo tablets too.
But Dr. Maki added that it can be a losing battle for the clinician if patients think their symptoms are related to taking a statin.
“We suggest that clinicians inform patients that most people can tolerate a statin – maybe with a different agent or an alternative dose – and it is really important to lower LDL cholesterol as that will lower the risk of MI and stroke, so we need to find a regimen that works for each individual,” he said. “Most people can find a regimen that works. If this means taking a lower dose of a statin, they can take some additional therapy as well. This is a better situation than stopping taking statins altogether and allowing ASCVD to progress.”
Dr. Maki stressed that statins should still be the first choice as they are effective, taken orally, and inexpensive.
“Other medications do not have all these advantages. For example, PCSK9 inhibitors are very effective but they are expensive and injectable,” he noted. “And while ezetimibe [Zetia] is now generic so inexpensive, it has a more modest effect on LDL-lowering compared to statins, so by itself it is not normally enough for most patients to get to their target LDL, but it is an option for use in combination with a statin.”
He added that the NLA message is to do everything possible to keep patients on a statin, especially patients with preexisting ASCVD.
“We would like these patients to be on high-intensity statins. If they really can’t tolerate this, then they could be on a low-intensity statin plus an additional agent.”
Commenting on the NLA statement, SAMSON study coauthor James Howard, MB BChir, PhD, Imperial College London, said he had reservations about some of the recommendations.
“Whilst I think it is great news that the existence and importance of the nocebo effect is increasingly recognized in international guidelines and statements, I think we need to be very careful about recommending reduced doses and frequencies of statins,” Dr. Howard said.
“Studies such as SAMSON and StatinWISE indicate the vast majority of side effects reported by patients taking statins are not caused by the statin molecule, but instead are caused by either the nocebo effect, or ever-present background symptoms that are wrongly attributed to the statins,” he commented. “Therefore, to recommend that the correct approach in a patient with a history of MI suffering symptoms on 80 mg of atorvastatin is to reduce the dose or try alternate daily dosing. This reinforces the view that these drugs are side-effect prone and need to be carefully titrated.”
Dr. Howard suggested that patients should be educated on the possibility of the nocebo effect or background symptoms and encouraged to retrial statins at the same dose. “If that doesn’t work, then formal recording with a symptom diary might help patients recognize background symptoms,” he added.
Dr. Howard noted that, if symptoms still persist, an “n-of-1” trial could be conducted, in which the patient rotates between multiple periods of taking a statin and a placebo, but he acknowledged that this is expensive and time consuming.
Also commenting, Steve Nissen, MD, Cleveland Clinic, said he thought the NLA statement was “reasonable and thoughtful.”
“Regardless of whether the symptoms are due to the nocebo effect or not, some patients will just not take a statin no matter how hard you try to convince them to persevere, so we do need alternatives,” Dr. Nissen said.
He noted that current alternatives would include the PCSK9 inhibitors and ezetimibe, but a future candidate could be the oral bempedoic acid (Nexletol), which is currently being evaluated in a large outcomes trial (CLEAR Outcomes).
A version of this article first appeared on Medscape.com.
The U.S. National Lipid Association has issued a new scientific statement on the management of patients with statin intolerance, which recommends different strategies to help patients stay on statin medications, and also suggests alternatives that can be used in patients who really cannot tolerate statin drugs.
The statement was published online in the Journal of Clinical Lipidology.
It notes that, although statins are generally well tolerated, statin intolerance is reported in 5%-30% of patients and contributes to reduced statin adherence and persistence, as well as higher risk for adverse cardiovascular outcomes.
The statement acknowledges the importance of identifying modifiable risk factors for statin intolerance and recognizes the possibility of a “nocebo” effect, basically the patient expectation of harm resulting in perceived side effects.
To identify a tolerable statin regimen, it recommends that clinicians consider using several different strategies (different statin, dose, and/or dosing frequency), and to classify a patient as having statin intolerance, a minimum of two statins should have been attempted, including at least one at the lowest-approved daily dosage.
The statement says that nonstatin therapy may be required for patients who cannot reach therapeutic objectives with lifestyle and maximal tolerated statin therapy, and in these cases, therapies with outcomes data from randomized trials showing reduced cardiovascular events are favored.
In high and very high-risk patients who are statin intolerant, clinicians should consider initiating nonstatin therapy while additional attempts are made to identify a tolerable statin in order to limit the time of exposure to elevated levels of atherogenic lipoproteins, it suggests.
“There is strong evidence that statins reduce risk of cardiovascular events particularly in patients with atherosclerotic cardiovascular disease, but recent research shows that only about half of patients with ASCVD are on a statin,” Kevin C. Maki, PhD, coauthor of the statement and current president of the National Lipid Association, said in an interview.
“There is an urgent problem with underutilization of statins and undertreatment of ASCVD. And we know that perceived side effects associated with statins are a common reason for discontinuation of these drugs and the consequent failure to manage ASCVD adequately,” he said.
Dr. Maki noted that the NLA’s first message is that, when experiencing symptoms taking statins, a large majority of patients can still tolerate a statin. “They can try a different agent or a different dose. But for those who still can’t tolerate a statin, we then recommend nonstatin therapies and we favor those therapies with evidence from randomized trials.”
He pointed out that many patients who believe they are experiencing side effects from taking statins still experience the same effects on a placebo, a condition known as the nocebo effect.
“Several studies have shown that the nocebo effect is very common and accounts for more than half of perceived statin side effects. It is therefore estimated that many of the complaints of statin intolerance are probably not directly related to the pharmacodynamic actions of the drugs,” Dr. Maki said.
One recent study on the nocebo effect, the SAMSON study, suggested that 90% of symptoms attributed to statins were elicited by placebo tablets too.
But Dr. Maki added that it can be a losing battle for the clinician if patients think their symptoms are related to taking a statin.
“We suggest that clinicians inform patients that most people can tolerate a statin – maybe with a different agent or an alternative dose – and it is really important to lower LDL cholesterol as that will lower the risk of MI and stroke, so we need to find a regimen that works for each individual,” he said. “Most people can find a regimen that works. If this means taking a lower dose of a statin, they can take some additional therapy as well. This is a better situation than stopping taking statins altogether and allowing ASCVD to progress.”
Dr. Maki stressed that statins should still be the first choice as they are effective, taken orally, and inexpensive.
“Other medications do not have all these advantages. For example, PCSK9 inhibitors are very effective but they are expensive and injectable,” he noted. “And while ezetimibe [Zetia] is now generic so inexpensive, it has a more modest effect on LDL-lowering compared to statins, so by itself it is not normally enough for most patients to get to their target LDL, but it is an option for use in combination with a statin.”
He added that the NLA message is to do everything possible to keep patients on a statin, especially patients with preexisting ASCVD.
“We would like these patients to be on high-intensity statins. If they really can’t tolerate this, then they could be on a low-intensity statin plus an additional agent.”
Commenting on the NLA statement, SAMSON study coauthor James Howard, MB BChir, PhD, Imperial College London, said he had reservations about some of the recommendations.
“Whilst I think it is great news that the existence and importance of the nocebo effect is increasingly recognized in international guidelines and statements, I think we need to be very careful about recommending reduced doses and frequencies of statins,” Dr. Howard said.
“Studies such as SAMSON and StatinWISE indicate the vast majority of side effects reported by patients taking statins are not caused by the statin molecule, but instead are caused by either the nocebo effect, or ever-present background symptoms that are wrongly attributed to the statins,” he commented. “Therefore, to recommend that the correct approach in a patient with a history of MI suffering symptoms on 80 mg of atorvastatin is to reduce the dose or try alternate daily dosing. This reinforces the view that these drugs are side-effect prone and need to be carefully titrated.”
Dr. Howard suggested that patients should be educated on the possibility of the nocebo effect or background symptoms and encouraged to retrial statins at the same dose. “If that doesn’t work, then formal recording with a symptom diary might help patients recognize background symptoms,” he added.
Dr. Howard noted that, if symptoms still persist, an “n-of-1” trial could be conducted, in which the patient rotates between multiple periods of taking a statin and a placebo, but he acknowledged that this is expensive and time consuming.
Also commenting, Steve Nissen, MD, Cleveland Clinic, said he thought the NLA statement was “reasonable and thoughtful.”
“Regardless of whether the symptoms are due to the nocebo effect or not, some patients will just not take a statin no matter how hard you try to convince them to persevere, so we do need alternatives,” Dr. Nissen said.
He noted that current alternatives would include the PCSK9 inhibitors and ezetimibe, but a future candidate could be the oral bempedoic acid (Nexletol), which is currently being evaluated in a large outcomes trial (CLEAR Outcomes).
A version of this article first appeared on Medscape.com.
The U.S. National Lipid Association has issued a new scientific statement on the management of patients with statin intolerance, which recommends different strategies to help patients stay on statin medications, and also suggests alternatives that can be used in patients who really cannot tolerate statin drugs.
The statement was published online in the Journal of Clinical Lipidology.
It notes that, although statins are generally well tolerated, statin intolerance is reported in 5%-30% of patients and contributes to reduced statin adherence and persistence, as well as higher risk for adverse cardiovascular outcomes.
The statement acknowledges the importance of identifying modifiable risk factors for statin intolerance and recognizes the possibility of a “nocebo” effect, basically the patient expectation of harm resulting in perceived side effects.
To identify a tolerable statin regimen, it recommends that clinicians consider using several different strategies (different statin, dose, and/or dosing frequency), and to classify a patient as having statin intolerance, a minimum of two statins should have been attempted, including at least one at the lowest-approved daily dosage.
The statement says that nonstatin therapy may be required for patients who cannot reach therapeutic objectives with lifestyle and maximal tolerated statin therapy, and in these cases, therapies with outcomes data from randomized trials showing reduced cardiovascular events are favored.
In high and very high-risk patients who are statin intolerant, clinicians should consider initiating nonstatin therapy while additional attempts are made to identify a tolerable statin in order to limit the time of exposure to elevated levels of atherogenic lipoproteins, it suggests.
“There is strong evidence that statins reduce risk of cardiovascular events particularly in patients with atherosclerotic cardiovascular disease, but recent research shows that only about half of patients with ASCVD are on a statin,” Kevin C. Maki, PhD, coauthor of the statement and current president of the National Lipid Association, said in an interview.
“There is an urgent problem with underutilization of statins and undertreatment of ASCVD. And we know that perceived side effects associated with statins are a common reason for discontinuation of these drugs and the consequent failure to manage ASCVD adequately,” he said.
Dr. Maki noted that the NLA’s first message is that, when experiencing symptoms taking statins, a large majority of patients can still tolerate a statin. “They can try a different agent or a different dose. But for those who still can’t tolerate a statin, we then recommend nonstatin therapies and we favor those therapies with evidence from randomized trials.”
He pointed out that many patients who believe they are experiencing side effects from taking statins still experience the same effects on a placebo, a condition known as the nocebo effect.
“Several studies have shown that the nocebo effect is very common and accounts for more than half of perceived statin side effects. It is therefore estimated that many of the complaints of statin intolerance are probably not directly related to the pharmacodynamic actions of the drugs,” Dr. Maki said.
One recent study on the nocebo effect, the SAMSON study, suggested that 90% of symptoms attributed to statins were elicited by placebo tablets too.
But Dr. Maki added that it can be a losing battle for the clinician if patients think their symptoms are related to taking a statin.
“We suggest that clinicians inform patients that most people can tolerate a statin – maybe with a different agent or an alternative dose – and it is really important to lower LDL cholesterol as that will lower the risk of MI and stroke, so we need to find a regimen that works for each individual,” he said. “Most people can find a regimen that works. If this means taking a lower dose of a statin, they can take some additional therapy as well. This is a better situation than stopping taking statins altogether and allowing ASCVD to progress.”
Dr. Maki stressed that statins should still be the first choice as they are effective, taken orally, and inexpensive.
“Other medications do not have all these advantages. For example, PCSK9 inhibitors are very effective but they are expensive and injectable,” he noted. “And while ezetimibe [Zetia] is now generic so inexpensive, it has a more modest effect on LDL-lowering compared to statins, so by itself it is not normally enough for most patients to get to their target LDL, but it is an option for use in combination with a statin.”
He added that the NLA message is to do everything possible to keep patients on a statin, especially patients with preexisting ASCVD.
“We would like these patients to be on high-intensity statins. If they really can’t tolerate this, then they could be on a low-intensity statin plus an additional agent.”
Commenting on the NLA statement, SAMSON study coauthor James Howard, MB BChir, PhD, Imperial College London, said he had reservations about some of the recommendations.
“Whilst I think it is great news that the existence and importance of the nocebo effect is increasingly recognized in international guidelines and statements, I think we need to be very careful about recommending reduced doses and frequencies of statins,” Dr. Howard said.
“Studies such as SAMSON and StatinWISE indicate the vast majority of side effects reported by patients taking statins are not caused by the statin molecule, but instead are caused by either the nocebo effect, or ever-present background symptoms that are wrongly attributed to the statins,” he commented. “Therefore, to recommend that the correct approach in a patient with a history of MI suffering symptoms on 80 mg of atorvastatin is to reduce the dose or try alternate daily dosing. This reinforces the view that these drugs are side-effect prone and need to be carefully titrated.”
Dr. Howard suggested that patients should be educated on the possibility of the nocebo effect or background symptoms and encouraged to retrial statins at the same dose. “If that doesn’t work, then formal recording with a symptom diary might help patients recognize background symptoms,” he added.
Dr. Howard noted that, if symptoms still persist, an “n-of-1” trial could be conducted, in which the patient rotates between multiple periods of taking a statin and a placebo, but he acknowledged that this is expensive and time consuming.
Also commenting, Steve Nissen, MD, Cleveland Clinic, said he thought the NLA statement was “reasonable and thoughtful.”
“Regardless of whether the symptoms are due to the nocebo effect or not, some patients will just not take a statin no matter how hard you try to convince them to persevere, so we do need alternatives,” Dr. Nissen said.
He noted that current alternatives would include the PCSK9 inhibitors and ezetimibe, but a future candidate could be the oral bempedoic acid (Nexletol), which is currently being evaluated in a large outcomes trial (CLEAR Outcomes).
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL LIPIDOLOGY
Microbiome’s new happy place: The beer gut
Your gut microbiome will thank you later
A healthy gut seems like the new catch-all to better overall health these days. Nutrition and diet culture has us drinking kombucha and ginger tea and coffee, but what if we told you that going to happy hour might also help?
In a recent double-blind study published in the Journal of Agricultural and Food Chemistry, 19 men were divided into two groups and asked to drink 11 ounces of alcoholic lager (5.2% by volume) or nonalcoholic lager with dinner for 4 weeks.
Beer? Yes. Beer.
We humans have trillions of microorganisms running rampant through our digestive tracts. When they’re happy, we have a lower chance of developing heart disease and diabetes. You know what else has millions of happy microorganisms from fermentation? Beer. It also has polyphenols that can help the body’s tissues fight cancers, as well as heart disease and inflammation. So beer is looking a little more healthy now, isn’t it?
In the study, the researchers found that both the alcoholic- and nonalcoholic-lager groups had a boost in bacterial diversity in the gut and higher fecal alkaline phosphatase levels, which showed improved intestinal health. They acknowledged, however, that the nonalcoholic route would be safer and healthier for overall health.
So add a lager to the list of gut-healthy foods that you should be consuming. It may give the phrase “beer gut” a whole new meaning.
We’ve lost our minds, but at least we know how fast they’re going
The phrase “quantum consciousness” sounds like something out of a particularly cheesy episode of Star Trek: “Oh no, Captain, the quantum consciousness has invaded our computer, and the only way to drive it out is to reverse the polarity of a focused tachyon beam.”
When it comes to understanding such basic existential issues as the origin of consciousness, however, quantum mechanics wasn’t off the table. The theory of the quantum origin of consciousness dates back to the 1990s (thanks in part to noted physician Roger Penrose), and goes something like this: There are microtubules within neurons in the brain that are small enough and isolated enough from the warm, wet, and chaotic brain environment where quantum effects can briefly come into play. We’re talking miniscule fractions of a second here, but still, long enough for quantum calculations to take place in the form of system wavefunction collapse, courtesy of gravity.
To plunge even deeper into the rabbit hole of quantum mechanics, the reason Schrödinger’s cat doesn’t occur in real life is wavefunction collapse; the more massive a quantum system is, the more likely it is to collapse into one state or another (alive or dead, in the cat’s case). The quantum origin of consciousness, or Orch OR theory, holds that human consciousness arises from electrical oscillations within the neuronal microtubules caused by the computations stemming from the collapse of small quantum systems.
That is an awful lot of overly simplified explanation, especially considering the study that just came out essentially disproved it. Oops. The research, published in Physics of Life Reviews, is pretty simple. The researchers went to a lab deep underground to avoid interference from cosmic rays, and sat around for months, observing a chunk of germanium for signs of spontaneous radiation, attributable to the same sort of wavefunction collapse that is supposedly occurring in our brains. They found nothing out of the ordinary, pretty definitively disproving most of Orch OR theory.
The researchers were unwilling to completely dismiss the idea (this is quantum mechanics, after all, uncertainty kind of goes with the territory), but it does seem like we’ll have to search elsewhere for sources of human consciousness. Personally, we’re big fans of the cymbal-playing monkey.
Missing links: A real fish story
Dear LOTME:
Ear’s a question that’s been keeping me up at night. Is the human middle ear the result of top-secret government experiments involving alien technology, Abraham Lincoln, and the Illuminati?
Restless in Roswell
Dear Restless:
The paleoanthropologic community has been sorting through this mystery for decades, and fossils discovered in China over the past 20 years finally provide a much less conspiratorially satisfying answer.
For some time now, experts in the field have believed that the bones of the human middle ear evolved from the spiracular gill of a fish. The spiracle is a small hole behind each eye that opens to the mouth in some fishes and was used to breathe air in the earliest, most primitive species. But how did we get from spiracle to ear?
The missing links come in the form of the cranial anatomy of Shuyu, a 438-million-year-old, fingernail-sized skull of a jawless fish, and the 419-million-year-old fossil of a completely preserved fish with gill filaments in the first branchial chamber.
“These fossils provided the first anatomical and fossil evidence for a vertebrate spiracle originating from fish gills,” senior author Gai Zhikun, PhD, of the Institute of Vertebrate Paleontology and Paleoanthropology, Beijing, said in a written statement.
In many ways, it seems, we are fish: “Many important structures of human beings can be traced back to our fish ancestors, such as our teeth, jaws, middle ears, etc,” added Zhu Min, PhD, also of the institute.
So, Restless, the next time you hear the soothing sounds of an angry mob storming the Capitol or you chew on a slab, slice, or chunk of mutant, laboratory-produced chicken in your favorite fast-food restaurant, be sure to thank Shuyu.
Can you lend me an ear?
If you thought locusts were only a nuisance, think again. They have their uses. If you take a locust’s ear and put it inside a robot, the robot will be able to hear and receive signals. Who knew?
Researchers from Tel Aviv University in Israel showed the robot’s hearing abilities by giving clap signals that told the robot what to do: One clap means go forward, two claps mean move back. What do you think the robot would do if it heard the clap break from Cha Cha Slide?
“Our task was to replace the robot’s electronic microphone with a dead insect’s ear, use the ear’s ability to detect the electrical signals from the environment, in this case vibrations in the air, and, using a special chip, convert the insect input to that of the robot,” Ben M. Maoz, PhD, said in a statement from the university.
And how does a dead locust ear work in a robot? Well, Dr. Maoz explained: “My laboratory has developed a special device – Ear-on-a-Chip – that allows the ear to be kept alive throughout the experiment by supplying oxygen and food to the organ while allowing the electrical signals to be taken out of the locust’s ear and amplified and transmitted to the robot.”
The research won’t stop at hearing, he said, as the other four senses also will be taken into consideration. This could help us sense dangers in the future, such as earthquakes or diseases. We said it before and we’ll say it again: We’re rooting for you, science!
Your gut microbiome will thank you later
A healthy gut seems like the new catch-all to better overall health these days. Nutrition and diet culture has us drinking kombucha and ginger tea and coffee, but what if we told you that going to happy hour might also help?
In a recent double-blind study published in the Journal of Agricultural and Food Chemistry, 19 men were divided into two groups and asked to drink 11 ounces of alcoholic lager (5.2% by volume) or nonalcoholic lager with dinner for 4 weeks.
Beer? Yes. Beer.
We humans have trillions of microorganisms running rampant through our digestive tracts. When they’re happy, we have a lower chance of developing heart disease and diabetes. You know what else has millions of happy microorganisms from fermentation? Beer. It also has polyphenols that can help the body’s tissues fight cancers, as well as heart disease and inflammation. So beer is looking a little more healthy now, isn’t it?
In the study, the researchers found that both the alcoholic- and nonalcoholic-lager groups had a boost in bacterial diversity in the gut and higher fecal alkaline phosphatase levels, which showed improved intestinal health. They acknowledged, however, that the nonalcoholic route would be safer and healthier for overall health.
So add a lager to the list of gut-healthy foods that you should be consuming. It may give the phrase “beer gut” a whole new meaning.
We’ve lost our minds, but at least we know how fast they’re going
The phrase “quantum consciousness” sounds like something out of a particularly cheesy episode of Star Trek: “Oh no, Captain, the quantum consciousness has invaded our computer, and the only way to drive it out is to reverse the polarity of a focused tachyon beam.”
When it comes to understanding such basic existential issues as the origin of consciousness, however, quantum mechanics wasn’t off the table. The theory of the quantum origin of consciousness dates back to the 1990s (thanks in part to noted physician Roger Penrose), and goes something like this: There are microtubules within neurons in the brain that are small enough and isolated enough from the warm, wet, and chaotic brain environment where quantum effects can briefly come into play. We’re talking miniscule fractions of a second here, but still, long enough for quantum calculations to take place in the form of system wavefunction collapse, courtesy of gravity.
To plunge even deeper into the rabbit hole of quantum mechanics, the reason Schrödinger’s cat doesn’t occur in real life is wavefunction collapse; the more massive a quantum system is, the more likely it is to collapse into one state or another (alive or dead, in the cat’s case). The quantum origin of consciousness, or Orch OR theory, holds that human consciousness arises from electrical oscillations within the neuronal microtubules caused by the computations stemming from the collapse of small quantum systems.
That is an awful lot of overly simplified explanation, especially considering the study that just came out essentially disproved it. Oops. The research, published in Physics of Life Reviews, is pretty simple. The researchers went to a lab deep underground to avoid interference from cosmic rays, and sat around for months, observing a chunk of germanium for signs of spontaneous radiation, attributable to the same sort of wavefunction collapse that is supposedly occurring in our brains. They found nothing out of the ordinary, pretty definitively disproving most of Orch OR theory.
The researchers were unwilling to completely dismiss the idea (this is quantum mechanics, after all, uncertainty kind of goes with the territory), but it does seem like we’ll have to search elsewhere for sources of human consciousness. Personally, we’re big fans of the cymbal-playing monkey.
Missing links: A real fish story
Dear LOTME:
Ear’s a question that’s been keeping me up at night. Is the human middle ear the result of top-secret government experiments involving alien technology, Abraham Lincoln, and the Illuminati?
Restless in Roswell
Dear Restless:
The paleoanthropologic community has been sorting through this mystery for decades, and fossils discovered in China over the past 20 years finally provide a much less conspiratorially satisfying answer.
For some time now, experts in the field have believed that the bones of the human middle ear evolved from the spiracular gill of a fish. The spiracle is a small hole behind each eye that opens to the mouth in some fishes and was used to breathe air in the earliest, most primitive species. But how did we get from spiracle to ear?
The missing links come in the form of the cranial anatomy of Shuyu, a 438-million-year-old, fingernail-sized skull of a jawless fish, and the 419-million-year-old fossil of a completely preserved fish with gill filaments in the first branchial chamber.
“These fossils provided the first anatomical and fossil evidence for a vertebrate spiracle originating from fish gills,” senior author Gai Zhikun, PhD, of the Institute of Vertebrate Paleontology and Paleoanthropology, Beijing, said in a written statement.
In many ways, it seems, we are fish: “Many important structures of human beings can be traced back to our fish ancestors, such as our teeth, jaws, middle ears, etc,” added Zhu Min, PhD, also of the institute.
So, Restless, the next time you hear the soothing sounds of an angry mob storming the Capitol or you chew on a slab, slice, or chunk of mutant, laboratory-produced chicken in your favorite fast-food restaurant, be sure to thank Shuyu.
Can you lend me an ear?
If you thought locusts were only a nuisance, think again. They have their uses. If you take a locust’s ear and put it inside a robot, the robot will be able to hear and receive signals. Who knew?
Researchers from Tel Aviv University in Israel showed the robot’s hearing abilities by giving clap signals that told the robot what to do: One clap means go forward, two claps mean move back. What do you think the robot would do if it heard the clap break from Cha Cha Slide?
“Our task was to replace the robot’s electronic microphone with a dead insect’s ear, use the ear’s ability to detect the electrical signals from the environment, in this case vibrations in the air, and, using a special chip, convert the insect input to that of the robot,” Ben M. Maoz, PhD, said in a statement from the university.
And how does a dead locust ear work in a robot? Well, Dr. Maoz explained: “My laboratory has developed a special device – Ear-on-a-Chip – that allows the ear to be kept alive throughout the experiment by supplying oxygen and food to the organ while allowing the electrical signals to be taken out of the locust’s ear and amplified and transmitted to the robot.”
The research won’t stop at hearing, he said, as the other four senses also will be taken into consideration. This could help us sense dangers in the future, such as earthquakes or diseases. We said it before and we’ll say it again: We’re rooting for you, science!
Your gut microbiome will thank you later
A healthy gut seems like the new catch-all to better overall health these days. Nutrition and diet culture has us drinking kombucha and ginger tea and coffee, but what if we told you that going to happy hour might also help?
In a recent double-blind study published in the Journal of Agricultural and Food Chemistry, 19 men were divided into two groups and asked to drink 11 ounces of alcoholic lager (5.2% by volume) or nonalcoholic lager with dinner for 4 weeks.
Beer? Yes. Beer.
We humans have trillions of microorganisms running rampant through our digestive tracts. When they’re happy, we have a lower chance of developing heart disease and diabetes. You know what else has millions of happy microorganisms from fermentation? Beer. It also has polyphenols that can help the body’s tissues fight cancers, as well as heart disease and inflammation. So beer is looking a little more healthy now, isn’t it?
In the study, the researchers found that both the alcoholic- and nonalcoholic-lager groups had a boost in bacterial diversity in the gut and higher fecal alkaline phosphatase levels, which showed improved intestinal health. They acknowledged, however, that the nonalcoholic route would be safer and healthier for overall health.
So add a lager to the list of gut-healthy foods that you should be consuming. It may give the phrase “beer gut” a whole new meaning.
We’ve lost our minds, but at least we know how fast they’re going
The phrase “quantum consciousness” sounds like something out of a particularly cheesy episode of Star Trek: “Oh no, Captain, the quantum consciousness has invaded our computer, and the only way to drive it out is to reverse the polarity of a focused tachyon beam.”
When it comes to understanding such basic existential issues as the origin of consciousness, however, quantum mechanics wasn’t off the table. The theory of the quantum origin of consciousness dates back to the 1990s (thanks in part to noted physician Roger Penrose), and goes something like this: There are microtubules within neurons in the brain that are small enough and isolated enough from the warm, wet, and chaotic brain environment where quantum effects can briefly come into play. We’re talking miniscule fractions of a second here, but still, long enough for quantum calculations to take place in the form of system wavefunction collapse, courtesy of gravity.
To plunge even deeper into the rabbit hole of quantum mechanics, the reason Schrödinger’s cat doesn’t occur in real life is wavefunction collapse; the more massive a quantum system is, the more likely it is to collapse into one state or another (alive or dead, in the cat’s case). The quantum origin of consciousness, or Orch OR theory, holds that human consciousness arises from electrical oscillations within the neuronal microtubules caused by the computations stemming from the collapse of small quantum systems.
That is an awful lot of overly simplified explanation, especially considering the study that just came out essentially disproved it. Oops. The research, published in Physics of Life Reviews, is pretty simple. The researchers went to a lab deep underground to avoid interference from cosmic rays, and sat around for months, observing a chunk of germanium for signs of spontaneous radiation, attributable to the same sort of wavefunction collapse that is supposedly occurring in our brains. They found nothing out of the ordinary, pretty definitively disproving most of Orch OR theory.
The researchers were unwilling to completely dismiss the idea (this is quantum mechanics, after all, uncertainty kind of goes with the territory), but it does seem like we’ll have to search elsewhere for sources of human consciousness. Personally, we’re big fans of the cymbal-playing monkey.
Missing links: A real fish story
Dear LOTME:
Ear’s a question that’s been keeping me up at night. Is the human middle ear the result of top-secret government experiments involving alien technology, Abraham Lincoln, and the Illuminati?
Restless in Roswell
Dear Restless:
The paleoanthropologic community has been sorting through this mystery for decades, and fossils discovered in China over the past 20 years finally provide a much less conspiratorially satisfying answer.
For some time now, experts in the field have believed that the bones of the human middle ear evolved from the spiracular gill of a fish. The spiracle is a small hole behind each eye that opens to the mouth in some fishes and was used to breathe air in the earliest, most primitive species. But how did we get from spiracle to ear?
The missing links come in the form of the cranial anatomy of Shuyu, a 438-million-year-old, fingernail-sized skull of a jawless fish, and the 419-million-year-old fossil of a completely preserved fish with gill filaments in the first branchial chamber.
“These fossils provided the first anatomical and fossil evidence for a vertebrate spiracle originating from fish gills,” senior author Gai Zhikun, PhD, of the Institute of Vertebrate Paleontology and Paleoanthropology, Beijing, said in a written statement.
In many ways, it seems, we are fish: “Many important structures of human beings can be traced back to our fish ancestors, such as our teeth, jaws, middle ears, etc,” added Zhu Min, PhD, also of the institute.
So, Restless, the next time you hear the soothing sounds of an angry mob storming the Capitol or you chew on a slab, slice, or chunk of mutant, laboratory-produced chicken in your favorite fast-food restaurant, be sure to thank Shuyu.
Can you lend me an ear?
If you thought locusts were only a nuisance, think again. They have their uses. If you take a locust’s ear and put it inside a robot, the robot will be able to hear and receive signals. Who knew?
Researchers from Tel Aviv University in Israel showed the robot’s hearing abilities by giving clap signals that told the robot what to do: One clap means go forward, two claps mean move back. What do you think the robot would do if it heard the clap break from Cha Cha Slide?
“Our task was to replace the robot’s electronic microphone with a dead insect’s ear, use the ear’s ability to detect the electrical signals from the environment, in this case vibrations in the air, and, using a special chip, convert the insect input to that of the robot,” Ben M. Maoz, PhD, said in a statement from the university.
And how does a dead locust ear work in a robot? Well, Dr. Maoz explained: “My laboratory has developed a special device – Ear-on-a-Chip – that allows the ear to be kept alive throughout the experiment by supplying oxygen and food to the organ while allowing the electrical signals to be taken out of the locust’s ear and amplified and transmitted to the robot.”
The research won’t stop at hearing, he said, as the other four senses also will be taken into consideration. This could help us sense dangers in the future, such as earthquakes or diseases. We said it before and we’ll say it again: We’re rooting for you, science!
Nonhormonal drug for menopause symptoms passes phase 3 test
A phase 3 trial has associated the neurokinin-3 (NK3)–receptor inhibitor fezolinetant, an oral therapy taken once daily, with substantial control over the symptoms of menopause, according to results of the randomized SKYLIGHT 2 trial.
The nonhormonal therapy has the potential to address an important unmet need, Genevieve Neal-Perry, MD, PhD, said at the annual meeting of the Endocrine Society.
The health risks of hormone therapy (HT) have “caused quite a few women to consider whether hormone replacement is right for them, and, in addition, there are other individuals who have hormone-responsive cancers or other disorders that might prohibit them [from using HT],” Dr. Neal-Perry said.
The NK3 receptor stimulates the thermoregulatory center in the hypothalamus. By blocking the NK3 receptor, vasodilation and other downstream effects are inhibited, explained Dr. Neal-Perry. She credited relatively recent advances in understanding the mechanisms of menopausal symptoms for identifying this and other potentially targetable mediators.
SKYLIGHT 2 trial: Two phases
In the double-blind multinational phase 3 SKYLIGHT 2 trial, 484 otherwise healthy symptomatic menopausal women were randomized to 30 mg of fezolinetant, 45 mg of fezolinetant, or placebo. The 120 participating centers were in North American and Europe.
In the first phase, safety and efficacy were evaluated over 12 weeks. In a second extension phase, placebo patients were rerandomized to one of the fezolinetant study doses. Those on active therapy remained in their assigned groups. All patients were then followed for an additional 40 weeks.
The coprimary endpoints were frequency and severity of moderate to severe vasomotor symptoms as reported by patients using an electronic diary. There were several secondary endpoints, including patient-reported outcomes regarding sleep quality.
As expected from other controlled trials, placebo patients achieved about a 40% reduction in moderate to severe vasomotor symptom frequency over the first 12 weeks. Relative to placebo, symptom frequency declined more quickly and steeply on fezolinetant. By week 12, both achieved reductions of about 60%. Statistical P values for the differences in the three arms were not provided, but Dr. Neal-Perry reported they were significant.
Vasomotor severity, like frequency, is reduced
The change in vasomotor severity, which subjects in the trial rated as better or worse, was also significant. The differences in the severity curves were less, but they separated in favor of the two active treatment arms by about 2 weeks, and the curves continued to show an advantage for fezolinetant over both the first 12 weeks and then the remaining 40 weeks.
Overall, the decline in vasomotor symptom frequency remained on a persistent downward slope on both doses of fezolinetant for the full 52 weeks of the study, so that the reduction at 52 weeks was on the order of 25% greater than that seen at 12 weeks.
At 52 weeks, “you can see that individuals on placebo who were crossed over to an active treatment had a significant reduction in their hot flashes and look very much like those who were randomized to fezolinetant at the beginning of the study,” said Dr. Neal-Perry, who is chair of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Other outcomes also favored fezolinetant over placebo. For example, a reduction in sleep disturbance observed at 12 weeks was sustained over the full 52 weeks of the study. The reduction in sleep symptoms appeared to be slightly greater on the higher dose, but the benefit at 52 weeks among patients after the crossover was similar on either active arm.
No serious side effects identified
There were no serious drug-related treatment-emergent adverse events in any treatment group. One patient in the placebo arm (< 1%), two patients in the 30-mg fezolinetant arm (1.2%), and five patients in the 45-mg arm (3%) discontinued therapy for an adverse event considered to be treatment related.
“The most common side effect associated with fezolinetant was headache. There were no other side effects that led patients to pull out of the study,” Dr. Neal-Perry reported at the meeting, which was held in Atlanta and virtually.
According to Dr. Neal-Perry the vasomotor symptoms relative to menopause, which occur in almost all women, are moderate to severe in an estimated 35%-45%. Some groups, such as those with an elevated body mass index and African Americans, appear to be at even greater risk. Study enrollment was specifically designed to include these high-risk groups, but the subgroup efficacy data have not yet been analyzed.
Other drugs with a similar mechanism of action have not been brought forward because of concern about elevated liver enzymes, but Dr. Neal-Perry said that this does not appear to be an issue for fezolinetant, which was designed with greater specificity for the NK3 target than previous treatments.
If fezolinetant is approved, Dr. Neal-Perry expects this agent to fulfill an important unmet need because of the limitations of other nonhormonal solutions for control of menopause symptoms.
HT alternatives limited
For control of many menopause symptoms, particularly hot flashes, hormone therapy (HT) is the most efficacious, but Richard J. Santen, MD, emeritus professor and an endocrinologist at the University of Virginia, Charlottesville, agreed there is a need for alternatives.
In addition to those who have contraindications for HT, Dr. Santen said in an interview that this option is not acceptable to others “for a variety of reasons.” The problem is that the alternatives are limited.
“The SSRI agents and gabapentin are alternative nonhormonal agents, but they have side effects and are not as effective,” he said. Hot flashes “can be a major disruptor of quality of life,” so he is intrigued with the positive results achieved with fezolinetant.
“A new drug such as reported at the Endocrine Society meeting would be an important new addition to the armamentarium,” he said.
Dr. Neal-Perry reports no conflicts of interest.
A phase 3 trial has associated the neurokinin-3 (NK3)–receptor inhibitor fezolinetant, an oral therapy taken once daily, with substantial control over the symptoms of menopause, according to results of the randomized SKYLIGHT 2 trial.
The nonhormonal therapy has the potential to address an important unmet need, Genevieve Neal-Perry, MD, PhD, said at the annual meeting of the Endocrine Society.
The health risks of hormone therapy (HT) have “caused quite a few women to consider whether hormone replacement is right for them, and, in addition, there are other individuals who have hormone-responsive cancers or other disorders that might prohibit them [from using HT],” Dr. Neal-Perry said.
The NK3 receptor stimulates the thermoregulatory center in the hypothalamus. By blocking the NK3 receptor, vasodilation and other downstream effects are inhibited, explained Dr. Neal-Perry. She credited relatively recent advances in understanding the mechanisms of menopausal symptoms for identifying this and other potentially targetable mediators.
SKYLIGHT 2 trial: Two phases
In the double-blind multinational phase 3 SKYLIGHT 2 trial, 484 otherwise healthy symptomatic menopausal women were randomized to 30 mg of fezolinetant, 45 mg of fezolinetant, or placebo. The 120 participating centers were in North American and Europe.
In the first phase, safety and efficacy were evaluated over 12 weeks. In a second extension phase, placebo patients were rerandomized to one of the fezolinetant study doses. Those on active therapy remained in their assigned groups. All patients were then followed for an additional 40 weeks.
The coprimary endpoints were frequency and severity of moderate to severe vasomotor symptoms as reported by patients using an electronic diary. There were several secondary endpoints, including patient-reported outcomes regarding sleep quality.
As expected from other controlled trials, placebo patients achieved about a 40% reduction in moderate to severe vasomotor symptom frequency over the first 12 weeks. Relative to placebo, symptom frequency declined more quickly and steeply on fezolinetant. By week 12, both achieved reductions of about 60%. Statistical P values for the differences in the three arms were not provided, but Dr. Neal-Perry reported they were significant.
Vasomotor severity, like frequency, is reduced
The change in vasomotor severity, which subjects in the trial rated as better or worse, was also significant. The differences in the severity curves were less, but they separated in favor of the two active treatment arms by about 2 weeks, and the curves continued to show an advantage for fezolinetant over both the first 12 weeks and then the remaining 40 weeks.
Overall, the decline in vasomotor symptom frequency remained on a persistent downward slope on both doses of fezolinetant for the full 52 weeks of the study, so that the reduction at 52 weeks was on the order of 25% greater than that seen at 12 weeks.
At 52 weeks, “you can see that individuals on placebo who were crossed over to an active treatment had a significant reduction in their hot flashes and look very much like those who were randomized to fezolinetant at the beginning of the study,” said Dr. Neal-Perry, who is chair of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Other outcomes also favored fezolinetant over placebo. For example, a reduction in sleep disturbance observed at 12 weeks was sustained over the full 52 weeks of the study. The reduction in sleep symptoms appeared to be slightly greater on the higher dose, but the benefit at 52 weeks among patients after the crossover was similar on either active arm.
No serious side effects identified
There were no serious drug-related treatment-emergent adverse events in any treatment group. One patient in the placebo arm (< 1%), two patients in the 30-mg fezolinetant arm (1.2%), and five patients in the 45-mg arm (3%) discontinued therapy for an adverse event considered to be treatment related.
“The most common side effect associated with fezolinetant was headache. There were no other side effects that led patients to pull out of the study,” Dr. Neal-Perry reported at the meeting, which was held in Atlanta and virtually.
According to Dr. Neal-Perry the vasomotor symptoms relative to menopause, which occur in almost all women, are moderate to severe in an estimated 35%-45%. Some groups, such as those with an elevated body mass index and African Americans, appear to be at even greater risk. Study enrollment was specifically designed to include these high-risk groups, but the subgroup efficacy data have not yet been analyzed.
Other drugs with a similar mechanism of action have not been brought forward because of concern about elevated liver enzymes, but Dr. Neal-Perry said that this does not appear to be an issue for fezolinetant, which was designed with greater specificity for the NK3 target than previous treatments.
If fezolinetant is approved, Dr. Neal-Perry expects this agent to fulfill an important unmet need because of the limitations of other nonhormonal solutions for control of menopause symptoms.
HT alternatives limited
For control of many menopause symptoms, particularly hot flashes, hormone therapy (HT) is the most efficacious, but Richard J. Santen, MD, emeritus professor and an endocrinologist at the University of Virginia, Charlottesville, agreed there is a need for alternatives.
In addition to those who have contraindications for HT, Dr. Santen said in an interview that this option is not acceptable to others “for a variety of reasons.” The problem is that the alternatives are limited.
“The SSRI agents and gabapentin are alternative nonhormonal agents, but they have side effects and are not as effective,” he said. Hot flashes “can be a major disruptor of quality of life,” so he is intrigued with the positive results achieved with fezolinetant.
“A new drug such as reported at the Endocrine Society meeting would be an important new addition to the armamentarium,” he said.
Dr. Neal-Perry reports no conflicts of interest.
A phase 3 trial has associated the neurokinin-3 (NK3)–receptor inhibitor fezolinetant, an oral therapy taken once daily, with substantial control over the symptoms of menopause, according to results of the randomized SKYLIGHT 2 trial.
The nonhormonal therapy has the potential to address an important unmet need, Genevieve Neal-Perry, MD, PhD, said at the annual meeting of the Endocrine Society.
The health risks of hormone therapy (HT) have “caused quite a few women to consider whether hormone replacement is right for them, and, in addition, there are other individuals who have hormone-responsive cancers or other disorders that might prohibit them [from using HT],” Dr. Neal-Perry said.
The NK3 receptor stimulates the thermoregulatory center in the hypothalamus. By blocking the NK3 receptor, vasodilation and other downstream effects are inhibited, explained Dr. Neal-Perry. She credited relatively recent advances in understanding the mechanisms of menopausal symptoms for identifying this and other potentially targetable mediators.
SKYLIGHT 2 trial: Two phases
In the double-blind multinational phase 3 SKYLIGHT 2 trial, 484 otherwise healthy symptomatic menopausal women were randomized to 30 mg of fezolinetant, 45 mg of fezolinetant, or placebo. The 120 participating centers were in North American and Europe.
In the first phase, safety and efficacy were evaluated over 12 weeks. In a second extension phase, placebo patients were rerandomized to one of the fezolinetant study doses. Those on active therapy remained in their assigned groups. All patients were then followed for an additional 40 weeks.
The coprimary endpoints were frequency and severity of moderate to severe vasomotor symptoms as reported by patients using an electronic diary. There were several secondary endpoints, including patient-reported outcomes regarding sleep quality.
As expected from other controlled trials, placebo patients achieved about a 40% reduction in moderate to severe vasomotor symptom frequency over the first 12 weeks. Relative to placebo, symptom frequency declined more quickly and steeply on fezolinetant. By week 12, both achieved reductions of about 60%. Statistical P values for the differences in the three arms were not provided, but Dr. Neal-Perry reported they were significant.
Vasomotor severity, like frequency, is reduced
The change in vasomotor severity, which subjects in the trial rated as better or worse, was also significant. The differences in the severity curves were less, but they separated in favor of the two active treatment arms by about 2 weeks, and the curves continued to show an advantage for fezolinetant over both the first 12 weeks and then the remaining 40 weeks.
Overall, the decline in vasomotor symptom frequency remained on a persistent downward slope on both doses of fezolinetant for the full 52 weeks of the study, so that the reduction at 52 weeks was on the order of 25% greater than that seen at 12 weeks.
At 52 weeks, “you can see that individuals on placebo who were crossed over to an active treatment had a significant reduction in their hot flashes and look very much like those who were randomized to fezolinetant at the beginning of the study,” said Dr. Neal-Perry, who is chair of the department of obstetrics and gynecology at the University of North Carolina at Chapel Hill.
Other outcomes also favored fezolinetant over placebo. For example, a reduction in sleep disturbance observed at 12 weeks was sustained over the full 52 weeks of the study. The reduction in sleep symptoms appeared to be slightly greater on the higher dose, but the benefit at 52 weeks among patients after the crossover was similar on either active arm.
No serious side effects identified
There were no serious drug-related treatment-emergent adverse events in any treatment group. One patient in the placebo arm (< 1%), two patients in the 30-mg fezolinetant arm (1.2%), and five patients in the 45-mg arm (3%) discontinued therapy for an adverse event considered to be treatment related.
“The most common side effect associated with fezolinetant was headache. There were no other side effects that led patients to pull out of the study,” Dr. Neal-Perry reported at the meeting, which was held in Atlanta and virtually.
According to Dr. Neal-Perry the vasomotor symptoms relative to menopause, which occur in almost all women, are moderate to severe in an estimated 35%-45%. Some groups, such as those with an elevated body mass index and African Americans, appear to be at even greater risk. Study enrollment was specifically designed to include these high-risk groups, but the subgroup efficacy data have not yet been analyzed.
Other drugs with a similar mechanism of action have not been brought forward because of concern about elevated liver enzymes, but Dr. Neal-Perry said that this does not appear to be an issue for fezolinetant, which was designed with greater specificity for the NK3 target than previous treatments.
If fezolinetant is approved, Dr. Neal-Perry expects this agent to fulfill an important unmet need because of the limitations of other nonhormonal solutions for control of menopause symptoms.
HT alternatives limited
For control of many menopause symptoms, particularly hot flashes, hormone therapy (HT) is the most efficacious, but Richard J. Santen, MD, emeritus professor and an endocrinologist at the University of Virginia, Charlottesville, agreed there is a need for alternatives.
In addition to those who have contraindications for HT, Dr. Santen said in an interview that this option is not acceptable to others “for a variety of reasons.” The problem is that the alternatives are limited.
“The SSRI agents and gabapentin are alternative nonhormonal agents, but they have side effects and are not as effective,” he said. Hot flashes “can be a major disruptor of quality of life,” so he is intrigued with the positive results achieved with fezolinetant.
“A new drug such as reported at the Endocrine Society meeting would be an important new addition to the armamentarium,” he said.
Dr. Neal-Perry reports no conflicts of interest.
FROM ENDO 2022
Exercise of any type boosts type 1 diabetes time in range
Adults with type 1 diabetes had significantly better glycemic control on days they exercised, regardless of exercise type, compared to days when they were inactive, according to a prospective study in nearly 500 individuals.
Different types of exercise, such as aerobic workouts, interval training, or resistance training, may have different immediate glycemic effects in adults with type 1 diabetes (T1D), but the impact of exercise type on the percentage of time diabetes patients maintain glucose in the 70-180 mg/dL range on days when they are active vs. inactive has not been well studied, Zoey Li said in a presentation at the annual scientific sessions of the American Diabetes Association.
In the Type 1 Diabetes Exercise Initiative (T1DEXI) study, Ms. Li and colleagues examined continuous glucose monitoring (CGM) data from 497 adults with T1D. The observational study included self-referred adults aged 18 years and older who had been living with T1D for at least 2 years. Participants were assigned to programs of aerobic exercise (defined as a target heart rate of 70%-80% of age-predicted maximum), interval exercise (defined as an interval heart rate of 80%-90% of age-predicted maximum), or resistance exercise (defined as muscle group fatigue after three sets of eight repetitions).
Participants completed the workouts at home via 30-minute videos at least six times over the 4-week study period. The study design involved an activity goal of at least 150 minutes per week, including the videos and self-reported usual activity, such as walking. The data were collected through an app designed for the study, a heart rate monitor, and a CGM.
The researchers compared glucose levels on days when the participants reported being active compared to days when they were sedentary. The goal of the study was to assess the effect of exercise type on time spent with glucose in the range of 70-180 mg/dL, defined as time in range (TIR).
The mean age of the participants was 37 years; 89% were White. The mean duration of diabetes was 18 years, and the mean hemoglobin A1c was 6.6%. “An astounding 95% were current continuous glucose monitoring [CGM] users,” said Ms. Li, a statistician at the Jaeb Center for Health Research in Tampa, Fla.
A total of 398 participants reported at least one exercise day and one sedentary day, for a total of 1,302 exercise days and 2,470 sedentary days.
Overall, the mean TIR was significantly higher on exercise days compared to sedentary days (75% vs. 70%, P < .001). The median time above 180 mg/dL also was significantly lower on exercise days compared to sedentary days (17% vs. 23%, P < .001), and mean glucose levels were 10 mg/dL lower on exercise days (145 mg/dL vs. 155 mg/dL)
“This all came with a slight hit to their time below range,” Ms. Li noted. The median time below 70 mg/dL was 1.1% on exercise days compared to 0.4% on sedentary days (P < .001). The percentage of days with hypoglycemic events was higher on exercise days compared to sedentary days (47% vs. 40%, P < .001), as they are related to time below 70 mg/dL, she added.
The differences for mean glucose level and TIR between exercise days and sedentary days were significant for each of the three exercise types, Ms. Li said.
“After establishing these glycemic trends, we looked at whether there were any factors that influenced the glycemic differences on exercise vs. sedentary days,” Ms. Li said.
Regardless of exercise type, age, sex, baseline A1c, diabetes duration, body mass index, insulin modality, CGM use, and percentage of time below range in the past 24 hours, there was higher TIR and higher hypoglycemia on exercise days compared to sedentary days.
Although the study was limited in part by the observational design, “with these data, we can better understand the glycemic benefits and disadvantages of exercise in adults with type 1 diabetes,” Ms. Li said.
Don’t forget the negative effects of exercise
“It is well known that the three types of exercise can modulate glucose levels. This can be very useful when attempting to reduce excessively high glucose levels, and when encouraging people to engage in frequent, regular, and consistent physical activity and exercise for general cardiovascular pulmonary and musculoskeletal health,” Helena W. Rodbard, MD, an endocrinologist in private practice in Rockville, Md., said in an interview.
“However, it was not known what effects various types of exercise would have on time in range (70-180 mg/dL) and time below range (< 70 mg/dL) measured over a full 24-hour period in people with type 1 diabetes,” said Dr. Rodbard, who was not involved with the study.
“I was surprised to see that the effect of the three different types of exercise were so similar,” Dr. Rodbard noted. “There had been previous reports suggesting that the time course of glucose could be different for these three types of exercise.”
The current study confirms prior knowledge that exercise can help reduce blood glucose, and increase TIR, said Dr. Rodbard. The study shows that TIR increases by roughly 5-7 percentage points (about 1 hour per day) and reduces mean glucose by 9-13 mg/dL irrespective of the three types of exercise,” she said. “There was a suggestion that the risk of increasing hypoglycemia below 70 mg/dL was less likely for resistance exercise than for the interval or aerobic types of exercise,” she noted.
As for additional research, “This study did not address the various ways in which one can mitigate the potentially deleterious effects of exercise, specifically with reference to rates of hypoglycemia, even mild symptomatic biochemical hypoglycemia,” said Dr. Rodbard. “Since the actual amount of time below 70 mg/dL is usually so small (0.3%-0.7% of the 1,440 minutes in the day, or about 5-10 minutes per day on average), it is difficult to measure and there is considerable variability between different people,” she emphasized. “Finding optimal and robust ways to achieve consistency in the reduction of glucose, between days within subjects, and between subjects, will need further examination of various types of protocols for diet, exercise and insulin administration, and of various methods for education of the patient,” she said.
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust. Ms. Li and Dr. Rodbard had no financial conflicts to disclose. Dr. Rodbard serves on the editorial advisory board of Clinical Endocrinology News.
Adults with type 1 diabetes had significantly better glycemic control on days they exercised, regardless of exercise type, compared to days when they were inactive, according to a prospective study in nearly 500 individuals.
Different types of exercise, such as aerobic workouts, interval training, or resistance training, may have different immediate glycemic effects in adults with type 1 diabetes (T1D), but the impact of exercise type on the percentage of time diabetes patients maintain glucose in the 70-180 mg/dL range on days when they are active vs. inactive has not been well studied, Zoey Li said in a presentation at the annual scientific sessions of the American Diabetes Association.
In the Type 1 Diabetes Exercise Initiative (T1DEXI) study, Ms. Li and colleagues examined continuous glucose monitoring (CGM) data from 497 adults with T1D. The observational study included self-referred adults aged 18 years and older who had been living with T1D for at least 2 years. Participants were assigned to programs of aerobic exercise (defined as a target heart rate of 70%-80% of age-predicted maximum), interval exercise (defined as an interval heart rate of 80%-90% of age-predicted maximum), or resistance exercise (defined as muscle group fatigue after three sets of eight repetitions).
Participants completed the workouts at home via 30-minute videos at least six times over the 4-week study period. The study design involved an activity goal of at least 150 minutes per week, including the videos and self-reported usual activity, such as walking. The data were collected through an app designed for the study, a heart rate monitor, and a CGM.
The researchers compared glucose levels on days when the participants reported being active compared to days when they were sedentary. The goal of the study was to assess the effect of exercise type on time spent with glucose in the range of 70-180 mg/dL, defined as time in range (TIR).
The mean age of the participants was 37 years; 89% were White. The mean duration of diabetes was 18 years, and the mean hemoglobin A1c was 6.6%. “An astounding 95% were current continuous glucose monitoring [CGM] users,” said Ms. Li, a statistician at the Jaeb Center for Health Research in Tampa, Fla.
A total of 398 participants reported at least one exercise day and one sedentary day, for a total of 1,302 exercise days and 2,470 sedentary days.
Overall, the mean TIR was significantly higher on exercise days compared to sedentary days (75% vs. 70%, P < .001). The median time above 180 mg/dL also was significantly lower on exercise days compared to sedentary days (17% vs. 23%, P < .001), and mean glucose levels were 10 mg/dL lower on exercise days (145 mg/dL vs. 155 mg/dL)
“This all came with a slight hit to their time below range,” Ms. Li noted. The median time below 70 mg/dL was 1.1% on exercise days compared to 0.4% on sedentary days (P < .001). The percentage of days with hypoglycemic events was higher on exercise days compared to sedentary days (47% vs. 40%, P < .001), as they are related to time below 70 mg/dL, she added.
The differences for mean glucose level and TIR between exercise days and sedentary days were significant for each of the three exercise types, Ms. Li said.
“After establishing these glycemic trends, we looked at whether there were any factors that influenced the glycemic differences on exercise vs. sedentary days,” Ms. Li said.
Regardless of exercise type, age, sex, baseline A1c, diabetes duration, body mass index, insulin modality, CGM use, and percentage of time below range in the past 24 hours, there was higher TIR and higher hypoglycemia on exercise days compared to sedentary days.
Although the study was limited in part by the observational design, “with these data, we can better understand the glycemic benefits and disadvantages of exercise in adults with type 1 diabetes,” Ms. Li said.
Don’t forget the negative effects of exercise
“It is well known that the three types of exercise can modulate glucose levels. This can be very useful when attempting to reduce excessively high glucose levels, and when encouraging people to engage in frequent, regular, and consistent physical activity and exercise for general cardiovascular pulmonary and musculoskeletal health,” Helena W. Rodbard, MD, an endocrinologist in private practice in Rockville, Md., said in an interview.
“However, it was not known what effects various types of exercise would have on time in range (70-180 mg/dL) and time below range (< 70 mg/dL) measured over a full 24-hour period in people with type 1 diabetes,” said Dr. Rodbard, who was not involved with the study.
“I was surprised to see that the effect of the three different types of exercise were so similar,” Dr. Rodbard noted. “There had been previous reports suggesting that the time course of glucose could be different for these three types of exercise.”
The current study confirms prior knowledge that exercise can help reduce blood glucose, and increase TIR, said Dr. Rodbard. The study shows that TIR increases by roughly 5-7 percentage points (about 1 hour per day) and reduces mean glucose by 9-13 mg/dL irrespective of the three types of exercise,” she said. “There was a suggestion that the risk of increasing hypoglycemia below 70 mg/dL was less likely for resistance exercise than for the interval or aerobic types of exercise,” she noted.
As for additional research, “This study did not address the various ways in which one can mitigate the potentially deleterious effects of exercise, specifically with reference to rates of hypoglycemia, even mild symptomatic biochemical hypoglycemia,” said Dr. Rodbard. “Since the actual amount of time below 70 mg/dL is usually so small (0.3%-0.7% of the 1,440 minutes in the day, or about 5-10 minutes per day on average), it is difficult to measure and there is considerable variability between different people,” she emphasized. “Finding optimal and robust ways to achieve consistency in the reduction of glucose, between days within subjects, and between subjects, will need further examination of various types of protocols for diet, exercise and insulin administration, and of various methods for education of the patient,” she said.
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust. Ms. Li and Dr. Rodbard had no financial conflicts to disclose. Dr. Rodbard serves on the editorial advisory board of Clinical Endocrinology News.
Adults with type 1 diabetes had significantly better glycemic control on days they exercised, regardless of exercise type, compared to days when they were inactive, according to a prospective study in nearly 500 individuals.
Different types of exercise, such as aerobic workouts, interval training, or resistance training, may have different immediate glycemic effects in adults with type 1 diabetes (T1D), but the impact of exercise type on the percentage of time diabetes patients maintain glucose in the 70-180 mg/dL range on days when they are active vs. inactive has not been well studied, Zoey Li said in a presentation at the annual scientific sessions of the American Diabetes Association.
In the Type 1 Diabetes Exercise Initiative (T1DEXI) study, Ms. Li and colleagues examined continuous glucose monitoring (CGM) data from 497 adults with T1D. The observational study included self-referred adults aged 18 years and older who had been living with T1D for at least 2 years. Participants were assigned to programs of aerobic exercise (defined as a target heart rate of 70%-80% of age-predicted maximum), interval exercise (defined as an interval heart rate of 80%-90% of age-predicted maximum), or resistance exercise (defined as muscle group fatigue after three sets of eight repetitions).
Participants completed the workouts at home via 30-minute videos at least six times over the 4-week study period. The study design involved an activity goal of at least 150 minutes per week, including the videos and self-reported usual activity, such as walking. The data were collected through an app designed for the study, a heart rate monitor, and a CGM.
The researchers compared glucose levels on days when the participants reported being active compared to days when they were sedentary. The goal of the study was to assess the effect of exercise type on time spent with glucose in the range of 70-180 mg/dL, defined as time in range (TIR).
The mean age of the participants was 37 years; 89% were White. The mean duration of diabetes was 18 years, and the mean hemoglobin A1c was 6.6%. “An astounding 95% were current continuous glucose monitoring [CGM] users,” said Ms. Li, a statistician at the Jaeb Center for Health Research in Tampa, Fla.
A total of 398 participants reported at least one exercise day and one sedentary day, for a total of 1,302 exercise days and 2,470 sedentary days.
Overall, the mean TIR was significantly higher on exercise days compared to sedentary days (75% vs. 70%, P < .001). The median time above 180 mg/dL also was significantly lower on exercise days compared to sedentary days (17% vs. 23%, P < .001), and mean glucose levels were 10 mg/dL lower on exercise days (145 mg/dL vs. 155 mg/dL)
“This all came with a slight hit to their time below range,” Ms. Li noted. The median time below 70 mg/dL was 1.1% on exercise days compared to 0.4% on sedentary days (P < .001). The percentage of days with hypoglycemic events was higher on exercise days compared to sedentary days (47% vs. 40%, P < .001), as they are related to time below 70 mg/dL, she added.
The differences for mean glucose level and TIR between exercise days and sedentary days were significant for each of the three exercise types, Ms. Li said.
“After establishing these glycemic trends, we looked at whether there were any factors that influenced the glycemic differences on exercise vs. sedentary days,” Ms. Li said.
Regardless of exercise type, age, sex, baseline A1c, diabetes duration, body mass index, insulin modality, CGM use, and percentage of time below range in the past 24 hours, there was higher TIR and higher hypoglycemia on exercise days compared to sedentary days.
Although the study was limited in part by the observational design, “with these data, we can better understand the glycemic benefits and disadvantages of exercise in adults with type 1 diabetes,” Ms. Li said.
Don’t forget the negative effects of exercise
“It is well known that the three types of exercise can modulate glucose levels. This can be very useful when attempting to reduce excessively high glucose levels, and when encouraging people to engage in frequent, regular, and consistent physical activity and exercise for general cardiovascular pulmonary and musculoskeletal health,” Helena W. Rodbard, MD, an endocrinologist in private practice in Rockville, Md., said in an interview.
“However, it was not known what effects various types of exercise would have on time in range (70-180 mg/dL) and time below range (< 70 mg/dL) measured over a full 24-hour period in people with type 1 diabetes,” said Dr. Rodbard, who was not involved with the study.
“I was surprised to see that the effect of the three different types of exercise were so similar,” Dr. Rodbard noted. “There had been previous reports suggesting that the time course of glucose could be different for these three types of exercise.”
The current study confirms prior knowledge that exercise can help reduce blood glucose, and increase TIR, said Dr. Rodbard. The study shows that TIR increases by roughly 5-7 percentage points (about 1 hour per day) and reduces mean glucose by 9-13 mg/dL irrespective of the three types of exercise,” she said. “There was a suggestion that the risk of increasing hypoglycemia below 70 mg/dL was less likely for resistance exercise than for the interval or aerobic types of exercise,” she noted.
As for additional research, “This study did not address the various ways in which one can mitigate the potentially deleterious effects of exercise, specifically with reference to rates of hypoglycemia, even mild symptomatic biochemical hypoglycemia,” said Dr. Rodbard. “Since the actual amount of time below 70 mg/dL is usually so small (0.3%-0.7% of the 1,440 minutes in the day, or about 5-10 minutes per day on average), it is difficult to measure and there is considerable variability between different people,” she emphasized. “Finding optimal and robust ways to achieve consistency in the reduction of glucose, between days within subjects, and between subjects, will need further examination of various types of protocols for diet, exercise and insulin administration, and of various methods for education of the patient,” she said.
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust. Ms. Li and Dr. Rodbard had no financial conflicts to disclose. Dr. Rodbard serves on the editorial advisory board of Clinical Endocrinology News.
FROM ADA 2022
‘Forever chemicals’ linked to hypertension in middle-aged women
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large, prospective study, researchers found an association between higher blood levels of PFAS and increased risk of hypertension in middle-aged women. Women in the highest tertile of overall PFAS concentrations had a 71% increased risk of developing hypertension.
“Our findings suggest that long-term cumulative exposure, even before midlife, may increase the risk of high blood pressure, and therefore, the benefit of reducing the population exposure to PFAS and potential prevention of high blood pressure and other health conditions would be enormous,” Sung Kyun Park, ScD, MPH, University of Michigan School of Public Health, Ann Arbor, said in an interview.
The study was published online in Hypertension.
Everywhere and forever
“PFAS are forever chemicals as well as everywhere chemicals,” Dr. Park noted.
Possible sources of PFAS exposure run the gamut from nonstick cookware, food wrappers, and waterproof fabrics to cosmetics and drinking water. They have been detected in the blood of most people and have been linked to a variety of health concerns.
“A few studies showed an association between PFAS and hypertension, but those were cross-sectional and examined prevalence of hypertension. It was unclear whether PFAS are associated with the development (incidence) of hypertension,” Dr. Park explained.
For their study, the researchers examined the association between serum concentrations of PFAS and risks of incident hypertension in 1,058 initially normotensive women participating in the Study of Women’s Health Across the Nation-Multi-Pollutant Study (SWAN-MPS). They were followed annually between 1999 and 2017.
During 11,722 person-years of follow-up, 470 of the women developed hypertension, at a rate of 40.1 cases per 1,000 person-years. Hypertension was defined as blood pressure of at least 140 mm Hg systolic or at least 90 mm Hg diastolic or receiving antihypertensive treatment.
Women in the highest tertile of baseline serum concentration of perfluorooctane sulfonate (PFOS) had a 42% higher risk of developing hypertension, compared with peers in the lowest tertile (adjusted hazard ratio, 1.42; 95% confidence interval, 1.19-1.68; P trend = .01).
Similar results were found for perfluorooctanoate (PFOA) and 2-N-ethyl-perfluorooctane sulfonamido acetate (EtFOSAA), with 47% (aHR, 1.47; 95% CI, 1.24-1.75; P trend = .01) and 42% (aHR, 1.42; 95% CI, 1.19-1.70; P trend = .01) higher risks of incident hypertension, comparing the highest to the lowest tertiles.
The risks persisted after adjusting for various factors, including race, study site, education, financial strain, smoking status, alcohol use, total calorie intake, and menopausal status.
In the PFAS “mixture” analysis, women in the highest tertile of overall PFAS concentrations were 71% more likely to develop hypertension during follow-up, compared with women in the lowest tertile (aHR, 1.71; 95% CI, 1.15-2.54; P trend = .008).
“These findings suggest that PFAS might be an underappreciated contributing factor to women’s cardiovascular disease risk,” the researchers write.
They caution that the study only included middle-aged women and that it is unclear whether the findings hold for middle-aged men.
“This is an important question, but the answer is that we do not know,” Dr. Park told this news organization.
“Women become more susceptible to metabolic changes and hypertension risk during the menopausal transition. Our findings suggest that PFAS may play a role in the development of hypertension in women during this critical life stage,” Dr. Park said.
The researchers say more research is needed to confirm and expand the findings and to find ways to reduce PFAS exposure.
“If confirmed in future studies, these findings suggest that understanding human exposure to PFAS and developing effective strategies to reduce PFAS exposure may help prevent the development of hypertension and thereby reduce the global burden of CVD,” the researchers write.
‘The more we learn, the worse it gets’
This is an “interesting” study and shows that “the more we learn about PFAS, the worse it seems to get,” Ankur Shah, MD, division of kidney disease and hypertension, Warren Alpert Medical School of Brown University, Providence, R.I., said in an interview.
“This multisite, multiracial and multiethnic, community-based longitudinal study establishes an association between PFAS and hypertension,” said Dr. Shah, who wasn’t involved in the study.
“This adds to a growing literature base of associations of PFAS with illnesses, including malignancy, thyroid disorders, diabetes, ulcerative colitis, hyperlipidemia, and pregnancy-induced hypertension,” he noted.
Dr. Shah also noted that the authors adjusted for race and ethnicity, study site, education, financial strain, smoking status, environmental tobacco smoke, alcohol consumption, total calorie intake, and menopausal status “and still found a strong association.”
“Still to be determined are both whether PFAS are the causative agent or if there is an unmeasured/unadjusted for entity which has resulted in both increased PFAS exposure and hypertension, as well as if PFAS are causative, if reduction in PFAS exposure would be result in blood pressure reduction,” Dr. Shah added.
The study had no sources of funding. Dr. Park and Dr. Shah have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
‘DIY’ artificial pancreas systems found to be safe, effective: CREATE trial
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADA 2022
A ‘crisis’ of suicidal thoughts, attempts in transgender youth
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
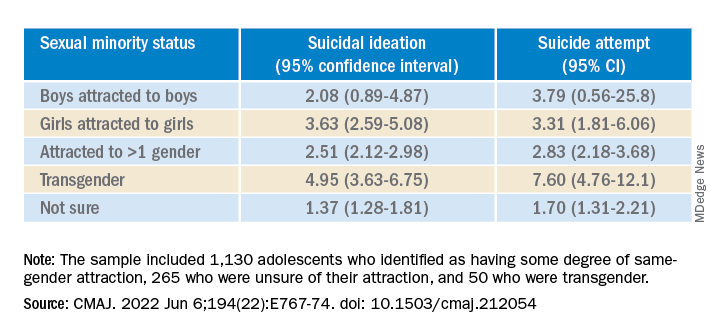
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
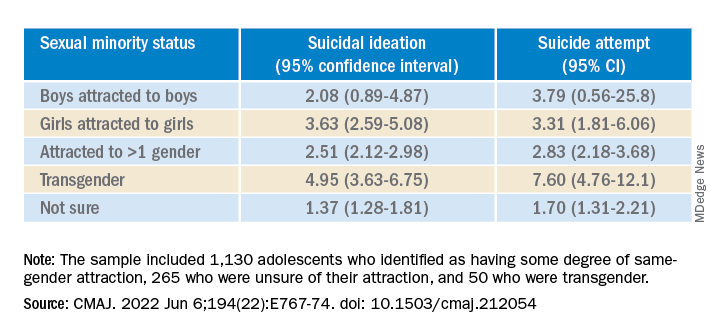
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Transgender youth are significantly more likely to consider suicide and attempt it, compared with their cisgender peers, new research shows.
In a large population-based study, investigators found the increased risk of suicidality is partly because of bullying and cyberbullying experienced by transgender teens.
The findings are “extremely concerning and should be a wake-up call,” Ian Colman, PhD, with the University of Ottawa School of Epidemiology and Public Health, said in an interview.
Young people who are exploring their sexual identities may suffer from depression and anxiety, both about the reactions of their peers and families, as well as their own sense of self.
“These youth are highly marginalized and stigmatized in many corners of our society, and these findings highlight just how distressing these experiences can be,” Dr. Colman said.
The study was published online in the Canadian Medical Association Journal.
Sevenfold increased risk of attempted suicide
The risk of suicidal thoughts and actions is not well studied in transgender and nonbinary youth.
To expand the evidence base, the researchers analyzed data for 6,800 adolescents aged 15-17 years from the 2019 Canadian Health Survey on Children and Youth.
The sample included 1,130 (16.5%) adolescents who identified as having some degree of same-gender attraction, 265 (4.3%) who were unsure of their attraction (“questioning”), and 50 (0.6%) who were transgender, meaning they identified as being of a gender different from that assigned at birth.
Overall, 980 (14.0%) adolescents reported having thoughts of suicide in the prior year, and 480 (6.8%) had attempted suicide in their life.
Transgender youth were five times more likely to think about suicide and more than seven times more likely to have ever attempted suicide than cisgender, heterosexual peers.
Among cisgender adolescents, girls who were attracted to girls had 3.6 times the risk of suicidal ideation and 3.3 times the risk of having ever attempted suicide, compared with their heterosexual peers.
Teens attracted to multiple genders had more than twice the risk of suicidal ideation and suicide attempt. Youth who were questioning their sexual orientation had twice the risk of having attempted suicide in their lifetime.
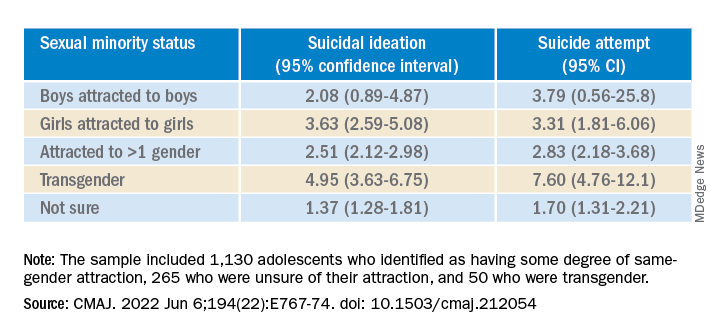
A crisis – with reason for hope
“This is a crisis, and it shows just how much more needs to be done to support transgender young people,” co-author Fae Johnstone, MSW, executive director, Wisdom2Action, who is a trans woman herself, said in the news release.
“Suicide prevention programs specifically targeted to transgender, nonbinary, and sexual minority adolescents, as well as gender-affirming care for transgender adolescents, may help reduce the burden of suicidality among this group,” Ms. Johnstone added.
“The most important thing that parents, teachers, and health care providers can do is to be supportive of these youth,” Dr. Colman told this news organization.
“Providing a safe place where gender and sexual minorities can explore and express themselves is crucial. The first step is to listen and to be compassionate,” Dr. Colman added.
Reached for comment, Jess Ting, MD, director of surgery at the Mount Sinai Center for Transgender Medicine and Surgery, New York, said the data from this study on suicidal thoughts and actions among sexual minority and transgender adolescents “mirror what we see and what we know” about suicidality in trans and nonbinary adults.
“The reasons for this are complex, and it’s hard for someone who doesn’t have a lived experience as a trans or nonbinary person to understand the reasons for suicidality,” he told this news organization.
“But we also know that there are higher rates of anxiety and depression and self-image issues and posttraumatic stress disorder, not to mention outside factors – marginalization, discrimination, violence, abuse. When you add up all these intrinsic and extrinsic factors, it’s not hard to believe that there is a high rate of suicidality,” Dr. Ting said.
“There have been studies that have shown that in children who are supported in their gender identity, the rates of depression and anxiety decreased to almost the same levels as non-trans and nonbinary children, so I think that gives cause for hope,” Dr. Ting added.
The study was funded in part by the Research Council of Norway through its Centres of Excellence funding scheme and by a Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Award. Ms. Johnstone reports consulting fees from Spectrum Waterloo and volunteer participation with the Youth Suicide Prevention Leadership Committee of Ontario. No other competing interests were declared. Dr. Ting has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
New studies show growing number of trans, nonbinary youth in U.S.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.
Two new studies point to an ever-increasing number of young people in the United States who identify as transgender and nonbinary, with the figures doubling among 18- to 24-year-olds in one institute’s research – from 0.66% of the population in 2016 to 1.3% (398,900) in 2022.
In addition, 1.4% (300,100) of 13- to 17-year-olds identify as trans or nonbinary, according to the report from that group, the Williams Institute at the University of California, Los Angeles, School of Law.
Williams, which conducts independent research on sexual orientation and gender identity law and public policy, did not contain data on 13- to 17-year-olds in its 2016 study, so the growth in that group over the past 5+ years is not as well documented.
Overall, some 1.6 million Americans older than age 13 now identify as transgender, reported the Williams researchers.
And in a new Pew Research Center survey, 2% of adults aged 18-29 identify as transgender and 3% identify as nonbinary, a far greater number than in other age cohorts.
These reports are likely underestimates. The Human Rights Campaign estimates that some 2 million Americans of all ages identify as transgender.
The Pew survey is weighted to be representative but still has limitations, said the organization. The Williams analysis, based on responses to two CDC surveys – the Behavioral Risk Factor Surveillance System (BRFSS) and Youth Risk Behavior Survey (YRBS) – is incomplete, say researchers, because not every state collects data on gender identity.
Transgender identities more predominant among youth
The Williams researchers report that 18.3% of those who identified as trans were 13- to 17-year-olds; that age group makes up 7.6% of the United States population 13 and older.
And despite not having firm figures from earlier reports, they comment: “Youth ages 13-17 comprise a larger share of the transgender-identified population than we previously estimated, currently comprising about 18% of the transgender-identified population in the United State, up from 10% previously.”
About one-quarter of those who identified as trans in the new 2022 report were aged 18-24; that age cohort accounts for 11% of Americans.
The number of older Americans who identify as trans are more proportionate to their representation in the population, according to Williams. Overall, about half of those who said they were trans were aged 25-64; that group accounts for 62% of the overall American population. Some 10% of trans-identified individuals were over age 65. About 20% of Americans are 65 or older, said the researchers.
The Pew research – based on the responses of 10,188 individuals surveyed in May – also found growing numbers of young people who identify as trans. “The share of U.S. adults who are transgender is particularly high among adults younger than 25,” reported Pew in a blog post.
In the 18- to 25-year-old group, 3.1% identified as a trans man or a trans woman, compared with just 0.5% of those ages 25-29.
That compares to 0.3% of those aged 30-49 and 0.2% of those older than 50.
Racial and state-by-state variation
Similar percentages of youth aged 13-17 of all races and ethnicities in the Williams study report they are transgender, ranging from 1% of those who are Asian, to 1.3% of White youth, 1.4% of Black youth, 1.8% of American Indian or Alaska Native, and 1.8% of Latinx youth. The institute reported that 1.5% of biracial and multiracial youth identified as transgender.
The researchers said, however, that “transgender-identified youth and adults appear more likely to report being Latinx and less likely to report being White, as compared to the United States population.”
Transgender individuals live in every state, with the greatest percentage of both youth and adults in the Northeast and West, and lesser percentages in the Midwest and South, reported the Williams Institute.
Williams estimates as many as 3% of 13- to 17-year-olds in New York identify as trans, while just 0.6% of that age group in Wyoming is transgender. A total of 2%-2.5% of those aged 13-17 are transgender in Hawaii, New Mexico, Maryland, and Washington, D.C.
Among the states with higher percentages of trans-identifying 18- to 24-year-olds: Arizona (1.9%), Arkansas (3.6%), Colorado (2%), Delaware (2.4%), Illinois (1.9%), Maryland (1.9%), North Carolina (2.5%), Oklahoma (2.5%), Massachusetts (2.3%), Rhode Island (2.1%), and Washington (2%).
A version of this article first appeared on Medscape.com.










