User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Pulse oximeters lead to less oxygen supplementation for people of color
The new research suggests that skin color–related differences in pulse oximeter readings are in fact impacting clinical decision-making, lead author Eric R. Gottlieb, MD, of Brigham and Women’s Hospital and Massachusetts Institute of Technology, both in Boston, and colleagues wrote. This suggests that technology needs to updated to improve health equity, they continued, in their paper published in JAMA Internal Medicine.
“It has been known for decades that these readings are affected by various surface pigmentations, including nail polish and skin melanin, which may affect light absorption and scattering,” the investigators wrote. “This increases the risk of hidden hypoxemia [among patients with darker skin], in which patients have falsely elevated SpO2 readings, usually defined as 92% or greater, with a blood hemoglobin oxygen saturation less than 88%.”
Although published reports on this phenomenon date back to the 1980s, clinical significance has been largely discounted, they said, citing a 2008 paper on the topic, which stated that “oximetry need not have exact accuracy” to determine if a patient needs oxygen supplementation.
‘We’re not providing equal care’
Questioning the validity of this statement, Dr. Gottlieb and colleagues conducted a retrospective cohort study involving 3,069 patients admitted to intensive care at the Beth Israel Deaconess Medical Center in Boston between 2008 and 2019, thereby excluding patients treated during the COVID-19 pandemic. The population consisted of four races/ethnicities: White (87%), Black (7%), Hispanic (4%), and Asian (3%).
Aligning with previous studies, multivariable linear regression analyses showed that Asian, Black, and Hispanic patients had significantly higher SpO2 readings than White patients in relation to hemoglobin oxygen saturation values, suggesting falsely elevated readings.
Further modeling showed that these same patient groups also received lower oxygen delivery rates, which were not explained directly by race/ethnicity, but instead were mediated by the discrepancy between SpO2 and hemoglobin oxygen saturation values. In other words, physicians were responding consistently to pulse oximetry readings, rather than exhibiting a direct racial/ethnic bias in their clinical decision-making.
“We’re not providing equal care,” Dr. Gottlieb said in an interview. “It’s not that the patients are sicker, or have other socioeconomic explanations for why this happens to them. It’s us. It’s our technology. And that’s something that really has to be fixed.”
The investigators offered a cautionary view of corrective algorithms, as these “have exacerbated disparities and are subject to ethical concerns;” for example, with glomerular filtration rate estimations in Black patients.
Dr. Gottlieb also cautioned against action by individual physicians, who may now be inclined to change how they interpret pulse oximeter readings based on a patient’s race or ethnicity.
“I don’t think that we can expect physicians, every time they see a patient, to be second guessing whether the number basically reflects the truth,” he said.
Instead, Dr. Gottlieb suggested that the burden of change rests upon the shoulders of institutions, including hospitals and device manufacturers, both of which “really need to take the responsibility” for making sure that pulse oximeters are “equitable and have similar performance across races.”
While Dr. Gottlieb said that skin color likely plays the greatest role in measurement discrepancies, he encouraged stakeholders “to think broadly about this, and not just assume that it’s entirely skin color,” noting a small amount of evidence indicating that blood chemistry may also play a role. Still, he predicted that colorimetry – the direct measurement of skin color – will probably be incorporated into pulse oximeters of the future.
Black patients 3X more likely to have hidden hypoxia than White patients
Michael Sjoding, MD, of the University of Michigan, Ann Arbor, was one of the first to raise awareness of skin color–related issues with pulse oximeters during the throes of the COVID-19 pandemic. His study, which involved more than 10,000 patients, showed that Black patients were threefold more likely to have hidden hypoxia than White patients.
The present study shows that such discrepancies are indeed clinically significant, Dr. Sjoding said in an interview. And these data are needed, he added, to bring about change.
“What is being asked is potentially a big deal,” Dr. Sjoding said. “Pulse oximeters are everywhere, and it would be a big undertaking to redesign pulse oximeters and purchase new pulse oximeters. You need a compelling body of evidence to do that. I think it’s there now, clearly. So I’m hopeful that we’re going to finally move forward, towards having devices that we are confident work accurately in everyone.”
Why it has taken so long to gather this evidence, however, is a thornier topic, considering race-related discrepancies in pulse oximeter readings were first documented more than 3 decades ago.
“We sort of rediscovered something that had been known and had been described in the past,” Dr. Sjoding said. He explained how he and many of his colleagues had completed pulmonary fellowships, yet none of them knew of these potential issues with pulse oximeters until they began to observe differences in their own patients during the pandemic.
“I’ll give previous generations of researchers the benefit of the doubt,” Dr. Sjoding said, pointing out that techniques in data gathering and analysis have advanced considerably over the years. “The types of studies that were done before were very different than what we did.”
Yet Dr. Sjoding entertained the possibility that other factors may have been at play.
“I think definitely there’s a social commentary on prioritization of research,” he said.
The study was supported by grants from the National Institutes of Health. The investigators and Dr. Sjoding reported no conflicts of interest.
The new research suggests that skin color–related differences in pulse oximeter readings are in fact impacting clinical decision-making, lead author Eric R. Gottlieb, MD, of Brigham and Women’s Hospital and Massachusetts Institute of Technology, both in Boston, and colleagues wrote. This suggests that technology needs to updated to improve health equity, they continued, in their paper published in JAMA Internal Medicine.
“It has been known for decades that these readings are affected by various surface pigmentations, including nail polish and skin melanin, which may affect light absorption and scattering,” the investigators wrote. “This increases the risk of hidden hypoxemia [among patients with darker skin], in which patients have falsely elevated SpO2 readings, usually defined as 92% or greater, with a blood hemoglobin oxygen saturation less than 88%.”
Although published reports on this phenomenon date back to the 1980s, clinical significance has been largely discounted, they said, citing a 2008 paper on the topic, which stated that “oximetry need not have exact accuracy” to determine if a patient needs oxygen supplementation.
‘We’re not providing equal care’
Questioning the validity of this statement, Dr. Gottlieb and colleagues conducted a retrospective cohort study involving 3,069 patients admitted to intensive care at the Beth Israel Deaconess Medical Center in Boston between 2008 and 2019, thereby excluding patients treated during the COVID-19 pandemic. The population consisted of four races/ethnicities: White (87%), Black (7%), Hispanic (4%), and Asian (3%).
Aligning with previous studies, multivariable linear regression analyses showed that Asian, Black, and Hispanic patients had significantly higher SpO2 readings than White patients in relation to hemoglobin oxygen saturation values, suggesting falsely elevated readings.
Further modeling showed that these same patient groups also received lower oxygen delivery rates, which were not explained directly by race/ethnicity, but instead were mediated by the discrepancy between SpO2 and hemoglobin oxygen saturation values. In other words, physicians were responding consistently to pulse oximetry readings, rather than exhibiting a direct racial/ethnic bias in their clinical decision-making.
“We’re not providing equal care,” Dr. Gottlieb said in an interview. “It’s not that the patients are sicker, or have other socioeconomic explanations for why this happens to them. It’s us. It’s our technology. And that’s something that really has to be fixed.”
The investigators offered a cautionary view of corrective algorithms, as these “have exacerbated disparities and are subject to ethical concerns;” for example, with glomerular filtration rate estimations in Black patients.
Dr. Gottlieb also cautioned against action by individual physicians, who may now be inclined to change how they interpret pulse oximeter readings based on a patient’s race or ethnicity.
“I don’t think that we can expect physicians, every time they see a patient, to be second guessing whether the number basically reflects the truth,” he said.
Instead, Dr. Gottlieb suggested that the burden of change rests upon the shoulders of institutions, including hospitals and device manufacturers, both of which “really need to take the responsibility” for making sure that pulse oximeters are “equitable and have similar performance across races.”
While Dr. Gottlieb said that skin color likely plays the greatest role in measurement discrepancies, he encouraged stakeholders “to think broadly about this, and not just assume that it’s entirely skin color,” noting a small amount of evidence indicating that blood chemistry may also play a role. Still, he predicted that colorimetry – the direct measurement of skin color – will probably be incorporated into pulse oximeters of the future.
Black patients 3X more likely to have hidden hypoxia than White patients
Michael Sjoding, MD, of the University of Michigan, Ann Arbor, was one of the first to raise awareness of skin color–related issues with pulse oximeters during the throes of the COVID-19 pandemic. His study, which involved more than 10,000 patients, showed that Black patients were threefold more likely to have hidden hypoxia than White patients.
The present study shows that such discrepancies are indeed clinically significant, Dr. Sjoding said in an interview. And these data are needed, he added, to bring about change.
“What is being asked is potentially a big deal,” Dr. Sjoding said. “Pulse oximeters are everywhere, and it would be a big undertaking to redesign pulse oximeters and purchase new pulse oximeters. You need a compelling body of evidence to do that. I think it’s there now, clearly. So I’m hopeful that we’re going to finally move forward, towards having devices that we are confident work accurately in everyone.”
Why it has taken so long to gather this evidence, however, is a thornier topic, considering race-related discrepancies in pulse oximeter readings were first documented more than 3 decades ago.
“We sort of rediscovered something that had been known and had been described in the past,” Dr. Sjoding said. He explained how he and many of his colleagues had completed pulmonary fellowships, yet none of them knew of these potential issues with pulse oximeters until they began to observe differences in their own patients during the pandemic.
“I’ll give previous generations of researchers the benefit of the doubt,” Dr. Sjoding said, pointing out that techniques in data gathering and analysis have advanced considerably over the years. “The types of studies that were done before were very different than what we did.”
Yet Dr. Sjoding entertained the possibility that other factors may have been at play.
“I think definitely there’s a social commentary on prioritization of research,” he said.
The study was supported by grants from the National Institutes of Health. The investigators and Dr. Sjoding reported no conflicts of interest.
The new research suggests that skin color–related differences in pulse oximeter readings are in fact impacting clinical decision-making, lead author Eric R. Gottlieb, MD, of Brigham and Women’s Hospital and Massachusetts Institute of Technology, both in Boston, and colleagues wrote. This suggests that technology needs to updated to improve health equity, they continued, in their paper published in JAMA Internal Medicine.
“It has been known for decades that these readings are affected by various surface pigmentations, including nail polish and skin melanin, which may affect light absorption and scattering,” the investigators wrote. “This increases the risk of hidden hypoxemia [among patients with darker skin], in which patients have falsely elevated SpO2 readings, usually defined as 92% or greater, with a blood hemoglobin oxygen saturation less than 88%.”
Although published reports on this phenomenon date back to the 1980s, clinical significance has been largely discounted, they said, citing a 2008 paper on the topic, which stated that “oximetry need not have exact accuracy” to determine if a patient needs oxygen supplementation.
‘We’re not providing equal care’
Questioning the validity of this statement, Dr. Gottlieb and colleagues conducted a retrospective cohort study involving 3,069 patients admitted to intensive care at the Beth Israel Deaconess Medical Center in Boston between 2008 and 2019, thereby excluding patients treated during the COVID-19 pandemic. The population consisted of four races/ethnicities: White (87%), Black (7%), Hispanic (4%), and Asian (3%).
Aligning with previous studies, multivariable linear regression analyses showed that Asian, Black, and Hispanic patients had significantly higher SpO2 readings than White patients in relation to hemoglobin oxygen saturation values, suggesting falsely elevated readings.
Further modeling showed that these same patient groups also received lower oxygen delivery rates, which were not explained directly by race/ethnicity, but instead were mediated by the discrepancy between SpO2 and hemoglobin oxygen saturation values. In other words, physicians were responding consistently to pulse oximetry readings, rather than exhibiting a direct racial/ethnic bias in their clinical decision-making.
“We’re not providing equal care,” Dr. Gottlieb said in an interview. “It’s not that the patients are sicker, or have other socioeconomic explanations for why this happens to them. It’s us. It’s our technology. And that’s something that really has to be fixed.”
The investigators offered a cautionary view of corrective algorithms, as these “have exacerbated disparities and are subject to ethical concerns;” for example, with glomerular filtration rate estimations in Black patients.
Dr. Gottlieb also cautioned against action by individual physicians, who may now be inclined to change how they interpret pulse oximeter readings based on a patient’s race or ethnicity.
“I don’t think that we can expect physicians, every time they see a patient, to be second guessing whether the number basically reflects the truth,” he said.
Instead, Dr. Gottlieb suggested that the burden of change rests upon the shoulders of institutions, including hospitals and device manufacturers, both of which “really need to take the responsibility” for making sure that pulse oximeters are “equitable and have similar performance across races.”
While Dr. Gottlieb said that skin color likely plays the greatest role in measurement discrepancies, he encouraged stakeholders “to think broadly about this, and not just assume that it’s entirely skin color,” noting a small amount of evidence indicating that blood chemistry may also play a role. Still, he predicted that colorimetry – the direct measurement of skin color – will probably be incorporated into pulse oximeters of the future.
Black patients 3X more likely to have hidden hypoxia than White patients
Michael Sjoding, MD, of the University of Michigan, Ann Arbor, was one of the first to raise awareness of skin color–related issues with pulse oximeters during the throes of the COVID-19 pandemic. His study, which involved more than 10,000 patients, showed that Black patients were threefold more likely to have hidden hypoxia than White patients.
The present study shows that such discrepancies are indeed clinically significant, Dr. Sjoding said in an interview. And these data are needed, he added, to bring about change.
“What is being asked is potentially a big deal,” Dr. Sjoding said. “Pulse oximeters are everywhere, and it would be a big undertaking to redesign pulse oximeters and purchase new pulse oximeters. You need a compelling body of evidence to do that. I think it’s there now, clearly. So I’m hopeful that we’re going to finally move forward, towards having devices that we are confident work accurately in everyone.”
Why it has taken so long to gather this evidence, however, is a thornier topic, considering race-related discrepancies in pulse oximeter readings were first documented more than 3 decades ago.
“We sort of rediscovered something that had been known and had been described in the past,” Dr. Sjoding said. He explained how he and many of his colleagues had completed pulmonary fellowships, yet none of them knew of these potential issues with pulse oximeters until they began to observe differences in their own patients during the pandemic.
“I’ll give previous generations of researchers the benefit of the doubt,” Dr. Sjoding said, pointing out that techniques in data gathering and analysis have advanced considerably over the years. “The types of studies that were done before were very different than what we did.”
Yet Dr. Sjoding entertained the possibility that other factors may have been at play.
“I think definitely there’s a social commentary on prioritization of research,” he said.
The study was supported by grants from the National Institutes of Health. The investigators and Dr. Sjoding reported no conflicts of interest.
FROM JAMA INTERNAL MEDICINE
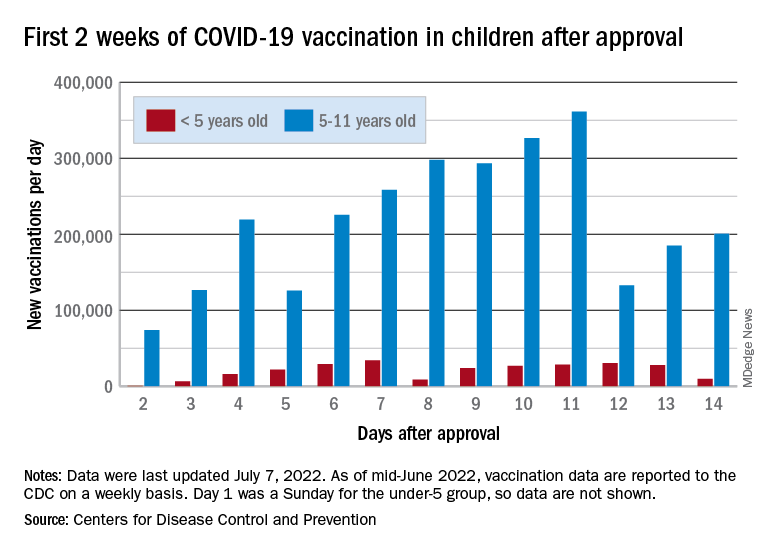
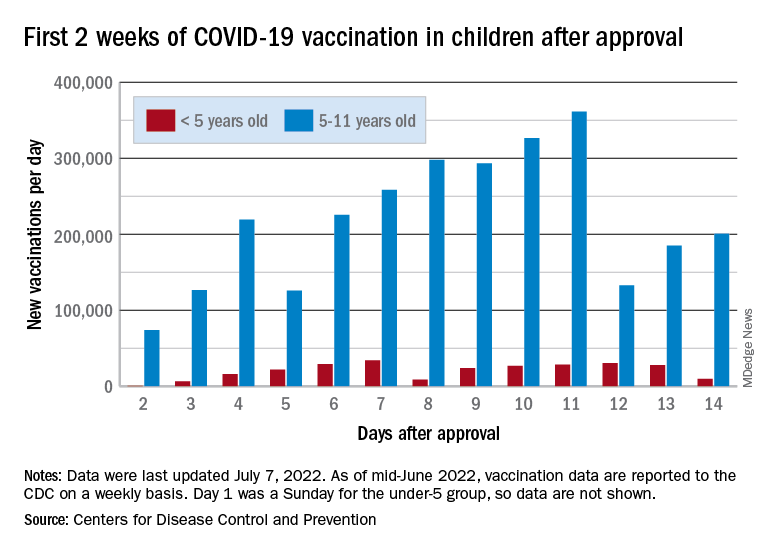
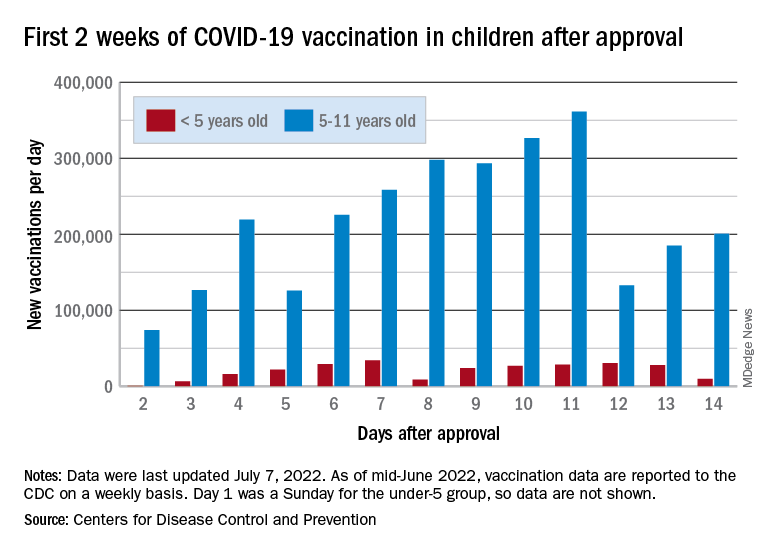
Children and COVID: Vaccination a harder sell in the summer
The COVID-19 vaccination effort in the youngest children has begun much more slowly than the most recent rollout for older children, according to the Centers for Disease Control and Prevention.
in early November of 2021, based on CDC data last updated on July 7.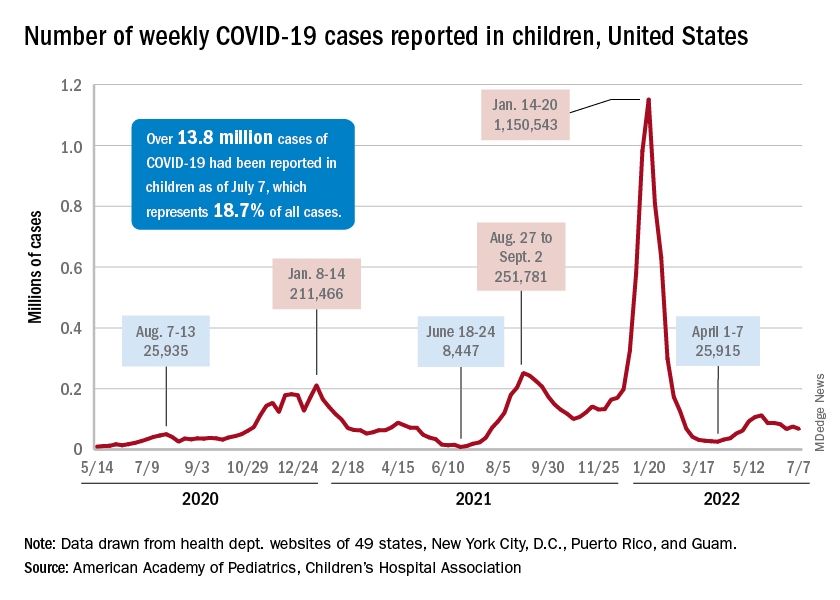
That approval, of course, came between the Delta and Omicron surges, when awareness was higher. The low initial uptake among those under age 5, however, was not unexpected by the Biden administration. “That number in and of itself is very much in line with our expectation, and we’re eager to continue working closely with partners to build on this start,” a senior administration official told ABC News.
With approval of the vaccine occurring after the school year was over, parents’ thoughts have been focused more on vacations and less on vaccinations. “Even before these vaccines officially became available, this was going to be a different rollout; it was going to take more time,” the official explained.
Incidence measures continue on different paths
New COVID-19 cases dropped during the latest reporting week (July 1-7), returning to the downward trend that began in late May and then stopped for 1 week (June 24-30), when cases were up by 12.4%, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Children also represent a smaller share of cases, probably because of underreporting. “There has been a notable decline in the portion of reported weekly COVID-19 cases that are children,” the two groups said in their weekly COVID report. Although “cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases.”
Other measures, however, have been rising slowly but steadily since the spring. New admissions of patients aged 0-17 years with confirmed COVID, which were down to 0.13 per 100,000 population in early April, had climbed to 0.39 per 100,000 by July 7, the CDC said on its COVID Data Tracker.
Emergency department visits continue to show the same upward trend, despite a small decline in early June. A COVID diagnosis was involved in just 0.5% of ED visits in children aged 0-11 years on March 26, but by July 6 the rate was 4.7%. Increases were not as high among older children: From 0.3% on March 26 to 2.5% on July 6 for those aged 12-15 and from 0.3% to 2.4% for 16- and 17-year-olds, according to the CDC.
The COVID-19 vaccination effort in the youngest children has begun much more slowly than the most recent rollout for older children, according to the Centers for Disease Control and Prevention.
in early November of 2021, based on CDC data last updated on July 7.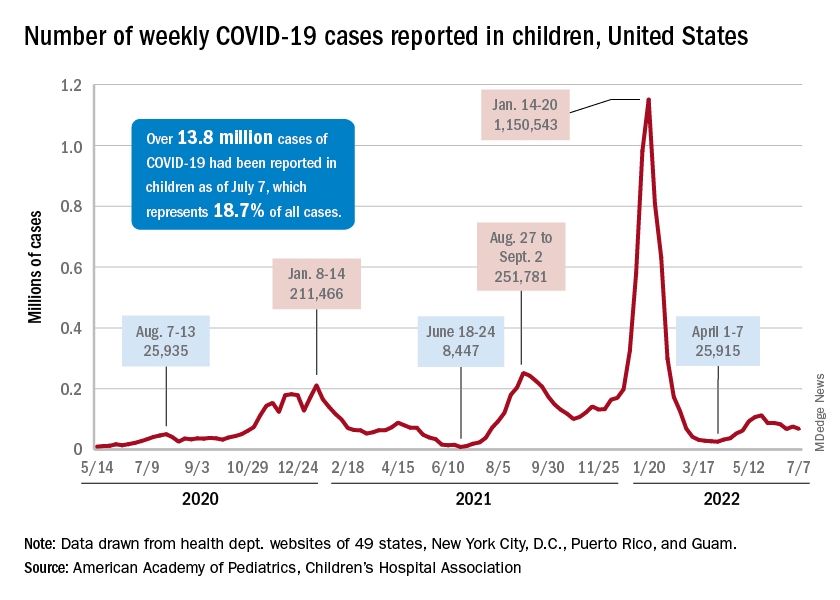
That approval, of course, came between the Delta and Omicron surges, when awareness was higher. The low initial uptake among those under age 5, however, was not unexpected by the Biden administration. “That number in and of itself is very much in line with our expectation, and we’re eager to continue working closely with partners to build on this start,” a senior administration official told ABC News.
With approval of the vaccine occurring after the school year was over, parents’ thoughts have been focused more on vacations and less on vaccinations. “Even before these vaccines officially became available, this was going to be a different rollout; it was going to take more time,” the official explained.
Incidence measures continue on different paths
New COVID-19 cases dropped during the latest reporting week (July 1-7), returning to the downward trend that began in late May and then stopped for 1 week (June 24-30), when cases were up by 12.4%, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Children also represent a smaller share of cases, probably because of underreporting. “There has been a notable decline in the portion of reported weekly COVID-19 cases that are children,” the two groups said in their weekly COVID report. Although “cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases.”
Other measures, however, have been rising slowly but steadily since the spring. New admissions of patients aged 0-17 years with confirmed COVID, which were down to 0.13 per 100,000 population in early April, had climbed to 0.39 per 100,000 by July 7, the CDC said on its COVID Data Tracker.
Emergency department visits continue to show the same upward trend, despite a small decline in early June. A COVID diagnosis was involved in just 0.5% of ED visits in children aged 0-11 years on March 26, but by July 6 the rate was 4.7%. Increases were not as high among older children: From 0.3% on March 26 to 2.5% on July 6 for those aged 12-15 and from 0.3% to 2.4% for 16- and 17-year-olds, according to the CDC.
The COVID-19 vaccination effort in the youngest children has begun much more slowly than the most recent rollout for older children, according to the Centers for Disease Control and Prevention.
in early November of 2021, based on CDC data last updated on July 7.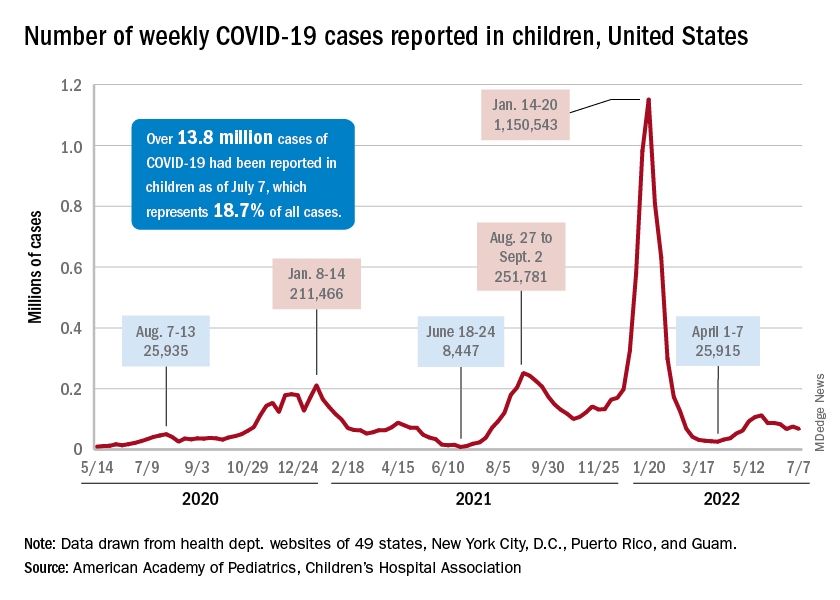
That approval, of course, came between the Delta and Omicron surges, when awareness was higher. The low initial uptake among those under age 5, however, was not unexpected by the Biden administration. “That number in and of itself is very much in line with our expectation, and we’re eager to continue working closely with partners to build on this start,” a senior administration official told ABC News.
With approval of the vaccine occurring after the school year was over, parents’ thoughts have been focused more on vacations and less on vaccinations. “Even before these vaccines officially became available, this was going to be a different rollout; it was going to take more time,” the official explained.
Incidence measures continue on different paths
New COVID-19 cases dropped during the latest reporting week (July 1-7), returning to the downward trend that began in late May and then stopped for 1 week (June 24-30), when cases were up by 12.4%, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Children also represent a smaller share of cases, probably because of underreporting. “There has been a notable decline in the portion of reported weekly COVID-19 cases that are children,” the two groups said in their weekly COVID report. Although “cases are likely increasingly underreported for all age groups, this decline indicates that children are disproportionately undercounted in reported COVID-19 cases.”
Other measures, however, have been rising slowly but steadily since the spring. New admissions of patients aged 0-17 years with confirmed COVID, which were down to 0.13 per 100,000 population in early April, had climbed to 0.39 per 100,000 by July 7, the CDC said on its COVID Data Tracker.
Emergency department visits continue to show the same upward trend, despite a small decline in early June. A COVID diagnosis was involved in just 0.5% of ED visits in children aged 0-11 years on March 26, but by July 6 the rate was 4.7%. Increases were not as high among older children: From 0.3% on March 26 to 2.5% on July 6 for those aged 12-15 and from 0.3% to 2.4% for 16- and 17-year-olds, according to the CDC.
Aggression toward health care providers common during pandemic
After an aggressive event or abuse occurred, 56% of providers considered changing their care tasks, and more than a third considered quitting their profession.
“Aggression of any sort against health care providers is not a new social phenomenon, and it has existed as far as medicine and health care is reported in literature. However, the phenomenon of aggression against health care providers during the pandemic grew worse,” senior study author Adrian Baranchuk, MD, a professor of medicine at Queen’s University, Kingston, Ont., told this news organization.
The study was published online in Current Problems in Cardiology
Survey snapshot
Dr. Baranchuk and colleagues, with the support of the Inter-American Society of Cardiology, developed a survey to characterize the frequency and types of abuse that frontline health professionals faced. They invited health care professionals from Latin America who had provided care since March 2020 to participate.
Between January and February 2022, 3,544 participants from 19 countries took the survey. Among them, 70.8% were physicians, 16% were nurses, and 13.2% were other health team members, such as administrative staff and technicians. About 58.5% were women, and 74.7% provided direct care to patients with COVID-19.
Overall, 54.8% of respondents reported acts of aggression. Of this group, 95.6% reported verbal abuse, 11.1% reported physical abuse, and 19.9% reported other types of abuse, including microaggressions.
About 13% of respondents reported experiencing some form of aggression daily, 26.4% experienced abuse weekly, and 38.8% reported violence a few times per month. Typically, the incidents involved patients’ relatives or both the patients and their relatives.
Nearly half of those who reported abuse experienced psychosomatic symptoms after the event, and 12% sought psychological care.
Administrative staff were 3.5 times more likely to experience abuse than other health care workers. Doctors and nurses were about twice as likely to experience abuse.
In addition, women, younger staff, and those who worked directly with COVID-19 patients were more likely to report abuse.
‘Shocking results’
Dr. Baranchuk, a native of Argentina, said people initially celebrated doctors and nurses for keeping communities safe. In several countries across Latin America, for instance, people lit candles, applauded at certain hours, and posted support on social media. As pandemic-related policies changed, however, health care providers faced unrest as people grew tired of wearing masks, maintaining social distance, and obeying restrictions at public spaces such as clubs and restaurants.
“This fatigue toward the social changes grew, but people didn’t have a specific target, and slowly and gradually, health care providers became the target of frustration and hate,” said Dr. Baranchuk. “In areas of the world where legislation is more flexible and less strict in charging individuals with poor or unacceptable behavior toward members of the health care team, aggression and microaggression became more frequent.”
“The results we obtained were more shocking than we expected,” Sebastián García-Zamora, MD, the lead study author and head of the coronary care unit at the Delta Clinic, Buenos Aires, said in an interview.
Dr. García-Zamora, also the coordinator of the International Society of Electrocardiology Young Community, noted the particularly high numbers of reports among young health care workers and women.
“Unfortunately, young women seem to be the most vulnerable staff to suffering violence, regardless of the work they perform in the health system,” he said. “Notably, less than one in four health team members that suffered workplace violence pursued legal action based on the events.”
The research team is now conducting additional analyses on the different types of aggression based on gender, region, and task performed by the health care team. They’re trying to understand who is most vulnerable to physical attacks, as well as the consequences.
“The most important thing to highlight is that this problem exists, it is more frequent than we think, and we can only solve it if we all get involved in it,” Dr. García-Zamora said.
‘Complete systematic failure’
Health care workers in certain communities faced more aggression as well. In a CMAJ Open study published in November 2021, Asian Canadian and Asian American health care workers experienced discrimination, racial microaggressions, threats of violence, and violent acts during the pandemic. Women and frontline workers with direct patient contact were more likely to face verbal and physical abuse.
“This highlights that we need to continue the fight against misogyny, racism, and health care worker discrimination,” lead study author Zhida Shang, a medical student at McGill University, Montreal, told this news organization.
“As we are managing to live with the COVID-19 pandemic, it is important to study our successes and shortcomings. I sincerely believe that during the pandemic, the treatment of various racialized communities, including Asian Americans and Asian Canadians, was a complete systematic failure,” he said. “It is crucial to continue to examine, reflect, and learn from these lessons so that there will be equitable outcomes during the next public health emergency.”
The study was conducted without funding support. Dr. Baranchuk, Dr. García-Zamora, and Ms. Shang report no relevant disclosures.
A version of this article first appeared on Medscape.com.
After an aggressive event or abuse occurred, 56% of providers considered changing their care tasks, and more than a third considered quitting their profession.
“Aggression of any sort against health care providers is not a new social phenomenon, and it has existed as far as medicine and health care is reported in literature. However, the phenomenon of aggression against health care providers during the pandemic grew worse,” senior study author Adrian Baranchuk, MD, a professor of medicine at Queen’s University, Kingston, Ont., told this news organization.
The study was published online in Current Problems in Cardiology
Survey snapshot
Dr. Baranchuk and colleagues, with the support of the Inter-American Society of Cardiology, developed a survey to characterize the frequency and types of abuse that frontline health professionals faced. They invited health care professionals from Latin America who had provided care since March 2020 to participate.
Between January and February 2022, 3,544 participants from 19 countries took the survey. Among them, 70.8% were physicians, 16% were nurses, and 13.2% were other health team members, such as administrative staff and technicians. About 58.5% were women, and 74.7% provided direct care to patients with COVID-19.
Overall, 54.8% of respondents reported acts of aggression. Of this group, 95.6% reported verbal abuse, 11.1% reported physical abuse, and 19.9% reported other types of abuse, including microaggressions.
About 13% of respondents reported experiencing some form of aggression daily, 26.4% experienced abuse weekly, and 38.8% reported violence a few times per month. Typically, the incidents involved patients’ relatives or both the patients and their relatives.
Nearly half of those who reported abuse experienced psychosomatic symptoms after the event, and 12% sought psychological care.
Administrative staff were 3.5 times more likely to experience abuse than other health care workers. Doctors and nurses were about twice as likely to experience abuse.
In addition, women, younger staff, and those who worked directly with COVID-19 patients were more likely to report abuse.
‘Shocking results’
Dr. Baranchuk, a native of Argentina, said people initially celebrated doctors and nurses for keeping communities safe. In several countries across Latin America, for instance, people lit candles, applauded at certain hours, and posted support on social media. As pandemic-related policies changed, however, health care providers faced unrest as people grew tired of wearing masks, maintaining social distance, and obeying restrictions at public spaces such as clubs and restaurants.
“This fatigue toward the social changes grew, but people didn’t have a specific target, and slowly and gradually, health care providers became the target of frustration and hate,” said Dr. Baranchuk. “In areas of the world where legislation is more flexible and less strict in charging individuals with poor or unacceptable behavior toward members of the health care team, aggression and microaggression became more frequent.”
“The results we obtained were more shocking than we expected,” Sebastián García-Zamora, MD, the lead study author and head of the coronary care unit at the Delta Clinic, Buenos Aires, said in an interview.
Dr. García-Zamora, also the coordinator of the International Society of Electrocardiology Young Community, noted the particularly high numbers of reports among young health care workers and women.
“Unfortunately, young women seem to be the most vulnerable staff to suffering violence, regardless of the work they perform in the health system,” he said. “Notably, less than one in four health team members that suffered workplace violence pursued legal action based on the events.”
The research team is now conducting additional analyses on the different types of aggression based on gender, region, and task performed by the health care team. They’re trying to understand who is most vulnerable to physical attacks, as well as the consequences.
“The most important thing to highlight is that this problem exists, it is more frequent than we think, and we can only solve it if we all get involved in it,” Dr. García-Zamora said.
‘Complete systematic failure’
Health care workers in certain communities faced more aggression as well. In a CMAJ Open study published in November 2021, Asian Canadian and Asian American health care workers experienced discrimination, racial microaggressions, threats of violence, and violent acts during the pandemic. Women and frontline workers with direct patient contact were more likely to face verbal and physical abuse.
“This highlights that we need to continue the fight against misogyny, racism, and health care worker discrimination,” lead study author Zhida Shang, a medical student at McGill University, Montreal, told this news organization.
“As we are managing to live with the COVID-19 pandemic, it is important to study our successes and shortcomings. I sincerely believe that during the pandemic, the treatment of various racialized communities, including Asian Americans and Asian Canadians, was a complete systematic failure,” he said. “It is crucial to continue to examine, reflect, and learn from these lessons so that there will be equitable outcomes during the next public health emergency.”
The study was conducted without funding support. Dr. Baranchuk, Dr. García-Zamora, and Ms. Shang report no relevant disclosures.
A version of this article first appeared on Medscape.com.
After an aggressive event or abuse occurred, 56% of providers considered changing their care tasks, and more than a third considered quitting their profession.
“Aggression of any sort against health care providers is not a new social phenomenon, and it has existed as far as medicine and health care is reported in literature. However, the phenomenon of aggression against health care providers during the pandemic grew worse,” senior study author Adrian Baranchuk, MD, a professor of medicine at Queen’s University, Kingston, Ont., told this news organization.
The study was published online in Current Problems in Cardiology
Survey snapshot
Dr. Baranchuk and colleagues, with the support of the Inter-American Society of Cardiology, developed a survey to characterize the frequency and types of abuse that frontline health professionals faced. They invited health care professionals from Latin America who had provided care since March 2020 to participate.
Between January and February 2022, 3,544 participants from 19 countries took the survey. Among them, 70.8% were physicians, 16% were nurses, and 13.2% were other health team members, such as administrative staff and technicians. About 58.5% were women, and 74.7% provided direct care to patients with COVID-19.
Overall, 54.8% of respondents reported acts of aggression. Of this group, 95.6% reported verbal abuse, 11.1% reported physical abuse, and 19.9% reported other types of abuse, including microaggressions.
About 13% of respondents reported experiencing some form of aggression daily, 26.4% experienced abuse weekly, and 38.8% reported violence a few times per month. Typically, the incidents involved patients’ relatives or both the patients and their relatives.
Nearly half of those who reported abuse experienced psychosomatic symptoms after the event, and 12% sought psychological care.
Administrative staff were 3.5 times more likely to experience abuse than other health care workers. Doctors and nurses were about twice as likely to experience abuse.
In addition, women, younger staff, and those who worked directly with COVID-19 patients were more likely to report abuse.
‘Shocking results’
Dr. Baranchuk, a native of Argentina, said people initially celebrated doctors and nurses for keeping communities safe. In several countries across Latin America, for instance, people lit candles, applauded at certain hours, and posted support on social media. As pandemic-related policies changed, however, health care providers faced unrest as people grew tired of wearing masks, maintaining social distance, and obeying restrictions at public spaces such as clubs and restaurants.
“This fatigue toward the social changes grew, but people didn’t have a specific target, and slowly and gradually, health care providers became the target of frustration and hate,” said Dr. Baranchuk. “In areas of the world where legislation is more flexible and less strict in charging individuals with poor or unacceptable behavior toward members of the health care team, aggression and microaggression became more frequent.”
“The results we obtained were more shocking than we expected,” Sebastián García-Zamora, MD, the lead study author and head of the coronary care unit at the Delta Clinic, Buenos Aires, said in an interview.
Dr. García-Zamora, also the coordinator of the International Society of Electrocardiology Young Community, noted the particularly high numbers of reports among young health care workers and women.
“Unfortunately, young women seem to be the most vulnerable staff to suffering violence, regardless of the work they perform in the health system,” he said. “Notably, less than one in four health team members that suffered workplace violence pursued legal action based on the events.”
The research team is now conducting additional analyses on the different types of aggression based on gender, region, and task performed by the health care team. They’re trying to understand who is most vulnerable to physical attacks, as well as the consequences.
“The most important thing to highlight is that this problem exists, it is more frequent than we think, and we can only solve it if we all get involved in it,” Dr. García-Zamora said.
‘Complete systematic failure’
Health care workers in certain communities faced more aggression as well. In a CMAJ Open study published in November 2021, Asian Canadian and Asian American health care workers experienced discrimination, racial microaggressions, threats of violence, and violent acts during the pandemic. Women and frontline workers with direct patient contact were more likely to face verbal and physical abuse.
“This highlights that we need to continue the fight against misogyny, racism, and health care worker discrimination,” lead study author Zhida Shang, a medical student at McGill University, Montreal, told this news organization.
“As we are managing to live with the COVID-19 pandemic, it is important to study our successes and shortcomings. I sincerely believe that during the pandemic, the treatment of various racialized communities, including Asian Americans and Asian Canadians, was a complete systematic failure,” he said. “It is crucial to continue to examine, reflect, and learn from these lessons so that there will be equitable outcomes during the next public health emergency.”
The study was conducted without funding support. Dr. Baranchuk, Dr. García-Zamora, and Ms. Shang report no relevant disclosures.
A version of this article first appeared on Medscape.com.
Inflation and health care: The prognosis for doctors
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Obesity links to faster fading of COVID vaccine protection
Researchers published the study covered in this summary on medRxiv.org as a preprint that has not yet been peer reviewed.
Key takeaways
- The study results suggest that
- The findings documented evidence of reduced neutralizing antibody capacity 6 months after primary vaccination in people with severe obesity.
- This was a large study involving about more than 3.5 million people who had received at least two doses of COVID-19 vaccine, including more than 650,000 with obesity.
Why this matters
- Obesity is associated with comorbidities that independently increase the risk for severe COVID-19, including type 2 diabetes, chronic kidney disease, and heart failure.
- The authors concluded that additional or more frequent booster doses are likely to be required to maintain protection among people with obesity against COVID-19.
Study design
- Prospective longitudinal study of the incidence and severity of COVID-19 infections and immune responses in a cohort of more than 3.5 million adults from a Scottish healthcare database who received two or three doses of COVID-19 vaccine. The data came from the study, centered at the University of Edinburgh.
- About 16% had obesity with a body mass index of 30-39.9 kg/m2, and an additional 3% had severe obesity with a BMI of 40 or greater.
- Although not specified in this preprint, another said that the vaccines administered in Scotland have been the Pfizer-BioNTech and Oxford-AstraZeneca formulations.
Key results
- Between Sept. 14, 2020, and March 19, 2022, 10,983 people (0.3% of the total cohort; 6.0 events per 1,000 person-years) had severe COVID-19, consisting of 9,733 who were hospitalized and 2,207 who died (957 of those hospitalized also died).
- People with obesity or severe obesity were at higher risk of hospitalization or death from COVID-19 after both a second and third (booster) dose of vaccine.
- Compared with those with normal weight, those with severe obesity (BMI higher than 40) were at significantly increased risk for severe COVID-19 after a second vaccine dose, with an adjusted rate ratio 1.76, whereas those with standard obesity (BMI, 30-40) were at a modestly but significantly increased risk with an adjusted rate ratio of 1.11.
- Breakthrough infections after the second dose for those with severe obesity, obesity, and normal weight occurred on average at 10 weeks, 15 weeks, and 20 weeks, respectively.
- Interaction testing showed that vaccine effectiveness significantly diminished over time across BMI groups, and protection waned more rapidly as BMI increased.
- Results from immunophenotyping studies run in a subgroup of several dozen subjects with severe obesity or normal weight showed significant decrements in the robustness of antibody responses in those with severe obesity 6 months after a second or third vaccine dose.
Limitations
- The authors did not specify any limitations.
Disclosures
- The study received no commercial funding.
- One author received funding from Wellcome.
This is a summary of a preprint research study , “Accelerated waning of the humoral response to SARS-CoV-2 vaccines in obesity,” published by researchers primarily at the University of Cambridge (England), on medRxiv. This study has not yet been peer reviewed. The full text of the study can be found on medRxiv.org.
A version of this article first appeared on Medscape.com.
Researchers published the study covered in this summary on medRxiv.org as a preprint that has not yet been peer reviewed.
Key takeaways
- The study results suggest that
- The findings documented evidence of reduced neutralizing antibody capacity 6 months after primary vaccination in people with severe obesity.
- This was a large study involving about more than 3.5 million people who had received at least two doses of COVID-19 vaccine, including more than 650,000 with obesity.
Why this matters
- Obesity is associated with comorbidities that independently increase the risk for severe COVID-19, including type 2 diabetes, chronic kidney disease, and heart failure.
- The authors concluded that additional or more frequent booster doses are likely to be required to maintain protection among people with obesity against COVID-19.
Study design
- Prospective longitudinal study of the incidence and severity of COVID-19 infections and immune responses in a cohort of more than 3.5 million adults from a Scottish healthcare database who received two or three doses of COVID-19 vaccine. The data came from the study, centered at the University of Edinburgh.
- About 16% had obesity with a body mass index of 30-39.9 kg/m2, and an additional 3% had severe obesity with a BMI of 40 or greater.
- Although not specified in this preprint, another said that the vaccines administered in Scotland have been the Pfizer-BioNTech and Oxford-AstraZeneca formulations.
Key results
- Between Sept. 14, 2020, and March 19, 2022, 10,983 people (0.3% of the total cohort; 6.0 events per 1,000 person-years) had severe COVID-19, consisting of 9,733 who were hospitalized and 2,207 who died (957 of those hospitalized also died).
- People with obesity or severe obesity were at higher risk of hospitalization or death from COVID-19 after both a second and third (booster) dose of vaccine.
- Compared with those with normal weight, those with severe obesity (BMI higher than 40) were at significantly increased risk for severe COVID-19 after a second vaccine dose, with an adjusted rate ratio 1.76, whereas those with standard obesity (BMI, 30-40) were at a modestly but significantly increased risk with an adjusted rate ratio of 1.11.
- Breakthrough infections after the second dose for those with severe obesity, obesity, and normal weight occurred on average at 10 weeks, 15 weeks, and 20 weeks, respectively.
- Interaction testing showed that vaccine effectiveness significantly diminished over time across BMI groups, and protection waned more rapidly as BMI increased.
- Results from immunophenotyping studies run in a subgroup of several dozen subjects with severe obesity or normal weight showed significant decrements in the robustness of antibody responses in those with severe obesity 6 months after a second or third vaccine dose.
Limitations
- The authors did not specify any limitations.
Disclosures
- The study received no commercial funding.
- One author received funding from Wellcome.
This is a summary of a preprint research study , “Accelerated waning of the humoral response to SARS-CoV-2 vaccines in obesity,” published by researchers primarily at the University of Cambridge (England), on medRxiv. This study has not yet been peer reviewed. The full text of the study can be found on medRxiv.org.
A version of this article first appeared on Medscape.com.
Researchers published the study covered in this summary on medRxiv.org as a preprint that has not yet been peer reviewed.
Key takeaways
- The study results suggest that
- The findings documented evidence of reduced neutralizing antibody capacity 6 months after primary vaccination in people with severe obesity.
- This was a large study involving about more than 3.5 million people who had received at least two doses of COVID-19 vaccine, including more than 650,000 with obesity.
Why this matters
- Obesity is associated with comorbidities that independently increase the risk for severe COVID-19, including type 2 diabetes, chronic kidney disease, and heart failure.
- The authors concluded that additional or more frequent booster doses are likely to be required to maintain protection among people with obesity against COVID-19.
Study design
- Prospective longitudinal study of the incidence and severity of COVID-19 infections and immune responses in a cohort of more than 3.5 million adults from a Scottish healthcare database who received two or three doses of COVID-19 vaccine. The data came from the study, centered at the University of Edinburgh.
- About 16% had obesity with a body mass index of 30-39.9 kg/m2, and an additional 3% had severe obesity with a BMI of 40 or greater.
- Although not specified in this preprint, another said that the vaccines administered in Scotland have been the Pfizer-BioNTech and Oxford-AstraZeneca formulations.
Key results
- Between Sept. 14, 2020, and March 19, 2022, 10,983 people (0.3% of the total cohort; 6.0 events per 1,000 person-years) had severe COVID-19, consisting of 9,733 who were hospitalized and 2,207 who died (957 of those hospitalized also died).
- People with obesity or severe obesity were at higher risk of hospitalization or death from COVID-19 after both a second and third (booster) dose of vaccine.
- Compared with those with normal weight, those with severe obesity (BMI higher than 40) were at significantly increased risk for severe COVID-19 after a second vaccine dose, with an adjusted rate ratio 1.76, whereas those with standard obesity (BMI, 30-40) were at a modestly but significantly increased risk with an adjusted rate ratio of 1.11.
- Breakthrough infections after the second dose for those with severe obesity, obesity, and normal weight occurred on average at 10 weeks, 15 weeks, and 20 weeks, respectively.
- Interaction testing showed that vaccine effectiveness significantly diminished over time across BMI groups, and protection waned more rapidly as BMI increased.
- Results from immunophenotyping studies run in a subgroup of several dozen subjects with severe obesity or normal weight showed significant decrements in the robustness of antibody responses in those with severe obesity 6 months after a second or third vaccine dose.
Limitations
- The authors did not specify any limitations.
Disclosures
- The study received no commercial funding.
- One author received funding from Wellcome.
This is a summary of a preprint research study , “Accelerated waning of the humoral response to SARS-CoV-2 vaccines in obesity,” published by researchers primarily at the University of Cambridge (England), on medRxiv. This study has not yet been peer reviewed. The full text of the study can be found on medRxiv.org.
A version of this article first appeared on Medscape.com.
Biologics reduce exacerbations in severe asthma
, based on data from more than 2,000 individuals.
The development of biologics to target specific inflammatory pathways “has transformed the management of uncontrolled SA,” but data on the real-world use of biologics in severe asthma patients treated by subspecialists are limited, wrote Reynold A. Panettieri, Jr., MD, of Rutgers, State University of New Jersey, New Brunswick, and colleagues.
In a study published in the Annals of Allergy, Asthma & Immunology, the researchers reviewed data from CHRONICLE, an ongoing, prospective, real-world noninterventional study of adults aged 18 years and older with severe asthma in the United States.
The study population included 2,847 patients enrolled in the CHRONICLE study between February 2018 and February 2021; 68.8% were women, 74.6% were White. The patients ranged in age from 18 to 89 years, with a mean age of 54.2 years.
Biologic use was defined as patients who started or had ongoing use of biologics between 12 months before enrollment and the patient’s most recent data collection. Switches were defined as stopping one biologic and starting another within 6 months; stops were defined as discontinuing a biologic without switching to another within 6 months. A total of 66% of the patients were using biologics at the time of study enrollment. The most common biologic was omalizumab (47%), followed by benralizumab (27%), mepolizumab (26%), and dupilumab (18%).
Overall, 89% of the patients had ongoing biologic use, 16% had biologic switches, and 13% had stops.
Patients who started biologics or switched biologics had significant reductions in asthma exacerbations at 6 months, compared with nonbiologic users of 58% (1.80 vs. 0.76 per patient-year) and 49% (1.47 vs. 0.75 per patient-year), respectively (P < .001 for both). Asthma exacerbations declined by 70% among biologics users for whom data were available for 12 months before and 12 months after starting biologics.
Exacerbations decreased at 6 months after biologic initiation across all subgroups of patients, notably patients with pre-biologic FEV1 < 80% and patients with FEV1 ≥ 80% (66% and 53%, respectively); never smokers and current/former smokers (63% and 50%, respectively); and patients with COPD and without COPD (58% and 52%, respectively).
The researchers also found a greater reduction in exacerbations among patients who switched from anti-IgE therapy to anti–IL-5/IL-5R/IL-4R therapy, compared with those who switched among anti–IL-5/IL-5R/IL-4R therapies (58% vs. 46%).
Patients who stopped or switched biologics appeared to have more severe or treatment-refractory disease than those with ongoing biologic use, the researchers noted. The most common reason for stopping or switching was worsening symptoms.
The study findings were limited by several factors, including the focus only on adults in the United States with subspecialist-treated SA, which may limit generalizability to children or other populations, the researchers noted. Other limitations included the variation in clinical decisions and insurance coverage and the inability to conduct longitudinal assessments, they said.
The results demonstrate that starting or switching biologics was consistently associated with fewer exacerbations in severe asthma. However, more research is needed to determine why some patients were not receiving biologics because they were not considered clinically eligible by their subspecialist health care providers, the researchers concluded.
The current study and the CHRONICLE study were supported by AstraZeneca. Lead author Dr. Panettieri disclosed serving on the advisory boards for and receiving grant support from AstraZeneca, Sanofi, Genentech, Regeneron, and Novartis.
, based on data from more than 2,000 individuals.
The development of biologics to target specific inflammatory pathways “has transformed the management of uncontrolled SA,” but data on the real-world use of biologics in severe asthma patients treated by subspecialists are limited, wrote Reynold A. Panettieri, Jr., MD, of Rutgers, State University of New Jersey, New Brunswick, and colleagues.
In a study published in the Annals of Allergy, Asthma & Immunology, the researchers reviewed data from CHRONICLE, an ongoing, prospective, real-world noninterventional study of adults aged 18 years and older with severe asthma in the United States.
The study population included 2,847 patients enrolled in the CHRONICLE study between February 2018 and February 2021; 68.8% were women, 74.6% were White. The patients ranged in age from 18 to 89 years, with a mean age of 54.2 years.
Biologic use was defined as patients who started or had ongoing use of biologics between 12 months before enrollment and the patient’s most recent data collection. Switches were defined as stopping one biologic and starting another within 6 months; stops were defined as discontinuing a biologic without switching to another within 6 months. A total of 66% of the patients were using biologics at the time of study enrollment. The most common biologic was omalizumab (47%), followed by benralizumab (27%), mepolizumab (26%), and dupilumab (18%).
Overall, 89% of the patients had ongoing biologic use, 16% had biologic switches, and 13% had stops.
Patients who started biologics or switched biologics had significant reductions in asthma exacerbations at 6 months, compared with nonbiologic users of 58% (1.80 vs. 0.76 per patient-year) and 49% (1.47 vs. 0.75 per patient-year), respectively (P < .001 for both). Asthma exacerbations declined by 70% among biologics users for whom data were available for 12 months before and 12 months after starting biologics.
Exacerbations decreased at 6 months after biologic initiation across all subgroups of patients, notably patients with pre-biologic FEV1 < 80% and patients with FEV1 ≥ 80% (66% and 53%, respectively); never smokers and current/former smokers (63% and 50%, respectively); and patients with COPD and without COPD (58% and 52%, respectively).
The researchers also found a greater reduction in exacerbations among patients who switched from anti-IgE therapy to anti–IL-5/IL-5R/IL-4R therapy, compared with those who switched among anti–IL-5/IL-5R/IL-4R therapies (58% vs. 46%).
Patients who stopped or switched biologics appeared to have more severe or treatment-refractory disease than those with ongoing biologic use, the researchers noted. The most common reason for stopping or switching was worsening symptoms.
The study findings were limited by several factors, including the focus only on adults in the United States with subspecialist-treated SA, which may limit generalizability to children or other populations, the researchers noted. Other limitations included the variation in clinical decisions and insurance coverage and the inability to conduct longitudinal assessments, they said.
The results demonstrate that starting or switching biologics was consistently associated with fewer exacerbations in severe asthma. However, more research is needed to determine why some patients were not receiving biologics because they were not considered clinically eligible by their subspecialist health care providers, the researchers concluded.
The current study and the CHRONICLE study were supported by AstraZeneca. Lead author Dr. Panettieri disclosed serving on the advisory boards for and receiving grant support from AstraZeneca, Sanofi, Genentech, Regeneron, and Novartis.
, based on data from more than 2,000 individuals.
The development of biologics to target specific inflammatory pathways “has transformed the management of uncontrolled SA,” but data on the real-world use of biologics in severe asthma patients treated by subspecialists are limited, wrote Reynold A. Panettieri, Jr., MD, of Rutgers, State University of New Jersey, New Brunswick, and colleagues.
In a study published in the Annals of Allergy, Asthma & Immunology, the researchers reviewed data from CHRONICLE, an ongoing, prospective, real-world noninterventional study of adults aged 18 years and older with severe asthma in the United States.
The study population included 2,847 patients enrolled in the CHRONICLE study between February 2018 and February 2021; 68.8% were women, 74.6% were White. The patients ranged in age from 18 to 89 years, with a mean age of 54.2 years.
Biologic use was defined as patients who started or had ongoing use of biologics between 12 months before enrollment and the patient’s most recent data collection. Switches were defined as stopping one biologic and starting another within 6 months; stops were defined as discontinuing a biologic without switching to another within 6 months. A total of 66% of the patients were using biologics at the time of study enrollment. The most common biologic was omalizumab (47%), followed by benralizumab (27%), mepolizumab (26%), and dupilumab (18%).
Overall, 89% of the patients had ongoing biologic use, 16% had biologic switches, and 13% had stops.
Patients who started biologics or switched biologics had significant reductions in asthma exacerbations at 6 months, compared with nonbiologic users of 58% (1.80 vs. 0.76 per patient-year) and 49% (1.47 vs. 0.75 per patient-year), respectively (P < .001 for both). Asthma exacerbations declined by 70% among biologics users for whom data were available for 12 months before and 12 months after starting biologics.
Exacerbations decreased at 6 months after biologic initiation across all subgroups of patients, notably patients with pre-biologic FEV1 < 80% and patients with FEV1 ≥ 80% (66% and 53%, respectively); never smokers and current/former smokers (63% and 50%, respectively); and patients with COPD and without COPD (58% and 52%, respectively).
The researchers also found a greater reduction in exacerbations among patients who switched from anti-IgE therapy to anti–IL-5/IL-5R/IL-4R therapy, compared with those who switched among anti–IL-5/IL-5R/IL-4R therapies (58% vs. 46%).
Patients who stopped or switched biologics appeared to have more severe or treatment-refractory disease than those with ongoing biologic use, the researchers noted. The most common reason for stopping or switching was worsening symptoms.
The study findings were limited by several factors, including the focus only on adults in the United States with subspecialist-treated SA, which may limit generalizability to children or other populations, the researchers noted. Other limitations included the variation in clinical decisions and insurance coverage and the inability to conduct longitudinal assessments, they said.
The results demonstrate that starting or switching biologics was consistently associated with fewer exacerbations in severe asthma. However, more research is needed to determine why some patients were not receiving biologics because they were not considered clinically eligible by their subspecialist health care providers, the researchers concluded.
The current study and the CHRONICLE study were supported by AstraZeneca. Lead author Dr. Panettieri disclosed serving on the advisory boards for and receiving grant support from AstraZeneca, Sanofi, Genentech, Regeneron, and Novartis.
FROM THE ANNALS OF ALLERGY, ASTHMA & IMMUNOLOGY
Adding salt to food linked to higher risk of premature death
in a new study.
In the study of more than 500,000 people, compared with those who never or rarely added salt, those who always added salt to their food had a 28% increased risk of dying prematurely (defined as death before the age of 75 years).
Results also showed that adding salt to food was linked to a lower life expectancy. At the age of 50 years, life expectancy was reduced by 1.5 years in women and by 2.28 years in men who always added salt to their food, compared with those who never or rarely did.
However, these increased risks appeared to be attenuated with increasing intakes of high-potassium foods (vegetables and fruits).
The study was published online in the European Heart Journal.
“As far as we are aware, this is the first study to analyze adding salt to meals as a unique measurement for dietary sodium intake. Such a measure is less likely affected by other dietary components, especially potassium intake,” senior author Lu Qi, MD, Tulane University, New Orleans, told this news organization.
“Our study provides supportive evidence from a novel perspective to show the adverse effects of high sodium intake on human health, which is still a controversial topic. Our findings support the advice that reduction of salt intake by reducing the salt added to meals may benefit health and improve life expectancy. Our results also suggest that high intakes of fruits and vegetables are beneficial regarding lowering the adverse effects of salt,” he added.
Link between dietary salt and health is subject of longstanding debate
The researchers explained that the relationship between dietary salt intake and health remains a subject of longstanding debate, with previous studies on the association between sodium intake and mortality having shown conflicting results.
They attributed the inconsistent results to the low accuracy of sodium measurement, noting that sodium intake varies widely from day to day, but the majority of previous studies have largely relied on a single day’s urine collection or dietary survey for estimating the sodium intake, which is inadequate to assess an individual’s usual consumption levels.
They also pointed out that it is difficult to separate the contributions of intakes of sodium and potassium to health based on current methods for measuring dietary sodium and potassium, and this may confound the association between sodium intake and health outcomes.
They noted that the hypothesis that a high-potassium intake may attenuate the adverse association of high-sodium intake with health outcomes has been proposed for many years, but studies assessing the interaction between sodium intake and potassium intake on the risk of mortality are scarce.
Adding salt to food at the table is a common eating behavior directly related to an individual’s long-term preference for salty tasting foods and habitual salt intake, the authors said, adding that commonly used table salt contains 97%-99% sodium chloride, minimizing the potential confounding effects of other dietary factors including potassium. “Therefore, adding salt to foods provides a unique assessment to evaluate the association between habitual sodium intake and mortality.”
UK Biobank study
For the current study Dr. Qi and colleagues analyzed data from 501,379 people taking part in the UK Biobank study. When joining the study between 2006 and 2010, the participants were asked whether they added salt to their foods never/rarely, sometimes, usually or always. Participants were then followed for a median of 9 years.
After adjustment for sex, age, race, smoking, moderate drinking, body mass index, physical activity, Townsend deprivation index, high cholesterol, chronic kidney disease, diabetes, cardiovascular disease, and cancer, results showed an increasing risk of all-cause premature mortality rose with increasing frequency of adding salt to foods.
The adjusted hazard ratios, compared with those who never or rarely added salt, were 1.02 (95% CI, 0.99-1.06) for those who added salt sometimes, 1.07 (95% CI, 1.02-1.11) for those who usually added salt, and 1.28 (95% CI, 1.20-1.35) for those who always added salt.
The researchers also estimated the lower survival time caused by the high frequency of adding salt to foods. At age 50, women who always added salt to foods had an average 1.50 fewer years of life expectancy, and men who always added salt had an average 2.28 fewer years of life expectancy, as compared with their counterparts who never/rarely added salt to foods.
For cause-specific premature mortality, results showed that higher frequency of adding salt to foods was significantly associated with a higher risk of cardiovascular mortality and cancer mortality, but not for dementia mortality or respiratory mortality. For the subtypes of cardiovascular mortality, adding salt to foods was significantly associated with higher risk of stroke mortality but not coronary heart disease mortality.
Other analyses suggested that the association of adding salt to foods with an increased risk of premature mortality appeared to be attenuated with increasing intake of food high in potassium (fruits and vegetables).
The authors point out that the amounts of discretionary sodium intake (the salt used at the table or in home cooking) have been largely overlooked in previous studies, even though adding salt to foods accounts for a considerable proportion of total sodium intake (6%-20%) in Western diets.
“Our findings also support the notion that even a modest reduction in sodium intake is likely to result in substantial health benefits, especially when it is achieved in the general population,” they conclude.
Conflicting information from different studies
But the current findings seem to directly contradict those from another recent study by Messerli and colleagues showing higher sodium intake correlates with improved life expectancy.
Addressing these contradictory results, Dr. Qi commented: “The study of Messerli et al. is based on an ecological design, in which the analysis is performed on country average sodium intake, rather than at the individual level. This type of ecological study has several major limitations, such as the lack of individuals’ sodium intake, uncontrolled confounding, and the cross-sectional nature. Typically, ecological studies are not considered useful for testing hypothesis in epidemiological studies.”
Dr. Qi noted that, in contrast, his current study analyzes individuals’ exposure, and has a prospective design. “Our findings are supported by previous large-scale observational studies and clinical trials which show the high intake of sodium may adversely affect chronic diseases such as cardiovascular disease and hypertension.” =
Lead author of the ecological study, Franz Messerli, MD, Bern (Switzerland) University Hospital, however, was not convinced by the findings from Dr. Qi’s study.
“The difference in 24-hour sodium intake between those who never/rarely added salt and those who always did is a minuscule 0.17 g. It is highly unlikely that such negligible quantity has any impact on blood pressure, not to mention cardiovascular mortality or life expectancy,” he commented in an interview.
He also pointed out that, in Dr. Qi’s study, people who added salt more frequently also consumed more red meat and processed meat, as well as less fish and less fruit and vegetables. “I would suggest that the bad habit of adding salt at the table is simply a powerful marker for an unhealthy diet.”
“There is no question that an excessive salt intake is harmful in hypertensive patients and increases the risk of stroke. But 0.17 g is not going to make any difference,” Dr. Messerli added.
What is the optimum level?
In an editorial accompanying the study by Dr. Qi and colleagues in the European Heart Journal, Annika Rosengren, MD, PhD, Sahlgrenska University Hospital, Gothenburg, Sweden, noted that guidelines recommend a salt intake below 5 g, or about a teaspoon, per day. But few individuals meet this recommendation.
Because several recent studies show a U- or J-shaped association between salt and atherosclerotic cardiovascular disease, reducing salt intake across the whole population may not be universally beneficial, Dr. Rosengren said.
“So far, what the collective evidence about salt seems to indicate is that healthy people consuming what constitutes normal levels of ordinary salt need not worry too much about their salt intake,” she wrote.
Instead, she advised a diet rich in fruit and vegetables should be a priority to counterbalance potentially harmful effects of salt, and for many other reasons.
And she added that people at high risk, such as those with hypertension who have a high salt intake, are probably well advised to cut down, and not adding extra salt to already prepared foods is one way of achieving this. However, at the individual level, the optimal salt consumption range, or the “sweet spot” remains to be determined.
“Not adding extra salt to food is unlikely to be harmful and could contribute to strategies to lower population blood pressure levels,” Dr. Rosengren concluded.
A version of this article first appeared on Medscape.com.
in a new study.
In the study of more than 500,000 people, compared with those who never or rarely added salt, those who always added salt to their food had a 28% increased risk of dying prematurely (defined as death before the age of 75 years).
Results also showed that adding salt to food was linked to a lower life expectancy. At the age of 50 years, life expectancy was reduced by 1.5 years in women and by 2.28 years in men who always added salt to their food, compared with those who never or rarely did.
However, these increased risks appeared to be attenuated with increasing intakes of high-potassium foods (vegetables and fruits).
The study was published online in the European Heart Journal.
“As far as we are aware, this is the first study to analyze adding salt to meals as a unique measurement for dietary sodium intake. Such a measure is less likely affected by other dietary components, especially potassium intake,” senior author Lu Qi, MD, Tulane University, New Orleans, told this news organization.
“Our study provides supportive evidence from a novel perspective to show the adverse effects of high sodium intake on human health, which is still a controversial topic. Our findings support the advice that reduction of salt intake by reducing the salt added to meals may benefit health and improve life expectancy. Our results also suggest that high intakes of fruits and vegetables are beneficial regarding lowering the adverse effects of salt,” he added.
Link between dietary salt and health is subject of longstanding debate
The researchers explained that the relationship between dietary salt intake and health remains a subject of longstanding debate, with previous studies on the association between sodium intake and mortality having shown conflicting results.
They attributed the inconsistent results to the low accuracy of sodium measurement, noting that sodium intake varies widely from day to day, but the majority of previous studies have largely relied on a single day’s urine collection or dietary survey for estimating the sodium intake, which is inadequate to assess an individual’s usual consumption levels.
They also pointed out that it is difficult to separate the contributions of intakes of sodium and potassium to health based on current methods for measuring dietary sodium and potassium, and this may confound the association between sodium intake and health outcomes.
They noted that the hypothesis that a high-potassium intake may attenuate the adverse association of high-sodium intake with health outcomes has been proposed for many years, but studies assessing the interaction between sodium intake and potassium intake on the risk of mortality are scarce.
Adding salt to food at the table is a common eating behavior directly related to an individual’s long-term preference for salty tasting foods and habitual salt intake, the authors said, adding that commonly used table salt contains 97%-99% sodium chloride, minimizing the potential confounding effects of other dietary factors including potassium. “Therefore, adding salt to foods provides a unique assessment to evaluate the association between habitual sodium intake and mortality.”
UK Biobank study
For the current study Dr. Qi and colleagues analyzed data from 501,379 people taking part in the UK Biobank study. When joining the study between 2006 and 2010, the participants were asked whether they added salt to their foods never/rarely, sometimes, usually or always. Participants were then followed for a median of 9 years.
After adjustment for sex, age, race, smoking, moderate drinking, body mass index, physical activity, Townsend deprivation index, high cholesterol, chronic kidney disease, diabetes, cardiovascular disease, and cancer, results showed an increasing risk of all-cause premature mortality rose with increasing frequency of adding salt to foods.
The adjusted hazard ratios, compared with those who never or rarely added salt, were 1.02 (95% CI, 0.99-1.06) for those who added salt sometimes, 1.07 (95% CI, 1.02-1.11) for those who usually added salt, and 1.28 (95% CI, 1.20-1.35) for those who always added salt.
The researchers also estimated the lower survival time caused by the high frequency of adding salt to foods. At age 50, women who always added salt to foods had an average 1.50 fewer years of life expectancy, and men who always added salt had an average 2.28 fewer years of life expectancy, as compared with their counterparts who never/rarely added salt to foods.
For cause-specific premature mortality, results showed that higher frequency of adding salt to foods was significantly associated with a higher risk of cardiovascular mortality and cancer mortality, but not for dementia mortality or respiratory mortality. For the subtypes of cardiovascular mortality, adding salt to foods was significantly associated with higher risk of stroke mortality but not coronary heart disease mortality.
Other analyses suggested that the association of adding salt to foods with an increased risk of premature mortality appeared to be attenuated with increasing intake of food high in potassium (fruits and vegetables).
The authors point out that the amounts of discretionary sodium intake (the salt used at the table or in home cooking) have been largely overlooked in previous studies, even though adding salt to foods accounts for a considerable proportion of total sodium intake (6%-20%) in Western diets.
“Our findings also support the notion that even a modest reduction in sodium intake is likely to result in substantial health benefits, especially when it is achieved in the general population,” they conclude.
Conflicting information from different studies
But the current findings seem to directly contradict those from another recent study by Messerli and colleagues showing higher sodium intake correlates with improved life expectancy.
Addressing these contradictory results, Dr. Qi commented: “The study of Messerli et al. is based on an ecological design, in which the analysis is performed on country average sodium intake, rather than at the individual level. This type of ecological study has several major limitations, such as the lack of individuals’ sodium intake, uncontrolled confounding, and the cross-sectional nature. Typically, ecological studies are not considered useful for testing hypothesis in epidemiological studies.”
Dr. Qi noted that, in contrast, his current study analyzes individuals’ exposure, and has a prospective design. “Our findings are supported by previous large-scale observational studies and clinical trials which show the high intake of sodium may adversely affect chronic diseases such as cardiovascular disease and hypertension.” =
Lead author of the ecological study, Franz Messerli, MD, Bern (Switzerland) University Hospital, however, was not convinced by the findings from Dr. Qi’s study.
“The difference in 24-hour sodium intake between those who never/rarely added salt and those who always did is a minuscule 0.17 g. It is highly unlikely that such negligible quantity has any impact on blood pressure, not to mention cardiovascular mortality or life expectancy,” he commented in an interview.
He also pointed out that, in Dr. Qi’s study, people who added salt more frequently also consumed more red meat and processed meat, as well as less fish and less fruit and vegetables. “I would suggest that the bad habit of adding salt at the table is simply a powerful marker for an unhealthy diet.”
“There is no question that an excessive salt intake is harmful in hypertensive patients and increases the risk of stroke. But 0.17 g is not going to make any difference,” Dr. Messerli added.
What is the optimum level?
In an editorial accompanying the study by Dr. Qi and colleagues in the European Heart Journal, Annika Rosengren, MD, PhD, Sahlgrenska University Hospital, Gothenburg, Sweden, noted that guidelines recommend a salt intake below 5 g, or about a teaspoon, per day. But few individuals meet this recommendation.
Because several recent studies show a U- or J-shaped association between salt and atherosclerotic cardiovascular disease, reducing salt intake across the whole population may not be universally beneficial, Dr. Rosengren said.
“So far, what the collective evidence about salt seems to indicate is that healthy people consuming what constitutes normal levels of ordinary salt need not worry too much about their salt intake,” she wrote.
Instead, she advised a diet rich in fruit and vegetables should be a priority to counterbalance potentially harmful effects of salt, and for many other reasons.
And she added that people at high risk, such as those with hypertension who have a high salt intake, are probably well advised to cut down, and not adding extra salt to already prepared foods is one way of achieving this. However, at the individual level, the optimal salt consumption range, or the “sweet spot” remains to be determined.
“Not adding extra salt to food is unlikely to be harmful and could contribute to strategies to lower population blood pressure levels,” Dr. Rosengren concluded.
A version of this article first appeared on Medscape.com.
in a new study.
In the study of more than 500,000 people, compared with those who never or rarely added salt, those who always added salt to their food had a 28% increased risk of dying prematurely (defined as death before the age of 75 years).
Results also showed that adding salt to food was linked to a lower life expectancy. At the age of 50 years, life expectancy was reduced by 1.5 years in women and by 2.28 years in men who always added salt to their food, compared with those who never or rarely did.
However, these increased risks appeared to be attenuated with increasing intakes of high-potassium foods (vegetables and fruits).
The study was published online in the European Heart Journal.
“As far as we are aware, this is the first study to analyze adding salt to meals as a unique measurement for dietary sodium intake. Such a measure is less likely affected by other dietary components, especially potassium intake,” senior author Lu Qi, MD, Tulane University, New Orleans, told this news organization.
“Our study provides supportive evidence from a novel perspective to show the adverse effects of high sodium intake on human health, which is still a controversial topic. Our findings support the advice that reduction of salt intake by reducing the salt added to meals may benefit health and improve life expectancy. Our results also suggest that high intakes of fruits and vegetables are beneficial regarding lowering the adverse effects of salt,” he added.
Link between dietary salt and health is subject of longstanding debate
The researchers explained that the relationship between dietary salt intake and health remains a subject of longstanding debate, with previous studies on the association between sodium intake and mortality having shown conflicting results.
They attributed the inconsistent results to the low accuracy of sodium measurement, noting that sodium intake varies widely from day to day, but the majority of previous studies have largely relied on a single day’s urine collection or dietary survey for estimating the sodium intake, which is inadequate to assess an individual’s usual consumption levels.
They also pointed out that it is difficult to separate the contributions of intakes of sodium and potassium to health based on current methods for measuring dietary sodium and potassium, and this may confound the association between sodium intake and health outcomes.
They noted that the hypothesis that a high-potassium intake may attenuate the adverse association of high-sodium intake with health outcomes has been proposed for many years, but studies assessing the interaction between sodium intake and potassium intake on the risk of mortality are scarce.
Adding salt to food at the table is a common eating behavior directly related to an individual’s long-term preference for salty tasting foods and habitual salt intake, the authors said, adding that commonly used table salt contains 97%-99% sodium chloride, minimizing the potential confounding effects of other dietary factors including potassium. “Therefore, adding salt to foods provides a unique assessment to evaluate the association between habitual sodium intake and mortality.”
UK Biobank study
For the current study Dr. Qi and colleagues analyzed data from 501,379 people taking part in the UK Biobank study. When joining the study between 2006 and 2010, the participants were asked whether they added salt to their foods never/rarely, sometimes, usually or always. Participants were then followed for a median of 9 years.
After adjustment for sex, age, race, smoking, moderate drinking, body mass index, physical activity, Townsend deprivation index, high cholesterol, chronic kidney disease, diabetes, cardiovascular disease, and cancer, results showed an increasing risk of all-cause premature mortality rose with increasing frequency of adding salt to foods.
The adjusted hazard ratios, compared with those who never or rarely added salt, were 1.02 (95% CI, 0.99-1.06) for those who added salt sometimes, 1.07 (95% CI, 1.02-1.11) for those who usually added salt, and 1.28 (95% CI, 1.20-1.35) for those who always added salt.
The researchers also estimated the lower survival time caused by the high frequency of adding salt to foods. At age 50, women who always added salt to foods had an average 1.50 fewer years of life expectancy, and men who always added salt had an average 2.28 fewer years of life expectancy, as compared with their counterparts who never/rarely added salt to foods.
For cause-specific premature mortality, results showed that higher frequency of adding salt to foods was significantly associated with a higher risk of cardiovascular mortality and cancer mortality, but not for dementia mortality or respiratory mortality. For the subtypes of cardiovascular mortality, adding salt to foods was significantly associated with higher risk of stroke mortality but not coronary heart disease mortality.
Other analyses suggested that the association of adding salt to foods with an increased risk of premature mortality appeared to be attenuated with increasing intake of food high in potassium (fruits and vegetables).
The authors point out that the amounts of discretionary sodium intake (the salt used at the table or in home cooking) have been largely overlooked in previous studies, even though adding salt to foods accounts for a considerable proportion of total sodium intake (6%-20%) in Western diets.
“Our findings also support the notion that even a modest reduction in sodium intake is likely to result in substantial health benefits, especially when it is achieved in the general population,” they conclude.
Conflicting information from different studies
But the current findings seem to directly contradict those from another recent study by Messerli and colleagues showing higher sodium intake correlates with improved life expectancy.
Addressing these contradictory results, Dr. Qi commented: “The study of Messerli et al. is based on an ecological design, in which the analysis is performed on country average sodium intake, rather than at the individual level. This type of ecological study has several major limitations, such as the lack of individuals’ sodium intake, uncontrolled confounding, and the cross-sectional nature. Typically, ecological studies are not considered useful for testing hypothesis in epidemiological studies.”
Dr. Qi noted that, in contrast, his current study analyzes individuals’ exposure, and has a prospective design. “Our findings are supported by previous large-scale observational studies and clinical trials which show the high intake of sodium may adversely affect chronic diseases such as cardiovascular disease and hypertension.” =
Lead author of the ecological study, Franz Messerli, MD, Bern (Switzerland) University Hospital, however, was not convinced by the findings from Dr. Qi’s study.
“The difference in 24-hour sodium intake between those who never/rarely added salt and those who always did is a minuscule 0.17 g. It is highly unlikely that such negligible quantity has any impact on blood pressure, not to mention cardiovascular mortality or life expectancy,” he commented in an interview.
He also pointed out that, in Dr. Qi’s study, people who added salt more frequently also consumed more red meat and processed meat, as well as less fish and less fruit and vegetables. “I would suggest that the bad habit of adding salt at the table is simply a powerful marker for an unhealthy diet.”
“There is no question that an excessive salt intake is harmful in hypertensive patients and increases the risk of stroke. But 0.17 g is not going to make any difference,” Dr. Messerli added.
What is the optimum level?
In an editorial accompanying the study by Dr. Qi and colleagues in the European Heart Journal, Annika Rosengren, MD, PhD, Sahlgrenska University Hospital, Gothenburg, Sweden, noted that guidelines recommend a salt intake below 5 g, or about a teaspoon, per day. But few individuals meet this recommendation.
Because several recent studies show a U- or J-shaped association between salt and atherosclerotic cardiovascular disease, reducing salt intake across the whole population may not be universally beneficial, Dr. Rosengren said.
“So far, what the collective evidence about salt seems to indicate is that healthy people consuming what constitutes normal levels of ordinary salt need not worry too much about their salt intake,” she wrote.
Instead, she advised a diet rich in fruit and vegetables should be a priority to counterbalance potentially harmful effects of salt, and for many other reasons.
And she added that people at high risk, such as those with hypertension who have a high salt intake, are probably well advised to cut down, and not adding extra salt to already prepared foods is one way of achieving this. However, at the individual level, the optimal salt consumption range, or the “sweet spot” remains to be determined.
“Not adding extra salt to food is unlikely to be harmful and could contribute to strategies to lower population blood pressure levels,” Dr. Rosengren concluded.
A version of this article first appeared on Medscape.com.
FROM THE EUROPEAN HEART JOURNAL
Zoster vaccination does not appear to increase flare risk in patients with immune-mediated inflammatory disease
, according to research published in Arthritis & Rheumatology.
The authors of the study noted that individuals with IMIDs are at increased risk for herpes zoster and related complications, including postherpetic neuralgia, and that vaccination has been recommended for certain groups of patients with rheumatoid arthritis, inflammatory bowel disease, and psoriasis, by the American College of Rheumatology and other professional organizations for individuals aged 50 and older.
The study investigators used medical claims from IBM MarketScan, which provided data on patients aged 50-64 years, and data from the Centers for Medicare and Medicaid Services’ Medicare on patients aged 65 and older.
They defined presumed flares in three ways: hospitalization/emergency department visits for IMIDs, steroid treatment with a short-acting oral glucocorticoid, or treatment with a parenteral glucocorticoid injection. The investigators conducted a self-controlled case series (SCCS) analysis to examine any temporal link between the RZV and disease flares.
Among enrollees with IMIDs, 14.8% of the 55,654 patients in the MarketScan database and 43.2% of the 160,545 patients in the Medicare database received at least one dose of RZV during 2018-2019. The two-dose series completion within 6 months was 76.6% in the MarketScan group (age range, 50-64 years) and 85.4% among Medicare enrollees (age range, 65 years and older). In the SCCS analysis, 10% and 13% of patients developed flares in the control group as compared to 9%, and 11%-12% in the risk window following one or two doses of RZV among MarketScan and Medicare enrollees, respectively.
Based on these findings, the investigators concluded there was no statistically significant increase in flares subsequent to RZV administration for any IMID in either patients aged 50-64 years or patients aged 65 years and older following the first dose or second dose.
Nilanjana Bose, MD, a rheumatologist with Lonestar Rheumatology, Houston, Texas, who was not involved with the study, said that the research addresses a topic where there is uneasiness, namely vaccination in patients with IMIDs.
“Anytime you are vaccinating a patient with an autoimmune disease, especially one on a biologic, you always worry about the risk of flares,” said Dr. Bose. “Any time you tamper with the immune system, there is a risk of flares.”
The study serves as a clarification for the primary care setting, said Dr. Bose. “A lot of the time, the shingles vaccine is administered not by rheumatology but by primary care or through the pharmacy,” she said. “This study puts them [primary care physicians] at ease.”
Findings from the study reflect that most RZV vaccinations were administered in pharmacies.
One of the weaknesses of the study is that the investigators did not include patients younger than 50 years old, said Dr. Bose. “It would have been nice if they could have looked at younger patients,” she said. “We try to vaccinate all our [immunocompromised] adult patients, even the younger ones, because they are also at risk for shingles.”
Given that there are increasing options of medical therapies in rheumatology that are immunomodulatory, the subject of vaccination for patients is often one of discussion, added Dr. Bose.
Arthur Kavanaugh, MD, professor of medicine, University of California San Diego (UCSD), La Jolla, Calif., and director of the Center for Innovative Therapy in the UCSD Division of Rheumatology, Allergy, and Immunology, told this news organization that a strength of the study is its large numbers of patients but noted the shortcoming of using claims data. “Claims data has inherent limitations, such as the lack of detailed granular data on the patients,” wrote Dr. Kavanaugh, who was not involved with the study. He described this investigation as “really about the first evidence that I am aware of addressing this issue.”
No funding source was listed. One author disclosed having received research grants and consulting fees received from Pfizer and GSK for unrelated work; the other authors had no disclosures. Dr. Bose and Dr. Kavanaugh had no relevant disclosures.
, according to research published in Arthritis & Rheumatology.
The authors of the study noted that individuals with IMIDs are at increased risk for herpes zoster and related complications, including postherpetic neuralgia, and that vaccination has been recommended for certain groups of patients with rheumatoid arthritis, inflammatory bowel disease, and psoriasis, by the American College of Rheumatology and other professional organizations for individuals aged 50 and older.
The study investigators used medical claims from IBM MarketScan, which provided data on patients aged 50-64 years, and data from the Centers for Medicare and Medicaid Services’ Medicare on patients aged 65 and older.
They defined presumed flares in three ways: hospitalization/emergency department visits for IMIDs, steroid treatment with a short-acting oral glucocorticoid, or treatment with a parenteral glucocorticoid injection. The investigators conducted a self-controlled case series (SCCS) analysis to examine any temporal link between the RZV and disease flares.
Among enrollees with IMIDs, 14.8% of the 55,654 patients in the MarketScan database and 43.2% of the 160,545 patients in the Medicare database received at least one dose of RZV during 2018-2019. The two-dose series completion within 6 months was 76.6% in the MarketScan group (age range, 50-64 years) and 85.4% among Medicare enrollees (age range, 65 years and older). In the SCCS analysis, 10% and 13% of patients developed flares in the control group as compared to 9%, and 11%-12% in the risk window following one or two doses of RZV among MarketScan and Medicare enrollees, respectively.
Based on these findings, the investigators concluded there was no statistically significant increase in flares subsequent to RZV administration for any IMID in either patients aged 50-64 years or patients aged 65 years and older following the first dose or second dose.
Nilanjana Bose, MD, a rheumatologist with Lonestar Rheumatology, Houston, Texas, who was not involved with the study, said that the research addresses a topic where there is uneasiness, namely vaccination in patients with IMIDs.
“Anytime you are vaccinating a patient with an autoimmune disease, especially one on a biologic, you always worry about the risk of flares,” said Dr. Bose. “Any time you tamper with the immune system, there is a risk of flares.”
The study serves as a clarification for the primary care setting, said Dr. Bose. “A lot of the time, the shingles vaccine is administered not by rheumatology but by primary care or through the pharmacy,” she said. “This study puts them [primary care physicians] at ease.”
Findings from the study reflect that most RZV vaccinations were administered in pharmacies.
One of the weaknesses of the study is that the investigators did not include patients younger than 50 years old, said Dr. Bose. “It would have been nice if they could have looked at younger patients,” she said. “We try to vaccinate all our [immunocompromised] adult patients, even the younger ones, because they are also at risk for shingles.”
Given that there are increasing options of medical therapies in rheumatology that are immunomodulatory, the subject of vaccination for patients is often one of discussion, added Dr. Bose.
Arthur Kavanaugh, MD, professor of medicine, University of California San Diego (UCSD), La Jolla, Calif., and director of the Center for Innovative Therapy in the UCSD Division of Rheumatology, Allergy, and Immunology, told this news organization that a strength of the study is its large numbers of patients but noted the shortcoming of using claims data. “Claims data has inherent limitations, such as the lack of detailed granular data on the patients,” wrote Dr. Kavanaugh, who was not involved with the study. He described this investigation as “really about the first evidence that I am aware of addressing this issue.”
No funding source was listed. One author disclosed having received research grants and consulting fees received from Pfizer and GSK for unrelated work; the other authors had no disclosures. Dr. Bose and Dr. Kavanaugh had no relevant disclosures.
, according to research published in Arthritis & Rheumatology.
The authors of the study noted that individuals with IMIDs are at increased risk for herpes zoster and related complications, including postherpetic neuralgia, and that vaccination has been recommended for certain groups of patients with rheumatoid arthritis, inflammatory bowel disease, and psoriasis, by the American College of Rheumatology and other professional organizations for individuals aged 50 and older.
The study investigators used medical claims from IBM MarketScan, which provided data on patients aged 50-64 years, and data from the Centers for Medicare and Medicaid Services’ Medicare on patients aged 65 and older.
They defined presumed flares in three ways: hospitalization/emergency department visits for IMIDs, steroid treatment with a short-acting oral glucocorticoid, or treatment with a parenteral glucocorticoid injection. The investigators conducted a self-controlled case series (SCCS) analysis to examine any temporal link between the RZV and disease flares.
Among enrollees with IMIDs, 14.8% of the 55,654 patients in the MarketScan database and 43.2% of the 160,545 patients in the Medicare database received at least one dose of RZV during 2018-2019. The two-dose series completion within 6 months was 76.6% in the MarketScan group (age range, 50-64 years) and 85.4% among Medicare enrollees (age range, 65 years and older). In the SCCS analysis, 10% and 13% of patients developed flares in the control group as compared to 9%, and 11%-12% in the risk window following one or two doses of RZV among MarketScan and Medicare enrollees, respectively.
Based on these findings, the investigators concluded there was no statistically significant increase in flares subsequent to RZV administration for any IMID in either patients aged 50-64 years or patients aged 65 years and older following the first dose or second dose.
Nilanjana Bose, MD, a rheumatologist with Lonestar Rheumatology, Houston, Texas, who was not involved with the study, said that the research addresses a topic where there is uneasiness, namely vaccination in patients with IMIDs.
“Anytime you are vaccinating a patient with an autoimmune disease, especially one on a biologic, you always worry about the risk of flares,” said Dr. Bose. “Any time you tamper with the immune system, there is a risk of flares.”
The study serves as a clarification for the primary care setting, said Dr. Bose. “A lot of the time, the shingles vaccine is administered not by rheumatology but by primary care or through the pharmacy,” she said. “This study puts them [primary care physicians] at ease.”
Findings from the study reflect that most RZV vaccinations were administered in pharmacies.
One of the weaknesses of the study is that the investigators did not include patients younger than 50 years old, said Dr. Bose. “It would have been nice if they could have looked at younger patients,” she said. “We try to vaccinate all our [immunocompromised] adult patients, even the younger ones, because they are also at risk for shingles.”
Given that there are increasing options of medical therapies in rheumatology that are immunomodulatory, the subject of vaccination for patients is often one of discussion, added Dr. Bose.
Arthur Kavanaugh, MD, professor of medicine, University of California San Diego (UCSD), La Jolla, Calif., and director of the Center for Innovative Therapy in the UCSD Division of Rheumatology, Allergy, and Immunology, told this news organization that a strength of the study is its large numbers of patients but noted the shortcoming of using claims data. “Claims data has inherent limitations, such as the lack of detailed granular data on the patients,” wrote Dr. Kavanaugh, who was not involved with the study. He described this investigation as “really about the first evidence that I am aware of addressing this issue.”
No funding source was listed. One author disclosed having received research grants and consulting fees received from Pfizer and GSK for unrelated work; the other authors had no disclosures. Dr. Bose and Dr. Kavanaugh had no relevant disclosures.
Sleep-deprived physicians less empathetic to patient pain?
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
Docs reveal perils of giving medical advice to friends and family
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.