User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Class I recall issued for intracranial pressure monitor
Integra is recalling the CereLink Intracranial Pressure (ICP) Monitor after reports that the device may display incorrect ICP values and out-of-range pressure readings.
The recall includes 388 monitors, with model numbers 826820 and 826820P. The devices were distributed between June 1, 2021 and May 31, 2022.
The U.S. Food and Drug Administration has identified this as a class I recall, the most serious type, because of the risk for serious injury or death.
The monitor is used in patients with head injuries and stroke as well as in surgical and postoperative neurosurgical patients and those with other conditions.
The device’s sensor is implanted in the brain and connected by a wire to an external monitor that displays ICP readings, which are used to both monitor and guide treatment.
If the CereLink ICP Monitor fails to function properly, the patient may have to undergo additional brain surgeries to replace it, which involves the risks for infection, bleeding, and damage to tissue. A malfunctioning device also creates a risk for serious injury or death, the MedWatch notes.
Global complaints
As of July 31, Integra has received 105 global complaints associated with this recall.
In addition,
According to the FDA, the patient death report in the MDR described a malfunctioning CereLink ICP Monitor during use in a critically injured patient, which was mitigated by replacing the ICP sensor.
“The cause of patient death was determined by Integra to be unrelated to the CereLink ICP Monitor malfunction,” the FDA said.
The manufacturer has sent a letter to customers advising them to stop using the recalled monitors “as soon as clinically possible.”
The letter states that continued use of a monitor already in place should be determined only by an individualized risk-benefit analysis by the attending clinician.
For any new patients, the company advises switching to an alternate patient-monitoring system.
Customers with questions or concerns about this recall should contact their Integra account manager, clinical specialist, or customer service by phone at 800-654-2873 or by email at [email protected].
Problems related to the CereLink ICP Monitor should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Integra is recalling the CereLink Intracranial Pressure (ICP) Monitor after reports that the device may display incorrect ICP values and out-of-range pressure readings.
The recall includes 388 monitors, with model numbers 826820 and 826820P. The devices were distributed between June 1, 2021 and May 31, 2022.
The U.S. Food and Drug Administration has identified this as a class I recall, the most serious type, because of the risk for serious injury or death.
The monitor is used in patients with head injuries and stroke as well as in surgical and postoperative neurosurgical patients and those with other conditions.
The device’s sensor is implanted in the brain and connected by a wire to an external monitor that displays ICP readings, which are used to both monitor and guide treatment.
If the CereLink ICP Monitor fails to function properly, the patient may have to undergo additional brain surgeries to replace it, which involves the risks for infection, bleeding, and damage to tissue. A malfunctioning device also creates a risk for serious injury or death, the MedWatch notes.
Global complaints
As of July 31, Integra has received 105 global complaints associated with this recall.
In addition,
According to the FDA, the patient death report in the MDR described a malfunctioning CereLink ICP Monitor during use in a critically injured patient, which was mitigated by replacing the ICP sensor.
“The cause of patient death was determined by Integra to be unrelated to the CereLink ICP Monitor malfunction,” the FDA said.
The manufacturer has sent a letter to customers advising them to stop using the recalled monitors “as soon as clinically possible.”
The letter states that continued use of a monitor already in place should be determined only by an individualized risk-benefit analysis by the attending clinician.
For any new patients, the company advises switching to an alternate patient-monitoring system.
Customers with questions or concerns about this recall should contact their Integra account manager, clinical specialist, or customer service by phone at 800-654-2873 or by email at [email protected].
Problems related to the CereLink ICP Monitor should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Integra is recalling the CereLink Intracranial Pressure (ICP) Monitor after reports that the device may display incorrect ICP values and out-of-range pressure readings.
The recall includes 388 monitors, with model numbers 826820 and 826820P. The devices were distributed between June 1, 2021 and May 31, 2022.
The U.S. Food and Drug Administration has identified this as a class I recall, the most serious type, because of the risk for serious injury or death.
The monitor is used in patients with head injuries and stroke as well as in surgical and postoperative neurosurgical patients and those with other conditions.
The device’s sensor is implanted in the brain and connected by a wire to an external monitor that displays ICP readings, which are used to both monitor and guide treatment.
If the CereLink ICP Monitor fails to function properly, the patient may have to undergo additional brain surgeries to replace it, which involves the risks for infection, bleeding, and damage to tissue. A malfunctioning device also creates a risk for serious injury or death, the MedWatch notes.
Global complaints
As of July 31, Integra has received 105 global complaints associated with this recall.
In addition,
According to the FDA, the patient death report in the MDR described a malfunctioning CereLink ICP Monitor during use in a critically injured patient, which was mitigated by replacing the ICP sensor.
“The cause of patient death was determined by Integra to be unrelated to the CereLink ICP Monitor malfunction,” the FDA said.
The manufacturer has sent a letter to customers advising them to stop using the recalled monitors “as soon as clinically possible.”
The letter states that continued use of a monitor already in place should be determined only by an individualized risk-benefit analysis by the attending clinician.
For any new patients, the company advises switching to an alternate patient-monitoring system.
Customers with questions or concerns about this recall should contact their Integra account manager, clinical specialist, or customer service by phone at 800-654-2873 or by email at [email protected].
Problems related to the CereLink ICP Monitor should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Real medical news: Many teens trust fake medical news
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
The kids aren’t alright (at identifying fake news online)
If there’s one thing today’s teenagers are good at, it’s the Internet. What with their TokTiks, Fortnights, and memes whose lifespans are measured in milliseconds, it’s only natural that a contingent of people who have never known a world where the Internet wasn’t omnipresent would be highly skilled at navigating the dense, labyrinthine virtual world and the many falsehoods contained within.
Ladies and gentlemen, we’ve been duped, bamboozled, and smeckledorfed. New research from Slovakia suggests the opposite, in fact: Teenagers are just as bad as the rest of us, if not worse, at distinguishing between fake and real online health messaging.
For the study, 300 teenagers aged 16-19 years old were shown a group of messages about the health-promoting effects of fruits and vegetables; these messages were either false, true and neutral, or true with some sort of editing (a clickbait title or grammar mistakes) to mask their trustworthiness. Just under half of the subjects identified and trusted the true neutral messages over fake messages, while 41% couldn’t tell the difference and 11% trusted the fake messages more. In addition, they couldn’t tell the difference between fake and true messages when the content seemed plausible.
In a bit of good news, teenagers were just as likely to trust the edited true messages as the true neutral ones, except in instances when the edited message had a clickbait title. They were much less likely to trust those.
Based on their subjects’ rather poor performance, the study authors suggested teenagers go through health literacy and media literacy training, as well as develop their analytical and scientific reasoning. The LOTME staff rather suspects the study authors have never met a teenager. The only thing teenagers are going to get out of health literacy training is fodder for memes to put up on Myspace. Myspace is still a thing, right? We’re not old, we swear.
Can a computer help deliver babies?
Delivering babies can be a complicated business. Most doctors and midwives rely on their years of experience and training to make certain decisions for mothers in labor, but an artificial intelligence (AI) algorithm could make the entire process easier and safer.
Researchers from the Mayo Clinic recently reported that using an AI to analyze women’s labor patterns was very successful in determining whether a vaginal or cesarean delivery was appropriate.
They examined over 700 factors and over 66,000 deliveries from the National Institute of Child Health and Human Development’s multicenter Consortium on Safe Labor database to produce a risk-prediction model that may “provide an alternative to conventional labor charts and promote individualization of clinical decisions using baseline and labor characteristics of each patient,” they said in a written statement from the clinic.
It is hoped that the AI will reduce the risk of possible complications and the costs associated with maternal mortality. The AI also could be a significant tool for doctors and midwives in rural areas to determine when a patient needs to be moved to a location with a higher level of care.
“We believe the algorithm will work in real time, meaning every input of new data during an expectant woman’s labor automatically recalculates the risk of adverse outcome,” said senior author Abimbola Famuyide, MD, of the Mayo Clinic.
If it all works out, many lives and dollars could be saved, thanks to science.
Democracy, meet COVID-19
Everywhere you look, it seems, someone is trying to keep someone else from doing something: Don’t carry a gun. Don’t get an abortion. Don’t drive so fast. Don’t inhale that whipped cream. Don’t get a vaccine. Don’t put that in your mouth.
One of the biggies these days is voting rights. Some people are trying to prevent other people from voting. But why? Well, turns out that turnout can be bad for your health … at least during a worldwide pandemic event.
The evidence for that claim comes from researchers who examined the Italian national constitutional referendum conducted in September 2020 along with elections for assembly representatives in 7 of the country’s 20 regions and for mayors in about 12% of municipalities. The combination mattered: Voter turnout was higher in the municipalities that voted for both the referendum and local elections (69%), compared with municipalities voting only for the referendum (47%), the investigators reported in the Journal of Economic Behavior & Organization.
Also occurring in September of 2020 was, as we mentioned, a worldwide pandemic event. You may have heard about it.
The investigators considered the differences in election turnout between the various municipalities and compared them with new weekly COVID-19 infections at the municipality level. “Our model shows that something as fundamental as casting a vote can come at a cost,” investigator Giuseppe Moscelli, PhD, of the University of Surrey (England) said in a written statement.
What was the cost? Each 1% increase in turnout, they found, amounted to an average 1.1% increase in COVID infections after the elections.
See? More people voting means more COVID, which is bad. Which brings us to today’s lesson in people preventing other people from doing something. Don’t let COVID win. Stay in your house and never come out. And get that smeckledorf out of your mouth. You don’t know where it’s been.
Many young kids with COVID may show no symptoms
BY WILL PASS
Just 14% of adults who tested positive for SARS-CoV-2 were asymptomatic, versus 37% of children aged 0-4 years, in the paper. This raises concern that parents, childcare providers, and preschools may be underestimating infection in seemingly healthy young kids who have been exposed to COVID, wrote lead author Ruth A. Karron, MD, and colleagues in JAMA Network Open.
Methods
The new research involved 690 individuals from 175 households in Maryland who were monitored closely between November 2020 and October 2021. Every week for 8 months, participants completed online symptom checks and underwent PCR testing using nasal swabs, with symptomatic individuals submitting additional swabs for analysis.
“What was different about our study [compared with previous studies] was the intensity of our collection, and the fact that we collected specimens from asymptomatic people,” said Dr. Karron, a pediatrician and professor in the department of international health, Johns Hopkins University, Baltimore, in an interview. “You shed more virus earlier in the infection than later, and the fact that we were sampling every single week meant that we could pick up those early infections.”
The study also stands out for its focus on young children, Dr. Karron said. Enrollment required all households to have at least one child aged 0-4 years, so 256 out of 690 participants (37.1%) were in this youngest age group. The remainder of the population consisted of 100 older children aged 5-17 years (14.5%) and 334 adults aged 18-74 years (48.4%).
Children 4 and under more than twice as likely to be asymptomatic
By the end of the study, 51 participants had tested positive for SARS-CoV-2, among whom 14 had no symptoms. A closer look showed that children 0-4 years of age who contracted COVID were more than twice as likely to be asymptomatic as infected adults (36.8% vs. 14.3%).
The relationship between symptoms and viral load also differed between adults and young children.
While adults with high viral loads – suggesting greater contagiousness – typically had more severe COVID symptoms, no correlation was found in young kids, meaning children with mild or no symptoms could still be highly contagious.
Dr. Karron said these findings should help parents and other stakeholders make better-informed decisions based on known risks. She recommended testing young, asymptomatic children for COVID if they have been exposed to infected individuals, then acting accordingly based on the results.
“If a family is infected with the virus, and the 2-year-old is asymptomatic, and people are thinking about a visit to elderly grandparents who may be frail, one shouldn’t assume that the 2-year-old is uninfected,” Dr. Karron said. “That child should be tested along with other family members.”
Testing should also be considered for young children exposed to COVID at childcare facilities, she added.
But not every expert consulted for this piece shared these opinions of Dr. Karron.
“I question whether that effort is worth it,” said Dean Blumberg, MD, professor and chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, Calif.
He noted that recent Food and Drug Administration guidance for COVID testing calls for three negative at-home antigen tests to confirm lack of infection.
“That would take 4 days to get those tests done,” he said. “So, it’s a lot of testing. It’s a lot of record keeping, it’s inconvenient, it’s uncomfortable to be tested, and I just question whether it’s worth that effort.”
Applicability of findings to today questioned
Dr. Blumberg also questioned whether the study, which was completed almost a year ago, reflects the current pandemic landscape.
“At the time this study was done, it was predominantly Delta [variant instead of Omicron],” Dr. Blumberg said. “The other issue [with the study] is that … most of the children didn’t have preexisting immunity, so you have to take that into account.”
Preexisting immunity – whether from exposure or vaccination – could lower viral loads, so asymptomatic children today really could be less contagious than they were when the study was done, according to Dr. Blumberg. Kids without symptoms are also less likely to spread the virus, because they aren’t coughing or sneezing, he added.
Sara R. Kim, MD, and Janet A. Englund, MD, of the Seattle Children’s Research Institute, University of Washington, said it’s challenging to know how applicable the findings are, although they sided more with the investigators than Dr. Blumberg.
“Given the higher rate of transmissibility and infectivity of the Omicron variant, it is difficult to make direct associations between findings reported during this study period and those present in the current era during which the Omicron variant is circulating,” they wrote in an accompanying editorial. “However, the higher rates of asymptomatic infection observed among children in this study are likely to be consistent with those observed for current and future viral variants.”
Although the experts offered different interpretations of the findings, they shared similar perspectives on vaccination.
“The most important thing that parents can do is get their kids vaccinated, be vaccinated themselves, and have everybody in the household vaccinated and up to date for all doses that are indicated,” Dr. Blumberg said.
Dr. Karron noted that vaccination will be increasingly important in the coming months.
“Summer is ending; school is starting,” she said. “We’re going to be in large groups indoors again very soon. To keep young children safe, I think it’s really important for them to get vaccinated.”
The study was funded by the CDC. The investigators disclosed no other relationships. Dr. Englund disclosed relationships with AstraZeneca, GlaxoSmithKline, Merck, and others. Dr. Kim and Dr. Blumberg disclosed no relevant conflicts of interest.
BY WILL PASS
Just 14% of adults who tested positive for SARS-CoV-2 were asymptomatic, versus 37% of children aged 0-4 years, in the paper. This raises concern that parents, childcare providers, and preschools may be underestimating infection in seemingly healthy young kids who have been exposed to COVID, wrote lead author Ruth A. Karron, MD, and colleagues in JAMA Network Open.
Methods
The new research involved 690 individuals from 175 households in Maryland who were monitored closely between November 2020 and October 2021. Every week for 8 months, participants completed online symptom checks and underwent PCR testing using nasal swabs, with symptomatic individuals submitting additional swabs for analysis.
“What was different about our study [compared with previous studies] was the intensity of our collection, and the fact that we collected specimens from asymptomatic people,” said Dr. Karron, a pediatrician and professor in the department of international health, Johns Hopkins University, Baltimore, in an interview. “You shed more virus earlier in the infection than later, and the fact that we were sampling every single week meant that we could pick up those early infections.”
The study also stands out for its focus on young children, Dr. Karron said. Enrollment required all households to have at least one child aged 0-4 years, so 256 out of 690 participants (37.1%) were in this youngest age group. The remainder of the population consisted of 100 older children aged 5-17 years (14.5%) and 334 adults aged 18-74 years (48.4%).
Children 4 and under more than twice as likely to be asymptomatic
By the end of the study, 51 participants had tested positive for SARS-CoV-2, among whom 14 had no symptoms. A closer look showed that children 0-4 years of age who contracted COVID were more than twice as likely to be asymptomatic as infected adults (36.8% vs. 14.3%).
The relationship between symptoms and viral load also differed between adults and young children.
While adults with high viral loads – suggesting greater contagiousness – typically had more severe COVID symptoms, no correlation was found in young kids, meaning children with mild or no symptoms could still be highly contagious.
Dr. Karron said these findings should help parents and other stakeholders make better-informed decisions based on known risks. She recommended testing young, asymptomatic children for COVID if they have been exposed to infected individuals, then acting accordingly based on the results.
“If a family is infected with the virus, and the 2-year-old is asymptomatic, and people are thinking about a visit to elderly grandparents who may be frail, one shouldn’t assume that the 2-year-old is uninfected,” Dr. Karron said. “That child should be tested along with other family members.”
Testing should also be considered for young children exposed to COVID at childcare facilities, she added.
But not every expert consulted for this piece shared these opinions of Dr. Karron.
“I question whether that effort is worth it,” said Dean Blumberg, MD, professor and chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, Calif.
He noted that recent Food and Drug Administration guidance for COVID testing calls for three negative at-home antigen tests to confirm lack of infection.
“That would take 4 days to get those tests done,” he said. “So, it’s a lot of testing. It’s a lot of record keeping, it’s inconvenient, it’s uncomfortable to be tested, and I just question whether it’s worth that effort.”
Applicability of findings to today questioned
Dr. Blumberg also questioned whether the study, which was completed almost a year ago, reflects the current pandemic landscape.
“At the time this study was done, it was predominantly Delta [variant instead of Omicron],” Dr. Blumberg said. “The other issue [with the study] is that … most of the children didn’t have preexisting immunity, so you have to take that into account.”
Preexisting immunity – whether from exposure or vaccination – could lower viral loads, so asymptomatic children today really could be less contagious than they were when the study was done, according to Dr. Blumberg. Kids without symptoms are also less likely to spread the virus, because they aren’t coughing or sneezing, he added.
Sara R. Kim, MD, and Janet A. Englund, MD, of the Seattle Children’s Research Institute, University of Washington, said it’s challenging to know how applicable the findings are, although they sided more with the investigators than Dr. Blumberg.
“Given the higher rate of transmissibility and infectivity of the Omicron variant, it is difficult to make direct associations between findings reported during this study period and those present in the current era during which the Omicron variant is circulating,” they wrote in an accompanying editorial. “However, the higher rates of asymptomatic infection observed among children in this study are likely to be consistent with those observed for current and future viral variants.”
Although the experts offered different interpretations of the findings, they shared similar perspectives on vaccination.
“The most important thing that parents can do is get their kids vaccinated, be vaccinated themselves, and have everybody in the household vaccinated and up to date for all doses that are indicated,” Dr. Blumberg said.
Dr. Karron noted that vaccination will be increasingly important in the coming months.
“Summer is ending; school is starting,” she said. “We’re going to be in large groups indoors again very soon. To keep young children safe, I think it’s really important for them to get vaccinated.”
The study was funded by the CDC. The investigators disclosed no other relationships. Dr. Englund disclosed relationships with AstraZeneca, GlaxoSmithKline, Merck, and others. Dr. Kim and Dr. Blumberg disclosed no relevant conflicts of interest.
BY WILL PASS
Just 14% of adults who tested positive for SARS-CoV-2 were asymptomatic, versus 37% of children aged 0-4 years, in the paper. This raises concern that parents, childcare providers, and preschools may be underestimating infection in seemingly healthy young kids who have been exposed to COVID, wrote lead author Ruth A. Karron, MD, and colleagues in JAMA Network Open.
Methods
The new research involved 690 individuals from 175 households in Maryland who were monitored closely between November 2020 and October 2021. Every week for 8 months, participants completed online symptom checks and underwent PCR testing using nasal swabs, with symptomatic individuals submitting additional swabs for analysis.
“What was different about our study [compared with previous studies] was the intensity of our collection, and the fact that we collected specimens from asymptomatic people,” said Dr. Karron, a pediatrician and professor in the department of international health, Johns Hopkins University, Baltimore, in an interview. “You shed more virus earlier in the infection than later, and the fact that we were sampling every single week meant that we could pick up those early infections.”
The study also stands out for its focus on young children, Dr. Karron said. Enrollment required all households to have at least one child aged 0-4 years, so 256 out of 690 participants (37.1%) were in this youngest age group. The remainder of the population consisted of 100 older children aged 5-17 years (14.5%) and 334 adults aged 18-74 years (48.4%).
Children 4 and under more than twice as likely to be asymptomatic
By the end of the study, 51 participants had tested positive for SARS-CoV-2, among whom 14 had no symptoms. A closer look showed that children 0-4 years of age who contracted COVID were more than twice as likely to be asymptomatic as infected adults (36.8% vs. 14.3%).
The relationship between symptoms and viral load also differed between adults and young children.
While adults with high viral loads – suggesting greater contagiousness – typically had more severe COVID symptoms, no correlation was found in young kids, meaning children with mild or no symptoms could still be highly contagious.
Dr. Karron said these findings should help parents and other stakeholders make better-informed decisions based on known risks. She recommended testing young, asymptomatic children for COVID if they have been exposed to infected individuals, then acting accordingly based on the results.
“If a family is infected with the virus, and the 2-year-old is asymptomatic, and people are thinking about a visit to elderly grandparents who may be frail, one shouldn’t assume that the 2-year-old is uninfected,” Dr. Karron said. “That child should be tested along with other family members.”
Testing should also be considered for young children exposed to COVID at childcare facilities, she added.
But not every expert consulted for this piece shared these opinions of Dr. Karron.
“I question whether that effort is worth it,” said Dean Blumberg, MD, professor and chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, Calif.
He noted that recent Food and Drug Administration guidance for COVID testing calls for three negative at-home antigen tests to confirm lack of infection.
“That would take 4 days to get those tests done,” he said. “So, it’s a lot of testing. It’s a lot of record keeping, it’s inconvenient, it’s uncomfortable to be tested, and I just question whether it’s worth that effort.”
Applicability of findings to today questioned
Dr. Blumberg also questioned whether the study, which was completed almost a year ago, reflects the current pandemic landscape.
“At the time this study was done, it was predominantly Delta [variant instead of Omicron],” Dr. Blumberg said. “The other issue [with the study] is that … most of the children didn’t have preexisting immunity, so you have to take that into account.”
Preexisting immunity – whether from exposure or vaccination – could lower viral loads, so asymptomatic children today really could be less contagious than they were when the study was done, according to Dr. Blumberg. Kids without symptoms are also less likely to spread the virus, because they aren’t coughing or sneezing, he added.
Sara R. Kim, MD, and Janet A. Englund, MD, of the Seattle Children’s Research Institute, University of Washington, said it’s challenging to know how applicable the findings are, although they sided more with the investigators than Dr. Blumberg.
“Given the higher rate of transmissibility and infectivity of the Omicron variant, it is difficult to make direct associations between findings reported during this study period and those present in the current era during which the Omicron variant is circulating,” they wrote in an accompanying editorial. “However, the higher rates of asymptomatic infection observed among children in this study are likely to be consistent with those observed for current and future viral variants.”
Although the experts offered different interpretations of the findings, they shared similar perspectives on vaccination.
“The most important thing that parents can do is get their kids vaccinated, be vaccinated themselves, and have everybody in the household vaccinated and up to date for all doses that are indicated,” Dr. Blumberg said.
Dr. Karron noted that vaccination will be increasingly important in the coming months.
“Summer is ending; school is starting,” she said. “We’re going to be in large groups indoors again very soon. To keep young children safe, I think it’s really important for them to get vaccinated.”
The study was funded by the CDC. The investigators disclosed no other relationships. Dr. Englund disclosed relationships with AstraZeneca, GlaxoSmithKline, Merck, and others. Dr. Kim and Dr. Blumberg disclosed no relevant conflicts of interest.
FROM JAMA NETWORK OPEN
FDA authorizes updated COVID boosters to target newest variants
The agency cited data to support the safety and efficacy of this next generation of mRNA vaccines targeted toward variants of concern.
The Pfizer EUA corresponds to the company’s combination booster shot that includes the original COVID-19 vaccine as well as a vaccine specifically designed to protect against the most recent Omicron variants, BA.4 and BA.5.
The Moderna combination vaccine will contain both the firm’s original COVID-19 vaccine and a vaccine to protect specifically against Omicron BA.4 and BA.5 subvariants.
As of Aug. 27, BA.4 and BA.4.6 account for about 11% of circulating variants and BA.5 accounts for almost all the remaining 89%, Centers for Disease Control and Prevention data show.
The next step will be review of the scientific data by the CDC’s Advisory Committee on Immunization Practices, which is set to meet Sept. 1 and 2. The final hurdle before distribution of the new vaccines will be sign-off on CDC recommendations for use by agency Director Rochelle Walensky, MD.
This is a developing story. A version of this article first appeared on WebMD.com.
The agency cited data to support the safety and efficacy of this next generation of mRNA vaccines targeted toward variants of concern.
The Pfizer EUA corresponds to the company’s combination booster shot that includes the original COVID-19 vaccine as well as a vaccine specifically designed to protect against the most recent Omicron variants, BA.4 and BA.5.
The Moderna combination vaccine will contain both the firm’s original COVID-19 vaccine and a vaccine to protect specifically against Omicron BA.4 and BA.5 subvariants.
As of Aug. 27, BA.4 and BA.4.6 account for about 11% of circulating variants and BA.5 accounts for almost all the remaining 89%, Centers for Disease Control and Prevention data show.
The next step will be review of the scientific data by the CDC’s Advisory Committee on Immunization Practices, which is set to meet Sept. 1 and 2. The final hurdle before distribution of the new vaccines will be sign-off on CDC recommendations for use by agency Director Rochelle Walensky, MD.
This is a developing story. A version of this article first appeared on WebMD.com.
The agency cited data to support the safety and efficacy of this next generation of mRNA vaccines targeted toward variants of concern.
The Pfizer EUA corresponds to the company’s combination booster shot that includes the original COVID-19 vaccine as well as a vaccine specifically designed to protect against the most recent Omicron variants, BA.4 and BA.5.
The Moderna combination vaccine will contain both the firm’s original COVID-19 vaccine and a vaccine to protect specifically against Omicron BA.4 and BA.5 subvariants.
As of Aug. 27, BA.4 and BA.4.6 account for about 11% of circulating variants and BA.5 accounts for almost all the remaining 89%, Centers for Disease Control and Prevention data show.
The next step will be review of the scientific data by the CDC’s Advisory Committee on Immunization Practices, which is set to meet Sept. 1 and 2. The final hurdle before distribution of the new vaccines will be sign-off on CDC recommendations for use by agency Director Rochelle Walensky, MD.
This is a developing story. A version of this article first appeared on WebMD.com.
Omega-3 fatty acids and depression: Are they protective?
New research is suggesting that there are “meaningful” associations between higher dietary intake of omega-3 fatty acids and lower risk for depressive episodes.
In addition, consumption of total fatty acids and alpha-linolenic acid was associated with a reduced risk for incident depressive episodes (9% and 29%, respectively).
“Our results showed an important protective effect from the consumption of omega-3,” Maria de Jesus Mendes da Fonseca, University of the State of Rio de Janeiro, and colleagues write.
The findings were published online in Nutrients.
Mixed bag of studies
Epidemiologic evidence suggests that deficient dietary omega-3 intake is a modifiable risk factor for depression and that individuals with low consumption of omega-3 food sources have more depressive symptoms.
However, the results are inconsistent, and few longitudinal studies have addressed this association, the investigators note.
The new analysis included 13,879 adults (aged 39-65 years or older) participating in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) from 2008 to 2014.
Data on depressive episodes were obtained with the Clinical Interview Schedule Revised (CIS-R), and food consumption was measured with the Food Frequency Questionnaire (FFQ).
The target dietary components were total polyunsaturated fatty acids (PUFA) and the omega-3 fatty acids: alpha-linolenic acid, eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and docosapentaenoic acid (DPA).
The majority of participants had adequate dietary intake of omega-3 fatty acids, and none was taking omega-3 supplements.
In the fully adjusted model, consumption of fatty acids from the omega-3 family had a protective effect against maintenance of depressive episodes, showing “important associations, although the significance levels are borderline, possibly due to the sample size,” the researchers report.
In regard to onset of depressive episodes, estimates from the fully adjusted model suggest that a higher consumption of omega-3 acids (total and subtypes) is associated with lower risk for depressive episodes – with significant associations for omega-3 and alpha-linolenic acid.
The investigators note that strengths of the study include “its originality, as it is the first to assess associations between maintenance and incidence of depressive episodes and consumption of omega-3, besides the use of data from the ELSA-Brasil Study, with rigorous data collection protocols and reliable and validated instruments, thus guaranteeing the quality of the sample and the data.”
A study limitation, however, was that the ELSA-Brasil sample consists only of public employees, with the potential for a selection bias such as healthy worker phenomenon, the researchers note. Another was the use of the FFQ, which may underestimate daily intake of foods and depends on individual participant recall – all of which could possibly lead to a differential classification bias.
Interpret cautiously
Commenting on the study, David Mischoulon, MD, PhD, professor of psychiatry, Harvard Medical School, and director of the depression clinical and research program at Massachusetts General Hospital, both in Boston, said that data on omega-3s in depression are “very mixed.”
“A lot of the studies don’t necessarily agree with each other. Certainly, in studies that try to seek an association between omega-3 use and depression, it’s always complicated because it can be difficult to control for all variables that could be contributing to the result that you get,” said Dr. Mischoulon, who is also a member of the Anxiety and Depression Association of America and was not involved in the research.
A caveat to the current study was that diet was assessed only at baseline, “so we don’t really know whether there were any substantial dietary changes over time, he noted.
He also cautioned that it is hard to draw any firm conclusions from this type of study.
“In general, in studies with a large sample, which this study has, it’s easier to find statistically significant differences. But you need to ask yourself: Does it really matter? Is it enough to have a clinical impact and make a difference?” Dr. Mischoulon said.
The ELSA-Brasil study was funded by the Brazilian Ministry of Science, Technology, and Innovation and by the Ministry of Health. The investigators have reported no relevant financial relationships. Dr. Mischoulon has received research support from Nordic Naturals and heckel medizintechnik GmbH and honoraria for speaking from the Massachusetts General Hospital Psychiatry Academy. He also works with the MGH Clinical Trials Network and Institute, which has received research funding from multiple pharmaceutical companies and the National Institute of Mental Health.
A version of this article first appeared on Medscape.com.
New research is suggesting that there are “meaningful” associations between higher dietary intake of omega-3 fatty acids and lower risk for depressive episodes.
In addition, consumption of total fatty acids and alpha-linolenic acid was associated with a reduced risk for incident depressive episodes (9% and 29%, respectively).
“Our results showed an important protective effect from the consumption of omega-3,” Maria de Jesus Mendes da Fonseca, University of the State of Rio de Janeiro, and colleagues write.
The findings were published online in Nutrients.
Mixed bag of studies
Epidemiologic evidence suggests that deficient dietary omega-3 intake is a modifiable risk factor for depression and that individuals with low consumption of omega-3 food sources have more depressive symptoms.
However, the results are inconsistent, and few longitudinal studies have addressed this association, the investigators note.
The new analysis included 13,879 adults (aged 39-65 years or older) participating in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) from 2008 to 2014.
Data on depressive episodes were obtained with the Clinical Interview Schedule Revised (CIS-R), and food consumption was measured with the Food Frequency Questionnaire (FFQ).
The target dietary components were total polyunsaturated fatty acids (PUFA) and the omega-3 fatty acids: alpha-linolenic acid, eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and docosapentaenoic acid (DPA).
The majority of participants had adequate dietary intake of omega-3 fatty acids, and none was taking omega-3 supplements.
In the fully adjusted model, consumption of fatty acids from the omega-3 family had a protective effect against maintenance of depressive episodes, showing “important associations, although the significance levels are borderline, possibly due to the sample size,” the researchers report.
In regard to onset of depressive episodes, estimates from the fully adjusted model suggest that a higher consumption of omega-3 acids (total and subtypes) is associated with lower risk for depressive episodes – with significant associations for omega-3 and alpha-linolenic acid.
The investigators note that strengths of the study include “its originality, as it is the first to assess associations between maintenance and incidence of depressive episodes and consumption of omega-3, besides the use of data from the ELSA-Brasil Study, with rigorous data collection protocols and reliable and validated instruments, thus guaranteeing the quality of the sample and the data.”
A study limitation, however, was that the ELSA-Brasil sample consists only of public employees, with the potential for a selection bias such as healthy worker phenomenon, the researchers note. Another was the use of the FFQ, which may underestimate daily intake of foods and depends on individual participant recall – all of which could possibly lead to a differential classification bias.
Interpret cautiously
Commenting on the study, David Mischoulon, MD, PhD, professor of psychiatry, Harvard Medical School, and director of the depression clinical and research program at Massachusetts General Hospital, both in Boston, said that data on omega-3s in depression are “very mixed.”
“A lot of the studies don’t necessarily agree with each other. Certainly, in studies that try to seek an association between omega-3 use and depression, it’s always complicated because it can be difficult to control for all variables that could be contributing to the result that you get,” said Dr. Mischoulon, who is also a member of the Anxiety and Depression Association of America and was not involved in the research.
A caveat to the current study was that diet was assessed only at baseline, “so we don’t really know whether there were any substantial dietary changes over time, he noted.
He also cautioned that it is hard to draw any firm conclusions from this type of study.
“In general, in studies with a large sample, which this study has, it’s easier to find statistically significant differences. But you need to ask yourself: Does it really matter? Is it enough to have a clinical impact and make a difference?” Dr. Mischoulon said.
The ELSA-Brasil study was funded by the Brazilian Ministry of Science, Technology, and Innovation and by the Ministry of Health. The investigators have reported no relevant financial relationships. Dr. Mischoulon has received research support from Nordic Naturals and heckel medizintechnik GmbH and honoraria for speaking from the Massachusetts General Hospital Psychiatry Academy. He also works with the MGH Clinical Trials Network and Institute, which has received research funding from multiple pharmaceutical companies and the National Institute of Mental Health.
A version of this article first appeared on Medscape.com.
New research is suggesting that there are “meaningful” associations between higher dietary intake of omega-3 fatty acids and lower risk for depressive episodes.
In addition, consumption of total fatty acids and alpha-linolenic acid was associated with a reduced risk for incident depressive episodes (9% and 29%, respectively).
“Our results showed an important protective effect from the consumption of omega-3,” Maria de Jesus Mendes da Fonseca, University of the State of Rio de Janeiro, and colleagues write.
The findings were published online in Nutrients.
Mixed bag of studies
Epidemiologic evidence suggests that deficient dietary omega-3 intake is a modifiable risk factor for depression and that individuals with low consumption of omega-3 food sources have more depressive symptoms.
However, the results are inconsistent, and few longitudinal studies have addressed this association, the investigators note.
The new analysis included 13,879 adults (aged 39-65 years or older) participating in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) from 2008 to 2014.
Data on depressive episodes were obtained with the Clinical Interview Schedule Revised (CIS-R), and food consumption was measured with the Food Frequency Questionnaire (FFQ).
The target dietary components were total polyunsaturated fatty acids (PUFA) and the omega-3 fatty acids: alpha-linolenic acid, eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and docosapentaenoic acid (DPA).
The majority of participants had adequate dietary intake of omega-3 fatty acids, and none was taking omega-3 supplements.
In the fully adjusted model, consumption of fatty acids from the omega-3 family had a protective effect against maintenance of depressive episodes, showing “important associations, although the significance levels are borderline, possibly due to the sample size,” the researchers report.
In regard to onset of depressive episodes, estimates from the fully adjusted model suggest that a higher consumption of omega-3 acids (total and subtypes) is associated with lower risk for depressive episodes – with significant associations for omega-3 and alpha-linolenic acid.
The investigators note that strengths of the study include “its originality, as it is the first to assess associations between maintenance and incidence of depressive episodes and consumption of omega-3, besides the use of data from the ELSA-Brasil Study, with rigorous data collection protocols and reliable and validated instruments, thus guaranteeing the quality of the sample and the data.”
A study limitation, however, was that the ELSA-Brasil sample consists only of public employees, with the potential for a selection bias such as healthy worker phenomenon, the researchers note. Another was the use of the FFQ, which may underestimate daily intake of foods and depends on individual participant recall – all of which could possibly lead to a differential classification bias.
Interpret cautiously
Commenting on the study, David Mischoulon, MD, PhD, professor of psychiatry, Harvard Medical School, and director of the depression clinical and research program at Massachusetts General Hospital, both in Boston, said that data on omega-3s in depression are “very mixed.”
“A lot of the studies don’t necessarily agree with each other. Certainly, in studies that try to seek an association between omega-3 use and depression, it’s always complicated because it can be difficult to control for all variables that could be contributing to the result that you get,” said Dr. Mischoulon, who is also a member of the Anxiety and Depression Association of America and was not involved in the research.
A caveat to the current study was that diet was assessed only at baseline, “so we don’t really know whether there were any substantial dietary changes over time, he noted.
He also cautioned that it is hard to draw any firm conclusions from this type of study.
“In general, in studies with a large sample, which this study has, it’s easier to find statistically significant differences. But you need to ask yourself: Does it really matter? Is it enough to have a clinical impact and make a difference?” Dr. Mischoulon said.
The ELSA-Brasil study was funded by the Brazilian Ministry of Science, Technology, and Innovation and by the Ministry of Health. The investigators have reported no relevant financial relationships. Dr. Mischoulon has received research support from Nordic Naturals and heckel medizintechnik GmbH and honoraria for speaking from the Massachusetts General Hospital Psychiatry Academy. He also works with the MGH Clinical Trials Network and Institute, which has received research funding from multiple pharmaceutical companies and the National Institute of Mental Health.
A version of this article first appeared on Medscape.com.
FROM NUTRIENTS
Children and COVID: New cases increase; hospital admissions could follow
New cases of COVID-19 in children were up again after 2 weeks of declines, and preliminary data suggest that hospitalizations may be on the rise as well.
, based on data collected by the American Academy of Pediatrics and the Children’s Hospital Association from state and territorial health departments.
A similar increase seems to be reflected by hospital-level data. The latest 7-day (Aug. 21-27) average is 305 new admissions with diagnosed COVID per day among children aged 0-17 years, compared with 290 per day for the week of Aug. 14-20, the Centers for Disease Control and Prevention reported, while also noting the potential for reporting delays in the most recent 7-day period.
Daily hospital admissions for COVID had been headed downward through the first half of August, falling from 0.46 per 100,000 population at the end of July to 0.40 on Aug. 19, the CDC said on its COVID Data Tracker. Since then, however, admissions have gone the other way, with the preliminary nature of the latest data suggesting that the numbers will be even higher as more hospitals report over the next few days.
Vaccine initiations continue to fall
Initiations among school-age children have fallen for 3 consecutive weeks since Aug. 3, when numbers receiving their first vaccinations reached late-summer highs for those aged 5-11 and 12-17 years. Children under age 5, included in the CDC data for the first time on Aug. 11 as separate groups – under 2 years and 2-4 years – have had vaccine initiations drop by 8.0% and 19.8% over the 2 following weeks, the CDC said.

Through their first 8 weeks of vaccine eligibility (June 19 to Aug. 15), 4.8% of children under 5 years of age had received a first vaccination and 1.0% were fully vaccinated. For the two other age groups (5-11 and 12-15) who became eligible after the very first emergency authorization back in 2020, the respective proportions were 25.0% and 16.0% (5-11) and 33.8% and 26.1% (12-15) through the first 8 weeks, according to CDC data.
New cases of COVID-19 in children were up again after 2 weeks of declines, and preliminary data suggest that hospitalizations may be on the rise as well.
, based on data collected by the American Academy of Pediatrics and the Children’s Hospital Association from state and territorial health departments.
A similar increase seems to be reflected by hospital-level data. The latest 7-day (Aug. 21-27) average is 305 new admissions with diagnosed COVID per day among children aged 0-17 years, compared with 290 per day for the week of Aug. 14-20, the Centers for Disease Control and Prevention reported, while also noting the potential for reporting delays in the most recent 7-day period.
Daily hospital admissions for COVID had been headed downward through the first half of August, falling from 0.46 per 100,000 population at the end of July to 0.40 on Aug. 19, the CDC said on its COVID Data Tracker. Since then, however, admissions have gone the other way, with the preliminary nature of the latest data suggesting that the numbers will be even higher as more hospitals report over the next few days.
Vaccine initiations continue to fall
Initiations among school-age children have fallen for 3 consecutive weeks since Aug. 3, when numbers receiving their first vaccinations reached late-summer highs for those aged 5-11 and 12-17 years. Children under age 5, included in the CDC data for the first time on Aug. 11 as separate groups – under 2 years and 2-4 years – have had vaccine initiations drop by 8.0% and 19.8% over the 2 following weeks, the CDC said.

Through their first 8 weeks of vaccine eligibility (June 19 to Aug. 15), 4.8% of children under 5 years of age had received a first vaccination and 1.0% were fully vaccinated. For the two other age groups (5-11 and 12-15) who became eligible after the very first emergency authorization back in 2020, the respective proportions were 25.0% and 16.0% (5-11) and 33.8% and 26.1% (12-15) through the first 8 weeks, according to CDC data.
New cases of COVID-19 in children were up again after 2 weeks of declines, and preliminary data suggest that hospitalizations may be on the rise as well.
, based on data collected by the American Academy of Pediatrics and the Children’s Hospital Association from state and territorial health departments.
A similar increase seems to be reflected by hospital-level data. The latest 7-day (Aug. 21-27) average is 305 new admissions with diagnosed COVID per day among children aged 0-17 years, compared with 290 per day for the week of Aug. 14-20, the Centers for Disease Control and Prevention reported, while also noting the potential for reporting delays in the most recent 7-day period.
Daily hospital admissions for COVID had been headed downward through the first half of August, falling from 0.46 per 100,000 population at the end of July to 0.40 on Aug. 19, the CDC said on its COVID Data Tracker. Since then, however, admissions have gone the other way, with the preliminary nature of the latest data suggesting that the numbers will be even higher as more hospitals report over the next few days.
Vaccine initiations continue to fall
Initiations among school-age children have fallen for 3 consecutive weeks since Aug. 3, when numbers receiving their first vaccinations reached late-summer highs for those aged 5-11 and 12-17 years. Children under age 5, included in the CDC data for the first time on Aug. 11 as separate groups – under 2 years and 2-4 years – have had vaccine initiations drop by 8.0% and 19.8% over the 2 following weeks, the CDC said.

Through their first 8 weeks of vaccine eligibility (June 19 to Aug. 15), 4.8% of children under 5 years of age had received a first vaccination and 1.0% were fully vaccinated. For the two other age groups (5-11 and 12-15) who became eligible after the very first emergency authorization back in 2020, the respective proportions were 25.0% and 16.0% (5-11) and 33.8% and 26.1% (12-15) through the first 8 weeks, according to CDC data.
‘Doomscrolling’ may be a significant driver of poor mental health
The past 2 years have been filled with worrisome global events, from the pandemic to the war in Ukraine, large-scale protests, mass shootings, and devastating wildfires. The 24-hour media coverage of these events can take a toll on “news addicts” who have an excessive urge to constantly check the news, researchers note.
Results from an online survey of more than 1,000 adults showed that nearly 17% showed signs of “severely problematic” news consumption.
These “doomscrollers” or “doomsurfers” scored high on all five problematic news consumption dimensions: being absorbed in news content, being consumed by thoughts about the news, attempting to alleviate feelings of threat by consuming more news, losing control over news consumption, and having news consumption interfere in daily life.
“We anticipated that a sizable portion of our sample would show signs of problematic news consumption. However, we were surprised to find that 17% of study participants suffer from the most severe level of problematic news consumption,” lead author Bryan McLaughlin, PhD, Texas Tech University, Lubbock, told this news organization. “This is certainly concerning and suggests the problem may be more widespread than we expected,” he said.
In addition, 74% of those with severe levels of problematic news consumption reported experiencing mental problems, and 61% reported physical problems.
“It’s important for health care providers to be aware that problematic news consumption may be a significant driver of mental and physical ill-being, especially because a lot of people might be unaware of the negative impact the news is having on their health,” Dr. McLaughlin said.
The findings were published online in Health Communication.
Emotionally invested
The researchers assessed data from an online survey of 1,100 adults (mean age, 40.5 years; 51% women) in the United States who were recruited in August 2021.
Among those surveyed, 27.3% reported “moderately problematic” news consumption, 27.5% reported minimally problematic news consumption, and 28.7% reported no problematic news consumption.
Perhaps not surprisingly, respondents with higher levels of problematic news consumption were significantly more likely to experience mental and physical ill-being than those with lower levels, even after accounting for demographics, personality traits, and overall news use, the researchers note.
Nearly three-quarters (74%) of those with severe levels of problematic news consumption reported experiencing mental ill-being “quite a bit” or “very much” – whereas frequent symptoms were only reported by 8% of all other study participants.
In addition, 61% of adults with severe problematic news consumption reported experiencing physical ill-being “quite a bit” or “very much,” compared with only 6.1% for all other study participants.
Dr. McLaughlin noted that one way to combat this problem is to help individuals develop a healthier relationship with the news – and mindfulness training may be one way to accomplish that.
“We have some preliminary evidence that individuals with high levels of mindfulness are much less susceptible to developing higher levels of problematic news consumption,” he said.
“Given this, mindfulness-based training could potentially help problematic news consumers follow the news without becoming so emotionally invested in it. We hope to examine the effectiveness of a mindfulness intervention in our future research,” he added.
Increased distress
Commenting on the study, Steven R. Thorp, PhD, ABPP, a professor at California School of Professional Psychology, Alliant International University, San Diego, said that he and his colleagues have noticed an increase in clients reporting distress about news consumption.
The survey by Dr. McLaughlin and colleagues “appears to be representative and has sufficient statistical power to address the issues,” said Dr. Thorp, who was not involved with the research.
“However, as the researchers note, it is a cross-sectional and correlational survey. So it’s possible that, as implied, people who ‘doomscroll’ are more likely to have physical and mental health problems that interfere with their functioning,” he added.
It is also possible that individuals with physical and mental health problems are more likely to be isolated and have restricted activities, thus leading to greater news consumption, Dr. Thorp noted. Alternatively, there could be an independent link between health and news consumption.
Most news is “sensational and not representative,” Dr. Thorp pointed out.
For example, “we are far more likely to hear about deaths from terrorist attacks or plane crashes than from heart attacks, though deaths from heart attacks are far more common,” he said.
“News also tends to be negative, rather than uplifting, and most news is not directly relevant to a person’s day-to-day functioning. Thus, for most people, the consumption of news may have more downsides than upsides,” Dr. Thorp added.
Still, many people want to stay informed about national and international events. So rather than following a “cold turkey” or abstinence model of stopping all news consumption, individuals could consider a “harm reduction” model of reducing time spent consuming news, Dr. Thorp noted.
Another thing to consider is the news source. “Some outlets and social media sites are designed to instill outrage, fear, or anger and to increase polarization, while others have been shown to provide balanced and less sensational coverage,” Dr. Thorp said.
“I also think it’s a good idea for providers to regularly ask about news consumption, along with learning about other daily activities that may enhance or diminish mental and physical health,” he added.
The research had no specific funding. Dr. McLaughlin and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The past 2 years have been filled with worrisome global events, from the pandemic to the war in Ukraine, large-scale protests, mass shootings, and devastating wildfires. The 24-hour media coverage of these events can take a toll on “news addicts” who have an excessive urge to constantly check the news, researchers note.
Results from an online survey of more than 1,000 adults showed that nearly 17% showed signs of “severely problematic” news consumption.
These “doomscrollers” or “doomsurfers” scored high on all five problematic news consumption dimensions: being absorbed in news content, being consumed by thoughts about the news, attempting to alleviate feelings of threat by consuming more news, losing control over news consumption, and having news consumption interfere in daily life.
“We anticipated that a sizable portion of our sample would show signs of problematic news consumption. However, we were surprised to find that 17% of study participants suffer from the most severe level of problematic news consumption,” lead author Bryan McLaughlin, PhD, Texas Tech University, Lubbock, told this news organization. “This is certainly concerning and suggests the problem may be more widespread than we expected,” he said.
In addition, 74% of those with severe levels of problematic news consumption reported experiencing mental problems, and 61% reported physical problems.
“It’s important for health care providers to be aware that problematic news consumption may be a significant driver of mental and physical ill-being, especially because a lot of people might be unaware of the negative impact the news is having on their health,” Dr. McLaughlin said.
The findings were published online in Health Communication.
Emotionally invested
The researchers assessed data from an online survey of 1,100 adults (mean age, 40.5 years; 51% women) in the United States who were recruited in August 2021.
Among those surveyed, 27.3% reported “moderately problematic” news consumption, 27.5% reported minimally problematic news consumption, and 28.7% reported no problematic news consumption.
Perhaps not surprisingly, respondents with higher levels of problematic news consumption were significantly more likely to experience mental and physical ill-being than those with lower levels, even after accounting for demographics, personality traits, and overall news use, the researchers note.
Nearly three-quarters (74%) of those with severe levels of problematic news consumption reported experiencing mental ill-being “quite a bit” or “very much” – whereas frequent symptoms were only reported by 8% of all other study participants.
In addition, 61% of adults with severe problematic news consumption reported experiencing physical ill-being “quite a bit” or “very much,” compared with only 6.1% for all other study participants.
Dr. McLaughlin noted that one way to combat this problem is to help individuals develop a healthier relationship with the news – and mindfulness training may be one way to accomplish that.
“We have some preliminary evidence that individuals with high levels of mindfulness are much less susceptible to developing higher levels of problematic news consumption,” he said.
“Given this, mindfulness-based training could potentially help problematic news consumers follow the news without becoming so emotionally invested in it. We hope to examine the effectiveness of a mindfulness intervention in our future research,” he added.
Increased distress
Commenting on the study, Steven R. Thorp, PhD, ABPP, a professor at California School of Professional Psychology, Alliant International University, San Diego, said that he and his colleagues have noticed an increase in clients reporting distress about news consumption.
The survey by Dr. McLaughlin and colleagues “appears to be representative and has sufficient statistical power to address the issues,” said Dr. Thorp, who was not involved with the research.
“However, as the researchers note, it is a cross-sectional and correlational survey. So it’s possible that, as implied, people who ‘doomscroll’ are more likely to have physical and mental health problems that interfere with their functioning,” he added.
It is also possible that individuals with physical and mental health problems are more likely to be isolated and have restricted activities, thus leading to greater news consumption, Dr. Thorp noted. Alternatively, there could be an independent link between health and news consumption.
Most news is “sensational and not representative,” Dr. Thorp pointed out.
For example, “we are far more likely to hear about deaths from terrorist attacks or plane crashes than from heart attacks, though deaths from heart attacks are far more common,” he said.
“News also tends to be negative, rather than uplifting, and most news is not directly relevant to a person’s day-to-day functioning. Thus, for most people, the consumption of news may have more downsides than upsides,” Dr. Thorp added.
Still, many people want to stay informed about national and international events. So rather than following a “cold turkey” or abstinence model of stopping all news consumption, individuals could consider a “harm reduction” model of reducing time spent consuming news, Dr. Thorp noted.
Another thing to consider is the news source. “Some outlets and social media sites are designed to instill outrage, fear, or anger and to increase polarization, while others have been shown to provide balanced and less sensational coverage,” Dr. Thorp said.
“I also think it’s a good idea for providers to regularly ask about news consumption, along with learning about other daily activities that may enhance or diminish mental and physical health,” he added.
The research had no specific funding. Dr. McLaughlin and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The past 2 years have been filled with worrisome global events, from the pandemic to the war in Ukraine, large-scale protests, mass shootings, and devastating wildfires. The 24-hour media coverage of these events can take a toll on “news addicts” who have an excessive urge to constantly check the news, researchers note.
Results from an online survey of more than 1,000 adults showed that nearly 17% showed signs of “severely problematic” news consumption.
These “doomscrollers” or “doomsurfers” scored high on all five problematic news consumption dimensions: being absorbed in news content, being consumed by thoughts about the news, attempting to alleviate feelings of threat by consuming more news, losing control over news consumption, and having news consumption interfere in daily life.
“We anticipated that a sizable portion of our sample would show signs of problematic news consumption. However, we were surprised to find that 17% of study participants suffer from the most severe level of problematic news consumption,” lead author Bryan McLaughlin, PhD, Texas Tech University, Lubbock, told this news organization. “This is certainly concerning and suggests the problem may be more widespread than we expected,” he said.
In addition, 74% of those with severe levels of problematic news consumption reported experiencing mental problems, and 61% reported physical problems.
“It’s important for health care providers to be aware that problematic news consumption may be a significant driver of mental and physical ill-being, especially because a lot of people might be unaware of the negative impact the news is having on their health,” Dr. McLaughlin said.
The findings were published online in Health Communication.
Emotionally invested
The researchers assessed data from an online survey of 1,100 adults (mean age, 40.5 years; 51% women) in the United States who were recruited in August 2021.
Among those surveyed, 27.3% reported “moderately problematic” news consumption, 27.5% reported minimally problematic news consumption, and 28.7% reported no problematic news consumption.
Perhaps not surprisingly, respondents with higher levels of problematic news consumption were significantly more likely to experience mental and physical ill-being than those with lower levels, even after accounting for demographics, personality traits, and overall news use, the researchers note.
Nearly three-quarters (74%) of those with severe levels of problematic news consumption reported experiencing mental ill-being “quite a bit” or “very much” – whereas frequent symptoms were only reported by 8% of all other study participants.
In addition, 61% of adults with severe problematic news consumption reported experiencing physical ill-being “quite a bit” or “very much,” compared with only 6.1% for all other study participants.
Dr. McLaughlin noted that one way to combat this problem is to help individuals develop a healthier relationship with the news – and mindfulness training may be one way to accomplish that.
“We have some preliminary evidence that individuals with high levels of mindfulness are much less susceptible to developing higher levels of problematic news consumption,” he said.
“Given this, mindfulness-based training could potentially help problematic news consumers follow the news without becoming so emotionally invested in it. We hope to examine the effectiveness of a mindfulness intervention in our future research,” he added.
Increased distress
Commenting on the study, Steven R. Thorp, PhD, ABPP, a professor at California School of Professional Psychology, Alliant International University, San Diego, said that he and his colleagues have noticed an increase in clients reporting distress about news consumption.
The survey by Dr. McLaughlin and colleagues “appears to be representative and has sufficient statistical power to address the issues,” said Dr. Thorp, who was not involved with the research.
“However, as the researchers note, it is a cross-sectional and correlational survey. So it’s possible that, as implied, people who ‘doomscroll’ are more likely to have physical and mental health problems that interfere with their functioning,” he added.
It is also possible that individuals with physical and mental health problems are more likely to be isolated and have restricted activities, thus leading to greater news consumption, Dr. Thorp noted. Alternatively, there could be an independent link between health and news consumption.
Most news is “sensational and not representative,” Dr. Thorp pointed out.
For example, “we are far more likely to hear about deaths from terrorist attacks or plane crashes than from heart attacks, though deaths from heart attacks are far more common,” he said.
“News also tends to be negative, rather than uplifting, and most news is not directly relevant to a person’s day-to-day functioning. Thus, for most people, the consumption of news may have more downsides than upsides,” Dr. Thorp added.
Still, many people want to stay informed about national and international events. So rather than following a “cold turkey” or abstinence model of stopping all news consumption, individuals could consider a “harm reduction” model of reducing time spent consuming news, Dr. Thorp noted.
Another thing to consider is the news source. “Some outlets and social media sites are designed to instill outrage, fear, or anger and to increase polarization, while others have been shown to provide balanced and less sensational coverage,” Dr. Thorp said.
“I also think it’s a good idea for providers to regularly ask about news consumption, along with learning about other daily activities that may enhance or diminish mental and physical health,” he added.
The research had no specific funding. Dr. McLaughlin and Dr. Thorp have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HEALTH COMMUNICATION
How do you live with COVID? One doctor’s personal experience
Early in 2020, Anne Peters, MD, caught COVID-19. The author of Medscape’s “Peters on Diabetes” column was sick in March 2020 before state-mandated lockdowns, and well before there were any vaccines.
She remembers sitting in a small exam room with two patients who had flown to her Los Angeles office from New York. The elderly couple had hearing difficulties, so Dr. Peters sat close to them, putting on a continuous glucose monitor. “At that time, we didn’t think of COVID-19 as being in L.A.,” Dr. Peters recalled, “so I think we were not terribly consistent at mask-wearing due to the need to educate.”
“Several days later, I got COVID, but I didn’t know I had COVID per se. I felt crappy, had a terrible sore throat, lost my sense of taste and smell [which was not yet described as a COVID symptom], was completely exhausted, but had no fever or cough, which were the only criteria for getting COVID tested at the time. I didn’t know I had been exposed until 2 weeks later, when the patient’s assistant returned the sensor warning us to ‘be careful’ with it because the patient and his wife were recovering from COVID.”
That early battle with COVID-19 was just the beginning of what would become a 2-year struggle, including familial loss amid her own health problems and concerns about the under-resourced patients she cares for. Here, she shares her journey through the pandemic with this news organization.
Question: Thanks for talking to us. Let’s discuss your journey over these past 2.5 years.
Answer: Everybody has their own COVID story because we all went through this together. Some of us have worse COVID stories, and some of us have better ones, but all have been impacted.
I’m not a sick person. I’m a very healthy person but COVID made me so unwell for 2 years. The brain fog and fatigue were nothing compared to the autonomic neuropathy that affected my heart. It was really limiting for me. And I still don’t know the long-term implications, looking 20-30 years from now.
Q: When you initially had COVID, what were your symptoms? What was the impact?
A: I had all the symptoms of COVID, except for a cough and fever. I lost my sense of taste and smell. I had a horrible headache, a sore throat, and I was exhausted. I couldn’t get tested because I didn’t have the right symptoms.
Despite being sick, I never stopped working but just switched to telemedicine. I also took my regular monthly trip to our cabin in Montana. I unknowingly flew on a plane with COVID. I wore a well-fitted N95 mask, so I don’t think I gave anybody COVID. I didn’t give COVID to my partner, Eric, which is hard to believe as – at 77 – he’s older than me. He has diabetes, heart disease, and every other high-risk characteristic. If he’d gotten COVID back then, it would have been terrible, as there were no treatments, but luckily he didn’t get it.
Q: When were you officially diagnosed?
A: Two or 3 months after I thought I might have had COVID, I checked my antibodies, which tested strongly positive for a prior COVID infection. That was when I knew all the symptoms I’d had were due to the disease.
Q: Not only were you dealing with your own illness, but also that of those close to you. Can you talk about that?
A: In April 2020, my mother who was in her 90s and otherwise healthy except for dementia, got COVID. She could have gotten it from me. I visited often but wore a mask. She had all the horrible pulmonary symptoms. In her advance directive, she didn’t want to be hospitalized so I kept her in her home. She died from COVID in her own bed. It was fairly brutal, but at least I kept her where she felt comforted.
My 91-year-old dad was living in a different residential facility. Throughout COVID he had become very depressed because his social patterns had changed. Prior to COVID, they all ate together, but during the pandemic they were unable to. He missed his social connections, disliked being isolated in his room, hated everyone in masks.
He was a bit demented, but not so much that he couldn’t communicate with me or remember where his grandson was going to law school. I wasn’t allowed inside the facility, which was hard on him. I hadn’t told him his wife died because the hospice social workers advised me that I shouldn’t give him news that he couldn’t process readily until I could spend time with him. Unfortunately, that time never came. In December 2020, he got COVID. One of the people in that facility had gone to the hospital, came back, and tested negative, but actually had COVID and gave it to my dad. The guy who gave it to my dad didn’t die but my dad was terribly ill. He died 2 weeks short of getting his vaccine. He was coherent enough to have a conversation. I asked him: ‘Do you want to go to the hospital?’ And he said: ‘No, because it would be too scary,’ since he couldn’t be with me. I put him on hospice and held his hand as he died from pulmonary COVID, which was awful. I couldn’t give him enough morphine or valium to ease his breathing. But his last words to me were “I love you,” and at the very end he seemed peaceful, which was a blessing.
I got an autopsy, because he wanted one. Nothing else was wrong with him other than COVID. It destroyed his lungs. The rest of him was fine – no heart disease, cancer, or anything else. He died of COVID-19, the same as my mother.
That same week, my aunt, my only surviving older relative, who was in Des Moines, Iowa, died of COVID-19. All three family members died before the vaccine came out.
It was hard to lose my parents. I’m the only surviving child because my sister died in her 20s. It’s not been an easy pandemic. But what pandemic is easy? I just happened to have lost more people than most. Ironically, my grandfather was one of the legionnaires at the Bellevue-Stratford Hotel in Philadelphia in 1976 and died of Legionnaire’s disease before we knew what was causing the outbreak.
Q: Were you still struggling with COVID?
A: COVID impacted my whole body. I lost a lot of weight. I didn’t want to eat, and my gastrointestinal system was not happy. It took a while for my sense of taste and smell to come back. Nothing tasted good. I’m not a foodie; I don’t really care about food. We could get takeout or whatever, but none of it appealed to me. I’m not so sure it was a taste thing, I just didn’t feel like eating.
I didn’t realize I had “brain fog” per se, because I felt stressed and overwhelmed by the pandemic and my patients’ concerns. But one day, about 3 months after I had developed COVID, I woke up without the fog. Which made me aware that I hadn’t been feeling right up until that point.
The worst symptoms, however, were cardiac. I noticed also immediately that my heart rate went up very quickly with minimal exertion. My pulse has always been in the 55-60 bpm range, and suddenly just walking across a room made it go up to over 140 bpm. If I did any aerobic activity, it went up over 160 and would be associated with dyspnea and chest pain. I believed these were all post-COVID symptoms and felt validated when reports of others having similar issues were published in the literature.
Q: Did you continue seeing patients?
A: Yes, of course. Patients never needed their doctors more. In East L.A., where patients don’t have easy access to telemedicine, I kept going into clinic throughout the pandemic. In the more affluent Westside of Los Angeles, we switched to telemedicine, which was quite effective for most. However, because diabetes was associated with an increased risk of hospitalization and death from COVID, my patients were understandably afraid. I’ve never been busier, but (like all health care providers), I became more of a COVID provider than a diabetologist.
Q: Do you feel your battle with COVID impacted your work?
A: It didn’t affect me at work. If I was sitting still, I was fine. Sitting at home at a desk, I didn’t notice any symptoms. But as a habitual stair-user, I would be gasping for breath in the stairwell because I couldn’t go up the stairs to my office as I once could.
I think you empathize more with people who had COVID (when you’ve had it yourself). There was such a huge patient burden. And I think that’s been the thing that’s affected health care providers the most – no matter what specialty we’re in – that nobody has answers.
Q: What happened after you had your vaccine?
A: The vaccine itself was fine. I didn’t have any reaction to the first two doses. But the first booster made my cardiac issues worse.
By this point, my cardiac problems stopped me from exercising. I even went to the ER with chest pain once because I was having palpitations and chest pressure caused by simply taking my morning shower. Fortunately, I wasn’t having an MI, but I certainly wasn’t “normal.”
My measure of my fitness is the cross-country skiing trail I use in Montana. I know exactly how far I can ski. Usually I can do the loop in 35 minutes. After COVID, I lasted 10 minutes. I would be tachycardic, short of breath with chest pain radiating down my left arm. I would rest and try to keep going. But with each rest period, I only got worse. I would be laying in the snow and strangers would ask if I needed help.
Q: What helped you?
A: I’ve read a lot about long COVID and have tried to learn from the experts. Of course, I never went to a doctor directly, although I did ask colleagues for advice. What I learned was to never push myself. I forced myself to create an exercise schedule where I only exercised three times a week with rest days in between. When exercising, the second my heart rate went above 140 bpm, I stopped until I could get it back down. I would push against this new limit, even though my limit was low.
Additionally, I worked on my breathing patterns and did meditative breathing for 10 minutes twice daily using a commercially available app.
Although progress was slow, I did improve, and by June 2022, I seemed back to normal. I was not as fit as I was prior to COVID and needed to improve, but the tachycardic response to exercise and cardiac symptoms were gone. I felt like my normal self. Normal enough to go on a spot packing trip in the Sierras in August. (Horses carried us and a mule carried the gear over the 12,000-foot pass into the mountains, and then left my friend and me high in the Sierras for a week.) We were camped above 10,000 feet and every day hiked up to another high mountain lake where we fly-fished for trout that we ate for dinner. The hikes were a challenge, but not abnormally so. Not as they would have been while I had long COVID.
Q: What is the current atmosphere in your clinic?
A: COVID is much milder now in my vaccinated patients, but I feel most health care providers are exhausted. Many of my staff left when COVID hit because they didn’t want to keep working. It made practicing medicine exhausting. There’s been a shortage of nurses, a shortage of everything. We’ve been required to do a whole lot more than we ever did before. It’s much harder to be a doctor. This pandemic is the first time I’ve ever thought of quitting. Granted, I lost my whole family, or at least the older generation, but it’s just been almost overwhelming.
On the plus side, almost every one of my patients has been vaccinated, because early on, people would ask: “Do you trust this vaccine?” I would reply: “I saw my parents die from COVID when they weren’t vaccinated, so you’re getting vaccinated. This is real and the vaccines help.” It made me very good at convincing people to get vaccines because I knew what it was like to see someone dying from COVID up close.
Q: What advice do you have for those struggling with the COVID pandemic?
A: People need to decide what their own risk is for getting sick and how many times they want to get COVID. At this point, I want people to go out, but safely. In the beginning, when my patients said, “can I go visit my granddaughter?” I said, “no,” but that was before we had the vaccine. Now I feel it is safe to go out using common sense. I still have my patients wear masks on planes. I still have patients try to eat outside as much as possible. And I tell people to take the precautions that make sense, but I tell them to go out and do things because life is short.
I had a patient in his 70s who has many risk factors like heart disease and diabetes. His granddaughter’s Bat Mitzvah in Florida was coming up. He asked: “Can I go?” I told him “Yes,” but to be safe – to wear an N95 mask on the plane and at the event, and stay in his own hotel room, rather than with the whole family. I said, “You need to do this.” Earlier in the pandemic, I saw people who literally died from loneliness and isolation.
He and his wife flew there. He sent me a picture of himself with his granddaughter. When he returned, he showed me a handwritten note from her that said, “I love you so much. Everyone else canceled, which made me cry. You’re the only one who came. You have no idea how much this meant to me.”
He’s back in L.A., and he didn’t get COVID. He said, “It was the best thing I’ve done in years.” That’s what I need to help people with, navigating this world with COVID and assessing risks and benefits. As with all of medicine, my advice is individualized. My advice changes based on the major circulating variant and the rates of the virus in the population, as well as the risk factors of the individual.
Q: What are you doing now?
A: I’m trying to avoid getting COVID again, or another booster. I could get pre-exposure monoclonal antibodies but am waiting to do anything further until I see what happens over the fall and winter. I still wear a mask inside but now do a mix of in-person and telemedicine visits. I still try to go to outdoor restaurants, which is easy in California. But I’m flying to see my son in New York and plan to go to Europe this fall for a meeting. I also go to my cabin in Montana every month to get my “dose” of the wilderness. Overall, I travel for conferences and speaking engagements much less because I have learned the joy of staying home.
Thinking back on my life as a doctor, my career began as an intern at Stanford rotating through Ward 5B, the AIDS unit at San Francisco General Hospital, and will likely end with COVID. In spite of all our medical advances, my generation of physicians, much as many generations before us, has a front-row seat to the vulnerability of humans to infectious diseases and how far we still need to go to protect our patients from communicable illness.
A version of this article first appeared on Medscape.com.
Anne L. Peters, MD, is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts; three books on diabetes; and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations.
Early in 2020, Anne Peters, MD, caught COVID-19. The author of Medscape’s “Peters on Diabetes” column was sick in March 2020 before state-mandated lockdowns, and well before there were any vaccines.
She remembers sitting in a small exam room with two patients who had flown to her Los Angeles office from New York. The elderly couple had hearing difficulties, so Dr. Peters sat close to them, putting on a continuous glucose monitor. “At that time, we didn’t think of COVID-19 as being in L.A.,” Dr. Peters recalled, “so I think we were not terribly consistent at mask-wearing due to the need to educate.”
“Several days later, I got COVID, but I didn’t know I had COVID per se. I felt crappy, had a terrible sore throat, lost my sense of taste and smell [which was not yet described as a COVID symptom], was completely exhausted, but had no fever or cough, which were the only criteria for getting COVID tested at the time. I didn’t know I had been exposed until 2 weeks later, when the patient’s assistant returned the sensor warning us to ‘be careful’ with it because the patient and his wife were recovering from COVID.”
That early battle with COVID-19 was just the beginning of what would become a 2-year struggle, including familial loss amid her own health problems and concerns about the under-resourced patients she cares for. Here, she shares her journey through the pandemic with this news organization.
Question: Thanks for talking to us. Let’s discuss your journey over these past 2.5 years.
Answer: Everybody has their own COVID story because we all went through this together. Some of us have worse COVID stories, and some of us have better ones, but all have been impacted.
I’m not a sick person. I’m a very healthy person but COVID made me so unwell for 2 years. The brain fog and fatigue were nothing compared to the autonomic neuropathy that affected my heart. It was really limiting for me. And I still don’t know the long-term implications, looking 20-30 years from now.
Q: When you initially had COVID, what were your symptoms? What was the impact?
A: I had all the symptoms of COVID, except for a cough and fever. I lost my sense of taste and smell. I had a horrible headache, a sore throat, and I was exhausted. I couldn’t get tested because I didn’t have the right symptoms.
Despite being sick, I never stopped working but just switched to telemedicine. I also took my regular monthly trip to our cabin in Montana. I unknowingly flew on a plane with COVID. I wore a well-fitted N95 mask, so I don’t think I gave anybody COVID. I didn’t give COVID to my partner, Eric, which is hard to believe as – at 77 – he’s older than me. He has diabetes, heart disease, and every other high-risk characteristic. If he’d gotten COVID back then, it would have been terrible, as there were no treatments, but luckily he didn’t get it.
Q: When were you officially diagnosed?
A: Two or 3 months after I thought I might have had COVID, I checked my antibodies, which tested strongly positive for a prior COVID infection. That was when I knew all the symptoms I’d had were due to the disease.
Q: Not only were you dealing with your own illness, but also that of those close to you. Can you talk about that?
A: In April 2020, my mother who was in her 90s and otherwise healthy except for dementia, got COVID. She could have gotten it from me. I visited often but wore a mask. She had all the horrible pulmonary symptoms. In her advance directive, she didn’t want to be hospitalized so I kept her in her home. She died from COVID in her own bed. It was fairly brutal, but at least I kept her where she felt comforted.
My 91-year-old dad was living in a different residential facility. Throughout COVID he had become very depressed because his social patterns had changed. Prior to COVID, they all ate together, but during the pandemic they were unable to. He missed his social connections, disliked being isolated in his room, hated everyone in masks.
He was a bit demented, but not so much that he couldn’t communicate with me or remember where his grandson was going to law school. I wasn’t allowed inside the facility, which was hard on him. I hadn’t told him his wife died because the hospice social workers advised me that I shouldn’t give him news that he couldn’t process readily until I could spend time with him. Unfortunately, that time never came. In December 2020, he got COVID. One of the people in that facility had gone to the hospital, came back, and tested negative, but actually had COVID and gave it to my dad. The guy who gave it to my dad didn’t die but my dad was terribly ill. He died 2 weeks short of getting his vaccine. He was coherent enough to have a conversation. I asked him: ‘Do you want to go to the hospital?’ And he said: ‘No, because it would be too scary,’ since he couldn’t be with me. I put him on hospice and held his hand as he died from pulmonary COVID, which was awful. I couldn’t give him enough morphine or valium to ease his breathing. But his last words to me were “I love you,” and at the very end he seemed peaceful, which was a blessing.
I got an autopsy, because he wanted one. Nothing else was wrong with him other than COVID. It destroyed his lungs. The rest of him was fine – no heart disease, cancer, or anything else. He died of COVID-19, the same as my mother.
That same week, my aunt, my only surviving older relative, who was in Des Moines, Iowa, died of COVID-19. All three family members died before the vaccine came out.
It was hard to lose my parents. I’m the only surviving child because my sister died in her 20s. It’s not been an easy pandemic. But what pandemic is easy? I just happened to have lost more people than most. Ironically, my grandfather was one of the legionnaires at the Bellevue-Stratford Hotel in Philadelphia in 1976 and died of Legionnaire’s disease before we knew what was causing the outbreak.
Q: Were you still struggling with COVID?
A: COVID impacted my whole body. I lost a lot of weight. I didn’t want to eat, and my gastrointestinal system was not happy. It took a while for my sense of taste and smell to come back. Nothing tasted good. I’m not a foodie; I don’t really care about food. We could get takeout or whatever, but none of it appealed to me. I’m not so sure it was a taste thing, I just didn’t feel like eating.
I didn’t realize I had “brain fog” per se, because I felt stressed and overwhelmed by the pandemic and my patients’ concerns. But one day, about 3 months after I had developed COVID, I woke up without the fog. Which made me aware that I hadn’t been feeling right up until that point.
The worst symptoms, however, were cardiac. I noticed also immediately that my heart rate went up very quickly with minimal exertion. My pulse has always been in the 55-60 bpm range, and suddenly just walking across a room made it go up to over 140 bpm. If I did any aerobic activity, it went up over 160 and would be associated with dyspnea and chest pain. I believed these were all post-COVID symptoms and felt validated when reports of others having similar issues were published in the literature.
Q: Did you continue seeing patients?
A: Yes, of course. Patients never needed their doctors more. In East L.A., where patients don’t have easy access to telemedicine, I kept going into clinic throughout the pandemic. In the more affluent Westside of Los Angeles, we switched to telemedicine, which was quite effective for most. However, because diabetes was associated with an increased risk of hospitalization and death from COVID, my patients were understandably afraid. I’ve never been busier, but (like all health care providers), I became more of a COVID provider than a diabetologist.
Q: Do you feel your battle with COVID impacted your work?
A: It didn’t affect me at work. If I was sitting still, I was fine. Sitting at home at a desk, I didn’t notice any symptoms. But as a habitual stair-user, I would be gasping for breath in the stairwell because I couldn’t go up the stairs to my office as I once could.
I think you empathize more with people who had COVID (when you’ve had it yourself). There was such a huge patient burden. And I think that’s been the thing that’s affected health care providers the most – no matter what specialty we’re in – that nobody has answers.
Q: What happened after you had your vaccine?
A: The vaccine itself was fine. I didn’t have any reaction to the first two doses. But the first booster made my cardiac issues worse.
By this point, my cardiac problems stopped me from exercising. I even went to the ER with chest pain once because I was having palpitations and chest pressure caused by simply taking my morning shower. Fortunately, I wasn’t having an MI, but I certainly wasn’t “normal.”
My measure of my fitness is the cross-country skiing trail I use in Montana. I know exactly how far I can ski. Usually I can do the loop in 35 minutes. After COVID, I lasted 10 minutes. I would be tachycardic, short of breath with chest pain radiating down my left arm. I would rest and try to keep going. But with each rest period, I only got worse. I would be laying in the snow and strangers would ask if I needed help.
Q: What helped you?
A: I’ve read a lot about long COVID and have tried to learn from the experts. Of course, I never went to a doctor directly, although I did ask colleagues for advice. What I learned was to never push myself. I forced myself to create an exercise schedule where I only exercised three times a week with rest days in between. When exercising, the second my heart rate went above 140 bpm, I stopped until I could get it back down. I would push against this new limit, even though my limit was low.
Additionally, I worked on my breathing patterns and did meditative breathing for 10 minutes twice daily using a commercially available app.
Although progress was slow, I did improve, and by June 2022, I seemed back to normal. I was not as fit as I was prior to COVID and needed to improve, but the tachycardic response to exercise and cardiac symptoms were gone. I felt like my normal self. Normal enough to go on a spot packing trip in the Sierras in August. (Horses carried us and a mule carried the gear over the 12,000-foot pass into the mountains, and then left my friend and me high in the Sierras for a week.) We were camped above 10,000 feet and every day hiked up to another high mountain lake where we fly-fished for trout that we ate for dinner. The hikes were a challenge, but not abnormally so. Not as they would have been while I had long COVID.
Q: What is the current atmosphere in your clinic?
A: COVID is much milder now in my vaccinated patients, but I feel most health care providers are exhausted. Many of my staff left when COVID hit because they didn’t want to keep working. It made practicing medicine exhausting. There’s been a shortage of nurses, a shortage of everything. We’ve been required to do a whole lot more than we ever did before. It’s much harder to be a doctor. This pandemic is the first time I’ve ever thought of quitting. Granted, I lost my whole family, or at least the older generation, but it’s just been almost overwhelming.
On the plus side, almost every one of my patients has been vaccinated, because early on, people would ask: “Do you trust this vaccine?” I would reply: “I saw my parents die from COVID when they weren’t vaccinated, so you’re getting vaccinated. This is real and the vaccines help.” It made me very good at convincing people to get vaccines because I knew what it was like to see someone dying from COVID up close.
Q: What advice do you have for those struggling with the COVID pandemic?
A: People need to decide what their own risk is for getting sick and how many times they want to get COVID. At this point, I want people to go out, but safely. In the beginning, when my patients said, “can I go visit my granddaughter?” I said, “no,” but that was before we had the vaccine. Now I feel it is safe to go out using common sense. I still have my patients wear masks on planes. I still have patients try to eat outside as much as possible. And I tell people to take the precautions that make sense, but I tell them to go out and do things because life is short.
I had a patient in his 70s who has many risk factors like heart disease and diabetes. His granddaughter’s Bat Mitzvah in Florida was coming up. He asked: “Can I go?” I told him “Yes,” but to be safe – to wear an N95 mask on the plane and at the event, and stay in his own hotel room, rather than with the whole family. I said, “You need to do this.” Earlier in the pandemic, I saw people who literally died from loneliness and isolation.
He and his wife flew there. He sent me a picture of himself with his granddaughter. When he returned, he showed me a handwritten note from her that said, “I love you so much. Everyone else canceled, which made me cry. You’re the only one who came. You have no idea how much this meant to me.”
He’s back in L.A., and he didn’t get COVID. He said, “It was the best thing I’ve done in years.” That’s what I need to help people with, navigating this world with COVID and assessing risks and benefits. As with all of medicine, my advice is individualized. My advice changes based on the major circulating variant and the rates of the virus in the population, as well as the risk factors of the individual.
Q: What are you doing now?
A: I’m trying to avoid getting COVID again, or another booster. I could get pre-exposure monoclonal antibodies but am waiting to do anything further until I see what happens over the fall and winter. I still wear a mask inside but now do a mix of in-person and telemedicine visits. I still try to go to outdoor restaurants, which is easy in California. But I’m flying to see my son in New York and plan to go to Europe this fall for a meeting. I also go to my cabin in Montana every month to get my “dose” of the wilderness. Overall, I travel for conferences and speaking engagements much less because I have learned the joy of staying home.
Thinking back on my life as a doctor, my career began as an intern at Stanford rotating through Ward 5B, the AIDS unit at San Francisco General Hospital, and will likely end with COVID. In spite of all our medical advances, my generation of physicians, much as many generations before us, has a front-row seat to the vulnerability of humans to infectious diseases and how far we still need to go to protect our patients from communicable illness.
A version of this article first appeared on Medscape.com.
Anne L. Peters, MD, is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts; three books on diabetes; and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations.
Early in 2020, Anne Peters, MD, caught COVID-19. The author of Medscape’s “Peters on Diabetes” column was sick in March 2020 before state-mandated lockdowns, and well before there were any vaccines.
She remembers sitting in a small exam room with two patients who had flown to her Los Angeles office from New York. The elderly couple had hearing difficulties, so Dr. Peters sat close to them, putting on a continuous glucose monitor. “At that time, we didn’t think of COVID-19 as being in L.A.,” Dr. Peters recalled, “so I think we were not terribly consistent at mask-wearing due to the need to educate.”
“Several days later, I got COVID, but I didn’t know I had COVID per se. I felt crappy, had a terrible sore throat, lost my sense of taste and smell [which was not yet described as a COVID symptom], was completely exhausted, but had no fever or cough, which were the only criteria for getting COVID tested at the time. I didn’t know I had been exposed until 2 weeks later, when the patient’s assistant returned the sensor warning us to ‘be careful’ with it because the patient and his wife were recovering from COVID.”
That early battle with COVID-19 was just the beginning of what would become a 2-year struggle, including familial loss amid her own health problems and concerns about the under-resourced patients she cares for. Here, she shares her journey through the pandemic with this news organization.
Question: Thanks for talking to us. Let’s discuss your journey over these past 2.5 years.
Answer: Everybody has their own COVID story because we all went through this together. Some of us have worse COVID stories, and some of us have better ones, but all have been impacted.
I’m not a sick person. I’m a very healthy person but COVID made me so unwell for 2 years. The brain fog and fatigue were nothing compared to the autonomic neuropathy that affected my heart. It was really limiting for me. And I still don’t know the long-term implications, looking 20-30 years from now.
Q: When you initially had COVID, what were your symptoms? What was the impact?
A: I had all the symptoms of COVID, except for a cough and fever. I lost my sense of taste and smell. I had a horrible headache, a sore throat, and I was exhausted. I couldn’t get tested because I didn’t have the right symptoms.
Despite being sick, I never stopped working but just switched to telemedicine. I also took my regular monthly trip to our cabin in Montana. I unknowingly flew on a plane with COVID. I wore a well-fitted N95 mask, so I don’t think I gave anybody COVID. I didn’t give COVID to my partner, Eric, which is hard to believe as – at 77 – he’s older than me. He has diabetes, heart disease, and every other high-risk characteristic. If he’d gotten COVID back then, it would have been terrible, as there were no treatments, but luckily he didn’t get it.
Q: When were you officially diagnosed?
A: Two or 3 months after I thought I might have had COVID, I checked my antibodies, which tested strongly positive for a prior COVID infection. That was when I knew all the symptoms I’d had were due to the disease.
Q: Not only were you dealing with your own illness, but also that of those close to you. Can you talk about that?
A: In April 2020, my mother who was in her 90s and otherwise healthy except for dementia, got COVID. She could have gotten it from me. I visited often but wore a mask. She had all the horrible pulmonary symptoms. In her advance directive, she didn’t want to be hospitalized so I kept her in her home. She died from COVID in her own bed. It was fairly brutal, but at least I kept her where she felt comforted.
My 91-year-old dad was living in a different residential facility. Throughout COVID he had become very depressed because his social patterns had changed. Prior to COVID, they all ate together, but during the pandemic they were unable to. He missed his social connections, disliked being isolated in his room, hated everyone in masks.
He was a bit demented, but not so much that he couldn’t communicate with me or remember where his grandson was going to law school. I wasn’t allowed inside the facility, which was hard on him. I hadn’t told him his wife died because the hospice social workers advised me that I shouldn’t give him news that he couldn’t process readily until I could spend time with him. Unfortunately, that time never came. In December 2020, he got COVID. One of the people in that facility had gone to the hospital, came back, and tested negative, but actually had COVID and gave it to my dad. The guy who gave it to my dad didn’t die but my dad was terribly ill. He died 2 weeks short of getting his vaccine. He was coherent enough to have a conversation. I asked him: ‘Do you want to go to the hospital?’ And he said: ‘No, because it would be too scary,’ since he couldn’t be with me. I put him on hospice and held his hand as he died from pulmonary COVID, which was awful. I couldn’t give him enough morphine or valium to ease his breathing. But his last words to me were “I love you,” and at the very end he seemed peaceful, which was a blessing.
I got an autopsy, because he wanted one. Nothing else was wrong with him other than COVID. It destroyed his lungs. The rest of him was fine – no heart disease, cancer, or anything else. He died of COVID-19, the same as my mother.
That same week, my aunt, my only surviving older relative, who was in Des Moines, Iowa, died of COVID-19. All three family members died before the vaccine came out.
It was hard to lose my parents. I’m the only surviving child because my sister died in her 20s. It’s not been an easy pandemic. But what pandemic is easy? I just happened to have lost more people than most. Ironically, my grandfather was one of the legionnaires at the Bellevue-Stratford Hotel in Philadelphia in 1976 and died of Legionnaire’s disease before we knew what was causing the outbreak.
Q: Were you still struggling with COVID?
A: COVID impacted my whole body. I lost a lot of weight. I didn’t want to eat, and my gastrointestinal system was not happy. It took a while for my sense of taste and smell to come back. Nothing tasted good. I’m not a foodie; I don’t really care about food. We could get takeout or whatever, but none of it appealed to me. I’m not so sure it was a taste thing, I just didn’t feel like eating.
I didn’t realize I had “brain fog” per se, because I felt stressed and overwhelmed by the pandemic and my patients’ concerns. But one day, about 3 months after I had developed COVID, I woke up without the fog. Which made me aware that I hadn’t been feeling right up until that point.
The worst symptoms, however, were cardiac. I noticed also immediately that my heart rate went up very quickly with minimal exertion. My pulse has always been in the 55-60 bpm range, and suddenly just walking across a room made it go up to over 140 bpm. If I did any aerobic activity, it went up over 160 and would be associated with dyspnea and chest pain. I believed these were all post-COVID symptoms and felt validated when reports of others having similar issues were published in the literature.
Q: Did you continue seeing patients?
A: Yes, of course. Patients never needed their doctors more. In East L.A., where patients don’t have easy access to telemedicine, I kept going into clinic throughout the pandemic. In the more affluent Westside of Los Angeles, we switched to telemedicine, which was quite effective for most. However, because diabetes was associated with an increased risk of hospitalization and death from COVID, my patients were understandably afraid. I’ve never been busier, but (like all health care providers), I became more of a COVID provider than a diabetologist.
Q: Do you feel your battle with COVID impacted your work?
A: It didn’t affect me at work. If I was sitting still, I was fine. Sitting at home at a desk, I didn’t notice any symptoms. But as a habitual stair-user, I would be gasping for breath in the stairwell because I couldn’t go up the stairs to my office as I once could.
I think you empathize more with people who had COVID (when you’ve had it yourself). There was such a huge patient burden. And I think that’s been the thing that’s affected health care providers the most – no matter what specialty we’re in – that nobody has answers.
Q: What happened after you had your vaccine?
A: The vaccine itself was fine. I didn’t have any reaction to the first two doses. But the first booster made my cardiac issues worse.
By this point, my cardiac problems stopped me from exercising. I even went to the ER with chest pain once because I was having palpitations and chest pressure caused by simply taking my morning shower. Fortunately, I wasn’t having an MI, but I certainly wasn’t “normal.”
My measure of my fitness is the cross-country skiing trail I use in Montana. I know exactly how far I can ski. Usually I can do the loop in 35 minutes. After COVID, I lasted 10 minutes. I would be tachycardic, short of breath with chest pain radiating down my left arm. I would rest and try to keep going. But with each rest period, I only got worse. I would be laying in the snow and strangers would ask if I needed help.
Q: What helped you?
A: I’ve read a lot about long COVID and have tried to learn from the experts. Of course, I never went to a doctor directly, although I did ask colleagues for advice. What I learned was to never push myself. I forced myself to create an exercise schedule where I only exercised three times a week with rest days in between. When exercising, the second my heart rate went above 140 bpm, I stopped until I could get it back down. I would push against this new limit, even though my limit was low.
Additionally, I worked on my breathing patterns and did meditative breathing for 10 minutes twice daily using a commercially available app.
Although progress was slow, I did improve, and by June 2022, I seemed back to normal. I was not as fit as I was prior to COVID and needed to improve, but the tachycardic response to exercise and cardiac symptoms were gone. I felt like my normal self. Normal enough to go on a spot packing trip in the Sierras in August. (Horses carried us and a mule carried the gear over the 12,000-foot pass into the mountains, and then left my friend and me high in the Sierras for a week.) We were camped above 10,000 feet and every day hiked up to another high mountain lake where we fly-fished for trout that we ate for dinner. The hikes were a challenge, but not abnormally so. Not as they would have been while I had long COVID.
Q: What is the current atmosphere in your clinic?
A: COVID is much milder now in my vaccinated patients, but I feel most health care providers are exhausted. Many of my staff left when COVID hit because they didn’t want to keep working. It made practicing medicine exhausting. There’s been a shortage of nurses, a shortage of everything. We’ve been required to do a whole lot more than we ever did before. It’s much harder to be a doctor. This pandemic is the first time I’ve ever thought of quitting. Granted, I lost my whole family, or at least the older generation, but it’s just been almost overwhelming.
On the plus side, almost every one of my patients has been vaccinated, because early on, people would ask: “Do you trust this vaccine?” I would reply: “I saw my parents die from COVID when they weren’t vaccinated, so you’re getting vaccinated. This is real and the vaccines help.” It made me very good at convincing people to get vaccines because I knew what it was like to see someone dying from COVID up close.
Q: What advice do you have for those struggling with the COVID pandemic?
A: People need to decide what their own risk is for getting sick and how many times they want to get COVID. At this point, I want people to go out, but safely. In the beginning, when my patients said, “can I go visit my granddaughter?” I said, “no,” but that was before we had the vaccine. Now I feel it is safe to go out using common sense. I still have my patients wear masks on planes. I still have patients try to eat outside as much as possible. And I tell people to take the precautions that make sense, but I tell them to go out and do things because life is short.
I had a patient in his 70s who has many risk factors like heart disease and diabetes. His granddaughter’s Bat Mitzvah in Florida was coming up. He asked: “Can I go?” I told him “Yes,” but to be safe – to wear an N95 mask on the plane and at the event, and stay in his own hotel room, rather than with the whole family. I said, “You need to do this.” Earlier in the pandemic, I saw people who literally died from loneliness and isolation.
He and his wife flew there. He sent me a picture of himself with his granddaughter. When he returned, he showed me a handwritten note from her that said, “I love you so much. Everyone else canceled, which made me cry. You’re the only one who came. You have no idea how much this meant to me.”
He’s back in L.A., and he didn’t get COVID. He said, “It was the best thing I’ve done in years.” That’s what I need to help people with, navigating this world with COVID and assessing risks and benefits. As with all of medicine, my advice is individualized. My advice changes based on the major circulating variant and the rates of the virus in the population, as well as the risk factors of the individual.
Q: What are you doing now?
A: I’m trying to avoid getting COVID again, or another booster. I could get pre-exposure monoclonal antibodies but am waiting to do anything further until I see what happens over the fall and winter. I still wear a mask inside but now do a mix of in-person and telemedicine visits. I still try to go to outdoor restaurants, which is easy in California. But I’m flying to see my son in New York and plan to go to Europe this fall for a meeting. I also go to my cabin in Montana every month to get my “dose” of the wilderness. Overall, I travel for conferences and speaking engagements much less because I have learned the joy of staying home.
Thinking back on my life as a doctor, my career began as an intern at Stanford rotating through Ward 5B, the AIDS unit at San Francisco General Hospital, and will likely end with COVID. In spite of all our medical advances, my generation of physicians, much as many generations before us, has a front-row seat to the vulnerability of humans to infectious diseases and how far we still need to go to protect our patients from communicable illness.
A version of this article first appeared on Medscape.com.
Anne L. Peters, MD, is a professor of medicine at the University of Southern California, Los Angeles, and director of the USC clinical diabetes programs. She has published more than 200 articles, reviews, and abstracts; three books on diabetes; and has been an investigator for more than 40 research studies. She has spoken internationally at over 400 programs and serves on many committees of several professional organizations.
Stable, long-term opioid therapy safer than tapering?
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
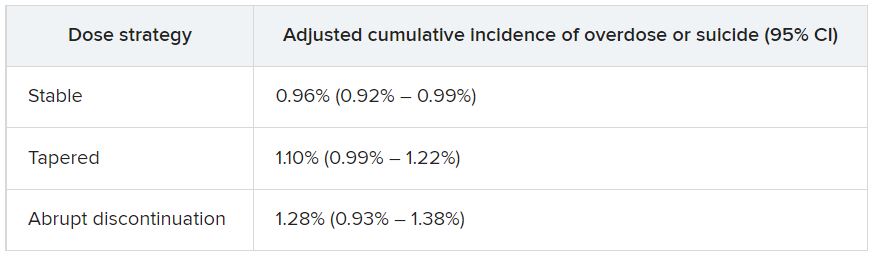
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
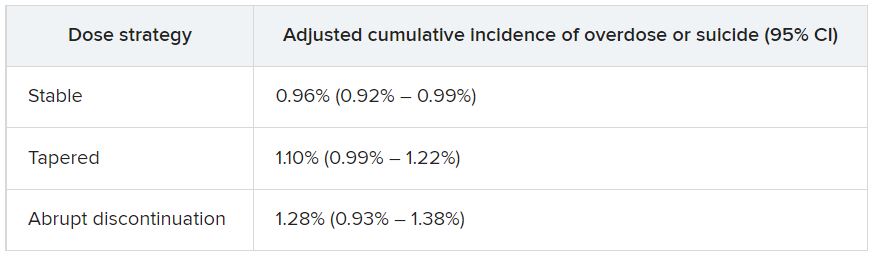
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed data for almost 200,000 patients who did not have signs of opioid use disorder (OUD) and were receiving opioid treatment. The investigators compared three dosing strategies: abrupt withdrawal, gradual tapering, and continuation of the current stable dosage.
Results showed a higher adjusted cumulative incidence of opioid overdose or suicide events 11 months after baseline among participants for whom a tapered dosing strategy was utilized, compared with those who continued taking a stable dosage. The risk difference was 0.15% between taper and stable dosage and 0.33% between abrupt discontinuation and stable dosage.
“This study identified a small absolute increase in risk of harms associated with opioid tapering compared with a stable opioid dosage,” Marc LaRochelle, MD, MPH, assistant professor, Boston University, and colleagues write.
“These results do not suggest that policies of mandatory dosage tapering for individuals receiving a stable long-term opioid dosage without evidence of opioid misuse will reduce short-term harm via suicide and overdose,” they add.
The findings were published online in JAMA Network Open.
Benefits vs. harms
The investigators note that the Centers for Disease Control and Prevention, in its 2016 Guideline for Prescribing Opioids for Chronic Pain, “recommended tapering opioid dosages if benefits no longer outweigh harms.”
In response, “some health systems and U.S. states enacted stringent dose limits that were applied with few exceptions, regardless of individual patients’ risk of harms,” they write. By contrast, there have been “increasing reports of patients experiencing adverse effects from forced opioid tapers.”
Previous studies that identified harms associated with opioid tapering and discontinuation had several limitations, including a focus on discontinuation, which is “likely more destabilizing than gradual tapering,” the researchers write. There is also “a high potential for confounding” in these studies, they add.
The investigators sought to fill the research gap by drawing on 8-year data (Jan. 1, 2010, to Dec. 31, 2018) from a large database that includes adjudicated pharmacy, outpatient, and inpatient medical claims for individuals with commercial or Medicare Advantage insurance encompassing all 50 states, the District of Columbia, and Puerto Rico.
Notably, individuals who had received a diagnosis of substance use, abuse, or dependence or for whom there were indicators consistent with OUD were excluded.
The researchers compared the three treatment strategies during a 4-month treatment strategy assignment period (“grace period”) after baseline. Tapering was defined as “2 consecutive months with a mean MME [morphine milligram equivalent] reduction of 15% or more compared with the baseline month.”
All estimates were adjusted for potential confounders, including demographic and treatment characteristics, baseline year, region, insurance plan type, comorbid psychiatric and medical conditions, and the prescribing of other psychiatric medications, such as benzodiazepines, gabapentin, or pregabalin.
Patient-centered approaches
The final cohort that met inclusion criteria consisted of 199,836 individuals (45.1% men; mean age, 56.9 years). Of the total group, 57.6% were aged 45-64 years. There were 415,123 qualifying long-term opioid therapy episodes.
The largest percentage of the cohort (41.2%) were receiving a baseline mean MME of 50-89 mg/day, while 34% were receiving 90-199 mg/day and 23.5% were receiving at least 200 mg/day.
During the 6-month eligibility assessment period, 34.8% of the cohort were receiving benzodiazepine prescriptions, 18% had been diagnosed with comorbid anxiety, and 19.7% had been diagnosed with comorbid depression.
After the treatment assignment period, most treatment episodes (87.1%) were considered stable, 11.1% were considered a taper, and 1.8% were considered abrupt discontinuation.
Eleven months after baseline, the adjusted cumulative incidence of opioid overdose or suicide events was lowest for those who continued to receive a stable dose.
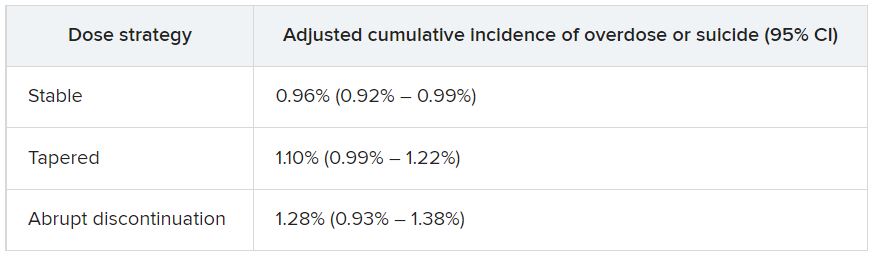
The risk differences between taper vs. stable dosage were 0.15% (95% confidence interval, 0.03%-0.26%), and the risk differences between abrupt discontinuation and stable dose were 0.33% (95% CI, −0.03%-0.74%). The risk ratios associated with taper vs. stable dosage and abrupt discontinuation vs. stable dosage were 1.15 (95% CI, 1.04-1.27) and 1.34 (95% CI, 0.97-1.79), respectively.
The adjusted cumulative incidence curves for overdose or suicide diverged at month 4 when comparing stable dosage and taper, with a higher incidence associated with the taper vs. stable dosage treatment strategies thereafter. However, when the researchers compared stable dosage with abrupt discontinuation, the event rates were similar.
A per protocol analysis, in which the researchers censored episodes involving lack of adherence to assigned treatment, yielded results similar to those of the main analysis.
“Policies establishing dosage thresholds or mandating tapers for all patients receiving long-term opioid therapy are not supported by existing data in terms of anticipated benefits even if, as we found, the rate of adverse outcomes is small,” the investigators write.
Instead, they encourage health care systems and clinicians to “continue to develop and implement patient-centered approaches to pain management for patients with established long-term opioid therapy.”
Protracted withdrawal?
Commenting on the study, A. Benjamin Srivastava, MD, assistant professor of clinical psychiatry, division on substance use disorders, Columbia University Medical Center, New York State Psychiatric Institute, New York, called the study “an important contribution to the literature” that “sheds further light on the risks associated with tapering.”
Dr. Srivastava, who was not involved with the research, noted that previous studies showing an increased prevalence of adverse events with tapering included participants with OUD or signs of opioid misuse, “potentially confounding findings.”
By contrast, the current study investigators specifically excluded patients with OUD/opioid misuse but still found a “slight increase in risk for opioid overdose and suicide, even when excluding for potential confounders,” he said.
Although causal implications require further investigation, “a source of these adverse outcomes may be unmanaged withdrawal that may be protracted,” Dr. Srivastava noted.
While abrupt discontinuation “may result in significant acute withdrawal symptoms, these should subside by 1-2 weeks at most,” he said.
Lowering the dose without discontinuation may lead to patients’ entering into “a dyshomeostatic state characterized by anxiety and dysphoria ... that may not be recognized by the prescribing clinician,” he added.
The brain “is still being primed by opioids [and] ‘wanting’ a higher dose. Thus, particular attention to withdrawal symptoms, both physical and psychiatric, is prudent when choosing to taper opioids vs. maintaining or discontinuing,” Dr. Srivastava said.
The study was funded by a grant from the CDC and a grant from the National Institute on Drug Abuse to one of the investigators. Dr. LaRochelle received grants from the CDC and NIDA during the conduct of the study and has received consulting fees for research paid to his institution from OptumLabs outside the submitted work. The other investigators’ disclosures are listed in the original article. Dr. Srivastava reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
How docs in firearm-friendly states talk gun safety
Samuel Mathis, MD, tries to cover a lot of ground during a wellness exam for his patients. Nutrition, immunizations, dental hygiene, and staying safe at school are a few of the topics on his list. And the Texas pediatrician asks one more question of children and their parents: “Are there any firearms in the house?”
If the answer is “yes,” Dr. Mathis discusses safety courses and other ideas with the families. “Rather than ask a bunch of questions, often I will say it’s recommended to keep them locked up and don’t forget toddlers can climb heights that you never would have envisioned,” said Dr. Mathis, an assistant professor at the University of Texas Medical Branch, Galveston.
Dr. Mathis said some of his physician colleagues are wary of bringing up the topic of guns in a state that leads the nation with more than 1 million registered firearms. “My discussion is more on firearm responsibility and just making sure they are taking extra steps to keep themselves and everyone around them safe. That works much better in these discussions.”
Gun safety: Public health concern, not politics
The statistics tell why:
- Unintentional shooting deaths by children rose by nearly one third in a 3-month period in 2020, compared with the same period in 2019.
- Of every 10 gun deaths in the United States, 6 are by suicide.
- As of July 28, 372 mass shootings have occured.
- Firearms now represent the leading cause of death among the nation’s youth.
In 2018, the editors of Annals of Internal Medicine urged physicians in the United States to sign a pledge to talk with their patients about guns in the home. To date, at least 3,664 have done so.
In 2019, the American Academy of Family Medicine, with other leading physician and public health organizations, issued a “call to action,” recommending ways to reduce firearm-related injury and death in the United States. Physicians can and should address the issue, it said, by counseling patients about firearm safety.
“This is just another part of healthcare,” said Sarah C. Nosal, MD, a member of the board of directors of the AAFP, who practices at the Urban Horizons Family Health Center, New York.
Dr. Nosal said she asks about firearms during every well-child visit. She also focuses on patients with a history of depression or suicide attempts and those who have experienced domestic violence.
Are physicians counseling patients about gun safety?
A 2018 survey of physicians found that 73% of the 71 who responded agreed to discuss gun safety with at-risk patients. But just 5% said they always talk to those at-risk patients, according to Melanie G. Hagen, MD, professor of internal medicine at the University of Florida, Gainesville, who led the study. While the overwhelming majority agreed that gun safety is a public health issue, only 55% said they felt comfortable initiating conversations about firearms with their patients.
Have things changed since then? “Probably not,” Dr. Hagen said in an interview. She cited some reasons, at least in her state.
One obstacle is that many people, including physicians, believe that Florida’s physician gag law, which prohibited physicians from asking about a patient’s firearm ownership, was still in effect. The law, passed in 2011, was overturned in 2017. In her survey, 76% said they were aware it had been overturned. But that awareness appears not to be universal, she said.
In a 2020 report about physician involvement in promoting gun safety, researchers noted four main challenges: lingering fears about the overturned law and potential liability from violating it, feeling unprepared, worry that patients don’t want to discuss the topic, and lack of time to talk about it during a rushed office visit.
But recent research suggests that patients are often open to talking about gun safety, and another study found that if physicians are given educational materials on firearm safety, more will counsel patients about gun safety.
Are patients and parents receptive?
Parents welcome discussion from health care providers about gun safety, according to a study from the University of Pennsylvania, Philadelphia.
Researchers asked roughly 100 parents to watch a short video about a firearm safety program designed to prevent accidents and suicides from guns. The program, still under study, involves a discussion between a parent and a pediatrician, with information given on secure storage of guns and the offering of a free cable lock.
The parents, about equally divided between gun owners and non–gun owners, said they were open to discussion about firearm safety, especially when the conversation involves their child’s pediatrician. Among the gun owners, only one in three said all their firearms were locked, unloaded, and stored properly. But after getting the safety information, 64% said they would change the way they stored their firearms.
A different program that offered pediatricians educational materials on firearm safety, as well as free firearm locks for distribution, increased the likelihood that the physicians would counsel patients on gun safety, other researchers reported.
Getting the conversation started
Some patients “bristle” when they’re asked about guns, Dr. Hagen said. Focusing on the “why” of the question can soften their response. One of her patients, a man in his 80s, had worked as a prison guard. After he was diagnosed with clinical depression, she asked him if he ever thought about ending his life. He said yes.
“And in Florida, I know a lot of people have guns,” she said. The state ranks second in the nation, with more than a half million registered weapons.
When Dr. Hagen asked him if he had firearms at home, he balked. Why did she need to know? “People do get defensive,” she said. “Luckily, I had a good relationship with this man, and he was willing to listen to me. If it’s someone I have a good relationship with, and I have this initial bristling, if I say: ‘I’m worried about you, I’m worried about your safety,’ that changes the entire conversation.”
She talked through the best plan for this patient, and he agreed to give his weapons to his son to keep.
Likewise, she talks with family members of dementia patients, urging them to be sure the weapons are stored and locked to prevent tragic accidents.
Dr. Nosal said reading the room is key. “Often, we are having the conversation with a parent with a child present,” she said. “Perhaps that is not the conversation the parent or guardian wanted to have with the child present.” In such a situation, she suggests asking the parent if they would talk about it solo.
“It can be a challenge to know the appropriate way to start the conversation,” Dr. Mathis said. The topic is not taught in medical school, although many experts think it should be. Dr. Hagen recently delivered a lecture to medical students about how to broach the topic with patients. She said she hopes it will become a regular event.
“It really comes down to being willing to be open and just ask that first question in a nonjudgmental way,” Dr. Mathis said. It helps, too, he said, for physicians to remember what he always tries to keep in mind: “My job isn’t politics, my job is health.”
Among the points Dr. Hagen makes in her lecture about talking to patients about guns are the following:
- Every day, more than 110 Americans are killed with guns.
- Gun violence accounts for just 1%-2% of those deaths, but mass shootings serve to shine a light on the issue of gun safety.
- 110,000 firearm injuries a year require medical or legal attention. Each year, more than 1,200 children in this country die from gun-related injuries.
- More than 33,000 people, on average, die in the United States each year from gun violence, including more than 21,000 from suicide.
- About 31% of all U.S. households have firearms; 22% of U.S. adults own one or more.
- Guns are 70% less likely to be stored locked and unloaded in homes where suicides or unintentional gun injuries occur.
- Action points: Identify risk, counsel patients at risk, act when someone is in imminent danger (such as unsafe practices or suicide threats).
- Focus on identifying adults who have a risk of inflicting violence on self or others.
- Focus on health and well-being with all; be conversational and educational.
- Clinicians should ask five crucial questions, all with an “L,” if firearms are in the home: Is it Loaded? Locked? Are Little children present? Is the owner feeling Low? Are they Learned [educated] in gun safety?
A version of this article first appeared on Medscape.com.
Samuel Mathis, MD, tries to cover a lot of ground during a wellness exam for his patients. Nutrition, immunizations, dental hygiene, and staying safe at school are a few of the topics on his list. And the Texas pediatrician asks one more question of children and their parents: “Are there any firearms in the house?”
If the answer is “yes,” Dr. Mathis discusses safety courses and other ideas with the families. “Rather than ask a bunch of questions, often I will say it’s recommended to keep them locked up and don’t forget toddlers can climb heights that you never would have envisioned,” said Dr. Mathis, an assistant professor at the University of Texas Medical Branch, Galveston.
Dr. Mathis said some of his physician colleagues are wary of bringing up the topic of guns in a state that leads the nation with more than 1 million registered firearms. “My discussion is more on firearm responsibility and just making sure they are taking extra steps to keep themselves and everyone around them safe. That works much better in these discussions.”
Gun safety: Public health concern, not politics
The statistics tell why:
- Unintentional shooting deaths by children rose by nearly one third in a 3-month period in 2020, compared with the same period in 2019.
- Of every 10 gun deaths in the United States, 6 are by suicide.
- As of July 28, 372 mass shootings have occured.
- Firearms now represent the leading cause of death among the nation’s youth.
In 2018, the editors of Annals of Internal Medicine urged physicians in the United States to sign a pledge to talk with their patients about guns in the home. To date, at least 3,664 have done so.
In 2019, the American Academy of Family Medicine, with other leading physician and public health organizations, issued a “call to action,” recommending ways to reduce firearm-related injury and death in the United States. Physicians can and should address the issue, it said, by counseling patients about firearm safety.
“This is just another part of healthcare,” said Sarah C. Nosal, MD, a member of the board of directors of the AAFP, who practices at the Urban Horizons Family Health Center, New York.
Dr. Nosal said she asks about firearms during every well-child visit. She also focuses on patients with a history of depression or suicide attempts and those who have experienced domestic violence.
Are physicians counseling patients about gun safety?
A 2018 survey of physicians found that 73% of the 71 who responded agreed to discuss gun safety with at-risk patients. But just 5% said they always talk to those at-risk patients, according to Melanie G. Hagen, MD, professor of internal medicine at the University of Florida, Gainesville, who led the study. While the overwhelming majority agreed that gun safety is a public health issue, only 55% said they felt comfortable initiating conversations about firearms with their patients.
Have things changed since then? “Probably not,” Dr. Hagen said in an interview. She cited some reasons, at least in her state.
One obstacle is that many people, including physicians, believe that Florida’s physician gag law, which prohibited physicians from asking about a patient’s firearm ownership, was still in effect. The law, passed in 2011, was overturned in 2017. In her survey, 76% said they were aware it had been overturned. But that awareness appears not to be universal, she said.
In a 2020 report about physician involvement in promoting gun safety, researchers noted four main challenges: lingering fears about the overturned law and potential liability from violating it, feeling unprepared, worry that patients don’t want to discuss the topic, and lack of time to talk about it during a rushed office visit.
But recent research suggests that patients are often open to talking about gun safety, and another study found that if physicians are given educational materials on firearm safety, more will counsel patients about gun safety.
Are patients and parents receptive?
Parents welcome discussion from health care providers about gun safety, according to a study from the University of Pennsylvania, Philadelphia.
Researchers asked roughly 100 parents to watch a short video about a firearm safety program designed to prevent accidents and suicides from guns. The program, still under study, involves a discussion between a parent and a pediatrician, with information given on secure storage of guns and the offering of a free cable lock.
The parents, about equally divided between gun owners and non–gun owners, said they were open to discussion about firearm safety, especially when the conversation involves their child’s pediatrician. Among the gun owners, only one in three said all their firearms were locked, unloaded, and stored properly. But after getting the safety information, 64% said they would change the way they stored their firearms.
A different program that offered pediatricians educational materials on firearm safety, as well as free firearm locks for distribution, increased the likelihood that the physicians would counsel patients on gun safety, other researchers reported.
Getting the conversation started
Some patients “bristle” when they’re asked about guns, Dr. Hagen said. Focusing on the “why” of the question can soften their response. One of her patients, a man in his 80s, had worked as a prison guard. After he was diagnosed with clinical depression, she asked him if he ever thought about ending his life. He said yes.
“And in Florida, I know a lot of people have guns,” she said. The state ranks second in the nation, with more than a half million registered weapons.
When Dr. Hagen asked him if he had firearms at home, he balked. Why did she need to know? “People do get defensive,” she said. “Luckily, I had a good relationship with this man, and he was willing to listen to me. If it’s someone I have a good relationship with, and I have this initial bristling, if I say: ‘I’m worried about you, I’m worried about your safety,’ that changes the entire conversation.”
She talked through the best plan for this patient, and he agreed to give his weapons to his son to keep.
Likewise, she talks with family members of dementia patients, urging them to be sure the weapons are stored and locked to prevent tragic accidents.
Dr. Nosal said reading the room is key. “Often, we are having the conversation with a parent with a child present,” she said. “Perhaps that is not the conversation the parent or guardian wanted to have with the child present.” In such a situation, she suggests asking the parent if they would talk about it solo.
“It can be a challenge to know the appropriate way to start the conversation,” Dr. Mathis said. The topic is not taught in medical school, although many experts think it should be. Dr. Hagen recently delivered a lecture to medical students about how to broach the topic with patients. She said she hopes it will become a regular event.
“It really comes down to being willing to be open and just ask that first question in a nonjudgmental way,” Dr. Mathis said. It helps, too, he said, for physicians to remember what he always tries to keep in mind: “My job isn’t politics, my job is health.”
Among the points Dr. Hagen makes in her lecture about talking to patients about guns are the following:
- Every day, more than 110 Americans are killed with guns.
- Gun violence accounts for just 1%-2% of those deaths, but mass shootings serve to shine a light on the issue of gun safety.
- 110,000 firearm injuries a year require medical or legal attention. Each year, more than 1,200 children in this country die from gun-related injuries.
- More than 33,000 people, on average, die in the United States each year from gun violence, including more than 21,000 from suicide.
- About 31% of all U.S. households have firearms; 22% of U.S. adults own one or more.
- Guns are 70% less likely to be stored locked and unloaded in homes where suicides or unintentional gun injuries occur.
- Action points: Identify risk, counsel patients at risk, act when someone is in imminent danger (such as unsafe practices or suicide threats).
- Focus on identifying adults who have a risk of inflicting violence on self or others.
- Focus on health and well-being with all; be conversational and educational.
- Clinicians should ask five crucial questions, all with an “L,” if firearms are in the home: Is it Loaded? Locked? Are Little children present? Is the owner feeling Low? Are they Learned [educated] in gun safety?
A version of this article first appeared on Medscape.com.
Samuel Mathis, MD, tries to cover a lot of ground during a wellness exam for his patients. Nutrition, immunizations, dental hygiene, and staying safe at school are a few of the topics on his list. And the Texas pediatrician asks one more question of children and their parents: “Are there any firearms in the house?”
If the answer is “yes,” Dr. Mathis discusses safety courses and other ideas with the families. “Rather than ask a bunch of questions, often I will say it’s recommended to keep them locked up and don’t forget toddlers can climb heights that you never would have envisioned,” said Dr. Mathis, an assistant professor at the University of Texas Medical Branch, Galveston.
Dr. Mathis said some of his physician colleagues are wary of bringing up the topic of guns in a state that leads the nation with more than 1 million registered firearms. “My discussion is more on firearm responsibility and just making sure they are taking extra steps to keep themselves and everyone around them safe. That works much better in these discussions.”
Gun safety: Public health concern, not politics
The statistics tell why:
- Unintentional shooting deaths by children rose by nearly one third in a 3-month period in 2020, compared with the same period in 2019.
- Of every 10 gun deaths in the United States, 6 are by suicide.
- As of July 28, 372 mass shootings have occured.
- Firearms now represent the leading cause of death among the nation’s youth.
In 2018, the editors of Annals of Internal Medicine urged physicians in the United States to sign a pledge to talk with their patients about guns in the home. To date, at least 3,664 have done so.
In 2019, the American Academy of Family Medicine, with other leading physician and public health organizations, issued a “call to action,” recommending ways to reduce firearm-related injury and death in the United States. Physicians can and should address the issue, it said, by counseling patients about firearm safety.
“This is just another part of healthcare,” said Sarah C. Nosal, MD, a member of the board of directors of the AAFP, who practices at the Urban Horizons Family Health Center, New York.
Dr. Nosal said she asks about firearms during every well-child visit. She also focuses on patients with a history of depression or suicide attempts and those who have experienced domestic violence.
Are physicians counseling patients about gun safety?
A 2018 survey of physicians found that 73% of the 71 who responded agreed to discuss gun safety with at-risk patients. But just 5% said they always talk to those at-risk patients, according to Melanie G. Hagen, MD, professor of internal medicine at the University of Florida, Gainesville, who led the study. While the overwhelming majority agreed that gun safety is a public health issue, only 55% said they felt comfortable initiating conversations about firearms with their patients.
Have things changed since then? “Probably not,” Dr. Hagen said in an interview. She cited some reasons, at least in her state.
One obstacle is that many people, including physicians, believe that Florida’s physician gag law, which prohibited physicians from asking about a patient’s firearm ownership, was still in effect. The law, passed in 2011, was overturned in 2017. In her survey, 76% said they were aware it had been overturned. But that awareness appears not to be universal, she said.
In a 2020 report about physician involvement in promoting gun safety, researchers noted four main challenges: lingering fears about the overturned law and potential liability from violating it, feeling unprepared, worry that patients don’t want to discuss the topic, and lack of time to talk about it during a rushed office visit.
But recent research suggests that patients are often open to talking about gun safety, and another study found that if physicians are given educational materials on firearm safety, more will counsel patients about gun safety.
Are patients and parents receptive?
Parents welcome discussion from health care providers about gun safety, according to a study from the University of Pennsylvania, Philadelphia.
Researchers asked roughly 100 parents to watch a short video about a firearm safety program designed to prevent accidents and suicides from guns. The program, still under study, involves a discussion between a parent and a pediatrician, with information given on secure storage of guns and the offering of a free cable lock.
The parents, about equally divided between gun owners and non–gun owners, said they were open to discussion about firearm safety, especially when the conversation involves their child’s pediatrician. Among the gun owners, only one in three said all their firearms were locked, unloaded, and stored properly. But after getting the safety information, 64% said they would change the way they stored their firearms.
A different program that offered pediatricians educational materials on firearm safety, as well as free firearm locks for distribution, increased the likelihood that the physicians would counsel patients on gun safety, other researchers reported.
Getting the conversation started
Some patients “bristle” when they’re asked about guns, Dr. Hagen said. Focusing on the “why” of the question can soften their response. One of her patients, a man in his 80s, had worked as a prison guard. After he was diagnosed with clinical depression, she asked him if he ever thought about ending his life. He said yes.
“And in Florida, I know a lot of people have guns,” she said. The state ranks second in the nation, with more than a half million registered weapons.
When Dr. Hagen asked him if he had firearms at home, he balked. Why did she need to know? “People do get defensive,” she said. “Luckily, I had a good relationship with this man, and he was willing to listen to me. If it’s someone I have a good relationship with, and I have this initial bristling, if I say: ‘I’m worried about you, I’m worried about your safety,’ that changes the entire conversation.”
She talked through the best plan for this patient, and he agreed to give his weapons to his son to keep.
Likewise, she talks with family members of dementia patients, urging them to be sure the weapons are stored and locked to prevent tragic accidents.
Dr. Nosal said reading the room is key. “Often, we are having the conversation with a parent with a child present,” she said. “Perhaps that is not the conversation the parent or guardian wanted to have with the child present.” In such a situation, she suggests asking the parent if they would talk about it solo.
“It can be a challenge to know the appropriate way to start the conversation,” Dr. Mathis said. The topic is not taught in medical school, although many experts think it should be. Dr. Hagen recently delivered a lecture to medical students about how to broach the topic with patients. She said she hopes it will become a regular event.
“It really comes down to being willing to be open and just ask that first question in a nonjudgmental way,” Dr. Mathis said. It helps, too, he said, for physicians to remember what he always tries to keep in mind: “My job isn’t politics, my job is health.”
Among the points Dr. Hagen makes in her lecture about talking to patients about guns are the following:
- Every day, more than 110 Americans are killed with guns.
- Gun violence accounts for just 1%-2% of those deaths, but mass shootings serve to shine a light on the issue of gun safety.
- 110,000 firearm injuries a year require medical or legal attention. Each year, more than 1,200 children in this country die from gun-related injuries.
- More than 33,000 people, on average, die in the United States each year from gun violence, including more than 21,000 from suicide.
- About 31% of all U.S. households have firearms; 22% of U.S. adults own one or more.
- Guns are 70% less likely to be stored locked and unloaded in homes where suicides or unintentional gun injuries occur.
- Action points: Identify risk, counsel patients at risk, act when someone is in imminent danger (such as unsafe practices or suicide threats).
- Focus on identifying adults who have a risk of inflicting violence on self or others.
- Focus on health and well-being with all; be conversational and educational.
- Clinicians should ask five crucial questions, all with an “L,” if firearms are in the home: Is it Loaded? Locked? Are Little children present? Is the owner feeling Low? Are they Learned [educated] in gun safety?
A version of this article first appeared on Medscape.com.













