User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Why people lie about COVID
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
Have you ever lied about COVID-19?
Before you get upset, before the “how dare you,” I want you to think carefully.
Did you have COVID-19 (or think you did) and not mention it to someone you were going to be with? Did you tell someone you were taking more COVID precautions than you really were? Did you tell someone you were vaccinated when you weren’t? Have you avoided getting a COVID test even though you knew you should have?
Researchers appreciated the fact that public health interventions in COVID are important but are only as good as the percentage of people who actually abide by them. So, they designed a survey to ask the questions that many people don’t want to hear the answer to.
A total of 1,733 participants – 80% of those invited – responded to the survey. By design, approximately one-third of respondents (477) had already had COVID, one-third (499) were vaccinated and not yet infected, and one-third (509) were unvaccinated and not yet infected.
Of those surveyed, 41.6% admitted that they lied about COVID or didn’t adhere to COVID guidelines - a conservative estimate, if you ask me.
Breaking down some of the results, about 20% of people who previously were infected with COVID said they didn’t mention it when meeting with someone. A similar number said they didn’t tell anyone when they were entering a public place. A bit more concerning to me, roughly 20% reported not disclosing their COVID-positive status when going to a health care provider’s office.
About 10% of those who had not been vaccinated reported lying about their vaccination status. That’s actually less than the 15% of vaccinated people who lied and told someone they weren’t vaccinated.
About 17% of people lied about the need to quarantine, and many more broke quarantine rules.
The authors tried to see if certain personal characteristics predicted people who were more likely to lie about COVID-19–related issues. Turns out there was only one thing that predicted honesty: age.
Older people were more honest about their COVID status and COVID habits. Other factors – gender, education, race, political affiliation, COVID-19 conspiracy beliefs, and where you got your COVID information – did not seem to make much of a difference. Why are older people more honest? Because older people take COVID more seriously. And they should; COVID is more severe in older people.
The problem arises, of course, because people who are at lower risk for COVID complications interact with people at higher risk – and in those situations, honesty matters more.
On the other hand, isn’t lying about COVID stuff inevitable? If you know that a positive test means you can’t go to work, and not going to work means you won’t get paid, might you not be more likely to lie about the test? Or not get the test at all?
The authors explored the reasons for dishonesty and they are fairly broad, ranging from the desire for life to feel normal (more than half of people who lied) to not believing that COVID was real (a whopping 30%). Some of the reasons for lying included:
- Wanted life to feel normal (50%).
- Freedom (45%).
- It’s no one’s business (40%).
- COVID isn’t real (30%).
In the end, though, we need to realize that public health recommendations are not going to be universally followed, and people may tell us they are following them when, in fact, they are not.
What this adds is another data point to a trend we’ve seen across the course of the pandemic, a shift from collective to individual responsibility. If you can’t be sure what others are doing in regard to COVID, you need to focus on protecting yourself. Perhaps that shift was inevitable. Doesn’t mean we have to like it.
A version of this article first appeared on Medscape.com.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and hosts a repository of his communication work at www.methodsman.com.
Epidemic of brain fog? Long COVID’s effects worry experts
Weeks after Jeannie Volpe caught COVID-19 in November 2020, she could no longer do her job running sexual assault support groups in Anniston, Ala., because she kept forgetting the details that survivors had shared with her. “People were telling me they were having to revisit their traumatic memories, which isn’t fair to anybody,” the 47-year-old says.
Ms. Volpe has been diagnosed with long-COVID autonomic dysfunction, which includes severe muscle pain, depression, anxiety, and a loss of thinking skills. Some of her symptoms are more commonly known as brain fog, and they’re among the most frequent problems reported by people who have long-term issues after a bout of COVID-19.
Many experts and medical professionals say they haven’t even begun to scratch the surface of what impact this will have in years to come.
“I’m very worried that we have an epidemic of neurologic dysfunction coming down the pike,” says Pamela Davis, MD, PhD, a research professor at Case Western Reserve University, Cleveland.
In the 2 years Ms. Volpe has been living with long COVID, her executive function – the mental processes that enable people to focus attention, retain information, and multitask – has been so diminished that she had to relearn to drive. One of the various doctors assessing her has suggested speech therapy to help Ms. Volpe relearn how to form words. “I can see the words I want to say in my mind, but I can’t make them come out of my mouth,” she says in a sluggish voice that gives away her condition.
All of those symptoms make it difficult for her to care for herself. Without a job and health insurance, Ms. Volpe says she’s researched assisted suicide in the states that allow it but has ultimately decided she wants to live.
“People tell you things like you should be grateful you survived it, and you should; but you shouldn’t expect somebody to not grieve after losing their autonomy, their career, their finances.”
The findings of researchers studying the brain effects of COVID-19 reinforce what people with long COVID have been dealing with from the start. Their experiences aren’t imaginary; they’re consistent with neurological disorders – including myalgic encephalomyelitis, also known as chronic fatigue syndrome, or ME/CFS – which carry much more weight in the public imagination than the term brain fog, which can often be used dismissively.
Studies have found that COVID-19 is linked to conditions such as strokes; seizures; and mood, memory, and movement disorders.
While there are still a lot of unanswered questions about exactly how COVID-19 affects the brain and what the long-term effects are, there’s enough reason to suggest people should be trying to avoid both infection and reinfection until researchers get more answers.
Worldwide, it’s estimated that COVID-19 has contributed to more than 40 million new cases of neurological disorders, says Ziyad Al-Aly, MD, a clinical epidemiologist and long COVID researcher at Washington University in St. Louis. In his latest study of 14 million medical records of the U.S. Department of Veterans Affairs, the country’s largest integrated health care system, researchers found that regardless of age, gender, race, and lifestyle,
He noted that some of the conditions, such as headaches and mild decline in memory and sharpness, may improve and go away over time. But others that showed up, such as stroke, encephalitis (inflammation of the brain), and Guillain-Barré syndrome (a rare disorder in which the body’s immune system attacks the nerves), often lead to lasting damage. Dr. Al-Aly’s team found that neurological conditions were 7% more likely in those who had COVID-19 than in those who had never been infected.
What’s more, researchers noticed that compared with control groups, the risk of post-COVID thinking problems was more pronounced in people in their 30s, 40s, and 50s – a group that usually would be very unlikely to have these problems. For those over the age of 60, the risks stood out less because at that stage of life, such thinking problems aren’t as rare.
Another study of the veterans system last year showed that COVID-19 survivors were at a 46% higher risk of considering suicide after 1 year.
“We need to be paying attention to this,” says Dr. Al-Aly. “What we’ve seen is really the tip of the iceberg.” He worries that millions of people, including youths, will lose out on employment and education while dealing with long-term disabilities – and the economic and societal implications of such a fallout. “What we will all be left with is the aftermath of sheer devastation in some people’s lives,” he says.
Igor Koralnik, MD, chief of neuro-infectious disease and global neurology at Northwestern University, Chicago, has been running a specialized long COVID clinic. His team published a paper in March 2021 detailing what they saw in their first 100 patients. “About half the population in the study missed at least 10 days of work. This is going to have persistent impact on the workforce,” Dr. Koralnik said in a podcast posted on the Northwestern website. “We have seen that not only [do] patients have symptoms, but they have decreased quality of life.”
For older people and their caregivers, the risk of potential neurodegenerative diseases that the virus has shown to accelerate, such as dementia, is also a big concern. Alzheimer’s is already the fifth leading cause of death for people 65 and older.
In a recent study of more than 6 million people over the age of 65, Dr. Davis and her team at Case Western found the risk of Alzheimer’s in the year after COVID-19 increased by 50%-80%. The chances were especially high for women older than 85.
To date, there are no good treatments for Alzheimer’s, yet total health care costs for long-term care and hospice services for people with dementia topped $300 billion in 2020. That doesn’t even include the related costs to families.
“The downstream effect of having someone with Alzheimer’s being taken care of by a family member can be devastating on everyone,” she says. “Sometimes the caregivers don’t weather that very well.”
When Dr. Davis’s own father got Alzheimer’s at age 86, her mother took care of him until she had a stroke one morning while making breakfast. Dr. Davis attributes the stroke to the stress of caregiving. That left Dr. Davis no choice but to seek housing where both her parents could get care.
Looking at the broader picture, Dr. Davis believes widespread isolation, loneliness, and grief during the pandemic, and the disease of COVID-19 itself, will continue to have a profound impact on psychiatric diagnoses. This in turn could trigger a wave of new substance abuse as a result of unchecked mental health problems.
Still, not all brain experts are jumping to worst-case scenarios, with a lot yet to be understood before sounding the alarm. Joanna Hellmuth, MD, a neurologist and researcher at the University of California, San Francisco, cautions against reading too much into early data, including any assumptions that COVID-19 causes neurodegeneration or irreversible damage in the brain.
Even with before-and-after brain scans by University of Oxford, England, researchers that show structural changes to the brain after infection, she points out that they didn’t actually study the clinical symptoms of the people in the study, so it’s too soon to reach conclusions about associated cognitive problems.
“It’s an important piece of the puzzle, but we don’t know how that fits together with everything else,” says Dr. Hellmuth. “Some of my patients get better. … I haven’t seen a single person get worse since the pandemic started, and so I’m hopeful.”
A version of this article first appeared on WebMD.com.
Weeks after Jeannie Volpe caught COVID-19 in November 2020, she could no longer do her job running sexual assault support groups in Anniston, Ala., because she kept forgetting the details that survivors had shared with her. “People were telling me they were having to revisit their traumatic memories, which isn’t fair to anybody,” the 47-year-old says.
Ms. Volpe has been diagnosed with long-COVID autonomic dysfunction, which includes severe muscle pain, depression, anxiety, and a loss of thinking skills. Some of her symptoms are more commonly known as brain fog, and they’re among the most frequent problems reported by people who have long-term issues after a bout of COVID-19.
Many experts and medical professionals say they haven’t even begun to scratch the surface of what impact this will have in years to come.
“I’m very worried that we have an epidemic of neurologic dysfunction coming down the pike,” says Pamela Davis, MD, PhD, a research professor at Case Western Reserve University, Cleveland.
In the 2 years Ms. Volpe has been living with long COVID, her executive function – the mental processes that enable people to focus attention, retain information, and multitask – has been so diminished that she had to relearn to drive. One of the various doctors assessing her has suggested speech therapy to help Ms. Volpe relearn how to form words. “I can see the words I want to say in my mind, but I can’t make them come out of my mouth,” she says in a sluggish voice that gives away her condition.
All of those symptoms make it difficult for her to care for herself. Without a job and health insurance, Ms. Volpe says she’s researched assisted suicide in the states that allow it but has ultimately decided she wants to live.
“People tell you things like you should be grateful you survived it, and you should; but you shouldn’t expect somebody to not grieve after losing their autonomy, their career, their finances.”
The findings of researchers studying the brain effects of COVID-19 reinforce what people with long COVID have been dealing with from the start. Their experiences aren’t imaginary; they’re consistent with neurological disorders – including myalgic encephalomyelitis, also known as chronic fatigue syndrome, or ME/CFS – which carry much more weight in the public imagination than the term brain fog, which can often be used dismissively.
Studies have found that COVID-19 is linked to conditions such as strokes; seizures; and mood, memory, and movement disorders.
While there are still a lot of unanswered questions about exactly how COVID-19 affects the brain and what the long-term effects are, there’s enough reason to suggest people should be trying to avoid both infection and reinfection until researchers get more answers.
Worldwide, it’s estimated that COVID-19 has contributed to more than 40 million new cases of neurological disorders, says Ziyad Al-Aly, MD, a clinical epidemiologist and long COVID researcher at Washington University in St. Louis. In his latest study of 14 million medical records of the U.S. Department of Veterans Affairs, the country’s largest integrated health care system, researchers found that regardless of age, gender, race, and lifestyle,
He noted that some of the conditions, such as headaches and mild decline in memory and sharpness, may improve and go away over time. But others that showed up, such as stroke, encephalitis (inflammation of the brain), and Guillain-Barré syndrome (a rare disorder in which the body’s immune system attacks the nerves), often lead to lasting damage. Dr. Al-Aly’s team found that neurological conditions were 7% more likely in those who had COVID-19 than in those who had never been infected.
What’s more, researchers noticed that compared with control groups, the risk of post-COVID thinking problems was more pronounced in people in their 30s, 40s, and 50s – a group that usually would be very unlikely to have these problems. For those over the age of 60, the risks stood out less because at that stage of life, such thinking problems aren’t as rare.
Another study of the veterans system last year showed that COVID-19 survivors were at a 46% higher risk of considering suicide after 1 year.
“We need to be paying attention to this,” says Dr. Al-Aly. “What we’ve seen is really the tip of the iceberg.” He worries that millions of people, including youths, will lose out on employment and education while dealing with long-term disabilities – and the economic and societal implications of such a fallout. “What we will all be left with is the aftermath of sheer devastation in some people’s lives,” he says.
Igor Koralnik, MD, chief of neuro-infectious disease and global neurology at Northwestern University, Chicago, has been running a specialized long COVID clinic. His team published a paper in March 2021 detailing what they saw in their first 100 patients. “About half the population in the study missed at least 10 days of work. This is going to have persistent impact on the workforce,” Dr. Koralnik said in a podcast posted on the Northwestern website. “We have seen that not only [do] patients have symptoms, but they have decreased quality of life.”
For older people and their caregivers, the risk of potential neurodegenerative diseases that the virus has shown to accelerate, such as dementia, is also a big concern. Alzheimer’s is already the fifth leading cause of death for people 65 and older.
In a recent study of more than 6 million people over the age of 65, Dr. Davis and her team at Case Western found the risk of Alzheimer’s in the year after COVID-19 increased by 50%-80%. The chances were especially high for women older than 85.
To date, there are no good treatments for Alzheimer’s, yet total health care costs for long-term care and hospice services for people with dementia topped $300 billion in 2020. That doesn’t even include the related costs to families.
“The downstream effect of having someone with Alzheimer’s being taken care of by a family member can be devastating on everyone,” she says. “Sometimes the caregivers don’t weather that very well.”
When Dr. Davis’s own father got Alzheimer’s at age 86, her mother took care of him until she had a stroke one morning while making breakfast. Dr. Davis attributes the stroke to the stress of caregiving. That left Dr. Davis no choice but to seek housing where both her parents could get care.
Looking at the broader picture, Dr. Davis believes widespread isolation, loneliness, and grief during the pandemic, and the disease of COVID-19 itself, will continue to have a profound impact on psychiatric diagnoses. This in turn could trigger a wave of new substance abuse as a result of unchecked mental health problems.
Still, not all brain experts are jumping to worst-case scenarios, with a lot yet to be understood before sounding the alarm. Joanna Hellmuth, MD, a neurologist and researcher at the University of California, San Francisco, cautions against reading too much into early data, including any assumptions that COVID-19 causes neurodegeneration or irreversible damage in the brain.
Even with before-and-after brain scans by University of Oxford, England, researchers that show structural changes to the brain after infection, she points out that they didn’t actually study the clinical symptoms of the people in the study, so it’s too soon to reach conclusions about associated cognitive problems.
“It’s an important piece of the puzzle, but we don’t know how that fits together with everything else,” says Dr. Hellmuth. “Some of my patients get better. … I haven’t seen a single person get worse since the pandemic started, and so I’m hopeful.”
A version of this article first appeared on WebMD.com.
Weeks after Jeannie Volpe caught COVID-19 in November 2020, she could no longer do her job running sexual assault support groups in Anniston, Ala., because she kept forgetting the details that survivors had shared with her. “People were telling me they were having to revisit their traumatic memories, which isn’t fair to anybody,” the 47-year-old says.
Ms. Volpe has been diagnosed with long-COVID autonomic dysfunction, which includes severe muscle pain, depression, anxiety, and a loss of thinking skills. Some of her symptoms are more commonly known as brain fog, and they’re among the most frequent problems reported by people who have long-term issues after a bout of COVID-19.
Many experts and medical professionals say they haven’t even begun to scratch the surface of what impact this will have in years to come.
“I’m very worried that we have an epidemic of neurologic dysfunction coming down the pike,” says Pamela Davis, MD, PhD, a research professor at Case Western Reserve University, Cleveland.
In the 2 years Ms. Volpe has been living with long COVID, her executive function – the mental processes that enable people to focus attention, retain information, and multitask – has been so diminished that she had to relearn to drive. One of the various doctors assessing her has suggested speech therapy to help Ms. Volpe relearn how to form words. “I can see the words I want to say in my mind, but I can’t make them come out of my mouth,” she says in a sluggish voice that gives away her condition.
All of those symptoms make it difficult for her to care for herself. Without a job and health insurance, Ms. Volpe says she’s researched assisted suicide in the states that allow it but has ultimately decided she wants to live.
“People tell you things like you should be grateful you survived it, and you should; but you shouldn’t expect somebody to not grieve after losing their autonomy, their career, their finances.”
The findings of researchers studying the brain effects of COVID-19 reinforce what people with long COVID have been dealing with from the start. Their experiences aren’t imaginary; they’re consistent with neurological disorders – including myalgic encephalomyelitis, also known as chronic fatigue syndrome, or ME/CFS – which carry much more weight in the public imagination than the term brain fog, which can often be used dismissively.
Studies have found that COVID-19 is linked to conditions such as strokes; seizures; and mood, memory, and movement disorders.
While there are still a lot of unanswered questions about exactly how COVID-19 affects the brain and what the long-term effects are, there’s enough reason to suggest people should be trying to avoid both infection and reinfection until researchers get more answers.
Worldwide, it’s estimated that COVID-19 has contributed to more than 40 million new cases of neurological disorders, says Ziyad Al-Aly, MD, a clinical epidemiologist and long COVID researcher at Washington University in St. Louis. In his latest study of 14 million medical records of the U.S. Department of Veterans Affairs, the country’s largest integrated health care system, researchers found that regardless of age, gender, race, and lifestyle,
He noted that some of the conditions, such as headaches and mild decline in memory and sharpness, may improve and go away over time. But others that showed up, such as stroke, encephalitis (inflammation of the brain), and Guillain-Barré syndrome (a rare disorder in which the body’s immune system attacks the nerves), often lead to lasting damage. Dr. Al-Aly’s team found that neurological conditions were 7% more likely in those who had COVID-19 than in those who had never been infected.
What’s more, researchers noticed that compared with control groups, the risk of post-COVID thinking problems was more pronounced in people in their 30s, 40s, and 50s – a group that usually would be very unlikely to have these problems. For those over the age of 60, the risks stood out less because at that stage of life, such thinking problems aren’t as rare.
Another study of the veterans system last year showed that COVID-19 survivors were at a 46% higher risk of considering suicide after 1 year.
“We need to be paying attention to this,” says Dr. Al-Aly. “What we’ve seen is really the tip of the iceberg.” He worries that millions of people, including youths, will lose out on employment and education while dealing with long-term disabilities – and the economic and societal implications of such a fallout. “What we will all be left with is the aftermath of sheer devastation in some people’s lives,” he says.
Igor Koralnik, MD, chief of neuro-infectious disease and global neurology at Northwestern University, Chicago, has been running a specialized long COVID clinic. His team published a paper in March 2021 detailing what they saw in their first 100 patients. “About half the population in the study missed at least 10 days of work. This is going to have persistent impact on the workforce,” Dr. Koralnik said in a podcast posted on the Northwestern website. “We have seen that not only [do] patients have symptoms, but they have decreased quality of life.”
For older people and their caregivers, the risk of potential neurodegenerative diseases that the virus has shown to accelerate, such as dementia, is also a big concern. Alzheimer’s is already the fifth leading cause of death for people 65 and older.
In a recent study of more than 6 million people over the age of 65, Dr. Davis and her team at Case Western found the risk of Alzheimer’s in the year after COVID-19 increased by 50%-80%. The chances were especially high for women older than 85.
To date, there are no good treatments for Alzheimer’s, yet total health care costs for long-term care and hospice services for people with dementia topped $300 billion in 2020. That doesn’t even include the related costs to families.
“The downstream effect of having someone with Alzheimer’s being taken care of by a family member can be devastating on everyone,” she says. “Sometimes the caregivers don’t weather that very well.”
When Dr. Davis’s own father got Alzheimer’s at age 86, her mother took care of him until she had a stroke one morning while making breakfast. Dr. Davis attributes the stroke to the stress of caregiving. That left Dr. Davis no choice but to seek housing where both her parents could get care.
Looking at the broader picture, Dr. Davis believes widespread isolation, loneliness, and grief during the pandemic, and the disease of COVID-19 itself, will continue to have a profound impact on psychiatric diagnoses. This in turn could trigger a wave of new substance abuse as a result of unchecked mental health problems.
Still, not all brain experts are jumping to worst-case scenarios, with a lot yet to be understood before sounding the alarm. Joanna Hellmuth, MD, a neurologist and researcher at the University of California, San Francisco, cautions against reading too much into early data, including any assumptions that COVID-19 causes neurodegeneration or irreversible damage in the brain.
Even with before-and-after brain scans by University of Oxford, England, researchers that show structural changes to the brain after infection, she points out that they didn’t actually study the clinical symptoms of the people in the study, so it’s too soon to reach conclusions about associated cognitive problems.
“It’s an important piece of the puzzle, but we don’t know how that fits together with everything else,” says Dr. Hellmuth. “Some of my patients get better. … I haven’t seen a single person get worse since the pandemic started, and so I’m hopeful.”
A version of this article first appeared on WebMD.com.
ACC issues guidance on ED evaluation of acute chest pain
Chest pain accounts for more than 7 million ED visits annually. A major challenge is to quickly identify the small number of patients with acute coronary syndrome (ACS) among the large number of patients who have noncardiac conditions.
The new document is intended to provide guidance on how to “practically apply” recommendations from the 2021 American Heart Association/American College of Cardiology Guideline for the Evaluation and Diagnosis of Chest Pain, focusing specifically on patients who present to the ED, the writing group explains.
“A systematic approach – both at the level of the institution and the individual patient – is essential to achieve optimal outcomes for patients presenting with chest pain to the ED,” say writing group chair Michael Kontos, MD, Virginia Commonwealth University, Richmond, and colleagues.
At the institution level, this decision pathway recommends high-sensitivity cardiac troponin (hs-cTn) assays coupled with a clinical decision pathway (CDP) to reduce ED “dwell” times and increase the number of patients with chest pain who can safely be discharged without additional testing. This will decrease ED crowding and limit unnecessary testing, they point out.
At the individual patient level, this document aims to provide structure for the ED evaluation of chest pain, accelerating the evaluation process and matching the intensity of testing and treatment to patient risk.
The 36-page document was published online in the Journal of the American College of Cardiology.
Key summary points in the document include the following:
- Electrocardiogram remains the best initial test for evaluation of chest pain in the ED and should be performed and interpreted within 10 minutes of ED arrival.
- In patients who arrive via ambulance, the prehospital ECG should be reviewed, because ischemic changes may have resolved before ED arrival.
- When the ECG shows evidence of acute infarction or ischemia, subsequent care should follow current guidelines for management of acute ST-segment elevation myocardial infarction (STEMI) and non–ST-segment elevation ACS (NSTE-ACS).
- Patients with a nonischemic ECG can enter an accelerated CDP designed to provide rapid risk assessment and exclusion of ACS.
- Patients who are hemodynamically unstable, have significant arrhythmias, or evidence of significant heart failure should be evaluated and treated appropriately and are not candidates for an accelerated CDP.
- High-sensitivity cardiac troponin T (hs-cTnT) and high-sensitivity cardiac troponin I (hs-cTnI) are the preferred biomarkers for evaluation of possible ACS.
- Patients classified as low risk (rule out) using the current hs-cTn-based CDPs can generally be discharged directly from the ED without additional testing, although outpatient testing may be considered in selected cases.
- Patients with substantially elevated initial hs-cTn values or those with significant dynamic changes over 1-3 hours are assigned to the abnormal/high-risk category and should be further classified according to the universal definition of myocardial infarction type 1 or 2 or acute or chronic nonischemic cardiac injury.
- High-risk patients should usually be admitted to an inpatient setting for further evaluation and treatment.
- Patients determined to be intermediate risk with the CDP should undergo additional observation with repeat hs-cTn measurements at 3-6 hours and risk assessment using either the modified HEART (history, ECG, age, risk factors, and troponin) score or the ED assessment of chest pain score (EDACS).
- Noninvasive testing should be considered for the intermediate-risk group unless low-risk features are identified using risk scores or noninvasive testing has been performed recently with normal or low-risk findings.
The writing group notes that “safe and efficient” management of chest pain in the ED requires appropriate follow-up after discharge. Timing of follow-up and referral for outpatient noninvasive testing should be influenced by patient risk and results of cardiac testing.
Disclosures for members of the writing group are available with the original article.
A version of this article first appeared on Medscape.com.
Chest pain accounts for more than 7 million ED visits annually. A major challenge is to quickly identify the small number of patients with acute coronary syndrome (ACS) among the large number of patients who have noncardiac conditions.
The new document is intended to provide guidance on how to “practically apply” recommendations from the 2021 American Heart Association/American College of Cardiology Guideline for the Evaluation and Diagnosis of Chest Pain, focusing specifically on patients who present to the ED, the writing group explains.
“A systematic approach – both at the level of the institution and the individual patient – is essential to achieve optimal outcomes for patients presenting with chest pain to the ED,” say writing group chair Michael Kontos, MD, Virginia Commonwealth University, Richmond, and colleagues.
At the institution level, this decision pathway recommends high-sensitivity cardiac troponin (hs-cTn) assays coupled with a clinical decision pathway (CDP) to reduce ED “dwell” times and increase the number of patients with chest pain who can safely be discharged without additional testing. This will decrease ED crowding and limit unnecessary testing, they point out.
At the individual patient level, this document aims to provide structure for the ED evaluation of chest pain, accelerating the evaluation process and matching the intensity of testing and treatment to patient risk.
The 36-page document was published online in the Journal of the American College of Cardiology.
Key summary points in the document include the following:
- Electrocardiogram remains the best initial test for evaluation of chest pain in the ED and should be performed and interpreted within 10 minutes of ED arrival.
- In patients who arrive via ambulance, the prehospital ECG should be reviewed, because ischemic changes may have resolved before ED arrival.
- When the ECG shows evidence of acute infarction or ischemia, subsequent care should follow current guidelines for management of acute ST-segment elevation myocardial infarction (STEMI) and non–ST-segment elevation ACS (NSTE-ACS).
- Patients with a nonischemic ECG can enter an accelerated CDP designed to provide rapid risk assessment and exclusion of ACS.
- Patients who are hemodynamically unstable, have significant arrhythmias, or evidence of significant heart failure should be evaluated and treated appropriately and are not candidates for an accelerated CDP.
- High-sensitivity cardiac troponin T (hs-cTnT) and high-sensitivity cardiac troponin I (hs-cTnI) are the preferred biomarkers for evaluation of possible ACS.
- Patients classified as low risk (rule out) using the current hs-cTn-based CDPs can generally be discharged directly from the ED without additional testing, although outpatient testing may be considered in selected cases.
- Patients with substantially elevated initial hs-cTn values or those with significant dynamic changes over 1-3 hours are assigned to the abnormal/high-risk category and should be further classified according to the universal definition of myocardial infarction type 1 or 2 or acute or chronic nonischemic cardiac injury.
- High-risk patients should usually be admitted to an inpatient setting for further evaluation and treatment.
- Patients determined to be intermediate risk with the CDP should undergo additional observation with repeat hs-cTn measurements at 3-6 hours and risk assessment using either the modified HEART (history, ECG, age, risk factors, and troponin) score or the ED assessment of chest pain score (EDACS).
- Noninvasive testing should be considered for the intermediate-risk group unless low-risk features are identified using risk scores or noninvasive testing has been performed recently with normal or low-risk findings.
The writing group notes that “safe and efficient” management of chest pain in the ED requires appropriate follow-up after discharge. Timing of follow-up and referral for outpatient noninvasive testing should be influenced by patient risk and results of cardiac testing.
Disclosures for members of the writing group are available with the original article.
A version of this article first appeared on Medscape.com.
Chest pain accounts for more than 7 million ED visits annually. A major challenge is to quickly identify the small number of patients with acute coronary syndrome (ACS) among the large number of patients who have noncardiac conditions.
The new document is intended to provide guidance on how to “practically apply” recommendations from the 2021 American Heart Association/American College of Cardiology Guideline for the Evaluation and Diagnosis of Chest Pain, focusing specifically on patients who present to the ED, the writing group explains.
“A systematic approach – both at the level of the institution and the individual patient – is essential to achieve optimal outcomes for patients presenting with chest pain to the ED,” say writing group chair Michael Kontos, MD, Virginia Commonwealth University, Richmond, and colleagues.
At the institution level, this decision pathway recommends high-sensitivity cardiac troponin (hs-cTn) assays coupled with a clinical decision pathway (CDP) to reduce ED “dwell” times and increase the number of patients with chest pain who can safely be discharged without additional testing. This will decrease ED crowding and limit unnecessary testing, they point out.
At the individual patient level, this document aims to provide structure for the ED evaluation of chest pain, accelerating the evaluation process and matching the intensity of testing and treatment to patient risk.
The 36-page document was published online in the Journal of the American College of Cardiology.
Key summary points in the document include the following:
- Electrocardiogram remains the best initial test for evaluation of chest pain in the ED and should be performed and interpreted within 10 minutes of ED arrival.
- In patients who arrive via ambulance, the prehospital ECG should be reviewed, because ischemic changes may have resolved before ED arrival.
- When the ECG shows evidence of acute infarction or ischemia, subsequent care should follow current guidelines for management of acute ST-segment elevation myocardial infarction (STEMI) and non–ST-segment elevation ACS (NSTE-ACS).
- Patients with a nonischemic ECG can enter an accelerated CDP designed to provide rapid risk assessment and exclusion of ACS.
- Patients who are hemodynamically unstable, have significant arrhythmias, or evidence of significant heart failure should be evaluated and treated appropriately and are not candidates for an accelerated CDP.
- High-sensitivity cardiac troponin T (hs-cTnT) and high-sensitivity cardiac troponin I (hs-cTnI) are the preferred biomarkers for evaluation of possible ACS.
- Patients classified as low risk (rule out) using the current hs-cTn-based CDPs can generally be discharged directly from the ED without additional testing, although outpatient testing may be considered in selected cases.
- Patients with substantially elevated initial hs-cTn values or those with significant dynamic changes over 1-3 hours are assigned to the abnormal/high-risk category and should be further classified according to the universal definition of myocardial infarction type 1 or 2 or acute or chronic nonischemic cardiac injury.
- High-risk patients should usually be admitted to an inpatient setting for further evaluation and treatment.
- Patients determined to be intermediate risk with the CDP should undergo additional observation with repeat hs-cTn measurements at 3-6 hours and risk assessment using either the modified HEART (history, ECG, age, risk factors, and troponin) score or the ED assessment of chest pain score (EDACS).
- Noninvasive testing should be considered for the intermediate-risk group unless low-risk features are identified using risk scores or noninvasive testing has been performed recently with normal or low-risk findings.
The writing group notes that “safe and efficient” management of chest pain in the ED requires appropriate follow-up after discharge. Timing of follow-up and referral for outpatient noninvasive testing should be influenced by patient risk and results of cardiac testing.
Disclosures for members of the writing group are available with the original article.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Opioids leading cause of poisoning deaths in young children
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
AT AAP 2022
At the front lines of long COVID, local clinics prove vital
Big-name hospital chains across the United States are opening dedicated centers to help patients dealing with long COVID. But so are the lower-profile clinics and hospitals run by cities, counties and states – including Harborview Medical Center in Seattle.
They serve areas ranging from Campbell County, Wyo., with 47,000 residents, to New York City, with its 8.4 million people. Many providers working there are searching for innovative ways to approach this lingering illness with its variety of symptoms, from brain fog to shortness of breath to depression and more.
Their efforts often fall below the radar, with still-scant serious media attention to long COVID or the public health employees working to treat ailing patients.
Why are state and local health agencies taking on these duties?
They’re leading the way in part because the federal government has made only limited efforts, said Lisa McCorkell, a cofounder of the Patient-Led Research Collaborative. The international group was founded in spring 2020 by researchers who are also long COVID patients.
“It’s a big reason why long COVID isn’t talked about as much,” Ms. McCorkell said. “It’s definitely a national issue. But it trickles down to state and local health departments, and there’s not enough resources.”
The government clinics may be accessible to people without insurance and often are cheaper than clinics at private hospitals.
Harborview has treated more than 1,000 patients with long COVID, and another 200 patients are awaiting treatment, said Jessica Bender, MD, a codirector of the University of Washington Post-COVID Rehabilitation and Recovery Clinic in Seattle’s First Hill neighborhood.
The group Survivor Corps offers lists by states of clinics. While the publicly run clinics may be less expensive or even free for some patients, methods of payment vary from clinic to clinic. Federally qualified health clinics offer treatment on a sliding scale. For instance, the Riverside University Health System in California has federally qualified centers. And other providers who are not federally qualified also offer care paid for on a sliding scale. They include Campbell County Health, where some residents are eligible for discounts of 25%-100%, said spokesperson Norberto Orellana.
At Harborview, Dr. Bender said the public hospital’s post-COVID clinic initially began with a staff of rehabilitation doctors but expanded in 2021 to include family and internal medicine doctors. And it offers mental health programs with rehabilitation psychologists who instruct on how to deal with doctors or loved ones who don’t believe that long COVID exists.
“I have patients who really have been devastated by the lack of support from coworkers [and] family,” Dr. Bender said.
In Campbell County, Wyo., the pandemic surge did not arrive in earnest until late 2021. Physical therapists at Campbell County’s Health Rehabilitation Services organized a rehabilitation program for residents with long COVID after recognizing the need, said Shannon Sorensen, rehabilitation director at Campbell County Health.
“We had patients coming in showing chest pain, or heart palpitations. There were people trying to get back to work. They were frustrated,” Ms. Sorensen said.
Myalgic encephalomyelitis and chronic fatigue syndrome activists have embraced the fight to recognize and help long COVID patients, noting the similarities between the conditions, and hope to help kickstart more organized research, treatment and benefits for long COVID sufferers and myalgic encephalomyelitis/chronic fatigue syndrome patients alike.
In Ft. Collins, Colo., disability activist Alison Sbrana has long had myalgic encephalomyelitis. She and other members of the local chapter of ME Action have met with state officials for several years and are finally seeing the results of those efforts.
Colorado Gov. Jared Polis has created the full-time position of policy adviser for long COVID and post–viral infection planning.
“This is one way forward of how state governments are (finally) paying attention to infection-triggered chronic illnesses and starting to think ahead on them,” Ms. Sbrana said.
New York City’s Health + Hospitals launched what may be the most expansive long COVID treatment program in the nation in April 2021. Called AfterCare, it provides physical and mental health services as well as community support systems and financial assistance.
A persistent issue for patients is that there isn’t yet a test for long COVID, like there is for COVID-19, said Amanda Johnson, MD, assistant vice president for ambulatory care and population health at New York Health + Hospitals. “It’s in many ways a diagnosis of exclusion. You have to make sure their shortness of breath isn’t caused by something else. The same with anemia,” she said.
California’s Department of Public Health has a detailed website devoted to the topic, including videos of “long haulers” describing their experiences.
Vermont is one of several states studying long COVID, said Mark Levine, MD, the state health commissioner. The state, in collaboration with the University of Vermont, has established a surveillance project to determine how many people have long COVID, as well as how severe it is, how long it lasts, and potential predispositions.
The University of Utah, Salt Lake City, established a comprehensive COVID-19 clinic more than a year ago that also handles long COVID patients, said Jeannette Brown, MD, PhD, an associate professor at the school and director of the COVID-19 clinic.
Jennifer Chevinsky, MD, MPH, already had a deep understanding of long COVID when she landed in Riverside County, Calif., in the summer of 2021. She came from Atlanta, where as part of her job as an epidemic intelligence service officer at the CDC, she heard stories of COVID-19 patients who were not getting better.
Now she is a deputy public health officer for Riverside County, in a region known for its deserts, sizzling summer temperatures and diverse populations. She said her department has helped launch programs such as post–COVID-19 follow-up phone calls and long COVID training programs that reach out to the many Latino residents in this county of 2.4 million people. It also includes Black and Native American residents.
“We’re making sure information is circulated with community and faith-based organizations, and community health workers,” she said.
Ms. McCorkell said there is still much work to do to raise public awareness of the risks of long COVID and how to obtain care for patients. She would like to see a national public health campaign about long COVID, possibly spearheaded by the Centers for Disease Control and Prevention in partnership with local health workers and community-based organizations.
“That,” she said, “could make a big difference.”
A version of this article first appeared on WebMD.com.
Big-name hospital chains across the United States are opening dedicated centers to help patients dealing with long COVID. But so are the lower-profile clinics and hospitals run by cities, counties and states – including Harborview Medical Center in Seattle.
They serve areas ranging from Campbell County, Wyo., with 47,000 residents, to New York City, with its 8.4 million people. Many providers working there are searching for innovative ways to approach this lingering illness with its variety of symptoms, from brain fog to shortness of breath to depression and more.
Their efforts often fall below the radar, with still-scant serious media attention to long COVID or the public health employees working to treat ailing patients.
Why are state and local health agencies taking on these duties?
They’re leading the way in part because the federal government has made only limited efforts, said Lisa McCorkell, a cofounder of the Patient-Led Research Collaborative. The international group was founded in spring 2020 by researchers who are also long COVID patients.
“It’s a big reason why long COVID isn’t talked about as much,” Ms. McCorkell said. “It’s definitely a national issue. But it trickles down to state and local health departments, and there’s not enough resources.”
The government clinics may be accessible to people without insurance and often are cheaper than clinics at private hospitals.
Harborview has treated more than 1,000 patients with long COVID, and another 200 patients are awaiting treatment, said Jessica Bender, MD, a codirector of the University of Washington Post-COVID Rehabilitation and Recovery Clinic in Seattle’s First Hill neighborhood.
The group Survivor Corps offers lists by states of clinics. While the publicly run clinics may be less expensive or even free for some patients, methods of payment vary from clinic to clinic. Federally qualified health clinics offer treatment on a sliding scale. For instance, the Riverside University Health System in California has federally qualified centers. And other providers who are not federally qualified also offer care paid for on a sliding scale. They include Campbell County Health, where some residents are eligible for discounts of 25%-100%, said spokesperson Norberto Orellana.
At Harborview, Dr. Bender said the public hospital’s post-COVID clinic initially began with a staff of rehabilitation doctors but expanded in 2021 to include family and internal medicine doctors. And it offers mental health programs with rehabilitation psychologists who instruct on how to deal with doctors or loved ones who don’t believe that long COVID exists.
“I have patients who really have been devastated by the lack of support from coworkers [and] family,” Dr. Bender said.
In Campbell County, Wyo., the pandemic surge did not arrive in earnest until late 2021. Physical therapists at Campbell County’s Health Rehabilitation Services organized a rehabilitation program for residents with long COVID after recognizing the need, said Shannon Sorensen, rehabilitation director at Campbell County Health.
“We had patients coming in showing chest pain, or heart palpitations. There were people trying to get back to work. They were frustrated,” Ms. Sorensen said.
Myalgic encephalomyelitis and chronic fatigue syndrome activists have embraced the fight to recognize and help long COVID patients, noting the similarities between the conditions, and hope to help kickstart more organized research, treatment and benefits for long COVID sufferers and myalgic encephalomyelitis/chronic fatigue syndrome patients alike.
In Ft. Collins, Colo., disability activist Alison Sbrana has long had myalgic encephalomyelitis. She and other members of the local chapter of ME Action have met with state officials for several years and are finally seeing the results of those efforts.
Colorado Gov. Jared Polis has created the full-time position of policy adviser for long COVID and post–viral infection planning.
“This is one way forward of how state governments are (finally) paying attention to infection-triggered chronic illnesses and starting to think ahead on them,” Ms. Sbrana said.
New York City’s Health + Hospitals launched what may be the most expansive long COVID treatment program in the nation in April 2021. Called AfterCare, it provides physical and mental health services as well as community support systems and financial assistance.
A persistent issue for patients is that there isn’t yet a test for long COVID, like there is for COVID-19, said Amanda Johnson, MD, assistant vice president for ambulatory care and population health at New York Health + Hospitals. “It’s in many ways a diagnosis of exclusion. You have to make sure their shortness of breath isn’t caused by something else. The same with anemia,” she said.
California’s Department of Public Health has a detailed website devoted to the topic, including videos of “long haulers” describing their experiences.
Vermont is one of several states studying long COVID, said Mark Levine, MD, the state health commissioner. The state, in collaboration with the University of Vermont, has established a surveillance project to determine how many people have long COVID, as well as how severe it is, how long it lasts, and potential predispositions.
The University of Utah, Salt Lake City, established a comprehensive COVID-19 clinic more than a year ago that also handles long COVID patients, said Jeannette Brown, MD, PhD, an associate professor at the school and director of the COVID-19 clinic.
Jennifer Chevinsky, MD, MPH, already had a deep understanding of long COVID when she landed in Riverside County, Calif., in the summer of 2021. She came from Atlanta, where as part of her job as an epidemic intelligence service officer at the CDC, she heard stories of COVID-19 patients who were not getting better.
Now she is a deputy public health officer for Riverside County, in a region known for its deserts, sizzling summer temperatures and diverse populations. She said her department has helped launch programs such as post–COVID-19 follow-up phone calls and long COVID training programs that reach out to the many Latino residents in this county of 2.4 million people. It also includes Black and Native American residents.
“We’re making sure information is circulated with community and faith-based organizations, and community health workers,” she said.
Ms. McCorkell said there is still much work to do to raise public awareness of the risks of long COVID and how to obtain care for patients. She would like to see a national public health campaign about long COVID, possibly spearheaded by the Centers for Disease Control and Prevention in partnership with local health workers and community-based organizations.
“That,” she said, “could make a big difference.”
A version of this article first appeared on WebMD.com.
Big-name hospital chains across the United States are opening dedicated centers to help patients dealing with long COVID. But so are the lower-profile clinics and hospitals run by cities, counties and states – including Harborview Medical Center in Seattle.
They serve areas ranging from Campbell County, Wyo., with 47,000 residents, to New York City, with its 8.4 million people. Many providers working there are searching for innovative ways to approach this lingering illness with its variety of symptoms, from brain fog to shortness of breath to depression and more.
Their efforts often fall below the radar, with still-scant serious media attention to long COVID or the public health employees working to treat ailing patients.
Why are state and local health agencies taking on these duties?
They’re leading the way in part because the federal government has made only limited efforts, said Lisa McCorkell, a cofounder of the Patient-Led Research Collaborative. The international group was founded in spring 2020 by researchers who are also long COVID patients.
“It’s a big reason why long COVID isn’t talked about as much,” Ms. McCorkell said. “It’s definitely a national issue. But it trickles down to state and local health departments, and there’s not enough resources.”
The government clinics may be accessible to people without insurance and often are cheaper than clinics at private hospitals.
Harborview has treated more than 1,000 patients with long COVID, and another 200 patients are awaiting treatment, said Jessica Bender, MD, a codirector of the University of Washington Post-COVID Rehabilitation and Recovery Clinic in Seattle’s First Hill neighborhood.
The group Survivor Corps offers lists by states of clinics. While the publicly run clinics may be less expensive or even free for some patients, methods of payment vary from clinic to clinic. Federally qualified health clinics offer treatment on a sliding scale. For instance, the Riverside University Health System in California has federally qualified centers. And other providers who are not federally qualified also offer care paid for on a sliding scale. They include Campbell County Health, where some residents are eligible for discounts of 25%-100%, said spokesperson Norberto Orellana.
At Harborview, Dr. Bender said the public hospital’s post-COVID clinic initially began with a staff of rehabilitation doctors but expanded in 2021 to include family and internal medicine doctors. And it offers mental health programs with rehabilitation psychologists who instruct on how to deal with doctors or loved ones who don’t believe that long COVID exists.
“I have patients who really have been devastated by the lack of support from coworkers [and] family,” Dr. Bender said.
In Campbell County, Wyo., the pandemic surge did not arrive in earnest until late 2021. Physical therapists at Campbell County’s Health Rehabilitation Services organized a rehabilitation program for residents with long COVID after recognizing the need, said Shannon Sorensen, rehabilitation director at Campbell County Health.
“We had patients coming in showing chest pain, or heart palpitations. There were people trying to get back to work. They were frustrated,” Ms. Sorensen said.
Myalgic encephalomyelitis and chronic fatigue syndrome activists have embraced the fight to recognize and help long COVID patients, noting the similarities between the conditions, and hope to help kickstart more organized research, treatment and benefits for long COVID sufferers and myalgic encephalomyelitis/chronic fatigue syndrome patients alike.
In Ft. Collins, Colo., disability activist Alison Sbrana has long had myalgic encephalomyelitis. She and other members of the local chapter of ME Action have met with state officials for several years and are finally seeing the results of those efforts.
Colorado Gov. Jared Polis has created the full-time position of policy adviser for long COVID and post–viral infection planning.
“This is one way forward of how state governments are (finally) paying attention to infection-triggered chronic illnesses and starting to think ahead on them,” Ms. Sbrana said.
New York City’s Health + Hospitals launched what may be the most expansive long COVID treatment program in the nation in April 2021. Called AfterCare, it provides physical and mental health services as well as community support systems and financial assistance.
A persistent issue for patients is that there isn’t yet a test for long COVID, like there is for COVID-19, said Amanda Johnson, MD, assistant vice president for ambulatory care and population health at New York Health + Hospitals. “It’s in many ways a diagnosis of exclusion. You have to make sure their shortness of breath isn’t caused by something else. The same with anemia,” she said.
California’s Department of Public Health has a detailed website devoted to the topic, including videos of “long haulers” describing their experiences.
Vermont is one of several states studying long COVID, said Mark Levine, MD, the state health commissioner. The state, in collaboration with the University of Vermont, has established a surveillance project to determine how many people have long COVID, as well as how severe it is, how long it lasts, and potential predispositions.
The University of Utah, Salt Lake City, established a comprehensive COVID-19 clinic more than a year ago that also handles long COVID patients, said Jeannette Brown, MD, PhD, an associate professor at the school and director of the COVID-19 clinic.
Jennifer Chevinsky, MD, MPH, already had a deep understanding of long COVID when she landed in Riverside County, Calif., in the summer of 2021. She came from Atlanta, where as part of her job as an epidemic intelligence service officer at the CDC, she heard stories of COVID-19 patients who were not getting better.
Now she is a deputy public health officer for Riverside County, in a region known for its deserts, sizzling summer temperatures and diverse populations. She said her department has helped launch programs such as post–COVID-19 follow-up phone calls and long COVID training programs that reach out to the many Latino residents in this county of 2.4 million people. It also includes Black and Native American residents.
“We’re making sure information is circulated with community and faith-based organizations, and community health workers,” she said.
Ms. McCorkell said there is still much work to do to raise public awareness of the risks of long COVID and how to obtain care for patients. She would like to see a national public health campaign about long COVID, possibly spearheaded by the Centers for Disease Control and Prevention in partnership with local health workers and community-based organizations.
“That,” she said, “could make a big difference.”
A version of this article first appeared on WebMD.com.
Children and COVID: Downward trend reverses with small increase in new cases
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.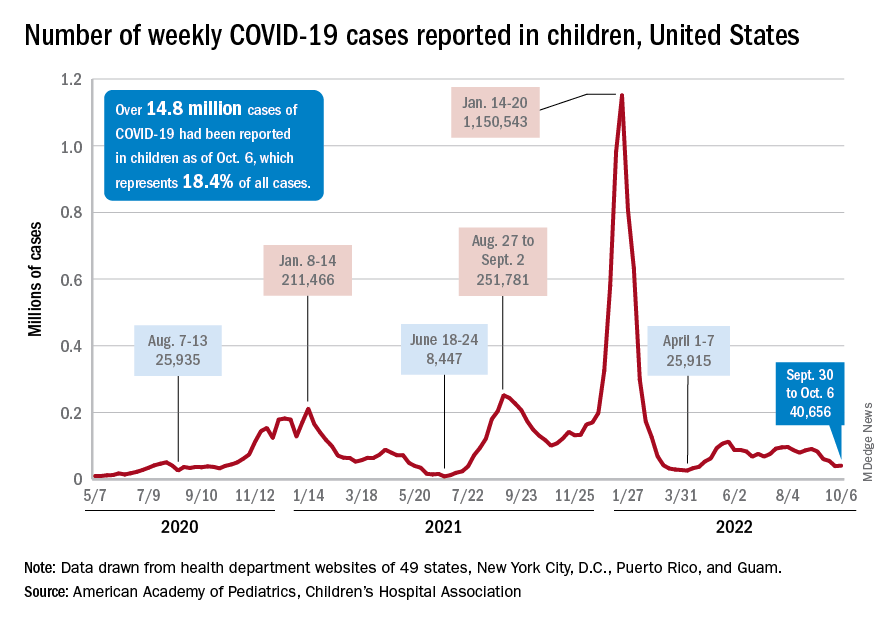
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
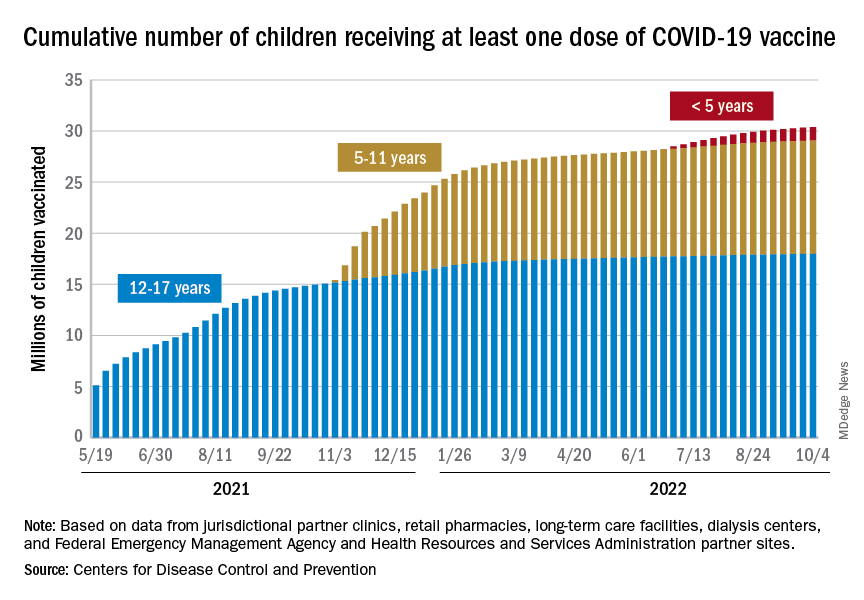
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.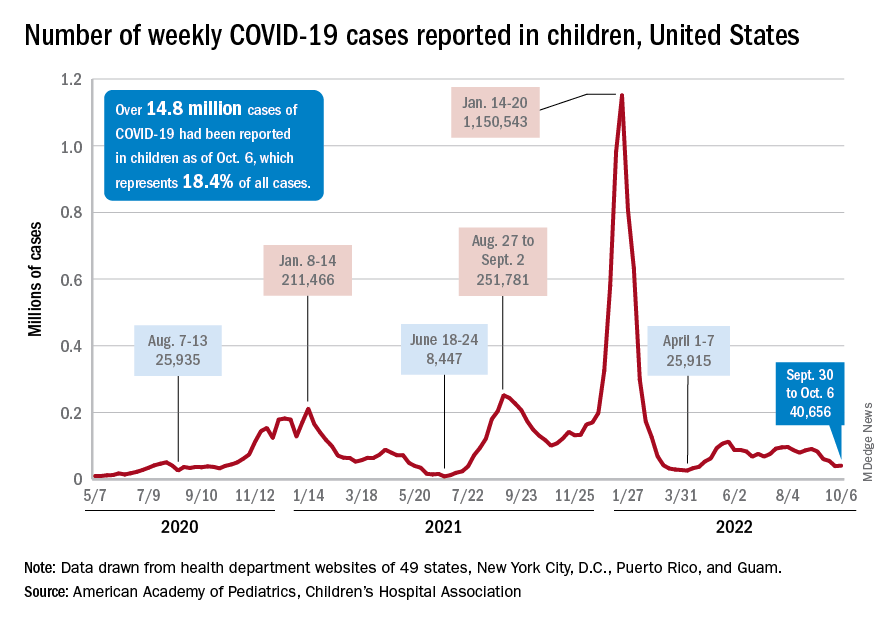
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
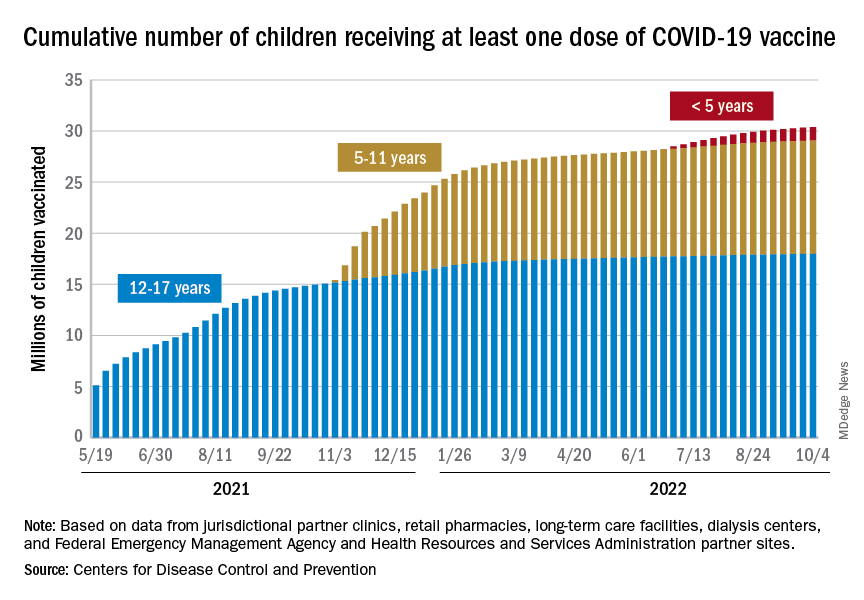
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.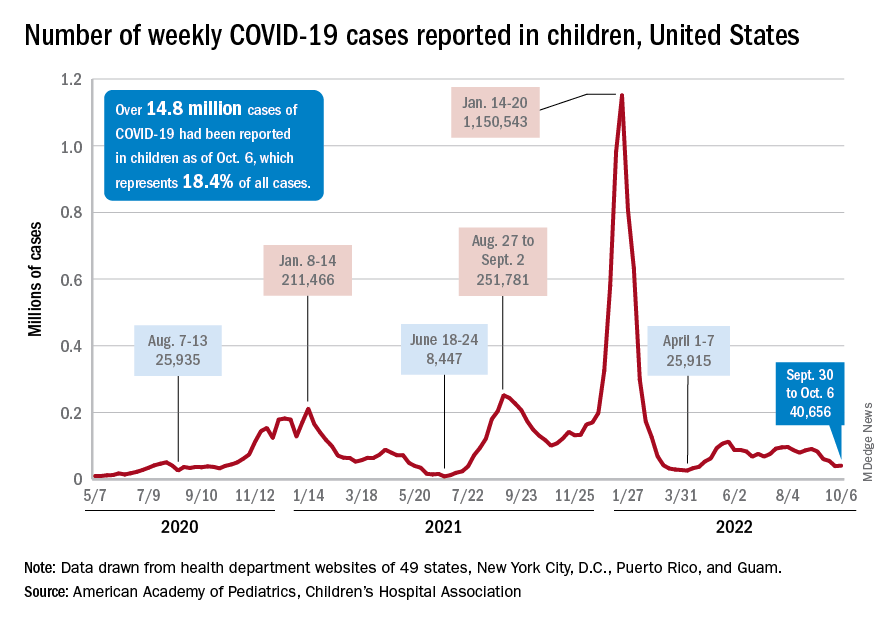
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
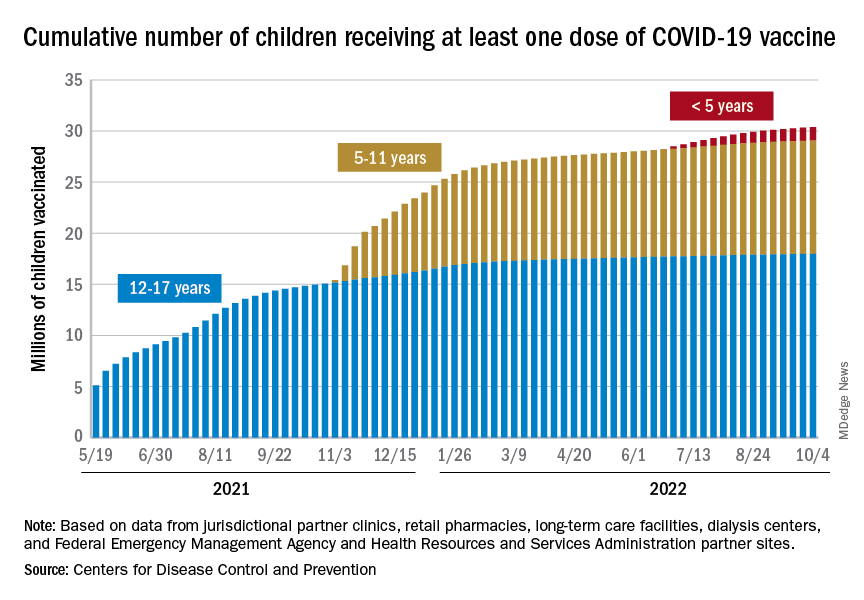
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
The truth about the ‘happy hormone’: Why we shouldn’t mess with dopamine
Google the word “dopamine” and you will learn that its nicknames are the “happy hormone” and the “pleasure molecule” and that it is among the most important chemicals in our brains. With The Guardian branding it “the Kim Kardashian of neurotransmitters,” dopamine has become a true pop-science darling – people across the globe have attempted to boost their mood with dopamine fasts and dopamine dressing.
A century ago, however, newly discovered dopamine was seen as an uninspiring chemical, nothing more than a precursor of noradrenaline. It took several stubborn and hardworking scientists to change that view.
Levodopa: An indifferent precursor
When Casimir Funk, PhD, a Polish biochemist and the discoverer of vitamins, first synthesized the dopamine precursor levodopa in 1911, he had no idea how important the molecule would prove to be in pharmacology and neurobiology. Nor did Markus Guggenheim, PhD, a Swiss biochemist, who isolated levodopa in 1913 from the seeds of a broad bean, Vicia faba. Dr. Guggenheim administered 1 g of levodopa to a rabbit, with no apparent negative consequences. He then prepared a larger dose (2.5 g) and tested it on himself. “Ten minutes after taking it, I felt very nauseous, I had to vomit twice,” he wrote in his paper. In the body, levodopa is converted into dopamine, which may act as an emetic – an effect Dr. Guggenheim didn’t understand. He simply abandoned his human study, erroneously concluding, on the basis of his animal research, that levodopa is “pharmacologically fairly indifferent.”
Around the same time, several scientists across Europe successfully synthesized dopamine, but those discoveries were shelved without much fanfare. For the next 3 decades, dopamine and levodopa were pushed into academic obscurity. Just before World War II, a group of German scientists showed that levodopa is metabolized to dopamine in the body, while another German researcher, Hermann Blaschko, MD, discovered that dopamine is an intermediary in the synthesis of noradrenaline. Even these findings, however, were not immediately accepted.
The dopamine story picked up pace in the post-war years with the observation that the hormone was present in various tissues and body fluids, although nowhere as abundantly as in the central nervous system. Intrigued, Dr. Blaschko, who (after escaping Nazi Germany, changing his name to Hugh, and starting work at Oxford [England] University) hypothesized that dopamine couldn’t be an unremarkable precursor of noradrenaline – it had to have some physiologic functions of its own. He asked his postdoctoral fellow, Oheh Hornykiewicz, MD, to test a few ideas. Dr. Hornykiewicz soon confirmed that dopamine lowered blood pressure in guinea pigs, proving that dopamine indeed had physiologic activity that was independent of other catecholamines.
Reserpine and rabbit ears
While Dr. Blaschko and Dr. Hornykiewicz were puzzling over dopamine’s physiologic role in the body, across the ocean at the National Heart Institute in Maryland, pharmacologist Bernard Brodie, PhD and colleagues were laying the groundwork for the discovery of dopamine’s starring role in the brain.
Spoiler alert: Dr. Brodie’s work showed that a new psychiatric drug known as reserpine was capable of fully depleting the brain’s stores of serotonin and – of greatest significance, as it turned out – mimicking the neuromuscular symptoms typical of Parkinson’s disease. The connection to dopamine would be made by new lab colleague Arvid Carlsson, MD, PhD, who would go on to win a Nobel Prize.
Derived from Rauwolfia serpentina (a plant that for centuries has been used in India for the treatment of mental illness, insomnia, and snake bites), reserpine was introduced in the West as a treatment for schizophrenia.
It worked marvels. In 1954, the press lauded the “dramatic” and seemingly “incredible”: results in treating “hopelessly insane patients.” Reserpine had a downside, however. Reports soon changed in tone regarding the drug’s severe side effects, including headaches, dizziness, vomiting, and, far more disturbingly, symptoms mimicking Parkinson’s disease, from muscular rigidity to tremors.
Dr. Brodie observed that, when reserpine was injected, animals became completely immobile. Serotonin nearly vanished from their brains, but bizarrely, drugs that spur serotonin production did not reverse the rabbits’ immobility.
Dr. Carlsson realized that other catecholamines must be involved in reserpine’s side effects, and he began to search for the culprits. He moved back to his native Sweden and ordered a spectrophotofluorimeter. In one of his experiments, Carlsson injected a pair of rabbits with reserpine, which caused the animals to become catatonic with flattened ears. After the researchers injected the animals with levodopa, within 15 minutes, the rabbits were hopping around, ears proudly vertical. “We were just as excited as the rabbits,” Dr. Carlsson later recalled in a 2016 interview. Dr. Carlsson realized that, because there was no noradrenaline in the rabbits’ brains, dopamine depletion must have been directly responsible for producing reserpine’s motor inhibitory effects.
Skeptics are silenced
In 1960, however, the medical community was not yet ready to accept that dopamine was anything but a boring intermediate between levodopa and noradrenaline. At a prestigious London symposium, Dr. Carlsson and his two colleagues presented their hypothesis that dopamine may be a neurotransmitter, thus implicating it in Parkinson’s disease. They were met with harsh criticism. Some of the experts said levodopa was nothing more than a poison. Dr. Carlsson later recalled facing “a profound and nearly unanimous skepticism regarding our points of view.”
That would soon change. Dr. Hornykiewicz, the biochemist who had earlier discovered dopamine’s BP-lowering effects, tested Dr. Carlsson’s ideas using the postmortem brains of Parkinson’s disease patients. It appeared Dr. Carlsson was right: Unlike in healthy brains, the striatum of patients with Parkinson’s disease contained almost no dopamine whatsoever. Beginning in 1961, in collaboration with neurologist Walther Birkmayer, MD, Hornykiewicz injected levodopa into 20 patients with Parkinson’s disease and observed a “miraculous” (albeit temporary) amelioration of rigidity, motionlessness, and speechlessness.
By the late 1960s, levodopa and dopamine were making headlines. A 1969 New York Times article described similar stunning improvements in patients with Parkinson’s disease who were treated with levodopa. A patient who had arrived at a hospital unable to speak, with hands clenched and rigid expression, was suddenly able to stride into his doctor’s office and even jog around. “I might say I’m a human being,” he told reporters. Although the treatment was expensive – equivalent to $210 in 2022 – physicians were deluged with requests for “dopa.” To this day, levodopa remains a gold standard in the treatment of Parkinson’s disease.
Still misunderstood
The history of dopamine, however, is not only about Parkinson’s disease but extends to the treatment of schizophrenia and addiction. When in the1940s a French military surgeon started giving a new antihistamine drug, promethazine, to prevent shock in soldiers undergoing surgery, he noticed a bizarre side effect: the soldiers would become euphoric yet oddly calm at the same time.
After the drug was modified by adding a chlorine atom and renamed chlorpromazine, it fast became a go-to treatment for psychosis. At the time, no one made the connection to dopamine. Contemporary doctors believed that it calmed people by lowering body temperature (common treatments for mental illness back in the day included swaddling patients in cold, wet sheets). Yet just like reserpine, chlorpromazine produced range of nasty side effects that closely mimicked Parkinson’s disease. This led a Dutch pharmacologist, Jacques van Rossum, to hypothesize that dopamine receptor blockade could explain chlorpromazine’s antipsychotic effects – an idea that remains widely accepted today.
In the 1970s, dopamine was linked with addiction through research on rodents, and this novel idea caught people’s imagination over the coming decades. A story on dopamine titled, “How We Get Addicted,” made the cover of Time in 1997.
Yet as the dopamine/addiction connection became widespread, it also became oversimplified. According to a 2015 article in Nature Reviews Neuroscience, a wave of low-quality research followed – nonreplicated, insufficient – which led the authors to conclude that we are “addicted to the dopamine theory of addiction.” Just about every pleasure under the sun was being attributed to dopamine, from eating delicious foods and playing computer games to sex, music, and hot showers. As recent science shows, however, dopamine is not simply about pleasure – it’s about reward prediction, response to stress, memory, learning, and even the functioning of the immune system. Since its first synthesis in the early 20th century, dopamine has often been misunderstood and oversimplified – and it seems the story is repeating itself now.
In one of his final interviews, Dr. Carlsson, who passed away in 2018 at the age of 95, warned about playing around with dopamine and, in particular, prescribing drugs that have an inhibitory action on this neurotransmitter. “Dopamine is involved in everything that happens in our brains – all its important functions,” he said.
We should be careful how we handle such a delicate and still little-known system.
A version of this article first appeared on Medscape.com.
Google the word “dopamine” and you will learn that its nicknames are the “happy hormone” and the “pleasure molecule” and that it is among the most important chemicals in our brains. With The Guardian branding it “the Kim Kardashian of neurotransmitters,” dopamine has become a true pop-science darling – people across the globe have attempted to boost their mood with dopamine fasts and dopamine dressing.
A century ago, however, newly discovered dopamine was seen as an uninspiring chemical, nothing more than a precursor of noradrenaline. It took several stubborn and hardworking scientists to change that view.
Levodopa: An indifferent precursor
When Casimir Funk, PhD, a Polish biochemist and the discoverer of vitamins, first synthesized the dopamine precursor levodopa in 1911, he had no idea how important the molecule would prove to be in pharmacology and neurobiology. Nor did Markus Guggenheim, PhD, a Swiss biochemist, who isolated levodopa in 1913 from the seeds of a broad bean, Vicia faba. Dr. Guggenheim administered 1 g of levodopa to a rabbit, with no apparent negative consequences. He then prepared a larger dose (2.5 g) and tested it on himself. “Ten minutes after taking it, I felt very nauseous, I had to vomit twice,” he wrote in his paper. In the body, levodopa is converted into dopamine, which may act as an emetic – an effect Dr. Guggenheim didn’t understand. He simply abandoned his human study, erroneously concluding, on the basis of his animal research, that levodopa is “pharmacologically fairly indifferent.”
Around the same time, several scientists across Europe successfully synthesized dopamine, but those discoveries were shelved without much fanfare. For the next 3 decades, dopamine and levodopa were pushed into academic obscurity. Just before World War II, a group of German scientists showed that levodopa is metabolized to dopamine in the body, while another German researcher, Hermann Blaschko, MD, discovered that dopamine is an intermediary in the synthesis of noradrenaline. Even these findings, however, were not immediately accepted.
The dopamine story picked up pace in the post-war years with the observation that the hormone was present in various tissues and body fluids, although nowhere as abundantly as in the central nervous system. Intrigued, Dr. Blaschko, who (after escaping Nazi Germany, changing his name to Hugh, and starting work at Oxford [England] University) hypothesized that dopamine couldn’t be an unremarkable precursor of noradrenaline – it had to have some physiologic functions of its own. He asked his postdoctoral fellow, Oheh Hornykiewicz, MD, to test a few ideas. Dr. Hornykiewicz soon confirmed that dopamine lowered blood pressure in guinea pigs, proving that dopamine indeed had physiologic activity that was independent of other catecholamines.
Reserpine and rabbit ears
While Dr. Blaschko and Dr. Hornykiewicz were puzzling over dopamine’s physiologic role in the body, across the ocean at the National Heart Institute in Maryland, pharmacologist Bernard Brodie, PhD and colleagues were laying the groundwork for the discovery of dopamine’s starring role in the brain.
Spoiler alert: Dr. Brodie’s work showed that a new psychiatric drug known as reserpine was capable of fully depleting the brain’s stores of serotonin and – of greatest significance, as it turned out – mimicking the neuromuscular symptoms typical of Parkinson’s disease. The connection to dopamine would be made by new lab colleague Arvid Carlsson, MD, PhD, who would go on to win a Nobel Prize.
Derived from Rauwolfia serpentina (a plant that for centuries has been used in India for the treatment of mental illness, insomnia, and snake bites), reserpine was introduced in the West as a treatment for schizophrenia.
It worked marvels. In 1954, the press lauded the “dramatic” and seemingly “incredible”: results in treating “hopelessly insane patients.” Reserpine had a downside, however. Reports soon changed in tone regarding the drug’s severe side effects, including headaches, dizziness, vomiting, and, far more disturbingly, symptoms mimicking Parkinson’s disease, from muscular rigidity to tremors.
Dr. Brodie observed that, when reserpine was injected, animals became completely immobile. Serotonin nearly vanished from their brains, but bizarrely, drugs that spur serotonin production did not reverse the rabbits’ immobility.
Dr. Carlsson realized that other catecholamines must be involved in reserpine’s side effects, and he began to search for the culprits. He moved back to his native Sweden and ordered a spectrophotofluorimeter. In one of his experiments, Carlsson injected a pair of rabbits with reserpine, which caused the animals to become catatonic with flattened ears. After the researchers injected the animals with levodopa, within 15 minutes, the rabbits were hopping around, ears proudly vertical. “We were just as excited as the rabbits,” Dr. Carlsson later recalled in a 2016 interview. Dr. Carlsson realized that, because there was no noradrenaline in the rabbits’ brains, dopamine depletion must have been directly responsible for producing reserpine’s motor inhibitory effects.
Skeptics are silenced
In 1960, however, the medical community was not yet ready to accept that dopamine was anything but a boring intermediate between levodopa and noradrenaline. At a prestigious London symposium, Dr. Carlsson and his two colleagues presented their hypothesis that dopamine may be a neurotransmitter, thus implicating it in Parkinson’s disease. They were met with harsh criticism. Some of the experts said levodopa was nothing more than a poison. Dr. Carlsson later recalled facing “a profound and nearly unanimous skepticism regarding our points of view.”
That would soon change. Dr. Hornykiewicz, the biochemist who had earlier discovered dopamine’s BP-lowering effects, tested Dr. Carlsson’s ideas using the postmortem brains of Parkinson’s disease patients. It appeared Dr. Carlsson was right: Unlike in healthy brains, the striatum of patients with Parkinson’s disease contained almost no dopamine whatsoever. Beginning in 1961, in collaboration with neurologist Walther Birkmayer, MD, Hornykiewicz injected levodopa into 20 patients with Parkinson’s disease and observed a “miraculous” (albeit temporary) amelioration of rigidity, motionlessness, and speechlessness.
By the late 1960s, levodopa and dopamine were making headlines. A 1969 New York Times article described similar stunning improvements in patients with Parkinson’s disease who were treated with levodopa. A patient who had arrived at a hospital unable to speak, with hands clenched and rigid expression, was suddenly able to stride into his doctor’s office and even jog around. “I might say I’m a human being,” he told reporters. Although the treatment was expensive – equivalent to $210 in 2022 – physicians were deluged with requests for “dopa.” To this day, levodopa remains a gold standard in the treatment of Parkinson’s disease.
Still misunderstood
The history of dopamine, however, is not only about Parkinson’s disease but extends to the treatment of schizophrenia and addiction. When in the1940s a French military surgeon started giving a new antihistamine drug, promethazine, to prevent shock in soldiers undergoing surgery, he noticed a bizarre side effect: the soldiers would become euphoric yet oddly calm at the same time.
After the drug was modified by adding a chlorine atom and renamed chlorpromazine, it fast became a go-to treatment for psychosis. At the time, no one made the connection to dopamine. Contemporary doctors believed that it calmed people by lowering body temperature (common treatments for mental illness back in the day included swaddling patients in cold, wet sheets). Yet just like reserpine, chlorpromazine produced range of nasty side effects that closely mimicked Parkinson’s disease. This led a Dutch pharmacologist, Jacques van Rossum, to hypothesize that dopamine receptor blockade could explain chlorpromazine’s antipsychotic effects – an idea that remains widely accepted today.
In the 1970s, dopamine was linked with addiction through research on rodents, and this novel idea caught people’s imagination over the coming decades. A story on dopamine titled, “How We Get Addicted,” made the cover of Time in 1997.
Yet as the dopamine/addiction connection became widespread, it also became oversimplified. According to a 2015 article in Nature Reviews Neuroscience, a wave of low-quality research followed – nonreplicated, insufficient – which led the authors to conclude that we are “addicted to the dopamine theory of addiction.” Just about every pleasure under the sun was being attributed to dopamine, from eating delicious foods and playing computer games to sex, music, and hot showers. As recent science shows, however, dopamine is not simply about pleasure – it’s about reward prediction, response to stress, memory, learning, and even the functioning of the immune system. Since its first synthesis in the early 20th century, dopamine has often been misunderstood and oversimplified – and it seems the story is repeating itself now.
In one of his final interviews, Dr. Carlsson, who passed away in 2018 at the age of 95, warned about playing around with dopamine and, in particular, prescribing drugs that have an inhibitory action on this neurotransmitter. “Dopamine is involved in everything that happens in our brains – all its important functions,” he said.
We should be careful how we handle such a delicate and still little-known system.
A version of this article first appeared on Medscape.com.
Google the word “dopamine” and you will learn that its nicknames are the “happy hormone” and the “pleasure molecule” and that it is among the most important chemicals in our brains. With The Guardian branding it “the Kim Kardashian of neurotransmitters,” dopamine has become a true pop-science darling – people across the globe have attempted to boost their mood with dopamine fasts and dopamine dressing.
A century ago, however, newly discovered dopamine was seen as an uninspiring chemical, nothing more than a precursor of noradrenaline. It took several stubborn and hardworking scientists to change that view.
Levodopa: An indifferent precursor
When Casimir Funk, PhD, a Polish biochemist and the discoverer of vitamins, first synthesized the dopamine precursor levodopa in 1911, he had no idea how important the molecule would prove to be in pharmacology and neurobiology. Nor did Markus Guggenheim, PhD, a Swiss biochemist, who isolated levodopa in 1913 from the seeds of a broad bean, Vicia faba. Dr. Guggenheim administered 1 g of levodopa to a rabbit, with no apparent negative consequences. He then prepared a larger dose (2.5 g) and tested it on himself. “Ten minutes after taking it, I felt very nauseous, I had to vomit twice,” he wrote in his paper. In the body, levodopa is converted into dopamine, which may act as an emetic – an effect Dr. Guggenheim didn’t understand. He simply abandoned his human study, erroneously concluding, on the basis of his animal research, that levodopa is “pharmacologically fairly indifferent.”
Around the same time, several scientists across Europe successfully synthesized dopamine, but those discoveries were shelved without much fanfare. For the next 3 decades, dopamine and levodopa were pushed into academic obscurity. Just before World War II, a group of German scientists showed that levodopa is metabolized to dopamine in the body, while another German researcher, Hermann Blaschko, MD, discovered that dopamine is an intermediary in the synthesis of noradrenaline. Even these findings, however, were not immediately accepted.
The dopamine story picked up pace in the post-war years with the observation that the hormone was present in various tissues and body fluids, although nowhere as abundantly as in the central nervous system. Intrigued, Dr. Blaschko, who (after escaping Nazi Germany, changing his name to Hugh, and starting work at Oxford [England] University) hypothesized that dopamine couldn’t be an unremarkable precursor of noradrenaline – it had to have some physiologic functions of its own. He asked his postdoctoral fellow, Oheh Hornykiewicz, MD, to test a few ideas. Dr. Hornykiewicz soon confirmed that dopamine lowered blood pressure in guinea pigs, proving that dopamine indeed had physiologic activity that was independent of other catecholamines.
Reserpine and rabbit ears
While Dr. Blaschko and Dr. Hornykiewicz were puzzling over dopamine’s physiologic role in the body, across the ocean at the National Heart Institute in Maryland, pharmacologist Bernard Brodie, PhD and colleagues were laying the groundwork for the discovery of dopamine’s starring role in the brain.
Spoiler alert: Dr. Brodie’s work showed that a new psychiatric drug known as reserpine was capable of fully depleting the brain’s stores of serotonin and – of greatest significance, as it turned out – mimicking the neuromuscular symptoms typical of Parkinson’s disease. The connection to dopamine would be made by new lab colleague Arvid Carlsson, MD, PhD, who would go on to win a Nobel Prize.
Derived from Rauwolfia serpentina (a plant that for centuries has been used in India for the treatment of mental illness, insomnia, and snake bites), reserpine was introduced in the West as a treatment for schizophrenia.
It worked marvels. In 1954, the press lauded the “dramatic” and seemingly “incredible”: results in treating “hopelessly insane patients.” Reserpine had a downside, however. Reports soon changed in tone regarding the drug’s severe side effects, including headaches, dizziness, vomiting, and, far more disturbingly, symptoms mimicking Parkinson’s disease, from muscular rigidity to tremors.
Dr. Brodie observed that, when reserpine was injected, animals became completely immobile. Serotonin nearly vanished from their brains, but bizarrely, drugs that spur serotonin production did not reverse the rabbits’ immobility.
Dr. Carlsson realized that other catecholamines must be involved in reserpine’s side effects, and he began to search for the culprits. He moved back to his native Sweden and ordered a spectrophotofluorimeter. In one of his experiments, Carlsson injected a pair of rabbits with reserpine, which caused the animals to become catatonic with flattened ears. After the researchers injected the animals with levodopa, within 15 minutes, the rabbits were hopping around, ears proudly vertical. “We were just as excited as the rabbits,” Dr. Carlsson later recalled in a 2016 interview. Dr. Carlsson realized that, because there was no noradrenaline in the rabbits’ brains, dopamine depletion must have been directly responsible for producing reserpine’s motor inhibitory effects.
Skeptics are silenced
In 1960, however, the medical community was not yet ready to accept that dopamine was anything but a boring intermediate between levodopa and noradrenaline. At a prestigious London symposium, Dr. Carlsson and his two colleagues presented their hypothesis that dopamine may be a neurotransmitter, thus implicating it in Parkinson’s disease. They were met with harsh criticism. Some of the experts said levodopa was nothing more than a poison. Dr. Carlsson later recalled facing “a profound and nearly unanimous skepticism regarding our points of view.”
That would soon change. Dr. Hornykiewicz, the biochemist who had earlier discovered dopamine’s BP-lowering effects, tested Dr. Carlsson’s ideas using the postmortem brains of Parkinson’s disease patients. It appeared Dr. Carlsson was right: Unlike in healthy brains, the striatum of patients with Parkinson’s disease contained almost no dopamine whatsoever. Beginning in 1961, in collaboration with neurologist Walther Birkmayer, MD, Hornykiewicz injected levodopa into 20 patients with Parkinson’s disease and observed a “miraculous” (albeit temporary) amelioration of rigidity, motionlessness, and speechlessness.
By the late 1960s, levodopa and dopamine were making headlines. A 1969 New York Times article described similar stunning improvements in patients with Parkinson’s disease who were treated with levodopa. A patient who had arrived at a hospital unable to speak, with hands clenched and rigid expression, was suddenly able to stride into his doctor’s office and even jog around. “I might say I’m a human being,” he told reporters. Although the treatment was expensive – equivalent to $210 in 2022 – physicians were deluged with requests for “dopa.” To this day, levodopa remains a gold standard in the treatment of Parkinson’s disease.
Still misunderstood
The history of dopamine, however, is not only about Parkinson’s disease but extends to the treatment of schizophrenia and addiction. When in the1940s a French military surgeon started giving a new antihistamine drug, promethazine, to prevent shock in soldiers undergoing surgery, he noticed a bizarre side effect: the soldiers would become euphoric yet oddly calm at the same time.
After the drug was modified by adding a chlorine atom and renamed chlorpromazine, it fast became a go-to treatment for psychosis. At the time, no one made the connection to dopamine. Contemporary doctors believed that it calmed people by lowering body temperature (common treatments for mental illness back in the day included swaddling patients in cold, wet sheets). Yet just like reserpine, chlorpromazine produced range of nasty side effects that closely mimicked Parkinson’s disease. This led a Dutch pharmacologist, Jacques van Rossum, to hypothesize that dopamine receptor blockade could explain chlorpromazine’s antipsychotic effects – an idea that remains widely accepted today.
In the 1970s, dopamine was linked with addiction through research on rodents, and this novel idea caught people’s imagination over the coming decades. A story on dopamine titled, “How We Get Addicted,” made the cover of Time in 1997.
Yet as the dopamine/addiction connection became widespread, it also became oversimplified. According to a 2015 article in Nature Reviews Neuroscience, a wave of low-quality research followed – nonreplicated, insufficient – which led the authors to conclude that we are “addicted to the dopamine theory of addiction.” Just about every pleasure under the sun was being attributed to dopamine, from eating delicious foods and playing computer games to sex, music, and hot showers. As recent science shows, however, dopamine is not simply about pleasure – it’s about reward prediction, response to stress, memory, learning, and even the functioning of the immune system. Since its first synthesis in the early 20th century, dopamine has often been misunderstood and oversimplified – and it seems the story is repeating itself now.
In one of his final interviews, Dr. Carlsson, who passed away in 2018 at the age of 95, warned about playing around with dopamine and, in particular, prescribing drugs that have an inhibitory action on this neurotransmitter. “Dopamine is involved in everything that happens in our brains – all its important functions,” he said.
We should be careful how we handle such a delicate and still little-known system.
A version of this article first appeared on Medscape.com.
Longer boarding times predict patient processing in ED
on the basis of data from nearly 900 facilities presented at the annual meeting of the American College of Emergency Physicians.
The study was important to conduct at this time because ED boarding is significantly limiting ED physicians to provide optimal care, said Camila Tyminski, MD, of Brown University, Providence, R.I., who presented the findings at the meeting.
“Boarding had steadily been rising prior to the COVID-19 pandemic due to increased ED use. As our data show, boarding had a detrimental impact on ED throughput measures, including increased door to provider time, increased length of stay of the patient discharged from the ED, and increased rate of patients that left before completion of treatment,” she said.
“It was important to understand these trends prior to 2019-2020 because the COVID-19 pandemic and national nursing shortage have drastically worsened boarding. This study provided a framework for future studies on boarding across ED’s nationally since the start of the pandemic,” she added.
“Post-pandemic, we have hit a crisis point,” lead author Anthony Napoli, MD, also of Brown University, said in an interview. “Boarding is largely a hospital capacity problem, but one key fix germane to EM [emergency medicine] is the provider in triage model (PIT). While PIT has been shown to improve efficiency of ED care, a single institution study demonstrated that it was unable to mitigate the effects of boarding. The study of the association of boarding and efficiency of ED operations and intake needed to be shown on a national scale,” he said.
The researchers reviewed cross-sectional ED operational data from the ED Department Benchmarking Alliance (EDBA), a voluntary database that includes self-reports of operational metrics from approximately half of EDs in the United States.
The data set included 892 EDs; freestanding and pediatric EDs, as well as those with missing boarding data, were excluded.
The primary outcome was boarding time, door-to-provider time (D2P), length of stay for discharged patients (LOSD) and the percentage of patients who left the hospital before treatment was complete (LBTC).
In a multivariate analysis, increased boarding time was significantly associated with longer D2P time, LOSD time, and rates of LBTC.
Overall, D2P and LOSD increased by 0.8 minutes and 2.8 minutes, respectively, for each additional 10 minutes of boarding time. LBTC rates increased by 0.1% for each additional 10 minutes of boarding time.
However, boarding did not have a significant impact on operational metrics among hospitals with fewer than 20,000 visits per year.
Although more research is needed, the results indicate that boarding reduces the throughput of nonboarded patients at a ratio of approximately 4:1. The limited impact of ED efficiency measures on operations highlights the need for hospital-based solutions to boarding, Dr. Tyminski concluded.
“Overall, we expected that there would be an association between boarding and reductions in ED intake and operational efficiency,” said Dr. Napoli in an interview. “However, we were surprised the relationship continued to be as strong in a national study of nearly a quarter of all EDs, as it did in our prior local study,” he said. “Every 10 minutes of boarding in an ED is associated with an approximate 0.1% increase in LWBS and a 3-minute increase in LOSD. Extrapolating this association across the country, we predicted that nearly one million patients may have potentially not received ED care due to boarding,” he explained. “Not only does this potentially have a huge impact on hospital finances but also the overall health of our patients,” he added.
The key takeaway from the study is that boarding is a hospital capacity management issue, said Dr. Napoli. Hospital leadership must be directly involved in plans to mitigate or eliminate it to the extent possible; until then, boarding will continue to result in inefficient ED operations, he explained.
“As ED providers, we are limited in what we can do, but one area where we might be able to make the most impact is to optimize the care and throughput of the LOSD patients,” Dr. Tyminski said. More research is needed to see if interventions to reduce boarding correspond with equivalent improvements in emergency department intake and improved ED throughput, she noted.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
on the basis of data from nearly 900 facilities presented at the annual meeting of the American College of Emergency Physicians.
The study was important to conduct at this time because ED boarding is significantly limiting ED physicians to provide optimal care, said Camila Tyminski, MD, of Brown University, Providence, R.I., who presented the findings at the meeting.
“Boarding had steadily been rising prior to the COVID-19 pandemic due to increased ED use. As our data show, boarding had a detrimental impact on ED throughput measures, including increased door to provider time, increased length of stay of the patient discharged from the ED, and increased rate of patients that left before completion of treatment,” she said.
“It was important to understand these trends prior to 2019-2020 because the COVID-19 pandemic and national nursing shortage have drastically worsened boarding. This study provided a framework for future studies on boarding across ED’s nationally since the start of the pandemic,” she added.
“Post-pandemic, we have hit a crisis point,” lead author Anthony Napoli, MD, also of Brown University, said in an interview. “Boarding is largely a hospital capacity problem, but one key fix germane to EM [emergency medicine] is the provider in triage model (PIT). While PIT has been shown to improve efficiency of ED care, a single institution study demonstrated that it was unable to mitigate the effects of boarding. The study of the association of boarding and efficiency of ED operations and intake needed to be shown on a national scale,” he said.
The researchers reviewed cross-sectional ED operational data from the ED Department Benchmarking Alliance (EDBA), a voluntary database that includes self-reports of operational metrics from approximately half of EDs in the United States.
The data set included 892 EDs; freestanding and pediatric EDs, as well as those with missing boarding data, were excluded.
The primary outcome was boarding time, door-to-provider time (D2P), length of stay for discharged patients (LOSD) and the percentage of patients who left the hospital before treatment was complete (LBTC).
In a multivariate analysis, increased boarding time was significantly associated with longer D2P time, LOSD time, and rates of LBTC.
Overall, D2P and LOSD increased by 0.8 minutes and 2.8 minutes, respectively, for each additional 10 minutes of boarding time. LBTC rates increased by 0.1% for each additional 10 minutes of boarding time.
However, boarding did not have a significant impact on operational metrics among hospitals with fewer than 20,000 visits per year.
Although more research is needed, the results indicate that boarding reduces the throughput of nonboarded patients at a ratio of approximately 4:1. The limited impact of ED efficiency measures on operations highlights the need for hospital-based solutions to boarding, Dr. Tyminski concluded.
“Overall, we expected that there would be an association between boarding and reductions in ED intake and operational efficiency,” said Dr. Napoli in an interview. “However, we were surprised the relationship continued to be as strong in a national study of nearly a quarter of all EDs, as it did in our prior local study,” he said. “Every 10 minutes of boarding in an ED is associated with an approximate 0.1% increase in LWBS and a 3-minute increase in LOSD. Extrapolating this association across the country, we predicted that nearly one million patients may have potentially not received ED care due to boarding,” he explained. “Not only does this potentially have a huge impact on hospital finances but also the overall health of our patients,” he added.
The key takeaway from the study is that boarding is a hospital capacity management issue, said Dr. Napoli. Hospital leadership must be directly involved in plans to mitigate or eliminate it to the extent possible; until then, boarding will continue to result in inefficient ED operations, he explained.
“As ED providers, we are limited in what we can do, but one area where we might be able to make the most impact is to optimize the care and throughput of the LOSD patients,” Dr. Tyminski said. More research is needed to see if interventions to reduce boarding correspond with equivalent improvements in emergency department intake and improved ED throughput, she noted.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
on the basis of data from nearly 900 facilities presented at the annual meeting of the American College of Emergency Physicians.
The study was important to conduct at this time because ED boarding is significantly limiting ED physicians to provide optimal care, said Camila Tyminski, MD, of Brown University, Providence, R.I., who presented the findings at the meeting.
“Boarding had steadily been rising prior to the COVID-19 pandemic due to increased ED use. As our data show, boarding had a detrimental impact on ED throughput measures, including increased door to provider time, increased length of stay of the patient discharged from the ED, and increased rate of patients that left before completion of treatment,” she said.
“It was important to understand these trends prior to 2019-2020 because the COVID-19 pandemic and national nursing shortage have drastically worsened boarding. This study provided a framework for future studies on boarding across ED’s nationally since the start of the pandemic,” she added.
“Post-pandemic, we have hit a crisis point,” lead author Anthony Napoli, MD, also of Brown University, said in an interview. “Boarding is largely a hospital capacity problem, but one key fix germane to EM [emergency medicine] is the provider in triage model (PIT). While PIT has been shown to improve efficiency of ED care, a single institution study demonstrated that it was unable to mitigate the effects of boarding. The study of the association of boarding and efficiency of ED operations and intake needed to be shown on a national scale,” he said.
The researchers reviewed cross-sectional ED operational data from the ED Department Benchmarking Alliance (EDBA), a voluntary database that includes self-reports of operational metrics from approximately half of EDs in the United States.
The data set included 892 EDs; freestanding and pediatric EDs, as well as those with missing boarding data, were excluded.
The primary outcome was boarding time, door-to-provider time (D2P), length of stay for discharged patients (LOSD) and the percentage of patients who left the hospital before treatment was complete (LBTC).
In a multivariate analysis, increased boarding time was significantly associated with longer D2P time, LOSD time, and rates of LBTC.
Overall, D2P and LOSD increased by 0.8 minutes and 2.8 minutes, respectively, for each additional 10 minutes of boarding time. LBTC rates increased by 0.1% for each additional 10 minutes of boarding time.
However, boarding did not have a significant impact on operational metrics among hospitals with fewer than 20,000 visits per year.
Although more research is needed, the results indicate that boarding reduces the throughput of nonboarded patients at a ratio of approximately 4:1. The limited impact of ED efficiency measures on operations highlights the need for hospital-based solutions to boarding, Dr. Tyminski concluded.
“Overall, we expected that there would be an association between boarding and reductions in ED intake and operational efficiency,” said Dr. Napoli in an interview. “However, we were surprised the relationship continued to be as strong in a national study of nearly a quarter of all EDs, as it did in our prior local study,” he said. “Every 10 minutes of boarding in an ED is associated with an approximate 0.1% increase in LWBS and a 3-minute increase in LOSD. Extrapolating this association across the country, we predicted that nearly one million patients may have potentially not received ED care due to boarding,” he explained. “Not only does this potentially have a huge impact on hospital finances but also the overall health of our patients,” he added.
The key takeaway from the study is that boarding is a hospital capacity management issue, said Dr. Napoli. Hospital leadership must be directly involved in plans to mitigate or eliminate it to the extent possible; until then, boarding will continue to result in inefficient ED operations, he explained.
“As ED providers, we are limited in what we can do, but one area where we might be able to make the most impact is to optimize the care and throughput of the LOSD patients,” Dr. Tyminski said. More research is needed to see if interventions to reduce boarding correspond with equivalent improvements in emergency department intake and improved ED throughput, she noted.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
Air pollution tied to stroke risk, subsequent CV events, and death
Results of a UK biobank study show high levels of air pollution were associated with an increased risk of transition from health to a first stroke and subsequent progression to cardiovascular (CV) events and death.
“These results indicate that understanding and reducing the effects of air pollutants on different transition stages in stroke will be beneficial in managing people’s health and preventing the occurrence and progression of stroke,” study investigator Hualiang Lin, PhD, of Sun Yat-sen University School of Public Health, Guangzhou, China, said in a news release.
The study was published online in the journal Neurology.
A way to stop stroke progression?
The researchers assessed air pollution exposure in 318,752 people (mean age, 56) from the UK biobank database. None had a history of stroke or heart disease at the start of the study. Annual concentrations of air pollution near where people lived were estimated through land-use regressions.
During an average follow-up of 12 years, 5,967 people had a stroke, 2,985 developed post-stroke CVD, and 1,020 died.
After adjusting for confounding factors, every 5 µg/m3 increase in exposure to fine particulate matter (PM2.5) was associated with a 24% increase in transition from healthy to first stroke (hazard ratio, 1.24; 95% confidence interval, 1.10-1.40) and a 30% increase in transition from being healthy to dying (HR, 1.30; 95% CI, 1.21-1.40).
PM2.5 is less than 2.5 microns in diameter and includes fly ash from coal combustion. The World Health Organization recommends that annual PM2.5 exposure should not exceed 5 µg/m3.
Those who had a stroke during the study had an average exposure of 10.03 µg/m3 of PM2.5, compared with 9.97 µg/m3 for those who did not have a stroke.
The air pollutants nitrogen oxide and nitrogen dioxide were also associated with an increased risk of stroke and death, but the associations were weaker.
“More research is needed, but it’s possible that decreasing exposure to heavy levels of air pollution could play a role in reducing the progression of stroke,” Dr. Lin said.
“People can reduce their exposure by staying indoors on heavy pollution days, reducing their outdoor exercise, wearing masks to filter out particulate matter, and using air purifiers,” Dr. Lin added.
Public policy implications
Reached for comment, Steffen E. Petersen, MD, MPH, professor of cardiovascular medicine, Barts Health NHS Trust, London, said the study “elegantly confirms the increased risk of stroke due to air pollution in the UK Biobank population study but interestingly suggests that the impact of air pollution may continue to adversely impact cardiovascular health even after the stroke occurred.”
“This is further evidence to inform policymakers to tackle air pollution and get levels below the recommended levels,” Dr. Petersen said.
“On a personal level, everyone, including stroke patients, may wish to consider personal measures to reduce exposure to air pollution, such as avoiding walking along polluted streets and rather take a less polluted route away from the main roads,” Dr. Petersen added.
The study had no targeted funding. Dr. Lin and Dr. Petersen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a UK biobank study show high levels of air pollution were associated with an increased risk of transition from health to a first stroke and subsequent progression to cardiovascular (CV) events and death.
“These results indicate that understanding and reducing the effects of air pollutants on different transition stages in stroke will be beneficial in managing people’s health and preventing the occurrence and progression of stroke,” study investigator Hualiang Lin, PhD, of Sun Yat-sen University School of Public Health, Guangzhou, China, said in a news release.
The study was published online in the journal Neurology.
A way to stop stroke progression?
The researchers assessed air pollution exposure in 318,752 people (mean age, 56) from the UK biobank database. None had a history of stroke or heart disease at the start of the study. Annual concentrations of air pollution near where people lived were estimated through land-use regressions.
During an average follow-up of 12 years, 5,967 people had a stroke, 2,985 developed post-stroke CVD, and 1,020 died.
After adjusting for confounding factors, every 5 µg/m3 increase in exposure to fine particulate matter (PM2.5) was associated with a 24% increase in transition from healthy to first stroke (hazard ratio, 1.24; 95% confidence interval, 1.10-1.40) and a 30% increase in transition from being healthy to dying (HR, 1.30; 95% CI, 1.21-1.40).
PM2.5 is less than 2.5 microns in diameter and includes fly ash from coal combustion. The World Health Organization recommends that annual PM2.5 exposure should not exceed 5 µg/m3.
Those who had a stroke during the study had an average exposure of 10.03 µg/m3 of PM2.5, compared with 9.97 µg/m3 for those who did not have a stroke.
The air pollutants nitrogen oxide and nitrogen dioxide were also associated with an increased risk of stroke and death, but the associations were weaker.
“More research is needed, but it’s possible that decreasing exposure to heavy levels of air pollution could play a role in reducing the progression of stroke,” Dr. Lin said.
“People can reduce their exposure by staying indoors on heavy pollution days, reducing their outdoor exercise, wearing masks to filter out particulate matter, and using air purifiers,” Dr. Lin added.
Public policy implications
Reached for comment, Steffen E. Petersen, MD, MPH, professor of cardiovascular medicine, Barts Health NHS Trust, London, said the study “elegantly confirms the increased risk of stroke due to air pollution in the UK Biobank population study but interestingly suggests that the impact of air pollution may continue to adversely impact cardiovascular health even after the stroke occurred.”
“This is further evidence to inform policymakers to tackle air pollution and get levels below the recommended levels,” Dr. Petersen said.
“On a personal level, everyone, including stroke patients, may wish to consider personal measures to reduce exposure to air pollution, such as avoiding walking along polluted streets and rather take a less polluted route away from the main roads,” Dr. Petersen added.
The study had no targeted funding. Dr. Lin and Dr. Petersen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a UK biobank study show high levels of air pollution were associated with an increased risk of transition from health to a first stroke and subsequent progression to cardiovascular (CV) events and death.
“These results indicate that understanding and reducing the effects of air pollutants on different transition stages in stroke will be beneficial in managing people’s health and preventing the occurrence and progression of stroke,” study investigator Hualiang Lin, PhD, of Sun Yat-sen University School of Public Health, Guangzhou, China, said in a news release.
The study was published online in the journal Neurology.
A way to stop stroke progression?
The researchers assessed air pollution exposure in 318,752 people (mean age, 56) from the UK biobank database. None had a history of stroke or heart disease at the start of the study. Annual concentrations of air pollution near where people lived were estimated through land-use regressions.
During an average follow-up of 12 years, 5,967 people had a stroke, 2,985 developed post-stroke CVD, and 1,020 died.
After adjusting for confounding factors, every 5 µg/m3 increase in exposure to fine particulate matter (PM2.5) was associated with a 24% increase in transition from healthy to first stroke (hazard ratio, 1.24; 95% confidence interval, 1.10-1.40) and a 30% increase in transition from being healthy to dying (HR, 1.30; 95% CI, 1.21-1.40).
PM2.5 is less than 2.5 microns in diameter and includes fly ash from coal combustion. The World Health Organization recommends that annual PM2.5 exposure should not exceed 5 µg/m3.
Those who had a stroke during the study had an average exposure of 10.03 µg/m3 of PM2.5, compared with 9.97 µg/m3 for those who did not have a stroke.
The air pollutants nitrogen oxide and nitrogen dioxide were also associated with an increased risk of stroke and death, but the associations were weaker.
“More research is needed, but it’s possible that decreasing exposure to heavy levels of air pollution could play a role in reducing the progression of stroke,” Dr. Lin said.
“People can reduce their exposure by staying indoors on heavy pollution days, reducing their outdoor exercise, wearing masks to filter out particulate matter, and using air purifiers,” Dr. Lin added.
Public policy implications
Reached for comment, Steffen E. Petersen, MD, MPH, professor of cardiovascular medicine, Barts Health NHS Trust, London, said the study “elegantly confirms the increased risk of stroke due to air pollution in the UK Biobank population study but interestingly suggests that the impact of air pollution may continue to adversely impact cardiovascular health even after the stroke occurred.”
“This is further evidence to inform policymakers to tackle air pollution and get levels below the recommended levels,” Dr. Petersen said.
“On a personal level, everyone, including stroke patients, may wish to consider personal measures to reduce exposure to air pollution, such as avoiding walking along polluted streets and rather take a less polluted route away from the main roads,” Dr. Petersen added.
The study had no targeted funding. Dr. Lin and Dr. Petersen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Youth killed by guns in U.S. equals classroom a day
according to the American Academy of Pediatrics.
Preventing firearm-related injuries and deaths in children and youth “demands a public safety approach like regulation of motor vehicles,” the group said.
The organization on Oct. 8 released an updated policy statement and technical report about gun violence and children at its 2022 annual meeting in Anaheim, Calif. The reports were published in the journal Pediatrics, and the authors plan to discuss them during the conference.
“Each day, 28 U.S. children and teens – the equivalent of a high school classroom – die from gun violence, making it the No. 1 killer of youth through age 24,” the AAP said in a statement about the reports. “The national death rate is significantly higher than all other high-income countries combined, largely due to an alarming increase in suicides and homicides that do not make national headlines.”
Firearms have become the leading cause of death among children in the United States.
In 2020, guns caused 10,197 deaths of Americans younger than 24, according to the Society for Adolescent Health and Medicine.
In 2015, more than 7,200 American youth were killed by firearms. That same year in 28 other high-income countries – which combined would have had a population twice that of the United States – just 685 youth were killed by firearms, according to the AAP.
Separately at the AAP conference, physicians are presenting new research about gun violence and children. And on Oct. 10, a pediatrician who was at Uvalde Memorial Hospital in Texas after the deadly school shooting in May is scheduled to address attendees. The doctor, Roy Guerrero, MD, testified on Capitol Hill to advocate for gun control after the shooting at Robb Elementary School, which killed 19 children and two adults.
“This is not a simple problem, and it cannot be fixed with a simple solution,” Lois K. Lee, MD, MPH, said in the AAP news release. Dr. Lee chairs the AAP Council on Injury, Violence, and Poison Prevention that wrote the new reports. “Pediatricians as a start can offer families guidance and education on more safely storing guns. AAP also calls for supporting legislation that, much like the common-sense requirements for obtaining a driver’s license, would improve gun ownership safety.”
Many deaths occur at home
The rate of homicide from firearms in U.S. youth, especially those aged 15-24 years, increased by 14% during the past decade, and the rate of suicide from firearms increased by 39%, according to the AAP.
Homicides account for 58% of youth firearm deaths, whereas suicides account for 37%. Another 2% of youth firearm deaths are unintentional, and 1% result from law enforcement actions, the group said.
Among children 12 years old and younger, about 85% of firearm deaths occur at home. Teen firearm deaths are about as likely to occur at home (39%) as on the street or sidewalk (38%), according to research based on 2014 data.
“School shootings represent a relatively new phenomenon over the last half-century, and the United States has the highest rate of school shootings in the world,” the AAP technical report noted. Between 1966 and 2008, according to the group, 44 such shootings occurred in the United States, or an average of about one per year. Fast forward a few years and the violence became dramatically worse: Between 2013 and 2015, officials counted 154 school shootings – or about one per week.
Still, school shootings are responsible for less than 1% of all firearm deaths among children 17 years or younger in the United States. While school shootings “receive a tremendous amount of attention,” the report stated, other child firearm deaths may be less likely to make national headlines.
“Many firearm tragedies escape public attention because they occur in a home, sometimes in a child’s own home or at a friend’s house, or their neighbor’s or grandparent’s residence,” Eric W. Fleegler, MD, MPH, Boston Children’s Hospital, a co-author of the new reports, said in a statement from AAP. “Research tells us that families tend to underestimate how children will behave when they encounter a gun and miscalculate the risks. Suicide risks are also a huge concern, especially in families where teens are struggling with their mental health.”
AAP-recommended actions include:
- Mental health screenings and safe gun storage education provided by clinicians as part of routine patient visits
- Increased funding for violence intervention programs in hospital and community settings
- Regulation of firearms like other consumer products, with national requirements that address training, licensing, insurance coverage, registration of individuals purchasing firearms, and safe storage
- The use of technology that allows only authorized users to pull the trigger
- Universal background checks that use federal databases and information from local police before all gun purchases
- Extreme risk protection order laws, or “red flag laws,” that prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm
- More funding for firearm injury and prevention research.
A noticeable increase in the ED
Irma Ugalde, MD, associate professor and director of pediatric emergency medicine research at McGovern Medical School at UTHealth Houston, noticed that firearm-related injuries in children at her hospital were more common during the COVID-19 pandemic, even as pediatric emergency department visits decreased overall.
She and her colleagues studied the trends and reported their findings at the AAP meeting.
“We saw a drop in pediatric admissions overall,” Dr. Ugalde said in a statement about the study. “But what was really noticeable was that trauma was still very prevalent – in fact probably more so – and we were seeing more firearm injuries.”
The researchers found that firearm injuries in children rose from 88 cases in 2019 to 118 in 2020. The number of incidents remained elevated in 2021, with 115 cases.
In addition, the researchers found an initial increase in injuries occurring at home where the shooter was a known family member or friend, and in cases involving firearms that were not properly stored.
By comparison, pediatric ED visits overall decreased by 34.2% from 2019 to 2020, and by 11.8% from 2019 to 2021.
The increase in firearm injuries coincided with an increase in gun sales in the United States, the researchers noted.
“National and statewide initiatives to mitigate the risk of firearm-related injury and death are necessary,” Dr. Ugalde’s group said. “We recommend that health care workers remain vigilant about screening for potential risk factors and safe storage of firearms.”
Accidental injuries
Daniel D. Guzman, MD, with Cook Children’s Health Care Center, Fort Worth, Tex., conducted a study focused on unintentional firearm injuries in children. Dr. Guzman’s group analyzed data from 204 patients younger than age 19 seen at Cook Children’s from January 2015 to June 2021.
Dr. Guzman and his colleagues examined outcomes for injuries caused by powder guns – shotguns, rifles, and handguns – and air-power guns that shoot BBs and pellets.
The researchers found that 29% of the unintentional firearm injuries occurred with powder guns and 71% with air-power weapons, often BB guns.
“It is important that all firearms, powdered and air-powered, be stored safely in a lock box or safe,” Dr. Guzman said in a statement. To that end, Cook Children’s has developed a program called Aim for Safety to teach children and parents about the dangers of unsupervised play with BB guns and pellet guns, as well as the importance of storing all firearms unloaded and in a locked safe.
A version of this article first appeared on Medscape.com.
according to the American Academy of Pediatrics.
Preventing firearm-related injuries and deaths in children and youth “demands a public safety approach like regulation of motor vehicles,” the group said.
The organization on Oct. 8 released an updated policy statement and technical report about gun violence and children at its 2022 annual meeting in Anaheim, Calif. The reports were published in the journal Pediatrics, and the authors plan to discuss them during the conference.
“Each day, 28 U.S. children and teens – the equivalent of a high school classroom – die from gun violence, making it the No. 1 killer of youth through age 24,” the AAP said in a statement about the reports. “The national death rate is significantly higher than all other high-income countries combined, largely due to an alarming increase in suicides and homicides that do not make national headlines.”
Firearms have become the leading cause of death among children in the United States.
In 2020, guns caused 10,197 deaths of Americans younger than 24, according to the Society for Adolescent Health and Medicine.
In 2015, more than 7,200 American youth were killed by firearms. That same year in 28 other high-income countries – which combined would have had a population twice that of the United States – just 685 youth were killed by firearms, according to the AAP.
Separately at the AAP conference, physicians are presenting new research about gun violence and children. And on Oct. 10, a pediatrician who was at Uvalde Memorial Hospital in Texas after the deadly school shooting in May is scheduled to address attendees. The doctor, Roy Guerrero, MD, testified on Capitol Hill to advocate for gun control after the shooting at Robb Elementary School, which killed 19 children and two adults.
“This is not a simple problem, and it cannot be fixed with a simple solution,” Lois K. Lee, MD, MPH, said in the AAP news release. Dr. Lee chairs the AAP Council on Injury, Violence, and Poison Prevention that wrote the new reports. “Pediatricians as a start can offer families guidance and education on more safely storing guns. AAP also calls for supporting legislation that, much like the common-sense requirements for obtaining a driver’s license, would improve gun ownership safety.”
Many deaths occur at home
The rate of homicide from firearms in U.S. youth, especially those aged 15-24 years, increased by 14% during the past decade, and the rate of suicide from firearms increased by 39%, according to the AAP.
Homicides account for 58% of youth firearm deaths, whereas suicides account for 37%. Another 2% of youth firearm deaths are unintentional, and 1% result from law enforcement actions, the group said.
Among children 12 years old and younger, about 85% of firearm deaths occur at home. Teen firearm deaths are about as likely to occur at home (39%) as on the street or sidewalk (38%), according to research based on 2014 data.
“School shootings represent a relatively new phenomenon over the last half-century, and the United States has the highest rate of school shootings in the world,” the AAP technical report noted. Between 1966 and 2008, according to the group, 44 such shootings occurred in the United States, or an average of about one per year. Fast forward a few years and the violence became dramatically worse: Between 2013 and 2015, officials counted 154 school shootings – or about one per week.
Still, school shootings are responsible for less than 1% of all firearm deaths among children 17 years or younger in the United States. While school shootings “receive a tremendous amount of attention,” the report stated, other child firearm deaths may be less likely to make national headlines.
“Many firearm tragedies escape public attention because they occur in a home, sometimes in a child’s own home or at a friend’s house, or their neighbor’s or grandparent’s residence,” Eric W. Fleegler, MD, MPH, Boston Children’s Hospital, a co-author of the new reports, said in a statement from AAP. “Research tells us that families tend to underestimate how children will behave when they encounter a gun and miscalculate the risks. Suicide risks are also a huge concern, especially in families where teens are struggling with their mental health.”
AAP-recommended actions include:
- Mental health screenings and safe gun storage education provided by clinicians as part of routine patient visits
- Increased funding for violence intervention programs in hospital and community settings
- Regulation of firearms like other consumer products, with national requirements that address training, licensing, insurance coverage, registration of individuals purchasing firearms, and safe storage
- The use of technology that allows only authorized users to pull the trigger
- Universal background checks that use federal databases and information from local police before all gun purchases
- Extreme risk protection order laws, or “red flag laws,” that prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm
- More funding for firearm injury and prevention research.
A noticeable increase in the ED
Irma Ugalde, MD, associate professor and director of pediatric emergency medicine research at McGovern Medical School at UTHealth Houston, noticed that firearm-related injuries in children at her hospital were more common during the COVID-19 pandemic, even as pediatric emergency department visits decreased overall.
She and her colleagues studied the trends and reported their findings at the AAP meeting.
“We saw a drop in pediatric admissions overall,” Dr. Ugalde said in a statement about the study. “But what was really noticeable was that trauma was still very prevalent – in fact probably more so – and we were seeing more firearm injuries.”
The researchers found that firearm injuries in children rose from 88 cases in 2019 to 118 in 2020. The number of incidents remained elevated in 2021, with 115 cases.
In addition, the researchers found an initial increase in injuries occurring at home where the shooter was a known family member or friend, and in cases involving firearms that were not properly stored.
By comparison, pediatric ED visits overall decreased by 34.2% from 2019 to 2020, and by 11.8% from 2019 to 2021.
The increase in firearm injuries coincided with an increase in gun sales in the United States, the researchers noted.
“National and statewide initiatives to mitigate the risk of firearm-related injury and death are necessary,” Dr. Ugalde’s group said. “We recommend that health care workers remain vigilant about screening for potential risk factors and safe storage of firearms.”
Accidental injuries
Daniel D. Guzman, MD, with Cook Children’s Health Care Center, Fort Worth, Tex., conducted a study focused on unintentional firearm injuries in children. Dr. Guzman’s group analyzed data from 204 patients younger than age 19 seen at Cook Children’s from January 2015 to June 2021.
Dr. Guzman and his colleagues examined outcomes for injuries caused by powder guns – shotguns, rifles, and handguns – and air-power guns that shoot BBs and pellets.
The researchers found that 29% of the unintentional firearm injuries occurred with powder guns and 71% with air-power weapons, often BB guns.
“It is important that all firearms, powdered and air-powered, be stored safely in a lock box or safe,” Dr. Guzman said in a statement. To that end, Cook Children’s has developed a program called Aim for Safety to teach children and parents about the dangers of unsupervised play with BB guns and pellet guns, as well as the importance of storing all firearms unloaded and in a locked safe.
A version of this article first appeared on Medscape.com.
according to the American Academy of Pediatrics.
Preventing firearm-related injuries and deaths in children and youth “demands a public safety approach like regulation of motor vehicles,” the group said.
The organization on Oct. 8 released an updated policy statement and technical report about gun violence and children at its 2022 annual meeting in Anaheim, Calif. The reports were published in the journal Pediatrics, and the authors plan to discuss them during the conference.
“Each day, 28 U.S. children and teens – the equivalent of a high school classroom – die from gun violence, making it the No. 1 killer of youth through age 24,” the AAP said in a statement about the reports. “The national death rate is significantly higher than all other high-income countries combined, largely due to an alarming increase in suicides and homicides that do not make national headlines.”
Firearms have become the leading cause of death among children in the United States.
In 2020, guns caused 10,197 deaths of Americans younger than 24, according to the Society for Adolescent Health and Medicine.
In 2015, more than 7,200 American youth were killed by firearms. That same year in 28 other high-income countries – which combined would have had a population twice that of the United States – just 685 youth were killed by firearms, according to the AAP.
Separately at the AAP conference, physicians are presenting new research about gun violence and children. And on Oct. 10, a pediatrician who was at Uvalde Memorial Hospital in Texas after the deadly school shooting in May is scheduled to address attendees. The doctor, Roy Guerrero, MD, testified on Capitol Hill to advocate for gun control after the shooting at Robb Elementary School, which killed 19 children and two adults.
“This is not a simple problem, and it cannot be fixed with a simple solution,” Lois K. Lee, MD, MPH, said in the AAP news release. Dr. Lee chairs the AAP Council on Injury, Violence, and Poison Prevention that wrote the new reports. “Pediatricians as a start can offer families guidance and education on more safely storing guns. AAP also calls for supporting legislation that, much like the common-sense requirements for obtaining a driver’s license, would improve gun ownership safety.”
Many deaths occur at home
The rate of homicide from firearms in U.S. youth, especially those aged 15-24 years, increased by 14% during the past decade, and the rate of suicide from firearms increased by 39%, according to the AAP.
Homicides account for 58% of youth firearm deaths, whereas suicides account for 37%. Another 2% of youth firearm deaths are unintentional, and 1% result from law enforcement actions, the group said.
Among children 12 years old and younger, about 85% of firearm deaths occur at home. Teen firearm deaths are about as likely to occur at home (39%) as on the street or sidewalk (38%), according to research based on 2014 data.
“School shootings represent a relatively new phenomenon over the last half-century, and the United States has the highest rate of school shootings in the world,” the AAP technical report noted. Between 1966 and 2008, according to the group, 44 such shootings occurred in the United States, or an average of about one per year. Fast forward a few years and the violence became dramatically worse: Between 2013 and 2015, officials counted 154 school shootings – or about one per week.
Still, school shootings are responsible for less than 1% of all firearm deaths among children 17 years or younger in the United States. While school shootings “receive a tremendous amount of attention,” the report stated, other child firearm deaths may be less likely to make national headlines.
“Many firearm tragedies escape public attention because they occur in a home, sometimes in a child’s own home or at a friend’s house, or their neighbor’s or grandparent’s residence,” Eric W. Fleegler, MD, MPH, Boston Children’s Hospital, a co-author of the new reports, said in a statement from AAP. “Research tells us that families tend to underestimate how children will behave when they encounter a gun and miscalculate the risks. Suicide risks are also a huge concern, especially in families where teens are struggling with their mental health.”
AAP-recommended actions include:
- Mental health screenings and safe gun storage education provided by clinicians as part of routine patient visits
- Increased funding for violence intervention programs in hospital and community settings
- Regulation of firearms like other consumer products, with national requirements that address training, licensing, insurance coverage, registration of individuals purchasing firearms, and safe storage
- The use of technology that allows only authorized users to pull the trigger
- Universal background checks that use federal databases and information from local police before all gun purchases
- Extreme risk protection order laws, or “red flag laws,” that prohibit individuals at risk for harming themselves or others from purchasing or owning a firearm
- More funding for firearm injury and prevention research.
A noticeable increase in the ED
Irma Ugalde, MD, associate professor and director of pediatric emergency medicine research at McGovern Medical School at UTHealth Houston, noticed that firearm-related injuries in children at her hospital were more common during the COVID-19 pandemic, even as pediatric emergency department visits decreased overall.
She and her colleagues studied the trends and reported their findings at the AAP meeting.
“We saw a drop in pediatric admissions overall,” Dr. Ugalde said in a statement about the study. “But what was really noticeable was that trauma was still very prevalent – in fact probably more so – and we were seeing more firearm injuries.”
The researchers found that firearm injuries in children rose from 88 cases in 2019 to 118 in 2020. The number of incidents remained elevated in 2021, with 115 cases.
In addition, the researchers found an initial increase in injuries occurring at home where the shooter was a known family member or friend, and in cases involving firearms that were not properly stored.
By comparison, pediatric ED visits overall decreased by 34.2% from 2019 to 2020, and by 11.8% from 2019 to 2021.
The increase in firearm injuries coincided with an increase in gun sales in the United States, the researchers noted.
“National and statewide initiatives to mitigate the risk of firearm-related injury and death are necessary,” Dr. Ugalde’s group said. “We recommend that health care workers remain vigilant about screening for potential risk factors and safe storage of firearms.”
Accidental injuries
Daniel D. Guzman, MD, with Cook Children’s Health Care Center, Fort Worth, Tex., conducted a study focused on unintentional firearm injuries in children. Dr. Guzman’s group analyzed data from 204 patients younger than age 19 seen at Cook Children’s from January 2015 to June 2021.
Dr. Guzman and his colleagues examined outcomes for injuries caused by powder guns – shotguns, rifles, and handguns – and air-power guns that shoot BBs and pellets.
The researchers found that 29% of the unintentional firearm injuries occurred with powder guns and 71% with air-power weapons, often BB guns.
“It is important that all firearms, powdered and air-powered, be stored safely in a lock box or safe,” Dr. Guzman said in a statement. To that end, Cook Children’s has developed a program called Aim for Safety to teach children and parents about the dangers of unsupervised play with BB guns and pellet guns, as well as the importance of storing all firearms unloaded and in a locked safe.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS


