User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Emerging invasive fungal infections call for multidisciplinary cooperation
BUENOS AIRES – Emerging invasive fungal infections represent a new diagnostic and therapeutic challenge. To address their growing clinical impact on immunocompromised patients requires better local epidemiologic records, said a specialist at the XXII Congress of the Argentine Society of Infectology.
“To know that these fungal infections exist, I believe that in this respect we are falling short,” said Javier Afeltra, PhD, a mycologist at the Ramos Mejía Hospital in Buenos Aires, professor of microbiology at the School of Medicine of the University of Buenos Aires, and coordinator of the commission of immunocompromised patients of the Argentine Society of Infectious Diseases.
“There is some change in mentality that encourages professionals to report the cases they detect – for example, in scientific meetings,” Dr. Afeltra told this news orgnization. “But the problem is that there is no unified registry.
“That’s what we lack: a place to record all those isolated cases. Records where clinical and microbiological data are together within a click. Perhaps the microbiologists report their findings to the Malbrán Institute, an Argentine reference center for infectious disease research, but we do not know what the patients had. And we doctors may get together to make records of what happens clinically with the patient, but the germ data are elsewhere. We need a common registry,” he stressed.
“The main importance of a registry of this type is that it would allow a diagnostic and therapeutic decision to be made that is appropriate to the epidemiological profile of the country and the region, not looking at what they do in the North. Most likely, the best antifungal treatment for our country differs from what is indicated in the guidelines written elsewhere,” said Dr. Afeltra.
Dr. Afeltra pointed out that in the United States, when an oncohematology patient does not respond to antimicrobial treatment, the first thing that doctors think is that the patient has aspergillosis or mucormycosis, in which the fungal infection is caused by filamentous fungi.
But an analysis of data from the REMINI registry – the only prospective, observational, multicenter surveillance registry for invasive mycoses in immunocompromised patients (excluding HIV infection) in Argentina, which has been in existence since 2010 – tells a different story. The most prevalent fungal infections turned out to be those caused by Aspergillus species, followed by Fusarium species. Together, they account for more than half of cases. Mucoral infections (mucormycosis) account for less than 6%. And the initial treatments for these diseases could be different.
Changes in the local epidemiology can occur because the behavior of phytopathogenic fungi found in the environment can be modified. For example, cases of chronic mucormycosis can be detected in China but are virtually nonexistent on this side of the Greenwich meridian, Dr. Afeltra said.
“Nature is not the same in geographical areas, and the fungi … we breathe are completely different, so patients have different infections and require different diagnostic and treatment approaches,” he stressed.
Dr. Afeltra mentioned different fungi that are emerging locally and globally, including yeasts, septate, dimorphic, and pigmented hyaline fungi, that have a variable response to antifungal drugs and are associated with high mortality, “which has a lot to do with a later diagnosis,” he said, noting that reports have increased worldwide. A barrier to sharing this information more widely with the professional community, in addition to the lack of records, is the difficulty in publishing cases or series of cases in indexed journals.
Another challenge in characterizing the phenomenon is in regard to taxonomic reclassifications of fungi. Such reclassifications can mean that “perhaps we are speaking of the same pathogen in similar situations, believing that we are referring to different pathogens,” said Dr. Afeltra.
Clinical pearls related to emerging fungal pathogens
Candida auris. This organism has emerged simultaneously on several continents. It has pathogenicity factors typical of the genus, such as biofilm formation and production of phospholipases and proteinases, although it has greater thermal tolerance. In hospitals, it colonizes for weeks and months. In Argentina, it is resistant to multiple antifungal agents. Sensitivity is variable in different geographical regions. Most strains are resistant to fluconazole, and there is variable resistance to the other triazoles [which are not normally used to treat candidemia]. In the United States, in vitro resistance to amphotericin B is up to 30%, and resistance to echinocandins is up to 5%. New drugs such as rezafungin and ibrexafungerp are being studied. Infection control is similar to that used to control Clostridium difficile.
Fusarium. This genus affects immunocompromised patients, including transplant recipients of solid organs and hematopoietic progenitor cells and patients with neutropenia. The genus has various species, included within complexes, such as F. solani SC, F. oxysporum SC, and F. fujikuroi SC, with clinical manifestations similar to those of aspergillosis. In addition to the pulmonary and disseminated forms, there may be skin involvement attributable to dissemination from a respiratory focus or by contiguity from a focus of onychomycosis. In general, mortality is high, and responses to antifungal agents are variable. Some species are more sensitive to voriconazole or posaconazole, and others less so. All show in vitro resistance to itraconazole. In Argentina, voriconazole is usually used as initial treatment, and in special cases, liposomal amphotericin B or combinations. Fosmanogepix is being evaluated for the future.
Azole-resistant aspergillosis. This infection has shown resistance to itraconazole and third-generation azole drugs. In immunocompromised patients, mortlaity is high. Early detection is key. It is sensitive to amphotericin B and echinocandins. It is generally treated with liposomal amphotericin B. Olorofim and fosmanogepix are being studied.
Pulmonary aspergillosis associated with COVID-19. This infection is associated with high mortality among intubated patients. Signs and symptoms include fever, pleural effusion, hemoptysis, and chest pain, with infiltrates or cavitations on imaging. Determining the diagnosis is difficult. “We couldn’t perform lung biopsies, and it was difficult for us to get patients out of intensive care units for CT scans. We treated the proven cases. We treated the probable cases, and those that had a very low certainty of disease were also treated. We came across this emergency and tried to do the best we could,” said Dr. Afeltra. A digital readout lateral flow trial (Sona Aspergillus Galactomannan LFA) for the quantification of galactomannan, a cell wall component of the Aspergillus genus, proved to be a useful tool for screening and diagnosing patients with probable pulmonary aspergillosis associated with COVID-19. The incidence of invasive mycosis was around 10% among 185 seriously ill COVID-19 patients, according to an Argentine multicenter prospective study in which Dr. Afeltra participated.
Scedosporium and Lomentospora. These genera are rarer septate hyaline fungi. Scedosporium is a complex of species. One species, S. apiospermum, can colonize pediatric patients with cystic fibrosis. Lomentospora prolificans is a multiresistant fungus. It produces pulmonary compromise or disseminated infection. The response to antifungal agents is variable, with a high minimum inhibitory concentration for amphotericin B and isavuconazole. Patients are usually treated with voriconazole alone or in combination with terbinafine or micafungin. Olorofim is emerging as a promising treatment.
Dr. Afeltra has received fees from Biotoscana, Gador, Pfizer, Merck, and Sandoz.
This article was translated from the Medscape Spanish edition, a version appeared on Medscape.com.
BUENOS AIRES – Emerging invasive fungal infections represent a new diagnostic and therapeutic challenge. To address their growing clinical impact on immunocompromised patients requires better local epidemiologic records, said a specialist at the XXII Congress of the Argentine Society of Infectology.
“To know that these fungal infections exist, I believe that in this respect we are falling short,” said Javier Afeltra, PhD, a mycologist at the Ramos Mejía Hospital in Buenos Aires, professor of microbiology at the School of Medicine of the University of Buenos Aires, and coordinator of the commission of immunocompromised patients of the Argentine Society of Infectious Diseases.
“There is some change in mentality that encourages professionals to report the cases they detect – for example, in scientific meetings,” Dr. Afeltra told this news orgnization. “But the problem is that there is no unified registry.
“That’s what we lack: a place to record all those isolated cases. Records where clinical and microbiological data are together within a click. Perhaps the microbiologists report their findings to the Malbrán Institute, an Argentine reference center for infectious disease research, but we do not know what the patients had. And we doctors may get together to make records of what happens clinically with the patient, but the germ data are elsewhere. We need a common registry,” he stressed.
“The main importance of a registry of this type is that it would allow a diagnostic and therapeutic decision to be made that is appropriate to the epidemiological profile of the country and the region, not looking at what they do in the North. Most likely, the best antifungal treatment for our country differs from what is indicated in the guidelines written elsewhere,” said Dr. Afeltra.
Dr. Afeltra pointed out that in the United States, when an oncohematology patient does not respond to antimicrobial treatment, the first thing that doctors think is that the patient has aspergillosis or mucormycosis, in which the fungal infection is caused by filamentous fungi.
But an analysis of data from the REMINI registry – the only prospective, observational, multicenter surveillance registry for invasive mycoses in immunocompromised patients (excluding HIV infection) in Argentina, which has been in existence since 2010 – tells a different story. The most prevalent fungal infections turned out to be those caused by Aspergillus species, followed by Fusarium species. Together, they account for more than half of cases. Mucoral infections (mucormycosis) account for less than 6%. And the initial treatments for these diseases could be different.
Changes in the local epidemiology can occur because the behavior of phytopathogenic fungi found in the environment can be modified. For example, cases of chronic mucormycosis can be detected in China but are virtually nonexistent on this side of the Greenwich meridian, Dr. Afeltra said.
“Nature is not the same in geographical areas, and the fungi … we breathe are completely different, so patients have different infections and require different diagnostic and treatment approaches,” he stressed.
Dr. Afeltra mentioned different fungi that are emerging locally and globally, including yeasts, septate, dimorphic, and pigmented hyaline fungi, that have a variable response to antifungal drugs and are associated with high mortality, “which has a lot to do with a later diagnosis,” he said, noting that reports have increased worldwide. A barrier to sharing this information more widely with the professional community, in addition to the lack of records, is the difficulty in publishing cases or series of cases in indexed journals.
Another challenge in characterizing the phenomenon is in regard to taxonomic reclassifications of fungi. Such reclassifications can mean that “perhaps we are speaking of the same pathogen in similar situations, believing that we are referring to different pathogens,” said Dr. Afeltra.
Clinical pearls related to emerging fungal pathogens
Candida auris. This organism has emerged simultaneously on several continents. It has pathogenicity factors typical of the genus, such as biofilm formation and production of phospholipases and proteinases, although it has greater thermal tolerance. In hospitals, it colonizes for weeks and months. In Argentina, it is resistant to multiple antifungal agents. Sensitivity is variable in different geographical regions. Most strains are resistant to fluconazole, and there is variable resistance to the other triazoles [which are not normally used to treat candidemia]. In the United States, in vitro resistance to amphotericin B is up to 30%, and resistance to echinocandins is up to 5%. New drugs such as rezafungin and ibrexafungerp are being studied. Infection control is similar to that used to control Clostridium difficile.
Fusarium. This genus affects immunocompromised patients, including transplant recipients of solid organs and hematopoietic progenitor cells and patients with neutropenia. The genus has various species, included within complexes, such as F. solani SC, F. oxysporum SC, and F. fujikuroi SC, with clinical manifestations similar to those of aspergillosis. In addition to the pulmonary and disseminated forms, there may be skin involvement attributable to dissemination from a respiratory focus or by contiguity from a focus of onychomycosis. In general, mortality is high, and responses to antifungal agents are variable. Some species are more sensitive to voriconazole or posaconazole, and others less so. All show in vitro resistance to itraconazole. In Argentina, voriconazole is usually used as initial treatment, and in special cases, liposomal amphotericin B or combinations. Fosmanogepix is being evaluated for the future.
Azole-resistant aspergillosis. This infection has shown resistance to itraconazole and third-generation azole drugs. In immunocompromised patients, mortlaity is high. Early detection is key. It is sensitive to amphotericin B and echinocandins. It is generally treated with liposomal amphotericin B. Olorofim and fosmanogepix are being studied.
Pulmonary aspergillosis associated with COVID-19. This infection is associated with high mortality among intubated patients. Signs and symptoms include fever, pleural effusion, hemoptysis, and chest pain, with infiltrates or cavitations on imaging. Determining the diagnosis is difficult. “We couldn’t perform lung biopsies, and it was difficult for us to get patients out of intensive care units for CT scans. We treated the proven cases. We treated the probable cases, and those that had a very low certainty of disease were also treated. We came across this emergency and tried to do the best we could,” said Dr. Afeltra. A digital readout lateral flow trial (Sona Aspergillus Galactomannan LFA) for the quantification of galactomannan, a cell wall component of the Aspergillus genus, proved to be a useful tool for screening and diagnosing patients with probable pulmonary aspergillosis associated with COVID-19. The incidence of invasive mycosis was around 10% among 185 seriously ill COVID-19 patients, according to an Argentine multicenter prospective study in which Dr. Afeltra participated.
Scedosporium and Lomentospora. These genera are rarer septate hyaline fungi. Scedosporium is a complex of species. One species, S. apiospermum, can colonize pediatric patients with cystic fibrosis. Lomentospora prolificans is a multiresistant fungus. It produces pulmonary compromise or disseminated infection. The response to antifungal agents is variable, with a high minimum inhibitory concentration for amphotericin B and isavuconazole. Patients are usually treated with voriconazole alone or in combination with terbinafine or micafungin. Olorofim is emerging as a promising treatment.
Dr. Afeltra has received fees from Biotoscana, Gador, Pfizer, Merck, and Sandoz.
This article was translated from the Medscape Spanish edition, a version appeared on Medscape.com.
BUENOS AIRES – Emerging invasive fungal infections represent a new diagnostic and therapeutic challenge. To address their growing clinical impact on immunocompromised patients requires better local epidemiologic records, said a specialist at the XXII Congress of the Argentine Society of Infectology.
“To know that these fungal infections exist, I believe that in this respect we are falling short,” said Javier Afeltra, PhD, a mycologist at the Ramos Mejía Hospital in Buenos Aires, professor of microbiology at the School of Medicine of the University of Buenos Aires, and coordinator of the commission of immunocompromised patients of the Argentine Society of Infectious Diseases.
“There is some change in mentality that encourages professionals to report the cases they detect – for example, in scientific meetings,” Dr. Afeltra told this news orgnization. “But the problem is that there is no unified registry.
“That’s what we lack: a place to record all those isolated cases. Records where clinical and microbiological data are together within a click. Perhaps the microbiologists report their findings to the Malbrán Institute, an Argentine reference center for infectious disease research, but we do not know what the patients had. And we doctors may get together to make records of what happens clinically with the patient, but the germ data are elsewhere. We need a common registry,” he stressed.
“The main importance of a registry of this type is that it would allow a diagnostic and therapeutic decision to be made that is appropriate to the epidemiological profile of the country and the region, not looking at what they do in the North. Most likely, the best antifungal treatment for our country differs from what is indicated in the guidelines written elsewhere,” said Dr. Afeltra.
Dr. Afeltra pointed out that in the United States, when an oncohematology patient does not respond to antimicrobial treatment, the first thing that doctors think is that the patient has aspergillosis or mucormycosis, in which the fungal infection is caused by filamentous fungi.
But an analysis of data from the REMINI registry – the only prospective, observational, multicenter surveillance registry for invasive mycoses in immunocompromised patients (excluding HIV infection) in Argentina, which has been in existence since 2010 – tells a different story. The most prevalent fungal infections turned out to be those caused by Aspergillus species, followed by Fusarium species. Together, they account for more than half of cases. Mucoral infections (mucormycosis) account for less than 6%. And the initial treatments for these diseases could be different.
Changes in the local epidemiology can occur because the behavior of phytopathogenic fungi found in the environment can be modified. For example, cases of chronic mucormycosis can be detected in China but are virtually nonexistent on this side of the Greenwich meridian, Dr. Afeltra said.
“Nature is not the same in geographical areas, and the fungi … we breathe are completely different, so patients have different infections and require different diagnostic and treatment approaches,” he stressed.
Dr. Afeltra mentioned different fungi that are emerging locally and globally, including yeasts, septate, dimorphic, and pigmented hyaline fungi, that have a variable response to antifungal drugs and are associated with high mortality, “which has a lot to do with a later diagnosis,” he said, noting that reports have increased worldwide. A barrier to sharing this information more widely with the professional community, in addition to the lack of records, is the difficulty in publishing cases or series of cases in indexed journals.
Another challenge in characterizing the phenomenon is in regard to taxonomic reclassifications of fungi. Such reclassifications can mean that “perhaps we are speaking of the same pathogen in similar situations, believing that we are referring to different pathogens,” said Dr. Afeltra.
Clinical pearls related to emerging fungal pathogens
Candida auris. This organism has emerged simultaneously on several continents. It has pathogenicity factors typical of the genus, such as biofilm formation and production of phospholipases and proteinases, although it has greater thermal tolerance. In hospitals, it colonizes for weeks and months. In Argentina, it is resistant to multiple antifungal agents. Sensitivity is variable in different geographical regions. Most strains are resistant to fluconazole, and there is variable resistance to the other triazoles [which are not normally used to treat candidemia]. In the United States, in vitro resistance to amphotericin B is up to 30%, and resistance to echinocandins is up to 5%. New drugs such as rezafungin and ibrexafungerp are being studied. Infection control is similar to that used to control Clostridium difficile.
Fusarium. This genus affects immunocompromised patients, including transplant recipients of solid organs and hematopoietic progenitor cells and patients with neutropenia. The genus has various species, included within complexes, such as F. solani SC, F. oxysporum SC, and F. fujikuroi SC, with clinical manifestations similar to those of aspergillosis. In addition to the pulmonary and disseminated forms, there may be skin involvement attributable to dissemination from a respiratory focus or by contiguity from a focus of onychomycosis. In general, mortality is high, and responses to antifungal agents are variable. Some species are more sensitive to voriconazole or posaconazole, and others less so. All show in vitro resistance to itraconazole. In Argentina, voriconazole is usually used as initial treatment, and in special cases, liposomal amphotericin B or combinations. Fosmanogepix is being evaluated for the future.
Azole-resistant aspergillosis. This infection has shown resistance to itraconazole and third-generation azole drugs. In immunocompromised patients, mortlaity is high. Early detection is key. It is sensitive to amphotericin B and echinocandins. It is generally treated with liposomal amphotericin B. Olorofim and fosmanogepix are being studied.
Pulmonary aspergillosis associated with COVID-19. This infection is associated with high mortality among intubated patients. Signs and symptoms include fever, pleural effusion, hemoptysis, and chest pain, with infiltrates or cavitations on imaging. Determining the diagnosis is difficult. “We couldn’t perform lung biopsies, and it was difficult for us to get patients out of intensive care units for CT scans. We treated the proven cases. We treated the probable cases, and those that had a very low certainty of disease were also treated. We came across this emergency and tried to do the best we could,” said Dr. Afeltra. A digital readout lateral flow trial (Sona Aspergillus Galactomannan LFA) for the quantification of galactomannan, a cell wall component of the Aspergillus genus, proved to be a useful tool for screening and diagnosing patients with probable pulmonary aspergillosis associated with COVID-19. The incidence of invasive mycosis was around 10% among 185 seriously ill COVID-19 patients, according to an Argentine multicenter prospective study in which Dr. Afeltra participated.
Scedosporium and Lomentospora. These genera are rarer septate hyaline fungi. Scedosporium is a complex of species. One species, S. apiospermum, can colonize pediatric patients with cystic fibrosis. Lomentospora prolificans is a multiresistant fungus. It produces pulmonary compromise or disseminated infection. The response to antifungal agents is variable, with a high minimum inhibitory concentration for amphotericin B and isavuconazole. Patients are usually treated with voriconazole alone or in combination with terbinafine or micafungin. Olorofim is emerging as a promising treatment.
Dr. Afeltra has received fees from Biotoscana, Gador, Pfizer, Merck, and Sandoz.
This article was translated from the Medscape Spanish edition, a version appeared on Medscape.com.
AT SADI 2022
Three COVID scenarios that could spell trouble for the fall
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As the United States enters a third fall with COVID-19, the virus for many is seemingly gone – or at least out of mind. But for those keeping watch, it is far from forgotten as deaths and infections continue to mount at a lower but steady pace.
What does that mean for the upcoming months? Experts predict different scenarios, some more dire than others – with one more encouraging.
In the United States, more than 300 people still die every day from COVID and more than 44,000 new daily cases are reported, according to the Centers for Disease Control and Prevention.
But progress is undeniable. The stark daily death tolls of 2020 have plummeted. Vaccines and treatments have dramatically reduced severe illness, and mask requirements have mostly turned to personal preference.
among them more-resistant variants coupled with waning immunity, the potential for a “twindemic” with a flu/COVID onslaught, and underuse of lifesaving vaccines and treatments.
Variants loom/waning immunity
Omicron variant BA.5 still makes up about 80% of infections in the United States, followed by BA4.6, according to the CDC, but other subvariants are emerging and showing signs of resistance to current antiviral treatments.
Eric Topol, MD, founder and director of the Scripps Research Translational Institute in San Diego, said about COVID this fall: “There will be another wave, magnitude unknown.”
He said subvariants XBB and BQ.1.1 “have extreme levels of immune evasion and both could pose a challenge,” explaining that XBB is more likely to cause trouble than BQ.1.1 because it is even more resistant to natural or vaccine-induced immunity.
Dr. Topol pointed to new research on those variants in a preprint posted on bioRxiv. The authors’ conclusion: “These results suggest that current herd immunity and BA.5 vaccine boosters may not provide sufficiently broad protection against infection.”
Another variant to watch, some experts say, is Omicron subvariant BA.2.75.2, which has shown resistance to antiviral treatments. It is also growing at a rather alarming rate, says Michael Sweat, PhD, director of the Medical University of South Carolina Center for Global Health in Charleston. That subvariant currently makes up under 2% of U.S. cases but has spread to at least 55 countries and 43 U.S. states after first appearing at the end of last year globally and in mid-June in the United States.
A non–peer-reviewed preprint study from Sweden found that the variant in blood samples was neutralized on average “at titers approximately 6.5 times lower than BA.5, making BA.2.75.2 the most [neutralization-resistant] variant evaluated to date.”
Katelyn Jetelina, PhD, assistant professor in the department of epidemiology at University of Texas Health Science Center, Houston, said in an interview the U.S. waves often follow Europe’s, and Europe has seen a recent spike in cases and hospitalizations not related to Omicron subvariants, but to weather changes, waning immunity, and changes in behavior.
The World Health Organization reported on Oct. 5 that, while cases were down in every other region of the world, Europe’s numbers stand out, with an 8% increase in cases from the week before.
Dr. Jetelina cited events such as Oktoberfest in Germany, which ended in the first week of October after drawing nearly 6 million people over 2 weeks, as a potential contributor, and people heading indoors as weather patterns change in Europe.
Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said in an interview he is less worried about the documented variants we know about than he is about the potential for a new immune-escape variety yet to emerge.
“Right now we know the Chinese are gearing up to open up the country, and because they have low immunity and little infection, we expect in China there will be a lot of spread of Omicron,” he said. “It’s possible because of the number of infections we could see a new variant.”
Dr. Mokdad said waning immunity could also leave populations vulnerable to variants.
“Even if you get infected, after about 5 months, you’re susceptible again. Remember, most of the infections from Omicron happened in January or February 2022, and we had two waves after that,” he said.
The new bivalent vaccines tweaked to target some Omicron variants will help, Dr. Mokdad said, but he noted, “people are very reluctant to take it.”
Jennifer Nuzzo, DrPH, professor of epidemiology and director of the Pandemic Center at Brown University, Providence, R.I., worries that in the United States we have less ability this year to track variants as funding has receded for testing kits and testing sites. Most people are testing at home – which doesn’t show up in the numbers – and the United States is relying more on other countries’ data to spot trends.
“I think we’re just going to have less visibility into the circulation of this virus,” she said in an interview.
‘Twindemic’: COVID and flu
Dr. Jetelina noted Australia and New Zealand just wrapped up a flu season that saw flu numbers returning to normal after a sharp drop in the last 2 years, and North America typically follows suit.
“We do expect flu will be here in the United States and probably at levels that we saw prepandemic. We’re all holding our breath to see how our health systems hold up with COVID-19 and flu. We haven’t really experienced that yet,” she said.
There is some disagreement, however, about the possibility of a so-called “twindemic” of influenza and COVID.
Richard Webby, PhD, an infectious disease specialist at St. Jude Children’s Research Hospital in Memphis, said in an interview he thinks the possibility of both viruses spiking at the same time is unlikely.
“That’s not to say we won’t get flu and COVID activity in the same winter,” he explained, “but I think both roaring at the same time is unlikely.”
As an indicator, he said, at the beginning of the flu season last year in the Northern Hemisphere, flu activity started to pick up, but when the Omicron variant came along, “flu just wasn’t able to compete in that same environment and flu numbers dropped right off.” Previous literature suggests that when one virus is spiking it’s hard for another respiratory virus to take hold.
Vaccine, treatment underuse
Another threat is vaccines, boosters, and treatments sitting on shelves.
Dr. Sweat referred to frustration with vaccine uptake that seems to be “frozen in amber.”
As of Oct. 4, only 5.3% of people in the United States who were eligible had received the updated booster launched in early September.
Dr. Nuzzo said boosters for people at least 65 years old will be key to severity of COVID this season.
“I think that’s probably the biggest factor going into the fall and winter,” she said.
Only 38% of people at least 50 years old and 45% of those at least 65 years old had gotten a second booster as of early October.
“If we do nothing else, we have to increase booster uptake in that group,” Dr. Nuzzo said.
She said the treatment nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is greatly underused, often because providers aren’t prescribing it because they don’t think it helps, are worried about drug interactions, or are worried about its “rebound” effect.
Dr. Nuzzo urged greater use of the drug and education on how to manage drug interactions.
“We have very strong data that it does help keep people out of hospital. Sure, there may be a rebound, but that pales in comparison to the risk of being hospitalized,” she said.
Calm COVID season?
Not all predictions are dire. There is another little-talked-about scenario, Dr. Sweat said – that we could be in for a calm COVID season, and those who seem to be only mildly concerned about COVID may find those thoughts justified in the numbers.
Omicron blew through with such strength, he noted, that it may have left wide immunity in its wake. Because variants seem to be staying in the Omicron family, that may signal optimism.
“If the next variant is a descendant of the Omicron lineage, I would suspect that all these people who just got infected will have some protection, not perfect, but quite a bit of protection,” Dr. Sweat said.
Dr. Topol, Dr. Nuzzo, Dr. Sweat, Dr. Webby, Dr. Mokdad, and Dr. Jetelina reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MD and APP-only care benefit patients in the ED
A provider-only patient care protocol was safe and efficient for delivery of emergency department care in response to pandemic-related staff shortages, based on data from nearly 3,000 patients.
The COVID-19 pandemic sparked a shortage of health care personnel, according to Tanveer Gaibi, MD, of INOVA Fairfax Hospital, Falls Church, Va., and colleagues. To help manage these challenges, the INOVA emergency department developed a Provider-Only Patients (POP) protocol for patients who required minimal nursing care.
In a study presented at the American College of Emergency Physicians 2022 Scientific Assembly, the researchers reported the outcomes of a cohort of patients with suspected COVID-19 who were treated in the emergency department using the POP protocol between Dec. 1, 2021, and Jan. 15, 2022. The patients ranged in age from 21 to 64, and all presented with COVID-19-related complaints, with an Emergency Severity Index (ESI) of 4 or 5, with 1 being the most urgent and 5 being the least urgent.
Patients were triaged by a physician or nurse to determine POP status. The researchers reviewed data from a total of 640 patients treated via the POP protocol and 2,386 patients who were not POP with ESI of 4 or 5.
Overall, the mean time from when a patient was initially seen by a provider to the discharge disposition was 48 minutes shorter for POP, and the mean time from discharge disposition placement to leaving the ED was 66 minutes shorter. None of the POP-protocol patients were readmitted within 72 hours of discharge. The researchers estimated that the 640 patients in the POP protocol saved approximately 1892.27 hours of nursing and 705.1 provider hours during the study period, and no additional physician hours or advanced-practice provider hours were needed.
The study findings suggest that POP holds up as a safe, efficient, and effective process that can reduce discharge length of stay and provider to disposition times. Although more research is needed, the POP model also may be considered to address staffing challenges unrelated to the pandemic, the researchers concluded.
“This study was conducted at [a] time when our emergency department was experiencing a sudden and disproportionate increase in volume related to the Omicron variant of COVID-19,” Dr. Gaibi told this news organization. “This novel process was developed by brainstorming untested ways of managing this increased demand. The research study was a natural outcome once the process was implemented,” he said.
“Once barriers to implementing this process were overcome, we were not surprised by the results,” Dr. Gaibi said. “Subtracting at the time for nursing process was anticipated to shorten cycle times.”
The clinical implications of POP relate to generalizability outside of the pandemic setting, Dr. Gaibi noted. “We anticipate that POP could be used for patients with minor complaints to greatly shorten their time in the emergency department,” he said.
“Potential barriers to the generalized use of POP relate, in part, to local administrative barriers related to nursing assessments,” Dr. Gaibi explained. “Further, POP patients should be simple and require little or no testing. Keeping to this strict definition of the provider-only patient may be a pitfall in terms of its hard wiring,” he added.
Looking ahead, more research is needed to study POP in ED patients with minor complaints not necessarily related to COVID-19, Dr. Gaibi said.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A provider-only patient care protocol was safe and efficient for delivery of emergency department care in response to pandemic-related staff shortages, based on data from nearly 3,000 patients.
The COVID-19 pandemic sparked a shortage of health care personnel, according to Tanveer Gaibi, MD, of INOVA Fairfax Hospital, Falls Church, Va., and colleagues. To help manage these challenges, the INOVA emergency department developed a Provider-Only Patients (POP) protocol for patients who required minimal nursing care.
In a study presented at the American College of Emergency Physicians 2022 Scientific Assembly, the researchers reported the outcomes of a cohort of patients with suspected COVID-19 who were treated in the emergency department using the POP protocol between Dec. 1, 2021, and Jan. 15, 2022. The patients ranged in age from 21 to 64, and all presented with COVID-19-related complaints, with an Emergency Severity Index (ESI) of 4 or 5, with 1 being the most urgent and 5 being the least urgent.
Patients were triaged by a physician or nurse to determine POP status. The researchers reviewed data from a total of 640 patients treated via the POP protocol and 2,386 patients who were not POP with ESI of 4 or 5.
Overall, the mean time from when a patient was initially seen by a provider to the discharge disposition was 48 minutes shorter for POP, and the mean time from discharge disposition placement to leaving the ED was 66 minutes shorter. None of the POP-protocol patients were readmitted within 72 hours of discharge. The researchers estimated that the 640 patients in the POP protocol saved approximately 1892.27 hours of nursing and 705.1 provider hours during the study period, and no additional physician hours or advanced-practice provider hours were needed.
The study findings suggest that POP holds up as a safe, efficient, and effective process that can reduce discharge length of stay and provider to disposition times. Although more research is needed, the POP model also may be considered to address staffing challenges unrelated to the pandemic, the researchers concluded.
“This study was conducted at [a] time when our emergency department was experiencing a sudden and disproportionate increase in volume related to the Omicron variant of COVID-19,” Dr. Gaibi told this news organization. “This novel process was developed by brainstorming untested ways of managing this increased demand. The research study was a natural outcome once the process was implemented,” he said.
“Once barriers to implementing this process were overcome, we were not surprised by the results,” Dr. Gaibi said. “Subtracting at the time for nursing process was anticipated to shorten cycle times.”
The clinical implications of POP relate to generalizability outside of the pandemic setting, Dr. Gaibi noted. “We anticipate that POP could be used for patients with minor complaints to greatly shorten their time in the emergency department,” he said.
“Potential barriers to the generalized use of POP relate, in part, to local administrative barriers related to nursing assessments,” Dr. Gaibi explained. “Further, POP patients should be simple and require little or no testing. Keeping to this strict definition of the provider-only patient may be a pitfall in terms of its hard wiring,” he added.
Looking ahead, more research is needed to study POP in ED patients with minor complaints not necessarily related to COVID-19, Dr. Gaibi said.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A provider-only patient care protocol was safe and efficient for delivery of emergency department care in response to pandemic-related staff shortages, based on data from nearly 3,000 patients.
The COVID-19 pandemic sparked a shortage of health care personnel, according to Tanveer Gaibi, MD, of INOVA Fairfax Hospital, Falls Church, Va., and colleagues. To help manage these challenges, the INOVA emergency department developed a Provider-Only Patients (POP) protocol for patients who required minimal nursing care.
In a study presented at the American College of Emergency Physicians 2022 Scientific Assembly, the researchers reported the outcomes of a cohort of patients with suspected COVID-19 who were treated in the emergency department using the POP protocol between Dec. 1, 2021, and Jan. 15, 2022. The patients ranged in age from 21 to 64, and all presented with COVID-19-related complaints, with an Emergency Severity Index (ESI) of 4 or 5, with 1 being the most urgent and 5 being the least urgent.
Patients were triaged by a physician or nurse to determine POP status. The researchers reviewed data from a total of 640 patients treated via the POP protocol and 2,386 patients who were not POP with ESI of 4 or 5.
Overall, the mean time from when a patient was initially seen by a provider to the discharge disposition was 48 minutes shorter for POP, and the mean time from discharge disposition placement to leaving the ED was 66 minutes shorter. None of the POP-protocol patients were readmitted within 72 hours of discharge. The researchers estimated that the 640 patients in the POP protocol saved approximately 1892.27 hours of nursing and 705.1 provider hours during the study period, and no additional physician hours or advanced-practice provider hours were needed.
The study findings suggest that POP holds up as a safe, efficient, and effective process that can reduce discharge length of stay and provider to disposition times. Although more research is needed, the POP model also may be considered to address staffing challenges unrelated to the pandemic, the researchers concluded.
“This study was conducted at [a] time when our emergency department was experiencing a sudden and disproportionate increase in volume related to the Omicron variant of COVID-19,” Dr. Gaibi told this news organization. “This novel process was developed by brainstorming untested ways of managing this increased demand. The research study was a natural outcome once the process was implemented,” he said.
“Once barriers to implementing this process were overcome, we were not surprised by the results,” Dr. Gaibi said. “Subtracting at the time for nursing process was anticipated to shorten cycle times.”
The clinical implications of POP relate to generalizability outside of the pandemic setting, Dr. Gaibi noted. “We anticipate that POP could be used for patients with minor complaints to greatly shorten their time in the emergency department,” he said.
“Potential barriers to the generalized use of POP relate, in part, to local administrative barriers related to nursing assessments,” Dr. Gaibi explained. “Further, POP patients should be simple and require little or no testing. Keeping to this strict definition of the provider-only patient may be a pitfall in terms of its hard wiring,” he added.
Looking ahead, more research is needed to study POP in ED patients with minor complaints not necessarily related to COVID-19, Dr. Gaibi said.
The study received no outside funding. The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACEP 2022
New technology a sepsis breakthrough?
Sepsis is among the most feared conditions for health care providers. These blood infections strike with such rapid intensity that treating them demands a mix of both clinical skill and luck – recognizing symptoms early enough while choosing the right drug to tame the bacterial culprit before the germs have overwhelmed the body’s immune system.
All too often, sepsis wins the race. According to the U.S. Centers for Disease Control and Prevention, at least 1.7 million people in this country develop sepsis annually. About 350,000 die during hospitalization or are discharged to hospice.
But new research, published in Proceedings of the National Academy of Sciences, offers hope that clinicians may one day be able to detect and treat sepsis more quickly.
The researchers broke down whole blood and dried it by heating, resulting in a solid porous structure with the bacterial DNA trapped inside. They then used chemicals – primers and enzymes – to reach inside the porous structure and amplify the target DNA.
The team was able to detect four causes of bloodstream infections – the bacteria methicillin-resistant Staphylococcus aureus (MRSA), methicillin-susceptible Staphylococcus aureus (MSSA), gram-negative Escherichia coli, and the fungal species Candida albicans. They validated their method against clinical laboratory results that used blood cultures and DNA analyses to detect sepsis.
The technique took just 2.5 hours and required roughly 1 mL of blood, according to the researchers.
“This technique can have broad applications in detection of bacterial infection and presence of bacteria in large values of blood,” Rashid Bashir, PhD, dean of the University of Illinois at Urbana-Champaign’s Grainger College of Engineering, and a co-author of the study, told this news organization.
While infection control experts and sepsis prevention advocates said the new study offers no clues about how to treat sepsis once detected, they hope the innovation eventually could save lives.
A rapid killer
Sepsis occurs when the body overreacts to an infection. The severe response can lead to tissue damage, organ failure, and death.
Thomas Heymann, MBA, president and CEO of Sepsis Alliance, an advocacy group, said mortality can rise 8% for each hour treatment is delayed.
Infants born prematurely are particularly vulnerable. Dr. Bashir and his colleagues noted that 25% of all infants admitted to the neonatal intensive care unit are diagnosed with sepsis. Of those, as many as 35% may die from infection. Sepsis is the most expensive condition treated in U.S. hospitals, accounting for $23.7 billion in costs annually, they added.
Despite high mortality rates and hospital costs, according to a Sepsis Alliance survey, only 66% of Americans are aware of the term sepsis. Only 19% can name the four primary signs of the condition: Altered body Temperature, an Infection, Mental decline, and feeling Extremely ill, or “TIME.”
Getting the appropriate antibiotics to sepsis patients quickly can greatly improve chances of survival, but Dr. Bashir said the current method of confirming the diagnosis is too slow.
Blood cultures too slow
Traditional blood cultures are among the most common methods of determining if a patient has a bloodstream infection. But the process takes about 24 hours for a culture to detect the category of bacteria and an additional day to determine exactly which bacteria is present, according to Cindy Hou, DO, infection control officer and medical director of research at Jefferson Health, Voorhees Township, New Jersey. At 72 hours, Dr. Hou said, a blood culture will finally be able to produce a “sensitivity” result, which tells doctors which antibiotics will be most effective against the pathogen.
By then, patients often are already past the point of saving. The bottom line, according to Dr. Bashir and his colleagues: Blood cultures are “too slow and cumbersome to allow for initial management of patients and thus contribute to high mortality.”
Dr. Hou called the ability to identify the type of infection in just 2.5 hours an “amazing” feat.
,” she said. “These researchers are pushing the bar for what rapid means.”
The new detection method is not yet available commercially. Dr. Bashir said he and his colleagues plan to scale their study and hope to find a way to bypass the long culture steps to identify target pathogens directly from a large volume of blood.
Dr. Hou said she believes a blood culture would still be necessary since clinicians would need sensitivity results to guide targeted treatment of infections.
“There is a lot more we need, but this paper is a call to arms for the field of rapid diagnostics to make rapid as fast as it really needs to be, but we still need to find solutions which are affordable,” Dr. Hou said.
Even without a blood culture, Dr. Bashir’s technology could improve care. Mr. Heymann said the technology could help convince clinicians worried about antibiotic resistance to prescribe treatment faster.
“We know we’re overusing antibiotics, and that’s creating a new big problem” when it comes to sepsis treatment, he said. “Getting a diagnostic read earlier is a game changer.”
Combined with a blood culture that can later confirm or help adjust the course of treatment, Dr. Hou said this new method of sepsis detection could improve care, especially in places where rapid diagnostics are not available and particularly if combined with physician education so they understand what treatment is best for various types of infection.
Mr. Heymann agreed. Sepsis Alliance also operates the Sepsis Innovation Collaborative, a group that supports public-private innovation on sepsis care.
“We’re losing someone every 90 seconds in the United States to sepsis,” Mr. Heymann said. “There is a huge opportunity to do better, and it’s this kind of innovation that is really inspiring.”
Dr. Hou is chief medical officer for Sepsis Alliance, a medical advisor for the Sepsis Innovation Collaborative, an advisor for Janssen, and a key opinion leader for T2 Biosystems. Dr. Bashir and Mr. Heymann report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sepsis is among the most feared conditions for health care providers. These blood infections strike with such rapid intensity that treating them demands a mix of both clinical skill and luck – recognizing symptoms early enough while choosing the right drug to tame the bacterial culprit before the germs have overwhelmed the body’s immune system.
All too often, sepsis wins the race. According to the U.S. Centers for Disease Control and Prevention, at least 1.7 million people in this country develop sepsis annually. About 350,000 die during hospitalization or are discharged to hospice.
But new research, published in Proceedings of the National Academy of Sciences, offers hope that clinicians may one day be able to detect and treat sepsis more quickly.
The researchers broke down whole blood and dried it by heating, resulting in a solid porous structure with the bacterial DNA trapped inside. They then used chemicals – primers and enzymes – to reach inside the porous structure and amplify the target DNA.
The team was able to detect four causes of bloodstream infections – the bacteria methicillin-resistant Staphylococcus aureus (MRSA), methicillin-susceptible Staphylococcus aureus (MSSA), gram-negative Escherichia coli, and the fungal species Candida albicans. They validated their method against clinical laboratory results that used blood cultures and DNA analyses to detect sepsis.
The technique took just 2.5 hours and required roughly 1 mL of blood, according to the researchers.
“This technique can have broad applications in detection of bacterial infection and presence of bacteria in large values of blood,” Rashid Bashir, PhD, dean of the University of Illinois at Urbana-Champaign’s Grainger College of Engineering, and a co-author of the study, told this news organization.
While infection control experts and sepsis prevention advocates said the new study offers no clues about how to treat sepsis once detected, they hope the innovation eventually could save lives.
A rapid killer
Sepsis occurs when the body overreacts to an infection. The severe response can lead to tissue damage, organ failure, and death.
Thomas Heymann, MBA, president and CEO of Sepsis Alliance, an advocacy group, said mortality can rise 8% for each hour treatment is delayed.
Infants born prematurely are particularly vulnerable. Dr. Bashir and his colleagues noted that 25% of all infants admitted to the neonatal intensive care unit are diagnosed with sepsis. Of those, as many as 35% may die from infection. Sepsis is the most expensive condition treated in U.S. hospitals, accounting for $23.7 billion in costs annually, they added.
Despite high mortality rates and hospital costs, according to a Sepsis Alliance survey, only 66% of Americans are aware of the term sepsis. Only 19% can name the four primary signs of the condition: Altered body Temperature, an Infection, Mental decline, and feeling Extremely ill, or “TIME.”
Getting the appropriate antibiotics to sepsis patients quickly can greatly improve chances of survival, but Dr. Bashir said the current method of confirming the diagnosis is too slow.
Blood cultures too slow
Traditional blood cultures are among the most common methods of determining if a patient has a bloodstream infection. But the process takes about 24 hours for a culture to detect the category of bacteria and an additional day to determine exactly which bacteria is present, according to Cindy Hou, DO, infection control officer and medical director of research at Jefferson Health, Voorhees Township, New Jersey. At 72 hours, Dr. Hou said, a blood culture will finally be able to produce a “sensitivity” result, which tells doctors which antibiotics will be most effective against the pathogen.
By then, patients often are already past the point of saving. The bottom line, according to Dr. Bashir and his colleagues: Blood cultures are “too slow and cumbersome to allow for initial management of patients and thus contribute to high mortality.”
Dr. Hou called the ability to identify the type of infection in just 2.5 hours an “amazing” feat.
,” she said. “These researchers are pushing the bar for what rapid means.”
The new detection method is not yet available commercially. Dr. Bashir said he and his colleagues plan to scale their study and hope to find a way to bypass the long culture steps to identify target pathogens directly from a large volume of blood.
Dr. Hou said she believes a blood culture would still be necessary since clinicians would need sensitivity results to guide targeted treatment of infections.
“There is a lot more we need, but this paper is a call to arms for the field of rapid diagnostics to make rapid as fast as it really needs to be, but we still need to find solutions which are affordable,” Dr. Hou said.
Even without a blood culture, Dr. Bashir’s technology could improve care. Mr. Heymann said the technology could help convince clinicians worried about antibiotic resistance to prescribe treatment faster.
“We know we’re overusing antibiotics, and that’s creating a new big problem” when it comes to sepsis treatment, he said. “Getting a diagnostic read earlier is a game changer.”
Combined with a blood culture that can later confirm or help adjust the course of treatment, Dr. Hou said this new method of sepsis detection could improve care, especially in places where rapid diagnostics are not available and particularly if combined with physician education so they understand what treatment is best for various types of infection.
Mr. Heymann agreed. Sepsis Alliance also operates the Sepsis Innovation Collaborative, a group that supports public-private innovation on sepsis care.
“We’re losing someone every 90 seconds in the United States to sepsis,” Mr. Heymann said. “There is a huge opportunity to do better, and it’s this kind of innovation that is really inspiring.”
Dr. Hou is chief medical officer for Sepsis Alliance, a medical advisor for the Sepsis Innovation Collaborative, an advisor for Janssen, and a key opinion leader for T2 Biosystems. Dr. Bashir and Mr. Heymann report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Sepsis is among the most feared conditions for health care providers. These blood infections strike with such rapid intensity that treating them demands a mix of both clinical skill and luck – recognizing symptoms early enough while choosing the right drug to tame the bacterial culprit before the germs have overwhelmed the body’s immune system.
All too often, sepsis wins the race. According to the U.S. Centers for Disease Control and Prevention, at least 1.7 million people in this country develop sepsis annually. About 350,000 die during hospitalization or are discharged to hospice.
But new research, published in Proceedings of the National Academy of Sciences, offers hope that clinicians may one day be able to detect and treat sepsis more quickly.
The researchers broke down whole blood and dried it by heating, resulting in a solid porous structure with the bacterial DNA trapped inside. They then used chemicals – primers and enzymes – to reach inside the porous structure and amplify the target DNA.
The team was able to detect four causes of bloodstream infections – the bacteria methicillin-resistant Staphylococcus aureus (MRSA), methicillin-susceptible Staphylococcus aureus (MSSA), gram-negative Escherichia coli, and the fungal species Candida albicans. They validated their method against clinical laboratory results that used blood cultures and DNA analyses to detect sepsis.
The technique took just 2.5 hours and required roughly 1 mL of blood, according to the researchers.
“This technique can have broad applications in detection of bacterial infection and presence of bacteria in large values of blood,” Rashid Bashir, PhD, dean of the University of Illinois at Urbana-Champaign’s Grainger College of Engineering, and a co-author of the study, told this news organization.
While infection control experts and sepsis prevention advocates said the new study offers no clues about how to treat sepsis once detected, they hope the innovation eventually could save lives.
A rapid killer
Sepsis occurs when the body overreacts to an infection. The severe response can lead to tissue damage, organ failure, and death.
Thomas Heymann, MBA, president and CEO of Sepsis Alliance, an advocacy group, said mortality can rise 8% for each hour treatment is delayed.
Infants born prematurely are particularly vulnerable. Dr. Bashir and his colleagues noted that 25% of all infants admitted to the neonatal intensive care unit are diagnosed with sepsis. Of those, as many as 35% may die from infection. Sepsis is the most expensive condition treated in U.S. hospitals, accounting for $23.7 billion in costs annually, they added.
Despite high mortality rates and hospital costs, according to a Sepsis Alliance survey, only 66% of Americans are aware of the term sepsis. Only 19% can name the four primary signs of the condition: Altered body Temperature, an Infection, Mental decline, and feeling Extremely ill, or “TIME.”
Getting the appropriate antibiotics to sepsis patients quickly can greatly improve chances of survival, but Dr. Bashir said the current method of confirming the diagnosis is too slow.
Blood cultures too slow
Traditional blood cultures are among the most common methods of determining if a patient has a bloodstream infection. But the process takes about 24 hours for a culture to detect the category of bacteria and an additional day to determine exactly which bacteria is present, according to Cindy Hou, DO, infection control officer and medical director of research at Jefferson Health, Voorhees Township, New Jersey. At 72 hours, Dr. Hou said, a blood culture will finally be able to produce a “sensitivity” result, which tells doctors which antibiotics will be most effective against the pathogen.
By then, patients often are already past the point of saving. The bottom line, according to Dr. Bashir and his colleagues: Blood cultures are “too slow and cumbersome to allow for initial management of patients and thus contribute to high mortality.”
Dr. Hou called the ability to identify the type of infection in just 2.5 hours an “amazing” feat.
,” she said. “These researchers are pushing the bar for what rapid means.”
The new detection method is not yet available commercially. Dr. Bashir said he and his colleagues plan to scale their study and hope to find a way to bypass the long culture steps to identify target pathogens directly from a large volume of blood.
Dr. Hou said she believes a blood culture would still be necessary since clinicians would need sensitivity results to guide targeted treatment of infections.
“There is a lot more we need, but this paper is a call to arms for the field of rapid diagnostics to make rapid as fast as it really needs to be, but we still need to find solutions which are affordable,” Dr. Hou said.
Even without a blood culture, Dr. Bashir’s technology could improve care. Mr. Heymann said the technology could help convince clinicians worried about antibiotic resistance to prescribe treatment faster.
“We know we’re overusing antibiotics, and that’s creating a new big problem” when it comes to sepsis treatment, he said. “Getting a diagnostic read earlier is a game changer.”
Combined with a blood culture that can later confirm or help adjust the course of treatment, Dr. Hou said this new method of sepsis detection could improve care, especially in places where rapid diagnostics are not available and particularly if combined with physician education so they understand what treatment is best for various types of infection.
Mr. Heymann agreed. Sepsis Alliance also operates the Sepsis Innovation Collaborative, a group that supports public-private innovation on sepsis care.
“We’re losing someone every 90 seconds in the United States to sepsis,” Mr. Heymann said. “There is a huge opportunity to do better, and it’s this kind of innovation that is really inspiring.”
Dr. Hou is chief medical officer for Sepsis Alliance, a medical advisor for the Sepsis Innovation Collaborative, an advisor for Janssen, and a key opinion leader for T2 Biosystems. Dr. Bashir and Mr. Heymann report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ED docs seek accountability for violence committed by patients
Acts of violence targeting the professionals who staff America’s emergency departments have gotten significantly worse since the COVID pandemic’s onset – with serious implications for the future provision of emergency medicine. Those are among the conclusions from a new poll conducted for the American College of Emergency Physicians and reported Sept. 22 in a virtual press briefing.
Among 2,712 physicians responding to the ACEP poll conducted from July 25 to Aug. 1, 45% said that violence in the ED has increased greatly and 40% said it has increased somewhat over the past 5 years, while 89% said they believe this violence has harmed patient care. And 55% reported that they personally had been assaulted in the ED – some of them on a weekly or more frequent basis.
That number is up from 49% in a similar poll conducted for ACEP in 2018. One-third (33%) of respondents said they were injured on the job from a workplace assault, up from 27% in 2018. Reported incidents include verbal assaults with the threat of violence as well as being hit, slapped, spit on, punched, kicked, scratched or bit, sexual assaults, and assaults with a weapon like a knife or gun.
Doctors often describe personal encounters that illustrate the survey results. Alex Skog, MD, an emergency physician in Oregon City and president-elect of ACEP’s Oregon state chapter, said that when he was asked to speak at the press briefing, he started reviewing past violent incidents from his own career. But in the weeks leading up to the briefing, two more horrific incidents occurred, highlighting how dire the situation has become for emergency personnel.
“Few memories are more painful to me than an evening about a month ago when an intoxicated patient started roaming down the halls, out of sight of nursing staff due to overcrowding,” Dr. Skog related at the press briefing. “I heard a scream. I was the second person into the room next door. I saw the male patient on the ground straddling a nurse I work with and repeatedly punching her in the head. I wrestled him off and was quickly joined by other staff,” he said.
“I consider the staff I work with not just colleagues but close friends. ... Emergency medicine is hemorrhaging doctors, nurses, and techs who can no longer accept the violence they experience daily. Violent incidents like these contribute to increased rates of burnout, turnover, and mental health issues for ED professionals.
A paralyzed ED
Dr. Skog described another very recent incident where an agitated patient, brought in by ambulance after an intervention involving multiple police and restraints to prevent him from attacking the paramedics transporting him, charged an ED technician, tearing his shirt and wrestling him to the ground.
While the physical trauma that results from events like this is unacceptable, other effects may be less obvious, Dr. Skog said. His department was essentially paralyzed by the turmoil in its ability to care for other emergency patients and had to go on ambulance diversion for several hours, causing delays in the treatment of other critically ill patients.
“The average emergency department clinician is well aware that violence today is completely different than it was 5 years ago, and this survey quantifies that,” Dr. Skog said. Clinicians need to understand how important it is to share their stories and get the word out. ED professionals often fail to report violent incidents because of the belief that nothing will be done about it.
“But without us making it known to everyone, it will be harder to call stakeholders to account to address the problem.” Those stakeholders include hospital administrators, law enforcement, and legislators, Dr. Skog added. “We need to find appropriate venues for holding the people who knowingly assault health care workers accountable.”
Legislative solutions proposed
Two bills now in Congress are designed to address the problem of ED violence. While it is late in the legislative season of an election year, ACEP is encouraging legislators to include ED violence as a component of any larger conversation about mental health, patients, and physicians.
The Workplace Violence Prevention Act for Health Care and Social Service Workers, H.R. 1195, which passed the House in 2021 and was introduced in the Senate by Sen. Tammy Baldwin (D-Wisc.), was highlighted in a press conference on the Senate lawn in May, cosponsored by ACEP and the Emergency Nurses Association (ED nurses may have even higher rates of violence on the job). It calls on the Occupational Safety and Health Administration to require employers in health care and social services to establish workplace violence prevention plans in accordance with OSHA’s 2016 “Guidelines for Preventing Workplace Violence for Healthcare and Social Service Workers.”
This bill is supported by the American Public Health Association, although the American Hospital Association opposes it based on increased costs for hospitals. AHA has stated that hospitals already strive to prevent violence in the workplace, although ACEP’s new study reinforces how this is not sufficient.
A recent article in Security suggests that hospitals could start implementing the features of H.R. 1195 even before it becomes law, given its important implications for hospital bottom lines, absenteeism, turnover, and morale.
A second bill, the Safety from Violence for Healthcare Employees Act, H.R. 7961, introduced in June by Rep. Madeleine Dean (D-Pa.) and Rep. Larry Bucshon, MD, (R-Ind.), would create federal penalties for violence against health care workers, similar to protections now in place for airport and airline personnel.
Violence’s vicious cycle
“This type of legislation is urgently needed to ensure the safety of all health care providers,” said Robert Glatter, MD, an emergency physician at Lenox Hill Hospital, New York.
“ED violence creates a vicious cycle affecting not only the long-term mental and physical health, but overall well-being and security of health care workers,” Dr. Glatter said in an interview. “It ultimately impacts their ability to perform their jobs in a confident and competent manner. The bottom line is that much more needs to be done to ensure that every member of the team in the ED can make patient care a priority, as opposed to worry and concerns about their own safety.”
The pandemic seriously eroded trust between patients and providers, Dr. Glatter said. This loss of trust is harmful not only to patient care, but to the long-term health and compliance of patients overall. It makes addressing the epidemic of ED violence crucial to all stakeholders, healthcare providers and patients alike.”
Experienced clinicians have a sense of what triggers patients to an act of violence, although that understanding may not help in a fast-moving crisis, Dr. Skog said. In addition to the lack of trust between patients and clinicians, frustrations over delays in treatment, obvious agitation, intoxication, and drug-seeking behavior may be warning signs. “I can see patients’ past violent behavior red-flagged in their chart, but they are still assaulting us.”
What else could help? More use of metal detectors and the 24-hour presence of security personnel able to rapidly respond to escalating situations can be great tools in specific situations, he said. But EDs vary widely in size and setting. Another tool is an emergency device that can alert the entire department in a crisis.
But for Dr. Skog, one of the most important responses is to actually hold patients accountable for their acts of violence – to report them to the police and the criminal justice system. According to the new poll, hospital security departments pressed charges for such incidents a mere 2% of the time.
In Oregon, it now is merely a misdemeanor to assault a hospital worker, he said. A bill proposing to change that just died in the state legislature.
ACEP engaged Marketing General Incorporated to replicate a brief polling survey originally conducted in 2018. Dr. Skog and Dr. Glatter disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Acts of violence targeting the professionals who staff America’s emergency departments have gotten significantly worse since the COVID pandemic’s onset – with serious implications for the future provision of emergency medicine. Those are among the conclusions from a new poll conducted for the American College of Emergency Physicians and reported Sept. 22 in a virtual press briefing.
Among 2,712 physicians responding to the ACEP poll conducted from July 25 to Aug. 1, 45% said that violence in the ED has increased greatly and 40% said it has increased somewhat over the past 5 years, while 89% said they believe this violence has harmed patient care. And 55% reported that they personally had been assaulted in the ED – some of them on a weekly or more frequent basis.
That number is up from 49% in a similar poll conducted for ACEP in 2018. One-third (33%) of respondents said they were injured on the job from a workplace assault, up from 27% in 2018. Reported incidents include verbal assaults with the threat of violence as well as being hit, slapped, spit on, punched, kicked, scratched or bit, sexual assaults, and assaults with a weapon like a knife or gun.
Doctors often describe personal encounters that illustrate the survey results. Alex Skog, MD, an emergency physician in Oregon City and president-elect of ACEP’s Oregon state chapter, said that when he was asked to speak at the press briefing, he started reviewing past violent incidents from his own career. But in the weeks leading up to the briefing, two more horrific incidents occurred, highlighting how dire the situation has become for emergency personnel.
“Few memories are more painful to me than an evening about a month ago when an intoxicated patient started roaming down the halls, out of sight of nursing staff due to overcrowding,” Dr. Skog related at the press briefing. “I heard a scream. I was the second person into the room next door. I saw the male patient on the ground straddling a nurse I work with and repeatedly punching her in the head. I wrestled him off and was quickly joined by other staff,” he said.
“I consider the staff I work with not just colleagues but close friends. ... Emergency medicine is hemorrhaging doctors, nurses, and techs who can no longer accept the violence they experience daily. Violent incidents like these contribute to increased rates of burnout, turnover, and mental health issues for ED professionals.
A paralyzed ED
Dr. Skog described another very recent incident where an agitated patient, brought in by ambulance after an intervention involving multiple police and restraints to prevent him from attacking the paramedics transporting him, charged an ED technician, tearing his shirt and wrestling him to the ground.
While the physical trauma that results from events like this is unacceptable, other effects may be less obvious, Dr. Skog said. His department was essentially paralyzed by the turmoil in its ability to care for other emergency patients and had to go on ambulance diversion for several hours, causing delays in the treatment of other critically ill patients.
“The average emergency department clinician is well aware that violence today is completely different than it was 5 years ago, and this survey quantifies that,” Dr. Skog said. Clinicians need to understand how important it is to share their stories and get the word out. ED professionals often fail to report violent incidents because of the belief that nothing will be done about it.
“But without us making it known to everyone, it will be harder to call stakeholders to account to address the problem.” Those stakeholders include hospital administrators, law enforcement, and legislators, Dr. Skog added. “We need to find appropriate venues for holding the people who knowingly assault health care workers accountable.”
Legislative solutions proposed
Two bills now in Congress are designed to address the problem of ED violence. While it is late in the legislative season of an election year, ACEP is encouraging legislators to include ED violence as a component of any larger conversation about mental health, patients, and physicians.
The Workplace Violence Prevention Act for Health Care and Social Service Workers, H.R. 1195, which passed the House in 2021 and was introduced in the Senate by Sen. Tammy Baldwin (D-Wisc.), was highlighted in a press conference on the Senate lawn in May, cosponsored by ACEP and the Emergency Nurses Association (ED nurses may have even higher rates of violence on the job). It calls on the Occupational Safety and Health Administration to require employers in health care and social services to establish workplace violence prevention plans in accordance with OSHA’s 2016 “Guidelines for Preventing Workplace Violence for Healthcare and Social Service Workers.”
This bill is supported by the American Public Health Association, although the American Hospital Association opposes it based on increased costs for hospitals. AHA has stated that hospitals already strive to prevent violence in the workplace, although ACEP’s new study reinforces how this is not sufficient.
A recent article in Security suggests that hospitals could start implementing the features of H.R. 1195 even before it becomes law, given its important implications for hospital bottom lines, absenteeism, turnover, and morale.
A second bill, the Safety from Violence for Healthcare Employees Act, H.R. 7961, introduced in June by Rep. Madeleine Dean (D-Pa.) and Rep. Larry Bucshon, MD, (R-Ind.), would create federal penalties for violence against health care workers, similar to protections now in place for airport and airline personnel.
Violence’s vicious cycle
“This type of legislation is urgently needed to ensure the safety of all health care providers,” said Robert Glatter, MD, an emergency physician at Lenox Hill Hospital, New York.
“ED violence creates a vicious cycle affecting not only the long-term mental and physical health, but overall well-being and security of health care workers,” Dr. Glatter said in an interview. “It ultimately impacts their ability to perform their jobs in a confident and competent manner. The bottom line is that much more needs to be done to ensure that every member of the team in the ED can make patient care a priority, as opposed to worry and concerns about their own safety.”
The pandemic seriously eroded trust between patients and providers, Dr. Glatter said. This loss of trust is harmful not only to patient care, but to the long-term health and compliance of patients overall. It makes addressing the epidemic of ED violence crucial to all stakeholders, healthcare providers and patients alike.”
Experienced clinicians have a sense of what triggers patients to an act of violence, although that understanding may not help in a fast-moving crisis, Dr. Skog said. In addition to the lack of trust between patients and clinicians, frustrations over delays in treatment, obvious agitation, intoxication, and drug-seeking behavior may be warning signs. “I can see patients’ past violent behavior red-flagged in their chart, but they are still assaulting us.”
What else could help? More use of metal detectors and the 24-hour presence of security personnel able to rapidly respond to escalating situations can be great tools in specific situations, he said. But EDs vary widely in size and setting. Another tool is an emergency device that can alert the entire department in a crisis.
But for Dr. Skog, one of the most important responses is to actually hold patients accountable for their acts of violence – to report them to the police and the criminal justice system. According to the new poll, hospital security departments pressed charges for such incidents a mere 2% of the time.
In Oregon, it now is merely a misdemeanor to assault a hospital worker, he said. A bill proposing to change that just died in the state legislature.
ACEP engaged Marketing General Incorporated to replicate a brief polling survey originally conducted in 2018. Dr. Skog and Dr. Glatter disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Acts of violence targeting the professionals who staff America’s emergency departments have gotten significantly worse since the COVID pandemic’s onset – with serious implications for the future provision of emergency medicine. Those are among the conclusions from a new poll conducted for the American College of Emergency Physicians and reported Sept. 22 in a virtual press briefing.
Among 2,712 physicians responding to the ACEP poll conducted from July 25 to Aug. 1, 45% said that violence in the ED has increased greatly and 40% said it has increased somewhat over the past 5 years, while 89% said they believe this violence has harmed patient care. And 55% reported that they personally had been assaulted in the ED – some of them on a weekly or more frequent basis.
That number is up from 49% in a similar poll conducted for ACEP in 2018. One-third (33%) of respondents said they were injured on the job from a workplace assault, up from 27% in 2018. Reported incidents include verbal assaults with the threat of violence as well as being hit, slapped, spit on, punched, kicked, scratched or bit, sexual assaults, and assaults with a weapon like a knife or gun.
Doctors often describe personal encounters that illustrate the survey results. Alex Skog, MD, an emergency physician in Oregon City and president-elect of ACEP’s Oregon state chapter, said that when he was asked to speak at the press briefing, he started reviewing past violent incidents from his own career. But in the weeks leading up to the briefing, two more horrific incidents occurred, highlighting how dire the situation has become for emergency personnel.
“Few memories are more painful to me than an evening about a month ago when an intoxicated patient started roaming down the halls, out of sight of nursing staff due to overcrowding,” Dr. Skog related at the press briefing. “I heard a scream. I was the second person into the room next door. I saw the male patient on the ground straddling a nurse I work with and repeatedly punching her in the head. I wrestled him off and was quickly joined by other staff,” he said.
“I consider the staff I work with not just colleagues but close friends. ... Emergency medicine is hemorrhaging doctors, nurses, and techs who can no longer accept the violence they experience daily. Violent incidents like these contribute to increased rates of burnout, turnover, and mental health issues for ED professionals.
A paralyzed ED
Dr. Skog described another very recent incident where an agitated patient, brought in by ambulance after an intervention involving multiple police and restraints to prevent him from attacking the paramedics transporting him, charged an ED technician, tearing his shirt and wrestling him to the ground.
While the physical trauma that results from events like this is unacceptable, other effects may be less obvious, Dr. Skog said. His department was essentially paralyzed by the turmoil in its ability to care for other emergency patients and had to go on ambulance diversion for several hours, causing delays in the treatment of other critically ill patients.
“The average emergency department clinician is well aware that violence today is completely different than it was 5 years ago, and this survey quantifies that,” Dr. Skog said. Clinicians need to understand how important it is to share their stories and get the word out. ED professionals often fail to report violent incidents because of the belief that nothing will be done about it.
“But without us making it known to everyone, it will be harder to call stakeholders to account to address the problem.” Those stakeholders include hospital administrators, law enforcement, and legislators, Dr. Skog added. “We need to find appropriate venues for holding the people who knowingly assault health care workers accountable.”
Legislative solutions proposed
Two bills now in Congress are designed to address the problem of ED violence. While it is late in the legislative season of an election year, ACEP is encouraging legislators to include ED violence as a component of any larger conversation about mental health, patients, and physicians.
The Workplace Violence Prevention Act for Health Care and Social Service Workers, H.R. 1195, which passed the House in 2021 and was introduced in the Senate by Sen. Tammy Baldwin (D-Wisc.), was highlighted in a press conference on the Senate lawn in May, cosponsored by ACEP and the Emergency Nurses Association (ED nurses may have even higher rates of violence on the job). It calls on the Occupational Safety and Health Administration to require employers in health care and social services to establish workplace violence prevention plans in accordance with OSHA’s 2016 “Guidelines for Preventing Workplace Violence for Healthcare and Social Service Workers.”
This bill is supported by the American Public Health Association, although the American Hospital Association opposes it based on increased costs for hospitals. AHA has stated that hospitals already strive to prevent violence in the workplace, although ACEP’s new study reinforces how this is not sufficient.
A recent article in Security suggests that hospitals could start implementing the features of H.R. 1195 even before it becomes law, given its important implications for hospital bottom lines, absenteeism, turnover, and morale.
A second bill, the Safety from Violence for Healthcare Employees Act, H.R. 7961, introduced in June by Rep. Madeleine Dean (D-Pa.) and Rep. Larry Bucshon, MD, (R-Ind.), would create federal penalties for violence against health care workers, similar to protections now in place for airport and airline personnel.
Violence’s vicious cycle
“This type of legislation is urgently needed to ensure the safety of all health care providers,” said Robert Glatter, MD, an emergency physician at Lenox Hill Hospital, New York.
“ED violence creates a vicious cycle affecting not only the long-term mental and physical health, but overall well-being and security of health care workers,” Dr. Glatter said in an interview. “It ultimately impacts their ability to perform their jobs in a confident and competent manner. The bottom line is that much more needs to be done to ensure that every member of the team in the ED can make patient care a priority, as opposed to worry and concerns about their own safety.”
The pandemic seriously eroded trust between patients and providers, Dr. Glatter said. This loss of trust is harmful not only to patient care, but to the long-term health and compliance of patients overall. It makes addressing the epidemic of ED violence crucial to all stakeholders, healthcare providers and patients alike.”
Experienced clinicians have a sense of what triggers patients to an act of violence, although that understanding may not help in a fast-moving crisis, Dr. Skog said. In addition to the lack of trust between patients and clinicians, frustrations over delays in treatment, obvious agitation, intoxication, and drug-seeking behavior may be warning signs. “I can see patients’ past violent behavior red-flagged in their chart, but they are still assaulting us.”
What else could help? More use of metal detectors and the 24-hour presence of security personnel able to rapidly respond to escalating situations can be great tools in specific situations, he said. But EDs vary widely in size and setting. Another tool is an emergency device that can alert the entire department in a crisis.
But for Dr. Skog, one of the most important responses is to actually hold patients accountable for their acts of violence – to report them to the police and the criminal justice system. According to the new poll, hospital security departments pressed charges for such incidents a mere 2% of the time.
In Oregon, it now is merely a misdemeanor to assault a hospital worker, he said. A bill proposing to change that just died in the state legislature.
ACEP engaged Marketing General Incorporated to replicate a brief polling survey originally conducted in 2018. Dr. Skog and Dr. Glatter disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nifedipine during labor controls BP in severe preeclampsia
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Women with preeclampsia with severe features benefit from treatment with oral nifedipine during labor and delivery, results of a randomized controlled trial suggest.
The study showed that intrapartum administration of extended-release oral nifedipine was safe and reduced the need for acute intravenous or immediate-release oral hypertensive therapy. There was a trend toward fewer cesarean deliveries and less need for neonatal intensive care.
The results suggest that providers “consider initiating long-acting nifedipine every 24 hours for individuals with preeclampsia with severe features who are undergoing induction of labor,” Erin M. Cleary, MD, with the Ohio State University, Columbus, told this news organization.
“There is no need to wait until patients require one or more doses of acute [antihypertensive] therapy before starting long-acting nifedipine, as long as they otherwise meet criteria for preeclampsia with severe features,” Dr. Cleary said.
The study was published online in Hypertension.
Clear benefits for mom and baby
Preeclampsia complicates up to 8% of pregnancies and often leads to significant maternal and perinatal morbidity.
“We know that bringing down very high blood pressure to a safer range will help prevent maternal and fetal complications. However, besides rapid-acting, intravenous medicines for severe hypertension during pregnancy, optimal management for hypertension during the labor and delivery process has not been studied,” Dr. Cleary explains in a news release.
In a randomized, triple-blind, placebo-controlled study, the researchers assessed whether treatment with long-acting nifedipine could prevent severe hypertension in women with a singleton or twin gestation and preeclampsia with severe features, as defined according to American College of Obstetrics and Gynecology criteria.
During induction of labor between 22 and 41 weeks’ gestation, 55 women were assigned to 30-mg oral extended-release nifedipine, and 55 received matching placebo, administered every 24 hours until delivery.
The primary outcome was receipt of one or more doses of acute hypertension therapy for blood pressure of at least 160/110 mm Hg that was sustained for 10 minutes or longer.
The primary outcome occurred in significantly fewer women in the nifedipine group than in the placebo group (34% vs. 55%; relative risk, 0.62; 95% CI, 0.39-0.97; number needed to treat, 4.7).
Fewer women in the nifedipine group than in the placebo group required cesarean delivery, although this difference did not meet statistical significance (21% vs. 35%; RR, 0.60; 95% CI, 0.31-1.15).
There was no between-group difference in the rate of hypotensive episodes, including symptomatic hypotension requiring phenylephrine for pressure support following neuraxial anesthesia (9.4% vs. 8.2%; RR, 1.15; 95% CI, 0.33-4.06).
After delivery, there was no difference in the rate of persistently severe blood pressure that required acute therapy and maintenance therapy at time of discharge home.
Birth weight and rates of births of neonates who were small for gestational age were similar in the two groups. There was a trend for decreased rates of neonatal intensive care unit admission among infants born to mothers who received nifedipine (29% vs. 47%; RR, 0.62; 95% CI, 0.37-1.02).
The neonatal composite outcome was also similar between the nifedipine group and the placebo group (36% vs. 41%; RR, 0.83; 95% CI, 0.51-1.37). The composite outcome included Apgar score of less than 7 at 5 minutes, hyperbilirubinemia requiring phototherapy, hypoglycemia requiring intravenous therapy, or supplemental oxygen therapy beyond the first 24 hours of life.
“Our findings support the growing trend in more active management of hypertension in pregnancy with daily maintenance medications,” Dr. Cleary and colleagues note in their article.
“Even in the absence of preeclampsia, emerging research suggests pregnant individuals may benefit from initiating and titrating antihypertensive therapy at goals similar to the nonobstetric population,” they add.
Potentially practice changing
Reached for comment, Vesna Garovic, MD, PhD, with Mayo Clinic, Rochester, Minn., said that this is an “important initial paper to start a very important conversation about blood pressure treatment goals in preeclampsia.”
Dr. Garovic noted that for chronic hypertension in pregnancy, the blood pressure treatment goal is now less than or equal to 140/90 mm Hg.
“However, this does not apply to preeclampsia, where quite high blood pressures, such 160/110 mm Hg or higher, are still allowed before treatment is considered,” Dr. Garovic said.
“This study shows that as soon as you reach that level, treatment with oral nifedipine should be initiated and that timely initiation of oral nifedipine may optimize blood pressure control and decrease the need for intravenous therapy subsequently, and that has good effects on the mother without adversely affecting the baby,” Dr. Garovic said.
“This is potentially practice changing,” Dr. Garovic added. “But the elephant in the room is the question of why we are waiting for blood pressure to reach such dangerous levels before initiating treatment, and whether initiating treatment at a blood pressure of 140/90 or higher may prevent blood pressure reaching these high levels and women developing complications that are the consequence of severe hypertension.”
The study was funded by the Ohio State University’s Department of Obstetrics and Gynecology. Dr. Cleary and Dr. Garovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
Too old to practice medicine?
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Unlike for many other professions, there is no age limit for practicing medicine. According to international standards, airplane pilots, for example, who are responsible for the safety of many human lives, must retire by the age of 60 if they work alone, or 65 if they have a copilot. In Brazil, however, this age limit does not exist for pilots or physicians.
The only restriction on professional practice within the medical context is the mandatory retirement imposed on medical professors who teach at public (state and federal) universities, starting at the age of 75. Nevertheless, these professionals can continue practicing administrative and research-related activities. After “expulsion,” as this mandatory retirement is often called, professors who stood out or contributed to the institution and science may receive the title of professor emeritus.
In the private sector, age limits are not formally set, but the hiring of middle-aged professionals is limited.
At the Heart Institute of the University of São Paulo (Brazil) School of Medicine Clinical Hospital (InCor/HCFMUSP), one of the world’s largest teaching and research centers for cardiovascular and pulmonary diseases, several octogenarian specialists lead studies and teams. One of these is Noedir Stolf, MD, an 82-year-old cardiovascular surgeon who operates almost every day and coordinates studies on transplants, mechanical circulatory support, and aortic surgery. There is also Protásio Lemos da Luz, MD, an 82-year-old clinical cardiologist who guides research on subjects including atherosclerosis, the endothelium, microbiota, and diabetes. The protective effect of wine on atherosclerosis is one of his best-known studies.
No longer working is also not in the cards for Angelita Habr-Gama, MD, who, at 89 years old, is one of the oldest physicians in current practice. With a career spanning more than 7 decades, she is a world reference in coloproctology. She was the first woman to become a surgical resident at the HCFMUSP, where she later founded the coloproctology specialty and created the first residency program for the specialty. In April 2022, Dr. Habr-Gama joined the ranks of the 100 most influential scientists in the world, nominated by researchers at Stanford (Calif.) University, and published in PLOS Biology.
In 2020, she was sedated, intubated, and hospitalized in the intensive care unit of the Oswaldo Cruz German Hospital for 54 days because of a SARS-CoV-2 infection. After her discharge, she went back to work in less than 10 days – and added chess classes to her routine. “To get up and go to work makes me very happy. Work is my greatest hobby. No one has ever heard me complain about my life,” Dr. Habr-Gama told this news organization after having rescheduled the interview twice because of emergency surgeries.
“Doctors have a professional longevity that does not exist for other professions in which the person retires and stops practicing their profession or goes on to do something else for entertainment. Doctors can retire from one place of employment or public practice and continue practicing medicine in the office as an administrator or consultant,” Ângelo Vattimo, first secretary of the state of São Paulo Regional Board of Medicine (CREMESP), stated. The board regularly organizes a ceremony to honor professionals who have been practicing for 50 years, awarding them a certificate and engraved medal. “Many of them are around 80 years old, working and teaching. This always makes us very happy. What profession has such exceptional compliance for so long?” said Mr. Vattimo.
In the medical field, the older the age range, the smaller the number of women. According to the 2020 Medical Demographics in Brazil survey, only 2 out of 10 practicing professionals older than 70 are women.
Not everyone over 80 has Dr. Habr-Gama’s vitality, because the impact of aging is not equal. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” stated Mark Katlic, MD, chief of surgery at LifeBridge Health System in the United States, who has dedicated his life to studying the subject. Dr. Katlic spoke on the subject in an interview that was published in the article “How Old Is Too Old to Work as a Doctor?” published by this news organization in April of 2022. The article discusses the evaluations of elderly physicians’ skills and competences that U.S. companies conduct. The subject has been leading to profound debate.
Dr. Katlic defends screening programs for elderly physicians, which already are in effect at the company for which he works, LifeBridge Health, and various others in the United States. “We do [screen elderly physicians at LifeBridge Health], and so do a few dozen other [U.S. institutions], but there are hundreds [of health care institutions] that do not conduct this screening,” he pointed out.
Age-related assessment faces great resistance in the United States. One physician who is against the initiative is Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist affiliated with Stanford (Calif.) University Health. “It’s age discrimination ... Physicians [in the United States] receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as physicians reach a certain age,” Dr. Stockdale told this news organization.
The U.S. initiative of instituting physician assessment programs for those of a certain age has even been tested in court. According to an article published in Medscape, “in New Haven, Connecticut, for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory late career practitioner policy.”
Also, according to the article, a similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
In Brazil, the subject is of interest to more than 34,571 physicians between 65 and 69 years of age and 34,237 physicians older than 70. In all, this population represents approximately 14.3% of the country’s active workforce, according to the 2020 Medical Demographics in Brazil survey.
The significant participation of health care professionals over age 50 in a survey conducted by this news organization to learn what physicians think about the age limit for practicing their professions is evidence that the subject is a present concern. Of a total of 1,641 participants, 57% were age 60 or older, 17% were between 50 and 59 years, and 12% were between 40 and 49 years. Among all participants, 51% were against these limitations, 17% approved of the idea for all specialties, and 32% believed the restriction was appropriate only for some specialties. Regarding the possibility of older physicians undergoing regular assessments, the opinions were divided: Thirty-one percent thought they should be assessed in all specialties. Furthermore, 31% believed that cognitive abilities should be regularly tested in all specialties, 31% thought this should take place for some specialties, and 38% were against this approach.
Professionals want to know, for example, how (and whether) advanced age can interfere with performance, what are the competences required to practice their activities, and if the criteria vary by specialty. “A psychiatrist doesn’t have to have perfect visual acuity, as required from a dermatologist, but it is important that they have good hearing, for example,” argued Clóvis Constantino, MD, former president of the São Paulo Regional Medical Board (CRM-SP) and former vice president of the Brazilian Federal Medical Board (CFM). “However, a surgeon has to stand for several hours in positions that may be uncomfortable. It’s not easy,” he told this news organization.
In the opinion of 82-year-old Henrique Klajner, MD, the oldest pediatrician in practice at the Albert Einstein Israeli Hospital in São Paulo, the physician cannot be subjected to the types of evaluations that have been applied in the United States. “Physicians should conduct constant self-evaluations to see if they have the competences and skills needed to practice their profession ... Moreover, this is not a matter of age. It is a matter of ethics,” said Dr. Klajner.
The ability to adapt to change and implement innovation is critical to professional longevity, he said. “Nowadays, when I admit patients, I no longer do hospital rounds, which requires a mobility equal to physical abuse for me. Therefore, I work with physicians who take care of my hospitalized patients.”
Dr. Klajner also feels there is a distinction between innovations learned through studies and what can be offered safely to patients. “If I have to care for a hospitalized patient with severe pneumonia, for example, since I am not up to date in this specialty, I am going to call upon a pulmonologist I trust and forgo my honorarium for this admission. But I will remain on the team, monitoring the patient’s progression,” he said.
During the COVID-19 pandemic, Dr. Klajner stopped seeing patients in person under the recommendation of his son, Sidney Klajner, MD, also a physician. The elder Dr. Klajner began exploring telemedicine, which opened a whole new world of possibilities. “I have conducted several online visits to provide educational instruction to mothers returning home post delivery, for example,” he told this news organization. The time to stop is not something that concerns Dr. Klajner. “I’m only going to stop when I have a really important reason to do so. For example, if I can no longer write or study, reading and rereading an article without being able to understand what is being said. At this time, none of that is happening.”
In the United States, as well as in Brazil, physicians rarely provide information to human resources departments on colleagues showing signs of cognitive or motor decline affecting their professional performance. “The expectation is that health care professionals will report colleagues with cognitive impairments, but that often does not happen,” Dr. Katlic said.
It is also not common for professionals to report their own deficits to their institutions. In large part, this is caused by a lack of well-defined policies for dealing with this issue. This news organization sought out several public and private hospitals in Brazil to see if there is any guidance on professional longevity: Most said that there is not. Only the A. C. Camargo Cancer Center reported, through its public relations team, that a committee is discussing the subject but that it is still in the early stages.
Brazilian specialist associations do not offer guidelines or instructions on the various aspects of professional longevity. Dr. Constantino tried to put the subject on the agenda during the years in which he was an administrator with the CFM. “We tried to open up discussions regarding truly elderly physicians, but the subject was not well received. I believe that it is precisely because there is a tradition of physicians working until they are no longer able that this is more difficult in Brazil ... No one exactly knows what to do in this respect.” Dr. Constantino is against the use of age as a criterion for quitting practice.
“Of course, this is a point that has to be considered, but I always defended the need for regular assessment of physicians, regardless of age range. And, although assessments are always welcome, in any profession, I also believe this would not be well received in Brazil.” He endorses an assessment of one’s knowledge and not of physical abilities, which are generally assessed through investigation when needed.
The absence of guidelines increases individual responsibility, as well as vulnerability. “Consciously, physicians will not put patients at risk if they do not have the competence to care for them or to perform a surgical procedure,” said Clystenes Odyr Soares Silva, MD, PhD, adjunct professor of pulmonology of the Federal University of São Paulo (Brazil) School of Medicine (UNIFESP). “Your peers will tell you if you are no longer able,” he added. The problem is that physicians rarely admit to or talk about their colleagues’ deficits, especially if they are in the spotlight because of advanced age. In this situation, the observation and opinion of family members regarding the health care professional’s competences and skills will hold more weight.
In case of health-related physical impairment, such as partial loss of hand movement, for example, “it is expected that this will set off an ethical warning in the person,” said Dr. Constantino. When this warning does not occur naturally, patients or colleagues can report the professional, and this may lead to the opening of an administrative investigation. If the report is found to be true, this investigation is used to suspend physicians who do not have the physical or mental ability to continue practicing medicine.
“If it’s something very serious, the physician’s license can be temporarily suspended while [the physician] is treated by a psychiatrist, with follow-up by the professional board. When discharged, the physician will get his or her [professional] license back and can go back to work,” Dr. Constantino explained. If an expert evaluation is needed, the physician will then be assessed by a forensic psychiatrist. One of the most in-demand forensic psychiatrists in Brazil is Guido Arturo Palomba, MD, 73 years old. “I have assessed some physicians for actions reported to see if they were normal people or not, but never for circumstances related to age,” Dr. Palomba said.
In practice, Brazilian medical entities do not have policies or programs to guide physicians who wish to grow old while they work or those who have started to notice they are not performing as they used to. “We have never lived as long; therefore, the quality of life in old age, as well as the concept of aging, are some of the most relevant questions of our time. These are subjects requiring additional discussion, broadening understanding and awareness in this regard,” observed Mr. Vattimo.
Dr. Constantino and Dr. Silva, who are completely against age-based assessments, believe that recertification of the specialist license every 5 years is the best path to confirming whether the physician is still able to practice. “A knowledge-based test every 5 years to recertify the specialist license has often been a topic of conversation. I think it’s an excellent idea. The person would provide a dossier of all they have done in terms of courses, conferences, and other activities, present it, and receive a score,” said Dr. Silva.
In practice, recertification of the specialist license is a topic of discussion that has been raised for years, and it is an idea that the Brazilian Medical Association (AMB) defends. In conjunction with the CFM, the association is studying a way to best implement this assessment. “It’s important to emphasize that this measure would not be retroactive at first. Instead, it would only be in effect for professionals licensed after the recertification requirement is established,” the AMB pointed out in a note sent to this news organization. Even so, the measure has faced significant resistance from a faction of the profession, and its enactment does not seem to be imminent.
The debate regarding professional longevity is taking place in various countries. In 2021, the American Medical Association Council on Medical Education released a report with a set of guidelines for the screening and assessment of physicians. The document is the product of a committee created in 2015 to study the subject. The AMA recommends that the assessment of elderly physicians be based on evidence and ethical, relevant, fair, equitable, transparent, verifiable, nonexhaustive principles, contemplating support and protecting against legal proceedings. In April of this year, a new AMA document highlighted the same principles.
Also in the United States, one of oldest initiatives created to support physicians in the process of recycling, the University of California San Diego Physician Assessment and Clinical Education Program (PACE), has a section focusing on the extended practice of medicine (Practicing Medicine Longer). For those wanting to learn more about discussions on this subject, there are online presentations on experiences in Quebec and Ontario with assessing aging physicians, neuropsychological perspectives on the aging medical population, and what to expect of healthy aging, among other subjects.
Created in 1996, PACE mostly provides services to physicians who need to address requirements of the state medical boards. Few physicians enroll on their own.
The first part of the program assesses knowledge and skills over approximately 2 days. In the second phase, the physician participates in a series of activities in a corresponding residency program. Depending on the results, the physician may have to go through a remedial program with varying activities to deal with performance deficiencies to clinical experiences at the residency level.
A version of this article first appeared on Medscape.com.
Salt pills for patients with acute decompensated heart failure?
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.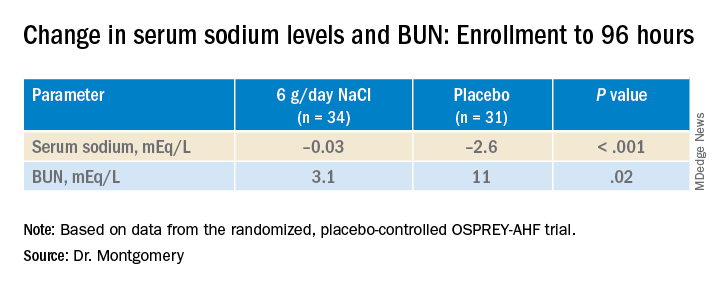
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.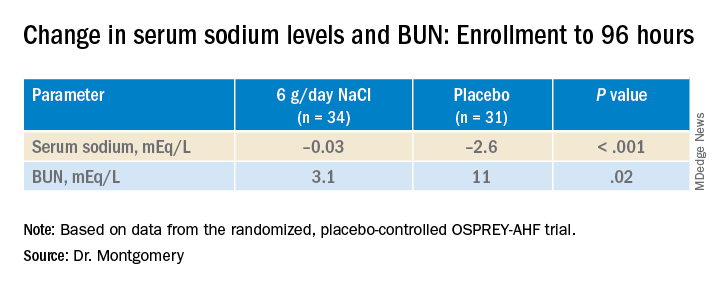
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.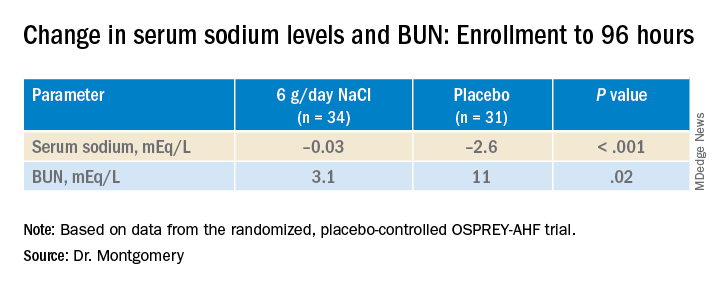
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HFSA 2022
Malaria vaccine gets special delivery by tiny health personnel
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Children and COVID: Weekly cases dropped by 57% in September
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.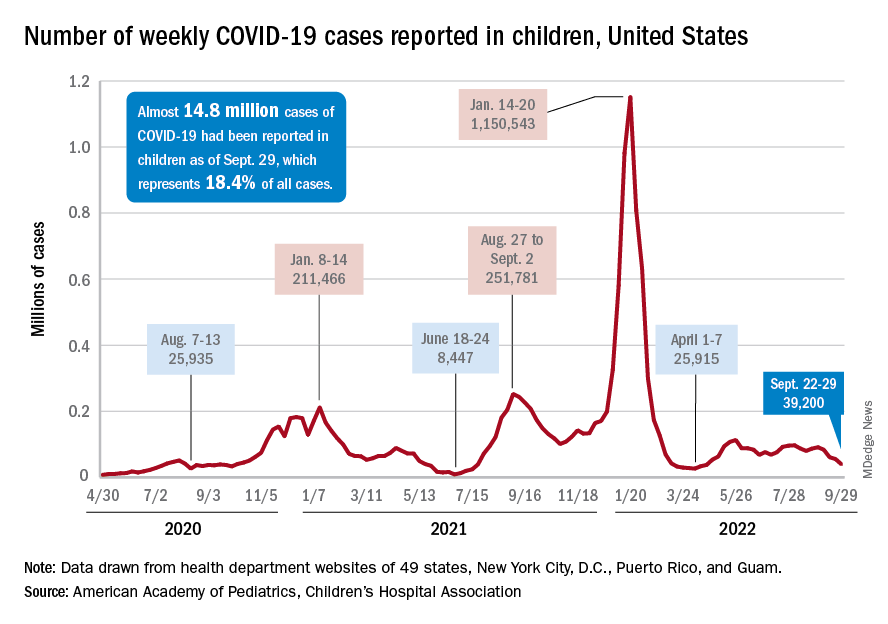
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.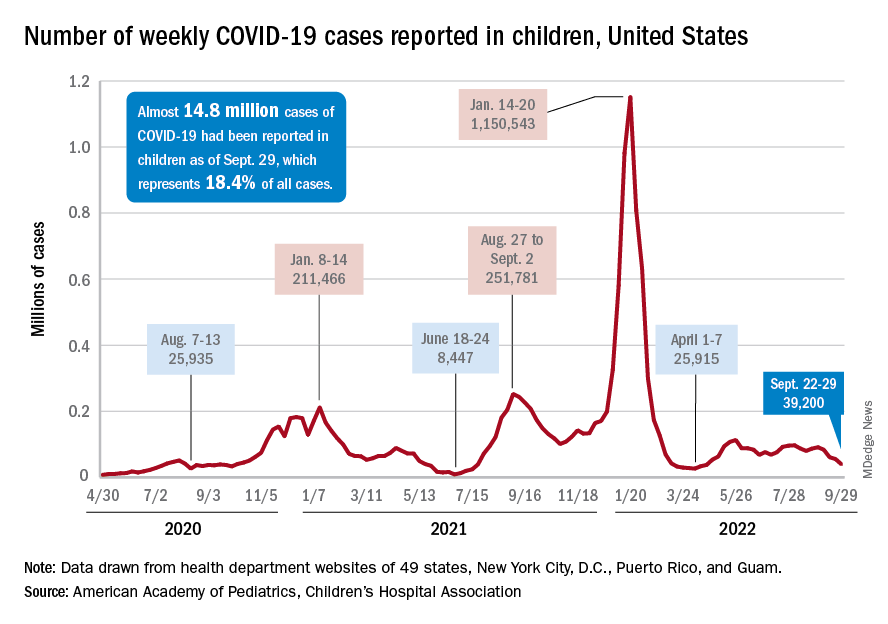
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.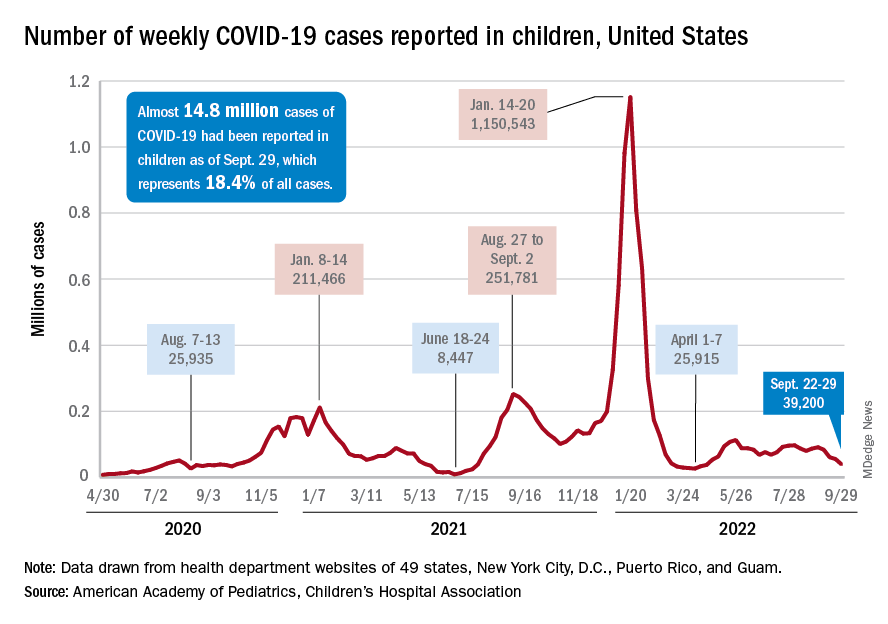
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.





