User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Ex-nursing assistant pleads guilty in West Virginia insulin deaths
A former nursing assistant and Army veteran pleaded guilty to federal murder charges this week in connection with the 2017-2018 deaths of seven patients in a West Virginia veteran’s hospital, according to news reports.
Prosecutors said in court documents filed on July 13 that Reta Mays, 46, injected lethal doses of insulin into seven veterans at the Louis A. Johnson VA Medical Center (VAMC) in rural Clarksburg, W.Va.
Their blood glucose levels plummeted, and each died shortly after their injections, according to the Tennessean.
An eighth patient, a 92-year-old man whom Mays is accused of assaulting with an insulin injection, initially survived after staff were able to stabilize him but died 2 weeks later at a nursing home, NPR reports.
According to NPR, US Attorney Jarod Douglas told the court Tuesday that the medical investigator could not determine whether the insulin contributed to the man’s death but that it was Mays’ intention to kill him.
“No one watched while she injected them with lethal doses of insulin during an 11-month killing rampage,” the Washington Post reported.
No motive offered
The Post article said no motive has been established, but after a 2-year investigation into a pattern of suspicious deaths that took the hospital almost a year to detect, Mays, who had denied any wrongdoing in multiple interviews with investigators, told a federal judge she preyed on some of the country›s most vulnerable service members.
An attorney for Mays, Brian Kornbrath, contacted by Medscape Medical News, said: “The defense team decided that we would have no public comment at this time.”
According to court documents from the Northern District of West Virginia, Mays was charged with seven counts of second-degree murder and one count of assault with intent to commit murder in connection with the patient who died later.
Mays was hired at the VAMC in Clarksburg in June 2015. She worked from 7:30 PM to 8:00 AM in the medical surgical unit, court documents say.
According to the documents, “VAMC Clarksburg did not require a nursing assistant to have a certification or licensure for initial appointment or as a condition of continuing employment.”
The documents indicate that in June 2018, a hospitalist employed by VAMC Clarksburg reported concern about several deaths from unexplained hypoglycemic events in the same ward and noted that many of the affected patients did not have diabetes.
By that time, according to the Tennessean, “at least eight patients had died under suspicious circumstances. Several had been embalmed and buried, destroying potential evidence. One veteran had been cremated.”
An internal investigation began, followed by a criminal investigation, and in July 2018, Mays was removed from patient care.
Mays fired in 2019 because of lies on resume; claims suffers from PTSD
The Post reports that Mays was fired from the hospital in 2019, 7 months after she was banned from patient care, «after it was discovered she had lied about her qualifications on her resume.»
Court documents indicate that her duties included acting as a sitter for patients, checking vital signs, intake and output, and testing blood glucose levels, but she was not qualified to administer medications, including insulin.
Similarities in the deaths were evident, the Post reported. Citing sources familiar with the case, the report said, “elderly patients in private rooms were injected in their abdomen and limbs with insulin the hospital had not ordered.”
The Post reported that Mays sobbed by the end of the hearing on Tuesday.
The article notes that Mays has three sons and served in the Army National Guard from November 2000 to April 2001 and again from February 2003 to May 2004, when she was deployed to Iraq and Kuwait. She told the judge she was taking medication for posttraumatic stress disorder.
By pleading guilty, she waived her right to have the case presented to a grand jury. A sentencing hearing has not been scheduled, the Post reports.
NPR notes that prosecutors have requested that Mays serve seven consecutive life sentences and an additional 20 years in prison.
“Our hearts go out to those affected by these tragic deaths”
A spokesman for VAMC Clarksburg said in a statement to Medscape Medical News: “Our hearts go out to those affected by these tragic deaths. Clarksburg VA Medical Center discovered these allegations and reported them to VA›s independent inspector general more than 2 years ago. Clarksburg VA Medical Center also fired the individual at the center of the allegations.
“We’re glad the Department of Justice stepped in to push this investigation across the finish line and hopeful our court system will deliver the justice Clarksburg-area Veterans and families deserve.”
According to the Tennessean, Michael Missal, inspector general for the Department of Veteran Affairs, said the agency is investigating the hospital’s practices, “including medication management and communications among staffers.”
This article first appeared on Medscape.com.
A former nursing assistant and Army veteran pleaded guilty to federal murder charges this week in connection with the 2017-2018 deaths of seven patients in a West Virginia veteran’s hospital, according to news reports.
Prosecutors said in court documents filed on July 13 that Reta Mays, 46, injected lethal doses of insulin into seven veterans at the Louis A. Johnson VA Medical Center (VAMC) in rural Clarksburg, W.Va.
Their blood glucose levels plummeted, and each died shortly after their injections, according to the Tennessean.
An eighth patient, a 92-year-old man whom Mays is accused of assaulting with an insulin injection, initially survived after staff were able to stabilize him but died 2 weeks later at a nursing home, NPR reports.
According to NPR, US Attorney Jarod Douglas told the court Tuesday that the medical investigator could not determine whether the insulin contributed to the man’s death but that it was Mays’ intention to kill him.
“No one watched while she injected them with lethal doses of insulin during an 11-month killing rampage,” the Washington Post reported.
No motive offered
The Post article said no motive has been established, but after a 2-year investigation into a pattern of suspicious deaths that took the hospital almost a year to detect, Mays, who had denied any wrongdoing in multiple interviews with investigators, told a federal judge she preyed on some of the country›s most vulnerable service members.
An attorney for Mays, Brian Kornbrath, contacted by Medscape Medical News, said: “The defense team decided that we would have no public comment at this time.”
According to court documents from the Northern District of West Virginia, Mays was charged with seven counts of second-degree murder and one count of assault with intent to commit murder in connection with the patient who died later.
Mays was hired at the VAMC in Clarksburg in June 2015. She worked from 7:30 PM to 8:00 AM in the medical surgical unit, court documents say.
According to the documents, “VAMC Clarksburg did not require a nursing assistant to have a certification or licensure for initial appointment or as a condition of continuing employment.”
The documents indicate that in June 2018, a hospitalist employed by VAMC Clarksburg reported concern about several deaths from unexplained hypoglycemic events in the same ward and noted that many of the affected patients did not have diabetes.
By that time, according to the Tennessean, “at least eight patients had died under suspicious circumstances. Several had been embalmed and buried, destroying potential evidence. One veteran had been cremated.”
An internal investigation began, followed by a criminal investigation, and in July 2018, Mays was removed from patient care.
Mays fired in 2019 because of lies on resume; claims suffers from PTSD
The Post reports that Mays was fired from the hospital in 2019, 7 months after she was banned from patient care, «after it was discovered she had lied about her qualifications on her resume.»
Court documents indicate that her duties included acting as a sitter for patients, checking vital signs, intake and output, and testing blood glucose levels, but she was not qualified to administer medications, including insulin.
Similarities in the deaths were evident, the Post reported. Citing sources familiar with the case, the report said, “elderly patients in private rooms were injected in their abdomen and limbs with insulin the hospital had not ordered.”
The Post reported that Mays sobbed by the end of the hearing on Tuesday.
The article notes that Mays has three sons and served in the Army National Guard from November 2000 to April 2001 and again from February 2003 to May 2004, when she was deployed to Iraq and Kuwait. She told the judge she was taking medication for posttraumatic stress disorder.
By pleading guilty, she waived her right to have the case presented to a grand jury. A sentencing hearing has not been scheduled, the Post reports.
NPR notes that prosecutors have requested that Mays serve seven consecutive life sentences and an additional 20 years in prison.
“Our hearts go out to those affected by these tragic deaths”
A spokesman for VAMC Clarksburg said in a statement to Medscape Medical News: “Our hearts go out to those affected by these tragic deaths. Clarksburg VA Medical Center discovered these allegations and reported them to VA›s independent inspector general more than 2 years ago. Clarksburg VA Medical Center also fired the individual at the center of the allegations.
“We’re glad the Department of Justice stepped in to push this investigation across the finish line and hopeful our court system will deliver the justice Clarksburg-area Veterans and families deserve.”
According to the Tennessean, Michael Missal, inspector general for the Department of Veteran Affairs, said the agency is investigating the hospital’s practices, “including medication management and communications among staffers.”
This article first appeared on Medscape.com.
A former nursing assistant and Army veteran pleaded guilty to federal murder charges this week in connection with the 2017-2018 deaths of seven patients in a West Virginia veteran’s hospital, according to news reports.
Prosecutors said in court documents filed on July 13 that Reta Mays, 46, injected lethal doses of insulin into seven veterans at the Louis A. Johnson VA Medical Center (VAMC) in rural Clarksburg, W.Va.
Their blood glucose levels plummeted, and each died shortly after their injections, according to the Tennessean.
An eighth patient, a 92-year-old man whom Mays is accused of assaulting with an insulin injection, initially survived after staff were able to stabilize him but died 2 weeks later at a nursing home, NPR reports.
According to NPR, US Attorney Jarod Douglas told the court Tuesday that the medical investigator could not determine whether the insulin contributed to the man’s death but that it was Mays’ intention to kill him.
“No one watched while she injected them with lethal doses of insulin during an 11-month killing rampage,” the Washington Post reported.
No motive offered
The Post article said no motive has been established, but after a 2-year investigation into a pattern of suspicious deaths that took the hospital almost a year to detect, Mays, who had denied any wrongdoing in multiple interviews with investigators, told a federal judge she preyed on some of the country›s most vulnerable service members.
An attorney for Mays, Brian Kornbrath, contacted by Medscape Medical News, said: “The defense team decided that we would have no public comment at this time.”
According to court documents from the Northern District of West Virginia, Mays was charged with seven counts of second-degree murder and one count of assault with intent to commit murder in connection with the patient who died later.
Mays was hired at the VAMC in Clarksburg in June 2015. She worked from 7:30 PM to 8:00 AM in the medical surgical unit, court documents say.
According to the documents, “VAMC Clarksburg did not require a nursing assistant to have a certification or licensure for initial appointment or as a condition of continuing employment.”
The documents indicate that in June 2018, a hospitalist employed by VAMC Clarksburg reported concern about several deaths from unexplained hypoglycemic events in the same ward and noted that many of the affected patients did not have diabetes.
By that time, according to the Tennessean, “at least eight patients had died under suspicious circumstances. Several had been embalmed and buried, destroying potential evidence. One veteran had been cremated.”
An internal investigation began, followed by a criminal investigation, and in July 2018, Mays was removed from patient care.
Mays fired in 2019 because of lies on resume; claims suffers from PTSD
The Post reports that Mays was fired from the hospital in 2019, 7 months after she was banned from patient care, «after it was discovered she had lied about her qualifications on her resume.»
Court documents indicate that her duties included acting as a sitter for patients, checking vital signs, intake and output, and testing blood glucose levels, but she was not qualified to administer medications, including insulin.
Similarities in the deaths were evident, the Post reported. Citing sources familiar with the case, the report said, “elderly patients in private rooms were injected in their abdomen and limbs with insulin the hospital had not ordered.”
The Post reported that Mays sobbed by the end of the hearing on Tuesday.
The article notes that Mays has three sons and served in the Army National Guard from November 2000 to April 2001 and again from February 2003 to May 2004, when she was deployed to Iraq and Kuwait. She told the judge she was taking medication for posttraumatic stress disorder.
By pleading guilty, she waived her right to have the case presented to a grand jury. A sentencing hearing has not been scheduled, the Post reports.
NPR notes that prosecutors have requested that Mays serve seven consecutive life sentences and an additional 20 years in prison.
“Our hearts go out to those affected by these tragic deaths”
A spokesman for VAMC Clarksburg said in a statement to Medscape Medical News: “Our hearts go out to those affected by these tragic deaths. Clarksburg VA Medical Center discovered these allegations and reported them to VA›s independent inspector general more than 2 years ago. Clarksburg VA Medical Center also fired the individual at the center of the allegations.
“We’re glad the Department of Justice stepped in to push this investigation across the finish line and hopeful our court system will deliver the justice Clarksburg-area Veterans and families deserve.”
According to the Tennessean, Michael Missal, inspector general for the Department of Veteran Affairs, said the agency is investigating the hospital’s practices, “including medication management and communications among staffers.”
This article first appeared on Medscape.com.
Schools can reopen safely with precautions, experts say
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
The absence of in-person school has harmed children in ways beyond loss of academic learning, according to Josh Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore. In addition to learning, school is a place where many children receive breakfast and lunch every day, as well as support services and the benefits of being in a safe and secure environment, Dr. Sharfstein said in a press briefing sponsored by Johns Hopkins University.
However, although it is an important priority for children to return to school, “we are in the midst of a pandemic that poses real risk,” he said.
In the press briefing, several experts shared ideas and considerations for safely reopening K-12 schools in the fall of 2020.
Data from other countries where schools have reopened, notably Austria and Denmark, have been reassuring about the lack of transmission of SARS-CoV-2 among children in a school setting, said Jennifer Nuzzo, DrPH, an epidemiologist at the Johns Hopkins Center for Health Security. However, other countries where schools have reopened successfully have reported low levels of viral transmission locally, and a responsible strategy for school reopening in the United States should follow a similar plan, she said. In areas where transmission and infection rates are increasing “it may not be safe to reopen,” but in areas where rates are declining or stable, schools could potentially reopen if they follow safety measures.
Dr. Nuzzo suggested that Considerations include protocols for handwashing and sanitation, and maintaining physical distance by creative use of outdoor classrooms (weather permitting) or other spaces within school buildings. Transportation to and from school also will be an issue to address, she noted.
None of the strategies being considered will completely eliminate risk of SARS-CoV-2 infection in school settings, so allowing parents and students to opt out and choose distance learning will be important as well, said Dr. Nuzzo. In addition, schools may need to consider alternative roles for teachers and staff who don’t feel comfortable being in contact with students and fellow staff members. “All of these things are going to be hard,” Dr. Nuzzo acknowledged. “Hard should not be a deterrent,” to reopening schools, but “we acknowledge the resources that schools will need in order to do this.”
At present, all 50 states and the District of Columbia have released some type of plan for reopening schools, said Megan Collins, MD, MPH, codirector the Johns Hopkins Consortium for School-Based Health Solutions.
Dr. Collins and colleagues have developed a school reopening tracker, which is “a national snapshot of current reopening plans that have been released,” she said. The tracker is being updated continuously as plans evolve. The eSchool+ K-12 School Reopening Tracker identifies 12 reopening categories that states could potentially address in the plans. These categories are divided into Operational and Ethics/Equity. The operational categories include:
- Core academics
- SARS-CoV-2 protection
- Before and after school programs
- School access and transportation
- Student health services
- Food and nutrition.
Ethics/equity categories include the following:
- Parent choice
- Teacher and staff choice
- Children of poverty and systemic disadvantage
- Children with special needs/English as second language/gifted and twice exceptional
- Privacy
- Engagement and transparency.
As of July 15, 2020, 16 states (Arizona, Colorado, Connecticut, Georgia, Maryland, Minnesota, New Mexico, North Carolina, North Dakota, Ohio, Rhode Island, Tennessee, Texas, Virginia, Washington, and Wisconsin) had addressed all 12 categories in their reopening plans, Dr. Collins said.
School reopening plans must take equity issues into account, said Annette Anderson, PhD, of the Johns Hopkins University School of Education.
Specifically, developing learning plans for special education students and others at the most risk for learning loss will be essential. “The digital divide has become a digital canyon” in some areas, Dr. Anderson noted, and schools need to rethink eligibility and work to provide access to devices for online learning for all students.
In addition, schools need to convince parents that schools are safe. She recommended that schools consider inviting parents and families to visit buildings in advance of reopening so they can see the safety measures, such as space between desks, cleaning stations, and other protective strategies.
The message to pediatricians and health care professionals when counseling families about returning individual children to school is to consider the risk to the child and the family directly in the context of the local plans, Dr. Sharfstein said during a question and answer session. “One school system’s plan is one school system’s plan,” he said, and added that families who are concerned about the risk should have an online option. However, “if you see a thoughtful approach” to reopening, with safety steps taken and parents informed, with protocols such as keeping small groups of children together to reduce transmission, “it is a pretty good trade-off,” and that is why the American Academy of Pediatrics currently favors children returning to school, he said.
The briefing participants had no relevant financial conflicts to disclose.
Why doctors keep monitoring kids who recover from mysterious COVID-linked illness
He’s a 5-year-old boy and would much rather talk about cartoons or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children (MIS-C). And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the long-term health effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at the Children’s Hospital at Montefiore, New York, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Marc Foca, MD, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Dr. Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Dr. Foca left. It’s his new sign-off, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself. And she’s also hoping that, after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough – and mysterious enough – that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Nadine Choueiter, MD, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104° F – but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the ED a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Ms. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Ms. Moholland grew frustrated. “I wish his pediatrician and [the ED and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Ms. Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community because of a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times – very uncertain times.”
Finally, the Children’s Hospital at Montefiore admitted Israel – and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms – which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immunoglobulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immunoglobulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Dr. Choueiter.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases – though not Israel’s – the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms – which can fatally rupture blood vessels – after the initial condition subsides.
Dr. Choueiter and colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania teen, the MIS-C diagnosis came much later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del.
Andrew had been a healthy 14-year-old boy before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Mrs. Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about 5 days in the pediatric ICU, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat, and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition – administering intravenous immunoglobulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Mrs. Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family – both parents, Andrew’s twin brother and two older siblings – all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Mrs. Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, push-ups, and sit-ups. A few weeks later, an ECG showed Andrew’s heart was “perfect,” Mr. Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every 3 months.
An eye on the long-term effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Dr. Choueiter hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first 6 weeks of the illness do well long-term,” said Dr. Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup 1 week after discharge, then after 1 month, 3 months, 6 months, and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Dr. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable with registries that exist for other diseases.
Ms. Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR, and Kaiser Health News. A version of this article originally appeared on Kaiser Health News.
He’s a 5-year-old boy and would much rather talk about cartoons or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children (MIS-C). And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the long-term health effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at the Children’s Hospital at Montefiore, New York, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Marc Foca, MD, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Dr. Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Dr. Foca left. It’s his new sign-off, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself. And she’s also hoping that, after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough – and mysterious enough – that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Nadine Choueiter, MD, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104° F – but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the ED a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Ms. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Ms. Moholland grew frustrated. “I wish his pediatrician and [the ED and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Ms. Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community because of a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times – very uncertain times.”
Finally, the Children’s Hospital at Montefiore admitted Israel – and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms – which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immunoglobulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immunoglobulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Dr. Choueiter.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases – though not Israel’s – the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms – which can fatally rupture blood vessels – after the initial condition subsides.
Dr. Choueiter and colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania teen, the MIS-C diagnosis came much later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del.
Andrew had been a healthy 14-year-old boy before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Mrs. Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about 5 days in the pediatric ICU, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat, and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition – administering intravenous immunoglobulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Mrs. Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family – both parents, Andrew’s twin brother and two older siblings – all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Mrs. Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, push-ups, and sit-ups. A few weeks later, an ECG showed Andrew’s heart was “perfect,” Mr. Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every 3 months.
An eye on the long-term effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Dr. Choueiter hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first 6 weeks of the illness do well long-term,” said Dr. Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup 1 week after discharge, then after 1 month, 3 months, 6 months, and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Dr. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable with registries that exist for other diseases.
Ms. Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR, and Kaiser Health News. A version of this article originally appeared on Kaiser Health News.
He’s a 5-year-old boy and would much rather talk about cartoons or the ideas for inventions that constantly pop into his head.
“Hold your horses, I think I know what I’m gonna make,” he said, holding up a finger in the middle of a conversation. “I’m gonna make something that lights up and attaches to things with glue, so if you don’t have a flashlight, you can just use it!”
In New York, at least 237 kids, including Israel, appear to have Multisystem Inflammatory Syndrome in Children (MIS-C). And state officials continue to track the syndrome, but the Centers for Disease Control and Prevention did not respond to repeated requests for information on how many children nationwide have been diagnosed so far with MIS-C.
A study published June 29 in the New England Journal of Medicine reported on 186 patients in 26 states who had been diagnosed with MIS-C. A researcher writing in the same issue added reports from other countries, finding that about 1,000 children worldwide have been diagnosed with MIS-C.
Tracking the long-term health effects of MIS-C
Israel is friendly and energetic, but he’s also really good at sitting still. During a recent checkup at the Children’s Hospital at Montefiore, New York, he had no complaints about all the stickers and wires a health aide attached to him for an EKG. And when Marc Foca, MD, an infectious disease specialist, came by to listen to his heart and lungs, and prod his abdomen, Israel barely seemed to notice.
There were still some tests pending, but overall, Dr. Foca said, “Israel looks like a totally healthy 5-year-old.”
“Stay safe!” Israel called out, as Dr. Foca left. It’s his new sign-off, instead of goodbye. His mother, Janelle Moholland, explained Israel came up with it himself. And she’s also hoping that, after a harrowing couple of weeks in early May, Israel himself will “stay safe.”
That’s why they’ve been returning to Montefiore for the periodic checkups, even though Israel seems to have recovered fully from both COVID-19 and MIS-C.
MIS-C is relatively rare, and it apparently responds well to treatment, but it is new enough – and mysterious enough – that doctors here want to make sure the children who recover don’t experience any related health complications in the future.
“We’ve seen these kids get really sick, and get better and recover and go home, yet we don’t know what the long-term outcomes are,” said Nadine Choueiter, MD, a pediatric cardiologist at Montefiore. “So that’s why we will be seeing them.”
When Israel first got sick at the end of April, his illness didn’t exactly look like COVID-19. He had persistent high fevers, with his temperature reaching 104° F – but no problems breathing. He wasn’t eating. He was barely drinking. He wasn’t using the bathroom. He had abdominal pains. His eyes were red.
They went to the ED a couple of times and visited an urgent care center, but the doctors sent them home without testing him for the coronavirus. Ms. Moholland, 29, said she felt powerless.
“There was nothing I could do but make him comfortable,” she said. “I literally had to just trust in a higher power and just hope that He would come through for us. It taught me a lot about patience and faith.”
As Israel grew sicker, and they still had no answers, Ms. Moholland grew frustrated. “I wish his pediatrician and [the ED and urgent care staff] had done what they were supposed to do and given him a test” when Israel first got sick, Ms. Moholland said. “What harm would it have done? He suffered for about 10 or 11 days that could have been avoided.”
In a later interview, she talked with NPR about how COVID-19 has disproportionately affected the African American community because of a combination of underlying health conditions and lack of access to good health care. She said she felt she, too, had fallen victim to those disparities.
“It affects me, personally, because I am African American, but you just never know,” she said. “It’s hard. We’re living in uncertain times – very uncertain times.”
Finally, the Children’s Hospital at Montefiore admitted Israel – and the test she’d been trying to get for days confirmed he had the virus.
“I was literally in tears, like begging them not to discharge me because I knew he was not fine,” she recalled.
Israel was in shock, and by the time he got to the hospital, doctors were on the lookout for MIS-C, so they recognized his symptoms – which were distinct from most people with COVID-19.
Doctors gave Israel fluids and intravenous immunoglobulin, a substance obtained from donated human plasma, which is used to treat deficiencies in the immune system.
Immunoglobulin has been effective in children like Israel because MIS-C appears to be caused by an immune overreaction to the initial coronavirus infection, according to Dr. Choueiter.
“The immune system starts attacking the body itself, including the arteries of the heart,” she said.
In some MIS-C cases – though not Israel’s – the attack occurs in the coronary arteries, inflaming and dilating them. That also happens in a different syndrome affecting children, Kawasaki disease. About 5% of Kawasaki patients experience aneurysms – which can fatally rupture blood vessels – after the initial condition subsides.
Dr. Choueiter and colleagues want to make sure MIS-C patients don’t face similar risks. So far, they’re cautiously optimistic.
“We have not seen any new decrease in heart function or any new coronary artery dilations,” she said. “When we check their blood, their inflammatory markers are back to normal. For the parents, the child is back to baseline, and it’s as if this illness is a nightmare that’s long gone.”
For a Pennsylvania teen, the MIS-C diagnosis came much later
Not every child who develops MIS-C tests positive for the coronavirus, though many will test positive for antibodies to the coronavirus, indicating they had been infected previously. That was the case with Andrew Lis, a boy from Pennsylvania who was the first MIS-C patient seen at the Nemours/Alfred I. duPont Hospital for Children in Wilmington, Del.
Andrew had been a healthy 14-year-old boy before he got sick. He and his twin brother love sports and video games. He said the first symptom was a bad headache. He developed a fever the next day, then constipation and intense stomach pain.
“It was terrible,” Andrew said. “It was unbearable. I couldn’t really move a lot.”
His mother, Ingrid Lis, said they were thinking appendicitis, not coronavirus, at first. In fact, she hesitated to take Andrew to the hospital, for fear of exposing him to the virus. But after Andrew stopped eating because of his headache and stomach discomfort, “I knew I couldn’t keep him home anymore,” Mrs. Lis said.
Andrew was admitted to the hospital April 12, but that was before reports of the mysterious syndrome had started trickling out of Europe.
Over about 5 days in the pediatric ICU, Andrew’s condition deteriorated rapidly, as doctors struggled to figure out what was wrong. Puzzled, they tried treatments for scarlet fever, strep throat, and toxic shock syndrome. Andrew’s body broke out in rashes, then his heart began failing and he was put on a ventilator. Andrew’s father, Ed Lis, said doctors told the family to brace for the worst: “We’ve got a healthy kid who a few days ago was just having these sort of strange symptoms. And now they’re telling us that we could lose him.”
Though Andrew’s symptoms were atypical for Kawasaki disease, doctors decided to give him the standard treatment for that condition – administering intravenous immunoglobulin, the same treatment Israel Shippy received.
“Within the 24 hours of the infusion, he was a different person,” Mrs. Lis said. Andrew was removed from the ventilator, and his appetite eventually returned. “That’s when we knew that we had turned that corner.”
It wasn’t until after Andrew’s discharge that his doctors learned about MIS-C from colleagues in Europe. They recommended the whole family be tested for antibodies to the coronavirus. Although Andrew tested positive, the rest of the family – both parents, Andrew’s twin brother and two older siblings – all tested negative. Andrew’s mother is still not sure how he was exposed since the family had been observing a strict lockdown since mid-March. Both she and her husband were working remotely from home, and she says they all wore masks and were conscientious about hand-washing when they ventured out for groceries. She thinks Andrew must have been exposed at least a month before his illness began.
And she’s puzzled why the rest of her close-knit family wasn’t infected as well. “We are a Latino family,” Mrs. Lis said. “We are very used to being together, clustering in the same room.” Even when Andrew was sick, she says, all six of them huddled in his bedroom to comfort him.
Meanwhile, Andrew has made a quick recovery. Not long after his discharge in April, he turned 15 and resumed an exercise routine involving running, push-ups, and sit-ups. A few weeks later, an ECG showed Andrew’s heart was “perfect,” Mr. Lis said. Still, doctors have asked Andrew to follow up with a cardiologist every 3 months.
An eye on the long-term effects
The medical team at Montefiore is tracking the 40 children they have already treated and discharged. With kids showing few symptoms in the immediate aftermath, Dr. Choueiter hopes the long-term trajectory after MIS-C will be similar to what happens after Kawasaki disease.
“Usually children who have had coronary artery dilations [from Kawasaki disease] that have resolved within the first 6 weeks of the illness do well long-term,” said Dr. Choueiter, who runs the Kawasaki disease program at Montefiore.
The Montefiore team is asking patients affected by MIS-C to return for a checkup 1 week after discharge, then after 1 month, 3 months, 6 months, and a year. They will be evaluated by pediatric cardiologists, hematologists, rheumatologists and infectious disease specialists.
Montefiore and other children’s hospitals around the country are sharing information. Dr. Choueiter wants to establish an even longer-term monitoring program for MIS-C, comparable with registries that exist for other diseases.
Ms. Moholland is glad the hospital is being vigilant.
“The uncertainty of not knowing whether it could come back in his future is a little unsettling,” she said. “But I am hopeful.”
This story is part of a partnership that includes WNYC, NPR, and Kaiser Health News. A version of this article originally appeared on Kaiser Health News.
Stillbirth incidence increases during COVID-19 pandemic
The incidence of stillbirth has increased since the COVID-19 pandemic began, according to a comparative study of pregnancy outcomes in a London hospital.
“The increase in stillbirths may have resulted from indirect effects such as reluctance to attend hospital when needed (e.g., with reduced fetal movements), fear of contracting infection, or not wanting to add to the National Health Service burden,” Asma Khalil, MD, of St George’s University of London and coauthors reported in JAMA.
To further assess reported changes in stillbirth and preterm delivery rates during the pandemic, the researchers began a retrospective study of pregnancy outcomes at St George’s University Hospital in London. They compared two periods: from Oct. 1, 2019, to Jan. 31, 2020 as the pre–COVID-19 period and from Feb. 1, 2020, to June 14, 2020 as the pandemic period. The median age of the mother at time of birth in both periods was 33 years. The prepandemic period had 1,681 births, and the pandemic period had 1,718 births.
Although there were found to be fewer nulliparous women and fewer women with hypertension in the pandemic period, the incidence of stillbirth in that period was significantly higher (n = 16 [9 per 1,000 births]) than in the prepandemic period (n = 4 [2 per 1,000 births]) (difference, 7 per 1,000 births; 95% confidence interval, 1.83-12.0; P = .01). The pandemic rate remained higher when late terminations for fetal abnormality were excluded (difference 6 per 1,000 births; 95% CI 1.54-10.1; P = .01).
None of the pregnant women who experienced stillbirth had COVID-19 symptoms, and none of the postmortems or placental exams indicated infection. There were no significant differences between the two periods in regard to births before 37 weeks’ gestation, births after 34 weeks’ gestation, neonatal unit admission, or cesarean delivery.
“It’s very important to highlight the effects of the pandemic on pregnant patients, even if they’re not infected with COVID-19,” Shannon Clark, MD, of the University of Texas Medical Branch in Galveston said in an interview.
She noted several COVID-related considerations that could have contributed to this increase: the reluctance of both low-risk and high-risk patients to enter a hospital setting during a pandemic, along with safety-centered changes made in antenatal services and care, which includes a reduced number of ultrasounds and screening exams.
“Checking a patient’s blood pressure, checking their weight changes, checking how the baby is growing,” she said. “They’re all simple things that just can’t be done via telemedicine.”
“We’ve thought a lot about the potential effects of getting COVID in pregnancy,” she added, “but it’s just as important to think about what might happen to those who don’t have it and are considered low risk otherwise.”
The study authors noted its limitations, including it being retrospective, analyzing a short time frame, and focusing on a single medical center. It also didn’t factor in the causes of the stillbirths, nor were the time periods precisely comparable, although they did add that “there is no seasonality to stillbirths in the UK.”
One doctor reported receiving grants outside of the submitted work. No other potential conflicts of interest were noted. Dr. Clark said she had no relevant financial disclosures.
SOURCE: Khalil A et al. JAMA. 2020 Jul. doi: 10.1001/jama.2020.12746.
The incidence of stillbirth has increased since the COVID-19 pandemic began, according to a comparative study of pregnancy outcomes in a London hospital.
“The increase in stillbirths may have resulted from indirect effects such as reluctance to attend hospital when needed (e.g., with reduced fetal movements), fear of contracting infection, or not wanting to add to the National Health Service burden,” Asma Khalil, MD, of St George’s University of London and coauthors reported in JAMA.
To further assess reported changes in stillbirth and preterm delivery rates during the pandemic, the researchers began a retrospective study of pregnancy outcomes at St George’s University Hospital in London. They compared two periods: from Oct. 1, 2019, to Jan. 31, 2020 as the pre–COVID-19 period and from Feb. 1, 2020, to June 14, 2020 as the pandemic period. The median age of the mother at time of birth in both periods was 33 years. The prepandemic period had 1,681 births, and the pandemic period had 1,718 births.
Although there were found to be fewer nulliparous women and fewer women with hypertension in the pandemic period, the incidence of stillbirth in that period was significantly higher (n = 16 [9 per 1,000 births]) than in the prepandemic period (n = 4 [2 per 1,000 births]) (difference, 7 per 1,000 births; 95% confidence interval, 1.83-12.0; P = .01). The pandemic rate remained higher when late terminations for fetal abnormality were excluded (difference 6 per 1,000 births; 95% CI 1.54-10.1; P = .01).
None of the pregnant women who experienced stillbirth had COVID-19 symptoms, and none of the postmortems or placental exams indicated infection. There were no significant differences between the two periods in regard to births before 37 weeks’ gestation, births after 34 weeks’ gestation, neonatal unit admission, or cesarean delivery.
“It’s very important to highlight the effects of the pandemic on pregnant patients, even if they’re not infected with COVID-19,” Shannon Clark, MD, of the University of Texas Medical Branch in Galveston said in an interview.
She noted several COVID-related considerations that could have contributed to this increase: the reluctance of both low-risk and high-risk patients to enter a hospital setting during a pandemic, along with safety-centered changes made in antenatal services and care, which includes a reduced number of ultrasounds and screening exams.
“Checking a patient’s blood pressure, checking their weight changes, checking how the baby is growing,” she said. “They’re all simple things that just can’t be done via telemedicine.”
“We’ve thought a lot about the potential effects of getting COVID in pregnancy,” she added, “but it’s just as important to think about what might happen to those who don’t have it and are considered low risk otherwise.”
The study authors noted its limitations, including it being retrospective, analyzing a short time frame, and focusing on a single medical center. It also didn’t factor in the causes of the stillbirths, nor were the time periods precisely comparable, although they did add that “there is no seasonality to stillbirths in the UK.”
One doctor reported receiving grants outside of the submitted work. No other potential conflicts of interest were noted. Dr. Clark said she had no relevant financial disclosures.
SOURCE: Khalil A et al. JAMA. 2020 Jul. doi: 10.1001/jama.2020.12746.
The incidence of stillbirth has increased since the COVID-19 pandemic began, according to a comparative study of pregnancy outcomes in a London hospital.
“The increase in stillbirths may have resulted from indirect effects such as reluctance to attend hospital when needed (e.g., with reduced fetal movements), fear of contracting infection, or not wanting to add to the National Health Service burden,” Asma Khalil, MD, of St George’s University of London and coauthors reported in JAMA.
To further assess reported changes in stillbirth and preterm delivery rates during the pandemic, the researchers began a retrospective study of pregnancy outcomes at St George’s University Hospital in London. They compared two periods: from Oct. 1, 2019, to Jan. 31, 2020 as the pre–COVID-19 period and from Feb. 1, 2020, to June 14, 2020 as the pandemic period. The median age of the mother at time of birth in both periods was 33 years. The prepandemic period had 1,681 births, and the pandemic period had 1,718 births.
Although there were found to be fewer nulliparous women and fewer women with hypertension in the pandemic period, the incidence of stillbirth in that period was significantly higher (n = 16 [9 per 1,000 births]) than in the prepandemic period (n = 4 [2 per 1,000 births]) (difference, 7 per 1,000 births; 95% confidence interval, 1.83-12.0; P = .01). The pandemic rate remained higher when late terminations for fetal abnormality were excluded (difference 6 per 1,000 births; 95% CI 1.54-10.1; P = .01).
None of the pregnant women who experienced stillbirth had COVID-19 symptoms, and none of the postmortems or placental exams indicated infection. There were no significant differences between the two periods in regard to births before 37 weeks’ gestation, births after 34 weeks’ gestation, neonatal unit admission, or cesarean delivery.
“It’s very important to highlight the effects of the pandemic on pregnant patients, even if they’re not infected with COVID-19,” Shannon Clark, MD, of the University of Texas Medical Branch in Galveston said in an interview.
She noted several COVID-related considerations that could have contributed to this increase: the reluctance of both low-risk and high-risk patients to enter a hospital setting during a pandemic, along with safety-centered changes made in antenatal services and care, which includes a reduced number of ultrasounds and screening exams.
“Checking a patient’s blood pressure, checking their weight changes, checking how the baby is growing,” she said. “They’re all simple things that just can’t be done via telemedicine.”
“We’ve thought a lot about the potential effects of getting COVID in pregnancy,” she added, “but it’s just as important to think about what might happen to those who don’t have it and are considered low risk otherwise.”
The study authors noted its limitations, including it being retrospective, analyzing a short time frame, and focusing on a single medical center. It also didn’t factor in the causes of the stillbirths, nor were the time periods precisely comparable, although they did add that “there is no seasonality to stillbirths in the UK.”
One doctor reported receiving grants outside of the submitted work. No other potential conflicts of interest were noted. Dr. Clark said she had no relevant financial disclosures.
SOURCE: Khalil A et al. JAMA. 2020 Jul. doi: 10.1001/jama.2020.12746.
FROM JAMA
Doctors say their COVID-19 protocol saves lives; others want proof
As COVID-19 cases mounted in Texas in late June, a local Houston news station shadowed Joseph Varon, MD, making rounds in the intensive care unit at United Memorial Medical Center in Houston. An unseen newscaster tells viewers that Varon credits his success against COVID-19 so far to an experimental and “controversial” drug protocol consisting of vitamins, steroids, and blood thinners.
“This is war. There’s no time to double-blind anything,” Varon tells the camera. “This is working. And if it’s working, I’m going to keep on doing it.”
But response to the protocol among other critical care physicians is mixed, with several physicians, in interviews with Medscape Medical News, urging caution because the benefits and relative risks of the combined medications have not been tested in randomized control trials.
From the earliest days of the pandemic, there’s been tension between the need for rigorous scientific study to understand a novel disease, which takes time, and the need to treat seriously ill patients immediately. Some treatments, like hydroxychloroquine, were promoted without randomized clinical trial data and then later were shown to be ineffective or even potentially harmful when tested.
“This pandemic has shown us there’s lots of ideas out there and they need to be tested and a theoretical basis is insufficient,” says Daniel Kaul, MD, a professor of infectious disease at the University of Michigan in Ann Arbor. The ups and downs with hydroxychloroquine offer a sobering example, he says. “I would argue we have an ethical obligation to do randomized controlled trials to see if our treatments work.”
Creating MATH+
MATH+ stands for methylprednisolone, ascorbic acid, thiamine, and heparin. The “+” holds a place for additional therapies like vitamin D, zinc, and melatonin. The protocol originated as a variation of the “HAT therapy,” a combination of hydrocortisone, ascorbic acid, and thiamine, which critical care specialist Paul Marik, MD, created for treating critically ill patients with sepsis.
Over a few weeks, the protocol evolved as Marik, chief of the division of pulmonary and critical care medicine at Eastern Virginia Medical School in Norfolk, emailed with a small group of colleagues about treatments and their observations of SARS-CoV-2 in action, swapping in methylprednisolone and adding the anticoagulant heparin.
When Marik and colleagues created the protocol in early March, many healthcare organizations like the World Health Organization (WHO) were advising against steroids for COVID-19 patients. The MATH+ physicians decided they needed to spread a different message, and began publicizing the protocol with a website and a small communications team.
Marik says they tried to get their protocol in front of healthcare organizations – including the WHO, the Centers for Disease Control and Prevention, and the National Institutes of Health – but received no response. Marik went on Newt Gingrich’s podcast to discuss the protocol in the hopes it would make its way to the White House.
Senator Ron Johnson of Wisconsin saw the protocol and invited Pierre Kory, MD, MPA, who practices in Johnson’s home state, to testify remotely in front of the Senate Homeland Security Committee. Kory is a pulmonary critical care specialist about to start a new job at Aurora St. Luke’s Medical Center in Milwaukee.
In his testimony, Kory shared his positive experience using the protocol to treat patients and expressed his dismay that national healthcare organizations came out against the use of corticosteroids for COVID-19 from the early days of the pandemic based on what he called a “tragic error in analysis of medical data.” Although an analysis by national organizations suggested corticosteroids might be dangerous in COVID-19 patients, one of his colleagues came to the opposite conclusion, he said. But these organizations advised supportive care only, and against steroids. “We think that is a fatal and tragic flaw,” Kory said.
“The problem with the protocol early on was that it was heresy,” says Kory, referring to the protocol’s inclusion of corticosteroids before official treatment guidelines. During the height of the pandemic in New York this spring, Kory spent 5 weeks working in the ICU at Mount Sinai Beth Israel in Manhattan. Seeing patients flounder on supportive care, Kory says he used MATH+ successfully during his time in New York, using escalating and pulse doses of corticosteroids to stabilize rapidly deteriorating patients.
The website’s home page initially included an invitation for visitors to donate money to support “getting word of this effective treatment protocol out to physicians and hospitals around the world.” After Medscape Medical News brought up the donation prompt in questions, the physicians decided to remove all calls for donations from the website and social media, communications representative Betsy Ashton said. “Critics are misinterpreting this as some kind of fund-raising operation, when that could hardly be the case,” Ashton said in an email. “They are horrified that anyone would impugn their motives.”
Donations paid for the website designer, webmaster, and her work, Ashton said, and the physicians now have donors who will support publicizing the protocol without online calls for donations. “We have no commercial or vested interest,” Marik said. “I’m not going to make a single cent out of this and it’s obviously very time-consuming.”
The basis for the protocol
The protocol is based on common sense, an understanding of scientific literature, and an understanding of COVID-19, Marik says. The website includes links to past research trials and observational studies examining ascorbic acid and thiamine in critically ill patients and early looks at anticoagulants in COVID-19 patients.
They chose methylprednisolone as their corticosteroid based on the expertise of group member G. Umberto Meduri, MD, professor of medicine at the University of Tennessee Health Science Center in Memphis, Tennessee, who had found the steroid effective in treating acute respiratory distress syndrome. On the MATH+ website, the physicians link to multiple observational studies posted on preprint servers in April and May that suggest methylprednisolone helped COVID-19 patients.
“What’s happened with time is all the elements have been validated by scientific studies, which makes this so cool,” says Marik. The RECOVERY Trial results in particular validated the push to use corticosteroids in COVID-19 patients, he says. But that study used a different steroid, dexamethasone, in much smaller doses than what MATH+ recommends. Revised guidance from the Infectious Diseases Society of America recommends dexamethasone for severely ill patients, but says methylprednisolone and prednisone can be used as substitutes at equivalent doses.
Marik and Kory say that mortality rates for COVID-19 patients at their respective hospitals decreased after they began using the protocol. The physicians have been collecting observational data on their patients, but have not yet published any, and do not plan to conduct a randomized trial.
Several physicians who were not involved in the creation of the protocol say the evidence the physicians cite is not robust enough to warrant the promotion of MATH+ and call for randomized controlled trials. Coming up with a protocol is fine, says Kaul, but “you have to do the hard work of doing a randomized control trial to determine if those drugs given in those combinations work or not.”
“When I looked at it, I thought it was actually not very evidence based,” says Michelle Gong, MD, chief of the Division of Critical Care Medicine at Montefiore Health System in New York City. “It is not something I would recommend for my doctors to do outside of a clinical trial.”
The protocol authors push back against the necessity and feasibility of randomized control trials.
There is no time for a randomized control trial right now, says Jose Iglesias, DO, associate professor at Hackensack Meridian School of Medicine at Seton Hall and critical care specialist at Community Medical Center and Jersey Shore University Medical Center in New Jersey. “Time is limited. We’re busy bedside clinicians taking care of patients, and patients who are dying.”
Marik argues there is not equipoise: It wouldn’t be ethical to randomize patients in a placebo group when the physicians are confident the steroids will help. And the protocol is personalized for each patient, making the standardization required for a randomized control trial incredibly difficult, he says. He also cites “the people who are unwilling to accept our results and just think it’s too good to be true.”
Hugh Cassiere, MD, director of critical care medicine at Northwell Health’s North Shore University Hospital in Manhasset, New York, said he finds it “very disturbing that this is being propagated.” In the context of a pandemic in which physicians from other specialties are helping out colleagues in ICUs and might follow the protocol uncritically, he worries, “this could potentially lead to harm.”
“I understand the intention; everybody wants to do something, these patients are so sick and the crisis so sharp that we all want to do something to make patients better,” Gong said. “But as physicians taking care of patients we need to make sure we separate the noise from the evidence.”
Peer review
The physicians who reviewed MATH+ for Medscape Medical News differed on which parts of the protocol they support and which parts they would change.
Dexamethasone should be the corticosteroid of choice over methylprednisolone, says Cassiere, because it has now been proven effective in the randomized RECOVERY Trial, which also tested dosing and a timetable for treatment.
But Sam Parnia, MD, PhD, associate professor of medicine and director of critical care and resuscitation research at NYU Langone, thinks methylprednisolone may be effective, and that even higher doses over longer periods of time may stave off recurring pneumonia, based on his experience using the steroid to treat COVID-19 patients in New York.
“What I really like about this protocol is, these guys are very smart, they recommend the need to treat multiple different things at the same time,” says Parnia. COVID-19 is a complex condition, he notes: If physicians are only focused on solving one problem, like hypoxia, patients could still be dying from blood clots.
Despite general concerns about the protocol, Cassiere says he was excited about the inclusion of heparin. Given the extreme levels of clotting seen in COVID-19 patients, he would have included specific D-dimer levels to guide treatment and explored antiplatelet therapies like aspirin. Gong, however, cautioned that she had seen her patients on anticoagulants develop gastrointestinal bleeding, and reiterated the need for clinical evidence. (At least one clinical trial is currently testing the risks and benefits of heparin as an antithrombotic therapy for COVID-19 patients.)
Perhaps the most divisive part of the protocol is the inclusion of ascorbic acid. “That’s the civil war,” says Kory. “It’s the most polarizing medicine.” The authors of the MATH+ protocol were close colleagues before COVID-19 in part because of a mutual research interest in ascorbic acid, he says. Other physicians, including Cassiere, are extremely skeptical that ascorbic acid has any effect, citing recently published studies in the Journal of the American Medical Association that found ascorbic acid ineffective for treating sepsis.
The MATH+ creators say they are working on a literature review of the research behind the protocol, and they plan to write up the observational impacts of the protocol. Marik says he’s not optimistic about getting the findings published in a high-impact journal given the observational nature of the research; the relatively small number of patients treated at hospitals using the protocol (140 patients at Marik’s hospital in Virginia and 180 at Varon’s in Houston, according to Marik); and the vast number of COVID-19 papers being submitted to scientific journals right now.
“This is not a remedy with expensive designer drugs,” Marik said. “No one has any interest in treating patients with cheap, safe, readily available drugs.”
“I hope they’re right if they’re saying this combination of medicines dramatically decreases mortality,” says Taison Bell, MD, director of the medical intensive care unit and assistant professor of medicine at UVA Health in Charlottesville, Virginia.
But physicians have hurt patients in the past with medications they hoped would work, he says. “We have to make sure we’re balancing the risk and the harm with that benefit, and the only way to protect patients from those biases is by doing a randomized controlled trial.”
This article first appeared on Medscape.com.
As COVID-19 cases mounted in Texas in late June, a local Houston news station shadowed Joseph Varon, MD, making rounds in the intensive care unit at United Memorial Medical Center in Houston. An unseen newscaster tells viewers that Varon credits his success against COVID-19 so far to an experimental and “controversial” drug protocol consisting of vitamins, steroids, and blood thinners.
“This is war. There’s no time to double-blind anything,” Varon tells the camera. “This is working. And if it’s working, I’m going to keep on doing it.”
But response to the protocol among other critical care physicians is mixed, with several physicians, in interviews with Medscape Medical News, urging caution because the benefits and relative risks of the combined medications have not been tested in randomized control trials.
From the earliest days of the pandemic, there’s been tension between the need for rigorous scientific study to understand a novel disease, which takes time, and the need to treat seriously ill patients immediately. Some treatments, like hydroxychloroquine, were promoted without randomized clinical trial data and then later were shown to be ineffective or even potentially harmful when tested.
“This pandemic has shown us there’s lots of ideas out there and they need to be tested and a theoretical basis is insufficient,” says Daniel Kaul, MD, a professor of infectious disease at the University of Michigan in Ann Arbor. The ups and downs with hydroxychloroquine offer a sobering example, he says. “I would argue we have an ethical obligation to do randomized controlled trials to see if our treatments work.”
Creating MATH+
MATH+ stands for methylprednisolone, ascorbic acid, thiamine, and heparin. The “+” holds a place for additional therapies like vitamin D, zinc, and melatonin. The protocol originated as a variation of the “HAT therapy,” a combination of hydrocortisone, ascorbic acid, and thiamine, which critical care specialist Paul Marik, MD, created for treating critically ill patients with sepsis.
Over a few weeks, the protocol evolved as Marik, chief of the division of pulmonary and critical care medicine at Eastern Virginia Medical School in Norfolk, emailed with a small group of colleagues about treatments and their observations of SARS-CoV-2 in action, swapping in methylprednisolone and adding the anticoagulant heparin.
When Marik and colleagues created the protocol in early March, many healthcare organizations like the World Health Organization (WHO) were advising against steroids for COVID-19 patients. The MATH+ physicians decided they needed to spread a different message, and began publicizing the protocol with a website and a small communications team.
Marik says they tried to get their protocol in front of healthcare organizations – including the WHO, the Centers for Disease Control and Prevention, and the National Institutes of Health – but received no response. Marik went on Newt Gingrich’s podcast to discuss the protocol in the hopes it would make its way to the White House.
Senator Ron Johnson of Wisconsin saw the protocol and invited Pierre Kory, MD, MPA, who practices in Johnson’s home state, to testify remotely in front of the Senate Homeland Security Committee. Kory is a pulmonary critical care specialist about to start a new job at Aurora St. Luke’s Medical Center in Milwaukee.
In his testimony, Kory shared his positive experience using the protocol to treat patients and expressed his dismay that national healthcare organizations came out against the use of corticosteroids for COVID-19 from the early days of the pandemic based on what he called a “tragic error in analysis of medical data.” Although an analysis by national organizations suggested corticosteroids might be dangerous in COVID-19 patients, one of his colleagues came to the opposite conclusion, he said. But these organizations advised supportive care only, and against steroids. “We think that is a fatal and tragic flaw,” Kory said.
“The problem with the protocol early on was that it was heresy,” says Kory, referring to the protocol’s inclusion of corticosteroids before official treatment guidelines. During the height of the pandemic in New York this spring, Kory spent 5 weeks working in the ICU at Mount Sinai Beth Israel in Manhattan. Seeing patients flounder on supportive care, Kory says he used MATH+ successfully during his time in New York, using escalating and pulse doses of corticosteroids to stabilize rapidly deteriorating patients.
The website’s home page initially included an invitation for visitors to donate money to support “getting word of this effective treatment protocol out to physicians and hospitals around the world.” After Medscape Medical News brought up the donation prompt in questions, the physicians decided to remove all calls for donations from the website and social media, communications representative Betsy Ashton said. “Critics are misinterpreting this as some kind of fund-raising operation, when that could hardly be the case,” Ashton said in an email. “They are horrified that anyone would impugn their motives.”
Donations paid for the website designer, webmaster, and her work, Ashton said, and the physicians now have donors who will support publicizing the protocol without online calls for donations. “We have no commercial or vested interest,” Marik said. “I’m not going to make a single cent out of this and it’s obviously very time-consuming.”
The basis for the protocol
The protocol is based on common sense, an understanding of scientific literature, and an understanding of COVID-19, Marik says. The website includes links to past research trials and observational studies examining ascorbic acid and thiamine in critically ill patients and early looks at anticoagulants in COVID-19 patients.
They chose methylprednisolone as their corticosteroid based on the expertise of group member G. Umberto Meduri, MD, professor of medicine at the University of Tennessee Health Science Center in Memphis, Tennessee, who had found the steroid effective in treating acute respiratory distress syndrome. On the MATH+ website, the physicians link to multiple observational studies posted on preprint servers in April and May that suggest methylprednisolone helped COVID-19 patients.
“What’s happened with time is all the elements have been validated by scientific studies, which makes this so cool,” says Marik. The RECOVERY Trial results in particular validated the push to use corticosteroids in COVID-19 patients, he says. But that study used a different steroid, dexamethasone, in much smaller doses than what MATH+ recommends. Revised guidance from the Infectious Diseases Society of America recommends dexamethasone for severely ill patients, but says methylprednisolone and prednisone can be used as substitutes at equivalent doses.
Marik and Kory say that mortality rates for COVID-19 patients at their respective hospitals decreased after they began using the protocol. The physicians have been collecting observational data on their patients, but have not yet published any, and do not plan to conduct a randomized trial.
Several physicians who were not involved in the creation of the protocol say the evidence the physicians cite is not robust enough to warrant the promotion of MATH+ and call for randomized controlled trials. Coming up with a protocol is fine, says Kaul, but “you have to do the hard work of doing a randomized control trial to determine if those drugs given in those combinations work or not.”
“When I looked at it, I thought it was actually not very evidence based,” says Michelle Gong, MD, chief of the Division of Critical Care Medicine at Montefiore Health System in New York City. “It is not something I would recommend for my doctors to do outside of a clinical trial.”
The protocol authors push back against the necessity and feasibility of randomized control trials.
There is no time for a randomized control trial right now, says Jose Iglesias, DO, associate professor at Hackensack Meridian School of Medicine at Seton Hall and critical care specialist at Community Medical Center and Jersey Shore University Medical Center in New Jersey. “Time is limited. We’re busy bedside clinicians taking care of patients, and patients who are dying.”
Marik argues there is not equipoise: It wouldn’t be ethical to randomize patients in a placebo group when the physicians are confident the steroids will help. And the protocol is personalized for each patient, making the standardization required for a randomized control trial incredibly difficult, he says. He also cites “the people who are unwilling to accept our results and just think it’s too good to be true.”
Hugh Cassiere, MD, director of critical care medicine at Northwell Health’s North Shore University Hospital in Manhasset, New York, said he finds it “very disturbing that this is being propagated.” In the context of a pandemic in which physicians from other specialties are helping out colleagues in ICUs and might follow the protocol uncritically, he worries, “this could potentially lead to harm.”
“I understand the intention; everybody wants to do something, these patients are so sick and the crisis so sharp that we all want to do something to make patients better,” Gong said. “But as physicians taking care of patients we need to make sure we separate the noise from the evidence.”
Peer review
The physicians who reviewed MATH+ for Medscape Medical News differed on which parts of the protocol they support and which parts they would change.
Dexamethasone should be the corticosteroid of choice over methylprednisolone, says Cassiere, because it has now been proven effective in the randomized RECOVERY Trial, which also tested dosing and a timetable for treatment.
But Sam Parnia, MD, PhD, associate professor of medicine and director of critical care and resuscitation research at NYU Langone, thinks methylprednisolone may be effective, and that even higher doses over longer periods of time may stave off recurring pneumonia, based on his experience using the steroid to treat COVID-19 patients in New York.
“What I really like about this protocol is, these guys are very smart, they recommend the need to treat multiple different things at the same time,” says Parnia. COVID-19 is a complex condition, he notes: If physicians are only focused on solving one problem, like hypoxia, patients could still be dying from blood clots.
Despite general concerns about the protocol, Cassiere says he was excited about the inclusion of heparin. Given the extreme levels of clotting seen in COVID-19 patients, he would have included specific D-dimer levels to guide treatment and explored antiplatelet therapies like aspirin. Gong, however, cautioned that she had seen her patients on anticoagulants develop gastrointestinal bleeding, and reiterated the need for clinical evidence. (At least one clinical trial is currently testing the risks and benefits of heparin as an antithrombotic therapy for COVID-19 patients.)
Perhaps the most divisive part of the protocol is the inclusion of ascorbic acid. “That’s the civil war,” says Kory. “It’s the most polarizing medicine.” The authors of the MATH+ protocol were close colleagues before COVID-19 in part because of a mutual research interest in ascorbic acid, he says. Other physicians, including Cassiere, are extremely skeptical that ascorbic acid has any effect, citing recently published studies in the Journal of the American Medical Association that found ascorbic acid ineffective for treating sepsis.
The MATH+ creators say they are working on a literature review of the research behind the protocol, and they plan to write up the observational impacts of the protocol. Marik says he’s not optimistic about getting the findings published in a high-impact journal given the observational nature of the research; the relatively small number of patients treated at hospitals using the protocol (140 patients at Marik’s hospital in Virginia and 180 at Varon’s in Houston, according to Marik); and the vast number of COVID-19 papers being submitted to scientific journals right now.
“This is not a remedy with expensive designer drugs,” Marik said. “No one has any interest in treating patients with cheap, safe, readily available drugs.”
“I hope they’re right if they’re saying this combination of medicines dramatically decreases mortality,” says Taison Bell, MD, director of the medical intensive care unit and assistant professor of medicine at UVA Health in Charlottesville, Virginia.
But physicians have hurt patients in the past with medications they hoped would work, he says. “We have to make sure we’re balancing the risk and the harm with that benefit, and the only way to protect patients from those biases is by doing a randomized controlled trial.”
This article first appeared on Medscape.com.
As COVID-19 cases mounted in Texas in late June, a local Houston news station shadowed Joseph Varon, MD, making rounds in the intensive care unit at United Memorial Medical Center in Houston. An unseen newscaster tells viewers that Varon credits his success against COVID-19 so far to an experimental and “controversial” drug protocol consisting of vitamins, steroids, and blood thinners.
“This is war. There’s no time to double-blind anything,” Varon tells the camera. “This is working. And if it’s working, I’m going to keep on doing it.”
But response to the protocol among other critical care physicians is mixed, with several physicians, in interviews with Medscape Medical News, urging caution because the benefits and relative risks of the combined medications have not been tested in randomized control trials.
From the earliest days of the pandemic, there’s been tension between the need for rigorous scientific study to understand a novel disease, which takes time, and the need to treat seriously ill patients immediately. Some treatments, like hydroxychloroquine, were promoted without randomized clinical trial data and then later were shown to be ineffective or even potentially harmful when tested.
“This pandemic has shown us there’s lots of ideas out there and they need to be tested and a theoretical basis is insufficient,” says Daniel Kaul, MD, a professor of infectious disease at the University of Michigan in Ann Arbor. The ups and downs with hydroxychloroquine offer a sobering example, he says. “I would argue we have an ethical obligation to do randomized controlled trials to see if our treatments work.”
Creating MATH+
MATH+ stands for methylprednisolone, ascorbic acid, thiamine, and heparin. The “+” holds a place for additional therapies like vitamin D, zinc, and melatonin. The protocol originated as a variation of the “HAT therapy,” a combination of hydrocortisone, ascorbic acid, and thiamine, which critical care specialist Paul Marik, MD, created for treating critically ill patients with sepsis.
Over a few weeks, the protocol evolved as Marik, chief of the division of pulmonary and critical care medicine at Eastern Virginia Medical School in Norfolk, emailed with a small group of colleagues about treatments and their observations of SARS-CoV-2 in action, swapping in methylprednisolone and adding the anticoagulant heparin.
When Marik and colleagues created the protocol in early March, many healthcare organizations like the World Health Organization (WHO) were advising against steroids for COVID-19 patients. The MATH+ physicians decided they needed to spread a different message, and began publicizing the protocol with a website and a small communications team.
Marik says they tried to get their protocol in front of healthcare organizations – including the WHO, the Centers for Disease Control and Prevention, and the National Institutes of Health – but received no response. Marik went on Newt Gingrich’s podcast to discuss the protocol in the hopes it would make its way to the White House.
Senator Ron Johnson of Wisconsin saw the protocol and invited Pierre Kory, MD, MPA, who practices in Johnson’s home state, to testify remotely in front of the Senate Homeland Security Committee. Kory is a pulmonary critical care specialist about to start a new job at Aurora St. Luke’s Medical Center in Milwaukee.
In his testimony, Kory shared his positive experience using the protocol to treat patients and expressed his dismay that national healthcare organizations came out against the use of corticosteroids for COVID-19 from the early days of the pandemic based on what he called a “tragic error in analysis of medical data.” Although an analysis by national organizations suggested corticosteroids might be dangerous in COVID-19 patients, one of his colleagues came to the opposite conclusion, he said. But these organizations advised supportive care only, and against steroids. “We think that is a fatal and tragic flaw,” Kory said.
“The problem with the protocol early on was that it was heresy,” says Kory, referring to the protocol’s inclusion of corticosteroids before official treatment guidelines. During the height of the pandemic in New York this spring, Kory spent 5 weeks working in the ICU at Mount Sinai Beth Israel in Manhattan. Seeing patients flounder on supportive care, Kory says he used MATH+ successfully during his time in New York, using escalating and pulse doses of corticosteroids to stabilize rapidly deteriorating patients.
The website’s home page initially included an invitation for visitors to donate money to support “getting word of this effective treatment protocol out to physicians and hospitals around the world.” After Medscape Medical News brought up the donation prompt in questions, the physicians decided to remove all calls for donations from the website and social media, communications representative Betsy Ashton said. “Critics are misinterpreting this as some kind of fund-raising operation, when that could hardly be the case,” Ashton said in an email. “They are horrified that anyone would impugn their motives.”
Donations paid for the website designer, webmaster, and her work, Ashton said, and the physicians now have donors who will support publicizing the protocol without online calls for donations. “We have no commercial or vested interest,” Marik said. “I’m not going to make a single cent out of this and it’s obviously very time-consuming.”
The basis for the protocol
The protocol is based on common sense, an understanding of scientific literature, and an understanding of COVID-19, Marik says. The website includes links to past research trials and observational studies examining ascorbic acid and thiamine in critically ill patients and early looks at anticoagulants in COVID-19 patients.
They chose methylprednisolone as their corticosteroid based on the expertise of group member G. Umberto Meduri, MD, professor of medicine at the University of Tennessee Health Science Center in Memphis, Tennessee, who had found the steroid effective in treating acute respiratory distress syndrome. On the MATH+ website, the physicians link to multiple observational studies posted on preprint servers in April and May that suggest methylprednisolone helped COVID-19 patients.
“What’s happened with time is all the elements have been validated by scientific studies, which makes this so cool,” says Marik. The RECOVERY Trial results in particular validated the push to use corticosteroids in COVID-19 patients, he says. But that study used a different steroid, dexamethasone, in much smaller doses than what MATH+ recommends. Revised guidance from the Infectious Diseases Society of America recommends dexamethasone for severely ill patients, but says methylprednisolone and prednisone can be used as substitutes at equivalent doses.
Marik and Kory say that mortality rates for COVID-19 patients at their respective hospitals decreased after they began using the protocol. The physicians have been collecting observational data on their patients, but have not yet published any, and do not plan to conduct a randomized trial.
Several physicians who were not involved in the creation of the protocol say the evidence the physicians cite is not robust enough to warrant the promotion of MATH+ and call for randomized controlled trials. Coming up with a protocol is fine, says Kaul, but “you have to do the hard work of doing a randomized control trial to determine if those drugs given in those combinations work or not.”
“When I looked at it, I thought it was actually not very evidence based,” says Michelle Gong, MD, chief of the Division of Critical Care Medicine at Montefiore Health System in New York City. “It is not something I would recommend for my doctors to do outside of a clinical trial.”
The protocol authors push back against the necessity and feasibility of randomized control trials.
There is no time for a randomized control trial right now, says Jose Iglesias, DO, associate professor at Hackensack Meridian School of Medicine at Seton Hall and critical care specialist at Community Medical Center and Jersey Shore University Medical Center in New Jersey. “Time is limited. We’re busy bedside clinicians taking care of patients, and patients who are dying.”
Marik argues there is not equipoise: It wouldn’t be ethical to randomize patients in a placebo group when the physicians are confident the steroids will help. And the protocol is personalized for each patient, making the standardization required for a randomized control trial incredibly difficult, he says. He also cites “the people who are unwilling to accept our results and just think it’s too good to be true.”
Hugh Cassiere, MD, director of critical care medicine at Northwell Health’s North Shore University Hospital in Manhasset, New York, said he finds it “very disturbing that this is being propagated.” In the context of a pandemic in which physicians from other specialties are helping out colleagues in ICUs and might follow the protocol uncritically, he worries, “this could potentially lead to harm.”
“I understand the intention; everybody wants to do something, these patients are so sick and the crisis so sharp that we all want to do something to make patients better,” Gong said. “But as physicians taking care of patients we need to make sure we separate the noise from the evidence.”
Peer review
The physicians who reviewed MATH+ for Medscape Medical News differed on which parts of the protocol they support and which parts they would change.
Dexamethasone should be the corticosteroid of choice over methylprednisolone, says Cassiere, because it has now been proven effective in the randomized RECOVERY Trial, which also tested dosing and a timetable for treatment.
But Sam Parnia, MD, PhD, associate professor of medicine and director of critical care and resuscitation research at NYU Langone, thinks methylprednisolone may be effective, and that even higher doses over longer periods of time may stave off recurring pneumonia, based on his experience using the steroid to treat COVID-19 patients in New York.
“What I really like about this protocol is, these guys are very smart, they recommend the need to treat multiple different things at the same time,” says Parnia. COVID-19 is a complex condition, he notes: If physicians are only focused on solving one problem, like hypoxia, patients could still be dying from blood clots.
Despite general concerns about the protocol, Cassiere says he was excited about the inclusion of heparin. Given the extreme levels of clotting seen in COVID-19 patients, he would have included specific D-dimer levels to guide treatment and explored antiplatelet therapies like aspirin. Gong, however, cautioned that she had seen her patients on anticoagulants develop gastrointestinal bleeding, and reiterated the need for clinical evidence. (At least one clinical trial is currently testing the risks and benefits of heparin as an antithrombotic therapy for COVID-19 patients.)
Perhaps the most divisive part of the protocol is the inclusion of ascorbic acid. “That’s the civil war,” says Kory. “It’s the most polarizing medicine.” The authors of the MATH+ protocol were close colleagues before COVID-19 in part because of a mutual research interest in ascorbic acid, he says. Other physicians, including Cassiere, are extremely skeptical that ascorbic acid has any effect, citing recently published studies in the Journal of the American Medical Association that found ascorbic acid ineffective for treating sepsis.
The MATH+ creators say they are working on a literature review of the research behind the protocol, and they plan to write up the observational impacts of the protocol. Marik says he’s not optimistic about getting the findings published in a high-impact journal given the observational nature of the research; the relatively small number of patients treated at hospitals using the protocol (140 patients at Marik’s hospital in Virginia and 180 at Varon’s in Houston, according to Marik); and the vast number of COVID-19 papers being submitted to scientific journals right now.
“This is not a remedy with expensive designer drugs,” Marik said. “No one has any interest in treating patients with cheap, safe, readily available drugs.”
“I hope they’re right if they’re saying this combination of medicines dramatically decreases mortality,” says Taison Bell, MD, director of the medical intensive care unit and assistant professor of medicine at UVA Health in Charlottesville, Virginia.
But physicians have hurt patients in the past with medications they hoped would work, he says. “We have to make sure we’re balancing the risk and the harm with that benefit, and the only way to protect patients from those biases is by doing a randomized controlled trial.”
This article first appeared on Medscape.com.
COVID-19 pandemic dictates reconsideration of pemphigus therapy
The Dedee F. Murrell, MD, said at the virtual annual meeting of the American Academy of Dermatology.
Together with physicians from the Mayo Clinic, Alexandria (Egypt) University, and Tehran (Iran) University, she recently published updated expert guidance for treatment of this severe, potentially fatal mucocutaneous autoimmune blistering disease, in a letter to the editor in the Journal of the American Academy of Dermatology. She presented some of the key recommendations at AAD 2020.
First off, rituximab (Rituxan), the only Food and Drug Administration–approved medication for moderate to severe pemphigus vulgaris and a biologic considered first-line therapy prepandemic, is ill-advised during the COVID-19 era. Its mechanism of benefit is through B-cell depletion. This is an irreversible effect, and reconstitution of B-cell immunity takes 6-12 months. The absence of this immunologic protection for such a long time poses potentially serious problems for pemphigus patients who become infected with SARS-CoV-2.
Also, the opportunity to administer intravenous infusions of the biologic becomes unpredictable during pandemic surges, when limitations on nonemergent medical care may be necessary, noted Dr. Murrell, professor of dermatology at the University of New South Wales and head of dermatology at St. George University Hospital, both in Sydney.
“We have taken the approach of postponing rituximab infusions temporarily, with the aim of delaying peak patient immunosuppression during peak COVID-19 incidence to reduce the risk of adverse outcomes,” Dr. Murrell and coauthors wrote in the letter (J Am Acad Dermatol. 2020 Jun;82[6]:e235-6).
The other traditional go-to therapy for pemphigus is corticosteroids. They’re effective, fast acting, and relatively inexpensive. But their nonselective immunosuppressive action boosts infection risk in general, and more specifically it increases the risk of developing severe forms of COVID-19 should a patient become infected with SARS-CoV-2.
“A basic therapeutic principle with particular importance during the pandemic is that glucocorticoids and steroid-sparing immunosuppressive agents, such as azathioprine and mycophenolate mofetil, should be tapered to the lowest effective dose. In active COVID-19 infection, immunosuppressive steroid-sparing medications should be discontinued when possible, although glucocorticoid cessation often cannot be considered due to risk for adrenal insufficiency,” the authors continued.
“Effective as adjuvant treatment in both pemphigus and COVID-19,intravenous immunoglobulin supports immunity and therefore may be useful in this setting,” they wrote. It’s not immunosuppressive, and, they noted, there’s good-quality evidence from a Japanese randomized, double-blind, controlled trial that a 5-day course of intravenous immunoglobulin is effective therapy for pemphigus (J Am Acad Dermatol. 2009 Apr;60[4]:595-603).
Moreover, intravenous immunoglobulin is also reportedly effective in severe COVID-19 (Open Forum Infect Dis. 2020 Mar 21. doi: 10.1093/ofid/ofaa102.).
Another option is to consider enrolling a patient with moderate or severe pemphigus vulgaris or foliaceus in the ongoing pivotal phase 3, international, double-blind, placebo-controlled PEGASUS trial of rilzabrutinib, a promising oral reversible Bruton tyrosine kinase inhibitor. The medication has a short half-life and a self-limited immunomodulatory effect. Moreover, the trial is set up for remote patient visits on an outpatient basis via teledermatology, so the 65-week study can continue despite the pandemic. Both newly diagnosed and relapsing patients are eligible for the trial, headed by Dr. Murrell. At AAD 2020 she reported encouraging results from a phase 2b trial of rilzabrutinib.
She is a consultant to Principia Biopharma, sponsor of the PEGASUS trial, and has received institutional research grants from numerous pharmaceutical companies.
The Dedee F. Murrell, MD, said at the virtual annual meeting of the American Academy of Dermatology.
Together with physicians from the Mayo Clinic, Alexandria (Egypt) University, and Tehran (Iran) University, she recently published updated expert guidance for treatment of this severe, potentially fatal mucocutaneous autoimmune blistering disease, in a letter to the editor in the Journal of the American Academy of Dermatology. She presented some of the key recommendations at AAD 2020.
First off, rituximab (Rituxan), the only Food and Drug Administration–approved medication for moderate to severe pemphigus vulgaris and a biologic considered first-line therapy prepandemic, is ill-advised during the COVID-19 era. Its mechanism of benefit is through B-cell depletion. This is an irreversible effect, and reconstitution of B-cell immunity takes 6-12 months. The absence of this immunologic protection for such a long time poses potentially serious problems for pemphigus patients who become infected with SARS-CoV-2.
Also, the opportunity to administer intravenous infusions of the biologic becomes unpredictable during pandemic surges, when limitations on nonemergent medical care may be necessary, noted Dr. Murrell, professor of dermatology at the University of New South Wales and head of dermatology at St. George University Hospital, both in Sydney.
“We have taken the approach of postponing rituximab infusions temporarily, with the aim of delaying peak patient immunosuppression during peak COVID-19 incidence to reduce the risk of adverse outcomes,” Dr. Murrell and coauthors wrote in the letter (J Am Acad Dermatol. 2020 Jun;82[6]:e235-6).
The other traditional go-to therapy for pemphigus is corticosteroids. They’re effective, fast acting, and relatively inexpensive. But their nonselective immunosuppressive action boosts infection risk in general, and more specifically it increases the risk of developing severe forms of COVID-19 should a patient become infected with SARS-CoV-2.
“A basic therapeutic principle with particular importance during the pandemic is that glucocorticoids and steroid-sparing immunosuppressive agents, such as azathioprine and mycophenolate mofetil, should be tapered to the lowest effective dose. In active COVID-19 infection, immunosuppressive steroid-sparing medications should be discontinued when possible, although glucocorticoid cessation often cannot be considered due to risk for adrenal insufficiency,” the authors continued.
“Effective as adjuvant treatment in both pemphigus and COVID-19,intravenous immunoglobulin supports immunity and therefore may be useful in this setting,” they wrote. It’s not immunosuppressive, and, they noted, there’s good-quality evidence from a Japanese randomized, double-blind, controlled trial that a 5-day course of intravenous immunoglobulin is effective therapy for pemphigus (J Am Acad Dermatol. 2009 Apr;60[4]:595-603).
Moreover, intravenous immunoglobulin is also reportedly effective in severe COVID-19 (Open Forum Infect Dis. 2020 Mar 21. doi: 10.1093/ofid/ofaa102.).
Another option is to consider enrolling a patient with moderate or severe pemphigus vulgaris or foliaceus in the ongoing pivotal phase 3, international, double-blind, placebo-controlled PEGASUS trial of rilzabrutinib, a promising oral reversible Bruton tyrosine kinase inhibitor. The medication has a short half-life and a self-limited immunomodulatory effect. Moreover, the trial is set up for remote patient visits on an outpatient basis via teledermatology, so the 65-week study can continue despite the pandemic. Both newly diagnosed and relapsing patients are eligible for the trial, headed by Dr. Murrell. At AAD 2020 she reported encouraging results from a phase 2b trial of rilzabrutinib.
She is a consultant to Principia Biopharma, sponsor of the PEGASUS trial, and has received institutional research grants from numerous pharmaceutical companies.
The Dedee F. Murrell, MD, said at the virtual annual meeting of the American Academy of Dermatology.
Together with physicians from the Mayo Clinic, Alexandria (Egypt) University, and Tehran (Iran) University, she recently published updated expert guidance for treatment of this severe, potentially fatal mucocutaneous autoimmune blistering disease, in a letter to the editor in the Journal of the American Academy of Dermatology. She presented some of the key recommendations at AAD 2020.
First off, rituximab (Rituxan), the only Food and Drug Administration–approved medication for moderate to severe pemphigus vulgaris and a biologic considered first-line therapy prepandemic, is ill-advised during the COVID-19 era. Its mechanism of benefit is through B-cell depletion. This is an irreversible effect, and reconstitution of B-cell immunity takes 6-12 months. The absence of this immunologic protection for such a long time poses potentially serious problems for pemphigus patients who become infected with SARS-CoV-2.
Also, the opportunity to administer intravenous infusions of the biologic becomes unpredictable during pandemic surges, when limitations on nonemergent medical care may be necessary, noted Dr. Murrell, professor of dermatology at the University of New South Wales and head of dermatology at St. George University Hospital, both in Sydney.
“We have taken the approach of postponing rituximab infusions temporarily, with the aim of delaying peak patient immunosuppression during peak COVID-19 incidence to reduce the risk of adverse outcomes,” Dr. Murrell and coauthors wrote in the letter (J Am Acad Dermatol. 2020 Jun;82[6]:e235-6).
The other traditional go-to therapy for pemphigus is corticosteroids. They’re effective, fast acting, and relatively inexpensive. But their nonselective immunosuppressive action boosts infection risk in general, and more specifically it increases the risk of developing severe forms of COVID-19 should a patient become infected with SARS-CoV-2.
“A basic therapeutic principle with particular importance during the pandemic is that glucocorticoids and steroid-sparing immunosuppressive agents, such as azathioprine and mycophenolate mofetil, should be tapered to the lowest effective dose. In active COVID-19 infection, immunosuppressive steroid-sparing medications should be discontinued when possible, although glucocorticoid cessation often cannot be considered due to risk for adrenal insufficiency,” the authors continued.
“Effective as adjuvant treatment in both pemphigus and COVID-19,intravenous immunoglobulin supports immunity and therefore may be useful in this setting,” they wrote. It’s not immunosuppressive, and, they noted, there’s good-quality evidence from a Japanese randomized, double-blind, controlled trial that a 5-day course of intravenous immunoglobulin is effective therapy for pemphigus (J Am Acad Dermatol. 2009 Apr;60[4]:595-603).
Moreover, intravenous immunoglobulin is also reportedly effective in severe COVID-19 (Open Forum Infect Dis. 2020 Mar 21. doi: 10.1093/ofid/ofaa102.).
Another option is to consider enrolling a patient with moderate or severe pemphigus vulgaris or foliaceus in the ongoing pivotal phase 3, international, double-blind, placebo-controlled PEGASUS trial of rilzabrutinib, a promising oral reversible Bruton tyrosine kinase inhibitor. The medication has a short half-life and a self-limited immunomodulatory effect. Moreover, the trial is set up for remote patient visits on an outpatient basis via teledermatology, so the 65-week study can continue despite the pandemic. Both newly diagnosed and relapsing patients are eligible for the trial, headed by Dr. Murrell. At AAD 2020 she reported encouraging results from a phase 2b trial of rilzabrutinib.
She is a consultant to Principia Biopharma, sponsor of the PEGASUS trial, and has received institutional research grants from numerous pharmaceutical companies.
FROM AAD 20
PCI or not, mortality climbs with post-ACS bleeding complications
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
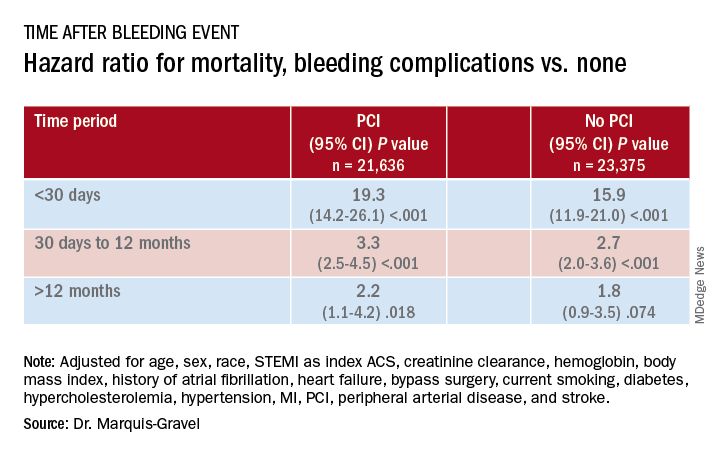
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
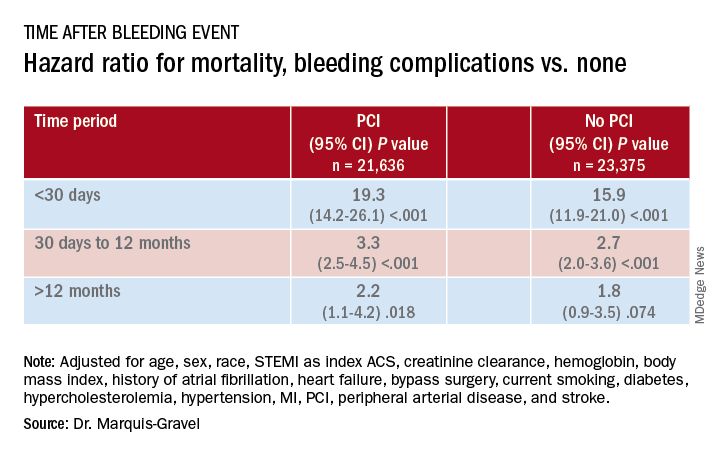
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
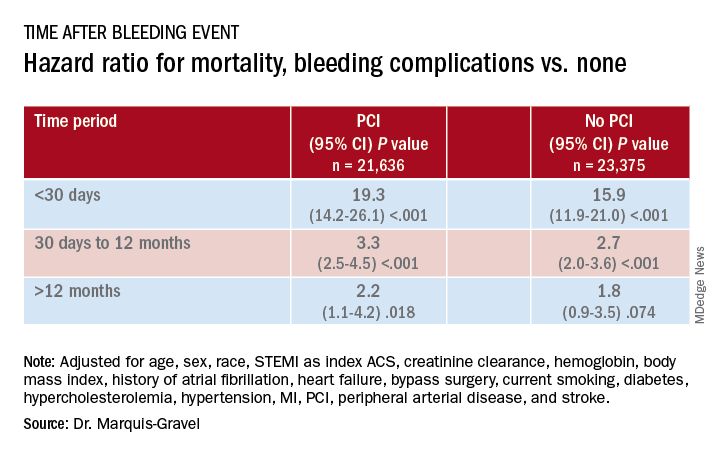
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
What have we learned from COVID?
In 2015, I proposed virtual care for the division of adolescent medicine, to the administration of our Midwestern children and adolescent hospital; they gladly listened and accepted a copy of the resources I provided. Virtual care was acknowledged to be the future direction of our and other organizations.
Four years later, virtual visits were introduced in the pediatric urgent care, but with little usability as families were slow to adopt this new form of medicine. Fast forward to the COVID-19 crisis in March 2020, and virtual medicine was the only option to meet the needs of patients and to stop the economic consequences. Unfortunately, the expedited rollout at our and many other hospitals may have resulted in limited program development and a lack of shared best practices.
Since March 2020, both patients and medical providers have accepted virtual care, but we now have an opportunity to review some of the limitations to offering virtual care. Work in primary care centers may see limitations using virtual medicine to meet the needs of all patients. Take into consideration the ability to offer confidential care. Confidential care has been a challenge virtually. For example, while completing a virtual visit with a 19-year-old female, it was apparent she was not alone and when asked a benign question the commotion in the background told the real story. The young woman began to laugh and said, “That was my dad running out of the room.” Despite requesting that parents leave the call, they can be heard within earshot of the caller.
On a televisit, written words appear backwards on the video, requiring written questions to be mirror images. When asking questions meant to be confidential, we have used note cards with a question mark. Verbal directions asking the adolescent to give a thumbs up or down to answer the question are required to maintain privacy from others in the room. If the patient responds thumbs up, this leads to additional questions with note cards. Although not ideal, this process gets to the answers, and the adolescent can disclose confidential information without concern about being overheard. Child abuse and neglect professionals have found similar challenges talking to caregivers or children as they are uncertain if others in the home are out of the screen but listening to the questions or prompting responses.
Obtaining vitals may be restricted and picking up hypertension or changes in weight has been limited to face to face visits. To continue to provide virtual care will require screening stations. I foresee a kiosk at the grocery or drugstore with a computer and the ability to obtain vitals or portions of an exam such as heart and lung evaluations. Patients could go at their convenience and the results could be sent to their providers. Technology already exists to use a cell phone to take photos of a toddler’s sore ear drum, and to obtain basic pulse oximetry and ECG, but these have a cost and may be available only to those able to afford these tools.
Billing issues have developed when patients go to a lab on the same day as a virtual visit. Completing a virtual visit for a sore throat thought to be streptococcal pharyngitis should not be finalized without access to a streptococcal throat swab. Until families have home kits to evaluate for strep throat, the families must bring the patient to a clinic or lab to obtain a pharyngeal culture. Furthermore, insurance reimbursement standards will need to be set for ongoing virtual health to become a sustainable option.
Workflows have been disrupted by balancing face to face visits with virtual visits. Unless the virtual visit has been set up for the medical team to access immediately, there are delays accessing the virtual platform, resulting in unnecessary gaps in care. Arranging schedules to separate face to face visits from virtual visits offers more efficiency. Creating a block of virtual visits separated from face-to-face visits or assigning providers to virtual-only schedules may be the best option for an efficient clinic flow. Telemedicine visit templates may need to be created as virtual visits become standard practice.
At present, virtual visits can only be offered to English-speaking patients. The inability to offer translators limits access to a small number of patients. Given COVID-19’s impact on the underserved communities, having a safe resource to reach these patients has been limited, leaving face-to-face visits as their only option. Requiring a face-to-face visit during peak illness has placed patients at risk. They have refused health care as opposed to exposure to the illness in health care settings.
We have innovative opportunities to create a new health care system. Despite the initial struggles with the adoption of virtual care, patients and providers have begun embracing the technology. Best practices and shared resources will be required to have a successful system before brick and mortar organizations can be reduced or insurance companies create their own health care systems which can branch across state lines.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She said she had no relevant financial disclosures. Email her at [email protected].
The article was updated 7/17/2020.
In 2015, I proposed virtual care for the division of adolescent medicine, to the administration of our Midwestern children and adolescent hospital; they gladly listened and accepted a copy of the resources I provided. Virtual care was acknowledged to be the future direction of our and other organizations.
Four years later, virtual visits were introduced in the pediatric urgent care, but with little usability as families were slow to adopt this new form of medicine. Fast forward to the COVID-19 crisis in March 2020, and virtual medicine was the only option to meet the needs of patients and to stop the economic consequences. Unfortunately, the expedited rollout at our and many other hospitals may have resulted in limited program development and a lack of shared best practices.
Since March 2020, both patients and medical providers have accepted virtual care, but we now have an opportunity to review some of the limitations to offering virtual care. Work in primary care centers may see limitations using virtual medicine to meet the needs of all patients. Take into consideration the ability to offer confidential care. Confidential care has been a challenge virtually. For example, while completing a virtual visit with a 19-year-old female, it was apparent she was not alone and when asked a benign question the commotion in the background told the real story. The young woman began to laugh and said, “That was my dad running out of the room.” Despite requesting that parents leave the call, they can be heard within earshot of the caller.
On a televisit, written words appear backwards on the video, requiring written questions to be mirror images. When asking questions meant to be confidential, we have used note cards with a question mark. Verbal directions asking the adolescent to give a thumbs up or down to answer the question are required to maintain privacy from others in the room. If the patient responds thumbs up, this leads to additional questions with note cards. Although not ideal, this process gets to the answers, and the adolescent can disclose confidential information without concern about being overheard. Child abuse and neglect professionals have found similar challenges talking to caregivers or children as they are uncertain if others in the home are out of the screen but listening to the questions or prompting responses.
Obtaining vitals may be restricted and picking up hypertension or changes in weight has been limited to face to face visits. To continue to provide virtual care will require screening stations. I foresee a kiosk at the grocery or drugstore with a computer and the ability to obtain vitals or portions of an exam such as heart and lung evaluations. Patients could go at their convenience and the results could be sent to their providers. Technology already exists to use a cell phone to take photos of a toddler’s sore ear drum, and to obtain basic pulse oximetry and ECG, but these have a cost and may be available only to those able to afford these tools.
Billing issues have developed when patients go to a lab on the same day as a virtual visit. Completing a virtual visit for a sore throat thought to be streptococcal pharyngitis should not be finalized without access to a streptococcal throat swab. Until families have home kits to evaluate for strep throat, the families must bring the patient to a clinic or lab to obtain a pharyngeal culture. Furthermore, insurance reimbursement standards will need to be set for ongoing virtual health to become a sustainable option.
Workflows have been disrupted by balancing face to face visits with virtual visits. Unless the virtual visit has been set up for the medical team to access immediately, there are delays accessing the virtual platform, resulting in unnecessary gaps in care. Arranging schedules to separate face to face visits from virtual visits offers more efficiency. Creating a block of virtual visits separated from face-to-face visits or assigning providers to virtual-only schedules may be the best option for an efficient clinic flow. Telemedicine visit templates may need to be created as virtual visits become standard practice.
At present, virtual visits can only be offered to English-speaking patients. The inability to offer translators limits access to a small number of patients. Given COVID-19’s impact on the underserved communities, having a safe resource to reach these patients has been limited, leaving face-to-face visits as their only option. Requiring a face-to-face visit during peak illness has placed patients at risk. They have refused health care as opposed to exposure to the illness in health care settings.
We have innovative opportunities to create a new health care system. Despite the initial struggles with the adoption of virtual care, patients and providers have begun embracing the technology. Best practices and shared resources will be required to have a successful system before brick and mortar organizations can be reduced or insurance companies create their own health care systems which can branch across state lines.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She said she had no relevant financial disclosures. Email her at [email protected].
The article was updated 7/17/2020.
In 2015, I proposed virtual care for the division of adolescent medicine, to the administration of our Midwestern children and adolescent hospital; they gladly listened and accepted a copy of the resources I provided. Virtual care was acknowledged to be the future direction of our and other organizations.
Four years later, virtual visits were introduced in the pediatric urgent care, but with little usability as families were slow to adopt this new form of medicine. Fast forward to the COVID-19 crisis in March 2020, and virtual medicine was the only option to meet the needs of patients and to stop the economic consequences. Unfortunately, the expedited rollout at our and many other hospitals may have resulted in limited program development and a lack of shared best practices.
Since March 2020, both patients and medical providers have accepted virtual care, but we now have an opportunity to review some of the limitations to offering virtual care. Work in primary care centers may see limitations using virtual medicine to meet the needs of all patients. Take into consideration the ability to offer confidential care. Confidential care has been a challenge virtually. For example, while completing a virtual visit with a 19-year-old female, it was apparent she was not alone and when asked a benign question the commotion in the background told the real story. The young woman began to laugh and said, “That was my dad running out of the room.” Despite requesting that parents leave the call, they can be heard within earshot of the caller.
On a televisit, written words appear backwards on the video, requiring written questions to be mirror images. When asking questions meant to be confidential, we have used note cards with a question mark. Verbal directions asking the adolescent to give a thumbs up or down to answer the question are required to maintain privacy from others in the room. If the patient responds thumbs up, this leads to additional questions with note cards. Although not ideal, this process gets to the answers, and the adolescent can disclose confidential information without concern about being overheard. Child abuse and neglect professionals have found similar challenges talking to caregivers or children as they are uncertain if others in the home are out of the screen but listening to the questions or prompting responses.
Obtaining vitals may be restricted and picking up hypertension or changes in weight has been limited to face to face visits. To continue to provide virtual care will require screening stations. I foresee a kiosk at the grocery or drugstore with a computer and the ability to obtain vitals or portions of an exam such as heart and lung evaluations. Patients could go at their convenience and the results could be sent to their providers. Technology already exists to use a cell phone to take photos of a toddler’s sore ear drum, and to obtain basic pulse oximetry and ECG, but these have a cost and may be available only to those able to afford these tools.
Billing issues have developed when patients go to a lab on the same day as a virtual visit. Completing a virtual visit for a sore throat thought to be streptococcal pharyngitis should not be finalized without access to a streptococcal throat swab. Until families have home kits to evaluate for strep throat, the families must bring the patient to a clinic or lab to obtain a pharyngeal culture. Furthermore, insurance reimbursement standards will need to be set for ongoing virtual health to become a sustainable option.
Workflows have been disrupted by balancing face to face visits with virtual visits. Unless the virtual visit has been set up for the medical team to access immediately, there are delays accessing the virtual platform, resulting in unnecessary gaps in care. Arranging schedules to separate face to face visits from virtual visits offers more efficiency. Creating a block of virtual visits separated from face-to-face visits or assigning providers to virtual-only schedules may be the best option for an efficient clinic flow. Telemedicine visit templates may need to be created as virtual visits become standard practice.
At present, virtual visits can only be offered to English-speaking patients. The inability to offer translators limits access to a small number of patients. Given COVID-19’s impact on the underserved communities, having a safe resource to reach these patients has been limited, leaving face-to-face visits as their only option. Requiring a face-to-face visit during peak illness has placed patients at risk. They have refused health care as opposed to exposure to the illness in health care settings.
We have innovative opportunities to create a new health care system. Despite the initial struggles with the adoption of virtual care, patients and providers have begun embracing the technology. Best practices and shared resources will be required to have a successful system before brick and mortar organizations can be reduced or insurance companies create their own health care systems which can branch across state lines.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She said she had no relevant financial disclosures. Email her at [email protected].
The article was updated 7/17/2020.
SGLT2 inhibitors, developed for T2D, now ‘belong to cardiologists and nephrologists’
It’s passé to think of the sodium-glucose cotransporter 2 (SGLT2) inhibitor drugs as agents that primarily treat hyperglycemia because their major clinical role has rapidly morphed into treating or preventing heart failure and chronic kidney disease.
This change suddenly thrust primary responsibility for prescribing these drug into the hands of cardiologists and nephrologists, though endocrinologists, diabetologists, and primary care physicians remain in the prescribing mix, experts agreed at the virtual annual scientific sessions of the American Diabetes Association.
“Glucose lowering plays little or no role in the cardiorenal protection from drugs in the sodium-glucose cotransporter 2 inhibitor class,” said David Z. Cherney, MD, a nephrologist and professor of medicine at the University of Toronto.
The SGLT2 inhibitor drugs “belong to cardiologists and nephrologists,” declared endocrinologist Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of The Metabolic Institute of America in Tarzana, Calif.
But therein lies a problem. “Cardiologists and nephrologists often say that they don’t want to start SGLT2 inhibitors because they do not want to interfere with the glucose reducing medications a patient takes,” Dr. Cherney added.
“Cardiologists are absolutely afraid to prescribe SGLT2 inhibitors,” claimed John J.V. McMurray MD, a professor of medical cardiology at the University of Glasgow. “Cardiologists need to talk with diabetologists about the importance of treating heart failure” in patients with type 2 diabetes (T2D), and diabetologists “need to help cardiologists understand how to use these and other effective glucose-lowering drugs that reduce cardiovascular disease risk,” said Dr. McMurray during the ADA sessions.
“I don’t think any medical specialty owns this drug class,” said Silvio E. Inzucchi, MD, professor of medicine at Yale University, New Haven, Conn., and director of the Yale Medicine Diabetes Center. “No permission is needed” from an endocrinologist for another specialist to prescribe an SGLT2 inhibitor to patients with T2D or to appropriate patients without diabetes, he maintained.
The need for greater involvement by cardiologists in prescribing SGLT2 inhibitors to patients with T2D was underscored in findings recently reported by Dr. Inzucchi and associates. They analyzed the physician encounters that patients with T2D had with cardiologists and endocrinologists during 2017 at two U.S. health systems: one centered around clinicians affiliated with Yale Medicine and Yale University, and a second with clinicians drawn from the staffs of the Saint Luke’s Health System, including Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
During 2017, the two systems has outpatient encounters with 109,747 patients with T2D, who averaged 67 years of age and were roughly evenly split between women and men: 43% had prevalent cardiovascular disease, including 30% with coronary artery disease and 15% with heart failure. These patients had more than 110,000 physician visits, and the number of these consultations with a cardiologist was double the number with an endocrinologist, Dr. Inzucchi and associates recently reported (Cardiovasc Endocrinol Metab. 2020 Jun;9[2]:56-9).
Among the 30% of T2D patients with prevalent cardiovascular disease, the consultation rate with a cardiologist was four times greater than with an endocrinologist; among the 15% with heart failure, a visit with a cardiologist was nearly seven times more common that with an endocrinologist.
“Based on these data, cardiovascular specialists encouraging the use of these medications, or, if comfortable, actually prescribing these medications, would likely significantly hasten the adoption of evidence-based glucose-lowering therapies in those patients most apt to benefit from them,” concluded the study’s authors.
Dr. Cherney has been a consultant to or has received honoraria from AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Merck, Mitsubishi Tanabe Pharma, and Sanofi. Dr. Handelsman has been a consultant to or speaker on behalf of Amarin, Amgen, Applied Therapeutic, AstraZeneca, Boehringer Ingelheim, Esperion, Gilead, Janssen, Merck, Merck-Pfizer, Novo Nordisk, Regeneron, and Sanofi. Dr. McMurray’s employer, the University of Glasgow, received payments from AstraZeneca for his involvement in trials involving dapagliflozin. Dr. Inzucchi has been a consultant to or helped run trials for Abbott, AstraZeneca, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
It’s passé to think of the sodium-glucose cotransporter 2 (SGLT2) inhibitor drugs as agents that primarily treat hyperglycemia because their major clinical role has rapidly morphed into treating or preventing heart failure and chronic kidney disease.
This change suddenly thrust primary responsibility for prescribing these drug into the hands of cardiologists and nephrologists, though endocrinologists, diabetologists, and primary care physicians remain in the prescribing mix, experts agreed at the virtual annual scientific sessions of the American Diabetes Association.
“Glucose lowering plays little or no role in the cardiorenal protection from drugs in the sodium-glucose cotransporter 2 inhibitor class,” said David Z. Cherney, MD, a nephrologist and professor of medicine at the University of Toronto.
The SGLT2 inhibitor drugs “belong to cardiologists and nephrologists,” declared endocrinologist Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of The Metabolic Institute of America in Tarzana, Calif.
But therein lies a problem. “Cardiologists and nephrologists often say that they don’t want to start SGLT2 inhibitors because they do not want to interfere with the glucose reducing medications a patient takes,” Dr. Cherney added.
“Cardiologists are absolutely afraid to prescribe SGLT2 inhibitors,” claimed John J.V. McMurray MD, a professor of medical cardiology at the University of Glasgow. “Cardiologists need to talk with diabetologists about the importance of treating heart failure” in patients with type 2 diabetes (T2D), and diabetologists “need to help cardiologists understand how to use these and other effective glucose-lowering drugs that reduce cardiovascular disease risk,” said Dr. McMurray during the ADA sessions.
“I don’t think any medical specialty owns this drug class,” said Silvio E. Inzucchi, MD, professor of medicine at Yale University, New Haven, Conn., and director of the Yale Medicine Diabetes Center. “No permission is needed” from an endocrinologist for another specialist to prescribe an SGLT2 inhibitor to patients with T2D or to appropriate patients without diabetes, he maintained.
The need for greater involvement by cardiologists in prescribing SGLT2 inhibitors to patients with T2D was underscored in findings recently reported by Dr. Inzucchi and associates. They analyzed the physician encounters that patients with T2D had with cardiologists and endocrinologists during 2017 at two U.S. health systems: one centered around clinicians affiliated with Yale Medicine and Yale University, and a second with clinicians drawn from the staffs of the Saint Luke’s Health System, including Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
During 2017, the two systems has outpatient encounters with 109,747 patients with T2D, who averaged 67 years of age and were roughly evenly split between women and men: 43% had prevalent cardiovascular disease, including 30% with coronary artery disease and 15% with heart failure. These patients had more than 110,000 physician visits, and the number of these consultations with a cardiologist was double the number with an endocrinologist, Dr. Inzucchi and associates recently reported (Cardiovasc Endocrinol Metab. 2020 Jun;9[2]:56-9).
Among the 30% of T2D patients with prevalent cardiovascular disease, the consultation rate with a cardiologist was four times greater than with an endocrinologist; among the 15% with heart failure, a visit with a cardiologist was nearly seven times more common that with an endocrinologist.
“Based on these data, cardiovascular specialists encouraging the use of these medications, or, if comfortable, actually prescribing these medications, would likely significantly hasten the adoption of evidence-based glucose-lowering therapies in those patients most apt to benefit from them,” concluded the study’s authors.
Dr. Cherney has been a consultant to or has received honoraria from AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Merck, Mitsubishi Tanabe Pharma, and Sanofi. Dr. Handelsman has been a consultant to or speaker on behalf of Amarin, Amgen, Applied Therapeutic, AstraZeneca, Boehringer Ingelheim, Esperion, Gilead, Janssen, Merck, Merck-Pfizer, Novo Nordisk, Regeneron, and Sanofi. Dr. McMurray’s employer, the University of Glasgow, received payments from AstraZeneca for his involvement in trials involving dapagliflozin. Dr. Inzucchi has been a consultant to or helped run trials for Abbott, AstraZeneca, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
It’s passé to think of the sodium-glucose cotransporter 2 (SGLT2) inhibitor drugs as agents that primarily treat hyperglycemia because their major clinical role has rapidly morphed into treating or preventing heart failure and chronic kidney disease.
This change suddenly thrust primary responsibility for prescribing these drug into the hands of cardiologists and nephrologists, though endocrinologists, diabetologists, and primary care physicians remain in the prescribing mix, experts agreed at the virtual annual scientific sessions of the American Diabetes Association.
“Glucose lowering plays little or no role in the cardiorenal protection from drugs in the sodium-glucose cotransporter 2 inhibitor class,” said David Z. Cherney, MD, a nephrologist and professor of medicine at the University of Toronto.
The SGLT2 inhibitor drugs “belong to cardiologists and nephrologists,” declared endocrinologist Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of The Metabolic Institute of America in Tarzana, Calif.
But therein lies a problem. “Cardiologists and nephrologists often say that they don’t want to start SGLT2 inhibitors because they do not want to interfere with the glucose reducing medications a patient takes,” Dr. Cherney added.
“Cardiologists are absolutely afraid to prescribe SGLT2 inhibitors,” claimed John J.V. McMurray MD, a professor of medical cardiology at the University of Glasgow. “Cardiologists need to talk with diabetologists about the importance of treating heart failure” in patients with type 2 diabetes (T2D), and diabetologists “need to help cardiologists understand how to use these and other effective glucose-lowering drugs that reduce cardiovascular disease risk,” said Dr. McMurray during the ADA sessions.
“I don’t think any medical specialty owns this drug class,” said Silvio E. Inzucchi, MD, professor of medicine at Yale University, New Haven, Conn., and director of the Yale Medicine Diabetes Center. “No permission is needed” from an endocrinologist for another specialist to prescribe an SGLT2 inhibitor to patients with T2D or to appropriate patients without diabetes, he maintained.
The need for greater involvement by cardiologists in prescribing SGLT2 inhibitors to patients with T2D was underscored in findings recently reported by Dr. Inzucchi and associates. They analyzed the physician encounters that patients with T2D had with cardiologists and endocrinologists during 2017 at two U.S. health systems: one centered around clinicians affiliated with Yale Medicine and Yale University, and a second with clinicians drawn from the staffs of the Saint Luke’s Health System, including Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
During 2017, the two systems has outpatient encounters with 109,747 patients with T2D, who averaged 67 years of age and were roughly evenly split between women and men: 43% had prevalent cardiovascular disease, including 30% with coronary artery disease and 15% with heart failure. These patients had more than 110,000 physician visits, and the number of these consultations with a cardiologist was double the number with an endocrinologist, Dr. Inzucchi and associates recently reported (Cardiovasc Endocrinol Metab. 2020 Jun;9[2]:56-9).
Among the 30% of T2D patients with prevalent cardiovascular disease, the consultation rate with a cardiologist was four times greater than with an endocrinologist; among the 15% with heart failure, a visit with a cardiologist was nearly seven times more common that with an endocrinologist.
“Based on these data, cardiovascular specialists encouraging the use of these medications, or, if comfortable, actually prescribing these medications, would likely significantly hasten the adoption of evidence-based glucose-lowering therapies in those patients most apt to benefit from them,” concluded the study’s authors.
Dr. Cherney has been a consultant to or has received honoraria from AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Merck, Mitsubishi Tanabe Pharma, and Sanofi. Dr. Handelsman has been a consultant to or speaker on behalf of Amarin, Amgen, Applied Therapeutic, AstraZeneca, Boehringer Ingelheim, Esperion, Gilead, Janssen, Merck, Merck-Pfizer, Novo Nordisk, Regeneron, and Sanofi. Dr. McMurray’s employer, the University of Glasgow, received payments from AstraZeneca for his involvement in trials involving dapagliflozin. Dr. Inzucchi has been a consultant to or helped run trials for Abbott, AstraZeneca, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
FROM ADA 2020
Provide support in uncertain times
A sense of safety and stability, both emotional and physical, is crucial in promoting the healthy development of youth. Between the global pandemic, need for social distancing, economic downturn, and increased awareness of racial disparities, for many this sense of stability has been rattled.
School closures have led to a loss of social interaction, challenges to continued academic growth, and, for some students, lack of access to nutrition and increased food insecurity. For students with learning or mental health challenges, closures may have eliminated or significantly reduced desperately needed supports received in school.1 While these trying circumstances have been difficult for many, the transition back to school in the fall also may be challenging because of the uncertainty about what this will look like and possible change in routine. Some students or their families may have anxiety about returning, either because of a history of adverse experiences at school such as bullying, or because of fears about exposure for themselves or others to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The past several months also brought about greater awareness of systemic racial disparities, whether as reflected in health care, education, or the criminal justice system. According to the Centers for Disease Control and Prevention data, Latinx and African-American individuals in the United States have had a threefold greater chance of contracting SARS-CoV-2 and have a twofold greater risk of death, compared with white people in the same communities.2 Other social determinants of health – economic stability, education, social factors such as incarceration and discrimination, and neighborhood factors including access to healthy food – play a role in this vulnerability.
The pandemic has resulted in a need for social distancing, and as a result, isolation. Children and teens exposed to the news may have anxiety about what they see or hear. Additional pressures in the family can include economic uncertainty, loss of employment for the primary wage earner of the household, or stress related to family members being first responders.
Any one of these factors is a potentially significant stressor, so how do we best support youth to help them survive and hopefully thrive during this time?
- It is important to establish a sense of routine; this can help create a sense of stability and safety. Recognizing that circumstances are not the same as they were 5 or 6 months ago, encouraging structure should not come at the cost of preserving connection.
- Note positive behavior and choices made by children and make sure they know it was observed.
- Many children have experienced increased screen time with the lack of structure of the traditional school day or summer camp and extracurricular activities. Limiting screen time and being mindful of its potential impact on mood is prudent.
- Self-care for parents and guardians is important. This time is stressful for the adults of the household, let alone children who are learning self-regulation skills.
- Listen to children’s or teens’ concerns and share information in developmentally appropriate ways. It is okay to not have all of the answers.
- Balance fostering a sense of gratitude with not invalidating a child’s or teen’s experience. Showing empathy during this time is vital. While there may be other soccer seasons, it is normal to experience grief about the loss of experiences during this time.
- Parents and guardians know their children best, so it is prudent for them to be mindful of concerning changes such as an increase in sadness, anxiety, or irritability that negatively impacts daily functioning such as sleeping, eating, or relationships with family and friends.
- Promote social interactions with appropriate safeguards in place. Unfortunately, the number of SARS-CoV-2 infections is increasing in multiple states, and there is the potential to return to some of the previous restrictions. However, encouraging social interaction while following local guidelines and with cautions such as limiting the number of people present, meeting outside, or considering interacting with others who are similarly social distancing can help foster social connection and development.
- Maintain connection digitally when in-person contact is not an option.3 Social groups, places of worship, and other activities have been agile in developing virtual communities. Communication by voice and/or video is thought to be more powerful than by written communication (text, email) alone.4 However, it is important to consider those who may have limited to no access to electronic methods.
- Encourage open communication with children about diversity and bias, and consider how our interactions with others may affect our children’s perspectives.5
- As providers, it is crucial that we address structural and institutional systems that negatively impact the health, safety, and access to care including our Black, indigenous, and people of color (BIPOC) and lesbian, gay, bisexual, transgender/transsexual, queer/questioning, intersex, and allied/asexual/aromantic/agender (LGBTQIA) patients.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. Dr. Strange has no relevant financial disclosures. Email her at [email protected].
Online resources for parents and families
- Child Mind Institute: Coping With the Coronavirus Crisis: Supporting Your Kids.
- American Psychological Association: Talking with children about discrimination.
- Common Sense Media: Help with determining appropriateness of media for children.
Hotlines
- National Suicide Prevention Hotline: 1-800-273-8255
- GLBT National Hotline: 888-843-4564
- The California Peer-Run Warm Line: 1-855-845-7415
- Trevor Project: 866-488-7386 or text TREVOR to 1-202-304-1200
- Trans Lifeline: 877-565-8860
- Crisis Text Line: Text HOME to 741741
References
1. JAMA Pediatr. 2020 Apr 14. doi: 10.1001/jamapediatrics.2020.1456.
2. CDC: COVID-19 in Racial and Ethnic Minority Groups.
3. JAMA. 2020 Mar 23. doi: 10.1001/jama.2020.4469.
4. JAMA Intern Med. 2020 Apr 10. doi: 10.1001/jamainternmed.2020.1562.
5. American Psychological Association: Talking with children about discrimination.
A sense of safety and stability, both emotional and physical, is crucial in promoting the healthy development of youth. Between the global pandemic, need for social distancing, economic downturn, and increased awareness of racial disparities, for many this sense of stability has been rattled.
School closures have led to a loss of social interaction, challenges to continued academic growth, and, for some students, lack of access to nutrition and increased food insecurity. For students with learning or mental health challenges, closures may have eliminated or significantly reduced desperately needed supports received in school.1 While these trying circumstances have been difficult for many, the transition back to school in the fall also may be challenging because of the uncertainty about what this will look like and possible change in routine. Some students or their families may have anxiety about returning, either because of a history of adverse experiences at school such as bullying, or because of fears about exposure for themselves or others to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The past several months also brought about greater awareness of systemic racial disparities, whether as reflected in health care, education, or the criminal justice system. According to the Centers for Disease Control and Prevention data, Latinx and African-American individuals in the United States have had a threefold greater chance of contracting SARS-CoV-2 and have a twofold greater risk of death, compared with white people in the same communities.2 Other social determinants of health – economic stability, education, social factors such as incarceration and discrimination, and neighborhood factors including access to healthy food – play a role in this vulnerability.
The pandemic has resulted in a need for social distancing, and as a result, isolation. Children and teens exposed to the news may have anxiety about what they see or hear. Additional pressures in the family can include economic uncertainty, loss of employment for the primary wage earner of the household, or stress related to family members being first responders.
Any one of these factors is a potentially significant stressor, so how do we best support youth to help them survive and hopefully thrive during this time?
- It is important to establish a sense of routine; this can help create a sense of stability and safety. Recognizing that circumstances are not the same as they were 5 or 6 months ago, encouraging structure should not come at the cost of preserving connection.
- Note positive behavior and choices made by children and make sure they know it was observed.
- Many children have experienced increased screen time with the lack of structure of the traditional school day or summer camp and extracurricular activities. Limiting screen time and being mindful of its potential impact on mood is prudent.
- Self-care for parents and guardians is important. This time is stressful for the adults of the household, let alone children who are learning self-regulation skills.
- Listen to children’s or teens’ concerns and share information in developmentally appropriate ways. It is okay to not have all of the answers.
- Balance fostering a sense of gratitude with not invalidating a child’s or teen’s experience. Showing empathy during this time is vital. While there may be other soccer seasons, it is normal to experience grief about the loss of experiences during this time.
- Parents and guardians know their children best, so it is prudent for them to be mindful of concerning changes such as an increase in sadness, anxiety, or irritability that negatively impacts daily functioning such as sleeping, eating, or relationships with family and friends.
- Promote social interactions with appropriate safeguards in place. Unfortunately, the number of SARS-CoV-2 infections is increasing in multiple states, and there is the potential to return to some of the previous restrictions. However, encouraging social interaction while following local guidelines and with cautions such as limiting the number of people present, meeting outside, or considering interacting with others who are similarly social distancing can help foster social connection and development.
- Maintain connection digitally when in-person contact is not an option.3 Social groups, places of worship, and other activities have been agile in developing virtual communities. Communication by voice and/or video is thought to be more powerful than by written communication (text, email) alone.4 However, it is important to consider those who may have limited to no access to electronic methods.
- Encourage open communication with children about diversity and bias, and consider how our interactions with others may affect our children’s perspectives.5
- As providers, it is crucial that we address structural and institutional systems that negatively impact the health, safety, and access to care including our Black, indigenous, and people of color (BIPOC) and lesbian, gay, bisexual, transgender/transsexual, queer/questioning, intersex, and allied/asexual/aromantic/agender (LGBTQIA) patients.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. Dr. Strange has no relevant financial disclosures. Email her at [email protected].
Online resources for parents and families
- Child Mind Institute: Coping With the Coronavirus Crisis: Supporting Your Kids.
- American Psychological Association: Talking with children about discrimination.
- Common Sense Media: Help with determining appropriateness of media for children.
Hotlines
- National Suicide Prevention Hotline: 1-800-273-8255
- GLBT National Hotline: 888-843-4564
- The California Peer-Run Warm Line: 1-855-845-7415
- Trevor Project: 866-488-7386 or text TREVOR to 1-202-304-1200
- Trans Lifeline: 877-565-8860
- Crisis Text Line: Text HOME to 741741
References
1. JAMA Pediatr. 2020 Apr 14. doi: 10.1001/jamapediatrics.2020.1456.
2. CDC: COVID-19 in Racial and Ethnic Minority Groups.
3. JAMA. 2020 Mar 23. doi: 10.1001/jama.2020.4469.
4. JAMA Intern Med. 2020 Apr 10. doi: 10.1001/jamainternmed.2020.1562.
5. American Psychological Association: Talking with children about discrimination.
A sense of safety and stability, both emotional and physical, is crucial in promoting the healthy development of youth. Between the global pandemic, need for social distancing, economic downturn, and increased awareness of racial disparities, for many this sense of stability has been rattled.
School closures have led to a loss of social interaction, challenges to continued academic growth, and, for some students, lack of access to nutrition and increased food insecurity. For students with learning or mental health challenges, closures may have eliminated or significantly reduced desperately needed supports received in school.1 While these trying circumstances have been difficult for many, the transition back to school in the fall also may be challenging because of the uncertainty about what this will look like and possible change in routine. Some students or their families may have anxiety about returning, either because of a history of adverse experiences at school such as bullying, or because of fears about exposure for themselves or others to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The past several months also brought about greater awareness of systemic racial disparities, whether as reflected in health care, education, or the criminal justice system. According to the Centers for Disease Control and Prevention data, Latinx and African-American individuals in the United States have had a threefold greater chance of contracting SARS-CoV-2 and have a twofold greater risk of death, compared with white people in the same communities.2 Other social determinants of health – economic stability, education, social factors such as incarceration and discrimination, and neighborhood factors including access to healthy food – play a role in this vulnerability.
The pandemic has resulted in a need for social distancing, and as a result, isolation. Children and teens exposed to the news may have anxiety about what they see or hear. Additional pressures in the family can include economic uncertainty, loss of employment for the primary wage earner of the household, or stress related to family members being first responders.
Any one of these factors is a potentially significant stressor, so how do we best support youth to help them survive and hopefully thrive during this time?
- It is important to establish a sense of routine; this can help create a sense of stability and safety. Recognizing that circumstances are not the same as they were 5 or 6 months ago, encouraging structure should not come at the cost of preserving connection.
- Note positive behavior and choices made by children and make sure they know it was observed.
- Many children have experienced increased screen time with the lack of structure of the traditional school day or summer camp and extracurricular activities. Limiting screen time and being mindful of its potential impact on mood is prudent.
- Self-care for parents and guardians is important. This time is stressful for the adults of the household, let alone children who are learning self-regulation skills.
- Listen to children’s or teens’ concerns and share information in developmentally appropriate ways. It is okay to not have all of the answers.
- Balance fostering a sense of gratitude with not invalidating a child’s or teen’s experience. Showing empathy during this time is vital. While there may be other soccer seasons, it is normal to experience grief about the loss of experiences during this time.
- Parents and guardians know their children best, so it is prudent for them to be mindful of concerning changes such as an increase in sadness, anxiety, or irritability that negatively impacts daily functioning such as sleeping, eating, or relationships with family and friends.
- Promote social interactions with appropriate safeguards in place. Unfortunately, the number of SARS-CoV-2 infections is increasing in multiple states, and there is the potential to return to some of the previous restrictions. However, encouraging social interaction while following local guidelines and with cautions such as limiting the number of people present, meeting outside, or considering interacting with others who are similarly social distancing can help foster social connection and development.
- Maintain connection digitally when in-person contact is not an option.3 Social groups, places of worship, and other activities have been agile in developing virtual communities. Communication by voice and/or video is thought to be more powerful than by written communication (text, email) alone.4 However, it is important to consider those who may have limited to no access to electronic methods.
- Encourage open communication with children about diversity and bias, and consider how our interactions with others may affect our children’s perspectives.5
- As providers, it is crucial that we address structural and institutional systems that negatively impact the health, safety, and access to care including our Black, indigenous, and people of color (BIPOC) and lesbian, gay, bisexual, transgender/transsexual, queer/questioning, intersex, and allied/asexual/aromantic/agender (LGBTQIA) patients.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. Dr. Strange has no relevant financial disclosures. Email her at [email protected].
Online resources for parents and families
- Child Mind Institute: Coping With the Coronavirus Crisis: Supporting Your Kids.
- American Psychological Association: Talking with children about discrimination.
- Common Sense Media: Help with determining appropriateness of media for children.
Hotlines
- National Suicide Prevention Hotline: 1-800-273-8255
- GLBT National Hotline: 888-843-4564
- The California Peer-Run Warm Line: 1-855-845-7415
- Trevor Project: 866-488-7386 or text TREVOR to 1-202-304-1200
- Trans Lifeline: 877-565-8860
- Crisis Text Line: Text HOME to 741741
References
1. JAMA Pediatr. 2020 Apr 14. doi: 10.1001/jamapediatrics.2020.1456.
2. CDC: COVID-19 in Racial and Ethnic Minority Groups.
3. JAMA. 2020 Mar 23. doi: 10.1001/jama.2020.4469.
4. JAMA Intern Med. 2020 Apr 10. doi: 10.1001/jamainternmed.2020.1562.
5. American Psychological Association: Talking with children about discrimination.









