User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Machine learning shows ability to predict diastolic dysfunction with ECG
A machine-learning model that uses readily available clinical and electrocardiography data may have the potential to identify left ventricular (LV) diastolic dysfunction, a key biomarker in predicting heart failure, without echocardiography, but a workable clinical platform is still far off, a team of North American researchers reported.
“This cost-effective strategy may be a valuable first clinical step for assessing the presence of LV dysfunction and may potentially aid in the early diagnosis and management of heart failure patients,” Nobuyuki Kagiyama, MD, PhD, of West Virginia University, Morgantown, and colleagues, wrote in the Journal of the American Academy of Cardiology.
The researchers reported on a multicenter, prospective study that evaluated 1,202 patients from three centers in the United States and one in Canada. To develop machine-learning models, the study pooled 814 patients from the U.S. institutions as an internal cohort. They were then randomly divided into a training set and an internal test set on an 80:20 basis (651 and 163). The 388 Canadian patients were reserved as an external set to test the model.
All patients had 12-lead ECG and simultaneous body surface signal-processed ECG (spECG) along with comprehensive two-dimensional Doppler ECG on the same day.
How the model works
The machine-learning model estimated echocardiographic LV relaxation velocities (e’) values using traditional ECG and spECG features. The model also took into account 10 basic clinical features: age; sex; systolic and diastolic blood pressure; and comorbid conditions such as cerebrovascular and cardiovascular disease, diabetes, hypertension, dyslipidemia, and chronic kidney disease.
Patient characteristics were starkly different between the internal (United States) and external (Canadian) cohorts, with the latter being 10 years older on average (65 vs. 44; P < .001), predominantly male (58.2% vs. 47.3%; P < .001) and with significantly lower rates of coronary artery disease (1.8% vs. 21.1%; P < .001), although average blood pressure was similar between the two groups.
The study used area under the curve (AUC) to calculate the predictability of the machine-learning estimated e’ values versus the guideline-based reduced e’, finding close correlation between the internal (AUC, 0.83; sensitivity, 78%; specificity, 77%; negative predictive value, 73%; and positive predictive value, 82%) and external test sets (AUC, 0.84; sensitivity, 90%; specificity, 61%; NPV, 81%; and PPV, 77%).
Similar variations between the two cohorts were reported for global LV diastolic dysfunction and reduced LV ejection fraction.
The final model used 18 features in all, including 3 clinical features (age, dyslipidemia, and hypertension), 7 scores from spECG features, and 8 from traditional ECG features.
Interpreting the results
Dr. Kagiyama and colleagues noted that, because impaired myocardial relaxation is an early sign of cardiac tissue deterioration, screening for it can aid in early detection of subclinical LVDD and earlier treatment for hypertension and diabetes. But they acknowledged that further studies are needed.
In an invited editorial, Khurram Nasir, MD, MPH, MSc, of Houston Methodist DeBakey Heart and Vascular Center and Rohan Khera, MD, MS, of Yale University, New Haven, Conn., wrote that the machine-learning model has a way to go.
They noted that the 73%-77% accuracy of the model in identifying diastolic dysfunction impedes its imminent use. “Although we are excited about the prospects of such developments, we hold out for better evidence for their actual use,” they wrote, adding that the algorithms have limited use in the clinic because most patients already get “definitive testing” if they need it.
Developing a machine-learning model that obviates the need for ECG for evaluating LV diastolic dysfunction seems dubious at this time, said Luigi Di Biase, MD, PhD, section head of electrophysiology and director of arrhythmia services at Montefiore Medical Center and professor at Albert Einstein College of Medicine, both in New York. “The echo is not a difficult test. It’s the most proven usable tool that we have in cardiology because it’s easy to reproduce, low cost, and noninvasive – so we have all that we want in medicine.”
But machine learning does have potential, added Dr. Di Biase, who’s also a member of the American College of Cardiology’s Electrophysiology Section Leadership Council. “If this application could predict the people that would develop diastolic dysfunction that leads to heart failure – because an echo at that time may be negative but there may be other features that tell me this patient will develop disease – then it would have a much different clinical impact.”
The National Science Foundation provided funding for the study. Heart Test Laboratories, doing business as Heart Sciences, provided funding and spECG devices. Dr. Kagiyama reported receiving a research grant from Hitachi Healthcare. A coauthor disclosed financial relationships with Heart Sciences, Ultronics, and Kencor Health.
Dr. Nasir, Dr. Khera, and Dr. Di Biase have no relevant financial relationships to disclose.
SOURCE: Kagiyama N et al. J Am Coll Cardiol. 2020;76:930-41.
A machine-learning model that uses readily available clinical and electrocardiography data may have the potential to identify left ventricular (LV) diastolic dysfunction, a key biomarker in predicting heart failure, without echocardiography, but a workable clinical platform is still far off, a team of North American researchers reported.
“This cost-effective strategy may be a valuable first clinical step for assessing the presence of LV dysfunction and may potentially aid in the early diagnosis and management of heart failure patients,” Nobuyuki Kagiyama, MD, PhD, of West Virginia University, Morgantown, and colleagues, wrote in the Journal of the American Academy of Cardiology.
The researchers reported on a multicenter, prospective study that evaluated 1,202 patients from three centers in the United States and one in Canada. To develop machine-learning models, the study pooled 814 patients from the U.S. institutions as an internal cohort. They were then randomly divided into a training set and an internal test set on an 80:20 basis (651 and 163). The 388 Canadian patients were reserved as an external set to test the model.
All patients had 12-lead ECG and simultaneous body surface signal-processed ECG (spECG) along with comprehensive two-dimensional Doppler ECG on the same day.
How the model works
The machine-learning model estimated echocardiographic LV relaxation velocities (e’) values using traditional ECG and spECG features. The model also took into account 10 basic clinical features: age; sex; systolic and diastolic blood pressure; and comorbid conditions such as cerebrovascular and cardiovascular disease, diabetes, hypertension, dyslipidemia, and chronic kidney disease.
Patient characteristics were starkly different between the internal (United States) and external (Canadian) cohorts, with the latter being 10 years older on average (65 vs. 44; P < .001), predominantly male (58.2% vs. 47.3%; P < .001) and with significantly lower rates of coronary artery disease (1.8% vs. 21.1%; P < .001), although average blood pressure was similar between the two groups.
The study used area under the curve (AUC) to calculate the predictability of the machine-learning estimated e’ values versus the guideline-based reduced e’, finding close correlation between the internal (AUC, 0.83; sensitivity, 78%; specificity, 77%; negative predictive value, 73%; and positive predictive value, 82%) and external test sets (AUC, 0.84; sensitivity, 90%; specificity, 61%; NPV, 81%; and PPV, 77%).
Similar variations between the two cohorts were reported for global LV diastolic dysfunction and reduced LV ejection fraction.
The final model used 18 features in all, including 3 clinical features (age, dyslipidemia, and hypertension), 7 scores from spECG features, and 8 from traditional ECG features.
Interpreting the results
Dr. Kagiyama and colleagues noted that, because impaired myocardial relaxation is an early sign of cardiac tissue deterioration, screening for it can aid in early detection of subclinical LVDD and earlier treatment for hypertension and diabetes. But they acknowledged that further studies are needed.
In an invited editorial, Khurram Nasir, MD, MPH, MSc, of Houston Methodist DeBakey Heart and Vascular Center and Rohan Khera, MD, MS, of Yale University, New Haven, Conn., wrote that the machine-learning model has a way to go.
They noted that the 73%-77% accuracy of the model in identifying diastolic dysfunction impedes its imminent use. “Although we are excited about the prospects of such developments, we hold out for better evidence for their actual use,” they wrote, adding that the algorithms have limited use in the clinic because most patients already get “definitive testing” if they need it.
Developing a machine-learning model that obviates the need for ECG for evaluating LV diastolic dysfunction seems dubious at this time, said Luigi Di Biase, MD, PhD, section head of electrophysiology and director of arrhythmia services at Montefiore Medical Center and professor at Albert Einstein College of Medicine, both in New York. “The echo is not a difficult test. It’s the most proven usable tool that we have in cardiology because it’s easy to reproduce, low cost, and noninvasive – so we have all that we want in medicine.”
But machine learning does have potential, added Dr. Di Biase, who’s also a member of the American College of Cardiology’s Electrophysiology Section Leadership Council. “If this application could predict the people that would develop diastolic dysfunction that leads to heart failure – because an echo at that time may be negative but there may be other features that tell me this patient will develop disease – then it would have a much different clinical impact.”
The National Science Foundation provided funding for the study. Heart Test Laboratories, doing business as Heart Sciences, provided funding and spECG devices. Dr. Kagiyama reported receiving a research grant from Hitachi Healthcare. A coauthor disclosed financial relationships with Heart Sciences, Ultronics, and Kencor Health.
Dr. Nasir, Dr. Khera, and Dr. Di Biase have no relevant financial relationships to disclose.
SOURCE: Kagiyama N et al. J Am Coll Cardiol. 2020;76:930-41.
A machine-learning model that uses readily available clinical and electrocardiography data may have the potential to identify left ventricular (LV) diastolic dysfunction, a key biomarker in predicting heart failure, without echocardiography, but a workable clinical platform is still far off, a team of North American researchers reported.
“This cost-effective strategy may be a valuable first clinical step for assessing the presence of LV dysfunction and may potentially aid in the early diagnosis and management of heart failure patients,” Nobuyuki Kagiyama, MD, PhD, of West Virginia University, Morgantown, and colleagues, wrote in the Journal of the American Academy of Cardiology.
The researchers reported on a multicenter, prospective study that evaluated 1,202 patients from three centers in the United States and one in Canada. To develop machine-learning models, the study pooled 814 patients from the U.S. institutions as an internal cohort. They were then randomly divided into a training set and an internal test set on an 80:20 basis (651 and 163). The 388 Canadian patients were reserved as an external set to test the model.
All patients had 12-lead ECG and simultaneous body surface signal-processed ECG (spECG) along with comprehensive two-dimensional Doppler ECG on the same day.
How the model works
The machine-learning model estimated echocardiographic LV relaxation velocities (e’) values using traditional ECG and spECG features. The model also took into account 10 basic clinical features: age; sex; systolic and diastolic blood pressure; and comorbid conditions such as cerebrovascular and cardiovascular disease, diabetes, hypertension, dyslipidemia, and chronic kidney disease.
Patient characteristics were starkly different between the internal (United States) and external (Canadian) cohorts, with the latter being 10 years older on average (65 vs. 44; P < .001), predominantly male (58.2% vs. 47.3%; P < .001) and with significantly lower rates of coronary artery disease (1.8% vs. 21.1%; P < .001), although average blood pressure was similar between the two groups.
The study used area under the curve (AUC) to calculate the predictability of the machine-learning estimated e’ values versus the guideline-based reduced e’, finding close correlation between the internal (AUC, 0.83; sensitivity, 78%; specificity, 77%; negative predictive value, 73%; and positive predictive value, 82%) and external test sets (AUC, 0.84; sensitivity, 90%; specificity, 61%; NPV, 81%; and PPV, 77%).
Similar variations between the two cohorts were reported for global LV diastolic dysfunction and reduced LV ejection fraction.
The final model used 18 features in all, including 3 clinical features (age, dyslipidemia, and hypertension), 7 scores from spECG features, and 8 from traditional ECG features.
Interpreting the results
Dr. Kagiyama and colleagues noted that, because impaired myocardial relaxation is an early sign of cardiac tissue deterioration, screening for it can aid in early detection of subclinical LVDD and earlier treatment for hypertension and diabetes. But they acknowledged that further studies are needed.
In an invited editorial, Khurram Nasir, MD, MPH, MSc, of Houston Methodist DeBakey Heart and Vascular Center and Rohan Khera, MD, MS, of Yale University, New Haven, Conn., wrote that the machine-learning model has a way to go.
They noted that the 73%-77% accuracy of the model in identifying diastolic dysfunction impedes its imminent use. “Although we are excited about the prospects of such developments, we hold out for better evidence for their actual use,” they wrote, adding that the algorithms have limited use in the clinic because most patients already get “definitive testing” if they need it.
Developing a machine-learning model that obviates the need for ECG for evaluating LV diastolic dysfunction seems dubious at this time, said Luigi Di Biase, MD, PhD, section head of electrophysiology and director of arrhythmia services at Montefiore Medical Center and professor at Albert Einstein College of Medicine, both in New York. “The echo is not a difficult test. It’s the most proven usable tool that we have in cardiology because it’s easy to reproduce, low cost, and noninvasive – so we have all that we want in medicine.”
But machine learning does have potential, added Dr. Di Biase, who’s also a member of the American College of Cardiology’s Electrophysiology Section Leadership Council. “If this application could predict the people that would develop diastolic dysfunction that leads to heart failure – because an echo at that time may be negative but there may be other features that tell me this patient will develop disease – then it would have a much different clinical impact.”
The National Science Foundation provided funding for the study. Heart Test Laboratories, doing business as Heart Sciences, provided funding and spECG devices. Dr. Kagiyama reported receiving a research grant from Hitachi Healthcare. A coauthor disclosed financial relationships with Heart Sciences, Ultronics, and Kencor Health.
Dr. Nasir, Dr. Khera, and Dr. Di Biase have no relevant financial relationships to disclose.
SOURCE: Kagiyama N et al. J Am Coll Cardiol. 2020;76:930-41.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
COVID-19 child case count now over 400,000
according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
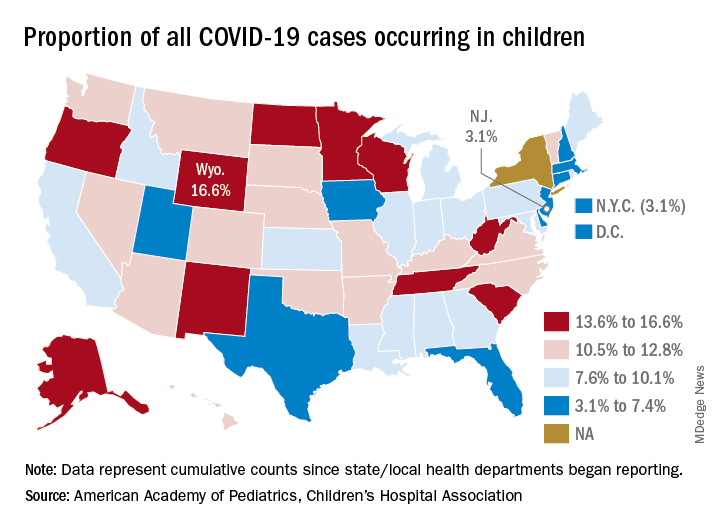
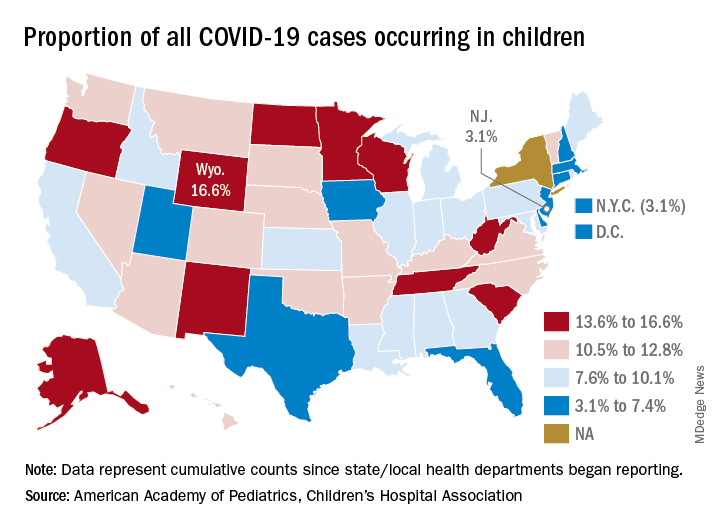
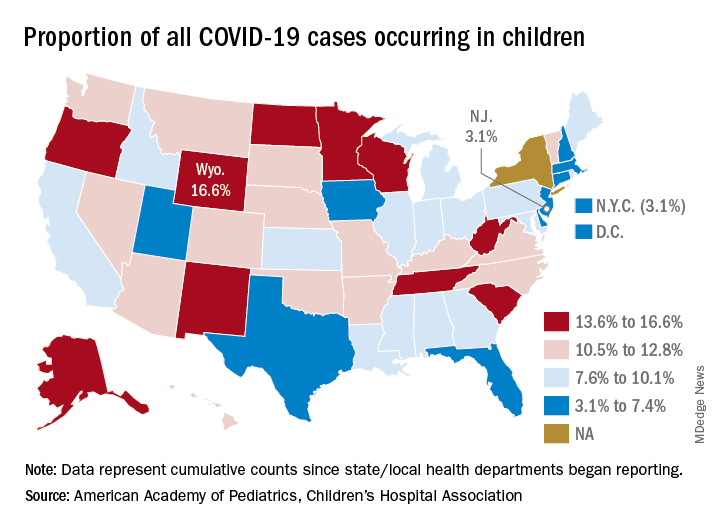
The 406,000 children who have tested positive for COVID-19 represent 9.1% of all cases reported so far by 49 states (New York does not provide age distribution), New York City, the District of Columbia, Puerto Rico, and Guam. Since the proportion of child cases also was 9.1% on Aug. 6, the most recent week is the first without an increase since tracking began in mid-April, the report shows.
State-level data show that Wyoming has the highest percentage of child cases (16.6%) after Alabama changed its “definition of child case from 0-24 to 0-17 years, resulting in a downward revision of cumulative child cases,” the AAP and the CHA said. Alabama’s proportion of such cases dropped from 22.5% to 9.0%.
New Jersey had the lowest rate (3.1%) again this week, along with New York City, but both were up slightly from the week before, when New Jersey was at 2.9% and N.Y.C. was 3.0%. The only states, other than Alabama, that saw declines over the last week were Arkansas, Massachusetts, Mississippi, South Dakota, Texas, and West Virginia. Texas, however, has reported age for only 8% of its confirmed cases, the report noted.
The overall rate of child COVID-19 cases as of Aug. 13 was 538 per 100,000 children, up from 500.7 per 100,000 a week earlier. Arizona was again highest among the states with a rate of 1,254 per 100,000 (up from 1,206) and Vermont was lowest at 121, although Puerto Rico (114) and Guam (88) were lower still, the AAP/CHA data indicate.
For the nine states that report testing information for children, Arizona has the highest positivity rate at 18.3% and West Virginia has the lowest at 3.6%. Data on hospitalizations – available from 21 states and N.Y.C. – show that 3,849 children have been admitted, with rates varying from 0.2% of children in Hawaii to 8.8% in the Big Apple, according to the report.
More specific information on child cases, such as symptoms or underlying conditions, is not being provided by states at this time, the AAP and CHA pointed out.
according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
The 406,000 children who have tested positive for COVID-19 represent 9.1% of all cases reported so far by 49 states (New York does not provide age distribution), New York City, the District of Columbia, Puerto Rico, and Guam. Since the proportion of child cases also was 9.1% on Aug. 6, the most recent week is the first without an increase since tracking began in mid-April, the report shows.
State-level data show that Wyoming has the highest percentage of child cases (16.6%) after Alabama changed its “definition of child case from 0-24 to 0-17 years, resulting in a downward revision of cumulative child cases,” the AAP and the CHA said. Alabama’s proportion of such cases dropped from 22.5% to 9.0%.
New Jersey had the lowest rate (3.1%) again this week, along with New York City, but both were up slightly from the week before, when New Jersey was at 2.9% and N.Y.C. was 3.0%. The only states, other than Alabama, that saw declines over the last week were Arkansas, Massachusetts, Mississippi, South Dakota, Texas, and West Virginia. Texas, however, has reported age for only 8% of its confirmed cases, the report noted.
The overall rate of child COVID-19 cases as of Aug. 13 was 538 per 100,000 children, up from 500.7 per 100,000 a week earlier. Arizona was again highest among the states with a rate of 1,254 per 100,000 (up from 1,206) and Vermont was lowest at 121, although Puerto Rico (114) and Guam (88) were lower still, the AAP/CHA data indicate.
For the nine states that report testing information for children, Arizona has the highest positivity rate at 18.3% and West Virginia has the lowest at 3.6%. Data on hospitalizations – available from 21 states and N.Y.C. – show that 3,849 children have been admitted, with rates varying from 0.2% of children in Hawaii to 8.8% in the Big Apple, according to the report.
More specific information on child cases, such as symptoms or underlying conditions, is not being provided by states at this time, the AAP and CHA pointed out.
according to a new report from the American Academy of Pediatrics and the Children’s Hospital Association.
The 406,000 children who have tested positive for COVID-19 represent 9.1% of all cases reported so far by 49 states (New York does not provide age distribution), New York City, the District of Columbia, Puerto Rico, and Guam. Since the proportion of child cases also was 9.1% on Aug. 6, the most recent week is the first without an increase since tracking began in mid-April, the report shows.
State-level data show that Wyoming has the highest percentage of child cases (16.6%) after Alabama changed its “definition of child case from 0-24 to 0-17 years, resulting in a downward revision of cumulative child cases,” the AAP and the CHA said. Alabama’s proportion of such cases dropped from 22.5% to 9.0%.
New Jersey had the lowest rate (3.1%) again this week, along with New York City, but both were up slightly from the week before, when New Jersey was at 2.9% and N.Y.C. was 3.0%. The only states, other than Alabama, that saw declines over the last week were Arkansas, Massachusetts, Mississippi, South Dakota, Texas, and West Virginia. Texas, however, has reported age for only 8% of its confirmed cases, the report noted.
The overall rate of child COVID-19 cases as of Aug. 13 was 538 per 100,000 children, up from 500.7 per 100,000 a week earlier. Arizona was again highest among the states with a rate of 1,254 per 100,000 (up from 1,206) and Vermont was lowest at 121, although Puerto Rico (114) and Guam (88) were lower still, the AAP/CHA data indicate.
For the nine states that report testing information for children, Arizona has the highest positivity rate at 18.3% and West Virginia has the lowest at 3.6%. Data on hospitalizations – available from 21 states and N.Y.C. – show that 3,849 children have been admitted, with rates varying from 0.2% of children in Hawaii to 8.8% in the Big Apple, according to the report.
More specific information on child cases, such as symptoms or underlying conditions, is not being provided by states at this time, the AAP and CHA pointed out.
Are aging physicians a burden?
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
The evaluation of physicians with alleged cognitive decline
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
Evidence mounts for COVID-19 effects on thyroid gland
Rates of thyrotoxicosis are significantly higher among patients who are critically ill with COVID-19 than among patients who are critically ill but who do not not have COVID-19, suggesting an atypical form of thyroiditis related to the novel coronavirus infection, according to new research.
“We suggest routine assessment of thyroid function in patients with COVID-19 requiring high-intensity care because they frequently present with thyrotoxicosis due to a form of subacute thyroiditis related to SARS-CoV-2,” the authors wrote in correspondence published online in The Lancet Diabetes and Endocrinology.
However, notably, the study – which compared critically ill ICU patients who had COVID-19 with those who did not have COVID-19 or who had milder cases of COVID-19 – indicates that thyroid disorders do not appear to increase the risk of developing COVID-19, first author Ilaria Muller, MD, PhD, of the department of endocrinology, IRCCS Fondazione Ca’ Granda Ospedale Maggiore Policlinico, Milan, said in an interview.
“It is important to highlight that we did not find an increased prevalence of preexisting thyroid disorders in COVID-19 patients (contrary to early media reports),” she said. “So far, clinical observations do not support this fear, and we need to reassure people with thyroid disorders, since such disorders are very common among the general population.”
Yet the findings add to emerging evidence of a COVID-19/thyroid relationship, Angela M. Leung, MD, said in an interview.
“Given the health care impacts of the current COVID-19 pandemic worldwide, this study provides some insight on the potential systemic inflammation, as well as thyroid-specific inflammation, of the SARS-Cov-2 virus that is described in some emerging reports,” she said.
“This study joins at least six others that have reported a clinical presentation resembling subacute thyroiditis in critically ill patients with COVID-19,” noted Dr. Leung, of the division of endocrinology, diabetes, and metabolism in the department of medicine at the University of California, Los Angeles.
Thyroid function analysis in those with severe COVID-19
Dr. Muller explained that preliminary data from her institution showed thyroid abnormalities in patients who were severely ill with COVID-19. She and her team extended the evaluation to include thyroid data and other data on 93 patients with COVID-19 who were admitted to high-intensity care units (HICUs) in Italy during the 2020 pandemic.
Those data were compared with data on 101 critically ill patients admitted to the same HICUs in 2019 who did not have COVID-19. A third group of 52 patients with COVID-19 who were admitted to low-intensity care units (LICUs) in Italy in 2020 were also included in the analysis.
The mean age of the patients in the HICU 2020 group was 65.3 years; in the HICU 2019 group, it was 73 years; and in the LICU group, it was 70 years (P = .001). In addition, the HICU 2020 group included more men than the other two groups (69% vs. 56% and 48%; P = .03).
Of note, only 9% of patients in the HICU 2020 group had preexisting thyroid disorders, compared with 21% in the LICU group and 23% in the HICU 2019 group (P = .017).
These findings suggest that “such conditions are not a risk factor for SARS-CoV-2 infection or severity of COVID-19,” the authors wrote.
The patients with the preexisting thyroid conditions were excluded from the thyroid function analysis.
A significantly higher proportion of patients in the HICU 2020 group (13; 15%) were thyrotoxic upon admission, compared with just 1 (1%) of 78 patients in the HICU 2019 group (P = .002) and one (2%) of 41 patients in the LICU group (P = .025).
Among the 14 patients in the two COVID-19 groups who had thyrotoxicosis, the majority were male (9; 64%)
Among those in the HICU 2020 group, serum thyroid-stimulating hormone concentrations were lower than in either of the other two groups (P = .018), and serum free thyroxine (free T4) concentrations were higher than in the LICU group (P = .016) but not the HICU 2019 group.
Differences compared with other infection-related thyroiditis
Although thyrotoxicosis relating to subacute viral thyroiditis can result from a wide variety of viral infections, there are some key differences with COVID-19, Dr. Muller said.
“Thyroid dysfunction related to SARS-CoV-2 seems to be milder than that of classic subacute thyroiditis due to other viruses,” she explained. Furthermore, thyroid dysfunction associated with other viral infections is more common in women, whereas there were more male patients with the COVID-19–related atypical thyroiditis.
In addition, the thyroid effects developed early with COVID-19, whereas they usually emerge after the infections by other viruses.
Patients did not demonstrate the neck pain that is common with classic viral thyroiditis, and the thyroid abnormalities appear to correlate with the severity of COVID-19, whereas they are seen even in patients with mild symptoms when other viral infections are the cause.
In addition to the risk for subacute viral thyroiditis, critically ill patients in general are at risk of developing nonthyroidal illness syndrome, with alterations in thyroid function. However, thyroid hormone measures in the patients severely ill with COVID-19 were not consistent with that syndrome.
A subanalysis of eight HICU 2020 patients with thyroid dysfunction who were followed for 55 days after discharge showed that two experienced hyperthyroidism but likely not from COVID-19; in the remaining six, thyroid function normalized.
Muller speculated that, when ill with COVID-19, the patients likely had a combination of SARS-CoV-2–related atypical thyroiditis and nonthyroidal illness syndrome, known as T4 toxicosis.
Will there be any long-term effects?
Importantly, it remains unknown whether the novel coronavirus has longer-term effects on the thyroid, Dr. Muller said.
“We cannot predict what will be the long-lasting thyroid effects after COVID-19,” she said.
With classic subacute viral thyroiditis, “After a few years ... 5%-20% of patients develop permanent hypothyroidism, [and] the same might happen in COVID-19 patients,” she hypothesized. “We will follow our patients long term to answer this question – this study is already ongoing.”
In the meantime, diagnosis of thyroid dysfunction in patients with COVID-19 is important, inasmuch as it could worsen the already critical conditions of patients, Muller stressed.
“The gold-standard treatment for thyroiditis is steroids, so the presence of thyroid dysfunction might represent an additional indication to such treatment in COVID-19 patients, to be verified in properly designed clinical trials,” she advised.
ACE2 cell receptors highly expressed in thyroid
Dr. Muller and colleagues also noted recent research showing that ACE2 – demonstrated to be a key host-cell entry receptor for both SARS-CoV and SARS-CoV-2 – is expressed in even higher levels in the thyroid than the lungs, where it causes COVID-19’s notorious pulmonary effects.
Dr. Muller said the implications of ACE2 expression in the thyroid remain to be elucidated.
“If ACE2 is confirmed to be expressed at higher levels, compared with the lungs in the thyroid gland and other tissues, i.e., small intestine, testis, kidney, heart, etc, dedicated studies will be needed to correlate ACE2 expression with the organs’ susceptibility to SARS-CoV-2 reflected by clinical presentation,” she said.
Dr. Leung added that, as a take-home message from these and the other thyroid/COVID-19 studies, “data are starting to show us that COVID-19 infection may cause thyrotoxicosis that is possibly related to thyroid and systemic inflammation. However, the serum thyroid function test abnormalities seen in COVID-19 patients with subacute thyroiditis are also likely exacerbated to a substantial extent by nonthyroidal illness physiology.”
The authors have disclosed no relevant financial relationships. Dr. Leung is on the advisory board of Medscape Diabetes and Endocrinology.
A version of this article originally appeared on Medscape.com.
Rates of thyrotoxicosis are significantly higher among patients who are critically ill with COVID-19 than among patients who are critically ill but who do not not have COVID-19, suggesting an atypical form of thyroiditis related to the novel coronavirus infection, according to new research.
“We suggest routine assessment of thyroid function in patients with COVID-19 requiring high-intensity care because they frequently present with thyrotoxicosis due to a form of subacute thyroiditis related to SARS-CoV-2,” the authors wrote in correspondence published online in The Lancet Diabetes and Endocrinology.
However, notably, the study – which compared critically ill ICU patients who had COVID-19 with those who did not have COVID-19 or who had milder cases of COVID-19 – indicates that thyroid disorders do not appear to increase the risk of developing COVID-19, first author Ilaria Muller, MD, PhD, of the department of endocrinology, IRCCS Fondazione Ca’ Granda Ospedale Maggiore Policlinico, Milan, said in an interview.
“It is important to highlight that we did not find an increased prevalence of preexisting thyroid disorders in COVID-19 patients (contrary to early media reports),” she said. “So far, clinical observations do not support this fear, and we need to reassure people with thyroid disorders, since such disorders are very common among the general population.”
Yet the findings add to emerging evidence of a COVID-19/thyroid relationship, Angela M. Leung, MD, said in an interview.
“Given the health care impacts of the current COVID-19 pandemic worldwide, this study provides some insight on the potential systemic inflammation, as well as thyroid-specific inflammation, of the SARS-Cov-2 virus that is described in some emerging reports,” she said.
“This study joins at least six others that have reported a clinical presentation resembling subacute thyroiditis in critically ill patients with COVID-19,” noted Dr. Leung, of the division of endocrinology, diabetes, and metabolism in the department of medicine at the University of California, Los Angeles.
Thyroid function analysis in those with severe COVID-19
Dr. Muller explained that preliminary data from her institution showed thyroid abnormalities in patients who were severely ill with COVID-19. She and her team extended the evaluation to include thyroid data and other data on 93 patients with COVID-19 who were admitted to high-intensity care units (HICUs) in Italy during the 2020 pandemic.
Those data were compared with data on 101 critically ill patients admitted to the same HICUs in 2019 who did not have COVID-19. A third group of 52 patients with COVID-19 who were admitted to low-intensity care units (LICUs) in Italy in 2020 were also included in the analysis.
The mean age of the patients in the HICU 2020 group was 65.3 years; in the HICU 2019 group, it was 73 years; and in the LICU group, it was 70 years (P = .001). In addition, the HICU 2020 group included more men than the other two groups (69% vs. 56% and 48%; P = .03).
Of note, only 9% of patients in the HICU 2020 group had preexisting thyroid disorders, compared with 21% in the LICU group and 23% in the HICU 2019 group (P = .017).
These findings suggest that “such conditions are not a risk factor for SARS-CoV-2 infection or severity of COVID-19,” the authors wrote.
The patients with the preexisting thyroid conditions were excluded from the thyroid function analysis.
A significantly higher proportion of patients in the HICU 2020 group (13; 15%) were thyrotoxic upon admission, compared with just 1 (1%) of 78 patients in the HICU 2019 group (P = .002) and one (2%) of 41 patients in the LICU group (P = .025).
Among the 14 patients in the two COVID-19 groups who had thyrotoxicosis, the majority were male (9; 64%)
Among those in the HICU 2020 group, serum thyroid-stimulating hormone concentrations were lower than in either of the other two groups (P = .018), and serum free thyroxine (free T4) concentrations were higher than in the LICU group (P = .016) but not the HICU 2019 group.
Differences compared with other infection-related thyroiditis
Although thyrotoxicosis relating to subacute viral thyroiditis can result from a wide variety of viral infections, there are some key differences with COVID-19, Dr. Muller said.
“Thyroid dysfunction related to SARS-CoV-2 seems to be milder than that of classic subacute thyroiditis due to other viruses,” she explained. Furthermore, thyroid dysfunction associated with other viral infections is more common in women, whereas there were more male patients with the COVID-19–related atypical thyroiditis.
In addition, the thyroid effects developed early with COVID-19, whereas they usually emerge after the infections by other viruses.
Patients did not demonstrate the neck pain that is common with classic viral thyroiditis, and the thyroid abnormalities appear to correlate with the severity of COVID-19, whereas they are seen even in patients with mild symptoms when other viral infections are the cause.
In addition to the risk for subacute viral thyroiditis, critically ill patients in general are at risk of developing nonthyroidal illness syndrome, with alterations in thyroid function. However, thyroid hormone measures in the patients severely ill with COVID-19 were not consistent with that syndrome.
A subanalysis of eight HICU 2020 patients with thyroid dysfunction who were followed for 55 days after discharge showed that two experienced hyperthyroidism but likely not from COVID-19; in the remaining six, thyroid function normalized.
Muller speculated that, when ill with COVID-19, the patients likely had a combination of SARS-CoV-2–related atypical thyroiditis and nonthyroidal illness syndrome, known as T4 toxicosis.
Will there be any long-term effects?
Importantly, it remains unknown whether the novel coronavirus has longer-term effects on the thyroid, Dr. Muller said.
“We cannot predict what will be the long-lasting thyroid effects after COVID-19,” she said.
With classic subacute viral thyroiditis, “After a few years ... 5%-20% of patients develop permanent hypothyroidism, [and] the same might happen in COVID-19 patients,” she hypothesized. “We will follow our patients long term to answer this question – this study is already ongoing.”
In the meantime, diagnosis of thyroid dysfunction in patients with COVID-19 is important, inasmuch as it could worsen the already critical conditions of patients, Muller stressed.
“The gold-standard treatment for thyroiditis is steroids, so the presence of thyroid dysfunction might represent an additional indication to such treatment in COVID-19 patients, to be verified in properly designed clinical trials,” she advised.
ACE2 cell receptors highly expressed in thyroid
Dr. Muller and colleagues also noted recent research showing that ACE2 – demonstrated to be a key host-cell entry receptor for both SARS-CoV and SARS-CoV-2 – is expressed in even higher levels in the thyroid than the lungs, where it causes COVID-19’s notorious pulmonary effects.
Dr. Muller said the implications of ACE2 expression in the thyroid remain to be elucidated.
“If ACE2 is confirmed to be expressed at higher levels, compared with the lungs in the thyroid gland and other tissues, i.e., small intestine, testis, kidney, heart, etc, dedicated studies will be needed to correlate ACE2 expression with the organs’ susceptibility to SARS-CoV-2 reflected by clinical presentation,” she said.
Dr. Leung added that, as a take-home message from these and the other thyroid/COVID-19 studies, “data are starting to show us that COVID-19 infection may cause thyrotoxicosis that is possibly related to thyroid and systemic inflammation. However, the serum thyroid function test abnormalities seen in COVID-19 patients with subacute thyroiditis are also likely exacerbated to a substantial extent by nonthyroidal illness physiology.”
The authors have disclosed no relevant financial relationships. Dr. Leung is on the advisory board of Medscape Diabetes and Endocrinology.
A version of this article originally appeared on Medscape.com.
Rates of thyrotoxicosis are significantly higher among patients who are critically ill with COVID-19 than among patients who are critically ill but who do not not have COVID-19, suggesting an atypical form of thyroiditis related to the novel coronavirus infection, according to new research.
“We suggest routine assessment of thyroid function in patients with COVID-19 requiring high-intensity care because they frequently present with thyrotoxicosis due to a form of subacute thyroiditis related to SARS-CoV-2,” the authors wrote in correspondence published online in The Lancet Diabetes and Endocrinology.
However, notably, the study – which compared critically ill ICU patients who had COVID-19 with those who did not have COVID-19 or who had milder cases of COVID-19 – indicates that thyroid disorders do not appear to increase the risk of developing COVID-19, first author Ilaria Muller, MD, PhD, of the department of endocrinology, IRCCS Fondazione Ca’ Granda Ospedale Maggiore Policlinico, Milan, said in an interview.
“It is important to highlight that we did not find an increased prevalence of preexisting thyroid disorders in COVID-19 patients (contrary to early media reports),” she said. “So far, clinical observations do not support this fear, and we need to reassure people with thyroid disorders, since such disorders are very common among the general population.”
Yet the findings add to emerging evidence of a COVID-19/thyroid relationship, Angela M. Leung, MD, said in an interview.
“Given the health care impacts of the current COVID-19 pandemic worldwide, this study provides some insight on the potential systemic inflammation, as well as thyroid-specific inflammation, of the SARS-Cov-2 virus that is described in some emerging reports,” she said.
“This study joins at least six others that have reported a clinical presentation resembling subacute thyroiditis in critically ill patients with COVID-19,” noted Dr. Leung, of the division of endocrinology, diabetes, and metabolism in the department of medicine at the University of California, Los Angeles.
Thyroid function analysis in those with severe COVID-19
Dr. Muller explained that preliminary data from her institution showed thyroid abnormalities in patients who were severely ill with COVID-19. She and her team extended the evaluation to include thyroid data and other data on 93 patients with COVID-19 who were admitted to high-intensity care units (HICUs) in Italy during the 2020 pandemic.
Those data were compared with data on 101 critically ill patients admitted to the same HICUs in 2019 who did not have COVID-19. A third group of 52 patients with COVID-19 who were admitted to low-intensity care units (LICUs) in Italy in 2020 were also included in the analysis.
The mean age of the patients in the HICU 2020 group was 65.3 years; in the HICU 2019 group, it was 73 years; and in the LICU group, it was 70 years (P = .001). In addition, the HICU 2020 group included more men than the other two groups (69% vs. 56% and 48%; P = .03).
Of note, only 9% of patients in the HICU 2020 group had preexisting thyroid disorders, compared with 21% in the LICU group and 23% in the HICU 2019 group (P = .017).
These findings suggest that “such conditions are not a risk factor for SARS-CoV-2 infection or severity of COVID-19,” the authors wrote.
The patients with the preexisting thyroid conditions were excluded from the thyroid function analysis.
A significantly higher proportion of patients in the HICU 2020 group (13; 15%) were thyrotoxic upon admission, compared with just 1 (1%) of 78 patients in the HICU 2019 group (P = .002) and one (2%) of 41 patients in the LICU group (P = .025).
Among the 14 patients in the two COVID-19 groups who had thyrotoxicosis, the majority were male (9; 64%)
Among those in the HICU 2020 group, serum thyroid-stimulating hormone concentrations were lower than in either of the other two groups (P = .018), and serum free thyroxine (free T4) concentrations were higher than in the LICU group (P = .016) but not the HICU 2019 group.
Differences compared with other infection-related thyroiditis
Although thyrotoxicosis relating to subacute viral thyroiditis can result from a wide variety of viral infections, there are some key differences with COVID-19, Dr. Muller said.
“Thyroid dysfunction related to SARS-CoV-2 seems to be milder than that of classic subacute thyroiditis due to other viruses,” she explained. Furthermore, thyroid dysfunction associated with other viral infections is more common in women, whereas there were more male patients with the COVID-19–related atypical thyroiditis.
In addition, the thyroid effects developed early with COVID-19, whereas they usually emerge after the infections by other viruses.
Patients did not demonstrate the neck pain that is common with classic viral thyroiditis, and the thyroid abnormalities appear to correlate with the severity of COVID-19, whereas they are seen even in patients with mild symptoms when other viral infections are the cause.
In addition to the risk for subacute viral thyroiditis, critically ill patients in general are at risk of developing nonthyroidal illness syndrome, with alterations in thyroid function. However, thyroid hormone measures in the patients severely ill with COVID-19 were not consistent with that syndrome.
A subanalysis of eight HICU 2020 patients with thyroid dysfunction who were followed for 55 days after discharge showed that two experienced hyperthyroidism but likely not from COVID-19; in the remaining six, thyroid function normalized.
Muller speculated that, when ill with COVID-19, the patients likely had a combination of SARS-CoV-2–related atypical thyroiditis and nonthyroidal illness syndrome, known as T4 toxicosis.
Will there be any long-term effects?
Importantly, it remains unknown whether the novel coronavirus has longer-term effects on the thyroid, Dr. Muller said.
“We cannot predict what will be the long-lasting thyroid effects after COVID-19,” she said.
With classic subacute viral thyroiditis, “After a few years ... 5%-20% of patients develop permanent hypothyroidism, [and] the same might happen in COVID-19 patients,” she hypothesized. “We will follow our patients long term to answer this question – this study is already ongoing.”
In the meantime, diagnosis of thyroid dysfunction in patients with COVID-19 is important, inasmuch as it could worsen the already critical conditions of patients, Muller stressed.
“The gold-standard treatment for thyroiditis is steroids, so the presence of thyroid dysfunction might represent an additional indication to such treatment in COVID-19 patients, to be verified in properly designed clinical trials,” she advised.
ACE2 cell receptors highly expressed in thyroid
Dr. Muller and colleagues also noted recent research showing that ACE2 – demonstrated to be a key host-cell entry receptor for both SARS-CoV and SARS-CoV-2 – is expressed in even higher levels in the thyroid than the lungs, where it causes COVID-19’s notorious pulmonary effects.
Dr. Muller said the implications of ACE2 expression in the thyroid remain to be elucidated.
“If ACE2 is confirmed to be expressed at higher levels, compared with the lungs in the thyroid gland and other tissues, i.e., small intestine, testis, kidney, heart, etc, dedicated studies will be needed to correlate ACE2 expression with the organs’ susceptibility to SARS-CoV-2 reflected by clinical presentation,” she said.
Dr. Leung added that, as a take-home message from these and the other thyroid/COVID-19 studies, “data are starting to show us that COVID-19 infection may cause thyrotoxicosis that is possibly related to thyroid and systemic inflammation. However, the serum thyroid function test abnormalities seen in COVID-19 patients with subacute thyroiditis are also likely exacerbated to a substantial extent by nonthyroidal illness physiology.”
The authors have disclosed no relevant financial relationships. Dr. Leung is on the advisory board of Medscape Diabetes and Endocrinology.
A version of this article originally appeared on Medscape.com.
Non-COVID-19 clinical trials grind to a halt during pandemic
The COVID-19 pandemic has created unique and unprecedented challenges for the clinical research world, with potentially long-lasting consequences.
A new analysis of the extent of disruption shows that the average rate of stopped trials nearly doubled during the first 5 months of 2020, compared with the 2 previous years.
“Typically, clinical research precedes clinical practice by several years, so this disruption we’re seeing now will be felt for many years to come,” said Mario Guadino, MD, of Weill Cornell Medicine, New York.
The analysis was published online July 31 in the Journal of the American College of Cardiology.
The researchers used Python software to query meta-data from all trials reported on ClinicalTrials.gov. Of 321,218 non-COVID-19 trials queried, 28,672 (8.9%) were reported as stopped, defined as a switch in trial status from “recruiting” to “active and not recruiting,” “completed,” “suspended,” “terminated,” or “withdrawn.”
The average rate of discontinuation was 638 trials/month from January 2017 to December 2019, rising to 1,147 trials/month between January 2020 and May 2020 (P < .001 for trend).
Once stopped (as opposed to paused), restarting a trial is a tricky prospect, said Dr. Guadino. “You can’t stop and restart a trial because it creates a lot of issues, so we should expect many of these stopped trials to never be completed.”
He said these figures likely represent an underestimate of the true impact of the pandemic because there is typically a delay in the updating of the status of a trial on ClinicalTrials.gov.
“We are likely looking only at the tip of the iceberg,” he added. “My impression is that the number of trials that will be affected and even canceled will be very high.”
As for cardiology trials, one of the report’s authors, Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, without naming specific trials, had this to say: “Several cardiovascular trials were paused, and some were permanently discontinued. It may be a while before we fully appreciate just how much information was lost and how much might be salvaged.”
He’s not worried, however, that upcoming cardiology meetings, which have moved online for the foreseeable future, might get a bit boring. “Fortunately, there is enough good work going on in the cardiovascular and cardiometabolic space that I believe there will still be ample randomized and observational data of high quality to present at the major meetings,” Dr. Bhatt said in an email.
The researchers found a weak correlation between the national population-adjusted numbers of COVID-19 cases and the proportion of non-COVID-19 trials stopped by country.
Even for trials that stopped recruiting for a period of time but are continuing, there are myriad issues involving compliance, data integrity, statistical interpretability, etc.
“Even if there is just a temporary disruption, that will most likely lead to reduced enrollment, missing follow-up visits, and protocol deviations, all things that would be red flags during normal times and impact the quality of the clinical trial,” said Dr. Guadino.
“And if your outcome of interest is mortality, well, how exactly do you measure that during a pandemic?” he added.
Stopped for lack of funding
Besides the logistical issues, another reason trials may be in jeopardy is funding. A warning early in the pandemic from the research community in Canada that funding was quickly drying up, leaving both jobs and data at risk, led to an aid package from the government to keep the lights on.
The National Institutes of Health (NIH), the Canadian Institutes of Health Research, and similar groups “have devoted large sums of money to research in COVID, which is of course very appropriate, but that clearly reduces the amount of funding that is available for other researchers,” said Dr. Guadino.
Some funding agencies around the world have canceled or put on hold all non-COVID-19 clinical trials still at the design state, Dr. Guadino said in an interview.
The NIH, he stressed, has not canceled funding and has been “extremely open and cooperative” in trying to help trialists navigate the many COVID-generated issues. They’ve even issued guidance on how to manage trials during COVID-19.
Of note, in the survey, the majority of the trials stopped (95.4%) had nongovernmental funding.
“The data are not very granular, so we’re only able to make some very simple, descriptive comments, but it does seem like the more fragile trials – those that are smaller and industry-funded – are the ones more likely to be disrupted,” said Dr. Guadino.
In some cases, he said, priorities have shifted to COVID-19. “If a small company is sponsoring a trial and they decide they want to sponsor something related to COVID, or they realize that because of the slow enrollment, the trial becomes too expensive to complete, they may opt to just abandon it,” said Dr. Guadino.
At what cost? It will take years to sort that out, he said.
This study received no funding. Dr. Guadino and Dr. Bhatt are both active trialists, participating in both industry- and government-sponsored clinical research.
A version of this article originally appeared on Medscape.com.
The COVID-19 pandemic has created unique and unprecedented challenges for the clinical research world, with potentially long-lasting consequences.
A new analysis of the extent of disruption shows that the average rate of stopped trials nearly doubled during the first 5 months of 2020, compared with the 2 previous years.
“Typically, clinical research precedes clinical practice by several years, so this disruption we’re seeing now will be felt for many years to come,” said Mario Guadino, MD, of Weill Cornell Medicine, New York.
The analysis was published online July 31 in the Journal of the American College of Cardiology.
The researchers used Python software to query meta-data from all trials reported on ClinicalTrials.gov. Of 321,218 non-COVID-19 trials queried, 28,672 (8.9%) were reported as stopped, defined as a switch in trial status from “recruiting” to “active and not recruiting,” “completed,” “suspended,” “terminated,” or “withdrawn.”
The average rate of discontinuation was 638 trials/month from January 2017 to December 2019, rising to 1,147 trials/month between January 2020 and May 2020 (P < .001 for trend).
Once stopped (as opposed to paused), restarting a trial is a tricky prospect, said Dr. Guadino. “You can’t stop and restart a trial because it creates a lot of issues, so we should expect many of these stopped trials to never be completed.”
He said these figures likely represent an underestimate of the true impact of the pandemic because there is typically a delay in the updating of the status of a trial on ClinicalTrials.gov.
“We are likely looking only at the tip of the iceberg,” he added. “My impression is that the number of trials that will be affected and even canceled will be very high.”
As for cardiology trials, one of the report’s authors, Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, without naming specific trials, had this to say: “Several cardiovascular trials were paused, and some were permanently discontinued. It may be a while before we fully appreciate just how much information was lost and how much might be salvaged.”
He’s not worried, however, that upcoming cardiology meetings, which have moved online for the foreseeable future, might get a bit boring. “Fortunately, there is enough good work going on in the cardiovascular and cardiometabolic space that I believe there will still be ample randomized and observational data of high quality to present at the major meetings,” Dr. Bhatt said in an email.
The researchers found a weak correlation between the national population-adjusted numbers of COVID-19 cases and the proportion of non-COVID-19 trials stopped by country.
Even for trials that stopped recruiting for a period of time but are continuing, there are myriad issues involving compliance, data integrity, statistical interpretability, etc.
“Even if there is just a temporary disruption, that will most likely lead to reduced enrollment, missing follow-up visits, and protocol deviations, all things that would be red flags during normal times and impact the quality of the clinical trial,” said Dr. Guadino.
“And if your outcome of interest is mortality, well, how exactly do you measure that during a pandemic?” he added.
Stopped for lack of funding
Besides the logistical issues, another reason trials may be in jeopardy is funding. A warning early in the pandemic from the research community in Canada that funding was quickly drying up, leaving both jobs and data at risk, led to an aid package from the government to keep the lights on.
The National Institutes of Health (NIH), the Canadian Institutes of Health Research, and similar groups “have devoted large sums of money to research in COVID, which is of course very appropriate, but that clearly reduces the amount of funding that is available for other researchers,” said Dr. Guadino.
Some funding agencies around the world have canceled or put on hold all non-COVID-19 clinical trials still at the design state, Dr. Guadino said in an interview.
The NIH, he stressed, has not canceled funding and has been “extremely open and cooperative” in trying to help trialists navigate the many COVID-generated issues. They’ve even issued guidance on how to manage trials during COVID-19.
Of note, in the survey, the majority of the trials stopped (95.4%) had nongovernmental funding.
“The data are not very granular, so we’re only able to make some very simple, descriptive comments, but it does seem like the more fragile trials – those that are smaller and industry-funded – are the ones more likely to be disrupted,” said Dr. Guadino.
In some cases, he said, priorities have shifted to COVID-19. “If a small company is sponsoring a trial and they decide they want to sponsor something related to COVID, or they realize that because of the slow enrollment, the trial becomes too expensive to complete, they may opt to just abandon it,” said Dr. Guadino.
At what cost? It will take years to sort that out, he said.
This study received no funding. Dr. Guadino and Dr. Bhatt are both active trialists, participating in both industry- and government-sponsored clinical research.
A version of this article originally appeared on Medscape.com.
The COVID-19 pandemic has created unique and unprecedented challenges for the clinical research world, with potentially long-lasting consequences.
A new analysis of the extent of disruption shows that the average rate of stopped trials nearly doubled during the first 5 months of 2020, compared with the 2 previous years.
“Typically, clinical research precedes clinical practice by several years, so this disruption we’re seeing now will be felt for many years to come,” said Mario Guadino, MD, of Weill Cornell Medicine, New York.
The analysis was published online July 31 in the Journal of the American College of Cardiology.
The researchers used Python software to query meta-data from all trials reported on ClinicalTrials.gov. Of 321,218 non-COVID-19 trials queried, 28,672 (8.9%) were reported as stopped, defined as a switch in trial status from “recruiting” to “active and not recruiting,” “completed,” “suspended,” “terminated,” or “withdrawn.”
The average rate of discontinuation was 638 trials/month from January 2017 to December 2019, rising to 1,147 trials/month between January 2020 and May 2020 (P < .001 for trend).
Once stopped (as opposed to paused), restarting a trial is a tricky prospect, said Dr. Guadino. “You can’t stop and restart a trial because it creates a lot of issues, so we should expect many of these stopped trials to never be completed.”
He said these figures likely represent an underestimate of the true impact of the pandemic because there is typically a delay in the updating of the status of a trial on ClinicalTrials.gov.
“We are likely looking only at the tip of the iceberg,” he added. “My impression is that the number of trials that will be affected and even canceled will be very high.”
As for cardiology trials, one of the report’s authors, Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, without naming specific trials, had this to say: “Several cardiovascular trials were paused, and some were permanently discontinued. It may be a while before we fully appreciate just how much information was lost and how much might be salvaged.”
He’s not worried, however, that upcoming cardiology meetings, which have moved online for the foreseeable future, might get a bit boring. “Fortunately, there is enough good work going on in the cardiovascular and cardiometabolic space that I believe there will still be ample randomized and observational data of high quality to present at the major meetings,” Dr. Bhatt said in an email.
The researchers found a weak correlation between the national population-adjusted numbers of COVID-19 cases and the proportion of non-COVID-19 trials stopped by country.
Even for trials that stopped recruiting for a period of time but are continuing, there are myriad issues involving compliance, data integrity, statistical interpretability, etc.
“Even if there is just a temporary disruption, that will most likely lead to reduced enrollment, missing follow-up visits, and protocol deviations, all things that would be red flags during normal times and impact the quality of the clinical trial,” said Dr. Guadino.
“And if your outcome of interest is mortality, well, how exactly do you measure that during a pandemic?” he added.
Stopped for lack of funding
Besides the logistical issues, another reason trials may be in jeopardy is funding. A warning early in the pandemic from the research community in Canada that funding was quickly drying up, leaving both jobs and data at risk, led to an aid package from the government to keep the lights on.
The National Institutes of Health (NIH), the Canadian Institutes of Health Research, and similar groups “have devoted large sums of money to research in COVID, which is of course very appropriate, but that clearly reduces the amount of funding that is available for other researchers,” said Dr. Guadino.
Some funding agencies around the world have canceled or put on hold all non-COVID-19 clinical trials still at the design state, Dr. Guadino said in an interview.
The NIH, he stressed, has not canceled funding and has been “extremely open and cooperative” in trying to help trialists navigate the many COVID-generated issues. They’ve even issued guidance on how to manage trials during COVID-19.
Of note, in the survey, the majority of the trials stopped (95.4%) had nongovernmental funding.
“The data are not very granular, so we’re only able to make some very simple, descriptive comments, but it does seem like the more fragile trials – those that are smaller and industry-funded – are the ones more likely to be disrupted,” said Dr. Guadino.
In some cases, he said, priorities have shifted to COVID-19. “If a small company is sponsoring a trial and they decide they want to sponsor something related to COVID, or they realize that because of the slow enrollment, the trial becomes too expensive to complete, they may opt to just abandon it,” said Dr. Guadino.
At what cost? It will take years to sort that out, he said.
This study received no funding. Dr. Guadino and Dr. Bhatt are both active trialists, participating in both industry- and government-sponsored clinical research.
A version of this article originally appeared on Medscape.com.
Send kids to school safely if possible, supplement virtually
The abrupt transition to online learning for American children in kindergarten through 12th grade has left educators and parents unprepared, but virtual learning can be a successful part of education going forward, according to a viewpoint published in JAMA Pediatrics. However, schools also can reopen safely if precautions are taken, and students would benefit in many ways, according to a second viewpoint.
“As policy makers, health care professionals, and parents prepare for the fall semester and as public and private schools grapple with how to make that possible, a better understanding of K-12 virtual learning options and outcomes may facilitate those difficult decisions,” wrote Erik Black, PhD, of the University of Florida, Gainesville; Richard Ferdig, PhD, of Kent State University, Ohio; and Lindsay A. Thompson, MD, of the University of Florida, Gainesville.
“Importantly, K-12 virtual schooling is not suited for all students or all families.”
In a viewpoint published in JAMA Pediatrics, the authors noted that virtual schooling has existed in the United States in various forms for some time. “Just like the myriad options that are available for face-to-face schooling in the U.S., virtual schooling exists in a complex landscape of for-profit, charter, and public options.”
Not all virtual schools are equal
Consequently, not all virtual schools are created equal, they emphasized. Virtual education can be successful for many students when presented by trained online instructors using a curriculum designed to be effective in an online venue.
“Parents need to seek reviews and ask for educational outcomes from each virtual school system to assess the quality of the provided education,” Dr. Black, Dr. Ferdig, and Dr. Thompson emphasized.
Key questions for parents to consider when faced with online learning include the type of technology needed to participate; whether their child can maintain a study schedule and complete assignments with limited supervision; whether their child could ask for help and communicate with teachers through technology including phone, text, email, or video; and whether their child has the basic reading, math, and computer literacy skills to engage in online learning, the authors said. Other questions include the school’s expectations for parents and caregivers, how student information may be shared, and how the virtual school lines up with state standards for K-12 educators (in the case of options outside the public school system).
“The COVID-19 pandemic offers a unique challenge for educators, policymakers, and health care professionals to partner with parents to make the best local and individual decisions for children,” Dr. Black, Dr. Ferdig, and Dr. Thompson concluded.
Schools may be able to open safely
Children continue to make up a low percentage of COVID-19 cases and appear less likely to experience illness, wrote C. Jason Wang, MD, PhD, and Henry Bair, BS, of Stanford (Calif.) University in a second viewpoint also published in JAMA Pediatrics. The impact of long-term school closures extends beyond education and can “exacerbate socioeconomic disparities, amplify existing educational inequalities, and aggravate food insecurity, domestic violence, and mental health disorders,” they wrote.
Dr. Wang and Mr. Bair proposed that school districts “engage key stakeholders to establish a COVID-19 task force, composed of the superintendent, members of the school board, teachers, parents, and health care professionals to develop policies and procedures,” that would allow schools to open safely.
The authors outlined strategies including adapting teaching spaces to accommodate physical distance, with the addition of temporary modular buildings if needed. They advised assigned seating on school buses, and acknowledged the need for the availability of protective equipment, including hand sanitizer and masks, as well as the possible use of transparent barriers on the sides of student desks.
“As the AAP [American Academy of Pediatrics] guidance suggests, teachers who must work closely with students with special needs or with students who are unable to wear masks should wear N95 masks if possible or wear face shields in addition to surgical masks,” Dr. Wang and Mr. Bair noted. Other elements of the AAP guidance include the creation of fixed cohorts of students and teachers to limit virus exposure.
“Even with all the precautions in place, COVID-19 outbreaks within schools are still likely,” they said. “Therefore, schools will need to remain flexible and consider temporary closures if there is an outbreak involving multiple students and/or staff and be ready to transition to online education.”
The AAP guidance does not address operational approaches to identifying signs and symptoms of COVID-19, the authors noted. “To address this, we recommend that schools implement multilevel screening for students and staff.”
“In summary, to maximize health and educational outcomes, school districts should adopt some or all of the measures of the AAP guidance and prioritize them after considering local COVID-19 incidence, key stakeholder input, and budgetary constraints,” Dr. Wang and Mr. Bair concluded.
Schools opening is a regional decision
“The mission of the AAP is to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents, and young adults,” Howard Smart, MD, said in an interview. The question of school reopening “is of national importance, and the AAP has a national role in making recommendations regarding national policy affecting the health of the children.”
“The decision to open schools will be made regionally, but it is important for a nonpolitical national voice to make expert recommendations,” he emphasized.
“Many of the recommendations are ideal goals,” noted Dr. Smart, chairman of the department of pediatrics at the Sharp Rees-Stealy Medical Group in San Diego. “It will be difficult, for example, to implement symptom screening every day before school, no matter where it is performed. Some of the measures may be quite costly, and take time to implement, or require expansion of school staff, for which there may be no budget.”
In addition, “[n]ot all students are likely to comply with masking, distance, and hand-washing recommendations. One student who is noncompliant will be able to infect many other students and staff, as has been seen in other countries.” Also, parental attitudes toward control measures are likely to affect student attitudes, he noted.
“I have interviewed many families at recent checkups, and most have felt that the rush to remote learning that occurred at the end of the last school year resulted in fairly disorganized instruction,” Dr. Smart said. “They are hoping that, having had the summer to plan ahead, the remote teaching will be handled better. Remote learning will certainly work best for self-motivated, organized students with good family support, as noted in the Black, Ferdig, and Thompson article,” he said.
Pediatricians can support the schools by being a source of evidence-based information for parents, Dr. Smart said. “Pediatricians with time and energy might want to volunteer to hold informational video conferences for parents and/or school personnel if they feel they are up to date on current COVID-19 science and want to handle potentially contentious questions.”
The decision parents make to send their children back to school comes down to a risk-benefit calculation. “In some communities this may be left to parents, while in other communities this will a public health decision,” he said. “It is still not clear whether having students attend school in person will result in increased spread of COVID-19 among the students, or in their communities. Although some evidence from early in the pandemic suggests that children may not spread the virus as much as adults, more recent evidence suggests that children 10 years and older do transmit the virus at least as much as adults.”
“The risk to the students and the community, therefore, is unknown,” and difficult to compare with the benefit of in-person schooling, Dr. Smart noted.
“We will learn quite a bit from communities where students do go back to in-person class, as we follow the progression of COVID-19 over the weeks following the resumption of instruction.” Ultimately, advice to parents will need to be tailored to the current conditions of COVID-19 transmission in the community, he concluded.
It’s not just about education
“The AAP released its guidance to ensure that as school districts were contemplating reopening they were considering the full array of risks for children and adolescents. These risks included not only those related to COVID-19, but also those related to the impact of not reopening in-person,” Nathaniel Beers, MD, president of the HSC Health Care System in Washington, said in an interview.
“Students and families are dependent on schools for much more than just an education, and those [elements] need to be factored into the decisions to reopen,” the pediatrician said.
However, “[t]he major barrier for schools is resources to safely reopen,” said Dr. Beers. “The additional staffing and supplies will require additional funding. There are increased demands regardless of whether students are learning in-person or virtually or through hybrid models.”
“Another significant barrier is ensuring that parents and staff are actively engaged in planning for the type of model being used,” he said.
“All of the models require buy-in by staff and parents. This will require significant outreach and strong communication plans. Schools also need to ensure they are planning not just for how to return students to schools, but what will happen when staff or students test positive for COVID-19. Students, families, and staff all will need to know what these plans are up front to feel confident in returning to school,” he emphasized.
“There are students who can thrive in a virtual learning environment,” Dr. Beers said. “There are also students who benefit from the virtual learning environment because of their own risk, or because of a family member’s risk for COVID-19 or the complications from it.”
“However, many children with disabilities have struggled in a virtual environment,” he said. “These students struggle to access the educational services without the adequate supports at home. They often receive additional services in school, such as speech, occupational therapy or physical therapy, or nursing services, that may not have transitioned to home but are critical for their health and development. Many students with disabilities are dependent on family members to successfully access the educational services they need.”
“Pediatricians can play a role in providing feedback on recommendations related to physical distancing and face coverings in particular,” said Dr. Beers. “In addition, they can be helpful in developing plans for children with disabilities as well as what the response plan should be for students who become sick during the school day.”
The Centers for Disease Control and Prevention released a decision tool for parents who are considering whether to send their child to in-person school, and pediatricians can help parents walk through these questions, Dr. Beers noted. “In addition, pediatricians play an important role in helping patients and families think about the risks of COVID for the patient and other family members, and this can be helpful in addressing the anxiety that parents and patients may be experiencing.”
Further information can be found in Return to School During COVID-19, which can be located at HealthyChildren.org, by the American Academy of Pediatrics.
The authors of the viewpoints had no relevant financial disclosures. Dr. Smart, a member of the Pediatric News editorial advisory board, had no relevant financial disclosures. Dr. Beers has served on the editorial advisory board of Pediatric News in the past, but had no relevant financial disclosures.
SOURCES: Black E, Ferdig R, Thompson LA. JAMA Pediatr. 2020 Aug 11. doi: 10.1001/jamapediatrics.2020.3800. Wang CJ and Bair H. JAMA Pediatr. Aug 11. doi: 10.1001/jamapediatrics.2020.3871.
The abrupt transition to online learning for American children in kindergarten through 12th grade has left educators and parents unprepared, but virtual learning can be a successful part of education going forward, according to a viewpoint published in JAMA Pediatrics. However, schools also can reopen safely if precautions are taken, and students would benefit in many ways, according to a second viewpoint.
“As policy makers, health care professionals, and parents prepare for the fall semester and as public and private schools grapple with how to make that possible, a better understanding of K-12 virtual learning options and outcomes may facilitate those difficult decisions,” wrote Erik Black, PhD, of the University of Florida, Gainesville; Richard Ferdig, PhD, of Kent State University, Ohio; and Lindsay A. Thompson, MD, of the University of Florida, Gainesville.
“Importantly, K-12 virtual schooling is not suited for all students or all families.”
In a viewpoint published in JAMA Pediatrics, the authors noted that virtual schooling has existed in the United States in various forms for some time. “Just like the myriad options that are available for face-to-face schooling in the U.S., virtual schooling exists in a complex landscape of for-profit, charter, and public options.”
Not all virtual schools are equal
Consequently, not all virtual schools are created equal, they emphasized. Virtual education can be successful for many students when presented by trained online instructors using a curriculum designed to be effective in an online venue.
“Parents need to seek reviews and ask for educational outcomes from each virtual school system to assess the quality of the provided education,” Dr. Black, Dr. Ferdig, and Dr. Thompson emphasized.
Key questions for parents to consider when faced with online learning include the type of technology needed to participate; whether their child can maintain a study schedule and complete assignments with limited supervision; whether their child could ask for help and communicate with teachers through technology including phone, text, email, or video; and whether their child has the basic reading, math, and computer literacy skills to engage in online learning, the authors said. Other questions include the school’s expectations for parents and caregivers, how student information may be shared, and how the virtual school lines up with state standards for K-12 educators (in the case of options outside the public school system).
“The COVID-19 pandemic offers a unique challenge for educators, policymakers, and health care professionals to partner with parents to make the best local and individual decisions for children,” Dr. Black, Dr. Ferdig, and Dr. Thompson concluded.
Schools may be able to open safely
Children continue to make up a low percentage of COVID-19 cases and appear less likely to experience illness, wrote C. Jason Wang, MD, PhD, and Henry Bair, BS, of Stanford (Calif.) University in a second viewpoint also published in JAMA Pediatrics. The impact of long-term school closures extends beyond education and can “exacerbate socioeconomic disparities, amplify existing educational inequalities, and aggravate food insecurity, domestic violence, and mental health disorders,” they wrote.
Dr. Wang and Mr. Bair proposed that school districts “engage key stakeholders to establish a COVID-19 task force, composed of the superintendent, members of the school board, teachers, parents, and health care professionals to develop policies and procedures,” that would allow schools to open safely.
The authors outlined strategies including adapting teaching spaces to accommodate physical distance, with the addition of temporary modular buildings if needed. They advised assigned seating on school buses, and acknowledged the need for the availability of protective equipment, including hand sanitizer and masks, as well as the possible use of transparent barriers on the sides of student desks.
“As the AAP [American Academy of Pediatrics] guidance suggests, teachers who must work closely with students with special needs or with students who are unable to wear masks should wear N95 masks if possible or wear face shields in addition to surgical masks,” Dr. Wang and Mr. Bair noted. Other elements of the AAP guidance include the creation of fixed cohorts of students and teachers to limit virus exposure.
“Even with all the precautions in place, COVID-19 outbreaks within schools are still likely,” they said. “Therefore, schools will need to remain flexible and consider temporary closures if there is an outbreak involving multiple students and/or staff and be ready to transition to online education.”
The AAP guidance does not address operational approaches to identifying signs and symptoms of COVID-19, the authors noted. “To address this, we recommend that schools implement multilevel screening for students and staff.”
“In summary, to maximize health and educational outcomes, school districts should adopt some or all of the measures of the AAP guidance and prioritize them after considering local COVID-19 incidence, key stakeholder input, and budgetary constraints,” Dr. Wang and Mr. Bair concluded.
Schools opening is a regional decision
“The mission of the AAP is to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents, and young adults,” Howard Smart, MD, said in an interview. The question of school reopening “is of national importance, and the AAP has a national role in making recommendations regarding national policy affecting the health of the children.”
“The decision to open schools will be made regionally, but it is important for a nonpolitical national voice to make expert recommendations,” he emphasized.
“Many of the recommendations are ideal goals,” noted Dr. Smart, chairman of the department of pediatrics at the Sharp Rees-Stealy Medical Group in San Diego. “It will be difficult, for example, to implement symptom screening every day before school, no matter where it is performed. Some of the measures may be quite costly, and take time to implement, or require expansion of school staff, for which there may be no budget.”
In addition, “[n]ot all students are likely to comply with masking, distance, and hand-washing recommendations. One student who is noncompliant will be able to infect many other students and staff, as has been seen in other countries.” Also, parental attitudes toward control measures are likely to affect student attitudes, he noted.
“I have interviewed many families at recent checkups, and most have felt that the rush to remote learning that occurred at the end of the last school year resulted in fairly disorganized instruction,” Dr. Smart said. “They are hoping that, having had the summer to plan ahead, the remote teaching will be handled better. Remote learning will certainly work best for self-motivated, organized students with good family support, as noted in the Black, Ferdig, and Thompson article,” he said.
Pediatricians can support the schools by being a source of evidence-based information for parents, Dr. Smart said. “Pediatricians with time and energy might want to volunteer to hold informational video conferences for parents and/or school personnel if they feel they are up to date on current COVID-19 science and want to handle potentially contentious questions.”
The decision parents make to send their children back to school comes down to a risk-benefit calculation. “In some communities this may be left to parents, while in other communities this will a public health decision,” he said. “It is still not clear whether having students attend school in person will result in increased spread of COVID-19 among the students, or in their communities. Although some evidence from early in the pandemic suggests that children may not spread the virus as much as adults, more recent evidence suggests that children 10 years and older do transmit the virus at least as much as adults.”
“The risk to the students and the community, therefore, is unknown,” and difficult to compare with the benefit of in-person schooling, Dr. Smart noted.
“We will learn quite a bit from communities where students do go back to in-person class, as we follow the progression of COVID-19 over the weeks following the resumption of instruction.” Ultimately, advice to parents will need to be tailored to the current conditions of COVID-19 transmission in the community, he concluded.
It’s not just about education
“The AAP released its guidance to ensure that as school districts were contemplating reopening they were considering the full array of risks for children and adolescents. These risks included not only those related to COVID-19, but also those related to the impact of not reopening in-person,” Nathaniel Beers, MD, president of the HSC Health Care System in Washington, said in an interview.
“Students and families are dependent on schools for much more than just an education, and those [elements] need to be factored into the decisions to reopen,” the pediatrician said.
However, “[t]he major barrier for schools is resources to safely reopen,” said Dr. Beers. “The additional staffing and supplies will require additional funding. There are increased demands regardless of whether students are learning in-person or virtually or through hybrid models.”
“Another significant barrier is ensuring that parents and staff are actively engaged in planning for the type of model being used,” he said.
“All of the models require buy-in by staff and parents. This will require significant outreach and strong communication plans. Schools also need to ensure they are planning not just for how to return students to schools, but what will happen when staff or students test positive for COVID-19. Students, families, and staff all will need to know what these plans are up front to feel confident in returning to school,” he emphasized.
“There are students who can thrive in a virtual learning environment,” Dr. Beers said. “There are also students who benefit from the virtual learning environment because of their own risk, or because of a family member’s risk for COVID-19 or the complications from it.”
“However, many children with disabilities have struggled in a virtual environment,” he said. “These students struggle to access the educational services without the adequate supports at home. They often receive additional services in school, such as speech, occupational therapy or physical therapy, or nursing services, that may not have transitioned to home but are critical for their health and development. Many students with disabilities are dependent on family members to successfully access the educational services they need.”
“Pediatricians can play a role in providing feedback on recommendations related to physical distancing and face coverings in particular,” said Dr. Beers. “In addition, they can be helpful in developing plans for children with disabilities as well as what the response plan should be for students who become sick during the school day.”
The Centers for Disease Control and Prevention released a decision tool for parents who are considering whether to send their child to in-person school, and pediatricians can help parents walk through these questions, Dr. Beers noted. “In addition, pediatricians play an important role in helping patients and families think about the risks of COVID for the patient and other family members, and this can be helpful in addressing the anxiety that parents and patients may be experiencing.”
Further information can be found in Return to School During COVID-19, which can be located at HealthyChildren.org, by the American Academy of Pediatrics.
The authors of the viewpoints had no relevant financial disclosures. Dr. Smart, a member of the Pediatric News editorial advisory board, had no relevant financial disclosures. Dr. Beers has served on the editorial advisory board of Pediatric News in the past, but had no relevant financial disclosures.
SOURCES: Black E, Ferdig R, Thompson LA. JAMA Pediatr. 2020 Aug 11. doi: 10.1001/jamapediatrics.2020.3800. Wang CJ and Bair H. JAMA Pediatr. Aug 11. doi: 10.1001/jamapediatrics.2020.3871.
The abrupt transition to online learning for American children in kindergarten through 12th grade has left educators and parents unprepared, but virtual learning can be a successful part of education going forward, according to a viewpoint published in JAMA Pediatrics. However, schools also can reopen safely if precautions are taken, and students would benefit in many ways, according to a second viewpoint.
“As policy makers, health care professionals, and parents prepare for the fall semester and as public and private schools grapple with how to make that possible, a better understanding of K-12 virtual learning options and outcomes may facilitate those difficult decisions,” wrote Erik Black, PhD, of the University of Florida, Gainesville; Richard Ferdig, PhD, of Kent State University, Ohio; and Lindsay A. Thompson, MD, of the University of Florida, Gainesville.
“Importantly, K-12 virtual schooling is not suited for all students or all families.”
In a viewpoint published in JAMA Pediatrics, the authors noted that virtual schooling has existed in the United States in various forms for some time. “Just like the myriad options that are available for face-to-face schooling in the U.S., virtual schooling exists in a complex landscape of for-profit, charter, and public options.”
Not all virtual schools are equal
Consequently, not all virtual schools are created equal, they emphasized. Virtual education can be successful for many students when presented by trained online instructors using a curriculum designed to be effective in an online venue.
“Parents need to seek reviews and ask for educational outcomes from each virtual school system to assess the quality of the provided education,” Dr. Black, Dr. Ferdig, and Dr. Thompson emphasized.
Key questions for parents to consider when faced with online learning include the type of technology needed to participate; whether their child can maintain a study schedule and complete assignments with limited supervision; whether their child could ask for help and communicate with teachers through technology including phone, text, email, or video; and whether their child has the basic reading, math, and computer literacy skills to engage in online learning, the authors said. Other questions include the school’s expectations for parents and caregivers, how student information may be shared, and how the virtual school lines up with state standards for K-12 educators (in the case of options outside the public school system).
“The COVID-19 pandemic offers a unique challenge for educators, policymakers, and health care professionals to partner with parents to make the best local and individual decisions for children,” Dr. Black, Dr. Ferdig, and Dr. Thompson concluded.
Schools may be able to open safely
Children continue to make up a low percentage of COVID-19 cases and appear less likely to experience illness, wrote C. Jason Wang, MD, PhD, and Henry Bair, BS, of Stanford (Calif.) University in a second viewpoint also published in JAMA Pediatrics. The impact of long-term school closures extends beyond education and can “exacerbate socioeconomic disparities, amplify existing educational inequalities, and aggravate food insecurity, domestic violence, and mental health disorders,” they wrote.
Dr. Wang and Mr. Bair proposed that school districts “engage key stakeholders to establish a COVID-19 task force, composed of the superintendent, members of the school board, teachers, parents, and health care professionals to develop policies and procedures,” that would allow schools to open safely.
The authors outlined strategies including adapting teaching spaces to accommodate physical distance, with the addition of temporary modular buildings if needed. They advised assigned seating on school buses, and acknowledged the need for the availability of protective equipment, including hand sanitizer and masks, as well as the possible use of transparent barriers on the sides of student desks.
“As the AAP [American Academy of Pediatrics] guidance suggests, teachers who must work closely with students with special needs or with students who are unable to wear masks should wear N95 masks if possible or wear face shields in addition to surgical masks,” Dr. Wang and Mr. Bair noted. Other elements of the AAP guidance include the creation of fixed cohorts of students and teachers to limit virus exposure.
“Even with all the precautions in place, COVID-19 outbreaks within schools are still likely,” they said. “Therefore, schools will need to remain flexible and consider temporary closures if there is an outbreak involving multiple students and/or staff and be ready to transition to online education.”
The AAP guidance does not address operational approaches to identifying signs and symptoms of COVID-19, the authors noted. “To address this, we recommend that schools implement multilevel screening for students and staff.”
“In summary, to maximize health and educational outcomes, school districts should adopt some or all of the measures of the AAP guidance and prioritize them after considering local COVID-19 incidence, key stakeholder input, and budgetary constraints,” Dr. Wang and Mr. Bair concluded.
Schools opening is a regional decision
“The mission of the AAP is to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents, and young adults,” Howard Smart, MD, said in an interview. The question of school reopening “is of national importance, and the AAP has a national role in making recommendations regarding national policy affecting the health of the children.”
“The decision to open schools will be made regionally, but it is important for a nonpolitical national voice to make expert recommendations,” he emphasized.
“Many of the recommendations are ideal goals,” noted Dr. Smart, chairman of the department of pediatrics at the Sharp Rees-Stealy Medical Group in San Diego. “It will be difficult, for example, to implement symptom screening every day before school, no matter where it is performed. Some of the measures may be quite costly, and take time to implement, or require expansion of school staff, for which there may be no budget.”
In addition, “[n]ot all students are likely to comply with masking, distance, and hand-washing recommendations. One student who is noncompliant will be able to infect many other students and staff, as has been seen in other countries.” Also, parental attitudes toward control measures are likely to affect student attitudes, he noted.
“I have interviewed many families at recent checkups, and most have felt that the rush to remote learning that occurred at the end of the last school year resulted in fairly disorganized instruction,” Dr. Smart said. “They are hoping that, having had the summer to plan ahead, the remote teaching will be handled better. Remote learning will certainly work best for self-motivated, organized students with good family support, as noted in the Black, Ferdig, and Thompson article,” he said.
Pediatricians can support the schools by being a source of evidence-based information for parents, Dr. Smart said. “Pediatricians with time and energy might want to volunteer to hold informational video conferences for parents and/or school personnel if they feel they are up to date on current COVID-19 science and want to handle potentially contentious questions.”
The decision parents make to send their children back to school comes down to a risk-benefit calculation. “In some communities this may be left to parents, while in other communities this will a public health decision,” he said. “It is still not clear whether having students attend school in person will result in increased spread of COVID-19 among the students, or in their communities. Although some evidence from early in the pandemic suggests that children may not spread the virus as much as adults, more recent evidence suggests that children 10 years and older do transmit the virus at least as much as adults.”
“The risk to the students and the community, therefore, is unknown,” and difficult to compare with the benefit of in-person schooling, Dr. Smart noted.
“We will learn quite a bit from communities where students do go back to in-person class, as we follow the progression of COVID-19 over the weeks following the resumption of instruction.” Ultimately, advice to parents will need to be tailored to the current conditions of COVID-19 transmission in the community, he concluded.
It’s not just about education
“The AAP released its guidance to ensure that as school districts were contemplating reopening they were considering the full array of risks for children and adolescents. These risks included not only those related to COVID-19, but also those related to the impact of not reopening in-person,” Nathaniel Beers, MD, president of the HSC Health Care System in Washington, said in an interview.
“Students and families are dependent on schools for much more than just an education, and those [elements] need to be factored into the decisions to reopen,” the pediatrician said.
However, “[t]he major barrier for schools is resources to safely reopen,” said Dr. Beers. “The additional staffing and supplies will require additional funding. There are increased demands regardless of whether students are learning in-person or virtually or through hybrid models.”
“Another significant barrier is ensuring that parents and staff are actively engaged in planning for the type of model being used,” he said.
“All of the models require buy-in by staff and parents. This will require significant outreach and strong communication plans. Schools also need to ensure they are planning not just for how to return students to schools, but what will happen when staff or students test positive for COVID-19. Students, families, and staff all will need to know what these plans are up front to feel confident in returning to school,” he emphasized.
“There are students who can thrive in a virtual learning environment,” Dr. Beers said. “There are also students who benefit from the virtual learning environment because of their own risk, or because of a family member’s risk for COVID-19 or the complications from it.”
“However, many children with disabilities have struggled in a virtual environment,” he said. “These students struggle to access the educational services without the adequate supports at home. They often receive additional services in school, such as speech, occupational therapy or physical therapy, or nursing services, that may not have transitioned to home but are critical for their health and development. Many students with disabilities are dependent on family members to successfully access the educational services they need.”
“Pediatricians can play a role in providing feedback on recommendations related to physical distancing and face coverings in particular,” said Dr. Beers. “In addition, they can be helpful in developing plans for children with disabilities as well as what the response plan should be for students who become sick during the school day.”
The Centers for Disease Control and Prevention released a decision tool for parents who are considering whether to send their child to in-person school, and pediatricians can help parents walk through these questions, Dr. Beers noted. “In addition, pediatricians play an important role in helping patients and families think about the risks of COVID for the patient and other family members, and this can be helpful in addressing the anxiety that parents and patients may be experiencing.”
Further information can be found in Return to School During COVID-19, which can be located at HealthyChildren.org, by the American Academy of Pediatrics.
The authors of the viewpoints had no relevant financial disclosures. Dr. Smart, a member of the Pediatric News editorial advisory board, had no relevant financial disclosures. Dr. Beers has served on the editorial advisory board of Pediatric News in the past, but had no relevant financial disclosures.
SOURCES: Black E, Ferdig R, Thompson LA. JAMA Pediatr. 2020 Aug 11. doi: 10.1001/jamapediatrics.2020.3800. Wang CJ and Bair H. JAMA Pediatr. Aug 11. doi: 10.1001/jamapediatrics.2020.3871.
FROM JAMA PEDIATRICS
Severe obesity ups risk for death in younger men with COVID-19
In a large California health care plan, among patients with COVID-19, men aged 60 years and younger had a much higher risk of dying within 3 weeks of diagnosis if they had severe obesity as opposed to being of normal weight, independently of other risk factors.
reported Sara Y. Tartof, PhD, MPH, Kaiser Permanente Southern California, Pasadena, Calif., and coauthors.
The data “highlight the leading role of severe obesity over correlated risk factors, providing a target for early intervention,” they concluded in an article published online Aug. 12 in Annals of Internal Medicine.
This work adds to nearly 300 articles that have shown that severe obesity is associated with an increased risk for morbidity and mortality from COVID-19.
In an accompanying editorial, David A. Kass, MD, said: “Consistency of this new study and prior research should put to rest the contention that obesity is common in severe COVID-19 because it is common in the population.”
Rather, these findings show that “obesity is an important independent risk factor for serious COVID-19 disease,” he pointed out.
On the basis of this evidence, “arguably the hardest question to answer is: What is to be done?” wondered Kass, of Johns Hopkins University, Baltimore.
Although data consistently show that a body mass index >35 kg/m2 is predictive of major health risks, “weight reduction at that level of obesity is difficult and certainly is not achieved rapidly,” Dr. Kass stressed.
“Therefore ... social distancing; altering behaviors to reduce viral exposure and transmission, such as wearing masks; and instituting policies and health care approaches that recognize the potential effects of obesity should be implemented,” he emphasized. “These actions should help and are certainly doable.”
Similarly, Dr. Tartof and colleagues said their “findings also reveal the distressing collision of two pandemics: COVID-19 and obesity.
“As COVID-19 continues to spread unabated, we must focus our immediate efforts on containing the crisis at hand,” they urged.
However, the findings also “underscore the need for future collective efforts to combat the equally devastating, and potentially synergistic, force of the obesity epidemic.”
COVID-19 pandemic collides with obesity epidemic
Previous studies of obesity and COVID-19 were small, did not adjust for multiple confounders, or did not include nonhospitalized patients, Dr. Tartof and coauthors wrote.
Their study included 6,916 members of the Kaiser Permanente Southern California health care plan who were diagnosed with COVID-19 from Feb. 13 to May 2, 2020.
The researchers calculated the risk for death at 21 days after a COVID-19 diagnosis; findings were corrected for age, sex, race/ethnicity, smoking, myocardial infarction, heart failure, peripheral vascular disease, cerebrovascular disease, chronic pulmonary disease, renal disease, metastatic tumor or malignancy, other immune disease, hyperlipidemia, hypertension, asthma, organ transplant, and diabetes status.
On the basis of BMI, the patients were classified as being underweight, of normal weight, overweight, or as having class 1, 2, or 3 obesity. BMI of 18.5 to 24 kg/m2 is defined as normal weight.
Class 3 obesity, also called severe obesity, included moderately severe obesity (BMI, 40-44 kg/m2) and extremely severe obesity (≥45 kg/m2).
A little more than half of the patients were women (55%), and more than 50% were Hispanic (54%).
A total of 206 patients (3%) died within 21 days of being diagnosed with COVID-19; of these, 67% had been hospitalized, and 43% had been intubated.
Overall, the COVID-19 patients with moderately severe or extremely severe obesity had a 2.7-fold and 4.2-fold increased risk for death, respectively, within 3 weeks compared with patients of normal weight.
Patients in the other BMI categories did not have a significantly higher risk of dying during follow-up.
However, each decade of increasing age after age 40 was associated with a stepwise increased risk for death within 3 weeks of the COVID-19 diagnosis.
Risk stratified by age and sex
Further analysis showed that, “most strikingly,” among patients aged 60 and younger, those with moderately severe obesity and extremely severe obesity had significant 17-fold and 12-fold higher risks of dying during follow-up, respectively, compared with patients of normal weight, the researchers reported.
In patients older than 60, moderately severe obesity did not confer a significant increased risk for imminent death from COVID-19; extremely severe obesity conferred a smaller, threefold increased risk for this.
“Our finding that severe obesity, particularly among younger patients, eclipses the mortality risk posed by other obesity-related conditions, such as history of myocardial infarction (MI), diabetes, hypertension, or hyperlipidemia, suggests a significant pathophysiologic link between excess adiposity and severe COVID-19 illness,” the researchers noted.
This independent increased risk for death with severe obesity was seen in men but not in women.
Men with moderately severe and extremely severe obesity had significant 4.8-fold and 10-fold higher risks of dying within 3 weeks, respectively, compared with men of normal weight.
“That the risks are higher in younger patients is probably not because obesity is particularly damaging in this age group; it is more likely that other serious comorbidities that evolve later in life take over as dominant risk factors,” Dr. Kass suggested in his editorial.
“That males are particularly affected may reflect their greater visceral adiposity over females, given that this fat is notably proinflammatory and contributes to metabolic and vascular disease,” he added.
“As a cardiologist who studies heart failure,” Dr. Kass wrote, “I am struck by how many of the mechanisms that are mentioned in reviews of obesity risk and heart disease are also mentioned in reviews of obesity and COVID-19.”
The study was funded by Roche-Genentech. Kass has disclosed no relevant financial relationships. Disclosures of the authors are listed in the article.
A version of this article originally appeared on Medscape.com.
In a large California health care plan, among patients with COVID-19, men aged 60 years and younger had a much higher risk of dying within 3 weeks of diagnosis if they had severe obesity as opposed to being of normal weight, independently of other risk factors.
reported Sara Y. Tartof, PhD, MPH, Kaiser Permanente Southern California, Pasadena, Calif., and coauthors.
The data “highlight the leading role of severe obesity over correlated risk factors, providing a target for early intervention,” they concluded in an article published online Aug. 12 in Annals of Internal Medicine.
This work adds to nearly 300 articles that have shown that severe obesity is associated with an increased risk for morbidity and mortality from COVID-19.
In an accompanying editorial, David A. Kass, MD, said: “Consistency of this new study and prior research should put to rest the contention that obesity is common in severe COVID-19 because it is common in the population.”
Rather, these findings show that “obesity is an important independent risk factor for serious COVID-19 disease,” he pointed out.
On the basis of this evidence, “arguably the hardest question to answer is: What is to be done?” wondered Kass, of Johns Hopkins University, Baltimore.
Although data consistently show that a body mass index >35 kg/m2 is predictive of major health risks, “weight reduction at that level of obesity is difficult and certainly is not achieved rapidly,” Dr. Kass stressed.
“Therefore ... social distancing; altering behaviors to reduce viral exposure and transmission, such as wearing masks; and instituting policies and health care approaches that recognize the potential effects of obesity should be implemented,” he emphasized. “These actions should help and are certainly doable.”
Similarly, Dr. Tartof and colleagues said their “findings also reveal the distressing collision of two pandemics: COVID-19 and obesity.
“As COVID-19 continues to spread unabated, we must focus our immediate efforts on containing the crisis at hand,” they urged.
However, the findings also “underscore the need for future collective efforts to combat the equally devastating, and potentially synergistic, force of the obesity epidemic.”
COVID-19 pandemic collides with obesity epidemic
Previous studies of obesity and COVID-19 were small, did not adjust for multiple confounders, or did not include nonhospitalized patients, Dr. Tartof and coauthors wrote.
Their study included 6,916 members of the Kaiser Permanente Southern California health care plan who were diagnosed with COVID-19 from Feb. 13 to May 2, 2020.
The researchers calculated the risk for death at 21 days after a COVID-19 diagnosis; findings were corrected for age, sex, race/ethnicity, smoking, myocardial infarction, heart failure, peripheral vascular disease, cerebrovascular disease, chronic pulmonary disease, renal disease, metastatic tumor or malignancy, other immune disease, hyperlipidemia, hypertension, asthma, organ transplant, and diabetes status.
On the basis of BMI, the patients were classified as being underweight, of normal weight, overweight, or as having class 1, 2, or 3 obesity. BMI of 18.5 to 24 kg/m2 is defined as normal weight.
Class 3 obesity, also called severe obesity, included moderately severe obesity (BMI, 40-44 kg/m2) and extremely severe obesity (≥45 kg/m2).
A little more than half of the patients were women (55%), and more than 50% were Hispanic (54%).
A total of 206 patients (3%) died within 21 days of being diagnosed with COVID-19; of these, 67% had been hospitalized, and 43% had been intubated.
Overall, the COVID-19 patients with moderately severe or extremely severe obesity had a 2.7-fold and 4.2-fold increased risk for death, respectively, within 3 weeks compared with patients of normal weight.
Patients in the other BMI categories did not have a significantly higher risk of dying during follow-up.
However, each decade of increasing age after age 40 was associated with a stepwise increased risk for death within 3 weeks of the COVID-19 diagnosis.
Risk stratified by age and sex
Further analysis showed that, “most strikingly,” among patients aged 60 and younger, those with moderately severe obesity and extremely severe obesity had significant 17-fold and 12-fold higher risks of dying during follow-up, respectively, compared with patients of normal weight, the researchers reported.
In patients older than 60, moderately severe obesity did not confer a significant increased risk for imminent death from COVID-19; extremely severe obesity conferred a smaller, threefold increased risk for this.
“Our finding that severe obesity, particularly among younger patients, eclipses the mortality risk posed by other obesity-related conditions, such as history of myocardial infarction (MI), diabetes, hypertension, or hyperlipidemia, suggests a significant pathophysiologic link between excess adiposity and severe COVID-19 illness,” the researchers noted.
This independent increased risk for death with severe obesity was seen in men but not in women.
Men with moderately severe and extremely severe obesity had significant 4.8-fold and 10-fold higher risks of dying within 3 weeks, respectively, compared with men of normal weight.
“That the risks are higher in younger patients is probably not because obesity is particularly damaging in this age group; it is more likely that other serious comorbidities that evolve later in life take over as dominant risk factors,” Dr. Kass suggested in his editorial.
“That males are particularly affected may reflect their greater visceral adiposity over females, given that this fat is notably proinflammatory and contributes to metabolic and vascular disease,” he added.
“As a cardiologist who studies heart failure,” Dr. Kass wrote, “I am struck by how many of the mechanisms that are mentioned in reviews of obesity risk and heart disease are also mentioned in reviews of obesity and COVID-19.”
The study was funded by Roche-Genentech. Kass has disclosed no relevant financial relationships. Disclosures of the authors are listed in the article.
A version of this article originally appeared on Medscape.com.
In a large California health care plan, among patients with COVID-19, men aged 60 years and younger had a much higher risk of dying within 3 weeks of diagnosis if they had severe obesity as opposed to being of normal weight, independently of other risk factors.
reported Sara Y. Tartof, PhD, MPH, Kaiser Permanente Southern California, Pasadena, Calif., and coauthors.
The data “highlight the leading role of severe obesity over correlated risk factors, providing a target for early intervention,” they concluded in an article published online Aug. 12 in Annals of Internal Medicine.
This work adds to nearly 300 articles that have shown that severe obesity is associated with an increased risk for morbidity and mortality from COVID-19.
In an accompanying editorial, David A. Kass, MD, said: “Consistency of this new study and prior research should put to rest the contention that obesity is common in severe COVID-19 because it is common in the population.”
Rather, these findings show that “obesity is an important independent risk factor for serious COVID-19 disease,” he pointed out.
On the basis of this evidence, “arguably the hardest question to answer is: What is to be done?” wondered Kass, of Johns Hopkins University, Baltimore.
Although data consistently show that a body mass index >35 kg/m2 is predictive of major health risks, “weight reduction at that level of obesity is difficult and certainly is not achieved rapidly,” Dr. Kass stressed.
“Therefore ... social distancing; altering behaviors to reduce viral exposure and transmission, such as wearing masks; and instituting policies and health care approaches that recognize the potential effects of obesity should be implemented,” he emphasized. “These actions should help and are certainly doable.”
Similarly, Dr. Tartof and colleagues said their “findings also reveal the distressing collision of two pandemics: COVID-19 and obesity.
“As COVID-19 continues to spread unabated, we must focus our immediate efforts on containing the crisis at hand,” they urged.
However, the findings also “underscore the need for future collective efforts to combat the equally devastating, and potentially synergistic, force of the obesity epidemic.”
COVID-19 pandemic collides with obesity epidemic
Previous studies of obesity and COVID-19 were small, did not adjust for multiple confounders, or did not include nonhospitalized patients, Dr. Tartof and coauthors wrote.
Their study included 6,916 members of the Kaiser Permanente Southern California health care plan who were diagnosed with COVID-19 from Feb. 13 to May 2, 2020.
The researchers calculated the risk for death at 21 days after a COVID-19 diagnosis; findings were corrected for age, sex, race/ethnicity, smoking, myocardial infarction, heart failure, peripheral vascular disease, cerebrovascular disease, chronic pulmonary disease, renal disease, metastatic tumor or malignancy, other immune disease, hyperlipidemia, hypertension, asthma, organ transplant, and diabetes status.
On the basis of BMI, the patients were classified as being underweight, of normal weight, overweight, or as having class 1, 2, or 3 obesity. BMI of 18.5 to 24 kg/m2 is defined as normal weight.
Class 3 obesity, also called severe obesity, included moderately severe obesity (BMI, 40-44 kg/m2) and extremely severe obesity (≥45 kg/m2).
A little more than half of the patients were women (55%), and more than 50% were Hispanic (54%).
A total of 206 patients (3%) died within 21 days of being diagnosed with COVID-19; of these, 67% had been hospitalized, and 43% had been intubated.
Overall, the COVID-19 patients with moderately severe or extremely severe obesity had a 2.7-fold and 4.2-fold increased risk for death, respectively, within 3 weeks compared with patients of normal weight.
Patients in the other BMI categories did not have a significantly higher risk of dying during follow-up.
However, each decade of increasing age after age 40 was associated with a stepwise increased risk for death within 3 weeks of the COVID-19 diagnosis.
Risk stratified by age and sex
Further analysis showed that, “most strikingly,” among patients aged 60 and younger, those with moderately severe obesity and extremely severe obesity had significant 17-fold and 12-fold higher risks of dying during follow-up, respectively, compared with patients of normal weight, the researchers reported.
In patients older than 60, moderately severe obesity did not confer a significant increased risk for imminent death from COVID-19; extremely severe obesity conferred a smaller, threefold increased risk for this.
“Our finding that severe obesity, particularly among younger patients, eclipses the mortality risk posed by other obesity-related conditions, such as history of myocardial infarction (MI), diabetes, hypertension, or hyperlipidemia, suggests a significant pathophysiologic link between excess adiposity and severe COVID-19 illness,” the researchers noted.
This independent increased risk for death with severe obesity was seen in men but not in women.
Men with moderately severe and extremely severe obesity had significant 4.8-fold and 10-fold higher risks of dying within 3 weeks, respectively, compared with men of normal weight.
“That the risks are higher in younger patients is probably not because obesity is particularly damaging in this age group; it is more likely that other serious comorbidities that evolve later in life take over as dominant risk factors,” Dr. Kass suggested in his editorial.
“That males are particularly affected may reflect their greater visceral adiposity over females, given that this fat is notably proinflammatory and contributes to metabolic and vascular disease,” he added.
“As a cardiologist who studies heart failure,” Dr. Kass wrote, “I am struck by how many of the mechanisms that are mentioned in reviews of obesity risk and heart disease are also mentioned in reviews of obesity and COVID-19.”
The study was funded by Roche-Genentech. Kass has disclosed no relevant financial relationships. Disclosures of the authors are listed in the article.
A version of this article originally appeared on Medscape.com.
Only 40% of residents said training prepped them for COVID-19
Most residents who were asked whether their training prepared them for COVID-19 in a Medscape survey said it had not or they weren’t sure.
Whereas 40% said they felt prepared, 30% said they did not feel prepared and 31% answered they were unsure. (Numbers were rounded, so some answers pushed above 100%.)
One quarter have $300,000 or more in student debt
The Medscape Residents Salary & Debt Report 2020, with data collected April 3 to June 1, found that nearly one in four residents (24%) had medical school debt of more than $300,000. Half (49%) had more than $200,000.
The data include answers from 1,659 U.S. medical residents.
For the sixth straight year, female residents were more satisfied with their pay than were their male colleagues. This year the satisfaction gap was 45% female compared with 42% male. That imbalance came despite their making nearly the same pay overall ($63,700 for men and $63,000 for women).
Among practicing physicians, the pay gap is much wider: Men make 25% more in primary care and 31% more in specialties.
Ten percent thought they should earn 76%-100% more.
For those not satisfied with pay, the top reasons were feeling the pay was too low for the hours worked (81%) or too low compared with other medical staff, such as physician assistants (PAs) or nurses (77% chose that answer).
As for hours worked, 31% of residents reported they spend more than 60 hours/week seeing patients.
The top-paying specialties, averaging $69,500, were allergy and immunology, hematology, plastic surgery, aesthetic medicine, rheumatology, and specialized surgery. The lowest paid were family medicine residents at $58,500.
In primary care, overall, most residents said they planned to specialize. Only 47% planned to continue to work in primary care. Male residents were much more likely to say they will subspecialize than were their female colleagues (52% vs. 35%).
More than 90% of residents say future pay has influenced their choice of specialty, though more men than women felt that way (93% vs. 86%).
Good relationships with others
Overall, residents reported good relationships with attending physicians and nurses.
Most (88%) said they had good or very good relationships with attending physicians, 10% said the relationships were fair, and 2% said they were poor.
In addition, 89% of residents said the amount of supervision was appropriate, 4% said there was too much, and 7% said there was too little.
Relationships with nurses/PAs were slightly less positive overall: Eighty-two percent reported good or very good relationships with nurses/PAs, 15% said those relationships were fair, and 3% said they were poor.
One respondent said: “Our relationships could be better, but I think everyone is just overwhelmed with COVID-19, so emotions are heightened.”
Another said: “It takes time to earn the respect from nurses.”
Seventy-seven percent said they were satisfied with their learning experience overall, 12% were neutral on the question, and 11% said they were dissatisfied or very dissatisfied.
Work-life balance is the top concern
Work-life balance continues to be the top concern for residents. More than one-quarter (27%) in residency years 1 through 4 listed that as the top concern, and even more (32%) of those in years 5 through 8 agreed.
That was followed by demands on time and fear of failure or making a serious mistake.
The survey indicates that benefit packages for residents have stayed much the same over the past 2 years with health insurance and paid time off for sick leave, vacation, and personal time most commonly reported at 89% and 87%, respectively.
Much less common were benefits including commuter assistance (parking, public transportation) at 24%, housing allowance (8%), and child care (4%).
The vast majority of residents reported doing scut work (unskilled tasks): More than half (54%) reported doing 1-10 hours/week and 22% did 11-20 hours/week. Regardless of the number of hours, however, 62% said the time spent performing these tasks was appropriate.
A version of this article originally appeared on Medscape.com.
Most residents who were asked whether their training prepared them for COVID-19 in a Medscape survey said it had not or they weren’t sure.
Whereas 40% said they felt prepared, 30% said they did not feel prepared and 31% answered they were unsure. (Numbers were rounded, so some answers pushed above 100%.)
One quarter have $300,000 or more in student debt
The Medscape Residents Salary & Debt Report 2020, with data collected April 3 to June 1, found that nearly one in four residents (24%) had medical school debt of more than $300,000. Half (49%) had more than $200,000.
The data include answers from 1,659 U.S. medical residents.
For the sixth straight year, female residents were more satisfied with their pay than were their male colleagues. This year the satisfaction gap was 45% female compared with 42% male. That imbalance came despite their making nearly the same pay overall ($63,700 for men and $63,000 for women).
Among practicing physicians, the pay gap is much wider: Men make 25% more in primary care and 31% more in specialties.
Ten percent thought they should earn 76%-100% more.
For those not satisfied with pay, the top reasons were feeling the pay was too low for the hours worked (81%) or too low compared with other medical staff, such as physician assistants (PAs) or nurses (77% chose that answer).
As for hours worked, 31% of residents reported they spend more than 60 hours/week seeing patients.
The top-paying specialties, averaging $69,500, were allergy and immunology, hematology, plastic surgery, aesthetic medicine, rheumatology, and specialized surgery. The lowest paid were family medicine residents at $58,500.
In primary care, overall, most residents said they planned to specialize. Only 47% planned to continue to work in primary care. Male residents were much more likely to say they will subspecialize than were their female colleagues (52% vs. 35%).
More than 90% of residents say future pay has influenced their choice of specialty, though more men than women felt that way (93% vs. 86%).
Good relationships with others
Overall, residents reported good relationships with attending physicians and nurses.
Most (88%) said they had good or very good relationships with attending physicians, 10% said the relationships were fair, and 2% said they were poor.
In addition, 89% of residents said the amount of supervision was appropriate, 4% said there was too much, and 7% said there was too little.
Relationships with nurses/PAs were slightly less positive overall: Eighty-two percent reported good or very good relationships with nurses/PAs, 15% said those relationships were fair, and 3% said they were poor.
One respondent said: “Our relationships could be better, but I think everyone is just overwhelmed with COVID-19, so emotions are heightened.”
Another said: “It takes time to earn the respect from nurses.”
Seventy-seven percent said they were satisfied with their learning experience overall, 12% were neutral on the question, and 11% said they were dissatisfied or very dissatisfied.
Work-life balance is the top concern
Work-life balance continues to be the top concern for residents. More than one-quarter (27%) in residency years 1 through 4 listed that as the top concern, and even more (32%) of those in years 5 through 8 agreed.
That was followed by demands on time and fear of failure or making a serious mistake.
The survey indicates that benefit packages for residents have stayed much the same over the past 2 years with health insurance and paid time off for sick leave, vacation, and personal time most commonly reported at 89% and 87%, respectively.
Much less common were benefits including commuter assistance (parking, public transportation) at 24%, housing allowance (8%), and child care (4%).
The vast majority of residents reported doing scut work (unskilled tasks): More than half (54%) reported doing 1-10 hours/week and 22% did 11-20 hours/week. Regardless of the number of hours, however, 62% said the time spent performing these tasks was appropriate.
A version of this article originally appeared on Medscape.com.
Most residents who were asked whether their training prepared them for COVID-19 in a Medscape survey said it had not or they weren’t sure.
Whereas 40% said they felt prepared, 30% said they did not feel prepared and 31% answered they were unsure. (Numbers were rounded, so some answers pushed above 100%.)
One quarter have $300,000 or more in student debt
The Medscape Residents Salary & Debt Report 2020, with data collected April 3 to June 1, found that nearly one in four residents (24%) had medical school debt of more than $300,000. Half (49%) had more than $200,000.
The data include answers from 1,659 U.S. medical residents.
For the sixth straight year, female residents were more satisfied with their pay than were their male colleagues. This year the satisfaction gap was 45% female compared with 42% male. That imbalance came despite their making nearly the same pay overall ($63,700 for men and $63,000 for women).
Among practicing physicians, the pay gap is much wider: Men make 25% more in primary care and 31% more in specialties.
Ten percent thought they should earn 76%-100% more.
For those not satisfied with pay, the top reasons were feeling the pay was too low for the hours worked (81%) or too low compared with other medical staff, such as physician assistants (PAs) or nurses (77% chose that answer).
As for hours worked, 31% of residents reported they spend more than 60 hours/week seeing patients.
The top-paying specialties, averaging $69,500, were allergy and immunology, hematology, plastic surgery, aesthetic medicine, rheumatology, and specialized surgery. The lowest paid were family medicine residents at $58,500.
In primary care, overall, most residents said they planned to specialize. Only 47% planned to continue to work in primary care. Male residents were much more likely to say they will subspecialize than were their female colleagues (52% vs. 35%).
More than 90% of residents say future pay has influenced their choice of specialty, though more men than women felt that way (93% vs. 86%).
Good relationships with others
Overall, residents reported good relationships with attending physicians and nurses.
Most (88%) said they had good or very good relationships with attending physicians, 10% said the relationships were fair, and 2% said they were poor.
In addition, 89% of residents said the amount of supervision was appropriate, 4% said there was too much, and 7% said there was too little.
Relationships with nurses/PAs were slightly less positive overall: Eighty-two percent reported good or very good relationships with nurses/PAs, 15% said those relationships were fair, and 3% said they were poor.
One respondent said: “Our relationships could be better, but I think everyone is just overwhelmed with COVID-19, so emotions are heightened.”
Another said: “It takes time to earn the respect from nurses.”
Seventy-seven percent said they were satisfied with their learning experience overall, 12% were neutral on the question, and 11% said they were dissatisfied or very dissatisfied.
Work-life balance is the top concern
Work-life balance continues to be the top concern for residents. More than one-quarter (27%) in residency years 1 through 4 listed that as the top concern, and even more (32%) of those in years 5 through 8 agreed.
That was followed by demands on time and fear of failure or making a serious mistake.
The survey indicates that benefit packages for residents have stayed much the same over the past 2 years with health insurance and paid time off for sick leave, vacation, and personal time most commonly reported at 89% and 87%, respectively.
Much less common were benefits including commuter assistance (parking, public transportation) at 24%, housing allowance (8%), and child care (4%).
The vast majority of residents reported doing scut work (unskilled tasks): More than half (54%) reported doing 1-10 hours/week and 22% did 11-20 hours/week. Regardless of the number of hours, however, 62% said the time spent performing these tasks was appropriate.
A version of this article originally appeared on Medscape.com.
Financial planning in the COVID-19 era
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
FDA authorizes new saliva COVID-19 test
The FDA authorized a new type of saliva-based coronavirus test on August 15 that could cut down on the cost of testing and the time it takes to process results.
The emergency use authorization is for SalivaDirect, a diagnostic test created by the Yale School of Public Health. The test doesn’t require a special type of swab or collection tube — saliva can be collected in any sterile container, according to the FDA announcement.
The new test is “yet another testing innovation game changer that will reduce the demand for scarce testing resources,” Admiral Brett Giroir, MD, the assistant secretary for health and the COVID-19 testing coordinator, said in the statement.
The test also doesn’t require a special type of extractor, which is helpful because the extraction kits used to process other tests have faced shortages during the pandemic. The test can be used with different types of reagents and instruments already found in labs.
“Providing this type of flexibility for processing saliva samples to test for COVID-19 infection is groundbreaking in terms of efficiency and avoiding shortages of crucial test components like reagents,” Stephen Hahn, MD, the FDA commissioner, also said in the statement.
Yale will provide the instructions to labs as an “open source” protocol. The test doesn’t require any proprietary equipment or testing components, so labs across the country can assemble and use it based on the FDA guidelines. The testing method is available immediately and could be scaled up quickly in the next few weeks, according to a statement from Yale.
“This is a huge step forward to make testing more accessible,” Chantal Vogels, a postdoctoral fellow at Yale who led the lab development and test validation efforts, said in the statement.
The Yale team is further testing whether the saliva method can be used to find coronavirus cases among people who don’t have any symptoms and has been working with players and staff from the NBA. So far, the results have been accurate and similar to the nasal swabs for COVID-19, according to a preprint study published on medRxiv.
The research team wanted to get rid of the expensive collection tubes that other companies use to preserve the virus during processing, according to the Yale statement. They found that the virus is stable in saliva for long periods of time at warm temperatures and that special tubes aren’t necessary.
The FDA has authorized other saliva-based tests, according to ABC News, but SalivaDirect is the first that doesn’t require the extraction process used to test viral genetic material. Instead, the Yale process breaks down the saliva with an enzyme and applied heat. This type of testing could cost about $10, the Yale researchers said, and people can collect the saliva themselves under supervision.
“This, I hope, is a turning point,” Anne Wyllie, PhD, one of the lead researchers at Yale, told the news station.* “Expand testing capacity, inspire creativity and we can take competition to those labs charging a lot and bring prices down.”
This article first appeared on WebMD.com.
Correction, 8/25/20: An earlier version of this article misstated Dr. Wylie's academic degree.
The FDA authorized a new type of saliva-based coronavirus test on August 15 that could cut down on the cost of testing and the time it takes to process results.
The emergency use authorization is for SalivaDirect, a diagnostic test created by the Yale School of Public Health. The test doesn’t require a special type of swab or collection tube — saliva can be collected in any sterile container, according to the FDA announcement.
The new test is “yet another testing innovation game changer that will reduce the demand for scarce testing resources,” Admiral Brett Giroir, MD, the assistant secretary for health and the COVID-19 testing coordinator, said in the statement.
The test also doesn’t require a special type of extractor, which is helpful because the extraction kits used to process other tests have faced shortages during the pandemic. The test can be used with different types of reagents and instruments already found in labs.
“Providing this type of flexibility for processing saliva samples to test for COVID-19 infection is groundbreaking in terms of efficiency and avoiding shortages of crucial test components like reagents,” Stephen Hahn, MD, the FDA commissioner, also said in the statement.
Yale will provide the instructions to labs as an “open source” protocol. The test doesn’t require any proprietary equipment or testing components, so labs across the country can assemble and use it based on the FDA guidelines. The testing method is available immediately and could be scaled up quickly in the next few weeks, according to a statement from Yale.
“This is a huge step forward to make testing more accessible,” Chantal Vogels, a postdoctoral fellow at Yale who led the lab development and test validation efforts, said in the statement.
The Yale team is further testing whether the saliva method can be used to find coronavirus cases among people who don’t have any symptoms and has been working with players and staff from the NBA. So far, the results have been accurate and similar to the nasal swabs for COVID-19, according to a preprint study published on medRxiv.
The research team wanted to get rid of the expensive collection tubes that other companies use to preserve the virus during processing, according to the Yale statement. They found that the virus is stable in saliva for long periods of time at warm temperatures and that special tubes aren’t necessary.
The FDA has authorized other saliva-based tests, according to ABC News, but SalivaDirect is the first that doesn’t require the extraction process used to test viral genetic material. Instead, the Yale process breaks down the saliva with an enzyme and applied heat. This type of testing could cost about $10, the Yale researchers said, and people can collect the saliva themselves under supervision.
“This, I hope, is a turning point,” Anne Wyllie, PhD, one of the lead researchers at Yale, told the news station.* “Expand testing capacity, inspire creativity and we can take competition to those labs charging a lot and bring prices down.”
This article first appeared on WebMD.com.
Correction, 8/25/20: An earlier version of this article misstated Dr. Wylie's academic degree.
The FDA authorized a new type of saliva-based coronavirus test on August 15 that could cut down on the cost of testing and the time it takes to process results.
The emergency use authorization is for SalivaDirect, a diagnostic test created by the Yale School of Public Health. The test doesn’t require a special type of swab or collection tube — saliva can be collected in any sterile container, according to the FDA announcement.
The new test is “yet another testing innovation game changer that will reduce the demand for scarce testing resources,” Admiral Brett Giroir, MD, the assistant secretary for health and the COVID-19 testing coordinator, said in the statement.
The test also doesn’t require a special type of extractor, which is helpful because the extraction kits used to process other tests have faced shortages during the pandemic. The test can be used with different types of reagents and instruments already found in labs.
“Providing this type of flexibility for processing saliva samples to test for COVID-19 infection is groundbreaking in terms of efficiency and avoiding shortages of crucial test components like reagents,” Stephen Hahn, MD, the FDA commissioner, also said in the statement.
Yale will provide the instructions to labs as an “open source” protocol. The test doesn’t require any proprietary equipment or testing components, so labs across the country can assemble and use it based on the FDA guidelines. The testing method is available immediately and could be scaled up quickly in the next few weeks, according to a statement from Yale.
“This is a huge step forward to make testing more accessible,” Chantal Vogels, a postdoctoral fellow at Yale who led the lab development and test validation efforts, said in the statement.
The Yale team is further testing whether the saliva method can be used to find coronavirus cases among people who don’t have any symptoms and has been working with players and staff from the NBA. So far, the results have been accurate and similar to the nasal swabs for COVID-19, according to a preprint study published on medRxiv.
The research team wanted to get rid of the expensive collection tubes that other companies use to preserve the virus during processing, according to the Yale statement. They found that the virus is stable in saliva for long periods of time at warm temperatures and that special tubes aren’t necessary.
The FDA has authorized other saliva-based tests, according to ABC News, but SalivaDirect is the first that doesn’t require the extraction process used to test viral genetic material. Instead, the Yale process breaks down the saliva with an enzyme and applied heat. This type of testing could cost about $10, the Yale researchers said, and people can collect the saliva themselves under supervision.
“This, I hope, is a turning point,” Anne Wyllie, PhD, one of the lead researchers at Yale, told the news station.* “Expand testing capacity, inspire creativity and we can take competition to those labs charging a lot and bring prices down.”
This article first appeared on WebMD.com.
Correction, 8/25/20: An earlier version of this article misstated Dr. Wylie's academic degree.








