User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
COVID-19 virus reinfections rare; riskiest after age 65
When researchers analyzed test results of 4 million people in Denmark, they found that less than 1% of those who tested positive experienced reinfection.
Initial infection was associated with about 80% protection overall against getting SARS-CoV-2 again. However, among those older than 65, the protection plummeted to 47%.
“Not everybody is protected against reinfection after a first infection. Older people are at higher risk of catching it again,” co–lead author Daniela Michlmayr, PhD, said in an interview. “Our findings emphasize the importance of policies to protect the elderly and of adhering to infection control measures and restrictions, even if previously infected with COVID-19.”
Verifying the need for vaccination
“The findings also highlight the need to vaccinate people who had COVID-19 before, as natural immunity to infection – especially among the elderly 65 and older – cannot be relied upon,” added Dr. Michlmayr, a researcher in the department of bacteria, parasites, and fungi at the Staten Serums Institut, Copenhagen.
The population-based observational study was published online March 17 in The Lancet.
“The findings make sense, as patients who are immunocompromised or of advanced age may not mount an immune response that is as long-lasting,” David Hirschwerk, MD, said in an interview. “It does underscore the importance of vaccination for people of more advanced age, even if they previously were infected with COVID.
“For those who were infected last spring and have not yet been vaccinated, this helps to support the value of still pursuing the vaccine,” added Dr. Hirschwerk, an infectious disease specialist at Northwell Health in Manhasset, N.Y.
Evidence on reinfection risk was limited prior to this study. “Little is known about protection against SARS-CoV-2 repeat infections, but two studies in the UK have found that immunity could last at least 5 to 6 months after infection,” the authors noted.
Along with co–lead author Christian Holm Hansen, PhD, Dr. Michlmayr and colleagues found that 2.11% of 525,339 individuals tested positive for SARS-CoV-2 during the first surge in Denmark from March to May 2020. Within this group, 0.65% tested positive during a second surge from September to December.
By the end of 2020, more than 10 million people had undergone free polymerase chain reaction testing by the Danish government or through the national TestDenmark program.
“My overall take is that it is great to have such a big dataset looking at this question,” E. John Wherry, PhD, said in an interview. The findings support “what we’ve seen in previous, smaller studies.”
Natural protection against reinfection of approximately 80% “is not as good as the vaccines, but not bad,” added Dr. Wherry, director of the Institute for Immunology at the University of Pennsylvania, Philadelphia.
Age alters immunity?
“Our finding that older people were more likely than younger people to test positive again if they had already tested positive could be explained by natural age-related changes in the immune system of older adults, also referred to as immune senescence,” the authors noted.
The investigators found no significant differences in reinfection rates between women and men.
As with the previous research, this study also indicates that an initial bout with SARS-CoV-2 infection appears to confer protection for at least 6 months. The researchers found no significant differences between people who were followed for 3-6 months and those followed for 7 months or longer.
Variants not included
To account for possible bias among people who got tested repeatedly, Dr. Michlmayr and colleagues performed a sensitivity analysis in a subgroup. They assessed reinfection rates among people who underwent testing frequently and routinely – nurses, doctors, social workers, and health care assistants – and found that 1.2% tested positive a second time during the second surge.
A limitation of the study was the inability to correlate symptoms with risk for reinfection. Also, the researchers did not account for SARS-CoV-2 variants, noting that “during the study period, such variants were not yet established in Denmark; although into 2021 this pattern is changing.”
Asked to speculate whether the results would be different had the study accounted for variants, Dr. Hirschwerk said, “It depends upon the variant, but certainly for the B.1.351 variant, there already has been data clearly demonstrating risk of reinfection with SARS-CoV-2 despite prior infection with the original strain of virus.”
The emergence of SARS-CoV-2 variants of concern that could escape natural and vaccine-related immunity “complicates matters further,” Rosemary J. Boyton, MBBS, and Daniel M. Altmann, PhD, both of Imperial College London, wrote in an accompanying comment in The Lancet.
“Emerging variants of concern might shift immunity below a protective margin, prompting the need for updated vaccines. Interestingly, vaccine responses even after single dose are substantially enhanced in individuals with a history of infection with SARS-CoV-2,” they added.
The current study confirms that “the hope of protective immunity through natural infections might not be within our reach, and a global vaccination program with high efficacy vaccines is the enduring solution,” Dr. Boyton and Dr. Altmann noted.
Cause for alarm?
Despite evidence that reinfection is relatively rare, “many will find the data reported by Hansen and colleagues about protection through natural infection relatively alarming,” Dr. Boyton and Dr. Altmann wrote in their commentary. The 80% protection rate from reinfection in general and the 47% rate among people aged 65 and older “are more concerning figures than offered by previous studies.”
Vaccines appear to provide better quality, quantity, and durability of protection against repeated infection – measured in terms of neutralizing antibodies and T cells – compared with previous infection with SARS-CoV-2, Dr. Boyton and Dr. Altmann wrote.
More research needed
The duration of natural protection against reinfection remains an unanswered question, the researchers noted, “because too little time has elapsed since the beginning of the pandemic.”
Future prospective and longitudinal cohort studies coupled with molecular surveillance are needed to characterize antibody titers and waning of protection against repeat infections, the authors noted. Furthermore, more answers are needed regarding how some virus variants might contribute to reinfection risk.
No funding for the study has been reported. Dr. Michlmayr, Dr. Hirschwerk, Dr. Wherry, Dr. Boyton, and Dr. Altmann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When researchers analyzed test results of 4 million people in Denmark, they found that less than 1% of those who tested positive experienced reinfection.
Initial infection was associated with about 80% protection overall against getting SARS-CoV-2 again. However, among those older than 65, the protection plummeted to 47%.
“Not everybody is protected against reinfection after a first infection. Older people are at higher risk of catching it again,” co–lead author Daniela Michlmayr, PhD, said in an interview. “Our findings emphasize the importance of policies to protect the elderly and of adhering to infection control measures and restrictions, even if previously infected with COVID-19.”
Verifying the need for vaccination
“The findings also highlight the need to vaccinate people who had COVID-19 before, as natural immunity to infection – especially among the elderly 65 and older – cannot be relied upon,” added Dr. Michlmayr, a researcher in the department of bacteria, parasites, and fungi at the Staten Serums Institut, Copenhagen.
The population-based observational study was published online March 17 in The Lancet.
“The findings make sense, as patients who are immunocompromised or of advanced age may not mount an immune response that is as long-lasting,” David Hirschwerk, MD, said in an interview. “It does underscore the importance of vaccination for people of more advanced age, even if they previously were infected with COVID.
“For those who were infected last spring and have not yet been vaccinated, this helps to support the value of still pursuing the vaccine,” added Dr. Hirschwerk, an infectious disease specialist at Northwell Health in Manhasset, N.Y.
Evidence on reinfection risk was limited prior to this study. “Little is known about protection against SARS-CoV-2 repeat infections, but two studies in the UK have found that immunity could last at least 5 to 6 months after infection,” the authors noted.
Along with co–lead author Christian Holm Hansen, PhD, Dr. Michlmayr and colleagues found that 2.11% of 525,339 individuals tested positive for SARS-CoV-2 during the first surge in Denmark from March to May 2020. Within this group, 0.65% tested positive during a second surge from September to December.
By the end of 2020, more than 10 million people had undergone free polymerase chain reaction testing by the Danish government or through the national TestDenmark program.
“My overall take is that it is great to have such a big dataset looking at this question,” E. John Wherry, PhD, said in an interview. The findings support “what we’ve seen in previous, smaller studies.”
Natural protection against reinfection of approximately 80% “is not as good as the vaccines, but not bad,” added Dr. Wherry, director of the Institute for Immunology at the University of Pennsylvania, Philadelphia.
Age alters immunity?
“Our finding that older people were more likely than younger people to test positive again if they had already tested positive could be explained by natural age-related changes in the immune system of older adults, also referred to as immune senescence,” the authors noted.
The investigators found no significant differences in reinfection rates between women and men.
As with the previous research, this study also indicates that an initial bout with SARS-CoV-2 infection appears to confer protection for at least 6 months. The researchers found no significant differences between people who were followed for 3-6 months and those followed for 7 months or longer.
Variants not included
To account for possible bias among people who got tested repeatedly, Dr. Michlmayr and colleagues performed a sensitivity analysis in a subgroup. They assessed reinfection rates among people who underwent testing frequently and routinely – nurses, doctors, social workers, and health care assistants – and found that 1.2% tested positive a second time during the second surge.
A limitation of the study was the inability to correlate symptoms with risk for reinfection. Also, the researchers did not account for SARS-CoV-2 variants, noting that “during the study period, such variants were not yet established in Denmark; although into 2021 this pattern is changing.”
Asked to speculate whether the results would be different had the study accounted for variants, Dr. Hirschwerk said, “It depends upon the variant, but certainly for the B.1.351 variant, there already has been data clearly demonstrating risk of reinfection with SARS-CoV-2 despite prior infection with the original strain of virus.”
The emergence of SARS-CoV-2 variants of concern that could escape natural and vaccine-related immunity “complicates matters further,” Rosemary J. Boyton, MBBS, and Daniel M. Altmann, PhD, both of Imperial College London, wrote in an accompanying comment in The Lancet.
“Emerging variants of concern might shift immunity below a protective margin, prompting the need for updated vaccines. Interestingly, vaccine responses even after single dose are substantially enhanced in individuals with a history of infection with SARS-CoV-2,” they added.
The current study confirms that “the hope of protective immunity through natural infections might not be within our reach, and a global vaccination program with high efficacy vaccines is the enduring solution,” Dr. Boyton and Dr. Altmann noted.
Cause for alarm?
Despite evidence that reinfection is relatively rare, “many will find the data reported by Hansen and colleagues about protection through natural infection relatively alarming,” Dr. Boyton and Dr. Altmann wrote in their commentary. The 80% protection rate from reinfection in general and the 47% rate among people aged 65 and older “are more concerning figures than offered by previous studies.”
Vaccines appear to provide better quality, quantity, and durability of protection against repeated infection – measured in terms of neutralizing antibodies and T cells – compared with previous infection with SARS-CoV-2, Dr. Boyton and Dr. Altmann wrote.
More research needed
The duration of natural protection against reinfection remains an unanswered question, the researchers noted, “because too little time has elapsed since the beginning of the pandemic.”
Future prospective and longitudinal cohort studies coupled with molecular surveillance are needed to characterize antibody titers and waning of protection against repeat infections, the authors noted. Furthermore, more answers are needed regarding how some virus variants might contribute to reinfection risk.
No funding for the study has been reported. Dr. Michlmayr, Dr. Hirschwerk, Dr. Wherry, Dr. Boyton, and Dr. Altmann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When researchers analyzed test results of 4 million people in Denmark, they found that less than 1% of those who tested positive experienced reinfection.
Initial infection was associated with about 80% protection overall against getting SARS-CoV-2 again. However, among those older than 65, the protection plummeted to 47%.
“Not everybody is protected against reinfection after a first infection. Older people are at higher risk of catching it again,” co–lead author Daniela Michlmayr, PhD, said in an interview. “Our findings emphasize the importance of policies to protect the elderly and of adhering to infection control measures and restrictions, even if previously infected with COVID-19.”
Verifying the need for vaccination
“The findings also highlight the need to vaccinate people who had COVID-19 before, as natural immunity to infection – especially among the elderly 65 and older – cannot be relied upon,” added Dr. Michlmayr, a researcher in the department of bacteria, parasites, and fungi at the Staten Serums Institut, Copenhagen.
The population-based observational study was published online March 17 in The Lancet.
“The findings make sense, as patients who are immunocompromised or of advanced age may not mount an immune response that is as long-lasting,” David Hirschwerk, MD, said in an interview. “It does underscore the importance of vaccination for people of more advanced age, even if they previously were infected with COVID.
“For those who were infected last spring and have not yet been vaccinated, this helps to support the value of still pursuing the vaccine,” added Dr. Hirschwerk, an infectious disease specialist at Northwell Health in Manhasset, N.Y.
Evidence on reinfection risk was limited prior to this study. “Little is known about protection against SARS-CoV-2 repeat infections, but two studies in the UK have found that immunity could last at least 5 to 6 months after infection,” the authors noted.
Along with co–lead author Christian Holm Hansen, PhD, Dr. Michlmayr and colleagues found that 2.11% of 525,339 individuals tested positive for SARS-CoV-2 during the first surge in Denmark from March to May 2020. Within this group, 0.65% tested positive during a second surge from September to December.
By the end of 2020, more than 10 million people had undergone free polymerase chain reaction testing by the Danish government or through the national TestDenmark program.
“My overall take is that it is great to have such a big dataset looking at this question,” E. John Wherry, PhD, said in an interview. The findings support “what we’ve seen in previous, smaller studies.”
Natural protection against reinfection of approximately 80% “is not as good as the vaccines, but not bad,” added Dr. Wherry, director of the Institute for Immunology at the University of Pennsylvania, Philadelphia.
Age alters immunity?
“Our finding that older people were more likely than younger people to test positive again if they had already tested positive could be explained by natural age-related changes in the immune system of older adults, also referred to as immune senescence,” the authors noted.
The investigators found no significant differences in reinfection rates between women and men.
As with the previous research, this study also indicates that an initial bout with SARS-CoV-2 infection appears to confer protection for at least 6 months. The researchers found no significant differences between people who were followed for 3-6 months and those followed for 7 months or longer.
Variants not included
To account for possible bias among people who got tested repeatedly, Dr. Michlmayr and colleagues performed a sensitivity analysis in a subgroup. They assessed reinfection rates among people who underwent testing frequently and routinely – nurses, doctors, social workers, and health care assistants – and found that 1.2% tested positive a second time during the second surge.
A limitation of the study was the inability to correlate symptoms with risk for reinfection. Also, the researchers did not account for SARS-CoV-2 variants, noting that “during the study period, such variants were not yet established in Denmark; although into 2021 this pattern is changing.”
Asked to speculate whether the results would be different had the study accounted for variants, Dr. Hirschwerk said, “It depends upon the variant, but certainly for the B.1.351 variant, there already has been data clearly demonstrating risk of reinfection with SARS-CoV-2 despite prior infection with the original strain of virus.”
The emergence of SARS-CoV-2 variants of concern that could escape natural and vaccine-related immunity “complicates matters further,” Rosemary J. Boyton, MBBS, and Daniel M. Altmann, PhD, both of Imperial College London, wrote in an accompanying comment in The Lancet.
“Emerging variants of concern might shift immunity below a protective margin, prompting the need for updated vaccines. Interestingly, vaccine responses even after single dose are substantially enhanced in individuals with a history of infection with SARS-CoV-2,” they added.
The current study confirms that “the hope of protective immunity through natural infections might not be within our reach, and a global vaccination program with high efficacy vaccines is the enduring solution,” Dr. Boyton and Dr. Altmann noted.
Cause for alarm?
Despite evidence that reinfection is relatively rare, “many will find the data reported by Hansen and colleagues about protection through natural infection relatively alarming,” Dr. Boyton and Dr. Altmann wrote in their commentary. The 80% protection rate from reinfection in general and the 47% rate among people aged 65 and older “are more concerning figures than offered by previous studies.”
Vaccines appear to provide better quality, quantity, and durability of protection against repeated infection – measured in terms of neutralizing antibodies and T cells – compared with previous infection with SARS-CoV-2, Dr. Boyton and Dr. Altmann wrote.
More research needed
The duration of natural protection against reinfection remains an unanswered question, the researchers noted, “because too little time has elapsed since the beginning of the pandemic.”
Future prospective and longitudinal cohort studies coupled with molecular surveillance are needed to characterize antibody titers and waning of protection against repeat infections, the authors noted. Furthermore, more answers are needed regarding how some virus variants might contribute to reinfection risk.
No funding for the study has been reported. Dr. Michlmayr, Dr. Hirschwerk, Dr. Wherry, Dr. Boyton, and Dr. Altmann have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for OUD may also mitigate risk with concomitant benzo, Z-drug use
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Colchicine before PCI for acute MI fails to improve major outcomes
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
In a placebo-controlled randomized trial, a preprocedural dose of colchicine administered immediately before percutaneous coronary intervention (PCI) for an acute ST-segment elevated myocardial infarction (STEMI) did not reduce the no-reflow phenomenon or improve outcomes.
No-reflow, in which insufficient myocardial perfusion is present even though the coronary artery appears patent, was the primary outcome, and the proportion of patients experiencing this event was exactly the same (14.4%) in the colchicine and placebo groups, reported Yaser Jenab, MD, at CRT 2021 sponsored by MedStar Heart & Vascular Institute.
The hypothesis that colchicine would offer benefit in this setting was largely based on the Colchicine Cardiovascular Outcomes Trial (COLCOT). In that study, colchicine was associated with a 23% reduction in risk for major adverse cardiovascular events (MACE) relative to placebo when administered within 30 days after a myocardial infarction (hazard ratio, 0.77; P = .02).
The benefit in that trial was attributed to an anti-inflammatory effect, according to Dr. Jenab, associate professor of cardiology at Tehran (Iran) Heart Center. In particular as it relates to vascular disease, he cited experimental studies associating colchicine with a reduction in neutrophil activation and adherence to vascular endothelium.
The rationale for a preprocedural approach to colchicine was supplied by a subsequent time-to-treatment COLCOT analysis. In this study, MACE risk reduction for colchicine climbed to 48% (HR 0.52) for those treated within 3 days of the MI but largely disappeared (HR 0.96) if treatment was started at least 8 days post MI.
PodCAST-PCI trial
In the preprocedural study, called the PodCAST-PCI trial, 321 acute STEMI patients were randomized. Patients received a 1-mg dose of oral colchicine or placebo at the time PCI was scheduled. Another dose of colchicine (0.5 mg) or placebo was administered 1 hour after the procedure.
Of secondary outcomes, which included MACE at 1 month and 1 year, ST-segment resolution at 1 month, and change in inflammatory markers at 1 month, none were significant. Few even trended for significance.
For MACE, which included cardiac death, stroke, nonfatal MI, new hospitalization due to heart failure, or target vessel revascularization, the rates were lower in the colchicine group at 1 month (4.3% vs. 7.5%) and 1 year (9.3% vs. 11.2%), but neither approached significance.
For ST-segment resolution, the proportions were generally comparable among the colchicine and placebo groups, respectively, for the proportion below 50% (18.6% vs. 23.1%), between 50% and 70% (16.8% vs. 15.6%), and above 70% (64.6% vs. 61.3%).
The average troponin levels were nonsignificantly lower at 6 hours (1,847 vs. 2,883 ng/mL) in the colchicine group but higher at 48 hours (1,197 vs. 1,147 ng/mL). The average C-reactive protein (CRP) levels at 48 hours were nonsignificantly lower on colchicine (176.5 vs. 244.5 mg/L).
There were no significant differences in postprocedural perfusion, as measured with TIMI blood flow, or in the rate of stent thrombosis, which occurred in roughly 3% of each group of patients.
The small sample size was one limitation of this study, Dr. Jenab acknowledged. For this and other reasons, he cautioned that these data are not definitive and do not preclude a benefit on clinical outcomes in a study with a larger size, a different design, or different dosing.
Timing might be the issue
However, even if colchicine has a potential benefit in this setting, timing might be a major obstacle, according to Binata Shah, MD, associate director of research for the Cardiac Catheterization Laboratory at New York University.
“We have learned from our rheumatology colleagues that peak plasma levels of colchicine are not achieved for at least 1 hour after the full loading dose,” Dr. Shah said. “With us moving so quickly in a primary PCI setting, it is hard to imagine that colchicine would have had time to really kick in and exert its anti-inflammatory effect.”
Indeed, the problem might be worse than reaching the peak plasma level.
“Even though peak plasma levels occur as early as 1 hour after a full loading dose, we see that it takes about 24 hours to really see the effects translate downstream into more systemic inflammatory markers such as CRP and interleukin-6,” she added. If lowering these signals of inflammation is predictive of benefit, than this might be the biggest obstacle to benefit from colchicine in an urgent treatment setting.
Dr. Jenab and Dr. Shah reported no potential conflicts of interest.
FROM CRT 2021
We’re all vaccinated: Can we go back to the office (unmasked) now?
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
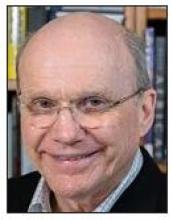
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Congratulations, you’ve been vaccinated!
It’s been a year like no other, and outpatient psychiatrists turned to Zoom and other telemental health platforms to provide treatment for our patients. Offices sit empty as the dust lands and the plants wilt. Perhaps a few patients are seen in person, masked and carefully distanced, after health screening and temperature checks, with surfaces sanitized between visits, all in accordance with health department regulations. But now the vaccine offers both safety and the promise of a return to a new normal, one that is certain to look different from the normal that was left behind.
I have been vaccinated and many of my patients have also been vaccinated. I began to wonder if it was safe to start seeing patients in person; could I see fully vaccinated patients, unmasked and without temperature checks and sanitizing? I started asking this question in February, and the response I got then was that it was too soon to tell; we did not have any data on whether vaccinated people could transmit the novel coronavirus. Two vaccinated people might be at risk of transmitting the virus and then infecting others, and the question of whether the vaccines would protect against illness caused by variants remained. Preliminary data out of Israel indicated that the vaccine did reduce transmission, but no one was saying that it was fine to see patients without masks, and video-conferencing remained the safest option.
On Monday, March 8, 2021, the Centers for Disease Control and Prevention released long-awaited interim public health guidelines for fully vaccinated people. The guidelines allowed for two vaccinated people to be in a room together unmasked, and for a fully-vaccinated person to be in a room unmasked with an unvaccinated person who did not have risk factors for becoming severely ill with COVID. Was this the green light that psychiatrists were waiting for? Was there new data about transmission, or was this part of the CDC’s effort to make vaccines more desirable?
Michael Chang, MD, is a pediatric infectious disease specialist at the University of Texas Health Science Center at Houston. We spoke 2 days after the CDC interim guidelines were released. Dr. Chang was optimistic.
“, including data about variants and about transmission. At some point, however, the risk is low enough, and we should probably start thinking about going back to in-person visits,” Dr. Chang said. He said he personally would feel safe meeting unmasked with a vaccinated patient, but noted that his institution still requires doctors to wear masks. “Most vaccinations reduce transmission of illness,” Dr. Chang said, “but SARS-CoV-2 continues to surprise us in many ways.”
Katelyn Jetelina, PhD, MPH, an epidemiologist at the University of Texas School of Public Health in Dallas, distributes a newsletter, “Your Local Epidemiologist,” where she discusses data pertaining to the pandemic. In her newsletter dated March 14, 2021, Dr. Jetelina wrote, “There are now 7 sub-studies/press releases that confirm a 50-95% reduced transmission after vaccination. This is a big range, which is typical for such drastically different scientific studies. Variability is likely due to different sample sizes, locations, vaccines, genetics, cultures, etc. It will be a while until we know the ‘true’ percentage for each vaccine.”
Leslie Walker, MD, is a fully vaccinated psychiatrist in private practice in Shaker Heights, Ohio. She has recently started seeing fully vaccinated patients in person.
“So far it’s only 1 or 2 patients a day. I’m leaving it up to the patient. If they prefer masks, we stay masked. I may reverse course, depending on what information comes out.” She went on to note, “There are benefits to being able to see someone’s full facial expressions and whether they match someone’s words and body language, so the benefit of “unmasking” extends beyond comfort and convenience and must be balanced against the theoretical risk of COVID exposure in the room.”
While the CDC has now said it is safe to meet, the state health departments also have guidelines for medical practices, and everyone is still worried about vulnerable people in their households and potential spread to the community at large.
In Maryland, where I work, Aliya Jones, MD, MBA, is the head of the Behavioral Health Administration (BHA) for the Maryland Department of Health. “It remains risky to not wear masks, however, the risk is low when both individuals are vaccinated,” Dr. Jones wrote. “BHA is not recommending that providers see clients without both parties wearing a mask. All of our general practice recommendations for infection control are unchanged. People should be screened before entering clinical practices and persons who are symptomatic, whether vaccinated or not, should not be seen face-to-face, except in cases of an emergency, in which case additional precautions should be taken.”
So is it safe for a fully-vaccinated psychiatrist to have a session with a fully-vaccinated patient sitting 8 feet apart without masks? I’m left with the idea that it is for those two people, but when it comes to unvaccinated people in their households, we want more certainty than we currently have. The messaging remains unclear. The CDC’s interim guidelines offer hope for a future, but the science is still catching up, and to feel safe enough, we may want to wait a little longer for more definitive data – or herd immunity – before we reveal our smiles.
Dr. Miller is a coauthor of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
Fauci worries about possible post–COVID-19 ‘mental health pandemic’
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
Anthony Fauci, MD, says he’s concerned about how Americans will react once the coronavirus pandemic is brought under control, CBS News reports.
Noting that an American Psychological Association survey showed people reporting high stress levels because of the pandemic, CBS’s Norah O’Donnell asked if Dr. Fauci was concerned about a possible “mental health pandemic.”
“Very much so,” Dr. Fauci, director of the National Institute of Allergy and Infectious Diseases and a top White House coronavirus adviser, replied.
“That’s the reason why I want to get the virological aspect of this pandemic behind us as quickly as we possibly can because the long-term ravages of this are so multifaceted,” Dr. Fauci said.
, he said.
“And then the other things: Not only the mental health effects, but many people have put off routine types of medical examinations that they normally would have done,” Dr. Fauci said.
“I hope we don’t see an increase in some preventable situations that would not have happened if people had the normal access to medical care, which clearly was interrupted by the shutdown associated with COVID-19,” he added.
The American Psychological Association released the survey results March 11 in what many people consider the 1-year anniversary of the start of the coronavirus pandemic.
“The prolonged stress experienced by adults, especially the high levels of stress reported by Americans directly linked to the pandemic, is seriously affecting mental and physical health, including changes to weight, sleep and alcohol use,” the APA said in a news release.
Some of the key findings of the survey include:
- 61% of respondents reported experiencing undesired weight changes since the start of the pandemic.
- 67% said their sleep habits changed, with 35% saying they slept more and 31% less.
- 23% reported drinking more alcohol to cope with stress.
- 47% said they delayed or canceled health care services because of the pandemic.
- 48% said their stress levels had increased.
A version of this article first appeared on Medscape.com.
‘Major update’ of BP guidance for kidney disease; treat to 120 mm Hg
The new 2021 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for blood pressure management for adults with chronic kidney disease (CKD) who are not receiving dialysis advises treating to a target systolic blood pressure of less than 120 mm Hg, provided measurements are “standardized” and that blood pressure is “measured properly.”
This blood pressure target – largely based on evidence from the Systolic Blood Pressure Intervention Trial (SPRINT) – represents “a major update” from the 2012 KDIGO guideline, which advised clinicians to treat to a target blood pressure of less than or equal to 130/80 mm Hg for patients with albuminuria or less than or equal to 140/90 mm Hg for patients without albuminuria.
The new goal is also lower than the less than 130/80 mm Hg target in the 2017 American College of Cardiology/American Heart Association guideline.
In a study of the public health implications of the guideline, Kathryn Foti, PhD, and colleagues determined that 70% of U.S. adults with CKD would now be eligible for treatment to lower blood pressure, as opposed to 50% under the previous KDIGO guideline and 56% under the ACC/AHA guideline.
“This is a major update of an influential set of guidelines for chronic kidney disease patients” at a time when blood pressure control is worsening in the United States, Dr. Foti, a postdoctoral researcher in the department of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in a statement from her institution.
The 2021 KDIGO blood pressure guideline and executive summary and the public health implications study are published online in Kidney International.
First, ‘take blood pressure well’
The cochair of the new KDIGO guidelines, Alfred K. Cheung, MD, from the University of Utah, Salt Lake City, said in an interview that the guideline has “two important points.”
First, “take that blood pressure well,” he said. “That has a lot to do with patient preparation rather than any fancy instrument,” he emphasized.
Second, the guideline proposes a systolic blood pressure target of less than 120 mm Hg for most people with CKD not receiving dialysis, except for children and kidney transplant recipients. This target is “contingent on ‘standardized’ blood pressure measurement.”
The document provides a checklist for obtaining a standardized blood pressure measurement, adapted from the 2017 ACC/AHA blood pressure guidelines. It starts with the patient relaxed and sitting on a chair for more than 5 minutes.
In contrast to this measurement, a “routine” or “casual” office blood pressure measurement could be off by plus or minus 10 mm Hg, Dr. Cheung noted.
In a typical scenario, he continued, a patient cannot find a place to park, rushes into the clinic, and has his or her blood pressure checked right away, which would provide a “totally unreliable” reading. Adding a “fudge factor” (correction factor) would not provide an accurate reading.
Clinicians “would not settle for a potassium measurement that is 5.0 mmol/L plus or minus a few decimal points” to guide treatment, he pointed out.
Second, target 120, properly measured
“The very first chapter of the guidelines is devoted to blood pressure measurement, because we recognize if we’re going to do 120 [mm Hg] – the emphasis is on 120 measured properly – so we try to drive that point home,” Tara I. Chang, MD, guideline second author and a coauthor of the public health implications study, pointed out in an interview.
“There are a lot of other things that we base clinical decisions on where we really require some degree of precision, and blood pressure is important enough that to us it’s kind of in the same boat,” said Dr. Chang, from Stanford (Calif.) University.
“In SPRINT, people were randomized to less than less than 120 vs. less than 140 (they weren’t randomized to <130),” she noted.
“The recommendation should be widely adopted in clinical practice,” the guideline authors write, “since accurate measurements will ensure that proper guidance is being applied to the management of BP, as it is to the management of other risk factors.”
Still need individual treatment
Nevertheless, patients still need individualized treatment, the document stresses. “Not every patient with CKD will be appropriate to target to less than 120,” Dr. Chang said. However, “we want people to at least consider less than 120,” she added, to avoid therapeutic inertia.
“If you take the blood pressure in a standardized manner – such as in the ACCORD trial and in the SPRINT trial – even patients over 75 years old, or people over 80 years old, they have very little side effects,” Dr. Cheung noted.
“In the overall cohort,” he continued, “they do not have a significant increase in serious adverse events, do not have adverse events of postural hypotension, syncope, bradycardia, injurious falls – so people are worried about it, but it’s not borne out by the data.
“That said, I have two cautions,” Dr. Cheung noted. “One. If you drop somebody’s blood pressure rapidly over a week, you may be more likely to get in trouble. If you drop the blood pressure gradually over several weeks, several months, you’re much less likely to get into trouble.”
“Two. If the patient is old, you know the patient has carotid stenosis and already has postural dizziness, you may not want to try on that patient – but just because the patient is old is not the reason not to target 120.”
ACE inhibitors and ARBs beneficial in albuminuria, underused
“How do you get to less than 120? The short answer is, use whatever medications you need to – there is no necessarily right cocktail,” Dr. Chang said.
“We’ve known that angiotensin-converting enzyme (ACE) inhibitors and ARBs [angiotensin II receptor blockers] are beneficial in patients with CKD and in particular those with heavier albuminuria,” she continued. “We’ve known this for over 20 years.”
Yet, the study identified underutilization – “a persistent gap, just like blood pressure control and awareness,” she noted. “We’re just not making much headway.
“We are not recommending ACE inhibitors or ARBs for all the patients,” Dr. Cheung clarified. “If you are diabetic and have heavy proteinuria, that’s when the use of ACE inhibitors and ARBs are most indicated.”
Public health implications
SPRINT showed that treating to a systolic blood pressure of less than 120 mm Hg vs. less than 140 mm Hg reduced the risk for cardiovascular disease by 25% and all-cause mortality by 27% for participants with and those without CKD, Dr. Foti and colleagues stress.
They aimed to estimate how the new guideline would affect (1) the number of U.S. patients with CKD who would be eligible for blood pressure lowering treatment, and (2) the proportion of those with albuminuria who would be eligible for an ACE inhibitor or an ARB.
The researchers analyzed data from 1,699 adults with CKD (estimated glomerular filtration rate, 15-59 mL/min/1.73 m2 or a urinary albumin-to-creatinine ratio of ≥30 mg/g) who participated in the 2015-2018 National Health and Nutrition Examination Survey.
Both the 2021 and 2012 KDIGO guidelines recommend that patients with albuminuria and blood pressure higher than the target value who are not kidney transplant recipients should be treated with an ACE inhibitor or an ARB.
On the basis of the new target, 78% of patients with CKD and albuminuria were eligible for ACE inhibitor/ARB treatment by the 2021 KDIGO guideline, compared with 71% by the 2012 KDIGO guideline. However, only 39% were taking one of these drugs.
These findings show that “with the new guideline and with the lower blood pressure target, you potentially have an even larger pool of people who have blood pressure that’s not under control, and a potential larger group of people who may benefit from ACE inhibitors and ARBs,” Dr. Chang said.
“Our paper is not the only one to show that we haven’t made a whole lot of progress,” she said, “and now that the bar has been lowered, there [have] to be some renewed efforts on controlling blood pressure, because we know that blood pressure control is such an important risk factor for cardiovascular outcomes.”
Dr. Foti is supported by an NIH/National Heart, Lung, and Blood Institute grant. Dr. Cheung has received consultancy fees from Amgen, Bard, Boehringer Ingelheim, Calliditas, Tricida, and UpToDate, and grant/research support from the National Institutes of Health for SPRINT (monies paid to institution). Dr. Chang has received consultancy fees from Bayer, Gilead, Janssen Research and Development, Novo Nordisk, Tricida, and Vascular Dynamics; grant/research support from AstraZeneca and Satellite Healthcare (monies paid to institution), the NIH, and the American Heart Association; is on advisory boards for AstraZeneca and Fresenius Medical Care Renal Therapies Group; and has received workshop honoraria from Fresenius. Disclosures of relevant financial relationships of the other authors are listed in the original articles.
A version of this article first appeared on Medscape.com.
The new 2021 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for blood pressure management for adults with chronic kidney disease (CKD) who are not receiving dialysis advises treating to a target systolic blood pressure of less than 120 mm Hg, provided measurements are “standardized” and that blood pressure is “measured properly.”
This blood pressure target – largely based on evidence from the Systolic Blood Pressure Intervention Trial (SPRINT) – represents “a major update” from the 2012 KDIGO guideline, which advised clinicians to treat to a target blood pressure of less than or equal to 130/80 mm Hg for patients with albuminuria or less than or equal to 140/90 mm Hg for patients without albuminuria.
The new goal is also lower than the less than 130/80 mm Hg target in the 2017 American College of Cardiology/American Heart Association guideline.
In a study of the public health implications of the guideline, Kathryn Foti, PhD, and colleagues determined that 70% of U.S. adults with CKD would now be eligible for treatment to lower blood pressure, as opposed to 50% under the previous KDIGO guideline and 56% under the ACC/AHA guideline.
“This is a major update of an influential set of guidelines for chronic kidney disease patients” at a time when blood pressure control is worsening in the United States, Dr. Foti, a postdoctoral researcher in the department of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in a statement from her institution.
The 2021 KDIGO blood pressure guideline and executive summary and the public health implications study are published online in Kidney International.
First, ‘take blood pressure well’
The cochair of the new KDIGO guidelines, Alfred K. Cheung, MD, from the University of Utah, Salt Lake City, said in an interview that the guideline has “two important points.”
First, “take that blood pressure well,” he said. “That has a lot to do with patient preparation rather than any fancy instrument,” he emphasized.
Second, the guideline proposes a systolic blood pressure target of less than 120 mm Hg for most people with CKD not receiving dialysis, except for children and kidney transplant recipients. This target is “contingent on ‘standardized’ blood pressure measurement.”
The document provides a checklist for obtaining a standardized blood pressure measurement, adapted from the 2017 ACC/AHA blood pressure guidelines. It starts with the patient relaxed and sitting on a chair for more than 5 minutes.
In contrast to this measurement, a “routine” or “casual” office blood pressure measurement could be off by plus or minus 10 mm Hg, Dr. Cheung noted.
In a typical scenario, he continued, a patient cannot find a place to park, rushes into the clinic, and has his or her blood pressure checked right away, which would provide a “totally unreliable” reading. Adding a “fudge factor” (correction factor) would not provide an accurate reading.
Clinicians “would not settle for a potassium measurement that is 5.0 mmol/L plus or minus a few decimal points” to guide treatment, he pointed out.
Second, target 120, properly measured
“The very first chapter of the guidelines is devoted to blood pressure measurement, because we recognize if we’re going to do 120 [mm Hg] – the emphasis is on 120 measured properly – so we try to drive that point home,” Tara I. Chang, MD, guideline second author and a coauthor of the public health implications study, pointed out in an interview.
“There are a lot of other things that we base clinical decisions on where we really require some degree of precision, and blood pressure is important enough that to us it’s kind of in the same boat,” said Dr. Chang, from Stanford (Calif.) University.
“In SPRINT, people were randomized to less than less than 120 vs. less than 140 (they weren’t randomized to <130),” she noted.
“The recommendation should be widely adopted in clinical practice,” the guideline authors write, “since accurate measurements will ensure that proper guidance is being applied to the management of BP, as it is to the management of other risk factors.”
Still need individual treatment
Nevertheless, patients still need individualized treatment, the document stresses. “Not every patient with CKD will be appropriate to target to less than 120,” Dr. Chang said. However, “we want people to at least consider less than 120,” she added, to avoid therapeutic inertia.
“If you take the blood pressure in a standardized manner – such as in the ACCORD trial and in the SPRINT trial – even patients over 75 years old, or people over 80 years old, they have very little side effects,” Dr. Cheung noted.
“In the overall cohort,” he continued, “they do not have a significant increase in serious adverse events, do not have adverse events of postural hypotension, syncope, bradycardia, injurious falls – so people are worried about it, but it’s not borne out by the data.
“That said, I have two cautions,” Dr. Cheung noted. “One. If you drop somebody’s blood pressure rapidly over a week, you may be more likely to get in trouble. If you drop the blood pressure gradually over several weeks, several months, you’re much less likely to get into trouble.”
“Two. If the patient is old, you know the patient has carotid stenosis and already has postural dizziness, you may not want to try on that patient – but just because the patient is old is not the reason not to target 120.”
ACE inhibitors and ARBs beneficial in albuminuria, underused
“How do you get to less than 120? The short answer is, use whatever medications you need to – there is no necessarily right cocktail,” Dr. Chang said.
“We’ve known that angiotensin-converting enzyme (ACE) inhibitors and ARBs [angiotensin II receptor blockers] are beneficial in patients with CKD and in particular those with heavier albuminuria,” she continued. “We’ve known this for over 20 years.”
Yet, the study identified underutilization – “a persistent gap, just like blood pressure control and awareness,” she noted. “We’re just not making much headway.
“We are not recommending ACE inhibitors or ARBs for all the patients,” Dr. Cheung clarified. “If you are diabetic and have heavy proteinuria, that’s when the use of ACE inhibitors and ARBs are most indicated.”
Public health implications
SPRINT showed that treating to a systolic blood pressure of less than 120 mm Hg vs. less than 140 mm Hg reduced the risk for cardiovascular disease by 25% and all-cause mortality by 27% for participants with and those without CKD, Dr. Foti and colleagues stress.
They aimed to estimate how the new guideline would affect (1) the number of U.S. patients with CKD who would be eligible for blood pressure lowering treatment, and (2) the proportion of those with albuminuria who would be eligible for an ACE inhibitor or an ARB.
The researchers analyzed data from 1,699 adults with CKD (estimated glomerular filtration rate, 15-59 mL/min/1.73 m2 or a urinary albumin-to-creatinine ratio of ≥30 mg/g) who participated in the 2015-2018 National Health and Nutrition Examination Survey.
Both the 2021 and 2012 KDIGO guidelines recommend that patients with albuminuria and blood pressure higher than the target value who are not kidney transplant recipients should be treated with an ACE inhibitor or an ARB.
On the basis of the new target, 78% of patients with CKD and albuminuria were eligible for ACE inhibitor/ARB treatment by the 2021 KDIGO guideline, compared with 71% by the 2012 KDIGO guideline. However, only 39% were taking one of these drugs.
These findings show that “with the new guideline and with the lower blood pressure target, you potentially have an even larger pool of people who have blood pressure that’s not under control, and a potential larger group of people who may benefit from ACE inhibitors and ARBs,” Dr. Chang said.
“Our paper is not the only one to show that we haven’t made a whole lot of progress,” she said, “and now that the bar has been lowered, there [have] to be some renewed efforts on controlling blood pressure, because we know that blood pressure control is such an important risk factor for cardiovascular outcomes.”
Dr. Foti is supported by an NIH/National Heart, Lung, and Blood Institute grant. Dr. Cheung has received consultancy fees from Amgen, Bard, Boehringer Ingelheim, Calliditas, Tricida, and UpToDate, and grant/research support from the National Institutes of Health for SPRINT (monies paid to institution). Dr. Chang has received consultancy fees from Bayer, Gilead, Janssen Research and Development, Novo Nordisk, Tricida, and Vascular Dynamics; grant/research support from AstraZeneca and Satellite Healthcare (monies paid to institution), the NIH, and the American Heart Association; is on advisory boards for AstraZeneca and Fresenius Medical Care Renal Therapies Group; and has received workshop honoraria from Fresenius. Disclosures of relevant financial relationships of the other authors are listed in the original articles.
A version of this article first appeared on Medscape.com.
The new 2021 Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guideline for blood pressure management for adults with chronic kidney disease (CKD) who are not receiving dialysis advises treating to a target systolic blood pressure of less than 120 mm Hg, provided measurements are “standardized” and that blood pressure is “measured properly.”
This blood pressure target – largely based on evidence from the Systolic Blood Pressure Intervention Trial (SPRINT) – represents “a major update” from the 2012 KDIGO guideline, which advised clinicians to treat to a target blood pressure of less than or equal to 130/80 mm Hg for patients with albuminuria or less than or equal to 140/90 mm Hg for patients without albuminuria.
The new goal is also lower than the less than 130/80 mm Hg target in the 2017 American College of Cardiology/American Heart Association guideline.
In a study of the public health implications of the guideline, Kathryn Foti, PhD, and colleagues determined that 70% of U.S. adults with CKD would now be eligible for treatment to lower blood pressure, as opposed to 50% under the previous KDIGO guideline and 56% under the ACC/AHA guideline.
“This is a major update of an influential set of guidelines for chronic kidney disease patients” at a time when blood pressure control is worsening in the United States, Dr. Foti, a postdoctoral researcher in the department of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, said in a statement from her institution.
The 2021 KDIGO blood pressure guideline and executive summary and the public health implications study are published online in Kidney International.
First, ‘take blood pressure well’
The cochair of the new KDIGO guidelines, Alfred K. Cheung, MD, from the University of Utah, Salt Lake City, said in an interview that the guideline has “two important points.”
First, “take that blood pressure well,” he said. “That has a lot to do with patient preparation rather than any fancy instrument,” he emphasized.
Second, the guideline proposes a systolic blood pressure target of less than 120 mm Hg for most people with CKD not receiving dialysis, except for children and kidney transplant recipients. This target is “contingent on ‘standardized’ blood pressure measurement.”
The document provides a checklist for obtaining a standardized blood pressure measurement, adapted from the 2017 ACC/AHA blood pressure guidelines. It starts with the patient relaxed and sitting on a chair for more than 5 minutes.
In contrast to this measurement, a “routine” or “casual” office blood pressure measurement could be off by plus or minus 10 mm Hg, Dr. Cheung noted.
In a typical scenario, he continued, a patient cannot find a place to park, rushes into the clinic, and has his or her blood pressure checked right away, which would provide a “totally unreliable” reading. Adding a “fudge factor” (correction factor) would not provide an accurate reading.
Clinicians “would not settle for a potassium measurement that is 5.0 mmol/L plus or minus a few decimal points” to guide treatment, he pointed out.
Second, target 120, properly measured
“The very first chapter of the guidelines is devoted to blood pressure measurement, because we recognize if we’re going to do 120 [mm Hg] – the emphasis is on 120 measured properly – so we try to drive that point home,” Tara I. Chang, MD, guideline second author and a coauthor of the public health implications study, pointed out in an interview.
“There are a lot of other things that we base clinical decisions on where we really require some degree of precision, and blood pressure is important enough that to us it’s kind of in the same boat,” said Dr. Chang, from Stanford (Calif.) University.
“In SPRINT, people were randomized to less than less than 120 vs. less than 140 (they weren’t randomized to <130),” she noted.
“The recommendation should be widely adopted in clinical practice,” the guideline authors write, “since accurate measurements will ensure that proper guidance is being applied to the management of BP, as it is to the management of other risk factors.”
Still need individual treatment
Nevertheless, patients still need individualized treatment, the document stresses. “Not every patient with CKD will be appropriate to target to less than 120,” Dr. Chang said. However, “we want people to at least consider less than 120,” she added, to avoid therapeutic inertia.
“If you take the blood pressure in a standardized manner – such as in the ACCORD trial and in the SPRINT trial – even patients over 75 years old, or people over 80 years old, they have very little side effects,” Dr. Cheung noted.
“In the overall cohort,” he continued, “they do not have a significant increase in serious adverse events, do not have adverse events of postural hypotension, syncope, bradycardia, injurious falls – so people are worried about it, but it’s not borne out by the data.
“That said, I have two cautions,” Dr. Cheung noted. “One. If you drop somebody’s blood pressure rapidly over a week, you may be more likely to get in trouble. If you drop the blood pressure gradually over several weeks, several months, you’re much less likely to get into trouble.”
“Two. If the patient is old, you know the patient has carotid stenosis and already has postural dizziness, you may not want to try on that patient – but just because the patient is old is not the reason not to target 120.”
ACE inhibitors and ARBs beneficial in albuminuria, underused
“How do you get to less than 120? The short answer is, use whatever medications you need to – there is no necessarily right cocktail,” Dr. Chang said.
“We’ve known that angiotensin-converting enzyme (ACE) inhibitors and ARBs [angiotensin II receptor blockers] are beneficial in patients with CKD and in particular those with heavier albuminuria,” she continued. “We’ve known this for over 20 years.”
Yet, the study identified underutilization – “a persistent gap, just like blood pressure control and awareness,” she noted. “We’re just not making much headway.
“We are not recommending ACE inhibitors or ARBs for all the patients,” Dr. Cheung clarified. “If you are diabetic and have heavy proteinuria, that’s when the use of ACE inhibitors and ARBs are most indicated.”
Public health implications
SPRINT showed that treating to a systolic blood pressure of less than 120 mm Hg vs. less than 140 mm Hg reduced the risk for cardiovascular disease by 25% and all-cause mortality by 27% for participants with and those without CKD, Dr. Foti and colleagues stress.
They aimed to estimate how the new guideline would affect (1) the number of U.S. patients with CKD who would be eligible for blood pressure lowering treatment, and (2) the proportion of those with albuminuria who would be eligible for an ACE inhibitor or an ARB.
The researchers analyzed data from 1,699 adults with CKD (estimated glomerular filtration rate, 15-59 mL/min/1.73 m2 or a urinary albumin-to-creatinine ratio of ≥30 mg/g) who participated in the 2015-2018 National Health and Nutrition Examination Survey.
Both the 2021 and 2012 KDIGO guidelines recommend that patients with albuminuria and blood pressure higher than the target value who are not kidney transplant recipients should be treated with an ACE inhibitor or an ARB.
On the basis of the new target, 78% of patients with CKD and albuminuria were eligible for ACE inhibitor/ARB treatment by the 2021 KDIGO guideline, compared with 71% by the 2012 KDIGO guideline. However, only 39% were taking one of these drugs.
These findings show that “with the new guideline and with the lower blood pressure target, you potentially have an even larger pool of people who have blood pressure that’s not under control, and a potential larger group of people who may benefit from ACE inhibitors and ARBs,” Dr. Chang said.
“Our paper is not the only one to show that we haven’t made a whole lot of progress,” she said, “and now that the bar has been lowered, there [have] to be some renewed efforts on controlling blood pressure, because we know that blood pressure control is such an important risk factor for cardiovascular outcomes.”
Dr. Foti is supported by an NIH/National Heart, Lung, and Blood Institute grant. Dr. Cheung has received consultancy fees from Amgen, Bard, Boehringer Ingelheim, Calliditas, Tricida, and UpToDate, and grant/research support from the National Institutes of Health for SPRINT (monies paid to institution). Dr. Chang has received consultancy fees from Bayer, Gilead, Janssen Research and Development, Novo Nordisk, Tricida, and Vascular Dynamics; grant/research support from AstraZeneca and Satellite Healthcare (monies paid to institution), the NIH, and the American Heart Association; is on advisory boards for AstraZeneca and Fresenius Medical Care Renal Therapies Group; and has received workshop honoraria from Fresenius. Disclosures of relevant financial relationships of the other authors are listed in the original articles.
A version of this article first appeared on Medscape.com.
Cannabinoids may pose death risk for older patients with COPD
, compared with nonusers, findings from a large study have shown.
Synthetic cannabinoids drugs, such as nabilone and dronabinol, have been approved by the Food and Drug Administration for nausea and vomiting caused by chemotherapy. But their off-label use by adults with COPD to help manage chronic musculoskeletal pain, insomnia, and refractory dyspnea is on the rise, wrote Nicholas T. Vozoris, MD, of the University of Toronto and colleagues.
Cannabinoids may actually contribute to negative respiratory outcomes among individuals with COPD through several possible mechanisms including causing sedation, inducing anxiety, and provoking respiratory muscle weakness, they said.
“Possible adverse respiratory effects of cannabinoids may occur with greater likelihood among older adults (in whom COPD is more prevalent), as this group is known to less efficiently metabolise drugs,” they noted.
In a retrospective, population-based cohort study published in Thorax the researchers identified 185,876 adults aged 66 years and older with COPD using health administrative database information from 2006 to 2016. New cannabinoid users (those starting nabilone or dronabinol) were matched with control nonusers (defined as new users of noncannabinoid drugs). Individuals receiving palliative care, or having a diagnosis of cancer or HIV, were excluded because these are settings where synthetic cannabinoids may be prescribed for nausea or vomiting, and these patients are more likely to be in a poorer state of health.
Overall, new cannabinoid users had significantly higher all-cause mortality rates, compared with nonusers (hazard ratio, 1.64). The effects was greater in high-dose users.
Daniel R. Ouellette, MD, associate professor of medicine at Wayne State University and a senior staff physician at Henry Ford Hospital, both in Detroit, commented that this study has value for clinicians. “Many states are liberalizing cannabinoid use, and it is important to know the health effects of this type of drug on patients with chronic respiratory disease,” he noted. “The study is somewhat surprising. While one might have expected adverse consequences in patients with COPD who inhaled smoke from cannabinoids, it is somewhat unexpected that oral use would be associated with adverse consequences.” He added, “Pain in older adults is a complex problem. Cannabinoids are often recommended for pain in the general community, but pain per se is not a primary symptom for most patients with COPD from their respiratory problems. Physicians treating patients with COPD should diagnose the cause of the pain and provide appropriate treatment.”
Dose makes a difference
All-cause mortality increased by 231% and hospitalization for COPD or pneumonia increased by 178% among new users of higher-dose cannabinoids, compared with nonusers. Higher dose was defined in this study as more than 1.5mg/day of nabilone. No significant differences appeared in new users vs. nonusers in hospitalization for COPD or pneumonia at lower doses, and no significant differences appeared overall in outpatient respiratory exacerbations, emergency department visits for COPD or pneumonia, or COPD- or pneumonia-related mortality.
Potential limitations and implications
“The fact that COPD- or pneumonia-related mortality was not observed to occur with significantly greater rates among cannabinoid users with COPD may suggest that the increased all-cause mortality finding was not being driven by adverse respiratory-related drug effects, as we hypothesized, and instead was possibly a result of unresolved confounding,” the researchers noted.
The study findings were limited by several factors including the inability to prove causation in an observational study, and the potential for confounding based on unmeasured differences between cannabinoid users and nonusers, the researchers said. “Our findings may not be generalizable to all individuals with COPD, as our study included only those aged 66 years and older, and our COPD identification algorithm, while highly specific, had modest sensitivity,” they added. However, the results were strengthened by the large study population and suggest that cannabinoids are not contraindicated for older adults with COPD, the researchers said. “There can be legitimate reasons for using cannabinoids in this population, such as to help treat chemotherapy-related nausea and vomiting, and possibly for end-of-life care,” they emphasized.
The study findings serve to inform clinicians of the significantly increased mortality risk when older adults with COPD initiate cannabinoids, and “this information should be discussed with patients and incorporated in prescribing decision-making and management plans,” along with consideration of using lower doses when possible to minimize adverse events, they concluded.
The study was supported by The Lung Association – Ontario Grant Review/Grant-In-Aid. The researchers had no financial conflicts to disclose.
, compared with nonusers, findings from a large study have shown.
Synthetic cannabinoids drugs, such as nabilone and dronabinol, have been approved by the Food and Drug Administration for nausea and vomiting caused by chemotherapy. But their off-label use by adults with COPD to help manage chronic musculoskeletal pain, insomnia, and refractory dyspnea is on the rise, wrote Nicholas T. Vozoris, MD, of the University of Toronto and colleagues.
Cannabinoids may actually contribute to negative respiratory outcomes among individuals with COPD through several possible mechanisms including causing sedation, inducing anxiety, and provoking respiratory muscle weakness, they said.
“Possible adverse respiratory effects of cannabinoids may occur with greater likelihood among older adults (in whom COPD is more prevalent), as this group is known to less efficiently metabolise drugs,” they noted.
In a retrospective, population-based cohort study published in Thorax the researchers identified 185,876 adults aged 66 years and older with COPD using health administrative database information from 2006 to 2016. New cannabinoid users (those starting nabilone or dronabinol) were matched with control nonusers (defined as new users of noncannabinoid drugs). Individuals receiving palliative care, or having a diagnosis of cancer or HIV, were excluded because these are settings where synthetic cannabinoids may be prescribed for nausea or vomiting, and these patients are more likely to be in a poorer state of health.
Overall, new cannabinoid users had significantly higher all-cause mortality rates, compared with nonusers (hazard ratio, 1.64). The effects was greater in high-dose users.
Daniel R. Ouellette, MD, associate professor of medicine at Wayne State University and a senior staff physician at Henry Ford Hospital, both in Detroit, commented that this study has value for clinicians. “Many states are liberalizing cannabinoid use, and it is important to know the health effects of this type of drug on patients with chronic respiratory disease,” he noted. “The study is somewhat surprising. While one might have expected adverse consequences in patients with COPD who inhaled smoke from cannabinoids, it is somewhat unexpected that oral use would be associated with adverse consequences.” He added, “Pain in older adults is a complex problem. Cannabinoids are often recommended for pain in the general community, but pain per se is not a primary symptom for most patients with COPD from their respiratory problems. Physicians treating patients with COPD should diagnose the cause of the pain and provide appropriate treatment.”
Dose makes a difference
All-cause mortality increased by 231% and hospitalization for COPD or pneumonia increased by 178% among new users of higher-dose cannabinoids, compared with nonusers. Higher dose was defined in this study as more than 1.5mg/day of nabilone. No significant differences appeared in new users vs. nonusers in hospitalization for COPD or pneumonia at lower doses, and no significant differences appeared overall in outpatient respiratory exacerbations, emergency department visits for COPD or pneumonia, or COPD- or pneumonia-related mortality.
Potential limitations and implications
“The fact that COPD- or pneumonia-related mortality was not observed to occur with significantly greater rates among cannabinoid users with COPD may suggest that the increased all-cause mortality finding was not being driven by adverse respiratory-related drug effects, as we hypothesized, and instead was possibly a result of unresolved confounding,” the researchers noted.
The study findings were limited by several factors including the inability to prove causation in an observational study, and the potential for confounding based on unmeasured differences between cannabinoid users and nonusers, the researchers said. “Our findings may not be generalizable to all individuals with COPD, as our study included only those aged 66 years and older, and our COPD identification algorithm, while highly specific, had modest sensitivity,” they added. However, the results were strengthened by the large study population and suggest that cannabinoids are not contraindicated for older adults with COPD, the researchers said. “There can be legitimate reasons for using cannabinoids in this population, such as to help treat chemotherapy-related nausea and vomiting, and possibly for end-of-life care,” they emphasized.
The study findings serve to inform clinicians of the significantly increased mortality risk when older adults with COPD initiate cannabinoids, and “this information should be discussed with patients and incorporated in prescribing decision-making and management plans,” along with consideration of using lower doses when possible to minimize adverse events, they concluded.
The study was supported by The Lung Association – Ontario Grant Review/Grant-In-Aid. The researchers had no financial conflicts to disclose.
, compared with nonusers, findings from a large study have shown.
Synthetic cannabinoids drugs, such as nabilone and dronabinol, have been approved by the Food and Drug Administration for nausea and vomiting caused by chemotherapy. But their off-label use by adults with COPD to help manage chronic musculoskeletal pain, insomnia, and refractory dyspnea is on the rise, wrote Nicholas T. Vozoris, MD, of the University of Toronto and colleagues.
Cannabinoids may actually contribute to negative respiratory outcomes among individuals with COPD through several possible mechanisms including causing sedation, inducing anxiety, and provoking respiratory muscle weakness, they said.
“Possible adverse respiratory effects of cannabinoids may occur with greater likelihood among older adults (in whom COPD is more prevalent), as this group is known to less efficiently metabolise drugs,” they noted.
In a retrospective, population-based cohort study published in Thorax the researchers identified 185,876 adults aged 66 years and older with COPD using health administrative database information from 2006 to 2016. New cannabinoid users (those starting nabilone or dronabinol) were matched with control nonusers (defined as new users of noncannabinoid drugs). Individuals receiving palliative care, or having a diagnosis of cancer or HIV, were excluded because these are settings where synthetic cannabinoids may be prescribed for nausea or vomiting, and these patients are more likely to be in a poorer state of health.
Overall, new cannabinoid users had significantly higher all-cause mortality rates, compared with nonusers (hazard ratio, 1.64). The effects was greater in high-dose users.
Daniel R. Ouellette, MD, associate professor of medicine at Wayne State University and a senior staff physician at Henry Ford Hospital, both in Detroit, commented that this study has value for clinicians. “Many states are liberalizing cannabinoid use, and it is important to know the health effects of this type of drug on patients with chronic respiratory disease,” he noted. “The study is somewhat surprising. While one might have expected adverse consequences in patients with COPD who inhaled smoke from cannabinoids, it is somewhat unexpected that oral use would be associated with adverse consequences.” He added, “Pain in older adults is a complex problem. Cannabinoids are often recommended for pain in the general community, but pain per se is not a primary symptom for most patients with COPD from their respiratory problems. Physicians treating patients with COPD should diagnose the cause of the pain and provide appropriate treatment.”
Dose makes a difference
All-cause mortality increased by 231% and hospitalization for COPD or pneumonia increased by 178% among new users of higher-dose cannabinoids, compared with nonusers. Higher dose was defined in this study as more than 1.5mg/day of nabilone. No significant differences appeared in new users vs. nonusers in hospitalization for COPD or pneumonia at lower doses, and no significant differences appeared overall in outpatient respiratory exacerbations, emergency department visits for COPD or pneumonia, or COPD- or pneumonia-related mortality.
Potential limitations and implications
“The fact that COPD- or pneumonia-related mortality was not observed to occur with significantly greater rates among cannabinoid users with COPD may suggest that the increased all-cause mortality finding was not being driven by adverse respiratory-related drug effects, as we hypothesized, and instead was possibly a result of unresolved confounding,” the researchers noted.
The study findings were limited by several factors including the inability to prove causation in an observational study, and the potential for confounding based on unmeasured differences between cannabinoid users and nonusers, the researchers said. “Our findings may not be generalizable to all individuals with COPD, as our study included only those aged 66 years and older, and our COPD identification algorithm, while highly specific, had modest sensitivity,” they added. However, the results were strengthened by the large study population and suggest that cannabinoids are not contraindicated for older adults with COPD, the researchers said. “There can be legitimate reasons for using cannabinoids in this population, such as to help treat chemotherapy-related nausea and vomiting, and possibly for end-of-life care,” they emphasized.
The study findings serve to inform clinicians of the significantly increased mortality risk when older adults with COPD initiate cannabinoids, and “this information should be discussed with patients and incorporated in prescribing decision-making and management plans,” along with consideration of using lower doses when possible to minimize adverse events, they concluded.
The study was supported by The Lung Association – Ontario Grant Review/Grant-In-Aid. The researchers had no financial conflicts to disclose.
FROM THORAX
Target-lesion failure reduced 2 years after MI with biodegradable stent
For a primary composite target-lesion failure outcome, a biodegradable polymer sirolimus-eluting stent showed superiority at 2 years over a durable polymer everolimus-eluting stent in patients undergoing percutaneous intervention (PCI) for an ST-segment elevated acute myocardial infarction (STEMI), according to a late-breaking trial presentation at CRT 2021.
As in the previously reported 1-year results from the BIOSTEMI trial, the advantage of the biodegradable device was “driven by lower rates of target-lesion revascularization,” reported Thomas Pilgrim, MD, of the University of Bern (Switzerland).
Drug-eluting stents have already been established as superior to bare-metal stents, but the question asked in this study is whether the polymer that carries antiproliferative drugs, such as sirolimus or everolimus, improves lesion-based outcomes if it is biodegradable rather than durable, Dr. Pilgrim explained.
The composite primary outcome was target-lesion failure defined by cardiac death, target-lesion MI, or clinically indicated target-lesion revascularization.
After 2 years of follow-up, the rates of target-lesion failure were 5.1% and 8.1% for the biodegradable and durable polymer stents, respectively. This 0.58 rate ratio was statistically significant, favoring the biodegradable stent.
The investigator-initiated BIOSTEMI trial randomized 1,300 patients to one of two drug-eluting stents with ultrathin struts. One was the Orsiro stent that employs a biodegradable polymer to deliver sirolimus. The other was the Xience Prime/Xpedition that uses a durable polymer stent to deliver everolimus.
The strut thicknesses of the Orsiro stent are 60 mcm for stents of 3.0 mm in diameter or smaller and 80 mcm for those with a larger diameter. The strut thickness of the Xience stent is 81 mcm regardless of diameter.
“Patients with an acute myocardial infarction are at increased risk of stent-related events due to exacerbated inflammatory response and delayed arterial healing,” Dr. Pilgrim said. The theoretical advantages of polymer that biodegrades include “mitigation of the arterial injury, facilitation of endothelialization, and reduced intimal hyperplasia,” he explained at the meeting sponsored by MedStar Heart & Vascular Institute.
The rates of cardiac death (2.9% vs. 3.2%) and target-vessel MI (2.9% vs. 3.2%) were lower for the biodegradable polymer stent, but not significantly. However, the rates of target-vessel revascularization at 2 years were 2.5% versus 5.1%. The associated rate ratio of 0.52 favoring the biodegradable stent was significant.
Similar results favoring the biodegradable polymer stent were observed at 1 year, but those earlier results factored in historical data from the BIOSCIENCE trial, using a Bayesian analysis, to improve the power of the comparison. In this 2-year analysis, the superiority of the biodegradable polymer stent to the durable polymer stent remained statistically significant even when excluding those historical controls.
The advantage of the biodegradable polymer stent was confined to “device-oriented” outcomes, according to Dr. Pilgrim. When compared for important patient-oriented outcomes at 2 years, there were no significant differences. Rather, several were numerically more common, including death (4.2% vs. 3.8%) and MI (3.7% vs. 3.1%) in those who were randomized to the biodegradable polymer stent.
But these types of clinical outcomes are not necessarily related to stent assignment because “up to one-half of all events over the 2 years of follow-up were unrelated to the stent implanted,” Dr. Pilgrim said. He noted that high rates of events unrelated to the implanted stent have also been seen in follow-up of other comparative stent trials.
The superiority of the biodegradable stent is noteworthy. Although Dr. Pilgrim described the BIOSTEMI trial as “the first head-to-head comparison of two new-generation drug-eluting stents in patients undergoing a primary percutaneous intervention for acute myocardial infarction,” there have been several studies comparing stents for other indications. Significant differences have been uncommon.
“Over the last 10 years, we have seen a number of noninferiority stent trials, but only now are we seeing some superiority differences. This is a move in the right direction,” commented Sripal Bangalore, MD, director of the cardiovascular outcomes group, New York University.
However, he, like others, questioned whether the difference in outcomes in this trial could be fully attributed to the type of polymer. He noted that all stents could be characterized by multiple small and large differences in design and composition. Any specific characteristic, such as biodegradable polymer, might be an important contributor but not an isolated factor in the outcomes observed.
On the day that the 2-year results of the BIOSTEMI trial were presented at the CRT 2021 meeting they were simultaneously published in JACC: Cardiovascular Interventions.
Dr. Pilgrim reports financial relationships with several companies that make stent devices, including Biotronik and Boston Scientific. Dr. Bangalore reports no potential conflicts of interest.
For a primary composite target-lesion failure outcome, a biodegradable polymer sirolimus-eluting stent showed superiority at 2 years over a durable polymer everolimus-eluting stent in patients undergoing percutaneous intervention (PCI) for an ST-segment elevated acute myocardial infarction (STEMI), according to a late-breaking trial presentation at CRT 2021.
As in the previously reported 1-year results from the BIOSTEMI trial, the advantage of the biodegradable device was “driven by lower rates of target-lesion revascularization,” reported Thomas Pilgrim, MD, of the University of Bern (Switzerland).
Drug-eluting stents have already been established as superior to bare-metal stents, but the question asked in this study is whether the polymer that carries antiproliferative drugs, such as sirolimus or everolimus, improves lesion-based outcomes if it is biodegradable rather than durable, Dr. Pilgrim explained.
The composite primary outcome was target-lesion failure defined by cardiac death, target-lesion MI, or clinically indicated target-lesion revascularization.
After 2 years of follow-up, the rates of target-lesion failure were 5.1% and 8.1% for the biodegradable and durable polymer stents, respectively. This 0.58 rate ratio was statistically significant, favoring the biodegradable stent.
The investigator-initiated BIOSTEMI trial randomized 1,300 patients to one of two drug-eluting stents with ultrathin struts. One was the Orsiro stent that employs a biodegradable polymer to deliver sirolimus. The other was the Xience Prime/Xpedition that uses a durable polymer stent to deliver everolimus.
The strut thicknesses of the Orsiro stent are 60 mcm for stents of 3.0 mm in diameter or smaller and 80 mcm for those with a larger diameter. The strut thickness of the Xience stent is 81 mcm regardless of diameter.
“Patients with an acute myocardial infarction are at increased risk of stent-related events due to exacerbated inflammatory response and delayed arterial healing,” Dr. Pilgrim said. The theoretical advantages of polymer that biodegrades include “mitigation of the arterial injury, facilitation of endothelialization, and reduced intimal hyperplasia,” he explained at the meeting sponsored by MedStar Heart & Vascular Institute.
The rates of cardiac death (2.9% vs. 3.2%) and target-vessel MI (2.9% vs. 3.2%) were lower for the biodegradable polymer stent, but not significantly. However, the rates of target-vessel revascularization at 2 years were 2.5% versus 5.1%. The associated rate ratio of 0.52 favoring the biodegradable stent was significant.
Similar results favoring the biodegradable polymer stent were observed at 1 year, but those earlier results factored in historical data from the BIOSCIENCE trial, using a Bayesian analysis, to improve the power of the comparison. In this 2-year analysis, the superiority of the biodegradable polymer stent to the durable polymer stent remained statistically significant even when excluding those historical controls.
The advantage of the biodegradable polymer stent was confined to “device-oriented” outcomes, according to Dr. Pilgrim. When compared for important patient-oriented outcomes at 2 years, there were no significant differences. Rather, several were numerically more common, including death (4.2% vs. 3.8%) and MI (3.7% vs. 3.1%) in those who were randomized to the biodegradable polymer stent.
But these types of clinical outcomes are not necessarily related to stent assignment because “up to one-half of all events over the 2 years of follow-up were unrelated to the stent implanted,” Dr. Pilgrim said. He noted that high rates of events unrelated to the implanted stent have also been seen in follow-up of other comparative stent trials.
The superiority of the biodegradable stent is noteworthy. Although Dr. Pilgrim described the BIOSTEMI trial as “the first head-to-head comparison of two new-generation drug-eluting stents in patients undergoing a primary percutaneous intervention for acute myocardial infarction,” there have been several studies comparing stents for other indications. Significant differences have been uncommon.
“Over the last 10 years, we have seen a number of noninferiority stent trials, but only now are we seeing some superiority differences. This is a move in the right direction,” commented Sripal Bangalore, MD, director of the cardiovascular outcomes group, New York University.
However, he, like others, questioned whether the difference in outcomes in this trial could be fully attributed to the type of polymer. He noted that all stents could be characterized by multiple small and large differences in design and composition. Any specific characteristic, such as biodegradable polymer, might be an important contributor but not an isolated factor in the outcomes observed.
On the day that the 2-year results of the BIOSTEMI trial were presented at the CRT 2021 meeting they were simultaneously published in JACC: Cardiovascular Interventions.
Dr. Pilgrim reports financial relationships with several companies that make stent devices, including Biotronik and Boston Scientific. Dr. Bangalore reports no potential conflicts of interest.
For a primary composite target-lesion failure outcome, a biodegradable polymer sirolimus-eluting stent showed superiority at 2 years over a durable polymer everolimus-eluting stent in patients undergoing percutaneous intervention (PCI) for an ST-segment elevated acute myocardial infarction (STEMI), according to a late-breaking trial presentation at CRT 2021.
As in the previously reported 1-year results from the BIOSTEMI trial, the advantage of the biodegradable device was “driven by lower rates of target-lesion revascularization,” reported Thomas Pilgrim, MD, of the University of Bern (Switzerland).
Drug-eluting stents have already been established as superior to bare-metal stents, but the question asked in this study is whether the polymer that carries antiproliferative drugs, such as sirolimus or everolimus, improves lesion-based outcomes if it is biodegradable rather than durable, Dr. Pilgrim explained.
The composite primary outcome was target-lesion failure defined by cardiac death, target-lesion MI, or clinically indicated target-lesion revascularization.
After 2 years of follow-up, the rates of target-lesion failure were 5.1% and 8.1% for the biodegradable and durable polymer stents, respectively. This 0.58 rate ratio was statistically significant, favoring the biodegradable stent.
The investigator-initiated BIOSTEMI trial randomized 1,300 patients to one of two drug-eluting stents with ultrathin struts. One was the Orsiro stent that employs a biodegradable polymer to deliver sirolimus. The other was the Xience Prime/Xpedition that uses a durable polymer stent to deliver everolimus.
The strut thicknesses of the Orsiro stent are 60 mcm for stents of 3.0 mm in diameter or smaller and 80 mcm for those with a larger diameter. The strut thickness of the Xience stent is 81 mcm regardless of diameter.
“Patients with an acute myocardial infarction are at increased risk of stent-related events due to exacerbated inflammatory response and delayed arterial healing,” Dr. Pilgrim said. The theoretical advantages of polymer that biodegrades include “mitigation of the arterial injury, facilitation of endothelialization, and reduced intimal hyperplasia,” he explained at the meeting sponsored by MedStar Heart & Vascular Institute.
The rates of cardiac death (2.9% vs. 3.2%) and target-vessel MI (2.9% vs. 3.2%) were lower for the biodegradable polymer stent, but not significantly. However, the rates of target-vessel revascularization at 2 years were 2.5% versus 5.1%. The associated rate ratio of 0.52 favoring the biodegradable stent was significant.
Similar results favoring the biodegradable polymer stent were observed at 1 year, but those earlier results factored in historical data from the BIOSCIENCE trial, using a Bayesian analysis, to improve the power of the comparison. In this 2-year analysis, the superiority of the biodegradable polymer stent to the durable polymer stent remained statistically significant even when excluding those historical controls.
The advantage of the biodegradable polymer stent was confined to “device-oriented” outcomes, according to Dr. Pilgrim. When compared for important patient-oriented outcomes at 2 years, there were no significant differences. Rather, several were numerically more common, including death (4.2% vs. 3.8%) and MI (3.7% vs. 3.1%) in those who were randomized to the biodegradable polymer stent.
But these types of clinical outcomes are not necessarily related to stent assignment because “up to one-half of all events over the 2 years of follow-up were unrelated to the stent implanted,” Dr. Pilgrim said. He noted that high rates of events unrelated to the implanted stent have also been seen in follow-up of other comparative stent trials.
The superiority of the biodegradable stent is noteworthy. Although Dr. Pilgrim described the BIOSTEMI trial as “the first head-to-head comparison of two new-generation drug-eluting stents in patients undergoing a primary percutaneous intervention for acute myocardial infarction,” there have been several studies comparing stents for other indications. Significant differences have been uncommon.
“Over the last 10 years, we have seen a number of noninferiority stent trials, but only now are we seeing some superiority differences. This is a move in the right direction,” commented Sripal Bangalore, MD, director of the cardiovascular outcomes group, New York University.
However, he, like others, questioned whether the difference in outcomes in this trial could be fully attributed to the type of polymer. He noted that all stents could be characterized by multiple small and large differences in design and composition. Any specific characteristic, such as biodegradable polymer, might be an important contributor but not an isolated factor in the outcomes observed.
On the day that the 2-year results of the BIOSTEMI trial were presented at the CRT 2021 meeting they were simultaneously published in JACC: Cardiovascular Interventions.
Dr. Pilgrim reports financial relationships with several companies that make stent devices, including Biotronik and Boston Scientific. Dr. Bangalore reports no potential conflicts of interest.
FROM CRT 2021
First pill for COVID-19 could be ready by year’s end
New pills to treat patients with COVID-19 are currently in midstage clinical trials and, if successful, could be ready by the end of the year.
Only one treatment – remdesivir (Veklury) – has been fully approved by the U.S. Food and Drug Administration for patients in the hospital and it must be administered intravenously.
Hopes for a day when patients with COVID-19 can take a pill to rid their bodies of the virus got a boost when early trial results were presented at a medical conference.
Interim phase 2 results for the oral experimental COVID-19 drug molnupiravir, designed to do for patients with COVID-19 what oseltamivir (Tamiflu) can do for patients with the flu, were presented at the Conference on Retroviruses and Opportunistic Infections 2021 Annual Meeting, as reported by this news organization.
In the small study, the pill significantly reduced infectious virus in patients who were symptomatic and had tested positive for COVID-19 during the previous 4 days but were not hospitalized.
After 5 days of treatment, no participants who received molnupiravir had detectable virus, whereas 24% who received placebo did.
Two other oral agents are being developed by RedHill Biopharma: one for severe COVID-19 infection for hospitalized patients and one for patients at home with mild infection.
The first, opaganib (Yeliva), proceeded to a phase 2/3 global trial for hospitalized patients after the company announced top-line safety and efficacy data in December. In phase 2, the drug was shown to be safe in patients requiring oxygen and effectively reduced the need for oxygen by the end of the treatment period.
A key feature is that it is both an antiviral and an anti-inflammatory, Gilead Raday, RedHill’s chief operating officer, said in an interview. Data are expected midyear on its performance in 464 patients. The drug is being tested on top of remdesivir or in addition to dexamethasone.
The second, upamostat (RHB-107), is currently undergoing a phase 2/3 trial in the United States and is being investigated for use in nonhospitalized COVID-19 patients.
“I would expect data to be available in the second half of this year,” Mr. Raday said.
Upamostat is a novel serine protease inhibitor expected to be effective against emerging variants because it targets human cell factors involved in viral entry, according to the company.
Other drugs are being investigated in trials that are in earlier stages.
Urgent need for oral agents
Infectious disease specialists are watching the move toward a COVID-19 pill enthusiastically.
“We badly need an oral treatment option for COVID,” said Sarah Doernberg, MD, an infectious disease specialist from the University of California, San Francisco.
“It’s a real gap in our armamentarium for COVID in outpatient treatment, which is where most who contract COVID-19 will seek care,” she said in an interview.
Although some studies have shown the benefit of monoclonal antibodies for prevention and early treatment, there are major logistical issues because all the current options require IV administration, she explained.
“If we had a pill to treat early COVID, especially in high-risk patients, it would fill a gap,” she said, noting that a pill could help people get better faster and prevent hospital stays.
Studies of molnupiravir suggest that it decreases viral shedding in the first few days after COVID infection, Dr. Doernberg reported.
There is excitement around the drug, but it will be important to see whether the results translate into fewer people requiring hospital admission and whether people feel better faster.
“I want to see the clinical data,” Dr. Doernberg said.
She will also be watching for the upamostat and opaganib results in the coming weeks.
“If these drugs are successful, I think it’s possible we could use them – maybe under an emergency use authorization – this year,” she said.
Once antiviral pills are a viable option for COVID-19 treatment, questions will arise about their use, she said.
One question is whether patients who are getting remdesivir in the hospital and are ready to leave after 5 days should continue treatment with antiviral pills at home.
Another is whether the pills – if they are shown to be effective – will be helpful for COVID post exposure. That use would be important for people who do not have COVID-19 but who are in close contact with someone who does, such as a member of their household.
“We have that model,” Dr. Doernberg said. “We know that oseltamivir can be used for postexposure prophylaxis and can help to prevent development of clinical disease.”
But she cautioned that a challenge with COVID is that people are contagious very early. A pill would need to come with the ability to test for COVID-19 early and get patients linked to care immediately.
“Those are not small challenges,” she said.
Vaccines alone won’t end the COVID threat
Treatments are part of the “belt-and-suspenders” approach, along with vaccines to combat COVID-19, Dr. Doernberg said.
“We’re not going to eradicate COVID,” she said. “We’re still going to need treatments for people who either don’t respond to the vaccine or haven’t gotten the vaccine or developed disease despite the vaccine.”
Oral formulations are desperately needed, agreed Kenneth Johnson, PhD, professor of molecular biosciences at the University of Texas at Austin.
Right now, remdesivir treatments involve patients being hooked up to an IV for 30-120 minutes each day for 5 days. And the cost of a 5-day course of remdesivir ranges from $2340 to $3120 in the United States.
“We’re hoping we can come up with something that is a little bit easier to administer, and without as many concerns for toxic side effects,” he said.
Dr. Johnson’s team at UT-Austin recently made a key discovery about the way remdesivir stops the replication of viral RNA.
The understanding of where the virus starts to replicate in the infection chain of events and how and where it reacts with remdesivir might lead to the development of better, more concentrated pill forms of antivirals in the future, with fewer toxicities, he said.
The team used a lab dish to recreate the step-by-step process that occurs when a patient who is infected with SARS-CoV-2 receives remdesivir.
The discovery was published online in Molecular Cell in January and will be printed in the April issue of the journal.
The discovery won’t lead to an effective COVID-19 pill for our current crisis, but will be important for the next generation of drugs needed to deal with future coronaviruses, Dr. Johnson explained.
And there will be other coronaviruses, he said, noting that this one is the third in 20 years to jump from animals to humans. “It’s just a matter of time,” he said.
A version of this article first appeared on Medscape.com.
New pills to treat patients with COVID-19 are currently in midstage clinical trials and, if successful, could be ready by the end of the year.
Only one treatment – remdesivir (Veklury) – has been fully approved by the U.S. Food and Drug Administration for patients in the hospital and it must be administered intravenously.
Hopes for a day when patients with COVID-19 can take a pill to rid their bodies of the virus got a boost when early trial results were presented at a medical conference.
Interim phase 2 results for the oral experimental COVID-19 drug molnupiravir, designed to do for patients with COVID-19 what oseltamivir (Tamiflu) can do for patients with the flu, were presented at the Conference on Retroviruses and Opportunistic Infections 2021 Annual Meeting, as reported by this news organization.
In the small study, the pill significantly reduced infectious virus in patients who were symptomatic and had tested positive for COVID-19 during the previous 4 days but were not hospitalized.
After 5 days of treatment, no participants who received molnupiravir had detectable virus, whereas 24% who received placebo did.
Two other oral agents are being developed by RedHill Biopharma: one for severe COVID-19 infection for hospitalized patients and one for patients at home with mild infection.
The first, opaganib (Yeliva), proceeded to a phase 2/3 global trial for hospitalized patients after the company announced top-line safety and efficacy data in December. In phase 2, the drug was shown to be safe in patients requiring oxygen and effectively reduced the need for oxygen by the end of the treatment period.
A key feature is that it is both an antiviral and an anti-inflammatory, Gilead Raday, RedHill’s chief operating officer, said in an interview. Data are expected midyear on its performance in 464 patients. The drug is being tested on top of remdesivir or in addition to dexamethasone.
The second, upamostat (RHB-107), is currently undergoing a phase 2/3 trial in the United States and is being investigated for use in nonhospitalized COVID-19 patients.
“I would expect data to be available in the second half of this year,” Mr. Raday said.
Upamostat is a novel serine protease inhibitor expected to be effective against emerging variants because it targets human cell factors involved in viral entry, according to the company.
Other drugs are being investigated in trials that are in earlier stages.
Urgent need for oral agents
Infectious disease specialists are watching the move toward a COVID-19 pill enthusiastically.
“We badly need an oral treatment option for COVID,” said Sarah Doernberg, MD, an infectious disease specialist from the University of California, San Francisco.
“It’s a real gap in our armamentarium for COVID in outpatient treatment, which is where most who contract COVID-19 will seek care,” she said in an interview.
Although some studies have shown the benefit of monoclonal antibodies for prevention and early treatment, there are major logistical issues because all the current options require IV administration, she explained.
“If we had a pill to treat early COVID, especially in high-risk patients, it would fill a gap,” she said, noting that a pill could help people get better faster and prevent hospital stays.
Studies of molnupiravir suggest that it decreases viral shedding in the first few days after COVID infection, Dr. Doernberg reported.
There is excitement around the drug, but it will be important to see whether the results translate into fewer people requiring hospital admission and whether people feel better faster.
“I want to see the clinical data,” Dr. Doernberg said.
She will also be watching for the upamostat and opaganib results in the coming weeks.
“If these drugs are successful, I think it’s possible we could use them – maybe under an emergency use authorization – this year,” she said.
Once antiviral pills are a viable option for COVID-19 treatment, questions will arise about their use, she said.
One question is whether patients who are getting remdesivir in the hospital and are ready to leave after 5 days should continue treatment with antiviral pills at home.
Another is whether the pills – if they are shown to be effective – will be helpful for COVID post exposure. That use would be important for people who do not have COVID-19 but who are in close contact with someone who does, such as a member of their household.
“We have that model,” Dr. Doernberg said. “We know that oseltamivir can be used for postexposure prophylaxis and can help to prevent development of clinical disease.”
But she cautioned that a challenge with COVID is that people are contagious very early. A pill would need to come with the ability to test for COVID-19 early and get patients linked to care immediately.
“Those are not small challenges,” she said.
Vaccines alone won’t end the COVID threat
Treatments are part of the “belt-and-suspenders” approach, along with vaccines to combat COVID-19, Dr. Doernberg said.
“We’re not going to eradicate COVID,” she said. “We’re still going to need treatments for people who either don’t respond to the vaccine or haven’t gotten the vaccine or developed disease despite the vaccine.”
Oral formulations are desperately needed, agreed Kenneth Johnson, PhD, professor of molecular biosciences at the University of Texas at Austin.
Right now, remdesivir treatments involve patients being hooked up to an IV for 30-120 minutes each day for 5 days. And the cost of a 5-day course of remdesivir ranges from $2340 to $3120 in the United States.
“We’re hoping we can come up with something that is a little bit easier to administer, and without as many concerns for toxic side effects,” he said.
Dr. Johnson’s team at UT-Austin recently made a key discovery about the way remdesivir stops the replication of viral RNA.
The understanding of where the virus starts to replicate in the infection chain of events and how and where it reacts with remdesivir might lead to the development of better, more concentrated pill forms of antivirals in the future, with fewer toxicities, he said.
The team used a lab dish to recreate the step-by-step process that occurs when a patient who is infected with SARS-CoV-2 receives remdesivir.
The discovery was published online in Molecular Cell in January and will be printed in the April issue of the journal.
The discovery won’t lead to an effective COVID-19 pill for our current crisis, but will be important for the next generation of drugs needed to deal with future coronaviruses, Dr. Johnson explained.
And there will be other coronaviruses, he said, noting that this one is the third in 20 years to jump from animals to humans. “It’s just a matter of time,” he said.
A version of this article first appeared on Medscape.com.
New pills to treat patients with COVID-19 are currently in midstage clinical trials and, if successful, could be ready by the end of the year.
Only one treatment – remdesivir (Veklury) – has been fully approved by the U.S. Food and Drug Administration for patients in the hospital and it must be administered intravenously.
Hopes for a day when patients with COVID-19 can take a pill to rid their bodies of the virus got a boost when early trial results were presented at a medical conference.
Interim phase 2 results for the oral experimental COVID-19 drug molnupiravir, designed to do for patients with COVID-19 what oseltamivir (Tamiflu) can do for patients with the flu, were presented at the Conference on Retroviruses and Opportunistic Infections 2021 Annual Meeting, as reported by this news organization.
In the small study, the pill significantly reduced infectious virus in patients who were symptomatic and had tested positive for COVID-19 during the previous 4 days but were not hospitalized.
After 5 days of treatment, no participants who received molnupiravir had detectable virus, whereas 24% who received placebo did.
Two other oral agents are being developed by RedHill Biopharma: one for severe COVID-19 infection for hospitalized patients and one for patients at home with mild infection.
The first, opaganib (Yeliva), proceeded to a phase 2/3 global trial for hospitalized patients after the company announced top-line safety and efficacy data in December. In phase 2, the drug was shown to be safe in patients requiring oxygen and effectively reduced the need for oxygen by the end of the treatment period.
A key feature is that it is both an antiviral and an anti-inflammatory, Gilead Raday, RedHill’s chief operating officer, said in an interview. Data are expected midyear on its performance in 464 patients. The drug is being tested on top of remdesivir or in addition to dexamethasone.
The second, upamostat (RHB-107), is currently undergoing a phase 2/3 trial in the United States and is being investigated for use in nonhospitalized COVID-19 patients.
“I would expect data to be available in the second half of this year,” Mr. Raday said.
Upamostat is a novel serine protease inhibitor expected to be effective against emerging variants because it targets human cell factors involved in viral entry, according to the company.
Other drugs are being investigated in trials that are in earlier stages.
Urgent need for oral agents
Infectious disease specialists are watching the move toward a COVID-19 pill enthusiastically.
“We badly need an oral treatment option for COVID,” said Sarah Doernberg, MD, an infectious disease specialist from the University of California, San Francisco.
“It’s a real gap in our armamentarium for COVID in outpatient treatment, which is where most who contract COVID-19 will seek care,” she said in an interview.
Although some studies have shown the benefit of monoclonal antibodies for prevention and early treatment, there are major logistical issues because all the current options require IV administration, she explained.
“If we had a pill to treat early COVID, especially in high-risk patients, it would fill a gap,” she said, noting that a pill could help people get better faster and prevent hospital stays.
Studies of molnupiravir suggest that it decreases viral shedding in the first few days after COVID infection, Dr. Doernberg reported.
There is excitement around the drug, but it will be important to see whether the results translate into fewer people requiring hospital admission and whether people feel better faster.
“I want to see the clinical data,” Dr. Doernberg said.
She will also be watching for the upamostat and opaganib results in the coming weeks.
“If these drugs are successful, I think it’s possible we could use them – maybe under an emergency use authorization – this year,” she said.
Once antiviral pills are a viable option for COVID-19 treatment, questions will arise about their use, she said.
One question is whether patients who are getting remdesivir in the hospital and are ready to leave after 5 days should continue treatment with antiviral pills at home.
Another is whether the pills – if they are shown to be effective – will be helpful for COVID post exposure. That use would be important for people who do not have COVID-19 but who are in close contact with someone who does, such as a member of their household.
“We have that model,” Dr. Doernberg said. “We know that oseltamivir can be used for postexposure prophylaxis and can help to prevent development of clinical disease.”
But she cautioned that a challenge with COVID is that people are contagious very early. A pill would need to come with the ability to test for COVID-19 early and get patients linked to care immediately.
“Those are not small challenges,” she said.
Vaccines alone won’t end the COVID threat
Treatments are part of the “belt-and-suspenders” approach, along with vaccines to combat COVID-19, Dr. Doernberg said.
“We’re not going to eradicate COVID,” she said. “We’re still going to need treatments for people who either don’t respond to the vaccine or haven’t gotten the vaccine or developed disease despite the vaccine.”
Oral formulations are desperately needed, agreed Kenneth Johnson, PhD, professor of molecular biosciences at the University of Texas at Austin.
Right now, remdesivir treatments involve patients being hooked up to an IV for 30-120 minutes each day for 5 days. And the cost of a 5-day course of remdesivir ranges from $2340 to $3120 in the United States.
“We’re hoping we can come up with something that is a little bit easier to administer, and without as many concerns for toxic side effects,” he said.
Dr. Johnson’s team at UT-Austin recently made a key discovery about the way remdesivir stops the replication of viral RNA.
The understanding of where the virus starts to replicate in the infection chain of events and how and where it reacts with remdesivir might lead to the development of better, more concentrated pill forms of antivirals in the future, with fewer toxicities, he said.
The team used a lab dish to recreate the step-by-step process that occurs when a patient who is infected with SARS-CoV-2 receives remdesivir.
The discovery was published online in Molecular Cell in January and will be printed in the April issue of the journal.
The discovery won’t lead to an effective COVID-19 pill for our current crisis, but will be important for the next generation of drugs needed to deal with future coronaviruses, Dr. Johnson explained.
And there will be other coronaviruses, he said, noting that this one is the third in 20 years to jump from animals to humans. “It’s just a matter of time,” he said.
A version of this article first appeared on Medscape.com.
Is pediatric subspecialty training financially worth it?
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pursuing fellowship training is often financially costly in terms of lifetime earnings, compared with starting a career as a general pediatrician immediately after residency, a report suggests.
Researchers found that most pediatric subspecialists – including those practicing neurology, pulmonology, and adolescent medicine – do not see a financial return from additional training because of the delays in receiving increased compensation and the repayment of educational debt.
“Most pediatric subspecialists don’t experience a relative increase in compensation after training compared to a general pediatrician, so there isn’t a financial benefit to additional training,” lead author Eva Catenaccio, MD, from the division of pediatric neurology, department of neurology, Johns Hopkins University, Baltimore, told this news organization.
The findings, published online March 8 in Pediatrics, contribute to the ongoing debate about the length of pediatric fellowship training programs. The data also provide evidence for the potential effect of a pediatric subspecialty loan repayment program.
Pediatric subspecialty training rarely pays off
However, not all practitioners in pediatric subspecialties would find themselves in the red relative to their generalist peers. Three subspecialties had a positive financial return: cardiology, critical care, and neonatology. Dr. Catenaccio explained that this may be because these subspecialties tend to be “inpatient procedure oriented, which are often more [lucrative] than outpatient cognitive–oriented subspecialties, such as pediatric infectious diseases, endocrinology, or adolescent medicine.”
Enrolling in a pediatric fellowship program resulted in lifetime financial returns that ranged from an increase of $852,129 for cardiology, relative to general pediatrics, to a loss of $1,594,366 for adolescent medicine, researchers found.
For the study, researchers calculated the financial returns of 15 pediatric subspecialties – emergency medicine, neurology, cardiology, critical care, neonatology, hematology and oncology, pulmonology, hospitalist medicine, allergy and immunology, gastroenterology, rheumatology, nephrology, adolescent medicine, infectious diseases, and endocrinology – in comparison with returns of private practice general pediatrics on the basis of 2018-2019 data on fellowship stipends, compensation, and educational debt.
They obtained most of the data from the Association of American Medical Colleges Survey of Resident/Fellow Stipends and Benefits, AAMC’s annual Medical School Faculty Salary Report, and the AAMC Medical School Graduation Questionnaire.
Richard Mink, MD, department of pediatrics, Harbor-UCLA Medical Center, Torrance, Calif., noted that it would have been helpful to have also compared the lifetime earnings of practitioners in pediatric subspecialties to academic general pediatricians and not just those in private practice.
The financial gap has worsened
To better understand which aspects of fellowship training have the greatest effect on lifetime compensation, Dr. Catenaccio and colleagues evaluated the potential effects of shortening fellowship length, eliminating school debt, and implementing a federal loan repayment plan. These changes enhanced the returns of cardiology, critical care, and neonatology – subspecialties that had already seen financial returns before these changes – and resulted in a positive financial return for emergency medicine.
The changes also narrowed the financial gap between subspecialties and general pediatrics. However, the remaining subspecialties still earned less than private practice pediatrics.
The new study is an update to a 2011 report, which reflected 2007-2008 data for 11 subspecialties. This time around, the researchers included the subspecialty of hospitalist medicine, which was approved as a board-certified subspecialty by the American Board of Pediatrics in 2014, as well as neurology, allergy and immunology, and adolescent medicine.
“I was most surprised that the additional pediatric subspecialties we included since the 2011 report followed the same general trend, with pediatric subspecialty training having a lower lifetime earning potential than general pediatrics,” Dr. Catenaccio said.
Comparing results from the two study periods showed that the financial gap between general pediatrics and subspecialty pediatrics worsened over time. For example, the financial return for pediatric endocrinology decreased an additional $500,000 between 2007 and 2018.
The researchers believe a combination of increased educational debt burden, slow growth in compensation, and changing interest rates over time have caused the financial differences between general pediatrics and subspecialty pediatrics to become more pronounced.
‘Pediatric subspecialty training is worth it!’
Despite the financial gaps, Dr. Catenaccio and colleagues say pediatric subspecialty training is still worthwhile but that policymakers should address these financial differences to help guide workforce distribution in a way that meets the needs of patients.
“I think pediatric subspecialty training is worth it,” said Dr. Catenaccio, who’s pursuing pediatric subspecialty training. “There are so many factors that go into choosing a specialty or subspecialty in medicine, including the desire to care for a particular patient population, interest in certain diseases or organ systems, lifestyle considerations, and research opportunities.”
But it’s also important for trainees to be aware of economic considerations in their decision-making.
Dr. Mink, who wrote an accompanying commentary, agrees that young clinicians should not make career decisions on the basis of metrics such as lifetime earning measures.
“I think people who go into pediatrics have decided that money is not the driving force,” said Dr. Mink. He noted that pediatricians are usually not paid well, compared with other specialists. “To me the important thing is you have to like what you’re doing.”
A 2020 study found that trainees who chose a career in pediatric pulmonology, a subspecialty, said that financial considerations were not the driving factor in their decision-making. Nevertheless, Dr. Mink also believes young clinicians should take into account their educational debt.
The further widening of the financial gap between general pediatrics and pediatric subspecialties could lead to shortages in the pediatric subspecialty workforce.
The authors and Dr. Mink have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.