User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Pancreatic involvement in COVID-19: What do we know?
MADRID – It involves the relationship between COVID-19 and new diagnoses of diabetes and blood glucose disorders, among others, in the post–COVID-19 period. These topics were addressed at the XXXIII National Congress of the Spanish Diabetes Society. They were also the central theme of the inaugural conference, Pancreatic Involvement During COVID-19: From Preclinical Studies to Clinical Relevance, which was led by Alexander Kleger, MD, PhD, head of the department of pancreatology at the Ulm (Germany) University Clinic for Internal Medicine.
The chair of the scientific committee of the congress, Franz Martín, MD, launched the conference by noting that the work of Dr. Kleger and his team has made it possible to ascertain that SARS-CoV-2 can infect pancreatic beta cells that produce insulin. This observation may help in understanding why patients with COVID-19 sometimes experience symptoms related to greater difficulty regulating blood glucose.
“In addition, the German expert and his group have described the abnormalities that occur in beta cells when they are infected by SARS-CoV-2, something especially important, given that knowledge of these abnormalities may be of great importance to understanding the possible appearance of more cases of diabetes in the future,” Dr. Martín added.
“Our data identify the human pancreas as a target of SARS-CoV-2 infection and suggest that pancreatic beta cell involvement could contribute to the metabolic dysregulation seen in COVID-19 patients,” Dr. Kleger pointed out.
In his speech, Dr. Kleger reviewed the evidence on the effects of SARS-CoV-2 that has been garnered since the start of the pandemic, and he presented his research group’s findings on the impact at the pancreatic level.
“Since March 2020, it has been seen that COVID-19 affected the pancreas, and studies published in August of that same year clearly spoke of both a worsening of diabetes and an increase in new cases of this disease diagnosed after SARS-CoV-2 infection. Also, the data showed how hospitalized patients with no previous history of diabetes experienced rapid increases in glucose levels 5 days after admission,” Dr. Kleger said.
Angiotensin-converting enzyme 2
As an example of the pace at which evidence on the pancreatic impact of this virus has been evolving, Dr. Kleger referred to early studies that found no angiotensin-converting enzyme 2 receptor on cells of the endocrine and exocrine pancreas. “To our surprise, in our work, we did observe the obvious presence of angiotensin-converting enzyme 2 specifically expressed in human pancreatic beta cells, something confirmed by other investigations. Another surprising aspect was verifying that the viral infection lasts longer in the pancreas than in the lungs,” said the expert.
These findings caused the researchers to realize that SARS-CoV-2 may be directly or indirectly associated with diabetes. “It is currently the subject of debate whether it may be a direct effect, infecting or directly reaching the pancreatic beta cells, or whether this involvement is a result of the effect of the infection at systemic level, in the context of the cytokine storm and the proinflammatory environment derived from it. Our current challenge is to confirm whether this virus can really replicate in pancreatic beta cells and to assess the possible existence of reinfections, among other aspects,” said Dr. Kleger.
Along with these “developing areas of knowledge,” there are several certainties regarding the link between diabetes and COVID-19. Dr. Kleger summarized the most relevant one. “Preexisting diabetes is known to be a highly prevalent comorbidity seen in 11%-22% of patients and increases the risk of severe disease and mortality.
“SARS-CoV-2 infection has also been shown to affect the exocrine pancreas, manifesting as pancreatitis in 5% of critically ill patients with COVID-19, as well as enlargement of the pancreas and abnormal levels of amylase or lipase in 7.5%-17% of patients.
“Furthermore, it is obvious that SARS-CoV-2 infection produces glycometabolic dysfunction in these patients, with increased hyperglycemia in people with type 2 diabetes and ketoacidosis in 2%-6.4% of patients with and without diabetes.”
After recovery
The most recent research reveals the persistence of this dysregulation long after recovery from COVID-19. “We’ve seen that in a significant proportion of patients, hyperglycemia is maintained for some time; in the specific case of hospitalized patients [without the need for assisted ventilation or other intensive care requirements], for up to more than 2 months after overcoming the illness.
“In the same way, there are studies that have shown that insulin resistance and hyperstimulation of pancreatic beta cells remain at pathological levels in the post–COVID-19 phase. And in line with increased insulin resistance, signs of hyperinflammation have also been detected in these patients.”
Dr. Kleger noted that another research area is the increased incidence of newly diagnosed diabetes after recovery from SARS-CoV-2 infection, “something that seems to be correlated with how severely the disease has been experienced and also depending on whether hospitalization or intensive care was needed. Likewise, retrospective studies have shown that the risk of developing type 2 diabetes is higher in COVID-19 patients, compared with those with other respiratory infections. Regarding the incidence of type 1 diabetes, there is evidence, particularly in the case of children, of a clear correlation between the pandemic waves and the increase in cases.
“Therefore, and in view of this data, we could say that, with regard to the involvement of SARS-CoV-2 in pancreatic beta cells, something is up, but we are not yet able to fully understand what it is. What can be confirmed based on the numerous studies carried out in this regard is that COVID-19 produces a metabolic dysregulation [hyperglycemia, insulin resistance, diabetic ketoacidosis] which in turn favors the development of diabetes in patients with no history of this disease,” said Dr. Kleger.
“Likewise, everything points to the existence of a definitively feasible infection in pancreatic beta cells associated with SARS-CoV-2, but there are still unknown aspects of the physiology that explain this effect that remain the subject of debate and deserve future studies,” he concluded.
Consequences of the pandemic
The experts agreed that, although COVID-19 is no longer at the center of specialist care, it is still a subject of investigation. On the conference’s opening day, an update was made on the approach to diabetes.
Care activity is gradually recovering as the time that professionals devote to COVID-19 care is reduced, “but it will take time to catch up with the care activities not carried out during the pandemic, and, unfortunately, in the coming years, we will see the repercussion of the lack or reduction of care during these years,” stressed the SED chair, Antonio Pérez Pérez, MD, director of endocrinology and nutrition of Hospital de la Santa Creu i Sant Pau, Barcelona.
Dr. Pérez stressed that the pandemic has revealed health system deficiencies in diabetes care. He added that the impact of COVID-19 on diabetes (resulting from the effects of the infection itself or from the inadequacy of prevention, diagnosis, and treatment measures) fostered a deterioration of metabolic control and a delay in the diagnosis of the disease and its complications.
“All this contributes to the fact that we currently continue to see patients with complications, especially in the case of type 2 diabetes, with more serious decompensations and diagnoses in more advanced stages of the disease. This impact has been more significant in older people from disadvantaged areas and with less capacity for self-monitoring and self-adjustment of treatment,” he added.
Describing lessons learned through the experiences accumulated in diabetes care during the pandemic, Dr. Pérez highlighted the push for virtual consultations, accessibility to drugs prescribed in electronic prescriptions, and the use of educational resources online and of telemedicine tools. “The need to invest in the health sector has also been assumed, endowing it with robustness in well-trained health personnel, to promote health education, boost efficient health organization, and invest in innovation aimed at facilitating care.”
Dr. Kleger and Dr. Pérez disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from the Medscape Spanish edition.
MADRID – It involves the relationship between COVID-19 and new diagnoses of diabetes and blood glucose disorders, among others, in the post–COVID-19 period. These topics were addressed at the XXXIII National Congress of the Spanish Diabetes Society. They were also the central theme of the inaugural conference, Pancreatic Involvement During COVID-19: From Preclinical Studies to Clinical Relevance, which was led by Alexander Kleger, MD, PhD, head of the department of pancreatology at the Ulm (Germany) University Clinic for Internal Medicine.
The chair of the scientific committee of the congress, Franz Martín, MD, launched the conference by noting that the work of Dr. Kleger and his team has made it possible to ascertain that SARS-CoV-2 can infect pancreatic beta cells that produce insulin. This observation may help in understanding why patients with COVID-19 sometimes experience symptoms related to greater difficulty regulating blood glucose.
“In addition, the German expert and his group have described the abnormalities that occur in beta cells when they are infected by SARS-CoV-2, something especially important, given that knowledge of these abnormalities may be of great importance to understanding the possible appearance of more cases of diabetes in the future,” Dr. Martín added.
“Our data identify the human pancreas as a target of SARS-CoV-2 infection and suggest that pancreatic beta cell involvement could contribute to the metabolic dysregulation seen in COVID-19 patients,” Dr. Kleger pointed out.
In his speech, Dr. Kleger reviewed the evidence on the effects of SARS-CoV-2 that has been garnered since the start of the pandemic, and he presented his research group’s findings on the impact at the pancreatic level.
“Since March 2020, it has been seen that COVID-19 affected the pancreas, and studies published in August of that same year clearly spoke of both a worsening of diabetes and an increase in new cases of this disease diagnosed after SARS-CoV-2 infection. Also, the data showed how hospitalized patients with no previous history of diabetes experienced rapid increases in glucose levels 5 days after admission,” Dr. Kleger said.
Angiotensin-converting enzyme 2
As an example of the pace at which evidence on the pancreatic impact of this virus has been evolving, Dr. Kleger referred to early studies that found no angiotensin-converting enzyme 2 receptor on cells of the endocrine and exocrine pancreas. “To our surprise, in our work, we did observe the obvious presence of angiotensin-converting enzyme 2 specifically expressed in human pancreatic beta cells, something confirmed by other investigations. Another surprising aspect was verifying that the viral infection lasts longer in the pancreas than in the lungs,” said the expert.
These findings caused the researchers to realize that SARS-CoV-2 may be directly or indirectly associated with diabetes. “It is currently the subject of debate whether it may be a direct effect, infecting or directly reaching the pancreatic beta cells, or whether this involvement is a result of the effect of the infection at systemic level, in the context of the cytokine storm and the proinflammatory environment derived from it. Our current challenge is to confirm whether this virus can really replicate in pancreatic beta cells and to assess the possible existence of reinfections, among other aspects,” said Dr. Kleger.
Along with these “developing areas of knowledge,” there are several certainties regarding the link between diabetes and COVID-19. Dr. Kleger summarized the most relevant one. “Preexisting diabetes is known to be a highly prevalent comorbidity seen in 11%-22% of patients and increases the risk of severe disease and mortality.
“SARS-CoV-2 infection has also been shown to affect the exocrine pancreas, manifesting as pancreatitis in 5% of critically ill patients with COVID-19, as well as enlargement of the pancreas and abnormal levels of amylase or lipase in 7.5%-17% of patients.
“Furthermore, it is obvious that SARS-CoV-2 infection produces glycometabolic dysfunction in these patients, with increased hyperglycemia in people with type 2 diabetes and ketoacidosis in 2%-6.4% of patients with and without diabetes.”
After recovery
The most recent research reveals the persistence of this dysregulation long after recovery from COVID-19. “We’ve seen that in a significant proportion of patients, hyperglycemia is maintained for some time; in the specific case of hospitalized patients [without the need for assisted ventilation or other intensive care requirements], for up to more than 2 months after overcoming the illness.
“In the same way, there are studies that have shown that insulin resistance and hyperstimulation of pancreatic beta cells remain at pathological levels in the post–COVID-19 phase. And in line with increased insulin resistance, signs of hyperinflammation have also been detected in these patients.”
Dr. Kleger noted that another research area is the increased incidence of newly diagnosed diabetes after recovery from SARS-CoV-2 infection, “something that seems to be correlated with how severely the disease has been experienced and also depending on whether hospitalization or intensive care was needed. Likewise, retrospective studies have shown that the risk of developing type 2 diabetes is higher in COVID-19 patients, compared with those with other respiratory infections. Regarding the incidence of type 1 diabetes, there is evidence, particularly in the case of children, of a clear correlation between the pandemic waves and the increase in cases.
“Therefore, and in view of this data, we could say that, with regard to the involvement of SARS-CoV-2 in pancreatic beta cells, something is up, but we are not yet able to fully understand what it is. What can be confirmed based on the numerous studies carried out in this regard is that COVID-19 produces a metabolic dysregulation [hyperglycemia, insulin resistance, diabetic ketoacidosis] which in turn favors the development of diabetes in patients with no history of this disease,” said Dr. Kleger.
“Likewise, everything points to the existence of a definitively feasible infection in pancreatic beta cells associated with SARS-CoV-2, but there are still unknown aspects of the physiology that explain this effect that remain the subject of debate and deserve future studies,” he concluded.
Consequences of the pandemic
The experts agreed that, although COVID-19 is no longer at the center of specialist care, it is still a subject of investigation. On the conference’s opening day, an update was made on the approach to diabetes.
Care activity is gradually recovering as the time that professionals devote to COVID-19 care is reduced, “but it will take time to catch up with the care activities not carried out during the pandemic, and, unfortunately, in the coming years, we will see the repercussion of the lack or reduction of care during these years,” stressed the SED chair, Antonio Pérez Pérez, MD, director of endocrinology and nutrition of Hospital de la Santa Creu i Sant Pau, Barcelona.
Dr. Pérez stressed that the pandemic has revealed health system deficiencies in diabetes care. He added that the impact of COVID-19 on diabetes (resulting from the effects of the infection itself or from the inadequacy of prevention, diagnosis, and treatment measures) fostered a deterioration of metabolic control and a delay in the diagnosis of the disease and its complications.
“All this contributes to the fact that we currently continue to see patients with complications, especially in the case of type 2 diabetes, with more serious decompensations and diagnoses in more advanced stages of the disease. This impact has been more significant in older people from disadvantaged areas and with less capacity for self-monitoring and self-adjustment of treatment,” he added.
Describing lessons learned through the experiences accumulated in diabetes care during the pandemic, Dr. Pérez highlighted the push for virtual consultations, accessibility to drugs prescribed in electronic prescriptions, and the use of educational resources online and of telemedicine tools. “The need to invest in the health sector has also been assumed, endowing it with robustness in well-trained health personnel, to promote health education, boost efficient health organization, and invest in innovation aimed at facilitating care.”
Dr. Kleger and Dr. Pérez disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from the Medscape Spanish edition.
MADRID – It involves the relationship between COVID-19 and new diagnoses of diabetes and blood glucose disorders, among others, in the post–COVID-19 period. These topics were addressed at the XXXIII National Congress of the Spanish Diabetes Society. They were also the central theme of the inaugural conference, Pancreatic Involvement During COVID-19: From Preclinical Studies to Clinical Relevance, which was led by Alexander Kleger, MD, PhD, head of the department of pancreatology at the Ulm (Germany) University Clinic for Internal Medicine.
The chair of the scientific committee of the congress, Franz Martín, MD, launched the conference by noting that the work of Dr. Kleger and his team has made it possible to ascertain that SARS-CoV-2 can infect pancreatic beta cells that produce insulin. This observation may help in understanding why patients with COVID-19 sometimes experience symptoms related to greater difficulty regulating blood glucose.
“In addition, the German expert and his group have described the abnormalities that occur in beta cells when they are infected by SARS-CoV-2, something especially important, given that knowledge of these abnormalities may be of great importance to understanding the possible appearance of more cases of diabetes in the future,” Dr. Martín added.
“Our data identify the human pancreas as a target of SARS-CoV-2 infection and suggest that pancreatic beta cell involvement could contribute to the metabolic dysregulation seen in COVID-19 patients,” Dr. Kleger pointed out.
In his speech, Dr. Kleger reviewed the evidence on the effects of SARS-CoV-2 that has been garnered since the start of the pandemic, and he presented his research group’s findings on the impact at the pancreatic level.
“Since March 2020, it has been seen that COVID-19 affected the pancreas, and studies published in August of that same year clearly spoke of both a worsening of diabetes and an increase in new cases of this disease diagnosed after SARS-CoV-2 infection. Also, the data showed how hospitalized patients with no previous history of diabetes experienced rapid increases in glucose levels 5 days after admission,” Dr. Kleger said.
Angiotensin-converting enzyme 2
As an example of the pace at which evidence on the pancreatic impact of this virus has been evolving, Dr. Kleger referred to early studies that found no angiotensin-converting enzyme 2 receptor on cells of the endocrine and exocrine pancreas. “To our surprise, in our work, we did observe the obvious presence of angiotensin-converting enzyme 2 specifically expressed in human pancreatic beta cells, something confirmed by other investigations. Another surprising aspect was verifying that the viral infection lasts longer in the pancreas than in the lungs,” said the expert.
These findings caused the researchers to realize that SARS-CoV-2 may be directly or indirectly associated with diabetes. “It is currently the subject of debate whether it may be a direct effect, infecting or directly reaching the pancreatic beta cells, or whether this involvement is a result of the effect of the infection at systemic level, in the context of the cytokine storm and the proinflammatory environment derived from it. Our current challenge is to confirm whether this virus can really replicate in pancreatic beta cells and to assess the possible existence of reinfections, among other aspects,” said Dr. Kleger.
Along with these “developing areas of knowledge,” there are several certainties regarding the link between diabetes and COVID-19. Dr. Kleger summarized the most relevant one. “Preexisting diabetes is known to be a highly prevalent comorbidity seen in 11%-22% of patients and increases the risk of severe disease and mortality.
“SARS-CoV-2 infection has also been shown to affect the exocrine pancreas, manifesting as pancreatitis in 5% of critically ill patients with COVID-19, as well as enlargement of the pancreas and abnormal levels of amylase or lipase in 7.5%-17% of patients.
“Furthermore, it is obvious that SARS-CoV-2 infection produces glycometabolic dysfunction in these patients, with increased hyperglycemia in people with type 2 diabetes and ketoacidosis in 2%-6.4% of patients with and without diabetes.”
After recovery
The most recent research reveals the persistence of this dysregulation long after recovery from COVID-19. “We’ve seen that in a significant proportion of patients, hyperglycemia is maintained for some time; in the specific case of hospitalized patients [without the need for assisted ventilation or other intensive care requirements], for up to more than 2 months after overcoming the illness.
“In the same way, there are studies that have shown that insulin resistance and hyperstimulation of pancreatic beta cells remain at pathological levels in the post–COVID-19 phase. And in line with increased insulin resistance, signs of hyperinflammation have also been detected in these patients.”
Dr. Kleger noted that another research area is the increased incidence of newly diagnosed diabetes after recovery from SARS-CoV-2 infection, “something that seems to be correlated with how severely the disease has been experienced and also depending on whether hospitalization or intensive care was needed. Likewise, retrospective studies have shown that the risk of developing type 2 diabetes is higher in COVID-19 patients, compared with those with other respiratory infections. Regarding the incidence of type 1 diabetes, there is evidence, particularly in the case of children, of a clear correlation between the pandemic waves and the increase in cases.
“Therefore, and in view of this data, we could say that, with regard to the involvement of SARS-CoV-2 in pancreatic beta cells, something is up, but we are not yet able to fully understand what it is. What can be confirmed based on the numerous studies carried out in this regard is that COVID-19 produces a metabolic dysregulation [hyperglycemia, insulin resistance, diabetic ketoacidosis] which in turn favors the development of diabetes in patients with no history of this disease,” said Dr. Kleger.
“Likewise, everything points to the existence of a definitively feasible infection in pancreatic beta cells associated with SARS-CoV-2, but there are still unknown aspects of the physiology that explain this effect that remain the subject of debate and deserve future studies,” he concluded.
Consequences of the pandemic
The experts agreed that, although COVID-19 is no longer at the center of specialist care, it is still a subject of investigation. On the conference’s opening day, an update was made on the approach to diabetes.
Care activity is gradually recovering as the time that professionals devote to COVID-19 care is reduced, “but it will take time to catch up with the care activities not carried out during the pandemic, and, unfortunately, in the coming years, we will see the repercussion of the lack or reduction of care during these years,” stressed the SED chair, Antonio Pérez Pérez, MD, director of endocrinology and nutrition of Hospital de la Santa Creu i Sant Pau, Barcelona.
Dr. Pérez stressed that the pandemic has revealed health system deficiencies in diabetes care. He added that the impact of COVID-19 on diabetes (resulting from the effects of the infection itself or from the inadequacy of prevention, diagnosis, and treatment measures) fostered a deterioration of metabolic control and a delay in the diagnosis of the disease and its complications.
“All this contributes to the fact that we currently continue to see patients with complications, especially in the case of type 2 diabetes, with more serious decompensations and diagnoses in more advanced stages of the disease. This impact has been more significant in older people from disadvantaged areas and with less capacity for self-monitoring and self-adjustment of treatment,” he added.
Describing lessons learned through the experiences accumulated in diabetes care during the pandemic, Dr. Pérez highlighted the push for virtual consultations, accessibility to drugs prescribed in electronic prescriptions, and the use of educational resources online and of telemedicine tools. “The need to invest in the health sector has also been assumed, endowing it with robustness in well-trained health personnel, to promote health education, boost efficient health organization, and invest in innovation aimed at facilitating care.”
Dr. Kleger and Dr. Pérez disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com. This article was translated from the Medscape Spanish edition.
AUA 2022: A report from the trenches
The annual meeting of the American Urological Association took place recently at the Ernest N. Morial Convention Center in New Orleans. Hundreds of talks and abstracts were presented over the 4 days in New Orleans; below is a summary of what I found to be the key scientific highlights.
1. Updates to the AUA’s guidelines for management of localized kidney cancer
The AUA’s recommendations for the treatment of localized kidney cancer have changed dramatically over the past few decades. Gone are the days of simply removing the entire kidney every time a mass is found. Today, a partial nephrectomy is preferred in most situations.
Our understanding that the prevalence of familial kidney cancer is much higher than previously thought has led to a change in the guidelines regarding which patients should receive genetic counseling. For the first time, the guidelines include the use of adjuvant medical treatment, such as pembrolizumab. A 2021 study in the New England Journal of Medicine showed a survival benefit for patients with high-risk disease who receive such therapies, so it›s not surprising that such treatments are now recommended.
The development of new second- and third-generation gadolinium contrast agents that spare the kidneys has dramatically increased the role for MRIs for patients with severe or even end-stage renal disease. As a result, the guidelines were updated to recommend the use of these agents. The role of a renal biopsy, which has always been limited, given the ability of cross-sectional imaging to diagnosis this disease, has further been constrained and should now be performed only when the results would clearly change a clinical decision, such as whether or not the lesion in question is a metastasis.
2. New and better ureteroscope technology
No one likes kidney stones, not the patient who deals with the incredible pain, nor the surgeon who has to remove them, given that these cases often present in the wee hours of the morning. The preferred surgical approach has changed dramatically over the past decade, moving away from extracorporeal shockwave lithotripsy toward flexible ureteroscope-based technology, which has a higher clearance rate and is more widely and more immediately available. Flexible ureteroscopy has been held back by technological barriers, including limited scope deflection and low laser power. The exceptionally high cost of repair and the tendency of the instruments to break haven’t helped, either. Although single-use ureteroscopes have been available for some time, it wasn’t until the recently introduced second-generation scopes became widely available that they have become popular. These new scopes have small external diameters, great optics, and can easily be used. Newer high-powered lasers and the change from holmium:YAG-based lasers to thulium technology is greatly increasing the size of stones that can be safely addressed ureteroscopically. The cost analysis of single-use technology versus reusable scopes tends to be site dependent but can be appealing in certain situations. Also, on the technology forefront, a new robotically assisted ureteroscope is being introduced that offers the chance for improved intrapelvic mobility and better ergonomics for the surgeon.
3. New options for the treatment of clinically localized prostate cancer
Since the guidelines were last updated in 2017, the definitive management of localized prostate cancer has changed dramatically. Although radical prostatectomy and radiotherapy remain the preferred options for men who choose treatment for their disease, the updated guidelines state that active surveillance is now the preferred approach for men with low-risk cancers.
Although the preferred surveillance protocol is still being debated, the consensus is that almost all men with low-risk disease can be safely monitored for some period. The imaging technology available to monitor patients is also radically changing with the rollout of prostate-specific membrane antigen–based PET technology. The increased sensitivity and specificity of this modality opens the door not only for better up-front staging of newly diagnosed patients with prostate cancer but also may allow clinicians to earlier identify and treat men with metastatic disease. The guidelines for the first time address the use of genetic markers to individualize treatment of men with advanced or metastatic prostate cancer. Exactly which treatments these patients need is still being debated, but the ability to use patient-specific genetic mutation information to customize treatment is potentially groundbreaking.
4. New treatment options for patients with high-grade non–muscle-invasive bladder cancer (NMIBC) refractory to bacille Calmette-Guérin (BCG) therapy
Patients with NMIBC who do not respond to BCG therapy are in a tough position. Cystectomy remains the preferred option as a second-line strategy, but the procedure has a complication rate approaching 30%. Further, many patients are not willing to have their bladder removed because of the life-altering changes that go along with having an urostomy or a neobladder. While intravesical treatments such as valrubicin, docetaxel, or gemcitabine have been available for many years, the success rates of those options are limited. The Food and Drug Administration recently approved the use of the immunotherapy-based treatment pembrolizumab. While none of these options is perfect, the fact that we now have at least some alternatives is a huge step in the right direction.
5. It’s all about the patient: Involving patients in designing the health care delivery system
Although it seems like an obvious concept, patients themselves have traditionally not been involved in designing the health care delivery system on which they rely. Research presented at the AUA shows that many health care outcomes improve when patients are actively involved in the process. For example, Angela Smith, MD, of the University of North Carolina at Chapel Hill, presented a study showing that including patients in the identification of possible research topics helps them feel engaged and more likely to participate in studies. Patients who are involved in advisory councils at the local hospital level are more likely to report having received high-quality care. And surveying patients on the goals of national health care policy helps them feel that the outcomes are more equitable.
As a small-town urologist who spends his days in the trenches of urology, I think the next time my group considers participating in new cancer research, I may talk to the local cancer support group first. If Dr. Smith’s data are correct, not only would our patients be better served, but we would also have an easier time filling the trial!
The 2023 AUA conference is going to be held in Chicago next spring. I hope to see you there!
A version of this article first appeared on Medscape.com.
The annual meeting of the American Urological Association took place recently at the Ernest N. Morial Convention Center in New Orleans. Hundreds of talks and abstracts were presented over the 4 days in New Orleans; below is a summary of what I found to be the key scientific highlights.
1. Updates to the AUA’s guidelines for management of localized kidney cancer
The AUA’s recommendations for the treatment of localized kidney cancer have changed dramatically over the past few decades. Gone are the days of simply removing the entire kidney every time a mass is found. Today, a partial nephrectomy is preferred in most situations.
Our understanding that the prevalence of familial kidney cancer is much higher than previously thought has led to a change in the guidelines regarding which patients should receive genetic counseling. For the first time, the guidelines include the use of adjuvant medical treatment, such as pembrolizumab. A 2021 study in the New England Journal of Medicine showed a survival benefit for patients with high-risk disease who receive such therapies, so it›s not surprising that such treatments are now recommended.
The development of new second- and third-generation gadolinium contrast agents that spare the kidneys has dramatically increased the role for MRIs for patients with severe or even end-stage renal disease. As a result, the guidelines were updated to recommend the use of these agents. The role of a renal biopsy, which has always been limited, given the ability of cross-sectional imaging to diagnosis this disease, has further been constrained and should now be performed only when the results would clearly change a clinical decision, such as whether or not the lesion in question is a metastasis.
2. New and better ureteroscope technology
No one likes kidney stones, not the patient who deals with the incredible pain, nor the surgeon who has to remove them, given that these cases often present in the wee hours of the morning. The preferred surgical approach has changed dramatically over the past decade, moving away from extracorporeal shockwave lithotripsy toward flexible ureteroscope-based technology, which has a higher clearance rate and is more widely and more immediately available. Flexible ureteroscopy has been held back by technological barriers, including limited scope deflection and low laser power. The exceptionally high cost of repair and the tendency of the instruments to break haven’t helped, either. Although single-use ureteroscopes have been available for some time, it wasn’t until the recently introduced second-generation scopes became widely available that they have become popular. These new scopes have small external diameters, great optics, and can easily be used. Newer high-powered lasers and the change from holmium:YAG-based lasers to thulium technology is greatly increasing the size of stones that can be safely addressed ureteroscopically. The cost analysis of single-use technology versus reusable scopes tends to be site dependent but can be appealing in certain situations. Also, on the technology forefront, a new robotically assisted ureteroscope is being introduced that offers the chance for improved intrapelvic mobility and better ergonomics for the surgeon.
3. New options for the treatment of clinically localized prostate cancer
Since the guidelines were last updated in 2017, the definitive management of localized prostate cancer has changed dramatically. Although radical prostatectomy and radiotherapy remain the preferred options for men who choose treatment for their disease, the updated guidelines state that active surveillance is now the preferred approach for men with low-risk cancers.
Although the preferred surveillance protocol is still being debated, the consensus is that almost all men with low-risk disease can be safely monitored for some period. The imaging technology available to monitor patients is also radically changing with the rollout of prostate-specific membrane antigen–based PET technology. The increased sensitivity and specificity of this modality opens the door not only for better up-front staging of newly diagnosed patients with prostate cancer but also may allow clinicians to earlier identify and treat men with metastatic disease. The guidelines for the first time address the use of genetic markers to individualize treatment of men with advanced or metastatic prostate cancer. Exactly which treatments these patients need is still being debated, but the ability to use patient-specific genetic mutation information to customize treatment is potentially groundbreaking.
4. New treatment options for patients with high-grade non–muscle-invasive bladder cancer (NMIBC) refractory to bacille Calmette-Guérin (BCG) therapy
Patients with NMIBC who do not respond to BCG therapy are in a tough position. Cystectomy remains the preferred option as a second-line strategy, but the procedure has a complication rate approaching 30%. Further, many patients are not willing to have their bladder removed because of the life-altering changes that go along with having an urostomy or a neobladder. While intravesical treatments such as valrubicin, docetaxel, or gemcitabine have been available for many years, the success rates of those options are limited. The Food and Drug Administration recently approved the use of the immunotherapy-based treatment pembrolizumab. While none of these options is perfect, the fact that we now have at least some alternatives is a huge step in the right direction.
5. It’s all about the patient: Involving patients in designing the health care delivery system
Although it seems like an obvious concept, patients themselves have traditionally not been involved in designing the health care delivery system on which they rely. Research presented at the AUA shows that many health care outcomes improve when patients are actively involved in the process. For example, Angela Smith, MD, of the University of North Carolina at Chapel Hill, presented a study showing that including patients in the identification of possible research topics helps them feel engaged and more likely to participate in studies. Patients who are involved in advisory councils at the local hospital level are more likely to report having received high-quality care. And surveying patients on the goals of national health care policy helps them feel that the outcomes are more equitable.
As a small-town urologist who spends his days in the trenches of urology, I think the next time my group considers participating in new cancer research, I may talk to the local cancer support group first. If Dr. Smith’s data are correct, not only would our patients be better served, but we would also have an easier time filling the trial!
The 2023 AUA conference is going to be held in Chicago next spring. I hope to see you there!
A version of this article first appeared on Medscape.com.
The annual meeting of the American Urological Association took place recently at the Ernest N. Morial Convention Center in New Orleans. Hundreds of talks and abstracts were presented over the 4 days in New Orleans; below is a summary of what I found to be the key scientific highlights.
1. Updates to the AUA’s guidelines for management of localized kidney cancer
The AUA’s recommendations for the treatment of localized kidney cancer have changed dramatically over the past few decades. Gone are the days of simply removing the entire kidney every time a mass is found. Today, a partial nephrectomy is preferred in most situations.
Our understanding that the prevalence of familial kidney cancer is much higher than previously thought has led to a change in the guidelines regarding which patients should receive genetic counseling. For the first time, the guidelines include the use of adjuvant medical treatment, such as pembrolizumab. A 2021 study in the New England Journal of Medicine showed a survival benefit for patients with high-risk disease who receive such therapies, so it›s not surprising that such treatments are now recommended.
The development of new second- and third-generation gadolinium contrast agents that spare the kidneys has dramatically increased the role for MRIs for patients with severe or even end-stage renal disease. As a result, the guidelines were updated to recommend the use of these agents. The role of a renal biopsy, which has always been limited, given the ability of cross-sectional imaging to diagnosis this disease, has further been constrained and should now be performed only when the results would clearly change a clinical decision, such as whether or not the lesion in question is a metastasis.
2. New and better ureteroscope technology
No one likes kidney stones, not the patient who deals with the incredible pain, nor the surgeon who has to remove them, given that these cases often present in the wee hours of the morning. The preferred surgical approach has changed dramatically over the past decade, moving away from extracorporeal shockwave lithotripsy toward flexible ureteroscope-based technology, which has a higher clearance rate and is more widely and more immediately available. Flexible ureteroscopy has been held back by technological barriers, including limited scope deflection and low laser power. The exceptionally high cost of repair and the tendency of the instruments to break haven’t helped, either. Although single-use ureteroscopes have been available for some time, it wasn’t until the recently introduced second-generation scopes became widely available that they have become popular. These new scopes have small external diameters, great optics, and can easily be used. Newer high-powered lasers and the change from holmium:YAG-based lasers to thulium technology is greatly increasing the size of stones that can be safely addressed ureteroscopically. The cost analysis of single-use technology versus reusable scopes tends to be site dependent but can be appealing in certain situations. Also, on the technology forefront, a new robotically assisted ureteroscope is being introduced that offers the chance for improved intrapelvic mobility and better ergonomics for the surgeon.
3. New options for the treatment of clinically localized prostate cancer
Since the guidelines were last updated in 2017, the definitive management of localized prostate cancer has changed dramatically. Although radical prostatectomy and radiotherapy remain the preferred options for men who choose treatment for their disease, the updated guidelines state that active surveillance is now the preferred approach for men with low-risk cancers.
Although the preferred surveillance protocol is still being debated, the consensus is that almost all men with low-risk disease can be safely monitored for some period. The imaging technology available to monitor patients is also radically changing with the rollout of prostate-specific membrane antigen–based PET technology. The increased sensitivity and specificity of this modality opens the door not only for better up-front staging of newly diagnosed patients with prostate cancer but also may allow clinicians to earlier identify and treat men with metastatic disease. The guidelines for the first time address the use of genetic markers to individualize treatment of men with advanced or metastatic prostate cancer. Exactly which treatments these patients need is still being debated, but the ability to use patient-specific genetic mutation information to customize treatment is potentially groundbreaking.
4. New treatment options for patients with high-grade non–muscle-invasive bladder cancer (NMIBC) refractory to bacille Calmette-Guérin (BCG) therapy
Patients with NMIBC who do not respond to BCG therapy are in a tough position. Cystectomy remains the preferred option as a second-line strategy, but the procedure has a complication rate approaching 30%. Further, many patients are not willing to have their bladder removed because of the life-altering changes that go along with having an urostomy or a neobladder. While intravesical treatments such as valrubicin, docetaxel, or gemcitabine have been available for many years, the success rates of those options are limited. The Food and Drug Administration recently approved the use of the immunotherapy-based treatment pembrolizumab. While none of these options is perfect, the fact that we now have at least some alternatives is a huge step in the right direction.
5. It’s all about the patient: Involving patients in designing the health care delivery system
Although it seems like an obvious concept, patients themselves have traditionally not been involved in designing the health care delivery system on which they rely. Research presented at the AUA shows that many health care outcomes improve when patients are actively involved in the process. For example, Angela Smith, MD, of the University of North Carolina at Chapel Hill, presented a study showing that including patients in the identification of possible research topics helps them feel engaged and more likely to participate in studies. Patients who are involved in advisory councils at the local hospital level are more likely to report having received high-quality care. And surveying patients on the goals of national health care policy helps them feel that the outcomes are more equitable.
As a small-town urologist who spends his days in the trenches of urology, I think the next time my group considers participating in new cancer research, I may talk to the local cancer support group first. If Dr. Smith’s data are correct, not only would our patients be better served, but we would also have an easier time filling the trial!
The 2023 AUA conference is going to be held in Chicago next spring. I hope to see you there!
A version of this article first appeared on Medscape.com.
FROM AUA 2022
Updated AHA/ASA guideline changes care for spontaneous intracerebral hemorrhage
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
NAVIGATOR steers uncontrolled asthma toward calmer seas
SAN FRANCISCO – Nearly half of all patients with severe, uncontrolled asthma who received a full course of the biologic agent tezepelumab (Tezspire) in the NAVIGATOR trial had a complete response to treatment at 1 year, results of a prespecified exploratory analysis indicated.
Among 471 patients assigned to tezepelumab who completed the on-treatment period of the phase 3 randomized trial, 46% had a complete response at 52 weeks, compared with 24% of patients assigned to placebo.
Complete response was defined as reduction in exacerbations of at least 50% over the previous year, improvement from baseline in Asthma Control Questionnaire 6 (ACQ-6) total score of at least 0.5 points, improvement in prebronchodilator forced expiratory volume in 1 second (pre-BD FEV1), and physician-assessed Clinical Global Impression measure of clinical change (CGI-C) score.
“These data further support the efficacy of tezepelumab in a broad population of patients with severe, uncontrolled asthma,” said Njira Lugogo, MD, of the division of pulmonary and critical care medicine at the University of Michigan, Ann Arbor.
Dr. Lugogo presented results of the exploratory analysis at the American Thoracic Society’s international conference.
Exacerbations reduced, lung function improved
Primary results from NAVIGATOR, published in The New England Journal of Medicine, showed that patients with severe, uncontrolled asthma randomly assigned to tezepelumab had fewer exacerbations and better lung function, asthma control, and health-related quality of life compared with patients assigned to placebo.
The investigators noted that approximately 10% of patients with asthma have symptoms and exacerbations despite maximal standard-of-care controller therapy.
Tezepelumab is a human monoclonal antibody that inhibits action of thymic stromal lymphopoietin (TSLP), an epithelial cytokine that is released in response to airborne triggers of asthma. TSLP is a major contributor to initiation and persistence of airway inflammation, Dr. Lugogo said.
The on-treatment analysis looked at all patients in the trial who completed 52 weeks of treatment and had complete data for all criteria studied.
The odds ratios (OR) for patients on tezepelumab achieving each of the response criteria are shown in the table.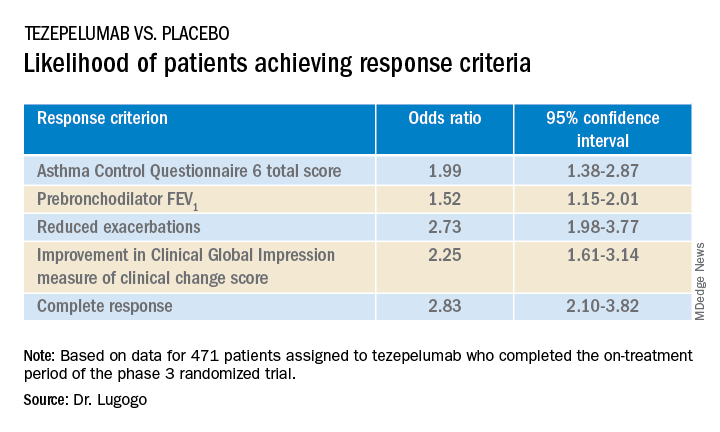
Exacerbations explored
In a separate presentation, Christopher S. Ambrose, MD, MBA, of AstraZeneca in Gaithersburg, Md., presented information from investigator-narrative descriptions of all hospitalization events related to asthma exacerbations (mild, moderate, or severe) that occurred while the investigator was blinded to each patient’s treatment assignment in NAVIGATOR.
In all, 39 of 531 patients (7.3%) assigned to placebo had a total of 78 exacerbations requiring hospitalization, compared with 13 of 528 patients (2.5%) assigned to tezepelumab. The latter group had a total of 14 exacerbations requiring hospitalization during the study.
Among hospitalized patients, 32 of the 39 assigned to placebo had severe, incapacitating exacerbations, compared with 5 of 13 assigned to tezepelumab.
Reported symptoms were generally similar between hospitalized patients in the two treatment groups, although there appeared to be trends toward lower incidence of dyspnea, fever, and tachycardia with tezepelumab.
Health care resource utilization, a surrogate marker for disease burden, was substantially lower for patients assigned to tezepelumab.
Infections were the most common triggers of exacerbations in both groups.
“These data provide further evidence that tezepelumab can reduce the burden of disease of severe uncontrolled asthma, both to patients and to health care systems,” Dr. Ambrose said.
Head-to-head studies needed
Although there have been no head-to-head comparisons of biologic agents for asthma to date, results of these studies suggest that tezepelumab has efficacy similar to that of other agents for reducing exacerbation, said Fernando Holguin, MD, MPH, from the University of Colorado at Denver, Aurora, who comoderated the oral session where the data were presented but was not involved in the study.
Biologic agents appear to be slightly more effective against type 2 inflammation in asthma, “but in general I think we give it to a broader severe population, so that’s exciting,” he told this news organization.
Comoderator Amisha Barochia, MBBS, MHS, of the National Institutes of Health, Bethesda, Md., told this news organization that head-to-head trials of biologic agents would provide important clinical information going forward.
“Should we switch to a different biologic or add a second biologic? Those are questions we need answers for,” she said.
The NAVIGATOR trial is funded by AstraZeneca and Amgen. Dr. Lugogo disclosed financial relationships with both companies. Dr. Holguin and Dr. Barochia have disclosed no financial relationships relevant to the studies presented.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – Nearly half of all patients with severe, uncontrolled asthma who received a full course of the biologic agent tezepelumab (Tezspire) in the NAVIGATOR trial had a complete response to treatment at 1 year, results of a prespecified exploratory analysis indicated.
Among 471 patients assigned to tezepelumab who completed the on-treatment period of the phase 3 randomized trial, 46% had a complete response at 52 weeks, compared with 24% of patients assigned to placebo.
Complete response was defined as reduction in exacerbations of at least 50% over the previous year, improvement from baseline in Asthma Control Questionnaire 6 (ACQ-6) total score of at least 0.5 points, improvement in prebronchodilator forced expiratory volume in 1 second (pre-BD FEV1), and physician-assessed Clinical Global Impression measure of clinical change (CGI-C) score.
“These data further support the efficacy of tezepelumab in a broad population of patients with severe, uncontrolled asthma,” said Njira Lugogo, MD, of the division of pulmonary and critical care medicine at the University of Michigan, Ann Arbor.
Dr. Lugogo presented results of the exploratory analysis at the American Thoracic Society’s international conference.
Exacerbations reduced, lung function improved
Primary results from NAVIGATOR, published in The New England Journal of Medicine, showed that patients with severe, uncontrolled asthma randomly assigned to tezepelumab had fewer exacerbations and better lung function, asthma control, and health-related quality of life compared with patients assigned to placebo.
The investigators noted that approximately 10% of patients with asthma have symptoms and exacerbations despite maximal standard-of-care controller therapy.
Tezepelumab is a human monoclonal antibody that inhibits action of thymic stromal lymphopoietin (TSLP), an epithelial cytokine that is released in response to airborne triggers of asthma. TSLP is a major contributor to initiation and persistence of airway inflammation, Dr. Lugogo said.
The on-treatment analysis looked at all patients in the trial who completed 52 weeks of treatment and had complete data for all criteria studied.
The odds ratios (OR) for patients on tezepelumab achieving each of the response criteria are shown in the table.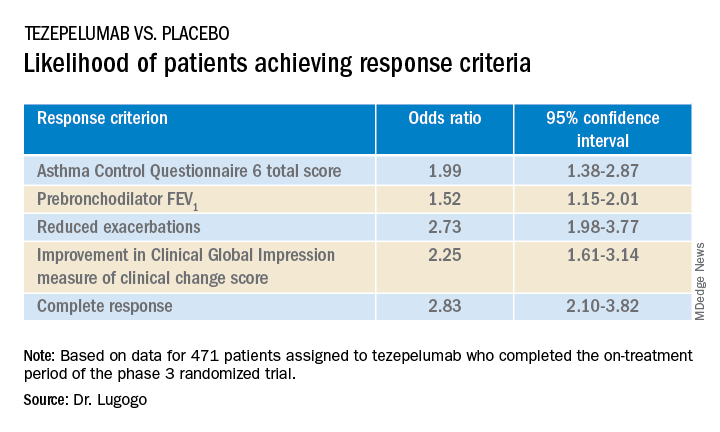
Exacerbations explored
In a separate presentation, Christopher S. Ambrose, MD, MBA, of AstraZeneca in Gaithersburg, Md., presented information from investigator-narrative descriptions of all hospitalization events related to asthma exacerbations (mild, moderate, or severe) that occurred while the investigator was blinded to each patient’s treatment assignment in NAVIGATOR.
In all, 39 of 531 patients (7.3%) assigned to placebo had a total of 78 exacerbations requiring hospitalization, compared with 13 of 528 patients (2.5%) assigned to tezepelumab. The latter group had a total of 14 exacerbations requiring hospitalization during the study.
Among hospitalized patients, 32 of the 39 assigned to placebo had severe, incapacitating exacerbations, compared with 5 of 13 assigned to tezepelumab.
Reported symptoms were generally similar between hospitalized patients in the two treatment groups, although there appeared to be trends toward lower incidence of dyspnea, fever, and tachycardia with tezepelumab.
Health care resource utilization, a surrogate marker for disease burden, was substantially lower for patients assigned to tezepelumab.
Infections were the most common triggers of exacerbations in both groups.
“These data provide further evidence that tezepelumab can reduce the burden of disease of severe uncontrolled asthma, both to patients and to health care systems,” Dr. Ambrose said.
Head-to-head studies needed
Although there have been no head-to-head comparisons of biologic agents for asthma to date, results of these studies suggest that tezepelumab has efficacy similar to that of other agents for reducing exacerbation, said Fernando Holguin, MD, MPH, from the University of Colorado at Denver, Aurora, who comoderated the oral session where the data were presented but was not involved in the study.
Biologic agents appear to be slightly more effective against type 2 inflammation in asthma, “but in general I think we give it to a broader severe population, so that’s exciting,” he told this news organization.
Comoderator Amisha Barochia, MBBS, MHS, of the National Institutes of Health, Bethesda, Md., told this news organization that head-to-head trials of biologic agents would provide important clinical information going forward.
“Should we switch to a different biologic or add a second biologic? Those are questions we need answers for,” she said.
The NAVIGATOR trial is funded by AstraZeneca and Amgen. Dr. Lugogo disclosed financial relationships with both companies. Dr. Holguin and Dr. Barochia have disclosed no financial relationships relevant to the studies presented.
A version of this article first appeared on Medscape.com.
SAN FRANCISCO – Nearly half of all patients with severe, uncontrolled asthma who received a full course of the biologic agent tezepelumab (Tezspire) in the NAVIGATOR trial had a complete response to treatment at 1 year, results of a prespecified exploratory analysis indicated.
Among 471 patients assigned to tezepelumab who completed the on-treatment period of the phase 3 randomized trial, 46% had a complete response at 52 weeks, compared with 24% of patients assigned to placebo.
Complete response was defined as reduction in exacerbations of at least 50% over the previous year, improvement from baseline in Asthma Control Questionnaire 6 (ACQ-6) total score of at least 0.5 points, improvement in prebronchodilator forced expiratory volume in 1 second (pre-BD FEV1), and physician-assessed Clinical Global Impression measure of clinical change (CGI-C) score.
“These data further support the efficacy of tezepelumab in a broad population of patients with severe, uncontrolled asthma,” said Njira Lugogo, MD, of the division of pulmonary and critical care medicine at the University of Michigan, Ann Arbor.
Dr. Lugogo presented results of the exploratory analysis at the American Thoracic Society’s international conference.
Exacerbations reduced, lung function improved
Primary results from NAVIGATOR, published in The New England Journal of Medicine, showed that patients with severe, uncontrolled asthma randomly assigned to tezepelumab had fewer exacerbations and better lung function, asthma control, and health-related quality of life compared with patients assigned to placebo.
The investigators noted that approximately 10% of patients with asthma have symptoms and exacerbations despite maximal standard-of-care controller therapy.
Tezepelumab is a human monoclonal antibody that inhibits action of thymic stromal lymphopoietin (TSLP), an epithelial cytokine that is released in response to airborne triggers of asthma. TSLP is a major contributor to initiation and persistence of airway inflammation, Dr. Lugogo said.
The on-treatment analysis looked at all patients in the trial who completed 52 weeks of treatment and had complete data for all criteria studied.
The odds ratios (OR) for patients on tezepelumab achieving each of the response criteria are shown in the table.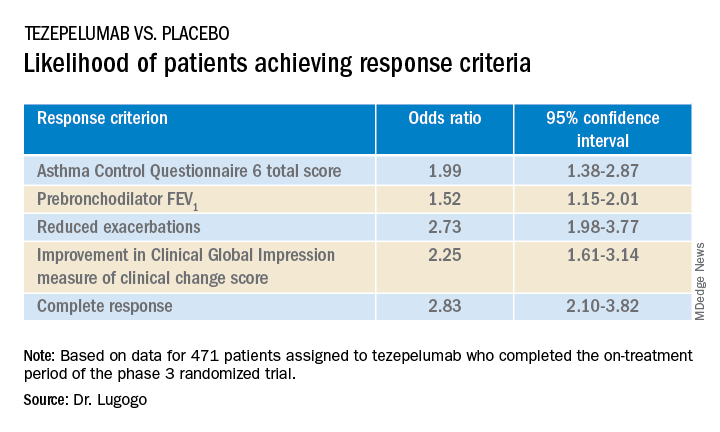
Exacerbations explored
In a separate presentation, Christopher S. Ambrose, MD, MBA, of AstraZeneca in Gaithersburg, Md., presented information from investigator-narrative descriptions of all hospitalization events related to asthma exacerbations (mild, moderate, or severe) that occurred while the investigator was blinded to each patient’s treatment assignment in NAVIGATOR.
In all, 39 of 531 patients (7.3%) assigned to placebo had a total of 78 exacerbations requiring hospitalization, compared with 13 of 528 patients (2.5%) assigned to tezepelumab. The latter group had a total of 14 exacerbations requiring hospitalization during the study.
Among hospitalized patients, 32 of the 39 assigned to placebo had severe, incapacitating exacerbations, compared with 5 of 13 assigned to tezepelumab.
Reported symptoms were generally similar between hospitalized patients in the two treatment groups, although there appeared to be trends toward lower incidence of dyspnea, fever, and tachycardia with tezepelumab.
Health care resource utilization, a surrogate marker for disease burden, was substantially lower for patients assigned to tezepelumab.
Infections were the most common triggers of exacerbations in both groups.
“These data provide further evidence that tezepelumab can reduce the burden of disease of severe uncontrolled asthma, both to patients and to health care systems,” Dr. Ambrose said.
Head-to-head studies needed
Although there have been no head-to-head comparisons of biologic agents for asthma to date, results of these studies suggest that tezepelumab has efficacy similar to that of other agents for reducing exacerbation, said Fernando Holguin, MD, MPH, from the University of Colorado at Denver, Aurora, who comoderated the oral session where the data were presented but was not involved in the study.
Biologic agents appear to be slightly more effective against type 2 inflammation in asthma, “but in general I think we give it to a broader severe population, so that’s exciting,” he told this news organization.
Comoderator Amisha Barochia, MBBS, MHS, of the National Institutes of Health, Bethesda, Md., told this news organization that head-to-head trials of biologic agents would provide important clinical information going forward.
“Should we switch to a different biologic or add a second biologic? Those are questions we need answers for,” she said.
The NAVIGATOR trial is funded by AstraZeneca and Amgen. Dr. Lugogo disclosed financial relationships with both companies. Dr. Holguin and Dr. Barochia have disclosed no financial relationships relevant to the studies presented.
A version of this article first appeared on Medscape.com.
AT ATS 2022
Cancer patients unaware of their increased thrombosis risk
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
FROM CANCER TREATMENT AND RESEARCH COMMUNICATIONS
Doc faces U.S. federal charges for hacking, ransomware
According to a statement from the U.S. Department of Justice, 55-year-old Moises Luis Zagala Gonzalez, MD, is charged with creating and distributing ransomware with a “doomsday” clock and sharing in profits from ransomware attacks.
Dr. Zagala, also known as “Nosophoros,” “Aesculapius,” and “Nebuchadnezzar,” is a citizen of France and Venezuela who currently lives in Ciudad Bolivar, Venezuela.
Breon Peace, U.S. attorney for the Eastern District of New York, and Michael J. Driscoll, assistant director in charge of the Federal Bureau of Investigaton’s New York Field Office, announced the charges.
“As alleged, the multitasking doctor treated patients, created and named his cyber tool after death, profited from a global ransomware ecosystem in which he sold the tools for conducting ransomware attacks, trained the attackers about how to extort victims, and then boasted about successful attacks, including by malicious actors associated with the government of Iran,” Mr. Peace said in the news release from the DOJ.
“We allege Zagala not only created and sold ransomware products to hackers, but also trained them in their use. Our actions today will prevent Zagala from further victimizing users,” Mr. Driscoll said. “However, many other malicious criminals are searching for businesses and organizations that haven’t taken steps to protect their systems – which is an incredibly vital step in stopping the next ransomware attack.”
Ransomware tools are malicious software that cybercriminals use to extort money from companies, nonprofits, and other institutions by encrypting their files and then demanding a ransom for the decryption keys.
One of Dr. Zagala’s early ransomware tools, called “Jigsaw v. 2,” had what Dr. Zagala described as a doomsday counter that kept track of how many times the user tried to remove the ransomware. “If the user kills the ransomware too many times, then it’s clear he won’t pay so better erase the whole hard drive,” Dr. Zagala wrote.
According to the DOJ, beginning in late 2019, Dr. Zagala began advertising a new tool as a “private ransomware builder,” which he called Thanos. The name appears to be in reference to a fictional villain responsible for destroying half of all life in the universe and to “Thanatos” from Greek mythology, who is associated with death.
Dr. Zagala’s Thanos software allows users to create their own unique ransomware software for personal use or to rent to other cybercriminals.
Dr. Zagala allegedly not only sold or rented out his ransomware tools to cybercriminals, but he also taught users how to deploy the tools, steal passwords from victim computers, and set up a Bitcoin address for ransom payments.
Dr. Zagala’s customers were happy with his products, the DOJ release noted. In a message posted in July 2020, one user said the ransomware was “very powerful” and claimed that he had used it to infect a network of roughly 3,000 computers.
In December 2020, another user wrote a post in Russian: “We have been working with this product for over a month now, we have a good profit! Best support I’ve met.”
Earlier in May, law enforcement agents interviewed a relative of Dr. Zagala who lives in Florida and whose PayPal account was used by Dr. Zagala to receive illicit proceeds.
According to the DOJ, the relative confirmed that Dr. Zagala lives in Venezuela and had taught himself computer programming. The relative also showed agents contact information for Dr. Zagala that matched the registered email for malicious infrastructure associated with the Thanos ransomware.
Dr. Zagala, who remains in Venezuela, faces up to 10 years in prison for attempted computer intrusions and conspiracy charges if brought to justice in the United States.
A version of this article first appeared on Medscape.com.
According to a statement from the U.S. Department of Justice, 55-year-old Moises Luis Zagala Gonzalez, MD, is charged with creating and distributing ransomware with a “doomsday” clock and sharing in profits from ransomware attacks.
Dr. Zagala, also known as “Nosophoros,” “Aesculapius,” and “Nebuchadnezzar,” is a citizen of France and Venezuela who currently lives in Ciudad Bolivar, Venezuela.
Breon Peace, U.S. attorney for the Eastern District of New York, and Michael J. Driscoll, assistant director in charge of the Federal Bureau of Investigaton’s New York Field Office, announced the charges.
“As alleged, the multitasking doctor treated patients, created and named his cyber tool after death, profited from a global ransomware ecosystem in which he sold the tools for conducting ransomware attacks, trained the attackers about how to extort victims, and then boasted about successful attacks, including by malicious actors associated with the government of Iran,” Mr. Peace said in the news release from the DOJ.
“We allege Zagala not only created and sold ransomware products to hackers, but also trained them in their use. Our actions today will prevent Zagala from further victimizing users,” Mr. Driscoll said. “However, many other malicious criminals are searching for businesses and organizations that haven’t taken steps to protect their systems – which is an incredibly vital step in stopping the next ransomware attack.”
Ransomware tools are malicious software that cybercriminals use to extort money from companies, nonprofits, and other institutions by encrypting their files and then demanding a ransom for the decryption keys.
One of Dr. Zagala’s early ransomware tools, called “Jigsaw v. 2,” had what Dr. Zagala described as a doomsday counter that kept track of how many times the user tried to remove the ransomware. “If the user kills the ransomware too many times, then it’s clear he won’t pay so better erase the whole hard drive,” Dr. Zagala wrote.
According to the DOJ, beginning in late 2019, Dr. Zagala began advertising a new tool as a “private ransomware builder,” which he called Thanos. The name appears to be in reference to a fictional villain responsible for destroying half of all life in the universe and to “Thanatos” from Greek mythology, who is associated with death.
Dr. Zagala’s Thanos software allows users to create their own unique ransomware software for personal use or to rent to other cybercriminals.
Dr. Zagala allegedly not only sold or rented out his ransomware tools to cybercriminals, but he also taught users how to deploy the tools, steal passwords from victim computers, and set up a Bitcoin address for ransom payments.
Dr. Zagala’s customers were happy with his products, the DOJ release noted. In a message posted in July 2020, one user said the ransomware was “very powerful” and claimed that he had used it to infect a network of roughly 3,000 computers.
In December 2020, another user wrote a post in Russian: “We have been working with this product for over a month now, we have a good profit! Best support I’ve met.”
Earlier in May, law enforcement agents interviewed a relative of Dr. Zagala who lives in Florida and whose PayPal account was used by Dr. Zagala to receive illicit proceeds.
According to the DOJ, the relative confirmed that Dr. Zagala lives in Venezuela and had taught himself computer programming. The relative also showed agents contact information for Dr. Zagala that matched the registered email for malicious infrastructure associated with the Thanos ransomware.
Dr. Zagala, who remains in Venezuela, faces up to 10 years in prison for attempted computer intrusions and conspiracy charges if brought to justice in the United States.
A version of this article first appeared on Medscape.com.
According to a statement from the U.S. Department of Justice, 55-year-old Moises Luis Zagala Gonzalez, MD, is charged with creating and distributing ransomware with a “doomsday” clock and sharing in profits from ransomware attacks.
Dr. Zagala, also known as “Nosophoros,” “Aesculapius,” and “Nebuchadnezzar,” is a citizen of France and Venezuela who currently lives in Ciudad Bolivar, Venezuela.
Breon Peace, U.S. attorney for the Eastern District of New York, and Michael J. Driscoll, assistant director in charge of the Federal Bureau of Investigaton’s New York Field Office, announced the charges.
“As alleged, the multitasking doctor treated patients, created and named his cyber tool after death, profited from a global ransomware ecosystem in which he sold the tools for conducting ransomware attacks, trained the attackers about how to extort victims, and then boasted about successful attacks, including by malicious actors associated with the government of Iran,” Mr. Peace said in the news release from the DOJ.
“We allege Zagala not only created and sold ransomware products to hackers, but also trained them in their use. Our actions today will prevent Zagala from further victimizing users,” Mr. Driscoll said. “However, many other malicious criminals are searching for businesses and organizations that haven’t taken steps to protect their systems – which is an incredibly vital step in stopping the next ransomware attack.”
Ransomware tools are malicious software that cybercriminals use to extort money from companies, nonprofits, and other institutions by encrypting their files and then demanding a ransom for the decryption keys.
One of Dr. Zagala’s early ransomware tools, called “Jigsaw v. 2,” had what Dr. Zagala described as a doomsday counter that kept track of how many times the user tried to remove the ransomware. “If the user kills the ransomware too many times, then it’s clear he won’t pay so better erase the whole hard drive,” Dr. Zagala wrote.
According to the DOJ, beginning in late 2019, Dr. Zagala began advertising a new tool as a “private ransomware builder,” which he called Thanos. The name appears to be in reference to a fictional villain responsible for destroying half of all life in the universe and to “Thanatos” from Greek mythology, who is associated with death.
Dr. Zagala’s Thanos software allows users to create their own unique ransomware software for personal use or to rent to other cybercriminals.
Dr. Zagala allegedly not only sold or rented out his ransomware tools to cybercriminals, but he also taught users how to deploy the tools, steal passwords from victim computers, and set up a Bitcoin address for ransom payments.
Dr. Zagala’s customers were happy with his products, the DOJ release noted. In a message posted in July 2020, one user said the ransomware was “very powerful” and claimed that he had used it to infect a network of roughly 3,000 computers.
In December 2020, another user wrote a post in Russian: “We have been working with this product for over a month now, we have a good profit! Best support I’ve met.”
Earlier in May, law enforcement agents interviewed a relative of Dr. Zagala who lives in Florida and whose PayPal account was used by Dr. Zagala to receive illicit proceeds.
According to the DOJ, the relative confirmed that Dr. Zagala lives in Venezuela and had taught himself computer programming. The relative also showed agents contact information for Dr. Zagala that matched the registered email for malicious infrastructure associated with the Thanos ransomware.
Dr. Zagala, who remains in Venezuela, faces up to 10 years in prison for attempted computer intrusions and conspiracy charges if brought to justice in the United States.
A version of this article first appeared on Medscape.com.
Does suicide risk show up in the blood?
Investigators found patients with MDD who died by suicide had a gene expression signature in blood distinct from patients with MDD who died by other means.
The signature included genes involved in stress response changes, including polyamine metabolism, circadian rhythm, immune dysregulation, and telomere maintenance.
“These blood biomarkers are an important step toward developing blood tests to identify patients with imminent risk of ending their lives,” study investigator Adolfo Sequeira, PhD, associate researcher in the department of psychiatry and human behavior, University of California, Irvine, said in a news release.
“To our knowledge, this is the first study to analyze blood and brain samples in a well-defined population of MDDs demonstrating significant differences in gene expression associated with completed suicide,” Dr. Sequeira added.
The findings were published online in Translational Psychiatry.
A pressing challenge
Suicide rates in the United States have jumped by more than 35% over the past 2 decades, with more than 48,000 deaths by suicide occurring just last year. MDD is the most common diagnosis among completed suicides, and identifying individuals at the highest risk for suicide remains a “pressing challenge,” the researchers noted.
They looked for changes in gene expression associated with suicide in archived postmortem blood and brain samples from adults with MDD who died by suicide (MDD-S) or by other means (MDD-NS), as well as a group of controls with no psychiatric illness.
In total, there were blood and brain samples for 45 adults, including 53 blood samples and 69 dorsolateral prefrontal cortex (DLPFC) tissue samples.
In blood, investigators identified 14 genes that significantly differentiated MDD-S from MDD-NS. The top six genes differentially expressed in blood were PER3, MTPAP, SLC25A26, CD19, SOX9, and GAR1.
In addition, four genes showed significant changes in brain and blood between the MDD-S and MDD-NS groups. SOX9 was decreased and PER3 was increased in MDD-S in both blood and brain samples, while CD19 and TERF1 were increased in blood but decreased in DLPFC.
SOX9, an astrocytic marker in the brain and B-cell marker in blood, has been shown to be decreased in MDD-S compared with controls in the prefrontal cortex.
In the current study, researchers found that SOX9 expression was significantly reduced both in blood and brain in MDD-S compared with MDD-NS, “suggesting similar immune/astrocytic dysregulations in suicide that could be further investigated.”
Potential signatures, potential targets
PER3 is a circadian rhythm gene implicated in sleep disorders associated with shifts in circadian rhythms and is thought to increase susceptibility to MDD.
Mutations in PER3 have been shown previously to alter multiple systems, including response to antidepressants; and increased blood expression of PER1 has been linked to suicidality in women, the researchers noted.
There also were significantly higher levels of two inflammatory markers (CD19 and CD6 genes) in blood of MDD-S patients compared to MDD-NS patients.
Another “significant” finding was the involvement of several mitochondrial genes in suicide, the researchers said.
Two nuclear genes coding for mitochondria-located proteins MTPAP (a mitochondrial poly(A) polymerase) and the mitochondrial polyamine transporter SLC25A26 were increased in blood in MDD-S compared with MDD-NS and controls, suggesting that “mitochondrial alterations could be used as potential signatures to differentiate MDD-S from MDD-NS patients and also from controls.”
The researchers added that the genes found to be dysregulated in suicide represent potential targets for future drug therapies to prevent suicide and could also be used to develop a molecular test to identify individuals at high risk for suicide.
The study was funded by the National Institute of Mental Health, the American Society for Suicide Prevention, and the Pritzker Family Philanthropic Fund. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators found patients with MDD who died by suicide had a gene expression signature in blood distinct from patients with MDD who died by other means.
The signature included genes involved in stress response changes, including polyamine metabolism, circadian rhythm, immune dysregulation, and telomere maintenance.
“These blood biomarkers are an important step toward developing blood tests to identify patients with imminent risk of ending their lives,” study investigator Adolfo Sequeira, PhD, associate researcher in the department of psychiatry and human behavior, University of California, Irvine, said in a news release.
“To our knowledge, this is the first study to analyze blood and brain samples in a well-defined population of MDDs demonstrating significant differences in gene expression associated with completed suicide,” Dr. Sequeira added.
The findings were published online in Translational Psychiatry.
A pressing challenge
Suicide rates in the United States have jumped by more than 35% over the past 2 decades, with more than 48,000 deaths by suicide occurring just last year. MDD is the most common diagnosis among completed suicides, and identifying individuals at the highest risk for suicide remains a “pressing challenge,” the researchers noted.
They looked for changes in gene expression associated with suicide in archived postmortem blood and brain samples from adults with MDD who died by suicide (MDD-S) or by other means (MDD-NS), as well as a group of controls with no psychiatric illness.
In total, there were blood and brain samples for 45 adults, including 53 blood samples and 69 dorsolateral prefrontal cortex (DLPFC) tissue samples.
In blood, investigators identified 14 genes that significantly differentiated MDD-S from MDD-NS. The top six genes differentially expressed in blood were PER3, MTPAP, SLC25A26, CD19, SOX9, and GAR1.
In addition, four genes showed significant changes in brain and blood between the MDD-S and MDD-NS groups. SOX9 was decreased and PER3 was increased in MDD-S in both blood and brain samples, while CD19 and TERF1 were increased in blood but decreased in DLPFC.
SOX9, an astrocytic marker in the brain and B-cell marker in blood, has been shown to be decreased in MDD-S compared with controls in the prefrontal cortex.
In the current study, researchers found that SOX9 expression was significantly reduced both in blood and brain in MDD-S compared with MDD-NS, “suggesting similar immune/astrocytic dysregulations in suicide that could be further investigated.”
Potential signatures, potential targets
PER3 is a circadian rhythm gene implicated in sleep disorders associated with shifts in circadian rhythms and is thought to increase susceptibility to MDD.
Mutations in PER3 have been shown previously to alter multiple systems, including response to antidepressants; and increased blood expression of PER1 has been linked to suicidality in women, the researchers noted.
There also were significantly higher levels of two inflammatory markers (CD19 and CD6 genes) in blood of MDD-S patients compared to MDD-NS patients.
Another “significant” finding was the involvement of several mitochondrial genes in suicide, the researchers said.
Two nuclear genes coding for mitochondria-located proteins MTPAP (a mitochondrial poly(A) polymerase) and the mitochondrial polyamine transporter SLC25A26 were increased in blood in MDD-S compared with MDD-NS and controls, suggesting that “mitochondrial alterations could be used as potential signatures to differentiate MDD-S from MDD-NS patients and also from controls.”
The researchers added that the genes found to be dysregulated in suicide represent potential targets for future drug therapies to prevent suicide and could also be used to develop a molecular test to identify individuals at high risk for suicide.
The study was funded by the National Institute of Mental Health, the American Society for Suicide Prevention, and the Pritzker Family Philanthropic Fund. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators found patients with MDD who died by suicide had a gene expression signature in blood distinct from patients with MDD who died by other means.
The signature included genes involved in stress response changes, including polyamine metabolism, circadian rhythm, immune dysregulation, and telomere maintenance.
“These blood biomarkers are an important step toward developing blood tests to identify patients with imminent risk of ending their lives,” study investigator Adolfo Sequeira, PhD, associate researcher in the department of psychiatry and human behavior, University of California, Irvine, said in a news release.
“To our knowledge, this is the first study to analyze blood and brain samples in a well-defined population of MDDs demonstrating significant differences in gene expression associated with completed suicide,” Dr. Sequeira added.
The findings were published online in Translational Psychiatry.
A pressing challenge
Suicide rates in the United States have jumped by more than 35% over the past 2 decades, with more than 48,000 deaths by suicide occurring just last year. MDD is the most common diagnosis among completed suicides, and identifying individuals at the highest risk for suicide remains a “pressing challenge,” the researchers noted.
They looked for changes in gene expression associated with suicide in archived postmortem blood and brain samples from adults with MDD who died by suicide (MDD-S) or by other means (MDD-NS), as well as a group of controls with no psychiatric illness.
In total, there were blood and brain samples for 45 adults, including 53 blood samples and 69 dorsolateral prefrontal cortex (DLPFC) tissue samples.
In blood, investigators identified 14 genes that significantly differentiated MDD-S from MDD-NS. The top six genes differentially expressed in blood were PER3, MTPAP, SLC25A26, CD19, SOX9, and GAR1.
In addition, four genes showed significant changes in brain and blood between the MDD-S and MDD-NS groups. SOX9 was decreased and PER3 was increased in MDD-S in both blood and brain samples, while CD19 and TERF1 were increased in blood but decreased in DLPFC.
SOX9, an astrocytic marker in the brain and B-cell marker in blood, has been shown to be decreased in MDD-S compared with controls in the prefrontal cortex.
In the current study, researchers found that SOX9 expression was significantly reduced both in blood and brain in MDD-S compared with MDD-NS, “suggesting similar immune/astrocytic dysregulations in suicide that could be further investigated.”
Potential signatures, potential targets
PER3 is a circadian rhythm gene implicated in sleep disorders associated with shifts in circadian rhythms and is thought to increase susceptibility to MDD.
Mutations in PER3 have been shown previously to alter multiple systems, including response to antidepressants; and increased blood expression of PER1 has been linked to suicidality in women, the researchers noted.
There also were significantly higher levels of two inflammatory markers (CD19 and CD6 genes) in blood of MDD-S patients compared to MDD-NS patients.
Another “significant” finding was the involvement of several mitochondrial genes in suicide, the researchers said.
Two nuclear genes coding for mitochondria-located proteins MTPAP (a mitochondrial poly(A) polymerase) and the mitochondrial polyamine transporter SLC25A26 were increased in blood in MDD-S compared with MDD-NS and controls, suggesting that “mitochondrial alterations could be used as potential signatures to differentiate MDD-S from MDD-NS patients and also from controls.”
The researchers added that the genes found to be dysregulated in suicide represent potential targets for future drug therapies to prevent suicide and could also be used to develop a molecular test to identify individuals at high risk for suicide.
The study was funded by the National Institute of Mental Health, the American Society for Suicide Prevention, and the Pritzker Family Philanthropic Fund. The investigators have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM TRANSLATIONAL PSYCHIATRY
Up in smoke: Cannabis-related ED visits increased 18-fold for older Californians
Researchers in California found an 18-fold increase in the rate of cannabis-related trips to the ED visits among adults over age 65 in the state from 2005 to 2019.
Addressing potential harms of cannabis use among older adults, who face heightened risk for adverse reactions to the substance, “is urgently required,” the researchers reported at the annual meeting of the American Geriatrics Society.
The researchers advised doctors to discuss cannabis use with older patients and screen older adults for cannabis use. Those living with multiple chronic conditions and taking multiple medications are especially likely to be at risk for harm, coinvestigator Benjamin Han, MD, MPH, a geriatrician at the University of California, San Diego, said in an interview.
Dr. Han added that “very little” is understood about the risks and benefits of cannabis use in the elderly, and more studies are needed “so that clinicians can have data-informed discussions with their patients.”
California legalized medical marijuana in 1996 and recreational marijuana in 2016.
The researchers used diagnostic code data from California’s nonmilitary acute care hospitals, collected by the state’s Department of Healthcare Access and Information, to calculate annual rates of cannabis-related visits per 10,000 ED visits.
ED trips up sharply among older adults
Rates of cannabis-related visits increased significantly for all older adult age ranges (P < .001), according to the researchers. Among those aged 65-74 years, the rate increased about 15-fold, from 44.9 per 10,000 visits in 2005 to 714.5 per 100,000 in 2019; for ages 75-84, the rate increased about 22-fold, from 8.4 to 193.9 per 10,000; and for those 85 and older the rate jumped nearly 18-fold, from 2.1 to 39.2 per 10,000.
The greatest increase occurred in visits categorized in diagnostic codes as cannabis abuse and unspecified use. Cannabis dependence and cannabis poisoning accounted for only a small fraction of cases, the investigators found.
The researchers did not have data on specific reasons for a visit, or whether patients had smoked or ingested marijuana products. They also could not discern whether patients had used delta-9-tetrahydrocannabinol, which has psychoactive properties, or cannabidiol, which typically does not have the same mind-altering effects.
Dr. Han said the data may not present a full picture of marijuana-related ED visits. “It is important to recognize that older adults have lived through the very putative language around drug use – including cannabis – as part of the racist war on drugs,” which could lead them to omit having used drugs during the intake process.
A 2017 study linked cannabis use among older adults with more injuries, which in turn led to greater emergency department use. Brian Kaskie, PhD, associate professor in health management and policy at the University of Iowa, Iowa City, said in an interview that the new findings show a state-specific, but alarming trend, and that more research is needed.
“Were these first-time users who were not familiar with anxiety-inducing aspects of cannabis use and took high potency products? Did they complete any education about how to use cannabis?” said Dr. Kaskie, who was not involved in the new study. “Were the ER visits for relatively benign, nonemergent reasons or were these ... visits an outcome of a tragic, harmful event like a car accident or overdose?”
Dr. Han and Dr. Kaskie disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in California found an 18-fold increase in the rate of cannabis-related trips to the ED visits among adults over age 65 in the state from 2005 to 2019.
Addressing potential harms of cannabis use among older adults, who face heightened risk for adverse reactions to the substance, “is urgently required,” the researchers reported at the annual meeting of the American Geriatrics Society.
The researchers advised doctors to discuss cannabis use with older patients and screen older adults for cannabis use. Those living with multiple chronic conditions and taking multiple medications are especially likely to be at risk for harm, coinvestigator Benjamin Han, MD, MPH, a geriatrician at the University of California, San Diego, said in an interview.
Dr. Han added that “very little” is understood about the risks and benefits of cannabis use in the elderly, and more studies are needed “so that clinicians can have data-informed discussions with their patients.”
California legalized medical marijuana in 1996 and recreational marijuana in 2016.
The researchers used diagnostic code data from California’s nonmilitary acute care hospitals, collected by the state’s Department of Healthcare Access and Information, to calculate annual rates of cannabis-related visits per 10,000 ED visits.
ED trips up sharply among older adults
Rates of cannabis-related visits increased significantly for all older adult age ranges (P < .001), according to the researchers. Among those aged 65-74 years, the rate increased about 15-fold, from 44.9 per 10,000 visits in 2005 to 714.5 per 100,000 in 2019; for ages 75-84, the rate increased about 22-fold, from 8.4 to 193.9 per 10,000; and for those 85 and older the rate jumped nearly 18-fold, from 2.1 to 39.2 per 10,000.
The greatest increase occurred in visits categorized in diagnostic codes as cannabis abuse and unspecified use. Cannabis dependence and cannabis poisoning accounted for only a small fraction of cases, the investigators found.
The researchers did not have data on specific reasons for a visit, or whether patients had smoked or ingested marijuana products. They also could not discern whether patients had used delta-9-tetrahydrocannabinol, which has psychoactive properties, or cannabidiol, which typically does not have the same mind-altering effects.
Dr. Han said the data may not present a full picture of marijuana-related ED visits. “It is important to recognize that older adults have lived through the very putative language around drug use – including cannabis – as part of the racist war on drugs,” which could lead them to omit having used drugs during the intake process.
A 2017 study linked cannabis use among older adults with more injuries, which in turn led to greater emergency department use. Brian Kaskie, PhD, associate professor in health management and policy at the University of Iowa, Iowa City, said in an interview that the new findings show a state-specific, but alarming trend, and that more research is needed.
“Were these first-time users who were not familiar with anxiety-inducing aspects of cannabis use and took high potency products? Did they complete any education about how to use cannabis?” said Dr. Kaskie, who was not involved in the new study. “Were the ER visits for relatively benign, nonemergent reasons or were these ... visits an outcome of a tragic, harmful event like a car accident or overdose?”
Dr. Han and Dr. Kaskie disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers in California found an 18-fold increase in the rate of cannabis-related trips to the ED visits among adults over age 65 in the state from 2005 to 2019.
Addressing potential harms of cannabis use among older adults, who face heightened risk for adverse reactions to the substance, “is urgently required,” the researchers reported at the annual meeting of the American Geriatrics Society.
The researchers advised doctors to discuss cannabis use with older patients and screen older adults for cannabis use. Those living with multiple chronic conditions and taking multiple medications are especially likely to be at risk for harm, coinvestigator Benjamin Han, MD, MPH, a geriatrician at the University of California, San Diego, said in an interview.
Dr. Han added that “very little” is understood about the risks and benefits of cannabis use in the elderly, and more studies are needed “so that clinicians can have data-informed discussions with their patients.”
California legalized medical marijuana in 1996 and recreational marijuana in 2016.
The researchers used diagnostic code data from California’s nonmilitary acute care hospitals, collected by the state’s Department of Healthcare Access and Information, to calculate annual rates of cannabis-related visits per 10,000 ED visits.
ED trips up sharply among older adults
Rates of cannabis-related visits increased significantly for all older adult age ranges (P < .001), according to the researchers. Among those aged 65-74 years, the rate increased about 15-fold, from 44.9 per 10,000 visits in 2005 to 714.5 per 100,000 in 2019; for ages 75-84, the rate increased about 22-fold, from 8.4 to 193.9 per 10,000; and for those 85 and older the rate jumped nearly 18-fold, from 2.1 to 39.2 per 10,000.
The greatest increase occurred in visits categorized in diagnostic codes as cannabis abuse and unspecified use. Cannabis dependence and cannabis poisoning accounted for only a small fraction of cases, the investigators found.
The researchers did not have data on specific reasons for a visit, or whether patients had smoked or ingested marijuana products. They also could not discern whether patients had used delta-9-tetrahydrocannabinol, which has psychoactive properties, or cannabidiol, which typically does not have the same mind-altering effects.
Dr. Han said the data may not present a full picture of marijuana-related ED visits. “It is important to recognize that older adults have lived through the very putative language around drug use – including cannabis – as part of the racist war on drugs,” which could lead them to omit having used drugs during the intake process.
A 2017 study linked cannabis use among older adults with more injuries, which in turn led to greater emergency department use. Brian Kaskie, PhD, associate professor in health management and policy at the University of Iowa, Iowa City, said in an interview that the new findings show a state-specific, but alarming trend, and that more research is needed.
“Were these first-time users who were not familiar with anxiety-inducing aspects of cannabis use and took high potency products? Did they complete any education about how to use cannabis?” said Dr. Kaskie, who was not involved in the new study. “Were the ER visits for relatively benign, nonemergent reasons or were these ... visits an outcome of a tragic, harmful event like a car accident or overdose?”
Dr. Han and Dr. Kaskie disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AGS 2022
Tool helps health system cut risky scripts for older adults
In the largest implementation yet of the tool, designed by the U.S. Department of Veterans Affairs to decrease the use of potentially inappropriate medications (PIMs), Lifespan, a nonprofit system whose partners include Brown University, Providence, R.I., reported a significant drop in the number of such prescriptions to older adults on discharge from the emergency department (ED).
The number of PIMs among monthly prescriptions fell by roughly 26% at Lifespan’s three adult acute care EDs after the system adopted EQUiPPED – Enhancing Quality of Prescribing Practices for Older Adults Discharged from the Emergency Department. The VA deployed a version of the tool in 2013 to address the lack of training most emergency clinicians receive in the management of geriatric medications.
The model “should be implemented in other states and, with greater replication, could shape national policy regarding quality of care for older adults,” according to the researchers, who reported the results May 12 at the American Geriatrics Society (AGS) 2022 Annual Scientific Meeting, Orlando.
Older adults are three times as likely as younger patients to wind up in an ED because of medication-related harms. This is in part due to the greater number of prescriptions U.S. adults older than 65 years take daily.
A key quality measure
Although the Centers for Medicare & Medicaid Services and other groups have deemed minimizing PIMs an important quality measure, most EDs lack an expert in geriatric prescribing, Elizabeth Goldberg, MD, an associate professor of emergency medicine at Brown University, told this news organization.
With EQUiPPED, clinicians receive access to geriatric medication order sets embedded in electronic health records, individualized benchmark reports, and education about medication safety in older adults. PIMs are defined by the American Geriatrics Society Beers Criteria and include drugs such as proton-pump inhibitors and antipsychotics.
Lifespan’s program involved 362 clinicians who treat about 230,000 patients annually – 40,000 of them aged 65 and older. Dr. Goldberg said implementing the program in such a large population could “really move the needle for older adults” by reducing falls, improving cognitive function, and preventing harm from the use of medication.
She and fellow researchers examined ED prescribing 13 months before and 16 months after they had implemented EQUiPPED, in August and September of 2019. Of clinicians who participated, 48% were attending physicians, 37% were residents, and 34% were advanced practice providers.
PIM prescribing dropped from 8.93% prior to implementation (95% confidence interval: 8.5%-9.36%) to 6.59% after (95% CI: 6.2%-6.98%; P < .001). Before implementation, 1,495 of 16,681 prescribed medications were considered inappropriate, compared with 1,044 of 15,818 medications after, according to the researchers. The biggest declines in prescribing involved antihistamines, muscle relaxants, and benzodiazepines.
Despite the improvements, the system did not meet a goal of reducing PIMs to less than 5%. Dr. Goldberg said educating the large number of clinicians, some of whom rotated in and out of the ED, proved particularly challenging. The COVID-19 pandemic also potentially diverted attention from the quality improvement project, she said.
In addition to its size, the project was notable because it was supported by Blue Cross & Blue Shield of Rhode Island. Dr. Goldberg said obtaining private funding proved to be a quicker and less competitive process than obtaining a government grant. Other institutions interested in running similar studies may need to find insurers that are in the Medicare Advantage market or that have a significant number of younger enrollees with chronic conditions, such as kidney disease, who may benefit from more careful prescribing practices, she said.
The new study builds on previous research, such as a 2017 study that showed that EQUiPPED reduced PIM prescribing at four VA hospitals. Findings from a more recent rollout at three academic health systems suggested that the model might also be effective in targeting the overuse of specific drugs in facilities in which PIM prescribing is already low.
A researcher in those earlier studies, Susan Nicole Hastings, MD, a geriatric medicine specialist at Duke University, Durham, N.C., and the Durham VA Health Care System, told this news organization that Lifespan’s experience supports the idea that “with the right attention to balancing fidelity and tailoring for the new setting, there is tremendous potential for moving successful programs from the VA to other health systems.”
Ann E. Vandenberg, PhD, MPH, a gerontologist at Emory University, Atlanta, said the fragmented nature of the American health care system makes it difficult to disseminate EQUiPPED widely, but interoperability applications that pull data from different electronic health records could help hospital systems to adopt the program without undergoing site-specific customization.
Dr. Hastings and Dr. Vandenberg have received research funding to study EQUiPPED from the Agency for Healthcare Research and Quality. Dr. Hastings also received research funding from the VA.
A version of this article first appeared on Medscape.com.
In the largest implementation yet of the tool, designed by the U.S. Department of Veterans Affairs to decrease the use of potentially inappropriate medications (PIMs), Lifespan, a nonprofit system whose partners include Brown University, Providence, R.I., reported a significant drop in the number of such prescriptions to older adults on discharge from the emergency department (ED).
The number of PIMs among monthly prescriptions fell by roughly 26% at Lifespan’s three adult acute care EDs after the system adopted EQUiPPED – Enhancing Quality of Prescribing Practices for Older Adults Discharged from the Emergency Department. The VA deployed a version of the tool in 2013 to address the lack of training most emergency clinicians receive in the management of geriatric medications.
The model “should be implemented in other states and, with greater replication, could shape national policy regarding quality of care for older adults,” according to the researchers, who reported the results May 12 at the American Geriatrics Society (AGS) 2022 Annual Scientific Meeting, Orlando.
Older adults are three times as likely as younger patients to wind up in an ED because of medication-related harms. This is in part due to the greater number of prescriptions U.S. adults older than 65 years take daily.
A key quality measure
Although the Centers for Medicare & Medicaid Services and other groups have deemed minimizing PIMs an important quality measure, most EDs lack an expert in geriatric prescribing, Elizabeth Goldberg, MD, an associate professor of emergency medicine at Brown University, told this news organization.
With EQUiPPED, clinicians receive access to geriatric medication order sets embedded in electronic health records, individualized benchmark reports, and education about medication safety in older adults. PIMs are defined by the American Geriatrics Society Beers Criteria and include drugs such as proton-pump inhibitors and antipsychotics.
Lifespan’s program involved 362 clinicians who treat about 230,000 patients annually – 40,000 of them aged 65 and older. Dr. Goldberg said implementing the program in such a large population could “really move the needle for older adults” by reducing falls, improving cognitive function, and preventing harm from the use of medication.
She and fellow researchers examined ED prescribing 13 months before and 16 months after they had implemented EQUiPPED, in August and September of 2019. Of clinicians who participated, 48% were attending physicians, 37% were residents, and 34% were advanced practice providers.
PIM prescribing dropped from 8.93% prior to implementation (95% confidence interval: 8.5%-9.36%) to 6.59% after (95% CI: 6.2%-6.98%; P < .001). Before implementation, 1,495 of 16,681 prescribed medications were considered inappropriate, compared with 1,044 of 15,818 medications after, according to the researchers. The biggest declines in prescribing involved antihistamines, muscle relaxants, and benzodiazepines.
Despite the improvements, the system did not meet a goal of reducing PIMs to less than 5%. Dr. Goldberg said educating the large number of clinicians, some of whom rotated in and out of the ED, proved particularly challenging. The COVID-19 pandemic also potentially diverted attention from the quality improvement project, she said.
In addition to its size, the project was notable because it was supported by Blue Cross & Blue Shield of Rhode Island. Dr. Goldberg said obtaining private funding proved to be a quicker and less competitive process than obtaining a government grant. Other institutions interested in running similar studies may need to find insurers that are in the Medicare Advantage market or that have a significant number of younger enrollees with chronic conditions, such as kidney disease, who may benefit from more careful prescribing practices, she said.
The new study builds on previous research, such as a 2017 study that showed that EQUiPPED reduced PIM prescribing at four VA hospitals. Findings from a more recent rollout at three academic health systems suggested that the model might also be effective in targeting the overuse of specific drugs in facilities in which PIM prescribing is already low.
A researcher in those earlier studies, Susan Nicole Hastings, MD, a geriatric medicine specialist at Duke University, Durham, N.C., and the Durham VA Health Care System, told this news organization that Lifespan’s experience supports the idea that “with the right attention to balancing fidelity and tailoring for the new setting, there is tremendous potential for moving successful programs from the VA to other health systems.”
Ann E. Vandenberg, PhD, MPH, a gerontologist at Emory University, Atlanta, said the fragmented nature of the American health care system makes it difficult to disseminate EQUiPPED widely, but interoperability applications that pull data from different electronic health records could help hospital systems to adopt the program without undergoing site-specific customization.
Dr. Hastings and Dr. Vandenberg have received research funding to study EQUiPPED from the Agency for Healthcare Research and Quality. Dr. Hastings also received research funding from the VA.
A version of this article first appeared on Medscape.com.
In the largest implementation yet of the tool, designed by the U.S. Department of Veterans Affairs to decrease the use of potentially inappropriate medications (PIMs), Lifespan, a nonprofit system whose partners include Brown University, Providence, R.I., reported a significant drop in the number of such prescriptions to older adults on discharge from the emergency department (ED).
The number of PIMs among monthly prescriptions fell by roughly 26% at Lifespan’s three adult acute care EDs after the system adopted EQUiPPED – Enhancing Quality of Prescribing Practices for Older Adults Discharged from the Emergency Department. The VA deployed a version of the tool in 2013 to address the lack of training most emergency clinicians receive in the management of geriatric medications.
The model “should be implemented in other states and, with greater replication, could shape national policy regarding quality of care for older adults,” according to the researchers, who reported the results May 12 at the American Geriatrics Society (AGS) 2022 Annual Scientific Meeting, Orlando.
Older adults are three times as likely as younger patients to wind up in an ED because of medication-related harms. This is in part due to the greater number of prescriptions U.S. adults older than 65 years take daily.
A key quality measure
Although the Centers for Medicare & Medicaid Services and other groups have deemed minimizing PIMs an important quality measure, most EDs lack an expert in geriatric prescribing, Elizabeth Goldberg, MD, an associate professor of emergency medicine at Brown University, told this news organization.
With EQUiPPED, clinicians receive access to geriatric medication order sets embedded in electronic health records, individualized benchmark reports, and education about medication safety in older adults. PIMs are defined by the American Geriatrics Society Beers Criteria and include drugs such as proton-pump inhibitors and antipsychotics.
Lifespan’s program involved 362 clinicians who treat about 230,000 patients annually – 40,000 of them aged 65 and older. Dr. Goldberg said implementing the program in such a large population could “really move the needle for older adults” by reducing falls, improving cognitive function, and preventing harm from the use of medication.
She and fellow researchers examined ED prescribing 13 months before and 16 months after they had implemented EQUiPPED, in August and September of 2019. Of clinicians who participated, 48% were attending physicians, 37% were residents, and 34% were advanced practice providers.
PIM prescribing dropped from 8.93% prior to implementation (95% confidence interval: 8.5%-9.36%) to 6.59% after (95% CI: 6.2%-6.98%; P < .001). Before implementation, 1,495 of 16,681 prescribed medications were considered inappropriate, compared with 1,044 of 15,818 medications after, according to the researchers. The biggest declines in prescribing involved antihistamines, muscle relaxants, and benzodiazepines.
Despite the improvements, the system did not meet a goal of reducing PIMs to less than 5%. Dr. Goldberg said educating the large number of clinicians, some of whom rotated in and out of the ED, proved particularly challenging. The COVID-19 pandemic also potentially diverted attention from the quality improvement project, she said.
In addition to its size, the project was notable because it was supported by Blue Cross & Blue Shield of Rhode Island. Dr. Goldberg said obtaining private funding proved to be a quicker and less competitive process than obtaining a government grant. Other institutions interested in running similar studies may need to find insurers that are in the Medicare Advantage market or that have a significant number of younger enrollees with chronic conditions, such as kidney disease, who may benefit from more careful prescribing practices, she said.
The new study builds on previous research, such as a 2017 study that showed that EQUiPPED reduced PIM prescribing at four VA hospitals. Findings from a more recent rollout at three academic health systems suggested that the model might also be effective in targeting the overuse of specific drugs in facilities in which PIM prescribing is already low.
A researcher in those earlier studies, Susan Nicole Hastings, MD, a geriatric medicine specialist at Duke University, Durham, N.C., and the Durham VA Health Care System, told this news organization that Lifespan’s experience supports the idea that “with the right attention to balancing fidelity and tailoring for the new setting, there is tremendous potential for moving successful programs from the VA to other health systems.”
Ann E. Vandenberg, PhD, MPH, a gerontologist at Emory University, Atlanta, said the fragmented nature of the American health care system makes it difficult to disseminate EQUiPPED widely, but interoperability applications that pull data from different electronic health records could help hospital systems to adopt the program without undergoing site-specific customization.
Dr. Hastings and Dr. Vandenberg have received research funding to study EQUiPPED from the Agency for Healthcare Research and Quality. Dr. Hastings also received research funding from the VA.
A version of this article first appeared on Medscape.com.
FROM AGS 2022
Health care facilities can prevent 35%-70% of infections. Here’s how
Good hand hygiene and other cost-effective infection prevention and control (IPC) practices can eliminate between 35% and 70% of health care–setting infections in all countries regardless of economic status, the World Health Organization reports.
IPC uses a practical, evidence-based approach to help patients, health care workers, and visitors to health care facilities avoid harmful infections, which can range from infections caused by localized antibiotic-resistant bacteria to pandemic viruses. The WHO calls the report the first global analysis of IPC implementation.
“Hospitals across the world saw increased rates of health care–associated infections (HAIs) during the COVID-19 pandemic. This included SARS-CoV-2 infections and other HAIs that increased as our health care systems were stretched to the breaking point and fewer resources were available for HAI prevention,” Daniel Diekema, MD, who was not involved in the report, said in an email.
“As we enter the third year of the pandemic, this WHO report should serve as an urgent call to action,” Dr. Diekema, a clinical professor of internal medicine at University of Iowa Health Care and an associate hospital epidemiologist with University of Iowa Hospitals and Clinics, both in Iowa City, noted. “Investing more resources in IPC programs will not only improve pandemic response, it will reduce morbidity, mortality, and global costs from all HAIs.”
No country or health system is free of HAIs
“Disparities in IPC investments between high- and low-income countries is the greatest challenge outlined in this report,” Dr. Diekema said in an email. “If the pandemic has taught us anything, it is that an infection spread anywhere in the world can soon become a problem everywhere. Thus, it is in everyone’s interest to ensure that IPC resources are more equitably distributed across the world.”
The report notes that HAIs are among the most common adverse events experienced in health care, and many HAIs are caused by multidrug-resistant organisms. The report includes these details:
It is predicted that of every 100 patients in acute-care hospitals, an average of 7 patients in high-income countries and 15 in low- and middle-income countries will acquire at least one HAI while hospitalized; as many as 30% of patients in intensive care encounter HAIs.
Of all cases of hospital-treated sepsis, 23.6% were linked to health care; 48.7% of all sepsis cases involving organ dysfunction treated in adult intensive care were acquired in the hospital; 24.4% of patients and 52.3% of those in intensive care who were affected by health care–associated sepsis died.
The European Centre for Disease Prevention and Control calculated that 4.5 million episodes of HAIs occurred each year among patients in acute-care hospitals in countries of the European Union and the European Economic Area.
The Centers for Disease Control and Prevention estimated that on any day, 1 in 31 hospital patients and 1 in 43 nursing home residents has an HAI.
Up to 41% of hospitalized patients with confirmed COVID-19 were infected with SARS-CoV-2 in health care settings.
Over roughly the first 18 months of the pandemic, COVID-19 killed between 80,000 and 180,000 health care workers worldwide.
The COVID-19 pandemic highlights the need for IPC
Despite the pandemic, high-income countries were eight times more likely to implement more advanced IPC than low-income countries, and IPC national programs in low- and middle-income countries improved only slightly.
Only 4 (3.8%) of the 106 evaluated countries met all the minimum requirements for IPC in place at the national level, and only 15.2% of health care facilities met all IPC minimum requirements.
Libby A. Richards, RN, MSN, PhD, CHES, an associate professor of nursing and the director of the PhD program in the Purdue University School of Nursing in West Lafayette, Ind., welcomed the report.
“While the principles of infection prevention and control have been fundamental for well over a hundred years, the COVID-19 pandemic brought these critical issues to everyone’s attention,” Dr. Richards, who was not involved in the report, said by email. “During the pandemic, the impact on our overburdened and understaffed health care system left little or no room for other acutely ill patients.
“This report brings timely attention to the importance of IPC across health care services,” she added.
Suzanne Wagester, RN, MSN, director of infection prevention at the University of Pittsburgh Medical Center, said in an email, “The pandemic has united us as a society as we recognize that infections impact us all. We struggle with the same universal challenges that directly impact the work of infection prevention.
“IPC programs are vital to facilities, patients, and countries,” Ms. Wagester, who also was not involved in the report, added. “The WHO report highlights the call to action that will hopefully ignite the movement to advance IPC programs across the globe to combat preventable infections.”
The WHO Global IPC Portal helps health care professionals in all countries analyze, track progress, and improve IPC at facility and national levels.
The report was funded by core WHO funds. The authors and Dr. Diekema, Dr. Richards, and Ms. Wagester have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Good hand hygiene and other cost-effective infection prevention and control (IPC) practices can eliminate between 35% and 70% of health care–setting infections in all countries regardless of economic status, the World Health Organization reports.
IPC uses a practical, evidence-based approach to help patients, health care workers, and visitors to health care facilities avoid harmful infections, which can range from infections caused by localized antibiotic-resistant bacteria to pandemic viruses. The WHO calls the report the first global analysis of IPC implementation.
“Hospitals across the world saw increased rates of health care–associated infections (HAIs) during the COVID-19 pandemic. This included SARS-CoV-2 infections and other HAIs that increased as our health care systems were stretched to the breaking point and fewer resources were available for HAI prevention,” Daniel Diekema, MD, who was not involved in the report, said in an email.
“As we enter the third year of the pandemic, this WHO report should serve as an urgent call to action,” Dr. Diekema, a clinical professor of internal medicine at University of Iowa Health Care and an associate hospital epidemiologist with University of Iowa Hospitals and Clinics, both in Iowa City, noted. “Investing more resources in IPC programs will not only improve pandemic response, it will reduce morbidity, mortality, and global costs from all HAIs.”
No country or health system is free of HAIs
“Disparities in IPC investments between high- and low-income countries is the greatest challenge outlined in this report,” Dr. Diekema said in an email. “If the pandemic has taught us anything, it is that an infection spread anywhere in the world can soon become a problem everywhere. Thus, it is in everyone’s interest to ensure that IPC resources are more equitably distributed across the world.”
The report notes that HAIs are among the most common adverse events experienced in health care, and many HAIs are caused by multidrug-resistant organisms. The report includes these details:
It is predicted that of every 100 patients in acute-care hospitals, an average of 7 patients in high-income countries and 15 in low- and middle-income countries will acquire at least one HAI while hospitalized; as many as 30% of patients in intensive care encounter HAIs.
Of all cases of hospital-treated sepsis, 23.6% were linked to health care; 48.7% of all sepsis cases involving organ dysfunction treated in adult intensive care were acquired in the hospital; 24.4% of patients and 52.3% of those in intensive care who were affected by health care–associated sepsis died.
The European Centre for Disease Prevention and Control calculated that 4.5 million episodes of HAIs occurred each year among patients in acute-care hospitals in countries of the European Union and the European Economic Area.
The Centers for Disease Control and Prevention estimated that on any day, 1 in 31 hospital patients and 1 in 43 nursing home residents has an HAI.
Up to 41% of hospitalized patients with confirmed COVID-19 were infected with SARS-CoV-2 in health care settings.
Over roughly the first 18 months of the pandemic, COVID-19 killed between 80,000 and 180,000 health care workers worldwide.
The COVID-19 pandemic highlights the need for IPC
Despite the pandemic, high-income countries were eight times more likely to implement more advanced IPC than low-income countries, and IPC national programs in low- and middle-income countries improved only slightly.
Only 4 (3.8%) of the 106 evaluated countries met all the minimum requirements for IPC in place at the national level, and only 15.2% of health care facilities met all IPC minimum requirements.
Libby A. Richards, RN, MSN, PhD, CHES, an associate professor of nursing and the director of the PhD program in the Purdue University School of Nursing in West Lafayette, Ind., welcomed the report.
“While the principles of infection prevention and control have been fundamental for well over a hundred years, the COVID-19 pandemic brought these critical issues to everyone’s attention,” Dr. Richards, who was not involved in the report, said by email. “During the pandemic, the impact on our overburdened and understaffed health care system left little or no room for other acutely ill patients.
“This report brings timely attention to the importance of IPC across health care services,” she added.
Suzanne Wagester, RN, MSN, director of infection prevention at the University of Pittsburgh Medical Center, said in an email, “The pandemic has united us as a society as we recognize that infections impact us all. We struggle with the same universal challenges that directly impact the work of infection prevention.
“IPC programs are vital to facilities, patients, and countries,” Ms. Wagester, who also was not involved in the report, added. “The WHO report highlights the call to action that will hopefully ignite the movement to advance IPC programs across the globe to combat preventable infections.”
The WHO Global IPC Portal helps health care professionals in all countries analyze, track progress, and improve IPC at facility and national levels.
The report was funded by core WHO funds. The authors and Dr. Diekema, Dr. Richards, and Ms. Wagester have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Good hand hygiene and other cost-effective infection prevention and control (IPC) practices can eliminate between 35% and 70% of health care–setting infections in all countries regardless of economic status, the World Health Organization reports.
IPC uses a practical, evidence-based approach to help patients, health care workers, and visitors to health care facilities avoid harmful infections, which can range from infections caused by localized antibiotic-resistant bacteria to pandemic viruses. The WHO calls the report the first global analysis of IPC implementation.
“Hospitals across the world saw increased rates of health care–associated infections (HAIs) during the COVID-19 pandemic. This included SARS-CoV-2 infections and other HAIs that increased as our health care systems were stretched to the breaking point and fewer resources were available for HAI prevention,” Daniel Diekema, MD, who was not involved in the report, said in an email.
“As we enter the third year of the pandemic, this WHO report should serve as an urgent call to action,” Dr. Diekema, a clinical professor of internal medicine at University of Iowa Health Care and an associate hospital epidemiologist with University of Iowa Hospitals and Clinics, both in Iowa City, noted. “Investing more resources in IPC programs will not only improve pandemic response, it will reduce morbidity, mortality, and global costs from all HAIs.”
No country or health system is free of HAIs
“Disparities in IPC investments between high- and low-income countries is the greatest challenge outlined in this report,” Dr. Diekema said in an email. “If the pandemic has taught us anything, it is that an infection spread anywhere in the world can soon become a problem everywhere. Thus, it is in everyone’s interest to ensure that IPC resources are more equitably distributed across the world.”
The report notes that HAIs are among the most common adverse events experienced in health care, and many HAIs are caused by multidrug-resistant organisms. The report includes these details:
It is predicted that of every 100 patients in acute-care hospitals, an average of 7 patients in high-income countries and 15 in low- and middle-income countries will acquire at least one HAI while hospitalized; as many as 30% of patients in intensive care encounter HAIs.
Of all cases of hospital-treated sepsis, 23.6% were linked to health care; 48.7% of all sepsis cases involving organ dysfunction treated in adult intensive care were acquired in the hospital; 24.4% of patients and 52.3% of those in intensive care who were affected by health care–associated sepsis died.
The European Centre for Disease Prevention and Control calculated that 4.5 million episodes of HAIs occurred each year among patients in acute-care hospitals in countries of the European Union and the European Economic Area.
The Centers for Disease Control and Prevention estimated that on any day, 1 in 31 hospital patients and 1 in 43 nursing home residents has an HAI.
Up to 41% of hospitalized patients with confirmed COVID-19 were infected with SARS-CoV-2 in health care settings.
Over roughly the first 18 months of the pandemic, COVID-19 killed between 80,000 and 180,000 health care workers worldwide.
The COVID-19 pandemic highlights the need for IPC
Despite the pandemic, high-income countries were eight times more likely to implement more advanced IPC than low-income countries, and IPC national programs in low- and middle-income countries improved only slightly.
Only 4 (3.8%) of the 106 evaluated countries met all the minimum requirements for IPC in place at the national level, and only 15.2% of health care facilities met all IPC minimum requirements.
Libby A. Richards, RN, MSN, PhD, CHES, an associate professor of nursing and the director of the PhD program in the Purdue University School of Nursing in West Lafayette, Ind., welcomed the report.
“While the principles of infection prevention and control have been fundamental for well over a hundred years, the COVID-19 pandemic brought these critical issues to everyone’s attention,” Dr. Richards, who was not involved in the report, said by email. “During the pandemic, the impact on our overburdened and understaffed health care system left little or no room for other acutely ill patients.
“This report brings timely attention to the importance of IPC across health care services,” she added.
Suzanne Wagester, RN, MSN, director of infection prevention at the University of Pittsburgh Medical Center, said in an email, “The pandemic has united us as a society as we recognize that infections impact us all. We struggle with the same universal challenges that directly impact the work of infection prevention.
“IPC programs are vital to facilities, patients, and countries,” Ms. Wagester, who also was not involved in the report, added. “The WHO report highlights the call to action that will hopefully ignite the movement to advance IPC programs across the globe to combat preventable infections.”
The WHO Global IPC Portal helps health care professionals in all countries analyze, track progress, and improve IPC at facility and national levels.
The report was funded by core WHO funds. The authors and Dr. Diekema, Dr. Richards, and Ms. Wagester have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.