User login
EMERGENCY MEDICINE is a practical, peer-reviewed monthly publication and Web site that meets the educational needs of emergency clinicians and urgent care clinicians for their practice.
Most cancer patients with breakthrough COVID-19 infection experience severe outcomes
Of 54 fully vaccinated patients with cancer and COVID-19, 35 (65%) were hospitalized, 10 (19%) were admitted to the intensive care unit or required mechanical ventilation, and 7 (13%) died within 30 days.
Although the study did not assess the rate of breakthrough infection among fully vaccinated patients with cancer, the findings do underscore the need for continued vigilance in protecting this vulnerable patient population by vaccinating close contacts, administering boosters, social distancing, and mask-wearing.
“Overall, vaccination remains an invaluable strategy in protecting vulnerable populations, including patients with cancer, against COVID-19. However, patients with cancer who develop breakthrough infection despite full vaccination remain at risk of severe outcomes,” Andrew L. Schmidt, MB, of Dana-Farber Cancer Institute, Boston, and associates wrote.
The analysis, which appeared online in Annals of Oncology Dec. 24 as a pre-proof but has not yet been peer reviewed, analyzed registry data from 1,787 adults with current or prior invasive cancer and laboratory-confirmed COVID-19 between Nov. 1, 2020, and May 31, 2021, before COVID vaccination was widespread. Of those, 1,656 (93%) were unvaccinated, 77 (4%) were partially vaccinated, and 54 (3%) were considered fully vaccinated at the time of COVID-19 infection.
Of the fully vaccinated patients with breakthrough infection, 52 (96%) experienced a severe outcome: two-thirds had to be hospitalized, nearly 1 in 5 went to the ICU or needed mechanical ventilation, and 13% died within 30 days.
“Comparable rates were observed in the unvaccinated group,” the investigators write, adding that there was no statistical difference in 30-day mortality between the fully vaccinated patients and the unvaccinated cohort (adjusted odds ratio, 1.08).
Factors associated with increased 30-day mortality among unvaccinated patients included lymphopenia (aOR, 1.68), comorbidities (aORs, 1.66-2.10), worse performance status (aORs, 2.26-4.34), and baseline cancer status (active/progressing vs. not active/ progressing, aOR, 6.07).
No significant differences were observed in ICU, mechanical ventilation, or hospitalization rates between the vaccinated and unvaccinated cohort after adjustment for confounders (aORs,1.13 and 1.25, respectively).
Notably, patients with an underlying hematologic malignancy were overrepresented among those with breakthrough COVID-19 (35% vs. 20%). Compared with those with solid cancers, patients with hematologic malignancies also had significantly higher rates of ICU admission, mechanical ventilation, and hospitalization.
This finding is “consistent with evidence that these patients may have a blunted serologic response to vaccination secondary to disease or therapy,” the authors note.
Although the investigators did not evaluate the risk of breakthrough infection post vaccination, recent research indicates that receiving a COVID-19 booster increases antibody levels among patients with cancer under active treatment and thus may provide additional protection against the virus.
Given the risk of breakthrough infection and severe outcomes in patients with cancer, the authors propose that “a mitigation approach that includes vaccination of close contacts, boosters, social distancing, and mask-wearing in public should be continued for the foreseeable future.” However, “additional research is needed to further categorize the patients that remain at risk of symptomatic COVID-19 following vaccination and test strategies that may reduce this risk.”
The findings are from a pre-proof that has not yet been peer reviewed or published. First author Dr. Schmidt reported nonfinancial support from Astellas, nonfinancial support from Pfizer, outside the submitted work. Other coauthors reported a range of disclosures as well. The full list can be found with the original article.
A version of this article first appeared on Medscape.com.
Of 54 fully vaccinated patients with cancer and COVID-19, 35 (65%) were hospitalized, 10 (19%) were admitted to the intensive care unit or required mechanical ventilation, and 7 (13%) died within 30 days.
Although the study did not assess the rate of breakthrough infection among fully vaccinated patients with cancer, the findings do underscore the need for continued vigilance in protecting this vulnerable patient population by vaccinating close contacts, administering boosters, social distancing, and mask-wearing.
“Overall, vaccination remains an invaluable strategy in protecting vulnerable populations, including patients with cancer, against COVID-19. However, patients with cancer who develop breakthrough infection despite full vaccination remain at risk of severe outcomes,” Andrew L. Schmidt, MB, of Dana-Farber Cancer Institute, Boston, and associates wrote.
The analysis, which appeared online in Annals of Oncology Dec. 24 as a pre-proof but has not yet been peer reviewed, analyzed registry data from 1,787 adults with current or prior invasive cancer and laboratory-confirmed COVID-19 between Nov. 1, 2020, and May 31, 2021, before COVID vaccination was widespread. Of those, 1,656 (93%) were unvaccinated, 77 (4%) were partially vaccinated, and 54 (3%) were considered fully vaccinated at the time of COVID-19 infection.
Of the fully vaccinated patients with breakthrough infection, 52 (96%) experienced a severe outcome: two-thirds had to be hospitalized, nearly 1 in 5 went to the ICU or needed mechanical ventilation, and 13% died within 30 days.
“Comparable rates were observed in the unvaccinated group,” the investigators write, adding that there was no statistical difference in 30-day mortality between the fully vaccinated patients and the unvaccinated cohort (adjusted odds ratio, 1.08).
Factors associated with increased 30-day mortality among unvaccinated patients included lymphopenia (aOR, 1.68), comorbidities (aORs, 1.66-2.10), worse performance status (aORs, 2.26-4.34), and baseline cancer status (active/progressing vs. not active/ progressing, aOR, 6.07).
No significant differences were observed in ICU, mechanical ventilation, or hospitalization rates between the vaccinated and unvaccinated cohort after adjustment for confounders (aORs,1.13 and 1.25, respectively).
Notably, patients with an underlying hematologic malignancy were overrepresented among those with breakthrough COVID-19 (35% vs. 20%). Compared with those with solid cancers, patients with hematologic malignancies also had significantly higher rates of ICU admission, mechanical ventilation, and hospitalization.
This finding is “consistent with evidence that these patients may have a blunted serologic response to vaccination secondary to disease or therapy,” the authors note.
Although the investigators did not evaluate the risk of breakthrough infection post vaccination, recent research indicates that receiving a COVID-19 booster increases antibody levels among patients with cancer under active treatment and thus may provide additional protection against the virus.
Given the risk of breakthrough infection and severe outcomes in patients with cancer, the authors propose that “a mitigation approach that includes vaccination of close contacts, boosters, social distancing, and mask-wearing in public should be continued for the foreseeable future.” However, “additional research is needed to further categorize the patients that remain at risk of symptomatic COVID-19 following vaccination and test strategies that may reduce this risk.”
The findings are from a pre-proof that has not yet been peer reviewed or published. First author Dr. Schmidt reported nonfinancial support from Astellas, nonfinancial support from Pfizer, outside the submitted work. Other coauthors reported a range of disclosures as well. The full list can be found with the original article.
A version of this article first appeared on Medscape.com.
Of 54 fully vaccinated patients with cancer and COVID-19, 35 (65%) were hospitalized, 10 (19%) were admitted to the intensive care unit or required mechanical ventilation, and 7 (13%) died within 30 days.
Although the study did not assess the rate of breakthrough infection among fully vaccinated patients with cancer, the findings do underscore the need for continued vigilance in protecting this vulnerable patient population by vaccinating close contacts, administering boosters, social distancing, and mask-wearing.
“Overall, vaccination remains an invaluable strategy in protecting vulnerable populations, including patients with cancer, against COVID-19. However, patients with cancer who develop breakthrough infection despite full vaccination remain at risk of severe outcomes,” Andrew L. Schmidt, MB, of Dana-Farber Cancer Institute, Boston, and associates wrote.
The analysis, which appeared online in Annals of Oncology Dec. 24 as a pre-proof but has not yet been peer reviewed, analyzed registry data from 1,787 adults with current or prior invasive cancer and laboratory-confirmed COVID-19 between Nov. 1, 2020, and May 31, 2021, before COVID vaccination was widespread. Of those, 1,656 (93%) were unvaccinated, 77 (4%) were partially vaccinated, and 54 (3%) were considered fully vaccinated at the time of COVID-19 infection.
Of the fully vaccinated patients with breakthrough infection, 52 (96%) experienced a severe outcome: two-thirds had to be hospitalized, nearly 1 in 5 went to the ICU or needed mechanical ventilation, and 13% died within 30 days.
“Comparable rates were observed in the unvaccinated group,” the investigators write, adding that there was no statistical difference in 30-day mortality between the fully vaccinated patients and the unvaccinated cohort (adjusted odds ratio, 1.08).
Factors associated with increased 30-day mortality among unvaccinated patients included lymphopenia (aOR, 1.68), comorbidities (aORs, 1.66-2.10), worse performance status (aORs, 2.26-4.34), and baseline cancer status (active/progressing vs. not active/ progressing, aOR, 6.07).
No significant differences were observed in ICU, mechanical ventilation, or hospitalization rates between the vaccinated and unvaccinated cohort after adjustment for confounders (aORs,1.13 and 1.25, respectively).
Notably, patients with an underlying hematologic malignancy were overrepresented among those with breakthrough COVID-19 (35% vs. 20%). Compared with those with solid cancers, patients with hematologic malignancies also had significantly higher rates of ICU admission, mechanical ventilation, and hospitalization.
This finding is “consistent with evidence that these patients may have a blunted serologic response to vaccination secondary to disease or therapy,” the authors note.
Although the investigators did not evaluate the risk of breakthrough infection post vaccination, recent research indicates that receiving a COVID-19 booster increases antibody levels among patients with cancer under active treatment and thus may provide additional protection against the virus.
Given the risk of breakthrough infection and severe outcomes in patients with cancer, the authors propose that “a mitigation approach that includes vaccination of close contacts, boosters, social distancing, and mask-wearing in public should be continued for the foreseeable future.” However, “additional research is needed to further categorize the patients that remain at risk of symptomatic COVID-19 following vaccination and test strategies that may reduce this risk.”
The findings are from a pre-proof that has not yet been peer reviewed or published. First author Dr. Schmidt reported nonfinancial support from Astellas, nonfinancial support from Pfizer, outside the submitted work. Other coauthors reported a range of disclosures as well. The full list can be found with the original article.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF ONCOLOGY
Is mindfulness key to helping physicians with mental health?
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
In 2011, the Mayo Clinic began surveying physicians about burnout and found 45% of physicians experienced at least one symptom, such as emotional exhaustion, finding work no longer meaningful, feelings of ineffectiveness, and depersonalizing patients. Associated manifestations can range from headache and insomnia to impaired memory and decreased attention.
Fast forward 10 years to the Medscape National Physician Burnout and Suicide Report, which found that a similar number of physicians (42%) feel burned out. The COVID-19 pandemic only added insult to injury. A Medscape survey that included nearly 5,000 U.S. physicians revealed that about two-thirds (64%) of them reported burnout had intensified during the crisis.
These elevated numbers are being labeled as “a public health crisis” for the impact widespread physician burnout could have on the health of the doctor and patient safety. The relatively consistent levels across the decade seem to suggest that, if health organizations are attempting to improve physician well-being, it doesn’t appear to be working, forcing doctors to find solutions for themselves.
Jill Wener, MD, considers herself part of the 45% burned out 10 years ago. She was working as an internist at Rush University Medical Center in Chicago, but the “existential reality of being a doctor in this world” was wearing on her. “Staying up with the literature, knowing that every day you’re going to go into work without knowing what you’re going to find, threats of lawsuits, the pressure of perfectionism,” Dr. Wener told this news organization. “By the time I hit burnout, everything made me feel like the world was crashing down on me.”
When Dr. Wener encountered someone who meditated twice a day, she was intrigued, even though the self-described “most Type-A, inside-the-box, nonspiritual type, anxious, linear-path doctor” didn’t think people like her could meditate. Dr. Wener is not alone in her hesitation to explore meditation as a means to help prevent burnout because the causes of burnout are primarily linked to external rather than internal factors. Issues including a loss of autonomy, the burden and distraction of electronic health records, and the intense pressure to comply with rules from the government are not things mindfulness can fix.
And because the sources of burnout are primarily environmental and inherent to the current medical system, the suggestion that physicians need to fix themselves with meditation can come as a slap in the face. However, when up against a system slow to change, mindfulness can provide physicians access to the one thing they can control: How they perceive and react to what’s in front of them.
At the recommendation of an acquaintance, Dr. Wener enrolled in a Vedic Meditation (also known as Conscious Health Meditation) course taught by Light Watkins, a well-known traveling instructor, author, and speaker. By the second meeting she was successfully practicing 20 minutes twice a day. This form of mediation traces its roots to the Vedas, ancient Indian texts (also the foundation for yoga), and uses a mantra to settle the mind, transitioning to an awake state of inner contentment.
Three weeks later, Dr. Wener’s daily crying jags ended as did her propensity for road rage. “I felt like I was on the cusp of something life-changing, I just didn’t understand it,” she recalled. “But I knew I was never going to give it up.”
Defining mindfulness
“Mindfulness is being able to be present in the moment that you’re in with acceptance of what it is and without judging it,” said Donna Rockwell, PsyD, a leading mindfulness meditation teacher. The practice of mindfulness is really meditation. Dr. Rockwell explained that the noise of our mind is most often focused on either the past or the future. “We’re either bemoaning something that happened earlier or we’re catastrophizing the future,” she said, which prevents us from being present in the moment.
Meditation allows you to notice when your mind has drifted from the present moment into the past or future. “You gently notice it, label it with a lot of self-compassion, and then bring your mind back by focusing on your breath – going out, going in – and the incoming stimuli through your five senses,” said Dr. Rockwell. “When you’re doing that, you can’t be in the past or future.”
Dr. Rockwell also pointed out that we constantly categorize incoming data of the moment as either “good for me or bad for me,” which gets in the way of simply being present for what you’re facing. “When you’re more fully present, you become more skillful and able to do what this moment is asking of you,” she said. Being mindful allows us to better navigate incoming stimuli, which could be a “code blue” in the ED or a patient who needs another 2 minutes during an office visit.
When Dr. Wener was burned out, she felt unable to adapt whenever something unexpected happened. “When you have no emotional reserves, everything feels like a big deal,” she said. “The meditation gave me what we call adaptation energy; it filled up my tank and kept me from feeling like I was going to lose it at 10 o’clock in the morning.”
Dr. Rockwell explained burnout as an overactive fight or flight response activated by the amygdala. It starts pumping cortisol, our pupils dilate, and our pores open. The prefrontal cortex is offline when we’re experiencing this physiological response because they both can’t be operational at the same time. “When we’re constantly in a ‘fight or flight’ response and don’t have any access to our prefrontal cortex, we are coming from a brain that is pumping cortisol and that leads to burnout,” said Dr. Rockwell.
“Any fight or flight response leaves a mark on your body,” Dr. Wener echoed. “When we go into our state of deep rest in the meditation practice, which is two to five times more restful than sleep, it heals those stress scars.”
Making time for mindfulness
Prescribing mindfulness for physicians is not new. Molecular biologist Jon Kabat-Zinn, PhD, developed Mindfulness-Based Stress Reduction (MBSR) in 1979, a practice that incorporates mindfulness exercises to help people become familiar with their behavior patterns in stressful situations. Thus, instead of reacting, they can respond with a clearer understanding of the circumstance. Dr. Kabat-Zinn initially targeted people with chronic health problems to help them cope with the effects of pain and the condition of their illness, but it has expanded to anyone experiencing challenges in their life, including physicians. A standard MBSR course runs 8 weeks, making it a commitment for most people.
Mindfulness training requires that physicians use what they already have so little of: time.
Dr. Wener was able to take a sabbatical, embarking on a 3-month trip to India to immerse herself in the study of Vedic Meditation. Upon her return, Dr. Wener took a position at Emory University, Atlanta, and has launched a number of CME-accredited meditation courses and retreats. Unlike Dr. Kabat-Zinn, her programs are by physicians and for physicians. She also created an online version of the meditation course to make it more accessible.
For these reasons, Kara Pepper, MD, an internist in outpatient primary care in Atlanta, was drawn to the meditation course. Dr. Pepper was 7 years into practice when she burned out. “The program dovetailed into my burnout recovery,” she said. “It allowed me space to separate myself from the thoughts I was having about work and just recognize them as just that – as thoughts.”
In the course, Dr. Wener teaches the REST Technique, which she says is different than mindfulness in that she encourages the mind to run rampant. “Trying to control the mind can feel very uncomfortable because we always have thoughts,” she says. “We can’t tell the mind to stop thinking just like we can’t tell the heart to stop beating.” Dr. Wener said the REST Technique lets “the mind swim downstream,” allowing the brain to go into a deep state of rest and start to heal from the scars caused by stress.
Dr. Pepper said the self-paced online course gave her all the tools she needed, and it was pragmatic and evidence based. “I didn’t feel ‘woo’ or like another gimmick,” she said. Pepper, who continues to practice medicine, became a life coach in 2019 to teach others the skills she uses daily.
An integrated strategy
In a review published in The American Journal of Medicine in 2019, Scott Yates, MD, MBA, from the Center for Executive Medicine in Plano, Tex., found that physicians who had adopted mediation and mindfulness training to decrease anxiety and perceived work stress only experienced modest benefits. In fact, Dr. Yates claims that there’s little data to suggest the long-term benefit of any particular stress management intervention in the prevention of burnout symptoms.
“The often-repeated goals of the Triple Aim [enhancing patient experience, improving population health, and reducing costs] may be unreachable until we recognize and address burnout in health care providers,” Dr. Yates wrote. He recommends adding a fourth goal to specifically address physician wellness, which certainly could include mindfulness training and meditation.
Burnout coach, trainer, and consultant Dike Drummond, MD, also professes that physician wellness must be added as the key fourth ingredient to improving health care. “Burnout is a dilemma, a balancing act,” he said. “It takes an integrated strategy.” The CEO and founder of TheHappyMD.com, Dr. Drummond’s integrated strategy to stop physician burnout has been taught to more than 40,000 physicians in 175 organizations, and one element of that strategy can be mindfulness training.
Dr. Drummond said he doesn’t use the word meditation “because that scares most people”; it takes a commitment and isn’t accessible for a lot of doctors. Instead, he coaches doctors to use a ‘single-breath’ technique to help them reset multiple times throughout the day. “I teach people how to breathe up to the top of their head and then down to the bottom of their feet,” Dr. Drummond said. He calls it the Squeegee Breath Technique because when they exhale, they “wipe away” anything that doesn’t need to be there right now. “If you happen to have a mindfulness practice like meditation, they work synergistically because the calmness you feel in your mediation is available to you at the bottom of these releasing breaths.”
Various studies and surveys provide great detail as to the “why” of physician burnout. And while mindfulness is not the sole answer, it’s something physicians can explore for themselves while health care as an industry looks for a more comprehensive solution.
“It’s not rocket science,” Dr. Drummond insisted. “You want a different result? You’re not satisfied with the way things are now and you want to feel different? You absolutely must do something different.”
A version of this article first appeared on Medscape.com.
Growing evidence supports repurposing antidepressants to treat COVID-19
Mounting evidence suggests selective serotonin reuptake inhibitors (SSRI) are associated with lower COVID-19 severity.
A large analysis of health records shows patients with COVID-19 taking an SSRI were significantly less likely to die of COVID-19 than a matched control group.
“We can’t tell if the drugs are causing these effects, but the statistical analysis is showing significant association. There’s power in the numbers,” Marina Sirota, PhD, University of California, San Francisco (UCSF), said in a statement.
The study was published online Nov. 15 in JAMA Network Open.
Data-driven approach
, including 3,401 patients who were prescribed SSRIs.
When compared with matched patients with COVID-19 taking SSRIs, patients taking fluoxetine were 28% less likely to die (relative risk, 0.72; 95% CI, 0.54-0.97; adjusted P = .03) and those taking either fluoxetine or fluvoxamine were 26% less likely to die (RR, 0.74; 95% CI, 0.55-0.99; adjusted P = .04) versus those not on these medications.
Patients with COVID-19 taking any kind of SSRI were 8% less likely to die than the matched controls (RR, 0.92; 95% CI, 0.85-0.99; adjusted P = .03).
“We observed a statistically significant reduction in mortality of COVID-19 patients who were already taking SSRIs. This is a demonstration of a data-driven approach for identifying new uses for existing drugs,” Dr. Sirota said in an interview.
“Our study simply shows an association between SSRIs and COVID-19 outcomes and doesn’t investigate the mechanism of action of why the drugs might work. Additional clinical trials need to be carried out before these drugs can be used in patients going forward,” she cautioned.
“There is currently an open-label trial investigating fluoxetine to reduce intubation and death after COVID-19. To our knowledge, there are no phase 3 randomized controlled trials taking place or planned,” study investigator Tomiko Oskotsky, MD, with UCSF, told this news organization.
Urgent need
The current results “confirm and expand on prior findings from observational, preclinical, and clinical studies suggesting that certain SSRI antidepressants, including fluoxetine or fluvoxamine, could be beneficial against COVID-19,” Nicolas Hoertel, MD, PhD, MPH, with Paris University and Corentin-Celton Hospital, France, writes in a linked editorial.
Dr. Hoertel notes that the anti-inflammatory properties of SSRIs may underlie their potential action against COVID-19, and other potential mechanisms may include reduction in platelet aggregation, decreased mast cell degranulation, increased melatonin levels, interference with endolysosomal viral trafficking, and antioxidant activities.
“Because most of the world’s population is currently unvaccinated and the COVID-19 pandemic is still active, effective treatments of COVID-19 – especially those that are easy to use, show good tolerability, can be administered orally, and have widespread availability at low cost to allow their use in resource-poor countries – are urgently needed to reduce COVID-19-related mortality and morbidity,” Dr. Hoertel points out.
“In this context, short-term use of fluoxetine or fluvoxamine, if proven effective, should be considered as a potential means of reaching this goal,” he adds.
The study was supported by the Christopher Hess Research Fund and, in part, by UCSF and the National Institutes of Health. Dr. Sirota has reported serving as a scientific advisor at Aria Pharmaceuticals. Dr. Hoertel has reported being listed as an inventor on a patent application related to methods of treating COVID-19, filed by Assistance Publique-Hopitaux de Paris, and receiving consulting fees and nonfinancial support from Lundbeck.
A version of this article first appeared on Medscape.com.
Mounting evidence suggests selective serotonin reuptake inhibitors (SSRI) are associated with lower COVID-19 severity.
A large analysis of health records shows patients with COVID-19 taking an SSRI were significantly less likely to die of COVID-19 than a matched control group.
“We can’t tell if the drugs are causing these effects, but the statistical analysis is showing significant association. There’s power in the numbers,” Marina Sirota, PhD, University of California, San Francisco (UCSF), said in a statement.
The study was published online Nov. 15 in JAMA Network Open.
Data-driven approach
, including 3,401 patients who were prescribed SSRIs.
When compared with matched patients with COVID-19 taking SSRIs, patients taking fluoxetine were 28% less likely to die (relative risk, 0.72; 95% CI, 0.54-0.97; adjusted P = .03) and those taking either fluoxetine or fluvoxamine were 26% less likely to die (RR, 0.74; 95% CI, 0.55-0.99; adjusted P = .04) versus those not on these medications.
Patients with COVID-19 taking any kind of SSRI were 8% less likely to die than the matched controls (RR, 0.92; 95% CI, 0.85-0.99; adjusted P = .03).
“We observed a statistically significant reduction in mortality of COVID-19 patients who were already taking SSRIs. This is a demonstration of a data-driven approach for identifying new uses for existing drugs,” Dr. Sirota said in an interview.
“Our study simply shows an association between SSRIs and COVID-19 outcomes and doesn’t investigate the mechanism of action of why the drugs might work. Additional clinical trials need to be carried out before these drugs can be used in patients going forward,” she cautioned.
“There is currently an open-label trial investigating fluoxetine to reduce intubation and death after COVID-19. To our knowledge, there are no phase 3 randomized controlled trials taking place or planned,” study investigator Tomiko Oskotsky, MD, with UCSF, told this news organization.
Urgent need
The current results “confirm and expand on prior findings from observational, preclinical, and clinical studies suggesting that certain SSRI antidepressants, including fluoxetine or fluvoxamine, could be beneficial against COVID-19,” Nicolas Hoertel, MD, PhD, MPH, with Paris University and Corentin-Celton Hospital, France, writes in a linked editorial.
Dr. Hoertel notes that the anti-inflammatory properties of SSRIs may underlie their potential action against COVID-19, and other potential mechanisms may include reduction in platelet aggregation, decreased mast cell degranulation, increased melatonin levels, interference with endolysosomal viral trafficking, and antioxidant activities.
“Because most of the world’s population is currently unvaccinated and the COVID-19 pandemic is still active, effective treatments of COVID-19 – especially those that are easy to use, show good tolerability, can be administered orally, and have widespread availability at low cost to allow their use in resource-poor countries – are urgently needed to reduce COVID-19-related mortality and morbidity,” Dr. Hoertel points out.
“In this context, short-term use of fluoxetine or fluvoxamine, if proven effective, should be considered as a potential means of reaching this goal,” he adds.
The study was supported by the Christopher Hess Research Fund and, in part, by UCSF and the National Institutes of Health. Dr. Sirota has reported serving as a scientific advisor at Aria Pharmaceuticals. Dr. Hoertel has reported being listed as an inventor on a patent application related to methods of treating COVID-19, filed by Assistance Publique-Hopitaux de Paris, and receiving consulting fees and nonfinancial support from Lundbeck.
A version of this article first appeared on Medscape.com.
Mounting evidence suggests selective serotonin reuptake inhibitors (SSRI) are associated with lower COVID-19 severity.
A large analysis of health records shows patients with COVID-19 taking an SSRI were significantly less likely to die of COVID-19 than a matched control group.
“We can’t tell if the drugs are causing these effects, but the statistical analysis is showing significant association. There’s power in the numbers,” Marina Sirota, PhD, University of California, San Francisco (UCSF), said in a statement.
The study was published online Nov. 15 in JAMA Network Open.
Data-driven approach
, including 3,401 patients who were prescribed SSRIs.
When compared with matched patients with COVID-19 taking SSRIs, patients taking fluoxetine were 28% less likely to die (relative risk, 0.72; 95% CI, 0.54-0.97; adjusted P = .03) and those taking either fluoxetine or fluvoxamine were 26% less likely to die (RR, 0.74; 95% CI, 0.55-0.99; adjusted P = .04) versus those not on these medications.
Patients with COVID-19 taking any kind of SSRI were 8% less likely to die than the matched controls (RR, 0.92; 95% CI, 0.85-0.99; adjusted P = .03).
“We observed a statistically significant reduction in mortality of COVID-19 patients who were already taking SSRIs. This is a demonstration of a data-driven approach for identifying new uses for existing drugs,” Dr. Sirota said in an interview.
“Our study simply shows an association between SSRIs and COVID-19 outcomes and doesn’t investigate the mechanism of action of why the drugs might work. Additional clinical trials need to be carried out before these drugs can be used in patients going forward,” she cautioned.
“There is currently an open-label trial investigating fluoxetine to reduce intubation and death after COVID-19. To our knowledge, there are no phase 3 randomized controlled trials taking place or planned,” study investigator Tomiko Oskotsky, MD, with UCSF, told this news organization.
Urgent need
The current results “confirm and expand on prior findings from observational, preclinical, and clinical studies suggesting that certain SSRI antidepressants, including fluoxetine or fluvoxamine, could be beneficial against COVID-19,” Nicolas Hoertel, MD, PhD, MPH, with Paris University and Corentin-Celton Hospital, France, writes in a linked editorial.
Dr. Hoertel notes that the anti-inflammatory properties of SSRIs may underlie their potential action against COVID-19, and other potential mechanisms may include reduction in platelet aggregation, decreased mast cell degranulation, increased melatonin levels, interference with endolysosomal viral trafficking, and antioxidant activities.
“Because most of the world’s population is currently unvaccinated and the COVID-19 pandemic is still active, effective treatments of COVID-19 – especially those that are easy to use, show good tolerability, can be administered orally, and have widespread availability at low cost to allow their use in resource-poor countries – are urgently needed to reduce COVID-19-related mortality and morbidity,” Dr. Hoertel points out.
“In this context, short-term use of fluoxetine or fluvoxamine, if proven effective, should be considered as a potential means of reaching this goal,” he adds.
The study was supported by the Christopher Hess Research Fund and, in part, by UCSF and the National Institutes of Health. Dr. Sirota has reported serving as a scientific advisor at Aria Pharmaceuticals. Dr. Hoertel has reported being listed as an inventor on a patent application related to methods of treating COVID-19, filed by Assistance Publique-Hopitaux de Paris, and receiving consulting fees and nonfinancial support from Lundbeck.
A version of this article first appeared on Medscape.com.
U.S. overdose deaths hit an all-time high
a 28.5% increase from the previous year.
Deaths in some states rose even more precipitously. Vermont saw an almost 70% increase, and drug overdose deaths in West Virginia increased by 62%. Many states, including Alabama, California, Kansas, Kentucky, Louisiana, Tennessee, and Washington, had a 45%-50% rise in overdose deaths.
The data released by the CDC was provisional, as there is generally a lag between a reported overdose and confirmation of the death to the National Vital Statistics System. The agency uses statistical models that render the counts almost 100% accurate, the CDC says.
The vast majority (73,757) of overdose deaths involved opioids – with most of those (62,338) involving synthetic opioids such as fentanyl. Federal officials said that one American died every 5 minutes from an overdose, or 265 a day.
“We have to acknowledge what this is – it is a crisis,” Department of Health & Human Services Secretary Xavier Becerra told reporters on a call.
“As much as the numbers speak so vividly, they don’t tell the whole story. We see it in the faces of grieving families and all those overworked caregivers. You hear it every time you get that panicked 911 phone call, you read it in obituaries of sons and daughters who left us way too soon,” Mr. Becerra said.
Rahul Gupta, MD, director of the White House Office of National Drug Control Policy, said that “this is unacceptable, and it requires an unprecedented response.”
Dr. Gupta, who noted that he has a waiver to treat substance use disorder patients with buprenorphine, said he’s seen “first-hand the heartbreak of the overdose epidemic,” adding that, with 23 years in practice, “I’ve learned that an overdose is a cry for help and for far too many people that cry goes unanswered.”
Both Mr. Becerra and Dr. Gupta called on Congress to pass President Joe Biden’s fiscal 2022 budget request, noting that it calls for $41 billion – a $669 million increase from fiscal year 2021 – to go to agencies working on drug interdiction and substance use prevention, treatment, and recovery support.
Dr. Gupta also announced that the administration was releasing a model law that could be used by state legislatures to help standardize policies on making the overdose antidote naloxone more accessible. Currently, such policies are a patchwork across the nation.
In addition, the federal government is newly supporting harm reduction, Mr. Becerra said. This means federal money can be used by clinics and outreach programs to buy fentanyl test strips, which they can then distribute to drug users.
“It’s important for Americans to have the ability to make sure that they can test for fentanyl in the substance,” Dr. Gupta said.
Fake pills, fentanyl a huge issue
Federal officials said that both fentanyl and methamphetamine are contributing to rising numbers of fatalities.
“Drug cartels in Mexico are mass-producing fentanyl and methamphetamine largely sourced from chemicals in China and they are distributing these substances throughout the United States,” Anne Milgram, administrator of the Drug Enforcement Administration, said on the call.
Ms. Milgram said the agency had seized 12,000 pounds of fentanyl in 2021, enough to provide every American with a lethal dose. Fentanyl is also mixed in with cocaine, heroin, methamphetamine, and marijuana – often in counterfeit pills, Ms. Milgram said.
The DEA and other law enforcement agencies have seized more than 14 million such pills in 2021. “These types of pills are easily accessible today on social media and e-commerce platforms, Ms. Milgram said.
“Drug dealers are now in our homes,” she said. “Wherever there is a smart phone or a computer, a dealer is one click away,” Ms. Milgram said.
National Institute on Drug Abuse Director Nora D. Volkow, MD, said that dealers will continue to push both fentanyl and methamphetamine because they are among the most addictive substances. They also are more profitable because they don’t require cultivation and harvesting, she said on the call.
Dr. Volkow also noted that naloxone is not as effective in reversing fentanyl overdoses because fentanyl is more potent than heroin and other opioids, and “it gets into the brain extremely rapidly.”
Ongoing research is aimed at developing a faster delivery mechanism and a longer-lasting formulation to counter overdoses, Dr. Volkow said.
A version of this article first appeared on Medscape.com.
a 28.5% increase from the previous year.
Deaths in some states rose even more precipitously. Vermont saw an almost 70% increase, and drug overdose deaths in West Virginia increased by 62%. Many states, including Alabama, California, Kansas, Kentucky, Louisiana, Tennessee, and Washington, had a 45%-50% rise in overdose deaths.
The data released by the CDC was provisional, as there is generally a lag between a reported overdose and confirmation of the death to the National Vital Statistics System. The agency uses statistical models that render the counts almost 100% accurate, the CDC says.
The vast majority (73,757) of overdose deaths involved opioids – with most of those (62,338) involving synthetic opioids such as fentanyl. Federal officials said that one American died every 5 minutes from an overdose, or 265 a day.
“We have to acknowledge what this is – it is a crisis,” Department of Health & Human Services Secretary Xavier Becerra told reporters on a call.
“As much as the numbers speak so vividly, they don’t tell the whole story. We see it in the faces of grieving families and all those overworked caregivers. You hear it every time you get that panicked 911 phone call, you read it in obituaries of sons and daughters who left us way too soon,” Mr. Becerra said.
Rahul Gupta, MD, director of the White House Office of National Drug Control Policy, said that “this is unacceptable, and it requires an unprecedented response.”
Dr. Gupta, who noted that he has a waiver to treat substance use disorder patients with buprenorphine, said he’s seen “first-hand the heartbreak of the overdose epidemic,” adding that, with 23 years in practice, “I’ve learned that an overdose is a cry for help and for far too many people that cry goes unanswered.”
Both Mr. Becerra and Dr. Gupta called on Congress to pass President Joe Biden’s fiscal 2022 budget request, noting that it calls for $41 billion – a $669 million increase from fiscal year 2021 – to go to agencies working on drug interdiction and substance use prevention, treatment, and recovery support.
Dr. Gupta also announced that the administration was releasing a model law that could be used by state legislatures to help standardize policies on making the overdose antidote naloxone more accessible. Currently, such policies are a patchwork across the nation.
In addition, the federal government is newly supporting harm reduction, Mr. Becerra said. This means federal money can be used by clinics and outreach programs to buy fentanyl test strips, which they can then distribute to drug users.
“It’s important for Americans to have the ability to make sure that they can test for fentanyl in the substance,” Dr. Gupta said.
Fake pills, fentanyl a huge issue
Federal officials said that both fentanyl and methamphetamine are contributing to rising numbers of fatalities.
“Drug cartels in Mexico are mass-producing fentanyl and methamphetamine largely sourced from chemicals in China and they are distributing these substances throughout the United States,” Anne Milgram, administrator of the Drug Enforcement Administration, said on the call.
Ms. Milgram said the agency had seized 12,000 pounds of fentanyl in 2021, enough to provide every American with a lethal dose. Fentanyl is also mixed in with cocaine, heroin, methamphetamine, and marijuana – often in counterfeit pills, Ms. Milgram said.
The DEA and other law enforcement agencies have seized more than 14 million such pills in 2021. “These types of pills are easily accessible today on social media and e-commerce platforms, Ms. Milgram said.
“Drug dealers are now in our homes,” she said. “Wherever there is a smart phone or a computer, a dealer is one click away,” Ms. Milgram said.
National Institute on Drug Abuse Director Nora D. Volkow, MD, said that dealers will continue to push both fentanyl and methamphetamine because they are among the most addictive substances. They also are more profitable because they don’t require cultivation and harvesting, she said on the call.
Dr. Volkow also noted that naloxone is not as effective in reversing fentanyl overdoses because fentanyl is more potent than heroin and other opioids, and “it gets into the brain extremely rapidly.”
Ongoing research is aimed at developing a faster delivery mechanism and a longer-lasting formulation to counter overdoses, Dr. Volkow said.
A version of this article first appeared on Medscape.com.
a 28.5% increase from the previous year.
Deaths in some states rose even more precipitously. Vermont saw an almost 70% increase, and drug overdose deaths in West Virginia increased by 62%. Many states, including Alabama, California, Kansas, Kentucky, Louisiana, Tennessee, and Washington, had a 45%-50% rise in overdose deaths.
The data released by the CDC was provisional, as there is generally a lag between a reported overdose and confirmation of the death to the National Vital Statistics System. The agency uses statistical models that render the counts almost 100% accurate, the CDC says.
The vast majority (73,757) of overdose deaths involved opioids – with most of those (62,338) involving synthetic opioids such as fentanyl. Federal officials said that one American died every 5 minutes from an overdose, or 265 a day.
“We have to acknowledge what this is – it is a crisis,” Department of Health & Human Services Secretary Xavier Becerra told reporters on a call.
“As much as the numbers speak so vividly, they don’t tell the whole story. We see it in the faces of grieving families and all those overworked caregivers. You hear it every time you get that panicked 911 phone call, you read it in obituaries of sons and daughters who left us way too soon,” Mr. Becerra said.
Rahul Gupta, MD, director of the White House Office of National Drug Control Policy, said that “this is unacceptable, and it requires an unprecedented response.”
Dr. Gupta, who noted that he has a waiver to treat substance use disorder patients with buprenorphine, said he’s seen “first-hand the heartbreak of the overdose epidemic,” adding that, with 23 years in practice, “I’ve learned that an overdose is a cry for help and for far too many people that cry goes unanswered.”
Both Mr. Becerra and Dr. Gupta called on Congress to pass President Joe Biden’s fiscal 2022 budget request, noting that it calls for $41 billion – a $669 million increase from fiscal year 2021 – to go to agencies working on drug interdiction and substance use prevention, treatment, and recovery support.
Dr. Gupta also announced that the administration was releasing a model law that could be used by state legislatures to help standardize policies on making the overdose antidote naloxone more accessible. Currently, such policies are a patchwork across the nation.
In addition, the federal government is newly supporting harm reduction, Mr. Becerra said. This means federal money can be used by clinics and outreach programs to buy fentanyl test strips, which they can then distribute to drug users.
“It’s important for Americans to have the ability to make sure that they can test for fentanyl in the substance,” Dr. Gupta said.
Fake pills, fentanyl a huge issue
Federal officials said that both fentanyl and methamphetamine are contributing to rising numbers of fatalities.
“Drug cartels in Mexico are mass-producing fentanyl and methamphetamine largely sourced from chemicals in China and they are distributing these substances throughout the United States,” Anne Milgram, administrator of the Drug Enforcement Administration, said on the call.
Ms. Milgram said the agency had seized 12,000 pounds of fentanyl in 2021, enough to provide every American with a lethal dose. Fentanyl is also mixed in with cocaine, heroin, methamphetamine, and marijuana – often in counterfeit pills, Ms. Milgram said.
The DEA and other law enforcement agencies have seized more than 14 million such pills in 2021. “These types of pills are easily accessible today on social media and e-commerce platforms, Ms. Milgram said.
“Drug dealers are now in our homes,” she said. “Wherever there is a smart phone or a computer, a dealer is one click away,” Ms. Milgram said.
National Institute on Drug Abuse Director Nora D. Volkow, MD, said that dealers will continue to push both fentanyl and methamphetamine because they are among the most addictive substances. They also are more profitable because they don’t require cultivation and harvesting, she said on the call.
Dr. Volkow also noted that naloxone is not as effective in reversing fentanyl overdoses because fentanyl is more potent than heroin and other opioids, and “it gets into the brain extremely rapidly.”
Ongoing research is aimed at developing a faster delivery mechanism and a longer-lasting formulation to counter overdoses, Dr. Volkow said.
A version of this article first appeared on Medscape.com.
Stroke thrombectomy alone fails noninferiority to bridging tPA
In the prospective, multicenter trial, the rate of good functional outcome was 57% for patients who underwent direct thrombectomy and 65% among patients who received IV thrombolysis before undergoing thrombectomy. This result failed to demonstrate noninferiority of direct mechanical thrombectomy compared to combination therapy, the researchers conclude.
“Good outcome was high in both treatment arms, with the point estimate in favor of the bridging cohort,” said lead investigator Urs Fischer, MD, co-chair of the stroke center at Inselspital, Bern University Hospital, Switzerland, during his presentation. “Postinterventional reperfusion was very high in both treatment arms and higher in patients with bridging thrombolysis, compared to direct mechanical thrombectomy.”
The findings were presented at the 13th World Stroke Congress (WSC) 2021.
Two views of thrombolysis
The value of bridging thrombolysis for patients who undergo mechanical thrombectomy is a matter of debate. One argument is that, for patients with large-vessel occlusion, IV thrombolysis may improve reperfusion before and after thrombectomy and yield better clinical outcomes. The opposing argument is that bridging thrombolysis may increase the risk for distal emboli, delay mechanical thrombectomy, and increase the rate of hemorrhage.
The researchers conducted the SWIFT DIRECT trial to investigate this question. They enrolled patients with acute ischemic stroke due to occlusion of the internal carotid artery or the M1 segment of the middle cerebral artery.
The trial was conducted at 48 sites in seven European countries and Canada. The investigators randomly assigned patients to receive IV alteplase (0.9 mg/kg) plus mechanical thrombectomy with the Solitaire device or to receive direct mechanical thrombectomy with the same device. Treatment was open label, but the assessment of endpoints was blinded.
Investigators assigned 423 patients to treatment, and 408 were included in the full analysis set. Of this group, 201 participants received direct mechanical thrombectomy, and 207 received IV thrombolysis plus thrombectomy. There were three crossovers in each treatment arm.
The primary outcome was functional independence, defined as a Modified Rankin Scale (mRS) score of 0-2, at 90 days. Secondary outcomes included mortality at 90 days, mRS shift, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, successful reperfusion, and symptomatic and asymptomatic intracranial hemorrhage (ICH).
Noninferiority not demonstrated
At baseline, patient characteristics were well balanced between the treatment groups. The median age of the patients was 72 years, and about 50% of participants were women. The median NIHSS score was 17 in both arms.
Approximately 57% of patients who underwent direct thrombectomy and 65% of those who received IV thrombolysis plus thrombectomy were functionally independent at 90 days, the primary outcome.
In addition, the researchers found no difference in mRS shift, mortality at 90 days, or change in NIHSS score at 24 hours. Postinterventional reperfusion was very high in both arms and was higher in patients who received IV tissue plasminogen activator, compared with those who received direct mechanical thrombectomy, said Dr. Fischer.
The rate of successful postinterventional reperfusion, however, was higher among patients who received thrombolysis than among those who underwent direct thrombectomy. The rate of symptomatic ICH was 1.5% in the direct thrombectomy group and 4.9% in the thrombolysis-plus-thrombectomy group.
New endpoints needed?
The investigators used noninferiority margins of 12%. “This question about the noninferiority margins, that’s a very tricky and difficult one in randomized clinical trials,” said Dr. Fischer. The investigators defined their margin using the 2015 HERMES data because no trials had yet compared direct mechanical thrombectomy and bridging thrombolysis at the time.
The researchers are performing a pooled analysis of all the trials that compared bridging thrombolysis with direct mechanical thrombectomy. “We are therefore looking at several margins, and I think this is the way we should look at these noninferiority margins,” said Dr. Fischer. “There’s not a clear-cut level which you can define.”
Enrollment in the trial was well balanced with respect to gender, which is not always the case in stroke studies, said Kevin Sheth, MD, professor of neurology and neurosurgery at Yale School of Medicine, New Haven, Conn., who commented on the study for this news organization.
The findings indicate that the likelihood of there being a difference between groups on this question is low, said Dr. Sheth. Both groups had large-vessel occlusion, both received thrombectomy, and both achieved reperfusion. But the higher rate of successful reperfusion in the bridging cohort was not reflected in any of the clinical endpoints that the investigators examined.
Observing a difference in this context will require very large trials or different endpoints that are more responsive to the intervention, said Dr. Sheth. “This is going to be a challenge for not just this but for any neuroprotection trial in the future,” he said.
The study was supported by Medtronic. Dr. Fischer has served as a consultant for Medtronic, Stryker, and CSL Behring. Dr. Sheth has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the prospective, multicenter trial, the rate of good functional outcome was 57% for patients who underwent direct thrombectomy and 65% among patients who received IV thrombolysis before undergoing thrombectomy. This result failed to demonstrate noninferiority of direct mechanical thrombectomy compared to combination therapy, the researchers conclude.
“Good outcome was high in both treatment arms, with the point estimate in favor of the bridging cohort,” said lead investigator Urs Fischer, MD, co-chair of the stroke center at Inselspital, Bern University Hospital, Switzerland, during his presentation. “Postinterventional reperfusion was very high in both treatment arms and higher in patients with bridging thrombolysis, compared to direct mechanical thrombectomy.”
The findings were presented at the 13th World Stroke Congress (WSC) 2021.
Two views of thrombolysis
The value of bridging thrombolysis for patients who undergo mechanical thrombectomy is a matter of debate. One argument is that, for patients with large-vessel occlusion, IV thrombolysis may improve reperfusion before and after thrombectomy and yield better clinical outcomes. The opposing argument is that bridging thrombolysis may increase the risk for distal emboli, delay mechanical thrombectomy, and increase the rate of hemorrhage.
The researchers conducted the SWIFT DIRECT trial to investigate this question. They enrolled patients with acute ischemic stroke due to occlusion of the internal carotid artery or the M1 segment of the middle cerebral artery.
The trial was conducted at 48 sites in seven European countries and Canada. The investigators randomly assigned patients to receive IV alteplase (0.9 mg/kg) plus mechanical thrombectomy with the Solitaire device or to receive direct mechanical thrombectomy with the same device. Treatment was open label, but the assessment of endpoints was blinded.
Investigators assigned 423 patients to treatment, and 408 were included in the full analysis set. Of this group, 201 participants received direct mechanical thrombectomy, and 207 received IV thrombolysis plus thrombectomy. There were three crossovers in each treatment arm.
The primary outcome was functional independence, defined as a Modified Rankin Scale (mRS) score of 0-2, at 90 days. Secondary outcomes included mortality at 90 days, mRS shift, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, successful reperfusion, and symptomatic and asymptomatic intracranial hemorrhage (ICH).
Noninferiority not demonstrated
At baseline, patient characteristics were well balanced between the treatment groups. The median age of the patients was 72 years, and about 50% of participants were women. The median NIHSS score was 17 in both arms.
Approximately 57% of patients who underwent direct thrombectomy and 65% of those who received IV thrombolysis plus thrombectomy were functionally independent at 90 days, the primary outcome.
In addition, the researchers found no difference in mRS shift, mortality at 90 days, or change in NIHSS score at 24 hours. Postinterventional reperfusion was very high in both arms and was higher in patients who received IV tissue plasminogen activator, compared with those who received direct mechanical thrombectomy, said Dr. Fischer.
The rate of successful postinterventional reperfusion, however, was higher among patients who received thrombolysis than among those who underwent direct thrombectomy. The rate of symptomatic ICH was 1.5% in the direct thrombectomy group and 4.9% in the thrombolysis-plus-thrombectomy group.
New endpoints needed?
The investigators used noninferiority margins of 12%. “This question about the noninferiority margins, that’s a very tricky and difficult one in randomized clinical trials,” said Dr. Fischer. The investigators defined their margin using the 2015 HERMES data because no trials had yet compared direct mechanical thrombectomy and bridging thrombolysis at the time.
The researchers are performing a pooled analysis of all the trials that compared bridging thrombolysis with direct mechanical thrombectomy. “We are therefore looking at several margins, and I think this is the way we should look at these noninferiority margins,” said Dr. Fischer. “There’s not a clear-cut level which you can define.”
Enrollment in the trial was well balanced with respect to gender, which is not always the case in stroke studies, said Kevin Sheth, MD, professor of neurology and neurosurgery at Yale School of Medicine, New Haven, Conn., who commented on the study for this news organization.
The findings indicate that the likelihood of there being a difference between groups on this question is low, said Dr. Sheth. Both groups had large-vessel occlusion, both received thrombectomy, and both achieved reperfusion. But the higher rate of successful reperfusion in the bridging cohort was not reflected in any of the clinical endpoints that the investigators examined.
Observing a difference in this context will require very large trials or different endpoints that are more responsive to the intervention, said Dr. Sheth. “This is going to be a challenge for not just this but for any neuroprotection trial in the future,” he said.
The study was supported by Medtronic. Dr. Fischer has served as a consultant for Medtronic, Stryker, and CSL Behring. Dr. Sheth has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the prospective, multicenter trial, the rate of good functional outcome was 57% for patients who underwent direct thrombectomy and 65% among patients who received IV thrombolysis before undergoing thrombectomy. This result failed to demonstrate noninferiority of direct mechanical thrombectomy compared to combination therapy, the researchers conclude.
“Good outcome was high in both treatment arms, with the point estimate in favor of the bridging cohort,” said lead investigator Urs Fischer, MD, co-chair of the stroke center at Inselspital, Bern University Hospital, Switzerland, during his presentation. “Postinterventional reperfusion was very high in both treatment arms and higher in patients with bridging thrombolysis, compared to direct mechanical thrombectomy.”
The findings were presented at the 13th World Stroke Congress (WSC) 2021.
Two views of thrombolysis
The value of bridging thrombolysis for patients who undergo mechanical thrombectomy is a matter of debate. One argument is that, for patients with large-vessel occlusion, IV thrombolysis may improve reperfusion before and after thrombectomy and yield better clinical outcomes. The opposing argument is that bridging thrombolysis may increase the risk for distal emboli, delay mechanical thrombectomy, and increase the rate of hemorrhage.
The researchers conducted the SWIFT DIRECT trial to investigate this question. They enrolled patients with acute ischemic stroke due to occlusion of the internal carotid artery or the M1 segment of the middle cerebral artery.
The trial was conducted at 48 sites in seven European countries and Canada. The investigators randomly assigned patients to receive IV alteplase (0.9 mg/kg) plus mechanical thrombectomy with the Solitaire device or to receive direct mechanical thrombectomy with the same device. Treatment was open label, but the assessment of endpoints was blinded.
Investigators assigned 423 patients to treatment, and 408 were included in the full analysis set. Of this group, 201 participants received direct mechanical thrombectomy, and 207 received IV thrombolysis plus thrombectomy. There were three crossovers in each treatment arm.
The primary outcome was functional independence, defined as a Modified Rankin Scale (mRS) score of 0-2, at 90 days. Secondary outcomes included mortality at 90 days, mRS shift, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, successful reperfusion, and symptomatic and asymptomatic intracranial hemorrhage (ICH).
Noninferiority not demonstrated
At baseline, patient characteristics were well balanced between the treatment groups. The median age of the patients was 72 years, and about 50% of participants were women. The median NIHSS score was 17 in both arms.
Approximately 57% of patients who underwent direct thrombectomy and 65% of those who received IV thrombolysis plus thrombectomy were functionally independent at 90 days, the primary outcome.
In addition, the researchers found no difference in mRS shift, mortality at 90 days, or change in NIHSS score at 24 hours. Postinterventional reperfusion was very high in both arms and was higher in patients who received IV tissue plasminogen activator, compared with those who received direct mechanical thrombectomy, said Dr. Fischer.
The rate of successful postinterventional reperfusion, however, was higher among patients who received thrombolysis than among those who underwent direct thrombectomy. The rate of symptomatic ICH was 1.5% in the direct thrombectomy group and 4.9% in the thrombolysis-plus-thrombectomy group.
New endpoints needed?
The investigators used noninferiority margins of 12%. “This question about the noninferiority margins, that’s a very tricky and difficult one in randomized clinical trials,” said Dr. Fischer. The investigators defined their margin using the 2015 HERMES data because no trials had yet compared direct mechanical thrombectomy and bridging thrombolysis at the time.
The researchers are performing a pooled analysis of all the trials that compared bridging thrombolysis with direct mechanical thrombectomy. “We are therefore looking at several margins, and I think this is the way we should look at these noninferiority margins,” said Dr. Fischer. “There’s not a clear-cut level which you can define.”
Enrollment in the trial was well balanced with respect to gender, which is not always the case in stroke studies, said Kevin Sheth, MD, professor of neurology and neurosurgery at Yale School of Medicine, New Haven, Conn., who commented on the study for this news organization.
The findings indicate that the likelihood of there being a difference between groups on this question is low, said Dr. Sheth. Both groups had large-vessel occlusion, both received thrombectomy, and both achieved reperfusion. But the higher rate of successful reperfusion in the bridging cohort was not reflected in any of the clinical endpoints that the investigators examined.
Observing a difference in this context will require very large trials or different endpoints that are more responsive to the intervention, said Dr. Sheth. “This is going to be a challenge for not just this but for any neuroprotection trial in the future,” he said.
The study was supported by Medtronic. Dr. Fischer has served as a consultant for Medtronic, Stryker, and CSL Behring. Dr. Sheth has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM WSC 2021
FDA clears first mobile rapid test for concussion
, the company has announced.
Eye-Sync is a virtual reality eye-tracking platform that provides objective measurements to aid in the assessment of concussion. It’s the first mobile, rapid test for concussion that has been cleared by the FDA, the company said.
As reported by this news organization, Eye-Sync received breakthrough designation from the FDA for this indication in March 2019.
The FDA initially cleared the Eye-Sync platform for recording, viewing, and analyzing eye movements to help clinicians identify visual tracking impairment.
The Eye-Sync technology uses a series of 60-second eye tracking assessments, neurocognitive batteries, symptom inventories, and standardized patient inventories to identify the type and severity of impairment after concussion.
“The platform generates customizable and interpretive reports that support clinical decision making and offers visual and vestibular therapies to remedy deficits and monitor improvement over time,” the company said.
In support of the application for use in concussion, SyncThink enrolled 1,655 children and adults into a clinical study that collected comprehensive patient and concussion-related data for over 12 months.
The company used these data to develop proprietary algorithms and deep learning models to identify a positive or negative indication of concussion.
The study showed that Eye-Sinc had sensitivity greater than 82% and specificity greater than 93%, “thereby providing clinicians with significant and actionable data when evaluating individuals with concussion,” the company said in a news release.
“The outcome of this study very clearly shows the effectiveness of our technology at detecting concussion and definitively demonstrates the clinical utility of Eye-Sinc,” SyncThink Chief Clinical Officer Scott Anderson said in the release.
“It also shows that the future of concussion diagnosis is no longer purely symptom-based but that of a technology driven multi-modal approach,” Mr. Anderson said.
A version of this article first appeared on Medscape.com.
, the company has announced.
Eye-Sync is a virtual reality eye-tracking platform that provides objective measurements to aid in the assessment of concussion. It’s the first mobile, rapid test for concussion that has been cleared by the FDA, the company said.
As reported by this news organization, Eye-Sync received breakthrough designation from the FDA for this indication in March 2019.
The FDA initially cleared the Eye-Sync platform for recording, viewing, and analyzing eye movements to help clinicians identify visual tracking impairment.
The Eye-Sync technology uses a series of 60-second eye tracking assessments, neurocognitive batteries, symptom inventories, and standardized patient inventories to identify the type and severity of impairment after concussion.
“The platform generates customizable and interpretive reports that support clinical decision making and offers visual and vestibular therapies to remedy deficits and monitor improvement over time,” the company said.
In support of the application for use in concussion, SyncThink enrolled 1,655 children and adults into a clinical study that collected comprehensive patient and concussion-related data for over 12 months.
The company used these data to develop proprietary algorithms and deep learning models to identify a positive or negative indication of concussion.
The study showed that Eye-Sinc had sensitivity greater than 82% and specificity greater than 93%, “thereby providing clinicians with significant and actionable data when evaluating individuals with concussion,” the company said in a news release.
“The outcome of this study very clearly shows the effectiveness of our technology at detecting concussion and definitively demonstrates the clinical utility of Eye-Sinc,” SyncThink Chief Clinical Officer Scott Anderson said in the release.
“It also shows that the future of concussion diagnosis is no longer purely symptom-based but that of a technology driven multi-modal approach,” Mr. Anderson said.
A version of this article first appeared on Medscape.com.
, the company has announced.
Eye-Sync is a virtual reality eye-tracking platform that provides objective measurements to aid in the assessment of concussion. It’s the first mobile, rapid test for concussion that has been cleared by the FDA, the company said.
As reported by this news organization, Eye-Sync received breakthrough designation from the FDA for this indication in March 2019.
The FDA initially cleared the Eye-Sync platform for recording, viewing, and analyzing eye movements to help clinicians identify visual tracking impairment.
The Eye-Sync technology uses a series of 60-second eye tracking assessments, neurocognitive batteries, symptom inventories, and standardized patient inventories to identify the type and severity of impairment after concussion.
“The platform generates customizable and interpretive reports that support clinical decision making and offers visual and vestibular therapies to remedy deficits and monitor improvement over time,” the company said.
In support of the application for use in concussion, SyncThink enrolled 1,655 children and adults into a clinical study that collected comprehensive patient and concussion-related data for over 12 months.
The company used these data to develop proprietary algorithms and deep learning models to identify a positive or negative indication of concussion.
The study showed that Eye-Sinc had sensitivity greater than 82% and specificity greater than 93%, “thereby providing clinicians with significant and actionable data when evaluating individuals with concussion,” the company said in a news release.
“The outcome of this study very clearly shows the effectiveness of our technology at detecting concussion and definitively demonstrates the clinical utility of Eye-Sinc,” SyncThink Chief Clinical Officer Scott Anderson said in the release.
“It also shows that the future of concussion diagnosis is no longer purely symptom-based but that of a technology driven multi-modal approach,” Mr. Anderson said.
A version of this article first appeared on Medscape.com.
‘Alarming’ increase in fake pills laced with fentanyl, methamphetamine, DEA warns
The U.S. Drug Enforcement Administration has issued a public safety alert over an “alarming” increase in fake prescription pills laced with the synthetic opioid fentanyl or the stimulant methamphetamine.
“The United States is facing an unprecedented crisis of overdose deaths fueled by illegally manufactured fentanyl and methamphetamine,” DEA Administrator Anne Milgram said in the alert.
“Counterfeit pills that contain these dangerous and extremely addictive drugs are more lethal and more accessible than ever before. DEA is focusing resources on taking down the violent drug traffickers causing the greatest harm and posing the greatest threat to the safety and health of Americans,” Ms. Milgram said.
Criminal drug networks are mass-producing fake fentanyl- and methamphetamine-laced pills and deceptively marketing them as legitimate prescription pills, the DEA warns.
such as oxycodone (Oxycontin, Percocet), hydrocodone (Vicodin), and alprazolam (Xanax); or stimulants like amphetamines (Adderall).
The agency has seized fake pills in every U.S. state. More than 9.5 million fake pills have been seized so far this year – more than the last 2 years combined.
The number of seized counterfeit pills with fentanyl has jumped nearly 430% since 2019. DEA lab tests reveal that two out of every five pills with fentanyl contain a potentially lethal dose.
These deadly pills are widely accessible and often sold on social media and e-commerce platforms – making them available to anyone with a smartphone, including minors, the DEA warns.
More than 93,000 people died of a drug overdose in the United States last year, according to federal statistics, and fentanyl is the primary driver of this alarming increase in overdose deaths, the DEA says.
The agency has launched a “One Pill Can Kill” public awareness campaign to educate the public of the dangers of counterfeit pills purchased outside of a licensed pharmacy. These pills are “illegal, dangerous, and potentially lethal,” the DEA warns.
This alert does not apply to legitimate pharmaceutical medications prescribed by doctors and dispensed by licensed pharmacists, the DEA says.
“The legitimate prescription supply chain is not impacted. Anyone filling a prescription at a licensed pharmacy can be confident that the medications they receive are safe when taken as directed by a medical professional,” the agency says.
A version of this article first appeared on Medscape.com.
The U.S. Drug Enforcement Administration has issued a public safety alert over an “alarming” increase in fake prescription pills laced with the synthetic opioid fentanyl or the stimulant methamphetamine.
“The United States is facing an unprecedented crisis of overdose deaths fueled by illegally manufactured fentanyl and methamphetamine,” DEA Administrator Anne Milgram said in the alert.
“Counterfeit pills that contain these dangerous and extremely addictive drugs are more lethal and more accessible than ever before. DEA is focusing resources on taking down the violent drug traffickers causing the greatest harm and posing the greatest threat to the safety and health of Americans,” Ms. Milgram said.
Criminal drug networks are mass-producing fake fentanyl- and methamphetamine-laced pills and deceptively marketing them as legitimate prescription pills, the DEA warns.
such as oxycodone (Oxycontin, Percocet), hydrocodone (Vicodin), and alprazolam (Xanax); or stimulants like amphetamines (Adderall).
The agency has seized fake pills in every U.S. state. More than 9.5 million fake pills have been seized so far this year – more than the last 2 years combined.
The number of seized counterfeit pills with fentanyl has jumped nearly 430% since 2019. DEA lab tests reveal that two out of every five pills with fentanyl contain a potentially lethal dose.
These deadly pills are widely accessible and often sold on social media and e-commerce platforms – making them available to anyone with a smartphone, including minors, the DEA warns.
More than 93,000 people died of a drug overdose in the United States last year, according to federal statistics, and fentanyl is the primary driver of this alarming increase in overdose deaths, the DEA says.
The agency has launched a “One Pill Can Kill” public awareness campaign to educate the public of the dangers of counterfeit pills purchased outside of a licensed pharmacy. These pills are “illegal, dangerous, and potentially lethal,” the DEA warns.
This alert does not apply to legitimate pharmaceutical medications prescribed by doctors and dispensed by licensed pharmacists, the DEA says.
“The legitimate prescription supply chain is not impacted. Anyone filling a prescription at a licensed pharmacy can be confident that the medications they receive are safe when taken as directed by a medical professional,” the agency says.
A version of this article first appeared on Medscape.com.
The U.S. Drug Enforcement Administration has issued a public safety alert over an “alarming” increase in fake prescription pills laced with the synthetic opioid fentanyl or the stimulant methamphetamine.
“The United States is facing an unprecedented crisis of overdose deaths fueled by illegally manufactured fentanyl and methamphetamine,” DEA Administrator Anne Milgram said in the alert.
“Counterfeit pills that contain these dangerous and extremely addictive drugs are more lethal and more accessible than ever before. DEA is focusing resources on taking down the violent drug traffickers causing the greatest harm and posing the greatest threat to the safety and health of Americans,” Ms. Milgram said.
Criminal drug networks are mass-producing fake fentanyl- and methamphetamine-laced pills and deceptively marketing them as legitimate prescription pills, the DEA warns.
such as oxycodone (Oxycontin, Percocet), hydrocodone (Vicodin), and alprazolam (Xanax); or stimulants like amphetamines (Adderall).
The agency has seized fake pills in every U.S. state. More than 9.5 million fake pills have been seized so far this year – more than the last 2 years combined.
The number of seized counterfeit pills with fentanyl has jumped nearly 430% since 2019. DEA lab tests reveal that two out of every five pills with fentanyl contain a potentially lethal dose.
These deadly pills are widely accessible and often sold on social media and e-commerce platforms – making them available to anyone with a smartphone, including minors, the DEA warns.
More than 93,000 people died of a drug overdose in the United States last year, according to federal statistics, and fentanyl is the primary driver of this alarming increase in overdose deaths, the DEA says.
The agency has launched a “One Pill Can Kill” public awareness campaign to educate the public of the dangers of counterfeit pills purchased outside of a licensed pharmacy. These pills are “illegal, dangerous, and potentially lethal,” the DEA warns.
This alert does not apply to legitimate pharmaceutical medications prescribed by doctors and dispensed by licensed pharmacists, the DEA says.
“The legitimate prescription supply chain is not impacted. Anyone filling a prescription at a licensed pharmacy can be confident that the medications they receive are safe when taken as directed by a medical professional,” the agency says.
A version of this article first appeared on Medscape.com.
Cavernous gender gap in Medicare payments to cardiologists
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
Women cardiologists receive dramatically smaller payments from the U.S. Centers for Medicare & Medicaid Services (CMS) than their male counterparts, new research suggests.
An analysis of 2016 claims data revealed male cardiologists received on average 45% more reimbursement than women in the inpatient setting, with the median payment 39% higher ($62,897 vs. $45,288).
In the outpatient setting, men received on average 62% more annual CMS payments, with the median payment 75% higher ($91,053 vs. $51,975; P < .001 for both).
The difference remained significant after the exclusion of the top and bottom 2.5% of earning physicians and cardiology subspecialties, like electrophysiology and interventional cardiology, with high procedural volumes and greater gender imbalances.
“This is one study among others which demonstrates a wage gap between men and women in medicine in cardiology,” lead author Inbar Raber, MD, Beth Israel Deaconess Medical Center, Boston, said in an interview. “I hope by increasing awareness [and] understanding of possible etiologies, it will enable some sustainable solutions, and those include access to additional support staff and equitable models surrounding parental leave and childcare support.”
The study, published online September 8 in JAMA Cardiology, comes on the heels of a recent cross-sectional analysis that put cardiology at the bottom of 13 internal medicine subspecialties with just 21% female faculty representation and one of only three specialties in which women’s median salaries did not reach 90% of men’s.
The new findings build on a 2017 report that showed Medicare payments to women physicians in 2013 were 55% of those to male physicians across all specialties.
“It can be disheartening, especially as an early career woman cardiologist, seeing these differences, but I think the responsibility on all of us is to take these observations and really try to understand more deeply why they exist,” Nosheen Reza, MD, from the University of Pennsylvania, Philadelphia, and coauthor of the cross-sectional analysis, told this news organization.
Several factors could be contributing to the disparity, but “it’s not gender discrimination from Medicare,” Dr. Raber said. “The gap in reimbursement is really driven by the types and the volume of charges submitted.”
Indeed, a direct comparison of the three most common inpatient and outpatient billing codes showed no difference in payments between the sexes.
Men, however, submitted 24% more median inpatient charges to CMS than women (1,190 vs. 959), and 94% more outpatient charges (1,685 vs. 870).
Men also submitted slightly more unique billing codes (median inpatient, 10 vs. 9; median outpatient, 11 vs. 8).
Notably, women made up just 13% of the 17,524 cardiologists who received CMS payments in the inpatient setting in 2016 and 13% of the 16,929 cardiologists who did so in the outpatient setting.
Louisiana had the dubious distinction of having the largest gender gap in mean CMS payments, with male cardiologists earning $145,323 (235%) more than women, whereas women cardiologists in Vermont out-earned men by $31,483 (38%).
Overall, male cardiologists had more years in practice than women cardiologists and cared for slightly older Medicare beneficiaries.
Differences in CMS payments persisted, however, after adjustment for years since graduation, physician subspecialty, number of charges, number of unique billing codes, and patient complexity. The resulting β coefficient was -0.06, which translates into women receiving an average of 94% of the CMS payments received by men.
“The first takeaway, if you were really crass and focused on the bottom line, might be: ‘Hey, let me get a few more male cardiologists because they’re going to bring more into the organization.’ But we shouldn’t do that because, unless you link these data with quality outcomes, they’re an interesting observation and hypothesis-generating,” said Sharonne Hayes, MD, coauthor of the 2017 report and professor of cardiovascular medicine at Mayo Clinic in Rochester, Minn., where she has served as director of diversity and inclusion for a decade.
She noted that there are multiple examples that the style of medicine women practice, on average, may be more effective, may be more outcomes based, and may save lives, as suggested by a recent analysis of hospitalized Medicare beneficiaries.
“The gap was not much different, like within 1% or so, but when you take that over the literally millions of Medicare patients cared for each year by hospitalists, that’s a substantial number of people,” Dr. Hayes said. “So, I think we need to take a step back, and we have to include these observations on studies like this and better understand the compensation gaps.”
She pointed out that the present study lacks data on full-time-equivalent status but that female physicians are more likely to work part-time, thus reducing the volume of claims.
Women might also care for different patient populations. “I practice in a women’s heart clinic and take care of [spontaneous coronary artery dissection] SCAD patients where the average age of SCAD is 42. So, the vast majority of patients I see on a day-to-day basis aren’t going to be Medicare age,” observed Dr. Hayes.
The differences in charges might also reflect the increased obligations in nonreimbursed work that women can have, Dr. Raber said. These can be things like mentoring, teaching roles, and serving on committees, which is a hypothesis supported by a 2021 study that showed women physicians spend more time on these “citizenship tasks” than men.
Finally, there could be organizational barriers that affect women’s clinical volumes, including less access to support from health care personnel. Added support is especially important, though, amid a 100-year pandemic, the women agreed.
“Within the first year of the pandemic, we saw women leaving the workforce in droves across all sectors, including medicine, including academic medicine. And, as the pandemic goes on without any signs of abatement, those threats continue to exist and continue to be amplified,” Dr. Reza said.
The groundswell of support surrounding the importance of diversity, equity, and inclusion initiatives across the board has helped bring attention to the issue, she said. Some institutions, including the National Institutes of Health, are making efforts to extend relief to women with young families, caregivers, or those in academic medicine who, for example, need extensions on grants or bridge funding.
“There’s certainly a lot left to do, but I do think within the last year, there’s been an acceleration of literature that has come out, not only pointing out the disparities, but pointing out that perhaps women physicians do have better outcomes and are better liked by their patients and that losing women in the workforce would be a huge detriment to the field overall,” Dr. Reza said.
Dr. Raber, Dr. Reza, and Dr. Hayes reports no relevant financial relationships. Coauthor conflict of interest disclosures are listed in the paper.
A version of this article first appeared on Medscape.com.
The trauma and healing of 9/11 echo in COVID-19
The scope and magnitude of the Sept. 11, 2001, attacks on the World Trade Center and the Pentagon were unprecedented in U.S. history. It was arguably the most serious trauma to beset Americans on U.S. soil. The 20th anniversary of 9/11 will take place during another crisis, not only in American history but also in world history – the COVID-19 pandemic.

“As different as these two events are, there are obvious points of comparison,” Jonathan DePierro, PhD, assistant professor of psychiatry, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Both were unprecedented life-threatening situations, presenting threats to individuals’ lives and profoundly traumatizing not only society as a whole but also first responders.”
Dr. DePierro, who is also the clinical director of the Center for Stress, Resilience, and Personal Growth at Mount Sinai, thinks there are many lessons to be learned from the mental health response to 9/11 that can inform our understanding of and response to the mental health needs of today’s first responders in the COVID-19 crisis, particularly health care professionals.
“Every one of our hospitals became a ‘ground zero’ early during the pandemic, and we see the numbers rising again and hospitals again overwhelmed, so he said.
Placing trauma within a new framework
According to Priscilla Dass-Brailsford, EdD, MPH, professor of psychology, department of psychiatry, Georgetown University, Washington, Sept. 11, 2001, “placed trauma within a new framework.”
“Prior to 9/11, crisis protocols and how to manage stress in the aftermath of violent events were uncommon,” Dr. Dass-Brailsford, a clinical psychologist with expertise in trauma who also chairs a clinical psychology program for the Chicago School of Professional Psychology, said in an interview.
As a first responder, she was involved in early interventions for survivors of 9/11. On Sept. 11, 2001, she had just resigned her position as coordinator of the community crisis response team – the first of its kind in the United States – through the Victims of Violence Program in Cambridge, in Cambridge, Mass.
The program responded to communities in which there were high rates of drive-by shootings and similar acts of violence. Because of her crisis experience, Dr. Dass-Brailsford was asked to conduct debriefings in Boston in the area where the 9/11 terrorists had stayed prior to boarding the planes that were used in the terrorist attacks. She subsequently went to New York City to conduct similar psychological debriefings with affected communities.
“What we’ve learned is that we had no crisis protocol on how to manage the stress in the aftermath of such a violent event, no standard operating procedures. There were very few people trained in crisis and trauma response at that time. Partially spurred by 9/11, trauma training programs became more prolific,” she said. Dr. Dass-Brailsford developed a trauma certification program at Lesley University in Cambridge, Mass., where she began to teach after 9/11. “I saw the importance of having clinicians trained to respond in a crisis, because responding to a crisis is very different from conducting regular mental health interventions.”
Short- and long-term interventions
Dr. DePierro said that Mount Sinai has a 20-year history of responding to the physical and mental health needs of 9/11 responders.
“We saw a number of first responders experiencing clinical depression, anxiety, a lot of worry, symptoms of posttraumatic stress disorder, and an increase in alcohol and/or substance use,” he recounted. In some, these responses were immediate; in others, the onset of symptoms was more gradual. Some responders had acute reactions that lasted for several months to a year, whereas for others, the reactions were prolonged, and they remained “chronically distressed long after the immediate exposure to the event,” he said.
Recent studies have shown that, during the COVID-19 pandemic, health care professionals and many essential workers have experienced similar symptoms, Dr. DePierro noted.
Mental health care professionals who provided interventions for workers involved in recovery and cleanup at the World Trade Center have highlighted the need for long-term monitoring of people on the front lines during the COVID-19 pandemic – especially health care workers, other essential personnel (for example, delivery, postal, and grocery store workers) and surviving family members. “Health monitoring and treatment efforts for 9/11 survivors and responders were put into place soon after the attacks and continue to this day,” using funding provided through the James Zadroga Act, Dr. DePierro said.
“Without similarly unified health registry and treatment services, many individuals – especially from underserved groups – will likely experience chronic mental health consequences and will be unable to access high-quality health care services,” he stated.
‘Psychological first aid’
“Although many people who go through a crisis – whether as a result of terrorism, such as 9/11, or a medical crisis, such as the current pandemic, or a natural disaster, such as Hurricane Katrina – experience PTSD, it’s important to note that not everyone who goes through a crisis and is traumatized will go on to develop PTSD,” Dr. Dass-Brailsford emphasized.
“To me, 9/11 placed psychological first aid on the map. Even if you are not a clinician, you can be trained to provide psychological first aid by becoming familiar with people’s reactions to trauma and how you can support them through it,” she continued.
For example, if a coworker is agitated or “seems to be having a meltdown, you can be there by offering support and getting them the appropriate help.” Research has suggested that having social support before and after a traumatic event can be helpful in determining vulnerability to the development of PTSD and in modulating the impact of the trauma.
Psychological first aid is helpful as an interim measure. “If you see a coworker holding their head in their hands all day and staring at the screen, identifying whether the person might be having a dissociative episode is critical. Providing some support is important, but if more intensive professional support is needed, determining that and making a referral becomes key,” Dr. Dass-Brailsford stated.
Dr. DePierro added: “One of the most important messages that I want health care workers to know from my years of working with 9/11 survivors is that feeling distressed after a traumatic event is very common, but with effective care, one doesn’t necessarily need to be in treatment for years.”
Danielle Ofri, MD, PhD, clinical professor, department of medicine, New York University, agreed. “It is important to continue keeping tabs on each other and remaining sensitive to the collateral struggles of our colleagues. Some have children who are struggling in school, others have parents who have lost a job. Continuing to check in on others and offer support is critical going forward,” she said in an interview.
Cohesiveness and volunteerism
One of the most powerful antidotes to long-term traumatization is a sense of community cohesiveness. This was the case following 9/11, and it is the case during the COVID-19 pandemic, according to Dr. Ofri, an internist at Bellevue Hospital in New York.
“There was an enormous mobilization. Bellevue is a city hospital with a level 1 trauma center, and we expected to be swamped, so the whole hospital shifted into gear,” said Dr. Ofri. “What would have been terrifying seemed tolerable because we felt that we were in it together. We discharged the inpatients to make beds available. Within hours, we had converted clinics into emergency departments and ICUs. We worked seamlessly, and the crisis brought us together ... but then, of course, no patients showed up.”
She described her relationship with her colleagues as “feeling almost like a family, especially during the pandemic, when so many others were in lockdown and feeling isolated and useless.”
She and her colleagues saw each other daily. Although the content of their tasks and responsibilities changed and people were redeployed to other areas, “our workday didn’t really change. It would have been overwhelming if we hadn’t had our daily meetings to regroup and assess where we were. Each day, everything we had learned or implemented the day before – treatment protocols, testing protocols, our understanding of how the virus was communicated – would change and need to be reevaluated. Those morning meetings were critical to staying centered. It felt as though we were building a plane and flying it at the same time, which felt both scary and heady. Luckily, it took place within the fraternity of a committed and caring group.”
Dr. Ofri recounted that, after 9/11, as well as during the pandemic, “professionals kept jumping in from the sidelines to volunteer. Within hours of the collapse of the towers, the ED had filled with staff. People came out of retirement and out from vacation and out of the woodwork. It was very heartening.”
Even more inspiring, “all the departmental barriers seemed to break down. People were willing to step out of their ordinary roles and check their egos at the door. Seasoned physicians were willing to function as medical interns.”
This generosity of time and spirit “helped keep us going,” she said.
Dr. DePierro agreed. “One of the things I’ve seen on medical floors is that COVID actually brought some units together, increasing their cohesion and mutual support and increasing the bonds between people.” These intensified bonds “increased the resilience of everyone involved.”
Commitment to the community
Dr. Ofri recalls families gathering at the hospital after 9/11, watching posters of missing people going up all over the hospital as well as on mailboxes and lampposts. Because the center for missing people was located right next door to Bellevue, there were long lines of families coming in to register. The chief medical office was there, and a huge tent was built to accommodate the families. The tent took up the entire block. “We felt a lot of ownership, because families were coming here,” she said.
The street remained closed even as the days, weeks, and years stretched on, and the tent remained. It was used as a reflection area for families. During the pandemic, that area was used for refrigerated trucks that served as temporary morgues.
“Both logistically and emotionally, we had a feeling during the pandemic of, ‘We’ve been here before, we’ll do it again and be there for the community,’ ” Dr. Ofri said.
She noted that the sense of commitment to the community carried her and fellow clinicians through the toughest parts of 9/11 and of the COVID-19 pandemic.
“People look to the medical system as a lodestar. ‘Where’s my family member? What should I do? Should I be tested? Vaccinated?’ We were there to be a steady presence for the community physically, psychologically, emotionally, and medically, which helped center us as well,” Dr. Ofri said. “If we didn’t have that, we might have all given in to existential panic.”
She added: “Although we had to work twice as hard, often amid great personal risk, we had the good fortune of having a sense of purpose, something to contribute, plus the community of colleagues we cared about and trusted with our lives.”
Crisis and personal growth
Dr. DePierro said that participants who went through 9/11 have been coming to Mount Sinai’s World Trade Center Health Program for care for nearly two decades. “Many are doing quite well, despite the emotional trauma and the dust and toxin exposure, which has given us a window into what makes people resilient.”
Social and community support are key factors in resilience. Another is recognizing opportunities for personal or professional growth during the crisis, according to Dr. DePierro.
During the pandemic, hospital staff were redeployed to departments where they didn’t typically work. They worked with new colleagues and used skills in patient care that they hadn’t needed for years or even decades. “Although this was stressful and distressing, quite a number said they came through with more medical knowledge than before and that they had forged relationships in the trenches that have been lasting and have become important to them,” he reported.
He noted that, during both crises, for first responders and health care practitioners, religious or spiritual faith was a source of resilience. “During the peak of the pandemic, chaplains provided an exorbitant amount of staff support as clinicians turned to the chaplain to help make sense of what they were going through and connect to something greater than themselves.” Similarly, during 9/11, police and fire department chaplains “played a huge role in supporting the first responders,” Dr. DePierro said.
He said that Mount Sinai holds resilience workshops “where we focus on these topics and teach health care workers how to build resilience in their lives, heal day-to-day stressors, and even grow from the experience.”
Dr. Ofri, who is the founder and editor-in-chief of the Bellevue Literary Review, added that the arts played an important role in bolstering resilience and providing a creative outlet for clinicians after 9/11 and again during the pandemic.
The publication is celebrating its twentieth anniversary – its first issue went to press in September 2001. The cover contained an acknowledgment of 9/11.
Dr. Ofri said that a gala event had been planned for Oct. 7, 2001, to celebrate the inaugural issue of the publication. She assumed no one would show up, given that the United States had invaded Afghanistan only hours earlier. To her surprise, over a hundred people attended, “which made me realize the role of the arts during trauma. People were seeking to come together and hear poetry, fiction, and creative nonfiction.”
Dr. Ofri has been “impressed by the amount of incredible creative writing of all sorts that has been submitted [to the publication] during the pandemic, an unexpected flowering of the arts.”
Unique challenges, unique opportunities
All three experts pointed to several noteworthy differences between the experiences of first responders following 9/11 and those of today’s health care professionals during the pandemic.
“What happened on Sept. 11 was one discrete event, and although it obviously led to years of recovering body parts and cleaning up Ground Zero, and on a national level it led to a war, it nevertheless was a single event,” Dr. DePierro observed. By contrast, the COVID-19 pandemic is ongoing, and for health care practitioners, “it’s by no means over. Again and again, they are being thrown back into battle, dealing with fatigue, weariness, and loss of life.”
Moreover, “it is my understanding that immediately following 9/11, there was a general coming together in our country, but it’s obvious that today, there’s a great deal of fractiousness, contention, disagreement, and disunity in our country when it comes to COVID-19,” Dr. DePierro continued.
“This takes a great toll, particularly on health care workers who are dealing with COVID-19 on a daily basis and experience a disconnect between what they see on their floors and ICUs of the hospital, experiencing loss of life they’ve likely never encountered in their careers, and what people are saying when they downplay the seriousness of COVID-19,” he said.
Dr. Ofri agreed. “The fragmentation of our country and the failure of leadership at the highest level to provide even the basics, such as PPE [personal protective equipment] for health care professionals, left us baffled, profoundly hurt, and angry.”
A positive difference between the COVID-19 pandemic and the aftermath of 9/11 is the development of sophisticated technology that allows interventions for traumatized individuals – both health care professionals and the general public – through telehealth, Dr. DePierro pointed out.
“I would say that these resources and technologies are a silver lining and should continue to be expanded on,” he said. “Now, busy health care workers can access all manner of supportive services, including teletherapy, right from home or between shifts.”
Another “silver lining” is that the pandemic has shone a spotlight on an issue that predated the pandemic – the mental health of health care professionals. Opening a discussion about this has reduced stigma and hopefully has paved the way for improved treatments and for providing resources.
Dr. Dass-Brailsford added that “it is important, going forward, for all of us to be trauma informed, to know how trauma and trauma-related stress unfolds in both other people and yourself, and to know what coping skills can be used to avoid crises from developing – a task that extends across all types of disasters.”
A version of this article first appeared on Medscape.com.
The scope and magnitude of the Sept. 11, 2001, attacks on the World Trade Center and the Pentagon were unprecedented in U.S. history. It was arguably the most serious trauma to beset Americans on U.S. soil. The 20th anniversary of 9/11 will take place during another crisis, not only in American history but also in world history – the COVID-19 pandemic.

“As different as these two events are, there are obvious points of comparison,” Jonathan DePierro, PhD, assistant professor of psychiatry, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Both were unprecedented life-threatening situations, presenting threats to individuals’ lives and profoundly traumatizing not only society as a whole but also first responders.”
Dr. DePierro, who is also the clinical director of the Center for Stress, Resilience, and Personal Growth at Mount Sinai, thinks there are many lessons to be learned from the mental health response to 9/11 that can inform our understanding of and response to the mental health needs of today’s first responders in the COVID-19 crisis, particularly health care professionals.
“Every one of our hospitals became a ‘ground zero’ early during the pandemic, and we see the numbers rising again and hospitals again overwhelmed, so he said.
Placing trauma within a new framework
According to Priscilla Dass-Brailsford, EdD, MPH, professor of psychology, department of psychiatry, Georgetown University, Washington, Sept. 11, 2001, “placed trauma within a new framework.”
“Prior to 9/11, crisis protocols and how to manage stress in the aftermath of violent events were uncommon,” Dr. Dass-Brailsford, a clinical psychologist with expertise in trauma who also chairs a clinical psychology program for the Chicago School of Professional Psychology, said in an interview.
As a first responder, she was involved in early interventions for survivors of 9/11. On Sept. 11, 2001, she had just resigned her position as coordinator of the community crisis response team – the first of its kind in the United States – through the Victims of Violence Program in Cambridge, in Cambridge, Mass.
The program responded to communities in which there were high rates of drive-by shootings and similar acts of violence. Because of her crisis experience, Dr. Dass-Brailsford was asked to conduct debriefings in Boston in the area where the 9/11 terrorists had stayed prior to boarding the planes that were used in the terrorist attacks. She subsequently went to New York City to conduct similar psychological debriefings with affected communities.
“What we’ve learned is that we had no crisis protocol on how to manage the stress in the aftermath of such a violent event, no standard operating procedures. There were very few people trained in crisis and trauma response at that time. Partially spurred by 9/11, trauma training programs became more prolific,” she said. Dr. Dass-Brailsford developed a trauma certification program at Lesley University in Cambridge, Mass., where she began to teach after 9/11. “I saw the importance of having clinicians trained to respond in a crisis, because responding to a crisis is very different from conducting regular mental health interventions.”
Short- and long-term interventions
Dr. DePierro said that Mount Sinai has a 20-year history of responding to the physical and mental health needs of 9/11 responders.
“We saw a number of first responders experiencing clinical depression, anxiety, a lot of worry, symptoms of posttraumatic stress disorder, and an increase in alcohol and/or substance use,” he recounted. In some, these responses were immediate; in others, the onset of symptoms was more gradual. Some responders had acute reactions that lasted for several months to a year, whereas for others, the reactions were prolonged, and they remained “chronically distressed long after the immediate exposure to the event,” he said.
Recent studies have shown that, during the COVID-19 pandemic, health care professionals and many essential workers have experienced similar symptoms, Dr. DePierro noted.
Mental health care professionals who provided interventions for workers involved in recovery and cleanup at the World Trade Center have highlighted the need for long-term monitoring of people on the front lines during the COVID-19 pandemic – especially health care workers, other essential personnel (for example, delivery, postal, and grocery store workers) and surviving family members. “Health monitoring and treatment efforts for 9/11 survivors and responders were put into place soon after the attacks and continue to this day,” using funding provided through the James Zadroga Act, Dr. DePierro said.
“Without similarly unified health registry and treatment services, many individuals – especially from underserved groups – will likely experience chronic mental health consequences and will be unable to access high-quality health care services,” he stated.
‘Psychological first aid’
“Although many people who go through a crisis – whether as a result of terrorism, such as 9/11, or a medical crisis, such as the current pandemic, or a natural disaster, such as Hurricane Katrina – experience PTSD, it’s important to note that not everyone who goes through a crisis and is traumatized will go on to develop PTSD,” Dr. Dass-Brailsford emphasized.
“To me, 9/11 placed psychological first aid on the map. Even if you are not a clinician, you can be trained to provide psychological first aid by becoming familiar with people’s reactions to trauma and how you can support them through it,” she continued.
For example, if a coworker is agitated or “seems to be having a meltdown, you can be there by offering support and getting them the appropriate help.” Research has suggested that having social support before and after a traumatic event can be helpful in determining vulnerability to the development of PTSD and in modulating the impact of the trauma.
Psychological first aid is helpful as an interim measure. “If you see a coworker holding their head in their hands all day and staring at the screen, identifying whether the person might be having a dissociative episode is critical. Providing some support is important, but if more intensive professional support is needed, determining that and making a referral becomes key,” Dr. Dass-Brailsford stated.
Dr. DePierro added: “One of the most important messages that I want health care workers to know from my years of working with 9/11 survivors is that feeling distressed after a traumatic event is very common, but with effective care, one doesn’t necessarily need to be in treatment for years.”
Danielle Ofri, MD, PhD, clinical professor, department of medicine, New York University, agreed. “It is important to continue keeping tabs on each other and remaining sensitive to the collateral struggles of our colleagues. Some have children who are struggling in school, others have parents who have lost a job. Continuing to check in on others and offer support is critical going forward,” she said in an interview.
Cohesiveness and volunteerism
One of the most powerful antidotes to long-term traumatization is a sense of community cohesiveness. This was the case following 9/11, and it is the case during the COVID-19 pandemic, according to Dr. Ofri, an internist at Bellevue Hospital in New York.
“There was an enormous mobilization. Bellevue is a city hospital with a level 1 trauma center, and we expected to be swamped, so the whole hospital shifted into gear,” said Dr. Ofri. “What would have been terrifying seemed tolerable because we felt that we were in it together. We discharged the inpatients to make beds available. Within hours, we had converted clinics into emergency departments and ICUs. We worked seamlessly, and the crisis brought us together ... but then, of course, no patients showed up.”
She described her relationship with her colleagues as “feeling almost like a family, especially during the pandemic, when so many others were in lockdown and feeling isolated and useless.”
She and her colleagues saw each other daily. Although the content of their tasks and responsibilities changed and people were redeployed to other areas, “our workday didn’t really change. It would have been overwhelming if we hadn’t had our daily meetings to regroup and assess where we were. Each day, everything we had learned or implemented the day before – treatment protocols, testing protocols, our understanding of how the virus was communicated – would change and need to be reevaluated. Those morning meetings were critical to staying centered. It felt as though we were building a plane and flying it at the same time, which felt both scary and heady. Luckily, it took place within the fraternity of a committed and caring group.”
Dr. Ofri recounted that, after 9/11, as well as during the pandemic, “professionals kept jumping in from the sidelines to volunteer. Within hours of the collapse of the towers, the ED had filled with staff. People came out of retirement and out from vacation and out of the woodwork. It was very heartening.”
Even more inspiring, “all the departmental barriers seemed to break down. People were willing to step out of their ordinary roles and check their egos at the door. Seasoned physicians were willing to function as medical interns.”
This generosity of time and spirit “helped keep us going,” she said.
Dr. DePierro agreed. “One of the things I’ve seen on medical floors is that COVID actually brought some units together, increasing their cohesion and mutual support and increasing the bonds between people.” These intensified bonds “increased the resilience of everyone involved.”
Commitment to the community
Dr. Ofri recalls families gathering at the hospital after 9/11, watching posters of missing people going up all over the hospital as well as on mailboxes and lampposts. Because the center for missing people was located right next door to Bellevue, there were long lines of families coming in to register. The chief medical office was there, and a huge tent was built to accommodate the families. The tent took up the entire block. “We felt a lot of ownership, because families were coming here,” she said.
The street remained closed even as the days, weeks, and years stretched on, and the tent remained. It was used as a reflection area for families. During the pandemic, that area was used for refrigerated trucks that served as temporary morgues.
“Both logistically and emotionally, we had a feeling during the pandemic of, ‘We’ve been here before, we’ll do it again and be there for the community,’ ” Dr. Ofri said.
She noted that the sense of commitment to the community carried her and fellow clinicians through the toughest parts of 9/11 and of the COVID-19 pandemic.
“People look to the medical system as a lodestar. ‘Where’s my family member? What should I do? Should I be tested? Vaccinated?’ We were there to be a steady presence for the community physically, psychologically, emotionally, and medically, which helped center us as well,” Dr. Ofri said. “If we didn’t have that, we might have all given in to existential panic.”
She added: “Although we had to work twice as hard, often amid great personal risk, we had the good fortune of having a sense of purpose, something to contribute, plus the community of colleagues we cared about and trusted with our lives.”
Crisis and personal growth
Dr. DePierro said that participants who went through 9/11 have been coming to Mount Sinai’s World Trade Center Health Program for care for nearly two decades. “Many are doing quite well, despite the emotional trauma and the dust and toxin exposure, which has given us a window into what makes people resilient.”
Social and community support are key factors in resilience. Another is recognizing opportunities for personal or professional growth during the crisis, according to Dr. DePierro.
During the pandemic, hospital staff were redeployed to departments where they didn’t typically work. They worked with new colleagues and used skills in patient care that they hadn’t needed for years or even decades. “Although this was stressful and distressing, quite a number said they came through with more medical knowledge than before and that they had forged relationships in the trenches that have been lasting and have become important to them,” he reported.
He noted that, during both crises, for first responders and health care practitioners, religious or spiritual faith was a source of resilience. “During the peak of the pandemic, chaplains provided an exorbitant amount of staff support as clinicians turned to the chaplain to help make sense of what they were going through and connect to something greater than themselves.” Similarly, during 9/11, police and fire department chaplains “played a huge role in supporting the first responders,” Dr. DePierro said.
He said that Mount Sinai holds resilience workshops “where we focus on these topics and teach health care workers how to build resilience in their lives, heal day-to-day stressors, and even grow from the experience.”
Dr. Ofri, who is the founder and editor-in-chief of the Bellevue Literary Review, added that the arts played an important role in bolstering resilience and providing a creative outlet for clinicians after 9/11 and again during the pandemic.
The publication is celebrating its twentieth anniversary – its first issue went to press in September 2001. The cover contained an acknowledgment of 9/11.
Dr. Ofri said that a gala event had been planned for Oct. 7, 2001, to celebrate the inaugural issue of the publication. She assumed no one would show up, given that the United States had invaded Afghanistan only hours earlier. To her surprise, over a hundred people attended, “which made me realize the role of the arts during trauma. People were seeking to come together and hear poetry, fiction, and creative nonfiction.”
Dr. Ofri has been “impressed by the amount of incredible creative writing of all sorts that has been submitted [to the publication] during the pandemic, an unexpected flowering of the arts.”
Unique challenges, unique opportunities
All three experts pointed to several noteworthy differences between the experiences of first responders following 9/11 and those of today’s health care professionals during the pandemic.
“What happened on Sept. 11 was one discrete event, and although it obviously led to years of recovering body parts and cleaning up Ground Zero, and on a national level it led to a war, it nevertheless was a single event,” Dr. DePierro observed. By contrast, the COVID-19 pandemic is ongoing, and for health care practitioners, “it’s by no means over. Again and again, they are being thrown back into battle, dealing with fatigue, weariness, and loss of life.”
Moreover, “it is my understanding that immediately following 9/11, there was a general coming together in our country, but it’s obvious that today, there’s a great deal of fractiousness, contention, disagreement, and disunity in our country when it comes to COVID-19,” Dr. DePierro continued.
“This takes a great toll, particularly on health care workers who are dealing with COVID-19 on a daily basis and experience a disconnect between what they see on their floors and ICUs of the hospital, experiencing loss of life they’ve likely never encountered in their careers, and what people are saying when they downplay the seriousness of COVID-19,” he said.
Dr. Ofri agreed. “The fragmentation of our country and the failure of leadership at the highest level to provide even the basics, such as PPE [personal protective equipment] for health care professionals, left us baffled, profoundly hurt, and angry.”
A positive difference between the COVID-19 pandemic and the aftermath of 9/11 is the development of sophisticated technology that allows interventions for traumatized individuals – both health care professionals and the general public – through telehealth, Dr. DePierro pointed out.
“I would say that these resources and technologies are a silver lining and should continue to be expanded on,” he said. “Now, busy health care workers can access all manner of supportive services, including teletherapy, right from home or between shifts.”
Another “silver lining” is that the pandemic has shone a spotlight on an issue that predated the pandemic – the mental health of health care professionals. Opening a discussion about this has reduced stigma and hopefully has paved the way for improved treatments and for providing resources.
Dr. Dass-Brailsford added that “it is important, going forward, for all of us to be trauma informed, to know how trauma and trauma-related stress unfolds in both other people and yourself, and to know what coping skills can be used to avoid crises from developing – a task that extends across all types of disasters.”
A version of this article first appeared on Medscape.com.
The scope and magnitude of the Sept. 11, 2001, attacks on the World Trade Center and the Pentagon were unprecedented in U.S. history. It was arguably the most serious trauma to beset Americans on U.S. soil. The 20th anniversary of 9/11 will take place during another crisis, not only in American history but also in world history – the COVID-19 pandemic.

“As different as these two events are, there are obvious points of comparison,” Jonathan DePierro, PhD, assistant professor of psychiatry, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Both were unprecedented life-threatening situations, presenting threats to individuals’ lives and profoundly traumatizing not only society as a whole but also first responders.”
Dr. DePierro, who is also the clinical director of the Center for Stress, Resilience, and Personal Growth at Mount Sinai, thinks there are many lessons to be learned from the mental health response to 9/11 that can inform our understanding of and response to the mental health needs of today’s first responders in the COVID-19 crisis, particularly health care professionals.
“Every one of our hospitals became a ‘ground zero’ early during the pandemic, and we see the numbers rising again and hospitals again overwhelmed, so he said.
Placing trauma within a new framework
According to Priscilla Dass-Brailsford, EdD, MPH, professor of psychology, department of psychiatry, Georgetown University, Washington, Sept. 11, 2001, “placed trauma within a new framework.”
“Prior to 9/11, crisis protocols and how to manage stress in the aftermath of violent events were uncommon,” Dr. Dass-Brailsford, a clinical psychologist with expertise in trauma who also chairs a clinical psychology program for the Chicago School of Professional Psychology, said in an interview.
As a first responder, she was involved in early interventions for survivors of 9/11. On Sept. 11, 2001, she had just resigned her position as coordinator of the community crisis response team – the first of its kind in the United States – through the Victims of Violence Program in Cambridge, in Cambridge, Mass.
The program responded to communities in which there were high rates of drive-by shootings and similar acts of violence. Because of her crisis experience, Dr. Dass-Brailsford was asked to conduct debriefings in Boston in the area where the 9/11 terrorists had stayed prior to boarding the planes that were used in the terrorist attacks. She subsequently went to New York City to conduct similar psychological debriefings with affected communities.
“What we’ve learned is that we had no crisis protocol on how to manage the stress in the aftermath of such a violent event, no standard operating procedures. There were very few people trained in crisis and trauma response at that time. Partially spurred by 9/11, trauma training programs became more prolific,” she said. Dr. Dass-Brailsford developed a trauma certification program at Lesley University in Cambridge, Mass., where she began to teach after 9/11. “I saw the importance of having clinicians trained to respond in a crisis, because responding to a crisis is very different from conducting regular mental health interventions.”
Short- and long-term interventions
Dr. DePierro said that Mount Sinai has a 20-year history of responding to the physical and mental health needs of 9/11 responders.
“We saw a number of first responders experiencing clinical depression, anxiety, a lot of worry, symptoms of posttraumatic stress disorder, and an increase in alcohol and/or substance use,” he recounted. In some, these responses were immediate; in others, the onset of symptoms was more gradual. Some responders had acute reactions that lasted for several months to a year, whereas for others, the reactions were prolonged, and they remained “chronically distressed long after the immediate exposure to the event,” he said.
Recent studies have shown that, during the COVID-19 pandemic, health care professionals and many essential workers have experienced similar symptoms, Dr. DePierro noted.
Mental health care professionals who provided interventions for workers involved in recovery and cleanup at the World Trade Center have highlighted the need for long-term monitoring of people on the front lines during the COVID-19 pandemic – especially health care workers, other essential personnel (for example, delivery, postal, and grocery store workers) and surviving family members. “Health monitoring and treatment efforts for 9/11 survivors and responders were put into place soon after the attacks and continue to this day,” using funding provided through the James Zadroga Act, Dr. DePierro said.
“Without similarly unified health registry and treatment services, many individuals – especially from underserved groups – will likely experience chronic mental health consequences and will be unable to access high-quality health care services,” he stated.
‘Psychological first aid’
“Although many people who go through a crisis – whether as a result of terrorism, such as 9/11, or a medical crisis, such as the current pandemic, or a natural disaster, such as Hurricane Katrina – experience PTSD, it’s important to note that not everyone who goes through a crisis and is traumatized will go on to develop PTSD,” Dr. Dass-Brailsford emphasized.
“To me, 9/11 placed psychological first aid on the map. Even if you are not a clinician, you can be trained to provide psychological first aid by becoming familiar with people’s reactions to trauma and how you can support them through it,” she continued.
For example, if a coworker is agitated or “seems to be having a meltdown, you can be there by offering support and getting them the appropriate help.” Research has suggested that having social support before and after a traumatic event can be helpful in determining vulnerability to the development of PTSD and in modulating the impact of the trauma.
Psychological first aid is helpful as an interim measure. “If you see a coworker holding their head in their hands all day and staring at the screen, identifying whether the person might be having a dissociative episode is critical. Providing some support is important, but if more intensive professional support is needed, determining that and making a referral becomes key,” Dr. Dass-Brailsford stated.
Dr. DePierro added: “One of the most important messages that I want health care workers to know from my years of working with 9/11 survivors is that feeling distressed after a traumatic event is very common, but with effective care, one doesn’t necessarily need to be in treatment for years.”
Danielle Ofri, MD, PhD, clinical professor, department of medicine, New York University, agreed. “It is important to continue keeping tabs on each other and remaining sensitive to the collateral struggles of our colleagues. Some have children who are struggling in school, others have parents who have lost a job. Continuing to check in on others and offer support is critical going forward,” she said in an interview.
Cohesiveness and volunteerism
One of the most powerful antidotes to long-term traumatization is a sense of community cohesiveness. This was the case following 9/11, and it is the case during the COVID-19 pandemic, according to Dr. Ofri, an internist at Bellevue Hospital in New York.
“There was an enormous mobilization. Bellevue is a city hospital with a level 1 trauma center, and we expected to be swamped, so the whole hospital shifted into gear,” said Dr. Ofri. “What would have been terrifying seemed tolerable because we felt that we were in it together. We discharged the inpatients to make beds available. Within hours, we had converted clinics into emergency departments and ICUs. We worked seamlessly, and the crisis brought us together ... but then, of course, no patients showed up.”
She described her relationship with her colleagues as “feeling almost like a family, especially during the pandemic, when so many others were in lockdown and feeling isolated and useless.”
She and her colleagues saw each other daily. Although the content of their tasks and responsibilities changed and people were redeployed to other areas, “our workday didn’t really change. It would have been overwhelming if we hadn’t had our daily meetings to regroup and assess where we were. Each day, everything we had learned or implemented the day before – treatment protocols, testing protocols, our understanding of how the virus was communicated – would change and need to be reevaluated. Those morning meetings were critical to staying centered. It felt as though we were building a plane and flying it at the same time, which felt both scary and heady. Luckily, it took place within the fraternity of a committed and caring group.”
Dr. Ofri recounted that, after 9/11, as well as during the pandemic, “professionals kept jumping in from the sidelines to volunteer. Within hours of the collapse of the towers, the ED had filled with staff. People came out of retirement and out from vacation and out of the woodwork. It was very heartening.”
Even more inspiring, “all the departmental barriers seemed to break down. People were willing to step out of their ordinary roles and check their egos at the door. Seasoned physicians were willing to function as medical interns.”
This generosity of time and spirit “helped keep us going,” she said.
Dr. DePierro agreed. “One of the things I’ve seen on medical floors is that COVID actually brought some units together, increasing their cohesion and mutual support and increasing the bonds between people.” These intensified bonds “increased the resilience of everyone involved.”
Commitment to the community
Dr. Ofri recalls families gathering at the hospital after 9/11, watching posters of missing people going up all over the hospital as well as on mailboxes and lampposts. Because the center for missing people was located right next door to Bellevue, there were long lines of families coming in to register. The chief medical office was there, and a huge tent was built to accommodate the families. The tent took up the entire block. “We felt a lot of ownership, because families were coming here,” she said.
The street remained closed even as the days, weeks, and years stretched on, and the tent remained. It was used as a reflection area for families. During the pandemic, that area was used for refrigerated trucks that served as temporary morgues.
“Both logistically and emotionally, we had a feeling during the pandemic of, ‘We’ve been here before, we’ll do it again and be there for the community,’ ” Dr. Ofri said.
She noted that the sense of commitment to the community carried her and fellow clinicians through the toughest parts of 9/11 and of the COVID-19 pandemic.
“People look to the medical system as a lodestar. ‘Where’s my family member? What should I do? Should I be tested? Vaccinated?’ We were there to be a steady presence for the community physically, psychologically, emotionally, and medically, which helped center us as well,” Dr. Ofri said. “If we didn’t have that, we might have all given in to existential panic.”
She added: “Although we had to work twice as hard, often amid great personal risk, we had the good fortune of having a sense of purpose, something to contribute, plus the community of colleagues we cared about and trusted with our lives.”
Crisis and personal growth
Dr. DePierro said that participants who went through 9/11 have been coming to Mount Sinai’s World Trade Center Health Program for care for nearly two decades. “Many are doing quite well, despite the emotional trauma and the dust and toxin exposure, which has given us a window into what makes people resilient.”
Social and community support are key factors in resilience. Another is recognizing opportunities for personal or professional growth during the crisis, according to Dr. DePierro.
During the pandemic, hospital staff were redeployed to departments where they didn’t typically work. They worked with new colleagues and used skills in patient care that they hadn’t needed for years or even decades. “Although this was stressful and distressing, quite a number said they came through with more medical knowledge than before and that they had forged relationships in the trenches that have been lasting and have become important to them,” he reported.
He noted that, during both crises, for first responders and health care practitioners, religious or spiritual faith was a source of resilience. “During the peak of the pandemic, chaplains provided an exorbitant amount of staff support as clinicians turned to the chaplain to help make sense of what they were going through and connect to something greater than themselves.” Similarly, during 9/11, police and fire department chaplains “played a huge role in supporting the first responders,” Dr. DePierro said.
He said that Mount Sinai holds resilience workshops “where we focus on these topics and teach health care workers how to build resilience in their lives, heal day-to-day stressors, and even grow from the experience.”
Dr. Ofri, who is the founder and editor-in-chief of the Bellevue Literary Review, added that the arts played an important role in bolstering resilience and providing a creative outlet for clinicians after 9/11 and again during the pandemic.
The publication is celebrating its twentieth anniversary – its first issue went to press in September 2001. The cover contained an acknowledgment of 9/11.
Dr. Ofri said that a gala event had been planned for Oct. 7, 2001, to celebrate the inaugural issue of the publication. She assumed no one would show up, given that the United States had invaded Afghanistan only hours earlier. To her surprise, over a hundred people attended, “which made me realize the role of the arts during trauma. People were seeking to come together and hear poetry, fiction, and creative nonfiction.”
Dr. Ofri has been “impressed by the amount of incredible creative writing of all sorts that has been submitted [to the publication] during the pandemic, an unexpected flowering of the arts.”
Unique challenges, unique opportunities
All three experts pointed to several noteworthy differences between the experiences of first responders following 9/11 and those of today’s health care professionals during the pandemic.
“What happened on Sept. 11 was one discrete event, and although it obviously led to years of recovering body parts and cleaning up Ground Zero, and on a national level it led to a war, it nevertheless was a single event,” Dr. DePierro observed. By contrast, the COVID-19 pandemic is ongoing, and for health care practitioners, “it’s by no means over. Again and again, they are being thrown back into battle, dealing with fatigue, weariness, and loss of life.”
Moreover, “it is my understanding that immediately following 9/11, there was a general coming together in our country, but it’s obvious that today, there’s a great deal of fractiousness, contention, disagreement, and disunity in our country when it comes to COVID-19,” Dr. DePierro continued.
“This takes a great toll, particularly on health care workers who are dealing with COVID-19 on a daily basis and experience a disconnect between what they see on their floors and ICUs of the hospital, experiencing loss of life they’ve likely never encountered in their careers, and what people are saying when they downplay the seriousness of COVID-19,” he said.
Dr. Ofri agreed. “The fragmentation of our country and the failure of leadership at the highest level to provide even the basics, such as PPE [personal protective equipment] for health care professionals, left us baffled, profoundly hurt, and angry.”
A positive difference between the COVID-19 pandemic and the aftermath of 9/11 is the development of sophisticated technology that allows interventions for traumatized individuals – both health care professionals and the general public – through telehealth, Dr. DePierro pointed out.
“I would say that these resources and technologies are a silver lining and should continue to be expanded on,” he said. “Now, busy health care workers can access all manner of supportive services, including teletherapy, right from home or between shifts.”
Another “silver lining” is that the pandemic has shone a spotlight on an issue that predated the pandemic – the mental health of health care professionals. Opening a discussion about this has reduced stigma and hopefully has paved the way for improved treatments and for providing resources.
Dr. Dass-Brailsford added that “it is important, going forward, for all of us to be trauma informed, to know how trauma and trauma-related stress unfolds in both other people and yourself, and to know what coping skills can be used to avoid crises from developing – a task that extends across all types of disasters.”
A version of this article first appeared on Medscape.com.
Low depression scores may miss seniors with suicidal intent
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
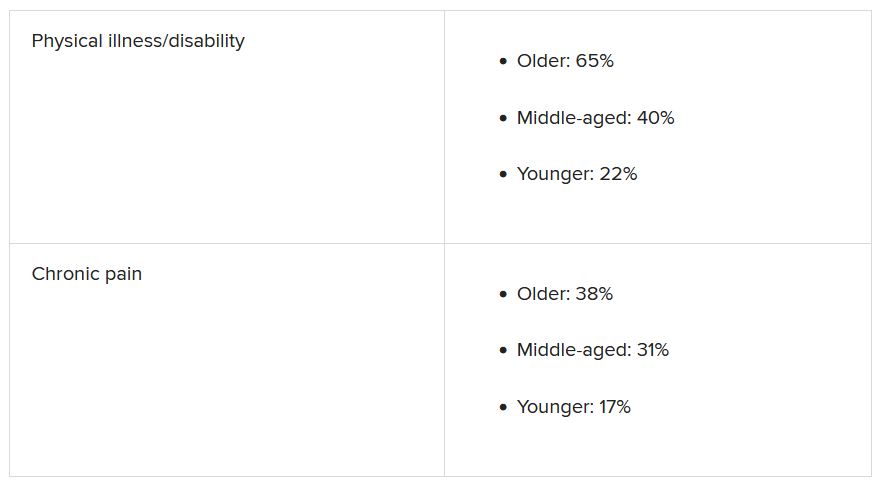
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
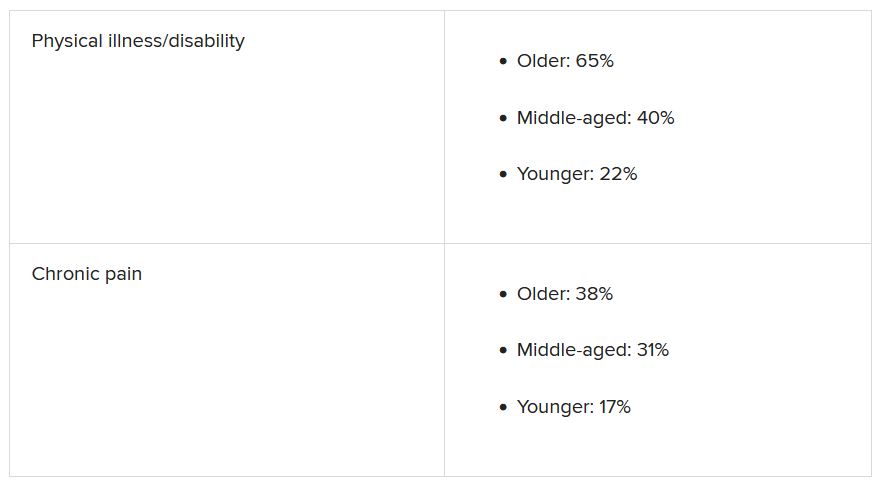
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
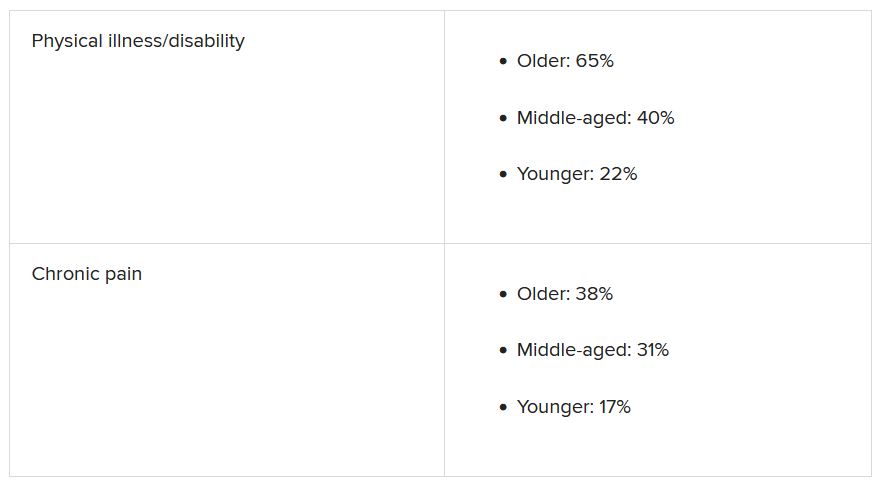
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.









