User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Face mask type matters when sterilizing, study finds
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
Hospitalist well-being during the pandemic
Navigating COVID-19 requires self-care
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
Navigating COVID-19 requires self-care
Navigating COVID-19 requires self-care
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
Persistent posttraumatic headache risk factors confirmed
It also revealed a surprisingly high frequency of misdiagnosis. The original sample included 500 patients drawn from the Stanford Research Repository Cohort Discovery Tool, but a review found 200 records that were misdiagnosed and had to be excluded.
“It’s very easy to label someone who suffered a head injury and say this is the reason why they have this (headache),” said lead author Tommy Chan, MBBS, a headache fellow in the department of neurology at Stanford (Calif.) University, in an interview. Such patients are often seen by ED or primary care physicians who do not have a lot of experience with posttraumatic headache, and that can lead to negative consequences if a low-pressure headache is mistaken as stemming from a skull fracture. “It’s a very different treatment plan for one versus the other,” said Dr. Chan in an interview.
He noted that it can help to take a patient history that includes the preaccident headache frequency and determine if there was a change in frequency post injury.
Dr. Chan presented the results at the virtual annual meeting of the American Headache Society.
“The results are what one might expect, although we haven’t studied it enough to really know. We haven’t systematically characterized these risk factors for chronic posttraumatic headache very well, [so] it’s useful to have this information,” said Andrew Charles, MD, professor neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program, who was not involved in the study. However, Dr. Charles emphasized the need to confirm the results prospectively.
Defining risk factors
The analysis found that a history of migraines, medication overuse, psychological disorders, and new posttraumatic headache–associated comorbidities were all associated with a greater risk for persistent posttraumatic headache. None of those came as a surprise, “but we live in a world where medicine is practiced based on evidence, and providers want to see data to support that. I think that this will help with resource allocation. It’s important to address [a patient’s] overuse of medications, or if they’re having psychological symptoms,” said Dr. Chan.
A total of 150 patients in the analysis had acute posttraumatic headache (mean duration, 0.7 months) while 150 had persistent posttraumatic headache (mean duration, 24 months; P < .00001). Clinical factors associated with risk of persistent headache included a history migraine (relative risk, 2.4; P < .0001), a previous head injury (odds ratio, 5.8; P < .0001), medication overuse (RR, 2.6; P < .0001), preexisting psychological history (OR, 5; P < .0001), and new posttraumatic headache–associated comorbidities, such as vertigo or posttraumatic stress disorder (RR, 9.8; P < .0001).
Identifying patient subgroups
The researchers also identified four subcategories of patients with persistent posttraumatic headache, each with differing risk factors and clinical characteristics. It’s too soon to use these identifiers to make clinical recommendations, but Dr. Chan hopes that further study of these groups will be informative. “It might point us toward (the idea) that each patient population is actually different, even within the chronic persistent posttraumatic headache population, we can’t group them all under the same umbrella term. If we can tease out that a patient has truly had a head injury, but no history of migraine, no overuse of medication, no psychological history, and no other associated symptoms, this would be a very interesting population to study because they would help us understand the pathophysiology [of persistent posttraumatic headache].”
Although the study was conducted by defining persistent posttraumatic headache as lasting at least 3 months, Dr. Chan took issue with that commonly held definition. That choice is arbitrary, with no pathophysiological basis or data to support it, and is based more on clinical trials testing preventative treatments. But when it is used in clinical practice, it can muddy communication with patients. “When this timeline is told to a patient, and when it’s not achieved, they might become disappointed. We should not put too much emphasis on time. Everybody is different,” he said.
The study did not receive any funding. Dr. Chan had no relevant financial disclosures. Dr. Charles consults for consults for Amgen, BioHaven, Eli Lilly, Novartis, and Lundbeck.
It also revealed a surprisingly high frequency of misdiagnosis. The original sample included 500 patients drawn from the Stanford Research Repository Cohort Discovery Tool, but a review found 200 records that were misdiagnosed and had to be excluded.
“It’s very easy to label someone who suffered a head injury and say this is the reason why they have this (headache),” said lead author Tommy Chan, MBBS, a headache fellow in the department of neurology at Stanford (Calif.) University, in an interview. Such patients are often seen by ED or primary care physicians who do not have a lot of experience with posttraumatic headache, and that can lead to negative consequences if a low-pressure headache is mistaken as stemming from a skull fracture. “It’s a very different treatment plan for one versus the other,” said Dr. Chan in an interview.
He noted that it can help to take a patient history that includes the preaccident headache frequency and determine if there was a change in frequency post injury.
Dr. Chan presented the results at the virtual annual meeting of the American Headache Society.
“The results are what one might expect, although we haven’t studied it enough to really know. We haven’t systematically characterized these risk factors for chronic posttraumatic headache very well, [so] it’s useful to have this information,” said Andrew Charles, MD, professor neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program, who was not involved in the study. However, Dr. Charles emphasized the need to confirm the results prospectively.
Defining risk factors
The analysis found that a history of migraines, medication overuse, psychological disorders, and new posttraumatic headache–associated comorbidities were all associated with a greater risk for persistent posttraumatic headache. None of those came as a surprise, “but we live in a world where medicine is practiced based on evidence, and providers want to see data to support that. I think that this will help with resource allocation. It’s important to address [a patient’s] overuse of medications, or if they’re having psychological symptoms,” said Dr. Chan.
A total of 150 patients in the analysis had acute posttraumatic headache (mean duration, 0.7 months) while 150 had persistent posttraumatic headache (mean duration, 24 months; P < .00001). Clinical factors associated with risk of persistent headache included a history migraine (relative risk, 2.4; P < .0001), a previous head injury (odds ratio, 5.8; P < .0001), medication overuse (RR, 2.6; P < .0001), preexisting psychological history (OR, 5; P < .0001), and new posttraumatic headache–associated comorbidities, such as vertigo or posttraumatic stress disorder (RR, 9.8; P < .0001).
Identifying patient subgroups
The researchers also identified four subcategories of patients with persistent posttraumatic headache, each with differing risk factors and clinical characteristics. It’s too soon to use these identifiers to make clinical recommendations, but Dr. Chan hopes that further study of these groups will be informative. “It might point us toward (the idea) that each patient population is actually different, even within the chronic persistent posttraumatic headache population, we can’t group them all under the same umbrella term. If we can tease out that a patient has truly had a head injury, but no history of migraine, no overuse of medication, no psychological history, and no other associated symptoms, this would be a very interesting population to study because they would help us understand the pathophysiology [of persistent posttraumatic headache].”
Although the study was conducted by defining persistent posttraumatic headache as lasting at least 3 months, Dr. Chan took issue with that commonly held definition. That choice is arbitrary, with no pathophysiological basis or data to support it, and is based more on clinical trials testing preventative treatments. But when it is used in clinical practice, it can muddy communication with patients. “When this timeline is told to a patient, and when it’s not achieved, they might become disappointed. We should not put too much emphasis on time. Everybody is different,” he said.
The study did not receive any funding. Dr. Chan had no relevant financial disclosures. Dr. Charles consults for consults for Amgen, BioHaven, Eli Lilly, Novartis, and Lundbeck.
It also revealed a surprisingly high frequency of misdiagnosis. The original sample included 500 patients drawn from the Stanford Research Repository Cohort Discovery Tool, but a review found 200 records that were misdiagnosed and had to be excluded.
“It’s very easy to label someone who suffered a head injury and say this is the reason why they have this (headache),” said lead author Tommy Chan, MBBS, a headache fellow in the department of neurology at Stanford (Calif.) University, in an interview. Such patients are often seen by ED or primary care physicians who do not have a lot of experience with posttraumatic headache, and that can lead to negative consequences if a low-pressure headache is mistaken as stemming from a skull fracture. “It’s a very different treatment plan for one versus the other,” said Dr. Chan in an interview.
He noted that it can help to take a patient history that includes the preaccident headache frequency and determine if there was a change in frequency post injury.
Dr. Chan presented the results at the virtual annual meeting of the American Headache Society.
“The results are what one might expect, although we haven’t studied it enough to really know. We haven’t systematically characterized these risk factors for chronic posttraumatic headache very well, [so] it’s useful to have this information,” said Andrew Charles, MD, professor neurology at the University of California, Los Angeles, and director of the UCLA Goldberg Migraine Program, who was not involved in the study. However, Dr. Charles emphasized the need to confirm the results prospectively.
Defining risk factors
The analysis found that a history of migraines, medication overuse, psychological disorders, and new posttraumatic headache–associated comorbidities were all associated with a greater risk for persistent posttraumatic headache. None of those came as a surprise, “but we live in a world where medicine is practiced based on evidence, and providers want to see data to support that. I think that this will help with resource allocation. It’s important to address [a patient’s] overuse of medications, or if they’re having psychological symptoms,” said Dr. Chan.
A total of 150 patients in the analysis had acute posttraumatic headache (mean duration, 0.7 months) while 150 had persistent posttraumatic headache (mean duration, 24 months; P < .00001). Clinical factors associated with risk of persistent headache included a history migraine (relative risk, 2.4; P < .0001), a previous head injury (odds ratio, 5.8; P < .0001), medication overuse (RR, 2.6; P < .0001), preexisting psychological history (OR, 5; P < .0001), and new posttraumatic headache–associated comorbidities, such as vertigo or posttraumatic stress disorder (RR, 9.8; P < .0001).
Identifying patient subgroups
The researchers also identified four subcategories of patients with persistent posttraumatic headache, each with differing risk factors and clinical characteristics. It’s too soon to use these identifiers to make clinical recommendations, but Dr. Chan hopes that further study of these groups will be informative. “It might point us toward (the idea) that each patient population is actually different, even within the chronic persistent posttraumatic headache population, we can’t group them all under the same umbrella term. If we can tease out that a patient has truly had a head injury, but no history of migraine, no overuse of medication, no psychological history, and no other associated symptoms, this would be a very interesting population to study because they would help us understand the pathophysiology [of persistent posttraumatic headache].”
Although the study was conducted by defining persistent posttraumatic headache as lasting at least 3 months, Dr. Chan took issue with that commonly held definition. That choice is arbitrary, with no pathophysiological basis or data to support it, and is based more on clinical trials testing preventative treatments. But when it is used in clinical practice, it can muddy communication with patients. “When this timeline is told to a patient, and when it’s not achieved, they might become disappointed. We should not put too much emphasis on time. Everybody is different,” he said.
The study did not receive any funding. Dr. Chan had no relevant financial disclosures. Dr. Charles consults for consults for Amgen, BioHaven, Eli Lilly, Novartis, and Lundbeck.
FROM AHS 2020
Preventive services coalition recommends routine anxiety screening for women
according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault, wrote Kimberly D. Gregory, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues on behalf of the Women’s Preventive Services Initiative (WPSI), a national coalition of women’s health professional organizations and patient representatives.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.”
“Effective screening may lead to earlier or timelier treatment (including behavioral and medical interventions) and result in improved clinical outcomes, such as symptoms, function, and quality of life. Screening may also lead to the detection of associated conditions, such as depression and posttraumatic stress disorder, which may also require treatment,” they wrote.
To support the recommendation, the researchers evaluated data from 33 studies and 2 systematic reviews for a total of 171 studies. Most studies included screening instruments that involved clinician- or patient-administered questionnaires designed for use in clinical practice. Although none of the studies evaluated the overall effectiveness versus harm of screening for anxiety, the strength of evidence for the effectiveness of anxiety treatment ranged from moderate to high, and the evidence of harms ranged from low for cognitive-behavioral therapy to moderate for anxiety medications.
“Overall, the WPSI determined that the balance of benefits and harms would likely be favorable on the basis of the high prevalence of anxiety in women; its substantial effect on health, function, and quality of life; and evidence on the accuracy of screening instruments in primary care settings and the effectiveness and harms of treatment,” the researchers wrote.
Although anxiety screening is not currently routine in clinical practice in the United States, such screening could be done quickly and efficiently as part of an intake visit in a primary care or obstetric setting, using a brief screening tool similar to those used for depression, the researchers wrote. The goal of anxiety screening, as with depression screening, is to identify those who need further evaluation to diagnose or rule out an anxiety disorder.
“A revised version [of the draft recommendation] was adopted by the Health Resources and Services Administration in December 2019; it will be incorporated into the summary of covered benefits for preventive services without cost sharing as required by the Patient Protection and Affordable Care Act immediately or no later than 1 January 2021, depending on individual coverage,” the researchers noted.
“Covered benefits apply to most group health plans and issuers of group and individual health insurance coverage, as well as to persons who qualify for Medicaid on the basis of Medicaid expansion under the Affordable Care Act,” they wrote.
“Because anxiety disorders can be successfully treated, early detection through the use of a brief questionnaire could prevent years of symptoms and impairment in the lives of women at every stage of life,” they concluded.
Aaron Sutton, LCSW, a behavioral health consultant at Abington (Pa.) Hospital–Jefferson Health, expressed support for the guidelines in an interview.
“With almost half of all women experiencing an anxiety disorder sometime in their life, effective recognition and treatment of anxiety disorders is needed,” he said.
Mr. Sutton described treatment as being “fairly benign” with the initial approach being cognitive-behavioral therapy, a form of psychological talk therapy, and first-line pharmacologic therapies being SSRIs and serotonin norepinephrine reuptake inhibitors.
Mr. Sutton also explained how he expects effective screening and treatment will benefit women with anxiety and the health care system.
“Women will see improvement in areas such as personal relationships, work, school, and social settings. The health care system will see benefits as costs related to anxiety disorders, be it direct or indirect, are in the billions of dollars,” he said.
Although screening for anxiety will increase the workload of primary care physicians, anxiety screening should be included and could perhaps be administered in conjunction with the routine depression screening already recommended as part of primary care visits, Mr. Sutton noted.
“Anxiety disorders can be successfully treated, and early detection can prevent years of symptoms and impairment,” he emphasized.
“Anxiety often occurs among adolescents and adult women and often becomes a chronic problem with impairments,” said Cynthia Pfeffer, MD, professor of psychiatry at Weill Cornell Medicine, New York, in an interview. “Screening for anxiety could identify and enable planning to decrease and prevent this impairing prevalent condition and its associated problems. For example, anxiety can impair adolescents’ academic and social functioning and if this is lasting also impair their success in work and future planning for families. There are successful treatments for anxiety and identification of individuals at an early time may prevent impairments in daily functioning.”
Dr. Pfeffer noted that steps to overcome barriers to prevention and treatment for anxiety include “educating health care professionals about the problems caused from anxiety, learning means to identify and diagnose anxiety, and developing proficiency in offering methods to prevent and intervene for women with symptoms of anxiety.”
The take-home message for clinicians is that anxiety is prevalent among females of all ages and often begins early and becomes chronic.
“There are excellent treatments including psychotherapy and medication that can decrease and prevent anxiety,” she emphasized. “Training practicing clinicians including MDs as well as other professionals in the health care system about anxiety will enhance the wellbeing of women.”
More research is needed to evaluate methods used during health care visits for anxiety screening and treatment in order to determine valid means of preventing the impairments associated with anxiety, Dr. Pfeffer said.
Mr. Sutton noted that no trials “have evaluated overall effectiveness or potential harms including labeling, misdiagnosis, and overdiagnosis.” Other areas in need of research include the changes in incidence and prevalence of anxiety over time, as well as specific risk factors including marriage, divorce, pregnancy, and childbirth, he added.
The research for the recommendation was supported by the Health Resources and Services Administration. The researchers had no financial conflicts to disclose. Mr. Sutton had no financial conflicts to disclose. Dr. Pfeffer has written extensively on depression and anxiety in children, adolescents, and adults. She had no financial conflicts to disclose.
SOURCE: Gregory KD et al. Ann Intern Med. 2020 June 9. doi: 10.7326/M20-0580.
according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault, wrote Kimberly D. Gregory, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues on behalf of the Women’s Preventive Services Initiative (WPSI), a national coalition of women’s health professional organizations and patient representatives.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.”
“Effective screening may lead to earlier or timelier treatment (including behavioral and medical interventions) and result in improved clinical outcomes, such as symptoms, function, and quality of life. Screening may also lead to the detection of associated conditions, such as depression and posttraumatic stress disorder, which may also require treatment,” they wrote.
To support the recommendation, the researchers evaluated data from 33 studies and 2 systematic reviews for a total of 171 studies. Most studies included screening instruments that involved clinician- or patient-administered questionnaires designed for use in clinical practice. Although none of the studies evaluated the overall effectiveness versus harm of screening for anxiety, the strength of evidence for the effectiveness of anxiety treatment ranged from moderate to high, and the evidence of harms ranged from low for cognitive-behavioral therapy to moderate for anxiety medications.
“Overall, the WPSI determined that the balance of benefits and harms would likely be favorable on the basis of the high prevalence of anxiety in women; its substantial effect on health, function, and quality of life; and evidence on the accuracy of screening instruments in primary care settings and the effectiveness and harms of treatment,” the researchers wrote.
Although anxiety screening is not currently routine in clinical practice in the United States, such screening could be done quickly and efficiently as part of an intake visit in a primary care or obstetric setting, using a brief screening tool similar to those used for depression, the researchers wrote. The goal of anxiety screening, as with depression screening, is to identify those who need further evaluation to diagnose or rule out an anxiety disorder.
“A revised version [of the draft recommendation] was adopted by the Health Resources and Services Administration in December 2019; it will be incorporated into the summary of covered benefits for preventive services without cost sharing as required by the Patient Protection and Affordable Care Act immediately or no later than 1 January 2021, depending on individual coverage,” the researchers noted.
“Covered benefits apply to most group health plans and issuers of group and individual health insurance coverage, as well as to persons who qualify for Medicaid on the basis of Medicaid expansion under the Affordable Care Act,” they wrote.
“Because anxiety disorders can be successfully treated, early detection through the use of a brief questionnaire could prevent years of symptoms and impairment in the lives of women at every stage of life,” they concluded.
Aaron Sutton, LCSW, a behavioral health consultant at Abington (Pa.) Hospital–Jefferson Health, expressed support for the guidelines in an interview.
“With almost half of all women experiencing an anxiety disorder sometime in their life, effective recognition and treatment of anxiety disorders is needed,” he said.
Mr. Sutton described treatment as being “fairly benign” with the initial approach being cognitive-behavioral therapy, a form of psychological talk therapy, and first-line pharmacologic therapies being SSRIs and serotonin norepinephrine reuptake inhibitors.
Mr. Sutton also explained how he expects effective screening and treatment will benefit women with anxiety and the health care system.
“Women will see improvement in areas such as personal relationships, work, school, and social settings. The health care system will see benefits as costs related to anxiety disorders, be it direct or indirect, are in the billions of dollars,” he said.
Although screening for anxiety will increase the workload of primary care physicians, anxiety screening should be included and could perhaps be administered in conjunction with the routine depression screening already recommended as part of primary care visits, Mr. Sutton noted.
“Anxiety disorders can be successfully treated, and early detection can prevent years of symptoms and impairment,” he emphasized.
“Anxiety often occurs among adolescents and adult women and often becomes a chronic problem with impairments,” said Cynthia Pfeffer, MD, professor of psychiatry at Weill Cornell Medicine, New York, in an interview. “Screening for anxiety could identify and enable planning to decrease and prevent this impairing prevalent condition and its associated problems. For example, anxiety can impair adolescents’ academic and social functioning and if this is lasting also impair their success in work and future planning for families. There are successful treatments for anxiety and identification of individuals at an early time may prevent impairments in daily functioning.”
Dr. Pfeffer noted that steps to overcome barriers to prevention and treatment for anxiety include “educating health care professionals about the problems caused from anxiety, learning means to identify and diagnose anxiety, and developing proficiency in offering methods to prevent and intervene for women with symptoms of anxiety.”
The take-home message for clinicians is that anxiety is prevalent among females of all ages and often begins early and becomes chronic.
“There are excellent treatments including psychotherapy and medication that can decrease and prevent anxiety,” she emphasized. “Training practicing clinicians including MDs as well as other professionals in the health care system about anxiety will enhance the wellbeing of women.”
More research is needed to evaluate methods used during health care visits for anxiety screening and treatment in order to determine valid means of preventing the impairments associated with anxiety, Dr. Pfeffer said.
Mr. Sutton noted that no trials “have evaluated overall effectiveness or potential harms including labeling, misdiagnosis, and overdiagnosis.” Other areas in need of research include the changes in incidence and prevalence of anxiety over time, as well as specific risk factors including marriage, divorce, pregnancy, and childbirth, he added.
The research for the recommendation was supported by the Health Resources and Services Administration. The researchers had no financial conflicts to disclose. Mr. Sutton had no financial conflicts to disclose. Dr. Pfeffer has written extensively on depression and anxiety in children, adolescents, and adults. She had no financial conflicts to disclose.
SOURCE: Gregory KD et al. Ann Intern Med. 2020 June 9. doi: 10.7326/M20-0580.
according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault, wrote Kimberly D. Gregory, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues on behalf of the Women’s Preventive Services Initiative (WPSI), a national coalition of women’s health professional organizations and patient representatives.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.”
“Effective screening may lead to earlier or timelier treatment (including behavioral and medical interventions) and result in improved clinical outcomes, such as symptoms, function, and quality of life. Screening may also lead to the detection of associated conditions, such as depression and posttraumatic stress disorder, which may also require treatment,” they wrote.
To support the recommendation, the researchers evaluated data from 33 studies and 2 systematic reviews for a total of 171 studies. Most studies included screening instruments that involved clinician- or patient-administered questionnaires designed for use in clinical practice. Although none of the studies evaluated the overall effectiveness versus harm of screening for anxiety, the strength of evidence for the effectiveness of anxiety treatment ranged from moderate to high, and the evidence of harms ranged from low for cognitive-behavioral therapy to moderate for anxiety medications.
“Overall, the WPSI determined that the balance of benefits and harms would likely be favorable on the basis of the high prevalence of anxiety in women; its substantial effect on health, function, and quality of life; and evidence on the accuracy of screening instruments in primary care settings and the effectiveness and harms of treatment,” the researchers wrote.
Although anxiety screening is not currently routine in clinical practice in the United States, such screening could be done quickly and efficiently as part of an intake visit in a primary care or obstetric setting, using a brief screening tool similar to those used for depression, the researchers wrote. The goal of anxiety screening, as with depression screening, is to identify those who need further evaluation to diagnose or rule out an anxiety disorder.
“A revised version [of the draft recommendation] was adopted by the Health Resources and Services Administration in December 2019; it will be incorporated into the summary of covered benefits for preventive services without cost sharing as required by the Patient Protection and Affordable Care Act immediately or no later than 1 January 2021, depending on individual coverage,” the researchers noted.
“Covered benefits apply to most group health plans and issuers of group and individual health insurance coverage, as well as to persons who qualify for Medicaid on the basis of Medicaid expansion under the Affordable Care Act,” they wrote.
“Because anxiety disorders can be successfully treated, early detection through the use of a brief questionnaire could prevent years of symptoms and impairment in the lives of women at every stage of life,” they concluded.
Aaron Sutton, LCSW, a behavioral health consultant at Abington (Pa.) Hospital–Jefferson Health, expressed support for the guidelines in an interview.
“With almost half of all women experiencing an anxiety disorder sometime in their life, effective recognition and treatment of anxiety disorders is needed,” he said.
Mr. Sutton described treatment as being “fairly benign” with the initial approach being cognitive-behavioral therapy, a form of psychological talk therapy, and first-line pharmacologic therapies being SSRIs and serotonin norepinephrine reuptake inhibitors.
Mr. Sutton also explained how he expects effective screening and treatment will benefit women with anxiety and the health care system.
“Women will see improvement in areas such as personal relationships, work, school, and social settings. The health care system will see benefits as costs related to anxiety disorders, be it direct or indirect, are in the billions of dollars,” he said.
Although screening for anxiety will increase the workload of primary care physicians, anxiety screening should be included and could perhaps be administered in conjunction with the routine depression screening already recommended as part of primary care visits, Mr. Sutton noted.
“Anxiety disorders can be successfully treated, and early detection can prevent years of symptoms and impairment,” he emphasized.
“Anxiety often occurs among adolescents and adult women and often becomes a chronic problem with impairments,” said Cynthia Pfeffer, MD, professor of psychiatry at Weill Cornell Medicine, New York, in an interview. “Screening for anxiety could identify and enable planning to decrease and prevent this impairing prevalent condition and its associated problems. For example, anxiety can impair adolescents’ academic and social functioning and if this is lasting also impair their success in work and future planning for families. There are successful treatments for anxiety and identification of individuals at an early time may prevent impairments in daily functioning.”
Dr. Pfeffer noted that steps to overcome barriers to prevention and treatment for anxiety include “educating health care professionals about the problems caused from anxiety, learning means to identify and diagnose anxiety, and developing proficiency in offering methods to prevent and intervene for women with symptoms of anxiety.”
The take-home message for clinicians is that anxiety is prevalent among females of all ages and often begins early and becomes chronic.
“There are excellent treatments including psychotherapy and medication that can decrease and prevent anxiety,” she emphasized. “Training practicing clinicians including MDs as well as other professionals in the health care system about anxiety will enhance the wellbeing of women.”
More research is needed to evaluate methods used during health care visits for anxiety screening and treatment in order to determine valid means of preventing the impairments associated with anxiety, Dr. Pfeffer said.
Mr. Sutton noted that no trials “have evaluated overall effectiveness or potential harms including labeling, misdiagnosis, and overdiagnosis.” Other areas in need of research include the changes in incidence and prevalence of anxiety over time, as well as specific risk factors including marriage, divorce, pregnancy, and childbirth, he added.
The research for the recommendation was supported by the Health Resources and Services Administration. The researchers had no financial conflicts to disclose. Mr. Sutton had no financial conflicts to disclose. Dr. Pfeffer has written extensively on depression and anxiety in children, adolescents, and adults. She had no financial conflicts to disclose.
SOURCE: Gregory KD et al. Ann Intern Med. 2020 June 9. doi: 10.7326/M20-0580.
FROM ANNALS OF INTERNAL MEDICINE
New guidance to help manage OCD during COVID-19
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Two international specialty societies have jointly released new guidance on management of obsessive-compulsive disorder (OCD) during the COVID-19 pandemic.
“Individuals with OCD, particularly those with contamination concerns or hypochondriacal kinds of worries associated with OCD, people who have perfectionistic type of rituals, or who worry about transmitting COVID-19 [to others] might be particularly vulnerable to this pandemic,” statement coauthor Michael Van Ameringen, MD, professor, of the department of psychiatry and behavioral neurosciences, McMaster University, Hamilton, Ont., said in an interview.
The guidance, issued by the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology, emphasizes the importance of using pharmacotherapy as a first-line approach, suspending or reducing exposure and response prevention (ERP), and offering psychoeducation.
The statement was published in the July issue of Comprehensive Psychiatry.
Confirm OCD diagnosis
A diagnosis of OCD should be confirmed, and it is important to clarify whether the current symptoms are a “rational or exaggerated response to recent highly stressful events” or a worsening of obsessive-compulsive symptomatology, the statement notes.
Some patients may experience an exacerbation of comorbid conditions such as anxiety disorder, depression, bipolar disorder, or posttraumatic stress disorder (PTSD), which may need to be managed separately.
The authors recommend consulting the World Health Organization (WHO) guidelines regarding mental health and psychosocial considerations during the COVID-19 outbreak.
“Several suicidal patients with OCD have come to the clinic during the pandemic,” reported Dr. Van Ameringen, director of the MacAnxiety Research Centre in Hamilton. “They felt overwhelmed and that they were contaminating themselves with everything they did, including breathing.”
The authors encourage clinicians to assess suicide risk using validated instruments, such as the Columbia Suicide Severity Rating Scale, and hospitalize patients if necessary.
Pharmacotherapy is “the most efficacious first-line treatment modality” for adults and children with OCD and contamination, washing, or cleaning symptoms during the pandemic, the authors note.
They recommend a stepwise pharmacotherapeutic approach:
Type of medication
- Selective serotonin reuptake inhibitor (SSRI) as first choice.
- Another SSRI if no response to first SSRI.
- Clomipramine as third choice.
Dosage
- Gradually increase suboptimal dose, paying attention to contraindications, adverse effects.
SSRI resistance
- Low-dose adjunctive antipsychotic (for example, aripiprazole, risperidone, quetiapine, olanzapine), for incomplete response, especially if tic is present.
Adherence
- Ensure patient can obtain an adequate supply of medication and is taking it regularly.
- Involve family/caregivers if adherence is problematic.
- Pill organizers and reminder apps may be helpful.
A role for CBT?
Under ordinary circumstances, CBT is considered a first-line intervention for OCD. However, there are risks associated specifically with ERP during the pandemic.
“In ERP, people are being exposed to things that trigger their OCD, so those with contamination fears may be asked to touch things in public places, then resist washing their hands, which would counter public health recommendations,” Dr. Van Ameringen said.
In vivo exposure should be paused, but some ERP interventions can be adapted or modified “on a case-by-case basis,” the authors state. For patients whose exposure is unrelated to contamination, other ERP treatment plans can be continued.
The authors recommend using therapy time to “prevent patients from deteriorating” by encouraging them to engage in activity scheduling and structuring the day to include physical activity, enjoyable activities, practices that enhance sleep, and mindfulness.
Limit news exposure
A central component of managing OCD during the pandemic is providing “balanced information” about the known risks and impact of COVID-19, the authors stated.
Dr. Van Ameringen recounted that he has seen patients who have washed their hands for hours and bleached or even boiled their hands.
“Some [patients with OCD] wonder if it’s safe to touch a newspaper or if they can catch the virus if they go outside, even if no one is around,” he reported. “Some wonder if they should ‘quarantine’ a package or wear gloves to bed.”
It has been helpful, for example, to show them the public health guidance of the WHO or CDC advising that 20 seconds of hand washing is adequate, he said.
“We have also seen that some of the sources of information about COVID-19 haven’t been factually correct and that people were watching the news all day and being bombarded with information from every source, which was making their symptoms a thousand times worse,” Dr. Van Ameringen reported.
Therefore, The authors also advise clinicians to “take a compassionate, calming,” and culturally sensitive approach to inform all interventions.
Unique anchor
Commenting on the statement in an interview, Debanjan Banerjee, MD, geriatric psychiatry senior resident, National Institute of Mental Health and Neurosciences, Bangalore, India, said that this “comprehensive guideline, based on expert experience, will serve as a guiding framework for physicians and psychiatrists globally.”
In the “absence of systemic data so far, this guideline can provide a unique anchor of a global consensus on how to take care of those with preexisting OCD or newly emergent cases” said Dr. Banerjee, who was not involved in authoring the statement.
Also commenting on the statement, Jonathan Abramowitz, PhD, professor of psychology and neuroscience, University of North Carolina at Chapel Hill, said that he “generally agrees” with these guidelines but disagrees with the “apparent recommendations to scale back” ERP.
“The fact is that effective and safe ERP is possible, even during this time, even following the scientific guidance,” stated Dr. Abramowitz, editor-in-chief of the Journal of Obsessive-Compulsive and Related Disorders. He was not involved in the statement.
He noted that the International OCD Foundation offers educational programs for clinicians regarding the safe use of ERP during this time.
The authors acknowledge that their guideline is “largely based on empirical evidence” and should be regarded as “preliminary.” The guidance “will be updated as new information arises.”
No specific source of funding for the statement is listed. Dr. Van Ameringen reports being on the advisory boards of Allergan, Almatica, Brainsway, Janssen, Lundbeck, Myriad Neuroscience, Otsuka, and Purdue Pharma (Canada); is on the speakers bureau for Allergan, Lundbeck, Otsuka, Pfizer, Purdue Pharma (Canada) and Takeda; and has received research support from Janssen, Purdue Pharma (Canada), the Canada Foundation for Innovation, and Hamilton Academic Health Sciences Organization. The other authors’ disclosures are listed on the original paper. Dr. Banerjee and Dr. Abramowitz have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Comorbidities increase COVID-19 deaths by factor of 12
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
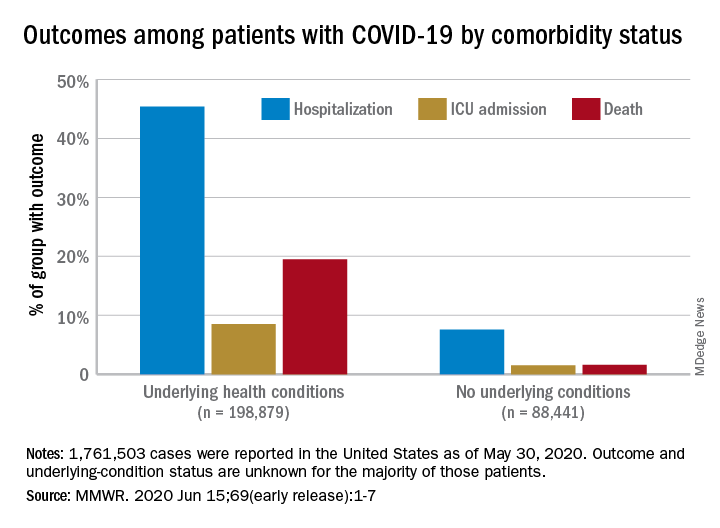
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
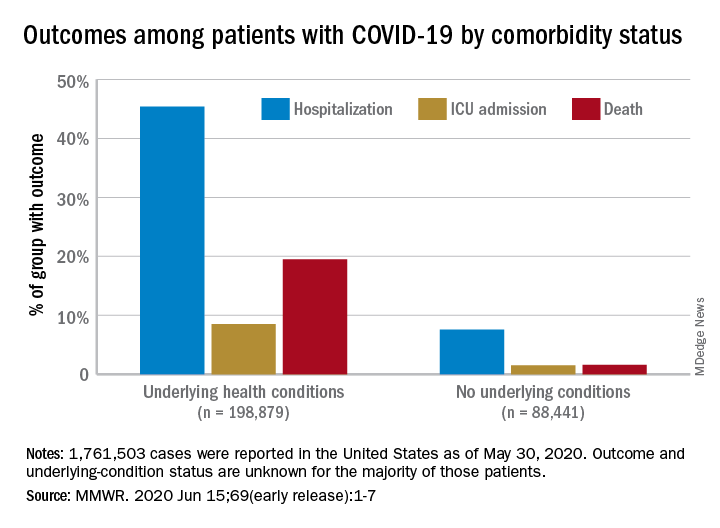
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
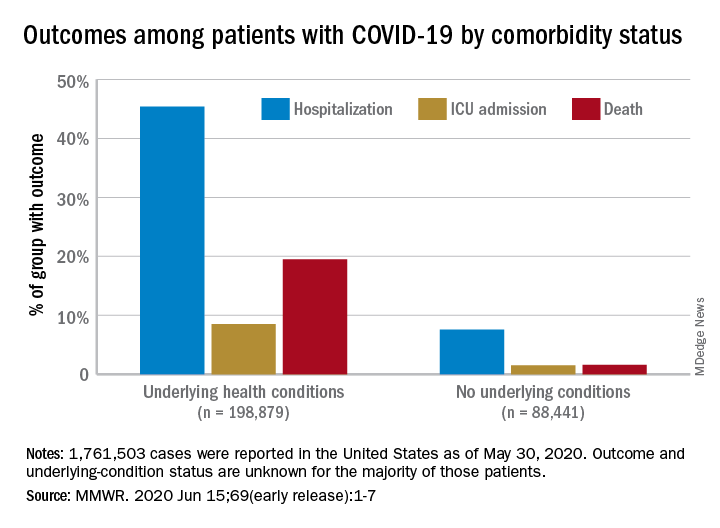
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
FROM MMWR
Population study supports migraine–dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
FROM AHS 2020
Health experts link rise in Arizona COVID cases to end of stay-at-home order
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Consider the stresses experienced by LGBTQ people of color
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
FDA revokes emergency use of hydroxychloroquine
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.
The U.S. Food and Drug Administration revoked its decision from March 28 allowing use of hydroxychloroquine and chloroquine to treat people hospitalized with COVID-19 under an emergency use authorization (EUA).
“Based on its ongoing analysis of the EUA and emerging scientific data, the FDA determined that chloroquine and hydroxychloroquine are unlikely to be effective in treating COVID-19 for the authorized uses in the EUA,” the agency announced in a June 15 statement.
The FDA also warned today that the use of hydroxychloroquine or chloroquine may have a potential drug interaction with the investigational antiviral drug remdesivir that limits its effectiveness against COVID-19.
Remdesivir was granted emergency use authorization by the FDA on May 1.
“Based on a recently completed nonclinical laboratory study, the FDA is revising the fact sheet for healthcare providers that accompanies the drug to state that coadministration of remdesivir and chloroquine phosphate or hydroxychloroquine sulfate is not recommended as it may result in reduced antiviral activity of remdesivir. The agency is not aware of instances of this reduced activity occurring in the clinical setting but is continuing to evaluate all data related to remdesivir,” the FDA said in a news release.
Controversy over hydroxychloroquine
Even with such federal permission, since late March the use of these two agents has been mired in controversy.
President Donald J. Trump promoted the use of hydroxychloroquine and chloroquine to treat Americans with COVID-19, while scientific studies raised questions about their safety and effectiveness. Recent research, for example, pointed to elevated cardiovascular risks, as reported by Medscape Medical News.
The FDA acknowledged this recent evidence. “Additionally, in light of ongoing serious cardiac adverse events and other potential serious side effects, the known and potential benefits of chloroquine and hydroxychloroquine no longer outweigh the known and potential risks for the authorized use.”
The full suspension of the EUA follows a warning the agency issued on April 24. The FDA’s Safety Communication cautioned against use of the two agents outside of a hospital setting, citing an increase in outpatient prescriptions and “reports of serious heart rhythm problems.”
“While additional clinical trials continue to evaluate the potential benefit of these drugs in treating or preventing COVID-19, we determined the emergency use authorization was no longer appropriate,” based on a rigorous assessment by scientists in our Center for Drug Evaluation and Research,” Patrizia Cavazzoni, MD, acting director of CDER, noted in the FDA statement.
This article first appeared on Medscape.com.