User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Understanding the enduring power of caste
Isabel Wilkerson’s naming of the malady facilitates space for a shift in thinking.
America has been struggling to understand its racial dynamics since the arrival of enslaved Africans more than 400 years ago. Today, with much of the world more polarized than ever, and certainly in our United States, there is a need for something to shift us from our fear and survival paranoid schizoid (us-vs.-them) position to an integrated form if we are to come out of this unusual democratic and societal unrest whole.
Yet, we’ve never had the lexicon to adequately describe the sociopolitical dynamics rooted in race and racism and their power to shape the thinking of all who originate in this country and all who enter its self-made borders whether forcefully or voluntarily. Enter Isabel Wilkerson, a Pulitzer Prize–winning, former New York Times Chicago bureau chief, and author of “The Warmth of Other Suns: The Epic Story of America’s Great Migration” (New York: Random House, 2010) with her second book, “Caste: The Origins of Our Discontents” (New York: Random House, 2020).
Ms. Wilkerson quickly gets to work in an engaging storytelling style of weaving past to present with ideas she supports with letters from the past, historians’ impressions, research studies, and data. Her observations and research are bookended by the lead up to the 2016 presidential election and its aftermath on the one end, and the impending 2020 presidential election on the other. In her view, the reemergence of violence that has accelerated in the 21st century and the renewed commitment to promote white supremacy can be understood if we expand our view of race and racism to consider the enduring power of caste. For, in Ms. Wilkerson’s view, the fear of the 2042 U.S. census (which is predicted to reflect for the first time a non-White majority) is a driving force behind the dominant caste’s determination to maintain the status quo power dynamics in the United States.
In an effort to explain American’s racial hierarchy, Ms. Wilkerson explains the need for a new lexicon “that may sound like a foreign language,” but this is intentional on her part. She writes:
“To recalibrate how we see ourselves, I use language that may be more commonly associated with people in other cultures, to suggest a new way of understanding our hierarchy: Dominant caste, ruling majority, favored caste, or upper caste, instead of, or in addition to, white. Middle castes instead of, or in addition to, Asian or Latino. Subordinate caste, lowest caste, bottom caste, disfavored caste, historically stigmatized instead of African-American. Original, conquered, or indigenous peoples instead of, or in addition to, Native American. Marginalized people in addition to, or instead of, women of any race, or minorities of any kind.”
Early in the book Ms. Wilkerson anchors her argument in Rev. Dr. Martin Luther King Jr.’s sojourn to India. Rather than focus on the known history of Dr. King’s admiration of Mohandas Gandhi, Ms. Wilkerson directs our attention to Dr. King’s discovery of his connection to Dalits, those who had been considered “untouchables” until Bhimrao Ramji Ambedkar, the Indian economist, jurist, social reformer, and Dalit leader, fiercely and successfully advocated for a rebranding of his caste of origin; instead of “untouchables” they would be considered Dalits or “broken people.” Dr. King did not meet Mr. Ambedkar, who died 3 years before this journey, but Ms. Wilkerson writes that Dr. King acknowledged the kinship, “And he said unto himself, Yes, I am an untouchable, and every Negro in the United States is an untouchable.” The Dalits and Dr. King recognized in each other their shared positions as subordinates in a global caste system.
In answering the question about the difference between racism and casteism, Ms. Wilkerson writes:
“Because caste and race are interwoven in America, it can be hard to separate the two. ... Casteism is the investment in keeping the hierarchy as it is in order to maintain your own ranking, advantage, privilege, or to elevate yourself above others or to keep others beneath you.”
Reading “Caste: The Origins of Our Discontents” is akin to the experience of gaining relief after struggling for years with a chronic malady that has a fluctuating course: Under the surface is low-grade pain that is compartmentalized and often met with denial or gaslighting when symptoms and systems are reported to members of the dominant caste. Yet, when there are acute flare-ups and increasingly frequent deadly encounters, the defenses of denial are painfully revealed; structures are broken and sometimes burned down. This has been the clinical course of racism, particularly in the United States. In that vein, an early reaction while reading “Caste” might be comparable to hearing an interpretation that educates, clarifies, resonates, and lands perfectly on the right diagnosis at the right moment.
Approach proves clarifying
In conceptualizing the malady as one of caste, Ms. Wilkerson achieves several things simultaneously – she names the malady, thus providing a lexicon, describes its symptoms, and most importantly, in our opinion, shares some of the compelling data from her field studies. By focusing on India, Nazi Germany, and the United States, she describes how easily one system influences another in the global effort to maintain power among the privileged.
This is not a new way of conceptualizing racial hierarchy; however, what is truly persuasive is Ms. Wilkerson’s ability to weave her rigorous research, sociopolitical analysis, and cogent psychological insights and interpretations to explain the 400-year trajectory of racialized caste in the United States. She achieves this exigent task with beautiful prose that motivates the reader to return time and time again to learn gut-wrenching painful historical details. She summarizes truths that have been unearthed (again) about Germany, India, and, in particular, the United States during her research and travels around the world. In doing so, she provides vivid examples of racism layered on caste. Consider the following:
“The Nazis were impressed by the American custom of lynching its subordinate caste of African-Americans, having become aware of the ritual torture and mutilations that typically accompanied them. Hitler especially marveled at the American ‘knack for maintaining an air of robust innocence in the wake of mass death.’ ” Ms. Wilkerson informs us that Hitler sent emissaries to study America’s Jim Crow system and then imported some features to orchestrate the Holocaust in Nazi Germany.
and a corresponding sense of inadequacy in the presence of someone who is considered to be from a higher caste.
A painful account of interpersonal racism is captured as Ms. Wilkerson recounts her experience after a routine business flight from Chicago to Detroit. She details her difficulty leaving a rental car parking lot because she had become so disoriented after being profiled and accosted by Drug Enforcement Administration agents who had intercepted her in the airport terminal and followed her onto the airport shuttle bus as she attempted to reach her destination. She provides a description of “getting turned around in a parking lot that I had been to dozens of times, going in circles, not able to get out, not registering the signs to the exit, not seeing how to get to Interstate 94, when I knew full well how to get to I-94 after all the times I’d driven it. ... This was the thievery of caste, stealing the time and psychic resources of the marginalized, draining energy in an already uphill competition. They were not, like me, frozen and disoriented, trying to make sense of a public violation that seemed all the more menacing now that I could see it in full. The quiet mundanity of that terror has never left me, the scars outliving the cut.”
This account is consistent with the dissociative, disorienting dynamics of race-based trauma. Her experience is not uncommon and helps to explain the activism of those in the subordinate caste who have attained some measure of wealth, power, and influence, and are motivated to expend their resources (energy, time, fame, and/or wealth) to raise awareness about social and political injustices by calling out structural racism in medicine, protesting police use of force by taking a knee, boycotting sporting events, and even demanding that football stadiums be used as polling sites. At the end of the day, all of us who have “made it” know that when we leave our homes, our relegation to the subordinate caste determines how we are perceived and what landmines we must navigate to make it through the day and that determine whether we will make it home.
This tour de force work of art has the potential to be a game changer in the way that we think about racial polarization in the United States. It is hoped that this new language opens up a space that allows each of us to explore this hegemony while identifying our placement and actions we take to maintain it, for each of us undeniably has a position in this caste system.
Having this new lexicon summons to mind the reactions of patients who gain immediate relief from having their illnesses named. In the case of the U.S. malady that has gripped us all, Ms. Wilkerson reiterates the importance of naming the condition. She writes:
“Because, to truly understand America, we must open our eyes to the hidden work of a caste system that has gone unnamed but prevails among us to our collective detriment, to see that we have more in common with each other and with cultures that we might otherwise dismiss, and to summon the courage to consider that therein may lie the answers.”
The naming allows both doctor and patient to have greater insight, understanding its origins and course, as well as having hope that there is a remedy. Naming facilitates the space for a shift in thinking and implementation of treatment protocols, such as Nazi Germany’s “zero tolerance policy” of swastikas in comparison to the ongoing U.S. controversy about the display of Confederate symbols. At this point in history, we welcome a diagnosis that has the potential to shift us from these poles of dominant and subordinate, black and white, good and bad, toward integration and wholeness of the individual psyche and collective global community. This is similar to what Melanie Klein calls the depressive position. Ms. Wilkerson suggests, in relinquishing these polar splits, we increase our capacity to shift to a space where our psychic integration occurs and our inextricable interdependence and responsibility for one another are honored.
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures. Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
Isabel Wilkerson’s naming of the malady facilitates space for a shift in thinking.
Isabel Wilkerson’s naming of the malady facilitates space for a shift in thinking.
America has been struggling to understand its racial dynamics since the arrival of enslaved Africans more than 400 years ago. Today, with much of the world more polarized than ever, and certainly in our United States, there is a need for something to shift us from our fear and survival paranoid schizoid (us-vs.-them) position to an integrated form if we are to come out of this unusual democratic and societal unrest whole.
Yet, we’ve never had the lexicon to adequately describe the sociopolitical dynamics rooted in race and racism and their power to shape the thinking of all who originate in this country and all who enter its self-made borders whether forcefully or voluntarily. Enter Isabel Wilkerson, a Pulitzer Prize–winning, former New York Times Chicago bureau chief, and author of “The Warmth of Other Suns: The Epic Story of America’s Great Migration” (New York: Random House, 2010) with her second book, “Caste: The Origins of Our Discontents” (New York: Random House, 2020).
Ms. Wilkerson quickly gets to work in an engaging storytelling style of weaving past to present with ideas she supports with letters from the past, historians’ impressions, research studies, and data. Her observations and research are bookended by the lead up to the 2016 presidential election and its aftermath on the one end, and the impending 2020 presidential election on the other. In her view, the reemergence of violence that has accelerated in the 21st century and the renewed commitment to promote white supremacy can be understood if we expand our view of race and racism to consider the enduring power of caste. For, in Ms. Wilkerson’s view, the fear of the 2042 U.S. census (which is predicted to reflect for the first time a non-White majority) is a driving force behind the dominant caste’s determination to maintain the status quo power dynamics in the United States.
In an effort to explain American’s racial hierarchy, Ms. Wilkerson explains the need for a new lexicon “that may sound like a foreign language,” but this is intentional on her part. She writes:
“To recalibrate how we see ourselves, I use language that may be more commonly associated with people in other cultures, to suggest a new way of understanding our hierarchy: Dominant caste, ruling majority, favored caste, or upper caste, instead of, or in addition to, white. Middle castes instead of, or in addition to, Asian or Latino. Subordinate caste, lowest caste, bottom caste, disfavored caste, historically stigmatized instead of African-American. Original, conquered, or indigenous peoples instead of, or in addition to, Native American. Marginalized people in addition to, or instead of, women of any race, or minorities of any kind.”
Early in the book Ms. Wilkerson anchors her argument in Rev. Dr. Martin Luther King Jr.’s sojourn to India. Rather than focus on the known history of Dr. King’s admiration of Mohandas Gandhi, Ms. Wilkerson directs our attention to Dr. King’s discovery of his connection to Dalits, those who had been considered “untouchables” until Bhimrao Ramji Ambedkar, the Indian economist, jurist, social reformer, and Dalit leader, fiercely and successfully advocated for a rebranding of his caste of origin; instead of “untouchables” they would be considered Dalits or “broken people.” Dr. King did not meet Mr. Ambedkar, who died 3 years before this journey, but Ms. Wilkerson writes that Dr. King acknowledged the kinship, “And he said unto himself, Yes, I am an untouchable, and every Negro in the United States is an untouchable.” The Dalits and Dr. King recognized in each other their shared positions as subordinates in a global caste system.
In answering the question about the difference between racism and casteism, Ms. Wilkerson writes:
“Because caste and race are interwoven in America, it can be hard to separate the two. ... Casteism is the investment in keeping the hierarchy as it is in order to maintain your own ranking, advantage, privilege, or to elevate yourself above others or to keep others beneath you.”
Reading “Caste: The Origins of Our Discontents” is akin to the experience of gaining relief after struggling for years with a chronic malady that has a fluctuating course: Under the surface is low-grade pain that is compartmentalized and often met with denial or gaslighting when symptoms and systems are reported to members of the dominant caste. Yet, when there are acute flare-ups and increasingly frequent deadly encounters, the defenses of denial are painfully revealed; structures are broken and sometimes burned down. This has been the clinical course of racism, particularly in the United States. In that vein, an early reaction while reading “Caste” might be comparable to hearing an interpretation that educates, clarifies, resonates, and lands perfectly on the right diagnosis at the right moment.
Approach proves clarifying
In conceptualizing the malady as one of caste, Ms. Wilkerson achieves several things simultaneously – she names the malady, thus providing a lexicon, describes its symptoms, and most importantly, in our opinion, shares some of the compelling data from her field studies. By focusing on India, Nazi Germany, and the United States, she describes how easily one system influences another in the global effort to maintain power among the privileged.
This is not a new way of conceptualizing racial hierarchy; however, what is truly persuasive is Ms. Wilkerson’s ability to weave her rigorous research, sociopolitical analysis, and cogent psychological insights and interpretations to explain the 400-year trajectory of racialized caste in the United States. She achieves this exigent task with beautiful prose that motivates the reader to return time and time again to learn gut-wrenching painful historical details. She summarizes truths that have been unearthed (again) about Germany, India, and, in particular, the United States during her research and travels around the world. In doing so, she provides vivid examples of racism layered on caste. Consider the following:
“The Nazis were impressed by the American custom of lynching its subordinate caste of African-Americans, having become aware of the ritual torture and mutilations that typically accompanied them. Hitler especially marveled at the American ‘knack for maintaining an air of robust innocence in the wake of mass death.’ ” Ms. Wilkerson informs us that Hitler sent emissaries to study America’s Jim Crow system and then imported some features to orchestrate the Holocaust in Nazi Germany.
and a corresponding sense of inadequacy in the presence of someone who is considered to be from a higher caste.
A painful account of interpersonal racism is captured as Ms. Wilkerson recounts her experience after a routine business flight from Chicago to Detroit. She details her difficulty leaving a rental car parking lot because she had become so disoriented after being profiled and accosted by Drug Enforcement Administration agents who had intercepted her in the airport terminal and followed her onto the airport shuttle bus as she attempted to reach her destination. She provides a description of “getting turned around in a parking lot that I had been to dozens of times, going in circles, not able to get out, not registering the signs to the exit, not seeing how to get to Interstate 94, when I knew full well how to get to I-94 after all the times I’d driven it. ... This was the thievery of caste, stealing the time and psychic resources of the marginalized, draining energy in an already uphill competition. They were not, like me, frozen and disoriented, trying to make sense of a public violation that seemed all the more menacing now that I could see it in full. The quiet mundanity of that terror has never left me, the scars outliving the cut.”
This account is consistent with the dissociative, disorienting dynamics of race-based trauma. Her experience is not uncommon and helps to explain the activism of those in the subordinate caste who have attained some measure of wealth, power, and influence, and are motivated to expend their resources (energy, time, fame, and/or wealth) to raise awareness about social and political injustices by calling out structural racism in medicine, protesting police use of force by taking a knee, boycotting sporting events, and even demanding that football stadiums be used as polling sites. At the end of the day, all of us who have “made it” know that when we leave our homes, our relegation to the subordinate caste determines how we are perceived and what landmines we must navigate to make it through the day and that determine whether we will make it home.
This tour de force work of art has the potential to be a game changer in the way that we think about racial polarization in the United States. It is hoped that this new language opens up a space that allows each of us to explore this hegemony while identifying our placement and actions we take to maintain it, for each of us undeniably has a position in this caste system.
Having this new lexicon summons to mind the reactions of patients who gain immediate relief from having their illnesses named. In the case of the U.S. malady that has gripped us all, Ms. Wilkerson reiterates the importance of naming the condition. She writes:
“Because, to truly understand America, we must open our eyes to the hidden work of a caste system that has gone unnamed but prevails among us to our collective detriment, to see that we have more in common with each other and with cultures that we might otherwise dismiss, and to summon the courage to consider that therein may lie the answers.”
The naming allows both doctor and patient to have greater insight, understanding its origins and course, as well as having hope that there is a remedy. Naming facilitates the space for a shift in thinking and implementation of treatment protocols, such as Nazi Germany’s “zero tolerance policy” of swastikas in comparison to the ongoing U.S. controversy about the display of Confederate symbols. At this point in history, we welcome a diagnosis that has the potential to shift us from these poles of dominant and subordinate, black and white, good and bad, toward integration and wholeness of the individual psyche and collective global community. This is similar to what Melanie Klein calls the depressive position. Ms. Wilkerson suggests, in relinquishing these polar splits, we increase our capacity to shift to a space where our psychic integration occurs and our inextricable interdependence and responsibility for one another are honored.
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures. Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
America has been struggling to understand its racial dynamics since the arrival of enslaved Africans more than 400 years ago. Today, with much of the world more polarized than ever, and certainly in our United States, there is a need for something to shift us from our fear and survival paranoid schizoid (us-vs.-them) position to an integrated form if we are to come out of this unusual democratic and societal unrest whole.
Yet, we’ve never had the lexicon to adequately describe the sociopolitical dynamics rooted in race and racism and their power to shape the thinking of all who originate in this country and all who enter its self-made borders whether forcefully or voluntarily. Enter Isabel Wilkerson, a Pulitzer Prize–winning, former New York Times Chicago bureau chief, and author of “The Warmth of Other Suns: The Epic Story of America’s Great Migration” (New York: Random House, 2010) with her second book, “Caste: The Origins of Our Discontents” (New York: Random House, 2020).
Ms. Wilkerson quickly gets to work in an engaging storytelling style of weaving past to present with ideas she supports with letters from the past, historians’ impressions, research studies, and data. Her observations and research are bookended by the lead up to the 2016 presidential election and its aftermath on the one end, and the impending 2020 presidential election on the other. In her view, the reemergence of violence that has accelerated in the 21st century and the renewed commitment to promote white supremacy can be understood if we expand our view of race and racism to consider the enduring power of caste. For, in Ms. Wilkerson’s view, the fear of the 2042 U.S. census (which is predicted to reflect for the first time a non-White majority) is a driving force behind the dominant caste’s determination to maintain the status quo power dynamics in the United States.
In an effort to explain American’s racial hierarchy, Ms. Wilkerson explains the need for a new lexicon “that may sound like a foreign language,” but this is intentional on her part. She writes:
“To recalibrate how we see ourselves, I use language that may be more commonly associated with people in other cultures, to suggest a new way of understanding our hierarchy: Dominant caste, ruling majority, favored caste, or upper caste, instead of, or in addition to, white. Middle castes instead of, or in addition to, Asian or Latino. Subordinate caste, lowest caste, bottom caste, disfavored caste, historically stigmatized instead of African-American. Original, conquered, or indigenous peoples instead of, or in addition to, Native American. Marginalized people in addition to, or instead of, women of any race, or minorities of any kind.”
Early in the book Ms. Wilkerson anchors her argument in Rev. Dr. Martin Luther King Jr.’s sojourn to India. Rather than focus on the known history of Dr. King’s admiration of Mohandas Gandhi, Ms. Wilkerson directs our attention to Dr. King’s discovery of his connection to Dalits, those who had been considered “untouchables” until Bhimrao Ramji Ambedkar, the Indian economist, jurist, social reformer, and Dalit leader, fiercely and successfully advocated for a rebranding of his caste of origin; instead of “untouchables” they would be considered Dalits or “broken people.” Dr. King did not meet Mr. Ambedkar, who died 3 years before this journey, but Ms. Wilkerson writes that Dr. King acknowledged the kinship, “And he said unto himself, Yes, I am an untouchable, and every Negro in the United States is an untouchable.” The Dalits and Dr. King recognized in each other their shared positions as subordinates in a global caste system.
In answering the question about the difference between racism and casteism, Ms. Wilkerson writes:
“Because caste and race are interwoven in America, it can be hard to separate the two. ... Casteism is the investment in keeping the hierarchy as it is in order to maintain your own ranking, advantage, privilege, or to elevate yourself above others or to keep others beneath you.”
Reading “Caste: The Origins of Our Discontents” is akin to the experience of gaining relief after struggling for years with a chronic malady that has a fluctuating course: Under the surface is low-grade pain that is compartmentalized and often met with denial or gaslighting when symptoms and systems are reported to members of the dominant caste. Yet, when there are acute flare-ups and increasingly frequent deadly encounters, the defenses of denial are painfully revealed; structures are broken and sometimes burned down. This has been the clinical course of racism, particularly in the United States. In that vein, an early reaction while reading “Caste” might be comparable to hearing an interpretation that educates, clarifies, resonates, and lands perfectly on the right diagnosis at the right moment.
Approach proves clarifying
In conceptualizing the malady as one of caste, Ms. Wilkerson achieves several things simultaneously – she names the malady, thus providing a lexicon, describes its symptoms, and most importantly, in our opinion, shares some of the compelling data from her field studies. By focusing on India, Nazi Germany, and the United States, she describes how easily one system influences another in the global effort to maintain power among the privileged.
This is not a new way of conceptualizing racial hierarchy; however, what is truly persuasive is Ms. Wilkerson’s ability to weave her rigorous research, sociopolitical analysis, and cogent psychological insights and interpretations to explain the 400-year trajectory of racialized caste in the United States. She achieves this exigent task with beautiful prose that motivates the reader to return time and time again to learn gut-wrenching painful historical details. She summarizes truths that have been unearthed (again) about Germany, India, and, in particular, the United States during her research and travels around the world. In doing so, she provides vivid examples of racism layered on caste. Consider the following:
“The Nazis were impressed by the American custom of lynching its subordinate caste of African-Americans, having become aware of the ritual torture and mutilations that typically accompanied them. Hitler especially marveled at the American ‘knack for maintaining an air of robust innocence in the wake of mass death.’ ” Ms. Wilkerson informs us that Hitler sent emissaries to study America’s Jim Crow system and then imported some features to orchestrate the Holocaust in Nazi Germany.
and a corresponding sense of inadequacy in the presence of someone who is considered to be from a higher caste.
A painful account of interpersonal racism is captured as Ms. Wilkerson recounts her experience after a routine business flight from Chicago to Detroit. She details her difficulty leaving a rental car parking lot because she had become so disoriented after being profiled and accosted by Drug Enforcement Administration agents who had intercepted her in the airport terminal and followed her onto the airport shuttle bus as she attempted to reach her destination. She provides a description of “getting turned around in a parking lot that I had been to dozens of times, going in circles, not able to get out, not registering the signs to the exit, not seeing how to get to Interstate 94, when I knew full well how to get to I-94 after all the times I’d driven it. ... This was the thievery of caste, stealing the time and psychic resources of the marginalized, draining energy in an already uphill competition. They were not, like me, frozen and disoriented, trying to make sense of a public violation that seemed all the more menacing now that I could see it in full. The quiet mundanity of that terror has never left me, the scars outliving the cut.”
This account is consistent with the dissociative, disorienting dynamics of race-based trauma. Her experience is not uncommon and helps to explain the activism of those in the subordinate caste who have attained some measure of wealth, power, and influence, and are motivated to expend their resources (energy, time, fame, and/or wealth) to raise awareness about social and political injustices by calling out structural racism in medicine, protesting police use of force by taking a knee, boycotting sporting events, and even demanding that football stadiums be used as polling sites. At the end of the day, all of us who have “made it” know that when we leave our homes, our relegation to the subordinate caste determines how we are perceived and what landmines we must navigate to make it through the day and that determine whether we will make it home.
This tour de force work of art has the potential to be a game changer in the way that we think about racial polarization in the United States. It is hoped that this new language opens up a space that allows each of us to explore this hegemony while identifying our placement and actions we take to maintain it, for each of us undeniably has a position in this caste system.
Having this new lexicon summons to mind the reactions of patients who gain immediate relief from having their illnesses named. In the case of the U.S. malady that has gripped us all, Ms. Wilkerson reiterates the importance of naming the condition. She writes:
“Because, to truly understand America, we must open our eyes to the hidden work of a caste system that has gone unnamed but prevails among us to our collective detriment, to see that we have more in common with each other and with cultures that we might otherwise dismiss, and to summon the courage to consider that therein may lie the answers.”
The naming allows both doctor and patient to have greater insight, understanding its origins and course, as well as having hope that there is a remedy. Naming facilitates the space for a shift in thinking and implementation of treatment protocols, such as Nazi Germany’s “zero tolerance policy” of swastikas in comparison to the ongoing U.S. controversy about the display of Confederate symbols. At this point in history, we welcome a diagnosis that has the potential to shift us from these poles of dominant and subordinate, black and white, good and bad, toward integration and wholeness of the individual psyche and collective global community. This is similar to what Melanie Klein calls the depressive position. Ms. Wilkerson suggests, in relinquishing these polar splits, we increase our capacity to shift to a space where our psychic integration occurs and our inextricable interdependence and responsibility for one another are honored.
Dr. Dunlap is a psychiatrist and psychoanalyst, and clinical professor of psychiatry and behavioral sciences at George Washington University. She is interested in the management of “difference” – race, gender, ethnicity, and intersectionality – in dyadic relationships and group dynamics; and the impact of racism on interpersonal relationships in institutional structures. Dr. Dunlap practices in Washington and has no disclosures. Dr. Dennis is a clinical psychologist and psychoanalyst. Her interests are in gender and ethnic diversity, health equity, and supervision and training. Dr. Dennis practices in Washington and has no disclosures.
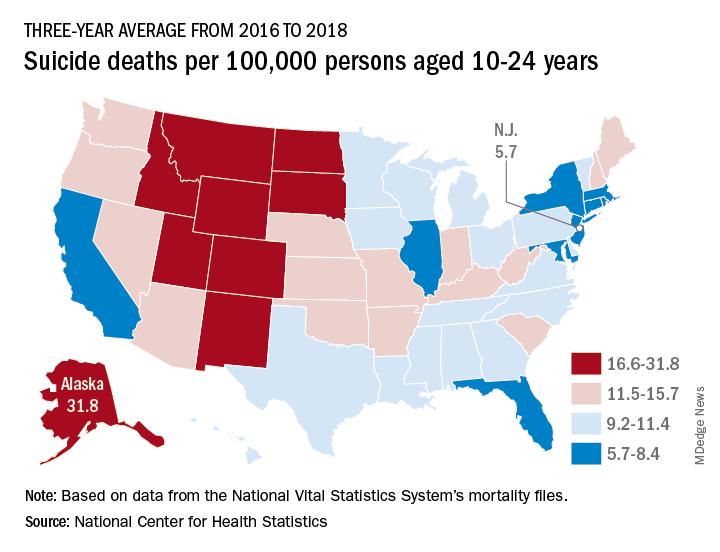
Suicide rates up significantly among adolescents, young adults
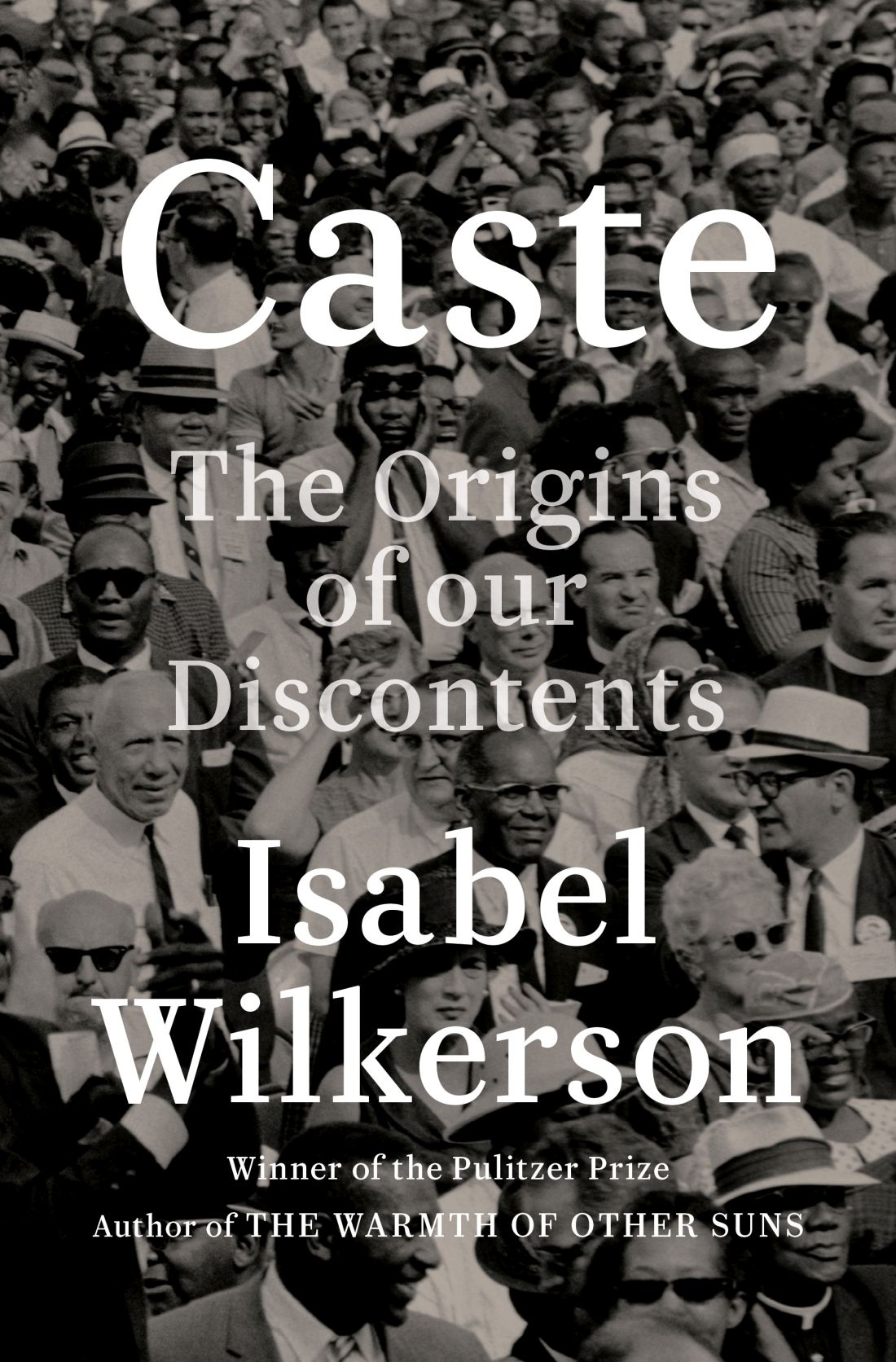
Suicide rates in young people aged 10-24 years increased significantly in 42 states from 2007-2009 to 2016-2018, according to a recent analysis from the National Center for Health Statistics.
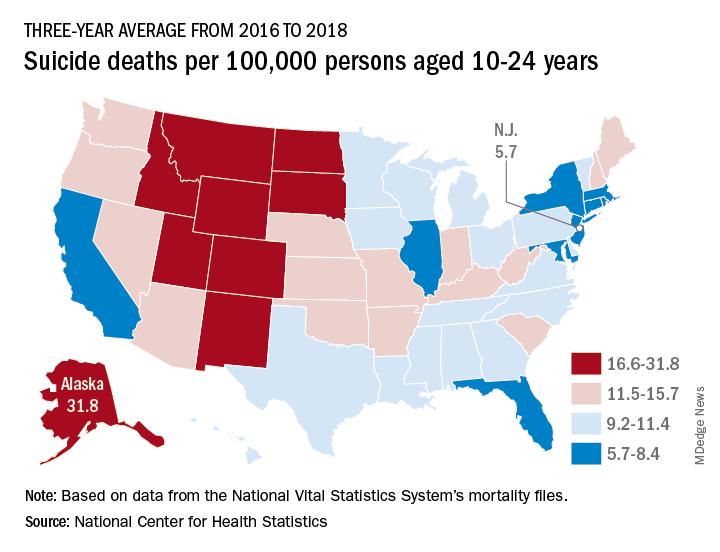
Nationally, the suicide rate jumped 47%, based on the averages for the two 3-year periods, rising from 7.0 per 100,000 persons aged 10-24 years to 10.3 per 100,000. For all ages, the corresponding increase was 47%, Sally C. Curtin, MA, of the NCHS, said in a National Vital Statistics Report.
There was no state with a decrease in suicide rates for adolescents and young adults, as the other eight all had nonsignificant increases, the smallest being 14% in South Dakota. Three-year averages were used to increase statistical power for states with relatively small numbers of deaths but were still not enough to show significance for some large increases, such as the 48% rise in Delaware, Ms. Curtin noted.
In 2016-2018, Alaska’s suicide rate of 31.8 per 100,000 persons aged 10-24 years was the highest in the country, followed by South Dakota (23.6), Montana (23.2), and Wyoming (20.5). New Jersey had the lowest rate at 5.7 per 100,000, with New York and Rhode Island both slightly higher at 5.9 and Connecticut at 6.3, based on data from the National Vital Statistics System.
Even the low numbers, however, hide some large changes, as New Jersey (up by 39%) and New York (up by 44%) were among the 42 states with statistically significant increases, which ranged from 21.7% in Maryland to 110% in New Hampshire, Ms. Curtin said in the report. The increases seen in this analysis contrast with data from the preceding time period, as “the suicide rate among persons aged 10-24 was statistically stable from 2000 to 2007.”
SOURCE: Curtin SC. National Vital Statistics Reports. 2020;69(11)1-9.
Suicide rates in young people aged 10-24 years increased significantly in 42 states from 2007-2009 to 2016-2018, according to a recent analysis from the National Center for Health Statistics.
Nationally, the suicide rate jumped 47%, based on the averages for the two 3-year periods, rising from 7.0 per 100,000 persons aged 10-24 years to 10.3 per 100,000. For all ages, the corresponding increase was 47%, Sally C. Curtin, MA, of the NCHS, said in a National Vital Statistics Report.
There was no state with a decrease in suicide rates for adolescents and young adults, as the other eight all had nonsignificant increases, the smallest being 14% in South Dakota. Three-year averages were used to increase statistical power for states with relatively small numbers of deaths but were still not enough to show significance for some large increases, such as the 48% rise in Delaware, Ms. Curtin noted.
In 2016-2018, Alaska’s suicide rate of 31.8 per 100,000 persons aged 10-24 years was the highest in the country, followed by South Dakota (23.6), Montana (23.2), and Wyoming (20.5). New Jersey had the lowest rate at 5.7 per 100,000, with New York and Rhode Island both slightly higher at 5.9 and Connecticut at 6.3, based on data from the National Vital Statistics System.
Even the low numbers, however, hide some large changes, as New Jersey (up by 39%) and New York (up by 44%) were among the 42 states with statistically significant increases, which ranged from 21.7% in Maryland to 110% in New Hampshire, Ms. Curtin said in the report. The increases seen in this analysis contrast with data from the preceding time period, as “the suicide rate among persons aged 10-24 was statistically stable from 2000 to 2007.”
SOURCE: Curtin SC. National Vital Statistics Reports. 2020;69(11)1-9.
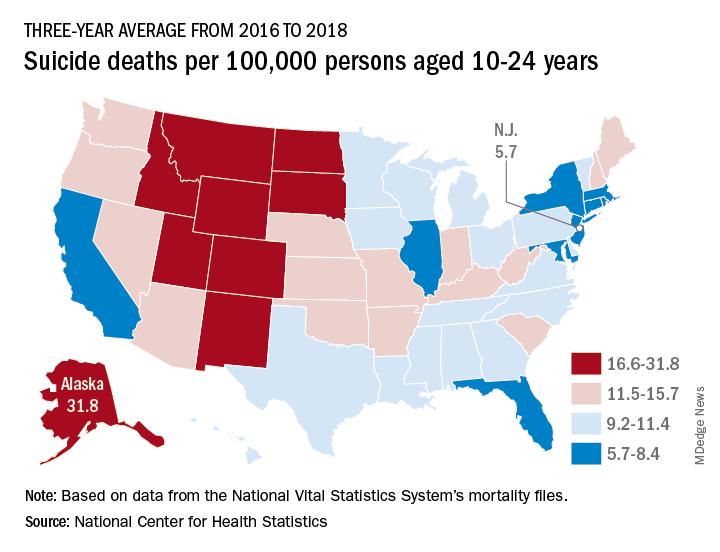
Suicide rates in young people aged 10-24 years increased significantly in 42 states from 2007-2009 to 2016-2018, according to a recent analysis from the National Center for Health Statistics.
Nationally, the suicide rate jumped 47%, based on the averages for the two 3-year periods, rising from 7.0 per 100,000 persons aged 10-24 years to 10.3 per 100,000. For all ages, the corresponding increase was 47%, Sally C. Curtin, MA, of the NCHS, said in a National Vital Statistics Report.
There was no state with a decrease in suicide rates for adolescents and young adults, as the other eight all had nonsignificant increases, the smallest being 14% in South Dakota. Three-year averages were used to increase statistical power for states with relatively small numbers of deaths but were still not enough to show significance for some large increases, such as the 48% rise in Delaware, Ms. Curtin noted.
In 2016-2018, Alaska’s suicide rate of 31.8 per 100,000 persons aged 10-24 years was the highest in the country, followed by South Dakota (23.6), Montana (23.2), and Wyoming (20.5). New Jersey had the lowest rate at 5.7 per 100,000, with New York and Rhode Island both slightly higher at 5.9 and Connecticut at 6.3, based on data from the National Vital Statistics System.
Even the low numbers, however, hide some large changes, as New Jersey (up by 39%) and New York (up by 44%) were among the 42 states with statistically significant increases, which ranged from 21.7% in Maryland to 110% in New Hampshire, Ms. Curtin said in the report. The increases seen in this analysis contrast with data from the preceding time period, as “the suicide rate among persons aged 10-24 was statistically stable from 2000 to 2007.”
SOURCE: Curtin SC. National Vital Statistics Reports. 2020;69(11)1-9.
Is psychiatry coddling the American mind?
A trainee recently observed that psychiatrists frequently seem motivated to protect patients from emotional and internal disruption. He suggested that we often did so by validating their maladaptive perspectives regarding their impaired relationships to society and close attachments. These maneuvers were justified by referring to the need to establish a therapeutic alliance and reduce patients’ suffering.
As an example, he mentioned a patient with alcohol use disorder. The patient came in with complaints that he could not stay sober with his current level of depression. The patient also complained of a family member who was setting limits. To the trainee’s surprise, the patient was not challenged on his perceived victimhood and his fantasy that a sober life should mean a life without negative effect. Instead, the patient was validated in his anger toward the family member. In addition, his medications were adjusted, seemingly confirming to the patient that one could only ask for sobriety once life is empty of pain.
The observation of the trainee reminded us of the three great “untruths” mentioned by Greg Lukianoff and Jonathan Haidt, PhD, in their famous book, “The Coddling of the American Mind.”1 In the book they warn against the idea of fragility – what doesn’t kill you makes you weaker; emotional reasoning – always trust your feelings; and us-versus-them thinking – life is a battle between good people and evil people. The authors compare these three great untruths with the cognitive distortions of cognitive-behavioral therapy.
We ponder the trainee’s observation that psychiatrists appear to encourage the untruths rather than challenge them. Part of psychiatric and all medical training involves learning nonjudgmental approaches to human suffering and an identification with individual needs over societal demands. Our suspicion is that a nonjudgmental approach to the understanding of the human condition generates a desire to protect patients from a moralistic shaming position. However, we wonder if, at times, psychiatry takes this approach too far.
Reconceptualizing shame
Shame can be a toxic presence in the overwhelmed superego of a patient, but it can serve an important role in psychic development and should not be avoided out of hand. We suggest that it can be appropriate for a patient with an alcohol use disorder to feel some shame for the harm caused by their drinking, and we question the limit of psychiatry’s current pursuit of incessant validation. As an extreme example, would modern psychiatry discourage a patient who killed someone while driving in an intoxicated state from feeling remorse and shame?
Modern psychiatry appears to have other examples of the three great untruths on display. In our work, we are often faced with patients who are prematurely placed on disability, an example of fragility. Instead of encouraging patients to return to the workforce, they are “protected” from the emotional difficulty of work. In many patients this results in a decline in functioning and worsening of psychiatric symptoms. We are also confronted with patients who define themselves by how they feel, an example of emotional reasoning. Instead of using our clinical judgments to define and assess symptoms, patients are left to decide for themselves through self-rated scales with questionable validity.2 This can result in patients having their emotional experiences not only validated when inappropriate but can also give emotional reasoning a false sense of medical legitimacy.
Finally, we commonly see patients who endlessly blame family members and others for any life difficulties, a form of us-versus-them thinking. Instead of acknowledging and then integrating life challenges to achieve recovery, patients are affirmed despite clinicians having little evidence on the veracity of the patients’ perspective. As a consequence, patients can be further isolated from their greatest source of support.
In some ways, a mindlessly validating approach in psychiatry is unexpected since the practice of psychiatry would seem to promote the development of strong attachments and resilience. After all, connections to family, employment, social institutions, and even religious worship are associated with vastly better outcomes. Those who have become alienated to these pillars of social cohesion fare much worse. One may deplore the static and at times oppressive nature of these institutions but the empirical experience of practicing psychiatry leads one to a healthy respect for the stabilizing influence they accord for individuals struggling with life’s vicissitudes, unpredictability, and loneliness. Overcoming the fear of responsibility, living up to the demands and expectations of society, and having the strength to overcome difficult emotions should be the standard goals of psychiatric treatment.
From the knowledge gained from working with patients struggling from psychic pain, we wonder how to encourage patients to pursue those adaptive approaches to life. We argue that a stoic emphasis on learning to manage one’s affective and mental response to the inevitable changes of life is key to achieving wisdom and stability in our humble lives. This perspective is a common denominator of multiple different psychotherapies. The goal is to provide patients with the ability to be in a place where they are engaged with the world in a meaningful way that is not overwhelmed by distorted, self-absorbed psychic anguish. This perspective discourages externalization as a relatively low-yield way to understand and overcome one’s problems. One identifies childhood experiences with one’s mother as a source of adult distress not for the purpose of blaming her, but for the purpose of recognizing one’s own childish motivations for making maladaptive decisions as an adult.
For many patients, the goal should be to emphasize an internal locus of control and responsibility. We should also avoid constantly relying on society and government’s role in helping the individual achieve a satisfactory life. We wonder if this endless pursuit of nonjudgment and validation corrupts the doctor-patient interaction. In other words, and individual responsibility for their own psychic development. Psychotherapy that ends with the patient being able to identify all the traumas that led to their sorrow has simply left the patient in the role of helpless and sorrowful victim. Instead, we should allow patients to proceed to the next step, which is empowerment and transformation. From this angle, the field of psychiatry should be cautious of encouraging movements that promote victimhood and grievance as a meaningful psychic position to take in society.
Mr. Lukianoff and Dr. Haidt use cognitive therapy as an analogy throughout their books for how to confront the great untruths. They perceive those modern forms of thinking as cognitive distortions, which can be remedied using the techniques of cognitive restructuring found in cognitive-behavioral therapy. They encourage us to recognize those maladaptive thoughts, and create more accurate and adaptive ways of viewing the world – a view that would be able to grow from challenges not just survive them; a view referred to as antifragile.3 We believe that those techniques and others would certainly be of assistance in our current times. However, the first step is to recognize our problem – a problem that is not rooted in the DSM, research, or biology but in an exaggerated intention to be patient centered. We should, however, remember that, when a patient has negative schemas, being too patient centered can be encouraging to maladaptive behaviors.
In conclusion, we wonder what modern psychiatry could look like if it made a concerted effort at also treating mental illness by reinforcing the importance of individual agency and responsibility. Modern psychiatry has been so focused on describing biological symptoms needing biological treatments that we sometimes forget that having no symptom (being asymptomatic) is not the only goal. Having a fulfilling and meaningful life, which is resilient to future symptoms is just as important to patients. We seem to have entrenched ourselves so deeply in an overly basic approach of problem-solution and diagnosis-treatment paradigm. However, we don’t need to renege on modern advances to promote the patient’s strength, adaptability, and antifragility. An emphasis on patient growth can complement the medical model. We wonder what effect such an approach would have if the trainee’s patient with alcohol use disorder was instead told: “Given the suffering you have and have caused because of your alcohol use disorder, how do you plan to make changes in your life to help the treatment plan we create together?”
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at UCSD and the University of San Diego. Dr. Badre can be reached at his website, BadreMD.com.
References
1. Lukianoff G, Haidt J. The Coddling of the American Mind: How Good Intentions and Bad Ideas are Setting Up a Generation for Failure. New York: Penguin Books, 2019.
2. Levis B et al. J Clin Epidemiol. 2020 Jun;122:115-128.e1.,
3. Taleb NN. Antifragile: Things That Gain from Disorder. Vol. 3. New York: Random House, 2012.
A trainee recently observed that psychiatrists frequently seem motivated to protect patients from emotional and internal disruption. He suggested that we often did so by validating their maladaptive perspectives regarding their impaired relationships to society and close attachments. These maneuvers were justified by referring to the need to establish a therapeutic alliance and reduce patients’ suffering.
As an example, he mentioned a patient with alcohol use disorder. The patient came in with complaints that he could not stay sober with his current level of depression. The patient also complained of a family member who was setting limits. To the trainee’s surprise, the patient was not challenged on his perceived victimhood and his fantasy that a sober life should mean a life without negative effect. Instead, the patient was validated in his anger toward the family member. In addition, his medications were adjusted, seemingly confirming to the patient that one could only ask for sobriety once life is empty of pain.
The observation of the trainee reminded us of the three great “untruths” mentioned by Greg Lukianoff and Jonathan Haidt, PhD, in their famous book, “The Coddling of the American Mind.”1 In the book they warn against the idea of fragility – what doesn’t kill you makes you weaker; emotional reasoning – always trust your feelings; and us-versus-them thinking – life is a battle between good people and evil people. The authors compare these three great untruths with the cognitive distortions of cognitive-behavioral therapy.
We ponder the trainee’s observation that psychiatrists appear to encourage the untruths rather than challenge them. Part of psychiatric and all medical training involves learning nonjudgmental approaches to human suffering and an identification with individual needs over societal demands. Our suspicion is that a nonjudgmental approach to the understanding of the human condition generates a desire to protect patients from a moralistic shaming position. However, we wonder if, at times, psychiatry takes this approach too far.
Reconceptualizing shame
Shame can be a toxic presence in the overwhelmed superego of a patient, but it can serve an important role in psychic development and should not be avoided out of hand. We suggest that it can be appropriate for a patient with an alcohol use disorder to feel some shame for the harm caused by their drinking, and we question the limit of psychiatry’s current pursuit of incessant validation. As an extreme example, would modern psychiatry discourage a patient who killed someone while driving in an intoxicated state from feeling remorse and shame?
Modern psychiatry appears to have other examples of the three great untruths on display. In our work, we are often faced with patients who are prematurely placed on disability, an example of fragility. Instead of encouraging patients to return to the workforce, they are “protected” from the emotional difficulty of work. In many patients this results in a decline in functioning and worsening of psychiatric symptoms. We are also confronted with patients who define themselves by how they feel, an example of emotional reasoning. Instead of using our clinical judgments to define and assess symptoms, patients are left to decide for themselves through self-rated scales with questionable validity.2 This can result in patients having their emotional experiences not only validated when inappropriate but can also give emotional reasoning a false sense of medical legitimacy.
Finally, we commonly see patients who endlessly blame family members and others for any life difficulties, a form of us-versus-them thinking. Instead of acknowledging and then integrating life challenges to achieve recovery, patients are affirmed despite clinicians having little evidence on the veracity of the patients’ perspective. As a consequence, patients can be further isolated from their greatest source of support.
In some ways, a mindlessly validating approach in psychiatry is unexpected since the practice of psychiatry would seem to promote the development of strong attachments and resilience. After all, connections to family, employment, social institutions, and even religious worship are associated with vastly better outcomes. Those who have become alienated to these pillars of social cohesion fare much worse. One may deplore the static and at times oppressive nature of these institutions but the empirical experience of practicing psychiatry leads one to a healthy respect for the stabilizing influence they accord for individuals struggling with life’s vicissitudes, unpredictability, and loneliness. Overcoming the fear of responsibility, living up to the demands and expectations of society, and having the strength to overcome difficult emotions should be the standard goals of psychiatric treatment.
From the knowledge gained from working with patients struggling from psychic pain, we wonder how to encourage patients to pursue those adaptive approaches to life. We argue that a stoic emphasis on learning to manage one’s affective and mental response to the inevitable changes of life is key to achieving wisdom and stability in our humble lives. This perspective is a common denominator of multiple different psychotherapies. The goal is to provide patients with the ability to be in a place where they are engaged with the world in a meaningful way that is not overwhelmed by distorted, self-absorbed psychic anguish. This perspective discourages externalization as a relatively low-yield way to understand and overcome one’s problems. One identifies childhood experiences with one’s mother as a source of adult distress not for the purpose of blaming her, but for the purpose of recognizing one’s own childish motivations for making maladaptive decisions as an adult.
For many patients, the goal should be to emphasize an internal locus of control and responsibility. We should also avoid constantly relying on society and government’s role in helping the individual achieve a satisfactory life. We wonder if this endless pursuit of nonjudgment and validation corrupts the doctor-patient interaction. In other words, and individual responsibility for their own psychic development. Psychotherapy that ends with the patient being able to identify all the traumas that led to their sorrow has simply left the patient in the role of helpless and sorrowful victim. Instead, we should allow patients to proceed to the next step, which is empowerment and transformation. From this angle, the field of psychiatry should be cautious of encouraging movements that promote victimhood and grievance as a meaningful psychic position to take in society.
Mr. Lukianoff and Dr. Haidt use cognitive therapy as an analogy throughout their books for how to confront the great untruths. They perceive those modern forms of thinking as cognitive distortions, which can be remedied using the techniques of cognitive restructuring found in cognitive-behavioral therapy. They encourage us to recognize those maladaptive thoughts, and create more accurate and adaptive ways of viewing the world – a view that would be able to grow from challenges not just survive them; a view referred to as antifragile.3 We believe that those techniques and others would certainly be of assistance in our current times. However, the first step is to recognize our problem – a problem that is not rooted in the DSM, research, or biology but in an exaggerated intention to be patient centered. We should, however, remember that, when a patient has negative schemas, being too patient centered can be encouraging to maladaptive behaviors.
In conclusion, we wonder what modern psychiatry could look like if it made a concerted effort at also treating mental illness by reinforcing the importance of individual agency and responsibility. Modern psychiatry has been so focused on describing biological symptoms needing biological treatments that we sometimes forget that having no symptom (being asymptomatic) is not the only goal. Having a fulfilling and meaningful life, which is resilient to future symptoms is just as important to patients. We seem to have entrenched ourselves so deeply in an overly basic approach of problem-solution and diagnosis-treatment paradigm. However, we don’t need to renege on modern advances to promote the patient’s strength, adaptability, and antifragility. An emphasis on patient growth can complement the medical model. We wonder what effect such an approach would have if the trainee’s patient with alcohol use disorder was instead told: “Given the suffering you have and have caused because of your alcohol use disorder, how do you plan to make changes in your life to help the treatment plan we create together?”
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at UCSD and the University of San Diego. Dr. Badre can be reached at his website, BadreMD.com.
References
1. Lukianoff G, Haidt J. The Coddling of the American Mind: How Good Intentions and Bad Ideas are Setting Up a Generation for Failure. New York: Penguin Books, 2019.
2. Levis B et al. J Clin Epidemiol. 2020 Jun;122:115-128.e1.,
3. Taleb NN. Antifragile: Things That Gain from Disorder. Vol. 3. New York: Random House, 2012.
A trainee recently observed that psychiatrists frequently seem motivated to protect patients from emotional and internal disruption. He suggested that we often did so by validating their maladaptive perspectives regarding their impaired relationships to society and close attachments. These maneuvers were justified by referring to the need to establish a therapeutic alliance and reduce patients’ suffering.
As an example, he mentioned a patient with alcohol use disorder. The patient came in with complaints that he could not stay sober with his current level of depression. The patient also complained of a family member who was setting limits. To the trainee’s surprise, the patient was not challenged on his perceived victimhood and his fantasy that a sober life should mean a life without negative effect. Instead, the patient was validated in his anger toward the family member. In addition, his medications were adjusted, seemingly confirming to the patient that one could only ask for sobriety once life is empty of pain.
The observation of the trainee reminded us of the three great “untruths” mentioned by Greg Lukianoff and Jonathan Haidt, PhD, in their famous book, “The Coddling of the American Mind.”1 In the book they warn against the idea of fragility – what doesn’t kill you makes you weaker; emotional reasoning – always trust your feelings; and us-versus-them thinking – life is a battle between good people and evil people. The authors compare these three great untruths with the cognitive distortions of cognitive-behavioral therapy.
We ponder the trainee’s observation that psychiatrists appear to encourage the untruths rather than challenge them. Part of psychiatric and all medical training involves learning nonjudgmental approaches to human suffering and an identification with individual needs over societal demands. Our suspicion is that a nonjudgmental approach to the understanding of the human condition generates a desire to protect patients from a moralistic shaming position. However, we wonder if, at times, psychiatry takes this approach too far.
Reconceptualizing shame
Shame can be a toxic presence in the overwhelmed superego of a patient, but it can serve an important role in psychic development and should not be avoided out of hand. We suggest that it can be appropriate for a patient with an alcohol use disorder to feel some shame for the harm caused by their drinking, and we question the limit of psychiatry’s current pursuit of incessant validation. As an extreme example, would modern psychiatry discourage a patient who killed someone while driving in an intoxicated state from feeling remorse and shame?
Modern psychiatry appears to have other examples of the three great untruths on display. In our work, we are often faced with patients who are prematurely placed on disability, an example of fragility. Instead of encouraging patients to return to the workforce, they are “protected” from the emotional difficulty of work. In many patients this results in a decline in functioning and worsening of psychiatric symptoms. We are also confronted with patients who define themselves by how they feel, an example of emotional reasoning. Instead of using our clinical judgments to define and assess symptoms, patients are left to decide for themselves through self-rated scales with questionable validity.2 This can result in patients having their emotional experiences not only validated when inappropriate but can also give emotional reasoning a false sense of medical legitimacy.
Finally, we commonly see patients who endlessly blame family members and others for any life difficulties, a form of us-versus-them thinking. Instead of acknowledging and then integrating life challenges to achieve recovery, patients are affirmed despite clinicians having little evidence on the veracity of the patients’ perspective. As a consequence, patients can be further isolated from their greatest source of support.
In some ways, a mindlessly validating approach in psychiatry is unexpected since the practice of psychiatry would seem to promote the development of strong attachments and resilience. After all, connections to family, employment, social institutions, and even religious worship are associated with vastly better outcomes. Those who have become alienated to these pillars of social cohesion fare much worse. One may deplore the static and at times oppressive nature of these institutions but the empirical experience of practicing psychiatry leads one to a healthy respect for the stabilizing influence they accord for individuals struggling with life’s vicissitudes, unpredictability, and loneliness. Overcoming the fear of responsibility, living up to the demands and expectations of society, and having the strength to overcome difficult emotions should be the standard goals of psychiatric treatment.
From the knowledge gained from working with patients struggling from psychic pain, we wonder how to encourage patients to pursue those adaptive approaches to life. We argue that a stoic emphasis on learning to manage one’s affective and mental response to the inevitable changes of life is key to achieving wisdom and stability in our humble lives. This perspective is a common denominator of multiple different psychotherapies. The goal is to provide patients with the ability to be in a place where they are engaged with the world in a meaningful way that is not overwhelmed by distorted, self-absorbed psychic anguish. This perspective discourages externalization as a relatively low-yield way to understand and overcome one’s problems. One identifies childhood experiences with one’s mother as a source of adult distress not for the purpose of blaming her, but for the purpose of recognizing one’s own childish motivations for making maladaptive decisions as an adult.
For many patients, the goal should be to emphasize an internal locus of control and responsibility. We should also avoid constantly relying on society and government’s role in helping the individual achieve a satisfactory life. We wonder if this endless pursuit of nonjudgment and validation corrupts the doctor-patient interaction. In other words, and individual responsibility for their own psychic development. Psychotherapy that ends with the patient being able to identify all the traumas that led to their sorrow has simply left the patient in the role of helpless and sorrowful victim. Instead, we should allow patients to proceed to the next step, which is empowerment and transformation. From this angle, the field of psychiatry should be cautious of encouraging movements that promote victimhood and grievance as a meaningful psychic position to take in society.
Mr. Lukianoff and Dr. Haidt use cognitive therapy as an analogy throughout their books for how to confront the great untruths. They perceive those modern forms of thinking as cognitive distortions, which can be remedied using the techniques of cognitive restructuring found in cognitive-behavioral therapy. They encourage us to recognize those maladaptive thoughts, and create more accurate and adaptive ways of viewing the world – a view that would be able to grow from challenges not just survive them; a view referred to as antifragile.3 We believe that those techniques and others would certainly be of assistance in our current times. However, the first step is to recognize our problem – a problem that is not rooted in the DSM, research, or biology but in an exaggerated intention to be patient centered. We should, however, remember that, when a patient has negative schemas, being too patient centered can be encouraging to maladaptive behaviors.
In conclusion, we wonder what modern psychiatry could look like if it made a concerted effort at also treating mental illness by reinforcing the importance of individual agency and responsibility. Modern psychiatry has been so focused on describing biological symptoms needing biological treatments that we sometimes forget that having no symptom (being asymptomatic) is not the only goal. Having a fulfilling and meaningful life, which is resilient to future symptoms is just as important to patients. We seem to have entrenched ourselves so deeply in an overly basic approach of problem-solution and diagnosis-treatment paradigm. However, we don’t need to renege on modern advances to promote the patient’s strength, adaptability, and antifragility. An emphasis on patient growth can complement the medical model. We wonder what effect such an approach would have if the trainee’s patient with alcohol use disorder was instead told: “Given the suffering you have and have caused because of your alcohol use disorder, how do you plan to make changes in your life to help the treatment plan we create together?”
Dr. Lehman is a professor of psychiatry at the University of California, San Diego. He is codirector of all acute and intensive psychiatric treatment at the Veterans Affairs Medical Center in San Diego, where he practices clinical psychiatry. He also is the course director for the UCSD third-year medical student psychiatry clerkship. Dr. Badre is a clinical and forensic psychiatrist in San Diego. He holds teaching positions at UCSD and the University of San Diego. Dr. Badre can be reached at his website, BadreMD.com.
References
1. Lukianoff G, Haidt J. The Coddling of the American Mind: How Good Intentions and Bad Ideas are Setting Up a Generation for Failure. New York: Penguin Books, 2019.
2. Levis B et al. J Clin Epidemiol. 2020 Jun;122:115-128.e1.,
3. Taleb NN. Antifragile: Things That Gain from Disorder. Vol. 3. New York: Random House, 2012.
CDC playbook prepares states for rollout of COVID-19 vaccine if one is approved
States have begun preparing to distribute a COVID-19 vaccine if one is approved, a CDC official said today.
The CDC released guidance for states on Sept. 16 titled COVID-19 Vaccination Program Interim Playbook for Jurisdiction Operations. The document discusses vaccine ordering, storage, and handling and says that states should submit their plans for vaccine distribution to the agency by Oct. 16.
“Every jurisdiction is heavily involved right now in their plan development,” CDC official Janell Routh, MD, told the Advisory Committee on Immunization Practices during its Sept. 22 meeting. “It was really impressive to me that, even though the playbook only went out last week, states and jurisdictions have been thinking about this for quite some time.”
However, one committee member suggested that setting a deadline before more safety, efficacy, and storage information is known may be premature.
“I cannot imagine that we will actually know the final storage requirements for this vaccine by Oct. 16, which makes me a little concerned about finalizing state plans,” said Helen “Keipp” Talbot, MD, MPH, associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. “We also don’t know the best populations yet when it comes to efficacy and safety.”
Dr. Routh said the CDC is asking states to plan on the basis of assumptions. “We know those plans will constantly be improving, changing, as we learn more information,” Dr. Routh said. States agreed to return a plan 30 days after the playbook was released, which is how the Oct. 16 deadline was established, she said.
States are encouraged to think broadly. Plans may include contingencies for a product that requires ultracold storage or for distributing more than one vaccine product, Dr. Routh said.
“One goal is to be ready on the first day that we can actually distribute vaccine,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the meeting. “Our colleagues in Operation Warp Speed say that they expect there will be vaccine as early as November, and therefore we need to be ready so there is no delay in distributing that vaccine. And that phase, that early phase, is really close upon us.”
Many states have already developed plans, and the CDC is providing technical assistance as needed to monitor the plans regularly, Dr. Routh said.
Key issues identified
From holding pilot meetings with five jurisdictions, officials learned that public confidence in the vaccine is among states’ greatest concerns, Dr. Routh said. In addition, distribution is resource intensive, and social distancing adds logistical complexity.
Specific guidance on whom to vaccinate in the early stages will smooth the process, officials suggested during the pilot meetings. For the first several weeks, vaccine doses may be limited to priority populations, such as health care workers.
“This interim playbook is a living document,” Dr. Routh emphasized. “We definitely plan to update the content regularly as we learn more information about what vaccines and when they will be released.”
During the early stages of COVID-19 vaccination, officials plan to implement an enhanced monitoring program in which vaccine recipients would complete surveys about adverse events, in addition to the traditional vaccine safety monitoring programs that already exist, officials said.
A version of this article originally appeared on Medscape.com.
States have begun preparing to distribute a COVID-19 vaccine if one is approved, a CDC official said today.
The CDC released guidance for states on Sept. 16 titled COVID-19 Vaccination Program Interim Playbook for Jurisdiction Operations. The document discusses vaccine ordering, storage, and handling and says that states should submit their plans for vaccine distribution to the agency by Oct. 16.
“Every jurisdiction is heavily involved right now in their plan development,” CDC official Janell Routh, MD, told the Advisory Committee on Immunization Practices during its Sept. 22 meeting. “It was really impressive to me that, even though the playbook only went out last week, states and jurisdictions have been thinking about this for quite some time.”
However, one committee member suggested that setting a deadline before more safety, efficacy, and storage information is known may be premature.
“I cannot imagine that we will actually know the final storage requirements for this vaccine by Oct. 16, which makes me a little concerned about finalizing state plans,” said Helen “Keipp” Talbot, MD, MPH, associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. “We also don’t know the best populations yet when it comes to efficacy and safety.”
Dr. Routh said the CDC is asking states to plan on the basis of assumptions. “We know those plans will constantly be improving, changing, as we learn more information,” Dr. Routh said. States agreed to return a plan 30 days after the playbook was released, which is how the Oct. 16 deadline was established, she said.
States are encouraged to think broadly. Plans may include contingencies for a product that requires ultracold storage or for distributing more than one vaccine product, Dr. Routh said.
“One goal is to be ready on the first day that we can actually distribute vaccine,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the meeting. “Our colleagues in Operation Warp Speed say that they expect there will be vaccine as early as November, and therefore we need to be ready so there is no delay in distributing that vaccine. And that phase, that early phase, is really close upon us.”
Many states have already developed plans, and the CDC is providing technical assistance as needed to monitor the plans regularly, Dr. Routh said.
Key issues identified
From holding pilot meetings with five jurisdictions, officials learned that public confidence in the vaccine is among states’ greatest concerns, Dr. Routh said. In addition, distribution is resource intensive, and social distancing adds logistical complexity.
Specific guidance on whom to vaccinate in the early stages will smooth the process, officials suggested during the pilot meetings. For the first several weeks, vaccine doses may be limited to priority populations, such as health care workers.
“This interim playbook is a living document,” Dr. Routh emphasized. “We definitely plan to update the content regularly as we learn more information about what vaccines and when they will be released.”
During the early stages of COVID-19 vaccination, officials plan to implement an enhanced monitoring program in which vaccine recipients would complete surveys about adverse events, in addition to the traditional vaccine safety monitoring programs that already exist, officials said.
A version of this article originally appeared on Medscape.com.
States have begun preparing to distribute a COVID-19 vaccine if one is approved, a CDC official said today.
The CDC released guidance for states on Sept. 16 titled COVID-19 Vaccination Program Interim Playbook for Jurisdiction Operations. The document discusses vaccine ordering, storage, and handling and says that states should submit their plans for vaccine distribution to the agency by Oct. 16.
“Every jurisdiction is heavily involved right now in their plan development,” CDC official Janell Routh, MD, told the Advisory Committee on Immunization Practices during its Sept. 22 meeting. “It was really impressive to me that, even though the playbook only went out last week, states and jurisdictions have been thinking about this for quite some time.”
However, one committee member suggested that setting a deadline before more safety, efficacy, and storage information is known may be premature.
“I cannot imagine that we will actually know the final storage requirements for this vaccine by Oct. 16, which makes me a little concerned about finalizing state plans,” said Helen “Keipp” Talbot, MD, MPH, associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn. “We also don’t know the best populations yet when it comes to efficacy and safety.”
Dr. Routh said the CDC is asking states to plan on the basis of assumptions. “We know those plans will constantly be improving, changing, as we learn more information,” Dr. Routh said. States agreed to return a plan 30 days after the playbook was released, which is how the Oct. 16 deadline was established, she said.
States are encouraged to think broadly. Plans may include contingencies for a product that requires ultracold storage or for distributing more than one vaccine product, Dr. Routh said.
“One goal is to be ready on the first day that we can actually distribute vaccine,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during the meeting. “Our colleagues in Operation Warp Speed say that they expect there will be vaccine as early as November, and therefore we need to be ready so there is no delay in distributing that vaccine. And that phase, that early phase, is really close upon us.”
Many states have already developed plans, and the CDC is providing technical assistance as needed to monitor the plans regularly, Dr. Routh said.
Key issues identified
From holding pilot meetings with five jurisdictions, officials learned that public confidence in the vaccine is among states’ greatest concerns, Dr. Routh said. In addition, distribution is resource intensive, and social distancing adds logistical complexity.
Specific guidance on whom to vaccinate in the early stages will smooth the process, officials suggested during the pilot meetings. For the first several weeks, vaccine doses may be limited to priority populations, such as health care workers.
“This interim playbook is a living document,” Dr. Routh emphasized. “We definitely plan to update the content regularly as we learn more information about what vaccines and when they will be released.”
During the early stages of COVID-19 vaccination, officials plan to implement an enhanced monitoring program in which vaccine recipients would complete surveys about adverse events, in addition to the traditional vaccine safety monitoring programs that already exist, officials said.
A version of this article originally appeared on Medscape.com.
Three major COVID vaccine developers release detailed trial protocols
Typically, manufacturers guard the specifics of preclinical vaccine trials. This rare move follows calls for greater transparency. For example, the American Medical Association wrote a letter in late August asking the Food and Drug Administration to keep physicians informed of their COVID-19 vaccine review process.
On September 17, ModernaTx released the phase 3 trial protocol for its mRNA-1273 SARS-CoV-2 vaccine. In short order, on September 19, Pfizer/BioNTech shared their phase 1/2/3 trial vaccine protocol. AstraZeneca, which is developing a vaccine along with Oxford University, also released its protocol.
The AstraZeneca vaccine trial made headlines recently for having to be temporarily halted because of unexpected illnesses that arose in two participants, according to the New York Times and other sources.
“I applaud the release of the clinical trial protocols by the companies. The public trust in any COVID-19 vaccine is paramount, especially given the fast timeline and perceived political pressures of these candidates,” Robert Kruse, MD, PhD, told Medscape Medical News when asked to comment.
AstraZeneca takes a shot at transparency
The three primary objectives of the AstraZeneca AZD1222 trial outlined in the 110-page protocol include estimating the efficacy, safety, tolerability, and reactogenicity associated with two intramuscular doses of the vaccine in comparison with placebo in adults.
The projected enrollment is 30,000 participants, and the estimated primary completion date is Dec. 2, 2020, according to information on clinicaltrials.gov.
“Given the unprecedented global impact of the coronavirus pandemic and the need for public information, AstraZeneca has published the detailed protocol and design of our AZD1222 clinical trial,” the company said in a statement. “As with most clinical development, protocols are not typically shared publicly due to the importance of maintaining confidentiality and integrity of trials.
“AstraZeneca continues to work with industry peers to ensure a consistent approach to sharing timely clinical trial information,” the company added.
Moderna methodology
The ModernaTX 135-page protocol outlines the primary trial objectives of evaluating efficacy, safety, and reactogenicity of two injections of the vaccine administered 28 days apart. Researchers also plan to randomly assign 30,000 adults to receive either vaccine or placebo. The estimated primary completion date is Oct. 27, 2022.
A statement that was requested from ModernaTX was not received by press time.
Pfizer protocol
In the Pfizer/BioNTech vaccine trial, researchers plan to evaluate different doses in different age groups in a multistep protocol. The trial features 20 primary safety objectives, which include reporting adverse events and serious adverse events, including any local or systemic events.
Efficacy endpoints are secondary objectives. The estimated enrollment is 29,481 adults; the estimated primary completion date is April 19, 2021.
“Pfizer and BioNTech recognize that the COVID-19 pandemic is a unique circumstance, and the need for transparency is clear,” Pfizer spokesperson Sharon Castillo told Medscape Medical News. By making the full protocol available, “we believe this will reinforce our long-standing commitment to scientific and regulatory rigor that benefits patients,” she said.
“Based on current infection rates, Pfizer and BioNTech continue to expect that a conclusive read-out on efficacy is likely by the end of October. Neither Pfizer nor the FDA can move faster than the data we are generating through our clinical trial,” Castillo said.
If clinical work and regulatory approval or authorization proceed as planned, Pfizer and BioNTech expect to supply up to 100 million doses worldwide by the end of 2020 and approximately 1.3 billion doses worldwide by the end of 2021.
Pfizer is not willing to sacrifice safety and efficacy in the name of expediency, Castillo said. “We will not cut corners in this pursuit. Patient safety is our highest priority, and Pfizer will not bring a vaccine to market without adequate evidence of safety and efficacy.”
A positive move
“COVID-19 vaccines will only be useful if many people are willing to receive them,” said Kruse, a postgraduate year 3 resident in the Department of Pathology at Johns Hopkins Medicine in Baltimore, Maryland.
“By giving the general public along with other scientists and physicians the opportunity to critique the protocols, everyone can understand what the metrics would be for an early look at efficacy,” Kruse said. He noted that information could help inform a potential FDA emergency use authorization.
Kruse has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Typically, manufacturers guard the specifics of preclinical vaccine trials. This rare move follows calls for greater transparency. For example, the American Medical Association wrote a letter in late August asking the Food and Drug Administration to keep physicians informed of their COVID-19 vaccine review process.
On September 17, ModernaTx released the phase 3 trial protocol for its mRNA-1273 SARS-CoV-2 vaccine. In short order, on September 19, Pfizer/BioNTech shared their phase 1/2/3 trial vaccine protocol. AstraZeneca, which is developing a vaccine along with Oxford University, also released its protocol.
The AstraZeneca vaccine trial made headlines recently for having to be temporarily halted because of unexpected illnesses that arose in two participants, according to the New York Times and other sources.
“I applaud the release of the clinical trial protocols by the companies. The public trust in any COVID-19 vaccine is paramount, especially given the fast timeline and perceived political pressures of these candidates,” Robert Kruse, MD, PhD, told Medscape Medical News when asked to comment.
AstraZeneca takes a shot at transparency
The three primary objectives of the AstraZeneca AZD1222 trial outlined in the 110-page protocol include estimating the efficacy, safety, tolerability, and reactogenicity associated with two intramuscular doses of the vaccine in comparison with placebo in adults.
The projected enrollment is 30,000 participants, and the estimated primary completion date is Dec. 2, 2020, according to information on clinicaltrials.gov.
“Given the unprecedented global impact of the coronavirus pandemic and the need for public information, AstraZeneca has published the detailed protocol and design of our AZD1222 clinical trial,” the company said in a statement. “As with most clinical development, protocols are not typically shared publicly due to the importance of maintaining confidentiality and integrity of trials.
“AstraZeneca continues to work with industry peers to ensure a consistent approach to sharing timely clinical trial information,” the company added.
Moderna methodology
The ModernaTX 135-page protocol outlines the primary trial objectives of evaluating efficacy, safety, and reactogenicity of two injections of the vaccine administered 28 days apart. Researchers also plan to randomly assign 30,000 adults to receive either vaccine or placebo. The estimated primary completion date is Oct. 27, 2022.
A statement that was requested from ModernaTX was not received by press time.
Pfizer protocol
In the Pfizer/BioNTech vaccine trial, researchers plan to evaluate different doses in different age groups in a multistep protocol. The trial features 20 primary safety objectives, which include reporting adverse events and serious adverse events, including any local or systemic events.
Efficacy endpoints are secondary objectives. The estimated enrollment is 29,481 adults; the estimated primary completion date is April 19, 2021.
“Pfizer and BioNTech recognize that the COVID-19 pandemic is a unique circumstance, and the need for transparency is clear,” Pfizer spokesperson Sharon Castillo told Medscape Medical News. By making the full protocol available, “we believe this will reinforce our long-standing commitment to scientific and regulatory rigor that benefits patients,” she said.
“Based on current infection rates, Pfizer and BioNTech continue to expect that a conclusive read-out on efficacy is likely by the end of October. Neither Pfizer nor the FDA can move faster than the data we are generating through our clinical trial,” Castillo said.
If clinical work and regulatory approval or authorization proceed as planned, Pfizer and BioNTech expect to supply up to 100 million doses worldwide by the end of 2020 and approximately 1.3 billion doses worldwide by the end of 2021.
Pfizer is not willing to sacrifice safety and efficacy in the name of expediency, Castillo said. “We will not cut corners in this pursuit. Patient safety is our highest priority, and Pfizer will not bring a vaccine to market without adequate evidence of safety and efficacy.”
A positive move
“COVID-19 vaccines will only be useful if many people are willing to receive them,” said Kruse, a postgraduate year 3 resident in the Department of Pathology at Johns Hopkins Medicine in Baltimore, Maryland.
“By giving the general public along with other scientists and physicians the opportunity to critique the protocols, everyone can understand what the metrics would be for an early look at efficacy,” Kruse said. He noted that information could help inform a potential FDA emergency use authorization.
Kruse has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Typically, manufacturers guard the specifics of preclinical vaccine trials. This rare move follows calls for greater transparency. For example, the American Medical Association wrote a letter in late August asking the Food and Drug Administration to keep physicians informed of their COVID-19 vaccine review process.
On September 17, ModernaTx released the phase 3 trial protocol for its mRNA-1273 SARS-CoV-2 vaccine. In short order, on September 19, Pfizer/BioNTech shared their phase 1/2/3 trial vaccine protocol. AstraZeneca, which is developing a vaccine along with Oxford University, also released its protocol.
The AstraZeneca vaccine trial made headlines recently for having to be temporarily halted because of unexpected illnesses that arose in two participants, according to the New York Times and other sources.
“I applaud the release of the clinical trial protocols by the companies. The public trust in any COVID-19 vaccine is paramount, especially given the fast timeline and perceived political pressures of these candidates,” Robert Kruse, MD, PhD, told Medscape Medical News when asked to comment.
AstraZeneca takes a shot at transparency
The three primary objectives of the AstraZeneca AZD1222 trial outlined in the 110-page protocol include estimating the efficacy, safety, tolerability, and reactogenicity associated with two intramuscular doses of the vaccine in comparison with placebo in adults.
The projected enrollment is 30,000 participants, and the estimated primary completion date is Dec. 2, 2020, according to information on clinicaltrials.gov.
“Given the unprecedented global impact of the coronavirus pandemic and the need for public information, AstraZeneca has published the detailed protocol and design of our AZD1222 clinical trial,” the company said in a statement. “As with most clinical development, protocols are not typically shared publicly due to the importance of maintaining confidentiality and integrity of trials.
“AstraZeneca continues to work with industry peers to ensure a consistent approach to sharing timely clinical trial information,” the company added.
Moderna methodology
The ModernaTX 135-page protocol outlines the primary trial objectives of evaluating efficacy, safety, and reactogenicity of two injections of the vaccine administered 28 days apart. Researchers also plan to randomly assign 30,000 adults to receive either vaccine or placebo. The estimated primary completion date is Oct. 27, 2022.
A statement that was requested from ModernaTX was not received by press time.
Pfizer protocol
In the Pfizer/BioNTech vaccine trial, researchers plan to evaluate different doses in different age groups in a multistep protocol. The trial features 20 primary safety objectives, which include reporting adverse events and serious adverse events, including any local or systemic events.
Efficacy endpoints are secondary objectives. The estimated enrollment is 29,481 adults; the estimated primary completion date is April 19, 2021.
“Pfizer and BioNTech recognize that the COVID-19 pandemic is a unique circumstance, and the need for transparency is clear,” Pfizer spokesperson Sharon Castillo told Medscape Medical News. By making the full protocol available, “we believe this will reinforce our long-standing commitment to scientific and regulatory rigor that benefits patients,” she said.
“Based on current infection rates, Pfizer and BioNTech continue to expect that a conclusive read-out on efficacy is likely by the end of October. Neither Pfizer nor the FDA can move faster than the data we are generating through our clinical trial,” Castillo said.
If clinical work and regulatory approval or authorization proceed as planned, Pfizer and BioNTech expect to supply up to 100 million doses worldwide by the end of 2020 and approximately 1.3 billion doses worldwide by the end of 2021.
Pfizer is not willing to sacrifice safety and efficacy in the name of expediency, Castillo said. “We will not cut corners in this pursuit. Patient safety is our highest priority, and Pfizer will not bring a vaccine to market without adequate evidence of safety and efficacy.”
A positive move
“COVID-19 vaccines will only be useful if many people are willing to receive them,” said Kruse, a postgraduate year 3 resident in the Department of Pathology at Johns Hopkins Medicine in Baltimore, Maryland.
“By giving the general public along with other scientists and physicians the opportunity to critique the protocols, everyone can understand what the metrics would be for an early look at efficacy,” Kruse said. He noted that information could help inform a potential FDA emergency use authorization.
Kruse has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Smart health devices – promises and pitfalls
What needs to be done before the data deluge hits the office
Hurricane Sally recently crossed the Gulf of Mexico and landed with torrential rainfalls along the Alabama coast. A little rainfall is important for crops; too much leads to devastation. As physicians, we need data in order to help manage patients’ illnesses and to help to keep them healthy. Our fear though is that too much data provided too quickly may have the opposite effect.
Personal monitoring devices
When I bought my first Fitbit 7 years ago, I was enamored with the technology. The Fitbit was little more than a step tracker, yet I proudly wore its black rubber strap on my wrist. It was my first foray into wearable technology, and it felt quite empowering to have an objective way to track my fitness beyond just using my bathroom scale. Now less than a decade later, that Fitbit looks archaic in comparison with the wrist-top technology currently available.
As I write this, the world’s largest technology company is in the process of releasing its sixth-generation Apple Watch. In addition to acting as a smartphone, this new device, which is barely larger than a postage stamp, offers GPS-based movement tracking, the ability to detect falls, continuous heart rate monitoring, a built-in EKG capable of diagnosing atrial fibrillation, and an oxygen saturation sensor. These features weren’t added thoughtlessly. Apple is marketing this as a health-focused device, with their primary advertising campaign claiming that “the future of health is on your wrist,” and they aren’t the only company making this play.
Along with Apple, Samsung, Withings, Fitbit, and other companies continue to bring products to market that monitor our activity and provide new insights into our health. Typically linked to smartphone-based apps, these devices record all of their measurements for later review, while software helps interpret the findings to make them actionable. From heart rate tracking to sleep analysis, these options now provide access to volumes of data that promise to improve our wellness and change our lives. Of course, those promises will only be fulfilled if our behavior is altered as a consequence of having more detailed information. Whether that will happen remains to be seen.
Health system–linked devices
Major advancements in medical monitoring technology are now enabling physicians to get much deeper insight into their patients’ health status. Internet-connected scales, blood pressure cuffs, and exercise equipment offer the ability to upload information into patient portals and integrate that information into EHRs. New devices provide access to information that previously was impossible to obtain. For example, wearable continuous blood glucose monitors, such as the FreeStyle Libre or DexCom’s G6, allow patients and physicians to follow blood sugar readings 24 hours a day. This provides unprecedented awareness of diabetes control and relieves the pain and inconvenience of finger sticks and blood draws. It also aids with compliance because patients don’t need to remember to check their sugar levels on a schedule.
Other compliance-boosting breakthroughs, such as Bluetooth-enabled asthma inhalers and cellular-connected continuous positive airway pressure machines, assist patients with managing chronic respiratory conditions. Many companies are developing technologies to manage acute conditions as well. One such company, an on-demand telemedicine provider called TytoCare, has developed a $299 suite of instruments that includes a digital stethoscope, thermometer, and camera-based otoscope. In concert with a virtual visit, their providers can remotely use these tools to examine and assess sick individuals. This virtual “laying on of hands” may have sounded like science fiction and likely would have been rejected by patients just a few years ago. Now it is becoming commonplace and will soon be an expectation of many seeking care.
But if we are to be successful, everyone must acknowledge that this revolution in health care brings many challenges along with it. One of those is the deluge of data that connected devices provide.
Information overload
There is such a thing as “too much of a good thing.” Described by journalist David Shenk as “data smog” in his 1997 book of the same name, the idea is clear: There is only so much information we can assimilate.
Even after years of using EHRs and with government-implemented incentives that promote “meaningful use,” physicians are still struggling with EHRs. Additionally, many have expressed frustration with the connectedness that EHRs provide and lament their inability to ever really “leave the office.” As more and more data become available to physicians, the challenge of how to assimilate and act on those data will continue to grow. The addition of patient-provided health statistics will only make information overload worse, with clinicians will feeling an ever-growing burden to know, understand, and act on this information.
Unless we develop systems to sort, filter, and prioritize the flow of information, there is potential for liability from not acting on the amount of virtual information doctors receive. This new risk for already fatigued and overburdened physicians combined with an increase in the amount of virtual information at doctors’ fingertips may lead to the value of patient data being lost.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
What needs to be done before the data deluge hits the office
What needs to be done before the data deluge hits the office
Hurricane Sally recently crossed the Gulf of Mexico and landed with torrential rainfalls along the Alabama coast. A little rainfall is important for crops; too much leads to devastation. As physicians, we need data in order to help manage patients’ illnesses and to help to keep them healthy. Our fear though is that too much data provided too quickly may have the opposite effect.
Personal monitoring devices
When I bought my first Fitbit 7 years ago, I was enamored with the technology. The Fitbit was little more than a step tracker, yet I proudly wore its black rubber strap on my wrist. It was my first foray into wearable technology, and it felt quite empowering to have an objective way to track my fitness beyond just using my bathroom scale. Now less than a decade later, that Fitbit looks archaic in comparison with the wrist-top technology currently available.
As I write this, the world’s largest technology company is in the process of releasing its sixth-generation Apple Watch. In addition to acting as a smartphone, this new device, which is barely larger than a postage stamp, offers GPS-based movement tracking, the ability to detect falls, continuous heart rate monitoring, a built-in EKG capable of diagnosing atrial fibrillation, and an oxygen saturation sensor. These features weren’t added thoughtlessly. Apple is marketing this as a health-focused device, with their primary advertising campaign claiming that “the future of health is on your wrist,” and they aren’t the only company making this play.
Along with Apple, Samsung, Withings, Fitbit, and other companies continue to bring products to market that monitor our activity and provide new insights into our health. Typically linked to smartphone-based apps, these devices record all of their measurements for later review, while software helps interpret the findings to make them actionable. From heart rate tracking to sleep analysis, these options now provide access to volumes of data that promise to improve our wellness and change our lives. Of course, those promises will only be fulfilled if our behavior is altered as a consequence of having more detailed information. Whether that will happen remains to be seen.
Health system–linked devices
Major advancements in medical monitoring technology are now enabling physicians to get much deeper insight into their patients’ health status. Internet-connected scales, blood pressure cuffs, and exercise equipment offer the ability to upload information into patient portals and integrate that information into EHRs. New devices provide access to information that previously was impossible to obtain. For example, wearable continuous blood glucose monitors, such as the FreeStyle Libre or DexCom’s G6, allow patients and physicians to follow blood sugar readings 24 hours a day. This provides unprecedented awareness of diabetes control and relieves the pain and inconvenience of finger sticks and blood draws. It also aids with compliance because patients don’t need to remember to check their sugar levels on a schedule.
Other compliance-boosting breakthroughs, such as Bluetooth-enabled asthma inhalers and cellular-connected continuous positive airway pressure machines, assist patients with managing chronic respiratory conditions. Many companies are developing technologies to manage acute conditions as well. One such company, an on-demand telemedicine provider called TytoCare, has developed a $299 suite of instruments that includes a digital stethoscope, thermometer, and camera-based otoscope. In concert with a virtual visit, their providers can remotely use these tools to examine and assess sick individuals. This virtual “laying on of hands” may have sounded like science fiction and likely would have been rejected by patients just a few years ago. Now it is becoming commonplace and will soon be an expectation of many seeking care.
But if we are to be successful, everyone must acknowledge that this revolution in health care brings many challenges along with it. One of those is the deluge of data that connected devices provide.
Information overload
There is such a thing as “too much of a good thing.” Described by journalist David Shenk as “data smog” in his 1997 book of the same name, the idea is clear: There is only so much information we can assimilate.
Even after years of using EHRs and with government-implemented incentives that promote “meaningful use,” physicians are still struggling with EHRs. Additionally, many have expressed frustration with the connectedness that EHRs provide and lament their inability to ever really “leave the office.” As more and more data become available to physicians, the challenge of how to assimilate and act on those data will continue to grow. The addition of patient-provided health statistics will only make information overload worse, with clinicians will feeling an ever-growing burden to know, understand, and act on this information.
Unless we develop systems to sort, filter, and prioritize the flow of information, there is potential for liability from not acting on the amount of virtual information doctors receive. This new risk for already fatigued and overburdened physicians combined with an increase in the amount of virtual information at doctors’ fingertips may lead to the value of patient data being lost.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
Hurricane Sally recently crossed the Gulf of Mexico and landed with torrential rainfalls along the Alabama coast. A little rainfall is important for crops; too much leads to devastation. As physicians, we need data in order to help manage patients’ illnesses and to help to keep them healthy. Our fear though is that too much data provided too quickly may have the opposite effect.
Personal monitoring devices
When I bought my first Fitbit 7 years ago, I was enamored with the technology. The Fitbit was little more than a step tracker, yet I proudly wore its black rubber strap on my wrist. It was my first foray into wearable technology, and it felt quite empowering to have an objective way to track my fitness beyond just using my bathroom scale. Now less than a decade later, that Fitbit looks archaic in comparison with the wrist-top technology currently available.
As I write this, the world’s largest technology company is in the process of releasing its sixth-generation Apple Watch. In addition to acting as a smartphone, this new device, which is barely larger than a postage stamp, offers GPS-based movement tracking, the ability to detect falls, continuous heart rate monitoring, a built-in EKG capable of diagnosing atrial fibrillation, and an oxygen saturation sensor. These features weren’t added thoughtlessly. Apple is marketing this as a health-focused device, with their primary advertising campaign claiming that “the future of health is on your wrist,” and they aren’t the only company making this play.
Along with Apple, Samsung, Withings, Fitbit, and other companies continue to bring products to market that monitor our activity and provide new insights into our health. Typically linked to smartphone-based apps, these devices record all of their measurements for later review, while software helps interpret the findings to make them actionable. From heart rate tracking to sleep analysis, these options now provide access to volumes of data that promise to improve our wellness and change our lives. Of course, those promises will only be fulfilled if our behavior is altered as a consequence of having more detailed information. Whether that will happen remains to be seen.
Health system–linked devices
Major advancements in medical monitoring technology are now enabling physicians to get much deeper insight into their patients’ health status. Internet-connected scales, blood pressure cuffs, and exercise equipment offer the ability to upload information into patient portals and integrate that information into EHRs. New devices provide access to information that previously was impossible to obtain. For example, wearable continuous blood glucose monitors, such as the FreeStyle Libre or DexCom’s G6, allow patients and physicians to follow blood sugar readings 24 hours a day. This provides unprecedented awareness of diabetes control and relieves the pain and inconvenience of finger sticks and blood draws. It also aids with compliance because patients don’t need to remember to check their sugar levels on a schedule.
Other compliance-boosting breakthroughs, such as Bluetooth-enabled asthma inhalers and cellular-connected continuous positive airway pressure machines, assist patients with managing chronic respiratory conditions. Many companies are developing technologies to manage acute conditions as well. One such company, an on-demand telemedicine provider called TytoCare, has developed a $299 suite of instruments that includes a digital stethoscope, thermometer, and camera-based otoscope. In concert with a virtual visit, their providers can remotely use these tools to examine and assess sick individuals. This virtual “laying on of hands” may have sounded like science fiction and likely would have been rejected by patients just a few years ago. Now it is becoming commonplace and will soon be an expectation of many seeking care.
But if we are to be successful, everyone must acknowledge that this revolution in health care brings many challenges along with it. One of those is the deluge of data that connected devices provide.
Information overload
There is such a thing as “too much of a good thing.” Described by journalist David Shenk as “data smog” in his 1997 book of the same name, the idea is clear: There is only so much information we can assimilate.
Even after years of using EHRs and with government-implemented incentives that promote “meaningful use,” physicians are still struggling with EHRs. Additionally, many have expressed frustration with the connectedness that EHRs provide and lament their inability to ever really “leave the office.” As more and more data become available to physicians, the challenge of how to assimilate and act on those data will continue to grow. The addition of patient-provided health statistics will only make information overload worse, with clinicians will feeling an ever-growing burden to know, understand, and act on this information.
Unless we develop systems to sort, filter, and prioritize the flow of information, there is potential for liability from not acting on the amount of virtual information doctors receive. This new risk for already fatigued and overburdened physicians combined with an increase in the amount of virtual information at doctors’ fingertips may lead to the value of patient data being lost.
Dr. Notte is a family physician and chief medical officer of Abington (Pa.) Hospital–Jefferson Health. Follow him on Twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health. They have no conflicts related to the content of this piece.
Vascular dementia risk particularly high in type 2 diabetes
Persons with type 2 diabetes may be at heightened risk for developing vascular dementia than other types of dementia, a team of international researchers has found.
Compared with a nondiabetic control population, those with type 2 diabetes had a statistically significant 35% increased chance of having vascular dementia in a large observational study.
By comparison, the risk for nonvascular dementia was increased by a “more modest” 8%, said the researchers from the University of Glasgow and the University of Gothenburg (Sweden), while the risk for Alzheimer’s dementia appeared to be reduced by 8%.
The link between type 2 diabetes and dementia is not new, observed Carlos Celis-Morales, PhD, who presented the study’s findings at the virtual annual meeting of the European Association for the Study of Diabetes. With people living longer thanks to improved preventative strategies and treatments, there is a risk for developing other chronic conditions, such as dementia.
“A third of all dementia cases may be attributable to modifiable risk factors, among them type 2 diabetes, which accounts for 3.2% of all dementia cases,” said Dr. Celis-Morales, a research fellow at the University of Glasgow’s Institute of Cardiovascular and Medical Sciences.
“Although we know that diabetes is linked to dementia, what we don’t know really well is how much of this association between diabetes and dementia outcomes are explained by modifiable and nonmodifiable risk factors,” Dr. Celis-Morales added.
“Diabetes and dementia share certain risk factors,” commented coinvestigator Naveed Sattar, MD, in a press release issued by the EASD. These include obesity, smoking, and lack of physical activity and might explain part of the association between the two conditions.
Dr. Sattar said that the heightened vascular dementia risk found in the study was “in itself an argument for preventive measures such as healthier lifestyle,” adding that “the importance of prevention is underscored by the fact that, for the majority of dementia diseases, there is no good treatment.”
Using data from the Swedish National Diabetes Register, the research team set out to determine the extent to which type 2 diabetes was associated with dementia and the incidence of different subtypes of dementia. They also looked to see if there were any associations with blood glucose control and what risk factors may be involved.
In total, data on 378,299 individuals with type 2 diabetes were compared with data on 1,886,022 similarly aged (average, 64 years) and gender-matched controls from the general population.
After a mean 7 years of follow-up, 10,143 people with and 46,479 people without type 2 diabetes developed dementia. Nonvascular dementia was the most common type of dementia recorded, followed by Alzheimer’s disease and then vascular dementia.
“Within type 2 diabetes individuals, poor glycemic [control] increased the risk of dementia especially for vascular dementia and nonvascular dementia. However, these associations were not as evident for Alzheimer’s disease,” Dr. Celis-Morales reported.
Comparing those with hemoglobin bA1c of less than 52 mmol/mol (7%) with those whose A1c was above 87 mmol/mol (10.1%), there was 93% increase in the risk for vascular dementia, a 67% increase in the risk for nonvascular dementia, and a 34% higher risk for Alzheimer’s disease–associated dementia.
“We have focused on high levels of HbA1c, but what happens if you have really low limits? It’s something we’re working on right now,” Dr. Celis-Morales said.
Importantly, cardiovascular-related risk factors – some of which, like systolic blood pressure and body weight, were potentially modifiable – accounted for more than 40% of the risk for dementia in type 2 diabetes. This suggests that a large percentage of the dementia risk could perhaps be addressed by identifying high-risk individuals and tailoring interventions accordingly.
“These are observational findings, so we need to be careful before we translate to any sort of recommendation,” Dr. Celis-Morales said.
The study was financed by the Swedish state under the agreement between the government and the county councils, the ALF agreement, as well as grant from the Novo Nordisk Foundation and the Swedish Association of Local Authorities and Regions. Dr. Celis-Morales and Dr. Sattar had no conflicts of interest.
SOURCE: Celis-Morales C et al. EASD 2020, Oral presentation 06.
Persons with type 2 diabetes may be at heightened risk for developing vascular dementia than other types of dementia, a team of international researchers has found.
Compared with a nondiabetic control population, those with type 2 diabetes had a statistically significant 35% increased chance of having vascular dementia in a large observational study.
By comparison, the risk for nonvascular dementia was increased by a “more modest” 8%, said the researchers from the University of Glasgow and the University of Gothenburg (Sweden), while the risk for Alzheimer’s dementia appeared to be reduced by 8%.
The link between type 2 diabetes and dementia is not new, observed Carlos Celis-Morales, PhD, who presented the study’s findings at the virtual annual meeting of the European Association for the Study of Diabetes. With people living longer thanks to improved preventative strategies and treatments, there is a risk for developing other chronic conditions, such as dementia.
“A third of all dementia cases may be attributable to modifiable risk factors, among them type 2 diabetes, which accounts for 3.2% of all dementia cases,” said Dr. Celis-Morales, a research fellow at the University of Glasgow’s Institute of Cardiovascular and Medical Sciences.
“Although we know that diabetes is linked to dementia, what we don’t know really well is how much of this association between diabetes and dementia outcomes are explained by modifiable and nonmodifiable risk factors,” Dr. Celis-Morales added.
“Diabetes and dementia share certain risk factors,” commented coinvestigator Naveed Sattar, MD, in a press release issued by the EASD. These include obesity, smoking, and lack of physical activity and might explain part of the association between the two conditions.
Dr. Sattar said that the heightened vascular dementia risk found in the study was “in itself an argument for preventive measures such as healthier lifestyle,” adding that “the importance of prevention is underscored by the fact that, for the majority of dementia diseases, there is no good treatment.”
Using data from the Swedish National Diabetes Register, the research team set out to determine the extent to which type 2 diabetes was associated with dementia and the incidence of different subtypes of dementia. They also looked to see if there were any associations with blood glucose control and what risk factors may be involved.
In total, data on 378,299 individuals with type 2 diabetes were compared with data on 1,886,022 similarly aged (average, 64 years) and gender-matched controls from the general population.
After a mean 7 years of follow-up, 10,143 people with and 46,479 people without type 2 diabetes developed dementia. Nonvascular dementia was the most common type of dementia recorded, followed by Alzheimer’s disease and then vascular dementia.
“Within type 2 diabetes individuals, poor glycemic [control] increased the risk of dementia especially for vascular dementia and nonvascular dementia. However, these associations were not as evident for Alzheimer’s disease,” Dr. Celis-Morales reported.
Comparing those with hemoglobin bA1c of less than 52 mmol/mol (7%) with those whose A1c was above 87 mmol/mol (10.1%), there was 93% increase in the risk for vascular dementia, a 67% increase in the risk for nonvascular dementia, and a 34% higher risk for Alzheimer’s disease–associated dementia.
“We have focused on high levels of HbA1c, but what happens if you have really low limits? It’s something we’re working on right now,” Dr. Celis-Morales said.
Importantly, cardiovascular-related risk factors – some of which, like systolic blood pressure and body weight, were potentially modifiable – accounted for more than 40% of the risk for dementia in type 2 diabetes. This suggests that a large percentage of the dementia risk could perhaps be addressed by identifying high-risk individuals and tailoring interventions accordingly.
“These are observational findings, so we need to be careful before we translate to any sort of recommendation,” Dr. Celis-Morales said.
The study was financed by the Swedish state under the agreement between the government and the county councils, the ALF agreement, as well as grant from the Novo Nordisk Foundation and the Swedish Association of Local Authorities and Regions. Dr. Celis-Morales and Dr. Sattar had no conflicts of interest.
SOURCE: Celis-Morales C et al. EASD 2020, Oral presentation 06.
Persons with type 2 diabetes may be at heightened risk for developing vascular dementia than other types of dementia, a team of international researchers has found.
Compared with a nondiabetic control population, those with type 2 diabetes had a statistically significant 35% increased chance of having vascular dementia in a large observational study.
By comparison, the risk for nonvascular dementia was increased by a “more modest” 8%, said the researchers from the University of Glasgow and the University of Gothenburg (Sweden), while the risk for Alzheimer’s dementia appeared to be reduced by 8%.
The link between type 2 diabetes and dementia is not new, observed Carlos Celis-Morales, PhD, who presented the study’s findings at the virtual annual meeting of the European Association for the Study of Diabetes. With people living longer thanks to improved preventative strategies and treatments, there is a risk for developing other chronic conditions, such as dementia.
“A third of all dementia cases may be attributable to modifiable risk factors, among them type 2 diabetes, which accounts for 3.2% of all dementia cases,” said Dr. Celis-Morales, a research fellow at the University of Glasgow’s Institute of Cardiovascular and Medical Sciences.
“Although we know that diabetes is linked to dementia, what we don’t know really well is how much of this association between diabetes and dementia outcomes are explained by modifiable and nonmodifiable risk factors,” Dr. Celis-Morales added.
“Diabetes and dementia share certain risk factors,” commented coinvestigator Naveed Sattar, MD, in a press release issued by the EASD. These include obesity, smoking, and lack of physical activity and might explain part of the association between the two conditions.
Dr. Sattar said that the heightened vascular dementia risk found in the study was “in itself an argument for preventive measures such as healthier lifestyle,” adding that “the importance of prevention is underscored by the fact that, for the majority of dementia diseases, there is no good treatment.”
Using data from the Swedish National Diabetes Register, the research team set out to determine the extent to which type 2 diabetes was associated with dementia and the incidence of different subtypes of dementia. They also looked to see if there were any associations with blood glucose control and what risk factors may be involved.
In total, data on 378,299 individuals with type 2 diabetes were compared with data on 1,886,022 similarly aged (average, 64 years) and gender-matched controls from the general population.
After a mean 7 years of follow-up, 10,143 people with and 46,479 people without type 2 diabetes developed dementia. Nonvascular dementia was the most common type of dementia recorded, followed by Alzheimer’s disease and then vascular dementia.
“Within type 2 diabetes individuals, poor glycemic [control] increased the risk of dementia especially for vascular dementia and nonvascular dementia. However, these associations were not as evident for Alzheimer’s disease,” Dr. Celis-Morales reported.
Comparing those with hemoglobin bA1c of less than 52 mmol/mol (7%) with those whose A1c was above 87 mmol/mol (10.1%), there was 93% increase in the risk for vascular dementia, a 67% increase in the risk for nonvascular dementia, and a 34% higher risk for Alzheimer’s disease–associated dementia.
“We have focused on high levels of HbA1c, but what happens if you have really low limits? It’s something we’re working on right now,” Dr. Celis-Morales said.
Importantly, cardiovascular-related risk factors – some of which, like systolic blood pressure and body weight, were potentially modifiable – accounted for more than 40% of the risk for dementia in type 2 diabetes. This suggests that a large percentage of the dementia risk could perhaps be addressed by identifying high-risk individuals and tailoring interventions accordingly.
“These are observational findings, so we need to be careful before we translate to any sort of recommendation,” Dr. Celis-Morales said.
The study was financed by the Swedish state under the agreement between the government and the county councils, the ALF agreement, as well as grant from the Novo Nordisk Foundation and the Swedish Association of Local Authorities and Regions. Dr. Celis-Morales and Dr. Sattar had no conflicts of interest.
SOURCE: Celis-Morales C et al. EASD 2020, Oral presentation 06.
FROM EASD 2020
Breathing enriched oxygen improves major depression
Maybe the hipsters patronizing trendy oxygen bars seeking elevation of mood back in the prepandemic era were actually onto something – because Israeli investigators have now shown in a pilot double-blind, placebo-controlled, randomized trial that breathing enriched oxygen on a nightly basis resulted in clinically meaningful symptomatic improvement in mild to moderate major depression.
“We saw a highly significant effect of normobaric hyperoxia therapy in lowering Hamilton Rating Scale for Depression scores,” R. Haim Belmaker, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
In addition, the patients on enriched oxygen also showed statistically significant and clinically meaningful improvements relative to sham-treated controls on the secondary endpoints of Clinical Global Impressions Scale, the World Health Organization–Five Well-Being Index, the Sheehan Disability Scale, and the Sense of Coherence Scale, added Dr. Belmaker, professor emeritus of psychiatry at the Ben Gurion University of the Negev in Beersheva, Israel.
Numerous PET imaging studies have documented diminished brain mitochondrial function in patients with depression or schizophrenia. And mitochondria need oxygen to do their work. Yet, the idea of administering enriched oxygen in an effort to boost mitochondrial energy metabolism has long been viewed with skepticism – even though it’s a simple and well-tolerated intervention – because of the fact that 90%-95% of the oxygen supply is carried bound to hemoglobin, and oxygen enrichment doesn’t further increase hemoglobin saturation in individuals with normal lung function. However, recently it has been shown that inspired enriched oxygen roughly doubles arterial oxygen tension, and while this doesn’t translate into anything close to a doubled oxygen supply to tissues, it may result in increased oxygen diffusion into brain tissue, the psychiatrist explained.
Normobaric hyperoxia therapy is not to be confused with hyperbaric oxygen therapy, which requires a special chamber to handle markedly increased atmospheric pressures and has some inherent dangers. Mobile bedside oxygen generator units for oxygen enrichment are commercially available over the counter. Those used in the Israeli study were about the size of a vacuum cleaner and weighed a little more than 40 lb. Much smaller, more convenient units are available as well, but are costlier.
Dr. Belmaker reported on 51 adults with mild or moderate symptoms of major depressive disorder and a mean 11-year disease history who were randomized double blind to breathe either 35% oxygen or normal air – that is, 21% oxygen – at 1 atm pressure delivered from an investigator-supplied oxygen generator through standard plastic nasal prongs at a flow rate of 5 L/min for 7 hours nightly for 1 month.
“Controls heard the same flow and felt the same feeling on the face but were receiving 21% oxygen,” he noted.
Oxygen generator units are capable of enriching air to more than 90% oxygen; however, the investigators wanted to be cautious in a pilot study of an untested therapy, and they found evidence from both animal and human studies that 40% oxygen is reassuringly safe. Study exclusion criteria included obesity, acute or chronic respiratory disease, psychosis, and suicidality.
The primary study endpoint was the change in Hamilton Rating Scale for Depression score at 1 month. From a mean baseline of 14.6, the score in the normobaric hyperoxia group dropped by more than 4 points while remaining unchanged in controls. In a subscale analysis, it was apparent that most of the improvement occurred in the anxiety and cognitive disturbance subscale domains, according to Dr. Belmaker.
Of note, all patients rated by blinded investigators as much improved or very much improved on the Clinical Global Impression scale came from the enriched oxygen group.
No treatment-related adverse events occurred in the study.
“We don’t know the mechanism of the benefit of oxygen on the brain. It’s complex. In stroke and acute MI we used to think oxygen was beneficial, but scientists now feel that it’s not,” the psychiatrist said. “This early data deserve replication with higher concentrations of oxygen, different time periods of application, and in different patient groups.”
He emphasized that, since individuals with physical illnesses – including sleep apnea and chronic obstructive pulmonary disease – were excluded from the study, it’s not possible to say whether normobaric hyperoxia therapy would have an antidepressant effect in such patients.
“I would be especially careful with the normobaric oxygen in any patients with any cardiovascular or hypertensive disease because the increased oxygen pressure can have the side effect of contracting cardiac capillaries as a reflex action. So I certainly cannot recommend applying this study in any patients with a physical disease at this point,” Dr. Belmaker emphasized.
He reported having no financial conflicts regarding the study, funded by a grant from the Brain and Behavior Research Foundation.
SOURCE: Belmaker RH. ECNP 2020, Session S.12.
Maybe the hipsters patronizing trendy oxygen bars seeking elevation of mood back in the prepandemic era were actually onto something – because Israeli investigators have now shown in a pilot double-blind, placebo-controlled, randomized trial that breathing enriched oxygen on a nightly basis resulted in clinically meaningful symptomatic improvement in mild to moderate major depression.
“We saw a highly significant effect of normobaric hyperoxia therapy in lowering Hamilton Rating Scale for Depression scores,” R. Haim Belmaker, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
In addition, the patients on enriched oxygen also showed statistically significant and clinically meaningful improvements relative to sham-treated controls on the secondary endpoints of Clinical Global Impressions Scale, the World Health Organization–Five Well-Being Index, the Sheehan Disability Scale, and the Sense of Coherence Scale, added Dr. Belmaker, professor emeritus of psychiatry at the Ben Gurion University of the Negev in Beersheva, Israel.
Numerous PET imaging studies have documented diminished brain mitochondrial function in patients with depression or schizophrenia. And mitochondria need oxygen to do their work. Yet, the idea of administering enriched oxygen in an effort to boost mitochondrial energy metabolism has long been viewed with skepticism – even though it’s a simple and well-tolerated intervention – because of the fact that 90%-95% of the oxygen supply is carried bound to hemoglobin, and oxygen enrichment doesn’t further increase hemoglobin saturation in individuals with normal lung function. However, recently it has been shown that inspired enriched oxygen roughly doubles arterial oxygen tension, and while this doesn’t translate into anything close to a doubled oxygen supply to tissues, it may result in increased oxygen diffusion into brain tissue, the psychiatrist explained.
Normobaric hyperoxia therapy is not to be confused with hyperbaric oxygen therapy, which requires a special chamber to handle markedly increased atmospheric pressures and has some inherent dangers. Mobile bedside oxygen generator units for oxygen enrichment are commercially available over the counter. Those used in the Israeli study were about the size of a vacuum cleaner and weighed a little more than 40 lb. Much smaller, more convenient units are available as well, but are costlier.
Dr. Belmaker reported on 51 adults with mild or moderate symptoms of major depressive disorder and a mean 11-year disease history who were randomized double blind to breathe either 35% oxygen or normal air – that is, 21% oxygen – at 1 atm pressure delivered from an investigator-supplied oxygen generator through standard plastic nasal prongs at a flow rate of 5 L/min for 7 hours nightly for 1 month.
“Controls heard the same flow and felt the same feeling on the face but were receiving 21% oxygen,” he noted.
Oxygen generator units are capable of enriching air to more than 90% oxygen; however, the investigators wanted to be cautious in a pilot study of an untested therapy, and they found evidence from both animal and human studies that 40% oxygen is reassuringly safe. Study exclusion criteria included obesity, acute or chronic respiratory disease, psychosis, and suicidality.
The primary study endpoint was the change in Hamilton Rating Scale for Depression score at 1 month. From a mean baseline of 14.6, the score in the normobaric hyperoxia group dropped by more than 4 points while remaining unchanged in controls. In a subscale analysis, it was apparent that most of the improvement occurred in the anxiety and cognitive disturbance subscale domains, according to Dr. Belmaker.
Of note, all patients rated by blinded investigators as much improved or very much improved on the Clinical Global Impression scale came from the enriched oxygen group.
No treatment-related adverse events occurred in the study.
“We don’t know the mechanism of the benefit of oxygen on the brain. It’s complex. In stroke and acute MI we used to think oxygen was beneficial, but scientists now feel that it’s not,” the psychiatrist said. “This early data deserve replication with higher concentrations of oxygen, different time periods of application, and in different patient groups.”
He emphasized that, since individuals with physical illnesses – including sleep apnea and chronic obstructive pulmonary disease – were excluded from the study, it’s not possible to say whether normobaric hyperoxia therapy would have an antidepressant effect in such patients.
“I would be especially careful with the normobaric oxygen in any patients with any cardiovascular or hypertensive disease because the increased oxygen pressure can have the side effect of contracting cardiac capillaries as a reflex action. So I certainly cannot recommend applying this study in any patients with a physical disease at this point,” Dr. Belmaker emphasized.
He reported having no financial conflicts regarding the study, funded by a grant from the Brain and Behavior Research Foundation.
SOURCE: Belmaker RH. ECNP 2020, Session S.12.
Maybe the hipsters patronizing trendy oxygen bars seeking elevation of mood back in the prepandemic era were actually onto something – because Israeli investigators have now shown in a pilot double-blind, placebo-controlled, randomized trial that breathing enriched oxygen on a nightly basis resulted in clinically meaningful symptomatic improvement in mild to moderate major depression.
“We saw a highly significant effect of normobaric hyperoxia therapy in lowering Hamilton Rating Scale for Depression scores,” R. Haim Belmaker, MD, reported at the virtual congress of the European College of Neuropsychopharmacology.
In addition, the patients on enriched oxygen also showed statistically significant and clinically meaningful improvements relative to sham-treated controls on the secondary endpoints of Clinical Global Impressions Scale, the World Health Organization–Five Well-Being Index, the Sheehan Disability Scale, and the Sense of Coherence Scale, added Dr. Belmaker, professor emeritus of psychiatry at the Ben Gurion University of the Negev in Beersheva, Israel.
Numerous PET imaging studies have documented diminished brain mitochondrial function in patients with depression or schizophrenia. And mitochondria need oxygen to do their work. Yet, the idea of administering enriched oxygen in an effort to boost mitochondrial energy metabolism has long been viewed with skepticism – even though it’s a simple and well-tolerated intervention – because of the fact that 90%-95% of the oxygen supply is carried bound to hemoglobin, and oxygen enrichment doesn’t further increase hemoglobin saturation in individuals with normal lung function. However, recently it has been shown that inspired enriched oxygen roughly doubles arterial oxygen tension, and while this doesn’t translate into anything close to a doubled oxygen supply to tissues, it may result in increased oxygen diffusion into brain tissue, the psychiatrist explained.
Normobaric hyperoxia therapy is not to be confused with hyperbaric oxygen therapy, which requires a special chamber to handle markedly increased atmospheric pressures and has some inherent dangers. Mobile bedside oxygen generator units for oxygen enrichment are commercially available over the counter. Those used in the Israeli study were about the size of a vacuum cleaner and weighed a little more than 40 lb. Much smaller, more convenient units are available as well, but are costlier.
Dr. Belmaker reported on 51 adults with mild or moderate symptoms of major depressive disorder and a mean 11-year disease history who were randomized double blind to breathe either 35% oxygen or normal air – that is, 21% oxygen – at 1 atm pressure delivered from an investigator-supplied oxygen generator through standard plastic nasal prongs at a flow rate of 5 L/min for 7 hours nightly for 1 month.
“Controls heard the same flow and felt the same feeling on the face but were receiving 21% oxygen,” he noted.
Oxygen generator units are capable of enriching air to more than 90% oxygen; however, the investigators wanted to be cautious in a pilot study of an untested therapy, and they found evidence from both animal and human studies that 40% oxygen is reassuringly safe. Study exclusion criteria included obesity, acute or chronic respiratory disease, psychosis, and suicidality.
The primary study endpoint was the change in Hamilton Rating Scale for Depression score at 1 month. From a mean baseline of 14.6, the score in the normobaric hyperoxia group dropped by more than 4 points while remaining unchanged in controls. In a subscale analysis, it was apparent that most of the improvement occurred in the anxiety and cognitive disturbance subscale domains, according to Dr. Belmaker.
Of note, all patients rated by blinded investigators as much improved or very much improved on the Clinical Global Impression scale came from the enriched oxygen group.
No treatment-related adverse events occurred in the study.
“We don’t know the mechanism of the benefit of oxygen on the brain. It’s complex. In stroke and acute MI we used to think oxygen was beneficial, but scientists now feel that it’s not,” the psychiatrist said. “This early data deserve replication with higher concentrations of oxygen, different time periods of application, and in different patient groups.”
He emphasized that, since individuals with physical illnesses – including sleep apnea and chronic obstructive pulmonary disease – were excluded from the study, it’s not possible to say whether normobaric hyperoxia therapy would have an antidepressant effect in such patients.
“I would be especially careful with the normobaric oxygen in any patients with any cardiovascular or hypertensive disease because the increased oxygen pressure can have the side effect of contracting cardiac capillaries as a reflex action. So I certainly cannot recommend applying this study in any patients with a physical disease at this point,” Dr. Belmaker emphasized.
He reported having no financial conflicts regarding the study, funded by a grant from the Brain and Behavior Research Foundation.
SOURCE: Belmaker RH. ECNP 2020, Session S.12.
FROM ECNP 2020
More female specialists, but gender gap persists in pay, survey finds
More female physicians are becoming specialists, a Medscape survey finds, and five specialties have seen particularly large increases during the last 5 years.
Obstetrician/gynecologists and pediatricians had the largest female representation at 58% and those percentages were both up from 50% in 2015, according to the Medscape Female Physician Compensation Report 2020.
Rheumatology saw a dramatic jump in numbers of women from 29% in 2015 to 54% now. Dermatology increased from 32% to 49%, and family medicine rose from 35% to 43% during that time.
Specialist pay gap narrows slightly
The gender gap was the same this year in primary care — women made 25% less ($212,000 vs. $264,000).
The gap in specialists narrowed slightly. Women made 31% less this year ($286,000 vs $375,000) instead of the 33% less reported in last year’s survey, a difference of $89,000 this year.
The gender pay gap was consistent across all race and age groups and was consistent in responses about net worth. Whereas 57% of male physicians had a net worth of $1 million or more, only 40% of female physicians did. Twice as many male physicians as female physicians had a net worth of more than $5 million (10% vs. 5%).
“Many physicians expect the gender pay gap to narrow in the coming years,” John Prescott, MD, chief academic officer of the Association of American Medical Colleges, said in an interview.
“Yet, it is a challenging task, requiring an institutional commitment to transparency, cross-campus collaboration, ongoing communication, dedicated resources, and enlightened leadership,” he said.
Female physicians working in office-based, solo practices made the most overall at $290,000; women in outpatient settings made the least at $223,000.
The survey included more than 4,500 responses. The responses were collected during the early part of the year and do not reflect changes in income expected from the COVID-19 pandemic.
An analysis in Health Affairs, for instance, predicted that primary care practices would lose $67,774 in gross revenue per full-time-equivalent physician in calendar year 2020 because of the pandemic.
Most physicians did not experience a significant financial loss in 2019, but COVID-19 may, at least temporarily, change those answers in next year’s report, physicians predicted.
Women more likely than men to live above their means
More women this year (39%) said they live below their means than answered that way last year (31%). Female physicians were more likely to say they lived above their means than were their male counterparts (8% vs. 6%).
Greenwald Wealth Management in St. Louis Park, Minn., says aiming for putting away 20% of total gross salary is a good financial goal.
Women in this year’s survey spent about 7% less time seeing patients than did their male counterparts (35.9 hours a week vs. 38.8). The average for all physicians was 37.8 hours a week. Add the 15.6 average hours per week physicians spend on paperwork, and they are putting in 53-hour workweeks on average overall.
Asked what parts of their job they found most rewarding, women were more likely than were men to say “gratitude/relationships with patients” (31% vs. 25%). They were less likely than were men to answer that the most rewarding part was “being very good at what I do/finding answers/diagnoses” (22% vs. 25%) or “making good money at a job I like” (9% vs. 13%).
Most female physicians — and physicians overall — said they would choose medicine again. But two specialties saw a substantial increase in that answer.
This year, 79% of those in physical medicine and rehabilitation said they would choose medicine again (compared with 66% last year) and 84% of gastroenterologists answered that way (compared with 76% in 2019).
Psychiatrists, however, were in the group least likely to say they would choose their specialty again along with those in internal medicine, family medicine, and diabetes and endocrinology.
Female physicians in orthopedics, radiology, and dermatology were most likely to choose their specialties again (91% - 92%).
Female physicians were less likely to use physician assistants in their practices than were their male colleagues (31% vs. 38%) but more likely to use NPs (52% vs. 50%). More than a third (38%) of male and female physicians reported they use neither.
A version of this article originally appeared on Medscape.com.
More female physicians are becoming specialists, a Medscape survey finds, and five specialties have seen particularly large increases during the last 5 years.
Obstetrician/gynecologists and pediatricians had the largest female representation at 58% and those percentages were both up from 50% in 2015, according to the Medscape Female Physician Compensation Report 2020.
Rheumatology saw a dramatic jump in numbers of women from 29% in 2015 to 54% now. Dermatology increased from 32% to 49%, and family medicine rose from 35% to 43% during that time.
Specialist pay gap narrows slightly
The gender gap was the same this year in primary care — women made 25% less ($212,000 vs. $264,000).
The gap in specialists narrowed slightly. Women made 31% less this year ($286,000 vs $375,000) instead of the 33% less reported in last year’s survey, a difference of $89,000 this year.
The gender pay gap was consistent across all race and age groups and was consistent in responses about net worth. Whereas 57% of male physicians had a net worth of $1 million or more, only 40% of female physicians did. Twice as many male physicians as female physicians had a net worth of more than $5 million (10% vs. 5%).
“Many physicians expect the gender pay gap to narrow in the coming years,” John Prescott, MD, chief academic officer of the Association of American Medical Colleges, said in an interview.
“Yet, it is a challenging task, requiring an institutional commitment to transparency, cross-campus collaboration, ongoing communication, dedicated resources, and enlightened leadership,” he said.
Female physicians working in office-based, solo practices made the most overall at $290,000; women in outpatient settings made the least at $223,000.
The survey included more than 4,500 responses. The responses were collected during the early part of the year and do not reflect changes in income expected from the COVID-19 pandemic.
An analysis in Health Affairs, for instance, predicted that primary care practices would lose $67,774 in gross revenue per full-time-equivalent physician in calendar year 2020 because of the pandemic.
Most physicians did not experience a significant financial loss in 2019, but COVID-19 may, at least temporarily, change those answers in next year’s report, physicians predicted.
Women more likely than men to live above their means
More women this year (39%) said they live below their means than answered that way last year (31%). Female physicians were more likely to say they lived above their means than were their male counterparts (8% vs. 6%).
Greenwald Wealth Management in St. Louis Park, Minn., says aiming for putting away 20% of total gross salary is a good financial goal.
Women in this year’s survey spent about 7% less time seeing patients than did their male counterparts (35.9 hours a week vs. 38.8). The average for all physicians was 37.8 hours a week. Add the 15.6 average hours per week physicians spend on paperwork, and they are putting in 53-hour workweeks on average overall.
Asked what parts of their job they found most rewarding, women were more likely than were men to say “gratitude/relationships with patients” (31% vs. 25%). They were less likely than were men to answer that the most rewarding part was “being very good at what I do/finding answers/diagnoses” (22% vs. 25%) or “making good money at a job I like” (9% vs. 13%).
Most female physicians — and physicians overall — said they would choose medicine again. But two specialties saw a substantial increase in that answer.
This year, 79% of those in physical medicine and rehabilitation said they would choose medicine again (compared with 66% last year) and 84% of gastroenterologists answered that way (compared with 76% in 2019).
Psychiatrists, however, were in the group least likely to say they would choose their specialty again along with those in internal medicine, family medicine, and diabetes and endocrinology.
Female physicians in orthopedics, radiology, and dermatology were most likely to choose their specialties again (91% - 92%).
Female physicians were less likely to use physician assistants in their practices than were their male colleagues (31% vs. 38%) but more likely to use NPs (52% vs. 50%). More than a third (38%) of male and female physicians reported they use neither.
A version of this article originally appeared on Medscape.com.
More female physicians are becoming specialists, a Medscape survey finds, and five specialties have seen particularly large increases during the last 5 years.
Obstetrician/gynecologists and pediatricians had the largest female representation at 58% and those percentages were both up from 50% in 2015, according to the Medscape Female Physician Compensation Report 2020.
Rheumatology saw a dramatic jump in numbers of women from 29% in 2015 to 54% now. Dermatology increased from 32% to 49%, and family medicine rose from 35% to 43% during that time.
Specialist pay gap narrows slightly
The gender gap was the same this year in primary care — women made 25% less ($212,000 vs. $264,000).
The gap in specialists narrowed slightly. Women made 31% less this year ($286,000 vs $375,000) instead of the 33% less reported in last year’s survey, a difference of $89,000 this year.
The gender pay gap was consistent across all race and age groups and was consistent in responses about net worth. Whereas 57% of male physicians had a net worth of $1 million or more, only 40% of female physicians did. Twice as many male physicians as female physicians had a net worth of more than $5 million (10% vs. 5%).
“Many physicians expect the gender pay gap to narrow in the coming years,” John Prescott, MD, chief academic officer of the Association of American Medical Colleges, said in an interview.
“Yet, it is a challenging task, requiring an institutional commitment to transparency, cross-campus collaboration, ongoing communication, dedicated resources, and enlightened leadership,” he said.
Female physicians working in office-based, solo practices made the most overall at $290,000; women in outpatient settings made the least at $223,000.
The survey included more than 4,500 responses. The responses were collected during the early part of the year and do not reflect changes in income expected from the COVID-19 pandemic.
An analysis in Health Affairs, for instance, predicted that primary care practices would lose $67,774 in gross revenue per full-time-equivalent physician in calendar year 2020 because of the pandemic.
Most physicians did not experience a significant financial loss in 2019, but COVID-19 may, at least temporarily, change those answers in next year’s report, physicians predicted.
Women more likely than men to live above their means
More women this year (39%) said they live below their means than answered that way last year (31%). Female physicians were more likely to say they lived above their means than were their male counterparts (8% vs. 6%).
Greenwald Wealth Management in St. Louis Park, Minn., says aiming for putting away 20% of total gross salary is a good financial goal.
Women in this year’s survey spent about 7% less time seeing patients than did their male counterparts (35.9 hours a week vs. 38.8). The average for all physicians was 37.8 hours a week. Add the 15.6 average hours per week physicians spend on paperwork, and they are putting in 53-hour workweeks on average overall.
Asked what parts of their job they found most rewarding, women were more likely than were men to say “gratitude/relationships with patients” (31% vs. 25%). They were less likely than were men to answer that the most rewarding part was “being very good at what I do/finding answers/diagnoses” (22% vs. 25%) or “making good money at a job I like” (9% vs. 13%).
Most female physicians — and physicians overall — said they would choose medicine again. But two specialties saw a substantial increase in that answer.
This year, 79% of those in physical medicine and rehabilitation said they would choose medicine again (compared with 66% last year) and 84% of gastroenterologists answered that way (compared with 76% in 2019).
Psychiatrists, however, were in the group least likely to say they would choose their specialty again along with those in internal medicine, family medicine, and diabetes and endocrinology.
Female physicians in orthopedics, radiology, and dermatology were most likely to choose their specialties again (91% - 92%).
Female physicians were less likely to use physician assistants in their practices than were their male colleagues (31% vs. 38%) but more likely to use NPs (52% vs. 50%). More than a third (38%) of male and female physicians reported they use neither.
A version of this article originally appeared on Medscape.com.
Signs of an ‘October vaccine surprise’ alarm career scientists
who have pledged not to release any vaccine unless it’s proved safe and effective.
In podcasts, public forums, social media and medical journals, a growing number of prominent health leaders say they fear that Mr. Trump – who has repeatedly signaled his desire for the swift approval of a vaccine and his displeasure with perceived delays at the FDA – will take matters into his own hands, running roughshod over the usual regulatory process.
It would reflect another attempt by a norm-breaking administration, poised to ram through a Supreme Court nominee opposed to existing abortion rights and the Affordable Care Act, to inject politics into sensitive public health decisions. Mr. Trump has repeatedly contradicted the advice of senior scientists on COVID-19 while pushing controversial treatments for the disease.
If the executive branch were to overrule the FDA’s scientific judgment, a vaccine of limited efficacy and, worse, unknown side effects could be rushed to market.
The worries intensified over the weekend, after Alex Azar, the administration’s secretary of Health & Human Services, asserted his agency’s rule-making authority over the FDA. HHS spokesperson Caitlin Oakley said Mr. Azar’s decision had no bearing on the vaccine approval process.
Vaccines are typically approved by the FDA. Alternatively, Mr. Azar – who reports directly to Mr. Trump – can issue an emergency use authorization, even before any vaccines have been shown to be safe and effective in late-stage clinical trials.
“Yes, this scenario is certainly possible legally and politically,” said Jerry Avorn, MD, a professor of medicine at Harvard Medical School, who outlined such an event in the New England Journal of Medicine. He said it “seems frighteningly more plausible each day.”
Vaccine experts and public health officials are particularly vexed by the possibility because it could ruin the fragile public confidence in a COVID-19 vaccine. It might put scientific authorities in the position of urging people not to be vaccinated after years of coaxing hesitant parents to ignore baseless fears.
Physicians might refuse to administer a vaccine approved with inadequate data, said Preeti Malani, MD, chief health officer and professor of medicine at the University of Michigan in Ann Arbor, in a recent webinar. “You could have a safe, effective vaccine that no one wants to take.” A recent KFF poll found that 54% of Americans would not submit to a COVID-19 vaccine authorized before Election Day.
After this story was published, an HHS official said that Mr. Azar “will defer completely to the FDA” as the agency weighs whether to approve a vaccine produced through the government’s Operation Warp Speed effort.
“The idea the Secretary would approve or authorize a vaccine over the FDA’s objections is preposterous and betrays ignorance of the transparent process that we’re following for the development of the OWS vaccines,” HHS chief of staff Brian Harrison wrote in an email.
White House spokesperson Judd Deere dismissed the scientists’ concerns, saying Trump cared only about the public’s safety and health. “This false narrative that the media and Democrats have created that politics is influencing approvals is not only false but is a danger to the American public,” he said.
Usually, the FDA approves vaccines only after companies submit years of data proving that a vaccine is safe and effective. But a 2004 law allows the FDA to issue an emergency use authorization with much less evidence, as long as the vaccine “may be effective” and its “known and potential benefits” outweigh its “known and potential risks.”
Many scientists doubt a vaccine could meet those criteria before the election. But the terms might be legally vague enough to allow the administration to take such steps.
Moncef Slaoui, chief scientific adviser to Operation Warp Speed, the government program aiming to more quickly develop COVID-19 vaccines, said it’s “extremely unlikely” that vaccine trial results will be ready before the end of October.
Mr. Trump, however, has insisted repeatedly that a vaccine to fight the pandemic that has claimed 200,000 American lives will be distributed starting next month. He reiterated that claim Saturday at a campaign rally in Fayetteville, N.C.
The vaccine will be ready “in a matter of weeks,” he said. “We will end the pandemic from China.”
Although pharmaceutical companies have launched three clinical trials in the United States, no one can say with certainty when those trials will have enough data to determine whether the vaccines are safe and effective.
Officials at Moderna, whose vaccine is being tested in 30,000 volunteers, have said their studies could produce a result by the end of the year, although the final analysis could take place next spring.
Pfizer executives, who have expanded their clinical trial to 44,000 participants, boast that they could know their vaccine works by the end of October.
AstraZeneca’s U.S. vaccine trial, which was scheduled to enroll 30,000 volunteers, is on hold pending an investigation of a possible vaccine-related illness.
Scientists have warned for months that the Trump administration could try to win the election with an “October surprise,” authorizing a vaccine that hasn’t been fully tested. “I don’t think people are crazy to be thinking about all of this,” said William Schultz, a partner in a Washington, D.C., law firm who served as a former FDA commissioner for policy and as general counsel for HHS.
“You’ve got a president saying you’ll have an approval in October. Everybody’s wondering how that could happen.”
In an opinion piece published in the Wall Street Journal, conservative former FDA commissioners Scott Gottlieb and Mark McClellan argued that presidential intrusion was unlikely because the FDA’s “thorough and transparent process doesn’t lend itself to meddling. Any deviation would quickly be apparent.”
But the administration has demonstrated a willingness to bend the agency to its will. The FDA has been criticized for issuing emergency authorizations for two COVID-19 treatments that were boosted by the president but lacked strong evidence to support them: hydroxychloroquine and convalescent plasma.
Mr. Azar has sidelined the FDA in other ways, such as by blocking the agency from regulating lab-developed tests, including tests for the novel coronavirus.
Although FDA Commissioner Stephen Hahn told the Financial Times he would be willing to approve emergency use of a vaccine before large-scale studies conclude, agency officials also have pledged to ensure the safety of any COVID-19 vaccines.
A senior FDA official who oversees vaccine approvals, Peter Marks, MD, has said he will quit if his agency rubber-stamps an unproven COVID-19 vaccine.
“I think there would be an outcry from the public health community second to none, which is my worst nightmare – my worst nightmare – because we will so confuse the public,” said Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, in his weekly podcast.
Still, “even if a company did not want it to be done, even if the FDA did not want it to be done, he could still do that,” said Dr. Osterholm, in his podcast. “I hope that we’d never see that happen, but we have to entertain that’s a possibility.”
In the New England Journal editorial, Dr. Avorn and coauthor Aaron Kesselheim, MD, wondered whether Mr. Trump might invoke the 1950 Defense Production Act to force reluctant drug companies to manufacture their vaccines.
But Mr. Trump would have to sue a company to enforce the Defense Production Act, and the company would have a strong case in refusing, said Lawrence Gostin, director of Georgetown’s O’Neill Institute for National and Global Health Law.
Also, he noted that Mr. Trump could not invoke the Defense Production Act unless a vaccine were “scientifically justified and approved by the FDA.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
who have pledged not to release any vaccine unless it’s proved safe and effective.
In podcasts, public forums, social media and medical journals, a growing number of prominent health leaders say they fear that Mr. Trump – who has repeatedly signaled his desire for the swift approval of a vaccine and his displeasure with perceived delays at the FDA – will take matters into his own hands, running roughshod over the usual regulatory process.
It would reflect another attempt by a norm-breaking administration, poised to ram through a Supreme Court nominee opposed to existing abortion rights and the Affordable Care Act, to inject politics into sensitive public health decisions. Mr. Trump has repeatedly contradicted the advice of senior scientists on COVID-19 while pushing controversial treatments for the disease.
If the executive branch were to overrule the FDA’s scientific judgment, a vaccine of limited efficacy and, worse, unknown side effects could be rushed to market.
The worries intensified over the weekend, after Alex Azar, the administration’s secretary of Health & Human Services, asserted his agency’s rule-making authority over the FDA. HHS spokesperson Caitlin Oakley said Mr. Azar’s decision had no bearing on the vaccine approval process.
Vaccines are typically approved by the FDA. Alternatively, Mr. Azar – who reports directly to Mr. Trump – can issue an emergency use authorization, even before any vaccines have been shown to be safe and effective in late-stage clinical trials.
“Yes, this scenario is certainly possible legally and politically,” said Jerry Avorn, MD, a professor of medicine at Harvard Medical School, who outlined such an event in the New England Journal of Medicine. He said it “seems frighteningly more plausible each day.”
Vaccine experts and public health officials are particularly vexed by the possibility because it could ruin the fragile public confidence in a COVID-19 vaccine. It might put scientific authorities in the position of urging people not to be vaccinated after years of coaxing hesitant parents to ignore baseless fears.
Physicians might refuse to administer a vaccine approved with inadequate data, said Preeti Malani, MD, chief health officer and professor of medicine at the University of Michigan in Ann Arbor, in a recent webinar. “You could have a safe, effective vaccine that no one wants to take.” A recent KFF poll found that 54% of Americans would not submit to a COVID-19 vaccine authorized before Election Day.
After this story was published, an HHS official said that Mr. Azar “will defer completely to the FDA” as the agency weighs whether to approve a vaccine produced through the government’s Operation Warp Speed effort.
“The idea the Secretary would approve or authorize a vaccine over the FDA’s objections is preposterous and betrays ignorance of the transparent process that we’re following for the development of the OWS vaccines,” HHS chief of staff Brian Harrison wrote in an email.
White House spokesperson Judd Deere dismissed the scientists’ concerns, saying Trump cared only about the public’s safety and health. “This false narrative that the media and Democrats have created that politics is influencing approvals is not only false but is a danger to the American public,” he said.
Usually, the FDA approves vaccines only after companies submit years of data proving that a vaccine is safe and effective. But a 2004 law allows the FDA to issue an emergency use authorization with much less evidence, as long as the vaccine “may be effective” and its “known and potential benefits” outweigh its “known and potential risks.”
Many scientists doubt a vaccine could meet those criteria before the election. But the terms might be legally vague enough to allow the administration to take such steps.
Moncef Slaoui, chief scientific adviser to Operation Warp Speed, the government program aiming to more quickly develop COVID-19 vaccines, said it’s “extremely unlikely” that vaccine trial results will be ready before the end of October.
Mr. Trump, however, has insisted repeatedly that a vaccine to fight the pandemic that has claimed 200,000 American lives will be distributed starting next month. He reiterated that claim Saturday at a campaign rally in Fayetteville, N.C.
The vaccine will be ready “in a matter of weeks,” he said. “We will end the pandemic from China.”
Although pharmaceutical companies have launched three clinical trials in the United States, no one can say with certainty when those trials will have enough data to determine whether the vaccines are safe and effective.
Officials at Moderna, whose vaccine is being tested in 30,000 volunteers, have said their studies could produce a result by the end of the year, although the final analysis could take place next spring.
Pfizer executives, who have expanded their clinical trial to 44,000 participants, boast that they could know their vaccine works by the end of October.
AstraZeneca’s U.S. vaccine trial, which was scheduled to enroll 30,000 volunteers, is on hold pending an investigation of a possible vaccine-related illness.
Scientists have warned for months that the Trump administration could try to win the election with an “October surprise,” authorizing a vaccine that hasn’t been fully tested. “I don’t think people are crazy to be thinking about all of this,” said William Schultz, a partner in a Washington, D.C., law firm who served as a former FDA commissioner for policy and as general counsel for HHS.
“You’ve got a president saying you’ll have an approval in October. Everybody’s wondering how that could happen.”
In an opinion piece published in the Wall Street Journal, conservative former FDA commissioners Scott Gottlieb and Mark McClellan argued that presidential intrusion was unlikely because the FDA’s “thorough and transparent process doesn’t lend itself to meddling. Any deviation would quickly be apparent.”
But the administration has demonstrated a willingness to bend the agency to its will. The FDA has been criticized for issuing emergency authorizations for two COVID-19 treatments that were boosted by the president but lacked strong evidence to support them: hydroxychloroquine and convalescent plasma.
Mr. Azar has sidelined the FDA in other ways, such as by blocking the agency from regulating lab-developed tests, including tests for the novel coronavirus.
Although FDA Commissioner Stephen Hahn told the Financial Times he would be willing to approve emergency use of a vaccine before large-scale studies conclude, agency officials also have pledged to ensure the safety of any COVID-19 vaccines.
A senior FDA official who oversees vaccine approvals, Peter Marks, MD, has said he will quit if his agency rubber-stamps an unproven COVID-19 vaccine.
“I think there would be an outcry from the public health community second to none, which is my worst nightmare – my worst nightmare – because we will so confuse the public,” said Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, in his weekly podcast.
Still, “even if a company did not want it to be done, even if the FDA did not want it to be done, he could still do that,” said Dr. Osterholm, in his podcast. “I hope that we’d never see that happen, but we have to entertain that’s a possibility.”
In the New England Journal editorial, Dr. Avorn and coauthor Aaron Kesselheim, MD, wondered whether Mr. Trump might invoke the 1950 Defense Production Act to force reluctant drug companies to manufacture their vaccines.
But Mr. Trump would have to sue a company to enforce the Defense Production Act, and the company would have a strong case in refusing, said Lawrence Gostin, director of Georgetown’s O’Neill Institute for National and Global Health Law.
Also, he noted that Mr. Trump could not invoke the Defense Production Act unless a vaccine were “scientifically justified and approved by the FDA.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
who have pledged not to release any vaccine unless it’s proved safe and effective.
In podcasts, public forums, social media and medical journals, a growing number of prominent health leaders say they fear that Mr. Trump – who has repeatedly signaled his desire for the swift approval of a vaccine and his displeasure with perceived delays at the FDA – will take matters into his own hands, running roughshod over the usual regulatory process.
It would reflect another attempt by a norm-breaking administration, poised to ram through a Supreme Court nominee opposed to existing abortion rights and the Affordable Care Act, to inject politics into sensitive public health decisions. Mr. Trump has repeatedly contradicted the advice of senior scientists on COVID-19 while pushing controversial treatments for the disease.
If the executive branch were to overrule the FDA’s scientific judgment, a vaccine of limited efficacy and, worse, unknown side effects could be rushed to market.
The worries intensified over the weekend, after Alex Azar, the administration’s secretary of Health & Human Services, asserted his agency’s rule-making authority over the FDA. HHS spokesperson Caitlin Oakley said Mr. Azar’s decision had no bearing on the vaccine approval process.
Vaccines are typically approved by the FDA. Alternatively, Mr. Azar – who reports directly to Mr. Trump – can issue an emergency use authorization, even before any vaccines have been shown to be safe and effective in late-stage clinical trials.
“Yes, this scenario is certainly possible legally and politically,” said Jerry Avorn, MD, a professor of medicine at Harvard Medical School, who outlined such an event in the New England Journal of Medicine. He said it “seems frighteningly more plausible each day.”
Vaccine experts and public health officials are particularly vexed by the possibility because it could ruin the fragile public confidence in a COVID-19 vaccine. It might put scientific authorities in the position of urging people not to be vaccinated after years of coaxing hesitant parents to ignore baseless fears.
Physicians might refuse to administer a vaccine approved with inadequate data, said Preeti Malani, MD, chief health officer and professor of medicine at the University of Michigan in Ann Arbor, in a recent webinar. “You could have a safe, effective vaccine that no one wants to take.” A recent KFF poll found that 54% of Americans would not submit to a COVID-19 vaccine authorized before Election Day.
After this story was published, an HHS official said that Mr. Azar “will defer completely to the FDA” as the agency weighs whether to approve a vaccine produced through the government’s Operation Warp Speed effort.
“The idea the Secretary would approve or authorize a vaccine over the FDA’s objections is preposterous and betrays ignorance of the transparent process that we’re following for the development of the OWS vaccines,” HHS chief of staff Brian Harrison wrote in an email.
White House spokesperson Judd Deere dismissed the scientists’ concerns, saying Trump cared only about the public’s safety and health. “This false narrative that the media and Democrats have created that politics is influencing approvals is not only false but is a danger to the American public,” he said.
Usually, the FDA approves vaccines only after companies submit years of data proving that a vaccine is safe and effective. But a 2004 law allows the FDA to issue an emergency use authorization with much less evidence, as long as the vaccine “may be effective” and its “known and potential benefits” outweigh its “known and potential risks.”
Many scientists doubt a vaccine could meet those criteria before the election. But the terms might be legally vague enough to allow the administration to take such steps.
Moncef Slaoui, chief scientific adviser to Operation Warp Speed, the government program aiming to more quickly develop COVID-19 vaccines, said it’s “extremely unlikely” that vaccine trial results will be ready before the end of October.
Mr. Trump, however, has insisted repeatedly that a vaccine to fight the pandemic that has claimed 200,000 American lives will be distributed starting next month. He reiterated that claim Saturday at a campaign rally in Fayetteville, N.C.
The vaccine will be ready “in a matter of weeks,” he said. “We will end the pandemic from China.”
Although pharmaceutical companies have launched three clinical trials in the United States, no one can say with certainty when those trials will have enough data to determine whether the vaccines are safe and effective.
Officials at Moderna, whose vaccine is being tested in 30,000 volunteers, have said their studies could produce a result by the end of the year, although the final analysis could take place next spring.
Pfizer executives, who have expanded their clinical trial to 44,000 participants, boast that they could know their vaccine works by the end of October.
AstraZeneca’s U.S. vaccine trial, which was scheduled to enroll 30,000 volunteers, is on hold pending an investigation of a possible vaccine-related illness.
Scientists have warned for months that the Trump administration could try to win the election with an “October surprise,” authorizing a vaccine that hasn’t been fully tested. “I don’t think people are crazy to be thinking about all of this,” said William Schultz, a partner in a Washington, D.C., law firm who served as a former FDA commissioner for policy and as general counsel for HHS.
“You’ve got a president saying you’ll have an approval in October. Everybody’s wondering how that could happen.”
In an opinion piece published in the Wall Street Journal, conservative former FDA commissioners Scott Gottlieb and Mark McClellan argued that presidential intrusion was unlikely because the FDA’s “thorough and transparent process doesn’t lend itself to meddling. Any deviation would quickly be apparent.”
But the administration has demonstrated a willingness to bend the agency to its will. The FDA has been criticized for issuing emergency authorizations for two COVID-19 treatments that were boosted by the president but lacked strong evidence to support them: hydroxychloroquine and convalescent plasma.
Mr. Azar has sidelined the FDA in other ways, such as by blocking the agency from regulating lab-developed tests, including tests for the novel coronavirus.
Although FDA Commissioner Stephen Hahn told the Financial Times he would be willing to approve emergency use of a vaccine before large-scale studies conclude, agency officials also have pledged to ensure the safety of any COVID-19 vaccines.
A senior FDA official who oversees vaccine approvals, Peter Marks, MD, has said he will quit if his agency rubber-stamps an unproven COVID-19 vaccine.
“I think there would be an outcry from the public health community second to none, which is my worst nightmare – my worst nightmare – because we will so confuse the public,” said Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, in his weekly podcast.
Still, “even if a company did not want it to be done, even if the FDA did not want it to be done, he could still do that,” said Dr. Osterholm, in his podcast. “I hope that we’d never see that happen, but we have to entertain that’s a possibility.”
In the New England Journal editorial, Dr. Avorn and coauthor Aaron Kesselheim, MD, wondered whether Mr. Trump might invoke the 1950 Defense Production Act to force reluctant drug companies to manufacture their vaccines.
But Mr. Trump would have to sue a company to enforce the Defense Production Act, and the company would have a strong case in refusing, said Lawrence Gostin, director of Georgetown’s O’Neill Institute for National and Global Health Law.
Also, he noted that Mr. Trump could not invoke the Defense Production Act unless a vaccine were “scientifically justified and approved by the FDA.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.