User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Fivefold Increase in Vaping During Adolescent Pregnancies
TOPLINE:
, according to research published online on December 13 in JAMA Network Open.
METHODOLOGY:
- Researchers analyzed data from the 2016-2021 Pregnancy Risk Assessment Monitoring System.
- They focused on 10,428 adolescents aged 10-19 years who had had a singleton birth and provided information about their use of e-cigarettes or cigarettes.
TAKEAWAY:
- Whereas the researchers found a roughly fivefold increase in the exclusive use of e-cigarettes, the percentage of patients using only cigarettes decreased from 9.2% in 2017 to 3.2% in 2021.
- The percentage of patients who both vaped and smoked fluctuated between 0.6% and 1.6%.
- The rate of small-for-gestational-age (SGA) births for adolescents who did not smoke or vape (12.9%) did not differ significantly from that among adolescents who exclusively used e-cigarettes (16.8%) or those who used both cigarettes and e-cigarettes (17.6%).
- The researchers found use of cigarettes only was associated with a significantly higher rate of SGA births: 24.6%.
IN PRACTICE:
“Exclusive e-cigarette use and dual use of cigarettes and e-cigarettes did not seem to be statistically significantly associated with SGA birth in our analysis, but this finding should be interpreted with caution given the low prevalence of use and the limited sample size,” the study authors wrote.
SOURCE:
Xiaozhong Wen, MD, PhD, with the Jacobs School of Medicine and Biomedical Sciences at the State University of New York at Buffalo, was the corresponding author of the study.
LIMITATIONS:
Participants may have underreported their use of e-cigarettes and cigarettes because of fears of social stigma. The researchers lacked information about vaping in the first and second trimesters, exposure to secondhand smoke, cannabis use, and diet.
DISCLOSURES:
The research was supported by the National Institute on Drug Abuse; the Food and Drug Administration Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the American Heart Association. A study coauthor has received grants from Pfizer and personal fees from Johnson & Johnson, the World Health Organization, and the Campaign for Tobacco-Free Kids.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to research published online on December 13 in JAMA Network Open.
METHODOLOGY:
- Researchers analyzed data from the 2016-2021 Pregnancy Risk Assessment Monitoring System.
- They focused on 10,428 adolescents aged 10-19 years who had had a singleton birth and provided information about their use of e-cigarettes or cigarettes.
TAKEAWAY:
- Whereas the researchers found a roughly fivefold increase in the exclusive use of e-cigarettes, the percentage of patients using only cigarettes decreased from 9.2% in 2017 to 3.2% in 2021.
- The percentage of patients who both vaped and smoked fluctuated between 0.6% and 1.6%.
- The rate of small-for-gestational-age (SGA) births for adolescents who did not smoke or vape (12.9%) did not differ significantly from that among adolescents who exclusively used e-cigarettes (16.8%) or those who used both cigarettes and e-cigarettes (17.6%).
- The researchers found use of cigarettes only was associated with a significantly higher rate of SGA births: 24.6%.
IN PRACTICE:
“Exclusive e-cigarette use and dual use of cigarettes and e-cigarettes did not seem to be statistically significantly associated with SGA birth in our analysis, but this finding should be interpreted with caution given the low prevalence of use and the limited sample size,” the study authors wrote.
SOURCE:
Xiaozhong Wen, MD, PhD, with the Jacobs School of Medicine and Biomedical Sciences at the State University of New York at Buffalo, was the corresponding author of the study.
LIMITATIONS:
Participants may have underreported their use of e-cigarettes and cigarettes because of fears of social stigma. The researchers lacked information about vaping in the first and second trimesters, exposure to secondhand smoke, cannabis use, and diet.
DISCLOSURES:
The research was supported by the National Institute on Drug Abuse; the Food and Drug Administration Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the American Heart Association. A study coauthor has received grants from Pfizer and personal fees from Johnson & Johnson, the World Health Organization, and the Campaign for Tobacco-Free Kids.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to research published online on December 13 in JAMA Network Open.
METHODOLOGY:
- Researchers analyzed data from the 2016-2021 Pregnancy Risk Assessment Monitoring System.
- They focused on 10,428 adolescents aged 10-19 years who had had a singleton birth and provided information about their use of e-cigarettes or cigarettes.
TAKEAWAY:
- Whereas the researchers found a roughly fivefold increase in the exclusive use of e-cigarettes, the percentage of patients using only cigarettes decreased from 9.2% in 2017 to 3.2% in 2021.
- The percentage of patients who both vaped and smoked fluctuated between 0.6% and 1.6%.
- The rate of small-for-gestational-age (SGA) births for adolescents who did not smoke or vape (12.9%) did not differ significantly from that among adolescents who exclusively used e-cigarettes (16.8%) or those who used both cigarettes and e-cigarettes (17.6%).
- The researchers found use of cigarettes only was associated with a significantly higher rate of SGA births: 24.6%.
IN PRACTICE:
“Exclusive e-cigarette use and dual use of cigarettes and e-cigarettes did not seem to be statistically significantly associated with SGA birth in our analysis, but this finding should be interpreted with caution given the low prevalence of use and the limited sample size,” the study authors wrote.
SOURCE:
Xiaozhong Wen, MD, PhD, with the Jacobs School of Medicine and Biomedical Sciences at the State University of New York at Buffalo, was the corresponding author of the study.
LIMITATIONS:
Participants may have underreported their use of e-cigarettes and cigarettes because of fears of social stigma. The researchers lacked information about vaping in the first and second trimesters, exposure to secondhand smoke, cannabis use, and diet.
DISCLOSURES:
The research was supported by the National Institute on Drug Abuse; the Food and Drug Administration Center for Tobacco Products; the National Heart, Lung, and Blood Institute; and the American Heart Association. A study coauthor has received grants from Pfizer and personal fees from Johnson & Johnson, the World Health Organization, and the Campaign for Tobacco-Free Kids.
A version of this article appeared on Medscape.com.
Federal program offers free COVID, flu at-home tests, treatments
The U.S. government has expanded a program offering free COVID-19 and flu tests and treatment.
The Home Test to Treat program is virtual and offers at-home rapid tests, telehealth sessions, and at-home treatments to people nationwide. The program is a collaboration among the National Institutes of Health, the Administration for Strategic Preparedness and Response, and the CDC. It began as a pilot program in some locations this year.
“With its expansion, the Home Test to Treat program will now offer free testing, telehealth and treatment for both COVID-19 and for influenza (flu) A and B,” the NIH said in a press release. “It is the first public health program that includes home testing technology at such a scale for both COVID-19 and flu.”
The news release says that anyone 18 or over with a current positive test for COVID-19 or flu can get free telehealth care and medicine delivered to their home.
Adults who don’t have COVID-19 or the flu can get free tests if they are uninsured or are enrolled in Medicare, Medicaid, the Veterans Affairs health care system, or Indian Health Services. If they test positive later, they can get free telehealth care and, if prescribed, treatment.
“I think that these [telehealth] delivery mechanisms are going to be absolutely crucial to unburden the in-person offices and the lines that we have and wait times,” said Michael Mina, MD, chief science officer at eMed, the company that helped implement the new Home Test to Treat program, to ABC News.
ABC notes that COVID tests can also be ordered at covidtests.gov – four tests per household or eight for those who have yet to order any this fall.
A version of this article appeared on WebMD.com .
The U.S. government has expanded a program offering free COVID-19 and flu tests and treatment.
The Home Test to Treat program is virtual and offers at-home rapid tests, telehealth sessions, and at-home treatments to people nationwide. The program is a collaboration among the National Institutes of Health, the Administration for Strategic Preparedness and Response, and the CDC. It began as a pilot program in some locations this year.
“With its expansion, the Home Test to Treat program will now offer free testing, telehealth and treatment for both COVID-19 and for influenza (flu) A and B,” the NIH said in a press release. “It is the first public health program that includes home testing technology at such a scale for both COVID-19 and flu.”
The news release says that anyone 18 or over with a current positive test for COVID-19 or flu can get free telehealth care and medicine delivered to their home.
Adults who don’t have COVID-19 or the flu can get free tests if they are uninsured or are enrolled in Medicare, Medicaid, the Veterans Affairs health care system, or Indian Health Services. If they test positive later, they can get free telehealth care and, if prescribed, treatment.
“I think that these [telehealth] delivery mechanisms are going to be absolutely crucial to unburden the in-person offices and the lines that we have and wait times,” said Michael Mina, MD, chief science officer at eMed, the company that helped implement the new Home Test to Treat program, to ABC News.
ABC notes that COVID tests can also be ordered at covidtests.gov – four tests per household or eight for those who have yet to order any this fall.
A version of this article appeared on WebMD.com .
The U.S. government has expanded a program offering free COVID-19 and flu tests and treatment.
The Home Test to Treat program is virtual and offers at-home rapid tests, telehealth sessions, and at-home treatments to people nationwide. The program is a collaboration among the National Institutes of Health, the Administration for Strategic Preparedness and Response, and the CDC. It began as a pilot program in some locations this year.
“With its expansion, the Home Test to Treat program will now offer free testing, telehealth and treatment for both COVID-19 and for influenza (flu) A and B,” the NIH said in a press release. “It is the first public health program that includes home testing technology at such a scale for both COVID-19 and flu.”
The news release says that anyone 18 or over with a current positive test for COVID-19 or flu can get free telehealth care and medicine delivered to their home.
Adults who don’t have COVID-19 or the flu can get free tests if they are uninsured or are enrolled in Medicare, Medicaid, the Veterans Affairs health care system, or Indian Health Services. If they test positive later, they can get free telehealth care and, if prescribed, treatment.
“I think that these [telehealth] delivery mechanisms are going to be absolutely crucial to unburden the in-person offices and the lines that we have and wait times,” said Michael Mina, MD, chief science officer at eMed, the company that helped implement the new Home Test to Treat program, to ABC News.
ABC notes that COVID tests can also be ordered at covidtests.gov – four tests per household or eight for those who have yet to order any this fall.
A version of this article appeared on WebMD.com .
Researchers making strides to better understand RA-associated interstitial lung disease
SAN DIEGO — Clinically significant interstitial lung disease (ILD) is believed to occur in 5%-10% of patients with rheumatoid arthritis (RA), but robust data are lacking on how to best predict which patients face the highest risk for RA-associated ILD. However, the results of several studies presented at the American College of Rheumatology annual meeting indicate that researchers are making strides in this field of rheumatologic care.
Adding Genetic Factors Improves ILD Risk Prediction
In the realm of risk stratification, Austin M. Wheeler, MD, a rheumatology fellow at the University of Nebraska Medical Center, Omaha, discussed the development and validation of a combined clinical and genetic risk score for ILD. “There is clear and well documented phenotypic and genetic overlap of ILD with idiopathic pulmonary fibrosis (IPF),” Dr. Wheeler said. “A number of clinical risk factors have been described for RA-ILD, including older age, male sex, smoking history, higher disease activity, and seropositivity. There are also well-documented genetic risk factors for RA-ILD. The MUC5B genetic variant is the strongest risk factor for IPF, and it’s been described in RA-ILD as well.”
A recently published study indicated that a genetic risk score without the MUC5B variant improved predictive ability for IPF and interstitial lung abnormalities better than using the MUC5B variant alone, “but no prior attempts have been made at developing a composite genetic risk score in RA-ILD” using both genetic and clinical risk factors, he said.
For the current study, Dr. Wheeler and colleagues drew from 2,386 participants in the Veterans Affairs Rheumatoid Arthritis (VARA) Registry, a multicenter, prospective cohort of US veterans with rheumatologist-diagnosed RA and who fulfilled the 1987 ACR classification criteria. The researchers validated ILD through a systematic review of medical records, including clinical diagnosis of ILD plus either imaging or lung biopsy findings, and collected whole genome data that included 12 single nucleotide polymorphisms (SNPs) previously identified to be associated with risk for RA-ILD. They then used a meta-analytic approach to create pooled associations for each of those respective SNPs using data from the VARA registry participants as well as participants from the past study where the SNPs were first identified. “Those pooled associations were what we used for our effects size within the genetic risk score,” which ended up using five of the SNPs, Dr. Wheeler explained. Next, he and his colleagues combined the genetic risk score with clinical risk factors including age, sex, smoking history, disease activity, and rheumatoid factor (RF) positivity to create their combined risk score.
The mean age of the cohort was 70 years, 89% were male, 78% had a smoking history, and 78% were anti–cyclic citrullinated peptide (CCP) antibody positive. Of the 2,386 participants, 224 (9.4%) had RA-ILD. The full composite risk score had the highest area under the receiver operating curve (AUC) of 0.67, compared with an AUC of 0.623 using the clinical factors alone, 0.651 using the clinical factors plus only the MUC5B variant, and 0.654 using the composite score minus only the MUC5B variant. These AUCs show that “the combined risk score performs better than clinical factors even without the inclusion of the MUC5B variant in the score, which is notable because it supports the importance of further investigation into polygenic risk scores in RA-ILD as there is clearly more at play in a patient’s overall genetic risk,” Dr. Wheeler said.
As an example of the composite score’s ability to discriminate between people with and without RA-ILD, a cutpoint of 0.05 gave a sensitivity of 90.2% and would have eliminated about 25% of the cohort from unnecessary high-resolution CT scans and pulmonary function tests, he said.
“This study demonstrates the potential utility of genetic risk scores in RA-ILD identification and supports further investigation into individual risk stratification and screening,” he concluded. “This isn’t ready for clinical applicability by any means, but I think it serves as a proof of concept of the idea of a genetic risk score in RA-ILD.”
Biomarker Score Investigated
In a separate abstract, Brent Luedders, MD, assistant professor of rheumatology and immunology at the University of Nebraska Medical Center, and colleagues set out to determine if a previously derived biomarker score is associated with prevalent and incident ILD in the same VARA Registry cohort. An abstract presented at the ACR 2022 annual meeting found that a panel derived from IPF peripheral biomarkers was significantly associated with RA-ILD, including matrix metalloproteinase (MMP)-2, -7, and -9, eotaxin, macrophage-derived chemokine (MDC), monocyte chemoattractant protein-1 (MCP-1), fms-like tyrosine kinase 3 ligand (Flt3L) and interleukin-8 (IL-8). For the current analysis, Dr. Luedders and colleagues measured the concentrations of seven biomarkers (MMP-7, MMP-9, eotaxin, MDC, MCP-1, Flt3L, IL-8) from serum/plasma samples collected from VARA’s participants at enrollment to develop a score based on the concentrations of each biomarker.
Baseline characteristics were similar between the groups, although those with prevalent RA-ILD were slightly older than those without ILD, and those who developed incident ILD during follow-up had slightly higher RA disease activity at the time of enrollment. When the researchers examined the association of the biomarker score with prevalent RA-ILD as a continuous measure, they found an adjusted OR of 1.08 for prevalent RA-ILD for each 1-point increase in the biomarker score. “When this was divided into quartiles, we found that the highest quartile of the biomarker score was associated with an adjusted odds ratio of 2.31 for prevalent RA-ILD,” Dr. Luedders said. “We saw a significant P for trend of < .001, suggesting a dose-response relationship, in which higher scores had higher risk.” Similar associations were observed for incident RA-ILD, in which participants with the highest quartile had an adjusted hazard ratio of 2.26 for incident RA-ILD.
The AUC of 0.653 that was obtained with clinical factors did not significantly improve with inclusion of the biomarker score, rising to only 0.669. “In receiver operating characteristic analysis, the addition of the biomarker score to clinical variables (age, sex, race, smoking status, anti-CCP positivity, and RA disease activity by DAS28) did not lead to a significant increase in the area under the curve. Therefore, further work is needed to identify combinations of clinical, biomarker, and other factors to accurately predict which people with RA will develop ILD,” he said.
Dr. Luedders acknowledged certain limitations of the results, including the fact that MMP-2 was not measured in this cohort and thus not included in the score. “This was an observational study with usual care; therefore, the absence of systemic evaluation for ILD may miss early or mild RA-ILD cases,” he added. “Similarly, a male predominance may limit the generalizability, and we have limited information on the RA-ILD pattern.” He concluded that the study results “support the shared pathogenesis of IPF and RA-ILD. However, we found that this score has limited discriminative performance, compared to clinical risk factors alone.”
Drilling Down on ILD Subtypes
In a poster abstract presentation at the meeting, Gregory Campbell McDermott, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, highlighted results from a study that investigated differences in demographic, serologic, and lifestyle factors for RA-ILD and the major subtypes of RA-ILD: usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP). “Historically, RA-ILD has been studied as a single entity, even though we increasingly recognized that there are lots of different subtypes that fall under the umbrella of RA-ILD,” Dr. McDermott said in an interview. “We are also learning that the different subtypes probably have both prognostic and potentially therapeutic implications. For example, the UIP subtype, which is the most fibrotic subtype, has the worst prognosis but also may be a potential target for antifibrotic therapies. We’ve been trying to see if we can identify factors that are associated with specific subtypes, in particular the UIP subtype which has the worst prognosis.”
He and his colleagues examined 208 patients with RA-ILD with a mean age of 51 years and 547 patients with RA but no ILD with a mean age of 49 years from two RA cohorts comprising 3,328 patients: the Mass General Brigham Biobank RA Cohort and the Brigham RA Sequential Study (BRASS). Of the 208 RA-ILD cases, nearly half (48%) were RA-UIP, 18% were RA-NSIP, 8% were organizing pneumonia, 3% were respiratory bronchiolitis-ILD, and 23% were other/indeterminate. After conducting multivariable adjusted analyses, the researchers found that RA-ILD was associated with male sex (OR, 1.58; 95% CI, 1.09-2.23), seropositivity for RF and/or anti-CCP (OR, 2.22; 95% CI, 1.51-3.24) and being an ever smoker (OR, 1.70; 95% CI, 1.13-2.54). Having all three of these risk factors was strongly associated with RA-ILD (OR, 6.04; 95% CI, 2.92-12.47) and with RA-UIP in particular (OR, 7.1). “We found that a lot of the traditional RA-ILD risk factors like male sex, history of smoking, and seropositive status were most strongly associated with a UIP pattern,” Dr. McDermott said. “We think this is a first step in trying to understand how these different ILD subtypes may have different risk factors, pathogenesis, and potentially different treatments, prevention, and screening strategies.”
While clinicians wait for guidelines on systemic autoimmune rheumatic disease-associated ILD that are expected to be published by the ACR in 2024, he added that “we probably shouldn’t screen every single person with RA for ILD, but we need to identify people who have symptoms or findings on clinical exam. This study wasn’t designed to look specifically at who is at high risk, but I think we are moving toward that question: Who is high risk, and who’s asymptomatic [but] may need more screening?”
He pointed out limitations of the study, including its retrospective design and the fact that imaging was done for clinical purposes, “so it’s probably a higher risk group to begin with than the whole RA population,” he said. “We also didn’t have data on RA disease activity or erosions, some of these other measures that we think are important for understanding the full RA disease phenotype in these patients.”
Dr. Wheeler reported having no disclosures. Dr. Luedders reported that his study was supported by the VA, the Rheumatology Research Foundation, and the University of Nebraska Medical Center Mentored Scholars Program. Dr. McDermott reported that his study was supported by the Rheumatology Research Foundation.
SAN DIEGO — Clinically significant interstitial lung disease (ILD) is believed to occur in 5%-10% of patients with rheumatoid arthritis (RA), but robust data are lacking on how to best predict which patients face the highest risk for RA-associated ILD. However, the results of several studies presented at the American College of Rheumatology annual meeting indicate that researchers are making strides in this field of rheumatologic care.
Adding Genetic Factors Improves ILD Risk Prediction
In the realm of risk stratification, Austin M. Wheeler, MD, a rheumatology fellow at the University of Nebraska Medical Center, Omaha, discussed the development and validation of a combined clinical and genetic risk score for ILD. “There is clear and well documented phenotypic and genetic overlap of ILD with idiopathic pulmonary fibrosis (IPF),” Dr. Wheeler said. “A number of clinical risk factors have been described for RA-ILD, including older age, male sex, smoking history, higher disease activity, and seropositivity. There are also well-documented genetic risk factors for RA-ILD. The MUC5B genetic variant is the strongest risk factor for IPF, and it’s been described in RA-ILD as well.”
A recently published study indicated that a genetic risk score without the MUC5B variant improved predictive ability for IPF and interstitial lung abnormalities better than using the MUC5B variant alone, “but no prior attempts have been made at developing a composite genetic risk score in RA-ILD” using both genetic and clinical risk factors, he said.
For the current study, Dr. Wheeler and colleagues drew from 2,386 participants in the Veterans Affairs Rheumatoid Arthritis (VARA) Registry, a multicenter, prospective cohort of US veterans with rheumatologist-diagnosed RA and who fulfilled the 1987 ACR classification criteria. The researchers validated ILD through a systematic review of medical records, including clinical diagnosis of ILD plus either imaging or lung biopsy findings, and collected whole genome data that included 12 single nucleotide polymorphisms (SNPs) previously identified to be associated with risk for RA-ILD. They then used a meta-analytic approach to create pooled associations for each of those respective SNPs using data from the VARA registry participants as well as participants from the past study where the SNPs were first identified. “Those pooled associations were what we used for our effects size within the genetic risk score,” which ended up using five of the SNPs, Dr. Wheeler explained. Next, he and his colleagues combined the genetic risk score with clinical risk factors including age, sex, smoking history, disease activity, and rheumatoid factor (RF) positivity to create their combined risk score.
The mean age of the cohort was 70 years, 89% were male, 78% had a smoking history, and 78% were anti–cyclic citrullinated peptide (CCP) antibody positive. Of the 2,386 participants, 224 (9.4%) had RA-ILD. The full composite risk score had the highest area under the receiver operating curve (AUC) of 0.67, compared with an AUC of 0.623 using the clinical factors alone, 0.651 using the clinical factors plus only the MUC5B variant, and 0.654 using the composite score minus only the MUC5B variant. These AUCs show that “the combined risk score performs better than clinical factors even without the inclusion of the MUC5B variant in the score, which is notable because it supports the importance of further investigation into polygenic risk scores in RA-ILD as there is clearly more at play in a patient’s overall genetic risk,” Dr. Wheeler said.
As an example of the composite score’s ability to discriminate between people with and without RA-ILD, a cutpoint of 0.05 gave a sensitivity of 90.2% and would have eliminated about 25% of the cohort from unnecessary high-resolution CT scans and pulmonary function tests, he said.
“This study demonstrates the potential utility of genetic risk scores in RA-ILD identification and supports further investigation into individual risk stratification and screening,” he concluded. “This isn’t ready for clinical applicability by any means, but I think it serves as a proof of concept of the idea of a genetic risk score in RA-ILD.”
Biomarker Score Investigated
In a separate abstract, Brent Luedders, MD, assistant professor of rheumatology and immunology at the University of Nebraska Medical Center, and colleagues set out to determine if a previously derived biomarker score is associated with prevalent and incident ILD in the same VARA Registry cohort. An abstract presented at the ACR 2022 annual meeting found that a panel derived from IPF peripheral biomarkers was significantly associated with RA-ILD, including matrix metalloproteinase (MMP)-2, -7, and -9, eotaxin, macrophage-derived chemokine (MDC), monocyte chemoattractant protein-1 (MCP-1), fms-like tyrosine kinase 3 ligand (Flt3L) and interleukin-8 (IL-8). For the current analysis, Dr. Luedders and colleagues measured the concentrations of seven biomarkers (MMP-7, MMP-9, eotaxin, MDC, MCP-1, Flt3L, IL-8) from serum/plasma samples collected from VARA’s participants at enrollment to develop a score based on the concentrations of each biomarker.
Baseline characteristics were similar between the groups, although those with prevalent RA-ILD were slightly older than those without ILD, and those who developed incident ILD during follow-up had slightly higher RA disease activity at the time of enrollment. When the researchers examined the association of the biomarker score with prevalent RA-ILD as a continuous measure, they found an adjusted OR of 1.08 for prevalent RA-ILD for each 1-point increase in the biomarker score. “When this was divided into quartiles, we found that the highest quartile of the biomarker score was associated with an adjusted odds ratio of 2.31 for prevalent RA-ILD,” Dr. Luedders said. “We saw a significant P for trend of < .001, suggesting a dose-response relationship, in which higher scores had higher risk.” Similar associations were observed for incident RA-ILD, in which participants with the highest quartile had an adjusted hazard ratio of 2.26 for incident RA-ILD.
The AUC of 0.653 that was obtained with clinical factors did not significantly improve with inclusion of the biomarker score, rising to only 0.669. “In receiver operating characteristic analysis, the addition of the biomarker score to clinical variables (age, sex, race, smoking status, anti-CCP positivity, and RA disease activity by DAS28) did not lead to a significant increase in the area under the curve. Therefore, further work is needed to identify combinations of clinical, biomarker, and other factors to accurately predict which people with RA will develop ILD,” he said.
Dr. Luedders acknowledged certain limitations of the results, including the fact that MMP-2 was not measured in this cohort and thus not included in the score. “This was an observational study with usual care; therefore, the absence of systemic evaluation for ILD may miss early or mild RA-ILD cases,” he added. “Similarly, a male predominance may limit the generalizability, and we have limited information on the RA-ILD pattern.” He concluded that the study results “support the shared pathogenesis of IPF and RA-ILD. However, we found that this score has limited discriminative performance, compared to clinical risk factors alone.”
Drilling Down on ILD Subtypes
In a poster abstract presentation at the meeting, Gregory Campbell McDermott, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, highlighted results from a study that investigated differences in demographic, serologic, and lifestyle factors for RA-ILD and the major subtypes of RA-ILD: usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP). “Historically, RA-ILD has been studied as a single entity, even though we increasingly recognized that there are lots of different subtypes that fall under the umbrella of RA-ILD,” Dr. McDermott said in an interview. “We are also learning that the different subtypes probably have both prognostic and potentially therapeutic implications. For example, the UIP subtype, which is the most fibrotic subtype, has the worst prognosis but also may be a potential target for antifibrotic therapies. We’ve been trying to see if we can identify factors that are associated with specific subtypes, in particular the UIP subtype which has the worst prognosis.”
He and his colleagues examined 208 patients with RA-ILD with a mean age of 51 years and 547 patients with RA but no ILD with a mean age of 49 years from two RA cohorts comprising 3,328 patients: the Mass General Brigham Biobank RA Cohort and the Brigham RA Sequential Study (BRASS). Of the 208 RA-ILD cases, nearly half (48%) were RA-UIP, 18% were RA-NSIP, 8% were organizing pneumonia, 3% were respiratory bronchiolitis-ILD, and 23% were other/indeterminate. After conducting multivariable adjusted analyses, the researchers found that RA-ILD was associated with male sex (OR, 1.58; 95% CI, 1.09-2.23), seropositivity for RF and/or anti-CCP (OR, 2.22; 95% CI, 1.51-3.24) and being an ever smoker (OR, 1.70; 95% CI, 1.13-2.54). Having all three of these risk factors was strongly associated with RA-ILD (OR, 6.04; 95% CI, 2.92-12.47) and with RA-UIP in particular (OR, 7.1). “We found that a lot of the traditional RA-ILD risk factors like male sex, history of smoking, and seropositive status were most strongly associated with a UIP pattern,” Dr. McDermott said. “We think this is a first step in trying to understand how these different ILD subtypes may have different risk factors, pathogenesis, and potentially different treatments, prevention, and screening strategies.”
While clinicians wait for guidelines on systemic autoimmune rheumatic disease-associated ILD that are expected to be published by the ACR in 2024, he added that “we probably shouldn’t screen every single person with RA for ILD, but we need to identify people who have symptoms or findings on clinical exam. This study wasn’t designed to look specifically at who is at high risk, but I think we are moving toward that question: Who is high risk, and who’s asymptomatic [but] may need more screening?”
He pointed out limitations of the study, including its retrospective design and the fact that imaging was done for clinical purposes, “so it’s probably a higher risk group to begin with than the whole RA population,” he said. “We also didn’t have data on RA disease activity or erosions, some of these other measures that we think are important for understanding the full RA disease phenotype in these patients.”
Dr. Wheeler reported having no disclosures. Dr. Luedders reported that his study was supported by the VA, the Rheumatology Research Foundation, and the University of Nebraska Medical Center Mentored Scholars Program. Dr. McDermott reported that his study was supported by the Rheumatology Research Foundation.
SAN DIEGO — Clinically significant interstitial lung disease (ILD) is believed to occur in 5%-10% of patients with rheumatoid arthritis (RA), but robust data are lacking on how to best predict which patients face the highest risk for RA-associated ILD. However, the results of several studies presented at the American College of Rheumatology annual meeting indicate that researchers are making strides in this field of rheumatologic care.
Adding Genetic Factors Improves ILD Risk Prediction
In the realm of risk stratification, Austin M. Wheeler, MD, a rheumatology fellow at the University of Nebraska Medical Center, Omaha, discussed the development and validation of a combined clinical and genetic risk score for ILD. “There is clear and well documented phenotypic and genetic overlap of ILD with idiopathic pulmonary fibrosis (IPF),” Dr. Wheeler said. “A number of clinical risk factors have been described for RA-ILD, including older age, male sex, smoking history, higher disease activity, and seropositivity. There are also well-documented genetic risk factors for RA-ILD. The MUC5B genetic variant is the strongest risk factor for IPF, and it’s been described in RA-ILD as well.”
A recently published study indicated that a genetic risk score without the MUC5B variant improved predictive ability for IPF and interstitial lung abnormalities better than using the MUC5B variant alone, “but no prior attempts have been made at developing a composite genetic risk score in RA-ILD” using both genetic and clinical risk factors, he said.
For the current study, Dr. Wheeler and colleagues drew from 2,386 participants in the Veterans Affairs Rheumatoid Arthritis (VARA) Registry, a multicenter, prospective cohort of US veterans with rheumatologist-diagnosed RA and who fulfilled the 1987 ACR classification criteria. The researchers validated ILD through a systematic review of medical records, including clinical diagnosis of ILD plus either imaging or lung biopsy findings, and collected whole genome data that included 12 single nucleotide polymorphisms (SNPs) previously identified to be associated with risk for RA-ILD. They then used a meta-analytic approach to create pooled associations for each of those respective SNPs using data from the VARA registry participants as well as participants from the past study where the SNPs were first identified. “Those pooled associations were what we used for our effects size within the genetic risk score,” which ended up using five of the SNPs, Dr. Wheeler explained. Next, he and his colleagues combined the genetic risk score with clinical risk factors including age, sex, smoking history, disease activity, and rheumatoid factor (RF) positivity to create their combined risk score.
The mean age of the cohort was 70 years, 89% were male, 78% had a smoking history, and 78% were anti–cyclic citrullinated peptide (CCP) antibody positive. Of the 2,386 participants, 224 (9.4%) had RA-ILD. The full composite risk score had the highest area under the receiver operating curve (AUC) of 0.67, compared with an AUC of 0.623 using the clinical factors alone, 0.651 using the clinical factors plus only the MUC5B variant, and 0.654 using the composite score minus only the MUC5B variant. These AUCs show that “the combined risk score performs better than clinical factors even without the inclusion of the MUC5B variant in the score, which is notable because it supports the importance of further investigation into polygenic risk scores in RA-ILD as there is clearly more at play in a patient’s overall genetic risk,” Dr. Wheeler said.
As an example of the composite score’s ability to discriminate between people with and without RA-ILD, a cutpoint of 0.05 gave a sensitivity of 90.2% and would have eliminated about 25% of the cohort from unnecessary high-resolution CT scans and pulmonary function tests, he said.
“This study demonstrates the potential utility of genetic risk scores in RA-ILD identification and supports further investigation into individual risk stratification and screening,” he concluded. “This isn’t ready for clinical applicability by any means, but I think it serves as a proof of concept of the idea of a genetic risk score in RA-ILD.”
Biomarker Score Investigated
In a separate abstract, Brent Luedders, MD, assistant professor of rheumatology and immunology at the University of Nebraska Medical Center, and colleagues set out to determine if a previously derived biomarker score is associated with prevalent and incident ILD in the same VARA Registry cohort. An abstract presented at the ACR 2022 annual meeting found that a panel derived from IPF peripheral biomarkers was significantly associated with RA-ILD, including matrix metalloproteinase (MMP)-2, -7, and -9, eotaxin, macrophage-derived chemokine (MDC), monocyte chemoattractant protein-1 (MCP-1), fms-like tyrosine kinase 3 ligand (Flt3L) and interleukin-8 (IL-8). For the current analysis, Dr. Luedders and colleagues measured the concentrations of seven biomarkers (MMP-7, MMP-9, eotaxin, MDC, MCP-1, Flt3L, IL-8) from serum/plasma samples collected from VARA’s participants at enrollment to develop a score based on the concentrations of each biomarker.
Baseline characteristics were similar between the groups, although those with prevalent RA-ILD were slightly older than those without ILD, and those who developed incident ILD during follow-up had slightly higher RA disease activity at the time of enrollment. When the researchers examined the association of the biomarker score with prevalent RA-ILD as a continuous measure, they found an adjusted OR of 1.08 for prevalent RA-ILD for each 1-point increase in the biomarker score. “When this was divided into quartiles, we found that the highest quartile of the biomarker score was associated with an adjusted odds ratio of 2.31 for prevalent RA-ILD,” Dr. Luedders said. “We saw a significant P for trend of < .001, suggesting a dose-response relationship, in which higher scores had higher risk.” Similar associations were observed for incident RA-ILD, in which participants with the highest quartile had an adjusted hazard ratio of 2.26 for incident RA-ILD.
The AUC of 0.653 that was obtained with clinical factors did not significantly improve with inclusion of the biomarker score, rising to only 0.669. “In receiver operating characteristic analysis, the addition of the biomarker score to clinical variables (age, sex, race, smoking status, anti-CCP positivity, and RA disease activity by DAS28) did not lead to a significant increase in the area under the curve. Therefore, further work is needed to identify combinations of clinical, biomarker, and other factors to accurately predict which people with RA will develop ILD,” he said.
Dr. Luedders acknowledged certain limitations of the results, including the fact that MMP-2 was not measured in this cohort and thus not included in the score. “This was an observational study with usual care; therefore, the absence of systemic evaluation for ILD may miss early or mild RA-ILD cases,” he added. “Similarly, a male predominance may limit the generalizability, and we have limited information on the RA-ILD pattern.” He concluded that the study results “support the shared pathogenesis of IPF and RA-ILD. However, we found that this score has limited discriminative performance, compared to clinical risk factors alone.”
Drilling Down on ILD Subtypes
In a poster abstract presentation at the meeting, Gregory Campbell McDermott, MD, MPH, a rheumatologist at Brigham and Women’s Hospital, Boston, highlighted results from a study that investigated differences in demographic, serologic, and lifestyle factors for RA-ILD and the major subtypes of RA-ILD: usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP). “Historically, RA-ILD has been studied as a single entity, even though we increasingly recognized that there are lots of different subtypes that fall under the umbrella of RA-ILD,” Dr. McDermott said in an interview. “We are also learning that the different subtypes probably have both prognostic and potentially therapeutic implications. For example, the UIP subtype, which is the most fibrotic subtype, has the worst prognosis but also may be a potential target for antifibrotic therapies. We’ve been trying to see if we can identify factors that are associated with specific subtypes, in particular the UIP subtype which has the worst prognosis.”
He and his colleagues examined 208 patients with RA-ILD with a mean age of 51 years and 547 patients with RA but no ILD with a mean age of 49 years from two RA cohorts comprising 3,328 patients: the Mass General Brigham Biobank RA Cohort and the Brigham RA Sequential Study (BRASS). Of the 208 RA-ILD cases, nearly half (48%) were RA-UIP, 18% were RA-NSIP, 8% were organizing pneumonia, 3% were respiratory bronchiolitis-ILD, and 23% were other/indeterminate. After conducting multivariable adjusted analyses, the researchers found that RA-ILD was associated with male sex (OR, 1.58; 95% CI, 1.09-2.23), seropositivity for RF and/or anti-CCP (OR, 2.22; 95% CI, 1.51-3.24) and being an ever smoker (OR, 1.70; 95% CI, 1.13-2.54). Having all three of these risk factors was strongly associated with RA-ILD (OR, 6.04; 95% CI, 2.92-12.47) and with RA-UIP in particular (OR, 7.1). “We found that a lot of the traditional RA-ILD risk factors like male sex, history of smoking, and seropositive status were most strongly associated with a UIP pattern,” Dr. McDermott said. “We think this is a first step in trying to understand how these different ILD subtypes may have different risk factors, pathogenesis, and potentially different treatments, prevention, and screening strategies.”
While clinicians wait for guidelines on systemic autoimmune rheumatic disease-associated ILD that are expected to be published by the ACR in 2024, he added that “we probably shouldn’t screen every single person with RA for ILD, but we need to identify people who have symptoms or findings on clinical exam. This study wasn’t designed to look specifically at who is at high risk, but I think we are moving toward that question: Who is high risk, and who’s asymptomatic [but] may need more screening?”
He pointed out limitations of the study, including its retrospective design and the fact that imaging was done for clinical purposes, “so it’s probably a higher risk group to begin with than the whole RA population,” he said. “We also didn’t have data on RA disease activity or erosions, some of these other measures that we think are important for understanding the full RA disease phenotype in these patients.”
Dr. Wheeler reported having no disclosures. Dr. Luedders reported that his study was supported by the VA, the Rheumatology Research Foundation, and the University of Nebraska Medical Center Mentored Scholars Program. Dr. McDermott reported that his study was supported by the Rheumatology Research Foundation.
FROM ACR 2023
Sotatercept Endorsed for PAH by ICER
In a new report, the Midwest Institute for Clinical and Economic Review’s (ICER) Comparative Effectiveness Public Advisory Council concluded that the Merck drug sotatercept, currently under review by the US Food and Drug Administration (FDA), has a high certainty of at least a small net health benefit to patients with pulmonary arterial hypertension (PAH) when added to background therapy. The limited availability of evidence means that the benefit could range from minimal to substantial, according to the authors.
Sotatercept, administered by injection every 3 weeks, is a first-in-class activin signaling inhibitor. It counters cell proliferation and decreases inflammation in vessel walls, which may lead to improved pulmonary blood flow. The US FDA is considering it for approval through a biologics license application, with a decision expected by March 26, 2024.
There remains a great deal of uncertainty surrounding the long-term benefits of sotatercept. It’s possible that the drug is disease-modifying, but there isn’t yet any proof, according to Greg Curfman, MD, who attended a virtual ICER public meeting on December 1 that summarized the report and accepted public comments. “I’m still wondering the extent to which disease-modifying issue here is more aspirational at this point than really documented,” said Dr. Curfman, who is an associated professor of medicine at Harvard Medical School and executive editor of the Journal of the American Medical Association.
Current PAH treatment consists of vasodilators, including phosphodiesterase-5 inhibitors (PDE5i), guanylate cyclase stimulators, endothelin receptor antagonists (ERA), prostacyclin analogues (prostanoids), and a prostacyclin receptor agonist. The 2022 European Society of Cardiology and the European Respiratory Society clinical practice guideline recommends that low- and intermediate-risk patients should be started on ERA/PDE5i combination therapy, while high-risk patients should also be given an intravenous or subcutaneous prostacyclin analogue, referred to as triple therapy.
Sotatercept’s regulatory approval hinges on the phase 3 STELLAR trial, which included 323 patients with World Health Organization functional class (WHO-FC) II and III PAH who were randomized to 0.75 mg/kg sotatercept in addition to background double or triple therapy, or background therapy alone. The mean age was 48 years, and the mean time since diagnosis was 8.8 years. About 40% received infused prostacyclin therapy at baseline. At 24 weeks, the median change in 6-min walking distance (6mWD) was 40.8 m longer in the sotatercept group. More patients in the sotatercept group experienced WHO-FC improvement (29.4% vs 13.8%). Those in the sotatercept group also experienced an 84% reduction in risk for clinical worsening or death. PAH-specific quality of life scales did not show a difference between the two groups. Open-label extension trials have shown that benefits are maintained for up to 2 years. Adverse events likely related to sotatercept included telangiectasias, increased hemoglobin levels, and bleeding events.
Along with its benefits, the report authors suggest that the subcutaneous delivery of sotatercept may be less burdensome to patients than some other PAH treatments, especially inhaled and intravenous prostanoids. “However, uncertainty remains about sotatercept’s efficacy in sicker populations and in those with connective tissue disease, and about the durability of effect,” the authors wrote.
A lack of long-term data leaves open the question of its effect on mortality and unknown adverse effects.
Using a de novo decision analytic model, the authors estimated that sotatercept treatment would lead to a longer time without symptoms at rest and more quality-adjusted life years, life years, and equal value life years. They determined the health benefit price benchmark for sotatercept to be between $18,700 and $36,200 per year. “The long-term conventional cost-effectiveness of sotatercept is largely dependent on the long-term effect of sotatercept on improving functional class and slowing the worsening in functional class; however, controlled trial evidence for sotatercept is limited to 24 weeks. Long-term data are necessary to reduce the uncertainty in sotatercept’s long-term effect on improving functional class and slowing the worsening in functional class,” the authors wrote.
During the online meeting, Dr. Curfman took note of the fact that the STELLAR trial reported a median value of increase in 6mWD, rather than a mean, and the 40-m improvement is close to the value accepted as clinically meaningful. “So that tells us that half the patients had less than a clinically important improvement in the six-minute walk distance. We should be putting that in perspective,” said Dr. Curfman.
Another attendee pointed out that the open-label PULSAR extension trial showed that the proportion of patients in the sotatercept arm who were functional class I rose from 7.5% at the end of the trial to 20.6% at the end of the open-label period and wondered if that could be a sign of disease-modifying activity. “I think that’s a remarkable piece of data. I don’t recall seeing that in any other open label [trial of a PAH therapy] — that much of an improvement in getting to our best functional status,” said Marc Simon, MD, professor of medicine and director of the Pulmonary Hypertension Center at the University of California, San Francisco, who was a coauthor of the report.
Dr. Curfman has no relevant financial disclosures. Dr. Simon has consulted for Merck.
A version of this article appeared on Medscape.com.
In a new report, the Midwest Institute for Clinical and Economic Review’s (ICER) Comparative Effectiveness Public Advisory Council concluded that the Merck drug sotatercept, currently under review by the US Food and Drug Administration (FDA), has a high certainty of at least a small net health benefit to patients with pulmonary arterial hypertension (PAH) when added to background therapy. The limited availability of evidence means that the benefit could range from minimal to substantial, according to the authors.
Sotatercept, administered by injection every 3 weeks, is a first-in-class activin signaling inhibitor. It counters cell proliferation and decreases inflammation in vessel walls, which may lead to improved pulmonary blood flow. The US FDA is considering it for approval through a biologics license application, with a decision expected by March 26, 2024.
There remains a great deal of uncertainty surrounding the long-term benefits of sotatercept. It’s possible that the drug is disease-modifying, but there isn’t yet any proof, according to Greg Curfman, MD, who attended a virtual ICER public meeting on December 1 that summarized the report and accepted public comments. “I’m still wondering the extent to which disease-modifying issue here is more aspirational at this point than really documented,” said Dr. Curfman, who is an associated professor of medicine at Harvard Medical School and executive editor of the Journal of the American Medical Association.
Current PAH treatment consists of vasodilators, including phosphodiesterase-5 inhibitors (PDE5i), guanylate cyclase stimulators, endothelin receptor antagonists (ERA), prostacyclin analogues (prostanoids), and a prostacyclin receptor agonist. The 2022 European Society of Cardiology and the European Respiratory Society clinical practice guideline recommends that low- and intermediate-risk patients should be started on ERA/PDE5i combination therapy, while high-risk patients should also be given an intravenous or subcutaneous prostacyclin analogue, referred to as triple therapy.
Sotatercept’s regulatory approval hinges on the phase 3 STELLAR trial, which included 323 patients with World Health Organization functional class (WHO-FC) II and III PAH who were randomized to 0.75 mg/kg sotatercept in addition to background double or triple therapy, or background therapy alone. The mean age was 48 years, and the mean time since diagnosis was 8.8 years. About 40% received infused prostacyclin therapy at baseline. At 24 weeks, the median change in 6-min walking distance (6mWD) was 40.8 m longer in the sotatercept group. More patients in the sotatercept group experienced WHO-FC improvement (29.4% vs 13.8%). Those in the sotatercept group also experienced an 84% reduction in risk for clinical worsening or death. PAH-specific quality of life scales did not show a difference between the two groups. Open-label extension trials have shown that benefits are maintained for up to 2 years. Adverse events likely related to sotatercept included telangiectasias, increased hemoglobin levels, and bleeding events.
Along with its benefits, the report authors suggest that the subcutaneous delivery of sotatercept may be less burdensome to patients than some other PAH treatments, especially inhaled and intravenous prostanoids. “However, uncertainty remains about sotatercept’s efficacy in sicker populations and in those with connective tissue disease, and about the durability of effect,” the authors wrote.
A lack of long-term data leaves open the question of its effect on mortality and unknown adverse effects.
Using a de novo decision analytic model, the authors estimated that sotatercept treatment would lead to a longer time without symptoms at rest and more quality-adjusted life years, life years, and equal value life years. They determined the health benefit price benchmark for sotatercept to be between $18,700 and $36,200 per year. “The long-term conventional cost-effectiveness of sotatercept is largely dependent on the long-term effect of sotatercept on improving functional class and slowing the worsening in functional class; however, controlled trial evidence for sotatercept is limited to 24 weeks. Long-term data are necessary to reduce the uncertainty in sotatercept’s long-term effect on improving functional class and slowing the worsening in functional class,” the authors wrote.
During the online meeting, Dr. Curfman took note of the fact that the STELLAR trial reported a median value of increase in 6mWD, rather than a mean, and the 40-m improvement is close to the value accepted as clinically meaningful. “So that tells us that half the patients had less than a clinically important improvement in the six-minute walk distance. We should be putting that in perspective,” said Dr. Curfman.
Another attendee pointed out that the open-label PULSAR extension trial showed that the proportion of patients in the sotatercept arm who were functional class I rose from 7.5% at the end of the trial to 20.6% at the end of the open-label period and wondered if that could be a sign of disease-modifying activity. “I think that’s a remarkable piece of data. I don’t recall seeing that in any other open label [trial of a PAH therapy] — that much of an improvement in getting to our best functional status,” said Marc Simon, MD, professor of medicine and director of the Pulmonary Hypertension Center at the University of California, San Francisco, who was a coauthor of the report.
Dr. Curfman has no relevant financial disclosures. Dr. Simon has consulted for Merck.
A version of this article appeared on Medscape.com.
In a new report, the Midwest Institute for Clinical and Economic Review’s (ICER) Comparative Effectiveness Public Advisory Council concluded that the Merck drug sotatercept, currently under review by the US Food and Drug Administration (FDA), has a high certainty of at least a small net health benefit to patients with pulmonary arterial hypertension (PAH) when added to background therapy. The limited availability of evidence means that the benefit could range from minimal to substantial, according to the authors.
Sotatercept, administered by injection every 3 weeks, is a first-in-class activin signaling inhibitor. It counters cell proliferation and decreases inflammation in vessel walls, which may lead to improved pulmonary blood flow. The US FDA is considering it for approval through a biologics license application, with a decision expected by March 26, 2024.
There remains a great deal of uncertainty surrounding the long-term benefits of sotatercept. It’s possible that the drug is disease-modifying, but there isn’t yet any proof, according to Greg Curfman, MD, who attended a virtual ICER public meeting on December 1 that summarized the report and accepted public comments. “I’m still wondering the extent to which disease-modifying issue here is more aspirational at this point than really documented,” said Dr. Curfman, who is an associated professor of medicine at Harvard Medical School and executive editor of the Journal of the American Medical Association.
Current PAH treatment consists of vasodilators, including phosphodiesterase-5 inhibitors (PDE5i), guanylate cyclase stimulators, endothelin receptor antagonists (ERA), prostacyclin analogues (prostanoids), and a prostacyclin receptor agonist. The 2022 European Society of Cardiology and the European Respiratory Society clinical practice guideline recommends that low- and intermediate-risk patients should be started on ERA/PDE5i combination therapy, while high-risk patients should also be given an intravenous or subcutaneous prostacyclin analogue, referred to as triple therapy.
Sotatercept’s regulatory approval hinges on the phase 3 STELLAR trial, which included 323 patients with World Health Organization functional class (WHO-FC) II and III PAH who were randomized to 0.75 mg/kg sotatercept in addition to background double or triple therapy, or background therapy alone. The mean age was 48 years, and the mean time since diagnosis was 8.8 years. About 40% received infused prostacyclin therapy at baseline. At 24 weeks, the median change in 6-min walking distance (6mWD) was 40.8 m longer in the sotatercept group. More patients in the sotatercept group experienced WHO-FC improvement (29.4% vs 13.8%). Those in the sotatercept group also experienced an 84% reduction in risk for clinical worsening or death. PAH-specific quality of life scales did not show a difference between the two groups. Open-label extension trials have shown that benefits are maintained for up to 2 years. Adverse events likely related to sotatercept included telangiectasias, increased hemoglobin levels, and bleeding events.
Along with its benefits, the report authors suggest that the subcutaneous delivery of sotatercept may be less burdensome to patients than some other PAH treatments, especially inhaled and intravenous prostanoids. “However, uncertainty remains about sotatercept’s efficacy in sicker populations and in those with connective tissue disease, and about the durability of effect,” the authors wrote.
A lack of long-term data leaves open the question of its effect on mortality and unknown adverse effects.
Using a de novo decision analytic model, the authors estimated that sotatercept treatment would lead to a longer time without symptoms at rest and more quality-adjusted life years, life years, and equal value life years. They determined the health benefit price benchmark for sotatercept to be between $18,700 and $36,200 per year. “The long-term conventional cost-effectiveness of sotatercept is largely dependent on the long-term effect of sotatercept on improving functional class and slowing the worsening in functional class; however, controlled trial evidence for sotatercept is limited to 24 weeks. Long-term data are necessary to reduce the uncertainty in sotatercept’s long-term effect on improving functional class and slowing the worsening in functional class,” the authors wrote.
During the online meeting, Dr. Curfman took note of the fact that the STELLAR trial reported a median value of increase in 6mWD, rather than a mean, and the 40-m improvement is close to the value accepted as clinically meaningful. “So that tells us that half the patients had less than a clinically important improvement in the six-minute walk distance. We should be putting that in perspective,” said Dr. Curfman.
Another attendee pointed out that the open-label PULSAR extension trial showed that the proportion of patients in the sotatercept arm who were functional class I rose from 7.5% at the end of the trial to 20.6% at the end of the open-label period and wondered if that could be a sign of disease-modifying activity. “I think that’s a remarkable piece of data. I don’t recall seeing that in any other open label [trial of a PAH therapy] — that much of an improvement in getting to our best functional status,” said Marc Simon, MD, professor of medicine and director of the Pulmonary Hypertension Center at the University of California, San Francisco, who was a coauthor of the report.
Dr. Curfman has no relevant financial disclosures. Dr. Simon has consulted for Merck.
A version of this article appeared on Medscape.com.
Some reasons to get off the fence about COVID booster
Though many people remain on the fence about getting the latest COVID vaccine booster, new research suggests a strong argument for getting the shot this winter: It sharply reduces the risk for COVID.
The risk reduction was 37% for those who received two doses. Experts say the research provides a strong argument for getting the vaccine, noting that about 10% of people infected with COVID go on to have long COVID, which can be debilitating for one quarter of those with long-lasting symptoms.
The data come from a systematic literature review and meta-analysis published in October in Antimicrobial Stewardship & Epidemiology. Researchers examined 32 studies published between December 2019 and June 2023, involving 775,931 adults. Twenty-four studies, encompassing 620,221 individuals, were included in the meta-analysis.
“The body of evidence from all these different studies converge on one single reality — that vaccines reduce the risk of long COVID, and people who keep up to date on their vaccinations also fared better than people who got it once or twice and didn’t follow up,” said Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University in St Louis.
Researchers have reported similar results for children. The National Institutes of Health RECOVER Initiative team found that vaccines are up to 42% effective in preventing long COVID in children, said Dr. Carlos Oliveira, MD, a pediatric infectious diseases specialist and Yale researcher who contributed to the study, which is in preprint.
Vaccines also protect children from multisystem inflammatory syndrome, a condition that can happen after COVID, as well as protect against other COVID-related problems, such as missed school days, Oliveira said. “Even if the vaccine doesn’t completely stop long COVID, it’s still good for kids to get vaccinated for all these other reasons.”
However, uptake for the latest boosters has been slow: the Centers for Disease Control and Prevention reported that by mid-November, less than 16% of people aged 18 years or older had received a shot. For children, the number was closer to 6%. A recent Kaiser Family Foundation survey found that booster rates for adults are similar to what it was 1 year ago.
The survey results suggest that people are no longer as worried about COVID, which is why there is less concerned about keeping up with boosters. Though the current mutation of the virus is not as debilitating as its predecessors, long COVID continues to be a problem: as of January 2023, 28% of people who had contracted the virus had experienced long-COVID symptoms. And though the mechanisms are still not fully understood, and researchers have yet to agree on a definition of long COVID, they are certain about this much: The best way to avoid it is to avoid getting infected to begin with.
The lack of a diagnostic test for long COVID and the fact that the symptoms mimic those of other diseases lead to inconsistency that can make studies hard to replicate. In the papers reviewed for the Antimicrobial Stewardship & Epidemiology study, long COVID was defined as having symptoms lasting from more than 4 weeks to more than 6 months. Alexandre Marra, MD, the lead author and a researcher at the Hospital Israelita Albert Einstein, in São Paulo, Brazil, and at the University of Iowa, said that a clear standard definition is needed to better understand the actual prevalence and evaluate vaccine effectiveness.
Al-Aly noted that there is a logical explanation for one finding in the paper: The percentage of individuals who had COVID and reported that long-COVID symptoms declined from 19% in June 2022 to 11% in January 2023.
Because a pandemic is a dynamic event, constantly producing different variants with different phenotypes, the prevalence of disease is naturally going to be affected. “People who got infected early in the pandemic may have a different long COVID profile and long COVID risk than people who got infected in the second or third year of the pandemic,” Al-Aly said.
Most of the studies reported data from before the Omicron-variant era. Only eight reported data during that era. Omicron was not as lethal as previous variants, and consequently, fewer patients developed long COVID during that time.
One of those who did is Yeng Chang, age 40 years, a family doctor who lives in Sherwood Park, Alberta, Canada. Chang developed long COVID during fall 2022 after getting the virus in June. By then, she’d been vaccinated three times, but she isn’t surprised that she got sick because each vaccine she had was developed before Omicron.
“When I had COVID I was really sick, but I was well enough to stay home,” she said. “I think if I didn’t have my immunizations, I might have been hospitalized, and I don’t know what would have happened.”
Long COVID has left Chang with brain fog, fatigue, and a lack of physical stamina that forced her to pause her medical practice. For the past year and a half, she’s spent more time as a patient than a physician.
Chang had her fifth COVID vaccination in the fall and recommends that others do the same. “The booster you got however many years ago was effective for the COVID of that time but there is a new COVID now. You can’t just say, ‘I had one and I’m fine forever.’”
A version of this article appeared on Medscape.com.
Though many people remain on the fence about getting the latest COVID vaccine booster, new research suggests a strong argument for getting the shot this winter: It sharply reduces the risk for COVID.
The risk reduction was 37% for those who received two doses. Experts say the research provides a strong argument for getting the vaccine, noting that about 10% of people infected with COVID go on to have long COVID, which can be debilitating for one quarter of those with long-lasting symptoms.
The data come from a systematic literature review and meta-analysis published in October in Antimicrobial Stewardship & Epidemiology. Researchers examined 32 studies published between December 2019 and June 2023, involving 775,931 adults. Twenty-four studies, encompassing 620,221 individuals, were included in the meta-analysis.
“The body of evidence from all these different studies converge on one single reality — that vaccines reduce the risk of long COVID, and people who keep up to date on their vaccinations also fared better than people who got it once or twice and didn’t follow up,” said Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University in St Louis.
Researchers have reported similar results for children. The National Institutes of Health RECOVER Initiative team found that vaccines are up to 42% effective in preventing long COVID in children, said Dr. Carlos Oliveira, MD, a pediatric infectious diseases specialist and Yale researcher who contributed to the study, which is in preprint.
Vaccines also protect children from multisystem inflammatory syndrome, a condition that can happen after COVID, as well as protect against other COVID-related problems, such as missed school days, Oliveira said. “Even if the vaccine doesn’t completely stop long COVID, it’s still good for kids to get vaccinated for all these other reasons.”
However, uptake for the latest boosters has been slow: the Centers for Disease Control and Prevention reported that by mid-November, less than 16% of people aged 18 years or older had received a shot. For children, the number was closer to 6%. A recent Kaiser Family Foundation survey found that booster rates for adults are similar to what it was 1 year ago.
The survey results suggest that people are no longer as worried about COVID, which is why there is less concerned about keeping up with boosters. Though the current mutation of the virus is not as debilitating as its predecessors, long COVID continues to be a problem: as of January 2023, 28% of people who had contracted the virus had experienced long-COVID symptoms. And though the mechanisms are still not fully understood, and researchers have yet to agree on a definition of long COVID, they are certain about this much: The best way to avoid it is to avoid getting infected to begin with.
The lack of a diagnostic test for long COVID and the fact that the symptoms mimic those of other diseases lead to inconsistency that can make studies hard to replicate. In the papers reviewed for the Antimicrobial Stewardship & Epidemiology study, long COVID was defined as having symptoms lasting from more than 4 weeks to more than 6 months. Alexandre Marra, MD, the lead author and a researcher at the Hospital Israelita Albert Einstein, in São Paulo, Brazil, and at the University of Iowa, said that a clear standard definition is needed to better understand the actual prevalence and evaluate vaccine effectiveness.
Al-Aly noted that there is a logical explanation for one finding in the paper: The percentage of individuals who had COVID and reported that long-COVID symptoms declined from 19% in June 2022 to 11% in January 2023.
Because a pandemic is a dynamic event, constantly producing different variants with different phenotypes, the prevalence of disease is naturally going to be affected. “People who got infected early in the pandemic may have a different long COVID profile and long COVID risk than people who got infected in the second or third year of the pandemic,” Al-Aly said.
Most of the studies reported data from before the Omicron-variant era. Only eight reported data during that era. Omicron was not as lethal as previous variants, and consequently, fewer patients developed long COVID during that time.
One of those who did is Yeng Chang, age 40 years, a family doctor who lives in Sherwood Park, Alberta, Canada. Chang developed long COVID during fall 2022 after getting the virus in June. By then, she’d been vaccinated three times, but she isn’t surprised that she got sick because each vaccine she had was developed before Omicron.
“When I had COVID I was really sick, but I was well enough to stay home,” she said. “I think if I didn’t have my immunizations, I might have been hospitalized, and I don’t know what would have happened.”
Long COVID has left Chang with brain fog, fatigue, and a lack of physical stamina that forced her to pause her medical practice. For the past year and a half, she’s spent more time as a patient than a physician.
Chang had her fifth COVID vaccination in the fall and recommends that others do the same. “The booster you got however many years ago was effective for the COVID of that time but there is a new COVID now. You can’t just say, ‘I had one and I’m fine forever.’”
A version of this article appeared on Medscape.com.
Though many people remain on the fence about getting the latest COVID vaccine booster, new research suggests a strong argument for getting the shot this winter: It sharply reduces the risk for COVID.
The risk reduction was 37% for those who received two doses. Experts say the research provides a strong argument for getting the vaccine, noting that about 10% of people infected with COVID go on to have long COVID, which can be debilitating for one quarter of those with long-lasting symptoms.
The data come from a systematic literature review and meta-analysis published in October in Antimicrobial Stewardship & Epidemiology. Researchers examined 32 studies published between December 2019 and June 2023, involving 775,931 adults. Twenty-four studies, encompassing 620,221 individuals, were included in the meta-analysis.
“The body of evidence from all these different studies converge on one single reality — that vaccines reduce the risk of long COVID, and people who keep up to date on their vaccinations also fared better than people who got it once or twice and didn’t follow up,” said Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University in St Louis.
Researchers have reported similar results for children. The National Institutes of Health RECOVER Initiative team found that vaccines are up to 42% effective in preventing long COVID in children, said Dr. Carlos Oliveira, MD, a pediatric infectious diseases specialist and Yale researcher who contributed to the study, which is in preprint.
Vaccines also protect children from multisystem inflammatory syndrome, a condition that can happen after COVID, as well as protect against other COVID-related problems, such as missed school days, Oliveira said. “Even if the vaccine doesn’t completely stop long COVID, it’s still good for kids to get vaccinated for all these other reasons.”
However, uptake for the latest boosters has been slow: the Centers for Disease Control and Prevention reported that by mid-November, less than 16% of people aged 18 years or older had received a shot. For children, the number was closer to 6%. A recent Kaiser Family Foundation survey found that booster rates for adults are similar to what it was 1 year ago.
The survey results suggest that people are no longer as worried about COVID, which is why there is less concerned about keeping up with boosters. Though the current mutation of the virus is not as debilitating as its predecessors, long COVID continues to be a problem: as of January 2023, 28% of people who had contracted the virus had experienced long-COVID symptoms. And though the mechanisms are still not fully understood, and researchers have yet to agree on a definition of long COVID, they are certain about this much: The best way to avoid it is to avoid getting infected to begin with.
The lack of a diagnostic test for long COVID and the fact that the symptoms mimic those of other diseases lead to inconsistency that can make studies hard to replicate. In the papers reviewed for the Antimicrobial Stewardship & Epidemiology study, long COVID was defined as having symptoms lasting from more than 4 weeks to more than 6 months. Alexandre Marra, MD, the lead author and a researcher at the Hospital Israelita Albert Einstein, in São Paulo, Brazil, and at the University of Iowa, said that a clear standard definition is needed to better understand the actual prevalence and evaluate vaccine effectiveness.
Al-Aly noted that there is a logical explanation for one finding in the paper: The percentage of individuals who had COVID and reported that long-COVID symptoms declined from 19% in June 2022 to 11% in January 2023.
Because a pandemic is a dynamic event, constantly producing different variants with different phenotypes, the prevalence of disease is naturally going to be affected. “People who got infected early in the pandemic may have a different long COVID profile and long COVID risk than people who got infected in the second or third year of the pandemic,” Al-Aly said.
Most of the studies reported data from before the Omicron-variant era. Only eight reported data during that era. Omicron was not as lethal as previous variants, and consequently, fewer patients developed long COVID during that time.
One of those who did is Yeng Chang, age 40 years, a family doctor who lives in Sherwood Park, Alberta, Canada. Chang developed long COVID during fall 2022 after getting the virus in June. By then, she’d been vaccinated three times, but she isn’t surprised that she got sick because each vaccine she had was developed before Omicron.
“When I had COVID I was really sick, but I was well enough to stay home,” she said. “I think if I didn’t have my immunizations, I might have been hospitalized, and I don’t know what would have happened.”
Long COVID has left Chang with brain fog, fatigue, and a lack of physical stamina that forced her to pause her medical practice. For the past year and a half, she’s spent more time as a patient than a physician.
Chang had her fifth COVID vaccination in the fall and recommends that others do the same. “The booster you got however many years ago was effective for the COVID of that time but there is a new COVID now. You can’t just say, ‘I had one and I’m fine forever.’”
A version of this article appeared on Medscape.com.
Pulmonary arterial hypertension: Promising results for investigational agents and catheter-based denervation
PHILADELPHIA — Promise that the unmet need for more effective pulmonary artery hypertension treatments may soon be met was in strong evidence in research into three strategies presented at this year’s recent American Heart Association scientific sessions; one was based on an ancient Chinese herb epimedium (yin yang huo or horny goat weed) commonly used for treating sexual dysfunction and directly related to the phosphodiesterase inhibitors sildenafil, vardenafil, and tadalafil (sold as Viagra, Levitra, and Cialis). A second studied sotatercept, an investigational, potential first-in-class activin signaling inhibitor biologic, and a third evaluated physically ablating the baroreceptor nerves that stimulate vasoconstriction of the pulmonary artery via catheter-based techniques.
Until as recently as the late 1970s, a pulmonary arterial hypertension diagnosis was a uniformly fatal one.1 While associated with pulmonary and right ventricle remodeling, and leads toward heart failure and death. The complex underlying pathogenesis was divided into six groups by the 6th World Symposium on Pulmonary Hypertension (WSPH) in 2018, and includes as its most common features pulmonary artery endothelial cell dysfunction, pulmonary artery smooth muscle cell proliferation and migration, and dysregulated fibroblast activity leading to dysregulated vasoconstriction, micro and in-situ vascular thrombosis, vascular fibrosis and pathogenic remodeling of pulmonary vessels.1 The threshold mean arterial pressure (mPAP) for pulmonary arterial hypertension was defined by the 6th [WSPH] at mPAP ≥ 20 mm Hg, twice the upper limit of a normal mPAP of 14.0 ± 3.3 mm Hg as reported by Kovacs et al. in 2018.2
Pathways for current therapies
Current drugs for pulmonary arterial hypertension focus on three signaling pathways, including the endothelin receptor, prostacyclin and nitric oxide pathways, stated Zhi-Cheng Jing, MD, professor of medicine, head of the cardiology department at Peking Union Medical College Hospital, Peking, China. While the phosphodiesterase 5 inhibitors sildenafil and tadalafil, which target the nitric oxide pathway, came into wide use after Food and Drug Administration approval, the need for higher PDE5-selectivity remains, Dr. Jing said. Structurally modified from the active ingredient in epimedium, TPN171H is an investigational PDE5 inhibitor which has shown several favorable features: a greater PDE5 selectivity than both sildenafil and tadalafil in vitro, an ability to decrease right ventricular systolic pressure and alleviate arterial remodeling in animal studies, and safety and tolerability in healthy human subjects.
The current randomized, double-blind, placebo-and active-controlled phase IIa study assessed the hemodynamic impact of a single oral dose of TPN171H in 60 pulmonary arterial hypertension patients (mean age ~34 years, 83.3% female), all with negative vasodilation test results and in WHO class 2 or 3. Only patients aged 18-75 years with group 1 pulmonary arterial hypertension of idiopathic, connective tissue disorder, or repaired congenital heart defects etiology were included. Patients were divided into six groups: placebo, TPN171H at 2.5, 5, and 10 milligrams, and tadalafil at 20 and 40 milligrams.
For the primary endpoint of maximum decrease in pulmonary vascular resistance (PVR), significant reductions vs. placebo were found only for the TPN171H 5-mg group (–41.2% vs. –24.4%; P = .008) and for the 20-mg (–39.8%) and 40-mg (–37.6%) tadalafil groups (both P < .05). What was not seen in the tadalafil groups, but was evident in the TPN171H 5-mg group, was a significant reduction in the secondary endpoint of PVR/SVR (systolic vascular resistance) at 2, 3, and 5 hours (all P < .05). “As we know,” Dr. Jing said in an interview, “the PDE5 inhibitor functions as a vasodilator, having an impact on both pulmonary circulation and systemic circulation. So, to evaluate the selectivity for pulmonary circulation is crucial when exploring a novel drug for pulmonary arterial hypertension. The change of PVR/SVR ratio from baseline is an indicator for selectivity for pulmonary circulation and implies that TPN171H has good PDE5 selectivity in the pulmonary vasculature,” Dr. Jing said.
TPN171H was well tolerated with no serious adverse effects (vomiting 10% and headache 10% were most common with no discontinuations).
TGF-signaling pathway
A meta-analysis of randomized controlled trials of sotatercept, an investigational fusion protein under priority FDA review that modulates the TGF-beta superfamily signaling pathway, looked at PVR, pulmonary arterial pressure (PAP), right arterial pressure (RAP) and N-terminal pro-brain natriuretic peptide (NT-proBNP). A literature search by corresponding author Vamsikalyan Borra, MD, Knapp Medical Center, Weslaco, Texas, and colleagues identified two trials (STELLAR and PULSAR) comprising 429 patients with pulmonary arterial hypertension. The experimental arms (sotatercept) had 237 patients (mean age ~49 years, ~82% female) and the placebo arm had 192 patients (mean age ~47 years, ~80% female).
A pooled analysis showed significant reductions with sotatercept in PVR (standardization mean difference [SMD] = –1.00, 95% confidence interval [CI] = –1.2, –.79, P < .001), PAP (SMD = –1.34, 95% CI = 1.6, –1.08, P < .001), RAP (SMD = –0.66, 95% CI = –0.93, –0.39, P < .001), and the levels of NT-proBNP (SMD = –0.64, 95% CI = –1.01, –0.27, P < .001) at 24 weeks from baseline. The sotatercept safety profile was favorable, with lower overall incidence of adverse events (84.8% vs. 87.5%) and fewer adverse events leading to death (0.4% vs. 3.1%) compared with placebo. Further investigation is needed, however, according to Dr. Borra, into the higher frequency of reported thrombocytopenia (71.7% vs. 20.8%) with sotatercept. “Our findings,” Dr. Borra said in a poster session, “suggest that sotatercept is an effective treatment option for pulmonary arterial hypertension, with the potential to improve both pulmonary and cardiac function.”
Denervation technique
Catheter-based ablation techniques, most commonly using thermal energy, target the afferent and efferent fibers of the baroreceptor reflex in the main pulmonary artery trunk and bifurcation involved in elevated pulmonary artery pressure. Mounica Vorla, MD, Carle Foundation Hospital, Urbana, Illinois, and colleagues conducted an updated systematic review and meta-analysis of the safety and efficacy of pulmonary artery denervation (PADN) for pulmonary arterial hypertension in seven clinical trials with 506 patients with moderate-severe pulmonary arterial hypertension conducted from 2013 to 2022.
Compared with placebo, PADN treatment was associated with a significant reduction in mean pulmonary artery pressure (weighted mean difference [WMD] = –6.9 mm Hg; 95% CI = –9.7, –4.1; P < .01; I2 = 61) and pulmonary vascular resistance (WMD = –3.2; 95% CI = –5.4, –0.9; P = .005). PADN improvements in cardiac output were also statistically significant (WMD = 0.3; 95% CI = 0.07, 0.6; P = .012), with numerical improvement in 6-minute walking distance (WMD = 67.7; 95% CI = –3.73, 139.2; P = .06) in the PADN group. Side effects were less common in the PADN group as compared with the placebo group, Dr. Vorla reported. She concluded, “This updated meta-analysis supports PADN as a safe and efficacious therapy for severe pulmonary arterial hypertension.” The authors noted limitations imposed by the small sample size, large data heterogeneity, and medium-quality literature. Larger randomized, controlled trials with clinical endpoints comparing PADN with optimal medical therapy are needed, they stated.
References
1. Shah AJ et al. New Drugs and Therapies in Pulmonary Arterial Hypertension. Int J Mol Sci. 2023 Mar 19;24(6):5850. doi: 10.3390/ijms24065850. PMID: 36982922; PMCID: PMC10058689.
2. Kovacs G et al. Pulmonary Vascular Involvement in Chronic Obstructive Pulmonary Disease. Is There a Pulmonary Vascular Phenotype? Am J Respir Crit Care Med. 2018 Oct 15;198(8):1000-11. doi: 10.1164/rccm.201801-0095PP. PMID: 29746142.
PHILADELPHIA — Promise that the unmet need for more effective pulmonary artery hypertension treatments may soon be met was in strong evidence in research into three strategies presented at this year’s recent American Heart Association scientific sessions; one was based on an ancient Chinese herb epimedium (yin yang huo or horny goat weed) commonly used for treating sexual dysfunction and directly related to the phosphodiesterase inhibitors sildenafil, vardenafil, and tadalafil (sold as Viagra, Levitra, and Cialis). A second studied sotatercept, an investigational, potential first-in-class activin signaling inhibitor biologic, and a third evaluated physically ablating the baroreceptor nerves that stimulate vasoconstriction of the pulmonary artery via catheter-based techniques.
Until as recently as the late 1970s, a pulmonary arterial hypertension diagnosis was a uniformly fatal one.1 While associated with pulmonary and right ventricle remodeling, and leads toward heart failure and death. The complex underlying pathogenesis was divided into six groups by the 6th World Symposium on Pulmonary Hypertension (WSPH) in 2018, and includes as its most common features pulmonary artery endothelial cell dysfunction, pulmonary artery smooth muscle cell proliferation and migration, and dysregulated fibroblast activity leading to dysregulated vasoconstriction, micro and in-situ vascular thrombosis, vascular fibrosis and pathogenic remodeling of pulmonary vessels.1 The threshold mean arterial pressure (mPAP) for pulmonary arterial hypertension was defined by the 6th [WSPH] at mPAP ≥ 20 mm Hg, twice the upper limit of a normal mPAP of 14.0 ± 3.3 mm Hg as reported by Kovacs et al. in 2018.2
Pathways for current therapies
Current drugs for pulmonary arterial hypertension focus on three signaling pathways, including the endothelin receptor, prostacyclin and nitric oxide pathways, stated Zhi-Cheng Jing, MD, professor of medicine, head of the cardiology department at Peking Union Medical College Hospital, Peking, China. While the phosphodiesterase 5 inhibitors sildenafil and tadalafil, which target the nitric oxide pathway, came into wide use after Food and Drug Administration approval, the need for higher PDE5-selectivity remains, Dr. Jing said. Structurally modified from the active ingredient in epimedium, TPN171H is an investigational PDE5 inhibitor which has shown several favorable features: a greater PDE5 selectivity than both sildenafil and tadalafil in vitro, an ability to decrease right ventricular systolic pressure and alleviate arterial remodeling in animal studies, and safety and tolerability in healthy human subjects.
The current randomized, double-blind, placebo-and active-controlled phase IIa study assessed the hemodynamic impact of a single oral dose of TPN171H in 60 pulmonary arterial hypertension patients (mean age ~34 years, 83.3% female), all with negative vasodilation test results and in WHO class 2 or 3. Only patients aged 18-75 years with group 1 pulmonary arterial hypertension of idiopathic, connective tissue disorder, or repaired congenital heart defects etiology were included. Patients were divided into six groups: placebo, TPN171H at 2.5, 5, and 10 milligrams, and tadalafil at 20 and 40 milligrams.
For the primary endpoint of maximum decrease in pulmonary vascular resistance (PVR), significant reductions vs. placebo were found only for the TPN171H 5-mg group (–41.2% vs. –24.4%; P = .008) and for the 20-mg (–39.8%) and 40-mg (–37.6%) tadalafil groups (both P < .05). What was not seen in the tadalafil groups, but was evident in the TPN171H 5-mg group, was a significant reduction in the secondary endpoint of PVR/SVR (systolic vascular resistance) at 2, 3, and 5 hours (all P < .05). “As we know,” Dr. Jing said in an interview, “the PDE5 inhibitor functions as a vasodilator, having an impact on both pulmonary circulation and systemic circulation. So, to evaluate the selectivity for pulmonary circulation is crucial when exploring a novel drug for pulmonary arterial hypertension. The change of PVR/SVR ratio from baseline is an indicator for selectivity for pulmonary circulation and implies that TPN171H has good PDE5 selectivity in the pulmonary vasculature,” Dr. Jing said.
TPN171H was well tolerated with no serious adverse effects (vomiting 10% and headache 10% were most common with no discontinuations).
TGF-signaling pathway
A meta-analysis of randomized controlled trials of sotatercept, an investigational fusion protein under priority FDA review that modulates the TGF-beta superfamily signaling pathway, looked at PVR, pulmonary arterial pressure (PAP), right arterial pressure (RAP) and N-terminal pro-brain natriuretic peptide (NT-proBNP). A literature search by corresponding author Vamsikalyan Borra, MD, Knapp Medical Center, Weslaco, Texas, and colleagues identified two trials (STELLAR and PULSAR) comprising 429 patients with pulmonary arterial hypertension. The experimental arms (sotatercept) had 237 patients (mean age ~49 years, ~82% female) and the placebo arm had 192 patients (mean age ~47 years, ~80% female).
A pooled analysis showed significant reductions with sotatercept in PVR (standardization mean difference [SMD] = –1.00, 95% confidence interval [CI] = –1.2, –.79, P < .001), PAP (SMD = –1.34, 95% CI = 1.6, –1.08, P < .001), RAP (SMD = –0.66, 95% CI = –0.93, –0.39, P < .001), and the levels of NT-proBNP (SMD = –0.64, 95% CI = –1.01, –0.27, P < .001) at 24 weeks from baseline. The sotatercept safety profile was favorable, with lower overall incidence of adverse events (84.8% vs. 87.5%) and fewer adverse events leading to death (0.4% vs. 3.1%) compared with placebo. Further investigation is needed, however, according to Dr. Borra, into the higher frequency of reported thrombocytopenia (71.7% vs. 20.8%) with sotatercept. “Our findings,” Dr. Borra said in a poster session, “suggest that sotatercept is an effective treatment option for pulmonary arterial hypertension, with the potential to improve both pulmonary and cardiac function.”
Denervation technique
Catheter-based ablation techniques, most commonly using thermal energy, target the afferent and efferent fibers of the baroreceptor reflex in the main pulmonary artery trunk and bifurcation involved in elevated pulmonary artery pressure. Mounica Vorla, MD, Carle Foundation Hospital, Urbana, Illinois, and colleagues conducted an updated systematic review and meta-analysis of the safety and efficacy of pulmonary artery denervation (PADN) for pulmonary arterial hypertension in seven clinical trials with 506 patients with moderate-severe pulmonary arterial hypertension conducted from 2013 to 2022.
Compared with placebo, PADN treatment was associated with a significant reduction in mean pulmonary artery pressure (weighted mean difference [WMD] = –6.9 mm Hg; 95% CI = –9.7, –4.1; P < .01; I2 = 61) and pulmonary vascular resistance (WMD = –3.2; 95% CI = –5.4, –0.9; P = .005). PADN improvements in cardiac output were also statistically significant (WMD = 0.3; 95% CI = 0.07, 0.6; P = .012), with numerical improvement in 6-minute walking distance (WMD = 67.7; 95% CI = –3.73, 139.2; P = .06) in the PADN group. Side effects were less common in the PADN group as compared with the placebo group, Dr. Vorla reported. She concluded, “This updated meta-analysis supports PADN as a safe and efficacious therapy for severe pulmonary arterial hypertension.” The authors noted limitations imposed by the small sample size, large data heterogeneity, and medium-quality literature. Larger randomized, controlled trials with clinical endpoints comparing PADN with optimal medical therapy are needed, they stated.
References
1. Shah AJ et al. New Drugs and Therapies in Pulmonary Arterial Hypertension. Int J Mol Sci. 2023 Mar 19;24(6):5850. doi: 10.3390/ijms24065850. PMID: 36982922; PMCID: PMC10058689.
2. Kovacs G et al. Pulmonary Vascular Involvement in Chronic Obstructive Pulmonary Disease. Is There a Pulmonary Vascular Phenotype? Am J Respir Crit Care Med. 2018 Oct 15;198(8):1000-11. doi: 10.1164/rccm.201801-0095PP. PMID: 29746142.
PHILADELPHIA — Promise that the unmet need for more effective pulmonary artery hypertension treatments may soon be met was in strong evidence in research into three strategies presented at this year’s recent American Heart Association scientific sessions; one was based on an ancient Chinese herb epimedium (yin yang huo or horny goat weed) commonly used for treating sexual dysfunction and directly related to the phosphodiesterase inhibitors sildenafil, vardenafil, and tadalafil (sold as Viagra, Levitra, and Cialis). A second studied sotatercept, an investigational, potential first-in-class activin signaling inhibitor biologic, and a third evaluated physically ablating the baroreceptor nerves that stimulate vasoconstriction of the pulmonary artery via catheter-based techniques.
Until as recently as the late 1970s, a pulmonary arterial hypertension diagnosis was a uniformly fatal one.1 While associated with pulmonary and right ventricle remodeling, and leads toward heart failure and death. The complex underlying pathogenesis was divided into six groups by the 6th World Symposium on Pulmonary Hypertension (WSPH) in 2018, and includes as its most common features pulmonary artery endothelial cell dysfunction, pulmonary artery smooth muscle cell proliferation and migration, and dysregulated fibroblast activity leading to dysregulated vasoconstriction, micro and in-situ vascular thrombosis, vascular fibrosis and pathogenic remodeling of pulmonary vessels.1 The threshold mean arterial pressure (mPAP) for pulmonary arterial hypertension was defined by the 6th [WSPH] at mPAP ≥ 20 mm Hg, twice the upper limit of a normal mPAP of 14.0 ± 3.3 mm Hg as reported by Kovacs et al. in 2018.2
Pathways for current therapies
Current drugs for pulmonary arterial hypertension focus on three signaling pathways, including the endothelin receptor, prostacyclin and nitric oxide pathways, stated Zhi-Cheng Jing, MD, professor of medicine, head of the cardiology department at Peking Union Medical College Hospital, Peking, China. While the phosphodiesterase 5 inhibitors sildenafil and tadalafil, which target the nitric oxide pathway, came into wide use after Food and Drug Administration approval, the need for higher PDE5-selectivity remains, Dr. Jing said. Structurally modified from the active ingredient in epimedium, TPN171H is an investigational PDE5 inhibitor which has shown several favorable features: a greater PDE5 selectivity than both sildenafil and tadalafil in vitro, an ability to decrease right ventricular systolic pressure and alleviate arterial remodeling in animal studies, and safety and tolerability in healthy human subjects.
The current randomized, double-blind, placebo-and active-controlled phase IIa study assessed the hemodynamic impact of a single oral dose of TPN171H in 60 pulmonary arterial hypertension patients (mean age ~34 years, 83.3% female), all with negative vasodilation test results and in WHO class 2 or 3. Only patients aged 18-75 years with group 1 pulmonary arterial hypertension of idiopathic, connective tissue disorder, or repaired congenital heart defects etiology were included. Patients were divided into six groups: placebo, TPN171H at 2.5, 5, and 10 milligrams, and tadalafil at 20 and 40 milligrams.
For the primary endpoint of maximum decrease in pulmonary vascular resistance (PVR), significant reductions vs. placebo were found only for the TPN171H 5-mg group (–41.2% vs. –24.4%; P = .008) and for the 20-mg (–39.8%) and 40-mg (–37.6%) tadalafil groups (both P < .05). What was not seen in the tadalafil groups, but was evident in the TPN171H 5-mg group, was a significant reduction in the secondary endpoint of PVR/SVR (systolic vascular resistance) at 2, 3, and 5 hours (all P < .05). “As we know,” Dr. Jing said in an interview, “the PDE5 inhibitor functions as a vasodilator, having an impact on both pulmonary circulation and systemic circulation. So, to evaluate the selectivity for pulmonary circulation is crucial when exploring a novel drug for pulmonary arterial hypertension. The change of PVR/SVR ratio from baseline is an indicator for selectivity for pulmonary circulation and implies that TPN171H has good PDE5 selectivity in the pulmonary vasculature,” Dr. Jing said.
TPN171H was well tolerated with no serious adverse effects (vomiting 10% and headache 10% were most common with no discontinuations).
TGF-signaling pathway
A meta-analysis of randomized controlled trials of sotatercept, an investigational fusion protein under priority FDA review that modulates the TGF-beta superfamily signaling pathway, looked at PVR, pulmonary arterial pressure (PAP), right arterial pressure (RAP) and N-terminal pro-brain natriuretic peptide (NT-proBNP). A literature search by corresponding author Vamsikalyan Borra, MD, Knapp Medical Center, Weslaco, Texas, and colleagues identified two trials (STELLAR and PULSAR) comprising 429 patients with pulmonary arterial hypertension. The experimental arms (sotatercept) had 237 patients (mean age ~49 years, ~82% female) and the placebo arm had 192 patients (mean age ~47 years, ~80% female).
A pooled analysis showed significant reductions with sotatercept in PVR (standardization mean difference [SMD] = –1.00, 95% confidence interval [CI] = –1.2, –.79, P < .001), PAP (SMD = –1.34, 95% CI = 1.6, –1.08, P < .001), RAP (SMD = –0.66, 95% CI = –0.93, –0.39, P < .001), and the levels of NT-proBNP (SMD = –0.64, 95% CI = –1.01, –0.27, P < .001) at 24 weeks from baseline. The sotatercept safety profile was favorable, with lower overall incidence of adverse events (84.8% vs. 87.5%) and fewer adverse events leading to death (0.4% vs. 3.1%) compared with placebo. Further investigation is needed, however, according to Dr. Borra, into the higher frequency of reported thrombocytopenia (71.7% vs. 20.8%) with sotatercept. “Our findings,” Dr. Borra said in a poster session, “suggest that sotatercept is an effective treatment option for pulmonary arterial hypertension, with the potential to improve both pulmonary and cardiac function.”
Denervation technique
Catheter-based ablation techniques, most commonly using thermal energy, target the afferent and efferent fibers of the baroreceptor reflex in the main pulmonary artery trunk and bifurcation involved in elevated pulmonary artery pressure. Mounica Vorla, MD, Carle Foundation Hospital, Urbana, Illinois, and colleagues conducted an updated systematic review and meta-analysis of the safety and efficacy of pulmonary artery denervation (PADN) for pulmonary arterial hypertension in seven clinical trials with 506 patients with moderate-severe pulmonary arterial hypertension conducted from 2013 to 2022.
Compared with placebo, PADN treatment was associated with a significant reduction in mean pulmonary artery pressure (weighted mean difference [WMD] = –6.9 mm Hg; 95% CI = –9.7, –4.1; P < .01; I2 = 61) and pulmonary vascular resistance (WMD = –3.2; 95% CI = –5.4, –0.9; P = .005). PADN improvements in cardiac output were also statistically significant (WMD = 0.3; 95% CI = 0.07, 0.6; P = .012), with numerical improvement in 6-minute walking distance (WMD = 67.7; 95% CI = –3.73, 139.2; P = .06) in the PADN group. Side effects were less common in the PADN group as compared with the placebo group, Dr. Vorla reported. She concluded, “This updated meta-analysis supports PADN as a safe and efficacious therapy for severe pulmonary arterial hypertension.” The authors noted limitations imposed by the small sample size, large data heterogeneity, and medium-quality literature. Larger randomized, controlled trials with clinical endpoints comparing PADN with optimal medical therapy are needed, they stated.
References
1. Shah AJ et al. New Drugs and Therapies in Pulmonary Arterial Hypertension. Int J Mol Sci. 2023 Mar 19;24(6):5850. doi: 10.3390/ijms24065850. PMID: 36982922; PMCID: PMC10058689.
2. Kovacs G et al. Pulmonary Vascular Involvement in Chronic Obstructive Pulmonary Disease. Is There a Pulmonary Vascular Phenotype? Am J Respir Crit Care Med. 2018 Oct 15;198(8):1000-11. doi: 10.1164/rccm.201801-0095PP. PMID: 29746142.
FROM AHA 2023
Are you sure your patient is alive?
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.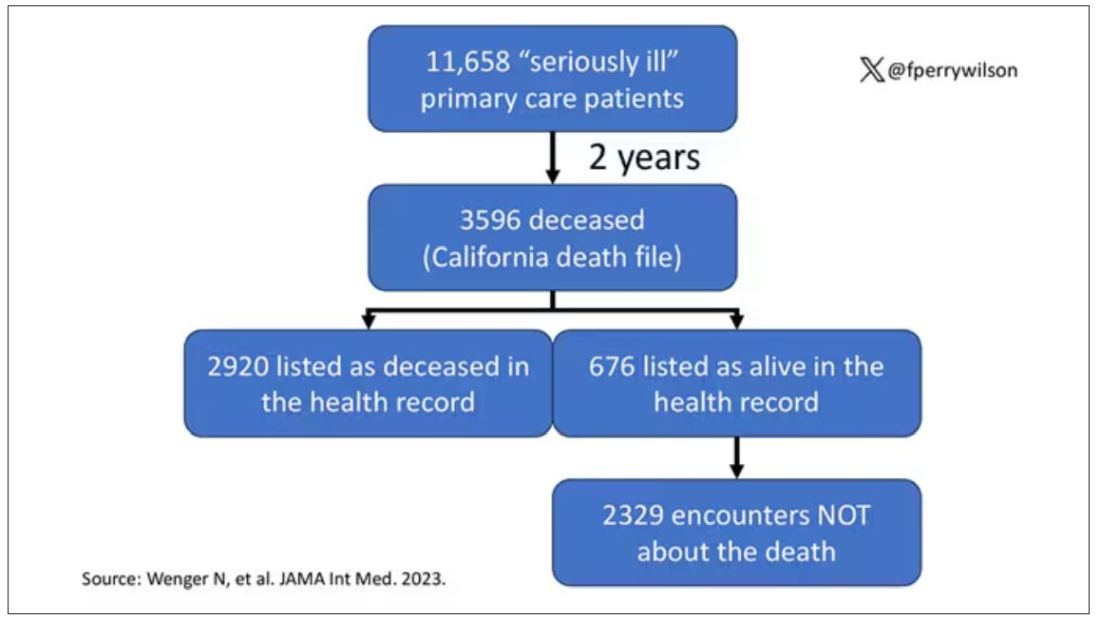
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.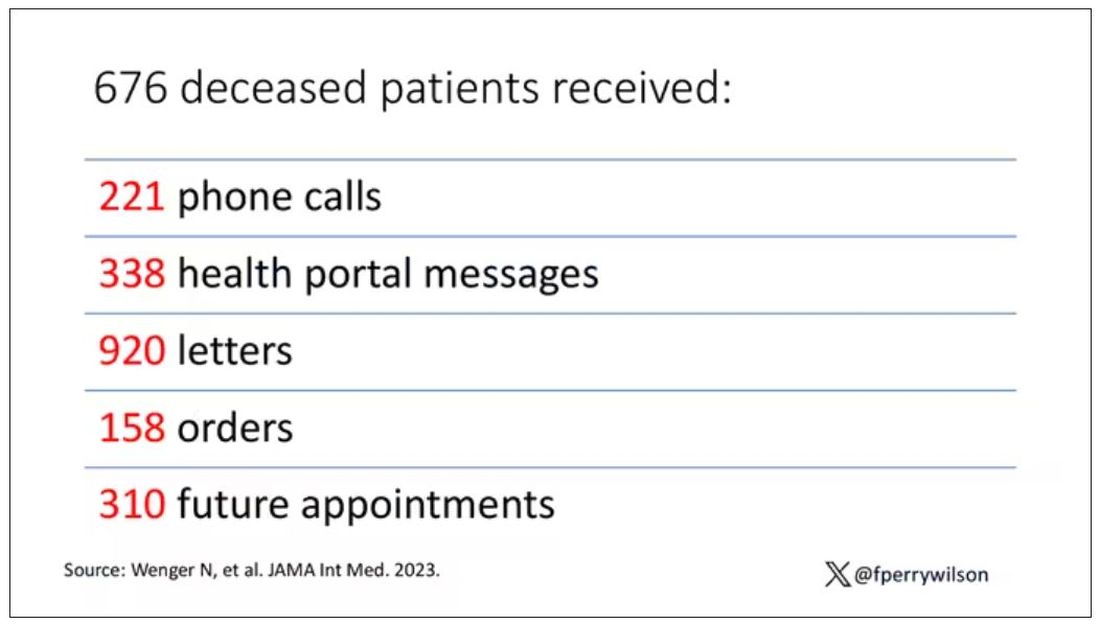
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.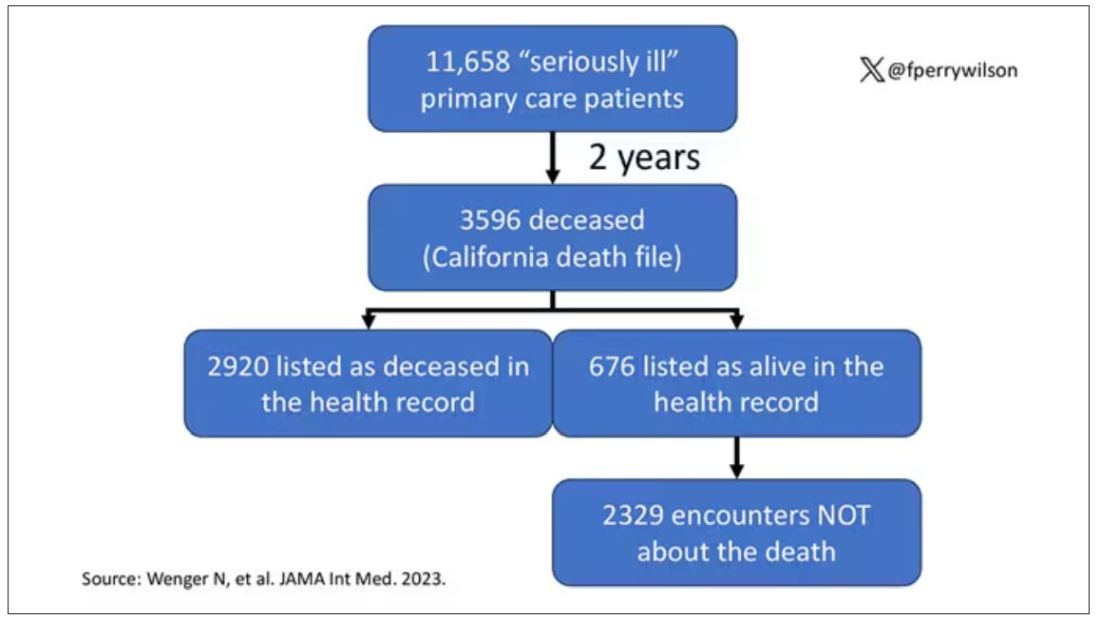
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.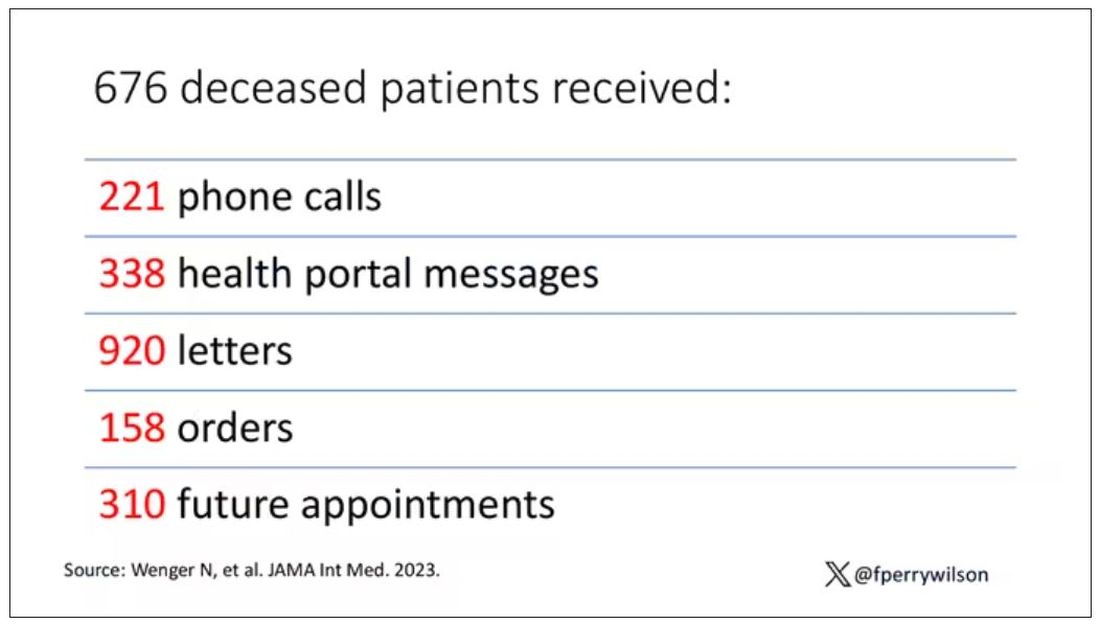
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.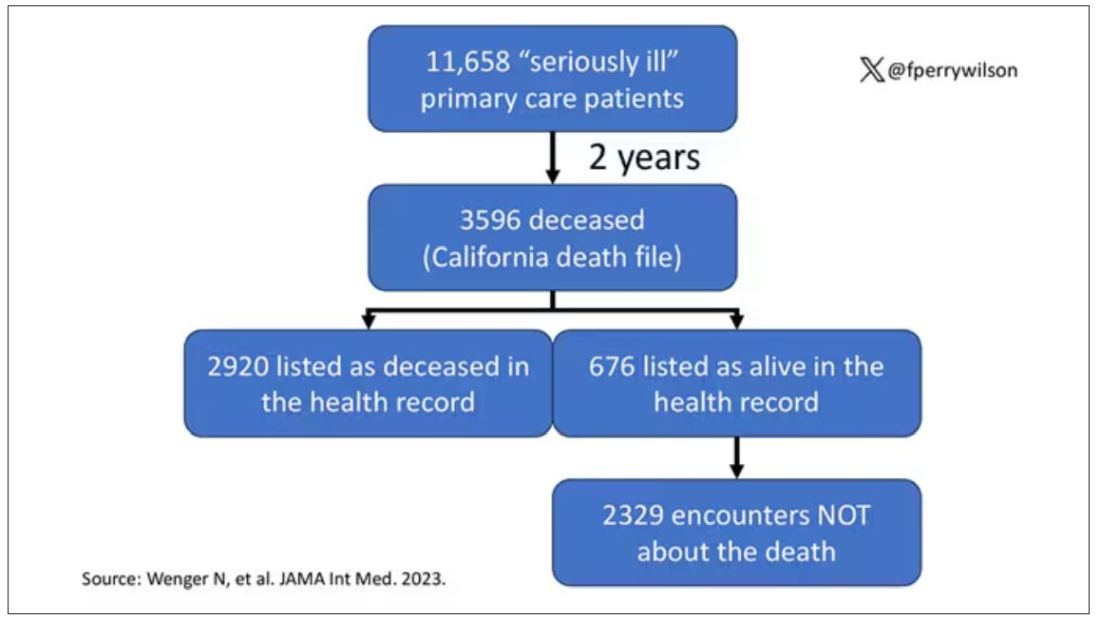
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.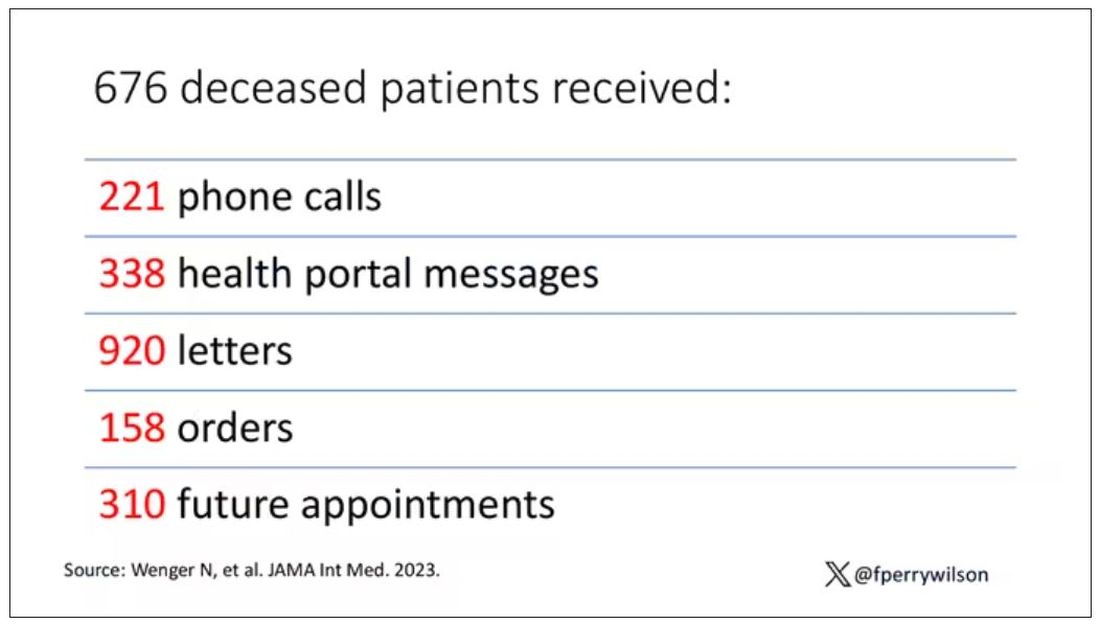
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
The prospect of a medication to treat OSA is getting closer
For researchers involved with sleep disorders, developing a pharmacologic treatment for obstructive sleep apnea (OSA) is a bit like searching for the holy grail. P K Schweitzer and colleagues have published the results of the randomized MARIPOSA study assessing a combination of two medicinal products known as AD109, one of the products having an antimuscarinic effect (aroxybutynin), and the other a noradrenergic effect (atomoxetine), in treating this condition.
MARIPOSA Methodology
The trial included 209 patients, 176 of whom completed the 4-week protocol. The trial was double-blinded according to four parallel arms: participants in the first and second arms received AD109 containing doses of 2.5 mg/75 mg and 5 mg/75 mg of aroxybutynin and atomoxetine, respectively. The third arm received atomoxetine alone (75 mg), and the fourth arm was given a placebo.
Two polysomnograms (PSGs) were carried out at the start and end of the trial, allowing researchers to calculate the apnea-hypopnea index (AHI) and to quantify nocturnal desaturation. The impact of these variables are now being deemed as the primary marker of the risk for cardiovascular complications secondary to OSA. Finally, questionnaires that evaluated excessive daytime sleepiness, fatigue, and sleep quality were completed.
The median age varied from 5 to 57 years, depending on the arm of the study, and body mass index varied between 31.2 and 34.5. Inclusion criteria comprised an AHI between 10 and 45 events per hour, of which, at least 75% were described as obstructive. Where continuous positive airway pressure (CPAP) was used (21%-30% of cases), it was abandoned during the trial (in a time frame that is perhaps too short to consider these patients as treatment naive).
Combination Brought Improvements
After the 4 weeks of treatment, the AHI measured via follow-up PSG went from a median of 20.5 to 10.8 (in arm one and from 19.4 to 9.5 in arm two (P < .0001 vs placebo in these two arms). For participants in arm three, AHI went from 19.0 to 11.8 (P < .01 vs placebo).
The rate of nocturnal desaturation (in percentage per hour) declined from -12.7 in arm one (P = .03), from -16.6 in arm two (P = .005), and from -5.2 in arm three (P = .003) compared with the placebo. The fatigue score was significantly improved by AD109 2.5 mg/75 mg. The use of atomoxetine alone slightly worsened the sleep disturbance score.
The main side effects were dry mouth sensation (which was markedly more common with AD109 5 mg/75 mg), difficulty passing urine in 7%-22% of cases, tachycardia in all trial arms, and increased diastolic blood pressure at the 2.5-mg/75-mg dose. The authors concluded that AD109, a combination of noradrenergic and antimuscarinic molecules, is effective in correcting mild to severe OSA.
The 2.5-mg/75-mg dose was as effective as the 5-mg/75-mg dose. Atomoxetine alone is less effective, has more side effects, and is associated with lower quality sleep. Finally, it is reported that compliance with oral treatment was not checked, yet the argument of patient noncompliance with CPAP is largely used by the authors in their presentation of their study. A phase 3 trial is underway.
Nevertheless, these results herald important scientific benefits if we consider that Colin Sullivan’s original 1981 research paper, which ushered in the CPAP era, presented the results of just five participants.
This article was translated from JIM, which is part of the Medscape professional network.
A version of this article appeared on Medscape.com.
For researchers involved with sleep disorders, developing a pharmacologic treatment for obstructive sleep apnea (OSA) is a bit like searching for the holy grail. P K Schweitzer and colleagues have published the results of the randomized MARIPOSA study assessing a combination of two medicinal products known as AD109, one of the products having an antimuscarinic effect (aroxybutynin), and the other a noradrenergic effect (atomoxetine), in treating this condition.
MARIPOSA Methodology
The trial included 209 patients, 176 of whom completed the 4-week protocol. The trial was double-blinded according to four parallel arms: participants in the first and second arms received AD109 containing doses of 2.5 mg/75 mg and 5 mg/75 mg of aroxybutynin and atomoxetine, respectively. The third arm received atomoxetine alone (75 mg), and the fourth arm was given a placebo.
Two polysomnograms (PSGs) were carried out at the start and end of the trial, allowing researchers to calculate the apnea-hypopnea index (AHI) and to quantify nocturnal desaturation. The impact of these variables are now being deemed as the primary marker of the risk for cardiovascular complications secondary to OSA. Finally, questionnaires that evaluated excessive daytime sleepiness, fatigue, and sleep quality were completed.
The median age varied from 5 to 57 years, depending on the arm of the study, and body mass index varied between 31.2 and 34.5. Inclusion criteria comprised an AHI between 10 and 45 events per hour, of which, at least 75% were described as obstructive. Where continuous positive airway pressure (CPAP) was used (21%-30% of cases), it was abandoned during the trial (in a time frame that is perhaps too short to consider these patients as treatment naive).
Combination Brought Improvements
After the 4 weeks of treatment, the AHI measured via follow-up PSG went from a median of 20.5 to 10.8 (in arm one and from 19.4 to 9.5 in arm two (P < .0001 vs placebo in these two arms). For participants in arm three, AHI went from 19.0 to 11.8 (P < .01 vs placebo).
The rate of nocturnal desaturation (in percentage per hour) declined from -12.7 in arm one (P = .03), from -16.6 in arm two (P = .005), and from -5.2 in arm three (P = .003) compared with the placebo. The fatigue score was significantly improved by AD109 2.5 mg/75 mg. The use of atomoxetine alone slightly worsened the sleep disturbance score.
The main side effects were dry mouth sensation (which was markedly more common with AD109 5 mg/75 mg), difficulty passing urine in 7%-22% of cases, tachycardia in all trial arms, and increased diastolic blood pressure at the 2.5-mg/75-mg dose. The authors concluded that AD109, a combination of noradrenergic and antimuscarinic molecules, is effective in correcting mild to severe OSA.
The 2.5-mg/75-mg dose was as effective as the 5-mg/75-mg dose. Atomoxetine alone is less effective, has more side effects, and is associated with lower quality sleep. Finally, it is reported that compliance with oral treatment was not checked, yet the argument of patient noncompliance with CPAP is largely used by the authors in their presentation of their study. A phase 3 trial is underway.
Nevertheless, these results herald important scientific benefits if we consider that Colin Sullivan’s original 1981 research paper, which ushered in the CPAP era, presented the results of just five participants.
This article was translated from JIM, which is part of the Medscape professional network.
A version of this article appeared on Medscape.com.
For researchers involved with sleep disorders, developing a pharmacologic treatment for obstructive sleep apnea (OSA) is a bit like searching for the holy grail. P K Schweitzer and colleagues have published the results of the randomized MARIPOSA study assessing a combination of two medicinal products known as AD109, one of the products having an antimuscarinic effect (aroxybutynin), and the other a noradrenergic effect (atomoxetine), in treating this condition.
MARIPOSA Methodology
The trial included 209 patients, 176 of whom completed the 4-week protocol. The trial was double-blinded according to four parallel arms: participants in the first and second arms received AD109 containing doses of 2.5 mg/75 mg and 5 mg/75 mg of aroxybutynin and atomoxetine, respectively. The third arm received atomoxetine alone (75 mg), and the fourth arm was given a placebo.
Two polysomnograms (PSGs) were carried out at the start and end of the trial, allowing researchers to calculate the apnea-hypopnea index (AHI) and to quantify nocturnal desaturation. The impact of these variables are now being deemed as the primary marker of the risk for cardiovascular complications secondary to OSA. Finally, questionnaires that evaluated excessive daytime sleepiness, fatigue, and sleep quality were completed.
The median age varied from 5 to 57 years, depending on the arm of the study, and body mass index varied between 31.2 and 34.5. Inclusion criteria comprised an AHI between 10 and 45 events per hour, of which, at least 75% were described as obstructive. Where continuous positive airway pressure (CPAP) was used (21%-30% of cases), it was abandoned during the trial (in a time frame that is perhaps too short to consider these patients as treatment naive).
Combination Brought Improvements
After the 4 weeks of treatment, the AHI measured via follow-up PSG went from a median of 20.5 to 10.8 (in arm one and from 19.4 to 9.5 in arm two (P < .0001 vs placebo in these two arms). For participants in arm three, AHI went from 19.0 to 11.8 (P < .01 vs placebo).
The rate of nocturnal desaturation (in percentage per hour) declined from -12.7 in arm one (P = .03), from -16.6 in arm two (P = .005), and from -5.2 in arm three (P = .003) compared with the placebo. The fatigue score was significantly improved by AD109 2.5 mg/75 mg. The use of atomoxetine alone slightly worsened the sleep disturbance score.
The main side effects were dry mouth sensation (which was markedly more common with AD109 5 mg/75 mg), difficulty passing urine in 7%-22% of cases, tachycardia in all trial arms, and increased diastolic blood pressure at the 2.5-mg/75-mg dose. The authors concluded that AD109, a combination of noradrenergic and antimuscarinic molecules, is effective in correcting mild to severe OSA.
The 2.5-mg/75-mg dose was as effective as the 5-mg/75-mg dose. Atomoxetine alone is less effective, has more side effects, and is associated with lower quality sleep. Finally, it is reported that compliance with oral treatment was not checked, yet the argument of patient noncompliance with CPAP is largely used by the authors in their presentation of their study. A phase 3 trial is underway.
Nevertheless, these results herald important scientific benefits if we consider that Colin Sullivan’s original 1981 research paper, which ushered in the CPAP era, presented the results of just five participants.
This article was translated from JIM, which is part of the Medscape professional network.
A version of this article appeared on Medscape.com.
Analysis supports link between psoriasis and obstructive sleep apnea
TOPLINE:
Patients with psoriasis had a 1.77-fold increased risk of having obstructive sleep apnea, in a study comparing patients with psoriasis with controls.
METHODOLOGY:
- Prior studies have established a link between psoriasis and obstructive sleep apnea (OSA), but some have suggested that confounders may drive the association.
- Using a case-control design, researchers analyzed data from 156,707 participants in the National Institutes of Health’s : 5140 with psoriasis and 151,567 controls.
- They used Pearson’s x 2 test to compare the prevalence of OSA among cases and controls, logistic regression to calculate odds ratios (ORs) in multivariable analysis, and two-sided t-tests to evaluate the significance between continuous variables.
TAKEAWAY:
- Compared with controls, patients with psoriasis were older (a mean of 62.4 vs 57.3 years, respectively), more likely to be White (86.1% vs 70.6%), reported higher annual household incomes (59.9% vs 52.6%), and were more likely to smoke (48.2% vs 43.4%).
- The rate of OSA was significantly higher among patients with psoriasis compared with controls (29.3% vs 17.1%; P < .001).
- On unadjusted multivariable logistic regression controlling for age, gender, and race, psoriasis was significantly associated with OSA (OR, 1.77, 95% CI, 1.66 - 1.89; P < .001).
- Psoriasis was also significantly associated with OSA in the adjusted model controlling for age, gender, race, BMI, and smoking status (OR, 1.66, 95% CI, 1.55 - 1.77; P < .001) and in the adjusted model controlling for age, gender, race, BMI, smoking status, type 2 diabetes, congestive heart failure, hypertension, history of myocardial infarction, angina, and peripheral artery disease (OR, 1.45, 95% CI, 1.35 - 1.55; P <.001).
IN PRACTICE:
“This study further substantiates the association between psoriasis and OSA, reinforcing the importance of evaluation for OSA when clinically appropriate given that both psoriasis and OSA contribute to adverse health outcomes,” the authors conclude.
SOURCE:
Corresponding author Jeffrey M. Cohen, MD, of the Department of Dermatology at Yale University, New Haven, Connecticut, led the research. The study was published online in the Journal of the American Academy of Dermatology.
LIMITATIONS:
Study limitations included the use of electronic health record data, a potential lack of generalizability to the US population, and reliance on survey data for certain variables such as income and smoking status.
DISCLOSURES:
The All of Us Research Program is supported by the National Institutes of Health. Cohen disclosed that he serves on a data safety and monitoring board for Advarra.
A version of this article appeared on Medscape.com.
TOPLINE:
Patients with psoriasis had a 1.77-fold increased risk of having obstructive sleep apnea, in a study comparing patients with psoriasis with controls.
METHODOLOGY:
- Prior studies have established a link between psoriasis and obstructive sleep apnea (OSA), but some have suggested that confounders may drive the association.
- Using a case-control design, researchers analyzed data from 156,707 participants in the National Institutes of Health’s : 5140 with psoriasis and 151,567 controls.
- They used Pearson’s x 2 test to compare the prevalence of OSA among cases and controls, logistic regression to calculate odds ratios (ORs) in multivariable analysis, and two-sided t-tests to evaluate the significance between continuous variables.
TAKEAWAY:
- Compared with controls, patients with psoriasis were older (a mean of 62.4 vs 57.3 years, respectively), more likely to be White (86.1% vs 70.6%), reported higher annual household incomes (59.9% vs 52.6%), and were more likely to smoke (48.2% vs 43.4%).
- The rate of OSA was significantly higher among patients with psoriasis compared with controls (29.3% vs 17.1%; P < .001).
- On unadjusted multivariable logistic regression controlling for age, gender, and race, psoriasis was significantly associated with OSA (OR, 1.77, 95% CI, 1.66 - 1.89; P < .001).
- Psoriasis was also significantly associated with OSA in the adjusted model controlling for age, gender, race, BMI, and smoking status (OR, 1.66, 95% CI, 1.55 - 1.77; P < .001) and in the adjusted model controlling for age, gender, race, BMI, smoking status, type 2 diabetes, congestive heart failure, hypertension, history of myocardial infarction, angina, and peripheral artery disease (OR, 1.45, 95% CI, 1.35 - 1.55; P <.001).
IN PRACTICE:
“This study further substantiates the association between psoriasis and OSA, reinforcing the importance of evaluation for OSA when clinically appropriate given that both psoriasis and OSA contribute to adverse health outcomes,” the authors conclude.
SOURCE:
Corresponding author Jeffrey M. Cohen, MD, of the Department of Dermatology at Yale University, New Haven, Connecticut, led the research. The study was published online in the Journal of the American Academy of Dermatology.
LIMITATIONS:
Study limitations included the use of electronic health record data, a potential lack of generalizability to the US population, and reliance on survey data for certain variables such as income and smoking status.
DISCLOSURES:
The All of Us Research Program is supported by the National Institutes of Health. Cohen disclosed that he serves on a data safety and monitoring board for Advarra.
A version of this article appeared on Medscape.com.
TOPLINE:
Patients with psoriasis had a 1.77-fold increased risk of having obstructive sleep apnea, in a study comparing patients with psoriasis with controls.
METHODOLOGY:
- Prior studies have established a link between psoriasis and obstructive sleep apnea (OSA), but some have suggested that confounders may drive the association.
- Using a case-control design, researchers analyzed data from 156,707 participants in the National Institutes of Health’s : 5140 with psoriasis and 151,567 controls.
- They used Pearson’s x 2 test to compare the prevalence of OSA among cases and controls, logistic regression to calculate odds ratios (ORs) in multivariable analysis, and two-sided t-tests to evaluate the significance between continuous variables.
TAKEAWAY:
- Compared with controls, patients with psoriasis were older (a mean of 62.4 vs 57.3 years, respectively), more likely to be White (86.1% vs 70.6%), reported higher annual household incomes (59.9% vs 52.6%), and were more likely to smoke (48.2% vs 43.4%).
- The rate of OSA was significantly higher among patients with psoriasis compared with controls (29.3% vs 17.1%; P < .001).
- On unadjusted multivariable logistic regression controlling for age, gender, and race, psoriasis was significantly associated with OSA (OR, 1.77, 95% CI, 1.66 - 1.89; P < .001).
- Psoriasis was also significantly associated with OSA in the adjusted model controlling for age, gender, race, BMI, and smoking status (OR, 1.66, 95% CI, 1.55 - 1.77; P < .001) and in the adjusted model controlling for age, gender, race, BMI, smoking status, type 2 diabetes, congestive heart failure, hypertension, history of myocardial infarction, angina, and peripheral artery disease (OR, 1.45, 95% CI, 1.35 - 1.55; P <.001).
IN PRACTICE:
“This study further substantiates the association between psoriasis and OSA, reinforcing the importance of evaluation for OSA when clinically appropriate given that both psoriasis and OSA contribute to adverse health outcomes,” the authors conclude.
SOURCE:
Corresponding author Jeffrey M. Cohen, MD, of the Department of Dermatology at Yale University, New Haven, Connecticut, led the research. The study was published online in the Journal of the American Academy of Dermatology.
LIMITATIONS:
Study limitations included the use of electronic health record data, a potential lack of generalizability to the US population, and reliance on survey data for certain variables such as income and smoking status.
DISCLOSURES:
The All of Us Research Program is supported by the National Institutes of Health. Cohen disclosed that he serves on a data safety and monitoring board for Advarra.
A version of this article appeared on Medscape.com.
Smoking alters salivary microbiota in potential path to disease risk
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
TOPLINE:
Salivary microbiota changes caused by cigarette smoking may affect metabolic pathways and increase disease risk.
METHODOLOGY:
The researchers analyzed health information and data on the composition of salivary microbiota from 1601 adult participants in the Cooperative Health Research in South Tyrol (CHRIS) microbiome study (CHRISMB); CHRIS is an ongoing study in Italy.
The average age of the study population was 45 years; 53% were female, and 45% were current or former smokers.
The researchers hypothesized that changes in salivary microbial composition would be associated with smoking, with more nitrate-reducing bacteria present, and that nitrate reduction pathways would be reduced in smokers.
TAKEAWAY:
The researchers identified 44 genera that differed in the salivary microbiota of current smokers and nonsmokers. In smokers, seven genera in the phylum Proteobacteria were decreased and six in the phylum Actinobacteria were increased compared with nonsmokers; these phyla contain primarily aerobic and anaerobic taxa, respectively.
Some microbiota changes were significantly associated with daily smoking intensity; genera from the classes Betaproteobacteria (Lautropia or Neisseria), Gammaproteobacteria (Cardiobacterium), and Flavobacteriia (Capnocytophaga) decreased significantly with increased grams of tobacco smoked per day, measured in 5-g increments.
Smoking was associated with changes in the salivary microbiota; the nitrate reduction pathway was significantly lower in smokers compared with nonsmokers, and these decreases were consistent with previous studies of decreased cardiovascular events in former smokers.
However, the salivary microbiota of smokers who had quit for at least 5 years resembled that of individuals who had never smoked.
IN PRACTICE:
“Decreased microbial nitrate reduction pathway abundance in smokers may provide an additional explanation for the effect of smoking on cardiovascular and periodontal diseases risk, a hypothesis which should be tested in future studies,” the researchers wrote.
SOURCE:
The lead author of the study was Giacomo Antonello, MD, of Eurac Research, Affiliated Institute of the University of Lübeck, Bolzano, Italy. The study was published online in Scientific Reports (a Nature journal) on November 2, 2023.
LIMITATIONS:
The cross-sectional design and lack of professional assessment of tooth and gum health were limiting factors, as were potential confounding factors including medication use, diet, and alcohol intake.
DISCLOSURES:
The study was supported by the Department of Innovation, Research and University of the Autonomous Province of Bolzano-South Tyrol and by the European Regional Development Fund. The CHRISMB microbiota data generation was funded by the National Institute of Dental and Craniofacial Research. The researchers had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.