User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


An update on the pharmacologic treatment of hypersomnia
The hypersomnias are an etiologically diverse group of disorders of wakefulness and sleep, characterized principally by excessive daytime sleepiness (EDS), often despite sufficient or even long total sleep durations. Hypersomnolence may be severely disabling and isolating for patients, is associated with decreased quality of life and economic disadvantage, and, in some cases, may pose a personal and public health danger through drowsy driving. Though historically, management of these patients has been principally supportive and aimed at reducing daytime functional impairment, new and evolving treatments are quickly changing management paradigms in this population. This brief review highlights some of the newest pharmacotherapeutic advances in this dynamic field.
Hypersomnolence is a common presenting concern primary care and sleep clinics, with an estimated prevalence of EDS in the general adult population of as high as 6%.1 The initial diagnosis of hypersomnia is, broadly, a clinical one, with careful consideration to the patient’s report of daytime sleepiness and functional impairment, sleep/wake cycle, and any medical comorbidities. The primary hypersomnias include narcolepsy type 1 (narcolepsy with cataplexy, NT1) and narcolepsy type 2 (without cataplexy, NT2), Kleine-Levin Syndrome (KLS), and idiopathic hypersomnia. Secondary hypersomnia disorders are more commonly encountered in clinical practice and include hypersomnia attributable to another medical condition (including psychiatric and neurologic disorders), hypersomnia related to medication effects, and EDS related to behaviorally insufficient sleep. Distinguishing primary and secondary etiologies, when possible, is important as treatment pathways may vary considerably between hypersomnias.
Generally, overnight in-lab polysomnography is warranted to exclude untreated or sub-optimally treated sleep-disordered breathing or movement disorders which may undermine sleep quality. In the absence of any such findings, this is usually followed by daytime multiple sleep latency testing (MSLT). The MSLT is comprised of four to five scheduled daytime naps in the sleep lab and is designed to quantify a patient’s propensity to sleep during the day and to identify architectural sleep abnormalities which indicate narcolepsy. Specifically, narcolepsy is identified by MSLT when a patient exhibits a sleep onset latency of ≤ 8 minutes and at least two sleep-onset REM periods (SOREMPs), or, one SOREMP on MSLT with a second noted on the preceding night’s PSG. Actigraphy or sleep logs may be helpful in quantifying a patient’s total sleep time in their home environment. Adjunctive laboratory tests for narcolepsy including HLA typing and CSF hypocretin testing may sometimes be indicated.
General hypersomnia management usually consists of the use of wakefulness promoting agents, such as stimulants (eg, dexmethylphenidate) and dopamine-modulating agents (eg, modafinil, armodafinil), and adjunctive supportive strategies, including planned daytime naps and elimination of modifiable secondary causes. In those patients with hypersomnolence associated with depression or anxiety, the use of antidepressants, including SSRI, SNRI, and DNRIs, is often effective, and these medications can also improve cataplexy symptoms in narcoleptics. KLS may respond to treatment with lithium, shortening the duration of the striking hypersomnolent episodes characteristic of this rare syndrome, and there is some indication that ketamine may also be a helpful adjunctive in some cases. In treatment-refractory cases of hypersomnolence associated with GABA-A receptor potentiation, drugs such as flumazenil and clarithromycin appear to improve subjective measures of hypersomnolence.2,3 In patients with narcolepsy, sodium oxybate (available as Xyrem and, more recently, as a generic medication) has proven to be clinically very useful, reducing EDS and the frequency and severity of cataplexy and sleep disturbance associated with this condition. In July 2020, the FDA approved a new, low-sodium formulation of sodium oxybate (Xywav) for patients 7 years of age and older with a diagnosis of narcolepsy, a helpful option in those patients with cardiovascular and renal disease.
Despite this broadening armamentarium, in many cases daytime sleepiness and functional impairment is refractory to typical pharmacotherapy. In this context, we would like to highlight two newer pharmacotherapeutic options, solriamfetol and pitolisant.
Solriamfetol
Solriamfetol (Sunosi) is a Schedule IV FDA-approved medication indicated for treatment of EDS in adults with narcolepsy or obstructive sleep apnea. The precise mechanism of action is unknown, but this medication is believed to inhibit both dopamine and norepinerphrine reuptake in the brain, similar to the widely-prescribed NDRI buproprion. In a 12-week RCT study on its effects on narcolepsy in adults, solriamfetol improved important measures of wakefulness and sleepiness, without associated polysomnographic evidence of significant sleep disruption.4 In another 12-week RCT study of solriamfetol in adult patients with EDS related to OSA, there was a dose-dependent improvement in measures of wakefulness.5 Some notable side-effects seen with this medication include anxiety and elevated mood, as well as increases in blood pressure. A subsequent study of this medication found that it was efficacious at maintenance of improvements at 6 months.6 Given the theorized mechanism of action as an NDRI, future observation and studies could provide insights on its effect on depression, as well.
Pitolisant
Histaminergic neurons within the CNS play an important role in the promotion of wakefulness. Pitolisant (Wakix) is an interesting wakefulness-promoting agent for adult patients with narcolepsy. It acts as an inverse agonist and antagonist of histamine H3 receptors, resulting in a reduction of the usual feedback inhibition effected through the H3 receptor, thereby enhancing CNS release of histamine and other neurotransmitters. This medication was approved by the FDA in August 2019 and is currently indicated for adult patients with narcolepsy. The HARMONY I trial comparing pitolisant with both placebo and modafinil in adults with narcolepsy and EDS demonstrated improvement in measures of sleepiness and maintenance of wakefulness over placebo, and noninferiority to modafinil.7 In addition, pitolisant had a favorable side-effect profile compared with modafinil. Subsequent studies have reaffirmed the safety profile of pitolisant, including its minimal abuse potential. In one recent placebo-controlled trial of the use of pitolisant in a population of 268 adults with positive airway pressure (PAP) non-adherence, pitolisant was found to improve measures of EDS and related patient-reported measurements in patients with OSA who were CPAP nonadherent.8 Though generally well-tolerated by patients, in initial clinical trials pitolisant was associated with increased headache, insomnia, and nausea relative to placebo, among other less commonly reported adverse effects. Pitolisant is QT interval-prolonging, so caution must be taken when using this medication in combination other medications which may induce QT interval prolongation, including SSRIs.
Future directions
Greater awareness of the hypersomnias and their management has led to improved outcomes and access to care for these patients, yet these disorders remain burdensome and the treatments imperfect. Looking forward, novel pharmacotherapies that target underlying mechanisms rather than symptom palliation will allow for more precise treatments. Ongoing investigations of hypocretin receptor agonists seek to target one critical central mediator of wakefulness. Recent studies have highlighted the association of dysautonomia with hypersomnia, offering interesting insight into possible future targets to improve the function and quality of life of these patients.9 Similarly, understanding of the interplay between psychiatric disorders and primary and secondary hypersomnias may offer new therapeutic pathways.
As treatment plans targeting hypersomnia become more comprehensive and holistic, with an increased emphasis on self-care, sleep hygiene, and mental health awareness, in addition to mechanism-specific treatments, we hope they will ultimately provide improved symptom and burden relief for our patients.
Dr. Shih Yee-Marie Tan Gipson is a psychiatrist and Dr. Kevin Gipson is a sleep medicine specialist, both with Massachusetts General Hospital, Boston.
References
1 Dauvilliers, et al. Hypersomnia. Dialogues Clin Neurosci. 2005;7(4):347-356.
2 Trotti, et al. Clarithromycin in gamma-aminobutyric acid-related hypersomnolence: A randomized, crossover trial. Ann Neurol. 2015;78(3):454-465. doi: 10.1002/ana.24459.
3 Trotti, et al. Flumazenil for the treatment of refractory hypersomnolence: Clinical experience with 153 patients. J Clin Sleep Med. 2016;12(10):1389-1394. doi: 10.5664/jcsm.6196.
4 Thorpy, et al. A randomized study of solriamfetol for excessive sleepiness in narcolepsy. Ann Neurol. 2019; 85(3):359-370. doi: 10.1002/ana.25423.
5 Schweitzer, et al. Solriamfetol for excessive sleepiness in obstructive sleep apnea (TONES 3): A randomized controlled trial. Am J Respir Crit Care Med. 2019;199(11):1421-1431. doi: 10.1164/rccm.201806-1100OC.
6 Malhotra, et al. Long-term study of the safety and maintenance of efficacy of solriamfetol (JZP-110) in the treatment of excessive sleepiness in participants with narcolepsy or obstructive sleep apnea. Sleep. 2020; 43(2): doi: 10.1093/sleep/zsz220.
7 Dauvilliers, et al. Pitolisant versus placebo or modafinil in patients with narcolepsy: a double-blind, randomised trial. Lancet Neurol. 2013;12(11):1068-1075. doi: 10.1016/S1474-4422(13)70225-4.
8 Dauvilliers, et al. Pitolisant for daytime sleepiness in obstructive sleep apnea patients refusing CPAP: A randomized trial. Am J Respir Crit Care Med. 2020. doi: 10.1164/rccm.201907-1284OC.
9 Miglis, et al. Frequency and severity of autonomic symptoms in idiopathic hypersomnia. J Clin Sleep Med. 2020; 16(5):749-756. doi: 10.5664/jcsm.8344.
The hypersomnias are an etiologically diverse group of disorders of wakefulness and sleep, characterized principally by excessive daytime sleepiness (EDS), often despite sufficient or even long total sleep durations. Hypersomnolence may be severely disabling and isolating for patients, is associated with decreased quality of life and economic disadvantage, and, in some cases, may pose a personal and public health danger through drowsy driving. Though historically, management of these patients has been principally supportive and aimed at reducing daytime functional impairment, new and evolving treatments are quickly changing management paradigms in this population. This brief review highlights some of the newest pharmacotherapeutic advances in this dynamic field.
Hypersomnolence is a common presenting concern primary care and sleep clinics, with an estimated prevalence of EDS in the general adult population of as high as 6%.1 The initial diagnosis of hypersomnia is, broadly, a clinical one, with careful consideration to the patient’s report of daytime sleepiness and functional impairment, sleep/wake cycle, and any medical comorbidities. The primary hypersomnias include narcolepsy type 1 (narcolepsy with cataplexy, NT1) and narcolepsy type 2 (without cataplexy, NT2), Kleine-Levin Syndrome (KLS), and idiopathic hypersomnia. Secondary hypersomnia disorders are more commonly encountered in clinical practice and include hypersomnia attributable to another medical condition (including psychiatric and neurologic disorders), hypersomnia related to medication effects, and EDS related to behaviorally insufficient sleep. Distinguishing primary and secondary etiologies, when possible, is important as treatment pathways may vary considerably between hypersomnias.
Generally, overnight in-lab polysomnography is warranted to exclude untreated or sub-optimally treated sleep-disordered breathing or movement disorders which may undermine sleep quality. In the absence of any such findings, this is usually followed by daytime multiple sleep latency testing (MSLT). The MSLT is comprised of four to five scheduled daytime naps in the sleep lab and is designed to quantify a patient’s propensity to sleep during the day and to identify architectural sleep abnormalities which indicate narcolepsy. Specifically, narcolepsy is identified by MSLT when a patient exhibits a sleep onset latency of ≤ 8 minutes and at least two sleep-onset REM periods (SOREMPs), or, one SOREMP on MSLT with a second noted on the preceding night’s PSG. Actigraphy or sleep logs may be helpful in quantifying a patient’s total sleep time in their home environment. Adjunctive laboratory tests for narcolepsy including HLA typing and CSF hypocretin testing may sometimes be indicated.
General hypersomnia management usually consists of the use of wakefulness promoting agents, such as stimulants (eg, dexmethylphenidate) and dopamine-modulating agents (eg, modafinil, armodafinil), and adjunctive supportive strategies, including planned daytime naps and elimination of modifiable secondary causes. In those patients with hypersomnolence associated with depression or anxiety, the use of antidepressants, including SSRI, SNRI, and DNRIs, is often effective, and these medications can also improve cataplexy symptoms in narcoleptics. KLS may respond to treatment with lithium, shortening the duration of the striking hypersomnolent episodes characteristic of this rare syndrome, and there is some indication that ketamine may also be a helpful adjunctive in some cases. In treatment-refractory cases of hypersomnolence associated with GABA-A receptor potentiation, drugs such as flumazenil and clarithromycin appear to improve subjective measures of hypersomnolence.2,3 In patients with narcolepsy, sodium oxybate (available as Xyrem and, more recently, as a generic medication) has proven to be clinically very useful, reducing EDS and the frequency and severity of cataplexy and sleep disturbance associated with this condition. In July 2020, the FDA approved a new, low-sodium formulation of sodium oxybate (Xywav) for patients 7 years of age and older with a diagnosis of narcolepsy, a helpful option in those patients with cardiovascular and renal disease.
Despite this broadening armamentarium, in many cases daytime sleepiness and functional impairment is refractory to typical pharmacotherapy. In this context, we would like to highlight two newer pharmacotherapeutic options, solriamfetol and pitolisant.
Solriamfetol
Solriamfetol (Sunosi) is a Schedule IV FDA-approved medication indicated for treatment of EDS in adults with narcolepsy or obstructive sleep apnea. The precise mechanism of action is unknown, but this medication is believed to inhibit both dopamine and norepinerphrine reuptake in the brain, similar to the widely-prescribed NDRI buproprion. In a 12-week RCT study on its effects on narcolepsy in adults, solriamfetol improved important measures of wakefulness and sleepiness, without associated polysomnographic evidence of significant sleep disruption.4 In another 12-week RCT study of solriamfetol in adult patients with EDS related to OSA, there was a dose-dependent improvement in measures of wakefulness.5 Some notable side-effects seen with this medication include anxiety and elevated mood, as well as increases in blood pressure. A subsequent study of this medication found that it was efficacious at maintenance of improvements at 6 months.6 Given the theorized mechanism of action as an NDRI, future observation and studies could provide insights on its effect on depression, as well.
Pitolisant
Histaminergic neurons within the CNS play an important role in the promotion of wakefulness. Pitolisant (Wakix) is an interesting wakefulness-promoting agent for adult patients with narcolepsy. It acts as an inverse agonist and antagonist of histamine H3 receptors, resulting in a reduction of the usual feedback inhibition effected through the H3 receptor, thereby enhancing CNS release of histamine and other neurotransmitters. This medication was approved by the FDA in August 2019 and is currently indicated for adult patients with narcolepsy. The HARMONY I trial comparing pitolisant with both placebo and modafinil in adults with narcolepsy and EDS demonstrated improvement in measures of sleepiness and maintenance of wakefulness over placebo, and noninferiority to modafinil.7 In addition, pitolisant had a favorable side-effect profile compared with modafinil. Subsequent studies have reaffirmed the safety profile of pitolisant, including its minimal abuse potential. In one recent placebo-controlled trial of the use of pitolisant in a population of 268 adults with positive airway pressure (PAP) non-adherence, pitolisant was found to improve measures of EDS and related patient-reported measurements in patients with OSA who were CPAP nonadherent.8 Though generally well-tolerated by patients, in initial clinical trials pitolisant was associated with increased headache, insomnia, and nausea relative to placebo, among other less commonly reported adverse effects. Pitolisant is QT interval-prolonging, so caution must be taken when using this medication in combination other medications which may induce QT interval prolongation, including SSRIs.
Future directions
Greater awareness of the hypersomnias and their management has led to improved outcomes and access to care for these patients, yet these disorders remain burdensome and the treatments imperfect. Looking forward, novel pharmacotherapies that target underlying mechanisms rather than symptom palliation will allow for more precise treatments. Ongoing investigations of hypocretin receptor agonists seek to target one critical central mediator of wakefulness. Recent studies have highlighted the association of dysautonomia with hypersomnia, offering interesting insight into possible future targets to improve the function and quality of life of these patients.9 Similarly, understanding of the interplay between psychiatric disorders and primary and secondary hypersomnias may offer new therapeutic pathways.
As treatment plans targeting hypersomnia become more comprehensive and holistic, with an increased emphasis on self-care, sleep hygiene, and mental health awareness, in addition to mechanism-specific treatments, we hope they will ultimately provide improved symptom and burden relief for our patients.
Dr. Shih Yee-Marie Tan Gipson is a psychiatrist and Dr. Kevin Gipson is a sleep medicine specialist, both with Massachusetts General Hospital, Boston.
References
1 Dauvilliers, et al. Hypersomnia. Dialogues Clin Neurosci. 2005;7(4):347-356.
2 Trotti, et al. Clarithromycin in gamma-aminobutyric acid-related hypersomnolence: A randomized, crossover trial. Ann Neurol. 2015;78(3):454-465. doi: 10.1002/ana.24459.
3 Trotti, et al. Flumazenil for the treatment of refractory hypersomnolence: Clinical experience with 153 patients. J Clin Sleep Med. 2016;12(10):1389-1394. doi: 10.5664/jcsm.6196.
4 Thorpy, et al. A randomized study of solriamfetol for excessive sleepiness in narcolepsy. Ann Neurol. 2019; 85(3):359-370. doi: 10.1002/ana.25423.
5 Schweitzer, et al. Solriamfetol for excessive sleepiness in obstructive sleep apnea (TONES 3): A randomized controlled trial. Am J Respir Crit Care Med. 2019;199(11):1421-1431. doi: 10.1164/rccm.201806-1100OC.
6 Malhotra, et al. Long-term study of the safety and maintenance of efficacy of solriamfetol (JZP-110) in the treatment of excessive sleepiness in participants with narcolepsy or obstructive sleep apnea. Sleep. 2020; 43(2): doi: 10.1093/sleep/zsz220.
7 Dauvilliers, et al. Pitolisant versus placebo or modafinil in patients with narcolepsy: a double-blind, randomised trial. Lancet Neurol. 2013;12(11):1068-1075. doi: 10.1016/S1474-4422(13)70225-4.
8 Dauvilliers, et al. Pitolisant for daytime sleepiness in obstructive sleep apnea patients refusing CPAP: A randomized trial. Am J Respir Crit Care Med. 2020. doi: 10.1164/rccm.201907-1284OC.
9 Miglis, et al. Frequency and severity of autonomic symptoms in idiopathic hypersomnia. J Clin Sleep Med. 2020; 16(5):749-756. doi: 10.5664/jcsm.8344.
The hypersomnias are an etiologically diverse group of disorders of wakefulness and sleep, characterized principally by excessive daytime sleepiness (EDS), often despite sufficient or even long total sleep durations. Hypersomnolence may be severely disabling and isolating for patients, is associated with decreased quality of life and economic disadvantage, and, in some cases, may pose a personal and public health danger through drowsy driving. Though historically, management of these patients has been principally supportive and aimed at reducing daytime functional impairment, new and evolving treatments are quickly changing management paradigms in this population. This brief review highlights some of the newest pharmacotherapeutic advances in this dynamic field.
Hypersomnolence is a common presenting concern primary care and sleep clinics, with an estimated prevalence of EDS in the general adult population of as high as 6%.1 The initial diagnosis of hypersomnia is, broadly, a clinical one, with careful consideration to the patient’s report of daytime sleepiness and functional impairment, sleep/wake cycle, and any medical comorbidities. The primary hypersomnias include narcolepsy type 1 (narcolepsy with cataplexy, NT1) and narcolepsy type 2 (without cataplexy, NT2), Kleine-Levin Syndrome (KLS), and idiopathic hypersomnia. Secondary hypersomnia disorders are more commonly encountered in clinical practice and include hypersomnia attributable to another medical condition (including psychiatric and neurologic disorders), hypersomnia related to medication effects, and EDS related to behaviorally insufficient sleep. Distinguishing primary and secondary etiologies, when possible, is important as treatment pathways may vary considerably between hypersomnias.
Generally, overnight in-lab polysomnography is warranted to exclude untreated or sub-optimally treated sleep-disordered breathing or movement disorders which may undermine sleep quality. In the absence of any such findings, this is usually followed by daytime multiple sleep latency testing (MSLT). The MSLT is comprised of four to five scheduled daytime naps in the sleep lab and is designed to quantify a patient’s propensity to sleep during the day and to identify architectural sleep abnormalities which indicate narcolepsy. Specifically, narcolepsy is identified by MSLT when a patient exhibits a sleep onset latency of ≤ 8 minutes and at least two sleep-onset REM periods (SOREMPs), or, one SOREMP on MSLT with a second noted on the preceding night’s PSG. Actigraphy or sleep logs may be helpful in quantifying a patient’s total sleep time in their home environment. Adjunctive laboratory tests for narcolepsy including HLA typing and CSF hypocretin testing may sometimes be indicated.
General hypersomnia management usually consists of the use of wakefulness promoting agents, such as stimulants (eg, dexmethylphenidate) and dopamine-modulating agents (eg, modafinil, armodafinil), and adjunctive supportive strategies, including planned daytime naps and elimination of modifiable secondary causes. In those patients with hypersomnolence associated with depression or anxiety, the use of antidepressants, including SSRI, SNRI, and DNRIs, is often effective, and these medications can also improve cataplexy symptoms in narcoleptics. KLS may respond to treatment with lithium, shortening the duration of the striking hypersomnolent episodes characteristic of this rare syndrome, and there is some indication that ketamine may also be a helpful adjunctive in some cases. In treatment-refractory cases of hypersomnolence associated with GABA-A receptor potentiation, drugs such as flumazenil and clarithromycin appear to improve subjective measures of hypersomnolence.2,3 In patients with narcolepsy, sodium oxybate (available as Xyrem and, more recently, as a generic medication) has proven to be clinically very useful, reducing EDS and the frequency and severity of cataplexy and sleep disturbance associated with this condition. In July 2020, the FDA approved a new, low-sodium formulation of sodium oxybate (Xywav) for patients 7 years of age and older with a diagnosis of narcolepsy, a helpful option in those patients with cardiovascular and renal disease.
Despite this broadening armamentarium, in many cases daytime sleepiness and functional impairment is refractory to typical pharmacotherapy. In this context, we would like to highlight two newer pharmacotherapeutic options, solriamfetol and pitolisant.
Solriamfetol
Solriamfetol (Sunosi) is a Schedule IV FDA-approved medication indicated for treatment of EDS in adults with narcolepsy or obstructive sleep apnea. The precise mechanism of action is unknown, but this medication is believed to inhibit both dopamine and norepinerphrine reuptake in the brain, similar to the widely-prescribed NDRI buproprion. In a 12-week RCT study on its effects on narcolepsy in adults, solriamfetol improved important measures of wakefulness and sleepiness, without associated polysomnographic evidence of significant sleep disruption.4 In another 12-week RCT study of solriamfetol in adult patients with EDS related to OSA, there was a dose-dependent improvement in measures of wakefulness.5 Some notable side-effects seen with this medication include anxiety and elevated mood, as well as increases in blood pressure. A subsequent study of this medication found that it was efficacious at maintenance of improvements at 6 months.6 Given the theorized mechanism of action as an NDRI, future observation and studies could provide insights on its effect on depression, as well.
Pitolisant
Histaminergic neurons within the CNS play an important role in the promotion of wakefulness. Pitolisant (Wakix) is an interesting wakefulness-promoting agent for adult patients with narcolepsy. It acts as an inverse agonist and antagonist of histamine H3 receptors, resulting in a reduction of the usual feedback inhibition effected through the H3 receptor, thereby enhancing CNS release of histamine and other neurotransmitters. This medication was approved by the FDA in August 2019 and is currently indicated for adult patients with narcolepsy. The HARMONY I trial comparing pitolisant with both placebo and modafinil in adults with narcolepsy and EDS demonstrated improvement in measures of sleepiness and maintenance of wakefulness over placebo, and noninferiority to modafinil.7 In addition, pitolisant had a favorable side-effect profile compared with modafinil. Subsequent studies have reaffirmed the safety profile of pitolisant, including its minimal abuse potential. In one recent placebo-controlled trial of the use of pitolisant in a population of 268 adults with positive airway pressure (PAP) non-adherence, pitolisant was found to improve measures of EDS and related patient-reported measurements in patients with OSA who were CPAP nonadherent.8 Though generally well-tolerated by patients, in initial clinical trials pitolisant was associated with increased headache, insomnia, and nausea relative to placebo, among other less commonly reported adverse effects. Pitolisant is QT interval-prolonging, so caution must be taken when using this medication in combination other medications which may induce QT interval prolongation, including SSRIs.
Future directions
Greater awareness of the hypersomnias and their management has led to improved outcomes and access to care for these patients, yet these disorders remain burdensome and the treatments imperfect. Looking forward, novel pharmacotherapies that target underlying mechanisms rather than symptom palliation will allow for more precise treatments. Ongoing investigations of hypocretin receptor agonists seek to target one critical central mediator of wakefulness. Recent studies have highlighted the association of dysautonomia with hypersomnia, offering interesting insight into possible future targets to improve the function and quality of life of these patients.9 Similarly, understanding of the interplay between psychiatric disorders and primary and secondary hypersomnias may offer new therapeutic pathways.
As treatment plans targeting hypersomnia become more comprehensive and holistic, with an increased emphasis on self-care, sleep hygiene, and mental health awareness, in addition to mechanism-specific treatments, we hope they will ultimately provide improved symptom and burden relief for our patients.
Dr. Shih Yee-Marie Tan Gipson is a psychiatrist and Dr. Kevin Gipson is a sleep medicine specialist, both with Massachusetts General Hospital, Boston.
References
1 Dauvilliers, et al. Hypersomnia. Dialogues Clin Neurosci. 2005;7(4):347-356.
2 Trotti, et al. Clarithromycin in gamma-aminobutyric acid-related hypersomnolence: A randomized, crossover trial. Ann Neurol. 2015;78(3):454-465. doi: 10.1002/ana.24459.
3 Trotti, et al. Flumazenil for the treatment of refractory hypersomnolence: Clinical experience with 153 patients. J Clin Sleep Med. 2016;12(10):1389-1394. doi: 10.5664/jcsm.6196.
4 Thorpy, et al. A randomized study of solriamfetol for excessive sleepiness in narcolepsy. Ann Neurol. 2019; 85(3):359-370. doi: 10.1002/ana.25423.
5 Schweitzer, et al. Solriamfetol for excessive sleepiness in obstructive sleep apnea (TONES 3): A randomized controlled trial. Am J Respir Crit Care Med. 2019;199(11):1421-1431. doi: 10.1164/rccm.201806-1100OC.
6 Malhotra, et al. Long-term study of the safety and maintenance of efficacy of solriamfetol (JZP-110) in the treatment of excessive sleepiness in participants with narcolepsy or obstructive sleep apnea. Sleep. 2020; 43(2): doi: 10.1093/sleep/zsz220.
7 Dauvilliers, et al. Pitolisant versus placebo or modafinil in patients with narcolepsy: a double-blind, randomised trial. Lancet Neurol. 2013;12(11):1068-1075. doi: 10.1016/S1474-4422(13)70225-4.
8 Dauvilliers, et al. Pitolisant for daytime sleepiness in obstructive sleep apnea patients refusing CPAP: A randomized trial. Am J Respir Crit Care Med. 2020. doi: 10.1164/rccm.201907-1284OC.
9 Miglis, et al. Frequency and severity of autonomic symptoms in idiopathic hypersomnia. J Clin Sleep Med. 2020; 16(5):749-756. doi: 10.5664/jcsm.8344.
Coronavirus-associated aspergillosis increased 30-day mortality risk
Researchers are beginning to make some headway in identifying the role of secondary infections in the course and outcomes of COVID-19.
Patients who are on ventilatory support for severe COVID-19 infections appear to be at high risk for invasive pulmonary aspergillosis, which in a small prospective study was associated with a more than threefold risk for 30-day mortality. The findings were published online in Clinical Infectious Diseases.
Among 108 patients with COVID-19 on mechanical ventilation in one of three intensive care units, 30 (27.7%) were diagnosed with coronavirus-associated pulmonary aspergillosis (CAPA) based on consensus definitions similar to those used to diagnose influenza-associated pulmonary aspergillosis (IAPA).
Of the patients with CAPA, 44% died within 30 days of ICU admission, compared with 19% of patients who did not meet the criteria for aspergillosis (P = .002). This difference translated into an odds ratio (OR) for death with CAPA of 3.55 (P = .014), reported Michele Bartoletti, MD, PhD, of the infectious diseases unit at Sant’Orsola Malpighi Hospital in Bologna, Italy, and colleagues.
When the investigators applied a proposed definition of putative invasive pulmonary aspergillosis, or “PIPA” to the same patients, the 30-day mortality rate jumped to 74% vs. 26% for patients without PIPA (P < .001), with an OR of 11.60 (P < .001). “We found a high incidence of CAPA among critically ill COVID-19 patients and that its occurrence seems to change the natural history of disease,” they wrote.
“[T]he study from Bartoletti et al. alerts the clinical audience to be aware of CAPA and take appropriate (and where needed repetitive) actions that fits their clinical setting,” Roger J. Brüggemann, PharmD, of the department of pharmacy, Radboud University Medical Center, Nijmegen, the Netherlands, and colleagues wrote in an editorial accompanying the study.
Diagnosis challenging
At the best of times, the diagnosis of pulmonary aspergillosis is difficult, subject to both false-positive and false-negative results, said a critical care specialist who was not involved in the study.
“Critically ill patients are susceptible to having aspergillus, so in reading the article, my only concerns are that I don’t know how accurate the testing is, and I don’t know if their population is truly different from a general population of patients in the ICU,” Daniel R. Ouellette, MD, FCCP, associate director of medical critical care at Henry Ford Hospital in Detroit, said in an interview.
As seen in ICU patients with severe influenza or other viral infections, patients with severe COVID-19 disease are susceptible to secondary infections, he said, making it difficult to know whether the worse outcomes seen in patients with COVID-19 and presumed aspergillosis are a reflection of their being more critically ill or whether the secondary infections themselves account for the difference in mortality.
Three ICUs
Dr. Bartoletti and colleagues conducted a study on all adult patients with microbiologically confirmed COVID-19 receiving mechanical ventilation in three ICUs in Bologna.
All patients included in the study were screened for invasive pulmonary aspergillosis with bronchoalveolar lavage and galactomannan detection and cultures. The lavage was performed on ICU admission, one day from the first day of mechanical ventilation, and if patients had evidence of clinical disease progression.
Samples that tested positive for galactomannan, a component of the aspergillus cell wall, were stored and later analyzed with a commercial quantitative real-time polymerase chain reaction assay for aspergillus; these results were not reported to clinicians on the patient floors.
The investigators defined invasive pulmonary aspergillosis according to a recently proposed definition for CAPA. This definition applies to COVID-19–positive patients admitted to an ICU with pulmonary infiltrates and at least one of the following:
- A serum galactomannan > 0.5.
- Bronchoalveolar lavage galactomannan > 1.0.
- Positive aspergillus bronchoalveolar lavage culture or cavitating infiltrate not attributed to another cause in the area of the pulmonary infiltrate.
They compared the CAPA diagnostic criteria with those of PIPA criteria as described by Stijn J. Blot, PhD, and colleagues in study published in the American Journal of Respiratory and Critical Care Medicine (2012 Jul 1;186(1):56-64).
A total of 108 patients were screened for aspergillosis, with a median age of 64. The majority of patients (78%) were male. The median age-adjusted Charlson Comorbidity Index was 2.5 (range 1-4). The median Sequential Organ Failure Assessment (SOFA) score at ICU admission was 4 (range 3-5).
As noted, probable aspergillosis by CAPA criteria was diagnosed in 30 patients (27.7%), with the diagnosis made after a median of 4 days after intubation and a median of 14 days from onset of COVID-19 symptoms.
The incidence rate of probable CAPA was 38.83 per 10,000 ICU patient days.
A comparison of clinical characteristics of patients with and without probable CAPA showed that only chronic steroid therapy at ≥ 16 mg/day prednisone for at least 15 days was significantly associated with risk for CAPA (P = .02).
At a median follow-up of 31 days, 54 patients (50%) had been discharged, 44 (41%) had died, and the remaining patients were still on follow-up.
As noted before, the mortality rate with 30 days of ICU admission was 44% for patients with probable CAPA vs. 19% for patients without. Among patients deemed to have PIPA, 74% died within 30 days of admission, compared with 26% without PIPA.
In a logistic regression model, the association of CAPA with increased risk for 30-day mortality remained even after adjustment for the need for renal replacement therapy (OR 3.02, P = .015) and SOFA score at ICU admission (OR 1.38, P = .004).
In a logistic regression using the PIPA rather than CAPA definition, the OR for 30-day mortality was 11.60 (P = .001).
Prognostic marker
The investigators noted that bronchoalveolar lavage galactomannan index appeared to be predictive of death. Each 1-point increase in the index was associated with 1.41-fold increase in the risk for 30-day mortality (P = .0070), a relationship that held up after adjustment for age, need for renal replacement therapy, and SOFA score.
Sixteen patients who met the CAPA definition received antifungal therapy, primarily voriconazole. The use of voriconazole was associated with a nonsignificant trend toward lower mortality.
They noted that the heavy use of immunomodulating agents in the patients in their study may have contributed to the high prevalence of CAPA.
Dr. Ouellette agreed that many of the therapies used to treat COVID-19 in the ICU are experimental, and that agents used to suppress the cytokine storm that is believed to contribute to disease severity may increase risk for secondary infections such as invasive aspergillosis.
“Many of our treatments may be associated with adverse consequences,” he said. “There is a trend toward treating patients with COVID-19 pneumonia with corticosteroids, and certainly that could have an immunosuppressant effect and predispose patients to secondary infections.”
He noted that the World Health Organization recommendations current in March 2020, when the pandemic began in earnest in the United States, advised against the use of corticosteroids, likely because of a lack of evidence of efficacy and concerns about risk for secondary infections.
“Regardless of the strategic choice made, all efforts should be put into improving our ability to reliably identify patients that may benefit from therapeutic interventions, which include host and risk factors, clinical factors and CAPA disease markers,” Dr. Brüggemann and colleagues wrote in their editorial.
The study was performed without external funding. The authors and Dr. Ouellette reported no conflicts of interest. Dr. Brüggemann and coauthors report grants and/or personal fees from various companies outside the submitted work.
SOURCE: Bartoletti M et al. Clin Infect Dis. 2020 Jul 28. doi: 10.1093/cid/ciaa1065.
Researchers are beginning to make some headway in identifying the role of secondary infections in the course and outcomes of COVID-19.
Patients who are on ventilatory support for severe COVID-19 infections appear to be at high risk for invasive pulmonary aspergillosis, which in a small prospective study was associated with a more than threefold risk for 30-day mortality. The findings were published online in Clinical Infectious Diseases.
Among 108 patients with COVID-19 on mechanical ventilation in one of three intensive care units, 30 (27.7%) were diagnosed with coronavirus-associated pulmonary aspergillosis (CAPA) based on consensus definitions similar to those used to diagnose influenza-associated pulmonary aspergillosis (IAPA).
Of the patients with CAPA, 44% died within 30 days of ICU admission, compared with 19% of patients who did not meet the criteria for aspergillosis (P = .002). This difference translated into an odds ratio (OR) for death with CAPA of 3.55 (P = .014), reported Michele Bartoletti, MD, PhD, of the infectious diseases unit at Sant’Orsola Malpighi Hospital in Bologna, Italy, and colleagues.
When the investigators applied a proposed definition of putative invasive pulmonary aspergillosis, or “PIPA” to the same patients, the 30-day mortality rate jumped to 74% vs. 26% for patients without PIPA (P < .001), with an OR of 11.60 (P < .001). “We found a high incidence of CAPA among critically ill COVID-19 patients and that its occurrence seems to change the natural history of disease,” they wrote.
“[T]he study from Bartoletti et al. alerts the clinical audience to be aware of CAPA and take appropriate (and where needed repetitive) actions that fits their clinical setting,” Roger J. Brüggemann, PharmD, of the department of pharmacy, Radboud University Medical Center, Nijmegen, the Netherlands, and colleagues wrote in an editorial accompanying the study.
Diagnosis challenging
At the best of times, the diagnosis of pulmonary aspergillosis is difficult, subject to both false-positive and false-negative results, said a critical care specialist who was not involved in the study.
“Critically ill patients are susceptible to having aspergillus, so in reading the article, my only concerns are that I don’t know how accurate the testing is, and I don’t know if their population is truly different from a general population of patients in the ICU,” Daniel R. Ouellette, MD, FCCP, associate director of medical critical care at Henry Ford Hospital in Detroit, said in an interview.
As seen in ICU patients with severe influenza or other viral infections, patients with severe COVID-19 disease are susceptible to secondary infections, he said, making it difficult to know whether the worse outcomes seen in patients with COVID-19 and presumed aspergillosis are a reflection of their being more critically ill or whether the secondary infections themselves account for the difference in mortality.
Three ICUs
Dr. Bartoletti and colleagues conducted a study on all adult patients with microbiologically confirmed COVID-19 receiving mechanical ventilation in three ICUs in Bologna.
All patients included in the study were screened for invasive pulmonary aspergillosis with bronchoalveolar lavage and galactomannan detection and cultures. The lavage was performed on ICU admission, one day from the first day of mechanical ventilation, and if patients had evidence of clinical disease progression.
Samples that tested positive for galactomannan, a component of the aspergillus cell wall, were stored and later analyzed with a commercial quantitative real-time polymerase chain reaction assay for aspergillus; these results were not reported to clinicians on the patient floors.
The investigators defined invasive pulmonary aspergillosis according to a recently proposed definition for CAPA. This definition applies to COVID-19–positive patients admitted to an ICU with pulmonary infiltrates and at least one of the following:
- A serum galactomannan > 0.5.
- Bronchoalveolar lavage galactomannan > 1.0.
- Positive aspergillus bronchoalveolar lavage culture or cavitating infiltrate not attributed to another cause in the area of the pulmonary infiltrate.
They compared the CAPA diagnostic criteria with those of PIPA criteria as described by Stijn J. Blot, PhD, and colleagues in study published in the American Journal of Respiratory and Critical Care Medicine (2012 Jul 1;186(1):56-64).
A total of 108 patients were screened for aspergillosis, with a median age of 64. The majority of patients (78%) were male. The median age-adjusted Charlson Comorbidity Index was 2.5 (range 1-4). The median Sequential Organ Failure Assessment (SOFA) score at ICU admission was 4 (range 3-5).
As noted, probable aspergillosis by CAPA criteria was diagnosed in 30 patients (27.7%), with the diagnosis made after a median of 4 days after intubation and a median of 14 days from onset of COVID-19 symptoms.
The incidence rate of probable CAPA was 38.83 per 10,000 ICU patient days.
A comparison of clinical characteristics of patients with and without probable CAPA showed that only chronic steroid therapy at ≥ 16 mg/day prednisone for at least 15 days was significantly associated with risk for CAPA (P = .02).
At a median follow-up of 31 days, 54 patients (50%) had been discharged, 44 (41%) had died, and the remaining patients were still on follow-up.
As noted before, the mortality rate with 30 days of ICU admission was 44% for patients with probable CAPA vs. 19% for patients without. Among patients deemed to have PIPA, 74% died within 30 days of admission, compared with 26% without PIPA.
In a logistic regression model, the association of CAPA with increased risk for 30-day mortality remained even after adjustment for the need for renal replacement therapy (OR 3.02, P = .015) and SOFA score at ICU admission (OR 1.38, P = .004).
In a logistic regression using the PIPA rather than CAPA definition, the OR for 30-day mortality was 11.60 (P = .001).
Prognostic marker
The investigators noted that bronchoalveolar lavage galactomannan index appeared to be predictive of death. Each 1-point increase in the index was associated with 1.41-fold increase in the risk for 30-day mortality (P = .0070), a relationship that held up after adjustment for age, need for renal replacement therapy, and SOFA score.
Sixteen patients who met the CAPA definition received antifungal therapy, primarily voriconazole. The use of voriconazole was associated with a nonsignificant trend toward lower mortality.
They noted that the heavy use of immunomodulating agents in the patients in their study may have contributed to the high prevalence of CAPA.
Dr. Ouellette agreed that many of the therapies used to treat COVID-19 in the ICU are experimental, and that agents used to suppress the cytokine storm that is believed to contribute to disease severity may increase risk for secondary infections such as invasive aspergillosis.
“Many of our treatments may be associated with adverse consequences,” he said. “There is a trend toward treating patients with COVID-19 pneumonia with corticosteroids, and certainly that could have an immunosuppressant effect and predispose patients to secondary infections.”
He noted that the World Health Organization recommendations current in March 2020, when the pandemic began in earnest in the United States, advised against the use of corticosteroids, likely because of a lack of evidence of efficacy and concerns about risk for secondary infections.
“Regardless of the strategic choice made, all efforts should be put into improving our ability to reliably identify patients that may benefit from therapeutic interventions, which include host and risk factors, clinical factors and CAPA disease markers,” Dr. Brüggemann and colleagues wrote in their editorial.
The study was performed without external funding. The authors and Dr. Ouellette reported no conflicts of interest. Dr. Brüggemann and coauthors report grants and/or personal fees from various companies outside the submitted work.
SOURCE: Bartoletti M et al. Clin Infect Dis. 2020 Jul 28. doi: 10.1093/cid/ciaa1065.
Researchers are beginning to make some headway in identifying the role of secondary infections in the course and outcomes of COVID-19.
Patients who are on ventilatory support for severe COVID-19 infections appear to be at high risk for invasive pulmonary aspergillosis, which in a small prospective study was associated with a more than threefold risk for 30-day mortality. The findings were published online in Clinical Infectious Diseases.
Among 108 patients with COVID-19 on mechanical ventilation in one of three intensive care units, 30 (27.7%) were diagnosed with coronavirus-associated pulmonary aspergillosis (CAPA) based on consensus definitions similar to those used to diagnose influenza-associated pulmonary aspergillosis (IAPA).
Of the patients with CAPA, 44% died within 30 days of ICU admission, compared with 19% of patients who did not meet the criteria for aspergillosis (P = .002). This difference translated into an odds ratio (OR) for death with CAPA of 3.55 (P = .014), reported Michele Bartoletti, MD, PhD, of the infectious diseases unit at Sant’Orsola Malpighi Hospital in Bologna, Italy, and colleagues.
When the investigators applied a proposed definition of putative invasive pulmonary aspergillosis, or “PIPA” to the same patients, the 30-day mortality rate jumped to 74% vs. 26% for patients without PIPA (P < .001), with an OR of 11.60 (P < .001). “We found a high incidence of CAPA among critically ill COVID-19 patients and that its occurrence seems to change the natural history of disease,” they wrote.
“[T]he study from Bartoletti et al. alerts the clinical audience to be aware of CAPA and take appropriate (and where needed repetitive) actions that fits their clinical setting,” Roger J. Brüggemann, PharmD, of the department of pharmacy, Radboud University Medical Center, Nijmegen, the Netherlands, and colleagues wrote in an editorial accompanying the study.
Diagnosis challenging
At the best of times, the diagnosis of pulmonary aspergillosis is difficult, subject to both false-positive and false-negative results, said a critical care specialist who was not involved in the study.
“Critically ill patients are susceptible to having aspergillus, so in reading the article, my only concerns are that I don’t know how accurate the testing is, and I don’t know if their population is truly different from a general population of patients in the ICU,” Daniel R. Ouellette, MD, FCCP, associate director of medical critical care at Henry Ford Hospital in Detroit, said in an interview.
As seen in ICU patients with severe influenza or other viral infections, patients with severe COVID-19 disease are susceptible to secondary infections, he said, making it difficult to know whether the worse outcomes seen in patients with COVID-19 and presumed aspergillosis are a reflection of their being more critically ill or whether the secondary infections themselves account for the difference in mortality.
Three ICUs
Dr. Bartoletti and colleagues conducted a study on all adult patients with microbiologically confirmed COVID-19 receiving mechanical ventilation in three ICUs in Bologna.
All patients included in the study were screened for invasive pulmonary aspergillosis with bronchoalveolar lavage and galactomannan detection and cultures. The lavage was performed on ICU admission, one day from the first day of mechanical ventilation, and if patients had evidence of clinical disease progression.
Samples that tested positive for galactomannan, a component of the aspergillus cell wall, were stored and later analyzed with a commercial quantitative real-time polymerase chain reaction assay for aspergillus; these results were not reported to clinicians on the patient floors.
The investigators defined invasive pulmonary aspergillosis according to a recently proposed definition for CAPA. This definition applies to COVID-19–positive patients admitted to an ICU with pulmonary infiltrates and at least one of the following:
- A serum galactomannan > 0.5.
- Bronchoalveolar lavage galactomannan > 1.0.
- Positive aspergillus bronchoalveolar lavage culture or cavitating infiltrate not attributed to another cause in the area of the pulmonary infiltrate.
They compared the CAPA diagnostic criteria with those of PIPA criteria as described by Stijn J. Blot, PhD, and colleagues in study published in the American Journal of Respiratory and Critical Care Medicine (2012 Jul 1;186(1):56-64).
A total of 108 patients were screened for aspergillosis, with a median age of 64. The majority of patients (78%) were male. The median age-adjusted Charlson Comorbidity Index was 2.5 (range 1-4). The median Sequential Organ Failure Assessment (SOFA) score at ICU admission was 4 (range 3-5).
As noted, probable aspergillosis by CAPA criteria was diagnosed in 30 patients (27.7%), with the diagnosis made after a median of 4 days after intubation and a median of 14 days from onset of COVID-19 symptoms.
The incidence rate of probable CAPA was 38.83 per 10,000 ICU patient days.
A comparison of clinical characteristics of patients with and without probable CAPA showed that only chronic steroid therapy at ≥ 16 mg/day prednisone for at least 15 days was significantly associated with risk for CAPA (P = .02).
At a median follow-up of 31 days, 54 patients (50%) had been discharged, 44 (41%) had died, and the remaining patients were still on follow-up.
As noted before, the mortality rate with 30 days of ICU admission was 44% for patients with probable CAPA vs. 19% for patients without. Among patients deemed to have PIPA, 74% died within 30 days of admission, compared with 26% without PIPA.
In a logistic regression model, the association of CAPA with increased risk for 30-day mortality remained even after adjustment for the need for renal replacement therapy (OR 3.02, P = .015) and SOFA score at ICU admission (OR 1.38, P = .004).
In a logistic regression using the PIPA rather than CAPA definition, the OR for 30-day mortality was 11.60 (P = .001).
Prognostic marker
The investigators noted that bronchoalveolar lavage galactomannan index appeared to be predictive of death. Each 1-point increase in the index was associated with 1.41-fold increase in the risk for 30-day mortality (P = .0070), a relationship that held up after adjustment for age, need for renal replacement therapy, and SOFA score.
Sixteen patients who met the CAPA definition received antifungal therapy, primarily voriconazole. The use of voriconazole was associated with a nonsignificant trend toward lower mortality.
They noted that the heavy use of immunomodulating agents in the patients in their study may have contributed to the high prevalence of CAPA.
Dr. Ouellette agreed that many of the therapies used to treat COVID-19 in the ICU are experimental, and that agents used to suppress the cytokine storm that is believed to contribute to disease severity may increase risk for secondary infections such as invasive aspergillosis.
“Many of our treatments may be associated with adverse consequences,” he said. “There is a trend toward treating patients with COVID-19 pneumonia with corticosteroids, and certainly that could have an immunosuppressant effect and predispose patients to secondary infections.”
He noted that the World Health Organization recommendations current in March 2020, when the pandemic began in earnest in the United States, advised against the use of corticosteroids, likely because of a lack of evidence of efficacy and concerns about risk for secondary infections.
“Regardless of the strategic choice made, all efforts should be put into improving our ability to reliably identify patients that may benefit from therapeutic interventions, which include host and risk factors, clinical factors and CAPA disease markers,” Dr. Brüggemann and colleagues wrote in their editorial.
The study was performed without external funding. The authors and Dr. Ouellette reported no conflicts of interest. Dr. Brüggemann and coauthors report grants and/or personal fees from various companies outside the submitted work.
SOURCE: Bartoletti M et al. Clin Infect Dis. 2020 Jul 28. doi: 10.1093/cid/ciaa1065.
FROM CLINICAL INFECTIOUS DISEASES
First evidence of SARS-CoV-2 in heart cells
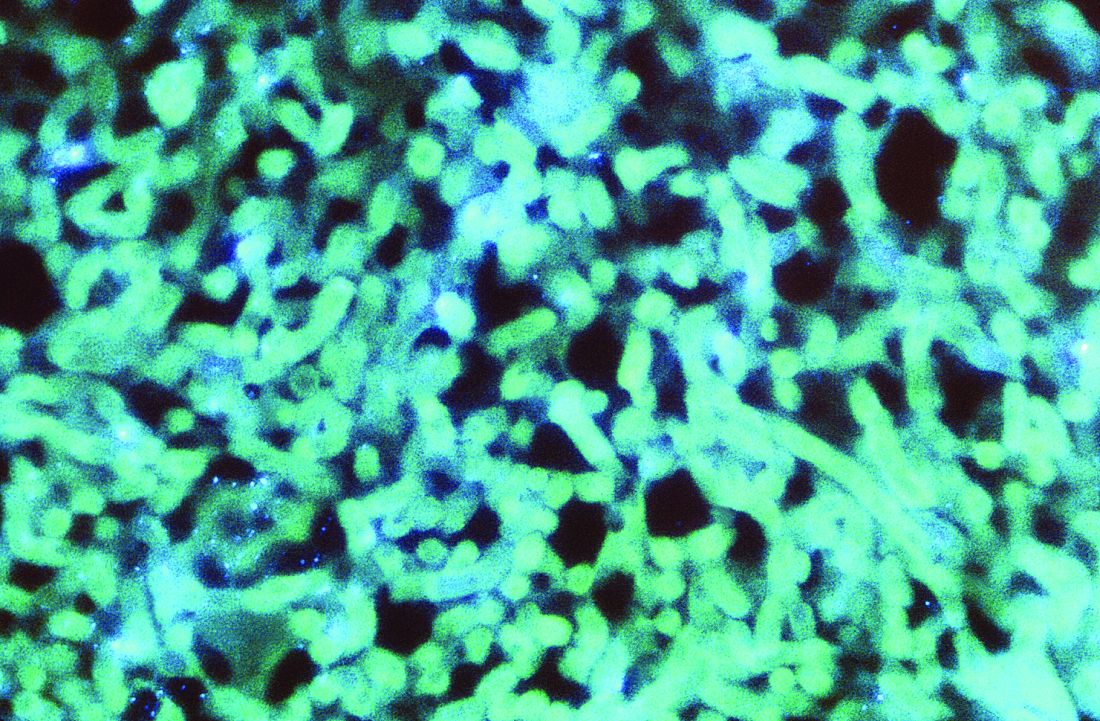
SARS-CoV-2 has been found in cardiac tissue of a child from Brazil with multisystem inflammatory syndrome (MIS-C) related to COVID-19 who presented with myocarditis and died of heart failure.
It’s believed to be the first evidence of direct infection of heart muscle cells by the virus; viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.
The case was described in a report published online August 20 in The Lancet Child & Adolescent Health.
“The presence of the virus in various cell types of cardiac tissue, as evidenced by electron microscopy, shows that myocarditis in this case is likely a direct inflammatory response to the virus infection in the heart,” first author Marisa Dolhnikoff, MD, department of pathology, University of São Paulo, said in an interview.
There have been previous reports in adults with COVID-19 of both SARS-CoV-2 RNA by reverse transcription–polymerase chain reaction (RT-PCR) and viral particles by electron microscopy in cardiac tissue from endomyocardial specimens, the researchers noted. One of these reports, published in April by Tavazzi and colleagues, “detected viral particles in cardiac macrophages in an adult patient with acute cardiac injury associated with COVID-19; no viral particles were seen in cardiomyocytes or endothelial cells.
“Our case report is the first to our knowledge to document the presence of viral particles in the cardiac tissue of a child affected by MIS-C,” they added. “Moreover, viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.”
‘Concerning’ case report
“This is a concerning report as it shows for the first time that the virus can actually invade the heart muscle cells themselves,” C. Michael Gibson, MD, CEO of the Baim Institute for Clinical Research in Boston, said in an interview.
“Previous reports of COVID-19 and the heart found that the virus was in the area outside the heart muscle cells. We do not know yet the relative contribution of the inflammatory cells invading the heart, the release of blood-borne inflammatory mediators, and the virus inside the heart muscle cells themselves to heart damage,” Dr. Gibson said.
The patient was a previously healthy 11-year-old girl of African descent with MIS-C related to COVID-19. She developed cardiac failure and died after 1 day in the hospital, despite aggressive treatment.
SARS-CoV-2 RNA was detected on a postmortem nasopharyngeal swab and in cardiac and pulmonary tissues by RT-PCR.
Postmortem ultrasound examination of the heart showed a “hyperechogenic and diffusely thickened endocardium (mean thickness, 10 mm), a thickened myocardium (18 mm thick in the left ventricle), and a small pericardial effusion,” Dr. Dolhnikoff and colleagues reported.
Histopathologic exam revealed myocarditis, pericarditis, and endocarditis characterized by infiltration of inflammatory cells. Inflammation was mainly interstitial and perivascular, associated with foci of cardiomyocyte necrosis and was mainly composed of CD68+ macrophages, a few CD45+ lymphocytes, and a few neutrophils and eosinophils.
Electron microscopy of cardiac tissue revealed spherical viral particles in shape and size consistent with the Coronaviridae family in the extracellular compartment and within cardiomyocytes, capillary endothelial cells, endocardium endothelial cells, macrophages, neutrophils, and fibroblasts.
Microthrombi in the pulmonary arterioles and renal glomerular capillaries were also seen at autopsy. SARS-CoV-2–associated pneumonia was mild.
Lymphoid depletion and signs of hemophagocytosis were observed in the spleen and lymph nodes. Acute tubular necrosis in the kidneys and hepatic centrilobular necrosis, secondary to shock, were also seen. Brain tissue showed microglial reactivity.
“Fortunately, MIS-C is a rare event and, although it can be severe and life threatening, most children recover,” Dr. Dolhnikoff commented.
“This case report comes at a time when the scientific community around the world calls attention to MIS-C and the need for it to be quickly recognized and treated by the pediatric community. Evidence of a direct relation between the virus and myocarditis confirms that MIS-C is one of the possible forms of presentation of COVID-19 and that the heart may be the target organ. It also alerts clinicians to possible cardiac sequelae in these children,” she added.
Experts weigh in
Scott Aydin, MD, medical director of pediatric cardiac intensive care, Mount Sinai Kravis Children’s Hospital in New York City, said that this case report is “unfortunately not all that surprising.
“Since the initial presentations of MIS-C several months ago, we have suspected mechanisms of direct and indirect injury to the myocardium. This important work is just the next step in further understanding the mechanisms of how COVID-19 creates havoc in the human body and the choices of possible therapies we have to treat children with COVID-19 and MIS-C,” said Dr. Aydin, who was not involved with the case report.
Anish Koka, MD, a cardiologist in private practice in Philadelphia, noted that, in these cases, endomyocardial biopsy is “rarely done because it is fairly invasive, but even when it has been done, the pathologic findings are of widespread inflammation rather than virus-induced cell necrosis.”
“While reports like this are sure to spawn viral tweets, it’s vital to understand that it’s not unusual to find widespread organ dissemination of virus in very sick patients. This does not mean that the virus is causing dysfunction of the organ it happens to be found in,” Dr. Koka said in an interview.
He noted that, in the case of the young girl who died, it took high PCR-cycle threshold values to isolate virus from the lung and heart samples.
“This means there was a low viral load in both organs, supporting the theory of SARS-CoV-2 as a potential trigger of a widespread inflammatory response that results in organ damage, rather than the virus itself infecting and destroying organs,” said Dr. Koka, who was also not associated with the case report.
This research had no specific funding. The authors declared no competing interests. Dr. Aydin disclosed no relevant financial relationships. Dr. Koka disclosed financial relationships with Boehringer Ingelheim and Jardiance.
This article first appeared on Medscape.com.
SARS-CoV-2 has been found in cardiac tissue of a child from Brazil with multisystem inflammatory syndrome (MIS-C) related to COVID-19 who presented with myocarditis and died of heart failure.
It’s believed to be the first evidence of direct infection of heart muscle cells by the virus; viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.
The case was described in a report published online August 20 in The Lancet Child & Adolescent Health.
“The presence of the virus in various cell types of cardiac tissue, as evidenced by electron microscopy, shows that myocarditis in this case is likely a direct inflammatory response to the virus infection in the heart,” first author Marisa Dolhnikoff, MD, department of pathology, University of São Paulo, said in an interview.
There have been previous reports in adults with COVID-19 of both SARS-CoV-2 RNA by reverse transcription–polymerase chain reaction (RT-PCR) and viral particles by electron microscopy in cardiac tissue from endomyocardial specimens, the researchers noted. One of these reports, published in April by Tavazzi and colleagues, “detected viral particles in cardiac macrophages in an adult patient with acute cardiac injury associated with COVID-19; no viral particles were seen in cardiomyocytes or endothelial cells.
“Our case report is the first to our knowledge to document the presence of viral particles in the cardiac tissue of a child affected by MIS-C,” they added. “Moreover, viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.”
‘Concerning’ case report
“This is a concerning report as it shows for the first time that the virus can actually invade the heart muscle cells themselves,” C. Michael Gibson, MD, CEO of the Baim Institute for Clinical Research in Boston, said in an interview.
“Previous reports of COVID-19 and the heart found that the virus was in the area outside the heart muscle cells. We do not know yet the relative contribution of the inflammatory cells invading the heart, the release of blood-borne inflammatory mediators, and the virus inside the heart muscle cells themselves to heart damage,” Dr. Gibson said.
The patient was a previously healthy 11-year-old girl of African descent with MIS-C related to COVID-19. She developed cardiac failure and died after 1 day in the hospital, despite aggressive treatment.
SARS-CoV-2 RNA was detected on a postmortem nasopharyngeal swab and in cardiac and pulmonary tissues by RT-PCR.
Postmortem ultrasound examination of the heart showed a “hyperechogenic and diffusely thickened endocardium (mean thickness, 10 mm), a thickened myocardium (18 mm thick in the left ventricle), and a small pericardial effusion,” Dr. Dolhnikoff and colleagues reported.
Histopathologic exam revealed myocarditis, pericarditis, and endocarditis characterized by infiltration of inflammatory cells. Inflammation was mainly interstitial and perivascular, associated with foci of cardiomyocyte necrosis and was mainly composed of CD68+ macrophages, a few CD45+ lymphocytes, and a few neutrophils and eosinophils.
Electron microscopy of cardiac tissue revealed spherical viral particles in shape and size consistent with the Coronaviridae family in the extracellular compartment and within cardiomyocytes, capillary endothelial cells, endocardium endothelial cells, macrophages, neutrophils, and fibroblasts.
Microthrombi in the pulmonary arterioles and renal glomerular capillaries were also seen at autopsy. SARS-CoV-2–associated pneumonia was mild.
Lymphoid depletion and signs of hemophagocytosis were observed in the spleen and lymph nodes. Acute tubular necrosis in the kidneys and hepatic centrilobular necrosis, secondary to shock, were also seen. Brain tissue showed microglial reactivity.
“Fortunately, MIS-C is a rare event and, although it can be severe and life threatening, most children recover,” Dr. Dolhnikoff commented.
“This case report comes at a time when the scientific community around the world calls attention to MIS-C and the need for it to be quickly recognized and treated by the pediatric community. Evidence of a direct relation between the virus and myocarditis confirms that MIS-C is one of the possible forms of presentation of COVID-19 and that the heart may be the target organ. It also alerts clinicians to possible cardiac sequelae in these children,” she added.
Experts weigh in
Scott Aydin, MD, medical director of pediatric cardiac intensive care, Mount Sinai Kravis Children’s Hospital in New York City, said that this case report is “unfortunately not all that surprising.
“Since the initial presentations of MIS-C several months ago, we have suspected mechanisms of direct and indirect injury to the myocardium. This important work is just the next step in further understanding the mechanisms of how COVID-19 creates havoc in the human body and the choices of possible therapies we have to treat children with COVID-19 and MIS-C,” said Dr. Aydin, who was not involved with the case report.
Anish Koka, MD, a cardiologist in private practice in Philadelphia, noted that, in these cases, endomyocardial biopsy is “rarely done because it is fairly invasive, but even when it has been done, the pathologic findings are of widespread inflammation rather than virus-induced cell necrosis.”
“While reports like this are sure to spawn viral tweets, it’s vital to understand that it’s not unusual to find widespread organ dissemination of virus in very sick patients. This does not mean that the virus is causing dysfunction of the organ it happens to be found in,” Dr. Koka said in an interview.
He noted that, in the case of the young girl who died, it took high PCR-cycle threshold values to isolate virus from the lung and heart samples.
“This means there was a low viral load in both organs, supporting the theory of SARS-CoV-2 as a potential trigger of a widespread inflammatory response that results in organ damage, rather than the virus itself infecting and destroying organs,” said Dr. Koka, who was also not associated with the case report.
This research had no specific funding. The authors declared no competing interests. Dr. Aydin disclosed no relevant financial relationships. Dr. Koka disclosed financial relationships with Boehringer Ingelheim and Jardiance.
This article first appeared on Medscape.com.
SARS-CoV-2 has been found in cardiac tissue of a child from Brazil with multisystem inflammatory syndrome (MIS-C) related to COVID-19 who presented with myocarditis and died of heart failure.
It’s believed to be the first evidence of direct infection of heart muscle cells by the virus; viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.
The case was described in a report published online August 20 in The Lancet Child & Adolescent Health.
“The presence of the virus in various cell types of cardiac tissue, as evidenced by electron microscopy, shows that myocarditis in this case is likely a direct inflammatory response to the virus infection in the heart,” first author Marisa Dolhnikoff, MD, department of pathology, University of São Paulo, said in an interview.
There have been previous reports in adults with COVID-19 of both SARS-CoV-2 RNA by reverse transcription–polymerase chain reaction (RT-PCR) and viral particles by electron microscopy in cardiac tissue from endomyocardial specimens, the researchers noted. One of these reports, published in April by Tavazzi and colleagues, “detected viral particles in cardiac macrophages in an adult patient with acute cardiac injury associated with COVID-19; no viral particles were seen in cardiomyocytes or endothelial cells.
“Our case report is the first to our knowledge to document the presence of viral particles in the cardiac tissue of a child affected by MIS-C,” they added. “Moreover, viral particles were identified in different cell lineages of the heart, including cardiomyocytes, endothelial cells, mesenchymal cells, and inflammatory cells.”
‘Concerning’ case report
“This is a concerning report as it shows for the first time that the virus can actually invade the heart muscle cells themselves,” C. Michael Gibson, MD, CEO of the Baim Institute for Clinical Research in Boston, said in an interview.
“Previous reports of COVID-19 and the heart found that the virus was in the area outside the heart muscle cells. We do not know yet the relative contribution of the inflammatory cells invading the heart, the release of blood-borne inflammatory mediators, and the virus inside the heart muscle cells themselves to heart damage,” Dr. Gibson said.
The patient was a previously healthy 11-year-old girl of African descent with MIS-C related to COVID-19. She developed cardiac failure and died after 1 day in the hospital, despite aggressive treatment.
SARS-CoV-2 RNA was detected on a postmortem nasopharyngeal swab and in cardiac and pulmonary tissues by RT-PCR.
Postmortem ultrasound examination of the heart showed a “hyperechogenic and diffusely thickened endocardium (mean thickness, 10 mm), a thickened myocardium (18 mm thick in the left ventricle), and a small pericardial effusion,” Dr. Dolhnikoff and colleagues reported.
Histopathologic exam revealed myocarditis, pericarditis, and endocarditis characterized by infiltration of inflammatory cells. Inflammation was mainly interstitial and perivascular, associated with foci of cardiomyocyte necrosis and was mainly composed of CD68+ macrophages, a few CD45+ lymphocytes, and a few neutrophils and eosinophils.
Electron microscopy of cardiac tissue revealed spherical viral particles in shape and size consistent with the Coronaviridae family in the extracellular compartment and within cardiomyocytes, capillary endothelial cells, endocardium endothelial cells, macrophages, neutrophils, and fibroblasts.
Microthrombi in the pulmonary arterioles and renal glomerular capillaries were also seen at autopsy. SARS-CoV-2–associated pneumonia was mild.
Lymphoid depletion and signs of hemophagocytosis were observed in the spleen and lymph nodes. Acute tubular necrosis in the kidneys and hepatic centrilobular necrosis, secondary to shock, were also seen. Brain tissue showed microglial reactivity.
“Fortunately, MIS-C is a rare event and, although it can be severe and life threatening, most children recover,” Dr. Dolhnikoff commented.
“This case report comes at a time when the scientific community around the world calls attention to MIS-C and the need for it to be quickly recognized and treated by the pediatric community. Evidence of a direct relation between the virus and myocarditis confirms that MIS-C is one of the possible forms of presentation of COVID-19 and that the heart may be the target organ. It also alerts clinicians to possible cardiac sequelae in these children,” she added.
Experts weigh in
Scott Aydin, MD, medical director of pediatric cardiac intensive care, Mount Sinai Kravis Children’s Hospital in New York City, said that this case report is “unfortunately not all that surprising.
“Since the initial presentations of MIS-C several months ago, we have suspected mechanisms of direct and indirect injury to the myocardium. This important work is just the next step in further understanding the mechanisms of how COVID-19 creates havoc in the human body and the choices of possible therapies we have to treat children with COVID-19 and MIS-C,” said Dr. Aydin, who was not involved with the case report.
Anish Koka, MD, a cardiologist in private practice in Philadelphia, noted that, in these cases, endomyocardial biopsy is “rarely done because it is fairly invasive, but even when it has been done, the pathologic findings are of widespread inflammation rather than virus-induced cell necrosis.”
“While reports like this are sure to spawn viral tweets, it’s vital to understand that it’s not unusual to find widespread organ dissemination of virus in very sick patients. This does not mean that the virus is causing dysfunction of the organ it happens to be found in,” Dr. Koka said in an interview.
He noted that, in the case of the young girl who died, it took high PCR-cycle threshold values to isolate virus from the lung and heart samples.
“This means there was a low viral load in both organs, supporting the theory of SARS-CoV-2 as a potential trigger of a widespread inflammatory response that results in organ damage, rather than the virus itself infecting and destroying organs,” said Dr. Koka, who was also not associated with the case report.
This research had no specific funding. The authors declared no competing interests. Dr. Aydin disclosed no relevant financial relationships. Dr. Koka disclosed financial relationships with Boehringer Ingelheim and Jardiance.
This article first appeared on Medscape.com.
Famotidine associated with benefits in hospitalized COVID patients in another trial
It also demonstrated lower levels of serum markers for severe disease.
The findings come from an observational study of 83 hospitalized patients that was published in the American Journal of Gastroenterology.
“The mechanism of exactly how famotidine works has yet to be proven,” lead study author Jeffrey F. Mather, MS, said in an interview. “There’s thought that it works directly on the virus, and there is thought that it works through inactivating certain proteases that are required for the virus infection, but I think the most interesting [hypothesis] is by Malone et al. “They’re looking at the blocking of the histamine-2 receptor causing a decrease in the amount of histamine. It’s all speculative, but it will be interesting if that gets worked out.”
In a study that largely mimicked that of an earlier, larger published observational study on the topic (doi: 10.1053/j.gastro.2020.05.053), Mr. Mather and colleagues retrospectively evaluated 878 patients who tested positive for SARS-CoV-2 and who required admission to Hartford (Conn.) Hospital between Feb. 24, 2020, and May 14, 2020. Patients were classified as receiving famotidine if they were treated with either oral or intravenous drug within 1 week of COVID-19 screening and/or hospital admission. Primary outcomes of interest were in-hospital death as recorded in the discharge of the patients, requirement for mechanical ventilation, and the composite of death or requirement for ventilation. Secondary outcomes of interest were several serum markers of disease activity including white blood cell count, lymphocyte count, and eosinophil count.
Famotidine was administered orally in 83% of the patients and intravenously in the remaining 17%. Mr. Mather, director of data management in the division of research management at Hartford Hospital, and his colleagues reported that 83 of the 878 patients studied (9.5%) received famotidine. Compared with patients not treated with famotidine, those who received the drug were slightly younger (a mean of 64 vs. 68 years, respectively; P = .021); otherwise, there were no differences between the two groups in baseline demographics or in preexisting comorbidities.
The use of famotidine was associated with a decreased risk of in-hospital mortality (odds ratio, 0.37; P = .021) as well as combined death or intubation (OR, 0.47; P = .040). The outcomes were similar when the researchers performed propensity score matching to adjust for age differences between groups.
In addition, the use of famotidine was associated with lower levels of serum markers for severe disease including lower median peak C-reactive protein levels (9.4 vs. 12.7 mg/dL; P =. 002), lower median procalcitonin levels (0.16 vs. 0.30 ng/mL; P = .004), and a nonsignificant trend to lower median mean ferritin levels (797.5 vs. 964 ng/mL; P = .076).
Logistic regression analysis revealed that use of famotidine was an independent predictor of both lower mortality and combined death/intubation. In addition, predictors of both adverse outcomes included older age, a body mass index of greater than 30 kg/m2, chronic kidney disease, the national early warning score, and a higher neutrophil-lymphocyte ratio.
“This is an important stepping stone, but until we have a randomized, controlled trial, we really can’t speak about causation; we can only speak about association, and that’s okay,” Brennan Spiegel, MD, MSHS, director of health services research at Cedars-Sinai, Los Angeles, who was not affiliated with the study, said in an interview. “There’s nothing wrong with association because finding associations can raise important hypotheses that can then be tested in prospective randomized trials, for example.”
In July 2020, Dr. Spiegel and his colleagues published a separate paper looking at proton pump inhibitors and the risk of COVID-19. “In that study we did look at H2 blockers, and we did find that they were slightly associated with a reduction in COVID-19,” he said. “It was a small effect, but it was a benefit. When we see consistency among studies, it’s a signal in the noise we can try and follow and see if there is something more to it.”
Mr. Mather acknowledged certain limitations of the study, including the fact that patients who did and did not receive famotidine were propensity-matched for age. “The risk factors that others have shown for adverse events are equivalent in the groups, but anytime you do a retrospective study like this there is the potential for underlying factors that may play a role in the outcomes that you’re not considering,” Mr. Mather said. “That’s why the gold standard is the randomized trial, to wash those effects out. There’s only an association here, and it supports the need for a randomized trial.”
Famotidine is currently being tested in a double-blind randomized clinical trial in combination with either hydroxychloroquine or remdesivir (NCT 04370262).
“It’s fascinating because famotidine is a safe medicine,” added Dr. Spiegel, who is also co–editor in chief of the American Journal of Gastroenterology. “There are very few side effects; it’s something we’ve been using for decades.”
Mr. Mather and his colleagues reported having no financial disclosures. Dr. Spiegel disclosed that he has served on advisory boards for Allergan, Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals.
SOURCE: Mather J et al. 2020 Aug 14. Am J Gastroenterol.
It also demonstrated lower levels of serum markers for severe disease.
The findings come from an observational study of 83 hospitalized patients that was published in the American Journal of Gastroenterology.
“The mechanism of exactly how famotidine works has yet to be proven,” lead study author Jeffrey F. Mather, MS, said in an interview. “There’s thought that it works directly on the virus, and there is thought that it works through inactivating certain proteases that are required for the virus infection, but I think the most interesting [hypothesis] is by Malone et al. “They’re looking at the blocking of the histamine-2 receptor causing a decrease in the amount of histamine. It’s all speculative, but it will be interesting if that gets worked out.”
In a study that largely mimicked that of an earlier, larger published observational study on the topic (doi: 10.1053/j.gastro.2020.05.053), Mr. Mather and colleagues retrospectively evaluated 878 patients who tested positive for SARS-CoV-2 and who required admission to Hartford (Conn.) Hospital between Feb. 24, 2020, and May 14, 2020. Patients were classified as receiving famotidine if they were treated with either oral or intravenous drug within 1 week of COVID-19 screening and/or hospital admission. Primary outcomes of interest were in-hospital death as recorded in the discharge of the patients, requirement for mechanical ventilation, and the composite of death or requirement for ventilation. Secondary outcomes of interest were several serum markers of disease activity including white blood cell count, lymphocyte count, and eosinophil count.
Famotidine was administered orally in 83% of the patients and intravenously in the remaining 17%. Mr. Mather, director of data management in the division of research management at Hartford Hospital, and his colleagues reported that 83 of the 878 patients studied (9.5%) received famotidine. Compared with patients not treated with famotidine, those who received the drug were slightly younger (a mean of 64 vs. 68 years, respectively; P = .021); otherwise, there were no differences between the two groups in baseline demographics or in preexisting comorbidities.
The use of famotidine was associated with a decreased risk of in-hospital mortality (odds ratio, 0.37; P = .021) as well as combined death or intubation (OR, 0.47; P = .040). The outcomes were similar when the researchers performed propensity score matching to adjust for age differences between groups.
In addition, the use of famotidine was associated with lower levels of serum markers for severe disease including lower median peak C-reactive protein levels (9.4 vs. 12.7 mg/dL; P =. 002), lower median procalcitonin levels (0.16 vs. 0.30 ng/mL; P = .004), and a nonsignificant trend to lower median mean ferritin levels (797.5 vs. 964 ng/mL; P = .076).
Logistic regression analysis revealed that use of famotidine was an independent predictor of both lower mortality and combined death/intubation. In addition, predictors of both adverse outcomes included older age, a body mass index of greater than 30 kg/m2, chronic kidney disease, the national early warning score, and a higher neutrophil-lymphocyte ratio.
“This is an important stepping stone, but until we have a randomized, controlled trial, we really can’t speak about causation; we can only speak about association, and that’s okay,” Brennan Spiegel, MD, MSHS, director of health services research at Cedars-Sinai, Los Angeles, who was not affiliated with the study, said in an interview. “There’s nothing wrong with association because finding associations can raise important hypotheses that can then be tested in prospective randomized trials, for example.”
In July 2020, Dr. Spiegel and his colleagues published a separate paper looking at proton pump inhibitors and the risk of COVID-19. “In that study we did look at H2 blockers, and we did find that they were slightly associated with a reduction in COVID-19,” he said. “It was a small effect, but it was a benefit. When we see consistency among studies, it’s a signal in the noise we can try and follow and see if there is something more to it.”
Mr. Mather acknowledged certain limitations of the study, including the fact that patients who did and did not receive famotidine were propensity-matched for age. “The risk factors that others have shown for adverse events are equivalent in the groups, but anytime you do a retrospective study like this there is the potential for underlying factors that may play a role in the outcomes that you’re not considering,” Mr. Mather said. “That’s why the gold standard is the randomized trial, to wash those effects out. There’s only an association here, and it supports the need for a randomized trial.”
Famotidine is currently being tested in a double-blind randomized clinical trial in combination with either hydroxychloroquine or remdesivir (NCT 04370262).
“It’s fascinating because famotidine is a safe medicine,” added Dr. Spiegel, who is also co–editor in chief of the American Journal of Gastroenterology. “There are very few side effects; it’s something we’ve been using for decades.”
Mr. Mather and his colleagues reported having no financial disclosures. Dr. Spiegel disclosed that he has served on advisory boards for Allergan, Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals.
SOURCE: Mather J et al. 2020 Aug 14. Am J Gastroenterol.
It also demonstrated lower levels of serum markers for severe disease.
The findings come from an observational study of 83 hospitalized patients that was published in the American Journal of Gastroenterology.
“The mechanism of exactly how famotidine works has yet to be proven,” lead study author Jeffrey F. Mather, MS, said in an interview. “There’s thought that it works directly on the virus, and there is thought that it works through inactivating certain proteases that are required for the virus infection, but I think the most interesting [hypothesis] is by Malone et al. “They’re looking at the blocking of the histamine-2 receptor causing a decrease in the amount of histamine. It’s all speculative, but it will be interesting if that gets worked out.”
In a study that largely mimicked that of an earlier, larger published observational study on the topic (doi: 10.1053/j.gastro.2020.05.053), Mr. Mather and colleagues retrospectively evaluated 878 patients who tested positive for SARS-CoV-2 and who required admission to Hartford (Conn.) Hospital between Feb. 24, 2020, and May 14, 2020. Patients were classified as receiving famotidine if they were treated with either oral or intravenous drug within 1 week of COVID-19 screening and/or hospital admission. Primary outcomes of interest were in-hospital death as recorded in the discharge of the patients, requirement for mechanical ventilation, and the composite of death or requirement for ventilation. Secondary outcomes of interest were several serum markers of disease activity including white blood cell count, lymphocyte count, and eosinophil count.
Famotidine was administered orally in 83% of the patients and intravenously in the remaining 17%. Mr. Mather, director of data management in the division of research management at Hartford Hospital, and his colleagues reported that 83 of the 878 patients studied (9.5%) received famotidine. Compared with patients not treated with famotidine, those who received the drug were slightly younger (a mean of 64 vs. 68 years, respectively; P = .021); otherwise, there were no differences between the two groups in baseline demographics or in preexisting comorbidities.
The use of famotidine was associated with a decreased risk of in-hospital mortality (odds ratio, 0.37; P = .021) as well as combined death or intubation (OR, 0.47; P = .040). The outcomes were similar when the researchers performed propensity score matching to adjust for age differences between groups.
In addition, the use of famotidine was associated with lower levels of serum markers for severe disease including lower median peak C-reactive protein levels (9.4 vs. 12.7 mg/dL; P =. 002), lower median procalcitonin levels (0.16 vs. 0.30 ng/mL; P = .004), and a nonsignificant trend to lower median mean ferritin levels (797.5 vs. 964 ng/mL; P = .076).
Logistic regression analysis revealed that use of famotidine was an independent predictor of both lower mortality and combined death/intubation. In addition, predictors of both adverse outcomes included older age, a body mass index of greater than 30 kg/m2, chronic kidney disease, the national early warning score, and a higher neutrophil-lymphocyte ratio.
“This is an important stepping stone, but until we have a randomized, controlled trial, we really can’t speak about causation; we can only speak about association, and that’s okay,” Brennan Spiegel, MD, MSHS, director of health services research at Cedars-Sinai, Los Angeles, who was not affiliated with the study, said in an interview. “There’s nothing wrong with association because finding associations can raise important hypotheses that can then be tested in prospective randomized trials, for example.”
In July 2020, Dr. Spiegel and his colleagues published a separate paper looking at proton pump inhibitors and the risk of COVID-19. “In that study we did look at H2 blockers, and we did find that they were slightly associated with a reduction in COVID-19,” he said. “It was a small effect, but it was a benefit. When we see consistency among studies, it’s a signal in the noise we can try and follow and see if there is something more to it.”
Mr. Mather acknowledged certain limitations of the study, including the fact that patients who did and did not receive famotidine were propensity-matched for age. “The risk factors that others have shown for adverse events are equivalent in the groups, but anytime you do a retrospective study like this there is the potential for underlying factors that may play a role in the outcomes that you’re not considering,” Mr. Mather said. “That’s why the gold standard is the randomized trial, to wash those effects out. There’s only an association here, and it supports the need for a randomized trial.”
Famotidine is currently being tested in a double-blind randomized clinical trial in combination with either hydroxychloroquine or remdesivir (NCT 04370262).
“It’s fascinating because famotidine is a safe medicine,” added Dr. Spiegel, who is also co–editor in chief of the American Journal of Gastroenterology. “There are very few side effects; it’s something we’ve been using for decades.”
Mr. Mather and his colleagues reported having no financial disclosures. Dr. Spiegel disclosed that he has served on advisory boards for Allergan, Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals.
SOURCE: Mather J et al. 2020 Aug 14. Am J Gastroenterol.
REPORTING FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Key clinical point: Among hospitalized COVID-19 patients, famotidine use was associated with a reduction in death and either death or intubation.
Major finding: The use of famotidine was associated with a decreased risk of in-hospital mortality (OR, 0.37; P = .021), as well as the combined endpoint of death or intubation (OR, 0.47; P = .040).
Study details: A single-center observational study of 83 patients hospitalized with COVID-19.
Disclosures: The researchers reported having no financial disclosures.
Source: Mather J et al. 2020 Aug 14. Am J Gastroenterol.
FDA approves clinical trials for cannabinoid drug designed to reduce COVID-19 lung inflammation
The US Food and Drug Administration has approved phase one clinical trials for a synthetic cannabinoid drug designed to treat acute respiratory distress syndrome (ARDS), a life-threatening lung condition which may occur in severe cases of the novel coronavirus, Forbes reported.
ARDS can be triggered by over-creation of cytokines, proteins which tell the body to produce more inflammation, Forbes said.
The drug going to clinical trials, ARDS-003, would “dampen the cytokine release” and prevent development of ARDS, Tetra Bio-Pharma company CEO and chief regulatory officer Guy Chamberland, MD, said in a news release.
Consequences of ARDS include scarring of the lungs and organ injury caused by the decrease in blood to the tissue, the release said.
“The FDA repeatedly stated that they want clinical trials for COVID-19 to begin as soon as possible, as long as they meet regulatory requirements,” the news release said. “The medical community is in urgent need of drugs that can reduce the strength and duration of the severe inflammation. It is anticipated that this type of new drug would favorably impact health care and possibly reduce the negative health outcomes post infection.”
ARDS-003 works by binding to CB2 receptors, one of two main receptors in the endocannabinoid system which modulate inflammation and cytokine activity, Forbes said. CB2 receptors don’t bring on a psychoactive high.
Phase one clinical trials would begin enrolling participants in December to determine if the drug is safe, Chamberland said, according to Forbes.
If phase one is successful, phase two would test the drug on a larger group in the second quarter of 2021 to assess safety and tolerability for people who have COVID-19.
If phase two is successful, the company may seek emergency authorization through the FDA, Chamberland said. Phase three would start at the end of 2021.
Tetra Bio-Pharma says it has already contracted with Dalton Pharma Services to manufacture the active pharmaceutical ingredient (API), HU-308, and the finished drug product ARDS-003.
This article first appeared on Medscape.com.
The US Food and Drug Administration has approved phase one clinical trials for a synthetic cannabinoid drug designed to treat acute respiratory distress syndrome (ARDS), a life-threatening lung condition which may occur in severe cases of the novel coronavirus, Forbes reported.
ARDS can be triggered by over-creation of cytokines, proteins which tell the body to produce more inflammation, Forbes said.
The drug going to clinical trials, ARDS-003, would “dampen the cytokine release” and prevent development of ARDS, Tetra Bio-Pharma company CEO and chief regulatory officer Guy Chamberland, MD, said in a news release.
Consequences of ARDS include scarring of the lungs and organ injury caused by the decrease in blood to the tissue, the release said.
“The FDA repeatedly stated that they want clinical trials for COVID-19 to begin as soon as possible, as long as they meet regulatory requirements,” the news release said. “The medical community is in urgent need of drugs that can reduce the strength and duration of the severe inflammation. It is anticipated that this type of new drug would favorably impact health care and possibly reduce the negative health outcomes post infection.”
ARDS-003 works by binding to CB2 receptors, one of two main receptors in the endocannabinoid system which modulate inflammation and cytokine activity, Forbes said. CB2 receptors don’t bring on a psychoactive high.
Phase one clinical trials would begin enrolling participants in December to determine if the drug is safe, Chamberland said, according to Forbes.
If phase one is successful, phase two would test the drug on a larger group in the second quarter of 2021 to assess safety and tolerability for people who have COVID-19.
If phase two is successful, the company may seek emergency authorization through the FDA, Chamberland said. Phase three would start at the end of 2021.
Tetra Bio-Pharma says it has already contracted with Dalton Pharma Services to manufacture the active pharmaceutical ingredient (API), HU-308, and the finished drug product ARDS-003.
This article first appeared on Medscape.com.
The US Food and Drug Administration has approved phase one clinical trials for a synthetic cannabinoid drug designed to treat acute respiratory distress syndrome (ARDS), a life-threatening lung condition which may occur in severe cases of the novel coronavirus, Forbes reported.
ARDS can be triggered by over-creation of cytokines, proteins which tell the body to produce more inflammation, Forbes said.
The drug going to clinical trials, ARDS-003, would “dampen the cytokine release” and prevent development of ARDS, Tetra Bio-Pharma company CEO and chief regulatory officer Guy Chamberland, MD, said in a news release.
Consequences of ARDS include scarring of the lungs and organ injury caused by the decrease in blood to the tissue, the release said.
“The FDA repeatedly stated that they want clinical trials for COVID-19 to begin as soon as possible, as long as they meet regulatory requirements,” the news release said. “The medical community is in urgent need of drugs that can reduce the strength and duration of the severe inflammation. It is anticipated that this type of new drug would favorably impact health care and possibly reduce the negative health outcomes post infection.”
ARDS-003 works by binding to CB2 receptors, one of two main receptors in the endocannabinoid system which modulate inflammation and cytokine activity, Forbes said. CB2 receptors don’t bring on a psychoactive high.
Phase one clinical trials would begin enrolling participants in December to determine if the drug is safe, Chamberland said, according to Forbes.
If phase one is successful, phase two would test the drug on a larger group in the second quarter of 2021 to assess safety and tolerability for people who have COVID-19.
If phase two is successful, the company may seek emergency authorization through the FDA, Chamberland said. Phase three would start at the end of 2021.
Tetra Bio-Pharma says it has already contracted with Dalton Pharma Services to manufacture the active pharmaceutical ingredient (API), HU-308, and the finished drug product ARDS-003.
This article first appeared on Medscape.com.
Study confirms it’s possible to catch COVID-19 twice
Researchers in Hong Kong say they’ve confirmed that a person can be infected with COVID-19 twice.
The new proof comes from a 33-year-old man in Hong Kong who first caught COVID-19 in March. He was tested for the coronavirus after he developed a cough, sore throat, fever, and a headache for 3 days. He stayed in the hospital until he twice tested negative for the virus in mid-April.
On Aug. 15, the man returned to Hong Kong from a recent trip to Spain and the United Kingdom, areas that have recently seen a resurgence of COVID-19 cases. At the airport, he was screened for COVID-19 with a test that checks saliva for the virus. He tested positive, but this time, had no symptoms. He was taken to the hospital for monitoring. His viral load – the amount of virus he had in his body – went down over time, suggesting that his immune system was taking care of the intrusion on its own.
The special thing about his case is that each time he was hospitalized, doctors sequenced the genome of the virus that infected him. It was slightly different from one infection to the next, suggesting that the virus had mutated – or changed – in the 4 months between his infections. It also proves that it’s possible for this coronavirus to infect the same person twice.
Experts with the World Health Organization responded to the case at a news briefing.
“What we are learning about infection is that people do develop an immune response. What is not completely clear yet is how strong that immune response is and for how long that immune response lasts,” said Maria Van Kerkhove, PhD, an infectious disease epidemiologist with the World Health Organization in Geneva, Switzerland.
A study on the man’s case is being prepared for publication in the journal Clinical Infectious Diseases. Experts say the finding shouldn’t cause alarm, but it does have important implications for the development of herd immunity and efforts to come up with vaccines and treatments.
“This appears to be pretty clear-cut evidence of reinfection because of sequencing and isolation of two different viruses,” said Gregory Poland, MD, an expert on vaccine development and immunology at the Mayo Clinic in Rochester, Minn. “The big unknown is how often is this happening,” he said. More studies are needed to learn whether this was a rare case or something that is happening often.
Past experience guides present
Until we know more, Dr. Poland said, the possibility of getting COVID-19 twice shouldn’t make anyone worry.
This also happens with other kinds of coronaviruses – the ones that cause common colds. Those coronaviruses change slightly each year as they circle the globe, which allows them to keep spreading and causing their more run-of-the-mill kind of misery.
It also happens with seasonal flu. It is the reason people have to get vaccinated against the flu year after year, and why the flu vaccine has to change slightly each year in an effort to keep up with the ever-evolving influenza virus.
“We’ve been making flu vaccines for 80 years, and there are clinical trials happening as we speak to find new and better influenza vaccines,” Dr. Poland said.
There has been other evidence the virus that causes COVID-19 can change this way, too. Researchers at Howard Hughes Medical Center, at Rockefeller University in New York, recently used a key piece of the SARS-CoV-2 virus – the genetic instructions for its spike protein – to repeatedly infect human cells. Scientists watched as each new generation of the virus went on to infect a new batch of cells. Over time, as it copied itself, some of the copies changed their genes to allow them to survive after scientists attacked them with neutralizing antibodies. Those antibodies are among the main weapons used by the immune system to recognize and disable a virus.
Though that study is still a preprint, which means it hasn’t yet been reviewed by outside experts, the authors wrote that their findings suggest the virus can change in ways that help it evade our immune system. If true, they wrote in mid-July, it means reinfection is possible, especially in people who have a weak immune response to the virus the first time they encounter it.
Good news
That seems to be true in the case of the man from Hong Kong. When doctors tested his blood to look for antibodies to the virus, they didn’t find any. That could mean that he either had a weak immune response to the virus the first time around, or that the antibodies he made during his first infection diminished over time. But during his second infection, he quickly developed more antibodies, suggesting that the second infection acted a little bit like a booster to fire up his immune system. That’s probably the reason he didn’t have any symptoms the second time, too.
That’s good news, Dr. Poland said. It means our bodies can get better at fighting off the COVID-19 virus and that catching it once means the second time might not be so bad.
But the fact that the virus can change quickly this way does have some impact on the effort to come up with a vaccine that works well.
“I think a potential implication of this is that we will have to give booster doses. The question is how frequently,” Dr. Poland said. That will depend on how fast the virus is changing, and how often reinfection is happening in the real world.
“I’m a little surprised at 4½ months,” Dr. Poland said, referencing the time between the Hong Kong man’s infections. “I’m not surprised by, you know, I got infected last winter and I got infected again this winter,” he said.
It also suggests that immune-based therapies such as convalescent plasma and monoclonal antibodies may be of limited help over time, since the virus might be changing in ways that help it outsmart those treatments.
Convalescent plasma is essentially a concentrated dose of antibodies from people who have recovered from a COVID-19 infection. As the virus changes, the antibodies in that plasma may not work as well for future infections.
Drug companies have learned to harness the power of monoclonal antibodies as powerful treatments against cancer and other diseases. Monoclonal antibodies, which are mass-produced in a lab, mimic the body’s natural defenses against a pathogen. Just like the virus can become resistant to natural immunity, it can change in ways that help it outsmart lab-created treatments. Some drug companies that are developing monoclonal antibodies to fight COVID-19 have already prepared for that possibility by making antibody cocktails that are designed to disable the virus by locking onto it in different places, which may help prevent it from developing resistance to those therapies.
“We have a lot to learn,” Dr. Poland said. “Now that the proof of principle has been established, and I would say it has with this man, and with our knowledge of seasonal coronaviruses, we need to look more aggressively to define how often this occurs.”
A version of this article originally appeared on WebMD.com.
Researchers in Hong Kong say they’ve confirmed that a person can be infected with COVID-19 twice.
The new proof comes from a 33-year-old man in Hong Kong who first caught COVID-19 in March. He was tested for the coronavirus after he developed a cough, sore throat, fever, and a headache for 3 days. He stayed in the hospital until he twice tested negative for the virus in mid-April.
On Aug. 15, the man returned to Hong Kong from a recent trip to Spain and the United Kingdom, areas that have recently seen a resurgence of COVID-19 cases. At the airport, he was screened for COVID-19 with a test that checks saliva for the virus. He tested positive, but this time, had no symptoms. He was taken to the hospital for monitoring. His viral load – the amount of virus he had in his body – went down over time, suggesting that his immune system was taking care of the intrusion on its own.
The special thing about his case is that each time he was hospitalized, doctors sequenced the genome of the virus that infected him. It was slightly different from one infection to the next, suggesting that the virus had mutated – or changed – in the 4 months between his infections. It also proves that it’s possible for this coronavirus to infect the same person twice.
Experts with the World Health Organization responded to the case at a news briefing.
“What we are learning about infection is that people do develop an immune response. What is not completely clear yet is how strong that immune response is and for how long that immune response lasts,” said Maria Van Kerkhove, PhD, an infectious disease epidemiologist with the World Health Organization in Geneva, Switzerland.
A study on the man’s case is being prepared for publication in the journal Clinical Infectious Diseases. Experts say the finding shouldn’t cause alarm, but it does have important implications for the development of herd immunity and efforts to come up with vaccines and treatments.
“This appears to be pretty clear-cut evidence of reinfection because of sequencing and isolation of two different viruses,” said Gregory Poland, MD, an expert on vaccine development and immunology at the Mayo Clinic in Rochester, Minn. “The big unknown is how often is this happening,” he said. More studies are needed to learn whether this was a rare case or something that is happening often.
Past experience guides present
Until we know more, Dr. Poland said, the possibility of getting COVID-19 twice shouldn’t make anyone worry.
This also happens with other kinds of coronaviruses – the ones that cause common colds. Those coronaviruses change slightly each year as they circle the globe, which allows them to keep spreading and causing their more run-of-the-mill kind of misery.
It also happens with seasonal flu. It is the reason people have to get vaccinated against the flu year after year, and why the flu vaccine has to change slightly each year in an effort to keep up with the ever-evolving influenza virus.
“We’ve been making flu vaccines for 80 years, and there are clinical trials happening as we speak to find new and better influenza vaccines,” Dr. Poland said.
There has been other evidence the virus that causes COVID-19 can change this way, too. Researchers at Howard Hughes Medical Center, at Rockefeller University in New York, recently used a key piece of the SARS-CoV-2 virus – the genetic instructions for its spike protein – to repeatedly infect human cells. Scientists watched as each new generation of the virus went on to infect a new batch of cells. Over time, as it copied itself, some of the copies changed their genes to allow them to survive after scientists attacked them with neutralizing antibodies. Those antibodies are among the main weapons used by the immune system to recognize and disable a virus.
Though that study is still a preprint, which means it hasn’t yet been reviewed by outside experts, the authors wrote that their findings suggest the virus can change in ways that help it evade our immune system. If true, they wrote in mid-July, it means reinfection is possible, especially in people who have a weak immune response to the virus the first time they encounter it.
Good news
That seems to be true in the case of the man from Hong Kong. When doctors tested his blood to look for antibodies to the virus, they didn’t find any. That could mean that he either had a weak immune response to the virus the first time around, or that the antibodies he made during his first infection diminished over time. But during his second infection, he quickly developed more antibodies, suggesting that the second infection acted a little bit like a booster to fire up his immune system. That’s probably the reason he didn’t have any symptoms the second time, too.
That’s good news, Dr. Poland said. It means our bodies can get better at fighting off the COVID-19 virus and that catching it once means the second time might not be so bad.
But the fact that the virus can change quickly this way does have some impact on the effort to come up with a vaccine that works well.
“I think a potential implication of this is that we will have to give booster doses. The question is how frequently,” Dr. Poland said. That will depend on how fast the virus is changing, and how often reinfection is happening in the real world.
“I’m a little surprised at 4½ months,” Dr. Poland said, referencing the time between the Hong Kong man’s infections. “I’m not surprised by, you know, I got infected last winter and I got infected again this winter,” he said.
It also suggests that immune-based therapies such as convalescent plasma and monoclonal antibodies may be of limited help over time, since the virus might be changing in ways that help it outsmart those treatments.
Convalescent plasma is essentially a concentrated dose of antibodies from people who have recovered from a COVID-19 infection. As the virus changes, the antibodies in that plasma may not work as well for future infections.
Drug companies have learned to harness the power of monoclonal antibodies as powerful treatments against cancer and other diseases. Monoclonal antibodies, which are mass-produced in a lab, mimic the body’s natural defenses against a pathogen. Just like the virus can become resistant to natural immunity, it can change in ways that help it outsmart lab-created treatments. Some drug companies that are developing monoclonal antibodies to fight COVID-19 have already prepared for that possibility by making antibody cocktails that are designed to disable the virus by locking onto it in different places, which may help prevent it from developing resistance to those therapies.
“We have a lot to learn,” Dr. Poland said. “Now that the proof of principle has been established, and I would say it has with this man, and with our knowledge of seasonal coronaviruses, we need to look more aggressively to define how often this occurs.”
A version of this article originally appeared on WebMD.com.
Researchers in Hong Kong say they’ve confirmed that a person can be infected with COVID-19 twice.
The new proof comes from a 33-year-old man in Hong Kong who first caught COVID-19 in March. He was tested for the coronavirus after he developed a cough, sore throat, fever, and a headache for 3 days. He stayed in the hospital until he twice tested negative for the virus in mid-April.
On Aug. 15, the man returned to Hong Kong from a recent trip to Spain and the United Kingdom, areas that have recently seen a resurgence of COVID-19 cases. At the airport, he was screened for COVID-19 with a test that checks saliva for the virus. He tested positive, but this time, had no symptoms. He was taken to the hospital for monitoring. His viral load – the amount of virus he had in his body – went down over time, suggesting that his immune system was taking care of the intrusion on its own.
The special thing about his case is that each time he was hospitalized, doctors sequenced the genome of the virus that infected him. It was slightly different from one infection to the next, suggesting that the virus had mutated – or changed – in the 4 months between his infections. It also proves that it’s possible for this coronavirus to infect the same person twice.
Experts with the World Health Organization responded to the case at a news briefing.
“What we are learning about infection is that people do develop an immune response. What is not completely clear yet is how strong that immune response is and for how long that immune response lasts,” said Maria Van Kerkhove, PhD, an infectious disease epidemiologist with the World Health Organization in Geneva, Switzerland.
A study on the man’s case is being prepared for publication in the journal Clinical Infectious Diseases. Experts say the finding shouldn’t cause alarm, but it does have important implications for the development of herd immunity and efforts to come up with vaccines and treatments.
“This appears to be pretty clear-cut evidence of reinfection because of sequencing and isolation of two different viruses,” said Gregory Poland, MD, an expert on vaccine development and immunology at the Mayo Clinic in Rochester, Minn. “The big unknown is how often is this happening,” he said. More studies are needed to learn whether this was a rare case or something that is happening often.
Past experience guides present
Until we know more, Dr. Poland said, the possibility of getting COVID-19 twice shouldn’t make anyone worry.
This also happens with other kinds of coronaviruses – the ones that cause common colds. Those coronaviruses change slightly each year as they circle the globe, which allows them to keep spreading and causing their more run-of-the-mill kind of misery.
It also happens with seasonal flu. It is the reason people have to get vaccinated against the flu year after year, and why the flu vaccine has to change slightly each year in an effort to keep up with the ever-evolving influenza virus.
“We’ve been making flu vaccines for 80 years, and there are clinical trials happening as we speak to find new and better influenza vaccines,” Dr. Poland said.
There has been other evidence the virus that causes COVID-19 can change this way, too. Researchers at Howard Hughes Medical Center, at Rockefeller University in New York, recently used a key piece of the SARS-CoV-2 virus – the genetic instructions for its spike protein – to repeatedly infect human cells. Scientists watched as each new generation of the virus went on to infect a new batch of cells. Over time, as it copied itself, some of the copies changed their genes to allow them to survive after scientists attacked them with neutralizing antibodies. Those antibodies are among the main weapons used by the immune system to recognize and disable a virus.
Though that study is still a preprint, which means it hasn’t yet been reviewed by outside experts, the authors wrote that their findings suggest the virus can change in ways that help it evade our immune system. If true, they wrote in mid-July, it means reinfection is possible, especially in people who have a weak immune response to the virus the first time they encounter it.
Good news
That seems to be true in the case of the man from Hong Kong. When doctors tested his blood to look for antibodies to the virus, they didn’t find any. That could mean that he either had a weak immune response to the virus the first time around, or that the antibodies he made during his first infection diminished over time. But during his second infection, he quickly developed more antibodies, suggesting that the second infection acted a little bit like a booster to fire up his immune system. That’s probably the reason he didn’t have any symptoms the second time, too.
That’s good news, Dr. Poland said. It means our bodies can get better at fighting off the COVID-19 virus and that catching it once means the second time might not be so bad.
But the fact that the virus can change quickly this way does have some impact on the effort to come up with a vaccine that works well.
“I think a potential implication of this is that we will have to give booster doses. The question is how frequently,” Dr. Poland said. That will depend on how fast the virus is changing, and how often reinfection is happening in the real world.
“I’m a little surprised at 4½ months,” Dr. Poland said, referencing the time between the Hong Kong man’s infections. “I’m not surprised by, you know, I got infected last winter and I got infected again this winter,” he said.
It also suggests that immune-based therapies such as convalescent plasma and monoclonal antibodies may be of limited help over time, since the virus might be changing in ways that help it outsmart those treatments.
Convalescent plasma is essentially a concentrated dose of antibodies from people who have recovered from a COVID-19 infection. As the virus changes, the antibodies in that plasma may not work as well for future infections.
Drug companies have learned to harness the power of monoclonal antibodies as powerful treatments against cancer and other diseases. Monoclonal antibodies, which are mass-produced in a lab, mimic the body’s natural defenses against a pathogen. Just like the virus can become resistant to natural immunity, it can change in ways that help it outsmart lab-created treatments. Some drug companies that are developing monoclonal antibodies to fight COVID-19 have already prepared for that possibility by making antibody cocktails that are designed to disable the virus by locking onto it in different places, which may help prevent it from developing resistance to those therapies.
“We have a lot to learn,” Dr. Poland said. “Now that the proof of principle has been established, and I would say it has with this man, and with our knowledge of seasonal coronaviruses, we need to look more aggressively to define how often this occurs.”
A version of this article originally appeared on WebMD.com.
Research examines links between ‘long COVID’ and ME/CFS
Some patients who had COVID-19 continue to have symptoms weeks to months later, even after they no longer test positive for the virus. In two recent reports – one published in JAMA in July and another published in Morbidity and Mortality Weekly Report in August – chronic fatigue was listed as the top symptom among individuals still feeling unwell beyond 2 weeks after COVID-19 onset.
Although some of the reported persistent symptoms appear specific to SARS-CoV-2 – such as cough, chest pain, and dyspnea – others overlap with the diagnostic criteria for ME/CFS, which is defined by substantial, profound fatigue for at least 6 months, postexertional malaise, unrefreshing sleep, and one or both of orthostatic intolerance and/or cognitive impairment. Although the etiology of ME/CFS is unclear, the condition commonly arises following a viral illness.
At the virtual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis August 21, the opening session was devoted to research documenting the extent to which COVID-19 survivors subsequently meet ME/CFS criteria, and to exploring underlying mechanisms.
“It offers a lot of opportunities for us to study potentially early ME/CFS and how it develops, but in addition, a lot of the research that has been done on ME/CFS may also provide answers for COVID-19,” IACFS/ME vice president Lily Chu, MD, said in an interview.
A hint from the SARS outbreak
This isn’t the first time researchers have seen a possible link between a coronavirus and ME/CFS, Harvey Moldofsky, MD, told attendees. To illustrate that point, Dr. Moldofsky, of the department of psychiatry (emeritus) at the University of Toronto, reviewed data from a previously published case-controlled study, which included 22 health care workers who had been infected in 2003 with SARS-CoV-1 and continued to report chronic fatigue, musculoskeletal pain, and disturbed and unrefreshing sleep with EEG-documented sleep disturbances 1-3 years following the illness. None had been able to return to work by 1 year.
“We’re looking at similar symptoms now” among survivors of COVID-19, Dr. Moldofsky said. “[T]he key issue is that we have no idea of its prevalence. … We need epidemiologic studies.”
Distinguishing ME/CFS from other post–COVID-19 symptoms
Not everyone who has persistent symptoms after COVID-19 will develop ME/CFS, and distinguishing between cases may be important.
Clinically, Dr. Chu said, one way to assess whether a patient with persistent COVID-19 symptoms might be progressing to ME/CFS is to ask him or her specifically about the level of fatigue following physical exertion and the timing of any fatigue. With ME/CFS, postexertional malaise often involves a dramatic exacerbation of symptoms such as fatigue, pain, and cognitive impairment a day or 2 after exertion rather than immediately following it. In contrast, shortness of breath during exertion isn’t typical of ME/CFS.
Objective measures of ME/CFS include low natural killer cell function (the test can be ordered from commercial labs but requires rapid transport of the blood sample), and autonomic dysfunction assessed by a tilt-table test.
While there is currently no cure for ME/CFS, diagnosing it allows for the patient to be taught “pacing” in which the person conserves his or her energy by balancing activity with rest. “That type of behavioral technique is valuable for everyone who suffers from a chronic disease with fatigue. It can help them be more functional,” Dr. Chu said.
If a patient appears to be exhibiting signs of ME/CFS, “don’t wait until they hit the 6-month mark to start helping them manage their symptoms,” she said. “Teaching pacing to COVID-19 patients who have a lot of fatigue isn’t going to harm them. As they get better they’re going to just naturally do more. But if they do have ME/CFS, [pacing] stresses their system less, since the data seem to be pointing to deficiencies in producing energy.”
Will COVID-19 unleash a new wave of ME/CFS patients?
Much of the session at the virtual meeting was devoted to ongoing studies. For example, Leonard Jason, PhD, of the Center for Community Research at DePaul University, Chicago, described a prospective study launched in 2014 that looked at risk factors for developing ME/CFS in college students who contracted infectious mononucleosis as a result of Epstein-Barr virus. Now, his team is also following students from the same cohort who develop COVID-19.
Because the study included collection of baseline biological samples, the results could help reveal predisposing factors associated with long-term illness from either virus.
Another project, funded by the Open Medicine Foundation, will follow patients who are discharged from the ICU following severe COVID-19 illness. Blood, urine, and cerebrospinal fluid will be collected from those with persistent symptoms at 6 months, along with questionnaire data. At 18-24 months, those who continue to report symptoms will undergo more intensive evaluation using genomics, metabolomics, and proteomics.
“We’re taking advantage of this horrible situation, hoping to understand how a serious viral infection might lead to ME/CFS,” said lead investigator Ronald Tompkins, MD, ScD, chief medical officer at the Open Medicine Foundation and a faculty member at Harvard Medical School, Boston. The results, he said, “might give us insight into potential drug targets or biomarkers useful for prevention and treatment strategies.”
Meanwhile, Sadie Whittaker, PhD, head of the Solve ME/CFS initiative, described her organization’s new plan to use their registry to prospectively track the impact of COVID-19 on people with ME/CFS.
She noted that they’ve also teamed up with “long-COVID” communities including Body Politic. “Our goal is to form a coalition to study together or at least harmonize data … and understand what’s going on through the power of bigger sample sizes,” Dr. Whittaker said.
None of the speakers disclosed relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Some patients who had COVID-19 continue to have symptoms weeks to months later, even after they no longer test positive for the virus. In two recent reports – one published in JAMA in July and another published in Morbidity and Mortality Weekly Report in August – chronic fatigue was listed as the top symptom among individuals still feeling unwell beyond 2 weeks after COVID-19 onset.
Although some of the reported persistent symptoms appear specific to SARS-CoV-2 – such as cough, chest pain, and dyspnea – others overlap with the diagnostic criteria for ME/CFS, which is defined by substantial, profound fatigue for at least 6 months, postexertional malaise, unrefreshing sleep, and one or both of orthostatic intolerance and/or cognitive impairment. Although the etiology of ME/CFS is unclear, the condition commonly arises following a viral illness.
At the virtual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis August 21, the opening session was devoted to research documenting the extent to which COVID-19 survivors subsequently meet ME/CFS criteria, and to exploring underlying mechanisms.
“It offers a lot of opportunities for us to study potentially early ME/CFS and how it develops, but in addition, a lot of the research that has been done on ME/CFS may also provide answers for COVID-19,” IACFS/ME vice president Lily Chu, MD, said in an interview.
A hint from the SARS outbreak
This isn’t the first time researchers have seen a possible link between a coronavirus and ME/CFS, Harvey Moldofsky, MD, told attendees. To illustrate that point, Dr. Moldofsky, of the department of psychiatry (emeritus) at the University of Toronto, reviewed data from a previously published case-controlled study, which included 22 health care workers who had been infected in 2003 with SARS-CoV-1 and continued to report chronic fatigue, musculoskeletal pain, and disturbed and unrefreshing sleep with EEG-documented sleep disturbances 1-3 years following the illness. None had been able to return to work by 1 year.
“We’re looking at similar symptoms now” among survivors of COVID-19, Dr. Moldofsky said. “[T]he key issue is that we have no idea of its prevalence. … We need epidemiologic studies.”
Distinguishing ME/CFS from other post–COVID-19 symptoms
Not everyone who has persistent symptoms after COVID-19 will develop ME/CFS, and distinguishing between cases may be important.
Clinically, Dr. Chu said, one way to assess whether a patient with persistent COVID-19 symptoms might be progressing to ME/CFS is to ask him or her specifically about the level of fatigue following physical exertion and the timing of any fatigue. With ME/CFS, postexertional malaise often involves a dramatic exacerbation of symptoms such as fatigue, pain, and cognitive impairment a day or 2 after exertion rather than immediately following it. In contrast, shortness of breath during exertion isn’t typical of ME/CFS.
Objective measures of ME/CFS include low natural killer cell function (the test can be ordered from commercial labs but requires rapid transport of the blood sample), and autonomic dysfunction assessed by a tilt-table test.
While there is currently no cure for ME/CFS, diagnosing it allows for the patient to be taught “pacing” in which the person conserves his or her energy by balancing activity with rest. “That type of behavioral technique is valuable for everyone who suffers from a chronic disease with fatigue. It can help them be more functional,” Dr. Chu said.
If a patient appears to be exhibiting signs of ME/CFS, “don’t wait until they hit the 6-month mark to start helping them manage their symptoms,” she said. “Teaching pacing to COVID-19 patients who have a lot of fatigue isn’t going to harm them. As they get better they’re going to just naturally do more. But if they do have ME/CFS, [pacing] stresses their system less, since the data seem to be pointing to deficiencies in producing energy.”
Will COVID-19 unleash a new wave of ME/CFS patients?
Much of the session at the virtual meeting was devoted to ongoing studies. For example, Leonard Jason, PhD, of the Center for Community Research at DePaul University, Chicago, described a prospective study launched in 2014 that looked at risk factors for developing ME/CFS in college students who contracted infectious mononucleosis as a result of Epstein-Barr virus. Now, his team is also following students from the same cohort who develop COVID-19.
Because the study included collection of baseline biological samples, the results could help reveal predisposing factors associated with long-term illness from either virus.
Another project, funded by the Open Medicine Foundation, will follow patients who are discharged from the ICU following severe COVID-19 illness. Blood, urine, and cerebrospinal fluid will be collected from those with persistent symptoms at 6 months, along with questionnaire data. At 18-24 months, those who continue to report symptoms will undergo more intensive evaluation using genomics, metabolomics, and proteomics.
“We’re taking advantage of this horrible situation, hoping to understand how a serious viral infection might lead to ME/CFS,” said lead investigator Ronald Tompkins, MD, ScD, chief medical officer at the Open Medicine Foundation and a faculty member at Harvard Medical School, Boston. The results, he said, “might give us insight into potential drug targets or biomarkers useful for prevention and treatment strategies.”
Meanwhile, Sadie Whittaker, PhD, head of the Solve ME/CFS initiative, described her organization’s new plan to use their registry to prospectively track the impact of COVID-19 on people with ME/CFS.
She noted that they’ve also teamed up with “long-COVID” communities including Body Politic. “Our goal is to form a coalition to study together or at least harmonize data … and understand what’s going on through the power of bigger sample sizes,” Dr. Whittaker said.
None of the speakers disclosed relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Some patients who had COVID-19 continue to have symptoms weeks to months later, even after they no longer test positive for the virus. In two recent reports – one published in JAMA in July and another published in Morbidity and Mortality Weekly Report in August – chronic fatigue was listed as the top symptom among individuals still feeling unwell beyond 2 weeks after COVID-19 onset.
Although some of the reported persistent symptoms appear specific to SARS-CoV-2 – such as cough, chest pain, and dyspnea – others overlap with the diagnostic criteria for ME/CFS, which is defined by substantial, profound fatigue for at least 6 months, postexertional malaise, unrefreshing sleep, and one or both of orthostatic intolerance and/or cognitive impairment. Although the etiology of ME/CFS is unclear, the condition commonly arises following a viral illness.
At the virtual meeting of the International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis August 21, the opening session was devoted to research documenting the extent to which COVID-19 survivors subsequently meet ME/CFS criteria, and to exploring underlying mechanisms.
“It offers a lot of opportunities for us to study potentially early ME/CFS and how it develops, but in addition, a lot of the research that has been done on ME/CFS may also provide answers for COVID-19,” IACFS/ME vice president Lily Chu, MD, said in an interview.
A hint from the SARS outbreak
This isn’t the first time researchers have seen a possible link between a coronavirus and ME/CFS, Harvey Moldofsky, MD, told attendees. To illustrate that point, Dr. Moldofsky, of the department of psychiatry (emeritus) at the University of Toronto, reviewed data from a previously published case-controlled study, which included 22 health care workers who had been infected in 2003 with SARS-CoV-1 and continued to report chronic fatigue, musculoskeletal pain, and disturbed and unrefreshing sleep with EEG-documented sleep disturbances 1-3 years following the illness. None had been able to return to work by 1 year.
“We’re looking at similar symptoms now” among survivors of COVID-19, Dr. Moldofsky said. “[T]he key issue is that we have no idea of its prevalence. … We need epidemiologic studies.”
Distinguishing ME/CFS from other post–COVID-19 symptoms
Not everyone who has persistent symptoms after COVID-19 will develop ME/CFS, and distinguishing between cases may be important.
Clinically, Dr. Chu said, one way to assess whether a patient with persistent COVID-19 symptoms might be progressing to ME/CFS is to ask him or her specifically about the level of fatigue following physical exertion and the timing of any fatigue. With ME/CFS, postexertional malaise often involves a dramatic exacerbation of symptoms such as fatigue, pain, and cognitive impairment a day or 2 after exertion rather than immediately following it. In contrast, shortness of breath during exertion isn’t typical of ME/CFS.
Objective measures of ME/CFS include low natural killer cell function (the test can be ordered from commercial labs but requires rapid transport of the blood sample), and autonomic dysfunction assessed by a tilt-table test.
While there is currently no cure for ME/CFS, diagnosing it allows for the patient to be taught “pacing” in which the person conserves his or her energy by balancing activity with rest. “That type of behavioral technique is valuable for everyone who suffers from a chronic disease with fatigue. It can help them be more functional,” Dr. Chu said.
If a patient appears to be exhibiting signs of ME/CFS, “don’t wait until they hit the 6-month mark to start helping them manage their symptoms,” she said. “Teaching pacing to COVID-19 patients who have a lot of fatigue isn’t going to harm them. As they get better they’re going to just naturally do more. But if they do have ME/CFS, [pacing] stresses their system less, since the data seem to be pointing to deficiencies in producing energy.”
Will COVID-19 unleash a new wave of ME/CFS patients?
Much of the session at the virtual meeting was devoted to ongoing studies. For example, Leonard Jason, PhD, of the Center for Community Research at DePaul University, Chicago, described a prospective study launched in 2014 that looked at risk factors for developing ME/CFS in college students who contracted infectious mononucleosis as a result of Epstein-Barr virus. Now, his team is also following students from the same cohort who develop COVID-19.
Because the study included collection of baseline biological samples, the results could help reveal predisposing factors associated with long-term illness from either virus.
Another project, funded by the Open Medicine Foundation, will follow patients who are discharged from the ICU following severe COVID-19 illness. Blood, urine, and cerebrospinal fluid will be collected from those with persistent symptoms at 6 months, along with questionnaire data. At 18-24 months, those who continue to report symptoms will undergo more intensive evaluation using genomics, metabolomics, and proteomics.
“We’re taking advantage of this horrible situation, hoping to understand how a serious viral infection might lead to ME/CFS,” said lead investigator Ronald Tompkins, MD, ScD, chief medical officer at the Open Medicine Foundation and a faculty member at Harvard Medical School, Boston. The results, he said, “might give us insight into potential drug targets or biomarkers useful for prevention and treatment strategies.”
Meanwhile, Sadie Whittaker, PhD, head of the Solve ME/CFS initiative, described her organization’s new plan to use their registry to prospectively track the impact of COVID-19 on people with ME/CFS.
She noted that they’ve also teamed up with “long-COVID” communities including Body Politic. “Our goal is to form a coalition to study together or at least harmonize data … and understand what’s going on through the power of bigger sample sizes,” Dr. Whittaker said.
None of the speakers disclosed relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FDA authorizes convalescent plasma for COVID-19
Convalescent plasma contains antibodies from the blood of recovered COVID-19 patients, which can be used to treat people with severe infections. Convalescent plasma has been used to treat patients for other infectious diseases. The authorization allows the plasma to be distributed in the United States and administered by health care providers.
“COVID-19 convalescent plasma is safe and shows promising efficacy,” Stephen Hahn, MD, commissioner of the FDA, said during a press briefing with President Donald Trump.
In April, the FDA approved a program to test convalescent plasma in COVID-19 patients at the Mayo Clinic, followed by other institutions. More than 90,000 patients have enrolled in the program, and 70,000 have received the treatment, Dr. Hahn said.
The data indicate that the plasma can reduce mortality in patients by 35%, particularly if patients are treated within 3 days of being diagnosed. Those who have benefited the most were under age 80 and not on artificial respiration, Alex Azar, the secretary for the Department of Health & Human Services, said during the briefing.
“We dream, in drug development, of something like a 35% mortality reduction,” he said.
But top scientists pushed back against the announcement.
Eric Topol, MD, director of the Scripps Research Translational Institute, professor of molecular medicine, and executive vice president of Scripps Research, said the data the FDA are relying on did not come from the rigorous randomized, double-blind placebo trials that best determine if a treatment is successful.
Still, convalescent plasma is “one more tool added to the arsenal” of combating COVID-19, Mr. Azar said. The FDA will continue to study convalescent plasma as a COVID-19 treatment, Dr. Hahn added.
“We’re waiting for more data. We’re going to continue to gather data,” Dr. Hahn said during the briefing, but the current results meet FDA criteria for issuing an emergency use authorization.
Convalescent plasma “may be effective in lessening the severity or shortening the length of COVID-19 illness in some hospitalized patients,” according to the FDA announcement. Potential side effects include allergic reactions, transfusion-transmitted infections, and transfusion-associated lung injury.
“We’ve seen a great deal of demand for this from doctors around the country,” Dr. Hahn said during the briefing. “The EUA … allows us to continue that and meet that demand.”
Dr. Topol, however, said it appears Trump and the FDA are playing politics with science.
“There’s no evidence to support any survival benefit,” Dr. Topol said on Twitter. “Two days ago [the] FDA’s website stated there was no evidence for an EUA.”
The American Red Cross and other blood centers put out a national call for blood donors in July, especially for patients who have recovered from COVID-19. Mr. Azar and Dr. Hahn emphasized the need for blood donors during the press briefing.
“If you donate plasma, you could save a life,” Mr. Azar said.
The study has not been peer reviewed and did not include a placebo group for comparison, STAT reported.
Last week several health officials warned that the scientific data were too weak to warrant an emergency authorization, the New York Times reported.
A version of this originally appeared on WebMD.com.
Convalescent plasma contains antibodies from the blood of recovered COVID-19 patients, which can be used to treat people with severe infections. Convalescent plasma has been used to treat patients for other infectious diseases. The authorization allows the plasma to be distributed in the United States and administered by health care providers.
“COVID-19 convalescent plasma is safe and shows promising efficacy,” Stephen Hahn, MD, commissioner of the FDA, said during a press briefing with President Donald Trump.
In April, the FDA approved a program to test convalescent plasma in COVID-19 patients at the Mayo Clinic, followed by other institutions. More than 90,000 patients have enrolled in the program, and 70,000 have received the treatment, Dr. Hahn said.
The data indicate that the plasma can reduce mortality in patients by 35%, particularly if patients are treated within 3 days of being diagnosed. Those who have benefited the most were under age 80 and not on artificial respiration, Alex Azar, the secretary for the Department of Health & Human Services, said during the briefing.
“We dream, in drug development, of something like a 35% mortality reduction,” he said.
But top scientists pushed back against the announcement.
Eric Topol, MD, director of the Scripps Research Translational Institute, professor of molecular medicine, and executive vice president of Scripps Research, said the data the FDA are relying on did not come from the rigorous randomized, double-blind placebo trials that best determine if a treatment is successful.
Still, convalescent plasma is “one more tool added to the arsenal” of combating COVID-19, Mr. Azar said. The FDA will continue to study convalescent plasma as a COVID-19 treatment, Dr. Hahn added.
“We’re waiting for more data. We’re going to continue to gather data,” Dr. Hahn said during the briefing, but the current results meet FDA criteria for issuing an emergency use authorization.
Convalescent plasma “may be effective in lessening the severity or shortening the length of COVID-19 illness in some hospitalized patients,” according to the FDA announcement. Potential side effects include allergic reactions, transfusion-transmitted infections, and transfusion-associated lung injury.
“We’ve seen a great deal of demand for this from doctors around the country,” Dr. Hahn said during the briefing. “The EUA … allows us to continue that and meet that demand.”
Dr. Topol, however, said it appears Trump and the FDA are playing politics with science.
“There’s no evidence to support any survival benefit,” Dr. Topol said on Twitter. “Two days ago [the] FDA’s website stated there was no evidence for an EUA.”
The American Red Cross and other blood centers put out a national call for blood donors in July, especially for patients who have recovered from COVID-19. Mr. Azar and Dr. Hahn emphasized the need for blood donors during the press briefing.
“If you donate plasma, you could save a life,” Mr. Azar said.
The study has not been peer reviewed and did not include a placebo group for comparison, STAT reported.
Last week several health officials warned that the scientific data were too weak to warrant an emergency authorization, the New York Times reported.
A version of this originally appeared on WebMD.com.
Convalescent plasma contains antibodies from the blood of recovered COVID-19 patients, which can be used to treat people with severe infections. Convalescent plasma has been used to treat patients for other infectious diseases. The authorization allows the plasma to be distributed in the United States and administered by health care providers.
“COVID-19 convalescent plasma is safe and shows promising efficacy,” Stephen Hahn, MD, commissioner of the FDA, said during a press briefing with President Donald Trump.
In April, the FDA approved a program to test convalescent plasma in COVID-19 patients at the Mayo Clinic, followed by other institutions. More than 90,000 patients have enrolled in the program, and 70,000 have received the treatment, Dr. Hahn said.
The data indicate that the plasma can reduce mortality in patients by 35%, particularly if patients are treated within 3 days of being diagnosed. Those who have benefited the most were under age 80 and not on artificial respiration, Alex Azar, the secretary for the Department of Health & Human Services, said during the briefing.
“We dream, in drug development, of something like a 35% mortality reduction,” he said.
But top scientists pushed back against the announcement.
Eric Topol, MD, director of the Scripps Research Translational Institute, professor of molecular medicine, and executive vice president of Scripps Research, said the data the FDA are relying on did not come from the rigorous randomized, double-blind placebo trials that best determine if a treatment is successful.
Still, convalescent plasma is “one more tool added to the arsenal” of combating COVID-19, Mr. Azar said. The FDA will continue to study convalescent plasma as a COVID-19 treatment, Dr. Hahn added.
“We’re waiting for more data. We’re going to continue to gather data,” Dr. Hahn said during the briefing, but the current results meet FDA criteria for issuing an emergency use authorization.
Convalescent plasma “may be effective in lessening the severity or shortening the length of COVID-19 illness in some hospitalized patients,” according to the FDA announcement. Potential side effects include allergic reactions, transfusion-transmitted infections, and transfusion-associated lung injury.
“We’ve seen a great deal of demand for this from doctors around the country,” Dr. Hahn said during the briefing. “The EUA … allows us to continue that and meet that demand.”
Dr. Topol, however, said it appears Trump and the FDA are playing politics with science.
“There’s no evidence to support any survival benefit,” Dr. Topol said on Twitter. “Two days ago [the] FDA’s website stated there was no evidence for an EUA.”
The American Red Cross and other blood centers put out a national call for blood donors in July, especially for patients who have recovered from COVID-19. Mr. Azar and Dr. Hahn emphasized the need for blood donors during the press briefing.
“If you donate plasma, you could save a life,” Mr. Azar said.
The study has not been peer reviewed and did not include a placebo group for comparison, STAT reported.
Last week several health officials warned that the scientific data were too weak to warrant an emergency authorization, the New York Times reported.
A version of this originally appeared on WebMD.com.
Near-hanging injuries: Critical care, psychiatric management
Suicide by hanging results in many deaths, and half of those survivors who are admitted later die from cardiac arrest.
Although hanging is a common form of suicide, studies of the clinical outcomes of near-hanging injury are rare. To address this void, Louise de Charentenay, MD, of the Medical-Surgical Intensive Care Unit, Centre Hospitalier de Versailles (France) and colleagues examined the vital and functional outcomes of more than 800 patients with suicidal near-hanging injury over 2 decades. Despite the high in-hospital mortality rate among survivors, those who do survive have an excellent chance of a full neurocognitive recovery. The investigators published their findings in Chest.
New data on near-hanging injuries
Near hanging refers to strangulation or hanging that doesn’t immediately lead to death. Little data have been available on this subject, particularly on the morbidity and mortality of patients admitted to the ICU following near-hanging injuries. In a retrospective analysis spanning 23 years (1992-2014), researchers looked at outcomes and early predictors of hospital deaths in patients with this injury. The study included 886 adult patients who were admitted to 31 university or university-affiliated ICUs in France and Belgium following successful resuscitation of suicidal near-hanging injury.
Investigators used logistic multivariate regression to report vital and functional outcomes at hospital discharge as a primary objective. They also aimed to identify predictors of hospital mortality in these patients.
Among all patients, 450 (50.8%) had hanging-induced cardiac arrest and of these, 371 (95.4%) eventually died. Although the rate of crude hospital deaths decreased over the 23-year period, hanging-induced cardiac arrest emerged as the strongest predictor of hospital mortality, followed by high blood lactate and hyperglycemia at ICU admission. “Hanging-induced cardiac arrest and worse consciousness impairment at ICU admission are directly related to the hanging, whereas higher glycemia and lactate levels at ICU admission represent biochemical markers of physiologic perturbation and injury severity that may suggest avenues for improvement in prehospital care,” wrote the investigators.
More than 56% of the patients survived to discharge, with a majority achieving favorable outcomes (a Glasgow Outcome Scale scores of 4 or 5 at discharge).
‘COVID-lateral’ damage and ICU management
Casey D. Bryant, MD, of the department of anesthesiology and the department of emergency medicine at Wake Forest Baptist Health, Winston-Salem, N.C., has treated these patients in the ICU and is prepared to see more of them in light of the current situation. He said in an interview, “The “COVID-lateral” damage being unleashed on the population as a result of increased isolation, lack of access to resources, higher unemployment, and increased substance abuse was detailed recently in an article by one of my colleagues, Dr. Seth Hawkins (Emerg Med News. 2020 Jun;42[6]:1,31-2). According to the Centers for Disease Control and Prevention, hanging is the second leading cause of suicide in the United States, and one can only assume that with increased mental health crises there will also be an increased number of hanging attempts.”
Dr. Bryant suggested that the first task of doctors who learn that a near-hanging patient has been admitted is to “recover from the gut-punch you feel when you learn that a fellow human has tried to take their own life.” Once one is composed, he said, the first order of business is to come up with a treatment plan, one that typically begins with the airway. “These patients are at a high risk for cervical vertebrae injury (e.g., hangman’s fracture), spinal cord injury, tracheal injury, and neck vessel injury or dissection, so care must be taken to maintain in-line stabilization and limit movement of the neck during intubation while also being prepared for all manner of airway disasters. After airway management, addressing traumatic injuries, and initial stabilization, the focus then shifts to ‘bread and butter’ critical care, including optimization of ventilator management, titration of analgosedation, providing adequate nutrition, and strict avoidance of hypoxia, hypotension, fever, and either hyper- or hypoglycemia.”
Dr. Bryant noted that targeted temperature management prescriptions remain an area of debate in those with comatose state after hanging, but fever should absolutely be avoided. He added: “As the path to recovery begins to be forged, the full gamut of mental health resources should be provided to the patients in order to give them the best chance for success once they leave the ICU, and ultimately the hospital.”
The different hospitals seemed to have varying degrees of success in saving these patients, which is surprising, Mangala Narasimhan, DO, FCCP, regional director of critical care, director of the acute lung injury/ECMO center at Northwell and a professor of medicine at the Hofstra/Northwell School of Medicine, New York, said in an interview. “Usually, the death rate for cardiac arrest is high and the death rate for hanging is high. But here, it was high in some places and low in others.” Different time frames from presenting from hanging and different treatments may explain this, said Dr. Narasimhan.
Patient characteristics
Consistent with previous research, near-hanging patients are predominantly male, have at least one psychiatric diagnosis and a previous suicidal attempt (rarely by hanging), and abuse substances such as an alcohol, Stéphane Legriel, MD, PhD, the study’s corresponding author, said in an interview. Overall, 67.7% of the patients had a diagnosed mental illness and 30% had previously attempted suicide. Most of the hangings took place at home (79%), while some took place in a hospital ward (6%), a correctional facility (7%), or outside (5%).
The study had several limitations: It applied only to near-hanging patients admitted to the ICU, and its long duration may have resulted in heterogeneity of the population and therapeutic interventions, and in some missing data. “However, the multivariate analysis was adjusted for the time period and we carried out a sensitivity analysis after multiple imputation for missing data by means of chained equations, which reinforces confidence in our findings,” Dr. Legriel said. Next steps are to conduct a prospective data collection.
Postdischarge recovery and psychiatric follow-up
Those left to treat survivors of near-hangings are psychiatrists and other mental health clinicians, Eric M. Plakun, MD, said in an interview.
“Some of these survivors will regret they survived and remain high suicide risks. Some will feel their lives are transformed or at least no longer as intensely drawn to suicide as a solution to a life filled with the impact of adversity, trauma, comorbidity, and other struggles – but even these individuals will still have to face the often complex underlying issues that led them to choose suicide as a solution,” said Dr. Plakun, medical director and CEO of the Austen Riggs Center in Stockbridge, Mass.
Patients with medically serious suicide attempts are seen a lot at Austen Riggs, he said, because acute inpatient settings are designed for brief, crisis-focused treatment of those for whom safety is an issue. After the crisis has been stabilized, patients are discharged, and then must begin to achieve recovery as outpatients, he said.
John Kruse, MD, PhD, a psychiatrist who practices in San Francisco, praised the size and the breath of the study. “One limitation was the reliance on hospital records, without an opportunity to directly evaluate or interview the patients involved.”
The authors disclosed no conflicts of interest. The study received grant support from the French public funding agency, Délégation la Recherche Clinique et de l’Innovation in Versailles, France.
SOURCE: de Charentenay L et al. 2020 Aug 3. doi: 10.1016/j.chest.2020.07.064
Suicide by hanging results in many deaths, and half of those survivors who are admitted later die from cardiac arrest.
Although hanging is a common form of suicide, studies of the clinical outcomes of near-hanging injury are rare. To address this void, Louise de Charentenay, MD, of the Medical-Surgical Intensive Care Unit, Centre Hospitalier de Versailles (France) and colleagues examined the vital and functional outcomes of more than 800 patients with suicidal near-hanging injury over 2 decades. Despite the high in-hospital mortality rate among survivors, those who do survive have an excellent chance of a full neurocognitive recovery. The investigators published their findings in Chest.
New data on near-hanging injuries
Near hanging refers to strangulation or hanging that doesn’t immediately lead to death. Little data have been available on this subject, particularly on the morbidity and mortality of patients admitted to the ICU following near-hanging injuries. In a retrospective analysis spanning 23 years (1992-2014), researchers looked at outcomes and early predictors of hospital deaths in patients with this injury. The study included 886 adult patients who were admitted to 31 university or university-affiliated ICUs in France and Belgium following successful resuscitation of suicidal near-hanging injury.
Investigators used logistic multivariate regression to report vital and functional outcomes at hospital discharge as a primary objective. They also aimed to identify predictors of hospital mortality in these patients.
Among all patients, 450 (50.8%) had hanging-induced cardiac arrest and of these, 371 (95.4%) eventually died. Although the rate of crude hospital deaths decreased over the 23-year period, hanging-induced cardiac arrest emerged as the strongest predictor of hospital mortality, followed by high blood lactate and hyperglycemia at ICU admission. “Hanging-induced cardiac arrest and worse consciousness impairment at ICU admission are directly related to the hanging, whereas higher glycemia and lactate levels at ICU admission represent biochemical markers of physiologic perturbation and injury severity that may suggest avenues for improvement in prehospital care,” wrote the investigators.
More than 56% of the patients survived to discharge, with a majority achieving favorable outcomes (a Glasgow Outcome Scale scores of 4 or 5 at discharge).
‘COVID-lateral’ damage and ICU management
Casey D. Bryant, MD, of the department of anesthesiology and the department of emergency medicine at Wake Forest Baptist Health, Winston-Salem, N.C., has treated these patients in the ICU and is prepared to see more of them in light of the current situation. He said in an interview, “The “COVID-lateral” damage being unleashed on the population as a result of increased isolation, lack of access to resources, higher unemployment, and increased substance abuse was detailed recently in an article by one of my colleagues, Dr. Seth Hawkins (Emerg Med News. 2020 Jun;42[6]:1,31-2). According to the Centers for Disease Control and Prevention, hanging is the second leading cause of suicide in the United States, and one can only assume that with increased mental health crises there will also be an increased number of hanging attempts.”
Dr. Bryant suggested that the first task of doctors who learn that a near-hanging patient has been admitted is to “recover from the gut-punch you feel when you learn that a fellow human has tried to take their own life.” Once one is composed, he said, the first order of business is to come up with a treatment plan, one that typically begins with the airway. “These patients are at a high risk for cervical vertebrae injury (e.g., hangman’s fracture), spinal cord injury, tracheal injury, and neck vessel injury or dissection, so care must be taken to maintain in-line stabilization and limit movement of the neck during intubation while also being prepared for all manner of airway disasters. After airway management, addressing traumatic injuries, and initial stabilization, the focus then shifts to ‘bread and butter’ critical care, including optimization of ventilator management, titration of analgosedation, providing adequate nutrition, and strict avoidance of hypoxia, hypotension, fever, and either hyper- or hypoglycemia.”
Dr. Bryant noted that targeted temperature management prescriptions remain an area of debate in those with comatose state after hanging, but fever should absolutely be avoided. He added: “As the path to recovery begins to be forged, the full gamut of mental health resources should be provided to the patients in order to give them the best chance for success once they leave the ICU, and ultimately the hospital.”
The different hospitals seemed to have varying degrees of success in saving these patients, which is surprising, Mangala Narasimhan, DO, FCCP, regional director of critical care, director of the acute lung injury/ECMO center at Northwell and a professor of medicine at the Hofstra/Northwell School of Medicine, New York, said in an interview. “Usually, the death rate for cardiac arrest is high and the death rate for hanging is high. But here, it was high in some places and low in others.” Different time frames from presenting from hanging and different treatments may explain this, said Dr. Narasimhan.
Patient characteristics
Consistent with previous research, near-hanging patients are predominantly male, have at least one psychiatric diagnosis and a previous suicidal attempt (rarely by hanging), and abuse substances such as an alcohol, Stéphane Legriel, MD, PhD, the study’s corresponding author, said in an interview. Overall, 67.7% of the patients had a diagnosed mental illness and 30% had previously attempted suicide. Most of the hangings took place at home (79%), while some took place in a hospital ward (6%), a correctional facility (7%), or outside (5%).
The study had several limitations: It applied only to near-hanging patients admitted to the ICU, and its long duration may have resulted in heterogeneity of the population and therapeutic interventions, and in some missing data. “However, the multivariate analysis was adjusted for the time period and we carried out a sensitivity analysis after multiple imputation for missing data by means of chained equations, which reinforces confidence in our findings,” Dr. Legriel said. Next steps are to conduct a prospective data collection.
Postdischarge recovery and psychiatric follow-up
Those left to treat survivors of near-hangings are psychiatrists and other mental health clinicians, Eric M. Plakun, MD, said in an interview.
“Some of these survivors will regret they survived and remain high suicide risks. Some will feel their lives are transformed or at least no longer as intensely drawn to suicide as a solution to a life filled with the impact of adversity, trauma, comorbidity, and other struggles – but even these individuals will still have to face the often complex underlying issues that led them to choose suicide as a solution,” said Dr. Plakun, medical director and CEO of the Austen Riggs Center in Stockbridge, Mass.
Patients with medically serious suicide attempts are seen a lot at Austen Riggs, he said, because acute inpatient settings are designed for brief, crisis-focused treatment of those for whom safety is an issue. After the crisis has been stabilized, patients are discharged, and then must begin to achieve recovery as outpatients, he said.
John Kruse, MD, PhD, a psychiatrist who practices in San Francisco, praised the size and the breath of the study. “One limitation was the reliance on hospital records, without an opportunity to directly evaluate or interview the patients involved.”
The authors disclosed no conflicts of interest. The study received grant support from the French public funding agency, Délégation la Recherche Clinique et de l’Innovation in Versailles, France.
SOURCE: de Charentenay L et al. 2020 Aug 3. doi: 10.1016/j.chest.2020.07.064
Suicide by hanging results in many deaths, and half of those survivors who are admitted later die from cardiac arrest.
Although hanging is a common form of suicide, studies of the clinical outcomes of near-hanging injury are rare. To address this void, Louise de Charentenay, MD, of the Medical-Surgical Intensive Care Unit, Centre Hospitalier de Versailles (France) and colleagues examined the vital and functional outcomes of more than 800 patients with suicidal near-hanging injury over 2 decades. Despite the high in-hospital mortality rate among survivors, those who do survive have an excellent chance of a full neurocognitive recovery. The investigators published their findings in Chest.
New data on near-hanging injuries
Near hanging refers to strangulation or hanging that doesn’t immediately lead to death. Little data have been available on this subject, particularly on the morbidity and mortality of patients admitted to the ICU following near-hanging injuries. In a retrospective analysis spanning 23 years (1992-2014), researchers looked at outcomes and early predictors of hospital deaths in patients with this injury. The study included 886 adult patients who were admitted to 31 university or university-affiliated ICUs in France and Belgium following successful resuscitation of suicidal near-hanging injury.
Investigators used logistic multivariate regression to report vital and functional outcomes at hospital discharge as a primary objective. They also aimed to identify predictors of hospital mortality in these patients.
Among all patients, 450 (50.8%) had hanging-induced cardiac arrest and of these, 371 (95.4%) eventually died. Although the rate of crude hospital deaths decreased over the 23-year period, hanging-induced cardiac arrest emerged as the strongest predictor of hospital mortality, followed by high blood lactate and hyperglycemia at ICU admission. “Hanging-induced cardiac arrest and worse consciousness impairment at ICU admission are directly related to the hanging, whereas higher glycemia and lactate levels at ICU admission represent biochemical markers of physiologic perturbation and injury severity that may suggest avenues for improvement in prehospital care,” wrote the investigators.
More than 56% of the patients survived to discharge, with a majority achieving favorable outcomes (a Glasgow Outcome Scale scores of 4 or 5 at discharge).
‘COVID-lateral’ damage and ICU management
Casey D. Bryant, MD, of the department of anesthesiology and the department of emergency medicine at Wake Forest Baptist Health, Winston-Salem, N.C., has treated these patients in the ICU and is prepared to see more of them in light of the current situation. He said in an interview, “The “COVID-lateral” damage being unleashed on the population as a result of increased isolation, lack of access to resources, higher unemployment, and increased substance abuse was detailed recently in an article by one of my colleagues, Dr. Seth Hawkins (Emerg Med News. 2020 Jun;42[6]:1,31-2). According to the Centers for Disease Control and Prevention, hanging is the second leading cause of suicide in the United States, and one can only assume that with increased mental health crises there will also be an increased number of hanging attempts.”
Dr. Bryant suggested that the first task of doctors who learn that a near-hanging patient has been admitted is to “recover from the gut-punch you feel when you learn that a fellow human has tried to take their own life.” Once one is composed, he said, the first order of business is to come up with a treatment plan, one that typically begins with the airway. “These patients are at a high risk for cervical vertebrae injury (e.g., hangman’s fracture), spinal cord injury, tracheal injury, and neck vessel injury or dissection, so care must be taken to maintain in-line stabilization and limit movement of the neck during intubation while also being prepared for all manner of airway disasters. After airway management, addressing traumatic injuries, and initial stabilization, the focus then shifts to ‘bread and butter’ critical care, including optimization of ventilator management, titration of analgosedation, providing adequate nutrition, and strict avoidance of hypoxia, hypotension, fever, and either hyper- or hypoglycemia.”
Dr. Bryant noted that targeted temperature management prescriptions remain an area of debate in those with comatose state after hanging, but fever should absolutely be avoided. He added: “As the path to recovery begins to be forged, the full gamut of mental health resources should be provided to the patients in order to give them the best chance for success once they leave the ICU, and ultimately the hospital.”
The different hospitals seemed to have varying degrees of success in saving these patients, which is surprising, Mangala Narasimhan, DO, FCCP, regional director of critical care, director of the acute lung injury/ECMO center at Northwell and a professor of medicine at the Hofstra/Northwell School of Medicine, New York, said in an interview. “Usually, the death rate for cardiac arrest is high and the death rate for hanging is high. But here, it was high in some places and low in others.” Different time frames from presenting from hanging and different treatments may explain this, said Dr. Narasimhan.
Patient characteristics
Consistent with previous research, near-hanging patients are predominantly male, have at least one psychiatric diagnosis and a previous suicidal attempt (rarely by hanging), and abuse substances such as an alcohol, Stéphane Legriel, MD, PhD, the study’s corresponding author, said in an interview. Overall, 67.7% of the patients had a diagnosed mental illness and 30% had previously attempted suicide. Most of the hangings took place at home (79%), while some took place in a hospital ward (6%), a correctional facility (7%), or outside (5%).
The study had several limitations: It applied only to near-hanging patients admitted to the ICU, and its long duration may have resulted in heterogeneity of the population and therapeutic interventions, and in some missing data. “However, the multivariate analysis was adjusted for the time period and we carried out a sensitivity analysis after multiple imputation for missing data by means of chained equations, which reinforces confidence in our findings,” Dr. Legriel said. Next steps are to conduct a prospective data collection.
Postdischarge recovery and psychiatric follow-up
Those left to treat survivors of near-hangings are psychiatrists and other mental health clinicians, Eric M. Plakun, MD, said in an interview.
“Some of these survivors will regret they survived and remain high suicide risks. Some will feel their lives are transformed or at least no longer as intensely drawn to suicide as a solution to a life filled with the impact of adversity, trauma, comorbidity, and other struggles – but even these individuals will still have to face the often complex underlying issues that led them to choose suicide as a solution,” said Dr. Plakun, medical director and CEO of the Austen Riggs Center in Stockbridge, Mass.
Patients with medically serious suicide attempts are seen a lot at Austen Riggs, he said, because acute inpatient settings are designed for brief, crisis-focused treatment of those for whom safety is an issue. After the crisis has been stabilized, patients are discharged, and then must begin to achieve recovery as outpatients, he said.
John Kruse, MD, PhD, a psychiatrist who practices in San Francisco, praised the size and the breath of the study. “One limitation was the reliance on hospital records, without an opportunity to directly evaluate or interview the patients involved.”
The authors disclosed no conflicts of interest. The study received grant support from the French public funding agency, Délégation la Recherche Clinique et de l’Innovation in Versailles, France.
SOURCE: de Charentenay L et al. 2020 Aug 3. doi: 10.1016/j.chest.2020.07.064
Black/White gap gone: ‘The only cancer where this has happened’
The historically higher incidence rates of lung cancer among Black men, compared with White men, in the United States have all but been eliminated, at least among most men in the younger age groups, a new analysis from the American Cancer Society (ACS) indicates.
Among women, the trend is even more impressive, as the Black/White gap in lung cancer incidence rates has actually reversed in younger women. Black women in certain age groups are now less likely to develop lung cancer than White women, the same study indicates.
These trends reflect the steeper declines in smoking rates among Blacks in the US, compared with comparably-aged Whites, say the authors.
“This is the only cancer where this has happened,” lead author Ahmedin Jemal, DVM, PhD, senior vice president for Data Science at the American Cancer Society, told Medscape Medical News.
“If you look at cancers that are affected by access to screening and treatment, the disparity between the Blacks and the Whites has been increasing over the years because tests and treatment require access to insurance, so the Whites are getting more of them than the Blacks,” Jemal explained.
“But for smoking, all you have to do for prevention is just don’t smoke, so this is a success story that really should be highlighted,” he emphasized.
The study was published online Aug. 20 in JNCI Cancer: Spectrum.
Nationwide Incidence Data
For this study, Jemal and colleagues collected nationwide incidence data on individuals between ages 30 and 54 who had been diagnosed with lung cancer between 1997 and 2016.
“We categorized age at diagnosis by 5-year age intervals (from 30-34 to 50-54 years) and year of diagnosis by 5-year calendar period (from 1997-2001 to 2012-2016),” the investigators explain.
Analyses showed that lung cancer incidence rates generally decreased among both Black and White men during the study interval but the decline in incidence rates was steeper in Black men than in White men. As a consequence, the Black-to-White incidence rate ratios (IRRs) became similar in men born between 1967 and 1972 and reversed in women born since about 1967. For example, the Black-to-White IRRs in men between the ages of 40 and 44 who were born between 1957 and 1972 declined from 1.92 to 1.03.
Similarly, lung cancer incidence rates during the study interval declined among both Black and White women between the ages of 30 and 49 but, again, the decline was “considerably larger” among Black women. As a consequence, the Black-to-White IRR in women age 45 to 49 dropped from 1.25 during the period 1997-2001 down to 0.83 during the period 2012-2016.
This is in stark contrast to historical trends in lung cancer incidence rates, which were over 30% higher among similarly aged Black women born in the late 1950s. Now, lung cancer incidence rates are about 30% lower for similarly aged Black women born in 1972, compared with White women.
For Black and White women between age 50 and 54, lung cancer incidence rates either declined only slightly or remained stable during the study interval, the investigators reported.
The one exception to the diminishing gap in lung cancer incidence rates between Black and White men was an observed increase in IRRs in men born around the period 1977-1982
Among this group of men, who were between age 30 and 39 in the years 2012-2016, lung cancer incidence rates were higher in Black men than in White men.
As the authors point out, this increase in lung cancer rates among young Black men likely reflects a rapid rise in smoking seen among Black youth in the 1990s.
This trend coincided with an R.J. Reynolds tobacco ad campaign in which African Americans were targeted; between 1991 and 1997, the prevalence of smoking among Black high school students doubled from 14.1% to 28.2%, the investigators point out, citing a 2008 Centers for Disease Control and Prevention report on cigarette use among US high school students.
Smoking Prevalence Rates
Smoking prevalence rates were derived from National Health Interview Survey data from 1970 to 2016.
Mirroring findings in the racial patterns of lung cancer incidence rates, smoking prevalence rates declined in successive birth cohorts in both Black and White males and females, but the decline was again steeper in Black men and women than it was in White men and women.
As a result, the historically higher sex-specific smoking prevalence rates seen historically in Blacks disappeared in men born around 1960, and reversed in women born at the same time, Jemal and colleagues point out.
As the authors explain, the more rapid decline in smoking prevalence after 1960 is likely a reflection of the “precipitous” drop in smoking initiation rates among Black teenagers starting about the late 1970s through to the early 1990s.
For example, among 12th graders, smoking prevalence rates between 1977 and 1992 dropped from 36.7% to 8.1% among Black teens. In stark contrast, they hardly changed at all among White teens, dropping only from 38.3% in 1977 to 31.8% in 1992.
Jemal suggested that steeper decline in smoking initiation rates seen between the late 1970s and early 90s reflects the fact that Black teenagers were deterred from smoking because the cost of cigarettes kept going up.
He also suggested that smoking is less acceptable in the Black community than it is in the White community, especially among churchgoers, where smoking is severely frowned upon and nonsmoking is the community “norm.”
Additionally, Black youth may simply be heeding government antismoking messages to a greater extent than White youth, Jemal suggested.
He wondered if there are parallels now in the current pandemic. “When I go to a store here in Georgia, I would say almost all Blacks are wearing a mask [even though masks are not mandatory in Georgia] whereas it’s amazing the number of Whites who don’t wear a mask,” he recounts.
“So it would seem that Whites feel that government is simply interfering with their lives, while Blacks have a better perspective of the harms of smoking, so they are listening to the government’s antismoking campaigns,” he speculated.
Some Isolated Areas
Asked to comment on the study’s findings, Otis Brawley, MD, Bloomberg, distinguished professor of oncology and epidemiology at Johns Hopkins University in Baltimore, said that, while overall Black smoking rates are declining, there are some isolated areas where they are still very high.
For example, in his hometown of Baltimore, recent prevalence rates indicate that over 30% of Blacks are still smoking, “so these areas with high usage are still areas to focus on,” he told Medscape Medical News.
On the other hand, the study also supports the benefits of local, state, and federal government efforts to promote antismoking messages and tobacco-control activities over the past number of years.
“It proves that tactics used to control tobacco use have had some effect [even though] the study also shows that the tobacco industry’s advertising tactics such as the R.J. Reynolds targeted ads in the 90s can have deleterious effects,” Brawley noted.
Lung cancer has traditionally been one of the biggest drivers in the Black/White cancer mortality gap, Brawley said, adding that steeper declines in smoking initiation rates among Blacks compared with Whites are the main reason why this disparity is decreasing.
The study was supported by the Intramural Research Department of the American Cancer Society. The study authors have disclosed no relevant financial relationships. Brawley declares he does some consulting work for pharmaceutical company Genentech.
This article first appeared on Medscape.com.
The historically higher incidence rates of lung cancer among Black men, compared with White men, in the United States have all but been eliminated, at least among most men in the younger age groups, a new analysis from the American Cancer Society (ACS) indicates.
Among women, the trend is even more impressive, as the Black/White gap in lung cancer incidence rates has actually reversed in younger women. Black women in certain age groups are now less likely to develop lung cancer than White women, the same study indicates.
These trends reflect the steeper declines in smoking rates among Blacks in the US, compared with comparably-aged Whites, say the authors.
“This is the only cancer where this has happened,” lead author Ahmedin Jemal, DVM, PhD, senior vice president for Data Science at the American Cancer Society, told Medscape Medical News.
“If you look at cancers that are affected by access to screening and treatment, the disparity between the Blacks and the Whites has been increasing over the years because tests and treatment require access to insurance, so the Whites are getting more of them than the Blacks,” Jemal explained.
“But for smoking, all you have to do for prevention is just don’t smoke, so this is a success story that really should be highlighted,” he emphasized.
The study was published online Aug. 20 in JNCI Cancer: Spectrum.
Nationwide Incidence Data
For this study, Jemal and colleagues collected nationwide incidence data on individuals between ages 30 and 54 who had been diagnosed with lung cancer between 1997 and 2016.
“We categorized age at diagnosis by 5-year age intervals (from 30-34 to 50-54 years) and year of diagnosis by 5-year calendar period (from 1997-2001 to 2012-2016),” the investigators explain.
Analyses showed that lung cancer incidence rates generally decreased among both Black and White men during the study interval but the decline in incidence rates was steeper in Black men than in White men. As a consequence, the Black-to-White incidence rate ratios (IRRs) became similar in men born between 1967 and 1972 and reversed in women born since about 1967. For example, the Black-to-White IRRs in men between the ages of 40 and 44 who were born between 1957 and 1972 declined from 1.92 to 1.03.
Similarly, lung cancer incidence rates during the study interval declined among both Black and White women between the ages of 30 and 49 but, again, the decline was “considerably larger” among Black women. As a consequence, the Black-to-White IRR in women age 45 to 49 dropped from 1.25 during the period 1997-2001 down to 0.83 during the period 2012-2016.
This is in stark contrast to historical trends in lung cancer incidence rates, which were over 30% higher among similarly aged Black women born in the late 1950s. Now, lung cancer incidence rates are about 30% lower for similarly aged Black women born in 1972, compared with White women.
For Black and White women between age 50 and 54, lung cancer incidence rates either declined only slightly or remained stable during the study interval, the investigators reported.
The one exception to the diminishing gap in lung cancer incidence rates between Black and White men was an observed increase in IRRs in men born around the period 1977-1982
Among this group of men, who were between age 30 and 39 in the years 2012-2016, lung cancer incidence rates were higher in Black men than in White men.
As the authors point out, this increase in lung cancer rates among young Black men likely reflects a rapid rise in smoking seen among Black youth in the 1990s.
This trend coincided with an R.J. Reynolds tobacco ad campaign in which African Americans were targeted; between 1991 and 1997, the prevalence of smoking among Black high school students doubled from 14.1% to 28.2%, the investigators point out, citing a 2008 Centers for Disease Control and Prevention report on cigarette use among US high school students.
Smoking Prevalence Rates
Smoking prevalence rates were derived from National Health Interview Survey data from 1970 to 2016.
Mirroring findings in the racial patterns of lung cancer incidence rates, smoking prevalence rates declined in successive birth cohorts in both Black and White males and females, but the decline was again steeper in Black men and women than it was in White men and women.
As a result, the historically higher sex-specific smoking prevalence rates seen historically in Blacks disappeared in men born around 1960, and reversed in women born at the same time, Jemal and colleagues point out.
As the authors explain, the more rapid decline in smoking prevalence after 1960 is likely a reflection of the “precipitous” drop in smoking initiation rates among Black teenagers starting about the late 1970s through to the early 1990s.
For example, among 12th graders, smoking prevalence rates between 1977 and 1992 dropped from 36.7% to 8.1% among Black teens. In stark contrast, they hardly changed at all among White teens, dropping only from 38.3% in 1977 to 31.8% in 1992.
Jemal suggested that steeper decline in smoking initiation rates seen between the late 1970s and early 90s reflects the fact that Black teenagers were deterred from smoking because the cost of cigarettes kept going up.
He also suggested that smoking is less acceptable in the Black community than it is in the White community, especially among churchgoers, where smoking is severely frowned upon and nonsmoking is the community “norm.”
Additionally, Black youth may simply be heeding government antismoking messages to a greater extent than White youth, Jemal suggested.
He wondered if there are parallels now in the current pandemic. “When I go to a store here in Georgia, I would say almost all Blacks are wearing a mask [even though masks are not mandatory in Georgia] whereas it’s amazing the number of Whites who don’t wear a mask,” he recounts.
“So it would seem that Whites feel that government is simply interfering with their lives, while Blacks have a better perspective of the harms of smoking, so they are listening to the government’s antismoking campaigns,” he speculated.
Some Isolated Areas
Asked to comment on the study’s findings, Otis Brawley, MD, Bloomberg, distinguished professor of oncology and epidemiology at Johns Hopkins University in Baltimore, said that, while overall Black smoking rates are declining, there are some isolated areas where they are still very high.
For example, in his hometown of Baltimore, recent prevalence rates indicate that over 30% of Blacks are still smoking, “so these areas with high usage are still areas to focus on,” he told Medscape Medical News.
On the other hand, the study also supports the benefits of local, state, and federal government efforts to promote antismoking messages and tobacco-control activities over the past number of years.
“It proves that tactics used to control tobacco use have had some effect [even though] the study also shows that the tobacco industry’s advertising tactics such as the R.J. Reynolds targeted ads in the 90s can have deleterious effects,” Brawley noted.
Lung cancer has traditionally been one of the biggest drivers in the Black/White cancer mortality gap, Brawley said, adding that steeper declines in smoking initiation rates among Blacks compared with Whites are the main reason why this disparity is decreasing.
The study was supported by the Intramural Research Department of the American Cancer Society. The study authors have disclosed no relevant financial relationships. Brawley declares he does some consulting work for pharmaceutical company Genentech.
This article first appeared on Medscape.com.
The historically higher incidence rates of lung cancer among Black men, compared with White men, in the United States have all but been eliminated, at least among most men in the younger age groups, a new analysis from the American Cancer Society (ACS) indicates.
Among women, the trend is even more impressive, as the Black/White gap in lung cancer incidence rates has actually reversed in younger women. Black women in certain age groups are now less likely to develop lung cancer than White women, the same study indicates.
These trends reflect the steeper declines in smoking rates among Blacks in the US, compared with comparably-aged Whites, say the authors.
“This is the only cancer where this has happened,” lead author Ahmedin Jemal, DVM, PhD, senior vice president for Data Science at the American Cancer Society, told Medscape Medical News.
“If you look at cancers that are affected by access to screening and treatment, the disparity between the Blacks and the Whites has been increasing over the years because tests and treatment require access to insurance, so the Whites are getting more of them than the Blacks,” Jemal explained.
“But for smoking, all you have to do for prevention is just don’t smoke, so this is a success story that really should be highlighted,” he emphasized.
The study was published online Aug. 20 in JNCI Cancer: Spectrum.
Nationwide Incidence Data
For this study, Jemal and colleagues collected nationwide incidence data on individuals between ages 30 and 54 who had been diagnosed with lung cancer between 1997 and 2016.
“We categorized age at diagnosis by 5-year age intervals (from 30-34 to 50-54 years) and year of diagnosis by 5-year calendar period (from 1997-2001 to 2012-2016),” the investigators explain.
Analyses showed that lung cancer incidence rates generally decreased among both Black and White men during the study interval but the decline in incidence rates was steeper in Black men than in White men. As a consequence, the Black-to-White incidence rate ratios (IRRs) became similar in men born between 1967 and 1972 and reversed in women born since about 1967. For example, the Black-to-White IRRs in men between the ages of 40 and 44 who were born between 1957 and 1972 declined from 1.92 to 1.03.
Similarly, lung cancer incidence rates during the study interval declined among both Black and White women between the ages of 30 and 49 but, again, the decline was “considerably larger” among Black women. As a consequence, the Black-to-White IRR in women age 45 to 49 dropped from 1.25 during the period 1997-2001 down to 0.83 during the period 2012-2016.
This is in stark contrast to historical trends in lung cancer incidence rates, which were over 30% higher among similarly aged Black women born in the late 1950s. Now, lung cancer incidence rates are about 30% lower for similarly aged Black women born in 1972, compared with White women.
For Black and White women between age 50 and 54, lung cancer incidence rates either declined only slightly or remained stable during the study interval, the investigators reported.
The one exception to the diminishing gap in lung cancer incidence rates between Black and White men was an observed increase in IRRs in men born around the period 1977-1982
Among this group of men, who were between age 30 and 39 in the years 2012-2016, lung cancer incidence rates were higher in Black men than in White men.
As the authors point out, this increase in lung cancer rates among young Black men likely reflects a rapid rise in smoking seen among Black youth in the 1990s.
This trend coincided with an R.J. Reynolds tobacco ad campaign in which African Americans were targeted; between 1991 and 1997, the prevalence of smoking among Black high school students doubled from 14.1% to 28.2%, the investigators point out, citing a 2008 Centers for Disease Control and Prevention report on cigarette use among US high school students.
Smoking Prevalence Rates
Smoking prevalence rates were derived from National Health Interview Survey data from 1970 to 2016.
Mirroring findings in the racial patterns of lung cancer incidence rates, smoking prevalence rates declined in successive birth cohorts in both Black and White males and females, but the decline was again steeper in Black men and women than it was in White men and women.
As a result, the historically higher sex-specific smoking prevalence rates seen historically in Blacks disappeared in men born around 1960, and reversed in women born at the same time, Jemal and colleagues point out.
As the authors explain, the more rapid decline in smoking prevalence after 1960 is likely a reflection of the “precipitous” drop in smoking initiation rates among Black teenagers starting about the late 1970s through to the early 1990s.
For example, among 12th graders, smoking prevalence rates between 1977 and 1992 dropped from 36.7% to 8.1% among Black teens. In stark contrast, they hardly changed at all among White teens, dropping only from 38.3% in 1977 to 31.8% in 1992.
Jemal suggested that steeper decline in smoking initiation rates seen between the late 1970s and early 90s reflects the fact that Black teenagers were deterred from smoking because the cost of cigarettes kept going up.
He also suggested that smoking is less acceptable in the Black community than it is in the White community, especially among churchgoers, where smoking is severely frowned upon and nonsmoking is the community “norm.”
Additionally, Black youth may simply be heeding government antismoking messages to a greater extent than White youth, Jemal suggested.
He wondered if there are parallels now in the current pandemic. “When I go to a store here in Georgia, I would say almost all Blacks are wearing a mask [even though masks are not mandatory in Georgia] whereas it’s amazing the number of Whites who don’t wear a mask,” he recounts.
“So it would seem that Whites feel that government is simply interfering with their lives, while Blacks have a better perspective of the harms of smoking, so they are listening to the government’s antismoking campaigns,” he speculated.
Some Isolated Areas
Asked to comment on the study’s findings, Otis Brawley, MD, Bloomberg, distinguished professor of oncology and epidemiology at Johns Hopkins University in Baltimore, said that, while overall Black smoking rates are declining, there are some isolated areas where they are still very high.
For example, in his hometown of Baltimore, recent prevalence rates indicate that over 30% of Blacks are still smoking, “so these areas with high usage are still areas to focus on,” he told Medscape Medical News.
On the other hand, the study also supports the benefits of local, state, and federal government efforts to promote antismoking messages and tobacco-control activities over the past number of years.
“It proves that tactics used to control tobacco use have had some effect [even though] the study also shows that the tobacco industry’s advertising tactics such as the R.J. Reynolds targeted ads in the 90s can have deleterious effects,” Brawley noted.
Lung cancer has traditionally been one of the biggest drivers in the Black/White cancer mortality gap, Brawley said, adding that steeper declines in smoking initiation rates among Blacks compared with Whites are the main reason why this disparity is decreasing.
The study was supported by the Intramural Research Department of the American Cancer Society. The study authors have disclosed no relevant financial relationships. Brawley declares he does some consulting work for pharmaceutical company Genentech.
This article first appeared on Medscape.com.