User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


‘Profound implications’: COVID ups diabetes risk 40% a year later
COVID-19 infection appears to significantly raise the risk for diabetes by about 40% at 1 year, indicate new data from a very large Veterans Administration population.
“If patients have a prior history of COVID-19, that’s a risk factor for diabetes and they should certainly be screened for diabetes,” study coauthor Ziyad Al-Aly, MD, a nephrologist and chief of research and development at VA St. Louis Health Care, told this news organization.
“It’s still premature to make guidelines. I think we have to process the data landscape to understand what this all really means, but it’s really, really clear that all these roads are pointing in one direction, that COVID-19 increases the risk of diabetes up to a year later. The risk is small but not negligible,” he said.
The database includes over 8 million people and 180,000 with a prior COVID-19 diagnosis. Significantly increased diabetes risks compared to those not infected ranging from 31% to more than double were found in an analysis of subgroups based on diabetes risk score, body mass index, age, race, prediabetes status, and deprivation level, even after adjustment for confounding factors.
There was a gradient of diabetes risk by COVID-19 severity – i.e., whether patients had not been hospitalized, had been hospitalized, or stayed in intensive care – but a significant excess diabetes burden was seen even among those with “mild” COVID-19. The diabetes risk was also elevated compared to both contemporary and historical controls.
The study was published March 21 in The Lancet Diabetes & Endocrinology, by Yan Xie, MPH, also of VA St Louis Health Care, along with Dr. Al-Aly.
The data align with those from another study just published from a nationwide German primary care database. That study was smaller and of shorter duration than the new VA study but consistent, said Dr. Al-Aly, a clinical epidemiologist at Washington University, St. Louis.
Millions more with new diabetes as late manifestation of COVID-19
“Millions of people in the U.S. have had COVID-19, so this is going to translate to literally millions more people with new-onset diabetes. Better to identify them early so they can be adequately treated,” Dr. Al-Aly said in an interview.
“The long-term implications of SARS-CoV-2 infection increasing diabetes risk are profound,” Venkat Narayan, MD, and Lisa R. Staimez, PhD, both of the Rollins School of Public Health and Emory Global Diabetes Research Center at Emory University, Atlanta, said in an accompanying editorial.
“With large and growing numbers of people worldwide infected with SARS-CoV-2 (434,154,739 cumulative cases by Feb. 28, 2022), any COVID-19-related increases in diabetes incidence could lead to unprecedented cases of diabetes worldwide – wreaking havoc on already over-stretched and under-resourced clinical and public health systems globally, with devastating tolls in terms of deaths and suffering,” they added.
Medscape Medical News contributor Eric Topol MD, of Scripps Research Institute, La Jolla, Calif., agrees. He said these new data “are most profound. The researchers found a 40% increase in diabetes that wasn’t present at 1 month after COVID-19 but at 1 year, it was. Some kind of late manifestation is happening here.”
Dr. Al-Aly told this news organization that the mechanisms for the association are unknown and likely to be heterogeneous. Among the people who already had risk factors for type 2 diabetes, such as obesity or metabolic syndrome, SARS-CoV-2 could simply accelerate that process and “put them over the edge” to overt diabetes.
However, for those without diabetes risk factors, “COVID-19 with all the inflammation it provokes in the body could be leading to de novo disease.” (Diabetes status was ascertained by ICD-10 codes and only about 0.70% of the total were recorded as type 1 diabetes. But, since autoantibody testing wasn’t routinely conducted, it’s unknown how many of the cases may have been type 1 misclassified as type 2, Dr. Al-Aly acknowledged.)
Diabetes risk significantly increased after COVID-19 in all analyses
The analysis included 181,280 patients in the U.S. Department of Veterans Affairs health care database with a COVID-19 diagnosis who survived for at least 30 days afterward during March 2020 through Sept. 30, 2021, with 4,118,441 contemporary controls without COVID-19 seen during 2019, and a historical control group of 4,286,911 people seen at the VA in 2017. Average follow-up was about a year.
Compared with the contemporary controls, the COVID-19 group had an excess diabetes burden of 13.46 per 1,000 person-years with a hazard ratio of 1.40. They had an increased 12.35 per 1,000 person-year risk for incident use of glucose-lowering medications, with a hazard ratio of 1.85. Similar results were seen with the historical controls.
Subgroup analyses showed an increased risk for diabetes following COVID-19 infection by age (≤ 65 years and > 65 years), race (White and Black), sex (male and female), BMI categories (> 18.5 to ≤ 25 kg/m², > 25 to ≤ 30 kg/m², and > 30 kg/m²), and area deprivation index quartiles. The increased risk was also seen across diabetes risk score quartiles.
Notably, COVID-19 significantly elevated the diabetes risk by 59% even for the subgroup with BMI between 18 and 25 kg/m², and by 38% among those with the lowest diabetes risk score quartile.
The COVID-19 population included 162,096 who were not hospitalized, 15,078 hospitalized, and 4,106 admitted to intensive care. Here, the hazard ratios for diabetes compared to the contemporary controls were 1.25, 2.73, and 3.76, respectively, all significant.
Dr. Al-Aly said that his group is now further analyzing the VA data for other outcomes including cardiovascular disease and kidney disease, as well as the now well-documented long COVID symptoms including fatigue, pain, and neurocognitive dysfunction.
They’re also investigating the impact of the COVID-19 vaccine to see whether the risks are mitigated in the case of breakthrough infections: “We’re doing a broad systematic assessment. The next paper will be more comprehensive.”
Dr. Narayan and Dr. Staimez wrote: “The potential connection between COVID-19 and diabetes highlights that infectious diseases (eg, SARS-CoV-2) and chronic diseases (eg, diabetes) cannot be viewed in siloes. When we emerge out of the pandemic, the much-neglected non-communicable diseases, such as type 2 diabetes, will continue their relentless trajectory, possibly in an accelerated manner, as the leading burdens of global health.”
Dr. Al-Aly declared support from the U.S. Department of Veterans Affairs for the submitted work. He has received consultation fees from Gilead Sciences and funding (unrelated to this work) from Tonix Pharmaceuticals. He is a member of the board of directors for Veterans Research and Education Foundation of Saint Louis, associate editor for the Journal of the American Society of Nephrology, and a member of multiple editorial boards. Dr. Narayan and Dr. Staimez have received support from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
COVID-19 infection appears to significantly raise the risk for diabetes by about 40% at 1 year, indicate new data from a very large Veterans Administration population.
“If patients have a prior history of COVID-19, that’s a risk factor for diabetes and they should certainly be screened for diabetes,” study coauthor Ziyad Al-Aly, MD, a nephrologist and chief of research and development at VA St. Louis Health Care, told this news organization.
“It’s still premature to make guidelines. I think we have to process the data landscape to understand what this all really means, but it’s really, really clear that all these roads are pointing in one direction, that COVID-19 increases the risk of diabetes up to a year later. The risk is small but not negligible,” he said.
The database includes over 8 million people and 180,000 with a prior COVID-19 diagnosis. Significantly increased diabetes risks compared to those not infected ranging from 31% to more than double were found in an analysis of subgroups based on diabetes risk score, body mass index, age, race, prediabetes status, and deprivation level, even after adjustment for confounding factors.
There was a gradient of diabetes risk by COVID-19 severity – i.e., whether patients had not been hospitalized, had been hospitalized, or stayed in intensive care – but a significant excess diabetes burden was seen even among those with “mild” COVID-19. The diabetes risk was also elevated compared to both contemporary and historical controls.
The study was published March 21 in The Lancet Diabetes & Endocrinology, by Yan Xie, MPH, also of VA St Louis Health Care, along with Dr. Al-Aly.
The data align with those from another study just published from a nationwide German primary care database. That study was smaller and of shorter duration than the new VA study but consistent, said Dr. Al-Aly, a clinical epidemiologist at Washington University, St. Louis.
Millions more with new diabetes as late manifestation of COVID-19
“Millions of people in the U.S. have had COVID-19, so this is going to translate to literally millions more people with new-onset diabetes. Better to identify them early so they can be adequately treated,” Dr. Al-Aly said in an interview.
“The long-term implications of SARS-CoV-2 infection increasing diabetes risk are profound,” Venkat Narayan, MD, and Lisa R. Staimez, PhD, both of the Rollins School of Public Health and Emory Global Diabetes Research Center at Emory University, Atlanta, said in an accompanying editorial.
“With large and growing numbers of people worldwide infected with SARS-CoV-2 (434,154,739 cumulative cases by Feb. 28, 2022), any COVID-19-related increases in diabetes incidence could lead to unprecedented cases of diabetes worldwide – wreaking havoc on already over-stretched and under-resourced clinical and public health systems globally, with devastating tolls in terms of deaths and suffering,” they added.
Medscape Medical News contributor Eric Topol MD, of Scripps Research Institute, La Jolla, Calif., agrees. He said these new data “are most profound. The researchers found a 40% increase in diabetes that wasn’t present at 1 month after COVID-19 but at 1 year, it was. Some kind of late manifestation is happening here.”
Dr. Al-Aly told this news organization that the mechanisms for the association are unknown and likely to be heterogeneous. Among the people who already had risk factors for type 2 diabetes, such as obesity or metabolic syndrome, SARS-CoV-2 could simply accelerate that process and “put them over the edge” to overt diabetes.
However, for those without diabetes risk factors, “COVID-19 with all the inflammation it provokes in the body could be leading to de novo disease.” (Diabetes status was ascertained by ICD-10 codes and only about 0.70% of the total were recorded as type 1 diabetes. But, since autoantibody testing wasn’t routinely conducted, it’s unknown how many of the cases may have been type 1 misclassified as type 2, Dr. Al-Aly acknowledged.)
Diabetes risk significantly increased after COVID-19 in all analyses
The analysis included 181,280 patients in the U.S. Department of Veterans Affairs health care database with a COVID-19 diagnosis who survived for at least 30 days afterward during March 2020 through Sept. 30, 2021, with 4,118,441 contemporary controls without COVID-19 seen during 2019, and a historical control group of 4,286,911 people seen at the VA in 2017. Average follow-up was about a year.
Compared with the contemporary controls, the COVID-19 group had an excess diabetes burden of 13.46 per 1,000 person-years with a hazard ratio of 1.40. They had an increased 12.35 per 1,000 person-year risk for incident use of glucose-lowering medications, with a hazard ratio of 1.85. Similar results were seen with the historical controls.
Subgroup analyses showed an increased risk for diabetes following COVID-19 infection by age (≤ 65 years and > 65 years), race (White and Black), sex (male and female), BMI categories (> 18.5 to ≤ 25 kg/m², > 25 to ≤ 30 kg/m², and > 30 kg/m²), and area deprivation index quartiles. The increased risk was also seen across diabetes risk score quartiles.
Notably, COVID-19 significantly elevated the diabetes risk by 59% even for the subgroup with BMI between 18 and 25 kg/m², and by 38% among those with the lowest diabetes risk score quartile.
The COVID-19 population included 162,096 who were not hospitalized, 15,078 hospitalized, and 4,106 admitted to intensive care. Here, the hazard ratios for diabetes compared to the contemporary controls were 1.25, 2.73, and 3.76, respectively, all significant.
Dr. Al-Aly said that his group is now further analyzing the VA data for other outcomes including cardiovascular disease and kidney disease, as well as the now well-documented long COVID symptoms including fatigue, pain, and neurocognitive dysfunction.
They’re also investigating the impact of the COVID-19 vaccine to see whether the risks are mitigated in the case of breakthrough infections: “We’re doing a broad systematic assessment. The next paper will be more comprehensive.”
Dr. Narayan and Dr. Staimez wrote: “The potential connection between COVID-19 and diabetes highlights that infectious diseases (eg, SARS-CoV-2) and chronic diseases (eg, diabetes) cannot be viewed in siloes. When we emerge out of the pandemic, the much-neglected non-communicable diseases, such as type 2 diabetes, will continue their relentless trajectory, possibly in an accelerated manner, as the leading burdens of global health.”
Dr. Al-Aly declared support from the U.S. Department of Veterans Affairs for the submitted work. He has received consultation fees from Gilead Sciences and funding (unrelated to this work) from Tonix Pharmaceuticals. He is a member of the board of directors for Veterans Research and Education Foundation of Saint Louis, associate editor for the Journal of the American Society of Nephrology, and a member of multiple editorial boards. Dr. Narayan and Dr. Staimez have received support from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
COVID-19 infection appears to significantly raise the risk for diabetes by about 40% at 1 year, indicate new data from a very large Veterans Administration population.
“If patients have a prior history of COVID-19, that’s a risk factor for diabetes and they should certainly be screened for diabetes,” study coauthor Ziyad Al-Aly, MD, a nephrologist and chief of research and development at VA St. Louis Health Care, told this news organization.
“It’s still premature to make guidelines. I think we have to process the data landscape to understand what this all really means, but it’s really, really clear that all these roads are pointing in one direction, that COVID-19 increases the risk of diabetes up to a year later. The risk is small but not negligible,” he said.
The database includes over 8 million people and 180,000 with a prior COVID-19 diagnosis. Significantly increased diabetes risks compared to those not infected ranging from 31% to more than double were found in an analysis of subgroups based on diabetes risk score, body mass index, age, race, prediabetes status, and deprivation level, even after adjustment for confounding factors.
There was a gradient of diabetes risk by COVID-19 severity – i.e., whether patients had not been hospitalized, had been hospitalized, or stayed in intensive care – but a significant excess diabetes burden was seen even among those with “mild” COVID-19. The diabetes risk was also elevated compared to both contemporary and historical controls.
The study was published March 21 in The Lancet Diabetes & Endocrinology, by Yan Xie, MPH, also of VA St Louis Health Care, along with Dr. Al-Aly.
The data align with those from another study just published from a nationwide German primary care database. That study was smaller and of shorter duration than the new VA study but consistent, said Dr. Al-Aly, a clinical epidemiologist at Washington University, St. Louis.
Millions more with new diabetes as late manifestation of COVID-19
“Millions of people in the U.S. have had COVID-19, so this is going to translate to literally millions more people with new-onset diabetes. Better to identify them early so they can be adequately treated,” Dr. Al-Aly said in an interview.
“The long-term implications of SARS-CoV-2 infection increasing diabetes risk are profound,” Venkat Narayan, MD, and Lisa R. Staimez, PhD, both of the Rollins School of Public Health and Emory Global Diabetes Research Center at Emory University, Atlanta, said in an accompanying editorial.
“With large and growing numbers of people worldwide infected with SARS-CoV-2 (434,154,739 cumulative cases by Feb. 28, 2022), any COVID-19-related increases in diabetes incidence could lead to unprecedented cases of diabetes worldwide – wreaking havoc on already over-stretched and under-resourced clinical and public health systems globally, with devastating tolls in terms of deaths and suffering,” they added.
Medscape Medical News contributor Eric Topol MD, of Scripps Research Institute, La Jolla, Calif., agrees. He said these new data “are most profound. The researchers found a 40% increase in diabetes that wasn’t present at 1 month after COVID-19 but at 1 year, it was. Some kind of late manifestation is happening here.”
Dr. Al-Aly told this news organization that the mechanisms for the association are unknown and likely to be heterogeneous. Among the people who already had risk factors for type 2 diabetes, such as obesity or metabolic syndrome, SARS-CoV-2 could simply accelerate that process and “put them over the edge” to overt diabetes.
However, for those without diabetes risk factors, “COVID-19 with all the inflammation it provokes in the body could be leading to de novo disease.” (Diabetes status was ascertained by ICD-10 codes and only about 0.70% of the total were recorded as type 1 diabetes. But, since autoantibody testing wasn’t routinely conducted, it’s unknown how many of the cases may have been type 1 misclassified as type 2, Dr. Al-Aly acknowledged.)
Diabetes risk significantly increased after COVID-19 in all analyses
The analysis included 181,280 patients in the U.S. Department of Veterans Affairs health care database with a COVID-19 diagnosis who survived for at least 30 days afterward during March 2020 through Sept. 30, 2021, with 4,118,441 contemporary controls without COVID-19 seen during 2019, and a historical control group of 4,286,911 people seen at the VA in 2017. Average follow-up was about a year.
Compared with the contemporary controls, the COVID-19 group had an excess diabetes burden of 13.46 per 1,000 person-years with a hazard ratio of 1.40. They had an increased 12.35 per 1,000 person-year risk for incident use of glucose-lowering medications, with a hazard ratio of 1.85. Similar results were seen with the historical controls.
Subgroup analyses showed an increased risk for diabetes following COVID-19 infection by age (≤ 65 years and > 65 years), race (White and Black), sex (male and female), BMI categories (> 18.5 to ≤ 25 kg/m², > 25 to ≤ 30 kg/m², and > 30 kg/m²), and area deprivation index quartiles. The increased risk was also seen across diabetes risk score quartiles.
Notably, COVID-19 significantly elevated the diabetes risk by 59% even for the subgroup with BMI between 18 and 25 kg/m², and by 38% among those with the lowest diabetes risk score quartile.
The COVID-19 population included 162,096 who were not hospitalized, 15,078 hospitalized, and 4,106 admitted to intensive care. Here, the hazard ratios for diabetes compared to the contemporary controls were 1.25, 2.73, and 3.76, respectively, all significant.
Dr. Al-Aly said that his group is now further analyzing the VA data for other outcomes including cardiovascular disease and kidney disease, as well as the now well-documented long COVID symptoms including fatigue, pain, and neurocognitive dysfunction.
They’re also investigating the impact of the COVID-19 vaccine to see whether the risks are mitigated in the case of breakthrough infections: “We’re doing a broad systematic assessment. The next paper will be more comprehensive.”
Dr. Narayan and Dr. Staimez wrote: “The potential connection between COVID-19 and diabetes highlights that infectious diseases (eg, SARS-CoV-2) and chronic diseases (eg, diabetes) cannot be viewed in siloes. When we emerge out of the pandemic, the much-neglected non-communicable diseases, such as type 2 diabetes, will continue their relentless trajectory, possibly in an accelerated manner, as the leading burdens of global health.”
Dr. Al-Aly declared support from the U.S. Department of Veterans Affairs for the submitted work. He has received consultation fees from Gilead Sciences and funding (unrelated to this work) from Tonix Pharmaceuticals. He is a member of the board of directors for Veterans Research and Education Foundation of Saint Louis, associate editor for the Journal of the American Society of Nephrology, and a member of multiple editorial boards. Dr. Narayan and Dr. Staimez have received support from the National Institutes of Health.
A version of this article first appeared on Medscape.com.
FROM THE LANCET DIABETES & ENDOCRINOLOGY
Children and COVID: CDC gives perspective on hospitalizations
New COVID-19 cases in children fell by 23% as the latest weekly count dropped to its lowest level since July of 2021, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
, when the early stages of the Delta surge led to 23,551 cases, the AAP and CHA said in their weekly COVID report.
The two organizations put the total number of cases at nearly 12.8 million from the start of the pandemic to March 17, with children representing 19.0% of cases among all ages. The Centers for Disease Control and Prevention puts the cumulative number of COVID-19 cases at almost 12.0 million as of March 21, or 17.5% of the nationwide total.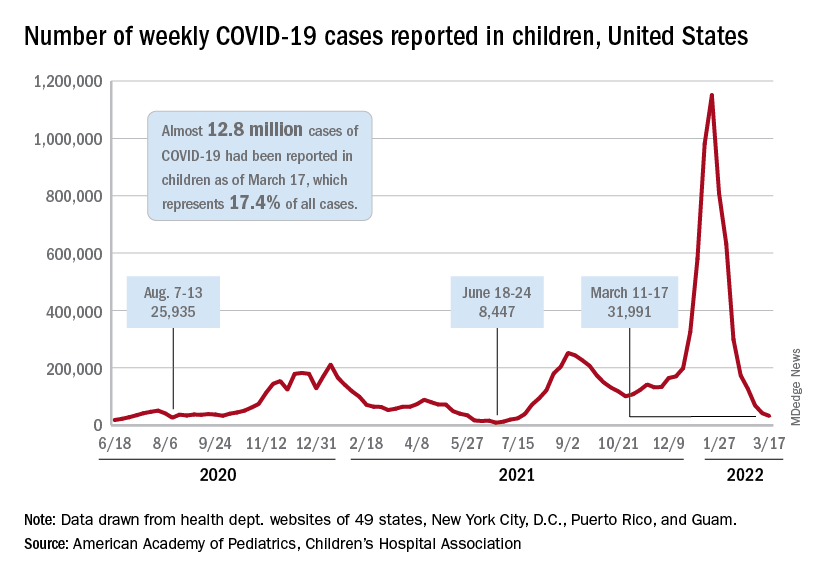
COVID-related hospitalizations also continue to fall, and two new studies from the CDC put children’s experiences during the Omicron surge and the larger pandemic into perspective.
One study showed that hospitalization rates for children aged 4 years and younger during the Omicron surge were five times higher than at the peak of the Delta surge, with the highest rates occurring in infants under 6 months of age. That report was based on the CDC’s COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), which covers 99 counties across 14 states (MMWR. 2022 March 18;71[11]:429-36).
The second study compared child hospitalizations during 1 year of the COVID pandemic (Oct. 1, 2020, to Sept. 30, 2021) with three influenza seasons (2017-2018 through 2019-2020). The pre-Omicron hospitalization rate for those under age 18 years, 48.2 per 100,000 children, was higher than any of the three flu seasons: 33.5 per 100,000 in 2017-2018, 33.8 in 2018-2019, and 41.7 for 2019-2020, the investigators said in a medRxiv preprint.
Most of the increased COVID burden fell on adolescents aged 12-17, they said. The COVID hospitalization rate for that age group was 59.9 per 100,000, versus 12.2-14.1 for influenza, while children aged 5-11 had a COVID-related rate of 25.0 and flu-related rates of 24.3-31.7, and those aged 0-4 had rates of 66.8 for COVID and 70.9-91.5 for the flu, Miranda J. Delahoy of the CDC’s COVID-19 Response Team and associates reported.
New COVID-19 cases in children fell by 23% as the latest weekly count dropped to its lowest level since July of 2021, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
, when the early stages of the Delta surge led to 23,551 cases, the AAP and CHA said in their weekly COVID report.
The two organizations put the total number of cases at nearly 12.8 million from the start of the pandemic to March 17, with children representing 19.0% of cases among all ages. The Centers for Disease Control and Prevention puts the cumulative number of COVID-19 cases at almost 12.0 million as of March 21, or 17.5% of the nationwide total.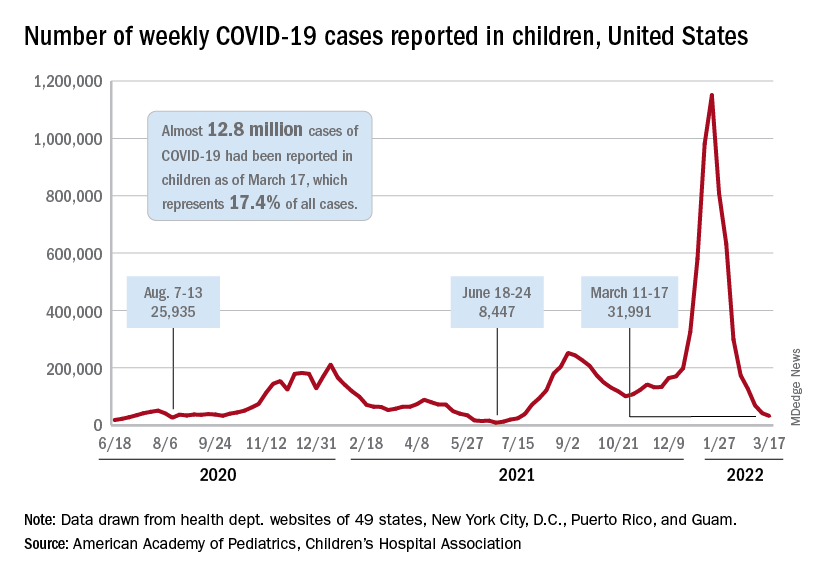
COVID-related hospitalizations also continue to fall, and two new studies from the CDC put children’s experiences during the Omicron surge and the larger pandemic into perspective.
One study showed that hospitalization rates for children aged 4 years and younger during the Omicron surge were five times higher than at the peak of the Delta surge, with the highest rates occurring in infants under 6 months of age. That report was based on the CDC’s COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), which covers 99 counties across 14 states (MMWR. 2022 March 18;71[11]:429-36).
The second study compared child hospitalizations during 1 year of the COVID pandemic (Oct. 1, 2020, to Sept. 30, 2021) with three influenza seasons (2017-2018 through 2019-2020). The pre-Omicron hospitalization rate for those under age 18 years, 48.2 per 100,000 children, was higher than any of the three flu seasons: 33.5 per 100,000 in 2017-2018, 33.8 in 2018-2019, and 41.7 for 2019-2020, the investigators said in a medRxiv preprint.
Most of the increased COVID burden fell on adolescents aged 12-17, they said. The COVID hospitalization rate for that age group was 59.9 per 100,000, versus 12.2-14.1 for influenza, while children aged 5-11 had a COVID-related rate of 25.0 and flu-related rates of 24.3-31.7, and those aged 0-4 had rates of 66.8 for COVID and 70.9-91.5 for the flu, Miranda J. Delahoy of the CDC’s COVID-19 Response Team and associates reported.
New COVID-19 cases in children fell by 23% as the latest weekly count dropped to its lowest level since July of 2021, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
, when the early stages of the Delta surge led to 23,551 cases, the AAP and CHA said in their weekly COVID report.
The two organizations put the total number of cases at nearly 12.8 million from the start of the pandemic to March 17, with children representing 19.0% of cases among all ages. The Centers for Disease Control and Prevention puts the cumulative number of COVID-19 cases at almost 12.0 million as of March 21, or 17.5% of the nationwide total.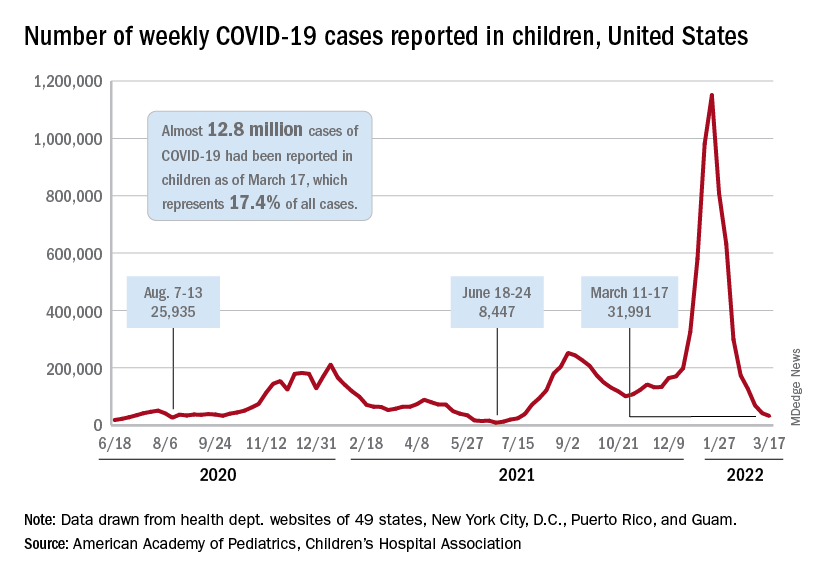
COVID-related hospitalizations also continue to fall, and two new studies from the CDC put children’s experiences during the Omicron surge and the larger pandemic into perspective.
One study showed that hospitalization rates for children aged 4 years and younger during the Omicron surge were five times higher than at the peak of the Delta surge, with the highest rates occurring in infants under 6 months of age. That report was based on the CDC’s COVID-19–Associated Hospitalization Surveillance Network (COVID-NET), which covers 99 counties across 14 states (MMWR. 2022 March 18;71[11]:429-36).
The second study compared child hospitalizations during 1 year of the COVID pandemic (Oct. 1, 2020, to Sept. 30, 2021) with three influenza seasons (2017-2018 through 2019-2020). The pre-Omicron hospitalization rate for those under age 18 years, 48.2 per 100,000 children, was higher than any of the three flu seasons: 33.5 per 100,000 in 2017-2018, 33.8 in 2018-2019, and 41.7 for 2019-2020, the investigators said in a medRxiv preprint.
Most of the increased COVID burden fell on adolescents aged 12-17, they said. The COVID hospitalization rate for that age group was 59.9 per 100,000, versus 12.2-14.1 for influenza, while children aged 5-11 had a COVID-related rate of 25.0 and flu-related rates of 24.3-31.7, and those aged 0-4 had rates of 66.8 for COVID and 70.9-91.5 for the flu, Miranda J. Delahoy of the CDC’s COVID-19 Response Team and associates reported.
Mild COVID-19 infection linked to later type 2 diabetes
People who recover from a mild case of COVID-19 appear to have an increased risk for subsequent new-onset type 2 diabetes but not other types of diabetes, new data suggest.
“If confirmed, the results of the present study indicate that diabetes screening in individuals who have recovered from even mild COVID-19 should be recommended,” say Wolfgang Rathmann, MD, of the Leibniz Center for Diabetes Research at Heinrich Heine University, Düsseldorf, Germany, and colleagues.
The findings, from a nationwide primary care database in Germany, were recently published in Diabetologia.
These primary care data align with those from other studies of more seriously ill patients with COVID-19 that found increased rates of type 2 diabetes diagnoses in the subsequent months following illness, they point out.
“COVID-19 infection may lead to diabetes by upregulation of the immune system after remission, which may induce pancreatic beta-cell dysfunction and insulin resistance, or patients may have been at risk for developing diabetes due to having obesity or prediabetes, and the stress COVID-19 put on their bodies sped it up,” said Dr. Rathmann in a press release.
However, because the patients with COVID-19 in the study were only followed for about 3 months, “further follow-up is needed to understand whether type 2 diabetes after mild COVID-19 is just temporary and can be reversed after they have fully recovered or whether it leads to a chronic condition,” he noted.
Increase in type 2 diabetes 3 months after mild COVID-19
The retrospective cohort analysis was performed using data from the Disease Analyzer, a representative panel of 1,171 physician practices in Germany, from March 2020 to January 2021, with follow-up through July 2021.
Individuals with a history of COVID-19 or diabetes and those taking corticosteroids within 30 days after the index dates were excluded.
A total of 35,865 patients with confirmed SARS-CoV-2 infection were propensity score-matched on a one-to-one basis for sex, age, health insurance, and comorbidities with those who had acute respiratory tract infections (controls) but were COVID-19 negative. Median follow-up was 119 days for the COVID-19 group and 161 days for controls.
There was a 28% increased risk of type 2 diabetes for those who had COVID-19 versus controls (15.8 per 1,000 person-years vs. 12.3 per 1,000 person-years, respectively, which was significantly different, and an incidence rate ratio of 1.28).
The incidence of other types of diabetes or unspecified diabetes for the COVID-19 and control groups did not differ significantly (4.3 per 1,000 person-years vs. 3.7 per 1,000 person-years; IRR, 1.17).
Similar findings were seen in sensitivity analyses by glucose-lowering medication prescriptions and by ICD-10 codes.
Although type 2 diabetes is not likely to be a problem for the vast majority of people who have mild COVID-19, the authors recommend that anyone who has recovered from COVID-19 be aware of the warning signs and symptoms such as fatigue, frequent urination, and increased thirst, and seek treatment right away.
CoviDiab registry tracking type 1 and type 2 diabetes
Over the course of the pandemic, there have been conflicting data on whether COVID-19 induces or reveals a propensity for type 1 and type 2 diabetes.
The CoviDiab global registry is tracking this and will include diabetes type for adults and children.
The aim is to have “as many as possible cases of new-onset diabetes for which we can have also a minimum set of clinical data including type of diabetes and A1c,” coprincipal investigator Francesco Rubino, MD, of King’s College London, previously told this news organization.
“By looking at this information we can infer whether a role of COVID-19 in triggering diabetes is clinically plausible – or not – and what type of diabetes is most frequently associated with COVID-19.”
Rubino said that the CoviDiab team is approaching the data with the assumption that, at least in adults diagnosed with type 2 diabetes, the explanation might be that the person already had undiagnosed diabetes or the hyperglycemia may be stress-induced and temporary.
The German Diabetes Center is funded by the German Federal Ministry of Health and the Ministry of Culture and Science of the State of North Rhine-Westphalia. Dr. Rathmann has reported receiving consulting fees for attending educational sessions or advisory boards for AstraZeneca, Boehringer Ingelheim, and Novo Nordisk and institutional research grants from Novo Nordisk outside of the topic of the current work.
A version of this article first appeared on Medscape.com.
People who recover from a mild case of COVID-19 appear to have an increased risk for subsequent new-onset type 2 diabetes but not other types of diabetes, new data suggest.
“If confirmed, the results of the present study indicate that diabetes screening in individuals who have recovered from even mild COVID-19 should be recommended,” say Wolfgang Rathmann, MD, of the Leibniz Center for Diabetes Research at Heinrich Heine University, Düsseldorf, Germany, and colleagues.
The findings, from a nationwide primary care database in Germany, were recently published in Diabetologia.
These primary care data align with those from other studies of more seriously ill patients with COVID-19 that found increased rates of type 2 diabetes diagnoses in the subsequent months following illness, they point out.
“COVID-19 infection may lead to diabetes by upregulation of the immune system after remission, which may induce pancreatic beta-cell dysfunction and insulin resistance, or patients may have been at risk for developing diabetes due to having obesity or prediabetes, and the stress COVID-19 put on their bodies sped it up,” said Dr. Rathmann in a press release.
However, because the patients with COVID-19 in the study were only followed for about 3 months, “further follow-up is needed to understand whether type 2 diabetes after mild COVID-19 is just temporary and can be reversed after they have fully recovered or whether it leads to a chronic condition,” he noted.
Increase in type 2 diabetes 3 months after mild COVID-19
The retrospective cohort analysis was performed using data from the Disease Analyzer, a representative panel of 1,171 physician practices in Germany, from March 2020 to January 2021, with follow-up through July 2021.
Individuals with a history of COVID-19 or diabetes and those taking corticosteroids within 30 days after the index dates were excluded.
A total of 35,865 patients with confirmed SARS-CoV-2 infection were propensity score-matched on a one-to-one basis for sex, age, health insurance, and comorbidities with those who had acute respiratory tract infections (controls) but were COVID-19 negative. Median follow-up was 119 days for the COVID-19 group and 161 days for controls.
There was a 28% increased risk of type 2 diabetes for those who had COVID-19 versus controls (15.8 per 1,000 person-years vs. 12.3 per 1,000 person-years, respectively, which was significantly different, and an incidence rate ratio of 1.28).
The incidence of other types of diabetes or unspecified diabetes for the COVID-19 and control groups did not differ significantly (4.3 per 1,000 person-years vs. 3.7 per 1,000 person-years; IRR, 1.17).
Similar findings were seen in sensitivity analyses by glucose-lowering medication prescriptions and by ICD-10 codes.
Although type 2 diabetes is not likely to be a problem for the vast majority of people who have mild COVID-19, the authors recommend that anyone who has recovered from COVID-19 be aware of the warning signs and symptoms such as fatigue, frequent urination, and increased thirst, and seek treatment right away.
CoviDiab registry tracking type 1 and type 2 diabetes
Over the course of the pandemic, there have been conflicting data on whether COVID-19 induces or reveals a propensity for type 1 and type 2 diabetes.
The CoviDiab global registry is tracking this and will include diabetes type for adults and children.
The aim is to have “as many as possible cases of new-onset diabetes for which we can have also a minimum set of clinical data including type of diabetes and A1c,” coprincipal investigator Francesco Rubino, MD, of King’s College London, previously told this news organization.
“By looking at this information we can infer whether a role of COVID-19 in triggering diabetes is clinically plausible – or not – and what type of diabetes is most frequently associated with COVID-19.”
Rubino said that the CoviDiab team is approaching the data with the assumption that, at least in adults diagnosed with type 2 diabetes, the explanation might be that the person already had undiagnosed diabetes or the hyperglycemia may be stress-induced and temporary.
The German Diabetes Center is funded by the German Federal Ministry of Health and the Ministry of Culture and Science of the State of North Rhine-Westphalia. Dr. Rathmann has reported receiving consulting fees for attending educational sessions or advisory boards for AstraZeneca, Boehringer Ingelheim, and Novo Nordisk and institutional research grants from Novo Nordisk outside of the topic of the current work.
A version of this article first appeared on Medscape.com.
People who recover from a mild case of COVID-19 appear to have an increased risk for subsequent new-onset type 2 diabetes but not other types of diabetes, new data suggest.
“If confirmed, the results of the present study indicate that diabetes screening in individuals who have recovered from even mild COVID-19 should be recommended,” say Wolfgang Rathmann, MD, of the Leibniz Center for Diabetes Research at Heinrich Heine University, Düsseldorf, Germany, and colleagues.
The findings, from a nationwide primary care database in Germany, were recently published in Diabetologia.
These primary care data align with those from other studies of more seriously ill patients with COVID-19 that found increased rates of type 2 diabetes diagnoses in the subsequent months following illness, they point out.
“COVID-19 infection may lead to diabetes by upregulation of the immune system after remission, which may induce pancreatic beta-cell dysfunction and insulin resistance, or patients may have been at risk for developing diabetes due to having obesity or prediabetes, and the stress COVID-19 put on their bodies sped it up,” said Dr. Rathmann in a press release.
However, because the patients with COVID-19 in the study were only followed for about 3 months, “further follow-up is needed to understand whether type 2 diabetes after mild COVID-19 is just temporary and can be reversed after they have fully recovered or whether it leads to a chronic condition,” he noted.
Increase in type 2 diabetes 3 months after mild COVID-19
The retrospective cohort analysis was performed using data from the Disease Analyzer, a representative panel of 1,171 physician practices in Germany, from March 2020 to January 2021, with follow-up through July 2021.
Individuals with a history of COVID-19 or diabetes and those taking corticosteroids within 30 days after the index dates were excluded.
A total of 35,865 patients with confirmed SARS-CoV-2 infection were propensity score-matched on a one-to-one basis for sex, age, health insurance, and comorbidities with those who had acute respiratory tract infections (controls) but were COVID-19 negative. Median follow-up was 119 days for the COVID-19 group and 161 days for controls.
There was a 28% increased risk of type 2 diabetes for those who had COVID-19 versus controls (15.8 per 1,000 person-years vs. 12.3 per 1,000 person-years, respectively, which was significantly different, and an incidence rate ratio of 1.28).
The incidence of other types of diabetes or unspecified diabetes for the COVID-19 and control groups did not differ significantly (4.3 per 1,000 person-years vs. 3.7 per 1,000 person-years; IRR, 1.17).
Similar findings were seen in sensitivity analyses by glucose-lowering medication prescriptions and by ICD-10 codes.
Although type 2 diabetes is not likely to be a problem for the vast majority of people who have mild COVID-19, the authors recommend that anyone who has recovered from COVID-19 be aware of the warning signs and symptoms such as fatigue, frequent urination, and increased thirst, and seek treatment right away.
CoviDiab registry tracking type 1 and type 2 diabetes
Over the course of the pandemic, there have been conflicting data on whether COVID-19 induces or reveals a propensity for type 1 and type 2 diabetes.
The CoviDiab global registry is tracking this and will include diabetes type for adults and children.
The aim is to have “as many as possible cases of new-onset diabetes for which we can have also a minimum set of clinical data including type of diabetes and A1c,” coprincipal investigator Francesco Rubino, MD, of King’s College London, previously told this news organization.
“By looking at this information we can infer whether a role of COVID-19 in triggering diabetes is clinically plausible – or not – and what type of diabetes is most frequently associated with COVID-19.”
Rubino said that the CoviDiab team is approaching the data with the assumption that, at least in adults diagnosed with type 2 diabetes, the explanation might be that the person already had undiagnosed diabetes or the hyperglycemia may be stress-induced and temporary.
The German Diabetes Center is funded by the German Federal Ministry of Health and the Ministry of Culture and Science of the State of North Rhine-Westphalia. Dr. Rathmann has reported receiving consulting fees for attending educational sessions or advisory boards for AstraZeneca, Boehringer Ingelheim, and Novo Nordisk and institutional research grants from Novo Nordisk outside of the topic of the current work.
A version of this article first appeared on Medscape.com.
FROM DIABETOLOGIA
WHO issues new TB guidelines for children and adolescents
The World Health Organization now recommends shortened treatment for children with mild tuberculosis, as well as two oral TB treatments (bedaquiline and delamanid) for use in children of all ages. The updated guidelines for TB management in children and adolescents were announced March 21 ahead of World Tuberculosis Day on March 24.
The agency also called for increased investment in global TB programs, noting that in 2020, TB deaths increased for the first time in over a decade. “We cannot falter in our commitment to reach and save every man, woman, child, family, and community impacted by this deadly disease,” said Tereza Kasaeva, MD, PhD, director of the WHO Global Tuberculosis Programme during a press conference.
TB is the 13th-leading cause of death and the second top infectious killer after COVID-19, with more than 4,100 people dying from TB every day. WHO estimates that 1.1 million children fall ill with TB each year.
Calls for investment
The increase in TB deaths from 1.4 million in 2019 to 1.5 million in 2020 was coupled with a decrease in funding. From 2019-2020, global spending for TB diagnostic, treatment, and prevention services fell from $5.8 billion to $5.3 billion. This is less than half of the $13 billion target funding amount for 2022, Dr. Kasaeva said.
Efforts to expand access to TB care have fallen short mainly because of this lack of funding, especially for children. In 2020, about 63% of children under 15 years of age with TB either did not receive or were not reported to have access to TB diagnosis and treatment services, which rose to 72% in children under age 5. Almost two-thirds of children under age 5 also did not receive TB preventive treatment in 2022, according to WHO statistics.
The socioeconomic ramifications of the COVID-19 pandemic as well as ongoing conflict in Eastern Europe, Africa, and the Middle East have “further exacerbated the situation,” Dr. Kasaeva said. “This conveys the urgent need to dramatically increase investments to ramp up the fight against TB and achieve commitments to end TB made by global leaders.”
Dr. Kasaeva laid out WHO’s main points for global investment in TB care:
- Increase domestic and international funding to close gaps in TB research and program implementation. For countries with smaller economies, increased international investment will be necessary in the short or medium term to help regain progress.
- Double funding for TB research, including vaccines.
- Invest in sustaining TB programs and services during the COVID-19 pandemic and ongoing crises so care is not disrupted.
New guidelines
Dr. Kasaeva also noted that adoption of WHO’s new guidelines for children and adolescents should be fast-tracked to improve access to and quality of care. The updates include:
- Rapid molecular tests called Xpert Ultra should be used as the initial test for TB in children and adolescents.
- Diagnostic testing can now include noninvasive specimens, like stool samples.
- Children with mild TB can be treated with a , rather than 6 months. This shortened regimen will allow children to return to school faster and save money for families and the health care system, said Kerri Viney, MD, PhD, a team lead for the WHO Tuberculosis Programme, with a focus on vulnerable populations, including children. She presented the new guidelines during the WHO press conference.
- The recommended treatment regimen for TB meningitis has also been shortened from 12 to 6 months.
Two oral medications for drug-resistant TB (bedaquiline and delamanid) are now recommended for use in children of all ages. “There is no longer a need for painful injections that can have serious side effects, including deafness,” Dr. Viney said.
Health systems should develop new models of decentralized and integrated TB care to bring TB care closer to where children live.
The guidelines are available on the WHO website.
“The WHO guidelines issued today are a game changer for children and adolescents with TB,” Dr. Kasaeva said. The next step is assisting countries in implementing these updates so that children and adolescents globally have access to high quality TB care,” Dr. Viney added. “We have the policy recommendations. We have the implementation guidance, we have child-friendly formulations of TB medicines,” she said. “Let us not wait any longer. Let us invest to end TB in children and adolescents.”
A version of this article first appeared on Medscape.com.
The World Health Organization now recommends shortened treatment for children with mild tuberculosis, as well as two oral TB treatments (bedaquiline and delamanid) for use in children of all ages. The updated guidelines for TB management in children and adolescents were announced March 21 ahead of World Tuberculosis Day on March 24.
The agency also called for increased investment in global TB programs, noting that in 2020, TB deaths increased for the first time in over a decade. “We cannot falter in our commitment to reach and save every man, woman, child, family, and community impacted by this deadly disease,” said Tereza Kasaeva, MD, PhD, director of the WHO Global Tuberculosis Programme during a press conference.
TB is the 13th-leading cause of death and the second top infectious killer after COVID-19, with more than 4,100 people dying from TB every day. WHO estimates that 1.1 million children fall ill with TB each year.
Calls for investment
The increase in TB deaths from 1.4 million in 2019 to 1.5 million in 2020 was coupled with a decrease in funding. From 2019-2020, global spending for TB diagnostic, treatment, and prevention services fell from $5.8 billion to $5.3 billion. This is less than half of the $13 billion target funding amount for 2022, Dr. Kasaeva said.
Efforts to expand access to TB care have fallen short mainly because of this lack of funding, especially for children. In 2020, about 63% of children under 15 years of age with TB either did not receive or were not reported to have access to TB diagnosis and treatment services, which rose to 72% in children under age 5. Almost two-thirds of children under age 5 also did not receive TB preventive treatment in 2022, according to WHO statistics.
The socioeconomic ramifications of the COVID-19 pandemic as well as ongoing conflict in Eastern Europe, Africa, and the Middle East have “further exacerbated the situation,” Dr. Kasaeva said. “This conveys the urgent need to dramatically increase investments to ramp up the fight against TB and achieve commitments to end TB made by global leaders.”
Dr. Kasaeva laid out WHO’s main points for global investment in TB care:
- Increase domestic and international funding to close gaps in TB research and program implementation. For countries with smaller economies, increased international investment will be necessary in the short or medium term to help regain progress.
- Double funding for TB research, including vaccines.
- Invest in sustaining TB programs and services during the COVID-19 pandemic and ongoing crises so care is not disrupted.
New guidelines
Dr. Kasaeva also noted that adoption of WHO’s new guidelines for children and adolescents should be fast-tracked to improve access to and quality of care. The updates include:
- Rapid molecular tests called Xpert Ultra should be used as the initial test for TB in children and adolescents.
- Diagnostic testing can now include noninvasive specimens, like stool samples.
- Children with mild TB can be treated with a , rather than 6 months. This shortened regimen will allow children to return to school faster and save money for families and the health care system, said Kerri Viney, MD, PhD, a team lead for the WHO Tuberculosis Programme, with a focus on vulnerable populations, including children. She presented the new guidelines during the WHO press conference.
- The recommended treatment regimen for TB meningitis has also been shortened from 12 to 6 months.
Two oral medications for drug-resistant TB (bedaquiline and delamanid) are now recommended for use in children of all ages. “There is no longer a need for painful injections that can have serious side effects, including deafness,” Dr. Viney said.
Health systems should develop new models of decentralized and integrated TB care to bring TB care closer to where children live.
The guidelines are available on the WHO website.
“The WHO guidelines issued today are a game changer for children and adolescents with TB,” Dr. Kasaeva said. The next step is assisting countries in implementing these updates so that children and adolescents globally have access to high quality TB care,” Dr. Viney added. “We have the policy recommendations. We have the implementation guidance, we have child-friendly formulations of TB medicines,” she said. “Let us not wait any longer. Let us invest to end TB in children and adolescents.”
A version of this article first appeared on Medscape.com.
The World Health Organization now recommends shortened treatment for children with mild tuberculosis, as well as two oral TB treatments (bedaquiline and delamanid) for use in children of all ages. The updated guidelines for TB management in children and adolescents were announced March 21 ahead of World Tuberculosis Day on March 24.
The agency also called for increased investment in global TB programs, noting that in 2020, TB deaths increased for the first time in over a decade. “We cannot falter in our commitment to reach and save every man, woman, child, family, and community impacted by this deadly disease,” said Tereza Kasaeva, MD, PhD, director of the WHO Global Tuberculosis Programme during a press conference.
TB is the 13th-leading cause of death and the second top infectious killer after COVID-19, with more than 4,100 people dying from TB every day. WHO estimates that 1.1 million children fall ill with TB each year.
Calls for investment
The increase in TB deaths from 1.4 million in 2019 to 1.5 million in 2020 was coupled with a decrease in funding. From 2019-2020, global spending for TB diagnostic, treatment, and prevention services fell from $5.8 billion to $5.3 billion. This is less than half of the $13 billion target funding amount for 2022, Dr. Kasaeva said.
Efforts to expand access to TB care have fallen short mainly because of this lack of funding, especially for children. In 2020, about 63% of children under 15 years of age with TB either did not receive or were not reported to have access to TB diagnosis and treatment services, which rose to 72% in children under age 5. Almost two-thirds of children under age 5 also did not receive TB preventive treatment in 2022, according to WHO statistics.
The socioeconomic ramifications of the COVID-19 pandemic as well as ongoing conflict in Eastern Europe, Africa, and the Middle East have “further exacerbated the situation,” Dr. Kasaeva said. “This conveys the urgent need to dramatically increase investments to ramp up the fight against TB and achieve commitments to end TB made by global leaders.”
Dr. Kasaeva laid out WHO’s main points for global investment in TB care:
- Increase domestic and international funding to close gaps in TB research and program implementation. For countries with smaller economies, increased international investment will be necessary in the short or medium term to help regain progress.
- Double funding for TB research, including vaccines.
- Invest in sustaining TB programs and services during the COVID-19 pandemic and ongoing crises so care is not disrupted.
New guidelines
Dr. Kasaeva also noted that adoption of WHO’s new guidelines for children and adolescents should be fast-tracked to improve access to and quality of care. The updates include:
- Rapid molecular tests called Xpert Ultra should be used as the initial test for TB in children and adolescents.
- Diagnostic testing can now include noninvasive specimens, like stool samples.
- Children with mild TB can be treated with a , rather than 6 months. This shortened regimen will allow children to return to school faster and save money for families and the health care system, said Kerri Viney, MD, PhD, a team lead for the WHO Tuberculosis Programme, with a focus on vulnerable populations, including children. She presented the new guidelines during the WHO press conference.
- The recommended treatment regimen for TB meningitis has also been shortened from 12 to 6 months.
Two oral medications for drug-resistant TB (bedaquiline and delamanid) are now recommended for use in children of all ages. “There is no longer a need for painful injections that can have serious side effects, including deafness,” Dr. Viney said.
Health systems should develop new models of decentralized and integrated TB care to bring TB care closer to where children live.
The guidelines are available on the WHO website.
“The WHO guidelines issued today are a game changer for children and adolescents with TB,” Dr. Kasaeva said. The next step is assisting countries in implementing these updates so that children and adolescents globally have access to high quality TB care,” Dr. Viney added. “We have the policy recommendations. We have the implementation guidance, we have child-friendly formulations of TB medicines,” she said. “Let us not wait any longer. Let us invest to end TB in children and adolescents.”
A version of this article first appeared on Medscape.com.
Lancet Commission reexamines the current approach to death
“The story of dying in the 21st century is a story of paradox.” This is the opening line of a report recently published in the Lancet, in which the Lancet Commission experts tackle what is, for many, a very sensitive topic: the end of life. The recommendations they present aim at “bringing death back into life.”
What makes the story a paradox is that, in end-of-life situations, many people are overtreated, and on the other hand, many people are undertreated.
In short, when all is said and done, “people die bad deaths.” A natural event, a natural part of life, has turned into something that people fear or, in some cases, refuse to even acknowledge or talk about.
This was the motivating factor for the Lancet Commission, a group of experts from various disciplines, to come together to try to better understand this complex concept. , as well as a balance between life and death.
This sensitive topic was explored by Marina Sozzi, PhD. She is the director of the Association for the Support and Assistance of People With Chronic and Oncological Diseases, a nonprofit organization that for more than 30 years has been dedicated to “providing palliative care and supporting individuals with oncological or other chronic and degenerative diseases.”
Call for rebalancing
To give people an idea of a better system in which life and death are in balance, the Lancet Commission experts described a realistic utopia, which they summarized in the following five principles:
- The social determinants of death, dying, and grieving are confronted.
- Dying is understood to be a relational and spiritual process rather than simply a physiological event.
- Networks of care provide support for people who are dying, those caring for them, and those grieving.
- Conversations and stories about everyday death, dying, and grief become common.
- Death is recognized as having value.
Achieving this utopia will not be easy, especially considering the current systems that are in place. “There have been tremendous medical advances over the last hundred years, particularly in increasing life expectancy and curing diseases that were once considered death sentences,” Dr. Sozzi explained. “Indeed, over the course of that time period, medical science acquired an enormous degree of social power, and matters of death – which in previous centuries had been within the purview of religions and houses of worship – were handed over to be handled by doctors and nurses.”
The COVID-19 pandemic has made the medical field’s role in matters of death more prominent: every day, people saw footage of dying people in hospital beds being cared for by health care professionals in masks and gowns. These patients were otherwise alone, their only contact with loved ones being over the phone or online. They died the ultimate medicalized deaths, stripped of almost all opportunities to get emotional support from family and friends.
New perspective needed
The Lancet Commission experts were certain about one point: The need to move away from the reductionist approach to death in order to integrate a more holistic approach, one that takes into account all of the dimensions of death without limiting itself only to the medical aspects.
“Medicine has its own take on the death phenomenon and on disease, which is a reductionist take,” said Dr. Sozzi, noting that, thanks to processes that make it possible to reduce phenomena to the measurable, medicine has managed to make tremendous progress. The same approach has been applied to the view of death, which has by and large become a biologic event.
“The problem is that, in reality, death is a much more complex phenomenon: cultural, social, involving families and society,” she explained. “Not all of these aspects are taken into consideration by medicine, and therefore, our culture has diminished its view of the death phenomenon.” Dr. Sozzi pointed out that, if looked upon more closely, the very question: “What did the person die of?” presupposes, in a certain sense, that it might have been possible to prevent that death – if only medicine had the right technology. So, death comes to be seen as something that could have been avoided.
Power of palliative care
Changing the approach to death requires a profound culture shift and, therefore, a lot of time. The good news is that, although there is still a long way to go, a few steps have been taken in this direction. “Talking about death, and even organizing courses aimed at health care professionals, is definitely easier these days than it was even just 10 years ago,” said Dr. Sozzi, citing, as an example, a project she developed for training nursing home operators in palliative care.
It is in palliative care where the greatest progress has been made in end-of-life matters. “The culture of palliative care allows us to think about death in very different terms and to recognize that moment when we should stop looking at curative care and direct our efforts at ‘comfort care.’ And this care of the dying has to be holistic,” Dr. Sozzi explained. She adds that we are increasingly talking about simultaneous palliative care – care that is not limited to the final days of a person’s life but that rather starts early on, when active treatments are still in place.
Dr. Sozzi mentioned Italy’s Law 38, which took effect in 2010. It regulates access to palliative care and pain management, expanding the right to receive these treatments to patients “in any health care setting, at any stage of life, and for any chronic or progressive condition which has no treatment or has a treatment that is not sufficient to stabilize it.”
A culture shift is also needed in this area; there has already been a movement away from general practitioners to health care professionals who can and must direct a patient to palliative care.
“We need to provide these doctors with more training and make them more aware of what a difference this kind of care can make throughout a patient’s life, not only during the final stages,” said Dr. Sozzi. Concerning training, she mentioned that Italy had recently introduced a specialization in palliative care for medical school graduates. This is another small step and one that adds a sense of dignity to this new approach to life and to death.
The experts’ recommendations
In attempting to find a balance between life and death, we must not look at the period prior to the 1900s as some kind of golden age. Dr. Sozzi explained that back then there was almost none of the medical technology now available to treat people at the end of life. “Palliative care has also set forth original technical aspects for eliminating pain. Without having eliminated a patient’s pain, I can hardly begin a discussion with them about spiritual aspects,” she said, emphasizing the importance of always contextualizing approaches to death.
The Lancet Commission experts assessed the approach to death in many different contexts. They recommended that, to best handle end-of-life matters in all their complexity, one should keep in mind the importance of relationships and networks across society.
They recommended that health care and social care professionals improve their skills and their capacity for taking care of dying patients and their families. When the patient has a life-limiting illness, a caring and compassionate approach should be taken when providing clear information about all interventions involved in palliative care, as well as when having conversations about death.
Governments and policy makers are advised to implement actions to allow all citizens to have the same access to necessary palliative care. In addition, all strategies and reports on social care and well-being more broadly should always include consideration of death, dying, and grieving. It’s an uphill climb, but one that must be made if we’re to build a new culture aimed at bringing death back into life. “As we continue stepping toward this new culture, let us each put a stone in place,” Dr. Sozzi concluded.
A version of this article first appeared on Medscape.com.
“The story of dying in the 21st century is a story of paradox.” This is the opening line of a report recently published in the Lancet, in which the Lancet Commission experts tackle what is, for many, a very sensitive topic: the end of life. The recommendations they present aim at “bringing death back into life.”
What makes the story a paradox is that, in end-of-life situations, many people are overtreated, and on the other hand, many people are undertreated.
In short, when all is said and done, “people die bad deaths.” A natural event, a natural part of life, has turned into something that people fear or, in some cases, refuse to even acknowledge or talk about.
This was the motivating factor for the Lancet Commission, a group of experts from various disciplines, to come together to try to better understand this complex concept. , as well as a balance between life and death.
This sensitive topic was explored by Marina Sozzi, PhD. She is the director of the Association for the Support and Assistance of People With Chronic and Oncological Diseases, a nonprofit organization that for more than 30 years has been dedicated to “providing palliative care and supporting individuals with oncological or other chronic and degenerative diseases.”
Call for rebalancing
To give people an idea of a better system in which life and death are in balance, the Lancet Commission experts described a realistic utopia, which they summarized in the following five principles:
- The social determinants of death, dying, and grieving are confronted.
- Dying is understood to be a relational and spiritual process rather than simply a physiological event.
- Networks of care provide support for people who are dying, those caring for them, and those grieving.
- Conversations and stories about everyday death, dying, and grief become common.
- Death is recognized as having value.
Achieving this utopia will not be easy, especially considering the current systems that are in place. “There have been tremendous medical advances over the last hundred years, particularly in increasing life expectancy and curing diseases that were once considered death sentences,” Dr. Sozzi explained. “Indeed, over the course of that time period, medical science acquired an enormous degree of social power, and matters of death – which in previous centuries had been within the purview of religions and houses of worship – were handed over to be handled by doctors and nurses.”
The COVID-19 pandemic has made the medical field’s role in matters of death more prominent: every day, people saw footage of dying people in hospital beds being cared for by health care professionals in masks and gowns. These patients were otherwise alone, their only contact with loved ones being over the phone or online. They died the ultimate medicalized deaths, stripped of almost all opportunities to get emotional support from family and friends.
New perspective needed
The Lancet Commission experts were certain about one point: The need to move away from the reductionist approach to death in order to integrate a more holistic approach, one that takes into account all of the dimensions of death without limiting itself only to the medical aspects.
“Medicine has its own take on the death phenomenon and on disease, which is a reductionist take,” said Dr. Sozzi, noting that, thanks to processes that make it possible to reduce phenomena to the measurable, medicine has managed to make tremendous progress. The same approach has been applied to the view of death, which has by and large become a biologic event.
“The problem is that, in reality, death is a much more complex phenomenon: cultural, social, involving families and society,” she explained. “Not all of these aspects are taken into consideration by medicine, and therefore, our culture has diminished its view of the death phenomenon.” Dr. Sozzi pointed out that, if looked upon more closely, the very question: “What did the person die of?” presupposes, in a certain sense, that it might have been possible to prevent that death – if only medicine had the right technology. So, death comes to be seen as something that could have been avoided.
Power of palliative care
Changing the approach to death requires a profound culture shift and, therefore, a lot of time. The good news is that, although there is still a long way to go, a few steps have been taken in this direction. “Talking about death, and even organizing courses aimed at health care professionals, is definitely easier these days than it was even just 10 years ago,” said Dr. Sozzi, citing, as an example, a project she developed for training nursing home operators in palliative care.
It is in palliative care where the greatest progress has been made in end-of-life matters. “The culture of palliative care allows us to think about death in very different terms and to recognize that moment when we should stop looking at curative care and direct our efforts at ‘comfort care.’ And this care of the dying has to be holistic,” Dr. Sozzi explained. She adds that we are increasingly talking about simultaneous palliative care – care that is not limited to the final days of a person’s life but that rather starts early on, when active treatments are still in place.
Dr. Sozzi mentioned Italy’s Law 38, which took effect in 2010. It regulates access to palliative care and pain management, expanding the right to receive these treatments to patients “in any health care setting, at any stage of life, and for any chronic or progressive condition which has no treatment or has a treatment that is not sufficient to stabilize it.”
A culture shift is also needed in this area; there has already been a movement away from general practitioners to health care professionals who can and must direct a patient to palliative care.
“We need to provide these doctors with more training and make them more aware of what a difference this kind of care can make throughout a patient’s life, not only during the final stages,” said Dr. Sozzi. Concerning training, she mentioned that Italy had recently introduced a specialization in palliative care for medical school graduates. This is another small step and one that adds a sense of dignity to this new approach to life and to death.
The experts’ recommendations
In attempting to find a balance between life and death, we must not look at the period prior to the 1900s as some kind of golden age. Dr. Sozzi explained that back then there was almost none of the medical technology now available to treat people at the end of life. “Palliative care has also set forth original technical aspects for eliminating pain. Without having eliminated a patient’s pain, I can hardly begin a discussion with them about spiritual aspects,” she said, emphasizing the importance of always contextualizing approaches to death.
The Lancet Commission experts assessed the approach to death in many different contexts. They recommended that, to best handle end-of-life matters in all their complexity, one should keep in mind the importance of relationships and networks across society.
They recommended that health care and social care professionals improve their skills and their capacity for taking care of dying patients and their families. When the patient has a life-limiting illness, a caring and compassionate approach should be taken when providing clear information about all interventions involved in palliative care, as well as when having conversations about death.
Governments and policy makers are advised to implement actions to allow all citizens to have the same access to necessary palliative care. In addition, all strategies and reports on social care and well-being more broadly should always include consideration of death, dying, and grieving. It’s an uphill climb, but one that must be made if we’re to build a new culture aimed at bringing death back into life. “As we continue stepping toward this new culture, let us each put a stone in place,” Dr. Sozzi concluded.
A version of this article first appeared on Medscape.com.
“The story of dying in the 21st century is a story of paradox.” This is the opening line of a report recently published in the Lancet, in which the Lancet Commission experts tackle what is, for many, a very sensitive topic: the end of life. The recommendations they present aim at “bringing death back into life.”
What makes the story a paradox is that, in end-of-life situations, many people are overtreated, and on the other hand, many people are undertreated.
In short, when all is said and done, “people die bad deaths.” A natural event, a natural part of life, has turned into something that people fear or, in some cases, refuse to even acknowledge or talk about.
This was the motivating factor for the Lancet Commission, a group of experts from various disciplines, to come together to try to better understand this complex concept. , as well as a balance between life and death.
This sensitive topic was explored by Marina Sozzi, PhD. She is the director of the Association for the Support and Assistance of People With Chronic and Oncological Diseases, a nonprofit organization that for more than 30 years has been dedicated to “providing palliative care and supporting individuals with oncological or other chronic and degenerative diseases.”
Call for rebalancing
To give people an idea of a better system in which life and death are in balance, the Lancet Commission experts described a realistic utopia, which they summarized in the following five principles:
- The social determinants of death, dying, and grieving are confronted.
- Dying is understood to be a relational and spiritual process rather than simply a physiological event.
- Networks of care provide support for people who are dying, those caring for them, and those grieving.
- Conversations and stories about everyday death, dying, and grief become common.
- Death is recognized as having value.
Achieving this utopia will not be easy, especially considering the current systems that are in place. “There have been tremendous medical advances over the last hundred years, particularly in increasing life expectancy and curing diseases that were once considered death sentences,” Dr. Sozzi explained. “Indeed, over the course of that time period, medical science acquired an enormous degree of social power, and matters of death – which in previous centuries had been within the purview of religions and houses of worship – were handed over to be handled by doctors and nurses.”
The COVID-19 pandemic has made the medical field’s role in matters of death more prominent: every day, people saw footage of dying people in hospital beds being cared for by health care professionals in masks and gowns. These patients were otherwise alone, their only contact with loved ones being over the phone or online. They died the ultimate medicalized deaths, stripped of almost all opportunities to get emotional support from family and friends.
New perspective needed
The Lancet Commission experts were certain about one point: The need to move away from the reductionist approach to death in order to integrate a more holistic approach, one that takes into account all of the dimensions of death without limiting itself only to the medical aspects.
“Medicine has its own take on the death phenomenon and on disease, which is a reductionist take,” said Dr. Sozzi, noting that, thanks to processes that make it possible to reduce phenomena to the measurable, medicine has managed to make tremendous progress. The same approach has been applied to the view of death, which has by and large become a biologic event.
“The problem is that, in reality, death is a much more complex phenomenon: cultural, social, involving families and society,” she explained. “Not all of these aspects are taken into consideration by medicine, and therefore, our culture has diminished its view of the death phenomenon.” Dr. Sozzi pointed out that, if looked upon more closely, the very question: “What did the person die of?” presupposes, in a certain sense, that it might have been possible to prevent that death – if only medicine had the right technology. So, death comes to be seen as something that could have been avoided.
Power of palliative care
Changing the approach to death requires a profound culture shift and, therefore, a lot of time. The good news is that, although there is still a long way to go, a few steps have been taken in this direction. “Talking about death, and even organizing courses aimed at health care professionals, is definitely easier these days than it was even just 10 years ago,” said Dr. Sozzi, citing, as an example, a project she developed for training nursing home operators in palliative care.
It is in palliative care where the greatest progress has been made in end-of-life matters. “The culture of palliative care allows us to think about death in very different terms and to recognize that moment when we should stop looking at curative care and direct our efforts at ‘comfort care.’ And this care of the dying has to be holistic,” Dr. Sozzi explained. She adds that we are increasingly talking about simultaneous palliative care – care that is not limited to the final days of a person’s life but that rather starts early on, when active treatments are still in place.
Dr. Sozzi mentioned Italy’s Law 38, which took effect in 2010. It regulates access to palliative care and pain management, expanding the right to receive these treatments to patients “in any health care setting, at any stage of life, and for any chronic or progressive condition which has no treatment or has a treatment that is not sufficient to stabilize it.”
A culture shift is also needed in this area; there has already been a movement away from general practitioners to health care professionals who can and must direct a patient to palliative care.
“We need to provide these doctors with more training and make them more aware of what a difference this kind of care can make throughout a patient’s life, not only during the final stages,” said Dr. Sozzi. Concerning training, she mentioned that Italy had recently introduced a specialization in palliative care for medical school graduates. This is another small step and one that adds a sense of dignity to this new approach to life and to death.
The experts’ recommendations
In attempting to find a balance between life and death, we must not look at the period prior to the 1900s as some kind of golden age. Dr. Sozzi explained that back then there was almost none of the medical technology now available to treat people at the end of life. “Palliative care has also set forth original technical aspects for eliminating pain. Without having eliminated a patient’s pain, I can hardly begin a discussion with them about spiritual aspects,” she said, emphasizing the importance of always contextualizing approaches to death.
The Lancet Commission experts assessed the approach to death in many different contexts. They recommended that, to best handle end-of-life matters in all their complexity, one should keep in mind the importance of relationships and networks across society.
They recommended that health care and social care professionals improve their skills and their capacity for taking care of dying patients and their families. When the patient has a life-limiting illness, a caring and compassionate approach should be taken when providing clear information about all interventions involved in palliative care, as well as when having conversations about death.
Governments and policy makers are advised to implement actions to allow all citizens to have the same access to necessary palliative care. In addition, all strategies and reports on social care and well-being more broadly should always include consideration of death, dying, and grieving. It’s an uphill climb, but one that must be made if we’re to build a new culture aimed at bringing death back into life. “As we continue stepping toward this new culture, let us each put a stone in place,” Dr. Sozzi concluded.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
U.S. health officials tracking COVID-19 increase in U.K.
according to NPR.
Daily cases counts have increased 38% in the past week, according to the latest data from the U.K. Health Security Agency. Hospitalizations are up about 25% as well.
“Over the last year or so, what happens in the U.K. usually happens here a few weeks later,” Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told NPR.
“And right now, the U.K. is seeing somewhat of a rebound in cases,” he said.
Health officials in the United Kingdom have noted the latest increase is likely due to the contagious BA.2 Omicron subvariant, the recent loosening of coronavirus restrictions, and waning immunity from vaccinations and infections.
“All three of those factors we have here in the United States,” Dr. Fauci said. “So I would not be surprised if, in the next few weeks, we see either a plateauing … of cases or even [the curve] rebounds and slightly goes up.”
Right now, COVID-19 cases in the United Stastes have dropped to their lowest levels since July 2021, according to the latest Centers for Disease Control and Prevention data, with fewer than 30,000 daily cases. At the same time, the rate of decline in cases has slowed significantly and is beginning to plateau.
Public health experts are also pointing to wastewater surveillance data that shows an uptick in viral activity across the country. The CDC’s wastewater dashboard indicates that about 35% of sites that monitor wastewater are seeing an increase, with consistent growth in Florida, Rhode Island, and West Virginia.
“The power of wastewater surveillance is that it’s an early warning system,” Amy Kirby, the program lead for the CDC’s National Wastewater Surveillance System, told NPR.
“We are seeing evidence of increases in some communities across the country,” she said. “What looked like noise at the beginning of the week is starting to look like a true signal here at the end of the week.”
The wastewater system doesn’t distinguish between Omicron and subvariants such as BA.2. However, other CDC data has found an increase in BA.2 cases in the United States, making up about a quarter of new COVID-19 cases.
The BA.2 variant has roughly doubled each week for the last month, which means it could become the dominant coronavirus strain in the United States in coming weeks, according to USA Today. Cases appear to be spreading more quickly in the Northeast and West, making up about 39% of cases in New York and New Jersey last week.
BA.2 also accounts for nearly 39% of cases across the Northeast, including Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island and Vermont, USA Today reported. In the West, which includes Arizona, California and Nevada, the subvariant makes up about 28% of new cases. In the upper West, which includes Alaska, Oregon and Washington, about 26% of cases are BA.2.
The good news is that BA.2 “doesn’t seem to evade our vaccines or immunity any more than the prior Omicron [variant]. And it doesn’t seem to lead to any more increased severity of disease,” Rochelle Walensky, MD, the CDC director, told NPR’s Morning Edition on March 18.
The effects of BA.2 will likely depend on the immunity profile in the United States, including how long it’s been since someone was vaccinated, boosted, or recovered from an infection, she said.
Health officials are watching other countries with BA.2 increases, such as Germany, Italy, and the Netherlands. Many European countries have been reporting an uptick but not implementing major restrictions or shutdowns, USA Today reported.
The BA.2 variant likely won’t lead to a major surge in severe disease or strict COVID-19 measures, Dr. Fauci told NPR, but some coronavirus protocols may need to be implemented again if cases grow dramatically.
“We must be ready to pivot and, if necessary, to go back to stricter mitigation with regard to masks,” he said.
A version of this article first appeared on WebMD.com.
according to NPR.
Daily cases counts have increased 38% in the past week, according to the latest data from the U.K. Health Security Agency. Hospitalizations are up about 25% as well.
“Over the last year or so, what happens in the U.K. usually happens here a few weeks later,” Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told NPR.
“And right now, the U.K. is seeing somewhat of a rebound in cases,” he said.
Health officials in the United Kingdom have noted the latest increase is likely due to the contagious BA.2 Omicron subvariant, the recent loosening of coronavirus restrictions, and waning immunity from vaccinations and infections.
“All three of those factors we have here in the United States,” Dr. Fauci said. “So I would not be surprised if, in the next few weeks, we see either a plateauing … of cases or even [the curve] rebounds and slightly goes up.”
Right now, COVID-19 cases in the United Stastes have dropped to their lowest levels since July 2021, according to the latest Centers for Disease Control and Prevention data, with fewer than 30,000 daily cases. At the same time, the rate of decline in cases has slowed significantly and is beginning to plateau.
Public health experts are also pointing to wastewater surveillance data that shows an uptick in viral activity across the country. The CDC’s wastewater dashboard indicates that about 35% of sites that monitor wastewater are seeing an increase, with consistent growth in Florida, Rhode Island, and West Virginia.
“The power of wastewater surveillance is that it’s an early warning system,” Amy Kirby, the program lead for the CDC’s National Wastewater Surveillance System, told NPR.
“We are seeing evidence of increases in some communities across the country,” she said. “What looked like noise at the beginning of the week is starting to look like a true signal here at the end of the week.”
The wastewater system doesn’t distinguish between Omicron and subvariants such as BA.2. However, other CDC data has found an increase in BA.2 cases in the United States, making up about a quarter of new COVID-19 cases.
The BA.2 variant has roughly doubled each week for the last month, which means it could become the dominant coronavirus strain in the United States in coming weeks, according to USA Today. Cases appear to be spreading more quickly in the Northeast and West, making up about 39% of cases in New York and New Jersey last week.
BA.2 also accounts for nearly 39% of cases across the Northeast, including Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island and Vermont, USA Today reported. In the West, which includes Arizona, California and Nevada, the subvariant makes up about 28% of new cases. In the upper West, which includes Alaska, Oregon and Washington, about 26% of cases are BA.2.
The good news is that BA.2 “doesn’t seem to evade our vaccines or immunity any more than the prior Omicron [variant]. And it doesn’t seem to lead to any more increased severity of disease,” Rochelle Walensky, MD, the CDC director, told NPR’s Morning Edition on March 18.
The effects of BA.2 will likely depend on the immunity profile in the United States, including how long it’s been since someone was vaccinated, boosted, or recovered from an infection, she said.
Health officials are watching other countries with BA.2 increases, such as Germany, Italy, and the Netherlands. Many European countries have been reporting an uptick but not implementing major restrictions or shutdowns, USA Today reported.
The BA.2 variant likely won’t lead to a major surge in severe disease or strict COVID-19 measures, Dr. Fauci told NPR, but some coronavirus protocols may need to be implemented again if cases grow dramatically.
“We must be ready to pivot and, if necessary, to go back to stricter mitigation with regard to masks,” he said.
A version of this article first appeared on WebMD.com.
according to NPR.
Daily cases counts have increased 38% in the past week, according to the latest data from the U.K. Health Security Agency. Hospitalizations are up about 25% as well.
“Over the last year or so, what happens in the U.K. usually happens here a few weeks later,” Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, told NPR.
“And right now, the U.K. is seeing somewhat of a rebound in cases,” he said.
Health officials in the United Kingdom have noted the latest increase is likely due to the contagious BA.2 Omicron subvariant, the recent loosening of coronavirus restrictions, and waning immunity from vaccinations and infections.
“All three of those factors we have here in the United States,” Dr. Fauci said. “So I would not be surprised if, in the next few weeks, we see either a plateauing … of cases or even [the curve] rebounds and slightly goes up.”
Right now, COVID-19 cases in the United Stastes have dropped to their lowest levels since July 2021, according to the latest Centers for Disease Control and Prevention data, with fewer than 30,000 daily cases. At the same time, the rate of decline in cases has slowed significantly and is beginning to plateau.
Public health experts are also pointing to wastewater surveillance data that shows an uptick in viral activity across the country. The CDC’s wastewater dashboard indicates that about 35% of sites that monitor wastewater are seeing an increase, with consistent growth in Florida, Rhode Island, and West Virginia.
“The power of wastewater surveillance is that it’s an early warning system,” Amy Kirby, the program lead for the CDC’s National Wastewater Surveillance System, told NPR.
“We are seeing evidence of increases in some communities across the country,” she said. “What looked like noise at the beginning of the week is starting to look like a true signal here at the end of the week.”
The wastewater system doesn’t distinguish between Omicron and subvariants such as BA.2. However, other CDC data has found an increase in BA.2 cases in the United States, making up about a quarter of new COVID-19 cases.
The BA.2 variant has roughly doubled each week for the last month, which means it could become the dominant coronavirus strain in the United States in coming weeks, according to USA Today. Cases appear to be spreading more quickly in the Northeast and West, making up about 39% of cases in New York and New Jersey last week.
BA.2 also accounts for nearly 39% of cases across the Northeast, including Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island and Vermont, USA Today reported. In the West, which includes Arizona, California and Nevada, the subvariant makes up about 28% of new cases. In the upper West, which includes Alaska, Oregon and Washington, about 26% of cases are BA.2.
The good news is that BA.2 “doesn’t seem to evade our vaccines or immunity any more than the prior Omicron [variant]. And it doesn’t seem to lead to any more increased severity of disease,” Rochelle Walensky, MD, the CDC director, told NPR’s Morning Edition on March 18.
The effects of BA.2 will likely depend on the immunity profile in the United States, including how long it’s been since someone was vaccinated, boosted, or recovered from an infection, she said.
Health officials are watching other countries with BA.2 increases, such as Germany, Italy, and the Netherlands. Many European countries have been reporting an uptick but not implementing major restrictions or shutdowns, USA Today reported.
The BA.2 variant likely won’t lead to a major surge in severe disease or strict COVID-19 measures, Dr. Fauci told NPR, but some coronavirus protocols may need to be implemented again if cases grow dramatically.
“We must be ready to pivot and, if necessary, to go back to stricter mitigation with regard to masks,” he said.
A version of this article first appeared on WebMD.com.
Step test signals exercise capacity in asthma patients
The incremental step test is a highly reliable measure of exercise capacity in patients with moderate to severe asthma, based on data from 50 individuals.
Asthma patients often limit their physical exercise to avoid respiratory symptoms, which creates a downward spiral of reduced exercise capacity and ability to perform activities of daily living, wrote Renata Cléia Claudino Barbosa of the University of Sao Paulo and colleagues. “However, exercise training has been shown to be an important adjunctive therapy for asthma treatment that improves exercise capacity and health-related quality of life,” they wrote.
Step tests have been identified as a simpler, less costly alternative to cardiopulmonary exercise tests to measure exercise capacity in patients with chronic obstructive pulmonary disease, but their effectiveness for asthma patients has not investigated, the researchers said.
In a study published in Pulmonology, the researchers recruited 50 adults with moderate or severe asthma during routine care at a university hospital. The participants had been clinically stable for at least 6 months, with no hospitalizations, emergency care, or medication changes in the past 30 days. All participants received short-acting and long-acting bronchodilators and inhaled corticosteroids. The patients ranged in age from 18 to 60 years, with body mass index measures from 20 kg/m2 to 40 kg/m2.
Participants were randomized to tests on 2 nonconsecutive days at least 48 hours apart. On the first day, patients completed asthma control questionnaires and lung function tests, then performed either a cardiopulmonary exercise test (CPET) or two incremental step tests (IST-1 and IST-2). On the second day, they performed the other test. Participants were instructed to use bronchodilators 15 minutes before each test.
The step test involved stepping up and down on a 20-cm high wooden bench.
Overall, the peak oxygen uptakes were 27.6 mL/kg per minute for the CPET, 22.3 mL/kg per minute for the first IST, and 23.3 mL/kg per minute for the second IST.
“The IST with better performance regarding the peak VO2 value was called the best IST (b-IST),” and these values were used for validity and interpretability analyses, the researchers wrote.
In a reliability analysis, the intraclass correlation coefficient (ICC) was 0.93, the measurement error was 2.5%, and the construct validity for peak VO2 was significantly more reliable than the CPET (P < 0.001), the researchers said. The ICC for total number of steps was 0.88.
Notably, “the present study also demonstrated that IST is not interchangeable with the CPET since the subjects with moderate to severe asthma did not reach the maximal exercise capacity,” the researchers said. However, “we believe that the IST is superior to walking tests in subjects with asthma because it is an activity that requires greater ventilation in a subject’s daily life,” they said.
The study findings were limited by several factors including the relatively small study population and the small number of male patients, which may limit generalizability to males with asthma or other asthma endotypes, the researchers said. However, the results were strengthened by the randomized design, and support the value of the IST as a cost-effective option for assessing exercise capacity, preferably with two step tests to minimize the learning effect, they said. Additional research is needed to determine whether IST can assess responsiveness to pharmacological and nonpharmalogical treatments in asthma patients, they noted.
The study was supported by the Sao Paulo Research Foundation, Conselho Nacional de Pesquisa, and Coordination of Improvement of Higher Level Personnel--Brazil. The researchers had no financial conflicts to disclose.
The incremental step test is a highly reliable measure of exercise capacity in patients with moderate to severe asthma, based on data from 50 individuals.
Asthma patients often limit their physical exercise to avoid respiratory symptoms, which creates a downward spiral of reduced exercise capacity and ability to perform activities of daily living, wrote Renata Cléia Claudino Barbosa of the University of Sao Paulo and colleagues. “However, exercise training has been shown to be an important adjunctive therapy for asthma treatment that improves exercise capacity and health-related quality of life,” they wrote.
Step tests have been identified as a simpler, less costly alternative to cardiopulmonary exercise tests to measure exercise capacity in patients with chronic obstructive pulmonary disease, but their effectiveness for asthma patients has not investigated, the researchers said.
In a study published in Pulmonology, the researchers recruited 50 adults with moderate or severe asthma during routine care at a university hospital. The participants had been clinically stable for at least 6 months, with no hospitalizations, emergency care, or medication changes in the past 30 days. All participants received short-acting and long-acting bronchodilators and inhaled corticosteroids. The patients ranged in age from 18 to 60 years, with body mass index measures from 20 kg/m2 to 40 kg/m2.
Participants were randomized to tests on 2 nonconsecutive days at least 48 hours apart. On the first day, patients completed asthma control questionnaires and lung function tests, then performed either a cardiopulmonary exercise test (CPET) or two incremental step tests (IST-1 and IST-2). On the second day, they performed the other test. Participants were instructed to use bronchodilators 15 minutes before each test.
The step test involved stepping up and down on a 20-cm high wooden bench.
Overall, the peak oxygen uptakes were 27.6 mL/kg per minute for the CPET, 22.3 mL/kg per minute for the first IST, and 23.3 mL/kg per minute for the second IST.
“The IST with better performance regarding the peak VO2 value was called the best IST (b-IST),” and these values were used for validity and interpretability analyses, the researchers wrote.
In a reliability analysis, the intraclass correlation coefficient (ICC) was 0.93, the measurement error was 2.5%, and the construct validity for peak VO2 was significantly more reliable than the CPET (P < 0.001), the researchers said. The ICC for total number of steps was 0.88.
Notably, “the present study also demonstrated that IST is not interchangeable with the CPET since the subjects with moderate to severe asthma did not reach the maximal exercise capacity,” the researchers said. However, “we believe that the IST is superior to walking tests in subjects with asthma because it is an activity that requires greater ventilation in a subject’s daily life,” they said.
The study findings were limited by several factors including the relatively small study population and the small number of male patients, which may limit generalizability to males with asthma or other asthma endotypes, the researchers said. However, the results were strengthened by the randomized design, and support the value of the IST as a cost-effective option for assessing exercise capacity, preferably with two step tests to minimize the learning effect, they said. Additional research is needed to determine whether IST can assess responsiveness to pharmacological and nonpharmalogical treatments in asthma patients, they noted.
The study was supported by the Sao Paulo Research Foundation, Conselho Nacional de Pesquisa, and Coordination of Improvement of Higher Level Personnel--Brazil. The researchers had no financial conflicts to disclose.
The incremental step test is a highly reliable measure of exercise capacity in patients with moderate to severe asthma, based on data from 50 individuals.
Asthma patients often limit their physical exercise to avoid respiratory symptoms, which creates a downward spiral of reduced exercise capacity and ability to perform activities of daily living, wrote Renata Cléia Claudino Barbosa of the University of Sao Paulo and colleagues. “However, exercise training has been shown to be an important adjunctive therapy for asthma treatment that improves exercise capacity and health-related quality of life,” they wrote.
Step tests have been identified as a simpler, less costly alternative to cardiopulmonary exercise tests to measure exercise capacity in patients with chronic obstructive pulmonary disease, but their effectiveness for asthma patients has not investigated, the researchers said.
In a study published in Pulmonology, the researchers recruited 50 adults with moderate or severe asthma during routine care at a university hospital. The participants had been clinically stable for at least 6 months, with no hospitalizations, emergency care, or medication changes in the past 30 days. All participants received short-acting and long-acting bronchodilators and inhaled corticosteroids. The patients ranged in age from 18 to 60 years, with body mass index measures from 20 kg/m2 to 40 kg/m2.
Participants were randomized to tests on 2 nonconsecutive days at least 48 hours apart. On the first day, patients completed asthma control questionnaires and lung function tests, then performed either a cardiopulmonary exercise test (CPET) or two incremental step tests (IST-1 and IST-2). On the second day, they performed the other test. Participants were instructed to use bronchodilators 15 minutes before each test.
The step test involved stepping up and down on a 20-cm high wooden bench.
Overall, the peak oxygen uptakes were 27.6 mL/kg per minute for the CPET, 22.3 mL/kg per minute for the first IST, and 23.3 mL/kg per minute for the second IST.
“The IST with better performance regarding the peak VO2 value was called the best IST (b-IST),” and these values were used for validity and interpretability analyses, the researchers wrote.
In a reliability analysis, the intraclass correlation coefficient (ICC) was 0.93, the measurement error was 2.5%, and the construct validity for peak VO2 was significantly more reliable than the CPET (P < 0.001), the researchers said. The ICC for total number of steps was 0.88.
Notably, “the present study also demonstrated that IST is not interchangeable with the CPET since the subjects with moderate to severe asthma did not reach the maximal exercise capacity,” the researchers said. However, “we believe that the IST is superior to walking tests in subjects with asthma because it is an activity that requires greater ventilation in a subject’s daily life,” they said.
The study findings were limited by several factors including the relatively small study population and the small number of male patients, which may limit generalizability to males with asthma or other asthma endotypes, the researchers said. However, the results were strengthened by the randomized design, and support the value of the IST as a cost-effective option for assessing exercise capacity, preferably with two step tests to minimize the learning effect, they said. Additional research is needed to determine whether IST can assess responsiveness to pharmacological and nonpharmalogical treatments in asthma patients, they noted.
The study was supported by the Sao Paulo Research Foundation, Conselho Nacional de Pesquisa, and Coordination of Improvement of Higher Level Personnel--Brazil. The researchers had no financial conflicts to disclose.
FROM PULMONOLOGY
‘Vast majority’ of COVID patients wake up after mechanical ventilation
COVID-19 patients who are successfully weaned off a ventilator may take days, or even weeks, to regain consciousness, especially those who experienced episodes of hypoxemia while intubated, a new study shows.
“As we started to see the first patients waking up after successful COVID-19 ICU treatments, we also encountered many patients who remained comatose for days and weeks and then regained consciousness to become fully oriented,” co-senior investigator Nicholas Schiff, MD, with NewYork-Presbyterian/Weill Cornell Medical Center, says in a news release.
The findings have immediate implications regarding life-sustaining therapies for unresponsive COVID-19 patients, the investigators note.
“In critical care medicine, one of our main tasks is to advise families about planning in the event a patient does not regain consciousness,” said co-senior author Jan Claassen, MD, with New York-Presbyterian/Columbia University Irving Medical Center.
“Our findings suggest that for patients with severe COVID, the decision to withdraw life support shouldn’t be based solely on prolonged periods of unconsciousness, as these patients may eventually recover,” Dr. Claassen adds.
The study was published online March 7 in Annals of Neurology.
Slow road back
The researchers examined 795 intubated patients with severe COVID-19 at three medical centers in New York during the first wave of the pandemic (March-July 2020). All patients had impaired consciousness (Glasgow Coma Scale [GCS] motor score less than 6) on day 7 of intubation.
A total of 571 patients (72%) survived and regained consciousness.
The median time to recovery of consciousness was 30 days. One-quarter of the patients recovered consciousness 10 days or longer after they stopped receiving ventilator support and 10% took 23 days or longer to recover.
Time to recovery of consciousness was associated with hypoxemia. The hazard ratio was 0.56 (95% confidence interval, 0.46-0.68) with arterial partial pressure of oxygen (PaO2) less than or equal to 55 mm Hg and 0.88 (95% CI, 0.85-0.91) with a PaO2 less than or equal to 70 mm Hg.
Each additional day of hypoxemia decreased the odds of recovery of consciousness after accounting for confounding factors including sedation.
These findings were confirmed among patients without any imaging evidence of structural brain injury and in a non-overlapping cohort of 427 patients from the second wave of the pandemic (October-April 2021).
“These findings provide us with more accurate information to guide families who are deciding whether to continue life-sustaining therapy in unconscious COVID-19 patients,” co-senior author Brian Edlow, MD, with Massachusetts General Hospital and Harvard Medical School in Boston, says in the news release.
“Encouragingly,” adds Dr. Claassen, “our study shows that the vast majority of unconscious COVID patients recover consciousness, but it is important to consider that we did not look at the quality of recovery. That’s something that should be the focus of long-term follow-up studies.”
The study was supported by the James S. McDonnell Foundation (JSMF). Dr. Schiff, Dr. Claassen, and Dr. Edlow have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 patients who are successfully weaned off a ventilator may take days, or even weeks, to regain consciousness, especially those who experienced episodes of hypoxemia while intubated, a new study shows.
“As we started to see the first patients waking up after successful COVID-19 ICU treatments, we also encountered many patients who remained comatose for days and weeks and then regained consciousness to become fully oriented,” co-senior investigator Nicholas Schiff, MD, with NewYork-Presbyterian/Weill Cornell Medical Center, says in a news release.
The findings have immediate implications regarding life-sustaining therapies for unresponsive COVID-19 patients, the investigators note.
“In critical care medicine, one of our main tasks is to advise families about planning in the event a patient does not regain consciousness,” said co-senior author Jan Claassen, MD, with New York-Presbyterian/Columbia University Irving Medical Center.
“Our findings suggest that for patients with severe COVID, the decision to withdraw life support shouldn’t be based solely on prolonged periods of unconsciousness, as these patients may eventually recover,” Dr. Claassen adds.
The study was published online March 7 in Annals of Neurology.
Slow road back
The researchers examined 795 intubated patients with severe COVID-19 at three medical centers in New York during the first wave of the pandemic (March-July 2020). All patients had impaired consciousness (Glasgow Coma Scale [GCS] motor score less than 6) on day 7 of intubation.
A total of 571 patients (72%) survived and regained consciousness.
The median time to recovery of consciousness was 30 days. One-quarter of the patients recovered consciousness 10 days or longer after they stopped receiving ventilator support and 10% took 23 days or longer to recover.
Time to recovery of consciousness was associated with hypoxemia. The hazard ratio was 0.56 (95% confidence interval, 0.46-0.68) with arterial partial pressure of oxygen (PaO2) less than or equal to 55 mm Hg and 0.88 (95% CI, 0.85-0.91) with a PaO2 less than or equal to 70 mm Hg.
Each additional day of hypoxemia decreased the odds of recovery of consciousness after accounting for confounding factors including sedation.
These findings were confirmed among patients without any imaging evidence of structural brain injury and in a non-overlapping cohort of 427 patients from the second wave of the pandemic (October-April 2021).
“These findings provide us with more accurate information to guide families who are deciding whether to continue life-sustaining therapy in unconscious COVID-19 patients,” co-senior author Brian Edlow, MD, with Massachusetts General Hospital and Harvard Medical School in Boston, says in the news release.
“Encouragingly,” adds Dr. Claassen, “our study shows that the vast majority of unconscious COVID patients recover consciousness, but it is important to consider that we did not look at the quality of recovery. That’s something that should be the focus of long-term follow-up studies.”
The study was supported by the James S. McDonnell Foundation (JSMF). Dr. Schiff, Dr. Claassen, and Dr. Edlow have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 patients who are successfully weaned off a ventilator may take days, or even weeks, to regain consciousness, especially those who experienced episodes of hypoxemia while intubated, a new study shows.
“As we started to see the first patients waking up after successful COVID-19 ICU treatments, we also encountered many patients who remained comatose for days and weeks and then regained consciousness to become fully oriented,” co-senior investigator Nicholas Schiff, MD, with NewYork-Presbyterian/Weill Cornell Medical Center, says in a news release.
The findings have immediate implications regarding life-sustaining therapies for unresponsive COVID-19 patients, the investigators note.
“In critical care medicine, one of our main tasks is to advise families about planning in the event a patient does not regain consciousness,” said co-senior author Jan Claassen, MD, with New York-Presbyterian/Columbia University Irving Medical Center.
“Our findings suggest that for patients with severe COVID, the decision to withdraw life support shouldn’t be based solely on prolonged periods of unconsciousness, as these patients may eventually recover,” Dr. Claassen adds.
The study was published online March 7 in Annals of Neurology.
Slow road back
The researchers examined 795 intubated patients with severe COVID-19 at three medical centers in New York during the first wave of the pandemic (March-July 2020). All patients had impaired consciousness (Glasgow Coma Scale [GCS] motor score less than 6) on day 7 of intubation.
A total of 571 patients (72%) survived and regained consciousness.
The median time to recovery of consciousness was 30 days. One-quarter of the patients recovered consciousness 10 days or longer after they stopped receiving ventilator support and 10% took 23 days or longer to recover.
Time to recovery of consciousness was associated with hypoxemia. The hazard ratio was 0.56 (95% confidence interval, 0.46-0.68) with arterial partial pressure of oxygen (PaO2) less than or equal to 55 mm Hg and 0.88 (95% CI, 0.85-0.91) with a PaO2 less than or equal to 70 mm Hg.
Each additional day of hypoxemia decreased the odds of recovery of consciousness after accounting for confounding factors including sedation.
These findings were confirmed among patients without any imaging evidence of structural brain injury and in a non-overlapping cohort of 427 patients from the second wave of the pandemic (October-April 2021).
“These findings provide us with more accurate information to guide families who are deciding whether to continue life-sustaining therapy in unconscious COVID-19 patients,” co-senior author Brian Edlow, MD, with Massachusetts General Hospital and Harvard Medical School in Boston, says in the news release.
“Encouragingly,” adds Dr. Claassen, “our study shows that the vast majority of unconscious COVID patients recover consciousness, but it is important to consider that we did not look at the quality of recovery. That’s something that should be the focus of long-term follow-up studies.”
The study was supported by the James S. McDonnell Foundation (JSMF). Dr. Schiff, Dr. Claassen, and Dr. Edlow have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF NEUROLOGY
Adverse skin effects of cancer immunotherapy reviewed
Immune checkpoint inhibitors (ICIs) have unquestionably revolutionized the care of patients with malignant melanoma, non-small cell lung cancer, and other types of cancer.
, according to members of a European Academy of Dermatology and Venereology (EADV) task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they write in a position statement on the management of ICI-derived dermatologic adverse events.
Recommendations from the EADV “Dermatology for Cancer Patients” task force have been published in the Journal of the European Academy of Dermatology and Venereology.
Task force members developed the recommendations based on clinical experience from published data and came up with specific recommendations for treating cutaneous toxicities associated with dermatologic immune-related adverse events (dirAEs) that occur in patients receiving immunotherapy with an ICI.
ICIs include the cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) inhibitor ipilimumab (Yervoy, Bristol Myers Squibb), and inhibitors of programmed death protein 1 (PD-1) and its ligand (PD-L1), including nivolumab (Opdivo, Bristol Myers Squibb), pembrolizumab (Keytruda, Merck), and other agents.
“The basic principle of management is that the interventions should be tailored to serve the equilibrium between patients’ relief from the symptoms and signs of skin toxicity and the preservation of an unimpeded oncologic treatment,” they write.
The recommendations are in line with those included in a 2021 update of the American Society of Clinical Oncology (ASCO) guidelines on the management of irAEs in patients treated with ICIs across the whole range of organ systems, said Milan J. Anadkat, MD, professor of dermatology and director of dermatology clinical trials at Washington University School of Medicine, St. Louis. Dr. Anadkat was a coauthor of the ASCO guideline update.
Although the European recommendations focus only on dermatologic side effects of ICIs in patients with cancer, “that doesn’t diminish their importance. They do a good job of summarizing how to approach and how to manage it depending on the severity of the toxicities and the various types of toxicities,” he told this news organization.
Having a paper focused exclusively on the dermatologic side effects of ICIs allows the inclusion of photographs that can help clinicians identify specific conditions that may require referral to a dermatologist, he said.
Both Dr. Anadkat and the authors of the European recommendations noted that dermatologic irAEs are more common with CTLA-4 inhibition than with PD-1/PD-L1 inhibition.
“It has to do with where the target is,” Dr. Anadkat said. “CTLA-4 inhibition works on a central aspect of the immune system, so it’s a much less specific site, whereas PD-1 affects an interaction at the site of the tumor cell itself, so it’s a little more specific.”
Pruritus
ICI-induced pruritus can occur without apparent skin changes, they write, noting that in a recent study of patients with dirAEs, about one-third had isolated pruritus.
The task force members cite a meta-analysis indicating a pruritus incidence of 13.2% for patients treated with nivolumab and 20.2% for patients treated with pembrolizumab but respective grade 3 pruritus rates of only 0.5% and 2.3%. The reported incidence of pruritus with ipilimumab was 47% in a different study.
Recommended treatments include topical moisturizers with or without medium-to-high potency corticosteroids for grade 1 reactions, non-sedating histamines and/or GABA agonists such as pregabalin, or gabapentin for grade 2 pruritus, and suspension of ICIs until pruritus improves in patients with grade 3 pruritus.
Maculopapular rash
Maculopapular or eczema-like rashes may occur in up to 68% of patients who receive a CTLA-4 inhibitor and up to 20% of those who receive a PD1/PD-L1 inhibitor, the authors note. Rashes commonly appear within 3-6 weeks of initiating therapy.
“The clinical presentation is nonspecific and consists of a rapid onset of multiple minimally scaly, erythematous macules and papules, congregating into plaques. Lesions are mostly located on trunk and extensor surfaces of the extremities and the face is generally spared,” they write.
Maculopapular rashes are typically accompanied by itching but could be asymptomatic, they noted.
Mild (grade 1) rashes may respond to moisturizers and topical potent or super-potent corticosteroids. Patients with grade 2 rash should also receive oral antihistamines. Systemic corticosteroids may be considered for patients with grade 3 rashes but only after other dirAEs that may require specific management, such as psoriasis, are ruled out.
Psoriasis-like rash
The most common form of psoriasis seen in patients treated with ICIs is psoriasis vulgaris with plaques, but other clinical variants are also seen, the authors note.
“Topical agents (corticosteroids, Vitamin D analogues) are prescribed in Grades 1/2 and supplementary” to systemic treatment for patients with grade 3 or recalcitrant lesions, they write. “If skin-directed therapies fail to provide symptomatic control,” systemic treatment and narrow band UVB phototherapy “should be considered,” they add.
Evidence regarding the use of systemic therapies to treat psoriasis-like rash associated with ICIs is sparse. Acitretin can be safely used in patients with cancer. Low-dose methotrexate is also safe to use except in patients with non-melanoma skin cancers. Cyclosporine, however, should be avoided because of the potential for tumor-promoting effects, they emphasized.
The recommendations also cover treatment of lichen planus-like and vitiligo-like rashes, as well as hair and nail changes, autoimmune bullous disorders, and oral mucosal dirAEs.
In addition, the recommendations cover severe cutaneous adverse reactions as well as serious, potentially life-threatening dirAEs, including Stevens-Johnson syndrome/TEN, acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome (DRESS/DIHS).
“The dose of corticosteroids may be adapted to the severity of DRESS. The therapeutic benefit of systemic corticosteroids in the management of SJS/TEN remains controversial, and some authors favor treatment with cyclosporine. However, the use of corticosteroids in this context of ICI treatment appears reasonable and should be proposed. Short courses of steroids seem also effective in AGEP,” the task force members write.
The recommendations did not have outside funding. Of the 19 authors, 6 disclosed relationships with various pharmaceutical companies, including AbbVie, Leo Pharma, Boehringer Ingelheim, Bristol Myers Squibb, and/or Janssen. Dr. Anadkat disclosed previous relationships with Merck, Bristol Myers Squibb, and current relationships with others.
A version of this article first appeared on Medscape.com.
Immune checkpoint inhibitors (ICIs) have unquestionably revolutionized the care of patients with malignant melanoma, non-small cell lung cancer, and other types of cancer.
, according to members of a European Academy of Dermatology and Venereology (EADV) task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they write in a position statement on the management of ICI-derived dermatologic adverse events.
Recommendations from the EADV “Dermatology for Cancer Patients” task force have been published in the Journal of the European Academy of Dermatology and Venereology.
Task force members developed the recommendations based on clinical experience from published data and came up with specific recommendations for treating cutaneous toxicities associated with dermatologic immune-related adverse events (dirAEs) that occur in patients receiving immunotherapy with an ICI.
ICIs include the cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) inhibitor ipilimumab (Yervoy, Bristol Myers Squibb), and inhibitors of programmed death protein 1 (PD-1) and its ligand (PD-L1), including nivolumab (Opdivo, Bristol Myers Squibb), pembrolizumab (Keytruda, Merck), and other agents.
“The basic principle of management is that the interventions should be tailored to serve the equilibrium between patients’ relief from the symptoms and signs of skin toxicity and the preservation of an unimpeded oncologic treatment,” they write.
The recommendations are in line with those included in a 2021 update of the American Society of Clinical Oncology (ASCO) guidelines on the management of irAEs in patients treated with ICIs across the whole range of organ systems, said Milan J. Anadkat, MD, professor of dermatology and director of dermatology clinical trials at Washington University School of Medicine, St. Louis. Dr. Anadkat was a coauthor of the ASCO guideline update.
Although the European recommendations focus only on dermatologic side effects of ICIs in patients with cancer, “that doesn’t diminish their importance. They do a good job of summarizing how to approach and how to manage it depending on the severity of the toxicities and the various types of toxicities,” he told this news organization.
Having a paper focused exclusively on the dermatologic side effects of ICIs allows the inclusion of photographs that can help clinicians identify specific conditions that may require referral to a dermatologist, he said.
Both Dr. Anadkat and the authors of the European recommendations noted that dermatologic irAEs are more common with CTLA-4 inhibition than with PD-1/PD-L1 inhibition.
“It has to do with where the target is,” Dr. Anadkat said. “CTLA-4 inhibition works on a central aspect of the immune system, so it’s a much less specific site, whereas PD-1 affects an interaction at the site of the tumor cell itself, so it’s a little more specific.”
Pruritus
ICI-induced pruritus can occur without apparent skin changes, they write, noting that in a recent study of patients with dirAEs, about one-third had isolated pruritus.
The task force members cite a meta-analysis indicating a pruritus incidence of 13.2% for patients treated with nivolumab and 20.2% for patients treated with pembrolizumab but respective grade 3 pruritus rates of only 0.5% and 2.3%. The reported incidence of pruritus with ipilimumab was 47% in a different study.
Recommended treatments include topical moisturizers with or without medium-to-high potency corticosteroids for grade 1 reactions, non-sedating histamines and/or GABA agonists such as pregabalin, or gabapentin for grade 2 pruritus, and suspension of ICIs until pruritus improves in patients with grade 3 pruritus.
Maculopapular rash
Maculopapular or eczema-like rashes may occur in up to 68% of patients who receive a CTLA-4 inhibitor and up to 20% of those who receive a PD1/PD-L1 inhibitor, the authors note. Rashes commonly appear within 3-6 weeks of initiating therapy.
“The clinical presentation is nonspecific and consists of a rapid onset of multiple minimally scaly, erythematous macules and papules, congregating into plaques. Lesions are mostly located on trunk and extensor surfaces of the extremities and the face is generally spared,” they write.
Maculopapular rashes are typically accompanied by itching but could be asymptomatic, they noted.
Mild (grade 1) rashes may respond to moisturizers and topical potent or super-potent corticosteroids. Patients with grade 2 rash should also receive oral antihistamines. Systemic corticosteroids may be considered for patients with grade 3 rashes but only after other dirAEs that may require specific management, such as psoriasis, are ruled out.
Psoriasis-like rash
The most common form of psoriasis seen in patients treated with ICIs is psoriasis vulgaris with plaques, but other clinical variants are also seen, the authors note.
“Topical agents (corticosteroids, Vitamin D analogues) are prescribed in Grades 1/2 and supplementary” to systemic treatment for patients with grade 3 or recalcitrant lesions, they write. “If skin-directed therapies fail to provide symptomatic control,” systemic treatment and narrow band UVB phototherapy “should be considered,” they add.
Evidence regarding the use of systemic therapies to treat psoriasis-like rash associated with ICIs is sparse. Acitretin can be safely used in patients with cancer. Low-dose methotrexate is also safe to use except in patients with non-melanoma skin cancers. Cyclosporine, however, should be avoided because of the potential for tumor-promoting effects, they emphasized.
The recommendations also cover treatment of lichen planus-like and vitiligo-like rashes, as well as hair and nail changes, autoimmune bullous disorders, and oral mucosal dirAEs.
In addition, the recommendations cover severe cutaneous adverse reactions as well as serious, potentially life-threatening dirAEs, including Stevens-Johnson syndrome/TEN, acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome (DRESS/DIHS).
“The dose of corticosteroids may be adapted to the severity of DRESS. The therapeutic benefit of systemic corticosteroids in the management of SJS/TEN remains controversial, and some authors favor treatment with cyclosporine. However, the use of corticosteroids in this context of ICI treatment appears reasonable and should be proposed. Short courses of steroids seem also effective in AGEP,” the task force members write.
The recommendations did not have outside funding. Of the 19 authors, 6 disclosed relationships with various pharmaceutical companies, including AbbVie, Leo Pharma, Boehringer Ingelheim, Bristol Myers Squibb, and/or Janssen. Dr. Anadkat disclosed previous relationships with Merck, Bristol Myers Squibb, and current relationships with others.
A version of this article first appeared on Medscape.com.
Immune checkpoint inhibitors (ICIs) have unquestionably revolutionized the care of patients with malignant melanoma, non-small cell lung cancer, and other types of cancer.
, according to members of a European Academy of Dermatology and Venereology (EADV) task force.
“The desirable, immune-mediated oncologic response is often achieved at the cost of immune-related adverse events (irAEs) that may potentially affect any organ system,” they write in a position statement on the management of ICI-derived dermatologic adverse events.
Recommendations from the EADV “Dermatology for Cancer Patients” task force have been published in the Journal of the European Academy of Dermatology and Venereology.
Task force members developed the recommendations based on clinical experience from published data and came up with specific recommendations for treating cutaneous toxicities associated with dermatologic immune-related adverse events (dirAEs) that occur in patients receiving immunotherapy with an ICI.
ICIs include the cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) inhibitor ipilimumab (Yervoy, Bristol Myers Squibb), and inhibitors of programmed death protein 1 (PD-1) and its ligand (PD-L1), including nivolumab (Opdivo, Bristol Myers Squibb), pembrolizumab (Keytruda, Merck), and other agents.
“The basic principle of management is that the interventions should be tailored to serve the equilibrium between patients’ relief from the symptoms and signs of skin toxicity and the preservation of an unimpeded oncologic treatment,” they write.
The recommendations are in line with those included in a 2021 update of the American Society of Clinical Oncology (ASCO) guidelines on the management of irAEs in patients treated with ICIs across the whole range of organ systems, said Milan J. Anadkat, MD, professor of dermatology and director of dermatology clinical trials at Washington University School of Medicine, St. Louis. Dr. Anadkat was a coauthor of the ASCO guideline update.
Although the European recommendations focus only on dermatologic side effects of ICIs in patients with cancer, “that doesn’t diminish their importance. They do a good job of summarizing how to approach and how to manage it depending on the severity of the toxicities and the various types of toxicities,” he told this news organization.
Having a paper focused exclusively on the dermatologic side effects of ICIs allows the inclusion of photographs that can help clinicians identify specific conditions that may require referral to a dermatologist, he said.
Both Dr. Anadkat and the authors of the European recommendations noted that dermatologic irAEs are more common with CTLA-4 inhibition than with PD-1/PD-L1 inhibition.
“It has to do with where the target is,” Dr. Anadkat said. “CTLA-4 inhibition works on a central aspect of the immune system, so it’s a much less specific site, whereas PD-1 affects an interaction at the site of the tumor cell itself, so it’s a little more specific.”
Pruritus
ICI-induced pruritus can occur without apparent skin changes, they write, noting that in a recent study of patients with dirAEs, about one-third had isolated pruritus.
The task force members cite a meta-analysis indicating a pruritus incidence of 13.2% for patients treated with nivolumab and 20.2% for patients treated with pembrolizumab but respective grade 3 pruritus rates of only 0.5% and 2.3%. The reported incidence of pruritus with ipilimumab was 47% in a different study.
Recommended treatments include topical moisturizers with or without medium-to-high potency corticosteroids for grade 1 reactions, non-sedating histamines and/or GABA agonists such as pregabalin, or gabapentin for grade 2 pruritus, and suspension of ICIs until pruritus improves in patients with grade 3 pruritus.
Maculopapular rash
Maculopapular or eczema-like rashes may occur in up to 68% of patients who receive a CTLA-4 inhibitor and up to 20% of those who receive a PD1/PD-L1 inhibitor, the authors note. Rashes commonly appear within 3-6 weeks of initiating therapy.
“The clinical presentation is nonspecific and consists of a rapid onset of multiple minimally scaly, erythematous macules and papules, congregating into plaques. Lesions are mostly located on trunk and extensor surfaces of the extremities and the face is generally spared,” they write.
Maculopapular rashes are typically accompanied by itching but could be asymptomatic, they noted.
Mild (grade 1) rashes may respond to moisturizers and topical potent or super-potent corticosteroids. Patients with grade 2 rash should also receive oral antihistamines. Systemic corticosteroids may be considered for patients with grade 3 rashes but only after other dirAEs that may require specific management, such as psoriasis, are ruled out.
Psoriasis-like rash
The most common form of psoriasis seen in patients treated with ICIs is psoriasis vulgaris with plaques, but other clinical variants are also seen, the authors note.
“Topical agents (corticosteroids, Vitamin D analogues) are prescribed in Grades 1/2 and supplementary” to systemic treatment for patients with grade 3 or recalcitrant lesions, they write. “If skin-directed therapies fail to provide symptomatic control,” systemic treatment and narrow band UVB phototherapy “should be considered,” they add.
Evidence regarding the use of systemic therapies to treat psoriasis-like rash associated with ICIs is sparse. Acitretin can be safely used in patients with cancer. Low-dose methotrexate is also safe to use except in patients with non-melanoma skin cancers. Cyclosporine, however, should be avoided because of the potential for tumor-promoting effects, they emphasized.
The recommendations also cover treatment of lichen planus-like and vitiligo-like rashes, as well as hair and nail changes, autoimmune bullous disorders, and oral mucosal dirAEs.
In addition, the recommendations cover severe cutaneous adverse reactions as well as serious, potentially life-threatening dirAEs, including Stevens-Johnson syndrome/TEN, acute generalized exanthematous pustulosis (AGEP), and drug reaction with eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome (DRESS/DIHS).
“The dose of corticosteroids may be adapted to the severity of DRESS. The therapeutic benefit of systemic corticosteroids in the management of SJS/TEN remains controversial, and some authors favor treatment with cyclosporine. However, the use of corticosteroids in this context of ICI treatment appears reasonable and should be proposed. Short courses of steroids seem also effective in AGEP,” the task force members write.
The recommendations did not have outside funding. Of the 19 authors, 6 disclosed relationships with various pharmaceutical companies, including AbbVie, Leo Pharma, Boehringer Ingelheim, Bristol Myers Squibb, and/or Janssen. Dr. Anadkat disclosed previous relationships with Merck, Bristol Myers Squibb, and current relationships with others.
A version of this article first appeared on Medscape.com.
Untargeted CT scans leads to overdiagnoses in lung cancer
Such overdiagnosis was illustrated in a recent study from JAMA Internal Medicine of women in Taiwan who were screened for lung cancer using low-dose CT (LDCT).
The study, and the accompanying editorial, pointed out the potential for large databases of routine clinical data to track long-term outcomes, and potentially identify patient subgroups that could benefit from early diagnosis using digital technologies.
The Taiwanese findings echo a similar trend identified in a 2018 post hoc analysis of the Danish Lung Cancer Screening Trial, which estimated that 67.2% of cancers found during that CT screening program for current or former smokers were overdiagnosed. The authors recommended that researchers report rates of overdiagnosis in future screening studies.
The authors of the Taiwan study noted that LDCT is low cost and is frequently offered to individuals who are not considered at high risk of lung cancer, and advertisements in Taiwan often target women, who rarely smoke. The researchers examined data from the Taiwan National Cancer Registry. They looked for evidence of an increased incidence of early-stage detection and reduced incidence of late-stage diagnosis. They found that, from 2004 to 2018, there was an increase of lung cancer incidence from 2.3 to 14.4 per 100,000 (difference, 12.1; 95% confidence interval, 11.3-12.8), but no significant difference in the incidence of late-stage disease (from 18.7 to 19.3 per 100,000; difference, 0.6; 95% CI, –0.5 to 1.7).
“This combination of findings, an additional 12.1 early-stage cancers per 100,000 population and no reduction in late-stage cancers, is strongly suggestive of overdiagnosis,” the authors wrote.
It can be difficult to convince people of the potential harms of overdiagnosis, especially when patients have a nodule removed and remain healthy years later. “It’s very counterintuitive, but it’s a reality, and I think this paper paints the reality very, very clearly,” said Daniel Capurro, MD, PhD, deputy director of the Centre for the Digital Transformation of Health at University of Melbourne, and an author of the editorial.
The issue is that some lung cancers progress so slowly that they may never cause a problem clinically, and their removal can lead to unnecessary cost and risk. And it’s not just cancer. “There are a bunch of other conditions that are defined by specific criteria, but we don’t add the prognosis to that definition. At the individual patient level, we don’t know the prognosis,” Dr. Capurro said.
Dr. Capurro discussed the increasing use of digital technologies like smartphone apps. Machine learning can potentially use such data to diagnose conditions like sleep or mood disorders before they become clinically significant, allowing earlier intervention, but they could also lead to overdiagnosis. Dr. Capurro proposed using longitudinal databases to track patient outcomes, which could be applied to digital screening technologies.
“You might be able to find unknown patterns that help discriminate between these pathological definitions. You should be able to train (digital screens) with the pathological definition plus the disease trajectory as a way to improve that label,” he said.
The study was funded by the Taiwan Ministry of Health and Welfare Clinical Trial Center.
Such overdiagnosis was illustrated in a recent study from JAMA Internal Medicine of women in Taiwan who were screened for lung cancer using low-dose CT (LDCT).
The study, and the accompanying editorial, pointed out the potential for large databases of routine clinical data to track long-term outcomes, and potentially identify patient subgroups that could benefit from early diagnosis using digital technologies.
The Taiwanese findings echo a similar trend identified in a 2018 post hoc analysis of the Danish Lung Cancer Screening Trial, which estimated that 67.2% of cancers found during that CT screening program for current or former smokers were overdiagnosed. The authors recommended that researchers report rates of overdiagnosis in future screening studies.
The authors of the Taiwan study noted that LDCT is low cost and is frequently offered to individuals who are not considered at high risk of lung cancer, and advertisements in Taiwan often target women, who rarely smoke. The researchers examined data from the Taiwan National Cancer Registry. They looked for evidence of an increased incidence of early-stage detection and reduced incidence of late-stage diagnosis. They found that, from 2004 to 2018, there was an increase of lung cancer incidence from 2.3 to 14.4 per 100,000 (difference, 12.1; 95% confidence interval, 11.3-12.8), but no significant difference in the incidence of late-stage disease (from 18.7 to 19.3 per 100,000; difference, 0.6; 95% CI, –0.5 to 1.7).
“This combination of findings, an additional 12.1 early-stage cancers per 100,000 population and no reduction in late-stage cancers, is strongly suggestive of overdiagnosis,” the authors wrote.
It can be difficult to convince people of the potential harms of overdiagnosis, especially when patients have a nodule removed and remain healthy years later. “It’s very counterintuitive, but it’s a reality, and I think this paper paints the reality very, very clearly,” said Daniel Capurro, MD, PhD, deputy director of the Centre for the Digital Transformation of Health at University of Melbourne, and an author of the editorial.
The issue is that some lung cancers progress so slowly that they may never cause a problem clinically, and their removal can lead to unnecessary cost and risk. And it’s not just cancer. “There are a bunch of other conditions that are defined by specific criteria, but we don’t add the prognosis to that definition. At the individual patient level, we don’t know the prognosis,” Dr. Capurro said.
Dr. Capurro discussed the increasing use of digital technologies like smartphone apps. Machine learning can potentially use such data to diagnose conditions like sleep or mood disorders before they become clinically significant, allowing earlier intervention, but they could also lead to overdiagnosis. Dr. Capurro proposed using longitudinal databases to track patient outcomes, which could be applied to digital screening technologies.
“You might be able to find unknown patterns that help discriminate between these pathological definitions. You should be able to train (digital screens) with the pathological definition plus the disease trajectory as a way to improve that label,” he said.
The study was funded by the Taiwan Ministry of Health and Welfare Clinical Trial Center.
Such overdiagnosis was illustrated in a recent study from JAMA Internal Medicine of women in Taiwan who were screened for lung cancer using low-dose CT (LDCT).
The study, and the accompanying editorial, pointed out the potential for large databases of routine clinical data to track long-term outcomes, and potentially identify patient subgroups that could benefit from early diagnosis using digital technologies.
The Taiwanese findings echo a similar trend identified in a 2018 post hoc analysis of the Danish Lung Cancer Screening Trial, which estimated that 67.2% of cancers found during that CT screening program for current or former smokers were overdiagnosed. The authors recommended that researchers report rates of overdiagnosis in future screening studies.
The authors of the Taiwan study noted that LDCT is low cost and is frequently offered to individuals who are not considered at high risk of lung cancer, and advertisements in Taiwan often target women, who rarely smoke. The researchers examined data from the Taiwan National Cancer Registry. They looked for evidence of an increased incidence of early-stage detection and reduced incidence of late-stage diagnosis. They found that, from 2004 to 2018, there was an increase of lung cancer incidence from 2.3 to 14.4 per 100,000 (difference, 12.1; 95% confidence interval, 11.3-12.8), but no significant difference in the incidence of late-stage disease (from 18.7 to 19.3 per 100,000; difference, 0.6; 95% CI, –0.5 to 1.7).
“This combination of findings, an additional 12.1 early-stage cancers per 100,000 population and no reduction in late-stage cancers, is strongly suggestive of overdiagnosis,” the authors wrote.
It can be difficult to convince people of the potential harms of overdiagnosis, especially when patients have a nodule removed and remain healthy years later. “It’s very counterintuitive, but it’s a reality, and I think this paper paints the reality very, very clearly,” said Daniel Capurro, MD, PhD, deputy director of the Centre for the Digital Transformation of Health at University of Melbourne, and an author of the editorial.
The issue is that some lung cancers progress so slowly that they may never cause a problem clinically, and their removal can lead to unnecessary cost and risk. And it’s not just cancer. “There are a bunch of other conditions that are defined by specific criteria, but we don’t add the prognosis to that definition. At the individual patient level, we don’t know the prognosis,” Dr. Capurro said.
Dr. Capurro discussed the increasing use of digital technologies like smartphone apps. Machine learning can potentially use such data to diagnose conditions like sleep or mood disorders before they become clinically significant, allowing earlier intervention, but they could also lead to overdiagnosis. Dr. Capurro proposed using longitudinal databases to track patient outcomes, which could be applied to digital screening technologies.
“You might be able to find unknown patterns that help discriminate between these pathological definitions. You should be able to train (digital screens) with the pathological definition plus the disease trajectory as a way to improve that label,” he said.
The study was funded by the Taiwan Ministry of Health and Welfare Clinical Trial Center.
FROM JAMA INTERNAL MEDICINE