User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Sleep Medicine Network
Respiratory-Related Sleep Disorders Section
Sleep health and fatigue mitigation during medical training
Medical trainees may experience acute or chronic sleep deprivation due to extended work hours and shift-work sleep schedules. Extended work hours may lead to serious medical errors, percutaneous injuries, prolonged task completion, and car crashes or near misses while driving (Landrigan, et al. N Engl J Med. 2004;351:1838; Ayas, et al. JAMA. 2006;296[9]:1055; Taffinder, et al. Lancet. 1998;352[9135]:1191; Barger, et al. N Engl J Med. 2005 Jan 13;352[2]:125).
Chronic sleep restriction also results in neurobehavioral and cognitive dysfunction without a proportionate increase in self-perceived sleepiness [Belenky, et al. J Sleep Res. 2003;12[1]:1; Van Dongen, et al. Sleep. 2003;26[2]:117). In 1987, when sleep deprivation was cited as a major cause of 18-year-old Libby Zion’s death, the ACGME restricted residents from working more than 80 hours per week. ACGME mandates that training programs provide yearly fatigue mitigation education.
A “Sleep Alertness and Fatigue Education in Residency” module may be purchased through the American Academy of Sleep Medicine. While one-time education opportunities are available, there remains a need for access to longitudinal, individualized tools during varying rotations and circumstances, as education alone has not been shown to improve sleep quality (Mazar D, et al. J Clin Sleep Med. 2021;17[6]:1211). The American Thoracic Society Early Career Professional Working Group offers individualized lectures to training programs. Wake Up and Learn is a sleep education program for children and teens that is currently being expanded for medical trainees.
Further data are needed to see if longitudinal and individualized support can promote better sleep quality among trainees.
Aesha Jobanputra, MD
Section Member
Sreelatha Naik, MD
Member-at-Large
Respiratory-Related Sleep Disorders Section
Sleep health and fatigue mitigation during medical training
Medical trainees may experience acute or chronic sleep deprivation due to extended work hours and shift-work sleep schedules. Extended work hours may lead to serious medical errors, percutaneous injuries, prolonged task completion, and car crashes or near misses while driving (Landrigan, et al. N Engl J Med. 2004;351:1838; Ayas, et al. JAMA. 2006;296[9]:1055; Taffinder, et al. Lancet. 1998;352[9135]:1191; Barger, et al. N Engl J Med. 2005 Jan 13;352[2]:125).
Chronic sleep restriction also results in neurobehavioral and cognitive dysfunction without a proportionate increase in self-perceived sleepiness [Belenky, et al. J Sleep Res. 2003;12[1]:1; Van Dongen, et al. Sleep. 2003;26[2]:117). In 1987, when sleep deprivation was cited as a major cause of 18-year-old Libby Zion’s death, the ACGME restricted residents from working more than 80 hours per week. ACGME mandates that training programs provide yearly fatigue mitigation education.
A “Sleep Alertness and Fatigue Education in Residency” module may be purchased through the American Academy of Sleep Medicine. While one-time education opportunities are available, there remains a need for access to longitudinal, individualized tools during varying rotations and circumstances, as education alone has not been shown to improve sleep quality (Mazar D, et al. J Clin Sleep Med. 2021;17[6]:1211). The American Thoracic Society Early Career Professional Working Group offers individualized lectures to training programs. Wake Up and Learn is a sleep education program for children and teens that is currently being expanded for medical trainees.
Further data are needed to see if longitudinal and individualized support can promote better sleep quality among trainees.
Aesha Jobanputra, MD
Section Member
Sreelatha Naik, MD
Member-at-Large
Respiratory-Related Sleep Disorders Section
Sleep health and fatigue mitigation during medical training
Medical trainees may experience acute or chronic sleep deprivation due to extended work hours and shift-work sleep schedules. Extended work hours may lead to serious medical errors, percutaneous injuries, prolonged task completion, and car crashes or near misses while driving (Landrigan, et al. N Engl J Med. 2004;351:1838; Ayas, et al. JAMA. 2006;296[9]:1055; Taffinder, et al. Lancet. 1998;352[9135]:1191; Barger, et al. N Engl J Med. 2005 Jan 13;352[2]:125).
Chronic sleep restriction also results in neurobehavioral and cognitive dysfunction without a proportionate increase in self-perceived sleepiness [Belenky, et al. J Sleep Res. 2003;12[1]:1; Van Dongen, et al. Sleep. 2003;26[2]:117). In 1987, when sleep deprivation was cited as a major cause of 18-year-old Libby Zion’s death, the ACGME restricted residents from working more than 80 hours per week. ACGME mandates that training programs provide yearly fatigue mitigation education.
A “Sleep Alertness and Fatigue Education in Residency” module may be purchased through the American Academy of Sleep Medicine. While one-time education opportunities are available, there remains a need for access to longitudinal, individualized tools during varying rotations and circumstances, as education alone has not been shown to improve sleep quality (Mazar D, et al. J Clin Sleep Med. 2021;17[6]:1211). The American Thoracic Society Early Career Professional Working Group offers individualized lectures to training programs. Wake Up and Learn is a sleep education program for children and teens that is currently being expanded for medical trainees.
Further data are needed to see if longitudinal and individualized support can promote better sleep quality among trainees.
Aesha Jobanputra, MD
Section Member
Sreelatha Naik, MD
Member-at-Large
Death of son reinforces flu vaccination message
“It was what the CDC [Centers for Disease Control and Prevention] would call classic influenza-like illness,” Dr. Teichman said. “It was too late to start antivirals, so I gave him advice on symptomatic treatment. We texted the next day, and I was glad to hear that his fever was trending down and that he was feeling a little bit better.”
Two days later, his son called again.
“He said he was having trouble breathing, and over the phone I could hear him hyperventilating.” The retired pediatrician and health care executive told his son to seek medical care.
“Then I got the call that no parent wants to get.”
Brent’s cousin Jake called saying he couldn’t wake Brent up.
“I called Jake back a few minutes later and asked him to hold up the phone,” Dr. Teichman said. “I listened to EMS working on my son, calling for round after round of many medications. He was in arrest and they couldn’t revive him.”
“To this day when I close my eyes at night, I still hear the beeping of those monitors.”
Brent had no health conditions to put him at higher risk for complications of the flu. “Brent was a wonderful son, brother, uncle, and friend. He had a passion for everything he did, and that included his chosen calling of the culinary arts but also included University of Kentucky sports,” Dr. Teichman said.
Brent planned to get a flu vaccine but had not done it yet. “In his obituary, we requested that, in lieu of flowers or donations, people go get their flu shot,” Dr. Teichman said.
“I’m here today to put a face on influenza,” Dr. Teichman said at a news briefing Oct. 4 on preventing the flu and pneumococcal disease, sponsored by the National Foundation for Infectious Diseases.
New survey numbers ‘alarming’
The NFID commissioned a national survey of more than 1,000 U.S. adults to better understand their knowledge and attitudes about the flu, pneumococcal disease, vaccines, and the impact of COVID-19.
“We were alarmed to learn that only 49% of U.S. adults plan to get their flu vaccine this season,” said Patricia A. “Patsy” Stinchfield, a registered nurse, NFID president, and moderator of the news briefing. “That is not good enough.”
In addition, 22% of people at higher risk for flu-related complications do not plan to get vaccinated this season. “That’s a dangerous risk to take,” Ms. Stinchfield said.
An encouraging finding, she said, is that 69% of adults surveyed recognize that an annual flu vaccination is the best way to prevent flu-related hospitalizations and death.
“So, most people know what to do. We just need to do it,” she said.
The top reason for not getting a flu shot in 2022 mentioned by 41% of people surveyed, is they do not think vaccines work very well. Another 39% are concerned about vaccine side effects, and 28% skip the vaccine because they “never get the flu.”
The experts on the panel emphasized the recommendation that all Americans 6 months or older get the flu vaccine, preferably by the end of October. Vaccination is especially important for those at higher risk of complications from the flu, including children under 5, pregnant women, people with one or more health conditions, the immunocompromised, and Americans 65 years and older.
Ms. Stinchfield acknowledged that the effectiveness of the flu vaccine varies season to season, but even if the vaccine does not completely match the circulating viruses, it can help prevent serious outcomes like hospitalization and death. One of the serious potential complications is pneumonia or “pneumococcal disease.”
“Our survey shows that only 29% of those at risk have been advised to receive a pneumococcal vaccine,” Ms. Stinchfield said. “The good news is that, among those who were advised to get the vaccine, 74% did receive their pneumococcal vaccine,” she said. “This underscores a key point to you, my fellow clinicians: As health professionals, our recommendations matter.”
Higher doses for 65+ Americans
The CDC updated recommendations this flu season for adults 65 and older to receive one of three preferentially recommended flu vaccines, said CDC Director Rochelle Walensky, MD. The CDC is recommending higher-dose, stronger vaccines for older Americans “based on a review of the available studies, which suggested that in this age group, these vaccines are potentially more effective than standard-dose ... vaccines.”
During most seasons, people 65 and older bear the greatest burden of severe flu disease, accounting for most flu-related hospitalizations and deaths.
“They are the largest vulnerable segment of our society,” Dr. Walensky said.
What will this flu season be like?
Health officials in the flu vaccine business also tend to be in the flu season prediction business. That includes Dr. Walensky.
“While we will never exactly know what each flu season will hold, we do know that every year, the best way you can protect yourself and those around you is to get your annual flu vaccine,” she said while taking part remotely in the briefing.
How severe will the flu season be in 2022-23? William Schaffner, MD, said he gets that question a lot. “Don’t think about that. Just focus on the fact that flu will be with us each year.
“We were a little bit spoiled. We’ve had two mild influenza seasons,” said Dr. Schaffner, medical director of NFID and a professor of infectious diseases and preventive medicine at Vanderbilt University, Nashville, Tenn. “I think with all the interest in COVID, people have rather forgotten about influenza. I’ve had to remind them that this is yet another serious winter respiratory virus.
“As I like to say, flu is fickle. It’s difficult to predict how serious this next outbreak of influenza this season is going to be. We could look at what happened in the Southern Hemisphere,” he said.
For example, Australia had the worst influenza season in the past 5 years, Schaffner said. “If you want a hint of what might happen here and you want yet another reason to be vaccinated, there it is.”
What we do know, Dr. Walensky said, is that the timing and severity of the past two flu seasons in the U.S. have been different than typical flu seasons. “And this is likely due to the COVID mitigation measures and other changes in circulating respiratory viruses.” Also, although last flu season was “relatively mild,” there was more flu activity than in the prior, 2020-21 season.
Also, Dr. Walensky said, last season’s flu cases began to increase in November and remained elevated until mid-June, “making it the latest season on record.”
The official cause of Brent Teichman’s death was multilobar pneumonia, cause undetermined. “But after 30-plus years as a pediatrician ... I know influenza when I see it,” Dr. Teichman said.
“There’s a hole in our hearts that will never heal. Loss of a child is devastating,” he said. The flu “can take the life of a healthy young person, as it did to my son.
“And for all those listening to my story who are vaccine hesitant, do it for those who love you. So that they won’t walk the path that we and many other families in this country have walked.”
To prove their point, Dr. Teichman and Ms. Stinchfield raised their sleeves and received flu shots during the news briefing.
“This one is for Brent,” Dr. Teichman said.
A version of this article first appeared on WebMD.com.
“It was what the CDC [Centers for Disease Control and Prevention] would call classic influenza-like illness,” Dr. Teichman said. “It was too late to start antivirals, so I gave him advice on symptomatic treatment. We texted the next day, and I was glad to hear that his fever was trending down and that he was feeling a little bit better.”
Two days later, his son called again.
“He said he was having trouble breathing, and over the phone I could hear him hyperventilating.” The retired pediatrician and health care executive told his son to seek medical care.
“Then I got the call that no parent wants to get.”
Brent’s cousin Jake called saying he couldn’t wake Brent up.
“I called Jake back a few minutes later and asked him to hold up the phone,” Dr. Teichman said. “I listened to EMS working on my son, calling for round after round of many medications. He was in arrest and they couldn’t revive him.”
“To this day when I close my eyes at night, I still hear the beeping of those monitors.”
Brent had no health conditions to put him at higher risk for complications of the flu. “Brent was a wonderful son, brother, uncle, and friend. He had a passion for everything he did, and that included his chosen calling of the culinary arts but also included University of Kentucky sports,” Dr. Teichman said.
Brent planned to get a flu vaccine but had not done it yet. “In his obituary, we requested that, in lieu of flowers or donations, people go get their flu shot,” Dr. Teichman said.
“I’m here today to put a face on influenza,” Dr. Teichman said at a news briefing Oct. 4 on preventing the flu and pneumococcal disease, sponsored by the National Foundation for Infectious Diseases.
New survey numbers ‘alarming’
The NFID commissioned a national survey of more than 1,000 U.S. adults to better understand their knowledge and attitudes about the flu, pneumococcal disease, vaccines, and the impact of COVID-19.
“We were alarmed to learn that only 49% of U.S. adults plan to get their flu vaccine this season,” said Patricia A. “Patsy” Stinchfield, a registered nurse, NFID president, and moderator of the news briefing. “That is not good enough.”
In addition, 22% of people at higher risk for flu-related complications do not plan to get vaccinated this season. “That’s a dangerous risk to take,” Ms. Stinchfield said.
An encouraging finding, she said, is that 69% of adults surveyed recognize that an annual flu vaccination is the best way to prevent flu-related hospitalizations and death.
“So, most people know what to do. We just need to do it,” she said.
The top reason for not getting a flu shot in 2022 mentioned by 41% of people surveyed, is they do not think vaccines work very well. Another 39% are concerned about vaccine side effects, and 28% skip the vaccine because they “never get the flu.”
The experts on the panel emphasized the recommendation that all Americans 6 months or older get the flu vaccine, preferably by the end of October. Vaccination is especially important for those at higher risk of complications from the flu, including children under 5, pregnant women, people with one or more health conditions, the immunocompromised, and Americans 65 years and older.
Ms. Stinchfield acknowledged that the effectiveness of the flu vaccine varies season to season, but even if the vaccine does not completely match the circulating viruses, it can help prevent serious outcomes like hospitalization and death. One of the serious potential complications is pneumonia or “pneumococcal disease.”
“Our survey shows that only 29% of those at risk have been advised to receive a pneumococcal vaccine,” Ms. Stinchfield said. “The good news is that, among those who were advised to get the vaccine, 74% did receive their pneumococcal vaccine,” she said. “This underscores a key point to you, my fellow clinicians: As health professionals, our recommendations matter.”
Higher doses for 65+ Americans
The CDC updated recommendations this flu season for adults 65 and older to receive one of three preferentially recommended flu vaccines, said CDC Director Rochelle Walensky, MD. The CDC is recommending higher-dose, stronger vaccines for older Americans “based on a review of the available studies, which suggested that in this age group, these vaccines are potentially more effective than standard-dose ... vaccines.”
During most seasons, people 65 and older bear the greatest burden of severe flu disease, accounting for most flu-related hospitalizations and deaths.
“They are the largest vulnerable segment of our society,” Dr. Walensky said.
What will this flu season be like?
Health officials in the flu vaccine business also tend to be in the flu season prediction business. That includes Dr. Walensky.
“While we will never exactly know what each flu season will hold, we do know that every year, the best way you can protect yourself and those around you is to get your annual flu vaccine,” she said while taking part remotely in the briefing.
How severe will the flu season be in 2022-23? William Schaffner, MD, said he gets that question a lot. “Don’t think about that. Just focus on the fact that flu will be with us each year.
“We were a little bit spoiled. We’ve had two mild influenza seasons,” said Dr. Schaffner, medical director of NFID and a professor of infectious diseases and preventive medicine at Vanderbilt University, Nashville, Tenn. “I think with all the interest in COVID, people have rather forgotten about influenza. I’ve had to remind them that this is yet another serious winter respiratory virus.
“As I like to say, flu is fickle. It’s difficult to predict how serious this next outbreak of influenza this season is going to be. We could look at what happened in the Southern Hemisphere,” he said.
For example, Australia had the worst influenza season in the past 5 years, Schaffner said. “If you want a hint of what might happen here and you want yet another reason to be vaccinated, there it is.”
What we do know, Dr. Walensky said, is that the timing and severity of the past two flu seasons in the U.S. have been different than typical flu seasons. “And this is likely due to the COVID mitigation measures and other changes in circulating respiratory viruses.” Also, although last flu season was “relatively mild,” there was more flu activity than in the prior, 2020-21 season.
Also, Dr. Walensky said, last season’s flu cases began to increase in November and remained elevated until mid-June, “making it the latest season on record.”
The official cause of Brent Teichman’s death was multilobar pneumonia, cause undetermined. “But after 30-plus years as a pediatrician ... I know influenza when I see it,” Dr. Teichman said.
“There’s a hole in our hearts that will never heal. Loss of a child is devastating,” he said. The flu “can take the life of a healthy young person, as it did to my son.
“And for all those listening to my story who are vaccine hesitant, do it for those who love you. So that they won’t walk the path that we and many other families in this country have walked.”
To prove their point, Dr. Teichman and Ms. Stinchfield raised their sleeves and received flu shots during the news briefing.
“This one is for Brent,” Dr. Teichman said.
A version of this article first appeared on WebMD.com.
“It was what the CDC [Centers for Disease Control and Prevention] would call classic influenza-like illness,” Dr. Teichman said. “It was too late to start antivirals, so I gave him advice on symptomatic treatment. We texted the next day, and I was glad to hear that his fever was trending down and that he was feeling a little bit better.”
Two days later, his son called again.
“He said he was having trouble breathing, and over the phone I could hear him hyperventilating.” The retired pediatrician and health care executive told his son to seek medical care.
“Then I got the call that no parent wants to get.”
Brent’s cousin Jake called saying he couldn’t wake Brent up.
“I called Jake back a few minutes later and asked him to hold up the phone,” Dr. Teichman said. “I listened to EMS working on my son, calling for round after round of many medications. He was in arrest and they couldn’t revive him.”
“To this day when I close my eyes at night, I still hear the beeping of those monitors.”
Brent had no health conditions to put him at higher risk for complications of the flu. “Brent was a wonderful son, brother, uncle, and friend. He had a passion for everything he did, and that included his chosen calling of the culinary arts but also included University of Kentucky sports,” Dr. Teichman said.
Brent planned to get a flu vaccine but had not done it yet. “In his obituary, we requested that, in lieu of flowers or donations, people go get their flu shot,” Dr. Teichman said.
“I’m here today to put a face on influenza,” Dr. Teichman said at a news briefing Oct. 4 on preventing the flu and pneumococcal disease, sponsored by the National Foundation for Infectious Diseases.
New survey numbers ‘alarming’
The NFID commissioned a national survey of more than 1,000 U.S. adults to better understand their knowledge and attitudes about the flu, pneumococcal disease, vaccines, and the impact of COVID-19.
“We were alarmed to learn that only 49% of U.S. adults plan to get their flu vaccine this season,” said Patricia A. “Patsy” Stinchfield, a registered nurse, NFID president, and moderator of the news briefing. “That is not good enough.”
In addition, 22% of people at higher risk for flu-related complications do not plan to get vaccinated this season. “That’s a dangerous risk to take,” Ms. Stinchfield said.
An encouraging finding, she said, is that 69% of adults surveyed recognize that an annual flu vaccination is the best way to prevent flu-related hospitalizations and death.
“So, most people know what to do. We just need to do it,” she said.
The top reason for not getting a flu shot in 2022 mentioned by 41% of people surveyed, is they do not think vaccines work very well. Another 39% are concerned about vaccine side effects, and 28% skip the vaccine because they “never get the flu.”
The experts on the panel emphasized the recommendation that all Americans 6 months or older get the flu vaccine, preferably by the end of October. Vaccination is especially important for those at higher risk of complications from the flu, including children under 5, pregnant women, people with one or more health conditions, the immunocompromised, and Americans 65 years and older.
Ms. Stinchfield acknowledged that the effectiveness of the flu vaccine varies season to season, but even if the vaccine does not completely match the circulating viruses, it can help prevent serious outcomes like hospitalization and death. One of the serious potential complications is pneumonia or “pneumococcal disease.”
“Our survey shows that only 29% of those at risk have been advised to receive a pneumococcal vaccine,” Ms. Stinchfield said. “The good news is that, among those who were advised to get the vaccine, 74% did receive their pneumococcal vaccine,” she said. “This underscores a key point to you, my fellow clinicians: As health professionals, our recommendations matter.”
Higher doses for 65+ Americans
The CDC updated recommendations this flu season for adults 65 and older to receive one of three preferentially recommended flu vaccines, said CDC Director Rochelle Walensky, MD. The CDC is recommending higher-dose, stronger vaccines for older Americans “based on a review of the available studies, which suggested that in this age group, these vaccines are potentially more effective than standard-dose ... vaccines.”
During most seasons, people 65 and older bear the greatest burden of severe flu disease, accounting for most flu-related hospitalizations and deaths.
“They are the largest vulnerable segment of our society,” Dr. Walensky said.
What will this flu season be like?
Health officials in the flu vaccine business also tend to be in the flu season prediction business. That includes Dr. Walensky.
“While we will never exactly know what each flu season will hold, we do know that every year, the best way you can protect yourself and those around you is to get your annual flu vaccine,” she said while taking part remotely in the briefing.
How severe will the flu season be in 2022-23? William Schaffner, MD, said he gets that question a lot. “Don’t think about that. Just focus on the fact that flu will be with us each year.
“We were a little bit spoiled. We’ve had two mild influenza seasons,” said Dr. Schaffner, medical director of NFID and a professor of infectious diseases and preventive medicine at Vanderbilt University, Nashville, Tenn. “I think with all the interest in COVID, people have rather forgotten about influenza. I’ve had to remind them that this is yet another serious winter respiratory virus.
“As I like to say, flu is fickle. It’s difficult to predict how serious this next outbreak of influenza this season is going to be. We could look at what happened in the Southern Hemisphere,” he said.
For example, Australia had the worst influenza season in the past 5 years, Schaffner said. “If you want a hint of what might happen here and you want yet another reason to be vaccinated, there it is.”
What we do know, Dr. Walensky said, is that the timing and severity of the past two flu seasons in the U.S. have been different than typical flu seasons. “And this is likely due to the COVID mitigation measures and other changes in circulating respiratory viruses.” Also, although last flu season was “relatively mild,” there was more flu activity than in the prior, 2020-21 season.
Also, Dr. Walensky said, last season’s flu cases began to increase in November and remained elevated until mid-June, “making it the latest season on record.”
The official cause of Brent Teichman’s death was multilobar pneumonia, cause undetermined. “But after 30-plus years as a pediatrician ... I know influenza when I see it,” Dr. Teichman said.
“There’s a hole in our hearts that will never heal. Loss of a child is devastating,” he said. The flu “can take the life of a healthy young person, as it did to my son.
“And for all those listening to my story who are vaccine hesitant, do it for those who love you. So that they won’t walk the path that we and many other families in this country have walked.”
To prove their point, Dr. Teichman and Ms. Stinchfield raised their sleeves and received flu shots during the news briefing.
“This one is for Brent,” Dr. Teichman said.
A version of this article first appeared on WebMD.com.
Thoracic Oncology and Chest Procedures Network
Pleural Disease Section
Aspirate or wait: changing the paradigm for PSP care
Although observation for small asymptomatic PSP is supported by current guidelines, management recommendations for larger PSP remains unclear (MacDuff, et al. Thorax. 2010;65[Suppl 2]:ii18-ii31; Tschopp JM, et al. Eur Respir J. 2015;46[2]:321). Two recent RCTs explore conservative vs intervention-based management in those with larger or symptomatic PSP. In the PSP trial, Brown and colleagues prospectively randomized 316 patients with moderate to large PSP to either conservative management (≥ 4 hour observation) or small-bore chest tube without suction (Brown, et al. N Engl J Med. 2020;382[5]:405). Although noninferiority criteria were met, the primary outcome of radiographic resolution of pneumothorax within 8 weeks of randomization was not statistically robust to conservative assumptions about missing data. They concluded that conservative management was noninferior to intervention, and it resulted in a lower risk of serious adverse events or PSP recurrence than interventional management. The multicenter randomized Ambulatory Management of Primary Pneumothorax (RAMPP) trial compared ambulatory management of PSP using an 8F drainage device to a guideline-driven approach (drainage, aspiration, or both) amongst 236 patients with symptomatic PSP. Intervention shortened length of hospital stay (median 0 vs 4 days, P<.0001), but the intervention arm experienced more adverse events (including enlargement of pneumothorax, as well as device malfunction) (Hallifax RJ, et al. Lancet. 2020;396[10243]:39). These two trials challenge the current guidelines for management for patients with PSP, but both had limitations. Though more data are needed to establish a clear consensus, these studies suggest that a conservative pathway for PSP warrants further consideration.
Tejaswi R. Nadig, MBBS
Member-at-Large
Yaron Gesthalter, MD
Member-at-Large
Priya P. Nath, MD
Member-at-Large
Pleural Disease Section
Aspirate or wait: changing the paradigm for PSP care
Although observation for small asymptomatic PSP is supported by current guidelines, management recommendations for larger PSP remains unclear (MacDuff, et al. Thorax. 2010;65[Suppl 2]:ii18-ii31; Tschopp JM, et al. Eur Respir J. 2015;46[2]:321). Two recent RCTs explore conservative vs intervention-based management in those with larger or symptomatic PSP. In the PSP trial, Brown and colleagues prospectively randomized 316 patients with moderate to large PSP to either conservative management (≥ 4 hour observation) or small-bore chest tube without suction (Brown, et al. N Engl J Med. 2020;382[5]:405). Although noninferiority criteria were met, the primary outcome of radiographic resolution of pneumothorax within 8 weeks of randomization was not statistically robust to conservative assumptions about missing data. They concluded that conservative management was noninferior to intervention, and it resulted in a lower risk of serious adverse events or PSP recurrence than interventional management. The multicenter randomized Ambulatory Management of Primary Pneumothorax (RAMPP) trial compared ambulatory management of PSP using an 8F drainage device to a guideline-driven approach (drainage, aspiration, or both) amongst 236 patients with symptomatic PSP. Intervention shortened length of hospital stay (median 0 vs 4 days, P<.0001), but the intervention arm experienced more adverse events (including enlargement of pneumothorax, as well as device malfunction) (Hallifax RJ, et al. Lancet. 2020;396[10243]:39). These two trials challenge the current guidelines for management for patients with PSP, but both had limitations. Though more data are needed to establish a clear consensus, these studies suggest that a conservative pathway for PSP warrants further consideration.
Tejaswi R. Nadig, MBBS
Member-at-Large
Yaron Gesthalter, MD
Member-at-Large
Priya P. Nath, MD
Member-at-Large
Pleural Disease Section
Aspirate or wait: changing the paradigm for PSP care
Although observation for small asymptomatic PSP is supported by current guidelines, management recommendations for larger PSP remains unclear (MacDuff, et al. Thorax. 2010;65[Suppl 2]:ii18-ii31; Tschopp JM, et al. Eur Respir J. 2015;46[2]:321). Two recent RCTs explore conservative vs intervention-based management in those with larger or symptomatic PSP. In the PSP trial, Brown and colleagues prospectively randomized 316 patients with moderate to large PSP to either conservative management (≥ 4 hour observation) or small-bore chest tube without suction (Brown, et al. N Engl J Med. 2020;382[5]:405). Although noninferiority criteria were met, the primary outcome of radiographic resolution of pneumothorax within 8 weeks of randomization was not statistically robust to conservative assumptions about missing data. They concluded that conservative management was noninferior to intervention, and it resulted in a lower risk of serious adverse events or PSP recurrence than interventional management. The multicenter randomized Ambulatory Management of Primary Pneumothorax (RAMPP) trial compared ambulatory management of PSP using an 8F drainage device to a guideline-driven approach (drainage, aspiration, or both) amongst 236 patients with symptomatic PSP. Intervention shortened length of hospital stay (median 0 vs 4 days, P<.0001), but the intervention arm experienced more adverse events (including enlargement of pneumothorax, as well as device malfunction) (Hallifax RJ, et al. Lancet. 2020;396[10243]:39). These two trials challenge the current guidelines for management for patients with PSP, but both had limitations. Though more data are needed to establish a clear consensus, these studies suggest that a conservative pathway for PSP warrants further consideration.
Tejaswi R. Nadig, MBBS
Member-at-Large
Yaron Gesthalter, MD
Member-at-Large
Priya P. Nath, MD
Member-at-Large
Malaria vaccine gets special delivery by tiny health personnel
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Don’t like needles? Have we got a vaccine for you
Here’s a quick question: How do you turn the most annoying thing ever into something positive?
No, we’re not talking about politicians this time. No, not Elon Musk, either. Infomercials? Guess again. Humidity? Nope, even more annoying than that.
Give up? The most annoying thing ever is mosquitoes. This time, however, NPR reports that mosquitoes have been used to deliver a vaccine for the very disease they’ve been transmitting to their human food sources all these years.
In a recent proof-of-concept trial, investigators used CRISPR technology to genetically modify malaria-causing Plasmodium falciparum sporozoites, which just happen to live in the salivary glands of Anopheles mosquitoes. And since the Plasmodium parasites are already in the mosquitoes, it made sense to use the buzzy little critters as the delivery device for the vaccine.
More sense than a syringe, you ask? Have you ever tried to poke a syringe into the salivary gland of a mosquito? No, we thought not. Well, we can tell you from experience that it’s really, really hard. Never mind how we know. We just do.
The 14 study volunteers – who were paid $4,100 for their participation – were first exposed to hundreds of mosquitoes carrying the altered Plasmodium parasites. Then, to test the vaccine, they were exposed to mosquitoes that had actual, malaria-carrying Plasmodium. Half of the subjects got malaria, so the vaccine was only 50% effective, meaning there’s still work to do.
Meanwhile, the scientists here at LOTMEco are all over this mosquito-delivery business, working on a vaccine to prevent Elon Musk. Plan B involves some sort of really big swatter.
Climate change: Sleeping your life away
It’s no secret that climate change is raising the temperature on everything. You may think you’re getting relief when the sun goes down, but in some places it’s still hot. A new survey conducted in central Japan shows how bad it can be and how higher nighttime temperatures can have a serious impact on people’s health.
That online survey, the Sleep Quality Index for Daily Sleep, enabled the investigators to correlate sleep quality with daily temperature for 1,284 adults in 2011 and 2012 who completed the survey over 10 days.
Not only was there a significant difference in sleep disturbance among younger men (higher) versus older men, but the prevalence of sleep disturbance went up when the daytime temperature was above 24.8° C. They also found that disability-adjusted life-years (DALYs), which measure time lost through premature death and time lived in certain conditions that put one’s health at risk, were 81.8 years for the city of Nagoya (population, 2.2 million) in 2012.
The damage to health from sleep disorders caused by daily temperatures higher than 25° C “is comparable to that of heatstroke and must be addressed,” lead author Tomohiko Ihara of the University of Tokyo said in a written statement.
The researchers hope that this information will help sway legislators to consider the impact of higher nighttime temperatures and that it can be used to provide guidance for better sleep. The solution for now? Sleep with the air conditioner on. Your energy bill might increase, but just think about those DALYs. If using the AC lowers DALYs and increases time lived, then we say it’s worth it.
Maybe it would have been a dragon WITH cancer
If you ask a random person on the street to tell you all they know about the country of Wales, they’ll probably mention two things: One, the contorted collection of jumbled-up letters that is the Welsh language (looking at you, Llanfairpwllgwyngyllgogerychwyrndrobwllllantysiliogogogoch) and, two, the association with dragons. The Welsh flag even has a dragon on it.
With that in mind, take a guess as to what sort of statue art dealer Simon Wingett wanted to build in the Welsh town of Wrexham. No, not a monument to the second-longest place name in the world. Try again. His dragon would not be some piddly little thing either; he wanted a virtual kaiju overlooking the town, with the whole statue to stand about 60 meters high. That’s taller than the original 1954 Godzilla.
Artistic masterpieces may sell for frankly insane prices, but art dealers themselves are not the wealthiest of individuals, so Mr. Wingett needed money to fund his dragon-based dream. Lucky for him, he also happened to be the manager of a cancer charity – initially set up by Mr. Wingett’s father, who had throat cancer – which nominally aimed to provide equipment and resources to cancer patients in the Wrexham area.
Yes, this is going precisely where you think it’s going. From 2011 to 2018, when the charity closed, Mr. Wingett used the charity’s donations to fund his dragon statue – which never actually got built, by the way – to the tune of over 400,000 pounds. Of course, Mr. Wingett came under scrutiny when people started to notice that his cancer charity hadn’t actually done anything charitable since 2011, and he was recently banned by the Welsh High Court from serving as trustee of any charity for 10 years. Oh no, tragedy and horror! Truly a punishment worse than death itself.
Okay fine, he also has to pay back 117,000 pounds to actual legitimate cancer charities. The astute mathematicians out there may notice that 117,000 is a lot less than 400,000. But it’s just as the old saying goes: One-quarter of crime doesn’t pay. You can keep three-quarters of it, though, that’s completely fine.
Children and COVID: Weekly cases dropped by 57% in September
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.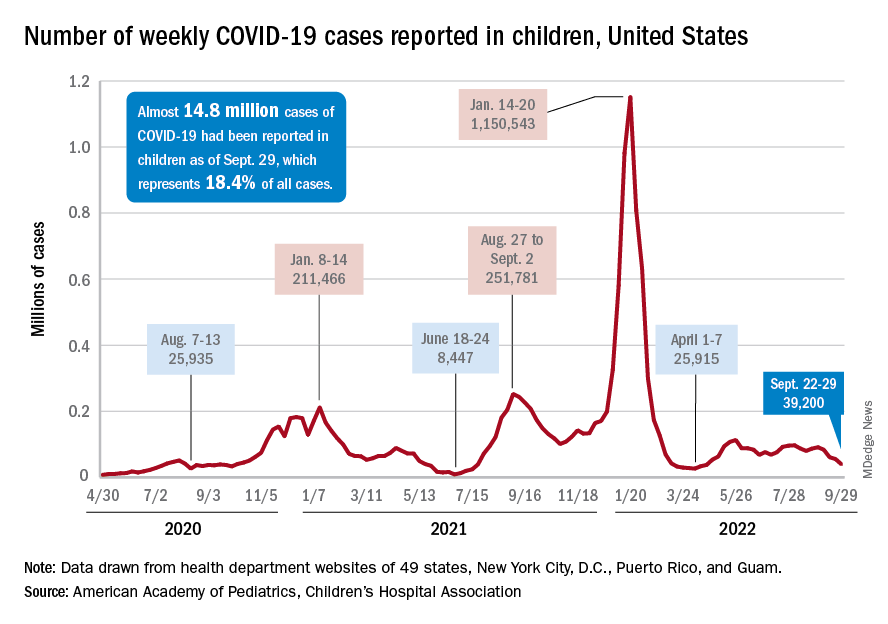
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.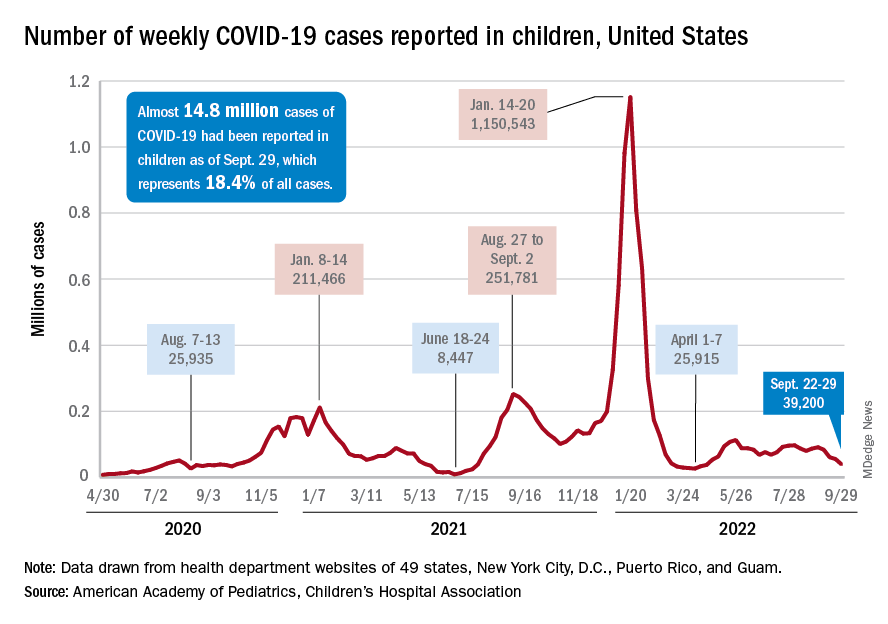
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
The last full week of September brought a 4th straight week of declines in the number of new COVID-19 cases reported among children, according to the American Academy of Pediatrics and the Children’s Hospital Association.
, with the month of September bringing a decline of about 57% in reported cases for the 45 states and territories that are still releasing pediatric COVID data on their health department websites, the AAP and CHA said in their joint weekly report.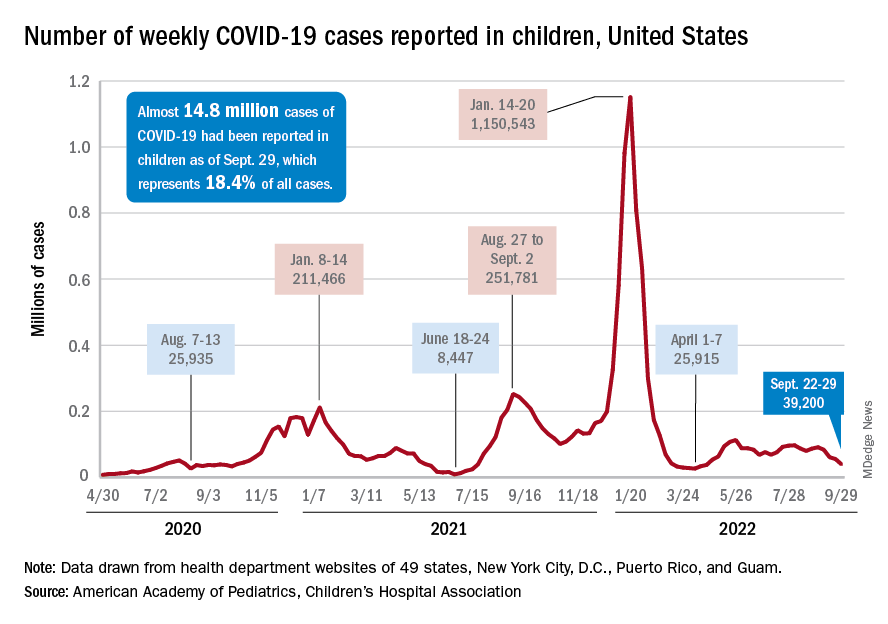
New cases dropped in all four regions after the Northeast and West had seen increases the previous week, and the distribution of cases for the latest week was fairly even, with the Midwest and Northeast right around 10,000, the South slightly over 10,000, and the West under 10,000 by about the same amount. At the state level, the largest increases – around 1.5% – over the last 2 weeks occurred in Kentucky and Nevada, the AAP/CHA data show.
The cumulative number of COVID-19 cases in children was almost 14.8 million as of Sept. 29, with children representing 18.4% of all cases since the pandemic began, the AAP and CHA said. The Centers for Disease Control and Prevention, which is able to use a uniform age range of 0-17 years, puts total cases at 15.2 million and the proportion of child cases at 17.4%. Total deaths in children from COVID as of Oct. 3 were 1,745, the CDC reported.
New vaccinations, in the meantime, are being added in numbers only slightly higher than new cases. Initial COVID vaccinations for the week of Sept. 22-28 were about 44,000 for children under 5 years of age (down from 51,000 the week before), 24,000 for children aged 5-11 years (down from 28,000), and 17,000 for those aged 12-17 (down from 18,000), the AAP said in its weekly vaccination report.
To look at it another way, the total proportion of children under 5 years of age who had received at least one dose of COVID vaccine as of Sept. 28 was 6.5%, compared with 6.4% on Sept. 21, while the corresponding rates for children aged 5-11 and 12-17 were unchanged at 38.5% and 70.9%. The 12- to 17-year-olds, in fact, have been stuck at 70.9% since Sept. 13, according to data from the CDC.
In a recent study published in Vaccine, investigators attributed the discrepancies between age groups at least partly to the acceptance of misinformation about vaccine safety in general and the COVID-19 vaccines in particular.
“All of the misconceptions we studied focused in one way or another on the safety of vaccination, and that explains why people’s misbeliefs about vaccinating kids are so highly related to their concerns about vaccines in general. Unfortunately, those concerns weigh even more heavily when adults consider vaccinating children,” lead author Dan Romer, PhD, of the University of Pennsylvania, Philadelphia, said in a written statement.
2022 billing and coding updates
Telehealth and Teaching Physician Services and ICD-10 codes updates
In my previous article in June, 2022, we plowed through the billing and coding updates regarding critical care services, and, I hope that it helped our readers get more acquainted with the nuances of billing and coding in the ICU. In this piece, I would like to briefly elucidate three other areas of practice, which will be relevant to all physicians across various specialties.
Telehealth services
(PHE). Initially, the plan was to remove these from the list of covered services by the latter end of the COVID-19 PHE, which, created some uncertainty, or by December 31, 2021. Fortunately, CMS finalized that they will extend it through the end of the calendar year (CY) 2023. So, now all the telehealth services will remain on the CMS list until December 31, 2023. The general principle behind this ruling is to allow for more time for CMS and stakeholders to gather data and to submit support for requesting these services to be permanently added to the Medicare telehealth services list.
Not only has CMS extended the deadline for telehealth services but also they have gone far and beyond to extend some of the codes for cardiac and intensive cardiac rehabilitation until December 31, 2023, as well.
There has been a lot of debate regarding the geographic restrictions when it comes to telehealth visits for diagnosis, evaluation, or treatment of a mental health disorder. As per the latest Consolidated Appropriations Act of 2021 (Section 123), the home of the patient is a permissible site. But, the caveat is that there must be an in-person service with the practitioner/physician within 6 months prior to the initial telehealth visit. Additionally, there has to be a set frequency for subsequent in-person visits. And, usually the subsequent visits will need to be provided at least every 12 months. These requirements are not set in stone and can be changed on a case-by-case basis provided there is appropriate documentation in the chart.
Lastly, it is important to understand and use the appropriate telecommunication systems for the telehealth visits and the modifiers that are associated with them. By definition, it has to be audio and video equipment that allows two-way, real-time interactive communication between the patient and the provider when used for telehealth services for the diagnosis, evaluation, or treatment of mental health disorders. But, CMS is in the process of amending it to include audio-only communications technology. At this time, the use of audio-only interactive telecommunications system is limited to practitioners who have the capability to provide two-way audio/video communications but, where the patient is not capable, or does not consent to, the use of two-way audio/video technology. Modifier FQ should be attached to all the mental health services that were furnished using audio-only communications. And, mental health services can include services for treatment of substance use disorders (SUD). Please do not confuse modifier FQ with modifier 93 as FQ is only for behavioral health services. And, remember that the totality of the communication of information exchanged between the provider and the patient during the course of the synchronous telemedicine service (rendered via telephone or other real-time interactive audio only telecommunication system) must be of an amount and nature that is sufficient to meet the key components and/or requirements of the same service when rendered via a face-to-face interaction.
Teaching physician services
As a general rule, a teaching physician can bill for the resident services only if they are present for the critical (key) portion of the service. But, there is one exception called the “primary care exception” under which in certain teaching hospital primary care centers, the teaching physician can bill for certain services as furnished independently by the resident without the teaching physician being physically present, but with the teaching physician’s review.
The current model to bill for office/outpatient E/M visit level is either based on either total time spent (personally) or medical-decision-making (MDM). When time is used to select the visit level only the time spent by the teaching physician in qualifying activities can be included for the purposes of the visit level selection. And, this includes the time the teaching physician was present with the resident performing those qualifying activities. Also, under the primary care exception, time cannot be used to select the visit level. This is to guard against the possibility of inappropriate coding that reflects residents’ inefficiencies rather than a measure of the total medically necessary time required to furnish the E/M services.
ICD-10 updates
Usually, the ICD-10 codes are updated annually and take effect every October 1. Some of the most relevant updates are as follows:
1. U09.9 Post COVID-19 condition, unspecified: This should be used to document sequelae of COVID-19 or “long COVID” conditions, after the acute illness has resolved. But, remember to code the conditions related to COVID-19 first and do not use this code with an active or current COVID-19 infection.
2. U07.0 Vaping-related disorder: This should be used for all vaping-related illnesses. However, additional codes for other diagnoses such as acute respiratory failure, acute respiratory distress syndrome, or pneumonitis can also be used with this code. Other respiratory signs and symptoms such as cough and shortness of breath should not be coded separately.
3. Cough is one of the most common reasons for referral to a pulmonologist. The CDC has expanded these codes so please remember to code the most specific diagnosis as deemed appropriate.
R05.1 Acute cough
R05.2 Subacute cough
R05.3 Chronic cough
R05.4 Cough, syncope
R05.8 Other specified cough
R05.9 Cough, unspecified
We will be back with some more exciting and intriguing billing and coding updates in our next article and hope to see everyone at CHEST 2022 in Nashville., TN.
Telehealth and Teaching Physician Services and ICD-10 codes updates
Telehealth and Teaching Physician Services and ICD-10 codes updates
In my previous article in June, 2022, we plowed through the billing and coding updates regarding critical care services, and, I hope that it helped our readers get more acquainted with the nuances of billing and coding in the ICU. In this piece, I would like to briefly elucidate three other areas of practice, which will be relevant to all physicians across various specialties.
Telehealth services
(PHE). Initially, the plan was to remove these from the list of covered services by the latter end of the COVID-19 PHE, which, created some uncertainty, or by December 31, 2021. Fortunately, CMS finalized that they will extend it through the end of the calendar year (CY) 2023. So, now all the telehealth services will remain on the CMS list until December 31, 2023. The general principle behind this ruling is to allow for more time for CMS and stakeholders to gather data and to submit support for requesting these services to be permanently added to the Medicare telehealth services list.
Not only has CMS extended the deadline for telehealth services but also they have gone far and beyond to extend some of the codes for cardiac and intensive cardiac rehabilitation until December 31, 2023, as well.
There has been a lot of debate regarding the geographic restrictions when it comes to telehealth visits for diagnosis, evaluation, or treatment of a mental health disorder. As per the latest Consolidated Appropriations Act of 2021 (Section 123), the home of the patient is a permissible site. But, the caveat is that there must be an in-person service with the practitioner/physician within 6 months prior to the initial telehealth visit. Additionally, there has to be a set frequency for subsequent in-person visits. And, usually the subsequent visits will need to be provided at least every 12 months. These requirements are not set in stone and can be changed on a case-by-case basis provided there is appropriate documentation in the chart.
Lastly, it is important to understand and use the appropriate telecommunication systems for the telehealth visits and the modifiers that are associated with them. By definition, it has to be audio and video equipment that allows two-way, real-time interactive communication between the patient and the provider when used for telehealth services for the diagnosis, evaluation, or treatment of mental health disorders. But, CMS is in the process of amending it to include audio-only communications technology. At this time, the use of audio-only interactive telecommunications system is limited to practitioners who have the capability to provide two-way audio/video communications but, where the patient is not capable, or does not consent to, the use of two-way audio/video technology. Modifier FQ should be attached to all the mental health services that were furnished using audio-only communications. And, mental health services can include services for treatment of substance use disorders (SUD). Please do not confuse modifier FQ with modifier 93 as FQ is only for behavioral health services. And, remember that the totality of the communication of information exchanged between the provider and the patient during the course of the synchronous telemedicine service (rendered via telephone or other real-time interactive audio only telecommunication system) must be of an amount and nature that is sufficient to meet the key components and/or requirements of the same service when rendered via a face-to-face interaction.
Teaching physician services
As a general rule, a teaching physician can bill for the resident services only if they are present for the critical (key) portion of the service. But, there is one exception called the “primary care exception” under which in certain teaching hospital primary care centers, the teaching physician can bill for certain services as furnished independently by the resident without the teaching physician being physically present, but with the teaching physician’s review.
The current model to bill for office/outpatient E/M visit level is either based on either total time spent (personally) or medical-decision-making (MDM). When time is used to select the visit level only the time spent by the teaching physician in qualifying activities can be included for the purposes of the visit level selection. And, this includes the time the teaching physician was present with the resident performing those qualifying activities. Also, under the primary care exception, time cannot be used to select the visit level. This is to guard against the possibility of inappropriate coding that reflects residents’ inefficiencies rather than a measure of the total medically necessary time required to furnish the E/M services.
ICD-10 updates
Usually, the ICD-10 codes are updated annually and take effect every October 1. Some of the most relevant updates are as follows:
1. U09.9 Post COVID-19 condition, unspecified: This should be used to document sequelae of COVID-19 or “long COVID” conditions, after the acute illness has resolved. But, remember to code the conditions related to COVID-19 first and do not use this code with an active or current COVID-19 infection.
2. U07.0 Vaping-related disorder: This should be used for all vaping-related illnesses. However, additional codes for other diagnoses such as acute respiratory failure, acute respiratory distress syndrome, or pneumonitis can also be used with this code. Other respiratory signs and symptoms such as cough and shortness of breath should not be coded separately.
3. Cough is one of the most common reasons for referral to a pulmonologist. The CDC has expanded these codes so please remember to code the most specific diagnosis as deemed appropriate.
R05.1 Acute cough
R05.2 Subacute cough
R05.3 Chronic cough
R05.4 Cough, syncope
R05.8 Other specified cough
R05.9 Cough, unspecified
We will be back with some more exciting and intriguing billing and coding updates in our next article and hope to see everyone at CHEST 2022 in Nashville., TN.
In my previous article in June, 2022, we plowed through the billing and coding updates regarding critical care services, and, I hope that it helped our readers get more acquainted with the nuances of billing and coding in the ICU. In this piece, I would like to briefly elucidate three other areas of practice, which will be relevant to all physicians across various specialties.
Telehealth services
(PHE). Initially, the plan was to remove these from the list of covered services by the latter end of the COVID-19 PHE, which, created some uncertainty, or by December 31, 2021. Fortunately, CMS finalized that they will extend it through the end of the calendar year (CY) 2023. So, now all the telehealth services will remain on the CMS list until December 31, 2023. The general principle behind this ruling is to allow for more time for CMS and stakeholders to gather data and to submit support for requesting these services to be permanently added to the Medicare telehealth services list.
Not only has CMS extended the deadline for telehealth services but also they have gone far and beyond to extend some of the codes for cardiac and intensive cardiac rehabilitation until December 31, 2023, as well.
There has been a lot of debate regarding the geographic restrictions when it comes to telehealth visits for diagnosis, evaluation, or treatment of a mental health disorder. As per the latest Consolidated Appropriations Act of 2021 (Section 123), the home of the patient is a permissible site. But, the caveat is that there must be an in-person service with the practitioner/physician within 6 months prior to the initial telehealth visit. Additionally, there has to be a set frequency for subsequent in-person visits. And, usually the subsequent visits will need to be provided at least every 12 months. These requirements are not set in stone and can be changed on a case-by-case basis provided there is appropriate documentation in the chart.
Lastly, it is important to understand and use the appropriate telecommunication systems for the telehealth visits and the modifiers that are associated with them. By definition, it has to be audio and video equipment that allows two-way, real-time interactive communication between the patient and the provider when used for telehealth services for the diagnosis, evaluation, or treatment of mental health disorders. But, CMS is in the process of amending it to include audio-only communications technology. At this time, the use of audio-only interactive telecommunications system is limited to practitioners who have the capability to provide two-way audio/video communications but, where the patient is not capable, or does not consent to, the use of two-way audio/video technology. Modifier FQ should be attached to all the mental health services that were furnished using audio-only communications. And, mental health services can include services for treatment of substance use disorders (SUD). Please do not confuse modifier FQ with modifier 93 as FQ is only for behavioral health services. And, remember that the totality of the communication of information exchanged between the provider and the patient during the course of the synchronous telemedicine service (rendered via telephone or other real-time interactive audio only telecommunication system) must be of an amount and nature that is sufficient to meet the key components and/or requirements of the same service when rendered via a face-to-face interaction.
Teaching physician services
As a general rule, a teaching physician can bill for the resident services only if they are present for the critical (key) portion of the service. But, there is one exception called the “primary care exception” under which in certain teaching hospital primary care centers, the teaching physician can bill for certain services as furnished independently by the resident without the teaching physician being physically present, but with the teaching physician’s review.
The current model to bill for office/outpatient E/M visit level is either based on either total time spent (personally) or medical-decision-making (MDM). When time is used to select the visit level only the time spent by the teaching physician in qualifying activities can be included for the purposes of the visit level selection. And, this includes the time the teaching physician was present with the resident performing those qualifying activities. Also, under the primary care exception, time cannot be used to select the visit level. This is to guard against the possibility of inappropriate coding that reflects residents’ inefficiencies rather than a measure of the total medically necessary time required to furnish the E/M services.
ICD-10 updates
Usually, the ICD-10 codes are updated annually and take effect every October 1. Some of the most relevant updates are as follows:
1. U09.9 Post COVID-19 condition, unspecified: This should be used to document sequelae of COVID-19 or “long COVID” conditions, after the acute illness has resolved. But, remember to code the conditions related to COVID-19 first and do not use this code with an active or current COVID-19 infection.
2. U07.0 Vaping-related disorder: This should be used for all vaping-related illnesses. However, additional codes for other diagnoses such as acute respiratory failure, acute respiratory distress syndrome, or pneumonitis can also be used with this code. Other respiratory signs and symptoms such as cough and shortness of breath should not be coded separately.
3. Cough is one of the most common reasons for referral to a pulmonologist. The CDC has expanded these codes so please remember to code the most specific diagnosis as deemed appropriate.
R05.1 Acute cough
R05.2 Subacute cough
R05.3 Chronic cough
R05.4 Cough, syncope
R05.8 Other specified cough
R05.9 Cough, unspecified
We will be back with some more exciting and intriguing billing and coding updates in our next article and hope to see everyone at CHEST 2022 in Nashville., TN.
Access unmatched asthma education from anywhere
CHEST is proud to announce the launch of the newest addition to our e-learning options: the CHEST Asthma Curriculum Pathway.
This unique offering combines a variety of bite-sized educational resources from among CHEST’s most popular and effective products, including case-based CHEST SEEK™ questions, podcasts and videos from asthma experts, the latest research from the journal CHEST®, and more.
The pathway comprises several different “paths,” or tracks, that enable clinicians to target their education based on their knowledge gaps and career level. Users can opt to follow the curriculum from start to finish to gain a comprehensive overview of asthma management. Or, they can select individual paths to focus their learning on topics including asthma pathophysiology, diagnosis and classification, exacerbations, phenotypes, and more.
According to early learners of the pathway: It helped a lot with the knowledge check-in.” Another commented: “It is very comprehensive on all aspects of asthma. I enjoyed the higher-level learning on the choice of biologics and asthma mimickers.” The education modalities were highlighted, as well, with this feedback: “I really enjoyed the variety of media (lectures, discussions, papers, games).”
Exploring the education
The Asthma Curriculum Pathway offers targeted education options to fit the career level and clinical interest of clinicians, ranging from trainees and early career physicians to experienced asthma specialists and advanced practice providers.
Paths include:
• Path 1: Pathophysiology
• Path 2: Diagnosis & Classification
• Path 3: Management
• Path 4: Mimickers
• Path 5: Comorbidities
• Path 6: Phenotypes
• Path 7: Exacerbations
• Path 8: Special Situations
Plus, each path offers claiming credit, including CME, for completion—all while driving clinicians to consistently advance best outcomes for their patients with asthma.
Visit (https://bit.ly/asthma-pathway) to access the best of CHEST’s asthma education with the new Asthma Curriculum Pathway, accessible via web or mobile device.
CHEST is proud to announce the launch of the newest addition to our e-learning options: the CHEST Asthma Curriculum Pathway.
This unique offering combines a variety of bite-sized educational resources from among CHEST’s most popular and effective products, including case-based CHEST SEEK™ questions, podcasts and videos from asthma experts, the latest research from the journal CHEST®, and more.
The pathway comprises several different “paths,” or tracks, that enable clinicians to target their education based on their knowledge gaps and career level. Users can opt to follow the curriculum from start to finish to gain a comprehensive overview of asthma management. Or, they can select individual paths to focus their learning on topics including asthma pathophysiology, diagnosis and classification, exacerbations, phenotypes, and more.
According to early learners of the pathway: It helped a lot with the knowledge check-in.” Another commented: “It is very comprehensive on all aspects of asthma. I enjoyed the higher-level learning on the choice of biologics and asthma mimickers.” The education modalities were highlighted, as well, with this feedback: “I really enjoyed the variety of media (lectures, discussions, papers, games).”
Exploring the education
The Asthma Curriculum Pathway offers targeted education options to fit the career level and clinical interest of clinicians, ranging from trainees and early career physicians to experienced asthma specialists and advanced practice providers.
Paths include:
• Path 1: Pathophysiology
• Path 2: Diagnosis & Classification
• Path 3: Management
• Path 4: Mimickers
• Path 5: Comorbidities
• Path 6: Phenotypes
• Path 7: Exacerbations
• Path 8: Special Situations
Plus, each path offers claiming credit, including CME, for completion—all while driving clinicians to consistently advance best outcomes for their patients with asthma.
Visit (https://bit.ly/asthma-pathway) to access the best of CHEST’s asthma education with the new Asthma Curriculum Pathway, accessible via web or mobile device.
CHEST is proud to announce the launch of the newest addition to our e-learning options: the CHEST Asthma Curriculum Pathway.
This unique offering combines a variety of bite-sized educational resources from among CHEST’s most popular and effective products, including case-based CHEST SEEK™ questions, podcasts and videos from asthma experts, the latest research from the journal CHEST®, and more.
The pathway comprises several different “paths,” or tracks, that enable clinicians to target their education based on their knowledge gaps and career level. Users can opt to follow the curriculum from start to finish to gain a comprehensive overview of asthma management. Or, they can select individual paths to focus their learning on topics including asthma pathophysiology, diagnosis and classification, exacerbations, phenotypes, and more.
According to early learners of the pathway: It helped a lot with the knowledge check-in.” Another commented: “It is very comprehensive on all aspects of asthma. I enjoyed the higher-level learning on the choice of biologics and asthma mimickers.” The education modalities were highlighted, as well, with this feedback: “I really enjoyed the variety of media (lectures, discussions, papers, games).”
Exploring the education
The Asthma Curriculum Pathway offers targeted education options to fit the career level and clinical interest of clinicians, ranging from trainees and early career physicians to experienced asthma specialists and advanced practice providers.
Paths include:
• Path 1: Pathophysiology
• Path 2: Diagnosis & Classification
• Path 3: Management
• Path 4: Mimickers
• Path 5: Comorbidities
• Path 6: Phenotypes
• Path 7: Exacerbations
• Path 8: Special Situations
Plus, each path offers claiming credit, including CME, for completion—all while driving clinicians to consistently advance best outcomes for their patients with asthma.
Visit (https://bit.ly/asthma-pathway) to access the best of CHEST’s asthma education with the new Asthma Curriculum Pathway, accessible via web or mobile device.
Advanced POCUS for us all?
Point-of-care ultrasound (POCUS) is a useful, practice-changing bedside tool that spans all medical and surgical specialties. While the definition of POCUS varies, most would agree it is an abbreviated exam that helps to answer a specific clinical question. With the expansion of POCUS training, the clinical questions being asked and answered have increased in scope and volume. The types of exams being utilized in “point of care ultrasound” have also increased and include transthoracic echocardiography; trans-esophageal echocardiography; and lung, gastric, abdominal, and ocular ultrasound. POCUS is used across multiple specialties, including critical care, anesthesiology, emergency medicine, and primary care.
Not only has POCUS become increasingly important clinically, but specialties now test these skills on their respective board examinations. Anesthesia is one of many such examples. The content outline for the American Board of Anesthesiology includes POCUS as a tested item on both the written and applied components of the exam. POCUS training must be directed toward both optimizing patient management and preparing learners for their board examination. A method for teaching this has yet to be defined (Naji A, et al. Cureus. 2021;13[5]:e15217).
One question – how should different specialties approach this educational challenge and should specialties train together? The answer is complicated. Many POCUS courses and certifications exist, and all vary in their content, didactics, and length. No true gold standard exists for POCUS certification for radiology or noncardiology providers. Additionally, there are no defined expectations or testing processes that certify a provider is “certified” to perform POCUS. While waiting for medical society guidelines to address these issues, many in graduate medical education (GME) are coming up with their own ways to incorporate POCUS into their respective training programs (Atkinson P, et al. CJEM. 2015 Mar;17[2]:161).
Who’s training whom?
Over the past decade, several expert committees, including those in critical care, have developed recommendations and consensus statements urging training facilities to independently create POCUS curriculums. The threshold for many programs to enter this realm of expertise is high and oftentimes unobtainable. We’ve seen emergency medicine and anesthesia raise the bar for ultrasound education in their residencies, but it’s unclear whether all fellowship-trained physicians can and should be tasked with obtaining official POCUS certification.
While specific specialties may require tailored certifications, there’s a considerable overlap in POCUS exam content across specialties. One approach to POCUS training could be developing and implementing a multidisciplinary curriculum. This would allow for pooling of resources (equipment, staff) and harnessing knowledge from providers familiar with different phases of patient care (ICU, perioperative, ED, outpatient clinics). By approaching POCUS from a multidisciplinary perspective, the quality of education may be enhanced (Mayo PH, et al. Intensive Care Med. 2014;40[5]:654). Is it then prudent for providers and trainees alike to share in didactics across all areas of the hospital and clinic? Would this close the knowledge gap between specialties who are facile with ultrasound and those not?
Determining the role of transesophageal echocardiography in a POCUS curriculum
This modality of imaging has been, until recently, reserved for cardiologists and anesthesiologists. More recently transesophageal echocardiography (TEE) has been utilized by emergency and critical care medicine physicians. TEE is part of recommended training for these specialties as a tool for diagnostic and rescue measures, including ventilator management, emergency procedures, and medication titration. Rescue TEE can also be utilized perioperatively where the transthoracic exam is limited by poor windows or the operative procedure precludes access to the chest. While transthoracic echocardiography (TTE) is often used in a point of care fashion, TEE is utilized less often. This may stem from the invasive nature of the procedure but likely also results from lack of equipment and training. Like POCUS overall, TEE POCUS will require incorporation into training programs to achieve widespread use and acceptance.
A deluge of research on TEE for the noncardiologist shows this modality is minimally invasive, safe, and effective. As it becomes more readily available and technology improves, there is no reason why an esophageal probe can’t be used in a patient with a secured airway (Wray TC, et al. J Intensive Care Med. 2021;36[1]:123).
Ultrasound for hemodynamic monitoring
There are many methods employed for hemodynamic monitoring in the ICU. Although echocardiographic and vascular parameters have been validated in the cardiac and perioperative fields, their application in the ICU setting for resuscitation and volume management remain somewhat controversial. The use of TEE and more advanced understanding of spectral doppler and pulmonary ultrasonography using TEE has revolutionized the way providers are managing critically ill patients. (Garcia YA, et al. Chest. 2017;152[4]:736).
In our opinion, physiology and imaging training for residents and fellows should be required for critical care medicine trainees. Delving into the nuances of frank-starling curves, stroke work, and diastolic function will enrich their understanding and highlight the applicability of ultrasonography. Furthermore, all clinicians caring for patients with critical illness should be privy to the nuances of physiologic derangement, and to that end, advanced echocardiographic principles and image acquisition. The heart-lung interactions are demonstrated in real time using POCUS and can clearly delineate treatment goals (Vieillard-Baron A, et al. Intensive Care Med. 2019;45[6]:770).
Documentation and billing
If clinicians are making medical decisions based off imaging gathered at the bedside and interpreted in real-time, documentation should reflect that. That documentation will invariably lead to billing and possibly audit or quality review by colleagues or other healthcare staff. Radiology and cardiology have perfected the billing process for image interpretation, but their form of documentation and interpretation may not easily be implemented in the perioperative or critical care settings. An abbreviated document with focused information should take the place of the formal study. With that, the credentialing and board certification process will allow providers to feel empowered to make clinical decisions based off these focused examinations.
Dr. Goertzen is Chief Fellow, Pulmonary/Critical Care; Dr. Knuf is Program Director, Department of Anesthesia; and Dr. Villalobos is Director of Medical ICU, Department of Internal Medicine, San Antonio Military Medical Center, San Antonio, Texas.
Point-of-care ultrasound (POCUS) is a useful, practice-changing bedside tool that spans all medical and surgical specialties. While the definition of POCUS varies, most would agree it is an abbreviated exam that helps to answer a specific clinical question. With the expansion of POCUS training, the clinical questions being asked and answered have increased in scope and volume. The types of exams being utilized in “point of care ultrasound” have also increased and include transthoracic echocardiography; trans-esophageal echocardiography; and lung, gastric, abdominal, and ocular ultrasound. POCUS is used across multiple specialties, including critical care, anesthesiology, emergency medicine, and primary care.
Not only has POCUS become increasingly important clinically, but specialties now test these skills on their respective board examinations. Anesthesia is one of many such examples. The content outline for the American Board of Anesthesiology includes POCUS as a tested item on both the written and applied components of the exam. POCUS training must be directed toward both optimizing patient management and preparing learners for their board examination. A method for teaching this has yet to be defined (Naji A, et al. Cureus. 2021;13[5]:e15217).
One question – how should different specialties approach this educational challenge and should specialties train together? The answer is complicated. Many POCUS courses and certifications exist, and all vary in their content, didactics, and length. No true gold standard exists for POCUS certification for radiology or noncardiology providers. Additionally, there are no defined expectations or testing processes that certify a provider is “certified” to perform POCUS. While waiting for medical society guidelines to address these issues, many in graduate medical education (GME) are coming up with their own ways to incorporate POCUS into their respective training programs (Atkinson P, et al. CJEM. 2015 Mar;17[2]:161).
Who’s training whom?
Over the past decade, several expert committees, including those in critical care, have developed recommendations and consensus statements urging training facilities to independently create POCUS curriculums. The threshold for many programs to enter this realm of expertise is high and oftentimes unobtainable. We’ve seen emergency medicine and anesthesia raise the bar for ultrasound education in their residencies, but it’s unclear whether all fellowship-trained physicians can and should be tasked with obtaining official POCUS certification.
While specific specialties may require tailored certifications, there’s a considerable overlap in POCUS exam content across specialties. One approach to POCUS training could be developing and implementing a multidisciplinary curriculum. This would allow for pooling of resources (equipment, staff) and harnessing knowledge from providers familiar with different phases of patient care (ICU, perioperative, ED, outpatient clinics). By approaching POCUS from a multidisciplinary perspective, the quality of education may be enhanced (Mayo PH, et al. Intensive Care Med. 2014;40[5]:654). Is it then prudent for providers and trainees alike to share in didactics across all areas of the hospital and clinic? Would this close the knowledge gap between specialties who are facile with ultrasound and those not?
Determining the role of transesophageal echocardiography in a POCUS curriculum
This modality of imaging has been, until recently, reserved for cardiologists and anesthesiologists. More recently transesophageal echocardiography (TEE) has been utilized by emergency and critical care medicine physicians. TEE is part of recommended training for these specialties as a tool for diagnostic and rescue measures, including ventilator management, emergency procedures, and medication titration. Rescue TEE can also be utilized perioperatively where the transthoracic exam is limited by poor windows or the operative procedure precludes access to the chest. While transthoracic echocardiography (TTE) is often used in a point of care fashion, TEE is utilized less often. This may stem from the invasive nature of the procedure but likely also results from lack of equipment and training. Like POCUS overall, TEE POCUS will require incorporation into training programs to achieve widespread use and acceptance.
A deluge of research on TEE for the noncardiologist shows this modality is minimally invasive, safe, and effective. As it becomes more readily available and technology improves, there is no reason why an esophageal probe can’t be used in a patient with a secured airway (Wray TC, et al. J Intensive Care Med. 2021;36[1]:123).
Ultrasound for hemodynamic monitoring
There are many methods employed for hemodynamic monitoring in the ICU. Although echocardiographic and vascular parameters have been validated in the cardiac and perioperative fields, their application in the ICU setting for resuscitation and volume management remain somewhat controversial. The use of TEE and more advanced understanding of spectral doppler and pulmonary ultrasonography using TEE has revolutionized the way providers are managing critically ill patients. (Garcia YA, et al. Chest. 2017;152[4]:736).
In our opinion, physiology and imaging training for residents and fellows should be required for critical care medicine trainees. Delving into the nuances of frank-starling curves, stroke work, and diastolic function will enrich their understanding and highlight the applicability of ultrasonography. Furthermore, all clinicians caring for patients with critical illness should be privy to the nuances of physiologic derangement, and to that end, advanced echocardiographic principles and image acquisition. The heart-lung interactions are demonstrated in real time using POCUS and can clearly delineate treatment goals (Vieillard-Baron A, et al. Intensive Care Med. 2019;45[6]:770).
Documentation and billing
If clinicians are making medical decisions based off imaging gathered at the bedside and interpreted in real-time, documentation should reflect that. That documentation will invariably lead to billing and possibly audit or quality review by colleagues or other healthcare staff. Radiology and cardiology have perfected the billing process for image interpretation, but their form of documentation and interpretation may not easily be implemented in the perioperative or critical care settings. An abbreviated document with focused information should take the place of the formal study. With that, the credentialing and board certification process will allow providers to feel empowered to make clinical decisions based off these focused examinations.
Dr. Goertzen is Chief Fellow, Pulmonary/Critical Care; Dr. Knuf is Program Director, Department of Anesthesia; and Dr. Villalobos is Director of Medical ICU, Department of Internal Medicine, San Antonio Military Medical Center, San Antonio, Texas.
Point-of-care ultrasound (POCUS) is a useful, practice-changing bedside tool that spans all medical and surgical specialties. While the definition of POCUS varies, most would agree it is an abbreviated exam that helps to answer a specific clinical question. With the expansion of POCUS training, the clinical questions being asked and answered have increased in scope and volume. The types of exams being utilized in “point of care ultrasound” have also increased and include transthoracic echocardiography; trans-esophageal echocardiography; and lung, gastric, abdominal, and ocular ultrasound. POCUS is used across multiple specialties, including critical care, anesthesiology, emergency medicine, and primary care.
Not only has POCUS become increasingly important clinically, but specialties now test these skills on their respective board examinations. Anesthesia is one of many such examples. The content outline for the American Board of Anesthesiology includes POCUS as a tested item on both the written and applied components of the exam. POCUS training must be directed toward both optimizing patient management and preparing learners for their board examination. A method for teaching this has yet to be defined (Naji A, et al. Cureus. 2021;13[5]:e15217).
One question – how should different specialties approach this educational challenge and should specialties train together? The answer is complicated. Many POCUS courses and certifications exist, and all vary in their content, didactics, and length. No true gold standard exists for POCUS certification for radiology or noncardiology providers. Additionally, there are no defined expectations or testing processes that certify a provider is “certified” to perform POCUS. While waiting for medical society guidelines to address these issues, many in graduate medical education (GME) are coming up with their own ways to incorporate POCUS into their respective training programs (Atkinson P, et al. CJEM. 2015 Mar;17[2]:161).
Who’s training whom?
Over the past decade, several expert committees, including those in critical care, have developed recommendations and consensus statements urging training facilities to independently create POCUS curriculums. The threshold for many programs to enter this realm of expertise is high and oftentimes unobtainable. We’ve seen emergency medicine and anesthesia raise the bar for ultrasound education in their residencies, but it’s unclear whether all fellowship-trained physicians can and should be tasked with obtaining official POCUS certification.
While specific specialties may require tailored certifications, there’s a considerable overlap in POCUS exam content across specialties. One approach to POCUS training could be developing and implementing a multidisciplinary curriculum. This would allow for pooling of resources (equipment, staff) and harnessing knowledge from providers familiar with different phases of patient care (ICU, perioperative, ED, outpatient clinics). By approaching POCUS from a multidisciplinary perspective, the quality of education may be enhanced (Mayo PH, et al. Intensive Care Med. 2014;40[5]:654). Is it then prudent for providers and trainees alike to share in didactics across all areas of the hospital and clinic? Would this close the knowledge gap between specialties who are facile with ultrasound and those not?
Determining the role of transesophageal echocardiography in a POCUS curriculum
This modality of imaging has been, until recently, reserved for cardiologists and anesthesiologists. More recently transesophageal echocardiography (TEE) has been utilized by emergency and critical care medicine physicians. TEE is part of recommended training for these specialties as a tool for diagnostic and rescue measures, including ventilator management, emergency procedures, and medication titration. Rescue TEE can also be utilized perioperatively where the transthoracic exam is limited by poor windows or the operative procedure precludes access to the chest. While transthoracic echocardiography (TTE) is often used in a point of care fashion, TEE is utilized less often. This may stem from the invasive nature of the procedure but likely also results from lack of equipment and training. Like POCUS overall, TEE POCUS will require incorporation into training programs to achieve widespread use and acceptance.
A deluge of research on TEE for the noncardiologist shows this modality is minimally invasive, safe, and effective. As it becomes more readily available and technology improves, there is no reason why an esophageal probe can’t be used in a patient with a secured airway (Wray TC, et al. J Intensive Care Med. 2021;36[1]:123).
Ultrasound for hemodynamic monitoring
There are many methods employed for hemodynamic monitoring in the ICU. Although echocardiographic and vascular parameters have been validated in the cardiac and perioperative fields, their application in the ICU setting for resuscitation and volume management remain somewhat controversial. The use of TEE and more advanced understanding of spectral doppler and pulmonary ultrasonography using TEE has revolutionized the way providers are managing critically ill patients. (Garcia YA, et al. Chest. 2017;152[4]:736).
In our opinion, physiology and imaging training for residents and fellows should be required for critical care medicine trainees. Delving into the nuances of frank-starling curves, stroke work, and diastolic function will enrich their understanding and highlight the applicability of ultrasonography. Furthermore, all clinicians caring for patients with critical illness should be privy to the nuances of physiologic derangement, and to that end, advanced echocardiographic principles and image acquisition. The heart-lung interactions are demonstrated in real time using POCUS and can clearly delineate treatment goals (Vieillard-Baron A, et al. Intensive Care Med. 2019;45[6]:770).
Documentation and billing
If clinicians are making medical decisions based off imaging gathered at the bedside and interpreted in real-time, documentation should reflect that. That documentation will invariably lead to billing and possibly audit or quality review by colleagues or other healthcare staff. Radiology and cardiology have perfected the billing process for image interpretation, but their form of documentation and interpretation may not easily be implemented in the perioperative or critical care settings. An abbreviated document with focused information should take the place of the formal study. With that, the credentialing and board certification process will allow providers to feel empowered to make clinical decisions based off these focused examinations.
Dr. Goertzen is Chief Fellow, Pulmonary/Critical Care; Dr. Knuf is Program Director, Department of Anesthesia; and Dr. Villalobos is Director of Medical ICU, Department of Internal Medicine, San Antonio Military Medical Center, San Antonio, Texas.
The possibilities are endless: A chat with the incoming CHEST Foundation President, Robert De Marco, MD, FCCP
As the presidency of the American College of Chest Physicians changes hands in January 2023, so will the role of President of the CHEST Foundation. To get to know the incoming President of the CHEST Foundation, we spoke with Robert (Bob) De Marco, MD, FCCP, about his philanthropy work and his goals for the philanthropic arm of CHEST.
Tell me about your history with philanthropy work.
My philanthropy work started long before the CHEST Foundation. While I’ve been a member of CHEST since my second year of fellowship, it wasn’t until much later that I became involved with the philanthropic side of the organization. Earlier in my career, I was involved more so with the American Cancer Society. I had gotten involved with them by chance – participating in an event of theirs – and was encouraged to get more involved by one of their board members. Being involved with them made a lot of sense seeing as a strong percentage of my patients at the time were being treated for lung cancer. My most notable accomplishments with the American Cancer Society were in serving as the Chairmen of my local Relay for Life program for 10 years, as a board member, and then as a president of my local chapter.
When did you get involved with the CHEST Foundation?
I had served in a handful of positions within CHEST, including Chair of the (since reinvented) Practice Management Committee, so I was deeply involved in the association, and I thought to myself, “I have experience in fundraising through my work with the American Cancer Society, why don’t I use it to help our association?” When I moved to Florida, I no longer had the local connection to the American Cancer Society, so it was an opportune time to transition over to the CHEST Foundation.
How has the Foundation changed in the time that you’ve been involved?
The Foundation has changed drastically since I first joined the Board of Trustees 9 years ago. When I first got involved, the primary goal of the Foundation was staying “out of the red.” At that time, we were an organization that gave away more than we made.
After years of building a corpus to fund our own projects, we’re in a really good place now with some phenomenal goals and some excellent initiatives to fundraise around, including a CHEST diversity initiative, First 5 Minutes™, and Bridging Specialties™: Timely Diagnosis for ILD Patients, which seeks to break down silos within medicine to improve patient care.
What will be a focus of your Foundation presidency?
You know, one thing I always appreciated about the American Cancer Society was that there were always notable accomplishments to point back to when supporting fundraising efforts. You could say, “Did you know that bone marrow transplantation was initially funded by the American Cancer Society?” and other examples that would truly inspire someone to want to get involved in supporting those efforts.
The CHEST Foundation may not have funded bone marrow transplantation, but in 25 years of awarding grants, there are equally good stories to share. The impact of the Foundation is tremendous, and we’ve only just begun to share examples of where grant recipients went with their research or community service projects.
A recent grant story that was shared with me was that of Panagis Galiatsatos, MD, MHS, who received a community service grant to start a program educating children in the Baltimore community about lung health. This program was so moving that it inspired one of the Baltimore teachers to pursue a career in medicine and that individual is now a practicing MD.
This is just one example of the Foundation’s impact and it’s through these stories that we share the “why” behind every dollar that is raised, and my first goal is to tell these stories.
Another key focus of not only my presidency, but Dr. Ian Nathanson’s, as well, as we collaborated a lot on our roles, will be on member involvement and awareness. Even I wasn’t involved in the CHEST Foundation until years into my CHEST membership, so I understand that there are competing demands. But I also know that there is a lot to be gained from the work with the Foundation. I want the CHEST members to be excited about the Foundation and to want to support its efforts.
These two goals go hand in hand, and I look forward to sharing the Foundation’s impact with a new audience and reinvigorating the support of our existing donors.
Is there anything else you’d like to say to the reader?
We cannot accomplish anything without the support of our donors, and I want to sincerely thank everyone who has donated to the CHEST Foundation. I also encourage those who have never donated or have yet to donate this year to visit the Foundation’s website (foundation.chestnet.org) and explore some of the inspiring initiatives you can support to strengthen the impact of the CHEST Foundation because the possibilities are truly endless.
As the presidency of the American College of Chest Physicians changes hands in January 2023, so will the role of President of the CHEST Foundation. To get to know the incoming President of the CHEST Foundation, we spoke with Robert (Bob) De Marco, MD, FCCP, about his philanthropy work and his goals for the philanthropic arm of CHEST.
Tell me about your history with philanthropy work.
My philanthropy work started long before the CHEST Foundation. While I’ve been a member of CHEST since my second year of fellowship, it wasn’t until much later that I became involved with the philanthropic side of the organization. Earlier in my career, I was involved more so with the American Cancer Society. I had gotten involved with them by chance – participating in an event of theirs – and was encouraged to get more involved by one of their board members. Being involved with them made a lot of sense seeing as a strong percentage of my patients at the time were being treated for lung cancer. My most notable accomplishments with the American Cancer Society were in serving as the Chairmen of my local Relay for Life program for 10 years, as a board member, and then as a president of my local chapter.
When did you get involved with the CHEST Foundation?
I had served in a handful of positions within CHEST, including Chair of the (since reinvented) Practice Management Committee, so I was deeply involved in the association, and I thought to myself, “I have experience in fundraising through my work with the American Cancer Society, why don’t I use it to help our association?” When I moved to Florida, I no longer had the local connection to the American Cancer Society, so it was an opportune time to transition over to the CHEST Foundation.
How has the Foundation changed in the time that you’ve been involved?
The Foundation has changed drastically since I first joined the Board of Trustees 9 years ago. When I first got involved, the primary goal of the Foundation was staying “out of the red.” At that time, we were an organization that gave away more than we made.
After years of building a corpus to fund our own projects, we’re in a really good place now with some phenomenal goals and some excellent initiatives to fundraise around, including a CHEST diversity initiative, First 5 Minutes™, and Bridging Specialties™: Timely Diagnosis for ILD Patients, which seeks to break down silos within medicine to improve patient care.
What will be a focus of your Foundation presidency?
You know, one thing I always appreciated about the American Cancer Society was that there were always notable accomplishments to point back to when supporting fundraising efforts. You could say, “Did you know that bone marrow transplantation was initially funded by the American Cancer Society?” and other examples that would truly inspire someone to want to get involved in supporting those efforts.
The CHEST Foundation may not have funded bone marrow transplantation, but in 25 years of awarding grants, there are equally good stories to share. The impact of the Foundation is tremendous, and we’ve only just begun to share examples of where grant recipients went with their research or community service projects.
A recent grant story that was shared with me was that of Panagis Galiatsatos, MD, MHS, who received a community service grant to start a program educating children in the Baltimore community about lung health. This program was so moving that it inspired one of the Baltimore teachers to pursue a career in medicine and that individual is now a practicing MD.
This is just one example of the Foundation’s impact and it’s through these stories that we share the “why” behind every dollar that is raised, and my first goal is to tell these stories.
Another key focus of not only my presidency, but Dr. Ian Nathanson’s, as well, as we collaborated a lot on our roles, will be on member involvement and awareness. Even I wasn’t involved in the CHEST Foundation until years into my CHEST membership, so I understand that there are competing demands. But I also know that there is a lot to be gained from the work with the Foundation. I want the CHEST members to be excited about the Foundation and to want to support its efforts.
These two goals go hand in hand, and I look forward to sharing the Foundation’s impact with a new audience and reinvigorating the support of our existing donors.
Is there anything else you’d like to say to the reader?
We cannot accomplish anything without the support of our donors, and I want to sincerely thank everyone who has donated to the CHEST Foundation. I also encourage those who have never donated or have yet to donate this year to visit the Foundation’s website (foundation.chestnet.org) and explore some of the inspiring initiatives you can support to strengthen the impact of the CHEST Foundation because the possibilities are truly endless.
As the presidency of the American College of Chest Physicians changes hands in January 2023, so will the role of President of the CHEST Foundation. To get to know the incoming President of the CHEST Foundation, we spoke with Robert (Bob) De Marco, MD, FCCP, about his philanthropy work and his goals for the philanthropic arm of CHEST.
Tell me about your history with philanthropy work.
My philanthropy work started long before the CHEST Foundation. While I’ve been a member of CHEST since my second year of fellowship, it wasn’t until much later that I became involved with the philanthropic side of the organization. Earlier in my career, I was involved more so with the American Cancer Society. I had gotten involved with them by chance – participating in an event of theirs – and was encouraged to get more involved by one of their board members. Being involved with them made a lot of sense seeing as a strong percentage of my patients at the time were being treated for lung cancer. My most notable accomplishments with the American Cancer Society were in serving as the Chairmen of my local Relay for Life program for 10 years, as a board member, and then as a president of my local chapter.
When did you get involved with the CHEST Foundation?
I had served in a handful of positions within CHEST, including Chair of the (since reinvented) Practice Management Committee, so I was deeply involved in the association, and I thought to myself, “I have experience in fundraising through my work with the American Cancer Society, why don’t I use it to help our association?” When I moved to Florida, I no longer had the local connection to the American Cancer Society, so it was an opportune time to transition over to the CHEST Foundation.
How has the Foundation changed in the time that you’ve been involved?
The Foundation has changed drastically since I first joined the Board of Trustees 9 years ago. When I first got involved, the primary goal of the Foundation was staying “out of the red.” At that time, we were an organization that gave away more than we made.
After years of building a corpus to fund our own projects, we’re in a really good place now with some phenomenal goals and some excellent initiatives to fundraise around, including a CHEST diversity initiative, First 5 Minutes™, and Bridging Specialties™: Timely Diagnosis for ILD Patients, which seeks to break down silos within medicine to improve patient care.
What will be a focus of your Foundation presidency?
You know, one thing I always appreciated about the American Cancer Society was that there were always notable accomplishments to point back to when supporting fundraising efforts. You could say, “Did you know that bone marrow transplantation was initially funded by the American Cancer Society?” and other examples that would truly inspire someone to want to get involved in supporting those efforts.
The CHEST Foundation may not have funded bone marrow transplantation, but in 25 years of awarding grants, there are equally good stories to share. The impact of the Foundation is tremendous, and we’ve only just begun to share examples of where grant recipients went with their research or community service projects.
A recent grant story that was shared with me was that of Panagis Galiatsatos, MD, MHS, who received a community service grant to start a program educating children in the Baltimore community about lung health. This program was so moving that it inspired one of the Baltimore teachers to pursue a career in medicine and that individual is now a practicing MD.
This is just one example of the Foundation’s impact and it’s through these stories that we share the “why” behind every dollar that is raised, and my first goal is to tell these stories.
Another key focus of not only my presidency, but Dr. Ian Nathanson’s, as well, as we collaborated a lot on our roles, will be on member involvement and awareness. Even I wasn’t involved in the CHEST Foundation until years into my CHEST membership, so I understand that there are competing demands. But I also know that there is a lot to be gained from the work with the Foundation. I want the CHEST members to be excited about the Foundation and to want to support its efforts.
These two goals go hand in hand, and I look forward to sharing the Foundation’s impact with a new audience and reinvigorating the support of our existing donors.
Is there anything else you’d like to say to the reader?
We cannot accomplish anything without the support of our donors, and I want to sincerely thank everyone who has donated to the CHEST Foundation. I also encourage those who have never donated or have yet to donate this year to visit the Foundation’s website (foundation.chestnet.org) and explore some of the inspiring initiatives you can support to strengthen the impact of the CHEST Foundation because the possibilities are truly endless.
Sore throat becoming dominant COVID symptom: Reports
according to recent reports in the United Kingdom.
The shift could be a cause of concern for the fall. As the main symptoms of the coronavirus change, people could spread the virus without realizing it.
“Many people are still using the government guidelines about symptoms, which are wrong,” Tim Spector, a professor of genetic epidemiology at King’s College London, told the Independent.
Prof. Spector cofounded the COVID ZOE app, which is part of the world’s largest COVID-19 study. Throughout the pandemic, researchers have used data from the app to track changes in symptoms.
“At the moment, COVID starts in two-thirds of people with a sore throat,” he said. “Fever and loss of smell are really rare now, so many old people may not think they’ve got COVID. They’d say it’s a cold and not be tested.”
COVID-19 infections in the United Kingdom increased 14% at the end of September, according to data from the U.K.’s Office for National Statistics. More than 1.1 million people tested positive during the week ending Sept. 20, up from 927,000 cases the week before. The numbers continue to increase in England and Wales, with an uncertain trend in Northern Ireland and Scotland.
The fall wave of infections has likely arrived in the United Kingdom, Prof. Spector told the Independent. Omicron variants continue to evolve and are escaping immunity from previous infection and vaccination, which he expects to continue into the winter.
But with reduced testing and surveillance of new variants, public health experts have voiced concerns about tracking the latest variants and COVID-19 trends.
“We can only detect variants or know what’s coming by doing sequencing from PCR testing, and that’s not going on anywhere near the extent it was a year ago,” Lawrence Young, a professor of virology at the University of Warwick, Coventry, England, told the Independent.
“People are going to get various infections over the winter but won’t know what they are because free tests aren’t available,” he said. “It’s going to be a problem.”
COVID-19 cases are also increasing across Europe, which could mark the first regional spike since the BA.5 wave, according to the latest data from the European CDC. (In the past, increases in Europe have signaled a trend to come in other regions.)
People aged 65 and older have been hit the hardest, the data shows, with cases rising 9% from the previous week. Hospitalizations remain stable for now, although 14 of 27 countries in the European region have noted an upward trend.
“Changes in population mixing following the summer break are likely to be the main driver of these increases, with no indication of changes in the distribution of circulating variants,” the European CDC said.
For now, most COVID-19 numbers are still falling in the United States, according to a weekly CDC update published Sept. 30. About 47,000 cases are being reported each day, marking a 13% decrease from the week before. Hospitalizations dropped 7%, and deaths dropped 6%.
At the same time, test positivity rose slightly last week, from 9.6% to 9.8%. Wastewater surveillance indicates that 53% of sites in the United States reported a decrease in virus levels, while 41% reported an increase last week.
The CDC encouraged people to get the updated Omicron-targeted booster shot for the fall. About 7.5 million Americans have received the updated vaccine. Half of the eligible population in the United States hasn’t received any booster dose yet.
“Bivalent boosters help restore protection that might have gone down since your last dose – and they also give extra protection for you and those around you against all lineages of the Omicron variant,” the CDC wrote. “The more people who stay up to date on vaccinations, the better chance we have of avoiding a possible surge in COVID-19 illness later this fall and winter.”
A version of this article first appeared on WebMD.com.
according to recent reports in the United Kingdom.
The shift could be a cause of concern for the fall. As the main symptoms of the coronavirus change, people could spread the virus without realizing it.
“Many people are still using the government guidelines about symptoms, which are wrong,” Tim Spector, a professor of genetic epidemiology at King’s College London, told the Independent.
Prof. Spector cofounded the COVID ZOE app, which is part of the world’s largest COVID-19 study. Throughout the pandemic, researchers have used data from the app to track changes in symptoms.
“At the moment, COVID starts in two-thirds of people with a sore throat,” he said. “Fever and loss of smell are really rare now, so many old people may not think they’ve got COVID. They’d say it’s a cold and not be tested.”
COVID-19 infections in the United Kingdom increased 14% at the end of September, according to data from the U.K.’s Office for National Statistics. More than 1.1 million people tested positive during the week ending Sept. 20, up from 927,000 cases the week before. The numbers continue to increase in England and Wales, with an uncertain trend in Northern Ireland and Scotland.
The fall wave of infections has likely arrived in the United Kingdom, Prof. Spector told the Independent. Omicron variants continue to evolve and are escaping immunity from previous infection and vaccination, which he expects to continue into the winter.
But with reduced testing and surveillance of new variants, public health experts have voiced concerns about tracking the latest variants and COVID-19 trends.
“We can only detect variants or know what’s coming by doing sequencing from PCR testing, and that’s not going on anywhere near the extent it was a year ago,” Lawrence Young, a professor of virology at the University of Warwick, Coventry, England, told the Independent.
“People are going to get various infections over the winter but won’t know what they are because free tests aren’t available,” he said. “It’s going to be a problem.”
COVID-19 cases are also increasing across Europe, which could mark the first regional spike since the BA.5 wave, according to the latest data from the European CDC. (In the past, increases in Europe have signaled a trend to come in other regions.)
People aged 65 and older have been hit the hardest, the data shows, with cases rising 9% from the previous week. Hospitalizations remain stable for now, although 14 of 27 countries in the European region have noted an upward trend.
“Changes in population mixing following the summer break are likely to be the main driver of these increases, with no indication of changes in the distribution of circulating variants,” the European CDC said.
For now, most COVID-19 numbers are still falling in the United States, according to a weekly CDC update published Sept. 30. About 47,000 cases are being reported each day, marking a 13% decrease from the week before. Hospitalizations dropped 7%, and deaths dropped 6%.
At the same time, test positivity rose slightly last week, from 9.6% to 9.8%. Wastewater surveillance indicates that 53% of sites in the United States reported a decrease in virus levels, while 41% reported an increase last week.
The CDC encouraged people to get the updated Omicron-targeted booster shot for the fall. About 7.5 million Americans have received the updated vaccine. Half of the eligible population in the United States hasn’t received any booster dose yet.
“Bivalent boosters help restore protection that might have gone down since your last dose – and they also give extra protection for you and those around you against all lineages of the Omicron variant,” the CDC wrote. “The more people who stay up to date on vaccinations, the better chance we have of avoiding a possible surge in COVID-19 illness later this fall and winter.”
A version of this article first appeared on WebMD.com.
according to recent reports in the United Kingdom.
The shift could be a cause of concern for the fall. As the main symptoms of the coronavirus change, people could spread the virus without realizing it.
“Many people are still using the government guidelines about symptoms, which are wrong,” Tim Spector, a professor of genetic epidemiology at King’s College London, told the Independent.
Prof. Spector cofounded the COVID ZOE app, which is part of the world’s largest COVID-19 study. Throughout the pandemic, researchers have used data from the app to track changes in symptoms.
“At the moment, COVID starts in two-thirds of people with a sore throat,” he said. “Fever and loss of smell are really rare now, so many old people may not think they’ve got COVID. They’d say it’s a cold and not be tested.”
COVID-19 infections in the United Kingdom increased 14% at the end of September, according to data from the U.K.’s Office for National Statistics. More than 1.1 million people tested positive during the week ending Sept. 20, up from 927,000 cases the week before. The numbers continue to increase in England and Wales, with an uncertain trend in Northern Ireland and Scotland.
The fall wave of infections has likely arrived in the United Kingdom, Prof. Spector told the Independent. Omicron variants continue to evolve and are escaping immunity from previous infection and vaccination, which he expects to continue into the winter.
But with reduced testing and surveillance of new variants, public health experts have voiced concerns about tracking the latest variants and COVID-19 trends.
“We can only detect variants or know what’s coming by doing sequencing from PCR testing, and that’s not going on anywhere near the extent it was a year ago,” Lawrence Young, a professor of virology at the University of Warwick, Coventry, England, told the Independent.
“People are going to get various infections over the winter but won’t know what they are because free tests aren’t available,” he said. “It’s going to be a problem.”
COVID-19 cases are also increasing across Europe, which could mark the first regional spike since the BA.5 wave, according to the latest data from the European CDC. (In the past, increases in Europe have signaled a trend to come in other regions.)
People aged 65 and older have been hit the hardest, the data shows, with cases rising 9% from the previous week. Hospitalizations remain stable for now, although 14 of 27 countries in the European region have noted an upward trend.
“Changes in population mixing following the summer break are likely to be the main driver of these increases, with no indication of changes in the distribution of circulating variants,” the European CDC said.
For now, most COVID-19 numbers are still falling in the United States, according to a weekly CDC update published Sept. 30. About 47,000 cases are being reported each day, marking a 13% decrease from the week before. Hospitalizations dropped 7%, and deaths dropped 6%.
At the same time, test positivity rose slightly last week, from 9.6% to 9.8%. Wastewater surveillance indicates that 53% of sites in the United States reported a decrease in virus levels, while 41% reported an increase last week.
The CDC encouraged people to get the updated Omicron-targeted booster shot for the fall. About 7.5 million Americans have received the updated vaccine. Half of the eligible population in the United States hasn’t received any booster dose yet.
“Bivalent boosters help restore protection that might have gone down since your last dose – and they also give extra protection for you and those around you against all lineages of the Omicron variant,” the CDC wrote. “The more people who stay up to date on vaccinations, the better chance we have of avoiding a possible surge in COVID-19 illness later this fall and winter.”
A version of this article first appeared on WebMD.com.









