User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Medical-level empathy? Yup, ChatGPT can fake that
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
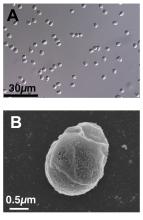
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
FDA approves first RSV vaccine for older adults
Arexvy, manufactured by GSK, is the world’s first RSV vaccine for adults aged 60 years and older, the company said in an announcement.
Every year, RSV is responsible for 60,000–120,000 hospitalizations and 6,000–10,000 deaths among U.S. adults older than age, according to the FDA. Older adults with underlying health conditions — such as diabetes, a weakened immune system, or lung or heart disease — are at high risk for severe disease. "Today’s approval of the first RSV vaccine is an important public health achievement to prevent a disease which can be life-threatening and reflects the FDA’s continued commitment to facilitating the development of safe and effective vaccines for use in the United States," said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in a statement.
The FDA approval of Arexvy was based on a clinical study of approximately 25,000 patients. Half of these patients received Arexvy, while the other half received a placebo. Researchers found that the RSV vaccine reduced RSV-associated lower respiratory tract disease (LRTD) by nearly 83% and reduced the risk of developing severe RSV-associated LRTD by 94%. The most commonly reported side effects were injection site pain, fatigue, muscle pain, headache, and joint stiffness/pain. Ten patients who received Arexvy and four patients who received placebo experienced atrial fibrillation within 30 days of vaccination. The company is planning to assess risk for atrial fibrillation in postmarking studies, the FDA said. The European Medicine Agency’s Committee for Medicinal Products for Human Use recommended approval of Arexvy on April 25, 2023, on the basis of data from the same clinical trial.
GSK said that the U.S. launch of Arexvy will occur sometime in the fall before the 2023/2024 RSV season, but the company did not provide exact dates. "Today marks a turning point in our effort to reduce the significant burden of RSV," said GSK’s chief scientific officer, Tony Wood, PhD, in a company statement. "Our focus now is to ensure eligible older adults in the U.S. can access the vaccine as quickly as possible and to progress regulatory review in other countries."
A version of this article first appeared on Medscape.com.
Arexvy, manufactured by GSK, is the world’s first RSV vaccine for adults aged 60 years and older, the company said in an announcement.
Every year, RSV is responsible for 60,000–120,000 hospitalizations and 6,000–10,000 deaths among U.S. adults older than age, according to the FDA. Older adults with underlying health conditions — such as diabetes, a weakened immune system, or lung or heart disease — are at high risk for severe disease. "Today’s approval of the first RSV vaccine is an important public health achievement to prevent a disease which can be life-threatening and reflects the FDA’s continued commitment to facilitating the development of safe and effective vaccines for use in the United States," said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in a statement.
The FDA approval of Arexvy was based on a clinical study of approximately 25,000 patients. Half of these patients received Arexvy, while the other half received a placebo. Researchers found that the RSV vaccine reduced RSV-associated lower respiratory tract disease (LRTD) by nearly 83% and reduced the risk of developing severe RSV-associated LRTD by 94%. The most commonly reported side effects were injection site pain, fatigue, muscle pain, headache, and joint stiffness/pain. Ten patients who received Arexvy and four patients who received placebo experienced atrial fibrillation within 30 days of vaccination. The company is planning to assess risk for atrial fibrillation in postmarking studies, the FDA said. The European Medicine Agency’s Committee for Medicinal Products for Human Use recommended approval of Arexvy on April 25, 2023, on the basis of data from the same clinical trial.
GSK said that the U.S. launch of Arexvy will occur sometime in the fall before the 2023/2024 RSV season, but the company did not provide exact dates. "Today marks a turning point in our effort to reduce the significant burden of RSV," said GSK’s chief scientific officer, Tony Wood, PhD, in a company statement. "Our focus now is to ensure eligible older adults in the U.S. can access the vaccine as quickly as possible and to progress regulatory review in other countries."
A version of this article first appeared on Medscape.com.
Arexvy, manufactured by GSK, is the world’s first RSV vaccine for adults aged 60 years and older, the company said in an announcement.
Every year, RSV is responsible for 60,000–120,000 hospitalizations and 6,000–10,000 deaths among U.S. adults older than age, according to the FDA. Older adults with underlying health conditions — such as diabetes, a weakened immune system, or lung or heart disease — are at high risk for severe disease. "Today’s approval of the first RSV vaccine is an important public health achievement to prevent a disease which can be life-threatening and reflects the FDA’s continued commitment to facilitating the development of safe and effective vaccines for use in the United States," said Peter Marks, MD, PhD, director of the FDA’s Center for Biologics Evaluation and Research, in a statement.
The FDA approval of Arexvy was based on a clinical study of approximately 25,000 patients. Half of these patients received Arexvy, while the other half received a placebo. Researchers found that the RSV vaccine reduced RSV-associated lower respiratory tract disease (LRTD) by nearly 83% and reduced the risk of developing severe RSV-associated LRTD by 94%. The most commonly reported side effects were injection site pain, fatigue, muscle pain, headache, and joint stiffness/pain. Ten patients who received Arexvy and four patients who received placebo experienced atrial fibrillation within 30 days of vaccination. The company is planning to assess risk for atrial fibrillation in postmarking studies, the FDA said. The European Medicine Agency’s Committee for Medicinal Products for Human Use recommended approval of Arexvy on April 25, 2023, on the basis of data from the same clinical trial.
GSK said that the U.S. launch of Arexvy will occur sometime in the fall before the 2023/2024 RSV season, but the company did not provide exact dates. "Today marks a turning point in our effort to reduce the significant burden of RSV," said GSK’s chief scientific officer, Tony Wood, PhD, in a company statement. "Our focus now is to ensure eligible older adults in the U.S. can access the vaccine as quickly as possible and to progress regulatory review in other countries."
A version of this article first appeared on Medscape.com.
Cancer pain declines with cannabis use
in a study.
Physician-prescribed cannabis, particularly cannabinoids, has been shown to ease cancer-related pain in adult cancer patients, who often find inadequate pain relief from medications including opioids, Saro Aprikian, MSc, a medical student at the Royal College of Surgeons, Dublin, and colleagues, wrote in their paper.
However, real-world data on the safety and effectiveness of cannabis in the cancer population and the impact on use of other medications are lacking, the researchers said.
In the study, published in BMJ Supportive & Palliative Care, the researchers reviewed data from 358 adults with cancer who were part of a multicenter cannabis registry in Canada between May 2015 and October 2018.
The average age of the patients was 57.6 years, and 48% were men. The top three cancer diagnoses in the study population were genitorurinary, breast, and colorectal.
Pain was the most common reason for obtaining a medical cannabis prescription, cited by 72.4% of patients.
Data were collected at follow-up visits conducted every 3 months over 1 year. Pain was assessed via the Brief Pain Inventory (BPI) and revised Edmonton Symptom Assessment System (ESAS-r) questionnaires and compared to baseline values. Patients rated their pain intensity on a sliding scale of 0 (none) to 10 (worst possible). Pain relief was rated on a scale of 0% (none) to 100% (complete).
Compared to baseline scores, patients showed significant decreases at 3, 6 and 9 months for BPI worst pain (5.5 at baseline, 3.6 for 3, 6, and 9 months) average pain (4.1 at baseline, 2.4, 2.3, and 2.7 for 3, 6, and 9 months, respectively), overall pain severity (2.7 at baseline, 2.3, 2.3, and 2.4 at 3, 6, and 9 months, respectively), and pain interference with daily life (4.3 at baseline, 2.4, 2.2, and 2.4 at 3, 6, and 9 months, respectively; P less than .01 for all four pain measures).
“Pain severity as reported in the ESAS-r decreased significantly at 3-month, 6-month and 9-month follow-ups,” the researchers noted.
In addition, total medication burden based on the medication quantification scale (MQS) and morphine equivalent daily dose (MEDD) were recorded at 3, 6, 9, and 12 months. MQS scores decreased compared to baseline at 3, 6, 9, and 12 months in 10%, 23.5%, 26.2%, and 31.6% of patients, respectively. Also compared with baseline, 11.1%, 31.3%, and 14.3% of patients reported decreases in MEDD scores at 3, 6, and 9 months, respectively.
Overall, products with equal amounts of active ingredients tetrahydrocannabinol (THC) and cannabidiol (CBD) were more effective than were those with a predominance of either THC or CBD, the researchers wrote.
Medical cannabis was well-tolerated; a total of 15 moderate to severe side effects were reported by 11 patients, 13 of which were minor. The most common side effects were sleepiness and fatigue, and five patients discontinued their medical cannabis because of side effects. The two serious side effects reported during the study period – pneumonia and a cardiovascular event – were deemed unlikely related to the patients’ medicinal cannabis use.
The findings were limited by several factors, including the observational design, which prevented conclusions about causality, the researchers noted. Other limitations included the loss of many patients to follow-up and incomplete data on other prescription medications in many cases.
The results support the use of medical cannabis by cancer patients as an adjunct pain relief strategy and a way to potentially reduce the use of other medications such as opioids, the authors concluded.
The study was supported by the Canadian Consortium for the Investigation of Cannabinoids, Collège des Médecins du Québec, and the Canopy Growth Corporation. The researchers had no financial conflicts to disclose.
in a study.
Physician-prescribed cannabis, particularly cannabinoids, has been shown to ease cancer-related pain in adult cancer patients, who often find inadequate pain relief from medications including opioids, Saro Aprikian, MSc, a medical student at the Royal College of Surgeons, Dublin, and colleagues, wrote in their paper.
However, real-world data on the safety and effectiveness of cannabis in the cancer population and the impact on use of other medications are lacking, the researchers said.
In the study, published in BMJ Supportive & Palliative Care, the researchers reviewed data from 358 adults with cancer who were part of a multicenter cannabis registry in Canada between May 2015 and October 2018.
The average age of the patients was 57.6 years, and 48% were men. The top three cancer diagnoses in the study population were genitorurinary, breast, and colorectal.
Pain was the most common reason for obtaining a medical cannabis prescription, cited by 72.4% of patients.
Data were collected at follow-up visits conducted every 3 months over 1 year. Pain was assessed via the Brief Pain Inventory (BPI) and revised Edmonton Symptom Assessment System (ESAS-r) questionnaires and compared to baseline values. Patients rated their pain intensity on a sliding scale of 0 (none) to 10 (worst possible). Pain relief was rated on a scale of 0% (none) to 100% (complete).
Compared to baseline scores, patients showed significant decreases at 3, 6 and 9 months for BPI worst pain (5.5 at baseline, 3.6 for 3, 6, and 9 months) average pain (4.1 at baseline, 2.4, 2.3, and 2.7 for 3, 6, and 9 months, respectively), overall pain severity (2.7 at baseline, 2.3, 2.3, and 2.4 at 3, 6, and 9 months, respectively), and pain interference with daily life (4.3 at baseline, 2.4, 2.2, and 2.4 at 3, 6, and 9 months, respectively; P less than .01 for all four pain measures).
“Pain severity as reported in the ESAS-r decreased significantly at 3-month, 6-month and 9-month follow-ups,” the researchers noted.
In addition, total medication burden based on the medication quantification scale (MQS) and morphine equivalent daily dose (MEDD) were recorded at 3, 6, 9, and 12 months. MQS scores decreased compared to baseline at 3, 6, 9, and 12 months in 10%, 23.5%, 26.2%, and 31.6% of patients, respectively. Also compared with baseline, 11.1%, 31.3%, and 14.3% of patients reported decreases in MEDD scores at 3, 6, and 9 months, respectively.
Overall, products with equal amounts of active ingredients tetrahydrocannabinol (THC) and cannabidiol (CBD) were more effective than were those with a predominance of either THC or CBD, the researchers wrote.
Medical cannabis was well-tolerated; a total of 15 moderate to severe side effects were reported by 11 patients, 13 of which were minor. The most common side effects were sleepiness and fatigue, and five patients discontinued their medical cannabis because of side effects. The two serious side effects reported during the study period – pneumonia and a cardiovascular event – were deemed unlikely related to the patients’ medicinal cannabis use.
The findings were limited by several factors, including the observational design, which prevented conclusions about causality, the researchers noted. Other limitations included the loss of many patients to follow-up and incomplete data on other prescription medications in many cases.
The results support the use of medical cannabis by cancer patients as an adjunct pain relief strategy and a way to potentially reduce the use of other medications such as opioids, the authors concluded.
The study was supported by the Canadian Consortium for the Investigation of Cannabinoids, Collège des Médecins du Québec, and the Canopy Growth Corporation. The researchers had no financial conflicts to disclose.
in a study.
Physician-prescribed cannabis, particularly cannabinoids, has been shown to ease cancer-related pain in adult cancer patients, who often find inadequate pain relief from medications including opioids, Saro Aprikian, MSc, a medical student at the Royal College of Surgeons, Dublin, and colleagues, wrote in their paper.
However, real-world data on the safety and effectiveness of cannabis in the cancer population and the impact on use of other medications are lacking, the researchers said.
In the study, published in BMJ Supportive & Palliative Care, the researchers reviewed data from 358 adults with cancer who were part of a multicenter cannabis registry in Canada between May 2015 and October 2018.
The average age of the patients was 57.6 years, and 48% were men. The top three cancer diagnoses in the study population were genitorurinary, breast, and colorectal.
Pain was the most common reason for obtaining a medical cannabis prescription, cited by 72.4% of patients.
Data were collected at follow-up visits conducted every 3 months over 1 year. Pain was assessed via the Brief Pain Inventory (BPI) and revised Edmonton Symptom Assessment System (ESAS-r) questionnaires and compared to baseline values. Patients rated their pain intensity on a sliding scale of 0 (none) to 10 (worst possible). Pain relief was rated on a scale of 0% (none) to 100% (complete).
Compared to baseline scores, patients showed significant decreases at 3, 6 and 9 months for BPI worst pain (5.5 at baseline, 3.6 for 3, 6, and 9 months) average pain (4.1 at baseline, 2.4, 2.3, and 2.7 for 3, 6, and 9 months, respectively), overall pain severity (2.7 at baseline, 2.3, 2.3, and 2.4 at 3, 6, and 9 months, respectively), and pain interference with daily life (4.3 at baseline, 2.4, 2.2, and 2.4 at 3, 6, and 9 months, respectively; P less than .01 for all four pain measures).
“Pain severity as reported in the ESAS-r decreased significantly at 3-month, 6-month and 9-month follow-ups,” the researchers noted.
In addition, total medication burden based on the medication quantification scale (MQS) and morphine equivalent daily dose (MEDD) were recorded at 3, 6, 9, and 12 months. MQS scores decreased compared to baseline at 3, 6, 9, and 12 months in 10%, 23.5%, 26.2%, and 31.6% of patients, respectively. Also compared with baseline, 11.1%, 31.3%, and 14.3% of patients reported decreases in MEDD scores at 3, 6, and 9 months, respectively.
Overall, products with equal amounts of active ingredients tetrahydrocannabinol (THC) and cannabidiol (CBD) were more effective than were those with a predominance of either THC or CBD, the researchers wrote.
Medical cannabis was well-tolerated; a total of 15 moderate to severe side effects were reported by 11 patients, 13 of which were minor. The most common side effects were sleepiness and fatigue, and five patients discontinued their medical cannabis because of side effects. The two serious side effects reported during the study period – pneumonia and a cardiovascular event – were deemed unlikely related to the patients’ medicinal cannabis use.
The findings were limited by several factors, including the observational design, which prevented conclusions about causality, the researchers noted. Other limitations included the loss of many patients to follow-up and incomplete data on other prescription medications in many cases.
The results support the use of medical cannabis by cancer patients as an adjunct pain relief strategy and a way to potentially reduce the use of other medications such as opioids, the authors concluded.
The study was supported by the Canadian Consortium for the Investigation of Cannabinoids, Collège des Médecins du Québec, and the Canopy Growth Corporation. The researchers had no financial conflicts to disclose.
FROM BMJ SUPPORTIVE & PALLIATIVE CARE
CPAP not only solution for sleep apnea
Although continuous positive airway pressure (CPAP) machines are the gold standard in the management of sleep apnea, several other treatments should be considered.
“Just because you have a hammer doesn’t mean everything is a nail,” Kimberly Hardin, MD, professor of clinical internal medicine at University of California, Davis, said at the annual meeting of the American College of Physicians.
“Sleep has been underestimated in the health arena for many, many years,” said Dr. Hardin, who likened sound sleep to the “sixth vital sign.” “We know that sleep plays an integral role in our health.”
Surgical options include nasal surgery and maxillomandibular advancement surgery, also known as double-jaw surgery. Such procedures should be considered only for patients who are unwilling or unable to use CPAP or other nonsurgical treatments.
Sleep apnea occurs in 4% of adult men and 2% of adult women aged 30-60. Most commonly, obstructive sleep apnea involves the cessation or significant decrease in airflow while sleeping. The Apnea Hypopnea Index (AHI) is the number of times a patient experiences apnea or hypopnea during one night divided by the hours of sleep. Normal sleep AHI is fewer than five events per hour on average; mild sleep apnea is five to 14 events; moderate, 15-29; and severe, at least 30 events.
To identify sleep apnea, physicians have several tools at their disposal, starting with preliminary questionnaires that query patients as to whether they are having trouble falling asleep, staying asleep, or are tired during the day. Additional assessment tools include sleep lab testing and at-home testing.
At-home testing has come to include more than the common devices that are worn around the chest and nose for a night.
“It’s not very fun looking,” Dr. Hardin said of the weighty, obtrusive monitoring devices. “So lots of folks have come up with some new ways of doing things.”
These new options incorporate headbands, wrist and finger devices, arterial tonometry, and sleep rings.
Studies show that U.S. adults do not get enough sleep, and poor-quality sleep is as inadequate as insufficient sleep. Barely a third of adults get the minimum 7 hours recommended by the Centers for Disease Control and Prevention. Non-Hispanic Black adults are less likely to report sleeping 7-9 hours and are more likely to report sleeping 6 or fewer hours than are non-Hispanic White and Hispanic adults.
Dr. Hardin said doctors can advise patients to keep their bedrooms quiet, dark, and cool with no TVs or electronics, to maintain regular wake and sleep times, and to stop consuming caffeine late in the day.
Insufficient or poor sleep can have wide-ranging implications on medical conditions such as diabetes, heart disease, obesity, immunodeficiency, cognitive function, mental health, and, ultimately, mortality, according to Dr. Hardin.
“Some people say, ‘Oh, never mind, I can sleep when I’m dead,’ “ Dr. Hardin said. But such a mentality can have a bearing on life expectancy.
A version of this article first appeared on Medscape.com.
Although continuous positive airway pressure (CPAP) machines are the gold standard in the management of sleep apnea, several other treatments should be considered.
“Just because you have a hammer doesn’t mean everything is a nail,” Kimberly Hardin, MD, professor of clinical internal medicine at University of California, Davis, said at the annual meeting of the American College of Physicians.
“Sleep has been underestimated in the health arena for many, many years,” said Dr. Hardin, who likened sound sleep to the “sixth vital sign.” “We know that sleep plays an integral role in our health.”
Surgical options include nasal surgery and maxillomandibular advancement surgery, also known as double-jaw surgery. Such procedures should be considered only for patients who are unwilling or unable to use CPAP or other nonsurgical treatments.
Sleep apnea occurs in 4% of adult men and 2% of adult women aged 30-60. Most commonly, obstructive sleep apnea involves the cessation or significant decrease in airflow while sleeping. The Apnea Hypopnea Index (AHI) is the number of times a patient experiences apnea or hypopnea during one night divided by the hours of sleep. Normal sleep AHI is fewer than five events per hour on average; mild sleep apnea is five to 14 events; moderate, 15-29; and severe, at least 30 events.
To identify sleep apnea, physicians have several tools at their disposal, starting with preliminary questionnaires that query patients as to whether they are having trouble falling asleep, staying asleep, or are tired during the day. Additional assessment tools include sleep lab testing and at-home testing.
At-home testing has come to include more than the common devices that are worn around the chest and nose for a night.
“It’s not very fun looking,” Dr. Hardin said of the weighty, obtrusive monitoring devices. “So lots of folks have come up with some new ways of doing things.”
These new options incorporate headbands, wrist and finger devices, arterial tonometry, and sleep rings.
Studies show that U.S. adults do not get enough sleep, and poor-quality sleep is as inadequate as insufficient sleep. Barely a third of adults get the minimum 7 hours recommended by the Centers for Disease Control and Prevention. Non-Hispanic Black adults are less likely to report sleeping 7-9 hours and are more likely to report sleeping 6 or fewer hours than are non-Hispanic White and Hispanic adults.
Dr. Hardin said doctors can advise patients to keep their bedrooms quiet, dark, and cool with no TVs or electronics, to maintain regular wake and sleep times, and to stop consuming caffeine late in the day.
Insufficient or poor sleep can have wide-ranging implications on medical conditions such as diabetes, heart disease, obesity, immunodeficiency, cognitive function, mental health, and, ultimately, mortality, according to Dr. Hardin.
“Some people say, ‘Oh, never mind, I can sleep when I’m dead,’ “ Dr. Hardin said. But such a mentality can have a bearing on life expectancy.
A version of this article first appeared on Medscape.com.
Although continuous positive airway pressure (CPAP) machines are the gold standard in the management of sleep apnea, several other treatments should be considered.
“Just because you have a hammer doesn’t mean everything is a nail,” Kimberly Hardin, MD, professor of clinical internal medicine at University of California, Davis, said at the annual meeting of the American College of Physicians.
“Sleep has been underestimated in the health arena for many, many years,” said Dr. Hardin, who likened sound sleep to the “sixth vital sign.” “We know that sleep plays an integral role in our health.”
Surgical options include nasal surgery and maxillomandibular advancement surgery, also known as double-jaw surgery. Such procedures should be considered only for patients who are unwilling or unable to use CPAP or other nonsurgical treatments.
Sleep apnea occurs in 4% of adult men and 2% of adult women aged 30-60. Most commonly, obstructive sleep apnea involves the cessation or significant decrease in airflow while sleeping. The Apnea Hypopnea Index (AHI) is the number of times a patient experiences apnea or hypopnea during one night divided by the hours of sleep. Normal sleep AHI is fewer than five events per hour on average; mild sleep apnea is five to 14 events; moderate, 15-29; and severe, at least 30 events.
To identify sleep apnea, physicians have several tools at their disposal, starting with preliminary questionnaires that query patients as to whether they are having trouble falling asleep, staying asleep, or are tired during the day. Additional assessment tools include sleep lab testing and at-home testing.
At-home testing has come to include more than the common devices that are worn around the chest and nose for a night.
“It’s not very fun looking,” Dr. Hardin said of the weighty, obtrusive monitoring devices. “So lots of folks have come up with some new ways of doing things.”
These new options incorporate headbands, wrist and finger devices, arterial tonometry, and sleep rings.
Studies show that U.S. adults do not get enough sleep, and poor-quality sleep is as inadequate as insufficient sleep. Barely a third of adults get the minimum 7 hours recommended by the Centers for Disease Control and Prevention. Non-Hispanic Black adults are less likely to report sleeping 7-9 hours and are more likely to report sleeping 6 or fewer hours than are non-Hispanic White and Hispanic adults.
Dr. Hardin said doctors can advise patients to keep their bedrooms quiet, dark, and cool with no TVs or electronics, to maintain regular wake and sleep times, and to stop consuming caffeine late in the day.
Insufficient or poor sleep can have wide-ranging implications on medical conditions such as diabetes, heart disease, obesity, immunodeficiency, cognitive function, mental health, and, ultimately, mortality, according to Dr. Hardin.
“Some people say, ‘Oh, never mind, I can sleep when I’m dead,’ “ Dr. Hardin said. But such a mentality can have a bearing on life expectancy.
A version of this article first appeared on Medscape.com.
FROM INTERNAL MEDICINE 2023
First guideline for treating oligometastatic NSCLC
The result of a joint effort by the American Society for Radiation Oncology and European Society for Radiotherapy and Oncology, the guidelines emphasizes the need for a multidisciplinary team approach to guide treatment decisions for oligometastatic disease.
Historically, treatment for oligometastatic NSCLC has involved systemic therapy including chemotherapy or immunotherapy, and local therapy was given only for palliation and symptom relief. But increasing evidence has demonstrated that definitive local therapy may have an additional role in controlling tumor growth and improving survival outcomes, and an increasing number of radiation oncologists and multidisciplinary teams are now using local therapy beyond palliative care for these patients, the authors noted.
“Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes, because it typically is more treatable than widely metastatic cancer,” said Puneeth Iyengar, MD, PhD, cochair of the guideline task force and an associate professor of radiation oncology at UT Southwestern Medical Center, Dallas.
“The research on local therapy for oligometastatic cancer is still at a relatively early stage, but we already see indicators of potential benefits for patients. Adding local therapy to systemic therapy may lead to more durable cancer control, potentially improving progression-free survival, overall survival and quality of life,” he said in a statement.
The new guideline is published in Practical Radiation Oncology.
The purpose of this joint guideline was to provide recommendations on local therapy use for oligometastatic NSCLC, along with a summary of the evidence justifying its incorporation into standard treatment paradigms.
Key recommendations
Owing to the lack of significant randomized phase 3 trials, the guideline task force strongly recommended a patient-centered, multidisciplinary approach for all decision-making regarding potential treatment. In addition, algorithms were also created for the optimal clinical scenarios for local therapy and the different types of local therapy that are available for these patients.
Key recommendations include:
- The integration of definitive local therapy is recommended only for patients who have five or fewer distant extracranial metastases, and only when technically feasible and clinically safe for all disease sites. Definitive local therapy is also conditionally recommended for carefully selected patients with synchronous oligometastatic, metachronous oligorecurrent, induced oligopersistent, or induced oligoprogressive conditions for extracranial NSCLC.
- Radiation and surgery are the only recommended modalities for definitive local treatment of oligometastatic NSCLC. Radiation is favored when multiple organ systems are being treated or when the clinical priority is to minimize breaks from systemic therapy, whereas surgery is favored when large tissue sampling is needed for molecular testing to guide systemic therapy.
- For sequencing and timing, there is an emphasis on upfront, definitive local treatment for symptomatic metastases. For asymptomatic patients with synchronous disease, at least 3 months of standard-of-care systemic therapy is recommended before starting definitive local therapy.
- For optimal staging, radiation dosing, treatment planning, and delivery techniques, there is a preference for hypofractionated radiation therapy or stereotactic body radiation therapy when appropriate. The task force also emphasizes the importance of appropriate imaging and comments that it “cannot be overstated” to diagnose oligometastatic disease; they recommend that care teams consult guidelines from groups such as the National Comprehensive Cancer Network and the European Organisation for Research and Treatment of Cancer.
- Patients who develop disease progression at a limited number of sites, so-called oligoprogression at previously treated sites, and/or de novo recurrences at new sites may benefit from repeat local definitive therapy performed with the aim of prolonging progression-free survival or delaying a switch in systemic therapies.
Matthias Guckenberger, MD, cochair of the guideline task force and a professor and chairman of radiation oncology at the University Hospital Zürich, cautioned that “despite the widespread enthusiasm in the field of oligometastatic disease, the quality of evidence supporting the integration of definitive local therapy into a multimodality treatment strategy is still lower as compared to indications such as locally advanced NSCLC.”
“To compensate for this lack of highest-quality evidence, recommendations of this guideline were established by a broad consensus involving experts from ASTRO and ESTRO, colleagues from the fields of thoracic surgery and medical oncology and a patient representative,” Dr. Guckenberger said in a statement.
The guideline task force also emphasized the need for equitable use of these techniques, noting that “a significant effort must be taken to ensure that the decisions regarding the use of local therapies for oligometastatic NSCLC be applied equally across all patients to avoid any health disparities.”
This work was funded by ASTRO. Dr. Iyengar reported no disclosures. Dr. Guckenberger reports relationships with the European Thoracic Oncology Platform, Varian, ViewRay, and ESTRO. Several of the coauthors disclosed relationships with industry.
A version of this article first appeared on Medscape.com.
The result of a joint effort by the American Society for Radiation Oncology and European Society for Radiotherapy and Oncology, the guidelines emphasizes the need for a multidisciplinary team approach to guide treatment decisions for oligometastatic disease.
Historically, treatment for oligometastatic NSCLC has involved systemic therapy including chemotherapy or immunotherapy, and local therapy was given only for palliation and symptom relief. But increasing evidence has demonstrated that definitive local therapy may have an additional role in controlling tumor growth and improving survival outcomes, and an increasing number of radiation oncologists and multidisciplinary teams are now using local therapy beyond palliative care for these patients, the authors noted.
“Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes, because it typically is more treatable than widely metastatic cancer,” said Puneeth Iyengar, MD, PhD, cochair of the guideline task force and an associate professor of radiation oncology at UT Southwestern Medical Center, Dallas.
“The research on local therapy for oligometastatic cancer is still at a relatively early stage, but we already see indicators of potential benefits for patients. Adding local therapy to systemic therapy may lead to more durable cancer control, potentially improving progression-free survival, overall survival and quality of life,” he said in a statement.
The new guideline is published in Practical Radiation Oncology.
The purpose of this joint guideline was to provide recommendations on local therapy use for oligometastatic NSCLC, along with a summary of the evidence justifying its incorporation into standard treatment paradigms.
Key recommendations
Owing to the lack of significant randomized phase 3 trials, the guideline task force strongly recommended a patient-centered, multidisciplinary approach for all decision-making regarding potential treatment. In addition, algorithms were also created for the optimal clinical scenarios for local therapy and the different types of local therapy that are available for these patients.
Key recommendations include:
- The integration of definitive local therapy is recommended only for patients who have five or fewer distant extracranial metastases, and only when technically feasible and clinically safe for all disease sites. Definitive local therapy is also conditionally recommended for carefully selected patients with synchronous oligometastatic, metachronous oligorecurrent, induced oligopersistent, or induced oligoprogressive conditions for extracranial NSCLC.
- Radiation and surgery are the only recommended modalities for definitive local treatment of oligometastatic NSCLC. Radiation is favored when multiple organ systems are being treated or when the clinical priority is to minimize breaks from systemic therapy, whereas surgery is favored when large tissue sampling is needed for molecular testing to guide systemic therapy.
- For sequencing and timing, there is an emphasis on upfront, definitive local treatment for symptomatic metastases. For asymptomatic patients with synchronous disease, at least 3 months of standard-of-care systemic therapy is recommended before starting definitive local therapy.
- For optimal staging, radiation dosing, treatment planning, and delivery techniques, there is a preference for hypofractionated radiation therapy or stereotactic body radiation therapy when appropriate. The task force also emphasizes the importance of appropriate imaging and comments that it “cannot be overstated” to diagnose oligometastatic disease; they recommend that care teams consult guidelines from groups such as the National Comprehensive Cancer Network and the European Organisation for Research and Treatment of Cancer.
- Patients who develop disease progression at a limited number of sites, so-called oligoprogression at previously treated sites, and/or de novo recurrences at new sites may benefit from repeat local definitive therapy performed with the aim of prolonging progression-free survival or delaying a switch in systemic therapies.
Matthias Guckenberger, MD, cochair of the guideline task force and a professor and chairman of radiation oncology at the University Hospital Zürich, cautioned that “despite the widespread enthusiasm in the field of oligometastatic disease, the quality of evidence supporting the integration of definitive local therapy into a multimodality treatment strategy is still lower as compared to indications such as locally advanced NSCLC.”
“To compensate for this lack of highest-quality evidence, recommendations of this guideline were established by a broad consensus involving experts from ASTRO and ESTRO, colleagues from the fields of thoracic surgery and medical oncology and a patient representative,” Dr. Guckenberger said in a statement.
The guideline task force also emphasized the need for equitable use of these techniques, noting that “a significant effort must be taken to ensure that the decisions regarding the use of local therapies for oligometastatic NSCLC be applied equally across all patients to avoid any health disparities.”
This work was funded by ASTRO. Dr. Iyengar reported no disclosures. Dr. Guckenberger reports relationships with the European Thoracic Oncology Platform, Varian, ViewRay, and ESTRO. Several of the coauthors disclosed relationships with industry.
A version of this article first appeared on Medscape.com.
The result of a joint effort by the American Society for Radiation Oncology and European Society for Radiotherapy and Oncology, the guidelines emphasizes the need for a multidisciplinary team approach to guide treatment decisions for oligometastatic disease.
Historically, treatment for oligometastatic NSCLC has involved systemic therapy including chemotherapy or immunotherapy, and local therapy was given only for palliation and symptom relief. But increasing evidence has demonstrated that definitive local therapy may have an additional role in controlling tumor growth and improving survival outcomes, and an increasing number of radiation oncologists and multidisciplinary teams are now using local therapy beyond palliative care for these patients, the authors noted.
“Oligometastatic NSCLC is a phase in lung cancer development that may offer us new opportunities to improve patient outcomes, because it typically is more treatable than widely metastatic cancer,” said Puneeth Iyengar, MD, PhD, cochair of the guideline task force and an associate professor of radiation oncology at UT Southwestern Medical Center, Dallas.
“The research on local therapy for oligometastatic cancer is still at a relatively early stage, but we already see indicators of potential benefits for patients. Adding local therapy to systemic therapy may lead to more durable cancer control, potentially improving progression-free survival, overall survival and quality of life,” he said in a statement.
The new guideline is published in Practical Radiation Oncology.
The purpose of this joint guideline was to provide recommendations on local therapy use for oligometastatic NSCLC, along with a summary of the evidence justifying its incorporation into standard treatment paradigms.
Key recommendations
Owing to the lack of significant randomized phase 3 trials, the guideline task force strongly recommended a patient-centered, multidisciplinary approach for all decision-making regarding potential treatment. In addition, algorithms were also created for the optimal clinical scenarios for local therapy and the different types of local therapy that are available for these patients.
Key recommendations include:
- The integration of definitive local therapy is recommended only for patients who have five or fewer distant extracranial metastases, and only when technically feasible and clinically safe for all disease sites. Definitive local therapy is also conditionally recommended for carefully selected patients with synchronous oligometastatic, metachronous oligorecurrent, induced oligopersistent, or induced oligoprogressive conditions for extracranial NSCLC.
- Radiation and surgery are the only recommended modalities for definitive local treatment of oligometastatic NSCLC. Radiation is favored when multiple organ systems are being treated or when the clinical priority is to minimize breaks from systemic therapy, whereas surgery is favored when large tissue sampling is needed for molecular testing to guide systemic therapy.
- For sequencing and timing, there is an emphasis on upfront, definitive local treatment for symptomatic metastases. For asymptomatic patients with synchronous disease, at least 3 months of standard-of-care systemic therapy is recommended before starting definitive local therapy.
- For optimal staging, radiation dosing, treatment planning, and delivery techniques, there is a preference for hypofractionated radiation therapy or stereotactic body radiation therapy when appropriate. The task force also emphasizes the importance of appropriate imaging and comments that it “cannot be overstated” to diagnose oligometastatic disease; they recommend that care teams consult guidelines from groups such as the National Comprehensive Cancer Network and the European Organisation for Research and Treatment of Cancer.
- Patients who develop disease progression at a limited number of sites, so-called oligoprogression at previously treated sites, and/or de novo recurrences at new sites may benefit from repeat local definitive therapy performed with the aim of prolonging progression-free survival or delaying a switch in systemic therapies.
Matthias Guckenberger, MD, cochair of the guideline task force and a professor and chairman of radiation oncology at the University Hospital Zürich, cautioned that “despite the widespread enthusiasm in the field of oligometastatic disease, the quality of evidence supporting the integration of definitive local therapy into a multimodality treatment strategy is still lower as compared to indications such as locally advanced NSCLC.”
“To compensate for this lack of highest-quality evidence, recommendations of this guideline were established by a broad consensus involving experts from ASTRO and ESTRO, colleagues from the fields of thoracic surgery and medical oncology and a patient representative,” Dr. Guckenberger said in a statement.
The guideline task force also emphasized the need for equitable use of these techniques, noting that “a significant effort must be taken to ensure that the decisions regarding the use of local therapies for oligometastatic NSCLC be applied equally across all patients to avoid any health disparities.”
This work was funded by ASTRO. Dr. Iyengar reported no disclosures. Dr. Guckenberger reports relationships with the European Thoracic Oncology Platform, Varian, ViewRay, and ESTRO. Several of the coauthors disclosed relationships with industry.
A version of this article first appeared on Medscape.com.
FROM PRACTICAL RADIATION ONCOLOGY
Long-COVID patients respond differently to COVID vaccines
A new study shows that people with long COVID respond differently to COVID vaccines and that the condition may be caused by a dysfunction of the immune system – possibly explaining why some people experience symptoms for months while others recover and resume normal lives.
The study compared people who already had long COVID with people who had recovered from the virus. Both groups had not yet been vaccinated prior to the study. When researchers analyzed blood samples after people received an initial vaccine dose, they found that people with long COVID and people who had already recovered from the virus had similar immune responses at first. But
The long-COVID group also showed an extra immune response that tried to fight the virus in a secondary way that researchers didn’t expect. Both groups showed an initial increase in their blood of antibodies that primarily target what’s known as the “spike” protein of the coronavirus, which allows the virus to invade healthy cells. But the long-COVID group also showed a prolonged increased immune response that tried to fight the part of the virus related to how it replicates.
“Theoretically, the production of these antibodies could mean that people are more protected from infection,” said researcher Catherine Le, MD, in a statement. “We also need to investigate if the elevated immune response corresponds with severity or number of long–COVID-19 symptoms.”
Dr. Le is codirector of the COVID-19 Recovery Program at Cedars-Sinai Medical Center in Los Angeles, where the study was conducted.
Study participants agreed in September 2020 to participate in long-term COVID research at Cedars-Sinai. The new analysis was published earlier this year in BMC Infectious Diseases and included 245 people who had long COVID and 86 health care workers who had recovered from COVID but did not have long-term symptoms.
For the study, long COVID was defined as having symptoms that lasted more than 12 weeks. Common long-COVID symptoms are fatigue, shortness of breath, and brain dysfunction such as confusion and forgetfulness.
The authors said it’s unclear why the two groups had different immune responses and also noted that their study was limited by a small sample size. Their research of blood samples is ongoing, with the goals of identifying a way to diagnose long COVID with a laboratory test and of better understanding what causes the condition.
A version of this article first appeared on WebMD.com.
A new study shows that people with long COVID respond differently to COVID vaccines and that the condition may be caused by a dysfunction of the immune system – possibly explaining why some people experience symptoms for months while others recover and resume normal lives.
The study compared people who already had long COVID with people who had recovered from the virus. Both groups had not yet been vaccinated prior to the study. When researchers analyzed blood samples after people received an initial vaccine dose, they found that people with long COVID and people who had already recovered from the virus had similar immune responses at first. But
The long-COVID group also showed an extra immune response that tried to fight the virus in a secondary way that researchers didn’t expect. Both groups showed an initial increase in their blood of antibodies that primarily target what’s known as the “spike” protein of the coronavirus, which allows the virus to invade healthy cells. But the long-COVID group also showed a prolonged increased immune response that tried to fight the part of the virus related to how it replicates.
“Theoretically, the production of these antibodies could mean that people are more protected from infection,” said researcher Catherine Le, MD, in a statement. “We also need to investigate if the elevated immune response corresponds with severity or number of long–COVID-19 symptoms.”
Dr. Le is codirector of the COVID-19 Recovery Program at Cedars-Sinai Medical Center in Los Angeles, where the study was conducted.
Study participants agreed in September 2020 to participate in long-term COVID research at Cedars-Sinai. The new analysis was published earlier this year in BMC Infectious Diseases and included 245 people who had long COVID and 86 health care workers who had recovered from COVID but did not have long-term symptoms.
For the study, long COVID was defined as having symptoms that lasted more than 12 weeks. Common long-COVID symptoms are fatigue, shortness of breath, and brain dysfunction such as confusion and forgetfulness.
The authors said it’s unclear why the two groups had different immune responses and also noted that their study was limited by a small sample size. Their research of blood samples is ongoing, with the goals of identifying a way to diagnose long COVID with a laboratory test and of better understanding what causes the condition.
A version of this article first appeared on WebMD.com.
A new study shows that people with long COVID respond differently to COVID vaccines and that the condition may be caused by a dysfunction of the immune system – possibly explaining why some people experience symptoms for months while others recover and resume normal lives.
The study compared people who already had long COVID with people who had recovered from the virus. Both groups had not yet been vaccinated prior to the study. When researchers analyzed blood samples after people received an initial vaccine dose, they found that people with long COVID and people who had already recovered from the virus had similar immune responses at first. But
The long-COVID group also showed an extra immune response that tried to fight the virus in a secondary way that researchers didn’t expect. Both groups showed an initial increase in their blood of antibodies that primarily target what’s known as the “spike” protein of the coronavirus, which allows the virus to invade healthy cells. But the long-COVID group also showed a prolonged increased immune response that tried to fight the part of the virus related to how it replicates.
“Theoretically, the production of these antibodies could mean that people are more protected from infection,” said researcher Catherine Le, MD, in a statement. “We also need to investigate if the elevated immune response corresponds with severity or number of long–COVID-19 symptoms.”
Dr. Le is codirector of the COVID-19 Recovery Program at Cedars-Sinai Medical Center in Los Angeles, where the study was conducted.
Study participants agreed in September 2020 to participate in long-term COVID research at Cedars-Sinai. The new analysis was published earlier this year in BMC Infectious Diseases and included 245 people who had long COVID and 86 health care workers who had recovered from COVID but did not have long-term symptoms.
For the study, long COVID was defined as having symptoms that lasted more than 12 weeks. Common long-COVID symptoms are fatigue, shortness of breath, and brain dysfunction such as confusion and forgetfulness.
The authors said it’s unclear why the two groups had different immune responses and also noted that their study was limited by a small sample size. Their research of blood samples is ongoing, with the goals of identifying a way to diagnose long COVID with a laboratory test and of better understanding what causes the condition.
A version of this article first appeared on WebMD.com.
Drive, chip, and putt your way to osteoarthritis relief
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Taking a swing against arthritis
Osteoarthritis is a tough disease to manage. Exercise helps ease the stiffness and pain of the joints, but at the same time, the disease makes it difficult to do that beneficial exercise. Even a relatively simple activity like jogging can hurt more than it helps. If only there were a low-impact exercise that was incredibly popular among the generally older population who are likely to have arthritis.
We love a good golf study here at LOTME, and a group of Australian and U.K. researchers have provided. Osteoarthritis affects 2 million people in the land down under, making it the most common source of disability there. In that population, only 64% reported their physical health to be good, very good, or excellent. Among the 459 golfers with OA that the study authors surveyed, however, the percentage reporting good health rose to more than 90%.
A similar story emerged when they looked at mental health. Nearly a quarter of nongolfers with OA reported high or very high levels of psychological distress, compared with just 8% of golfers. This pattern of improved physical and mental health remained when the researchers looked at the general, non-OA population.
This isn’t the first time golf’s been connected with improved health, and previous studies have shown golf to reduce the risks of cardiovascular disease, diabetes, and obesity, among other things. Just walking one 18-hole round significantly exceeds the CDC’s recommended 150 minutes of physical activity per week. Go out multiple times a week – leaving the cart and beer at home, American golfers – and you’ll be fit for a lifetime.
The golfers on our staff, however, are still waiting for those mental health benefits to kick in. Because when we’re adding up our scorecard after that string of four double bogeys to end the round, we’re most definitely thinking: “Yes, this sport is reducing my psychological distress. I am having fun right now.”
Battle of the sexes’ intestines
There are, we’re sure you’ve noticed, some differences between males and females. Females, for one thing, have longer small intestines than males. Everybody knows that, right? You didn’t know? Really? … Really?
Well, then, we’re guessing you haven’t read “Hidden diversity: Comparative functional morphology of humans and other species” by Erin A. McKenney, PhD, of North Carolina State University, Raleigh, and associates, which just appeared in PeerJ. We couldn’t put it down, even in the shower – a real page-turner/scroller. (It’s a great way to clean a phone, for those who also like to scroll, text, or talk on the toilet.)
The researchers got out their rulers, calipers, and string and took many measurements of the digestive systems of 45 human cadavers (21 female and 24 male), which were compared with data from 10 rats, 10 pigs, and 10 bullfrogs, which had been collected (the measurements, not the animals) by undergraduate students enrolled in a comparative anatomy laboratory course at the university.
There was little intestinal-length variation among the four-legged subjects, but when it comes to humans, females have “consistently and significantly longer small intestines than males,” the investigators noted.
The women’s small intestines, almost 14 feet long on average, were about a foot longer than the men’s, which suggests that women are better able to extract nutrients from food and “supports the canalization hypothesis, which posits that women are better able to survive during periods of stress,” coauthor Amanda Hale said in a written statement from the school. The way to a man’s heart may be through his stomach, but the way to a woman’s heart is through her duodenum, it seems.
Fascinating stuff, to be sure, but the thing that really caught our eye in the PeerJ article was the authors’ suggestion “that organs behave independently of one another, both within and across species.” Organs behaving independently? A somewhat ominous concept, no doubt, but it does explain a lot of the sounds we hear coming from our guts, which can get pretty frightening, especially on chili night.
Dog walking is dangerous business
Yes, you did read that right. A lot of strange things can send you to the emergency department. Go ahead and add dog walking onto that list.
Investigators from Johns Hopkins University estimate that over 422,000 adults presented to U.S. emergency departments with leash-dependent dog walking-related injuries between 2001 and 2020.
With almost 53% of U.S. households owning at least one dog in 2021-2022 in the wake of the COVID pet boom, this kind of occurrence is becoming more common than you think. The annual number of dog-walking injuries more than quadrupled from 7,300 to 32,000 over the course of the study, and the researchers link that spike to the promotion of dog walking for fitness, along with the boost of ownership itself.
The most common injuries listed in the National Electronic Injury Surveillance System database were finger fracture, traumatic brain injury, and shoulder sprain or strain. These mostly involved falls from being pulled, tripped, or tangled up in the leash while walking. For those aged 65 years and older, traumatic brain injury and hip fracture were the most common.
Women were 50% more likely to sustain a fracture than were men, and dog owners aged 65 and older were three times as likely to fall, twice as likely to get a fracture, and 60% more likely to have brain injury than were younger people. Now, that’s not to say younger people don’t also get hurt. After all, dogs aren’t ageists. The researchers have that data but it’s coming out later.
Meanwhile, the pitfalls involved with just trying to get our daily steps in while letting Muffin do her business have us on the lookout for random squirrels.
Proposed Medicare bill would raise docs’ pay with inflation
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Introduced by four physician U.S. House representatives, HR 2474 would link Medicare fee schedule updates to the Medicare Economic Index, a measure of inflation related to physicians’ practice costs and wages.
That’s a long-sought goal of the American Medical Association, which is leading 120 state medical societies and medical specialty groups in championing the bill.
The legislation is essential to enabling physician practices to better absorb payment distributions triggered by budget neutrality rules, performance adjustments, and periods of high inflation, the groups wrote in a joint letter sent to the bill’s sponsors. The sponsors say they hope the legislation will improve access to care, as low reimbursements cause some physicians to limit their number of Medicare patients.
Physicians groups for years have urged federal lawmakers to scrap short-term fixes staving off Medicare pay cuts in favor of permanent reforms. Unlike nearly all other Medicare clinicians including hospitals, physicians’ Medicare payment updates aren’t currently tied to inflation.
Adjusted for inflation, Medicare payments to physicians have declined 26% between 2001 and 2023, including a 2% payment reduction in 2023, according to the AMA. Small and rural physician practices have been disproportionately affected by these reductions, as have doctors treating low-income or uninsured patients, the AMA said.
Last month, an influential federal advisory panel recommended permanently tying Medicare physician pay increases to inflation. Clinicians’ cost of providing services, measured by the Medicare Economic Index, rose by 2.6% in 2021 and are estimated to have risen 4.7% in 2022, significantly more than in recent years, the Medicare Payment Advisory Commission said.
A version of this article originally appeared on Medscape.com.
Surgeons, intensivists earn more than do colleagues from private insurance
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
General and orthopedic surgeons and intensivists earn the highest net reimbursements from private U.S. insurers, a new report estimates.
On average in 2021, they were paid $5.8 million, $4.9 million, and $3.3 million, respectively, according to figures compiled by AMN Healthcare, a Dallas-based health staffing company.
None of 15 other physician specialties topped $3 million in net reimbursement on average, and three – dermatology, pediatrics, and family medicine – didn’t reach $1 million.
The report doesn’t include data about reimbursement from Medicare and Medicaid, and its numbers assume that 50% of insurance claims are denied. Denial rates differ from practice to practice.
Still, the findings offer a “benchmark tool” to help clinicians understand how they rank against their peers, Linda Murphy, president of AMN Healthcare’s Revenue Cycle Solutions division, said in an interview.
This is the first year that the company has calculated physician reimbursement levels by using claim and clearinghouse data, Ms. Murphy said. Previously, a division of the firm compiled data by surveying chief financial officers from hospitals.
The report’s estimate that insurers deny 50% of claims is “conservative,” Ms. Murphy said. Miscoding is a significant factor behind that number.
The estimated 2021 net private insurance reimbursements by specialty for direct services, assuming a 50% denial rate:
- Anesthesiology: $1,665,510
- Cardiology: $1,703,013
- Critical Care (intensivist): $3,338,656
- Dermatology: $729,107
- Family medicine: $697,094
- Gastroenterology: $2,765,110
- Internal medicine: $1,297,200
- Neurology: $1,390,181
- Obstetrician/gynecology: $1,880,888
- Otolaryngology: $2,095,277
- Pediatrics: $661,552
- Psychiatry: $1,348,730
- Pulmonology: $1,561,617
- Radiology: $1,015,750
- Rheumatology: $1,705,140
- General surgery: $5,834,508
- Orthopedic surgery: $4,904,757
- Urology: $2,943,381
Among 18 physician specialties overall, the report estimated that the average net reimbursement in 2021 was $1.9 million.
The report also estimated that the net reimbursement amounts at $875,140 for certified registered nurse anesthetists and $388,696 for nurse practitioners.
Surprisingly, Ms. Murphy said, there’s “a really large swing” among reimbursement levels for individual specialties. The quartile of cardiologists with the lowest level of reimbursement, for example, submitted $2.1 million in claims in 2021, netting about $1 million at a 50% denial rate versus the $7.3 million made by those in the highest quartile, netting about $3.6 million.
The gap seems to be due to regional variations, she said, adding that a rural cardiologist will have different billing practices than does one practicing in New York City.
The quartile of general surgeons with the highest reimbursement levels billed for $21.1 million on average in 2021, making about $10.5 million at a 50% denial rate. The lowest quartile billed for $5.5 million, making about $2.7 million at a 50% denial rate.
The report noted that primary care physicians – that is, family medicine, internal medicine, and pediatrics specialists – have much lower levels of reimbursement, compared with most other specialties. But the work of primary care physicians “may lead to considerable ‘downstream revenue’ through the hospital admissions, tests and treatment they order.”
A previous analysis by a division of AMN Healthcare found that primary care physicians, on average, generate $2,113,273 a year in net annual revenue for their affiliated hospitals, nearing the $2,446,429 in net annual hospital revenue generated by specialists.
AMN Healthcare is preparing another report that will examine Medicare reimbursements, Ms. Murphy said. According to the new report, payments by nonprivate insurers amount to about one-third of the total amount of reimbursement by commercial insurers.
A version of this article originally appeared on Medscape.com.
Long COVID mobile monitoring study hunts for answers
A new federal research project aims to answer lingering questions about long COVID using mobile monitoring devices to help track the condition.
The federally funded RECOVER Initiative expects to give out 10,000 sensors to people with long COVID to collect data in real time.
The hope is that researchers will be able to provide doctors and patients with a wealth of information to address gaps in knowledge about long COVID.
The project takes advantage of the approach other researchers have used to track patients’ health data on heart rate, exercise, and more using mobile monitoring devices such as Fitbits, smartwatches, and other remote sensors.
Researchers believe the initiative could be particularly useful for people with long COVID – whose symptoms come and go. They can use a wristband sensor to passively collect data in real time.
For a condition defined by its symptoms, that kind of data promises to be useful, experts said.
But not everyone has room in their budget for a smartwatch or a fitness tracker. Until recently, most clinical trials were BYOD: Bring your own device. At a time when researchers are trying to make sure that clinical trials reflect the diversity of the population, that leaves a lot of people out.
So, researchers are starting to supply subjects with their own monitors. The RECOVER Initiative expects to give out 10,000 sensors to people who are eligible based on race/ethnicity, income, and other demographic factors (rural residents for example). After 2 months, all people in the RECOVER study over the age of 13 will be eligible for the sensors.
The federal program builds on earlier research at places like The Scripps Institute, a center of research into remote monitoring. The institute supplied 7,000 monitors to people in an arm of the All of Us study, a 5-year-old multisite cohort that aims to collect medical information from 1 million people.
The devices went to people who have been historically underrepresented in biomedical research, said Scripps researchers, who plan to give out more this year.
In March of 2023, Scripps researchers published a study on the tracking data that found a significant post-COVID-19 drop in physical activity. But the data are incomplete because many people can’t always afford these devices. Most of the people in the study were “White, young, and active,” they wrote.
Researchers at an All of Us site at Vanderbilt University, which also used a BYOD approach, realized that they produced biased results. They reported their findings at the Pacific Symposium on Biocomputing in January.
“[The] majority of participants who provided Fitbit data reported being White and employed for wages,” they said. “However, these data represent participants who had their own Fitbit devices and consented to share EHR [electronic health record] data.”
Their solution: The program has begun providing Fitbit devices to all study participants who do not own one or cannot afford one.
Now, the web page for the All of Us study asks visitors to “Learn about the All of Us WEAR study. You could get a Fitbit at no cost! … As a part of the WEAR Study, you could receive a new Fitbit to wear at no cost to you. All of Us will be able to get the data the Fitbit collects. This data may help us understand how behavior impacts health.”
Jennifer Radin, PhD, an epidemiologist at Scripps Research Translational Institute, is heading up the DETECT study, which is a remote monitoring research project that has enrolled over 40,000 people who have their own sensors – be it a smartwatch or Fitbit. She was looking at remote monitoring for disease before COVID emerged.
Dr. Radin said she began researching remote sensing after working in public health and dealing with outdated data collection systems.
“They typically rely on case reports that are recorded by pen and paper and faxed or mailed in,” she said. “Then, they have to be entered into a database. “
In addition to offering objective data on a subject’s physical response to the infection, she said, the data collection can be long-term and continuous.
DETECT collects data on resting heart rate, which is unique to every person, and activity levels. Both measures are meaningful for those with long COVID. Her research found differences in sleep, heart rate, and activity between those with COVID and those without.
Joseph Kvedar, MD, is a Harvard Medical School researcher and the editor of NPJ Digital Medicine. He’s been studying digital health systems and called clinical research a “beachhead” for the use of data from monitors. But he also said problems remain that need to be worked out. The quality of the devices and their Bluetooth connections are better. But different devices measure different things, and a counted step can vary from person to person, he said. And the problems of the early days of electronic health records have not been fully resolved.
“We haven’t gotten to this universal language to connect all these things and make them relevant,” he said.
The All of Us researchers are working with the RECOVER project to address some of those issues. Usually not focused on a single condition, the All of Us researchers are testing a machine-learning approach for identifying long COVID.
A version of this article originally appeared on WebMD.com.
A new federal research project aims to answer lingering questions about long COVID using mobile monitoring devices to help track the condition.
The federally funded RECOVER Initiative expects to give out 10,000 sensors to people with long COVID to collect data in real time.
The hope is that researchers will be able to provide doctors and patients with a wealth of information to address gaps in knowledge about long COVID.
The project takes advantage of the approach other researchers have used to track patients’ health data on heart rate, exercise, and more using mobile monitoring devices such as Fitbits, smartwatches, and other remote sensors.
Researchers believe the initiative could be particularly useful for people with long COVID – whose symptoms come and go. They can use a wristband sensor to passively collect data in real time.
For a condition defined by its symptoms, that kind of data promises to be useful, experts said.
But not everyone has room in their budget for a smartwatch or a fitness tracker. Until recently, most clinical trials were BYOD: Bring your own device. At a time when researchers are trying to make sure that clinical trials reflect the diversity of the population, that leaves a lot of people out.
So, researchers are starting to supply subjects with their own monitors. The RECOVER Initiative expects to give out 10,000 sensors to people who are eligible based on race/ethnicity, income, and other demographic factors (rural residents for example). After 2 months, all people in the RECOVER study over the age of 13 will be eligible for the sensors.
The federal program builds on earlier research at places like The Scripps Institute, a center of research into remote monitoring. The institute supplied 7,000 monitors to people in an arm of the All of Us study, a 5-year-old multisite cohort that aims to collect medical information from 1 million people.
The devices went to people who have been historically underrepresented in biomedical research, said Scripps researchers, who plan to give out more this year.
In March of 2023, Scripps researchers published a study on the tracking data that found a significant post-COVID-19 drop in physical activity. But the data are incomplete because many people can’t always afford these devices. Most of the people in the study were “White, young, and active,” they wrote.
Researchers at an All of Us site at Vanderbilt University, which also used a BYOD approach, realized that they produced biased results. They reported their findings at the Pacific Symposium on Biocomputing in January.
“[The] majority of participants who provided Fitbit data reported being White and employed for wages,” they said. “However, these data represent participants who had their own Fitbit devices and consented to share EHR [electronic health record] data.”
Their solution: The program has begun providing Fitbit devices to all study participants who do not own one or cannot afford one.
Now, the web page for the All of Us study asks visitors to “Learn about the All of Us WEAR study. You could get a Fitbit at no cost! … As a part of the WEAR Study, you could receive a new Fitbit to wear at no cost to you. All of Us will be able to get the data the Fitbit collects. This data may help us understand how behavior impacts health.”
Jennifer Radin, PhD, an epidemiologist at Scripps Research Translational Institute, is heading up the DETECT study, which is a remote monitoring research project that has enrolled over 40,000 people who have their own sensors – be it a smartwatch or Fitbit. She was looking at remote monitoring for disease before COVID emerged.
Dr. Radin said she began researching remote sensing after working in public health and dealing with outdated data collection systems.
“They typically rely on case reports that are recorded by pen and paper and faxed or mailed in,” she said. “Then, they have to be entered into a database. “
In addition to offering objective data on a subject’s physical response to the infection, she said, the data collection can be long-term and continuous.
DETECT collects data on resting heart rate, which is unique to every person, and activity levels. Both measures are meaningful for those with long COVID. Her research found differences in sleep, heart rate, and activity between those with COVID and those without.
Joseph Kvedar, MD, is a Harvard Medical School researcher and the editor of NPJ Digital Medicine. He’s been studying digital health systems and called clinical research a “beachhead” for the use of data from monitors. But he also said problems remain that need to be worked out. The quality of the devices and their Bluetooth connections are better. But different devices measure different things, and a counted step can vary from person to person, he said. And the problems of the early days of electronic health records have not been fully resolved.
“We haven’t gotten to this universal language to connect all these things and make them relevant,” he said.
The All of Us researchers are working with the RECOVER project to address some of those issues. Usually not focused on a single condition, the All of Us researchers are testing a machine-learning approach for identifying long COVID.
A version of this article originally appeared on WebMD.com.
A new federal research project aims to answer lingering questions about long COVID using mobile monitoring devices to help track the condition.
The federally funded RECOVER Initiative expects to give out 10,000 sensors to people with long COVID to collect data in real time.
The hope is that researchers will be able to provide doctors and patients with a wealth of information to address gaps in knowledge about long COVID.
The project takes advantage of the approach other researchers have used to track patients’ health data on heart rate, exercise, and more using mobile monitoring devices such as Fitbits, smartwatches, and other remote sensors.
Researchers believe the initiative could be particularly useful for people with long COVID – whose symptoms come and go. They can use a wristband sensor to passively collect data in real time.
For a condition defined by its symptoms, that kind of data promises to be useful, experts said.
But not everyone has room in their budget for a smartwatch or a fitness tracker. Until recently, most clinical trials were BYOD: Bring your own device. At a time when researchers are trying to make sure that clinical trials reflect the diversity of the population, that leaves a lot of people out.
So, researchers are starting to supply subjects with their own monitors. The RECOVER Initiative expects to give out 10,000 sensors to people who are eligible based on race/ethnicity, income, and other demographic factors (rural residents for example). After 2 months, all people in the RECOVER study over the age of 13 will be eligible for the sensors.
The federal program builds on earlier research at places like The Scripps Institute, a center of research into remote monitoring. The institute supplied 7,000 monitors to people in an arm of the All of Us study, a 5-year-old multisite cohort that aims to collect medical information from 1 million people.
The devices went to people who have been historically underrepresented in biomedical research, said Scripps researchers, who plan to give out more this year.
In March of 2023, Scripps researchers published a study on the tracking data that found a significant post-COVID-19 drop in physical activity. But the data are incomplete because many people can’t always afford these devices. Most of the people in the study were “White, young, and active,” they wrote.
Researchers at an All of Us site at Vanderbilt University, which also used a BYOD approach, realized that they produced biased results. They reported their findings at the Pacific Symposium on Biocomputing in January.
“[The] majority of participants who provided Fitbit data reported being White and employed for wages,” they said. “However, these data represent participants who had their own Fitbit devices and consented to share EHR [electronic health record] data.”
Their solution: The program has begun providing Fitbit devices to all study participants who do not own one or cannot afford one.
Now, the web page for the All of Us study asks visitors to “Learn about the All of Us WEAR study. You could get a Fitbit at no cost! … As a part of the WEAR Study, you could receive a new Fitbit to wear at no cost to you. All of Us will be able to get the data the Fitbit collects. This data may help us understand how behavior impacts health.”
Jennifer Radin, PhD, an epidemiologist at Scripps Research Translational Institute, is heading up the DETECT study, which is a remote monitoring research project that has enrolled over 40,000 people who have their own sensors – be it a smartwatch or Fitbit. She was looking at remote monitoring for disease before COVID emerged.
Dr. Radin said she began researching remote sensing after working in public health and dealing with outdated data collection systems.
“They typically rely on case reports that are recorded by pen and paper and faxed or mailed in,” she said. “Then, they have to be entered into a database. “
In addition to offering objective data on a subject’s physical response to the infection, she said, the data collection can be long-term and continuous.
DETECT collects data on resting heart rate, which is unique to every person, and activity levels. Both measures are meaningful for those with long COVID. Her research found differences in sleep, heart rate, and activity between those with COVID and those without.
Joseph Kvedar, MD, is a Harvard Medical School researcher and the editor of NPJ Digital Medicine. He’s been studying digital health systems and called clinical research a “beachhead” for the use of data from monitors. But he also said problems remain that need to be worked out. The quality of the devices and their Bluetooth connections are better. But different devices measure different things, and a counted step can vary from person to person, he said. And the problems of the early days of electronic health records have not been fully resolved.
“We haven’t gotten to this universal language to connect all these things and make them relevant,” he said.
The All of Us researchers are working with the RECOVER project to address some of those issues. Usually not focused on a single condition, the All of Us researchers are testing a machine-learning approach for identifying long COVID.
A version of this article originally appeared on WebMD.com.