User login
Breast cancer trials enrolling now: Could your patient benefit?
• Menopausal women at moderate risk of developing breast cancer. A phase 2 study sponsored by the National Cancer Institute is seeking women aged 45-60 in late menopause or post menopause who are at “moderate” risk of developing breast cancer. Examples of criteria for moderate risk include prior proliferative disease on breast biopsy or having a first- or second-degree relative who developed breast cancer at aged 60 or younger. Researchers are looking for a signal that bazedoxifene plus conjugated estrogens (Duavee), a hot-flash therapy, could prevent breast cancer in at-risk people. Participants in the active-therapy group will receive once-daily oral medication for 6 months. The control patients will have the option of taking the medication after 6 months. The trial aims to enroll 120 participants. It began recruiting on Dec. 2, 2021, at the University of Kansas Medical Center; sites in California, Illinois, and Massachusetts are planned. The primary outcome is the change in fibroglandular volume. Overall survival (OS) and quality of life (QOL) will not be measured. More details at clinicaltrials.gov.
• Early high-risk nonmetastatic HER2+ breast cancer with no prior treatment. Adults with this type of breast cancer are invited to join a phase 3 trial of trastuzumab deruxtecan (T-DXd; Enhertu) as neoadjuvant therapy. T-DXd is currently approved for patients with advanced disease, so this study could lead to a new indication. Participants will receive standard intravenous regimens of either T-DXd monotherapy; T-DXd followed by paclitaxel (Taxol), trastuzumab (Herceptin), and pertuzumab (Perjeta), referred to as the THP regime; or doxorubicin plus cyclophosphamide followed by THP. The primary outcome is rate of pathologic complete response, and a secondary outcome is OS over approximately 5 years. QOL won’t be measured. The study opened on Oct. 25, 2021, and eventually hopes to recruit 624 participants in 19 countries and 15 U.S. states. More details at clinicaltrials.gov.
“[This is an] important early trial to move trastuzumab deruxtecan to early disease. If successful as monotherapy, this would be a big win for patients,” commented Kathy Miller, MD, professor of oncology and medicine at Indiana University, Indianapolis, a contributor to this news organization. She cautioned that monitoring rates of pneumonitis will be important in this curable setting.
• Locally advanced unresectable or metastatic HER2+ breast cancer with no prior tyrosine-kinase inhibitor therapy. Adult patients with these clinical features are eligible for a phase 3 study that is also testing a drug in an earlier setting than its current label – tucatinib (Tukysa) as first-line anti-HER2 therapy in advanced disease. Tucatinib was approved in April 2020 by the U.S. Food and Drug Administration as second-line therapy in such patients, so this study could also lead to a new indication. Participants in the experimental arm will receive tucatinib tablets twice daily and a combination of trastuzumab and pertuzumab intravenously or subcutaneously every 3 weeks for up to approximately 3 years. Patients in the control arm will take a placebo instead of tucatinib. Seven sites across Florida, Kentucky, Maryland, and South Carolina aim to start recruiting 650 participants on Feb. 28, 2022. The primary outcome is progression-free survival (PFS). OS and QoL will be tracked. More details at clinicaltrials.gov.
“Tucatinib has real activity,” commented Dr. Miller, adding that “we haven’t [yet] found the best way to exploit that activity for our patients.”
• Inoperable or metastatic HR+ HER2– breast cancer after one or two lines of systemic chemotherapy. Adults with this type of breast cancer are being recruited for a phase 3 study to compare datopotamab deruxtecan (Dato-DXd), an experimental antibody-drug conjugate (ADC), against a range of standard single-agent chemotherapies. Participants will receive either intravenous Dato-DXd or investigator’s choice of one of four chemotherapies: oral capecitabine (Xeloda), IV gemcitabine (Gemzar), IV eribulin (Halaven), or IV vinorelbine (Navelbine). The trial began recruiting for 700 participants at sites worldwide on Oct. 18, 2021. U.S. sites are in Michigan and California; trial centers in 15 other states are planned. Primary outcomes are OS over approximately 3.5 years and PFS over approximately 2 years. QOL is tracked. More details at clinicaltrials.gov.
Commenting on this trial, Dr. Miller said: “ADCs will play an expanded role in our management. This may be one of the first to move into the ER+ population.”
• Advanced ER+, HER2– breast cancer. Adult patients with this type of cancer can join a phase 3 trial testing oral imlunestrant, an experimental selective estrogen-receptor degrader (SERD), against standard endocrine therapy. For up to 3 years, people in the study will take either daily tablets of imlunestrant or once-daily pills of imlunestrant and another SERD, abemaciclib (Verzenio). A third group of participants will receive their investigator’s choice of either daily tablets of exemestane (Aromasin) or monthly intramuscular injections of fulvestrant (Faslodex). The study opened to 800 participants on Oct. 4, 2021, at sites in 11 U.S. states and worldwide. The primary outcome is PFS over approximately 3 years; 5-year OS is a secondary outcome. QOL is not assessed. More details at clinicaltrials.gov
Dr. Miller predicted that “oral SERDs will replace fulvestrant in the future: We already have positive phase 3 data with elacestrant.”
Dr. Miller has a regular column with this news organization, Miller on Oncology. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
• Menopausal women at moderate risk of developing breast cancer. A phase 2 study sponsored by the National Cancer Institute is seeking women aged 45-60 in late menopause or post menopause who are at “moderate” risk of developing breast cancer. Examples of criteria for moderate risk include prior proliferative disease on breast biopsy or having a first- or second-degree relative who developed breast cancer at aged 60 or younger. Researchers are looking for a signal that bazedoxifene plus conjugated estrogens (Duavee), a hot-flash therapy, could prevent breast cancer in at-risk people. Participants in the active-therapy group will receive once-daily oral medication for 6 months. The control patients will have the option of taking the medication after 6 months. The trial aims to enroll 120 participants. It began recruiting on Dec. 2, 2021, at the University of Kansas Medical Center; sites in California, Illinois, and Massachusetts are planned. The primary outcome is the change in fibroglandular volume. Overall survival (OS) and quality of life (QOL) will not be measured. More details at clinicaltrials.gov.
• Early high-risk nonmetastatic HER2+ breast cancer with no prior treatment. Adults with this type of breast cancer are invited to join a phase 3 trial of trastuzumab deruxtecan (T-DXd; Enhertu) as neoadjuvant therapy. T-DXd is currently approved for patients with advanced disease, so this study could lead to a new indication. Participants will receive standard intravenous regimens of either T-DXd monotherapy; T-DXd followed by paclitaxel (Taxol), trastuzumab (Herceptin), and pertuzumab (Perjeta), referred to as the THP regime; or doxorubicin plus cyclophosphamide followed by THP. The primary outcome is rate of pathologic complete response, and a secondary outcome is OS over approximately 5 years. QOL won’t be measured. The study opened on Oct. 25, 2021, and eventually hopes to recruit 624 participants in 19 countries and 15 U.S. states. More details at clinicaltrials.gov.
“[This is an] important early trial to move trastuzumab deruxtecan to early disease. If successful as monotherapy, this would be a big win for patients,” commented Kathy Miller, MD, professor of oncology and medicine at Indiana University, Indianapolis, a contributor to this news organization. She cautioned that monitoring rates of pneumonitis will be important in this curable setting.
• Locally advanced unresectable or metastatic HER2+ breast cancer with no prior tyrosine-kinase inhibitor therapy. Adult patients with these clinical features are eligible for a phase 3 study that is also testing a drug in an earlier setting than its current label – tucatinib (Tukysa) as first-line anti-HER2 therapy in advanced disease. Tucatinib was approved in April 2020 by the U.S. Food and Drug Administration as second-line therapy in such patients, so this study could also lead to a new indication. Participants in the experimental arm will receive tucatinib tablets twice daily and a combination of trastuzumab and pertuzumab intravenously or subcutaneously every 3 weeks for up to approximately 3 years. Patients in the control arm will take a placebo instead of tucatinib. Seven sites across Florida, Kentucky, Maryland, and South Carolina aim to start recruiting 650 participants on Feb. 28, 2022. The primary outcome is progression-free survival (PFS). OS and QoL will be tracked. More details at clinicaltrials.gov.
“Tucatinib has real activity,” commented Dr. Miller, adding that “we haven’t [yet] found the best way to exploit that activity for our patients.”
• Inoperable or metastatic HR+ HER2– breast cancer after one or two lines of systemic chemotherapy. Adults with this type of breast cancer are being recruited for a phase 3 study to compare datopotamab deruxtecan (Dato-DXd), an experimental antibody-drug conjugate (ADC), against a range of standard single-agent chemotherapies. Participants will receive either intravenous Dato-DXd or investigator’s choice of one of four chemotherapies: oral capecitabine (Xeloda), IV gemcitabine (Gemzar), IV eribulin (Halaven), or IV vinorelbine (Navelbine). The trial began recruiting for 700 participants at sites worldwide on Oct. 18, 2021. U.S. sites are in Michigan and California; trial centers in 15 other states are planned. Primary outcomes are OS over approximately 3.5 years and PFS over approximately 2 years. QOL is tracked. More details at clinicaltrials.gov.
Commenting on this trial, Dr. Miller said: “ADCs will play an expanded role in our management. This may be one of the first to move into the ER+ population.”
• Advanced ER+, HER2– breast cancer. Adult patients with this type of cancer can join a phase 3 trial testing oral imlunestrant, an experimental selective estrogen-receptor degrader (SERD), against standard endocrine therapy. For up to 3 years, people in the study will take either daily tablets of imlunestrant or once-daily pills of imlunestrant and another SERD, abemaciclib (Verzenio). A third group of participants will receive their investigator’s choice of either daily tablets of exemestane (Aromasin) or monthly intramuscular injections of fulvestrant (Faslodex). The study opened to 800 participants on Oct. 4, 2021, at sites in 11 U.S. states and worldwide. The primary outcome is PFS over approximately 3 years; 5-year OS is a secondary outcome. QOL is not assessed. More details at clinicaltrials.gov
Dr. Miller predicted that “oral SERDs will replace fulvestrant in the future: We already have positive phase 3 data with elacestrant.”
Dr. Miller has a regular column with this news organization, Miller on Oncology. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
• Menopausal women at moderate risk of developing breast cancer. A phase 2 study sponsored by the National Cancer Institute is seeking women aged 45-60 in late menopause or post menopause who are at “moderate” risk of developing breast cancer. Examples of criteria for moderate risk include prior proliferative disease on breast biopsy or having a first- or second-degree relative who developed breast cancer at aged 60 or younger. Researchers are looking for a signal that bazedoxifene plus conjugated estrogens (Duavee), a hot-flash therapy, could prevent breast cancer in at-risk people. Participants in the active-therapy group will receive once-daily oral medication for 6 months. The control patients will have the option of taking the medication after 6 months. The trial aims to enroll 120 participants. It began recruiting on Dec. 2, 2021, at the University of Kansas Medical Center; sites in California, Illinois, and Massachusetts are planned. The primary outcome is the change in fibroglandular volume. Overall survival (OS) and quality of life (QOL) will not be measured. More details at clinicaltrials.gov.
• Early high-risk nonmetastatic HER2+ breast cancer with no prior treatment. Adults with this type of breast cancer are invited to join a phase 3 trial of trastuzumab deruxtecan (T-DXd; Enhertu) as neoadjuvant therapy. T-DXd is currently approved for patients with advanced disease, so this study could lead to a new indication. Participants will receive standard intravenous regimens of either T-DXd monotherapy; T-DXd followed by paclitaxel (Taxol), trastuzumab (Herceptin), and pertuzumab (Perjeta), referred to as the THP regime; or doxorubicin plus cyclophosphamide followed by THP. The primary outcome is rate of pathologic complete response, and a secondary outcome is OS over approximately 5 years. QOL won’t be measured. The study opened on Oct. 25, 2021, and eventually hopes to recruit 624 participants in 19 countries and 15 U.S. states. More details at clinicaltrials.gov.
“[This is an] important early trial to move trastuzumab deruxtecan to early disease. If successful as monotherapy, this would be a big win for patients,” commented Kathy Miller, MD, professor of oncology and medicine at Indiana University, Indianapolis, a contributor to this news organization. She cautioned that monitoring rates of pneumonitis will be important in this curable setting.
• Locally advanced unresectable or metastatic HER2+ breast cancer with no prior tyrosine-kinase inhibitor therapy. Adult patients with these clinical features are eligible for a phase 3 study that is also testing a drug in an earlier setting than its current label – tucatinib (Tukysa) as first-line anti-HER2 therapy in advanced disease. Tucatinib was approved in April 2020 by the U.S. Food and Drug Administration as second-line therapy in such patients, so this study could also lead to a new indication. Participants in the experimental arm will receive tucatinib tablets twice daily and a combination of trastuzumab and pertuzumab intravenously or subcutaneously every 3 weeks for up to approximately 3 years. Patients in the control arm will take a placebo instead of tucatinib. Seven sites across Florida, Kentucky, Maryland, and South Carolina aim to start recruiting 650 participants on Feb. 28, 2022. The primary outcome is progression-free survival (PFS). OS and QoL will be tracked. More details at clinicaltrials.gov.
“Tucatinib has real activity,” commented Dr. Miller, adding that “we haven’t [yet] found the best way to exploit that activity for our patients.”
• Inoperable or metastatic HR+ HER2– breast cancer after one or two lines of systemic chemotherapy. Adults with this type of breast cancer are being recruited for a phase 3 study to compare datopotamab deruxtecan (Dato-DXd), an experimental antibody-drug conjugate (ADC), against a range of standard single-agent chemotherapies. Participants will receive either intravenous Dato-DXd or investigator’s choice of one of four chemotherapies: oral capecitabine (Xeloda), IV gemcitabine (Gemzar), IV eribulin (Halaven), or IV vinorelbine (Navelbine). The trial began recruiting for 700 participants at sites worldwide on Oct. 18, 2021. U.S. sites are in Michigan and California; trial centers in 15 other states are planned. Primary outcomes are OS over approximately 3.5 years and PFS over approximately 2 years. QOL is tracked. More details at clinicaltrials.gov.
Commenting on this trial, Dr. Miller said: “ADCs will play an expanded role in our management. This may be one of the first to move into the ER+ population.”
• Advanced ER+, HER2– breast cancer. Adult patients with this type of cancer can join a phase 3 trial testing oral imlunestrant, an experimental selective estrogen-receptor degrader (SERD), against standard endocrine therapy. For up to 3 years, people in the study will take either daily tablets of imlunestrant or once-daily pills of imlunestrant and another SERD, abemaciclib (Verzenio). A third group of participants will receive their investigator’s choice of either daily tablets of exemestane (Aromasin) or monthly intramuscular injections of fulvestrant (Faslodex). The study opened to 800 participants on Oct. 4, 2021, at sites in 11 U.S. states and worldwide. The primary outcome is PFS over approximately 3 years; 5-year OS is a secondary outcome. QOL is not assessed. More details at clinicaltrials.gov
Dr. Miller predicted that “oral SERDs will replace fulvestrant in the future: We already have positive phase 3 data with elacestrant.”
Dr. Miller has a regular column with this news organization, Miller on Oncology. She has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
Experimental breast cancer immunotherapy treatment passes important hurdle in pilot study
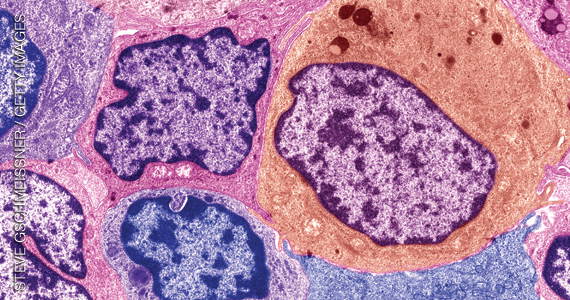
Three of 6 patients treated had a response, including one that lasted more than five years. TILs were expanded ex vivo, and patients treated with lymphodepleting chemotherapy before the infusion, along with the checkpoint inhibitor pembrolizumab (Keytruda, Merck).
The results pave the way for recruitment of more patients as researchers at the National Cancer Institute ramp up the experimental treatment. They also help to overturn the long-held dogma that breast cancer is not immunogenic, according to lead researcher Steven A. Rosenberg, MD, PhD, who is chief of the surgery branch of the National Cancer Institute.
Although common hormone positive breast cancer doesn’t respond to immunotherapy, the study found that two-thirds of patients with metastatic breast cancer have mutations recognized by TILs. “We can identify the antigens [that] T cells recognize,” said Dr. Rosenberg, who is the lead author on a paper describing the pilot study, published online Feb. 1 in the Journal of Clinical Oncology.
There has been wide speculation that some solid tumors, including common hormone-positive breast cancers, are not immunogenic, because they don’t respond to cancer vaccines or checkpoint inhibitors. However, newer research has unearthed an explanation: Patients with these solid tumors produce immunogenic antigens, but they differ from patient to patient. There was not a single shared antigen among the 42 patients in the study. “Every patient reacts with a unique antigen, so the treatments have to be highly personalized,” said Dr. Rosenberg.
In the phase 2 study, the researchers recruited 42 participants, who underwent screening for novel tumor antigens. Sixty percent were hormone-receptor positive and HER2 negative, 26% were triple negative, and 14% were HER2 enriched.
Of 42 patients, 28 (67%) had at least one detectable, immunogenic tumor antigen, including 46% of HR+/Her2– patients, 32% of triple-negative patients, and 21% of HER2-enriched patients. Thirteen patients had a positive TIL screen, making them candidates for treatment.
Six patients underwent the procedure. Researchers selected TIL culture fragments that responded when stimulated with mutant peptides. They expanded those cells externally over 24 days and then administered lymphodepleting chemotherapy 1 week before the infusion of the expanded TILs. Patients received aldesleukin (Proleukin, Prometheus Laboratories) every 8 hours after TIL infusion, as tolerated. Patients also received pembrolizumab 2 days before the TIL infusion and up to three more doses at 3-week intervals.
Three patients experienced objective tumor regression, including a complete response that has lasted for 5.5 years. Two had partial responses that lasted 6 and 10 months. One patient with a partial response had a limited recurrence that could be excised, followed by further regression of other lesions, and was disease free 2 years after treatment.
The National Cancer Institute has just constructed a new building on the National Institutes of Health campus to pursue this research, and Dr. Rosenberg is actively recruiting patients to further study the treatment protocol. “We’re prepared to start treating large numbers of breast cancer patients with this. It’s highly experimental, it needs to be improved, it’s not ready for primetime. But we have now a signal that it can work,” said Dr. Rosenberg.
The study was funded by the National Cancer Institute. Dr. Rosenberg has received research funding from Kite, Iovance Biotherapeutics, and ZIOPHARM Oncology.
Three of 6 patients treated had a response, including one that lasted more than five years. TILs were expanded ex vivo, and patients treated with lymphodepleting chemotherapy before the infusion, along with the checkpoint inhibitor pembrolizumab (Keytruda, Merck).
The results pave the way for recruitment of more patients as researchers at the National Cancer Institute ramp up the experimental treatment. They also help to overturn the long-held dogma that breast cancer is not immunogenic, according to lead researcher Steven A. Rosenberg, MD, PhD, who is chief of the surgery branch of the National Cancer Institute.
Although common hormone positive breast cancer doesn’t respond to immunotherapy, the study found that two-thirds of patients with metastatic breast cancer have mutations recognized by TILs. “We can identify the antigens [that] T cells recognize,” said Dr. Rosenberg, who is the lead author on a paper describing the pilot study, published online Feb. 1 in the Journal of Clinical Oncology.
There has been wide speculation that some solid tumors, including common hormone-positive breast cancers, are not immunogenic, because they don’t respond to cancer vaccines or checkpoint inhibitors. However, newer research has unearthed an explanation: Patients with these solid tumors produce immunogenic antigens, but they differ from patient to patient. There was not a single shared antigen among the 42 patients in the study. “Every patient reacts with a unique antigen, so the treatments have to be highly personalized,” said Dr. Rosenberg.
In the phase 2 study, the researchers recruited 42 participants, who underwent screening for novel tumor antigens. Sixty percent were hormone-receptor positive and HER2 negative, 26% were triple negative, and 14% were HER2 enriched.
Of 42 patients, 28 (67%) had at least one detectable, immunogenic tumor antigen, including 46% of HR+/Her2– patients, 32% of triple-negative patients, and 21% of HER2-enriched patients. Thirteen patients had a positive TIL screen, making them candidates for treatment.
Six patients underwent the procedure. Researchers selected TIL culture fragments that responded when stimulated with mutant peptides. They expanded those cells externally over 24 days and then administered lymphodepleting chemotherapy 1 week before the infusion of the expanded TILs. Patients received aldesleukin (Proleukin, Prometheus Laboratories) every 8 hours after TIL infusion, as tolerated. Patients also received pembrolizumab 2 days before the TIL infusion and up to three more doses at 3-week intervals.
Three patients experienced objective tumor regression, including a complete response that has lasted for 5.5 years. Two had partial responses that lasted 6 and 10 months. One patient with a partial response had a limited recurrence that could be excised, followed by further regression of other lesions, and was disease free 2 years after treatment.
The National Cancer Institute has just constructed a new building on the National Institutes of Health campus to pursue this research, and Dr. Rosenberg is actively recruiting patients to further study the treatment protocol. “We’re prepared to start treating large numbers of breast cancer patients with this. It’s highly experimental, it needs to be improved, it’s not ready for primetime. But we have now a signal that it can work,” said Dr. Rosenberg.
The study was funded by the National Cancer Institute. Dr. Rosenberg has received research funding from Kite, Iovance Biotherapeutics, and ZIOPHARM Oncology.
Three of 6 patients treated had a response, including one that lasted more than five years. TILs were expanded ex vivo, and patients treated with lymphodepleting chemotherapy before the infusion, along with the checkpoint inhibitor pembrolizumab (Keytruda, Merck).
The results pave the way for recruitment of more patients as researchers at the National Cancer Institute ramp up the experimental treatment. They also help to overturn the long-held dogma that breast cancer is not immunogenic, according to lead researcher Steven A. Rosenberg, MD, PhD, who is chief of the surgery branch of the National Cancer Institute.
Although common hormone positive breast cancer doesn’t respond to immunotherapy, the study found that two-thirds of patients with metastatic breast cancer have mutations recognized by TILs. “We can identify the antigens [that] T cells recognize,” said Dr. Rosenberg, who is the lead author on a paper describing the pilot study, published online Feb. 1 in the Journal of Clinical Oncology.
There has been wide speculation that some solid tumors, including common hormone-positive breast cancers, are not immunogenic, because they don’t respond to cancer vaccines or checkpoint inhibitors. However, newer research has unearthed an explanation: Patients with these solid tumors produce immunogenic antigens, but they differ from patient to patient. There was not a single shared antigen among the 42 patients in the study. “Every patient reacts with a unique antigen, so the treatments have to be highly personalized,” said Dr. Rosenberg.
In the phase 2 study, the researchers recruited 42 participants, who underwent screening for novel tumor antigens. Sixty percent were hormone-receptor positive and HER2 negative, 26% were triple negative, and 14% were HER2 enriched.
Of 42 patients, 28 (67%) had at least one detectable, immunogenic tumor antigen, including 46% of HR+/Her2– patients, 32% of triple-negative patients, and 21% of HER2-enriched patients. Thirteen patients had a positive TIL screen, making them candidates for treatment.
Six patients underwent the procedure. Researchers selected TIL culture fragments that responded when stimulated with mutant peptides. They expanded those cells externally over 24 days and then administered lymphodepleting chemotherapy 1 week before the infusion of the expanded TILs. Patients received aldesleukin (Proleukin, Prometheus Laboratories) every 8 hours after TIL infusion, as tolerated. Patients also received pembrolizumab 2 days before the TIL infusion and up to three more doses at 3-week intervals.
Three patients experienced objective tumor regression, including a complete response that has lasted for 5.5 years. Two had partial responses that lasted 6 and 10 months. One patient with a partial response had a limited recurrence that could be excised, followed by further regression of other lesions, and was disease free 2 years after treatment.
The National Cancer Institute has just constructed a new building on the National Institutes of Health campus to pursue this research, and Dr. Rosenberg is actively recruiting patients to further study the treatment protocol. “We’re prepared to start treating large numbers of breast cancer patients with this. It’s highly experimental, it needs to be improved, it’s not ready for primetime. But we have now a signal that it can work,” said Dr. Rosenberg.
The study was funded by the National Cancer Institute. Dr. Rosenberg has received research funding from Kite, Iovance Biotherapeutics, and ZIOPHARM Oncology.
FROM JOURNAL OF CLINICAL ONCOLOGY
Brain tumors exact higher mortality toll in men than women
And, researchers say, it’s not exactly clear why.
Differences in treatment may mediate some of the association, but biologic sex itself appears to be a stronger risk factor for death, according to the study published online Feb. 8 in Cancer.
The excess in male deaths is “concerning, and we need more clinical data and more biological tumor data within each histologic type of brain tumor to understand why these young adult men who would be otherwise healthy are dying of these brain tumors,” study author Lindsay Williams, PhD, MPH, with the division of epidemiology and clinical research, University of Minnesota, Minneapolis, told this news organization.
Central nervous system tumors rank among the top five cancers diagnosed in young adults aged 20-39 years.
Dr. Williams and her colleagues previously showed that men are more likely to develop brain tumors. Their latest study shows that men die more frequently from brain tumors as well.
Using the National Cancer Database, they identified 47,560 young adults aged 20-39 (47% male) diagnosed with a CNS tumor between 2004 and 2016.
After adjusting for relevant factors, males had a 47% increased risk of dying after a brain tumor diagnosis compared with females (hazard ratio, 1.47; 95% confidence interval, 1.41-1.53).
Males had significantly worse overall survival than females for all CNS tumors combined and for nine of 16 histologic types – namely, diffuse astrocytoma (HR, 1.30), anaplastic astrocytoma (HR, 1.25), glioblastoma (HR, 1.14), oligodendroglioma (HR, 1.37), oligoastrocytic tumors (HR, 1.22), ependymal tumors (HR, 1.29), other malignant gliomas (HR, 1.43), neuronal and mixed neuronal-glial tumors (HR, 1.52), and meningioma (HR, 2.01; all P < .05).
The researchers identified no histologies where females had worse survival.
Five-year survival differed between females and males by at least 5% for all histologies combined (83.2% female and 71.2% male) as well as for diffuse astrocytoma (75.1% vs. 68.5%), anaplastic astrocytoma (63.5% vs. 57.5%), oligoastrocytic tumors (80.2% vs. 74.7%), other malignant gliomas (74.1% vs. 64.9%), and germ cell tumors (92.4% vs. 86.5%).
The researchers estimated that had survival in men been equal to that of women over the study period, 20% of total deaths and 34% of male deaths could have been avoided.
They say future population-based studies are needed to confirm these findings and determine whether tumor biology or responses to therapy are driving forces of the observed male excess in death from brain tumors.
“We cannot discount the role of sex differences in diagnosis, treatment, or behavioral risk factors that may underlie the better survival for women after a brain tumor diagnosis,” they write.
“Hopefully, our research will increase awareness of sex differences in brain tumor outcomes in young adults and encourage other researchers with similar datasets to look at this same question and see if they observe a similar trend,” Dr. Williams said in an interview.
The study was supported by the National Cancer Institute. Dr. Williams has no relevant disclosures. One author, Christopher L. Moertel, MD, is chief medical officer for OX2 Therapeutics, has stock in OX2 Therapeutics, and reports patents relevant to his relationship with OX2 Therapeutics.
A version of this article first appeared on Medscape.com.
And, researchers say, it’s not exactly clear why.
Differences in treatment may mediate some of the association, but biologic sex itself appears to be a stronger risk factor for death, according to the study published online Feb. 8 in Cancer.
The excess in male deaths is “concerning, and we need more clinical data and more biological tumor data within each histologic type of brain tumor to understand why these young adult men who would be otherwise healthy are dying of these brain tumors,” study author Lindsay Williams, PhD, MPH, with the division of epidemiology and clinical research, University of Minnesota, Minneapolis, told this news organization.
Central nervous system tumors rank among the top five cancers diagnosed in young adults aged 20-39 years.
Dr. Williams and her colleagues previously showed that men are more likely to develop brain tumors. Their latest study shows that men die more frequently from brain tumors as well.
Using the National Cancer Database, they identified 47,560 young adults aged 20-39 (47% male) diagnosed with a CNS tumor between 2004 and 2016.
After adjusting for relevant factors, males had a 47% increased risk of dying after a brain tumor diagnosis compared with females (hazard ratio, 1.47; 95% confidence interval, 1.41-1.53).
Males had significantly worse overall survival than females for all CNS tumors combined and for nine of 16 histologic types – namely, diffuse astrocytoma (HR, 1.30), anaplastic astrocytoma (HR, 1.25), glioblastoma (HR, 1.14), oligodendroglioma (HR, 1.37), oligoastrocytic tumors (HR, 1.22), ependymal tumors (HR, 1.29), other malignant gliomas (HR, 1.43), neuronal and mixed neuronal-glial tumors (HR, 1.52), and meningioma (HR, 2.01; all P < .05).
The researchers identified no histologies where females had worse survival.
Five-year survival differed between females and males by at least 5% for all histologies combined (83.2% female and 71.2% male) as well as for diffuse astrocytoma (75.1% vs. 68.5%), anaplastic astrocytoma (63.5% vs. 57.5%), oligoastrocytic tumors (80.2% vs. 74.7%), other malignant gliomas (74.1% vs. 64.9%), and germ cell tumors (92.4% vs. 86.5%).
The researchers estimated that had survival in men been equal to that of women over the study period, 20% of total deaths and 34% of male deaths could have been avoided.
They say future population-based studies are needed to confirm these findings and determine whether tumor biology or responses to therapy are driving forces of the observed male excess in death from brain tumors.
“We cannot discount the role of sex differences in diagnosis, treatment, or behavioral risk factors that may underlie the better survival for women after a brain tumor diagnosis,” they write.
“Hopefully, our research will increase awareness of sex differences in brain tumor outcomes in young adults and encourage other researchers with similar datasets to look at this same question and see if they observe a similar trend,” Dr. Williams said in an interview.
The study was supported by the National Cancer Institute. Dr. Williams has no relevant disclosures. One author, Christopher L. Moertel, MD, is chief medical officer for OX2 Therapeutics, has stock in OX2 Therapeutics, and reports patents relevant to his relationship with OX2 Therapeutics.
A version of this article first appeared on Medscape.com.
And, researchers say, it’s not exactly clear why.
Differences in treatment may mediate some of the association, but biologic sex itself appears to be a stronger risk factor for death, according to the study published online Feb. 8 in Cancer.
The excess in male deaths is “concerning, and we need more clinical data and more biological tumor data within each histologic type of brain tumor to understand why these young adult men who would be otherwise healthy are dying of these brain tumors,” study author Lindsay Williams, PhD, MPH, with the division of epidemiology and clinical research, University of Minnesota, Minneapolis, told this news organization.
Central nervous system tumors rank among the top five cancers diagnosed in young adults aged 20-39 years.
Dr. Williams and her colleagues previously showed that men are more likely to develop brain tumors. Their latest study shows that men die more frequently from brain tumors as well.
Using the National Cancer Database, they identified 47,560 young adults aged 20-39 (47% male) diagnosed with a CNS tumor between 2004 and 2016.
After adjusting for relevant factors, males had a 47% increased risk of dying after a brain tumor diagnosis compared with females (hazard ratio, 1.47; 95% confidence interval, 1.41-1.53).
Males had significantly worse overall survival than females for all CNS tumors combined and for nine of 16 histologic types – namely, diffuse astrocytoma (HR, 1.30), anaplastic astrocytoma (HR, 1.25), glioblastoma (HR, 1.14), oligodendroglioma (HR, 1.37), oligoastrocytic tumors (HR, 1.22), ependymal tumors (HR, 1.29), other malignant gliomas (HR, 1.43), neuronal and mixed neuronal-glial tumors (HR, 1.52), and meningioma (HR, 2.01; all P < .05).
The researchers identified no histologies where females had worse survival.
Five-year survival differed between females and males by at least 5% for all histologies combined (83.2% female and 71.2% male) as well as for diffuse astrocytoma (75.1% vs. 68.5%), anaplastic astrocytoma (63.5% vs. 57.5%), oligoastrocytic tumors (80.2% vs. 74.7%), other malignant gliomas (74.1% vs. 64.9%), and germ cell tumors (92.4% vs. 86.5%).
The researchers estimated that had survival in men been equal to that of women over the study period, 20% of total deaths and 34% of male deaths could have been avoided.
They say future population-based studies are needed to confirm these findings and determine whether tumor biology or responses to therapy are driving forces of the observed male excess in death from brain tumors.
“We cannot discount the role of sex differences in diagnosis, treatment, or behavioral risk factors that may underlie the better survival for women after a brain tumor diagnosis,” they write.
“Hopefully, our research will increase awareness of sex differences in brain tumor outcomes in young adults and encourage other researchers with similar datasets to look at this same question and see if they observe a similar trend,” Dr. Williams said in an interview.
The study was supported by the National Cancer Institute. Dr. Williams has no relevant disclosures. One author, Christopher L. Moertel, MD, is chief medical officer for OX2 Therapeutics, has stock in OX2 Therapeutics, and reports patents relevant to his relationship with OX2 Therapeutics.
A version of this article first appeared on Medscape.com.
FROM CANCER
Increase in late-stage cancer diagnoses after pandemic
at Moores Cancer Center in La Jolla, Calif., according to a research letter in JAMA Network Open.
“The number of patients presenting at late, incurable stages is increasing,” say the authors, led by Jade Zifei Zhou, MD, PhD, a hematology/oncology fellow at the center, which is affiliated with the University of California, San Diego.
As the pandemic unfolded and much of routine medicine was put on hold, the postponement or delay in mammograms, colonoscopies, and other screenings led many cancer experts to warn of trouble ahead. In June 2020, for instance, the National Cancer Institute predicted tens of thousands of excess cancer deaths through 2030 because of missed screenings and delays in care.
The message now, Dr. Zhou and colleagues say, is that “patients who have delayed preventative care during the pandemic should be encouraged to resume treatment as soon as possible.”
The team compared the number of people presenting to their cancer center with stage I and IV disease, either for a new diagnosis or a second opinion, during 2019 and with the number during 2020, the first year of the pandemic. The review included over 500 patients, almost 90% of whom were women aged 58 years on average.
While 63.9% of patients with breast cancer presented with stage I disease in 2019, 51.3% did so in 2020. Conversely, while just 1.9% presented with stage IV breast cancer in 2019, the number went up to 6.2% in 2020.
The numbers were even worse from January through March 2021, with only 41.9% of women presenting with stage I and 8% presenting with stage IV breast cancer.
It was the same story for colon cancer, but because of smaller numbers, the findings were not statistically significant.
After the start of the pandemic, the number of patients presenting with stage I colon cancer fell from 17.8% (eight patients) to 14.6% (six patients), while stage IV presentations climbed from 6.7% (three) to 19.5% (eight).
Across all cancer types, stage I presentations fell from 31.9% in 2019 to 29% in 2020, while stage IV presentations rose from 26% to 26.4%.
One of the study limitations is that the patients who came in for a second opinion could have been newly diagnosed but might also have been referred for refractory disease, the authors comment.
No funding for this study was reported. Senior author Kathryn Ann Gold, MD, reported personal fees from AstraZeneca, Takeda, Rakuten, and Regeneron as well as grants from Pfizer and Pharmacyclics.
A version of this article first appeared on Medscape.com.
at Moores Cancer Center in La Jolla, Calif., according to a research letter in JAMA Network Open.
“The number of patients presenting at late, incurable stages is increasing,” say the authors, led by Jade Zifei Zhou, MD, PhD, a hematology/oncology fellow at the center, which is affiliated with the University of California, San Diego.
As the pandemic unfolded and much of routine medicine was put on hold, the postponement or delay in mammograms, colonoscopies, and other screenings led many cancer experts to warn of trouble ahead. In June 2020, for instance, the National Cancer Institute predicted tens of thousands of excess cancer deaths through 2030 because of missed screenings and delays in care.
The message now, Dr. Zhou and colleagues say, is that “patients who have delayed preventative care during the pandemic should be encouraged to resume treatment as soon as possible.”
The team compared the number of people presenting to their cancer center with stage I and IV disease, either for a new diagnosis or a second opinion, during 2019 and with the number during 2020, the first year of the pandemic. The review included over 500 patients, almost 90% of whom were women aged 58 years on average.
While 63.9% of patients with breast cancer presented with stage I disease in 2019, 51.3% did so in 2020. Conversely, while just 1.9% presented with stage IV breast cancer in 2019, the number went up to 6.2% in 2020.
The numbers were even worse from January through March 2021, with only 41.9% of women presenting with stage I and 8% presenting with stage IV breast cancer.
It was the same story for colon cancer, but because of smaller numbers, the findings were not statistically significant.
After the start of the pandemic, the number of patients presenting with stage I colon cancer fell from 17.8% (eight patients) to 14.6% (six patients), while stage IV presentations climbed from 6.7% (three) to 19.5% (eight).
Across all cancer types, stage I presentations fell from 31.9% in 2019 to 29% in 2020, while stage IV presentations rose from 26% to 26.4%.
One of the study limitations is that the patients who came in for a second opinion could have been newly diagnosed but might also have been referred for refractory disease, the authors comment.
No funding for this study was reported. Senior author Kathryn Ann Gold, MD, reported personal fees from AstraZeneca, Takeda, Rakuten, and Regeneron as well as grants from Pfizer and Pharmacyclics.
A version of this article first appeared on Medscape.com.
at Moores Cancer Center in La Jolla, Calif., according to a research letter in JAMA Network Open.
“The number of patients presenting at late, incurable stages is increasing,” say the authors, led by Jade Zifei Zhou, MD, PhD, a hematology/oncology fellow at the center, which is affiliated with the University of California, San Diego.
As the pandemic unfolded and much of routine medicine was put on hold, the postponement or delay in mammograms, colonoscopies, and other screenings led many cancer experts to warn of trouble ahead. In June 2020, for instance, the National Cancer Institute predicted tens of thousands of excess cancer deaths through 2030 because of missed screenings and delays in care.
The message now, Dr. Zhou and colleagues say, is that “patients who have delayed preventative care during the pandemic should be encouraged to resume treatment as soon as possible.”
The team compared the number of people presenting to their cancer center with stage I and IV disease, either for a new diagnosis or a second opinion, during 2019 and with the number during 2020, the first year of the pandemic. The review included over 500 patients, almost 90% of whom were women aged 58 years on average.
While 63.9% of patients with breast cancer presented with stage I disease in 2019, 51.3% did so in 2020. Conversely, while just 1.9% presented with stage IV breast cancer in 2019, the number went up to 6.2% in 2020.
The numbers were even worse from January through March 2021, with only 41.9% of women presenting with stage I and 8% presenting with stage IV breast cancer.
It was the same story for colon cancer, but because of smaller numbers, the findings were not statistically significant.
After the start of the pandemic, the number of patients presenting with stage I colon cancer fell from 17.8% (eight patients) to 14.6% (six patients), while stage IV presentations climbed from 6.7% (three) to 19.5% (eight).
Across all cancer types, stage I presentations fell from 31.9% in 2019 to 29% in 2020, while stage IV presentations rose from 26% to 26.4%.
One of the study limitations is that the patients who came in for a second opinion could have been newly diagnosed but might also have been referred for refractory disease, the authors comment.
No funding for this study was reported. Senior author Kathryn Ann Gold, MD, reported personal fees from AstraZeneca, Takeda, Rakuten, and Regeneron as well as grants from Pfizer and Pharmacyclics.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Late-onset recurrence in breast cancer: Implications for women’s health clinicians in survivorship care
Improved treatments for breast cancer (BC) and effective screening programs have resulted in a BC mortality rate reduction of 41% since 1989.1 Because BC is the leading cause of cancer in women, these mortality improvements have resulted in more than 3 million BC survivors in the United States.2,3 With longer-term survival, there is increasing interest in late-onset recurrences.4,5 A recent study has provided an improved understanding of the risk of lateonset recurrence in women with 10 years of disease-free survival, an important finding for women’s health providers because oncologists do not typically follow survivors after 10 years of disease-free survival.4
Recent study looks at incidence of late-onset recurrence
Pederson and colleagues evaluated all patients diagnosed with BC in Denmark from 1987 through 2004.4 Those patients without evidence of recurrence at 10 years were then followed utilizing population-based linked registries to identify patients who subsequently developed a local, regional, or distant late-onset recurrence. The authors evaluated the frequency of late recurrence and identified associations with demographic and tumor characteristics.
What they found
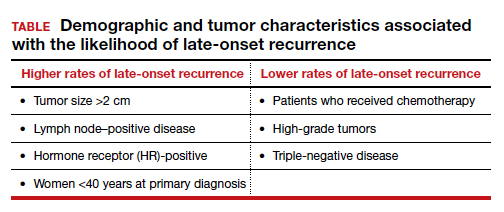
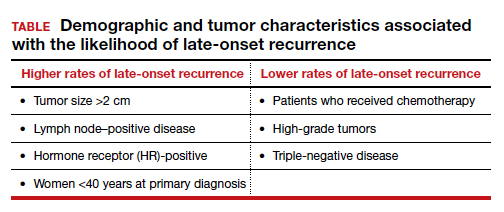
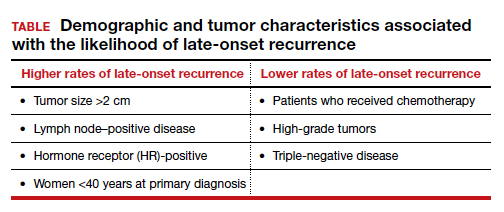
A total of 36,920 patients were diagnosed with BC in Denmark between 1987-2004, of whom 20,315 (55%) were identified as disease free for at least 10 years. Late-onset recurrence occurred in 2,595 (12.8%) with the strongest associations of recurrence seen in patients who had a tumor size >2 cm and lymph node‒positive (involving 4 or more nodes) disease (24.6%), compared with 12.7% in patients with tumors <2 cm and node-negative disease. Several other factors were associated with a higher risk of late-onset recurrence and are included in the TABLE. Half of the recurrences occurred between 10 and 15 years after the primary diagnosis.
Prior research
These findings are consistent with another recent study showing that BC patients have a 1% to 2%/year risk of recurrence after 10 disease-free years.5 Strengths of this study include:
- population-based, including all women with BC
- long-term follow-up for up to 32 years
- universal health care in Denmark, which results in robust and linked databases and very few missing data points.
There were two notable weaknesses to consider:
- Treatment regimens changed considerably during the time frame of the study (1997-2018), particularly the duration of tamoxifen use in patients with HR-positive disease. In this study nearly all patients received 5 years or less of tamoxifen. Since the mid-2010s, 10 years of hormonal adjuvant therapy has become routine in HR-positive BC, which reduces recurrences, including late-onset recurrence.6 The effect of 10 years of tamoxifen would very likely have resulted in less late-onset recurrence in the HR-positive population in this study.
- There is a lack of racial diversity in the Danish population, and the study findings may not translate to Black patients who have a higher frequency of triple-negative BC with a different risk of late-onset recurrence.7
Practice takeaways
Cancer surveillance. There are 3+ million BC survivors in the United States, and a 55%+ likelihood that they will be disease free for 10 years. This is clearly an important population to the women’s health care provider. This study, and previous research, suggests that among 10-year-disease-free survivors, 1% to 2% will recur annually, with higher rates amongst HR-positive, lymph-node positive women under age 40, and in the first 5 years following the 10-year post–initial diagnosis mark, so ongoing surveillance is imperative. Annual clinical breast examinations along with annual (not biennial) mammography should be performed.8 Digital breast tomosynthesis has improved specificity and sensitivity for BC detection and is the preferred modality when it is available.
Management of menopausal symptoms. These findings also have implications for menopausal hormone therapy for patients with symptoms. Because HR-positive patients have an increased risk of late-onset recurrence, nonhormonal therapies should be considered as first-line therapy for patients with menopausal symptoms. If hormone therapy is being considered, providers and patients should use shared decision making to balance the potential benefits (reduction in symptoms, possible cardiovascular benefits, and reduction in bone loss) with the risks (increased risk of recurrence and venous thromboembolism), even if patients are remote from the original diagnosis (ie, 10-year disease-free survival).
Topical estrogen therapies would be preferred for patients with significant urogenital atrophic symptoms who fail nonhormonal therapies due to substantially less systemic absorption and the lack of need to add a progestin.9,10 If oral therapy is being considered, I carefully counsel these women about the likely increased risk of recurrence and, if possible, include their breast oncologist in the discussion. ●
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7-33. doi: 10.3322/caac.21654.
- de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22:561- 570. doi: 10.1158/1055-9965.EPI-12-1356.
- Carreira H, Williams R, Funston G, et al. Associations between breast cancer survivorship and adverse mental health outcomes: a matched population-based cohort study in the United Kingdom. PLOS Med. 2021;18:e1003504. doi: 10.1371/journal.pmed.1003504.
- Pedersen RN, Esen BÖ, Mellemkjær L, et al. The incidence of breast cancer recurrence 10-32 years after primary diagnosis. J Natl Cancer Inst. November 8, 2021. doi: 10.1093/jnci/djab202.
- Pan H, Gray R, Braybrooke J, et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377:1836- 1846. doi: 10.1056/NEJMoa1701830.
- Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805-816. doi: 10.1016/S0140-6736(12)61963-1.
- Scott LC, Mobley LR, Kuo TM, et al. Update on triple‐negative breast cancer disparities for the United States: a population‐based study from the United States Cancer Statistics database, 2010 through 2014. Cancer. 2019;125:3412-3417. doi: 10.1002/cncr.32207.
- NCCN Clinical Practice Guidelines in Oncology: Breast Cancer. 2021; Version 2.2022.
- Crandall CJ, Diamant A, Santoro N. Safety of vaginal estrogens: a systematic review. Menopause. 2020;27:339-360. doi: 10.1097 /GME.0000000000001468.
- Treatment of urogenital symptoms in individuals with a history of estrogen-dependent breast cancer: clinical consensus. Obstet Gynecol. 2021;138:950-960. doi: 10.1097/AOG .0000000000004601.
Improved treatments for breast cancer (BC) and effective screening programs have resulted in a BC mortality rate reduction of 41% since 1989.1 Because BC is the leading cause of cancer in women, these mortality improvements have resulted in more than 3 million BC survivors in the United States.2,3 With longer-term survival, there is increasing interest in late-onset recurrences.4,5 A recent study has provided an improved understanding of the risk of lateonset recurrence in women with 10 years of disease-free survival, an important finding for women’s health providers because oncologists do not typically follow survivors after 10 years of disease-free survival.4
Recent study looks at incidence of late-onset recurrence
Pederson and colleagues evaluated all patients diagnosed with BC in Denmark from 1987 through 2004.4 Those patients without evidence of recurrence at 10 years were then followed utilizing population-based linked registries to identify patients who subsequently developed a local, regional, or distant late-onset recurrence. The authors evaluated the frequency of late recurrence and identified associations with demographic and tumor characteristics.
What they found
A total of 36,920 patients were diagnosed with BC in Denmark between 1987-2004, of whom 20,315 (55%) were identified as disease free for at least 10 years. Late-onset recurrence occurred in 2,595 (12.8%) with the strongest associations of recurrence seen in patients who had a tumor size >2 cm and lymph node‒positive (involving 4 or more nodes) disease (24.6%), compared with 12.7% in patients with tumors <2 cm and node-negative disease. Several other factors were associated with a higher risk of late-onset recurrence and are included in the TABLE. Half of the recurrences occurred between 10 and 15 years after the primary diagnosis.
Prior research
These findings are consistent with another recent study showing that BC patients have a 1% to 2%/year risk of recurrence after 10 disease-free years.5 Strengths of this study include:
- population-based, including all women with BC
- long-term follow-up for up to 32 years
- universal health care in Denmark, which results in robust and linked databases and very few missing data points.
There were two notable weaknesses to consider:
- Treatment regimens changed considerably during the time frame of the study (1997-2018), particularly the duration of tamoxifen use in patients with HR-positive disease. In this study nearly all patients received 5 years or less of tamoxifen. Since the mid-2010s, 10 years of hormonal adjuvant therapy has become routine in HR-positive BC, which reduces recurrences, including late-onset recurrence.6 The effect of 10 years of tamoxifen would very likely have resulted in less late-onset recurrence in the HR-positive population in this study.
- There is a lack of racial diversity in the Danish population, and the study findings may not translate to Black patients who have a higher frequency of triple-negative BC with a different risk of late-onset recurrence.7
Practice takeaways
Cancer surveillance. There are 3+ million BC survivors in the United States, and a 55%+ likelihood that they will be disease free for 10 years. This is clearly an important population to the women’s health care provider. This study, and previous research, suggests that among 10-year-disease-free survivors, 1% to 2% will recur annually, with higher rates amongst HR-positive, lymph-node positive women under age 40, and in the first 5 years following the 10-year post–initial diagnosis mark, so ongoing surveillance is imperative. Annual clinical breast examinations along with annual (not biennial) mammography should be performed.8 Digital breast tomosynthesis has improved specificity and sensitivity for BC detection and is the preferred modality when it is available.
Management of menopausal symptoms. These findings also have implications for menopausal hormone therapy for patients with symptoms. Because HR-positive patients have an increased risk of late-onset recurrence, nonhormonal therapies should be considered as first-line therapy for patients with menopausal symptoms. If hormone therapy is being considered, providers and patients should use shared decision making to balance the potential benefits (reduction in symptoms, possible cardiovascular benefits, and reduction in bone loss) with the risks (increased risk of recurrence and venous thromboembolism), even if patients are remote from the original diagnosis (ie, 10-year disease-free survival).
Topical estrogen therapies would be preferred for patients with significant urogenital atrophic symptoms who fail nonhormonal therapies due to substantially less systemic absorption and the lack of need to add a progestin.9,10 If oral therapy is being considered, I carefully counsel these women about the likely increased risk of recurrence and, if possible, include their breast oncologist in the discussion. ●
Improved treatments for breast cancer (BC) and effective screening programs have resulted in a BC mortality rate reduction of 41% since 1989.1 Because BC is the leading cause of cancer in women, these mortality improvements have resulted in more than 3 million BC survivors in the United States.2,3 With longer-term survival, there is increasing interest in late-onset recurrences.4,5 A recent study has provided an improved understanding of the risk of lateonset recurrence in women with 10 years of disease-free survival, an important finding for women’s health providers because oncologists do not typically follow survivors after 10 years of disease-free survival.4
Recent study looks at incidence of late-onset recurrence
Pederson and colleagues evaluated all patients diagnosed with BC in Denmark from 1987 through 2004.4 Those patients without evidence of recurrence at 10 years were then followed utilizing population-based linked registries to identify patients who subsequently developed a local, regional, or distant late-onset recurrence. The authors evaluated the frequency of late recurrence and identified associations with demographic and tumor characteristics.
What they found
A total of 36,920 patients were diagnosed with BC in Denmark between 1987-2004, of whom 20,315 (55%) were identified as disease free for at least 10 years. Late-onset recurrence occurred in 2,595 (12.8%) with the strongest associations of recurrence seen in patients who had a tumor size >2 cm and lymph node‒positive (involving 4 or more nodes) disease (24.6%), compared with 12.7% in patients with tumors <2 cm and node-negative disease. Several other factors were associated with a higher risk of late-onset recurrence and are included in the TABLE. Half of the recurrences occurred between 10 and 15 years after the primary diagnosis.
Prior research
These findings are consistent with another recent study showing that BC patients have a 1% to 2%/year risk of recurrence after 10 disease-free years.5 Strengths of this study include:
- population-based, including all women with BC
- long-term follow-up for up to 32 years
- universal health care in Denmark, which results in robust and linked databases and very few missing data points.
There were two notable weaknesses to consider:
- Treatment regimens changed considerably during the time frame of the study (1997-2018), particularly the duration of tamoxifen use in patients with HR-positive disease. In this study nearly all patients received 5 years or less of tamoxifen. Since the mid-2010s, 10 years of hormonal adjuvant therapy has become routine in HR-positive BC, which reduces recurrences, including late-onset recurrence.6 The effect of 10 years of tamoxifen would very likely have resulted in less late-onset recurrence in the HR-positive population in this study.
- There is a lack of racial diversity in the Danish population, and the study findings may not translate to Black patients who have a higher frequency of triple-negative BC with a different risk of late-onset recurrence.7
Practice takeaways
Cancer surveillance. There are 3+ million BC survivors in the United States, and a 55%+ likelihood that they will be disease free for 10 years. This is clearly an important population to the women’s health care provider. This study, and previous research, suggests that among 10-year-disease-free survivors, 1% to 2% will recur annually, with higher rates amongst HR-positive, lymph-node positive women under age 40, and in the first 5 years following the 10-year post–initial diagnosis mark, so ongoing surveillance is imperative. Annual clinical breast examinations along with annual (not biennial) mammography should be performed.8 Digital breast tomosynthesis has improved specificity and sensitivity for BC detection and is the preferred modality when it is available.
Management of menopausal symptoms. These findings also have implications for menopausal hormone therapy for patients with symptoms. Because HR-positive patients have an increased risk of late-onset recurrence, nonhormonal therapies should be considered as first-line therapy for patients with menopausal symptoms. If hormone therapy is being considered, providers and patients should use shared decision making to balance the potential benefits (reduction in symptoms, possible cardiovascular benefits, and reduction in bone loss) with the risks (increased risk of recurrence and venous thromboembolism), even if patients are remote from the original diagnosis (ie, 10-year disease-free survival).
Topical estrogen therapies would be preferred for patients with significant urogenital atrophic symptoms who fail nonhormonal therapies due to substantially less systemic absorption and the lack of need to add a progestin.9,10 If oral therapy is being considered, I carefully counsel these women about the likely increased risk of recurrence and, if possible, include their breast oncologist in the discussion. ●
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7-33. doi: 10.3322/caac.21654.
- de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22:561- 570. doi: 10.1158/1055-9965.EPI-12-1356.
- Carreira H, Williams R, Funston G, et al. Associations between breast cancer survivorship and adverse mental health outcomes: a matched population-based cohort study in the United Kingdom. PLOS Med. 2021;18:e1003504. doi: 10.1371/journal.pmed.1003504.
- Pedersen RN, Esen BÖ, Mellemkjær L, et al. The incidence of breast cancer recurrence 10-32 years after primary diagnosis. J Natl Cancer Inst. November 8, 2021. doi: 10.1093/jnci/djab202.
- Pan H, Gray R, Braybrooke J, et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377:1836- 1846. doi: 10.1056/NEJMoa1701830.
- Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805-816. doi: 10.1016/S0140-6736(12)61963-1.
- Scott LC, Mobley LR, Kuo TM, et al. Update on triple‐negative breast cancer disparities for the United States: a population‐based study from the United States Cancer Statistics database, 2010 through 2014. Cancer. 2019;125:3412-3417. doi: 10.1002/cncr.32207.
- NCCN Clinical Practice Guidelines in Oncology: Breast Cancer. 2021; Version 2.2022.
- Crandall CJ, Diamant A, Santoro N. Safety of vaginal estrogens: a systematic review. Menopause. 2020;27:339-360. doi: 10.1097 /GME.0000000000001468.
- Treatment of urogenital symptoms in individuals with a history of estrogen-dependent breast cancer: clinical consensus. Obstet Gynecol. 2021;138:950-960. doi: 10.1097/AOG .0000000000004601.
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7-33. doi: 10.3322/caac.21654.
- de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22:561- 570. doi: 10.1158/1055-9965.EPI-12-1356.
- Carreira H, Williams R, Funston G, et al. Associations between breast cancer survivorship and adverse mental health outcomes: a matched population-based cohort study in the United Kingdom. PLOS Med. 2021;18:e1003504. doi: 10.1371/journal.pmed.1003504.
- Pedersen RN, Esen BÖ, Mellemkjær L, et al. The incidence of breast cancer recurrence 10-32 years after primary diagnosis. J Natl Cancer Inst. November 8, 2021. doi: 10.1093/jnci/djab202.
- Pan H, Gray R, Braybrooke J, et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377:1836- 1846. doi: 10.1056/NEJMoa1701830.
- Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805-816. doi: 10.1016/S0140-6736(12)61963-1.
- Scott LC, Mobley LR, Kuo TM, et al. Update on triple‐negative breast cancer disparities for the United States: a population‐based study from the United States Cancer Statistics database, 2010 through 2014. Cancer. 2019;125:3412-3417. doi: 10.1002/cncr.32207.
- NCCN Clinical Practice Guidelines in Oncology: Breast Cancer. 2021; Version 2.2022.
- Crandall CJ, Diamant A, Santoro N. Safety of vaginal estrogens: a systematic review. Menopause. 2020;27:339-360. doi: 10.1097 /GME.0000000000001468.
- Treatment of urogenital symptoms in individuals with a history of estrogen-dependent breast cancer: clinical consensus. Obstet Gynecol. 2021;138:950-960. doi: 10.1097/AOG .0000000000004601.
Is mild cognitive impairment reversible?
new research shows.
The investigators found individuals with these factors, which are all markers of cognitive reserve, had a significantly greater chance of reversion from MCI to normal cognition (NC) than progression from MCI to dementia.
In a cohort study of more than 600 women aged 75 years or older, about a third of those with MCI reverted to NC at some point during follow-up, which sends “an encouraging message,” study author Suzanne Tyas, PhD, associate professor, University of Waterloo (Ont.), said in an interview.
“That’s a positive thing for people to keep in mind when they’re thinking about prognosis. Some of these novel characteristics we’ve identified might be useful in thinking about how likely a particular patient might be to improve versus decline cognitively,” Dr. Tyas added.
The findings were published online Feb. 4, 2022, in the journal Neurology.
Highly educated cohort
As the population ages, the number of individuals experiencing age-related conditions, including dementia, increases. There is no cure for most dementia types so prevention is key – and preventing dementia requires understanding its risk factors, Dr. Tyas noted.
The analysis included participants from the Nun Study, a longitudinal study of aging and cognition among members of the School Sisters of Notre Dame in the United States. All were 75 and older at baseline, which was from 1991 to 1993; about 14.5% were older than 90 years.
Participants were generally highly educated, with 84.5% attaining an undergraduate or graduate degree. They also had a similar socioeconomic status, level of social supports, marital and reproductive history, and alcohol and tobacco use.
Researchers examined cognitive function at baseline and then about annually until death or end of the 12th round of assessments. They used five measures from the Consortium to Establish a Registry for Alzheimer’s Disease neuropsychological battery to categorize subjects into NC, MCI, or dementia: Delayed Word Recall, Verbal Fluency, Boston Naming, Constructional Praxis, and the Mini-Mental State Exam.
The current analysis focused on the 619 participants with data on apolipoprotein E (apo E) epsilon-4 genotyping and education. From convent archives, investigators also had access to the nuns’ early high school academic performance in English, Latin, algebra, and geometry.
“Typically we only have data for [overall] education. But I know from teaching that there’s a difference between people who just pass my courses and graduate with a university degree versus those who really excel,” Dr. Tyas said.
The researchers also assessed handwriting samples from before the participants entered the religious order. From these, they scored “idea density,” which is the number of ideas contained in the writing and “grammatical complexity,” which includes structure, use of clauses, subclauses, and so on.
Dementia not inevitable
Results showed 472 of the 619 participants had MCI during the study period. About 30.3% of these showed at least one reverse transition from MCI to NC during a mean follow-up of 8.6 years; 83.9% went on to develop dementia.
This shows converting from MCI to NC occurs relatively frequently, Dr. Tyas noted.
“This is encouraging because some people think that if they have a diagnosis of MCI they are inevitably going to decline to dementia,” she added.
The researchers also used complicated modeling of transition rates over time between NC, MCI, and dementia and adjusted for participants who died. They estimated relative risk of reversion versus progression for age, apo E, and potential cognitive reserve indicators.
Not surprisingly, younger age (90 years or less) and absence of apo E epsilon-4 allele contributed to a significantly higher rate for reversion from MCI to NC versus progression from MCI to dementia.
However, although age and apo E are known risk factors for dementia, these have not been examined in the context of whether individuals with MCI are more likely to improve or decline, said Dr. Tyas.
Higher educational attainment, the traditional indicator of cognitive reserve, was associated with a significantly higher relative risk for reversion from MCI to NC versus progression from MCI to dementia (RR, 2.6) for a bachelor’s degree versus less education.
There was a greater RR for even higher education after adjusting for age and apo E epsilon-4 status.
Language skills key
Interestingly, the investigators also found a significant association with good grades in high school English but not other subjects (RR for higher vs. lower English grades, 1.83; 95% confidence interval, 1.07-3.14).
In addition, they found both characteristics of written language skills (idea density and grammatical complexity) were significant predictors of conversion to NC.
“Those with high levels of idea density were four times more likely to improve to normal cognition than progress to dementia, and the effect was even stronger for grammatical structure. Those individuals with higher levels were almost six times more likely to improve than decline,” Dr. Tyas reported.
The RR for higher versus lower idea density was 3.93 (95% CI, 1.3-11.9) and the RR for higher versus lower grammatical complexity was 5.78 (95% CI, 1.56-21.42).
These new results could be useful when planning future clinical trials, Dr. Tyas noted. “MCI in some people is going to improve even without any treatment, and this should be taken into consideration when recruiting participants to a study and when interpreting the results.
“You don’t want something to look like it’s a benefit of the treatment when in fact these individuals would have just reverted on their own,” she added.
Research implications
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, noted that, in “this study of highly educated, older women,” transitions from MCI to NC “were about equally common” as transitions from MCI to dementia.
“As advances are made in early detection of dementia, and treatments are developed and marketed for people living with MCI, this article’s findings are important to inform discussions of prognosis with patients and [to the] design of clinical trials,” Dr. Sexton said.
The study was funded by the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. Funding for the Nun Study at the University of Kentucky was provided by the U.S. National Institute of Aging and the Kleberg Foundation. Dr. Tyas has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows.
The investigators found individuals with these factors, which are all markers of cognitive reserve, had a significantly greater chance of reversion from MCI to normal cognition (NC) than progression from MCI to dementia.
In a cohort study of more than 600 women aged 75 years or older, about a third of those with MCI reverted to NC at some point during follow-up, which sends “an encouraging message,” study author Suzanne Tyas, PhD, associate professor, University of Waterloo (Ont.), said in an interview.
“That’s a positive thing for people to keep in mind when they’re thinking about prognosis. Some of these novel characteristics we’ve identified might be useful in thinking about how likely a particular patient might be to improve versus decline cognitively,” Dr. Tyas added.
The findings were published online Feb. 4, 2022, in the journal Neurology.
Highly educated cohort
As the population ages, the number of individuals experiencing age-related conditions, including dementia, increases. There is no cure for most dementia types so prevention is key – and preventing dementia requires understanding its risk factors, Dr. Tyas noted.
The analysis included participants from the Nun Study, a longitudinal study of aging and cognition among members of the School Sisters of Notre Dame in the United States. All were 75 and older at baseline, which was from 1991 to 1993; about 14.5% were older than 90 years.
Participants were generally highly educated, with 84.5% attaining an undergraduate or graduate degree. They also had a similar socioeconomic status, level of social supports, marital and reproductive history, and alcohol and tobacco use.
Researchers examined cognitive function at baseline and then about annually until death or end of the 12th round of assessments. They used five measures from the Consortium to Establish a Registry for Alzheimer’s Disease neuropsychological battery to categorize subjects into NC, MCI, or dementia: Delayed Word Recall, Verbal Fluency, Boston Naming, Constructional Praxis, and the Mini-Mental State Exam.
The current analysis focused on the 619 participants with data on apolipoprotein E (apo E) epsilon-4 genotyping and education. From convent archives, investigators also had access to the nuns’ early high school academic performance in English, Latin, algebra, and geometry.
“Typically we only have data for [overall] education. But I know from teaching that there’s a difference between people who just pass my courses and graduate with a university degree versus those who really excel,” Dr. Tyas said.
The researchers also assessed handwriting samples from before the participants entered the religious order. From these, they scored “idea density,” which is the number of ideas contained in the writing and “grammatical complexity,” which includes structure, use of clauses, subclauses, and so on.
Dementia not inevitable
Results showed 472 of the 619 participants had MCI during the study period. About 30.3% of these showed at least one reverse transition from MCI to NC during a mean follow-up of 8.6 years; 83.9% went on to develop dementia.
This shows converting from MCI to NC occurs relatively frequently, Dr. Tyas noted.
“This is encouraging because some people think that if they have a diagnosis of MCI they are inevitably going to decline to dementia,” she added.
The researchers also used complicated modeling of transition rates over time between NC, MCI, and dementia and adjusted for participants who died. They estimated relative risk of reversion versus progression for age, apo E, and potential cognitive reserve indicators.
Not surprisingly, younger age (90 years or less) and absence of apo E epsilon-4 allele contributed to a significantly higher rate for reversion from MCI to NC versus progression from MCI to dementia.
However, although age and apo E are known risk factors for dementia, these have not been examined in the context of whether individuals with MCI are more likely to improve or decline, said Dr. Tyas.
Higher educational attainment, the traditional indicator of cognitive reserve, was associated with a significantly higher relative risk for reversion from MCI to NC versus progression from MCI to dementia (RR, 2.6) for a bachelor’s degree versus less education.
There was a greater RR for even higher education after adjusting for age and apo E epsilon-4 status.
Language skills key
Interestingly, the investigators also found a significant association with good grades in high school English but not other subjects (RR for higher vs. lower English grades, 1.83; 95% confidence interval, 1.07-3.14).
In addition, they found both characteristics of written language skills (idea density and grammatical complexity) were significant predictors of conversion to NC.
“Those with high levels of idea density were four times more likely to improve to normal cognition than progress to dementia, and the effect was even stronger for grammatical structure. Those individuals with higher levels were almost six times more likely to improve than decline,” Dr. Tyas reported.
The RR for higher versus lower idea density was 3.93 (95% CI, 1.3-11.9) and the RR for higher versus lower grammatical complexity was 5.78 (95% CI, 1.56-21.42).
These new results could be useful when planning future clinical trials, Dr. Tyas noted. “MCI in some people is going to improve even without any treatment, and this should be taken into consideration when recruiting participants to a study and when interpreting the results.
“You don’t want something to look like it’s a benefit of the treatment when in fact these individuals would have just reverted on their own,” she added.
Research implications
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, noted that, in “this study of highly educated, older women,” transitions from MCI to NC “were about equally common” as transitions from MCI to dementia.
“As advances are made in early detection of dementia, and treatments are developed and marketed for people living with MCI, this article’s findings are important to inform discussions of prognosis with patients and [to the] design of clinical trials,” Dr. Sexton said.
The study was funded by the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. Funding for the Nun Study at the University of Kentucky was provided by the U.S. National Institute of Aging and the Kleberg Foundation. Dr. Tyas has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows.
The investigators found individuals with these factors, which are all markers of cognitive reserve, had a significantly greater chance of reversion from MCI to normal cognition (NC) than progression from MCI to dementia.
In a cohort study of more than 600 women aged 75 years or older, about a third of those with MCI reverted to NC at some point during follow-up, which sends “an encouraging message,” study author Suzanne Tyas, PhD, associate professor, University of Waterloo (Ont.), said in an interview.
“That’s a positive thing for people to keep in mind when they’re thinking about prognosis. Some of these novel characteristics we’ve identified might be useful in thinking about how likely a particular patient might be to improve versus decline cognitively,” Dr. Tyas added.
The findings were published online Feb. 4, 2022, in the journal Neurology.
Highly educated cohort
As the population ages, the number of individuals experiencing age-related conditions, including dementia, increases. There is no cure for most dementia types so prevention is key – and preventing dementia requires understanding its risk factors, Dr. Tyas noted.
The analysis included participants from the Nun Study, a longitudinal study of aging and cognition among members of the School Sisters of Notre Dame in the United States. All were 75 and older at baseline, which was from 1991 to 1993; about 14.5% were older than 90 years.
Participants were generally highly educated, with 84.5% attaining an undergraduate or graduate degree. They also had a similar socioeconomic status, level of social supports, marital and reproductive history, and alcohol and tobacco use.
Researchers examined cognitive function at baseline and then about annually until death or end of the 12th round of assessments. They used five measures from the Consortium to Establish a Registry for Alzheimer’s Disease neuropsychological battery to categorize subjects into NC, MCI, or dementia: Delayed Word Recall, Verbal Fluency, Boston Naming, Constructional Praxis, and the Mini-Mental State Exam.
The current analysis focused on the 619 participants with data on apolipoprotein E (apo E) epsilon-4 genotyping and education. From convent archives, investigators also had access to the nuns’ early high school academic performance in English, Latin, algebra, and geometry.
“Typically we only have data for [overall] education. But I know from teaching that there’s a difference between people who just pass my courses and graduate with a university degree versus those who really excel,” Dr. Tyas said.
The researchers also assessed handwriting samples from before the participants entered the religious order. From these, they scored “idea density,” which is the number of ideas contained in the writing and “grammatical complexity,” which includes structure, use of clauses, subclauses, and so on.
Dementia not inevitable
Results showed 472 of the 619 participants had MCI during the study period. About 30.3% of these showed at least one reverse transition from MCI to NC during a mean follow-up of 8.6 years; 83.9% went on to develop dementia.
This shows converting from MCI to NC occurs relatively frequently, Dr. Tyas noted.
“This is encouraging because some people think that if they have a diagnosis of MCI they are inevitably going to decline to dementia,” she added.
The researchers also used complicated modeling of transition rates over time between NC, MCI, and dementia and adjusted for participants who died. They estimated relative risk of reversion versus progression for age, apo E, and potential cognitive reserve indicators.
Not surprisingly, younger age (90 years or less) and absence of apo E epsilon-4 allele contributed to a significantly higher rate for reversion from MCI to NC versus progression from MCI to dementia.
However, although age and apo E are known risk factors for dementia, these have not been examined in the context of whether individuals with MCI are more likely to improve or decline, said Dr. Tyas.
Higher educational attainment, the traditional indicator of cognitive reserve, was associated with a significantly higher relative risk for reversion from MCI to NC versus progression from MCI to dementia (RR, 2.6) for a bachelor’s degree versus less education.
There was a greater RR for even higher education after adjusting for age and apo E epsilon-4 status.
Language skills key
Interestingly, the investigators also found a significant association with good grades in high school English but not other subjects (RR for higher vs. lower English grades, 1.83; 95% confidence interval, 1.07-3.14).
In addition, they found both characteristics of written language skills (idea density and grammatical complexity) were significant predictors of conversion to NC.
“Those with high levels of idea density were four times more likely to improve to normal cognition than progress to dementia, and the effect was even stronger for grammatical structure. Those individuals with higher levels were almost six times more likely to improve than decline,” Dr. Tyas reported.
The RR for higher versus lower idea density was 3.93 (95% CI, 1.3-11.9) and the RR for higher versus lower grammatical complexity was 5.78 (95% CI, 1.56-21.42).
These new results could be useful when planning future clinical trials, Dr. Tyas noted. “MCI in some people is going to improve even without any treatment, and this should be taken into consideration when recruiting participants to a study and when interpreting the results.
“You don’t want something to look like it’s a benefit of the treatment when in fact these individuals would have just reverted on their own,” she added.
Research implications
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, noted that, in “this study of highly educated, older women,” transitions from MCI to NC “were about equally common” as transitions from MCI to dementia.
“As advances are made in early detection of dementia, and treatments are developed and marketed for people living with MCI, this article’s findings are important to inform discussions of prognosis with patients and [to the] design of clinical trials,” Dr. Sexton said.
The study was funded by the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. Funding for the Nun Study at the University of Kentucky was provided by the U.S. National Institute of Aging and the Kleberg Foundation. Dr. Tyas has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ILAE offers first guide to treating depression in epilepsy
The new guidance highlights the high prevalence of depression among patients with epilepsy while offering the first systematic approach to treatment, reported lead author Marco Mula, MD, PhD, of Atkinson Morley Regional Neuroscience Centre at St George’s University Hospital, London, and colleagues.
“Despite evidence that depression represents a frequently encountered comorbidity [among patients with epilepsy], data on the treatment of depression in epilepsy [are] still limited and recommendations rely mostly on individual clinical experience and expertise,” the investigators wrote in Epilepsia.
Recommendations cover first-line treatment of unipolar depression in epilepsy without other psychiatric disorders.
For patients with mild depression, the guidance supports psychological intervention without pharmacologic therapy; however, if the patient wishes to use medication, has had a positive response to medication in the past, or nonpharmacologic treatments have previously failed or are unavailable, then SSRIs should be considered first-choice therapy. For moderate to severe depression, SSRIs are the first choice, according to Dr. Mula and colleagues.
“It has to be acknowledged that there is considerable debate in the psychiatric literature about the treatment of mild depression in adults,” the investigators noted. “A patient-level meta-analysis pointed out that the magnitude of benefit of antidepressant medications compared with placebo increases with severity of depression symptoms and it may be minimal or nonexistent, on average, in patients with mild or moderate symptoms.”
If a patient does not respond to first-line therapy, then venlafaxine should be considered, according to the guidance. When a patient does respond to therapy, treatment should be continued for at least 6 months, and when residual symptoms persist, treatment should be continued until resolution.
“In people with depression it is established that around two-thirds of patients do not achieve full remission with first-line treatment,” Dr. Mula and colleagues wrote. “In people with epilepsy, current data show that up to 50% of patients do not achieve full remission from depression. For this reason, augmentation strategies are often needed. They should be adopted by psychiatrists, neuropsychiatrists, or mental health professionals familiar with such therapeutic strategies.”
Beyond these key recommendations, the guidance covers a range of additional topics, including other pharmacologic options, medication discontinuation strategies, electroconvulsive therapy, light therapy, exercise training, vagus nerve stimulation, and repetitive transcranial magnetic stimulation.
Useful advice that counters common misconceptions
According to Jacqueline A. French, MD, a professor at NYU Langone Medical Center, Dr. Mula and colleagues are “top notch,” and their recommendations “hit every nail on the head.”
Dr. French, chief medical officer of The Epilepsy Foundation, emphasized the importance of the publication, which addresses two common misconceptions within the medical community: First, that standard antidepressants are insufficient to treat depression in patients with epilepsy, and second, that antidepressants may trigger seizures.
“The first purpose [of the publication] is to say, yes, these antidepressants do work,” Dr. French said, “and no, they don’t worsen seizures, and you can use them safely, and they are appropriate to use.”
Dr. French explained that managing depression remains a practice gap among epileptologists and neurologists because it is a diagnosis that doesn’t traditionally fall into their purview, yet many patients with epilepsy forgo visiting their primary care providers, who more frequently diagnose and manage depression. Dr. French agreed with the guidance that epilepsy specialists should fill this gap.
“We need to at least be able to take people through their first antidepressant, even though we were not trained to be psychiatrists,” Dr. French said. “That’s part of the best care of our patients.”
Imad Najm, MD, director of the Charles Shor Epilepsy Center, Cleveland Clinic, said the recommendations are a step forward in the field, as they are supported by clinical data, instead of just clinical experience and expertise.
Still, Dr. Najm noted that more work is needed to stratify risk of depression in epilepsy and evaluate a possible causal relationship between epilepsy therapies and depression.
He went on to emphasizes the scale of issue at hand, and the stakes involved.
“Depression, anxiety, and psychosis affect a large number of patients with epilepsy,” Dr. Najm said. “Clinical screening and recognition of these comorbidities leads to the institution of treatment options and significant improvement in quality of life. Mental health professionals should be an integral part of any comprehensive epilepsy center.”
The investigators disclosed relationships with Esai, UCB, Elsevier, and others. Dr. French is indirectly involved with multiple pharmaceutical companies developing epilepsy drugs through her role as director of The Epilepsy Study Consortium, a nonprofit organization. Dr. Najm reported no conflicts of interest.
The new guidance highlights the high prevalence of depression among patients with epilepsy while offering the first systematic approach to treatment, reported lead author Marco Mula, MD, PhD, of Atkinson Morley Regional Neuroscience Centre at St George’s University Hospital, London, and colleagues.
“Despite evidence that depression represents a frequently encountered comorbidity [among patients with epilepsy], data on the treatment of depression in epilepsy [are] still limited and recommendations rely mostly on individual clinical experience and expertise,” the investigators wrote in Epilepsia.
Recommendations cover first-line treatment of unipolar depression in epilepsy without other psychiatric disorders.
For patients with mild depression, the guidance supports psychological intervention without pharmacologic therapy; however, if the patient wishes to use medication, has had a positive response to medication in the past, or nonpharmacologic treatments have previously failed or are unavailable, then SSRIs should be considered first-choice therapy. For moderate to severe depression, SSRIs are the first choice, according to Dr. Mula and colleagues.
“It has to be acknowledged that there is considerable debate in the psychiatric literature about the treatment of mild depression in adults,” the investigators noted. “A patient-level meta-analysis pointed out that the magnitude of benefit of antidepressant medications compared with placebo increases with severity of depression symptoms and it may be minimal or nonexistent, on average, in patients with mild or moderate symptoms.”
If a patient does not respond to first-line therapy, then venlafaxine should be considered, according to the guidance. When a patient does respond to therapy, treatment should be continued for at least 6 months, and when residual symptoms persist, treatment should be continued until resolution.
“In people with depression it is established that around two-thirds of patients do not achieve full remission with first-line treatment,” Dr. Mula and colleagues wrote. “In people with epilepsy, current data show that up to 50% of patients do not achieve full remission from depression. For this reason, augmentation strategies are often needed. They should be adopted by psychiatrists, neuropsychiatrists, or mental health professionals familiar with such therapeutic strategies.”
Beyond these key recommendations, the guidance covers a range of additional topics, including other pharmacologic options, medication discontinuation strategies, electroconvulsive therapy, light therapy, exercise training, vagus nerve stimulation, and repetitive transcranial magnetic stimulation.
Useful advice that counters common misconceptions
According to Jacqueline A. French, MD, a professor at NYU Langone Medical Center, Dr. Mula and colleagues are “top notch,” and their recommendations “hit every nail on the head.”
Dr. French, chief medical officer of The Epilepsy Foundation, emphasized the importance of the publication, which addresses two common misconceptions within the medical community: First, that standard antidepressants are insufficient to treat depression in patients with epilepsy, and second, that antidepressants may trigger seizures.
“The first purpose [of the publication] is to say, yes, these antidepressants do work,” Dr. French said, “and no, they don’t worsen seizures, and you can use them safely, and they are appropriate to use.”
Dr. French explained that managing depression remains a practice gap among epileptologists and neurologists because it is a diagnosis that doesn’t traditionally fall into their purview, yet many patients with epilepsy forgo visiting their primary care providers, who more frequently diagnose and manage depression. Dr. French agreed with the guidance that epilepsy specialists should fill this gap.
“We need to at least be able to take people through their first antidepressant, even though we were not trained to be psychiatrists,” Dr. French said. “That’s part of the best care of our patients.”
Imad Najm, MD, director of the Charles Shor Epilepsy Center, Cleveland Clinic, said the recommendations are a step forward in the field, as they are supported by clinical data, instead of just clinical experience and expertise.
Still, Dr. Najm noted that more work is needed to stratify risk of depression in epilepsy and evaluate a possible causal relationship between epilepsy therapies and depression.
He went on to emphasizes the scale of issue at hand, and the stakes involved.
“Depression, anxiety, and psychosis affect a large number of patients with epilepsy,” Dr. Najm said. “Clinical screening and recognition of these comorbidities leads to the institution of treatment options and significant improvement in quality of life. Mental health professionals should be an integral part of any comprehensive epilepsy center.”
The investigators disclosed relationships with Esai, UCB, Elsevier, and others. Dr. French is indirectly involved with multiple pharmaceutical companies developing epilepsy drugs through her role as director of The Epilepsy Study Consortium, a nonprofit organization. Dr. Najm reported no conflicts of interest.
The new guidance highlights the high prevalence of depression among patients with epilepsy while offering the first systematic approach to treatment, reported lead author Marco Mula, MD, PhD, of Atkinson Morley Regional Neuroscience Centre at St George’s University Hospital, London, and colleagues.
“Despite evidence that depression represents a frequently encountered comorbidity [among patients with epilepsy], data on the treatment of depression in epilepsy [are] still limited and recommendations rely mostly on individual clinical experience and expertise,” the investigators wrote in Epilepsia.
Recommendations cover first-line treatment of unipolar depression in epilepsy without other psychiatric disorders.
For patients with mild depression, the guidance supports psychological intervention without pharmacologic therapy; however, if the patient wishes to use medication, has had a positive response to medication in the past, or nonpharmacologic treatments have previously failed or are unavailable, then SSRIs should be considered first-choice therapy. For moderate to severe depression, SSRIs are the first choice, according to Dr. Mula and colleagues.
“It has to be acknowledged that there is considerable debate in the psychiatric literature about the treatment of mild depression in adults,” the investigators noted. “A patient-level meta-analysis pointed out that the magnitude of benefit of antidepressant medications compared with placebo increases with severity of depression symptoms and it may be minimal or nonexistent, on average, in patients with mild or moderate symptoms.”
If a patient does not respond to first-line therapy, then venlafaxine should be considered, according to the guidance. When a patient does respond to therapy, treatment should be continued for at least 6 months, and when residual symptoms persist, treatment should be continued until resolution.
“In people with depression it is established that around two-thirds of patients do not achieve full remission with first-line treatment,” Dr. Mula and colleagues wrote. “In people with epilepsy, current data show that up to 50% of patients do not achieve full remission from depression. For this reason, augmentation strategies are often needed. They should be adopted by psychiatrists, neuropsychiatrists, or mental health professionals familiar with such therapeutic strategies.”
Beyond these key recommendations, the guidance covers a range of additional topics, including other pharmacologic options, medication discontinuation strategies, electroconvulsive therapy, light therapy, exercise training, vagus nerve stimulation, and repetitive transcranial magnetic stimulation.
Useful advice that counters common misconceptions
According to Jacqueline A. French, MD, a professor at NYU Langone Medical Center, Dr. Mula and colleagues are “top notch,” and their recommendations “hit every nail on the head.”
Dr. French, chief medical officer of The Epilepsy Foundation, emphasized the importance of the publication, which addresses two common misconceptions within the medical community: First, that standard antidepressants are insufficient to treat depression in patients with epilepsy, and second, that antidepressants may trigger seizures.
“The first purpose [of the publication] is to say, yes, these antidepressants do work,” Dr. French said, “and no, they don’t worsen seizures, and you can use them safely, and they are appropriate to use.”
Dr. French explained that managing depression remains a practice gap among epileptologists and neurologists because it is a diagnosis that doesn’t traditionally fall into their purview, yet many patients with epilepsy forgo visiting their primary care providers, who more frequently diagnose and manage depression. Dr. French agreed with the guidance that epilepsy specialists should fill this gap.
“We need to at least be able to take people through their first antidepressant, even though we were not trained to be psychiatrists,” Dr. French said. “That’s part of the best care of our patients.”
Imad Najm, MD, director of the Charles Shor Epilepsy Center, Cleveland Clinic, said the recommendations are a step forward in the field, as they are supported by clinical data, instead of just clinical experience and expertise.
Still, Dr. Najm noted that more work is needed to stratify risk of depression in epilepsy and evaluate a possible causal relationship between epilepsy therapies and depression.
He went on to emphasizes the scale of issue at hand, and the stakes involved.
“Depression, anxiety, and psychosis affect a large number of patients with epilepsy,” Dr. Najm said. “Clinical screening and recognition of these comorbidities leads to the institution of treatment options and significant improvement in quality of life. Mental health professionals should be an integral part of any comprehensive epilepsy center.”
The investigators disclosed relationships with Esai, UCB, Elsevier, and others. Dr. French is indirectly involved with multiple pharmaceutical companies developing epilepsy drugs through her role as director of The Epilepsy Study Consortium, a nonprofit organization. Dr. Najm reported no conflicts of interest.
FROM EPILEPSIA
PACAP38- and VIP-induced cluster headache attacks do not appear to alter CGRP levels
such as tryptase and histamine, a new study has found.
“Whether cluster headache attacks provoked by CGRP and PACAP38/VIP are mediated by distinct signaling pathways will be worth investigating in forthcoming studies,” wrote Lanfranco Pellesi, MD, of the Danish Headache Center at the University of Copenhagen, and his coauthors. The study was published in Cephalalgia.
To assess how these biochemical variables might contribute to cluster headache attacks, the researchers launched a randomized, double-blind trial of data from 44 Danish participants with cluster headache. The average age of the patients was 38 years; 14 had active episodic cluster headache, 15 had episodic cluster headache in remission, and 15 had chronic cluster headache.
All patients received a continuous infusion of either PACAP38 (10 pmol/kg per minute) or VIP (8 pmol/kg per minute) over a 20-minute period, using a time- and volume-controlled infusion pump. Blood was collected for analysis at fixed time points, including at baseline, at the end of the infusion, 10 minutes after the infusion, and 70 minutes after the infusion. Technical problems led to missing values in 285 out of 1,144 planned plasma samples.
PACAP38 infusion resulted in a cluster headache attack in 13 of the 44 participants and VIP induced an attack in 12 of the 44. No differences in plasma CGRP (P = .7074), tryptase (P = .6673), and histamine (P = .4792) levels were found between patients who developed attacks and those who did not, and the plasma concentrations did not differ among the various blood-drawing time points.
There was also no difference in plasma CGRP levels between patients with active episodic cluster headache, those with episodic cluster headache in remission, and those with chronic cluster headache. After post hoc analysis, plasma tryptase and plasma histamine levels were similar among the three cluster headache patient groups.
The final link to the cluster headache puzzle has not yet been found
“We know a lot about cluster headache: how it presents, how we can stop it acutely, and how we can stop it preventively. But we don’t know everything about all the neurotransmitters involved, the triggers that start an attack, or the causes of pain,” Alan Rapoport, MD, professor of neurology at the University of California, Los Angeles (UCLA), and past president of the International Headache Society, said in an interview. “This study was performed to find the answer to a small piece of the puzzle. Is CGRP the missing link for patients who begin a cluster attack, or should we be looking elsewhere?
“I would be cautious and say it appears that it doesn’t seem to be related, but further studies may show something different,” he added. “The reason for my qualification: There is a monoclonal antibody [galcanezumab], which grabs CGRP and prevents it from docking on its receptor, that has been approved for preventive treatment of episodic cluster headache. When you have episodic cluster, go into a cluster period, and take galcanezumab, it could and should decrease the number of attacks that you would ordinarily have had. That means it is related somewhat. But it certainly doesn’t work for everyone, so more investigations like this are needed.”
“What’s important about this study is that it opens up the possibility that there is another way into the cluster attack that could be operationalized for therapeutic purposes,” Peter Goadsby, MD, PhD, professor of neurology at UCLA and president of the American Headache Society, said in an interview.
When asked about the authors’ stated interest in investigating “if monoclonal antibodies targeting the CGRP pathway prevent PACAP38- or VIP-induced cluster headache attacks” as a follow-up, Dr. Goadsby strongly backed the idea. “If I sound excited about actually exploring whether that was a useful treatment or not, it’s because cluster headache is a dreadful condition. And the sooner you could work out whether it was useful or put the money into something else, well, that’s where I’d go.
“I think the principle here of doing experimental medicine, getting into human work with targets like this at the earliest possible time, is something that is not done as often as would be appropriate,” he added. “There is not enough investment, in my view, in early phase experimental work, which really just gets to that next step. Broadly speaking, the encouragement and support of experimental medicine is crucial to developing new therapies.”
The authors recognized their study’s potential limitations, including it’s being an exploratory study with results that should be interpreted cautiously. They acknowledged discrepancies with previous studies of plasma CGRP during cluster headache attacks, offering “different methodologies, including intra-assay differences and the location of blood sampling” as a possible reason. They also explained that some of the data are missing “completely at random” due to their policy of discarding all observations with incomplete laboratory measurements, adding that the impact on their sample size was “only modest.”
“In spite of these limitations,” Dr. Rapoport said, “this is an excellent study that shows us that PACAP38- and VIP-induced cluster headache attacks are not associated with alterations in plasma CGRP or in histamine and tryptase.”
Regarding potential conflicts of interest, one author reported being employed at the testing lab where the histamine measurements were conducted, as did another author who serves as the lab’s scientific adviser. A third author reported receiving personal fees from various pharmaceutical companies.
such as tryptase and histamine, a new study has found.
“Whether cluster headache attacks provoked by CGRP and PACAP38/VIP are mediated by distinct signaling pathways will be worth investigating in forthcoming studies,” wrote Lanfranco Pellesi, MD, of the Danish Headache Center at the University of Copenhagen, and his coauthors. The study was published in Cephalalgia.
To assess how these biochemical variables might contribute to cluster headache attacks, the researchers launched a randomized, double-blind trial of data from 44 Danish participants with cluster headache. The average age of the patients was 38 years; 14 had active episodic cluster headache, 15 had episodic cluster headache in remission, and 15 had chronic cluster headache.
All patients received a continuous infusion of either PACAP38 (10 pmol/kg per minute) or VIP (8 pmol/kg per minute) over a 20-minute period, using a time- and volume-controlled infusion pump. Blood was collected for analysis at fixed time points, including at baseline, at the end of the infusion, 10 minutes after the infusion, and 70 minutes after the infusion. Technical problems led to missing values in 285 out of 1,144 planned plasma samples.
PACAP38 infusion resulted in a cluster headache attack in 13 of the 44 participants and VIP induced an attack in 12 of the 44. No differences in plasma CGRP (P = .7074), tryptase (P = .6673), and histamine (P = .4792) levels were found between patients who developed attacks and those who did not, and the plasma concentrations did not differ among the various blood-drawing time points.
There was also no difference in plasma CGRP levels between patients with active episodic cluster headache, those with episodic cluster headache in remission, and those with chronic cluster headache. After post hoc analysis, plasma tryptase and plasma histamine levels were similar among the three cluster headache patient groups.
The final link to the cluster headache puzzle has not yet been found
“We know a lot about cluster headache: how it presents, how we can stop it acutely, and how we can stop it preventively. But we don’t know everything about all the neurotransmitters involved, the triggers that start an attack, or the causes of pain,” Alan Rapoport, MD, professor of neurology at the University of California, Los Angeles (UCLA), and past president of the International Headache Society, said in an interview. “This study was performed to find the answer to a small piece of the puzzle. Is CGRP the missing link for patients who begin a cluster attack, or should we be looking elsewhere?
“I would be cautious and say it appears that it doesn’t seem to be related, but further studies may show something different,” he added. “The reason for my qualification: There is a monoclonal antibody [galcanezumab], which grabs CGRP and prevents it from docking on its receptor, that has been approved for preventive treatment of episodic cluster headache. When you have episodic cluster, go into a cluster period, and take galcanezumab, it could and should decrease the number of attacks that you would ordinarily have had. That means it is related somewhat. But it certainly doesn’t work for everyone, so more investigations like this are needed.”
“What’s important about this study is that it opens up the possibility that there is another way into the cluster attack that could be operationalized for therapeutic purposes,” Peter Goadsby, MD, PhD, professor of neurology at UCLA and president of the American Headache Society, said in an interview.
When asked about the authors’ stated interest in investigating “if monoclonal antibodies targeting the CGRP pathway prevent PACAP38- or VIP-induced cluster headache attacks” as a follow-up, Dr. Goadsby strongly backed the idea. “If I sound excited about actually exploring whether that was a useful treatment or not, it’s because cluster headache is a dreadful condition. And the sooner you could work out whether it was useful or put the money into something else, well, that’s where I’d go.
“I think the principle here of doing experimental medicine, getting into human work with targets like this at the earliest possible time, is something that is not done as often as would be appropriate,” he added. “There is not enough investment, in my view, in early phase experimental work, which really just gets to that next step. Broadly speaking, the encouragement and support of experimental medicine is crucial to developing new therapies.”
The authors recognized their study’s potential limitations, including it’s being an exploratory study with results that should be interpreted cautiously. They acknowledged discrepancies with previous studies of plasma CGRP during cluster headache attacks, offering “different methodologies, including intra-assay differences and the location of blood sampling” as a possible reason. They also explained that some of the data are missing “completely at random” due to their policy of discarding all observations with incomplete laboratory measurements, adding that the impact on their sample size was “only modest.”
“In spite of these limitations,” Dr. Rapoport said, “this is an excellent study that shows us that PACAP38- and VIP-induced cluster headache attacks are not associated with alterations in plasma CGRP or in histamine and tryptase.”
Regarding potential conflicts of interest, one author reported being employed at the testing lab where the histamine measurements were conducted, as did another author who serves as the lab’s scientific adviser. A third author reported receiving personal fees from various pharmaceutical companies.
such as tryptase and histamine, a new study has found.
“Whether cluster headache attacks provoked by CGRP and PACAP38/VIP are mediated by distinct signaling pathways will be worth investigating in forthcoming studies,” wrote Lanfranco Pellesi, MD, of the Danish Headache Center at the University of Copenhagen, and his coauthors. The study was published in Cephalalgia.
To assess how these biochemical variables might contribute to cluster headache attacks, the researchers launched a randomized, double-blind trial of data from 44 Danish participants with cluster headache. The average age of the patients was 38 years; 14 had active episodic cluster headache, 15 had episodic cluster headache in remission, and 15 had chronic cluster headache.
All patients received a continuous infusion of either PACAP38 (10 pmol/kg per minute) or VIP (8 pmol/kg per minute) over a 20-minute period, using a time- and volume-controlled infusion pump. Blood was collected for analysis at fixed time points, including at baseline, at the end of the infusion, 10 minutes after the infusion, and 70 minutes after the infusion. Technical problems led to missing values in 285 out of 1,144 planned plasma samples.
PACAP38 infusion resulted in a cluster headache attack in 13 of the 44 participants and VIP induced an attack in 12 of the 44. No differences in plasma CGRP (P = .7074), tryptase (P = .6673), and histamine (P = .4792) levels were found between patients who developed attacks and those who did not, and the plasma concentrations did not differ among the various blood-drawing time points.
There was also no difference in plasma CGRP levels between patients with active episodic cluster headache, those with episodic cluster headache in remission, and those with chronic cluster headache. After post hoc analysis, plasma tryptase and plasma histamine levels were similar among the three cluster headache patient groups.
The final link to the cluster headache puzzle has not yet been found
“We know a lot about cluster headache: how it presents, how we can stop it acutely, and how we can stop it preventively. But we don’t know everything about all the neurotransmitters involved, the triggers that start an attack, or the causes of pain,” Alan Rapoport, MD, professor of neurology at the University of California, Los Angeles (UCLA), and past president of the International Headache Society, said in an interview. “This study was performed to find the answer to a small piece of the puzzle. Is CGRP the missing link for patients who begin a cluster attack, or should we be looking elsewhere?
“I would be cautious and say it appears that it doesn’t seem to be related, but further studies may show something different,” he added. “The reason for my qualification: There is a monoclonal antibody [galcanezumab], which grabs CGRP and prevents it from docking on its receptor, that has been approved for preventive treatment of episodic cluster headache. When you have episodic cluster, go into a cluster period, and take galcanezumab, it could and should decrease the number of attacks that you would ordinarily have had. That means it is related somewhat. But it certainly doesn’t work for everyone, so more investigations like this are needed.”
“What’s important about this study is that it opens up the possibility that there is another way into the cluster attack that could be operationalized for therapeutic purposes,” Peter Goadsby, MD, PhD, professor of neurology at UCLA and president of the American Headache Society, said in an interview.
When asked about the authors’ stated interest in investigating “if monoclonal antibodies targeting the CGRP pathway prevent PACAP38- or VIP-induced cluster headache attacks” as a follow-up, Dr. Goadsby strongly backed the idea. “If I sound excited about actually exploring whether that was a useful treatment or not, it’s because cluster headache is a dreadful condition. And the sooner you could work out whether it was useful or put the money into something else, well, that’s where I’d go.
“I think the principle here of doing experimental medicine, getting into human work with targets like this at the earliest possible time, is something that is not done as often as would be appropriate,” he added. “There is not enough investment, in my view, in early phase experimental work, which really just gets to that next step. Broadly speaking, the encouragement and support of experimental medicine is crucial to developing new therapies.”
The authors recognized their study’s potential limitations, including it’s being an exploratory study with results that should be interpreted cautiously. They acknowledged discrepancies with previous studies of plasma CGRP during cluster headache attacks, offering “different methodologies, including intra-assay differences and the location of blood sampling” as a possible reason. They also explained that some of the data are missing “completely at random” due to their policy of discarding all observations with incomplete laboratory measurements, adding that the impact on their sample size was “only modest.”
“In spite of these limitations,” Dr. Rapoport said, “this is an excellent study that shows us that PACAP38- and VIP-induced cluster headache attacks are not associated with alterations in plasma CGRP or in histamine and tryptase.”
Regarding potential conflicts of interest, one author reported being employed at the testing lab where the histamine measurements were conducted, as did another author who serves as the lab’s scientific adviser. A third author reported receiving personal fees from various pharmaceutical companies.
FROM CEPHALALGIA
Perinatal deaths from COVID show ‘extensive’ placental damage
Recent evidence has shown that women who contract COVID-19 during pregnancy are at increased risk for pregnancy loss and neonatal death. Now, an analysis of pathology data from dozens of perinatal deaths shows how.
Unlike numerous pathogens that kill the fetus by infecting it directly, SARS-CoV-2 causes “widespread and severe” destruction of the placenta that deprives the fetus of oxygen, a team of 44 researchers in 12 countries concluded after examining 64 stillbirths and four neonatal deaths in which the placentas were infected with the virus. They noted that such damage occurs in a small percentage of pregnant women with COVID and that all the women in the study had not been vaccinated against the disease.
The findings were published online Feb. 10 in the Archives of Pathology & Laboratory Medicine.
Nearly all placentas had each of three features that pathologists have dubbed SARS-CoV-2 placentitis: large deposits of fibrin, a clotting protein that obstructs the flow of blood, death of cells in the trophoblast, and an unusual form of inflammation called chronic histiocytic intervillositis. Some had other abnormalities that could have exacerbated the condition.
The researchers called the extent of damage “striking,” affecting 77.7% of the placenta on average. The virus did not appear to harm fetal tissue, but placental damage “was extensive and highly destructive,” they write. Notably, none of the women in the analysis were known to have severe COVID.
Virus seen ‘chewing up the placenta’
David Schwartz, MD, a pathologist in Atlanta, and the lead author of the study, said COVID appears to be unique in destroying the placenta.
“I don’t know of any infection that does that to this degree or with this uniformity,” Dr. Schwartz told this news organization. “The simple message is that this infection is chewing up the placenta and destroying its capability to oxygenate the fetus.”
In November, the Centers for Disease Control and Prevention reported that maternal COVID increases the risk of losing a pregnancy. From March 2020 to September 2021, 8,154 stillbirths were reported, affecting 0.65% of births by women without COVID and 1.26% of births by women with COVID, for a relative risk of 1.90 (95% confidence interval, 1.69-2.15).
Delta, the variant that dominated in mid-2021, appears to have been particularly harmful. The CDC reported that the relative risk for stillbirth for mothers with COVID-19 during that period increased to 4.04 (95% CI, 3.28-4.97). Many cases in the new analysis coincided with Delta.
Dr. Schwartz and his colleagues said immunization, along with antiviral therapy, might reduce the chance of SARS-CoV-2 infecting the placenta. None of the mothers in the analysis was vaccinated, and Dr. Schwartz said he is not aware of a single case in a vaccinated woman.
The analysis comes on the heels of a study from the National Institutes of Health linking severe to moderate COVID infection to greater risk of other pregnancy complications: cesarean and preterm delivery, death during childbirth, postpartum hemorrhaging, and non-COVID infections.
Diana Bianchi, MD, director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, said those findings underscore the need for pregnant women to be vaccinated. (The shots have been shown to be safe for pregnant women.)
Denise Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the new analysis, said the findings may have important clinical implications. In addition to ensuring that pregnant patients are fully vaccinated, she said “there may be opportunities to more closely monitor the placenta during pregnancy using imaging modalities such as ultrasound.”
Even in the presence of severe abnormalities, a fetus that has reached a viable gestational age could potentially be delivered prior to stillbirth, Dr. Jamieson said. The 64 stillbirths in the analysis ranged from 15 to 39.2 weeks of gestation, with an average of 30 weeks. Eight were delivered at full term.
However, additional studies are needed to support monitoring of placental changes, she said: “It is not ready for prime time now.”
Christopher Zahn, MD, vice president of practice activities the American College of Obstetricians and Gynecologists, cautioned that data on COVID and pregnancy complications remain limited.
The findings in this analysis “do not prove the association between COVID-19 infection and neonatal outcomes,” Dr. Zahn said. “While stillbirth could potentially be another adverse outcome for pregnant people who contract COVID-19, currently we don’t have enough data to confirm that a COVID-19 infection at any point in pregnancy indicates increased risk of stillbirth.”
He added that ACOG continues to strongly recommend vaccination against COVID for women who are pregnant, recently pregnant, or planning to be pregnant.
Dr. Schwartz and Dr. Jamieson have disclosed no relevant financial relationships. One author reported receiving financial support from the Slovak Research and Development Agency. Another reported funding from the Belgian Fund for Scientific Research and the Fetus for Life charity.
A version of this article first appeared on Medscape.com.
Recent evidence has shown that women who contract COVID-19 during pregnancy are at increased risk for pregnancy loss and neonatal death. Now, an analysis of pathology data from dozens of perinatal deaths shows how.
Unlike numerous pathogens that kill the fetus by infecting it directly, SARS-CoV-2 causes “widespread and severe” destruction of the placenta that deprives the fetus of oxygen, a team of 44 researchers in 12 countries concluded after examining 64 stillbirths and four neonatal deaths in which the placentas were infected with the virus. They noted that such damage occurs in a small percentage of pregnant women with COVID and that all the women in the study had not been vaccinated against the disease.
The findings were published online Feb. 10 in the Archives of Pathology & Laboratory Medicine.
Nearly all placentas had each of three features that pathologists have dubbed SARS-CoV-2 placentitis: large deposits of fibrin, a clotting protein that obstructs the flow of blood, death of cells in the trophoblast, and an unusual form of inflammation called chronic histiocytic intervillositis. Some had other abnormalities that could have exacerbated the condition.
The researchers called the extent of damage “striking,” affecting 77.7% of the placenta on average. The virus did not appear to harm fetal tissue, but placental damage “was extensive and highly destructive,” they write. Notably, none of the women in the analysis were known to have severe COVID.
Virus seen ‘chewing up the placenta’
David Schwartz, MD, a pathologist in Atlanta, and the lead author of the study, said COVID appears to be unique in destroying the placenta.
“I don’t know of any infection that does that to this degree or with this uniformity,” Dr. Schwartz told this news organization. “The simple message is that this infection is chewing up the placenta and destroying its capability to oxygenate the fetus.”
In November, the Centers for Disease Control and Prevention reported that maternal COVID increases the risk of losing a pregnancy. From March 2020 to September 2021, 8,154 stillbirths were reported, affecting 0.65% of births by women without COVID and 1.26% of births by women with COVID, for a relative risk of 1.90 (95% confidence interval, 1.69-2.15).
Delta, the variant that dominated in mid-2021, appears to have been particularly harmful. The CDC reported that the relative risk for stillbirth for mothers with COVID-19 during that period increased to 4.04 (95% CI, 3.28-4.97). Many cases in the new analysis coincided with Delta.
Dr. Schwartz and his colleagues said immunization, along with antiviral therapy, might reduce the chance of SARS-CoV-2 infecting the placenta. None of the mothers in the analysis was vaccinated, and Dr. Schwartz said he is not aware of a single case in a vaccinated woman.
The analysis comes on the heels of a study from the National Institutes of Health linking severe to moderate COVID infection to greater risk of other pregnancy complications: cesarean and preterm delivery, death during childbirth, postpartum hemorrhaging, and non-COVID infections.
Diana Bianchi, MD, director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, said those findings underscore the need for pregnant women to be vaccinated. (The shots have been shown to be safe for pregnant women.)
Denise Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the new analysis, said the findings may have important clinical implications. In addition to ensuring that pregnant patients are fully vaccinated, she said “there may be opportunities to more closely monitor the placenta during pregnancy using imaging modalities such as ultrasound.”
Even in the presence of severe abnormalities, a fetus that has reached a viable gestational age could potentially be delivered prior to stillbirth, Dr. Jamieson said. The 64 stillbirths in the analysis ranged from 15 to 39.2 weeks of gestation, with an average of 30 weeks. Eight were delivered at full term.
However, additional studies are needed to support monitoring of placental changes, she said: “It is not ready for prime time now.”
Christopher Zahn, MD, vice president of practice activities the American College of Obstetricians and Gynecologists, cautioned that data on COVID and pregnancy complications remain limited.
The findings in this analysis “do not prove the association between COVID-19 infection and neonatal outcomes,” Dr. Zahn said. “While stillbirth could potentially be another adverse outcome for pregnant people who contract COVID-19, currently we don’t have enough data to confirm that a COVID-19 infection at any point in pregnancy indicates increased risk of stillbirth.”
He added that ACOG continues to strongly recommend vaccination against COVID for women who are pregnant, recently pregnant, or planning to be pregnant.
Dr. Schwartz and Dr. Jamieson have disclosed no relevant financial relationships. One author reported receiving financial support from the Slovak Research and Development Agency. Another reported funding from the Belgian Fund for Scientific Research and the Fetus for Life charity.
A version of this article first appeared on Medscape.com.
Recent evidence has shown that women who contract COVID-19 during pregnancy are at increased risk for pregnancy loss and neonatal death. Now, an analysis of pathology data from dozens of perinatal deaths shows how.
Unlike numerous pathogens that kill the fetus by infecting it directly, SARS-CoV-2 causes “widespread and severe” destruction of the placenta that deprives the fetus of oxygen, a team of 44 researchers in 12 countries concluded after examining 64 stillbirths and four neonatal deaths in which the placentas were infected with the virus. They noted that such damage occurs in a small percentage of pregnant women with COVID and that all the women in the study had not been vaccinated against the disease.
The findings were published online Feb. 10 in the Archives of Pathology & Laboratory Medicine.
Nearly all placentas had each of three features that pathologists have dubbed SARS-CoV-2 placentitis: large deposits of fibrin, a clotting protein that obstructs the flow of blood, death of cells in the trophoblast, and an unusual form of inflammation called chronic histiocytic intervillositis. Some had other abnormalities that could have exacerbated the condition.
The researchers called the extent of damage “striking,” affecting 77.7% of the placenta on average. The virus did not appear to harm fetal tissue, but placental damage “was extensive and highly destructive,” they write. Notably, none of the women in the analysis were known to have severe COVID.
Virus seen ‘chewing up the placenta’
David Schwartz, MD, a pathologist in Atlanta, and the lead author of the study, said COVID appears to be unique in destroying the placenta.
“I don’t know of any infection that does that to this degree or with this uniformity,” Dr. Schwartz told this news organization. “The simple message is that this infection is chewing up the placenta and destroying its capability to oxygenate the fetus.”
In November, the Centers for Disease Control and Prevention reported that maternal COVID increases the risk of losing a pregnancy. From March 2020 to September 2021, 8,154 stillbirths were reported, affecting 0.65% of births by women without COVID and 1.26% of births by women with COVID, for a relative risk of 1.90 (95% confidence interval, 1.69-2.15).
Delta, the variant that dominated in mid-2021, appears to have been particularly harmful. The CDC reported that the relative risk for stillbirth for mothers with COVID-19 during that period increased to 4.04 (95% CI, 3.28-4.97). Many cases in the new analysis coincided with Delta.
Dr. Schwartz and his colleagues said immunization, along with antiviral therapy, might reduce the chance of SARS-CoV-2 infecting the placenta. None of the mothers in the analysis was vaccinated, and Dr. Schwartz said he is not aware of a single case in a vaccinated woman.
The analysis comes on the heels of a study from the National Institutes of Health linking severe to moderate COVID infection to greater risk of other pregnancy complications: cesarean and preterm delivery, death during childbirth, postpartum hemorrhaging, and non-COVID infections.
Diana Bianchi, MD, director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, said those findings underscore the need for pregnant women to be vaccinated. (The shots have been shown to be safe for pregnant women.)
Denise Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the new analysis, said the findings may have important clinical implications. In addition to ensuring that pregnant patients are fully vaccinated, she said “there may be opportunities to more closely monitor the placenta during pregnancy using imaging modalities such as ultrasound.”
Even in the presence of severe abnormalities, a fetus that has reached a viable gestational age could potentially be delivered prior to stillbirth, Dr. Jamieson said. The 64 stillbirths in the analysis ranged from 15 to 39.2 weeks of gestation, with an average of 30 weeks. Eight were delivered at full term.
However, additional studies are needed to support monitoring of placental changes, she said: “It is not ready for prime time now.”
Christopher Zahn, MD, vice president of practice activities the American College of Obstetricians and Gynecologists, cautioned that data on COVID and pregnancy complications remain limited.
The findings in this analysis “do not prove the association between COVID-19 infection and neonatal outcomes,” Dr. Zahn said. “While stillbirth could potentially be another adverse outcome for pregnant people who contract COVID-19, currently we don’t have enough data to confirm that a COVID-19 infection at any point in pregnancy indicates increased risk of stillbirth.”
He added that ACOG continues to strongly recommend vaccination against COVID for women who are pregnant, recently pregnant, or planning to be pregnant.
Dr. Schwartz and Dr. Jamieson have disclosed no relevant financial relationships. One author reported receiving financial support from the Slovak Research and Development Agency. Another reported funding from the Belgian Fund for Scientific Research and the Fetus for Life charity.
A version of this article first appeared on Medscape.com.
Breast cancer now leading cause of cancer death in Black women
Breast cancer has replaced lung cancer as the leading cause of cancer-related death among Black women, but lung cancer remains the leading cause of cancer death in Black men, according to a new report from the American Cancer Society (ACS).
Lung cancer remains the second most commonly diagnosed cancer in both Black women and Black men.
These are among the key findings of the report, Cancer Statistics for African American/Black People 2022 – a triannual compilation of U.S. data on cancer incidence, mortality, survival, screening, and risk factors for Black people – and it marks a major shift as of 2019.
“African American/Black people have a disproportionately high cancer burden compared to other population groups. According to the report, the risk of cancer death for Black individuals remains 19% higher for men and 12% higher for women compared to White individuals,” the ACS says in a statement.
“The gap for breast cancer is more alarming,” it adds. “Black women are 41% more likely to die from breast cancer than White women despite a lower risk of being diagnosed with the disease.”
The new report, published online on Feb. 10 in CA: A Cancer Journal for Clinicians, also notes the following:
An estimated 224,080 new cancer cases and 73,680 cancer deaths will occur among Black people in 2022.
Over the past 5 data years, Black women had an 8% lower overall cancer incidence than White women but 12% higher mortality; Black men have 6% higher cancer incidence than White men but 19% higher cancer mortality.
Prostate cancer mortality among Black men decreased by 1.3% per year from 2015 to 2019 despite a 5% increase in the diagnosis of distant-stage prostate cancer annually since 2012, but the decline was slower than the 5% per year decline from 2010 to 2014.
The overall cancer mortality gap between Black and White people is narrowing. This is due to a steeper drop in prostate, lung, and other smoking-related cancers among Black people.
Colorectal cancer incidence and mortality rates are 21% and 44% higher, respectively, in Black men in comparison with White men and 18% and 31% higher, respectively, in Black women in comparison with White women.
The reasons for the disparities are complex but “largely stem from less access to high-quality care and optimal treatment as a repercussion of long-standing institutional racism,” the report concludes.
“We must address structural racism as a public health issue to close the gaps and advance health equity,” Tawana Thomas-Johnson, senior vice president and chief diversity officer at the ACS, said in the press release.
A version of this article first appeared on Medscape.com.
Breast cancer has replaced lung cancer as the leading cause of cancer-related death among Black women, but lung cancer remains the leading cause of cancer death in Black men, according to a new report from the American Cancer Society (ACS).
Lung cancer remains the second most commonly diagnosed cancer in both Black women and Black men.
These are among the key findings of the report, Cancer Statistics for African American/Black People 2022 – a triannual compilation of U.S. data on cancer incidence, mortality, survival, screening, and risk factors for Black people – and it marks a major shift as of 2019.
“African American/Black people have a disproportionately high cancer burden compared to other population groups. According to the report, the risk of cancer death for Black individuals remains 19% higher for men and 12% higher for women compared to White individuals,” the ACS says in a statement.
“The gap for breast cancer is more alarming,” it adds. “Black women are 41% more likely to die from breast cancer than White women despite a lower risk of being diagnosed with the disease.”
The new report, published online on Feb. 10 in CA: A Cancer Journal for Clinicians, also notes the following:
An estimated 224,080 new cancer cases and 73,680 cancer deaths will occur among Black people in 2022.
Over the past 5 data years, Black women had an 8% lower overall cancer incidence than White women but 12% higher mortality; Black men have 6% higher cancer incidence than White men but 19% higher cancer mortality.
Prostate cancer mortality among Black men decreased by 1.3% per year from 2015 to 2019 despite a 5% increase in the diagnosis of distant-stage prostate cancer annually since 2012, but the decline was slower than the 5% per year decline from 2010 to 2014.
The overall cancer mortality gap between Black and White people is narrowing. This is due to a steeper drop in prostate, lung, and other smoking-related cancers among Black people.
Colorectal cancer incidence and mortality rates are 21% and 44% higher, respectively, in Black men in comparison with White men and 18% and 31% higher, respectively, in Black women in comparison with White women.
The reasons for the disparities are complex but “largely stem from less access to high-quality care and optimal treatment as a repercussion of long-standing institutional racism,” the report concludes.
“We must address structural racism as a public health issue to close the gaps and advance health equity,” Tawana Thomas-Johnson, senior vice president and chief diversity officer at the ACS, said in the press release.
A version of this article first appeared on Medscape.com.
Breast cancer has replaced lung cancer as the leading cause of cancer-related death among Black women, but lung cancer remains the leading cause of cancer death in Black men, according to a new report from the American Cancer Society (ACS).
Lung cancer remains the second most commonly diagnosed cancer in both Black women and Black men.
These are among the key findings of the report, Cancer Statistics for African American/Black People 2022 – a triannual compilation of U.S. data on cancer incidence, mortality, survival, screening, and risk factors for Black people – and it marks a major shift as of 2019.
“African American/Black people have a disproportionately high cancer burden compared to other population groups. According to the report, the risk of cancer death for Black individuals remains 19% higher for men and 12% higher for women compared to White individuals,” the ACS says in a statement.
“The gap for breast cancer is more alarming,” it adds. “Black women are 41% more likely to die from breast cancer than White women despite a lower risk of being diagnosed with the disease.”
The new report, published online on Feb. 10 in CA: A Cancer Journal for Clinicians, also notes the following:
An estimated 224,080 new cancer cases and 73,680 cancer deaths will occur among Black people in 2022.
Over the past 5 data years, Black women had an 8% lower overall cancer incidence than White women but 12% higher mortality; Black men have 6% higher cancer incidence than White men but 19% higher cancer mortality.
Prostate cancer mortality among Black men decreased by 1.3% per year from 2015 to 2019 despite a 5% increase in the diagnosis of distant-stage prostate cancer annually since 2012, but the decline was slower than the 5% per year decline from 2010 to 2014.
The overall cancer mortality gap between Black and White people is narrowing. This is due to a steeper drop in prostate, lung, and other smoking-related cancers among Black people.
Colorectal cancer incidence and mortality rates are 21% and 44% higher, respectively, in Black men in comparison with White men and 18% and 31% higher, respectively, in Black women in comparison with White women.
The reasons for the disparities are complex but “largely stem from less access to high-quality care and optimal treatment as a repercussion of long-standing institutional racism,” the report concludes.
“We must address structural racism as a public health issue to close the gaps and advance health equity,” Tawana Thomas-Johnson, senior vice president and chief diversity officer at the ACS, said in the press release.
A version of this article first appeared on Medscape.com.