User login
The future of GI: A choice between ‘care assembly’ or skilled risk management
BOSTON – Gastroenterology is becoming a game of risk: It’s either learn to leverage risk through the creation of advanced alternative payment methods (APM) under Medicare’s new Quality Payment Program or risk losing money through the commoditization of the field, according to an expert.
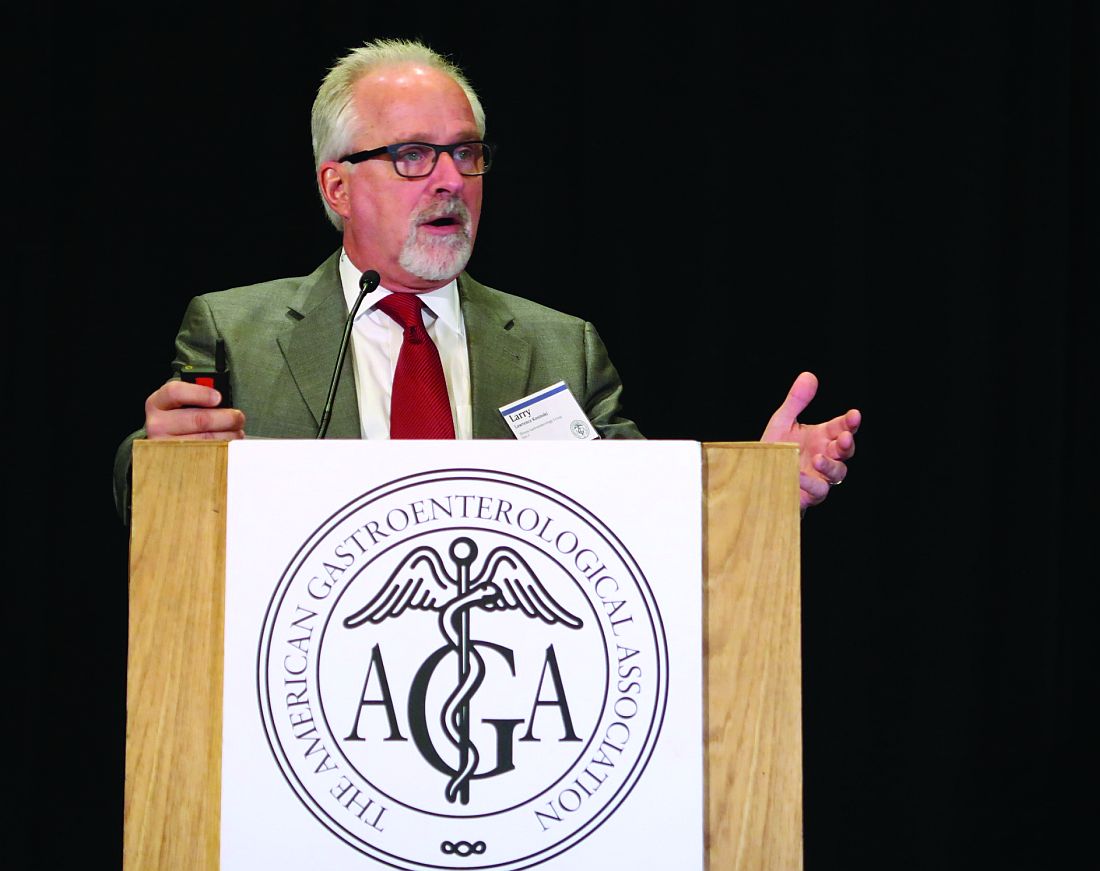
“Our culture right now is one where we get paid for making widgets,” said Lawrence Kosinski, MD, a practice councilor on the American Gastroenterological Association Governing Board and former chairman of its Practice Management and Economics Committee. He made his remarks in an interview in advance of his presentation at the 2017 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. “The more colonoscopies we do, the more money we make. The more we can charge for those colonoscopies and get collected, the better things are for us.”
“Over 80% of the cost of health care is for the management of chronic disease. We happen to have a very expensive set of chronic diseases that we take care of in GI, very complicated illnesses. We need to leverage the management of those patients, but we need to be able to show how our work decreases the overall cost of care so that we can get a piece of that risk premium,” he said.
In his own practice, Dr. Kosinski and his colleagues have created an APM – the first novel APM to be recommended to the Centers for Medicare & Medicaid Services for approval by the Physician-Focused Payment Model Technical Advisory Committee – that is based on better patient risk assessment, combined with earlier patient engagement.
After discovering in 2013 that one of his payers was spending $24,000 annually on patients with inflammatory bowel disease and that two-thirds of patients with inflammatory bowel disease who are admitted to the hospital had not had a CPT code issued in the 30 days before admission, Dr. Kosinski and his colleagues wanted to see if they could offer the insurer value by decreasing that hospitalization rate.
Using proprietary algorithms rooted in thorough patient risk assessment according to published guidelines for the management of patients with Crohn’s disease, they created a patient platform – coined ProjectSonar – that alerts their Crohn’s patients on their smart phones, engages them in a short survey, and provides them with instant feedback on their disease status and care needs based on their responses. Survey results are sent to the Web and to nurse case managers at the practice, who follow up with the patient accordingly.
A year-long pilot program of the patient portal with 50 people in the study population showed more than a 600% return on the cost of investment in the proprietary software, with an average of $6,000 in medical savings for test subjects who responded to texts, compared with controls who did not receive smart phone texts, for a total savings of more than half a million dollars. “All of the savings come from the patients who respond,” Dr. Kosinski said, noting that, in his practice, they now have a sustained patient response rate of more than 80% and that it helps to have the physician emphasize use of the platform to the patient.
“Patients love it. It is almost like chronic disease concierge medicine they don’t have to pay for,” Dr. Kosinski said during his presentation at the meeting, adding that the insurer likes it because it cuts costs, and physicians like it because they don’t have to take less reimbursement to help the insurer realize gains.
“We risk assess every patient, something the majority of doctors don’t do but [that] insurance companies do all the time,” Dr. Kosinski said in an interview after his presentation. “Then we apply the appropriate treatment using the scientific methods in the published guidelines. Then we analyze the data, which helps us refine our assessments and predict our costs of care in this population.”
Knowing the base cost of care for specific patient populations helps define the margin of financial risk he and his colleagues can tolerate. A gastroenterology practice that operates as a risk-bearing entity could theoretically offer to contract with affordable care organizations to manage IBD or other GI-type conditions, he said.
By learning to assess, measure, and leverage risk, gastroenterologists can become sought after for the value they provide rather than for the care they “assemble,” something Dr. Kosinski said is of rising concern as the Affordable Care Act has driven a lot of consolidation, with hospital systems buying up primary care physicians and specialists.
Otherwise, he said, “We’re just going to be commoditized proceduralists.”
Dr. Kosinski is president of SonarMDTM.
[email protected]
On Twitter @whitneymcknight
BOSTON – Gastroenterology is becoming a game of risk: It’s either learn to leverage risk through the creation of advanced alternative payment methods (APM) under Medicare’s new Quality Payment Program or risk losing money through the commoditization of the field, according to an expert.
“Our culture right now is one where we get paid for making widgets,” said Lawrence Kosinski, MD, a practice councilor on the American Gastroenterological Association Governing Board and former chairman of its Practice Management and Economics Committee. He made his remarks in an interview in advance of his presentation at the 2017 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. “The more colonoscopies we do, the more money we make. The more we can charge for those colonoscopies and get collected, the better things are for us.”
“Over 80% of the cost of health care is for the management of chronic disease. We happen to have a very expensive set of chronic diseases that we take care of in GI, very complicated illnesses. We need to leverage the management of those patients, but we need to be able to show how our work decreases the overall cost of care so that we can get a piece of that risk premium,” he said.
In his own practice, Dr. Kosinski and his colleagues have created an APM – the first novel APM to be recommended to the Centers for Medicare & Medicaid Services for approval by the Physician-Focused Payment Model Technical Advisory Committee – that is based on better patient risk assessment, combined with earlier patient engagement.
After discovering in 2013 that one of his payers was spending $24,000 annually on patients with inflammatory bowel disease and that two-thirds of patients with inflammatory bowel disease who are admitted to the hospital had not had a CPT code issued in the 30 days before admission, Dr. Kosinski and his colleagues wanted to see if they could offer the insurer value by decreasing that hospitalization rate.
Using proprietary algorithms rooted in thorough patient risk assessment according to published guidelines for the management of patients with Crohn’s disease, they created a patient platform – coined ProjectSonar – that alerts their Crohn’s patients on their smart phones, engages them in a short survey, and provides them with instant feedback on their disease status and care needs based on their responses. Survey results are sent to the Web and to nurse case managers at the practice, who follow up with the patient accordingly.
A year-long pilot program of the patient portal with 50 people in the study population showed more than a 600% return on the cost of investment in the proprietary software, with an average of $6,000 in medical savings for test subjects who responded to texts, compared with controls who did not receive smart phone texts, for a total savings of more than half a million dollars. “All of the savings come from the patients who respond,” Dr. Kosinski said, noting that, in his practice, they now have a sustained patient response rate of more than 80% and that it helps to have the physician emphasize use of the platform to the patient.
“Patients love it. It is almost like chronic disease concierge medicine they don’t have to pay for,” Dr. Kosinski said during his presentation at the meeting, adding that the insurer likes it because it cuts costs, and physicians like it because they don’t have to take less reimbursement to help the insurer realize gains.
“We risk assess every patient, something the majority of doctors don’t do but [that] insurance companies do all the time,” Dr. Kosinski said in an interview after his presentation. “Then we apply the appropriate treatment using the scientific methods in the published guidelines. Then we analyze the data, which helps us refine our assessments and predict our costs of care in this population.”
Knowing the base cost of care for specific patient populations helps define the margin of financial risk he and his colleagues can tolerate. A gastroenterology practice that operates as a risk-bearing entity could theoretically offer to contract with affordable care organizations to manage IBD or other GI-type conditions, he said.
By learning to assess, measure, and leverage risk, gastroenterologists can become sought after for the value they provide rather than for the care they “assemble,” something Dr. Kosinski said is of rising concern as the Affordable Care Act has driven a lot of consolidation, with hospital systems buying up primary care physicians and specialists.
Otherwise, he said, “We’re just going to be commoditized proceduralists.”
Dr. Kosinski is president of SonarMDTM.
[email protected]
On Twitter @whitneymcknight
BOSTON – Gastroenterology is becoming a game of risk: It’s either learn to leverage risk through the creation of advanced alternative payment methods (APM) under Medicare’s new Quality Payment Program or risk losing money through the commoditization of the field, according to an expert.
“Our culture right now is one where we get paid for making widgets,” said Lawrence Kosinski, MD, a practice councilor on the American Gastroenterological Association Governing Board and former chairman of its Practice Management and Economics Committee. He made his remarks in an interview in advance of his presentation at the 2017 AGA Tech Summit sponsored by the AGA Center for GI Innovation and Technology. “The more colonoscopies we do, the more money we make. The more we can charge for those colonoscopies and get collected, the better things are for us.”
“Over 80% of the cost of health care is for the management of chronic disease. We happen to have a very expensive set of chronic diseases that we take care of in GI, very complicated illnesses. We need to leverage the management of those patients, but we need to be able to show how our work decreases the overall cost of care so that we can get a piece of that risk premium,” he said.
In his own practice, Dr. Kosinski and his colleagues have created an APM – the first novel APM to be recommended to the Centers for Medicare & Medicaid Services for approval by the Physician-Focused Payment Model Technical Advisory Committee – that is based on better patient risk assessment, combined with earlier patient engagement.
After discovering in 2013 that one of his payers was spending $24,000 annually on patients with inflammatory bowel disease and that two-thirds of patients with inflammatory bowel disease who are admitted to the hospital had not had a CPT code issued in the 30 days before admission, Dr. Kosinski and his colleagues wanted to see if they could offer the insurer value by decreasing that hospitalization rate.
Using proprietary algorithms rooted in thorough patient risk assessment according to published guidelines for the management of patients with Crohn’s disease, they created a patient platform – coined ProjectSonar – that alerts their Crohn’s patients on their smart phones, engages them in a short survey, and provides them with instant feedback on their disease status and care needs based on their responses. Survey results are sent to the Web and to nurse case managers at the practice, who follow up with the patient accordingly.
A year-long pilot program of the patient portal with 50 people in the study population showed more than a 600% return on the cost of investment in the proprietary software, with an average of $6,000 in medical savings for test subjects who responded to texts, compared with controls who did not receive smart phone texts, for a total savings of more than half a million dollars. “All of the savings come from the patients who respond,” Dr. Kosinski said, noting that, in his practice, they now have a sustained patient response rate of more than 80% and that it helps to have the physician emphasize use of the platform to the patient.
“Patients love it. It is almost like chronic disease concierge medicine they don’t have to pay for,” Dr. Kosinski said during his presentation at the meeting, adding that the insurer likes it because it cuts costs, and physicians like it because they don’t have to take less reimbursement to help the insurer realize gains.
“We risk assess every patient, something the majority of doctors don’t do but [that] insurance companies do all the time,” Dr. Kosinski said in an interview after his presentation. “Then we apply the appropriate treatment using the scientific methods in the published guidelines. Then we analyze the data, which helps us refine our assessments and predict our costs of care in this population.”
Knowing the base cost of care for specific patient populations helps define the margin of financial risk he and his colleagues can tolerate. A gastroenterology practice that operates as a risk-bearing entity could theoretically offer to contract with affordable care organizations to manage IBD or other GI-type conditions, he said.
By learning to assess, measure, and leverage risk, gastroenterologists can become sought after for the value they provide rather than for the care they “assemble,” something Dr. Kosinski said is of rising concern as the Affordable Care Act has driven a lot of consolidation, with hospital systems buying up primary care physicians and specialists.
Otherwise, he said, “We’re just going to be commoditized proceduralists.”
Dr. Kosinski is president of SonarMDTM.
[email protected]
On Twitter @whitneymcknight
FROM THE 2017 AGA TECH SUMMIT
FDA warns against use of codeine, tramadol in children
The Food and Drug Administration is restricting the use of two opiates – codeine and tramadol – in children, and also warns they are potentially dangerous to infants of breastfeeding women.
Codeine is approved to treat pain and cough; tramadol is approved to treat pain.
“We understand that there are limited options when it comes to treating pain or cough in children, and that these changes may raise some questions for health care providers and parents. However, please know that our decision today was made based on the latest evidence and with this goal in mind: keeping our kids safe,” Douglas Throckmorton, MD, the deputy center director for regulatory programs at the FDA Center for Drug Evaluation and Research, said in a statement.
In 2013, the FDA updated prescription codeine labeling to contain a boxed warning and contraindication for children up to age 18 years regarding the risk of slowed breathing from codeine prescribed after tonsillectomy and/or adenoidectomy. And in 2015, the agency issued warnings about the risk of serious breathing problems in children who had ultrarapid metabolism of codeine and tramadol.
In the current safety statement, the FDA said it will require additional labeling changes, including contraindications for use of codeine or tramadol in all children younger than 12 years of age and a new contraindication for tramadol in children younger than 18 years being treated for pain after tonsillectomy and/or adenoidectomy, warnings about their use in children 12-18 years of age with certain medical conditions, and a stronger warning recommending against their use in nursing mothers.
Single-ingredient codeine and all tramadol-containing products are FDA-approved only for use in adults, the agency noted.
The agency cited particular concerns over those who are “ultra-rapid metabolizers” of substrates of the cytochrome P450 isoenzyme 2D6 (CYP2D6) genotype. These people more quickly convert codeine into potentially dangerously high levels of morphine, which can lead to fatal respiratory depression.
Supporting the restrictions and warning were data on 64 cases of respiratory depression that occurred worldwide between 1969 and 2015, when a codeine-based medicine was used in children younger than 18 years. Twenty-four of these children died.
The most frequently cited medicines in the cases were acetaminophen with codeine and promethazine with codeine with or without phenylephrine, either given to soothe postoperative pain, general pain, sore or strep throat pain, or cough and cold.
Ten of the 64 cases implicated the CYP2D6 genotype. Seven of the patients were “ultrarapid metabolizers,” five of whom died.
Data cited on tramadol included nine worldwide cases of tramadol-related respiratory depression occurring between 1969 and 2016, resulting in the deaths of three children, all under the age of 6 years, and all of whom were taking the drug for postoperative pain or fever.
All but one case of respiratory depression occurred within the first 24 hours of taking the drug. One of the patients was genotyped for CYP2D6, and found to have three functional alleles consistent with ultrarapid metabolism.
Mothers who are ultrarapid metabolizers of codeine can have high levels of morphine in their breast milk that are dangerous to their breastfed infants, whereas there is less of a threat posed by women with normal codeine metabolism because the amount of codeine secreted into the breast milk is low and dose dependent.
The FDA stated that data reveal numerous reports of respiratory depression and at least one death in infants of breastfeeding mothers taking these medicines, particularly mothers with the CYP2D6 genotype. Although there are FDA-cleared tests for ultrarapid metabolism, they are not commonly used.
The agency stated that breastfeeding women taking any opioid pain medicine, including codeine or tramadol should contact their health care provider if they notice the infant is sleeping more than 4 hours at a time, or if the infant is having difficulty breastfeeding or seems limp.
Clinicians are urged to report side effects that occur while using codeine or tramadol to the FDA’s MedWatch Adverse Event Reporting program.
[email protected]
On Twitter @whitneymcknight
The Food and Drug Administration is restricting the use of two opiates – codeine and tramadol – in children, and also warns they are potentially dangerous to infants of breastfeeding women.
Codeine is approved to treat pain and cough; tramadol is approved to treat pain.
“We understand that there are limited options when it comes to treating pain or cough in children, and that these changes may raise some questions for health care providers and parents. However, please know that our decision today was made based on the latest evidence and with this goal in mind: keeping our kids safe,” Douglas Throckmorton, MD, the deputy center director for regulatory programs at the FDA Center for Drug Evaluation and Research, said in a statement.
In 2013, the FDA updated prescription codeine labeling to contain a boxed warning and contraindication for children up to age 18 years regarding the risk of slowed breathing from codeine prescribed after tonsillectomy and/or adenoidectomy. And in 2015, the agency issued warnings about the risk of serious breathing problems in children who had ultrarapid metabolism of codeine and tramadol.
In the current safety statement, the FDA said it will require additional labeling changes, including contraindications for use of codeine or tramadol in all children younger than 12 years of age and a new contraindication for tramadol in children younger than 18 years being treated for pain after tonsillectomy and/or adenoidectomy, warnings about their use in children 12-18 years of age with certain medical conditions, and a stronger warning recommending against their use in nursing mothers.
Single-ingredient codeine and all tramadol-containing products are FDA-approved only for use in adults, the agency noted.
The agency cited particular concerns over those who are “ultra-rapid metabolizers” of substrates of the cytochrome P450 isoenzyme 2D6 (CYP2D6) genotype. These people more quickly convert codeine into potentially dangerously high levels of morphine, which can lead to fatal respiratory depression.
Supporting the restrictions and warning were data on 64 cases of respiratory depression that occurred worldwide between 1969 and 2015, when a codeine-based medicine was used in children younger than 18 years. Twenty-four of these children died.
The most frequently cited medicines in the cases were acetaminophen with codeine and promethazine with codeine with or without phenylephrine, either given to soothe postoperative pain, general pain, sore or strep throat pain, or cough and cold.
Ten of the 64 cases implicated the CYP2D6 genotype. Seven of the patients were “ultrarapid metabolizers,” five of whom died.
Data cited on tramadol included nine worldwide cases of tramadol-related respiratory depression occurring between 1969 and 2016, resulting in the deaths of three children, all under the age of 6 years, and all of whom were taking the drug for postoperative pain or fever.
All but one case of respiratory depression occurred within the first 24 hours of taking the drug. One of the patients was genotyped for CYP2D6, and found to have three functional alleles consistent with ultrarapid metabolism.
Mothers who are ultrarapid metabolizers of codeine can have high levels of morphine in their breast milk that are dangerous to their breastfed infants, whereas there is less of a threat posed by women with normal codeine metabolism because the amount of codeine secreted into the breast milk is low and dose dependent.
The FDA stated that data reveal numerous reports of respiratory depression and at least one death in infants of breastfeeding mothers taking these medicines, particularly mothers with the CYP2D6 genotype. Although there are FDA-cleared tests for ultrarapid metabolism, they are not commonly used.
The agency stated that breastfeeding women taking any opioid pain medicine, including codeine or tramadol should contact their health care provider if they notice the infant is sleeping more than 4 hours at a time, or if the infant is having difficulty breastfeeding or seems limp.
Clinicians are urged to report side effects that occur while using codeine or tramadol to the FDA’s MedWatch Adverse Event Reporting program.
[email protected]
On Twitter @whitneymcknight
The Food and Drug Administration is restricting the use of two opiates – codeine and tramadol – in children, and also warns they are potentially dangerous to infants of breastfeeding women.
Codeine is approved to treat pain and cough; tramadol is approved to treat pain.
“We understand that there are limited options when it comes to treating pain or cough in children, and that these changes may raise some questions for health care providers and parents. However, please know that our decision today was made based on the latest evidence and with this goal in mind: keeping our kids safe,” Douglas Throckmorton, MD, the deputy center director for regulatory programs at the FDA Center for Drug Evaluation and Research, said in a statement.
In 2013, the FDA updated prescription codeine labeling to contain a boxed warning and contraindication for children up to age 18 years regarding the risk of slowed breathing from codeine prescribed after tonsillectomy and/or adenoidectomy. And in 2015, the agency issued warnings about the risk of serious breathing problems in children who had ultrarapid metabolism of codeine and tramadol.
In the current safety statement, the FDA said it will require additional labeling changes, including contraindications for use of codeine or tramadol in all children younger than 12 years of age and a new contraindication for tramadol in children younger than 18 years being treated for pain after tonsillectomy and/or adenoidectomy, warnings about their use in children 12-18 years of age with certain medical conditions, and a stronger warning recommending against their use in nursing mothers.
Single-ingredient codeine and all tramadol-containing products are FDA-approved only for use in adults, the agency noted.
The agency cited particular concerns over those who are “ultra-rapid metabolizers” of substrates of the cytochrome P450 isoenzyme 2D6 (CYP2D6) genotype. These people more quickly convert codeine into potentially dangerously high levels of morphine, which can lead to fatal respiratory depression.
Supporting the restrictions and warning were data on 64 cases of respiratory depression that occurred worldwide between 1969 and 2015, when a codeine-based medicine was used in children younger than 18 years. Twenty-four of these children died.
The most frequently cited medicines in the cases were acetaminophen with codeine and promethazine with codeine with or without phenylephrine, either given to soothe postoperative pain, general pain, sore or strep throat pain, or cough and cold.
Ten of the 64 cases implicated the CYP2D6 genotype. Seven of the patients were “ultrarapid metabolizers,” five of whom died.
Data cited on tramadol included nine worldwide cases of tramadol-related respiratory depression occurring between 1969 and 2016, resulting in the deaths of three children, all under the age of 6 years, and all of whom were taking the drug for postoperative pain or fever.
All but one case of respiratory depression occurred within the first 24 hours of taking the drug. One of the patients was genotyped for CYP2D6, and found to have three functional alleles consistent with ultrarapid metabolism.
Mothers who are ultrarapid metabolizers of codeine can have high levels of morphine in their breast milk that are dangerous to their breastfed infants, whereas there is less of a threat posed by women with normal codeine metabolism because the amount of codeine secreted into the breast milk is low and dose dependent.
The FDA stated that data reveal numerous reports of respiratory depression and at least one death in infants of breastfeeding mothers taking these medicines, particularly mothers with the CYP2D6 genotype. Although there are FDA-cleared tests for ultrarapid metabolism, they are not commonly used.
The agency stated that breastfeeding women taking any opioid pain medicine, including codeine or tramadol should contact their health care provider if they notice the infant is sleeping more than 4 hours at a time, or if the infant is having difficulty breastfeeding or seems limp.
Clinicians are urged to report side effects that occur while using codeine or tramadol to the FDA’s MedWatch Adverse Event Reporting program.
[email protected]
On Twitter @whitneymcknight
Empirical evidence lags behind rise in preadolescents presenting with gender dysphoria
SCOTTSDALE, ARIZ. – The treatment of preadolescents who present with gender questions is often complicated by the absence of evidence-based data on who is most likely to remain gender dysphoric into adulthood and who is not, an expert said at the annual meeting of the American College of Psychiatrists.
“There are some [clinicians] who believe they can predict who will persist and who will not. But they have not published, to my satisfaction, a way to show anyone else how to tell the difference,” said Jack Drescher, MD, a member of the World Health Organization’s (WHO’s) Working Group on the Classification of Sexual Disorders and Sexual Health and clinical professor of psychiatry and behavioral sciences at New York Medical College, Valhalla.
The WHO working group was tasked with categorizing sex and gender diagnoses in the forthcoming International Classification of Diseases (ICD-11). Dr. Drescher said that he and his fellow WHO working group members have identified at least three discrete transgender populations.
“There are persisters, desisters, and those who first develop gender dysphoria in adolescence and adulthood,” he said. “It would be a clinical mistake to think that there is a seamless transition from childhood gender dysphoria into adolescent and adult gender dysphoria.”
Dr. Drescher said that he believes the Dutch model for treating younger children diagnosed with what is interchangeably referred to as gender dysphoria or gender variance demonstrates the greatest sensitivity to how fluid the situation can be for many of these children. The absence of biomarkers for dysphoria that will persist into adulthood and the finding that a minority of prepubescent gender dysphoria diagnoses persist into adolescence inform the Dutch approach.
This approach, which originated at the VU University Medical Center Amsterdam, is based on 2 decades of research and practice. It assumes that it is better not to actively transition a child socially but to remain neutral to the way in which the child expresses gender identity. If children persist into late adolescence in this model, they are assisted in transitioning. If not, they are supported socially as they adjust to their natal gender. Puberty may sometimes have to be suppressed until the time one of the two paths has been decided.
“In my opinion, it is the most conservative approach,” Dr. Drescher said of the Dutch model. “They are the most cognizant of how much we don’t know, and they do a lot of good research.”
An approach originating at the Child and Adolescent Gender Center Clinic, which is affiliated with the University of California, San Francisco, supports a child socially into a cross-gendered role without medical or surgical intervention but also suppresses puberty. This method is based on the presumption of an adult transgender outcome, despite the absence of a way to predict results, said Dr. Drescher, who also cautions about the iatrogenic effects of such a presumption. “It takes a lot of work to socially transition a child in one direction. It would take a lot to transition back in the other direction, and there is no good empirical data as to whether this is entirely a benign process,” he said.
A third method originated in Toronto at the Centre for Addiction and Mental Health. This method actively discourages a child’s atypical gender interests and views transsexualism as an undesirable outcome that can be prevented, despite what Dr. Drescher said is a complete lack of evidence to either support or refute this claim. This method largely has been abandoned, in part since Ontario and five U.S. states and the District of Columbia have passed laws banning efforts to change a minor’s sexual orientation or gender identity. This method does have puberty suppression in children whose gender dysphoria appears to be persisting into adolescence in common with the other two.
Dr. Drescher said puberty suppression has helped decrease the levels of anxiety, depression, and suicidal ideation typically associated with this cohort. Postponing the development of secondary sexual characteristics gives those who ultimately will desist from their dysphoria more time to let it run its course. The Dutch first initiated this procedure 2 decades ago and have shown that any possible future side effects are outweighed by the psychosocial advantages it provides in the present.
The clinical view of gender dysphoria probably will get a jolt in 2018 upon publication of the ICD-11. In an interview, Dr. Drescher said that, if the condition is no longer categorized by the WHO as a mental disorder and is instead called “gender incongruence” in a chapter dedicated to gender and sexuality issues as currently planned, “it is likely the [American Psychiatric Association] will follow suit and remove gender dysphoria from the DSM. However, I don’t know how long that will take,” he said.
In his presentation, Dr. Drescher said that the causes for gender dysphoria remain unknown, as do the ways in which gender identity develops. It is also unclear how biological, psychosocial, and environmental factors affect gender dysphoria. What is clear, he said, is that “we have to rethink our developmental literature.”
Meanwhile, although gender dysphoria affects a relatively small percentage of the population – less than 1% of “nonreferred” children and adolescents, according to the DSM-5 – the number of prepubescent children presenting to gender clinics is on the rise. This increase might be driven more by social forces than by scientific ones. Dr. Drescher made an anecdotal observation during the presentation that more children are presenting to gender clinics already socially transitioned by their parents than there are children in the research literature on persisters and desisters.
Dr. Drescher recalled in the interview that, during the public comment period for the DSM-5, gender dysphoria elicited the third most responses, compared with other diagnoses, despite its rarity as a condition. “Interest in the subject far outweighs its prevalence.”
Gender-related glossary of terms
"There are so many moving parts to our understanding of gender," said Jack Drescher, MD, during a plenary session at the annual meeting of the American College of Psychiatrists. For that reason, "language is very important" when addressing children who might have questions about their gender identity, he said.
To help establish as much clarity as possible when discussing gender in the clinical setting, Dr. Drescher offered the following glossary of terms. These are not listed alphabetically but in a stepwise fashion aimed at leading to a clearer understanding of successive terms.
Sex: The biological attributes of being male or female. This includes sex chromosomes, gonads, sex hormones, and nonambiguous internal and external genitalia.
Gender: The public - and typically the legal - recognition of one's lived role as a boy, girl, man, woman or of other biological factors in combination with psychosocial factors that are seen as contributing to identity development.
Sexual orientation: A person's erotic response tendency or sexual attractions, either directed toward individuals of the same sex (homosexual), the other sex (heterosexual), or both sexes (bisexual).
Gender identity: Often an independent variable from sexual orientation, this refers to how an individual identifies as either male, female, or, in some cases, some other category.
Gender assignment: The natal presentation as either male or female. The historical terms are "biological male" or "biological female"; also occasionally known as "birth assigned male" or "birth assigned female."
Gender atypical: The somatic features or behaviors not statistically typical in individuals with the same assigned gender in a given society or era.
Gender nonconforming: Typically used as an alternative descriptive term for "gender atypical".
Gender dysphoria: The conflict between a person's assigned gender and that person's gender identity and expression; replaced "gender identity disorder" in the DSM-5.
Gender variant: Often used by those who are concerned the term "gender dysphoria" will unnecessarily pathologize a child.
Gender expression: How an individual demonstrates gender to others, including by way of dress, behavior, and appearance. Increasingly, the term is used in antidiscrimination documents.
Desister: Prepubescent children who present with gender dysphoria but who do not become transgender adults.
Persister: This refers to children who present with gender dysphoria and progress to a transgender adulthood.
Gender reassignment: An official - and often legal - change of gender by way of cross-sex endocrine therapy and/or gender reassignment surgery.
Transsexual: An individual who modifies the body via endocrine and/or surgical means to conform with gender identity either partially or completely.
Transwoman: A person, such as Caitlyn Jenner, who transitions from a male sex assignment to become female.
Transman: A person who transitions from a female sex assignment to become male.
Transgender: The "T" in the acronym LGBT; the popular - not scientific - inclusive term for those whose gender identity, gender expression, or behavior does not conform to that which is typically associated with the natal sex assignment.
Cisgender: From the Latin for "on the same side"; used in the transgender community to describe those whose gender identities align with their natal assignment.
Gender beliefs: Used to refer to the implicit, typically binary, cultural views on the "essential" qualities of men and women.
[email protected]
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – The treatment of preadolescents who present with gender questions is often complicated by the absence of evidence-based data on who is most likely to remain gender dysphoric into adulthood and who is not, an expert said at the annual meeting of the American College of Psychiatrists.
“There are some [clinicians] who believe they can predict who will persist and who will not. But they have not published, to my satisfaction, a way to show anyone else how to tell the difference,” said Jack Drescher, MD, a member of the World Health Organization’s (WHO’s) Working Group on the Classification of Sexual Disorders and Sexual Health and clinical professor of psychiatry and behavioral sciences at New York Medical College, Valhalla.
The WHO working group was tasked with categorizing sex and gender diagnoses in the forthcoming International Classification of Diseases (ICD-11). Dr. Drescher said that he and his fellow WHO working group members have identified at least three discrete transgender populations.
“There are persisters, desisters, and those who first develop gender dysphoria in adolescence and adulthood,” he said. “It would be a clinical mistake to think that there is a seamless transition from childhood gender dysphoria into adolescent and adult gender dysphoria.”
Dr. Drescher said that he believes the Dutch model for treating younger children diagnosed with what is interchangeably referred to as gender dysphoria or gender variance demonstrates the greatest sensitivity to how fluid the situation can be for many of these children. The absence of biomarkers for dysphoria that will persist into adulthood and the finding that a minority of prepubescent gender dysphoria diagnoses persist into adolescence inform the Dutch approach.
This approach, which originated at the VU University Medical Center Amsterdam, is based on 2 decades of research and practice. It assumes that it is better not to actively transition a child socially but to remain neutral to the way in which the child expresses gender identity. If children persist into late adolescence in this model, they are assisted in transitioning. If not, they are supported socially as they adjust to their natal gender. Puberty may sometimes have to be suppressed until the time one of the two paths has been decided.
“In my opinion, it is the most conservative approach,” Dr. Drescher said of the Dutch model. “They are the most cognizant of how much we don’t know, and they do a lot of good research.”
An approach originating at the Child and Adolescent Gender Center Clinic, which is affiliated with the University of California, San Francisco, supports a child socially into a cross-gendered role without medical or surgical intervention but also suppresses puberty. This method is based on the presumption of an adult transgender outcome, despite the absence of a way to predict results, said Dr. Drescher, who also cautions about the iatrogenic effects of such a presumption. “It takes a lot of work to socially transition a child in one direction. It would take a lot to transition back in the other direction, and there is no good empirical data as to whether this is entirely a benign process,” he said.
A third method originated in Toronto at the Centre for Addiction and Mental Health. This method actively discourages a child’s atypical gender interests and views transsexualism as an undesirable outcome that can be prevented, despite what Dr. Drescher said is a complete lack of evidence to either support or refute this claim. This method largely has been abandoned, in part since Ontario and five U.S. states and the District of Columbia have passed laws banning efforts to change a minor’s sexual orientation or gender identity. This method does have puberty suppression in children whose gender dysphoria appears to be persisting into adolescence in common with the other two.
Dr. Drescher said puberty suppression has helped decrease the levels of anxiety, depression, and suicidal ideation typically associated with this cohort. Postponing the development of secondary sexual characteristics gives those who ultimately will desist from their dysphoria more time to let it run its course. The Dutch first initiated this procedure 2 decades ago and have shown that any possible future side effects are outweighed by the psychosocial advantages it provides in the present.
The clinical view of gender dysphoria probably will get a jolt in 2018 upon publication of the ICD-11. In an interview, Dr. Drescher said that, if the condition is no longer categorized by the WHO as a mental disorder and is instead called “gender incongruence” in a chapter dedicated to gender and sexuality issues as currently planned, “it is likely the [American Psychiatric Association] will follow suit and remove gender dysphoria from the DSM. However, I don’t know how long that will take,” he said.
In his presentation, Dr. Drescher said that the causes for gender dysphoria remain unknown, as do the ways in which gender identity develops. It is also unclear how biological, psychosocial, and environmental factors affect gender dysphoria. What is clear, he said, is that “we have to rethink our developmental literature.”
Meanwhile, although gender dysphoria affects a relatively small percentage of the population – less than 1% of “nonreferred” children and adolescents, according to the DSM-5 – the number of prepubescent children presenting to gender clinics is on the rise. This increase might be driven more by social forces than by scientific ones. Dr. Drescher made an anecdotal observation during the presentation that more children are presenting to gender clinics already socially transitioned by their parents than there are children in the research literature on persisters and desisters.
Dr. Drescher recalled in the interview that, during the public comment period for the DSM-5, gender dysphoria elicited the third most responses, compared with other diagnoses, despite its rarity as a condition. “Interest in the subject far outweighs its prevalence.”
Gender-related glossary of terms
"There are so many moving parts to our understanding of gender," said Jack Drescher, MD, during a plenary session at the annual meeting of the American College of Psychiatrists. For that reason, "language is very important" when addressing children who might have questions about their gender identity, he said.
To help establish as much clarity as possible when discussing gender in the clinical setting, Dr. Drescher offered the following glossary of terms. These are not listed alphabetically but in a stepwise fashion aimed at leading to a clearer understanding of successive terms.
Sex: The biological attributes of being male or female. This includes sex chromosomes, gonads, sex hormones, and nonambiguous internal and external genitalia.
Gender: The public - and typically the legal - recognition of one's lived role as a boy, girl, man, woman or of other biological factors in combination with psychosocial factors that are seen as contributing to identity development.
Sexual orientation: A person's erotic response tendency or sexual attractions, either directed toward individuals of the same sex (homosexual), the other sex (heterosexual), or both sexes (bisexual).
Gender identity: Often an independent variable from sexual orientation, this refers to how an individual identifies as either male, female, or, in some cases, some other category.
Gender assignment: The natal presentation as either male or female. The historical terms are "biological male" or "biological female"; also occasionally known as "birth assigned male" or "birth assigned female."
Gender atypical: The somatic features or behaviors not statistically typical in individuals with the same assigned gender in a given society or era.
Gender nonconforming: Typically used as an alternative descriptive term for "gender atypical".
Gender dysphoria: The conflict between a person's assigned gender and that person's gender identity and expression; replaced "gender identity disorder" in the DSM-5.
Gender variant: Often used by those who are concerned the term "gender dysphoria" will unnecessarily pathologize a child.
Gender expression: How an individual demonstrates gender to others, including by way of dress, behavior, and appearance. Increasingly, the term is used in antidiscrimination documents.
Desister: Prepubescent children who present with gender dysphoria but who do not become transgender adults.
Persister: This refers to children who present with gender dysphoria and progress to a transgender adulthood.
Gender reassignment: An official - and often legal - change of gender by way of cross-sex endocrine therapy and/or gender reassignment surgery.
Transsexual: An individual who modifies the body via endocrine and/or surgical means to conform with gender identity either partially or completely.
Transwoman: A person, such as Caitlyn Jenner, who transitions from a male sex assignment to become female.
Transman: A person who transitions from a female sex assignment to become male.
Transgender: The "T" in the acronym LGBT; the popular - not scientific - inclusive term for those whose gender identity, gender expression, or behavior does not conform to that which is typically associated with the natal sex assignment.
Cisgender: From the Latin for "on the same side"; used in the transgender community to describe those whose gender identities align with their natal assignment.
Gender beliefs: Used to refer to the implicit, typically binary, cultural views on the "essential" qualities of men and women.
[email protected]
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – The treatment of preadolescents who present with gender questions is often complicated by the absence of evidence-based data on who is most likely to remain gender dysphoric into adulthood and who is not, an expert said at the annual meeting of the American College of Psychiatrists.
“There are some [clinicians] who believe they can predict who will persist and who will not. But they have not published, to my satisfaction, a way to show anyone else how to tell the difference,” said Jack Drescher, MD, a member of the World Health Organization’s (WHO’s) Working Group on the Classification of Sexual Disorders and Sexual Health and clinical professor of psychiatry and behavioral sciences at New York Medical College, Valhalla.
The WHO working group was tasked with categorizing sex and gender diagnoses in the forthcoming International Classification of Diseases (ICD-11). Dr. Drescher said that he and his fellow WHO working group members have identified at least three discrete transgender populations.
“There are persisters, desisters, and those who first develop gender dysphoria in adolescence and adulthood,” he said. “It would be a clinical mistake to think that there is a seamless transition from childhood gender dysphoria into adolescent and adult gender dysphoria.”
Dr. Drescher said that he believes the Dutch model for treating younger children diagnosed with what is interchangeably referred to as gender dysphoria or gender variance demonstrates the greatest sensitivity to how fluid the situation can be for many of these children. The absence of biomarkers for dysphoria that will persist into adulthood and the finding that a minority of prepubescent gender dysphoria diagnoses persist into adolescence inform the Dutch approach.
This approach, which originated at the VU University Medical Center Amsterdam, is based on 2 decades of research and practice. It assumes that it is better not to actively transition a child socially but to remain neutral to the way in which the child expresses gender identity. If children persist into late adolescence in this model, they are assisted in transitioning. If not, they are supported socially as they adjust to their natal gender. Puberty may sometimes have to be suppressed until the time one of the two paths has been decided.
“In my opinion, it is the most conservative approach,” Dr. Drescher said of the Dutch model. “They are the most cognizant of how much we don’t know, and they do a lot of good research.”
An approach originating at the Child and Adolescent Gender Center Clinic, which is affiliated with the University of California, San Francisco, supports a child socially into a cross-gendered role without medical or surgical intervention but also suppresses puberty. This method is based on the presumption of an adult transgender outcome, despite the absence of a way to predict results, said Dr. Drescher, who also cautions about the iatrogenic effects of such a presumption. “It takes a lot of work to socially transition a child in one direction. It would take a lot to transition back in the other direction, and there is no good empirical data as to whether this is entirely a benign process,” he said.
A third method originated in Toronto at the Centre for Addiction and Mental Health. This method actively discourages a child’s atypical gender interests and views transsexualism as an undesirable outcome that can be prevented, despite what Dr. Drescher said is a complete lack of evidence to either support or refute this claim. This method largely has been abandoned, in part since Ontario and five U.S. states and the District of Columbia have passed laws banning efforts to change a minor’s sexual orientation or gender identity. This method does have puberty suppression in children whose gender dysphoria appears to be persisting into adolescence in common with the other two.
Dr. Drescher said puberty suppression has helped decrease the levels of anxiety, depression, and suicidal ideation typically associated with this cohort. Postponing the development of secondary sexual characteristics gives those who ultimately will desist from their dysphoria more time to let it run its course. The Dutch first initiated this procedure 2 decades ago and have shown that any possible future side effects are outweighed by the psychosocial advantages it provides in the present.
The clinical view of gender dysphoria probably will get a jolt in 2018 upon publication of the ICD-11. In an interview, Dr. Drescher said that, if the condition is no longer categorized by the WHO as a mental disorder and is instead called “gender incongruence” in a chapter dedicated to gender and sexuality issues as currently planned, “it is likely the [American Psychiatric Association] will follow suit and remove gender dysphoria from the DSM. However, I don’t know how long that will take,” he said.
In his presentation, Dr. Drescher said that the causes for gender dysphoria remain unknown, as do the ways in which gender identity develops. It is also unclear how biological, psychosocial, and environmental factors affect gender dysphoria. What is clear, he said, is that “we have to rethink our developmental literature.”
Meanwhile, although gender dysphoria affects a relatively small percentage of the population – less than 1% of “nonreferred” children and adolescents, according to the DSM-5 – the number of prepubescent children presenting to gender clinics is on the rise. This increase might be driven more by social forces than by scientific ones. Dr. Drescher made an anecdotal observation during the presentation that more children are presenting to gender clinics already socially transitioned by their parents than there are children in the research literature on persisters and desisters.
Dr. Drescher recalled in the interview that, during the public comment period for the DSM-5, gender dysphoria elicited the third most responses, compared with other diagnoses, despite its rarity as a condition. “Interest in the subject far outweighs its prevalence.”
Gender-related glossary of terms
"There are so many moving parts to our understanding of gender," said Jack Drescher, MD, during a plenary session at the annual meeting of the American College of Psychiatrists. For that reason, "language is very important" when addressing children who might have questions about their gender identity, he said.
To help establish as much clarity as possible when discussing gender in the clinical setting, Dr. Drescher offered the following glossary of terms. These are not listed alphabetically but in a stepwise fashion aimed at leading to a clearer understanding of successive terms.
Sex: The biological attributes of being male or female. This includes sex chromosomes, gonads, sex hormones, and nonambiguous internal and external genitalia.
Gender: The public - and typically the legal - recognition of one's lived role as a boy, girl, man, woman or of other biological factors in combination with psychosocial factors that are seen as contributing to identity development.
Sexual orientation: A person's erotic response tendency or sexual attractions, either directed toward individuals of the same sex (homosexual), the other sex (heterosexual), or both sexes (bisexual).
Gender identity: Often an independent variable from sexual orientation, this refers to how an individual identifies as either male, female, or, in some cases, some other category.
Gender assignment: The natal presentation as either male or female. The historical terms are "biological male" or "biological female"; also occasionally known as "birth assigned male" or "birth assigned female."
Gender atypical: The somatic features or behaviors not statistically typical in individuals with the same assigned gender in a given society or era.
Gender nonconforming: Typically used as an alternative descriptive term for "gender atypical".
Gender dysphoria: The conflict between a person's assigned gender and that person's gender identity and expression; replaced "gender identity disorder" in the DSM-5.
Gender variant: Often used by those who are concerned the term "gender dysphoria" will unnecessarily pathologize a child.
Gender expression: How an individual demonstrates gender to others, including by way of dress, behavior, and appearance. Increasingly, the term is used in antidiscrimination documents.
Desister: Prepubescent children who present with gender dysphoria but who do not become transgender adults.
Persister: This refers to children who present with gender dysphoria and progress to a transgender adulthood.
Gender reassignment: An official - and often legal - change of gender by way of cross-sex endocrine therapy and/or gender reassignment surgery.
Transsexual: An individual who modifies the body via endocrine and/or surgical means to conform with gender identity either partially or completely.
Transwoman: A person, such as Caitlyn Jenner, who transitions from a male sex assignment to become female.
Transman: A person who transitions from a female sex assignment to become male.
Transgender: The "T" in the acronym LGBT; the popular - not scientific - inclusive term for those whose gender identity, gender expression, or behavior does not conform to that which is typically associated with the natal sex assignment.
Cisgender: From the Latin for "on the same side"; used in the transgender community to describe those whose gender identities align with their natal assignment.
Gender beliefs: Used to refer to the implicit, typically binary, cultural views on the "essential" qualities of men and women.
[email protected]
On Twitter @whitneymcknight
EXPERT ANALYSIS AT THE AMERICAN COLLEGE OF PSYCHIATRISTS ANNUAL MEETING
Novel antifungal had favorable safety, efficacy profile for onychomycosis in phase IIB study
ORLANDO – A novel orally administered antifungal showed a favorable safety and efficacy profile in the treatment of distal lateral subungual onychomycosis, in a phase IIB study presented at the annual meeting of the American Academy of Dermatology.
In the RENOVATE (Restoring Nail: An Oral VT-1161 Tablet Evaluation) study, a randomized, double-blind, placebo-controlled, dose-ranging trial, 259 adults with moderate to severe distal lateral subungual onychomycosis of the large toenail were assigned to either one of four treatment arms. They were given the antifungal, currently named VT-1161, a selective CYP51 inhibitor, at doses of 300 mg or 600 mg once weekly for 10 or 22 weeks, after receiving daily loading doses for the initial 2 weeks. The trial evaluated two dose levels of VT-1161 (300 mg and 600 mg) administered once weekly for either 10 or 22 weeks following an initial 2-week, once-daily loading dose period.
At baseline, the average involvement of the large toenail was 46%, with an average of 4.6 toenails affected. In the intent-to-treat analysis, at 48 weeks, complete cure rates in the four study drug arms ranged from 32% to 42%, compared with 0% in the placebo arm.
Amir Tavakkol, PhD, chief development officer at Viamet Pharmaceuticals, which is developing VT01161, presented the study findings during a late breaking clinical session at the meeting.
Adverse event rates and discontinuation rates were comparable to placebo through week 60, with no patients discontinuing due to any laboratory abnormalities. Nausea and muscle spasms were the most commonly reported adverse events, which Dr. Tavakkol said seemed to occur in patients given the higher doses. VT-1161 is also being studied for treatment of vulvovaginal candidiasis. In October 2016, the FDA granted the drug Qualified Infectious Disease Product and Fast Track designations for the treatment of recurrent vulvovaginal candidiasis, according to the company.
Viamet sponsored the study and Dr. Tavakkol is an employee of the company.
[email protected]
On Twitter @whitneymcknight
ORLANDO – A novel orally administered antifungal showed a favorable safety and efficacy profile in the treatment of distal lateral subungual onychomycosis, in a phase IIB study presented at the annual meeting of the American Academy of Dermatology.
In the RENOVATE (Restoring Nail: An Oral VT-1161 Tablet Evaluation) study, a randomized, double-blind, placebo-controlled, dose-ranging trial, 259 adults with moderate to severe distal lateral subungual onychomycosis of the large toenail were assigned to either one of four treatment arms. They were given the antifungal, currently named VT-1161, a selective CYP51 inhibitor, at doses of 300 mg or 600 mg once weekly for 10 or 22 weeks, after receiving daily loading doses for the initial 2 weeks. The trial evaluated two dose levels of VT-1161 (300 mg and 600 mg) administered once weekly for either 10 or 22 weeks following an initial 2-week, once-daily loading dose period.
At baseline, the average involvement of the large toenail was 46%, with an average of 4.6 toenails affected. In the intent-to-treat analysis, at 48 weeks, complete cure rates in the four study drug arms ranged from 32% to 42%, compared with 0% in the placebo arm.
Amir Tavakkol, PhD, chief development officer at Viamet Pharmaceuticals, which is developing VT01161, presented the study findings during a late breaking clinical session at the meeting.
Adverse event rates and discontinuation rates were comparable to placebo through week 60, with no patients discontinuing due to any laboratory abnormalities. Nausea and muscle spasms were the most commonly reported adverse events, which Dr. Tavakkol said seemed to occur in patients given the higher doses. VT-1161 is also being studied for treatment of vulvovaginal candidiasis. In October 2016, the FDA granted the drug Qualified Infectious Disease Product and Fast Track designations for the treatment of recurrent vulvovaginal candidiasis, according to the company.
Viamet sponsored the study and Dr. Tavakkol is an employee of the company.
[email protected]
On Twitter @whitneymcknight
ORLANDO – A novel orally administered antifungal showed a favorable safety and efficacy profile in the treatment of distal lateral subungual onychomycosis, in a phase IIB study presented at the annual meeting of the American Academy of Dermatology.
In the RENOVATE (Restoring Nail: An Oral VT-1161 Tablet Evaluation) study, a randomized, double-blind, placebo-controlled, dose-ranging trial, 259 adults with moderate to severe distal lateral subungual onychomycosis of the large toenail were assigned to either one of four treatment arms. They were given the antifungal, currently named VT-1161, a selective CYP51 inhibitor, at doses of 300 mg or 600 mg once weekly for 10 or 22 weeks, after receiving daily loading doses for the initial 2 weeks. The trial evaluated two dose levels of VT-1161 (300 mg and 600 mg) administered once weekly for either 10 or 22 weeks following an initial 2-week, once-daily loading dose period.
At baseline, the average involvement of the large toenail was 46%, with an average of 4.6 toenails affected. In the intent-to-treat analysis, at 48 weeks, complete cure rates in the four study drug arms ranged from 32% to 42%, compared with 0% in the placebo arm.
Amir Tavakkol, PhD, chief development officer at Viamet Pharmaceuticals, which is developing VT01161, presented the study findings during a late breaking clinical session at the meeting.
Adverse event rates and discontinuation rates were comparable to placebo through week 60, with no patients discontinuing due to any laboratory abnormalities. Nausea and muscle spasms were the most commonly reported adverse events, which Dr. Tavakkol said seemed to occur in patients given the higher doses. VT-1161 is also being studied for treatment of vulvovaginal candidiasis. In October 2016, the FDA granted the drug Qualified Infectious Disease Product and Fast Track designations for the treatment of recurrent vulvovaginal candidiasis, according to the company.
Viamet sponsored the study and Dr. Tavakkol is an employee of the company.
[email protected]
On Twitter @whitneymcknight
AT AAD 17
Key clinical point:
Major finding: A new selective CYP51 inhibitor, administered orally, met the primary endpoint of complete cure rates at 48 weeks.
Data source: A phase IIB, randomized, double-blind, placebo-controlled, dose-ranging study of 259 adults with moderate-to-severe distal lateral subungual onychomycosis of the large toenail.
Disclosures: Dr. Tavakkol is the chief development officer of Viamet Pharmaceuticals, the sponsor of this trial.
Ixekizumab found superior to ustekinumab in psoriasis at 24 weeks
ORLANDO – The interleukin-17A inhibitor ixekizumab was associated with superior efficacy and safety when compared with ustekinumab at 24 weeks, a head-to-head trial of the two monoclonal antibodies in plaque psoriasis has shown.
The 24-week data from the IXORA-S trial were presented during a late-breaking clinical trial session at the annual meeting of the American Academy of Dermatology by Kristian Reich, MD, PhD, a founder of SCIderm in Hamburg, Germany.
At 24 weeks, 49% in the ixekizumab arm achieved a Psoriasis Area and Severity Index (PASI) 100 level of skin clearance, compared with 24% in the ustekinumab arm (P = .001). Ixekizumab treatment also reached significantly higher skin clearances than ustekinumab at 24 weeks at the level of PASI 90 (83% vs. 59%; P less than .001) and PASI 75 (91% vs. 82%; P = .015).
Treatment with ixekizumab produced a Static Physician’s Global Assessment (sPGA) score of 0 in 54% at 24 weeks, compared with 24% with ustekinumab (P less than .001). A sPGA score of 0 or 1 occurred in 87% of patients who took ixekizumab and in 59% of the ustekinumab group.
An improvement of 4 or more points in the pruritus Numeric Rating Scale was reported by 86% of ixekizumab patients at 24 weeks, compared with 72% of those who took ustekinumab (P = .018).
Dr. Reich reported that there were no deaths or any significant differences in overall treatment-related adverse events across both arms, although he cautioned against putting too much stock in 24-week safety data. “I hesitate to show safety data for only 300 patients at 24 weeks, but it’s good to see here that there doesn’t seem to be a difference. I still would want to see larger patient numbers and more long-term data,” he said.
Dr. Reich had numerous disclosures, including honoraria for serving as a speaker for Eli Lilly, the sponsor of this trial.
[email protected]
On Twitter @whitneymcknight
ORLANDO – The interleukin-17A inhibitor ixekizumab was associated with superior efficacy and safety when compared with ustekinumab at 24 weeks, a head-to-head trial of the two monoclonal antibodies in plaque psoriasis has shown.
The 24-week data from the IXORA-S trial were presented during a late-breaking clinical trial session at the annual meeting of the American Academy of Dermatology by Kristian Reich, MD, PhD, a founder of SCIderm in Hamburg, Germany.
At 24 weeks, 49% in the ixekizumab arm achieved a Psoriasis Area and Severity Index (PASI) 100 level of skin clearance, compared with 24% in the ustekinumab arm (P = .001). Ixekizumab treatment also reached significantly higher skin clearances than ustekinumab at 24 weeks at the level of PASI 90 (83% vs. 59%; P less than .001) and PASI 75 (91% vs. 82%; P = .015).
Treatment with ixekizumab produced a Static Physician’s Global Assessment (sPGA) score of 0 in 54% at 24 weeks, compared with 24% with ustekinumab (P less than .001). A sPGA score of 0 or 1 occurred in 87% of patients who took ixekizumab and in 59% of the ustekinumab group.
An improvement of 4 or more points in the pruritus Numeric Rating Scale was reported by 86% of ixekizumab patients at 24 weeks, compared with 72% of those who took ustekinumab (P = .018).
Dr. Reich reported that there were no deaths or any significant differences in overall treatment-related adverse events across both arms, although he cautioned against putting too much stock in 24-week safety data. “I hesitate to show safety data for only 300 patients at 24 weeks, but it’s good to see here that there doesn’t seem to be a difference. I still would want to see larger patient numbers and more long-term data,” he said.
Dr. Reich had numerous disclosures, including honoraria for serving as a speaker for Eli Lilly, the sponsor of this trial.
[email protected]
On Twitter @whitneymcknight
ORLANDO – The interleukin-17A inhibitor ixekizumab was associated with superior efficacy and safety when compared with ustekinumab at 24 weeks, a head-to-head trial of the two monoclonal antibodies in plaque psoriasis has shown.
The 24-week data from the IXORA-S trial were presented during a late-breaking clinical trial session at the annual meeting of the American Academy of Dermatology by Kristian Reich, MD, PhD, a founder of SCIderm in Hamburg, Germany.
At 24 weeks, 49% in the ixekizumab arm achieved a Psoriasis Area and Severity Index (PASI) 100 level of skin clearance, compared with 24% in the ustekinumab arm (P = .001). Ixekizumab treatment also reached significantly higher skin clearances than ustekinumab at 24 weeks at the level of PASI 90 (83% vs. 59%; P less than .001) and PASI 75 (91% vs. 82%; P = .015).
Treatment with ixekizumab produced a Static Physician’s Global Assessment (sPGA) score of 0 in 54% at 24 weeks, compared with 24% with ustekinumab (P less than .001). A sPGA score of 0 or 1 occurred in 87% of patients who took ixekizumab and in 59% of the ustekinumab group.
An improvement of 4 or more points in the pruritus Numeric Rating Scale was reported by 86% of ixekizumab patients at 24 weeks, compared with 72% of those who took ustekinumab (P = .018).
Dr. Reich reported that there were no deaths or any significant differences in overall treatment-related adverse events across both arms, although he cautioned against putting too much stock in 24-week safety data. “I hesitate to show safety data for only 300 patients at 24 weeks, but it’s good to see here that there doesn’t seem to be a difference. I still would want to see larger patient numbers and more long-term data,” he said.
Dr. Reich had numerous disclosures, including honoraria for serving as a speaker for Eli Lilly, the sponsor of this trial.
[email protected]
On Twitter @whitneymcknight
AT AAD 2017
Key clinical point:
Major finding: At 24 weeks, ixekizumab was associated with significantly better PASI response rates and reduction in itch than ustekinumab in patients with moderate to severe plaque psoriasis.
Data source: Head-to-head trial of 302 adults with moderate to severe plaque psoriasis treated with either ixekizumab or ustekinumab.
Disclosures: Dr. Reich had numerous disclosures, including honoraria for serving as a speaker for Eli Lilly, the sponsor of this trial.
Dupilumab improved eczema scores in children in open label trial
ORLANDO – Treatment with dupilumab in children and adolescents with moderate to severe atopic dermatitis (AD) reduced severity and pruritus scores from baseline and was well tolerated, in a multicenter, open-label trial of 78 children and adolescents.
Dupilumab’s “powerful ability” to block interleukin-4 and interleukin-13 pathways of inflammation is “especially exciting because AD is even more Th-2 cell driven in children,” said Michael J. Cork, MD, PhD, head of dermatologic research at the University of Sheffield (England), who presented the findings during a late-breaking research session at the annual meeting of the American Academy of Dermatology.
The study assessed the pharmacokinetics, safety, and efficacy of dupilumab and was conducted with 38 children, aged 6-11 years, and 40 adolescents, aged 12-17 years, with moderate to severe AD. All had failed topical corticosteroid therapy. Some of the children (16%) and adolescents (22.5%) had failed at least one systemic therapy.
Both age groups were given either a 2 mg/kg or a 4 mg/kg dose of dupilumab (administered subcutaneously), nothing for 8 weeks, followed by 4 weekly doses of their respective regimens. Mean Eczema Area and Severity Index (EASI) scores at baseline were 31.7 among the adolescents and 35.9 among the children.
At week 12, mean scores in the younger cohort given either 2 mg/kg or 4 mg/kg had improved by 76.2% and 63.4%, respectively, from baseline. In the adolescents, EASI scores at week 12 had improved by a mean of 66.4% in the 2-mg/kg group and 69.7% in the 4-mg/kg group.
Itch also improved “dramatically,” according to Dr. Cork. In the younger children, peak pruritus Numerical Rating Scale scores improved from baseline by a mean of 41.6% in the lower-dose group and 39.6% in the higher-dose group. In the older cohort, pruritus scores improved from baseline by a mean of 30.8% in the lower-dose group and 37.6% in the higher-dose group.
Treatment was well tolerated across the study, and adverse events were “mild, transient, and unrelated,” Dr. Cork said. “I would like to emphasize that these were not related to dupilumab, as they occurred during the period of time after the first dose, in weeks 6 and 7,” he commented. He attributed AD flares experienced in the study to the quick clearance of the drug in the first few weeks.
Dr. Cork reported numerous disclosures, including serving as an adviser, consultant, and investigator for Regeneron, the sponsor of the trial, and Sanofi; the companies developing dupilumab.
[email protected]
On Twitter @whitneymcknight
ORLANDO – Treatment with dupilumab in children and adolescents with moderate to severe atopic dermatitis (AD) reduced severity and pruritus scores from baseline and was well tolerated, in a multicenter, open-label trial of 78 children and adolescents.
Dupilumab’s “powerful ability” to block interleukin-4 and interleukin-13 pathways of inflammation is “especially exciting because AD is even more Th-2 cell driven in children,” said Michael J. Cork, MD, PhD, head of dermatologic research at the University of Sheffield (England), who presented the findings during a late-breaking research session at the annual meeting of the American Academy of Dermatology.
The study assessed the pharmacokinetics, safety, and efficacy of dupilumab and was conducted with 38 children, aged 6-11 years, and 40 adolescents, aged 12-17 years, with moderate to severe AD. All had failed topical corticosteroid therapy. Some of the children (16%) and adolescents (22.5%) had failed at least one systemic therapy.
Both age groups were given either a 2 mg/kg or a 4 mg/kg dose of dupilumab (administered subcutaneously), nothing for 8 weeks, followed by 4 weekly doses of their respective regimens. Mean Eczema Area and Severity Index (EASI) scores at baseline were 31.7 among the adolescents and 35.9 among the children.
At week 12, mean scores in the younger cohort given either 2 mg/kg or 4 mg/kg had improved by 76.2% and 63.4%, respectively, from baseline. In the adolescents, EASI scores at week 12 had improved by a mean of 66.4% in the 2-mg/kg group and 69.7% in the 4-mg/kg group.
Itch also improved “dramatically,” according to Dr. Cork. In the younger children, peak pruritus Numerical Rating Scale scores improved from baseline by a mean of 41.6% in the lower-dose group and 39.6% in the higher-dose group. In the older cohort, pruritus scores improved from baseline by a mean of 30.8% in the lower-dose group and 37.6% in the higher-dose group.
Treatment was well tolerated across the study, and adverse events were “mild, transient, and unrelated,” Dr. Cork said. “I would like to emphasize that these were not related to dupilumab, as they occurred during the period of time after the first dose, in weeks 6 and 7,” he commented. He attributed AD flares experienced in the study to the quick clearance of the drug in the first few weeks.
Dr. Cork reported numerous disclosures, including serving as an adviser, consultant, and investigator for Regeneron, the sponsor of the trial, and Sanofi; the companies developing dupilumab.
[email protected]
On Twitter @whitneymcknight
ORLANDO – Treatment with dupilumab in children and adolescents with moderate to severe atopic dermatitis (AD) reduced severity and pruritus scores from baseline and was well tolerated, in a multicenter, open-label trial of 78 children and adolescents.
Dupilumab’s “powerful ability” to block interleukin-4 and interleukin-13 pathways of inflammation is “especially exciting because AD is even more Th-2 cell driven in children,” said Michael J. Cork, MD, PhD, head of dermatologic research at the University of Sheffield (England), who presented the findings during a late-breaking research session at the annual meeting of the American Academy of Dermatology.
The study assessed the pharmacokinetics, safety, and efficacy of dupilumab and was conducted with 38 children, aged 6-11 years, and 40 adolescents, aged 12-17 years, with moderate to severe AD. All had failed topical corticosteroid therapy. Some of the children (16%) and adolescents (22.5%) had failed at least one systemic therapy.
Both age groups were given either a 2 mg/kg or a 4 mg/kg dose of dupilumab (administered subcutaneously), nothing for 8 weeks, followed by 4 weekly doses of their respective regimens. Mean Eczema Area and Severity Index (EASI) scores at baseline were 31.7 among the adolescents and 35.9 among the children.
At week 12, mean scores in the younger cohort given either 2 mg/kg or 4 mg/kg had improved by 76.2% and 63.4%, respectively, from baseline. In the adolescents, EASI scores at week 12 had improved by a mean of 66.4% in the 2-mg/kg group and 69.7% in the 4-mg/kg group.
Itch also improved “dramatically,” according to Dr. Cork. In the younger children, peak pruritus Numerical Rating Scale scores improved from baseline by a mean of 41.6% in the lower-dose group and 39.6% in the higher-dose group. In the older cohort, pruritus scores improved from baseline by a mean of 30.8% in the lower-dose group and 37.6% in the higher-dose group.
Treatment was well tolerated across the study, and adverse events were “mild, transient, and unrelated,” Dr. Cork said. “I would like to emphasize that these were not related to dupilumab, as they occurred during the period of time after the first dose, in weeks 6 and 7,” he commented. He attributed AD flares experienced in the study to the quick clearance of the drug in the first few weeks.
Dr. Cork reported numerous disclosures, including serving as an adviser, consultant, and investigator for Regeneron, the sponsor of the trial, and Sanofi; the companies developing dupilumab.
[email protected]
On Twitter @whitneymcknight
AT AAD 17
Key clinical point: Data on dupilumab for treating moderate to severe atopic dermatitis in children and adolescents are promising.
Major finding: At week 12, treatment with dupilumab at 2 mg/kg and 4 mg/kg doses, across 8 weeks in two pediatric cohorts improved baseline EASI scores by 69.7% and pruritus scores by a third and was well tolerated.
Data source: A phase IIa, multicenter, open label pharmacokinetics, safety, and efficacy trial evaluating two dosing regimens of dupilumab in 78 children with moderate to severe AD.
Disclosures: Dr. Cork reported numerous disclosures, including serving as an adviser, consultant, and investigator for Regeneron, the sponsor of the trial, and Sanofi – the two companies developing dupilumab.
Are new medications on horizon for patients with depression, inflammation?
SCOTTSDALE, ARIZ. – Inflammation is inextricably linked to depression in a subset of patients who differ from other depressed patients in their responses to certain interventions, according to Charles L. Raison, MD.
“The brains of people who are depressed and who have inflammation look very different from those of people who are depressed without inflammation,” Dr. Raison said in an interview at the annual meeting of the American College of Psychiatrists. “They have different connectivity patterns, different glutaminergic patterns, different signaling. It seems that inflammatory processes change the way different parts of the brain talk to each other and seem to do so in consistent ways.”
Dr. Raison, the Mary Sue and Mike Shannon Chair for Healthy Minds, Children & Families at the University of Wisconsin–Madison, told a plenary audience at the meeting: “We [psychiatrists] are so brain centric, it’s easy to forget how much the immune system drives us. It’s either like a second brain, or it is at least part of the brain.”
Over the years, Dr. Raison and his colleagues have observed how inflammation can interfere with mood, leading to depression in people who previously did not report or describe depressive symptoms.
In the early 2000s, Dr. Raison and others such as Andrew H. Miller, MD, a psychiatric oncologist, investigated the inflammatory response and levels of depression in people treated with interferon-alpha for hepatitis C infection (J Clin Psychiatry. 2005 Jan;66[1]:41-8). They found that more than half of people who had not reported or described depressive symptoms at baseline subsequently reported depressive symptoms. “In a nutshell, we found that interferon-alpha induces every single brain-body function associated with regular old major depression,” said Dr. Raison, also a professor of psychiatry at the university.
In another study, this one led by neuropsychosomatic specialist Dominique L. Musselman, MD, a similar cohort of hepatitis C patients assessed for baseline depression was randomly assigned to either placebo or paroxetine during the course of interferon-alpha treatment. Patients treated with placebo had a 0.24 relative risk (95% confidence interval, 0.08-0.93) of developing depression, compared with the paroxetine group (N Eng J Med. 2001;344:961-6).
The real “breakthrough” in understanding the role of inflammation in depression, Dr. Raison said, came from studies that made the association between early-life adversity, depression, and inflammation. In one particular study, Dr. Raison and colleagues found that stress-induced spikes in interleukin-6 and NF-kappaB DNA-binding were greater in patients with higher baseline levels of depression and higher levels of early life stress (Am J Psychiatry. 2006 Sep;163[9]:1630-3).
Spikes in the inflammatory response independently correlated with depression severity but not with early life stress, which Dr. Raison said suggests that adversity likely can cause inflammation – and thus predisposes people to depression, and not necessarily vice versa.
“Something about early adversity in life programs the brain-body complex to run inflammatory systems hot, probably because it’s an effective way to be ready for [a stream of] unpredictable miseries,” Dr. Raison said during the session. “Chronic, elevated inflammation [early on] seems to predict increased depression later.”
Now that the link has been established between some depression and inflammation, the next step for science is to tease out who is most likely to respond to anti-inflammatory interventions for depression, Dr. Raison said.
“Something that is just starting to emerge is that maybe the relationship between inflammation and depression is not a straight line but a U-shaped curve, such that if you have too much inflammation, you’re in trouble, and if you have too little, you’re also in trouble,” he said in the interview, citing a study he and others conducted into blocking the inflammatory response. In that study, people with major depression who were otherwise medically healthy received either three infusions of the anti-inflammatory tumor necrosis factor–alpha antagonist infliximab (5 mg/kg), or of salt water. The investigators found that placebo worked just as well as infliximab. But patients with lower levels of inflammation at baseline had the greatest improvements in their Hamilton Rating Scale for Depression scores with placebo when compared with treatment (JAMA Psychiatry. 2013 Jan;70[1]:31-41).
Data are not yet conclusive, but Dr. Raison said the field soon could use biomarkers such as levels of C-reactive protein to determine whether patients will respond to anti-inflammatories such as omega-3 essential fatty acids. “Everyone in psychiatry is desperate to find clear, unambiguous answers. We’re right on the edge, but we’re not there yet.”
Until then, Dr. Raison cautioned against the “indiscriminate” use of anti-inflammatories, lest they exacerbate patients’ depressive symptoms. “For instance, omega-3 fatty acids might actually be counterproductive in a lot of depressed people,” he said. Still, he believes that “developing and studying anti-inflammatory strategies is probably going to lead to a novel way of treating depression in some people. What is beautiful is that if these studies continue, we might actually be able – for the first time – to target a subgroup of patients for a specific treatment.”
Dr. Raison is on the scientific advisory board of the Usona Institute, a nonprofit medical research firm.
[email protected]
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – Inflammation is inextricably linked to depression in a subset of patients who differ from other depressed patients in their responses to certain interventions, according to Charles L. Raison, MD.
“The brains of people who are depressed and who have inflammation look very different from those of people who are depressed without inflammation,” Dr. Raison said in an interview at the annual meeting of the American College of Psychiatrists. “They have different connectivity patterns, different glutaminergic patterns, different signaling. It seems that inflammatory processes change the way different parts of the brain talk to each other and seem to do so in consistent ways.”
Dr. Raison, the Mary Sue and Mike Shannon Chair for Healthy Minds, Children & Families at the University of Wisconsin–Madison, told a plenary audience at the meeting: “We [psychiatrists] are so brain centric, it’s easy to forget how much the immune system drives us. It’s either like a second brain, or it is at least part of the brain.”
Over the years, Dr. Raison and his colleagues have observed how inflammation can interfere with mood, leading to depression in people who previously did not report or describe depressive symptoms.
In the early 2000s, Dr. Raison and others such as Andrew H. Miller, MD, a psychiatric oncologist, investigated the inflammatory response and levels of depression in people treated with interferon-alpha for hepatitis C infection (J Clin Psychiatry. 2005 Jan;66[1]:41-8). They found that more than half of people who had not reported or described depressive symptoms at baseline subsequently reported depressive symptoms. “In a nutshell, we found that interferon-alpha induces every single brain-body function associated with regular old major depression,” said Dr. Raison, also a professor of psychiatry at the university.
In another study, this one led by neuropsychosomatic specialist Dominique L. Musselman, MD, a similar cohort of hepatitis C patients assessed for baseline depression was randomly assigned to either placebo or paroxetine during the course of interferon-alpha treatment. Patients treated with placebo had a 0.24 relative risk (95% confidence interval, 0.08-0.93) of developing depression, compared with the paroxetine group (N Eng J Med. 2001;344:961-6).
The real “breakthrough” in understanding the role of inflammation in depression, Dr. Raison said, came from studies that made the association between early-life adversity, depression, and inflammation. In one particular study, Dr. Raison and colleagues found that stress-induced spikes in interleukin-6 and NF-kappaB DNA-binding were greater in patients with higher baseline levels of depression and higher levels of early life stress (Am J Psychiatry. 2006 Sep;163[9]:1630-3).
Spikes in the inflammatory response independently correlated with depression severity but not with early life stress, which Dr. Raison said suggests that adversity likely can cause inflammation – and thus predisposes people to depression, and not necessarily vice versa.
“Something about early adversity in life programs the brain-body complex to run inflammatory systems hot, probably because it’s an effective way to be ready for [a stream of] unpredictable miseries,” Dr. Raison said during the session. “Chronic, elevated inflammation [early on] seems to predict increased depression later.”
Now that the link has been established between some depression and inflammation, the next step for science is to tease out who is most likely to respond to anti-inflammatory interventions for depression, Dr. Raison said.
“Something that is just starting to emerge is that maybe the relationship between inflammation and depression is not a straight line but a U-shaped curve, such that if you have too much inflammation, you’re in trouble, and if you have too little, you’re also in trouble,” he said in the interview, citing a study he and others conducted into blocking the inflammatory response. In that study, people with major depression who were otherwise medically healthy received either three infusions of the anti-inflammatory tumor necrosis factor–alpha antagonist infliximab (5 mg/kg), or of salt water. The investigators found that placebo worked just as well as infliximab. But patients with lower levels of inflammation at baseline had the greatest improvements in their Hamilton Rating Scale for Depression scores with placebo when compared with treatment (JAMA Psychiatry. 2013 Jan;70[1]:31-41).
Data are not yet conclusive, but Dr. Raison said the field soon could use biomarkers such as levels of C-reactive protein to determine whether patients will respond to anti-inflammatories such as omega-3 essential fatty acids. “Everyone in psychiatry is desperate to find clear, unambiguous answers. We’re right on the edge, but we’re not there yet.”
Until then, Dr. Raison cautioned against the “indiscriminate” use of anti-inflammatories, lest they exacerbate patients’ depressive symptoms. “For instance, omega-3 fatty acids might actually be counterproductive in a lot of depressed people,” he said. Still, he believes that “developing and studying anti-inflammatory strategies is probably going to lead to a novel way of treating depression in some people. What is beautiful is that if these studies continue, we might actually be able – for the first time – to target a subgroup of patients for a specific treatment.”
Dr. Raison is on the scientific advisory board of the Usona Institute, a nonprofit medical research firm.
[email protected]
On Twitter @whitneymcknight
SCOTTSDALE, ARIZ. – Inflammation is inextricably linked to depression in a subset of patients who differ from other depressed patients in their responses to certain interventions, according to Charles L. Raison, MD.
“The brains of people who are depressed and who have inflammation look very different from those of people who are depressed without inflammation,” Dr. Raison said in an interview at the annual meeting of the American College of Psychiatrists. “They have different connectivity patterns, different glutaminergic patterns, different signaling. It seems that inflammatory processes change the way different parts of the brain talk to each other and seem to do so in consistent ways.”
Dr. Raison, the Mary Sue and Mike Shannon Chair for Healthy Minds, Children & Families at the University of Wisconsin–Madison, told a plenary audience at the meeting: “We [psychiatrists] are so brain centric, it’s easy to forget how much the immune system drives us. It’s either like a second brain, or it is at least part of the brain.”
Over the years, Dr. Raison and his colleagues have observed how inflammation can interfere with mood, leading to depression in people who previously did not report or describe depressive symptoms.
In the early 2000s, Dr. Raison and others such as Andrew H. Miller, MD, a psychiatric oncologist, investigated the inflammatory response and levels of depression in people treated with interferon-alpha for hepatitis C infection (J Clin Psychiatry. 2005 Jan;66[1]:41-8). They found that more than half of people who had not reported or described depressive symptoms at baseline subsequently reported depressive symptoms. “In a nutshell, we found that interferon-alpha induces every single brain-body function associated with regular old major depression,” said Dr. Raison, also a professor of psychiatry at the university.
In another study, this one led by neuropsychosomatic specialist Dominique L. Musselman, MD, a similar cohort of hepatitis C patients assessed for baseline depression was randomly assigned to either placebo or paroxetine during the course of interferon-alpha treatment. Patients treated with placebo had a 0.24 relative risk (95% confidence interval, 0.08-0.93) of developing depression, compared with the paroxetine group (N Eng J Med. 2001;344:961-6).
The real “breakthrough” in understanding the role of inflammation in depression, Dr. Raison said, came from studies that made the association between early-life adversity, depression, and inflammation. In one particular study, Dr. Raison and colleagues found that stress-induced spikes in interleukin-6 and NF-kappaB DNA-binding were greater in patients with higher baseline levels of depression and higher levels of early life stress (Am J Psychiatry. 2006 Sep;163[9]:1630-3).
Spikes in the inflammatory response independently correlated with depression severity but not with early life stress, which Dr. Raison said suggests that adversity likely can cause inflammation – and thus predisposes people to depression, and not necessarily vice versa.
“Something about early adversity in life programs the brain-body complex to run inflammatory systems hot, probably because it’s an effective way to be ready for [a stream of] unpredictable miseries,” Dr. Raison said during the session. “Chronic, elevated inflammation [early on] seems to predict increased depression later.”
Now that the link has been established between some depression and inflammation, the next step for science is to tease out who is most likely to respond to anti-inflammatory interventions for depression, Dr. Raison said.
“Something that is just starting to emerge is that maybe the relationship between inflammation and depression is not a straight line but a U-shaped curve, such that if you have too much inflammation, you’re in trouble, and if you have too little, you’re also in trouble,” he said in the interview, citing a study he and others conducted into blocking the inflammatory response. In that study, people with major depression who were otherwise medically healthy received either three infusions of the anti-inflammatory tumor necrosis factor–alpha antagonist infliximab (5 mg/kg), or of salt water. The investigators found that placebo worked just as well as infliximab. But patients with lower levels of inflammation at baseline had the greatest improvements in their Hamilton Rating Scale for Depression scores with placebo when compared with treatment (JAMA Psychiatry. 2013 Jan;70[1]:31-41).
Data are not yet conclusive, but Dr. Raison said the field soon could use biomarkers such as levels of C-reactive protein to determine whether patients will respond to anti-inflammatories such as omega-3 essential fatty acids. “Everyone in psychiatry is desperate to find clear, unambiguous answers. We’re right on the edge, but we’re not there yet.”
Until then, Dr. Raison cautioned against the “indiscriminate” use of anti-inflammatories, lest they exacerbate patients’ depressive symptoms. “For instance, omega-3 fatty acids might actually be counterproductive in a lot of depressed people,” he said. Still, he believes that “developing and studying anti-inflammatory strategies is probably going to lead to a novel way of treating depression in some people. What is beautiful is that if these studies continue, we might actually be able – for the first time – to target a subgroup of patients for a specific treatment.”
Dr. Raison is on the scientific advisory board of the Usona Institute, a nonprofit medical research firm.
[email protected]
On Twitter @whitneymcknight
EXPERT OPINION FROM THE AMERICAN COLLEGE OF PSYCHIATRISTS MEETING
Adalimumab for psoriasis: Blocking TNF-alpha had no effect on vascular inflammation
ORLANDO – Vascular inflammation was no different in patients with moderate to severe psoriasis after 16 weeks of treatment with adalimumab than in untreated controls, according to a study that evaluated the impact of blocking tumor necrosis factor–alpha on vascular inflammation.
Further, there was a modest increase in vascular inflammation in carotid arteries after 52 weeks of treatment with the tumor necrosis factor (TNF) alpha-antagonist adalimumab, Robert Bissonnette, MD, president of Innovaderm Research, Montreal, reported in a late-breaking session at the annual meeting of the American Academy of Dermatology.
At 16 weeks, there were no significant differences in vascular inflammation between the treatment and control arms, based on the change from baseline in the vessel wall target to background ratio from the ascending aorta (the primary endpoint). In the carotid arteries at 16 weeks, differences in vascular inflammation between the adalimumab group and control group were also not significant.
At 52 weeks, there was no significant change in target to background ratio from the ascending aorta between baseline and the start of adalimumab, although in the carotid arteries, there was a modest increase in vascular inflammation.
Several previous studies have suggested that reducing inflammation in psoriasis can also reduce the risk of some cardiovascular events. As to why this study did not demonstrate a correlation between vascular inflammation and treatment, Dr. Bissonnette said during the question and answer portion of the presentation that “either the dose of adalimumab that is used for psoriasis has no impact on vascular inflammation or it may be possible that levels of interleukin-6, a key cytokine correlated with vascular inflammation, were very low in our study.”
Interleukin-6 typically is increased in patients with psoriatic arthritis, he explained, noting that in this study, only 7.5% of patients in the treatment group and about 10% of those in the control group had a history of psoriatic arthritis.
Additionally, at baseline, high-sensitivity C-reactive protein levels were significantly higher in controls: 5.32, compared with 2.72 in the treatment arm (P = .003).
Another possible reason for the results could be the molecule size of adalimumab, session comoderator Joel Gelfand, MD, noted in an interview. “The drug may not penetrate the aorta. These are large molecules. It also might be that [TNF–alpha] is not the main driver of aortic inflammation in people with psoriasis. Increasingly, we think of people with psoriasis as an IL-23 and IL-17 disease, so maybe that is part of it,” said Dr. Gelfand, professor of dermatology and epidemiology at the University of Pennsylvania, Philadelphia. He also directs the psoriasis and phototherapy treatment center at the university.
In addition to being presented at the meeting, the results were published in the Journal of Investigative Dermatology (2017 Feb 7. doi: 10.1016/j.jid.2017.02.977).
Adalimumab is marketed as Humira by Abbvie; a biosimilar version, adalimumab-atto (Amjevita), was approved in the United States in 2016.
Dr. Bissonnette’s disclosures included serving as an adviser and consultant to Abbvie, which sponsored the study, as well as relationships with other companies, including Amgen, Celgene, Janssen, and Novartis. Dr. Gelfand’s disclosures included serving as a consultant and investigator for Abbvie, and serving as an investigator, speaker, and/or consultant for other companies, including Eli Lilly, Janssen, and Novartis.
[email protected]
On Twitter @whitneymcknight
ORLANDO – Vascular inflammation was no different in patients with moderate to severe psoriasis after 16 weeks of treatment with adalimumab than in untreated controls, according to a study that evaluated the impact of blocking tumor necrosis factor–alpha on vascular inflammation.
Further, there was a modest increase in vascular inflammation in carotid arteries after 52 weeks of treatment with the tumor necrosis factor (TNF) alpha-antagonist adalimumab, Robert Bissonnette, MD, president of Innovaderm Research, Montreal, reported in a late-breaking session at the annual meeting of the American Academy of Dermatology.
At 16 weeks, there were no significant differences in vascular inflammation between the treatment and control arms, based on the change from baseline in the vessel wall target to background ratio from the ascending aorta (the primary endpoint). In the carotid arteries at 16 weeks, differences in vascular inflammation between the adalimumab group and control group were also not significant.
At 52 weeks, there was no significant change in target to background ratio from the ascending aorta between baseline and the start of adalimumab, although in the carotid arteries, there was a modest increase in vascular inflammation.
Several previous studies have suggested that reducing inflammation in psoriasis can also reduce the risk of some cardiovascular events. As to why this study did not demonstrate a correlation between vascular inflammation and treatment, Dr. Bissonnette said during the question and answer portion of the presentation that “either the dose of adalimumab that is used for psoriasis has no impact on vascular inflammation or it may be possible that levels of interleukin-6, a key cytokine correlated with vascular inflammation, were very low in our study.”
Interleukin-6 typically is increased in patients with psoriatic arthritis, he explained, noting that in this study, only 7.5% of patients in the treatment group and about 10% of those in the control group had a history of psoriatic arthritis.
Additionally, at baseline, high-sensitivity C-reactive protein levels were significantly higher in controls: 5.32, compared with 2.72 in the treatment arm (P = .003).
Another possible reason for the results could be the molecule size of adalimumab, session comoderator Joel Gelfand, MD, noted in an interview. “The drug may not penetrate the aorta. These are large molecules. It also might be that [TNF–alpha] is not the main driver of aortic inflammation in people with psoriasis. Increasingly, we think of people with psoriasis as an IL-23 and IL-17 disease, so maybe that is part of it,” said Dr. Gelfand, professor of dermatology and epidemiology at the University of Pennsylvania, Philadelphia. He also directs the psoriasis and phototherapy treatment center at the university.
In addition to being presented at the meeting, the results were published in the Journal of Investigative Dermatology (2017 Feb 7. doi: 10.1016/j.jid.2017.02.977).
Adalimumab is marketed as Humira by Abbvie; a biosimilar version, adalimumab-atto (Amjevita), was approved in the United States in 2016.
Dr. Bissonnette’s disclosures included serving as an adviser and consultant to Abbvie, which sponsored the study, as well as relationships with other companies, including Amgen, Celgene, Janssen, and Novartis. Dr. Gelfand’s disclosures included serving as a consultant and investigator for Abbvie, and serving as an investigator, speaker, and/or consultant for other companies, including Eli Lilly, Janssen, and Novartis.
[email protected]
On Twitter @whitneymcknight
ORLANDO – Vascular inflammation was no different in patients with moderate to severe psoriasis after 16 weeks of treatment with adalimumab than in untreated controls, according to a study that evaluated the impact of blocking tumor necrosis factor–alpha on vascular inflammation.
Further, there was a modest increase in vascular inflammation in carotid arteries after 52 weeks of treatment with the tumor necrosis factor (TNF) alpha-antagonist adalimumab, Robert Bissonnette, MD, president of Innovaderm Research, Montreal, reported in a late-breaking session at the annual meeting of the American Academy of Dermatology.
At 16 weeks, there were no significant differences in vascular inflammation between the treatment and control arms, based on the change from baseline in the vessel wall target to background ratio from the ascending aorta (the primary endpoint). In the carotid arteries at 16 weeks, differences in vascular inflammation between the adalimumab group and control group were also not significant.
At 52 weeks, there was no significant change in target to background ratio from the ascending aorta between baseline and the start of adalimumab, although in the carotid arteries, there was a modest increase in vascular inflammation.
Several previous studies have suggested that reducing inflammation in psoriasis can also reduce the risk of some cardiovascular events. As to why this study did not demonstrate a correlation between vascular inflammation and treatment, Dr. Bissonnette said during the question and answer portion of the presentation that “either the dose of adalimumab that is used for psoriasis has no impact on vascular inflammation or it may be possible that levels of interleukin-6, a key cytokine correlated with vascular inflammation, were very low in our study.”
Interleukin-6 typically is increased in patients with psoriatic arthritis, he explained, noting that in this study, only 7.5% of patients in the treatment group and about 10% of those in the control group had a history of psoriatic arthritis.
Additionally, at baseline, high-sensitivity C-reactive protein levels were significantly higher in controls: 5.32, compared with 2.72 in the treatment arm (P = .003).
Another possible reason for the results could be the molecule size of adalimumab, session comoderator Joel Gelfand, MD, noted in an interview. “The drug may not penetrate the aorta. These are large molecules. It also might be that [TNF–alpha] is not the main driver of aortic inflammation in people with psoriasis. Increasingly, we think of people with psoriasis as an IL-23 and IL-17 disease, so maybe that is part of it,” said Dr. Gelfand, professor of dermatology and epidemiology at the University of Pennsylvania, Philadelphia. He also directs the psoriasis and phototherapy treatment center at the university.
In addition to being presented at the meeting, the results were published in the Journal of Investigative Dermatology (2017 Feb 7. doi: 10.1016/j.jid.2017.02.977).
Adalimumab is marketed as Humira by Abbvie; a biosimilar version, adalimumab-atto (Amjevita), was approved in the United States in 2016.
Dr. Bissonnette’s disclosures included serving as an adviser and consultant to Abbvie, which sponsored the study, as well as relationships with other companies, including Amgen, Celgene, Janssen, and Novartis. Dr. Gelfand’s disclosures included serving as a consultant and investigator for Abbvie, and serving as an investigator, speaker, and/or consultant for other companies, including Eli Lilly, Janssen, and Novartis.
[email protected]
On Twitter @whitneymcknight
Key clinical point:
Major finding: At 16 weeks, there were no significant differences in aortic and carotid inflammation in the change from baseline in moderate psoriasis patients given adalimumab and controls.
Data source: A randomized, double-blind multicenter study that used PET-CT scans to evaluate the impact of treatment on vascular inflammation in 107 adults with moderate to severe psoriasis.
Disclosures: Dr. Bissonnette’s disclosures included serving as an adviser and consultant to Abbvie, which sponsored the study, as well as relationships with other companies, including Amgen, Celgene, Janssen, and Novartis. Dr. Gelfand’s disclosures included serving as a consultant and investigator for Abbvie, and serving as an investigator, speaker, and/or consultant for other companies, including Eli Lilly, Janssen, and Novartis.
VIDEO: Stress alleviation strategies boost inflammatory skin treatment regimens
ORLANDO – “Consider the effects of the mind on the skin when treating patients with some skin diseases.” That was the message of several speakers during a session titled “The Skin and the Mind” at the annual meeting of the American Academy of Dermatology.
“I certainly believe that the time has come to use stress alleviation techniques, at least for selected patients, and this should certainly be part of our armamentarium in the clinic,” said Richard D. Granstein, MD, George W. Hambrick Jr. professor and chairman of the department of dermatology, Cornell University, New York. During the session, he spoke about the emerging science of stress in dermatology.
While it has long been believed that stress exacerbates different skin diseases, the connection has been difficult to prove scientifically, he pointed out. However, “the overwhelming number of reports and studies indicate that stress probably does exacerbate a number of inflammatory skin diseases,” he added.
In a video interview at the meeting, Dr. Granstein notes that a number of pathways that help explain this link have now been identified and discusses one of those pathways, which involves neuropeptides and future directions in understanding the relationship between stress and inflammatory skin diseases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Granstein disclosed serving as an advisor to Castle Biosciences, Elysium Health, Galderma Laboratories, and Velius.
[email protected]
On Twitter @whitneymcknight
ORLANDO – “Consider the effects of the mind on the skin when treating patients with some skin diseases.” That was the message of several speakers during a session titled “The Skin and the Mind” at the annual meeting of the American Academy of Dermatology.
“I certainly believe that the time has come to use stress alleviation techniques, at least for selected patients, and this should certainly be part of our armamentarium in the clinic,” said Richard D. Granstein, MD, George W. Hambrick Jr. professor and chairman of the department of dermatology, Cornell University, New York. During the session, he spoke about the emerging science of stress in dermatology.
While it has long been believed that stress exacerbates different skin diseases, the connection has been difficult to prove scientifically, he pointed out. However, “the overwhelming number of reports and studies indicate that stress probably does exacerbate a number of inflammatory skin diseases,” he added.
In a video interview at the meeting, Dr. Granstein notes that a number of pathways that help explain this link have now been identified and discusses one of those pathways, which involves neuropeptides and future directions in understanding the relationship between stress and inflammatory skin diseases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Granstein disclosed serving as an advisor to Castle Biosciences, Elysium Health, Galderma Laboratories, and Velius.
[email protected]
On Twitter @whitneymcknight
ORLANDO – “Consider the effects of the mind on the skin when treating patients with some skin diseases.” That was the message of several speakers during a session titled “The Skin and the Mind” at the annual meeting of the American Academy of Dermatology.
“I certainly believe that the time has come to use stress alleviation techniques, at least for selected patients, and this should certainly be part of our armamentarium in the clinic,” said Richard D. Granstein, MD, George W. Hambrick Jr. professor and chairman of the department of dermatology, Cornell University, New York. During the session, he spoke about the emerging science of stress in dermatology.
While it has long been believed that stress exacerbates different skin diseases, the connection has been difficult to prove scientifically, he pointed out. However, “the overwhelming number of reports and studies indicate that stress probably does exacerbate a number of inflammatory skin diseases,” he added.
In a video interview at the meeting, Dr. Granstein notes that a number of pathways that help explain this link have now been identified and discusses one of those pathways, which involves neuropeptides and future directions in understanding the relationship between stress and inflammatory skin diseases.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Granstein disclosed serving as an advisor to Castle Biosciences, Elysium Health, Galderma Laboratories, and Velius.
[email protected]
On Twitter @whitneymcknight
AT AAD 17
VIDEO: Consider alopecia ‘camouflage kits’ to boost patients’ self-esteem
ORLANDO – The hair loss encounter – which can be challenging for both physicians and patients – should address the negative psychological effects of hair loss, including ways to camouflage hair loss, advised Adriana N. Schmidt, MD, a dermatologist in Santa Monica, Calif.
Dermatologists may spend so much time on the work-up – reviewing history regarding medication, lab values, and hair care practices – that they do not spend time to simply say to patients, “I want to help you feel better about yourself, and here’s how,” she said in a video interview at the annual meeting of the American Academy of Dermatology.
“What we can do is offer them a way to camouflage the hair loss,” Dr. Schmidt said. She shared tips that include creating a kit to keep in the office filled with lists of reputable hairpiece vendors and tattoo specialists in the community, as well as sample wigs, cosmetic powders, and other items to show to patients during hair loss consultations. She also offers thoughts on working with new hair styles and stylists to help improve the self-esteem of alopecia patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Schmidt had no relevant disclosures.
[email protected]
On Twitter @whitneymcknight
ORLANDO – The hair loss encounter – which can be challenging for both physicians and patients – should address the negative psychological effects of hair loss, including ways to camouflage hair loss, advised Adriana N. Schmidt, MD, a dermatologist in Santa Monica, Calif.
Dermatologists may spend so much time on the work-up – reviewing history regarding medication, lab values, and hair care practices – that they do not spend time to simply say to patients, “I want to help you feel better about yourself, and here’s how,” she said in a video interview at the annual meeting of the American Academy of Dermatology.
“What we can do is offer them a way to camouflage the hair loss,” Dr. Schmidt said. She shared tips that include creating a kit to keep in the office filled with lists of reputable hairpiece vendors and tattoo specialists in the community, as well as sample wigs, cosmetic powders, and other items to show to patients during hair loss consultations. She also offers thoughts on working with new hair styles and stylists to help improve the self-esteem of alopecia patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Schmidt had no relevant disclosures.
[email protected]
On Twitter @whitneymcknight
ORLANDO – The hair loss encounter – which can be challenging for both physicians and patients – should address the negative psychological effects of hair loss, including ways to camouflage hair loss, advised Adriana N. Schmidt, MD, a dermatologist in Santa Monica, Calif.
Dermatologists may spend so much time on the work-up – reviewing history regarding medication, lab values, and hair care practices – that they do not spend time to simply say to patients, “I want to help you feel better about yourself, and here’s how,” she said in a video interview at the annual meeting of the American Academy of Dermatology.
“What we can do is offer them a way to camouflage the hair loss,” Dr. Schmidt said. She shared tips that include creating a kit to keep in the office filled with lists of reputable hairpiece vendors and tattoo specialists in the community, as well as sample wigs, cosmetic powders, and other items to show to patients during hair loss consultations. She also offers thoughts on working with new hair styles and stylists to help improve the self-esteem of alopecia patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Schmidt had no relevant disclosures.
[email protected]
On Twitter @whitneymcknight
AT AAD 2017