User login
Warn patients about illicit drugs doctored with fentanyl
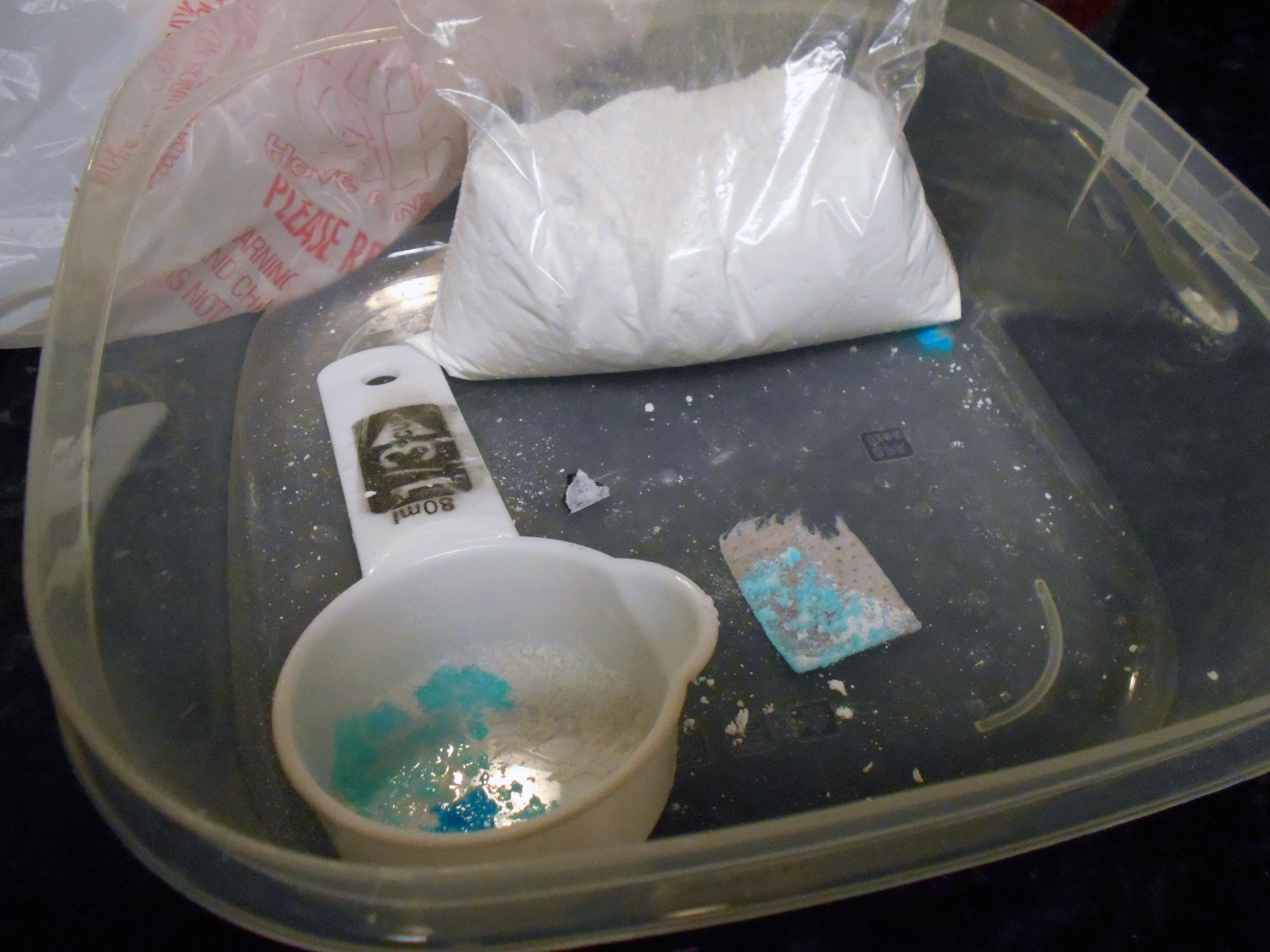
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
Fentanyl is now threatening overdoses in patients exposed to essentially any of the full array of recreational drugs – not just opioids – that are being sold illicitly, according to an overview of the problem presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“Fentanyl can now be found in cocaine and methamphetamine. At this point, there is really no way to predict what is in a [street] drug,” Edwin A. Salsitz, MD, said at the meeting, sponsored by Medscape Live. He is associate clinical professor of medicine who works in the division of chemical dependency at Mount Sinai Beth Israel Medical Center in New York.
As proof of the frequency with which fentanyl is now being used as an additive, most patients with a drug use disorder, regardless of their drug of choice, are testing positive for fentanyl at Dr. Salsitz’s center. Many of those with positive fentanyl tests are unaware that their drugs had been doctored with this agent.
Relative to drugs sold as an opioid, such as heroin or oxycodone, the fentanyl dose in nonopioid drugs is typically more modest, but Dr. Salsitz pointed out that those expecting cocaine or methamphetamine often “have no heroin tolerance, so they are more vulnerable” to the adverse effects of fentanyl, including an overdose.
Although opioid tolerance might improve the chances for surviving a fentanyl overdose, the toxicology of fentanyl is not the same as other opioids. Death from heroin is typically a result of respiratory depression, but the onset is relatively slow, providing a greater opportunity to administer a reversal agent, such as naloxone.
Fentanyl not only produces respiratory depression but skeletal muscle rigidity. The rapid onset of “wooden chest syndrome” can occur within minutes, making the opportunity for intervention much smaller, Dr. Salsitz said.
To illustrate the phenomenon, Dr. Salsitz recounted a case.
After an argument with his mother, a 26-year-old male with a long history of intravenous drug use went to his bedroom. His mother, responding to the sound of a loud thud, rushed to the bedroom to find her son on the floor with a needle still in his arm. Resuscitation efforts by the mother and by the emergency responders, who arrived quickly, failed.
“The speed of his death made it clear that it was fentanyl related, and the postmortem toxicology confirmed that the exposure involved both heroin and fentanyl,” Dr. Salsitz said.
After the first wave of deaths in the opioid epidemic, which was attributed to inappropriate use of prescription opioids, the second wave was driven by heroin. In that wave, patients who became addicted to prescription opioids but were having more difficulty gaining access to them, turned to far cheaper and readily available street heroin. The third wave, driven by fentanyl, began several years ago when sellers of heroin began adding this synthetic opioid, which is relatively cheap, to intensify the high.
It is not expected to end quickly. The fentanyl added to heroin was never a prescription version. Rather, Dr. Salsitz said, it is synthesized in laboratories in China, Mexico, and the United States. It is relatively easy to produce and compact, which makes it easy to transport.
Exacerbating the risks that fentanyl poses when added to street drugs, even more potent versions, such as carfentanil, are also being added to cocaine, methamphetamines, and other nonopioid illicit drugs. When compared on a per-milligram basis, fentanyl is about 100 times more potent than heroin, but carfentanil is about 100 times more potent than fentanyl, according to Dr. Salsitz.
When the third wave of deaths in the opioid epidemic began around 2013, prescriptions of fentanyl, like many other opioid-type therapies were declining. The “perfect storm” that initiated the opioid epidemic was a product of intense focus on pain control and a misperception that prescription opioids posed a low risk of abuse potential, Dr. Salsitz said. By the time fentanyl was driving opioid deaths, the risks of opioids were widely appreciated and their use for prescription analgesia was declining.
Citing several cases, Dr. Salsitz noted that only 20 years after clinicians were being successfully sued for not offering enough analgesia, they were now going to jail for prescribing these drugs too liberally.
According to Dr. Salsitz, While psychiatrists might not have a role in this issue, Dr. Salsitz did see a role for these specialists in protecting patients from the adverse consequences of using illicit drugs doctored with fentanyl.
Noting that individuals with psychiatric disorders are more likely than the general population to self-medicate with drugs purchased illegally, Dr. Salsitz encouraged psychiatrists “to get involved” in asking about drug use and counseling patients on the risks of fentanyl substitution or additives.
“The message is that no one knows what are in these drugs, anymore,” he said.
In addition to making patients aware that many street drugs are now contaminated with fentanyl, Dr. Salsitz provided some safety tips. He suggested instructing patients to take a low dose of any newly acquired drug to gauge its effect, to avoid taking drugs alone, and to avoid mixing drugs. He also recommended using rapid fentanyl test strips in order to detect fentanyl contamination.
Even for the many psychiatrists who do not feel comfortable managing addiction, Dr. Salsitz recommended a proactive approach to address the current threat.
Test strips as an intervention
The seriousness of fentanyl contamination of illicit drugs, including cocaine and methamphetamine, was corroborated by two investigators at the School of Public Health and the Albert Einstein Medical School of Brown University, Providence, R.I. Brandon D.L. Marshall, PhD, associate professor of epidemiology in the School of Public Health, called fentanyl-contaminated cannabis “extremely rare,” but he said that it is being found in counterfeit prescription pills as well as in crystal methamphetamine and in both crack and powder cocaine.
He also advocated the use of fentanyl test strips.
“Test strips are an efficient, inexpensive, and effective way to determine whether fentanyl or related analogs are present in illicit drugs,” he said, noting that he is involved in a trial designed to determine whether fentanyl test strips can reduce the risk of fatal and nonfatal overdoses.
In a pilot study conducted in Baltimore, 69% of the 103 participants engaged in harm reduction behavior after using a fentanyl test strip and receiving a positive result (Addict Behav. 2020;110:106529). It is notable that 86% of the participants had a least one positive result when using the strips. More than half were surprised by the result.
One of the findings from this study was “that the lasting benefit of fentanyl test strip distribution is the opportunity to engage in discussions around safety and relationship building with historically underserved communities,” said the lead author, Ju Nyeong Park, PhD, assistant professor of medicine and epidemiology at Brown University. She moved to Brown after performing this work at Johns Hopkins University, Baltimore.
Dr. Park noted that “many patients in the community already know that they are using drugs containing fentanyl,” but for those who are concerned and wish to avoid contaminated drugs, fentanyl test strips “are a quick screening tool.” However, while the strips are helpful, she cautioned that they cannot be considered a definitive tool for detecting harm in illicit drugs.
“There may also be other chemicals present in tested drugs that confer risk,” she said.
Medscape Live and this news organization are owned by the same parent company. Dr. Salsitz, Dr. Marshall, and Dr. Park reported no potential conflicts of interest.
FROM PSYCHOPHARMACOLOGY UPDATE
Cannabis use: Messages remain mixed across diagnoses
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
Marijuana use is now a legal activity in many parts of the United States, but those managing patients with psychiatric disorders are in the difficult position of determining whether this use is helpful, harmful, or irrelevant to the underlying illness on the basis of limited and largely incomplete data, according to an overview of this issue presented at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
While there is clear evidence that cannabis use relative to the general population “is more prevalent among patients with psychiatric disorders,” it is less certain how often this use is risky, said Diana M. Martinez, MD, professor of psychiatry at Columbia University in New York.
Independent of euphoric effects, cannabis can be perceived by individuals with psychiatric diagnosis as self-medication for feelings of stress, social anxiety, and insomnia, among other symptoms. These are the same reasons why many individuals without psychiatric conditions use cannabis-containing products.
The perception that cannabis use is generally benign presumably explains the successful efforts at legalization, but there are risks for those with or without psychiatric illnesses, Dr. Martinez pointed out at the meeting, sponsored by Medscape Live. Not least, about 20% of regular users of cannabis develop cannabis use disorder (CUD), a condition defined in the DSM-5 as the continued use of cannabis despite adverse consequences, such as dependence.
Impact of severe CUD ‘incapacitating’
“Of those who meet criteria for CUD, 23% have severe CUD, which is an incapacitating form,” reported Dr. Martinez, citing work led by Deborah Hasin, PhD, professor of clinical epidemiology at Columbia University.
However, relative to otherwise healthy individuals, those with a psychiatric diagnosis might face greater benefits or greater risks from cannabis use, according to Dr. Martinez, who cited a 2017 report from the National Academies of Science, Engineering, and Medicine (NASEM).
This report evaluated the potential risks and benefits on the basis of published studies.
There is limited evidence that regular cannabis increases rather than modifies symptoms of mania and hypomania in patients with bipolar disorder, according to the report. The report also cited limited evidence that cannabis use increases severity of posttraumatic stress disorder (PTSD). There was limited evidence of adverse effects on symptoms of anxiety, although this appeared to depend on daily or nearly daily use.
The report found no data of acceptable quality to draw conclusions about the effect of cannabis use on symptoms of depression.
In patients with attention-deficit/hyperactivity disorder (ADHD), “a recent study showed that daily but not occasional use of cannabis increased impulsivity but not inattention, working memory, or verbal intelligence,” said Dr. Martinez, citing a study published this year.
Some evidence also suggests that patients with a psychiatric disorder might benefit from cannabis use, but, again, this evidence is limited. For one example, it includes a potential reduction in symptoms of obsessive-compulsive disorder, Dr. Martinez said.
More support for cannabis in medical disease
Relative to the quality of evidence supporting benefit from cannabis in psychiatric disease, the data appear to be stronger for patients with medical illnesses, such as cancer. For example, Dr. Martinez cited evidence that tetrahydrocannabinol (THC), a major active ingredient in cannabis, improves sleep in the context of a medical illnesses. There is also evidence for anxiolytic effects in patients with a medical illness, although that is weaker.
In patients with or without a psychiatric disorder, marijuana does pose a risk of substance abuse disorder, and it shares the risks of intoxicants, such as inattention leading to increased risk of accidents, including motor vehicle accidents. This pertains to those with or without a psychiatric or medical condition, Dr. Martinez said.
While intermittent light use of cannabis appears to pose no risk or a very low risk of long-term adverse effects on cognition, at least in patients without psychiatric disorders, Dr. Martinez indicated that the risk-benefit ratio for any individual is use dependent. The risk of CUD, for example, increases with the frequency of exposure and the potency of the cannabis.
Empirical evidence for therapeutic role
In published studies, other researchers have expressed interest in a potential therapeutic role of cannabis for psychiatric disorders, but there appears to be a general consensus that the supportive data remain weak. One expert who has written on this topic, Jerome Sarris, PhD, professor of integrative mental health, NICM Health Research Institute, Western Sydney University, Westmead, Australia, said that empirical evidence does support a benefit in selected patients.
“Of course, high THC forms are strongly discouraged in people with schizophrenia or high risk of developing psychotic disorder, or in youths,” Dr. Sarris explained. “However, there is a potential role for use in people with sleep and pain issues, and many find it beneficial to also assist with affective disorder symptoms.”
In a systematic review he led that was published last year, the evidence to support cannabis for psychiatric disorders was characterized as “embryonic.” However, small studies and case reports appear to support benefit for such indications as ADHD if precautions are taken.
“I certainly would not discourage use of prescribed standardized medicinal cannabis therapeutics for all people with psychiatric disorders,” Dr. Sarris said. He suggested that attention should be made to the THC potency and terpene composition of the products that patients with psychiatric disorders are taking.
FROM PSYCHOPHARMACOLOGY UPDATE
Major increase seen in cosmeceutical alternatives to topical hydroquinone
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
along with new strategies to improve their efficacy, according to a report at the Skin of Color Update 2021.
“Ten or 15 years ago, I was showing a slide with five [alternatives to hydroquinone]. Now there are dozens,” reported Heather Woolery-Lloyd, MD, director of the skin of color division in the department of dermatology at the University of Miami.
The growth in alternatives to hydroquinone is timely. After threats to do so for more than a decade, the Food and Drug Administration finally banned hydroquinone from OTC products in 2020. The ban was folded into the Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March of 2020 and then implemented the following September.
Until the ban of hydroquinone, OTC products with this compound were widely sought by many individuals with darker skin tones to self-treat melasma and other forms of hyperpigmentation, according to Dr. Woolery-Lloyd. Hydroquinone is still available in prescription products, but she is often asked for OTC alternatives, and she says the list is long and getting longer.
Niacinamide
Detailing the products she has been recommending most frequently as substitutes, Dr. Woolery-Lloyd reported that several are supported by high quality studies. One example is niacinamide.
Of the several controlled studies she cited, one double-blind randomized trial found niacinamide to be equivalent to hydroquinone for melasma on the basis of colorimetric measures. The study compared 4% niacinamide cream applied on one side of the face with 4% hydroquinone cream applied on the other side in 27 patients with melasma. Although the proportion of responses rated good or excellent on a subjective basis was lower with niacinamide (44% vs. 55%), the difference was not statistically significant and niacinamide cream was clearly active, producing objective improvements in mast cell infiltrate and solar elastosis in melasma skin as well. Both were well tolerated.
In other studies, niacinamide has been shown to be effective in the treatment of melasma when combined with other active agents such as tranexamic acid, said Dr. Woolery-Lloyd, who added that OTC products containing niacinamide are now “among my favorites” when directing patients to cosmeceuticals for hyperpigmentation.
Topical vitamin C
Topical vitamin C or ascorbic acid is another. Like niacinamide, topical vitamin C has also been compared with hydroquinone in a double-blind, randomized trial. Although the niacinamide trial and this study were performed 10 or more years ago, these data have new relevance with the ban of OTC hydroquinone.
In the study, 5% ascorbic acid cream on one side of the face was compared with 4% hydroquinone cream, applied on the other side, in 16 women with melasma. Again, there were no statistical differences in colorimetric measures, but good to excellent results were reported for 93% of the sides of the face treated with hydroquinone versus 62.5% of the sides treated with vitamin C (P < .05). “Hydroquinone performed better, but the vitamin C was active and very well tolerated,” Dr. Woolery-Lloyd said.
However, the ascorbic acid cream was better tolerated, with a far lower rate of adverse events (6.2% vs. 68.7%), an advantage that makes it easy to recommend to patients, said Dr. Woolery-Lloyd, who now uses it frequently in her own practice.
Liquiritin, a licorice extract, is another lightening agent increasingly included in OTC products that she also recommends. In two older studies in medical journals published in Pakistan, both the 2% and 4% strengths of liquiritin cream outperformed hydroquinone on the basis of a Melasma Area and Severity Index (MASI) rating. The liquiritin cream was well tolerated in both studies.
Azelaic acid, tranexamic acid
OTC products containing azelaic acid are also effective for hyperpigmentation based on published trials in which they were compared with hydroquinone for treating melasma. In one study of 29 women with melasma cited by Dr. Woolery-Lloyd, 20% azelaic acid cream was more effective than hydroquinone 4% cream after 2 months of treatment on the basis of the mean MASI score (6.2 vs. 3.8).
The list also includes cysteamine, silymarin, and tranexamic acid.
In the case of tranexamic acid, Dr. Woolery-Lloyd cited a relatively recent study of 60 patients with melasma, comparing two strategies for applying tranexamic acid to treatment with hydroquinone over 12 weeks. Compared with 2% hydroquinone (applied nightly) or 1.8% liposomal tranexamic acid (applied twice a day), 5% tranexamic acid solution with microneedling (weekly) had a slightly greater rate of success defined as more than a 50% improvement in hyperpigmentation in an Asian population (30%, 27.8%, and 33.3%, respectively).
“Microneedling is a newer technology that appears to be effective at improving absorption,” said Dr. Woolery-Lloyd. She predicts that microneedling will be used with increasing frequency in combination with topical cosmeceuticals.
She also predicted that these topical agents will be increasingly employed in combinations as the field of cosmeceuticals becomes increasingly more sophisticated. “When it comes to skin quality, cosmeceuticals remain our first-line therapy, especially in skin of color,” she said.
The rapid growth and utility of OTC cosmeceuticals is an area that dermatologists need to be following, according to Darius Mehregan, MD, chair of the department of dermatology, Wayne State University, Detroit, who was senior author of an article published last year that reviewed the ingredients of popular OTC cosmeceuticals.
“Our patients have a great interest in cosmeceuticals and are looking to us for guidance. I think we have a responsibility to help them identify products supported by evidence and to warn them about potential side effects,” Dr. Mehregan, who was not at the meeting, said in an interview.
He agreed that the removal of hydroquinone from OTC products will create a specific need in the area of cosmeceuticals.
“Hydroquinone has for a long time been one of the most effective agents in OTC products for melasma, so patients are going to be looking for alternatives. Identifying which drugs have shown efficacy in controlled studies will be very helpful,” he said.
Dr. Woolery-Lloyd reports financial relationships with Ortho Dermatologics, L’Oréal, Galderma, Allergan, and Somabella Laboratories. Dr. Mehregan reports no potential conflicts of interest.
FROM SOC 2021
In atopic dermatitis trial, abrocitinib offers faster itch relief than dupilumab
), in a multicenter randomized trial presented as a late breaker at the annual meeting of the European Academy of Dermatology and Venereology.
The earlier onset of action with the JAK inhibitor was achieved even though most patients in both arms were on topical corticosteroids, a design element that “is clinically relevant” for a practical comparison of these two agents, according to Kristian Reich, MD, PhD, Center for Translational Research in Inflammatory Skin Diseases, University Medical Center, Hamburg-Eppendorf, Germany.
The goal of this phase 3b trial, called JADE DARE, was to compare relative safety and efficacy of these strategies over the early course of treatment, he said.
Over 700 patients randomized
JADE DARE enrolled 727 patients over age 18 years who previously had an inadequate response to conventional topical therapies. All had moderate to severe AD defined by criteria such as body surface area greater than or equal to 10% and Eczema Area Severity Index (EASI) greater than or equal to 16. They were randomly assigned to 200 mg oral abrocitinib once daily or 300 mg subcutaneous dupilumab (after a loading dose of 600 mg) every 2 weeks. A double-dummy design preserved blinding.
The coprimary endpoints were at least a 4-point improvement in pruritus as measured with the Peak Pruritus Numerical Rating Scale (PP-NRS) score at week 2 and at least a 90% improvement in the EASI (EASI 90) at week 4.
The primary endpoint for pruritus at 2 weeks was reached by nearly twice as many patients randomly assigned to abrocitinib (46.2% vs. 25.5%; P < .001). The proportion of those meeting the EASI 90 endpoint at week 4 was also superior on abrocitinib (28.5% vs. 14.6%; P < .001)
Advantage for pruritus control dissipates
For the pruritus endpoint, the advantage of abrocitinib slowly diminished over time after the peak difference observed at 2 weeks. Although the advantage at week 4 (58.1% vs. 40.8%) and week 8 (65.8% vs. 52.7%) remained sizable, there were very small differences thereafter. However, Dr. Reich pointed out that the percentages continued to favor abrocitinib at least numerically through the 26 weeks of follow-up completed so far.
The pattern of response on EASI 90 was not the same. After demonstrating superiority at the 4-week timepoint, the advantage of abrocitinib persisted. When compared at week 16, which was a secondary endpoint of the JADE DARE trial, the advantage of abrocitinib remained significant (54.3% vs. 41.9%; P < .001). The advantage of abrocitinib narrowed but remained numerically superior at 26 weeks (54.6% vs. 47.6%).
Based on the data collected to date, “abrocitinib is clearly superior early on,” Dr. Reich said. Moreover, he reiterated that topical corticosteroids were allowed as background therapy in both arms.
“It is difficult to show an advantage for one active therapy over the other in patients on background corticosteroids,” Dr. Reich maintained.
Both drugs are well tolerated
The drugs were similarly well tolerated. Serious adverse events were uncommon in either arm. The rate of study dropouts due to an adverse event potentially related to treatment assignment was 3% in each group.
Nausea (19% vs. 2%), acne (13.5% vs. 2%), and headache (13% vs. 7.5%) were all more common in patients randomly assigned to abrocitinib. Conjunctivitis was more common in the group randomly assigned to dupilumab (10% vs. 2%).
The two deaths that occurred during this study were in the abrocitinib arm, but one was the result of COVID-19 infection and the other was a cardiovascular event in a patient with risk factors. Neither was considered to be treatment-related.
Abrocitinib’s relative selectivity for the JAK1 inhibitor is a potential differentiator from other currently available JAK inhibitors, although direct comparisons of these therapies for clinical activity in AD as well as most other diseases remains limited.
The relatively rapid relief of pruritus with the JAK inhibitor relative to the monoclonal antibody in the JADE DARE trial is likely to be perceived as clinically significant by patients with AD, according to Sonja Ständer, MD, professor of dermatology and neurodermatology at the University Hospital Münster, Germany.
“One of the highest needs of patients with atopic dermatitis is a rapid and profound relief of itch,” Dr. Ständer, who wrote a review article on AD earlier this year, said in an interview.
Although several current therapies are effective against pruritus, Dr. Ständer believes that the higher proportion of patients achieving itch control at 2 weeks on abrocitinib “will attract the attention of affected patients.”
However, she added that patients need to take both benefits and risks into account, indicating that clinical utility cannot be judged on a single outcome. In selecting one drug over the others, she advised “a balanced use of therapies.”
Abrocitinib was first approved in the United Kingdom in early September, followed by Japan last Thursday, for the treatment of moderate to severe AD in patients ages 12 and older. It is under review elsewhere, including in the United States and the European Union for AD.
In September, the FDA approved the first JAK inhibitor for treating AD – a topical JAK inhibitor, ruxolitinib.
Dr. Reich reports financial relationships with 20 pharmaceutical companies, including Pfizer, which provided funding for the JADE DARE trial. Dr. Ständer reports financial relationships with Beiersdorf AG, Galderma, Kliniska, Lilly, Pfizer, and Sanofi.
A version of this article first appeared on Medscape.com.
), in a multicenter randomized trial presented as a late breaker at the annual meeting of the European Academy of Dermatology and Venereology.
The earlier onset of action with the JAK inhibitor was achieved even though most patients in both arms were on topical corticosteroids, a design element that “is clinically relevant” for a practical comparison of these two agents, according to Kristian Reich, MD, PhD, Center for Translational Research in Inflammatory Skin Diseases, University Medical Center, Hamburg-Eppendorf, Germany.
The goal of this phase 3b trial, called JADE DARE, was to compare relative safety and efficacy of these strategies over the early course of treatment, he said.
Over 700 patients randomized
JADE DARE enrolled 727 patients over age 18 years who previously had an inadequate response to conventional topical therapies. All had moderate to severe AD defined by criteria such as body surface area greater than or equal to 10% and Eczema Area Severity Index (EASI) greater than or equal to 16. They were randomly assigned to 200 mg oral abrocitinib once daily or 300 mg subcutaneous dupilumab (after a loading dose of 600 mg) every 2 weeks. A double-dummy design preserved blinding.
The coprimary endpoints were at least a 4-point improvement in pruritus as measured with the Peak Pruritus Numerical Rating Scale (PP-NRS) score at week 2 and at least a 90% improvement in the EASI (EASI 90) at week 4.
The primary endpoint for pruritus at 2 weeks was reached by nearly twice as many patients randomly assigned to abrocitinib (46.2% vs. 25.5%; P < .001). The proportion of those meeting the EASI 90 endpoint at week 4 was also superior on abrocitinib (28.5% vs. 14.6%; P < .001)
Advantage for pruritus control dissipates
For the pruritus endpoint, the advantage of abrocitinib slowly diminished over time after the peak difference observed at 2 weeks. Although the advantage at week 4 (58.1% vs. 40.8%) and week 8 (65.8% vs. 52.7%) remained sizable, there were very small differences thereafter. However, Dr. Reich pointed out that the percentages continued to favor abrocitinib at least numerically through the 26 weeks of follow-up completed so far.
The pattern of response on EASI 90 was not the same. After demonstrating superiority at the 4-week timepoint, the advantage of abrocitinib persisted. When compared at week 16, which was a secondary endpoint of the JADE DARE trial, the advantage of abrocitinib remained significant (54.3% vs. 41.9%; P < .001). The advantage of abrocitinib narrowed but remained numerically superior at 26 weeks (54.6% vs. 47.6%).
Based on the data collected to date, “abrocitinib is clearly superior early on,” Dr. Reich said. Moreover, he reiterated that topical corticosteroids were allowed as background therapy in both arms.
“It is difficult to show an advantage for one active therapy over the other in patients on background corticosteroids,” Dr. Reich maintained.
Both drugs are well tolerated
The drugs were similarly well tolerated. Serious adverse events were uncommon in either arm. The rate of study dropouts due to an adverse event potentially related to treatment assignment was 3% in each group.
Nausea (19% vs. 2%), acne (13.5% vs. 2%), and headache (13% vs. 7.5%) were all more common in patients randomly assigned to abrocitinib. Conjunctivitis was more common in the group randomly assigned to dupilumab (10% vs. 2%).
The two deaths that occurred during this study were in the abrocitinib arm, but one was the result of COVID-19 infection and the other was a cardiovascular event in a patient with risk factors. Neither was considered to be treatment-related.
Abrocitinib’s relative selectivity for the JAK1 inhibitor is a potential differentiator from other currently available JAK inhibitors, although direct comparisons of these therapies for clinical activity in AD as well as most other diseases remains limited.
The relatively rapid relief of pruritus with the JAK inhibitor relative to the monoclonal antibody in the JADE DARE trial is likely to be perceived as clinically significant by patients with AD, according to Sonja Ständer, MD, professor of dermatology and neurodermatology at the University Hospital Münster, Germany.
“One of the highest needs of patients with atopic dermatitis is a rapid and profound relief of itch,” Dr. Ständer, who wrote a review article on AD earlier this year, said in an interview.
Although several current therapies are effective against pruritus, Dr. Ständer believes that the higher proportion of patients achieving itch control at 2 weeks on abrocitinib “will attract the attention of affected patients.”
However, she added that patients need to take both benefits and risks into account, indicating that clinical utility cannot be judged on a single outcome. In selecting one drug over the others, she advised “a balanced use of therapies.”
Abrocitinib was first approved in the United Kingdom in early September, followed by Japan last Thursday, for the treatment of moderate to severe AD in patients ages 12 and older. It is under review elsewhere, including in the United States and the European Union for AD.
In September, the FDA approved the first JAK inhibitor for treating AD – a topical JAK inhibitor, ruxolitinib.
Dr. Reich reports financial relationships with 20 pharmaceutical companies, including Pfizer, which provided funding for the JADE DARE trial. Dr. Ständer reports financial relationships with Beiersdorf AG, Galderma, Kliniska, Lilly, Pfizer, and Sanofi.
A version of this article first appeared on Medscape.com.
), in a multicenter randomized trial presented as a late breaker at the annual meeting of the European Academy of Dermatology and Venereology.
The earlier onset of action with the JAK inhibitor was achieved even though most patients in both arms were on topical corticosteroids, a design element that “is clinically relevant” for a practical comparison of these two agents, according to Kristian Reich, MD, PhD, Center for Translational Research in Inflammatory Skin Diseases, University Medical Center, Hamburg-Eppendorf, Germany.
The goal of this phase 3b trial, called JADE DARE, was to compare relative safety and efficacy of these strategies over the early course of treatment, he said.
Over 700 patients randomized
JADE DARE enrolled 727 patients over age 18 years who previously had an inadequate response to conventional topical therapies. All had moderate to severe AD defined by criteria such as body surface area greater than or equal to 10% and Eczema Area Severity Index (EASI) greater than or equal to 16. They were randomly assigned to 200 mg oral abrocitinib once daily or 300 mg subcutaneous dupilumab (after a loading dose of 600 mg) every 2 weeks. A double-dummy design preserved blinding.
The coprimary endpoints were at least a 4-point improvement in pruritus as measured with the Peak Pruritus Numerical Rating Scale (PP-NRS) score at week 2 and at least a 90% improvement in the EASI (EASI 90) at week 4.
The primary endpoint for pruritus at 2 weeks was reached by nearly twice as many patients randomly assigned to abrocitinib (46.2% vs. 25.5%; P < .001). The proportion of those meeting the EASI 90 endpoint at week 4 was also superior on abrocitinib (28.5% vs. 14.6%; P < .001)
Advantage for pruritus control dissipates
For the pruritus endpoint, the advantage of abrocitinib slowly diminished over time after the peak difference observed at 2 weeks. Although the advantage at week 4 (58.1% vs. 40.8%) and week 8 (65.8% vs. 52.7%) remained sizable, there were very small differences thereafter. However, Dr. Reich pointed out that the percentages continued to favor abrocitinib at least numerically through the 26 weeks of follow-up completed so far.
The pattern of response on EASI 90 was not the same. After demonstrating superiority at the 4-week timepoint, the advantage of abrocitinib persisted. When compared at week 16, which was a secondary endpoint of the JADE DARE trial, the advantage of abrocitinib remained significant (54.3% vs. 41.9%; P < .001). The advantage of abrocitinib narrowed but remained numerically superior at 26 weeks (54.6% vs. 47.6%).
Based on the data collected to date, “abrocitinib is clearly superior early on,” Dr. Reich said. Moreover, he reiterated that topical corticosteroids were allowed as background therapy in both arms.
“It is difficult to show an advantage for one active therapy over the other in patients on background corticosteroids,” Dr. Reich maintained.
Both drugs are well tolerated
The drugs were similarly well tolerated. Serious adverse events were uncommon in either arm. The rate of study dropouts due to an adverse event potentially related to treatment assignment was 3% in each group.
Nausea (19% vs. 2%), acne (13.5% vs. 2%), and headache (13% vs. 7.5%) were all more common in patients randomly assigned to abrocitinib. Conjunctivitis was more common in the group randomly assigned to dupilumab (10% vs. 2%).
The two deaths that occurred during this study were in the abrocitinib arm, but one was the result of COVID-19 infection and the other was a cardiovascular event in a patient with risk factors. Neither was considered to be treatment-related.
Abrocitinib’s relative selectivity for the JAK1 inhibitor is a potential differentiator from other currently available JAK inhibitors, although direct comparisons of these therapies for clinical activity in AD as well as most other diseases remains limited.
The relatively rapid relief of pruritus with the JAK inhibitor relative to the monoclonal antibody in the JADE DARE trial is likely to be perceived as clinically significant by patients with AD, according to Sonja Ständer, MD, professor of dermatology and neurodermatology at the University Hospital Münster, Germany.
“One of the highest needs of patients with atopic dermatitis is a rapid and profound relief of itch,” Dr. Ständer, who wrote a review article on AD earlier this year, said in an interview.
Although several current therapies are effective against pruritus, Dr. Ständer believes that the higher proportion of patients achieving itch control at 2 weeks on abrocitinib “will attract the attention of affected patients.”
However, she added that patients need to take both benefits and risks into account, indicating that clinical utility cannot be judged on a single outcome. In selecting one drug over the others, she advised “a balanced use of therapies.”
Abrocitinib was first approved in the United Kingdom in early September, followed by Japan last Thursday, for the treatment of moderate to severe AD in patients ages 12 and older. It is under review elsewhere, including in the United States and the European Union for AD.
In September, the FDA approved the first JAK inhibitor for treating AD – a topical JAK inhibitor, ruxolitinib.
Dr. Reich reports financial relationships with 20 pharmaceutical companies, including Pfizer, which provided funding for the JADE DARE trial. Dr. Ständer reports financial relationships with Beiersdorf AG, Galderma, Kliniska, Lilly, Pfizer, and Sanofi.
A version of this article first appeared on Medscape.com.
Lessons from an ethnic skin center: Awareness and respect for diversity
With the strong likelihood that , according to a dermatologist with expertise in these types of cases who spoke at the Skin of Color Update 2021.
“Instead of avoiding the discussion of cultural practices, we should discuss them and be open about them. It fosters a comfortable environment, trust, and better compliance,” reported Neelam Ajit Vashi, MD, founding director of the Boston University Center for Ethnic Skin.
Out of fear of causing offense, a desire to be discreet, or of personal discomfort with foreign cultural practices, some clinicians might elect to limit themselves to the information that the patient volunteers, which is a mistake, according to Dr. Vashi.
“The avoidance of topics around culture actually limits the ability to have a successful relationship,” she maintained.
Successful encounters are not just based on a willingness to listen, Dr. Vashi said. Clinicians should be seeking a base of knowledge. With growing globalization and widespread immigration, “it is increasingly important for dermatologists in the U.S. to understand the role of cultural practices [in creating skin problems] and recognize the sequelae,” Dr. Vashi said.
Taking some common examples of dermatologic complaints created by cosmetic practices originating elsewhere, Dr. Vashi described key clinical points in addressing complications related to henna, hair removal through threading, and placement of decorative adornments on the forehead, called bindi. In addition, she pointed out common issues with facial and body marking created with kumkum powder, hair oils, and skin lightening agents.
Black henna
For cosmetic enhancement, henna is relatively benign. It is also no longer confined to the south Asian communities where it originated. However, Dr. Vashi pointed out that patients of south Asian origin or descent might be more likely to use black henna, a variety with more risks.
Black henna contains additives, such as diaminobenzenes and p-phenylenediamine (PPD), to darken the tone of the product as well as provide other desired characteristics, such as an accelerated drying time. While some patients do develop reactions to conventional henna, the risks of black henna are greater.
“The acute contact dermatitis reactions can include dyspigmentation, leukoderma, and keloids,” Dr. Vashi said. Other complications include erythema multiforme, temporary hypertrichosis, and systemic allergic reactions, such as angioedema.
While those who have had a reaction to henna should avoid further contact, Dr. Vashi warned that sequelae can include cross reactions with latex and rubber as well as some pharmaceutical agents, such as sulfonamides. When taking a patient history, she noted, be aware that risks of henna extend to the hairdressers and cosmeticians who sometimes apply these products on others.
Hair threading, bindi, and kumkum
Hair threading, another practice popularized in south Asia and now growing in popularity globally, involves capturing hairs between cotton threads for removal of both the hair and its follicle. It is a relatively rapid and efficient method of permanent depilation. In addition to pain and erythema, Dr. Vashi reported that the complications associated with hair threading include pigmentary changes, infections such as bullous impetigo, and lesions of koebnerization – such as vitiligo and lichen planus.
Bindi, a Hindi tradition that involves placing adornments between the eyebrows, and kumkum, a powder typically made from turmeric to be employed for decorative markings, have also spread to use outside of their cultural context, according to Dr. Vashi. She said that the complications of these two cosmetic practices are shared, and stem largely from contact dermatitis.
In the case of bindi, para-tertiary-butylphenol in adhesives is one source of reactions, whereas kumkum itself can be an irritant. As these are typically local to the site of application, the diagnosis is not difficult, but treatment can be more challenging for patients unwilling to abandon the practice.
Hair oils, skin-lightening agents
Culturally-linked hair oils among patients from south Asia or Africa – or descendants from these areas – can damage hair in a variety of ways as well as cause contact dermatitis. The oils can also exacerbate existing skin diseases.
“Oils with high oleic acid, such as coconut or olive oils or shea butter, can worsen seborrheic dermatitis,” Dr. Vashi cautioned.
Of this list of dermatologic issues induced by culturally linked cosmetic practices, skin lightening agents might pose the most risk for permanent and irreversible complications. Dr. Vashi said that up to 70% of patients using lighteners develop complications, and there is a relationship between the severity of side effects as duration of use increases.
“The problem is that ingredients of many of these products, which are imported illegally and sold on the black market, are often not disclosed,” Dr. Vashi said. Some contain a high content of metals such as lead, copper, and iron, whether they are added intentionally or end up in the product because of poor quality control. For those developing adverse events associated with the products, the obvious treatment is discontinuation.
When patients are unwilling to discontinue any of the products that have led to dermatologic issues, Dr. Vashi encouraged physicians “to take a middle ground.” Simple avoidance can be challenging for practices that are culturally meaningful. In respecting cultural differences, she encouraged tolerance and compromise.
“Often these patients will be doing an alternative medication or intervention, but this does not mean that they are not accepting what we have to offer,” she said. She indicated that mutual respect will lead to better solutions.
The awareness of common cultural practices that can have a harmful impact on the skin is an area of practice that deserves more attention, Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology at Weill Cornell Medical Center, New York, said in an interview.
He said that he agreed with Dr. Vashi that understanding the role of cultural practices leading to dermatoses is not enough.
“Advising patients to alter or discontinue a specific cultural practice due to a dermatologic complication should be done with respect, humility, and understanding that may be challenging,” said Dr. Alexis.
While being aware of the specific cultural practices that might be causing or exacerbating dermatoses is important for accurate diagnosis, he said he believes that “partnering with the patient to modify the cultural practices in question” is important for a clinical outcome acceptable to the patient.
“Educational resources to inform clinicians of dermatoses associated with cultural practices are available and can be helpful for dermatologists in any practice setting,” he said.
Dr. Vashi reports that she has no relevant financial relationships to disclose. Dr. Alexis reports financial relationships with Abbvie, Allergan, Almirall, Amgen, Arcutis, AstraZeneca, Bristol-Myers Squibb, Cara, Galderma, Genzyme, Janssen, Leo, Menlo, Novartis, Regeneron, Sanofi, and Valeant.
With the strong likelihood that , according to a dermatologist with expertise in these types of cases who spoke at the Skin of Color Update 2021.
“Instead of avoiding the discussion of cultural practices, we should discuss them and be open about them. It fosters a comfortable environment, trust, and better compliance,” reported Neelam Ajit Vashi, MD, founding director of the Boston University Center for Ethnic Skin.
Out of fear of causing offense, a desire to be discreet, or of personal discomfort with foreign cultural practices, some clinicians might elect to limit themselves to the information that the patient volunteers, which is a mistake, according to Dr. Vashi.
“The avoidance of topics around culture actually limits the ability to have a successful relationship,” she maintained.
Successful encounters are not just based on a willingness to listen, Dr. Vashi said. Clinicians should be seeking a base of knowledge. With growing globalization and widespread immigration, “it is increasingly important for dermatologists in the U.S. to understand the role of cultural practices [in creating skin problems] and recognize the sequelae,” Dr. Vashi said.
Taking some common examples of dermatologic complaints created by cosmetic practices originating elsewhere, Dr. Vashi described key clinical points in addressing complications related to henna, hair removal through threading, and placement of decorative adornments on the forehead, called bindi. In addition, she pointed out common issues with facial and body marking created with kumkum powder, hair oils, and skin lightening agents.
Black henna
For cosmetic enhancement, henna is relatively benign. It is also no longer confined to the south Asian communities where it originated. However, Dr. Vashi pointed out that patients of south Asian origin or descent might be more likely to use black henna, a variety with more risks.
Black henna contains additives, such as diaminobenzenes and p-phenylenediamine (PPD), to darken the tone of the product as well as provide other desired characteristics, such as an accelerated drying time. While some patients do develop reactions to conventional henna, the risks of black henna are greater.
“The acute contact dermatitis reactions can include dyspigmentation, leukoderma, and keloids,” Dr. Vashi said. Other complications include erythema multiforme, temporary hypertrichosis, and systemic allergic reactions, such as angioedema.
While those who have had a reaction to henna should avoid further contact, Dr. Vashi warned that sequelae can include cross reactions with latex and rubber as well as some pharmaceutical agents, such as sulfonamides. When taking a patient history, she noted, be aware that risks of henna extend to the hairdressers and cosmeticians who sometimes apply these products on others.
Hair threading, bindi, and kumkum
Hair threading, another practice popularized in south Asia and now growing in popularity globally, involves capturing hairs between cotton threads for removal of both the hair and its follicle. It is a relatively rapid and efficient method of permanent depilation. In addition to pain and erythema, Dr. Vashi reported that the complications associated with hair threading include pigmentary changes, infections such as bullous impetigo, and lesions of koebnerization – such as vitiligo and lichen planus.
Bindi, a Hindi tradition that involves placing adornments between the eyebrows, and kumkum, a powder typically made from turmeric to be employed for decorative markings, have also spread to use outside of their cultural context, according to Dr. Vashi. She said that the complications of these two cosmetic practices are shared, and stem largely from contact dermatitis.
In the case of bindi, para-tertiary-butylphenol in adhesives is one source of reactions, whereas kumkum itself can be an irritant. As these are typically local to the site of application, the diagnosis is not difficult, but treatment can be more challenging for patients unwilling to abandon the practice.
Hair oils, skin-lightening agents
Culturally-linked hair oils among patients from south Asia or Africa – or descendants from these areas – can damage hair in a variety of ways as well as cause contact dermatitis. The oils can also exacerbate existing skin diseases.
“Oils with high oleic acid, such as coconut or olive oils or shea butter, can worsen seborrheic dermatitis,” Dr. Vashi cautioned.
Of this list of dermatologic issues induced by culturally linked cosmetic practices, skin lightening agents might pose the most risk for permanent and irreversible complications. Dr. Vashi said that up to 70% of patients using lighteners develop complications, and there is a relationship between the severity of side effects as duration of use increases.
“The problem is that ingredients of many of these products, which are imported illegally and sold on the black market, are often not disclosed,” Dr. Vashi said. Some contain a high content of metals such as lead, copper, and iron, whether they are added intentionally or end up in the product because of poor quality control. For those developing adverse events associated with the products, the obvious treatment is discontinuation.
When patients are unwilling to discontinue any of the products that have led to dermatologic issues, Dr. Vashi encouraged physicians “to take a middle ground.” Simple avoidance can be challenging for practices that are culturally meaningful. In respecting cultural differences, she encouraged tolerance and compromise.
“Often these patients will be doing an alternative medication or intervention, but this does not mean that they are not accepting what we have to offer,” she said. She indicated that mutual respect will lead to better solutions.
The awareness of common cultural practices that can have a harmful impact on the skin is an area of practice that deserves more attention, Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology at Weill Cornell Medical Center, New York, said in an interview.
He said that he agreed with Dr. Vashi that understanding the role of cultural practices leading to dermatoses is not enough.
“Advising patients to alter or discontinue a specific cultural practice due to a dermatologic complication should be done with respect, humility, and understanding that may be challenging,” said Dr. Alexis.
While being aware of the specific cultural practices that might be causing or exacerbating dermatoses is important for accurate diagnosis, he said he believes that “partnering with the patient to modify the cultural practices in question” is important for a clinical outcome acceptable to the patient.
“Educational resources to inform clinicians of dermatoses associated with cultural practices are available and can be helpful for dermatologists in any practice setting,” he said.
Dr. Vashi reports that she has no relevant financial relationships to disclose. Dr. Alexis reports financial relationships with Abbvie, Allergan, Almirall, Amgen, Arcutis, AstraZeneca, Bristol-Myers Squibb, Cara, Galderma, Genzyme, Janssen, Leo, Menlo, Novartis, Regeneron, Sanofi, and Valeant.
With the strong likelihood that , according to a dermatologist with expertise in these types of cases who spoke at the Skin of Color Update 2021.
“Instead of avoiding the discussion of cultural practices, we should discuss them and be open about them. It fosters a comfortable environment, trust, and better compliance,” reported Neelam Ajit Vashi, MD, founding director of the Boston University Center for Ethnic Skin.
Out of fear of causing offense, a desire to be discreet, or of personal discomfort with foreign cultural practices, some clinicians might elect to limit themselves to the information that the patient volunteers, which is a mistake, according to Dr. Vashi.
“The avoidance of topics around culture actually limits the ability to have a successful relationship,” she maintained.
Successful encounters are not just based on a willingness to listen, Dr. Vashi said. Clinicians should be seeking a base of knowledge. With growing globalization and widespread immigration, “it is increasingly important for dermatologists in the U.S. to understand the role of cultural practices [in creating skin problems] and recognize the sequelae,” Dr. Vashi said.
Taking some common examples of dermatologic complaints created by cosmetic practices originating elsewhere, Dr. Vashi described key clinical points in addressing complications related to henna, hair removal through threading, and placement of decorative adornments on the forehead, called bindi. In addition, she pointed out common issues with facial and body marking created with kumkum powder, hair oils, and skin lightening agents.
Black henna
For cosmetic enhancement, henna is relatively benign. It is also no longer confined to the south Asian communities where it originated. However, Dr. Vashi pointed out that patients of south Asian origin or descent might be more likely to use black henna, a variety with more risks.
Black henna contains additives, such as diaminobenzenes and p-phenylenediamine (PPD), to darken the tone of the product as well as provide other desired characteristics, such as an accelerated drying time. While some patients do develop reactions to conventional henna, the risks of black henna are greater.
“The acute contact dermatitis reactions can include dyspigmentation, leukoderma, and keloids,” Dr. Vashi said. Other complications include erythema multiforme, temporary hypertrichosis, and systemic allergic reactions, such as angioedema.
While those who have had a reaction to henna should avoid further contact, Dr. Vashi warned that sequelae can include cross reactions with latex and rubber as well as some pharmaceutical agents, such as sulfonamides. When taking a patient history, she noted, be aware that risks of henna extend to the hairdressers and cosmeticians who sometimes apply these products on others.
Hair threading, bindi, and kumkum
Hair threading, another practice popularized in south Asia and now growing in popularity globally, involves capturing hairs between cotton threads for removal of both the hair and its follicle. It is a relatively rapid and efficient method of permanent depilation. In addition to pain and erythema, Dr. Vashi reported that the complications associated with hair threading include pigmentary changes, infections such as bullous impetigo, and lesions of koebnerization – such as vitiligo and lichen planus.
Bindi, a Hindi tradition that involves placing adornments between the eyebrows, and kumkum, a powder typically made from turmeric to be employed for decorative markings, have also spread to use outside of their cultural context, according to Dr. Vashi. She said that the complications of these two cosmetic practices are shared, and stem largely from contact dermatitis.
In the case of bindi, para-tertiary-butylphenol in adhesives is one source of reactions, whereas kumkum itself can be an irritant. As these are typically local to the site of application, the diagnosis is not difficult, but treatment can be more challenging for patients unwilling to abandon the practice.
Hair oils, skin-lightening agents
Culturally-linked hair oils among patients from south Asia or Africa – or descendants from these areas – can damage hair in a variety of ways as well as cause contact dermatitis. The oils can also exacerbate existing skin diseases.
“Oils with high oleic acid, such as coconut or olive oils or shea butter, can worsen seborrheic dermatitis,” Dr. Vashi cautioned.
Of this list of dermatologic issues induced by culturally linked cosmetic practices, skin lightening agents might pose the most risk for permanent and irreversible complications. Dr. Vashi said that up to 70% of patients using lighteners develop complications, and there is a relationship between the severity of side effects as duration of use increases.
“The problem is that ingredients of many of these products, which are imported illegally and sold on the black market, are often not disclosed,” Dr. Vashi said. Some contain a high content of metals such as lead, copper, and iron, whether they are added intentionally or end up in the product because of poor quality control. For those developing adverse events associated with the products, the obvious treatment is discontinuation.
When patients are unwilling to discontinue any of the products that have led to dermatologic issues, Dr. Vashi encouraged physicians “to take a middle ground.” Simple avoidance can be challenging for practices that are culturally meaningful. In respecting cultural differences, she encouraged tolerance and compromise.
“Often these patients will be doing an alternative medication or intervention, but this does not mean that they are not accepting what we have to offer,” she said. She indicated that mutual respect will lead to better solutions.
The awareness of common cultural practices that can have a harmful impact on the skin is an area of practice that deserves more attention, Andrew F. Alexis, MD, vice-chair for diversity and inclusion in the department of dermatology at Weill Cornell Medical Center, New York, said in an interview.
He said that he agreed with Dr. Vashi that understanding the role of cultural practices leading to dermatoses is not enough.
“Advising patients to alter or discontinue a specific cultural practice due to a dermatologic complication should be done with respect, humility, and understanding that may be challenging,” said Dr. Alexis.
While being aware of the specific cultural practices that might be causing or exacerbating dermatoses is important for accurate diagnosis, he said he believes that “partnering with the patient to modify the cultural practices in question” is important for a clinical outcome acceptable to the patient.
“Educational resources to inform clinicians of dermatoses associated with cultural practices are available and can be helpful for dermatologists in any practice setting,” he said.
Dr. Vashi reports that she has no relevant financial relationships to disclose. Dr. Alexis reports financial relationships with Abbvie, Allergan, Almirall, Amgen, Arcutis, AstraZeneca, Bristol-Myers Squibb, Cara, Galderma, Genzyme, Janssen, Leo, Menlo, Novartis, Regeneron, Sanofi, and Valeant.
FROM SOC 2021
JAK inhibitor provides impressive hair growth for patients with alopecia areata
, according to the results of two phase 3 trials presented at the European Academy of Dermatology and Venereology (EADV) 2021 Annual Meeting.
In both trials, severe alopecia areata, defined as a SALT (Severity of Alopecia Tool) score of greater than or equal to 50, was an enrollment requirement. The primary endpoint was a SALT score of less than or equal to 20, signifying 80% scalp coverage.
“The mean SALT score at entry was 85,” reported Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Conn. He explained that the SALT scale extends from 0 (no hair loss) to 100 (complete hair loss). About 45% of patients in the phase 3 trials had alopecia universalis.
In both trials, called BRAVE-AA1 and BRAVE-AA2, a response was seen with baricitinib after about 4 weeks. Response increased steadily through the entire 36 weeks of treatment. At the end of 36 weeks, when response curves still had an upward trajectory, the proportion of those treated with the 4-mg dose of baricitinib who had achieved a SALT score of less than or equal to 20 had reached 35.2% in BRAVE-AA1 and 32.5% in BRAVE-AA2.
The nearly identical BRAVE-AA1 and BRAVE-AA2 trials enrolled 654 and 546 patients, respectively. The patients were randomly assigned in a 3:2:2 ratio to receive baricitinib 4 mg, baricitinib 2 mg, or placebo. All treatments were taken once daily. Regrowth of eyebrow and eyelash hair were secondary outcomes.
There was a clear dose effect; hair growth increased more quickly with the 4-mg dose of baricitinib than with the 2-mg dose. The difference between the active therapy and placebo was significant by 16 weeks with the 4-mg dose. By 24 weeks, the advantage of the 2-mg dose over placebo also reached significance. The response rate with the 4-mg dose was nearly twice as great.
At the end of the 36-week trials, the proportion of patients treated with baricitinib 2 mg who achieved the primary endpoint was 21.7% and 17.3% in the BRAVE-AA1 and BRAVE-AA2 trials, respectively. Among patients taking placebo, the primary endpoint was met by 5.3% and 2.6%, respectively, at the end of the two trials.
The differences in responses with the 4-mg and the 2-mg doses were significantly higher compared with placebo (P ≤ .001 for both doses vs. placebo).
Using a scoring system for eyebrow and eyelash hair loss, the proportion of patients who achieved a score of 0 (full coverage) or 1 (minimal gaps) was again superior in both trials for patients taking the higher dose of baricitinib. This level of response was reached by about 31% to 35% of those taking the 4-mg dose in BRAVE-AA1 and BRAVE-AA2 (P ≤ .001 vs. placebo). With the lower dose, the rates were 19.1% and 13.5%, respectively. This endpoint was reached in only about 3% of patients who took placebo.
Rates of adverse events were modestly higher in the two active treatment groups in comparison with the group taking placebo. The most commonly occurring adverse events with baricitinib included upper respiratory tract infections, nasopharyngitis, urinary tract infections, and headache, according to Dr. King.
“Most of the adverse events were mild to moderate,” he said. He also reported that none of these adverse events occurred in more than 10% of patients, and there were no cases of other opportunistic infections, thromboembolic events, or gastrointestinal perforations. The discontinuation rates because of adverse events with active therapy were less than 3% in both trials.
JAK inhibitors are currently employed in the treatment of a variety of inflammatory diseases. Baricitinib is currently approved for the treatment of rheumatoid arthritis. Because specificity differs markedly for their inhibition of JAK kinases (JAK1, JAK2, JAK3, and Tyk2), these drugs do not appear to be interchangeable with regard to clinical effect.
Several case reports of hair regrowth with baricitinib led to a phase 2 trial, which was recently published in the Journal of the American Academy of Dermatology. In this trial, the therapy also yielded substantial benefit for patients with alopecia areata. The benefit of baricitinib is attributed to inhibition of JAK1 and JAK2 signaling, which has been implicated in cytokine-mediated immune dysfunction leading to damage of hair follicles.
Alopecia areata is a common disorder that can have a large adverse impact on quality of life, Dr. King noted. There is no approved therapy for this condition, so there is a large unmet need. Although longer follow-up is needed to gauge sustained efficacy and safety, he considers these results promising for a therapy with clinically meaningful benefit.
This point was reiterated by Yolanda Gilaberte Calzada, MD, PhD, head of the Dermatology Service, University Hospital Miguel Servet, Zaragoza, Spain, who was moderator of the session in which Dr. King presented these data. She expressed excitement about the promise of baricitinib, particularly with regard to the substantial proportion of patients who achieved meaningful degrees of hair regrowth.
“All of us will be happy to have options for alopecia areata,” said Dr. Calzada, who predicted that the higher dose of baricitinib will be selected for clinical development, given its greater efficacy with little increase in safety concerns.
Eli Lilly provided funding for the BRAVE-AA1 and -AA2 trials. Dr. King has financial relationships with Arena, Aclaris, Bristol-Myers Squibb, Concert, Pfizer, Regeneron, Sanofi Genzyme, and Eli Lilly. Dr. Calzada has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to the results of two phase 3 trials presented at the European Academy of Dermatology and Venereology (EADV) 2021 Annual Meeting.
In both trials, severe alopecia areata, defined as a SALT (Severity of Alopecia Tool) score of greater than or equal to 50, was an enrollment requirement. The primary endpoint was a SALT score of less than or equal to 20, signifying 80% scalp coverage.
“The mean SALT score at entry was 85,” reported Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Conn. He explained that the SALT scale extends from 0 (no hair loss) to 100 (complete hair loss). About 45% of patients in the phase 3 trials had alopecia universalis.
In both trials, called BRAVE-AA1 and BRAVE-AA2, a response was seen with baricitinib after about 4 weeks. Response increased steadily through the entire 36 weeks of treatment. At the end of 36 weeks, when response curves still had an upward trajectory, the proportion of those treated with the 4-mg dose of baricitinib who had achieved a SALT score of less than or equal to 20 had reached 35.2% in BRAVE-AA1 and 32.5% in BRAVE-AA2.
The nearly identical BRAVE-AA1 and BRAVE-AA2 trials enrolled 654 and 546 patients, respectively. The patients were randomly assigned in a 3:2:2 ratio to receive baricitinib 4 mg, baricitinib 2 mg, or placebo. All treatments were taken once daily. Regrowth of eyebrow and eyelash hair were secondary outcomes.
There was a clear dose effect; hair growth increased more quickly with the 4-mg dose of baricitinib than with the 2-mg dose. The difference between the active therapy and placebo was significant by 16 weeks with the 4-mg dose. By 24 weeks, the advantage of the 2-mg dose over placebo also reached significance. The response rate with the 4-mg dose was nearly twice as great.
At the end of the 36-week trials, the proportion of patients treated with baricitinib 2 mg who achieved the primary endpoint was 21.7% and 17.3% in the BRAVE-AA1 and BRAVE-AA2 trials, respectively. Among patients taking placebo, the primary endpoint was met by 5.3% and 2.6%, respectively, at the end of the two trials.
The differences in responses with the 4-mg and the 2-mg doses were significantly higher compared with placebo (P ≤ .001 for both doses vs. placebo).
Using a scoring system for eyebrow and eyelash hair loss, the proportion of patients who achieved a score of 0 (full coverage) or 1 (minimal gaps) was again superior in both trials for patients taking the higher dose of baricitinib. This level of response was reached by about 31% to 35% of those taking the 4-mg dose in BRAVE-AA1 and BRAVE-AA2 (P ≤ .001 vs. placebo). With the lower dose, the rates were 19.1% and 13.5%, respectively. This endpoint was reached in only about 3% of patients who took placebo.
Rates of adverse events were modestly higher in the two active treatment groups in comparison with the group taking placebo. The most commonly occurring adverse events with baricitinib included upper respiratory tract infections, nasopharyngitis, urinary tract infections, and headache, according to Dr. King.
“Most of the adverse events were mild to moderate,” he said. He also reported that none of these adverse events occurred in more than 10% of patients, and there were no cases of other opportunistic infections, thromboembolic events, or gastrointestinal perforations. The discontinuation rates because of adverse events with active therapy were less than 3% in both trials.
JAK inhibitors are currently employed in the treatment of a variety of inflammatory diseases. Baricitinib is currently approved for the treatment of rheumatoid arthritis. Because specificity differs markedly for their inhibition of JAK kinases (JAK1, JAK2, JAK3, and Tyk2), these drugs do not appear to be interchangeable with regard to clinical effect.
Several case reports of hair regrowth with baricitinib led to a phase 2 trial, which was recently published in the Journal of the American Academy of Dermatology. In this trial, the therapy also yielded substantial benefit for patients with alopecia areata. The benefit of baricitinib is attributed to inhibition of JAK1 and JAK2 signaling, which has been implicated in cytokine-mediated immune dysfunction leading to damage of hair follicles.
Alopecia areata is a common disorder that can have a large adverse impact on quality of life, Dr. King noted. There is no approved therapy for this condition, so there is a large unmet need. Although longer follow-up is needed to gauge sustained efficacy and safety, he considers these results promising for a therapy with clinically meaningful benefit.
This point was reiterated by Yolanda Gilaberte Calzada, MD, PhD, head of the Dermatology Service, University Hospital Miguel Servet, Zaragoza, Spain, who was moderator of the session in which Dr. King presented these data. She expressed excitement about the promise of baricitinib, particularly with regard to the substantial proportion of patients who achieved meaningful degrees of hair regrowth.
“All of us will be happy to have options for alopecia areata,” said Dr. Calzada, who predicted that the higher dose of baricitinib will be selected for clinical development, given its greater efficacy with little increase in safety concerns.
Eli Lilly provided funding for the BRAVE-AA1 and -AA2 trials. Dr. King has financial relationships with Arena, Aclaris, Bristol-Myers Squibb, Concert, Pfizer, Regeneron, Sanofi Genzyme, and Eli Lilly. Dr. Calzada has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to the results of two phase 3 trials presented at the European Academy of Dermatology and Venereology (EADV) 2021 Annual Meeting.
In both trials, severe alopecia areata, defined as a SALT (Severity of Alopecia Tool) score of greater than or equal to 50, was an enrollment requirement. The primary endpoint was a SALT score of less than or equal to 20, signifying 80% scalp coverage.
“The mean SALT score at entry was 85,” reported Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Conn. He explained that the SALT scale extends from 0 (no hair loss) to 100 (complete hair loss). About 45% of patients in the phase 3 trials had alopecia universalis.
In both trials, called BRAVE-AA1 and BRAVE-AA2, a response was seen with baricitinib after about 4 weeks. Response increased steadily through the entire 36 weeks of treatment. At the end of 36 weeks, when response curves still had an upward trajectory, the proportion of those treated with the 4-mg dose of baricitinib who had achieved a SALT score of less than or equal to 20 had reached 35.2% in BRAVE-AA1 and 32.5% in BRAVE-AA2.
The nearly identical BRAVE-AA1 and BRAVE-AA2 trials enrolled 654 and 546 patients, respectively. The patients were randomly assigned in a 3:2:2 ratio to receive baricitinib 4 mg, baricitinib 2 mg, or placebo. All treatments were taken once daily. Regrowth of eyebrow and eyelash hair were secondary outcomes.
There was a clear dose effect; hair growth increased more quickly with the 4-mg dose of baricitinib than with the 2-mg dose. The difference between the active therapy and placebo was significant by 16 weeks with the 4-mg dose. By 24 weeks, the advantage of the 2-mg dose over placebo also reached significance. The response rate with the 4-mg dose was nearly twice as great.
At the end of the 36-week trials, the proportion of patients treated with baricitinib 2 mg who achieved the primary endpoint was 21.7% and 17.3% in the BRAVE-AA1 and BRAVE-AA2 trials, respectively. Among patients taking placebo, the primary endpoint was met by 5.3% and 2.6%, respectively, at the end of the two trials.
The differences in responses with the 4-mg and the 2-mg doses were significantly higher compared with placebo (P ≤ .001 for both doses vs. placebo).
Using a scoring system for eyebrow and eyelash hair loss, the proportion of patients who achieved a score of 0 (full coverage) or 1 (minimal gaps) was again superior in both trials for patients taking the higher dose of baricitinib. This level of response was reached by about 31% to 35% of those taking the 4-mg dose in BRAVE-AA1 and BRAVE-AA2 (P ≤ .001 vs. placebo). With the lower dose, the rates were 19.1% and 13.5%, respectively. This endpoint was reached in only about 3% of patients who took placebo.
Rates of adverse events were modestly higher in the two active treatment groups in comparison with the group taking placebo. The most commonly occurring adverse events with baricitinib included upper respiratory tract infections, nasopharyngitis, urinary tract infections, and headache, according to Dr. King.
“Most of the adverse events were mild to moderate,” he said. He also reported that none of these adverse events occurred in more than 10% of patients, and there were no cases of other opportunistic infections, thromboembolic events, or gastrointestinal perforations. The discontinuation rates because of adverse events with active therapy were less than 3% in both trials.
JAK inhibitors are currently employed in the treatment of a variety of inflammatory diseases. Baricitinib is currently approved for the treatment of rheumatoid arthritis. Because specificity differs markedly for their inhibition of JAK kinases (JAK1, JAK2, JAK3, and Tyk2), these drugs do not appear to be interchangeable with regard to clinical effect.
Several case reports of hair regrowth with baricitinib led to a phase 2 trial, which was recently published in the Journal of the American Academy of Dermatology. In this trial, the therapy also yielded substantial benefit for patients with alopecia areata. The benefit of baricitinib is attributed to inhibition of JAK1 and JAK2 signaling, which has been implicated in cytokine-mediated immune dysfunction leading to damage of hair follicles.
Alopecia areata is a common disorder that can have a large adverse impact on quality of life, Dr. King noted. There is no approved therapy for this condition, so there is a large unmet need. Although longer follow-up is needed to gauge sustained efficacy and safety, he considers these results promising for a therapy with clinically meaningful benefit.
This point was reiterated by Yolanda Gilaberte Calzada, MD, PhD, head of the Dermatology Service, University Hospital Miguel Servet, Zaragoza, Spain, who was moderator of the session in which Dr. King presented these data. She expressed excitement about the promise of baricitinib, particularly with regard to the substantial proportion of patients who achieved meaningful degrees of hair regrowth.
“All of us will be happy to have options for alopecia areata,” said Dr. Calzada, who predicted that the higher dose of baricitinib will be selected for clinical development, given its greater efficacy with little increase in safety concerns.
Eli Lilly provided funding for the BRAVE-AA1 and -AA2 trials. Dr. King has financial relationships with Arena, Aclaris, Bristol-Myers Squibb, Concert, Pfizer, Regeneron, Sanofi Genzyme, and Eli Lilly. Dr. Calzada has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ruxolitinib cream meets primary endpoints in phase 3 vitiligo trial
presented together at the annual meeting of the European Academy of Dermatology and Venereology.
On the primary endpoint of F-VASI 75 (75% improvement in the Facial and Vitiligo Scoring Index), rates were nearly four times higher at 24 weeks in one trial (29.9% vs. 7.5%; P < .0001) and more than twice as great in the other (29.9% vs. 12.9%; P < .01).
“The larger phase 3 trials confirm the previous phase 2 findings,” reported David Rosmarin, MD, vice chairman for research and education, department of dermatology, Tufts Medical Center, Boston. These findings not only include substantial clinical efficacy but good tolerability with “no serious treatment-related adverse events,” he noted.
600 patients randomized
In one of the trials, called TRuE-V1, 330 patients with vitiligo were randomly assigned in a 2:1 ratio to 1.5% ruxolitinib or vehicle applied twice daily. In the other trial, called TRuE-V2, 344 patients were randomly assigned. The participating centers were in Europe and North America.
Patients aged 12 years or older with nonsegmental vitiligo and depigmentation covering no more than 10% of the total body surface area were eligible. The mean baseline F-VASI values were 1.0. The mean total VASI (T-FASI) values were 6.5. On those enrolled, half were female, 11% were adolescents, and 73% had Fitzpatrick skin phototypes III-VI.
Ruxolitinib cream provided near-complete vitiligo clearance (F-VASI 90) on the face at 24 weeks in only about 15% of patients, but this was several times higher than the 2% achieved on vehicle in the TRuE-V1 (P < .01) and the TRuE-V2 trials (P < .05), respectively.
F-VASI 50 response rates greater than 50%
For F-VASI 50, the response rate with ruxolitinib in both studies was approximately 51%. Relative to the 17.2% response on vehicle in TRuE-v1 and 23.4% in TRuE-V2 (both P < .0001 vs. active therapy), the advantage of the topical JAK inhibitor was considered to be a clinically meaningful, not just significant from a statistical standpoint.
In fact, improvement on the 5-point Vitiligo Noticeability Scale “also supported a clinically meaningful benefit,” Dr. Rosmarin reported. When those achieving a score of 4 (much less noticeable) or 5 (no longer noticeable), the response rates at 24 weeks were 24.5% and 21.6% in the TRuE-V1 and TRuE-V2 trials, respectively. Again, these response rates were several times greater than the 3.3% (P < .001) and 6.6% (P < .01) observed in the vehicle arms of TRuE-V1 and TRuE-V2 (P < .01), respectively.
Treatment-related adverse events were infrequent. The most common were acne at the application site, which occurred in about 5% of patients receiving ruxolitinib (vs. 2% or fewer of those receiving vehicle) and pruritus, which also occurred in about 5% of patients. However, the rates of pruritus among those on placebo reached 4% in TRuE-V1 and 2% in TRuE-V2 trials.
In vitiligo, where there has been recent progress in understanding the pathophysiology, loss of melanocytes in immune dysregulation has been linked to activation of the JAK signaling pathway, according to Dr. Rosmarin. In the 52-week phase 2 trial with 205 patients, ruxolitinib was associated with a sustained response and no serious treatment-related adverse events.
52-week data might show more benefit
Patients are continuing to be followed in the TRuE-V1 and TRuE-V-2 trials. Based on the phase 2 data and on the progressive improvement still being observed at the end of 24 weeks in the phase 3 trials, Dr. Rosmarin expects 52-week results be valuable in understanding the clinical role of ruxolitinib.
“We will be looking for further improvement in response as we follow these patients out to 1 year,” he said.
This further follow-up is important, agreed Iltefat Hamzavi, MD, senior staff physician, department of dermatology, Henry Ford Hospital, Detroit.
Despite the promise of perhaps other JAK inhibitors, “we still need to understand how long it will take for the drug to offer optimal results. We already know that is more than 24 weeks,” said Dr. Hamzavi, who has been involved in the clinical trials with this drug but was not involved with the TRuE-V1 or -V2 trials.
He also said more follow-up is needed to understand the duration of effect. He is, however, optimistic about the clinical role of this mechanism for treatment of vitiligo.
“I do think that JAK inhibitors show a lot of promise [in vitiligo] for certain locations of the body,” he said.
Given the limited treatment options for effective and prolonged improvement in vitiligo, both Dr. Hamzavi and Dr. Rosmarin indicated an effective topical cream is likely to be considered by physicians and patients to be a substantial advance.
On Sept. 21, ruxolitinib (Opzelura) 1.5% cream was approved by the Food and Drug Administration for the short-term treatment of mild to moderate atopic dermatitis in children and adults ages 12 years and older – the first FDA approval of this product.
Dr. Rosmarin reported financial relationships with more than 20 pharmaceutical companies, including Incyte, which provided funding for the TRuE-V1 and -V2 trials. Dr. Hamzavi reported financial relationships with more than 15 companies with pharmaceutical or cosmetic products, including Incyte.
A version of this article first appeared on Medscape.com.
presented together at the annual meeting of the European Academy of Dermatology and Venereology.
On the primary endpoint of F-VASI 75 (75% improvement in the Facial and Vitiligo Scoring Index), rates were nearly four times higher at 24 weeks in one trial (29.9% vs. 7.5%; P < .0001) and more than twice as great in the other (29.9% vs. 12.9%; P < .01).
“The larger phase 3 trials confirm the previous phase 2 findings,” reported David Rosmarin, MD, vice chairman for research and education, department of dermatology, Tufts Medical Center, Boston. These findings not only include substantial clinical efficacy but good tolerability with “no serious treatment-related adverse events,” he noted.
600 patients randomized
In one of the trials, called TRuE-V1, 330 patients with vitiligo were randomly assigned in a 2:1 ratio to 1.5% ruxolitinib or vehicle applied twice daily. In the other trial, called TRuE-V2, 344 patients were randomly assigned. The participating centers were in Europe and North America.
Patients aged 12 years or older with nonsegmental vitiligo and depigmentation covering no more than 10% of the total body surface area were eligible. The mean baseline F-VASI values were 1.0. The mean total VASI (T-FASI) values were 6.5. On those enrolled, half were female, 11% were adolescents, and 73% had Fitzpatrick skin phototypes III-VI.
Ruxolitinib cream provided near-complete vitiligo clearance (F-VASI 90) on the face at 24 weeks in only about 15% of patients, but this was several times higher than the 2% achieved on vehicle in the TRuE-V1 (P < .01) and the TRuE-V2 trials (P < .05), respectively.
F-VASI 50 response rates greater than 50%
For F-VASI 50, the response rate with ruxolitinib in both studies was approximately 51%. Relative to the 17.2% response on vehicle in TRuE-v1 and 23.4% in TRuE-V2 (both P < .0001 vs. active therapy), the advantage of the topical JAK inhibitor was considered to be a clinically meaningful, not just significant from a statistical standpoint.
In fact, improvement on the 5-point Vitiligo Noticeability Scale “also supported a clinically meaningful benefit,” Dr. Rosmarin reported. When those achieving a score of 4 (much less noticeable) or 5 (no longer noticeable), the response rates at 24 weeks were 24.5% and 21.6% in the TRuE-V1 and TRuE-V2 trials, respectively. Again, these response rates were several times greater than the 3.3% (P < .001) and 6.6% (P < .01) observed in the vehicle arms of TRuE-V1 and TRuE-V2 (P < .01), respectively.
Treatment-related adverse events were infrequent. The most common were acne at the application site, which occurred in about 5% of patients receiving ruxolitinib (vs. 2% or fewer of those receiving vehicle) and pruritus, which also occurred in about 5% of patients. However, the rates of pruritus among those on placebo reached 4% in TRuE-V1 and 2% in TRuE-V2 trials.
In vitiligo, where there has been recent progress in understanding the pathophysiology, loss of melanocytes in immune dysregulation has been linked to activation of the JAK signaling pathway, according to Dr. Rosmarin. In the 52-week phase 2 trial with 205 patients, ruxolitinib was associated with a sustained response and no serious treatment-related adverse events.
52-week data might show more benefit
Patients are continuing to be followed in the TRuE-V1 and TRuE-V-2 trials. Based on the phase 2 data and on the progressive improvement still being observed at the end of 24 weeks in the phase 3 trials, Dr. Rosmarin expects 52-week results be valuable in understanding the clinical role of ruxolitinib.
“We will be looking for further improvement in response as we follow these patients out to 1 year,” he said.
This further follow-up is important, agreed Iltefat Hamzavi, MD, senior staff physician, department of dermatology, Henry Ford Hospital, Detroit.
Despite the promise of perhaps other JAK inhibitors, “we still need to understand how long it will take for the drug to offer optimal results. We already know that is more than 24 weeks,” said Dr. Hamzavi, who has been involved in the clinical trials with this drug but was not involved with the TRuE-V1 or -V2 trials.
He also said more follow-up is needed to understand the duration of effect. He is, however, optimistic about the clinical role of this mechanism for treatment of vitiligo.
“I do think that JAK inhibitors show a lot of promise [in vitiligo] for certain locations of the body,” he said.
Given the limited treatment options for effective and prolonged improvement in vitiligo, both Dr. Hamzavi and Dr. Rosmarin indicated an effective topical cream is likely to be considered by physicians and patients to be a substantial advance.
On Sept. 21, ruxolitinib (Opzelura) 1.5% cream was approved by the Food and Drug Administration for the short-term treatment of mild to moderate atopic dermatitis in children and adults ages 12 years and older – the first FDA approval of this product.
Dr. Rosmarin reported financial relationships with more than 20 pharmaceutical companies, including Incyte, which provided funding for the TRuE-V1 and -V2 trials. Dr. Hamzavi reported financial relationships with more than 15 companies with pharmaceutical or cosmetic products, including Incyte.
A version of this article first appeared on Medscape.com.
presented together at the annual meeting of the European Academy of Dermatology and Venereology.
On the primary endpoint of F-VASI 75 (75% improvement in the Facial and Vitiligo Scoring Index), rates were nearly four times higher at 24 weeks in one trial (29.9% vs. 7.5%; P < .0001) and more than twice as great in the other (29.9% vs. 12.9%; P < .01).
“The larger phase 3 trials confirm the previous phase 2 findings,” reported David Rosmarin, MD, vice chairman for research and education, department of dermatology, Tufts Medical Center, Boston. These findings not only include substantial clinical efficacy but good tolerability with “no serious treatment-related adverse events,” he noted.
600 patients randomized
In one of the trials, called TRuE-V1, 330 patients with vitiligo were randomly assigned in a 2:1 ratio to 1.5% ruxolitinib or vehicle applied twice daily. In the other trial, called TRuE-V2, 344 patients were randomly assigned. The participating centers were in Europe and North America.
Patients aged 12 years or older with nonsegmental vitiligo and depigmentation covering no more than 10% of the total body surface area were eligible. The mean baseline F-VASI values were 1.0. The mean total VASI (T-FASI) values were 6.5. On those enrolled, half were female, 11% were adolescents, and 73% had Fitzpatrick skin phototypes III-VI.
Ruxolitinib cream provided near-complete vitiligo clearance (F-VASI 90) on the face at 24 weeks in only about 15% of patients, but this was several times higher than the 2% achieved on vehicle in the TRuE-V1 (P < .01) and the TRuE-V2 trials (P < .05), respectively.
F-VASI 50 response rates greater than 50%
For F-VASI 50, the response rate with ruxolitinib in both studies was approximately 51%. Relative to the 17.2% response on vehicle in TRuE-v1 and 23.4% in TRuE-V2 (both P < .0001 vs. active therapy), the advantage of the topical JAK inhibitor was considered to be a clinically meaningful, not just significant from a statistical standpoint.
In fact, improvement on the 5-point Vitiligo Noticeability Scale “also supported a clinically meaningful benefit,” Dr. Rosmarin reported. When those achieving a score of 4 (much less noticeable) or 5 (no longer noticeable), the response rates at 24 weeks were 24.5% and 21.6% in the TRuE-V1 and TRuE-V2 trials, respectively. Again, these response rates were several times greater than the 3.3% (P < .001) and 6.6% (P < .01) observed in the vehicle arms of TRuE-V1 and TRuE-V2 (P < .01), respectively.
Treatment-related adverse events were infrequent. The most common were acne at the application site, which occurred in about 5% of patients receiving ruxolitinib (vs. 2% or fewer of those receiving vehicle) and pruritus, which also occurred in about 5% of patients. However, the rates of pruritus among those on placebo reached 4% in TRuE-V1 and 2% in TRuE-V2 trials.
In vitiligo, where there has been recent progress in understanding the pathophysiology, loss of melanocytes in immune dysregulation has been linked to activation of the JAK signaling pathway, according to Dr. Rosmarin. In the 52-week phase 2 trial with 205 patients, ruxolitinib was associated with a sustained response and no serious treatment-related adverse events.
52-week data might show more benefit
Patients are continuing to be followed in the TRuE-V1 and TRuE-V-2 trials. Based on the phase 2 data and on the progressive improvement still being observed at the end of 24 weeks in the phase 3 trials, Dr. Rosmarin expects 52-week results be valuable in understanding the clinical role of ruxolitinib.
“We will be looking for further improvement in response as we follow these patients out to 1 year,” he said.
This further follow-up is important, agreed Iltefat Hamzavi, MD, senior staff physician, department of dermatology, Henry Ford Hospital, Detroit.
Despite the promise of perhaps other JAK inhibitors, “we still need to understand how long it will take for the drug to offer optimal results. We already know that is more than 24 weeks,” said Dr. Hamzavi, who has been involved in the clinical trials with this drug but was not involved with the TRuE-V1 or -V2 trials.
He also said more follow-up is needed to understand the duration of effect. He is, however, optimistic about the clinical role of this mechanism for treatment of vitiligo.
“I do think that JAK inhibitors show a lot of promise [in vitiligo] for certain locations of the body,” he said.
Given the limited treatment options for effective and prolonged improvement in vitiligo, both Dr. Hamzavi and Dr. Rosmarin indicated an effective topical cream is likely to be considered by physicians and patients to be a substantial advance.
On Sept. 21, ruxolitinib (Opzelura) 1.5% cream was approved by the Food and Drug Administration for the short-term treatment of mild to moderate atopic dermatitis in children and adults ages 12 years and older – the first FDA approval of this product.
Dr. Rosmarin reported financial relationships with more than 20 pharmaceutical companies, including Incyte, which provided funding for the TRuE-V1 and -V2 trials. Dr. Hamzavi reported financial relationships with more than 15 companies with pharmaceutical or cosmetic products, including Incyte.
A version of this article first appeared on Medscape.com.
Rapid response needed for rare filler injection complications
if not promptly addressed, according to an expert explaining the signs of an impending disaster at the Skin of Color Update 2021.
The most serious of the adverse events stem from vascular compromise, which is often signaled immediately by sharp pain and blanching of the skin, according to Hassan Galadari, MD, assistant professor of dermatology at the United Arab Emirates University, Dubai.
“Swift and aggressive treatment is required to avoid irreversible changes,” said Dr. Galadari, warning that blindness and vision impairment can be permanent, and that other events associated with vascular compromise include stroke and other types of embolism, as well as tissue necrosis.
To be swift, Dr. Galadari advised an immediate halt of injections and then a series of steps to abort the vascular insult. The goal is to encourage blood flow to prevent clotting and dissipate the filler.
“Massage the area like crazy. Keep on massaging. The more you massage the better. You are recruiting blood into that area so it remains viable,” Dr. Galadari said.
Hyaluronidase injections helpful
Warm compresses should also be applied for periods ranging from 5 minutes up to an hour, he added. In patients treated with hyaluronic acid, he also commonly introduces hyaluronidase injections of 200-500 IU diluted in lidocaine or saline. The injections are placed 2-3 cm apart and repeated every hour until signs and symptoms improve.
“Flush all of the filler out,” he said, emphasizing the urgency for reversing risk of vascular adverse events.
To sustain blood flow and avoid clots, he also recommends initiating aspirin with maintenance doses sustained over several days. Sildenafil to further improve conditions of blood perfusion can be “considered.”
The risks of vascular compromise, like other complications from filler injections, are low, but they are not zero, and the opportunity to prevent irreversible changes depends on acting quickly, according to Dr. Galadari.
“To prevent embolism, recognize the danger zones,” he advised, identifying the glabella region as the site of highest risk. The risk of vascular compromise from injections into the nasal region is lower but higher than injections of the nasolabial fold and forehead, which are associated with a relatively low risk.
Slow injections reduce risks
Some basic strategies he recommended for preventing vascular compromise included slow injections while keeping pressure low and using small volumes of filler per shot. Fractionated treatment and microdroplet techniques can be appropriate depending on the site of injection.
“Delivery of the filler by cannulas rather than by needles is preferable,” according to Dr. Galadari, who noted that a task force from the American Society for Dermatologic Surgery recently endorsed this approach as part of other recommendations to avoid complications of injectable fillers.
The Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database suggests that adverse events of any substantial severity from filler injections, not just those involving vascular compromise, occur at a rate of 1 per 3,600 cases. However, MAUDE is a passive surveillance system dependent on reports provided by clinicians and others, so this event rate might be an underrepresentation.
In the MAUDE database, complication rates are listed for each of the available filler products and show a variation in rates not just overall but also for each of the major types of complications, which include skin-specific complications such as nodules, discoloration, and inflammation, as well as neurologic adverse events, infection, and vascular compromise, Dr. Galadari reported.
Filler products are not interchangeable
Again, because of passive data collection, it is not clear whether the differences between products is a true representation of relative risk. Nevertheless, Dr. Galadari cautioned that these products are not necessarily interchangeable, advising clinicians to avoid products without an established safety track record.
There are a wide variety of fillers, including biostimulatory products, such as poly-L-lactic acid and calcium hydroxyapatite, and permanent fillers, such as silicone, in addition to collagen and hyaluronic acid, which function as temporary fillers, according to Dr. Galadari. He emphasized that the specific risks of each filler vary, but clinicians should always respond quickly whenever there is an adverse reaction or evidence of vascular compromise.
In flushing out filler, Cheryl M. Burgess, MD, of the Center for Dermatology and Dermatologic Surgery, Washington, who spoke at the meeting, also emphasized a prompt response. She too employs hyaluronidase injections to break down excess hyaluronic acid in the event of complications related to this filler.
Importantly, Dr. Burgess pointed out that hyaluronic acid can be considered safe for darker skin types, including Fitzpatrick skin types IV, V, and VI, but she added that speed of injection might be a particularly important variable for cosmetic procedures in skin of color.
“There is less postinflammatory hyperpigmentation with slower injection times and more with serial or multiple puncture injection technique,” she cautioned.
She further concurred with the value of cannulas over needles in most instances for facial contouring applications with filler, but she encouraged clinicians not to be overly ambitious and to move gradually toward goals.
“The desired outcome may require multiple sessions with conservative measures,” she said, indicating that conservative measures also represent a strategy to avoid adverse events.
if not promptly addressed, according to an expert explaining the signs of an impending disaster at the Skin of Color Update 2021.
The most serious of the adverse events stem from vascular compromise, which is often signaled immediately by sharp pain and blanching of the skin, according to Hassan Galadari, MD, assistant professor of dermatology at the United Arab Emirates University, Dubai.
“Swift and aggressive treatment is required to avoid irreversible changes,” said Dr. Galadari, warning that blindness and vision impairment can be permanent, and that other events associated with vascular compromise include stroke and other types of embolism, as well as tissue necrosis.
To be swift, Dr. Galadari advised an immediate halt of injections and then a series of steps to abort the vascular insult. The goal is to encourage blood flow to prevent clotting and dissipate the filler.
“Massage the area like crazy. Keep on massaging. The more you massage the better. You are recruiting blood into that area so it remains viable,” Dr. Galadari said.
Hyaluronidase injections helpful
Warm compresses should also be applied for periods ranging from 5 minutes up to an hour, he added. In patients treated with hyaluronic acid, he also commonly introduces hyaluronidase injections of 200-500 IU diluted in lidocaine or saline. The injections are placed 2-3 cm apart and repeated every hour until signs and symptoms improve.
“Flush all of the filler out,” he said, emphasizing the urgency for reversing risk of vascular adverse events.
To sustain blood flow and avoid clots, he also recommends initiating aspirin with maintenance doses sustained over several days. Sildenafil to further improve conditions of blood perfusion can be “considered.”
The risks of vascular compromise, like other complications from filler injections, are low, but they are not zero, and the opportunity to prevent irreversible changes depends on acting quickly, according to Dr. Galadari.
“To prevent embolism, recognize the danger zones,” he advised, identifying the glabella region as the site of highest risk. The risk of vascular compromise from injections into the nasal region is lower but higher than injections of the nasolabial fold and forehead, which are associated with a relatively low risk.
Slow injections reduce risks
Some basic strategies he recommended for preventing vascular compromise included slow injections while keeping pressure low and using small volumes of filler per shot. Fractionated treatment and microdroplet techniques can be appropriate depending on the site of injection.
“Delivery of the filler by cannulas rather than by needles is preferable,” according to Dr. Galadari, who noted that a task force from the American Society for Dermatologic Surgery recently endorsed this approach as part of other recommendations to avoid complications of injectable fillers.
The Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database suggests that adverse events of any substantial severity from filler injections, not just those involving vascular compromise, occur at a rate of 1 per 3,600 cases. However, MAUDE is a passive surveillance system dependent on reports provided by clinicians and others, so this event rate might be an underrepresentation.
In the MAUDE database, complication rates are listed for each of the available filler products and show a variation in rates not just overall but also for each of the major types of complications, which include skin-specific complications such as nodules, discoloration, and inflammation, as well as neurologic adverse events, infection, and vascular compromise, Dr. Galadari reported.
Filler products are not interchangeable
Again, because of passive data collection, it is not clear whether the differences between products is a true representation of relative risk. Nevertheless, Dr. Galadari cautioned that these products are not necessarily interchangeable, advising clinicians to avoid products without an established safety track record.
There are a wide variety of fillers, including biostimulatory products, such as poly-L-lactic acid and calcium hydroxyapatite, and permanent fillers, such as silicone, in addition to collagen and hyaluronic acid, which function as temporary fillers, according to Dr. Galadari. He emphasized that the specific risks of each filler vary, but clinicians should always respond quickly whenever there is an adverse reaction or evidence of vascular compromise.
In flushing out filler, Cheryl M. Burgess, MD, of the Center for Dermatology and Dermatologic Surgery, Washington, who spoke at the meeting, also emphasized a prompt response. She too employs hyaluronidase injections to break down excess hyaluronic acid in the event of complications related to this filler.
Importantly, Dr. Burgess pointed out that hyaluronic acid can be considered safe for darker skin types, including Fitzpatrick skin types IV, V, and VI, but she added that speed of injection might be a particularly important variable for cosmetic procedures in skin of color.
“There is less postinflammatory hyperpigmentation with slower injection times and more with serial or multiple puncture injection technique,” she cautioned.
She further concurred with the value of cannulas over needles in most instances for facial contouring applications with filler, but she encouraged clinicians not to be overly ambitious and to move gradually toward goals.
“The desired outcome may require multiple sessions with conservative measures,” she said, indicating that conservative measures also represent a strategy to avoid adverse events.
if not promptly addressed, according to an expert explaining the signs of an impending disaster at the Skin of Color Update 2021.
The most serious of the adverse events stem from vascular compromise, which is often signaled immediately by sharp pain and blanching of the skin, according to Hassan Galadari, MD, assistant professor of dermatology at the United Arab Emirates University, Dubai.
“Swift and aggressive treatment is required to avoid irreversible changes,” said Dr. Galadari, warning that blindness and vision impairment can be permanent, and that other events associated with vascular compromise include stroke and other types of embolism, as well as tissue necrosis.
To be swift, Dr. Galadari advised an immediate halt of injections and then a series of steps to abort the vascular insult. The goal is to encourage blood flow to prevent clotting and dissipate the filler.
“Massage the area like crazy. Keep on massaging. The more you massage the better. You are recruiting blood into that area so it remains viable,” Dr. Galadari said.
Hyaluronidase injections helpful
Warm compresses should also be applied for periods ranging from 5 minutes up to an hour, he added. In patients treated with hyaluronic acid, he also commonly introduces hyaluronidase injections of 200-500 IU diluted in lidocaine or saline. The injections are placed 2-3 cm apart and repeated every hour until signs and symptoms improve.
“Flush all of the filler out,” he said, emphasizing the urgency for reversing risk of vascular adverse events.
To sustain blood flow and avoid clots, he also recommends initiating aspirin with maintenance doses sustained over several days. Sildenafil to further improve conditions of blood perfusion can be “considered.”
The risks of vascular compromise, like other complications from filler injections, are low, but they are not zero, and the opportunity to prevent irreversible changes depends on acting quickly, according to Dr. Galadari.
“To prevent embolism, recognize the danger zones,” he advised, identifying the glabella region as the site of highest risk. The risk of vascular compromise from injections into the nasal region is lower but higher than injections of the nasolabial fold and forehead, which are associated with a relatively low risk.
Slow injections reduce risks
Some basic strategies he recommended for preventing vascular compromise included slow injections while keeping pressure low and using small volumes of filler per shot. Fractionated treatment and microdroplet techniques can be appropriate depending on the site of injection.
“Delivery of the filler by cannulas rather than by needles is preferable,” according to Dr. Galadari, who noted that a task force from the American Society for Dermatologic Surgery recently endorsed this approach as part of other recommendations to avoid complications of injectable fillers.
The Food and Drug Administration’s Manufacturer and User Facility Device Experience (MAUDE) database suggests that adverse events of any substantial severity from filler injections, not just those involving vascular compromise, occur at a rate of 1 per 3,600 cases. However, MAUDE is a passive surveillance system dependent on reports provided by clinicians and others, so this event rate might be an underrepresentation.
In the MAUDE database, complication rates are listed for each of the available filler products and show a variation in rates not just overall but also for each of the major types of complications, which include skin-specific complications such as nodules, discoloration, and inflammation, as well as neurologic adverse events, infection, and vascular compromise, Dr. Galadari reported.
Filler products are not interchangeable
Again, because of passive data collection, it is not clear whether the differences between products is a true representation of relative risk. Nevertheless, Dr. Galadari cautioned that these products are not necessarily interchangeable, advising clinicians to avoid products without an established safety track record.
There are a wide variety of fillers, including biostimulatory products, such as poly-L-lactic acid and calcium hydroxyapatite, and permanent fillers, such as silicone, in addition to collagen and hyaluronic acid, which function as temporary fillers, according to Dr. Galadari. He emphasized that the specific risks of each filler vary, but clinicians should always respond quickly whenever there is an adverse reaction or evidence of vascular compromise.
In flushing out filler, Cheryl M. Burgess, MD, of the Center for Dermatology and Dermatologic Surgery, Washington, who spoke at the meeting, also emphasized a prompt response. She too employs hyaluronidase injections to break down excess hyaluronic acid in the event of complications related to this filler.
Importantly, Dr. Burgess pointed out that hyaluronic acid can be considered safe for darker skin types, including Fitzpatrick skin types IV, V, and VI, but she added that speed of injection might be a particularly important variable for cosmetic procedures in skin of color.
“There is less postinflammatory hyperpigmentation with slower injection times and more with serial or multiple puncture injection technique,” she cautioned.
She further concurred with the value of cannulas over needles in most instances for facial contouring applications with filler, but she encouraged clinicians not to be overly ambitious and to move gradually toward goals.
“The desired outcome may require multiple sessions with conservative measures,” she said, indicating that conservative measures also represent a strategy to avoid adverse events.
FROM SOC 2021
Nonsteroidal topical found effective for psoriasis in 52-week study
Treatment with presented as a late-breaker at the virtual annual congress of the European Academy of Dermatology and Venereology.
The drug has several unique features with meaningful clinical differences from other topical psoriasis therapies, according to Linda Stein Gold, MD, director of dermatology clinical research, Henry Ford Health System, Detroit.
“The currently available nonsteroidal topical therapies are typically associated with significant irritation. We did not see that with tapinarof,” said Dr. Stein Gold. This is one of several reasons she believes this drug will be a valuable addition if it receives regulatory approval.
Tapinarof is a small-molecule aryl hydrocarbon receptor (AhR) modulating agent. AhR is widely expressed in immune cells, including macrophages, mast cells, and antigen-presenting cells. It is believed that modulation of AhR signaling by tapinarof reverses immune dysregulation that is involved in the formation of psoriatic lesions.
The newly presented PSOARING 3 data with tapinarof 1% build on the data from the 12-week PSOARING 1 and PSOARING 2 trials, which were released in August 2020 but have yet to be published.
The primary endpoint in both of the 12-week trials, each of which enrolled about 500 patients with plaque psoriasis, was a Physician Global Assessment (PGA) score of 0 (clear) or 1 (almost clear). Relative to a placebo response rate of about 6% in both trials, the proportion of patients who achieved scores of 0/1 with tapinarof 1% was 35.4% and 40.2% in the PSOARING 1 and PSOARING 2 trials, respectively (P < .0001 vs. placebo in both studies).
For the key secondary endpoint of at least 75% improvement in the Psoriasis Area and Severity Index (PASI 75), the relative advantage for tapinarof over placebo was similar. The results were highly statistically significant (P < .0001) in both of the 12-week trials.
More than 90% of the patients who participated in PSOARING 1 and PSOARING 2 and were eligible for the open-label PSOARING 3 extension trial, according to Dr. Stein Gold.
For the 79 patients with a score of 0 at the time of enrollment, tapinarof 1% was reapplied only if the PGA score reached at least 2 during the course of the study. For the 680 patients who entered with a PGA score of at least 1, once-daily applications of tapinarof 1% cream were maintained until a PGA score of 0 was achieved.
In the outcome analysis, response was defined as the proportion of patients with an initial PGA score of at least2 who achieved PGA 0. A remittive effect was defined as duration of a PGA score of 0 or 1 while off therapy after achieving a PGA score of 0. Durability of response was defined as the proportion of patients who achieved a PGA sore of 0 or 1 at least once during the study while on therapy. This last outcome provided a test of tachyphylaxis.
“Overall, 40.9% of patients achieved complete disease clearance at least once during the trial, and 58.2% who entered the study with a PGA score of 2 or higher achieved a PGA score of 0 or 1,” Dr. Stein Gold reported.
For the 79 patients who entered PSOARING 3 with a PGA score of 0 and were off treatment, the median duration of a remittive effect was 115 days. For the patients who entered the trial with a higher PGA score but who achieved a score of 0 during the study (312 patients), the mean remittive effect after discontinuing therapy was 130 days.
There was no evidence of tachyphylaxis. Rather, “there was no loss of effect despite intermittent therapy observed over the course of the trial,” Dr. Stein Gold reported.
The most common treatment-emergent adverse events in PSOARING 3, as in the previous PSOARING studies, were folliculitis, which was observed in 24.0% of patients; contact dermatitis, which occurred in 5.9% of patients; and headache, which was reported in 2%. Rates of study drug discontinuations for folliculitis and contact dermatitis were 1.2% and 1.4%, respectively. Headache did not lead to any study discontinuations.
Calling tapinarof a “first-in-class nonsteroidal,” Dr. Stein Gold suggested that this is likely to be a useful adjunctive therapy for psoriasis control. It avoids the adverse events associated with long-term topical steroid use, and its tolerability might be particularly attractive for use in sensitive areas.
“This is likely to be very useful in patients who are looking for a topical therapy for skin folds or the face, where there is a need for well-tolerated topical treatments,” Dr. Stein Gold said.
There are a lot of reasons to be positive about a new, well-tolerated topical agent for psoriasis, particularly as an alternative to topical steroids, agreed Adam Friedman, MD, director of translational research and professor and chair of the department of dermatology at George Washington University, Washington. He considers the data with tapinarof promising in general, but he also likes any new, effective topical psoriasis therapy.
“Patients and physicians are always hungry for new options, especially psoriasis patients, given many have ‘been there and done that’ with topical steroids,” Dr. Friedman said.
“Topical steroids are not irritating, but long-term use beyond recommended dosing can lead to skin thinning, lightening, tachyphylaxis, and, if really abused, HPA [hypothalamic-pituitary-adrenal] axis suppression and adrenal insufficiency,” he observed.
A topical therapy with a durable effect is particularly intriguing.
“The other issue with topical steroids is that psoriatic plaques return rather easily after stopping. The data I have seen with tapinarof show more sustainability after cessation, owing to its mechanism of action,” Dr. Friedman said. Rather than its potential for application to sensitive areas, such as the face, the durability “to me is more interesting.”
He suspects that, owing to “the incurable steroid phobia that haunts many of our patients,” an effective nonsteroidal topical option is also likely to lead to better compliance with topical treatment over time.
“A well-tolerated nonsteroidal topical drug will probably find an important place in the future management of chronic inflammatory diseases,” Marius-Anton Ionescu, MD, PhD, a dermatologist at the Hôpital Saint Louis, Paris, said in an interview. He referred to the positive effects of treatment with tapinarof in clinical trials in adults with atopic dermatitis, in addition to psoriasis.
Tapinarof 1% is also being investigated in a phase 3 study involving patients with moderate to severe atopic dermatitis. In that study, patients are as young as age 2 years. The drug is under review at the Food and Drug Administration for the plaque psoriasis indication in adults.
Dr. Stein Gold has financial relationships with Arcutis, Amgen, Bristol-Myers Squibb, Eli Lilly, Leo Pharma Ortho Dermatologic, UCB, and Dermavant Sciences, which is developing tapinarof and is provided funding for the PSOARING 3 trial. Dr. Friedman reported financial relationships with Amgen, Biogen, Encore, Galderma, GlaxoSmithKline, IntraDerm, Johnson & Johnson, Nerium, Novartis, Oculus, Onset, Pfizer, Sanova, and Valeant Pharmaceuticals. Dr. Ionescu has been a speaker or investigator (honoraria) for Celgene, Novartis, Lilly, and Uriage Cosmetics.
A version of this article first appeared on Medscape.com.
Treatment with presented as a late-breaker at the virtual annual congress of the European Academy of Dermatology and Venereology.
The drug has several unique features with meaningful clinical differences from other topical psoriasis therapies, according to Linda Stein Gold, MD, director of dermatology clinical research, Henry Ford Health System, Detroit.
“The currently available nonsteroidal topical therapies are typically associated with significant irritation. We did not see that with tapinarof,” said Dr. Stein Gold. This is one of several reasons she believes this drug will be a valuable addition if it receives regulatory approval.
Tapinarof is a small-molecule aryl hydrocarbon receptor (AhR) modulating agent. AhR is widely expressed in immune cells, including macrophages, mast cells, and antigen-presenting cells. It is believed that modulation of AhR signaling by tapinarof reverses immune dysregulation that is involved in the formation of psoriatic lesions.
The newly presented PSOARING 3 data with tapinarof 1% build on the data from the 12-week PSOARING 1 and PSOARING 2 trials, which were released in August 2020 but have yet to be published.
The primary endpoint in both of the 12-week trials, each of which enrolled about 500 patients with plaque psoriasis, was a Physician Global Assessment (PGA) score of 0 (clear) or 1 (almost clear). Relative to a placebo response rate of about 6% in both trials, the proportion of patients who achieved scores of 0/1 with tapinarof 1% was 35.4% and 40.2% in the PSOARING 1 and PSOARING 2 trials, respectively (P < .0001 vs. placebo in both studies).
For the key secondary endpoint of at least 75% improvement in the Psoriasis Area and Severity Index (PASI 75), the relative advantage for tapinarof over placebo was similar. The results were highly statistically significant (P < .0001) in both of the 12-week trials.
More than 90% of the patients who participated in PSOARING 1 and PSOARING 2 and were eligible for the open-label PSOARING 3 extension trial, according to Dr. Stein Gold.
For the 79 patients with a score of 0 at the time of enrollment, tapinarof 1% was reapplied only if the PGA score reached at least 2 during the course of the study. For the 680 patients who entered with a PGA score of at least 1, once-daily applications of tapinarof 1% cream were maintained until a PGA score of 0 was achieved.
In the outcome analysis, response was defined as the proportion of patients with an initial PGA score of at least2 who achieved PGA 0. A remittive effect was defined as duration of a PGA score of 0 or 1 while off therapy after achieving a PGA score of 0. Durability of response was defined as the proportion of patients who achieved a PGA sore of 0 or 1 at least once during the study while on therapy. This last outcome provided a test of tachyphylaxis.
“Overall, 40.9% of patients achieved complete disease clearance at least once during the trial, and 58.2% who entered the study with a PGA score of 2 or higher achieved a PGA score of 0 or 1,” Dr. Stein Gold reported.
For the 79 patients who entered PSOARING 3 with a PGA score of 0 and were off treatment, the median duration of a remittive effect was 115 days. For the patients who entered the trial with a higher PGA score but who achieved a score of 0 during the study (312 patients), the mean remittive effect after discontinuing therapy was 130 days.
There was no evidence of tachyphylaxis. Rather, “there was no loss of effect despite intermittent therapy observed over the course of the trial,” Dr. Stein Gold reported.
The most common treatment-emergent adverse events in PSOARING 3, as in the previous PSOARING studies, were folliculitis, which was observed in 24.0% of patients; contact dermatitis, which occurred in 5.9% of patients; and headache, which was reported in 2%. Rates of study drug discontinuations for folliculitis and contact dermatitis were 1.2% and 1.4%, respectively. Headache did not lead to any study discontinuations.
Calling tapinarof a “first-in-class nonsteroidal,” Dr. Stein Gold suggested that this is likely to be a useful adjunctive therapy for psoriasis control. It avoids the adverse events associated with long-term topical steroid use, and its tolerability might be particularly attractive for use in sensitive areas.
“This is likely to be very useful in patients who are looking for a topical therapy for skin folds or the face, where there is a need for well-tolerated topical treatments,” Dr. Stein Gold said.
There are a lot of reasons to be positive about a new, well-tolerated topical agent for psoriasis, particularly as an alternative to topical steroids, agreed Adam Friedman, MD, director of translational research and professor and chair of the department of dermatology at George Washington University, Washington. He considers the data with tapinarof promising in general, but he also likes any new, effective topical psoriasis therapy.
“Patients and physicians are always hungry for new options, especially psoriasis patients, given many have ‘been there and done that’ with topical steroids,” Dr. Friedman said.
“Topical steroids are not irritating, but long-term use beyond recommended dosing can lead to skin thinning, lightening, tachyphylaxis, and, if really abused, HPA [hypothalamic-pituitary-adrenal] axis suppression and adrenal insufficiency,” he observed.
A topical therapy with a durable effect is particularly intriguing.
“The other issue with topical steroids is that psoriatic plaques return rather easily after stopping. The data I have seen with tapinarof show more sustainability after cessation, owing to its mechanism of action,” Dr. Friedman said. Rather than its potential for application to sensitive areas, such as the face, the durability “to me is more interesting.”
He suspects that, owing to “the incurable steroid phobia that haunts many of our patients,” an effective nonsteroidal topical option is also likely to lead to better compliance with topical treatment over time.
“A well-tolerated nonsteroidal topical drug will probably find an important place in the future management of chronic inflammatory diseases,” Marius-Anton Ionescu, MD, PhD, a dermatologist at the Hôpital Saint Louis, Paris, said in an interview. He referred to the positive effects of treatment with tapinarof in clinical trials in adults with atopic dermatitis, in addition to psoriasis.
Tapinarof 1% is also being investigated in a phase 3 study involving patients with moderate to severe atopic dermatitis. In that study, patients are as young as age 2 years. The drug is under review at the Food and Drug Administration for the plaque psoriasis indication in adults.
Dr. Stein Gold has financial relationships with Arcutis, Amgen, Bristol-Myers Squibb, Eli Lilly, Leo Pharma Ortho Dermatologic, UCB, and Dermavant Sciences, which is developing tapinarof and is provided funding for the PSOARING 3 trial. Dr. Friedman reported financial relationships with Amgen, Biogen, Encore, Galderma, GlaxoSmithKline, IntraDerm, Johnson & Johnson, Nerium, Novartis, Oculus, Onset, Pfizer, Sanova, and Valeant Pharmaceuticals. Dr. Ionescu has been a speaker or investigator (honoraria) for Celgene, Novartis, Lilly, and Uriage Cosmetics.
A version of this article first appeared on Medscape.com.
Treatment with presented as a late-breaker at the virtual annual congress of the European Academy of Dermatology and Venereology.
The drug has several unique features with meaningful clinical differences from other topical psoriasis therapies, according to Linda Stein Gold, MD, director of dermatology clinical research, Henry Ford Health System, Detroit.
“The currently available nonsteroidal topical therapies are typically associated with significant irritation. We did not see that with tapinarof,” said Dr. Stein Gold. This is one of several reasons she believes this drug will be a valuable addition if it receives regulatory approval.
Tapinarof is a small-molecule aryl hydrocarbon receptor (AhR) modulating agent. AhR is widely expressed in immune cells, including macrophages, mast cells, and antigen-presenting cells. It is believed that modulation of AhR signaling by tapinarof reverses immune dysregulation that is involved in the formation of psoriatic lesions.
The newly presented PSOARING 3 data with tapinarof 1% build on the data from the 12-week PSOARING 1 and PSOARING 2 trials, which were released in August 2020 but have yet to be published.
The primary endpoint in both of the 12-week trials, each of which enrolled about 500 patients with plaque psoriasis, was a Physician Global Assessment (PGA) score of 0 (clear) or 1 (almost clear). Relative to a placebo response rate of about 6% in both trials, the proportion of patients who achieved scores of 0/1 with tapinarof 1% was 35.4% and 40.2% in the PSOARING 1 and PSOARING 2 trials, respectively (P < .0001 vs. placebo in both studies).
For the key secondary endpoint of at least 75% improvement in the Psoriasis Area and Severity Index (PASI 75), the relative advantage for tapinarof over placebo was similar. The results were highly statistically significant (P < .0001) in both of the 12-week trials.
More than 90% of the patients who participated in PSOARING 1 and PSOARING 2 and were eligible for the open-label PSOARING 3 extension trial, according to Dr. Stein Gold.
For the 79 patients with a score of 0 at the time of enrollment, tapinarof 1% was reapplied only if the PGA score reached at least 2 during the course of the study. For the 680 patients who entered with a PGA score of at least 1, once-daily applications of tapinarof 1% cream were maintained until a PGA score of 0 was achieved.
In the outcome analysis, response was defined as the proportion of patients with an initial PGA score of at least2 who achieved PGA 0. A remittive effect was defined as duration of a PGA score of 0 or 1 while off therapy after achieving a PGA score of 0. Durability of response was defined as the proportion of patients who achieved a PGA sore of 0 or 1 at least once during the study while on therapy. This last outcome provided a test of tachyphylaxis.
“Overall, 40.9% of patients achieved complete disease clearance at least once during the trial, and 58.2% who entered the study with a PGA score of 2 or higher achieved a PGA score of 0 or 1,” Dr. Stein Gold reported.
For the 79 patients who entered PSOARING 3 with a PGA score of 0 and were off treatment, the median duration of a remittive effect was 115 days. For the patients who entered the trial with a higher PGA score but who achieved a score of 0 during the study (312 patients), the mean remittive effect after discontinuing therapy was 130 days.
There was no evidence of tachyphylaxis. Rather, “there was no loss of effect despite intermittent therapy observed over the course of the trial,” Dr. Stein Gold reported.
The most common treatment-emergent adverse events in PSOARING 3, as in the previous PSOARING studies, were folliculitis, which was observed in 24.0% of patients; contact dermatitis, which occurred in 5.9% of patients; and headache, which was reported in 2%. Rates of study drug discontinuations for folliculitis and contact dermatitis were 1.2% and 1.4%, respectively. Headache did not lead to any study discontinuations.
Calling tapinarof a “first-in-class nonsteroidal,” Dr. Stein Gold suggested that this is likely to be a useful adjunctive therapy for psoriasis control. It avoids the adverse events associated with long-term topical steroid use, and its tolerability might be particularly attractive for use in sensitive areas.
“This is likely to be very useful in patients who are looking for a topical therapy for skin folds or the face, where there is a need for well-tolerated topical treatments,” Dr. Stein Gold said.
There are a lot of reasons to be positive about a new, well-tolerated topical agent for psoriasis, particularly as an alternative to topical steroids, agreed Adam Friedman, MD, director of translational research and professor and chair of the department of dermatology at George Washington University, Washington. He considers the data with tapinarof promising in general, but he also likes any new, effective topical psoriasis therapy.
“Patients and physicians are always hungry for new options, especially psoriasis patients, given many have ‘been there and done that’ with topical steroids,” Dr. Friedman said.
“Topical steroids are not irritating, but long-term use beyond recommended dosing can lead to skin thinning, lightening, tachyphylaxis, and, if really abused, HPA [hypothalamic-pituitary-adrenal] axis suppression and adrenal insufficiency,” he observed.
A topical therapy with a durable effect is particularly intriguing.
“The other issue with topical steroids is that psoriatic plaques return rather easily after stopping. The data I have seen with tapinarof show more sustainability after cessation, owing to its mechanism of action,” Dr. Friedman said. Rather than its potential for application to sensitive areas, such as the face, the durability “to me is more interesting.”
He suspects that, owing to “the incurable steroid phobia that haunts many of our patients,” an effective nonsteroidal topical option is also likely to lead to better compliance with topical treatment over time.
“A well-tolerated nonsteroidal topical drug will probably find an important place in the future management of chronic inflammatory diseases,” Marius-Anton Ionescu, MD, PhD, a dermatologist at the Hôpital Saint Louis, Paris, said in an interview. He referred to the positive effects of treatment with tapinarof in clinical trials in adults with atopic dermatitis, in addition to psoriasis.
Tapinarof 1% is also being investigated in a phase 3 study involving patients with moderate to severe atopic dermatitis. In that study, patients are as young as age 2 years. The drug is under review at the Food and Drug Administration for the plaque psoriasis indication in adults.
Dr. Stein Gold has financial relationships with Arcutis, Amgen, Bristol-Myers Squibb, Eli Lilly, Leo Pharma Ortho Dermatologic, UCB, and Dermavant Sciences, which is developing tapinarof and is provided funding for the PSOARING 3 trial. Dr. Friedman reported financial relationships with Amgen, Biogen, Encore, Galderma, GlaxoSmithKline, IntraDerm, Johnson & Johnson, Nerium, Novartis, Oculus, Onset, Pfizer, Sanova, and Valeant Pharmaceuticals. Dr. Ionescu has been a speaker or investigator (honoraria) for Celgene, Novartis, Lilly, and Uriage Cosmetics.
A version of this article first appeared on Medscape.com.
Ketosis, including ketogenic diets, implicated in prurigo pigmentosa
, according to a dermatologist, who reviewed skin conditions common to patients of Asian descent at the Skin of Color Update 2021.
“Ketogenic diets are gaining popularity globally for weight loss. After 2-4 weeks [on a strict ketogenic diet], some patients start to notice very pruritic papules on their trunk, the so-called keto rash,” reported Hye Jin Chung, MD, director of the Asian Skin Clinic, Beth Israel Deaconess Medical Center, Boston. “Keto rash is actually prurigo pigmentosa.”
The exact pathogenesis of prurigo pigmentosa, a highly pruritic macular and papular rash with gross reticular pigmentation, is unclear, but Dr. Chung reported that the strong link with ketosis might explain why more cases are now being encountered outside of east Asia. Ketosis or conditions associated with a high risk for ketosis, such as anorexia nervosa, diabetes mellitus, or recent bariatric surgery, have been linked to prurigo pigmentosa in all skin types and ethnicities.
“I tell my residents that this is a disease you will never forget after your first case,” she said.
The differential diagnosis includes contact dermatitis and other inflammatory disorders, but Dr. Chung said that the reticular pattern of the lesions is a relatively unique feature. Confluent and reticulated papillomatosis (CARP) shares a pattern of reticulated lesions, but Dr. Chung said it lacks the inflammatory erythematous papules and the severe pruritus common to prurigo pigmentosa.
Histologically, the pattern evolves. It begins as a perivascular infiltration dominated by neutrophils and eosinophils with hyperkeratosis, acanthosis, and spongiosis. Over time, Dr. Chung said that the histologic picture shows an increasing degree of dyskeratosis as keratinocytes die.
Prurigo pigmentosa was first described 50 years ago by Masaji Nagashima, MD, who published a report on eight patients in Japan with a pruriginous truncal dermatosis featuring symmetrical pigmentation. Most subsequent reports were also from Japan or other east Asian countries, but it has since spread.
This global spread was captured in a recently published review of 115 published studies and case reports from 24 countries. In this review, the proportion of studies from Europe (36.5%) approached that of those from east Asia (38.2%), even if 76% of the patients for whom race was reported were of Asian ethnicity.
Of the 369 patients evaluated in these studies and case reports, 72.1% were female. The mean age was 25.6 years. In the studies originating outside of Asia, prurigo pigmentosa was reported in a spectrum of skin types and ethnicities, including Whites, Blacks, and Hispanics. The lowest reported incidence has been in the latter two groups, but the authors of the review speculated that this condition is likely being underdiagnosed in non-Asian individuals.
Dr. Chung agreed, and she cautioned that the consequences typically result in a significant delay for achieving disease control. In recounting a recent case of prurigo pigmentosa at her center, she said that the 59-year-old Asian patient had been initiated on topical steroids and oral antihistamines by her primary care physician before she was referred. This is a common and reasonable strategy for a highly pruritic rash potentially caused by contact dermatitis, but it is ineffective for this disorder.
“Prurigo pigmentosa requires anti-inflammatory agents,” she explained. She said that doxycycline and minocycline are the treatments of choice, but noted that there are also reports of efficacy with dapsone, macrolide antibiotics, and isotretinoin.
In her most recent case, she initiated the patient on 100 mg of doxycycline twice daily. There was significant improvement within 2 weeks, and the rash resolved within a month with no relapse in follow-up that now exceeds 12 months, Dr. Chung said.
According to Dr. Chung, Asian-Americans are the most rapidly growing ethnic group in the United States, making it increasingly important to be familiar with conditions common or unique to Asian skin, but prurigo pigmentosa is no longer confined to those of Asian descent. She encouraged clinicians to recognize this disorder to reduce the common delays to effective treatment.
The senior author of the recently published review of studies, Jensen Yeung, MD, of the department of dermatology, University of Toronto, agreed. He, too, believes that dermatologists need to increase their awareness of the signs and symptoms of prurigo pigmentosa – and not just in Asian patients or patients of Asian descent.
“This diagnosis is often missed,” he contended in an interview. “This condition has become more common in the past 5 years in my clinical experience.” He added that the increasing incidence might not just be related to better diagnostic accuracy, although the most significant of other possible explanations “is not yet well understood.”
Dr. Chung reports that she has no relevant financial relationships to disclose. Dr. Yeung reports financial relationships with more than 25 pharmaceutical companies, some of which produce treatments employed in the control of prurigo pigmentosa.
, according to a dermatologist, who reviewed skin conditions common to patients of Asian descent at the Skin of Color Update 2021.
“Ketogenic diets are gaining popularity globally for weight loss. After 2-4 weeks [on a strict ketogenic diet], some patients start to notice very pruritic papules on their trunk, the so-called keto rash,” reported Hye Jin Chung, MD, director of the Asian Skin Clinic, Beth Israel Deaconess Medical Center, Boston. “Keto rash is actually prurigo pigmentosa.”
The exact pathogenesis of prurigo pigmentosa, a highly pruritic macular and papular rash with gross reticular pigmentation, is unclear, but Dr. Chung reported that the strong link with ketosis might explain why more cases are now being encountered outside of east Asia. Ketosis or conditions associated with a high risk for ketosis, such as anorexia nervosa, diabetes mellitus, or recent bariatric surgery, have been linked to prurigo pigmentosa in all skin types and ethnicities.
“I tell my residents that this is a disease you will never forget after your first case,” she said.
The differential diagnosis includes contact dermatitis and other inflammatory disorders, but Dr. Chung said that the reticular pattern of the lesions is a relatively unique feature. Confluent and reticulated papillomatosis (CARP) shares a pattern of reticulated lesions, but Dr. Chung said it lacks the inflammatory erythematous papules and the severe pruritus common to prurigo pigmentosa.
Histologically, the pattern evolves. It begins as a perivascular infiltration dominated by neutrophils and eosinophils with hyperkeratosis, acanthosis, and spongiosis. Over time, Dr. Chung said that the histologic picture shows an increasing degree of dyskeratosis as keratinocytes die.
Prurigo pigmentosa was first described 50 years ago by Masaji Nagashima, MD, who published a report on eight patients in Japan with a pruriginous truncal dermatosis featuring symmetrical pigmentation. Most subsequent reports were also from Japan or other east Asian countries, but it has since spread.
This global spread was captured in a recently published review of 115 published studies and case reports from 24 countries. In this review, the proportion of studies from Europe (36.5%) approached that of those from east Asia (38.2%), even if 76% of the patients for whom race was reported were of Asian ethnicity.
Of the 369 patients evaluated in these studies and case reports, 72.1% were female. The mean age was 25.6 years. In the studies originating outside of Asia, prurigo pigmentosa was reported in a spectrum of skin types and ethnicities, including Whites, Blacks, and Hispanics. The lowest reported incidence has been in the latter two groups, but the authors of the review speculated that this condition is likely being underdiagnosed in non-Asian individuals.
Dr. Chung agreed, and she cautioned that the consequences typically result in a significant delay for achieving disease control. In recounting a recent case of prurigo pigmentosa at her center, she said that the 59-year-old Asian patient had been initiated on topical steroids and oral antihistamines by her primary care physician before she was referred. This is a common and reasonable strategy for a highly pruritic rash potentially caused by contact dermatitis, but it is ineffective for this disorder.
“Prurigo pigmentosa requires anti-inflammatory agents,” she explained. She said that doxycycline and minocycline are the treatments of choice, but noted that there are also reports of efficacy with dapsone, macrolide antibiotics, and isotretinoin.
In her most recent case, she initiated the patient on 100 mg of doxycycline twice daily. There was significant improvement within 2 weeks, and the rash resolved within a month with no relapse in follow-up that now exceeds 12 months, Dr. Chung said.
According to Dr. Chung, Asian-Americans are the most rapidly growing ethnic group in the United States, making it increasingly important to be familiar with conditions common or unique to Asian skin, but prurigo pigmentosa is no longer confined to those of Asian descent. She encouraged clinicians to recognize this disorder to reduce the common delays to effective treatment.
The senior author of the recently published review of studies, Jensen Yeung, MD, of the department of dermatology, University of Toronto, agreed. He, too, believes that dermatologists need to increase their awareness of the signs and symptoms of prurigo pigmentosa – and not just in Asian patients or patients of Asian descent.
“This diagnosis is often missed,” he contended in an interview. “This condition has become more common in the past 5 years in my clinical experience.” He added that the increasing incidence might not just be related to better diagnostic accuracy, although the most significant of other possible explanations “is not yet well understood.”
Dr. Chung reports that she has no relevant financial relationships to disclose. Dr. Yeung reports financial relationships with more than 25 pharmaceutical companies, some of which produce treatments employed in the control of prurigo pigmentosa.
, according to a dermatologist, who reviewed skin conditions common to patients of Asian descent at the Skin of Color Update 2021.
“Ketogenic diets are gaining popularity globally for weight loss. After 2-4 weeks [on a strict ketogenic diet], some patients start to notice very pruritic papules on their trunk, the so-called keto rash,” reported Hye Jin Chung, MD, director of the Asian Skin Clinic, Beth Israel Deaconess Medical Center, Boston. “Keto rash is actually prurigo pigmentosa.”
The exact pathogenesis of prurigo pigmentosa, a highly pruritic macular and papular rash with gross reticular pigmentation, is unclear, but Dr. Chung reported that the strong link with ketosis might explain why more cases are now being encountered outside of east Asia. Ketosis or conditions associated with a high risk for ketosis, such as anorexia nervosa, diabetes mellitus, or recent bariatric surgery, have been linked to prurigo pigmentosa in all skin types and ethnicities.
“I tell my residents that this is a disease you will never forget after your first case,” she said.
The differential diagnosis includes contact dermatitis and other inflammatory disorders, but Dr. Chung said that the reticular pattern of the lesions is a relatively unique feature. Confluent and reticulated papillomatosis (CARP) shares a pattern of reticulated lesions, but Dr. Chung said it lacks the inflammatory erythematous papules and the severe pruritus common to prurigo pigmentosa.
Histologically, the pattern evolves. It begins as a perivascular infiltration dominated by neutrophils and eosinophils with hyperkeratosis, acanthosis, and spongiosis. Over time, Dr. Chung said that the histologic picture shows an increasing degree of dyskeratosis as keratinocytes die.
Prurigo pigmentosa was first described 50 years ago by Masaji Nagashima, MD, who published a report on eight patients in Japan with a pruriginous truncal dermatosis featuring symmetrical pigmentation. Most subsequent reports were also from Japan or other east Asian countries, but it has since spread.
This global spread was captured in a recently published review of 115 published studies and case reports from 24 countries. In this review, the proportion of studies from Europe (36.5%) approached that of those from east Asia (38.2%), even if 76% of the patients for whom race was reported were of Asian ethnicity.
Of the 369 patients evaluated in these studies and case reports, 72.1% were female. The mean age was 25.6 years. In the studies originating outside of Asia, prurigo pigmentosa was reported in a spectrum of skin types and ethnicities, including Whites, Blacks, and Hispanics. The lowest reported incidence has been in the latter two groups, but the authors of the review speculated that this condition is likely being underdiagnosed in non-Asian individuals.
Dr. Chung agreed, and she cautioned that the consequences typically result in a significant delay for achieving disease control. In recounting a recent case of prurigo pigmentosa at her center, she said that the 59-year-old Asian patient had been initiated on topical steroids and oral antihistamines by her primary care physician before she was referred. This is a common and reasonable strategy for a highly pruritic rash potentially caused by contact dermatitis, but it is ineffective for this disorder.
“Prurigo pigmentosa requires anti-inflammatory agents,” she explained. She said that doxycycline and minocycline are the treatments of choice, but noted that there are also reports of efficacy with dapsone, macrolide antibiotics, and isotretinoin.
In her most recent case, she initiated the patient on 100 mg of doxycycline twice daily. There was significant improvement within 2 weeks, and the rash resolved within a month with no relapse in follow-up that now exceeds 12 months, Dr. Chung said.
According to Dr. Chung, Asian-Americans are the most rapidly growing ethnic group in the United States, making it increasingly important to be familiar with conditions common or unique to Asian skin, but prurigo pigmentosa is no longer confined to those of Asian descent. She encouraged clinicians to recognize this disorder to reduce the common delays to effective treatment.
The senior author of the recently published review of studies, Jensen Yeung, MD, of the department of dermatology, University of Toronto, agreed. He, too, believes that dermatologists need to increase their awareness of the signs and symptoms of prurigo pigmentosa – and not just in Asian patients or patients of Asian descent.
“This diagnosis is often missed,” he contended in an interview. “This condition has become more common in the past 5 years in my clinical experience.” He added that the increasing incidence might not just be related to better diagnostic accuracy, although the most significant of other possible explanations “is not yet well understood.”
Dr. Chung reports that she has no relevant financial relationships to disclose. Dr. Yeung reports financial relationships with more than 25 pharmaceutical companies, some of which produce treatments employed in the control of prurigo pigmentosa.
FROM SOC 2021