User login
Antenatal steroids for preterm birth is cost effective
Administering antenatal corticosteroids to pregnant women at high risk for preterm birth was a cost-effective intervention that improved infant respiratory outcomes, according to a new study.
“This intervention has a potential cost saving in the United States of approximately $100 million dollars annually from the benefit in the immediate neonatal outcome alone,” Cynthia Gyamfi-Bannerman, MD, of Columbia University, New York, and her associates reported in JAMA Pediatrics. “Because late preterm birth comprises a large proportion of all preterm births, our findings have the potential for a large influence on public health.”
The researchers conducted a retrospective secondary analysis of the randomized Antenatal Late Preterm Steroids (ALPS) clinical trial October 2010 to February 2015. The trial enrolled randomly assigned antenatal administration of betamethasone or placebo to women pregnant with a singleton and at high risk for preterm birth while between 34 weeks, 6 days, and 36 weeks, 0 days, of gestation.
Antenatal corticosteroid administration was regarded as effective if a newborn did not require treatment in the first 72 hours for respiratory distress or illness. Treatment could include “continuous positive airway pressure or high-flow nasal cannula for 2 hours or more, supplemental oxygen with a fraction of inspired oxygen of 30% or more for 4 hours or more, and extracorporeal membrane oxygenation or mechanical ventilation,” Dr. Gyamfi-Bannerman and her associates wrote.
To tally the costs, the researchers used Medicaid rates to estimate the total in 2015 U.S. dollars for betamethasone, outpatient visits or inpatient stays to administer it, and all direct newborn care costs, including neonatal ICU daily costs stratified by respiratory illness severity. Betamethasone administration included an initial 12-mg intramuscular dose followed by another after 24 hours if the infant had not been delivered.
“Because therapy often persists for longer than this 72-hour duration, we measured costs through hospital discharge,” the authors wrote. “The analysis took the perspective of a third-party payer in which we included direct medical costs and associated overhead accruing to hospitals and medical payers for the care of enrolled patients and their infants.”
Among 2,821 mothers not lost to follow-up during the secondary analysis, 1,426 received betamethasone and 1,395 received placebo. For mothers who received betamethasone antenatally, the total mean cost was $4,681 per mother-infant pair. Total mean cost for those in the placebo group was $5,379 per pair, resulting in a significant mean $698 savings (P = .02). Respiratory morbidity was 2.9% lower in infants whose mothers received antenatal corticosteroid treatment.
“Thus, because the treated group had lower costs and this strategy was more effective, administration of betamethasone to women at risk for late preterm birth was judged to be a dominant strategy, which is defined as one in which costs are lower and effectiveness is higher than a comparator (incremental cost-effectiveness ratio [ICER], −23 986),” Dr. Gyamfi-Bannerman and her associates reported. ICER is defined as the difference in mean total cost per patient in the betamethasone and placebo arms divided by the difference in the effectiveness.
Study limitations were an inability to estimate costs according to quality-adjusted life years or to include families’/caregivers’ costs.
SOURCE: Gyamfi-Bannerman C. JAMA Pediatr. 2019 Mar 11. doi: 10.1001/jamapediatrics.2019.0032.
Administering antenatal corticosteroids to pregnant women at high risk for preterm birth was a cost-effective intervention that improved infant respiratory outcomes, according to a new study.
“This intervention has a potential cost saving in the United States of approximately $100 million dollars annually from the benefit in the immediate neonatal outcome alone,” Cynthia Gyamfi-Bannerman, MD, of Columbia University, New York, and her associates reported in JAMA Pediatrics. “Because late preterm birth comprises a large proportion of all preterm births, our findings have the potential for a large influence on public health.”
The researchers conducted a retrospective secondary analysis of the randomized Antenatal Late Preterm Steroids (ALPS) clinical trial October 2010 to February 2015. The trial enrolled randomly assigned antenatal administration of betamethasone or placebo to women pregnant with a singleton and at high risk for preterm birth while between 34 weeks, 6 days, and 36 weeks, 0 days, of gestation.
Antenatal corticosteroid administration was regarded as effective if a newborn did not require treatment in the first 72 hours for respiratory distress or illness. Treatment could include “continuous positive airway pressure or high-flow nasal cannula for 2 hours or more, supplemental oxygen with a fraction of inspired oxygen of 30% or more for 4 hours or more, and extracorporeal membrane oxygenation or mechanical ventilation,” Dr. Gyamfi-Bannerman and her associates wrote.
To tally the costs, the researchers used Medicaid rates to estimate the total in 2015 U.S. dollars for betamethasone, outpatient visits or inpatient stays to administer it, and all direct newborn care costs, including neonatal ICU daily costs stratified by respiratory illness severity. Betamethasone administration included an initial 12-mg intramuscular dose followed by another after 24 hours if the infant had not been delivered.
“Because therapy often persists for longer than this 72-hour duration, we measured costs through hospital discharge,” the authors wrote. “The analysis took the perspective of a third-party payer in which we included direct medical costs and associated overhead accruing to hospitals and medical payers for the care of enrolled patients and their infants.”
Among 2,821 mothers not lost to follow-up during the secondary analysis, 1,426 received betamethasone and 1,395 received placebo. For mothers who received betamethasone antenatally, the total mean cost was $4,681 per mother-infant pair. Total mean cost for those in the placebo group was $5,379 per pair, resulting in a significant mean $698 savings (P = .02). Respiratory morbidity was 2.9% lower in infants whose mothers received antenatal corticosteroid treatment.
“Thus, because the treated group had lower costs and this strategy was more effective, administration of betamethasone to women at risk for late preterm birth was judged to be a dominant strategy, which is defined as one in which costs are lower and effectiveness is higher than a comparator (incremental cost-effectiveness ratio [ICER], −23 986),” Dr. Gyamfi-Bannerman and her associates reported. ICER is defined as the difference in mean total cost per patient in the betamethasone and placebo arms divided by the difference in the effectiveness.
Study limitations were an inability to estimate costs according to quality-adjusted life years or to include families’/caregivers’ costs.
SOURCE: Gyamfi-Bannerman C. JAMA Pediatr. 2019 Mar 11. doi: 10.1001/jamapediatrics.2019.0032.
Administering antenatal corticosteroids to pregnant women at high risk for preterm birth was a cost-effective intervention that improved infant respiratory outcomes, according to a new study.
“This intervention has a potential cost saving in the United States of approximately $100 million dollars annually from the benefit in the immediate neonatal outcome alone,” Cynthia Gyamfi-Bannerman, MD, of Columbia University, New York, and her associates reported in JAMA Pediatrics. “Because late preterm birth comprises a large proportion of all preterm births, our findings have the potential for a large influence on public health.”
The researchers conducted a retrospective secondary analysis of the randomized Antenatal Late Preterm Steroids (ALPS) clinical trial October 2010 to February 2015. The trial enrolled randomly assigned antenatal administration of betamethasone or placebo to women pregnant with a singleton and at high risk for preterm birth while between 34 weeks, 6 days, and 36 weeks, 0 days, of gestation.
Antenatal corticosteroid administration was regarded as effective if a newborn did not require treatment in the first 72 hours for respiratory distress or illness. Treatment could include “continuous positive airway pressure or high-flow nasal cannula for 2 hours or more, supplemental oxygen with a fraction of inspired oxygen of 30% or more for 4 hours or more, and extracorporeal membrane oxygenation or mechanical ventilation,” Dr. Gyamfi-Bannerman and her associates wrote.
To tally the costs, the researchers used Medicaid rates to estimate the total in 2015 U.S. dollars for betamethasone, outpatient visits or inpatient stays to administer it, and all direct newborn care costs, including neonatal ICU daily costs stratified by respiratory illness severity. Betamethasone administration included an initial 12-mg intramuscular dose followed by another after 24 hours if the infant had not been delivered.
“Because therapy often persists for longer than this 72-hour duration, we measured costs through hospital discharge,” the authors wrote. “The analysis took the perspective of a third-party payer in which we included direct medical costs and associated overhead accruing to hospitals and medical payers for the care of enrolled patients and their infants.”
Among 2,821 mothers not lost to follow-up during the secondary analysis, 1,426 received betamethasone and 1,395 received placebo. For mothers who received betamethasone antenatally, the total mean cost was $4,681 per mother-infant pair. Total mean cost for those in the placebo group was $5,379 per pair, resulting in a significant mean $698 savings (P = .02). Respiratory morbidity was 2.9% lower in infants whose mothers received antenatal corticosteroid treatment.
“Thus, because the treated group had lower costs and this strategy was more effective, administration of betamethasone to women at risk for late preterm birth was judged to be a dominant strategy, which is defined as one in which costs are lower and effectiveness is higher than a comparator (incremental cost-effectiveness ratio [ICER], −23 986),” Dr. Gyamfi-Bannerman and her associates reported. ICER is defined as the difference in mean total cost per patient in the betamethasone and placebo arms divided by the difference in the effectiveness.
Study limitations were an inability to estimate costs according to quality-adjusted life years or to include families’/caregivers’ costs.
SOURCE: Gyamfi-Bannerman C. JAMA Pediatr. 2019 Mar 11. doi: 10.1001/jamapediatrics.2019.0032.
FROM JAMA PEDIATRICS
Daily aspirin associated with lower risk of COPD flareup
Daily aspirin use could reduce the risk of acute exacerbations of chronic obstructive pulmonary disease, new data suggest.
Researchers reported the outcomes of an observational cohort study of 1,698 individuals with COPD, 45% of whom said they were taking daily aspirin at baseline. Their findings were published in Chest.
After a median follow up of 2.7 years, aspirin users had an overall 22% lower incidence of acute COPD exacerbations compared with nonusers. This was largely accounted for by a 25% reduction in moderate exacerbations, but there was no significant difference between aspirin users and nonusers in severe exacerbations.
A similar pattern was seen after just 1 year of follow-up, with an overall 30% reduction in the incidence of exacerbations, a 37% reduction in moderate exacerbations, but no significant reduction in severe exacerbations.
“Though aspirin use has previously been linked with reduced mortality risk in patients with COPD, to our knowledge, this is the first study to investigate the association of daily aspirin use with respiratory morbidity in COPD,” wrote Ashraf Fawzy, MD, of the division of pulmonary and critical care medicine at Johns Hopkins University, Baltimore, and his coauthors.
The association between aspirin use and reduced incidence of exacerbations was stronger among individuals with chronic bronchitis, which prompted the authors to suggest that future studies of aspirin in COPD should focus on participants with chronic bronchitis.
However, the association was not affected by COPD severity, emphysema presence or severity, or cardiometabolic phenotype.
Aspirin users reported better respiratory-specific quality of life than that of nonusers, including 34% lower odds of reporting moderate to severe dyspnea, and better baseline COPD health status.
“Findings of this study add to the existing literature by highlighting that aspirin use is also associated with reduced respiratory morbidity across several domains – including exacerbation risk, quality of life, and dyspnea – factors related to patient well-being and healthcare utilization,” the authors wrote.
Aspirin users were more likely to be white, male, and obese, and less likely to be smokers. They had better lung function but more cardiovascular comorbidities at baseline, although the aspirin users and nonusers were matched on baseline characteristics.
Speculating on the mechanisms by which aspirin might impact COPD exacerbations, the authors noted that the drug has both systemic and local pulmonary mechanisms of action.
For example, a pathway that results in elevated levels of a urinary metabolite in patients with COPD is irreversibly blocked by aspirin. Aspirin also attenuates the elevation of inflammatory markers interleukin-6 and C-reactive protein, which are part of the inflammatory phenotype of COPD. Aspirin has been shown to reduce proinflammatory cytokines in the lung.
The authors did note that aspirin use was self-reported, so they did not have data on dosage or duration of use.
The National Institutes of Health funded the study. Six authors declared advisory board positions, research support, and other funding from the pharmaceutical sector. One author was also a founder of a company commercializing lung image analysis software. No other conflicts of interest were declared.
SOURCE: Fawzy A et al. Chest. 2019 Mar;155(3): 519-27. doi: 10.1016/j.chest.2018.11.028.
Daily aspirin use could reduce the risk of acute exacerbations of chronic obstructive pulmonary disease, new data suggest.
Researchers reported the outcomes of an observational cohort study of 1,698 individuals with COPD, 45% of whom said they were taking daily aspirin at baseline. Their findings were published in Chest.
After a median follow up of 2.7 years, aspirin users had an overall 22% lower incidence of acute COPD exacerbations compared with nonusers. This was largely accounted for by a 25% reduction in moderate exacerbations, but there was no significant difference between aspirin users and nonusers in severe exacerbations.
A similar pattern was seen after just 1 year of follow-up, with an overall 30% reduction in the incidence of exacerbations, a 37% reduction in moderate exacerbations, but no significant reduction in severe exacerbations.
“Though aspirin use has previously been linked with reduced mortality risk in patients with COPD, to our knowledge, this is the first study to investigate the association of daily aspirin use with respiratory morbidity in COPD,” wrote Ashraf Fawzy, MD, of the division of pulmonary and critical care medicine at Johns Hopkins University, Baltimore, and his coauthors.
The association between aspirin use and reduced incidence of exacerbations was stronger among individuals with chronic bronchitis, which prompted the authors to suggest that future studies of aspirin in COPD should focus on participants with chronic bronchitis.
However, the association was not affected by COPD severity, emphysema presence or severity, or cardiometabolic phenotype.
Aspirin users reported better respiratory-specific quality of life than that of nonusers, including 34% lower odds of reporting moderate to severe dyspnea, and better baseline COPD health status.
“Findings of this study add to the existing literature by highlighting that aspirin use is also associated with reduced respiratory morbidity across several domains – including exacerbation risk, quality of life, and dyspnea – factors related to patient well-being and healthcare utilization,” the authors wrote.
Aspirin users were more likely to be white, male, and obese, and less likely to be smokers. They had better lung function but more cardiovascular comorbidities at baseline, although the aspirin users and nonusers were matched on baseline characteristics.
Speculating on the mechanisms by which aspirin might impact COPD exacerbations, the authors noted that the drug has both systemic and local pulmonary mechanisms of action.
For example, a pathway that results in elevated levels of a urinary metabolite in patients with COPD is irreversibly blocked by aspirin. Aspirin also attenuates the elevation of inflammatory markers interleukin-6 and C-reactive protein, which are part of the inflammatory phenotype of COPD. Aspirin has been shown to reduce proinflammatory cytokines in the lung.
The authors did note that aspirin use was self-reported, so they did not have data on dosage or duration of use.
The National Institutes of Health funded the study. Six authors declared advisory board positions, research support, and other funding from the pharmaceutical sector. One author was also a founder of a company commercializing lung image analysis software. No other conflicts of interest were declared.
SOURCE: Fawzy A et al. Chest. 2019 Mar;155(3): 519-27. doi: 10.1016/j.chest.2018.11.028.
Daily aspirin use could reduce the risk of acute exacerbations of chronic obstructive pulmonary disease, new data suggest.
Researchers reported the outcomes of an observational cohort study of 1,698 individuals with COPD, 45% of whom said they were taking daily aspirin at baseline. Their findings were published in Chest.
After a median follow up of 2.7 years, aspirin users had an overall 22% lower incidence of acute COPD exacerbations compared with nonusers. This was largely accounted for by a 25% reduction in moderate exacerbations, but there was no significant difference between aspirin users and nonusers in severe exacerbations.
A similar pattern was seen after just 1 year of follow-up, with an overall 30% reduction in the incidence of exacerbations, a 37% reduction in moderate exacerbations, but no significant reduction in severe exacerbations.
“Though aspirin use has previously been linked with reduced mortality risk in patients with COPD, to our knowledge, this is the first study to investigate the association of daily aspirin use with respiratory morbidity in COPD,” wrote Ashraf Fawzy, MD, of the division of pulmonary and critical care medicine at Johns Hopkins University, Baltimore, and his coauthors.
The association between aspirin use and reduced incidence of exacerbations was stronger among individuals with chronic bronchitis, which prompted the authors to suggest that future studies of aspirin in COPD should focus on participants with chronic bronchitis.
However, the association was not affected by COPD severity, emphysema presence or severity, or cardiometabolic phenotype.
Aspirin users reported better respiratory-specific quality of life than that of nonusers, including 34% lower odds of reporting moderate to severe dyspnea, and better baseline COPD health status.
“Findings of this study add to the existing literature by highlighting that aspirin use is also associated with reduced respiratory morbidity across several domains – including exacerbation risk, quality of life, and dyspnea – factors related to patient well-being and healthcare utilization,” the authors wrote.
Aspirin users were more likely to be white, male, and obese, and less likely to be smokers. They had better lung function but more cardiovascular comorbidities at baseline, although the aspirin users and nonusers were matched on baseline characteristics.
Speculating on the mechanisms by which aspirin might impact COPD exacerbations, the authors noted that the drug has both systemic and local pulmonary mechanisms of action.
For example, a pathway that results in elevated levels of a urinary metabolite in patients with COPD is irreversibly blocked by aspirin. Aspirin also attenuates the elevation of inflammatory markers interleukin-6 and C-reactive protein, which are part of the inflammatory phenotype of COPD. Aspirin has been shown to reduce proinflammatory cytokines in the lung.
The authors did note that aspirin use was self-reported, so they did not have data on dosage or duration of use.
The National Institutes of Health funded the study. Six authors declared advisory board positions, research support, and other funding from the pharmaceutical sector. One author was also a founder of a company commercializing lung image analysis software. No other conflicts of interest were declared.
SOURCE: Fawzy A et al. Chest. 2019 Mar;155(3): 519-27. doi: 10.1016/j.chest.2018.11.028.
FROM CHEST
Quitting smoking during pregnancy cuts SUID risk
Odds of sudden unexpected infant death (SUID) more than doubled with maternal prenatal smoking and increased linearly with each additional cigarette mothers smoked during pregnancy, but quitting smoking during pregnancy cut SUID risk, according to a new study in Pediatrics.
“As prevalence of prone sleeping has declined, the relative contribution of prenatal maternal smoking to the risk of sudden infant death has increased,” Tatiana M. Anderson, PhD, of the Seattle Children’s Research Institute and her associates reported. When the researchers considered causality, they estimated that approximately 800 infants (22% of all SUID cases) per year in the United States could be attributed to maternal smoking during pregnancy.
The researchers analyzed 19,127 SUID cases among 20,685,463 births included in the Centers for Disease Control and Prevention Birth Cohort Linked Birth/Infant Death Data Set for 2007-2011. A SUID diagnosis included sudden infant death syndrome, infant death from ill-defined or unknown cause, and accidental suffocation or strangulation in bed for any infants under 1 year old.
When the authors calculated odds related to prenatal maternal smoking and SUID, they adjusted for infant sex and birth weight, gestational length of pregnancy, delivery method (vaginal or cesarean), total prenatal visits, live birth order, maternal marital status and education, and maternal and paternal age and race/ethnicity.
Any maternal smoking at all during pregnancy was associated with more than twice the odds of SUID (adjusted odds ratio, 2.44). Odds of SUID also doubled for smoking one cigarette daily during pregnancy versus smoking none. For each additional cigarette smoked daily during pregnancy, odds of SUID increased by 0.07 up until 20 cigarettes, when the risk evened out, which suggests “that smoking cessation efforts may have greater impact on decreasing SUID rates when directed toward those who smoke fewer than 1 pack per day versus the more traditionally targeted heavy ([more than] 20 cigarettes per day) smokers,” the authors wrote.
Odds of SUID dropped 12% when mothers cut down on smoking during pregnancy and dropped 23% when they quit altogether (aORs, 0.88 and 0.77, respectively). “However, there may be some selection bias because the group who reduced smoking started at a higher average number of cigarettes in the first trimester, whereas those who successfully quit smoked fewer cigarettes in the first trimester,” the authors noted.
Among the 11.6% of mothers who said in 2011 that they smoked in the 3 months leading up to pregnancy, only a quarter quit while pregnant, the authors wrote. Quitting after having smoked before pregnancy was linked to a 47% increased risk of SUID, although the researchers noted that second- and third-hand smoke may have played a role since mothers who smoke may begin smoking again post partum and/or often have a partner who smokes.
“This group may have also included women who stopped smoking as soon as they knew they were pregnant and thus reported that they were nonsmokers in the first trimester, but the fetus had been exposed to maternal smoking during the period before pregnancy was diagnosed,” the authors wrote. They also acknowledged the possibility of residual confounding, particularly from socioeconomic factors or alcohol consumption during pregnancy.
The research was funded by the National Institutes of Health, Microsoft, and the Aaron Matthew Sudden Infant Death Syndrome Research Guild. One author has testified as a paid expert in a SUID case. No other authors reported conflicts of interest.
SOURCE: Anderson TM et al. Pediatrics. 2019 March 11. doi: 10.1542/peds.2018-3325.
Odds of sudden unexpected infant death (SUID) more than doubled with maternal prenatal smoking and increased linearly with each additional cigarette mothers smoked during pregnancy, but quitting smoking during pregnancy cut SUID risk, according to a new study in Pediatrics.
“As prevalence of prone sleeping has declined, the relative contribution of prenatal maternal smoking to the risk of sudden infant death has increased,” Tatiana M. Anderson, PhD, of the Seattle Children’s Research Institute and her associates reported. When the researchers considered causality, they estimated that approximately 800 infants (22% of all SUID cases) per year in the United States could be attributed to maternal smoking during pregnancy.
The researchers analyzed 19,127 SUID cases among 20,685,463 births included in the Centers for Disease Control and Prevention Birth Cohort Linked Birth/Infant Death Data Set for 2007-2011. A SUID diagnosis included sudden infant death syndrome, infant death from ill-defined or unknown cause, and accidental suffocation or strangulation in bed for any infants under 1 year old.
When the authors calculated odds related to prenatal maternal smoking and SUID, they adjusted for infant sex and birth weight, gestational length of pregnancy, delivery method (vaginal or cesarean), total prenatal visits, live birth order, maternal marital status and education, and maternal and paternal age and race/ethnicity.
Any maternal smoking at all during pregnancy was associated with more than twice the odds of SUID (adjusted odds ratio, 2.44). Odds of SUID also doubled for smoking one cigarette daily during pregnancy versus smoking none. For each additional cigarette smoked daily during pregnancy, odds of SUID increased by 0.07 up until 20 cigarettes, when the risk evened out, which suggests “that smoking cessation efforts may have greater impact on decreasing SUID rates when directed toward those who smoke fewer than 1 pack per day versus the more traditionally targeted heavy ([more than] 20 cigarettes per day) smokers,” the authors wrote.
Odds of SUID dropped 12% when mothers cut down on smoking during pregnancy and dropped 23% when they quit altogether (aORs, 0.88 and 0.77, respectively). “However, there may be some selection bias because the group who reduced smoking started at a higher average number of cigarettes in the first trimester, whereas those who successfully quit smoked fewer cigarettes in the first trimester,” the authors noted.
Among the 11.6% of mothers who said in 2011 that they smoked in the 3 months leading up to pregnancy, only a quarter quit while pregnant, the authors wrote. Quitting after having smoked before pregnancy was linked to a 47% increased risk of SUID, although the researchers noted that second- and third-hand smoke may have played a role since mothers who smoke may begin smoking again post partum and/or often have a partner who smokes.
“This group may have also included women who stopped smoking as soon as they knew they were pregnant and thus reported that they were nonsmokers in the first trimester, but the fetus had been exposed to maternal smoking during the period before pregnancy was diagnosed,” the authors wrote. They also acknowledged the possibility of residual confounding, particularly from socioeconomic factors or alcohol consumption during pregnancy.
The research was funded by the National Institutes of Health, Microsoft, and the Aaron Matthew Sudden Infant Death Syndrome Research Guild. One author has testified as a paid expert in a SUID case. No other authors reported conflicts of interest.
SOURCE: Anderson TM et al. Pediatrics. 2019 March 11. doi: 10.1542/peds.2018-3325.
Odds of sudden unexpected infant death (SUID) more than doubled with maternal prenatal smoking and increased linearly with each additional cigarette mothers smoked during pregnancy, but quitting smoking during pregnancy cut SUID risk, according to a new study in Pediatrics.
“As prevalence of prone sleeping has declined, the relative contribution of prenatal maternal smoking to the risk of sudden infant death has increased,” Tatiana M. Anderson, PhD, of the Seattle Children’s Research Institute and her associates reported. When the researchers considered causality, they estimated that approximately 800 infants (22% of all SUID cases) per year in the United States could be attributed to maternal smoking during pregnancy.
The researchers analyzed 19,127 SUID cases among 20,685,463 births included in the Centers for Disease Control and Prevention Birth Cohort Linked Birth/Infant Death Data Set for 2007-2011. A SUID diagnosis included sudden infant death syndrome, infant death from ill-defined or unknown cause, and accidental suffocation or strangulation in bed for any infants under 1 year old.
When the authors calculated odds related to prenatal maternal smoking and SUID, they adjusted for infant sex and birth weight, gestational length of pregnancy, delivery method (vaginal or cesarean), total prenatal visits, live birth order, maternal marital status and education, and maternal and paternal age and race/ethnicity.
Any maternal smoking at all during pregnancy was associated with more than twice the odds of SUID (adjusted odds ratio, 2.44). Odds of SUID also doubled for smoking one cigarette daily during pregnancy versus smoking none. For each additional cigarette smoked daily during pregnancy, odds of SUID increased by 0.07 up until 20 cigarettes, when the risk evened out, which suggests “that smoking cessation efforts may have greater impact on decreasing SUID rates when directed toward those who smoke fewer than 1 pack per day versus the more traditionally targeted heavy ([more than] 20 cigarettes per day) smokers,” the authors wrote.
Odds of SUID dropped 12% when mothers cut down on smoking during pregnancy and dropped 23% when they quit altogether (aORs, 0.88 and 0.77, respectively). “However, there may be some selection bias because the group who reduced smoking started at a higher average number of cigarettes in the first trimester, whereas those who successfully quit smoked fewer cigarettes in the first trimester,” the authors noted.
Among the 11.6% of mothers who said in 2011 that they smoked in the 3 months leading up to pregnancy, only a quarter quit while pregnant, the authors wrote. Quitting after having smoked before pregnancy was linked to a 47% increased risk of SUID, although the researchers noted that second- and third-hand smoke may have played a role since mothers who smoke may begin smoking again post partum and/or often have a partner who smokes.
“This group may have also included women who stopped smoking as soon as they knew they were pregnant and thus reported that they were nonsmokers in the first trimester, but the fetus had been exposed to maternal smoking during the period before pregnancy was diagnosed,” the authors wrote. They also acknowledged the possibility of residual confounding, particularly from socioeconomic factors or alcohol consumption during pregnancy.
The research was funded by the National Institutes of Health, Microsoft, and the Aaron Matthew Sudden Infant Death Syndrome Research Guild. One author has testified as a paid expert in a SUID case. No other authors reported conflicts of interest.
SOURCE: Anderson TM et al. Pediatrics. 2019 March 11. doi: 10.1542/peds.2018-3325.
FROM PEDIATRICS
Prenatal betamethasone not linked to later adverse neurocognitive problems
Administering prenatal corticosteroids to women at risk for preterm birth does not appear to contribute to adverse neurocognitive function in children 6-8 years later, regardless of whether they had fetal growth restriction, a new study found.
Women at less than 32 weeks’ gestation are recommended to receive multiple betamethasone doses if they have a high ongoing risk of preterm birth. However, concern existed regarding possible effects of these steroid doses on the infant in later childhood, particularly in cases of fetal growth restriction (FGR) because of “animal studies suggesting long-term adverse effects of treatment on neurosensory function,” Robert D. Cartwright of the University of Auckland (New Zealand), and his associates reported in JAMA Network Open.
Yet no such effects were identified in this preplanned follow-up analysis of the placebo-controlled, randomized Australasian Collaborative Trial of Repeat Doses of Corticosteroids (ACTORDS). “Physicians should use repeated doses of antenatal corticosteroids when indicated before preterm birth, regardless of fetal growth restriction, in view of the associated neonatal benefits and absence of later adverse effects,” the authors concluded.
The original ACTORDS study involved 982 women pregnant with 1,146 fetuses at 23 hospitals throughout Australia and New Zealand, enrolled from April 1998 to July 2004. All enrolled women were less than 32 weeks’ gestation, had received an initial course of corticosteroids, and had an ongoing risk of preterm birth at least 7 days later.
Women were randomly assigned to receive an intramuscular dose of betamethasone or saline placebo weekly until birth or preterm birth risk abated. The current follow-up, when children were 6-8 years old, was planned during the 2-year follow-up. Children underwent a pediatrician’s physical and neurologic exam, vision and hearing screening, and fine and gross motor testing. A psychologist tested children’s IQ, attention, executive function, and academic skills using standardized, validated assessment tools. Caregivers also rated children’s behavioral and emotional problems, executive function abilities, and attention in questionnaires.
Among 988 of 1,059 surviving children assessed, FGR occurred in 28% of children exposed to betamethasone and 25% in the placebo group.
For the primary outcomes, rates of disability-free survival were similar in both the placebo and betamethasone groups for children with (odds ratio, 1.1) and without FGR (OR, 1.0). Rates also were similar for death or survival with moderate to severe disability (FGR: OR, 0.9; and non-FGR: OR, 0.8).
“Some evidence suggested a differential effect for several secondary outcomes, with better scores for selective and divided attention after exposure to repeated antenatal betamethasone in children with FGR, but poorer scores for impulse control in children without FGR,” Dr. Cartwright and his associates reported. “These effects were small and of uncertain clinical significance and may reflect type I error.
“For all other measures of neurocognitive function and learning, exposure to repeated antenatal betamethasone treatment did not alter performance in midchildhood, even in the presence of FGR,” they added.
Children with FGR had an increased risk of death or moderate to severe disability, compared with children without FGR, regardless of treatment group. Those with FGR also had greater risk of motor impairment.
One possible reason for not finding adverse neurocognitive effects in the betamethasone group is “that infants with fetal growth restriction appeared to have greater benefit from repeated antenatal corticosteroid therapy, with a nearly twofold reduction in serious neonatal morbidity,” the authors surmised. “Thus, the decrease in serious postnatal complications may have counteracted any potential adverse effects of corticosteroid exposure.” But they noted a continuing concern about whether “repeated antenatal corticosteroids in FGR could increase the risk of ADHD.”
The research was funded by the National Health Medical Research Council of Australia, the Health Research Council of New Zealand and the Auckland Medical Research Foundation. One coauthor reported receiving grants from National Health and Medical Research Council of Australia, and a second coauthor received grants from the Auckland Medical Research Foundation.
SOURCE: Cartwright RD et al. JAMA Netw Open. 2019 Feb 1. doi:10.1001/jamanetworkopen.2018.7636.
Administering prenatal corticosteroids to women at risk for preterm birth does not appear to contribute to adverse neurocognitive function in children 6-8 years later, regardless of whether they had fetal growth restriction, a new study found.
Women at less than 32 weeks’ gestation are recommended to receive multiple betamethasone doses if they have a high ongoing risk of preterm birth. However, concern existed regarding possible effects of these steroid doses on the infant in later childhood, particularly in cases of fetal growth restriction (FGR) because of “animal studies suggesting long-term adverse effects of treatment on neurosensory function,” Robert D. Cartwright of the University of Auckland (New Zealand), and his associates reported in JAMA Network Open.
Yet no such effects were identified in this preplanned follow-up analysis of the placebo-controlled, randomized Australasian Collaborative Trial of Repeat Doses of Corticosteroids (ACTORDS). “Physicians should use repeated doses of antenatal corticosteroids when indicated before preterm birth, regardless of fetal growth restriction, in view of the associated neonatal benefits and absence of later adverse effects,” the authors concluded.
The original ACTORDS study involved 982 women pregnant with 1,146 fetuses at 23 hospitals throughout Australia and New Zealand, enrolled from April 1998 to July 2004. All enrolled women were less than 32 weeks’ gestation, had received an initial course of corticosteroids, and had an ongoing risk of preterm birth at least 7 days later.
Women were randomly assigned to receive an intramuscular dose of betamethasone or saline placebo weekly until birth or preterm birth risk abated. The current follow-up, when children were 6-8 years old, was planned during the 2-year follow-up. Children underwent a pediatrician’s physical and neurologic exam, vision and hearing screening, and fine and gross motor testing. A psychologist tested children’s IQ, attention, executive function, and academic skills using standardized, validated assessment tools. Caregivers also rated children’s behavioral and emotional problems, executive function abilities, and attention in questionnaires.
Among 988 of 1,059 surviving children assessed, FGR occurred in 28% of children exposed to betamethasone and 25% in the placebo group.
For the primary outcomes, rates of disability-free survival were similar in both the placebo and betamethasone groups for children with (odds ratio, 1.1) and without FGR (OR, 1.0). Rates also were similar for death or survival with moderate to severe disability (FGR: OR, 0.9; and non-FGR: OR, 0.8).
“Some evidence suggested a differential effect for several secondary outcomes, with better scores for selective and divided attention after exposure to repeated antenatal betamethasone in children with FGR, but poorer scores for impulse control in children without FGR,” Dr. Cartwright and his associates reported. “These effects were small and of uncertain clinical significance and may reflect type I error.
“For all other measures of neurocognitive function and learning, exposure to repeated antenatal betamethasone treatment did not alter performance in midchildhood, even in the presence of FGR,” they added.
Children with FGR had an increased risk of death or moderate to severe disability, compared with children without FGR, regardless of treatment group. Those with FGR also had greater risk of motor impairment.
One possible reason for not finding adverse neurocognitive effects in the betamethasone group is “that infants with fetal growth restriction appeared to have greater benefit from repeated antenatal corticosteroid therapy, with a nearly twofold reduction in serious neonatal morbidity,” the authors surmised. “Thus, the decrease in serious postnatal complications may have counteracted any potential adverse effects of corticosteroid exposure.” But they noted a continuing concern about whether “repeated antenatal corticosteroids in FGR could increase the risk of ADHD.”
The research was funded by the National Health Medical Research Council of Australia, the Health Research Council of New Zealand and the Auckland Medical Research Foundation. One coauthor reported receiving grants from National Health and Medical Research Council of Australia, and a second coauthor received grants from the Auckland Medical Research Foundation.
SOURCE: Cartwright RD et al. JAMA Netw Open. 2019 Feb 1. doi:10.1001/jamanetworkopen.2018.7636.
Administering prenatal corticosteroids to women at risk for preterm birth does not appear to contribute to adverse neurocognitive function in children 6-8 years later, regardless of whether they had fetal growth restriction, a new study found.
Women at less than 32 weeks’ gestation are recommended to receive multiple betamethasone doses if they have a high ongoing risk of preterm birth. However, concern existed regarding possible effects of these steroid doses on the infant in later childhood, particularly in cases of fetal growth restriction (FGR) because of “animal studies suggesting long-term adverse effects of treatment on neurosensory function,” Robert D. Cartwright of the University of Auckland (New Zealand), and his associates reported in JAMA Network Open.
Yet no such effects were identified in this preplanned follow-up analysis of the placebo-controlled, randomized Australasian Collaborative Trial of Repeat Doses of Corticosteroids (ACTORDS). “Physicians should use repeated doses of antenatal corticosteroids when indicated before preterm birth, regardless of fetal growth restriction, in view of the associated neonatal benefits and absence of later adverse effects,” the authors concluded.
The original ACTORDS study involved 982 women pregnant with 1,146 fetuses at 23 hospitals throughout Australia and New Zealand, enrolled from April 1998 to July 2004. All enrolled women were less than 32 weeks’ gestation, had received an initial course of corticosteroids, and had an ongoing risk of preterm birth at least 7 days later.
Women were randomly assigned to receive an intramuscular dose of betamethasone or saline placebo weekly until birth or preterm birth risk abated. The current follow-up, when children were 6-8 years old, was planned during the 2-year follow-up. Children underwent a pediatrician’s physical and neurologic exam, vision and hearing screening, and fine and gross motor testing. A psychologist tested children’s IQ, attention, executive function, and academic skills using standardized, validated assessment tools. Caregivers also rated children’s behavioral and emotional problems, executive function abilities, and attention in questionnaires.
Among 988 of 1,059 surviving children assessed, FGR occurred in 28% of children exposed to betamethasone and 25% in the placebo group.
For the primary outcomes, rates of disability-free survival were similar in both the placebo and betamethasone groups for children with (odds ratio, 1.1) and without FGR (OR, 1.0). Rates also were similar for death or survival with moderate to severe disability (FGR: OR, 0.9; and non-FGR: OR, 0.8).
“Some evidence suggested a differential effect for several secondary outcomes, with better scores for selective and divided attention after exposure to repeated antenatal betamethasone in children with FGR, but poorer scores for impulse control in children without FGR,” Dr. Cartwright and his associates reported. “These effects were small and of uncertain clinical significance and may reflect type I error.
“For all other measures of neurocognitive function and learning, exposure to repeated antenatal betamethasone treatment did not alter performance in midchildhood, even in the presence of FGR,” they added.
Children with FGR had an increased risk of death or moderate to severe disability, compared with children without FGR, regardless of treatment group. Those with FGR also had greater risk of motor impairment.
One possible reason for not finding adverse neurocognitive effects in the betamethasone group is “that infants with fetal growth restriction appeared to have greater benefit from repeated antenatal corticosteroid therapy, with a nearly twofold reduction in serious neonatal morbidity,” the authors surmised. “Thus, the decrease in serious postnatal complications may have counteracted any potential adverse effects of corticosteroid exposure.” But they noted a continuing concern about whether “repeated antenatal corticosteroids in FGR could increase the risk of ADHD.”
The research was funded by the National Health Medical Research Council of Australia, the Health Research Council of New Zealand and the Auckland Medical Research Foundation. One coauthor reported receiving grants from National Health and Medical Research Council of Australia, and a second coauthor received grants from the Auckland Medical Research Foundation.
SOURCE: Cartwright RD et al. JAMA Netw Open. 2019 Feb 1. doi:10.1001/jamanetworkopen.2018.7636.
FROM JAMA NETWORK OPEN
‘Telereferrals’ improved mental health referral follow-through
Children referred for mental health services in Los Angeles County using a telehealth referral were three times more likely to complete a community mental health clinic (CMHC) screening than children receiving conventional mental health referrals, a study found.
“Our findings highlight the importance of this initial access point for a successful referral to the CHMC,” Tumaini R. Coker, MD, MBA, of the University of Washington, Seattle, and Seattle Children’s Research Institute, and her colleagues wrote in Pediatrics. “We can hypothesize that the assistance from the telehealth care coordinator may have played an important role in access for families.”
Although this study was not powered to compare psychological health or quality-of-life differences, a larger study with a longer follow-up period may allow study of “variation in health outcomes … among a sample of all who were initially referred, particularly if the higher rates of access for children in the intervention translate into a greater proportion of children receiving services,” the authors wrote.
The research group partnered with two community mental health clinics (CMHCs) and six federally qualified health center clinics, the latter randomly assigned as control or intervention. The telehealth-enhanced referral process developed by the researchers involved patients at the intervention clinics viewing a video orientation to the CMHC and then participating in a live video conference for screening. Completion of the referral screening visit was the measure for CMHC access as a primary endpoint.
Among the 342 children, aged 5-12 years (average, 9 years), enrolled in the study, 87% were Latino, and 62% were boys.
Of children using the telehealth referral process, 80% completed an initial CMHC screening, compared to 64% of children receiving referrals via usual care procedures, resulting in three-times greater odds of a screening in the intervention group (adjusted odds ratio, 3.02).
It took approximately 6 more days for the telehealth-referred children to complete the screening.
“The increased time to the initial access point was anticipated for the intervention clinics because the telehealth care coordinator and CMHC staff held all the videoconference screening visits on a single preselected day each week,” which thereby limited availability of slots for screenings, Dr. Coker and her associates wrote.
Children who received telehealth-enabled referrals reported higher satisfaction levels with the referral system and with care, compared with those using usual care methods. Of the 342 children in the study, 213 were considered eligible to receive CMHC services. Reasons for ineligibility for services included presence of a developmental disability, lack of an mental health need, private health insurance coverage, a zip code outside of the CMHC’s catchment area, and not meeting income requirements.
Of those 213, 80% of the intervention group and 84% of controls subsequently had a mental health visit.
A study limitation is its personalization to the community partners involved, which may require different procedures in other settings, the authors noted. The study also did not look at the quality of mental health services received after initial screenings, precluding the ability to assess clinical outcomes. In addition, “the CMHCs did not involve the payers of mental health care for this population, limiting our capacity to identify barriers and system solutions that may improve the intervention’s sustainability,” the authors wrote.
The research was funded by grants from the Patient-Centered Outcomes Research Institute and the California Community Foundation. The authors reported having no relevant financial disclosures.
SOURCE: Coker TR et al. Pediatrics. 2019 Feb 15. doi: 10.1542/peds.2018-2738.
Despite the challenges of meeting patients’ and their families’ mental and behavioral needs, Coker et al. “had the courage to think outside the box to solve a practice and community need,” Susan J. Kressly, MD, is in private practice in Warrington, Pa., wrote in an accompanying editorial.
Some practices have been able to fully integrate a mental health service within their practice, usually on-site, but that model does not work for everyone. Space and privacy can be problematic, depending on the practice, and payment models can become complex, especially when mental health benefits are not managed by the same payer or through the same plan as other health insurance benefits, Dr. Kressly noted.
“The innovative model in this study combines a ‘soft hand-off’ referral model and takes advantage of telehealth technology for implementation,” she wrote. Families frequently do not follow through on recommendations and referrals, but practices can improve follow-through when they make personal introductions and appointments from their own practice. And using technology to do so can particularly resonate with the generations of children and parents now coming to pediatric practices.
“As pediatricians, we have a unique opportunity to provide care to families who are digital natives,” Dr. Kressly wrote. “As part of the family’s health care team, if we truly decide to put the patient and family at the center, pediatricians should examine their own hesitancy and trepidation regarding telehealth and technology-enabled communications and work to overcome them.”
Other ways to use telehealth beyond the referral system described by Coker et al. might include providing actual telepsychiatry visits at the child’s medical home or connecting families to local resources.
“Those practices that innovate to solve their problems by extending their medical home to include care teams outside their practice walls will likely see improved family satisfaction and, hopefully, improved outcomes,” Dr. Kressly suggested.
Dr. Kressly is in private practice in Warrington, Pa. She used no external funding and has no financial conflicts to report. These comments are condensed and summarized from her editorial accompanying the article by Coker et al (Pediatrics. 2019 Feb 15. doi: 10.1542/peds.2018-3765).
Despite the challenges of meeting patients’ and their families’ mental and behavioral needs, Coker et al. “had the courage to think outside the box to solve a practice and community need,” Susan J. Kressly, MD, is in private practice in Warrington, Pa., wrote in an accompanying editorial.
Some practices have been able to fully integrate a mental health service within their practice, usually on-site, but that model does not work for everyone. Space and privacy can be problematic, depending on the practice, and payment models can become complex, especially when mental health benefits are not managed by the same payer or through the same plan as other health insurance benefits, Dr. Kressly noted.
“The innovative model in this study combines a ‘soft hand-off’ referral model and takes advantage of telehealth technology for implementation,” she wrote. Families frequently do not follow through on recommendations and referrals, but practices can improve follow-through when they make personal introductions and appointments from their own practice. And using technology to do so can particularly resonate with the generations of children and parents now coming to pediatric practices.
“As pediatricians, we have a unique opportunity to provide care to families who are digital natives,” Dr. Kressly wrote. “As part of the family’s health care team, if we truly decide to put the patient and family at the center, pediatricians should examine their own hesitancy and trepidation regarding telehealth and technology-enabled communications and work to overcome them.”
Other ways to use telehealth beyond the referral system described by Coker et al. might include providing actual telepsychiatry visits at the child’s medical home or connecting families to local resources.
“Those practices that innovate to solve their problems by extending their medical home to include care teams outside their practice walls will likely see improved family satisfaction and, hopefully, improved outcomes,” Dr. Kressly suggested.
Dr. Kressly is in private practice in Warrington, Pa. She used no external funding and has no financial conflicts to report. These comments are condensed and summarized from her editorial accompanying the article by Coker et al (Pediatrics. 2019 Feb 15. doi: 10.1542/peds.2018-3765).
Despite the challenges of meeting patients’ and their families’ mental and behavioral needs, Coker et al. “had the courage to think outside the box to solve a practice and community need,” Susan J. Kressly, MD, is in private practice in Warrington, Pa., wrote in an accompanying editorial.
Some practices have been able to fully integrate a mental health service within their practice, usually on-site, but that model does not work for everyone. Space and privacy can be problematic, depending on the practice, and payment models can become complex, especially when mental health benefits are not managed by the same payer or through the same plan as other health insurance benefits, Dr. Kressly noted.
“The innovative model in this study combines a ‘soft hand-off’ referral model and takes advantage of telehealth technology for implementation,” she wrote. Families frequently do not follow through on recommendations and referrals, but practices can improve follow-through when they make personal introductions and appointments from their own practice. And using technology to do so can particularly resonate with the generations of children and parents now coming to pediatric practices.
“As pediatricians, we have a unique opportunity to provide care to families who are digital natives,” Dr. Kressly wrote. “As part of the family’s health care team, if we truly decide to put the patient and family at the center, pediatricians should examine their own hesitancy and trepidation regarding telehealth and technology-enabled communications and work to overcome them.”
Other ways to use telehealth beyond the referral system described by Coker et al. might include providing actual telepsychiatry visits at the child’s medical home or connecting families to local resources.
“Those practices that innovate to solve their problems by extending their medical home to include care teams outside their practice walls will likely see improved family satisfaction and, hopefully, improved outcomes,” Dr. Kressly suggested.
Dr. Kressly is in private practice in Warrington, Pa. She used no external funding and has no financial conflicts to report. These comments are condensed and summarized from her editorial accompanying the article by Coker et al (Pediatrics. 2019 Feb 15. doi: 10.1542/peds.2018-3765).
Children referred for mental health services in Los Angeles County using a telehealth referral were three times more likely to complete a community mental health clinic (CMHC) screening than children receiving conventional mental health referrals, a study found.
“Our findings highlight the importance of this initial access point for a successful referral to the CHMC,” Tumaini R. Coker, MD, MBA, of the University of Washington, Seattle, and Seattle Children’s Research Institute, and her colleagues wrote in Pediatrics. “We can hypothesize that the assistance from the telehealth care coordinator may have played an important role in access for families.”
Although this study was not powered to compare psychological health or quality-of-life differences, a larger study with a longer follow-up period may allow study of “variation in health outcomes … among a sample of all who were initially referred, particularly if the higher rates of access for children in the intervention translate into a greater proportion of children receiving services,” the authors wrote.
The research group partnered with two community mental health clinics (CMHCs) and six federally qualified health center clinics, the latter randomly assigned as control or intervention. The telehealth-enhanced referral process developed by the researchers involved patients at the intervention clinics viewing a video orientation to the CMHC and then participating in a live video conference for screening. Completion of the referral screening visit was the measure for CMHC access as a primary endpoint.
Among the 342 children, aged 5-12 years (average, 9 years), enrolled in the study, 87% were Latino, and 62% were boys.
Of children using the telehealth referral process, 80% completed an initial CMHC screening, compared to 64% of children receiving referrals via usual care procedures, resulting in three-times greater odds of a screening in the intervention group (adjusted odds ratio, 3.02).
It took approximately 6 more days for the telehealth-referred children to complete the screening.
“The increased time to the initial access point was anticipated for the intervention clinics because the telehealth care coordinator and CMHC staff held all the videoconference screening visits on a single preselected day each week,” which thereby limited availability of slots for screenings, Dr. Coker and her associates wrote.
Children who received telehealth-enabled referrals reported higher satisfaction levels with the referral system and with care, compared with those using usual care methods. Of the 342 children in the study, 213 were considered eligible to receive CMHC services. Reasons for ineligibility for services included presence of a developmental disability, lack of an mental health need, private health insurance coverage, a zip code outside of the CMHC’s catchment area, and not meeting income requirements.
Of those 213, 80% of the intervention group and 84% of controls subsequently had a mental health visit.
A study limitation is its personalization to the community partners involved, which may require different procedures in other settings, the authors noted. The study also did not look at the quality of mental health services received after initial screenings, precluding the ability to assess clinical outcomes. In addition, “the CMHCs did not involve the payers of mental health care for this population, limiting our capacity to identify barriers and system solutions that may improve the intervention’s sustainability,” the authors wrote.
The research was funded by grants from the Patient-Centered Outcomes Research Institute and the California Community Foundation. The authors reported having no relevant financial disclosures.
SOURCE: Coker TR et al. Pediatrics. 2019 Feb 15. doi: 10.1542/peds.2018-2738.
Children referred for mental health services in Los Angeles County using a telehealth referral were three times more likely to complete a community mental health clinic (CMHC) screening than children receiving conventional mental health referrals, a study found.
“Our findings highlight the importance of this initial access point for a successful referral to the CHMC,” Tumaini R. Coker, MD, MBA, of the University of Washington, Seattle, and Seattle Children’s Research Institute, and her colleagues wrote in Pediatrics. “We can hypothesize that the assistance from the telehealth care coordinator may have played an important role in access for families.”
Although this study was not powered to compare psychological health or quality-of-life differences, a larger study with a longer follow-up period may allow study of “variation in health outcomes … among a sample of all who were initially referred, particularly if the higher rates of access for children in the intervention translate into a greater proportion of children receiving services,” the authors wrote.
The research group partnered with two community mental health clinics (CMHCs) and six federally qualified health center clinics, the latter randomly assigned as control or intervention. The telehealth-enhanced referral process developed by the researchers involved patients at the intervention clinics viewing a video orientation to the CMHC and then participating in a live video conference for screening. Completion of the referral screening visit was the measure for CMHC access as a primary endpoint.
Among the 342 children, aged 5-12 years (average, 9 years), enrolled in the study, 87% were Latino, and 62% were boys.
Of children using the telehealth referral process, 80% completed an initial CMHC screening, compared to 64% of children receiving referrals via usual care procedures, resulting in three-times greater odds of a screening in the intervention group (adjusted odds ratio, 3.02).
It took approximately 6 more days for the telehealth-referred children to complete the screening.
“The increased time to the initial access point was anticipated for the intervention clinics because the telehealth care coordinator and CMHC staff held all the videoconference screening visits on a single preselected day each week,” which thereby limited availability of slots for screenings, Dr. Coker and her associates wrote.
Children who received telehealth-enabled referrals reported higher satisfaction levels with the referral system and with care, compared with those using usual care methods. Of the 342 children in the study, 213 were considered eligible to receive CMHC services. Reasons for ineligibility for services included presence of a developmental disability, lack of an mental health need, private health insurance coverage, a zip code outside of the CMHC’s catchment area, and not meeting income requirements.
Of those 213, 80% of the intervention group and 84% of controls subsequently had a mental health visit.
A study limitation is its personalization to the community partners involved, which may require different procedures in other settings, the authors noted. The study also did not look at the quality of mental health services received after initial screenings, precluding the ability to assess clinical outcomes. In addition, “the CMHCs did not involve the payers of mental health care for this population, limiting our capacity to identify barriers and system solutions that may improve the intervention’s sustainability,” the authors wrote.
The research was funded by grants from the Patient-Centered Outcomes Research Institute and the California Community Foundation. The authors reported having no relevant financial disclosures.
SOURCE: Coker TR et al. Pediatrics. 2019 Feb 15. doi: 10.1542/peds.2018-2738.
FROM PEDIATRICS
Key clinical point: Use of telehealth referrals increased children’s access to mental health services in an urban county.
Major finding:
Study details: The findings are based on a multisite, randomized, controlled trial that included 342 children, aged 5-12 years, at two community mental health clinics and six federally qualified health center clinics in Los Angeles County.
Disclosures: The research was funded by the Patient-Centered Outcomes Research Institute and the California Community Foundation. The authors reported having no relevant financial disclosures.
Source: Coker TR et al. Pediatrics. 2019 Feb 15. doi: 10.1542/peds.2018-2738.
High prevalence of sleep problems in children with autism spectrum disorder
Children with a diagnosis of autism spectrum disorder or another developmental delay or disorder that includes autistic characteristics are twice as likely to have sleeping problems, a multisite case-control study has found.
The findings match up with previous similar studies, but this study is among the largest to measure sleeping problems in children with autism spectrum disorder (ASD) with two control groups.
“ including physiologic differences, sleep disorders, developmental comorbidities, medical comorbidities causing sleep disruption, communication impairments, and behavioral disturbances,” Ann M. Reynolds, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and her associates reported in Pediatrics.
“Children with ASD are more likely to have anxiety, which may predispose them to sleep problems,” the authors added.
The study evaluated sleep habits and problems in 1,987 children aged 2-5 years. The study population included 522 children with ASD, 228 children with other developmental delays and disorders that have ASD characteristics, 534 children with other developmental delays and disorders, and 703 children from the general population.
Parents completed the Children Sleep Habits Questionnaire (CSHQ), a 33-item assessment tool typically used with a total score cutoff of 41 and above for identification of children with sleep disorders. The researchers also used a second, more conservative cutoff of 48 – the cutoff for the highest quartile in the general population group – to avoid overidentification with the lower cutoff.
Scores were adjusted for maternal education and race/ethnicity, family income, child age and sex, and child cognitive scores on the Mullen Scales of Early Learning (MSEL). The researchers also adjusted for genetic and/or neurologic diagnoses, including Down syndrome, fragile X, Rett syndrome, tuberous sclerosis, cerebral palsy, and neurofibromatosis.
Autistic children tended to have lower MSEL scores than the other children. Both the autistic children and those with other developmental disorders and delays were more likely than those in the general population to have neurologic or genetic conditions.
Based on a cutoff score of 48, autistic children had more than double the odds of sleep problems, compared with children in the general population (adjusted odds ratio, 2.37; P = .001) and children with other developmental delays (aOR, 2.12; P = .001).
With a cutoff of 41, ASD children’s odds of sleep problems were 1.45 times greater than the general population (P = .023) and 1.75 times greater than those with developmental delays (P = .001).
But children with developmental delays who displayed autistic characteristics did not have not significantly different prevalence of sleep problems than children with ASD had.
“The phenotypic overlay between children with ASD and children with developmental delay with ASD [characteristics] may explain the similarities in sleep disturbance among these two groups,” the authors wrote. Both groups have “higher rates of obsessive-compulsive symptoms, self-injurious behavior, ADHD symptoms, and developmental and communication impairments” than children with developmental delays without autistic characteristics.
The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
SOURCE: Reynolds AM et al. Pediatrics. 2019 Feb. 11. doi: 10.1542/peds.2018-0492.
We can help reduce night waking and improve sleep onset within 5-15 weeks after parents have been trained. “Successful behavioral programs include bedtime fading, teaching healthy sleep practices, and increasing a child’s physical activity during the day,” Catherine Lord, PhD, wrote. Although research supports melatonin as an effective intervention for helping children fall asleep and sleep longer, the high percentage of children in the study already taking melatonin reveals its limitations. “Thus, it is recommended that families try behavioral programs before trials with melatonin,” she wrote.
But families and providers can only work together to address sleep issues if providers ask about sleep concerns, help families implement interventions, and follow up with progress. “In most cases, this help does not have to come from sleep experts, but does require dedicated time and effort using the now-growing base of evidence about effective interventions,” she concluded.
These comments are condensed from an editorial (Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-2629) by Dr. Lord , a professor of psychiatry and biobehavioral sciences at the University of California Los Angeles. Dr. Lord reports royalties from diagnostic instruments used in this study that were donated to a not-for-profit agency. She is supported by grants from the National Institutes of Health and Simons Foundation Autism Research Initiative.
We can help reduce night waking and improve sleep onset within 5-15 weeks after parents have been trained. “Successful behavioral programs include bedtime fading, teaching healthy sleep practices, and increasing a child’s physical activity during the day,” Catherine Lord, PhD, wrote. Although research supports melatonin as an effective intervention for helping children fall asleep and sleep longer, the high percentage of children in the study already taking melatonin reveals its limitations. “Thus, it is recommended that families try behavioral programs before trials with melatonin,” she wrote.
But families and providers can only work together to address sleep issues if providers ask about sleep concerns, help families implement interventions, and follow up with progress. “In most cases, this help does not have to come from sleep experts, but does require dedicated time and effort using the now-growing base of evidence about effective interventions,” she concluded.
These comments are condensed from an editorial (Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-2629) by Dr. Lord , a professor of psychiatry and biobehavioral sciences at the University of California Los Angeles. Dr. Lord reports royalties from diagnostic instruments used in this study that were donated to a not-for-profit agency. She is supported by grants from the National Institutes of Health and Simons Foundation Autism Research Initiative.
We can help reduce night waking and improve sleep onset within 5-15 weeks after parents have been trained. “Successful behavioral programs include bedtime fading, teaching healthy sleep practices, and increasing a child’s physical activity during the day,” Catherine Lord, PhD, wrote. Although research supports melatonin as an effective intervention for helping children fall asleep and sleep longer, the high percentage of children in the study already taking melatonin reveals its limitations. “Thus, it is recommended that families try behavioral programs before trials with melatonin,” she wrote.
But families and providers can only work together to address sleep issues if providers ask about sleep concerns, help families implement interventions, and follow up with progress. “In most cases, this help does not have to come from sleep experts, but does require dedicated time and effort using the now-growing base of evidence about effective interventions,” she concluded.
These comments are condensed from an editorial (Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-2629) by Dr. Lord , a professor of psychiatry and biobehavioral sciences at the University of California Los Angeles. Dr. Lord reports royalties from diagnostic instruments used in this study that were donated to a not-for-profit agency. She is supported by grants from the National Institutes of Health and Simons Foundation Autism Research Initiative.
Children with a diagnosis of autism spectrum disorder or another developmental delay or disorder that includes autistic characteristics are twice as likely to have sleeping problems, a multisite case-control study has found.
The findings match up with previous similar studies, but this study is among the largest to measure sleeping problems in children with autism spectrum disorder (ASD) with two control groups.
“ including physiologic differences, sleep disorders, developmental comorbidities, medical comorbidities causing sleep disruption, communication impairments, and behavioral disturbances,” Ann M. Reynolds, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and her associates reported in Pediatrics.
“Children with ASD are more likely to have anxiety, which may predispose them to sleep problems,” the authors added.
The study evaluated sleep habits and problems in 1,987 children aged 2-5 years. The study population included 522 children with ASD, 228 children with other developmental delays and disorders that have ASD characteristics, 534 children with other developmental delays and disorders, and 703 children from the general population.
Parents completed the Children Sleep Habits Questionnaire (CSHQ), a 33-item assessment tool typically used with a total score cutoff of 41 and above for identification of children with sleep disorders. The researchers also used a second, more conservative cutoff of 48 – the cutoff for the highest quartile in the general population group – to avoid overidentification with the lower cutoff.
Scores were adjusted for maternal education and race/ethnicity, family income, child age and sex, and child cognitive scores on the Mullen Scales of Early Learning (MSEL). The researchers also adjusted for genetic and/or neurologic diagnoses, including Down syndrome, fragile X, Rett syndrome, tuberous sclerosis, cerebral palsy, and neurofibromatosis.
Autistic children tended to have lower MSEL scores than the other children. Both the autistic children and those with other developmental disorders and delays were more likely than those in the general population to have neurologic or genetic conditions.
Based on a cutoff score of 48, autistic children had more than double the odds of sleep problems, compared with children in the general population (adjusted odds ratio, 2.37; P = .001) and children with other developmental delays (aOR, 2.12; P = .001).
With a cutoff of 41, ASD children’s odds of sleep problems were 1.45 times greater than the general population (P = .023) and 1.75 times greater than those with developmental delays (P = .001).
But children with developmental delays who displayed autistic characteristics did not have not significantly different prevalence of sleep problems than children with ASD had.
“The phenotypic overlay between children with ASD and children with developmental delay with ASD [characteristics] may explain the similarities in sleep disturbance among these two groups,” the authors wrote. Both groups have “higher rates of obsessive-compulsive symptoms, self-injurious behavior, ADHD symptoms, and developmental and communication impairments” than children with developmental delays without autistic characteristics.
The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
SOURCE: Reynolds AM et al. Pediatrics. 2019 Feb. 11. doi: 10.1542/peds.2018-0492.
Children with a diagnosis of autism spectrum disorder or another developmental delay or disorder that includes autistic characteristics are twice as likely to have sleeping problems, a multisite case-control study has found.
The findings match up with previous similar studies, but this study is among the largest to measure sleeping problems in children with autism spectrum disorder (ASD) with two control groups.
“ including physiologic differences, sleep disorders, developmental comorbidities, medical comorbidities causing sleep disruption, communication impairments, and behavioral disturbances,” Ann M. Reynolds, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and her associates reported in Pediatrics.
“Children with ASD are more likely to have anxiety, which may predispose them to sleep problems,” the authors added.
The study evaluated sleep habits and problems in 1,987 children aged 2-5 years. The study population included 522 children with ASD, 228 children with other developmental delays and disorders that have ASD characteristics, 534 children with other developmental delays and disorders, and 703 children from the general population.
Parents completed the Children Sleep Habits Questionnaire (CSHQ), a 33-item assessment tool typically used with a total score cutoff of 41 and above for identification of children with sleep disorders. The researchers also used a second, more conservative cutoff of 48 – the cutoff for the highest quartile in the general population group – to avoid overidentification with the lower cutoff.
Scores were adjusted for maternal education and race/ethnicity, family income, child age and sex, and child cognitive scores on the Mullen Scales of Early Learning (MSEL). The researchers also adjusted for genetic and/or neurologic diagnoses, including Down syndrome, fragile X, Rett syndrome, tuberous sclerosis, cerebral palsy, and neurofibromatosis.
Autistic children tended to have lower MSEL scores than the other children. Both the autistic children and those with other developmental disorders and delays were more likely than those in the general population to have neurologic or genetic conditions.
Based on a cutoff score of 48, autistic children had more than double the odds of sleep problems, compared with children in the general population (adjusted odds ratio, 2.37; P = .001) and children with other developmental delays (aOR, 2.12; P = .001).
With a cutoff of 41, ASD children’s odds of sleep problems were 1.45 times greater than the general population (P = .023) and 1.75 times greater than those with developmental delays (P = .001).
But children with developmental delays who displayed autistic characteristics did not have not significantly different prevalence of sleep problems than children with ASD had.
“The phenotypic overlay between children with ASD and children with developmental delay with ASD [characteristics] may explain the similarities in sleep disturbance among these two groups,” the authors wrote. Both groups have “higher rates of obsessive-compulsive symptoms, self-injurious behavior, ADHD symptoms, and developmental and communication impairments” than children with developmental delays without autistic characteristics.
The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
SOURCE: Reynolds AM et al. Pediatrics. 2019 Feb. 11. doi: 10.1542/peds.2018-0492.
FROM PEDIATRICS
Key clinical point: Sleeping problems are over twice as common in autistic children than in children in the general population.
Major finding: Children with ASD had 2.37 greater odds of sleep problems than did typically developing children.
Study details: Data from the Children Sleep Habits Questionnaire for 1,987 children, either typically developing, diagnosed with autism spectrum disorder, or diagnosed with other developmental disabilities.
Disclosures: The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr. Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
Source: Reynolds AM et al. Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-0492.
No increase in severe community-acquired pneumonia after PCV13
Despite concern about the rise of nonvaccine serotypes following widespread PCV13 immunization, cases of community-acquired pneumonia (CAP) remain nearly as low as after initial implementation of the vaccine and severe cases have not risen at all.
This was the finding of a prospective time-series analysis study from eight French pediatric emergency departments between June 2009 and May 2017.
The 12,587 children with CAP enrolled in the study between June 2009 and May 2017 were all aged 15 years or younger and came from one of eight French pediatric EDs.
Pediatric pneumonia cases per 1,000 ED visits dropped 44% after PCV13 was implemented, a decrease from 6.3 to 3.5 cases of CAP per 1,000 pediatric visits from June 2011 to May 2014, with a slight but statistically significant increase to 3.8 cases of CAP per 1,000 pediatric visits from June 2014 to May 2017. However, there was no statistically significant increase in cases with pleural effusion, hospitalization, or high inflammatory biomarkers.
“These results contrast with the recent increase in frequency of invasive pneumococcal disease observed in several countries during the same period linked to serotype replacement beyond 5 years after PCV13 implementation,” reported Naïm Ouldali, MD, of the Association Clinique et Thérapeutique Infantile du Val-de-Marne in France, and associates. The report is in JAMA Pediatrics.
“This difference in the trends suggests different consequences of serotype replacement on pneumococcal CAP vs invasive pneumococcal disease,” they wrote. “The recent slight increase in the number of all CAP cases and virus involvement may reflect changes in the epidemiology of other pathogens and/or serotype replacement with less pathogenic serotypes.”
This latter point arose from discovering no dominant serotype during the study period. Of the 11 serotypes not covered by PCV13, none appeared in more than four cases.
“The implementation of PCV13 has led to the quasi-disappearance of the more invasive serotypes and increase in others in nasopharyngeal flora, which greatly reduces the frequency of the more severe forms of CAP, but could also play a role in the slight increase in frequency of the more benign forms,” the authors reported.
Among the study’s limitations was lack of a control group, precluding the ability to attribute findings to any changes in case reporting. And “participating physicians were encouraged to not change their practice, including test use, and no other potential interfering intervention.”
Funding sources for this study included the Pediatric Infectious Diseases Group of the French Pediatrics Society, Association Clinique et Thérapeutique Infantile du Val-de-Marne, the Foundation for Medical Research and a Pfizer Investigator Initiated Research grant.
Dr Ouldali has received grants from GlaxoSmithKline, and many of the authors have financial ties and/or have received non-financial support from AstraZeneca, Biocodex, GlaxoSmithKline, Merck, Novartis, Pfizer and/or Sanofi Pasteur.
SOURCE: Ouldali N et al. JAMA Pediatrics. 2019 Feb 4. doi: 10.1001/jamapediatrics.2018.5273.
Despite concern about the rise of nonvaccine serotypes following widespread PCV13 immunization, cases of community-acquired pneumonia (CAP) remain nearly as low as after initial implementation of the vaccine and severe cases have not risen at all.
This was the finding of a prospective time-series analysis study from eight French pediatric emergency departments between June 2009 and May 2017.
The 12,587 children with CAP enrolled in the study between June 2009 and May 2017 were all aged 15 years or younger and came from one of eight French pediatric EDs.
Pediatric pneumonia cases per 1,000 ED visits dropped 44% after PCV13 was implemented, a decrease from 6.3 to 3.5 cases of CAP per 1,000 pediatric visits from June 2011 to May 2014, with a slight but statistically significant increase to 3.8 cases of CAP per 1,000 pediatric visits from June 2014 to May 2017. However, there was no statistically significant increase in cases with pleural effusion, hospitalization, or high inflammatory biomarkers.
“These results contrast with the recent increase in frequency of invasive pneumococcal disease observed in several countries during the same period linked to serotype replacement beyond 5 years after PCV13 implementation,” reported Naïm Ouldali, MD, of the Association Clinique et Thérapeutique Infantile du Val-de-Marne in France, and associates. The report is in JAMA Pediatrics.
“This difference in the trends suggests different consequences of serotype replacement on pneumococcal CAP vs invasive pneumococcal disease,” they wrote. “The recent slight increase in the number of all CAP cases and virus involvement may reflect changes in the epidemiology of other pathogens and/or serotype replacement with less pathogenic serotypes.”
This latter point arose from discovering no dominant serotype during the study period. Of the 11 serotypes not covered by PCV13, none appeared in more than four cases.
“The implementation of PCV13 has led to the quasi-disappearance of the more invasive serotypes and increase in others in nasopharyngeal flora, which greatly reduces the frequency of the more severe forms of CAP, but could also play a role in the slight increase in frequency of the more benign forms,” the authors reported.
Among the study’s limitations was lack of a control group, precluding the ability to attribute findings to any changes in case reporting. And “participating physicians were encouraged to not change their practice, including test use, and no other potential interfering intervention.”
Funding sources for this study included the Pediatric Infectious Diseases Group of the French Pediatrics Society, Association Clinique et Thérapeutique Infantile du Val-de-Marne, the Foundation for Medical Research and a Pfizer Investigator Initiated Research grant.
Dr Ouldali has received grants from GlaxoSmithKline, and many of the authors have financial ties and/or have received non-financial support from AstraZeneca, Biocodex, GlaxoSmithKline, Merck, Novartis, Pfizer and/or Sanofi Pasteur.
SOURCE: Ouldali N et al. JAMA Pediatrics. 2019 Feb 4. doi: 10.1001/jamapediatrics.2018.5273.
Despite concern about the rise of nonvaccine serotypes following widespread PCV13 immunization, cases of community-acquired pneumonia (CAP) remain nearly as low as after initial implementation of the vaccine and severe cases have not risen at all.
This was the finding of a prospective time-series analysis study from eight French pediatric emergency departments between June 2009 and May 2017.
The 12,587 children with CAP enrolled in the study between June 2009 and May 2017 were all aged 15 years or younger and came from one of eight French pediatric EDs.
Pediatric pneumonia cases per 1,000 ED visits dropped 44% after PCV13 was implemented, a decrease from 6.3 to 3.5 cases of CAP per 1,000 pediatric visits from June 2011 to May 2014, with a slight but statistically significant increase to 3.8 cases of CAP per 1,000 pediatric visits from June 2014 to May 2017. However, there was no statistically significant increase in cases with pleural effusion, hospitalization, or high inflammatory biomarkers.
“These results contrast with the recent increase in frequency of invasive pneumococcal disease observed in several countries during the same period linked to serotype replacement beyond 5 years after PCV13 implementation,” reported Naïm Ouldali, MD, of the Association Clinique et Thérapeutique Infantile du Val-de-Marne in France, and associates. The report is in JAMA Pediatrics.
“This difference in the trends suggests different consequences of serotype replacement on pneumococcal CAP vs invasive pneumococcal disease,” they wrote. “The recent slight increase in the number of all CAP cases and virus involvement may reflect changes in the epidemiology of other pathogens and/or serotype replacement with less pathogenic serotypes.”
This latter point arose from discovering no dominant serotype during the study period. Of the 11 serotypes not covered by PCV13, none appeared in more than four cases.
“The implementation of PCV13 has led to the quasi-disappearance of the more invasive serotypes and increase in others in nasopharyngeal flora, which greatly reduces the frequency of the more severe forms of CAP, but could also play a role in the slight increase in frequency of the more benign forms,” the authors reported.
Among the study’s limitations was lack of a control group, precluding the ability to attribute findings to any changes in case reporting. And “participating physicians were encouraged to not change their practice, including test use, and no other potential interfering intervention.”
Funding sources for this study included the Pediatric Infectious Diseases Group of the French Pediatrics Society, Association Clinique et Thérapeutique Infantile du Val-de-Marne, the Foundation for Medical Research and a Pfizer Investigator Initiated Research grant.
Dr Ouldali has received grants from GlaxoSmithKline, and many of the authors have financial ties and/or have received non-financial support from AstraZeneca, Biocodex, GlaxoSmithKline, Merck, Novartis, Pfizer and/or Sanofi Pasteur.
SOURCE: Ouldali N et al. JAMA Pediatrics. 2019 Feb 4. doi: 10.1001/jamapediatrics.2018.5273.
FROM JAMA PEDIATRICS
Key clinical point:
Major finding: Pediatric community-acquired pneumonia cases dropped from 6.3 to 3.5 cases per 1,000 visits from 2010 to 2014 and increased to 3.8 cases per 1,000 visits in May 2017.
Study details: The findings are based on a prospective time series analysis of 12,587 pediatric pneumonia cases (under 15 years old) in eight French emergency departments from June 2009 to May 2017.
Disclosures: Funding sources for this study included the Pediatric Infectious Diseases Group of the French Pediatrics Society, Association Clinique et Thérapeutique Infantile du Val-de-Marne, the Foundation for Medical Research, and a Pfizer Investigator Initiated Research grant. Dr. Ouldali has received grants from GlaxoSmithKline, and many of the authors have financial ties and/or have received nonfinancial support from AstraZeneca, Biocodex, GlaxoSmithKline, Merck, Novartis, Pfizer, and/or Sanofi Pasteur.
Source: Ouldali N et al. JAMA Pediatrics. 2019 Feb 4. doi: 10.1001/jamapediatrics.2018.5273.
Anxiety, depression, burnout higher in physician mothers caring for others at home
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Physicians who are also mothers have a higher risk of burnout and mood and anxiety disorders if they are also caring for someone with a serious illness or disability outside of work, according to a cross-sectional survey reported in a letter in JAMA Internal Medicine.
“Our findings highlight the additional caregiving responsibilities of some women physicians and the potential consequences of these additional responsibilities for their behavioral health and careers,” wrote Veronica Yank, MD, of the department of medicine at the University of California, San Francisco, and her colleagues.
“To reduce burnout and improve workforce retention, health care systems should develop new approaches to identify and address the needs of these physician mothers,” they wrote.
The researchers used data from a June-July 2016 online survey of respondents from the Physicians Moms Group online community. Approximately 16,059 members saw the posting for the survey, and 5,613 United States–based mothers participated.
Among the questions was one on non–work related caregiving responsibilities that asked whether the respondent provided “regular care or assistance to a friend or family member with a serious health problem, long-term illness or disability” during the last year. Other questions assessed alcohol and drug use, history of a mood or anxiety disorder, career satisfaction and burnout.
Among the 16.4% of respondents who had additional caregiving responsibilities outside of work for someone chronically or seriously ill or disabled, nearly half (48.3%) said they cared for ill parents, 16.9% for children or infants, 7.7% for a partner, and 28.6% for another relative. In addition, 16.7% of respondents had such caregiving responsibilities for more than one person.
The women with these extra caregiving responsibilities were 21% more likely to have a mood or anxiety disorder (adjusted relative risk, 1.21; P = .02) and 25% more likely to report burnout (aRR, 1.25; P = .007), compared with those who did not have such extra responsibilities.
There were no significant differences, however, on rates of career satisfaction, risky drinking behaviors, or substance abuse between physician mothers who did have additional caregiving responsibilities and those who did not.
Among the study’s limitations were its cross-sectional nature, use of a convenience sample that may not be generalizable or representative, and lack of data on fathers or non-parent physicians for comparison.
SOURCE: Yank V et al. JAMA Intern Med. 2019 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: Risk of anxiety and mood disorders is 21% higher and burnout is 25% higher among physician mothers with extra caregiving at home.
Study details: The findings are based on an online cross-sectional survey of 5,613 United States–based physician mothers conducted from June to July 2016.
Disclosures: No single entity directly funded the study, but the authors were supported by a variety of grants from foundations and the National Institutes of Health at the time it was completed. One coauthor is founder of Equity Quotient, a company that provides gender equity culture analytics for institutions, and another has consulted for Amgen and Vizient and receives stock options as an Equity Quotient advisory board member.
Source: Yank V et al. JAMA Internal Medicine. 2018 Jan 28. doi: 10.1001/jamainternmed.2018.6411.
Family handgun ownership linked to young children’s gun deaths
A recent increase in U.S. handgun ownership among white families tracks with a similar trend of recently rising gun deaths among young white children, a new study found. This association held even after adjustments for multiple sociodemographic variables that research previously had linked to higher gun ownership and higher firearm mortality.
“Indeed, firearm ownership, generally, was positively associated with firearm-related mortality among 1- to 5-year-old white children, but this correlation was primarily driven by changes in the proportion of families who owned handguns: firearms more often stored unsecured and loaded,” wrote Kate C. Prickett, PhD, of the Victoria University of Wellington (New Zealand) and her associates in Pediatrics.
“These findings suggest that ease of access and use may be an important consideration when examining firearm-related fatality risk among young children,” they continued. Given the lack of attenuation in the relationship from controlling for sociodemographic variables, they add, “this finding is in line with research documenting that the presence of a firearm in the home matters above and beyond other risk factors associated with child injury.”
Even though U.S. gun ownership and pediatric firearm mortality overall have been dropping over the past several decades, the latter has stagnated recently, and gun deaths among children aged 1-4 years nearly doubled between 2006-2016, the researchers noted.
Given the counterintuitive increase in young children’s gun deaths while overall gun ownership kept dropping, the researchers took a closer look at the relationship between gun deaths among children aged 1-5 years and specific types of firearm ownership among families with children under age 5 years in the home. They relied on household data from the nationally representative General Social Survey and on fatality statistics from the National Vital Statistics System from 1976-2016.
Over those 4 decades, gun ownership in white families with small children decreased from 50% to 45% and in black families with small children from 38% to 6%.
Simultaneously, however, handgun ownership increased from 25% to 32% among white families with young children. In fact, most firearm-owning white families (72%) owned a handgun in 2016 while rifle ownership had declined substantially.
Meanwhile, “firearm-related mortality rate among young white children declined from historic highs in the late 1970s to early 1980s until 2001,” the authors reported. “After 2004, however, the mortality rate began to rise, reaching mid-1980s levels.” Further, gun deaths constituted 2% of young children’s injury deaths in 1976 but nearly 5% in 2016.
When the researchers compared these findings, they found a positive, significant association between white child firearm mortality and the proportion of white families who owned a handgun but not a rifle or shotgun.
The association remained after the researchers adjusted for several covariates already established in the evidence base to have associations with firearm ownership, child injury risk and/or firearm mortality: living in a rural area, living in the South, neither parent having a college degree, and a household income in the bottom quartile nationally. In addition, “the annual national unemployment rate by race was included as an indicator of the broader economic context,” the authors wrote.
Although young black children die from guns nearly three times more frequently than white children, the authors were unable to present detailed findings on associations with gun ownership because of small sample sizes. They noted, however, that handgun ownership actually declined during the study period from 15% to 6% in black families with young children.
The researchers concluded that the recent increase in young children’s gun deaths may be partly driven by an increase in handgun ownership, even as overall gun ownership (primarily rifles and shotguns) has continued dropping.
“For young children, shootings are more likely to be unintentional, making the ease at which firearms can be accessed and used a more important determinant of mortality than perhaps for older children,” the authors wrote. “Moreover, relative to other firearms like hunting rifles, handguns, because they are more likely to be purchased for personal protection, are more likely to be stored loaded with ammunition, unlocked, and in a more easily accessible place, such as a bedroom drawer.”
The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
SOURCE: Prickett KC et al. Pediatrics. 2019;143(2):e20181171.
The “unique and important approach” used by Prickett et al. to investigate an association between gun ownership and children’s gun deaths is “novel” because of their focus on firearm types and the youngest children, wrote Shilpa J. Patel, MD; Monika K. Goyal, MD; and Kavita Parikh, MD, all with the Children’s National Health System in Washington, DC, in an editorial published with the study (Pediatrics. 2018 Jan 28. doi: 10.1542/peds.2018-3611).
The findings are particularly relevant to pediatricians’ conversations with families about safe firearm storage practices. The American Academy of Pediatrics recommends all firearms are stored locked and unloaded with ammunition stored separately.
For families who find these guidelines difficult because they keep handguns at the ready for protection, “it is important to note that the risk of unintentional or intentional injury from a household firearm is much greater than the likelihood of providing protection for self-defense,” the editorial’s authors wrote. But they advocate for personalized safe storage strategies and shared decision making based on families’ needs and values.
“This study is a loud and compelling call to action for all pediatricians to start open discussions around firearm ownership with all families and to share data on the significant risks associated with unsafe storage,” they wrote. “It is an even louder call to firearm manufacturers to step up and innovate, test, and design smart handguns that are inoperable by young children to prevent unintentional injury.”
Although having no firearms in the home is the most effective way to reduce children’s risk of gun-related injuries and deaths, developing effective safety controls on guns could also substantially curtail young children’s gun deaths. “We as a society should be advocating for continued research to childproof firearms so that if families choose to have firearms in the home, the safety of their children is not compromised,” they wrote.
Dr. Parikh is a hospitalist, Dr. Goyal is assistant division chief or emergency medicine, and Dr. Patel is an emergency medicine specialist, all with Children’s National Health System in Washington, DC. They reported no funding and no disclosures.
The “unique and important approach” used by Prickett et al. to investigate an association between gun ownership and children’s gun deaths is “novel” because of their focus on firearm types and the youngest children, wrote Shilpa J. Patel, MD; Monika K. Goyal, MD; and Kavita Parikh, MD, all with the Children’s National Health System in Washington, DC, in an editorial published with the study (Pediatrics. 2018 Jan 28. doi: 10.1542/peds.2018-3611).
The findings are particularly relevant to pediatricians’ conversations with families about safe firearm storage practices. The American Academy of Pediatrics recommends all firearms are stored locked and unloaded with ammunition stored separately.
For families who find these guidelines difficult because they keep handguns at the ready for protection, “it is important to note that the risk of unintentional or intentional injury from a household firearm is much greater than the likelihood of providing protection for self-defense,” the editorial’s authors wrote. But they advocate for personalized safe storage strategies and shared decision making based on families’ needs and values.
“This study is a loud and compelling call to action for all pediatricians to start open discussions around firearm ownership with all families and to share data on the significant risks associated with unsafe storage,” they wrote. “It is an even louder call to firearm manufacturers to step up and innovate, test, and design smart handguns that are inoperable by young children to prevent unintentional injury.”
Although having no firearms in the home is the most effective way to reduce children’s risk of gun-related injuries and deaths, developing effective safety controls on guns could also substantially curtail young children’s gun deaths. “We as a society should be advocating for continued research to childproof firearms so that if families choose to have firearms in the home, the safety of their children is not compromised,” they wrote.
Dr. Parikh is a hospitalist, Dr. Goyal is assistant division chief or emergency medicine, and Dr. Patel is an emergency medicine specialist, all with Children’s National Health System in Washington, DC. They reported no funding and no disclosures.
The “unique and important approach” used by Prickett et al. to investigate an association between gun ownership and children’s gun deaths is “novel” because of their focus on firearm types and the youngest children, wrote Shilpa J. Patel, MD; Monika K. Goyal, MD; and Kavita Parikh, MD, all with the Children’s National Health System in Washington, DC, in an editorial published with the study (Pediatrics. 2018 Jan 28. doi: 10.1542/peds.2018-3611).
The findings are particularly relevant to pediatricians’ conversations with families about safe firearm storage practices. The American Academy of Pediatrics recommends all firearms are stored locked and unloaded with ammunition stored separately.
For families who find these guidelines difficult because they keep handguns at the ready for protection, “it is important to note that the risk of unintentional or intentional injury from a household firearm is much greater than the likelihood of providing protection for self-defense,” the editorial’s authors wrote. But they advocate for personalized safe storage strategies and shared decision making based on families’ needs and values.
“This study is a loud and compelling call to action for all pediatricians to start open discussions around firearm ownership with all families and to share data on the significant risks associated with unsafe storage,” they wrote. “It is an even louder call to firearm manufacturers to step up and innovate, test, and design smart handguns that are inoperable by young children to prevent unintentional injury.”
Although having no firearms in the home is the most effective way to reduce children’s risk of gun-related injuries and deaths, developing effective safety controls on guns could also substantially curtail young children’s gun deaths. “We as a society should be advocating for continued research to childproof firearms so that if families choose to have firearms in the home, the safety of their children is not compromised,” they wrote.
Dr. Parikh is a hospitalist, Dr. Goyal is assistant division chief or emergency medicine, and Dr. Patel is an emergency medicine specialist, all with Children’s National Health System in Washington, DC. They reported no funding and no disclosures.
A recent increase in U.S. handgun ownership among white families tracks with a similar trend of recently rising gun deaths among young white children, a new study found. This association held even after adjustments for multiple sociodemographic variables that research previously had linked to higher gun ownership and higher firearm mortality.
“Indeed, firearm ownership, generally, was positively associated with firearm-related mortality among 1- to 5-year-old white children, but this correlation was primarily driven by changes in the proportion of families who owned handguns: firearms more often stored unsecured and loaded,” wrote Kate C. Prickett, PhD, of the Victoria University of Wellington (New Zealand) and her associates in Pediatrics.
“These findings suggest that ease of access and use may be an important consideration when examining firearm-related fatality risk among young children,” they continued. Given the lack of attenuation in the relationship from controlling for sociodemographic variables, they add, “this finding is in line with research documenting that the presence of a firearm in the home matters above and beyond other risk factors associated with child injury.”
Even though U.S. gun ownership and pediatric firearm mortality overall have been dropping over the past several decades, the latter has stagnated recently, and gun deaths among children aged 1-4 years nearly doubled between 2006-2016, the researchers noted.
Given the counterintuitive increase in young children’s gun deaths while overall gun ownership kept dropping, the researchers took a closer look at the relationship between gun deaths among children aged 1-5 years and specific types of firearm ownership among families with children under age 5 years in the home. They relied on household data from the nationally representative General Social Survey and on fatality statistics from the National Vital Statistics System from 1976-2016.
Over those 4 decades, gun ownership in white families with small children decreased from 50% to 45% and in black families with small children from 38% to 6%.
Simultaneously, however, handgun ownership increased from 25% to 32% among white families with young children. In fact, most firearm-owning white families (72%) owned a handgun in 2016 while rifle ownership had declined substantially.
Meanwhile, “firearm-related mortality rate among young white children declined from historic highs in the late 1970s to early 1980s until 2001,” the authors reported. “After 2004, however, the mortality rate began to rise, reaching mid-1980s levels.” Further, gun deaths constituted 2% of young children’s injury deaths in 1976 but nearly 5% in 2016.
When the researchers compared these findings, they found a positive, significant association between white child firearm mortality and the proportion of white families who owned a handgun but not a rifle or shotgun.
The association remained after the researchers adjusted for several covariates already established in the evidence base to have associations with firearm ownership, child injury risk and/or firearm mortality: living in a rural area, living in the South, neither parent having a college degree, and a household income in the bottom quartile nationally. In addition, “the annual national unemployment rate by race was included as an indicator of the broader economic context,” the authors wrote.
Although young black children die from guns nearly three times more frequently than white children, the authors were unable to present detailed findings on associations with gun ownership because of small sample sizes. They noted, however, that handgun ownership actually declined during the study period from 15% to 6% in black families with young children.
The researchers concluded that the recent increase in young children’s gun deaths may be partly driven by an increase in handgun ownership, even as overall gun ownership (primarily rifles and shotguns) has continued dropping.
“For young children, shootings are more likely to be unintentional, making the ease at which firearms can be accessed and used a more important determinant of mortality than perhaps for older children,” the authors wrote. “Moreover, relative to other firearms like hunting rifles, handguns, because they are more likely to be purchased for personal protection, are more likely to be stored loaded with ammunition, unlocked, and in a more easily accessible place, such as a bedroom drawer.”
The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
SOURCE: Prickett KC et al. Pediatrics. 2019;143(2):e20181171.
A recent increase in U.S. handgun ownership among white families tracks with a similar trend of recently rising gun deaths among young white children, a new study found. This association held even after adjustments for multiple sociodemographic variables that research previously had linked to higher gun ownership and higher firearm mortality.
“Indeed, firearm ownership, generally, was positively associated with firearm-related mortality among 1- to 5-year-old white children, but this correlation was primarily driven by changes in the proportion of families who owned handguns: firearms more often stored unsecured and loaded,” wrote Kate C. Prickett, PhD, of the Victoria University of Wellington (New Zealand) and her associates in Pediatrics.
“These findings suggest that ease of access and use may be an important consideration when examining firearm-related fatality risk among young children,” they continued. Given the lack of attenuation in the relationship from controlling for sociodemographic variables, they add, “this finding is in line with research documenting that the presence of a firearm in the home matters above and beyond other risk factors associated with child injury.”
Even though U.S. gun ownership and pediatric firearm mortality overall have been dropping over the past several decades, the latter has stagnated recently, and gun deaths among children aged 1-4 years nearly doubled between 2006-2016, the researchers noted.
Given the counterintuitive increase in young children’s gun deaths while overall gun ownership kept dropping, the researchers took a closer look at the relationship between gun deaths among children aged 1-5 years and specific types of firearm ownership among families with children under age 5 years in the home. They relied on household data from the nationally representative General Social Survey and on fatality statistics from the National Vital Statistics System from 1976-2016.
Over those 4 decades, gun ownership in white families with small children decreased from 50% to 45% and in black families with small children from 38% to 6%.
Simultaneously, however, handgun ownership increased from 25% to 32% among white families with young children. In fact, most firearm-owning white families (72%) owned a handgun in 2016 while rifle ownership had declined substantially.
Meanwhile, “firearm-related mortality rate among young white children declined from historic highs in the late 1970s to early 1980s until 2001,” the authors reported. “After 2004, however, the mortality rate began to rise, reaching mid-1980s levels.” Further, gun deaths constituted 2% of young children’s injury deaths in 1976 but nearly 5% in 2016.
When the researchers compared these findings, they found a positive, significant association between white child firearm mortality and the proportion of white families who owned a handgun but not a rifle or shotgun.
The association remained after the researchers adjusted for several covariates already established in the evidence base to have associations with firearm ownership, child injury risk and/or firearm mortality: living in a rural area, living in the South, neither parent having a college degree, and a household income in the bottom quartile nationally. In addition, “the annual national unemployment rate by race was included as an indicator of the broader economic context,” the authors wrote.
Although young black children die from guns nearly three times more frequently than white children, the authors were unable to present detailed findings on associations with gun ownership because of small sample sizes. They noted, however, that handgun ownership actually declined during the study period from 15% to 6% in black families with young children.
The researchers concluded that the recent increase in young children’s gun deaths may be partly driven by an increase in handgun ownership, even as overall gun ownership (primarily rifles and shotguns) has continued dropping.
“For young children, shootings are more likely to be unintentional, making the ease at which firearms can be accessed and used a more important determinant of mortality than perhaps for older children,” the authors wrote. “Moreover, relative to other firearms like hunting rifles, handguns, because they are more likely to be purchased for personal protection, are more likely to be stored loaded with ammunition, unlocked, and in a more easily accessible place, such as a bedroom drawer.”
The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
SOURCE: Prickett KC et al. Pediatrics. 2019;143(2):e20181171.
FROM PEDIATRICS
Key clinical point: Greater handgun ownership in families may increase young children’s risk of gun death.
Major finding: Handgun ownership in white families with young children rose from 25% to 32% during 1976-2016, alongside increasing rates of firearm deaths in young white children.
Study details: The findings are based on analysis of data on U.S. family firearm ownership and pediatric gun deaths in the General Social Study and National Vital Statistics System from 1976-2016.
Disclosures: The research was funded by the National Institute of Child Health and Human Development. The authors reported having no conflicts of interest.
Source: Prickett KC et al. Pediatrics. 2019 Jan 28;143(2):e20181171.
Unintentional injuries top killer of U.S. children
Unintentional injuries accounted for more than half of all deaths among U.S. children aged 1-19 years in 2016, according to a new study based on data from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (WONDER) database. 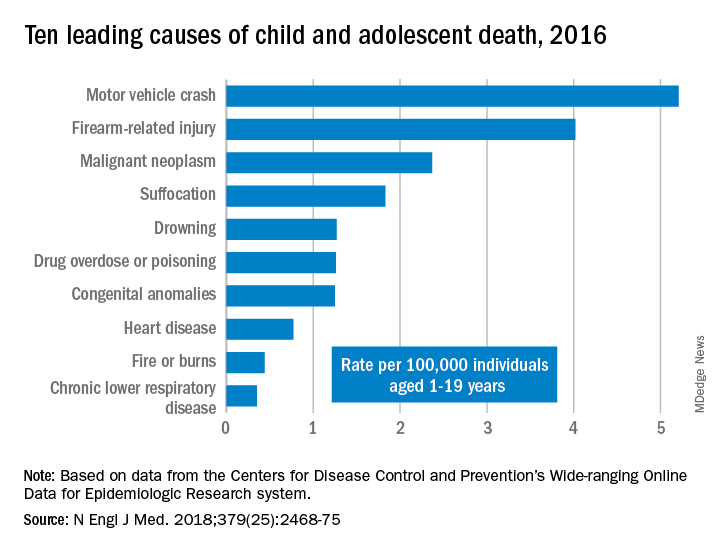
WONDER collects data from U.S. death certificates for 57 vital-statistics jurisdictions, and the 2016 data included 20,360 deaths. Injuries accounted for 12,336 deaths; unintentional injuries accounted for 57% or 7,057 deaths. Approximately one in five U.S. youth deaths (21%) were suicides, and another one in five (20%) were homicides.
Motor vehicle accidents, also responsible for one in five (20%) of all deaths, were the leading cause of accidental deaths, followed by firearm-related injuries, which accounted for 15% of all deaths. Of the firearm-related deaths, 59% were homicides, 35% suicides, 4% accidental, and 2% undetermined.
The only high-ranking noninjury cause of death overall was neoplasms, yet childhood cancer accounted for just 9% of all deaths. Suffocation was the cause of 7% of deaths, and included homicides, suicides and unintentional injuries.
The remaining causes included drowning (5.9%), drug overdose or poisoning (4.8%), congenital anomalies (4.8%), heart disease (2.9%), fire or burns (1.7%) and chronic lower respiratory disease (1.3%).
“Progress toward further reducing deaths among children and adolescents will require a shift in public perceptions so that injury deaths are viewed not as ‘accidents,’ but rather as social ecologic phenomena that are amenable to prevention,” wrote Rebecca M. Cunningham, MD, and her colleagues at the University of Michigan, Ann Arbor (N Engl J Med. 2018 Dec 20. doi: 10.1056/NEJMsr1804754). The findings “highlight the need to implement public health strategies that are tailored according to age, underlying developmental factors, and injury-related intent” to reduce the risk for death in children.”
“The sad fact is that a child or adolescent in the United States is 57% more likely to die by the age of 19 years than those in other wealthy nations,” Edward W. Campion, MD, executive editor and online editor of the New England Journal of Medicine, wrote in an editorial that accompanied the study (N Engl J Med. 2018 Dec. 20;379[25]:2466-7. doi: 10.1056/NEJMe1814600). “Children in America are dying or being killed at rates that are shameful.
“Our country has led the way in so much medical research, but the facts summarized by Cunningham et al. reveal a need to invest far more in research on the prevention of the injuries that threaten the lives of children and adolescents,” he said.
In an interview, Ben Hoffman, MD, professor of pediatrics at Oregon Health and Science University, Portland, said the only thing surprising in this report is that nothing is surprising.
“This is the stuff that those of us in injury prevention have been screaming about for decades,” said Dr. Hoffman, also medical director of the Tom Sargent Safety Center at OHSU Doernbecher Children’s Hospital.
“Unintentional injuries are what kill kids. We have made such tremendous progress in other areas, and we’ve made progress in terms of preventing injuries, but what we see is unacceptable,” he said. “The fact that [injuries] remain such an issue is a testament to the fact that our collective will [to address these issues] has failed us.”
Among children aged 1-4, drowning was the leading cause of death, followed by congenital anomalies and motor vehicle crashes.
Mandated four-sided fencing around pools is a highly effective intervention for reducing drowning risks, Dr. Hoffman said.
Children aged 5-9 represented the smallest proportion of all youth deaths (12%) and were the only age group not to have injuries as the leading cause of death. Malignant neoplasms led the causes of death in this group, followed by car accidents and congenital anomalies.
Adolescents aged 10-19, the widest age range, comprised 68% of all youth deaths, led by motor vehicle accidents, firearms, and suffocation.
“These findings reflect social and developmental factors that are associated with adolescence, including increased risk-taking behavior, differential peer and parental influence, and initiation of substance use,” Dr. Cunningham and her colleagues wrote.
The most concerning trends, according to Dr. Hoffman, were the upticks in motor vehicle deaths, suffocation, and poisonings, the latter driven largely by opioid overdoses, which were responsible for more than half of all overdoses in adolescents.
Addressing these issues “will require an investment in kids, which is not something that our society does really well,” Dr. Hoffman said. “We talk about it, we tiptoe around it, but when push comes to shove, nobody is really willing to support and fund the efforts to do it.”
In his editorial, Dr. Campion observed that despite a decades-long trend of decreasing mortality from car accidents, these deaths began steadily increasing from 2013 to 2016.
Previous gains in this area came from “the widespread adoption of seat belts and appropriate child safety seats, the production of cars with improved safety standards, better constructed roads, graduated driver-licensing programs, and a focus on reducing teen drinking and driving,” the authors stated. Multiple reasons likely account for the reversal, including distracted driving and possibly marijuana use, though the latter requires more data.
Firearm deaths increased by 28% from 2013 to 2016, driven by suicides (a 26% increase) and homicides (a 32% increase), including increasing school shootings.
Dr. Hoffman acknowledged the complexities of addressing firearm deaths, but “there are effective common sense interventions that could be made ... there’s just not the will.” An example is passing child access prevention (CAP) laws, such as mandating safe storage of guns and imposing criminal liability when children negligently acquire access to firearms. While a variety of small groups address child injury issues, a large, coordinated, centralized national advocacy for kids is lacking, he added.
“The approach to this underrecognized public health problem has to be social as well as technological, and the risks are highest in areas of poverty and social isolation,” Dr. Campion wrote. “We are living in a divisive era in which there are few areas of consensus and agreement. Perhaps one of the few core beliefs that all can agree on is that deaths in childhood and adolescence are tragedies that we must find ways to prevent.”
“Every day, 10 babies die in their sleep, 1.7 kids under age 4 drown, and 4 kids over the age of 1 die in car crashes,” Dr. Hoffman said. “We need to acknowledge the impact of unintentional and intentional injuries and recognize that there are things we can do, that we’re complicit in all of those deaths because in every circumstance, there is something we as a society could have done.”
SOURCE: Cunningham et al. N Engl J Med. 2018 Dec 20;379(25):2468-75. doi: 10.1056/NEJMsr1804754.
Unintentional injuries accounted for more than half of all deaths among U.S. children aged 1-19 years in 2016, according to a new study based on data from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (WONDER) database. 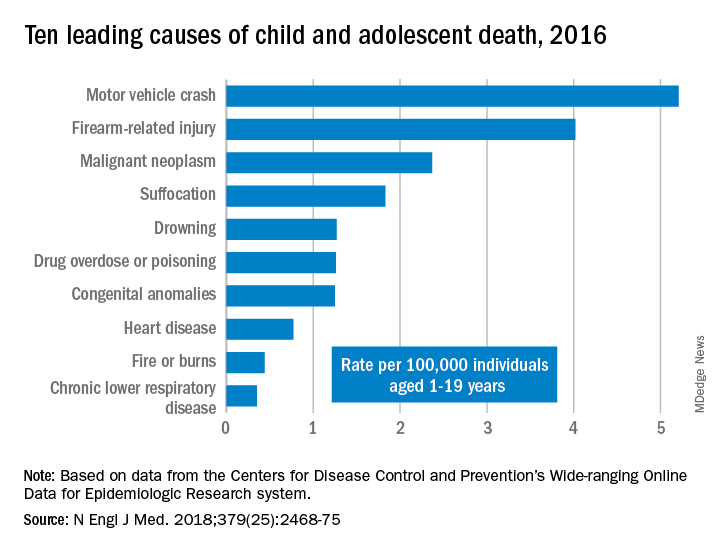
WONDER collects data from U.S. death certificates for 57 vital-statistics jurisdictions, and the 2016 data included 20,360 deaths. Injuries accounted for 12,336 deaths; unintentional injuries accounted for 57% or 7,057 deaths. Approximately one in five U.S. youth deaths (21%) were suicides, and another one in five (20%) were homicides.
Motor vehicle accidents, also responsible for one in five (20%) of all deaths, were the leading cause of accidental deaths, followed by firearm-related injuries, which accounted for 15% of all deaths. Of the firearm-related deaths, 59% were homicides, 35% suicides, 4% accidental, and 2% undetermined.
The only high-ranking noninjury cause of death overall was neoplasms, yet childhood cancer accounted for just 9% of all deaths. Suffocation was the cause of 7% of deaths, and included homicides, suicides and unintentional injuries.
The remaining causes included drowning (5.9%), drug overdose or poisoning (4.8%), congenital anomalies (4.8%), heart disease (2.9%), fire or burns (1.7%) and chronic lower respiratory disease (1.3%).
“Progress toward further reducing deaths among children and adolescents will require a shift in public perceptions so that injury deaths are viewed not as ‘accidents,’ but rather as social ecologic phenomena that are amenable to prevention,” wrote Rebecca M. Cunningham, MD, and her colleagues at the University of Michigan, Ann Arbor (N Engl J Med. 2018 Dec 20. doi: 10.1056/NEJMsr1804754). The findings “highlight the need to implement public health strategies that are tailored according to age, underlying developmental factors, and injury-related intent” to reduce the risk for death in children.”
“The sad fact is that a child or adolescent in the United States is 57% more likely to die by the age of 19 years than those in other wealthy nations,” Edward W. Campion, MD, executive editor and online editor of the New England Journal of Medicine, wrote in an editorial that accompanied the study (N Engl J Med. 2018 Dec. 20;379[25]:2466-7. doi: 10.1056/NEJMe1814600). “Children in America are dying or being killed at rates that are shameful.
“Our country has led the way in so much medical research, but the facts summarized by Cunningham et al. reveal a need to invest far more in research on the prevention of the injuries that threaten the lives of children and adolescents,” he said.
In an interview, Ben Hoffman, MD, professor of pediatrics at Oregon Health and Science University, Portland, said the only thing surprising in this report is that nothing is surprising.
“This is the stuff that those of us in injury prevention have been screaming about for decades,” said Dr. Hoffman, also medical director of the Tom Sargent Safety Center at OHSU Doernbecher Children’s Hospital.
“Unintentional injuries are what kill kids. We have made such tremendous progress in other areas, and we’ve made progress in terms of preventing injuries, but what we see is unacceptable,” he said. “The fact that [injuries] remain such an issue is a testament to the fact that our collective will [to address these issues] has failed us.”
Among children aged 1-4, drowning was the leading cause of death, followed by congenital anomalies and motor vehicle crashes.
Mandated four-sided fencing around pools is a highly effective intervention for reducing drowning risks, Dr. Hoffman said.
Children aged 5-9 represented the smallest proportion of all youth deaths (12%) and were the only age group not to have injuries as the leading cause of death. Malignant neoplasms led the causes of death in this group, followed by car accidents and congenital anomalies.
Adolescents aged 10-19, the widest age range, comprised 68% of all youth deaths, led by motor vehicle accidents, firearms, and suffocation.
“These findings reflect social and developmental factors that are associated with adolescence, including increased risk-taking behavior, differential peer and parental influence, and initiation of substance use,” Dr. Cunningham and her colleagues wrote.
The most concerning trends, according to Dr. Hoffman, were the upticks in motor vehicle deaths, suffocation, and poisonings, the latter driven largely by opioid overdoses, which were responsible for more than half of all overdoses in adolescents.
Addressing these issues “will require an investment in kids, which is not something that our society does really well,” Dr. Hoffman said. “We talk about it, we tiptoe around it, but when push comes to shove, nobody is really willing to support and fund the efforts to do it.”
In his editorial, Dr. Campion observed that despite a decades-long trend of decreasing mortality from car accidents, these deaths began steadily increasing from 2013 to 2016.
Previous gains in this area came from “the widespread adoption of seat belts and appropriate child safety seats, the production of cars with improved safety standards, better constructed roads, graduated driver-licensing programs, and a focus on reducing teen drinking and driving,” the authors stated. Multiple reasons likely account for the reversal, including distracted driving and possibly marijuana use, though the latter requires more data.
Firearm deaths increased by 28% from 2013 to 2016, driven by suicides (a 26% increase) and homicides (a 32% increase), including increasing school shootings.
Dr. Hoffman acknowledged the complexities of addressing firearm deaths, but “there are effective common sense interventions that could be made ... there’s just not the will.” An example is passing child access prevention (CAP) laws, such as mandating safe storage of guns and imposing criminal liability when children negligently acquire access to firearms. While a variety of small groups address child injury issues, a large, coordinated, centralized national advocacy for kids is lacking, he added.
“The approach to this underrecognized public health problem has to be social as well as technological, and the risks are highest in areas of poverty and social isolation,” Dr. Campion wrote. “We are living in a divisive era in which there are few areas of consensus and agreement. Perhaps one of the few core beliefs that all can agree on is that deaths in childhood and adolescence are tragedies that we must find ways to prevent.”
“Every day, 10 babies die in their sleep, 1.7 kids under age 4 drown, and 4 kids over the age of 1 die in car crashes,” Dr. Hoffman said. “We need to acknowledge the impact of unintentional and intentional injuries and recognize that there are things we can do, that we’re complicit in all of those deaths because in every circumstance, there is something we as a society could have done.”
SOURCE: Cunningham et al. N Engl J Med. 2018 Dec 20;379(25):2468-75. doi: 10.1056/NEJMsr1804754.
Unintentional injuries accounted for more than half of all deaths among U.S. children aged 1-19 years in 2016, according to a new study based on data from the Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (WONDER) database. 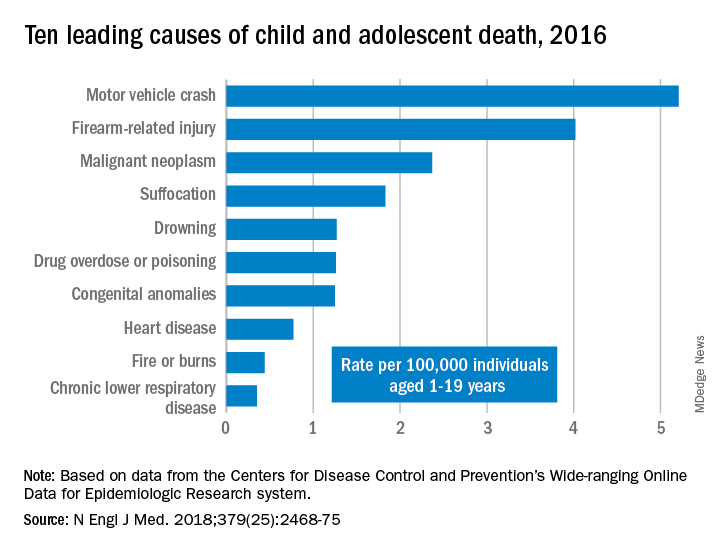
WONDER collects data from U.S. death certificates for 57 vital-statistics jurisdictions, and the 2016 data included 20,360 deaths. Injuries accounted for 12,336 deaths; unintentional injuries accounted for 57% or 7,057 deaths. Approximately one in five U.S. youth deaths (21%) were suicides, and another one in five (20%) were homicides.
Motor vehicle accidents, also responsible for one in five (20%) of all deaths, were the leading cause of accidental deaths, followed by firearm-related injuries, which accounted for 15% of all deaths. Of the firearm-related deaths, 59% were homicides, 35% suicides, 4% accidental, and 2% undetermined.
The only high-ranking noninjury cause of death overall was neoplasms, yet childhood cancer accounted for just 9% of all deaths. Suffocation was the cause of 7% of deaths, and included homicides, suicides and unintentional injuries.
The remaining causes included drowning (5.9%), drug overdose or poisoning (4.8%), congenital anomalies (4.8%), heart disease (2.9%), fire or burns (1.7%) and chronic lower respiratory disease (1.3%).
“Progress toward further reducing deaths among children and adolescents will require a shift in public perceptions so that injury deaths are viewed not as ‘accidents,’ but rather as social ecologic phenomena that are amenable to prevention,” wrote Rebecca M. Cunningham, MD, and her colleagues at the University of Michigan, Ann Arbor (N Engl J Med. 2018 Dec 20. doi: 10.1056/NEJMsr1804754). The findings “highlight the need to implement public health strategies that are tailored according to age, underlying developmental factors, and injury-related intent” to reduce the risk for death in children.”
“The sad fact is that a child or adolescent in the United States is 57% more likely to die by the age of 19 years than those in other wealthy nations,” Edward W. Campion, MD, executive editor and online editor of the New England Journal of Medicine, wrote in an editorial that accompanied the study (N Engl J Med. 2018 Dec. 20;379[25]:2466-7. doi: 10.1056/NEJMe1814600). “Children in America are dying or being killed at rates that are shameful.
“Our country has led the way in so much medical research, but the facts summarized by Cunningham et al. reveal a need to invest far more in research on the prevention of the injuries that threaten the lives of children and adolescents,” he said.
In an interview, Ben Hoffman, MD, professor of pediatrics at Oregon Health and Science University, Portland, said the only thing surprising in this report is that nothing is surprising.
“This is the stuff that those of us in injury prevention have been screaming about for decades,” said Dr. Hoffman, also medical director of the Tom Sargent Safety Center at OHSU Doernbecher Children’s Hospital.
“Unintentional injuries are what kill kids. We have made such tremendous progress in other areas, and we’ve made progress in terms of preventing injuries, but what we see is unacceptable,” he said. “The fact that [injuries] remain such an issue is a testament to the fact that our collective will [to address these issues] has failed us.”
Among children aged 1-4, drowning was the leading cause of death, followed by congenital anomalies and motor vehicle crashes.
Mandated four-sided fencing around pools is a highly effective intervention for reducing drowning risks, Dr. Hoffman said.
Children aged 5-9 represented the smallest proportion of all youth deaths (12%) and were the only age group not to have injuries as the leading cause of death. Malignant neoplasms led the causes of death in this group, followed by car accidents and congenital anomalies.
Adolescents aged 10-19, the widest age range, comprised 68% of all youth deaths, led by motor vehicle accidents, firearms, and suffocation.
“These findings reflect social and developmental factors that are associated with adolescence, including increased risk-taking behavior, differential peer and parental influence, and initiation of substance use,” Dr. Cunningham and her colleagues wrote.
The most concerning trends, according to Dr. Hoffman, were the upticks in motor vehicle deaths, suffocation, and poisonings, the latter driven largely by opioid overdoses, which were responsible for more than half of all overdoses in adolescents.
Addressing these issues “will require an investment in kids, which is not something that our society does really well,” Dr. Hoffman said. “We talk about it, we tiptoe around it, but when push comes to shove, nobody is really willing to support and fund the efforts to do it.”
In his editorial, Dr. Campion observed that despite a decades-long trend of decreasing mortality from car accidents, these deaths began steadily increasing from 2013 to 2016.
Previous gains in this area came from “the widespread adoption of seat belts and appropriate child safety seats, the production of cars with improved safety standards, better constructed roads, graduated driver-licensing programs, and a focus on reducing teen drinking and driving,” the authors stated. Multiple reasons likely account for the reversal, including distracted driving and possibly marijuana use, though the latter requires more data.
Firearm deaths increased by 28% from 2013 to 2016, driven by suicides (a 26% increase) and homicides (a 32% increase), including increasing school shootings.
Dr. Hoffman acknowledged the complexities of addressing firearm deaths, but “there are effective common sense interventions that could be made ... there’s just not the will.” An example is passing child access prevention (CAP) laws, such as mandating safe storage of guns and imposing criminal liability when children negligently acquire access to firearms. While a variety of small groups address child injury issues, a large, coordinated, centralized national advocacy for kids is lacking, he added.
“The approach to this underrecognized public health problem has to be social as well as technological, and the risks are highest in areas of poverty and social isolation,” Dr. Campion wrote. “We are living in a divisive era in which there are few areas of consensus and agreement. Perhaps one of the few core beliefs that all can agree on is that deaths in childhood and adolescence are tragedies that we must find ways to prevent.”
“Every day, 10 babies die in their sleep, 1.7 kids under age 4 drown, and 4 kids over the age of 1 die in car crashes,” Dr. Hoffman said. “We need to acknowledge the impact of unintentional and intentional injuries and recognize that there are things we can do, that we’re complicit in all of those deaths because in every circumstance, there is something we as a society could have done.”
SOURCE: Cunningham et al. N Engl J Med. 2018 Dec 20;379(25):2468-75. doi: 10.1056/NEJMsr1804754.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Injury prevention efforts are needed to address unintentional injuries, the leading cause of death in U.S. children.
Major finding: Unintentional injuries were the cause of death for 57% of U.S. children aged 1-19 in 2016.
Study details: The findings are based on an analysis of the CDC WONDER database mortality data on 20,360 deaths of U.S. youth aged 1-19.
Disclosures: No external funding was noted. The authors and Dr. Hoffman had no relevant financial disclosures. Dr. Campion is executive editor of the New England Journal of Medicine.
Source: Cunningham et al. N Engl J Med. 2018 Dec 20;379(25):2468-75. doi: 10.1056/NEJMsr1804754.
















